User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Understanding the new CMS bundle model
Hospitalists have been among the highest-volume participants in Medicare’s Bundled Payments for Care Improvement (BPCI) demonstration model, initiating over 200,000 episodes representing $4.7 billion in spending since the model began.1 On Jan. 9, the Centers for Medicare & Medicaid Services announced BPCI’s follow-on model, “BPCI Advanced.”2
BPCI launched in October 2013 and sunsets at the end of Q3 2018. BPCI Advanced starts immediately upon conclusion of BPCI (Q4 2018) and is slated to finish at year-end 2023.
CMS intends for the program to qualify as an Advanced Alternative Payment Model (APM). As BPCI Advanced focuses on episodes of care involving an inpatient stay (It also includes three outpatient episodes.) and the subsequent 90-day recovery period, it represents the first large-scale opportunity for hospitalists to meet criteria for Advanced APM participation. Qualifying for the Advanced APM track of the Quality Payment Program – which involves meeting patient volume or payment thresholds3 – comes with a 5% lump-sum bonus based on Medicare Part B fees and avoids exposure to penalties and reporting requirements of the Merit-based Incentive Payment System (MIPS).
Key program features
Acute care hospitals and physician groups may initiate episodes under BPCI Advanced, assuming financial risk under the model. Similar to its predecessor, BPCI Advanced assigns a target price based on past claims payments associated with the “episode initiator.”
During the performance period, if the initiator can beat the price in the aggregate for its bundles, it can keep the difference, and if it comes in over the price, it must pay the difference back to Medicare. Medicare discounts the target price by 3%, effectively paying itself that amount. After that, there is no sharing of savings with Medicare, as opposed to the permanent ACO programs, where there is sharing after the ACO meets the minimum savings rate.
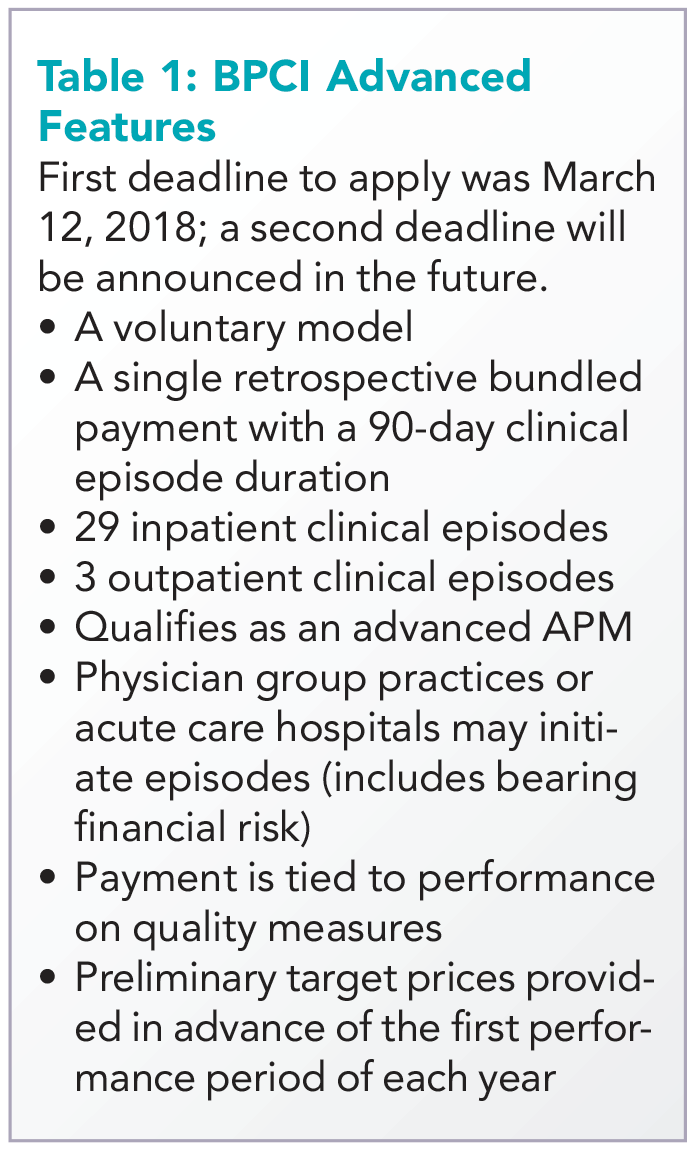
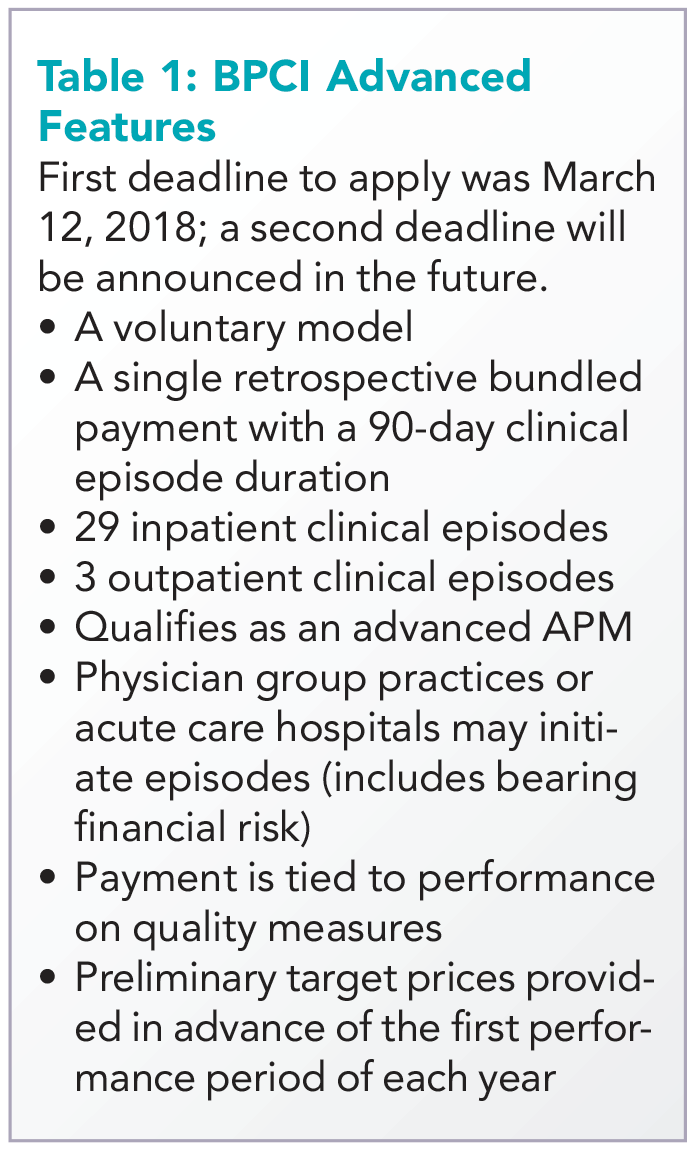
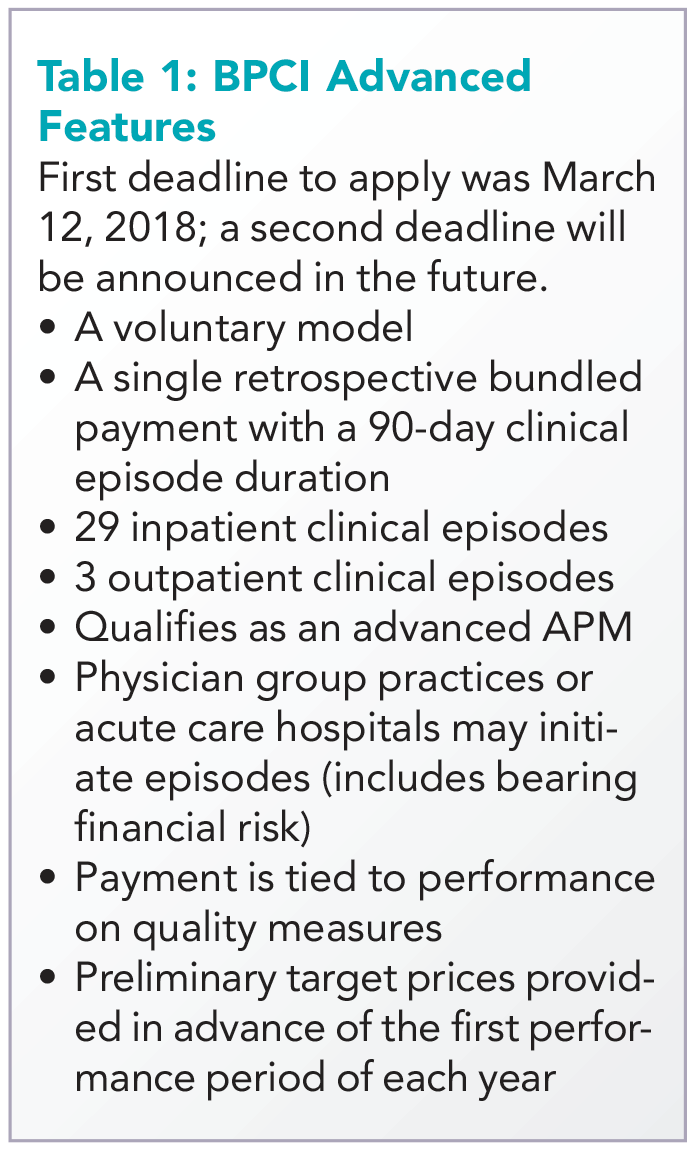
The program allows physician groups and hospital initiators to go it alone or to work with a “convener,” which may share risk and reward with initiators, and may provide software, analytics, networks of high-performing providers like nursing facilities, and knowledge of specific care redesign approaches to enable program success. See Table 1 for a listing of other notable features of BPCI Advanced.
Quality measures
BPCI Advanced qualifies as an Advanced APM in part because payment is tied to performance on a set of quality measures (see Table 2). There are two measures applied to all episodes: all-cause hospital readmissions and advance care plan. These are notable because hospitalists may be especially focused on improvement activities in these areas.
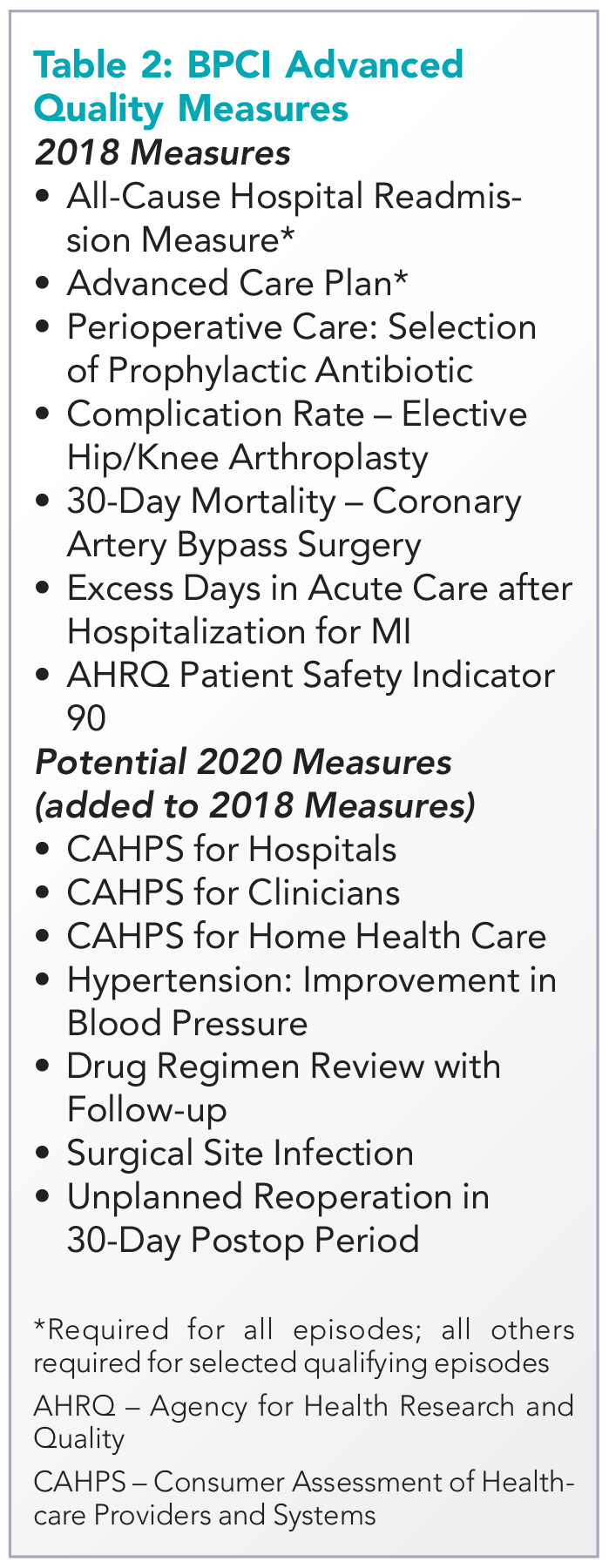
While the advance care plan measure refers to a process reflected by record documentation and is therefore directly under the control of hospitalists, readmissions – and most of the other measures – require a team approach. Because the outcome measures are risk adjusted, accurate and complete clinical documentation is crucial, as it drives how risk is adjusted. Of note, all the 2018 measures, collected directly through claims, will place no additional administrative burden for collection on providers.
Two ways for hospitalists to participate
Hospitalist groups – whether independent or employed – may be episode initiators in BPCI Advanced. In this case, any episodes in which the group participates that carry the name of a member of the hospitalist group in the “Attending Provider” field on the hospital bill claim form to Medicare (and the associated carrier claim) are attributed to that member’s physician group.
For example, if the group has chosen heart failure as an episode in which to participate at the program’s outset, a hospitalization is assigned the heart failure DRG (diagnosis-related group) and a group member is the Attending Provider on the claim form (and submits a claim for the physician services), then the episode is attributed to that group. This means that the group is responsible for payments represented by Medicare Part A and Part B claims (with a few exclusions like trauma and cancer) against the target price for the initial hospitalization and subsequent 90-day period. In practice, hospitalists are rewarded for actions aimed at optimizing location after discharge,4 avoiding readmissions, choosing efficient nursing facilities, and helping patients to maximize functional status.
The other way hospitalists may participate is through an agreement to share in savings with a hospital or physician group episode initiator. This requires hospitalist individuals or groups to enter into a contract with the initiator that meets certain program requirements – for example, report quality measures, engage in care redesign, use certified EHR technology (hospital-based clinicians automatically fulfill this criterion).
If there is broad participation, BPCI Advanced could represent a key milestone for hospitalists, as they seek to be recognized for the value they confer to the system as a whole instead of simply their professional billings. While there are legitimate concerns about the effect MIPS may have on health care value and the complexity of participation in APMs, barring a repeal of the law that created them, hospitalists now have the chance to extend their influence within and outside the hospital’s four walls and be more fairly rewarded for it.
Dr. Whitcomb is chief medical officer at Remedy Partners in Darien, Conn., and cofounder and past president of the Society of Hospital Medicine. Contact him at [email protected]. Disclosure: The author’s employer, Remedy Partners, is an Awardee Convener for the BPCI initiative and intends to apply as a Convener in BPCI Advanced.
References
1. Based on BPCI awardee convener Remedy Partners claims analysis.
2. https://innovation.cms.gov/initiatives/bpci-advanced.
3. https://qpp.cms.gov/apms/overview.
4. Whitcomb W. Choosing location after discharge wisely. The-hospitalist.org. 2018 Jan 3. Digital edition. Accessed Jan 13, 2018.
Hospitalists have been among the highest-volume participants in Medicare’s Bundled Payments for Care Improvement (BPCI) demonstration model, initiating over 200,000 episodes representing $4.7 billion in spending since the model began.1 On Jan. 9, the Centers for Medicare & Medicaid Services announced BPCI’s follow-on model, “BPCI Advanced.”2
BPCI launched in October 2013 and sunsets at the end of Q3 2018. BPCI Advanced starts immediately upon conclusion of BPCI (Q4 2018) and is slated to finish at year-end 2023.
CMS intends for the program to qualify as an Advanced Alternative Payment Model (APM). As BPCI Advanced focuses on episodes of care involving an inpatient stay (It also includes three outpatient episodes.) and the subsequent 90-day recovery period, it represents the first large-scale opportunity for hospitalists to meet criteria for Advanced APM participation. Qualifying for the Advanced APM track of the Quality Payment Program – which involves meeting patient volume or payment thresholds3 – comes with a 5% lump-sum bonus based on Medicare Part B fees and avoids exposure to penalties and reporting requirements of the Merit-based Incentive Payment System (MIPS).
Key program features
Acute care hospitals and physician groups may initiate episodes under BPCI Advanced, assuming financial risk under the model. Similar to its predecessor, BPCI Advanced assigns a target price based on past claims payments associated with the “episode initiator.”
During the performance period, if the initiator can beat the price in the aggregate for its bundles, it can keep the difference, and if it comes in over the price, it must pay the difference back to Medicare. Medicare discounts the target price by 3%, effectively paying itself that amount. After that, there is no sharing of savings with Medicare, as opposed to the permanent ACO programs, where there is sharing after the ACO meets the minimum savings rate.
The program allows physician groups and hospital initiators to go it alone or to work with a “convener,” which may share risk and reward with initiators, and may provide software, analytics, networks of high-performing providers like nursing facilities, and knowledge of specific care redesign approaches to enable program success. See Table 1 for a listing of other notable features of BPCI Advanced.
Quality measures
BPCI Advanced qualifies as an Advanced APM in part because payment is tied to performance on a set of quality measures (see Table 2). There are two measures applied to all episodes: all-cause hospital readmissions and advance care plan. These are notable because hospitalists may be especially focused on improvement activities in these areas.
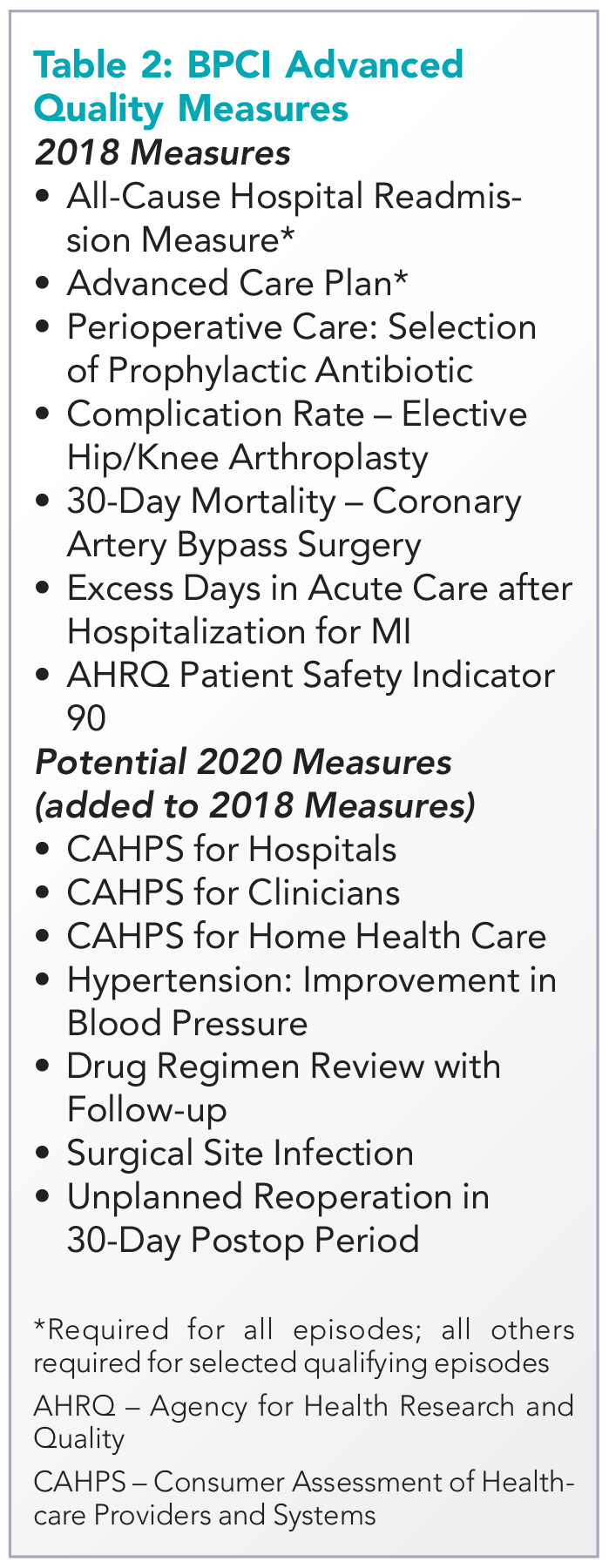
While the advance care plan measure refers to a process reflected by record documentation and is therefore directly under the control of hospitalists, readmissions – and most of the other measures – require a team approach. Because the outcome measures are risk adjusted, accurate and complete clinical documentation is crucial, as it drives how risk is adjusted. Of note, all the 2018 measures, collected directly through claims, will place no additional administrative burden for collection on providers.
Two ways for hospitalists to participate
Hospitalist groups – whether independent or employed – may be episode initiators in BPCI Advanced. In this case, any episodes in which the group participates that carry the name of a member of the hospitalist group in the “Attending Provider” field on the hospital bill claim form to Medicare (and the associated carrier claim) are attributed to that member’s physician group.
For example, if the group has chosen heart failure as an episode in which to participate at the program’s outset, a hospitalization is assigned the heart failure DRG (diagnosis-related group) and a group member is the Attending Provider on the claim form (and submits a claim for the physician services), then the episode is attributed to that group. This means that the group is responsible for payments represented by Medicare Part A and Part B claims (with a few exclusions like trauma and cancer) against the target price for the initial hospitalization and subsequent 90-day period. In practice, hospitalists are rewarded for actions aimed at optimizing location after discharge,4 avoiding readmissions, choosing efficient nursing facilities, and helping patients to maximize functional status.
The other way hospitalists may participate is through an agreement to share in savings with a hospital or physician group episode initiator. This requires hospitalist individuals or groups to enter into a contract with the initiator that meets certain program requirements – for example, report quality measures, engage in care redesign, use certified EHR technology (hospital-based clinicians automatically fulfill this criterion).
If there is broad participation, BPCI Advanced could represent a key milestone for hospitalists, as they seek to be recognized for the value they confer to the system as a whole instead of simply their professional billings. While there are legitimate concerns about the effect MIPS may have on health care value and the complexity of participation in APMs, barring a repeal of the law that created them, hospitalists now have the chance to extend their influence within and outside the hospital’s four walls and be more fairly rewarded for it.
Dr. Whitcomb is chief medical officer at Remedy Partners in Darien, Conn., and cofounder and past president of the Society of Hospital Medicine. Contact him at [email protected]. Disclosure: The author’s employer, Remedy Partners, is an Awardee Convener for the BPCI initiative and intends to apply as a Convener in BPCI Advanced.
References
1. Based on BPCI awardee convener Remedy Partners claims analysis.
2. https://innovation.cms.gov/initiatives/bpci-advanced.
3. https://qpp.cms.gov/apms/overview.
4. Whitcomb W. Choosing location after discharge wisely. The-hospitalist.org. 2018 Jan 3. Digital edition. Accessed Jan 13, 2018.
Hospitalists have been among the highest-volume participants in Medicare’s Bundled Payments for Care Improvement (BPCI) demonstration model, initiating over 200,000 episodes representing $4.7 billion in spending since the model began.1 On Jan. 9, the Centers for Medicare & Medicaid Services announced BPCI’s follow-on model, “BPCI Advanced.”2
BPCI launched in October 2013 and sunsets at the end of Q3 2018. BPCI Advanced starts immediately upon conclusion of BPCI (Q4 2018) and is slated to finish at year-end 2023.
CMS intends for the program to qualify as an Advanced Alternative Payment Model (APM). As BPCI Advanced focuses on episodes of care involving an inpatient stay (It also includes three outpatient episodes.) and the subsequent 90-day recovery period, it represents the first large-scale opportunity for hospitalists to meet criteria for Advanced APM participation. Qualifying for the Advanced APM track of the Quality Payment Program – which involves meeting patient volume or payment thresholds3 – comes with a 5% lump-sum bonus based on Medicare Part B fees and avoids exposure to penalties and reporting requirements of the Merit-based Incentive Payment System (MIPS).
Key program features
Acute care hospitals and physician groups may initiate episodes under BPCI Advanced, assuming financial risk under the model. Similar to its predecessor, BPCI Advanced assigns a target price based on past claims payments associated with the “episode initiator.”
During the performance period, if the initiator can beat the price in the aggregate for its bundles, it can keep the difference, and if it comes in over the price, it must pay the difference back to Medicare. Medicare discounts the target price by 3%, effectively paying itself that amount. After that, there is no sharing of savings with Medicare, as opposed to the permanent ACO programs, where there is sharing after the ACO meets the minimum savings rate.
The program allows physician groups and hospital initiators to go it alone or to work with a “convener,” which may share risk and reward with initiators, and may provide software, analytics, networks of high-performing providers like nursing facilities, and knowledge of specific care redesign approaches to enable program success. See Table 1 for a listing of other notable features of BPCI Advanced.
Quality measures
BPCI Advanced qualifies as an Advanced APM in part because payment is tied to performance on a set of quality measures (see Table 2). There are two measures applied to all episodes: all-cause hospital readmissions and advance care plan. These are notable because hospitalists may be especially focused on improvement activities in these areas.
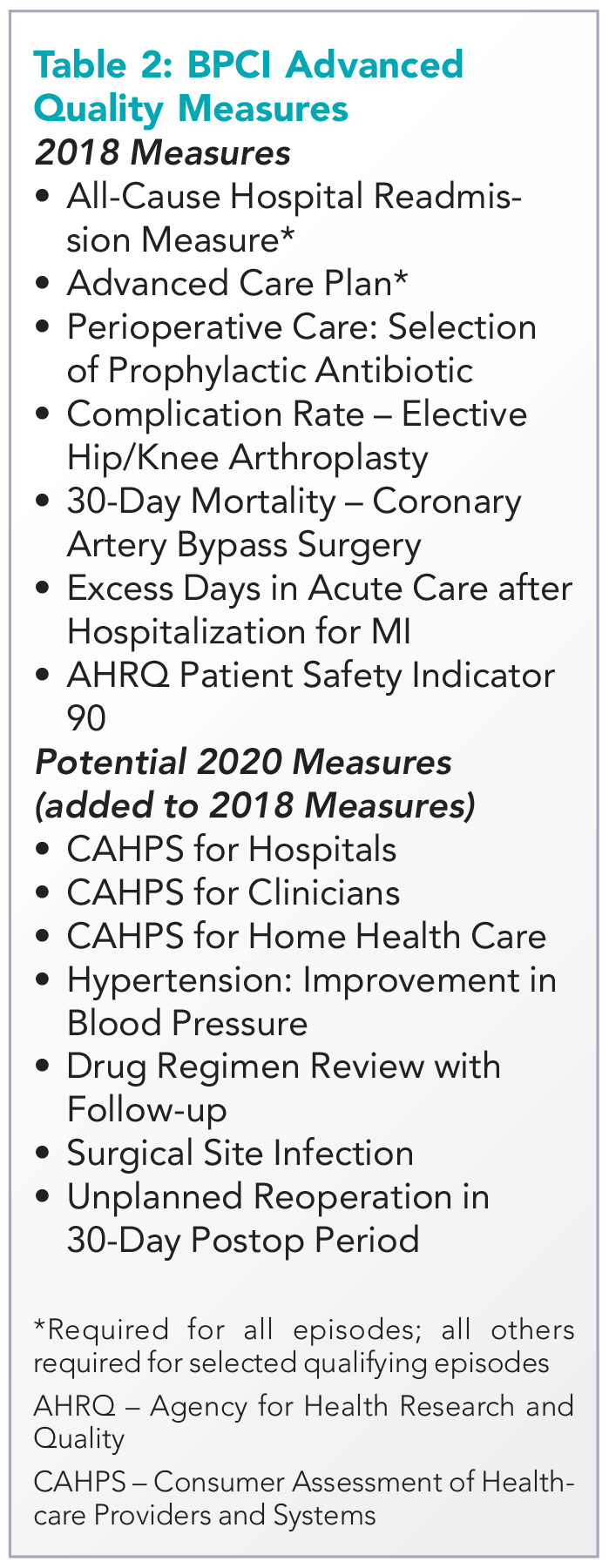
While the advance care plan measure refers to a process reflected by record documentation and is therefore directly under the control of hospitalists, readmissions – and most of the other measures – require a team approach. Because the outcome measures are risk adjusted, accurate and complete clinical documentation is crucial, as it drives how risk is adjusted. Of note, all the 2018 measures, collected directly through claims, will place no additional administrative burden for collection on providers.
Two ways for hospitalists to participate
Hospitalist groups – whether independent or employed – may be episode initiators in BPCI Advanced. In this case, any episodes in which the group participates that carry the name of a member of the hospitalist group in the “Attending Provider” field on the hospital bill claim form to Medicare (and the associated carrier claim) are attributed to that member’s physician group.
For example, if the group has chosen heart failure as an episode in which to participate at the program’s outset, a hospitalization is assigned the heart failure DRG (diagnosis-related group) and a group member is the Attending Provider on the claim form (and submits a claim for the physician services), then the episode is attributed to that group. This means that the group is responsible for payments represented by Medicare Part A and Part B claims (with a few exclusions like trauma and cancer) against the target price for the initial hospitalization and subsequent 90-day period. In practice, hospitalists are rewarded for actions aimed at optimizing location after discharge,4 avoiding readmissions, choosing efficient nursing facilities, and helping patients to maximize functional status.
The other way hospitalists may participate is through an agreement to share in savings with a hospital or physician group episode initiator. This requires hospitalist individuals or groups to enter into a contract with the initiator that meets certain program requirements – for example, report quality measures, engage in care redesign, use certified EHR technology (hospital-based clinicians automatically fulfill this criterion).
If there is broad participation, BPCI Advanced could represent a key milestone for hospitalists, as they seek to be recognized for the value they confer to the system as a whole instead of simply their professional billings. While there are legitimate concerns about the effect MIPS may have on health care value and the complexity of participation in APMs, barring a repeal of the law that created them, hospitalists now have the chance to extend their influence within and outside the hospital’s four walls and be more fairly rewarded for it.
Dr. Whitcomb is chief medical officer at Remedy Partners in Darien, Conn., and cofounder and past president of the Society of Hospital Medicine. Contact him at [email protected]. Disclosure: The author’s employer, Remedy Partners, is an Awardee Convener for the BPCI initiative and intends to apply as a Convener in BPCI Advanced.
References
1. Based on BPCI awardee convener Remedy Partners claims analysis.
2. https://innovation.cms.gov/initiatives/bpci-advanced.
3. https://qpp.cms.gov/apms/overview.
4. Whitcomb W. Choosing location after discharge wisely. The-hospitalist.org. 2018 Jan 3. Digital edition. Accessed Jan 13, 2018.
A public health approach to gun violence
In 2014, 33,594 people were killed by firearms in the United States. More than 21,000 of these deaths were suicides. The rest were primarily homicides and accidental shootings. Meanwhile, firearm deaths represented nearly 17% of injury deaths that year.1,2
In a 2015 Perspective published in the New England Journal of Medicine, author Chana Sacks, MD, pointed out that 20 children and adolescents are sent to the hospital daily for firearm injuries and 2,000 people each year suffer gunshot-related spinal cord injuries and “become lifelong patients.”3
At the same time, Federal Bureau of Investigation data show that the number of active shooter situations rose between 2000 and 2013, with an average of 6.4 incidents a year for the first 7 years of the study, conducted in 2013, and an average of 16.4 in the last 7 years of the study. More than 1,000 people were wounded or killed across 160 active shooter incidents, defined as an individual or individuals actively engaged in killing or trying to kill people in a populous area.4
“Gun violence is undeniably a public health issue,” said Dr. Sacks, a hospitalist at Massachusetts General Hospital and instructor at Harvard Medical School, both in Boston, and a vocal proponent of addressing firearms in the public health sphere. Her cousin’s 7-year-old son, Daniel Barden, was fatally shot at Sandy Hook Elementary School in Newtown, Conn., in December 2012.
Yet, the notion of firearm injuries and deaths as a public health issue is, in America, an issue of contention. How can hospitalists and other health care providers avoid wading into the political thicket while also looking out for their patients?
For one, it’s not the only controversial issue with which providers are confronted, Dr. Sacks and others say. From taking sexual histories, counseling patients about abortion and adoption, and discussing end-of-life issues, clinicians may routinely face uncomfortable interactions in the name of patient care.
“It’s not a question about their right to a weapon; it’s about how individuals can stay as safe as possible and keep their families as safe as possible,” said Dr. Sacks, who also wrote in a January 2017 opinion for the American Medical Association that: “Counseling about gun safety is not political – no more so than a physician counseling a patient about cutting down on sugary beverages is an act of declaring support for New York City’s attempted ban on large-sized sodas.”5
This idea is echoed by David Hemenway, PhD, director of the Harvard Injury Control Research Center, Boston. “You can talk about wearing your seat belt without advocating for mandatory seat belt laws,” he said.
Yet in a 2014 survey of internist members of the American College of Physicians, only 66% of respondents said they believed physicians have the right to counsel patients on gun violence prevention and 58% said they never ask patients about guns in their home. That same survey showed the public is also split: While two-thirds of respondents said it was at least sometimes appropriate for providers to ask about firearms during a visit, one-third believed it was never appropriate.6
In fact, Barbara Meyer, MD, MPH, a family physician in Seattle, said she once had a patient walk out of the office when he encountered a question about firearms on the intake forms for the health system at which she was employed at the time. Today, at NeighborCare Health, the presence of firearms in the home is a question in the well-child electronic health record.
The Harvard Injury Control Research Center runs a campaign called Means Matter, designed to address suicide by firearm, the most common method of suicide in America. The campaign – backed by decades of some of the best research available – reports that people die of suicide by gun more than all other methods combined, that suicide attempts using a firearm are almost always fatal, and that firearms used by youths who commit suicide almost always belong to a parent.
“Suicide is often an impulsive act,” said Dr. Sacks, which means preventing access to firearms for patients at risk can be a matter of life and death. “There is potential for intervention there … what can be more clearly medical than suicide prevention?”
For her, that means eliminating the partisan component and equipping providers with the best evidence-based research available and with best practices. Reliable studies show that having guns at home increases the danger to families, said Dr. Hemenway, and places with fewer guns and stronger gun laws are correlated with fewer gun fatalities.7,8
“In accordance with guidelines and the best evidence out there, we should be screening patients who might be at risk for gun violence,” he said. “In some cases, interventions can be as simple and straightforward as informing patients where to get gun locks and talking to them about how to store firearms safely.”
At Massachusetts General Hospital, Dr. Sacks helped found the Gun Violence Prevention Coalition, an interdisciplinary group of physicians, nurses, physical therapists, and others committed to raising awareness and preparing providers to address gun violence. She believes strongly that physicians can act locally to help address the issue.
In Seattle, Dr. Meyer has been involved with a local group called Washington Ceasefire, prompted both by her experience as a resident in Detroit – where she was routinely exposed to the traumas of gun violence – as well as a shooting that occurred outside her daughter’s high school in Seattle years ago. The group has recently begun advocating for smart guns, which are designed to be fired only by an authorized user.
Indeed, Dr. Hemenway said research by his group suggests 300,000-500,000 guns are stolen every year, though he points out that we know almost nothing about “who, what, when, why, and where.” That’s largely because of an effective ban on gun violence research, enacted by Congress in the 1990s.9
“It’s not like there’s no evidence, but compared to the size of the problem, you want good evidence,” Dr. Hemenway said. “America has lots of guns. How can we learn to live with them?”
Gun violence affects not just those shot and killed by firearms, but also those affected by the trauma it can leave in its wake. Dr. Sacks recounts a recent visit to Massachusetts General by survivors of the Pulse Nightclub shooting in Orlando, Fla., which took place on June 12, 2016.
“It was a moving, intense event where we all sat around and talked about this issue,” Dr. Sacks said. “The number of people dying is horrific enough, but it’s not just that. Here were a number of young people who survived and yet whose lives will never be the same. We are undercounting the number of people affected by gun violence.”
Studies also estimate the cost of medical care related to gun violence to be roughly $620 million per year, averaging between $9,000 and $18,000 per patient in 2014.10
Despite some arguments to the contrary, addressing gun violence as a public health issue is not a distraction from other important public health issues such as opioid abuse. “It is entirely a false choice that we must only take on one issue or another,” Dr. Sacks said.
Nor should efforts to address gun violence focus only on individuals, said Dr. Hemenway, who told the Harvard T.H. Chan School of Public Health in October 2017 that: “A lesson from public health is that it is usually more effective to change the environment than to try to change people. The U.S. should use the same harm reduction approach to gun violence that it uses to treat other public health threats, like automobile crashes or air pollution, employing a wide variety of methods to reduce the problem.”
The issue must be reframed, said Dr. Sacks. This remains one of her biggest goals. “If we can find a way to act and intervene and lower [the] number [of people affected by gun violence], what could be more fundamentally in line with what we try to do every day as physicians?” she asked. “How can we reduce morbidity and mortality? That’s an answerable question and we can make sure we have pathways and approaches we can put in place to understand this. This is a solvable problem.”
1. Centers for Disease Control and Prevention, National Center for Health Statistics. FastStats. Injuries. https://www.cdc.gov/nchs/fastats/injury.htm. Accessed Nov 20, 2017.
2. Centers for Disease Control and Prevention, National Center for Health Statistics. FastStats. Suicide. https://www.cdc.gov/nchs/fastats/suicide.htm. Accessed Nov 20, 2017.
3. Sacks CA. In memory of Daniel – Reviving research to prevent gun violence. N Engl J Med. 2015; 372:800-801. doi: 10.1056/NEJMp1415128.
4. U.S. Department of Justice, Federal Bureau of Investigation. A study of active shooter incidents in the United States between 2000 and 2013. Published Sept 16, 2013. Accessed Nov 20, 2017.
5. Sacks CA. The role of physicians in preventing firearm suicides. JAMA Int Med. doi: 10.001/jamainternmed.2016.6715. Published Nov 14, 2016. Accessed Nov 20, 2017.
6. Butkus R, Weissman A. Internists’ attitudes toward prevention of firearm injury. Ann Intern Med. 2014;160(12):821-827. doi: 10.7326/M13-1960.
7. Fleegler EW, Lee LK, Monuteaux MC, et al. Firearm Legislation and Firearm-Related Fatalities in the United States. JAMA Intern Med. 2013; 173(9):732-740. doi: 10.1001/jamaimternmed.2013.1286.
8. American Academy of Pediatricians. Addressing gun violence. The federal level. https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Pages/Gun-Violence-Matrix--Intentional-(Federal).aspx. Accessed Nov 20, 2017.
9. Rubin R. Tale of 2 agencies: CDC avoids gun violence research bit NIH funds it. JAMA. 2016;315(16):1689-1692. doi:10.1001/jama.2016.1707.
10. Howell E and Gangopadhyaya A. State variation in the hospital costs of gun violence, 2010 and 2014. The Urban Institute, Health Policy Center.
In 2014, 33,594 people were killed by firearms in the United States. More than 21,000 of these deaths were suicides. The rest were primarily homicides and accidental shootings. Meanwhile, firearm deaths represented nearly 17% of injury deaths that year.1,2
In a 2015 Perspective published in the New England Journal of Medicine, author Chana Sacks, MD, pointed out that 20 children and adolescents are sent to the hospital daily for firearm injuries and 2,000 people each year suffer gunshot-related spinal cord injuries and “become lifelong patients.”3
At the same time, Federal Bureau of Investigation data show that the number of active shooter situations rose between 2000 and 2013, with an average of 6.4 incidents a year for the first 7 years of the study, conducted in 2013, and an average of 16.4 in the last 7 years of the study. More than 1,000 people were wounded or killed across 160 active shooter incidents, defined as an individual or individuals actively engaged in killing or trying to kill people in a populous area.4
“Gun violence is undeniably a public health issue,” said Dr. Sacks, a hospitalist at Massachusetts General Hospital and instructor at Harvard Medical School, both in Boston, and a vocal proponent of addressing firearms in the public health sphere. Her cousin’s 7-year-old son, Daniel Barden, was fatally shot at Sandy Hook Elementary School in Newtown, Conn., in December 2012.
Yet, the notion of firearm injuries and deaths as a public health issue is, in America, an issue of contention. How can hospitalists and other health care providers avoid wading into the political thicket while also looking out for their patients?
For one, it’s not the only controversial issue with which providers are confronted, Dr. Sacks and others say. From taking sexual histories, counseling patients about abortion and adoption, and discussing end-of-life issues, clinicians may routinely face uncomfortable interactions in the name of patient care.
“It’s not a question about their right to a weapon; it’s about how individuals can stay as safe as possible and keep their families as safe as possible,” said Dr. Sacks, who also wrote in a January 2017 opinion for the American Medical Association that: “Counseling about gun safety is not political – no more so than a physician counseling a patient about cutting down on sugary beverages is an act of declaring support for New York City’s attempted ban on large-sized sodas.”5
This idea is echoed by David Hemenway, PhD, director of the Harvard Injury Control Research Center, Boston. “You can talk about wearing your seat belt without advocating for mandatory seat belt laws,” he said.
Yet in a 2014 survey of internist members of the American College of Physicians, only 66% of respondents said they believed physicians have the right to counsel patients on gun violence prevention and 58% said they never ask patients about guns in their home. That same survey showed the public is also split: While two-thirds of respondents said it was at least sometimes appropriate for providers to ask about firearms during a visit, one-third believed it was never appropriate.6
In fact, Barbara Meyer, MD, MPH, a family physician in Seattle, said she once had a patient walk out of the office when he encountered a question about firearms on the intake forms for the health system at which she was employed at the time. Today, at NeighborCare Health, the presence of firearms in the home is a question in the well-child electronic health record.
The Harvard Injury Control Research Center runs a campaign called Means Matter, designed to address suicide by firearm, the most common method of suicide in America. The campaign – backed by decades of some of the best research available – reports that people die of suicide by gun more than all other methods combined, that suicide attempts using a firearm are almost always fatal, and that firearms used by youths who commit suicide almost always belong to a parent.
“Suicide is often an impulsive act,” said Dr. Sacks, which means preventing access to firearms for patients at risk can be a matter of life and death. “There is potential for intervention there … what can be more clearly medical than suicide prevention?”
For her, that means eliminating the partisan component and equipping providers with the best evidence-based research available and with best practices. Reliable studies show that having guns at home increases the danger to families, said Dr. Hemenway, and places with fewer guns and stronger gun laws are correlated with fewer gun fatalities.7,8
“In accordance with guidelines and the best evidence out there, we should be screening patients who might be at risk for gun violence,” he said. “In some cases, interventions can be as simple and straightforward as informing patients where to get gun locks and talking to them about how to store firearms safely.”
At Massachusetts General Hospital, Dr. Sacks helped found the Gun Violence Prevention Coalition, an interdisciplinary group of physicians, nurses, physical therapists, and others committed to raising awareness and preparing providers to address gun violence. She believes strongly that physicians can act locally to help address the issue.
In Seattle, Dr. Meyer has been involved with a local group called Washington Ceasefire, prompted both by her experience as a resident in Detroit – where she was routinely exposed to the traumas of gun violence – as well as a shooting that occurred outside her daughter’s high school in Seattle years ago. The group has recently begun advocating for smart guns, which are designed to be fired only by an authorized user.
Indeed, Dr. Hemenway said research by his group suggests 300,000-500,000 guns are stolen every year, though he points out that we know almost nothing about “who, what, when, why, and where.” That’s largely because of an effective ban on gun violence research, enacted by Congress in the 1990s.9
“It’s not like there’s no evidence, but compared to the size of the problem, you want good evidence,” Dr. Hemenway said. “America has lots of guns. How can we learn to live with them?”
Gun violence affects not just those shot and killed by firearms, but also those affected by the trauma it can leave in its wake. Dr. Sacks recounts a recent visit to Massachusetts General by survivors of the Pulse Nightclub shooting in Orlando, Fla., which took place on June 12, 2016.
“It was a moving, intense event where we all sat around and talked about this issue,” Dr. Sacks said. “The number of people dying is horrific enough, but it’s not just that. Here were a number of young people who survived and yet whose lives will never be the same. We are undercounting the number of people affected by gun violence.”
Studies also estimate the cost of medical care related to gun violence to be roughly $620 million per year, averaging between $9,000 and $18,000 per patient in 2014.10
Despite some arguments to the contrary, addressing gun violence as a public health issue is not a distraction from other important public health issues such as opioid abuse. “It is entirely a false choice that we must only take on one issue or another,” Dr. Sacks said.
Nor should efforts to address gun violence focus only on individuals, said Dr. Hemenway, who told the Harvard T.H. Chan School of Public Health in October 2017 that: “A lesson from public health is that it is usually more effective to change the environment than to try to change people. The U.S. should use the same harm reduction approach to gun violence that it uses to treat other public health threats, like automobile crashes or air pollution, employing a wide variety of methods to reduce the problem.”
The issue must be reframed, said Dr. Sacks. This remains one of her biggest goals. “If we can find a way to act and intervene and lower [the] number [of people affected by gun violence], what could be more fundamentally in line with what we try to do every day as physicians?” she asked. “How can we reduce morbidity and mortality? That’s an answerable question and we can make sure we have pathways and approaches we can put in place to understand this. This is a solvable problem.”
In 2014, 33,594 people were killed by firearms in the United States. More than 21,000 of these deaths were suicides. The rest were primarily homicides and accidental shootings. Meanwhile, firearm deaths represented nearly 17% of injury deaths that year.1,2
In a 2015 Perspective published in the New England Journal of Medicine, author Chana Sacks, MD, pointed out that 20 children and adolescents are sent to the hospital daily for firearm injuries and 2,000 people each year suffer gunshot-related spinal cord injuries and “become lifelong patients.”3
At the same time, Federal Bureau of Investigation data show that the number of active shooter situations rose between 2000 and 2013, with an average of 6.4 incidents a year for the first 7 years of the study, conducted in 2013, and an average of 16.4 in the last 7 years of the study. More than 1,000 people were wounded or killed across 160 active shooter incidents, defined as an individual or individuals actively engaged in killing or trying to kill people in a populous area.4
“Gun violence is undeniably a public health issue,” said Dr. Sacks, a hospitalist at Massachusetts General Hospital and instructor at Harvard Medical School, both in Boston, and a vocal proponent of addressing firearms in the public health sphere. Her cousin’s 7-year-old son, Daniel Barden, was fatally shot at Sandy Hook Elementary School in Newtown, Conn., in December 2012.
Yet, the notion of firearm injuries and deaths as a public health issue is, in America, an issue of contention. How can hospitalists and other health care providers avoid wading into the political thicket while also looking out for their patients?
For one, it’s not the only controversial issue with which providers are confronted, Dr. Sacks and others say. From taking sexual histories, counseling patients about abortion and adoption, and discussing end-of-life issues, clinicians may routinely face uncomfortable interactions in the name of patient care.
“It’s not a question about their right to a weapon; it’s about how individuals can stay as safe as possible and keep their families as safe as possible,” said Dr. Sacks, who also wrote in a January 2017 opinion for the American Medical Association that: “Counseling about gun safety is not political – no more so than a physician counseling a patient about cutting down on sugary beverages is an act of declaring support for New York City’s attempted ban on large-sized sodas.”5
This idea is echoed by David Hemenway, PhD, director of the Harvard Injury Control Research Center, Boston. “You can talk about wearing your seat belt without advocating for mandatory seat belt laws,” he said.
Yet in a 2014 survey of internist members of the American College of Physicians, only 66% of respondents said they believed physicians have the right to counsel patients on gun violence prevention and 58% said they never ask patients about guns in their home. That same survey showed the public is also split: While two-thirds of respondents said it was at least sometimes appropriate for providers to ask about firearms during a visit, one-third believed it was never appropriate.6
In fact, Barbara Meyer, MD, MPH, a family physician in Seattle, said she once had a patient walk out of the office when he encountered a question about firearms on the intake forms for the health system at which she was employed at the time. Today, at NeighborCare Health, the presence of firearms in the home is a question in the well-child electronic health record.
The Harvard Injury Control Research Center runs a campaign called Means Matter, designed to address suicide by firearm, the most common method of suicide in America. The campaign – backed by decades of some of the best research available – reports that people die of suicide by gun more than all other methods combined, that suicide attempts using a firearm are almost always fatal, and that firearms used by youths who commit suicide almost always belong to a parent.
“Suicide is often an impulsive act,” said Dr. Sacks, which means preventing access to firearms for patients at risk can be a matter of life and death. “There is potential for intervention there … what can be more clearly medical than suicide prevention?”
For her, that means eliminating the partisan component and equipping providers with the best evidence-based research available and with best practices. Reliable studies show that having guns at home increases the danger to families, said Dr. Hemenway, and places with fewer guns and stronger gun laws are correlated with fewer gun fatalities.7,8
“In accordance with guidelines and the best evidence out there, we should be screening patients who might be at risk for gun violence,” he said. “In some cases, interventions can be as simple and straightforward as informing patients where to get gun locks and talking to them about how to store firearms safely.”
At Massachusetts General Hospital, Dr. Sacks helped found the Gun Violence Prevention Coalition, an interdisciplinary group of physicians, nurses, physical therapists, and others committed to raising awareness and preparing providers to address gun violence. She believes strongly that physicians can act locally to help address the issue.
In Seattle, Dr. Meyer has been involved with a local group called Washington Ceasefire, prompted both by her experience as a resident in Detroit – where she was routinely exposed to the traumas of gun violence – as well as a shooting that occurred outside her daughter’s high school in Seattle years ago. The group has recently begun advocating for smart guns, which are designed to be fired only by an authorized user.
Indeed, Dr. Hemenway said research by his group suggests 300,000-500,000 guns are stolen every year, though he points out that we know almost nothing about “who, what, when, why, and where.” That’s largely because of an effective ban on gun violence research, enacted by Congress in the 1990s.9
“It’s not like there’s no evidence, but compared to the size of the problem, you want good evidence,” Dr. Hemenway said. “America has lots of guns. How can we learn to live with them?”
Gun violence affects not just those shot and killed by firearms, but also those affected by the trauma it can leave in its wake. Dr. Sacks recounts a recent visit to Massachusetts General by survivors of the Pulse Nightclub shooting in Orlando, Fla., which took place on June 12, 2016.
“It was a moving, intense event where we all sat around and talked about this issue,” Dr. Sacks said. “The number of people dying is horrific enough, but it’s not just that. Here were a number of young people who survived and yet whose lives will never be the same. We are undercounting the number of people affected by gun violence.”
Studies also estimate the cost of medical care related to gun violence to be roughly $620 million per year, averaging between $9,000 and $18,000 per patient in 2014.10
Despite some arguments to the contrary, addressing gun violence as a public health issue is not a distraction from other important public health issues such as opioid abuse. “It is entirely a false choice that we must only take on one issue or another,” Dr. Sacks said.
Nor should efforts to address gun violence focus only on individuals, said Dr. Hemenway, who told the Harvard T.H. Chan School of Public Health in October 2017 that: “A lesson from public health is that it is usually more effective to change the environment than to try to change people. The U.S. should use the same harm reduction approach to gun violence that it uses to treat other public health threats, like automobile crashes or air pollution, employing a wide variety of methods to reduce the problem.”
The issue must be reframed, said Dr. Sacks. This remains one of her biggest goals. “If we can find a way to act and intervene and lower [the] number [of people affected by gun violence], what could be more fundamentally in line with what we try to do every day as physicians?” she asked. “How can we reduce morbidity and mortality? That’s an answerable question and we can make sure we have pathways and approaches we can put in place to understand this. This is a solvable problem.”
1. Centers for Disease Control and Prevention, National Center for Health Statistics. FastStats. Injuries. https://www.cdc.gov/nchs/fastats/injury.htm. Accessed Nov 20, 2017.
2. Centers for Disease Control and Prevention, National Center for Health Statistics. FastStats. Suicide. https://www.cdc.gov/nchs/fastats/suicide.htm. Accessed Nov 20, 2017.
3. Sacks CA. In memory of Daniel – Reviving research to prevent gun violence. N Engl J Med. 2015; 372:800-801. doi: 10.1056/NEJMp1415128.
4. U.S. Department of Justice, Federal Bureau of Investigation. A study of active shooter incidents in the United States between 2000 and 2013. Published Sept 16, 2013. Accessed Nov 20, 2017.
5. Sacks CA. The role of physicians in preventing firearm suicides. JAMA Int Med. doi: 10.001/jamainternmed.2016.6715. Published Nov 14, 2016. Accessed Nov 20, 2017.
6. Butkus R, Weissman A. Internists’ attitudes toward prevention of firearm injury. Ann Intern Med. 2014;160(12):821-827. doi: 10.7326/M13-1960.
7. Fleegler EW, Lee LK, Monuteaux MC, et al. Firearm Legislation and Firearm-Related Fatalities in the United States. JAMA Intern Med. 2013; 173(9):732-740. doi: 10.1001/jamaimternmed.2013.1286.
8. American Academy of Pediatricians. Addressing gun violence. The federal level. https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Pages/Gun-Violence-Matrix--Intentional-(Federal).aspx. Accessed Nov 20, 2017.
9. Rubin R. Tale of 2 agencies: CDC avoids gun violence research bit NIH funds it. JAMA. 2016;315(16):1689-1692. doi:10.1001/jama.2016.1707.
10. Howell E and Gangopadhyaya A. State variation in the hospital costs of gun violence, 2010 and 2014. The Urban Institute, Health Policy Center.
1. Centers for Disease Control and Prevention, National Center for Health Statistics. FastStats. Injuries. https://www.cdc.gov/nchs/fastats/injury.htm. Accessed Nov 20, 2017.
2. Centers for Disease Control and Prevention, National Center for Health Statistics. FastStats. Suicide. https://www.cdc.gov/nchs/fastats/suicide.htm. Accessed Nov 20, 2017.
3. Sacks CA. In memory of Daniel – Reviving research to prevent gun violence. N Engl J Med. 2015; 372:800-801. doi: 10.1056/NEJMp1415128.
4. U.S. Department of Justice, Federal Bureau of Investigation. A study of active shooter incidents in the United States between 2000 and 2013. Published Sept 16, 2013. Accessed Nov 20, 2017.
5. Sacks CA. The role of physicians in preventing firearm suicides. JAMA Int Med. doi: 10.001/jamainternmed.2016.6715. Published Nov 14, 2016. Accessed Nov 20, 2017.
6. Butkus R, Weissman A. Internists’ attitudes toward prevention of firearm injury. Ann Intern Med. 2014;160(12):821-827. doi: 10.7326/M13-1960.
7. Fleegler EW, Lee LK, Monuteaux MC, et al. Firearm Legislation and Firearm-Related Fatalities in the United States. JAMA Intern Med. 2013; 173(9):732-740. doi: 10.1001/jamaimternmed.2013.1286.
8. American Academy of Pediatricians. Addressing gun violence. The federal level. https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Pages/Gun-Violence-Matrix--Intentional-(Federal).aspx. Accessed Nov 20, 2017.
9. Rubin R. Tale of 2 agencies: CDC avoids gun violence research bit NIH funds it. JAMA. 2016;315(16):1689-1692. doi:10.1001/jama.2016.1707.
10. Howell E and Gangopadhyaya A. State variation in the hospital costs of gun violence, 2010 and 2014. The Urban Institute, Health Policy Center.
Synthetic opioids drive increase in overdose deaths
Opioid-related drug overdose deaths jumped 28% from 2015 to 2016, with the largest increase coming from synthetic opioids, such as illicitly manufactured fentanyl, according to the Centers for Disease Control and Prevention.
The age-adjusted death rate for opioid overdoses increased from 10.4 per 100,000 population in 2015 to 13.3 per 100,000 in 2016, and the 42,249 opioid deaths in 2016 represented more than 66% of all overdose deaths that year, Puja Seth, PhD, and her associates at the CDC reported in the Morbidity and Mortality Weekly Report.
Illegally manufactured fentanyl “is now being mixed into counterfeit opioid and benzodiazepine pills, heroin, and cocaine, likely contributing to increases in overdose death rates involving other substances,” they wrote. To illustrate that point, they reported that cocaine overdose deaths increased 52.4% from 2.1 per 100,000 in 2015 to 3.2 in 2016. The death rate for the other drug category covered in the report – psychostimulants with abuse potential – climbed from 1.8 per 100,000 in 2015 to 2.4 in 2016, for an increase of 33.3%, Dr. Seth and her associates noted.
Data presented from 31 states and the District of Columbia show that
CDC Principal Deputy Director Anne Schuchat, MD, said in a written statement.
Death rates from overdoses involving synthetic opioids increased in 21 states, with 10 states doubling their rates from 2015 to 2016, and 14 states had significant increases in death rates involving heroin. In D.C., for example, the death rate increased 392% (3.9 per 100,000 to 19.2) from synthetic opioid overdoses and 75% (9.9 per 100,000 to 17.3) for deaths related to heroin, the report showed.
“Effective, synchronized programs to prevent drug overdoses will require coordination of law enforcement, first responders, mental health/substance-abuse providers, public health agencies, and community partners,” Dr. Seth and her associates said.
SOURCE: Seth P et al. MMWR. 2018 Mar 30;67(12):349-58.
Opioid-related drug overdose deaths jumped 28% from 2015 to 2016, with the largest increase coming from synthetic opioids, such as illicitly manufactured fentanyl, according to the Centers for Disease Control and Prevention.
The age-adjusted death rate for opioid overdoses increased from 10.4 per 100,000 population in 2015 to 13.3 per 100,000 in 2016, and the 42,249 opioid deaths in 2016 represented more than 66% of all overdose deaths that year, Puja Seth, PhD, and her associates at the CDC reported in the Morbidity and Mortality Weekly Report.
Illegally manufactured fentanyl “is now being mixed into counterfeit opioid and benzodiazepine pills, heroin, and cocaine, likely contributing to increases in overdose death rates involving other substances,” they wrote. To illustrate that point, they reported that cocaine overdose deaths increased 52.4% from 2.1 per 100,000 in 2015 to 3.2 in 2016. The death rate for the other drug category covered in the report – psychostimulants with abuse potential – climbed from 1.8 per 100,000 in 2015 to 2.4 in 2016, for an increase of 33.3%, Dr. Seth and her associates noted.
Data presented from 31 states and the District of Columbia show that
CDC Principal Deputy Director Anne Schuchat, MD, said in a written statement.
Death rates from overdoses involving synthetic opioids increased in 21 states, with 10 states doubling their rates from 2015 to 2016, and 14 states had significant increases in death rates involving heroin. In D.C., for example, the death rate increased 392% (3.9 per 100,000 to 19.2) from synthetic opioid overdoses and 75% (9.9 per 100,000 to 17.3) for deaths related to heroin, the report showed.
“Effective, synchronized programs to prevent drug overdoses will require coordination of law enforcement, first responders, mental health/substance-abuse providers, public health agencies, and community partners,” Dr. Seth and her associates said.
SOURCE: Seth P et al. MMWR. 2018 Mar 30;67(12):349-58.
Opioid-related drug overdose deaths jumped 28% from 2015 to 2016, with the largest increase coming from synthetic opioids, such as illicitly manufactured fentanyl, according to the Centers for Disease Control and Prevention.
The age-adjusted death rate for opioid overdoses increased from 10.4 per 100,000 population in 2015 to 13.3 per 100,000 in 2016, and the 42,249 opioid deaths in 2016 represented more than 66% of all overdose deaths that year, Puja Seth, PhD, and her associates at the CDC reported in the Morbidity and Mortality Weekly Report.
Illegally manufactured fentanyl “is now being mixed into counterfeit opioid and benzodiazepine pills, heroin, and cocaine, likely contributing to increases in overdose death rates involving other substances,” they wrote. To illustrate that point, they reported that cocaine overdose deaths increased 52.4% from 2.1 per 100,000 in 2015 to 3.2 in 2016. The death rate for the other drug category covered in the report – psychostimulants with abuse potential – climbed from 1.8 per 100,000 in 2015 to 2.4 in 2016, for an increase of 33.3%, Dr. Seth and her associates noted.
Data presented from 31 states and the District of Columbia show that
CDC Principal Deputy Director Anne Schuchat, MD, said in a written statement.
Death rates from overdoses involving synthetic opioids increased in 21 states, with 10 states doubling their rates from 2015 to 2016, and 14 states had significant increases in death rates involving heroin. In D.C., for example, the death rate increased 392% (3.9 per 100,000 to 19.2) from synthetic opioid overdoses and 75% (9.9 per 100,000 to 17.3) for deaths related to heroin, the report showed.
“Effective, synchronized programs to prevent drug overdoses will require coordination of law enforcement, first responders, mental health/substance-abuse providers, public health agencies, and community partners,” Dr. Seth and her associates said.
SOURCE: Seth P et al. MMWR. 2018 Mar 30;67(12):349-58.
FROM MMWR
Many VTE patients live in fear of the next event
SAN DIEGO – An estimated 41% of patients who experienced a venous thromboembolism (VTE) fear another clot often or almost all the time. In addition, about 25% report abnormal levels of anxiety, and 12% have abnormal depression scores.
Those are key findings from a large survey that set out to estimate the number of bleeding harms and emotional harms experienced by a U.S. population of adults who have experienced a VTE.
“There is emerging research in Europe that shows high levels of stress and anxiety in people who have a thrombosis event,” lead study author Michael Feehan, PhD, said in an interview at the biennial summit of the Thrombosis & Hemostasis Societies of North America. “We interviewed people around the country and found that a lot of them were living with fear, anxiety, and distress. We did a projective exercise and asked, ‘If VTE was an animal, what would it be?’ Many responded with snakes and bears, hostile things. Snakes came up a lot. Snakes can be dormant, and then they can suddenly come out and bite you. That was the kind of language they were using.”
In what he said is the largest study of its kind, Dr. Feehan, a psychologist in the College of Pharmacy at the University of Utah, Salt Lake City, and his associates conducted an online survey of 907 patients aged 18 and older who had experienced a VTE event in the previous 24 months.
The survey was administered in May 2016 and excluded patients with cancer-related VTE. It took about 30 minutes to complete and included questions about the bleeding harms that have occurred since their VTE diagnosis, such as nosebleeds or a cut difficult to control, excessive bruising, vomiting blood, bloody urine, and blood in stools. It also included standardized measures of anxiety, depression, cognitive function, and ratings on eight items of current distress, feeling tense, anxious, confused, depressed, afraid, angry, frustrated, or annoyed.
Self-reported bleeding events included excessive bruising (45%), bleeding from cuts difficult to control (33%), and epistaxis (16%). As for emotional harm, 41% of respondents lived in fear of getting another clot “often” or “almost all the time,” while 25% experienced abnormally high levels of anxiety, and 12% experienced abnormally high levels of depression.
A multivariate structural equation model revealed the following principal factors significantly associated with a composite latent variable of emotional harm: poor health literacy, younger age, the lack of perceived self-control over one’s health, history of medical mistakes in care, and overt barriers to health care access such as transportation limitations and financial limitations (P less than .05 for all associations).
“If you’re working with patients who believe they don’t have any control over their own care, or if they’re younger or have other disease states, or if they have difficulty getting to and from the hospital, all of those things contribute to elevated emotional harms,” Dr. Feehan said. “That level of emotional harm is clinically relevant.”
After the research team shared the study results with staff of the university’s thrombosis services, clinicians started changing how they interview patients. “For example, instead of asking just ‘Have you experienced any VTE symptoms?’ they now ask things like, ‘How are you feeling?’ or ‘How are things going for you living with the disease?’” Dr. Feehan noted. “Then, patients might say, ‘I’m actually quite worried.’ Such questions can help patients open up about how they feel and foster a better relationship with their provider. A better relationship with their provider might help them feel more in control.”
The study was supported by Pfizer Independent Grants for Learning & Change, Bristol-Myers Squibb Independent Medical Education, the Joint Commission, the National Eye Institute, and an unrestricted grant from Research to Prevent Blindness. Dr. Feehan disclosed that he has consulted for Pfizer in the past.
SOURCE: Feehan et al. THSNA 2018, Poster 75.
SAN DIEGO – An estimated 41% of patients who experienced a venous thromboembolism (VTE) fear another clot often or almost all the time. In addition, about 25% report abnormal levels of anxiety, and 12% have abnormal depression scores.
Those are key findings from a large survey that set out to estimate the number of bleeding harms and emotional harms experienced by a U.S. population of adults who have experienced a VTE.
“There is emerging research in Europe that shows high levels of stress and anxiety in people who have a thrombosis event,” lead study author Michael Feehan, PhD, said in an interview at the biennial summit of the Thrombosis & Hemostasis Societies of North America. “We interviewed people around the country and found that a lot of them were living with fear, anxiety, and distress. We did a projective exercise and asked, ‘If VTE was an animal, what would it be?’ Many responded with snakes and bears, hostile things. Snakes came up a lot. Snakes can be dormant, and then they can suddenly come out and bite you. That was the kind of language they were using.”
In what he said is the largest study of its kind, Dr. Feehan, a psychologist in the College of Pharmacy at the University of Utah, Salt Lake City, and his associates conducted an online survey of 907 patients aged 18 and older who had experienced a VTE event in the previous 24 months.
The survey was administered in May 2016 and excluded patients with cancer-related VTE. It took about 30 minutes to complete and included questions about the bleeding harms that have occurred since their VTE diagnosis, such as nosebleeds or a cut difficult to control, excessive bruising, vomiting blood, bloody urine, and blood in stools. It also included standardized measures of anxiety, depression, cognitive function, and ratings on eight items of current distress, feeling tense, anxious, confused, depressed, afraid, angry, frustrated, or annoyed.
Self-reported bleeding events included excessive bruising (45%), bleeding from cuts difficult to control (33%), and epistaxis (16%). As for emotional harm, 41% of respondents lived in fear of getting another clot “often” or “almost all the time,” while 25% experienced abnormally high levels of anxiety, and 12% experienced abnormally high levels of depression.
A multivariate structural equation model revealed the following principal factors significantly associated with a composite latent variable of emotional harm: poor health literacy, younger age, the lack of perceived self-control over one’s health, history of medical mistakes in care, and overt barriers to health care access such as transportation limitations and financial limitations (P less than .05 for all associations).
“If you’re working with patients who believe they don’t have any control over their own care, or if they’re younger or have other disease states, or if they have difficulty getting to and from the hospital, all of those things contribute to elevated emotional harms,” Dr. Feehan said. “That level of emotional harm is clinically relevant.”
After the research team shared the study results with staff of the university’s thrombosis services, clinicians started changing how they interview patients. “For example, instead of asking just ‘Have you experienced any VTE symptoms?’ they now ask things like, ‘How are you feeling?’ or ‘How are things going for you living with the disease?’” Dr. Feehan noted. “Then, patients might say, ‘I’m actually quite worried.’ Such questions can help patients open up about how they feel and foster a better relationship with their provider. A better relationship with their provider might help them feel more in control.”
The study was supported by Pfizer Independent Grants for Learning & Change, Bristol-Myers Squibb Independent Medical Education, the Joint Commission, the National Eye Institute, and an unrestricted grant from Research to Prevent Blindness. Dr. Feehan disclosed that he has consulted for Pfizer in the past.
SOURCE: Feehan et al. THSNA 2018, Poster 75.
SAN DIEGO – An estimated 41% of patients who experienced a venous thromboembolism (VTE) fear another clot often or almost all the time. In addition, about 25% report abnormal levels of anxiety, and 12% have abnormal depression scores.
Those are key findings from a large survey that set out to estimate the number of bleeding harms and emotional harms experienced by a U.S. population of adults who have experienced a VTE.
“There is emerging research in Europe that shows high levels of stress and anxiety in people who have a thrombosis event,” lead study author Michael Feehan, PhD, said in an interview at the biennial summit of the Thrombosis & Hemostasis Societies of North America. “We interviewed people around the country and found that a lot of them were living with fear, anxiety, and distress. We did a projective exercise and asked, ‘If VTE was an animal, what would it be?’ Many responded with snakes and bears, hostile things. Snakes came up a lot. Snakes can be dormant, and then they can suddenly come out and bite you. That was the kind of language they were using.”
In what he said is the largest study of its kind, Dr. Feehan, a psychologist in the College of Pharmacy at the University of Utah, Salt Lake City, and his associates conducted an online survey of 907 patients aged 18 and older who had experienced a VTE event in the previous 24 months.
The survey was administered in May 2016 and excluded patients with cancer-related VTE. It took about 30 minutes to complete and included questions about the bleeding harms that have occurred since their VTE diagnosis, such as nosebleeds or a cut difficult to control, excessive bruising, vomiting blood, bloody urine, and blood in stools. It also included standardized measures of anxiety, depression, cognitive function, and ratings on eight items of current distress, feeling tense, anxious, confused, depressed, afraid, angry, frustrated, or annoyed.
Self-reported bleeding events included excessive bruising (45%), bleeding from cuts difficult to control (33%), and epistaxis (16%). As for emotional harm, 41% of respondents lived in fear of getting another clot “often” or “almost all the time,” while 25% experienced abnormally high levels of anxiety, and 12% experienced abnormally high levels of depression.
A multivariate structural equation model revealed the following principal factors significantly associated with a composite latent variable of emotional harm: poor health literacy, younger age, the lack of perceived self-control over one’s health, history of medical mistakes in care, and overt barriers to health care access such as transportation limitations and financial limitations (P less than .05 for all associations).
“If you’re working with patients who believe they don’t have any control over their own care, or if they’re younger or have other disease states, or if they have difficulty getting to and from the hospital, all of those things contribute to elevated emotional harms,” Dr. Feehan said. “That level of emotional harm is clinically relevant.”
After the research team shared the study results with staff of the university’s thrombosis services, clinicians started changing how they interview patients. “For example, instead of asking just ‘Have you experienced any VTE symptoms?’ they now ask things like, ‘How are you feeling?’ or ‘How are things going for you living with the disease?’” Dr. Feehan noted. “Then, patients might say, ‘I’m actually quite worried.’ Such questions can help patients open up about how they feel and foster a better relationship with their provider. A better relationship with their provider might help them feel more in control.”
The study was supported by Pfizer Independent Grants for Learning & Change, Bristol-Myers Squibb Independent Medical Education, the Joint Commission, the National Eye Institute, and an unrestricted grant from Research to Prevent Blindness. Dr. Feehan disclosed that he has consulted for Pfizer in the past.
SOURCE: Feehan et al. THSNA 2018, Poster 75.
REPORTING FROM THSNA 2018
Key clinical point: Consider asking VTE patients how living with their disease affects them from an emotional standpoint.
Major finding: Of 907 survey respondents, 41% said they live in fear of getting another clot “often” or “almost all the time.”
Study details: An online survey of 907 patients aged 18 and older who had experienced a VTE event in the previous 24 months.
Disclosures: The study was supported by Pfizer Independent Grants for Learning & Change, Bristol-Myers Squibb Independent Medical Education, the Joint Commission, the National Eye Institute, and an unrestricted grant from Research to Prevent Blindness. Dr. Feehan disclosed that he has consulted for Pfizer in the past.
Source: Feehan M et al. THSNA 2018, Poster 75.
Are higher rifampin doses for pulmonary TB more effective?
BOSTON – Current daily doses of rifampin for treating pulmonary tuberculosis may be too low and could be safely increased, results of a randomized phase 2 study suggest.
“Back in the 1970s, rifampin was an expensive drug, and attempts to shorten TB therapy using higher but intermittent doses of rifampin were unsuccessful at that time because of increased toxicity. That line of inquiry was essentially dormant for 40 years,” said Gustavo Velásquez, MD, from Brigham & Women’s Hospital in Boston.
To get a better idea of optimal rifampin dosing for the treatment of pulmonary TB, Dr. Velásquez and his colleagues conducted the HIRIF (High-Dose Rifampin in Patients With TB) trial. The phase 2 study was designed to evaluate the pharmacokinetics, efficacy, and safety of higher daily rifampin doses for pulmonary TB.
They looked at the three parameters across three treatments arms: 10 mg/kg rifampin (the current standard of care), 15 mg/kg, or 20 mg/kg.
Patients in Peru were screened, enrolled, and randomized in cohorts of 60 patients each to one of the three specified dose levels, which they received either as additional rifampin tablets or placebo for the first 8 weeks of treatment, after which all patients were continued on rifampin 10 mg/kg to complete a 6-month regimen. All patients were followed for an additional 6 months to for assessment of TB recurrence.
Rifampin total doses ranged from as low as 300 mg for patients in the 30 kg-37 kg weight range, to as high as 1,500 mg for those weighing more than 70 kg.
The efficacy analysis was by modified intention to treat, excluding 6 patients who had insufficient log10 colony-forming units (CFUs) of TB, and a per-protocol analysis excluding an additional 42 patients whose doses of rifampin were affected by three study halts for adverse events. After each halt and review by the data-safety monitoring board, the trial was allowed to resume, but because enrollment and experimental dosing also were suspended, patients in the 15- and 20-mg/kg arms received 10 mg/kg during the 2-5 week halts. The number of patients in the 10-, 15-, and 20-mg/kg doses included in the per-protocol analysis were 56, 38, and 38, respectively,
Pharmacokinetic evidence from this study, previously published, showed that the median maximum drug concentration (Cmax) in serum in the experimental arms reached the lower end of the targeted range of 8 mcg/mL or greater, whereas the median in the standard-of-care arm was 6.2 mcg/mL. Only 33% of patients in the 10-mg/kg arm reached the minimum 8-mcg/mL level, Dr. Velásquez noted, vs. 72% and 81% of patients in the 15- and 20-mg/kg doses, respectively.
In the modified intention-to-treat population, for every 5-mg/kg increase in rifampin dose, there was a nonsignificant trend toward faster decline in TB CFUs in sputum. Similarly, for every 1-log increase in rifampin AUC/MIC, there was a trend, albeit nonsignificant, toward faster decline.
However, in patients in the per-protocol analysis, every 5-mg/kg dose increase and 1-log increase in rifampin AUC was associated with significantly faster declines in CFUs (P = .022 and .011, respectively).
An analysis of treatment outcomes at 12 months, a secondary endpoint, showed that there were five cases of treatment failure, including three in the control arm and one each in 15- and 20-mg/kg arms, and six cases of recurrence after cure, which occurred in three, one, and two patients, respectively,
The safety analysis by intention-to-treat showed that the incidence of grade 2 or greater rifampin-related adverse events (AEs) were 43.3%, 51.7%, and 38.3% in the 10-, 15-, and 20-mg/kg doses, differences that were not statistically significant.
In addition, there were no significant differences among the treatment arms in either time to first grade 2 or greater rifampin-related AEs, the occurrence of one or more grade 2 or greater hepatic rifampin-AEs, or time to first hepatic rifampin-related AEs of grade 2 or above.
Dr. Velásquez noted that the study was limited by the possibility that the study halts could have biased efficacy effect estimates toward null and by differences in weight distribution among the three treatment arms.
“This actually is the first trial that shows not only a dose response of rifampin but also an exposure response of rifampin in combination therapy,” he said. “Our study supports that even higher doses of rifampin beyond what we studied of 20 mg/kg should be studied for potential treatment shortening.” The evidence also suggests that the current 10-mg/kg dose is low and could be safely increased to a 15- or 20-mg/kg dose, he concluded.
In a media briefing following the presentation, moderator Constance Benson, MD, from the University of California San Diego, who was not involved in the study, commented that with “high-dose rifampin, I think we have a really very robust body of literature to which this study can be added, demonstrating the safety of high-dose rifampin in the context of TB treatment.”
“There are some circumstances where I think using a much higher dose than we’ve been using would be an appropriate thing to do,” she added.
Examples of patients who might benefit include patients with disseminated TB or people with more serious TB than the average case, she said.
The study was supported by the National Institute of Allergy and Infectious Diseases. Dr. Velásquez and Dr. Benson reported no relevant conflicts of interest.
SOURCE: Velásquez GE et al. CROI 2018, Abstract 39LB.
BOSTON – Current daily doses of rifampin for treating pulmonary tuberculosis may be too low and could be safely increased, results of a randomized phase 2 study suggest.
“Back in the 1970s, rifampin was an expensive drug, and attempts to shorten TB therapy using higher but intermittent doses of rifampin were unsuccessful at that time because of increased toxicity. That line of inquiry was essentially dormant for 40 years,” said Gustavo Velásquez, MD, from Brigham & Women’s Hospital in Boston.
To get a better idea of optimal rifampin dosing for the treatment of pulmonary TB, Dr. Velásquez and his colleagues conducted the HIRIF (High-Dose Rifampin in Patients With TB) trial. The phase 2 study was designed to evaluate the pharmacokinetics, efficacy, and safety of higher daily rifampin doses for pulmonary TB.
They looked at the three parameters across three treatments arms: 10 mg/kg rifampin (the current standard of care), 15 mg/kg, or 20 mg/kg.
Patients in Peru were screened, enrolled, and randomized in cohorts of 60 patients each to one of the three specified dose levels, which they received either as additional rifampin tablets or placebo for the first 8 weeks of treatment, after which all patients were continued on rifampin 10 mg/kg to complete a 6-month regimen. All patients were followed for an additional 6 months to for assessment of TB recurrence.
Rifampin total doses ranged from as low as 300 mg for patients in the 30 kg-37 kg weight range, to as high as 1,500 mg for those weighing more than 70 kg.
The efficacy analysis was by modified intention to treat, excluding 6 patients who had insufficient log10 colony-forming units (CFUs) of TB, and a per-protocol analysis excluding an additional 42 patients whose doses of rifampin were affected by three study halts for adverse events. After each halt and review by the data-safety monitoring board, the trial was allowed to resume, but because enrollment and experimental dosing also were suspended, patients in the 15- and 20-mg/kg arms received 10 mg/kg during the 2-5 week halts. The number of patients in the 10-, 15-, and 20-mg/kg doses included in the per-protocol analysis were 56, 38, and 38, respectively,
Pharmacokinetic evidence from this study, previously published, showed that the median maximum drug concentration (Cmax) in serum in the experimental arms reached the lower end of the targeted range of 8 mcg/mL or greater, whereas the median in the standard-of-care arm was 6.2 mcg/mL. Only 33% of patients in the 10-mg/kg arm reached the minimum 8-mcg/mL level, Dr. Velásquez noted, vs. 72% and 81% of patients in the 15- and 20-mg/kg doses, respectively.
In the modified intention-to-treat population, for every 5-mg/kg increase in rifampin dose, there was a nonsignificant trend toward faster decline in TB CFUs in sputum. Similarly, for every 1-log increase in rifampin AUC/MIC, there was a trend, albeit nonsignificant, toward faster decline.
However, in patients in the per-protocol analysis, every 5-mg/kg dose increase and 1-log increase in rifampin AUC was associated with significantly faster declines in CFUs (P = .022 and .011, respectively).
An analysis of treatment outcomes at 12 months, a secondary endpoint, showed that there were five cases of treatment failure, including three in the control arm and one each in 15- and 20-mg/kg arms, and six cases of recurrence after cure, which occurred in three, one, and two patients, respectively,
The safety analysis by intention-to-treat showed that the incidence of grade 2 or greater rifampin-related adverse events (AEs) were 43.3%, 51.7%, and 38.3% in the 10-, 15-, and 20-mg/kg doses, differences that were not statistically significant.
In addition, there were no significant differences among the treatment arms in either time to first grade 2 or greater rifampin-related AEs, the occurrence of one or more grade 2 or greater hepatic rifampin-AEs, or time to first hepatic rifampin-related AEs of grade 2 or above.
Dr. Velásquez noted that the study was limited by the possibility that the study halts could have biased efficacy effect estimates toward null and by differences in weight distribution among the three treatment arms.
“This actually is the first trial that shows not only a dose response of rifampin but also an exposure response of rifampin in combination therapy,” he said. “Our study supports that even higher doses of rifampin beyond what we studied of 20 mg/kg should be studied for potential treatment shortening.” The evidence also suggests that the current 10-mg/kg dose is low and could be safely increased to a 15- or 20-mg/kg dose, he concluded.
In a media briefing following the presentation, moderator Constance Benson, MD, from the University of California San Diego, who was not involved in the study, commented that with “high-dose rifampin, I think we have a really very robust body of literature to which this study can be added, demonstrating the safety of high-dose rifampin in the context of TB treatment.”
“There are some circumstances where I think using a much higher dose than we’ve been using would be an appropriate thing to do,” she added.
Examples of patients who might benefit include patients with disseminated TB or people with more serious TB than the average case, she said.
The study was supported by the National Institute of Allergy and Infectious Diseases. Dr. Velásquez and Dr. Benson reported no relevant conflicts of interest.
SOURCE: Velásquez GE et al. CROI 2018, Abstract 39LB.
BOSTON – Current daily doses of rifampin for treating pulmonary tuberculosis may be too low and could be safely increased, results of a randomized phase 2 study suggest.
“Back in the 1970s, rifampin was an expensive drug, and attempts to shorten TB therapy using higher but intermittent doses of rifampin were unsuccessful at that time because of increased toxicity. That line of inquiry was essentially dormant for 40 years,” said Gustavo Velásquez, MD, from Brigham & Women’s Hospital in Boston.
To get a better idea of optimal rifampin dosing for the treatment of pulmonary TB, Dr. Velásquez and his colleagues conducted the HIRIF (High-Dose Rifampin in Patients With TB) trial. The phase 2 study was designed to evaluate the pharmacokinetics, efficacy, and safety of higher daily rifampin doses for pulmonary TB.
They looked at the three parameters across three treatments arms: 10 mg/kg rifampin (the current standard of care), 15 mg/kg, or 20 mg/kg.
Patients in Peru were screened, enrolled, and randomized in cohorts of 60 patients each to one of the three specified dose levels, which they received either as additional rifampin tablets or placebo for the first 8 weeks of treatment, after which all patients were continued on rifampin 10 mg/kg to complete a 6-month regimen. All patients were followed for an additional 6 months to for assessment of TB recurrence.
Rifampin total doses ranged from as low as 300 mg for patients in the 30 kg-37 kg weight range, to as high as 1,500 mg for those weighing more than 70 kg.
The efficacy analysis was by modified intention to treat, excluding 6 patients who had insufficient log10 colony-forming units (CFUs) of TB, and a per-protocol analysis excluding an additional 42 patients whose doses of rifampin were affected by three study halts for adverse events. After each halt and review by the data-safety monitoring board, the trial was allowed to resume, but because enrollment and experimental dosing also were suspended, patients in the 15- and 20-mg/kg arms received 10 mg/kg during the 2-5 week halts. The number of patients in the 10-, 15-, and 20-mg/kg doses included in the per-protocol analysis were 56, 38, and 38, respectively,
Pharmacokinetic evidence from this study, previously published, showed that the median maximum drug concentration (Cmax) in serum in the experimental arms reached the lower end of the targeted range of 8 mcg/mL or greater, whereas the median in the standard-of-care arm was 6.2 mcg/mL. Only 33% of patients in the 10-mg/kg arm reached the minimum 8-mcg/mL level, Dr. Velásquez noted, vs. 72% and 81% of patients in the 15- and 20-mg/kg doses, respectively.
In the modified intention-to-treat population, for every 5-mg/kg increase in rifampin dose, there was a nonsignificant trend toward faster decline in TB CFUs in sputum. Similarly, for every 1-log increase in rifampin AUC/MIC, there was a trend, albeit nonsignificant, toward faster decline.
However, in patients in the per-protocol analysis, every 5-mg/kg dose increase and 1-log increase in rifampin AUC was associated with significantly faster declines in CFUs (P = .022 and .011, respectively).
An analysis of treatment outcomes at 12 months, a secondary endpoint, showed that there were five cases of treatment failure, including three in the control arm and one each in 15- and 20-mg/kg arms, and six cases of recurrence after cure, which occurred in three, one, and two patients, respectively,
The safety analysis by intention-to-treat showed that the incidence of grade 2 or greater rifampin-related adverse events (AEs) were 43.3%, 51.7%, and 38.3% in the 10-, 15-, and 20-mg/kg doses, differences that were not statistically significant.
In addition, there were no significant differences among the treatment arms in either time to first grade 2 or greater rifampin-related AEs, the occurrence of one or more grade 2 or greater hepatic rifampin-AEs, or time to first hepatic rifampin-related AEs of grade 2 or above.
Dr. Velásquez noted that the study was limited by the possibility that the study halts could have biased efficacy effect estimates toward null and by differences in weight distribution among the three treatment arms.
“This actually is the first trial that shows not only a dose response of rifampin but also an exposure response of rifampin in combination therapy,” he said. “Our study supports that even higher doses of rifampin beyond what we studied of 20 mg/kg should be studied for potential treatment shortening.” The evidence also suggests that the current 10-mg/kg dose is low and could be safely increased to a 15- or 20-mg/kg dose, he concluded.
In a media briefing following the presentation, moderator Constance Benson, MD, from the University of California San Diego, who was not involved in the study, commented that with “high-dose rifampin, I think we have a really very robust body of literature to which this study can be added, demonstrating the safety of high-dose rifampin in the context of TB treatment.”
“There are some circumstances where I think using a much higher dose than we’ve been using would be an appropriate thing to do,” she added.
Examples of patients who might benefit include patients with disseminated TB or people with more serious TB than the average case, she said.
The study was supported by the National Institute of Allergy and Infectious Diseases. Dr. Velásquez and Dr. Benson reported no relevant conflicts of interest.
SOURCE: Velásquez GE et al. CROI 2018, Abstract 39LB.
REPORTING FROM CROI 2018
Key clinical point: Higher rifampin doses than customarily used offer better control of TB with safety, investigators say.
Major finding: In a per-protocol analysis, reduction in TB colony-forming units was significantly faster with 15- or 20-mg/kg rifampin dose vs. the standard 10-mg/kg dose.
Data source: Randomized, controlled trial in 180 Peruvian patients with pulmonary tuberculosis.
Disclosures: The study was supported by the National Institute of Allergy and Infectious Diseases. Dr. Velásquez and Dr. Benson reported no relevant conflicts of interest.
Source: Velásquez GE et al. CROI 2018, Abstract 39LB.
SHM to induct new Masters in Hospital Medicine
The Society of Hospital Medicine will induct four new Masters in Hospital Medicine (MHM), the society’s highest professional honor, at HM18. Recipients are distinguished by the excellence and significance of their contributions to the field of hospital medicine and health care overall, said Larry Wellikson, MD, MHM, CEO of the Society of Hospital Medicine. They have been selected because of personal character; positions of honor; contributions toward furthering the society’s goals; distinction in practice, education, medical research; and other achievements in science or in the art of hospital medicine.
MHM nominees must be highly accomplished individuals in the hospital medicine specialty. Evidence of their achievements can come from many types of activities, such as excellence in clinical care, health care initiatives, education, research, writing and publication, volunteerism, and administrative positions. Current members of the society’s board are not eligible for nomination or selection.
This is truly the Hall of Fame for hospital medicine. Congratulations to this year’s MHMs.
Andrew Auerbach, MD, MPH, MHM, is professor of medicine in residence at the University of California, San Francisco, where he also serves as director of innovation research for the Center for Digital Health and Innovation. He was one of the first 200 members of the Society of Hospital Medicine when it was first called the National Association of Inpatient Physicians. “I have contributed to the field and society through my research and national role as a hospitalist in high-profile policy and guideline initiatives,” he said. These include formulating guidelines for the Institute of Medicine, American College of Cardiology, and Agency for Healthcare Research and Quality.
Dr. Auerbach has been deeply involved with the society through his role as chair of its Research Committee and Academic Hospitalist Committee for several years. Other accomplishments include being a founding framer of the Academic Hospitalist Academy, contributing to white papers outlining academic hospitalists’ needs, cofounding a national research network for hospitalists, and serving as editor-in-chief of the Journal of Hospital Medicine for 7 years.
“Being named an MHM is wonderful recognition,” he said. “I just hope it does not represent a ‘lifetime achievement’ award – I still have many things I want to accomplish in my career!”
Daniel J. Brotman, MD, MHM, professor of medicine, director of the hospitalist program at Johns Hopkins Hospital, Baltimore, and a member of the Society of Hospital Medicine since 2000, has served in many roles at the organization. These include being a member of the Annual Meeting Planning Committee (2007-2016), course director for the annual meeting (2013, 2014), chair of the Education Committee (2012-2016), and a member of the Research Committee (2008-2015). Dr. Brotman also won the society’s Research Award in 2015. He has been a staple of the editorial team at the Journal of Hospital Medicine since its founding in 2006.
“I am truly honored to be recognized for my participation and leadership in the field of hospital medicine and the society,” he said. “I am humbled to be included among the many luminaries who have won the award in prior years.”
He has been in his current role at Johns Hopkins since 2005, where he has more than tripled the program’s size and grown its academic profile.
“I have had the good fortune to work with a lot of talented faculty members and have helped them advance professionally and academically, while they pushed me to be a better leader,” Dr. Brotman said. “I encourage my team members to participate in the Society of Hospital Medicine; it is a fabulous way to gain leadership opportunities while staying abreast of the most important developments in the field.”
Bob Harrington, MD, MHM, is president and chief medical officer, SurveyVitals, an organization that provides digital patient experience and Consumer Assessment of Healthcare Providers and Systems (CAHPS) surveys nationwide to hospitals, health care systems, and physician practices. He believes he is an award recipient because he is a long-time advocate for hospitalists trained in family medicine (HTFMs). “I have always looked for ways to level the playing field for clinical and leadership opportunities for HTFMs,” he said.
Dr. Harrington first became involved with the Society of Hospital Medicine as chair of its Family Medicine Committee in the late 1990s. In that role, his committee looked at unique needs of HTFMs, including hiring practices, providing education to potential employers, and assisting HTFM members in career advancement.
“Our efforts resulted in tremendous growth of the HTFM membership, as these physicians began to view the society as their professional home and not as an internal medicine–dominant organization,” he said. He went on to become the first HTFM to serve on the society’s board and then became the first HTFM to be its president.
“This award is the greatest professional honor that I have received,” Dr. Harrington said. “It is especially important to me, because it is from a group of people whom I hold in the highest professional regard. They always put quality and patients first. I have been privileged to play a small part in that.”
Janet Nagamine, MD, BSN, MHM, is a hospitalist in the department of hospital-based specialty and inpatient palliative care at Kaiser Permanente Hospital in Santa Clara, Calif.
Dr. Nagamine was one of the first 200 people to join the Society of Hospital Medicine. Among her many roles within the society were serving on its board of directors from 2009 to 2014 and chairing the Quality and Safety committee for 5 years.
“I’m honored to be acknowledged in this formal and prestigious way, because my career path hasn’t always followed the traditional course of recipients who receive this type of award,” commented Dr. Nagamine, who has worked in a community hospital for the last 18 years. “This speaks volumes to the type of organization that the Society of Hospital Medicine is, and it makes me proud.”
She started her career as an ICU nurse and spent the last 30 years in various institutional and organizational roles trying to make hospitals a better place.
“At times, I was juggling family responsibilities and had to defer the fancy titles, but I always found a way to contribute meaningfully through my work with the Society of Hospital Medicine.”
The Society of Hospital Medicine will induct four new Masters in Hospital Medicine (MHM), the society’s highest professional honor, at HM18. Recipients are distinguished by the excellence and significance of their contributions to the field of hospital medicine and health care overall, said Larry Wellikson, MD, MHM, CEO of the Society of Hospital Medicine. They have been selected because of personal character; positions of honor; contributions toward furthering the society’s goals; distinction in practice, education, medical research; and other achievements in science or in the art of hospital medicine.
MHM nominees must be highly accomplished individuals in the hospital medicine specialty. Evidence of their achievements can come from many types of activities, such as excellence in clinical care, health care initiatives, education, research, writing and publication, volunteerism, and administrative positions. Current members of the society’s board are not eligible for nomination or selection.
This is truly the Hall of Fame for hospital medicine. Congratulations to this year’s MHMs.
Andrew Auerbach, MD, MPH, MHM, is professor of medicine in residence at the University of California, San Francisco, where he also serves as director of innovation research for the Center for Digital Health and Innovation. He was one of the first 200 members of the Society of Hospital Medicine when it was first called the National Association of Inpatient Physicians. “I have contributed to the field and society through my research and national role as a hospitalist in high-profile policy and guideline initiatives,” he said. These include formulating guidelines for the Institute of Medicine, American College of Cardiology, and Agency for Healthcare Research and Quality.
Dr. Auerbach has been deeply involved with the society through his role as chair of its Research Committee and Academic Hospitalist Committee for several years. Other accomplishments include being a founding framer of the Academic Hospitalist Academy, contributing to white papers outlining academic hospitalists’ needs, cofounding a national research network for hospitalists, and serving as editor-in-chief of the Journal of Hospital Medicine for 7 years.
“Being named an MHM is wonderful recognition,” he said. “I just hope it does not represent a ‘lifetime achievement’ award – I still have many things I want to accomplish in my career!”
Daniel J. Brotman, MD, MHM, professor of medicine, director of the hospitalist program at Johns Hopkins Hospital, Baltimore, and a member of the Society of Hospital Medicine since 2000, has served in many roles at the organization. These include being a member of the Annual Meeting Planning Committee (2007-2016), course director for the annual meeting (2013, 2014), chair of the Education Committee (2012-2016), and a member of the Research Committee (2008-2015). Dr. Brotman also won the society’s Research Award in 2015. He has been a staple of the editorial team at the Journal of Hospital Medicine since its founding in 2006.
“I am truly honored to be recognized for my participation and leadership in the field of hospital medicine and the society,” he said. “I am humbled to be included among the many luminaries who have won the award in prior years.”
He has been in his current role at Johns Hopkins since 2005, where he has more than tripled the program’s size and grown its academic profile.
“I have had the good fortune to work with a lot of talented faculty members and have helped them advance professionally and academically, while they pushed me to be a better leader,” Dr. Brotman said. “I encourage my team members to participate in the Society of Hospital Medicine; it is a fabulous way to gain leadership opportunities while staying abreast of the most important developments in the field.”
Bob Harrington, MD, MHM, is president and chief medical officer, SurveyVitals, an organization that provides digital patient experience and Consumer Assessment of Healthcare Providers and Systems (CAHPS) surveys nationwide to hospitals, health care systems, and physician practices. He believes he is an award recipient because he is a long-time advocate for hospitalists trained in family medicine (HTFMs). “I have always looked for ways to level the playing field for clinical and leadership opportunities for HTFMs,” he said.
Dr. Harrington first became involved with the Society of Hospital Medicine as chair of its Family Medicine Committee in the late 1990s. In that role, his committee looked at unique needs of HTFMs, including hiring practices, providing education to potential employers, and assisting HTFM members in career advancement.
“Our efforts resulted in tremendous growth of the HTFM membership, as these physicians began to view the society as their professional home and not as an internal medicine–dominant organization,” he said. He went on to become the first HTFM to serve on the society’s board and then became the first HTFM to be its president.
“This award is the greatest professional honor that I have received,” Dr. Harrington said. “It is especially important to me, because it is from a group of people whom I hold in the highest professional regard. They always put quality and patients first. I have been privileged to play a small part in that.”
Janet Nagamine, MD, BSN, MHM, is a hospitalist in the department of hospital-based specialty and inpatient palliative care at Kaiser Permanente Hospital in Santa Clara, Calif.
Dr. Nagamine was one of the first 200 people to join the Society of Hospital Medicine. Among her many roles within the society were serving on its board of directors from 2009 to 2014 and chairing the Quality and Safety committee for 5 years.
“I’m honored to be acknowledged in this formal and prestigious way, because my career path hasn’t always followed the traditional course of recipients who receive this type of award,” commented Dr. Nagamine, who has worked in a community hospital for the last 18 years. “This speaks volumes to the type of organization that the Society of Hospital Medicine is, and it makes me proud.”
She started her career as an ICU nurse and spent the last 30 years in various institutional and organizational roles trying to make hospitals a better place.
“At times, I was juggling family responsibilities and had to defer the fancy titles, but I always found a way to contribute meaningfully through my work with the Society of Hospital Medicine.”
The Society of Hospital Medicine will induct four new Masters in Hospital Medicine (MHM), the society’s highest professional honor, at HM18. Recipients are distinguished by the excellence and significance of their contributions to the field of hospital medicine and health care overall, said Larry Wellikson, MD, MHM, CEO of the Society of Hospital Medicine. They have been selected because of personal character; positions of honor; contributions toward furthering the society’s goals; distinction in practice, education, medical research; and other achievements in science or in the art of hospital medicine.
MHM nominees must be highly accomplished individuals in the hospital medicine specialty. Evidence of their achievements can come from many types of activities, such as excellence in clinical care, health care initiatives, education, research, writing and publication, volunteerism, and administrative positions. Current members of the society’s board are not eligible for nomination or selection.
This is truly the Hall of Fame for hospital medicine. Congratulations to this year’s MHMs.
Andrew Auerbach, MD, MPH, MHM, is professor of medicine in residence at the University of California, San Francisco, where he also serves as director of innovation research for the Center for Digital Health and Innovation. He was one of the first 200 members of the Society of Hospital Medicine when it was first called the National Association of Inpatient Physicians. “I have contributed to the field and society through my research and national role as a hospitalist in high-profile policy and guideline initiatives,” he said. These include formulating guidelines for the Institute of Medicine, American College of Cardiology, and Agency for Healthcare Research and Quality.
Dr. Auerbach has been deeply involved with the society through his role as chair of its Research Committee and Academic Hospitalist Committee for several years. Other accomplishments include being a founding framer of the Academic Hospitalist Academy, contributing to white papers outlining academic hospitalists’ needs, cofounding a national research network for hospitalists, and serving as editor-in-chief of the Journal of Hospital Medicine for 7 years.
“Being named an MHM is wonderful recognition,” he said. “I just hope it does not represent a ‘lifetime achievement’ award – I still have many things I want to accomplish in my career!”
Daniel J. Brotman, MD, MHM, professor of medicine, director of the hospitalist program at Johns Hopkins Hospital, Baltimore, and a member of the Society of Hospital Medicine since 2000, has served in many roles at the organization. These include being a member of the Annual Meeting Planning Committee (2007-2016), course director for the annual meeting (2013, 2014), chair of the Education Committee (2012-2016), and a member of the Research Committee (2008-2015). Dr. Brotman also won the society’s Research Award in 2015. He has been a staple of the editorial team at the Journal of Hospital Medicine since its founding in 2006.
“I am truly honored to be recognized for my participation and leadership in the field of hospital medicine and the society,” he said. “I am humbled to be included among the many luminaries who have won the award in prior years.”
He has been in his current role at Johns Hopkins since 2005, where he has more than tripled the program’s size and grown its academic profile.
“I have had the good fortune to work with a lot of talented faculty members and have helped them advance professionally and academically, while they pushed me to be a better leader,” Dr. Brotman said. “I encourage my team members to participate in the Society of Hospital Medicine; it is a fabulous way to gain leadership opportunities while staying abreast of the most important developments in the field.”
Bob Harrington, MD, MHM, is president and chief medical officer, SurveyVitals, an organization that provides digital patient experience and Consumer Assessment of Healthcare Providers and Systems (CAHPS) surveys nationwide to hospitals, health care systems, and physician practices. He believes he is an award recipient because he is a long-time advocate for hospitalists trained in family medicine (HTFMs). “I have always looked for ways to level the playing field for clinical and leadership opportunities for HTFMs,” he said.
Dr. Harrington first became involved with the Society of Hospital Medicine as chair of its Family Medicine Committee in the late 1990s. In that role, his committee looked at unique needs of HTFMs, including hiring practices, providing education to potential employers, and assisting HTFM members in career advancement.
“Our efforts resulted in tremendous growth of the HTFM membership, as these physicians began to view the society as their professional home and not as an internal medicine–dominant organization,” he said. He went on to become the first HTFM to serve on the society’s board and then became the first HTFM to be its president.
“This award is the greatest professional honor that I have received,” Dr. Harrington said. “It is especially important to me, because it is from a group of people whom I hold in the highest professional regard. They always put quality and patients first. I have been privileged to play a small part in that.”
Janet Nagamine, MD, BSN, MHM, is a hospitalist in the department of hospital-based specialty and inpatient palliative care at Kaiser Permanente Hospital in Santa Clara, Calif.
Dr. Nagamine was one of the first 200 people to join the Society of Hospital Medicine. Among her many roles within the society were serving on its board of directors from 2009 to 2014 and chairing the Quality and Safety committee for 5 years.
“I’m honored to be acknowledged in this formal and prestigious way, because my career path hasn’t always followed the traditional course of recipients who receive this type of award,” commented Dr. Nagamine, who has worked in a community hospital for the last 18 years. “This speaks volumes to the type of organization that the Society of Hospital Medicine is, and it makes me proud.”
She started her career as an ICU nurse and spent the last 30 years in various institutional and organizational roles trying to make hospitals a better place.
“At times, I was juggling family responsibilities and had to defer the fancy titles, but I always found a way to contribute meaningfully through my work with the Society of Hospital Medicine.”
HM18 satellite symposia schedule, information
From Hospital Admission to Home: New Standards for Extended Duration VTE Prophylaxis in Acutely Ill Medical Patients
Sunday, April 8
5:30 – 7:30 p.m., Canary Room 1-2
Dinner provided at 5:30 p.m.
Learning Objective: To educate on the risk of VTE in acutely ill medical patients, APEX clinical trial results, and Bevyxxa (betrixaban).
Overview:
- Review the burden of VTE in acutely ill medical patients.
- Provide an overview of the unmet need for extended-duration VTE prophylaxis from hospital admission to home.
- Review the APEX clinical trial data.
- Provide an overview of Bevyxxa (betrixaban) indication, safety information, dosing, and appropriate patient types.
Presenter: Hameed Ali, DO, FHM, clinical assistant professor of medicine and hospitalist, Baylor Scott and White Health Hospital, Temple, Tex.
This program is supported by Portola Pharmaceuticals.
Reducing COPD-related Readmissions through Individualized Maintenance Therapy and Increased Patient Engagement
Sunday, April 8
5:30 – 7:30 p.m., Canary Room 3-4
Dinner provided at 5:30 p.m.
Overview: Hospitals are a critical point of intervention in the care pathway of chronic obstructive pulmonary disease (COPD). Clinicians in this setting must be well versed in current treatment guidelines, as well as the full spectrum of medications and delivery devices, to provide disease management tailored to the physical and cognitive needs of each patient. Moreover, hospital clinicians also need to be adept at communicating with patients and engaging them in the management of their own disease. Collectively, these measures can significantly reduce symptom severity and the risk for future exacerbations, increase physical activity, and improve overall quality of life in patients with COPD. This program will improve the knowledge and competence of clinicians who care for patients with COPD.
Learning objectives: Upon completion of this educational activity, participants should be able to:
- Identify long-term treatment strategies to reduce hospital readmissions for COPD exacerbations.
- Review the clinical evidence regarding the efficacy and safety of long-acting maintenance regimens for COPD.
- Select medication delivery devices for patients with COPD based upon individual physical and cognitive characteristics.
- Outline a transitional care plan that promotes patient self-management to reduce the risk for future exacerbations and hospital readmissions.
Presenters: Stanley B. Fiel, MD, regional chair in the department of medicine, Atlantic Health System, and the deNeufville Professor, chairman of the department of medicine, Morristown (NJ) Medical Center; José Luis González, MD, assistant professor of internal medicine, department of internal medicine, University of Southern California, and primary care physician, department of primary care, LAC+USC Medical Center, Los Angeles.
Accreditation statement: Integrity Continuing Education, Inc. is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
Credit designation: Integrity Continuing Education, Inc. designates this live activity for a maximum of 1.5 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
A Physician’s Keys to Locking Out Lawsuits and Reducing Taxes
Monday, April 9
Noon – 1:00 p.m., Anaheim/Atlanta/Boston Room
Lunch provided at noon.
Objectives:
- Protect your license from negative reports to the National Practitioner Data Bank (NPDB) following a settlement from your insurance company. If there is no NPDB report, it’s unlikely that a board investigation into the legal matter will materialize. Preventing any sanctions from the state licensing board.
- Show how to structure: C-corps, S-corps, FLPs, LLCs, etc.
- Teach the use of legal tools that will protect their professional and personal assets from lawsuits. (Statistically, not even 1 in 100,000 are using these tools in the right way.)
- Learn how to protect business, property, and personal assets in the event of a judgment in excess of liability insurance.
- Learn how to protect your license from negative reports to the NPDB following a settlement from your insurance company. If there is no NPDB report, it’s unlikely that a board investigation into the legal matter will materialize. Preventing any sanctions from the state licensing board.
- Learn the best business structure for income tax reduction. Learn the new tax laws passed in 2017 and how they can benefit you.
Faculty: Art McOmber
Sponsored by Legally Mine.
Community-Acquired Bacterial Pneumonia (CABP) in the Hospital Setting: Why Are Patients Not Getting Better?
Monday, April 9
7:30 – 9:30 p.m., Canary Room 1-2
Dinner provided at 7:30 p.m.
Program Summary: Appropriate management of pneumonia in the hospital setting can have a substantial impact on patient outcomes and hospital measures such as readmission rates and length of stay. Community-acquired bacterial pneumonia (CABP) is one of the most common infectious diseases, one of the most frequent infections requiring antibiotics, and remains a leading cause of death in the United States. During this presentation, we will review current CABP guidelines from IDSA (the Infectious Diseases Society of America) and discuss the importance of appropriate antibiotic selection as it relates to the tenets of antimicrobial stewardship. The faculty will present two case studies and will solicit audience participation with a focus on antibiotic resistance and the importance of transition of care.
Chair: William Ford, MD, SFHM, Abington Jefferson Health, Abington, Penn.
Faculty: Mauricio Pinto, MD, St. David’s Round Rock Medical Center, Round Rock, Tex.; Sumeet Shetty, MD, MBA, FHM, Axel Health, Fort Meyers, Fla.
This program is supported by Nabriva Therapeutics, plc.
Register: [email protected] www.nabrivaevents.com/SHM/Symposium, or call 877-547-5640.
Direct Oral Anticoagulants (DOACs): Current Evidence for Extended VTE Prophylaxis in Medically Ill Patients and Reversal
Monday, April 9
7:30 – 9:30 p.m., Canary Room 3-4
Dinner provided at 7:30 p.m.
Overview: Patients hospitalized for an acute medical illness are at an increased risk for venous thromboembolism (VTE). With increasingly shortened hospital stays, acutely ill hospitalized patients are at an increased risk of developing VTE both in the hospital and after discharge. Outpatient VTE episodes often occur within 30 days of hospital discharge and fewer than half of those discharged patients receive VTE prophylaxis. Therefore, it is important for clinicians to be able to risk-stratify patients and provide extended prophylaxis for medical patients at increased risk for VTE.
This symposium will discuss the risk factors and burden of VTE and review ACCP guideline recommendations for VTE prophylaxis in acutely ill hospitalized medical patients. Faculty will assess the safety and efficacy of direct oral anticoagulants (DOACs) for extended VTE prophylaxis, explain the stratification of VTE and bleeding risk, as well as the process for devising evidence-based antithrombotic regimens. The presentation also will include an outline of current and emerging options for reversal of direct oral anticoagulants.
Learning objectives:
- Outline the risk factors and burden of VTE in medically ill patients post hospitalization.
- Review ACCP and ASH guideline recommendations for VTE prophylaxis in acutely ill hospitalized medical patients.
- Assess the safety and efficacy of DOACs for extended VTE prophylaxis in medically ill patients.
- Devise evidence-based antithrombotic regimens for medically ill patients taking into consideration patient-specific factors that impact VTE and bleeding risk
- Outline current and emerging options for reversal of DOACs
Faculty: Amir K. Jaffer, MD, MBA, chief medical officer, New York Presbyterian Queens Hospital, New York; Alex C. Spyropoulos, MD, FACP, FCCP, FRCPC, professor of medicine, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, system director – anticoagulation and clinical thrombosis services, Northwell Health at Lenox Hill Hospital, New York, NY; and Alan Jacobson, MD, FACC, assistant professor of medicine, Loma Linda University School of Medicine, director of anticoagulation services, Loma Linda VA Medical Center, Calif.
Target audience: Hospitalists, internists, nurse practitioners (NPs), physician assistants (PAs) who practice in a hospital setting.
Credit designation: Horizon CME designates this live activity for a maximum of 1.5 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Accreditation statement: This activity has been planned and implemented in accordance with the accreditation requirements and policies of the Accreditation Council for Continuing Medical Education (ACCME) through the providership of Horizon CME. Horizon CME is accredited by the ACCME to provide continuing medical education for physicians.
ABIM MOC statement: Successful completion of this CME activity, which includes participation in the evaluation component, enables the participant to earn up to 1.5 Medical Knowledge MOC points in the American Board of Internal Medicine’s (ABIM) Maintenance of Certification (MOC) program.
Participants will earn MOC points equivalent to the amount of CME credits claimed for the activity. It is the CME activity provider’s responsibility to submit participant completion information to ACCME for the purpose of granting ABIM MOC credit.
Supporter statement: This activity is supported by an independent educational grant from Portola Pharmaceuticals.
Register: http://bit.ly/2EoP1tb
From Hospital Admission to Home: New Standards for Extended Duration VTE Prophylaxis in Acutely Ill Medical Patients
Sunday, April 8
5:30 – 7:30 p.m., Canary Room 1-2
Dinner provided at 5:30 p.m.
Learning Objective: To educate on the risk of VTE in acutely ill medical patients, APEX clinical trial results, and Bevyxxa (betrixaban).
Overview:
- Review the burden of VTE in acutely ill medical patients.
- Provide an overview of the unmet need for extended-duration VTE prophylaxis from hospital admission to home.
- Review the APEX clinical trial data.
- Provide an overview of Bevyxxa (betrixaban) indication, safety information, dosing, and appropriate patient types.
Presenter: Hameed Ali, DO, FHM, clinical assistant professor of medicine and hospitalist, Baylor Scott and White Health Hospital, Temple, Tex.
This program is supported by Portola Pharmaceuticals.
Reducing COPD-related Readmissions through Individualized Maintenance Therapy and Increased Patient Engagement
Sunday, April 8
5:30 – 7:30 p.m., Canary Room 3-4
Dinner provided at 5:30 p.m.
Overview: Hospitals are a critical point of intervention in the care pathway of chronic obstructive pulmonary disease (COPD). Clinicians in this setting must be well versed in current treatment guidelines, as well as the full spectrum of medications and delivery devices, to provide disease management tailored to the physical and cognitive needs of each patient. Moreover, hospital clinicians also need to be adept at communicating with patients and engaging them in the management of their own disease. Collectively, these measures can significantly reduce symptom severity and the risk for future exacerbations, increase physical activity, and improve overall quality of life in patients with COPD. This program will improve the knowledge and competence of clinicians who care for patients with COPD.
Learning objectives: Upon completion of this educational activity, participants should be able to:
- Identify long-term treatment strategies to reduce hospital readmissions for COPD exacerbations.
- Review the clinical evidence regarding the efficacy and safety of long-acting maintenance regimens for COPD.
- Select medication delivery devices for patients with COPD based upon individual physical and cognitive characteristics.
- Outline a transitional care plan that promotes patient self-management to reduce the risk for future exacerbations and hospital readmissions.
Presenters: Stanley B. Fiel, MD, regional chair in the department of medicine, Atlantic Health System, and the deNeufville Professor, chairman of the department of medicine, Morristown (NJ) Medical Center; José Luis González, MD, assistant professor of internal medicine, department of internal medicine, University of Southern California, and primary care physician, department of primary care, LAC+USC Medical Center, Los Angeles.
Accreditation statement: Integrity Continuing Education, Inc. is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
Credit designation: Integrity Continuing Education, Inc. designates this live activity for a maximum of 1.5 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
A Physician’s Keys to Locking Out Lawsuits and Reducing Taxes
Monday, April 9
Noon – 1:00 p.m., Anaheim/Atlanta/Boston Room
Lunch provided at noon.
Objectives:
- Protect your license from negative reports to the National Practitioner Data Bank (NPDB) following a settlement from your insurance company. If there is no NPDB report, it’s unlikely that a board investigation into the legal matter will materialize. Preventing any sanctions from the state licensing board.
- Show how to structure: C-corps, S-corps, FLPs, LLCs, etc.
- Teach the use of legal tools that will protect their professional and personal assets from lawsuits. (Statistically, not even 1 in 100,000 are using these tools in the right way.)
- Learn how to protect business, property, and personal assets in the event of a judgment in excess of liability insurance.
- Learn how to protect your license from negative reports to the NPDB following a settlement from your insurance company. If there is no NPDB report, it’s unlikely that a board investigation into the legal matter will materialize. Preventing any sanctions from the state licensing board.
- Learn the best business structure for income tax reduction. Learn the new tax laws passed in 2017 and how they can benefit you.
Faculty: Art McOmber
Sponsored by Legally Mine.
Community-Acquired Bacterial Pneumonia (CABP) in the Hospital Setting: Why Are Patients Not Getting Better?
Monday, April 9
7:30 – 9:30 p.m., Canary Room 1-2
Dinner provided at 7:30 p.m.
Program Summary: Appropriate management of pneumonia in the hospital setting can have a substantial impact on patient outcomes and hospital measures such as readmission rates and length of stay. Community-acquired bacterial pneumonia (CABP) is one of the most common infectious diseases, one of the most frequent infections requiring antibiotics, and remains a leading cause of death in the United States. During this presentation, we will review current CABP guidelines from IDSA (the Infectious Diseases Society of America) and discuss the importance of appropriate antibiotic selection as it relates to the tenets of antimicrobial stewardship. The faculty will present two case studies and will solicit audience participation with a focus on antibiotic resistance and the importance of transition of care.
Chair: William Ford, MD, SFHM, Abington Jefferson Health, Abington, Penn.
Faculty: Mauricio Pinto, MD, St. David’s Round Rock Medical Center, Round Rock, Tex.; Sumeet Shetty, MD, MBA, FHM, Axel Health, Fort Meyers, Fla.
This program is supported by Nabriva Therapeutics, plc.
Register: [email protected] www.nabrivaevents.com/SHM/Symposium, or call 877-547-5640.
Direct Oral Anticoagulants (DOACs): Current Evidence for Extended VTE Prophylaxis in Medically Ill Patients and Reversal
Monday, April 9
7:30 – 9:30 p.m., Canary Room 3-4
Dinner provided at 7:30 p.m.
Overview: Patients hospitalized for an acute medical illness are at an increased risk for venous thromboembolism (VTE). With increasingly shortened hospital stays, acutely ill hospitalized patients are at an increased risk of developing VTE both in the hospital and after discharge. Outpatient VTE episodes often occur within 30 days of hospital discharge and fewer than half of those discharged patients receive VTE prophylaxis. Therefore, it is important for clinicians to be able to risk-stratify patients and provide extended prophylaxis for medical patients at increased risk for VTE.
This symposium will discuss the risk factors and burden of VTE and review ACCP guideline recommendations for VTE prophylaxis in acutely ill hospitalized medical patients. Faculty will assess the safety and efficacy of direct oral anticoagulants (DOACs) for extended VTE prophylaxis, explain the stratification of VTE and bleeding risk, as well as the process for devising evidence-based antithrombotic regimens. The presentation also will include an outline of current and emerging options for reversal of direct oral anticoagulants.
Learning objectives:
- Outline the risk factors and burden of VTE in medically ill patients post hospitalization.
- Review ACCP and ASH guideline recommendations for VTE prophylaxis in acutely ill hospitalized medical patients.
- Assess the safety and efficacy of DOACs for extended VTE prophylaxis in medically ill patients.
- Devise evidence-based antithrombotic regimens for medically ill patients taking into consideration patient-specific factors that impact VTE and bleeding risk
- Outline current and emerging options for reversal of DOACs
Faculty: Amir K. Jaffer, MD, MBA, chief medical officer, New York Presbyterian Queens Hospital, New York; Alex C. Spyropoulos, MD, FACP, FCCP, FRCPC, professor of medicine, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, system director – anticoagulation and clinical thrombosis services, Northwell Health at Lenox Hill Hospital, New York, NY; and Alan Jacobson, MD, FACC, assistant professor of medicine, Loma Linda University School of Medicine, director of anticoagulation services, Loma Linda VA Medical Center, Calif.
Target audience: Hospitalists, internists, nurse practitioners (NPs), physician assistants (PAs) who practice in a hospital setting.
Credit designation: Horizon CME designates this live activity for a maximum of 1.5 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Accreditation statement: This activity has been planned and implemented in accordance with the accreditation requirements and policies of the Accreditation Council for Continuing Medical Education (ACCME) through the providership of Horizon CME. Horizon CME is accredited by the ACCME to provide continuing medical education for physicians.
ABIM MOC statement: Successful completion of this CME activity, which includes participation in the evaluation component, enables the participant to earn up to 1.5 Medical Knowledge MOC points in the American Board of Internal Medicine’s (ABIM) Maintenance of Certification (MOC) program.
Participants will earn MOC points equivalent to the amount of CME credits claimed for the activity. It is the CME activity provider’s responsibility to submit participant completion information to ACCME for the purpose of granting ABIM MOC credit.
Supporter statement: This activity is supported by an independent educational grant from Portola Pharmaceuticals.
Register: http://bit.ly/2EoP1tb
From Hospital Admission to Home: New Standards for Extended Duration VTE Prophylaxis in Acutely Ill Medical Patients
Sunday, April 8
5:30 – 7:30 p.m., Canary Room 1-2
Dinner provided at 5:30 p.m.
Learning Objective: To educate on the risk of VTE in acutely ill medical patients, APEX clinical trial results, and Bevyxxa (betrixaban).
Overview:
- Review the burden of VTE in acutely ill medical patients.
- Provide an overview of the unmet need for extended-duration VTE prophylaxis from hospital admission to home.
- Review the APEX clinical trial data.
- Provide an overview of Bevyxxa (betrixaban) indication, safety information, dosing, and appropriate patient types.
Presenter: Hameed Ali, DO, FHM, clinical assistant professor of medicine and hospitalist, Baylor Scott and White Health Hospital, Temple, Tex.
This program is supported by Portola Pharmaceuticals.
Reducing COPD-related Readmissions through Individualized Maintenance Therapy and Increased Patient Engagement
Sunday, April 8
5:30 – 7:30 p.m., Canary Room 3-4
Dinner provided at 5:30 p.m.
Overview: Hospitals are a critical point of intervention in the care pathway of chronic obstructive pulmonary disease (COPD). Clinicians in this setting must be well versed in current treatment guidelines, as well as the full spectrum of medications and delivery devices, to provide disease management tailored to the physical and cognitive needs of each patient. Moreover, hospital clinicians also need to be adept at communicating with patients and engaging them in the management of their own disease. Collectively, these measures can significantly reduce symptom severity and the risk for future exacerbations, increase physical activity, and improve overall quality of life in patients with COPD. This program will improve the knowledge and competence of clinicians who care for patients with COPD.
Learning objectives: Upon completion of this educational activity, participants should be able to:
- Identify long-term treatment strategies to reduce hospital readmissions for COPD exacerbations.
- Review the clinical evidence regarding the efficacy and safety of long-acting maintenance regimens for COPD.
- Select medication delivery devices for patients with COPD based upon individual physical and cognitive characteristics.
- Outline a transitional care plan that promotes patient self-management to reduce the risk for future exacerbations and hospital readmissions.
Presenters: Stanley B. Fiel, MD, regional chair in the department of medicine, Atlantic Health System, and the deNeufville Professor, chairman of the department of medicine, Morristown (NJ) Medical Center; José Luis González, MD, assistant professor of internal medicine, department of internal medicine, University of Southern California, and primary care physician, department of primary care, LAC+USC Medical Center, Los Angeles.
Accreditation statement: Integrity Continuing Education, Inc. is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
Credit designation: Integrity Continuing Education, Inc. designates this live activity for a maximum of 1.5 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
A Physician’s Keys to Locking Out Lawsuits and Reducing Taxes
Monday, April 9
Noon – 1:00 p.m., Anaheim/Atlanta/Boston Room
Lunch provided at noon.
Objectives:
- Protect your license from negative reports to the National Practitioner Data Bank (NPDB) following a settlement from your insurance company. If there is no NPDB report, it’s unlikely that a board investigation into the legal matter will materialize. Preventing any sanctions from the state licensing board.
- Show how to structure: C-corps, S-corps, FLPs, LLCs, etc.
- Teach the use of legal tools that will protect their professional and personal assets from lawsuits. (Statistically, not even 1 in 100,000 are using these tools in the right way.)
- Learn how to protect business, property, and personal assets in the event of a judgment in excess of liability insurance.
- Learn how to protect your license from negative reports to the NPDB following a settlement from your insurance company. If there is no NPDB report, it’s unlikely that a board investigation into the legal matter will materialize. Preventing any sanctions from the state licensing board.
- Learn the best business structure for income tax reduction. Learn the new tax laws passed in 2017 and how they can benefit you.
Faculty: Art McOmber
Sponsored by Legally Mine.
Community-Acquired Bacterial Pneumonia (CABP) in the Hospital Setting: Why Are Patients Not Getting Better?
Monday, April 9
7:30 – 9:30 p.m., Canary Room 1-2
Dinner provided at 7:30 p.m.
Program Summary: Appropriate management of pneumonia in the hospital setting can have a substantial impact on patient outcomes and hospital measures such as readmission rates and length of stay. Community-acquired bacterial pneumonia (CABP) is one of the most common infectious diseases, one of the most frequent infections requiring antibiotics, and remains a leading cause of death in the United States. During this presentation, we will review current CABP guidelines from IDSA (the Infectious Diseases Society of America) and discuss the importance of appropriate antibiotic selection as it relates to the tenets of antimicrobial stewardship. The faculty will present two case studies and will solicit audience participation with a focus on antibiotic resistance and the importance of transition of care.
Chair: William Ford, MD, SFHM, Abington Jefferson Health, Abington, Penn.
Faculty: Mauricio Pinto, MD, St. David’s Round Rock Medical Center, Round Rock, Tex.; Sumeet Shetty, MD, MBA, FHM, Axel Health, Fort Meyers, Fla.
This program is supported by Nabriva Therapeutics, plc.
Register: [email protected] www.nabrivaevents.com/SHM/Symposium, or call 877-547-5640.
Direct Oral Anticoagulants (DOACs): Current Evidence for Extended VTE Prophylaxis in Medically Ill Patients and Reversal
Monday, April 9
7:30 – 9:30 p.m., Canary Room 3-4
Dinner provided at 7:30 p.m.
Overview: Patients hospitalized for an acute medical illness are at an increased risk for venous thromboembolism (VTE). With increasingly shortened hospital stays, acutely ill hospitalized patients are at an increased risk of developing VTE both in the hospital and after discharge. Outpatient VTE episodes often occur within 30 days of hospital discharge and fewer than half of those discharged patients receive VTE prophylaxis. Therefore, it is important for clinicians to be able to risk-stratify patients and provide extended prophylaxis for medical patients at increased risk for VTE.
This symposium will discuss the risk factors and burden of VTE and review ACCP guideline recommendations for VTE prophylaxis in acutely ill hospitalized medical patients. Faculty will assess the safety and efficacy of direct oral anticoagulants (DOACs) for extended VTE prophylaxis, explain the stratification of VTE and bleeding risk, as well as the process for devising evidence-based antithrombotic regimens. The presentation also will include an outline of current and emerging options for reversal of direct oral anticoagulants.
Learning objectives:
- Outline the risk factors and burden of VTE in medically ill patients post hospitalization.
- Review ACCP and ASH guideline recommendations for VTE prophylaxis in acutely ill hospitalized medical patients.
- Assess the safety and efficacy of DOACs for extended VTE prophylaxis in medically ill patients.
- Devise evidence-based antithrombotic regimens for medically ill patients taking into consideration patient-specific factors that impact VTE and bleeding risk
- Outline current and emerging options for reversal of DOACs
Faculty: Amir K. Jaffer, MD, MBA, chief medical officer, New York Presbyterian Queens Hospital, New York; Alex C. Spyropoulos, MD, FACP, FCCP, FRCPC, professor of medicine, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, system director – anticoagulation and clinical thrombosis services, Northwell Health at Lenox Hill Hospital, New York, NY; and Alan Jacobson, MD, FACC, assistant professor of medicine, Loma Linda University School of Medicine, director of anticoagulation services, Loma Linda VA Medical Center, Calif.
Target audience: Hospitalists, internists, nurse practitioners (NPs), physician assistants (PAs) who practice in a hospital setting.
Credit designation: Horizon CME designates this live activity for a maximum of 1.5 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Accreditation statement: This activity has been planned and implemented in accordance with the accreditation requirements and policies of the Accreditation Council for Continuing Medical Education (ACCME) through the providership of Horizon CME. Horizon CME is accredited by the ACCME to provide continuing medical education for physicians.
ABIM MOC statement: Successful completion of this CME activity, which includes participation in the evaluation component, enables the participant to earn up to 1.5 Medical Knowledge MOC points in the American Board of Internal Medicine’s (ABIM) Maintenance of Certification (MOC) program.
Participants will earn MOC points equivalent to the amount of CME credits claimed for the activity. It is the CME activity provider’s responsibility to submit participant completion information to ACCME for the purpose of granting ABIM MOC credit.
Supporter statement: This activity is supported by an independent educational grant from Portola Pharmaceuticals.
Register: http://bit.ly/2EoP1tb
HM18 Special Interest Forums
The Society of Hospital Medicine presents a variety of special interest forums during its annual conference. The small-group sessions take place Monday, April 9, 4:30-5:25 p.m.
Academic and Research
Greg Seymann, MD, SFHM; Nicole Adler, MD, FHM
Grand Ballroom 12-14
The Academic and Research Forum brings together faculty and researchers to discuss topics of interest to the academic hospital medicine community, such as mentorship, research support, and professional development. Join this collaborative offering of the Academic and Research Committees.
Advocacy & Public Policy
Joshua Lenchus, DO, RPh, SFHM; Josh Boswell
Key Biscayne Room
During this forum with SHM’s Advocacy leaders and staff, you will learn about the direction of SHM’s Advocacy & Public Policy work and how you can help. Discussion will focus on SHM’s new Advocacy & Public Policy Section, its role, and how you can participate and share your own ideas.
Canadian Hospitalists
Serge Soolsma, MD
Key Largo Room
This forum provides a unique setting for hospitalists based in Canada to gather as an organized group, network with each other, and discuss the common issues with which they are faced.
Care for Vulnerable Populations
Mara Bann, MD; Pallabi Sanyal-Day, MD
Key West Room
SHM’s Caring for Vulnerable Populations Section aims to increase awareness and improve quality of care for vulnerable and underserved patient populations in the hospital setting. The principles and skills needed to care effectively for vulnerable patients span practitioners across all health systems, although they are important particularly for hospitalists practicing in safety-net and resource-limited settings.
Community-Based Hospitalists
Steve Behnke, MD; Jason Robertson, MD, SFHM
Sawgrass Room
This session provides a forum for sharing principles of successful clinical practices, quality care, and professional sustainability, as well as other “hot” topics of interest to the community-based hospitalist.
NEW: Critical Care
David Aymond, MD
Grand Ballroom 4-6
This special interest forum seeks to convene hospitalists charged with providing some level of critical care at their institution. Participants should come prepared to discuss and share their own experiences, including their current role in providing critical care, facing institutional barriers, and dealing with gaps in training.
NEW: Diversity and Inclusion
Marisha Burden, MD, SFHM; Flora Kisuule, MD, SFHM
Grand Ballroom 7A
SHM is committed to a diverse and inclusive membership that works to provide high-quality, equitable care to diverse populations. This forum invites hospitalists from any underrepresented group to discuss issues, concerns, and solutions to improve workforce diversity and their own career opportunities. In addition, this forum would be for HM leaders who would like to discuss strategies and opportunities for expanding the diversity and inclusion of their HM groups.
NEW: Ethics in Hospital Medicine
David Alfandre, MD, MSPH
West Indies Room
This forum serves as a resource for discussion, coaching, and mentorship regarding common and challenging ethical concerns that hospitalists face. We aim to support SHM members in collaborating on ethics scholarships and projects that address ethics in clinical care, education, and policy.
Global Health and Human Rights
Brett Hendel-Paterson, MD, FHM
Harbor Beach Room
SHM’s Global Health and Human Rights Section has been established to build interest and engagement in global health and human rights work among hospitalists so they can share their expertise. The section also plans to build long-term collaborations in the United States and abroad.
Hospitalists Trained in Family Medicine
David Goldstein, MD; Patricia Seymour, MD
Anaheim Room
Participants will network and discuss their training, how they’ve achieved recognition and access in the job market, as well as national trends related to hospitalists trained in family medicine.
Information Technology
Cheng-Kai Kao, MD; Andrew Young, DO
St. Thomas Room
This forum provides an opportunity for attendees to provide SHM and the IT Committee with input on what would be most beneficial regarding implementing, managing, and participating in health/hospital IT initiatives.
International Hospital Medicine
Guillherme Barcellos, MD, SFHM; Rafaela Dal Molin, MD, MEd, FHM; Nerea Fernandez, MEd, PhD
Crystal Ballroom G1/A&B
This forum is designed to provide an opportunity for attendees who practice hospital medicine outside of North America to share their ideas and discuss issues they’ve faced.
Leadership in Hospital Medicine
Thomas McIlraith, MD, SFHM, CLHM; Rob Zipper, MD, MMM, SFHM
Marco Island Room
Want to be a better leader? A better coach and mentor? Do you want to drive quality improvement (QI) at your hospital? Developing ourselves and our teams is what we are all here to do! We will review, discuss, and shape the resources and programmatic offerings that are needed to promote leadership skills development at all levels. We will also review SHMs existing programs, including the Leadership Academies, the Leadership Certificate Program, e-learning opportunities, and the HMX: Leadership Alumni Forum.
Med-Peds Hospitalists
Heather Toth, MD, SFHM; Carrie Herzke, MD, SFHM
Crystal Ballroom H
This special interest forum will explore the role of Med-Peds physicians in hospitalist medicine. Discussion items may include personal experiences, how to create more Med-Peds jobs, and how to succeed as a Med-Peds hospitalist.
Multi-Site HMG Leaders
Leslie Flores, MHA, SFHM; Ryan Brown, MD, FHM
Grand Ballroom 1-3
This forum is for physician and administrative leaders who are responsible for managing multiple hospitalist practice sites within the same health system. The number of people with this role has increased significantly in the last few years and comes with challenges that are different from those faced by the lead hospitalist at a single-practice site.
Nurse Practitioners and Physician Assistants
Emilie Davis, PA-C, FHM; Noam Shabani, MS, PA-C
Vinoy Room
Share best practices and challenges. Learn about SHM resources for NPs and PAs in practice, as well as onboarding and recruitment resources. Network with peers and help build membership engagement.
Oncology Hospitalists
Maria Campagna, MD, FHM; Barbara Egan, MD, SFHM; Kerry Reynolds, MD
Aruba Room
This special interest forum will explore the role of hospitalists in oncology services. Discussion items may include personal experiences and how to succeed as an oncology hospitalist.
Palliative Care
Rab Razzak, MBBS, MD; Jeffrey Frank, MD, MBA
Bahamas Room
This special interest forum seeks to convene hospitalists charged with providing some level of palliative care at their institution. Participants should come prepared to discuss and share their own experiences, including their current role in providing palliative care, facing institutional barriers, and dealing with gaps in training.
Patient Experience
Mark Rudolph, MD, SFHM; Patrick Kneeland, MD
Grand Ballroom 7B
Join the Patient Experience Forum to exchange ideas about how hospitalists can enhance patients’ care experiences while also improving professional satisfaction. Learn about the work of SHM’s Patient Experience Committee and opportunities for getting involved in SHM’s patient experience initiatives.
Pediatric Hospitalists
Sandy Gage, MD, SFHM
Grand Ballroom 9-11
This special interest forum will provide an opportunity for pediatric hospitalists to network, share, and discuss topics and issues of particular interest to them. Topics will include an updates on SHM’s pediatric activities, on potential paths to specialty certification, and about the relationships between SHM, AAP, APA, PRIS, and the Joint Council on Pediatric Hospital Medicine.
NEW: Perioperative Care
Steven Cohn, MD, SFHM; Kurt Pfeifer, MD
San Francisco Room
In this special interest forum, learn about guideline updates and recent literature while communicating controversial or difficult patient management issues around perioperative medicine.
Point-of-Care Ultrasound (POCUS)
Benji Mathews, MD, CLHM, SFHM; Gordon Johnson, MD, FHM
Atlanta Room
This special interest forum will discuss opportunities to collaborate and standardize processes for POCUS certification, including what resources already exist. In addition, discussion will revolve around privileging at your own institution, gaining skills, and the challenges and successes of procedural teams in the hospital.
Post-Acute Care Providers
Robert Reynolds, MD
Puerto Rico Room
This forum provides opportunities for hospitalists who practice in or are interested in learning more about working in or becoming more involved in the post-acute care arena, such as SNFs, LTACs, and rehab facilities.
Practice Administrators
Tiffani Panek, CLHM; Roberta Himebaugh, MBA, SFHM
Boston Room
Practice administrators are important members of the hospitalist team, providing key management and organizational skills. In this forum, administrators can voice their unique perspectives and hear from their peers.
Quality Improvement
Mangla Gulati, MD, MBBS, CPPS, SFHM; Jenna Goldstein
Grand Cayman Room
Hospitalists are at the center of the national quality and patient safety movement and are increasingly responsible for performance at their institutions. This forum provides a venue for connecting with SHM’s QI and patient safety community and for engaging with leaders, peers, and collaborators to share ideas and inform SHM’s QI efforts. Discussion during the forum will focus on what hospitalists need to know to become involved with QI at SHM or locally. Hear about SHM’s plans for future QI initiatives, and share your own ideas.
NEW: Residents & Medical Students
Aram Namavar, MS; Chris Bartlett, MD, MPH
New Orleans Room
This forum provides opportunities in networking and discussion for physicians in training who are contemplating a career in hospital medicine.
Rural Hospitalists
Ken Simone, DO, SFHM; Michael Sullivan, MD
Los Angeles Room
Hospital medicine groups in rural areas face some unique problems, from recruitment, night call, and staffing to communicating with geographically dispersed primary care physicians. Rural hospitalists may also face clinical challenges because of limited technological resources and/or limited access to specialists. This forum provides an opportunity for hospitalists in rural areas to share their issues and concerns and to see how others have solved similar problems.
Veterans Affairs Hospitalists
Kathlyn Fletcher, MD, FHM; Peter Kaboli, MD, FHM
Miami Room
This forum provides opportunities in networking and discussion for hospitalists who work at the VA. Issues unique to VA hospitalists will be discussed.
Women in Hospital Medicine
Melissa Mattison, MD, SFHM; Cory Ritter, MD, FHM
New York Room
This forum provides an opportunity to discuss issues relevant to women in hospital medicine and strategies for success/coping. Topics may include career satisfaction, occupational stresses, opportunities for change, promotion of leadership, and identification of resources.
The Society of Hospital Medicine presents a variety of special interest forums during its annual conference. The small-group sessions take place Monday, April 9, 4:30-5:25 p.m.
Academic and Research
Greg Seymann, MD, SFHM; Nicole Adler, MD, FHM
Grand Ballroom 12-14
The Academic and Research Forum brings together faculty and researchers to discuss topics of interest to the academic hospital medicine community, such as mentorship, research support, and professional development. Join this collaborative offering of the Academic and Research Committees.
Advocacy & Public Policy
Joshua Lenchus, DO, RPh, SFHM; Josh Boswell
Key Biscayne Room
During this forum with SHM’s Advocacy leaders and staff, you will learn about the direction of SHM’s Advocacy & Public Policy work and how you can help. Discussion will focus on SHM’s new Advocacy & Public Policy Section, its role, and how you can participate and share your own ideas.
Canadian Hospitalists
Serge Soolsma, MD
Key Largo Room
This forum provides a unique setting for hospitalists based in Canada to gather as an organized group, network with each other, and discuss the common issues with which they are faced.
Care for Vulnerable Populations
Mara Bann, MD; Pallabi Sanyal-Day, MD
Key West Room
SHM’s Caring for Vulnerable Populations Section aims to increase awareness and improve quality of care for vulnerable and underserved patient populations in the hospital setting. The principles and skills needed to care effectively for vulnerable patients span practitioners across all health systems, although they are important particularly for hospitalists practicing in safety-net and resource-limited settings.
Community-Based Hospitalists
Steve Behnke, MD; Jason Robertson, MD, SFHM
Sawgrass Room
This session provides a forum for sharing principles of successful clinical practices, quality care, and professional sustainability, as well as other “hot” topics of interest to the community-based hospitalist.
NEW: Critical Care
David Aymond, MD
Grand Ballroom 4-6
This special interest forum seeks to convene hospitalists charged with providing some level of critical care at their institution. Participants should come prepared to discuss and share their own experiences, including their current role in providing critical care, facing institutional barriers, and dealing with gaps in training.
NEW: Diversity and Inclusion
Marisha Burden, MD, SFHM; Flora Kisuule, MD, SFHM
Grand Ballroom 7A
SHM is committed to a diverse and inclusive membership that works to provide high-quality, equitable care to diverse populations. This forum invites hospitalists from any underrepresented group to discuss issues, concerns, and solutions to improve workforce diversity and their own career opportunities. In addition, this forum would be for HM leaders who would like to discuss strategies and opportunities for expanding the diversity and inclusion of their HM groups.
NEW: Ethics in Hospital Medicine
David Alfandre, MD, MSPH
West Indies Room
This forum serves as a resource for discussion, coaching, and mentorship regarding common and challenging ethical concerns that hospitalists face. We aim to support SHM members in collaborating on ethics scholarships and projects that address ethics in clinical care, education, and policy.
Global Health and Human Rights
Brett Hendel-Paterson, MD, FHM
Harbor Beach Room
SHM’s Global Health and Human Rights Section has been established to build interest and engagement in global health and human rights work among hospitalists so they can share their expertise. The section also plans to build long-term collaborations in the United States and abroad.
Hospitalists Trained in Family Medicine
David Goldstein, MD; Patricia Seymour, MD
Anaheim Room
Participants will network and discuss their training, how they’ve achieved recognition and access in the job market, as well as national trends related to hospitalists trained in family medicine.
Information Technology
Cheng-Kai Kao, MD; Andrew Young, DO
St. Thomas Room
This forum provides an opportunity for attendees to provide SHM and the IT Committee with input on what would be most beneficial regarding implementing, managing, and participating in health/hospital IT initiatives.
International Hospital Medicine
Guillherme Barcellos, MD, SFHM; Rafaela Dal Molin, MD, MEd, FHM; Nerea Fernandez, MEd, PhD
Crystal Ballroom G1/A&B
This forum is designed to provide an opportunity for attendees who practice hospital medicine outside of North America to share their ideas and discuss issues they’ve faced.
Leadership in Hospital Medicine
Thomas McIlraith, MD, SFHM, CLHM; Rob Zipper, MD, MMM, SFHM
Marco Island Room
Want to be a better leader? A better coach and mentor? Do you want to drive quality improvement (QI) at your hospital? Developing ourselves and our teams is what we are all here to do! We will review, discuss, and shape the resources and programmatic offerings that are needed to promote leadership skills development at all levels. We will also review SHMs existing programs, including the Leadership Academies, the Leadership Certificate Program, e-learning opportunities, and the HMX: Leadership Alumni Forum.
Med-Peds Hospitalists
Heather Toth, MD, SFHM; Carrie Herzke, MD, SFHM
Crystal Ballroom H
This special interest forum will explore the role of Med-Peds physicians in hospitalist medicine. Discussion items may include personal experiences, how to create more Med-Peds jobs, and how to succeed as a Med-Peds hospitalist.
Multi-Site HMG Leaders
Leslie Flores, MHA, SFHM; Ryan Brown, MD, FHM
Grand Ballroom 1-3
This forum is for physician and administrative leaders who are responsible for managing multiple hospitalist practice sites within the same health system. The number of people with this role has increased significantly in the last few years and comes with challenges that are different from those faced by the lead hospitalist at a single-practice site.
Nurse Practitioners and Physician Assistants
Emilie Davis, PA-C, FHM; Noam Shabani, MS, PA-C
Vinoy Room
Share best practices and challenges. Learn about SHM resources for NPs and PAs in practice, as well as onboarding and recruitment resources. Network with peers and help build membership engagement.
Oncology Hospitalists
Maria Campagna, MD, FHM; Barbara Egan, MD, SFHM; Kerry Reynolds, MD
Aruba Room
This special interest forum will explore the role of hospitalists in oncology services. Discussion items may include personal experiences and how to succeed as an oncology hospitalist.
Palliative Care
Rab Razzak, MBBS, MD; Jeffrey Frank, MD, MBA
Bahamas Room
This special interest forum seeks to convene hospitalists charged with providing some level of palliative care at their institution. Participants should come prepared to discuss and share their own experiences, including their current role in providing palliative care, facing institutional barriers, and dealing with gaps in training.
Patient Experience
Mark Rudolph, MD, SFHM; Patrick Kneeland, MD
Grand Ballroom 7B
Join the Patient Experience Forum to exchange ideas about how hospitalists can enhance patients’ care experiences while also improving professional satisfaction. Learn about the work of SHM’s Patient Experience Committee and opportunities for getting involved in SHM’s patient experience initiatives.
Pediatric Hospitalists
Sandy Gage, MD, SFHM
Grand Ballroom 9-11
This special interest forum will provide an opportunity for pediatric hospitalists to network, share, and discuss topics and issues of particular interest to them. Topics will include an updates on SHM’s pediatric activities, on potential paths to specialty certification, and about the relationships between SHM, AAP, APA, PRIS, and the Joint Council on Pediatric Hospital Medicine.
NEW: Perioperative Care
Steven Cohn, MD, SFHM; Kurt Pfeifer, MD
San Francisco Room
In this special interest forum, learn about guideline updates and recent literature while communicating controversial or difficult patient management issues around perioperative medicine.
Point-of-Care Ultrasound (POCUS)
Benji Mathews, MD, CLHM, SFHM; Gordon Johnson, MD, FHM
Atlanta Room
This special interest forum will discuss opportunities to collaborate and standardize processes for POCUS certification, including what resources already exist. In addition, discussion will revolve around privileging at your own institution, gaining skills, and the challenges and successes of procedural teams in the hospital.
Post-Acute Care Providers
Robert Reynolds, MD
Puerto Rico Room
This forum provides opportunities for hospitalists who practice in or are interested in learning more about working in or becoming more involved in the post-acute care arena, such as SNFs, LTACs, and rehab facilities.
Practice Administrators
Tiffani Panek, CLHM; Roberta Himebaugh, MBA, SFHM
Boston Room
Practice administrators are important members of the hospitalist team, providing key management and organizational skills. In this forum, administrators can voice their unique perspectives and hear from their peers.
Quality Improvement
Mangla Gulati, MD, MBBS, CPPS, SFHM; Jenna Goldstein
Grand Cayman Room
Hospitalists are at the center of the national quality and patient safety movement and are increasingly responsible for performance at their institutions. This forum provides a venue for connecting with SHM’s QI and patient safety community and for engaging with leaders, peers, and collaborators to share ideas and inform SHM’s QI efforts. Discussion during the forum will focus on what hospitalists need to know to become involved with QI at SHM or locally. Hear about SHM’s plans for future QI initiatives, and share your own ideas.
NEW: Residents & Medical Students
Aram Namavar, MS; Chris Bartlett, MD, MPH
New Orleans Room
This forum provides opportunities in networking and discussion for physicians in training who are contemplating a career in hospital medicine.
Rural Hospitalists
Ken Simone, DO, SFHM; Michael Sullivan, MD
Los Angeles Room
Hospital medicine groups in rural areas face some unique problems, from recruitment, night call, and staffing to communicating with geographically dispersed primary care physicians. Rural hospitalists may also face clinical challenges because of limited technological resources and/or limited access to specialists. This forum provides an opportunity for hospitalists in rural areas to share their issues and concerns and to see how others have solved similar problems.
Veterans Affairs Hospitalists
Kathlyn Fletcher, MD, FHM; Peter Kaboli, MD, FHM
Miami Room
This forum provides opportunities in networking and discussion for hospitalists who work at the VA. Issues unique to VA hospitalists will be discussed.
Women in Hospital Medicine
Melissa Mattison, MD, SFHM; Cory Ritter, MD, FHM
New York Room
This forum provides an opportunity to discuss issues relevant to women in hospital medicine and strategies for success/coping. Topics may include career satisfaction, occupational stresses, opportunities for change, promotion of leadership, and identification of resources.
The Society of Hospital Medicine presents a variety of special interest forums during its annual conference. The small-group sessions take place Monday, April 9, 4:30-5:25 p.m.
Academic and Research
Greg Seymann, MD, SFHM; Nicole Adler, MD, FHM
Grand Ballroom 12-14
The Academic and Research Forum brings together faculty and researchers to discuss topics of interest to the academic hospital medicine community, such as mentorship, research support, and professional development. Join this collaborative offering of the Academic and Research Committees.
Advocacy & Public Policy
Joshua Lenchus, DO, RPh, SFHM; Josh Boswell
Key Biscayne Room
During this forum with SHM’s Advocacy leaders and staff, you will learn about the direction of SHM’s Advocacy & Public Policy work and how you can help. Discussion will focus on SHM’s new Advocacy & Public Policy Section, its role, and how you can participate and share your own ideas.
Canadian Hospitalists
Serge Soolsma, MD
Key Largo Room
This forum provides a unique setting for hospitalists based in Canada to gather as an organized group, network with each other, and discuss the common issues with which they are faced.
Care for Vulnerable Populations
Mara Bann, MD; Pallabi Sanyal-Day, MD
Key West Room
SHM’s Caring for Vulnerable Populations Section aims to increase awareness and improve quality of care for vulnerable and underserved patient populations in the hospital setting. The principles and skills needed to care effectively for vulnerable patients span practitioners across all health systems, although they are important particularly for hospitalists practicing in safety-net and resource-limited settings.
Community-Based Hospitalists
Steve Behnke, MD; Jason Robertson, MD, SFHM
Sawgrass Room
This session provides a forum for sharing principles of successful clinical practices, quality care, and professional sustainability, as well as other “hot” topics of interest to the community-based hospitalist.
NEW: Critical Care
David Aymond, MD
Grand Ballroom 4-6
This special interest forum seeks to convene hospitalists charged with providing some level of critical care at their institution. Participants should come prepared to discuss and share their own experiences, including their current role in providing critical care, facing institutional barriers, and dealing with gaps in training.
NEW: Diversity and Inclusion
Marisha Burden, MD, SFHM; Flora Kisuule, MD, SFHM
Grand Ballroom 7A
SHM is committed to a diverse and inclusive membership that works to provide high-quality, equitable care to diverse populations. This forum invites hospitalists from any underrepresented group to discuss issues, concerns, and solutions to improve workforce diversity and their own career opportunities. In addition, this forum would be for HM leaders who would like to discuss strategies and opportunities for expanding the diversity and inclusion of their HM groups.
NEW: Ethics in Hospital Medicine
David Alfandre, MD, MSPH
West Indies Room
This forum serves as a resource for discussion, coaching, and mentorship regarding common and challenging ethical concerns that hospitalists face. We aim to support SHM members in collaborating on ethics scholarships and projects that address ethics in clinical care, education, and policy.
Global Health and Human Rights
Brett Hendel-Paterson, MD, FHM
Harbor Beach Room
SHM’s Global Health and Human Rights Section has been established to build interest and engagement in global health and human rights work among hospitalists so they can share their expertise. The section also plans to build long-term collaborations in the United States and abroad.
Hospitalists Trained in Family Medicine
David Goldstein, MD; Patricia Seymour, MD
Anaheim Room
Participants will network and discuss their training, how they’ve achieved recognition and access in the job market, as well as national trends related to hospitalists trained in family medicine.
Information Technology
Cheng-Kai Kao, MD; Andrew Young, DO
St. Thomas Room
This forum provides an opportunity for attendees to provide SHM and the IT Committee with input on what would be most beneficial regarding implementing, managing, and participating in health/hospital IT initiatives.
International Hospital Medicine
Guillherme Barcellos, MD, SFHM; Rafaela Dal Molin, MD, MEd, FHM; Nerea Fernandez, MEd, PhD
Crystal Ballroom G1/A&B
This forum is designed to provide an opportunity for attendees who practice hospital medicine outside of North America to share their ideas and discuss issues they’ve faced.
Leadership in Hospital Medicine
Thomas McIlraith, MD, SFHM, CLHM; Rob Zipper, MD, MMM, SFHM
Marco Island Room
Want to be a better leader? A better coach and mentor? Do you want to drive quality improvement (QI) at your hospital? Developing ourselves and our teams is what we are all here to do! We will review, discuss, and shape the resources and programmatic offerings that are needed to promote leadership skills development at all levels. We will also review SHMs existing programs, including the Leadership Academies, the Leadership Certificate Program, e-learning opportunities, and the HMX: Leadership Alumni Forum.
Med-Peds Hospitalists
Heather Toth, MD, SFHM; Carrie Herzke, MD, SFHM
Crystal Ballroom H
This special interest forum will explore the role of Med-Peds physicians in hospitalist medicine. Discussion items may include personal experiences, how to create more Med-Peds jobs, and how to succeed as a Med-Peds hospitalist.
Multi-Site HMG Leaders
Leslie Flores, MHA, SFHM; Ryan Brown, MD, FHM
Grand Ballroom 1-3
This forum is for physician and administrative leaders who are responsible for managing multiple hospitalist practice sites within the same health system. The number of people with this role has increased significantly in the last few years and comes with challenges that are different from those faced by the lead hospitalist at a single-practice site.
Nurse Practitioners and Physician Assistants
Emilie Davis, PA-C, FHM; Noam Shabani, MS, PA-C
Vinoy Room
Share best practices and challenges. Learn about SHM resources for NPs and PAs in practice, as well as onboarding and recruitment resources. Network with peers and help build membership engagement.
Oncology Hospitalists
Maria Campagna, MD, FHM; Barbara Egan, MD, SFHM; Kerry Reynolds, MD
Aruba Room
This special interest forum will explore the role of hospitalists in oncology services. Discussion items may include personal experiences and how to succeed as an oncology hospitalist.
Palliative Care
Rab Razzak, MBBS, MD; Jeffrey Frank, MD, MBA
Bahamas Room
This special interest forum seeks to convene hospitalists charged with providing some level of palliative care at their institution. Participants should come prepared to discuss and share their own experiences, including their current role in providing palliative care, facing institutional barriers, and dealing with gaps in training.
Patient Experience
Mark Rudolph, MD, SFHM; Patrick Kneeland, MD
Grand Ballroom 7B
Join the Patient Experience Forum to exchange ideas about how hospitalists can enhance patients’ care experiences while also improving professional satisfaction. Learn about the work of SHM’s Patient Experience Committee and opportunities for getting involved in SHM’s patient experience initiatives.
Pediatric Hospitalists
Sandy Gage, MD, SFHM
Grand Ballroom 9-11
This special interest forum will provide an opportunity for pediatric hospitalists to network, share, and discuss topics and issues of particular interest to them. Topics will include an updates on SHM’s pediatric activities, on potential paths to specialty certification, and about the relationships between SHM, AAP, APA, PRIS, and the Joint Council on Pediatric Hospital Medicine.
NEW: Perioperative Care
Steven Cohn, MD, SFHM; Kurt Pfeifer, MD
San Francisco Room
In this special interest forum, learn about guideline updates and recent literature while communicating controversial or difficult patient management issues around perioperative medicine.
Point-of-Care Ultrasound (POCUS)
Benji Mathews, MD, CLHM, SFHM; Gordon Johnson, MD, FHM
Atlanta Room
This special interest forum will discuss opportunities to collaborate and standardize processes for POCUS certification, including what resources already exist. In addition, discussion will revolve around privileging at your own institution, gaining skills, and the challenges and successes of procedural teams in the hospital.
Post-Acute Care Providers
Robert Reynolds, MD
Puerto Rico Room
This forum provides opportunities for hospitalists who practice in or are interested in learning more about working in or becoming more involved in the post-acute care arena, such as SNFs, LTACs, and rehab facilities.
Practice Administrators
Tiffani Panek, CLHM; Roberta Himebaugh, MBA, SFHM
Boston Room
Practice administrators are important members of the hospitalist team, providing key management and organizational skills. In this forum, administrators can voice their unique perspectives and hear from their peers.
Quality Improvement
Mangla Gulati, MD, MBBS, CPPS, SFHM; Jenna Goldstein
Grand Cayman Room
Hospitalists are at the center of the national quality and patient safety movement and are increasingly responsible for performance at their institutions. This forum provides a venue for connecting with SHM’s QI and patient safety community and for engaging with leaders, peers, and collaborators to share ideas and inform SHM’s QI efforts. Discussion during the forum will focus on what hospitalists need to know to become involved with QI at SHM or locally. Hear about SHM’s plans for future QI initiatives, and share your own ideas.
NEW: Residents & Medical Students
Aram Namavar, MS; Chris Bartlett, MD, MPH
New Orleans Room
This forum provides opportunities in networking and discussion for physicians in training who are contemplating a career in hospital medicine.
Rural Hospitalists
Ken Simone, DO, SFHM; Michael Sullivan, MD
Los Angeles Room
Hospital medicine groups in rural areas face some unique problems, from recruitment, night call, and staffing to communicating with geographically dispersed primary care physicians. Rural hospitalists may also face clinical challenges because of limited technological resources and/or limited access to specialists. This forum provides an opportunity for hospitalists in rural areas to share their issues and concerns and to see how others have solved similar problems.
Veterans Affairs Hospitalists
Kathlyn Fletcher, MD, FHM; Peter Kaboli, MD, FHM
Miami Room
This forum provides opportunities in networking and discussion for hospitalists who work at the VA. Issues unique to VA hospitalists will be discussed.
Women in Hospital Medicine
Melissa Mattison, MD, SFHM; Cory Ritter, MD, FHM
New York Room
This forum provides an opportunity to discuss issues relevant to women in hospital medicine and strategies for success/coping. Topics may include career satisfaction, occupational stresses, opportunities for change, promotion of leadership, and identification of resources.
SHM Loyalty Partners at HM18
The Society of Hospital Medicine is grateful for the loyal support of the following companies:
Platinum Level
Aurora Health Care
Baylor Scott & White Health
BMS/Pfizer
Boehringer Ingelheim Pharmaceuticals, Inc.
Community Hospitalists
CompHealth
D&Y
Emory
Envision Physician Services
In Compass Health, Inc.
Ingenious Med, Inc.
Kaiser Permanente
Lightning Bolt Solutions, Inc.
Medstaff National Medical Staffing
NEJM Group
PeaceHealth
PracticeLink
Schumacher Clinical Partners
Sound Physicians
Staff Care, Inc.
TeamHealth
The Delta Companies
Today’s Hospitalist
University of Tennessee Physician Executive MBA Program
VEP Healthcare
VISTA Staffing Solutions
Vituity
Gold Level
Allergan USA, Inc.
American Board of Internal Medicine (ABIM)
Billings Clinic; Billings, Montana
Hospitalists Plus
Jackson & Coker
Janssen Pharmaceuticals, Inc.
Locum Leaders
MedAptus
MediMobile
Mountain States Health Alliance
PatientKeeper
Sonosite FujiFilm
Sutter Health Sacramento Sierra Region
Texas Health Resources
The Doctors Company
Weatherby Healthcare
Silver Level
Adventist Health System
Agency for Healthcare Research and Quality
Apogee Physicians
Banner Health
Calmoseptine, Inc.
Community Health Systems
Geisinger
Global Medical Staffing
LocumTenens.com
Mayo Clinic
MedData, Inc.
Medicus Healthcare Solutions
Mint Physician Staffing
PracticeMatch
Providence St Joseph Health (aka Providence Health & Services)
QGenda, LLC
Quest Healthcare Solutions
ScribeAmerica
Shift Administrators
TIVA Healthcare, Inc.
VITAS Healthcare
Wellstar Health System
Bronze Level
AAPA Center for Healthcare Leadership & Management
Alteon Health
ApolloMD
Aspirus Clinics
BioFire Diagnostics, Inc.
Carnegie Mellon University Master of Medical Management
Carolinas HealthCare System
Center to Advance Palliative Care (CAPC)
DaVita Medical Group
Drwanted.com
ICON Medical Network
Indiana University Kelley School of Business, Business of Medicine MBA
Integrity Locums
Melinta Therapeutics
Mercy Health
Northwell
Nova Biomedical
Pinnacle Health Group Remedy Partners
The Ohio State University Division of Hospital Medicine
The Society of Hospital Medicine is grateful for the loyal support of the following companies:
Platinum Level
Aurora Health Care
Baylor Scott & White Health
BMS/Pfizer
Boehringer Ingelheim Pharmaceuticals, Inc.
Community Hospitalists
CompHealth
D&Y
Emory
Envision Physician Services
In Compass Health, Inc.
Ingenious Med, Inc.
Kaiser Permanente
Lightning Bolt Solutions, Inc.
Medstaff National Medical Staffing
NEJM Group
PeaceHealth
PracticeLink
Schumacher Clinical Partners
Sound Physicians
Staff Care, Inc.
TeamHealth
The Delta Companies
Today’s Hospitalist
University of Tennessee Physician Executive MBA Program
VEP Healthcare
VISTA Staffing Solutions
Vituity
Gold Level
Allergan USA, Inc.
American Board of Internal Medicine (ABIM)
Billings Clinic; Billings, Montana
Hospitalists Plus
Jackson & Coker
Janssen Pharmaceuticals, Inc.
Locum Leaders
MedAptus
MediMobile
Mountain States Health Alliance
PatientKeeper
Sonosite FujiFilm
Sutter Health Sacramento Sierra Region
Texas Health Resources
The Doctors Company
Weatherby Healthcare
Silver Level
Adventist Health System
Agency for Healthcare Research and Quality
Apogee Physicians
Banner Health
Calmoseptine, Inc.
Community Health Systems
Geisinger
Global Medical Staffing
LocumTenens.com
Mayo Clinic
MedData, Inc.
Medicus Healthcare Solutions
Mint Physician Staffing
PracticeMatch
Providence St Joseph Health (aka Providence Health & Services)
QGenda, LLC
Quest Healthcare Solutions
ScribeAmerica
Shift Administrators
TIVA Healthcare, Inc.
VITAS Healthcare
Wellstar Health System
Bronze Level
AAPA Center for Healthcare Leadership & Management
Alteon Health
ApolloMD
Aspirus Clinics
BioFire Diagnostics, Inc.
Carnegie Mellon University Master of Medical Management
Carolinas HealthCare System
Center to Advance Palliative Care (CAPC)
DaVita Medical Group
Drwanted.com
ICON Medical Network
Indiana University Kelley School of Business, Business of Medicine MBA
Integrity Locums
Melinta Therapeutics
Mercy Health
Northwell
Nova Biomedical
Pinnacle Health Group Remedy Partners
The Ohio State University Division of Hospital Medicine
The Society of Hospital Medicine is grateful for the loyal support of the following companies:
Platinum Level
Aurora Health Care
Baylor Scott & White Health
BMS/Pfizer
Boehringer Ingelheim Pharmaceuticals, Inc.
Community Hospitalists
CompHealth
D&Y
Emory
Envision Physician Services
In Compass Health, Inc.
Ingenious Med, Inc.
Kaiser Permanente
Lightning Bolt Solutions, Inc.
Medstaff National Medical Staffing
NEJM Group
PeaceHealth
PracticeLink
Schumacher Clinical Partners
Sound Physicians
Staff Care, Inc.
TeamHealth
The Delta Companies
Today’s Hospitalist
University of Tennessee Physician Executive MBA Program
VEP Healthcare
VISTA Staffing Solutions
Vituity
Gold Level
Allergan USA, Inc.
American Board of Internal Medicine (ABIM)
Billings Clinic; Billings, Montana
Hospitalists Plus
Jackson & Coker
Janssen Pharmaceuticals, Inc.
Locum Leaders
MedAptus
MediMobile
Mountain States Health Alliance
PatientKeeper
Sonosite FujiFilm
Sutter Health Sacramento Sierra Region
Texas Health Resources
The Doctors Company
Weatherby Healthcare
Silver Level
Adventist Health System
Agency for Healthcare Research and Quality
Apogee Physicians
Banner Health
Calmoseptine, Inc.
Community Health Systems
Geisinger
Global Medical Staffing
LocumTenens.com
Mayo Clinic
MedData, Inc.
Medicus Healthcare Solutions
Mint Physician Staffing
PracticeMatch
Providence St Joseph Health (aka Providence Health & Services)
QGenda, LLC
Quest Healthcare Solutions
ScribeAmerica
Shift Administrators
TIVA Healthcare, Inc.
VITAS Healthcare
Wellstar Health System
Bronze Level
AAPA Center for Healthcare Leadership & Management
Alteon Health
ApolloMD
Aspirus Clinics
BioFire Diagnostics, Inc.
Carnegie Mellon University Master of Medical Management
Carolinas HealthCare System
Center to Advance Palliative Care (CAPC)
DaVita Medical Group
Drwanted.com
ICON Medical Network
Indiana University Kelley School of Business, Business of Medicine MBA
Integrity Locums
Melinta Therapeutics
Mercy Health
Northwell
Nova Biomedical
Pinnacle Health Group Remedy Partners
The Ohio State University Division of Hospital Medicine
Stay on top of perioperative medicine
The fluid, evolving nature of perioperative medicine lends itself to a lively literature review and research update, according to Steven L. Cohn, MD, SFHM, a presenter of “ ‘A Whole New World’ of Perioperative Medicine: The 2018 Update” on Monday, April 9, at HM18.
The perioperative medicine update has been a fixture at the SHM annual conference for several years and provides an opportunity to highlight articles that may affect practice, said Dr. Cohn of the University of Miami in an interview. “Our goals are to familiarize the attendees with this new data so they are aware, so they can review the key articles in detail on their own, and so they can then apply the new information in their clinical practices,” he said.
The agenda for the session involves a presentation of 10-15 articles published since HM17. Dr. Cohn and presenter Paul J. Grant, MD, SFHM, the director of the consultative and perioperative medicine program and an associate chief medical information officer at Michigan Medicine, Ann Arbor, will briefly review the objectives and methods of each study before moving on to focus primarily on the result and conclusions.
“The top take-home message is to try to keep up with the perioperative literature, particularly in cardiology, because the evidence base keeps expanding and changing,” said Dr. Cohn. “This session is designed to deliver new information and also to stimulate the attendees to periodically review the literature on their own during the year,” he said.
This year’s collection of articles will address a range of topics, Dr. Cohn said, but he highlighted several articles “that will be thought provoking and potentially impact clinical practice regarding perioperative surveillance with the new fifth generation high sensitivity troponin assay and management of myocardial injury after noncardiac surgery. In particular, results from the MANAGE trial that was presented as a late-breaking trial at the American College of Cardiology meeting in March will be of interest to anyone involved in perioperative medicine,” he noted.
Dr. Cohn and Dr. Grant had no relevant financial conflicts to disclose.
“A Whole New World” of Perioperative Medicine: The 2018 Update
Monday, April 9, 2:00-2:40 p.m.
Crystal Ballroom G2/C-F
The fluid, evolving nature of perioperative medicine lends itself to a lively literature review and research update, according to Steven L. Cohn, MD, SFHM, a presenter of “ ‘A Whole New World’ of Perioperative Medicine: The 2018 Update” on Monday, April 9, at HM18.
The perioperative medicine update has been a fixture at the SHM annual conference for several years and provides an opportunity to highlight articles that may affect practice, said Dr. Cohn of the University of Miami in an interview. “Our goals are to familiarize the attendees with this new data so they are aware, so they can review the key articles in detail on their own, and so they can then apply the new information in their clinical practices,” he said.
The agenda for the session involves a presentation of 10-15 articles published since HM17. Dr. Cohn and presenter Paul J. Grant, MD, SFHM, the director of the consultative and perioperative medicine program and an associate chief medical information officer at Michigan Medicine, Ann Arbor, will briefly review the objectives and methods of each study before moving on to focus primarily on the result and conclusions.
“The top take-home message is to try to keep up with the perioperative literature, particularly in cardiology, because the evidence base keeps expanding and changing,” said Dr. Cohn. “This session is designed to deliver new information and also to stimulate the attendees to periodically review the literature on their own during the year,” he said.
This year’s collection of articles will address a range of topics, Dr. Cohn said, but he highlighted several articles “that will be thought provoking and potentially impact clinical practice regarding perioperative surveillance with the new fifth generation high sensitivity troponin assay and management of myocardial injury after noncardiac surgery. In particular, results from the MANAGE trial that was presented as a late-breaking trial at the American College of Cardiology meeting in March will be of interest to anyone involved in perioperative medicine,” he noted.
Dr. Cohn and Dr. Grant had no relevant financial conflicts to disclose.
“A Whole New World” of Perioperative Medicine: The 2018 Update
Monday, April 9, 2:00-2:40 p.m.
Crystal Ballroom G2/C-F
The fluid, evolving nature of perioperative medicine lends itself to a lively literature review and research update, according to Steven L. Cohn, MD, SFHM, a presenter of “ ‘A Whole New World’ of Perioperative Medicine: The 2018 Update” on Monday, April 9, at HM18.
The perioperative medicine update has been a fixture at the SHM annual conference for several years and provides an opportunity to highlight articles that may affect practice, said Dr. Cohn of the University of Miami in an interview. “Our goals are to familiarize the attendees with this new data so they are aware, so they can review the key articles in detail on their own, and so they can then apply the new information in their clinical practices,” he said.
The agenda for the session involves a presentation of 10-15 articles published since HM17. Dr. Cohn and presenter Paul J. Grant, MD, SFHM, the director of the consultative and perioperative medicine program and an associate chief medical information officer at Michigan Medicine, Ann Arbor, will briefly review the objectives and methods of each study before moving on to focus primarily on the result and conclusions.
“The top take-home message is to try to keep up with the perioperative literature, particularly in cardiology, because the evidence base keeps expanding and changing,” said Dr. Cohn. “This session is designed to deliver new information and also to stimulate the attendees to periodically review the literature on their own during the year,” he said.
This year’s collection of articles will address a range of topics, Dr. Cohn said, but he highlighted several articles “that will be thought provoking and potentially impact clinical practice regarding perioperative surveillance with the new fifth generation high sensitivity troponin assay and management of myocardial injury after noncardiac surgery. In particular, results from the MANAGE trial that was presented as a late-breaking trial at the American College of Cardiology meeting in March will be of interest to anyone involved in perioperative medicine,” he noted.
Dr. Cohn and Dr. Grant had no relevant financial conflicts to disclose.
“A Whole New World” of Perioperative Medicine: The 2018 Update
Monday, April 9, 2:00-2:40 p.m.
Crystal Ballroom G2/C-F