User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


SHM welcomes its newest members - January 2017
Justin Kimsey, Alabama
Mohammed N.Y. Shah, MD, Alaska
Katharina Beeler, MD, Arizona
Khoi Nguyen, MD, Arizona
Vinay Saini, MD, Arizona
Maria Aceves, PA-C, California
Sarvenaz Alibeigi, California
Peter Cadman, MD, California
Katrina Chapman, DO, MPH, California
Cheryll Gallardo-Villena, MD, California
Sripriya Ganesan, California
Alice Gong, MD, California
Henry Kwang, MD, California
Kevin Li, California
Anthony Murphy, MD, California
Dan Nguyen, California
Daniel Oh, California
Joon Parle, California
Katie Raffel, California
Darshana Sarathchandra, MD, California
Lifang Zhang, California
Jaime Baker, MD, Colorado
Eric Johnson, PA-C, Colorado
Juan Lessing, MD, Colorado
Benjamin Ruckman, DO, Colorado
Rehaan Shaffie, MD, Colorado
Deborah Casey, MD, Connecticut
Daniel Heacock, PA-C, Connecticut
Shabana Ansari, DO, Delaware
Madhu Prattipati, MD, Delaware
Pallavi Aneja, MD, Florida
Satcha Borgella, MD, Florida
Thendrex H. Estrella, MD, Florida
Abid Hussain, MD, Florida
Daphnee Hutchinson, DO, Florida
Muhammad Jaffer, Florida
Sue Lee, ANP, Florida
Melissa Odermann, DO, Florida
Jose Guillermo Revelo Paiz, MD, Florida
Rafael J. Rolon Rivera, MD, Florida
Eleonor Rongo, Florida
Esther Roth, Florida
Shitaye Argaw, MD, Georgia
Taryn DeGrazia, Georgia
Becca Feistritzer, Georgia
Jamal Fitts, Georgia
Kristen Flint, Georgia
Zachary Hermes, Georgia
Mukesh Kumar, Georgia
Kajal Patel, Georgia
Madeline Smith, Georgia
Wade Flowers, PharmD, Idaho
Ajay Bhandare, Illinois
Kimberly Brighton, Illinois
Hristo D. Hristov, MD, Illinois
Sidney Iriana, Illinois
Aurelian Ivan, Illinois
Ming Lee, MD, Illinois
Michelle Lundholm, Illinois
Idrees Mohiuddin, MD, Illinois
Murr Murray, Illinois
Tad Nair, MD, Illinois
Shalini Reddy, MD, Illinois
Richard Rethorst, MD, Illinois
Kelly Robertshaw, Illinois
Gracelene Wegrzyn, Illinois
Evan Yates, Illinois
Lora J. Jones McClure, MD, Indiana
Carleigh Wilson, DO, Indiana
Erin Brown, ARNP, Iowa
Adam Gray, Iowa
Paul Greco, MD, Iowa
Shelly McGurk, ACNP, ARNP, Iowa
Julie Stanik-Hutt, ACNP, CNS, PhD, Iowa
Elizabeth Cozad, DO, Kansas
Roshan Pais, Kentucky
Mark Youssef, MD, Kentucky
Heather Kahn, MD, Louisiana
Danielle Parrott, PA-C, Maine
Erica Lafferty, ACNP, Maryland
Andrea Limpuangthip, Maryland
Steven Schwartz, CCM, MD, Maryland
Eisha Azhar, MBBS, Massachusetts
Badal Kalamkar, MD, MPH, Massachusetts
Bhavya Rajanna, MD, Massachusetts
Sahib Baljinder Singh, MD, Massachusetts
Kathryn Adams, Michigan
Haseeb Aslam, MD, MBBS, Michigan
Hilda Crispin, MD, Michigan
Sharmistha Dev, MD, Michigan
Tristan Feierabend, MD, Michigan
Sonal Kamalia, MD, MBBS, Michigan
Matthew Luzum, MD, Michigan
Daniel Mitzel, MD, Michigan
Richard Raad, Michigan
Mythri Ramegowda, MD, Michigan
Katie Scally, MD, Michigan
Linden Spital, MSN, NP, Michigan
Porama Koy Thanaporn, MD, Michigan
Chanteil Ulatowski, Michigan
Tingting Xiong, MD, Michigan
Adam Zahr, Michigan
Mike Beste, MD, Minnesota
Elise Haupt, PA-C, Minnesota
Lobsang Trasar, MD, Minnesota
Kari Goan, DO, Mississippi
David C. Pierre, Mississippi
Sudheer Tangella, MD, Mississippi
Tahani Atieh, Missouri
Nicholas Arnold, Missouri
Amanda Calhoun, Missouri
Jyotirmoy Das, Missouri
Umber Dube, Missouri
Daniel Gaughan, Missouri
Woojin Joo, Missouri
Khaled Jumean, MBBS, Missouri
Salma Kazmi, MBBS, MD, Missouri
Yoon Kook (Danny) Kim, Missouri
Ryan Kronen, Missouri
Alyssa Kroner, Missouri
Randy Laine, Missouri
Edward Lee, Missouri
Cerena Leung, Missouri
Patricia Lithrow, Missouri
Brandt Lydon, Missouri
Mary Morgan Scott, Missouri
Jay Patel, Missouri
Justin Porter, Missouri
Danelle Reagin, FNP-C, Missouri
Amanda Reis, Missouri
Awik Som, Missouri
Abby Sung, Missouri
Mary Sutherland, Missouri
Maggie Wang, Missouri
Noah Wasserman, Missouri
Alexis Webber, Missouri
Ryan White, Missouri
Amy Xu, Missouri
Ran Xu, Missouri
Michael Yang, Missouri
Christopher Dietrich, MD, Montana
Jason Kunz, DO, Montana
Jodi Cantrell, MD, Nebraska
Steven Hart, MD, Nebraska
Kurt Kapels, MD, Nebraska
Brian Keegan, MD, Nebraska
Shaun Jang, MD, Nevada
Gurpinder Singh, MD, New Hampshire
Pragati Banda, MD, New Jersey
Sahai Donaldson, MBBS, New Jersey
Ashesha Mechineni, MD, New Jersey
Alisa Clark, New Mexico
Prajit Arora, MBBS, New Mexico
Crystal Cardwell, New Mexico
Landon Casaus, New Mexico
Tapuwa Mupfumira, MD, New Mexico
Eric Rightley, New Mexico
David S. Anderson, New York
Joan Bosco, MD, New York
Jessica Caro, New York
Anna Dewan, New York
Amrita Dhillon, MBBS, New York
Julia Frydman, New York
Radhika Gali, MBBS, MDS, New York
Allison Guttmann, MD, New York
Aryles Hedjar, MD, New York
Peter Janes, New York
Nadine Kalavazoff, New York
Jeffrey Lach, DO, New York
Keron Lezama, MD, New York
Yingheng Liu, New York
Taimur Mirza, New York
Cyrus Nensey, MD, New York
Nekee Pandya, MD, New York
Thushara Paul, MD, New York
Yu Sung, New York
Joel Boggan, MD, North Carolina
Angela Fletcher, North Carolina
Rebecca Gimpert, PA-C, North Carolina
Samantha Levering, PA-C, North Carolina
Nancy Martin, North Carolina
Richard Sherwood, North Carolina
Kranthi K. Sitammagari, MD, North Carolina
Aaron Swedberg, MPAS, PA-C, North Carolina
Yih-Cherng Tsai, North Carolina
Richard Bakker, MD, PhD, Ohio
Matthew Broderick, MD, Ohio
Subbaraju Budharaju, MD, MS, Ohio
Steven Bumb, MD, Ohio
Ahmed Eltelbany, MD, Ohio
Tracey Hardin, MS, Ohio
Patricia Hardman, APRN, Ohio
Michael Lewis, MD, Ohio
Volodymyr Manko, Ohio
Rebecca Stone, Ohio
Chaitanya Valluri, Ohio
Holly Wierzbicki, CNP, Ohio
Jamie Yockey, APRN, CNP, Ohio
Mahdi Mussa, MD, Oklahoma
Monica Saemz, DO, Oklahoma
Peter Ganter, MD, Oregon
Bethany Roy, MD, Oregon
Mary Clare Bohnett, Oregon
Molly Rabinowitz, Oregon
Abdullateef Abdulkareem, MD, MPH, Pennsylvania
David Ahamba, MD, MPH, Pennsylvania
David Chin, MD, Pennsylvania
Thomas Conlon, Pennsylvania
Dan Giesler, MD, Pennsylvania
Umair Randhawa, MD, Pennsylvania
Syed Yusuf, MBBS, Pennsylvania
Michael Rigatti, Pennsylvania
Thaylon Barreto, Rhode Island
Jessica Cook, MD, South Carolina
Robin Malik, MD, South Carolina
John Busigin, Tennessee
Shefali Paranjape, MD, Tennessee
Thai Dang, MD, Texas
Matthew Glover, MD, Texas
Snigdha Jain, MD, Texas
David Kellenberger, Texas
Sumeet Kumar, Texas
Kyle McClendon, PA-C, Texas
Sowjanya Mohan, Texas
Akhil D. Vats, MD, Texas
Samatha Vellanki, Texas
Lee-Anna Burgess, MD, Vermont
Rick Hildebrant, MD, Vermont
Matthew Backens, MD, Virginia
Megan Coe, Virginia
Kevin Dehaan, Virginia
Stephen Fox, Virginia
Amber Inofuentes, MD, Virginia
Jessica Keiser, MD, Virginia
Joseph Perez, MD, FAAFP, MBA, Virginia
Kanwapreet S. Saini, MD, Virginia
Erin Vipler, MD, Virginia
Naveen Voore, MBBS, Virginia
Abhishek Agarwal, MD, MBBS, Washington
Robert Cooney, MD, Washington
Cynthia Horton, MD, Washington
Rich A. Kukreja, MD, Washington
Ji Young Nam, MD, Washington
Kai Wilhelm, MD, Washington
In Kyu Yoo, Washington
Temu Brown, Wisconsin
Pablo Colon Nieves, Wisconsin
Christina Evans, PAC, Wisconsin
Swetha Karturi, MBBS, Wisconsin
Mark Babcock, DO, Wyoming
Ahmad Von Schlegell, Canada
Anand Kartha, Japan
Mohamed Sadek, Qatar
Amine Rakab, MD, Qatar
Abazar Saeed, Qatar
Joao Guerra, MD
Justin Kimsey, Alabama
Mohammed N.Y. Shah, MD, Alaska
Katharina Beeler, MD, Arizona
Khoi Nguyen, MD, Arizona
Vinay Saini, MD, Arizona
Maria Aceves, PA-C, California
Sarvenaz Alibeigi, California
Peter Cadman, MD, California
Katrina Chapman, DO, MPH, California
Cheryll Gallardo-Villena, MD, California
Sripriya Ganesan, California
Alice Gong, MD, California
Henry Kwang, MD, California
Kevin Li, California
Anthony Murphy, MD, California
Dan Nguyen, California
Daniel Oh, California
Joon Parle, California
Katie Raffel, California
Darshana Sarathchandra, MD, California
Lifang Zhang, California
Jaime Baker, MD, Colorado
Eric Johnson, PA-C, Colorado
Juan Lessing, MD, Colorado
Benjamin Ruckman, DO, Colorado
Rehaan Shaffie, MD, Colorado
Deborah Casey, MD, Connecticut
Daniel Heacock, PA-C, Connecticut
Shabana Ansari, DO, Delaware
Madhu Prattipati, MD, Delaware
Pallavi Aneja, MD, Florida
Satcha Borgella, MD, Florida
Thendrex H. Estrella, MD, Florida
Abid Hussain, MD, Florida
Daphnee Hutchinson, DO, Florida
Muhammad Jaffer, Florida
Sue Lee, ANP, Florida
Melissa Odermann, DO, Florida
Jose Guillermo Revelo Paiz, MD, Florida
Rafael J. Rolon Rivera, MD, Florida
Eleonor Rongo, Florida
Esther Roth, Florida
Shitaye Argaw, MD, Georgia
Taryn DeGrazia, Georgia
Becca Feistritzer, Georgia
Jamal Fitts, Georgia
Kristen Flint, Georgia
Zachary Hermes, Georgia
Mukesh Kumar, Georgia
Kajal Patel, Georgia
Madeline Smith, Georgia
Wade Flowers, PharmD, Idaho
Ajay Bhandare, Illinois
Kimberly Brighton, Illinois
Hristo D. Hristov, MD, Illinois
Sidney Iriana, Illinois
Aurelian Ivan, Illinois
Ming Lee, MD, Illinois
Michelle Lundholm, Illinois
Idrees Mohiuddin, MD, Illinois
Murr Murray, Illinois
Tad Nair, MD, Illinois
Shalini Reddy, MD, Illinois
Richard Rethorst, MD, Illinois
Kelly Robertshaw, Illinois
Gracelene Wegrzyn, Illinois
Evan Yates, Illinois
Lora J. Jones McClure, MD, Indiana
Carleigh Wilson, DO, Indiana
Erin Brown, ARNP, Iowa
Adam Gray, Iowa
Paul Greco, MD, Iowa
Shelly McGurk, ACNP, ARNP, Iowa
Julie Stanik-Hutt, ACNP, CNS, PhD, Iowa
Elizabeth Cozad, DO, Kansas
Roshan Pais, Kentucky
Mark Youssef, MD, Kentucky
Heather Kahn, MD, Louisiana
Danielle Parrott, PA-C, Maine
Erica Lafferty, ACNP, Maryland
Andrea Limpuangthip, Maryland
Steven Schwartz, CCM, MD, Maryland
Eisha Azhar, MBBS, Massachusetts
Badal Kalamkar, MD, MPH, Massachusetts
Bhavya Rajanna, MD, Massachusetts
Sahib Baljinder Singh, MD, Massachusetts
Kathryn Adams, Michigan
Haseeb Aslam, MD, MBBS, Michigan
Hilda Crispin, MD, Michigan
Sharmistha Dev, MD, Michigan
Tristan Feierabend, MD, Michigan
Sonal Kamalia, MD, MBBS, Michigan
Matthew Luzum, MD, Michigan
Daniel Mitzel, MD, Michigan
Richard Raad, Michigan
Mythri Ramegowda, MD, Michigan
Katie Scally, MD, Michigan
Linden Spital, MSN, NP, Michigan
Porama Koy Thanaporn, MD, Michigan
Chanteil Ulatowski, Michigan
Tingting Xiong, MD, Michigan
Adam Zahr, Michigan
Mike Beste, MD, Minnesota
Elise Haupt, PA-C, Minnesota
Lobsang Trasar, MD, Minnesota
Kari Goan, DO, Mississippi
David C. Pierre, Mississippi
Sudheer Tangella, MD, Mississippi
Tahani Atieh, Missouri
Nicholas Arnold, Missouri
Amanda Calhoun, Missouri
Jyotirmoy Das, Missouri
Umber Dube, Missouri
Daniel Gaughan, Missouri
Woojin Joo, Missouri
Khaled Jumean, MBBS, Missouri
Salma Kazmi, MBBS, MD, Missouri
Yoon Kook (Danny) Kim, Missouri
Ryan Kronen, Missouri
Alyssa Kroner, Missouri
Randy Laine, Missouri
Edward Lee, Missouri
Cerena Leung, Missouri
Patricia Lithrow, Missouri
Brandt Lydon, Missouri
Mary Morgan Scott, Missouri
Jay Patel, Missouri
Justin Porter, Missouri
Danelle Reagin, FNP-C, Missouri
Amanda Reis, Missouri
Awik Som, Missouri
Abby Sung, Missouri
Mary Sutherland, Missouri
Maggie Wang, Missouri
Noah Wasserman, Missouri
Alexis Webber, Missouri
Ryan White, Missouri
Amy Xu, Missouri
Ran Xu, Missouri
Michael Yang, Missouri
Christopher Dietrich, MD, Montana
Jason Kunz, DO, Montana
Jodi Cantrell, MD, Nebraska
Steven Hart, MD, Nebraska
Kurt Kapels, MD, Nebraska
Brian Keegan, MD, Nebraska
Shaun Jang, MD, Nevada
Gurpinder Singh, MD, New Hampshire
Pragati Banda, MD, New Jersey
Sahai Donaldson, MBBS, New Jersey
Ashesha Mechineni, MD, New Jersey
Alisa Clark, New Mexico
Prajit Arora, MBBS, New Mexico
Crystal Cardwell, New Mexico
Landon Casaus, New Mexico
Tapuwa Mupfumira, MD, New Mexico
Eric Rightley, New Mexico
David S. Anderson, New York
Joan Bosco, MD, New York
Jessica Caro, New York
Anna Dewan, New York
Amrita Dhillon, MBBS, New York
Julia Frydman, New York
Radhika Gali, MBBS, MDS, New York
Allison Guttmann, MD, New York
Aryles Hedjar, MD, New York
Peter Janes, New York
Nadine Kalavazoff, New York
Jeffrey Lach, DO, New York
Keron Lezama, MD, New York
Yingheng Liu, New York
Taimur Mirza, New York
Cyrus Nensey, MD, New York
Nekee Pandya, MD, New York
Thushara Paul, MD, New York
Yu Sung, New York
Joel Boggan, MD, North Carolina
Angela Fletcher, North Carolina
Rebecca Gimpert, PA-C, North Carolina
Samantha Levering, PA-C, North Carolina
Nancy Martin, North Carolina
Richard Sherwood, North Carolina
Kranthi K. Sitammagari, MD, North Carolina
Aaron Swedberg, MPAS, PA-C, North Carolina
Yih-Cherng Tsai, North Carolina
Richard Bakker, MD, PhD, Ohio
Matthew Broderick, MD, Ohio
Subbaraju Budharaju, MD, MS, Ohio
Steven Bumb, MD, Ohio
Ahmed Eltelbany, MD, Ohio
Tracey Hardin, MS, Ohio
Patricia Hardman, APRN, Ohio
Michael Lewis, MD, Ohio
Volodymyr Manko, Ohio
Rebecca Stone, Ohio
Chaitanya Valluri, Ohio
Holly Wierzbicki, CNP, Ohio
Jamie Yockey, APRN, CNP, Ohio
Mahdi Mussa, MD, Oklahoma
Monica Saemz, DO, Oklahoma
Peter Ganter, MD, Oregon
Bethany Roy, MD, Oregon
Mary Clare Bohnett, Oregon
Molly Rabinowitz, Oregon
Abdullateef Abdulkareem, MD, MPH, Pennsylvania
David Ahamba, MD, MPH, Pennsylvania
David Chin, MD, Pennsylvania
Thomas Conlon, Pennsylvania
Dan Giesler, MD, Pennsylvania
Umair Randhawa, MD, Pennsylvania
Syed Yusuf, MBBS, Pennsylvania
Michael Rigatti, Pennsylvania
Thaylon Barreto, Rhode Island
Jessica Cook, MD, South Carolina
Robin Malik, MD, South Carolina
John Busigin, Tennessee
Shefali Paranjape, MD, Tennessee
Thai Dang, MD, Texas
Matthew Glover, MD, Texas
Snigdha Jain, MD, Texas
David Kellenberger, Texas
Sumeet Kumar, Texas
Kyle McClendon, PA-C, Texas
Sowjanya Mohan, Texas
Akhil D. Vats, MD, Texas
Samatha Vellanki, Texas
Lee-Anna Burgess, MD, Vermont
Rick Hildebrant, MD, Vermont
Matthew Backens, MD, Virginia
Megan Coe, Virginia
Kevin Dehaan, Virginia
Stephen Fox, Virginia
Amber Inofuentes, MD, Virginia
Jessica Keiser, MD, Virginia
Joseph Perez, MD, FAAFP, MBA, Virginia
Kanwapreet S. Saini, MD, Virginia
Erin Vipler, MD, Virginia
Naveen Voore, MBBS, Virginia
Abhishek Agarwal, MD, MBBS, Washington
Robert Cooney, MD, Washington
Cynthia Horton, MD, Washington
Rich A. Kukreja, MD, Washington
Ji Young Nam, MD, Washington
Kai Wilhelm, MD, Washington
In Kyu Yoo, Washington
Temu Brown, Wisconsin
Pablo Colon Nieves, Wisconsin
Christina Evans, PAC, Wisconsin
Swetha Karturi, MBBS, Wisconsin
Mark Babcock, DO, Wyoming
Ahmad Von Schlegell, Canada
Anand Kartha, Japan
Mohamed Sadek, Qatar
Amine Rakab, MD, Qatar
Abazar Saeed, Qatar
Joao Guerra, MD
Justin Kimsey, Alabama
Mohammed N.Y. Shah, MD, Alaska
Katharina Beeler, MD, Arizona
Khoi Nguyen, MD, Arizona
Vinay Saini, MD, Arizona
Maria Aceves, PA-C, California
Sarvenaz Alibeigi, California
Peter Cadman, MD, California
Katrina Chapman, DO, MPH, California
Cheryll Gallardo-Villena, MD, California
Sripriya Ganesan, California
Alice Gong, MD, California
Henry Kwang, MD, California
Kevin Li, California
Anthony Murphy, MD, California
Dan Nguyen, California
Daniel Oh, California
Joon Parle, California
Katie Raffel, California
Darshana Sarathchandra, MD, California
Lifang Zhang, California
Jaime Baker, MD, Colorado
Eric Johnson, PA-C, Colorado
Juan Lessing, MD, Colorado
Benjamin Ruckman, DO, Colorado
Rehaan Shaffie, MD, Colorado
Deborah Casey, MD, Connecticut
Daniel Heacock, PA-C, Connecticut
Shabana Ansari, DO, Delaware
Madhu Prattipati, MD, Delaware
Pallavi Aneja, MD, Florida
Satcha Borgella, MD, Florida
Thendrex H. Estrella, MD, Florida
Abid Hussain, MD, Florida
Daphnee Hutchinson, DO, Florida
Muhammad Jaffer, Florida
Sue Lee, ANP, Florida
Melissa Odermann, DO, Florida
Jose Guillermo Revelo Paiz, MD, Florida
Rafael J. Rolon Rivera, MD, Florida
Eleonor Rongo, Florida
Esther Roth, Florida
Shitaye Argaw, MD, Georgia
Taryn DeGrazia, Georgia
Becca Feistritzer, Georgia
Jamal Fitts, Georgia
Kristen Flint, Georgia
Zachary Hermes, Georgia
Mukesh Kumar, Georgia
Kajal Patel, Georgia
Madeline Smith, Georgia
Wade Flowers, PharmD, Idaho
Ajay Bhandare, Illinois
Kimberly Brighton, Illinois
Hristo D. Hristov, MD, Illinois
Sidney Iriana, Illinois
Aurelian Ivan, Illinois
Ming Lee, MD, Illinois
Michelle Lundholm, Illinois
Idrees Mohiuddin, MD, Illinois
Murr Murray, Illinois
Tad Nair, MD, Illinois
Shalini Reddy, MD, Illinois
Richard Rethorst, MD, Illinois
Kelly Robertshaw, Illinois
Gracelene Wegrzyn, Illinois
Evan Yates, Illinois
Lora J. Jones McClure, MD, Indiana
Carleigh Wilson, DO, Indiana
Erin Brown, ARNP, Iowa
Adam Gray, Iowa
Paul Greco, MD, Iowa
Shelly McGurk, ACNP, ARNP, Iowa
Julie Stanik-Hutt, ACNP, CNS, PhD, Iowa
Elizabeth Cozad, DO, Kansas
Roshan Pais, Kentucky
Mark Youssef, MD, Kentucky
Heather Kahn, MD, Louisiana
Danielle Parrott, PA-C, Maine
Erica Lafferty, ACNP, Maryland
Andrea Limpuangthip, Maryland
Steven Schwartz, CCM, MD, Maryland
Eisha Azhar, MBBS, Massachusetts
Badal Kalamkar, MD, MPH, Massachusetts
Bhavya Rajanna, MD, Massachusetts
Sahib Baljinder Singh, MD, Massachusetts
Kathryn Adams, Michigan
Haseeb Aslam, MD, MBBS, Michigan
Hilda Crispin, MD, Michigan
Sharmistha Dev, MD, Michigan
Tristan Feierabend, MD, Michigan
Sonal Kamalia, MD, MBBS, Michigan
Matthew Luzum, MD, Michigan
Daniel Mitzel, MD, Michigan
Richard Raad, Michigan
Mythri Ramegowda, MD, Michigan
Katie Scally, MD, Michigan
Linden Spital, MSN, NP, Michigan
Porama Koy Thanaporn, MD, Michigan
Chanteil Ulatowski, Michigan
Tingting Xiong, MD, Michigan
Adam Zahr, Michigan
Mike Beste, MD, Minnesota
Elise Haupt, PA-C, Minnesota
Lobsang Trasar, MD, Minnesota
Kari Goan, DO, Mississippi
David C. Pierre, Mississippi
Sudheer Tangella, MD, Mississippi
Tahani Atieh, Missouri
Nicholas Arnold, Missouri
Amanda Calhoun, Missouri
Jyotirmoy Das, Missouri
Umber Dube, Missouri
Daniel Gaughan, Missouri
Woojin Joo, Missouri
Khaled Jumean, MBBS, Missouri
Salma Kazmi, MBBS, MD, Missouri
Yoon Kook (Danny) Kim, Missouri
Ryan Kronen, Missouri
Alyssa Kroner, Missouri
Randy Laine, Missouri
Edward Lee, Missouri
Cerena Leung, Missouri
Patricia Lithrow, Missouri
Brandt Lydon, Missouri
Mary Morgan Scott, Missouri
Jay Patel, Missouri
Justin Porter, Missouri
Danelle Reagin, FNP-C, Missouri
Amanda Reis, Missouri
Awik Som, Missouri
Abby Sung, Missouri
Mary Sutherland, Missouri
Maggie Wang, Missouri
Noah Wasserman, Missouri
Alexis Webber, Missouri
Ryan White, Missouri
Amy Xu, Missouri
Ran Xu, Missouri
Michael Yang, Missouri
Christopher Dietrich, MD, Montana
Jason Kunz, DO, Montana
Jodi Cantrell, MD, Nebraska
Steven Hart, MD, Nebraska
Kurt Kapels, MD, Nebraska
Brian Keegan, MD, Nebraska
Shaun Jang, MD, Nevada
Gurpinder Singh, MD, New Hampshire
Pragati Banda, MD, New Jersey
Sahai Donaldson, MBBS, New Jersey
Ashesha Mechineni, MD, New Jersey
Alisa Clark, New Mexico
Prajit Arora, MBBS, New Mexico
Crystal Cardwell, New Mexico
Landon Casaus, New Mexico
Tapuwa Mupfumira, MD, New Mexico
Eric Rightley, New Mexico
David S. Anderson, New York
Joan Bosco, MD, New York
Jessica Caro, New York
Anna Dewan, New York
Amrita Dhillon, MBBS, New York
Julia Frydman, New York
Radhika Gali, MBBS, MDS, New York
Allison Guttmann, MD, New York
Aryles Hedjar, MD, New York
Peter Janes, New York
Nadine Kalavazoff, New York
Jeffrey Lach, DO, New York
Keron Lezama, MD, New York
Yingheng Liu, New York
Taimur Mirza, New York
Cyrus Nensey, MD, New York
Nekee Pandya, MD, New York
Thushara Paul, MD, New York
Yu Sung, New York
Joel Boggan, MD, North Carolina
Angela Fletcher, North Carolina
Rebecca Gimpert, PA-C, North Carolina
Samantha Levering, PA-C, North Carolina
Nancy Martin, North Carolina
Richard Sherwood, North Carolina
Kranthi K. Sitammagari, MD, North Carolina
Aaron Swedberg, MPAS, PA-C, North Carolina
Yih-Cherng Tsai, North Carolina
Richard Bakker, MD, PhD, Ohio
Matthew Broderick, MD, Ohio
Subbaraju Budharaju, MD, MS, Ohio
Steven Bumb, MD, Ohio
Ahmed Eltelbany, MD, Ohio
Tracey Hardin, MS, Ohio
Patricia Hardman, APRN, Ohio
Michael Lewis, MD, Ohio
Volodymyr Manko, Ohio
Rebecca Stone, Ohio
Chaitanya Valluri, Ohio
Holly Wierzbicki, CNP, Ohio
Jamie Yockey, APRN, CNP, Ohio
Mahdi Mussa, MD, Oklahoma
Monica Saemz, DO, Oklahoma
Peter Ganter, MD, Oregon
Bethany Roy, MD, Oregon
Mary Clare Bohnett, Oregon
Molly Rabinowitz, Oregon
Abdullateef Abdulkareem, MD, MPH, Pennsylvania
David Ahamba, MD, MPH, Pennsylvania
David Chin, MD, Pennsylvania
Thomas Conlon, Pennsylvania
Dan Giesler, MD, Pennsylvania
Umair Randhawa, MD, Pennsylvania
Syed Yusuf, MBBS, Pennsylvania
Michael Rigatti, Pennsylvania
Thaylon Barreto, Rhode Island
Jessica Cook, MD, South Carolina
Robin Malik, MD, South Carolina
John Busigin, Tennessee
Shefali Paranjape, MD, Tennessee
Thai Dang, MD, Texas
Matthew Glover, MD, Texas
Snigdha Jain, MD, Texas
David Kellenberger, Texas
Sumeet Kumar, Texas
Kyle McClendon, PA-C, Texas
Sowjanya Mohan, Texas
Akhil D. Vats, MD, Texas
Samatha Vellanki, Texas
Lee-Anna Burgess, MD, Vermont
Rick Hildebrant, MD, Vermont
Matthew Backens, MD, Virginia
Megan Coe, Virginia
Kevin Dehaan, Virginia
Stephen Fox, Virginia
Amber Inofuentes, MD, Virginia
Jessica Keiser, MD, Virginia
Joseph Perez, MD, FAAFP, MBA, Virginia
Kanwapreet S. Saini, MD, Virginia
Erin Vipler, MD, Virginia
Naveen Voore, MBBS, Virginia
Abhishek Agarwal, MD, MBBS, Washington
Robert Cooney, MD, Washington
Cynthia Horton, MD, Washington
Rich A. Kukreja, MD, Washington
Ji Young Nam, MD, Washington
Kai Wilhelm, MD, Washington
In Kyu Yoo, Washington
Temu Brown, Wisconsin
Pablo Colon Nieves, Wisconsin
Christina Evans, PAC, Wisconsin
Swetha Karturi, MBBS, Wisconsin
Mark Babcock, DO, Wyoming
Ahmad Von Schlegell, Canada
Anand Kartha, Japan
Mohamed Sadek, Qatar
Amine Rakab, MD, Qatar
Abazar Saeed, Qatar
Joao Guerra, MD
Inhalers used incorrectly at least one-third of time
Clinical question: What are the most common errors in inhaler use over the past 40 years?
Background: One of the reasons for poor asthma and COPD control is incorrect inhaler use. Problems with technique have been recognized since the launch of the metered-dose inhaler (MDI) in the 1960s. Multiple initiatives have been implemented, including the design of the dry powder inhaler (DPI); however, problems persist despite all corrective measures.
Study design: Meta-analysis.
Synopsis: The most frequent MDI errors were lack of initial full expiration (48%), inadequate coordination (45%), and no postinhalation breath hold (46%). DPI errors were lower, compared with MDI errors: incorrect preparation (29%), no initial full expiration before inhalation (46%), and no postinhalation breath hold (37%).
The overall prevalence of correct technique was the same as poor technique (31%). There was no difference in the rates of incorrect inhaler use between the first and second 20-year periods of investigation.
Bottom line: Incorrect inhaler use in patients with asthma and COPD persists over time despite multiple implemented strategies.
Citation: Sanchis J, Gich I, Pedersen S, Aerosol Drug Management Improvement Team. Systematic review of errors in inhaler use: has the patient technique improved over time? Chest. 2016;150(2):394-406.
Dr. Florindez is an assistant professor at the University of Miami Miller School of Medicine and a hospitalist at University of Miami Hospital and Jackson Memorial Hospital.
Clinical question: What are the most common errors in inhaler use over the past 40 years?
Background: One of the reasons for poor asthma and COPD control is incorrect inhaler use. Problems with technique have been recognized since the launch of the metered-dose inhaler (MDI) in the 1960s. Multiple initiatives have been implemented, including the design of the dry powder inhaler (DPI); however, problems persist despite all corrective measures.
Study design: Meta-analysis.
Synopsis: The most frequent MDI errors were lack of initial full expiration (48%), inadequate coordination (45%), and no postinhalation breath hold (46%). DPI errors were lower, compared with MDI errors: incorrect preparation (29%), no initial full expiration before inhalation (46%), and no postinhalation breath hold (37%).
The overall prevalence of correct technique was the same as poor technique (31%). There was no difference in the rates of incorrect inhaler use between the first and second 20-year periods of investigation.
Bottom line: Incorrect inhaler use in patients with asthma and COPD persists over time despite multiple implemented strategies.
Citation: Sanchis J, Gich I, Pedersen S, Aerosol Drug Management Improvement Team. Systematic review of errors in inhaler use: has the patient technique improved over time? Chest. 2016;150(2):394-406.
Dr. Florindez is an assistant professor at the University of Miami Miller School of Medicine and a hospitalist at University of Miami Hospital and Jackson Memorial Hospital.
Clinical question: What are the most common errors in inhaler use over the past 40 years?
Background: One of the reasons for poor asthma and COPD control is incorrect inhaler use. Problems with technique have been recognized since the launch of the metered-dose inhaler (MDI) in the 1960s. Multiple initiatives have been implemented, including the design of the dry powder inhaler (DPI); however, problems persist despite all corrective measures.
Study design: Meta-analysis.
Synopsis: The most frequent MDI errors were lack of initial full expiration (48%), inadequate coordination (45%), and no postinhalation breath hold (46%). DPI errors were lower, compared with MDI errors: incorrect preparation (29%), no initial full expiration before inhalation (46%), and no postinhalation breath hold (37%).
The overall prevalence of correct technique was the same as poor technique (31%). There was no difference in the rates of incorrect inhaler use between the first and second 20-year periods of investigation.
Bottom line: Incorrect inhaler use in patients with asthma and COPD persists over time despite multiple implemented strategies.
Citation: Sanchis J, Gich I, Pedersen S, Aerosol Drug Management Improvement Team. Systematic review of errors in inhaler use: has the patient technique improved over time? Chest. 2016;150(2):394-406.
Dr. Florindez is an assistant professor at the University of Miami Miller School of Medicine and a hospitalist at University of Miami Hospital and Jackson Memorial Hospital.
Blood thinning with bioprosthetic valves
Clinical question: Does anticoagulation prevent thromboembolic events in patients undergoing bioprosthetic valve implantation?
Background: The main advantage of bioprosthetic valves, compared with mechanical valves, is the avoidance of long-term anticoagulation. Current guidelines recommend the use of vitamin K antagonist (VKA) during the first 3 months after surgery, which remains controversial. Two randomized controlled trials (RCTs) showed no benefit of using VKA in the first 3 months; however, other studies have reported conflicting results.
Study design: Meta-analysis and systematic review.
Setting: Multicenter.
Synopsis: This meta-analysis included two RCTs and 12 observational studies that compared the outcomes in group I (VKA) versus group II (antiplatelet therapy/no treatment). There was no difference in thromboembolic events between group I (1%) and group II (1.5%), but there were more bleeding events in group I (2.6%) versus group II (1.1%). In addition, no differences in all-cause of mortality rate and need for redo surgery were found between the two groups.
Bottom line: The use of VKA in the first 3 months after a bioprosthetic valve implantation does not decrease the rate of thromboembolic events or mortality, but it is associated with increased risk of major bleeding.
Citation: Masri A, Gillinov M, Johnston DM, et al. Anticoagulation versus antiplatelet or no therapy in patients undergoing bioprosthetic valve implantation: a systematic review and meta-analysis [published online ahead of print Aug. 3, 2016]. Heart. doi: 10.1136/heartjnl-2016-309630
Dr. Florindez is an assistant professor at the University of Miami Miller School of Medicine and a hospitalist at University of Miami Hospital and Jackson Memorial Hospital.
Clinical question: Does anticoagulation prevent thromboembolic events in patients undergoing bioprosthetic valve implantation?
Background: The main advantage of bioprosthetic valves, compared with mechanical valves, is the avoidance of long-term anticoagulation. Current guidelines recommend the use of vitamin K antagonist (VKA) during the first 3 months after surgery, which remains controversial. Two randomized controlled trials (RCTs) showed no benefit of using VKA in the first 3 months; however, other studies have reported conflicting results.
Study design: Meta-analysis and systematic review.
Setting: Multicenter.
Synopsis: This meta-analysis included two RCTs and 12 observational studies that compared the outcomes in group I (VKA) versus group II (antiplatelet therapy/no treatment). There was no difference in thromboembolic events between group I (1%) and group II (1.5%), but there were more bleeding events in group I (2.6%) versus group II (1.1%). In addition, no differences in all-cause of mortality rate and need for redo surgery were found between the two groups.
Bottom line: The use of VKA in the first 3 months after a bioprosthetic valve implantation does not decrease the rate of thromboembolic events or mortality, but it is associated with increased risk of major bleeding.
Citation: Masri A, Gillinov M, Johnston DM, et al. Anticoagulation versus antiplatelet or no therapy in patients undergoing bioprosthetic valve implantation: a systematic review and meta-analysis [published online ahead of print Aug. 3, 2016]. Heart. doi: 10.1136/heartjnl-2016-309630
Dr. Florindez is an assistant professor at the University of Miami Miller School of Medicine and a hospitalist at University of Miami Hospital and Jackson Memorial Hospital.
Clinical question: Does anticoagulation prevent thromboembolic events in patients undergoing bioprosthetic valve implantation?
Background: The main advantage of bioprosthetic valves, compared with mechanical valves, is the avoidance of long-term anticoagulation. Current guidelines recommend the use of vitamin K antagonist (VKA) during the first 3 months after surgery, which remains controversial. Two randomized controlled trials (RCTs) showed no benefit of using VKA in the first 3 months; however, other studies have reported conflicting results.
Study design: Meta-analysis and systematic review.
Setting: Multicenter.
Synopsis: This meta-analysis included two RCTs and 12 observational studies that compared the outcomes in group I (VKA) versus group II (antiplatelet therapy/no treatment). There was no difference in thromboembolic events between group I (1%) and group II (1.5%), but there were more bleeding events in group I (2.6%) versus group II (1.1%). In addition, no differences in all-cause of mortality rate and need for redo surgery were found between the two groups.
Bottom line: The use of VKA in the first 3 months after a bioprosthetic valve implantation does not decrease the rate of thromboembolic events or mortality, but it is associated with increased risk of major bleeding.
Citation: Masri A, Gillinov M, Johnston DM, et al. Anticoagulation versus antiplatelet or no therapy in patients undergoing bioprosthetic valve implantation: a systematic review and meta-analysis [published online ahead of print Aug. 3, 2016]. Heart. doi: 10.1136/heartjnl-2016-309630
Dr. Florindez is an assistant professor at the University of Miami Miller School of Medicine and a hospitalist at University of Miami Hospital and Jackson Memorial Hospital.
Instability of INRs
Clinical question: Does an initial stable international normalized ratio (INR) predict long-term stability?
Background: Warfarin decreases stroke risk among patients with atrial fibrillation; however, it interacts with food and drugs and requires monitoring to achieve a therapeutic INR. It is unclear if patients on warfarin with an initial stable INR value remain stable over time. Additionally, it is controversial whether patients on warfarin with previously stable INRs should benefit from switching to a non–vitamin K oral anticoagulant.
Study design: Retrospective study.
Setting: Outpatient clinics.
Synopsis: Data were collected from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation. Included in the study were patients taking warfarin at baseline with three or more INR values in the first 6 months and six or more INR values in the subsequent year. Stability was defined as 80% or more INRs in therapeutic range (2.0-3.0).
Only 26% of patients taking warfarin had a stable INR during the first 6 months, and only 34% continued to have a stable INR in the subsequent year.
Bottom line: Initial stable INR within the first 6 months among patients taking warfarin does not predict long-term INR stability in the subsequent year.
Citation: Pokorney SD, Simon DN, Thomas L, et al. Stability of international normalized ratios in patients taking long-term warfarin therapy. JAMA.2016;316(6):661-663
Dr. Florindez is an assistant professor at the University of Miami Miller School of Medicine and a hospitalist at University of Miami Hospital and Jackson Memorial Hospital.
Clinical question: Does an initial stable international normalized ratio (INR) predict long-term stability?
Background: Warfarin decreases stroke risk among patients with atrial fibrillation; however, it interacts with food and drugs and requires monitoring to achieve a therapeutic INR. It is unclear if patients on warfarin with an initial stable INR value remain stable over time. Additionally, it is controversial whether patients on warfarin with previously stable INRs should benefit from switching to a non–vitamin K oral anticoagulant.
Study design: Retrospective study.
Setting: Outpatient clinics.
Synopsis: Data were collected from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation. Included in the study were patients taking warfarin at baseline with three or more INR values in the first 6 months and six or more INR values in the subsequent year. Stability was defined as 80% or more INRs in therapeutic range (2.0-3.0).
Only 26% of patients taking warfarin had a stable INR during the first 6 months, and only 34% continued to have a stable INR in the subsequent year.
Bottom line: Initial stable INR within the first 6 months among patients taking warfarin does not predict long-term INR stability in the subsequent year.
Citation: Pokorney SD, Simon DN, Thomas L, et al. Stability of international normalized ratios in patients taking long-term warfarin therapy. JAMA.2016;316(6):661-663
Dr. Florindez is an assistant professor at the University of Miami Miller School of Medicine and a hospitalist at University of Miami Hospital and Jackson Memorial Hospital.
Clinical question: Does an initial stable international normalized ratio (INR) predict long-term stability?
Background: Warfarin decreases stroke risk among patients with atrial fibrillation; however, it interacts with food and drugs and requires monitoring to achieve a therapeutic INR. It is unclear if patients on warfarin with an initial stable INR value remain stable over time. Additionally, it is controversial whether patients on warfarin with previously stable INRs should benefit from switching to a non–vitamin K oral anticoagulant.
Study design: Retrospective study.
Setting: Outpatient clinics.
Synopsis: Data were collected from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation. Included in the study were patients taking warfarin at baseline with three or more INR values in the first 6 months and six or more INR values in the subsequent year. Stability was defined as 80% or more INRs in therapeutic range (2.0-3.0).
Only 26% of patients taking warfarin had a stable INR during the first 6 months, and only 34% continued to have a stable INR in the subsequent year.
Bottom line: Initial stable INR within the first 6 months among patients taking warfarin does not predict long-term INR stability in the subsequent year.
Citation: Pokorney SD, Simon DN, Thomas L, et al. Stability of international normalized ratios in patients taking long-term warfarin therapy. JAMA.2016;316(6):661-663
Dr. Florindez is an assistant professor at the University of Miami Miller School of Medicine and a hospitalist at University of Miami Hospital and Jackson Memorial Hospital.
Inpatient antibiotic use has not declined
Clinical question: How has inpatient antibiotic use changed in the United States in recent years?
Study design: Retrospective analysis.
Setting: Adult and pediatric data from 300 acute-care hospitals, 2006-2012.
Synopsis: Weighted extrapolation of data from a database was used to estimate national antibiotic use. Overall, 55.1% of discharged patients received antibiotics. The rate of antibiotic use was 755/1,000 patient-days over the study period. The small increase in antibiotic use over the years (5.6 days of therapy/1,000 patient-days increase; 95% CI, –18.9 to 30.1; P = .65) was not statistically significant. There was a significant decrease in the use of aminoglycosides, first- and second-generation cephalosporins, fluoroquinolones, sulfonamide, metronidazole, and penicillins. The use of third- and fourth-generation cephalosporins, macrolides, glycopeptides, beta-lactam/beta-lactamase inhibitor, carbapenems, and tetracyclines has increased significantly.
Limitations of the study include underrepresentation of pediatric hospitals and certain geographic regions.
Bottom line: Antibiotic-use rates have not changed during 2006-2012. However, broad-spectrum antibiotic use has increased significantly.
Citation: Baggs J, Fridkin SK, Pollack LA, Srinivasan A, Jernigan JA. Estimating national trends in inpatient antibiotic use among US hospitals from 2006 to 2012. JAMA Intern Med. 2016;176(11):1639-1648.
Dr. Menon is an assistant professor at the University of Miami Miller School of Medicine and a hospitalist at University of Miami Hospital and Jackson Memorial Hospital.
Clinical question: How has inpatient antibiotic use changed in the United States in recent years?
Study design: Retrospective analysis.
Setting: Adult and pediatric data from 300 acute-care hospitals, 2006-2012.
Synopsis: Weighted extrapolation of data from a database was used to estimate national antibiotic use. Overall, 55.1% of discharged patients received antibiotics. The rate of antibiotic use was 755/1,000 patient-days over the study period. The small increase in antibiotic use over the years (5.6 days of therapy/1,000 patient-days increase; 95% CI, –18.9 to 30.1; P = .65) was not statistically significant. There was a significant decrease in the use of aminoglycosides, first- and second-generation cephalosporins, fluoroquinolones, sulfonamide, metronidazole, and penicillins. The use of third- and fourth-generation cephalosporins, macrolides, glycopeptides, beta-lactam/beta-lactamase inhibitor, carbapenems, and tetracyclines has increased significantly.
Limitations of the study include underrepresentation of pediatric hospitals and certain geographic regions.
Bottom line: Antibiotic-use rates have not changed during 2006-2012. However, broad-spectrum antibiotic use has increased significantly.
Citation: Baggs J, Fridkin SK, Pollack LA, Srinivasan A, Jernigan JA. Estimating national trends in inpatient antibiotic use among US hospitals from 2006 to 2012. JAMA Intern Med. 2016;176(11):1639-1648.
Dr. Menon is an assistant professor at the University of Miami Miller School of Medicine and a hospitalist at University of Miami Hospital and Jackson Memorial Hospital.
Clinical question: How has inpatient antibiotic use changed in the United States in recent years?
Study design: Retrospective analysis.
Setting: Adult and pediatric data from 300 acute-care hospitals, 2006-2012.
Synopsis: Weighted extrapolation of data from a database was used to estimate national antibiotic use. Overall, 55.1% of discharged patients received antibiotics. The rate of antibiotic use was 755/1,000 patient-days over the study period. The small increase in antibiotic use over the years (5.6 days of therapy/1,000 patient-days increase; 95% CI, –18.9 to 30.1; P = .65) was not statistically significant. There was a significant decrease in the use of aminoglycosides, first- and second-generation cephalosporins, fluoroquinolones, sulfonamide, metronidazole, and penicillins. The use of third- and fourth-generation cephalosporins, macrolides, glycopeptides, beta-lactam/beta-lactamase inhibitor, carbapenems, and tetracyclines has increased significantly.
Limitations of the study include underrepresentation of pediatric hospitals and certain geographic regions.
Bottom line: Antibiotic-use rates have not changed during 2006-2012. However, broad-spectrum antibiotic use has increased significantly.
Citation: Baggs J, Fridkin SK, Pollack LA, Srinivasan A, Jernigan JA. Estimating national trends in inpatient antibiotic use among US hospitals from 2006 to 2012. JAMA Intern Med. 2016;176(11):1639-1648.
Dr. Menon is an assistant professor at the University of Miami Miller School of Medicine and a hospitalist at University of Miami Hospital and Jackson Memorial Hospital.
Evaluating the qSOF
Clinical question: How does the quick Sepsis-Related Organ Failure Assessment (qSOFA) compare with other sepsis scoring tools?
Study design: Single-center, retrospective analysis.
Setting: Hospital ED in China.
Synopsis: A total of 516 adult ED patients with clinically diagnosed infections were followed for 28 days. Calculated scores for qSOFA, SOFA, Mortality in ED Sepsis (MEDS), and Acute Physiology and Chronic Health Evaluation (APACHE) II were compared using ROC curves.
qSOFA was similar to the other scoring systems to predict ICU admission.
The area under the curve for qSOFA to predict 28-day mortality was lower than all other scoring systems but was statistically significant only when compared to MEDS. A qSOFA score of 2 had a positive likelihood ratio of 2.47 to predict mortality (95% CI, 2.3-5.4) and a positive likelihood ratio of 2.08 (95% CI, 1.7-4.1) to predict ICU admission.
Bottom line: qSOFA was similar to other scoring systems to predict 28-day mortality and ICU admission but slightly inferior than MEDS to predict mortality.
Citation: Wang JY, Chen YX, Guo SB, Mei X, Yang P. Predictive performance of quick sepsis-related organ failure assessment for mortality and ICU admission in patients with infection at the ED. Am J Em Med. 2016;34(9):1788-1793
Clinical question: How does the quick Sepsis-Related Organ Failure Assessment (qSOFA) compare with other sepsis scoring tools?
Study design: Single-center, retrospective analysis.
Setting: Hospital ED in China.
Synopsis: A total of 516 adult ED patients with clinically diagnosed infections were followed for 28 days. Calculated scores for qSOFA, SOFA, Mortality in ED Sepsis (MEDS), and Acute Physiology and Chronic Health Evaluation (APACHE) II were compared using ROC curves.
qSOFA was similar to the other scoring systems to predict ICU admission.
The area under the curve for qSOFA to predict 28-day mortality was lower than all other scoring systems but was statistically significant only when compared to MEDS. A qSOFA score of 2 had a positive likelihood ratio of 2.47 to predict mortality (95% CI, 2.3-5.4) and a positive likelihood ratio of 2.08 (95% CI, 1.7-4.1) to predict ICU admission.
Bottom line: qSOFA was similar to other scoring systems to predict 28-day mortality and ICU admission but slightly inferior than MEDS to predict mortality.
Citation: Wang JY, Chen YX, Guo SB, Mei X, Yang P. Predictive performance of quick sepsis-related organ failure assessment for mortality and ICU admission in patients with infection at the ED. Am J Em Med. 2016;34(9):1788-1793
Clinical question: How does the quick Sepsis-Related Organ Failure Assessment (qSOFA) compare with other sepsis scoring tools?
Study design: Single-center, retrospective analysis.
Setting: Hospital ED in China.
Synopsis: A total of 516 adult ED patients with clinically diagnosed infections were followed for 28 days. Calculated scores for qSOFA, SOFA, Mortality in ED Sepsis (MEDS), and Acute Physiology and Chronic Health Evaluation (APACHE) II were compared using ROC curves.
qSOFA was similar to the other scoring systems to predict ICU admission.
The area under the curve for qSOFA to predict 28-day mortality was lower than all other scoring systems but was statistically significant only when compared to MEDS. A qSOFA score of 2 had a positive likelihood ratio of 2.47 to predict mortality (95% CI, 2.3-5.4) and a positive likelihood ratio of 2.08 (95% CI, 1.7-4.1) to predict ICU admission.
Bottom line: qSOFA was similar to other scoring systems to predict 28-day mortality and ICU admission but slightly inferior than MEDS to predict mortality.
Citation: Wang JY, Chen YX, Guo SB, Mei X, Yang P. Predictive performance of quick sepsis-related organ failure assessment for mortality and ICU admission in patients with infection at the ED. Am J Em Med. 2016;34(9):1788-1793
Pulmonary embolism in COPD exacerbations
Clinical question: How frequent is pulmonary embolism (PE) in patients with unexplained acute chronic obstructive pulmonary disease (COPD) exacerbation?
Study design: Systematic review.
Setting: U.S. hospitals and EDs.
Synopsis: PE prevalence was 16.1% (95% CI, 8.3%-25.8%) in patients with unexplained COPD exacerbations. Thirty-two percent were subsegmental, 35% affected one of the main pulmonary arteries, and 32% were located in the lobar and interlobar arteries. Heterogeneity between the included studies was high. In-hospital and 1-year mortality were increased in patients with PE and COPD exacerbations in one study but not in another.
Signs of cardiac failure, hypotension, and syncope were more frequently found in patients with COPD exacerbation and PE, compared with patients with COPD exacerbation without PE.
Bottom line: PE is a common occurrence in patients with unexplained COPD exacerbations; two-thirds of those emboli involved segmental circulation and therefore were clinically relevant.
Citation: Aleva FE, Voets LW, Simons SO, de Mast Q, van der Ven A, Heijdra YF. Prevalence and localization of pulmonary embolism in unexplained acute exacerbations of COPD: a systematic review and meta-analysis [published online ahead of print Aug. 11, 2016]. Chest. doi: 10.1016/j.chest.2016.07.034.
Clinical question: How frequent is pulmonary embolism (PE) in patients with unexplained acute chronic obstructive pulmonary disease (COPD) exacerbation?
Study design: Systematic review.
Setting: U.S. hospitals and EDs.
Synopsis: PE prevalence was 16.1% (95% CI, 8.3%-25.8%) in patients with unexplained COPD exacerbations. Thirty-two percent were subsegmental, 35% affected one of the main pulmonary arteries, and 32% were located in the lobar and interlobar arteries. Heterogeneity between the included studies was high. In-hospital and 1-year mortality were increased in patients with PE and COPD exacerbations in one study but not in another.
Signs of cardiac failure, hypotension, and syncope were more frequently found in patients with COPD exacerbation and PE, compared with patients with COPD exacerbation without PE.
Bottom line: PE is a common occurrence in patients with unexplained COPD exacerbations; two-thirds of those emboli involved segmental circulation and therefore were clinically relevant.
Citation: Aleva FE, Voets LW, Simons SO, de Mast Q, van der Ven A, Heijdra YF. Prevalence and localization of pulmonary embolism in unexplained acute exacerbations of COPD: a systematic review and meta-analysis [published online ahead of print Aug. 11, 2016]. Chest. doi: 10.1016/j.chest.2016.07.034.
Clinical question: How frequent is pulmonary embolism (PE) in patients with unexplained acute chronic obstructive pulmonary disease (COPD) exacerbation?
Study design: Systematic review.
Setting: U.S. hospitals and EDs.
Synopsis: PE prevalence was 16.1% (95% CI, 8.3%-25.8%) in patients with unexplained COPD exacerbations. Thirty-two percent were subsegmental, 35% affected one of the main pulmonary arteries, and 32% were located in the lobar and interlobar arteries. Heterogeneity between the included studies was high. In-hospital and 1-year mortality were increased in patients with PE and COPD exacerbations in one study but not in another.
Signs of cardiac failure, hypotension, and syncope were more frequently found in patients with COPD exacerbation and PE, compared with patients with COPD exacerbation without PE.
Bottom line: PE is a common occurrence in patients with unexplained COPD exacerbations; two-thirds of those emboli involved segmental circulation and therefore were clinically relevant.
Citation: Aleva FE, Voets LW, Simons SO, de Mast Q, van der Ven A, Heijdra YF. Prevalence and localization of pulmonary embolism in unexplained acute exacerbations of COPD: a systematic review and meta-analysis [published online ahead of print Aug. 11, 2016]. Chest. doi: 10.1016/j.chest.2016.07.034.
Have you Googled yourself lately?
The online rating business is proliferating in the medical industry. This should really come as no surprise as health care is a service industry and online ratings have long been a staple in most other service industries. It has become routine practice for most of us to search such online reviews when seeking a pair of shoes, a toaster, or a restaurant; we almost can’t help but scour these sites to help us make the best decision possible.
Not dissimilarly, patients these days seek care and make decisions by using a variety of inputs, including:
- Anticipated cost (is the physician or practice in or out of network?).
- Availability or access to the service (location of the practice and how long it will take to be seen).
- How good the services and care will be when they get there.
That same article found that for those who used online physician ratings, about one-third had selected a physician based on good ratings, and about one-third had avoided a physician based on poor ratings. So patients do seem to be paying attention to these sites and seeking or avoiding care based on what information they find.
Based on that evidence, it is not surprising that so many physician rating sites have sprung up; not only is there a market demand for the availability of this information, the rating sites are also profitable for the host companies. Vitals.com, for example, makes most of its revenue from advertisements and turns a sizable profit every year. Other profitable health care rating sites include Healthgrades, Yelp, Zocdoc, and WebMD.
When I Google my own name, for example, Vitals.com is the first ratings website that appears in the search results. The first pop-up asks you to rate me and then it takes you to a site with all sorts of facts about me (most of which are notably inaccurate). If I had any online ratings (which I do not currently), you would then see my star ratings and any comments.
The second rating site that comes up for me via Google search is PhysicianWiki.com.There is a whole host of information on me (most of which is accurate), along with a set of personal ratings, including my office, my staff, and my waiting times (which, of course, do not make any sense given I am a hospitalist!). It is unclear how those ratings were generated or what volume of responses they represent.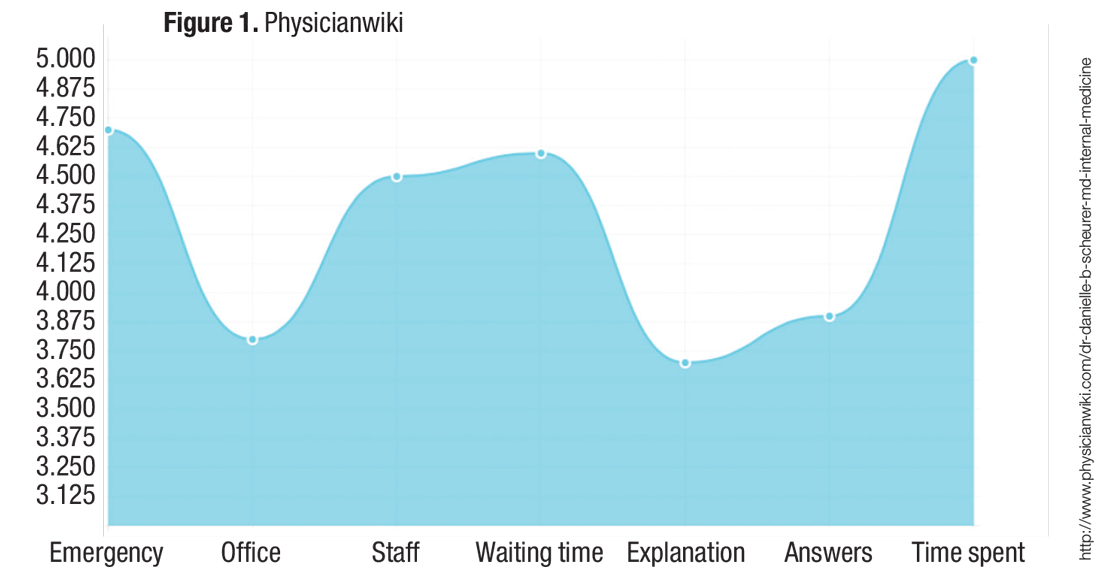
My health care system proposed rolling out a similar online rating system, and it was met with great skepticism from many physicians. There were two primary concerns:
- They felt it was “tacky” and that the profession of medicine should not be relegated to oversimplified service ratings. They worried that they would feel pressured to please the patient rather than “do the right thing” for the patient. For example, they would be less likely to give difficult advice (such as lose weight or stop smoking) or to resist prescribing medications that they deemed unnecessary or frankly dangerous (for example, antibiotics or narcotics).
Although these are valid concerns, it is hard to ignore the proliferation and traffic of these online websites. For you and your team, I would recommend taking a look at what is online about the members of your group and thinking about online strategies to take control of the conversation.
I don’t think the controversy over online physician ratings will wane anytime soon, but there is no doubt that they are profitable for companies and are therefore highly likely to continue to multiply.
References
1.Hanauer DA, Zheng K, Singer DC, Gebremariam A, Davis MM. Public awareness, perception, and use of online physician rating sites. JAMA. 2014;311(7):734-735. 2. A to Z provider listing: find a U of U Health Care physician by last name. University of Utah website. Available at http://healthcare.utah.edu/fad. Accessed Nov. 16, 2016.
Danielle Scheurer, MD, MSc, SFHM, is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
The online rating business is proliferating in the medical industry. This should really come as no surprise as health care is a service industry and online ratings have long been a staple in most other service industries. It has become routine practice for most of us to search such online reviews when seeking a pair of shoes, a toaster, or a restaurant; we almost can’t help but scour these sites to help us make the best decision possible.
Not dissimilarly, patients these days seek care and make decisions by using a variety of inputs, including:
- Anticipated cost (is the physician or practice in or out of network?).
- Availability or access to the service (location of the practice and how long it will take to be seen).
- How good the services and care will be when they get there.
That same article found that for those who used online physician ratings, about one-third had selected a physician based on good ratings, and about one-third had avoided a physician based on poor ratings. So patients do seem to be paying attention to these sites and seeking or avoiding care based on what information they find.
Based on that evidence, it is not surprising that so many physician rating sites have sprung up; not only is there a market demand for the availability of this information, the rating sites are also profitable for the host companies. Vitals.com, for example, makes most of its revenue from advertisements and turns a sizable profit every year. Other profitable health care rating sites include Healthgrades, Yelp, Zocdoc, and WebMD.
When I Google my own name, for example, Vitals.com is the first ratings website that appears in the search results. The first pop-up asks you to rate me and then it takes you to a site with all sorts of facts about me (most of which are notably inaccurate). If I had any online ratings (which I do not currently), you would then see my star ratings and any comments.
The second rating site that comes up for me via Google search is PhysicianWiki.com.There is a whole host of information on me (most of which is accurate), along with a set of personal ratings, including my office, my staff, and my waiting times (which, of course, do not make any sense given I am a hospitalist!). It is unclear how those ratings were generated or what volume of responses they represent.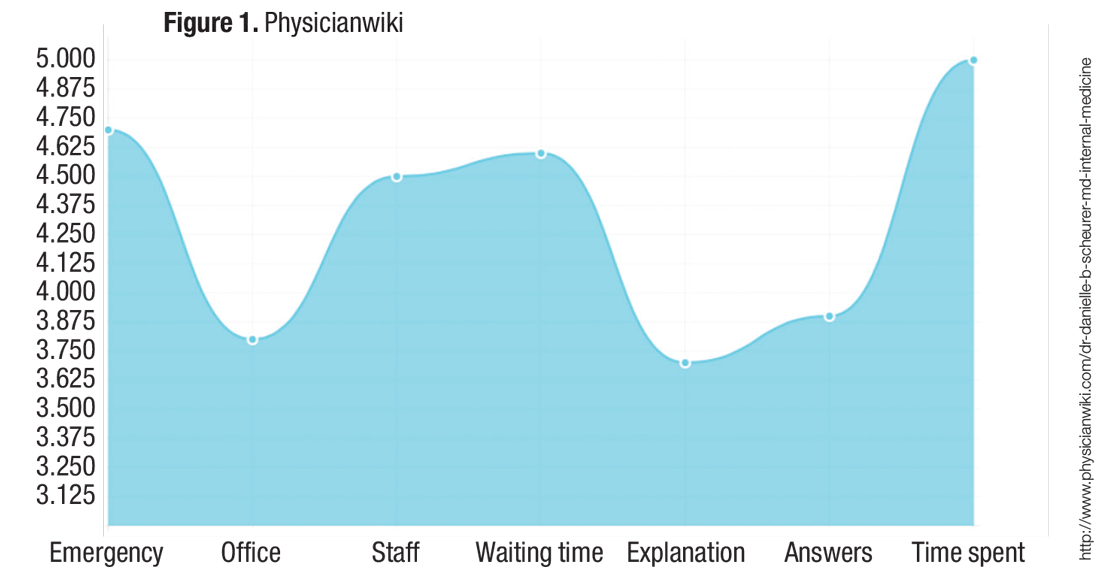
My health care system proposed rolling out a similar online rating system, and it was met with great skepticism from many physicians. There were two primary concerns:
- They felt it was “tacky” and that the profession of medicine should not be relegated to oversimplified service ratings. They worried that they would feel pressured to please the patient rather than “do the right thing” for the patient. For example, they would be less likely to give difficult advice (such as lose weight or stop smoking) or to resist prescribing medications that they deemed unnecessary or frankly dangerous (for example, antibiotics or narcotics).
Although these are valid concerns, it is hard to ignore the proliferation and traffic of these online websites. For you and your team, I would recommend taking a look at what is online about the members of your group and thinking about online strategies to take control of the conversation.
I don’t think the controversy over online physician ratings will wane anytime soon, but there is no doubt that they are profitable for companies and are therefore highly likely to continue to multiply.
References
1.Hanauer DA, Zheng K, Singer DC, Gebremariam A, Davis MM. Public awareness, perception, and use of online physician rating sites. JAMA. 2014;311(7):734-735. 2. A to Z provider listing: find a U of U Health Care physician by last name. University of Utah website. Available at http://healthcare.utah.edu/fad. Accessed Nov. 16, 2016.
Danielle Scheurer, MD, MSc, SFHM, is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
The online rating business is proliferating in the medical industry. This should really come as no surprise as health care is a service industry and online ratings have long been a staple in most other service industries. It has become routine practice for most of us to search such online reviews when seeking a pair of shoes, a toaster, or a restaurant; we almost can’t help but scour these sites to help us make the best decision possible.
Not dissimilarly, patients these days seek care and make decisions by using a variety of inputs, including:
- Anticipated cost (is the physician or practice in or out of network?).
- Availability or access to the service (location of the practice and how long it will take to be seen).
- How good the services and care will be when they get there.
That same article found that for those who used online physician ratings, about one-third had selected a physician based on good ratings, and about one-third had avoided a physician based on poor ratings. So patients do seem to be paying attention to these sites and seeking or avoiding care based on what information they find.
Based on that evidence, it is not surprising that so many physician rating sites have sprung up; not only is there a market demand for the availability of this information, the rating sites are also profitable for the host companies. Vitals.com, for example, makes most of its revenue from advertisements and turns a sizable profit every year. Other profitable health care rating sites include Healthgrades, Yelp, Zocdoc, and WebMD.
When I Google my own name, for example, Vitals.com is the first ratings website that appears in the search results. The first pop-up asks you to rate me and then it takes you to a site with all sorts of facts about me (most of which are notably inaccurate). If I had any online ratings (which I do not currently), you would then see my star ratings and any comments.
The second rating site that comes up for me via Google search is PhysicianWiki.com.There is a whole host of information on me (most of which is accurate), along with a set of personal ratings, including my office, my staff, and my waiting times (which, of course, do not make any sense given I am a hospitalist!). It is unclear how those ratings were generated or what volume of responses they represent.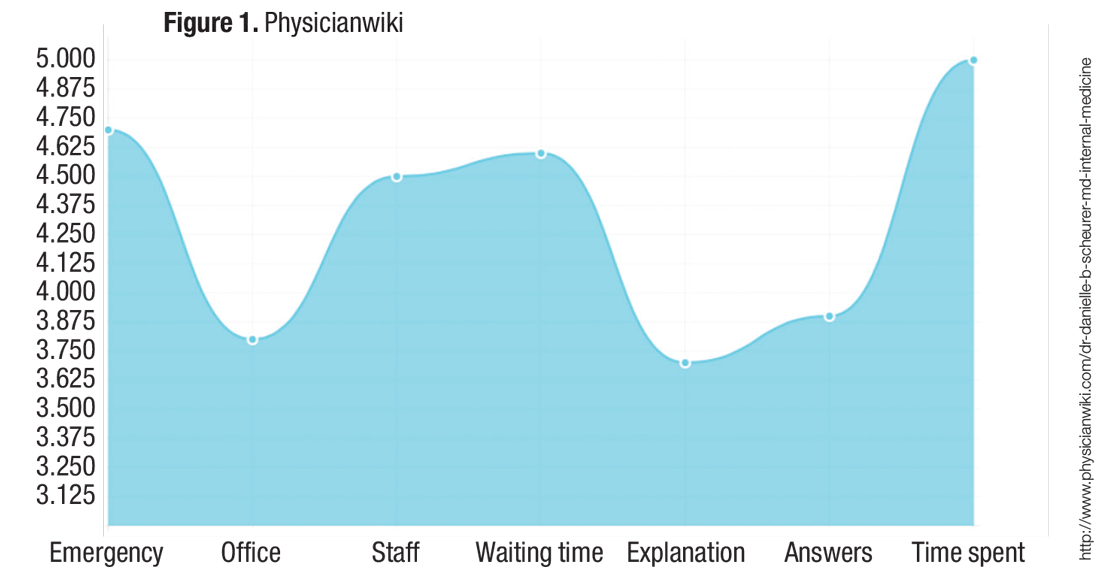
My health care system proposed rolling out a similar online rating system, and it was met with great skepticism from many physicians. There were two primary concerns:
- They felt it was “tacky” and that the profession of medicine should not be relegated to oversimplified service ratings. They worried that they would feel pressured to please the patient rather than “do the right thing” for the patient. For example, they would be less likely to give difficult advice (such as lose weight or stop smoking) or to resist prescribing medications that they deemed unnecessary or frankly dangerous (for example, antibiotics or narcotics).
Although these are valid concerns, it is hard to ignore the proliferation and traffic of these online websites. For you and your team, I would recommend taking a look at what is online about the members of your group and thinking about online strategies to take control of the conversation.
I don’t think the controversy over online physician ratings will wane anytime soon, but there is no doubt that they are profitable for companies and are therefore highly likely to continue to multiply.
References
1.Hanauer DA, Zheng K, Singer DC, Gebremariam A, Davis MM. Public awareness, perception, and use of online physician rating sites. JAMA. 2014;311(7):734-735. 2. A to Z provider listing: find a U of U Health Care physician by last name. University of Utah website. Available at http://healthcare.utah.edu/fad. Accessed Nov. 16, 2016.
Danielle Scheurer, MD, MSc, SFHM, is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
U.S. health care policy: What lies ahead?
The New Year brings new leadership in the United States, with President-elect Donald Trump taking office later this month. With a Republican-controlled Congress, party leaders have the opportunity to shape the nation’s policies around conservative ideals. This includes health care.
Since the Affordable Care Act (ACA) was passed in 2010, Republicans have vowed to repeal and replace it. This could be their opportunity.
However, “there is no clear coalescence around specific policy reforms that would replace the Affordable Care Act,” says Christine Eibner, PhD, a senior economist at Rand and a professor at the Pardee Rand Graduate School.
As a candidate, Trump did little to advance policy ideas around health care. Meanwhile, House Speaker Paul Ryan (R-Wis.) and others have, over the years, proposed reforms with which Trump may or may not agree.
“The Republicans now have a hard issue in their hands,” says Allison Hoffman, JD, professor of law at UCLA School of Law and an expert on health care law and policy. “It was hard before the Affordable Care Act, and it will be hard after. There is not an easy solution.”
By 2016, the ACA had expanded health coverage to 20 million people through Medicaid and private insurance on health care marketplaces. It extended the solvency of the Medicare Hospital Insurance Trust Fund. It accelerated the pace of delivery system and payment reform through creation of the Center for Medicare & Medicaid Innovation.
The law, however, has not been without its challenges.
“It was a strong achievement to get 20 million people insured, but it’s not clear that it bent the cost curve,” says Dr. Eibner. “There are high premiums on the individual market and still 31 million people without coverage. There is still opportunity to improve.”
Where we stand January 2017
Whether the Republicans can or will repeal the ACA in its entirety and improve it remains unknown. But, the experts say, the landmark law has left its mark on the American health care system.
“Everyone is complaining about the uncertainty created by the election, but we have been dealing with a highly uncertain environment for many years,” says Ron Greeno, MD, FCCP, MHM, senior advisor for medical affairs at TeamHealth, chair of the SHM Public Policy Committee, and SHM president-elect. “There will be changes, but things were going to change no matter the outcome of the election. It continues to require tolerance for change and tolerance for uncertainty.”
In an analysis for the Commonwealth Fund, Dr. Eibner investigated the economic implications of aspects of Trump’s plans as a candidate. Using a computer model that incorporates economic theory and data to simulate the effects of health policy changes, Dr. Eibner found that Trump’s plans (full repeal alone or repeal with tax deductions for health care premiums, Medicaid block grants, or selling health insurance across state lines) would increase the number of uninsured people by 16 million to 25 million, disproportionately impact low-income and sicker patients, expose individual market enrollees to higher out-of-pocket costs, and increase the federal deficit by $0.5 billion to $41 billion.1 The Congressional Budget Office (CBO) estimates full repeal could increase the federal deficit by $137 billion to $353 billion by 2025.2 Rep. Ryan’s plan, A Better Way, proposes providing people more control over their health care, giving tax credits instead of subsidies for premiums, capping the employer-sponsored health insurance tax exclusion, and expanding use of health savings accounts.3 However, Rep. Ryan’s plan “doesn’t reduce the cost of health care. It puts more onus on individuals, and their costs go up,” Ms. Hoffman says. “The weight of that will be more on people who have preexisting conditions.”
Joshua Lenchus, DO, RPh, FACP, SFHM, a member of SHM’s Public Policy Committee and hospitalist at the University of Miami/Jackson Memorial Hospital in Florida, is no fan of entitlement programs like Medicaid but says, “The safety-net hospital where I work would rather have people covered with something than nothing.”
Dr. Lenchus is optimistic that economic reforms under Trump will lead to more jobs, increasing the number of people covered by employer plans. “The economy drives health care reform,” he says. “He has to up his ante now and show people that he can stimulate job growth in this country so we don’t have this middle class that is continuously squeezed.”
Dr. Greeno and Ms. Hoffman, who is also a faculty associate at the UCLA Center for Health Policy Research and vice chair of the Insurance Law Section of the Association of American Law Schools, suggest hospitalists get involved as rules are being shaped and written.
“We want to help reform the delivery system, and we want it to be done right and to be done fairly. We want to have say in how our patients are treated,” Dr. Greeno says.
Key provisions: A delicate balance
Many people equate the ACA with the individual mandate, which requires nearly all Americans to purchase health insurance or pay a fine. The federal government provides subsidies to enrollees between 138% and 400% of the federal poverty level so their out-of-pocket costs never exceed a defined threshold even if premiums go up. These could be on the chopping block.
“The last bill Congress passed to repeal the Affordable Care Act, which Obama vetoed, repealed the individual mandate and subsidies for people to buy insurance,” Ms. Hoffman says. “If they do repeal it, private insurance through the exchanges will crumble.”
Mr. Trump’s tax deductions to offset premium costs are based on income, making them more generous for higher-income earners than low-income ones, Hoffman adds.
As a result, she says, people may choose high-deductible plans and face high out-of-pocket costs if they do seek care.
“It’s asking individuals to save by deciding how they’re going to ration care, where someone says they’re not going to go to the doctor today or fill a prescription drug they need,” Ms. Hoffman says.
Meanwhile, Mr. Trump has said he would like to keep the provision of the ACA that bans insurers from denying individuals with preexisting conditions. This, experts agree, may not be possible if other parts of the law are repealed and not replaced with similar protections for insurers.
“If you try to keep the rules about not including preexisting conditions and get rid of subsidies and the individual mandate, it just won’t work,” Ms. Hoffman says. “You end up with extraordinarily expensive health insurance.”
Rep. Ryan’s plan would prohibit insurers from denying patients with preexisting conditions but only if patients maintain continuous coverage, with a single open-enrollment period. He has promised to provide at least $25 billion in federal funding for state high-risk pools.
Prior to the passage of the ACA, 35 states offered high-risk pools to people excluded from the individual market. The Kaiser Family Foundation shows the net annual losses in these states averaged $5,510 per enrollee in 2011. Premiums ranged from 100% to 200% higher than non–high-risk group coverage. Government subsidies to cover losses amounted to $1 billion in each state.4
Meanwhile, both Mr. Trump and Rep. Ryan have proposed profound changes for Medicaid. Dr. Greeno calls this a “massive political challenge” unless they can provide an alternative way to cover people who currently rely on the federal-state entitlement, as well as those who gained coverage through ACA expansion. Currently, 70 million people are enrolled in Medicaid and the Children’s Health Insurance Program.5 Through Mr. Trump’s suggested block grants, states would receive a fixed amount of money to administer their program with increased flexibility. Rep. Ryan’s plan calls for enrollment caps that would distribute a dollar amount to each participant in the program with no limit on the number of enrollees. Either would be adjusted for inflation.
States could implement work requirements for beneficiaries or ask them to pay a small amount toward their premiums. Expansion states could also lower the Medicaid threshold below 138%.
Some states will struggle to provide for all their enrollees, Ms. Hoffman says, particularly since health spending generally outpaces inflation. Dr. Lenchus is more optimistic. “I believe states that didn’t expand Medicaid, one way or another, will figure out a way to deal with that population,” he says.
And … Medicare
The other entitlement program facing abrupt change is Medicare, typically considered the third rail of American politics.
“This is the hot political moment,” Ms. Hoffman says. “This is the point where the Republicans think they can tick off their wish list. For many Republicans, this kind of entitlement program is the opposite of what they believe in.”
Though Mr. Trump has said before he would not alter Medicare, he remained quiet on this point in the aftermath of the election. Repealing the ACA would affect Medicare by potentially reopening the Part D prescription drug doughnut hole and eliminating some of the savings provisions in the law. In fact, the CBO estimates Medicare’s direct spending would increase $802 billion between 2016 and 2025.1 Rep. Ryan has talked about privatizing Medicare by offering seniors who rely on it vouchers to apply toward private insurance.
“At the highest level, it’s moving Medicare from a defined benefit to a defined contribution program,” Ms. Hoffman says. “It shifts financial risk from the federal government onto beneficiaries. If Medicare spending continues to grow faster than the rest of the economy, Medicare beneficiaries will pay more and more.”
Seniors may also find themselves rationing or skimping on care.
Despite Rep. Ryan’s statements to the contrary, Medicare is not broken because of the ACA, Ms. Hoffman says. Its solvency has been prolonged, and though the reasons are not clear, Medicare spending has slowed since the passage of the ACA.6
MACRA launch
Another key factor in the health care policy landscape is MACRA, the Medicare Access and CHIP Reauthorization Act, which fundamentally shifts the way the government administrates and reimburses physicians for health care. MACRA begins in 2017. Dr. Greeno is concerned that changes to the ACA will impact the testing of payment models CMS is testing.
“There are hundreds of hospitals and thousands of physicians already invested in different models, so I don’t expect anybody has any desire to pull the rug from under physicians who are testing alternative payment models [APMs],” he says. “MACRA was passed on a strong bipartisan vote, and it created an APM track. Obviously, Congress intended APM models to continue to expand.”
Dr. Greeno says hospitalists are helping “shape these models,” working with the CMS and the Physician-Focused Payment Model Technical Advisory Committee (PTAC) “to ensure physicians participate in APMs and feel engaged rather than being a worker in a model someone else controls.”
On the campaign trail, Mr. Trump spoke of importing pharmaceuticals from overseas in an effort to control high prices. This policy is no longer part of his online plan. He also proposes allowing the sale of health insurance across state lines.
“It would be giving enrollees in states with stricter regulations the opportunity to circumvent to a looser state, which undermines the state with the stricter regulations,” Dr. Eibner says. “That would really create winners and losers. People who are healthy can buy a policy in a state with looser regulations, and their costs would likely fall. But someone sicker and older, it would be harder.”
Ms. Hoffman defines such a plan as a “race to the bottom.” Without well-established networks of physicians and hospitals, startup costs in new states are prohibitive, and many insurers may not wish to compete across state lines, she adds.
Repeal of the ACA could also limit some of the health benefits it required of plans on the individual market. For example, policymakers might be allowed to strip the contraceptive coverage regulation, which provides for free birth control.
“The reality is a lot of things changing in health care now were changing before the Affordable Care Act passed – PQRS, value-based purchasing, hospital-acquired infections,” Dr. Greeno says. “MACRA will continue the journey away from fee-for-service toward outcome-based models.”
At such a pivotal time, he strongly encourages hospitalists to join SHM if they are not already members and to get involved in SHM’s Grassroots Network.
“For a society of our age – young – and size, we’ve been tremendously impactful in helping with delivery system reform,” Dr. Greeno says. “I think it’s because we’re supporting change, not trying to stop it. We just want it to be intelligent change.”
He also is “convinced” hospitalists will be “critical to the redesign of the health care system. Since we are going to be taking care of the majority of hospitalized adult patients in hospitals, hospitalists want to have our say.”
Kelly April Tyrrell is a freelance writer in Madison, Wis.
References
1. Eibner C. Donald Trump’s health care reform proposals: Anticipated effects on insurance coverage, out-of-pocket costs, and the federal deficit. The Commonweath Fund website. Available at: http://www.commonwealthfund.org/publications/issue-briefs/2016/sep/trump-presidential-health-care-proposal. Accessed Nov. 17, 2016.
2. Budgetary and economic effects of repealing the Affordable Care Act. Congressional Budget Office website. Available at: https://www.cbo.gov/sites/default/files/114th-congress-2015-2016/reports/50252-Effects_of_ACA_Repeal.pdf. Accessed Nov. 15, 2016.
3. Our vision for a confident America. A Better Way website. Available at: http://abetterway.speaker.gov. Accessed Nov. 17, 2016.
4. Pollitz K. High-risk pools for uninsurable individuals. Kaiser Family Foundation website. Available at: http://kff.org/health-reform/issue-brief/high-risk-pools-for-uninsurable-individuals/. Accessed Nov. 17, 2016.
5. How accessible is individual health insurance for consumers in less-than-ideal health? Kaiser Family Foundation website. Available at: https://kaiserfamilyfoundation.files.wordpress.com/2013/01/how-accessible-is-individual-health-insurance-for-consumer-in-less-than-perfect-health-report.pdf. Accessed Nov. 17, 2016.
6. The Affordable Care Act and Medicare. The Commonwealth Fund website. Available at: http://www.commonwealthfund.org/publications/fund-reports/2015/jun/medicare-affordable-care-act Accessed Nov. 17, 2016.
The New Year brings new leadership in the United States, with President-elect Donald Trump taking office later this month. With a Republican-controlled Congress, party leaders have the opportunity to shape the nation’s policies around conservative ideals. This includes health care.
Since the Affordable Care Act (ACA) was passed in 2010, Republicans have vowed to repeal and replace it. This could be their opportunity.
However, “there is no clear coalescence around specific policy reforms that would replace the Affordable Care Act,” says Christine Eibner, PhD, a senior economist at Rand and a professor at the Pardee Rand Graduate School.
As a candidate, Trump did little to advance policy ideas around health care. Meanwhile, House Speaker Paul Ryan (R-Wis.) and others have, over the years, proposed reforms with which Trump may or may not agree.
“The Republicans now have a hard issue in their hands,” says Allison Hoffman, JD, professor of law at UCLA School of Law and an expert on health care law and policy. “It was hard before the Affordable Care Act, and it will be hard after. There is not an easy solution.”
By 2016, the ACA had expanded health coverage to 20 million people through Medicaid and private insurance on health care marketplaces. It extended the solvency of the Medicare Hospital Insurance Trust Fund. It accelerated the pace of delivery system and payment reform through creation of the Center for Medicare & Medicaid Innovation.
The law, however, has not been without its challenges.
“It was a strong achievement to get 20 million people insured, but it’s not clear that it bent the cost curve,” says Dr. Eibner. “There are high premiums on the individual market and still 31 million people without coverage. There is still opportunity to improve.”
Where we stand January 2017
Whether the Republicans can or will repeal the ACA in its entirety and improve it remains unknown. But, the experts say, the landmark law has left its mark on the American health care system.
“Everyone is complaining about the uncertainty created by the election, but we have been dealing with a highly uncertain environment for many years,” says Ron Greeno, MD, FCCP, MHM, senior advisor for medical affairs at TeamHealth, chair of the SHM Public Policy Committee, and SHM president-elect. “There will be changes, but things were going to change no matter the outcome of the election. It continues to require tolerance for change and tolerance for uncertainty.”
In an analysis for the Commonwealth Fund, Dr. Eibner investigated the economic implications of aspects of Trump’s plans as a candidate. Using a computer model that incorporates economic theory and data to simulate the effects of health policy changes, Dr. Eibner found that Trump’s plans (full repeal alone or repeal with tax deductions for health care premiums, Medicaid block grants, or selling health insurance across state lines) would increase the number of uninsured people by 16 million to 25 million, disproportionately impact low-income and sicker patients, expose individual market enrollees to higher out-of-pocket costs, and increase the federal deficit by $0.5 billion to $41 billion.1 The Congressional Budget Office (CBO) estimates full repeal could increase the federal deficit by $137 billion to $353 billion by 2025.2 Rep. Ryan’s plan, A Better Way, proposes providing people more control over their health care, giving tax credits instead of subsidies for premiums, capping the employer-sponsored health insurance tax exclusion, and expanding use of health savings accounts.3 However, Rep. Ryan’s plan “doesn’t reduce the cost of health care. It puts more onus on individuals, and their costs go up,” Ms. Hoffman says. “The weight of that will be more on people who have preexisting conditions.”
Joshua Lenchus, DO, RPh, FACP, SFHM, a member of SHM’s Public Policy Committee and hospitalist at the University of Miami/Jackson Memorial Hospital in Florida, is no fan of entitlement programs like Medicaid but says, “The safety-net hospital where I work would rather have people covered with something than nothing.”
Dr. Lenchus is optimistic that economic reforms under Trump will lead to more jobs, increasing the number of people covered by employer plans. “The economy drives health care reform,” he says. “He has to up his ante now and show people that he can stimulate job growth in this country so we don’t have this middle class that is continuously squeezed.”
Dr. Greeno and Ms. Hoffman, who is also a faculty associate at the UCLA Center for Health Policy Research and vice chair of the Insurance Law Section of the Association of American Law Schools, suggest hospitalists get involved as rules are being shaped and written.
“We want to help reform the delivery system, and we want it to be done right and to be done fairly. We want to have say in how our patients are treated,” Dr. Greeno says.
Key provisions: A delicate balance
Many people equate the ACA with the individual mandate, which requires nearly all Americans to purchase health insurance or pay a fine. The federal government provides subsidies to enrollees between 138% and 400% of the federal poverty level so their out-of-pocket costs never exceed a defined threshold even if premiums go up. These could be on the chopping block.
“The last bill Congress passed to repeal the Affordable Care Act, which Obama vetoed, repealed the individual mandate and subsidies for people to buy insurance,” Ms. Hoffman says. “If they do repeal it, private insurance through the exchanges will crumble.”
Mr. Trump’s tax deductions to offset premium costs are based on income, making them more generous for higher-income earners than low-income ones, Hoffman adds.
As a result, she says, people may choose high-deductible plans and face high out-of-pocket costs if they do seek care.
“It’s asking individuals to save by deciding how they’re going to ration care, where someone says they’re not going to go to the doctor today or fill a prescription drug they need,” Ms. Hoffman says.
Meanwhile, Mr. Trump has said he would like to keep the provision of the ACA that bans insurers from denying individuals with preexisting conditions. This, experts agree, may not be possible if other parts of the law are repealed and not replaced with similar protections for insurers.
“If you try to keep the rules about not including preexisting conditions and get rid of subsidies and the individual mandate, it just won’t work,” Ms. Hoffman says. “You end up with extraordinarily expensive health insurance.”
Rep. Ryan’s plan would prohibit insurers from denying patients with preexisting conditions but only if patients maintain continuous coverage, with a single open-enrollment period. He has promised to provide at least $25 billion in federal funding for state high-risk pools.
Prior to the passage of the ACA, 35 states offered high-risk pools to people excluded from the individual market. The Kaiser Family Foundation shows the net annual losses in these states averaged $5,510 per enrollee in 2011. Premiums ranged from 100% to 200% higher than non–high-risk group coverage. Government subsidies to cover losses amounted to $1 billion in each state.4
Meanwhile, both Mr. Trump and Rep. Ryan have proposed profound changes for Medicaid. Dr. Greeno calls this a “massive political challenge” unless they can provide an alternative way to cover people who currently rely on the federal-state entitlement, as well as those who gained coverage through ACA expansion. Currently, 70 million people are enrolled in Medicaid and the Children’s Health Insurance Program.5 Through Mr. Trump’s suggested block grants, states would receive a fixed amount of money to administer their program with increased flexibility. Rep. Ryan’s plan calls for enrollment caps that would distribute a dollar amount to each participant in the program with no limit on the number of enrollees. Either would be adjusted for inflation.
States could implement work requirements for beneficiaries or ask them to pay a small amount toward their premiums. Expansion states could also lower the Medicaid threshold below 138%.
Some states will struggle to provide for all their enrollees, Ms. Hoffman says, particularly since health spending generally outpaces inflation. Dr. Lenchus is more optimistic. “I believe states that didn’t expand Medicaid, one way or another, will figure out a way to deal with that population,” he says.
And … Medicare
The other entitlement program facing abrupt change is Medicare, typically considered the third rail of American politics.
“This is the hot political moment,” Ms. Hoffman says. “This is the point where the Republicans think they can tick off their wish list. For many Republicans, this kind of entitlement program is the opposite of what they believe in.”
Though Mr. Trump has said before he would not alter Medicare, he remained quiet on this point in the aftermath of the election. Repealing the ACA would affect Medicare by potentially reopening the Part D prescription drug doughnut hole and eliminating some of the savings provisions in the law. In fact, the CBO estimates Medicare’s direct spending would increase $802 billion between 2016 and 2025.1 Rep. Ryan has talked about privatizing Medicare by offering seniors who rely on it vouchers to apply toward private insurance.
“At the highest level, it’s moving Medicare from a defined benefit to a defined contribution program,” Ms. Hoffman says. “It shifts financial risk from the federal government onto beneficiaries. If Medicare spending continues to grow faster than the rest of the economy, Medicare beneficiaries will pay more and more.”
Seniors may also find themselves rationing or skimping on care.
Despite Rep. Ryan’s statements to the contrary, Medicare is not broken because of the ACA, Ms. Hoffman says. Its solvency has been prolonged, and though the reasons are not clear, Medicare spending has slowed since the passage of the ACA.6
MACRA launch
Another key factor in the health care policy landscape is MACRA, the Medicare Access and CHIP Reauthorization Act, which fundamentally shifts the way the government administrates and reimburses physicians for health care. MACRA begins in 2017. Dr. Greeno is concerned that changes to the ACA will impact the testing of payment models CMS is testing.
“There are hundreds of hospitals and thousands of physicians already invested in different models, so I don’t expect anybody has any desire to pull the rug from under physicians who are testing alternative payment models [APMs],” he says. “MACRA was passed on a strong bipartisan vote, and it created an APM track. Obviously, Congress intended APM models to continue to expand.”
Dr. Greeno says hospitalists are helping “shape these models,” working with the CMS and the Physician-Focused Payment Model Technical Advisory Committee (PTAC) “to ensure physicians participate in APMs and feel engaged rather than being a worker in a model someone else controls.”
On the campaign trail, Mr. Trump spoke of importing pharmaceuticals from overseas in an effort to control high prices. This policy is no longer part of his online plan. He also proposes allowing the sale of health insurance across state lines.
“It would be giving enrollees in states with stricter regulations the opportunity to circumvent to a looser state, which undermines the state with the stricter regulations,” Dr. Eibner says. “That would really create winners and losers. People who are healthy can buy a policy in a state with looser regulations, and their costs would likely fall. But someone sicker and older, it would be harder.”
Ms. Hoffman defines such a plan as a “race to the bottom.” Without well-established networks of physicians and hospitals, startup costs in new states are prohibitive, and many insurers may not wish to compete across state lines, she adds.
Repeal of the ACA could also limit some of the health benefits it required of plans on the individual market. For example, policymakers might be allowed to strip the contraceptive coverage regulation, which provides for free birth control.
“The reality is a lot of things changing in health care now were changing before the Affordable Care Act passed – PQRS, value-based purchasing, hospital-acquired infections,” Dr. Greeno says. “MACRA will continue the journey away from fee-for-service toward outcome-based models.”
At such a pivotal time, he strongly encourages hospitalists to join SHM if they are not already members and to get involved in SHM’s Grassroots Network.
“For a society of our age – young – and size, we’ve been tremendously impactful in helping with delivery system reform,” Dr. Greeno says. “I think it’s because we’re supporting change, not trying to stop it. We just want it to be intelligent change.”
He also is “convinced” hospitalists will be “critical to the redesign of the health care system. Since we are going to be taking care of the majority of hospitalized adult patients in hospitals, hospitalists want to have our say.”
Kelly April Tyrrell is a freelance writer in Madison, Wis.
References
1. Eibner C. Donald Trump’s health care reform proposals: Anticipated effects on insurance coverage, out-of-pocket costs, and the federal deficit. The Commonweath Fund website. Available at: http://www.commonwealthfund.org/publications/issue-briefs/2016/sep/trump-presidential-health-care-proposal. Accessed Nov. 17, 2016.
2. Budgetary and economic effects of repealing the Affordable Care Act. Congressional Budget Office website. Available at: https://www.cbo.gov/sites/default/files/114th-congress-2015-2016/reports/50252-Effects_of_ACA_Repeal.pdf. Accessed Nov. 15, 2016.
3. Our vision for a confident America. A Better Way website. Available at: http://abetterway.speaker.gov. Accessed Nov. 17, 2016.
4. Pollitz K. High-risk pools for uninsurable individuals. Kaiser Family Foundation website. Available at: http://kff.org/health-reform/issue-brief/high-risk-pools-for-uninsurable-individuals/. Accessed Nov. 17, 2016.
5. How accessible is individual health insurance for consumers in less-than-ideal health? Kaiser Family Foundation website. Available at: https://kaiserfamilyfoundation.files.wordpress.com/2013/01/how-accessible-is-individual-health-insurance-for-consumer-in-less-than-perfect-health-report.pdf. Accessed Nov. 17, 2016.
6. The Affordable Care Act and Medicare. The Commonwealth Fund website. Available at: http://www.commonwealthfund.org/publications/fund-reports/2015/jun/medicare-affordable-care-act Accessed Nov. 17, 2016.
The New Year brings new leadership in the United States, with President-elect Donald Trump taking office later this month. With a Republican-controlled Congress, party leaders have the opportunity to shape the nation’s policies around conservative ideals. This includes health care.
Since the Affordable Care Act (ACA) was passed in 2010, Republicans have vowed to repeal and replace it. This could be their opportunity.
However, “there is no clear coalescence around specific policy reforms that would replace the Affordable Care Act,” says Christine Eibner, PhD, a senior economist at Rand and a professor at the Pardee Rand Graduate School.
As a candidate, Trump did little to advance policy ideas around health care. Meanwhile, House Speaker Paul Ryan (R-Wis.) and others have, over the years, proposed reforms with which Trump may or may not agree.
“The Republicans now have a hard issue in their hands,” says Allison Hoffman, JD, professor of law at UCLA School of Law and an expert on health care law and policy. “It was hard before the Affordable Care Act, and it will be hard after. There is not an easy solution.”
By 2016, the ACA had expanded health coverage to 20 million people through Medicaid and private insurance on health care marketplaces. It extended the solvency of the Medicare Hospital Insurance Trust Fund. It accelerated the pace of delivery system and payment reform through creation of the Center for Medicare & Medicaid Innovation.
The law, however, has not been without its challenges.
“It was a strong achievement to get 20 million people insured, but it’s not clear that it bent the cost curve,” says Dr. Eibner. “There are high premiums on the individual market and still 31 million people without coverage. There is still opportunity to improve.”
Where we stand January 2017
Whether the Republicans can or will repeal the ACA in its entirety and improve it remains unknown. But, the experts say, the landmark law has left its mark on the American health care system.
“Everyone is complaining about the uncertainty created by the election, but we have been dealing with a highly uncertain environment for many years,” says Ron Greeno, MD, FCCP, MHM, senior advisor for medical affairs at TeamHealth, chair of the SHM Public Policy Committee, and SHM president-elect. “There will be changes, but things were going to change no matter the outcome of the election. It continues to require tolerance for change and tolerance for uncertainty.”
In an analysis for the Commonwealth Fund, Dr. Eibner investigated the economic implications of aspects of Trump’s plans as a candidate. Using a computer model that incorporates economic theory and data to simulate the effects of health policy changes, Dr. Eibner found that Trump’s plans (full repeal alone or repeal with tax deductions for health care premiums, Medicaid block grants, or selling health insurance across state lines) would increase the number of uninsured people by 16 million to 25 million, disproportionately impact low-income and sicker patients, expose individual market enrollees to higher out-of-pocket costs, and increase the federal deficit by $0.5 billion to $41 billion.1 The Congressional Budget Office (CBO) estimates full repeal could increase the federal deficit by $137 billion to $353 billion by 2025.2 Rep. Ryan’s plan, A Better Way, proposes providing people more control over their health care, giving tax credits instead of subsidies for premiums, capping the employer-sponsored health insurance tax exclusion, and expanding use of health savings accounts.3 However, Rep. Ryan’s plan “doesn’t reduce the cost of health care. It puts more onus on individuals, and their costs go up,” Ms. Hoffman says. “The weight of that will be more on people who have preexisting conditions.”
Joshua Lenchus, DO, RPh, FACP, SFHM, a member of SHM’s Public Policy Committee and hospitalist at the University of Miami/Jackson Memorial Hospital in Florida, is no fan of entitlement programs like Medicaid but says, “The safety-net hospital where I work would rather have people covered with something than nothing.”
Dr. Lenchus is optimistic that economic reforms under Trump will lead to more jobs, increasing the number of people covered by employer plans. “The economy drives health care reform,” he says. “He has to up his ante now and show people that he can stimulate job growth in this country so we don’t have this middle class that is continuously squeezed.”
Dr. Greeno and Ms. Hoffman, who is also a faculty associate at the UCLA Center for Health Policy Research and vice chair of the Insurance Law Section of the Association of American Law Schools, suggest hospitalists get involved as rules are being shaped and written.
“We want to help reform the delivery system, and we want it to be done right and to be done fairly. We want to have say in how our patients are treated,” Dr. Greeno says.
Key provisions: A delicate balance
Many people equate the ACA with the individual mandate, which requires nearly all Americans to purchase health insurance or pay a fine. The federal government provides subsidies to enrollees between 138% and 400% of the federal poverty level so their out-of-pocket costs never exceed a defined threshold even if premiums go up. These could be on the chopping block.
“The last bill Congress passed to repeal the Affordable Care Act, which Obama vetoed, repealed the individual mandate and subsidies for people to buy insurance,” Ms. Hoffman says. “If they do repeal it, private insurance through the exchanges will crumble.”
Mr. Trump’s tax deductions to offset premium costs are based on income, making them more generous for higher-income earners than low-income ones, Hoffman adds.
As a result, she says, people may choose high-deductible plans and face high out-of-pocket costs if they do seek care.
“It’s asking individuals to save by deciding how they’re going to ration care, where someone says they’re not going to go to the doctor today or fill a prescription drug they need,” Ms. Hoffman says.
Meanwhile, Mr. Trump has said he would like to keep the provision of the ACA that bans insurers from denying individuals with preexisting conditions. This, experts agree, may not be possible if other parts of the law are repealed and not replaced with similar protections for insurers.
“If you try to keep the rules about not including preexisting conditions and get rid of subsidies and the individual mandate, it just won’t work,” Ms. Hoffman says. “You end up with extraordinarily expensive health insurance.”
Rep. Ryan’s plan would prohibit insurers from denying patients with preexisting conditions but only if patients maintain continuous coverage, with a single open-enrollment period. He has promised to provide at least $25 billion in federal funding for state high-risk pools.
Prior to the passage of the ACA, 35 states offered high-risk pools to people excluded from the individual market. The Kaiser Family Foundation shows the net annual losses in these states averaged $5,510 per enrollee in 2011. Premiums ranged from 100% to 200% higher than non–high-risk group coverage. Government subsidies to cover losses amounted to $1 billion in each state.4
Meanwhile, both Mr. Trump and Rep. Ryan have proposed profound changes for Medicaid. Dr. Greeno calls this a “massive political challenge” unless they can provide an alternative way to cover people who currently rely on the federal-state entitlement, as well as those who gained coverage through ACA expansion. Currently, 70 million people are enrolled in Medicaid and the Children’s Health Insurance Program.5 Through Mr. Trump’s suggested block grants, states would receive a fixed amount of money to administer their program with increased flexibility. Rep. Ryan’s plan calls for enrollment caps that would distribute a dollar amount to each participant in the program with no limit on the number of enrollees. Either would be adjusted for inflation.
States could implement work requirements for beneficiaries or ask them to pay a small amount toward their premiums. Expansion states could also lower the Medicaid threshold below 138%.
Some states will struggle to provide for all their enrollees, Ms. Hoffman says, particularly since health spending generally outpaces inflation. Dr. Lenchus is more optimistic. “I believe states that didn’t expand Medicaid, one way or another, will figure out a way to deal with that population,” he says.
And … Medicare
The other entitlement program facing abrupt change is Medicare, typically considered the third rail of American politics.
“This is the hot political moment,” Ms. Hoffman says. “This is the point where the Republicans think they can tick off their wish list. For many Republicans, this kind of entitlement program is the opposite of what they believe in.”
Though Mr. Trump has said before he would not alter Medicare, he remained quiet on this point in the aftermath of the election. Repealing the ACA would affect Medicare by potentially reopening the Part D prescription drug doughnut hole and eliminating some of the savings provisions in the law. In fact, the CBO estimates Medicare’s direct spending would increase $802 billion between 2016 and 2025.1 Rep. Ryan has talked about privatizing Medicare by offering seniors who rely on it vouchers to apply toward private insurance.
“At the highest level, it’s moving Medicare from a defined benefit to a defined contribution program,” Ms. Hoffman says. “It shifts financial risk from the federal government onto beneficiaries. If Medicare spending continues to grow faster than the rest of the economy, Medicare beneficiaries will pay more and more.”
Seniors may also find themselves rationing or skimping on care.
Despite Rep. Ryan’s statements to the contrary, Medicare is not broken because of the ACA, Ms. Hoffman says. Its solvency has been prolonged, and though the reasons are not clear, Medicare spending has slowed since the passage of the ACA.6
MACRA launch
Another key factor in the health care policy landscape is MACRA, the Medicare Access and CHIP Reauthorization Act, which fundamentally shifts the way the government administrates and reimburses physicians for health care. MACRA begins in 2017. Dr. Greeno is concerned that changes to the ACA will impact the testing of payment models CMS is testing.
“There are hundreds of hospitals and thousands of physicians already invested in different models, so I don’t expect anybody has any desire to pull the rug from under physicians who are testing alternative payment models [APMs],” he says. “MACRA was passed on a strong bipartisan vote, and it created an APM track. Obviously, Congress intended APM models to continue to expand.”
Dr. Greeno says hospitalists are helping “shape these models,” working with the CMS and the Physician-Focused Payment Model Technical Advisory Committee (PTAC) “to ensure physicians participate in APMs and feel engaged rather than being a worker in a model someone else controls.”
On the campaign trail, Mr. Trump spoke of importing pharmaceuticals from overseas in an effort to control high prices. This policy is no longer part of his online plan. He also proposes allowing the sale of health insurance across state lines.
“It would be giving enrollees in states with stricter regulations the opportunity to circumvent to a looser state, which undermines the state with the stricter regulations,” Dr. Eibner says. “That would really create winners and losers. People who are healthy can buy a policy in a state with looser regulations, and their costs would likely fall. But someone sicker and older, it would be harder.”
Ms. Hoffman defines such a plan as a “race to the bottom.” Without well-established networks of physicians and hospitals, startup costs in new states are prohibitive, and many insurers may not wish to compete across state lines, she adds.
Repeal of the ACA could also limit some of the health benefits it required of plans on the individual market. For example, policymakers might be allowed to strip the contraceptive coverage regulation, which provides for free birth control.
“The reality is a lot of things changing in health care now were changing before the Affordable Care Act passed – PQRS, value-based purchasing, hospital-acquired infections,” Dr. Greeno says. “MACRA will continue the journey away from fee-for-service toward outcome-based models.”
At such a pivotal time, he strongly encourages hospitalists to join SHM if they are not already members and to get involved in SHM’s Grassroots Network.
“For a society of our age – young – and size, we’ve been tremendously impactful in helping with delivery system reform,” Dr. Greeno says. “I think it’s because we’re supporting change, not trying to stop it. We just want it to be intelligent change.”
He also is “convinced” hospitalists will be “critical to the redesign of the health care system. Since we are going to be taking care of the majority of hospitalized adult patients in hospitals, hospitalists want to have our say.”
Kelly April Tyrrell is a freelance writer in Madison, Wis.
References
1. Eibner C. Donald Trump’s health care reform proposals: Anticipated effects on insurance coverage, out-of-pocket costs, and the federal deficit. The Commonweath Fund website. Available at: http://www.commonwealthfund.org/publications/issue-briefs/2016/sep/trump-presidential-health-care-proposal. Accessed Nov. 17, 2016.
2. Budgetary and economic effects of repealing the Affordable Care Act. Congressional Budget Office website. Available at: https://www.cbo.gov/sites/default/files/114th-congress-2015-2016/reports/50252-Effects_of_ACA_Repeal.pdf. Accessed Nov. 15, 2016.
3. Our vision for a confident America. A Better Way website. Available at: http://abetterway.speaker.gov. Accessed Nov. 17, 2016.
4. Pollitz K. High-risk pools for uninsurable individuals. Kaiser Family Foundation website. Available at: http://kff.org/health-reform/issue-brief/high-risk-pools-for-uninsurable-individuals/. Accessed Nov. 17, 2016.
5. How accessible is individual health insurance for consumers in less-than-ideal health? Kaiser Family Foundation website. Available at: https://kaiserfamilyfoundation.files.wordpress.com/2013/01/how-accessible-is-individual-health-insurance-for-consumer-in-less-than-perfect-health-report.pdf. Accessed Nov. 17, 2016.
6. The Affordable Care Act and Medicare. The Commonwealth Fund website. Available at: http://www.commonwealthfund.org/publications/fund-reports/2015/jun/medicare-affordable-care-act Accessed Nov. 17, 2016.







