User login
Welcome to Current Psychiatry, a leading source of information, online and in print, for practitioners of psychiatry and its related subspecialties, including addiction psychiatry, child and adolescent psychiatry, and geriatric psychiatry. This Web site contains evidence-based reviews of the prevention, diagnosis, and treatment of mental illness and psychological disorders; case reports; updates on psychopharmacology; news about the specialty of psychiatry; pearls for practice; and other topics of interest and use to this audience.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-current-psychiatry')]
div[contains(@class, 'pane-pub-home-current-psychiatry')]
div[contains(@class, 'pane-pub-topic-current-psychiatry')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
2019 Peer Reviewers
Aparna Atluru, MD
Stanford Medicine
Anjan Bhattacharyya, MD
Saint Louis University
Caroline Bonham, MD
The University of New Mexico
Catherine Crone, MD
Inova Health System
Sheila Dowd, PhD
Rush Medical College
Ahmed Z. Elmaadawi, MD
Indiana University School of Medicine
Donald Gilbert, MD, MS
Cincinnati Children’s Hospital Medical Center
Mark Gold, MD
Washington University in St. Louis
Elana Harris, MD, PhD
Cincinnati Children’s Hospital
Susan Hatters-Friedman, MD
Case Western Reserve University
Faisal Islam, MD, MBA
Greenvale, New York
Kaustubh G. Joshi, MD
University of South Carolina School of Medicine
Rita Khoury, MD
Saint George Hospital University Medical Center
Suneeta Kumari, MD, MPH
Howard University Hospital
Michelle Magid, MD
Austin PsychCare PA
Michael Maksimowski, MD
Wayne State University
Jose Maldonado, MD
Stanford University
Thomas W. Meeks, MD
Portland VA Medical Center
John Miller, MD
University of South Florida
Armando Morera-Fumero, MD, PhD
Universidad de La Laguna
Mary K. Morreale, MD
Wayne State University
Philip Muskin, MD
Columbia University College of Physicians and Surgeons
Katharine Nelson, MD
University of Minnesota
Carol North, MD
University of Texas Southwestern Medical Center at Dallas
Douglas Opler, MD
Rutgers University School of Medicine
Joseph Pierre, MD
University of California, Los Angeles
Jerrold Pollak, PhD, ABN, ABPP
Seacoast Mental Health Center
Edwin Raffi, MD, MPH
Massachusetts General Hospital Center for Women’s Mental Health
Y. Pritham Raj, MD
Oregon Health and Science University
Jeffrey Rakofsky, MD
Emory University School of Medicine
Laura Ramsey, PhD
Cincinnati Children’s Hospital Medical Center
Erica Rapp, MD
University of Colorado School of Medicine
Abhishek Reddy, MD
The University of Alabama at Birmingham
Eduardo Rueda Vasquez, MD
Williamsport, Pennsylvania
Stephen Saklad, PharmD, BCPP
The University of Texas at Austin
Lauren Schwarz, PhD, ABPP-CN
Saint Louis University School of Medicine
Andreas Sidiropoulos, MD
University of Michigan
Shirshendu Sinha, MD
Mayo Clinic Health System and Mayo Clinic
Cornel Stanciu, MD
Dartmouth’s Geisel School of Medicine
Jeffrey Sung, MD
University of Washington
Thida Thant, MD
University of Colorado at Denver
Adele Viguera, MD
Cleveland Clinic Lerner College of Medicine
Aparna Atluru, MD
Stanford Medicine
Anjan Bhattacharyya, MD
Saint Louis University
Caroline Bonham, MD
The University of New Mexico
Catherine Crone, MD
Inova Health System
Sheila Dowd, PhD
Rush Medical College
Ahmed Z. Elmaadawi, MD
Indiana University School of Medicine
Donald Gilbert, MD, MS
Cincinnati Children’s Hospital Medical Center
Mark Gold, MD
Washington University in St. Louis
Elana Harris, MD, PhD
Cincinnati Children’s Hospital
Susan Hatters-Friedman, MD
Case Western Reserve University
Faisal Islam, MD, MBA
Greenvale, New York
Kaustubh G. Joshi, MD
University of South Carolina School of Medicine
Rita Khoury, MD
Saint George Hospital University Medical Center
Suneeta Kumari, MD, MPH
Howard University Hospital
Michelle Magid, MD
Austin PsychCare PA
Michael Maksimowski, MD
Wayne State University
Jose Maldonado, MD
Stanford University
Thomas W. Meeks, MD
Portland VA Medical Center
John Miller, MD
University of South Florida
Armando Morera-Fumero, MD, PhD
Universidad de La Laguna
Mary K. Morreale, MD
Wayne State University
Philip Muskin, MD
Columbia University College of Physicians and Surgeons
Katharine Nelson, MD
University of Minnesota
Carol North, MD
University of Texas Southwestern Medical Center at Dallas
Douglas Opler, MD
Rutgers University School of Medicine
Joseph Pierre, MD
University of California, Los Angeles
Jerrold Pollak, PhD, ABN, ABPP
Seacoast Mental Health Center
Edwin Raffi, MD, MPH
Massachusetts General Hospital Center for Women’s Mental Health
Y. Pritham Raj, MD
Oregon Health and Science University
Jeffrey Rakofsky, MD
Emory University School of Medicine
Laura Ramsey, PhD
Cincinnati Children’s Hospital Medical Center
Erica Rapp, MD
University of Colorado School of Medicine
Abhishek Reddy, MD
The University of Alabama at Birmingham
Eduardo Rueda Vasquez, MD
Williamsport, Pennsylvania
Stephen Saklad, PharmD, BCPP
The University of Texas at Austin
Lauren Schwarz, PhD, ABPP-CN
Saint Louis University School of Medicine
Andreas Sidiropoulos, MD
University of Michigan
Shirshendu Sinha, MD
Mayo Clinic Health System and Mayo Clinic
Cornel Stanciu, MD
Dartmouth’s Geisel School of Medicine
Jeffrey Sung, MD
University of Washington
Thida Thant, MD
University of Colorado at Denver
Adele Viguera, MD
Cleveland Clinic Lerner College of Medicine
Aparna Atluru, MD
Stanford Medicine
Anjan Bhattacharyya, MD
Saint Louis University
Caroline Bonham, MD
The University of New Mexico
Catherine Crone, MD
Inova Health System
Sheila Dowd, PhD
Rush Medical College
Ahmed Z. Elmaadawi, MD
Indiana University School of Medicine
Donald Gilbert, MD, MS
Cincinnati Children’s Hospital Medical Center
Mark Gold, MD
Washington University in St. Louis
Elana Harris, MD, PhD
Cincinnati Children’s Hospital
Susan Hatters-Friedman, MD
Case Western Reserve University
Faisal Islam, MD, MBA
Greenvale, New York
Kaustubh G. Joshi, MD
University of South Carolina School of Medicine
Rita Khoury, MD
Saint George Hospital University Medical Center
Suneeta Kumari, MD, MPH
Howard University Hospital
Michelle Magid, MD
Austin PsychCare PA
Michael Maksimowski, MD
Wayne State University
Jose Maldonado, MD
Stanford University
Thomas W. Meeks, MD
Portland VA Medical Center
John Miller, MD
University of South Florida
Armando Morera-Fumero, MD, PhD
Universidad de La Laguna
Mary K. Morreale, MD
Wayne State University
Philip Muskin, MD
Columbia University College of Physicians and Surgeons
Katharine Nelson, MD
University of Minnesota
Carol North, MD
University of Texas Southwestern Medical Center at Dallas
Douglas Opler, MD
Rutgers University School of Medicine
Joseph Pierre, MD
University of California, Los Angeles
Jerrold Pollak, PhD, ABN, ABPP
Seacoast Mental Health Center
Edwin Raffi, MD, MPH
Massachusetts General Hospital Center for Women’s Mental Health
Y. Pritham Raj, MD
Oregon Health and Science University
Jeffrey Rakofsky, MD
Emory University School of Medicine
Laura Ramsey, PhD
Cincinnati Children’s Hospital Medical Center
Erica Rapp, MD
University of Colorado School of Medicine
Abhishek Reddy, MD
The University of Alabama at Birmingham
Eduardo Rueda Vasquez, MD
Williamsport, Pennsylvania
Stephen Saklad, PharmD, BCPP
The University of Texas at Austin
Lauren Schwarz, PhD, ABPP-CN
Saint Louis University School of Medicine
Andreas Sidiropoulos, MD
University of Michigan
Shirshendu Sinha, MD
Mayo Clinic Health System and Mayo Clinic
Cornel Stanciu, MD
Dartmouth’s Geisel School of Medicine
Jeffrey Sung, MD
University of Washington
Thida Thant, MD
University of Colorado at Denver
Adele Viguera, MD
Cleveland Clinic Lerner College of Medicine
AI and machine learning
Recent advances in neuroscience and genetics are providing a new view of brain function in health and disease.1 As discussed in Drs. Hripsime Kalanderian and Henry Nasrallah’s article “Artificial intelligence in psychiatry” (Evidence-Based Reviews,
In a 2016 article, Dr. Arshya Vahabzadeh2 wrote, “In the near term, humans will continue to make the majority of psychiatric diagnoses and provide treatment.” He predicted that data science—specifically machine learning—will help revolutionize how we diagnose, treat, and monitor depression. He foresees a future where AI machines or learning machines will more accurately diagnose and treat depression.
These predictions remind us of the promises made with the introduction of psychoactive drugs to the practice of psychiatry. In the 1970s, the increased emphasis on neurotransmitters led to new biologic models of mental illness and the expansion of the Diagnostic and Statistical Manual of Mental Disorders. The increased use of psychoactive medications relegated the practice of psychotherapy to other mental health professionals. Psychiatry became a “drug-intensive” specialty, and psychiatrists saw themselves as psychopharmacologists.3 During this time, psychiatry became progressively dominated by the pharmaceutical industry. The deregulation of the markets and the for-profit ideology of the pharmaceutical industry resulted in an economically and mutually beneficial alliance between pharmaceutical companies, academic faculty, and individual psychiatrists.
Using the same for-profit ideology and ethics of the pharmaceutical industry, technology-based corporations are making massive investments in the application of these technologies in neuroscience research and clinical practice. The “promise” that AI will diagnose and treat depression more accurately than clinicians will again radically change the psychiatrist’s role. Most of a psychiatrist’s clinical work eventually will be replicated by machine learning and technicians. The human-to-human encounter that is at core of the profession will be replaced by the machine-to-human encounter.4
From the social economic perspective, the American health care system is designed to increase profit and maximize the earnings of the industries.5 Unless social policy changes, expensive new technologies will increase the cost and limit accessibility to health care, benefiting the few at the expense of the majority of people. These technologies will produce a robust return on investment, but the wealth they create will benefit fewer and fewer people.
Several writers have called attention to the social, economic, and ethical consequences of these advances and recommended that the academics and technologists who support AI and machine learning in medicine must “receive sufficient training in ethics” and gain exposure to social and economic issues.6 Darcy et al7 warns of the risks of introducing these advanced technologies in medicine: “As machine learning enters the state-of-the-art clinical practice, medicine thus has the immense obligation to ensure that this technology is harnessed for societal and individual good, fulfilling the ethical basis of the profession.… Ethical design thinking is essential at every stage of development and application of machine learning in advancing health. Toward this
Marco T. Carpio, MD
Psychiatrist, Private Practice
Lynbrook, New York
Disclosure: The author reports no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
1. Bargeman CI. How the new neuroscience will advance medicine. JAMA. 2015;314(3):221-222.
2. Vahabzadeh A. Can machine learning decode depression? Psychiatric News. https://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2016.4a3. Published April 11, 2016. Accessed October 16, 2019.
3. Angell M. The illusions of psychiatry. The New York Review. https://www.nybooks.com/articles/2011/07/14/illusions-of-psychiatry/. Published July 14, 2011. Accessed October 16, 2019.
4. Heath I, Nessa J. Objectification of physicians and loss of therapeutic power. Lancet. 2007;369(9565):886-888.
5. Wang D. Health care, American style: how did we arrive? Where will we go? Psychiatric Annals. 2014;44(7):342-348.
6. Nourbakhsh IR. The coming robot dystopia. Foreign Affairs. https://www.foreignaffairs.com/articles/2015-06-16/coming-robot-dystopia. Published July 2015. Accessed October 16, 2019.
7. Darcy AM, Louie AK, Roberts LW. Machine learning and the profession of medicine. JAMA. 2016;315(6):551-552.
Recent advances in neuroscience and genetics are providing a new view of brain function in health and disease.1 As discussed in Drs. Hripsime Kalanderian and Henry Nasrallah’s article “Artificial intelligence in psychiatry” (Evidence-Based Reviews,
In a 2016 article, Dr. Arshya Vahabzadeh2 wrote, “In the near term, humans will continue to make the majority of psychiatric diagnoses and provide treatment.” He predicted that data science—specifically machine learning—will help revolutionize how we diagnose, treat, and monitor depression. He foresees a future where AI machines or learning machines will more accurately diagnose and treat depression.
These predictions remind us of the promises made with the introduction of psychoactive drugs to the practice of psychiatry. In the 1970s, the increased emphasis on neurotransmitters led to new biologic models of mental illness and the expansion of the Diagnostic and Statistical Manual of Mental Disorders. The increased use of psychoactive medications relegated the practice of psychotherapy to other mental health professionals. Psychiatry became a “drug-intensive” specialty, and psychiatrists saw themselves as psychopharmacologists.3 During this time, psychiatry became progressively dominated by the pharmaceutical industry. The deregulation of the markets and the for-profit ideology of the pharmaceutical industry resulted in an economically and mutually beneficial alliance between pharmaceutical companies, academic faculty, and individual psychiatrists.
Using the same for-profit ideology and ethics of the pharmaceutical industry, technology-based corporations are making massive investments in the application of these technologies in neuroscience research and clinical practice. The “promise” that AI will diagnose and treat depression more accurately than clinicians will again radically change the psychiatrist’s role. Most of a psychiatrist’s clinical work eventually will be replicated by machine learning and technicians. The human-to-human encounter that is at core of the profession will be replaced by the machine-to-human encounter.4
From the social economic perspective, the American health care system is designed to increase profit and maximize the earnings of the industries.5 Unless social policy changes, expensive new technologies will increase the cost and limit accessibility to health care, benefiting the few at the expense of the majority of people. These technologies will produce a robust return on investment, but the wealth they create will benefit fewer and fewer people.
Several writers have called attention to the social, economic, and ethical consequences of these advances and recommended that the academics and technologists who support AI and machine learning in medicine must “receive sufficient training in ethics” and gain exposure to social and economic issues.6 Darcy et al7 warns of the risks of introducing these advanced technologies in medicine: “As machine learning enters the state-of-the-art clinical practice, medicine thus has the immense obligation to ensure that this technology is harnessed for societal and individual good, fulfilling the ethical basis of the profession.… Ethical design thinking is essential at every stage of development and application of machine learning in advancing health. Toward this
Marco T. Carpio, MD
Psychiatrist, Private Practice
Lynbrook, New York
Disclosure: The author reports no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
Recent advances in neuroscience and genetics are providing a new view of brain function in health and disease.1 As discussed in Drs. Hripsime Kalanderian and Henry Nasrallah’s article “Artificial intelligence in psychiatry” (Evidence-Based Reviews,
In a 2016 article, Dr. Arshya Vahabzadeh2 wrote, “In the near term, humans will continue to make the majority of psychiatric diagnoses and provide treatment.” He predicted that data science—specifically machine learning—will help revolutionize how we diagnose, treat, and monitor depression. He foresees a future where AI machines or learning machines will more accurately diagnose and treat depression.
These predictions remind us of the promises made with the introduction of psychoactive drugs to the practice of psychiatry. In the 1970s, the increased emphasis on neurotransmitters led to new biologic models of mental illness and the expansion of the Diagnostic and Statistical Manual of Mental Disorders. The increased use of psychoactive medications relegated the practice of psychotherapy to other mental health professionals. Psychiatry became a “drug-intensive” specialty, and psychiatrists saw themselves as psychopharmacologists.3 During this time, psychiatry became progressively dominated by the pharmaceutical industry. The deregulation of the markets and the for-profit ideology of the pharmaceutical industry resulted in an economically and mutually beneficial alliance between pharmaceutical companies, academic faculty, and individual psychiatrists.
Using the same for-profit ideology and ethics of the pharmaceutical industry, technology-based corporations are making massive investments in the application of these technologies in neuroscience research and clinical practice. The “promise” that AI will diagnose and treat depression more accurately than clinicians will again radically change the psychiatrist’s role. Most of a psychiatrist’s clinical work eventually will be replicated by machine learning and technicians. The human-to-human encounter that is at core of the profession will be replaced by the machine-to-human encounter.4
From the social economic perspective, the American health care system is designed to increase profit and maximize the earnings of the industries.5 Unless social policy changes, expensive new technologies will increase the cost and limit accessibility to health care, benefiting the few at the expense of the majority of people. These technologies will produce a robust return on investment, but the wealth they create will benefit fewer and fewer people.
Several writers have called attention to the social, economic, and ethical consequences of these advances and recommended that the academics and technologists who support AI and machine learning in medicine must “receive sufficient training in ethics” and gain exposure to social and economic issues.6 Darcy et al7 warns of the risks of introducing these advanced technologies in medicine: “As machine learning enters the state-of-the-art clinical practice, medicine thus has the immense obligation to ensure that this technology is harnessed for societal and individual good, fulfilling the ethical basis of the profession.… Ethical design thinking is essential at every stage of development and application of machine learning in advancing health. Toward this
Marco T. Carpio, MD
Psychiatrist, Private Practice
Lynbrook, New York
Disclosure: The author reports no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
1. Bargeman CI. How the new neuroscience will advance medicine. JAMA. 2015;314(3):221-222.
2. Vahabzadeh A. Can machine learning decode depression? Psychiatric News. https://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2016.4a3. Published April 11, 2016. Accessed October 16, 2019.
3. Angell M. The illusions of psychiatry. The New York Review. https://www.nybooks.com/articles/2011/07/14/illusions-of-psychiatry/. Published July 14, 2011. Accessed October 16, 2019.
4. Heath I, Nessa J. Objectification of physicians and loss of therapeutic power. Lancet. 2007;369(9565):886-888.
5. Wang D. Health care, American style: how did we arrive? Where will we go? Psychiatric Annals. 2014;44(7):342-348.
6. Nourbakhsh IR. The coming robot dystopia. Foreign Affairs. https://www.foreignaffairs.com/articles/2015-06-16/coming-robot-dystopia. Published July 2015. Accessed October 16, 2019.
7. Darcy AM, Louie AK, Roberts LW. Machine learning and the profession of medicine. JAMA. 2016;315(6):551-552.
1. Bargeman CI. How the new neuroscience will advance medicine. JAMA. 2015;314(3):221-222.
2. Vahabzadeh A. Can machine learning decode depression? Psychiatric News. https://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2016.4a3. Published April 11, 2016. Accessed October 16, 2019.
3. Angell M. The illusions of psychiatry. The New York Review. https://www.nybooks.com/articles/2011/07/14/illusions-of-psychiatry/. Published July 14, 2011. Accessed October 16, 2019.
4. Heath I, Nessa J. Objectification of physicians and loss of therapeutic power. Lancet. 2007;369(9565):886-888.
5. Wang D. Health care, American style: how did we arrive? Where will we go? Psychiatric Annals. 2014;44(7):342-348.
6. Nourbakhsh IR. The coming robot dystopia. Foreign Affairs. https://www.foreignaffairs.com/articles/2015-06-16/coming-robot-dystopia. Published July 2015. Accessed October 16, 2019.
7. Darcy AM, Louie AK, Roberts LW. Machine learning and the profession of medicine. JAMA. 2016;315(6):551-552.
The woman who couldn’t stop eating
CASE Uncontrollable eating and weight gain
Ms. C, age 33, presents to an outpatient clinic with complaints of weight gain and “uncontrollable eating.” Ms. C says she’s gained >50 lb over the last year. She describes progressively frequent episodes of overeating during which she feels that she has no control over the amount of food she consumes. She reports eating as often as 10 times a day, and overeating to the point of physical discomfort during most meals. She gives an example of having recently consumed a large pizza, several portions of Chinese food, approximately 20 chicken wings, and half a chocolate cake for dinner. Ms. C admits that on several occasions she has vomited after meals due to feeling extremely full; however, she denies having done so intentionally. She also denies restricting her food intake, misusing laxatives or diuretics, or exercising excessively.
Ms. C expresses frustration and embarrassment with her eating and resulting weight gain. She says she has poor self-esteem, low energy and motivation, and poor concentration. She feels that her condition has significantly impacted her social life, romantic relationships, and family life. She admits she’s been avoiding dating and seeing friends due to her weight gain, and has been irritable with her teenage daughter.
During her initial evaluation, Ms. C is alert and oriented, with a linear and goal-directed thought process. She is somewhat irritable and guarded, wearing large sunglasses that cover most of her face, but is not overtly paranoid. Although she appears frustrated when discussing her condition, she denies feeling hopeless or helpless.
HISTORY Thyroid cancer and mood swings
Ms. C, who is single and unemployed, lives in an apartment with her teenage daughter, with whom she describes having a good relationship. She has been receiving disability benefits for the past 2 years after a motor vehicle accident resulted in multiple fractures of her arm and elbow, and subsequent chronic pain. Ms. C reports a distant history of “problems with alcohol,” but denies drinking any alcohol since being charged with driving under the influence several years ago. She has a 10 pack-year history of smoking and denies any history of illicit drug use.
Two years ago, Ms. C was diagnosed with thyroid carcinoma, and treated with surgical resection and a course of radiation. She has regular visits with her endocrinologist and has been prescribed oral levothyroxine, 150 mcg/d.
Ms. C reports a history of “mood swings” characterized by “snapping at people” and becoming irritable in response to stressful situations, but denies any past symptoms consistent with a manic or hypomanic episode. Ms. C has not been admitted to a psychiatric hospital, nor has she received any prior psychiatric treatment. She reluctantly discloses that approximately 3 years ago she had a less severe episode of uncontrollable eating and weight gain (20 to 30 lb). At that time, she was able to regain her desired physical appearance by going on the “Subway diet” and undergoing liposuction and plastic surgery.
At her current outpatient clinic visit, Ms. C expresses an interest in exploring bariatric surgery as a potential solution to her weight gain.
[polldaddy:10446186]
Continue to: EVALUATION Obese; stable thyroid function
EVALUATION Obese; stable thyroid function
We refer Ms. C for a physical examination and routine blood analysis to rule out any medical contributors to her condition. Her physical examination is reported as normal, with no signs of skin changes, goiter, or exophthalmos. Ms. C is noted to be obese, with a body mass index of 37.2 kg/m2, and an abdominal circumference of 38.5 in.
A blood analysis shows that Ms. C has elevated triglyceride levels (202 mg/dL) and elevated cholesterol levels (210 mg/dL). Her thyroid function tests are within normal limits based on the dose of levothyroxine she’s been receiving. A pregnancy test is negative.
Ms. C gives the team at the clinic permission to contact her endocrinologist, who reports that he does not suspect that Ms. C’s drastic weight gain and abnormal eating patterns are attributable to her history of thyroid carcinoma because her thyroid function tests have been stable on her current regimen.
The authors’ observations
Based on Ms. C’s initial presentation, we strongly suspected a diagnosis of binge eating disorder (BED). Several differential diagnoses were considered and carefully ruled out; Ms. C’s medical workup did not suggest that her weight gain was due to an active medical condition, and she did not meet DSM-5 criteria for a mood or psychotic disorder or anorexia nervosa or bulimia nervosa.
With an estimated lifetime prevalence in the United States of 2.6%, BED is the most prevalent eating disorder (compared with 0.6% for anorexia nervosa and 1% for bulimia nervosa).1 BED is more prevalent in women than in men, and the mean age of onset is mid-20s.
Continue to: BED may be difficult...
BED may be difficult to detect because patients may feel ashamed or guilty and are often hesitant to disclose and discuss their symptoms. Furthermore, they are frequently frustrated by the subjective loss of control over their behaviors. Patients with BED often present to medical facilities seeking weight loss solutions rather than to psychiatric clinics.
Screening for eating disorders
Several screening instruments have been developed to help clinicians identify patients who may need further evaluation for possible diagnosis of an eating disorder, including anorexia nervosa, bulimia nervosa, and BED.2 The SCOFF questionnaire is composed of 5 brief clinician-administered questions to screen for eating disorders.2 The 7-item Binge Eating Disorder Screener (BED-7) is a screening instrument specific for BED that examines a patient’s eating patterns and behaviors during the past 3 months.3
In general, suspect BED in patients who have significant weight dissatisfaction, fluctuation in weight, and depressive symptoms. The DSM-5 criteria for binge eating disorder are shown in Table 14.
BED and comorbid psychiatric disorders
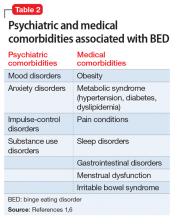
Patients with BED are more likely than the general population to have comorbid psychiatric disorders, including mood and anxiety disorders, attention-deficit/hyperactivity disorder, posttraumatic stress disorder, and substance use disorders. Swanson et al5 found that 83.5% of adolescents who met criteria for BED also met criteria for at least 1 other psychiatric disorder, and 37% endorsed >3 concurrent psychiatric conditions. Once BED is confirmed, it is important to screen for other psychiatric and medical comorbidities that are often present in individuals with BED (Table 21,6).
The rates of diagnosis and treatment of BED remain low. This is likely due to patient factors such as shame and fear of stigma and clinician factors such as lack of awareness, ineffective communication, hesitation to discuss the sensitive topic, or insufficient knowledge about treatment options once BED is diagnosed.
[polldaddy:10446187]
Continue to: TREATMENT Combination therapy
TREATMENT Combination therapy
Ms. C is ambivalent about her BED diagnosis, and becomes angry about it when the proposed treatments do not involve bariatric surgery or cosmetic procedures. Ms. C is enrolled in weekly individual psychotherapy, where she receives a combination of CBT and psychodynamic therapy; however, her attendance is inconsistent. Ms. C is offered a trial of fluoxetine, but adamantly refuses, citing a relative who experienced adverse effects while receiving this type of antidepressant. Ms. C also refuses a trial of topiramate due to concerns of feeling sedated. Finally, she is offered a trial of lisdexamfetamine, 30 mg/d, which was FDA-approved in 2015 to treat moderate to severe BED. We discuss the risks, benefits, and adverse effects of lisdexamfetamine with Ms. C; however, she is hesitant to start this medication and expresses increasing interest in obtaining a consultation for bariatric surgery. Ms. C is provided with extensive education about the risks and dangers of surgery before addressing her eating patterns, and the clinician provides validation, verbal support, and counseling. Ms. C eventually agrees to a trial of lisdexamfetamine, but her insurance denies coverage of this medication.
The authors’ observations
When developing an individualized treatment plan for a patient with BED, the patient’s psychiatric and medical comorbidities should be considered. Treatment goals for patients with BED include:
- abstinence from binge eating
- sustainable weight loss and metabolic health
- reduction in symptoms associated with comorbid conditions
- improvement in self-esteem and overall quality of life.
A 2015 comparative effectiveness review of management and outcomes for patients with BED evaluated pharmacologic, psychologic, behavioral, and combined approaches for treating patients with BED.7 The results suggested that second-generation antidepressants, topiramate, and lisdexamfetamine were superior to placebo in reducing binge-eating episodes and achieving abstinence from binge-eating. Weight reduction was also achieved with topiramate and lisdexamfetamine, and antidepressants helped relieve symptoms of comorbid depression.
Various formats of CBT, including therapist-led and guided self-help, were also superior to placebo in reducing the frequency of binge-eating and promoting abstinence; however, they were generally not effective in treating depression or reducing patients’ weight.7
OUTCOME Fixated on surgery
We appeal the decision of Ms. C’s insurance company; however, during the appeals process, Ms. C becomes increasingly irritable and informs us that she has changed her mind and, with the reported support of her medical doctors, wishes to undergo bariatric surgery. Although we made multiple attempts to engage Ms. C in further treatment, she is lost to follow-up.
Continue to: Bottom Line
Bottom Line
Diagnosing and managing patients with binge eating disorder (BED) can be challenging because patients may hesitate to seek help, and/or have psychiatric and medical comorbidities. They often present to medical facilities seeking weight loss solutions rather than to psychiatric clinics. Once BED is confirmed, screen for other psychiatric and medical comorbidities. A combination of pharmacologic and psychotherapeutic interventions can benefit some patients with BED, but treatment should be individualized.
Related Resources
- National Eating Disorders Association. NEDA. www.nationaleatingdisorders.org/.
- Safer D, Telch C, Chen EY. Dialectical behavior therapy for binge eating and bulimia. New York, NY: Guilford Press; 2017.
Drug Brand Names
Fluoxetine • Prozac
Levothyroxine • Synthroid
Lisdexamfetamine • Vyvanse
Topiramate • Topamax
1. Hudson JI, Hiripi E, Pope HG Jr, et al. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61(3):348-358.
2. Morgan JF, Reid F, Lacey JH. The SCOFF questionnaire: assessment of a new screening tool for eating disorders. BMJ. 1999;319(7223):1467-1468.
3. Herman BK, Deal LS, DiBenedetti DB, et al. Development of the 7-Item Binge-Eating Disorder screener (BEDS-7). Prim Care Companion CNS Disord. 2016;18(2):10.4088/PCC.15m01896. doi:10.4088/PCC.15m01896.
4. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
5. Swanson SA, Crow SJ, Le Grange D, et al. Prevalence and correlates of eating disorders in adolescents. Results from the national comorbidity survey replication adolescent supplement. Arch Gen Psychiatry. 2011;68(7):714.
6. Guerdjikova AI, Mori N, Casuto LS, et al. Binge eating disorder. Psychiatric Clinics of North America. 2017;40(2):255-266.
7. Berkman ND, Brownley KA, Peat CM, et al. Management and outcomes of binge-eating disorder. Comparative Effectiveness Reviews, No. 160. Agency for Healthcare Research and Quality (US). https://www.ncbi.nlm.nih.gov/books/NBK338312/. Published December 2015. Accessed July 29, 2019.
CASE Uncontrollable eating and weight gain
Ms. C, age 33, presents to an outpatient clinic with complaints of weight gain and “uncontrollable eating.” Ms. C says she’s gained >50 lb over the last year. She describes progressively frequent episodes of overeating during which she feels that she has no control over the amount of food she consumes. She reports eating as often as 10 times a day, and overeating to the point of physical discomfort during most meals. She gives an example of having recently consumed a large pizza, several portions of Chinese food, approximately 20 chicken wings, and half a chocolate cake for dinner. Ms. C admits that on several occasions she has vomited after meals due to feeling extremely full; however, she denies having done so intentionally. She also denies restricting her food intake, misusing laxatives or diuretics, or exercising excessively.
Ms. C expresses frustration and embarrassment with her eating and resulting weight gain. She says she has poor self-esteem, low energy and motivation, and poor concentration. She feels that her condition has significantly impacted her social life, romantic relationships, and family life. She admits she’s been avoiding dating and seeing friends due to her weight gain, and has been irritable with her teenage daughter.
During her initial evaluation, Ms. C is alert and oriented, with a linear and goal-directed thought process. She is somewhat irritable and guarded, wearing large sunglasses that cover most of her face, but is not overtly paranoid. Although she appears frustrated when discussing her condition, she denies feeling hopeless or helpless.
HISTORY Thyroid cancer and mood swings
Ms. C, who is single and unemployed, lives in an apartment with her teenage daughter, with whom she describes having a good relationship. She has been receiving disability benefits for the past 2 years after a motor vehicle accident resulted in multiple fractures of her arm and elbow, and subsequent chronic pain. Ms. C reports a distant history of “problems with alcohol,” but denies drinking any alcohol since being charged with driving under the influence several years ago. She has a 10 pack-year history of smoking and denies any history of illicit drug use.
Two years ago, Ms. C was diagnosed with thyroid carcinoma, and treated with surgical resection and a course of radiation. She has regular visits with her endocrinologist and has been prescribed oral levothyroxine, 150 mcg/d.
Ms. C reports a history of “mood swings” characterized by “snapping at people” and becoming irritable in response to stressful situations, but denies any past symptoms consistent with a manic or hypomanic episode. Ms. C has not been admitted to a psychiatric hospital, nor has she received any prior psychiatric treatment. She reluctantly discloses that approximately 3 years ago she had a less severe episode of uncontrollable eating and weight gain (20 to 30 lb). At that time, she was able to regain her desired physical appearance by going on the “Subway diet” and undergoing liposuction and plastic surgery.
At her current outpatient clinic visit, Ms. C expresses an interest in exploring bariatric surgery as a potential solution to her weight gain.
[polldaddy:10446186]
Continue to: EVALUATION Obese; stable thyroid function
EVALUATION Obese; stable thyroid function
We refer Ms. C for a physical examination and routine blood analysis to rule out any medical contributors to her condition. Her physical examination is reported as normal, with no signs of skin changes, goiter, or exophthalmos. Ms. C is noted to be obese, with a body mass index of 37.2 kg/m2, and an abdominal circumference of 38.5 in.
A blood analysis shows that Ms. C has elevated triglyceride levels (202 mg/dL) and elevated cholesterol levels (210 mg/dL). Her thyroid function tests are within normal limits based on the dose of levothyroxine she’s been receiving. A pregnancy test is negative.
Ms. C gives the team at the clinic permission to contact her endocrinologist, who reports that he does not suspect that Ms. C’s drastic weight gain and abnormal eating patterns are attributable to her history of thyroid carcinoma because her thyroid function tests have been stable on her current regimen.
The authors’ observations
Based on Ms. C’s initial presentation, we strongly suspected a diagnosis of binge eating disorder (BED). Several differential diagnoses were considered and carefully ruled out; Ms. C’s medical workup did not suggest that her weight gain was due to an active medical condition, and she did not meet DSM-5 criteria for a mood or psychotic disorder or anorexia nervosa or bulimia nervosa.
With an estimated lifetime prevalence in the United States of 2.6%, BED is the most prevalent eating disorder (compared with 0.6% for anorexia nervosa and 1% for bulimia nervosa).1 BED is more prevalent in women than in men, and the mean age of onset is mid-20s.
Continue to: BED may be difficult...
BED may be difficult to detect because patients may feel ashamed or guilty and are often hesitant to disclose and discuss their symptoms. Furthermore, they are frequently frustrated by the subjective loss of control over their behaviors. Patients with BED often present to medical facilities seeking weight loss solutions rather than to psychiatric clinics.
Screening for eating disorders
Several screening instruments have been developed to help clinicians identify patients who may need further evaluation for possible diagnosis of an eating disorder, including anorexia nervosa, bulimia nervosa, and BED.2 The SCOFF questionnaire is composed of 5 brief clinician-administered questions to screen for eating disorders.2 The 7-item Binge Eating Disorder Screener (BED-7) is a screening instrument specific for BED that examines a patient’s eating patterns and behaviors during the past 3 months.3
In general, suspect BED in patients who have significant weight dissatisfaction, fluctuation in weight, and depressive symptoms. The DSM-5 criteria for binge eating disorder are shown in Table 14.
BED and comorbid psychiatric disorders
Patients with BED are more likely than the general population to have comorbid psychiatric disorders, including mood and anxiety disorders, attention-deficit/hyperactivity disorder, posttraumatic stress disorder, and substance use disorders. Swanson et al5 found that 83.5% of adolescents who met criteria for BED also met criteria for at least 1 other psychiatric disorder, and 37% endorsed >3 concurrent psychiatric conditions. Once BED is confirmed, it is important to screen for other psychiatric and medical comorbidities that are often present in individuals with BED (Table 21,6).
The rates of diagnosis and treatment of BED remain low. This is likely due to patient factors such as shame and fear of stigma and clinician factors such as lack of awareness, ineffective communication, hesitation to discuss the sensitive topic, or insufficient knowledge about treatment options once BED is diagnosed.
[polldaddy:10446187]
Continue to: TREATMENT Combination therapy
TREATMENT Combination therapy
Ms. C is ambivalent about her BED diagnosis, and becomes angry about it when the proposed treatments do not involve bariatric surgery or cosmetic procedures. Ms. C is enrolled in weekly individual psychotherapy, where she receives a combination of CBT and psychodynamic therapy; however, her attendance is inconsistent. Ms. C is offered a trial of fluoxetine, but adamantly refuses, citing a relative who experienced adverse effects while receiving this type of antidepressant. Ms. C also refuses a trial of topiramate due to concerns of feeling sedated. Finally, she is offered a trial of lisdexamfetamine, 30 mg/d, which was FDA-approved in 2015 to treat moderate to severe BED. We discuss the risks, benefits, and adverse effects of lisdexamfetamine with Ms. C; however, she is hesitant to start this medication and expresses increasing interest in obtaining a consultation for bariatric surgery. Ms. C is provided with extensive education about the risks and dangers of surgery before addressing her eating patterns, and the clinician provides validation, verbal support, and counseling. Ms. C eventually agrees to a trial of lisdexamfetamine, but her insurance denies coverage of this medication.
The authors’ observations
When developing an individualized treatment plan for a patient with BED, the patient’s psychiatric and medical comorbidities should be considered. Treatment goals for patients with BED include:
- abstinence from binge eating
- sustainable weight loss and metabolic health
- reduction in symptoms associated with comorbid conditions
- improvement in self-esteem and overall quality of life.
A 2015 comparative effectiveness review of management and outcomes for patients with BED evaluated pharmacologic, psychologic, behavioral, and combined approaches for treating patients with BED.7 The results suggested that second-generation antidepressants, topiramate, and lisdexamfetamine were superior to placebo in reducing binge-eating episodes and achieving abstinence from binge-eating. Weight reduction was also achieved with topiramate and lisdexamfetamine, and antidepressants helped relieve symptoms of comorbid depression.
Various formats of CBT, including therapist-led and guided self-help, were also superior to placebo in reducing the frequency of binge-eating and promoting abstinence; however, they were generally not effective in treating depression or reducing patients’ weight.7
OUTCOME Fixated on surgery
We appeal the decision of Ms. C’s insurance company; however, during the appeals process, Ms. C becomes increasingly irritable and informs us that she has changed her mind and, with the reported support of her medical doctors, wishes to undergo bariatric surgery. Although we made multiple attempts to engage Ms. C in further treatment, she is lost to follow-up.
Continue to: Bottom Line
Bottom Line
Diagnosing and managing patients with binge eating disorder (BED) can be challenging because patients may hesitate to seek help, and/or have psychiatric and medical comorbidities. They often present to medical facilities seeking weight loss solutions rather than to psychiatric clinics. Once BED is confirmed, screen for other psychiatric and medical comorbidities. A combination of pharmacologic and psychotherapeutic interventions can benefit some patients with BED, but treatment should be individualized.
Related Resources
- National Eating Disorders Association. NEDA. www.nationaleatingdisorders.org/.
- Safer D, Telch C, Chen EY. Dialectical behavior therapy for binge eating and bulimia. New York, NY: Guilford Press; 2017.
Drug Brand Names
Fluoxetine • Prozac
Levothyroxine • Synthroid
Lisdexamfetamine • Vyvanse
Topiramate • Topamax
CASE Uncontrollable eating and weight gain
Ms. C, age 33, presents to an outpatient clinic with complaints of weight gain and “uncontrollable eating.” Ms. C says she’s gained >50 lb over the last year. She describes progressively frequent episodes of overeating during which she feels that she has no control over the amount of food she consumes. She reports eating as often as 10 times a day, and overeating to the point of physical discomfort during most meals. She gives an example of having recently consumed a large pizza, several portions of Chinese food, approximately 20 chicken wings, and half a chocolate cake for dinner. Ms. C admits that on several occasions she has vomited after meals due to feeling extremely full; however, she denies having done so intentionally. She also denies restricting her food intake, misusing laxatives or diuretics, or exercising excessively.
Ms. C expresses frustration and embarrassment with her eating and resulting weight gain. She says she has poor self-esteem, low energy and motivation, and poor concentration. She feels that her condition has significantly impacted her social life, romantic relationships, and family life. She admits she’s been avoiding dating and seeing friends due to her weight gain, and has been irritable with her teenage daughter.
During her initial evaluation, Ms. C is alert and oriented, with a linear and goal-directed thought process. She is somewhat irritable and guarded, wearing large sunglasses that cover most of her face, but is not overtly paranoid. Although she appears frustrated when discussing her condition, she denies feeling hopeless or helpless.
HISTORY Thyroid cancer and mood swings
Ms. C, who is single and unemployed, lives in an apartment with her teenage daughter, with whom she describes having a good relationship. She has been receiving disability benefits for the past 2 years after a motor vehicle accident resulted in multiple fractures of her arm and elbow, and subsequent chronic pain. Ms. C reports a distant history of “problems with alcohol,” but denies drinking any alcohol since being charged with driving under the influence several years ago. She has a 10 pack-year history of smoking and denies any history of illicit drug use.
Two years ago, Ms. C was diagnosed with thyroid carcinoma, and treated with surgical resection and a course of radiation. She has regular visits with her endocrinologist and has been prescribed oral levothyroxine, 150 mcg/d.
Ms. C reports a history of “mood swings” characterized by “snapping at people” and becoming irritable in response to stressful situations, but denies any past symptoms consistent with a manic or hypomanic episode. Ms. C has not been admitted to a psychiatric hospital, nor has she received any prior psychiatric treatment. She reluctantly discloses that approximately 3 years ago she had a less severe episode of uncontrollable eating and weight gain (20 to 30 lb). At that time, she was able to regain her desired physical appearance by going on the “Subway diet” and undergoing liposuction and plastic surgery.
At her current outpatient clinic visit, Ms. C expresses an interest in exploring bariatric surgery as a potential solution to her weight gain.
[polldaddy:10446186]
Continue to: EVALUATION Obese; stable thyroid function
EVALUATION Obese; stable thyroid function
We refer Ms. C for a physical examination and routine blood analysis to rule out any medical contributors to her condition. Her physical examination is reported as normal, with no signs of skin changes, goiter, or exophthalmos. Ms. C is noted to be obese, with a body mass index of 37.2 kg/m2, and an abdominal circumference of 38.5 in.
A blood analysis shows that Ms. C has elevated triglyceride levels (202 mg/dL) and elevated cholesterol levels (210 mg/dL). Her thyroid function tests are within normal limits based on the dose of levothyroxine she’s been receiving. A pregnancy test is negative.
Ms. C gives the team at the clinic permission to contact her endocrinologist, who reports that he does not suspect that Ms. C’s drastic weight gain and abnormal eating patterns are attributable to her history of thyroid carcinoma because her thyroid function tests have been stable on her current regimen.
The authors’ observations
Based on Ms. C’s initial presentation, we strongly suspected a diagnosis of binge eating disorder (BED). Several differential diagnoses were considered and carefully ruled out; Ms. C’s medical workup did not suggest that her weight gain was due to an active medical condition, and she did not meet DSM-5 criteria for a mood or psychotic disorder or anorexia nervosa or bulimia nervosa.
With an estimated lifetime prevalence in the United States of 2.6%, BED is the most prevalent eating disorder (compared with 0.6% for anorexia nervosa and 1% for bulimia nervosa).1 BED is more prevalent in women than in men, and the mean age of onset is mid-20s.
Continue to: BED may be difficult...
BED may be difficult to detect because patients may feel ashamed or guilty and are often hesitant to disclose and discuss their symptoms. Furthermore, they are frequently frustrated by the subjective loss of control over their behaviors. Patients with BED often present to medical facilities seeking weight loss solutions rather than to psychiatric clinics.
Screening for eating disorders
Several screening instruments have been developed to help clinicians identify patients who may need further evaluation for possible diagnosis of an eating disorder, including anorexia nervosa, bulimia nervosa, and BED.2 The SCOFF questionnaire is composed of 5 brief clinician-administered questions to screen for eating disorders.2 The 7-item Binge Eating Disorder Screener (BED-7) is a screening instrument specific for BED that examines a patient’s eating patterns and behaviors during the past 3 months.3
In general, suspect BED in patients who have significant weight dissatisfaction, fluctuation in weight, and depressive symptoms. The DSM-5 criteria for binge eating disorder are shown in Table 14.
BED and comorbid psychiatric disorders
Patients with BED are more likely than the general population to have comorbid psychiatric disorders, including mood and anxiety disorders, attention-deficit/hyperactivity disorder, posttraumatic stress disorder, and substance use disorders. Swanson et al5 found that 83.5% of adolescents who met criteria for BED also met criteria for at least 1 other psychiatric disorder, and 37% endorsed >3 concurrent psychiatric conditions. Once BED is confirmed, it is important to screen for other psychiatric and medical comorbidities that are often present in individuals with BED (Table 21,6).
The rates of diagnosis and treatment of BED remain low. This is likely due to patient factors such as shame and fear of stigma and clinician factors such as lack of awareness, ineffective communication, hesitation to discuss the sensitive topic, or insufficient knowledge about treatment options once BED is diagnosed.
[polldaddy:10446187]
Continue to: TREATMENT Combination therapy
TREATMENT Combination therapy
Ms. C is ambivalent about her BED diagnosis, and becomes angry about it when the proposed treatments do not involve bariatric surgery or cosmetic procedures. Ms. C is enrolled in weekly individual psychotherapy, where she receives a combination of CBT and psychodynamic therapy; however, her attendance is inconsistent. Ms. C is offered a trial of fluoxetine, but adamantly refuses, citing a relative who experienced adverse effects while receiving this type of antidepressant. Ms. C also refuses a trial of topiramate due to concerns of feeling sedated. Finally, she is offered a trial of lisdexamfetamine, 30 mg/d, which was FDA-approved in 2015 to treat moderate to severe BED. We discuss the risks, benefits, and adverse effects of lisdexamfetamine with Ms. C; however, she is hesitant to start this medication and expresses increasing interest in obtaining a consultation for bariatric surgery. Ms. C is provided with extensive education about the risks and dangers of surgery before addressing her eating patterns, and the clinician provides validation, verbal support, and counseling. Ms. C eventually agrees to a trial of lisdexamfetamine, but her insurance denies coverage of this medication.
The authors’ observations
When developing an individualized treatment plan for a patient with BED, the patient’s psychiatric and medical comorbidities should be considered. Treatment goals for patients with BED include:
- abstinence from binge eating
- sustainable weight loss and metabolic health
- reduction in symptoms associated with comorbid conditions
- improvement in self-esteem and overall quality of life.
A 2015 comparative effectiveness review of management and outcomes for patients with BED evaluated pharmacologic, psychologic, behavioral, and combined approaches for treating patients with BED.7 The results suggested that second-generation antidepressants, topiramate, and lisdexamfetamine were superior to placebo in reducing binge-eating episodes and achieving abstinence from binge-eating. Weight reduction was also achieved with topiramate and lisdexamfetamine, and antidepressants helped relieve symptoms of comorbid depression.
Various formats of CBT, including therapist-led and guided self-help, were also superior to placebo in reducing the frequency of binge-eating and promoting abstinence; however, they were generally not effective in treating depression or reducing patients’ weight.7
OUTCOME Fixated on surgery
We appeal the decision of Ms. C’s insurance company; however, during the appeals process, Ms. C becomes increasingly irritable and informs us that she has changed her mind and, with the reported support of her medical doctors, wishes to undergo bariatric surgery. Although we made multiple attempts to engage Ms. C in further treatment, she is lost to follow-up.
Continue to: Bottom Line
Bottom Line
Diagnosing and managing patients with binge eating disorder (BED) can be challenging because patients may hesitate to seek help, and/or have psychiatric and medical comorbidities. They often present to medical facilities seeking weight loss solutions rather than to psychiatric clinics. Once BED is confirmed, screen for other psychiatric and medical comorbidities. A combination of pharmacologic and psychotherapeutic interventions can benefit some patients with BED, but treatment should be individualized.
Related Resources
- National Eating Disorders Association. NEDA. www.nationaleatingdisorders.org/.
- Safer D, Telch C, Chen EY. Dialectical behavior therapy for binge eating and bulimia. New York, NY: Guilford Press; 2017.
Drug Brand Names
Fluoxetine • Prozac
Levothyroxine • Synthroid
Lisdexamfetamine • Vyvanse
Topiramate • Topamax
1. Hudson JI, Hiripi E, Pope HG Jr, et al. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61(3):348-358.
2. Morgan JF, Reid F, Lacey JH. The SCOFF questionnaire: assessment of a new screening tool for eating disorders. BMJ. 1999;319(7223):1467-1468.
3. Herman BK, Deal LS, DiBenedetti DB, et al. Development of the 7-Item Binge-Eating Disorder screener (BEDS-7). Prim Care Companion CNS Disord. 2016;18(2):10.4088/PCC.15m01896. doi:10.4088/PCC.15m01896.
4. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
5. Swanson SA, Crow SJ, Le Grange D, et al. Prevalence and correlates of eating disorders in adolescents. Results from the national comorbidity survey replication adolescent supplement. Arch Gen Psychiatry. 2011;68(7):714.
6. Guerdjikova AI, Mori N, Casuto LS, et al. Binge eating disorder. Psychiatric Clinics of North America. 2017;40(2):255-266.
7. Berkman ND, Brownley KA, Peat CM, et al. Management and outcomes of binge-eating disorder. Comparative Effectiveness Reviews, No. 160. Agency for Healthcare Research and Quality (US). https://www.ncbi.nlm.nih.gov/books/NBK338312/. Published December 2015. Accessed July 29, 2019.
1. Hudson JI, Hiripi E, Pope HG Jr, et al. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61(3):348-358.
2. Morgan JF, Reid F, Lacey JH. The SCOFF questionnaire: assessment of a new screening tool for eating disorders. BMJ. 1999;319(7223):1467-1468.
3. Herman BK, Deal LS, DiBenedetti DB, et al. Development of the 7-Item Binge-Eating Disorder screener (BEDS-7). Prim Care Companion CNS Disord. 2016;18(2):10.4088/PCC.15m01896. doi:10.4088/PCC.15m01896.
4. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
5. Swanson SA, Crow SJ, Le Grange D, et al. Prevalence and correlates of eating disorders in adolescents. Results from the national comorbidity survey replication adolescent supplement. Arch Gen Psychiatry. 2011;68(7):714.
6. Guerdjikova AI, Mori N, Casuto LS, et al. Binge eating disorder. Psychiatric Clinics of North America. 2017;40(2):255-266.
7. Berkman ND, Brownley KA, Peat CM, et al. Management and outcomes of binge-eating disorder. Comparative Effectiveness Reviews, No. 160. Agency for Healthcare Research and Quality (US). https://www.ncbi.nlm.nih.gov/books/NBK338312/. Published December 2015. Accessed July 29, 2019.
Effects of psychotropic medications on thyroid function
Ms. L, age 53, presents to an inpatient psychiatric unit with depression, difficulty concentrating, fatigue, cognitive blunting, loss of appetite, increased alcohol intake, and recent suicidal ideation. Her symptoms began 3 months ago and gradually worsened. Her medical and psychiatric history is significant for hypertension, fibromyalgia, and chronic pain (back and neck), major depressive disorder (MDD; recurrent, severe), and generalized anxiety disorder (GAD). Ms. L’s current medication regimen includes lisinopril, 40 mg daily; fluoxetine, 60 mg daily; mirtazapine, 30 mg at bedtime; gabapentin, 300 mg twice daily; alprazolam, 0.5 mg twice daily as needed for anxiety; and oral docusate, 100 mg twice daily as needed. Her blood pressure is 124/85 mm Hg, heart rate is 66 beats per minute, and an electrocardiogram is normal. Laboratory workup reveals a potassium level of 4.4 mEq/L, blood urea nitrogen level of 20 mg/dL, serum creatinine level of 0.8 mg/dL, estimated creatinine clearance of 89.6 mL/min, free triiodothyronine (T3) levels of 2.7 pg/mL, thyroid-stimulating hormone (TSH) level of 7.68 mIU/L, free thyroxine (T4) level of 1.3 ng/dL, and blood ethanol level <10 mg/dL. In addition to the symptoms Ms. L initially described, a review of systems reveals word-finding difficulty, cold intolerance, constipation, hair loss, brittle nails, and dry skin.
To target Ms. L’s MDD, GAD, fibromyalgia, and chronic pain, fluoxetine, 60 mg daily is cross titrated beginning on Day 1 to duloxetine, 60 mg twice daily, over 4 days. Mirtazapine is decreased on Day 3 to 7.5 mg at bedtime to target Ms. L’s sleep and appetite. Due to the presence of several symptoms associated with hypothyroidism and a slightly elevated TSH level, on Day 6 we initiate adjunctive levothyroxine, 50 mcg daily each morning to target symptomatic subclinical hypothyroidism, and to potentially augment the other medications prescribed to address Ms. L’s MDD.
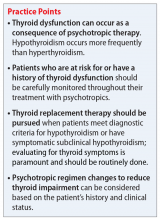
Thyroid hormone function is a complex physiological process controlled through the hypothalamic-pituitary-thyroid (HPT) axis. Psychotropic medications can impact thyroid hormone function and contribute to aberrations in thyroid physiology.1 Because patients with mental illness may require multiple psychotropic medications, it is imperative to understand the potential effects of these agents.
Antidepressants can induce hypothyroidism along multiple points of hormonal synthesis and iodine utilization. Tricyclic antidepressants have been implicated in the development of drug-iodide complexes, thus reducing biologically active iodine.2 Tricyclic antidepressants also can bind thyroid peroxidase, an enzyme necessary in the production of T4 and T3, altering hormonal production, resulting in a hypothyroid state.1 Non-tricyclic antidepressants (ie, selective serotonin reuptake inhibitors [SSRIs] and non-SSRIs [including serotonin-norepinephrine reuptake inhibitors and mirtazapine]) have also been implicated in thyroid dysfunction. Selective serotonin reuptake inhibitors have the propensity to induce hypothyroidism through inhibition of thyroid hormones T4 and T3.1,3 This inhibition is not always seen with concurrent reductions in TSH levels. Conversely, non-SSRIs can influence thyroid hormone levels with great variation, leading to thyroid hormone levels that are increased, decreased, or unchanged.1 Patients with a history of thyroid dysfunction should receive close thyroid function monitoring, especially while taking antidepressants.
Antipsychotics have a proclivity to induce hypothyroidism by means similar to antidepressants via hormonal manipulation and immunogenicity. Phenothiazines impact thyroid function through hormonal activation and degradation, and induction of autoimmunity.1 Autoimmunity may develop by means of antibody production or antigen immunization through the major histocompatibility complex.2 Other first-generation antipsychotics (FGAs) (eg, haloperidol and loxapine) are known to antagonize dopamine receptors in the tuberoinfundibular pathway, resulting in increased prolactin levels. Hyperprolactinemia may result in increased TSH levels through HPT axis activation.1 Additionally, FGAs can induce an immunogenic effect through production of antithyroid antibodies.1 Similar to FGAs, second-generation antipsychotics (SGAs) can increase TSH levels through hyperprolactinemia. Further research focused on SGAs is needed to determine how profound this effect may be.
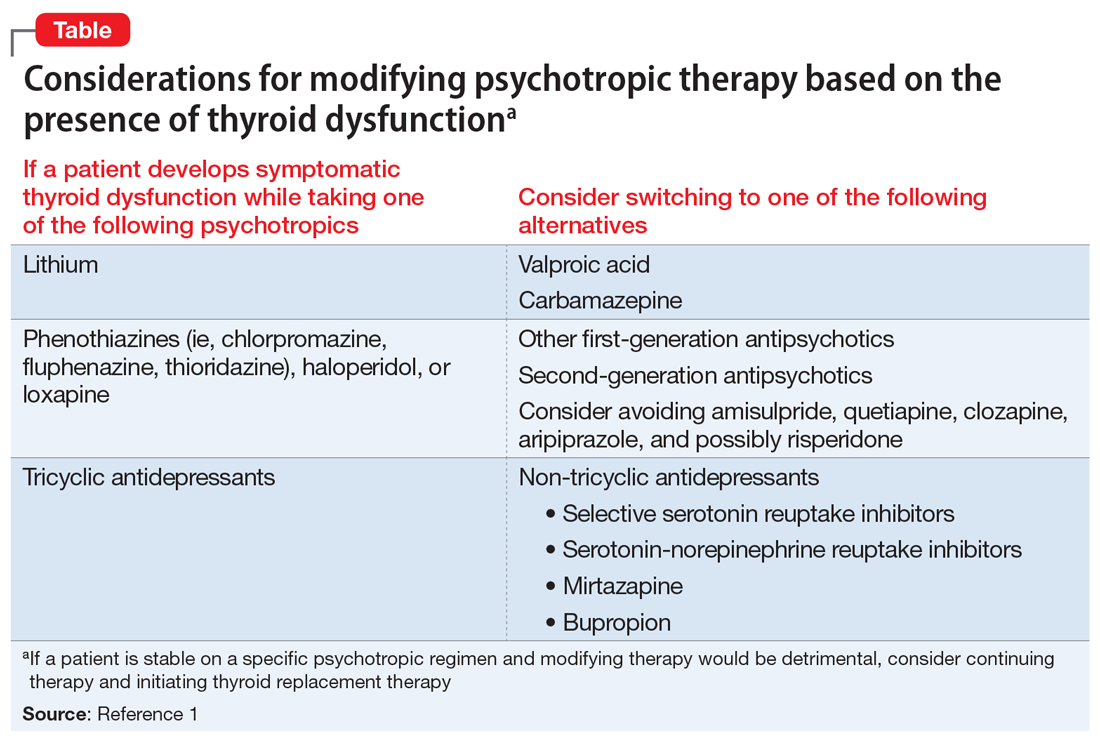
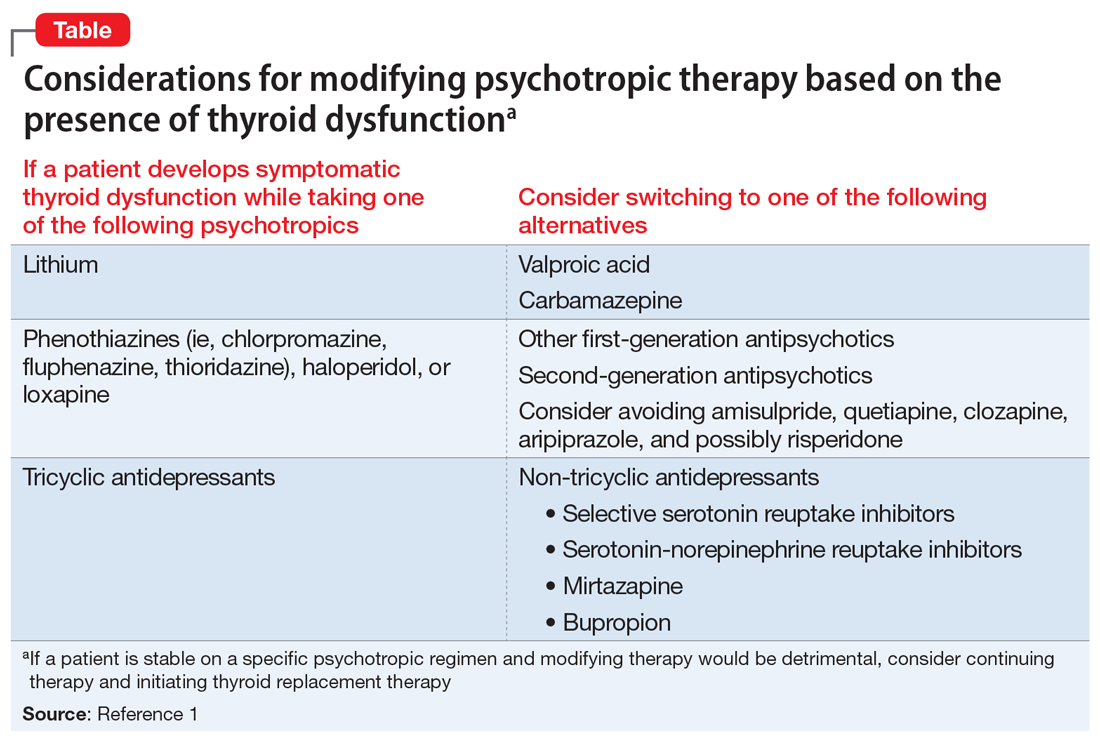
The Table1 outlines considerations for modifying psychotropic therapy based on the presence of concurrent thyroid dysfunction. Thyroid function should be routinely assessed in patients treated with antipsychotics.
Mood stabilizers are capable of altering thyroid function and inducing a hypothyroid state. Lithium has been implicated in both hypothyroidism and hyperthyroidism due to its inhibition of hormonal secretion, and toxicity to thyroid cells with chronic use, respectively.1,4 Hypothyroidism can develop shortly after initiating lithium; women tend to have a greater predilection for thyroid dysfunction than men.1 Carbamazepine (CBZ) can reduce thyroid hormone levels without having a direct effect on TSH or thyroid dysfunction.1 As with lithium, women tend to be more susceptible to this effect. Valproic acid (VPA) has been shown to either increase, decrease, or have no impact on thyroid hormone levels, with little effect on TSH.1 When VPA is given in combination with CBZ, significant reductions in thyroid levels with a concurrent increase in TSH can occur.1 In patients with preexisting thyroid dysfunction, the combination of VPA and CBZ should be used with caution.
Continue to: CASE
CASE CONTINUED
By Day 8, Ms. L reports less fatigue, clearer thinking, improved concentration, and less pain. She also no longer reports suicidal ideation, and demonstrates improved appetite and mood. She is discharged on Day 9 of her hospitalization.
The treatment team refers Ms. L for outpatient follow-up in 4 weeks, with a goal TSH level <3.0. Unfortunately, the effects of levothyroxine on Ms. L’s TSH level could not be determined during her hospital stay, and she has not returned to the facility since the initial presentation.
Thyroid function and mood
Ms. L’s case illustrates how thyroid function, pain, cognition, and mood may be interconnected. It is important to address all potential underlying comorbidities and establish appropriate outpatient care and follow-up so that patients may experience a more robust recovery. Further, this case highlights the importance of ruling out other potential medical causes of MDD during the initial diagnosis, and during times of recurrence or relapse, especially when a recent stressor, medication changes, or medication nonadherence cannot be identified as potential contributors.
Related Resources
- Cojić M, Cvejanov-Kezunović L. Subclinical hypothyroidism – whether and when to start treatment? Open Access Maced J Med Sci. 2017;5(7):1042-1046.
- Garber JR, Cobin RH, Gharib H, et al. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Thyroid. 2012;22(12):1200-1235.
- Iosifescu DV. ‘Supercharge’ antidepressants by adding thyroid hormones. Current Psychiatry. 2006;5(7):15-20,25.
Drug Brand Names
Alprazolam • Xanax
Aripiprazole • Abilify
Bupropion • Wellbutrin
Carbamazepine • Carbatrol, Tegretol
Chlorpromazine • Thorazine
Clozapine • Clozaril
Duloxetine • Cymbalta
Fluoxetine • Prozac
Fluphenazine • Prolixin
Gabapentin • Neurontin
Haloperidol • Haldol
Levothyroxine • Synthroid
Lisinopril • Prinivil, Zestril
Lithium • Eskalith, Lithobid
Loxapine • Loxitane
Mirtazapine • Remeron
Quetiapine • Seroquel
Risperidone • Risperdal
Thioridazine • Mellaril
Valproic acid • Depakote
1. Bou Khalil R, Richa S. Thyroid adverse effect of psychotropic drugs: a review. Clin Neuropharm. 2001;34(6):248-255.
2. Sauvage MF, Marquet P, Rousseau A, et al. Relationship between psychotropic drugs and thyroid function: a review. Toxicol Appl Pharmacol. 1998;149(2):127-135.
3. Shelton RC, Winn S, Ekhatore N, et al. The effects of antidepressants on the thyroid axis in depression. Biol Psychiatry. 1993;33(2):120-126.
4. Kundra P, Burman KD. The effect of medications on thyroid function tests. Med Clin North Am. 2012;96(2):283-295.
Ms. L, age 53, presents to an inpatient psychiatric unit with depression, difficulty concentrating, fatigue, cognitive blunting, loss of appetite, increased alcohol intake, and recent suicidal ideation. Her symptoms began 3 months ago and gradually worsened. Her medical and psychiatric history is significant for hypertension, fibromyalgia, and chronic pain (back and neck), major depressive disorder (MDD; recurrent, severe), and generalized anxiety disorder (GAD). Ms. L’s current medication regimen includes lisinopril, 40 mg daily; fluoxetine, 60 mg daily; mirtazapine, 30 mg at bedtime; gabapentin, 300 mg twice daily; alprazolam, 0.5 mg twice daily as needed for anxiety; and oral docusate, 100 mg twice daily as needed. Her blood pressure is 124/85 mm Hg, heart rate is 66 beats per minute, and an electrocardiogram is normal. Laboratory workup reveals a potassium level of 4.4 mEq/L, blood urea nitrogen level of 20 mg/dL, serum creatinine level of 0.8 mg/dL, estimated creatinine clearance of 89.6 mL/min, free triiodothyronine (T3) levels of 2.7 pg/mL, thyroid-stimulating hormone (TSH) level of 7.68 mIU/L, free thyroxine (T4) level of 1.3 ng/dL, and blood ethanol level <10 mg/dL. In addition to the symptoms Ms. L initially described, a review of systems reveals word-finding difficulty, cold intolerance, constipation, hair loss, brittle nails, and dry skin.
To target Ms. L’s MDD, GAD, fibromyalgia, and chronic pain, fluoxetine, 60 mg daily is cross titrated beginning on Day 1 to duloxetine, 60 mg twice daily, over 4 days. Mirtazapine is decreased on Day 3 to 7.5 mg at bedtime to target Ms. L’s sleep and appetite. Due to the presence of several symptoms associated with hypothyroidism and a slightly elevated TSH level, on Day 6 we initiate adjunctive levothyroxine, 50 mcg daily each morning to target symptomatic subclinical hypothyroidism, and to potentially augment the other medications prescribed to address Ms. L’s MDD.
Thyroid hormone function is a complex physiological process controlled through the hypothalamic-pituitary-thyroid (HPT) axis. Psychotropic medications can impact thyroid hormone function and contribute to aberrations in thyroid physiology.1 Because patients with mental illness may require multiple psychotropic medications, it is imperative to understand the potential effects of these agents.
Antidepressants can induce hypothyroidism along multiple points of hormonal synthesis and iodine utilization. Tricyclic antidepressants have been implicated in the development of drug-iodide complexes, thus reducing biologically active iodine.2 Tricyclic antidepressants also can bind thyroid peroxidase, an enzyme necessary in the production of T4 and T3, altering hormonal production, resulting in a hypothyroid state.1 Non-tricyclic antidepressants (ie, selective serotonin reuptake inhibitors [SSRIs] and non-SSRIs [including serotonin-norepinephrine reuptake inhibitors and mirtazapine]) have also been implicated in thyroid dysfunction. Selective serotonin reuptake inhibitors have the propensity to induce hypothyroidism through inhibition of thyroid hormones T4 and T3.1,3 This inhibition is not always seen with concurrent reductions in TSH levels. Conversely, non-SSRIs can influence thyroid hormone levels with great variation, leading to thyroid hormone levels that are increased, decreased, or unchanged.1 Patients with a history of thyroid dysfunction should receive close thyroid function monitoring, especially while taking antidepressants.
Antipsychotics have a proclivity to induce hypothyroidism by means similar to antidepressants via hormonal manipulation and immunogenicity. Phenothiazines impact thyroid function through hormonal activation and degradation, and induction of autoimmunity.1 Autoimmunity may develop by means of antibody production or antigen immunization through the major histocompatibility complex.2 Other first-generation antipsychotics (FGAs) (eg, haloperidol and loxapine) are known to antagonize dopamine receptors in the tuberoinfundibular pathway, resulting in increased prolactin levels. Hyperprolactinemia may result in increased TSH levels through HPT axis activation.1 Additionally, FGAs can induce an immunogenic effect through production of antithyroid antibodies.1 Similar to FGAs, second-generation antipsychotics (SGAs) can increase TSH levels through hyperprolactinemia. Further research focused on SGAs is needed to determine how profound this effect may be.
The Table1 outlines considerations for modifying psychotropic therapy based on the presence of concurrent thyroid dysfunction. Thyroid function should be routinely assessed in patients treated with antipsychotics.
Mood stabilizers are capable of altering thyroid function and inducing a hypothyroid state. Lithium has been implicated in both hypothyroidism and hyperthyroidism due to its inhibition of hormonal secretion, and toxicity to thyroid cells with chronic use, respectively.1,4 Hypothyroidism can develop shortly after initiating lithium; women tend to have a greater predilection for thyroid dysfunction than men.1 Carbamazepine (CBZ) can reduce thyroid hormone levels without having a direct effect on TSH or thyroid dysfunction.1 As with lithium, women tend to be more susceptible to this effect. Valproic acid (VPA) has been shown to either increase, decrease, or have no impact on thyroid hormone levels, with little effect on TSH.1 When VPA is given in combination with CBZ, significant reductions in thyroid levels with a concurrent increase in TSH can occur.1 In patients with preexisting thyroid dysfunction, the combination of VPA and CBZ should be used with caution.
Continue to: CASE
CASE CONTINUED
By Day 8, Ms. L reports less fatigue, clearer thinking, improved concentration, and less pain. She also no longer reports suicidal ideation, and demonstrates improved appetite and mood. She is discharged on Day 9 of her hospitalization.
The treatment team refers Ms. L for outpatient follow-up in 4 weeks, with a goal TSH level <3.0. Unfortunately, the effects of levothyroxine on Ms. L’s TSH level could not be determined during her hospital stay, and she has not returned to the facility since the initial presentation.
Thyroid function and mood
Ms. L’s case illustrates how thyroid function, pain, cognition, and mood may be interconnected. It is important to address all potential underlying comorbidities and establish appropriate outpatient care and follow-up so that patients may experience a more robust recovery. Further, this case highlights the importance of ruling out other potential medical causes of MDD during the initial diagnosis, and during times of recurrence or relapse, especially when a recent stressor, medication changes, or medication nonadherence cannot be identified as potential contributors.
Related Resources
- Cojić M, Cvejanov-Kezunović L. Subclinical hypothyroidism – whether and when to start treatment? Open Access Maced J Med Sci. 2017;5(7):1042-1046.
- Garber JR, Cobin RH, Gharib H, et al. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Thyroid. 2012;22(12):1200-1235.
- Iosifescu DV. ‘Supercharge’ antidepressants by adding thyroid hormones. Current Psychiatry. 2006;5(7):15-20,25.
Drug Brand Names
Alprazolam • Xanax
Aripiprazole • Abilify
Bupropion • Wellbutrin
Carbamazepine • Carbatrol, Tegretol
Chlorpromazine • Thorazine
Clozapine • Clozaril
Duloxetine • Cymbalta
Fluoxetine • Prozac
Fluphenazine • Prolixin
Gabapentin • Neurontin
Haloperidol • Haldol
Levothyroxine • Synthroid
Lisinopril • Prinivil, Zestril
Lithium • Eskalith, Lithobid
Loxapine • Loxitane
Mirtazapine • Remeron
Quetiapine • Seroquel
Risperidone • Risperdal
Thioridazine • Mellaril
Valproic acid • Depakote
Ms. L, age 53, presents to an inpatient psychiatric unit with depression, difficulty concentrating, fatigue, cognitive blunting, loss of appetite, increased alcohol intake, and recent suicidal ideation. Her symptoms began 3 months ago and gradually worsened. Her medical and psychiatric history is significant for hypertension, fibromyalgia, and chronic pain (back and neck), major depressive disorder (MDD; recurrent, severe), and generalized anxiety disorder (GAD). Ms. L’s current medication regimen includes lisinopril, 40 mg daily; fluoxetine, 60 mg daily; mirtazapine, 30 mg at bedtime; gabapentin, 300 mg twice daily; alprazolam, 0.5 mg twice daily as needed for anxiety; and oral docusate, 100 mg twice daily as needed. Her blood pressure is 124/85 mm Hg, heart rate is 66 beats per minute, and an electrocardiogram is normal. Laboratory workup reveals a potassium level of 4.4 mEq/L, blood urea nitrogen level of 20 mg/dL, serum creatinine level of 0.8 mg/dL, estimated creatinine clearance of 89.6 mL/min, free triiodothyronine (T3) levels of 2.7 pg/mL, thyroid-stimulating hormone (TSH) level of 7.68 mIU/L, free thyroxine (T4) level of 1.3 ng/dL, and blood ethanol level <10 mg/dL. In addition to the symptoms Ms. L initially described, a review of systems reveals word-finding difficulty, cold intolerance, constipation, hair loss, brittle nails, and dry skin.
To target Ms. L’s MDD, GAD, fibromyalgia, and chronic pain, fluoxetine, 60 mg daily is cross titrated beginning on Day 1 to duloxetine, 60 mg twice daily, over 4 days. Mirtazapine is decreased on Day 3 to 7.5 mg at bedtime to target Ms. L’s sleep and appetite. Due to the presence of several symptoms associated with hypothyroidism and a slightly elevated TSH level, on Day 6 we initiate adjunctive levothyroxine, 50 mcg daily each morning to target symptomatic subclinical hypothyroidism, and to potentially augment the other medications prescribed to address Ms. L’s MDD.
Thyroid hormone function is a complex physiological process controlled through the hypothalamic-pituitary-thyroid (HPT) axis. Psychotropic medications can impact thyroid hormone function and contribute to aberrations in thyroid physiology.1 Because patients with mental illness may require multiple psychotropic medications, it is imperative to understand the potential effects of these agents.
Antidepressants can induce hypothyroidism along multiple points of hormonal synthesis and iodine utilization. Tricyclic antidepressants have been implicated in the development of drug-iodide complexes, thus reducing biologically active iodine.2 Tricyclic antidepressants also can bind thyroid peroxidase, an enzyme necessary in the production of T4 and T3, altering hormonal production, resulting in a hypothyroid state.1 Non-tricyclic antidepressants (ie, selective serotonin reuptake inhibitors [SSRIs] and non-SSRIs [including serotonin-norepinephrine reuptake inhibitors and mirtazapine]) have also been implicated in thyroid dysfunction. Selective serotonin reuptake inhibitors have the propensity to induce hypothyroidism through inhibition of thyroid hormones T4 and T3.1,3 This inhibition is not always seen with concurrent reductions in TSH levels. Conversely, non-SSRIs can influence thyroid hormone levels with great variation, leading to thyroid hormone levels that are increased, decreased, or unchanged.1 Patients with a history of thyroid dysfunction should receive close thyroid function monitoring, especially while taking antidepressants.
Antipsychotics have a proclivity to induce hypothyroidism by means similar to antidepressants via hormonal manipulation and immunogenicity. Phenothiazines impact thyroid function through hormonal activation and degradation, and induction of autoimmunity.1 Autoimmunity may develop by means of antibody production or antigen immunization through the major histocompatibility complex.2 Other first-generation antipsychotics (FGAs) (eg, haloperidol and loxapine) are known to antagonize dopamine receptors in the tuberoinfundibular pathway, resulting in increased prolactin levels. Hyperprolactinemia may result in increased TSH levels through HPT axis activation.1 Additionally, FGAs can induce an immunogenic effect through production of antithyroid antibodies.1 Similar to FGAs, second-generation antipsychotics (SGAs) can increase TSH levels through hyperprolactinemia. Further research focused on SGAs is needed to determine how profound this effect may be.
The Table1 outlines considerations for modifying psychotropic therapy based on the presence of concurrent thyroid dysfunction. Thyroid function should be routinely assessed in patients treated with antipsychotics.
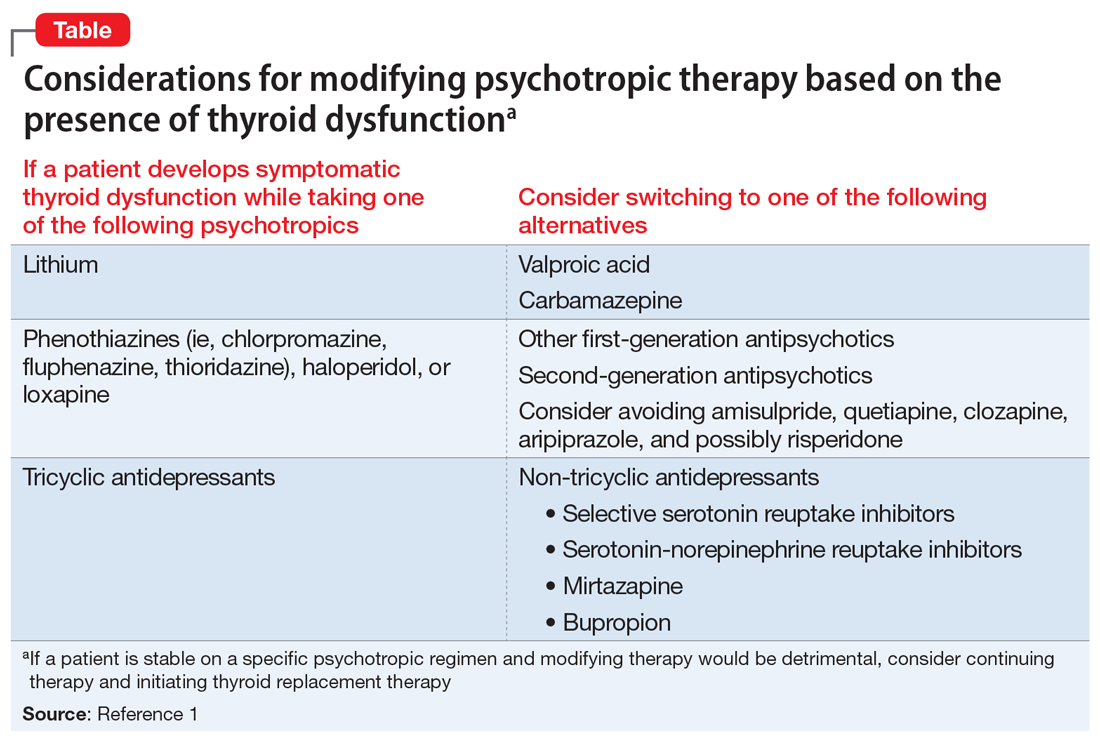
Mood stabilizers are capable of altering thyroid function and inducing a hypothyroid state. Lithium has been implicated in both hypothyroidism and hyperthyroidism due to its inhibition of hormonal secretion, and toxicity to thyroid cells with chronic use, respectively.1,4 Hypothyroidism can develop shortly after initiating lithium; women tend to have a greater predilection for thyroid dysfunction than men.1 Carbamazepine (CBZ) can reduce thyroid hormone levels without having a direct effect on TSH or thyroid dysfunction.1 As with lithium, women tend to be more susceptible to this effect. Valproic acid (VPA) has been shown to either increase, decrease, or have no impact on thyroid hormone levels, with little effect on TSH.1 When VPA is given in combination with CBZ, significant reductions in thyroid levels with a concurrent increase in TSH can occur.1 In patients with preexisting thyroid dysfunction, the combination of VPA and CBZ should be used with caution.
Continue to: CASE
CASE CONTINUED
By Day 8, Ms. L reports less fatigue, clearer thinking, improved concentration, and less pain. She also no longer reports suicidal ideation, and demonstrates improved appetite and mood. She is discharged on Day 9 of her hospitalization.
The treatment team refers Ms. L for outpatient follow-up in 4 weeks, with a goal TSH level <3.0. Unfortunately, the effects of levothyroxine on Ms. L’s TSH level could not be determined during her hospital stay, and she has not returned to the facility since the initial presentation.
Thyroid function and mood
Ms. L’s case illustrates how thyroid function, pain, cognition, and mood may be interconnected. It is important to address all potential underlying comorbidities and establish appropriate outpatient care and follow-up so that patients may experience a more robust recovery. Further, this case highlights the importance of ruling out other potential medical causes of MDD during the initial diagnosis, and during times of recurrence or relapse, especially when a recent stressor, medication changes, or medication nonadherence cannot be identified as potential contributors.
Related Resources
- Cojić M, Cvejanov-Kezunović L. Subclinical hypothyroidism – whether and when to start treatment? Open Access Maced J Med Sci. 2017;5(7):1042-1046.
- Garber JR, Cobin RH, Gharib H, et al. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Thyroid. 2012;22(12):1200-1235.
- Iosifescu DV. ‘Supercharge’ antidepressants by adding thyroid hormones. Current Psychiatry. 2006;5(7):15-20,25.
Drug Brand Names
Alprazolam • Xanax
Aripiprazole • Abilify
Bupropion • Wellbutrin
Carbamazepine • Carbatrol, Tegretol
Chlorpromazine • Thorazine
Clozapine • Clozaril
Duloxetine • Cymbalta
Fluoxetine • Prozac
Fluphenazine • Prolixin
Gabapentin • Neurontin
Haloperidol • Haldol
Levothyroxine • Synthroid
Lisinopril • Prinivil, Zestril
Lithium • Eskalith, Lithobid
Loxapine • Loxitane
Mirtazapine • Remeron
Quetiapine • Seroquel
Risperidone • Risperdal
Thioridazine • Mellaril
Valproic acid • Depakote
1. Bou Khalil R, Richa S. Thyroid adverse effect of psychotropic drugs: a review. Clin Neuropharm. 2001;34(6):248-255.
2. Sauvage MF, Marquet P, Rousseau A, et al. Relationship between psychotropic drugs and thyroid function: a review. Toxicol Appl Pharmacol. 1998;149(2):127-135.
3. Shelton RC, Winn S, Ekhatore N, et al. The effects of antidepressants on the thyroid axis in depression. Biol Psychiatry. 1993;33(2):120-126.
4. Kundra P, Burman KD. The effect of medications on thyroid function tests. Med Clin North Am. 2012;96(2):283-295.
1. Bou Khalil R, Richa S. Thyroid adverse effect of psychotropic drugs: a review. Clin Neuropharm. 2001;34(6):248-255.
2. Sauvage MF, Marquet P, Rousseau A, et al. Relationship between psychotropic drugs and thyroid function: a review. Toxicol Appl Pharmacol. 1998;149(2):127-135.
3. Shelton RC, Winn S, Ekhatore N, et al. The effects of antidepressants on the thyroid axis in depression. Biol Psychiatry. 1993;33(2):120-126.
4. Kundra P, Burman KD. The effect of medications on thyroid function tests. Med Clin North Am. 2012;96(2):283-295.
Prescribing medications in an emergency situation? Document your rationale
Emergent medication use is indicated in numerous clinical scenarios, including psychotic agitation, physical aggression, or withdrawal from substances. While there is plenty of literature to help clinicians with medical record documentation in various other settings,1-3 there is minimal guidance on how to document your rationale for using psychiatric medications in emergency situations.
I have designed a template for structuring progress notes that has helped me to quickly explain my decision-making for using psychiatric medications during an emergency. When writing a progress note to justify your clinical actions in these situations, ask yourself the following questions:
- What symptoms/behaviors needed to be emergently treated? (Use direct quotes from the patient.)
- Which nonpharmacologic interventions were attempted prior to using a medication?
- Does the patient have any medication allergies? (Document if you were unable to assess for allergies.)
- Why did you select this specific route for medication administration?
- What was your rationale for using the specific medication(s)?
- What was the rationale for the selected dose?
- Who was present during medication administration?
- Which (if any) concurrent interventions did you order during or after medication administration?
- Were any safety follow-up checks ordered after medication administration?
A sample progress note
To help illustrate how these questions could guide a clinician’s writing, the following is a progress note I created using this template:
“Patient woke up at 3:15
1. Gutheil TG. Fundamentals of medical record documentation. Psychiatry (Edgmont). 2004;1(3):26-28.
2. Guth T, Morrissey T. Medical documentation and ED charting. Clerkship Directors in Emergency Medicine. https://saem.org/cdem/education/online-education/m3-curriculum/documentation/documentation-of-em-encounters. Updated 2015. Accessed October 10, 2019.
3. Aftab A, Latorre S, Nagle-Yang S. Effective note-writing: a primer for psychiatry residents. Psychiatric Times. http://www.psychiatrictimes.com/couch-crisis/effective-note-writing-primer-psychiatry-residents. Published January 13, 2017. Accessed October 10, 2019.
Emergent medication use is indicated in numerous clinical scenarios, including psychotic agitation, physical aggression, or withdrawal from substances. While there is plenty of literature to help clinicians with medical record documentation in various other settings,1-3 there is minimal guidance on how to document your rationale for using psychiatric medications in emergency situations.
I have designed a template for structuring progress notes that has helped me to quickly explain my decision-making for using psychiatric medications during an emergency. When writing a progress note to justify your clinical actions in these situations, ask yourself the following questions:
- What symptoms/behaviors needed to be emergently treated? (Use direct quotes from the patient.)
- Which nonpharmacologic interventions were attempted prior to using a medication?
- Does the patient have any medication allergies? (Document if you were unable to assess for allergies.)
- Why did you select this specific route for medication administration?
- What was your rationale for using the specific medication(s)?
- What was the rationale for the selected dose?
- Who was present during medication administration?
- Which (if any) concurrent interventions did you order during or after medication administration?
- Were any safety follow-up checks ordered after medication administration?
A sample progress note
To help illustrate how these questions could guide a clinician’s writing, the following is a progress note I created using this template:
“Patient woke up at 3:15
Emergent medication use is indicated in numerous clinical scenarios, including psychotic agitation, physical aggression, or withdrawal from substances. While there is plenty of literature to help clinicians with medical record documentation in various other settings,1-3 there is minimal guidance on how to document your rationale for using psychiatric medications in emergency situations.
I have designed a template for structuring progress notes that has helped me to quickly explain my decision-making for using psychiatric medications during an emergency. When writing a progress note to justify your clinical actions in these situations, ask yourself the following questions:
- What symptoms/behaviors needed to be emergently treated? (Use direct quotes from the patient.)
- Which nonpharmacologic interventions were attempted prior to using a medication?
- Does the patient have any medication allergies? (Document if you were unable to assess for allergies.)
- Why did you select this specific route for medication administration?
- What was your rationale for using the specific medication(s)?
- What was the rationale for the selected dose?
- Who was present during medication administration?
- Which (if any) concurrent interventions did you order during or after medication administration?
- Were any safety follow-up checks ordered after medication administration?
A sample progress note
To help illustrate how these questions could guide a clinician’s writing, the following is a progress note I created using this template:
“Patient woke up at 3:15
1. Gutheil TG. Fundamentals of medical record documentation. Psychiatry (Edgmont). 2004;1(3):26-28.
2. Guth T, Morrissey T. Medical documentation and ED charting. Clerkship Directors in Emergency Medicine. https://saem.org/cdem/education/online-education/m3-curriculum/documentation/documentation-of-em-encounters. Updated 2015. Accessed October 10, 2019.
3. Aftab A, Latorre S, Nagle-Yang S. Effective note-writing: a primer for psychiatry residents. Psychiatric Times. http://www.psychiatrictimes.com/couch-crisis/effective-note-writing-primer-psychiatry-residents. Published January 13, 2017. Accessed October 10, 2019.
1. Gutheil TG. Fundamentals of medical record documentation. Psychiatry (Edgmont). 2004;1(3):26-28.
2. Guth T, Morrissey T. Medical documentation and ED charting. Clerkship Directors in Emergency Medicine. https://saem.org/cdem/education/online-education/m3-curriculum/documentation/documentation-of-em-encounters. Updated 2015. Accessed October 10, 2019.
3. Aftab A, Latorre S, Nagle-Yang S. Effective note-writing: a primer for psychiatry residents. Psychiatric Times. http://www.psychiatrictimes.com/couch-crisis/effective-note-writing-primer-psychiatry-residents. Published January 13, 2017. Accessed October 10, 2019.
Dealing with deception: How to manage patients who are ‘faking it’
Patients who fabricate or exaggerate psychiatric symptoms for primary or secondary gain may elicit negative responses from health care professionals. As clinicians, we may believe that such patients are wasting our time and taking resources away from other patients who are genuinely struggling with mental illness and are more deserving of assistance. However, patients who are fabricating or exaggerating their symptoms have legitimate clinical needs that we should strive to understand. If we view them as having reasons for their actions without becoming complicit in their deception, we may find it easier to work with them.
Managing patients who are fabricating or exaggerating
Caring for patients who attempt to mislead us is a challenging proposition. The relevant research is scarce, and there are few recommended interventions for managing patients who fabricate or exaggerate symptoms.1 Direct confrontation and accusation are often unproductive and should be used sparingly. Indirect approaches tend to be more effective.
It is important to manage our countertransference at the outset while establishing and maintaining rapport. Although we may become frustrated, we should avoid using sarcasm or overt skepticism; instead, we should validate these patients’ emotions because their emotional turmoil could be driving their fabrication or exaggeration. We should attempt to explore their specific motivations by focusing our questions on detecting the underlying stressors or conditions.2
To assess our patients’ motives, consider asking the following:
- What kind of problems have these symptoms caused you in your day-to-day life?
- What would make life better for you?
- What are you hoping I can do for you today?
We should ask open-ended questions as well as interview patients over a long period of time and on multiple occasions to observe the consistency of their reported symptoms. In addition, we should take good notes and document our observations to compare what our patients tell us during their appointments.
Addressing inconsistencies
While exploring our patients’ motives, when it is appropriate, we can gently confront discrepancies in their report by asking:
- I am confused about your symptoms. Help me understand what is happening. Can you tell me more? (Then ask specific follow-up questions based on their answer.)
- What do you mean when you say you are experiencing this symptom?
- I am not sure if I understand what you said correctly. These symptoms do not typically occur in the way that you described. Could you tell me more?
- The symptoms you described are unusual to me. Is there something else going on that I am not aware of?
- Do you think these symptoms have been coming up because you are under stress?
- Is it possible that you want to (avoid work, avoid jail, be prescribed a specific medication, etc.) and that this is the only way you could think of to get what you need?
- Is it possible that you are describing what you are experiencing so that you can convince others that you are having problems?
Despite our best efforts, some patients may not drop their guard and will continue to fabricate or exaggerate their symptoms. However, establishing and maintaining rapport, exploring our patients’ potential motives to mislead, and gently confronting discrepancies in their report may maximize the chances of successfully engaging them and developing appropriate treatment plans.
1. Brady MC, Scher LM, Newman W. “I just saw Big Bird. He was 100 feet tall!” Malingering in the emergency room. Current Psychiatry. 2013;12(10):33-40.
2. Schnellbacher S, O’Mara H. Identifying and managing malingering and factitious disorder in the military. Curr Psychiatry Rep. 2016;18(11):105.
Patients who fabricate or exaggerate psychiatric symptoms for primary or secondary gain may elicit negative responses from health care professionals. As clinicians, we may believe that such patients are wasting our time and taking resources away from other patients who are genuinely struggling with mental illness and are more deserving of assistance. However, patients who are fabricating or exaggerating their symptoms have legitimate clinical needs that we should strive to understand. If we view them as having reasons for their actions without becoming complicit in their deception, we may find it easier to work with them.
Managing patients who are fabricating or exaggerating
Caring for patients who attempt to mislead us is a challenging proposition. The relevant research is scarce, and there are few recommended interventions for managing patients who fabricate or exaggerate symptoms.1 Direct confrontation and accusation are often unproductive and should be used sparingly. Indirect approaches tend to be more effective.
It is important to manage our countertransference at the outset while establishing and maintaining rapport. Although we may become frustrated, we should avoid using sarcasm or overt skepticism; instead, we should validate these patients’ emotions because their emotional turmoil could be driving their fabrication or exaggeration. We should attempt to explore their specific motivations by focusing our questions on detecting the underlying stressors or conditions.2
To assess our patients’ motives, consider asking the following:
- What kind of problems have these symptoms caused you in your day-to-day life?
- What would make life better for you?
- What are you hoping I can do for you today?
We should ask open-ended questions as well as interview patients over a long period of time and on multiple occasions to observe the consistency of their reported symptoms. In addition, we should take good notes and document our observations to compare what our patients tell us during their appointments.
Addressing inconsistencies
While exploring our patients’ motives, when it is appropriate, we can gently confront discrepancies in their report by asking:
- I am confused about your symptoms. Help me understand what is happening. Can you tell me more? (Then ask specific follow-up questions based on their answer.)
- What do you mean when you say you are experiencing this symptom?
- I am not sure if I understand what you said correctly. These symptoms do not typically occur in the way that you described. Could you tell me more?
- The symptoms you described are unusual to me. Is there something else going on that I am not aware of?
- Do you think these symptoms have been coming up because you are under stress?
- Is it possible that you want to (avoid work, avoid jail, be prescribed a specific medication, etc.) and that this is the only way you could think of to get what you need?
- Is it possible that you are describing what you are experiencing so that you can convince others that you are having problems?
Despite our best efforts, some patients may not drop their guard and will continue to fabricate or exaggerate their symptoms. However, establishing and maintaining rapport, exploring our patients’ potential motives to mislead, and gently confronting discrepancies in their report may maximize the chances of successfully engaging them and developing appropriate treatment plans.
Patients who fabricate or exaggerate psychiatric symptoms for primary or secondary gain may elicit negative responses from health care professionals. As clinicians, we may believe that such patients are wasting our time and taking resources away from other patients who are genuinely struggling with mental illness and are more deserving of assistance. However, patients who are fabricating or exaggerating their symptoms have legitimate clinical needs that we should strive to understand. If we view them as having reasons for their actions without becoming complicit in their deception, we may find it easier to work with them.
Managing patients who are fabricating or exaggerating
Caring for patients who attempt to mislead us is a challenging proposition. The relevant research is scarce, and there are few recommended interventions for managing patients who fabricate or exaggerate symptoms.1 Direct confrontation and accusation are often unproductive and should be used sparingly. Indirect approaches tend to be more effective.
It is important to manage our countertransference at the outset while establishing and maintaining rapport. Although we may become frustrated, we should avoid using sarcasm or overt skepticism; instead, we should validate these patients’ emotions because their emotional turmoil could be driving their fabrication or exaggeration. We should attempt to explore their specific motivations by focusing our questions on detecting the underlying stressors or conditions.2
To assess our patients’ motives, consider asking the following:
- What kind of problems have these symptoms caused you in your day-to-day life?
- What would make life better for you?
- What are you hoping I can do for you today?
We should ask open-ended questions as well as interview patients over a long period of time and on multiple occasions to observe the consistency of their reported symptoms. In addition, we should take good notes and document our observations to compare what our patients tell us during their appointments.
Addressing inconsistencies
While exploring our patients’ motives, when it is appropriate, we can gently confront discrepancies in their report by asking:
- I am confused about your symptoms. Help me understand what is happening. Can you tell me more? (Then ask specific follow-up questions based on their answer.)
- What do you mean when you say you are experiencing this symptom?
- I am not sure if I understand what you said correctly. These symptoms do not typically occur in the way that you described. Could you tell me more?
- The symptoms you described are unusual to me. Is there something else going on that I am not aware of?
- Do you think these symptoms have been coming up because you are under stress?
- Is it possible that you want to (avoid work, avoid jail, be prescribed a specific medication, etc.) and that this is the only way you could think of to get what you need?
- Is it possible that you are describing what you are experiencing so that you can convince others that you are having problems?
Despite our best efforts, some patients may not drop their guard and will continue to fabricate or exaggerate their symptoms. However, establishing and maintaining rapport, exploring our patients’ potential motives to mislead, and gently confronting discrepancies in their report may maximize the chances of successfully engaging them and developing appropriate treatment plans.
1. Brady MC, Scher LM, Newman W. “I just saw Big Bird. He was 100 feet tall!” Malingering in the emergency room. Current Psychiatry. 2013;12(10):33-40.
2. Schnellbacher S, O’Mara H. Identifying and managing malingering and factitious disorder in the military. Curr Psychiatry Rep. 2016;18(11):105.
1. Brady MC, Scher LM, Newman W. “I just saw Big Bird. He was 100 feet tall!” Malingering in the emergency room. Current Psychiatry. 2013;12(10):33-40.
2. Schnellbacher S, O’Mara H. Identifying and managing malingering and factitious disorder in the military. Curr Psychiatry Rep. 2016;18(11):105.
Anathemas of psychiatric practice
The quarterly report of the State Medical Board can be a sobering read. In addition to the usual updates about new regulations or requirements for licensed physicians, there is always the disciplinary actions “blacklist” of dozens of medical practitioners in all specialties whose licenses were revoked or suspended due to a shocking array of serious violations.
Those infractions range from Medicare billing fraud to prescribing narcotics to fictitious patients to engaging in sex with a patient to walking into the operating room drunk. It is truly disheartening to see dozens of physicians destroy their careers by committing a panoply of odious, repugnant, or illegal actions.
The term “anathema” comes to mind when I read about those miscreants. This Greek term is occasionally used in scholarly or religious publications, but rarely in everyday conversations or articles. Anathema refers to something detested, shunned, or denounced. When used by the clergy, it connotes something to condemn, such as a sinful or evil act.
Like all other medical specialists, we psychiatrists have a noble mission of treating and relieving the suffering of those afflicted with brain disorders that manifest as mood, thought, perceptual, behavioral, or cognitive abnormalities. Our main goal is to restore health, wellness, and quality of life to the millions of individuals who buckle under the weight of genetic redispersion, adverse environmental events, or both. So psychiatrists do a lot of “good,” which benefits all those who live with mental illness. However, psychiatric practice may have some pitfalls that occasionally lead to anathemas, no matter how diligently a practitioner tries to avoid them. The code of psychiatric ethics is a shield that can preempt anathemas from contaminating clinical practice, but human error will occur when the ethical compass fails.
Here are some examples of anathemas that may rear their ugly heads if a practitioner is not constantly on the alert. It is likely you, the readers of
- Sexual contact with a patient. This major anathema must not occur under any circumstance. It will have grave professional consequences for the practitioner and serious emotional repercussions for the patient.
- Breach of confidentiality. This is a sacred rule in psychiatric practice that must not be broken under any circumstance. Breaching confidentiality will rupture the therapeutic bond and trust that a patient has with a psychiatrist (or psychiatric nurse practitioner).
- Causing physical or emotional harm. This anathema can have serious legal implications in addition to being an unacceptable professional violation.
- Failure to assess patients for suicidal or homicidal risk. The life of the patient, and others, may be at stake if this critical component is missing in the evaluation of psychiatric patients, even if they appear “stable.”
- Irrational and hazardous polypharmacy. This type of harm must never occur during medical management of psychiatric patients, and may have legal consequences.
- Not seeking collateral information. This may seem like a “minor” anathema, but it can have major repercussions if a gap of clinically important data about the patient leads to erroneous diagnosis or inappropriate treatment. Regrettably, informants are sometimes unavailable.
- Assessing patients from the neck up only. Psychiatrists are, first and foremost, physicians who must evaluate the entire medical status of the patient, not just his/her mind. There are numerous bidirectional effects between the body and the brain that can influence diagnosis, holistic treatment, medical outcomes, and prognosis.
- Treating patients with medication only, without any concomitant psychotherapy. Such a suboptimal practice is an anathema that is not excusable due to a “lack of time.” Every psychiatric patient deserves a biopsychosocial treatment approach.
- Not inquiring about adherence at every visit. It is impossible to assess the effectiveness of treatment if adherence is partial or poor. Patients must be constantly reminded that while their psychiatrists are committed to their care, full adherence is a vital responsibility for them to fulfill to ensure optimal outcome.
- Ignoring the patient’s cues, both verbal and nonverbal. Being rushed by a large workload, a full schedule, or the demands of electronic medical records that distract a psychiatrist from fully attending to what the patient’s words, facial expressions, or body language convey can lead to a failure to meet the patient’s needs. Even worse, it may lead to missing a serious message a patient is consciously or unconsciously trying to relay.
- Lowering expectations. Nothing is more devastating for patients than to feel that the psychiatrist does not believe he/she will ever achieve wellness, or that they are beyond help and will never improve, recover, or overcome disabling psychiatric illness. This will generate profound hopelessness in vulnerable patients, who crave having a normal life free from illness or disability.
- Using the same medication for all patients. This is an anathema because one size does not fit all, and patients deserve to have their psychiatrists customize their pharmacotherapy to match their medical status and tolerability. For example, the 11 FDA-approved second-generation antipsychotics are not all the same, and a psychiatrist must select the member of that class that is most likely to be a good match for each patient based on that patient’s medical history and the safety/tolerability profile of each antipsychotic.
- Not continuously upgrading one’s practice to incorporate new evidence-based findings of more effective therapeutic strategies. It is an anathema to continue practicing what was learned in residency 25 to 30 years ago when there’s new knowledge and many advances permeating psychiatric practice today.
- Using alcohol or recreational drugs during a shift in the clinic or the hospital. No explanation is needed for this anathema!
- Prescribing for patients without a full evaluation. That’s poor clinical practice, and also is illegal.
- Billing for patients who were never examined. That’s fraudulent, and stupid!
In an editorial I wrote last year intended for graduates of psychiatry residency training programs about the “DNA of psychiatric practice,” I described what comprises good psychiatric practice.1 Anathemas can be regarded as “mutations” within the DNA of psychiatric practice. It is always my hope that none of the freshly minted psychiatrists going into practice will ever commit an anathema, and end up on the “list of shame” in their State Medical Board’s quarterly report….
1. Nasrallah HA. The DNA of psychiatric practice: a covenant with our patients. Current Psychiatry. 2018;17(5):20,22.
The quarterly report of the State Medical Board can be a sobering read. In addition to the usual updates about new regulations or requirements for licensed physicians, there is always the disciplinary actions “blacklist” of dozens of medical practitioners in all specialties whose licenses were revoked or suspended due to a shocking array of serious violations.
Those infractions range from Medicare billing fraud to prescribing narcotics to fictitious patients to engaging in sex with a patient to walking into the operating room drunk. It is truly disheartening to see dozens of physicians destroy their careers by committing a panoply of odious, repugnant, or illegal actions.
The term “anathema” comes to mind when I read about those miscreants. This Greek term is occasionally used in scholarly or religious publications, but rarely in everyday conversations or articles. Anathema refers to something detested, shunned, or denounced. When used by the clergy, it connotes something to condemn, such as a sinful or evil act.
Like all other medical specialists, we psychiatrists have a noble mission of treating and relieving the suffering of those afflicted with brain disorders that manifest as mood, thought, perceptual, behavioral, or cognitive abnormalities. Our main goal is to restore health, wellness, and quality of life to the millions of individuals who buckle under the weight of genetic redispersion, adverse environmental events, or both. So psychiatrists do a lot of “good,” which benefits all those who live with mental illness. However, psychiatric practice may have some pitfalls that occasionally lead to anathemas, no matter how diligently a practitioner tries to avoid them. The code of psychiatric ethics is a shield that can preempt anathemas from contaminating clinical practice, but human error will occur when the ethical compass fails.
Here are some examples of anathemas that may rear their ugly heads if a practitioner is not constantly on the alert. It is likely you, the readers of
- Sexual contact with a patient. This major anathema must not occur under any circumstance. It will have grave professional consequences for the practitioner and serious emotional repercussions for the patient.
- Breach of confidentiality. This is a sacred rule in psychiatric practice that must not be broken under any circumstance. Breaching confidentiality will rupture the therapeutic bond and trust that a patient has with a psychiatrist (or psychiatric nurse practitioner).
- Causing physical or emotional harm. This anathema can have serious legal implications in addition to being an unacceptable professional violation.
- Failure to assess patients for suicidal or homicidal risk. The life of the patient, and others, may be at stake if this critical component is missing in the evaluation of psychiatric patients, even if they appear “stable.”
- Irrational and hazardous polypharmacy. This type of harm must never occur during medical management of psychiatric patients, and may have legal consequences.
- Not seeking collateral information. This may seem like a “minor” anathema, but it can have major repercussions if a gap of clinically important data about the patient leads to erroneous diagnosis or inappropriate treatment. Regrettably, informants are sometimes unavailable.
- Assessing patients from the neck up only. Psychiatrists are, first and foremost, physicians who must evaluate the entire medical status of the patient, not just his/her mind. There are numerous bidirectional effects between the body and the brain that can influence diagnosis, holistic treatment, medical outcomes, and prognosis.
- Treating patients with medication only, without any concomitant psychotherapy. Such a suboptimal practice is an anathema that is not excusable due to a “lack of time.” Every psychiatric patient deserves a biopsychosocial treatment approach.
- Not inquiring about adherence at every visit. It is impossible to assess the effectiveness of treatment if adherence is partial or poor. Patients must be constantly reminded that while their psychiatrists are committed to their care, full adherence is a vital responsibility for them to fulfill to ensure optimal outcome.
- Ignoring the patient’s cues, both verbal and nonverbal. Being rushed by a large workload, a full schedule, or the demands of electronic medical records that distract a psychiatrist from fully attending to what the patient’s words, facial expressions, or body language convey can lead to a failure to meet the patient’s needs. Even worse, it may lead to missing a serious message a patient is consciously or unconsciously trying to relay.
- Lowering expectations. Nothing is more devastating for patients than to feel that the psychiatrist does not believe he/she will ever achieve wellness, or that they are beyond help and will never improve, recover, or overcome disabling psychiatric illness. This will generate profound hopelessness in vulnerable patients, who crave having a normal life free from illness or disability.
- Using the same medication for all patients. This is an anathema because one size does not fit all, and patients deserve to have their psychiatrists customize their pharmacotherapy to match their medical status and tolerability. For example, the 11 FDA-approved second-generation antipsychotics are not all the same, and a psychiatrist must select the member of that class that is most likely to be a good match for each patient based on that patient’s medical history and the safety/tolerability profile of each antipsychotic.
- Not continuously upgrading one’s practice to incorporate new evidence-based findings of more effective therapeutic strategies. It is an anathema to continue practicing what was learned in residency 25 to 30 years ago when there’s new knowledge and many advances permeating psychiatric practice today.
- Using alcohol or recreational drugs during a shift in the clinic or the hospital. No explanation is needed for this anathema!
- Prescribing for patients without a full evaluation. That’s poor clinical practice, and also is illegal.
- Billing for patients who were never examined. That’s fraudulent, and stupid!
In an editorial I wrote last year intended for graduates of psychiatry residency training programs about the “DNA of psychiatric practice,” I described what comprises good psychiatric practice.1 Anathemas can be regarded as “mutations” within the DNA of psychiatric practice. It is always my hope that none of the freshly minted psychiatrists going into practice will ever commit an anathema, and end up on the “list of shame” in their State Medical Board’s quarterly report….
The quarterly report of the State Medical Board can be a sobering read. In addition to the usual updates about new regulations or requirements for licensed physicians, there is always the disciplinary actions “blacklist” of dozens of medical practitioners in all specialties whose licenses were revoked or suspended due to a shocking array of serious violations.
Those infractions range from Medicare billing fraud to prescribing narcotics to fictitious patients to engaging in sex with a patient to walking into the operating room drunk. It is truly disheartening to see dozens of physicians destroy their careers by committing a panoply of odious, repugnant, or illegal actions.
The term “anathema” comes to mind when I read about those miscreants. This Greek term is occasionally used in scholarly or religious publications, but rarely in everyday conversations or articles. Anathema refers to something detested, shunned, or denounced. When used by the clergy, it connotes something to condemn, such as a sinful or evil act.
Like all other medical specialists, we psychiatrists have a noble mission of treating and relieving the suffering of those afflicted with brain disorders that manifest as mood, thought, perceptual, behavioral, or cognitive abnormalities. Our main goal is to restore health, wellness, and quality of life to the millions of individuals who buckle under the weight of genetic redispersion, adverse environmental events, or both. So psychiatrists do a lot of “good,” which benefits all those who live with mental illness. However, psychiatric practice may have some pitfalls that occasionally lead to anathemas, no matter how diligently a practitioner tries to avoid them. The code of psychiatric ethics is a shield that can preempt anathemas from contaminating clinical practice, but human error will occur when the ethical compass fails.
Here are some examples of anathemas that may rear their ugly heads if a practitioner is not constantly on the alert. It is likely you, the readers of
- Sexual contact with a patient. This major anathema must not occur under any circumstance. It will have grave professional consequences for the practitioner and serious emotional repercussions for the patient.
- Breach of confidentiality. This is a sacred rule in psychiatric practice that must not be broken under any circumstance. Breaching confidentiality will rupture the therapeutic bond and trust that a patient has with a psychiatrist (or psychiatric nurse practitioner).
- Causing physical or emotional harm. This anathema can have serious legal implications in addition to being an unacceptable professional violation.
- Failure to assess patients for suicidal or homicidal risk. The life of the patient, and others, may be at stake if this critical component is missing in the evaluation of psychiatric patients, even if they appear “stable.”
- Irrational and hazardous polypharmacy. This type of harm must never occur during medical management of psychiatric patients, and may have legal consequences.
- Not seeking collateral information. This may seem like a “minor” anathema, but it can have major repercussions if a gap of clinically important data about the patient leads to erroneous diagnosis or inappropriate treatment. Regrettably, informants are sometimes unavailable.
- Assessing patients from the neck up only. Psychiatrists are, first and foremost, physicians who must evaluate the entire medical status of the patient, not just his/her mind. There are numerous bidirectional effects between the body and the brain that can influence diagnosis, holistic treatment, medical outcomes, and prognosis.
- Treating patients with medication only, without any concomitant psychotherapy. Such a suboptimal practice is an anathema that is not excusable due to a “lack of time.” Every psychiatric patient deserves a biopsychosocial treatment approach.
- Not inquiring about adherence at every visit. It is impossible to assess the effectiveness of treatment if adherence is partial or poor. Patients must be constantly reminded that while their psychiatrists are committed to their care, full adherence is a vital responsibility for them to fulfill to ensure optimal outcome.
- Ignoring the patient’s cues, both verbal and nonverbal. Being rushed by a large workload, a full schedule, or the demands of electronic medical records that distract a psychiatrist from fully attending to what the patient’s words, facial expressions, or body language convey can lead to a failure to meet the patient’s needs. Even worse, it may lead to missing a serious message a patient is consciously or unconsciously trying to relay.
- Lowering expectations. Nothing is more devastating for patients than to feel that the psychiatrist does not believe he/she will ever achieve wellness, or that they are beyond help and will never improve, recover, or overcome disabling psychiatric illness. This will generate profound hopelessness in vulnerable patients, who crave having a normal life free from illness or disability.
- Using the same medication for all patients. This is an anathema because one size does not fit all, and patients deserve to have their psychiatrists customize their pharmacotherapy to match their medical status and tolerability. For example, the 11 FDA-approved second-generation antipsychotics are not all the same, and a psychiatrist must select the member of that class that is most likely to be a good match for each patient based on that patient’s medical history and the safety/tolerability profile of each antipsychotic.
- Not continuously upgrading one’s practice to incorporate new evidence-based findings of more effective therapeutic strategies. It is an anathema to continue practicing what was learned in residency 25 to 30 years ago when there’s new knowledge and many advances permeating psychiatric practice today.
- Using alcohol or recreational drugs during a shift in the clinic or the hospital. No explanation is needed for this anathema!
- Prescribing for patients without a full evaluation. That’s poor clinical practice, and also is illegal.
- Billing for patients who were never examined. That’s fraudulent, and stupid!
In an editorial I wrote last year intended for graduates of psychiatry residency training programs about the “DNA of psychiatric practice,” I described what comprises good psychiatric practice.1 Anathemas can be regarded as “mutations” within the DNA of psychiatric practice. It is always my hope that none of the freshly minted psychiatrists going into practice will ever commit an anathema, and end up on the “list of shame” in their State Medical Board’s quarterly report….
1. Nasrallah HA. The DNA of psychiatric practice: a covenant with our patients. Current Psychiatry. 2018;17(5):20,22.
1. Nasrallah HA. The DNA of psychiatric practice: a covenant with our patients. Current Psychiatry. 2018;17(5):20,22.
Should psychiatrists prescribe nonpsychotropic medications?
In our experience, most psychiatrists are uncomfortable with prescribing a medication when they feel that doing so would be outside their scope of practice. But there are many situations when prescribing a nonpsychotropic medication would be the correct choice. In this article, we discuss the scope of psychiatric practice, and present 4 case studies that illustrate situations in which psychiatrists should feel comfortable prescribing nonpsychotropic medications.
Defining the scope of practice
What is the scope of a psychiatrist’s practice? Scope of practice usually describes activities that a health care practitioner is allowed to undertake as defined by the terms of his/her license. A license to practice medicine does not include any stipulation restricting practice to a specific medical specialty. However, a local entity may delineate scope of practice within its organization. For instance, local practice standards held by the Detroit Wayne Mental Health Authority (DWMHA) state “Psychiatrists…shall not exceed their scope of practice as per DWMHA credentialing and privileging. For example, a Psychiatrist…who [has] not been appropriately privileged to deliver services to children shall not treat children, excepting crisis situations.”1
Like physicians in other specialties, psychiatrists are not limited to prescribing only a subset of medications commonly associated with their specialty. But for many psychiatrists, prescribing nonpsychotropic medications is complicated by individual and local factors. On one hand, some psychiatrists do not feel it is their role to prescribe nonpsychotropic medications,2 or even some psychotropic medications that may be more complex to prescribe, such as lithium, clozapine, or monoamine oxidase inhibitors.3-5 However, many feel comfortable prescribing complex combinations of psychotropic medications, or prescribing in a way that does not necessarily make sense (eg, prescribing benztropine as prophylaxis for dystonia when starting an antipsychotic).
Reviewing an average day at one urban psychiatric clinic, these questions seem to come up in half of the patient population, especially in patients with chronic mental illness, multiple medical comorbidities, and limited access to health care. When a young patient walks in without an appointment with an acute dystonic reaction secondary to the initiation of antipsychotics a couple of days ago, there is no hesitation to swiftly and appropriately prescribe an IM anticholinergic medication. But why are psychiatrists often hesitant to prescribe nonpsychotropic medications to treat other adverse effects of medications? Lack of knowledge? Lack of training?
Psychiatrists who practice in hospital systems often have immediate access to consultants, and this availability may encourage them to defer to the consultant for treatment of certain adverse effects. We have seen psychiatrists consult Neurology regarding the prescription of donepezil for mild neurocognitive disorder due to Alzheimer’s disease, or Endocrinology regarding prescription of levothyroxine for lithium-induced hypothyroidism.
However, there are numerous scenarios in which psychiatrists should feel comfortable prescribing nonpsychotropic medications or managing medication adverse effects, regardless of whether they consider it to be within or outside their scope of practice. The following case examples illustrate several such situations.
CASE 1
Ms. W, age 30, has been diagnosed with schizophrenia. She requests a refill of quetiapine, 800 mg/d. This medication has been clearly beneficial in alleviating her psychotic symptoms. However, since her last visit 3 months ago, her face appears more round, and she has gained 9 kg. Further evaluation indicates that she has developed metabolic syndrome and pre-diabetes.
Continue to: Metabolic adverse effects
Metabolic adverse effects, such as metabolic syndrome, diabetic ketoacidosis, and cardiovascular disease, are well-known risks of prescribing second-generation antipsychotics.6 In such situations, psychiatrists often advise patients to modify their diet, increase physical activity, and follow up with their primary care physician to determine if other medications are needed. However, getting a patient with a serious mental illness to exercise and modify her/his diet is difficult, and many of these patients do not have a primary care physician.
For patients such as Ms. W, a psychiatrist should consider prescribing metformin. Wu et al7 found that in addition to lifestyle modifications, metformin had the greatest effect on antipsychotic-induced weight gain. In this study, metformin alone had more impact on reversing weight gain and increasing insulin sensitivity than lifestyle modifications alone.7 This is crucial because these patients are especially vulnerable to cardiac disease.8 Metformin is well tolerated and has a low risk of causing hypoglycemia. Concerns regarding lactic acidosis have abated to the extent that the estimated glomerular filtration rate (eGFR) limits for using metformin have been lowered significantly. After reviewing the contraindications, the only knowledge needed to prescribe metformin is the patient’s kidney function and a brief understanding of the titration needed to minimize gastrointestinal adverse effects.9 Thus, prescribing metformin would be a fairly logical and easy first step for managing metabolic syndrome, especially in a patient whose motivation for increasing physical activity and modifying his/her diet is doubtful.
CASE 2
Mr. B, age 45, has major depressive disorder that has been well-controlled on paroxetine, 40 mg/d, for the past 2 years. He has no history of physical illness. On his most recent visit, he appears uncomfortable and nervous. After a long discussion, he discloses that his sex life isn’t what it used to be since starting paroxetine. He is bothered by erectile problems and asks whether he can “get some Viagra.”
Sexual adverse effects, such as erectile dysfunction, are frequently associated with the use of selective serotonin reuptake inhibitors.10 Although managing these adverse effects requires careful evaluation, in most cases, psychiatrists should be able to treat them.10 The logical choice in this case would be to prescribe one of the 4 FDA-approved phosphodiesterase-5 inhibitors (sildenafil [Viagra], tadalafil [Cialis], vardenafil [Levitra], and avanafil [Stendra]. However, Balon et al11 found that few psychiatrists prescribe phosphodiesterase-5 inhibitors, although they believed that they should be prescribing to treat their patients’ sexual dysfunction. Managing these adverse effects is important not only for the patient’s quality of life and relationship with his/her partner, but also for the therapeutic alliance. In a systematic review of 23 trials, Taylor et al12 examined >1,800 patients who were prescribed a medication to address sexual dysfunction secondary to antidepressants. They found that for men, adding a phosphodiesterase-5 inhibitor was appropriate and effective, and for women, adding bupropion at high doses should be considered.12 Like many other adverse effects, sexual adverse effects surely play a role in medication compliance. Dording et al13 found that the addition of sildenafil, 50 to 100 mg as needed, resulted in increased treatment satisfaction and overall contentment in 102 patients who complained of sexual dysfunction in the follow-up phase of the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) antidepressant trials. In most cases, with proper psychoeducation, prescription of
CASE 3
Ms. G, age 22, was recently discharged from an inpatient psychiatric unit after an episode of mania. She was prescribed carbamazepine, 600 mg/d, and ziprasidone, 40 mg twice a day, and appears to be doing well on this regimen. When asked about what led to her admission, she recalls having an elevated mood, increased energy, hypersexuality, impulsivity, and poor judgment. She reveals that she had several sexual partners during her manic episode, and worries that if such behavior occurs again, she may get pregnant. Yet Ms. G was not prescribed birth control upon discharge.
Continue to: Contraception
Contraception. We believe that psychiatrists have an obligation to protect patients from consequences of mental illness. Much the same way that psychiatrists hope to prevent suicide in a patient who has depression, patients should be protected from risks encountered in the manic phase of bipolar disorder. Another reason to prescribe contraceptives in such patients is the teratogenic effects of mood stabilizers. Pagano et al14 reviewed 6 studies that examined common forms of hormonal birth control to determine their safety in patients with depression or bipolar disorder. They found that overall, use of hormonal contraception was not associated with a worse clinical course of disease.
Many available forms of birth control are available. When prescribing in an outpatient setting, a daily oral medication or a monthly depot injection are convenient options.
CASE 4
Mr. P, age 65, has bipolar I disorder and is stable on risperidone long-acting injection, 37.7 mg bimonthly, and lithium, 1,200 mg/d. He reports that he is doing well but has noticed a recent decrease in energy and weight gain without any change in mood. Laboratory testing conducted prior to this visit revealed a thyroid-stimulating hormone (TSH) level of 4 mU/L (normal range: 0.4 to 4.0 mU/L). Six months ago, Mr. P’s TSH level was 2.8 mU/L. The resident supervisor suggests discussing the case with an endocrinologist.
Thyroid function. The impact of lithium on the thyroid gland is well established; however, psychiatrists’ response to such changes are not.15 Gitlin16 reviewed the many adverse effects of lithium and presented various management strategies to address findings such as Mr. P’s. Two important points are that lithium should not be discontinued in light of hypothyroidism, and synthetic thyroxine (levothyroxine) can be initiated and titrated to return TSH levels to a normal range.16 Levothyroxine can be started at low doses (eg, 25 to 50 mcg/d) and increased every 6 weeks until a normal TSH level is achieved.17 Managing lithium-induced clinical or subclinical hypothyroidism can prevent further pathology and possible relapse to depression.
Incorporating integrated care
In all these cases, the prescription of a medication with which some psychiatrists are not comfortable prescribing would have been the logical, easiest, and preferable choice. Of course, when initiating any medication, boxed warnings, contraindications, and drug–drug interactions should be reviewed. Initial dosages and titration schedules can be found in every medication’s FDA-approved prescribing information document (package insert), as well as in numerous reference books and articles.
Continue to: We acknowledge...
We acknowledge that prescribing a nonpsychotropic medication is not always a psychiatrist’s best choice, and that in patients with multiple medical comorbidities and drug–drug interactions that are not clearly defined, referring to or consulting a specialist is appropriate. We in no way support reckless prescribing, but instead present an opportunity to expand the perception of what should be considered within a psychiatrist’s scope of practice, and call for further education of psychiatrists so that they are more comfortable managing these adverse effects and/or prescribing at least some nonpsychotropic medications.
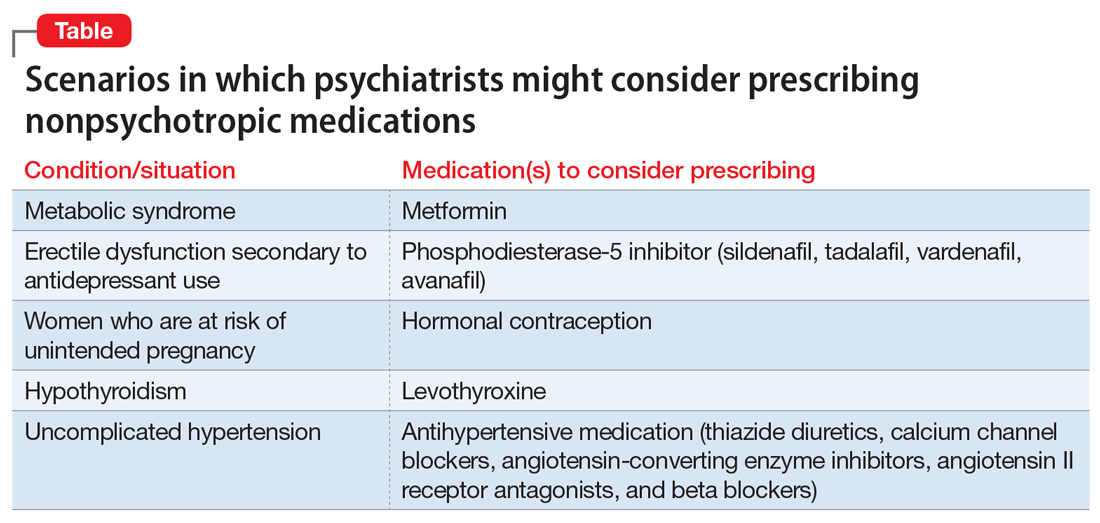
We exhort integrated medical care during this time of a physician shortage; however, we do not practice this way. Interestingly, physicians in primary care, such as those in family medicine or obstetrics and gynecology, frequently attempt to treat patients with psychiatric conditions in an attempt to provide integrated care. Numerous articles have discussed these efforts.18-20 However, this type of integrated care seems less frequent in psychiatry, even though the practice of modern psychiatry in the United States shows substantial overlap with the practice of physicians in primary care specialties.21 There are few articles or practical guidelines for psychiatrists who wish to treat patients’ physical illnesses, particularly patients with severe mental illness (see Related Resources, page 56). If we practice in an integrated manner to treat one of the simple conditions we described above, we can eliminate the need for a patient to visit a second physician, pay another co-pay, pay another bus fare, and take another day off work. This can be particularly helpful for patients who at times have to decide between paying for groceries or for medications. Having one clinician manage a patient’s medications also can decrease the risk of polypharmacy.
In addition to the case scenarios described in this article, there are more clinical situations and nonpsychotropic medications that psychiatrists could manage. Considering them outside the scope of psychiatric practice and being uncomfortable or ambivalent about them is not an excuse. We hope that psychiatrists can increase their expertise in this area, and can start to practice as the primary care physicians they claim they are, and should be.
Bottom Line
Many psychiatrists are uncomfortable prescribing nonpsychotropic medications, but there are numerous clinical scenarios in which the practice would make sense. This could include cases of metabolic syndrome, sexual dysfunction secondary to antidepressant use, or other adverse effects of commonly prescribed psychotropic medications.
Related Resources
- McCarron RM, Xiong GL, Keenan CR, et al. Preventive medical care in psychiatry. A practical guide for clinicians. Arlington, VA: American Psychiatric Association Publishing; 2015.
- McCarron RM, Xiong GL, Keenan CR, et al. Study guide to preventive medical care in psychiatry. Arlington, VA: American Psychiatric Association Publishing; 2017.
- Goldberg JF, Ernst CL. Managing the side effects of psychotropic medications. Washington, DC: American Psychiatric Association Publishing; 2019.
Drug Brand Names
Avanafil • Stendra
Benztropine • Cogentin
Bupropion • Wellbutrin, Zyban
Carbamazepine • Carbatrol, Tegretol
Clozapine • Clozaril
Donepezil • Aricept
Levothyroxine • Levoxyl, Synthroid
Lithium • Eskalith, Lithobid
Metformin • Fortamet, Glucophage
Paroxetine • Paxil
Quetiapine • Seroquel
Risperidone long-acting injection • Risperdal Consta
Sildenafil • Viagra
Tadalafil • Cialis
Vardenafil • Levitra
Ziprasidone • Geodon
1. Detroit Wayne Integrated Health Network. DWMHA psychiatric practice standards. http://dwihn.org/files/2015/6451/9628/Psychiatric_Practice_Standards.pdf. Revised June 2018. Accessed October 8, 2019.
2. Seaman JJ, Cornfield RM, Cummings DM, et al. Exploring psychiatric prescribing practices: the relationship between the role of the provider and the appropriateness of prescribing. Gen Hosp Psychiatry. 1987;9(3):220-224.
3. Zivanovic O. Lithium: a classic drug—frequently discussed, but, sadly, seldom prescribed! Aust N Z J Psychiatry. 2017;51(9):886-896.
4. Stroup TS, Gerhard T, Crystal S, et al. Geographic and clinical variation in clozapine use in the United States. Psychiatric Services. 2014;65(2):186-192.
5. Balon R, Mufti R, Arfken C. A survey of prescribing practices for monoamine oxidase inhibitors. Psychiatric Services. 1999;50(7):945-947.
6. Rummel-Kluge C, Komossa K, Schwarz S, et al. Head-to-head comparisons of metabolic side effects of second generation antipsychotics in the treatment of schizophrenia: a systematic review and meta-analysis. Schizophr Res. 2010;123(2-3):225-233.
7. Wu RR, Zhao JP, Jin H, et al. Lifestyle intervention and metformin for treatment of antipsychotic-induced weight gain: a randomized controlled trial. JAMA. 2008;299(2):185-193.
8. De Hert M, Correll CU, Bobes J, et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry. 2011;10(1):52-77.
9. Kirpichnikov D, McFarlane SI, Sowers JR. Metformin: an update. Ann Internal Med. 2002;137(1):25-33.
10. Balon R. SSRI-associated sexual dysfunction. Am J Psychiatry. 2006;163(9):1504-1509.
11. Balon R, Morreale MK, Segraves RT. Prescribing of phosphodiesterase-5 inhibitors among psychiatrists. J Sex Marital Ther. 2014;40(3):165-169.
12. Taylor MJ, Rudkin L, Bullemor-Day P, et al. Strategies for managing sexual dysfunction induced by antidepressant medication. Cochrane Database Syst Rev. 2013;(5):CD003382.
13. Dording CM, LaRocca RA, Hails KA, et al. The effect of sildenafil on quality of life. Ann Clin Psychiatry. 2013;25(1):3-10.
14. Pagano HP, Zapata LB, Berry-Bibee EN, et al. Safety of hormonal contraception and intrauterine devices among women with depressive and bipolar disorders: a systematic review. Contraception. 2016;94(6):641-649.
15. Kibirige D, Luzinda K, Ssekitoleko R. Spectrum of lithium induced thyroid abnormalities: a current perspective. Thyroid Res. 2013;6(1):3.
16. Gitlin M. Lithium side effects and toxicity: prevalence and management strategies. Int J Bipolar Disord. 2016;4(1):27.
17. Devdhar M, Ousman YH, Burman KD. Hypothyroidism. Endocrinol Metab Clin North Am. 2007;36(3):595-615.
18. Hackley B, Sharma C, Kedzior A, et al. Managing mental health conditions in primary care settings. J Midwifery Women’s Health. 2010;55(1):9-19.
19. Fitelson E, McGibbon C. Evaluation and management of behavioral health disorders in women: an overview of major depression, bipolar disorder, anxiety disorders, and sleep in the primary care setting. Obstet Gynecol Clin North Am. 2016;43(2):231-246.
20. Colorafi K, Vanselow J, Nelson T. Treating anxiety and depression in primary care: reducing barriers to access. Fam Pract Manag. 2017;24(4):11-16.
21. McCall WV. Defining the unique scope of psychiatric practice in 2015. J ECT. 2015;31(4):203-204.
In our experience, most psychiatrists are uncomfortable with prescribing a medication when they feel that doing so would be outside their scope of practice. But there are many situations when prescribing a nonpsychotropic medication would be the correct choice. In this article, we discuss the scope of psychiatric practice, and present 4 case studies that illustrate situations in which psychiatrists should feel comfortable prescribing nonpsychotropic medications.
Defining the scope of practice
What is the scope of a psychiatrist’s practice? Scope of practice usually describes activities that a health care practitioner is allowed to undertake as defined by the terms of his/her license. A license to practice medicine does not include any stipulation restricting practice to a specific medical specialty. However, a local entity may delineate scope of practice within its organization. For instance, local practice standards held by the Detroit Wayne Mental Health Authority (DWMHA) state “Psychiatrists…shall not exceed their scope of practice as per DWMHA credentialing and privileging. For example, a Psychiatrist…who [has] not been appropriately privileged to deliver services to children shall not treat children, excepting crisis situations.”1
Like physicians in other specialties, psychiatrists are not limited to prescribing only a subset of medications commonly associated with their specialty. But for many psychiatrists, prescribing nonpsychotropic medications is complicated by individual and local factors. On one hand, some psychiatrists do not feel it is their role to prescribe nonpsychotropic medications,2 or even some psychotropic medications that may be more complex to prescribe, such as lithium, clozapine, or monoamine oxidase inhibitors.3-5 However, many feel comfortable prescribing complex combinations of psychotropic medications, or prescribing in a way that does not necessarily make sense (eg, prescribing benztropine as prophylaxis for dystonia when starting an antipsychotic).
Reviewing an average day at one urban psychiatric clinic, these questions seem to come up in half of the patient population, especially in patients with chronic mental illness, multiple medical comorbidities, and limited access to health care. When a young patient walks in without an appointment with an acute dystonic reaction secondary to the initiation of antipsychotics a couple of days ago, there is no hesitation to swiftly and appropriately prescribe an IM anticholinergic medication. But why are psychiatrists often hesitant to prescribe nonpsychotropic medications to treat other adverse effects of medications? Lack of knowledge? Lack of training?
Psychiatrists who practice in hospital systems often have immediate access to consultants, and this availability may encourage them to defer to the consultant for treatment of certain adverse effects. We have seen psychiatrists consult Neurology regarding the prescription of donepezil for mild neurocognitive disorder due to Alzheimer’s disease, or Endocrinology regarding prescription of levothyroxine for lithium-induced hypothyroidism.
However, there are numerous scenarios in which psychiatrists should feel comfortable prescribing nonpsychotropic medications or managing medication adverse effects, regardless of whether they consider it to be within or outside their scope of practice. The following case examples illustrate several such situations.
CASE 1
Ms. W, age 30, has been diagnosed with schizophrenia. She requests a refill of quetiapine, 800 mg/d. This medication has been clearly beneficial in alleviating her psychotic symptoms. However, since her last visit 3 months ago, her face appears more round, and she has gained 9 kg. Further evaluation indicates that she has developed metabolic syndrome and pre-diabetes.
Continue to: Metabolic adverse effects
Metabolic adverse effects, such as metabolic syndrome, diabetic ketoacidosis, and cardiovascular disease, are well-known risks of prescribing second-generation antipsychotics.6 In such situations, psychiatrists often advise patients to modify their diet, increase physical activity, and follow up with their primary care physician to determine if other medications are needed. However, getting a patient with a serious mental illness to exercise and modify her/his diet is difficult, and many of these patients do not have a primary care physician.
For patients such as Ms. W, a psychiatrist should consider prescribing metformin. Wu et al7 found that in addition to lifestyle modifications, metformin had the greatest effect on antipsychotic-induced weight gain. In this study, metformin alone had more impact on reversing weight gain and increasing insulin sensitivity than lifestyle modifications alone.7 This is crucial because these patients are especially vulnerable to cardiac disease.8 Metformin is well tolerated and has a low risk of causing hypoglycemia. Concerns regarding lactic acidosis have abated to the extent that the estimated glomerular filtration rate (eGFR) limits for using metformin have been lowered significantly. After reviewing the contraindications, the only knowledge needed to prescribe metformin is the patient’s kidney function and a brief understanding of the titration needed to minimize gastrointestinal adverse effects.9 Thus, prescribing metformin would be a fairly logical and easy first step for managing metabolic syndrome, especially in a patient whose motivation for increasing physical activity and modifying his/her diet is doubtful.
CASE 2
Mr. B, age 45, has major depressive disorder that has been well-controlled on paroxetine, 40 mg/d, for the past 2 years. He has no history of physical illness. On his most recent visit, he appears uncomfortable and nervous. After a long discussion, he discloses that his sex life isn’t what it used to be since starting paroxetine. He is bothered by erectile problems and asks whether he can “get some Viagra.”
Sexual adverse effects, such as erectile dysfunction, are frequently associated with the use of selective serotonin reuptake inhibitors.10 Although managing these adverse effects requires careful evaluation, in most cases, psychiatrists should be able to treat them.10 The logical choice in this case would be to prescribe one of the 4 FDA-approved phosphodiesterase-5 inhibitors (sildenafil [Viagra], tadalafil [Cialis], vardenafil [Levitra], and avanafil [Stendra]. However, Balon et al11 found that few psychiatrists prescribe phosphodiesterase-5 inhibitors, although they believed that they should be prescribing to treat their patients’ sexual dysfunction. Managing these adverse effects is important not only for the patient’s quality of life and relationship with his/her partner, but also for the therapeutic alliance. In a systematic review of 23 trials, Taylor et al12 examined >1,800 patients who were prescribed a medication to address sexual dysfunction secondary to antidepressants. They found that for men, adding a phosphodiesterase-5 inhibitor was appropriate and effective, and for women, adding bupropion at high doses should be considered.12 Like many other adverse effects, sexual adverse effects surely play a role in medication compliance. Dording et al13 found that the addition of sildenafil, 50 to 100 mg as needed, resulted in increased treatment satisfaction and overall contentment in 102 patients who complained of sexual dysfunction in the follow-up phase of the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) antidepressant trials. In most cases, with proper psychoeducation, prescription of
CASE 3
Ms. G, age 22, was recently discharged from an inpatient psychiatric unit after an episode of mania. She was prescribed carbamazepine, 600 mg/d, and ziprasidone, 40 mg twice a day, and appears to be doing well on this regimen. When asked about what led to her admission, she recalls having an elevated mood, increased energy, hypersexuality, impulsivity, and poor judgment. She reveals that she had several sexual partners during her manic episode, and worries that if such behavior occurs again, she may get pregnant. Yet Ms. G was not prescribed birth control upon discharge.
Continue to: Contraception
Contraception. We believe that psychiatrists have an obligation to protect patients from consequences of mental illness. Much the same way that psychiatrists hope to prevent suicide in a patient who has depression, patients should be protected from risks encountered in the manic phase of bipolar disorder. Another reason to prescribe contraceptives in such patients is the teratogenic effects of mood stabilizers. Pagano et al14 reviewed 6 studies that examined common forms of hormonal birth control to determine their safety in patients with depression or bipolar disorder. They found that overall, use of hormonal contraception was not associated with a worse clinical course of disease.
Many available forms of birth control are available. When prescribing in an outpatient setting, a daily oral medication or a monthly depot injection are convenient options.
CASE 4
Mr. P, age 65, has bipolar I disorder and is stable on risperidone long-acting injection, 37.7 mg bimonthly, and lithium, 1,200 mg/d. He reports that he is doing well but has noticed a recent decrease in energy and weight gain without any change in mood. Laboratory testing conducted prior to this visit revealed a thyroid-stimulating hormone (TSH) level of 4 mU/L (normal range: 0.4 to 4.0 mU/L). Six months ago, Mr. P’s TSH level was 2.8 mU/L. The resident supervisor suggests discussing the case with an endocrinologist.
Thyroid function. The impact of lithium on the thyroid gland is well established; however, psychiatrists’ response to such changes are not.15 Gitlin16 reviewed the many adverse effects of lithium and presented various management strategies to address findings such as Mr. P’s. Two important points are that lithium should not be discontinued in light of hypothyroidism, and synthetic thyroxine (levothyroxine) can be initiated and titrated to return TSH levels to a normal range.16 Levothyroxine can be started at low doses (eg, 25 to 50 mcg/d) and increased every 6 weeks until a normal TSH level is achieved.17 Managing lithium-induced clinical or subclinical hypothyroidism can prevent further pathology and possible relapse to depression.
Incorporating integrated care
In all these cases, the prescription of a medication with which some psychiatrists are not comfortable prescribing would have been the logical, easiest, and preferable choice. Of course, when initiating any medication, boxed warnings, contraindications, and drug–drug interactions should be reviewed. Initial dosages and titration schedules can be found in every medication’s FDA-approved prescribing information document (package insert), as well as in numerous reference books and articles.
Continue to: We acknowledge...
We acknowledge that prescribing a nonpsychotropic medication is not always a psychiatrist’s best choice, and that in patients with multiple medical comorbidities and drug–drug interactions that are not clearly defined, referring to or consulting a specialist is appropriate. We in no way support reckless prescribing, but instead present an opportunity to expand the perception of what should be considered within a psychiatrist’s scope of practice, and call for further education of psychiatrists so that they are more comfortable managing these adverse effects and/or prescribing at least some nonpsychotropic medications.
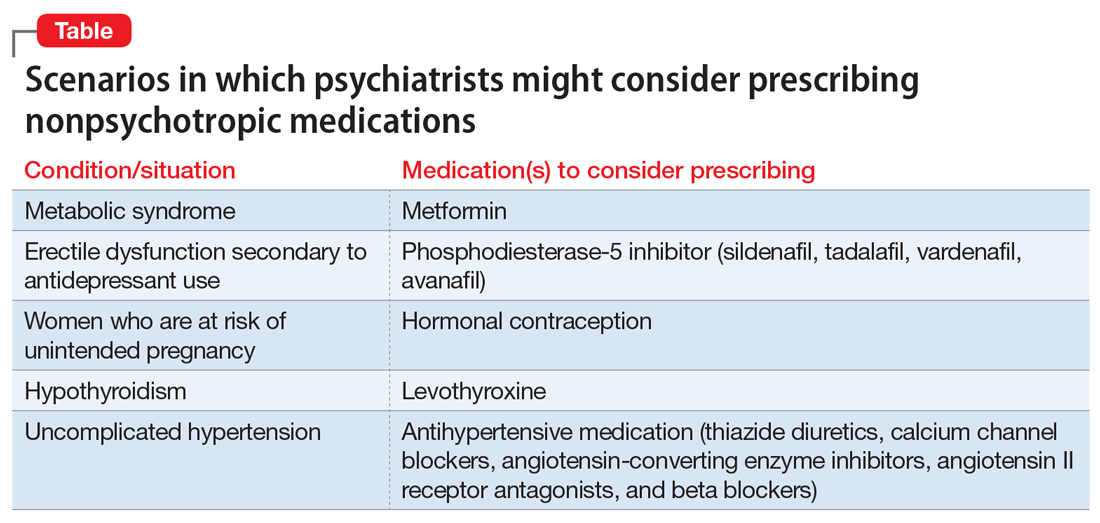
We exhort integrated medical care during this time of a physician shortage; however, we do not practice this way. Interestingly, physicians in primary care, such as those in family medicine or obstetrics and gynecology, frequently attempt to treat patients with psychiatric conditions in an attempt to provide integrated care. Numerous articles have discussed these efforts.18-20 However, this type of integrated care seems less frequent in psychiatry, even though the practice of modern psychiatry in the United States shows substantial overlap with the practice of physicians in primary care specialties.21 There are few articles or practical guidelines for psychiatrists who wish to treat patients’ physical illnesses, particularly patients with severe mental illness (see Related Resources, page 56). If we practice in an integrated manner to treat one of the simple conditions we described above, we can eliminate the need for a patient to visit a second physician, pay another co-pay, pay another bus fare, and take another day off work. This can be particularly helpful for patients who at times have to decide between paying for groceries or for medications. Having one clinician manage a patient’s medications also can decrease the risk of polypharmacy.
In addition to the case scenarios described in this article, there are more clinical situations and nonpsychotropic medications that psychiatrists could manage. Considering them outside the scope of psychiatric practice and being uncomfortable or ambivalent about them is not an excuse. We hope that psychiatrists can increase their expertise in this area, and can start to practice as the primary care physicians they claim they are, and should be.
Bottom Line
Many psychiatrists are uncomfortable prescribing nonpsychotropic medications, but there are numerous clinical scenarios in which the practice would make sense. This could include cases of metabolic syndrome, sexual dysfunction secondary to antidepressant use, or other adverse effects of commonly prescribed psychotropic medications.
Related Resources
- McCarron RM, Xiong GL, Keenan CR, et al. Preventive medical care in psychiatry. A practical guide for clinicians. Arlington, VA: American Psychiatric Association Publishing; 2015.
- McCarron RM, Xiong GL, Keenan CR, et al. Study guide to preventive medical care in psychiatry. Arlington, VA: American Psychiatric Association Publishing; 2017.
- Goldberg JF, Ernst CL. Managing the side effects of psychotropic medications. Washington, DC: American Psychiatric Association Publishing; 2019.
Drug Brand Names
Avanafil • Stendra
Benztropine • Cogentin
Bupropion • Wellbutrin, Zyban
Carbamazepine • Carbatrol, Tegretol
Clozapine • Clozaril
Donepezil • Aricept
Levothyroxine • Levoxyl, Synthroid
Lithium • Eskalith, Lithobid
Metformin • Fortamet, Glucophage
Paroxetine • Paxil
Quetiapine • Seroquel
Risperidone long-acting injection • Risperdal Consta
Sildenafil • Viagra
Tadalafil • Cialis
Vardenafil • Levitra
Ziprasidone • Geodon
In our experience, most psychiatrists are uncomfortable with prescribing a medication when they feel that doing so would be outside their scope of practice. But there are many situations when prescribing a nonpsychotropic medication would be the correct choice. In this article, we discuss the scope of psychiatric practice, and present 4 case studies that illustrate situations in which psychiatrists should feel comfortable prescribing nonpsychotropic medications.
Defining the scope of practice
What is the scope of a psychiatrist’s practice? Scope of practice usually describes activities that a health care practitioner is allowed to undertake as defined by the terms of his/her license. A license to practice medicine does not include any stipulation restricting practice to a specific medical specialty. However, a local entity may delineate scope of practice within its organization. For instance, local practice standards held by the Detroit Wayne Mental Health Authority (DWMHA) state “Psychiatrists…shall not exceed their scope of practice as per DWMHA credentialing and privileging. For example, a Psychiatrist…who [has] not been appropriately privileged to deliver services to children shall not treat children, excepting crisis situations.”1
Like physicians in other specialties, psychiatrists are not limited to prescribing only a subset of medications commonly associated with their specialty. But for many psychiatrists, prescribing nonpsychotropic medications is complicated by individual and local factors. On one hand, some psychiatrists do not feel it is their role to prescribe nonpsychotropic medications,2 or even some psychotropic medications that may be more complex to prescribe, such as lithium, clozapine, or monoamine oxidase inhibitors.3-5 However, many feel comfortable prescribing complex combinations of psychotropic medications, or prescribing in a way that does not necessarily make sense (eg, prescribing benztropine as prophylaxis for dystonia when starting an antipsychotic).
Reviewing an average day at one urban psychiatric clinic, these questions seem to come up in half of the patient population, especially in patients with chronic mental illness, multiple medical comorbidities, and limited access to health care. When a young patient walks in without an appointment with an acute dystonic reaction secondary to the initiation of antipsychotics a couple of days ago, there is no hesitation to swiftly and appropriately prescribe an IM anticholinergic medication. But why are psychiatrists often hesitant to prescribe nonpsychotropic medications to treat other adverse effects of medications? Lack of knowledge? Lack of training?
Psychiatrists who practice in hospital systems often have immediate access to consultants, and this availability may encourage them to defer to the consultant for treatment of certain adverse effects. We have seen psychiatrists consult Neurology regarding the prescription of donepezil for mild neurocognitive disorder due to Alzheimer’s disease, or Endocrinology regarding prescription of levothyroxine for lithium-induced hypothyroidism.
However, there are numerous scenarios in which psychiatrists should feel comfortable prescribing nonpsychotropic medications or managing medication adverse effects, regardless of whether they consider it to be within or outside their scope of practice. The following case examples illustrate several such situations.
CASE 1
Ms. W, age 30, has been diagnosed with schizophrenia. She requests a refill of quetiapine, 800 mg/d. This medication has been clearly beneficial in alleviating her psychotic symptoms. However, since her last visit 3 months ago, her face appears more round, and she has gained 9 kg. Further evaluation indicates that she has developed metabolic syndrome and pre-diabetes.
Continue to: Metabolic adverse effects
Metabolic adverse effects, such as metabolic syndrome, diabetic ketoacidosis, and cardiovascular disease, are well-known risks of prescribing second-generation antipsychotics.6 In such situations, psychiatrists often advise patients to modify their diet, increase physical activity, and follow up with their primary care physician to determine if other medications are needed. However, getting a patient with a serious mental illness to exercise and modify her/his diet is difficult, and many of these patients do not have a primary care physician.
For patients such as Ms. W, a psychiatrist should consider prescribing metformin. Wu et al7 found that in addition to lifestyle modifications, metformin had the greatest effect on antipsychotic-induced weight gain. In this study, metformin alone had more impact on reversing weight gain and increasing insulin sensitivity than lifestyle modifications alone.7 This is crucial because these patients are especially vulnerable to cardiac disease.8 Metformin is well tolerated and has a low risk of causing hypoglycemia. Concerns regarding lactic acidosis have abated to the extent that the estimated glomerular filtration rate (eGFR) limits for using metformin have been lowered significantly. After reviewing the contraindications, the only knowledge needed to prescribe metformin is the patient’s kidney function and a brief understanding of the titration needed to minimize gastrointestinal adverse effects.9 Thus, prescribing metformin would be a fairly logical and easy first step for managing metabolic syndrome, especially in a patient whose motivation for increasing physical activity and modifying his/her diet is doubtful.
CASE 2
Mr. B, age 45, has major depressive disorder that has been well-controlled on paroxetine, 40 mg/d, for the past 2 years. He has no history of physical illness. On his most recent visit, he appears uncomfortable and nervous. After a long discussion, he discloses that his sex life isn’t what it used to be since starting paroxetine. He is bothered by erectile problems and asks whether he can “get some Viagra.”
Sexual adverse effects, such as erectile dysfunction, are frequently associated with the use of selective serotonin reuptake inhibitors.10 Although managing these adverse effects requires careful evaluation, in most cases, psychiatrists should be able to treat them.10 The logical choice in this case would be to prescribe one of the 4 FDA-approved phosphodiesterase-5 inhibitors (sildenafil [Viagra], tadalafil [Cialis], vardenafil [Levitra], and avanafil [Stendra]. However, Balon et al11 found that few psychiatrists prescribe phosphodiesterase-5 inhibitors, although they believed that they should be prescribing to treat their patients’ sexual dysfunction. Managing these adverse effects is important not only for the patient’s quality of life and relationship with his/her partner, but also for the therapeutic alliance. In a systematic review of 23 trials, Taylor et al12 examined >1,800 patients who were prescribed a medication to address sexual dysfunction secondary to antidepressants. They found that for men, adding a phosphodiesterase-5 inhibitor was appropriate and effective, and for women, adding bupropion at high doses should be considered.12 Like many other adverse effects, sexual adverse effects surely play a role in medication compliance. Dording et al13 found that the addition of sildenafil, 50 to 100 mg as needed, resulted in increased treatment satisfaction and overall contentment in 102 patients who complained of sexual dysfunction in the follow-up phase of the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) antidepressant trials. In most cases, with proper psychoeducation, prescription of
CASE 3
Ms. G, age 22, was recently discharged from an inpatient psychiatric unit after an episode of mania. She was prescribed carbamazepine, 600 mg/d, and ziprasidone, 40 mg twice a day, and appears to be doing well on this regimen. When asked about what led to her admission, she recalls having an elevated mood, increased energy, hypersexuality, impulsivity, and poor judgment. She reveals that she had several sexual partners during her manic episode, and worries that if such behavior occurs again, she may get pregnant. Yet Ms. G was not prescribed birth control upon discharge.
Continue to: Contraception
Contraception. We believe that psychiatrists have an obligation to protect patients from consequences of mental illness. Much the same way that psychiatrists hope to prevent suicide in a patient who has depression, patients should be protected from risks encountered in the manic phase of bipolar disorder. Another reason to prescribe contraceptives in such patients is the teratogenic effects of mood stabilizers. Pagano et al14 reviewed 6 studies that examined common forms of hormonal birth control to determine their safety in patients with depression or bipolar disorder. They found that overall, use of hormonal contraception was not associated with a worse clinical course of disease.
Many available forms of birth control are available. When prescribing in an outpatient setting, a daily oral medication or a monthly depot injection are convenient options.
CASE 4
Mr. P, age 65, has bipolar I disorder and is stable on risperidone long-acting injection, 37.7 mg bimonthly, and lithium, 1,200 mg/d. He reports that he is doing well but has noticed a recent decrease in energy and weight gain without any change in mood. Laboratory testing conducted prior to this visit revealed a thyroid-stimulating hormone (TSH) level of 4 mU/L (normal range: 0.4 to 4.0 mU/L). Six months ago, Mr. P’s TSH level was 2.8 mU/L. The resident supervisor suggests discussing the case with an endocrinologist.
Thyroid function. The impact of lithium on the thyroid gland is well established; however, psychiatrists’ response to such changes are not.15 Gitlin16 reviewed the many adverse effects of lithium and presented various management strategies to address findings such as Mr. P’s. Two important points are that lithium should not be discontinued in light of hypothyroidism, and synthetic thyroxine (levothyroxine) can be initiated and titrated to return TSH levels to a normal range.16 Levothyroxine can be started at low doses (eg, 25 to 50 mcg/d) and increased every 6 weeks until a normal TSH level is achieved.17 Managing lithium-induced clinical or subclinical hypothyroidism can prevent further pathology and possible relapse to depression.
Incorporating integrated care
In all these cases, the prescription of a medication with which some psychiatrists are not comfortable prescribing would have been the logical, easiest, and preferable choice. Of course, when initiating any medication, boxed warnings, contraindications, and drug–drug interactions should be reviewed. Initial dosages and titration schedules can be found in every medication’s FDA-approved prescribing information document (package insert), as well as in numerous reference books and articles.
Continue to: We acknowledge...
We acknowledge that prescribing a nonpsychotropic medication is not always a psychiatrist’s best choice, and that in patients with multiple medical comorbidities and drug–drug interactions that are not clearly defined, referring to or consulting a specialist is appropriate. We in no way support reckless prescribing, but instead present an opportunity to expand the perception of what should be considered within a psychiatrist’s scope of practice, and call for further education of psychiatrists so that they are more comfortable managing these adverse effects and/or prescribing at least some nonpsychotropic medications.
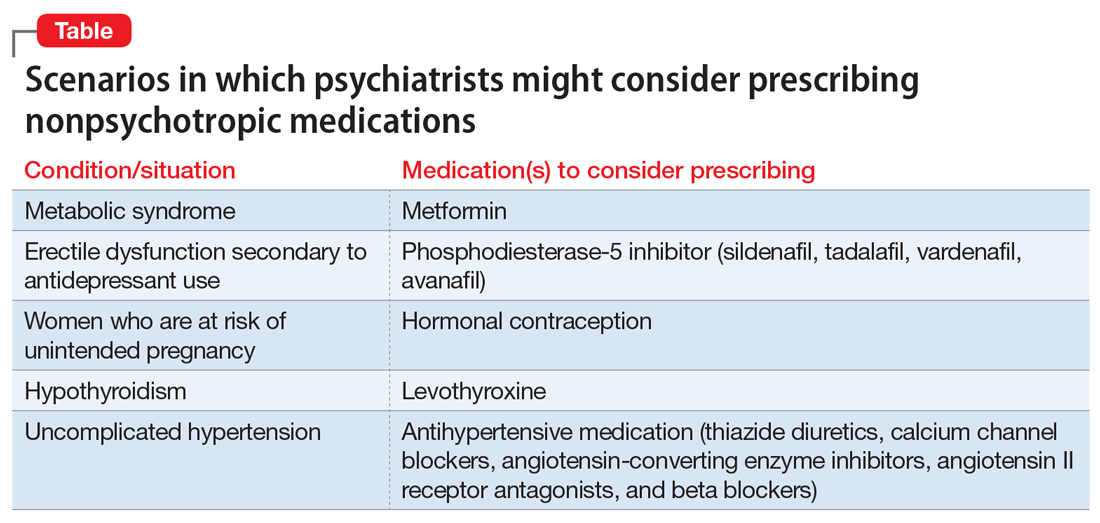
We exhort integrated medical care during this time of a physician shortage; however, we do not practice this way. Interestingly, physicians in primary care, such as those in family medicine or obstetrics and gynecology, frequently attempt to treat patients with psychiatric conditions in an attempt to provide integrated care. Numerous articles have discussed these efforts.18-20 However, this type of integrated care seems less frequent in psychiatry, even though the practice of modern psychiatry in the United States shows substantial overlap with the practice of physicians in primary care specialties.21 There are few articles or practical guidelines for psychiatrists who wish to treat patients’ physical illnesses, particularly patients with severe mental illness (see Related Resources, page 56). If we practice in an integrated manner to treat one of the simple conditions we described above, we can eliminate the need for a patient to visit a second physician, pay another co-pay, pay another bus fare, and take another day off work. This can be particularly helpful for patients who at times have to decide between paying for groceries or for medications. Having one clinician manage a patient’s medications also can decrease the risk of polypharmacy.
In addition to the case scenarios described in this article, there are more clinical situations and nonpsychotropic medications that psychiatrists could manage. Considering them outside the scope of psychiatric practice and being uncomfortable or ambivalent about them is not an excuse. We hope that psychiatrists can increase their expertise in this area, and can start to practice as the primary care physicians they claim they are, and should be.
Bottom Line
Many psychiatrists are uncomfortable prescribing nonpsychotropic medications, but there are numerous clinical scenarios in which the practice would make sense. This could include cases of metabolic syndrome, sexual dysfunction secondary to antidepressant use, or other adverse effects of commonly prescribed psychotropic medications.
Related Resources
- McCarron RM, Xiong GL, Keenan CR, et al. Preventive medical care in psychiatry. A practical guide for clinicians. Arlington, VA: American Psychiatric Association Publishing; 2015.
- McCarron RM, Xiong GL, Keenan CR, et al. Study guide to preventive medical care in psychiatry. Arlington, VA: American Psychiatric Association Publishing; 2017.
- Goldberg JF, Ernst CL. Managing the side effects of psychotropic medications. Washington, DC: American Psychiatric Association Publishing; 2019.
Drug Brand Names
Avanafil • Stendra
Benztropine • Cogentin
Bupropion • Wellbutrin, Zyban
Carbamazepine • Carbatrol, Tegretol
Clozapine • Clozaril
Donepezil • Aricept
Levothyroxine • Levoxyl, Synthroid
Lithium • Eskalith, Lithobid
Metformin • Fortamet, Glucophage
Paroxetine • Paxil
Quetiapine • Seroquel
Risperidone long-acting injection • Risperdal Consta
Sildenafil • Viagra
Tadalafil • Cialis
Vardenafil • Levitra
Ziprasidone • Geodon
1. Detroit Wayne Integrated Health Network. DWMHA psychiatric practice standards. http://dwihn.org/files/2015/6451/9628/Psychiatric_Practice_Standards.pdf. Revised June 2018. Accessed October 8, 2019.
2. Seaman JJ, Cornfield RM, Cummings DM, et al. Exploring psychiatric prescribing practices: the relationship between the role of the provider and the appropriateness of prescribing. Gen Hosp Psychiatry. 1987;9(3):220-224.
3. Zivanovic O. Lithium: a classic drug—frequently discussed, but, sadly, seldom prescribed! Aust N Z J Psychiatry. 2017;51(9):886-896.
4. Stroup TS, Gerhard T, Crystal S, et al. Geographic and clinical variation in clozapine use in the United States. Psychiatric Services. 2014;65(2):186-192.
5. Balon R, Mufti R, Arfken C. A survey of prescribing practices for monoamine oxidase inhibitors. Psychiatric Services. 1999;50(7):945-947.
6. Rummel-Kluge C, Komossa K, Schwarz S, et al. Head-to-head comparisons of metabolic side effects of second generation antipsychotics in the treatment of schizophrenia: a systematic review and meta-analysis. Schizophr Res. 2010;123(2-3):225-233.
7. Wu RR, Zhao JP, Jin H, et al. Lifestyle intervention and metformin for treatment of antipsychotic-induced weight gain: a randomized controlled trial. JAMA. 2008;299(2):185-193.
8. De Hert M, Correll CU, Bobes J, et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry. 2011;10(1):52-77.
9. Kirpichnikov D, McFarlane SI, Sowers JR. Metformin: an update. Ann Internal Med. 2002;137(1):25-33.
10. Balon R. SSRI-associated sexual dysfunction. Am J Psychiatry. 2006;163(9):1504-1509.
11. Balon R, Morreale MK, Segraves RT. Prescribing of phosphodiesterase-5 inhibitors among psychiatrists. J Sex Marital Ther. 2014;40(3):165-169.
12. Taylor MJ, Rudkin L, Bullemor-Day P, et al. Strategies for managing sexual dysfunction induced by antidepressant medication. Cochrane Database Syst Rev. 2013;(5):CD003382.
13. Dording CM, LaRocca RA, Hails KA, et al. The effect of sildenafil on quality of life. Ann Clin Psychiatry. 2013;25(1):3-10.
14. Pagano HP, Zapata LB, Berry-Bibee EN, et al. Safety of hormonal contraception and intrauterine devices among women with depressive and bipolar disorders: a systematic review. Contraception. 2016;94(6):641-649.
15. Kibirige D, Luzinda K, Ssekitoleko R. Spectrum of lithium induced thyroid abnormalities: a current perspective. Thyroid Res. 2013;6(1):3.
16. Gitlin M. Lithium side effects and toxicity: prevalence and management strategies. Int J Bipolar Disord. 2016;4(1):27.
17. Devdhar M, Ousman YH, Burman KD. Hypothyroidism. Endocrinol Metab Clin North Am. 2007;36(3):595-615.
18. Hackley B, Sharma C, Kedzior A, et al. Managing mental health conditions in primary care settings. J Midwifery Women’s Health. 2010;55(1):9-19.
19. Fitelson E, McGibbon C. Evaluation and management of behavioral health disorders in women: an overview of major depression, bipolar disorder, anxiety disorders, and sleep in the primary care setting. Obstet Gynecol Clin North Am. 2016;43(2):231-246.
20. Colorafi K, Vanselow J, Nelson T. Treating anxiety and depression in primary care: reducing barriers to access. Fam Pract Manag. 2017;24(4):11-16.
21. McCall WV. Defining the unique scope of psychiatric practice in 2015. J ECT. 2015;31(4):203-204.
1. Detroit Wayne Integrated Health Network. DWMHA psychiatric practice standards. http://dwihn.org/files/2015/6451/9628/Psychiatric_Practice_Standards.pdf. Revised June 2018. Accessed October 8, 2019.
2. Seaman JJ, Cornfield RM, Cummings DM, et al. Exploring psychiatric prescribing practices: the relationship between the role of the provider and the appropriateness of prescribing. Gen Hosp Psychiatry. 1987;9(3):220-224.
3. Zivanovic O. Lithium: a classic drug—frequently discussed, but, sadly, seldom prescribed! Aust N Z J Psychiatry. 2017;51(9):886-896.
4. Stroup TS, Gerhard T, Crystal S, et al. Geographic and clinical variation in clozapine use in the United States. Psychiatric Services. 2014;65(2):186-192.
5. Balon R, Mufti R, Arfken C. A survey of prescribing practices for monoamine oxidase inhibitors. Psychiatric Services. 1999;50(7):945-947.
6. Rummel-Kluge C, Komossa K, Schwarz S, et al. Head-to-head comparisons of metabolic side effects of second generation antipsychotics in the treatment of schizophrenia: a systematic review and meta-analysis. Schizophr Res. 2010;123(2-3):225-233.
7. Wu RR, Zhao JP, Jin H, et al. Lifestyle intervention and metformin for treatment of antipsychotic-induced weight gain: a randomized controlled trial. JAMA. 2008;299(2):185-193.
8. De Hert M, Correll CU, Bobes J, et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry. 2011;10(1):52-77.
9. Kirpichnikov D, McFarlane SI, Sowers JR. Metformin: an update. Ann Internal Med. 2002;137(1):25-33.
10. Balon R. SSRI-associated sexual dysfunction. Am J Psychiatry. 2006;163(9):1504-1509.
11. Balon R, Morreale MK, Segraves RT. Prescribing of phosphodiesterase-5 inhibitors among psychiatrists. J Sex Marital Ther. 2014;40(3):165-169.
12. Taylor MJ, Rudkin L, Bullemor-Day P, et al. Strategies for managing sexual dysfunction induced by antidepressant medication. Cochrane Database Syst Rev. 2013;(5):CD003382.
13. Dording CM, LaRocca RA, Hails KA, et al. The effect of sildenafil on quality of life. Ann Clin Psychiatry. 2013;25(1):3-10.
14. Pagano HP, Zapata LB, Berry-Bibee EN, et al. Safety of hormonal contraception and intrauterine devices among women with depressive and bipolar disorders: a systematic review. Contraception. 2016;94(6):641-649.
15. Kibirige D, Luzinda K, Ssekitoleko R. Spectrum of lithium induced thyroid abnormalities: a current perspective. Thyroid Res. 2013;6(1):3.
16. Gitlin M. Lithium side effects and toxicity: prevalence and management strategies. Int J Bipolar Disord. 2016;4(1):27.
17. Devdhar M, Ousman YH, Burman KD. Hypothyroidism. Endocrinol Metab Clin North Am. 2007;36(3):595-615.
18. Hackley B, Sharma C, Kedzior A, et al. Managing mental health conditions in primary care settings. J Midwifery Women’s Health. 2010;55(1):9-19.
19. Fitelson E, McGibbon C. Evaluation and management of behavioral health disorders in women: an overview of major depression, bipolar disorder, anxiety disorders, and sleep in the primary care setting. Obstet Gynecol Clin North Am. 2016;43(2):231-246.
20. Colorafi K, Vanselow J, Nelson T. Treating anxiety and depression in primary care: reducing barriers to access. Fam Pract Manag. 2017;24(4):11-16.
21. McCall WV. Defining the unique scope of psychiatric practice in 2015. J ECT. 2015;31(4):203-204.
A reflection on Ghana’s mental health system
In recent years, the delivery of mental health services in Ghana has expanded substantially, especially since the passing of the Mental Health Act in 2012. In this article, I reflect on my experience as a visiting psychiatry resident in August 2018 at 2 Ghanaian hospitals located in Accra and Navrongo. Evident strengths of the mental health system were family support for patients and the scope of psychiatrists, while the most prominent weakness was the inadequate funding. As treatment of mental illness expands, more funding, psychiatrists, and mental health workers will be critical for the continued success of Ghana’s mental health system.
Psychiatric treatment in Ghana
Ghana has a population of approximately 28 million people, yet the country has an estimated 18 to 25 psychiatrists, up from 11 psychiatrists in 2011.1-3 Compared with the United States, which has 10.54 psychiatrists per 100,000 people (approximately 1 psychiatrist per 9,500 people), Ghana has .058 psychiatrists per 100,000 people (approximately 1 psychiatrist per 1.7 million people).4 In Ghana, most psychiatric care is delivered by mental health nurses, community mental health officers (CMHOs), and clinical psychiatric officers; supervision by psychiatrists is limited.3 Due to low public awareness, a scarcity of clinicians, and limited access to diagnostic services and medications, individuals with psychiatric illness in Ghana are often stigmatized, undertreated, and mistreated. To address this, in March 2012, Ghana passed Mental Health Act 846, which established a mental health commission and outlined protections for individuals with mental health needs.5 Since then, the number of people seeking treatment and the number of clinicians have expanded, but there are still significant challenges, such as a lack of funding for medications and facilities, and limited clinicians.6
During my last year of psychiatry residency at Mount Sinai Hospital in New York, I spent several weeks in Ghana at 2 institutions, observing and supervising the provision of psychiatric services. This was my first experience with the country’s health care system; therefore, my objectives were to:
- assess the current state of psychiatric services through observation and interviews with clinical staff
- provide instruction to clinicians in areas of need.
Two-thirds of my time was spent at the Accra Psychiatric Hospital, 1 of only 3 psychiatric hospitals in Ghana, all of which are located in the southern region of the country. The remainder of my time was spent at the Navrongo War Memorial Hospital in Ghana’s Northern Region.
The Accra Psychiatric Hospital is a sprawling complex near the center of the capital city. Every morning I walked through a large outdoor waiting area to the examination room, which was filled with at least 30 patients by 9
Navrongo War Memorial Hospital. There are no practicing psychiatrists in the northern region of the country; therefore, all mental health care is delivered by mental health nurses and CMHOs. CMHOs have 1 year of training plus a minimum of 2 years of service. They focus on identifying psychiatric cases in the community and coordinating treatment. Nurses have prescribing rights. A psychiatrist should be scheduled to visit the various districts in the region every 6 months to provide supervision, but this is not always feasible.
When I visited, I was the only psychiatrist who had been to this hospital in more than 1 year. During my time there, I reviewed the treatment protocols and gave lectures on the management of psychiatric emergencies and motivational interviewing, because addiction to alcohol and tramadol are 2 of the most pressing mental health problems in the country.7 I also saw patients with nurses, and supervised them on their assessment and treatment.
Continue to: In Ghana...
In Ghana, psychiatric services are often delivered using the community mental health model, in which many patients are visited in their homes. One morning, we went to a prayer camp to see if there were any individuals who would benefit from psychiatric services. There were no cases that day, but during the visit I sat under a tree where a few years before it was not uncommon to find a person who was psychotic or agitated chained to the tree. Several years of outreach by the local nurses has resulted in the camp leaders better recognizing mental illness early and contacting the nurses, as opposed to locking a person in chains for an extended period.
On one occasion, we answered a crisis call where a person experiencing a psychotic episode had locked himself in his house. The team talked with the individual through a locked screen door for 30 minutes, after which he eventually came out of the home to speak with us. A few days later, the patient accepted fluphenazine decanoate injection at his home. Two weeks later, he came to the outpatient clinic to continue treatment. Four months later, the patient was still in treatment and had started an apprenticeship for repairing cars.
As I was walking out of the hospital on my last day, I was called back to see a woman with a seizure who had been brought to the hospital. Unfortunately, there was no more diazepam in stock with which to treat her. This event highlighted the lack of resources available in this setting.
3 Take-home messages
My experience at both hospitals led me to reflect on 3 important factors impacting the mental health system in Ghana:
Family support. For at least 80% of appointments, patients were accompanied by family members or friends. The family hierarchy is still dominant in the Ghanaian culture, and clinicians often need the buy-in of the family, especially when financial support is required. More often than not, families enhanced patients’ treatment, but in some instances, they were a barrier.
Continue to: The types of cases
The types of cases. Most of the patients coming to both hospitals had diagnoses of bipolar disorder, schizophrenia, substance use disorder, or epilepsy. My impression was that patients or family members sought treatment for disorders that were conspicuous. I saw <5 cases of depression or anxiety. I wonder if this was because:
- patients with these disorders were referred to psychologists
- patients sought out faith-based treatment
- there was a lower incidence of these disorders, or these disorders were detected less frequently.
Inadequate funding. Despite the clinicians’ astute observations and diagnoses, they faced challenges, including a lack of access to medications because pharmacies were out of stock, or the patient or hospital could not afford the medication. At times, these challenges resulted in patients admitted to the hospital not receiving medications. When Mental Health Act 846 was implemented, it was widely purported that mental health care would be available to everyone, but the funding mechanism was not firmly established.8,9 Currently, laboratory workup, mental health treatment, and medications are not covered by health insurance, and government funding for mental health is insufficient. Therefore, in most areas, the entire cost burden of psychiatric care falls on patients and their families, or on hospitals.
Making progress despite barriers
In her inaugural address, former American Psychiatric Association President Altha J. Stewart, MD, named expanding the organization’s work in global mental health as one of her 3 primary goals.10 There are several means by which American psychiatrists can support the work of psychiatrists in Ghana and elsewhere. One way is by helping the mental health commission and other entities within the country petition the government and health insurance companies to expand coverage for mental health services. Teleconferencing, in which psychiatrists in Ghana or other parts of the world provide supervision to mid-level clinicians, has been piloted in other countries such as Liberia and could be implemented to address the critical shortages of psychiatrists in certain regions.11
In the past 7 years, Ghana has made significant strides in destigmatizing mental illness, and as a result more individuals are seeking treatment and more clinicians at all levels are being trained. Despite significant barriers, physicians, nurses, and other mental health workers deliver empathic and evidence-based treatment in a manner that defies the mental health system’s current limitations.
1. Ofori-Atta A, Attafuah J, Jack H, et al. Joining psychiatric care and faith healing in a prayer camp in Ghana: randomised trial. Br J Psychiatry. 2018;212(1):34-41.
2. Ghana has only 18 psychiatrists; experts beg government for more funds. GhanaWeb. https://www.ghanaweb.com/GhanaHomePage/NewsArchive/Ghana-has-only-18-psychiatrists-experts-beg-government-for-more-funds-591732. Published October 17, 2017. Accessed July 24, 2019.
3. Agyapong VIO, Farren C, McAuliffe E. Improving Ghana’s mental healthcare through task-shifting-psychiatrists and health policy directors perceptions about government’s commitment and the role of community mental health workers. Global Health. 2016;12:57.
4. World Health Organization. Global Health Observatory data repository. http://apps.who.int/gho/data/node.main.MHHR?lang=en. Published April 25, 2019. Accessed July 24, 2019.
5. Walker GH, Osei A. Mental health law in Ghana. BJPsych Int. 2017;14(2):38-39.
6. Doku VC, Wusu-Takyi A, Awakame J. Implementing the Mental Health Act in Ghana: any challenges ahead? Ghana Med J. 2012;46(4):241-250.
7. Kissiedu E. High dose Tramadol floods market. Business Day. http://businessdayghana.com/high-dose-tramadol-floods-market/. Published September 25, 2017. Accessed July 24, 2019.
8. Badu E, O’Brien AP, Mitchell R. An integrative review of potential enablers and barriers to accessing mental health services in Ghana. Health Res Policy Syst. 2018;16(1):110.
9. Ghana mental health care delivery risks collapse for lack of funds. News Ghana. https://www.newsghana.com.gh/ghana-mental-health-care-delivery-risks-collapse-for-lack-of-funds/. Published May 29, 2018. Accessed July 24, 2019.
10. Stewart AJ. Response to the Presidential Address. Am J Psychiatry. 2018;175(8):726-727.
11. Katz, CL, Washington FB, Sacco M, et al. A resident-based telepsychiatry supervision pilot program in Liberia. Psychiatr Serv. 2018;70(3):243-246.
In recent years, the delivery of mental health services in Ghana has expanded substantially, especially since the passing of the Mental Health Act in 2012. In this article, I reflect on my experience as a visiting psychiatry resident in August 2018 at 2 Ghanaian hospitals located in Accra and Navrongo. Evident strengths of the mental health system were family support for patients and the scope of psychiatrists, while the most prominent weakness was the inadequate funding. As treatment of mental illness expands, more funding, psychiatrists, and mental health workers will be critical for the continued success of Ghana’s mental health system.
Psychiatric treatment in Ghana
Ghana has a population of approximately 28 million people, yet the country has an estimated 18 to 25 psychiatrists, up from 11 psychiatrists in 2011.1-3 Compared with the United States, which has 10.54 psychiatrists per 100,000 people (approximately 1 psychiatrist per 9,500 people), Ghana has .058 psychiatrists per 100,000 people (approximately 1 psychiatrist per 1.7 million people).4 In Ghana, most psychiatric care is delivered by mental health nurses, community mental health officers (CMHOs), and clinical psychiatric officers; supervision by psychiatrists is limited.3 Due to low public awareness, a scarcity of clinicians, and limited access to diagnostic services and medications, individuals with psychiatric illness in Ghana are often stigmatized, undertreated, and mistreated. To address this, in March 2012, Ghana passed Mental Health Act 846, which established a mental health commission and outlined protections for individuals with mental health needs.5 Since then, the number of people seeking treatment and the number of clinicians have expanded, but there are still significant challenges, such as a lack of funding for medications and facilities, and limited clinicians.6
During my last year of psychiatry residency at Mount Sinai Hospital in New York, I spent several weeks in Ghana at 2 institutions, observing and supervising the provision of psychiatric services. This was my first experience with the country’s health care system; therefore, my objectives were to:
- assess the current state of psychiatric services through observation and interviews with clinical staff
- provide instruction to clinicians in areas of need.
Two-thirds of my time was spent at the Accra Psychiatric Hospital, 1 of only 3 psychiatric hospitals in Ghana, all of which are located in the southern region of the country. The remainder of my time was spent at the Navrongo War Memorial Hospital in Ghana’s Northern Region.
The Accra Psychiatric Hospital is a sprawling complex near the center of the capital city. Every morning I walked through a large outdoor waiting area to the examination room, which was filled with at least 30 patients by 9
Navrongo War Memorial Hospital. There are no practicing psychiatrists in the northern region of the country; therefore, all mental health care is delivered by mental health nurses and CMHOs. CMHOs have 1 year of training plus a minimum of 2 years of service. They focus on identifying psychiatric cases in the community and coordinating treatment. Nurses have prescribing rights. A psychiatrist should be scheduled to visit the various districts in the region every 6 months to provide supervision, but this is not always feasible.
When I visited, I was the only psychiatrist who had been to this hospital in more than 1 year. During my time there, I reviewed the treatment protocols and gave lectures on the management of psychiatric emergencies and motivational interviewing, because addiction to alcohol and tramadol are 2 of the most pressing mental health problems in the country.7 I also saw patients with nurses, and supervised them on their assessment and treatment.
Continue to: In Ghana...
In Ghana, psychiatric services are often delivered using the community mental health model, in which many patients are visited in their homes. One morning, we went to a prayer camp to see if there were any individuals who would benefit from psychiatric services. There were no cases that day, but during the visit I sat under a tree where a few years before it was not uncommon to find a person who was psychotic or agitated chained to the tree. Several years of outreach by the local nurses has resulted in the camp leaders better recognizing mental illness early and contacting the nurses, as opposed to locking a person in chains for an extended period.
On one occasion, we answered a crisis call where a person experiencing a psychotic episode had locked himself in his house. The team talked with the individual through a locked screen door for 30 minutes, after which he eventually came out of the home to speak with us. A few days later, the patient accepted fluphenazine decanoate injection at his home. Two weeks later, he came to the outpatient clinic to continue treatment. Four months later, the patient was still in treatment and had started an apprenticeship for repairing cars.
As I was walking out of the hospital on my last day, I was called back to see a woman with a seizure who had been brought to the hospital. Unfortunately, there was no more diazepam in stock with which to treat her. This event highlighted the lack of resources available in this setting.
3 Take-home messages
My experience at both hospitals led me to reflect on 3 important factors impacting the mental health system in Ghana:
Family support. For at least 80% of appointments, patients were accompanied by family members or friends. The family hierarchy is still dominant in the Ghanaian culture, and clinicians often need the buy-in of the family, especially when financial support is required. More often than not, families enhanced patients’ treatment, but in some instances, they were a barrier.
Continue to: The types of cases
The types of cases. Most of the patients coming to both hospitals had diagnoses of bipolar disorder, schizophrenia, substance use disorder, or epilepsy. My impression was that patients or family members sought treatment for disorders that were conspicuous. I saw <5 cases of depression or anxiety. I wonder if this was because:
- patients with these disorders were referred to psychologists
- patients sought out faith-based treatment
- there was a lower incidence of these disorders, or these disorders were detected less frequently.
Inadequate funding. Despite the clinicians’ astute observations and diagnoses, they faced challenges, including a lack of access to medications because pharmacies were out of stock, or the patient or hospital could not afford the medication. At times, these challenges resulted in patients admitted to the hospital not receiving medications. When Mental Health Act 846 was implemented, it was widely purported that mental health care would be available to everyone, but the funding mechanism was not firmly established.8,9 Currently, laboratory workup, mental health treatment, and medications are not covered by health insurance, and government funding for mental health is insufficient. Therefore, in most areas, the entire cost burden of psychiatric care falls on patients and their families, or on hospitals.
Making progress despite barriers
In her inaugural address, former American Psychiatric Association President Altha J. Stewart, MD, named expanding the organization’s work in global mental health as one of her 3 primary goals.10 There are several means by which American psychiatrists can support the work of psychiatrists in Ghana and elsewhere. One way is by helping the mental health commission and other entities within the country petition the government and health insurance companies to expand coverage for mental health services. Teleconferencing, in which psychiatrists in Ghana or other parts of the world provide supervision to mid-level clinicians, has been piloted in other countries such as Liberia and could be implemented to address the critical shortages of psychiatrists in certain regions.11
In the past 7 years, Ghana has made significant strides in destigmatizing mental illness, and as a result more individuals are seeking treatment and more clinicians at all levels are being trained. Despite significant barriers, physicians, nurses, and other mental health workers deliver empathic and evidence-based treatment in a manner that defies the mental health system’s current limitations.
In recent years, the delivery of mental health services in Ghana has expanded substantially, especially since the passing of the Mental Health Act in 2012. In this article, I reflect on my experience as a visiting psychiatry resident in August 2018 at 2 Ghanaian hospitals located in Accra and Navrongo. Evident strengths of the mental health system were family support for patients and the scope of psychiatrists, while the most prominent weakness was the inadequate funding. As treatment of mental illness expands, more funding, psychiatrists, and mental health workers will be critical for the continued success of Ghana’s mental health system.
Psychiatric treatment in Ghana
Ghana has a population of approximately 28 million people, yet the country has an estimated 18 to 25 psychiatrists, up from 11 psychiatrists in 2011.1-3 Compared with the United States, which has 10.54 psychiatrists per 100,000 people (approximately 1 psychiatrist per 9,500 people), Ghana has .058 psychiatrists per 100,000 people (approximately 1 psychiatrist per 1.7 million people).4 In Ghana, most psychiatric care is delivered by mental health nurses, community mental health officers (CMHOs), and clinical psychiatric officers; supervision by psychiatrists is limited.3 Due to low public awareness, a scarcity of clinicians, and limited access to diagnostic services and medications, individuals with psychiatric illness in Ghana are often stigmatized, undertreated, and mistreated. To address this, in March 2012, Ghana passed Mental Health Act 846, which established a mental health commission and outlined protections for individuals with mental health needs.5 Since then, the number of people seeking treatment and the number of clinicians have expanded, but there are still significant challenges, such as a lack of funding for medications and facilities, and limited clinicians.6
During my last year of psychiatry residency at Mount Sinai Hospital in New York, I spent several weeks in Ghana at 2 institutions, observing and supervising the provision of psychiatric services. This was my first experience with the country’s health care system; therefore, my objectives were to:
- assess the current state of psychiatric services through observation and interviews with clinical staff
- provide instruction to clinicians in areas of need.
Two-thirds of my time was spent at the Accra Psychiatric Hospital, 1 of only 3 psychiatric hospitals in Ghana, all of which are located in the southern region of the country. The remainder of my time was spent at the Navrongo War Memorial Hospital in Ghana’s Northern Region.
The Accra Psychiatric Hospital is a sprawling complex near the center of the capital city. Every morning I walked through a large outdoor waiting area to the examination room, which was filled with at least 30 patients by 9
Navrongo War Memorial Hospital. There are no practicing psychiatrists in the northern region of the country; therefore, all mental health care is delivered by mental health nurses and CMHOs. CMHOs have 1 year of training plus a minimum of 2 years of service. They focus on identifying psychiatric cases in the community and coordinating treatment. Nurses have prescribing rights. A psychiatrist should be scheduled to visit the various districts in the region every 6 months to provide supervision, but this is not always feasible.
When I visited, I was the only psychiatrist who had been to this hospital in more than 1 year. During my time there, I reviewed the treatment protocols and gave lectures on the management of psychiatric emergencies and motivational interviewing, because addiction to alcohol and tramadol are 2 of the most pressing mental health problems in the country.7 I also saw patients with nurses, and supervised them on their assessment and treatment.
Continue to: In Ghana...
In Ghana, psychiatric services are often delivered using the community mental health model, in which many patients are visited in their homes. One morning, we went to a prayer camp to see if there were any individuals who would benefit from psychiatric services. There were no cases that day, but during the visit I sat under a tree where a few years before it was not uncommon to find a person who was psychotic or agitated chained to the tree. Several years of outreach by the local nurses has resulted in the camp leaders better recognizing mental illness early and contacting the nurses, as opposed to locking a person in chains for an extended period.
On one occasion, we answered a crisis call where a person experiencing a psychotic episode had locked himself in his house. The team talked with the individual through a locked screen door for 30 minutes, after which he eventually came out of the home to speak with us. A few days later, the patient accepted fluphenazine decanoate injection at his home. Two weeks later, he came to the outpatient clinic to continue treatment. Four months later, the patient was still in treatment and had started an apprenticeship for repairing cars.
As I was walking out of the hospital on my last day, I was called back to see a woman with a seizure who had been brought to the hospital. Unfortunately, there was no more diazepam in stock with which to treat her. This event highlighted the lack of resources available in this setting.
3 Take-home messages
My experience at both hospitals led me to reflect on 3 important factors impacting the mental health system in Ghana:
Family support. For at least 80% of appointments, patients were accompanied by family members or friends. The family hierarchy is still dominant in the Ghanaian culture, and clinicians often need the buy-in of the family, especially when financial support is required. More often than not, families enhanced patients’ treatment, but in some instances, they were a barrier.
Continue to: The types of cases
The types of cases. Most of the patients coming to both hospitals had diagnoses of bipolar disorder, schizophrenia, substance use disorder, or epilepsy. My impression was that patients or family members sought treatment for disorders that were conspicuous. I saw <5 cases of depression or anxiety. I wonder if this was because:
- patients with these disorders were referred to psychologists
- patients sought out faith-based treatment
- there was a lower incidence of these disorders, or these disorders were detected less frequently.
Inadequate funding. Despite the clinicians’ astute observations and diagnoses, they faced challenges, including a lack of access to medications because pharmacies were out of stock, or the patient or hospital could not afford the medication. At times, these challenges resulted in patients admitted to the hospital not receiving medications. When Mental Health Act 846 was implemented, it was widely purported that mental health care would be available to everyone, but the funding mechanism was not firmly established.8,9 Currently, laboratory workup, mental health treatment, and medications are not covered by health insurance, and government funding for mental health is insufficient. Therefore, in most areas, the entire cost burden of psychiatric care falls on patients and their families, or on hospitals.
Making progress despite barriers
In her inaugural address, former American Psychiatric Association President Altha J. Stewart, MD, named expanding the organization’s work in global mental health as one of her 3 primary goals.10 There are several means by which American psychiatrists can support the work of psychiatrists in Ghana and elsewhere. One way is by helping the mental health commission and other entities within the country petition the government and health insurance companies to expand coverage for mental health services. Teleconferencing, in which psychiatrists in Ghana or other parts of the world provide supervision to mid-level clinicians, has been piloted in other countries such as Liberia and could be implemented to address the critical shortages of psychiatrists in certain regions.11
In the past 7 years, Ghana has made significant strides in destigmatizing mental illness, and as a result more individuals are seeking treatment and more clinicians at all levels are being trained. Despite significant barriers, physicians, nurses, and other mental health workers deliver empathic and evidence-based treatment in a manner that defies the mental health system’s current limitations.
1. Ofori-Atta A, Attafuah J, Jack H, et al. Joining psychiatric care and faith healing in a prayer camp in Ghana: randomised trial. Br J Psychiatry. 2018;212(1):34-41.
2. Ghana has only 18 psychiatrists; experts beg government for more funds. GhanaWeb. https://www.ghanaweb.com/GhanaHomePage/NewsArchive/Ghana-has-only-18-psychiatrists-experts-beg-government-for-more-funds-591732. Published October 17, 2017. Accessed July 24, 2019.
3. Agyapong VIO, Farren C, McAuliffe E. Improving Ghana’s mental healthcare through task-shifting-psychiatrists and health policy directors perceptions about government’s commitment and the role of community mental health workers. Global Health. 2016;12:57.
4. World Health Organization. Global Health Observatory data repository. http://apps.who.int/gho/data/node.main.MHHR?lang=en. Published April 25, 2019. Accessed July 24, 2019.
5. Walker GH, Osei A. Mental health law in Ghana. BJPsych Int. 2017;14(2):38-39.
6. Doku VC, Wusu-Takyi A, Awakame J. Implementing the Mental Health Act in Ghana: any challenges ahead? Ghana Med J. 2012;46(4):241-250.
7. Kissiedu E. High dose Tramadol floods market. Business Day. http://businessdayghana.com/high-dose-tramadol-floods-market/. Published September 25, 2017. Accessed July 24, 2019.
8. Badu E, O’Brien AP, Mitchell R. An integrative review of potential enablers and barriers to accessing mental health services in Ghana. Health Res Policy Syst. 2018;16(1):110.
9. Ghana mental health care delivery risks collapse for lack of funds. News Ghana. https://www.newsghana.com.gh/ghana-mental-health-care-delivery-risks-collapse-for-lack-of-funds/. Published May 29, 2018. Accessed July 24, 2019.
10. Stewart AJ. Response to the Presidential Address. Am J Psychiatry. 2018;175(8):726-727.
11. Katz, CL, Washington FB, Sacco M, et al. A resident-based telepsychiatry supervision pilot program in Liberia. Psychiatr Serv. 2018;70(3):243-246.
1. Ofori-Atta A, Attafuah J, Jack H, et al. Joining psychiatric care and faith healing in a prayer camp in Ghana: randomised trial. Br J Psychiatry. 2018;212(1):34-41.
2. Ghana has only 18 psychiatrists; experts beg government for more funds. GhanaWeb. https://www.ghanaweb.com/GhanaHomePage/NewsArchive/Ghana-has-only-18-psychiatrists-experts-beg-government-for-more-funds-591732. Published October 17, 2017. Accessed July 24, 2019.
3. Agyapong VIO, Farren C, McAuliffe E. Improving Ghana’s mental healthcare through task-shifting-psychiatrists and health policy directors perceptions about government’s commitment and the role of community mental health workers. Global Health. 2016;12:57.
4. World Health Organization. Global Health Observatory data repository. http://apps.who.int/gho/data/node.main.MHHR?lang=en. Published April 25, 2019. Accessed July 24, 2019.
5. Walker GH, Osei A. Mental health law in Ghana. BJPsych Int. 2017;14(2):38-39.
6. Doku VC, Wusu-Takyi A, Awakame J. Implementing the Mental Health Act in Ghana: any challenges ahead? Ghana Med J. 2012;46(4):241-250.
7. Kissiedu E. High dose Tramadol floods market. Business Day. http://businessdayghana.com/high-dose-tramadol-floods-market/. Published September 25, 2017. Accessed July 24, 2019.
8. Badu E, O’Brien AP, Mitchell R. An integrative review of potential enablers and barriers to accessing mental health services in Ghana. Health Res Policy Syst. 2018;16(1):110.
9. Ghana mental health care delivery risks collapse for lack of funds. News Ghana. https://www.newsghana.com.gh/ghana-mental-health-care-delivery-risks-collapse-for-lack-of-funds/. Published May 29, 2018. Accessed July 24, 2019.
10. Stewart AJ. Response to the Presidential Address. Am J Psychiatry. 2018;175(8):726-727.
11. Katz, CL, Washington FB, Sacco M, et al. A resident-based telepsychiatry supervision pilot program in Liberia. Psychiatr Serv. 2018;70(3):243-246.