User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Treat sleep apnea with positive airway pressure, but don’t expect it to prevent heart attacks
Clinical question: In patients with sleep apnea, does using positive airway pressure (PAP) treatment prevent adverse cardiovascular events and death?
Background: Previous observational studies have suggested that untreated sleep apnea is a factor in cardiopulmonary morbidity as well as cerebrovascular events. Guidelines advise its use for prevention of cerebrovascular events. However, not enough is known from trials about its impact on prevention of cardiovascular events.
Synopsis: The authors analyzed 10 randomized-controlled trials encompassing 7,266 patients with sleep apnea. They examined instances of major adverse cardiovascular events (MACE; acute coronary syndrome, stroke, cardiovascular death) as well as hospitalization for unstable angina and all-cause deaths, among others. They found no association between treatment with positive airway pressure and MACEs (169 events vs. 187 events, with a relative risk of 0.77; 95% confidence interval, 0.53-1.13) or all-cause death (324 events vs. 289 events, RR 1.13; 95% CI,0.99-1.29).
Bottom line: Positive airway pressure treatment for patients with sleep apnea is not an intervention to prevent cardiovascular morbidity.
Citation: Yu J et al. Association of positive airway pressure with cardiovascular events and death in adults with sleep apnea. JAMA. 2017 Jul 11;318(2):156-66.
Dr. Sata is a medical instructor, Duke University Hospital.
Clinical question: In patients with sleep apnea, does using positive airway pressure (PAP) treatment prevent adverse cardiovascular events and death?
Background: Previous observational studies have suggested that untreated sleep apnea is a factor in cardiopulmonary morbidity as well as cerebrovascular events. Guidelines advise its use for prevention of cerebrovascular events. However, not enough is known from trials about its impact on prevention of cardiovascular events.
Synopsis: The authors analyzed 10 randomized-controlled trials encompassing 7,266 patients with sleep apnea. They examined instances of major adverse cardiovascular events (MACE; acute coronary syndrome, stroke, cardiovascular death) as well as hospitalization for unstable angina and all-cause deaths, among others. They found no association between treatment with positive airway pressure and MACEs (169 events vs. 187 events, with a relative risk of 0.77; 95% confidence interval, 0.53-1.13) or all-cause death (324 events vs. 289 events, RR 1.13; 95% CI,0.99-1.29).
Bottom line: Positive airway pressure treatment for patients with sleep apnea is not an intervention to prevent cardiovascular morbidity.
Citation: Yu J et al. Association of positive airway pressure with cardiovascular events and death in adults with sleep apnea. JAMA. 2017 Jul 11;318(2):156-66.
Dr. Sata is a medical instructor, Duke University Hospital.
Clinical question: In patients with sleep apnea, does using positive airway pressure (PAP) treatment prevent adverse cardiovascular events and death?
Background: Previous observational studies have suggested that untreated sleep apnea is a factor in cardiopulmonary morbidity as well as cerebrovascular events. Guidelines advise its use for prevention of cerebrovascular events. However, not enough is known from trials about its impact on prevention of cardiovascular events.
Synopsis: The authors analyzed 10 randomized-controlled trials encompassing 7,266 patients with sleep apnea. They examined instances of major adverse cardiovascular events (MACE; acute coronary syndrome, stroke, cardiovascular death) as well as hospitalization for unstable angina and all-cause deaths, among others. They found no association between treatment with positive airway pressure and MACEs (169 events vs. 187 events, with a relative risk of 0.77; 95% confidence interval, 0.53-1.13) or all-cause death (324 events vs. 289 events, RR 1.13; 95% CI,0.99-1.29).
Bottom line: Positive airway pressure treatment for patients with sleep apnea is not an intervention to prevent cardiovascular morbidity.
Citation: Yu J et al. Association of positive airway pressure with cardiovascular events and death in adults with sleep apnea. JAMA. 2017 Jul 11;318(2):156-66.
Dr. Sata is a medical instructor, Duke University Hospital.
Different perspectives on the care delivery process
Editor’s note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform health care and revolutionize patient care. The program has been expanded for the 2017-18 year, offering two options for students to receive funding and engage in scholarly work during their first, second and third years of medical school. As a part of the longitudinal (18-month) program, recipients are required to write about their experience on a monthly basis.
Last month I was able to conduct five interviews with key stakeholders, generate the patient flow diagram, define the problems, and propose potential interventions. The project is on time for the allotted time frame.
Interviewees include physicians and managers from infectious disease, hospital medicine, psychiatry and care management. They represent the services which admitted IVDU patients have contacts with: inpatient primary team, inpatient ID consult time, BIT (behavior intervention team), and OPAT (Outpatient Parenteral Antibiotic Therapy) program. I asked each interviewee about the specific challenges of care delivery during the inpatient, discharge, and outpatient follow up process.
It is not surprising that most would agree that discharge was the most difficult part. The ID service showed me data that those with IVDU history may have a one-time longer length of stay compared to the average. The social-psychological issues, including medication compliance, insurance coverage, and mental health comorbidities, are the most commonly mentioned factor for delayed discharge.
When asked about a suggestion for a particular area for quality improvement, different services came up with different recommendations. ID suggested looking at availability of community resources and improving patients’ access to them. Psychiatry has been trying to screen all admitted patients for substance use disorders, with an intention of early intervention. Hospital medicine and care management were contemplating the potential means for a repatriation program, i.e., making the transferring acute care facility agree to receive patients back once tertiary care was complete. Given that Dartmouth-Hitchcock Medical Center has a few satellite community hospitals, it would make sense to establish some institutional protocol to optimize patient flow within the system.
My next step would be to pursue one or two areas for improvement from the above options. I will work with the relevant stakeholders to define the problems and come up with a plan. I am excited about moving forward to the next phase.
My research approach has changed slightly during the process. Initially I was narrowly focused on the desired outcomes of decreasing length of stay and readmission rate. Dr. Huntington challenged me to understand the whole process thoroughly as well as to spend time on defining the problems before diving into interventions. I enjoyed my role of being a learner, researcher, and consultant in this project. I gained a very in-depth perspective on how each service operates and coordinates. Also, it is both challenging and fun to coming up with an improvement plan. In my future residency and physician career, I am definitely going to pursue more care improvement initiatives.
Yun Li is an MD/MBA student attending Geisel School of Medicine and Tuck School of Business at Dartmouth. She obtained her Bachelor of Arts degree from Hanover College double-majoring in Economics and Biological Chemistry. Ms. Li participated in research in injury epidemiology and genetics, and has conducted studies on traditional Tibetan medicine, rural health, health NGOs, and digital health. Her career interest is practicing hospital medicine and geriatrics as a clinician/administrator, either in the US or China. Ms. Li is a student member of the Society of Hospital Medicine.
Editor’s note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform health care and revolutionize patient care. The program has been expanded for the 2017-18 year, offering two options for students to receive funding and engage in scholarly work during their first, second and third years of medical school. As a part of the longitudinal (18-month) program, recipients are required to write about their experience on a monthly basis.
Last month I was able to conduct five interviews with key stakeholders, generate the patient flow diagram, define the problems, and propose potential interventions. The project is on time for the allotted time frame.
Interviewees include physicians and managers from infectious disease, hospital medicine, psychiatry and care management. They represent the services which admitted IVDU patients have contacts with: inpatient primary team, inpatient ID consult time, BIT (behavior intervention team), and OPAT (Outpatient Parenteral Antibiotic Therapy) program. I asked each interviewee about the specific challenges of care delivery during the inpatient, discharge, and outpatient follow up process.
It is not surprising that most would agree that discharge was the most difficult part. The ID service showed me data that those with IVDU history may have a one-time longer length of stay compared to the average. The social-psychological issues, including medication compliance, insurance coverage, and mental health comorbidities, are the most commonly mentioned factor for delayed discharge.
When asked about a suggestion for a particular area for quality improvement, different services came up with different recommendations. ID suggested looking at availability of community resources and improving patients’ access to them. Psychiatry has been trying to screen all admitted patients for substance use disorders, with an intention of early intervention. Hospital medicine and care management were contemplating the potential means for a repatriation program, i.e., making the transferring acute care facility agree to receive patients back once tertiary care was complete. Given that Dartmouth-Hitchcock Medical Center has a few satellite community hospitals, it would make sense to establish some institutional protocol to optimize patient flow within the system.
My next step would be to pursue one or two areas for improvement from the above options. I will work with the relevant stakeholders to define the problems and come up with a plan. I am excited about moving forward to the next phase.
My research approach has changed slightly during the process. Initially I was narrowly focused on the desired outcomes of decreasing length of stay and readmission rate. Dr. Huntington challenged me to understand the whole process thoroughly as well as to spend time on defining the problems before diving into interventions. I enjoyed my role of being a learner, researcher, and consultant in this project. I gained a very in-depth perspective on how each service operates and coordinates. Also, it is both challenging and fun to coming up with an improvement plan. In my future residency and physician career, I am definitely going to pursue more care improvement initiatives.
Yun Li is an MD/MBA student attending Geisel School of Medicine and Tuck School of Business at Dartmouth. She obtained her Bachelor of Arts degree from Hanover College double-majoring in Economics and Biological Chemistry. Ms. Li participated in research in injury epidemiology and genetics, and has conducted studies on traditional Tibetan medicine, rural health, health NGOs, and digital health. Her career interest is practicing hospital medicine and geriatrics as a clinician/administrator, either in the US or China. Ms. Li is a student member of the Society of Hospital Medicine.
Editor’s note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform health care and revolutionize patient care. The program has been expanded for the 2017-18 year, offering two options for students to receive funding and engage in scholarly work during their first, second and third years of medical school. As a part of the longitudinal (18-month) program, recipients are required to write about their experience on a monthly basis.
Last month I was able to conduct five interviews with key stakeholders, generate the patient flow diagram, define the problems, and propose potential interventions. The project is on time for the allotted time frame.
Interviewees include physicians and managers from infectious disease, hospital medicine, psychiatry and care management. They represent the services which admitted IVDU patients have contacts with: inpatient primary team, inpatient ID consult time, BIT (behavior intervention team), and OPAT (Outpatient Parenteral Antibiotic Therapy) program. I asked each interviewee about the specific challenges of care delivery during the inpatient, discharge, and outpatient follow up process.
It is not surprising that most would agree that discharge was the most difficult part. The ID service showed me data that those with IVDU history may have a one-time longer length of stay compared to the average. The social-psychological issues, including medication compliance, insurance coverage, and mental health comorbidities, are the most commonly mentioned factor for delayed discharge.
When asked about a suggestion for a particular area for quality improvement, different services came up with different recommendations. ID suggested looking at availability of community resources and improving patients’ access to them. Psychiatry has been trying to screen all admitted patients for substance use disorders, with an intention of early intervention. Hospital medicine and care management were contemplating the potential means for a repatriation program, i.e., making the transferring acute care facility agree to receive patients back once tertiary care was complete. Given that Dartmouth-Hitchcock Medical Center has a few satellite community hospitals, it would make sense to establish some institutional protocol to optimize patient flow within the system.
My next step would be to pursue one or two areas for improvement from the above options. I will work with the relevant stakeholders to define the problems and come up with a plan. I am excited about moving forward to the next phase.
My research approach has changed slightly during the process. Initially I was narrowly focused on the desired outcomes of decreasing length of stay and readmission rate. Dr. Huntington challenged me to understand the whole process thoroughly as well as to spend time on defining the problems before diving into interventions. I enjoyed my role of being a learner, researcher, and consultant in this project. I gained a very in-depth perspective on how each service operates and coordinates. Also, it is both challenging and fun to coming up with an improvement plan. In my future residency and physician career, I am definitely going to pursue more care improvement initiatives.
Yun Li is an MD/MBA student attending Geisel School of Medicine and Tuck School of Business at Dartmouth. She obtained her Bachelor of Arts degree from Hanover College double-majoring in Economics and Biological Chemistry. Ms. Li participated in research in injury epidemiology and genetics, and has conducted studies on traditional Tibetan medicine, rural health, health NGOs, and digital health. Her career interest is practicing hospital medicine and geriatrics as a clinician/administrator, either in the US or China. Ms. Li is a student member of the Society of Hospital Medicine.
Transition in care from the MICU to the ward
Editor’s Note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform healthcare and revolutionize patient care. The program has been expanded for the 2017-18 year, offering two options for students to receive funding and engage in scholarly work during their first, second and third years of medical school. As a part of the program, recipients are required to write about their experience on a biweekly basis.
This summer, my research project focused on the highly vulnerable patients who are transferred from the medical intensive care unit to the general floor. Patients who are readmitted tend to have worse health outcomes, longer stays, higher mortality rates, and higher health care costs. Previous research shows that higher quality handoffs, where receiving and transferring providers share the same shared mental model, result in better outcomes. We were interested in learning whether these shared mental models are being formed as a result of handoffs between the ward and the MICU.
The current results reveal that 18% of MICU teams shared a complete mental model, 25% shared a strong shared mental model, 9% shared a weak mental model, 30% shared no mental model, and 18% of patient encounters did not have a sufficient number of MICU respondents. Regarding inter-team communication, 7% shared a full shared mental model, 49% shared a partial mental model, 30% shared no shared mental model, and 14% of unique patient encounters did not have enough respondents.
With complex patient cases, it can be difficult to identify the most important factor of care for a particular patient. However, I think this information would be very useful in identifying whether these exchanges result in individuals prioritizing the same factor of care for their respective patient. I think this information would be very useful in future quality improvement, and seeing whether this communication results in the formation of shared mental models.
Anton Garazha is a medical student at Chicago Medical School at Rosalind Franklin University in North Chicago. He received his bachelor of science degree in biology from Loyola University in Chicago in 2015 and his master of biomedical science degree from Rosalind Franklin University in 2016. Anton is very interested in community outreach and quality improvement, and in his spare time tutors students in science-based subjects.
Editor’s Note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform healthcare and revolutionize patient care. The program has been expanded for the 2017-18 year, offering two options for students to receive funding and engage in scholarly work during their first, second and third years of medical school. As a part of the program, recipients are required to write about their experience on a biweekly basis.
This summer, my research project focused on the highly vulnerable patients who are transferred from the medical intensive care unit to the general floor. Patients who are readmitted tend to have worse health outcomes, longer stays, higher mortality rates, and higher health care costs. Previous research shows that higher quality handoffs, where receiving and transferring providers share the same shared mental model, result in better outcomes. We were interested in learning whether these shared mental models are being formed as a result of handoffs between the ward and the MICU.
The current results reveal that 18% of MICU teams shared a complete mental model, 25% shared a strong shared mental model, 9% shared a weak mental model, 30% shared no mental model, and 18% of patient encounters did not have a sufficient number of MICU respondents. Regarding inter-team communication, 7% shared a full shared mental model, 49% shared a partial mental model, 30% shared no shared mental model, and 14% of unique patient encounters did not have enough respondents.
With complex patient cases, it can be difficult to identify the most important factor of care for a particular patient. However, I think this information would be very useful in identifying whether these exchanges result in individuals prioritizing the same factor of care for their respective patient. I think this information would be very useful in future quality improvement, and seeing whether this communication results in the formation of shared mental models.
Anton Garazha is a medical student at Chicago Medical School at Rosalind Franklin University in North Chicago. He received his bachelor of science degree in biology from Loyola University in Chicago in 2015 and his master of biomedical science degree from Rosalind Franklin University in 2016. Anton is very interested in community outreach and quality improvement, and in his spare time tutors students in science-based subjects.
Editor’s Note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform healthcare and revolutionize patient care. The program has been expanded for the 2017-18 year, offering two options for students to receive funding and engage in scholarly work during their first, second and third years of medical school. As a part of the program, recipients are required to write about their experience on a biweekly basis.
This summer, my research project focused on the highly vulnerable patients who are transferred from the medical intensive care unit to the general floor. Patients who are readmitted tend to have worse health outcomes, longer stays, higher mortality rates, and higher health care costs. Previous research shows that higher quality handoffs, where receiving and transferring providers share the same shared mental model, result in better outcomes. We were interested in learning whether these shared mental models are being formed as a result of handoffs between the ward and the MICU.
The current results reveal that 18% of MICU teams shared a complete mental model, 25% shared a strong shared mental model, 9% shared a weak mental model, 30% shared no mental model, and 18% of patient encounters did not have a sufficient number of MICU respondents. Regarding inter-team communication, 7% shared a full shared mental model, 49% shared a partial mental model, 30% shared no shared mental model, and 14% of unique patient encounters did not have enough respondents.
With complex patient cases, it can be difficult to identify the most important factor of care for a particular patient. However, I think this information would be very useful in identifying whether these exchanges result in individuals prioritizing the same factor of care for their respective patient. I think this information would be very useful in future quality improvement, and seeing whether this communication results in the formation of shared mental models.
Anton Garazha is a medical student at Chicago Medical School at Rosalind Franklin University in North Chicago. He received his bachelor of science degree in biology from Loyola University in Chicago in 2015 and his master of biomedical science degree from Rosalind Franklin University in 2016. Anton is very interested in community outreach and quality improvement, and in his spare time tutors students in science-based subjects.
You aren’t (necessarily) a walking petri dish!
Clinical question: Does exposure to a patient with a multidrug-resistant organism result in colonization of a health care provider?
Background: Multidrug-resistant organisms (MDROs) are growing threats in our hospitals, particularly vancomycin-resistant enterococci (VRE) and resistant gram-negative bacteria. The role of the health care team in preventing infection transmission is paramount. If a team member who is caring for a patient with an MDRO or handling lab specimens becomes colonized with these bacteria, he or she could potentially transmit them to the next patient.
Setting: Large academic research hospital.
Synopsis: Staff submitted self-collected rectal swabs, which were then cultured for MDROs. 379 health care personnel (which they defined as having had self-reported exposure to MDROs) were compared with 376 staff members in the control group, who reported no exposure to MDROs. There was a nonsignificant difference between growth of multidrug-resistant organisms between the groups (4.0% vs 3.2%).
Bottom line: This study suggests that occupational exposure to an MDRO does not result in subsequent colonization of the health care provider and may not be a major risk factor for nosocomial transmission.
Citation: Decker BK et al. Healthcare personnel intestinal colonization with multidrug-resistant organisms. Clin Microbiol Infect. 2017 May 12. pii:S1198-743X(17)30270-7.
Dr. Sata is a medical instructor, Duke University Hospital.
Clinical question: Does exposure to a patient with a multidrug-resistant organism result in colonization of a health care provider?
Background: Multidrug-resistant organisms (MDROs) are growing threats in our hospitals, particularly vancomycin-resistant enterococci (VRE) and resistant gram-negative bacteria. The role of the health care team in preventing infection transmission is paramount. If a team member who is caring for a patient with an MDRO or handling lab specimens becomes colonized with these bacteria, he or she could potentially transmit them to the next patient.
Setting: Large academic research hospital.
Synopsis: Staff submitted self-collected rectal swabs, which were then cultured for MDROs. 379 health care personnel (which they defined as having had self-reported exposure to MDROs) were compared with 376 staff members in the control group, who reported no exposure to MDROs. There was a nonsignificant difference between growth of multidrug-resistant organisms between the groups (4.0% vs 3.2%).
Bottom line: This study suggests that occupational exposure to an MDRO does not result in subsequent colonization of the health care provider and may not be a major risk factor for nosocomial transmission.
Citation: Decker BK et al. Healthcare personnel intestinal colonization with multidrug-resistant organisms. Clin Microbiol Infect. 2017 May 12. pii:S1198-743X(17)30270-7.
Dr. Sata is a medical instructor, Duke University Hospital.
Clinical question: Does exposure to a patient with a multidrug-resistant organism result in colonization of a health care provider?
Background: Multidrug-resistant organisms (MDROs) are growing threats in our hospitals, particularly vancomycin-resistant enterococci (VRE) and resistant gram-negative bacteria. The role of the health care team in preventing infection transmission is paramount. If a team member who is caring for a patient with an MDRO or handling lab specimens becomes colonized with these bacteria, he or she could potentially transmit them to the next patient.
Setting: Large academic research hospital.
Synopsis: Staff submitted self-collected rectal swabs, which were then cultured for MDROs. 379 health care personnel (which they defined as having had self-reported exposure to MDROs) were compared with 376 staff members in the control group, who reported no exposure to MDROs. There was a nonsignificant difference between growth of multidrug-resistant organisms between the groups (4.0% vs 3.2%).
Bottom line: This study suggests that occupational exposure to an MDRO does not result in subsequent colonization of the health care provider and may not be a major risk factor for nosocomial transmission.
Citation: Decker BK et al. Healthcare personnel intestinal colonization with multidrug-resistant organisms. Clin Microbiol Infect. 2017 May 12. pii:S1198-743X(17)30270-7.
Dr. Sata is a medical instructor, Duke University Hospital.
Inpatient antiviral treatment reduces ICU admissions among influenza patients
SAN DIEGO – Administering inpatient antiviral influenza treatment may reduce admissions to the ICU among adults hospitalized with flu, according to a study presented at ID Week 2017, an infectious diseases meeting.
While interventions did not directly affect flu-related deaths, lower ICU admission rates could reduce morbidity as well as ease the financial burden felt during the influenza season.
Investigators retrospectively studied 4,679 influenza patients admitted to Canadian Immunization Research Network Serious Outcomes Surveillance (SOS) Network hospitals during 2011-2014. Of the 54% of patients given inpatient antiviral treatment, the risk of being admitted to the ICU was reduced by 90% (odds ratio, 0.10;95% confidence interval, 0.08-0.13; P less than .001).
Antiviral treatment was not protective against death outcomes in patients with either influenza A or influenza B (OR, 0.9; 95% CI, 0.7-1.2; P =.454).
The median age of patients was 70 years, with a majority older than 75 years(41%); the majority presented with one or more comorbidities (89%), and had influenza A (72%).
Researchers found that, of the 4,679 patients studied, 798 (16%) were admitted to the ICU, 511 (11%) required mechanical ventilation, and the average length of hospital stay was 11 days.
Of those studied, 444 (9%) died within 30 days of discharge.
Researchers also found that only 38% of those studied had received the current seasonal vaccine upon admittance. However, these numbers may be skewed from the general population, because patients who have not taken the vaccine are more likely to be hospitalized.
Along with the results of antivirals on hospitalized patients, researchers wanted to uncover how the effectiveness of inpatient vaccine administration would vary based on treatment timing, said presenter Zach Shaffelburg of the Canadian Center for Vaccinology, Dalhousie University, Halifax, NS.
Even when administered 4.28 days after symptom onset, antiviral treatments in patients proved to be associated with significant reductions in ICU admissions and the need for mechanical ventilation.
The investigators concluded that antivirals show a strong association with positive effects on serious, influenza-related outcomes in hospitalized patients and, while therapy remained effective with later treatment start, patients would benefit the most from initiation as soon as possible.
Currently, the U.S. Centers for Disease Control and Prevention and the Canadian Immunization Research Network (CIRN) have guidelines instructing best practice for inpatient antiviral treatment, however the number of hospitalized patients given treatment has declined in Canada since 2009, according to Mr. Shaffelburg.
The reason more patients were not receiving inpatient antiviral treatment may be related to studies of different populations that failed to show significant impact, Mr. Shaffelburg suggested during a question and answer session following the presentation: “I think a lot of that comes from outpatient studies that involve patients who are younger and quite healthy [who received] antivirals, and it showed a very minimal impact,” Mr. Shaffelburg said. “So a lot of people saw that study and thought, ‘What’s that point of giving it if it’s not going to make an impact?’ ”
Mr. Shaffelburg and his colleagues are planning to continue their study of inpatient antiviral treatment, focusing more on the effectiveness of treatment in relation to time administered after onset.
Mr. Shaffelburg reported having no disclosures. The study was funded by the CIRN SOS network, Canadian Institutes for Health Research, and a partnership with GlaxoSmithKline Biologicals. Some of the investigators were GSK employees or received grant funding from the company.
SOURCE: Shaffelburg Z et al. IDWeek 2017 Abstract 890.
SAN DIEGO – Administering inpatient antiviral influenza treatment may reduce admissions to the ICU among adults hospitalized with flu, according to a study presented at ID Week 2017, an infectious diseases meeting.
While interventions did not directly affect flu-related deaths, lower ICU admission rates could reduce morbidity as well as ease the financial burden felt during the influenza season.
Investigators retrospectively studied 4,679 influenza patients admitted to Canadian Immunization Research Network Serious Outcomes Surveillance (SOS) Network hospitals during 2011-2014. Of the 54% of patients given inpatient antiviral treatment, the risk of being admitted to the ICU was reduced by 90% (odds ratio, 0.10;95% confidence interval, 0.08-0.13; P less than .001).
Antiviral treatment was not protective against death outcomes in patients with either influenza A or influenza B (OR, 0.9; 95% CI, 0.7-1.2; P =.454).
The median age of patients was 70 years, with a majority older than 75 years(41%); the majority presented with one or more comorbidities (89%), and had influenza A (72%).
Researchers found that, of the 4,679 patients studied, 798 (16%) were admitted to the ICU, 511 (11%) required mechanical ventilation, and the average length of hospital stay was 11 days.
Of those studied, 444 (9%) died within 30 days of discharge.
Researchers also found that only 38% of those studied had received the current seasonal vaccine upon admittance. However, these numbers may be skewed from the general population, because patients who have not taken the vaccine are more likely to be hospitalized.
Along with the results of antivirals on hospitalized patients, researchers wanted to uncover how the effectiveness of inpatient vaccine administration would vary based on treatment timing, said presenter Zach Shaffelburg of the Canadian Center for Vaccinology, Dalhousie University, Halifax, NS.
Even when administered 4.28 days after symptom onset, antiviral treatments in patients proved to be associated with significant reductions in ICU admissions and the need for mechanical ventilation.
The investigators concluded that antivirals show a strong association with positive effects on serious, influenza-related outcomes in hospitalized patients and, while therapy remained effective with later treatment start, patients would benefit the most from initiation as soon as possible.
Currently, the U.S. Centers for Disease Control and Prevention and the Canadian Immunization Research Network (CIRN) have guidelines instructing best practice for inpatient antiviral treatment, however the number of hospitalized patients given treatment has declined in Canada since 2009, according to Mr. Shaffelburg.
The reason more patients were not receiving inpatient antiviral treatment may be related to studies of different populations that failed to show significant impact, Mr. Shaffelburg suggested during a question and answer session following the presentation: “I think a lot of that comes from outpatient studies that involve patients who are younger and quite healthy [who received] antivirals, and it showed a very minimal impact,” Mr. Shaffelburg said. “So a lot of people saw that study and thought, ‘What’s that point of giving it if it’s not going to make an impact?’ ”
Mr. Shaffelburg and his colleagues are planning to continue their study of inpatient antiviral treatment, focusing more on the effectiveness of treatment in relation to time administered after onset.
Mr. Shaffelburg reported having no disclosures. The study was funded by the CIRN SOS network, Canadian Institutes for Health Research, and a partnership with GlaxoSmithKline Biologicals. Some of the investigators were GSK employees or received grant funding from the company.
SOURCE: Shaffelburg Z et al. IDWeek 2017 Abstract 890.
SAN DIEGO – Administering inpatient antiviral influenza treatment may reduce admissions to the ICU among adults hospitalized with flu, according to a study presented at ID Week 2017, an infectious diseases meeting.
While interventions did not directly affect flu-related deaths, lower ICU admission rates could reduce morbidity as well as ease the financial burden felt during the influenza season.
Investigators retrospectively studied 4,679 influenza patients admitted to Canadian Immunization Research Network Serious Outcomes Surveillance (SOS) Network hospitals during 2011-2014. Of the 54% of patients given inpatient antiviral treatment, the risk of being admitted to the ICU was reduced by 90% (odds ratio, 0.10;95% confidence interval, 0.08-0.13; P less than .001).
Antiviral treatment was not protective against death outcomes in patients with either influenza A or influenza B (OR, 0.9; 95% CI, 0.7-1.2; P =.454).
The median age of patients was 70 years, with a majority older than 75 years(41%); the majority presented with one or more comorbidities (89%), and had influenza A (72%).
Researchers found that, of the 4,679 patients studied, 798 (16%) were admitted to the ICU, 511 (11%) required mechanical ventilation, and the average length of hospital stay was 11 days.
Of those studied, 444 (9%) died within 30 days of discharge.
Researchers also found that only 38% of those studied had received the current seasonal vaccine upon admittance. However, these numbers may be skewed from the general population, because patients who have not taken the vaccine are more likely to be hospitalized.
Along with the results of antivirals on hospitalized patients, researchers wanted to uncover how the effectiveness of inpatient vaccine administration would vary based on treatment timing, said presenter Zach Shaffelburg of the Canadian Center for Vaccinology, Dalhousie University, Halifax, NS.
Even when administered 4.28 days after symptom onset, antiviral treatments in patients proved to be associated with significant reductions in ICU admissions and the need for mechanical ventilation.
The investigators concluded that antivirals show a strong association with positive effects on serious, influenza-related outcomes in hospitalized patients and, while therapy remained effective with later treatment start, patients would benefit the most from initiation as soon as possible.
Currently, the U.S. Centers for Disease Control and Prevention and the Canadian Immunization Research Network (CIRN) have guidelines instructing best practice for inpatient antiviral treatment, however the number of hospitalized patients given treatment has declined in Canada since 2009, according to Mr. Shaffelburg.
The reason more patients were not receiving inpatient antiviral treatment may be related to studies of different populations that failed to show significant impact, Mr. Shaffelburg suggested during a question and answer session following the presentation: “I think a lot of that comes from outpatient studies that involve patients who are younger and quite healthy [who received] antivirals, and it showed a very minimal impact,” Mr. Shaffelburg said. “So a lot of people saw that study and thought, ‘What’s that point of giving it if it’s not going to make an impact?’ ”
Mr. Shaffelburg and his colleagues are planning to continue their study of inpatient antiviral treatment, focusing more on the effectiveness of treatment in relation to time administered after onset.
Mr. Shaffelburg reported having no disclosures. The study was funded by the CIRN SOS network, Canadian Institutes for Health Research, and a partnership with GlaxoSmithKline Biologicals. Some of the investigators were GSK employees or received grant funding from the company.
SOURCE: Shaffelburg Z et al. IDWeek 2017 Abstract 890.
REPORTING FROM ID WEEK 2017
Key clinical point:
Major finding: Patients who received antiviral treatment were significantly less likely to go to the ICU or need mechanical ventilation (OR, 0.10; 95% CI, 0.08-0.13; P less than .001).
Study details: Study of 4,679 hospitalized influenza patients admitted to the Canadian Immunization Research Network Serious Outcomes Surveillance (CIRN SOS) network hospitals between 2011 to 2014.
Disclosures: Mr. Shaffelburg reported having no disclosures. The study was funded by the CIRN SOS network, Canadian Institutes for Health Research, and a partnership with GlaxoSmithKline Biologicals. Some of the investigators were GSK employees or received grant funding from the company.
Source: Shaffelburg Z et al. IDWeek 2017 Abstract 890.
Idarucizumab reverses anticoagulation effects of dabigatran
Clinical question: Can idarucizumab reverse anticoagulation effects of dabigatran in a timely manner for urgent surgery or in the event of bleeding?
Background: Reversing the anticoagulant properties of anticoagulants can be important in the event of a life-threatening bleed, or if patients taking these medications need urgent surgery or other interventions. Idarucizumab, a humanized monoclonal antibody fragment, can reverse anticoagulant activity of dabigatran, increasing its acceptance for prescribing physicians as well as patients.
Study design: Multicenter prospective single cohort study.
Setting: 173 sites, 39 countries.
Synopsis: Among 503 patients (median age, 78 years, indication for dabigatran included stroke prophylaxis in setting of atrial fibrillation for most) who had either uncontrolled bleeding (n = 301) or needing emergent surgery (n = 202), a single 5-g dose of idarucizumab was able to reverse anticoagulation rapidly and completely in more than 98% of these patients independent of age, sex, renal function, and dabigatran concentration at baseline. Specifically in 68% of the patients in the bleeding group (excluding intracranial hemorrhage) median time to the cessation of bleeding was 2.5 hours and median time to the initiation of the procedure in the emergent surgery group was 1.6 hours. Study limited by lack of control group.
Bottom line: Idarucizumab can be effective for dabigatran reversal among patients who have uncontrolled bleeding or need to undergo urgent surgery.
Citation: Pollack CV Jr. et al. Idarucizumab for dabigatran reversal: Full cohort analysis. N Engl J Med. 2017 Aug 3;377(5):431-41.
Dr. Kamath is a hospitalist and medical director of quality and patient safety, Duke Regional Hospital, Duke University Health System.
Clinical question: Can idarucizumab reverse anticoagulation effects of dabigatran in a timely manner for urgent surgery or in the event of bleeding?
Background: Reversing the anticoagulant properties of anticoagulants can be important in the event of a life-threatening bleed, or if patients taking these medications need urgent surgery or other interventions. Idarucizumab, a humanized monoclonal antibody fragment, can reverse anticoagulant activity of dabigatran, increasing its acceptance for prescribing physicians as well as patients.
Study design: Multicenter prospective single cohort study.
Setting: 173 sites, 39 countries.
Synopsis: Among 503 patients (median age, 78 years, indication for dabigatran included stroke prophylaxis in setting of atrial fibrillation for most) who had either uncontrolled bleeding (n = 301) or needing emergent surgery (n = 202), a single 5-g dose of idarucizumab was able to reverse anticoagulation rapidly and completely in more than 98% of these patients independent of age, sex, renal function, and dabigatran concentration at baseline. Specifically in 68% of the patients in the bleeding group (excluding intracranial hemorrhage) median time to the cessation of bleeding was 2.5 hours and median time to the initiation of the procedure in the emergent surgery group was 1.6 hours. Study limited by lack of control group.
Bottom line: Idarucizumab can be effective for dabigatran reversal among patients who have uncontrolled bleeding or need to undergo urgent surgery.
Citation: Pollack CV Jr. et al. Idarucizumab for dabigatran reversal: Full cohort analysis. N Engl J Med. 2017 Aug 3;377(5):431-41.
Dr. Kamath is a hospitalist and medical director of quality and patient safety, Duke Regional Hospital, Duke University Health System.
Clinical question: Can idarucizumab reverse anticoagulation effects of dabigatran in a timely manner for urgent surgery or in the event of bleeding?
Background: Reversing the anticoagulant properties of anticoagulants can be important in the event of a life-threatening bleed, or if patients taking these medications need urgent surgery or other interventions. Idarucizumab, a humanized monoclonal antibody fragment, can reverse anticoagulant activity of dabigatran, increasing its acceptance for prescribing physicians as well as patients.
Study design: Multicenter prospective single cohort study.
Setting: 173 sites, 39 countries.
Synopsis: Among 503 patients (median age, 78 years, indication for dabigatran included stroke prophylaxis in setting of atrial fibrillation for most) who had either uncontrolled bleeding (n = 301) or needing emergent surgery (n = 202), a single 5-g dose of idarucizumab was able to reverse anticoagulation rapidly and completely in more than 98% of these patients independent of age, sex, renal function, and dabigatran concentration at baseline. Specifically in 68% of the patients in the bleeding group (excluding intracranial hemorrhage) median time to the cessation of bleeding was 2.5 hours and median time to the initiation of the procedure in the emergent surgery group was 1.6 hours. Study limited by lack of control group.
Bottom line: Idarucizumab can be effective for dabigatran reversal among patients who have uncontrolled bleeding or need to undergo urgent surgery.
Citation: Pollack CV Jr. et al. Idarucizumab for dabigatran reversal: Full cohort analysis. N Engl J Med. 2017 Aug 3;377(5):431-41.
Dr. Kamath is a hospitalist and medical director of quality and patient safety, Duke Regional Hospital, Duke University Health System.
Here’s what’s trending at SHM – Dec. 2017
State of Hospital Medicine Survey opens next month!
The 2018 State of Hospital Medicine Survey will begin in January and last through March with the release of the report in September 2018. Whether you are in a hospital medicine group in an academic or community setting, employed by a hospital or health system, a management company, a private group, or you serve adult or pediatric patients (or both), we need your participation.
Help us help you have the most comprehensive, up-to-date landscape of hospital medicine at your fingertips by participating. As a thank-you for your participation, your group will receive a free copy of the report. Sign up at hospitalmedicine.org/survey.
Apply for SHM’s MARQUIS Med Rec Collaborative kicking off in February 2018
SHM’s MARQUIS Med Rec Collaborative is designed to help hospitals across the United States implement evidence-based best practice medication reconciliation process change and improvement. The collaborative is a 14-month program, spanning from prelaunch to completion.
The staff has the expertise and experience of having completed two previous mentored implementation studies, involving 23 sites and thousands of patients. The collaborative also offers numerous resources, including training materials, project management and process improvement tools for hospitals to use to adapt for their needs to improve the medication reconciliation process. Visit hospitalmedicine.org/MARQUISrecruit to learn more.
Get engaged with public policy
Health care legislation is constantly evolving, and hospitalists play an important role in advocating for hospitalized patients and the hospital medicine movement. SHM is an active voice in many conversations on policy development and reform. Visit hospitalmedicine.org and sign up for the Grassroots Network to stay updated on developments in health care policy, share your experiences with health care programs and participate in policy forums.
Develop your career at Hospital Medicine 2018
Don’t miss SHM’s Annual Conference, Hospital Medicine 2018, to be held April 8-11, 2018. in Orlando. This year, the program was created to help you develop your hospital medicine career, no matter what stage you are in. Two new tracks include Seasoning Your Career and the Career Development Workshops.
Seasoning Your Career focuses on didactics designed to augment those committed to a career in hospital medicine, including topics such as career growth and development, resiliency, work-life balance, and how practical work matters such as schedules affect your career.
The new Career Development Workshops track includes six sessions that aim to help you use skills that will advance your career, such as: Leadership Essentials for Success in Hospital Medicine; Being Female in Hospital Medicine: Overcoming Individual and Institutional Barriers in the Workplace; Do You Have a Minute to Talk? Peer-to-Peer Feedback, and more.
Just starting out in hospital medicine? Back by popular demand, The Early-Career Hospitalists track has been designed for new hospitalists, resident physicians, and medical students interested in pursuing a career in hospital medicine. Designed by SHM’s Physicians-in-Training Committee, which includes nationally recognized hospitalists with expertise in scholarship, career development and medical education, this track aims to inspire future hospitalist leaders.
Visit shmannualconference.org/schedule to learn more.
Two new modules debut on SHM’s Learning Portal
SHM members have access to free continuing medical education (CME) and Maintenance of Certification (MOC) points with the SHM Learning Portal. Don’t miss two new modules: Role of the Medical Consultant and Anesthesia for Internists.
Medical consultation is an important clinical component for most hospitalists. Today, hospitalists also are asked to provide both “curbside” advice and more comprehensive comanagement of medical problems. Hospitalists who are effective consultants communicate skillfully and act professionally. The Role of the Medical Consultant module describes the different roles that hospitalists can perform as medical consultants and provides strategies for improving communications and referring physician satisfaction.
Looking for up-to-date information about surgical anesthesia? The Anesthesia for Internists module discusses the basic forms of surgical anesthesia and contraindications to each, as well as the most commonly used anesthetic drugs, their mechanisms of actions, and side effects.
Both modules are free for SHM members and $45.00 per module for nonmembers. Earn 2 AMA PRA Category 1 Credits™ and 2 MOC points per each module. Visit shmlearningportal.org to get started today.
Not a member? Join the movement today
More than 15,000 members have joined SHM to show their commitment to revolutionizing patient care. As a member, you will be connected with a wealth of opportunities designed to help you grow professionally, network with colleagues nationwide, and shape the practice of hospital medicine. See a full list of member benefits or become a member today at hospitalmedicine.org/join.
Join a chapter and connect to your local hospital medicine community
SHM hosts more than 50 local chapters nationwide to encourage networking, collaboration, and innovation within the hospital medicine community. Getting involved with your local chapter allows you to share knowledge, engage with colleagues, and stay current on the latest developments in hospital medicine.
Visit hospitalmedicine.org/chapters to find a chapter in your area.
Mr. Radler is marketing communications manager at the Society of Hospital Medicine.
State of Hospital Medicine Survey opens next month!
The 2018 State of Hospital Medicine Survey will begin in January and last through March with the release of the report in September 2018. Whether you are in a hospital medicine group in an academic or community setting, employed by a hospital or health system, a management company, a private group, or you serve adult or pediatric patients (or both), we need your participation.
Help us help you have the most comprehensive, up-to-date landscape of hospital medicine at your fingertips by participating. As a thank-you for your participation, your group will receive a free copy of the report. Sign up at hospitalmedicine.org/survey.
Apply for SHM’s MARQUIS Med Rec Collaborative kicking off in February 2018
SHM’s MARQUIS Med Rec Collaborative is designed to help hospitals across the United States implement evidence-based best practice medication reconciliation process change and improvement. The collaborative is a 14-month program, spanning from prelaunch to completion.
The staff has the expertise and experience of having completed two previous mentored implementation studies, involving 23 sites and thousands of patients. The collaborative also offers numerous resources, including training materials, project management and process improvement tools for hospitals to use to adapt for their needs to improve the medication reconciliation process. Visit hospitalmedicine.org/MARQUISrecruit to learn more.
Get engaged with public policy
Health care legislation is constantly evolving, and hospitalists play an important role in advocating for hospitalized patients and the hospital medicine movement. SHM is an active voice in many conversations on policy development and reform. Visit hospitalmedicine.org and sign up for the Grassroots Network to stay updated on developments in health care policy, share your experiences with health care programs and participate in policy forums.
Develop your career at Hospital Medicine 2018
Don’t miss SHM’s Annual Conference, Hospital Medicine 2018, to be held April 8-11, 2018. in Orlando. This year, the program was created to help you develop your hospital medicine career, no matter what stage you are in. Two new tracks include Seasoning Your Career and the Career Development Workshops.
Seasoning Your Career focuses on didactics designed to augment those committed to a career in hospital medicine, including topics such as career growth and development, resiliency, work-life balance, and how practical work matters such as schedules affect your career.
The new Career Development Workshops track includes six sessions that aim to help you use skills that will advance your career, such as: Leadership Essentials for Success in Hospital Medicine; Being Female in Hospital Medicine: Overcoming Individual and Institutional Barriers in the Workplace; Do You Have a Minute to Talk? Peer-to-Peer Feedback, and more.
Just starting out in hospital medicine? Back by popular demand, The Early-Career Hospitalists track has been designed for new hospitalists, resident physicians, and medical students interested in pursuing a career in hospital medicine. Designed by SHM’s Physicians-in-Training Committee, which includes nationally recognized hospitalists with expertise in scholarship, career development and medical education, this track aims to inspire future hospitalist leaders.
Visit shmannualconference.org/schedule to learn more.
Two new modules debut on SHM’s Learning Portal
SHM members have access to free continuing medical education (CME) and Maintenance of Certification (MOC) points with the SHM Learning Portal. Don’t miss two new modules: Role of the Medical Consultant and Anesthesia for Internists.
Medical consultation is an important clinical component for most hospitalists. Today, hospitalists also are asked to provide both “curbside” advice and more comprehensive comanagement of medical problems. Hospitalists who are effective consultants communicate skillfully and act professionally. The Role of the Medical Consultant module describes the different roles that hospitalists can perform as medical consultants and provides strategies for improving communications and referring physician satisfaction.
Looking for up-to-date information about surgical anesthesia? The Anesthesia for Internists module discusses the basic forms of surgical anesthesia and contraindications to each, as well as the most commonly used anesthetic drugs, their mechanisms of actions, and side effects.
Both modules are free for SHM members and $45.00 per module for nonmembers. Earn 2 AMA PRA Category 1 Credits™ and 2 MOC points per each module. Visit shmlearningportal.org to get started today.
Not a member? Join the movement today
More than 15,000 members have joined SHM to show their commitment to revolutionizing patient care. As a member, you will be connected with a wealth of opportunities designed to help you grow professionally, network with colleagues nationwide, and shape the practice of hospital medicine. See a full list of member benefits or become a member today at hospitalmedicine.org/join.
Join a chapter and connect to your local hospital medicine community
SHM hosts more than 50 local chapters nationwide to encourage networking, collaboration, and innovation within the hospital medicine community. Getting involved with your local chapter allows you to share knowledge, engage with colleagues, and stay current on the latest developments in hospital medicine.
Visit hospitalmedicine.org/chapters to find a chapter in your area.
Mr. Radler is marketing communications manager at the Society of Hospital Medicine.
State of Hospital Medicine Survey opens next month!
The 2018 State of Hospital Medicine Survey will begin in January and last through March with the release of the report in September 2018. Whether you are in a hospital medicine group in an academic or community setting, employed by a hospital or health system, a management company, a private group, or you serve adult or pediatric patients (or both), we need your participation.
Help us help you have the most comprehensive, up-to-date landscape of hospital medicine at your fingertips by participating. As a thank-you for your participation, your group will receive a free copy of the report. Sign up at hospitalmedicine.org/survey.
Apply for SHM’s MARQUIS Med Rec Collaborative kicking off in February 2018
SHM’s MARQUIS Med Rec Collaborative is designed to help hospitals across the United States implement evidence-based best practice medication reconciliation process change and improvement. The collaborative is a 14-month program, spanning from prelaunch to completion.
The staff has the expertise and experience of having completed two previous mentored implementation studies, involving 23 sites and thousands of patients. The collaborative also offers numerous resources, including training materials, project management and process improvement tools for hospitals to use to adapt for their needs to improve the medication reconciliation process. Visit hospitalmedicine.org/MARQUISrecruit to learn more.
Get engaged with public policy
Health care legislation is constantly evolving, and hospitalists play an important role in advocating for hospitalized patients and the hospital medicine movement. SHM is an active voice in many conversations on policy development and reform. Visit hospitalmedicine.org and sign up for the Grassroots Network to stay updated on developments in health care policy, share your experiences with health care programs and participate in policy forums.
Develop your career at Hospital Medicine 2018
Don’t miss SHM’s Annual Conference, Hospital Medicine 2018, to be held April 8-11, 2018. in Orlando. This year, the program was created to help you develop your hospital medicine career, no matter what stage you are in. Two new tracks include Seasoning Your Career and the Career Development Workshops.
Seasoning Your Career focuses on didactics designed to augment those committed to a career in hospital medicine, including topics such as career growth and development, resiliency, work-life balance, and how practical work matters such as schedules affect your career.
The new Career Development Workshops track includes six sessions that aim to help you use skills that will advance your career, such as: Leadership Essentials for Success in Hospital Medicine; Being Female in Hospital Medicine: Overcoming Individual and Institutional Barriers in the Workplace; Do You Have a Minute to Talk? Peer-to-Peer Feedback, and more.
Just starting out in hospital medicine? Back by popular demand, The Early-Career Hospitalists track has been designed for new hospitalists, resident physicians, and medical students interested in pursuing a career in hospital medicine. Designed by SHM’s Physicians-in-Training Committee, which includes nationally recognized hospitalists with expertise in scholarship, career development and medical education, this track aims to inspire future hospitalist leaders.
Visit shmannualconference.org/schedule to learn more.
Two new modules debut on SHM’s Learning Portal
SHM members have access to free continuing medical education (CME) and Maintenance of Certification (MOC) points with the SHM Learning Portal. Don’t miss two new modules: Role of the Medical Consultant and Anesthesia for Internists.
Medical consultation is an important clinical component for most hospitalists. Today, hospitalists also are asked to provide both “curbside” advice and more comprehensive comanagement of medical problems. Hospitalists who are effective consultants communicate skillfully and act professionally. The Role of the Medical Consultant module describes the different roles that hospitalists can perform as medical consultants and provides strategies for improving communications and referring physician satisfaction.
Looking for up-to-date information about surgical anesthesia? The Anesthesia for Internists module discusses the basic forms of surgical anesthesia and contraindications to each, as well as the most commonly used anesthetic drugs, their mechanisms of actions, and side effects.
Both modules are free for SHM members and $45.00 per module for nonmembers. Earn 2 AMA PRA Category 1 Credits™ and 2 MOC points per each module. Visit shmlearningportal.org to get started today.
Not a member? Join the movement today
More than 15,000 members have joined SHM to show their commitment to revolutionizing patient care. As a member, you will be connected with a wealth of opportunities designed to help you grow professionally, network with colleagues nationwide, and shape the practice of hospital medicine. See a full list of member benefits or become a member today at hospitalmedicine.org/join.
Join a chapter and connect to your local hospital medicine community
SHM hosts more than 50 local chapters nationwide to encourage networking, collaboration, and innovation within the hospital medicine community. Getting involved with your local chapter allows you to share knowledge, engage with colleagues, and stay current on the latest developments in hospital medicine.
Visit hospitalmedicine.org/chapters to find a chapter in your area.
Mr. Radler is marketing communications manager at the Society of Hospital Medicine.
Helping patients with addictions get, stay clean
Roughly 6 months ago, a primary care physician referred a patient to our clinic for an assessment for opioid use disorder and a recommendation for treatment. The patient estimated, likely underestimated, his daily heroin use to five bags and dropped positive, in addition to heroin, for benzodiazepines, amphetamines, and cannabis. He was in a profession in which public safety was a critical concern, and he refused to notify his employer’s employee assistance program. He also declined to voluntarily admit himself for detox and treatment at the local, fully accredited addiction program, which was affiliated with a major university medical center. Instead, after an Internet search, the patient opted for an opioid treatment center featuring massage therapy, acupuncture, a stable, a sweat lodge – and a magnificent view of the Pacific Ocean.
Mental health professionals and lay people alike are aware of the “opioid crisis” – the derailment of lives, the devastation to communities, the death toll. But despite proposals to increase research funding, policies aimed at tightening the prescribing of opioids, and pledges to ramp up interdiction of heroin traffic, there is often an ignorance and confusion regarding the best, evidence-based approaches to getting patients with substance use disorders clean and keeping them clean.
Unfortunately, as with any crisis, there will be opportunists preying on vulnerable patients and their families. And this travesty has reportedly escalated, as outpatient treatment centers take advantage of laws guaranteeing mental health parity and insurance companies paying out tens of thousands of dollars for residential and outpatient opioid treatment. The potential for significant profit is plainly illustrated by the influx of private equity firms, such as Bain Capital, that are investing heavily in treatment centers.
Reports of malfeasance and misconduct, by owners, operators, staff, and others connected with the industry are beginning to get the attention of authorities. There have been reports of outpatient treatment centers that spend lavishly on furnishing, on BMWs and signed art, yet are understaffed, leading to inadequate one-on-one counseling and even sexual transgressions between residents. There are centers that have been investigated for insurance fraud, such as illegally waiving a copay or a deductible or for charging up to $5,000 for a simple urine five drug screen, often multiple times a day. And there is evidence of “junkie hunters” who cruise for people with addictions and brokers who provide such people with fake addresses in order to qualify for insurance plans with excellent benefits for addiction treatment.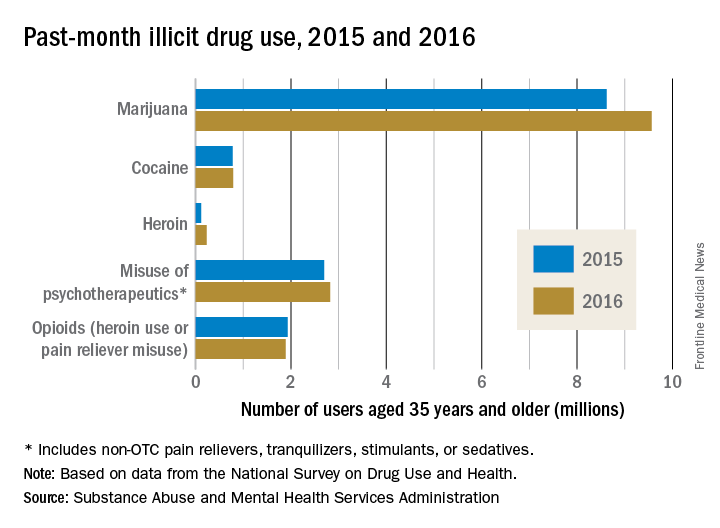
Probably the best means to find a suitable outpatient treatment center is by way of a local, experienced, and respected chemical dependency counselor or physician certified in addiction medicine. If people with substance use disorders and their families want to independently conduct a search, as a good rule of thumb, they should be advised to consider programs affiliated with major medical centers and hospitals or outpatient treatment centers that have been established in good standing for years, in contrast to the rash of pop-up, for-profit programs. Of equal, or even greater importance, is that the prospective center ought to be accredited by a national organization, for example, The Joint Commission, and its staff ought to be licensed and credentialed as well.
In addition, there is merit if the staff has been educated, trained, and supervised under the direction of a respected institution. Needless to add, an outpatient treatment center must use evidence-based practices as the bedrock of treatment; this includes pharmacotherapies such as Suboxone and naltrexone (Vivitrol), and behavioral therapies such as cognitive-behavioral therapy, contingency management, and motivational enhancement. To date, massage and essential oils might be relaxing and pleasurable, but they are not considered accepted standard of care.
It is crucial, too, that an outpatient treatment center have both the resources to reliably handle acute medical detox, which can be a potentially life-threatening emergency, and the medical personnel who can assess and treat such medical conditions as hypertension as well as psychiatric illnesses such as bipolar and generalized anxiety disorders. A prospective patient also should inquire whether any of the staff has been the subject of disciplinary action by a licensing board or whether the center has been investigated by the state or a national accrediting organization.
Because addiction so often has facets rooted in the family system, and recovery so often depends on family support, an outpatient treatment center should provide a structured family program integrated into the patient’s treatment and emphasize the importance of continued family involvement after discharge.
Lastly, the best treatment centers often regularly update a patient’s local therapist and physician, spell out the elements of successful aftercare (12-step programs, and so on), and provide amenities, such as calls to a recently discharged patient and an alumni support network.
Dr. Marseille is a psychiatrist who works on the staff of a clinic in Wheaton, Ill. His special interests include adolescent and addiction medicine, eating disorders, trauma, bipolar disorder, and the psychiatric manifestations of acute and chronic medical conditions.
This article was updated 12/15/17.
Roughly 6 months ago, a primary care physician referred a patient to our clinic for an assessment for opioid use disorder and a recommendation for treatment. The patient estimated, likely underestimated, his daily heroin use to five bags and dropped positive, in addition to heroin, for benzodiazepines, amphetamines, and cannabis. He was in a profession in which public safety was a critical concern, and he refused to notify his employer’s employee assistance program. He also declined to voluntarily admit himself for detox and treatment at the local, fully accredited addiction program, which was affiliated with a major university medical center. Instead, after an Internet search, the patient opted for an opioid treatment center featuring massage therapy, acupuncture, a stable, a sweat lodge – and a magnificent view of the Pacific Ocean.
Mental health professionals and lay people alike are aware of the “opioid crisis” – the derailment of lives, the devastation to communities, the death toll. But despite proposals to increase research funding, policies aimed at tightening the prescribing of opioids, and pledges to ramp up interdiction of heroin traffic, there is often an ignorance and confusion regarding the best, evidence-based approaches to getting patients with substance use disorders clean and keeping them clean.
Unfortunately, as with any crisis, there will be opportunists preying on vulnerable patients and their families. And this travesty has reportedly escalated, as outpatient treatment centers take advantage of laws guaranteeing mental health parity and insurance companies paying out tens of thousands of dollars for residential and outpatient opioid treatment. The potential for significant profit is plainly illustrated by the influx of private equity firms, such as Bain Capital, that are investing heavily in treatment centers.
Reports of malfeasance and misconduct, by owners, operators, staff, and others connected with the industry are beginning to get the attention of authorities. There have been reports of outpatient treatment centers that spend lavishly on furnishing, on BMWs and signed art, yet are understaffed, leading to inadequate one-on-one counseling and even sexual transgressions between residents. There are centers that have been investigated for insurance fraud, such as illegally waiving a copay or a deductible or for charging up to $5,000 for a simple urine five drug screen, often multiple times a day. And there is evidence of “junkie hunters” who cruise for people with addictions and brokers who provide such people with fake addresses in order to qualify for insurance plans with excellent benefits for addiction treatment.
Probably the best means to find a suitable outpatient treatment center is by way of a local, experienced, and respected chemical dependency counselor or physician certified in addiction medicine. If people with substance use disorders and their families want to independently conduct a search, as a good rule of thumb, they should be advised to consider programs affiliated with major medical centers and hospitals or outpatient treatment centers that have been established in good standing for years, in contrast to the rash of pop-up, for-profit programs. Of equal, or even greater importance, is that the prospective center ought to be accredited by a national organization, for example, The Joint Commission, and its staff ought to be licensed and credentialed as well.
In addition, there is merit if the staff has been educated, trained, and supervised under the direction of a respected institution. Needless to add, an outpatient treatment center must use evidence-based practices as the bedrock of treatment; this includes pharmacotherapies such as Suboxone and naltrexone (Vivitrol), and behavioral therapies such as cognitive-behavioral therapy, contingency management, and motivational enhancement. To date, massage and essential oils might be relaxing and pleasurable, but they are not considered accepted standard of care.
It is crucial, too, that an outpatient treatment center have both the resources to reliably handle acute medical detox, which can be a potentially life-threatening emergency, and the medical personnel who can assess and treat such medical conditions as hypertension as well as psychiatric illnesses such as bipolar and generalized anxiety disorders. A prospective patient also should inquire whether any of the staff has been the subject of disciplinary action by a licensing board or whether the center has been investigated by the state or a national accrediting organization.
Because addiction so often has facets rooted in the family system, and recovery so often depends on family support, an outpatient treatment center should provide a structured family program integrated into the patient’s treatment and emphasize the importance of continued family involvement after discharge.
Lastly, the best treatment centers often regularly update a patient’s local therapist and physician, spell out the elements of successful aftercare (12-step programs, and so on), and provide amenities, such as calls to a recently discharged patient and an alumni support network.
Dr. Marseille is a psychiatrist who works on the staff of a clinic in Wheaton, Ill. His special interests include adolescent and addiction medicine, eating disorders, trauma, bipolar disorder, and the psychiatric manifestations of acute and chronic medical conditions.
This article was updated 12/15/17.
Roughly 6 months ago, a primary care physician referred a patient to our clinic for an assessment for opioid use disorder and a recommendation for treatment. The patient estimated, likely underestimated, his daily heroin use to five bags and dropped positive, in addition to heroin, for benzodiazepines, amphetamines, and cannabis. He was in a profession in which public safety was a critical concern, and he refused to notify his employer’s employee assistance program. He also declined to voluntarily admit himself for detox and treatment at the local, fully accredited addiction program, which was affiliated with a major university medical center. Instead, after an Internet search, the patient opted for an opioid treatment center featuring massage therapy, acupuncture, a stable, a sweat lodge – and a magnificent view of the Pacific Ocean.
Mental health professionals and lay people alike are aware of the “opioid crisis” – the derailment of lives, the devastation to communities, the death toll. But despite proposals to increase research funding, policies aimed at tightening the prescribing of opioids, and pledges to ramp up interdiction of heroin traffic, there is often an ignorance and confusion regarding the best, evidence-based approaches to getting patients with substance use disorders clean and keeping them clean.
Unfortunately, as with any crisis, there will be opportunists preying on vulnerable patients and their families. And this travesty has reportedly escalated, as outpatient treatment centers take advantage of laws guaranteeing mental health parity and insurance companies paying out tens of thousands of dollars for residential and outpatient opioid treatment. The potential for significant profit is plainly illustrated by the influx of private equity firms, such as Bain Capital, that are investing heavily in treatment centers.
Reports of malfeasance and misconduct, by owners, operators, staff, and others connected with the industry are beginning to get the attention of authorities. There have been reports of outpatient treatment centers that spend lavishly on furnishing, on BMWs and signed art, yet are understaffed, leading to inadequate one-on-one counseling and even sexual transgressions between residents. There are centers that have been investigated for insurance fraud, such as illegally waiving a copay or a deductible or for charging up to $5,000 for a simple urine five drug screen, often multiple times a day. And there is evidence of “junkie hunters” who cruise for people with addictions and brokers who provide such people with fake addresses in order to qualify for insurance plans with excellent benefits for addiction treatment.
Probably the best means to find a suitable outpatient treatment center is by way of a local, experienced, and respected chemical dependency counselor or physician certified in addiction medicine. If people with substance use disorders and their families want to independently conduct a search, as a good rule of thumb, they should be advised to consider programs affiliated with major medical centers and hospitals or outpatient treatment centers that have been established in good standing for years, in contrast to the rash of pop-up, for-profit programs. Of equal, or even greater importance, is that the prospective center ought to be accredited by a national organization, for example, The Joint Commission, and its staff ought to be licensed and credentialed as well.
In addition, there is merit if the staff has been educated, trained, and supervised under the direction of a respected institution. Needless to add, an outpatient treatment center must use evidence-based practices as the bedrock of treatment; this includes pharmacotherapies such as Suboxone and naltrexone (Vivitrol), and behavioral therapies such as cognitive-behavioral therapy, contingency management, and motivational enhancement. To date, massage and essential oils might be relaxing and pleasurable, but they are not considered accepted standard of care.
It is crucial, too, that an outpatient treatment center have both the resources to reliably handle acute medical detox, which can be a potentially life-threatening emergency, and the medical personnel who can assess and treat such medical conditions as hypertension as well as psychiatric illnesses such as bipolar and generalized anxiety disorders. A prospective patient also should inquire whether any of the staff has been the subject of disciplinary action by a licensing board or whether the center has been investigated by the state or a national accrediting organization.
Because addiction so often has facets rooted in the family system, and recovery so often depends on family support, an outpatient treatment center should provide a structured family program integrated into the patient’s treatment and emphasize the importance of continued family involvement after discharge.
Lastly, the best treatment centers often regularly update a patient’s local therapist and physician, spell out the elements of successful aftercare (12-step programs, and so on), and provide amenities, such as calls to a recently discharged patient and an alumni support network.
Dr. Marseille is a psychiatrist who works on the staff of a clinic in Wheaton, Ill. His special interests include adolescent and addiction medicine, eating disorders, trauma, bipolar disorder, and the psychiatric manifestations of acute and chronic medical conditions.
This article was updated 12/15/17.
FDA approves premixed, low-volume colon-cleansing solution
in adults preparing to undergo colonoscopy, according to Ferring Pharmaceuticals.
The sodium picosulfate, magnesium oxide, and anhydrous citric acid oral solution is a relatively low-volume, premixed, cranberry-flavored solution, making it easier to use and more palatable for patients.
The oral solution is approved with two dosing options: split dose, one dose the evening prior and one dose the morning of the procedure, or the day before dose, which involves taking both doses the day prior to the procedure. Day before dosing is an alternative and should be used when split dosing is not appropriate. After each dose of sodium picosulfate, magnesium oxide, and anhydrous citric acid oral solution, clear liquids should be consumed based on the dosing recommendation. The American College of Gastroenterology recommends the split-dose regimen because of its improved cleansing quality of the colon and better tolerability of the liquid volume by patients.
Patients with impaired renal function should exercise caution if using sodium picosulfate, magnesium oxide, and anhydrous citric acid oral solution as it may effect renal function. A more comprehensive list of safety information is available at www.clenpiq.com.
in adults preparing to undergo colonoscopy, according to Ferring Pharmaceuticals.
The sodium picosulfate, magnesium oxide, and anhydrous citric acid oral solution is a relatively low-volume, premixed, cranberry-flavored solution, making it easier to use and more palatable for patients.
The oral solution is approved with two dosing options: split dose, one dose the evening prior and one dose the morning of the procedure, or the day before dose, which involves taking both doses the day prior to the procedure. Day before dosing is an alternative and should be used when split dosing is not appropriate. After each dose of sodium picosulfate, magnesium oxide, and anhydrous citric acid oral solution, clear liquids should be consumed based on the dosing recommendation. The American College of Gastroenterology recommends the split-dose regimen because of its improved cleansing quality of the colon and better tolerability of the liquid volume by patients.
Patients with impaired renal function should exercise caution if using sodium picosulfate, magnesium oxide, and anhydrous citric acid oral solution as it may effect renal function. A more comprehensive list of safety information is available at www.clenpiq.com.
in adults preparing to undergo colonoscopy, according to Ferring Pharmaceuticals.
The sodium picosulfate, magnesium oxide, and anhydrous citric acid oral solution is a relatively low-volume, premixed, cranberry-flavored solution, making it easier to use and more palatable for patients.
The oral solution is approved with two dosing options: split dose, one dose the evening prior and one dose the morning of the procedure, or the day before dose, which involves taking both doses the day prior to the procedure. Day before dosing is an alternative and should be used when split dosing is not appropriate. After each dose of sodium picosulfate, magnesium oxide, and anhydrous citric acid oral solution, clear liquids should be consumed based on the dosing recommendation. The American College of Gastroenterology recommends the split-dose regimen because of its improved cleansing quality of the colon and better tolerability of the liquid volume by patients.
Patients with impaired renal function should exercise caution if using sodium picosulfate, magnesium oxide, and anhydrous citric acid oral solution as it may effect renal function. A more comprehensive list of safety information is available at www.clenpiq.com.
Reducing outpatient medication costs
For many patients, paying for medication presents a serious challenge. Studies show that up to 45% of Americans do not fill prescriptions secondary to cost, and medication nonadherence leads to morbidity and mortality, with costs from $100 billion to $300 billion annually.
One way to address the problem is by empowering clinicians to reduce patient outpatient medication costs – the goal described in a recent abstract.
Initial testing was promising. One patient, admitted for the fourth time in 14 months for hypertriglyceridemia-induced pancreatitis secondary to medication nonadherence, was able to reduce 90-day outpatient medication cost by 95%, from $1,287.00 to $61.79. By reducing his readmissions, the institution saved more than $20,000 a year.
The researchers secured internal grant funding to develop an automated version of the tool. “We currently have technology that can dramatically reduce the cost of many medications with early promising results for patient outcomes, readmissions rates and overall systemic cost,” Dr. Kubey said. “We are working rapidly to further develop and study our tool and, if prospective results confirm our initial findings, we will seek to provide this tool to clinicians broadly.”
Such tools are a true win-win. Hospitalists using them help ensure that discharged patients are able to afford the often life-saving medications that will keep them healthy and out of the hospital, improve readmission rates, patient satisfaction metrics, total system cost, and, most important, do right by our patients in need for whom we are charged to care, Dr. Kubey said.
“Hospitalists first must be aware that savings of 90% or more are possible for many medications and that medication nonadherence because of cost is a serious issue affecting nearly half the patients we see,” he said. “The first step is simply asking patients if medication cost is proving troublesome – we cannot address what we do not see. The second step is to use current discount tools such as GoodRx, NeedyMeds, and the like – and, we hope, in the not too distant future, our tool, which we plan to integrate into EHR prescribing to make it easy and nearly instantaneous for hospitalists to prescribe the most high-value, low-cost medication regimen for each individual patient at discharge.”
Reference
Kubey A et al. Expensive free hospitalizations – A novel approach to reducing outpatient medication cost [abstract]. J Hosp Med. 2017; 12 (suppl 2). Accessed Aug. 7, 2017.
For many patients, paying for medication presents a serious challenge. Studies show that up to 45% of Americans do not fill prescriptions secondary to cost, and medication nonadherence leads to morbidity and mortality, with costs from $100 billion to $300 billion annually.
One way to address the problem is by empowering clinicians to reduce patient outpatient medication costs – the goal described in a recent abstract.
Initial testing was promising. One patient, admitted for the fourth time in 14 months for hypertriglyceridemia-induced pancreatitis secondary to medication nonadherence, was able to reduce 90-day outpatient medication cost by 95%, from $1,287.00 to $61.79. By reducing his readmissions, the institution saved more than $20,000 a year.
The researchers secured internal grant funding to develop an automated version of the tool. “We currently have technology that can dramatically reduce the cost of many medications with early promising results for patient outcomes, readmissions rates and overall systemic cost,” Dr. Kubey said. “We are working rapidly to further develop and study our tool and, if prospective results confirm our initial findings, we will seek to provide this tool to clinicians broadly.”
Such tools are a true win-win. Hospitalists using them help ensure that discharged patients are able to afford the often life-saving medications that will keep them healthy and out of the hospital, improve readmission rates, patient satisfaction metrics, total system cost, and, most important, do right by our patients in need for whom we are charged to care, Dr. Kubey said.
“Hospitalists first must be aware that savings of 90% or more are possible for many medications and that medication nonadherence because of cost is a serious issue affecting nearly half the patients we see,” he said. “The first step is simply asking patients if medication cost is proving troublesome – we cannot address what we do not see. The second step is to use current discount tools such as GoodRx, NeedyMeds, and the like – and, we hope, in the not too distant future, our tool, which we plan to integrate into EHR prescribing to make it easy and nearly instantaneous for hospitalists to prescribe the most high-value, low-cost medication regimen for each individual patient at discharge.”
Reference
Kubey A et al. Expensive free hospitalizations – A novel approach to reducing outpatient medication cost [abstract]. J Hosp Med. 2017; 12 (suppl 2). Accessed Aug. 7, 2017.
For many patients, paying for medication presents a serious challenge. Studies show that up to 45% of Americans do not fill prescriptions secondary to cost, and medication nonadherence leads to morbidity and mortality, with costs from $100 billion to $300 billion annually.
One way to address the problem is by empowering clinicians to reduce patient outpatient medication costs – the goal described in a recent abstract.
Initial testing was promising. One patient, admitted for the fourth time in 14 months for hypertriglyceridemia-induced pancreatitis secondary to medication nonadherence, was able to reduce 90-day outpatient medication cost by 95%, from $1,287.00 to $61.79. By reducing his readmissions, the institution saved more than $20,000 a year.
The researchers secured internal grant funding to develop an automated version of the tool. “We currently have technology that can dramatically reduce the cost of many medications with early promising results for patient outcomes, readmissions rates and overall systemic cost,” Dr. Kubey said. “We are working rapidly to further develop and study our tool and, if prospective results confirm our initial findings, we will seek to provide this tool to clinicians broadly.”
Such tools are a true win-win. Hospitalists using them help ensure that discharged patients are able to afford the often life-saving medications that will keep them healthy and out of the hospital, improve readmission rates, patient satisfaction metrics, total system cost, and, most important, do right by our patients in need for whom we are charged to care, Dr. Kubey said.
“Hospitalists first must be aware that savings of 90% or more are possible for many medications and that medication nonadherence because of cost is a serious issue affecting nearly half the patients we see,” he said. “The first step is simply asking patients if medication cost is proving troublesome – we cannot address what we do not see. The second step is to use current discount tools such as GoodRx, NeedyMeds, and the like – and, we hope, in the not too distant future, our tool, which we plan to integrate into EHR prescribing to make it easy and nearly instantaneous for hospitalists to prescribe the most high-value, low-cost medication regimen for each individual patient at discharge.”
Reference
Kubey A et al. Expensive free hospitalizations – A novel approach to reducing outpatient medication cost [abstract]. J Hosp Med. 2017; 12 (suppl 2). Accessed Aug. 7, 2017.