User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


SHM launches Chapter Development Fund to enhance reach, impact of chapters
As hospital medicine continues to experience unparalleled growth, the Society of Hospital Medicine (SHM) seeks to supplement its chapter program via a new $100,000 Chapter Development Fund. The monies will be used to further enhance the reach and impact of SHM’s 50 regional chapters.
Chapters can request up to $5,000 from the fund annually to support projects that promote networking, education, leadership opportunities, and improvements in health care delivery. In addition to growing the chapters, SHM expects that the additional resources will help facilitate relationships with local hospitals and medical schools, and demonstrate the value of membership.
“Chapters that were struggling now feel that they have the support they need to improve, and the ones that have figured out the basics can push their creative limits. That innovation can be passed along and benefit [all chapters],” Dr. Thompson said.
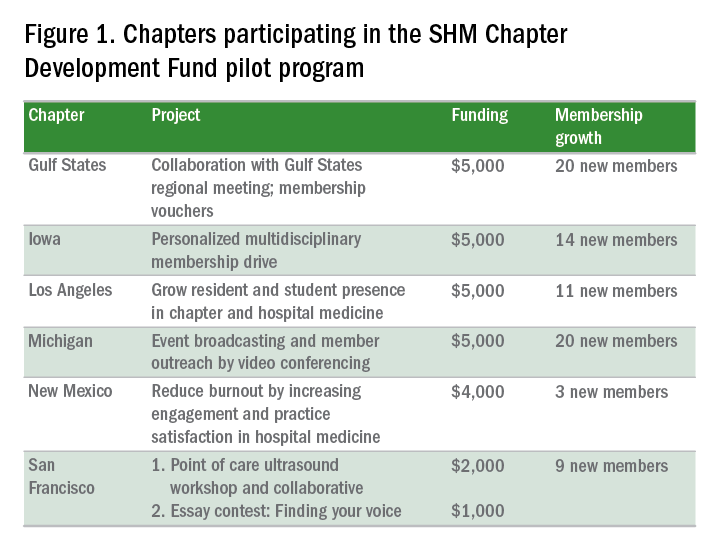
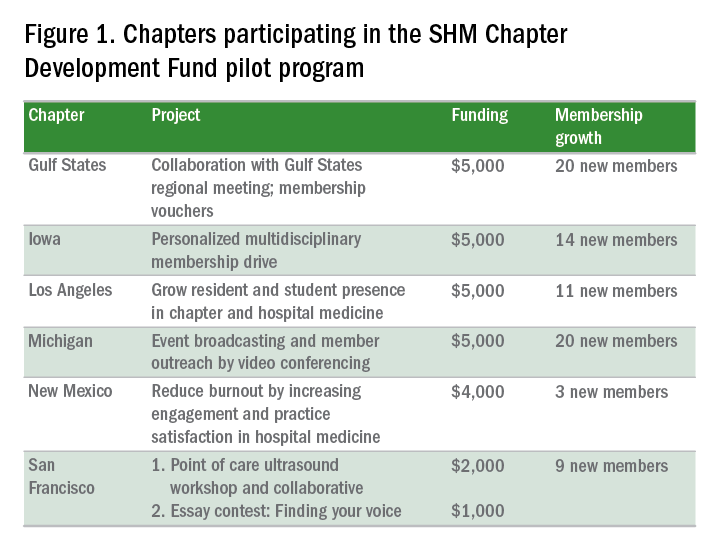
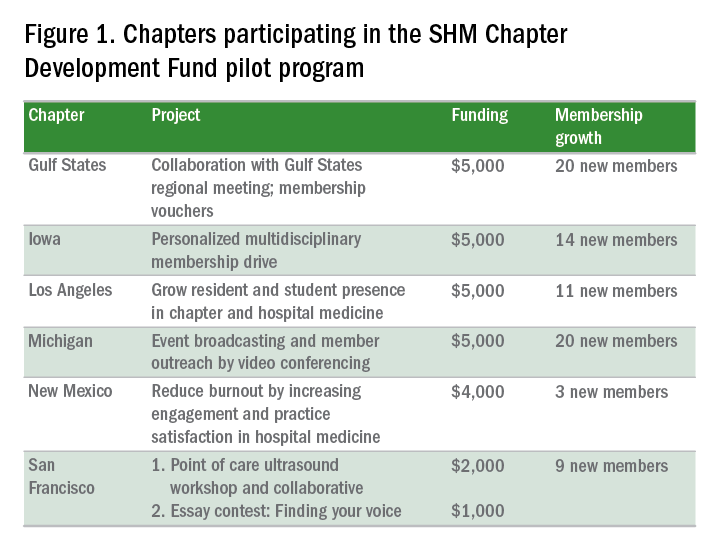
Fund usage already has led to a number of success stories (see Figure 1). During the program’s pilot phase, six chapters – Gulf States, Iowa, Los Angeles, Michigan, New Mexico, and San Francisco – acquired 77 new SHM members through a variety of innovative methods.
“We were struggling in recruitment, and saw this as an opportunity to attract members,” said chapter leader Venkataraman Palabindala, MD. “We used the funds to create 15 ‘coupons’ for membership. The rest of the money [was used] to start a regional meeting … where chapter leaders were invited to lead talks. [The meeting] really helped us.”
Another example of success comes from the Iowa Chapter, which attracted 14 new members through a multidisciplinary membership drive.
“We … requested funding for a few specific areas. One was marketing, where we had fliers written up to target specific groups, including … students, APPs (advanced practice practitioners), residents, students, and pharmacists, as well as other physicians,” said chapter leader Melinda Johnson, MD, SFHM.
The Iowa Chapter also used funding for SHM-branded “giveaways” (coffee mugs, portable chargers, etc.) to leave behind during meetings with prospective members. Vouchers, offering a 50% discount on a 1-year membership for new members during the pilot program, were especially effective. The combined activities “really increased visibility for SHM within our state and with disciplines besides physicians,” Dr. Johnson said.
Chapters can apply for support on a rolling basis by submitting a proposal to the Chapter Support Committee. For the full details, visit www.hospitalmedicine.org/chapterdevelopment.
When thinking about ideas, Dr. Thompson advises chapters to begin with “a brainstorm of all of the … exciting things that you have wanted to do for your membership. Then think about the ones that are attainable, and map out how to get there. The pilot showed that in a short time, you can reach many people when you plan your project out with timing and specific goals … and let the committee support you.”
In addition to a financial boost, fund recipients enjoy personalized mentorship from the committee, a benefit that both Dr. Johnson and Dr. Palabindala found invaluable. For new and developing chapters, “the support you get, the money, as well as the goal setting and feedback, is amazing,” Dr. Palabindala said.
Chapters, Dr. Johnson said, provide members with networking and leadership opportunities – and ensure that the unique, localized needs of their communities are represented at SHM.
“They become your professional home, providing opportunities,” she said, “that improve personal and professional satisfaction. Anyone is welcome to participate in the conversation.”
For more information on how you can become involved in an SHM chapter, visit www.hospitalmedicine.org/chapters.
Claudia Stahl is a content manager for the Society of Hospital Medicine.
As hospital medicine continues to experience unparalleled growth, the Society of Hospital Medicine (SHM) seeks to supplement its chapter program via a new $100,000 Chapter Development Fund. The monies will be used to further enhance the reach and impact of SHM’s 50 regional chapters.
Chapters can request up to $5,000 from the fund annually to support projects that promote networking, education, leadership opportunities, and improvements in health care delivery. In addition to growing the chapters, SHM expects that the additional resources will help facilitate relationships with local hospitals and medical schools, and demonstrate the value of membership.
“Chapters that were struggling now feel that they have the support they need to improve, and the ones that have figured out the basics can push their creative limits. That innovation can be passed along and benefit [all chapters],” Dr. Thompson said.
Fund usage already has led to a number of success stories (see Figure 1). During the program’s pilot phase, six chapters – Gulf States, Iowa, Los Angeles, Michigan, New Mexico, and San Francisco – acquired 77 new SHM members through a variety of innovative methods.
“We were struggling in recruitment, and saw this as an opportunity to attract members,” said chapter leader Venkataraman Palabindala, MD. “We used the funds to create 15 ‘coupons’ for membership. The rest of the money [was used] to start a regional meeting … where chapter leaders were invited to lead talks. [The meeting] really helped us.”
Another example of success comes from the Iowa Chapter, which attracted 14 new members through a multidisciplinary membership drive.
“We … requested funding for a few specific areas. One was marketing, where we had fliers written up to target specific groups, including … students, APPs (advanced practice practitioners), residents, students, and pharmacists, as well as other physicians,” said chapter leader Melinda Johnson, MD, SFHM.
The Iowa Chapter also used funding for SHM-branded “giveaways” (coffee mugs, portable chargers, etc.) to leave behind during meetings with prospective members. Vouchers, offering a 50% discount on a 1-year membership for new members during the pilot program, were especially effective. The combined activities “really increased visibility for SHM within our state and with disciplines besides physicians,” Dr. Johnson said.
Chapters can apply for support on a rolling basis by submitting a proposal to the Chapter Support Committee. For the full details, visit www.hospitalmedicine.org/chapterdevelopment.
When thinking about ideas, Dr. Thompson advises chapters to begin with “a brainstorm of all of the … exciting things that you have wanted to do for your membership. Then think about the ones that are attainable, and map out how to get there. The pilot showed that in a short time, you can reach many people when you plan your project out with timing and specific goals … and let the committee support you.”
In addition to a financial boost, fund recipients enjoy personalized mentorship from the committee, a benefit that both Dr. Johnson and Dr. Palabindala found invaluable. For new and developing chapters, “the support you get, the money, as well as the goal setting and feedback, is amazing,” Dr. Palabindala said.
Chapters, Dr. Johnson said, provide members with networking and leadership opportunities – and ensure that the unique, localized needs of their communities are represented at SHM.
“They become your professional home, providing opportunities,” she said, “that improve personal and professional satisfaction. Anyone is welcome to participate in the conversation.”
For more information on how you can become involved in an SHM chapter, visit www.hospitalmedicine.org/chapters.
Claudia Stahl is a content manager for the Society of Hospital Medicine.
As hospital medicine continues to experience unparalleled growth, the Society of Hospital Medicine (SHM) seeks to supplement its chapter program via a new $100,000 Chapter Development Fund. The monies will be used to further enhance the reach and impact of SHM’s 50 regional chapters.
Chapters can request up to $5,000 from the fund annually to support projects that promote networking, education, leadership opportunities, and improvements in health care delivery. In addition to growing the chapters, SHM expects that the additional resources will help facilitate relationships with local hospitals and medical schools, and demonstrate the value of membership.
“Chapters that were struggling now feel that they have the support they need to improve, and the ones that have figured out the basics can push their creative limits. That innovation can be passed along and benefit [all chapters],” Dr. Thompson said.
Fund usage already has led to a number of success stories (see Figure 1). During the program’s pilot phase, six chapters – Gulf States, Iowa, Los Angeles, Michigan, New Mexico, and San Francisco – acquired 77 new SHM members through a variety of innovative methods.
“We were struggling in recruitment, and saw this as an opportunity to attract members,” said chapter leader Venkataraman Palabindala, MD. “We used the funds to create 15 ‘coupons’ for membership. The rest of the money [was used] to start a regional meeting … where chapter leaders were invited to lead talks. [The meeting] really helped us.”
Another example of success comes from the Iowa Chapter, which attracted 14 new members through a multidisciplinary membership drive.
“We … requested funding for a few specific areas. One was marketing, where we had fliers written up to target specific groups, including … students, APPs (advanced practice practitioners), residents, students, and pharmacists, as well as other physicians,” said chapter leader Melinda Johnson, MD, SFHM.
The Iowa Chapter also used funding for SHM-branded “giveaways” (coffee mugs, portable chargers, etc.) to leave behind during meetings with prospective members. Vouchers, offering a 50% discount on a 1-year membership for new members during the pilot program, were especially effective. The combined activities “really increased visibility for SHM within our state and with disciplines besides physicians,” Dr. Johnson said.
Chapters can apply for support on a rolling basis by submitting a proposal to the Chapter Support Committee. For the full details, visit www.hospitalmedicine.org/chapterdevelopment.
When thinking about ideas, Dr. Thompson advises chapters to begin with “a brainstorm of all of the … exciting things that you have wanted to do for your membership. Then think about the ones that are attainable, and map out how to get there. The pilot showed that in a short time, you can reach many people when you plan your project out with timing and specific goals … and let the committee support you.”
In addition to a financial boost, fund recipients enjoy personalized mentorship from the committee, a benefit that both Dr. Johnson and Dr. Palabindala found invaluable. For new and developing chapters, “the support you get, the money, as well as the goal setting and feedback, is amazing,” Dr. Palabindala said.
Chapters, Dr. Johnson said, provide members with networking and leadership opportunities – and ensure that the unique, localized needs of their communities are represented at SHM.
“They become your professional home, providing opportunities,” she said, “that improve personal and professional satisfaction. Anyone is welcome to participate in the conversation.”
For more information on how you can become involved in an SHM chapter, visit www.hospitalmedicine.org/chapters.
Claudia Stahl is a content manager for the Society of Hospital Medicine.
Do not overtreat febrile neutropenia
Clinical question: Does emergency department management of patients with febrile neutropenia (FN) follow current guidelines?
Background: Chemotherapy-related FN is an oncologic emergency frequently leading to hospitalization and intravenous antibiotics. Familiarity with FN guidelines allows risk stratification for inpatient versus outpatient therapy.
Study design: Single-center, retrospective, cohort study.
Setting: Large, urban, tertiary-care academic hospital.
Synopsis: Of 173 patient visits, 25% were risk stratified as eligible for outpatient treatment and 75% as inpatient care. All patient care was assessed for guideline concordance at the time of ED disposition and therapy.
Primary outcome analysis demonstrated management was guideline discordant in 98% of low-risk patients versus 7% of high-risk patients. Secondary 30-day clinical outcomes showed high-risk patients were more likely to have positive blood cultures (54%), sepsis-induced hypotension (9.3%), and death (5.4%). Seventeen percent of all patients who received IV antibiotics were prescribed vancomycin without guideline support.
Bottom line: Low-risk FN patients in the ED received more aggressive treatment than recommended. Further research is needed to strategize means of better aligning FN management with standards of care.
Citation: Baugh CW, Wang TJ, Caterino JM, et al. ED management of patients with febrile neutropenia: guideline concordant or overly aggressive [published online ahead of print Sept. 9, 2016]? Acad Emerg Med. doi: 10.1111/acem.13079.
Dr. Zuleta is an assistant professor and associate program director of the Jackson Memorial/University of Miami Internal Medicine residency training program and the site director of the program at University of Miami Hospital.
Clinical question: Does emergency department management of patients with febrile neutropenia (FN) follow current guidelines?
Background: Chemotherapy-related FN is an oncologic emergency frequently leading to hospitalization and intravenous antibiotics. Familiarity with FN guidelines allows risk stratification for inpatient versus outpatient therapy.
Study design: Single-center, retrospective, cohort study.
Setting: Large, urban, tertiary-care academic hospital.
Synopsis: Of 173 patient visits, 25% were risk stratified as eligible for outpatient treatment and 75% as inpatient care. All patient care was assessed for guideline concordance at the time of ED disposition and therapy.
Primary outcome analysis demonstrated management was guideline discordant in 98% of low-risk patients versus 7% of high-risk patients. Secondary 30-day clinical outcomes showed high-risk patients were more likely to have positive blood cultures (54%), sepsis-induced hypotension (9.3%), and death (5.4%). Seventeen percent of all patients who received IV antibiotics were prescribed vancomycin without guideline support.
Bottom line: Low-risk FN patients in the ED received more aggressive treatment than recommended. Further research is needed to strategize means of better aligning FN management with standards of care.
Citation: Baugh CW, Wang TJ, Caterino JM, et al. ED management of patients with febrile neutropenia: guideline concordant or overly aggressive [published online ahead of print Sept. 9, 2016]? Acad Emerg Med. doi: 10.1111/acem.13079.
Dr. Zuleta is an assistant professor and associate program director of the Jackson Memorial/University of Miami Internal Medicine residency training program and the site director of the program at University of Miami Hospital.
Clinical question: Does emergency department management of patients with febrile neutropenia (FN) follow current guidelines?
Background: Chemotherapy-related FN is an oncologic emergency frequently leading to hospitalization and intravenous antibiotics. Familiarity with FN guidelines allows risk stratification for inpatient versus outpatient therapy.
Study design: Single-center, retrospective, cohort study.
Setting: Large, urban, tertiary-care academic hospital.
Synopsis: Of 173 patient visits, 25% were risk stratified as eligible for outpatient treatment and 75% as inpatient care. All patient care was assessed for guideline concordance at the time of ED disposition and therapy.
Primary outcome analysis demonstrated management was guideline discordant in 98% of low-risk patients versus 7% of high-risk patients. Secondary 30-day clinical outcomes showed high-risk patients were more likely to have positive blood cultures (54%), sepsis-induced hypotension (9.3%), and death (5.4%). Seventeen percent of all patients who received IV antibiotics were prescribed vancomycin without guideline support.
Bottom line: Low-risk FN patients in the ED received more aggressive treatment than recommended. Further research is needed to strategize means of better aligning FN management with standards of care.
Citation: Baugh CW, Wang TJ, Caterino JM, et al. ED management of patients with febrile neutropenia: guideline concordant or overly aggressive [published online ahead of print Sept. 9, 2016]? Acad Emerg Med. doi: 10.1111/acem.13079.
Dr. Zuleta is an assistant professor and associate program director of the Jackson Memorial/University of Miami Internal Medicine residency training program and the site director of the program at University of Miami Hospital.
What to do with isolated calf DVT
Clinical question: Does therapeutic anticoagulation of isolated calf deep vein thrombosis (DVT) decrease risk for proximal DVT or PE?
Background: Optimal management of isolated calf DVT lacks consensus.
Study design: Single-center, retrospective, cohort study.
Setting: Large academic hospital.
Nevertheless, 9.2% of control patients and 3.3% of exposure patients developed a proximal DVT or PE. The anticoagulation group was associated with lower likelihood of proximal DVT or PE (risk ratio 0.36; 95% CI, 0.15-0.84) but an increased risk of bleeding (8.6%), compared with the nonexposure group (2.2%). Sensitivity analysis did not alter the observed association.
Bottom line: Therapeutic anticoagulation for isolated calf DVT may be warranted to decrease the risk for proximal DVT or PE but with an increased risk of bleeding. Randomized trials are needed to clarify the risk versus benefit.
Citation: Utter GH, Dhillon TS, Salcedo ES, et al. Therapeutic anticoagulation for isolated calf deep vein thrombosis. JAMA Surg. 2016;151(9):e161770. doi: 10.1001/jamasurg.2016.1770.
Dr. Zuleta is an assistant professor and associate program director of the Jackson Memorial/University of Miami Internal Medicine residency training program and the site director of the program at University of Miami Hospital.
Clinical question: Does therapeutic anticoagulation of isolated calf deep vein thrombosis (DVT) decrease risk for proximal DVT or PE?
Background: Optimal management of isolated calf DVT lacks consensus.
Study design: Single-center, retrospective, cohort study.
Setting: Large academic hospital.
Nevertheless, 9.2% of control patients and 3.3% of exposure patients developed a proximal DVT or PE. The anticoagulation group was associated with lower likelihood of proximal DVT or PE (risk ratio 0.36; 95% CI, 0.15-0.84) but an increased risk of bleeding (8.6%), compared with the nonexposure group (2.2%). Sensitivity analysis did not alter the observed association.
Bottom line: Therapeutic anticoagulation for isolated calf DVT may be warranted to decrease the risk for proximal DVT or PE but with an increased risk of bleeding. Randomized trials are needed to clarify the risk versus benefit.
Citation: Utter GH, Dhillon TS, Salcedo ES, et al. Therapeutic anticoagulation for isolated calf deep vein thrombosis. JAMA Surg. 2016;151(9):e161770. doi: 10.1001/jamasurg.2016.1770.
Dr. Zuleta is an assistant professor and associate program director of the Jackson Memorial/University of Miami Internal Medicine residency training program and the site director of the program at University of Miami Hospital.
Clinical question: Does therapeutic anticoagulation of isolated calf deep vein thrombosis (DVT) decrease risk for proximal DVT or PE?
Background: Optimal management of isolated calf DVT lacks consensus.
Study design: Single-center, retrospective, cohort study.
Setting: Large academic hospital.
Nevertheless, 9.2% of control patients and 3.3% of exposure patients developed a proximal DVT or PE. The anticoagulation group was associated with lower likelihood of proximal DVT or PE (risk ratio 0.36; 95% CI, 0.15-0.84) but an increased risk of bleeding (8.6%), compared with the nonexposure group (2.2%). Sensitivity analysis did not alter the observed association.
Bottom line: Therapeutic anticoagulation for isolated calf DVT may be warranted to decrease the risk for proximal DVT or PE but with an increased risk of bleeding. Randomized trials are needed to clarify the risk versus benefit.
Citation: Utter GH, Dhillon TS, Salcedo ES, et al. Therapeutic anticoagulation for isolated calf deep vein thrombosis. JAMA Surg. 2016;151(9):e161770. doi: 10.1001/jamasurg.2016.1770.
Dr. Zuleta is an assistant professor and associate program director of the Jackson Memorial/University of Miami Internal Medicine residency training program and the site director of the program at University of Miami Hospital.
SHM Practice Administrators’ Mentor Program benefits both parties
Editor’s note: Each month, SHM puts the spotlight on our most active members and explores how they are making substantial contributions to hospital medicine. Visit www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise and help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Alessandra G. Cornelio, MPH, the acquisition manager at Hartford Healthcare Medical Group in Connecticut. Ms. Cornelio is an active member of SHM’s Practice Administrators Committee. She developed and now directs the Practice Administrators’ Mentor Program.
Answer: I was finishing my internship at the Middlesex Hospital Cancer Center. I was interested in hospital administration and learning more about the inpatient side of health care. I chose to work within hospital medicine because I wanted to help build a team of compassionate doctors who could provide an excellent patient experience while maintaining an environment with safe, high-quality care.
To complement my career goals, SHM helped my professional growth by exposing me to the variety of topics and issues that practice administrators deal with regularly in their practices. I was also able to review and learn from the many resources available on the SHM website, such as white papers and articles, which were extremely useful for a new administrator.
Q: What prompted you to join the Practice Administrators Committee? What are some of the most impactful projects the committee is currently working on?
A: Within my first year of being a practice administrator, I attended a practice administrators’ forum at the SHM annual meeting in Washington. I found that the information was relevant to my daily functions as an administrator, and I was also able to meet and share ideas with other practice administrators from throughout the country. Down the line, I learned that SHM needed new members for the Practice Administrators Committee. I wanted to become more involved in a meaningful way, so I decided to apply.
The Practice Administrators Committee is a hardworking committee that takes on many meaningful projects. Most recently, the team has been working on developing a more user-friendly website for practice administrators, and a subgroup of the committee has cross-referenced “The Key Principles and Characteristics of an Effective Hospital Medicine Group” with existing resources, which will prove valuable to all administrators in the final product.
Q: Can you discuss how you began leading the work group for the Practice Administrators’ Mentor Program and how it has evolved since its inception?
A: As part of the committee’s initiative to help fellow practice administrators, we formed a subcommittee to begin developing a mentor program. (Former SHM staffer) Joseph Miller and I worked together to create an appropriate program model through research and brainstorming. We also utilized the HMX Practice Administrators Community to ask fellow practice administrators what they would expect from a mentor program and if they would participate. There was a strong favorable response rate, and we were able to implement a pilot program.
We implemented two different tracks for the program – the buddy system track and the career development track. The buddy system track is for those of any level of expertise or experience who are more interested in short-term assistance or in need of a sounding board. The career development track is a more traditional approach, matching a seasoned practice administrator with a less experienced practice administrator.
The program was designed to have annual cohorts, with the Practice Administrators Committee members as mentors. There is a detailed application process to ensure that each mentee is matched with an appropriate mentor, based on their interests and needs. We provide an orientation webinar to both parties before kicking off the relationship to present program expectations. The pilot program used this model, and comments from 6-month and annual evaluations showed tremendous satisfaction with the structure and value of this program.
There were approximately 16 pairs during the pilot year, and the following year, we grew to almost 20 pairs. Our goal as a committee is to maintain this program year after year, and in order to expand, we’ll need more than just the committee members to volunteer as mentors. There are so many talented practice administrators, and it would be wonderful to fold them into this gratifying program to pay it forward.
Many mentors, including myself, found value in acting as a mentor. I learned from my mentees as well as made connections and friendships with other professionals in the field.
Q: Given your intimate involvement, how have you seen the Practice Administrators’ Mentor Program benefit both the mentors and the mentees? Can you provide any specific examples?
A: Mentees are able to connect with seasoned mentors and can ask specific questions about career development and any issues they may be experiencing. Mentors are able to share their experiences and pass along important and valuable lessons learned to mentees. I served as a mentor, even though I did not yet consider myself a qualified candidate. However, I found that I was more equipped than I had realized, and I was able to assist my mentee with many aspects of career development (i.e., resume building, discussions with the C-suite, etc.).
My mentee was a practice coordinator who had only been in hospital medicine for 1 year. She had little experience hiring hospitalists, so this was a major area that we worked on together during our yearlong connection. I introduced her to collaborating with her HR department when posting positions, as well as working with permanent placement agencies. Her service was also undergoing a change in leadership, which can be difficult for any service line to experience. We discussed ways in which she could present important information to the new medical director that would produce a meaningful conversation.
In turn, my mentee introduced me to new online resources and was able to connect me with the manager of her practice, who assisted me with streamlining the payroll structure in my practice. I truly enjoyed my experience developing and participating in the program.
Felicia Steele is SHM’s communications coordinator.
Learn more about how you can benefit from the Practice Administrators’ Mentor program via the SHM website.
Editor’s note: Each month, SHM puts the spotlight on our most active members and explores how they are making substantial contributions to hospital medicine. Visit www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise and help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Alessandra G. Cornelio, MPH, the acquisition manager at Hartford Healthcare Medical Group in Connecticut. Ms. Cornelio is an active member of SHM’s Practice Administrators Committee. She developed and now directs the Practice Administrators’ Mentor Program.
Answer: I was finishing my internship at the Middlesex Hospital Cancer Center. I was interested in hospital administration and learning more about the inpatient side of health care. I chose to work within hospital medicine because I wanted to help build a team of compassionate doctors who could provide an excellent patient experience while maintaining an environment with safe, high-quality care.
To complement my career goals, SHM helped my professional growth by exposing me to the variety of topics and issues that practice administrators deal with regularly in their practices. I was also able to review and learn from the many resources available on the SHM website, such as white papers and articles, which were extremely useful for a new administrator.
Q: What prompted you to join the Practice Administrators Committee? What are some of the most impactful projects the committee is currently working on?
A: Within my first year of being a practice administrator, I attended a practice administrators’ forum at the SHM annual meeting in Washington. I found that the information was relevant to my daily functions as an administrator, and I was also able to meet and share ideas with other practice administrators from throughout the country. Down the line, I learned that SHM needed new members for the Practice Administrators Committee. I wanted to become more involved in a meaningful way, so I decided to apply.
The Practice Administrators Committee is a hardworking committee that takes on many meaningful projects. Most recently, the team has been working on developing a more user-friendly website for practice administrators, and a subgroup of the committee has cross-referenced “The Key Principles and Characteristics of an Effective Hospital Medicine Group” with existing resources, which will prove valuable to all administrators in the final product.
Q: Can you discuss how you began leading the work group for the Practice Administrators’ Mentor Program and how it has evolved since its inception?
A: As part of the committee’s initiative to help fellow practice administrators, we formed a subcommittee to begin developing a mentor program. (Former SHM staffer) Joseph Miller and I worked together to create an appropriate program model through research and brainstorming. We also utilized the HMX Practice Administrators Community to ask fellow practice administrators what they would expect from a mentor program and if they would participate. There was a strong favorable response rate, and we were able to implement a pilot program.
We implemented two different tracks for the program – the buddy system track and the career development track. The buddy system track is for those of any level of expertise or experience who are more interested in short-term assistance or in need of a sounding board. The career development track is a more traditional approach, matching a seasoned practice administrator with a less experienced practice administrator.
The program was designed to have annual cohorts, with the Practice Administrators Committee members as mentors. There is a detailed application process to ensure that each mentee is matched with an appropriate mentor, based on their interests and needs. We provide an orientation webinar to both parties before kicking off the relationship to present program expectations. The pilot program used this model, and comments from 6-month and annual evaluations showed tremendous satisfaction with the structure and value of this program.
There were approximately 16 pairs during the pilot year, and the following year, we grew to almost 20 pairs. Our goal as a committee is to maintain this program year after year, and in order to expand, we’ll need more than just the committee members to volunteer as mentors. There are so many talented practice administrators, and it would be wonderful to fold them into this gratifying program to pay it forward.
Many mentors, including myself, found value in acting as a mentor. I learned from my mentees as well as made connections and friendships with other professionals in the field.
Q: Given your intimate involvement, how have you seen the Practice Administrators’ Mentor Program benefit both the mentors and the mentees? Can you provide any specific examples?
A: Mentees are able to connect with seasoned mentors and can ask specific questions about career development and any issues they may be experiencing. Mentors are able to share their experiences and pass along important and valuable lessons learned to mentees. I served as a mentor, even though I did not yet consider myself a qualified candidate. However, I found that I was more equipped than I had realized, and I was able to assist my mentee with many aspects of career development (i.e., resume building, discussions with the C-suite, etc.).
My mentee was a practice coordinator who had only been in hospital medicine for 1 year. She had little experience hiring hospitalists, so this was a major area that we worked on together during our yearlong connection. I introduced her to collaborating with her HR department when posting positions, as well as working with permanent placement agencies. Her service was also undergoing a change in leadership, which can be difficult for any service line to experience. We discussed ways in which she could present important information to the new medical director that would produce a meaningful conversation.
In turn, my mentee introduced me to new online resources and was able to connect me with the manager of her practice, who assisted me with streamlining the payroll structure in my practice. I truly enjoyed my experience developing and participating in the program.
Felicia Steele is SHM’s communications coordinator.
Learn more about how you can benefit from the Practice Administrators’ Mentor program via the SHM website.
Editor’s note: Each month, SHM puts the spotlight on our most active members and explores how they are making substantial contributions to hospital medicine. Visit www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise and help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Alessandra G. Cornelio, MPH, the acquisition manager at Hartford Healthcare Medical Group in Connecticut. Ms. Cornelio is an active member of SHM’s Practice Administrators Committee. She developed and now directs the Practice Administrators’ Mentor Program.
Answer: I was finishing my internship at the Middlesex Hospital Cancer Center. I was interested in hospital administration and learning more about the inpatient side of health care. I chose to work within hospital medicine because I wanted to help build a team of compassionate doctors who could provide an excellent patient experience while maintaining an environment with safe, high-quality care.
To complement my career goals, SHM helped my professional growth by exposing me to the variety of topics and issues that practice administrators deal with regularly in their practices. I was also able to review and learn from the many resources available on the SHM website, such as white papers and articles, which were extremely useful for a new administrator.
Q: What prompted you to join the Practice Administrators Committee? What are some of the most impactful projects the committee is currently working on?
A: Within my first year of being a practice administrator, I attended a practice administrators’ forum at the SHM annual meeting in Washington. I found that the information was relevant to my daily functions as an administrator, and I was also able to meet and share ideas with other practice administrators from throughout the country. Down the line, I learned that SHM needed new members for the Practice Administrators Committee. I wanted to become more involved in a meaningful way, so I decided to apply.
The Practice Administrators Committee is a hardworking committee that takes on many meaningful projects. Most recently, the team has been working on developing a more user-friendly website for practice administrators, and a subgroup of the committee has cross-referenced “The Key Principles and Characteristics of an Effective Hospital Medicine Group” with existing resources, which will prove valuable to all administrators in the final product.
Q: Can you discuss how you began leading the work group for the Practice Administrators’ Mentor Program and how it has evolved since its inception?
A: As part of the committee’s initiative to help fellow practice administrators, we formed a subcommittee to begin developing a mentor program. (Former SHM staffer) Joseph Miller and I worked together to create an appropriate program model through research and brainstorming. We also utilized the HMX Practice Administrators Community to ask fellow practice administrators what they would expect from a mentor program and if they would participate. There was a strong favorable response rate, and we were able to implement a pilot program.
We implemented two different tracks for the program – the buddy system track and the career development track. The buddy system track is for those of any level of expertise or experience who are more interested in short-term assistance or in need of a sounding board. The career development track is a more traditional approach, matching a seasoned practice administrator with a less experienced practice administrator.
The program was designed to have annual cohorts, with the Practice Administrators Committee members as mentors. There is a detailed application process to ensure that each mentee is matched with an appropriate mentor, based on their interests and needs. We provide an orientation webinar to both parties before kicking off the relationship to present program expectations. The pilot program used this model, and comments from 6-month and annual evaluations showed tremendous satisfaction with the structure and value of this program.
There were approximately 16 pairs during the pilot year, and the following year, we grew to almost 20 pairs. Our goal as a committee is to maintain this program year after year, and in order to expand, we’ll need more than just the committee members to volunteer as mentors. There are so many talented practice administrators, and it would be wonderful to fold them into this gratifying program to pay it forward.
Many mentors, including myself, found value in acting as a mentor. I learned from my mentees as well as made connections and friendships with other professionals in the field.
Q: Given your intimate involvement, how have you seen the Practice Administrators’ Mentor Program benefit both the mentors and the mentees? Can you provide any specific examples?
A: Mentees are able to connect with seasoned mentors and can ask specific questions about career development and any issues they may be experiencing. Mentors are able to share their experiences and pass along important and valuable lessons learned to mentees. I served as a mentor, even though I did not yet consider myself a qualified candidate. However, I found that I was more equipped than I had realized, and I was able to assist my mentee with many aspects of career development (i.e., resume building, discussions with the C-suite, etc.).
My mentee was a practice coordinator who had only been in hospital medicine for 1 year. She had little experience hiring hospitalists, so this was a major area that we worked on together during our yearlong connection. I introduced her to collaborating with her HR department when posting positions, as well as working with permanent placement agencies. Her service was also undergoing a change in leadership, which can be difficult for any service line to experience. We discussed ways in which she could present important information to the new medical director that would produce a meaningful conversation.
In turn, my mentee introduced me to new online resources and was able to connect me with the manager of her practice, who assisted me with streamlining the payroll structure in my practice. I truly enjoyed my experience developing and participating in the program.
Felicia Steele is SHM’s communications coordinator.
Learn more about how you can benefit from the Practice Administrators’ Mentor program via the SHM website.
Vent bundles and ventilator-associated pneumonia outcomes
Clinical question: Are the components of the ventilator bundles (VBs) associated with better outcomes for patients?
Background: VBs have been shown to prevent ventilator-associated pneumonia (VAP). However, most of the studies have analyzed outcomes based on the whole bundle without considering each individual component.
Study design: Retrospective cohort study.
Setting: Brigham and Women’s Hospital in Boston.
Spontaneous breathing trials were associated with lower hazards for VAEs (HR, 0.55; 95% CI, 0.40-0.76; P less than .001) and infection-related ventilator-associated complications (IVACs) (HR, 0.60; 95% CI, 0.37-1.00; P = .05). Head-of-bed elevation (HR, 1.38; 95% CI, 1.14-1.68; P = 0.001) and thromboembolism prophylaxis (HR, 2.57; 95% CI, 1.80-3.66; P less than .001) were associated with less time to extubation.
Oral care with chlorhexidine was associated with lower hazards for IVACs (HR, 0.60; 95% CI 0.36-1.00; P = .05) and for VAPs (HR, 0.55; 95% CI, 0.27-1.14; P = .11) but an increased risk for ventilator mortality (HR, 1.63; 95% CI, 1.15-2.31; P = .006). Stress ulcer prophylaxis was associated with higher risk for VAP (HR, 7.69; 95% CI, 1.44-41.10; P = .02).
Bottom line: Standard VB components merit revision to increase emphasis on beneficial components and eliminate potentially harmful ones.
Citation: Klompas M, Li L, Kleinman K, Szumita PM, Massaro AF. Association between ventilator bundle components and outcomes. JAMA Intern Med. 2016;176(9):1277-1283.
Dr. Mosetti is an assistant professor at the University of Miami Miller School of Medicine and a hospitalist at University of Miami Hospital and Jackson Memorial Hospital.
Clinical question: Are the components of the ventilator bundles (VBs) associated with better outcomes for patients?
Background: VBs have been shown to prevent ventilator-associated pneumonia (VAP). However, most of the studies have analyzed outcomes based on the whole bundle without considering each individual component.
Study design: Retrospective cohort study.
Setting: Brigham and Women’s Hospital in Boston.
Spontaneous breathing trials were associated with lower hazards for VAEs (HR, 0.55; 95% CI, 0.40-0.76; P less than .001) and infection-related ventilator-associated complications (IVACs) (HR, 0.60; 95% CI, 0.37-1.00; P = .05). Head-of-bed elevation (HR, 1.38; 95% CI, 1.14-1.68; P = 0.001) and thromboembolism prophylaxis (HR, 2.57; 95% CI, 1.80-3.66; P less than .001) were associated with less time to extubation.
Oral care with chlorhexidine was associated with lower hazards for IVACs (HR, 0.60; 95% CI 0.36-1.00; P = .05) and for VAPs (HR, 0.55; 95% CI, 0.27-1.14; P = .11) but an increased risk for ventilator mortality (HR, 1.63; 95% CI, 1.15-2.31; P = .006). Stress ulcer prophylaxis was associated with higher risk for VAP (HR, 7.69; 95% CI, 1.44-41.10; P = .02).
Bottom line: Standard VB components merit revision to increase emphasis on beneficial components and eliminate potentially harmful ones.
Citation: Klompas M, Li L, Kleinman K, Szumita PM, Massaro AF. Association between ventilator bundle components and outcomes. JAMA Intern Med. 2016;176(9):1277-1283.
Dr. Mosetti is an assistant professor at the University of Miami Miller School of Medicine and a hospitalist at University of Miami Hospital and Jackson Memorial Hospital.
Clinical question: Are the components of the ventilator bundles (VBs) associated with better outcomes for patients?
Background: VBs have been shown to prevent ventilator-associated pneumonia (VAP). However, most of the studies have analyzed outcomes based on the whole bundle without considering each individual component.
Study design: Retrospective cohort study.
Setting: Brigham and Women’s Hospital in Boston.
Spontaneous breathing trials were associated with lower hazards for VAEs (HR, 0.55; 95% CI, 0.40-0.76; P less than .001) and infection-related ventilator-associated complications (IVACs) (HR, 0.60; 95% CI, 0.37-1.00; P = .05). Head-of-bed elevation (HR, 1.38; 95% CI, 1.14-1.68; P = 0.001) and thromboembolism prophylaxis (HR, 2.57; 95% CI, 1.80-3.66; P less than .001) were associated with less time to extubation.
Oral care with chlorhexidine was associated with lower hazards for IVACs (HR, 0.60; 95% CI 0.36-1.00; P = .05) and for VAPs (HR, 0.55; 95% CI, 0.27-1.14; P = .11) but an increased risk for ventilator mortality (HR, 1.63; 95% CI, 1.15-2.31; P = .006). Stress ulcer prophylaxis was associated with higher risk for VAP (HR, 7.69; 95% CI, 1.44-41.10; P = .02).
Bottom line: Standard VB components merit revision to increase emphasis on beneficial components and eliminate potentially harmful ones.
Citation: Klompas M, Li L, Kleinman K, Szumita PM, Massaro AF. Association between ventilator bundle components and outcomes. JAMA Intern Med. 2016;176(9):1277-1283.
Dr. Mosetti is an assistant professor at the University of Miami Miller School of Medicine and a hospitalist at University of Miami Hospital and Jackson Memorial Hospital.
Overnight extubations associated with worse outcomes
Clinical question: Are overnight extubations in intensive care units associated with higher mortality rate?
Background: Little is known about the frequency, safety, and effectiveness of overnight extubations in the ICU.
Study design: Retrospective cohort study.
Setting: One-hundred sixty-five ICUs in the United States.
Synopsis: Using the Project IMPACT database, 97,844 adults undergoing mechanical ventilation (MV) admitted to ICUs were studied. Overnight extubation was defined as occurring between 7 p.m. and 6:59 a.m. Primary outcome was reintubation; secondary outcomes were ICU and hospital mortality and ICU and hospital length of stay.
Only one-fifth of patients with MV underwent overnight extubations. For MV duration of at least 12 hours, rates of reintubation were higher for patients undergoing overnight extubation (14.6% vs. 12.4%; P less than .001). Mortality was significantly higher for patients undergoing overnight versus daytime extubation in the ICU (11.2% vs. 6.1%; P less than.001) and in the hospital (16.0% vs. 11.1%; P less than .001). Length of ICU and hospital stays did not differ.
Bottom line: Overnight extubations occur in one of five patients in U.S. ICUs and are associated with worse outcomes, compared with daytime extubations.
Citation: Gershengorn HB, Scales DC, Kramer A, Wunsch H. Association between overnight extubations and outcomes in the intensive care unit. JAMA Intern Med. 2016;176(11):1651-1660.
Dr. Mosetti is an assistant professor at the University of Miami Miller School of Medicine and a hospitalist at University of Miami Hospital and Jackson Memorial Hospital.
Clinical question: Are overnight extubations in intensive care units associated with higher mortality rate?
Background: Little is known about the frequency, safety, and effectiveness of overnight extubations in the ICU.
Study design: Retrospective cohort study.
Setting: One-hundred sixty-five ICUs in the United States.
Synopsis: Using the Project IMPACT database, 97,844 adults undergoing mechanical ventilation (MV) admitted to ICUs were studied. Overnight extubation was defined as occurring between 7 p.m. and 6:59 a.m. Primary outcome was reintubation; secondary outcomes were ICU and hospital mortality and ICU and hospital length of stay.
Only one-fifth of patients with MV underwent overnight extubations. For MV duration of at least 12 hours, rates of reintubation were higher for patients undergoing overnight extubation (14.6% vs. 12.4%; P less than .001). Mortality was significantly higher for patients undergoing overnight versus daytime extubation in the ICU (11.2% vs. 6.1%; P less than.001) and in the hospital (16.0% vs. 11.1%; P less than .001). Length of ICU and hospital stays did not differ.
Bottom line: Overnight extubations occur in one of five patients in U.S. ICUs and are associated with worse outcomes, compared with daytime extubations.
Citation: Gershengorn HB, Scales DC, Kramer A, Wunsch H. Association between overnight extubations and outcomes in the intensive care unit. JAMA Intern Med. 2016;176(11):1651-1660.
Dr. Mosetti is an assistant professor at the University of Miami Miller School of Medicine and a hospitalist at University of Miami Hospital and Jackson Memorial Hospital.
Clinical question: Are overnight extubations in intensive care units associated with higher mortality rate?
Background: Little is known about the frequency, safety, and effectiveness of overnight extubations in the ICU.
Study design: Retrospective cohort study.
Setting: One-hundred sixty-five ICUs in the United States.
Synopsis: Using the Project IMPACT database, 97,844 adults undergoing mechanical ventilation (MV) admitted to ICUs were studied. Overnight extubation was defined as occurring between 7 p.m. and 6:59 a.m. Primary outcome was reintubation; secondary outcomes were ICU and hospital mortality and ICU and hospital length of stay.
Only one-fifth of patients with MV underwent overnight extubations. For MV duration of at least 12 hours, rates of reintubation were higher for patients undergoing overnight extubation (14.6% vs. 12.4%; P less than .001). Mortality was significantly higher for patients undergoing overnight versus daytime extubation in the ICU (11.2% vs. 6.1%; P less than.001) and in the hospital (16.0% vs. 11.1%; P less than .001). Length of ICU and hospital stays did not differ.
Bottom line: Overnight extubations occur in one of five patients in U.S. ICUs and are associated with worse outcomes, compared with daytime extubations.
Citation: Gershengorn HB, Scales DC, Kramer A, Wunsch H. Association between overnight extubations and outcomes in the intensive care unit. JAMA Intern Med. 2016;176(11):1651-1660.
Dr. Mosetti is an assistant professor at the University of Miami Miller School of Medicine and a hospitalist at University of Miami Hospital and Jackson Memorial Hospital.
Fecal transplant efficacy for Clostridium difficile infections
Clinical question: Is fecal microbiota transplantation (FMT) an efficacious and safe treatment approach for patients with recurrent Clostridium difficile infection (CDI)?
Background: FMT restores the normal composition of gut microbiota and is recommended when antibiotics fail to clear CDI. To date, only case series and open-labeled clinical trials support the use of FMT.
Study design: Randomized, controlled, double-blinded clinical trial.
Setting: Academic medical centers.
The primary endpoint was resolution of diarrhea without anti-CDI therapy after 8 weeks of follow-up. In the donor FMT group, 90.9% achieved clinical cure, compared with 62.5% in the autologous group. Patients who developed recurrent CDI were free of further disease after subsequent donor FMT.
The study included only patients who experienced three or more recurrences but excluded immunocompromised and older patients (older than 75 years of age).
Bottom line: Donor stool administered via colonoscopy was more effective than autologous FMT in preventing further CDI episodes.
Citation: Kelly CR, Khoruts A, Staley C, et al. Effect of fecal microbiota transplantation on recurrence in multiply recurrent Clostridium difficile infection: a randomized trial. Ann Intern Med. 2016;165(9):609-616.
Dr. Fernandez de la Vara is an instructor at the University of Miami Miller School of Medicine and chief medical resident at the University of Miami Hospital.
Clinical question: Is fecal microbiota transplantation (FMT) an efficacious and safe treatment approach for patients with recurrent Clostridium difficile infection (CDI)?
Background: FMT restores the normal composition of gut microbiota and is recommended when antibiotics fail to clear CDI. To date, only case series and open-labeled clinical trials support the use of FMT.
Study design: Randomized, controlled, double-blinded clinical trial.
Setting: Academic medical centers.
The primary endpoint was resolution of diarrhea without anti-CDI therapy after 8 weeks of follow-up. In the donor FMT group, 90.9% achieved clinical cure, compared with 62.5% in the autologous group. Patients who developed recurrent CDI were free of further disease after subsequent donor FMT.
The study included only patients who experienced three or more recurrences but excluded immunocompromised and older patients (older than 75 years of age).
Bottom line: Donor stool administered via colonoscopy was more effective than autologous FMT in preventing further CDI episodes.
Citation: Kelly CR, Khoruts A, Staley C, et al. Effect of fecal microbiota transplantation on recurrence in multiply recurrent Clostridium difficile infection: a randomized trial. Ann Intern Med. 2016;165(9):609-616.
Dr. Fernandez de la Vara is an instructor at the University of Miami Miller School of Medicine and chief medical resident at the University of Miami Hospital.
Clinical question: Is fecal microbiota transplantation (FMT) an efficacious and safe treatment approach for patients with recurrent Clostridium difficile infection (CDI)?
Background: FMT restores the normal composition of gut microbiota and is recommended when antibiotics fail to clear CDI. To date, only case series and open-labeled clinical trials support the use of FMT.
Study design: Randomized, controlled, double-blinded clinical trial.
Setting: Academic medical centers.
The primary endpoint was resolution of diarrhea without anti-CDI therapy after 8 weeks of follow-up. In the donor FMT group, 90.9% achieved clinical cure, compared with 62.5% in the autologous group. Patients who developed recurrent CDI were free of further disease after subsequent donor FMT.
The study included only patients who experienced three or more recurrences but excluded immunocompromised and older patients (older than 75 years of age).
Bottom line: Donor stool administered via colonoscopy was more effective than autologous FMT in preventing further CDI episodes.
Citation: Kelly CR, Khoruts A, Staley C, et al. Effect of fecal microbiota transplantation on recurrence in multiply recurrent Clostridium difficile infection: a randomized trial. Ann Intern Med. 2016;165(9):609-616.
Dr. Fernandez de la Vara is an instructor at the University of Miami Miller School of Medicine and chief medical resident at the University of Miami Hospital.
Non–vitamin K antagonist oral anticoagulants for planned atrial fibrillation cardioversions
Clinical question: How does edoxaban compare with enoxaparin-warfarin in patients with nonvalvular atrial fibrillation undergoing cardioversion?
Background: Studies on non–vitamin K antagonist oral anticoagulants (NOACs) for patients with nonvalvular atrial fibrillation undergoing cardioversion are limited.
Study design: Multicenter, prospective, randomized trial.
Setting: Nineteen countries at 239 study sites.
Synopsis: This trial compared edoxaban with enoxaparin-warfarin. The study was stratified by cardioversion approach, anticoagulant experience, selected edoxaban dose, and region. There were 2,199 patients, mean age was 64, mean CHA2DS2-VASc score was 2.6, and mean therapeutic time on warfarin was 70.8%.
The primary efficacy endpoint was a composite of stroke, systemic emboli, myocardial infarction, and cardiovascular mortality, which occurred in 5 (1%) patients in the edoxaban group versus 11 (1%) in the enoxaparin-warfarin group (odds ratio, 0.46; 95% CI, 0.12-1.43).
The primary safety endpoint was major and clinically relevant nonmajor bleeding for patients receiving at least one dose of the study drug, occurring in 16 (1%) of 1,067 patients given edoxaban versus 11 (1%) of 1,082 patients given enoxaparin-warfarin (OR, 1.48; 95% CI, 0.64-3.55).
Bottom line: In patients with nonvalvular atrial fibrillation undergoing cardioversion, edoxaban had low rates of major bleeding and thromboembolism similar to enoxaparin-warfarin therapy.
Citation: Goette A, Merino JL, Ezekowitz MD, et al. Edoxaban versus enoxaparin-warfarin in patients undergoing cardioversion of atrial fibrillation (ENSURE-AF): a randomised, open-label, phase 3b trial. Lancet. 2016;388(10055):1995-2003.
Dr. Fernandez de la Vara is an instructor at the University of Miami Miller School of Medicine and chief medical resident at the University of Miami Hospital.
Clinical question: How does edoxaban compare with enoxaparin-warfarin in patients with nonvalvular atrial fibrillation undergoing cardioversion?
Background: Studies on non–vitamin K antagonist oral anticoagulants (NOACs) for patients with nonvalvular atrial fibrillation undergoing cardioversion are limited.
Study design: Multicenter, prospective, randomized trial.
Setting: Nineteen countries at 239 study sites.
Synopsis: This trial compared edoxaban with enoxaparin-warfarin. The study was stratified by cardioversion approach, anticoagulant experience, selected edoxaban dose, and region. There were 2,199 patients, mean age was 64, mean CHA2DS2-VASc score was 2.6, and mean therapeutic time on warfarin was 70.8%.
The primary efficacy endpoint was a composite of stroke, systemic emboli, myocardial infarction, and cardiovascular mortality, which occurred in 5 (1%) patients in the edoxaban group versus 11 (1%) in the enoxaparin-warfarin group (odds ratio, 0.46; 95% CI, 0.12-1.43).
The primary safety endpoint was major and clinically relevant nonmajor bleeding for patients receiving at least one dose of the study drug, occurring in 16 (1%) of 1,067 patients given edoxaban versus 11 (1%) of 1,082 patients given enoxaparin-warfarin (OR, 1.48; 95% CI, 0.64-3.55).
Bottom line: In patients with nonvalvular atrial fibrillation undergoing cardioversion, edoxaban had low rates of major bleeding and thromboembolism similar to enoxaparin-warfarin therapy.
Citation: Goette A, Merino JL, Ezekowitz MD, et al. Edoxaban versus enoxaparin-warfarin in patients undergoing cardioversion of atrial fibrillation (ENSURE-AF): a randomised, open-label, phase 3b trial. Lancet. 2016;388(10055):1995-2003.
Dr. Fernandez de la Vara is an instructor at the University of Miami Miller School of Medicine and chief medical resident at the University of Miami Hospital.
Clinical question: How does edoxaban compare with enoxaparin-warfarin in patients with nonvalvular atrial fibrillation undergoing cardioversion?
Background: Studies on non–vitamin K antagonist oral anticoagulants (NOACs) for patients with nonvalvular atrial fibrillation undergoing cardioversion are limited.
Study design: Multicenter, prospective, randomized trial.
Setting: Nineteen countries at 239 study sites.
Synopsis: This trial compared edoxaban with enoxaparin-warfarin. The study was stratified by cardioversion approach, anticoagulant experience, selected edoxaban dose, and region. There were 2,199 patients, mean age was 64, mean CHA2DS2-VASc score was 2.6, and mean therapeutic time on warfarin was 70.8%.
The primary efficacy endpoint was a composite of stroke, systemic emboli, myocardial infarction, and cardiovascular mortality, which occurred in 5 (1%) patients in the edoxaban group versus 11 (1%) in the enoxaparin-warfarin group (odds ratio, 0.46; 95% CI, 0.12-1.43).
The primary safety endpoint was major and clinically relevant nonmajor bleeding for patients receiving at least one dose of the study drug, occurring in 16 (1%) of 1,067 patients given edoxaban versus 11 (1%) of 1,082 patients given enoxaparin-warfarin (OR, 1.48; 95% CI, 0.64-3.55).
Bottom line: In patients with nonvalvular atrial fibrillation undergoing cardioversion, edoxaban had low rates of major bleeding and thromboembolism similar to enoxaparin-warfarin therapy.
Citation: Goette A, Merino JL, Ezekowitz MD, et al. Edoxaban versus enoxaparin-warfarin in patients undergoing cardioversion of atrial fibrillation (ENSURE-AF): a randomised, open-label, phase 3b trial. Lancet. 2016;388(10055):1995-2003.
Dr. Fernandez de la Vara is an instructor at the University of Miami Miller School of Medicine and chief medical resident at the University of Miami Hospital.
Home treatment of PE remains rare
Clinical question: What is the prevalence of outpatient treatment of acute pulmonary embolism (PE)?
Background: PE traditionally is perceived as a serious condition requiring hospitalization. Many studies, however, have shown that outpatient treatment of PE in low-risk, compliant patients is safe. Several scoring systems have been derived to identify patients with PE who are at low risk of adverse events and may be candidates for home treatment.
Setting: Five U.S. EDs.
Synopsis: Among 983 patients diagnosed with acute PE, 237 (24.1%) were unstable and hypoxic. Only a small proportion of patients (1.7%) were eligible for outpatient therapy, and an additional 16.2% of hospitalized patients were discharged early (2 days or less). Novel oral anticoagulants were administered to fewer than one-third of patients.
Bottom line: In the era of novel anticoagulants, the majority of patients with acute PE were hospitalized, and home treatment was infrequently selected for stable low-risk patients.
Citation: Stein PD, Matta F, Hughes PG, et al. Home treatment of pulmonary embolism in the era of novel oral anticoagulants. Am J Med. 2016;129(9):974-977.
Dr. Gummalla is an assistant professor at the University of Miami Miller School of Medicine and a hospitalist at University of Miami Hospital and Jackson Memorial Hospital.
Clinical question: What is the prevalence of outpatient treatment of acute pulmonary embolism (PE)?
Background: PE traditionally is perceived as a serious condition requiring hospitalization. Many studies, however, have shown that outpatient treatment of PE in low-risk, compliant patients is safe. Several scoring systems have been derived to identify patients with PE who are at low risk of adverse events and may be candidates for home treatment.
Setting: Five U.S. EDs.
Synopsis: Among 983 patients diagnosed with acute PE, 237 (24.1%) were unstable and hypoxic. Only a small proportion of patients (1.7%) were eligible for outpatient therapy, and an additional 16.2% of hospitalized patients were discharged early (2 days or less). Novel oral anticoagulants were administered to fewer than one-third of patients.
Bottom line: In the era of novel anticoagulants, the majority of patients with acute PE were hospitalized, and home treatment was infrequently selected for stable low-risk patients.
Citation: Stein PD, Matta F, Hughes PG, et al. Home treatment of pulmonary embolism in the era of novel oral anticoagulants. Am J Med. 2016;129(9):974-977.
Dr. Gummalla is an assistant professor at the University of Miami Miller School of Medicine and a hospitalist at University of Miami Hospital and Jackson Memorial Hospital.
Clinical question: What is the prevalence of outpatient treatment of acute pulmonary embolism (PE)?
Background: PE traditionally is perceived as a serious condition requiring hospitalization. Many studies, however, have shown that outpatient treatment of PE in low-risk, compliant patients is safe. Several scoring systems have been derived to identify patients with PE who are at low risk of adverse events and may be candidates for home treatment.
Setting: Five U.S. EDs.
Synopsis: Among 983 patients diagnosed with acute PE, 237 (24.1%) were unstable and hypoxic. Only a small proportion of patients (1.7%) were eligible for outpatient therapy, and an additional 16.2% of hospitalized patients were discharged early (2 days or less). Novel oral anticoagulants were administered to fewer than one-third of patients.
Bottom line: In the era of novel anticoagulants, the majority of patients with acute PE were hospitalized, and home treatment was infrequently selected for stable low-risk patients.
Citation: Stein PD, Matta F, Hughes PG, et al. Home treatment of pulmonary embolism in the era of novel oral anticoagulants. Am J Med. 2016;129(9):974-977.
Dr. Gummalla is an assistant professor at the University of Miami Miller School of Medicine and a hospitalist at University of Miami Hospital and Jackson Memorial Hospital.
Updated recommendations for managing gout
Clinical question: What are the new treatment options for gout?
Background: The 2006 European League Against Rheumatism (EULAR) guidelines recommend that acute flares of gout be treated as early as possible with either oral colchicine, oral corticosteroids, or intra-articular corticosteroids. Experts recommend starting urate-lowering therapy (ULT) only when certain severe clinical features occur, such as recurrent acute attacks and tophi.
Study design: Systematic review.
Setting: EULAR task force members from 12 European countries.
Synopsis: Since the last guidelines, interleukin-1 blockers (IL-1) were found to play a crucial role in crystal-induced inflammation. IL-1, NSAIDs, and corticosteroids should be considered in patients with frequent flares and contraindications to colchicine.
Unlike in the previous guidelines, ULT should be considered from first presentation of gout; for severe disease, serum uric acid (SUA) levels should be maintained at less than 6 mg/dL and less than 5 mg/dL.
Allopurinol is recommended for first-line ULT, and if the SUA target cannot be reached, it should be switched to another xanthine oxidase inhibitor (febuxostat) or a uricosuric or combined with a uricosuric.
Pegloticase is recommended for refractory gout.
Bottom line: The updated 2016 EULAR guidelines recommend new treatment options for gout and updated indications for ULT.
Citation: Richette P, Doherty M, Pascual E, et al. 2016 updated EULAR evidence-based recommendations for the management of gout [published online ahead of print July 25, 2016]. Ann Rheum Dis. doi: 10.1136/annrheumdis-2016-209707.
Dr. Gummalla is an assistant professor at the University of Miami Miller School of Medicine and a hospitalist at University of Miami Hospital and Jackson Memorial Hospital.
Clinical question: What are the new treatment options for gout?
Background: The 2006 European League Against Rheumatism (EULAR) guidelines recommend that acute flares of gout be treated as early as possible with either oral colchicine, oral corticosteroids, or intra-articular corticosteroids. Experts recommend starting urate-lowering therapy (ULT) only when certain severe clinical features occur, such as recurrent acute attacks and tophi.
Study design: Systematic review.
Setting: EULAR task force members from 12 European countries.
Synopsis: Since the last guidelines, interleukin-1 blockers (IL-1) were found to play a crucial role in crystal-induced inflammation. IL-1, NSAIDs, and corticosteroids should be considered in patients with frequent flares and contraindications to colchicine.
Unlike in the previous guidelines, ULT should be considered from first presentation of gout; for severe disease, serum uric acid (SUA) levels should be maintained at less than 6 mg/dL and less than 5 mg/dL.
Allopurinol is recommended for first-line ULT, and if the SUA target cannot be reached, it should be switched to another xanthine oxidase inhibitor (febuxostat) or a uricosuric or combined with a uricosuric.
Pegloticase is recommended for refractory gout.
Bottom line: The updated 2016 EULAR guidelines recommend new treatment options for gout and updated indications for ULT.
Citation: Richette P, Doherty M, Pascual E, et al. 2016 updated EULAR evidence-based recommendations for the management of gout [published online ahead of print July 25, 2016]. Ann Rheum Dis. doi: 10.1136/annrheumdis-2016-209707.
Dr. Gummalla is an assistant professor at the University of Miami Miller School of Medicine and a hospitalist at University of Miami Hospital and Jackson Memorial Hospital.
Clinical question: What are the new treatment options for gout?
Background: The 2006 European League Against Rheumatism (EULAR) guidelines recommend that acute flares of gout be treated as early as possible with either oral colchicine, oral corticosteroids, or intra-articular corticosteroids. Experts recommend starting urate-lowering therapy (ULT) only when certain severe clinical features occur, such as recurrent acute attacks and tophi.
Study design: Systematic review.
Setting: EULAR task force members from 12 European countries.
Synopsis: Since the last guidelines, interleukin-1 blockers (IL-1) were found to play a crucial role in crystal-induced inflammation. IL-1, NSAIDs, and corticosteroids should be considered in patients with frequent flares and contraindications to colchicine.
Unlike in the previous guidelines, ULT should be considered from first presentation of gout; for severe disease, serum uric acid (SUA) levels should be maintained at less than 6 mg/dL and less than 5 mg/dL.
Allopurinol is recommended for first-line ULT, and if the SUA target cannot be reached, it should be switched to another xanthine oxidase inhibitor (febuxostat) or a uricosuric or combined with a uricosuric.
Pegloticase is recommended for refractory gout.
Bottom line: The updated 2016 EULAR guidelines recommend new treatment options for gout and updated indications for ULT.
Citation: Richette P, Doherty M, Pascual E, et al. 2016 updated EULAR evidence-based recommendations for the management of gout [published online ahead of print July 25, 2016]. Ann Rheum Dis. doi: 10.1136/annrheumdis-2016-209707.
Dr. Gummalla is an assistant professor at the University of Miami Miller School of Medicine and a hospitalist at University of Miami Hospital and Jackson Memorial Hospital.





