User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


VIDEO: What’s new in AAP’s pediatric hypertension guidelines
SAN FRANCISCO – The American Academy of Pediatrics recently released new hypertension guidelines for children and adolescents.
Some of the advice is similar to the group’s last effort in 2004, but there are a few key changes that clinicians need to know, according to lead author Joseph Flynn, MD, professor of pediatrics and chief of nephrology at Seattle Children’s Hospital. He explained what they are, and the reasons behind them, in an interview at the joint hypertension scientific sessions sponsored by the American Heart Association and the American Society of Hypertension (Pediatrics. 2017 Aug 21. doi: 10.1542/peds.2017-1904).
The prevalence of pediatric hypertension, he said, now rivals asthma.
SAN FRANCISCO – The American Academy of Pediatrics recently released new hypertension guidelines for children and adolescents.
Some of the advice is similar to the group’s last effort in 2004, but there are a few key changes that clinicians need to know, according to lead author Joseph Flynn, MD, professor of pediatrics and chief of nephrology at Seattle Children’s Hospital. He explained what they are, and the reasons behind them, in an interview at the joint hypertension scientific sessions sponsored by the American Heart Association and the American Society of Hypertension (Pediatrics. 2017 Aug 21. doi: 10.1542/peds.2017-1904).
The prevalence of pediatric hypertension, he said, now rivals asthma.
SAN FRANCISCO – The American Academy of Pediatrics recently released new hypertension guidelines for children and adolescents.
Some of the advice is similar to the group’s last effort in 2004, but there are a few key changes that clinicians need to know, according to lead author Joseph Flynn, MD, professor of pediatrics and chief of nephrology at Seattle Children’s Hospital. He explained what they are, and the reasons behind them, in an interview at the joint hypertension scientific sessions sponsored by the American Heart Association and the American Society of Hypertension (Pediatrics. 2017 Aug 21. doi: 10.1542/peds.2017-1904).
The prevalence of pediatric hypertension, he said, now rivals asthma.
EXPERT ANALYSIS FROM THE AHA/ASH JOINT SCIENTIFIC SESSIONS
Increase in sepsis incidence stable from 2009 to 2014
The trend for sepsis incidence from 2009 to 2014, “calculated relative to the observed 2014 rates,” was a stable increase of 0.6% per year using the more accurate of two forms of analysis, investigators reported.
The incidence of sepsis was an adjusted 5.9% among hospitalized adults in 2014, with in-hospital mortality of 15%, according to a retrospective cohort study published online Sept. 13 in JAMA.
“Most studies [of sepsis incidence] have used claims data, but increasing clinical awareness, changes in diagnosis and coding practices, and variable definitions have led to uncertainty about the accuracy of reported trends,” wrote Chanu Rhee, MD, of Harvard Medical School, Boston, and his associates (JAMA. 2017 Sep 13. doi: 10.1001/jama.2017.13836).
They used two methods – one involving claims-based estimates using ICD-9-CM codes and the other based on clinical data from electronic health records (EHRs) – to analyze data for more than 2.9 million adults admitted to 409 U.S. academic, community, and federal acute-care hospitals in 2014. The claims-based “explicit-codes” approach used discharge diagnoses of severe sepsis (995.92) or septic shock (785.52), while the EHR-based, clinical-criteria method included blood cultures, antibiotics, and concurrent organ dysfunction with or without the criterion of a lactate level of 2.0 mmol/L or greater, the investigators said.
The explicit-codes approach produced an increase of 10.3% per year in sepsis incidence from 2009 to 2014, compared with 0.6% per year for the clinical-criteria approach, while in-hospital mortality declined by 7% a year using explicit codes and 3.3% using clinical criteria, Dr. Rhee and his associates reported.
“EHR-based criteria were more sensitive than explicit sepsis codes on medical record review, with comparable [positive predictive value]; EHR-based criteria had similar sensitivity to implicit or explicit codes combined but higher [positive predictive value],” they said.
The estimates provided by Dr. Rhee and his associates provide “a clearer understanding of trends in the incidence and mortality of sepsis in the United States but also a better understanding of the challenges in improving ICD coding to accurately document the global burden of sepsis,” Kristina E. Rudd, MD, of the University of Washington, Seattle, and her associates said in an editorial (JAMA 2017 Sep 13. doi: 10.1001/jama.2017.13697).
The study was funded by the Centers for Disease Control and Prevention, Agency for Healthcare Research and Quality, National Institutes of Health, Department of Veterans Affairs, National Institutes of Health Clinical Center, and National Institute of Allergy and Infectious Diseases. Three of Dr. Rhee’s associates reported receiving personal fees from private companies or serving on advisory boards or as consultants. No other authors reported disclosures. Dr. Rudd and her associates had no conflicts of interest to report.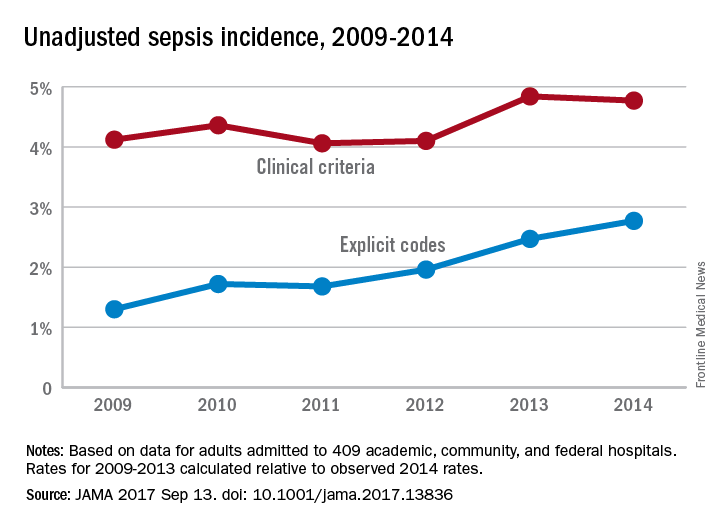
The trend for sepsis incidence from 2009 to 2014, “calculated relative to the observed 2014 rates,” was a stable increase of 0.6% per year using the more accurate of two forms of analysis, investigators reported.
The incidence of sepsis was an adjusted 5.9% among hospitalized adults in 2014, with in-hospital mortality of 15%, according to a retrospective cohort study published online Sept. 13 in JAMA.
“Most studies [of sepsis incidence] have used claims data, but increasing clinical awareness, changes in diagnosis and coding practices, and variable definitions have led to uncertainty about the accuracy of reported trends,” wrote Chanu Rhee, MD, of Harvard Medical School, Boston, and his associates (JAMA. 2017 Sep 13. doi: 10.1001/jama.2017.13836).
They used two methods – one involving claims-based estimates using ICD-9-CM codes and the other based on clinical data from electronic health records (EHRs) – to analyze data for more than 2.9 million adults admitted to 409 U.S. academic, community, and federal acute-care hospitals in 2014. The claims-based “explicit-codes” approach used discharge diagnoses of severe sepsis (995.92) or septic shock (785.52), while the EHR-based, clinical-criteria method included blood cultures, antibiotics, and concurrent organ dysfunction with or without the criterion of a lactate level of 2.0 mmol/L or greater, the investigators said.
The explicit-codes approach produced an increase of 10.3% per year in sepsis incidence from 2009 to 2014, compared with 0.6% per year for the clinical-criteria approach, while in-hospital mortality declined by 7% a year using explicit codes and 3.3% using clinical criteria, Dr. Rhee and his associates reported.
“EHR-based criteria were more sensitive than explicit sepsis codes on medical record review, with comparable [positive predictive value]; EHR-based criteria had similar sensitivity to implicit or explicit codes combined but higher [positive predictive value],” they said.
The estimates provided by Dr. Rhee and his associates provide “a clearer understanding of trends in the incidence and mortality of sepsis in the United States but also a better understanding of the challenges in improving ICD coding to accurately document the global burden of sepsis,” Kristina E. Rudd, MD, of the University of Washington, Seattle, and her associates said in an editorial (JAMA 2017 Sep 13. doi: 10.1001/jama.2017.13697).
The study was funded by the Centers for Disease Control and Prevention, Agency for Healthcare Research and Quality, National Institutes of Health, Department of Veterans Affairs, National Institutes of Health Clinical Center, and National Institute of Allergy and Infectious Diseases. Three of Dr. Rhee’s associates reported receiving personal fees from private companies or serving on advisory boards or as consultants. No other authors reported disclosures. Dr. Rudd and her associates had no conflicts of interest to report.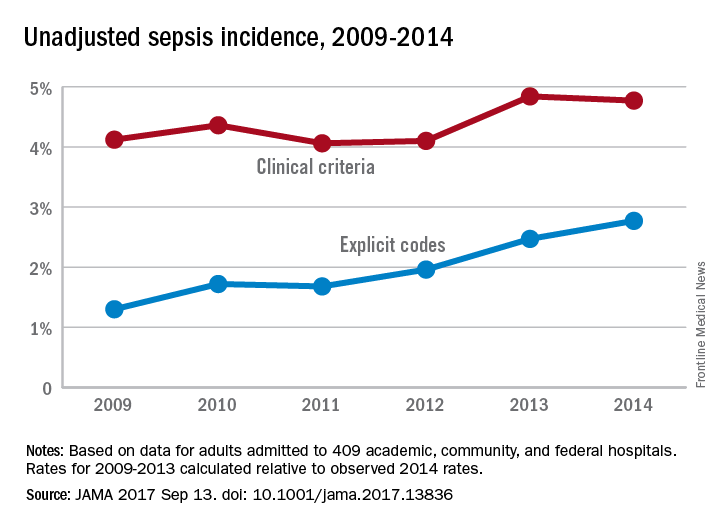
The trend for sepsis incidence from 2009 to 2014, “calculated relative to the observed 2014 rates,” was a stable increase of 0.6% per year using the more accurate of two forms of analysis, investigators reported.
The incidence of sepsis was an adjusted 5.9% among hospitalized adults in 2014, with in-hospital mortality of 15%, according to a retrospective cohort study published online Sept. 13 in JAMA.
“Most studies [of sepsis incidence] have used claims data, but increasing clinical awareness, changes in diagnosis and coding practices, and variable definitions have led to uncertainty about the accuracy of reported trends,” wrote Chanu Rhee, MD, of Harvard Medical School, Boston, and his associates (JAMA. 2017 Sep 13. doi: 10.1001/jama.2017.13836).
They used two methods – one involving claims-based estimates using ICD-9-CM codes and the other based on clinical data from electronic health records (EHRs) – to analyze data for more than 2.9 million adults admitted to 409 U.S. academic, community, and federal acute-care hospitals in 2014. The claims-based “explicit-codes” approach used discharge diagnoses of severe sepsis (995.92) or septic shock (785.52), while the EHR-based, clinical-criteria method included blood cultures, antibiotics, and concurrent organ dysfunction with or without the criterion of a lactate level of 2.0 mmol/L or greater, the investigators said.
The explicit-codes approach produced an increase of 10.3% per year in sepsis incidence from 2009 to 2014, compared with 0.6% per year for the clinical-criteria approach, while in-hospital mortality declined by 7% a year using explicit codes and 3.3% using clinical criteria, Dr. Rhee and his associates reported.
“EHR-based criteria were more sensitive than explicit sepsis codes on medical record review, with comparable [positive predictive value]; EHR-based criteria had similar sensitivity to implicit or explicit codes combined but higher [positive predictive value],” they said.
The estimates provided by Dr. Rhee and his associates provide “a clearer understanding of trends in the incidence and mortality of sepsis in the United States but also a better understanding of the challenges in improving ICD coding to accurately document the global burden of sepsis,” Kristina E. Rudd, MD, of the University of Washington, Seattle, and her associates said in an editorial (JAMA 2017 Sep 13. doi: 10.1001/jama.2017.13697).
The study was funded by the Centers for Disease Control and Prevention, Agency for Healthcare Research and Quality, National Institutes of Health, Department of Veterans Affairs, National Institutes of Health Clinical Center, and National Institute of Allergy and Infectious Diseases. Three of Dr. Rhee’s associates reported receiving personal fees from private companies or serving on advisory boards or as consultants. No other authors reported disclosures. Dr. Rudd and her associates had no conflicts of interest to report.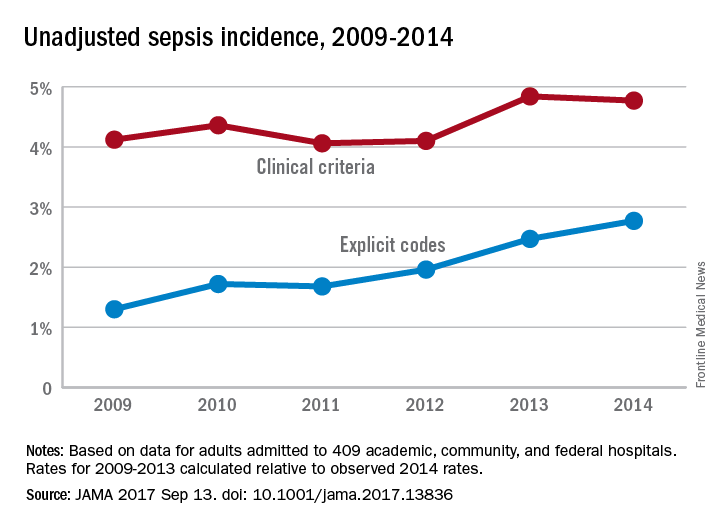
FROM JAMA
Identifying clinical pathways for injection drug–related infectious sequelae
Editor’s Note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform health care and revolutionize patient care. The program has been expanded for the 2017-18 year, offering two options for students to receive funding and engage in scholarly work during their first, second and third years of medical school. As a part of the longitudinal (18-month) program, recipients are required to write about their experience on a monthly basis.
It is not surprising that my medical school – home to a group of passionate thought leaders in health service and policy research, including the Dartmouth Atlas and Accountable Care Organization – required all first-year medical students to take a course called “health care delivery science.”
The course offered me the first glimpse into quality improvement. However, because of a lack of clinical context, much of the course remained theoretical until my clinical years. During the hospital medicine rotation, I took care of a 40-year old patient who was newly diagnosed with metastatic pancreatic cancer. It was challenging to deliver devastatingly bad news. The patient and family, however, were most confused and frustrated by the roles of different specialists and care providers, the purpose and scheduling of procedures, and diet arrangement. I wondered how I could make their experience better.
After several meetings with my mentor, Professor Jonathan Huntington, a hospitalist, MD-PhD researcher, and director of Care Coordination Center at Dartmouth-Hitchcock Medical Center (DHMC), we identified a research area that has rising interest, importance, and relevance to the rural New Hampshire population. It is about identifying a clinical pathway for injection drug–related infectious sequelae.
Because of the unique bio-socio-psycho needs of injection drug users, hospitalizations due to injection-related infection sequelae often contribute to increased length of stay, readmission rates, and expenses out of state and federal health care funding. Prolonged stays also result in the waste of tertiary care resources for nontertiary needs, underutilization of regional care resources such as community and critical access hospitals, and increased care burden, as most patients travel long distances to obtain care.
We will pilot and implement a clinical pathway in the medicine units and measure length of stay, readmission rate, patient satisfaction rating, infectious disease provider follow-up rate, and hospitalization cost. I appreciate the grant support from SHM, and am looking forward to working with Dr. Huntington and other providers at DHMC, as well as developing myself professionally.
Yun Li is an MD/MBA student attending Geisel School of Medicine and Tuck School of Business at Dartmouth, Hanover, N.H. She obtained her Bachelor of Arts degree from Hanover College double-majoring in Economics and Biological Chemistry. Ms. Li participated in research in injury epidemiology and genetics, and has conducted studies on traditional Tibetan medicine, rural health, health NGOs, and digital health. Her career interest is practicing hospital medicine and geriatrics as a clinician/administrator, either in the United States or China. Ms. Li is a student member of the Society of Hospital Medicine.
Editor’s Note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform health care and revolutionize patient care. The program has been expanded for the 2017-18 year, offering two options for students to receive funding and engage in scholarly work during their first, second and third years of medical school. As a part of the longitudinal (18-month) program, recipients are required to write about their experience on a monthly basis.
It is not surprising that my medical school – home to a group of passionate thought leaders in health service and policy research, including the Dartmouth Atlas and Accountable Care Organization – required all first-year medical students to take a course called “health care delivery science.”
The course offered me the first glimpse into quality improvement. However, because of a lack of clinical context, much of the course remained theoretical until my clinical years. During the hospital medicine rotation, I took care of a 40-year old patient who was newly diagnosed with metastatic pancreatic cancer. It was challenging to deliver devastatingly bad news. The patient and family, however, were most confused and frustrated by the roles of different specialists and care providers, the purpose and scheduling of procedures, and diet arrangement. I wondered how I could make their experience better.
After several meetings with my mentor, Professor Jonathan Huntington, a hospitalist, MD-PhD researcher, and director of Care Coordination Center at Dartmouth-Hitchcock Medical Center (DHMC), we identified a research area that has rising interest, importance, and relevance to the rural New Hampshire population. It is about identifying a clinical pathway for injection drug–related infectious sequelae.
Because of the unique bio-socio-psycho needs of injection drug users, hospitalizations due to injection-related infection sequelae often contribute to increased length of stay, readmission rates, and expenses out of state and federal health care funding. Prolonged stays also result in the waste of tertiary care resources for nontertiary needs, underutilization of regional care resources such as community and critical access hospitals, and increased care burden, as most patients travel long distances to obtain care.
We will pilot and implement a clinical pathway in the medicine units and measure length of stay, readmission rate, patient satisfaction rating, infectious disease provider follow-up rate, and hospitalization cost. I appreciate the grant support from SHM, and am looking forward to working with Dr. Huntington and other providers at DHMC, as well as developing myself professionally.
Yun Li is an MD/MBA student attending Geisel School of Medicine and Tuck School of Business at Dartmouth, Hanover, N.H. She obtained her Bachelor of Arts degree from Hanover College double-majoring in Economics and Biological Chemistry. Ms. Li participated in research in injury epidemiology and genetics, and has conducted studies on traditional Tibetan medicine, rural health, health NGOs, and digital health. Her career interest is practicing hospital medicine and geriatrics as a clinician/administrator, either in the United States or China. Ms. Li is a student member of the Society of Hospital Medicine.
Editor’s Note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform health care and revolutionize patient care. The program has been expanded for the 2017-18 year, offering two options for students to receive funding and engage in scholarly work during their first, second and third years of medical school. As a part of the longitudinal (18-month) program, recipients are required to write about their experience on a monthly basis.
It is not surprising that my medical school – home to a group of passionate thought leaders in health service and policy research, including the Dartmouth Atlas and Accountable Care Organization – required all first-year medical students to take a course called “health care delivery science.”
The course offered me the first glimpse into quality improvement. However, because of a lack of clinical context, much of the course remained theoretical until my clinical years. During the hospital medicine rotation, I took care of a 40-year old patient who was newly diagnosed with metastatic pancreatic cancer. It was challenging to deliver devastatingly bad news. The patient and family, however, were most confused and frustrated by the roles of different specialists and care providers, the purpose and scheduling of procedures, and diet arrangement. I wondered how I could make their experience better.
After several meetings with my mentor, Professor Jonathan Huntington, a hospitalist, MD-PhD researcher, and director of Care Coordination Center at Dartmouth-Hitchcock Medical Center (DHMC), we identified a research area that has rising interest, importance, and relevance to the rural New Hampshire population. It is about identifying a clinical pathway for injection drug–related infectious sequelae.
Because of the unique bio-socio-psycho needs of injection drug users, hospitalizations due to injection-related infection sequelae often contribute to increased length of stay, readmission rates, and expenses out of state and federal health care funding. Prolonged stays also result in the waste of tertiary care resources for nontertiary needs, underutilization of regional care resources such as community and critical access hospitals, and increased care burden, as most patients travel long distances to obtain care.
We will pilot and implement a clinical pathway in the medicine units and measure length of stay, readmission rate, patient satisfaction rating, infectious disease provider follow-up rate, and hospitalization cost. I appreciate the grant support from SHM, and am looking forward to working with Dr. Huntington and other providers at DHMC, as well as developing myself professionally.
Yun Li is an MD/MBA student attending Geisel School of Medicine and Tuck School of Business at Dartmouth, Hanover, N.H. She obtained her Bachelor of Arts degree from Hanover College double-majoring in Economics and Biological Chemistry. Ms. Li participated in research in injury epidemiology and genetics, and has conducted studies on traditional Tibetan medicine, rural health, health NGOs, and digital health. Her career interest is practicing hospital medicine and geriatrics as a clinician/administrator, either in the United States or China. Ms. Li is a student member of the Society of Hospital Medicine.
Student Hospitalist Scholars: The importance of shared mental models
Editor’s Note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform healthcare and revolutionize patient care. The program has been expanded for the 2017-18 year, offering two options for students to receive funding and engage in scholarly work during their first, second and third years of medical school. As a part of the program, recipients are required to write about their experience on a biweekly basis.
As I walk the University of Chicago Hospital observing various health care practitioners, I am continually impressed with the businesslike approach and productivity of each individual. The hospital staff is composed of highly intelligent, experienced, and talented physicians, but I have come to understand that in this large system it can be difficult to maintain quality patient care with both increased census and increased handoffs.
The research project I am working on focuses on shared mental models between the MICU and the general floor on what the most important factor of care is while they are on the floor, and to identify how prominent it is for shared mental models to be present between the transferring and receiving teams. After reading various papers, I am beginning to understand the various complexities present in translating information when transferring patients from any department onto the floor.
I continue to discuss these topics with my mentors, Dr. Vineet Arora and Dr. Juan Rojas, in order to appropriately categorize all survey responses and identify whether there is concordance between teams. I am glad to be able to rely on their insight concerning methods of coding the data, as well as what type of medical care each responding individual receives, and remaining on track with my estimated timeline of completion.
Past research supports the idea that increased times, distractions, and workloads in regard to handoffs result in potential errors, decreasing the quality of patient care and potentially resulting in worse patient outcomes. MICU patients are at a particular risk, since ineffective communication could lead to readmission, which could result in worsened health outcomes.
I believe that this current research project is highly significant since it highlights whether effective communication is occurring in the first place, and whether teams are appropriately communicating patient plans for this group of higher-acuity patients. As I continue my research at the university, I hope to further identify whether effective communication is taking place for this at-risk group of floor patients.
Anton Garazha is a medical student at Chicago Medical School at Rosalind Franklin University in North Chicago. He received his bachelor of science degree in biology from Loyola University in Chicago in 2015 and his master of biomedical science degree from Rosalind Franklin University in 2016. Anton is very interested in community outreach and quality improvement, and in his spare time tutors students in science-based subjects.
Editor’s Note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform healthcare and revolutionize patient care. The program has been expanded for the 2017-18 year, offering two options for students to receive funding and engage in scholarly work during their first, second and third years of medical school. As a part of the program, recipients are required to write about their experience on a biweekly basis.
As I walk the University of Chicago Hospital observing various health care practitioners, I am continually impressed with the businesslike approach and productivity of each individual. The hospital staff is composed of highly intelligent, experienced, and talented physicians, but I have come to understand that in this large system it can be difficult to maintain quality patient care with both increased census and increased handoffs.
The research project I am working on focuses on shared mental models between the MICU and the general floor on what the most important factor of care is while they are on the floor, and to identify how prominent it is for shared mental models to be present between the transferring and receiving teams. After reading various papers, I am beginning to understand the various complexities present in translating information when transferring patients from any department onto the floor.
I continue to discuss these topics with my mentors, Dr. Vineet Arora and Dr. Juan Rojas, in order to appropriately categorize all survey responses and identify whether there is concordance between teams. I am glad to be able to rely on their insight concerning methods of coding the data, as well as what type of medical care each responding individual receives, and remaining on track with my estimated timeline of completion.
Past research supports the idea that increased times, distractions, and workloads in regard to handoffs result in potential errors, decreasing the quality of patient care and potentially resulting in worse patient outcomes. MICU patients are at a particular risk, since ineffective communication could lead to readmission, which could result in worsened health outcomes.
I believe that this current research project is highly significant since it highlights whether effective communication is occurring in the first place, and whether teams are appropriately communicating patient plans for this group of higher-acuity patients. As I continue my research at the university, I hope to further identify whether effective communication is taking place for this at-risk group of floor patients.
Anton Garazha is a medical student at Chicago Medical School at Rosalind Franklin University in North Chicago. He received his bachelor of science degree in biology from Loyola University in Chicago in 2015 and his master of biomedical science degree from Rosalind Franklin University in 2016. Anton is very interested in community outreach and quality improvement, and in his spare time tutors students in science-based subjects.
Editor’s Note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform healthcare and revolutionize patient care. The program has been expanded for the 2017-18 year, offering two options for students to receive funding and engage in scholarly work during their first, second and third years of medical school. As a part of the program, recipients are required to write about their experience on a biweekly basis.
As I walk the University of Chicago Hospital observing various health care practitioners, I am continually impressed with the businesslike approach and productivity of each individual. The hospital staff is composed of highly intelligent, experienced, and talented physicians, but I have come to understand that in this large system it can be difficult to maintain quality patient care with both increased census and increased handoffs.
The research project I am working on focuses on shared mental models between the MICU and the general floor on what the most important factor of care is while they are on the floor, and to identify how prominent it is for shared mental models to be present between the transferring and receiving teams. After reading various papers, I am beginning to understand the various complexities present in translating information when transferring patients from any department onto the floor.
I continue to discuss these topics with my mentors, Dr. Vineet Arora and Dr. Juan Rojas, in order to appropriately categorize all survey responses and identify whether there is concordance between teams. I am glad to be able to rely on their insight concerning methods of coding the data, as well as what type of medical care each responding individual receives, and remaining on track with my estimated timeline of completion.
Past research supports the idea that increased times, distractions, and workloads in regard to handoffs result in potential errors, decreasing the quality of patient care and potentially resulting in worse patient outcomes. MICU patients are at a particular risk, since ineffective communication could lead to readmission, which could result in worsened health outcomes.
I believe that this current research project is highly significant since it highlights whether effective communication is occurring in the first place, and whether teams are appropriately communicating patient plans for this group of higher-acuity patients. As I continue my research at the university, I hope to further identify whether effective communication is taking place for this at-risk group of floor patients.
Anton Garazha is a medical student at Chicago Medical School at Rosalind Franklin University in North Chicago. He received his bachelor of science degree in biology from Loyola University in Chicago in 2015 and his master of biomedical science degree from Rosalind Franklin University in 2016. Anton is very interested in community outreach and quality improvement, and in his spare time tutors students in science-based subjects.
Here’s what’s trending at SHM - Sept. 2017
Early decision for Fellows applications is Sept. 15. Apply now!
SHM’s Fellows designation is a prestigious way to differentiate yourself among your peers in hospital medicine. There are currently over 2,000 hospitalists who have earned the Fellow in Hospital Medicine (FHM) or Senior Fellow in Hospital Medicine (SFHM) designation by demonstrating core values of leadership, teamwork, and quality improvement.
“I was encouraged to consider SHM’s Fellow designation by other members of an SHM committee that I belonged to. Although reluctant at first, I realized that this was an opportunity to really confirm that I was a career hospitalist. The application process itself allowed me to objectively evaluate the work I had done to date and how it fit into my overall career plan. I believe that this FHM designation has fostered connections in the HM community and within my own institution that may not have been open to me before.” – Dr. Patricia Seymour, MD, FAAFP, FHM
Got research? Get noticed at HM18!
Don’t miss your chance to present your research to a national audience. SHM’s scientific abstract and poster competition, known as Research, Innovations, and Clinical Vignettes (RIV), is one of the most popular events at SHM’s annual meeting, enabling hospitalists from across the country to discuss emerging scientific and clinical cases, share feedback, and make valuable professional connections.
Hospital Medicine 2018 (HM18) will be held April 8-11, 2018 at the Orlando World Center Marriott. Many cutting-edge abstracts first presented at SHM’s RIV sessions go on to be published in respected medical journals. Yours could be next.
For more details, visit hospitalmedicine2018.org.
Know someone with exceptional achievements in Hospital Medicine?
SHM’s prestigious Awards of Excellence recognize exceptional achievements in the field of hospital medicine in the following categories:
• Excellence in Research.
• Management Excellence in Hospital Medicine.
• Outstanding Service in Hospital Medicine.
• Excellence in Teaching.
• Clinical Excellence for Physicians.
• Clinical Excellence for Nurse Practitioners and Physician Assistants.
• Excellence in Humanitarian Services.
• Excellence in Teamwork.
Awards of Excellence nominations are due on Oct. 2, 2017. Nominate yourself or a colleague today at hospitalmedicine.org/awards.
Invest in your career with SPARK ONE
SPARK ONE, SHM’s premier online self-assessment created specifically for hospital medicine professionals, is the perfect tool to help you reach your goals. The activity contains 450+ vignette-style multiple-choice questions covering 100% of the American Board of Internal Medicine’s Focused Practice in Hospital Medicine (FPHM) exam blueprint.
This online tool is your complete resource for successfully preparing for the FPHM exam or assessing your general knowledge in hospital medicine. Used as a self-paced study guide, it engages learners through an open-book format, allowing users to review detailed learning objectives and discussion points, and define individual areas of strengths and weaknesses. Earn up to 23 AMA PRA Category 1 Credit™ and 23 MOC points.
Learn more at hospitalmedicine.org/sparkone.
Strengthen your knowledge & skills in practice administration
Get involved in the SHM Practice Administrators’ Committee 2018 Mentor/Mentee Program.
This program helps you create relationships and serves as an outlet for you to pose questions or ideas to a seasoned hospital medicine group administrator. There are two different ways you can participate: as a less experienced administrator looking for a mentor or as a more experienced administrator looking to be paired with a peer. This program is free to members only. Not a member? Join today at hospitalmedicine.org/join.
Learn more about the program and submit your application at hospitalmedicine.org/pamentor.
Obtain an extensive insight into Hospital Medicine groups configuration and operation
SHM’s State of Hospital Medicine Report includes data collected from 600 hospital medicine groups (HMGs) representing 9,000 providers to keep you current on hospitalist compensation and production, in addition to cutting-edge knowledge covering practice demographics, staffing levels, turnover, staff growth, compensation methods, and financial support for solid, evidence-based management decisions.
The 2016 State of Hospital Medicine Report is not only in print but also available in an enhanced, fully searchable digital version. Order your copy at hospitalmedicine.org/sohm.
Mr. Radler is marketing communications manager at the Society of Hospital Medicine.
Early decision for Fellows applications is Sept. 15. Apply now!
SHM’s Fellows designation is a prestigious way to differentiate yourself among your peers in hospital medicine. There are currently over 2,000 hospitalists who have earned the Fellow in Hospital Medicine (FHM) or Senior Fellow in Hospital Medicine (SFHM) designation by demonstrating core values of leadership, teamwork, and quality improvement.
“I was encouraged to consider SHM’s Fellow designation by other members of an SHM committee that I belonged to. Although reluctant at first, I realized that this was an opportunity to really confirm that I was a career hospitalist. The application process itself allowed me to objectively evaluate the work I had done to date and how it fit into my overall career plan. I believe that this FHM designation has fostered connections in the HM community and within my own institution that may not have been open to me before.” – Dr. Patricia Seymour, MD, FAAFP, FHM
Got research? Get noticed at HM18!
Don’t miss your chance to present your research to a national audience. SHM’s scientific abstract and poster competition, known as Research, Innovations, and Clinical Vignettes (RIV), is one of the most popular events at SHM’s annual meeting, enabling hospitalists from across the country to discuss emerging scientific and clinical cases, share feedback, and make valuable professional connections.
Hospital Medicine 2018 (HM18) will be held April 8-11, 2018 at the Orlando World Center Marriott. Many cutting-edge abstracts first presented at SHM’s RIV sessions go on to be published in respected medical journals. Yours could be next.
For more details, visit hospitalmedicine2018.org.
Know someone with exceptional achievements in Hospital Medicine?
SHM’s prestigious Awards of Excellence recognize exceptional achievements in the field of hospital medicine in the following categories:
• Excellence in Research.
• Management Excellence in Hospital Medicine.
• Outstanding Service in Hospital Medicine.
• Excellence in Teaching.
• Clinical Excellence for Physicians.
• Clinical Excellence for Nurse Practitioners and Physician Assistants.
• Excellence in Humanitarian Services.
• Excellence in Teamwork.
Awards of Excellence nominations are due on Oct. 2, 2017. Nominate yourself or a colleague today at hospitalmedicine.org/awards.
Invest in your career with SPARK ONE
SPARK ONE, SHM’s premier online self-assessment created specifically for hospital medicine professionals, is the perfect tool to help you reach your goals. The activity contains 450+ vignette-style multiple-choice questions covering 100% of the American Board of Internal Medicine’s Focused Practice in Hospital Medicine (FPHM) exam blueprint.
This online tool is your complete resource for successfully preparing for the FPHM exam or assessing your general knowledge in hospital medicine. Used as a self-paced study guide, it engages learners through an open-book format, allowing users to review detailed learning objectives and discussion points, and define individual areas of strengths and weaknesses. Earn up to 23 AMA PRA Category 1 Credit™ and 23 MOC points.
Learn more at hospitalmedicine.org/sparkone.
Strengthen your knowledge & skills in practice administration
Get involved in the SHM Practice Administrators’ Committee 2018 Mentor/Mentee Program.
This program helps you create relationships and serves as an outlet for you to pose questions or ideas to a seasoned hospital medicine group administrator. There are two different ways you can participate: as a less experienced administrator looking for a mentor or as a more experienced administrator looking to be paired with a peer. This program is free to members only. Not a member? Join today at hospitalmedicine.org/join.
Learn more about the program and submit your application at hospitalmedicine.org/pamentor.
Obtain an extensive insight into Hospital Medicine groups configuration and operation
SHM’s State of Hospital Medicine Report includes data collected from 600 hospital medicine groups (HMGs) representing 9,000 providers to keep you current on hospitalist compensation and production, in addition to cutting-edge knowledge covering practice demographics, staffing levels, turnover, staff growth, compensation methods, and financial support for solid, evidence-based management decisions.
The 2016 State of Hospital Medicine Report is not only in print but also available in an enhanced, fully searchable digital version. Order your copy at hospitalmedicine.org/sohm.
Mr. Radler is marketing communications manager at the Society of Hospital Medicine.
Early decision for Fellows applications is Sept. 15. Apply now!
SHM’s Fellows designation is a prestigious way to differentiate yourself among your peers in hospital medicine. There are currently over 2,000 hospitalists who have earned the Fellow in Hospital Medicine (FHM) or Senior Fellow in Hospital Medicine (SFHM) designation by demonstrating core values of leadership, teamwork, and quality improvement.
“I was encouraged to consider SHM’s Fellow designation by other members of an SHM committee that I belonged to. Although reluctant at first, I realized that this was an opportunity to really confirm that I was a career hospitalist. The application process itself allowed me to objectively evaluate the work I had done to date and how it fit into my overall career plan. I believe that this FHM designation has fostered connections in the HM community and within my own institution that may not have been open to me before.” – Dr. Patricia Seymour, MD, FAAFP, FHM
Got research? Get noticed at HM18!
Don’t miss your chance to present your research to a national audience. SHM’s scientific abstract and poster competition, known as Research, Innovations, and Clinical Vignettes (RIV), is one of the most popular events at SHM’s annual meeting, enabling hospitalists from across the country to discuss emerging scientific and clinical cases, share feedback, and make valuable professional connections.
Hospital Medicine 2018 (HM18) will be held April 8-11, 2018 at the Orlando World Center Marriott. Many cutting-edge abstracts first presented at SHM’s RIV sessions go on to be published in respected medical journals. Yours could be next.
For more details, visit hospitalmedicine2018.org.
Know someone with exceptional achievements in Hospital Medicine?
SHM’s prestigious Awards of Excellence recognize exceptional achievements in the field of hospital medicine in the following categories:
• Excellence in Research.
• Management Excellence in Hospital Medicine.
• Outstanding Service in Hospital Medicine.
• Excellence in Teaching.
• Clinical Excellence for Physicians.
• Clinical Excellence for Nurse Practitioners and Physician Assistants.
• Excellence in Humanitarian Services.
• Excellence in Teamwork.
Awards of Excellence nominations are due on Oct. 2, 2017. Nominate yourself or a colleague today at hospitalmedicine.org/awards.
Invest in your career with SPARK ONE
SPARK ONE, SHM’s premier online self-assessment created specifically for hospital medicine professionals, is the perfect tool to help you reach your goals. The activity contains 450+ vignette-style multiple-choice questions covering 100% of the American Board of Internal Medicine’s Focused Practice in Hospital Medicine (FPHM) exam blueprint.
This online tool is your complete resource for successfully preparing for the FPHM exam or assessing your general knowledge in hospital medicine. Used as a self-paced study guide, it engages learners through an open-book format, allowing users to review detailed learning objectives and discussion points, and define individual areas of strengths and weaknesses. Earn up to 23 AMA PRA Category 1 Credit™ and 23 MOC points.
Learn more at hospitalmedicine.org/sparkone.
Strengthen your knowledge & skills in practice administration
Get involved in the SHM Practice Administrators’ Committee 2018 Mentor/Mentee Program.
This program helps you create relationships and serves as an outlet for you to pose questions or ideas to a seasoned hospital medicine group administrator. There are two different ways you can participate: as a less experienced administrator looking for a mentor or as a more experienced administrator looking to be paired with a peer. This program is free to members only. Not a member? Join today at hospitalmedicine.org/join.
Learn more about the program and submit your application at hospitalmedicine.org/pamentor.
Obtain an extensive insight into Hospital Medicine groups configuration and operation
SHM’s State of Hospital Medicine Report includes data collected from 600 hospital medicine groups (HMGs) representing 9,000 providers to keep you current on hospitalist compensation and production, in addition to cutting-edge knowledge covering practice demographics, staffing levels, turnover, staff growth, compensation methods, and financial support for solid, evidence-based management decisions.
The 2016 State of Hospital Medicine Report is not only in print but also available in an enhanced, fully searchable digital version. Order your copy at hospitalmedicine.org/sohm.
Mr. Radler is marketing communications manager at the Society of Hospital Medicine.
Letter: Working together to empower our next generation of leaders
Editor:
Dr. Nasim Afsar’s article of June 2, 2017 (“A case for building our leadership skills”) calls for the integration of leadership skills into medical training, and we at the University of Colorado wholeheartedly agree. There are several institutions around the country that are already addressing this problem head on, and we write this letter to highlight a few educational programs we’ve created that demonstrate the power of arming our trainees with this skill set. Furthermore, we wish to encourage collaboration between educators and institutions that are engaged in similar work in the hopes of moving this field forward.
Here at the University of Colorado, a team of Hospital Medicine faculty has created a number of programs to address the leadership education gap in learners at the undergraduate medical education,1 graduate medical education,2 and fellowship levels – creating a pipeline for developing leaders in hospital medicine. These programs include an immersive medical student elective, a dedicated leadership track in the Internal Medicine Residency Program, and a fellowship program in Hospital Medicine focused on Quality Improvement and Health Systems Leadership. Our goal in each of these programs to equip trainees across the spectrum of medical education with the knowledge, attitudes, and skills needed to lead high-functioning teams.
In our 5-year experience with our leadership training pipeline, we’ve learned a few important lessons. First, medical trainees are rarely exposed to the leadership skill set elsewhere in medical training, and are eager to learn new approaches to common problems that they encounter on a daily basis: How do I negotiate with a colleague? How can I motivate team members to change behavior to accomplish a goal? How can I use data to support requests for resources?
Secondly, trainees who are exposed to leadership concepts and who are given the opportunity to practice them through challenging project work in the live system routinely make meaningful changes to the health system. Our trainees have revamped our process of managing interhospital transfers, have decreased rates of inappropriate antibiotic usage, and have enhanced the patient experience in our stroke units. Further, our recent graduates have positioned themselves as leaders in health systems. Our graduates are leading a QI program at a major academic center, being promoted to educational leadership roles such as assistant program director within a residency training program, directing process improvement in a developing country, and leading the operations unit of a large physician group.
As Dr. Afsar highlights, there is much work to be done to better equip trainees with the skill set to lead. We strongly encourage other training programs to develop strategies to teach leadership and create forums for trainees to practice their burgeoning skill set. In addition to responding to Dr. Afsar’s call to develop programs, we should form collaborative working groups through our regional and national organizations to develop comprehensive leadership programs for medical trainees at all levels. Collaborating to empower the next generation of providers is critical to our future as hospitalists as we continue to take the lead in improving and shaping our health care systems.
Tyler Anstett, DO
Manuel Diaz, MD
Emily Gottenborg, MD
University of Colorado School of Medicine, Anschutz Medical Campus, Aurora, Colo.
References
1. Sweigart JR, Tad-Y D, Kneeland P, Williams MV, Glasheen JJ. Hospital Medicine Resident Training Tracks: Developing the Hospital Medicine Pipeline. J Hosp Med. 2017 Mar;12(3):173-176. doi: 10.12788/jhm.2703.
2. Tad-y D, Price L, Cumbler E, Levin D, Wald H, Glasheen J. An experiential quality improvement curriculum for the inpatient setting – part 1: design phase of a QI project. MedEdPORTAL Publications. 2014;10:9841. http://doi.org/10.15766/mep_2374-8265.9841.
Editor:
Dr. Nasim Afsar’s article of June 2, 2017 (“A case for building our leadership skills”) calls for the integration of leadership skills into medical training, and we at the University of Colorado wholeheartedly agree. There are several institutions around the country that are already addressing this problem head on, and we write this letter to highlight a few educational programs we’ve created that demonstrate the power of arming our trainees with this skill set. Furthermore, we wish to encourage collaboration between educators and institutions that are engaged in similar work in the hopes of moving this field forward.
Here at the University of Colorado, a team of Hospital Medicine faculty has created a number of programs to address the leadership education gap in learners at the undergraduate medical education,1 graduate medical education,2 and fellowship levels – creating a pipeline for developing leaders in hospital medicine. These programs include an immersive medical student elective, a dedicated leadership track in the Internal Medicine Residency Program, and a fellowship program in Hospital Medicine focused on Quality Improvement and Health Systems Leadership. Our goal in each of these programs to equip trainees across the spectrum of medical education with the knowledge, attitudes, and skills needed to lead high-functioning teams.
In our 5-year experience with our leadership training pipeline, we’ve learned a few important lessons. First, medical trainees are rarely exposed to the leadership skill set elsewhere in medical training, and are eager to learn new approaches to common problems that they encounter on a daily basis: How do I negotiate with a colleague? How can I motivate team members to change behavior to accomplish a goal? How can I use data to support requests for resources?
Secondly, trainees who are exposed to leadership concepts and who are given the opportunity to practice them through challenging project work in the live system routinely make meaningful changes to the health system. Our trainees have revamped our process of managing interhospital transfers, have decreased rates of inappropriate antibiotic usage, and have enhanced the patient experience in our stroke units. Further, our recent graduates have positioned themselves as leaders in health systems. Our graduates are leading a QI program at a major academic center, being promoted to educational leadership roles such as assistant program director within a residency training program, directing process improvement in a developing country, and leading the operations unit of a large physician group.
As Dr. Afsar highlights, there is much work to be done to better equip trainees with the skill set to lead. We strongly encourage other training programs to develop strategies to teach leadership and create forums for trainees to practice their burgeoning skill set. In addition to responding to Dr. Afsar’s call to develop programs, we should form collaborative working groups through our regional and national organizations to develop comprehensive leadership programs for medical trainees at all levels. Collaborating to empower the next generation of providers is critical to our future as hospitalists as we continue to take the lead in improving and shaping our health care systems.
Tyler Anstett, DO
Manuel Diaz, MD
Emily Gottenborg, MD
University of Colorado School of Medicine, Anschutz Medical Campus, Aurora, Colo.
References
1. Sweigart JR, Tad-Y D, Kneeland P, Williams MV, Glasheen JJ. Hospital Medicine Resident Training Tracks: Developing the Hospital Medicine Pipeline. J Hosp Med. 2017 Mar;12(3):173-176. doi: 10.12788/jhm.2703.
2. Tad-y D, Price L, Cumbler E, Levin D, Wald H, Glasheen J. An experiential quality improvement curriculum for the inpatient setting – part 1: design phase of a QI project. MedEdPORTAL Publications. 2014;10:9841. http://doi.org/10.15766/mep_2374-8265.9841.
Editor:
Dr. Nasim Afsar’s article of June 2, 2017 (“A case for building our leadership skills”) calls for the integration of leadership skills into medical training, and we at the University of Colorado wholeheartedly agree. There are several institutions around the country that are already addressing this problem head on, and we write this letter to highlight a few educational programs we’ve created that demonstrate the power of arming our trainees with this skill set. Furthermore, we wish to encourage collaboration between educators and institutions that are engaged in similar work in the hopes of moving this field forward.
Here at the University of Colorado, a team of Hospital Medicine faculty has created a number of programs to address the leadership education gap in learners at the undergraduate medical education,1 graduate medical education,2 and fellowship levels – creating a pipeline for developing leaders in hospital medicine. These programs include an immersive medical student elective, a dedicated leadership track in the Internal Medicine Residency Program, and a fellowship program in Hospital Medicine focused on Quality Improvement and Health Systems Leadership. Our goal in each of these programs to equip trainees across the spectrum of medical education with the knowledge, attitudes, and skills needed to lead high-functioning teams.
In our 5-year experience with our leadership training pipeline, we’ve learned a few important lessons. First, medical trainees are rarely exposed to the leadership skill set elsewhere in medical training, and are eager to learn new approaches to common problems that they encounter on a daily basis: How do I negotiate with a colleague? How can I motivate team members to change behavior to accomplish a goal? How can I use data to support requests for resources?
Secondly, trainees who are exposed to leadership concepts and who are given the opportunity to practice them through challenging project work in the live system routinely make meaningful changes to the health system. Our trainees have revamped our process of managing interhospital transfers, have decreased rates of inappropriate antibiotic usage, and have enhanced the patient experience in our stroke units. Further, our recent graduates have positioned themselves as leaders in health systems. Our graduates are leading a QI program at a major academic center, being promoted to educational leadership roles such as assistant program director within a residency training program, directing process improvement in a developing country, and leading the operations unit of a large physician group.
As Dr. Afsar highlights, there is much work to be done to better equip trainees with the skill set to lead. We strongly encourage other training programs to develop strategies to teach leadership and create forums for trainees to practice their burgeoning skill set. In addition to responding to Dr. Afsar’s call to develop programs, we should form collaborative working groups through our regional and national organizations to develop comprehensive leadership programs for medical trainees at all levels. Collaborating to empower the next generation of providers is critical to our future as hospitalists as we continue to take the lead in improving and shaping our health care systems.
Tyler Anstett, DO
Manuel Diaz, MD
Emily Gottenborg, MD
University of Colorado School of Medicine, Anschutz Medical Campus, Aurora, Colo.
References
1. Sweigart JR, Tad-Y D, Kneeland P, Williams MV, Glasheen JJ. Hospital Medicine Resident Training Tracks: Developing the Hospital Medicine Pipeline. J Hosp Med. 2017 Mar;12(3):173-176. doi: 10.12788/jhm.2703.
2. Tad-y D, Price L, Cumbler E, Levin D, Wald H, Glasheen J. An experiential quality improvement curriculum for the inpatient setting – part 1: design phase of a QI project. MedEdPORTAL Publications. 2014;10:9841. http://doi.org/10.15766/mep_2374-8265.9841.
More studies show Medicaid expansion has benefited hospitals
In 2016, a series of studies showed the impact of Medicaid expansion on hospitals.1 The news was good: Hospitals in states that accepted Medicaid expansion through the Affordable Care Act saw dramatic reductions in their uninsured patient populations, increases in their Medicaid stays, and reductions in uncompensated care costs.1,2
In 2017, additional data continue to show that Medicaid expansion has been a boon to hospitals, including an April 2017 report published by the Urban Institute and a May 2017 analysis from The Commonwealth Fund.3,4 Both show that some of the hospitals that need it most are reaping the greatest benefits of expansion.
At the same time, Craig Garthwaite, PhD, MPP, lead author of The Commonwealth Fund report, said Medicaid expansion “wiped out roughly half of the uncompensated care faced by hospitals, with relatively little or no decline in nonexpansion states.” To date, 19 states have not expanded Medicaid.
With Medicaid facing an uncertain future, Dr. Blavin said some experts are concerned about what could happen to vulnerable hospitals if Medicaid expansion is repealed or scaled back. Indeed, President Trump and Congressional Republicans have proposed significantly altering Medicaid by either transitioning it to block grants or by capping federal funding for the entitlement.6,7
“We wanted to give people a sense of the stakes of what you’re talking about with repeal of the Affordable Care Act and go back to a system where patients are able to get emergency care at the hospital but not the complete care they get if they’re insured. We’re not going to be paying hospitals for that care, so the hospital has that coming out of their profit margin,” said Dr. Garthwaite, professor of strategy and codirector of the Health Enterprise Management Program in the Kellogg School of Management at Northwestern University, Evanston, Ill.
The Commonwealth Fund report used data from the Centers for Medicare & Medicaid Services (CMS) Hospital Cost Reports to examine 1,154 hospitals in expansion and nonexpansion states. It built on a Health Affairs study Dr. Garthwaite and his coauthors published in 2016.2 The analysis found that between 2013 and 2014, uncompensated care costs declined dramatically in expansion states and continued into 2015, falling from 3.9% to 2.3% of operating costs. Meanwhile, hospitals in nonexpansion states saw uncompensated care costs drop just 0.3-0.4 percentage points. The largest reductions were seen by hospitals providing the highest proportion of care to low-income and uninsured patients and overall savings to hospitals in expansion states amounted to $6.2 billion.
“Any contraction of the Medicaid expansion will reduce overall health insurance coverage and could have important financial implications for hospitals,” Dr. Blavin said. “We are likely to see large increases in expenses attributable to uninsured patients, declines in Medicaid revenue, and increases in uncompensated care burdens that can be a significant financial strain to hospitals.”
As part of a project supported by the Robert Wood Johnson Foundation, the Urban Institute in May 2011 began to track and study the impact of health reform. The report Dr. Blavin authored is part of this endeavor and utilized data from the American Hospital Association Annual Survey and the CMS Health Care Cost Reports to update the 2016 JAMA study. It compared hospitals in expansion states to those in nonexpansion states between fiscal years 2011 and 2015, excluding hospitals in states that expanded before January 2014. It examined hospital-reported data on uncompensated care, uncompensated care as a percentage of total hospital expenses, Medicaid revenue, Medicaid as a percentage of total revenue, operating margins, and excess margins.
The analysis found that Medicaid expansion resulted in a $3.2 million reduction in uncompensated care and a $5.0 million increase in mean annual Medicaid revenue per hospital. Expansion-state hospitals also saw improvements in excess and operating margins relative to nonexpansion state hospitals.
In Connecticut, Medicaid reimbursement rates are among the lowest in the country.8 The state uses a provider tax to finance Medicaid but, facing a budget deficit, state leaders have dramatically reduced the amount of money returned to hospitals in recent years.9
“Our Medicaid patient volume has gone up but our margins have declined because the return on investment is so low,” added Dr. Kumar, a practicing hospitalist and member of the SHM Public Policy Committee. He is concerned about what happens if Medicaid is capped or transitioned to a block grant, since “block grants have not been favorable so far … It would further squeeze us.”
In Arizona, Steve Narang, MD, MHCM, a hospitalist and CEO of Banner–University Medical Center Phoenix (B-UMCP), already knows what it’s like when Medicaid funding expands and then contracts. In 2001, the state expanded Medicaid to 100% of the federal poverty level for childless adults but then in 2011, in the throes of recession, the state froze its match on federal dollars. Prior to the freeze, charity care and bad debt made up 9% of B-UMCP’s net revenue. After the state cut to Medicaid, the hospital’s uncompensated care doubled; charity care and bad debt spiked to 20% of net revenue. Once the freeze was lifted and the state expanded Medicaid through the ACA in 2014, bad debt and charity care plummeted to 7% of revenue and remains in the single digits, Dr. Narang said.
“You hear a lot, especially in debates, about Medicaid being bad coverage … From a hospital perspective, if you’re taking care of a patient who is uninsured versus a patient with Medicaid coverage, that hospital is likely better off financially treating the patient with Medicaid coverage,” said Dr. Blavin.
“From a basic commitment to our fellow human beings, are we doing the right thing as a country?” he asked, noting that states and the federal government must address the economic realities of health care while also providing safety nets for patients. “We have to do both. But I have faith that the state and federal government will find a model and we will continue to focus on what we can control.”
References
1. Tyrrell K. Benefits of Medicaid Expansion for Hospitalists. The Hospitalist. 2016 March;2016(3). http://www.the-hospitalist.org/hospitalist/article/121832/benefits-medicaid-expansion-hospitalists. Accessed May 25, 2017.
2. Dranove D., Garthwaite C., Ody C. Uncompensated Care Decreased at Hospitals in Medicaid Expansion States but Not at Hospitals in Nonexpansion States. Health Affairs, Aug. 2016 35(8):1471-9. http://content.healthaffairs.org/content/35/8/1471.abstract. Accessed May 25, 2017.
3. Blavin F. How Has the ACA Changed Finances for Different Types of Hospitals? Updated Insights from 2015 Cost Report Data. Urban Institute. Published April 2017. Accessed May 25, 2017. http://www.urban.org/sites/default/files/publication/89446/2001215-how-has-the-aca-changed-finances-for-different-types-of-hospitals.pdf.
4. Dranove D., Garthwaite C., Ody C. The Impact of the ACA’s Medicaid Expansion on Hospitals’ Uncompensated Care Burden and the Potential Effects of Repeal. Published May 3, 2017. Accessed May 25, 2017. http://www.commonwealthfund.org/publications/issue-briefs/2017/may/aca-medicaid-expansion-hospital-uncompensated-care.
5. Blavin F. Association Between the 2014 Medicaid Expansion and US Hospital Finances. http://jamanetwork.com/journals/jama/fullarticle/2565750. JAMA 2016;316(14):1475-1483. doi:10.1001/jama.2016.14765
6. President Trump’s 2018 Budget Proposal Reduces Federal Funding for Coverage of Children in Medicaid and CHIP. Kaiser Family Foundation. Published March 23, 2017. Accessed May 25, 2017. http://kff.org/medicaid/fact-sheet/presidents-2018-budget-proposal-reduces-federal-funding-for-coverage-of-children-in-medicaid-and-chip/
7. Paradise J. Restructuring Medicaid in the American Health Care Act: Five Key Considerations. Kaiser Family Foundation. Published March 15, 2017. Accessed May 25, 2017. http://kff.org/medicaid/issue-brief/restructuring-medicaid-in-the-american-health-care-act-five-key-considerations/
8. Medicaid Hospital Payment: A comparison across states and to Medicare. MACPAC Issue Brief. Published April 2017.
9. Levin Becker A. Hospitals blast Malloy’s proposal to subject them to property taxes. Published Feb. 8, 2017. Accessed May 25, 2017. https://ctmirror.org/2017/02/08/hospitals-blast-malloys-proposal-to-subject-them-to-property-taxes/
In 2016, a series of studies showed the impact of Medicaid expansion on hospitals.1 The news was good: Hospitals in states that accepted Medicaid expansion through the Affordable Care Act saw dramatic reductions in their uninsured patient populations, increases in their Medicaid stays, and reductions in uncompensated care costs.1,2
In 2017, additional data continue to show that Medicaid expansion has been a boon to hospitals, including an April 2017 report published by the Urban Institute and a May 2017 analysis from The Commonwealth Fund.3,4 Both show that some of the hospitals that need it most are reaping the greatest benefits of expansion.
At the same time, Craig Garthwaite, PhD, MPP, lead author of The Commonwealth Fund report, said Medicaid expansion “wiped out roughly half of the uncompensated care faced by hospitals, with relatively little or no decline in nonexpansion states.” To date, 19 states have not expanded Medicaid.
With Medicaid facing an uncertain future, Dr. Blavin said some experts are concerned about what could happen to vulnerable hospitals if Medicaid expansion is repealed or scaled back. Indeed, President Trump and Congressional Republicans have proposed significantly altering Medicaid by either transitioning it to block grants or by capping federal funding for the entitlement.6,7
“We wanted to give people a sense of the stakes of what you’re talking about with repeal of the Affordable Care Act and go back to a system where patients are able to get emergency care at the hospital but not the complete care they get if they’re insured. We’re not going to be paying hospitals for that care, so the hospital has that coming out of their profit margin,” said Dr. Garthwaite, professor of strategy and codirector of the Health Enterprise Management Program in the Kellogg School of Management at Northwestern University, Evanston, Ill.
The Commonwealth Fund report used data from the Centers for Medicare & Medicaid Services (CMS) Hospital Cost Reports to examine 1,154 hospitals in expansion and nonexpansion states. It built on a Health Affairs study Dr. Garthwaite and his coauthors published in 2016.2 The analysis found that between 2013 and 2014, uncompensated care costs declined dramatically in expansion states and continued into 2015, falling from 3.9% to 2.3% of operating costs. Meanwhile, hospitals in nonexpansion states saw uncompensated care costs drop just 0.3-0.4 percentage points. The largest reductions were seen by hospitals providing the highest proportion of care to low-income and uninsured patients and overall savings to hospitals in expansion states amounted to $6.2 billion.
“Any contraction of the Medicaid expansion will reduce overall health insurance coverage and could have important financial implications for hospitals,” Dr. Blavin said. “We are likely to see large increases in expenses attributable to uninsured patients, declines in Medicaid revenue, and increases in uncompensated care burdens that can be a significant financial strain to hospitals.”
As part of a project supported by the Robert Wood Johnson Foundation, the Urban Institute in May 2011 began to track and study the impact of health reform. The report Dr. Blavin authored is part of this endeavor and utilized data from the American Hospital Association Annual Survey and the CMS Health Care Cost Reports to update the 2016 JAMA study. It compared hospitals in expansion states to those in nonexpansion states between fiscal years 2011 and 2015, excluding hospitals in states that expanded before January 2014. It examined hospital-reported data on uncompensated care, uncompensated care as a percentage of total hospital expenses, Medicaid revenue, Medicaid as a percentage of total revenue, operating margins, and excess margins.
The analysis found that Medicaid expansion resulted in a $3.2 million reduction in uncompensated care and a $5.0 million increase in mean annual Medicaid revenue per hospital. Expansion-state hospitals also saw improvements in excess and operating margins relative to nonexpansion state hospitals.
In Connecticut, Medicaid reimbursement rates are among the lowest in the country.8 The state uses a provider tax to finance Medicaid but, facing a budget deficit, state leaders have dramatically reduced the amount of money returned to hospitals in recent years.9
“Our Medicaid patient volume has gone up but our margins have declined because the return on investment is so low,” added Dr. Kumar, a practicing hospitalist and member of the SHM Public Policy Committee. He is concerned about what happens if Medicaid is capped or transitioned to a block grant, since “block grants have not been favorable so far … It would further squeeze us.”
In Arizona, Steve Narang, MD, MHCM, a hospitalist and CEO of Banner–University Medical Center Phoenix (B-UMCP), already knows what it’s like when Medicaid funding expands and then contracts. In 2001, the state expanded Medicaid to 100% of the federal poverty level for childless adults but then in 2011, in the throes of recession, the state froze its match on federal dollars. Prior to the freeze, charity care and bad debt made up 9% of B-UMCP’s net revenue. After the state cut to Medicaid, the hospital’s uncompensated care doubled; charity care and bad debt spiked to 20% of net revenue. Once the freeze was lifted and the state expanded Medicaid through the ACA in 2014, bad debt and charity care plummeted to 7% of revenue and remains in the single digits, Dr. Narang said.
“You hear a lot, especially in debates, about Medicaid being bad coverage … From a hospital perspective, if you’re taking care of a patient who is uninsured versus a patient with Medicaid coverage, that hospital is likely better off financially treating the patient with Medicaid coverage,” said Dr. Blavin.
“From a basic commitment to our fellow human beings, are we doing the right thing as a country?” he asked, noting that states and the federal government must address the economic realities of health care while also providing safety nets for patients. “We have to do both. But I have faith that the state and federal government will find a model and we will continue to focus on what we can control.”
References
1. Tyrrell K. Benefits of Medicaid Expansion for Hospitalists. The Hospitalist. 2016 March;2016(3). http://www.the-hospitalist.org/hospitalist/article/121832/benefits-medicaid-expansion-hospitalists. Accessed May 25, 2017.
2. Dranove D., Garthwaite C., Ody C. Uncompensated Care Decreased at Hospitals in Medicaid Expansion States but Not at Hospitals in Nonexpansion States. Health Affairs, Aug. 2016 35(8):1471-9. http://content.healthaffairs.org/content/35/8/1471.abstract. Accessed May 25, 2017.
3. Blavin F. How Has the ACA Changed Finances for Different Types of Hospitals? Updated Insights from 2015 Cost Report Data. Urban Institute. Published April 2017. Accessed May 25, 2017. http://www.urban.org/sites/default/files/publication/89446/2001215-how-has-the-aca-changed-finances-for-different-types-of-hospitals.pdf.
4. Dranove D., Garthwaite C., Ody C. The Impact of the ACA’s Medicaid Expansion on Hospitals’ Uncompensated Care Burden and the Potential Effects of Repeal. Published May 3, 2017. Accessed May 25, 2017. http://www.commonwealthfund.org/publications/issue-briefs/2017/may/aca-medicaid-expansion-hospital-uncompensated-care.
5. Blavin F. Association Between the 2014 Medicaid Expansion and US Hospital Finances. http://jamanetwork.com/journals/jama/fullarticle/2565750. JAMA 2016;316(14):1475-1483. doi:10.1001/jama.2016.14765
6. President Trump’s 2018 Budget Proposal Reduces Federal Funding for Coverage of Children in Medicaid and CHIP. Kaiser Family Foundation. Published March 23, 2017. Accessed May 25, 2017. http://kff.org/medicaid/fact-sheet/presidents-2018-budget-proposal-reduces-federal-funding-for-coverage-of-children-in-medicaid-and-chip/
7. Paradise J. Restructuring Medicaid in the American Health Care Act: Five Key Considerations. Kaiser Family Foundation. Published March 15, 2017. Accessed May 25, 2017. http://kff.org/medicaid/issue-brief/restructuring-medicaid-in-the-american-health-care-act-five-key-considerations/
8. Medicaid Hospital Payment: A comparison across states and to Medicare. MACPAC Issue Brief. Published April 2017.
9. Levin Becker A. Hospitals blast Malloy’s proposal to subject them to property taxes. Published Feb. 8, 2017. Accessed May 25, 2017. https://ctmirror.org/2017/02/08/hospitals-blast-malloys-proposal-to-subject-them-to-property-taxes/
In 2016, a series of studies showed the impact of Medicaid expansion on hospitals.1 The news was good: Hospitals in states that accepted Medicaid expansion through the Affordable Care Act saw dramatic reductions in their uninsured patient populations, increases in their Medicaid stays, and reductions in uncompensated care costs.1,2
In 2017, additional data continue to show that Medicaid expansion has been a boon to hospitals, including an April 2017 report published by the Urban Institute and a May 2017 analysis from The Commonwealth Fund.3,4 Both show that some of the hospitals that need it most are reaping the greatest benefits of expansion.
At the same time, Craig Garthwaite, PhD, MPP, lead author of The Commonwealth Fund report, said Medicaid expansion “wiped out roughly half of the uncompensated care faced by hospitals, with relatively little or no decline in nonexpansion states.” To date, 19 states have not expanded Medicaid.
With Medicaid facing an uncertain future, Dr. Blavin said some experts are concerned about what could happen to vulnerable hospitals if Medicaid expansion is repealed or scaled back. Indeed, President Trump and Congressional Republicans have proposed significantly altering Medicaid by either transitioning it to block grants or by capping federal funding for the entitlement.6,7
“We wanted to give people a sense of the stakes of what you’re talking about with repeal of the Affordable Care Act and go back to a system where patients are able to get emergency care at the hospital but not the complete care they get if they’re insured. We’re not going to be paying hospitals for that care, so the hospital has that coming out of their profit margin,” said Dr. Garthwaite, professor of strategy and codirector of the Health Enterprise Management Program in the Kellogg School of Management at Northwestern University, Evanston, Ill.
The Commonwealth Fund report used data from the Centers for Medicare & Medicaid Services (CMS) Hospital Cost Reports to examine 1,154 hospitals in expansion and nonexpansion states. It built on a Health Affairs study Dr. Garthwaite and his coauthors published in 2016.2 The analysis found that between 2013 and 2014, uncompensated care costs declined dramatically in expansion states and continued into 2015, falling from 3.9% to 2.3% of operating costs. Meanwhile, hospitals in nonexpansion states saw uncompensated care costs drop just 0.3-0.4 percentage points. The largest reductions were seen by hospitals providing the highest proportion of care to low-income and uninsured patients and overall savings to hospitals in expansion states amounted to $6.2 billion.
“Any contraction of the Medicaid expansion will reduce overall health insurance coverage and could have important financial implications for hospitals,” Dr. Blavin said. “We are likely to see large increases in expenses attributable to uninsured patients, declines in Medicaid revenue, and increases in uncompensated care burdens that can be a significant financial strain to hospitals.”
As part of a project supported by the Robert Wood Johnson Foundation, the Urban Institute in May 2011 began to track and study the impact of health reform. The report Dr. Blavin authored is part of this endeavor and utilized data from the American Hospital Association Annual Survey and the CMS Health Care Cost Reports to update the 2016 JAMA study. It compared hospitals in expansion states to those in nonexpansion states between fiscal years 2011 and 2015, excluding hospitals in states that expanded before January 2014. It examined hospital-reported data on uncompensated care, uncompensated care as a percentage of total hospital expenses, Medicaid revenue, Medicaid as a percentage of total revenue, operating margins, and excess margins.
The analysis found that Medicaid expansion resulted in a $3.2 million reduction in uncompensated care and a $5.0 million increase in mean annual Medicaid revenue per hospital. Expansion-state hospitals also saw improvements in excess and operating margins relative to nonexpansion state hospitals.
In Connecticut, Medicaid reimbursement rates are among the lowest in the country.8 The state uses a provider tax to finance Medicaid but, facing a budget deficit, state leaders have dramatically reduced the amount of money returned to hospitals in recent years.9
“Our Medicaid patient volume has gone up but our margins have declined because the return on investment is so low,” added Dr. Kumar, a practicing hospitalist and member of the SHM Public Policy Committee. He is concerned about what happens if Medicaid is capped or transitioned to a block grant, since “block grants have not been favorable so far … It would further squeeze us.”
In Arizona, Steve Narang, MD, MHCM, a hospitalist and CEO of Banner–University Medical Center Phoenix (B-UMCP), already knows what it’s like when Medicaid funding expands and then contracts. In 2001, the state expanded Medicaid to 100% of the federal poverty level for childless adults but then in 2011, in the throes of recession, the state froze its match on federal dollars. Prior to the freeze, charity care and bad debt made up 9% of B-UMCP’s net revenue. After the state cut to Medicaid, the hospital’s uncompensated care doubled; charity care and bad debt spiked to 20% of net revenue. Once the freeze was lifted and the state expanded Medicaid through the ACA in 2014, bad debt and charity care plummeted to 7% of revenue and remains in the single digits, Dr. Narang said.
“You hear a lot, especially in debates, about Medicaid being bad coverage … From a hospital perspective, if you’re taking care of a patient who is uninsured versus a patient with Medicaid coverage, that hospital is likely better off financially treating the patient with Medicaid coverage,” said Dr. Blavin.
“From a basic commitment to our fellow human beings, are we doing the right thing as a country?” he asked, noting that states and the federal government must address the economic realities of health care while also providing safety nets for patients. “We have to do both. But I have faith that the state and federal government will find a model and we will continue to focus on what we can control.”
References
1. Tyrrell K. Benefits of Medicaid Expansion for Hospitalists. The Hospitalist. 2016 March;2016(3). http://www.the-hospitalist.org/hospitalist/article/121832/benefits-medicaid-expansion-hospitalists. Accessed May 25, 2017.
2. Dranove D., Garthwaite C., Ody C. Uncompensated Care Decreased at Hospitals in Medicaid Expansion States but Not at Hospitals in Nonexpansion States. Health Affairs, Aug. 2016 35(8):1471-9. http://content.healthaffairs.org/content/35/8/1471.abstract. Accessed May 25, 2017.
3. Blavin F. How Has the ACA Changed Finances for Different Types of Hospitals? Updated Insights from 2015 Cost Report Data. Urban Institute. Published April 2017. Accessed May 25, 2017. http://www.urban.org/sites/default/files/publication/89446/2001215-how-has-the-aca-changed-finances-for-different-types-of-hospitals.pdf.
4. Dranove D., Garthwaite C., Ody C. The Impact of the ACA’s Medicaid Expansion on Hospitals’ Uncompensated Care Burden and the Potential Effects of Repeal. Published May 3, 2017. Accessed May 25, 2017. http://www.commonwealthfund.org/publications/issue-briefs/2017/may/aca-medicaid-expansion-hospital-uncompensated-care.
5. Blavin F. Association Between the 2014 Medicaid Expansion and US Hospital Finances. http://jamanetwork.com/journals/jama/fullarticle/2565750. JAMA 2016;316(14):1475-1483. doi:10.1001/jama.2016.14765
6. President Trump’s 2018 Budget Proposal Reduces Federal Funding for Coverage of Children in Medicaid and CHIP. Kaiser Family Foundation. Published March 23, 2017. Accessed May 25, 2017. http://kff.org/medicaid/fact-sheet/presidents-2018-budget-proposal-reduces-federal-funding-for-coverage-of-children-in-medicaid-and-chip/
7. Paradise J. Restructuring Medicaid in the American Health Care Act: Five Key Considerations. Kaiser Family Foundation. Published March 15, 2017. Accessed May 25, 2017. http://kff.org/medicaid/issue-brief/restructuring-medicaid-in-the-american-health-care-act-five-key-considerations/
8. Medicaid Hospital Payment: A comparison across states and to Medicare. MACPAC Issue Brief. Published April 2017.
9. Levin Becker A. Hospitals blast Malloy’s proposal to subject them to property taxes. Published Feb. 8, 2017. Accessed May 25, 2017. https://ctmirror.org/2017/02/08/hospitals-blast-malloys-proposal-to-subject-them-to-property-taxes/
Bezlotoxumab may lower risk of C. difficile readmissions
Clostridium difficile infection (CDI) patients treated with bezlotoxumab were less likely to be readmitted for recurring symptoms within 30 days of discharge, according to a phase 3 trial funded by Merck.
Recurrent CDI is a burden on both patients and providers, increasing health risks with each recurrence and eating through hospital resources, according to Vimalanand S. Prabhu, PhD, associate principal scientist for Merck.
In a randomized, double-blind, placebo-controlled, study of 1,050 CDI patients, a total of 27 (5%) of 530 of those given bezlotoxumab were re-hospitalized 30 days after discharge, compared with 58 (11%) of 520 patients in the placebo group (Clin Infect Dis. 2017 Aug 11. doi. 10.1093/cid/cix523).
Patients were gathered from 322 sites across 30 countries between November 2011 and May 2015.
When measuring CDI-related readmissions, the investigators found use of bezlotoxumab reduced rCDI hospitalizations by 6%, and by approximately 8% in high-risk patients, such as those over 65 years old or with severe CDI.
Bezlotoxumab works by binding to CDI toxin B, a primary cause of CDI symptoms, according to Dr. Prabhu and fellow investigators. The researchers suggested that bezlotoxumab could be a prevailing factor in fighting the rate of CDI infections, which accounted for 29,000 deaths in 2011 (N Engl J Med. 2015 Jun 11;372[24]:2368-9).
Investigators acknowledged that patients admitted for the study may be healthier than the real-world CDI population.
All investigators reported some financial involvement, whether being a full-time employee or acting as a consultant, for Merck, which funded the study. Individually, investigators reported financial ties to similar medical companies, such as Pfizer and AstraZeneca.
[email protected]
On Twitter @eaztweets
Clostridium difficile infection (CDI) patients treated with bezlotoxumab were less likely to be readmitted for recurring symptoms within 30 days of discharge, according to a phase 3 trial funded by Merck.
Recurrent CDI is a burden on both patients and providers, increasing health risks with each recurrence and eating through hospital resources, according to Vimalanand S. Prabhu, PhD, associate principal scientist for Merck.
In a randomized, double-blind, placebo-controlled, study of 1,050 CDI patients, a total of 27 (5%) of 530 of those given bezlotoxumab were re-hospitalized 30 days after discharge, compared with 58 (11%) of 520 patients in the placebo group (Clin Infect Dis. 2017 Aug 11. doi. 10.1093/cid/cix523).
Patients were gathered from 322 sites across 30 countries between November 2011 and May 2015.
When measuring CDI-related readmissions, the investigators found use of bezlotoxumab reduced rCDI hospitalizations by 6%, and by approximately 8% in high-risk patients, such as those over 65 years old or with severe CDI.
Bezlotoxumab works by binding to CDI toxin B, a primary cause of CDI symptoms, according to Dr. Prabhu and fellow investigators. The researchers suggested that bezlotoxumab could be a prevailing factor in fighting the rate of CDI infections, which accounted for 29,000 deaths in 2011 (N Engl J Med. 2015 Jun 11;372[24]:2368-9).
Investigators acknowledged that patients admitted for the study may be healthier than the real-world CDI population.
All investigators reported some financial involvement, whether being a full-time employee or acting as a consultant, for Merck, which funded the study. Individually, investigators reported financial ties to similar medical companies, such as Pfizer and AstraZeneca.
[email protected]
On Twitter @eaztweets
Clostridium difficile infection (CDI) patients treated with bezlotoxumab were less likely to be readmitted for recurring symptoms within 30 days of discharge, according to a phase 3 trial funded by Merck.
Recurrent CDI is a burden on both patients and providers, increasing health risks with each recurrence and eating through hospital resources, according to Vimalanand S. Prabhu, PhD, associate principal scientist for Merck.
In a randomized, double-blind, placebo-controlled, study of 1,050 CDI patients, a total of 27 (5%) of 530 of those given bezlotoxumab were re-hospitalized 30 days after discharge, compared with 58 (11%) of 520 patients in the placebo group (Clin Infect Dis. 2017 Aug 11. doi. 10.1093/cid/cix523).
Patients were gathered from 322 sites across 30 countries between November 2011 and May 2015.
When measuring CDI-related readmissions, the investigators found use of bezlotoxumab reduced rCDI hospitalizations by 6%, and by approximately 8% in high-risk patients, such as those over 65 years old or with severe CDI.
Bezlotoxumab works by binding to CDI toxin B, a primary cause of CDI symptoms, according to Dr. Prabhu and fellow investigators. The researchers suggested that bezlotoxumab could be a prevailing factor in fighting the rate of CDI infections, which accounted for 29,000 deaths in 2011 (N Engl J Med. 2015 Jun 11;372[24]:2368-9).
Investigators acknowledged that patients admitted for the study may be healthier than the real-world CDI population.
All investigators reported some financial involvement, whether being a full-time employee or acting as a consultant, for Merck, which funded the study. Individually, investigators reported financial ties to similar medical companies, such as Pfizer and AstraZeneca.
[email protected]
On Twitter @eaztweets
FROM CLINICAL INFECTIOUS DISEASES
Key clinical point:
Major finding: A total of 27 of 530 (5%) bezlotoxumab patients were readmitted within 30 days of discharge compared with 58 of 520 (11%) placebo patients.
Data source: Randomized, double-blind, placebo-controlled, multicenter, global phase 3 trials conducted from November 2011-May 2015 at 322 sites in 30 countries.
Disclosures: All investigators report employment or financial support with Merck and have individually reported financial ties to similar companies like Astellas, AstraZeneca, Pfizer, and others.
News Flash! Nocturnists are in high demand
Over 70% of all hospitalist programs have nocturnists, according to the 2016 State of Hospital Medicine Report. For adult-only practices, this has increased to 72.3% from 46.1% in the 2012 State of Hospital Medicine Report.
While one can assert that most hospital medicine practices have nocturnists, not all nights are covered by nocturnists. Thirty-nine percent (39%) of adult practices report that nocturnists cover 100% of nights, and 9.2% report that less than 25% of nights are covered by nocturnists. So, there remains a great deal of variability in the widespread use of nocturnists for nighttime coverage.
Categorically, nocturnists are hospitalists who work primarily at night, providing in-house coverage for hospitalist admissions and coverage for patients cared for by the hospitalist group.
Other clinicians, such as nurses, patient care technicians, medical technologists, and radiology technologists, have worked night shifts for many, many years. The phenomenon of hospital-based physicians and advanced practice clinicians working only at night is reflective of the needs in an acute care environment.
There are many lifestyle benefits to being a nocturnist – raising a family during the day while working at night, working fewer hours for more pay, and being in high demand.
Nocturnists can also allow a hospitalist group to offer more flexible scheduling options and create career longevity within the group. Having a nocturnist can allow a group to offer other hospitalists a “day shift only” option and other flexible scheduling options that many seasoned hospitalists are looking for.
Demand
Because of the increasing demand, it’s becoming more difficult to find long-term nocturnists, and therefore permanent nocturnists are expensive to hire. As reported in the 2016 State of Hospital Medicine Report, groups with nocturnists may offer either a differential in the hours or shifts worked, or compensation, or a combination of both.
About half of nocturnists work fewer shifts, compared with non-nocturnists. Equally stated, about half of nocturnists work the same number of shifts as their day-only counterparts. Of those groups whose nocturnists work fewer shifts than their daytime counterparts, about 60% work 1%-20% fewer shifts.
Nearly 70% of groups with nocturnists pay nocturnists differently. The median pay differential is 15%. While this compensation differential is an increase since the 2014 report, it is on par with the 2012 report.
It should not be construed that every practice with hospitalists offers both fewer shifts and more compensation. In fact, there are many who may offer neither and develop other, more creative ways of recognizing the nocturnist differently, such as evaluating scheduled hours per shift (e.g., 8 vs. 10 vs. 12).
Responsibility
With more adaptation and remuneration for nocturnists comes more responsibility.
Working as a nocturnist can be grueling work. Many times nocturnists may be working alone, and with less support from consultants and fewer hospital resources at night. On the other hand, it’s quieter at night and there can be a strong camaraderie from the smaller team at the hospital at night.
Nocturnists, many times, must be comfortable working alone; they must have strong clinical skills, and may need to seek extra training. In fact, in some hospitals the nocturnists may be the primary, or only, physician covering in-house codes.
Nocturnists must also take responsibility to remain abreast of the quality initiatives of the hospitalist group and hospital, since many of the quality committee meetings and hospitalist group meetings typically occur during daytime hours. Nocturnists may need to make an extra effort to feel a part of the group by voluntarily participating in daytime group activities, so that they don’t feel like an outsider.
Nocturnists should take the lead in receiving hand-off each evening, and handing off each morning to the day shift. This will likely mean handing off valuable patient care information with more than a few of their hospitalist colleagues. This is so immensely important that national patient safety-focused organizations have emphasized it for many years.
Since four out of five hospitalist programs have a hospitalist on site at night, and the majority of those programs have at least some nocturnist coverage, designing hospitalist programs and staffing models that meet the patient care need of 24/7 in-house coverage is a necessity. Also, given the strong demand for nocturnists, more and more program leaders are being challenged to evaluate creative alternatives to provide sustainable hospitalist services.
Some examples of creative solutions for in-house night coverage are implementing telemedicine for admissions, cross cover, or both; expanding coverage by advanced practice clinicians; and staggering shifts to cover late evenings and early mornings.
Perhaps we’ll see more questions about how hospitalist groups are addressing this need in future surveys?
Amanda Trask, MBA, MHA, FACHE, CMPE, SFHM, is national vice president, Hospital Medicine Service Line, at Catholic Health Initiatives, Englewood, Colo.
Over 70% of all hospitalist programs have nocturnists, according to the 2016 State of Hospital Medicine Report. For adult-only practices, this has increased to 72.3% from 46.1% in the 2012 State of Hospital Medicine Report.
While one can assert that most hospital medicine practices have nocturnists, not all nights are covered by nocturnists. Thirty-nine percent (39%) of adult practices report that nocturnists cover 100% of nights, and 9.2% report that less than 25% of nights are covered by nocturnists. So, there remains a great deal of variability in the widespread use of nocturnists for nighttime coverage.
Categorically, nocturnists are hospitalists who work primarily at night, providing in-house coverage for hospitalist admissions and coverage for patients cared for by the hospitalist group.
Other clinicians, such as nurses, patient care technicians, medical technologists, and radiology technologists, have worked night shifts for many, many years. The phenomenon of hospital-based physicians and advanced practice clinicians working only at night is reflective of the needs in an acute care environment.
There are many lifestyle benefits to being a nocturnist – raising a family during the day while working at night, working fewer hours for more pay, and being in high demand.
Nocturnists can also allow a hospitalist group to offer more flexible scheduling options and create career longevity within the group. Having a nocturnist can allow a group to offer other hospitalists a “day shift only” option and other flexible scheduling options that many seasoned hospitalists are looking for.
Demand
Because of the increasing demand, it’s becoming more difficult to find long-term nocturnists, and therefore permanent nocturnists are expensive to hire. As reported in the 2016 State of Hospital Medicine Report, groups with nocturnists may offer either a differential in the hours or shifts worked, or compensation, or a combination of both.
About half of nocturnists work fewer shifts, compared with non-nocturnists. Equally stated, about half of nocturnists work the same number of shifts as their day-only counterparts. Of those groups whose nocturnists work fewer shifts than their daytime counterparts, about 60% work 1%-20% fewer shifts.
Nearly 70% of groups with nocturnists pay nocturnists differently. The median pay differential is 15%. While this compensation differential is an increase since the 2014 report, it is on par with the 2012 report.
It should not be construed that every practice with hospitalists offers both fewer shifts and more compensation. In fact, there are many who may offer neither and develop other, more creative ways of recognizing the nocturnist differently, such as evaluating scheduled hours per shift (e.g., 8 vs. 10 vs. 12).
Responsibility
With more adaptation and remuneration for nocturnists comes more responsibility.
Working as a nocturnist can be grueling work. Many times nocturnists may be working alone, and with less support from consultants and fewer hospital resources at night. On the other hand, it’s quieter at night and there can be a strong camaraderie from the smaller team at the hospital at night.
Nocturnists, many times, must be comfortable working alone; they must have strong clinical skills, and may need to seek extra training. In fact, in some hospitals the nocturnists may be the primary, or only, physician covering in-house codes.
Nocturnists must also take responsibility to remain abreast of the quality initiatives of the hospitalist group and hospital, since many of the quality committee meetings and hospitalist group meetings typically occur during daytime hours. Nocturnists may need to make an extra effort to feel a part of the group by voluntarily participating in daytime group activities, so that they don’t feel like an outsider.
Nocturnists should take the lead in receiving hand-off each evening, and handing off each morning to the day shift. This will likely mean handing off valuable patient care information with more than a few of their hospitalist colleagues. This is so immensely important that national patient safety-focused organizations have emphasized it for many years.
Since four out of five hospitalist programs have a hospitalist on site at night, and the majority of those programs have at least some nocturnist coverage, designing hospitalist programs and staffing models that meet the patient care need of 24/7 in-house coverage is a necessity. Also, given the strong demand for nocturnists, more and more program leaders are being challenged to evaluate creative alternatives to provide sustainable hospitalist services.
Some examples of creative solutions for in-house night coverage are implementing telemedicine for admissions, cross cover, or both; expanding coverage by advanced practice clinicians; and staggering shifts to cover late evenings and early mornings.
Perhaps we’ll see more questions about how hospitalist groups are addressing this need in future surveys?
Amanda Trask, MBA, MHA, FACHE, CMPE, SFHM, is national vice president, Hospital Medicine Service Line, at Catholic Health Initiatives, Englewood, Colo.
Over 70% of all hospitalist programs have nocturnists, according to the 2016 State of Hospital Medicine Report. For adult-only practices, this has increased to 72.3% from 46.1% in the 2012 State of Hospital Medicine Report.
While one can assert that most hospital medicine practices have nocturnists, not all nights are covered by nocturnists. Thirty-nine percent (39%) of adult practices report that nocturnists cover 100% of nights, and 9.2% report that less than 25% of nights are covered by nocturnists. So, there remains a great deal of variability in the widespread use of nocturnists for nighttime coverage.
Categorically, nocturnists are hospitalists who work primarily at night, providing in-house coverage for hospitalist admissions and coverage for patients cared for by the hospitalist group.
Other clinicians, such as nurses, patient care technicians, medical technologists, and radiology technologists, have worked night shifts for many, many years. The phenomenon of hospital-based physicians and advanced practice clinicians working only at night is reflective of the needs in an acute care environment.
There are many lifestyle benefits to being a nocturnist – raising a family during the day while working at night, working fewer hours for more pay, and being in high demand.
Nocturnists can also allow a hospitalist group to offer more flexible scheduling options and create career longevity within the group. Having a nocturnist can allow a group to offer other hospitalists a “day shift only” option and other flexible scheduling options that many seasoned hospitalists are looking for.
Demand
Because of the increasing demand, it’s becoming more difficult to find long-term nocturnists, and therefore permanent nocturnists are expensive to hire. As reported in the 2016 State of Hospital Medicine Report, groups with nocturnists may offer either a differential in the hours or shifts worked, or compensation, or a combination of both.
About half of nocturnists work fewer shifts, compared with non-nocturnists. Equally stated, about half of nocturnists work the same number of shifts as their day-only counterparts. Of those groups whose nocturnists work fewer shifts than their daytime counterparts, about 60% work 1%-20% fewer shifts.
Nearly 70% of groups with nocturnists pay nocturnists differently. The median pay differential is 15%. While this compensation differential is an increase since the 2014 report, it is on par with the 2012 report.
It should not be construed that every practice with hospitalists offers both fewer shifts and more compensation. In fact, there are many who may offer neither and develop other, more creative ways of recognizing the nocturnist differently, such as evaluating scheduled hours per shift (e.g., 8 vs. 10 vs. 12).
Responsibility
With more adaptation and remuneration for nocturnists comes more responsibility.
Working as a nocturnist can be grueling work. Many times nocturnists may be working alone, and with less support from consultants and fewer hospital resources at night. On the other hand, it’s quieter at night and there can be a strong camaraderie from the smaller team at the hospital at night.
Nocturnists, many times, must be comfortable working alone; they must have strong clinical skills, and may need to seek extra training. In fact, in some hospitals the nocturnists may be the primary, or only, physician covering in-house codes.
Nocturnists must also take responsibility to remain abreast of the quality initiatives of the hospitalist group and hospital, since many of the quality committee meetings and hospitalist group meetings typically occur during daytime hours. Nocturnists may need to make an extra effort to feel a part of the group by voluntarily participating in daytime group activities, so that they don’t feel like an outsider.
Nocturnists should take the lead in receiving hand-off each evening, and handing off each morning to the day shift. This will likely mean handing off valuable patient care information with more than a few of their hospitalist colleagues. This is so immensely important that national patient safety-focused organizations have emphasized it for many years.
Since four out of five hospitalist programs have a hospitalist on site at night, and the majority of those programs have at least some nocturnist coverage, designing hospitalist programs and staffing models that meet the patient care need of 24/7 in-house coverage is a necessity. Also, given the strong demand for nocturnists, more and more program leaders are being challenged to evaluate creative alternatives to provide sustainable hospitalist services.
Some examples of creative solutions for in-house night coverage are implementing telemedicine for admissions, cross cover, or both; expanding coverage by advanced practice clinicians; and staggering shifts to cover late evenings and early mornings.
Perhaps we’ll see more questions about how hospitalist groups are addressing this need in future surveys?
Amanda Trask, MBA, MHA, FACHE, CMPE, SFHM, is national vice president, Hospital Medicine Service Line, at Catholic Health Initiatives, Englewood, Colo.
Alcohol misuse universal screening effective and efficient
Universal screening for alcohol misuse in acute medical admissions is feasible and can reduce readmissions for liver disease, according to a new study.
Detecting patients’ alcohol misuse early can help treat or prevent alcohol-related liver disease, such as cirrhosis; however, screening is not being used in a routine, effective way, according to Greta Westwood, PhD, head of Nursing, Midwifery, and AHP Research at Portsmouth (England) Hospitals and her fellow investigators.
“In primary care, screening is highly variable, and treatment rates are low, often focusing on patients who already have advanced psychiatric or physical illness,” Dr. Westwood and her colleagues wrote. “In addition, many patients with alcohol use disorders do not fully engage with primary care services for a variety of reasons, often leading to excessive use of the hospital ED as the first point of contact.”
Investigators conducted a retrospective, observational study of 53,165 patients who were admitted to the acute medical unit at Queen Alexandra Hospital, Portsmouth, England, between July 2011 and March 2014 (J Hepatol. 2017 Sep;67[3]:559-67).
More than half of patients were male (52%), the average patient age was 67 years, and the patients had an average of three previous hospital admissions.
Of the patients observed, 48,211 (90.68%) completed the screening test, while the remaining 4,934 (9.32%) did not.
Those who were not screened had a higher mortality rate than did those who were (8.30% vs 6.17%; P less than .001), were more likely to be discharged the same day (3.37% vs. 1.87%; P less than .001), and were more likely to discharge themselves (29.67% vs. 13.31%; P less than .001).
The screening process, an electronic modified version of the Paddington Alcohol Test, consisted of the nurses’ asking a series of questions about types of alcohol consumed, frequency and maximum daily amount, whether the admission was considered alcohol related, and they documented signs of alcohol withdrawal.
Patients were then given a score based on how the answers compared with the healthy level of alcohol consumption, with 0-2 points considered “low risk,” 3-5 points considered “increasing risk,” and 6-10 points considered “high risk.”
Those assigned a low-risk status were not referred to intervention, but doctors recommended increasing-risk patients attend a community alcohol intervention team for brief intervention, while high-risk patients were automatically referred to an Alcohol Specialist Nursing Service (ASNS).
Of those screened, there were 1,135 patients (2.33%) considered at increasing risk of alcohol misuse and 1,921 (3.98%) at high risk.
While 68.5% of patients with a high-risk score were referred to the ASNS, all those who were referred completed the medical detoxification course, according to investigators.
High-risk patients were found to have had, on average, more hospital visits than increasing- and low-risk patients – 4.74 visits, compared with 2.92 and 3.00, respectively; they also reported more ED trips – 7.68 visits, compared with 3.81 and 2.64, respectively.
Dr. Westwood and her colleagues found that, when using the screening tool, investigators were more likely to find signs of alcohol-related liver disease among those with higher scores.
Liver, pancreatic, and digestive disorders accounted for 22.1% of primary admission codes of high-risk patients, compared with 3.2% of low-risk patients.
Investigators wrote that this tool can help doctors identify at-risk patients early and attack the problem of alcohol misuse head on and in a timely manner.
“It is vital that patients with cirrhosis who continue to drink are identified and referred to dedicated hospital alcohol care teams,” Dr. Westwood and her colleagues wrote. “Screening can identify patients at an increased risk of alcohol-related harm whose range of diagnoses is not dissimilar to lower-risk patients and whose misuse of alcohol might otherwise have not been identified.”
Investigators did not account for decreased scores or testing effectiveness in patients readmitted and retested. Additionally, the long-term impact of ASNS care is still being studied.
Two investigators reported affiliations with the Learning Clinic, which created and licensed the analysis program that is part of the screening tool. All other investigators, including Dr. Westwood, reported no relevant financial disclosures.
[email protected]
On Twitter @eaztweets
Universal screening for alcohol misuse in acute medical admissions is feasible and can reduce readmissions for liver disease, according to a new study.
Detecting patients’ alcohol misuse early can help treat or prevent alcohol-related liver disease, such as cirrhosis; however, screening is not being used in a routine, effective way, according to Greta Westwood, PhD, head of Nursing, Midwifery, and AHP Research at Portsmouth (England) Hospitals and her fellow investigators.
“In primary care, screening is highly variable, and treatment rates are low, often focusing on patients who already have advanced psychiatric or physical illness,” Dr. Westwood and her colleagues wrote. “In addition, many patients with alcohol use disorders do not fully engage with primary care services for a variety of reasons, often leading to excessive use of the hospital ED as the first point of contact.”
Investigators conducted a retrospective, observational study of 53,165 patients who were admitted to the acute medical unit at Queen Alexandra Hospital, Portsmouth, England, between July 2011 and March 2014 (J Hepatol. 2017 Sep;67[3]:559-67).
More than half of patients were male (52%), the average patient age was 67 years, and the patients had an average of three previous hospital admissions.
Of the patients observed, 48,211 (90.68%) completed the screening test, while the remaining 4,934 (9.32%) did not.
Those who were not screened had a higher mortality rate than did those who were (8.30% vs 6.17%; P less than .001), were more likely to be discharged the same day (3.37% vs. 1.87%; P less than .001), and were more likely to discharge themselves (29.67% vs. 13.31%; P less than .001).
The screening process, an electronic modified version of the Paddington Alcohol Test, consisted of the nurses’ asking a series of questions about types of alcohol consumed, frequency and maximum daily amount, whether the admission was considered alcohol related, and they documented signs of alcohol withdrawal.
Patients were then given a score based on how the answers compared with the healthy level of alcohol consumption, with 0-2 points considered “low risk,” 3-5 points considered “increasing risk,” and 6-10 points considered “high risk.”
Those assigned a low-risk status were not referred to intervention, but doctors recommended increasing-risk patients attend a community alcohol intervention team for brief intervention, while high-risk patients were automatically referred to an Alcohol Specialist Nursing Service (ASNS).
Of those screened, there were 1,135 patients (2.33%) considered at increasing risk of alcohol misuse and 1,921 (3.98%) at high risk.
While 68.5% of patients with a high-risk score were referred to the ASNS, all those who were referred completed the medical detoxification course, according to investigators.
High-risk patients were found to have had, on average, more hospital visits than increasing- and low-risk patients – 4.74 visits, compared with 2.92 and 3.00, respectively; they also reported more ED trips – 7.68 visits, compared with 3.81 and 2.64, respectively.
Dr. Westwood and her colleagues found that, when using the screening tool, investigators were more likely to find signs of alcohol-related liver disease among those with higher scores.
Liver, pancreatic, and digestive disorders accounted for 22.1% of primary admission codes of high-risk patients, compared with 3.2% of low-risk patients.
Investigators wrote that this tool can help doctors identify at-risk patients early and attack the problem of alcohol misuse head on and in a timely manner.
“It is vital that patients with cirrhosis who continue to drink are identified and referred to dedicated hospital alcohol care teams,” Dr. Westwood and her colleagues wrote. “Screening can identify patients at an increased risk of alcohol-related harm whose range of diagnoses is not dissimilar to lower-risk patients and whose misuse of alcohol might otherwise have not been identified.”
Investigators did not account for decreased scores or testing effectiveness in patients readmitted and retested. Additionally, the long-term impact of ASNS care is still being studied.
Two investigators reported affiliations with the Learning Clinic, which created and licensed the analysis program that is part of the screening tool. All other investigators, including Dr. Westwood, reported no relevant financial disclosures.
[email protected]
On Twitter @eaztweets
Universal screening for alcohol misuse in acute medical admissions is feasible and can reduce readmissions for liver disease, according to a new study.
Detecting patients’ alcohol misuse early can help treat or prevent alcohol-related liver disease, such as cirrhosis; however, screening is not being used in a routine, effective way, according to Greta Westwood, PhD, head of Nursing, Midwifery, and AHP Research at Portsmouth (England) Hospitals and her fellow investigators.
“In primary care, screening is highly variable, and treatment rates are low, often focusing on patients who already have advanced psychiatric or physical illness,” Dr. Westwood and her colleagues wrote. “In addition, many patients with alcohol use disorders do not fully engage with primary care services for a variety of reasons, often leading to excessive use of the hospital ED as the first point of contact.”
Investigators conducted a retrospective, observational study of 53,165 patients who were admitted to the acute medical unit at Queen Alexandra Hospital, Portsmouth, England, between July 2011 and March 2014 (J Hepatol. 2017 Sep;67[3]:559-67).
More than half of patients were male (52%), the average patient age was 67 years, and the patients had an average of three previous hospital admissions.
Of the patients observed, 48,211 (90.68%) completed the screening test, while the remaining 4,934 (9.32%) did not.
Those who were not screened had a higher mortality rate than did those who were (8.30% vs 6.17%; P less than .001), were more likely to be discharged the same day (3.37% vs. 1.87%; P less than .001), and were more likely to discharge themselves (29.67% vs. 13.31%; P less than .001).
The screening process, an electronic modified version of the Paddington Alcohol Test, consisted of the nurses’ asking a series of questions about types of alcohol consumed, frequency and maximum daily amount, whether the admission was considered alcohol related, and they documented signs of alcohol withdrawal.
Patients were then given a score based on how the answers compared with the healthy level of alcohol consumption, with 0-2 points considered “low risk,” 3-5 points considered “increasing risk,” and 6-10 points considered “high risk.”
Those assigned a low-risk status were not referred to intervention, but doctors recommended increasing-risk patients attend a community alcohol intervention team for brief intervention, while high-risk patients were automatically referred to an Alcohol Specialist Nursing Service (ASNS).
Of those screened, there were 1,135 patients (2.33%) considered at increasing risk of alcohol misuse and 1,921 (3.98%) at high risk.
While 68.5% of patients with a high-risk score were referred to the ASNS, all those who were referred completed the medical detoxification course, according to investigators.
High-risk patients were found to have had, on average, more hospital visits than increasing- and low-risk patients – 4.74 visits, compared with 2.92 and 3.00, respectively; they also reported more ED trips – 7.68 visits, compared with 3.81 and 2.64, respectively.
Dr. Westwood and her colleagues found that, when using the screening tool, investigators were more likely to find signs of alcohol-related liver disease among those with higher scores.
Liver, pancreatic, and digestive disorders accounted for 22.1% of primary admission codes of high-risk patients, compared with 3.2% of low-risk patients.
Investigators wrote that this tool can help doctors identify at-risk patients early and attack the problem of alcohol misuse head on and in a timely manner.
“It is vital that patients with cirrhosis who continue to drink are identified and referred to dedicated hospital alcohol care teams,” Dr. Westwood and her colleagues wrote. “Screening can identify patients at an increased risk of alcohol-related harm whose range of diagnoses is not dissimilar to lower-risk patients and whose misuse of alcohol might otherwise have not been identified.”
Investigators did not account for decreased scores or testing effectiveness in patients readmitted and retested. Additionally, the long-term impact of ASNS care is still being studied.
Two investigators reported affiliations with the Learning Clinic, which created and licensed the analysis program that is part of the screening tool. All other investigators, including Dr. Westwood, reported no relevant financial disclosures.
[email protected]
On Twitter @eaztweets
FROM JOURNAL OF HEPATOLOGY
Key clinical point:
Major finding: Patients who were admitted and were not screened for alcohol misuse risk had a higher mortality rate, compared with those who were screened (8.3% vs. 6.17%; P less than .001).
Data source: Retrospective observational study of 53,165 patients admitted to the acute medical clinic of the Queen Alexandra Hospital, Portsmouth, England, between July 2011 and March 2014.
Disclosures: Two investigators reported affiliations with the Learning Clinic, which created and licensed the analysis program that is part of the screening tool. All other investigators, including Dr. Westwood, reported no relevant financial disclosures.