User login
Welcome to Current Psychiatry, a leading source of information, online and in print, for practitioners of psychiatry and its related subspecialties, including addiction psychiatry, child and adolescent psychiatry, and geriatric psychiatry. This Web site contains evidence-based reviews of the prevention, diagnosis, and treatment of mental illness and psychological disorders; case reports; updates on psychopharmacology; news about the specialty of psychiatry; pearls for practice; and other topics of interest and use to this audience.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-current-psychiatry')]
div[contains(@class, 'pane-pub-home-current-psychiatry')]
div[contains(@class, 'pane-pub-topic-current-psychiatry')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
High-dose antipsychotics
Pierre et al and Preskorn (Current Psychiatry, August 2004) address an important treatment issue that has not been well investigated. Titrating an antipsychotic dosage too high and too soon is common in many settings, especially where treatment-resistant patients are numerous.1 But while I advise trainees to use the lowest effective antipsychotic dosage, several justifications exist for exceeding what is arbitrarily regarded as the “approved” dose range:
- FDA registration trials of antipsychotics exclude treatment-resistant/refractory patients. Thus, the “approved” dose range applies only to those with good or adequate treatment response.
- Smoking induces the cytochrome P-450 1A2 isoenzyme, which oxidizes olanzapine. Thus, heavy smokers—especially those who are rapid metabolizers—may need much higher olanzapine dosages to compensate for the rapid clearance.
- The number of dopamine (D2) receptors varies among patients even at psychosis onset. Kapur et al2 gave a fixed dose of haloperidol to 22 subjects with first-episode psychosis. Only a few developed extrapyramidal symptoms (ie, achieved >78% D2receptor occupancy). D2receptor occupancy ranged from 38% to 87%, suggesting that while some patients with relatively few D2 receptors may respond to lower dosages, others may need higher dosages to achieve response (<65% D2 receptor occupancy).
- Different dosages may be needed at different phases of the illness. For example, much higher antipsychotic (or lithium) dosages are needed for acute mania than for maintenance.
- A psychotropic may sometimes exert different neurochemical effects at high vs low dosages. For example, a typical antipsychotic’s serotonin antagonist effects may be more apparent at lower dosages, while the dopamine antagonist effect is more prominent at higher dosages.
- In the United States, roughly 35% of persons with schizophrenia receive two or more concomitant antipsychotics. Although no controlled studies have shown that combination antipsychotic therapy is superior to monotherapy, many clinicians claim that some patients respond better to two atypicals than to one. This may be because of a net higher antipsychotic dosage, which may be therapeutic for treatment-resistant patients.
Use of antipsychotic dosages beyond the FDA-approved range is poorly studied and not evidence-based, but may be justified in some patients despite the higher risk of adverse events. Controlled trials addressing this issue are needed to help clinicians manage patients who perpetually fail to respond to approved dosage ranges. Treatment-resistant patients may be a biologically different subtype than responsive patients3 and may need a different class of drug with another mechanism of action. Until that drug is discovered, empirical trials of higher antipsychotic dosages cannot be overlooked as a clinical option.
Henry A. Nasrallah, MD
Professor of psychiatry, neurology and neuroscience
University of Cincinnati College of Medicine
- Pierre JM, Wirshing DA, Cannell J, et al. High-dose quetiapine in treatment-refractory schizophrenia. Schizophr Res 2003;60(supp):299.
- Kapur S, Zipursky R, Jones C et al. Relationship between dopamine D 2 occupancy, clinical response, and side-effects: A double-blind PET study of first-episode schizophrenia. Am J Psychiatry 2000;157:514–20.
- Nasrallah HA, Garver DL, Zhu M. The apoptosis executioner caspase—3 levels are low in rapid-responders and elevated in treatment-refractory schizophrenia. Int J Neuropsychopharm 2004;7(supp):431.
The authors respond
Dr. Preskorn’s and Dr. Nasrallah’s commentaries temper the cautionary tone of our article, which reviewed the “evidence-basis” of high-dose antipsychotic therapy (HDAT). Our tone stems from a lack of controlled research establishing HDAT’s efficacy, a respect for potentially serious antipsychotic side effects, and our belief that clozapine—despite established efficacy in treatment-resistant schizophrenia—is underutilized.
Both colleagues outline several theoretical reasons why HDAT may help some treatment-resistant patients. As we noted, however, similar theories and clinical observations were used to defend rapid neuroleptization, which has been shown to be ineffective with an increased side-effect risk.
The observation that smoking can decrease olanzapine plasma levels is valid, yet existing olanzapine dosing guidelines are based on clinical trials involving subjects with schizophrenia who most likely were smokers.
While we agree that HDAT has theoretical appeal and may prove effective in some patients, we are concerned that clinicians are routinely escalating the dosage after only 1 to 2 weeks of nonresponse to recommended doses. Although high rates of treatment-refractory illness may justify this clinical practice, we find it alarming that clozapine use is so disproportionately low.
As proponents of evidence-based medicine, we note that the lack of data does not mean that HDAT is not effective, but we share the call for well-designed clinical trials to address this issue. Future research may indeed vindicate HDAT, but until then—while we do employ HDAT in some situations—we also typically proceed with clozapine before resorting to desperation measures.
Joseph M. Pierre, MD
Donna A. Wirshing, MD
William C. Wirshing, MD
Geffen School of Medicine
University of California-Los Angeles
Pierre et al and Preskorn (Current Psychiatry, August 2004) address an important treatment issue that has not been well investigated. Titrating an antipsychotic dosage too high and too soon is common in many settings, especially where treatment-resistant patients are numerous.1 But while I advise trainees to use the lowest effective antipsychotic dosage, several justifications exist for exceeding what is arbitrarily regarded as the “approved” dose range:
- FDA registration trials of antipsychotics exclude treatment-resistant/refractory patients. Thus, the “approved” dose range applies only to those with good or adequate treatment response.
- Smoking induces the cytochrome P-450 1A2 isoenzyme, which oxidizes olanzapine. Thus, heavy smokers—especially those who are rapid metabolizers—may need much higher olanzapine dosages to compensate for the rapid clearance.
- The number of dopamine (D2) receptors varies among patients even at psychosis onset. Kapur et al2 gave a fixed dose of haloperidol to 22 subjects with first-episode psychosis. Only a few developed extrapyramidal symptoms (ie, achieved >78% D2receptor occupancy). D2receptor occupancy ranged from 38% to 87%, suggesting that while some patients with relatively few D2 receptors may respond to lower dosages, others may need higher dosages to achieve response (<65% D2 receptor occupancy).
- Different dosages may be needed at different phases of the illness. For example, much higher antipsychotic (or lithium) dosages are needed for acute mania than for maintenance.
- A psychotropic may sometimes exert different neurochemical effects at high vs low dosages. For example, a typical antipsychotic’s serotonin antagonist effects may be more apparent at lower dosages, while the dopamine antagonist effect is more prominent at higher dosages.
- In the United States, roughly 35% of persons with schizophrenia receive two or more concomitant antipsychotics. Although no controlled studies have shown that combination antipsychotic therapy is superior to monotherapy, many clinicians claim that some patients respond better to two atypicals than to one. This may be because of a net higher antipsychotic dosage, which may be therapeutic for treatment-resistant patients.
Use of antipsychotic dosages beyond the FDA-approved range is poorly studied and not evidence-based, but may be justified in some patients despite the higher risk of adverse events. Controlled trials addressing this issue are needed to help clinicians manage patients who perpetually fail to respond to approved dosage ranges. Treatment-resistant patients may be a biologically different subtype than responsive patients3 and may need a different class of drug with another mechanism of action. Until that drug is discovered, empirical trials of higher antipsychotic dosages cannot be overlooked as a clinical option.
Henry A. Nasrallah, MD
Professor of psychiatry, neurology and neuroscience
University of Cincinnati College of Medicine
- Pierre JM, Wirshing DA, Cannell J, et al. High-dose quetiapine in treatment-refractory schizophrenia. Schizophr Res 2003;60(supp):299.
- Kapur S, Zipursky R, Jones C et al. Relationship between dopamine D 2 occupancy, clinical response, and side-effects: A double-blind PET study of first-episode schizophrenia. Am J Psychiatry 2000;157:514–20.
- Nasrallah HA, Garver DL, Zhu M. The apoptosis executioner caspase—3 levels are low in rapid-responders and elevated in treatment-refractory schizophrenia. Int J Neuropsychopharm 2004;7(supp):431.
The authors respond
Dr. Preskorn’s and Dr. Nasrallah’s commentaries temper the cautionary tone of our article, which reviewed the “evidence-basis” of high-dose antipsychotic therapy (HDAT). Our tone stems from a lack of controlled research establishing HDAT’s efficacy, a respect for potentially serious antipsychotic side effects, and our belief that clozapine—despite established efficacy in treatment-resistant schizophrenia—is underutilized.
Both colleagues outline several theoretical reasons why HDAT may help some treatment-resistant patients. As we noted, however, similar theories and clinical observations were used to defend rapid neuroleptization, which has been shown to be ineffective with an increased side-effect risk.
The observation that smoking can decrease olanzapine plasma levels is valid, yet existing olanzapine dosing guidelines are based on clinical trials involving subjects with schizophrenia who most likely were smokers.
While we agree that HDAT has theoretical appeal and may prove effective in some patients, we are concerned that clinicians are routinely escalating the dosage after only 1 to 2 weeks of nonresponse to recommended doses. Although high rates of treatment-refractory illness may justify this clinical practice, we find it alarming that clozapine use is so disproportionately low.
As proponents of evidence-based medicine, we note that the lack of data does not mean that HDAT is not effective, but we share the call for well-designed clinical trials to address this issue. Future research may indeed vindicate HDAT, but until then—while we do employ HDAT in some situations—we also typically proceed with clozapine before resorting to desperation measures.
Joseph M. Pierre, MD
Donna A. Wirshing, MD
William C. Wirshing, MD
Geffen School of Medicine
University of California-Los Angeles
Pierre et al and Preskorn (Current Psychiatry, August 2004) address an important treatment issue that has not been well investigated. Titrating an antipsychotic dosage too high and too soon is common in many settings, especially where treatment-resistant patients are numerous.1 But while I advise trainees to use the lowest effective antipsychotic dosage, several justifications exist for exceeding what is arbitrarily regarded as the “approved” dose range:
- FDA registration trials of antipsychotics exclude treatment-resistant/refractory patients. Thus, the “approved” dose range applies only to those with good or adequate treatment response.
- Smoking induces the cytochrome P-450 1A2 isoenzyme, which oxidizes olanzapine. Thus, heavy smokers—especially those who are rapid metabolizers—may need much higher olanzapine dosages to compensate for the rapid clearance.
- The number of dopamine (D2) receptors varies among patients even at psychosis onset. Kapur et al2 gave a fixed dose of haloperidol to 22 subjects with first-episode psychosis. Only a few developed extrapyramidal symptoms (ie, achieved >78% D2receptor occupancy). D2receptor occupancy ranged from 38% to 87%, suggesting that while some patients with relatively few D2 receptors may respond to lower dosages, others may need higher dosages to achieve response (<65% D2 receptor occupancy).
- Different dosages may be needed at different phases of the illness. For example, much higher antipsychotic (or lithium) dosages are needed for acute mania than for maintenance.
- A psychotropic may sometimes exert different neurochemical effects at high vs low dosages. For example, a typical antipsychotic’s serotonin antagonist effects may be more apparent at lower dosages, while the dopamine antagonist effect is more prominent at higher dosages.
- In the United States, roughly 35% of persons with schizophrenia receive two or more concomitant antipsychotics. Although no controlled studies have shown that combination antipsychotic therapy is superior to monotherapy, many clinicians claim that some patients respond better to two atypicals than to one. This may be because of a net higher antipsychotic dosage, which may be therapeutic for treatment-resistant patients.
Use of antipsychotic dosages beyond the FDA-approved range is poorly studied and not evidence-based, but may be justified in some patients despite the higher risk of adverse events. Controlled trials addressing this issue are needed to help clinicians manage patients who perpetually fail to respond to approved dosage ranges. Treatment-resistant patients may be a biologically different subtype than responsive patients3 and may need a different class of drug with another mechanism of action. Until that drug is discovered, empirical trials of higher antipsychotic dosages cannot be overlooked as a clinical option.
Henry A. Nasrallah, MD
Professor of psychiatry, neurology and neuroscience
University of Cincinnati College of Medicine
- Pierre JM, Wirshing DA, Cannell J, et al. High-dose quetiapine in treatment-refractory schizophrenia. Schizophr Res 2003;60(supp):299.
- Kapur S, Zipursky R, Jones C et al. Relationship between dopamine D 2 occupancy, clinical response, and side-effects: A double-blind PET study of first-episode schizophrenia. Am J Psychiatry 2000;157:514–20.
- Nasrallah HA, Garver DL, Zhu M. The apoptosis executioner caspase—3 levels are low in rapid-responders and elevated in treatment-refractory schizophrenia. Int J Neuropsychopharm 2004;7(supp):431.
The authors respond
Dr. Preskorn’s and Dr. Nasrallah’s commentaries temper the cautionary tone of our article, which reviewed the “evidence-basis” of high-dose antipsychotic therapy (HDAT). Our tone stems from a lack of controlled research establishing HDAT’s efficacy, a respect for potentially serious antipsychotic side effects, and our belief that clozapine—despite established efficacy in treatment-resistant schizophrenia—is underutilized.
Both colleagues outline several theoretical reasons why HDAT may help some treatment-resistant patients. As we noted, however, similar theories and clinical observations were used to defend rapid neuroleptization, which has been shown to be ineffective with an increased side-effect risk.
The observation that smoking can decrease olanzapine plasma levels is valid, yet existing olanzapine dosing guidelines are based on clinical trials involving subjects with schizophrenia who most likely were smokers.
While we agree that HDAT has theoretical appeal and may prove effective in some patients, we are concerned that clinicians are routinely escalating the dosage after only 1 to 2 weeks of nonresponse to recommended doses. Although high rates of treatment-refractory illness may justify this clinical practice, we find it alarming that clozapine use is so disproportionately low.
As proponents of evidence-based medicine, we note that the lack of data does not mean that HDAT is not effective, but we share the call for well-designed clinical trials to address this issue. Future research may indeed vindicate HDAT, but until then—while we do employ HDAT in some situations—we also typically proceed with clozapine before resorting to desperation measures.
Joseph M. Pierre, MD
Donna A. Wirshing, MD
William C. Wirshing, MD
Geffen School of Medicine
University of California-Los Angeles
Recovery and reintegration
The case that accompanies “Recovery from Schizophrenia: Fact or Fiction” does not reflect the typical patient with schizophrenia. The affective symptoms, onset at age 15, and the fact that Ms. J was effectively maintained on lamotrigine, 300 mg/d, and olanzapine, 5 mg/d, suggest that she suffered from bipolar disorder. Paranoid delusions can appear in the context of mania.
Also, Ms. J had been taking haloperidol, 50 mg/d, which is excessive regardless of diagnosis. Insufficient or excessive dosing is detrimental, and overmedication can impede recovery. Ms. J was lucky to have avoided tardive dyskinesia.
Some thoughts about the role of vocational rehabilitation: Rule of thumb is that during recovery from schizophrenia, vocational goals should be set one step below the achievement or the potential that existed before illness onset. When onset occurs before the patient fulfills his or her vocational potential—as often happens—potential may have to be substituted for achievement.
Joseph More, MD
Attending psychiatrist, forensic division
Connecticut Valley Hospital
Middletown, CT
Dr. Martens responds
Ms. J’s symptoms were consistent with schizophrenia, bipolar type. Vocational goals for schizophrenic patients in remission might be set one step below the achievement or potential that existed before onset. Medication might enhance or hinder the patient’s creative, cognitive and intellectual abilities. Increased responsibilities, work stress, and career promotion can increase psychotic symptoms; relapse should be avoided by reducing vocational activities.
Willem HJ Martens, MD, PhD
Director, W. Kahn Institute of Theoretical Psychiatry and Neuroscience
Elst (Utrecht), The Netherlands
The case that accompanies “Recovery from Schizophrenia: Fact or Fiction” does not reflect the typical patient with schizophrenia. The affective symptoms, onset at age 15, and the fact that Ms. J was effectively maintained on lamotrigine, 300 mg/d, and olanzapine, 5 mg/d, suggest that she suffered from bipolar disorder. Paranoid delusions can appear in the context of mania.
Also, Ms. J had been taking haloperidol, 50 mg/d, which is excessive regardless of diagnosis. Insufficient or excessive dosing is detrimental, and overmedication can impede recovery. Ms. J was lucky to have avoided tardive dyskinesia.
Some thoughts about the role of vocational rehabilitation: Rule of thumb is that during recovery from schizophrenia, vocational goals should be set one step below the achievement or the potential that existed before illness onset. When onset occurs before the patient fulfills his or her vocational potential—as often happens—potential may have to be substituted for achievement.
Joseph More, MD
Attending psychiatrist, forensic division
Connecticut Valley Hospital
Middletown, CT
Dr. Martens responds
Ms. J’s symptoms were consistent with schizophrenia, bipolar type. Vocational goals for schizophrenic patients in remission might be set one step below the achievement or potential that existed before onset. Medication might enhance or hinder the patient’s creative, cognitive and intellectual abilities. Increased responsibilities, work stress, and career promotion can increase psychotic symptoms; relapse should be avoided by reducing vocational activities.
Willem HJ Martens, MD, PhD
Director, W. Kahn Institute of Theoretical Psychiatry and Neuroscience
Elst (Utrecht), The Netherlands
The case that accompanies “Recovery from Schizophrenia: Fact or Fiction” does not reflect the typical patient with schizophrenia. The affective symptoms, onset at age 15, and the fact that Ms. J was effectively maintained on lamotrigine, 300 mg/d, and olanzapine, 5 mg/d, suggest that she suffered from bipolar disorder. Paranoid delusions can appear in the context of mania.
Also, Ms. J had been taking haloperidol, 50 mg/d, which is excessive regardless of diagnosis. Insufficient or excessive dosing is detrimental, and overmedication can impede recovery. Ms. J was lucky to have avoided tardive dyskinesia.
Some thoughts about the role of vocational rehabilitation: Rule of thumb is that during recovery from schizophrenia, vocational goals should be set one step below the achievement or the potential that existed before illness onset. When onset occurs before the patient fulfills his or her vocational potential—as often happens—potential may have to be substituted for achievement.
Joseph More, MD
Attending psychiatrist, forensic division
Connecticut Valley Hospital
Middletown, CT
Dr. Martens responds
Ms. J’s symptoms were consistent with schizophrenia, bipolar type. Vocational goals for schizophrenic patients in remission might be set one step below the achievement or potential that existed before onset. Medication might enhance or hinder the patient’s creative, cognitive and intellectual abilities. Increased responsibilities, work stress, and career promotion can increase psychotic symptoms; relapse should be avoided by reducing vocational activities.
Willem HJ Martens, MD, PhD
Director, W. Kahn Institute of Theoretical Psychiatry and Neuroscience
Elst (Utrecht), The Netherlands
Antipsychotic dosing for schizophrenia
Dr. Willem Martens’ article, “Recovery from Schizophrenia: Fact or Fiction” (Current Psychiatry, July 2004), presents inaccurate and misleading information about quetiapine dosing during recovery.
Although quetiapine dosing during schizophrenia’s maintenance phase has not been systematically addressed in blinded studies, Buckley1 presented results from open-label extensions to three 6-week, double-blind, randomized trials of quetiapine in patients with schizophrenia. During these extension periods, which averaged 36 months, clinicians were encouraged to adjust the dosage to optimize efficacy and tolerability. The mean quetiapine dosage during these periods was 439 mg/d, and mean Brief Psychiatric Rating Scale scores continued to decline (13.94 to 9.04).
These findings suggest that patients who continued to do well on quetiapine did so on dosages similar to initial acute dosing. This information is critical to preventing relapse and providing longterm benefits to patients taking quetiapine.
Jeffrey M. Goldstein, PhD
Director clinical science
Wayne Macfadden, MD
U.S. medical director, Seroquel
AstraZeneca LP, Wilmington, DE
- Buckley PF. Maintenance treatment for schizophrenia with quetiapine. Hum Psychopharmacol 2004;19:121–4.
In “Recovery from Schizophrenia: Fact or Fiction,” the dosage range for risperidone cited in Table 3 does not reflect oral risperidone dosing.
The Dosing and Administration section of the U.S. Risperdal tablets/oral solution package insert states: “Efficacy in schizophrenia was demonstrated (at) 4 to 16 mg/d…however, maximal effect was generally seen (at) 4 to 8 mg/d.” Dosages >6 mg/d bid were not shown to be “more efficacious than lower doses, were associated with more extrapyramidal symptoms and other adverse effects, and are not generally recommended.”
Recommended dosing for risperidone long-acting IM injection—as stated in the package insert—is 25 mg every 2 weeks. The insert’s U.S. Dosing and Administration section further states: “Although dose response for effectiveness has not been established, some patients not responding to 25 mg may benefit from…37.5 mg or 50 mg. (The) dose should not exceed 50 mg every 2 weeks.”
Also, the listing of potential antipsychotic side effects in Table 3 does not reflect side effects reported in the current literature, clinical trials involving risperidone, or the U.S. prescribing information for risperidone oral and IM formulations. Clinicians should refer to these package inserts.
The 2004 American Psychiatric Association “Practice Guidelines for the Treatment of Patients with Schizophrenia” also addresses side effects and dosing guidelines for atypical antipsychotics, including risperidone. To obtain this resource, visit http://www.psych.org/psych_pract/treatg/pg/prac_ guide.cfm.
Patricia A. Wilkinson, PharmD, MS, BCPP
Associate director, medical services
Janssen Medical Affairs, LLC,
Titusville, NJ
Dr. Willem Martens’ article, “Recovery from Schizophrenia: Fact or Fiction” (Current Psychiatry, July 2004), presents inaccurate and misleading information about quetiapine dosing during recovery.
Although quetiapine dosing during schizophrenia’s maintenance phase has not been systematically addressed in blinded studies, Buckley1 presented results from open-label extensions to three 6-week, double-blind, randomized trials of quetiapine in patients with schizophrenia. During these extension periods, which averaged 36 months, clinicians were encouraged to adjust the dosage to optimize efficacy and tolerability. The mean quetiapine dosage during these periods was 439 mg/d, and mean Brief Psychiatric Rating Scale scores continued to decline (13.94 to 9.04).
These findings suggest that patients who continued to do well on quetiapine did so on dosages similar to initial acute dosing. This information is critical to preventing relapse and providing longterm benefits to patients taking quetiapine.
Jeffrey M. Goldstein, PhD
Director clinical science
Wayne Macfadden, MD
U.S. medical director, Seroquel
AstraZeneca LP, Wilmington, DE
- Buckley PF. Maintenance treatment for schizophrenia with quetiapine. Hum Psychopharmacol 2004;19:121–4.
In “Recovery from Schizophrenia: Fact or Fiction,” the dosage range for risperidone cited in Table 3 does not reflect oral risperidone dosing.
The Dosing and Administration section of the U.S. Risperdal tablets/oral solution package insert states: “Efficacy in schizophrenia was demonstrated (at) 4 to 16 mg/d…however, maximal effect was generally seen (at) 4 to 8 mg/d.” Dosages >6 mg/d bid were not shown to be “more efficacious than lower doses, were associated with more extrapyramidal symptoms and other adverse effects, and are not generally recommended.”
Recommended dosing for risperidone long-acting IM injection—as stated in the package insert—is 25 mg every 2 weeks. The insert’s U.S. Dosing and Administration section further states: “Although dose response for effectiveness has not been established, some patients not responding to 25 mg may benefit from…37.5 mg or 50 mg. (The) dose should not exceed 50 mg every 2 weeks.”
Also, the listing of potential antipsychotic side effects in Table 3 does not reflect side effects reported in the current literature, clinical trials involving risperidone, or the U.S. prescribing information for risperidone oral and IM formulations. Clinicians should refer to these package inserts.
The 2004 American Psychiatric Association “Practice Guidelines for the Treatment of Patients with Schizophrenia” also addresses side effects and dosing guidelines for atypical antipsychotics, including risperidone. To obtain this resource, visit http://www.psych.org/psych_pract/treatg/pg/prac_ guide.cfm.
Patricia A. Wilkinson, PharmD, MS, BCPP
Associate director, medical services
Janssen Medical Affairs, LLC,
Titusville, NJ
Dr. Willem Martens’ article, “Recovery from Schizophrenia: Fact or Fiction” (Current Psychiatry, July 2004), presents inaccurate and misleading information about quetiapine dosing during recovery.
Although quetiapine dosing during schizophrenia’s maintenance phase has not been systematically addressed in blinded studies, Buckley1 presented results from open-label extensions to three 6-week, double-blind, randomized trials of quetiapine in patients with schizophrenia. During these extension periods, which averaged 36 months, clinicians were encouraged to adjust the dosage to optimize efficacy and tolerability. The mean quetiapine dosage during these periods was 439 mg/d, and mean Brief Psychiatric Rating Scale scores continued to decline (13.94 to 9.04).
These findings suggest that patients who continued to do well on quetiapine did so on dosages similar to initial acute dosing. This information is critical to preventing relapse and providing longterm benefits to patients taking quetiapine.
Jeffrey M. Goldstein, PhD
Director clinical science
Wayne Macfadden, MD
U.S. medical director, Seroquel
AstraZeneca LP, Wilmington, DE
- Buckley PF. Maintenance treatment for schizophrenia with quetiapine. Hum Psychopharmacol 2004;19:121–4.
In “Recovery from Schizophrenia: Fact or Fiction,” the dosage range for risperidone cited in Table 3 does not reflect oral risperidone dosing.
The Dosing and Administration section of the U.S. Risperdal tablets/oral solution package insert states: “Efficacy in schizophrenia was demonstrated (at) 4 to 16 mg/d…however, maximal effect was generally seen (at) 4 to 8 mg/d.” Dosages >6 mg/d bid were not shown to be “more efficacious than lower doses, were associated with more extrapyramidal symptoms and other adverse effects, and are not generally recommended.”
Recommended dosing for risperidone long-acting IM injection—as stated in the package insert—is 25 mg every 2 weeks. The insert’s U.S. Dosing and Administration section further states: “Although dose response for effectiveness has not been established, some patients not responding to 25 mg may benefit from…37.5 mg or 50 mg. (The) dose should not exceed 50 mg every 2 weeks.”
Also, the listing of potential antipsychotic side effects in Table 3 does not reflect side effects reported in the current literature, clinical trials involving risperidone, or the U.S. prescribing information for risperidone oral and IM formulations. Clinicians should refer to these package inserts.
The 2004 American Psychiatric Association “Practice Guidelines for the Treatment of Patients with Schizophrenia” also addresses side effects and dosing guidelines for atypical antipsychotics, including risperidone. To obtain this resource, visit http://www.psych.org/psych_pract/treatg/pg/prac_ guide.cfm.
Patricia A. Wilkinson, PharmD, MS, BCPP
Associate director, medical services
Janssen Medical Affairs, LLC,
Titusville, NJ
Taking the mystery out of missing persons
A patient with schizophrenia or Alzheimer’s disease can function at home, but his family fears he would suddenly “run off”—potentially harming himself or others—unless he is watched around the clock. Can this patient avoid more-restrictive, institutionalized care without burdening the family?
Enter global positioning and radio frequency tracking technologies that are gaining wider acceptance and could one day play a role in caring for the chronically mentally ill.
Tracking technologies
The global positioning system (GPS) was created in 1993, when the United States Air Force launched the 24 th Navstar satellite.1 The system contains both military and civilian signals, but civilian accuracy initially was limited to 100 feet compared with 60 feet for the military signals. This limitation has since been lifted from civilian devices.
At first, GPS technology was used to navigate vehicles; later, specialized handheld devices provide navigation for hikers.
Today, GPS receivers are available for personal digital assistants, as are specialized wrist devices. Wherify Wireless offers GPS wrist devices, including GPS Locator for Kids, which allows parents or guardians to locate children within minutes and relay a message telling them to come home. GPS devices are increasingly popular and are used in the game of Geocaching,2 where players use GPS technology to hunt for a cache.
Radio frequency identification devices (RFIDs) are microchips the size of a grain of rice that allow retailers to track goods from warehouse to retail shelf. The chip contains no power source, but utilizes the energy within the initial radio signal.
RFID tags do not harbor information other than an identification number, which can be linked to a medical record or other database. Unlike bar codes, which require direct exposure to scan, hidden RFIDs broadcast themselves when activated by the radio signal, making transactions faster and more convenient.
RFIDs have caught on. Cards with RFID tags have been used at the Academy Awards ceremony to control access. Guards at jails throughout the United States use RFID tags to verify inmates’ whereabouts. Customers at Exxon and Mobil gasoline stations use RFID devices (called Speedpass) to facilitate purchases at the pump or register.
In 2002, RFID implants became available at medical clinics3 and are beginning to reach the mainstream. At the Baja Beach nightclub in Barcelona, for example, guests with the implant in their arms gain access to VIP areas once they pass through the scanner (which automatically assesses the cover charge to their tab).4
Approximately 1,000 persons have received VeriChip RFID implants over 2 years.5
How GPS, RFID can help caretakers
GPS. Caretakers can use GPS tracking devices to track a patient with a chronic mental disorder.
For example, the patient can wear a Wherify Wireless GPS locator wristwatch. To track the patient, the caretaker would log on to Wherify’s demo Web site (http://www.wherifywireless.com/demo.htm) and enter the device’s ID number. After clicking on the “locate” button, the locator device is contacted and its position and time of position is displayed on a map. Alternately, subscribers can call an 800 number and ask the operator to relay the locator address.
The wristwatch or locator phone costs about $200, and a monthly subscription ranges from $20 to $45 depending on number of location queries. The wristwatch comes with a remote-activated safety lock feature to prevent the patient from taking it off.
RFID. VeriChip implants are geared for indoor use, but can supplement a GPS device to track a chronically mentally ill patient.
The 11-millimeter chip, commonly used for standard security applications, is injected into the fatty tissue of the right tricep. When the recipient is near a VeriChip scanning device, the chip radios an ID number to the scanner. If the number matches an ID number in the database, the person with the implant can enter a secured room or complete a financial transaction.5
The FDA is reviewing whether hospitals can use RFID implants to identify patients and allow staff access to medical records without violating patients’ privacy.5
RFID tags located in wristbands could be used to identify hospitalized patients and prevent medication errors. RFID-tagged identification cards could help authenticate staff for access to the electronic medical record. Tags embedded in the bottle cap could measure medication compliance,6 and blister packs reveal when the medication was last taken.7 Special probes also could determine if the medication has expired or been stored properly.
Inviting ‘Big Brother’?
Critics, however, say use of GPS or RFID technology threatens privacy. The group Consumers Against Supermarket Privacy Invasion and Numbering (CASPIAN) complains that unique ID tags identify who purchased which product and where. Because the monitoring is passive via radio waves, these tags can be hidden and read at a distance—meaning that people can be monitored without their knowledge or consent. Critics also fear that the radio waves may pose a health hazard.8
Accuracy is another concern. Although GPS technology provides location information, the locator device still depends on cellular phone technology to transmit the information. Poor cellular coverage areas may decrease the device’s usefulness. More importantly, because GPS devices require a clear view of the sky to access the satellites, they do not work indoors. Thus, a patient must have escaped the house for the device to work.
Related Resources
- World Research Group: Leveraging RFID for hospitals. http://www.worldrg.com/HW455/agenda.asp
Disclosure
Dr. Luo reports no financial relationship with any company whose products are mentioned in this article. The opinions expressed by Dr. Luo in this column are his own and do not necessarily reflect those of CURRENT PSYCHIATRY.
(accessed Sept. 20, 2004)
1. National Academy of Sciences. The global positioning system: The role of atomic clocks-introduction. http://www.beyonddiscovery.org/content/view.page.asp?I=1275
2. Groundspeak Inc.—Geocaching. http://www.geocaching.com
3. ABC News: Meet the Chipsons. http://abcnews.go.com/sections/scitech/TechTV/techtv_chipfamily020510.html
4. VIP microchip launched in Baja Beach Club, Barcelona. http://www.niburu.nl/index.php?showarticle.php?articleID=2638
5. Kanellos M. Under-the-skin ID chips move toward U.S. hospitals. CNET news.com July 27, 2004. http://news.com.com/Under-the-kin+ID+chips+move+toward+U.S.+hospital+use/2100-7337_3-5285815.html?tag=alert
6. Information Mediary Corp. Med-ic eCap Compliance Monitor. http://informationmediary.com/ecap/
7. Ibid. http://informationmediary.com/certiscan.htm
8. CASPIAN. Stop RFID. www.stoprfid.org
A patient with schizophrenia or Alzheimer’s disease can function at home, but his family fears he would suddenly “run off”—potentially harming himself or others—unless he is watched around the clock. Can this patient avoid more-restrictive, institutionalized care without burdening the family?
Enter global positioning and radio frequency tracking technologies that are gaining wider acceptance and could one day play a role in caring for the chronically mentally ill.
Tracking technologies
The global positioning system (GPS) was created in 1993, when the United States Air Force launched the 24 th Navstar satellite.1 The system contains both military and civilian signals, but civilian accuracy initially was limited to 100 feet compared with 60 feet for the military signals. This limitation has since been lifted from civilian devices.
At first, GPS technology was used to navigate vehicles; later, specialized handheld devices provide navigation for hikers.
Today, GPS receivers are available for personal digital assistants, as are specialized wrist devices. Wherify Wireless offers GPS wrist devices, including GPS Locator for Kids, which allows parents or guardians to locate children within minutes and relay a message telling them to come home. GPS devices are increasingly popular and are used in the game of Geocaching,2 where players use GPS technology to hunt for a cache.
Radio frequency identification devices (RFIDs) are microchips the size of a grain of rice that allow retailers to track goods from warehouse to retail shelf. The chip contains no power source, but utilizes the energy within the initial radio signal.
RFID tags do not harbor information other than an identification number, which can be linked to a medical record or other database. Unlike bar codes, which require direct exposure to scan, hidden RFIDs broadcast themselves when activated by the radio signal, making transactions faster and more convenient.
RFIDs have caught on. Cards with RFID tags have been used at the Academy Awards ceremony to control access. Guards at jails throughout the United States use RFID tags to verify inmates’ whereabouts. Customers at Exxon and Mobil gasoline stations use RFID devices (called Speedpass) to facilitate purchases at the pump or register.
In 2002, RFID implants became available at medical clinics3 and are beginning to reach the mainstream. At the Baja Beach nightclub in Barcelona, for example, guests with the implant in their arms gain access to VIP areas once they pass through the scanner (which automatically assesses the cover charge to their tab).4
Approximately 1,000 persons have received VeriChip RFID implants over 2 years.5
How GPS, RFID can help caretakers
GPS. Caretakers can use GPS tracking devices to track a patient with a chronic mental disorder.
For example, the patient can wear a Wherify Wireless GPS locator wristwatch. To track the patient, the caretaker would log on to Wherify’s demo Web site (http://www.wherifywireless.com/demo.htm) and enter the device’s ID number. After clicking on the “locate” button, the locator device is contacted and its position and time of position is displayed on a map. Alternately, subscribers can call an 800 number and ask the operator to relay the locator address.
The wristwatch or locator phone costs about $200, and a monthly subscription ranges from $20 to $45 depending on number of location queries. The wristwatch comes with a remote-activated safety lock feature to prevent the patient from taking it off.
RFID. VeriChip implants are geared for indoor use, but can supplement a GPS device to track a chronically mentally ill patient.
The 11-millimeter chip, commonly used for standard security applications, is injected into the fatty tissue of the right tricep. When the recipient is near a VeriChip scanning device, the chip radios an ID number to the scanner. If the number matches an ID number in the database, the person with the implant can enter a secured room or complete a financial transaction.5
The FDA is reviewing whether hospitals can use RFID implants to identify patients and allow staff access to medical records without violating patients’ privacy.5
RFID tags located in wristbands could be used to identify hospitalized patients and prevent medication errors. RFID-tagged identification cards could help authenticate staff for access to the electronic medical record. Tags embedded in the bottle cap could measure medication compliance,6 and blister packs reveal when the medication was last taken.7 Special probes also could determine if the medication has expired or been stored properly.
Inviting ‘Big Brother’?
Critics, however, say use of GPS or RFID technology threatens privacy. The group Consumers Against Supermarket Privacy Invasion and Numbering (CASPIAN) complains that unique ID tags identify who purchased which product and where. Because the monitoring is passive via radio waves, these tags can be hidden and read at a distance—meaning that people can be monitored without their knowledge or consent. Critics also fear that the radio waves may pose a health hazard.8
Accuracy is another concern. Although GPS technology provides location information, the locator device still depends on cellular phone technology to transmit the information. Poor cellular coverage areas may decrease the device’s usefulness. More importantly, because GPS devices require a clear view of the sky to access the satellites, they do not work indoors. Thus, a patient must have escaped the house for the device to work.
Related Resources
- World Research Group: Leveraging RFID for hospitals. http://www.worldrg.com/HW455/agenda.asp
Disclosure
Dr. Luo reports no financial relationship with any company whose products are mentioned in this article. The opinions expressed by Dr. Luo in this column are his own and do not necessarily reflect those of CURRENT PSYCHIATRY.
A patient with schizophrenia or Alzheimer’s disease can function at home, but his family fears he would suddenly “run off”—potentially harming himself or others—unless he is watched around the clock. Can this patient avoid more-restrictive, institutionalized care without burdening the family?
Enter global positioning and radio frequency tracking technologies that are gaining wider acceptance and could one day play a role in caring for the chronically mentally ill.
Tracking technologies
The global positioning system (GPS) was created in 1993, when the United States Air Force launched the 24 th Navstar satellite.1 The system contains both military and civilian signals, but civilian accuracy initially was limited to 100 feet compared with 60 feet for the military signals. This limitation has since been lifted from civilian devices.
At first, GPS technology was used to navigate vehicles; later, specialized handheld devices provide navigation for hikers.
Today, GPS receivers are available for personal digital assistants, as are specialized wrist devices. Wherify Wireless offers GPS wrist devices, including GPS Locator for Kids, which allows parents or guardians to locate children within minutes and relay a message telling them to come home. GPS devices are increasingly popular and are used in the game of Geocaching,2 where players use GPS technology to hunt for a cache.
Radio frequency identification devices (RFIDs) are microchips the size of a grain of rice that allow retailers to track goods from warehouse to retail shelf. The chip contains no power source, but utilizes the energy within the initial radio signal.
RFID tags do not harbor information other than an identification number, which can be linked to a medical record or other database. Unlike bar codes, which require direct exposure to scan, hidden RFIDs broadcast themselves when activated by the radio signal, making transactions faster and more convenient.
RFIDs have caught on. Cards with RFID tags have been used at the Academy Awards ceremony to control access. Guards at jails throughout the United States use RFID tags to verify inmates’ whereabouts. Customers at Exxon and Mobil gasoline stations use RFID devices (called Speedpass) to facilitate purchases at the pump or register.
In 2002, RFID implants became available at medical clinics3 and are beginning to reach the mainstream. At the Baja Beach nightclub in Barcelona, for example, guests with the implant in their arms gain access to VIP areas once they pass through the scanner (which automatically assesses the cover charge to their tab).4
Approximately 1,000 persons have received VeriChip RFID implants over 2 years.5
How GPS, RFID can help caretakers
GPS. Caretakers can use GPS tracking devices to track a patient with a chronic mental disorder.
For example, the patient can wear a Wherify Wireless GPS locator wristwatch. To track the patient, the caretaker would log on to Wherify’s demo Web site (http://www.wherifywireless.com/demo.htm) and enter the device’s ID number. After clicking on the “locate” button, the locator device is contacted and its position and time of position is displayed on a map. Alternately, subscribers can call an 800 number and ask the operator to relay the locator address.
The wristwatch or locator phone costs about $200, and a monthly subscription ranges from $20 to $45 depending on number of location queries. The wristwatch comes with a remote-activated safety lock feature to prevent the patient from taking it off.
RFID. VeriChip implants are geared for indoor use, but can supplement a GPS device to track a chronically mentally ill patient.
The 11-millimeter chip, commonly used for standard security applications, is injected into the fatty tissue of the right tricep. When the recipient is near a VeriChip scanning device, the chip radios an ID number to the scanner. If the number matches an ID number in the database, the person with the implant can enter a secured room or complete a financial transaction.5
The FDA is reviewing whether hospitals can use RFID implants to identify patients and allow staff access to medical records without violating patients’ privacy.5
RFID tags located in wristbands could be used to identify hospitalized patients and prevent medication errors. RFID-tagged identification cards could help authenticate staff for access to the electronic medical record. Tags embedded in the bottle cap could measure medication compliance,6 and blister packs reveal when the medication was last taken.7 Special probes also could determine if the medication has expired or been stored properly.
Inviting ‘Big Brother’?
Critics, however, say use of GPS or RFID technology threatens privacy. The group Consumers Against Supermarket Privacy Invasion and Numbering (CASPIAN) complains that unique ID tags identify who purchased which product and where. Because the monitoring is passive via radio waves, these tags can be hidden and read at a distance—meaning that people can be monitored without their knowledge or consent. Critics also fear that the radio waves may pose a health hazard.8
Accuracy is another concern. Although GPS technology provides location information, the locator device still depends on cellular phone technology to transmit the information. Poor cellular coverage areas may decrease the device’s usefulness. More importantly, because GPS devices require a clear view of the sky to access the satellites, they do not work indoors. Thus, a patient must have escaped the house for the device to work.
Related Resources
- World Research Group: Leveraging RFID for hospitals. http://www.worldrg.com/HW455/agenda.asp
Disclosure
Dr. Luo reports no financial relationship with any company whose products are mentioned in this article. The opinions expressed by Dr. Luo in this column are his own and do not necessarily reflect those of CURRENT PSYCHIATRY.
(accessed Sept. 20, 2004)
1. National Academy of Sciences. The global positioning system: The role of atomic clocks-introduction. http://www.beyonddiscovery.org/content/view.page.asp?I=1275
2. Groundspeak Inc.—Geocaching. http://www.geocaching.com
3. ABC News: Meet the Chipsons. http://abcnews.go.com/sections/scitech/TechTV/techtv_chipfamily020510.html
4. VIP microchip launched in Baja Beach Club, Barcelona. http://www.niburu.nl/index.php?showarticle.php?articleID=2638
5. Kanellos M. Under-the-skin ID chips move toward U.S. hospitals. CNET news.com July 27, 2004. http://news.com.com/Under-the-kin+ID+chips+move+toward+U.S.+hospital+use/2100-7337_3-5285815.html?tag=alert
6. Information Mediary Corp. Med-ic eCap Compliance Monitor. http://informationmediary.com/ecap/
7. Ibid. http://informationmediary.com/certiscan.htm
8. CASPIAN. Stop RFID. www.stoprfid.org
(accessed Sept. 20, 2004)
1. National Academy of Sciences. The global positioning system: The role of atomic clocks-introduction. http://www.beyonddiscovery.org/content/view.page.asp?I=1275
2. Groundspeak Inc.—Geocaching. http://www.geocaching.com
3. ABC News: Meet the Chipsons. http://abcnews.go.com/sections/scitech/TechTV/techtv_chipfamily020510.html
4. VIP microchip launched in Baja Beach Club, Barcelona. http://www.niburu.nl/index.php?showarticle.php?articleID=2638
5. Kanellos M. Under-the-skin ID chips move toward U.S. hospitals. CNET news.com July 27, 2004. http://news.com.com/Under-the-kin+ID+chips+move+toward+U.S.+hospital+use/2100-7337_3-5285815.html?tag=alert
6. Information Mediary Corp. Med-ic eCap Compliance Monitor. http://informationmediary.com/ecap/
7. Ibid. http://informationmediary.com/certiscan.htm
8. CASPIAN. Stop RFID. www.stoprfid.org
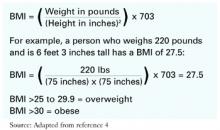
Choose precise BMI charts to track youths’ weight gain
Children and adolescents with a chronic mental illness face a much higher risk for obesity than do healthy youths. Use of one or more psychotropics associated with weight gain compounds common adolescent risk factors, including:
- increased eating
- reduced physical activity
- genetic, developmental, and environmental factors.
Use of body mass index (BMI) measurements based on sex and age in percentiles—instead of the usual height and weight—can help psychiatrists more accurately monitor psychotropic-induced weight gain and the effects of diet and exercise in youths.
Why: sex/age percentiles?
Child/adolescent growth charts show considerable BMI variations based on sex and age. Simply recording height, weight and serial BMI changes—as is done for adults—does not adequately reflect deviations from expected growth patterns. Trying to determine medication effect by combining height and weight measurements of youths of differing sex and age is particularly misleading.
Consider these examples, based on the Centers for Disease Control and Prevention (CDC) growth chart for boys ages 2 to 20 years:
- A BMI of 18 kg/m2would place a 5-year-old boy at the 95th percentile (obese), an 8-year-boy at the 85th percentile (overweight), and a 16.5-year-old boy at the 10th percentile (underweight).
- An 8.5-year-old boy with a BMI of 16 kg/m2 is in the 50th percentile, meaning his weight is normal for his age and gender. To remain in the 50th percentile at age 16, his BMI must increase to 20.5 kg/m2.
Available: tools
CDC publishes sex- and age-specific growth charts (www.cdc.gov/growthcharts) that are easy to understand and use.
CDC considers children and adolescents with BMIs at or above the 95th percentile as “overweight,” and those between the 85th and 95th percentiles as “at risk for overweight.” Others use the terms “obese” and “overweight” for these same percentiles.
For greater precision, CDC also offers free Epi Info software downloads (www.cdc.gov/epi-info). This includes the NutStat anthropometric program, which calculates percentiles and Z scores—number of standard deviations from the mean—from CDC’s 2000 growth charts.
Using NutStat and patient age, clinicians can quickly calculate BMI, percentile, and Z score. Staff can enter height, weight, date of birth, and date of measurement into the module and generate these numbers for clinical decision making and documentation.
Suggested reading
Committee on Nutrition. American Academy of Pediatrics. Policy statement. Prevention of pediatric overweight and obesity. Pediatrics 2003;112:424-30.
The authors are faculty members in the department of psychiatry, Medical College of Virginia, Virginia Commonwealth University, Richmond.
Children and adolescents with a chronic mental illness face a much higher risk for obesity than do healthy youths. Use of one or more psychotropics associated with weight gain compounds common adolescent risk factors, including:
- increased eating
- reduced physical activity
- genetic, developmental, and environmental factors.
Use of body mass index (BMI) measurements based on sex and age in percentiles—instead of the usual height and weight—can help psychiatrists more accurately monitor psychotropic-induced weight gain and the effects of diet and exercise in youths.
Why: sex/age percentiles?
Child/adolescent growth charts show considerable BMI variations based on sex and age. Simply recording height, weight and serial BMI changes—as is done for adults—does not adequately reflect deviations from expected growth patterns. Trying to determine medication effect by combining height and weight measurements of youths of differing sex and age is particularly misleading.
Consider these examples, based on the Centers for Disease Control and Prevention (CDC) growth chart for boys ages 2 to 20 years:
- A BMI of 18 kg/m2would place a 5-year-old boy at the 95th percentile (obese), an 8-year-boy at the 85th percentile (overweight), and a 16.5-year-old boy at the 10th percentile (underweight).
- An 8.5-year-old boy with a BMI of 16 kg/m2 is in the 50th percentile, meaning his weight is normal for his age and gender. To remain in the 50th percentile at age 16, his BMI must increase to 20.5 kg/m2.
Available: tools
CDC publishes sex- and age-specific growth charts (www.cdc.gov/growthcharts) that are easy to understand and use.
CDC considers children and adolescents with BMIs at or above the 95th percentile as “overweight,” and those between the 85th and 95th percentiles as “at risk for overweight.” Others use the terms “obese” and “overweight” for these same percentiles.
For greater precision, CDC also offers free Epi Info software downloads (www.cdc.gov/epi-info). This includes the NutStat anthropometric program, which calculates percentiles and Z scores—number of standard deviations from the mean—from CDC’s 2000 growth charts.
Using NutStat and patient age, clinicians can quickly calculate BMI, percentile, and Z score. Staff can enter height, weight, date of birth, and date of measurement into the module and generate these numbers for clinical decision making and documentation.
Children and adolescents with a chronic mental illness face a much higher risk for obesity than do healthy youths. Use of one or more psychotropics associated with weight gain compounds common adolescent risk factors, including:
- increased eating
- reduced physical activity
- genetic, developmental, and environmental factors.
Use of body mass index (BMI) measurements based on sex and age in percentiles—instead of the usual height and weight—can help psychiatrists more accurately monitor psychotropic-induced weight gain and the effects of diet and exercise in youths.
Why: sex/age percentiles?
Child/adolescent growth charts show considerable BMI variations based on sex and age. Simply recording height, weight and serial BMI changes—as is done for adults—does not adequately reflect deviations from expected growth patterns. Trying to determine medication effect by combining height and weight measurements of youths of differing sex and age is particularly misleading.
Consider these examples, based on the Centers for Disease Control and Prevention (CDC) growth chart for boys ages 2 to 20 years:
- A BMI of 18 kg/m2would place a 5-year-old boy at the 95th percentile (obese), an 8-year-boy at the 85th percentile (overweight), and a 16.5-year-old boy at the 10th percentile (underweight).
- An 8.5-year-old boy with a BMI of 16 kg/m2 is in the 50th percentile, meaning his weight is normal for his age and gender. To remain in the 50th percentile at age 16, his BMI must increase to 20.5 kg/m2.
Available: tools
CDC publishes sex- and age-specific growth charts (www.cdc.gov/growthcharts) that are easy to understand and use.
CDC considers children and adolescents with BMIs at or above the 95th percentile as “overweight,” and those between the 85th and 95th percentiles as “at risk for overweight.” Others use the terms “obese” and “overweight” for these same percentiles.
For greater precision, CDC also offers free Epi Info software downloads (www.cdc.gov/epi-info). This includes the NutStat anthropometric program, which calculates percentiles and Z scores—number of standard deviations from the mean—from CDC’s 2000 growth charts.
Using NutStat and patient age, clinicians can quickly calculate BMI, percentile, and Z score. Staff can enter height, weight, date of birth, and date of measurement into the module and generate these numbers for clinical decision making and documentation.
Suggested reading
Committee on Nutrition. American Academy of Pediatrics. Policy statement. Prevention of pediatric overweight and obesity. Pediatrics 2003;112:424-30.
The authors are faculty members in the department of psychiatry, Medical College of Virginia, Virginia Commonwealth University, Richmond.
Suggested reading
Committee on Nutrition. American Academy of Pediatrics. Policy statement. Prevention of pediatric overweight and obesity. Pediatrics 2003;112:424-30.
The authors are faculty members in the department of psychiatry, Medical College of Virginia, Virginia Commonwealth University, Richmond.
Lab tests in psychiatry: How much is enough?
Here’s a horrifying thought: What if psychiatrists were internists? Only by historical accident is psychiatry its own specialty, separate from internal medicine.
Our 19th- and 20th-century predecessors practiced in state mental hospitals and treated most patients with psychotherapy rather than drugs. Today, most inpatient psychiatry is practiced in general hospitals, and we do at least as much pharmacotherapy as psychotherapy. If psychiatry were getting started today, it probably would an internal medicine subspecialty.
When I was in medical school, one psychiatry attending had been a surgeon before his psychiatry residency. When I said his two specialties seemed very different, his response was, “Not really.” Psychiatrists and surgeons “treat patients,” whereas other specialists—say, internists—prefer to “solve problems.”
During my residency, the surgeons called internists “fleas” because all they seemed to do was hop around in packs drawing blood. This stereotype—if it was ever true—is probably less accurate today, with so many internists becoming proceduralists rather than cognitive specialists.
But still . . . if we were internists, we undoubtedly would do more diagnostic tests. Psychiatry’s standard of care is to do lab tests when patients are hospitalized but very seldom in outpatient settings. If we were internists, we would do lab tests before starting any outpatient on any treatment. Everyone would get an extensive “workup” to “rule out” numerous highly improbable diagnoses.
The article in this issue by Drs. Richard Rosse and Stephen Deutsch addresses intelligent lab testing before starting patients on psychotropics. I do not want to give away the ending, but these authors recommend more testing than most of us do and less than we probably would be doing if we were—horror of horrors!—internists.
Here’s a horrifying thought: What if psychiatrists were internists? Only by historical accident is psychiatry its own specialty, separate from internal medicine.
Our 19th- and 20th-century predecessors practiced in state mental hospitals and treated most patients with psychotherapy rather than drugs. Today, most inpatient psychiatry is practiced in general hospitals, and we do at least as much pharmacotherapy as psychotherapy. If psychiatry were getting started today, it probably would an internal medicine subspecialty.
When I was in medical school, one psychiatry attending had been a surgeon before his psychiatry residency. When I said his two specialties seemed very different, his response was, “Not really.” Psychiatrists and surgeons “treat patients,” whereas other specialists—say, internists—prefer to “solve problems.”
During my residency, the surgeons called internists “fleas” because all they seemed to do was hop around in packs drawing blood. This stereotype—if it was ever true—is probably less accurate today, with so many internists becoming proceduralists rather than cognitive specialists.
But still . . . if we were internists, we undoubtedly would do more diagnostic tests. Psychiatry’s standard of care is to do lab tests when patients are hospitalized but very seldom in outpatient settings. If we were internists, we would do lab tests before starting any outpatient on any treatment. Everyone would get an extensive “workup” to “rule out” numerous highly improbable diagnoses.
The article in this issue by Drs. Richard Rosse and Stephen Deutsch addresses intelligent lab testing before starting patients on psychotropics. I do not want to give away the ending, but these authors recommend more testing than most of us do and less than we probably would be doing if we were—horror of horrors!—internists.
Here’s a horrifying thought: What if psychiatrists were internists? Only by historical accident is psychiatry its own specialty, separate from internal medicine.
Our 19th- and 20th-century predecessors practiced in state mental hospitals and treated most patients with psychotherapy rather than drugs. Today, most inpatient psychiatry is practiced in general hospitals, and we do at least as much pharmacotherapy as psychotherapy. If psychiatry were getting started today, it probably would an internal medicine subspecialty.
When I was in medical school, one psychiatry attending had been a surgeon before his psychiatry residency. When I said his two specialties seemed very different, his response was, “Not really.” Psychiatrists and surgeons “treat patients,” whereas other specialists—say, internists—prefer to “solve problems.”
During my residency, the surgeons called internists “fleas” because all they seemed to do was hop around in packs drawing blood. This stereotype—if it was ever true—is probably less accurate today, with so many internists becoming proceduralists rather than cognitive specialists.
But still . . . if we were internists, we undoubtedly would do more diagnostic tests. Psychiatry’s standard of care is to do lab tests when patients are hospitalized but very seldom in outpatient settings. If we were internists, we would do lab tests before starting any outpatient on any treatment. Everyone would get an extensive “workup” to “rule out” numerous highly improbable diagnoses.
The article in this issue by Drs. Richard Rosse and Stephen Deutsch addresses intelligent lab testing before starting patients on psychotropics. I do not want to give away the ending, but these authors recommend more testing than most of us do and less than we probably would be doing if we were—horror of horrors!—internists.
Sobering facts about a missed diagnosis
HISTORY: TOO MUCH FOR TOO LONG
Mrs. B, age 73, has been alcohol-dependent for 20 years. Since her husband’s death 5 years ago, she has been drinking 1 to 2 liters of vodka a week. At her family’s insistence, she checks into a tertiary-care hospital for worsening alcohol use, memory problems, and increasing confusion.
Mrs. B’s family removed her car because of her alcohol and cognitive problems, but she walks half a mile to buy alcohol. She lives alone in an assisted-living facility and has been hospitalized for detoxification 3 times within 2 years.
At intake, her judgment and abstract thinking are impaired. She has poor insight into her condition. Physical examination reveals fine hand tremors. Lab test results and vital signs are normal. Mrs. B was previously diagnosed with bipolar disorder and takes divalproex, 250 each morning and 500 mg at bedtime, and paroxetine, 20 mg/d.
Mrs. B’s Folstein Mini-Mental State Examination (MMSE) score 1 week after admission was 5/30, indicating severe cognitive deficits. Her mood was euthymic, speech and motor activity were normal, and thought process was logical with intact associations. She exhibited no delusions or hallucinations but was disoriented, with a short attention span and poor concentration.
The authors’ observations
Mrs. B’s confusion has increased in recent weeks. Hand tremors could signal a neurologic problem triggered by a vascular event or alcohol use. Include dementia in the differential diagnosis.
Distinguishing between vascular dementia and alcohol-induced persisting dementia requires a thorough history, neurologic exam, and lab testing.
Vascular dementia. Cognition deteriorates step by step. Patients with this dementia have multiple vascular risk factors and display evidence of cerebrovascular events on physical examination or imaging studies. Watch for high blood pressure, high cholesterol, or obesity; history of diabetes, cardiac arrythmias, or strokes; or other vascular changes in the brain.
Alcohol-induced persisting dementia. Patients usually have abused alcohol for years, and memory slowly deteriorates. Vascular events that would explain cognitive deficits are not found. Such patients usually do not have vascular and cerebrovascular risk factors, but may exhibit worsening cognition in the context of alcohol use. Watch for mean corpuscular volume >100 femtoliters, gamma glutamyl transferase >50 U/L, and elevated liver function tests.
For Mrs. B, both dementia types were ruled out. Her memory problems were mild, and she had been functioning independently at the assisted-living facility. Dementia is not characterized by clouding of consciousness, and her disorder’s progression was fast. Mrs. B’s bipolar disorder was not a factor because she did not have significant depressive or manic symptoms.
Amnestic disorder. Mrs. B’s worsening mental status and neurologic signs after admission suggest amnestic disorder. Patients with amnestic disorder have trouble learning or recalling new information and forming new memories, although they can talk coherently and appropriately.
Injury to the diencephalic and medial temporal lobe structures triggers amnestic disorder. Head trauma, cerebral infections, and infarctions can damage these structures, but alcoholism is the most common cause.
ADMISSION: INCREASING CONFUSION
Mrs. B was admitted to the dual diagnosis unit for patients with substance use and psychiatric disorders. Although confused, she could eat and walk.
For 2 days, Mrs. B received chlordiazepoxide, 200 mg/d, for detoxification; a multivitamin tablet; and oral vitamin B1 (thiamine), 100 mg once daily. She also continued her divalproex/paroxetine regimen. Chlordiazepoxide was tapered and discontinued over 4 days. Vital signs remained normal.
Two days after starting detox, Mrs. B’s condition began to worsen. She became incontinent of urine and feces, had trouble eating, and required extensive assistance with activities of daily living.
On examination by the geriatric psychiatry team, Mrs. B appeared very confused. She was confabulating, had hand tremors, and was ataxic, with nystagmus on lateral gaze. Coordination was poor. Because she reported visual hallucinations and appeared delirious, divalproex sodium and paroxetine—which can worsen delirium—were stopped.
Head MRI with contrast revealed sulcal space prominence in the cerebral and cerebellar hemispheres, suggesting minimal volume loss, and nonspecific bilateral periventricular punctuate flairs and T2 hypodensities, indicating small-vessel ischemic disease. EEG showed moderate rhythm slowing. Blood and urine tests showed no infectious disease or metabolic abnormalities.
Lesions associated with Wernicke’s encephalopathy (WE) usually are found in the third ventricle, cerebral aqueduct, fourth ventricle, mamillary bodies, periaqueductal gray matter, dorsomedial thalamus, septal region, and oculomotor nuclei.
In approximately 50% of cases, damage to the cerebellum also occurs. Such damage is usually symmetrical and shows diffuse, patchy endothelial prominence, proliferation of microglia, and petechial hemorrhage.
In chronic cases, demyelination and gliosis occur. Neuronal loss is prominent in the medial thalamus. Atrophy of the mamillary bodies indicates chronic WE.
Source: References 8-10.
The authors’ observations
Mrs. B’s presentation suggests Wernicke’s encephalopathy (WE), an acute amnestic disorder caused by thiamine deficiency.
WE lesions are seen on autopsy in approximately 12.5% of alcohol abusers.1 Although alcoholism is more prevalent in men age 65, women are more likely to develop WE and cognitive dysfunction secondary to alcohol use.2
Alcoholism accounts for 77% of WE cases,3 although malnutrition caused by infection, cancer, gastric surgery, hemodialysis, hyperemesis, or starvation is another cause.
Clinical features of WE include confusion and disorientation (80% of cases, with stupor in 5%), ataxia (23%), and ocular abnormalities (29%). Nystagmus, especially to lateral gaze but also in vertical and other forms, is most common.4 Because less than one-third of patients with WE exhibit all 3 symptoms,5 the diagnosis is often missed. In studies, 15% of WE cases were diagnosed antemortem.1,6
Imaging studies. Brain MRI is more sensitive than computed tomography (CT) in detecting diencephalic, periventricular, and periaqueductal lesions (Box).7 Because of costs, physicians tend to order CT more often than MRI. CT can help rule out gross structural and vascular defects but is less adequate for evaluating specific lesions. In detecting WE lesions, MRI’s sensitivity is 53% and its specificity is 93%.7
Thiamine deficiency can occur when the liver can no longer absorb or store thiamine. Enzyme systems involved in the citric acid cycle and pentose phosphate pathway malfunction, and lactic acid production is increased. The associated pH change damages the apoenzymes. Glutamate accumulates, leading to production of free radicals, which cause cellular damage.11
Circulating thiamine levels are low (<50 ng/mL) in 30% to 80% of persons with alcoholism, putting them at risk for WE.12 Malnutrition secondary to alcoholism reduces thiamine absorption from the gut by 70%. Alcohol alone can reduce thiamine absorption by nearly 50%.13
WE lesions usually shrink within 48 to 72 hours of treatment with parenteral thiamine. Lactate <3.3 mg/dL or >14.9 mg/dL, and pyruvate <0.37 mg/dL or >0.75 mg/dL, indicate abnormal thiamine levels.14
Mrs. B’s confusion, hallucinations, and clouding of consciousness suggested DT, but this was ruled out because she had normal vital signs, classic eye signs of WE, no autonomic instability, and had been adequately tapered off alcohol.
TREATMENT: SHAKING ALCOHOL’S GRIP
A consulting neurologist confirmed a tentative diagnosis of WE.
Mrs. B’s oral thiamine was increased to 100 mg tid. She also received IM thiamine, 100 mg once daily for 5 days; risperidone, 0.5 mg every 4 hours as needed; and trazodone, 50 mg at bedtime as needed for irritability, agitation, and poor sleep. Multivitamins and folic acid were continued.
One week after starting IM thiamine, Mrs. B’s gait steadied, her coordination improved, and tremors and nystagmus stopped. She became more adept at eating. Cognitive impairment continued, but she confabulated less frequently. Her insight into her condition was improving.
Over the next 10 days, Mrs. B continued to improve, although neuropsychological assessment revealed major deficits in visuospatial function, attention, concentration, and memory. Repeat EEG showed diffuse slowing with frontal intermittent rhythmic delta activity, consistent with diffuse toxic metabolic encephalopathy.
Three weeks after admission, Mrs. B was discharged to her assisted-living facility, where she receives follow-up medical and psychiatric care. Her MMSE score at discharge was 12/30, indicating moderately severe cognitive impairment. Motor function has improved, although Mrs. B remains confused and needs help with daily living.
One month after discharge, Mrs. B’s diet was much improved; thiamine was reduced to 100 mg once daily. She has stayed sober but has repeatedly tried to drink. She was referred to a 12-step program but has not complied.
Table 1
Clinical features of WE, Korsakoff’s psychosis
| Wernicke’s encephalopathy | Korsakoff’s psychosis |
|---|---|
| Acute onset | Subacute or chronic onset |
| Clouding of conciousness common | Consciousness usually clear |
| Ataxia, nystagmus, ophthalmoplegiao usually present | Ataxia, nystagmus, ophthalmoplegia not common |
| Impaired anterograde, retrograde memory; confabulation is rare | Impaired anterograde, retrograde memory with prominent confabulation |
| Without adequate treatment, >80% progress to Korsakoff’s psychosis; death rate is 20% | >80% progress to alcohol induced persisting dementia; nursing home admission rate is 25% |
| Source: Reference 14. | |
The authors’ observations
Suspect WE in all patients with alcohol abuse disorder who are malnourished and/or elderly and whose dietary history is unclear. Early detection and treatment are crucial to preventing WE from becoming chronic. WE progresses to Korsakoff’s psychosis—a form of permanent short-term memory loss—in up to 80% of patients.5
Because Korsakoff’s psychosis carries an 8% death rate, consider the disorder in the differential diagnosis (Table). The disorder was ruled out in Mrs. B because of clouding of consciousness, ataxia, nystagmus, and shorter symptom duration.
Thiamine should be given IV, but can be given IM if unit nurses are not certified to give IV injections. Oral thiamine cannot generate the high thiamine blood concentrations (>50 ng/mL within the first 12 hours of treatment) needed to prevent irreversible damage.
Parenteral thiamine, 100 mg/d for 5 to 7 days, is given for acute WE. Some patients who are genetically predisposed to thiamine deficiency may need up to 1,000 mg/d. Continue oral thiamine, 100 mg/d, after parenteral dosing.
Although anaphylaxis risk during a 10-minute thiamine infusion is less than 1 in 1 million, make sure cardiopulmonary resuscitation is available during treatment. Glucose load can precipitate or worsen WE in a thiamine-deficient patient, so give thiamine before giving glucose in any form, including everyday foods.
Watch for other vitamin and magnesium deficiencies common to patients with alcoholism, as these might compromise response to IV/IM thiamine.15 Also rule out stroke in men age >65 who present with signs of hemiparesis.
Related resources
- Stern Y, Sackheim HA. Neuropsychiatric aspects of memory and amnesia. In: Yudofsky SC, Hales RE, (eds). Essentials of neuropsychiatry and clinical neurosciences. Washington, DC: American Psychiatric Publishing, 2004:201-38.
- National Institute of Neurological Disorders and Stroke. http://www.ninds.nih.gov/health_and_medical/disorders/wernicke-korsakoff.htm
Drug brand names
- Chlordiazepoxide • Libritabs, Lithium
- Divalproex sodium • Depakote
- Paroxetine • Paxil
- Risperidone • Risperdal
- Trazodone • Desyrel
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgment
Dr. Tampi’s efforts were supported by funds from the Division of State, Community, and Public Health, Bureau of Health Professions, Health Resources and Services Administration, Department of Health and Human Services, under grant number 1 K01 HP 00071-01, and the Geriatric Academic Career Award ($57,007). The information is that of Dr. Tampi and should not be construed as the official position or policy of, nor should any endorsements be inferred by, the aforementioned departments or the United States government.
1. Torvik A, Lindboe CF, Rodge S. Brain lesions in alcoholics. A neuropathological study with clinical correlations. J Neurol Sci 1982;56:233-48.
2. Grant BF. Prevalence and correlates of alcohol use and DSM IV dependence in the United States: results of the National Longitudinal Alcohol Epidemiological Survey. J Stud Alcohol 1997;58:464-73.
3. Lindboe CF, Loberg EM. Wernicke’s encephalopathy in non-alcoholics. An autopsy study. J Neurol Sci 1989;90:125-9
4. Harper CG, Giles M, Finlay-Jones R. Clinical signs in the Wernicke-Korsakoff complex: a retrospective analysis of 131 cases diagnosed at necropsy. J Neurol Neurosurg Psychiatry 1986;49:341-5.
5. Thompson AD, Cook CCH, Touquet R, Henry JA. The Royal College of Physicians Report on Alcohol: guidelines for managing Wernicke’s encephalopathy in the accident and emergency department. Alcohol Alcohol 2002;37(6):513-21.
6. Blansjaar BA, Van Dijk JG. Korsakoff minus Wernicke syndrome. Alcohol Alcohol 1992;27:435-7.
7. Antunez E, Estruch R, Cardenal C, et al. Usefulness of CT and MR imaging in the diagnosis of acute Wernicke’s encephalopathy. AJR Am J Roentgenol 1998;171:1131-7.
8. Charness ME. Intracranial voyeurism: revealing the mamillary bodies in alcoholism. Alcohol Clin Exp Res 1999;23:1941-4.
9. Victor M, Adams RD, Collins GH. The Wernicke-Korsakoff syndrome. A clinical and pathological study of 245 patients, 82 with post-mortem examinations. Contemp Neurol Ser 1971;7:1-206.
10. Weidauer S, Nichtweiss M, Lanfermann H, Zanella FE. Wernicke encephalopathy. MR findings and clinical presentation. Eur Radiol 2003;13(5):1001-9.
11. Hazell AS, Todd KG, Butterworth RF. Mechanism of neuronal cell death in Wernicke’s encephalopathy. Metab Brain Dis 1998;13(2):97-122.
12. Cook CC, Hallwood PM, Thomson AD. B vitamin deficiency and neuropsychiatric syndromes in alcohol misuse. Alcohol Alcohol 1998;33:317-36.
13. Thomson AD. Mechanisms of vitamin deficiency in chronic alcohol misusers and the development of the Wernicke-Korsakoff syndrome. Alcohol Alcohol 2000;35(suppl 1):2-7.
14. Victor M, Adams RA, Collins GH. The Wernicke-Korsakoff syndrome and related disorders due to alcoholism and malnutrition. Philadelphia: FA Davis, 1989.
15. Traviesa DC. Magnesium deficiency: a possible cause of thiamine refractoriness in Wernicke-Korsakoff encephalopathy. J Neurol Neurosurg Psychiatry 1974;37:959-62.
HISTORY: TOO MUCH FOR TOO LONG
Mrs. B, age 73, has been alcohol-dependent for 20 years. Since her husband’s death 5 years ago, she has been drinking 1 to 2 liters of vodka a week. At her family’s insistence, she checks into a tertiary-care hospital for worsening alcohol use, memory problems, and increasing confusion.
Mrs. B’s family removed her car because of her alcohol and cognitive problems, but she walks half a mile to buy alcohol. She lives alone in an assisted-living facility and has been hospitalized for detoxification 3 times within 2 years.
At intake, her judgment and abstract thinking are impaired. She has poor insight into her condition. Physical examination reveals fine hand tremors. Lab test results and vital signs are normal. Mrs. B was previously diagnosed with bipolar disorder and takes divalproex, 250 each morning and 500 mg at bedtime, and paroxetine, 20 mg/d.
Mrs. B’s Folstein Mini-Mental State Examination (MMSE) score 1 week after admission was 5/30, indicating severe cognitive deficits. Her mood was euthymic, speech and motor activity were normal, and thought process was logical with intact associations. She exhibited no delusions or hallucinations but was disoriented, with a short attention span and poor concentration.
The authors’ observations
Mrs. B’s confusion has increased in recent weeks. Hand tremors could signal a neurologic problem triggered by a vascular event or alcohol use. Include dementia in the differential diagnosis.
Distinguishing between vascular dementia and alcohol-induced persisting dementia requires a thorough history, neurologic exam, and lab testing.
Vascular dementia. Cognition deteriorates step by step. Patients with this dementia have multiple vascular risk factors and display evidence of cerebrovascular events on physical examination or imaging studies. Watch for high blood pressure, high cholesterol, or obesity; history of diabetes, cardiac arrythmias, or strokes; or other vascular changes in the brain.
Alcohol-induced persisting dementia. Patients usually have abused alcohol for years, and memory slowly deteriorates. Vascular events that would explain cognitive deficits are not found. Such patients usually do not have vascular and cerebrovascular risk factors, but may exhibit worsening cognition in the context of alcohol use. Watch for mean corpuscular volume >100 femtoliters, gamma glutamyl transferase >50 U/L, and elevated liver function tests.
For Mrs. B, both dementia types were ruled out. Her memory problems were mild, and she had been functioning independently at the assisted-living facility. Dementia is not characterized by clouding of consciousness, and her disorder’s progression was fast. Mrs. B’s bipolar disorder was not a factor because she did not have significant depressive or manic symptoms.
Amnestic disorder. Mrs. B’s worsening mental status and neurologic signs after admission suggest amnestic disorder. Patients with amnestic disorder have trouble learning or recalling new information and forming new memories, although they can talk coherently and appropriately.
Injury to the diencephalic and medial temporal lobe structures triggers amnestic disorder. Head trauma, cerebral infections, and infarctions can damage these structures, but alcoholism is the most common cause.
ADMISSION: INCREASING CONFUSION
Mrs. B was admitted to the dual diagnosis unit for patients with substance use and psychiatric disorders. Although confused, she could eat and walk.
For 2 days, Mrs. B received chlordiazepoxide, 200 mg/d, for detoxification; a multivitamin tablet; and oral vitamin B1 (thiamine), 100 mg once daily. She also continued her divalproex/paroxetine regimen. Chlordiazepoxide was tapered and discontinued over 4 days. Vital signs remained normal.
Two days after starting detox, Mrs. B’s condition began to worsen. She became incontinent of urine and feces, had trouble eating, and required extensive assistance with activities of daily living.
On examination by the geriatric psychiatry team, Mrs. B appeared very confused. She was confabulating, had hand tremors, and was ataxic, with nystagmus on lateral gaze. Coordination was poor. Because she reported visual hallucinations and appeared delirious, divalproex sodium and paroxetine—which can worsen delirium—were stopped.
Head MRI with contrast revealed sulcal space prominence in the cerebral and cerebellar hemispheres, suggesting minimal volume loss, and nonspecific bilateral periventricular punctuate flairs and T2 hypodensities, indicating small-vessel ischemic disease. EEG showed moderate rhythm slowing. Blood and urine tests showed no infectious disease or metabolic abnormalities.
Lesions associated with Wernicke’s encephalopathy (WE) usually are found in the third ventricle, cerebral aqueduct, fourth ventricle, mamillary bodies, periaqueductal gray matter, dorsomedial thalamus, septal region, and oculomotor nuclei.
In approximately 50% of cases, damage to the cerebellum also occurs. Such damage is usually symmetrical and shows diffuse, patchy endothelial prominence, proliferation of microglia, and petechial hemorrhage.
In chronic cases, demyelination and gliosis occur. Neuronal loss is prominent in the medial thalamus. Atrophy of the mamillary bodies indicates chronic WE.
Source: References 8-10.
The authors’ observations
Mrs. B’s presentation suggests Wernicke’s encephalopathy (WE), an acute amnestic disorder caused by thiamine deficiency.
WE lesions are seen on autopsy in approximately 12.5% of alcohol abusers.1 Although alcoholism is more prevalent in men age 65, women are more likely to develop WE and cognitive dysfunction secondary to alcohol use.2
Alcoholism accounts for 77% of WE cases,3 although malnutrition caused by infection, cancer, gastric surgery, hemodialysis, hyperemesis, or starvation is another cause.
Clinical features of WE include confusion and disorientation (80% of cases, with stupor in 5%), ataxia (23%), and ocular abnormalities (29%). Nystagmus, especially to lateral gaze but also in vertical and other forms, is most common.4 Because less than one-third of patients with WE exhibit all 3 symptoms,5 the diagnosis is often missed. In studies, 15% of WE cases were diagnosed antemortem.1,6
Imaging studies. Brain MRI is more sensitive than computed tomography (CT) in detecting diencephalic, periventricular, and periaqueductal lesions (Box).7 Because of costs, physicians tend to order CT more often than MRI. CT can help rule out gross structural and vascular defects but is less adequate for evaluating specific lesions. In detecting WE lesions, MRI’s sensitivity is 53% and its specificity is 93%.7
Thiamine deficiency can occur when the liver can no longer absorb or store thiamine. Enzyme systems involved in the citric acid cycle and pentose phosphate pathway malfunction, and lactic acid production is increased. The associated pH change damages the apoenzymes. Glutamate accumulates, leading to production of free radicals, which cause cellular damage.11
Circulating thiamine levels are low (<50 ng/mL) in 30% to 80% of persons with alcoholism, putting them at risk for WE.12 Malnutrition secondary to alcoholism reduces thiamine absorption from the gut by 70%. Alcohol alone can reduce thiamine absorption by nearly 50%.13
WE lesions usually shrink within 48 to 72 hours of treatment with parenteral thiamine. Lactate <3.3 mg/dL or >14.9 mg/dL, and pyruvate <0.37 mg/dL or >0.75 mg/dL, indicate abnormal thiamine levels.14
Mrs. B’s confusion, hallucinations, and clouding of consciousness suggested DT, but this was ruled out because she had normal vital signs, classic eye signs of WE, no autonomic instability, and had been adequately tapered off alcohol.
TREATMENT: SHAKING ALCOHOL’S GRIP
A consulting neurologist confirmed a tentative diagnosis of WE.
Mrs. B’s oral thiamine was increased to 100 mg tid. She also received IM thiamine, 100 mg once daily for 5 days; risperidone, 0.5 mg every 4 hours as needed; and trazodone, 50 mg at bedtime as needed for irritability, agitation, and poor sleep. Multivitamins and folic acid were continued.
One week after starting IM thiamine, Mrs. B’s gait steadied, her coordination improved, and tremors and nystagmus stopped. She became more adept at eating. Cognitive impairment continued, but she confabulated less frequently. Her insight into her condition was improving.
Over the next 10 days, Mrs. B continued to improve, although neuropsychological assessment revealed major deficits in visuospatial function, attention, concentration, and memory. Repeat EEG showed diffuse slowing with frontal intermittent rhythmic delta activity, consistent with diffuse toxic metabolic encephalopathy.
Three weeks after admission, Mrs. B was discharged to her assisted-living facility, where she receives follow-up medical and psychiatric care. Her MMSE score at discharge was 12/30, indicating moderately severe cognitive impairment. Motor function has improved, although Mrs. B remains confused and needs help with daily living.
One month after discharge, Mrs. B’s diet was much improved; thiamine was reduced to 100 mg once daily. She has stayed sober but has repeatedly tried to drink. She was referred to a 12-step program but has not complied.
Table 1
Clinical features of WE, Korsakoff’s psychosis
| Wernicke’s encephalopathy | Korsakoff’s psychosis |
|---|---|
| Acute onset | Subacute or chronic onset |
| Clouding of conciousness common | Consciousness usually clear |
| Ataxia, nystagmus, ophthalmoplegiao usually present | Ataxia, nystagmus, ophthalmoplegia not common |
| Impaired anterograde, retrograde memory; confabulation is rare | Impaired anterograde, retrograde memory with prominent confabulation |
| Without adequate treatment, >80% progress to Korsakoff’s psychosis; death rate is 20% | >80% progress to alcohol induced persisting dementia; nursing home admission rate is 25% |
| Source: Reference 14. | |
The authors’ observations
Suspect WE in all patients with alcohol abuse disorder who are malnourished and/or elderly and whose dietary history is unclear. Early detection and treatment are crucial to preventing WE from becoming chronic. WE progresses to Korsakoff’s psychosis—a form of permanent short-term memory loss—in up to 80% of patients.5
Because Korsakoff’s psychosis carries an 8% death rate, consider the disorder in the differential diagnosis (Table). The disorder was ruled out in Mrs. B because of clouding of consciousness, ataxia, nystagmus, and shorter symptom duration.
Thiamine should be given IV, but can be given IM if unit nurses are not certified to give IV injections. Oral thiamine cannot generate the high thiamine blood concentrations (>50 ng/mL within the first 12 hours of treatment) needed to prevent irreversible damage.
Parenteral thiamine, 100 mg/d for 5 to 7 days, is given for acute WE. Some patients who are genetically predisposed to thiamine deficiency may need up to 1,000 mg/d. Continue oral thiamine, 100 mg/d, after parenteral dosing.
Although anaphylaxis risk during a 10-minute thiamine infusion is less than 1 in 1 million, make sure cardiopulmonary resuscitation is available during treatment. Glucose load can precipitate or worsen WE in a thiamine-deficient patient, so give thiamine before giving glucose in any form, including everyday foods.
Watch for other vitamin and magnesium deficiencies common to patients with alcoholism, as these might compromise response to IV/IM thiamine.15 Also rule out stroke in men age >65 who present with signs of hemiparesis.
Related resources
- Stern Y, Sackheim HA. Neuropsychiatric aspects of memory and amnesia. In: Yudofsky SC, Hales RE, (eds). Essentials of neuropsychiatry and clinical neurosciences. Washington, DC: American Psychiatric Publishing, 2004:201-38.
- National Institute of Neurological Disorders and Stroke. http://www.ninds.nih.gov/health_and_medical/disorders/wernicke-korsakoff.htm
Drug brand names
- Chlordiazepoxide • Libritabs, Lithium
- Divalproex sodium • Depakote
- Paroxetine • Paxil
- Risperidone • Risperdal
- Trazodone • Desyrel
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgment
Dr. Tampi’s efforts were supported by funds from the Division of State, Community, and Public Health, Bureau of Health Professions, Health Resources and Services Administration, Department of Health and Human Services, under grant number 1 K01 HP 00071-01, and the Geriatric Academic Career Award ($57,007). The information is that of Dr. Tampi and should not be construed as the official position or policy of, nor should any endorsements be inferred by, the aforementioned departments or the United States government.
HISTORY: TOO MUCH FOR TOO LONG
Mrs. B, age 73, has been alcohol-dependent for 20 years. Since her husband’s death 5 years ago, she has been drinking 1 to 2 liters of vodka a week. At her family’s insistence, she checks into a tertiary-care hospital for worsening alcohol use, memory problems, and increasing confusion.
Mrs. B’s family removed her car because of her alcohol and cognitive problems, but she walks half a mile to buy alcohol. She lives alone in an assisted-living facility and has been hospitalized for detoxification 3 times within 2 years.
At intake, her judgment and abstract thinking are impaired. She has poor insight into her condition. Physical examination reveals fine hand tremors. Lab test results and vital signs are normal. Mrs. B was previously diagnosed with bipolar disorder and takes divalproex, 250 each morning and 500 mg at bedtime, and paroxetine, 20 mg/d.
Mrs. B’s Folstein Mini-Mental State Examination (MMSE) score 1 week after admission was 5/30, indicating severe cognitive deficits. Her mood was euthymic, speech and motor activity were normal, and thought process was logical with intact associations. She exhibited no delusions or hallucinations but was disoriented, with a short attention span and poor concentration.
The authors’ observations
Mrs. B’s confusion has increased in recent weeks. Hand tremors could signal a neurologic problem triggered by a vascular event or alcohol use. Include dementia in the differential diagnosis.
Distinguishing between vascular dementia and alcohol-induced persisting dementia requires a thorough history, neurologic exam, and lab testing.
Vascular dementia. Cognition deteriorates step by step. Patients with this dementia have multiple vascular risk factors and display evidence of cerebrovascular events on physical examination or imaging studies. Watch for high blood pressure, high cholesterol, or obesity; history of diabetes, cardiac arrythmias, or strokes; or other vascular changes in the brain.
Alcohol-induced persisting dementia. Patients usually have abused alcohol for years, and memory slowly deteriorates. Vascular events that would explain cognitive deficits are not found. Such patients usually do not have vascular and cerebrovascular risk factors, but may exhibit worsening cognition in the context of alcohol use. Watch for mean corpuscular volume >100 femtoliters, gamma glutamyl transferase >50 U/L, and elevated liver function tests.
For Mrs. B, both dementia types were ruled out. Her memory problems were mild, and she had been functioning independently at the assisted-living facility. Dementia is not characterized by clouding of consciousness, and her disorder’s progression was fast. Mrs. B’s bipolar disorder was not a factor because she did not have significant depressive or manic symptoms.
Amnestic disorder. Mrs. B’s worsening mental status and neurologic signs after admission suggest amnestic disorder. Patients with amnestic disorder have trouble learning or recalling new information and forming new memories, although they can talk coherently and appropriately.
Injury to the diencephalic and medial temporal lobe structures triggers amnestic disorder. Head trauma, cerebral infections, and infarctions can damage these structures, but alcoholism is the most common cause.
ADMISSION: INCREASING CONFUSION
Mrs. B was admitted to the dual diagnosis unit for patients with substance use and psychiatric disorders. Although confused, she could eat and walk.
For 2 days, Mrs. B received chlordiazepoxide, 200 mg/d, for detoxification; a multivitamin tablet; and oral vitamin B1 (thiamine), 100 mg once daily. She also continued her divalproex/paroxetine regimen. Chlordiazepoxide was tapered and discontinued over 4 days. Vital signs remained normal.
Two days after starting detox, Mrs. B’s condition began to worsen. She became incontinent of urine and feces, had trouble eating, and required extensive assistance with activities of daily living.
On examination by the geriatric psychiatry team, Mrs. B appeared very confused. She was confabulating, had hand tremors, and was ataxic, with nystagmus on lateral gaze. Coordination was poor. Because she reported visual hallucinations and appeared delirious, divalproex sodium and paroxetine—which can worsen delirium—were stopped.
Head MRI with contrast revealed sulcal space prominence in the cerebral and cerebellar hemispheres, suggesting minimal volume loss, and nonspecific bilateral periventricular punctuate flairs and T2 hypodensities, indicating small-vessel ischemic disease. EEG showed moderate rhythm slowing. Blood and urine tests showed no infectious disease or metabolic abnormalities.
Lesions associated with Wernicke’s encephalopathy (WE) usually are found in the third ventricle, cerebral aqueduct, fourth ventricle, mamillary bodies, periaqueductal gray matter, dorsomedial thalamus, septal region, and oculomotor nuclei.
In approximately 50% of cases, damage to the cerebellum also occurs. Such damage is usually symmetrical and shows diffuse, patchy endothelial prominence, proliferation of microglia, and petechial hemorrhage.
In chronic cases, demyelination and gliosis occur. Neuronal loss is prominent in the medial thalamus. Atrophy of the mamillary bodies indicates chronic WE.
Source: References 8-10.
The authors’ observations
Mrs. B’s presentation suggests Wernicke’s encephalopathy (WE), an acute amnestic disorder caused by thiamine deficiency.
WE lesions are seen on autopsy in approximately 12.5% of alcohol abusers.1 Although alcoholism is more prevalent in men age 65, women are more likely to develop WE and cognitive dysfunction secondary to alcohol use.2
Alcoholism accounts for 77% of WE cases,3 although malnutrition caused by infection, cancer, gastric surgery, hemodialysis, hyperemesis, or starvation is another cause.
Clinical features of WE include confusion and disorientation (80% of cases, with stupor in 5%), ataxia (23%), and ocular abnormalities (29%). Nystagmus, especially to lateral gaze but also in vertical and other forms, is most common.4 Because less than one-third of patients with WE exhibit all 3 symptoms,5 the diagnosis is often missed. In studies, 15% of WE cases were diagnosed antemortem.1,6
Imaging studies. Brain MRI is more sensitive than computed tomography (CT) in detecting diencephalic, periventricular, and periaqueductal lesions (Box).7 Because of costs, physicians tend to order CT more often than MRI. CT can help rule out gross structural and vascular defects but is less adequate for evaluating specific lesions. In detecting WE lesions, MRI’s sensitivity is 53% and its specificity is 93%.7
Thiamine deficiency can occur when the liver can no longer absorb or store thiamine. Enzyme systems involved in the citric acid cycle and pentose phosphate pathway malfunction, and lactic acid production is increased. The associated pH change damages the apoenzymes. Glutamate accumulates, leading to production of free radicals, which cause cellular damage.11
Circulating thiamine levels are low (<50 ng/mL) in 30% to 80% of persons with alcoholism, putting them at risk for WE.12 Malnutrition secondary to alcoholism reduces thiamine absorption from the gut by 70%. Alcohol alone can reduce thiamine absorption by nearly 50%.13
WE lesions usually shrink within 48 to 72 hours of treatment with parenteral thiamine. Lactate <3.3 mg/dL or >14.9 mg/dL, and pyruvate <0.37 mg/dL or >0.75 mg/dL, indicate abnormal thiamine levels.14
Mrs. B’s confusion, hallucinations, and clouding of consciousness suggested DT, but this was ruled out because she had normal vital signs, classic eye signs of WE, no autonomic instability, and had been adequately tapered off alcohol.
TREATMENT: SHAKING ALCOHOL’S GRIP
A consulting neurologist confirmed a tentative diagnosis of WE.
Mrs. B’s oral thiamine was increased to 100 mg tid. She also received IM thiamine, 100 mg once daily for 5 days; risperidone, 0.5 mg every 4 hours as needed; and trazodone, 50 mg at bedtime as needed for irritability, agitation, and poor sleep. Multivitamins and folic acid were continued.
One week after starting IM thiamine, Mrs. B’s gait steadied, her coordination improved, and tremors and nystagmus stopped. She became more adept at eating. Cognitive impairment continued, but she confabulated less frequently. Her insight into her condition was improving.
Over the next 10 days, Mrs. B continued to improve, although neuropsychological assessment revealed major deficits in visuospatial function, attention, concentration, and memory. Repeat EEG showed diffuse slowing with frontal intermittent rhythmic delta activity, consistent with diffuse toxic metabolic encephalopathy.
Three weeks after admission, Mrs. B was discharged to her assisted-living facility, where she receives follow-up medical and psychiatric care. Her MMSE score at discharge was 12/30, indicating moderately severe cognitive impairment. Motor function has improved, although Mrs. B remains confused and needs help with daily living.
One month after discharge, Mrs. B’s diet was much improved; thiamine was reduced to 100 mg once daily. She has stayed sober but has repeatedly tried to drink. She was referred to a 12-step program but has not complied.
Table 1
Clinical features of WE, Korsakoff’s psychosis
| Wernicke’s encephalopathy | Korsakoff’s psychosis |
|---|---|
| Acute onset | Subacute or chronic onset |
| Clouding of conciousness common | Consciousness usually clear |
| Ataxia, nystagmus, ophthalmoplegiao usually present | Ataxia, nystagmus, ophthalmoplegia not common |
| Impaired anterograde, retrograde memory; confabulation is rare | Impaired anterograde, retrograde memory with prominent confabulation |
| Without adequate treatment, >80% progress to Korsakoff’s psychosis; death rate is 20% | >80% progress to alcohol induced persisting dementia; nursing home admission rate is 25% |
| Source: Reference 14. | |
The authors’ observations
Suspect WE in all patients with alcohol abuse disorder who are malnourished and/or elderly and whose dietary history is unclear. Early detection and treatment are crucial to preventing WE from becoming chronic. WE progresses to Korsakoff’s psychosis—a form of permanent short-term memory loss—in up to 80% of patients.5
Because Korsakoff’s psychosis carries an 8% death rate, consider the disorder in the differential diagnosis (Table). The disorder was ruled out in Mrs. B because of clouding of consciousness, ataxia, nystagmus, and shorter symptom duration.
Thiamine should be given IV, but can be given IM if unit nurses are not certified to give IV injections. Oral thiamine cannot generate the high thiamine blood concentrations (>50 ng/mL within the first 12 hours of treatment) needed to prevent irreversible damage.
Parenteral thiamine, 100 mg/d for 5 to 7 days, is given for acute WE. Some patients who are genetically predisposed to thiamine deficiency may need up to 1,000 mg/d. Continue oral thiamine, 100 mg/d, after parenteral dosing.
Although anaphylaxis risk during a 10-minute thiamine infusion is less than 1 in 1 million, make sure cardiopulmonary resuscitation is available during treatment. Glucose load can precipitate or worsen WE in a thiamine-deficient patient, so give thiamine before giving glucose in any form, including everyday foods.
Watch for other vitamin and magnesium deficiencies common to patients with alcoholism, as these might compromise response to IV/IM thiamine.15 Also rule out stroke in men age >65 who present with signs of hemiparesis.
Related resources
- Stern Y, Sackheim HA. Neuropsychiatric aspects of memory and amnesia. In: Yudofsky SC, Hales RE, (eds). Essentials of neuropsychiatry and clinical neurosciences. Washington, DC: American Psychiatric Publishing, 2004:201-38.
- National Institute of Neurological Disorders and Stroke. http://www.ninds.nih.gov/health_and_medical/disorders/wernicke-korsakoff.htm
Drug brand names
- Chlordiazepoxide • Libritabs, Lithium
- Divalproex sodium • Depakote
- Paroxetine • Paxil
- Risperidone • Risperdal
- Trazodone • Desyrel
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgment
Dr. Tampi’s efforts were supported by funds from the Division of State, Community, and Public Health, Bureau of Health Professions, Health Resources and Services Administration, Department of Health and Human Services, under grant number 1 K01 HP 00071-01, and the Geriatric Academic Career Award ($57,007). The information is that of Dr. Tampi and should not be construed as the official position or policy of, nor should any endorsements be inferred by, the aforementioned departments or the United States government.
1. Torvik A, Lindboe CF, Rodge S. Brain lesions in alcoholics. A neuropathological study with clinical correlations. J Neurol Sci 1982;56:233-48.
2. Grant BF. Prevalence and correlates of alcohol use and DSM IV dependence in the United States: results of the National Longitudinal Alcohol Epidemiological Survey. J Stud Alcohol 1997;58:464-73.
3. Lindboe CF, Loberg EM. Wernicke’s encephalopathy in non-alcoholics. An autopsy study. J Neurol Sci 1989;90:125-9
4. Harper CG, Giles M, Finlay-Jones R. Clinical signs in the Wernicke-Korsakoff complex: a retrospective analysis of 131 cases diagnosed at necropsy. J Neurol Neurosurg Psychiatry 1986;49:341-5.
5. Thompson AD, Cook CCH, Touquet R, Henry JA. The Royal College of Physicians Report on Alcohol: guidelines for managing Wernicke’s encephalopathy in the accident and emergency department. Alcohol Alcohol 2002;37(6):513-21.
6. Blansjaar BA, Van Dijk JG. Korsakoff minus Wernicke syndrome. Alcohol Alcohol 1992;27:435-7.
7. Antunez E, Estruch R, Cardenal C, et al. Usefulness of CT and MR imaging in the diagnosis of acute Wernicke’s encephalopathy. AJR Am J Roentgenol 1998;171:1131-7.
8. Charness ME. Intracranial voyeurism: revealing the mamillary bodies in alcoholism. Alcohol Clin Exp Res 1999;23:1941-4.
9. Victor M, Adams RD, Collins GH. The Wernicke-Korsakoff syndrome. A clinical and pathological study of 245 patients, 82 with post-mortem examinations. Contemp Neurol Ser 1971;7:1-206.
10. Weidauer S, Nichtweiss M, Lanfermann H, Zanella FE. Wernicke encephalopathy. MR findings and clinical presentation. Eur Radiol 2003;13(5):1001-9.
11. Hazell AS, Todd KG, Butterworth RF. Mechanism of neuronal cell death in Wernicke’s encephalopathy. Metab Brain Dis 1998;13(2):97-122.
12. Cook CC, Hallwood PM, Thomson AD. B vitamin deficiency and neuropsychiatric syndromes in alcohol misuse. Alcohol Alcohol 1998;33:317-36.
13. Thomson AD. Mechanisms of vitamin deficiency in chronic alcohol misusers and the development of the Wernicke-Korsakoff syndrome. Alcohol Alcohol 2000;35(suppl 1):2-7.
14. Victor M, Adams RA, Collins GH. The Wernicke-Korsakoff syndrome and related disorders due to alcoholism and malnutrition. Philadelphia: FA Davis, 1989.
15. Traviesa DC. Magnesium deficiency: a possible cause of thiamine refractoriness in Wernicke-Korsakoff encephalopathy. J Neurol Neurosurg Psychiatry 1974;37:959-62.
1. Torvik A, Lindboe CF, Rodge S. Brain lesions in alcoholics. A neuropathological study with clinical correlations. J Neurol Sci 1982;56:233-48.
2. Grant BF. Prevalence and correlates of alcohol use and DSM IV dependence in the United States: results of the National Longitudinal Alcohol Epidemiological Survey. J Stud Alcohol 1997;58:464-73.
3. Lindboe CF, Loberg EM. Wernicke’s encephalopathy in non-alcoholics. An autopsy study. J Neurol Sci 1989;90:125-9
4. Harper CG, Giles M, Finlay-Jones R. Clinical signs in the Wernicke-Korsakoff complex: a retrospective analysis of 131 cases diagnosed at necropsy. J Neurol Neurosurg Psychiatry 1986;49:341-5.
5. Thompson AD, Cook CCH, Touquet R, Henry JA. The Royal College of Physicians Report on Alcohol: guidelines for managing Wernicke’s encephalopathy in the accident and emergency department. Alcohol Alcohol 2002;37(6):513-21.
6. Blansjaar BA, Van Dijk JG. Korsakoff minus Wernicke syndrome. Alcohol Alcohol 1992;27:435-7.
7. Antunez E, Estruch R, Cardenal C, et al. Usefulness of CT and MR imaging in the diagnosis of acute Wernicke’s encephalopathy. AJR Am J Roentgenol 1998;171:1131-7.
8. Charness ME. Intracranial voyeurism: revealing the mamillary bodies in alcoholism. Alcohol Clin Exp Res 1999;23:1941-4.
9. Victor M, Adams RD, Collins GH. The Wernicke-Korsakoff syndrome. A clinical and pathological study of 245 patients, 82 with post-mortem examinations. Contemp Neurol Ser 1971;7:1-206.
10. Weidauer S, Nichtweiss M, Lanfermann H, Zanella FE. Wernicke encephalopathy. MR findings and clinical presentation. Eur Radiol 2003;13(5):1001-9.
11. Hazell AS, Todd KG, Butterworth RF. Mechanism of neuronal cell death in Wernicke’s encephalopathy. Metab Brain Dis 1998;13(2):97-122.
12. Cook CC, Hallwood PM, Thomson AD. B vitamin deficiency and neuropsychiatric syndromes in alcohol misuse. Alcohol Alcohol 1998;33:317-36.
13. Thomson AD. Mechanisms of vitamin deficiency in chronic alcohol misusers and the development of the Wernicke-Korsakoff syndrome. Alcohol Alcohol 2000;35(suppl 1):2-7.
14. Victor M, Adams RA, Collins GH. The Wernicke-Korsakoff syndrome and related disorders due to alcoholism and malnutrition. Philadelphia: FA Davis, 1989.
15. Traviesa DC. Magnesium deficiency: a possible cause of thiamine refractoriness in Wernicke-Korsakoff encephalopathy. J Neurol Neurosurg Psychiatry 1974;37:959-62.
Secondary amenorrhea: Don’t dismiss it as ‘normal’
A young or middle-aged patient who stops menstruating may be pregnant or have an underlying medical problem that, left undiagnosed, could cause obesity, sexual dysfunction, infertility, osteoporosis, endometrial hyperplasia, or endometrial cancer.
Yet clinicians too often dismiss secondary amenorrhea as a “normal” result of a mental disorder or psychotropic. Psychiatrists need to:
- identify when a psychiatric disorder or drug disrupts menses
- diagnose medical causes, including thyroid dysfunction, pituitary adenomas, and polycystic ovary syndrome (PCOS).
This article outlines the most common and serious causes of secondary amenorrhea among psychiatric patients, and offers an algorithm for ruling out medical problems in nonpregnant women of child-bearing age who have stopped menstruating for 3 months. The diagnostic approach described here does not apply to women with primary amenorrhea (have never menstruated).
Table 1
Psychotropics that may cause amenorrhea
| Effect | Drug/class |
|---|---|
| Prolactin elevation | Antipsychotics (chlorpromazine, haloperidol, risperidone) SSRIs (citalopram, escitalopram, fluoxetine) |
| Sex hormone-binding globulin elevation | Carbamazepine |
| Association with PCOS unknown mechanism | Valproic acid |
| SSRIs: Selective serotonin reuptake inhibitors | |
| PCOS: Polycystic ovary syndrome | |
CASE REPORT: NO PREGNANCY, NO PERIOD
Two years ago Ms. J, age 28, was diagnosed with depression. Her psychiatrist prescribed fluoxetine, 20 mg/d titrated across 4 weeks to 40 mg/d. About 4 months later, she experienced her first manic episode. The psychiatrist changed the diagnosis to bipolar I disorder and added risperidone, 2 mg/d, to manage her mania.
Ms. J’s bipolar disorder has been under control for 1 year, but she reports that her menstruation stopped 6 months ago. She is sexually active; she and her partner use spermicide-coated condoms. She does not want to be pregnant now but might want to bear a child within the next year. Several home pregnancy tests across 6 months were negative.
The patient is obese (5 feet, 5 inches, 186 lbs, body mass index 31) and has gained about 30 pounds during the past year. Vital signs are normal; psychiatric examination indicates normal mood and affect. Skin exam reveals mild papular acne on her face and back and increased hair growth on her chin. Other physical findings—including cardiac, lung, and neurologic examinations—are normal.
Laboratory evaluation reveals a prolactin level of 105 ng/mL, a negative serum ß-Hcg reading, and normal TSH, FSH, DHEA-S and testosterone levels.
Discussion. Ms. J’s history, physical examination, and laboratory tests suggest several possible causes of secondary amenorrhea:
- Are psychotropics or a prolactin-secreting tumor elevating her prolactin level?
- Does she have PCOS, as her weight gain, hirsutism, and acne might indicate?
- Is her bipolar disorder a factor? Consider psychiatric illness, medication side effects, and medical causes when evaluating secondary amenorrhea.
PSYCHIATRIC ILLNESS
Patients with high emotional stress may have amenorrhea or menstrual irregularities related to hypothalamic dysfunction.1 Also:
Anorexia nervosa has been shown to cause hypothalamic dysfunction, leading to amenorrhea.2 A correlation exists between weight loss and menses cessation, and between regain of weight and menses resumption.2
Depression. Estradiol levels are lower in depressed women than in euthymic women, probably because of altered hypothalamic-pituitary axis (HPA) function. Also, physical distress is correlated with menses disruption.3
In a 3-year study of women ages 36 to 45,4 those with a history of depression exhibited 1.2 times the rate of perimenopause as nondepressed women. Subjects with Hamilton Rating Scale for Depression scores >8 at enrollment had twice the rate of perimenopause after 3 years compared with nondepressed women. The findings suggest that depression might increase a woman’s risk of ceasing ovarian function in her 30s or 40s. Natural menopause on average begins at age 51.5
In another study,6 16 of 32 women with PCOS had Center for Epidemiological Studies-Depression Rating Scale scores indicating depression (≥16). The study suggests a high prevalence of depression among women with PCOS, but was limited by possible selection bias, no further diagnostic evaluation for depression, small sample size, and lack of an age-matched control group.
Bipolar disorder. High rates of menstrual disturbances have been reported among women with bipolar disorder.7 Although the mechanism has not been ascertained, disruption of HPA function similar to that seen in depression is likely.7
MEDICATIONS AND AMENORRHEA
Medications can cause amenorrhea, primarily through hyperprolactinemia—although other mechanisms may be involved (Table 1). Prolactin suppresses hypothalamic luteinizing hormone-releasing hormone (LHRH) production, leading to decreased follicle-stimulating hormone (FSH) and luteinizing hormone (LH), thus reducing circulating estrogen. Prolactin-secreting pituitary tumors and drug side effects mostly commonly cause hyperprolactinemia.
Antipsychotics. Phenothiazines such as chlorpromazine, butyrophenones such as haloperidol, and the atypical antipsychotic risperidone raise prolactin levels via dopamine-receptor antagonism.
Other atypical antipsychotics—including aripiprazole, clozapine, olanzapine, quetiapine, and ziprasidone—are associated with lower serum prolactin levels than risperidone.8,9 Preliminary studies suggest, for example, that switching patients from risperidone to quetiapine may help resume menstruation without worsening psychotic symptoms,10 and that amenorrhea often resolves after the patient is switched to another atypical antipsychotic.11
SSRIs. All selective serotonin reuptake inhibitors except sertraline are associated with hyperprolactinemia and can lead to amenorrhea in some patients.12
Table 2
Differential diagnosis of secondary amenorrhea
Ovarian causes
|
Hypothalamic causes
|
Hyperprolactinemia
|
Uterine causes
|
| * Turner’s syndrome: A rare chromosomal disorder characterized by short stature, lack of sexual development at puberty. |
| † Asherman’s syndrome: Endometrial adhesions, scar tissue that develop after uterine curettage or infections. |
Anticonvulsants used as mood stabilizers to treat bipolar disorder may cause menstrual irregularities, although most data relate to women with seizure disorders.
Valproic acid has been associated with PCOS in patients with epilepsy,13 although it is unknown whether the agent’s androgenizing effects vary with age. Carbamazepine, which increases sex hormone-binding globulin, may also lead to menstrual disorders by decreasing bioavailability of circulating estrogen.14 Consider switching a patient with disrupted menses to lithium, lamotrigine, or oxcarbazepine, which have not been associated with menstrual dysfunction.
MEDICAL CAUSES
Pregnancy is the most common cause of menses cessation, followed by ovarian, hypothalamic, pituitary, or uterine dysfunction (Table 2). Hypothalamic and pituitary dysfunction often cause amenorrhea in psychiatric patients, whereas ovarian causes are common among all patients with secondary amenorrhea.15
Ovarian. In PCOS, the ovaries and sometimes the adrenal glands produce excess androgens, leading to infrequent or light periods (oligomenorrhea) or amenorrhea.
Patients with depression are prone to ovarian failure in their 30s or 40s, possibly because of chronic HPA disruption.4 Premature ovarian failure also is common among patients with Turner’s syndrome, a rare chromosomal disorder characterized by short stature and lack of sexual development at puberty. Ovarian failure also can occur spontaneously.
Hypothalamic. Functional hypothalamic amenorrhea occurs in mood and eating disorders. Emotional stress, excessive physical exercise, and nutritional deficiencies reduce LHRH secretion by the hypothalamus, which interrupts the reproductive cycle. Cardiovascular disease, respiratory disease, cancer, and other acute and chronic medical illnesses can cause significant physiologic stress, thus leading to HPA dysfunction. Hypothalamic amenorrhea is treated by targeting the underlying psychiatric or medical condition.
Pituitary. Prolactin-secreting pituitary tumors, such as a pituitary adenoma, must be ruled out in patients whose prolactin levels remain high after a medication change.15 Hypothyroidism also can trigger hyperprolactinemia by causing pituitary gland hyperplasia.
Uterine. Women who have had uterine curettage or infections can develop adhesions and scar tissue that ablate the endometrial lining. This condition, called Asherman’s syndrome, is the most common uterine cause of menstrual disruption.
EVALUATING SECONDARY AMENORRHEA
When a patient presents with secondary amenorrhea, immediately rule out pregnancy because psychiatric disorders often are managed differently in pregnant than in nonpregnant women.16
Next, take a thorough patient history to determine whether referral is necessary. Ask about weight loss (intentional or unintentional), increased stressors, or a medical illness that may point to functional hypothalamic amenorrhea. Galactorrhea or vision changes—particularly loss of peripheral vision—could suggest a pituitary tumor. Skin changes, cold intolerance, fatigue, or constipation could indicate hypothyroidism.
Menopausal symptoms such as hot flashes and vaginal dryness could point to premature ovarian failure. Galactorrhea may indicate high prolactin levels. Obesity, hirsutism, or acne could point to PCOS. Consider Asherman’s syndrome in patients with endometritis or who have had a uterine dilation and curettage.
Laboratory testing. Once pregnancy is ruled out, measure prolactin. If it exceeds 25 ng/mL by 15 ng/mL or more, do a confirmative second prolactin test. If a patient is taking a prolactin-raising medication and her prolactin was not gauged before treatment, change to a prolactin-sparing agent, then measure her prolactin 2 weeks later.17
When to refer. If prolactin persistently exceeds 50 ng/mL even after changing medications, refer the patient for brain MRI to rule out a pituitary tumor.
Tests for other underlying medical causes of secondary amenorrhea—and when to perform them—are shown in the algorithm. Psychiatrists can give these tests or refer the patient to her primary care physician.
Algorithm Laboratory evaluation of secondary amenorrhea
Communication between care team members is key to determining treatment. If a medical problem arises during psychiatric treatment, call the patient’s primary care physician or send a letter describing the problem. Also send the referring physician available lab reports.
CASE CONTINUED: TREATMENT CHANGE
Ms. J’s psychiatrist tapered risperidone to 1 mg/d for 2 weeks, then switched to olanzapine, 5 mg/d. Three weeks later, her prolactin decreased to 25 ng/mL. She continued fluoxetine, 40 mg/d, and tolerated the change in antipsychotics.
Ms. J’s bipolar disorder remains well-controlled, but menses had not resumed for another 2 months, so the psychiatrist referred Ms. J back to her primary care physician. Androgenizing and pituitary tumors were ruled out based on normal TSH, prolactin, and testosterone levels. Ms. J was diagnosed as having PCOS based on her constellation of signs and symptoms. She was started on metformin, an insulin sensitizer used to treat PCOS, and was referred to a dietitian to help her lose weight.
One year later, Ms. J still struggles with weight control, but menstruation is back to normal.
Related resources
- Lean M, De Smedt G. Schizophrenia and osteoporosis. Int Clin Psychopharmacol 2004;19:31-5.
- Berga SL, Marcus MD, Loucks TL, et al. Recovery of ovarian activity in women with functional hypothalamic amenorrhea who were treated with cognitive behavior therapy. Fertil Steril 2003;80:976-81.
- Carr BR, Bradshaw KD. Disturbances of menstruation and other common gynecologic complaints in women. In: Braunwald E, Hauser SL, Fauci AS, et al (eds). Harrison’s principles of internal medicine(15th ed). New York: McGraw-Hill, 2001:Chapter 52.
Drug brand names
- Aripiprazole • Abilify
- Carbamazepine • Tegretol
- Chlorpromazine • Thorazine
- Clozapine • Clozaril
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Haloperidol • Haldol
- Lamotrigine • Lamictal
- Lithium • Eskalith, others
- Metformin • Glucovance, others
- Olanzapine • Zyprexa
- Oxcarbazepine • Trileptal
- Paroxetine • Paxil
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Sertraline • Zoloft
- Valproic acid • Depakene
- Ziprasidone • Geodon
Disclosure
The author reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Kaplan JR, Manuck SB. Ovarian dysfunction, stress, and disease: a primate continuum. ILAR J 2004;45(2):89-115.
2. Mitan LA. Menstrual dysfunction in anorexia nervosa. J Pediatr Adolesc Gynecol 2004;17:81-85.
3. Young EA, Korzun A. The hypothalamic-pituitary-gonadal axis in mood disorders. Endocrinol Metab Clin North Am 2002;31(1):63-78.
4. Harlow BL, Wise LA, Otto MW, et al. Depression and its influence on reproductive endocrine and menstrual cycle markers associated with perimenopause. The Harvard Study of Moods and Cycles. Arch Gen Psychiatry 2003;60:29-36.
5. Brizendine L. Minding menopause. Psychotropics vs. estrogen? What you need to know now. Current Psychiatry 2003;2(10):12-31.
6. Rasgon NL, Rao RC, Hwang S, et al. Depression in women with polycystic ovary syndrome: clinical and biochemical correlates. J Affect Disord 2003;74(3):299-304.
7. Rasgon NL, Altshuler LL, Gundeman D, et al. Medication status and polycystic ovary syndrome in women with bipolar disorder: a preliminary report. J Clin Psychiatry 2000;61(3):173-8.
8. Kim KS, Pae CU, Chae JH, et al. Effects of olanzapine on prolactin levels of female patients with schizophrenia treated with risperidone. J Clin Psychiatry 2002;63(5):408-13.
9. Goodnick PJ, Rodriguez L, Santana O. Antipsychotics: impact on prolactin levels. Expert Opin Pharmacother 2002;3(10):1381-91.
10. Takahashi H, Higuchi H, Kamata M, et al. Effectiveness of switching to quetiapine for neuroleptic-induced amenorrhea. J Neuropsychiatry Clin Neurosci 2003;15:375-7.
11. Knegtering H, van der Moolen AE, Castelien S, et al. What are the effects of antipsychotics on sexual dysfunctions and endocrine functioning? Psychoneuroendocrinology 2003;28(suppl 2):109-23.
12. Goodnick PJ, Chaudry T, Artadi J, Arcey S. Women’s issues in mood disorders. Expert Opin Pharmacother 2000;1(5):903-16.
13. Isojarvi JI, Laatikainen TJ, Pakarinen AJ, et al. Polycystic ovaries and hyperandrogenism in women taking valproate for epilepsy. N Engl J Med 1993;329(19):1383-8.
14. Isojarvi JI. Reproductive dysfunction in women with epilepsy. Neurology 2003;61(6 Suppl 2):S27-S34.
15. Reindollar RH, Novak M, Tho SP, McDonough PG. Adult-onset amenorrhea: a study of 262 patients. Am J Obstet Gynecol 1986;155(3):531-43.
16. Altshuler L, Richards M, Yonkers K. Treating bipolar disorder during pregnancy. Current Psychiatry 2003;2(7):14-26.
17. Barbieri RL. Etiology, diagnosis and treatment of secondary amenorrhea. UpToDate 2003;12:1.-
A young or middle-aged patient who stops menstruating may be pregnant or have an underlying medical problem that, left undiagnosed, could cause obesity, sexual dysfunction, infertility, osteoporosis, endometrial hyperplasia, or endometrial cancer.
Yet clinicians too often dismiss secondary amenorrhea as a “normal” result of a mental disorder or psychotropic. Psychiatrists need to:
- identify when a psychiatric disorder or drug disrupts menses
- diagnose medical causes, including thyroid dysfunction, pituitary adenomas, and polycystic ovary syndrome (PCOS).
This article outlines the most common and serious causes of secondary amenorrhea among psychiatric patients, and offers an algorithm for ruling out medical problems in nonpregnant women of child-bearing age who have stopped menstruating for 3 months. The diagnostic approach described here does not apply to women with primary amenorrhea (have never menstruated).
Table 1
Psychotropics that may cause amenorrhea
| Effect | Drug/class |
|---|---|
| Prolactin elevation | Antipsychotics (chlorpromazine, haloperidol, risperidone) SSRIs (citalopram, escitalopram, fluoxetine) |
| Sex hormone-binding globulin elevation | Carbamazepine |
| Association with PCOS unknown mechanism | Valproic acid |
| SSRIs: Selective serotonin reuptake inhibitors | |
| PCOS: Polycystic ovary syndrome | |
CASE REPORT: NO PREGNANCY, NO PERIOD
Two years ago Ms. J, age 28, was diagnosed with depression. Her psychiatrist prescribed fluoxetine, 20 mg/d titrated across 4 weeks to 40 mg/d. About 4 months later, she experienced her first manic episode. The psychiatrist changed the diagnosis to bipolar I disorder and added risperidone, 2 mg/d, to manage her mania.
Ms. J’s bipolar disorder has been under control for 1 year, but she reports that her menstruation stopped 6 months ago. She is sexually active; she and her partner use spermicide-coated condoms. She does not want to be pregnant now but might want to bear a child within the next year. Several home pregnancy tests across 6 months were negative.
The patient is obese (5 feet, 5 inches, 186 lbs, body mass index 31) and has gained about 30 pounds during the past year. Vital signs are normal; psychiatric examination indicates normal mood and affect. Skin exam reveals mild papular acne on her face and back and increased hair growth on her chin. Other physical findings—including cardiac, lung, and neurologic examinations—are normal.
Laboratory evaluation reveals a prolactin level of 105 ng/mL, a negative serum ß-Hcg reading, and normal TSH, FSH, DHEA-S and testosterone levels.
Discussion. Ms. J’s history, physical examination, and laboratory tests suggest several possible causes of secondary amenorrhea:
- Are psychotropics or a prolactin-secreting tumor elevating her prolactin level?
- Does she have PCOS, as her weight gain, hirsutism, and acne might indicate?
- Is her bipolar disorder a factor? Consider psychiatric illness, medication side effects, and medical causes when evaluating secondary amenorrhea.
PSYCHIATRIC ILLNESS
Patients with high emotional stress may have amenorrhea or menstrual irregularities related to hypothalamic dysfunction.1 Also:
Anorexia nervosa has been shown to cause hypothalamic dysfunction, leading to amenorrhea.2 A correlation exists between weight loss and menses cessation, and between regain of weight and menses resumption.2
Depression. Estradiol levels are lower in depressed women than in euthymic women, probably because of altered hypothalamic-pituitary axis (HPA) function. Also, physical distress is correlated with menses disruption.3
In a 3-year study of women ages 36 to 45,4 those with a history of depression exhibited 1.2 times the rate of perimenopause as nondepressed women. Subjects with Hamilton Rating Scale for Depression scores >8 at enrollment had twice the rate of perimenopause after 3 years compared with nondepressed women. The findings suggest that depression might increase a woman’s risk of ceasing ovarian function in her 30s or 40s. Natural menopause on average begins at age 51.5
In another study,6 16 of 32 women with PCOS had Center for Epidemiological Studies-Depression Rating Scale scores indicating depression (≥16). The study suggests a high prevalence of depression among women with PCOS, but was limited by possible selection bias, no further diagnostic evaluation for depression, small sample size, and lack of an age-matched control group.
Bipolar disorder. High rates of menstrual disturbances have been reported among women with bipolar disorder.7 Although the mechanism has not been ascertained, disruption of HPA function similar to that seen in depression is likely.7
MEDICATIONS AND AMENORRHEA
Medications can cause amenorrhea, primarily through hyperprolactinemia—although other mechanisms may be involved (Table 1). Prolactin suppresses hypothalamic luteinizing hormone-releasing hormone (LHRH) production, leading to decreased follicle-stimulating hormone (FSH) and luteinizing hormone (LH), thus reducing circulating estrogen. Prolactin-secreting pituitary tumors and drug side effects mostly commonly cause hyperprolactinemia.
Antipsychotics. Phenothiazines such as chlorpromazine, butyrophenones such as haloperidol, and the atypical antipsychotic risperidone raise prolactin levels via dopamine-receptor antagonism.
Other atypical antipsychotics—including aripiprazole, clozapine, olanzapine, quetiapine, and ziprasidone—are associated with lower serum prolactin levels than risperidone.8,9 Preliminary studies suggest, for example, that switching patients from risperidone to quetiapine may help resume menstruation without worsening psychotic symptoms,10 and that amenorrhea often resolves after the patient is switched to another atypical antipsychotic.11
SSRIs. All selective serotonin reuptake inhibitors except sertraline are associated with hyperprolactinemia and can lead to amenorrhea in some patients.12
Table 2
Differential diagnosis of secondary amenorrhea
Ovarian causes
|
Hypothalamic causes
|
Hyperprolactinemia
|
Uterine causes
|
| * Turner’s syndrome: A rare chromosomal disorder characterized by short stature, lack of sexual development at puberty. |
| † Asherman’s syndrome: Endometrial adhesions, scar tissue that develop after uterine curettage or infections. |
Anticonvulsants used as mood stabilizers to treat bipolar disorder may cause menstrual irregularities, although most data relate to women with seizure disorders.
Valproic acid has been associated with PCOS in patients with epilepsy,13 although it is unknown whether the agent’s androgenizing effects vary with age. Carbamazepine, which increases sex hormone-binding globulin, may also lead to menstrual disorders by decreasing bioavailability of circulating estrogen.14 Consider switching a patient with disrupted menses to lithium, lamotrigine, or oxcarbazepine, which have not been associated with menstrual dysfunction.
MEDICAL CAUSES
Pregnancy is the most common cause of menses cessation, followed by ovarian, hypothalamic, pituitary, or uterine dysfunction (Table 2). Hypothalamic and pituitary dysfunction often cause amenorrhea in psychiatric patients, whereas ovarian causes are common among all patients with secondary amenorrhea.15
Ovarian. In PCOS, the ovaries and sometimes the adrenal glands produce excess androgens, leading to infrequent or light periods (oligomenorrhea) or amenorrhea.
Patients with depression are prone to ovarian failure in their 30s or 40s, possibly because of chronic HPA disruption.4 Premature ovarian failure also is common among patients with Turner’s syndrome, a rare chromosomal disorder characterized by short stature and lack of sexual development at puberty. Ovarian failure also can occur spontaneously.
Hypothalamic. Functional hypothalamic amenorrhea occurs in mood and eating disorders. Emotional stress, excessive physical exercise, and nutritional deficiencies reduce LHRH secretion by the hypothalamus, which interrupts the reproductive cycle. Cardiovascular disease, respiratory disease, cancer, and other acute and chronic medical illnesses can cause significant physiologic stress, thus leading to HPA dysfunction. Hypothalamic amenorrhea is treated by targeting the underlying psychiatric or medical condition.
Pituitary. Prolactin-secreting pituitary tumors, such as a pituitary adenoma, must be ruled out in patients whose prolactin levels remain high after a medication change.15 Hypothyroidism also can trigger hyperprolactinemia by causing pituitary gland hyperplasia.
Uterine. Women who have had uterine curettage or infections can develop adhesions and scar tissue that ablate the endometrial lining. This condition, called Asherman’s syndrome, is the most common uterine cause of menstrual disruption.
EVALUATING SECONDARY AMENORRHEA
When a patient presents with secondary amenorrhea, immediately rule out pregnancy because psychiatric disorders often are managed differently in pregnant than in nonpregnant women.16
Next, take a thorough patient history to determine whether referral is necessary. Ask about weight loss (intentional or unintentional), increased stressors, or a medical illness that may point to functional hypothalamic amenorrhea. Galactorrhea or vision changes—particularly loss of peripheral vision—could suggest a pituitary tumor. Skin changes, cold intolerance, fatigue, or constipation could indicate hypothyroidism.
Menopausal symptoms such as hot flashes and vaginal dryness could point to premature ovarian failure. Galactorrhea may indicate high prolactin levels. Obesity, hirsutism, or acne could point to PCOS. Consider Asherman’s syndrome in patients with endometritis or who have had a uterine dilation and curettage.
Laboratory testing. Once pregnancy is ruled out, measure prolactin. If it exceeds 25 ng/mL by 15 ng/mL or more, do a confirmative second prolactin test. If a patient is taking a prolactin-raising medication and her prolactin was not gauged before treatment, change to a prolactin-sparing agent, then measure her prolactin 2 weeks later.17
When to refer. If prolactin persistently exceeds 50 ng/mL even after changing medications, refer the patient for brain MRI to rule out a pituitary tumor.
Tests for other underlying medical causes of secondary amenorrhea—and when to perform them—are shown in the algorithm. Psychiatrists can give these tests or refer the patient to her primary care physician.
Algorithm Laboratory evaluation of secondary amenorrhea
Communication between care team members is key to determining treatment. If a medical problem arises during psychiatric treatment, call the patient’s primary care physician or send a letter describing the problem. Also send the referring physician available lab reports.
CASE CONTINUED: TREATMENT CHANGE
Ms. J’s psychiatrist tapered risperidone to 1 mg/d for 2 weeks, then switched to olanzapine, 5 mg/d. Three weeks later, her prolactin decreased to 25 ng/mL. She continued fluoxetine, 40 mg/d, and tolerated the change in antipsychotics.
Ms. J’s bipolar disorder remains well-controlled, but menses had not resumed for another 2 months, so the psychiatrist referred Ms. J back to her primary care physician. Androgenizing and pituitary tumors were ruled out based on normal TSH, prolactin, and testosterone levels. Ms. J was diagnosed as having PCOS based on her constellation of signs and symptoms. She was started on metformin, an insulin sensitizer used to treat PCOS, and was referred to a dietitian to help her lose weight.
One year later, Ms. J still struggles with weight control, but menstruation is back to normal.
Related resources
- Lean M, De Smedt G. Schizophrenia and osteoporosis. Int Clin Psychopharmacol 2004;19:31-5.
- Berga SL, Marcus MD, Loucks TL, et al. Recovery of ovarian activity in women with functional hypothalamic amenorrhea who were treated with cognitive behavior therapy. Fertil Steril 2003;80:976-81.
- Carr BR, Bradshaw KD. Disturbances of menstruation and other common gynecologic complaints in women. In: Braunwald E, Hauser SL, Fauci AS, et al (eds). Harrison’s principles of internal medicine(15th ed). New York: McGraw-Hill, 2001:Chapter 52.
Drug brand names
- Aripiprazole • Abilify
- Carbamazepine • Tegretol
- Chlorpromazine • Thorazine
- Clozapine • Clozaril
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Haloperidol • Haldol
- Lamotrigine • Lamictal
- Lithium • Eskalith, others
- Metformin • Glucovance, others
- Olanzapine • Zyprexa
- Oxcarbazepine • Trileptal
- Paroxetine • Paxil
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Sertraline • Zoloft
- Valproic acid • Depakene
- Ziprasidone • Geodon
Disclosure
The author reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
A young or middle-aged patient who stops menstruating may be pregnant or have an underlying medical problem that, left undiagnosed, could cause obesity, sexual dysfunction, infertility, osteoporosis, endometrial hyperplasia, or endometrial cancer.
Yet clinicians too often dismiss secondary amenorrhea as a “normal” result of a mental disorder or psychotropic. Psychiatrists need to:
- identify when a psychiatric disorder or drug disrupts menses
- diagnose medical causes, including thyroid dysfunction, pituitary adenomas, and polycystic ovary syndrome (PCOS).
This article outlines the most common and serious causes of secondary amenorrhea among psychiatric patients, and offers an algorithm for ruling out medical problems in nonpregnant women of child-bearing age who have stopped menstruating for 3 months. The diagnostic approach described here does not apply to women with primary amenorrhea (have never menstruated).
Table 1
Psychotropics that may cause amenorrhea
| Effect | Drug/class |
|---|---|
| Prolactin elevation | Antipsychotics (chlorpromazine, haloperidol, risperidone) SSRIs (citalopram, escitalopram, fluoxetine) |
| Sex hormone-binding globulin elevation | Carbamazepine |
| Association with PCOS unknown mechanism | Valproic acid |
| SSRIs: Selective serotonin reuptake inhibitors | |
| PCOS: Polycystic ovary syndrome | |
CASE REPORT: NO PREGNANCY, NO PERIOD
Two years ago Ms. J, age 28, was diagnosed with depression. Her psychiatrist prescribed fluoxetine, 20 mg/d titrated across 4 weeks to 40 mg/d. About 4 months later, she experienced her first manic episode. The psychiatrist changed the diagnosis to bipolar I disorder and added risperidone, 2 mg/d, to manage her mania.
Ms. J’s bipolar disorder has been under control for 1 year, but she reports that her menstruation stopped 6 months ago. She is sexually active; she and her partner use spermicide-coated condoms. She does not want to be pregnant now but might want to bear a child within the next year. Several home pregnancy tests across 6 months were negative.
The patient is obese (5 feet, 5 inches, 186 lbs, body mass index 31) and has gained about 30 pounds during the past year. Vital signs are normal; psychiatric examination indicates normal mood and affect. Skin exam reveals mild papular acne on her face and back and increased hair growth on her chin. Other physical findings—including cardiac, lung, and neurologic examinations—are normal.
Laboratory evaluation reveals a prolactin level of 105 ng/mL, a negative serum ß-Hcg reading, and normal TSH, FSH, DHEA-S and testosterone levels.
Discussion. Ms. J’s history, physical examination, and laboratory tests suggest several possible causes of secondary amenorrhea:
- Are psychotropics or a prolactin-secreting tumor elevating her prolactin level?
- Does she have PCOS, as her weight gain, hirsutism, and acne might indicate?
- Is her bipolar disorder a factor? Consider psychiatric illness, medication side effects, and medical causes when evaluating secondary amenorrhea.
PSYCHIATRIC ILLNESS
Patients with high emotional stress may have amenorrhea or menstrual irregularities related to hypothalamic dysfunction.1 Also:
Anorexia nervosa has been shown to cause hypothalamic dysfunction, leading to amenorrhea.2 A correlation exists between weight loss and menses cessation, and between regain of weight and menses resumption.2
Depression. Estradiol levels are lower in depressed women than in euthymic women, probably because of altered hypothalamic-pituitary axis (HPA) function. Also, physical distress is correlated with menses disruption.3
In a 3-year study of women ages 36 to 45,4 those with a history of depression exhibited 1.2 times the rate of perimenopause as nondepressed women. Subjects with Hamilton Rating Scale for Depression scores >8 at enrollment had twice the rate of perimenopause after 3 years compared with nondepressed women. The findings suggest that depression might increase a woman’s risk of ceasing ovarian function in her 30s or 40s. Natural menopause on average begins at age 51.5
In another study,6 16 of 32 women with PCOS had Center for Epidemiological Studies-Depression Rating Scale scores indicating depression (≥16). The study suggests a high prevalence of depression among women with PCOS, but was limited by possible selection bias, no further diagnostic evaluation for depression, small sample size, and lack of an age-matched control group.
Bipolar disorder. High rates of menstrual disturbances have been reported among women with bipolar disorder.7 Although the mechanism has not been ascertained, disruption of HPA function similar to that seen in depression is likely.7
MEDICATIONS AND AMENORRHEA
Medications can cause amenorrhea, primarily through hyperprolactinemia—although other mechanisms may be involved (Table 1). Prolactin suppresses hypothalamic luteinizing hormone-releasing hormone (LHRH) production, leading to decreased follicle-stimulating hormone (FSH) and luteinizing hormone (LH), thus reducing circulating estrogen. Prolactin-secreting pituitary tumors and drug side effects mostly commonly cause hyperprolactinemia.
Antipsychotics. Phenothiazines such as chlorpromazine, butyrophenones such as haloperidol, and the atypical antipsychotic risperidone raise prolactin levels via dopamine-receptor antagonism.
Other atypical antipsychotics—including aripiprazole, clozapine, olanzapine, quetiapine, and ziprasidone—are associated with lower serum prolactin levels than risperidone.8,9 Preliminary studies suggest, for example, that switching patients from risperidone to quetiapine may help resume menstruation without worsening psychotic symptoms,10 and that amenorrhea often resolves after the patient is switched to another atypical antipsychotic.11
SSRIs. All selective serotonin reuptake inhibitors except sertraline are associated with hyperprolactinemia and can lead to amenorrhea in some patients.12
Table 2
Differential diagnosis of secondary amenorrhea
Ovarian causes
|
Hypothalamic causes
|
Hyperprolactinemia
|
Uterine causes
|
| * Turner’s syndrome: A rare chromosomal disorder characterized by short stature, lack of sexual development at puberty. |
| † Asherman’s syndrome: Endometrial adhesions, scar tissue that develop after uterine curettage or infections. |
Anticonvulsants used as mood stabilizers to treat bipolar disorder may cause menstrual irregularities, although most data relate to women with seizure disorders.
Valproic acid has been associated with PCOS in patients with epilepsy,13 although it is unknown whether the agent’s androgenizing effects vary with age. Carbamazepine, which increases sex hormone-binding globulin, may also lead to menstrual disorders by decreasing bioavailability of circulating estrogen.14 Consider switching a patient with disrupted menses to lithium, lamotrigine, or oxcarbazepine, which have not been associated with menstrual dysfunction.
MEDICAL CAUSES
Pregnancy is the most common cause of menses cessation, followed by ovarian, hypothalamic, pituitary, or uterine dysfunction (Table 2). Hypothalamic and pituitary dysfunction often cause amenorrhea in psychiatric patients, whereas ovarian causes are common among all patients with secondary amenorrhea.15
Ovarian. In PCOS, the ovaries and sometimes the adrenal glands produce excess androgens, leading to infrequent or light periods (oligomenorrhea) or amenorrhea.
Patients with depression are prone to ovarian failure in their 30s or 40s, possibly because of chronic HPA disruption.4 Premature ovarian failure also is common among patients with Turner’s syndrome, a rare chromosomal disorder characterized by short stature and lack of sexual development at puberty. Ovarian failure also can occur spontaneously.
Hypothalamic. Functional hypothalamic amenorrhea occurs in mood and eating disorders. Emotional stress, excessive physical exercise, and nutritional deficiencies reduce LHRH secretion by the hypothalamus, which interrupts the reproductive cycle. Cardiovascular disease, respiratory disease, cancer, and other acute and chronic medical illnesses can cause significant physiologic stress, thus leading to HPA dysfunction. Hypothalamic amenorrhea is treated by targeting the underlying psychiatric or medical condition.
Pituitary. Prolactin-secreting pituitary tumors, such as a pituitary adenoma, must be ruled out in patients whose prolactin levels remain high after a medication change.15 Hypothyroidism also can trigger hyperprolactinemia by causing pituitary gland hyperplasia.
Uterine. Women who have had uterine curettage or infections can develop adhesions and scar tissue that ablate the endometrial lining. This condition, called Asherman’s syndrome, is the most common uterine cause of menstrual disruption.
EVALUATING SECONDARY AMENORRHEA
When a patient presents with secondary amenorrhea, immediately rule out pregnancy because psychiatric disorders often are managed differently in pregnant than in nonpregnant women.16
Next, take a thorough patient history to determine whether referral is necessary. Ask about weight loss (intentional or unintentional), increased stressors, or a medical illness that may point to functional hypothalamic amenorrhea. Galactorrhea or vision changes—particularly loss of peripheral vision—could suggest a pituitary tumor. Skin changes, cold intolerance, fatigue, or constipation could indicate hypothyroidism.
Menopausal symptoms such as hot flashes and vaginal dryness could point to premature ovarian failure. Galactorrhea may indicate high prolactin levels. Obesity, hirsutism, or acne could point to PCOS. Consider Asherman’s syndrome in patients with endometritis or who have had a uterine dilation and curettage.
Laboratory testing. Once pregnancy is ruled out, measure prolactin. If it exceeds 25 ng/mL by 15 ng/mL or more, do a confirmative second prolactin test. If a patient is taking a prolactin-raising medication and her prolactin was not gauged before treatment, change to a prolactin-sparing agent, then measure her prolactin 2 weeks later.17
When to refer. If prolactin persistently exceeds 50 ng/mL even after changing medications, refer the patient for brain MRI to rule out a pituitary tumor.
Tests for other underlying medical causes of secondary amenorrhea—and when to perform them—are shown in the algorithm. Psychiatrists can give these tests or refer the patient to her primary care physician.
Algorithm Laboratory evaluation of secondary amenorrhea
Communication between care team members is key to determining treatment. If a medical problem arises during psychiatric treatment, call the patient’s primary care physician or send a letter describing the problem. Also send the referring physician available lab reports.
CASE CONTINUED: TREATMENT CHANGE
Ms. J’s psychiatrist tapered risperidone to 1 mg/d for 2 weeks, then switched to olanzapine, 5 mg/d. Three weeks later, her prolactin decreased to 25 ng/mL. She continued fluoxetine, 40 mg/d, and tolerated the change in antipsychotics.
Ms. J’s bipolar disorder remains well-controlled, but menses had not resumed for another 2 months, so the psychiatrist referred Ms. J back to her primary care physician. Androgenizing and pituitary tumors were ruled out based on normal TSH, prolactin, and testosterone levels. Ms. J was diagnosed as having PCOS based on her constellation of signs and symptoms. She was started on metformin, an insulin sensitizer used to treat PCOS, and was referred to a dietitian to help her lose weight.
One year later, Ms. J still struggles with weight control, but menstruation is back to normal.
Related resources
- Lean M, De Smedt G. Schizophrenia and osteoporosis. Int Clin Psychopharmacol 2004;19:31-5.
- Berga SL, Marcus MD, Loucks TL, et al. Recovery of ovarian activity in women with functional hypothalamic amenorrhea who were treated with cognitive behavior therapy. Fertil Steril 2003;80:976-81.
- Carr BR, Bradshaw KD. Disturbances of menstruation and other common gynecologic complaints in women. In: Braunwald E, Hauser SL, Fauci AS, et al (eds). Harrison’s principles of internal medicine(15th ed). New York: McGraw-Hill, 2001:Chapter 52.
Drug brand names
- Aripiprazole • Abilify
- Carbamazepine • Tegretol
- Chlorpromazine • Thorazine
- Clozapine • Clozaril
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Haloperidol • Haldol
- Lamotrigine • Lamictal
- Lithium • Eskalith, others
- Metformin • Glucovance, others
- Olanzapine • Zyprexa
- Oxcarbazepine • Trileptal
- Paroxetine • Paxil
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Sertraline • Zoloft
- Valproic acid • Depakene
- Ziprasidone • Geodon
Disclosure
The author reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Kaplan JR, Manuck SB. Ovarian dysfunction, stress, and disease: a primate continuum. ILAR J 2004;45(2):89-115.
2. Mitan LA. Menstrual dysfunction in anorexia nervosa. J Pediatr Adolesc Gynecol 2004;17:81-85.
3. Young EA, Korzun A. The hypothalamic-pituitary-gonadal axis in mood disorders. Endocrinol Metab Clin North Am 2002;31(1):63-78.
4. Harlow BL, Wise LA, Otto MW, et al. Depression and its influence on reproductive endocrine and menstrual cycle markers associated with perimenopause. The Harvard Study of Moods and Cycles. Arch Gen Psychiatry 2003;60:29-36.
5. Brizendine L. Minding menopause. Psychotropics vs. estrogen? What you need to know now. Current Psychiatry 2003;2(10):12-31.
6. Rasgon NL, Rao RC, Hwang S, et al. Depression in women with polycystic ovary syndrome: clinical and biochemical correlates. J Affect Disord 2003;74(3):299-304.
7. Rasgon NL, Altshuler LL, Gundeman D, et al. Medication status and polycystic ovary syndrome in women with bipolar disorder: a preliminary report. J Clin Psychiatry 2000;61(3):173-8.
8. Kim KS, Pae CU, Chae JH, et al. Effects of olanzapine on prolactin levels of female patients with schizophrenia treated with risperidone. J Clin Psychiatry 2002;63(5):408-13.
9. Goodnick PJ, Rodriguez L, Santana O. Antipsychotics: impact on prolactin levels. Expert Opin Pharmacother 2002;3(10):1381-91.
10. Takahashi H, Higuchi H, Kamata M, et al. Effectiveness of switching to quetiapine for neuroleptic-induced amenorrhea. J Neuropsychiatry Clin Neurosci 2003;15:375-7.
11. Knegtering H, van der Moolen AE, Castelien S, et al. What are the effects of antipsychotics on sexual dysfunctions and endocrine functioning? Psychoneuroendocrinology 2003;28(suppl 2):109-23.
12. Goodnick PJ, Chaudry T, Artadi J, Arcey S. Women’s issues in mood disorders. Expert Opin Pharmacother 2000;1(5):903-16.
13. Isojarvi JI, Laatikainen TJ, Pakarinen AJ, et al. Polycystic ovaries and hyperandrogenism in women taking valproate for epilepsy. N Engl J Med 1993;329(19):1383-8.
14. Isojarvi JI. Reproductive dysfunction in women with epilepsy. Neurology 2003;61(6 Suppl 2):S27-S34.
15. Reindollar RH, Novak M, Tho SP, McDonough PG. Adult-onset amenorrhea: a study of 262 patients. Am J Obstet Gynecol 1986;155(3):531-43.
16. Altshuler L, Richards M, Yonkers K. Treating bipolar disorder during pregnancy. Current Psychiatry 2003;2(7):14-26.
17. Barbieri RL. Etiology, diagnosis and treatment of secondary amenorrhea. UpToDate 2003;12:1.-
1. Kaplan JR, Manuck SB. Ovarian dysfunction, stress, and disease: a primate continuum. ILAR J 2004;45(2):89-115.
2. Mitan LA. Menstrual dysfunction in anorexia nervosa. J Pediatr Adolesc Gynecol 2004;17:81-85.
3. Young EA, Korzun A. The hypothalamic-pituitary-gonadal axis in mood disorders. Endocrinol Metab Clin North Am 2002;31(1):63-78.
4. Harlow BL, Wise LA, Otto MW, et al. Depression and its influence on reproductive endocrine and menstrual cycle markers associated with perimenopause. The Harvard Study of Moods and Cycles. Arch Gen Psychiatry 2003;60:29-36.
5. Brizendine L. Minding menopause. Psychotropics vs. estrogen? What you need to know now. Current Psychiatry 2003;2(10):12-31.
6. Rasgon NL, Rao RC, Hwang S, et al. Depression in women with polycystic ovary syndrome: clinical and biochemical correlates. J Affect Disord 2003;74(3):299-304.
7. Rasgon NL, Altshuler LL, Gundeman D, et al. Medication status and polycystic ovary syndrome in women with bipolar disorder: a preliminary report. J Clin Psychiatry 2000;61(3):173-8.
8. Kim KS, Pae CU, Chae JH, et al. Effects of olanzapine on prolactin levels of female patients with schizophrenia treated with risperidone. J Clin Psychiatry 2002;63(5):408-13.
9. Goodnick PJ, Rodriguez L, Santana O. Antipsychotics: impact on prolactin levels. Expert Opin Pharmacother 2002;3(10):1381-91.
10. Takahashi H, Higuchi H, Kamata M, et al. Effectiveness of switching to quetiapine for neuroleptic-induced amenorrhea. J Neuropsychiatry Clin Neurosci 2003;15:375-7.
11. Knegtering H, van der Moolen AE, Castelien S, et al. What are the effects of antipsychotics on sexual dysfunctions and endocrine functioning? Psychoneuroendocrinology 2003;28(suppl 2):109-23.
12. Goodnick PJ, Chaudry T, Artadi J, Arcey S. Women’s issues in mood disorders. Expert Opin Pharmacother 2000;1(5):903-16.
13. Isojarvi JI, Laatikainen TJ, Pakarinen AJ, et al. Polycystic ovaries and hyperandrogenism in women taking valproate for epilepsy. N Engl J Med 1993;329(19):1383-8.
14. Isojarvi JI. Reproductive dysfunction in women with epilepsy. Neurology 2003;61(6 Suppl 2):S27-S34.
15. Reindollar RH, Novak M, Tho SP, McDonough PG. Adult-onset amenorrhea: a study of 262 patients. Am J Obstet Gynecol 1986;155(3):531-43.
16. Altshuler L, Richards M, Yonkers K. Treating bipolar disorder during pregnancy. Current Psychiatry 2003;2(7):14-26.
17. Barbieri RL. Etiology, diagnosis and treatment of secondary amenorrhea. UpToDate 2003;12:1.-
Prudent prescribing: Intelligent use of lab tests and other diagnostics
Evidence that atypical antipsychotics can increase risk of diabetes and heart disease is changing psychiatry’s approach to laboratory testing. The need for careful psychotropic prescribing—with intelligent use of diagnostic testing—has been emphasized by:
- four medical associations recommending that physicians screen and monitor patients taking atypical antipsychotics.
- FDA requiring antipsychotic labeling to describe increased risk of hyperglycemia and diabetes
- medical malpractice lawyers using television and Internet ads to seek clients who might have developed diabetes while taking antipsychotics.
This article offers information you need to detect emerging metabolic problems in patients taking atypical antipsychotics. We also discuss five other clinical situations where laboratory testing can help you:
- rule out organic illness
- perform therapeutic drug monitoring
- protect the heart when prescribing
- watch for clozapine’s side effects
- monitor for substance abuse.
Table 1
Lab testing with atypical antipsychotics*
Obtain baseline values before or as soon as possible after starting the antipsychotic:
Also note patient/family histories of obesity, diabetes, hypertension, hyperlipidemia, heart disease† |
Repeat diabetes monitoring with fasting blood glucose and/or Hb A1c after 3 months of treatment, then at least annually. More-frequent monitoring (quarterly or monthly) may be indicated for patients with:
|
Consider switching to a medication with less weight-gain liability‡ for patients:
|
| Identify patients with metabolic syndrome,§ and ensure that they are carefully monitored by a primary care clinician. Check weight (with BMI) monthly for all patients for the first 6 months, then every 3 months thereafter |
| Repeat fasting lipid profile after 3 months, then every 2 years if serum lipids are normal or every 6 months in consultation with primary care clinician if LDL >130 mg/dL |
| * Individualize to particular patients’ needs. |
| † Patients with schizophrenia are at increased risk of coronary heart disease. |
| ‡ Weight gain liability = clozapine, olanzapine > risperidone, quetiapine > aripiprazole, ziprasidone |
| § Metabolic syndrome: A proinflammatory, prothrombotic state described by a cluster of abnormalities including abdominal obesity, hypertriglyceridemia, insulin resistance, hypertension, and low HDL cholesterol. Can be exacerbated by atypical antipsychotics. |
| Source: Adapted from reference 3. |
DIABETES RISK
New monitoring standards. The American Psychiatric Association set a new standard of care by collaborating with the American Diabetes Association and others in recommending how to manage the potential for increased risk of obesity, diabetes, and lipid disorders when using atypical antipsychotics.2 The February 2004 APA/ADA report cites olanzapine and clozapine as the atypicals most likely to cause metabolic changes that increase heart disease risk. It also notes, however, that atypicals’ potential benefits to certain patients outweigh the risks.
Because of this report, psychiatrists who prescribe atypicals are now obligated to document baseline lab values and monitor patients for potential side effects (Table 1).1 We recommend that you also note patient race, as certain ethnic populations (such as African-American, Hispanic, Native American, Asian, Pacific Islander) are at elevated risk for diabetes.
Determining BMI. When starting patients on atypical antipsychotics, calculate baseline body mass index (BMI) with the simple formula in Table 2 or by using BMI tables (see Related resources).4 Determine BMI before starting a new atypical antipsychotic, at every visit for the first 6 months, and then quarterly when the dosage is stable.
A BMI increase of 1 unit warrants medical intervention, including increased weight monitoring and placing the patient in a weight-management program and switching to another antipsychotic.3
Table 2 An easy formula to calculate body mass index (BMI)
The increasing incidence of diabetes in the U.S. population makes it difficult to assess the relationship between atypical antipsychotic use and blood glucose abnormalities. Moreover, the risk of diabetes may be elevated in patients with schizophrenia, whether or not they are receiving medications. Diabetes and disturbed carbohydrate metabolism may be an integral component of schizophrenia itself.1
RULING OUT ORGANIC ILLNESS
A classic role of laboratory and diagnostic testing in psychiatry is to exclude organic illness that may be causing or exacerbating psychiatric symptoms. For a patient presenting with serious psychiatric symptoms, most sources recommend a standard battery of screening tests (Table 3).
Of course, the DSM-IV-TR “mental disorder due to a general medical condition” should be included in the differential diagnosis of any psychiatric presentation. DSM-IV-TR also calls for disease-specific tests, such as polysomnography in certain sleep disorders, CT for enlarged ventricles in schizophrenia, and electrolyte analysis in patients with anorexia nervosa.5 Order other tests as indicated, depending on patients’ medical conditions.
THERAPEUTIC DRUG MONITORING
Therapeutic drug monitoring (TDM) is used to optimize treatment with medications for which therapeutic blood levels for psychiatric disorders have been described.6 These include lithium, valproate, carbamazepine, clozapine, and tricyclic antidepressants.
Keep in mind that “therapeutic” blood levels have been determined in “usual” patients in controlled clinical trials and may not apply to the many “unusual” patients who metabolize drugs differently because of genetic variation, age, and concomitant diseases, diet, or medications.7
Lithium. A therapeutic blood level is typically 0.6 to 1.2 mEq/L, and—although the dosage must be individualized—900 to 1,200 mg/d in divided doses usually maintains this blood level. Lower levels between 0.4 mEq/L and 0.8 mEq/L have been described for the elderly.8
In uncomplicated cases, monitor lithium levels at least every 2 months during maintenance therapy. Draw blood immediately before a scheduled dose—such as 8 to 12 hours after the previous dose—when lithium concentrations are relatively stable.
Consider both clinical signs and serum levels when dosing, as patients unusually sensitive to lithium may exhibit toxic signs at <1.0 mEq/L. Elderly patients often respond to reduced dosages and may exhibit signs of toxicity—such as gastric upset and confusion—at serum levels most younger patients can tolerate.
Valproate. For seizure and bipolar disorders, the therapeutic blood level is 50 to 100 mcg/mL. Potential hematologic complications include thrombocytopenia; indigestion and nausea are common side effects. Typical practice is to obtain levels weekly for the first few weeks and then quarterly thereafter.
Carbamazepine. Plasma carbamazepine concentrations have not been correlated with response in bipolar disorder but are measured to prevent or identify toxicity. Dosages of 600 to 1,200 mg/d usually produce nontoxic levels of 4 to 12 mcg/mL. Carbamazepine interacts with many drugs that affect or are affected by hepatic metabolism. Blood dyscrasias including aplastic anemia are rare side effects.
Clozapine. Consensus is lacking on the optimal clozapine plasma level needed to achieve a therapeutic response. For some patients, it may be 200 to 350 ng/mL, which usually corresponds to 200 to 400 mg/d. Dosing must be individualized, however, because clozapine levels can vary almost 50-fold among patients taking the same dosage.9 Other studies10 and at least one recent textbook11 have reported therapeutic response most associated with clozapine levels >350 ng/mL, although adverse effects may be more likely at this higher dosage.
PROTECTING THE HEART
Before you prescribe any psychotropic with potential cardiotoxic effects, we recommend a baseline ECG for patients with cardiac risk factors, including:
- history of heart disease or ECG abnormalities
- history of syncope
- family history of sudden death before age 40, especially if both parents had sudden death
- history of prolonged QTc interval, such as congenital long QT syndrome.
Cardiotoxic effects such as QTc interval prolongation and torsades de pointes have been associated with thioridazine, mesoridazine, and pimozide. On ECG, a QTc interval >500 msec suggests an increased risk of potentially fatal arrhythmias. Do not prescribe medications associated with QTc interval prolongation to patients with this ECG finding.
Table 3
Screening tests most sources recommend for psychiatric practice
| Blood |
| Complete blood count (CBC) |
| Serum chemistry panel (“CHEM-20,” including liver function tests) |
| Lipid panels |
| Thyroid function tests (TFTs, TSH) |
| Screening tests for HIV, hepatitis C, syphilis |
| Serum B12 |
| Pregnancy tests in women of childbearing age and potential |
| Blood alcohol level in alcohol-intoxicated patient |
| Urine |
| Urine drug toxicology screen for substance abuse |
| Urinalysis |
| Cardiac |
| ECG |
| Imaging |
| Brain CT or MRI (preferred) if clinically indicated* |
| Chest radiography |
| Others |
| Serum medication levels† |
| Erythrocyte sedimentation rate or urine heavy metal screen, as indicated by medical history |
| Erythrocyte uroporphyrinogen-1-synthase |
| Urine uroporphyrins |
| EEG |
| Skull radiography |
| * Such as patient with disorientation, confusion, or abnormal neurologic exam |
| † When therapeutic/toxic blood levels are available for patient’s medications, such as theophylline, tricyclics, digoxin |
ECG is also indicated in patients who experience symptoms associated with a prolonged QT interval—such as dizziness or syncope—while taking antipsychotics. If ziprasidone is prescribed for patients with any of the risk factors described above, we recommend a baseline ECG before treatment begins, with a follow-up ECG if the patient experiences dizziness or syncope.4
Table 4
Screening tests for a patient beginning substance abuse treatment
|
WHEN USING CLOZAPINE
Clozapine is the only antipsychotic shown to improve neuroleptic-resistant symptoms12 and reduce suicidality13 in patients with schizophrenia. Unfortunately, clozapine’s potential side effects—including potentially life-threatening agranulocytosis—are legion, but careful monitoring with necessary lab testing can allow its benefits to outweigh the risks.
Agranulocytosis. Obtain white blood cell (WBC) count and differential at baseline, during treatment, and for 4 weeks after discontinuing clozapine, following the distribution program’s required schedule. Advise patients to immediately report flu-like complaints or signs that might suggest infection, such as lethargy, weakness, fever, sore throat, malaise, or mucous membrane ulceration.
Eosinophilia. In clinical trials, 1% of patients developed eosinophilia, which can be substantial in rare cases. If a differential count reveals a total eosinophil count >4,000/mm3 , stop clozapine therapy until the eosinophil count falls below 3,000/mm3 .
Myocarditis. Clozapine-treated patients are at much greater risk for developing myocarditis and of dying from it—especially during the first 6 weeks of therapy—than is the general population.3 Tachycardia can be a presenting sign.
Abnormal laboratory findings associated with clozapine-induced myocarditis may include increased WBC count, eosinophilia, increased erythrocyte sedimentation rate, and increased cardiac enzyme levels and plasma troponin. Because the mortality rate of clozapine-induced myocarditis approaches 40%, stop clozapine and refer the patient for medical evaluation as soon as possible when you suspect myocarditis.3
Endocrine and hepatic effects. Severe hyperglycemia, sometimes leading to ketoacidosis, can occur during clozapine treatment in patients without a history of hyperglycemia. Ketoacidosis symptoms include rapid breathing, nausea, vomiting, clouding of sensorium (even coma), weight loss, polyuria, polydipsia, and dehydration. Monitoring for blood glucose changes, as described in Table 1, is recommended with clozapine as with all other atypical antipsychotics.
Hepatitis during clozapine therapy has been reported in patients with baseline normal or preexisting abnormal liver function. After baseline liver function tests, we suggest follow-up LFTs:
- annually for patients with normal baseline values
- every 6 months for patients with minimally abnormal values
- every 3 months for patients with liver disease.
MONITORING SUBSTANCE ABUSE
Substance abuse is often associated with medical comorbidities that require laboratory workup and monitoring. These include overdose sequelae, sexual assault, cirrhosis, endocarditis, HIV infection, viral hepatitis, tuberculosis, and syphilis. Some testing is mandated by federal law for patients in methadone maintenance or opioid agonist therapy programs with methadone.
We recommend that new patients with substance abuse be screened for organic illness as described above, plus the workup in Table 4. Also gather a careful history for hepatitis, pancreatitis, diabetes, cirrhosis, unusual infections (cellulitis, endocarditis, atypical pneumonias, HIV), frequent hospitalizations, falls, injuries, and blackouts.
Obtain a blood alcohol level in alcohol-intoxicated patients and urine toxicology to screen for locally-available street drugs (typically marijuana, sedative/hypnotics, amphetamines, cocaine, opiates, and phencyclidine).
Confer with your laboratory staff about the capabilities and sensitivities of their drug testing methods. Marijuana may be detected for 3 days to 4 weeks, depending on level of use. Cocaine can be detected for up to 2 to 4 days in urine.
- Rosse RB, Deutsch LH, Deutsch SI. Medical assessment and laboratory testing in psychiatry. In: Sadock B, Kaplan HI (eds). Comprehensive textbook of psychiatry, 6th ed. Baltimore: Lippincott, Williams & Wilkins 1995:601-19.
- National Institute of Diabetes and Digestive and Kidney Diseases. Body mass index tables. www.niddk.nih.gov/health/nutrit/pubs/statobes.htm#table.
- National Cholesterol Education Program. Guidelines for managing patients at risk for coronary heart disease. www.nhlbi.nih.gov/about/ncep/
- Food and Drug Administration. Guidelines on hyperglycemia associated with atypical antipsychotics [example]. www.fda.gov/medwatch/SAFETY/2004/Clozaril-deardoc.pdf
Drug brand names
- Carbamazepine • Carbatrol, others
- Clozapine • Clozaril
- Lithium • Lithobid, others
- Mesoridazine • Serentil
- Pimozide • Orap
- Thioridazine • Mellaril
- Valproate • Depakote, Depakene
- Ziprasidone • Geodon
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Kohen D. Diabetes mellitus and schizophrenia: historical perspective. Br J Psychiatry 2004;47(Apr):S64-S66.
2. Association of Clinical Endocrinologists, North merican Association for the Study of Obesity. Consensus Development Conference on Antipsychotic Drugs and Obesity and Diabetes. Diabetes Care 2004;27:596-601.
3. Marder SR, Essock SM, Miller AL, et al. Physical health monitoring of patients with schizophrenia. Am J Psychiatry 2004;161:1334-49.
4. Work Group on Schizophrenia. Practice guideline for the treatment of patients with schizophrenia (2nd ed). Am J Psychiatry 2004, 161:2(suppl). For BMI information related to this guideline, see http://www.cdc.gov/nccdphp/dnpa/bmi/bmi-adult-formula.htm.
5. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed., text rev). Washington, DC: American Psychiatric Association, 2000.
6. Preskorn SH, Fast GA. Therapeutic drug monitoring for antidepressants: efficacy, safety, and cost effectiveness. J Clin Psychiatry 1991;(52 suppl):23-33.
7. Preskorn SH. Why patients may not respond to usual recommended dosages: 3 variables to consider when prescribing antipsychotics [commentary]. Current Psychiatry 2004;3(8):38-43.
8. Price DG, Ghaemi SN. Lithium. In: Stern TA., Herman JB (eds). The Massachusetts General Hospital psychiatry update and board preparation (2nd ed). New York: McGraw-Hill, 2004:355.
9. Kronig MH, Munne RA, Szymanski S, et al. Plasma clozapine levels and clinical response for treatment-refractory schizophrenic patients. Am J Psychiatry 1995;152(2):179-82.
10. Schulte P. What is an adequate trial with clozapine? Therapeutic drug monitoring and time to response in treatment-refractory schizophrenia. Clin Pharmacokinet 2003;42(7):607-18.
11. Henderson DC, Kunkel L, Goff DC. Antipsychotic drugs. In: Stern TA., Herman JB (eds). The Massachusetts General Hospital psychiatry update and board preparation (2nd ed). New York: McGraw-Hill, 2004;338-9.
12. Meltzer HY, Alphs L, Green AI, et al. International Suicide Prevention Trial Study Group. Clozapine treatment for suicidality in schizophrenia: International Suicide Prevention Trial (InterSePT). Arch Gen Psychiatry 2003;60(1):82-91.
13. Meltzer HY. Suicide in schizophrenia: risk factors and clozapine treatment. J Clin Psychiatry. 1998;59(suppl 3):15-20.
Evidence that atypical antipsychotics can increase risk of diabetes and heart disease is changing psychiatry’s approach to laboratory testing. The need for careful psychotropic prescribing—with intelligent use of diagnostic testing—has been emphasized by:
- four medical associations recommending that physicians screen and monitor patients taking atypical antipsychotics.
- FDA requiring antipsychotic labeling to describe increased risk of hyperglycemia and diabetes
- medical malpractice lawyers using television and Internet ads to seek clients who might have developed diabetes while taking antipsychotics.
This article offers information you need to detect emerging metabolic problems in patients taking atypical antipsychotics. We also discuss five other clinical situations where laboratory testing can help you:
- rule out organic illness
- perform therapeutic drug monitoring
- protect the heart when prescribing
- watch for clozapine’s side effects
- monitor for substance abuse.
Table 1
Lab testing with atypical antipsychotics*
Obtain baseline values before or as soon as possible after starting the antipsychotic:
Also note patient/family histories of obesity, diabetes, hypertension, hyperlipidemia, heart disease† |
Repeat diabetes monitoring with fasting blood glucose and/or Hb A1c after 3 months of treatment, then at least annually. More-frequent monitoring (quarterly or monthly) may be indicated for patients with:
|
Consider switching to a medication with less weight-gain liability‡ for patients:
|
| Identify patients with metabolic syndrome,§ and ensure that they are carefully monitored by a primary care clinician. Check weight (with BMI) monthly for all patients for the first 6 months, then every 3 months thereafter |
| Repeat fasting lipid profile after 3 months, then every 2 years if serum lipids are normal or every 6 months in consultation with primary care clinician if LDL >130 mg/dL |
| * Individualize to particular patients’ needs. |
| † Patients with schizophrenia are at increased risk of coronary heart disease. |
| ‡ Weight gain liability = clozapine, olanzapine > risperidone, quetiapine > aripiprazole, ziprasidone |
| § Metabolic syndrome: A proinflammatory, prothrombotic state described by a cluster of abnormalities including abdominal obesity, hypertriglyceridemia, insulin resistance, hypertension, and low HDL cholesterol. Can be exacerbated by atypical antipsychotics. |
| Source: Adapted from reference 3. |
DIABETES RISK
New monitoring standards. The American Psychiatric Association set a new standard of care by collaborating with the American Diabetes Association and others in recommending how to manage the potential for increased risk of obesity, diabetes, and lipid disorders when using atypical antipsychotics.2 The February 2004 APA/ADA report cites olanzapine and clozapine as the atypicals most likely to cause metabolic changes that increase heart disease risk. It also notes, however, that atypicals’ potential benefits to certain patients outweigh the risks.
Because of this report, psychiatrists who prescribe atypicals are now obligated to document baseline lab values and monitor patients for potential side effects (Table 1).1 We recommend that you also note patient race, as certain ethnic populations (such as African-American, Hispanic, Native American, Asian, Pacific Islander) are at elevated risk for diabetes.
Determining BMI. When starting patients on atypical antipsychotics, calculate baseline body mass index (BMI) with the simple formula in Table 2 or by using BMI tables (see Related resources).4 Determine BMI before starting a new atypical antipsychotic, at every visit for the first 6 months, and then quarterly when the dosage is stable.
A BMI increase of 1 unit warrants medical intervention, including increased weight monitoring and placing the patient in a weight-management program and switching to another antipsychotic.3
Table 2 An easy formula to calculate body mass index (BMI)
The increasing incidence of diabetes in the U.S. population makes it difficult to assess the relationship between atypical antipsychotic use and blood glucose abnormalities. Moreover, the risk of diabetes may be elevated in patients with schizophrenia, whether or not they are receiving medications. Diabetes and disturbed carbohydrate metabolism may be an integral component of schizophrenia itself.1
RULING OUT ORGANIC ILLNESS
A classic role of laboratory and diagnostic testing in psychiatry is to exclude organic illness that may be causing or exacerbating psychiatric symptoms. For a patient presenting with serious psychiatric symptoms, most sources recommend a standard battery of screening tests (Table 3).
Of course, the DSM-IV-TR “mental disorder due to a general medical condition” should be included in the differential diagnosis of any psychiatric presentation. DSM-IV-TR also calls for disease-specific tests, such as polysomnography in certain sleep disorders, CT for enlarged ventricles in schizophrenia, and electrolyte analysis in patients with anorexia nervosa.5 Order other tests as indicated, depending on patients’ medical conditions.
THERAPEUTIC DRUG MONITORING
Therapeutic drug monitoring (TDM) is used to optimize treatment with medications for which therapeutic blood levels for psychiatric disorders have been described.6 These include lithium, valproate, carbamazepine, clozapine, and tricyclic antidepressants.
Keep in mind that “therapeutic” blood levels have been determined in “usual” patients in controlled clinical trials and may not apply to the many “unusual” patients who metabolize drugs differently because of genetic variation, age, and concomitant diseases, diet, or medications.7
Lithium. A therapeutic blood level is typically 0.6 to 1.2 mEq/L, and—although the dosage must be individualized—900 to 1,200 mg/d in divided doses usually maintains this blood level. Lower levels between 0.4 mEq/L and 0.8 mEq/L have been described for the elderly.8
In uncomplicated cases, monitor lithium levels at least every 2 months during maintenance therapy. Draw blood immediately before a scheduled dose—such as 8 to 12 hours after the previous dose—when lithium concentrations are relatively stable.
Consider both clinical signs and serum levels when dosing, as patients unusually sensitive to lithium may exhibit toxic signs at <1.0 mEq/L. Elderly patients often respond to reduced dosages and may exhibit signs of toxicity—such as gastric upset and confusion—at serum levels most younger patients can tolerate.
Valproate. For seizure and bipolar disorders, the therapeutic blood level is 50 to 100 mcg/mL. Potential hematologic complications include thrombocytopenia; indigestion and nausea are common side effects. Typical practice is to obtain levels weekly for the first few weeks and then quarterly thereafter.
Carbamazepine. Plasma carbamazepine concentrations have not been correlated with response in bipolar disorder but are measured to prevent or identify toxicity. Dosages of 600 to 1,200 mg/d usually produce nontoxic levels of 4 to 12 mcg/mL. Carbamazepine interacts with many drugs that affect or are affected by hepatic metabolism. Blood dyscrasias including aplastic anemia are rare side effects.
Clozapine. Consensus is lacking on the optimal clozapine plasma level needed to achieve a therapeutic response. For some patients, it may be 200 to 350 ng/mL, which usually corresponds to 200 to 400 mg/d. Dosing must be individualized, however, because clozapine levels can vary almost 50-fold among patients taking the same dosage.9 Other studies10 and at least one recent textbook11 have reported therapeutic response most associated with clozapine levels >350 ng/mL, although adverse effects may be more likely at this higher dosage.
PROTECTING THE HEART
Before you prescribe any psychotropic with potential cardiotoxic effects, we recommend a baseline ECG for patients with cardiac risk factors, including:
- history of heart disease or ECG abnormalities
- history of syncope
- family history of sudden death before age 40, especially if both parents had sudden death
- history of prolonged QTc interval, such as congenital long QT syndrome.
Cardiotoxic effects such as QTc interval prolongation and torsades de pointes have been associated with thioridazine, mesoridazine, and pimozide. On ECG, a QTc interval >500 msec suggests an increased risk of potentially fatal arrhythmias. Do not prescribe medications associated with QTc interval prolongation to patients with this ECG finding.
Table 3
Screening tests most sources recommend for psychiatric practice
| Blood |
| Complete blood count (CBC) |
| Serum chemistry panel (“CHEM-20,” including liver function tests) |
| Lipid panels |
| Thyroid function tests (TFTs, TSH) |
| Screening tests for HIV, hepatitis C, syphilis |
| Serum B12 |
| Pregnancy tests in women of childbearing age and potential |
| Blood alcohol level in alcohol-intoxicated patient |
| Urine |
| Urine drug toxicology screen for substance abuse |
| Urinalysis |
| Cardiac |
| ECG |
| Imaging |
| Brain CT or MRI (preferred) if clinically indicated* |
| Chest radiography |
| Others |
| Serum medication levels† |
| Erythrocyte sedimentation rate or urine heavy metal screen, as indicated by medical history |
| Erythrocyte uroporphyrinogen-1-synthase |
| Urine uroporphyrins |
| EEG |
| Skull radiography |
| * Such as patient with disorientation, confusion, or abnormal neurologic exam |
| † When therapeutic/toxic blood levels are available for patient’s medications, such as theophylline, tricyclics, digoxin |
ECG is also indicated in patients who experience symptoms associated with a prolonged QT interval—such as dizziness or syncope—while taking antipsychotics. If ziprasidone is prescribed for patients with any of the risk factors described above, we recommend a baseline ECG before treatment begins, with a follow-up ECG if the patient experiences dizziness or syncope.4
Table 4
Screening tests for a patient beginning substance abuse treatment
|
WHEN USING CLOZAPINE
Clozapine is the only antipsychotic shown to improve neuroleptic-resistant symptoms12 and reduce suicidality13 in patients with schizophrenia. Unfortunately, clozapine’s potential side effects—including potentially life-threatening agranulocytosis—are legion, but careful monitoring with necessary lab testing can allow its benefits to outweigh the risks.
Agranulocytosis. Obtain white blood cell (WBC) count and differential at baseline, during treatment, and for 4 weeks after discontinuing clozapine, following the distribution program’s required schedule. Advise patients to immediately report flu-like complaints or signs that might suggest infection, such as lethargy, weakness, fever, sore throat, malaise, or mucous membrane ulceration.
Eosinophilia. In clinical trials, 1% of patients developed eosinophilia, which can be substantial in rare cases. If a differential count reveals a total eosinophil count >4,000/mm3 , stop clozapine therapy until the eosinophil count falls below 3,000/mm3 .
Myocarditis. Clozapine-treated patients are at much greater risk for developing myocarditis and of dying from it—especially during the first 6 weeks of therapy—than is the general population.3 Tachycardia can be a presenting sign.
Abnormal laboratory findings associated with clozapine-induced myocarditis may include increased WBC count, eosinophilia, increased erythrocyte sedimentation rate, and increased cardiac enzyme levels and plasma troponin. Because the mortality rate of clozapine-induced myocarditis approaches 40%, stop clozapine and refer the patient for medical evaluation as soon as possible when you suspect myocarditis.3
Endocrine and hepatic effects. Severe hyperglycemia, sometimes leading to ketoacidosis, can occur during clozapine treatment in patients without a history of hyperglycemia. Ketoacidosis symptoms include rapid breathing, nausea, vomiting, clouding of sensorium (even coma), weight loss, polyuria, polydipsia, and dehydration. Monitoring for blood glucose changes, as described in Table 1, is recommended with clozapine as with all other atypical antipsychotics.
Hepatitis during clozapine therapy has been reported in patients with baseline normal or preexisting abnormal liver function. After baseline liver function tests, we suggest follow-up LFTs:
- annually for patients with normal baseline values
- every 6 months for patients with minimally abnormal values
- every 3 months for patients with liver disease.
MONITORING SUBSTANCE ABUSE
Substance abuse is often associated with medical comorbidities that require laboratory workup and monitoring. These include overdose sequelae, sexual assault, cirrhosis, endocarditis, HIV infection, viral hepatitis, tuberculosis, and syphilis. Some testing is mandated by federal law for patients in methadone maintenance or opioid agonist therapy programs with methadone.
We recommend that new patients with substance abuse be screened for organic illness as described above, plus the workup in Table 4. Also gather a careful history for hepatitis, pancreatitis, diabetes, cirrhosis, unusual infections (cellulitis, endocarditis, atypical pneumonias, HIV), frequent hospitalizations, falls, injuries, and blackouts.
Obtain a blood alcohol level in alcohol-intoxicated patients and urine toxicology to screen for locally-available street drugs (typically marijuana, sedative/hypnotics, amphetamines, cocaine, opiates, and phencyclidine).
Confer with your laboratory staff about the capabilities and sensitivities of their drug testing methods. Marijuana may be detected for 3 days to 4 weeks, depending on level of use. Cocaine can be detected for up to 2 to 4 days in urine.
- Rosse RB, Deutsch LH, Deutsch SI. Medical assessment and laboratory testing in psychiatry. In: Sadock B, Kaplan HI (eds). Comprehensive textbook of psychiatry, 6th ed. Baltimore: Lippincott, Williams & Wilkins 1995:601-19.
- National Institute of Diabetes and Digestive and Kidney Diseases. Body mass index tables. www.niddk.nih.gov/health/nutrit/pubs/statobes.htm#table.
- National Cholesterol Education Program. Guidelines for managing patients at risk for coronary heart disease. www.nhlbi.nih.gov/about/ncep/
- Food and Drug Administration. Guidelines on hyperglycemia associated with atypical antipsychotics [example]. www.fda.gov/medwatch/SAFETY/2004/Clozaril-deardoc.pdf
Drug brand names
- Carbamazepine • Carbatrol, others
- Clozapine • Clozaril
- Lithium • Lithobid, others
- Mesoridazine • Serentil
- Pimozide • Orap
- Thioridazine • Mellaril
- Valproate • Depakote, Depakene
- Ziprasidone • Geodon
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Evidence that atypical antipsychotics can increase risk of diabetes and heart disease is changing psychiatry’s approach to laboratory testing. The need for careful psychotropic prescribing—with intelligent use of diagnostic testing—has been emphasized by:
- four medical associations recommending that physicians screen and monitor patients taking atypical antipsychotics.
- FDA requiring antipsychotic labeling to describe increased risk of hyperglycemia and diabetes
- medical malpractice lawyers using television and Internet ads to seek clients who might have developed diabetes while taking antipsychotics.
This article offers information you need to detect emerging metabolic problems in patients taking atypical antipsychotics. We also discuss five other clinical situations where laboratory testing can help you:
- rule out organic illness
- perform therapeutic drug monitoring
- protect the heart when prescribing
- watch for clozapine’s side effects
- monitor for substance abuse.
Table 1
Lab testing with atypical antipsychotics*
Obtain baseline values before or as soon as possible after starting the antipsychotic:
Also note patient/family histories of obesity, diabetes, hypertension, hyperlipidemia, heart disease† |
Repeat diabetes monitoring with fasting blood glucose and/or Hb A1c after 3 months of treatment, then at least annually. More-frequent monitoring (quarterly or monthly) may be indicated for patients with:
|
Consider switching to a medication with less weight-gain liability‡ for patients:
|
| Identify patients with metabolic syndrome,§ and ensure that they are carefully monitored by a primary care clinician. Check weight (with BMI) monthly for all patients for the first 6 months, then every 3 months thereafter |
| Repeat fasting lipid profile after 3 months, then every 2 years if serum lipids are normal or every 6 months in consultation with primary care clinician if LDL >130 mg/dL |
| * Individualize to particular patients’ needs. |
| † Patients with schizophrenia are at increased risk of coronary heart disease. |
| ‡ Weight gain liability = clozapine, olanzapine > risperidone, quetiapine > aripiprazole, ziprasidone |
| § Metabolic syndrome: A proinflammatory, prothrombotic state described by a cluster of abnormalities including abdominal obesity, hypertriglyceridemia, insulin resistance, hypertension, and low HDL cholesterol. Can be exacerbated by atypical antipsychotics. |
| Source: Adapted from reference 3. |
DIABETES RISK
New monitoring standards. The American Psychiatric Association set a new standard of care by collaborating with the American Diabetes Association and others in recommending how to manage the potential for increased risk of obesity, diabetes, and lipid disorders when using atypical antipsychotics.2 The February 2004 APA/ADA report cites olanzapine and clozapine as the atypicals most likely to cause metabolic changes that increase heart disease risk. It also notes, however, that atypicals’ potential benefits to certain patients outweigh the risks.
Because of this report, psychiatrists who prescribe atypicals are now obligated to document baseline lab values and monitor patients for potential side effects (Table 1).1 We recommend that you also note patient race, as certain ethnic populations (such as African-American, Hispanic, Native American, Asian, Pacific Islander) are at elevated risk for diabetes.
Determining BMI. When starting patients on atypical antipsychotics, calculate baseline body mass index (BMI) with the simple formula in Table 2 or by using BMI tables (see Related resources).4 Determine BMI before starting a new atypical antipsychotic, at every visit for the first 6 months, and then quarterly when the dosage is stable.
A BMI increase of 1 unit warrants medical intervention, including increased weight monitoring and placing the patient in a weight-management program and switching to another antipsychotic.3
Table 2 An easy formula to calculate body mass index (BMI)
The increasing incidence of diabetes in the U.S. population makes it difficult to assess the relationship between atypical antipsychotic use and blood glucose abnormalities. Moreover, the risk of diabetes may be elevated in patients with schizophrenia, whether or not they are receiving medications. Diabetes and disturbed carbohydrate metabolism may be an integral component of schizophrenia itself.1
RULING OUT ORGANIC ILLNESS
A classic role of laboratory and diagnostic testing in psychiatry is to exclude organic illness that may be causing or exacerbating psychiatric symptoms. For a patient presenting with serious psychiatric symptoms, most sources recommend a standard battery of screening tests (Table 3).
Of course, the DSM-IV-TR “mental disorder due to a general medical condition” should be included in the differential diagnosis of any psychiatric presentation. DSM-IV-TR also calls for disease-specific tests, such as polysomnography in certain sleep disorders, CT for enlarged ventricles in schizophrenia, and electrolyte analysis in patients with anorexia nervosa.5 Order other tests as indicated, depending on patients’ medical conditions.
THERAPEUTIC DRUG MONITORING
Therapeutic drug monitoring (TDM) is used to optimize treatment with medications for which therapeutic blood levels for psychiatric disorders have been described.6 These include lithium, valproate, carbamazepine, clozapine, and tricyclic antidepressants.
Keep in mind that “therapeutic” blood levels have been determined in “usual” patients in controlled clinical trials and may not apply to the many “unusual” patients who metabolize drugs differently because of genetic variation, age, and concomitant diseases, diet, or medications.7
Lithium. A therapeutic blood level is typically 0.6 to 1.2 mEq/L, and—although the dosage must be individualized—900 to 1,200 mg/d in divided doses usually maintains this blood level. Lower levels between 0.4 mEq/L and 0.8 mEq/L have been described for the elderly.8
In uncomplicated cases, monitor lithium levels at least every 2 months during maintenance therapy. Draw blood immediately before a scheduled dose—such as 8 to 12 hours after the previous dose—when lithium concentrations are relatively stable.
Consider both clinical signs and serum levels when dosing, as patients unusually sensitive to lithium may exhibit toxic signs at <1.0 mEq/L. Elderly patients often respond to reduced dosages and may exhibit signs of toxicity—such as gastric upset and confusion—at serum levels most younger patients can tolerate.
Valproate. For seizure and bipolar disorders, the therapeutic blood level is 50 to 100 mcg/mL. Potential hematologic complications include thrombocytopenia; indigestion and nausea are common side effects. Typical practice is to obtain levels weekly for the first few weeks and then quarterly thereafter.
Carbamazepine. Plasma carbamazepine concentrations have not been correlated with response in bipolar disorder but are measured to prevent or identify toxicity. Dosages of 600 to 1,200 mg/d usually produce nontoxic levels of 4 to 12 mcg/mL. Carbamazepine interacts with many drugs that affect or are affected by hepatic metabolism. Blood dyscrasias including aplastic anemia are rare side effects.
Clozapine. Consensus is lacking on the optimal clozapine plasma level needed to achieve a therapeutic response. For some patients, it may be 200 to 350 ng/mL, which usually corresponds to 200 to 400 mg/d. Dosing must be individualized, however, because clozapine levels can vary almost 50-fold among patients taking the same dosage.9 Other studies10 and at least one recent textbook11 have reported therapeutic response most associated with clozapine levels >350 ng/mL, although adverse effects may be more likely at this higher dosage.
PROTECTING THE HEART
Before you prescribe any psychotropic with potential cardiotoxic effects, we recommend a baseline ECG for patients with cardiac risk factors, including:
- history of heart disease or ECG abnormalities
- history of syncope
- family history of sudden death before age 40, especially if both parents had sudden death
- history of prolonged QTc interval, such as congenital long QT syndrome.
Cardiotoxic effects such as QTc interval prolongation and torsades de pointes have been associated with thioridazine, mesoridazine, and pimozide. On ECG, a QTc interval >500 msec suggests an increased risk of potentially fatal arrhythmias. Do not prescribe medications associated with QTc interval prolongation to patients with this ECG finding.
Table 3
Screening tests most sources recommend for psychiatric practice
| Blood |
| Complete blood count (CBC) |
| Serum chemistry panel (“CHEM-20,” including liver function tests) |
| Lipid panels |
| Thyroid function tests (TFTs, TSH) |
| Screening tests for HIV, hepatitis C, syphilis |
| Serum B12 |
| Pregnancy tests in women of childbearing age and potential |
| Blood alcohol level in alcohol-intoxicated patient |
| Urine |
| Urine drug toxicology screen for substance abuse |
| Urinalysis |
| Cardiac |
| ECG |
| Imaging |
| Brain CT or MRI (preferred) if clinically indicated* |
| Chest radiography |
| Others |
| Serum medication levels† |
| Erythrocyte sedimentation rate or urine heavy metal screen, as indicated by medical history |
| Erythrocyte uroporphyrinogen-1-synthase |
| Urine uroporphyrins |
| EEG |
| Skull radiography |
| * Such as patient with disorientation, confusion, or abnormal neurologic exam |
| † When therapeutic/toxic blood levels are available for patient’s medications, such as theophylline, tricyclics, digoxin |
ECG is also indicated in patients who experience symptoms associated with a prolonged QT interval—such as dizziness or syncope—while taking antipsychotics. If ziprasidone is prescribed for patients with any of the risk factors described above, we recommend a baseline ECG before treatment begins, with a follow-up ECG if the patient experiences dizziness or syncope.4
Table 4
Screening tests for a patient beginning substance abuse treatment
|
WHEN USING CLOZAPINE
Clozapine is the only antipsychotic shown to improve neuroleptic-resistant symptoms12 and reduce suicidality13 in patients with schizophrenia. Unfortunately, clozapine’s potential side effects—including potentially life-threatening agranulocytosis—are legion, but careful monitoring with necessary lab testing can allow its benefits to outweigh the risks.
Agranulocytosis. Obtain white blood cell (WBC) count and differential at baseline, during treatment, and for 4 weeks after discontinuing clozapine, following the distribution program’s required schedule. Advise patients to immediately report flu-like complaints or signs that might suggest infection, such as lethargy, weakness, fever, sore throat, malaise, or mucous membrane ulceration.
Eosinophilia. In clinical trials, 1% of patients developed eosinophilia, which can be substantial in rare cases. If a differential count reveals a total eosinophil count >4,000/mm3 , stop clozapine therapy until the eosinophil count falls below 3,000/mm3 .
Myocarditis. Clozapine-treated patients are at much greater risk for developing myocarditis and of dying from it—especially during the first 6 weeks of therapy—than is the general population.3 Tachycardia can be a presenting sign.
Abnormal laboratory findings associated with clozapine-induced myocarditis may include increased WBC count, eosinophilia, increased erythrocyte sedimentation rate, and increased cardiac enzyme levels and plasma troponin. Because the mortality rate of clozapine-induced myocarditis approaches 40%, stop clozapine and refer the patient for medical evaluation as soon as possible when you suspect myocarditis.3
Endocrine and hepatic effects. Severe hyperglycemia, sometimes leading to ketoacidosis, can occur during clozapine treatment in patients without a history of hyperglycemia. Ketoacidosis symptoms include rapid breathing, nausea, vomiting, clouding of sensorium (even coma), weight loss, polyuria, polydipsia, and dehydration. Monitoring for blood glucose changes, as described in Table 1, is recommended with clozapine as with all other atypical antipsychotics.
Hepatitis during clozapine therapy has been reported in patients with baseline normal or preexisting abnormal liver function. After baseline liver function tests, we suggest follow-up LFTs:
- annually for patients with normal baseline values
- every 6 months for patients with minimally abnormal values
- every 3 months for patients with liver disease.
MONITORING SUBSTANCE ABUSE
Substance abuse is often associated with medical comorbidities that require laboratory workup and monitoring. These include overdose sequelae, sexual assault, cirrhosis, endocarditis, HIV infection, viral hepatitis, tuberculosis, and syphilis. Some testing is mandated by federal law for patients in methadone maintenance or opioid agonist therapy programs with methadone.
We recommend that new patients with substance abuse be screened for organic illness as described above, plus the workup in Table 4. Also gather a careful history for hepatitis, pancreatitis, diabetes, cirrhosis, unusual infections (cellulitis, endocarditis, atypical pneumonias, HIV), frequent hospitalizations, falls, injuries, and blackouts.
Obtain a blood alcohol level in alcohol-intoxicated patients and urine toxicology to screen for locally-available street drugs (typically marijuana, sedative/hypnotics, amphetamines, cocaine, opiates, and phencyclidine).
Confer with your laboratory staff about the capabilities and sensitivities of their drug testing methods. Marijuana may be detected for 3 days to 4 weeks, depending on level of use. Cocaine can be detected for up to 2 to 4 days in urine.
- Rosse RB, Deutsch LH, Deutsch SI. Medical assessment and laboratory testing in psychiatry. In: Sadock B, Kaplan HI (eds). Comprehensive textbook of psychiatry, 6th ed. Baltimore: Lippincott, Williams & Wilkins 1995:601-19.
- National Institute of Diabetes and Digestive and Kidney Diseases. Body mass index tables. www.niddk.nih.gov/health/nutrit/pubs/statobes.htm#table.
- National Cholesterol Education Program. Guidelines for managing patients at risk for coronary heart disease. www.nhlbi.nih.gov/about/ncep/
- Food and Drug Administration. Guidelines on hyperglycemia associated with atypical antipsychotics [example]. www.fda.gov/medwatch/SAFETY/2004/Clozaril-deardoc.pdf
Drug brand names
- Carbamazepine • Carbatrol, others
- Clozapine • Clozaril
- Lithium • Lithobid, others
- Mesoridazine • Serentil
- Pimozide • Orap
- Thioridazine • Mellaril
- Valproate • Depakote, Depakene
- Ziprasidone • Geodon
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Kohen D. Diabetes mellitus and schizophrenia: historical perspective. Br J Psychiatry 2004;47(Apr):S64-S66.
2. Association of Clinical Endocrinologists, North merican Association for the Study of Obesity. Consensus Development Conference on Antipsychotic Drugs and Obesity and Diabetes. Diabetes Care 2004;27:596-601.
3. Marder SR, Essock SM, Miller AL, et al. Physical health monitoring of patients with schizophrenia. Am J Psychiatry 2004;161:1334-49.
4. Work Group on Schizophrenia. Practice guideline for the treatment of patients with schizophrenia (2nd ed). Am J Psychiatry 2004, 161:2(suppl). For BMI information related to this guideline, see http://www.cdc.gov/nccdphp/dnpa/bmi/bmi-adult-formula.htm.
5. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed., text rev). Washington, DC: American Psychiatric Association, 2000.
6. Preskorn SH, Fast GA. Therapeutic drug monitoring for antidepressants: efficacy, safety, and cost effectiveness. J Clin Psychiatry 1991;(52 suppl):23-33.
7. Preskorn SH. Why patients may not respond to usual recommended dosages: 3 variables to consider when prescribing antipsychotics [commentary]. Current Psychiatry 2004;3(8):38-43.
8. Price DG, Ghaemi SN. Lithium. In: Stern TA., Herman JB (eds). The Massachusetts General Hospital psychiatry update and board preparation (2nd ed). New York: McGraw-Hill, 2004:355.
9. Kronig MH, Munne RA, Szymanski S, et al. Plasma clozapine levels and clinical response for treatment-refractory schizophrenic patients. Am J Psychiatry 1995;152(2):179-82.
10. Schulte P. What is an adequate trial with clozapine? Therapeutic drug monitoring and time to response in treatment-refractory schizophrenia. Clin Pharmacokinet 2003;42(7):607-18.
11. Henderson DC, Kunkel L, Goff DC. Antipsychotic drugs. In: Stern TA., Herman JB (eds). The Massachusetts General Hospital psychiatry update and board preparation (2nd ed). New York: McGraw-Hill, 2004;338-9.
12. Meltzer HY, Alphs L, Green AI, et al. International Suicide Prevention Trial Study Group. Clozapine treatment for suicidality in schizophrenia: International Suicide Prevention Trial (InterSePT). Arch Gen Psychiatry 2003;60(1):82-91.
13. Meltzer HY. Suicide in schizophrenia: risk factors and clozapine treatment. J Clin Psychiatry. 1998;59(suppl 3):15-20.
1. Kohen D. Diabetes mellitus and schizophrenia: historical perspective. Br J Psychiatry 2004;47(Apr):S64-S66.
2. Association of Clinical Endocrinologists, North merican Association for the Study of Obesity. Consensus Development Conference on Antipsychotic Drugs and Obesity and Diabetes. Diabetes Care 2004;27:596-601.
3. Marder SR, Essock SM, Miller AL, et al. Physical health monitoring of patients with schizophrenia. Am J Psychiatry 2004;161:1334-49.
4. Work Group on Schizophrenia. Practice guideline for the treatment of patients with schizophrenia (2nd ed). Am J Psychiatry 2004, 161:2(suppl). For BMI information related to this guideline, see http://www.cdc.gov/nccdphp/dnpa/bmi/bmi-adult-formula.htm.
5. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed., text rev). Washington, DC: American Psychiatric Association, 2000.
6. Preskorn SH, Fast GA. Therapeutic drug monitoring for antidepressants: efficacy, safety, and cost effectiveness. J Clin Psychiatry 1991;(52 suppl):23-33.
7. Preskorn SH. Why patients may not respond to usual recommended dosages: 3 variables to consider when prescribing antipsychotics [commentary]. Current Psychiatry 2004;3(8):38-43.
8. Price DG, Ghaemi SN. Lithium. In: Stern TA., Herman JB (eds). The Massachusetts General Hospital psychiatry update and board preparation (2nd ed). New York: McGraw-Hill, 2004:355.
9. Kronig MH, Munne RA, Szymanski S, et al. Plasma clozapine levels and clinical response for treatment-refractory schizophrenic patients. Am J Psychiatry 1995;152(2):179-82.
10. Schulte P. What is an adequate trial with clozapine? Therapeutic drug monitoring and time to response in treatment-refractory schizophrenia. Clin Pharmacokinet 2003;42(7):607-18.
11. Henderson DC, Kunkel L, Goff DC. Antipsychotic drugs. In: Stern TA., Herman JB (eds). The Massachusetts General Hospital psychiatry update and board preparation (2nd ed). New York: McGraw-Hill, 2004;338-9.
12. Meltzer HY, Alphs L, Green AI, et al. International Suicide Prevention Trial Study Group. Clozapine treatment for suicidality in schizophrenia: International Suicide Prevention Trial (InterSePT). Arch Gen Psychiatry 2003;60(1):82-91.
13. Meltzer HY. Suicide in schizophrenia: risk factors and clozapine treatment. J Clin Psychiatry. 1998;59(suppl 3):15-20.
Commentary: Clinical perspective on pediatric depression
With “black box” warnings expected, prescribing antidepressants to children and adolescents is changing. In the past year, information from previously unpublished studies has shown the drugs’ risks to be greater and benefits less in pediatric patients than doctors had believed.
As this article went to press, the FDA said it would adopt tougher labeling for antidepressants, as recommended by its Psychopharmacologic Drugs and Pediatric advisory committees. The advisors voted 15 to 8 at a Sept. 14 hearing in favor of a “black box” for all antidepressants, warning of increased risk of suicidality in pediatric patients.
We reported on the FDA’s Feb. 2 public hearing on increased risk of suicidality with antidepressants (CURRENT PSYCHIATRY, March 2004).1 This commentary provides a follow-up perspective on:
- the Columbia group’s report on classifying suicidality in SSRI clinical trial data
- how undisclosed clinical trial data tipped the SSRI risk-benefit balance in pediatric patients
- new data on using SSRIs plus psychotherapy for depressed adolescents.
WHAT THE COLUMBIA GROUP FOUND
In March, the FDA requested a warning label on SSRIs and related antidepressants that all patients be “monitored closely for worsening depression or the emergence of suicidality.” The advisory’s text and supporting information is available on the FDA’s Web site.2
The FDA also contracted with Columbia University to classify SSRI clinical trial events—first analyzed by FDA senior epidemiologist Dr. Andrew D. Mosholder—that might represent suicidality. Dr. Mosholder had reviewed pharmaceutical industry data from 22 placebo-controlled trials involving 4,250 pediatric patients and found that youths given antidepressants were nearly twice as likely to become suicidal as those given placebo (Box 1). Suicidality has historically been attributed to depressive illness rather than antidepressant use. Therefore, FDA officials cancelled Dr. Mosholder’s scheduled testimony at the Feb. 2 hearing—a decision that triggered congressional investigations—to allow for further analysis.
Nearly 2 years ago, FDA senior epidemiologist Dr. Andrew Mosholder requested that paroxetine’s manufacturer analyze suicidal behaviors in its pediatric clinical trial database. In July 2003, the same analysis was requested for eight other antidepressants (bupropion, mirtazapine, fluoxetine, nefazodone, fluvoxamine, sertraline, citalopram, venlafaxine).
The pharmaceutical manufacturers subsequently analyzed data from 22 short-term, placebo-controlled trials involving 4,250 youths—2,298 treated with antidepressants and 1,952 given placebo. Dr. Mosholder reviewed the analyses in September 2003 and found that youths taking antidepressants were nearly twice as likely to become suicidal as those taking placebo. Statistically, the risk of suicide-related events was significantly higher with venlafaxine and paroxetine than with placebo, and data for citalopram approached statistical significance on one measure.
Relative risks for suicide-related events were 0.9 with fluoxetine and 0.5 with mirtazapine, suggesting a possible protective effect (although mirtazapine’s analysis was based on a very small number of events). For all other drugs, relative-risk estimates were >1 or undefined because of lack of events. This association between suicide-related events and active drug treatment was observed only in major depressive disorder treatment trials.
The analyses had limitations; the trials reflected short-term antidepressant use, and each sponsor analyzed its data separately. Based on the evidence, Dr. Mosholder recommended that the FDA discourage use of antidepressants other than fluoxetine in children.
As of Aug. 21, the Columbia group had analyzed data from 25 studies and reviewed 423 adverse events that occurred during the trials’ randomized double-blind phase and/or within 30 days of the last dose of randomized treatment.3 These events included intentional self-injury, suicidal ideation, suicide attempts, accidental injuries, and accidental overdose.
The preliminary evidence suggests that young antidepressant users were 1.8 times more likely to have suicidal thoughts or behaviors compared with patients given placebo4—the same conclusion Dr. Mosholder reached nearly 1 year earlier.
RISK VERSUS BENEFIT
Are SSRIs safe in children? In the United Kingdom, a review by the Medicines and Healthcare Products Regulatory Agency (MHRA) of data submitted by paroxetine’s manufacturer revealed an unfavorable risk-to-benefit ratio in children and adolescents. Review of other data on other antidepressants soon followed.
Last December, the MHRA’s Committee on Safety of Medicines and its Expert Working Group on SSRIs advised that the risks and benefits of treating major depressive disorder in patients younger than age 18 were unfavorable for sertraline, citalopram, paroxetine, and escitalopram, and could not be assessed for fluvoxamine.5 The MHRA warned British physicians against prescribing paroxetine to depressed patients younger than age 18 and ordered labeling changes for paroxetine contraindicating its use in pediatric major depression.
Fluoxetine is the only SSRI for which the committee considers the risk-benefit balance to be favorable. It cautions British physicians, however, that fluoxetine may benefit only an estimated 1 in 10 pediatric patients.5
Are SSRIs effective in children? To be labeled for treating depression in children and adolescents, an SSRI must have proven efficacy (statistically and clinically significant improvement) in two independently conducted, double-blind, placebo-controlled trials. Five trials have met this standard—fluoxetine (2),6,7 sertraline (1),8 paroxetine (1-adolescents only),9 and citalopram (1)10—and three trials have not—paroxetine (2) and citalopram (1).11 Thus, only fluoxetine is FDA-approved for treating depressed children and adolescents.
However, lacking two positive trials does not necessarily indicate that a medication is not effective, especially when only two trials were conducted.12 Also, unpublished data now becoming available show inconsistencies with the published data.13
PUBLISHED VS. UNPUBLISHED DATA
In a meta-analysis by Whittington et al,13 data from five published, randomized, controlled trials of SSRIs (fluoxetine, paroxetine, sertraline and venlafaxine) were compared with data from unpublished reports found in the United Kingdom’s Committee on Safety of Medicines’ review. In the unpublished data, for example, paroxetine had a significantly lower response rate and more-pronounced placebo effect than the published data indicated.
As a result, these investigators concluded that the favorable risk-benefit profiles of paroxetine, sertraline, and venlafaxine for children and adolescents should be switched to unfavorable. They recommended against using these three antidepressants in youth because of possible increased risk of suicidal ideation and serious adverse events—findings that corresponded to the MHRA’s 2003 decisions.
Tipping the balance? Discrepancies between published and unpublished data raise alarms about nonreporting of negative trials. Except for one paroxetine trial, one early fluoxetine trial, and one more-recent fluoxetine trial funded by the National Institute of Mental Health (NIMH),14 the FDA’s “pediatric rule” of 1997 has produced all emerging data on SSRIs in children and adolescents. This rule gives pharmaceutical companies an additional 6 months of patent protection (which translates to millions of dollars) for conducting minimal research to collect data on medications’ safety in pediatric populations.
The subsequent Pediatric Research Equity Act of 2003 (PREA) requires pharmaceutical companies to conduct pediatric studies as part of nearly every new drug application filed since Jan. 1, 1999. Unfortunately, PREA does not regulate the quality of that research nor require that negative studies be disclosed.
TADS: FLUOXETINE PLUS CBT
The recently reported Treatment for Adolescents with Depression Study (TADS)14—funded by the NIMH—showed the benefit of combining fluoxetine with cognitive-behavioral therapy (CBT) for depressed children and adolescents. In the 12-week, multi-site, double-blind, placebo-controlled trial, 439 adolescents ages 12 to 17 diagnosed with major depressive disorder received fluoxetine, 10 to 40 mg/d; CBT alone; CBT with fluoxetine, 10 to 40 mg/d; or placebo. Response rates were:
- fluoxetine alone, 61% (95% confidence interval [CI], 51-70%)
- CBT alone, 43% (95% CI, 34-52%)
- fluoxetine with CBT, 71% (95% CI, 62- 80%)
- placebo, 34.8% (95% CI, 26-44%).
The two treatments containing fluoxetine were statistically more effective than CBT alone or placebo, as measured by the Clinical Global Impression scale. Clinically significant suicidal thinking—in 29% of the adolescents at baseline—improved significantly in all treatment groups, with fluoxetine plus CBT showing the greatest reduction (P = 0.02). Seven of 439 patients (1.6%) attempted suicide; there were no completed suicides.
An association between SSRIs and suicidal ideation in children and adolescents was first reported in the early 1990s.15 In theory, agitation and nervousness that occur in some children treated with SSRIs might increase their risk of self-injury or of harming others. Agitation, hyperkinesia, mania, and hypomania tend to be more frequent among patients treated with SSRIs (including fluoxetine) than among those receiving placebo (1 to 6% vs 0 to 4%).16
Clinicians should watch carefully for activation during SSRI treatment. The following symptoms may occur in activation syndromes: anxiety, agitation, panic attacks, hostility, impulsivity, akathisia (severe restlessness), insomnia, hypomania, irritability, or mania.17
On the other hand, no evidence has shown that increased agitation with SSRIs is synonymous with suicidal behavior, and no suicides have occurred in more than 4,000 children and adolescents studied in SSRI clinical trials. In fact, increased SSRI prescribing for children ages 10 to 19 appears to parallel a significant decrease in suicide in this population. With each 1% increase in SSRI use among adolescents, the number of suicides has declined by 0.23 per 100,000 adolescents per year.18 continued
WHAT ARE CLINICIANS TO DO?
Depression is a known risk factor for suicidal ideation or behavior, and subjects with serious suicidal ideation or suicide attempts are always excluded from clinical trials of antidepressant therapy. Suicide is also relatively rare. Thus, a strong association between SSRI treatment and suicide is difficult to demonstrate. Dozens of controlled trials with thousands of pediatric subjects would be required to show definitively that suicide is associated with antidepressant use.
Recently, a panel of psychiatrists and primary care physicians discussed the FDA’s earlier advisory and its effect on depression treatment.15 Overall, the FDA findings seemed not to have convinced these clinicians of a link between suicide and SSRIs. They commented that:
- the FDA has not established a “firm causal connection” between suicide and SSRIs but uses the term “activation syndrome” (Box 2)15-18
- “activation” may give some depressed patients “the energy to carry out things they have been somewhat inhibited from doing”
- “antidepressant jitteriness syndrome” has been observed more frequently in patients diagnosed with panic disorder or somatizing anxiety than with major depressive disorder, and very little evidence exists to link this syndrome with suicide risk.
Recommendations. As this dialogue continues, how should clinicians care for pediatric patients with major depressive disorder? We suggest the following approach:
- For patients taking antidepressants, recommend that they not stop the medication abruptly, as this may result in severe withdrawal syndrome and increase the risk of depressive relapse. If you discontinue SSRI therapy, taper the dosage over 1 to 2 weeks while monitoring for risky and suicidal behavior.
- For patients newly diagnosed with severe depression, fluoxetine remains an option to use with caution. This includes making an accurate diagnosis, monitoring for suicidality, minimizing side effects, and preventing drug interactions.1
Children with depression often exhibit somatic symptoms such as abdominal pain, headaches, or irritability. Adolescents are more similar to adults, exhibiting sad mood, boredom, apathy, lack of energy, and vegetative signs. Girls and boys are equally at risk for depression until puberty, when prevalence rates for girls begin to rise above those for boys.
Up to 6% of teens meet criteria for major depressive disorder, and up to 25% are affected by it by late adolescence.19 Untreated pediatric depression is associated with substantial morbidity, reduced academic performance, substance abuse, interpersonal problems, social withdrawal, and a poor quality of life.20,21 Depression is a major risk factor for suicide, the third-leading cause of death among U.S. teenagers.
Because treating bipolar depression with antidepressants can cause switching to mania, rule out bipolar depression and mixed episodes before prescribing antidepressants. Bipolar illness may be characterized by marked irritability—also seen in depressed children and adolescents (Box 3).19,21
Informed consent. Inform the patient and parents of antidepressants’ labeling and side effects. Discuss the possibility of disinhibition and impulsivity during initial therapy, which may increase the risk of suicidal ideation or suicide attempts.
Dosing. Although SSRIs do not show a clear dose-response relationship, their side effects are considered dose-dependent.22 Therefore, start children on lower dosages than are used in adolescents and adults, and monitor very closely.
Nondrug intervention. CBT and other psychotherapies have shown short-term benefits for depressed children.23 Therefore, to improve SSRIs’ risk-benefit ratio, you may wish to reserve antidepressants for youths:
- with moderate to severe depression, recurrent depression, or a three-generation family history of depression
- who are unlikely to respond to psychotherapy alone, behavioral or environmental change, or general emotional support.
CONCLUSION
Deciding to start, continue, or discontinue SSRIs and other antidepressants in depressed children and adolescents is difficult for clinicians, patients, and their families. Despite data showing increased suicidal behavior in some pediatric patients, SSRIs—when used with caution—remain an important depression treatment in this population.
Related resources
Drug brand names
- Bupropion • Wellbutrin
- Citalopram • Celexa
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Mirtazapine • Remeron
- Nefazodone • Serzone
- Paroxetine • Paxil
- Sertraline • Zoloft
- Venlafaxine • Effexor
Disclosure
Dr. Elizabeth Weller receives research/grant support from Forest Pharmaceuticals, Organon, and Wyeth Pharmaceuticals and is a consultant to Johnson & Johnson, Novartis Pharmaceuticals Corp., AstraZeneca Pharmaceuticals, and Otsuka Pharmaceutical.
Joon Kang reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Ronald Weller receives research/grant support from Wyeth Pharmaceuticals, Organon, and Forest Pharmaceuticals.
1. Sood AB, Weller EB, Weller RA. SSRIs in children and adolescents: where do we stand? Current Psychiatry 2004;3(3):83-9.
2. Food and Drug Administration. Center for Drug Evaluation and Research. Antidepressant use in children, adolescents, and adults. Available at: http://www.fda.gov/cder/drug/antidepressants/default.htm. Accessed Sept. 2, 2004.
3. Department of Health and Human Services. Public Health Service. Report of the audit of the Columbia suicidality classification methodology [memorandum]. Aug. 16, 2004. Available at: http://www.fda.gov/ohrms/dockets/ac/04/briefing/2004-4065b1-09-TAB07-Iyasu-Audit_report.htm. Accessed Sept. 2, 2004.
4. Neergaard L. Suicide risk may prompt antidepressant warnings. Associated Press Aug. 21, 2004. Available at: http://chron.com (search archive). Accessed Sept. 15, 2004.
5. Medicines and Healthcare Products Regulatory Agency (UK). Use of selective serotonin reuptake inhibitors (SSRIs) in children and adolescents with major depressive disorder (MDD). Dec. 10, 2003. Available at: www.mhra.gov.uk/news/2003.htm#ssri. Accessed Sept. 2, 2004.
6. Emslie GJ, Rush AJ, Weinberg WA, et al. A double-blind, randomized, placebo controlled trial of fluoxetine in children and adolescents with depression. Arch Gen Psychiatry 1997;54(11):1031-7
7. Emslie GJ, Heiligenstein JH, Wagner KD, et al. Fluoxetine for acute treatment of depression in children and adolescents: a placebo-controlled, randomized clinical trial. J Am Acad Child Adolesc Psychiatry 2002;41(10):1205-15.
8. Wagner KD, Ambrosini P, Rynn M, et al. Efficacy of sertraline in the treatment of children and adolescents with major depressive disorder: two randomized controlled trials. JAMA 2003;290(8):1033-41.
9. Keller MB, Ryan ND, Strober M, et al. Efficacy of paroxetine in the treatment of adolescent major depression: a randomized, controlled study. J Am Acad Child Adolesc Psychiatry 2001;40:762-72.
10. Wagner KD, Robb AS, Findling RL, et al. A randomized, placebo-controlled trial of citalopram for the treatment of major depression in children and adolescents. Am J Psychiatry 2004;161(6):1079-83.
11. Laughren T. Background comments for Feb. 2, 2004 meeting of Psychopharmacological Drugs Advisory Committee (PDAC) and Pediatric Subcommittee of the Anti-Infective Drugs Advisory Committee (PedsAC). Available at: http://www.fda.gov/ohrms/dockets/ac/04/brief-ing/4006B1_03_Background Memo 01-05-04.doc. Accessed Sept. 15, 2004.
12. Emslie GJ. Making sense of the research puzzle. AACAP News 2004;35(2):
13. Whittington CJ, Kendall T, Fonagy P, et al. Selective serotonin reuptake inhibitors in childhood depression: Systematic review of published versus unpublished data. Lancet 2004;363:1341-5.Also available at: http://www.thelancet.com/journal/vol363/iss9418 (scroll to article title). Accessed Sept. 2, 2004.
14. Treatment for Adolescents with Depression Study (TADS) team. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression, JAMA 2004;922(7):807-20.
15. Vorstman J, Lahuis B, Buitelaar JK. SSRIs associated with behavioral activation and suicidal ideation. J Am Acad Child Adol Psychiatry 2001;40:1364-5.
16. Food and Drug Administration. Psychopharmacologic Drugs Advisory Committee and the Anti-Infective Drugs Advisory Committee. Briefing information for public hearing Feb. 2, 2004. Available at: www.fda.gov/ohrms/dockets/ac/04/briefing/4006b1.htm. Accessed Sept. 2, 2004.
17. Culpepper L, Davidson JR, Dietrich AJ, et al. Suicidality as a possible side effect of antidepressant treatment. Primary Care Companion: J Clin Psychiatry 2004;6(2):79-86.
18. Olfson M, Gameroff MJ, Marcus SC, Waslic BD. Outpatient treatment of child and adolescent depression in the United States. Arch Gen Psychiatry 2003;60:1236-42.
19. Kressler RC, Avenevoli S, Merikangas KR. Mood disorders in children and adolescents: an epidemiological perspective. Biol Psychiatry 2001;49:1002-14.
20. Shaffer D, Fisher P, Dulcan MK, et al. The NIMH Diagnostic Interview Schedule for Children, Version 2.3 (DISC-2.3): description, acceptability, prevalence rates, and performance in the MECA Study. Methods for the Epidemiology of Child and Adolescent Mental Disorders Study. J Am Acad Child Adolesc Psychiatry 1996;35:865-77.
21. Harrington R, Bredenkamp D, Groothues C, et al. Adult outcomes of child and adolescent depression. III: Links with suicidal behaviors. J Child Psychol Psychiatry 1994;35:1309-19.
22. Preskorn SH. Outpatient management of depression: a guide for the practitioner(2nd ed). Caddo, OK: Professional Publications, 1999.
23. Lewinsohn PM, Clarke GN. Psychosocial treatments for adolescent depression. Clin Psychol Rev 1999;19:329-42.
With “black box” warnings expected, prescribing antidepressants to children and adolescents is changing. In the past year, information from previously unpublished studies has shown the drugs’ risks to be greater and benefits less in pediatric patients than doctors had believed.
As this article went to press, the FDA said it would adopt tougher labeling for antidepressants, as recommended by its Psychopharmacologic Drugs and Pediatric advisory committees. The advisors voted 15 to 8 at a Sept. 14 hearing in favor of a “black box” for all antidepressants, warning of increased risk of suicidality in pediatric patients.
We reported on the FDA’s Feb. 2 public hearing on increased risk of suicidality with antidepressants (CURRENT PSYCHIATRY, March 2004).1 This commentary provides a follow-up perspective on:
- the Columbia group’s report on classifying suicidality in SSRI clinical trial data
- how undisclosed clinical trial data tipped the SSRI risk-benefit balance in pediatric patients
- new data on using SSRIs plus psychotherapy for depressed adolescents.
WHAT THE COLUMBIA GROUP FOUND
In March, the FDA requested a warning label on SSRIs and related antidepressants that all patients be “monitored closely for worsening depression or the emergence of suicidality.” The advisory’s text and supporting information is available on the FDA’s Web site.2
The FDA also contracted with Columbia University to classify SSRI clinical trial events—first analyzed by FDA senior epidemiologist Dr. Andrew D. Mosholder—that might represent suicidality. Dr. Mosholder had reviewed pharmaceutical industry data from 22 placebo-controlled trials involving 4,250 pediatric patients and found that youths given antidepressants were nearly twice as likely to become suicidal as those given placebo (Box 1). Suicidality has historically been attributed to depressive illness rather than antidepressant use. Therefore, FDA officials cancelled Dr. Mosholder’s scheduled testimony at the Feb. 2 hearing—a decision that triggered congressional investigations—to allow for further analysis.
Nearly 2 years ago, FDA senior epidemiologist Dr. Andrew Mosholder requested that paroxetine’s manufacturer analyze suicidal behaviors in its pediatric clinical trial database. In July 2003, the same analysis was requested for eight other antidepressants (bupropion, mirtazapine, fluoxetine, nefazodone, fluvoxamine, sertraline, citalopram, venlafaxine).
The pharmaceutical manufacturers subsequently analyzed data from 22 short-term, placebo-controlled trials involving 4,250 youths—2,298 treated with antidepressants and 1,952 given placebo. Dr. Mosholder reviewed the analyses in September 2003 and found that youths taking antidepressants were nearly twice as likely to become suicidal as those taking placebo. Statistically, the risk of suicide-related events was significantly higher with venlafaxine and paroxetine than with placebo, and data for citalopram approached statistical significance on one measure.
Relative risks for suicide-related events were 0.9 with fluoxetine and 0.5 with mirtazapine, suggesting a possible protective effect (although mirtazapine’s analysis was based on a very small number of events). For all other drugs, relative-risk estimates were >1 or undefined because of lack of events. This association between suicide-related events and active drug treatment was observed only in major depressive disorder treatment trials.
The analyses had limitations; the trials reflected short-term antidepressant use, and each sponsor analyzed its data separately. Based on the evidence, Dr. Mosholder recommended that the FDA discourage use of antidepressants other than fluoxetine in children.
As of Aug. 21, the Columbia group had analyzed data from 25 studies and reviewed 423 adverse events that occurred during the trials’ randomized double-blind phase and/or within 30 days of the last dose of randomized treatment.3 These events included intentional self-injury, suicidal ideation, suicide attempts, accidental injuries, and accidental overdose.
The preliminary evidence suggests that young antidepressant users were 1.8 times more likely to have suicidal thoughts or behaviors compared with patients given placebo4—the same conclusion Dr. Mosholder reached nearly 1 year earlier.
RISK VERSUS BENEFIT
Are SSRIs safe in children? In the United Kingdom, a review by the Medicines and Healthcare Products Regulatory Agency (MHRA) of data submitted by paroxetine’s manufacturer revealed an unfavorable risk-to-benefit ratio in children and adolescents. Review of other data on other antidepressants soon followed.
Last December, the MHRA’s Committee on Safety of Medicines and its Expert Working Group on SSRIs advised that the risks and benefits of treating major depressive disorder in patients younger than age 18 were unfavorable for sertraline, citalopram, paroxetine, and escitalopram, and could not be assessed for fluvoxamine.5 The MHRA warned British physicians against prescribing paroxetine to depressed patients younger than age 18 and ordered labeling changes for paroxetine contraindicating its use in pediatric major depression.
Fluoxetine is the only SSRI for which the committee considers the risk-benefit balance to be favorable. It cautions British physicians, however, that fluoxetine may benefit only an estimated 1 in 10 pediatric patients.5
Are SSRIs effective in children? To be labeled for treating depression in children and adolescents, an SSRI must have proven efficacy (statistically and clinically significant improvement) in two independently conducted, double-blind, placebo-controlled trials. Five trials have met this standard—fluoxetine (2),6,7 sertraline (1),8 paroxetine (1-adolescents only),9 and citalopram (1)10—and three trials have not—paroxetine (2) and citalopram (1).11 Thus, only fluoxetine is FDA-approved for treating depressed children and adolescents.
However, lacking two positive trials does not necessarily indicate that a medication is not effective, especially when only two trials were conducted.12 Also, unpublished data now becoming available show inconsistencies with the published data.13
PUBLISHED VS. UNPUBLISHED DATA
In a meta-analysis by Whittington et al,13 data from five published, randomized, controlled trials of SSRIs (fluoxetine, paroxetine, sertraline and venlafaxine) were compared with data from unpublished reports found in the United Kingdom’s Committee on Safety of Medicines’ review. In the unpublished data, for example, paroxetine had a significantly lower response rate and more-pronounced placebo effect than the published data indicated.
As a result, these investigators concluded that the favorable risk-benefit profiles of paroxetine, sertraline, and venlafaxine for children and adolescents should be switched to unfavorable. They recommended against using these three antidepressants in youth because of possible increased risk of suicidal ideation and serious adverse events—findings that corresponded to the MHRA’s 2003 decisions.
Tipping the balance? Discrepancies between published and unpublished data raise alarms about nonreporting of negative trials. Except for one paroxetine trial, one early fluoxetine trial, and one more-recent fluoxetine trial funded by the National Institute of Mental Health (NIMH),14 the FDA’s “pediatric rule” of 1997 has produced all emerging data on SSRIs in children and adolescents. This rule gives pharmaceutical companies an additional 6 months of patent protection (which translates to millions of dollars) for conducting minimal research to collect data on medications’ safety in pediatric populations.
The subsequent Pediatric Research Equity Act of 2003 (PREA) requires pharmaceutical companies to conduct pediatric studies as part of nearly every new drug application filed since Jan. 1, 1999. Unfortunately, PREA does not regulate the quality of that research nor require that negative studies be disclosed.
TADS: FLUOXETINE PLUS CBT
The recently reported Treatment for Adolescents with Depression Study (TADS)14—funded by the NIMH—showed the benefit of combining fluoxetine with cognitive-behavioral therapy (CBT) for depressed children and adolescents. In the 12-week, multi-site, double-blind, placebo-controlled trial, 439 adolescents ages 12 to 17 diagnosed with major depressive disorder received fluoxetine, 10 to 40 mg/d; CBT alone; CBT with fluoxetine, 10 to 40 mg/d; or placebo. Response rates were:
- fluoxetine alone, 61% (95% confidence interval [CI], 51-70%)
- CBT alone, 43% (95% CI, 34-52%)
- fluoxetine with CBT, 71% (95% CI, 62- 80%)
- placebo, 34.8% (95% CI, 26-44%).
The two treatments containing fluoxetine were statistically more effective than CBT alone or placebo, as measured by the Clinical Global Impression scale. Clinically significant suicidal thinking—in 29% of the adolescents at baseline—improved significantly in all treatment groups, with fluoxetine plus CBT showing the greatest reduction (P = 0.02). Seven of 439 patients (1.6%) attempted suicide; there were no completed suicides.
An association between SSRIs and suicidal ideation in children and adolescents was first reported in the early 1990s.15 In theory, agitation and nervousness that occur in some children treated with SSRIs might increase their risk of self-injury or of harming others. Agitation, hyperkinesia, mania, and hypomania tend to be more frequent among patients treated with SSRIs (including fluoxetine) than among those receiving placebo (1 to 6% vs 0 to 4%).16
Clinicians should watch carefully for activation during SSRI treatment. The following symptoms may occur in activation syndromes: anxiety, agitation, panic attacks, hostility, impulsivity, akathisia (severe restlessness), insomnia, hypomania, irritability, or mania.17
On the other hand, no evidence has shown that increased agitation with SSRIs is synonymous with suicidal behavior, and no suicides have occurred in more than 4,000 children and adolescents studied in SSRI clinical trials. In fact, increased SSRI prescribing for children ages 10 to 19 appears to parallel a significant decrease in suicide in this population. With each 1% increase in SSRI use among adolescents, the number of suicides has declined by 0.23 per 100,000 adolescents per year.18 continued
WHAT ARE CLINICIANS TO DO?
Depression is a known risk factor for suicidal ideation or behavior, and subjects with serious suicidal ideation or suicide attempts are always excluded from clinical trials of antidepressant therapy. Suicide is also relatively rare. Thus, a strong association between SSRI treatment and suicide is difficult to demonstrate. Dozens of controlled trials with thousands of pediatric subjects would be required to show definitively that suicide is associated with antidepressant use.
Recently, a panel of psychiatrists and primary care physicians discussed the FDA’s earlier advisory and its effect on depression treatment.15 Overall, the FDA findings seemed not to have convinced these clinicians of a link between suicide and SSRIs. They commented that:
- the FDA has not established a “firm causal connection” between suicide and SSRIs but uses the term “activation syndrome” (Box 2)15-18
- “activation” may give some depressed patients “the energy to carry out things they have been somewhat inhibited from doing”
- “antidepressant jitteriness syndrome” has been observed more frequently in patients diagnosed with panic disorder or somatizing anxiety than with major depressive disorder, and very little evidence exists to link this syndrome with suicide risk.
Recommendations. As this dialogue continues, how should clinicians care for pediatric patients with major depressive disorder? We suggest the following approach:
- For patients taking antidepressants, recommend that they not stop the medication abruptly, as this may result in severe withdrawal syndrome and increase the risk of depressive relapse. If you discontinue SSRI therapy, taper the dosage over 1 to 2 weeks while monitoring for risky and suicidal behavior.
- For patients newly diagnosed with severe depression, fluoxetine remains an option to use with caution. This includes making an accurate diagnosis, monitoring for suicidality, minimizing side effects, and preventing drug interactions.1
Children with depression often exhibit somatic symptoms such as abdominal pain, headaches, or irritability. Adolescents are more similar to adults, exhibiting sad mood, boredom, apathy, lack of energy, and vegetative signs. Girls and boys are equally at risk for depression until puberty, when prevalence rates for girls begin to rise above those for boys.
Up to 6% of teens meet criteria for major depressive disorder, and up to 25% are affected by it by late adolescence.19 Untreated pediatric depression is associated with substantial morbidity, reduced academic performance, substance abuse, interpersonal problems, social withdrawal, and a poor quality of life.20,21 Depression is a major risk factor for suicide, the third-leading cause of death among U.S. teenagers.
Because treating bipolar depression with antidepressants can cause switching to mania, rule out bipolar depression and mixed episodes before prescribing antidepressants. Bipolar illness may be characterized by marked irritability—also seen in depressed children and adolescents (Box 3).19,21
Informed consent. Inform the patient and parents of antidepressants’ labeling and side effects. Discuss the possibility of disinhibition and impulsivity during initial therapy, which may increase the risk of suicidal ideation or suicide attempts.
Dosing. Although SSRIs do not show a clear dose-response relationship, their side effects are considered dose-dependent.22 Therefore, start children on lower dosages than are used in adolescents and adults, and monitor very closely.
Nondrug intervention. CBT and other psychotherapies have shown short-term benefits for depressed children.23 Therefore, to improve SSRIs’ risk-benefit ratio, you may wish to reserve antidepressants for youths:
- with moderate to severe depression, recurrent depression, or a three-generation family history of depression
- who are unlikely to respond to psychotherapy alone, behavioral or environmental change, or general emotional support.
CONCLUSION
Deciding to start, continue, or discontinue SSRIs and other antidepressants in depressed children and adolescents is difficult for clinicians, patients, and their families. Despite data showing increased suicidal behavior in some pediatric patients, SSRIs—when used with caution—remain an important depression treatment in this population.
Related resources
Drug brand names
- Bupropion • Wellbutrin
- Citalopram • Celexa
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Mirtazapine • Remeron
- Nefazodone • Serzone
- Paroxetine • Paxil
- Sertraline • Zoloft
- Venlafaxine • Effexor
Disclosure
Dr. Elizabeth Weller receives research/grant support from Forest Pharmaceuticals, Organon, and Wyeth Pharmaceuticals and is a consultant to Johnson & Johnson, Novartis Pharmaceuticals Corp., AstraZeneca Pharmaceuticals, and Otsuka Pharmaceutical.
Joon Kang reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Ronald Weller receives research/grant support from Wyeth Pharmaceuticals, Organon, and Forest Pharmaceuticals.
With “black box” warnings expected, prescribing antidepressants to children and adolescents is changing. In the past year, information from previously unpublished studies has shown the drugs’ risks to be greater and benefits less in pediatric patients than doctors had believed.
As this article went to press, the FDA said it would adopt tougher labeling for antidepressants, as recommended by its Psychopharmacologic Drugs and Pediatric advisory committees. The advisors voted 15 to 8 at a Sept. 14 hearing in favor of a “black box” for all antidepressants, warning of increased risk of suicidality in pediatric patients.
We reported on the FDA’s Feb. 2 public hearing on increased risk of suicidality with antidepressants (CURRENT PSYCHIATRY, March 2004).1 This commentary provides a follow-up perspective on:
- the Columbia group’s report on classifying suicidality in SSRI clinical trial data
- how undisclosed clinical trial data tipped the SSRI risk-benefit balance in pediatric patients
- new data on using SSRIs plus psychotherapy for depressed adolescents.
WHAT THE COLUMBIA GROUP FOUND
In March, the FDA requested a warning label on SSRIs and related antidepressants that all patients be “monitored closely for worsening depression or the emergence of suicidality.” The advisory’s text and supporting information is available on the FDA’s Web site.2
The FDA also contracted with Columbia University to classify SSRI clinical trial events—first analyzed by FDA senior epidemiologist Dr. Andrew D. Mosholder—that might represent suicidality. Dr. Mosholder had reviewed pharmaceutical industry data from 22 placebo-controlled trials involving 4,250 pediatric patients and found that youths given antidepressants were nearly twice as likely to become suicidal as those given placebo (Box 1). Suicidality has historically been attributed to depressive illness rather than antidepressant use. Therefore, FDA officials cancelled Dr. Mosholder’s scheduled testimony at the Feb. 2 hearing—a decision that triggered congressional investigations—to allow for further analysis.
Nearly 2 years ago, FDA senior epidemiologist Dr. Andrew Mosholder requested that paroxetine’s manufacturer analyze suicidal behaviors in its pediatric clinical trial database. In July 2003, the same analysis was requested for eight other antidepressants (bupropion, mirtazapine, fluoxetine, nefazodone, fluvoxamine, sertraline, citalopram, venlafaxine).
The pharmaceutical manufacturers subsequently analyzed data from 22 short-term, placebo-controlled trials involving 4,250 youths—2,298 treated with antidepressants and 1,952 given placebo. Dr. Mosholder reviewed the analyses in September 2003 and found that youths taking antidepressants were nearly twice as likely to become suicidal as those taking placebo. Statistically, the risk of suicide-related events was significantly higher with venlafaxine and paroxetine than with placebo, and data for citalopram approached statistical significance on one measure.
Relative risks for suicide-related events were 0.9 with fluoxetine and 0.5 with mirtazapine, suggesting a possible protective effect (although mirtazapine’s analysis was based on a very small number of events). For all other drugs, relative-risk estimates were >1 or undefined because of lack of events. This association between suicide-related events and active drug treatment was observed only in major depressive disorder treatment trials.
The analyses had limitations; the trials reflected short-term antidepressant use, and each sponsor analyzed its data separately. Based on the evidence, Dr. Mosholder recommended that the FDA discourage use of antidepressants other than fluoxetine in children.
As of Aug. 21, the Columbia group had analyzed data from 25 studies and reviewed 423 adverse events that occurred during the trials’ randomized double-blind phase and/or within 30 days of the last dose of randomized treatment.3 These events included intentional self-injury, suicidal ideation, suicide attempts, accidental injuries, and accidental overdose.
The preliminary evidence suggests that young antidepressant users were 1.8 times more likely to have suicidal thoughts or behaviors compared with patients given placebo4—the same conclusion Dr. Mosholder reached nearly 1 year earlier.
RISK VERSUS BENEFIT
Are SSRIs safe in children? In the United Kingdom, a review by the Medicines and Healthcare Products Regulatory Agency (MHRA) of data submitted by paroxetine’s manufacturer revealed an unfavorable risk-to-benefit ratio in children and adolescents. Review of other data on other antidepressants soon followed.
Last December, the MHRA’s Committee on Safety of Medicines and its Expert Working Group on SSRIs advised that the risks and benefits of treating major depressive disorder in patients younger than age 18 were unfavorable for sertraline, citalopram, paroxetine, and escitalopram, and could not be assessed for fluvoxamine.5 The MHRA warned British physicians against prescribing paroxetine to depressed patients younger than age 18 and ordered labeling changes for paroxetine contraindicating its use in pediatric major depression.
Fluoxetine is the only SSRI for which the committee considers the risk-benefit balance to be favorable. It cautions British physicians, however, that fluoxetine may benefit only an estimated 1 in 10 pediatric patients.5
Are SSRIs effective in children? To be labeled for treating depression in children and adolescents, an SSRI must have proven efficacy (statistically and clinically significant improvement) in two independently conducted, double-blind, placebo-controlled trials. Five trials have met this standard—fluoxetine (2),6,7 sertraline (1),8 paroxetine (1-adolescents only),9 and citalopram (1)10—and three trials have not—paroxetine (2) and citalopram (1).11 Thus, only fluoxetine is FDA-approved for treating depressed children and adolescents.
However, lacking two positive trials does not necessarily indicate that a medication is not effective, especially when only two trials were conducted.12 Also, unpublished data now becoming available show inconsistencies with the published data.13
PUBLISHED VS. UNPUBLISHED DATA
In a meta-analysis by Whittington et al,13 data from five published, randomized, controlled trials of SSRIs (fluoxetine, paroxetine, sertraline and venlafaxine) were compared with data from unpublished reports found in the United Kingdom’s Committee on Safety of Medicines’ review. In the unpublished data, for example, paroxetine had a significantly lower response rate and more-pronounced placebo effect than the published data indicated.
As a result, these investigators concluded that the favorable risk-benefit profiles of paroxetine, sertraline, and venlafaxine for children and adolescents should be switched to unfavorable. They recommended against using these three antidepressants in youth because of possible increased risk of suicidal ideation and serious adverse events—findings that corresponded to the MHRA’s 2003 decisions.
Tipping the balance? Discrepancies between published and unpublished data raise alarms about nonreporting of negative trials. Except for one paroxetine trial, one early fluoxetine trial, and one more-recent fluoxetine trial funded by the National Institute of Mental Health (NIMH),14 the FDA’s “pediatric rule” of 1997 has produced all emerging data on SSRIs in children and adolescents. This rule gives pharmaceutical companies an additional 6 months of patent protection (which translates to millions of dollars) for conducting minimal research to collect data on medications’ safety in pediatric populations.
The subsequent Pediatric Research Equity Act of 2003 (PREA) requires pharmaceutical companies to conduct pediatric studies as part of nearly every new drug application filed since Jan. 1, 1999. Unfortunately, PREA does not regulate the quality of that research nor require that negative studies be disclosed.
TADS: FLUOXETINE PLUS CBT
The recently reported Treatment for Adolescents with Depression Study (TADS)14—funded by the NIMH—showed the benefit of combining fluoxetine with cognitive-behavioral therapy (CBT) for depressed children and adolescents. In the 12-week, multi-site, double-blind, placebo-controlled trial, 439 adolescents ages 12 to 17 diagnosed with major depressive disorder received fluoxetine, 10 to 40 mg/d; CBT alone; CBT with fluoxetine, 10 to 40 mg/d; or placebo. Response rates were:
- fluoxetine alone, 61% (95% confidence interval [CI], 51-70%)
- CBT alone, 43% (95% CI, 34-52%)
- fluoxetine with CBT, 71% (95% CI, 62- 80%)
- placebo, 34.8% (95% CI, 26-44%).
The two treatments containing fluoxetine were statistically more effective than CBT alone or placebo, as measured by the Clinical Global Impression scale. Clinically significant suicidal thinking—in 29% of the adolescents at baseline—improved significantly in all treatment groups, with fluoxetine plus CBT showing the greatest reduction (P = 0.02). Seven of 439 patients (1.6%) attempted suicide; there were no completed suicides.
An association between SSRIs and suicidal ideation in children and adolescents was first reported in the early 1990s.15 In theory, agitation and nervousness that occur in some children treated with SSRIs might increase their risk of self-injury or of harming others. Agitation, hyperkinesia, mania, and hypomania tend to be more frequent among patients treated with SSRIs (including fluoxetine) than among those receiving placebo (1 to 6% vs 0 to 4%).16
Clinicians should watch carefully for activation during SSRI treatment. The following symptoms may occur in activation syndromes: anxiety, agitation, panic attacks, hostility, impulsivity, akathisia (severe restlessness), insomnia, hypomania, irritability, or mania.17
On the other hand, no evidence has shown that increased agitation with SSRIs is synonymous with suicidal behavior, and no suicides have occurred in more than 4,000 children and adolescents studied in SSRI clinical trials. In fact, increased SSRI prescribing for children ages 10 to 19 appears to parallel a significant decrease in suicide in this population. With each 1% increase in SSRI use among adolescents, the number of suicides has declined by 0.23 per 100,000 adolescents per year.18 continued
WHAT ARE CLINICIANS TO DO?
Depression is a known risk factor for suicidal ideation or behavior, and subjects with serious suicidal ideation or suicide attempts are always excluded from clinical trials of antidepressant therapy. Suicide is also relatively rare. Thus, a strong association between SSRI treatment and suicide is difficult to demonstrate. Dozens of controlled trials with thousands of pediatric subjects would be required to show definitively that suicide is associated with antidepressant use.
Recently, a panel of psychiatrists and primary care physicians discussed the FDA’s earlier advisory and its effect on depression treatment.15 Overall, the FDA findings seemed not to have convinced these clinicians of a link between suicide and SSRIs. They commented that:
- the FDA has not established a “firm causal connection” between suicide and SSRIs but uses the term “activation syndrome” (Box 2)15-18
- “activation” may give some depressed patients “the energy to carry out things they have been somewhat inhibited from doing”
- “antidepressant jitteriness syndrome” has been observed more frequently in patients diagnosed with panic disorder or somatizing anxiety than with major depressive disorder, and very little evidence exists to link this syndrome with suicide risk.
Recommendations. As this dialogue continues, how should clinicians care for pediatric patients with major depressive disorder? We suggest the following approach:
- For patients taking antidepressants, recommend that they not stop the medication abruptly, as this may result in severe withdrawal syndrome and increase the risk of depressive relapse. If you discontinue SSRI therapy, taper the dosage over 1 to 2 weeks while monitoring for risky and suicidal behavior.
- For patients newly diagnosed with severe depression, fluoxetine remains an option to use with caution. This includes making an accurate diagnosis, monitoring for suicidality, minimizing side effects, and preventing drug interactions.1
Children with depression often exhibit somatic symptoms such as abdominal pain, headaches, or irritability. Adolescents are more similar to adults, exhibiting sad mood, boredom, apathy, lack of energy, and vegetative signs. Girls and boys are equally at risk for depression until puberty, when prevalence rates for girls begin to rise above those for boys.
Up to 6% of teens meet criteria for major depressive disorder, and up to 25% are affected by it by late adolescence.19 Untreated pediatric depression is associated with substantial morbidity, reduced academic performance, substance abuse, interpersonal problems, social withdrawal, and a poor quality of life.20,21 Depression is a major risk factor for suicide, the third-leading cause of death among U.S. teenagers.
Because treating bipolar depression with antidepressants can cause switching to mania, rule out bipolar depression and mixed episodes before prescribing antidepressants. Bipolar illness may be characterized by marked irritability—also seen in depressed children and adolescents (Box 3).19,21
Informed consent. Inform the patient and parents of antidepressants’ labeling and side effects. Discuss the possibility of disinhibition and impulsivity during initial therapy, which may increase the risk of suicidal ideation or suicide attempts.
Dosing. Although SSRIs do not show a clear dose-response relationship, their side effects are considered dose-dependent.22 Therefore, start children on lower dosages than are used in adolescents and adults, and monitor very closely.
Nondrug intervention. CBT and other psychotherapies have shown short-term benefits for depressed children.23 Therefore, to improve SSRIs’ risk-benefit ratio, you may wish to reserve antidepressants for youths:
- with moderate to severe depression, recurrent depression, or a three-generation family history of depression
- who are unlikely to respond to psychotherapy alone, behavioral or environmental change, or general emotional support.
CONCLUSION
Deciding to start, continue, or discontinue SSRIs and other antidepressants in depressed children and adolescents is difficult for clinicians, patients, and their families. Despite data showing increased suicidal behavior in some pediatric patients, SSRIs—when used with caution—remain an important depression treatment in this population.
Related resources
Drug brand names
- Bupropion • Wellbutrin
- Citalopram • Celexa
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Mirtazapine • Remeron
- Nefazodone • Serzone
- Paroxetine • Paxil
- Sertraline • Zoloft
- Venlafaxine • Effexor
Disclosure
Dr. Elizabeth Weller receives research/grant support from Forest Pharmaceuticals, Organon, and Wyeth Pharmaceuticals and is a consultant to Johnson & Johnson, Novartis Pharmaceuticals Corp., AstraZeneca Pharmaceuticals, and Otsuka Pharmaceutical.
Joon Kang reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Ronald Weller receives research/grant support from Wyeth Pharmaceuticals, Organon, and Forest Pharmaceuticals.
1. Sood AB, Weller EB, Weller RA. SSRIs in children and adolescents: where do we stand? Current Psychiatry 2004;3(3):83-9.
2. Food and Drug Administration. Center for Drug Evaluation and Research. Antidepressant use in children, adolescents, and adults. Available at: http://www.fda.gov/cder/drug/antidepressants/default.htm. Accessed Sept. 2, 2004.
3. Department of Health and Human Services. Public Health Service. Report of the audit of the Columbia suicidality classification methodology [memorandum]. Aug. 16, 2004. Available at: http://www.fda.gov/ohrms/dockets/ac/04/briefing/2004-4065b1-09-TAB07-Iyasu-Audit_report.htm. Accessed Sept. 2, 2004.
4. Neergaard L. Suicide risk may prompt antidepressant warnings. Associated Press Aug. 21, 2004. Available at: http://chron.com (search archive). Accessed Sept. 15, 2004.
5. Medicines and Healthcare Products Regulatory Agency (UK). Use of selective serotonin reuptake inhibitors (SSRIs) in children and adolescents with major depressive disorder (MDD). Dec. 10, 2003. Available at: www.mhra.gov.uk/news/2003.htm#ssri. Accessed Sept. 2, 2004.
6. Emslie GJ, Rush AJ, Weinberg WA, et al. A double-blind, randomized, placebo controlled trial of fluoxetine in children and adolescents with depression. Arch Gen Psychiatry 1997;54(11):1031-7
7. Emslie GJ, Heiligenstein JH, Wagner KD, et al. Fluoxetine for acute treatment of depression in children and adolescents: a placebo-controlled, randomized clinical trial. J Am Acad Child Adolesc Psychiatry 2002;41(10):1205-15.
8. Wagner KD, Ambrosini P, Rynn M, et al. Efficacy of sertraline in the treatment of children and adolescents with major depressive disorder: two randomized controlled trials. JAMA 2003;290(8):1033-41.
9. Keller MB, Ryan ND, Strober M, et al. Efficacy of paroxetine in the treatment of adolescent major depression: a randomized, controlled study. J Am Acad Child Adolesc Psychiatry 2001;40:762-72.
10. Wagner KD, Robb AS, Findling RL, et al. A randomized, placebo-controlled trial of citalopram for the treatment of major depression in children and adolescents. Am J Psychiatry 2004;161(6):1079-83.
11. Laughren T. Background comments for Feb. 2, 2004 meeting of Psychopharmacological Drugs Advisory Committee (PDAC) and Pediatric Subcommittee of the Anti-Infective Drugs Advisory Committee (PedsAC). Available at: http://www.fda.gov/ohrms/dockets/ac/04/brief-ing/4006B1_03_Background Memo 01-05-04.doc. Accessed Sept. 15, 2004.
12. Emslie GJ. Making sense of the research puzzle. AACAP News 2004;35(2):
13. Whittington CJ, Kendall T, Fonagy P, et al. Selective serotonin reuptake inhibitors in childhood depression: Systematic review of published versus unpublished data. Lancet 2004;363:1341-5.Also available at: http://www.thelancet.com/journal/vol363/iss9418 (scroll to article title). Accessed Sept. 2, 2004.
14. Treatment for Adolescents with Depression Study (TADS) team. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression, JAMA 2004;922(7):807-20.
15. Vorstman J, Lahuis B, Buitelaar JK. SSRIs associated with behavioral activation and suicidal ideation. J Am Acad Child Adol Psychiatry 2001;40:1364-5.
16. Food and Drug Administration. Psychopharmacologic Drugs Advisory Committee and the Anti-Infective Drugs Advisory Committee. Briefing information for public hearing Feb. 2, 2004. Available at: www.fda.gov/ohrms/dockets/ac/04/briefing/4006b1.htm. Accessed Sept. 2, 2004.
17. Culpepper L, Davidson JR, Dietrich AJ, et al. Suicidality as a possible side effect of antidepressant treatment. Primary Care Companion: J Clin Psychiatry 2004;6(2):79-86.
18. Olfson M, Gameroff MJ, Marcus SC, Waslic BD. Outpatient treatment of child and adolescent depression in the United States. Arch Gen Psychiatry 2003;60:1236-42.
19. Kressler RC, Avenevoli S, Merikangas KR. Mood disorders in children and adolescents: an epidemiological perspective. Biol Psychiatry 2001;49:1002-14.
20. Shaffer D, Fisher P, Dulcan MK, et al. The NIMH Diagnostic Interview Schedule for Children, Version 2.3 (DISC-2.3): description, acceptability, prevalence rates, and performance in the MECA Study. Methods for the Epidemiology of Child and Adolescent Mental Disorders Study. J Am Acad Child Adolesc Psychiatry 1996;35:865-77.
21. Harrington R, Bredenkamp D, Groothues C, et al. Adult outcomes of child and adolescent depression. III: Links with suicidal behaviors. J Child Psychol Psychiatry 1994;35:1309-19.
22. Preskorn SH. Outpatient management of depression: a guide for the practitioner(2nd ed). Caddo, OK: Professional Publications, 1999.
23. Lewinsohn PM, Clarke GN. Psychosocial treatments for adolescent depression. Clin Psychol Rev 1999;19:329-42.
1. Sood AB, Weller EB, Weller RA. SSRIs in children and adolescents: where do we stand? Current Psychiatry 2004;3(3):83-9.
2. Food and Drug Administration. Center for Drug Evaluation and Research. Antidepressant use in children, adolescents, and adults. Available at: http://www.fda.gov/cder/drug/antidepressants/default.htm. Accessed Sept. 2, 2004.
3. Department of Health and Human Services. Public Health Service. Report of the audit of the Columbia suicidality classification methodology [memorandum]. Aug. 16, 2004. Available at: http://www.fda.gov/ohrms/dockets/ac/04/briefing/2004-4065b1-09-TAB07-Iyasu-Audit_report.htm. Accessed Sept. 2, 2004.
4. Neergaard L. Suicide risk may prompt antidepressant warnings. Associated Press Aug. 21, 2004. Available at: http://chron.com (search archive). Accessed Sept. 15, 2004.
5. Medicines and Healthcare Products Regulatory Agency (UK). Use of selective serotonin reuptake inhibitors (SSRIs) in children and adolescents with major depressive disorder (MDD). Dec. 10, 2003. Available at: www.mhra.gov.uk/news/2003.htm#ssri. Accessed Sept. 2, 2004.
6. Emslie GJ, Rush AJ, Weinberg WA, et al. A double-blind, randomized, placebo controlled trial of fluoxetine in children and adolescents with depression. Arch Gen Psychiatry 1997;54(11):1031-7
7. Emslie GJ, Heiligenstein JH, Wagner KD, et al. Fluoxetine for acute treatment of depression in children and adolescents: a placebo-controlled, randomized clinical trial. J Am Acad Child Adolesc Psychiatry 2002;41(10):1205-15.
8. Wagner KD, Ambrosini P, Rynn M, et al. Efficacy of sertraline in the treatment of children and adolescents with major depressive disorder: two randomized controlled trials. JAMA 2003;290(8):1033-41.
9. Keller MB, Ryan ND, Strober M, et al. Efficacy of paroxetine in the treatment of adolescent major depression: a randomized, controlled study. J Am Acad Child Adolesc Psychiatry 2001;40:762-72.
10. Wagner KD, Robb AS, Findling RL, et al. A randomized, placebo-controlled trial of citalopram for the treatment of major depression in children and adolescents. Am J Psychiatry 2004;161(6):1079-83.
11. Laughren T. Background comments for Feb. 2, 2004 meeting of Psychopharmacological Drugs Advisory Committee (PDAC) and Pediatric Subcommittee of the Anti-Infective Drugs Advisory Committee (PedsAC). Available at: http://www.fda.gov/ohrms/dockets/ac/04/brief-ing/4006B1_03_Background Memo 01-05-04.doc. Accessed Sept. 15, 2004.
12. Emslie GJ. Making sense of the research puzzle. AACAP News 2004;35(2):
13. Whittington CJ, Kendall T, Fonagy P, et al. Selective serotonin reuptake inhibitors in childhood depression: Systematic review of published versus unpublished data. Lancet 2004;363:1341-5.Also available at: http://www.thelancet.com/journal/vol363/iss9418 (scroll to article title). Accessed Sept. 2, 2004.
14. Treatment for Adolescents with Depression Study (TADS) team. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression, JAMA 2004;922(7):807-20.
15. Vorstman J, Lahuis B, Buitelaar JK. SSRIs associated with behavioral activation and suicidal ideation. J Am Acad Child Adol Psychiatry 2001;40:1364-5.
16. Food and Drug Administration. Psychopharmacologic Drugs Advisory Committee and the Anti-Infective Drugs Advisory Committee. Briefing information for public hearing Feb. 2, 2004. Available at: www.fda.gov/ohrms/dockets/ac/04/briefing/4006b1.htm. Accessed Sept. 2, 2004.
17. Culpepper L, Davidson JR, Dietrich AJ, et al. Suicidality as a possible side effect of antidepressant treatment. Primary Care Companion: J Clin Psychiatry 2004;6(2):79-86.
18. Olfson M, Gameroff MJ, Marcus SC, Waslic BD. Outpatient treatment of child and adolescent depression in the United States. Arch Gen Psychiatry 2003;60:1236-42.
19. Kressler RC, Avenevoli S, Merikangas KR. Mood disorders in children and adolescents: an epidemiological perspective. Biol Psychiatry 2001;49:1002-14.
20. Shaffer D, Fisher P, Dulcan MK, et al. The NIMH Diagnostic Interview Schedule for Children, Version 2.3 (DISC-2.3): description, acceptability, prevalence rates, and performance in the MECA Study. Methods for the Epidemiology of Child and Adolescent Mental Disorders Study. J Am Acad Child Adolesc Psychiatry 1996;35:865-77.
21. Harrington R, Bredenkamp D, Groothues C, et al. Adult outcomes of child and adolescent depression. III: Links with suicidal behaviors. J Child Psychol Psychiatry 1994;35:1309-19.
22. Preskorn SH. Outpatient management of depression: a guide for the practitioner(2nd ed). Caddo, OK: Professional Publications, 1999.
23. Lewinsohn PM, Clarke GN. Psychosocial treatments for adolescent depression. Clin Psychol Rev 1999;19:329-42.