User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


A game of telephone?
Editor’s Note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform healthcare and revolutionize patient care. The program has been expanded for the 2017-18 year, offering two options for students to receive funding and engage in scholarly work during their first, second and third years of medical school. As a part of the program, recipients are required to write about their experience on a biweekly basis.
The transfer of information from floor to the MICU team is a very interesting process: outside of the patient record, the person performing the handoff is highly responsible in the appropriate transfer of information.
One of the challenges encountered within the project is the way in which we are categorizing agreement between groups. Previously, we created a set of categories based upon recurring themes present within the free-text provider responses, and created categories, such as “cardiac management” and “diabetes management.” Upon creating these categories, I would then group them based upon concordance. However, responses such as “bipap during the night” and “not giving her bipap” would both be coded under “respiratory management,” but those two responses would not show the providers being in concordance. Upon consulting with my mentors Dr. Vineet Arora and Dr. Juan Rojas, we decided that it would be more accurate to categorize concordance based upon the original answers, keeping the breadth of the original data intact.
As I continue to organize the data based on concordance, I have to modify my frame of thought and focus on appropriately representing the responses. There is no such thing as perfect data, and this project is no exception; in this case, not every provider was able to be reached for a response, which requires more nuance as I categorize the degree of concordance within the data and think of appropriate categories. I am very glad to learn the skill of appropriate data representation, as we want it to demonstrate both the potential lack or presence of clarity in handoffs, as well as the represented responding providers.
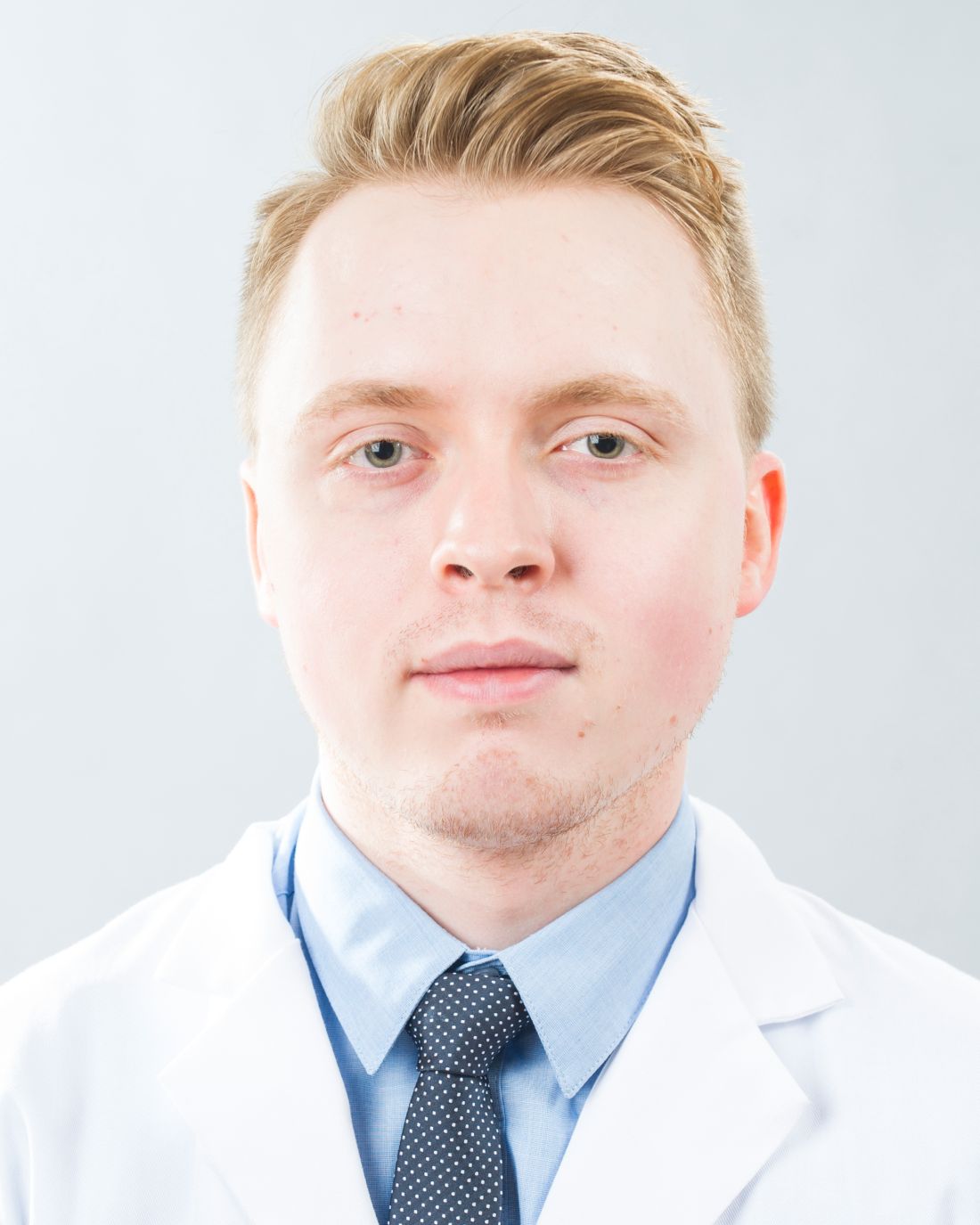
Anton Garazha is a medical student at Chicago Medical School at Rosalind Franklin University in North Chicago. He received his bachelor of science degree in biology from Loyola University in Chicago in 2015 and his master of biomedical science degree from Rosalind Franklin University in 2016. Anton is very interested in community outreach and quality improvement, and in his spare time tutors students in science-based subjects.
Editor’s Note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform healthcare and revolutionize patient care. The program has been expanded for the 2017-18 year, offering two options for students to receive funding and engage in scholarly work during their first, second and third years of medical school. As a part of the program, recipients are required to write about their experience on a biweekly basis.
The transfer of information from floor to the MICU team is a very interesting process: outside of the patient record, the person performing the handoff is highly responsible in the appropriate transfer of information.
One of the challenges encountered within the project is the way in which we are categorizing agreement between groups. Previously, we created a set of categories based upon recurring themes present within the free-text provider responses, and created categories, such as “cardiac management” and “diabetes management.” Upon creating these categories, I would then group them based upon concordance. However, responses such as “bipap during the night” and “not giving her bipap” would both be coded under “respiratory management,” but those two responses would not show the providers being in concordance. Upon consulting with my mentors Dr. Vineet Arora and Dr. Juan Rojas, we decided that it would be more accurate to categorize concordance based upon the original answers, keeping the breadth of the original data intact.
As I continue to organize the data based on concordance, I have to modify my frame of thought and focus on appropriately representing the responses. There is no such thing as perfect data, and this project is no exception; in this case, not every provider was able to be reached for a response, which requires more nuance as I categorize the degree of concordance within the data and think of appropriate categories. I am very glad to learn the skill of appropriate data representation, as we want it to demonstrate both the potential lack or presence of clarity in handoffs, as well as the represented responding providers.
Anton Garazha is a medical student at Chicago Medical School at Rosalind Franklin University in North Chicago. He received his bachelor of science degree in biology from Loyola University in Chicago in 2015 and his master of biomedical science degree from Rosalind Franklin University in 2016. Anton is very interested in community outreach and quality improvement, and in his spare time tutors students in science-based subjects.
Editor’s Note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform healthcare and revolutionize patient care. The program has been expanded for the 2017-18 year, offering two options for students to receive funding and engage in scholarly work during their first, second and third years of medical school. As a part of the program, recipients are required to write about their experience on a biweekly basis.
The transfer of information from floor to the MICU team is a very interesting process: outside of the patient record, the person performing the handoff is highly responsible in the appropriate transfer of information.
One of the challenges encountered within the project is the way in which we are categorizing agreement between groups. Previously, we created a set of categories based upon recurring themes present within the free-text provider responses, and created categories, such as “cardiac management” and “diabetes management.” Upon creating these categories, I would then group them based upon concordance. However, responses such as “bipap during the night” and “not giving her bipap” would both be coded under “respiratory management,” but those two responses would not show the providers being in concordance. Upon consulting with my mentors Dr. Vineet Arora and Dr. Juan Rojas, we decided that it would be more accurate to categorize concordance based upon the original answers, keeping the breadth of the original data intact.
As I continue to organize the data based on concordance, I have to modify my frame of thought and focus on appropriately representing the responses. There is no such thing as perfect data, and this project is no exception; in this case, not every provider was able to be reached for a response, which requires more nuance as I categorize the degree of concordance within the data and think of appropriate categories. I am very glad to learn the skill of appropriate data representation, as we want it to demonstrate both the potential lack or presence of clarity in handoffs, as well as the represented responding providers.
Anton Garazha is a medical student at Chicago Medical School at Rosalind Franklin University in North Chicago. He received his bachelor of science degree in biology from Loyola University in Chicago in 2015 and his master of biomedical science degree from Rosalind Franklin University in 2016. Anton is very interested in community outreach and quality improvement, and in his spare time tutors students in science-based subjects.
Thinking about the basic science of quality improvement
Editor’s note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform health care and revolutionize patient care. The program has been expanded for the 2017-18 year, offering two options for students to receive funding and engage in scholarly work during their first, second and third years of medical school. As a part of the longitudinal (18-month) program, recipients are required to write about their experience on a monthly basis.
I reviewed recent literature about my research topic, which is clinical pathways for hospitalized injection drug users due to injection-related infection sequelae and came up with my research proposal. As part of a scholarly pursuit, I believe having a theoretical background of quality improvement to be important. Before further diving into the research topic, I also generated a small reading list of the “basic science” of quality improvement, which covers topics of general operational science and those in health care applications.
What makes standardization in health care difficult? In my operations class at Tuck School of Business, we watched a video showing former Soviet Union ophthalmologists performing “assembly line” cataract surgery. It includes multiple surgeons sitting around multiple rotating tables, each surgeon performing exactly one step of the cataract surgery. I recall all my classmates were amused by the video, because it appeared both impractical (as one surgeon was almost chasing the table) as well as slightly de-humanizing. In the health care setting, standardization can be difficult. The service is intrinsically complex, it is difficult to define processes and to measure outcomes, and standardization can create tension secondary to physician autonomy and organizational culture.
In service delivery, the person (the patient in health care organizations) is part of the production process. Patients by nature are not standard inputs. They assume different pre-existing conditions and have different preferences for clinical and non-clinical services/processes. The medical service itself, consisting of both clinical and operational processes, sometimes can be difficult to qualify and measure. A hospital can control patient flow by managing appointment and beds allocation. Clinical pathways can be defined for different diseases. However, patients can encounter undiscovered diseases or complications during the treatment, making the clinical service different and unpredictable.
Lastly standardization can encounter resistance from physicians and other health care providers. “Patients are not cars” is a phrase commonly used when discussing standardization. A health care organization needs to have not only tools, but also the cultural and managerial foundations to carry out changes. I am looking forward to using this project opportunity to further explore the local application of quality improvement.
Yun Li is an MD/MBA student attending Geisel School of Medicine and Tuck School of Business at Dartmouth. She obtained her Bachelor of Arts degree from Hanover College double-majoring in Economics and Biological Chemistry. Ms. Li participated in research in injury epidemiology and genetics, and has conducted studies on traditional Tibetan medicine, rural health, health NGOs, and digital health. Her career interest is practicing hospital medicine and geriatrics as a clinician/administrator, either in the US or China. Ms. Li is a student member of the Society of Hospital Medicine.
Editor’s note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform health care and revolutionize patient care. The program has been expanded for the 2017-18 year, offering two options for students to receive funding and engage in scholarly work during their first, second and third years of medical school. As a part of the longitudinal (18-month) program, recipients are required to write about their experience on a monthly basis.
I reviewed recent literature about my research topic, which is clinical pathways for hospitalized injection drug users due to injection-related infection sequelae and came up with my research proposal. As part of a scholarly pursuit, I believe having a theoretical background of quality improvement to be important. Before further diving into the research topic, I also generated a small reading list of the “basic science” of quality improvement, which covers topics of general operational science and those in health care applications.
What makes standardization in health care difficult? In my operations class at Tuck School of Business, we watched a video showing former Soviet Union ophthalmologists performing “assembly line” cataract surgery. It includes multiple surgeons sitting around multiple rotating tables, each surgeon performing exactly one step of the cataract surgery. I recall all my classmates were amused by the video, because it appeared both impractical (as one surgeon was almost chasing the table) as well as slightly de-humanizing. In the health care setting, standardization can be difficult. The service is intrinsically complex, it is difficult to define processes and to measure outcomes, and standardization can create tension secondary to physician autonomy and organizational culture.
In service delivery, the person (the patient in health care organizations) is part of the production process. Patients by nature are not standard inputs. They assume different pre-existing conditions and have different preferences for clinical and non-clinical services/processes. The medical service itself, consisting of both clinical and operational processes, sometimes can be difficult to qualify and measure. A hospital can control patient flow by managing appointment and beds allocation. Clinical pathways can be defined for different diseases. However, patients can encounter undiscovered diseases or complications during the treatment, making the clinical service different and unpredictable.
Lastly standardization can encounter resistance from physicians and other health care providers. “Patients are not cars” is a phrase commonly used when discussing standardization. A health care organization needs to have not only tools, but also the cultural and managerial foundations to carry out changes. I am looking forward to using this project opportunity to further explore the local application of quality improvement.
Yun Li is an MD/MBA student attending Geisel School of Medicine and Tuck School of Business at Dartmouth. She obtained her Bachelor of Arts degree from Hanover College double-majoring in Economics and Biological Chemistry. Ms. Li participated in research in injury epidemiology and genetics, and has conducted studies on traditional Tibetan medicine, rural health, health NGOs, and digital health. Her career interest is practicing hospital medicine and geriatrics as a clinician/administrator, either in the US or China. Ms. Li is a student member of the Society of Hospital Medicine.
Editor’s note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform health care and revolutionize patient care. The program has been expanded for the 2017-18 year, offering two options for students to receive funding and engage in scholarly work during their first, second and third years of medical school. As a part of the longitudinal (18-month) program, recipients are required to write about their experience on a monthly basis.
I reviewed recent literature about my research topic, which is clinical pathways for hospitalized injection drug users due to injection-related infection sequelae and came up with my research proposal. As part of a scholarly pursuit, I believe having a theoretical background of quality improvement to be important. Before further diving into the research topic, I also generated a small reading list of the “basic science” of quality improvement, which covers topics of general operational science and those in health care applications.
What makes standardization in health care difficult? In my operations class at Tuck School of Business, we watched a video showing former Soviet Union ophthalmologists performing “assembly line” cataract surgery. It includes multiple surgeons sitting around multiple rotating tables, each surgeon performing exactly one step of the cataract surgery. I recall all my classmates were amused by the video, because it appeared both impractical (as one surgeon was almost chasing the table) as well as slightly de-humanizing. In the health care setting, standardization can be difficult. The service is intrinsically complex, it is difficult to define processes and to measure outcomes, and standardization can create tension secondary to physician autonomy and organizational culture.
In service delivery, the person (the patient in health care organizations) is part of the production process. Patients by nature are not standard inputs. They assume different pre-existing conditions and have different preferences for clinical and non-clinical services/processes. The medical service itself, consisting of both clinical and operational processes, sometimes can be difficult to qualify and measure. A hospital can control patient flow by managing appointment and beds allocation. Clinical pathways can be defined for different diseases. However, patients can encounter undiscovered diseases or complications during the treatment, making the clinical service different and unpredictable.
Lastly standardization can encounter resistance from physicians and other health care providers. “Patients are not cars” is a phrase commonly used when discussing standardization. A health care organization needs to have not only tools, but also the cultural and managerial foundations to carry out changes. I am looking forward to using this project opportunity to further explore the local application of quality improvement.
Yun Li is an MD/MBA student attending Geisel School of Medicine and Tuck School of Business at Dartmouth. She obtained her Bachelor of Arts degree from Hanover College double-majoring in Economics and Biological Chemistry. Ms. Li participated in research in injury epidemiology and genetics, and has conducted studies on traditional Tibetan medicine, rural health, health NGOs, and digital health. Her career interest is practicing hospital medicine and geriatrics as a clinician/administrator, either in the US or China. Ms. Li is a student member of the Society of Hospital Medicine.
Steroids underused in bacterial meningitis despite low risk
SAN DIEGO – Physicians often skipped out on using steroids when treating bacterial meningitis even though the benefits clearly outweigh the risks, Cinthia Gallegos, MD, reported during an oral presentation at an annual meeting on infectious diseases.
In a recent multicenter retrospective cohort study, only 40% of adults with bacterial meningitis received steroids within 4 hours of hospital admission, as recommended by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID), and only 14% received steroids concomitantly or 10-20 minutes prior to antibiotic initiation, as recommended by the Infectious Diseases Society of America (IDSA), said Dr. Gallegos, an infectious disease fellow at University of Texas, Houston.
“Steroids are being underutilized in our patient population,” she said. “And when steroids are used, they are being used later than is recommended.”
To evaluate the prevalence of guideline-concordant steroid use, Dr. Gallegos and her associates analyzed the medical records of 120 adults with culture-confirmed, community-acquired bacterial meningitis treated at 10 Houston-area hospitals between 2008 and 2016.
Median duration of steroid therapy was 4 hours, which is consistent with IDSA guidelines, she noted.
Among the five patients (4%) who developed delayed cerebral thrombosis, three had Streptococcus pneumoniae meningitis, one had methicillin-resistant Staphylococcus aureus meningitis, and one had Listeria meningitis. All had received either dexamethasone monotherapy or dexamethasone and methylprednisolone within 4 hours of antibiotic initiation. They showed an initial improvement in clinical course, including normal CT and MRI, but their clinical condition deteriorated between 5 and 12 days later. “Repeat imaging showed thrombosis of different areas of the brain,” Dr. Gallegos said. Two patients died, two developed moderate or severe disability, and one fully recovered. The patients ranged in age from 26 to 69; three were male, and two were female.
The 4% rate closely resembles what is seen in the Netherlands, said Diederik van de Beek, MD, PhD, of the Academic Medical Center in Amsterdam, who comoderated the session at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. “We have some recent data where we did autopsies of cases and we saw a huge amount of bacterial fragments around the blood vessels,” he said. “We have seen this in previous autopsy studies, but here it was a massive amount of bacterial fragments.”
Researchers have suggested that delayed cerebral thrombosis in bacterial meningitis results from increases in C5a and C5b-9 levels in the cerebrospinal fluid and from an increase in the tissue factor VII pathway, Dr. Gallegos said.
Researchers think that these patients historically developed vasculitis, but that this complication “has disappeared somewhat in the dexamethasone era,” said Dr. van de Beek, lead author of the 2016 ESCMID guidelines on bacterial meningitis. “It appears that some patients are ‘pro-inflammatory’ and still react 7-9 days after treatment,” he said. “The difficult question is whether we give 4 days of steroids or longer. A clinical trial is not feasible, so we [recommend] 4 days.”
Left untreated, bacterial meningitis is fatal in up to 70% of cases, and about one in five survivors faces limb loss or neurologic disability, according to the Centers for Disease Control and Prevention. The advent of penicillin and other antibiotics dramatically improved survival, but death rates remained around 10% for meningitis associated with Neisseria meningitides and Haemophilus influenza infection, and often exceeded 30% for S. pneumoniae meningitis. “That’s important because besides antibiotics, the only treatment that decreases mortality has been shown to be steroids,” Dr. Gallegos said.
High-quality evidence supports their use. In a double-blind, randomized, multicenter trial of 301 adults with bacterial meningitis, adjunctive dexamethasone was associated with a 50% improvement in mortality, compared with adjunctive placebo (N Engl J Med. 2002 Nov 14;347[20]:1549-56). Other data confirm that steroids do not prevent vancomycin from concentrating in CSF or increase the risk of hippocampal apoptosis. But although both IDSA and ESCMID endorse steroids as adjunctive therapy to help control intracranial pressure in patients with bacterial meningitis, studies have shown much higher rates of steroid use in the Netherlands, Sweden, and Denmark than in the United States.
The Grant A. Starr Foundation provided funding. The investigators had no conflicts of interest.
SAN DIEGO – Physicians often skipped out on using steroids when treating bacterial meningitis even though the benefits clearly outweigh the risks, Cinthia Gallegos, MD, reported during an oral presentation at an annual meeting on infectious diseases.
In a recent multicenter retrospective cohort study, only 40% of adults with bacterial meningitis received steroids within 4 hours of hospital admission, as recommended by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID), and only 14% received steroids concomitantly or 10-20 minutes prior to antibiotic initiation, as recommended by the Infectious Diseases Society of America (IDSA), said Dr. Gallegos, an infectious disease fellow at University of Texas, Houston.
“Steroids are being underutilized in our patient population,” she said. “And when steroids are used, they are being used later than is recommended.”
To evaluate the prevalence of guideline-concordant steroid use, Dr. Gallegos and her associates analyzed the medical records of 120 adults with culture-confirmed, community-acquired bacterial meningitis treated at 10 Houston-area hospitals between 2008 and 2016.
Median duration of steroid therapy was 4 hours, which is consistent with IDSA guidelines, she noted.
Among the five patients (4%) who developed delayed cerebral thrombosis, three had Streptococcus pneumoniae meningitis, one had methicillin-resistant Staphylococcus aureus meningitis, and one had Listeria meningitis. All had received either dexamethasone monotherapy or dexamethasone and methylprednisolone within 4 hours of antibiotic initiation. They showed an initial improvement in clinical course, including normal CT and MRI, but their clinical condition deteriorated between 5 and 12 days later. “Repeat imaging showed thrombosis of different areas of the brain,” Dr. Gallegos said. Two patients died, two developed moderate or severe disability, and one fully recovered. The patients ranged in age from 26 to 69; three were male, and two were female.
The 4% rate closely resembles what is seen in the Netherlands, said Diederik van de Beek, MD, PhD, of the Academic Medical Center in Amsterdam, who comoderated the session at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. “We have some recent data where we did autopsies of cases and we saw a huge amount of bacterial fragments around the blood vessels,” he said. “We have seen this in previous autopsy studies, but here it was a massive amount of bacterial fragments.”
Researchers have suggested that delayed cerebral thrombosis in bacterial meningitis results from increases in C5a and C5b-9 levels in the cerebrospinal fluid and from an increase in the tissue factor VII pathway, Dr. Gallegos said.
Researchers think that these patients historically developed vasculitis, but that this complication “has disappeared somewhat in the dexamethasone era,” said Dr. van de Beek, lead author of the 2016 ESCMID guidelines on bacterial meningitis. “It appears that some patients are ‘pro-inflammatory’ and still react 7-9 days after treatment,” he said. “The difficult question is whether we give 4 days of steroids or longer. A clinical trial is not feasible, so we [recommend] 4 days.”
Left untreated, bacterial meningitis is fatal in up to 70% of cases, and about one in five survivors faces limb loss or neurologic disability, according to the Centers for Disease Control and Prevention. The advent of penicillin and other antibiotics dramatically improved survival, but death rates remained around 10% for meningitis associated with Neisseria meningitides and Haemophilus influenza infection, and often exceeded 30% for S. pneumoniae meningitis. “That’s important because besides antibiotics, the only treatment that decreases mortality has been shown to be steroids,” Dr. Gallegos said.
High-quality evidence supports their use. In a double-blind, randomized, multicenter trial of 301 adults with bacterial meningitis, adjunctive dexamethasone was associated with a 50% improvement in mortality, compared with adjunctive placebo (N Engl J Med. 2002 Nov 14;347[20]:1549-56). Other data confirm that steroids do not prevent vancomycin from concentrating in CSF or increase the risk of hippocampal apoptosis. But although both IDSA and ESCMID endorse steroids as adjunctive therapy to help control intracranial pressure in patients with bacterial meningitis, studies have shown much higher rates of steroid use in the Netherlands, Sweden, and Denmark than in the United States.
The Grant A. Starr Foundation provided funding. The investigators had no conflicts of interest.
SAN DIEGO – Physicians often skipped out on using steroids when treating bacterial meningitis even though the benefits clearly outweigh the risks, Cinthia Gallegos, MD, reported during an oral presentation at an annual meeting on infectious diseases.
In a recent multicenter retrospective cohort study, only 40% of adults with bacterial meningitis received steroids within 4 hours of hospital admission, as recommended by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID), and only 14% received steroids concomitantly or 10-20 minutes prior to antibiotic initiation, as recommended by the Infectious Diseases Society of America (IDSA), said Dr. Gallegos, an infectious disease fellow at University of Texas, Houston.
“Steroids are being underutilized in our patient population,” she said. “And when steroids are used, they are being used later than is recommended.”
To evaluate the prevalence of guideline-concordant steroid use, Dr. Gallegos and her associates analyzed the medical records of 120 adults with culture-confirmed, community-acquired bacterial meningitis treated at 10 Houston-area hospitals between 2008 and 2016.
Median duration of steroid therapy was 4 hours, which is consistent with IDSA guidelines, she noted.
Among the five patients (4%) who developed delayed cerebral thrombosis, three had Streptococcus pneumoniae meningitis, one had methicillin-resistant Staphylococcus aureus meningitis, and one had Listeria meningitis. All had received either dexamethasone monotherapy or dexamethasone and methylprednisolone within 4 hours of antibiotic initiation. They showed an initial improvement in clinical course, including normal CT and MRI, but their clinical condition deteriorated between 5 and 12 days later. “Repeat imaging showed thrombosis of different areas of the brain,” Dr. Gallegos said. Two patients died, two developed moderate or severe disability, and one fully recovered. The patients ranged in age from 26 to 69; three were male, and two were female.
The 4% rate closely resembles what is seen in the Netherlands, said Diederik van de Beek, MD, PhD, of the Academic Medical Center in Amsterdam, who comoderated the session at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. “We have some recent data where we did autopsies of cases and we saw a huge amount of bacterial fragments around the blood vessels,” he said. “We have seen this in previous autopsy studies, but here it was a massive amount of bacterial fragments.”
Researchers have suggested that delayed cerebral thrombosis in bacterial meningitis results from increases in C5a and C5b-9 levels in the cerebrospinal fluid and from an increase in the tissue factor VII pathway, Dr. Gallegos said.
Researchers think that these patients historically developed vasculitis, but that this complication “has disappeared somewhat in the dexamethasone era,” said Dr. van de Beek, lead author of the 2016 ESCMID guidelines on bacterial meningitis. “It appears that some patients are ‘pro-inflammatory’ and still react 7-9 days after treatment,” he said. “The difficult question is whether we give 4 days of steroids or longer. A clinical trial is not feasible, so we [recommend] 4 days.”
Left untreated, bacterial meningitis is fatal in up to 70% of cases, and about one in five survivors faces limb loss or neurologic disability, according to the Centers for Disease Control and Prevention. The advent of penicillin and other antibiotics dramatically improved survival, but death rates remained around 10% for meningitis associated with Neisseria meningitides and Haemophilus influenza infection, and often exceeded 30% for S. pneumoniae meningitis. “That’s important because besides antibiotics, the only treatment that decreases mortality has been shown to be steroids,” Dr. Gallegos said.
High-quality evidence supports their use. In a double-blind, randomized, multicenter trial of 301 adults with bacterial meningitis, adjunctive dexamethasone was associated with a 50% improvement in mortality, compared with adjunctive placebo (N Engl J Med. 2002 Nov 14;347[20]:1549-56). Other data confirm that steroids do not prevent vancomycin from concentrating in CSF or increase the risk of hippocampal apoptosis. But although both IDSA and ESCMID endorse steroids as adjunctive therapy to help control intracranial pressure in patients with bacterial meningitis, studies have shown much higher rates of steroid use in the Netherlands, Sweden, and Denmark than in the United States.
The Grant A. Starr Foundation provided funding. The investigators had no conflicts of interest.
AT IDWEEK 2017
Key clinical point:
Major finding: Five of 120 (4%) of patients developed delayed cerebral thrombosis. Only 40% received steroids within the maximum recommended time frame.
Data source: A retrospective multicenter study of 120 adults with culture-confirmed bacterial meningitis.
Disclosures: The Grant A. Starr Foundation provided funding. The investigators had no conflicts of interest.
Negative nasal swabs reliably predicted no MRSA infection
SAN DIEGO – , said Darunee Chotiprasitsakul, MD, of Johns Hopkins Medicine in Baltimore.
But physicians often prescribed vancomycin anyway, accumulating nearly 7,400 potentially avoidable treatment days over a 19-month period, she said during an oral presentation at an annual meeting on infectious diseases.
Current guidelines recommend empiric vancomycin to cover MRSA infection when ill patients have a history of MRSA colonization or recent hospitalization or exposure to antibiotics. Patients whose nasal screening swabs are negative for MRSA have been shown to be at low risk of subsequent infection, but guidelines don’t address how to use swab results to guide decisions about empiric vancomycin, Dr. Chotiprasitsakul said.
Therefore, she and her associates studied 11,882 adults without historical MRSA infection or colonization who received nasal swabs for routine surveillance in adult ICUs at Johns Hopkins. A total of 441 patients (4%) had positive swabs, while 96% tested negative.
Among patients with negative swabs, only 25 (0.22%) developed MRSA infection requiring treatment. Thus, the negative predictive value of a nasal swab for MRSA was 99%, making the probability of infection despite a negative swab “exceedingly low,” Dr. Chotiprasitsakul said.
But clinicians seemed not to use negative swab results to curtail vancomycin therapy, she found. Rates of empiric vancomycin use were 36% among patients with positive swabs and 39% among those with negative swabs. Over 19 months, ICU patients received 7,371 avoidable days of vancomycin, a median of 3 days per patient.
Matching patients by ICU and days at risk identified no significant predictors of MRSA infection, Dr. Chotiprasitsakul said. Johns Hopkins Medicine has robust infection control practices, high compliance with hand hygiene and contact precautions, and low rates of nosocomial MRSA transmission, she noted. The predictive value of a negative MRSA nasal swab could be lower at institutions where that isn’t the case, she said.
Johns Hopkins is working to curtail unnecessary use of vancomycin, said senior author Sara Cosgrove, MD, professor of medicine in infectious diseases and director of the department of antimicrobial stewardship. The team has added the findings to its guidelines for antibiotic use, which are available in an app for Johns Hopkins providers, she said in an interview.
The stewardship also highlights the data when discussing starting and stopping vancomycin in patients at very low risk for MRSA infections, she said. “In general, providers have responded favorably to acting upon this new information,” Dr. Cosgrove noted.
Johns Hopkins continues to track median days of vancomycin use per patient and per 1,000 days in its units. “[We] will assess if there is an impact on vancomycin use over the coming year,” said Dr. Cosgrove.
The investigators had no conflicts of interest. The event marked the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
SAN DIEGO – , said Darunee Chotiprasitsakul, MD, of Johns Hopkins Medicine in Baltimore.
But physicians often prescribed vancomycin anyway, accumulating nearly 7,400 potentially avoidable treatment days over a 19-month period, she said during an oral presentation at an annual meeting on infectious diseases.
Current guidelines recommend empiric vancomycin to cover MRSA infection when ill patients have a history of MRSA colonization or recent hospitalization or exposure to antibiotics. Patients whose nasal screening swabs are negative for MRSA have been shown to be at low risk of subsequent infection, but guidelines don’t address how to use swab results to guide decisions about empiric vancomycin, Dr. Chotiprasitsakul said.
Therefore, she and her associates studied 11,882 adults without historical MRSA infection or colonization who received nasal swabs for routine surveillance in adult ICUs at Johns Hopkins. A total of 441 patients (4%) had positive swabs, while 96% tested negative.
Among patients with negative swabs, only 25 (0.22%) developed MRSA infection requiring treatment. Thus, the negative predictive value of a nasal swab for MRSA was 99%, making the probability of infection despite a negative swab “exceedingly low,” Dr. Chotiprasitsakul said.
But clinicians seemed not to use negative swab results to curtail vancomycin therapy, she found. Rates of empiric vancomycin use were 36% among patients with positive swabs and 39% among those with negative swabs. Over 19 months, ICU patients received 7,371 avoidable days of vancomycin, a median of 3 days per patient.
Matching patients by ICU and days at risk identified no significant predictors of MRSA infection, Dr. Chotiprasitsakul said. Johns Hopkins Medicine has robust infection control practices, high compliance with hand hygiene and contact precautions, and low rates of nosocomial MRSA transmission, she noted. The predictive value of a negative MRSA nasal swab could be lower at institutions where that isn’t the case, she said.
Johns Hopkins is working to curtail unnecessary use of vancomycin, said senior author Sara Cosgrove, MD, professor of medicine in infectious diseases and director of the department of antimicrobial stewardship. The team has added the findings to its guidelines for antibiotic use, which are available in an app for Johns Hopkins providers, she said in an interview.
The stewardship also highlights the data when discussing starting and stopping vancomycin in patients at very low risk for MRSA infections, she said. “In general, providers have responded favorably to acting upon this new information,” Dr. Cosgrove noted.
Johns Hopkins continues to track median days of vancomycin use per patient and per 1,000 days in its units. “[We] will assess if there is an impact on vancomycin use over the coming year,” said Dr. Cosgrove.
The investigators had no conflicts of interest. The event marked the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
SAN DIEGO – , said Darunee Chotiprasitsakul, MD, of Johns Hopkins Medicine in Baltimore.
But physicians often prescribed vancomycin anyway, accumulating nearly 7,400 potentially avoidable treatment days over a 19-month period, she said during an oral presentation at an annual meeting on infectious diseases.
Current guidelines recommend empiric vancomycin to cover MRSA infection when ill patients have a history of MRSA colonization or recent hospitalization or exposure to antibiotics. Patients whose nasal screening swabs are negative for MRSA have been shown to be at low risk of subsequent infection, but guidelines don’t address how to use swab results to guide decisions about empiric vancomycin, Dr. Chotiprasitsakul said.
Therefore, she and her associates studied 11,882 adults without historical MRSA infection or colonization who received nasal swabs for routine surveillance in adult ICUs at Johns Hopkins. A total of 441 patients (4%) had positive swabs, while 96% tested negative.
Among patients with negative swabs, only 25 (0.22%) developed MRSA infection requiring treatment. Thus, the negative predictive value of a nasal swab for MRSA was 99%, making the probability of infection despite a negative swab “exceedingly low,” Dr. Chotiprasitsakul said.
But clinicians seemed not to use negative swab results to curtail vancomycin therapy, she found. Rates of empiric vancomycin use were 36% among patients with positive swabs and 39% among those with negative swabs. Over 19 months, ICU patients received 7,371 avoidable days of vancomycin, a median of 3 days per patient.
Matching patients by ICU and days at risk identified no significant predictors of MRSA infection, Dr. Chotiprasitsakul said. Johns Hopkins Medicine has robust infection control practices, high compliance with hand hygiene and contact precautions, and low rates of nosocomial MRSA transmission, she noted. The predictive value of a negative MRSA nasal swab could be lower at institutions where that isn’t the case, she said.
Johns Hopkins is working to curtail unnecessary use of vancomycin, said senior author Sara Cosgrove, MD, professor of medicine in infectious diseases and director of the department of antimicrobial stewardship. The team has added the findings to its guidelines for antibiotic use, which are available in an app for Johns Hopkins providers, she said in an interview.
The stewardship also highlights the data when discussing starting and stopping vancomycin in patients at very low risk for MRSA infections, she said. “In general, providers have responded favorably to acting upon this new information,” Dr. Cosgrove noted.
Johns Hopkins continues to track median days of vancomycin use per patient and per 1,000 days in its units. “[We] will assess if there is an impact on vancomycin use over the coming year,” said Dr. Cosgrove.
The investigators had no conflicts of interest. The event marked the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
AT IDWEEK 2017
Key clinical point: Only 0.2% of ICU patients with negative surveillance nasal swabs developed MRSA infections during the same hospitalization.
Major finding: The predictive value of a negative swab was 99%.
Data source: A study of 11,882 adults without historical MRSA infection or colonization who received nasal swabs for routine surveillance.
Disclosures: The investigators had no conflicts of interest.
SHM pushes to protect patients from ‘surprise’ out-of-network expenses
Patients entering a hospital should not be on the hook for costs related to out-of-network insurance coverage when that hospital is in-network, according to the Society of Hospital Medicine and other major medical societies, especially if it is an emergency situation and the patient is unable to make an informed choice regarding who is administering care to them.
“We want to see it come to a resolution that does not put patients in jeopardy for paying these extra costs when they are going a hospital that is in-network, and they assume that the physicians are in-network,” Ron Greeno, MD, FCCP, MHM, president of the Society of Hospital Medicine, said in an interview.
Other groups signing onto the resolution include the American College of Emergency Physicians, the American Academy of Orthopedic Surgeons, the American College of Radiology, the American Society of Anesthesiologists, the College of American Pathologists, the American Association of Neurological Surgeons, and the Congress of Neurological Surgeons.
“States are tackling this on a state-by-state basis and creating laws that are meant to protect patients from being placed in legal jeopardy,” Dr. Greeno said. “But you still want to maintain the rights of the health plan and the physicians to negotiate in good faith. That is basically the stance we take.”
According to Dr. Greeno, the joint resolution passed at the AMA meeting was “designed to make recommendations to states who are considering such laws.” The medical societies want to provide guidance on what to include in those laws that will make the process fair. “If you have a law that says ‘out of network doctors cannot balance bill at a hospital that is in-network,’ then the health plans have no reason to negotiate in good faith,” he said. “They will just pay those doctors whatever they feel like paying them.”
Ultimately, though, the resolution was about medical societies affirming their desire to protect patients from burdensome, unexpected bills.
“We want to make sure whatever laws are passed that they actually protect the patients while maintaining the ability of physicians and health plans to negotiate in good faith to a mutual resolution,” Dr. Greeno said.
Patients entering a hospital should not be on the hook for costs related to out-of-network insurance coverage when that hospital is in-network, according to the Society of Hospital Medicine and other major medical societies, especially if it is an emergency situation and the patient is unable to make an informed choice regarding who is administering care to them.
“We want to see it come to a resolution that does not put patients in jeopardy for paying these extra costs when they are going a hospital that is in-network, and they assume that the physicians are in-network,” Ron Greeno, MD, FCCP, MHM, president of the Society of Hospital Medicine, said in an interview.
Other groups signing onto the resolution include the American College of Emergency Physicians, the American Academy of Orthopedic Surgeons, the American College of Radiology, the American Society of Anesthesiologists, the College of American Pathologists, the American Association of Neurological Surgeons, and the Congress of Neurological Surgeons.
“States are tackling this on a state-by-state basis and creating laws that are meant to protect patients from being placed in legal jeopardy,” Dr. Greeno said. “But you still want to maintain the rights of the health plan and the physicians to negotiate in good faith. That is basically the stance we take.”
According to Dr. Greeno, the joint resolution passed at the AMA meeting was “designed to make recommendations to states who are considering such laws.” The medical societies want to provide guidance on what to include in those laws that will make the process fair. “If you have a law that says ‘out of network doctors cannot balance bill at a hospital that is in-network,’ then the health plans have no reason to negotiate in good faith,” he said. “They will just pay those doctors whatever they feel like paying them.”
Ultimately, though, the resolution was about medical societies affirming their desire to protect patients from burdensome, unexpected bills.
“We want to make sure whatever laws are passed that they actually protect the patients while maintaining the ability of physicians and health plans to negotiate in good faith to a mutual resolution,” Dr. Greeno said.
Patients entering a hospital should not be on the hook for costs related to out-of-network insurance coverage when that hospital is in-network, according to the Society of Hospital Medicine and other major medical societies, especially if it is an emergency situation and the patient is unable to make an informed choice regarding who is administering care to them.
“We want to see it come to a resolution that does not put patients in jeopardy for paying these extra costs when they are going a hospital that is in-network, and they assume that the physicians are in-network,” Ron Greeno, MD, FCCP, MHM, president of the Society of Hospital Medicine, said in an interview.
Other groups signing onto the resolution include the American College of Emergency Physicians, the American Academy of Orthopedic Surgeons, the American College of Radiology, the American Society of Anesthesiologists, the College of American Pathologists, the American Association of Neurological Surgeons, and the Congress of Neurological Surgeons.
“States are tackling this on a state-by-state basis and creating laws that are meant to protect patients from being placed in legal jeopardy,” Dr. Greeno said. “But you still want to maintain the rights of the health plan and the physicians to negotiate in good faith. That is basically the stance we take.”
According to Dr. Greeno, the joint resolution passed at the AMA meeting was “designed to make recommendations to states who are considering such laws.” The medical societies want to provide guidance on what to include in those laws that will make the process fair. “If you have a law that says ‘out of network doctors cannot balance bill at a hospital that is in-network,’ then the health plans have no reason to negotiate in good faith,” he said. “They will just pay those doctors whatever they feel like paying them.”
Ultimately, though, the resolution was about medical societies affirming their desire to protect patients from burdensome, unexpected bills.
“We want to make sure whatever laws are passed that they actually protect the patients while maintaining the ability of physicians and health plans to negotiate in good faith to a mutual resolution,” Dr. Greeno said.
VA study finds high MRSA infection risk among those colonized with the bacterium
SAN DIEGO – Patients colonized with MRSA are at high risk of MRSA infection both in the predischarge and postdischarge time periods, results from an 8-year Veterans Affairs study showed.
“MRSA colonization is recognized as being a strong predictor of subsequent infection,” Richard E. Nelson, PhD, said at an annual scientific meeting on infectious diseases. “What’s less understood is, are there differences in infection rates among patients who are colonized at different times? And, is there a difference between patients who import colonization with them to a hospital versus those who acquire it during a hospital stay? In addition, infection control efforts mainly focus on the predischarge time period. What about infections that develop post discharge?”
In an effort to investigate these questions, Dr. Nelson of the VA Salt Lake City Healthcare System, and his associates, evaluated more than 1.3 million acute care inpatient admissions to 125 VA hospitals nationwide from January 2008 through December 2015 who had surveillance tests performed for MRSA carriage.
The researchers restricted admissions to individuals with at least 365 days of VA activity prior to admission and categorized them into three groups: no colonization (defined as those who had no positive surveillance tests (n = 1,196,928); importation (defined as those who tested positive for MRSA colonization on admission (n = 95,833); and acquisition (defined as those who did not test positive for MRSA on admission but tested positive on a subsequent surveillance test during their admission (n = 15,146). Next, they captured MRSA infections in these individuals prior to discharge and at 30 and 90 days post discharge. Infections were defined as positive MRSA cultures taken from sterile sites, including blood, catheter site, or bone.
Overall, patients were in their mid-60s, and those who imported MRSA and those who acquired it were more likely to be male, less likely to be married, and more likely to not have health insurance. , which peaked in 2010 and declined through 2015,” said Dr. Nelson, who also holds a faculty position in University of Utah’s department of internal medicine, in the division of epidemiology. Specifically, the proportion of predischarge MRSA infections, compared with 30 days post discharge, were 40.4% vs. 59.6%, respectively, in the no colonization group; 63% vs. 37% in the importation group, and 80.8% vs. 19.2% in the acquisition group.
He also reported that the proportion of predischarge MRSA infections, compared with 90 days post discharge, were 20.5% vs. 79.5%, respectively, in the no colonization group; 47.3% vs. 52.7% in the importation group, and 70.5% vs. 29.5% in the acquisition group. The time from acquisition to infection was a mean of 8.7 days in the 30-day analysis and a mean of 22.4 days in the 90-day analysis.
Multivariate logistic regression revealed that the impact of colonization status on infection was highest in the acquisition group, compared with the importation group. Specifically, the odds ratio of developing a MRSA infection among the importation group was 29.22 in the predischarge period, OR 10.87 at post discharge 30 days, and OR 7.64 at post discharge 90 days (P less than .001 for all). Meanwhile, the OR among the acquisition group was 85.19 in the predischarge period, OR 13.01 at post discharge 30 days, and OR 8.26 at post discharge 90 days (P less than .001 for all).
Dr. Nelson acknowledged certain limitations of the study, including the fact that it only identified postdischarge infections that were detected in a VA facility. “This is likely an underestimate of postdischarge infections, because we’re missing the infection that occur in non-VA facilities,” he said at the event, which marked the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. “Also, patients can be colonized in many different body locations, but the VA protocol is that the surveillance test be done in the nostrils. So we may have misclassified patients who were colonized in a different body location as being uncolonized, when in fact they were colonized.”
The study was funded by a grant from the VA. Dr. Nelson reported having no financial disclosures.
SAN DIEGO – Patients colonized with MRSA are at high risk of MRSA infection both in the predischarge and postdischarge time periods, results from an 8-year Veterans Affairs study showed.
“MRSA colonization is recognized as being a strong predictor of subsequent infection,” Richard E. Nelson, PhD, said at an annual scientific meeting on infectious diseases. “What’s less understood is, are there differences in infection rates among patients who are colonized at different times? And, is there a difference between patients who import colonization with them to a hospital versus those who acquire it during a hospital stay? In addition, infection control efforts mainly focus on the predischarge time period. What about infections that develop post discharge?”
In an effort to investigate these questions, Dr. Nelson of the VA Salt Lake City Healthcare System, and his associates, evaluated more than 1.3 million acute care inpatient admissions to 125 VA hospitals nationwide from January 2008 through December 2015 who had surveillance tests performed for MRSA carriage.
The researchers restricted admissions to individuals with at least 365 days of VA activity prior to admission and categorized them into three groups: no colonization (defined as those who had no positive surveillance tests (n = 1,196,928); importation (defined as those who tested positive for MRSA colonization on admission (n = 95,833); and acquisition (defined as those who did not test positive for MRSA on admission but tested positive on a subsequent surveillance test during their admission (n = 15,146). Next, they captured MRSA infections in these individuals prior to discharge and at 30 and 90 days post discharge. Infections were defined as positive MRSA cultures taken from sterile sites, including blood, catheter site, or bone.
Overall, patients were in their mid-60s, and those who imported MRSA and those who acquired it were more likely to be male, less likely to be married, and more likely to not have health insurance. , which peaked in 2010 and declined through 2015,” said Dr. Nelson, who also holds a faculty position in University of Utah’s department of internal medicine, in the division of epidemiology. Specifically, the proportion of predischarge MRSA infections, compared with 30 days post discharge, were 40.4% vs. 59.6%, respectively, in the no colonization group; 63% vs. 37% in the importation group, and 80.8% vs. 19.2% in the acquisition group.
He also reported that the proportion of predischarge MRSA infections, compared with 90 days post discharge, were 20.5% vs. 79.5%, respectively, in the no colonization group; 47.3% vs. 52.7% in the importation group, and 70.5% vs. 29.5% in the acquisition group. The time from acquisition to infection was a mean of 8.7 days in the 30-day analysis and a mean of 22.4 days in the 90-day analysis.
Multivariate logistic regression revealed that the impact of colonization status on infection was highest in the acquisition group, compared with the importation group. Specifically, the odds ratio of developing a MRSA infection among the importation group was 29.22 in the predischarge period, OR 10.87 at post discharge 30 days, and OR 7.64 at post discharge 90 days (P less than .001 for all). Meanwhile, the OR among the acquisition group was 85.19 in the predischarge period, OR 13.01 at post discharge 30 days, and OR 8.26 at post discharge 90 days (P less than .001 for all).
Dr. Nelson acknowledged certain limitations of the study, including the fact that it only identified postdischarge infections that were detected in a VA facility. “This is likely an underestimate of postdischarge infections, because we’re missing the infection that occur in non-VA facilities,” he said at the event, which marked the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. “Also, patients can be colonized in many different body locations, but the VA protocol is that the surveillance test be done in the nostrils. So we may have misclassified patients who were colonized in a different body location as being uncolonized, when in fact they were colonized.”
The study was funded by a grant from the VA. Dr. Nelson reported having no financial disclosures.
SAN DIEGO – Patients colonized with MRSA are at high risk of MRSA infection both in the predischarge and postdischarge time periods, results from an 8-year Veterans Affairs study showed.
“MRSA colonization is recognized as being a strong predictor of subsequent infection,” Richard E. Nelson, PhD, said at an annual scientific meeting on infectious diseases. “What’s less understood is, are there differences in infection rates among patients who are colonized at different times? And, is there a difference between patients who import colonization with them to a hospital versus those who acquire it during a hospital stay? In addition, infection control efforts mainly focus on the predischarge time period. What about infections that develop post discharge?”
In an effort to investigate these questions, Dr. Nelson of the VA Salt Lake City Healthcare System, and his associates, evaluated more than 1.3 million acute care inpatient admissions to 125 VA hospitals nationwide from January 2008 through December 2015 who had surveillance tests performed for MRSA carriage.
The researchers restricted admissions to individuals with at least 365 days of VA activity prior to admission and categorized them into three groups: no colonization (defined as those who had no positive surveillance tests (n = 1,196,928); importation (defined as those who tested positive for MRSA colonization on admission (n = 95,833); and acquisition (defined as those who did not test positive for MRSA on admission but tested positive on a subsequent surveillance test during their admission (n = 15,146). Next, they captured MRSA infections in these individuals prior to discharge and at 30 and 90 days post discharge. Infections were defined as positive MRSA cultures taken from sterile sites, including blood, catheter site, or bone.
Overall, patients were in their mid-60s, and those who imported MRSA and those who acquired it were more likely to be male, less likely to be married, and more likely to not have health insurance. , which peaked in 2010 and declined through 2015,” said Dr. Nelson, who also holds a faculty position in University of Utah’s department of internal medicine, in the division of epidemiology. Specifically, the proportion of predischarge MRSA infections, compared with 30 days post discharge, were 40.4% vs. 59.6%, respectively, in the no colonization group; 63% vs. 37% in the importation group, and 80.8% vs. 19.2% in the acquisition group.
He also reported that the proportion of predischarge MRSA infections, compared with 90 days post discharge, were 20.5% vs. 79.5%, respectively, in the no colonization group; 47.3% vs. 52.7% in the importation group, and 70.5% vs. 29.5% in the acquisition group. The time from acquisition to infection was a mean of 8.7 days in the 30-day analysis and a mean of 22.4 days in the 90-day analysis.
Multivariate logistic regression revealed that the impact of colonization status on infection was highest in the acquisition group, compared with the importation group. Specifically, the odds ratio of developing a MRSA infection among the importation group was 29.22 in the predischarge period, OR 10.87 at post discharge 30 days, and OR 7.64 at post discharge 90 days (P less than .001 for all). Meanwhile, the OR among the acquisition group was 85.19 in the predischarge period, OR 13.01 at post discharge 30 days, and OR 8.26 at post discharge 90 days (P less than .001 for all).
Dr. Nelson acknowledged certain limitations of the study, including the fact that it only identified postdischarge infections that were detected in a VA facility. “This is likely an underestimate of postdischarge infections, because we’re missing the infection that occur in non-VA facilities,” he said at the event, which marked the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. “Also, patients can be colonized in many different body locations, but the VA protocol is that the surveillance test be done in the nostrils. So we may have misclassified patients who were colonized in a different body location as being uncolonized, when in fact they were colonized.”
The study was funded by a grant from the VA. Dr. Nelson reported having no financial disclosures.
REPORTING FROM ID WEEK 2017
Key clinical point: About half of postdischarge MRSA infections were in patients who acquired the organism before discharge.
Major finding: The proportion of predischarge MRSA infections, compared with 30 days post discharge, were 40.4% vs. 59.6%, respectively, in the no colonization group; 63% vs. 37% in the importation group, and 80.8% vs. 19.2% in the acquisition group.
Study details: An analysis of more than 1.3 million acute care inpatient admissions to 125 VA hospitals nationwide from January 2008 through December 2015.
Disclosures: The study was funded by a grant from the VA. Dr. Nelson reported having no financial disclosures.
Advance care planning benefit presents challenges
When Donna Sweet, MD, sees patients for routine exams, death and dying are often the furthest thing from their minds. Regardless of age or health status, however, Dr. Sweet regularly asks patients about end-of-life care and whether they’ve considered their options.
In the past, physicians had to be creative in how they coded for such conversations, but Medicare’s newish advance care planning benefit is changing that.
Staring in 2016, the Centers for Medicare & Medicaid Services began reimbursing physicians for advance care planning discussions with the approval of two new codes: 99497 and 99498. The codes pay about $86 for the first 30-minutes of a face-to-face conversation with a patient, family member, and/or surrogate and about $75 for additional sessions. Services can be furnished in both inpatient and ambulatory settings, and payment is not limited to particular physician specialties.
Dr. Sweet said that she uses these codes a couple times a week when patients visit for reasons such as routine hypertension or diabetes exams or annual Medicare wellness visits. To broach the subject, Dr. Sweet said it helps to have literature about advance care planning in the room that patients can review.
“It’s just a matter of bringing it up,” she said. “Considering some of the other codes, the advance care planning code is really pretty simple.”
However, doctors like Dr. Sweet appear to be in the minority when it comes to providing this service. Of the nearly 57 million beneficiaries enrolled in Medicare at the end of 2016, only about 1% received advance care planning sessions, according to analysis of Medicare data posted by Kaiser Health News. Nationwide, health providers submitted about $93 million in charges, of which $43 million was paid by Medicare.
Challenges deter conversations
During a recent visit with a 72-year-old cancer patient, Bridget Fahy, MD, a surgical oncologist at the University of New Mexico, Albuquerque, spent time discussing advance directives and the importance of naming a surrogate decision maker. Dr. Fahy had treated the patient for two different cancers over the course of 4 years, and he was now diagnosed with a third, she recalled during an interview. Figuring out an advance care plan, though, proved complicated: The man was not married, had no children, and had no family members who lived in the state.
Although Dr. Fahy was aware of the Medicare advance care planning codes, she did not bill the session as such.
“Even in the course of having that conversation, I’m more apt to bill on time than I am specifically to meet the Medicare requirements for the documentation for [the benefit],” she said.
“There are two pieces required to take advantage of the advance care planning benefit code: having the conversation and documenting it,” Dr. Fahy noted. “What I write at the end of a resident note or an advanced practice provider note is going to be more focused on the counseling I had with the patient about their condition, the evaluation, and what the treatment plan is going to be. For surgeons to utilize the advance care planning codes, they have to have knowledge of the code, which many do not; they must know the requirements for documenting the conversation; and they have to have the time needed to have the conversation while also addressing all of the surgery-specific issues that need to be covered during the visit. There are a number of hurdles to overcome.”
Danielle B. Scheurer, MD, a hospitalist and chief quality officer at the Medical University of South Carolina, Charleston, said that she, too, has not used advance care planning codes. The reimbursement tool is a positive step forward, she said, but so far, it’s not an easy insert into a hospitalist’s practice.
“It’s not top of mind as far as a billing practice,” she said. “It’s not built into the typical work flow. Obviously, it’s not every patient, it’s not everyday, so you have to remember to put it into your work flow. That’s probably the biggest barrier for most hospitalists: either not knowing about it at all or not yet figuring out how to weave it into what they already do.”
Overcoming hurdles through experience
Using the advance care planning benefit has been easier said than done in his practice, according to Carl R. Olden, MD, a family physician in Yakima, Wash. The logistics of scheduling and patient reluctance are contributing to low usage of the new codes, said Dr. Olden, a member of the American Academy of Family Physicians board of directors.
Between Sept. 1, 2016, and Aug. 31, 2017, the family medicine, primary care, internal medicine, and pulmonary medicine members of Dr. Olden’s network who provide end-of-life counseling submitted billing for a total of 106,160 Medicare visits. Of those visits, the 99497 code was submitted only 32 times, according to data provided by Dr. Olden.
At Dr. Olden’s 16-physician practice, there are no registered nurses to help set up and start Medicare wellness visits, which the advance care planning session benefit is designed to fit within, he said.
“Most of those Medicare wellness visits are driven by having a registered nurse do most of the work,” he said. “[For us] to schedule a wellness visit, it’s mostly physician work and to do a 30-minute wellness visit, most of us can see three patients in that 30-minute slot, so it ends up not being very cost effective.”
“Most of my Medicare patients are folks that have four to five chronic medical conditions, and for them to make a 30-minute visit to the office and not talk about any of those conditions but to talk about home safety and advance directives and fall prevention, it’s hard for them to understand that,” he said.
Dr. Newman stresses that while the billing approach takes time to learn, the codes can be weaved into regular practice with some preparation and planning. At her practice, she primarily uses the codes for patients with challenging changes in their health status, sometimes setting up meetings in advance and, other times, conducting a spur-of-the-moment conversation.
“It’s a wonderful benefit,” she said. “I’m not surprised it’s taking awhile to take hold. The reason is you have to prepare for these visits. It takes preparation, including a chart review.”
A common misconception is that the visit must be scheduled separately and cannot be added to another visit, she said. Doctors can bill the advance care planning codes on the same day as an evaluation and management service. For instance, if a patient is accompanied by a family member and seen for routine follow-up, the physician can discuss the medical conditions first and later have a discussion about advance care planning. When billing, the physician can then use an evaluation and management code for the part of the visit related to the patient’s medical conditions and also bill for the advance care planning discussion using the new Medicare codes, Dr. Newman said.
“You’re allowed to use a modifier to attach to it to get paid for both on the same day,” she said. She suggested checking local Medicare policy for the use of the appropriate modifier, usually 26. “One thing that’s important to understand is there’s a lot of short discussions about advanced care planning that doesn’t fit the code. So if a patient wants to have a 5-minute conversation – that happens a lot – these will not be billable or counted under this new benefit. Fifteen minutes is the least amount of time that qualifies for 99497.”
Dr. Sweet said that she expects greater use of the codes as more doctors become aware of how they can be used.
“Once people use it a time or two, they will use it a lot more,” Dr. Sweet said. “It takes time to change, and it takes time to make time to do the things we need to do. But especially, as we move into high-value care, something like this hopefully, [doctors] will embrace.”
[email protected]
On Twitter @legal_med
When Donna Sweet, MD, sees patients for routine exams, death and dying are often the furthest thing from their minds. Regardless of age or health status, however, Dr. Sweet regularly asks patients about end-of-life care and whether they’ve considered their options.
In the past, physicians had to be creative in how they coded for such conversations, but Medicare’s newish advance care planning benefit is changing that.
Staring in 2016, the Centers for Medicare & Medicaid Services began reimbursing physicians for advance care planning discussions with the approval of two new codes: 99497 and 99498. The codes pay about $86 for the first 30-minutes of a face-to-face conversation with a patient, family member, and/or surrogate and about $75 for additional sessions. Services can be furnished in both inpatient and ambulatory settings, and payment is not limited to particular physician specialties.
Dr. Sweet said that she uses these codes a couple times a week when patients visit for reasons such as routine hypertension or diabetes exams or annual Medicare wellness visits. To broach the subject, Dr. Sweet said it helps to have literature about advance care planning in the room that patients can review.
“It’s just a matter of bringing it up,” she said. “Considering some of the other codes, the advance care planning code is really pretty simple.”
However, doctors like Dr. Sweet appear to be in the minority when it comes to providing this service. Of the nearly 57 million beneficiaries enrolled in Medicare at the end of 2016, only about 1% received advance care planning sessions, according to analysis of Medicare data posted by Kaiser Health News. Nationwide, health providers submitted about $93 million in charges, of which $43 million was paid by Medicare.
Challenges deter conversations
During a recent visit with a 72-year-old cancer patient, Bridget Fahy, MD, a surgical oncologist at the University of New Mexico, Albuquerque, spent time discussing advance directives and the importance of naming a surrogate decision maker. Dr. Fahy had treated the patient for two different cancers over the course of 4 years, and he was now diagnosed with a third, she recalled during an interview. Figuring out an advance care plan, though, proved complicated: The man was not married, had no children, and had no family members who lived in the state.
Although Dr. Fahy was aware of the Medicare advance care planning codes, she did not bill the session as such.
“Even in the course of having that conversation, I’m more apt to bill on time than I am specifically to meet the Medicare requirements for the documentation for [the benefit],” she said.
“There are two pieces required to take advantage of the advance care planning benefit code: having the conversation and documenting it,” Dr. Fahy noted. “What I write at the end of a resident note or an advanced practice provider note is going to be more focused on the counseling I had with the patient about their condition, the evaluation, and what the treatment plan is going to be. For surgeons to utilize the advance care planning codes, they have to have knowledge of the code, which many do not; they must know the requirements for documenting the conversation; and they have to have the time needed to have the conversation while also addressing all of the surgery-specific issues that need to be covered during the visit. There are a number of hurdles to overcome.”
Danielle B. Scheurer, MD, a hospitalist and chief quality officer at the Medical University of South Carolina, Charleston, said that she, too, has not used advance care planning codes. The reimbursement tool is a positive step forward, she said, but so far, it’s not an easy insert into a hospitalist’s practice.
“It’s not top of mind as far as a billing practice,” she said. “It’s not built into the typical work flow. Obviously, it’s not every patient, it’s not everyday, so you have to remember to put it into your work flow. That’s probably the biggest barrier for most hospitalists: either not knowing about it at all or not yet figuring out how to weave it into what they already do.”
Overcoming hurdles through experience
Using the advance care planning benefit has been easier said than done in his practice, according to Carl R. Olden, MD, a family physician in Yakima, Wash. The logistics of scheduling and patient reluctance are contributing to low usage of the new codes, said Dr. Olden, a member of the American Academy of Family Physicians board of directors.
Between Sept. 1, 2016, and Aug. 31, 2017, the family medicine, primary care, internal medicine, and pulmonary medicine members of Dr. Olden’s network who provide end-of-life counseling submitted billing for a total of 106,160 Medicare visits. Of those visits, the 99497 code was submitted only 32 times, according to data provided by Dr. Olden.
At Dr. Olden’s 16-physician practice, there are no registered nurses to help set up and start Medicare wellness visits, which the advance care planning session benefit is designed to fit within, he said.
“Most of those Medicare wellness visits are driven by having a registered nurse do most of the work,” he said. “[For us] to schedule a wellness visit, it’s mostly physician work and to do a 30-minute wellness visit, most of us can see three patients in that 30-minute slot, so it ends up not being very cost effective.”
“Most of my Medicare patients are folks that have four to five chronic medical conditions, and for them to make a 30-minute visit to the office and not talk about any of those conditions but to talk about home safety and advance directives and fall prevention, it’s hard for them to understand that,” he said.
Dr. Newman stresses that while the billing approach takes time to learn, the codes can be weaved into regular practice with some preparation and planning. At her practice, she primarily uses the codes for patients with challenging changes in their health status, sometimes setting up meetings in advance and, other times, conducting a spur-of-the-moment conversation.
“It’s a wonderful benefit,” she said. “I’m not surprised it’s taking awhile to take hold. The reason is you have to prepare for these visits. It takes preparation, including a chart review.”
A common misconception is that the visit must be scheduled separately and cannot be added to another visit, she said. Doctors can bill the advance care planning codes on the same day as an evaluation and management service. For instance, if a patient is accompanied by a family member and seen for routine follow-up, the physician can discuss the medical conditions first and later have a discussion about advance care planning. When billing, the physician can then use an evaluation and management code for the part of the visit related to the patient’s medical conditions and also bill for the advance care planning discussion using the new Medicare codes, Dr. Newman said.
“You’re allowed to use a modifier to attach to it to get paid for both on the same day,” she said. She suggested checking local Medicare policy for the use of the appropriate modifier, usually 26. “One thing that’s important to understand is there’s a lot of short discussions about advanced care planning that doesn’t fit the code. So if a patient wants to have a 5-minute conversation – that happens a lot – these will not be billable or counted under this new benefit. Fifteen minutes is the least amount of time that qualifies for 99497.”
Dr. Sweet said that she expects greater use of the codes as more doctors become aware of how they can be used.
“Once people use it a time or two, they will use it a lot more,” Dr. Sweet said. “It takes time to change, and it takes time to make time to do the things we need to do. But especially, as we move into high-value care, something like this hopefully, [doctors] will embrace.”
[email protected]
On Twitter @legal_med
When Donna Sweet, MD, sees patients for routine exams, death and dying are often the furthest thing from their minds. Regardless of age or health status, however, Dr. Sweet regularly asks patients about end-of-life care and whether they’ve considered their options.
In the past, physicians had to be creative in how they coded for such conversations, but Medicare’s newish advance care planning benefit is changing that.
Staring in 2016, the Centers for Medicare & Medicaid Services began reimbursing physicians for advance care planning discussions with the approval of two new codes: 99497 and 99498. The codes pay about $86 for the first 30-minutes of a face-to-face conversation with a patient, family member, and/or surrogate and about $75 for additional sessions. Services can be furnished in both inpatient and ambulatory settings, and payment is not limited to particular physician specialties.
Dr. Sweet said that she uses these codes a couple times a week when patients visit for reasons such as routine hypertension or diabetes exams or annual Medicare wellness visits. To broach the subject, Dr. Sweet said it helps to have literature about advance care planning in the room that patients can review.
“It’s just a matter of bringing it up,” she said. “Considering some of the other codes, the advance care planning code is really pretty simple.”
However, doctors like Dr. Sweet appear to be in the minority when it comes to providing this service. Of the nearly 57 million beneficiaries enrolled in Medicare at the end of 2016, only about 1% received advance care planning sessions, according to analysis of Medicare data posted by Kaiser Health News. Nationwide, health providers submitted about $93 million in charges, of which $43 million was paid by Medicare.
Challenges deter conversations
During a recent visit with a 72-year-old cancer patient, Bridget Fahy, MD, a surgical oncologist at the University of New Mexico, Albuquerque, spent time discussing advance directives and the importance of naming a surrogate decision maker. Dr. Fahy had treated the patient for two different cancers over the course of 4 years, and he was now diagnosed with a third, she recalled during an interview. Figuring out an advance care plan, though, proved complicated: The man was not married, had no children, and had no family members who lived in the state.
Although Dr. Fahy was aware of the Medicare advance care planning codes, she did not bill the session as such.
“Even in the course of having that conversation, I’m more apt to bill on time than I am specifically to meet the Medicare requirements for the documentation for [the benefit],” she said.
“There are two pieces required to take advantage of the advance care planning benefit code: having the conversation and documenting it,” Dr. Fahy noted. “What I write at the end of a resident note or an advanced practice provider note is going to be more focused on the counseling I had with the patient about their condition, the evaluation, and what the treatment plan is going to be. For surgeons to utilize the advance care planning codes, they have to have knowledge of the code, which many do not; they must know the requirements for documenting the conversation; and they have to have the time needed to have the conversation while also addressing all of the surgery-specific issues that need to be covered during the visit. There are a number of hurdles to overcome.”
Danielle B. Scheurer, MD, a hospitalist and chief quality officer at the Medical University of South Carolina, Charleston, said that she, too, has not used advance care planning codes. The reimbursement tool is a positive step forward, she said, but so far, it’s not an easy insert into a hospitalist’s practice.
“It’s not top of mind as far as a billing practice,” she said. “It’s not built into the typical work flow. Obviously, it’s not every patient, it’s not everyday, so you have to remember to put it into your work flow. That’s probably the biggest barrier for most hospitalists: either not knowing about it at all or not yet figuring out how to weave it into what they already do.”
Overcoming hurdles through experience
Using the advance care planning benefit has been easier said than done in his practice, according to Carl R. Olden, MD, a family physician in Yakima, Wash. The logistics of scheduling and patient reluctance are contributing to low usage of the new codes, said Dr. Olden, a member of the American Academy of Family Physicians board of directors.
Between Sept. 1, 2016, and Aug. 31, 2017, the family medicine, primary care, internal medicine, and pulmonary medicine members of Dr. Olden’s network who provide end-of-life counseling submitted billing for a total of 106,160 Medicare visits. Of those visits, the 99497 code was submitted only 32 times, according to data provided by Dr. Olden.
At Dr. Olden’s 16-physician practice, there are no registered nurses to help set up and start Medicare wellness visits, which the advance care planning session benefit is designed to fit within, he said.
“Most of those Medicare wellness visits are driven by having a registered nurse do most of the work,” he said. “[For us] to schedule a wellness visit, it’s mostly physician work and to do a 30-minute wellness visit, most of us can see three patients in that 30-minute slot, so it ends up not being very cost effective.”
“Most of my Medicare patients are folks that have four to five chronic medical conditions, and for them to make a 30-minute visit to the office and not talk about any of those conditions but to talk about home safety and advance directives and fall prevention, it’s hard for them to understand that,” he said.
Dr. Newman stresses that while the billing approach takes time to learn, the codes can be weaved into regular practice with some preparation and planning. At her practice, she primarily uses the codes for patients with challenging changes in their health status, sometimes setting up meetings in advance and, other times, conducting a spur-of-the-moment conversation.
“It’s a wonderful benefit,” she said. “I’m not surprised it’s taking awhile to take hold. The reason is you have to prepare for these visits. It takes preparation, including a chart review.”
A common misconception is that the visit must be scheduled separately and cannot be added to another visit, she said. Doctors can bill the advance care planning codes on the same day as an evaluation and management service. For instance, if a patient is accompanied by a family member and seen for routine follow-up, the physician can discuss the medical conditions first and later have a discussion about advance care planning. When billing, the physician can then use an evaluation and management code for the part of the visit related to the patient’s medical conditions and also bill for the advance care planning discussion using the new Medicare codes, Dr. Newman said.
“You’re allowed to use a modifier to attach to it to get paid for both on the same day,” she said. She suggested checking local Medicare policy for the use of the appropriate modifier, usually 26. “One thing that’s important to understand is there’s a lot of short discussions about advanced care planning that doesn’t fit the code. So if a patient wants to have a 5-minute conversation – that happens a lot – these will not be billable or counted under this new benefit. Fifteen minutes is the least amount of time that qualifies for 99497.”
Dr. Sweet said that she expects greater use of the codes as more doctors become aware of how they can be used.
“Once people use it a time or two, they will use it a lot more,” Dr. Sweet said. “It takes time to change, and it takes time to make time to do the things we need to do. But especially, as we move into high-value care, something like this hopefully, [doctors] will embrace.”
[email protected]
On Twitter @legal_med
VIDEO: Intermittent furosemide during acute HFpEF favors kidneys
DALLAS – Patients with heart failure with preserved ejection fraction who were hospitalized for acute decompensation had a significantly smaller rise in serum creatinine when treated with intermittent, bolus doses of furosemide, compared with patients who received a continuous furosemide infusion in a single-center, randomized trial with 90 patients.
Intermittent furosemide also resulted in many fewer episodes of worsening renal function. In the trial, 12% of patients who received bolus furosemide doses developed worsening renal function during hospitalization compared with 36% of patients treated with a continuous furosemide infusion, Kavita Sharma, MD, said at the annual scientific meeting of the Heart Failure Society of America.
While acknowledging that this finding is preliminary because it was made in a relatively small, single-center study, “I’d be cautious about continuous infusion” in acute decompensated patients with heart failure with preserved ejection fraction (HFpEF); “bolus is preferred,” Dr. Sharma said in a video interview.
Results from the prior Diuretic Optimization Strategies Evaluation (DOSE) trial, published in 2011, had shown no significant difference in renal function in hospitalized heart failure patients randomized to receive either bolus or continuous furosemide, but that study largely enrolled patients with heart failure with reduced ejection fraction (HFrEF) (N Engl J Med. 2011 Mar 3;364[9]:797-805).
“When patients with HFpEF are hospitalized with acute heart failure there is a high rate of kidney injury, that often results in slowing diuresis leading to longer hospital stays. With adjustment for changes in blood pressure and volume of diuresis we saw a fourfold increase in worsening renal failure [with continuous infusion], so you should think twice before using continuous dosing,” said Dr. Sharma, a heart failure cardiologist at Johns Hopkins Medicine in Baltimore.
She presented results from Diuretics and Dopamine in Heart Failure With Preserved Ejection Fraction (ROPA-DOP), which randomized 90 hospitalized heart failure patients with a left ventricular ejection fraction of at least 50% and an estimated glomerular filtration rate of more than 15 mL/min/1.73 m2. The enrolled patients averaged 66 years old, 61% were women, their average body mass index was 41 kg/m2, and their average estimated glomerular filtration rate was 58 mL/min/1.73 m2.
The study’s primary endpoint was percent change in creatinine during hospitalization, which rose by an average 5% in the patients who received intermittent bolus furosemide and by an average 16% in patient who received a continuous infusion, a statistically significant difference. In a regression analysis that controlled for between-group differences in patient’s age, sex, race, body mass index, smoking status, changes in systolic blood pressure, heart rate, fluid balance after 72 hours, and other variables, patients treated with continuous furosemide infusion averaged an 11% greater increase in serum creatinine, Dr. Sharma reported. After similar adjustments, the secondary endpoint rate of worsening renal function was more than four times more likely to occur in the patients on continuous infusion compared with those who received intermittent bolus treatment, she said.
A second aspect of the ROPA-DOP trial randomized the same patients to received either low dose (3 mcg/kg per min) dopamine or placebo during hospitalization. The results showed that low-dose dopamine had no significant impact on either change in creatinine levels or on the incidence of worsening renal function compared with placebo, though dopamine treatment did link with a nonsignificant trend toward somewhat greater diuresis. These results were consistent with prior findings in the Renal Optimization Strategies Evaluation (ROSE) trial (JAMA. 2013 Nov 18;310[23]:2533-43), which used a mixed population of patients with HFpEF or HFrEF but predominantly patients with HFrEF, Dr. Sharma noted.
“It was a neutral finding [for dopamine in ROPA-DOP], and while there was no harm from dopamine there was clearly no benefit,” she said. It is possible that HFpEF patients with right ventricular dysfunction secondary to pulmonary hypertension might benefit from low-dose dopamine, but this needs further study, Dr. Sharma said.
[email protected]
On Twitter @mitchelzoler
In the Diuretic Optimization Strategies Evaluation (DOSE) trial, we enrolled heart failure patients with a mix of reduced ejection fraction and preserved ejection fraction. The DOSE results showed no relationship between ejection fraction and the response to furosemide treatment by intermittent bolus or by continuous infusion in patients hospitalized with acute decompensated heart failure. The results also showed that continuous infusion was no better than intermittent bolus treatment, and following our report in 2011 (N Engl J Med. 2011 Mar 3;364[9]:797-805), many centers that had previously relied on continuous furosemide switched to use of bolus doses primarily because continuous infusion is much less convenient.
But it is important to keep in mind that trial results focus on averages and populations of patients. Anecdotally, we see some acute heart failure patients who seem to respond better to continuous infusion, and so some clinicians switch patients who do not respond well to bolus treatment to continuous infusion. In DOSE, we only tested the efficacy of the initial strategy; we have no evidence on whether or not changing the dosing strategy helps patients who do not respond adequately to an initial strategy of intermittent bolus doses.
G. Michael Felker, MD , professor of medicine at Duke University, Durham, N.C., made these comments in an interview. He has been a consultant to Amgen, Bristol-Myers Squibb, GlaxoSmithKline, Medtronic, MyoKardia, Novartis, Stealth, and Trevena.
In the Diuretic Optimization Strategies Evaluation (DOSE) trial, we enrolled heart failure patients with a mix of reduced ejection fraction and preserved ejection fraction. The DOSE results showed no relationship between ejection fraction and the response to furosemide treatment by intermittent bolus or by continuous infusion in patients hospitalized with acute decompensated heart failure. The results also showed that continuous infusion was no better than intermittent bolus treatment, and following our report in 2011 (N Engl J Med. 2011 Mar 3;364[9]:797-805), many centers that had previously relied on continuous furosemide switched to use of bolus doses primarily because continuous infusion is much less convenient.
But it is important to keep in mind that trial results focus on averages and populations of patients. Anecdotally, we see some acute heart failure patients who seem to respond better to continuous infusion, and so some clinicians switch patients who do not respond well to bolus treatment to continuous infusion. In DOSE, we only tested the efficacy of the initial strategy; we have no evidence on whether or not changing the dosing strategy helps patients who do not respond adequately to an initial strategy of intermittent bolus doses.
G. Michael Felker, MD , professor of medicine at Duke University, Durham, N.C., made these comments in an interview. He has been a consultant to Amgen, Bristol-Myers Squibb, GlaxoSmithKline, Medtronic, MyoKardia, Novartis, Stealth, and Trevena.
In the Diuretic Optimization Strategies Evaluation (DOSE) trial, we enrolled heart failure patients with a mix of reduced ejection fraction and preserved ejection fraction. The DOSE results showed no relationship between ejection fraction and the response to furosemide treatment by intermittent bolus or by continuous infusion in patients hospitalized with acute decompensated heart failure. The results also showed that continuous infusion was no better than intermittent bolus treatment, and following our report in 2011 (N Engl J Med. 2011 Mar 3;364[9]:797-805), many centers that had previously relied on continuous furosemide switched to use of bolus doses primarily because continuous infusion is much less convenient.
But it is important to keep in mind that trial results focus on averages and populations of patients. Anecdotally, we see some acute heart failure patients who seem to respond better to continuous infusion, and so some clinicians switch patients who do not respond well to bolus treatment to continuous infusion. In DOSE, we only tested the efficacy of the initial strategy; we have no evidence on whether or not changing the dosing strategy helps patients who do not respond adequately to an initial strategy of intermittent bolus doses.
G. Michael Felker, MD , professor of medicine at Duke University, Durham, N.C., made these comments in an interview. He has been a consultant to Amgen, Bristol-Myers Squibb, GlaxoSmithKline, Medtronic, MyoKardia, Novartis, Stealth, and Trevena.
DALLAS – Patients with heart failure with preserved ejection fraction who were hospitalized for acute decompensation had a significantly smaller rise in serum creatinine when treated with intermittent, bolus doses of furosemide, compared with patients who received a continuous furosemide infusion in a single-center, randomized trial with 90 patients.
Intermittent furosemide also resulted in many fewer episodes of worsening renal function. In the trial, 12% of patients who received bolus furosemide doses developed worsening renal function during hospitalization compared with 36% of patients treated with a continuous furosemide infusion, Kavita Sharma, MD, said at the annual scientific meeting of the Heart Failure Society of America.
While acknowledging that this finding is preliminary because it was made in a relatively small, single-center study, “I’d be cautious about continuous infusion” in acute decompensated patients with heart failure with preserved ejection fraction (HFpEF); “bolus is preferred,” Dr. Sharma said in a video interview.
Results from the prior Diuretic Optimization Strategies Evaluation (DOSE) trial, published in 2011, had shown no significant difference in renal function in hospitalized heart failure patients randomized to receive either bolus or continuous furosemide, but that study largely enrolled patients with heart failure with reduced ejection fraction (HFrEF) (N Engl J Med. 2011 Mar 3;364[9]:797-805).
“When patients with HFpEF are hospitalized with acute heart failure there is a high rate of kidney injury, that often results in slowing diuresis leading to longer hospital stays. With adjustment for changes in blood pressure and volume of diuresis we saw a fourfold increase in worsening renal failure [with continuous infusion], so you should think twice before using continuous dosing,” said Dr. Sharma, a heart failure cardiologist at Johns Hopkins Medicine in Baltimore.
She presented results from Diuretics and Dopamine in Heart Failure With Preserved Ejection Fraction (ROPA-DOP), which randomized 90 hospitalized heart failure patients with a left ventricular ejection fraction of at least 50% and an estimated glomerular filtration rate of more than 15 mL/min/1.73 m2. The enrolled patients averaged 66 years old, 61% were women, their average body mass index was 41 kg/m2, and their average estimated glomerular filtration rate was 58 mL/min/1.73 m2.
The study’s primary endpoint was percent change in creatinine during hospitalization, which rose by an average 5% in the patients who received intermittent bolus furosemide and by an average 16% in patient who received a continuous infusion, a statistically significant difference. In a regression analysis that controlled for between-group differences in patient’s age, sex, race, body mass index, smoking status, changes in systolic blood pressure, heart rate, fluid balance after 72 hours, and other variables, patients treated with continuous furosemide infusion averaged an 11% greater increase in serum creatinine, Dr. Sharma reported. After similar adjustments, the secondary endpoint rate of worsening renal function was more than four times more likely to occur in the patients on continuous infusion compared with those who received intermittent bolus treatment, she said.
A second aspect of the ROPA-DOP trial randomized the same patients to received either low dose (3 mcg/kg per min) dopamine or placebo during hospitalization. The results showed that low-dose dopamine had no significant impact on either change in creatinine levels or on the incidence of worsening renal function compared with placebo, though dopamine treatment did link with a nonsignificant trend toward somewhat greater diuresis. These results were consistent with prior findings in the Renal Optimization Strategies Evaluation (ROSE) trial (JAMA. 2013 Nov 18;310[23]:2533-43), which used a mixed population of patients with HFpEF or HFrEF but predominantly patients with HFrEF, Dr. Sharma noted.
“It was a neutral finding [for dopamine in ROPA-DOP], and while there was no harm from dopamine there was clearly no benefit,” she said. It is possible that HFpEF patients with right ventricular dysfunction secondary to pulmonary hypertension might benefit from low-dose dopamine, but this needs further study, Dr. Sharma said.
[email protected]
On Twitter @mitchelzoler
DALLAS – Patients with heart failure with preserved ejection fraction who were hospitalized for acute decompensation had a significantly smaller rise in serum creatinine when treated with intermittent, bolus doses of furosemide, compared with patients who received a continuous furosemide infusion in a single-center, randomized trial with 90 patients.
Intermittent furosemide also resulted in many fewer episodes of worsening renal function. In the trial, 12% of patients who received bolus furosemide doses developed worsening renal function during hospitalization compared with 36% of patients treated with a continuous furosemide infusion, Kavita Sharma, MD, said at the annual scientific meeting of the Heart Failure Society of America.
While acknowledging that this finding is preliminary because it was made in a relatively small, single-center study, “I’d be cautious about continuous infusion” in acute decompensated patients with heart failure with preserved ejection fraction (HFpEF); “bolus is preferred,” Dr. Sharma said in a video interview.
Results from the prior Diuretic Optimization Strategies Evaluation (DOSE) trial, published in 2011, had shown no significant difference in renal function in hospitalized heart failure patients randomized to receive either bolus or continuous furosemide, but that study largely enrolled patients with heart failure with reduced ejection fraction (HFrEF) (N Engl J Med. 2011 Mar 3;364[9]:797-805).
“When patients with HFpEF are hospitalized with acute heart failure there is a high rate of kidney injury, that often results in slowing diuresis leading to longer hospital stays. With adjustment for changes in blood pressure and volume of diuresis we saw a fourfold increase in worsening renal failure [with continuous infusion], so you should think twice before using continuous dosing,” said Dr. Sharma, a heart failure cardiologist at Johns Hopkins Medicine in Baltimore.
She presented results from Diuretics and Dopamine in Heart Failure With Preserved Ejection Fraction (ROPA-DOP), which randomized 90 hospitalized heart failure patients with a left ventricular ejection fraction of at least 50% and an estimated glomerular filtration rate of more than 15 mL/min/1.73 m2. The enrolled patients averaged 66 years old, 61% were women, their average body mass index was 41 kg/m2, and their average estimated glomerular filtration rate was 58 mL/min/1.73 m2.
The study’s primary endpoint was percent change in creatinine during hospitalization, which rose by an average 5% in the patients who received intermittent bolus furosemide and by an average 16% in patient who received a continuous infusion, a statistically significant difference. In a regression analysis that controlled for between-group differences in patient’s age, sex, race, body mass index, smoking status, changes in systolic blood pressure, heart rate, fluid balance after 72 hours, and other variables, patients treated with continuous furosemide infusion averaged an 11% greater increase in serum creatinine, Dr. Sharma reported. After similar adjustments, the secondary endpoint rate of worsening renal function was more than four times more likely to occur in the patients on continuous infusion compared with those who received intermittent bolus treatment, she said.
A second aspect of the ROPA-DOP trial randomized the same patients to received either low dose (3 mcg/kg per min) dopamine or placebo during hospitalization. The results showed that low-dose dopamine had no significant impact on either change in creatinine levels or on the incidence of worsening renal function compared with placebo, though dopamine treatment did link with a nonsignificant trend toward somewhat greater diuresis. These results were consistent with prior findings in the Renal Optimization Strategies Evaluation (ROSE) trial (JAMA. 2013 Nov 18;310[23]:2533-43), which used a mixed population of patients with HFpEF or HFrEF but predominantly patients with HFrEF, Dr. Sharma noted.
“It was a neutral finding [for dopamine in ROPA-DOP], and while there was no harm from dopamine there was clearly no benefit,” she said. It is possible that HFpEF patients with right ventricular dysfunction secondary to pulmonary hypertension might benefit from low-dose dopamine, but this needs further study, Dr. Sharma said.
[email protected]
On Twitter @mitchelzoler
AT THE HFSA ANNUAL SCIENTIFIC MEETING
Key clinical point:
Major finding: Serum creatinine rose by an average 5% with intermittent bolus furosemide and by 16% with continuous infusion.
Data source: ROPA-DOP, a single-center randomized trial with 90 patients.
Disclosures: Dr. Sharma had no disclosures.
Walking the halls of power
Hospital medicine may be a young specialty, but it is already playing a significant role in both front-line patient care and, increasingly, in shaping public policy. Case in point: Two hospitalists serving currently in key roles in the federal government, and two former top civil servants, each of whom are examples of the growing influence of the hospitalist perspective.
“The hospitalist viewpoint of the health care system is a unique one, and it lends itself very well to the challenges of our current delivery system reform. We’re reforming the health care system to deliver care more cost effectively,” said Ron Greeno, MD, FCCP, MHM, SHM president and chair of the SHM Public Policy committee. “Hospitalists are trained to do that – they go to work every day to do that.”
Leading the FDA
“He’s the perfect person for that job and is looking to shake things up,” Dr. Greeno said. “There are a lot of things that can improve in terms of how drugs get to market, including lower cost generic drugs.” That’s an issue Dr. Gottlieb has been championing for years, and his understanding of the issue also makes him well prepared to take this position now, Dr. Greeno said.
“Dr. Gottlieb’s nomination comes at a momentous time for the agency, which Mr. Trump has promised to significantly remake,” the New York Times wrote on March 29, prior to his confirmation. “The next commissioner will be charged with putting into practice a far-reaching law, passed in December, aimed at bringing drugs to market more quickly.”
In addition to his work at the AEI, Dr. Gottlieb served on SHM’s Public Policy committee. He was a clinical assistant professor at New York University School of Medicine and advised the U.S. Department of Health and Human Services as a member of the Federal Health IT Policy committee.
Steering national quality programs
Kate Goodrich’s preparation for her government role included experience with several sides of the health care system: Dr. Goodrich, MD, MHS, was the director of the Division of Hospital Medicine at George Washington University Hospital, one of the first hospitalist programs in the Washington area. She worked at an inpatient rehab facility and has practiced in ambulatory care.
Now, as chief medical officer of CMS and director of the Center for Clinical Standards and Quality (CCSQ), she’s helping drive those policy decisions, overseeing multiple quality measurement and value-based purchasing programs and health and safety standards for hospitals.
Dr. Goodrich still makes rounds at George Washington Hospital on weekends. “It allows me to have a sort of in-your-bones understanding of the challenges of frontline providers,” she said. “I’m able to understand the clinician point of view in our policy decisions.” She’s also able to see first-hand the effects of those policy decisions on clinicians, patients, and health care systems.
As physician leaders within their organizations, hospitalists fit naturally into other leadership positions, she said. “Hospitalists often take leadership roles around quality of care and efficiency and flow and those sorts of thing,” Dr. Goodrich said. “I think it is a very natural progression for hospitalists to get interested in health care and medicine from that viewpoint, which then might allow them to make a leap into another type of field.”
An innovator at CMS
Until very recently, pediatric hospitalist Patrick Conway, MD, FAAP, MHM, served as deputy administrator for Innovation and Quality at the Centers for Medicare & Medicaid Services and director of the Center for Medicare and Medicaid Innovation. On Oct. 1, he took on a new challenge, becoming president and CEO of Blue Cross and Blue Shield of North Carolina (Blue Cross NC).
Dr. Conway was selected as a Master of Hospital Medicine by SHM, and received the HHS Secretary’s Award for Distinguished Service, the Secretary’s highest distinction for excellence. The Patient Safety Movement Foundation gave him their Humanitarian Award, and in February 2017, he received the AMA’s Dr. Nathan Davis Award for Outstanding Government Service. He also was elected to the Health and Medicine Division of the National Academies of Sciences, Engineering, and Medicine in 2014.
Prior to joining CMS, Dr. Conway oversaw clinical operations and research at Cincinnati Children’s Hospital Medical Center as director of hospital medicine, with a focus on improving patient outcomes across the health system.
Improving the country’s health
Obesity, tobacco-related disease, mental illness, and addiction are some of the issues Vivek H. Murthy, MD, MBA, targeted while serving as the 19th U.S. Surgeon General. He was appointed to the position by President Obama in 2014, and was relieved of his duties by President Trump in April 2017.
Dr. Murthy has said that addiction should be seen as a chronic illness, not a character flaw, and last year sent a letter to 2.3 million health care providers nationwide, encouraging them to join a national effort to reform prescribing practices.
According to Dr. Greeno, each of these hospitalists illuminates new paths for others in the field. “I think for young people who are trying to identify what career path they want to pursue, this is something that can’t be anything but good for our specialty – and good for the health system,” he said. “Hospitalists have the perfect clinical background and mindset to help our health care system get to where it needs to go. It’s a huge challenge. It’s going to be a ton of work, and the stakes are very, very high.”
Reference
1. Thomas K. F.D.A. Nominee, Paid Millions by Industry, Says He’ll Recuse Himself if Needed. New York Times. March 29, 2017. https://www.nytimes.com/2017/03/29/health/fda-nominee-scott-gottlieb-recuse-conflicts.html?_r=0. Accessed March 31, 2017.
Hospital medicine may be a young specialty, but it is already playing a significant role in both front-line patient care and, increasingly, in shaping public policy. Case in point: Two hospitalists serving currently in key roles in the federal government, and two former top civil servants, each of whom are examples of the growing influence of the hospitalist perspective.
“The hospitalist viewpoint of the health care system is a unique one, and it lends itself very well to the challenges of our current delivery system reform. We’re reforming the health care system to deliver care more cost effectively,” said Ron Greeno, MD, FCCP, MHM, SHM president and chair of the SHM Public Policy committee. “Hospitalists are trained to do that – they go to work every day to do that.”
Leading the FDA
“He’s the perfect person for that job and is looking to shake things up,” Dr. Greeno said. “There are a lot of things that can improve in terms of how drugs get to market, including lower cost generic drugs.” That’s an issue Dr. Gottlieb has been championing for years, and his understanding of the issue also makes him well prepared to take this position now, Dr. Greeno said.
“Dr. Gottlieb’s nomination comes at a momentous time for the agency, which Mr. Trump has promised to significantly remake,” the New York Times wrote on March 29, prior to his confirmation. “The next commissioner will be charged with putting into practice a far-reaching law, passed in December, aimed at bringing drugs to market more quickly.”
In addition to his work at the AEI, Dr. Gottlieb served on SHM’s Public Policy committee. He was a clinical assistant professor at New York University School of Medicine and advised the U.S. Department of Health and Human Services as a member of the Federal Health IT Policy committee.
Steering national quality programs
Kate Goodrich’s preparation for her government role included experience with several sides of the health care system: Dr. Goodrich, MD, MHS, was the director of the Division of Hospital Medicine at George Washington University Hospital, one of the first hospitalist programs in the Washington area. She worked at an inpatient rehab facility and has practiced in ambulatory care.
Now, as chief medical officer of CMS and director of the Center for Clinical Standards and Quality (CCSQ), she’s helping drive those policy decisions, overseeing multiple quality measurement and value-based purchasing programs and health and safety standards for hospitals.
Dr. Goodrich still makes rounds at George Washington Hospital on weekends. “It allows me to have a sort of in-your-bones understanding of the challenges of frontline providers,” she said. “I’m able to understand the clinician point of view in our policy decisions.” She’s also able to see first-hand the effects of those policy decisions on clinicians, patients, and health care systems.
As physician leaders within their organizations, hospitalists fit naturally into other leadership positions, she said. “Hospitalists often take leadership roles around quality of care and efficiency and flow and those sorts of thing,” Dr. Goodrich said. “I think it is a very natural progression for hospitalists to get interested in health care and medicine from that viewpoint, which then might allow them to make a leap into another type of field.”
An innovator at CMS
Until very recently, pediatric hospitalist Patrick Conway, MD, FAAP, MHM, served as deputy administrator for Innovation and Quality at the Centers for Medicare & Medicaid Services and director of the Center for Medicare and Medicaid Innovation. On Oct. 1, he took on a new challenge, becoming president and CEO of Blue Cross and Blue Shield of North Carolina (Blue Cross NC).
Dr. Conway was selected as a Master of Hospital Medicine by SHM, and received the HHS Secretary’s Award for Distinguished Service, the Secretary’s highest distinction for excellence. The Patient Safety Movement Foundation gave him their Humanitarian Award, and in February 2017, he received the AMA’s Dr. Nathan Davis Award for Outstanding Government Service. He also was elected to the Health and Medicine Division of the National Academies of Sciences, Engineering, and Medicine in 2014.
Prior to joining CMS, Dr. Conway oversaw clinical operations and research at Cincinnati Children’s Hospital Medical Center as director of hospital medicine, with a focus on improving patient outcomes across the health system.
Improving the country’s health
Obesity, tobacco-related disease, mental illness, and addiction are some of the issues Vivek H. Murthy, MD, MBA, targeted while serving as the 19th U.S. Surgeon General. He was appointed to the position by President Obama in 2014, and was relieved of his duties by President Trump in April 2017.
Dr. Murthy has said that addiction should be seen as a chronic illness, not a character flaw, and last year sent a letter to 2.3 million health care providers nationwide, encouraging them to join a national effort to reform prescribing practices.
According to Dr. Greeno, each of these hospitalists illuminates new paths for others in the field. “I think for young people who are trying to identify what career path they want to pursue, this is something that can’t be anything but good for our specialty – and good for the health system,” he said. “Hospitalists have the perfect clinical background and mindset to help our health care system get to where it needs to go. It’s a huge challenge. It’s going to be a ton of work, and the stakes are very, very high.”
Reference
1. Thomas K. F.D.A. Nominee, Paid Millions by Industry, Says He’ll Recuse Himself if Needed. New York Times. March 29, 2017. https://www.nytimes.com/2017/03/29/health/fda-nominee-scott-gottlieb-recuse-conflicts.html?_r=0. Accessed March 31, 2017.
Hospital medicine may be a young specialty, but it is already playing a significant role in both front-line patient care and, increasingly, in shaping public policy. Case in point: Two hospitalists serving currently in key roles in the federal government, and two former top civil servants, each of whom are examples of the growing influence of the hospitalist perspective.
“The hospitalist viewpoint of the health care system is a unique one, and it lends itself very well to the challenges of our current delivery system reform. We’re reforming the health care system to deliver care more cost effectively,” said Ron Greeno, MD, FCCP, MHM, SHM president and chair of the SHM Public Policy committee. “Hospitalists are trained to do that – they go to work every day to do that.”
Leading the FDA
“He’s the perfect person for that job and is looking to shake things up,” Dr. Greeno said. “There are a lot of things that can improve in terms of how drugs get to market, including lower cost generic drugs.” That’s an issue Dr. Gottlieb has been championing for years, and his understanding of the issue also makes him well prepared to take this position now, Dr. Greeno said.
“Dr. Gottlieb’s nomination comes at a momentous time for the agency, which Mr. Trump has promised to significantly remake,” the New York Times wrote on March 29, prior to his confirmation. “The next commissioner will be charged with putting into practice a far-reaching law, passed in December, aimed at bringing drugs to market more quickly.”
In addition to his work at the AEI, Dr. Gottlieb served on SHM’s Public Policy committee. He was a clinical assistant professor at New York University School of Medicine and advised the U.S. Department of Health and Human Services as a member of the Federal Health IT Policy committee.
Steering national quality programs
Kate Goodrich’s preparation for her government role included experience with several sides of the health care system: Dr. Goodrich, MD, MHS, was the director of the Division of Hospital Medicine at George Washington University Hospital, one of the first hospitalist programs in the Washington area. She worked at an inpatient rehab facility and has practiced in ambulatory care.
Now, as chief medical officer of CMS and director of the Center for Clinical Standards and Quality (CCSQ), she’s helping drive those policy decisions, overseeing multiple quality measurement and value-based purchasing programs and health and safety standards for hospitals.
Dr. Goodrich still makes rounds at George Washington Hospital on weekends. “It allows me to have a sort of in-your-bones understanding of the challenges of frontline providers,” she said. “I’m able to understand the clinician point of view in our policy decisions.” She’s also able to see first-hand the effects of those policy decisions on clinicians, patients, and health care systems.
As physician leaders within their organizations, hospitalists fit naturally into other leadership positions, she said. “Hospitalists often take leadership roles around quality of care and efficiency and flow and those sorts of thing,” Dr. Goodrich said. “I think it is a very natural progression for hospitalists to get interested in health care and medicine from that viewpoint, which then might allow them to make a leap into another type of field.”
An innovator at CMS
Until very recently, pediatric hospitalist Patrick Conway, MD, FAAP, MHM, served as deputy administrator for Innovation and Quality at the Centers for Medicare & Medicaid Services and director of the Center for Medicare and Medicaid Innovation. On Oct. 1, he took on a new challenge, becoming president and CEO of Blue Cross and Blue Shield of North Carolina (Blue Cross NC).
Dr. Conway was selected as a Master of Hospital Medicine by SHM, and received the HHS Secretary’s Award for Distinguished Service, the Secretary’s highest distinction for excellence. The Patient Safety Movement Foundation gave him their Humanitarian Award, and in February 2017, he received the AMA’s Dr. Nathan Davis Award for Outstanding Government Service. He also was elected to the Health and Medicine Division of the National Academies of Sciences, Engineering, and Medicine in 2014.
Prior to joining CMS, Dr. Conway oversaw clinical operations and research at Cincinnati Children’s Hospital Medical Center as director of hospital medicine, with a focus on improving patient outcomes across the health system.
Improving the country’s health
Obesity, tobacco-related disease, mental illness, and addiction are some of the issues Vivek H. Murthy, MD, MBA, targeted while serving as the 19th U.S. Surgeon General. He was appointed to the position by President Obama in 2014, and was relieved of his duties by President Trump in April 2017.
Dr. Murthy has said that addiction should be seen as a chronic illness, not a character flaw, and last year sent a letter to 2.3 million health care providers nationwide, encouraging them to join a national effort to reform prescribing practices.
According to Dr. Greeno, each of these hospitalists illuminates new paths for others in the field. “I think for young people who are trying to identify what career path they want to pursue, this is something that can’t be anything but good for our specialty – and good for the health system,” he said. “Hospitalists have the perfect clinical background and mindset to help our health care system get to where it needs to go. It’s a huge challenge. It’s going to be a ton of work, and the stakes are very, very high.”
Reference
1. Thomas K. F.D.A. Nominee, Paid Millions by Industry, Says He’ll Recuse Himself if Needed. New York Times. March 29, 2017. https://www.nytimes.com/2017/03/29/health/fda-nominee-scott-gottlieb-recuse-conflicts.html?_r=0. Accessed March 31, 2017.
Sneak Peek: Journal of Hospital Medicine – Oct. 2017
BACKGROUND: Hospitalized patients frequently report poor sleep, partly due to the inpatient environment. In-hospital sound and light levels are not well described on non–intensive care unit (non-ICU) wards. Although non-ICU wards may have lower average and peak noise levels, sound level changes (SLCs), which are important in disrupting sleep, may still be a substantial problem.
OBJECTIVE: To compare ambient sound and light levels, including SLCs, in ICU and non-ICU environments.
DESIGN: Observational study.
SETTING: Tertiary-care hospital.
MEASUREMENTS: Sound measurements of 0.5 Hz were analyzed to provide average hourly sound levels, sound peaks, and SLCs greater than or equal to 17.5 decibels (dB). For light data, measurements taken at 2-minute intervals provided average and maximum light levels.
RESULTS: The ICU rooms were louder than non-ICU wards; hourly averages ranged from 56.1 plus or minus 1.3 dB to 60.3 plus or minus 1.7 dB in the ICU, 47.3 plus or minus 3.7 dB to 55.1 plus or minus 3.7 dB on the telemetry floor, and 44.6 plus or minus 2.1 dB to 53.7 plus or minus 3.6 dB on the general ward. However, SLCs greater than or equal to 17.5 dB were not statistically different (ICU, 203.9 plus or minus 28.8 times; non-ICU, 270.9 plus or minus 39.5; P = 0.11). In both ICU and non-ICU wards, average daytime light levels were less than 250 lux, and peak light levels occurred in the afternoon and early evening.
CONCLUSIONS: While quieter, non-ICU wards have as many SLCs as ICUs do, which has implications for quality improvement measurements. Efforts to further reduce average noise levels might be counterproductive. Light levels in the hospital (ICU and non-ICU) may not be optimal for maintenance of a normal circadian rhythm for most people.
Read the entire article in the Journal of Hospital Medicine.
Also in JHM this month
Associations of physician empathy with patient anxiety and ratings of communication in hospital admission encounters
AUTHORS: Rachel Weiss, MD, Eric Vittinghoff, PhD, MPH, Margaret C. Fang, MD, MPH, Jenica E. W. Cimino, Kristen Adams Chasteen, MD, Robert M. Arnold, MD, Andrew D. Auerbach, MD, Wendy G. Anderson, MD, MS
A concise tool for measuring care coordination from the provider’s perspective in the hospital setting
AUTHORS: Christine M. Weston, PhD, and Sehyo Yune, MD, Eric B. Bass, MD, MPH, Scott A. Berkowitz, MD, MBA, Daniel J. Brotman, MD, Amy Deutschendorf, MS, RN, ACNS-BC, Eric E. Howell, MD, Melissa B. Richardson, MBA Carol Sylvester, RN, MS, Albert W. Wu, MD, MPH
Post–intensive care unit psychiatric comorbidity and quality of life
AUTHORS: Sophia Wang, MD, and Chris Mosher, MD, Anthony J. Perkins, MS, Sujuan Gao, PhD, Sue Lasiter, RN, PhD, Sikandar Khan, MD, Malaz Boustani, MD, MPH, Babar Khan, MD, MS
An opportunity to improve Medicare’s planned readmissions measure
AUTHORS: Chad Ellimoottil, MD, MS, Roger K. Khouri Jr., MD, Apoorv Dhir, BA, Hechuan Hou, MS, David C. Miller, MD, MPH, James M. Dupree, MD, MPH
Against medical advice discharges
AUTHORS: David Alfandre, MD, MSPH, Jay Brenner, MD, Eberechukwu Onukwugha, MS, PhD
BACKGROUND: Hospitalized patients frequently report poor sleep, partly due to the inpatient environment. In-hospital sound and light levels are not well described on non–intensive care unit (non-ICU) wards. Although non-ICU wards may have lower average and peak noise levels, sound level changes (SLCs), which are important in disrupting sleep, may still be a substantial problem.
OBJECTIVE: To compare ambient sound and light levels, including SLCs, in ICU and non-ICU environments.
DESIGN: Observational study.
SETTING: Tertiary-care hospital.
MEASUREMENTS: Sound measurements of 0.5 Hz were analyzed to provide average hourly sound levels, sound peaks, and SLCs greater than or equal to 17.5 decibels (dB). For light data, measurements taken at 2-minute intervals provided average and maximum light levels.
RESULTS: The ICU rooms were louder than non-ICU wards; hourly averages ranged from 56.1 plus or minus 1.3 dB to 60.3 plus or minus 1.7 dB in the ICU, 47.3 plus or minus 3.7 dB to 55.1 plus or minus 3.7 dB on the telemetry floor, and 44.6 plus or minus 2.1 dB to 53.7 plus or minus 3.6 dB on the general ward. However, SLCs greater than or equal to 17.5 dB were not statistically different (ICU, 203.9 plus or minus 28.8 times; non-ICU, 270.9 plus or minus 39.5; P = 0.11). In both ICU and non-ICU wards, average daytime light levels were less than 250 lux, and peak light levels occurred in the afternoon and early evening.
CONCLUSIONS: While quieter, non-ICU wards have as many SLCs as ICUs do, which has implications for quality improvement measurements. Efforts to further reduce average noise levels might be counterproductive. Light levels in the hospital (ICU and non-ICU) may not be optimal for maintenance of a normal circadian rhythm for most people.
Read the entire article in the Journal of Hospital Medicine.
Also in JHM this month
Associations of physician empathy with patient anxiety and ratings of communication in hospital admission encounters
AUTHORS: Rachel Weiss, MD, Eric Vittinghoff, PhD, MPH, Margaret C. Fang, MD, MPH, Jenica E. W. Cimino, Kristen Adams Chasteen, MD, Robert M. Arnold, MD, Andrew D. Auerbach, MD, Wendy G. Anderson, MD, MS
A concise tool for measuring care coordination from the provider’s perspective in the hospital setting
AUTHORS: Christine M. Weston, PhD, and Sehyo Yune, MD, Eric B. Bass, MD, MPH, Scott A. Berkowitz, MD, MBA, Daniel J. Brotman, MD, Amy Deutschendorf, MS, RN, ACNS-BC, Eric E. Howell, MD, Melissa B. Richardson, MBA Carol Sylvester, RN, MS, Albert W. Wu, MD, MPH
Post–intensive care unit psychiatric comorbidity and quality of life
AUTHORS: Sophia Wang, MD, and Chris Mosher, MD, Anthony J. Perkins, MS, Sujuan Gao, PhD, Sue Lasiter, RN, PhD, Sikandar Khan, MD, Malaz Boustani, MD, MPH, Babar Khan, MD, MS
An opportunity to improve Medicare’s planned readmissions measure
AUTHORS: Chad Ellimoottil, MD, MS, Roger K. Khouri Jr., MD, Apoorv Dhir, BA, Hechuan Hou, MS, David C. Miller, MD, MPH, James M. Dupree, MD, MPH
Against medical advice discharges
AUTHORS: David Alfandre, MD, MSPH, Jay Brenner, MD, Eberechukwu Onukwugha, MS, PhD
BACKGROUND: Hospitalized patients frequently report poor sleep, partly due to the inpatient environment. In-hospital sound and light levels are not well described on non–intensive care unit (non-ICU) wards. Although non-ICU wards may have lower average and peak noise levels, sound level changes (SLCs), which are important in disrupting sleep, may still be a substantial problem.
OBJECTIVE: To compare ambient sound and light levels, including SLCs, in ICU and non-ICU environments.
DESIGN: Observational study.
SETTING: Tertiary-care hospital.
MEASUREMENTS: Sound measurements of 0.5 Hz were analyzed to provide average hourly sound levels, sound peaks, and SLCs greater than or equal to 17.5 decibels (dB). For light data, measurements taken at 2-minute intervals provided average and maximum light levels.
RESULTS: The ICU rooms were louder than non-ICU wards; hourly averages ranged from 56.1 plus or minus 1.3 dB to 60.3 plus or minus 1.7 dB in the ICU, 47.3 plus or minus 3.7 dB to 55.1 plus or minus 3.7 dB on the telemetry floor, and 44.6 plus or minus 2.1 dB to 53.7 plus or minus 3.6 dB on the general ward. However, SLCs greater than or equal to 17.5 dB were not statistically different (ICU, 203.9 plus or minus 28.8 times; non-ICU, 270.9 plus or minus 39.5; P = 0.11). In both ICU and non-ICU wards, average daytime light levels were less than 250 lux, and peak light levels occurred in the afternoon and early evening.
CONCLUSIONS: While quieter, non-ICU wards have as many SLCs as ICUs do, which has implications for quality improvement measurements. Efforts to further reduce average noise levels might be counterproductive. Light levels in the hospital (ICU and non-ICU) may not be optimal for maintenance of a normal circadian rhythm for most people.
Read the entire article in the Journal of Hospital Medicine.
Also in JHM this month
Associations of physician empathy with patient anxiety and ratings of communication in hospital admission encounters
AUTHORS: Rachel Weiss, MD, Eric Vittinghoff, PhD, MPH, Margaret C. Fang, MD, MPH, Jenica E. W. Cimino, Kristen Adams Chasteen, MD, Robert M. Arnold, MD, Andrew D. Auerbach, MD, Wendy G. Anderson, MD, MS
A concise tool for measuring care coordination from the provider’s perspective in the hospital setting
AUTHORS: Christine M. Weston, PhD, and Sehyo Yune, MD, Eric B. Bass, MD, MPH, Scott A. Berkowitz, MD, MBA, Daniel J. Brotman, MD, Amy Deutschendorf, MS, RN, ACNS-BC, Eric E. Howell, MD, Melissa B. Richardson, MBA Carol Sylvester, RN, MS, Albert W. Wu, MD, MPH
Post–intensive care unit psychiatric comorbidity and quality of life
AUTHORS: Sophia Wang, MD, and Chris Mosher, MD, Anthony J. Perkins, MS, Sujuan Gao, PhD, Sue Lasiter, RN, PhD, Sikandar Khan, MD, Malaz Boustani, MD, MPH, Babar Khan, MD, MS
An opportunity to improve Medicare’s planned readmissions measure
AUTHORS: Chad Ellimoottil, MD, MS, Roger K. Khouri Jr., MD, Apoorv Dhir, BA, Hechuan Hou, MS, David C. Miller, MD, MPH, James M. Dupree, MD, MPH
Against medical advice discharges
AUTHORS: David Alfandre, MD, MSPH, Jay Brenner, MD, Eberechukwu Onukwugha, MS, PhD