User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Uptake of new heart failure drugs slow despite guidelines
SNOWMASS, COLO. – As William T. Abraham, MD, speaks to colleagues around the country about heart failure therapy, he has noticed that the first-in-class drug ivabradine remains below the radar of most physicians.
“I’ve found that this is an agent that very few people know about, even though it’s been FDA [Food and Drug Administration] approved for about 3 years. It’s used fairly extensively in Europe because that’s where the pivotal SHIFT trial was done, but not very much in the United States,” according to Dr. Abraham, professor of medicine, physiology, and cell biology and director of the division of cardiovascular medicine at Ohio State University in Columbus.
That’s likely to change as word spreads about the May 2016 update of the American College of Cardiology/American Heart Association Guideline for the Management of Heart Failure. The update incorporated evidence-based recommendations on the use of two important new heart failure medications: ivabradine (Corlanor), which received a moderate class IIa recommendation, meaning the drug “should be considered,” and sacubitril/valsartan (Entresto), which received the strongest class I recommendation.
In the right patients, these two oral medications improve heart failure morbidity and mortality significantly beyond what’s achievable with what has been the gold standard, guideline-directed medical therapy. Dr. Abraham described how to get started using the two medications at the Annual Cardiovascular Conference at Snowmass.
Ivabradine
Ivabradine is a selective inhibitor of the sinoatrial pacemaker modulating I(f) current. It acts by slowing the sinus rate without reducing myocardial contractility.
“This agent does one thing and one thing alone: It lowers heart rate,” the cardiologist explained.
And that, he added, was sufficient to significantly reduce the risks of death due to heart failure and recurrent hospitalization for worsening heart failure in the pivotal SHIFT trial.
SHIFT included 6,505 patients with moderate to severe heart failure with reduced left ventricular ejection fraction (LVEF) and a resting heart rate above 70 bpm despite background guideline-directed medical therapy. Participants were randomized double blind to ivabradine titrated to a maximum of 7.5 mg twice daily or placebo and followed for a median of about 23 months. The rate of death due to heart failure was 3% with ivabradine and 5% with placebo, for a statistically significant 26% relative risk reduction favoring ivabradine.
But the drug’s main benefit was in reducing recurrent hospitalizations for heart failure, an endpoint of particular interest to health policy officials given that heart failure hospitalizations chew up a substantial proportion of the Medicare budget. Ivabradine reduced first hospitalizations for heart failure during the study period by 25%, second hospitalizations by 34%, and third hospitalizations by 29% (Eur Heart J. 2012 Nov;33[22]:2813-20).
The ACC/AHA guideline update stresses the importance of reserving ivabradine for heart failure patients whose resting heart rate exceeds 70 bpm, despite being on their maximum tolerated dose of a beta-blocker, Dr. Abraham noted.
Ivabradine is contraindicated in the setting of acute decompensated heart failure, severe liver disease, or hypotension, in patients on any of the numerous agents that strongly inhibit the enzyme cytochrome P450 3A4, and in those who have sick sinus syndrome, have sinoatrial block, or are pacemaker dependent.
Sacubitril/valsartan
Sacubitril inhibits neprilysin, an enzyme that blocks the action of endogenous vasoactive peptides including bradykinin, substance P, and natriuretic peptides, all of which counter important maladaptive mechanisms in heart failure. Sacubitril has been combined with the angiotensin receptor blocker valsartan to form the first-in-class angiotensin receptor neprilysin inhibitor, or ARNI, formerly known as LCZ696 and now marketed as Entresto.
In the pivotal double-blind PARADIGM-HF trial, 8,442 patients with heart failure with reduced ejection fraction were randomized to the ARNI at 200 mg b.i.d. or to enalapril at 10 mg b.i.d. on top of background guideline-directed medical therapy. The trial was stopped early because of evidence of overwhelming benefit: a 20% relative risk reduction in cardiovascular death and a 21% decrease in the risk of heart failure hospitalizations in the sacubitril/valsartan group, as well as significant reductions in heart failure symptoms and physical limitations (N Engl J Med. 2014 Sep 11;371[11]:993-1004).
The updated heart failure guidelines strongly recommend that patients with heart failure should be treated with either an ACE inhibitor, an angiotensin receptor blocker, or an ARNI. Further, patients who remain symptomatic on an ACE inhibitor or angiotensin receptor blocker should be switched to an ARNI; that’s a class Ib recommendation based upon the results of PARADIGM-HF.
In getting started using the ARNI, Dr. Abraham said it’s important to understand as background the selective nature of the PARADIGM-HF study design. During the single-blind run-in period of 5-8 weeks, roughly 10% of patients dropped out because they couldn’t tolerate enalapril at 10 mg b.i.d., and a similar percentage dropped out during the ARNI run-in. Thus, patients who couldn’t tolerate a low dose of an ACE inhibitor weren’t in the study. And patients capable of tolerating guideline-recommended full-dose ACE inhibitor therapy were not specifically sought for participation.
“So there are some unanswered questions about the ARNI. If you’re just getting started with this compound in treating your heart failure patients, my own feeling is you should maybe aim for the type of patient that was included in this trial: patients who could tolerate a moderate dose of an ACE inhibitor and had generally good blood pressure. That’s a great way to begin to get experience with this agent in heart failure,” the cardiologist advised.
He reported serving as a consultant to Abbott Vascular, Medtronic, Novartis, and St. Jude Medical.
SNOWMASS, COLO. – As William T. Abraham, MD, speaks to colleagues around the country about heart failure therapy, he has noticed that the first-in-class drug ivabradine remains below the radar of most physicians.
“I’ve found that this is an agent that very few people know about, even though it’s been FDA [Food and Drug Administration] approved for about 3 years. It’s used fairly extensively in Europe because that’s where the pivotal SHIFT trial was done, but not very much in the United States,” according to Dr. Abraham, professor of medicine, physiology, and cell biology and director of the division of cardiovascular medicine at Ohio State University in Columbus.
That’s likely to change as word spreads about the May 2016 update of the American College of Cardiology/American Heart Association Guideline for the Management of Heart Failure. The update incorporated evidence-based recommendations on the use of two important new heart failure medications: ivabradine (Corlanor), which received a moderate class IIa recommendation, meaning the drug “should be considered,” and sacubitril/valsartan (Entresto), which received the strongest class I recommendation.
In the right patients, these two oral medications improve heart failure morbidity and mortality significantly beyond what’s achievable with what has been the gold standard, guideline-directed medical therapy. Dr. Abraham described how to get started using the two medications at the Annual Cardiovascular Conference at Snowmass.
Ivabradine
Ivabradine is a selective inhibitor of the sinoatrial pacemaker modulating I(f) current. It acts by slowing the sinus rate without reducing myocardial contractility.
“This agent does one thing and one thing alone: It lowers heart rate,” the cardiologist explained.
And that, he added, was sufficient to significantly reduce the risks of death due to heart failure and recurrent hospitalization for worsening heart failure in the pivotal SHIFT trial.
SHIFT included 6,505 patients with moderate to severe heart failure with reduced left ventricular ejection fraction (LVEF) and a resting heart rate above 70 bpm despite background guideline-directed medical therapy. Participants were randomized double blind to ivabradine titrated to a maximum of 7.5 mg twice daily or placebo and followed for a median of about 23 months. The rate of death due to heart failure was 3% with ivabradine and 5% with placebo, for a statistically significant 26% relative risk reduction favoring ivabradine.
But the drug’s main benefit was in reducing recurrent hospitalizations for heart failure, an endpoint of particular interest to health policy officials given that heart failure hospitalizations chew up a substantial proportion of the Medicare budget. Ivabradine reduced first hospitalizations for heart failure during the study period by 25%, second hospitalizations by 34%, and third hospitalizations by 29% (Eur Heart J. 2012 Nov;33[22]:2813-20).
The ACC/AHA guideline update stresses the importance of reserving ivabradine for heart failure patients whose resting heart rate exceeds 70 bpm, despite being on their maximum tolerated dose of a beta-blocker, Dr. Abraham noted.
Ivabradine is contraindicated in the setting of acute decompensated heart failure, severe liver disease, or hypotension, in patients on any of the numerous agents that strongly inhibit the enzyme cytochrome P450 3A4, and in those who have sick sinus syndrome, have sinoatrial block, or are pacemaker dependent.
Sacubitril/valsartan
Sacubitril inhibits neprilysin, an enzyme that blocks the action of endogenous vasoactive peptides including bradykinin, substance P, and natriuretic peptides, all of which counter important maladaptive mechanisms in heart failure. Sacubitril has been combined with the angiotensin receptor blocker valsartan to form the first-in-class angiotensin receptor neprilysin inhibitor, or ARNI, formerly known as LCZ696 and now marketed as Entresto.
In the pivotal double-blind PARADIGM-HF trial, 8,442 patients with heart failure with reduced ejection fraction were randomized to the ARNI at 200 mg b.i.d. or to enalapril at 10 mg b.i.d. on top of background guideline-directed medical therapy. The trial was stopped early because of evidence of overwhelming benefit: a 20% relative risk reduction in cardiovascular death and a 21% decrease in the risk of heart failure hospitalizations in the sacubitril/valsartan group, as well as significant reductions in heart failure symptoms and physical limitations (N Engl J Med. 2014 Sep 11;371[11]:993-1004).
The updated heart failure guidelines strongly recommend that patients with heart failure should be treated with either an ACE inhibitor, an angiotensin receptor blocker, or an ARNI. Further, patients who remain symptomatic on an ACE inhibitor or angiotensin receptor blocker should be switched to an ARNI; that’s a class Ib recommendation based upon the results of PARADIGM-HF.
In getting started using the ARNI, Dr. Abraham said it’s important to understand as background the selective nature of the PARADIGM-HF study design. During the single-blind run-in period of 5-8 weeks, roughly 10% of patients dropped out because they couldn’t tolerate enalapril at 10 mg b.i.d., and a similar percentage dropped out during the ARNI run-in. Thus, patients who couldn’t tolerate a low dose of an ACE inhibitor weren’t in the study. And patients capable of tolerating guideline-recommended full-dose ACE inhibitor therapy were not specifically sought for participation.
“So there are some unanswered questions about the ARNI. If you’re just getting started with this compound in treating your heart failure patients, my own feeling is you should maybe aim for the type of patient that was included in this trial: patients who could tolerate a moderate dose of an ACE inhibitor and had generally good blood pressure. That’s a great way to begin to get experience with this agent in heart failure,” the cardiologist advised.
He reported serving as a consultant to Abbott Vascular, Medtronic, Novartis, and St. Jude Medical.
SNOWMASS, COLO. – As William T. Abraham, MD, speaks to colleagues around the country about heart failure therapy, he has noticed that the first-in-class drug ivabradine remains below the radar of most physicians.
“I’ve found that this is an agent that very few people know about, even though it’s been FDA [Food and Drug Administration] approved for about 3 years. It’s used fairly extensively in Europe because that’s where the pivotal SHIFT trial was done, but not very much in the United States,” according to Dr. Abraham, professor of medicine, physiology, and cell biology and director of the division of cardiovascular medicine at Ohio State University in Columbus.
That’s likely to change as word spreads about the May 2016 update of the American College of Cardiology/American Heart Association Guideline for the Management of Heart Failure. The update incorporated evidence-based recommendations on the use of two important new heart failure medications: ivabradine (Corlanor), which received a moderate class IIa recommendation, meaning the drug “should be considered,” and sacubitril/valsartan (Entresto), which received the strongest class I recommendation.
In the right patients, these two oral medications improve heart failure morbidity and mortality significantly beyond what’s achievable with what has been the gold standard, guideline-directed medical therapy. Dr. Abraham described how to get started using the two medications at the Annual Cardiovascular Conference at Snowmass.
Ivabradine
Ivabradine is a selective inhibitor of the sinoatrial pacemaker modulating I(f) current. It acts by slowing the sinus rate without reducing myocardial contractility.
“This agent does one thing and one thing alone: It lowers heart rate,” the cardiologist explained.
And that, he added, was sufficient to significantly reduce the risks of death due to heart failure and recurrent hospitalization for worsening heart failure in the pivotal SHIFT trial.
SHIFT included 6,505 patients with moderate to severe heart failure with reduced left ventricular ejection fraction (LVEF) and a resting heart rate above 70 bpm despite background guideline-directed medical therapy. Participants were randomized double blind to ivabradine titrated to a maximum of 7.5 mg twice daily or placebo and followed for a median of about 23 months. The rate of death due to heart failure was 3% with ivabradine and 5% with placebo, for a statistically significant 26% relative risk reduction favoring ivabradine.
But the drug’s main benefit was in reducing recurrent hospitalizations for heart failure, an endpoint of particular interest to health policy officials given that heart failure hospitalizations chew up a substantial proportion of the Medicare budget. Ivabradine reduced first hospitalizations for heart failure during the study period by 25%, second hospitalizations by 34%, and third hospitalizations by 29% (Eur Heart J. 2012 Nov;33[22]:2813-20).
The ACC/AHA guideline update stresses the importance of reserving ivabradine for heart failure patients whose resting heart rate exceeds 70 bpm, despite being on their maximum tolerated dose of a beta-blocker, Dr. Abraham noted.
Ivabradine is contraindicated in the setting of acute decompensated heart failure, severe liver disease, or hypotension, in patients on any of the numerous agents that strongly inhibit the enzyme cytochrome P450 3A4, and in those who have sick sinus syndrome, have sinoatrial block, or are pacemaker dependent.
Sacubitril/valsartan
Sacubitril inhibits neprilysin, an enzyme that blocks the action of endogenous vasoactive peptides including bradykinin, substance P, and natriuretic peptides, all of which counter important maladaptive mechanisms in heart failure. Sacubitril has been combined with the angiotensin receptor blocker valsartan to form the first-in-class angiotensin receptor neprilysin inhibitor, or ARNI, formerly known as LCZ696 and now marketed as Entresto.
In the pivotal double-blind PARADIGM-HF trial, 8,442 patients with heart failure with reduced ejection fraction were randomized to the ARNI at 200 mg b.i.d. or to enalapril at 10 mg b.i.d. on top of background guideline-directed medical therapy. The trial was stopped early because of evidence of overwhelming benefit: a 20% relative risk reduction in cardiovascular death and a 21% decrease in the risk of heart failure hospitalizations in the sacubitril/valsartan group, as well as significant reductions in heart failure symptoms and physical limitations (N Engl J Med. 2014 Sep 11;371[11]:993-1004).
The updated heart failure guidelines strongly recommend that patients with heart failure should be treated with either an ACE inhibitor, an angiotensin receptor blocker, or an ARNI. Further, patients who remain symptomatic on an ACE inhibitor or angiotensin receptor blocker should be switched to an ARNI; that’s a class Ib recommendation based upon the results of PARADIGM-HF.
In getting started using the ARNI, Dr. Abraham said it’s important to understand as background the selective nature of the PARADIGM-HF study design. During the single-blind run-in period of 5-8 weeks, roughly 10% of patients dropped out because they couldn’t tolerate enalapril at 10 mg b.i.d., and a similar percentage dropped out during the ARNI run-in. Thus, patients who couldn’t tolerate a low dose of an ACE inhibitor weren’t in the study. And patients capable of tolerating guideline-recommended full-dose ACE inhibitor therapy were not specifically sought for participation.
“So there are some unanswered questions about the ARNI. If you’re just getting started with this compound in treating your heart failure patients, my own feeling is you should maybe aim for the type of patient that was included in this trial: patients who could tolerate a moderate dose of an ACE inhibitor and had generally good blood pressure. That’s a great way to begin to get experience with this agent in heart failure,” the cardiologist advised.
He reported serving as a consultant to Abbott Vascular, Medtronic, Novartis, and St. Jude Medical.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
Tips from 'the father of modern networking'
Ivan Misner once spent one week on Necker Island – the tony 74-acre island in the British Virgin Islands that is entirely owned by billionaire Sir Richard Branson – because he met a guy at a convention.
And Misner is really good at networking.
“I stayed in touch with the person, and when there was an opportunity, I got invited to this incredible ethics program on Necker where I had a chance to meet Sir Richard. It all comes from building relationships with people,” said Misner, founder and chairman of BNI (Business Network International), a 32-year-old global business networking platform based in Charlotte, N.C., that has led CNN to call him “the father of modern networking.”
The why doesn’t matter most, Misner said. A person’s approach to networking, regardless of the hoped-for outcome, should always remain the same.
“The two key themes that I would address would be the mindset and the skill set,” he said.
The mindset is making sure one’s approach doesn’t “feel artificial,” Misner said.
“A lot of people, when they go to some kind of networking environment, they feel like they need to get a shower afterwards and think, ‘Ick, I don’t like that,’” Misner said. “The best way to become an effective networker is to go to networking events with the idea of being willing to help people and really believe in that and practice that. I’ve been doing this a long time and where I see it done wrong is when people use face-to-face networking as a cold-calling opportunity.”
Instead, Misner suggests, approach networking like it is “more about farming than it is about hunting.” Cultivate relationships with time and tenacity and don’t just expect them to be instant. Once the approach is set, Misner has a process he calls VCP – visibility, credibility, and profitability.
“Credibility is what takes time,” he said. “You really want to build credibility with somebody. It doesn’t happen overnight. People have to get to know, like, and trust you. It is the most time consuming portion of the VCP process... then, and only then, can you get to profitability. Where people know who you are, they know what you do, they know you’re good at it, and they’re willing to refer a business to you. They’re willing to put you in touch with other people.”
But even when a relationship gets struck early on, networking must be more than a few minutes at an SHM conference, a local chapter mixer, or a medical school reunion.
It’s the follow-up that makes all the impact. Misner calls that process 24/7/30.
Within 24 hours, send the person a note. An email, or even the seemingly lost art of a hand-written card. (If your handwriting is sloppy, Misner often recommends services that will send out legible notes on your behalf.)
Within a week, connect on social media. Focus on whatever platform that person has on their business card, or email signature. Connect where they like to connect to show the person you’re willing to make the effort.
Within a month, reach out to the person and set a time to talk, either face-to-face or via a telecommunication service like Skype.
“It’s these touch points that you make with people that build the relationship,” Misner said. “Without building a real relationship, there is almost no value in the networking effort because you basically are just waiting to stumble upon opportunities as opposed to building relationships and opportunities. It has to be more than just bumping into somebody at a meeting... otherwise you’re really wasting your time.”
Misner also notes that the point of networking is collaboration at some point. That partnership could be working on a research paper or a pilot project. Or just even getting a phone call returned to talk about something important to you.
“It’s not what you know or who you know, it’s how well you know each other that really counts,” he added. “And meeting people at events like HM17 is only the start of the process. It’s not the end of the process by any means, if you want to do this well.”
Ivan Misner once spent one week on Necker Island – the tony 74-acre island in the British Virgin Islands that is entirely owned by billionaire Sir Richard Branson – because he met a guy at a convention.
And Misner is really good at networking.
“I stayed in touch with the person, and when there was an opportunity, I got invited to this incredible ethics program on Necker where I had a chance to meet Sir Richard. It all comes from building relationships with people,” said Misner, founder and chairman of BNI (Business Network International), a 32-year-old global business networking platform based in Charlotte, N.C., that has led CNN to call him “the father of modern networking.”
The why doesn’t matter most, Misner said. A person’s approach to networking, regardless of the hoped-for outcome, should always remain the same.
“The two key themes that I would address would be the mindset and the skill set,” he said.
The mindset is making sure one’s approach doesn’t “feel artificial,” Misner said.
“A lot of people, when they go to some kind of networking environment, they feel like they need to get a shower afterwards and think, ‘Ick, I don’t like that,’” Misner said. “The best way to become an effective networker is to go to networking events with the idea of being willing to help people and really believe in that and practice that. I’ve been doing this a long time and where I see it done wrong is when people use face-to-face networking as a cold-calling opportunity.”
Instead, Misner suggests, approach networking like it is “more about farming than it is about hunting.” Cultivate relationships with time and tenacity and don’t just expect them to be instant. Once the approach is set, Misner has a process he calls VCP – visibility, credibility, and profitability.
“Credibility is what takes time,” he said. “You really want to build credibility with somebody. It doesn’t happen overnight. People have to get to know, like, and trust you. It is the most time consuming portion of the VCP process... then, and only then, can you get to profitability. Where people know who you are, they know what you do, they know you’re good at it, and they’re willing to refer a business to you. They’re willing to put you in touch with other people.”
But even when a relationship gets struck early on, networking must be more than a few minutes at an SHM conference, a local chapter mixer, or a medical school reunion.
It’s the follow-up that makes all the impact. Misner calls that process 24/7/30.
Within 24 hours, send the person a note. An email, or even the seemingly lost art of a hand-written card. (If your handwriting is sloppy, Misner often recommends services that will send out legible notes on your behalf.)
Within a week, connect on social media. Focus on whatever platform that person has on their business card, or email signature. Connect where they like to connect to show the person you’re willing to make the effort.
Within a month, reach out to the person and set a time to talk, either face-to-face or via a telecommunication service like Skype.
“It’s these touch points that you make with people that build the relationship,” Misner said. “Without building a real relationship, there is almost no value in the networking effort because you basically are just waiting to stumble upon opportunities as opposed to building relationships and opportunities. It has to be more than just bumping into somebody at a meeting... otherwise you’re really wasting your time.”
Misner also notes that the point of networking is collaboration at some point. That partnership could be working on a research paper or a pilot project. Or just even getting a phone call returned to talk about something important to you.
“It’s not what you know or who you know, it’s how well you know each other that really counts,” he added. “And meeting people at events like HM17 is only the start of the process. It’s not the end of the process by any means, if you want to do this well.”
Ivan Misner once spent one week on Necker Island – the tony 74-acre island in the British Virgin Islands that is entirely owned by billionaire Sir Richard Branson – because he met a guy at a convention.
And Misner is really good at networking.
“I stayed in touch with the person, and when there was an opportunity, I got invited to this incredible ethics program on Necker where I had a chance to meet Sir Richard. It all comes from building relationships with people,” said Misner, founder and chairman of BNI (Business Network International), a 32-year-old global business networking platform based in Charlotte, N.C., that has led CNN to call him “the father of modern networking.”
The why doesn’t matter most, Misner said. A person’s approach to networking, regardless of the hoped-for outcome, should always remain the same.
“The two key themes that I would address would be the mindset and the skill set,” he said.
The mindset is making sure one’s approach doesn’t “feel artificial,” Misner said.
“A lot of people, when they go to some kind of networking environment, they feel like they need to get a shower afterwards and think, ‘Ick, I don’t like that,’” Misner said. “The best way to become an effective networker is to go to networking events with the idea of being willing to help people and really believe in that and practice that. I’ve been doing this a long time and where I see it done wrong is when people use face-to-face networking as a cold-calling opportunity.”
Instead, Misner suggests, approach networking like it is “more about farming than it is about hunting.” Cultivate relationships with time and tenacity and don’t just expect them to be instant. Once the approach is set, Misner has a process he calls VCP – visibility, credibility, and profitability.
“Credibility is what takes time,” he said. “You really want to build credibility with somebody. It doesn’t happen overnight. People have to get to know, like, and trust you. It is the most time consuming portion of the VCP process... then, and only then, can you get to profitability. Where people know who you are, they know what you do, they know you’re good at it, and they’re willing to refer a business to you. They’re willing to put you in touch with other people.”
But even when a relationship gets struck early on, networking must be more than a few minutes at an SHM conference, a local chapter mixer, or a medical school reunion.
It’s the follow-up that makes all the impact. Misner calls that process 24/7/30.
Within 24 hours, send the person a note. An email, or even the seemingly lost art of a hand-written card. (If your handwriting is sloppy, Misner often recommends services that will send out legible notes on your behalf.)
Within a week, connect on social media. Focus on whatever platform that person has on their business card, or email signature. Connect where they like to connect to show the person you’re willing to make the effort.
Within a month, reach out to the person and set a time to talk, either face-to-face or via a telecommunication service like Skype.
“It’s these touch points that you make with people that build the relationship,” Misner said. “Without building a real relationship, there is almost no value in the networking effort because you basically are just waiting to stumble upon opportunities as opposed to building relationships and opportunities. It has to be more than just bumping into somebody at a meeting... otherwise you’re really wasting your time.”
Misner also notes that the point of networking is collaboration at some point. That partnership could be working on a research paper or a pilot project. Or just even getting a phone call returned to talk about something important to you.
“It’s not what you know or who you know, it’s how well you know each other that really counts,” he added. “And meeting people at events like HM17 is only the start of the process. It’s not the end of the process by any means, if you want to do this well.”
Transitioning from your current medical practice: an abbreviated step-by-step guide
You have decided it is time to move on from your current hospital or medical group position and transition into a new role. While this decision is exciting and well-earned after years of hard work, it is critical that you make a plan and take specific steps to ensure that the transition is seamless.
The steps below are recommendations to make this process smoother.
Step 1: Determine how you are leaving the practice and your proposed timeline
Before anything else, you should decide how you are leaving your practice. Are you leaving the practice of medicine altogether, or are you simply leaving your current position for a different position elsewhere? This distinction will dictate what steps are necessary. Timing is also critical when leaving a practice, as it will dictate what steps should be taken and when. Having specific but realistic goals is imperative. Select a goal date for leaving the practice, but be aware that this goal may need to be adjusted.
Step 2: Create your team of advisers
Whether you are leaving your current practice or transitioning to a different position, it is extremely important to have the right individuals on your team. You should consider enlisting an attorney, a financial adviser, and an accountant to help facilitate the process. Enlisting lawyers with certain areas of expertise, such as in the areas of employment restrictive covenants, health care, or tax, may also be extremely beneficial and helpful throughout the process.
Step 3: Review your current employment agreement
It is quite likely that at the onset of your current employment arrangement, you signed an employment agreement with your hospital or group. You will want to carefully review this agreement, as it may contain provisions that can affect the steps you should take before you leave your current practice and work elsewhere. These provisions include the following:
a) Noncompetition provisions
It is critical to determine whether or not there are any restrictive covenants in your employment agreement that limit where you can work after you transition from your current practice into a new role. Restrictive covenants include noncompetition and nonsolicitation provisions, and prohibit employees from working at certain places or in certain geographic areas after they leave their current place of employment. Rules surrounding restrictive covenants vary from state to state. If there are restrictive covenants in your agreement, be sure to understand the scope of the covenant, including the geographic and temporal scope, as well as the types of medicine you are prohibited from practicing. If the covenants seem too broad or unnecessarily restrictive, consult with an attorney, as overly broad or unduly burdensome covenants are often unenforceable. However, a state-by-state analysis is required.
b) Notice and termination provisions
It is important to review whether or not there are any notice requirements in your employment agreement, which may require you to notify your employer in advance of a departure. Make sure to comply with the time requirements in the notice provision to avoid a breach of the agreement. It is also critical to determine whether terminating an agreement early will result in any termination penalties. At times, employers will impose a penalty if an employee prematurely terminates a working relationship. Understanding the penalties associated with terminating your agreement will allow you to decide whether you want to cancel the agreement and pay the penalty or push back your timeline until the end of the agreement’s term to avoid termination fees.
Step 4: Licensure obligations
Further, if your practice bills Medicare, you will want to file certain forms with Medicare to show that you are either changing your practice location or leaving medicine. For example, if you are leaving the hospital or group to practice elsewhere, you will need to fill out forms in order for your old group to submit claims and receive payments for Medicare services you provided while you were still part of that group. Furthermore, you will need to file reassignment forms to allow your new practice to bill on your behalf. Understanding which forms to complete can be confusing, so enlisting the help of a healthcare attorney may be worthwhile.
Step 5: Discuss your transition with your insurance representative
Even after you leave your current practice, you may be exposed to litigation for services you provided while you were employed or otherwise retained by such practice. To ensure that you are protected, discuss your insurance policy with your insurance representative. Review whether your insurance policy is “occurrence” or “claims-made.” If you have an occurrence policy, you are protected from covered incidents that occur during the policy period, regardless if your policy is still in existence. Claims-made policies only provide coverage for claims where both the incident and the claim occur during the policy period. For example, if you cancel your policy on March 1, and are sued on April 1 for an incident that allegedly occurred on Feb. 1, your claims-made insurance policy will not protect you. Therefore, it is important to analyze your policies to determine if tail insurance is needed.
There are a number of other issues you will want to address before you leave your practice, including financial responsibilities and medical record and privacy obligations. To ensure that you leave your practice properly, you should contact an experienced lawyer who can help you navigate this process.
Steven M. Harris is a nationally recognized health care attorney and a member of the law firm McDonald Hopkins LLC in Chicago. Write to him at [email protected].
You have decided it is time to move on from your current hospital or medical group position and transition into a new role. While this decision is exciting and well-earned after years of hard work, it is critical that you make a plan and take specific steps to ensure that the transition is seamless.
The steps below are recommendations to make this process smoother.
Step 1: Determine how you are leaving the practice and your proposed timeline
Before anything else, you should decide how you are leaving your practice. Are you leaving the practice of medicine altogether, or are you simply leaving your current position for a different position elsewhere? This distinction will dictate what steps are necessary. Timing is also critical when leaving a practice, as it will dictate what steps should be taken and when. Having specific but realistic goals is imperative. Select a goal date for leaving the practice, but be aware that this goal may need to be adjusted.
Step 2: Create your team of advisers
Whether you are leaving your current practice or transitioning to a different position, it is extremely important to have the right individuals on your team. You should consider enlisting an attorney, a financial adviser, and an accountant to help facilitate the process. Enlisting lawyers with certain areas of expertise, such as in the areas of employment restrictive covenants, health care, or tax, may also be extremely beneficial and helpful throughout the process.
Step 3: Review your current employment agreement
It is quite likely that at the onset of your current employment arrangement, you signed an employment agreement with your hospital or group. You will want to carefully review this agreement, as it may contain provisions that can affect the steps you should take before you leave your current practice and work elsewhere. These provisions include the following:
a) Noncompetition provisions
It is critical to determine whether or not there are any restrictive covenants in your employment agreement that limit where you can work after you transition from your current practice into a new role. Restrictive covenants include noncompetition and nonsolicitation provisions, and prohibit employees from working at certain places or in certain geographic areas after they leave their current place of employment. Rules surrounding restrictive covenants vary from state to state. If there are restrictive covenants in your agreement, be sure to understand the scope of the covenant, including the geographic and temporal scope, as well as the types of medicine you are prohibited from practicing. If the covenants seem too broad or unnecessarily restrictive, consult with an attorney, as overly broad or unduly burdensome covenants are often unenforceable. However, a state-by-state analysis is required.
b) Notice and termination provisions
It is important to review whether or not there are any notice requirements in your employment agreement, which may require you to notify your employer in advance of a departure. Make sure to comply with the time requirements in the notice provision to avoid a breach of the agreement. It is also critical to determine whether terminating an agreement early will result in any termination penalties. At times, employers will impose a penalty if an employee prematurely terminates a working relationship. Understanding the penalties associated with terminating your agreement will allow you to decide whether you want to cancel the agreement and pay the penalty or push back your timeline until the end of the agreement’s term to avoid termination fees.
Step 4: Licensure obligations
Further, if your practice bills Medicare, you will want to file certain forms with Medicare to show that you are either changing your practice location or leaving medicine. For example, if you are leaving the hospital or group to practice elsewhere, you will need to fill out forms in order for your old group to submit claims and receive payments for Medicare services you provided while you were still part of that group. Furthermore, you will need to file reassignment forms to allow your new practice to bill on your behalf. Understanding which forms to complete can be confusing, so enlisting the help of a healthcare attorney may be worthwhile.
Step 5: Discuss your transition with your insurance representative
Even after you leave your current practice, you may be exposed to litigation for services you provided while you were employed or otherwise retained by such practice. To ensure that you are protected, discuss your insurance policy with your insurance representative. Review whether your insurance policy is “occurrence” or “claims-made.” If you have an occurrence policy, you are protected from covered incidents that occur during the policy period, regardless if your policy is still in existence. Claims-made policies only provide coverage for claims where both the incident and the claim occur during the policy period. For example, if you cancel your policy on March 1, and are sued on April 1 for an incident that allegedly occurred on Feb. 1, your claims-made insurance policy will not protect you. Therefore, it is important to analyze your policies to determine if tail insurance is needed.
There are a number of other issues you will want to address before you leave your practice, including financial responsibilities and medical record and privacy obligations. To ensure that you leave your practice properly, you should contact an experienced lawyer who can help you navigate this process.
Steven M. Harris is a nationally recognized health care attorney and a member of the law firm McDonald Hopkins LLC in Chicago. Write to him at [email protected].
You have decided it is time to move on from your current hospital or medical group position and transition into a new role. While this decision is exciting and well-earned after years of hard work, it is critical that you make a plan and take specific steps to ensure that the transition is seamless.
The steps below are recommendations to make this process smoother.
Step 1: Determine how you are leaving the practice and your proposed timeline
Before anything else, you should decide how you are leaving your practice. Are you leaving the practice of medicine altogether, or are you simply leaving your current position for a different position elsewhere? This distinction will dictate what steps are necessary. Timing is also critical when leaving a practice, as it will dictate what steps should be taken and when. Having specific but realistic goals is imperative. Select a goal date for leaving the practice, but be aware that this goal may need to be adjusted.
Step 2: Create your team of advisers
Whether you are leaving your current practice or transitioning to a different position, it is extremely important to have the right individuals on your team. You should consider enlisting an attorney, a financial adviser, and an accountant to help facilitate the process. Enlisting lawyers with certain areas of expertise, such as in the areas of employment restrictive covenants, health care, or tax, may also be extremely beneficial and helpful throughout the process.
Step 3: Review your current employment agreement
It is quite likely that at the onset of your current employment arrangement, you signed an employment agreement with your hospital or group. You will want to carefully review this agreement, as it may contain provisions that can affect the steps you should take before you leave your current practice and work elsewhere. These provisions include the following:
a) Noncompetition provisions
It is critical to determine whether or not there are any restrictive covenants in your employment agreement that limit where you can work after you transition from your current practice into a new role. Restrictive covenants include noncompetition and nonsolicitation provisions, and prohibit employees from working at certain places or in certain geographic areas after they leave their current place of employment. Rules surrounding restrictive covenants vary from state to state. If there are restrictive covenants in your agreement, be sure to understand the scope of the covenant, including the geographic and temporal scope, as well as the types of medicine you are prohibited from practicing. If the covenants seem too broad or unnecessarily restrictive, consult with an attorney, as overly broad or unduly burdensome covenants are often unenforceable. However, a state-by-state analysis is required.
b) Notice and termination provisions
It is important to review whether or not there are any notice requirements in your employment agreement, which may require you to notify your employer in advance of a departure. Make sure to comply with the time requirements in the notice provision to avoid a breach of the agreement. It is also critical to determine whether terminating an agreement early will result in any termination penalties. At times, employers will impose a penalty if an employee prematurely terminates a working relationship. Understanding the penalties associated with terminating your agreement will allow you to decide whether you want to cancel the agreement and pay the penalty or push back your timeline until the end of the agreement’s term to avoid termination fees.
Step 4: Licensure obligations
Further, if your practice bills Medicare, you will want to file certain forms with Medicare to show that you are either changing your practice location or leaving medicine. For example, if you are leaving the hospital or group to practice elsewhere, you will need to fill out forms in order for your old group to submit claims and receive payments for Medicare services you provided while you were still part of that group. Furthermore, you will need to file reassignment forms to allow your new practice to bill on your behalf. Understanding which forms to complete can be confusing, so enlisting the help of a healthcare attorney may be worthwhile.
Step 5: Discuss your transition with your insurance representative
Even after you leave your current practice, you may be exposed to litigation for services you provided while you were employed or otherwise retained by such practice. To ensure that you are protected, discuss your insurance policy with your insurance representative. Review whether your insurance policy is “occurrence” or “claims-made.” If you have an occurrence policy, you are protected from covered incidents that occur during the policy period, regardless if your policy is still in existence. Claims-made policies only provide coverage for claims where both the incident and the claim occur during the policy period. For example, if you cancel your policy on March 1, and are sued on April 1 for an incident that allegedly occurred on Feb. 1, your claims-made insurance policy will not protect you. Therefore, it is important to analyze your policies to determine if tail insurance is needed.
There are a number of other issues you will want to address before you leave your practice, including financial responsibilities and medical record and privacy obligations. To ensure that you leave your practice properly, you should contact an experienced lawyer who can help you navigate this process.
Steven M. Harris is a nationally recognized health care attorney and a member of the law firm McDonald Hopkins LLC in Chicago. Write to him at [email protected].
New-onset AF boosts bad HFrEF outcomes
WASHINGTON – New onset atrial fibrillation more than doubled the rate of adverse outcomes in patients with heart failure with reduced ejection fraction in a review of more than 15,000 such patients.
In 9,934 patients with heart failure with reduced ejection fraction (HFrEF) and no history of atrial fibrillation (AF), development of new-onset AF was linked with a greater than twofold increased risk of cardiovascular disease death or hospitalization for heart failure during follow-up, compared with HFrEF patients who did not initially have or later develop heart failure, after adjustment for several demographic and clinical variables, John J.V. McMurray, MD, said at the annual meeting of the American College of Cardiology. This difference for the primary endpoint of his analysis was statistically significant.
The 1,645 patients with paroxysmal AF at the start of their follow-up also had a significantly increased rate of cardiovascular death or heart failure hospitalization, but their increased risk when compared with HFrEF patients who didn’t develop AF was a much more modest 20% in his fully adjusted analysis. The patients who began follow-up with paroxysmal AF also had a relatively increased relative stroke rate of 33% when compared with HFrEF patients without AF at baseline who remained AF free, but the all-cause mortality rate among those with paroxysmal AF wasn’t significantly elevated, compared with the comparator group.
The 3,770 patients with persistent or permanent AF at baseline showed no statistically significant spike in their adverse event rates, compared with patients without AF, for any of the examined endpoints. The study group also included 66 patients with an undefined form of AF who weren’t included in these analyses.
“It’s the first episodes and paroxysmal episodes that cause trouble, and the trouble they cause is stroke,” Dr. McMurray said in an interview. Their stroke risk gets exacerbated in clinical practice, because these patients often don’t receive the stroke prevention they need in the form of anticoagulation treatment.
“We find over and over that patients with paroxysmal AF are not anticoagulated as frequently as they should be,” Dr. McMurray said. And HFrEF patients with a first AF episode need anticoagulation, too, as soon as AF is diagnosed, he advised.
He went a step further and speculated that the reason why HFrEF patients with new onset AF did so poorly in his analysis was because they already had several prior, brief AF episodes that had gone undetected. “Many of these patients probably had undiagnosed, clinically unapparent AF episodes” that then resulted in strokes, he suggested.
The upshot is that patients with HFrEF may need more aggressive monitoring for new-onset AF, possibly in the form of small, implanted arrhythmia-detection devices. Dr. McMurray said that he and other researchers are currently testing whether this hypothesis is correct. “We and others are now looking at this because these new data are convincing that new-onset AF is bad news [for HFrEF patients].”
In the analysis, “we looked only at clinically recognized and adjudicated new-onset AF. Goodness knows how many HFrEF patients are having unrecognized paroxysmal AF. Almost certainly there is a lot that is unrecognized” that potentially could be detected using a small implanted arrhythmia monitor, which could then lead to earlier anticoagulant treatment as well as possible treatment with antiarrhythmic drugs or with catheter ablation, Dr. McMurray said. Looking for undetected AF in HFrEF patients “is where the science is moving.”
The findings that Dr. McMurray reported are “something we should act on,” commented Adrian F. Hernandez, MD, professor of medicine and a cardiologist at Duke University in Durham, N.C. The comorbidity of AF in HFrEF patients requires “aggressive anticoagulation, and also a review of their heart failure medical treatment to be sure that is optimized, because AF could be a sign of worsening heart failure,” Dr. Hernandez said in an interview. “We may need to more aggressively get HFrEF patients with AF into normal sinus rhythm.”
When Mikhail Kosiborod, MD, treats HFrEF patients with a high risk for AF, such as patients with lower ejection fractions, a dilated left ventricle, or a dilated atrium, “I frequently do 30-day loop recordings in these patients because of their risk for incident AF,” Dr. Kosiborod said in an interview. “We don’t yet have convincing evidence for this, but it makes sense.”
Another finding from his analysis was that the HFrEF patients enrolled in these two trials did not get treatment with a mineralocorticoid receptor antagonist – spironolactone or eplerenone – “as often as they should,” with treatment rates of 44%-48%, compared with use of a beta-blocker in 92%-95% of patients. Treatment with eplerenone (Inspra) “has been shown to reduce the risk for new onset AF, so adding eplerenone or spironolactone is an important step that could be taken to try to prevent AF as well as treat the HFrEF and reduce mortality,” Dr. McMurray said.
PARADIGM-HF and ATMOSPHERE were funded by Novartis. Dr. McMurray has been a consultant to and has received travel and research support from Novartis, and he has received research and travel support from Amgen. Dr. Hernandez has received honoraria from Amgen, AstraZeneca, Janssen, Merck, and Novartis, and has received research support from Amgen, Bayer, Merck, and Portola. Dr. Kosiborod has been a consultant to several drug companies, and he has received research funding from AstraZeneca, Boehringer Ingelheim, Gilead, and Sanofi-Aventis.
[email protected]
On Twitter @mitchelzoler
WASHINGTON – New onset atrial fibrillation more than doubled the rate of adverse outcomes in patients with heart failure with reduced ejection fraction in a review of more than 15,000 such patients.
In 9,934 patients with heart failure with reduced ejection fraction (HFrEF) and no history of atrial fibrillation (AF), development of new-onset AF was linked with a greater than twofold increased risk of cardiovascular disease death or hospitalization for heart failure during follow-up, compared with HFrEF patients who did not initially have or later develop heart failure, after adjustment for several demographic and clinical variables, John J.V. McMurray, MD, said at the annual meeting of the American College of Cardiology. This difference for the primary endpoint of his analysis was statistically significant.
The 1,645 patients with paroxysmal AF at the start of their follow-up also had a significantly increased rate of cardiovascular death or heart failure hospitalization, but their increased risk when compared with HFrEF patients who didn’t develop AF was a much more modest 20% in his fully adjusted analysis. The patients who began follow-up with paroxysmal AF also had a relatively increased relative stroke rate of 33% when compared with HFrEF patients without AF at baseline who remained AF free, but the all-cause mortality rate among those with paroxysmal AF wasn’t significantly elevated, compared with the comparator group.
The 3,770 patients with persistent or permanent AF at baseline showed no statistically significant spike in their adverse event rates, compared with patients without AF, for any of the examined endpoints. The study group also included 66 patients with an undefined form of AF who weren’t included in these analyses.
“It’s the first episodes and paroxysmal episodes that cause trouble, and the trouble they cause is stroke,” Dr. McMurray said in an interview. Their stroke risk gets exacerbated in clinical practice, because these patients often don’t receive the stroke prevention they need in the form of anticoagulation treatment.
“We find over and over that patients with paroxysmal AF are not anticoagulated as frequently as they should be,” Dr. McMurray said. And HFrEF patients with a first AF episode need anticoagulation, too, as soon as AF is diagnosed, he advised.
He went a step further and speculated that the reason why HFrEF patients with new onset AF did so poorly in his analysis was because they already had several prior, brief AF episodes that had gone undetected. “Many of these patients probably had undiagnosed, clinically unapparent AF episodes” that then resulted in strokes, he suggested.
The upshot is that patients with HFrEF may need more aggressive monitoring for new-onset AF, possibly in the form of small, implanted arrhythmia-detection devices. Dr. McMurray said that he and other researchers are currently testing whether this hypothesis is correct. “We and others are now looking at this because these new data are convincing that new-onset AF is bad news [for HFrEF patients].”
In the analysis, “we looked only at clinically recognized and adjudicated new-onset AF. Goodness knows how many HFrEF patients are having unrecognized paroxysmal AF. Almost certainly there is a lot that is unrecognized” that potentially could be detected using a small implanted arrhythmia monitor, which could then lead to earlier anticoagulant treatment as well as possible treatment with antiarrhythmic drugs or with catheter ablation, Dr. McMurray said. Looking for undetected AF in HFrEF patients “is where the science is moving.”
The findings that Dr. McMurray reported are “something we should act on,” commented Adrian F. Hernandez, MD, professor of medicine and a cardiologist at Duke University in Durham, N.C. The comorbidity of AF in HFrEF patients requires “aggressive anticoagulation, and also a review of their heart failure medical treatment to be sure that is optimized, because AF could be a sign of worsening heart failure,” Dr. Hernandez said in an interview. “We may need to more aggressively get HFrEF patients with AF into normal sinus rhythm.”
When Mikhail Kosiborod, MD, treats HFrEF patients with a high risk for AF, such as patients with lower ejection fractions, a dilated left ventricle, or a dilated atrium, “I frequently do 30-day loop recordings in these patients because of their risk for incident AF,” Dr. Kosiborod said in an interview. “We don’t yet have convincing evidence for this, but it makes sense.”
Another finding from his analysis was that the HFrEF patients enrolled in these two trials did not get treatment with a mineralocorticoid receptor antagonist – spironolactone or eplerenone – “as often as they should,” with treatment rates of 44%-48%, compared with use of a beta-blocker in 92%-95% of patients. Treatment with eplerenone (Inspra) “has been shown to reduce the risk for new onset AF, so adding eplerenone or spironolactone is an important step that could be taken to try to prevent AF as well as treat the HFrEF and reduce mortality,” Dr. McMurray said.
PARADIGM-HF and ATMOSPHERE were funded by Novartis. Dr. McMurray has been a consultant to and has received travel and research support from Novartis, and he has received research and travel support from Amgen. Dr. Hernandez has received honoraria from Amgen, AstraZeneca, Janssen, Merck, and Novartis, and has received research support from Amgen, Bayer, Merck, and Portola. Dr. Kosiborod has been a consultant to several drug companies, and he has received research funding from AstraZeneca, Boehringer Ingelheim, Gilead, and Sanofi-Aventis.
[email protected]
On Twitter @mitchelzoler
WASHINGTON – New onset atrial fibrillation more than doubled the rate of adverse outcomes in patients with heart failure with reduced ejection fraction in a review of more than 15,000 such patients.
In 9,934 patients with heart failure with reduced ejection fraction (HFrEF) and no history of atrial fibrillation (AF), development of new-onset AF was linked with a greater than twofold increased risk of cardiovascular disease death or hospitalization for heart failure during follow-up, compared with HFrEF patients who did not initially have or later develop heart failure, after adjustment for several demographic and clinical variables, John J.V. McMurray, MD, said at the annual meeting of the American College of Cardiology. This difference for the primary endpoint of his analysis was statistically significant.
The 1,645 patients with paroxysmal AF at the start of their follow-up also had a significantly increased rate of cardiovascular death or heart failure hospitalization, but their increased risk when compared with HFrEF patients who didn’t develop AF was a much more modest 20% in his fully adjusted analysis. The patients who began follow-up with paroxysmal AF also had a relatively increased relative stroke rate of 33% when compared with HFrEF patients without AF at baseline who remained AF free, but the all-cause mortality rate among those with paroxysmal AF wasn’t significantly elevated, compared with the comparator group.
The 3,770 patients with persistent or permanent AF at baseline showed no statistically significant spike in their adverse event rates, compared with patients without AF, for any of the examined endpoints. The study group also included 66 patients with an undefined form of AF who weren’t included in these analyses.
“It’s the first episodes and paroxysmal episodes that cause trouble, and the trouble they cause is stroke,” Dr. McMurray said in an interview. Their stroke risk gets exacerbated in clinical practice, because these patients often don’t receive the stroke prevention they need in the form of anticoagulation treatment.
“We find over and over that patients with paroxysmal AF are not anticoagulated as frequently as they should be,” Dr. McMurray said. And HFrEF patients with a first AF episode need anticoagulation, too, as soon as AF is diagnosed, he advised.
He went a step further and speculated that the reason why HFrEF patients with new onset AF did so poorly in his analysis was because they already had several prior, brief AF episodes that had gone undetected. “Many of these patients probably had undiagnosed, clinically unapparent AF episodes” that then resulted in strokes, he suggested.
The upshot is that patients with HFrEF may need more aggressive monitoring for new-onset AF, possibly in the form of small, implanted arrhythmia-detection devices. Dr. McMurray said that he and other researchers are currently testing whether this hypothesis is correct. “We and others are now looking at this because these new data are convincing that new-onset AF is bad news [for HFrEF patients].”
In the analysis, “we looked only at clinically recognized and adjudicated new-onset AF. Goodness knows how many HFrEF patients are having unrecognized paroxysmal AF. Almost certainly there is a lot that is unrecognized” that potentially could be detected using a small implanted arrhythmia monitor, which could then lead to earlier anticoagulant treatment as well as possible treatment with antiarrhythmic drugs or with catheter ablation, Dr. McMurray said. Looking for undetected AF in HFrEF patients “is where the science is moving.”
The findings that Dr. McMurray reported are “something we should act on,” commented Adrian F. Hernandez, MD, professor of medicine and a cardiologist at Duke University in Durham, N.C. The comorbidity of AF in HFrEF patients requires “aggressive anticoagulation, and also a review of their heart failure medical treatment to be sure that is optimized, because AF could be a sign of worsening heart failure,” Dr. Hernandez said in an interview. “We may need to more aggressively get HFrEF patients with AF into normal sinus rhythm.”
When Mikhail Kosiborod, MD, treats HFrEF patients with a high risk for AF, such as patients with lower ejection fractions, a dilated left ventricle, or a dilated atrium, “I frequently do 30-day loop recordings in these patients because of their risk for incident AF,” Dr. Kosiborod said in an interview. “We don’t yet have convincing evidence for this, but it makes sense.”
Another finding from his analysis was that the HFrEF patients enrolled in these two trials did not get treatment with a mineralocorticoid receptor antagonist – spironolactone or eplerenone – “as often as they should,” with treatment rates of 44%-48%, compared with use of a beta-blocker in 92%-95% of patients. Treatment with eplerenone (Inspra) “has been shown to reduce the risk for new onset AF, so adding eplerenone or spironolactone is an important step that could be taken to try to prevent AF as well as treat the HFrEF and reduce mortality,” Dr. McMurray said.
PARADIGM-HF and ATMOSPHERE were funded by Novartis. Dr. McMurray has been a consultant to and has received travel and research support from Novartis, and he has received research and travel support from Amgen. Dr. Hernandez has received honoraria from Amgen, AstraZeneca, Janssen, Merck, and Novartis, and has received research support from Amgen, Bayer, Merck, and Portola. Dr. Kosiborod has been a consultant to several drug companies, and he has received research funding from AstraZeneca, Boehringer Ingelheim, Gilead, and Sanofi-Aventis.
[email protected]
On Twitter @mitchelzoler
AT ACC 17
Key clinical point:
Major finding: Adverse outcomes were more than twice as frequent in HFrEF patients with incident atrial fibrillation, compared with those without AF.
Data source: Post hoc analysis of 15,415 heart failure patients enrolled in the PARADIGM-HF and ATMOSPHERE trials.
Disclosures: PARADIGM-HF and ATMOSPHERE were funded by Novartis. Dr. McMurray has been a consultant to and has received travel and research support from Novartis, and he has received research and travel support from Amgen.
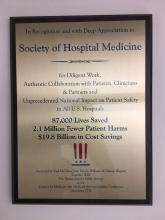
Evolution of a movement
One of the most enduring lessons I have learned during my time in hospital medicine is that hospitalists are always evolving, much like the specialty and healthcare system of which they are a part. And during my time as president of the Society of Hospital Medicine (SHM), I have come to realize how SHM provides its members with the resources to help us continue that evolution through our career journeys as a part of the hospital medicine movement.
Over a year ago, I ascended to president of SHM’s board of directors at HM16, the annual meeting in San Diego. Now, I am eagerly looking forward to HM17 next month, in Las Vegas, which we expect to be, yet again, the biggest, best, most innovative and most energetic gathering of hospitalists. As that meeting will mark the end of my tenure as president of the board, I’m also inclined to look back and survey what has happened over the last year, both personally and professionally.
The personal perspective is easy. I have a different position within my organization: president of Cleveland Clinic Akron General and the Southern Region, one which I would and could never have anticipated a year ago. It challenges, exhausts, exhilarates, and teaches me every day. I am also celebrating my 15th wedding anniversary and have three amazing children who seem to evolve in front of my eyes every day.
And, professionally, at HM16 (and on these pages a year ago), I framed what I felt were four critical directions for SHM and have a few thoughts on the work we have done over the last year.
1. Expand and engage SHM’s membership. SHM continues to be the envy of professional organizations, growing each year. More important than sole growth is our pursuit of connecting hospitalists to SHM’s resources and to each other; we have been incredibly active this past year. For instance, SHM is embarking on an engagement survey of HM groups, and is investing in new technologies to support membership. We are now a CME-accrediting organization and are moving the SHM Learning Portal to a new, enhanced platform. We launched a long-term communications strategy that is tied to engagement and a more nimble and mobile experience for our members. The SHM Leadership Academy sold out. HM17 is poised to be another success. And finally, we are increasingly appreciating that a strong SHM must have a vibrant chapter structure to ensure connections between our membership, staff, and board.
2. Focus on patient- and family-centered care. A look at the HM17 curriculum reinforces SHM’s awareness that patients and hospitalists must be more assertive in developing skills in communication and empathy. By doing so, they support a culture and environment wherein patients are active participants their care. Members of our Patient Experience Committee are presenting courses and workshops in Las Vegas, and last year’s annual meeting featured an entire pre-course on communication skills. Hospitalists play a signature role in the Cleveland Clinic’s national conference on improving the patient experience, and the committee has an advisory council of patients and advocates to guide their work.
3. Move assertively to define our role in an era of risk and reform. Last year’s national election will probably create policy upheavals that are difficult to either anticipate or plan for. However, the evolution of Medicare, Medicaid, and commercial payers toward passing risk (and reward) onto physicians, hospitals, and systems, likely is unstoppable. SHM held a board retreat with key hospital leaders (including Patrick Conway, MD, MSc, MHM, deputy administrator for Innovation and Quality at CMS and director of the Center for Medicare and Medicaid Innovation, and a keynote speaker at HM17) to outline a framework to engage and educate our membership by leveraging the work of our Public Policy, Education, and Practice Management committees.
4. Define our stance regarding specialty recognition: The complexities of this issue are political as well as logistical. SHM has continued to build out the infrastructure for Recognition of Focused Practice with the launch of SPARK ONE (our Focused Practice in Hospital Medicine exam preparation product), but the gaps between the curricula of internal medicine and family medicine residencies, and our daily clinical realities, will continue to exist for the foreseeable future. Pediatrics has established a board requirement for pediatric hospital medicine, but it is still unclear if this is the future of adult hospital medicine.
In sum
As I prepare to the pass to baton to Dr. Ron Greeno for 2017-18, I am reminded of one of the pearls of a former boss and mentor of mine who preached that career satisfaction comes from finding opportunities to achieve three goals: addressing meaningful challenges, working with compelling individuals, and learning something new every day. I would like to thank the board, SHM CEO Larry Wellikson, MD, MHM, and the society staff and volunteers, and, most of all, the many SHM members with whom I have met and spoken over the last year for providing me with exactly that opportunity.
I look forward to continuing to serve an active role in SHM, an organization that can provide you with those same opportunities and resources to help you grow, evolve and be an active participant in the hospital medicine movement.
One of the most enduring lessons I have learned during my time in hospital medicine is that hospitalists are always evolving, much like the specialty and healthcare system of which they are a part. And during my time as president of the Society of Hospital Medicine (SHM), I have come to realize how SHM provides its members with the resources to help us continue that evolution through our career journeys as a part of the hospital medicine movement.
Over a year ago, I ascended to president of SHM’s board of directors at HM16, the annual meeting in San Diego. Now, I am eagerly looking forward to HM17 next month, in Las Vegas, which we expect to be, yet again, the biggest, best, most innovative and most energetic gathering of hospitalists. As that meeting will mark the end of my tenure as president of the board, I’m also inclined to look back and survey what has happened over the last year, both personally and professionally.
The personal perspective is easy. I have a different position within my organization: president of Cleveland Clinic Akron General and the Southern Region, one which I would and could never have anticipated a year ago. It challenges, exhausts, exhilarates, and teaches me every day. I am also celebrating my 15th wedding anniversary and have three amazing children who seem to evolve in front of my eyes every day.
And, professionally, at HM16 (and on these pages a year ago), I framed what I felt were four critical directions for SHM and have a few thoughts on the work we have done over the last year.
1. Expand and engage SHM’s membership. SHM continues to be the envy of professional organizations, growing each year. More important than sole growth is our pursuit of connecting hospitalists to SHM’s resources and to each other; we have been incredibly active this past year. For instance, SHM is embarking on an engagement survey of HM groups, and is investing in new technologies to support membership. We are now a CME-accrediting organization and are moving the SHM Learning Portal to a new, enhanced platform. We launched a long-term communications strategy that is tied to engagement and a more nimble and mobile experience for our members. The SHM Leadership Academy sold out. HM17 is poised to be another success. And finally, we are increasingly appreciating that a strong SHM must have a vibrant chapter structure to ensure connections between our membership, staff, and board.
2. Focus on patient- and family-centered care. A look at the HM17 curriculum reinforces SHM’s awareness that patients and hospitalists must be more assertive in developing skills in communication and empathy. By doing so, they support a culture and environment wherein patients are active participants their care. Members of our Patient Experience Committee are presenting courses and workshops in Las Vegas, and last year’s annual meeting featured an entire pre-course on communication skills. Hospitalists play a signature role in the Cleveland Clinic’s national conference on improving the patient experience, and the committee has an advisory council of patients and advocates to guide their work.
3. Move assertively to define our role in an era of risk and reform. Last year’s national election will probably create policy upheavals that are difficult to either anticipate or plan for. However, the evolution of Medicare, Medicaid, and commercial payers toward passing risk (and reward) onto physicians, hospitals, and systems, likely is unstoppable. SHM held a board retreat with key hospital leaders (including Patrick Conway, MD, MSc, MHM, deputy administrator for Innovation and Quality at CMS and director of the Center for Medicare and Medicaid Innovation, and a keynote speaker at HM17) to outline a framework to engage and educate our membership by leveraging the work of our Public Policy, Education, and Practice Management committees.
4. Define our stance regarding specialty recognition: The complexities of this issue are political as well as logistical. SHM has continued to build out the infrastructure for Recognition of Focused Practice with the launch of SPARK ONE (our Focused Practice in Hospital Medicine exam preparation product), but the gaps between the curricula of internal medicine and family medicine residencies, and our daily clinical realities, will continue to exist for the foreseeable future. Pediatrics has established a board requirement for pediatric hospital medicine, but it is still unclear if this is the future of adult hospital medicine.
In sum
As I prepare to the pass to baton to Dr. Ron Greeno for 2017-18, I am reminded of one of the pearls of a former boss and mentor of mine who preached that career satisfaction comes from finding opportunities to achieve three goals: addressing meaningful challenges, working with compelling individuals, and learning something new every day. I would like to thank the board, SHM CEO Larry Wellikson, MD, MHM, and the society staff and volunteers, and, most of all, the many SHM members with whom I have met and spoken over the last year for providing me with exactly that opportunity.
I look forward to continuing to serve an active role in SHM, an organization that can provide you with those same opportunities and resources to help you grow, evolve and be an active participant in the hospital medicine movement.
One of the most enduring lessons I have learned during my time in hospital medicine is that hospitalists are always evolving, much like the specialty and healthcare system of which they are a part. And during my time as president of the Society of Hospital Medicine (SHM), I have come to realize how SHM provides its members with the resources to help us continue that evolution through our career journeys as a part of the hospital medicine movement.
Over a year ago, I ascended to president of SHM’s board of directors at HM16, the annual meeting in San Diego. Now, I am eagerly looking forward to HM17 next month, in Las Vegas, which we expect to be, yet again, the biggest, best, most innovative and most energetic gathering of hospitalists. As that meeting will mark the end of my tenure as president of the board, I’m also inclined to look back and survey what has happened over the last year, both personally and professionally.
The personal perspective is easy. I have a different position within my organization: president of Cleveland Clinic Akron General and the Southern Region, one which I would and could never have anticipated a year ago. It challenges, exhausts, exhilarates, and teaches me every day. I am also celebrating my 15th wedding anniversary and have three amazing children who seem to evolve in front of my eyes every day.
And, professionally, at HM16 (and on these pages a year ago), I framed what I felt were four critical directions for SHM and have a few thoughts on the work we have done over the last year.
1. Expand and engage SHM’s membership. SHM continues to be the envy of professional organizations, growing each year. More important than sole growth is our pursuit of connecting hospitalists to SHM’s resources and to each other; we have been incredibly active this past year. For instance, SHM is embarking on an engagement survey of HM groups, and is investing in new technologies to support membership. We are now a CME-accrediting organization and are moving the SHM Learning Portal to a new, enhanced platform. We launched a long-term communications strategy that is tied to engagement and a more nimble and mobile experience for our members. The SHM Leadership Academy sold out. HM17 is poised to be another success. And finally, we are increasingly appreciating that a strong SHM must have a vibrant chapter structure to ensure connections between our membership, staff, and board.
2. Focus on patient- and family-centered care. A look at the HM17 curriculum reinforces SHM’s awareness that patients and hospitalists must be more assertive in developing skills in communication and empathy. By doing so, they support a culture and environment wherein patients are active participants their care. Members of our Patient Experience Committee are presenting courses and workshops in Las Vegas, and last year’s annual meeting featured an entire pre-course on communication skills. Hospitalists play a signature role in the Cleveland Clinic’s national conference on improving the patient experience, and the committee has an advisory council of patients and advocates to guide their work.
3. Move assertively to define our role in an era of risk and reform. Last year’s national election will probably create policy upheavals that are difficult to either anticipate or plan for. However, the evolution of Medicare, Medicaid, and commercial payers toward passing risk (and reward) onto physicians, hospitals, and systems, likely is unstoppable. SHM held a board retreat with key hospital leaders (including Patrick Conway, MD, MSc, MHM, deputy administrator for Innovation and Quality at CMS and director of the Center for Medicare and Medicaid Innovation, and a keynote speaker at HM17) to outline a framework to engage and educate our membership by leveraging the work of our Public Policy, Education, and Practice Management committees.
4. Define our stance regarding specialty recognition: The complexities of this issue are political as well as logistical. SHM has continued to build out the infrastructure for Recognition of Focused Practice with the launch of SPARK ONE (our Focused Practice in Hospital Medicine exam preparation product), but the gaps between the curricula of internal medicine and family medicine residencies, and our daily clinical realities, will continue to exist for the foreseeable future. Pediatrics has established a board requirement for pediatric hospital medicine, but it is still unclear if this is the future of adult hospital medicine.
In sum
As I prepare to the pass to baton to Dr. Ron Greeno for 2017-18, I am reminded of one of the pearls of a former boss and mentor of mine who preached that career satisfaction comes from finding opportunities to achieve three goals: addressing meaningful challenges, working with compelling individuals, and learning something new every day. I would like to thank the board, SHM CEO Larry Wellikson, MD, MHM, and the society staff and volunteers, and, most of all, the many SHM members with whom I have met and spoken over the last year for providing me with exactly that opportunity.
I look forward to continuing to serve an active role in SHM, an organization that can provide you with those same opportunities and resources to help you grow, evolve and be an active participant in the hospital medicine movement.
CMS recognizes Society of Hospital Medicine’s Center for Quality Improvement
PHILADELPHIA – The Society of Hospital Medicine (SHM)’s Center for Quality Improvement (QI) has been distinguished by the Centers for Medicare & Medicaid Services for maintaining an ongoing collaborative partnership with CMS to enhance patient safety.
The letter of recognition from Paul McGann, MD, Jean Moody-Williams, RN, MPP, and Dennis Wagner, MPA, of the CMS, to Jenna Goldstein, MA, director of SHM’s Center for QI, and Kevin Vuernick, MPA, senior project manager, noted: “Over the last several years, our team has been privileged to partner with you and the Society of Hospital Medicine on the work of quality improvement and patient safety. Without relationships like these, the results in the reduction of patient harm we have seen at a national scale, saving 87,000 lives and nearly $20 billion in cost savings, would never have been possible.”
In August 2016, CMS’ Hospital Improvement Innovation Networks contacted SHM to participate in their weekly Partnership for Patients (PfP) Pacing Event webinar to present strategies for reducing opioid use and preventing adverse drug events, including SHM’s Mentored Implementation pilot program on Reducing Adverse Drug Events Related to Opioids (RADEO). SHM’s contribution to this webinar was twofold: Thomas W. Frederickson, MD, the lead author of the RADEO guide and one of two program mentors, spoke about the development of the RADEO program and its importance in the acute care setting. Matthew Jared, MD, a hospitalist at St. Anthony Hospital in Oklahoma City, one of the five pilot RADEO sites, discussed his experience implementing specific RADEO interventions as well as the mentoring provided by Dr. Frederickson of the department of hospital medicine at CHI Health in Omaha, Neb.
As a result of this successful partnership, SHM was contacted in January to provide its perspective on best practices in managing inpatients receiving opioids and adverse drug event data collection. At that time, Mr. Vuernick discussed the lessons learned between RADEO’s pilot program and the second iteration of RADEO, which launched in November 2016.
For more information about SHM’s Center for QI, please visit www.hospitalmedicine.org/QI. For more information about SHM and hospital medicine, visit www.hospitalmedicine.org and follow SHM on Twitter at @SHMLive.
PHILADELPHIA – The Society of Hospital Medicine (SHM)’s Center for Quality Improvement (QI) has been distinguished by the Centers for Medicare & Medicaid Services for maintaining an ongoing collaborative partnership with CMS to enhance patient safety.
The letter of recognition from Paul McGann, MD, Jean Moody-Williams, RN, MPP, and Dennis Wagner, MPA, of the CMS, to Jenna Goldstein, MA, director of SHM’s Center for QI, and Kevin Vuernick, MPA, senior project manager, noted: “Over the last several years, our team has been privileged to partner with you and the Society of Hospital Medicine on the work of quality improvement and patient safety. Without relationships like these, the results in the reduction of patient harm we have seen at a national scale, saving 87,000 lives and nearly $20 billion in cost savings, would never have been possible.”
In August 2016, CMS’ Hospital Improvement Innovation Networks contacted SHM to participate in their weekly Partnership for Patients (PfP) Pacing Event webinar to present strategies for reducing opioid use and preventing adverse drug events, including SHM’s Mentored Implementation pilot program on Reducing Adverse Drug Events Related to Opioids (RADEO). SHM’s contribution to this webinar was twofold: Thomas W. Frederickson, MD, the lead author of the RADEO guide and one of two program mentors, spoke about the development of the RADEO program and its importance in the acute care setting. Matthew Jared, MD, a hospitalist at St. Anthony Hospital in Oklahoma City, one of the five pilot RADEO sites, discussed his experience implementing specific RADEO interventions as well as the mentoring provided by Dr. Frederickson of the department of hospital medicine at CHI Health in Omaha, Neb.
As a result of this successful partnership, SHM was contacted in January to provide its perspective on best practices in managing inpatients receiving opioids and adverse drug event data collection. At that time, Mr. Vuernick discussed the lessons learned between RADEO’s pilot program and the second iteration of RADEO, which launched in November 2016.
For more information about SHM’s Center for QI, please visit www.hospitalmedicine.org/QI. For more information about SHM and hospital medicine, visit www.hospitalmedicine.org and follow SHM on Twitter at @SHMLive.
PHILADELPHIA – The Society of Hospital Medicine (SHM)’s Center for Quality Improvement (QI) has been distinguished by the Centers for Medicare & Medicaid Services for maintaining an ongoing collaborative partnership with CMS to enhance patient safety.
The letter of recognition from Paul McGann, MD, Jean Moody-Williams, RN, MPP, and Dennis Wagner, MPA, of the CMS, to Jenna Goldstein, MA, director of SHM’s Center for QI, and Kevin Vuernick, MPA, senior project manager, noted: “Over the last several years, our team has been privileged to partner with you and the Society of Hospital Medicine on the work of quality improvement and patient safety. Without relationships like these, the results in the reduction of patient harm we have seen at a national scale, saving 87,000 lives and nearly $20 billion in cost savings, would never have been possible.”
In August 2016, CMS’ Hospital Improvement Innovation Networks contacted SHM to participate in their weekly Partnership for Patients (PfP) Pacing Event webinar to present strategies for reducing opioid use and preventing adverse drug events, including SHM’s Mentored Implementation pilot program on Reducing Adverse Drug Events Related to Opioids (RADEO). SHM’s contribution to this webinar was twofold: Thomas W. Frederickson, MD, the lead author of the RADEO guide and one of two program mentors, spoke about the development of the RADEO program and its importance in the acute care setting. Matthew Jared, MD, a hospitalist at St. Anthony Hospital in Oklahoma City, one of the five pilot RADEO sites, discussed his experience implementing specific RADEO interventions as well as the mentoring provided by Dr. Frederickson of the department of hospital medicine at CHI Health in Omaha, Neb.
As a result of this successful partnership, SHM was contacted in January to provide its perspective on best practices in managing inpatients receiving opioids and adverse drug event data collection. At that time, Mr. Vuernick discussed the lessons learned between RADEO’s pilot program and the second iteration of RADEO, which launched in November 2016.
For more information about SHM’s Center for QI, please visit www.hospitalmedicine.org/QI. For more information about SHM and hospital medicine, visit www.hospitalmedicine.org and follow SHM on Twitter at @SHMLive.
Here’s what’s trending at SHM
Hospitalist specialty code becomes official designation
On April 3, 2017, “hospitalist” becomes an official specialty designation under Medicare – the code itself is C6. Starting on that date, hospitalists can change their specialty designation on the Medicare enrollment application. Specialty codes are self-designated and describe the kind of medicine that health care providers practice. Appropriate use of specialty codes helps distinguish differences among providers and improves the quality of utilization data. SHM applied for a specialty code for hospitalists nearly 3 years ago, and the Centers for Medicare & Medicaid Services approved the application in February 2016.
Stand with your fellow hospitalists and make sure to declare “I’m a C6.”
Assess your knowledge in hospital medicine with SPARK ONE
SHM recently launched SPARK ONE, a comprehensive online self-assessment tool created specifically for hospital medicine professionals. The activity contains 450-plus vignette-style multiple-choice questions covering 100% of the American Board of Internal Medicine’s Focused Practice in Hospital Medicine (FPHM) exam blueprint. This online tool is your complete resource for successfully preparing for the FPHM exam, or assessing your general knowledge in hospital medicine.
White paper now available: Hospitalist Attitudes Toward Electronic Medical Records
SHM’s Health Information Technology Committee diligently analyzed survey results that captured hospitalists’ attitudes towards electronic medical records, resulting in a white paper now available. The purpose of this paper is to effect change on EHR systems by informing conversations with decision makers and to provide hospital medicine a definitive voice in the landscape of the tumultuous world of electronic medical record systems.
SHM believes hospitalists are especially qualified to evaluate these systems, and the survey results paint a grim picture of the effectiveness and usability of the systems that hospitalists spend the majority of their time interacting with. These results should serve as a call to action to accelerate the pace of advancement and innovation in health care technology.
By sharing these results, SHM hopes to raise awareness of the unacceptable performance of existing systems that contributes to slower-than-desired improvement in quality and safety as well as increasing provider frustration. SHM strongly believes that health care needs a renewed focus on initial goals of technology adoption. View the white paper at hospitalmedicine.org/EHR.
Join the Early-Career Academic Hospitalist Speed Mentoring Session at Hospital Medicine 2017
The SHM “speed mentoring” session, held on Tuesday, May 2 from noon to 1:00 p.m. at Hospital Medicine 2017, is designed to assist early-career hospitalists in specific areas of career development by providing a fresh perspective and rapid advice.
Early-career hospitalists will be matched with three senior advisors by area of interest. The “mentee” will spend 10-15 minutes with each advisor and will then rotate to the next advisor. After the session, there will be time for additional informal discussion and networking among advisors and peers.
Pre-registration by March 31, 2017 is required; it will not be possible to register for this activity on-site at HM17. There is no additional fee to register. Registration will be limited to the first 20 participants. Visit hospitalmedicine2017.org/academic today.
Now available: 4 new antimicrobial stewardship modules
SHM has developed four new antimicrobial stewardship modules to help you demonstrate an understanding of best practices to optimize and improve antimicrobial prescribing within your hospital:
1. Optimizing Antibiotic Use for Hospitalized Patients
2. Best Practices in Treatment of UTIs: “Low-Hanging Fruit”
3. Best Practices in Acute Bacterial Skin Infection
4. Antibiotic Use for Inpatient Respiratory Infections
View these resources at hospitalmedicine.org/abx.
Network with the largest gathering of pediatric hospital medicine professionals
Pediatric Hospital Medicine 2017 (PHM 2017) will be held July 20-23 at the Omni Nashville located in Nashville, Tenn. PHM 2017 offers an all-inclusive arrangement of educational and networking opportunities planned specifically for the pediatric hospital medicine professional. More than 100 concurrent sessions to choose from over the 4 days of the conference allow participants to get the best out of their PHM 2017 experience.
Earn free CME in the enhanced SHM Learning Portal
You asked, and we listened: Introducing the enhanced SHM Learning Portal! The SHM Learning Portal, the online learning home for hospitalists with all eLearning initiatives in one place, just launched a brand-new responsive design in March 2016.
Launching this summer, SHM’s new Learning Portal will offer a better way to access and track online CME, with member discounts to a growing library of content. For more information, visit www.shmlearningportal.org.
Bringing SHM to you with local chapter meetings
Attend a chapter meeting and experience SHM locally. Chapters provide focused educational topics through key speakers and presentations and the opportunity to network with other hospitalists in your area. Find a chapter meeting close to you at hospitalmedicine.org/chapters.
A new look for SHM’s Center for Hospital Innovation & Improvement
Just as hospital medicine is evolving, so is SHM’s group dedicated to developing quality improvement safety tools and programs to meet health care’s changing needs. SHM is proud to unveil a new look for its Center for Hospital Innovation & Improvement this month. Stay tuned for more, and visit hospitalmedicine.org/QI for the latest offerings in a variety of quality improvement topics and clinical areas.
Stand out as a leader with the Fellow in Hospital Medicine designation
Applications for SHM’s Fellow in Hospital Medicine designation open on April 17, 2017. You may be eligible if you have been a member of SHM for at least 3 years and have been involved in key quality improvement programs and leadership roles in hospital medicine. Learn more and apply at hospitalmedicine.org/fellows.
Mr. Radler is Communications Specialist at the Society of Hospital Medicine.
Hospitalist specialty code becomes official designation
On April 3, 2017, “hospitalist” becomes an official specialty designation under Medicare – the code itself is C6. Starting on that date, hospitalists can change their specialty designation on the Medicare enrollment application. Specialty codes are self-designated and describe the kind of medicine that health care providers practice. Appropriate use of specialty codes helps distinguish differences among providers and improves the quality of utilization data. SHM applied for a specialty code for hospitalists nearly 3 years ago, and the Centers for Medicare & Medicaid Services approved the application in February 2016.
Stand with your fellow hospitalists and make sure to declare “I’m a C6.”
Assess your knowledge in hospital medicine with SPARK ONE
SHM recently launched SPARK ONE, a comprehensive online self-assessment tool created specifically for hospital medicine professionals. The activity contains 450-plus vignette-style multiple-choice questions covering 100% of the American Board of Internal Medicine’s Focused Practice in Hospital Medicine (FPHM) exam blueprint. This online tool is your complete resource for successfully preparing for the FPHM exam, or assessing your general knowledge in hospital medicine.
White paper now available: Hospitalist Attitudes Toward Electronic Medical Records
SHM’s Health Information Technology Committee diligently analyzed survey results that captured hospitalists’ attitudes towards electronic medical records, resulting in a white paper now available. The purpose of this paper is to effect change on EHR systems by informing conversations with decision makers and to provide hospital medicine a definitive voice in the landscape of the tumultuous world of electronic medical record systems.
SHM believes hospitalists are especially qualified to evaluate these systems, and the survey results paint a grim picture of the effectiveness and usability of the systems that hospitalists spend the majority of their time interacting with. These results should serve as a call to action to accelerate the pace of advancement and innovation in health care technology.
By sharing these results, SHM hopes to raise awareness of the unacceptable performance of existing systems that contributes to slower-than-desired improvement in quality and safety as well as increasing provider frustration. SHM strongly believes that health care needs a renewed focus on initial goals of technology adoption. View the white paper at hospitalmedicine.org/EHR.
Join the Early-Career Academic Hospitalist Speed Mentoring Session at Hospital Medicine 2017
The SHM “speed mentoring” session, held on Tuesday, May 2 from noon to 1:00 p.m. at Hospital Medicine 2017, is designed to assist early-career hospitalists in specific areas of career development by providing a fresh perspective and rapid advice.
Early-career hospitalists will be matched with three senior advisors by area of interest. The “mentee” will spend 10-15 minutes with each advisor and will then rotate to the next advisor. After the session, there will be time for additional informal discussion and networking among advisors and peers.
Pre-registration by March 31, 2017 is required; it will not be possible to register for this activity on-site at HM17. There is no additional fee to register. Registration will be limited to the first 20 participants. Visit hospitalmedicine2017.org/academic today.
Now available: 4 new antimicrobial stewardship modules
SHM has developed four new antimicrobial stewardship modules to help you demonstrate an understanding of best practices to optimize and improve antimicrobial prescribing within your hospital:
1. Optimizing Antibiotic Use for Hospitalized Patients
2. Best Practices in Treatment of UTIs: “Low-Hanging Fruit”
3. Best Practices in Acute Bacterial Skin Infection
4. Antibiotic Use for Inpatient Respiratory Infections
View these resources at hospitalmedicine.org/abx.
Network with the largest gathering of pediatric hospital medicine professionals
Pediatric Hospital Medicine 2017 (PHM 2017) will be held July 20-23 at the Omni Nashville located in Nashville, Tenn. PHM 2017 offers an all-inclusive arrangement of educational and networking opportunities planned specifically for the pediatric hospital medicine professional. More than 100 concurrent sessions to choose from over the 4 days of the conference allow participants to get the best out of their PHM 2017 experience.
Earn free CME in the enhanced SHM Learning Portal
You asked, and we listened: Introducing the enhanced SHM Learning Portal! The SHM Learning Portal, the online learning home for hospitalists with all eLearning initiatives in one place, just launched a brand-new responsive design in March 2016.
Launching this summer, SHM’s new Learning Portal will offer a better way to access and track online CME, with member discounts to a growing library of content. For more information, visit www.shmlearningportal.org.
Bringing SHM to you with local chapter meetings
Attend a chapter meeting and experience SHM locally. Chapters provide focused educational topics through key speakers and presentations and the opportunity to network with other hospitalists in your area. Find a chapter meeting close to you at hospitalmedicine.org/chapters.
A new look for SHM’s Center for Hospital Innovation & Improvement
Just as hospital medicine is evolving, so is SHM’s group dedicated to developing quality improvement safety tools and programs to meet health care’s changing needs. SHM is proud to unveil a new look for its Center for Hospital Innovation & Improvement this month. Stay tuned for more, and visit hospitalmedicine.org/QI for the latest offerings in a variety of quality improvement topics and clinical areas.
Stand out as a leader with the Fellow in Hospital Medicine designation
Applications for SHM’s Fellow in Hospital Medicine designation open on April 17, 2017. You may be eligible if you have been a member of SHM for at least 3 years and have been involved in key quality improvement programs and leadership roles in hospital medicine. Learn more and apply at hospitalmedicine.org/fellows.
Mr. Radler is Communications Specialist at the Society of Hospital Medicine.
Hospitalist specialty code becomes official designation
On April 3, 2017, “hospitalist” becomes an official specialty designation under Medicare – the code itself is C6. Starting on that date, hospitalists can change their specialty designation on the Medicare enrollment application. Specialty codes are self-designated and describe the kind of medicine that health care providers practice. Appropriate use of specialty codes helps distinguish differences among providers and improves the quality of utilization data. SHM applied for a specialty code for hospitalists nearly 3 years ago, and the Centers for Medicare & Medicaid Services approved the application in February 2016.
Stand with your fellow hospitalists and make sure to declare “I’m a C6.”
Assess your knowledge in hospital medicine with SPARK ONE
SHM recently launched SPARK ONE, a comprehensive online self-assessment tool created specifically for hospital medicine professionals. The activity contains 450-plus vignette-style multiple-choice questions covering 100% of the American Board of Internal Medicine’s Focused Practice in Hospital Medicine (FPHM) exam blueprint. This online tool is your complete resource for successfully preparing for the FPHM exam, or assessing your general knowledge in hospital medicine.
White paper now available: Hospitalist Attitudes Toward Electronic Medical Records
SHM’s Health Information Technology Committee diligently analyzed survey results that captured hospitalists’ attitudes towards electronic medical records, resulting in a white paper now available. The purpose of this paper is to effect change on EHR systems by informing conversations with decision makers and to provide hospital medicine a definitive voice in the landscape of the tumultuous world of electronic medical record systems.
SHM believes hospitalists are especially qualified to evaluate these systems, and the survey results paint a grim picture of the effectiveness and usability of the systems that hospitalists spend the majority of their time interacting with. These results should serve as a call to action to accelerate the pace of advancement and innovation in health care technology.
By sharing these results, SHM hopes to raise awareness of the unacceptable performance of existing systems that contributes to slower-than-desired improvement in quality and safety as well as increasing provider frustration. SHM strongly believes that health care needs a renewed focus on initial goals of technology adoption. View the white paper at hospitalmedicine.org/EHR.
Join the Early-Career Academic Hospitalist Speed Mentoring Session at Hospital Medicine 2017
The SHM “speed mentoring” session, held on Tuesday, May 2 from noon to 1:00 p.m. at Hospital Medicine 2017, is designed to assist early-career hospitalists in specific areas of career development by providing a fresh perspective and rapid advice.
Early-career hospitalists will be matched with three senior advisors by area of interest. The “mentee” will spend 10-15 minutes with each advisor and will then rotate to the next advisor. After the session, there will be time for additional informal discussion and networking among advisors and peers.
Pre-registration by March 31, 2017 is required; it will not be possible to register for this activity on-site at HM17. There is no additional fee to register. Registration will be limited to the first 20 participants. Visit hospitalmedicine2017.org/academic today.
Now available: 4 new antimicrobial stewardship modules
SHM has developed four new antimicrobial stewardship modules to help you demonstrate an understanding of best practices to optimize and improve antimicrobial prescribing within your hospital:
1. Optimizing Antibiotic Use for Hospitalized Patients
2. Best Practices in Treatment of UTIs: “Low-Hanging Fruit”
3. Best Practices in Acute Bacterial Skin Infection
4. Antibiotic Use for Inpatient Respiratory Infections
View these resources at hospitalmedicine.org/abx.
Network with the largest gathering of pediatric hospital medicine professionals
Pediatric Hospital Medicine 2017 (PHM 2017) will be held July 20-23 at the Omni Nashville located in Nashville, Tenn. PHM 2017 offers an all-inclusive arrangement of educational and networking opportunities planned specifically for the pediatric hospital medicine professional. More than 100 concurrent sessions to choose from over the 4 days of the conference allow participants to get the best out of their PHM 2017 experience.
Earn free CME in the enhanced SHM Learning Portal
You asked, and we listened: Introducing the enhanced SHM Learning Portal! The SHM Learning Portal, the online learning home for hospitalists with all eLearning initiatives in one place, just launched a brand-new responsive design in March 2016.
Launching this summer, SHM’s new Learning Portal will offer a better way to access and track online CME, with member discounts to a growing library of content. For more information, visit www.shmlearningportal.org.
Bringing SHM to you with local chapter meetings
Attend a chapter meeting and experience SHM locally. Chapters provide focused educational topics through key speakers and presentations and the opportunity to network with other hospitalists in your area. Find a chapter meeting close to you at hospitalmedicine.org/chapters.
A new look for SHM’s Center for Hospital Innovation & Improvement
Just as hospital medicine is evolving, so is SHM’s group dedicated to developing quality improvement safety tools and programs to meet health care’s changing needs. SHM is proud to unveil a new look for its Center for Hospital Innovation & Improvement this month. Stay tuned for more, and visit hospitalmedicine.org/QI for the latest offerings in a variety of quality improvement topics and clinical areas.
Stand out as a leader with the Fellow in Hospital Medicine designation
Applications for SHM’s Fellow in Hospital Medicine designation open on April 17, 2017. You may be eligible if you have been a member of SHM for at least 3 years and have been involved in key quality improvement programs and leadership roles in hospital medicine. Learn more and apply at hospitalmedicine.org/fellows.
Mr. Radler is Communications Specialist at the Society of Hospital Medicine.
Data-driven HR, RR parameters might help reduce alarm fatigue
Clinical question: Can alarm fatigue in pediatric inpatient settings be safely mitigated by modifying alarm limits with data-driven vital sign reference ranges?
Background: The management of patient alarms in the hospital is a significant safety issue, with the large majority of alarms (85%-99%) either false or not clinically significant. This leads to provider desensitization or alarm fatigue, which has been shown to contribute to adverse events.
In 2014, the Joint Commission made the issue of alarm system safety and alarm fatigue a priority for hospitals.1 Multiple studies have been published addressing alarm fatigue in hospitalized adult patients, but this issue is less well studied in pediatrics, including little guidance on optimizing alarm parameters. Widely used reference ranges and guides are based on limited evidence, primarily based on observational data in healthy outpatients or consensus data.
A 2013 study used vital sign data from hospitalized children to develop percentile curves for heart rate (HR) and respiratory rate (RR) and estimated that 54% of vital sign measurements in hospitalized children are out of range using currently accepted reference ranges.2
To safely decrease the number of out-of-range vital sign measurements resulting from current reference ranges, this study used data from non–critically ill hospitalized children to develop HR and RR percentile charts, and then performed retrospective safety analysis by evaluating effects of modifying the alarm limits on identification of cardiorespiratory arrests (CRA) and rapid response team (RRT) activations.
Study Design: Retrospective, cross-sectional study.
Setting: Single-site, 311-bed quaternary-care academic hospital, both general medical and surgical units.
Synopsis: Vital signs were extracted from the institution’s electronic health record (EHR) for all general medical and surgical patients discharged between Jan. 1, 3013, and May 3, 2014, excluding critically ill children and physiologically implausible vital signs. Two different sets were used, a training set (patients discharged between Jan. 1, 2013, and Dec. 31, 2013) and a validation set (Jan. 1, 2014-May 3, 2014). One HR and RR pair was randomly selected for each 4-hour interval during hospitalization, with a maximum of 10 HR and RR pairs per patient. Age-stratified percentiles were calculated using this data. The 5th and 95th percentile limits using the study data were compared with the 5th and 95th percentile values in the 2013 study, and the reference ranges currently in use at the institution (2004 National Institutes of Health ranges).2
The training set used 62,508 vital sign measurements for 7,202 patients to calculate percentiles for HR and RR among 14 different age groups. The validation set consisted of 82,993 vital sign measurements for 2,287 patients. Using the 5th and 95th percentiles for HR and RR resulted in 24,045 (55.6%) fewer out-of-range measurements in the validation set compared to NIH reference ranges (45% fewer HR values, 61% fewer RR values). This finding, as well as the vital sign percentile ranges, was consistent with the data published in the 2013 study.2
Data for all 148 out-of-ICU RRT and CRA events during the same time period were reviewed using manual chart review. Evaluating vital signs within the 12 hours preceding the events, 144 patients had out-of-range HR or RR measurements using NIH ranges. One hundred thirty-six (94.4%) of these 144 patients also had out-of-range measurements using the study-derived 5th and 95th percentile values.
Manual chart review of the remaining eight patients who had normal HR or RR demonstrated that the RRT or CRA interventions occurred for clinical indications that did no rely on HR or RR measurement (for example, desaturations, difficulty breathing, hematemesis), so the data-driven parameters did not miss any of these events.
Bottom line: In this retrospective study, using data-driven HR and RR parameters was at least as safe as the NIH-published reference ranges currently in use in this hospital. In addition to maintaining safety related to RRT and CRA events, use of the data-driven parameters resulted in 55.6% fewer out-of-range vital sign measurements in the studied population. This may reduce the frequency of false alarms and improve alarm fatigue, and should be studied prospectively in the future.
Citation: Goel VV, Poole SF, Longhurst CA, et al. Safety analysis of proposed data-driven physiologic alarm parameters for hospitalized children. J Hosp Med. 2016;11(12):817-823.
Dr. Galloway is a pediatric hospitalist at Sanford Children’s Hospital in Sioux Falls, S.D., assistant professor of pediatrics at the University of South Dakota Sanford School of Medicine, and vice chief of the division of hospital pediatrics at USD SSOM and Sanford Children’s Hospital.
References
1. The Joint Commission. Alarm system safety. Available at: https://www.jointcommission.org/assets/1/18/R3_Report_Issue_5_12_2_13_Final.pdf. Published December 11, 2013.
2. Bonafide CP, Brady PW, Keren R, Conway PH, Marsolo K, Daymont C. Development of heart and respiratory rate percentile curves for hospitalized children. Pediatrics. 2013;131(4):e1150-1157.
Clinical question: Can alarm fatigue in pediatric inpatient settings be safely mitigated by modifying alarm limits with data-driven vital sign reference ranges?
Background: The management of patient alarms in the hospital is a significant safety issue, with the large majority of alarms (85%-99%) either false or not clinically significant. This leads to provider desensitization or alarm fatigue, which has been shown to contribute to adverse events.
In 2014, the Joint Commission made the issue of alarm system safety and alarm fatigue a priority for hospitals.1 Multiple studies have been published addressing alarm fatigue in hospitalized adult patients, but this issue is less well studied in pediatrics, including little guidance on optimizing alarm parameters. Widely used reference ranges and guides are based on limited evidence, primarily based on observational data in healthy outpatients or consensus data.
A 2013 study used vital sign data from hospitalized children to develop percentile curves for heart rate (HR) and respiratory rate (RR) and estimated that 54% of vital sign measurements in hospitalized children are out of range using currently accepted reference ranges.2
To safely decrease the number of out-of-range vital sign measurements resulting from current reference ranges, this study used data from non–critically ill hospitalized children to develop HR and RR percentile charts, and then performed retrospective safety analysis by evaluating effects of modifying the alarm limits on identification of cardiorespiratory arrests (CRA) and rapid response team (RRT) activations.
Study Design: Retrospective, cross-sectional study.
Setting: Single-site, 311-bed quaternary-care academic hospital, both general medical and surgical units.
Synopsis: Vital signs were extracted from the institution’s electronic health record (EHR) for all general medical and surgical patients discharged between Jan. 1, 3013, and May 3, 2014, excluding critically ill children and physiologically implausible vital signs. Two different sets were used, a training set (patients discharged between Jan. 1, 2013, and Dec. 31, 2013) and a validation set (Jan. 1, 2014-May 3, 2014). One HR and RR pair was randomly selected for each 4-hour interval during hospitalization, with a maximum of 10 HR and RR pairs per patient. Age-stratified percentiles were calculated using this data. The 5th and 95th percentile limits using the study data were compared with the 5th and 95th percentile values in the 2013 study, and the reference ranges currently in use at the institution (2004 National Institutes of Health ranges).2
The training set used 62,508 vital sign measurements for 7,202 patients to calculate percentiles for HR and RR among 14 different age groups. The validation set consisted of 82,993 vital sign measurements for 2,287 patients. Using the 5th and 95th percentiles for HR and RR resulted in 24,045 (55.6%) fewer out-of-range measurements in the validation set compared to NIH reference ranges (45% fewer HR values, 61% fewer RR values). This finding, as well as the vital sign percentile ranges, was consistent with the data published in the 2013 study.2
Data for all 148 out-of-ICU RRT and CRA events during the same time period were reviewed using manual chart review. Evaluating vital signs within the 12 hours preceding the events, 144 patients had out-of-range HR or RR measurements using NIH ranges. One hundred thirty-six (94.4%) of these 144 patients also had out-of-range measurements using the study-derived 5th and 95th percentile values.
Manual chart review of the remaining eight patients who had normal HR or RR demonstrated that the RRT or CRA interventions occurred for clinical indications that did no rely on HR or RR measurement (for example, desaturations, difficulty breathing, hematemesis), so the data-driven parameters did not miss any of these events.
Bottom line: In this retrospective study, using data-driven HR and RR parameters was at least as safe as the NIH-published reference ranges currently in use in this hospital. In addition to maintaining safety related to RRT and CRA events, use of the data-driven parameters resulted in 55.6% fewer out-of-range vital sign measurements in the studied population. This may reduce the frequency of false alarms and improve alarm fatigue, and should be studied prospectively in the future.
Citation: Goel VV, Poole SF, Longhurst CA, et al. Safety analysis of proposed data-driven physiologic alarm parameters for hospitalized children. J Hosp Med. 2016;11(12):817-823.
Dr. Galloway is a pediatric hospitalist at Sanford Children’s Hospital in Sioux Falls, S.D., assistant professor of pediatrics at the University of South Dakota Sanford School of Medicine, and vice chief of the division of hospital pediatrics at USD SSOM and Sanford Children’s Hospital.
References
1. The Joint Commission. Alarm system safety. Available at: https://www.jointcommission.org/assets/1/18/R3_Report_Issue_5_12_2_13_Final.pdf. Published December 11, 2013.
2. Bonafide CP, Brady PW, Keren R, Conway PH, Marsolo K, Daymont C. Development of heart and respiratory rate percentile curves for hospitalized children. Pediatrics. 2013;131(4):e1150-1157.
Clinical question: Can alarm fatigue in pediatric inpatient settings be safely mitigated by modifying alarm limits with data-driven vital sign reference ranges?
Background: The management of patient alarms in the hospital is a significant safety issue, with the large majority of alarms (85%-99%) either false or not clinically significant. This leads to provider desensitization or alarm fatigue, which has been shown to contribute to adverse events.
In 2014, the Joint Commission made the issue of alarm system safety and alarm fatigue a priority for hospitals.1 Multiple studies have been published addressing alarm fatigue in hospitalized adult patients, but this issue is less well studied in pediatrics, including little guidance on optimizing alarm parameters. Widely used reference ranges and guides are based on limited evidence, primarily based on observational data in healthy outpatients or consensus data.
A 2013 study used vital sign data from hospitalized children to develop percentile curves for heart rate (HR) and respiratory rate (RR) and estimated that 54% of vital sign measurements in hospitalized children are out of range using currently accepted reference ranges.2
To safely decrease the number of out-of-range vital sign measurements resulting from current reference ranges, this study used data from non–critically ill hospitalized children to develop HR and RR percentile charts, and then performed retrospective safety analysis by evaluating effects of modifying the alarm limits on identification of cardiorespiratory arrests (CRA) and rapid response team (RRT) activations.
Study Design: Retrospective, cross-sectional study.
Setting: Single-site, 311-bed quaternary-care academic hospital, both general medical and surgical units.
Synopsis: Vital signs were extracted from the institution’s electronic health record (EHR) for all general medical and surgical patients discharged between Jan. 1, 3013, and May 3, 2014, excluding critically ill children and physiologically implausible vital signs. Two different sets were used, a training set (patients discharged between Jan. 1, 2013, and Dec. 31, 2013) and a validation set (Jan. 1, 2014-May 3, 2014). One HR and RR pair was randomly selected for each 4-hour interval during hospitalization, with a maximum of 10 HR and RR pairs per patient. Age-stratified percentiles were calculated using this data. The 5th and 95th percentile limits using the study data were compared with the 5th and 95th percentile values in the 2013 study, and the reference ranges currently in use at the institution (2004 National Institutes of Health ranges).2
The training set used 62,508 vital sign measurements for 7,202 patients to calculate percentiles for HR and RR among 14 different age groups. The validation set consisted of 82,993 vital sign measurements for 2,287 patients. Using the 5th and 95th percentiles for HR and RR resulted in 24,045 (55.6%) fewer out-of-range measurements in the validation set compared to NIH reference ranges (45% fewer HR values, 61% fewer RR values). This finding, as well as the vital sign percentile ranges, was consistent with the data published in the 2013 study.2
Data for all 148 out-of-ICU RRT and CRA events during the same time period were reviewed using manual chart review. Evaluating vital signs within the 12 hours preceding the events, 144 patients had out-of-range HR or RR measurements using NIH ranges. One hundred thirty-six (94.4%) of these 144 patients also had out-of-range measurements using the study-derived 5th and 95th percentile values.
Manual chart review of the remaining eight patients who had normal HR or RR demonstrated that the RRT or CRA interventions occurred for clinical indications that did no rely on HR or RR measurement (for example, desaturations, difficulty breathing, hematemesis), so the data-driven parameters did not miss any of these events.
Bottom line: In this retrospective study, using data-driven HR and RR parameters was at least as safe as the NIH-published reference ranges currently in use in this hospital. In addition to maintaining safety related to RRT and CRA events, use of the data-driven parameters resulted in 55.6% fewer out-of-range vital sign measurements in the studied population. This may reduce the frequency of false alarms and improve alarm fatigue, and should be studied prospectively in the future.
Citation: Goel VV, Poole SF, Longhurst CA, et al. Safety analysis of proposed data-driven physiologic alarm parameters for hospitalized children. J Hosp Med. 2016;11(12):817-823.
Dr. Galloway is a pediatric hospitalist at Sanford Children’s Hospital in Sioux Falls, S.D., assistant professor of pediatrics at the University of South Dakota Sanford School of Medicine, and vice chief of the division of hospital pediatrics at USD SSOM and Sanford Children’s Hospital.
References
1. The Joint Commission. Alarm system safety. Available at: https://www.jointcommission.org/assets/1/18/R3_Report_Issue_5_12_2_13_Final.pdf. Published December 11, 2013.
2. Bonafide CP, Brady PW, Keren R, Conway PH, Marsolo K, Daymont C. Development of heart and respiratory rate percentile curves for hospitalized children. Pediatrics. 2013;131(4):e1150-1157.
Sneak Peak: The Hospital Leader Blog
FEATURED POST: “A Renewed Call to Overhaul Hospital Observation Care”
In response to concerns about Medicare beneficiary out-of-pocket financial risk, Congress unanimously passed the NOTICE Act, which President Obama signed into law August 5, 2015. This law states that all Medicare beneficiaries hospitalized for 24 hours or more as outpatients under observation must to be notified in writing that they are outpatients “not later than 36 hours after the time such individual begins receiving such services” as well as the associated “implications for cost-sharing.” Last month, the Centers for Medicare & Medicaid Services (CMS) released the final Medicare Outpatient Observation Notice (MOON) that hospitals will start delivering to patients no later than March 8, 2017 to comply with the law. Patients or their representatives must sign the form to acknowledge receipt.
First, Medicare beneficiaries are notified after they have been hospitalized, certainly after they could make an informed decision about accepting observation care. Second, patients or their representative must sign the form, yet it is unclear if this signature holds the patient financially liable, particularly if signed by a representative with no legal authority over the patient’s financial affairs. Third, the form does nothing for a patient’s right to appeal their status. And because observation is a billing distinction, the field at the top of the form requiring hospitals to specify why the patient is not an inpatient is circular reasoning, as patients are outpatients only when they fail to meet Medicare inpatient billing criteria.
Perhaps most importantly, the primary purpose of the NOTICE Act – to inform beneficiaries of the “implications for cost-sharing” when hospitalized under observation – cannot truly be accomplished.
On December 19, 2016, the Department of Health and Human Services Office of Inspector General (OIG) issued the best cost-sharing data available to date describing observation hospital care under the 2-midnight rule. In their report, the OIG used FY 2014 data to compare cost of short outpatient and inpatient stays with similar diagnoses. But because hospitalized outpatients under observation pay a copayment for each individual hospital service, financial risk is not directly correlated with a diagnosis but instead the result of the number, cost, and complexity of services rendered in the hospital, with no limit on the additive amount of per-service deductibles. In contrast, the inpatient deductible is finite per benefit period.
As the OIG report does not provide an accounting of services rendered nor comparison based on equivalent services, it isn’t clear how these cost estimates will help inform discussions when my observation patients receive their MOON.
Dr. Sheehy is a physician and associate professor at the University of Wisconsin School of Medicine and Public Health.
Read the full text of this blog post at http://blogs.hospitalmedicine.org/Blog/a-renewed-call-to-overhaul-hospital-observation-care/
Also on The Hospital Leader…
• New ABIM MOC Two-Year Plan for Internal Medicine Threatens the Focused Practice in Hospital Medicine By Burke Kealey, MD, SFHM
• The Nursing Home Get Out of Jail Card (“We Don’t Want Our Patient Back”). It’s Now Adios. By Brad Flansbaum, DO, MPH, MHM
• The Inmates Are Running the Asylum By Tracy Cardin, ACNP-BC, SFHM
• Do Clinicians Understand Quality Metric Data? By Danielle Scheurer, MD, MSCR, SFHM
• Fake News! Get Your Fake News Here! By Jordan Messler, MD, SFHM
FEATURED POST: “A Renewed Call to Overhaul Hospital Observation Care”
In response to concerns about Medicare beneficiary out-of-pocket financial risk, Congress unanimously passed the NOTICE Act, which President Obama signed into law August 5, 2015. This law states that all Medicare beneficiaries hospitalized for 24 hours or more as outpatients under observation must to be notified in writing that they are outpatients “not later than 36 hours after the time such individual begins receiving such services” as well as the associated “implications for cost-sharing.” Last month, the Centers for Medicare & Medicaid Services (CMS) released the final Medicare Outpatient Observation Notice (MOON) that hospitals will start delivering to patients no later than March 8, 2017 to comply with the law. Patients or their representatives must sign the form to acknowledge receipt.
First, Medicare beneficiaries are notified after they have been hospitalized, certainly after they could make an informed decision about accepting observation care. Second, patients or their representative must sign the form, yet it is unclear if this signature holds the patient financially liable, particularly if signed by a representative with no legal authority over the patient’s financial affairs. Third, the form does nothing for a patient’s right to appeal their status. And because observation is a billing distinction, the field at the top of the form requiring hospitals to specify why the patient is not an inpatient is circular reasoning, as patients are outpatients only when they fail to meet Medicare inpatient billing criteria.
Perhaps most importantly, the primary purpose of the NOTICE Act – to inform beneficiaries of the “implications for cost-sharing” when hospitalized under observation – cannot truly be accomplished.
On December 19, 2016, the Department of Health and Human Services Office of Inspector General (OIG) issued the best cost-sharing data available to date describing observation hospital care under the 2-midnight rule. In their report, the OIG used FY 2014 data to compare cost of short outpatient and inpatient stays with similar diagnoses. But because hospitalized outpatients under observation pay a copayment for each individual hospital service, financial risk is not directly correlated with a diagnosis but instead the result of the number, cost, and complexity of services rendered in the hospital, with no limit on the additive amount of per-service deductibles. In contrast, the inpatient deductible is finite per benefit period.
As the OIG report does not provide an accounting of services rendered nor comparison based on equivalent services, it isn’t clear how these cost estimates will help inform discussions when my observation patients receive their MOON.
Dr. Sheehy is a physician and associate professor at the University of Wisconsin School of Medicine and Public Health.
Read the full text of this blog post at http://blogs.hospitalmedicine.org/Blog/a-renewed-call-to-overhaul-hospital-observation-care/
Also on The Hospital Leader…
• New ABIM MOC Two-Year Plan for Internal Medicine Threatens the Focused Practice in Hospital Medicine By Burke Kealey, MD, SFHM
• The Nursing Home Get Out of Jail Card (“We Don’t Want Our Patient Back”). It’s Now Adios. By Brad Flansbaum, DO, MPH, MHM
• The Inmates Are Running the Asylum By Tracy Cardin, ACNP-BC, SFHM
• Do Clinicians Understand Quality Metric Data? By Danielle Scheurer, MD, MSCR, SFHM
• Fake News! Get Your Fake News Here! By Jordan Messler, MD, SFHM
FEATURED POST: “A Renewed Call to Overhaul Hospital Observation Care”
In response to concerns about Medicare beneficiary out-of-pocket financial risk, Congress unanimously passed the NOTICE Act, which President Obama signed into law August 5, 2015. This law states that all Medicare beneficiaries hospitalized for 24 hours or more as outpatients under observation must to be notified in writing that they are outpatients “not later than 36 hours after the time such individual begins receiving such services” as well as the associated “implications for cost-sharing.” Last month, the Centers for Medicare & Medicaid Services (CMS) released the final Medicare Outpatient Observation Notice (MOON) that hospitals will start delivering to patients no later than March 8, 2017 to comply with the law. Patients or their representatives must sign the form to acknowledge receipt.
First, Medicare beneficiaries are notified after they have been hospitalized, certainly after they could make an informed decision about accepting observation care. Second, patients or their representative must sign the form, yet it is unclear if this signature holds the patient financially liable, particularly if signed by a representative with no legal authority over the patient’s financial affairs. Third, the form does nothing for a patient’s right to appeal their status. And because observation is a billing distinction, the field at the top of the form requiring hospitals to specify why the patient is not an inpatient is circular reasoning, as patients are outpatients only when they fail to meet Medicare inpatient billing criteria.
Perhaps most importantly, the primary purpose of the NOTICE Act – to inform beneficiaries of the “implications for cost-sharing” when hospitalized under observation – cannot truly be accomplished.
On December 19, 2016, the Department of Health and Human Services Office of Inspector General (OIG) issued the best cost-sharing data available to date describing observation hospital care under the 2-midnight rule. In their report, the OIG used FY 2014 data to compare cost of short outpatient and inpatient stays with similar diagnoses. But because hospitalized outpatients under observation pay a copayment for each individual hospital service, financial risk is not directly correlated with a diagnosis but instead the result of the number, cost, and complexity of services rendered in the hospital, with no limit on the additive amount of per-service deductibles. In contrast, the inpatient deductible is finite per benefit period.
As the OIG report does not provide an accounting of services rendered nor comparison based on equivalent services, it isn’t clear how these cost estimates will help inform discussions when my observation patients receive their MOON.
Dr. Sheehy is a physician and associate professor at the University of Wisconsin School of Medicine and Public Health.
Read the full text of this blog post at http://blogs.hospitalmedicine.org/Blog/a-renewed-call-to-overhaul-hospital-observation-care/
Also on The Hospital Leader…
• New ABIM MOC Two-Year Plan for Internal Medicine Threatens the Focused Practice in Hospital Medicine By Burke Kealey, MD, SFHM
• The Nursing Home Get Out of Jail Card (“We Don’t Want Our Patient Back”). It’s Now Adios. By Brad Flansbaum, DO, MPH, MHM
• The Inmates Are Running the Asylum By Tracy Cardin, ACNP-BC, SFHM
• Do Clinicians Understand Quality Metric Data? By Danielle Scheurer, MD, MSCR, SFHM
• Fake News! Get Your Fake News Here! By Jordan Messler, MD, SFHM
What’s new at HM17
There is only one annual meeting dedicated to hospitalists, designed by hospitalists, and focusing purely on issues important to hospitalists. But even that isn’t enough to make sure more hospitalists show up every year.
That’s because a yearly conference can’t just be a rehash of the last one.
A valuable conference, certainly one worth spending the bulk of a continuing medical budget on, offers something new every year. Or, to look at the schedule for HM17, a lot of new every year.
That’s an unlikely complaint this year. The annual meeting schedule for May 1-4 at Mandalay Bay Resort and Casino includes five new educational tracks: High Value Care, Clinical Updates, Health Policy, Diagnostic Reasoning, and Medical Education.
“We’re really excited to be able to offer more clinical content,” said HM17 course director Lenny Feldman, MD, FAAP, FACP, SFHM.
Dr. Feldman sees each of the new tracks as filling separate and specific needs of HM attendees who vary from nonphysician providers to hospitalists to medical students.
Take, for instance, the High Value Care, Clinical Updates, and Diagnostic Reasoning sessions that are debuting.
“We wanted to make sure that we had as many clinically oriented sessions as possible,” Dr. Feldman said. “Which meant we needed to increase the amount of clinical content we have offered compared to the past few years. The new clinical track allows us to add probably 12 or so different sessions that will fill the needs of our attendees.”
The Diagnostic Reasoning and High Value Care tracks, in particular, highlight the annual meeting’s continued evolution toward a focus on evidence-based care, as that mantra becomes a bedrock of clinical treatment.
“Training our hospitalists to use the best dialogistic reasoning in their approach to their patients is a big push in hospital medicine right now,” Dr. Feldman said, “Hopefully, a track on that topic will excite people who love thinking about medicine, who got into medicine because of the mystery and want a renewed focus on how to be a great diagnostician.”
Dr. Feldman also noted that the High Value Care track should be a hot topic, as hospitalists want to learn how to provide high quality and high value care to patients at the same time. The new tracks should appeal to different groups and make the annual meeting more appealing to a variety of attendees, not just rank-and-file doctors.
The mini Medical Education track, for instance, is a subset of a half-dozen sessions tailored directly to medical educators in academic settings who face different challenges than their counterparts in community settings. The same goes for the Health Policy track, which will offer a handful of sessions suitable for novices looking to learn more in an age of reform, or policy wonks hoping to expand their knowledge.
Meeting evolving needs
New offerings aren’t limited to the main conference schedule. The 2017 roster of pre-courses includes one titled, “Bugs, Drugs and You: Infectious Diseases ‘Boot Camp’ for Hospitalists.” This daylong session hasn’t been held since 2013, and copresenter Jennifer Hanrahan, DO, associate professor of medicine at Case Western Reserve University in Cleveland, says the timing is good.
“I don’t know that the percentage of people hospitalized for infection has increased,” she said. “Because we are doing things more quickly than we did in the past, length of stays are shorter and there is a lot of pressure to get patients out of the hospital. There is a lot of consultation with Infectious Disease.”
Dr. Hanrahan, who also serves as medical director of infection prevention at Cleveland’s MetroHealth Medical Center, says that with so many patients hospitalized for infections, the value of updating one’s knowledge every few years is critical.
“I’ve been an infectious disease physician for 18 years and I’m also a hospitalist,” she said. “The types of questions I get vary a great deal depending on the experience of the hospitalist. My hope would be that we would be able to provide a basic level of understanding so that people would be more confident in approaching these problems.”
Another new feature this year is offer some of the most popular sessions at multiple times. In years past, popular sessions – such as “Update and Pearls in Infectious Diseases” and “Non–Evidence-Based Medicine: Things We Do for No Reason” – are standing room only events with attendees sitting on floors or gathered to eavesdrop from doorways.
“That says something about the content that’s being delivered, but that’s not very comfortable for folks who want to sit through a session,” Dr. Feldman said. “We’ve decided to add repeat sessions of popular presentations. We want everyone to be comfortable while they’re learning the important clinical content that’s being delivered at these sessions.”
The 2017 focus on healthcare policy is also new. Educational sessions on the policy landscape will be formally buttressed by plenary presentations from Patrick Conway, MD, MSc, MHM, deputy administrator for Innovation and Quality at the Centers for Medicare & Medicaid Services and director of the Center for Medicare and Medicaid Innovation, and Karen DeSalvo, MD, MPH, MSc, a former acting assistant secretary for health at the U.S. Department of Health and Human Services and national coordinator for health information technology.
“There’s a thirst for (policy news) among members of the Society of Hospital Medicine,” Dr. Feldman said. “It is easy to get lost in the day-to-day work that we do, but I think most of us really enjoy hearing about the bigger picture, especially when the bigger picture is in flux.”
“Right now, this is critical,” added Dr. Finn. “Health insurance coverage has a huge impact on hospitals. I think all practicing hospitalists will need to engage with the hospital C-suite if insurance and coverage changes. Since we are hospital based, we are directly tied to anything that the federal government does in terms of health care changes. It’s important for hospitalists to be knowledgeable about health policy.”
One major highlight of the meeting calendar – less new and more historically under-appreciated, in Dr. Feldman’s view – should be the 18 workshop presentations, which are essentially 90-minute dissertations, whittled down from roughly 150 submissions.
“These are the best submissions that we received,” Dr. Feldman said. “We worked hard to make sure that the workshops encompass the breadth and depth of hospital medicine. It is not just one area that’s covered in every workshop. We’ll have workshops ranging from clinical reasoning and communication with patients, to quality improvement issues and high value care discussions, as well as a case-based approach to inpatient dermatology.”
While annual meetings’ new offerings are always an important draw, Dr. Feldman says that the annual “standbys,” such as practice management and pediatrics, are necessary to keep attendees up to date on best practices in changing times.
“It’s pretty self-evident that if we’re going to be an important specialty, we need to serve those who are caring for patients day in and day out, as well as folks who are researching how we can do it better,” he said. “Then we must make sure that data is disseminated to all of us who are taking care of patients. That’s one of the really important parts of this meeting: dissemination of the important work.”
There is only one annual meeting dedicated to hospitalists, designed by hospitalists, and focusing purely on issues important to hospitalists. But even that isn’t enough to make sure more hospitalists show up every year.
That’s because a yearly conference can’t just be a rehash of the last one.
A valuable conference, certainly one worth spending the bulk of a continuing medical budget on, offers something new every year. Or, to look at the schedule for HM17, a lot of new every year.
That’s an unlikely complaint this year. The annual meeting schedule for May 1-4 at Mandalay Bay Resort and Casino includes five new educational tracks: High Value Care, Clinical Updates, Health Policy, Diagnostic Reasoning, and Medical Education.
“We’re really excited to be able to offer more clinical content,” said HM17 course director Lenny Feldman, MD, FAAP, FACP, SFHM.
Dr. Feldman sees each of the new tracks as filling separate and specific needs of HM attendees who vary from nonphysician providers to hospitalists to medical students.
Take, for instance, the High Value Care, Clinical Updates, and Diagnostic Reasoning sessions that are debuting.
“We wanted to make sure that we had as many clinically oriented sessions as possible,” Dr. Feldman said. “Which meant we needed to increase the amount of clinical content we have offered compared to the past few years. The new clinical track allows us to add probably 12 or so different sessions that will fill the needs of our attendees.”
The Diagnostic Reasoning and High Value Care tracks, in particular, highlight the annual meeting’s continued evolution toward a focus on evidence-based care, as that mantra becomes a bedrock of clinical treatment.
“Training our hospitalists to use the best dialogistic reasoning in their approach to their patients is a big push in hospital medicine right now,” Dr. Feldman said, “Hopefully, a track on that topic will excite people who love thinking about medicine, who got into medicine because of the mystery and want a renewed focus on how to be a great diagnostician.”
Dr. Feldman also noted that the High Value Care track should be a hot topic, as hospitalists want to learn how to provide high quality and high value care to patients at the same time. The new tracks should appeal to different groups and make the annual meeting more appealing to a variety of attendees, not just rank-and-file doctors.
The mini Medical Education track, for instance, is a subset of a half-dozen sessions tailored directly to medical educators in academic settings who face different challenges than their counterparts in community settings. The same goes for the Health Policy track, which will offer a handful of sessions suitable for novices looking to learn more in an age of reform, or policy wonks hoping to expand their knowledge.
Meeting evolving needs
New offerings aren’t limited to the main conference schedule. The 2017 roster of pre-courses includes one titled, “Bugs, Drugs and You: Infectious Diseases ‘Boot Camp’ for Hospitalists.” This daylong session hasn’t been held since 2013, and copresenter Jennifer Hanrahan, DO, associate professor of medicine at Case Western Reserve University in Cleveland, says the timing is good.
“I don’t know that the percentage of people hospitalized for infection has increased,” she said. “Because we are doing things more quickly than we did in the past, length of stays are shorter and there is a lot of pressure to get patients out of the hospital. There is a lot of consultation with Infectious Disease.”
Dr. Hanrahan, who also serves as medical director of infection prevention at Cleveland’s MetroHealth Medical Center, says that with so many patients hospitalized for infections, the value of updating one’s knowledge every few years is critical.
“I’ve been an infectious disease physician for 18 years and I’m also a hospitalist,” she said. “The types of questions I get vary a great deal depending on the experience of the hospitalist. My hope would be that we would be able to provide a basic level of understanding so that people would be more confident in approaching these problems.”
Another new feature this year is offer some of the most popular sessions at multiple times. In years past, popular sessions – such as “Update and Pearls in Infectious Diseases” and “Non–Evidence-Based Medicine: Things We Do for No Reason” – are standing room only events with attendees sitting on floors or gathered to eavesdrop from doorways.
“That says something about the content that’s being delivered, but that’s not very comfortable for folks who want to sit through a session,” Dr. Feldman said. “We’ve decided to add repeat sessions of popular presentations. We want everyone to be comfortable while they’re learning the important clinical content that’s being delivered at these sessions.”
The 2017 focus on healthcare policy is also new. Educational sessions on the policy landscape will be formally buttressed by plenary presentations from Patrick Conway, MD, MSc, MHM, deputy administrator for Innovation and Quality at the Centers for Medicare & Medicaid Services and director of the Center for Medicare and Medicaid Innovation, and Karen DeSalvo, MD, MPH, MSc, a former acting assistant secretary for health at the U.S. Department of Health and Human Services and national coordinator for health information technology.
“There’s a thirst for (policy news) among members of the Society of Hospital Medicine,” Dr. Feldman said. “It is easy to get lost in the day-to-day work that we do, but I think most of us really enjoy hearing about the bigger picture, especially when the bigger picture is in flux.”
“Right now, this is critical,” added Dr. Finn. “Health insurance coverage has a huge impact on hospitals. I think all practicing hospitalists will need to engage with the hospital C-suite if insurance and coverage changes. Since we are hospital based, we are directly tied to anything that the federal government does in terms of health care changes. It’s important for hospitalists to be knowledgeable about health policy.”
One major highlight of the meeting calendar – less new and more historically under-appreciated, in Dr. Feldman’s view – should be the 18 workshop presentations, which are essentially 90-minute dissertations, whittled down from roughly 150 submissions.
“These are the best submissions that we received,” Dr. Feldman said. “We worked hard to make sure that the workshops encompass the breadth and depth of hospital medicine. It is not just one area that’s covered in every workshop. We’ll have workshops ranging from clinical reasoning and communication with patients, to quality improvement issues and high value care discussions, as well as a case-based approach to inpatient dermatology.”
While annual meetings’ new offerings are always an important draw, Dr. Feldman says that the annual “standbys,” such as practice management and pediatrics, are necessary to keep attendees up to date on best practices in changing times.
“It’s pretty self-evident that if we’re going to be an important specialty, we need to serve those who are caring for patients day in and day out, as well as folks who are researching how we can do it better,” he said. “Then we must make sure that data is disseminated to all of us who are taking care of patients. That’s one of the really important parts of this meeting: dissemination of the important work.”
There is only one annual meeting dedicated to hospitalists, designed by hospitalists, and focusing purely on issues important to hospitalists. But even that isn’t enough to make sure more hospitalists show up every year.
That’s because a yearly conference can’t just be a rehash of the last one.
A valuable conference, certainly one worth spending the bulk of a continuing medical budget on, offers something new every year. Or, to look at the schedule for HM17, a lot of new every year.
That’s an unlikely complaint this year. The annual meeting schedule for May 1-4 at Mandalay Bay Resort and Casino includes five new educational tracks: High Value Care, Clinical Updates, Health Policy, Diagnostic Reasoning, and Medical Education.
“We’re really excited to be able to offer more clinical content,” said HM17 course director Lenny Feldman, MD, FAAP, FACP, SFHM.
Dr. Feldman sees each of the new tracks as filling separate and specific needs of HM attendees who vary from nonphysician providers to hospitalists to medical students.
Take, for instance, the High Value Care, Clinical Updates, and Diagnostic Reasoning sessions that are debuting.
“We wanted to make sure that we had as many clinically oriented sessions as possible,” Dr. Feldman said. “Which meant we needed to increase the amount of clinical content we have offered compared to the past few years. The new clinical track allows us to add probably 12 or so different sessions that will fill the needs of our attendees.”
The Diagnostic Reasoning and High Value Care tracks, in particular, highlight the annual meeting’s continued evolution toward a focus on evidence-based care, as that mantra becomes a bedrock of clinical treatment.
“Training our hospitalists to use the best dialogistic reasoning in their approach to their patients is a big push in hospital medicine right now,” Dr. Feldman said, “Hopefully, a track on that topic will excite people who love thinking about medicine, who got into medicine because of the mystery and want a renewed focus on how to be a great diagnostician.”
Dr. Feldman also noted that the High Value Care track should be a hot topic, as hospitalists want to learn how to provide high quality and high value care to patients at the same time. The new tracks should appeal to different groups and make the annual meeting more appealing to a variety of attendees, not just rank-and-file doctors.
The mini Medical Education track, for instance, is a subset of a half-dozen sessions tailored directly to medical educators in academic settings who face different challenges than their counterparts in community settings. The same goes for the Health Policy track, which will offer a handful of sessions suitable for novices looking to learn more in an age of reform, or policy wonks hoping to expand their knowledge.
Meeting evolving needs
New offerings aren’t limited to the main conference schedule. The 2017 roster of pre-courses includes one titled, “Bugs, Drugs and You: Infectious Diseases ‘Boot Camp’ for Hospitalists.” This daylong session hasn’t been held since 2013, and copresenter Jennifer Hanrahan, DO, associate professor of medicine at Case Western Reserve University in Cleveland, says the timing is good.
“I don’t know that the percentage of people hospitalized for infection has increased,” she said. “Because we are doing things more quickly than we did in the past, length of stays are shorter and there is a lot of pressure to get patients out of the hospital. There is a lot of consultation with Infectious Disease.”
Dr. Hanrahan, who also serves as medical director of infection prevention at Cleveland’s MetroHealth Medical Center, says that with so many patients hospitalized for infections, the value of updating one’s knowledge every few years is critical.
“I’ve been an infectious disease physician for 18 years and I’m also a hospitalist,” she said. “The types of questions I get vary a great deal depending on the experience of the hospitalist. My hope would be that we would be able to provide a basic level of understanding so that people would be more confident in approaching these problems.”
Another new feature this year is offer some of the most popular sessions at multiple times. In years past, popular sessions – such as “Update and Pearls in Infectious Diseases” and “Non–Evidence-Based Medicine: Things We Do for No Reason” – are standing room only events with attendees sitting on floors or gathered to eavesdrop from doorways.
“That says something about the content that’s being delivered, but that’s not very comfortable for folks who want to sit through a session,” Dr. Feldman said. “We’ve decided to add repeat sessions of popular presentations. We want everyone to be comfortable while they’re learning the important clinical content that’s being delivered at these sessions.”
The 2017 focus on healthcare policy is also new. Educational sessions on the policy landscape will be formally buttressed by plenary presentations from Patrick Conway, MD, MSc, MHM, deputy administrator for Innovation and Quality at the Centers for Medicare & Medicaid Services and director of the Center for Medicare and Medicaid Innovation, and Karen DeSalvo, MD, MPH, MSc, a former acting assistant secretary for health at the U.S. Department of Health and Human Services and national coordinator for health information technology.
“There’s a thirst for (policy news) among members of the Society of Hospital Medicine,” Dr. Feldman said. “It is easy to get lost in the day-to-day work that we do, but I think most of us really enjoy hearing about the bigger picture, especially when the bigger picture is in flux.”
“Right now, this is critical,” added Dr. Finn. “Health insurance coverage has a huge impact on hospitals. I think all practicing hospitalists will need to engage with the hospital C-suite if insurance and coverage changes. Since we are hospital based, we are directly tied to anything that the federal government does in terms of health care changes. It’s important for hospitalists to be knowledgeable about health policy.”
One major highlight of the meeting calendar – less new and more historically under-appreciated, in Dr. Feldman’s view – should be the 18 workshop presentations, which are essentially 90-minute dissertations, whittled down from roughly 150 submissions.
“These are the best submissions that we received,” Dr. Feldman said. “We worked hard to make sure that the workshops encompass the breadth and depth of hospital medicine. It is not just one area that’s covered in every workshop. We’ll have workshops ranging from clinical reasoning and communication with patients, to quality improvement issues and high value care discussions, as well as a case-based approach to inpatient dermatology.”
While annual meetings’ new offerings are always an important draw, Dr. Feldman says that the annual “standbys,” such as practice management and pediatrics, are necessary to keep attendees up to date on best practices in changing times.
“It’s pretty self-evident that if we’re going to be an important specialty, we need to serve those who are caring for patients day in and day out, as well as folks who are researching how we can do it better,” he said. “Then we must make sure that data is disseminated to all of us who are taking care of patients. That’s one of the really important parts of this meeting: dissemination of the important work.”