User login
ID Practitioner is an independent news source that provides infectious disease specialists with timely and relevant news and commentary about clinical developments and the impact of health care policy on the infectious disease specialist’s practice. Specialty focus topics include antimicrobial resistance, emerging infections, global ID, hepatitis, HIV, hospital-acquired infections, immunizations and vaccines, influenza, mycoses, pediatric infections, and STIs. Infectious Diseases News is owned by Frontline Medical Communications.
sofosbuvir
ritonavir with dasabuvir
discount
support path
program
ritonavir
greedy
ledipasvir
assistance
viekira pak
vpak
advocacy
needy
protest
abbvie
paritaprevir
ombitasvir
direct-acting antivirals
dasabuvir
gilead
fake-ovir
support
v pak
oasis
harvoni
section[contains(@class, 'footer-nav-section-wrapper')]
div[contains(@class, 'pane-pub-article-idp')]
div[contains(@class, 'pane-medstat-latest-articles-articles-section')]
div[contains(@class, 'pane-pub-home-idp')]
div[contains(@class, 'pane-pub-topic-idp')]
Sepsis too often neglected in hospitals
according to a recent survey by the Centers for Disease Control and Prevention.
For the hospitals that do have sepsis teams, only 55% of them report that their team leaders get dedicated time to manage their sepsis programs.
“One in three people who dies in a hospital has sepsis during that hospitalization,” CDC Director Mandy Cohen, MD, MPH, noted in a statement. “That’s why CDC is calling on all U.S. hospitals to have a sepsis program and raise the bar on sepsis care by incorporating seven core elements.”
The sepsis seven
- Leadership: Dedicating the necessary human, financial, and information technology resources.
- Accountability: Appointing a leader responsible for program outcomes and setting concrete goals.
- Multiprofessional: Engaging key partners throughout the organization.
- Action: Implementing structures and processes to improve the identification, management, and recovery from sepsis.
- Tracking: Measuring sepsis epidemiology, outcomes, and progress toward program goals and the impact of sepsis initiatives.
- Reporting: Providing usable information on sepsis treatment and outcomes to relevant partners.
- Education: Providing sepsis education to health care professionals during onboarding and annually.
Craig Weinert, MD, MPH, a pulmonologist and critical care physician and professor of medicine at the University of Minnesota, Minneapolis, says the point the CDC is making with the announcement is that when these sepsis programs have been implemented at hospitals, they have been successful at reducing mortality. And now, the agency is urging all hospitals to implement them and support them properly.
“It’s not asking hospitals to develop new, innovative kinds of sepsis programs. This is not about new drugs or new antibiotics or new devices,” Dr. Weinert says. “This is about having hospitals dedicate organizational resources to implementing sepsis programs.”
The CDC’s announcement is aimed toward hospital administrators, Dr. Weinert adds. The agency is making the case that sepsis needs more funding in hospitals that either don’t have the programs or aren’t supporting them with dedicated resources.
There’s another message as well, Dr. Weinert says.
“COVID basically obliterated sepsis programs for two and a half years,” he says. Now the CDC is saying it’s time to divert staff back to sepsis care.
Stepping up sepsis care
Raymund Dantes, MD, assistant professor of medicine at Emory University, Atlanta, one of the developers of the core elements, says this is like a recipe for sepsis care.
Dr. Dantes compares the instructions for hospitals with getting a good restaurant up and running. And in the restaurant business, “you need more than the recipes. You need a leader or manager to ensure you have the right people working together, with the right supplies, getting the right feedback on their work to continuously improve,” he explains.
Dr. Dantes, who is also the physician lead for the Emory Healthcare Sepsis Program, says the approach is meant to be flexible to the size of the hospital, population served, and available resources.
He points out that a well-run sepsis program at a 25-bed rural hospital will look very different from the program at a 1,000-bed tertiary care hospital.
Some hospitals, Dr. Dantes says, will be starting from scratch when getting a sepsis program, and for those hospitals, the developers included a “Getting Started” section as part of the detailed, 29-page full report.
In September, Sepsis Awareness Month, the CDC will provide educational information to health care professionals, patients, families, and caregivers about preventing infections that can lead to sepsis through its ongoing Get Ahead of Sepsis campaign.
A version of this article first appeared on Medscape.com.
according to a recent survey by the Centers for Disease Control and Prevention.
For the hospitals that do have sepsis teams, only 55% of them report that their team leaders get dedicated time to manage their sepsis programs.
“One in three people who dies in a hospital has sepsis during that hospitalization,” CDC Director Mandy Cohen, MD, MPH, noted in a statement. “That’s why CDC is calling on all U.S. hospitals to have a sepsis program and raise the bar on sepsis care by incorporating seven core elements.”
The sepsis seven
- Leadership: Dedicating the necessary human, financial, and information technology resources.
- Accountability: Appointing a leader responsible for program outcomes and setting concrete goals.
- Multiprofessional: Engaging key partners throughout the organization.
- Action: Implementing structures and processes to improve the identification, management, and recovery from sepsis.
- Tracking: Measuring sepsis epidemiology, outcomes, and progress toward program goals and the impact of sepsis initiatives.
- Reporting: Providing usable information on sepsis treatment and outcomes to relevant partners.
- Education: Providing sepsis education to health care professionals during onboarding and annually.
Craig Weinert, MD, MPH, a pulmonologist and critical care physician and professor of medicine at the University of Minnesota, Minneapolis, says the point the CDC is making with the announcement is that when these sepsis programs have been implemented at hospitals, they have been successful at reducing mortality. And now, the agency is urging all hospitals to implement them and support them properly.
“It’s not asking hospitals to develop new, innovative kinds of sepsis programs. This is not about new drugs or new antibiotics or new devices,” Dr. Weinert says. “This is about having hospitals dedicate organizational resources to implementing sepsis programs.”
The CDC’s announcement is aimed toward hospital administrators, Dr. Weinert adds. The agency is making the case that sepsis needs more funding in hospitals that either don’t have the programs or aren’t supporting them with dedicated resources.
There’s another message as well, Dr. Weinert says.
“COVID basically obliterated sepsis programs for two and a half years,” he says. Now the CDC is saying it’s time to divert staff back to sepsis care.
Stepping up sepsis care
Raymund Dantes, MD, assistant professor of medicine at Emory University, Atlanta, one of the developers of the core elements, says this is like a recipe for sepsis care.
Dr. Dantes compares the instructions for hospitals with getting a good restaurant up and running. And in the restaurant business, “you need more than the recipes. You need a leader or manager to ensure you have the right people working together, with the right supplies, getting the right feedback on their work to continuously improve,” he explains.
Dr. Dantes, who is also the physician lead for the Emory Healthcare Sepsis Program, says the approach is meant to be flexible to the size of the hospital, population served, and available resources.
He points out that a well-run sepsis program at a 25-bed rural hospital will look very different from the program at a 1,000-bed tertiary care hospital.
Some hospitals, Dr. Dantes says, will be starting from scratch when getting a sepsis program, and for those hospitals, the developers included a “Getting Started” section as part of the detailed, 29-page full report.
In September, Sepsis Awareness Month, the CDC will provide educational information to health care professionals, patients, families, and caregivers about preventing infections that can lead to sepsis through its ongoing Get Ahead of Sepsis campaign.
A version of this article first appeared on Medscape.com.
according to a recent survey by the Centers for Disease Control and Prevention.
For the hospitals that do have sepsis teams, only 55% of them report that their team leaders get dedicated time to manage their sepsis programs.
“One in three people who dies in a hospital has sepsis during that hospitalization,” CDC Director Mandy Cohen, MD, MPH, noted in a statement. “That’s why CDC is calling on all U.S. hospitals to have a sepsis program and raise the bar on sepsis care by incorporating seven core elements.”
The sepsis seven
- Leadership: Dedicating the necessary human, financial, and information technology resources.
- Accountability: Appointing a leader responsible for program outcomes and setting concrete goals.
- Multiprofessional: Engaging key partners throughout the organization.
- Action: Implementing structures and processes to improve the identification, management, and recovery from sepsis.
- Tracking: Measuring sepsis epidemiology, outcomes, and progress toward program goals and the impact of sepsis initiatives.
- Reporting: Providing usable information on sepsis treatment and outcomes to relevant partners.
- Education: Providing sepsis education to health care professionals during onboarding and annually.
Craig Weinert, MD, MPH, a pulmonologist and critical care physician and professor of medicine at the University of Minnesota, Minneapolis, says the point the CDC is making with the announcement is that when these sepsis programs have been implemented at hospitals, they have been successful at reducing mortality. And now, the agency is urging all hospitals to implement them and support them properly.
“It’s not asking hospitals to develop new, innovative kinds of sepsis programs. This is not about new drugs or new antibiotics or new devices,” Dr. Weinert says. “This is about having hospitals dedicate organizational resources to implementing sepsis programs.”
The CDC’s announcement is aimed toward hospital administrators, Dr. Weinert adds. The agency is making the case that sepsis needs more funding in hospitals that either don’t have the programs or aren’t supporting them with dedicated resources.
There’s another message as well, Dr. Weinert says.
“COVID basically obliterated sepsis programs for two and a half years,” he says. Now the CDC is saying it’s time to divert staff back to sepsis care.
Stepping up sepsis care
Raymund Dantes, MD, assistant professor of medicine at Emory University, Atlanta, one of the developers of the core elements, says this is like a recipe for sepsis care.
Dr. Dantes compares the instructions for hospitals with getting a good restaurant up and running. And in the restaurant business, “you need more than the recipes. You need a leader or manager to ensure you have the right people working together, with the right supplies, getting the right feedback on their work to continuously improve,” he explains.
Dr. Dantes, who is also the physician lead for the Emory Healthcare Sepsis Program, says the approach is meant to be flexible to the size of the hospital, population served, and available resources.
He points out that a well-run sepsis program at a 25-bed rural hospital will look very different from the program at a 1,000-bed tertiary care hospital.
Some hospitals, Dr. Dantes says, will be starting from scratch when getting a sepsis program, and for those hospitals, the developers included a “Getting Started” section as part of the detailed, 29-page full report.
In September, Sepsis Awareness Month, the CDC will provide educational information to health care professionals, patients, families, and caregivers about preventing infections that can lead to sepsis through its ongoing Get Ahead of Sepsis campaign.
A version of this article first appeared on Medscape.com.
Five ways to avert a malpractice lawsuit with better EHR techniques
Although most physicians have gotten used to working with EHRs, despite their irritations, the use of EHRs has contributed to a growing number of malpractice lawsuits. Defense attorneys say that
According to a study in the Journal of Patient Safety, more than 30% of all EHR-related malpractice cases are associated with medication errors; 28% with diagnosis; and 31% with a complication of treatment, such as entering wrong information, entering information in the wrong place, and overlooking EHR flags and warnings for interactions or contraindications.
The study gave these examples of EHR-related errors that led to patient harm and ultimately to malpractice lawsuits:
- A discharge order omitted a patient’s medication that prevented strokes; the patient had a stroke days later.
- An electronic order for morphine failed to state the upper dose limit; the patient died.
- A physician meant to click on “discontinue” for an anticoagulant but mistakenly clicked on “continue” for home use.
Catching potential issues such as drug interactions or critical medical history that should inform treatment is more important than ever. “We know from safety engineering principles that just relying on vigilance is not a long-term safety strategy,” says Aaron Zach Hettinger, MD, chief research information officer at MedStar Health Research Institute, Washington, D.C. “So, it’s critical that we design these safe systems and leverage the data that’s in them.”
Here are five smart EHR practices to help protect your patients’ health and your own liability.
1. Double-check dropdown boxes
When it comes to user error, it’s easy to click the wrong choice from a drop-down menu. Better to take the time to explain your answer in a box, even if it takes a few more minutes. Or if you are choosing from a menu, proofread any information it auto-fills in the chart.
Dr. Hettinger says you can strike a balance between these templated approaches to diagnosis and long-term care by working with third-party systems and your organization or vendor IT department to help with follow-up questions to keep populated data in check.
“Make sure you have a back-end system that can help monitor that structured data,” says Dr. Hettinger. Structured data are the patient’s demographic information, like name, address, age, height, weight, vital signs, and data elements like diagnosis, medications, and lab results. “Wherever you can leverage the underlying tools that are part of the electronic health record to make sure that we’re constantly checking the right results, that helps reduce the workload so that clinicians can focus on taking care of the patients and doing the right thing and not be as focused on entering data into the system.”
2. Supplement EHR notes with direct communication
The failure to diagnose cancer because one physician doesn’t know what another physician saw in an imaging report is one of the most common claims in the cases he tries, says Aaron Boeder, a plaintiff’s medical negligence lawyer in Chicago.
Physicians often assume that if they put a note in the electronic chart, others will look for it, but Mr. Boeder says it’s far more prudent to communicate directly.
“Let’s say a radiologist interprets a scan and sees what might be cancer,” he says. “If the ordering doctor is an orthopedist who’s ordered a CT scan for DVT, there’s going to be a report for that scan. It’s going to get auto-populated back into that physician’s note,” says Mr. Boeder.
The physician may or may not look at it, but it will be in their note, and they’re supposed to follow up on it because they ordered the scan. “But they may not follow up on it, and they may not get a call from the radiologist,” he says.
“Next thing you know, 2 or 3 years later, that patient is diagnosed with very advanced cancer.”
3. Tailor auto-fill information to your common practices
Suppose, as a physician, you find that you need to change a default setting time and time again. Dr. Hettinger says it’s worth your time to take an extra couple of minutes to work with your vendor or your health system to try and make changes to auto-population settings that align with your practices.
“Let’s say a default dose of 20 milligrams of a medication is what automatically pops up, but in reality, your practice is to use a smaller dose because it’s safer, even though they’re all within the acceptable realm of what you would order,” he says. “Rather than have the default to the higher dose, see if you can change the default to a lower dose. And that way, you don’t have to catch yourself every time.”
If your auto-fills are amounts that constantly need changing, an interruption could easily knock you off course before you make that correction.
“If there are ways to have the system defaults be safer or more in line with your clinical practice, and especially across a group, then you’re designing a safer system and not relying on vigilance or memory prone to interruptions,” says Dr. Hettinger.
4. Curb the copy and paste
It’s tempting to copy a note from a previous patient visit and make only minimal changes as needed, but you risk including outdated information if you do. Even if you’re repeating questions asked by the intake nurse, it is safer to not to rely on that information, says Beth Kanik, a defense medical malpractice attorney in Atlanta.
“If it later goes into litigation, the argument then becomes that it looks like you didn’t do your job,” says Ms. Kanik. “Instead, try to ask questions in a way that would elicit responses that may be a little different than what the nurse got, so that it’s clear you asked the questions and didn’t just simply rely upon someone else’s information.”
5. Separate typing from listening
While EHR may be an excellent tool for data collection and safety checking, it’s not a stand-in for doctor-patient interaction. As technology practices push medicine toward more and more efficiency, Mr. Boeder says it’s most often listening over all else that makes the difference in the quality of care. And good listening requires full attention.
“A real concern for physicians is the number of visits they’re expected to accomplish in a set amount of time,” says Mr. Boeder. “Often this translates into a doctor talking to a patient while typing notes or while reading a note from the last time the patient was in.”
Taking the time to pause after entering data and briefly reviewing your understanding of what your patient has told you can be invaluable and may save you – and your patient – problems later.
“In so many cases, it comes down to people not being heard,” says Mr. Boeder. “So listen to what your patients are saying.”
A version of this article first appeared on Medscape.com.
Although most physicians have gotten used to working with EHRs, despite their irritations, the use of EHRs has contributed to a growing number of malpractice lawsuits. Defense attorneys say that
According to a study in the Journal of Patient Safety, more than 30% of all EHR-related malpractice cases are associated with medication errors; 28% with diagnosis; and 31% with a complication of treatment, such as entering wrong information, entering information in the wrong place, and overlooking EHR flags and warnings for interactions or contraindications.
The study gave these examples of EHR-related errors that led to patient harm and ultimately to malpractice lawsuits:
- A discharge order omitted a patient’s medication that prevented strokes; the patient had a stroke days later.
- An electronic order for morphine failed to state the upper dose limit; the patient died.
- A physician meant to click on “discontinue” for an anticoagulant but mistakenly clicked on “continue” for home use.
Catching potential issues such as drug interactions or critical medical history that should inform treatment is more important than ever. “We know from safety engineering principles that just relying on vigilance is not a long-term safety strategy,” says Aaron Zach Hettinger, MD, chief research information officer at MedStar Health Research Institute, Washington, D.C. “So, it’s critical that we design these safe systems and leverage the data that’s in them.”
Here are five smart EHR practices to help protect your patients’ health and your own liability.
1. Double-check dropdown boxes
When it comes to user error, it’s easy to click the wrong choice from a drop-down menu. Better to take the time to explain your answer in a box, even if it takes a few more minutes. Or if you are choosing from a menu, proofread any information it auto-fills in the chart.
Dr. Hettinger says you can strike a balance between these templated approaches to diagnosis and long-term care by working with third-party systems and your organization or vendor IT department to help with follow-up questions to keep populated data in check.
“Make sure you have a back-end system that can help monitor that structured data,” says Dr. Hettinger. Structured data are the patient’s demographic information, like name, address, age, height, weight, vital signs, and data elements like diagnosis, medications, and lab results. “Wherever you can leverage the underlying tools that are part of the electronic health record to make sure that we’re constantly checking the right results, that helps reduce the workload so that clinicians can focus on taking care of the patients and doing the right thing and not be as focused on entering data into the system.”
2. Supplement EHR notes with direct communication
The failure to diagnose cancer because one physician doesn’t know what another physician saw in an imaging report is one of the most common claims in the cases he tries, says Aaron Boeder, a plaintiff’s medical negligence lawyer in Chicago.
Physicians often assume that if they put a note in the electronic chart, others will look for it, but Mr. Boeder says it’s far more prudent to communicate directly.
“Let’s say a radiologist interprets a scan and sees what might be cancer,” he says. “If the ordering doctor is an orthopedist who’s ordered a CT scan for DVT, there’s going to be a report for that scan. It’s going to get auto-populated back into that physician’s note,” says Mr. Boeder.
The physician may or may not look at it, but it will be in their note, and they’re supposed to follow up on it because they ordered the scan. “But they may not follow up on it, and they may not get a call from the radiologist,” he says.
“Next thing you know, 2 or 3 years later, that patient is diagnosed with very advanced cancer.”
3. Tailor auto-fill information to your common practices
Suppose, as a physician, you find that you need to change a default setting time and time again. Dr. Hettinger says it’s worth your time to take an extra couple of minutes to work with your vendor or your health system to try and make changes to auto-population settings that align with your practices.
“Let’s say a default dose of 20 milligrams of a medication is what automatically pops up, but in reality, your practice is to use a smaller dose because it’s safer, even though they’re all within the acceptable realm of what you would order,” he says. “Rather than have the default to the higher dose, see if you can change the default to a lower dose. And that way, you don’t have to catch yourself every time.”
If your auto-fills are amounts that constantly need changing, an interruption could easily knock you off course before you make that correction.
“If there are ways to have the system defaults be safer or more in line with your clinical practice, and especially across a group, then you’re designing a safer system and not relying on vigilance or memory prone to interruptions,” says Dr. Hettinger.
4. Curb the copy and paste
It’s tempting to copy a note from a previous patient visit and make only minimal changes as needed, but you risk including outdated information if you do. Even if you’re repeating questions asked by the intake nurse, it is safer to not to rely on that information, says Beth Kanik, a defense medical malpractice attorney in Atlanta.
“If it later goes into litigation, the argument then becomes that it looks like you didn’t do your job,” says Ms. Kanik. “Instead, try to ask questions in a way that would elicit responses that may be a little different than what the nurse got, so that it’s clear you asked the questions and didn’t just simply rely upon someone else’s information.”
5. Separate typing from listening
While EHR may be an excellent tool for data collection and safety checking, it’s not a stand-in for doctor-patient interaction. As technology practices push medicine toward more and more efficiency, Mr. Boeder says it’s most often listening over all else that makes the difference in the quality of care. And good listening requires full attention.
“A real concern for physicians is the number of visits they’re expected to accomplish in a set amount of time,” says Mr. Boeder. “Often this translates into a doctor talking to a patient while typing notes or while reading a note from the last time the patient was in.”
Taking the time to pause after entering data and briefly reviewing your understanding of what your patient has told you can be invaluable and may save you – and your patient – problems later.
“In so many cases, it comes down to people not being heard,” says Mr. Boeder. “So listen to what your patients are saying.”
A version of this article first appeared on Medscape.com.
Although most physicians have gotten used to working with EHRs, despite their irritations, the use of EHRs has contributed to a growing number of malpractice lawsuits. Defense attorneys say that
According to a study in the Journal of Patient Safety, more than 30% of all EHR-related malpractice cases are associated with medication errors; 28% with diagnosis; and 31% with a complication of treatment, such as entering wrong information, entering information in the wrong place, and overlooking EHR flags and warnings for interactions or contraindications.
The study gave these examples of EHR-related errors that led to patient harm and ultimately to malpractice lawsuits:
- A discharge order omitted a patient’s medication that prevented strokes; the patient had a stroke days later.
- An electronic order for morphine failed to state the upper dose limit; the patient died.
- A physician meant to click on “discontinue” for an anticoagulant but mistakenly clicked on “continue” for home use.
Catching potential issues such as drug interactions or critical medical history that should inform treatment is more important than ever. “We know from safety engineering principles that just relying on vigilance is not a long-term safety strategy,” says Aaron Zach Hettinger, MD, chief research information officer at MedStar Health Research Institute, Washington, D.C. “So, it’s critical that we design these safe systems and leverage the data that’s in them.”
Here are five smart EHR practices to help protect your patients’ health and your own liability.
1. Double-check dropdown boxes
When it comes to user error, it’s easy to click the wrong choice from a drop-down menu. Better to take the time to explain your answer in a box, even if it takes a few more minutes. Or if you are choosing from a menu, proofread any information it auto-fills in the chart.
Dr. Hettinger says you can strike a balance between these templated approaches to diagnosis and long-term care by working with third-party systems and your organization or vendor IT department to help with follow-up questions to keep populated data in check.
“Make sure you have a back-end system that can help monitor that structured data,” says Dr. Hettinger. Structured data are the patient’s demographic information, like name, address, age, height, weight, vital signs, and data elements like diagnosis, medications, and lab results. “Wherever you can leverage the underlying tools that are part of the electronic health record to make sure that we’re constantly checking the right results, that helps reduce the workload so that clinicians can focus on taking care of the patients and doing the right thing and not be as focused on entering data into the system.”
2. Supplement EHR notes with direct communication
The failure to diagnose cancer because one physician doesn’t know what another physician saw in an imaging report is one of the most common claims in the cases he tries, says Aaron Boeder, a plaintiff’s medical negligence lawyer in Chicago.
Physicians often assume that if they put a note in the electronic chart, others will look for it, but Mr. Boeder says it’s far more prudent to communicate directly.
“Let’s say a radiologist interprets a scan and sees what might be cancer,” he says. “If the ordering doctor is an orthopedist who’s ordered a CT scan for DVT, there’s going to be a report for that scan. It’s going to get auto-populated back into that physician’s note,” says Mr. Boeder.
The physician may or may not look at it, but it will be in their note, and they’re supposed to follow up on it because they ordered the scan. “But they may not follow up on it, and they may not get a call from the radiologist,” he says.
“Next thing you know, 2 or 3 years later, that patient is diagnosed with very advanced cancer.”
3. Tailor auto-fill information to your common practices
Suppose, as a physician, you find that you need to change a default setting time and time again. Dr. Hettinger says it’s worth your time to take an extra couple of minutes to work with your vendor or your health system to try and make changes to auto-population settings that align with your practices.
“Let’s say a default dose of 20 milligrams of a medication is what automatically pops up, but in reality, your practice is to use a smaller dose because it’s safer, even though they’re all within the acceptable realm of what you would order,” he says. “Rather than have the default to the higher dose, see if you can change the default to a lower dose. And that way, you don’t have to catch yourself every time.”
If your auto-fills are amounts that constantly need changing, an interruption could easily knock you off course before you make that correction.
“If there are ways to have the system defaults be safer or more in line with your clinical practice, and especially across a group, then you’re designing a safer system and not relying on vigilance or memory prone to interruptions,” says Dr. Hettinger.
4. Curb the copy and paste
It’s tempting to copy a note from a previous patient visit and make only minimal changes as needed, but you risk including outdated information if you do. Even if you’re repeating questions asked by the intake nurse, it is safer to not to rely on that information, says Beth Kanik, a defense medical malpractice attorney in Atlanta.
“If it later goes into litigation, the argument then becomes that it looks like you didn’t do your job,” says Ms. Kanik. “Instead, try to ask questions in a way that would elicit responses that may be a little different than what the nurse got, so that it’s clear you asked the questions and didn’t just simply rely upon someone else’s information.”
5. Separate typing from listening
While EHR may be an excellent tool for data collection and safety checking, it’s not a stand-in for doctor-patient interaction. As technology practices push medicine toward more and more efficiency, Mr. Boeder says it’s most often listening over all else that makes the difference in the quality of care. And good listening requires full attention.
“A real concern for physicians is the number of visits they’re expected to accomplish in a set amount of time,” says Mr. Boeder. “Often this translates into a doctor talking to a patient while typing notes or while reading a note from the last time the patient was in.”
Taking the time to pause after entering data and briefly reviewing your understanding of what your patient has told you can be invaluable and may save you – and your patient – problems later.
“In so many cases, it comes down to people not being heard,” says Mr. Boeder. “So listen to what your patients are saying.”
A version of this article first appeared on Medscape.com.
Domestic violence in health care is real and underreported
To protect survivors’ identities, some names have been changed or shortened.
Natasha Abadilla, MD, met the man who would become her abuser while working abroad for a public health nonprofit. When he began emotionally and physically abusing her, she did everything she could to hide it.
“My coworkers knew nothing of the abuse. I became an expert in applying makeup to hide the bruises,” recalls Dr. Abadilla, now a second-year resident and pediatric neurologist at Lucile Packard Children’s Hospital at Stanford.
Dr. Abadilla says she strongly identifies as a hard worker and – to this day – hopes her work did not falter despite her partner’s constant drain on her. But the impact of the abuse continued to affect her for years. Like many survivors of domestic violence, she struggled with PTSD and depression.
Health care workers are often the first point of contact for survivors of domestic violence. Experts and advocates continue to push for more training for clinicians to identify and respond to signs among their patients. Often missing from this conversation is the reality that those tasked with screening can also be victims of intimate partner violence themselves.
What’s more: The very strengths that medical professionals often pride themselves on – perfectionism, empathy, grit – can make it harder for them to identify abuse in their own relationships and push through humiliation and shame to seek help.
Dr. Abadilla is exceptional among survivors in the medical field. Rather than keep her experience quiet, she has shared it publicly.
Awareness, she believes, can save lives.
An understudied problem in an underserved group
The majority of research on health care workers in this area has focused on workplace violence, which 62% experience worldwide. But intimate partner violence remains understudied and underdiscussed. Some medical professionals are even saddled with a “double burden,” facing trauma at work and at home, note the authors of a 2022 meta-analysis published in the journal Trauma, Violence, & Abuse.
The problem has had dire consequences. In recent years, many health care workers have been killed by their abusers:
- In 2016, Casey M. Drawert, MD, a Texas-based critical care anesthesiologist, was fatally shot by her husband in a murder-suicide.
- In 2018, Tamara O’Neal, MD, an ER physician, and Dayna Less, a first-year pharmacy resident, were killed by Dr. O’Neal’s ex-fiancé at Mercy Hospital in Chicago.
- In 2019, Sarah Hawley, MD, a first-year University of Utah resident, was fatally shot by her boyfriend in a murder-suicide.
- In 2021, Moria Kinsey, a nurse practitioner in Tahlequah, Okla., was murdered by a physician.
- In July of 2023, Gwendolyn Lavonne Riddick, DO, an ob.gyn. in North Carolina, was fatally shot by the father of her 3-year-old son.
There are others.
In the wake of these tragedies, calls for health care workers to screen each other as well as patients have grown. But for an untold number of survivors, breaking the silence is still not possible due to concerns about their reputation, professional consequences, the threat of harassment from abusers who are often in the same field, a medical culture of selfless endurance, and a lack of appropriate resources.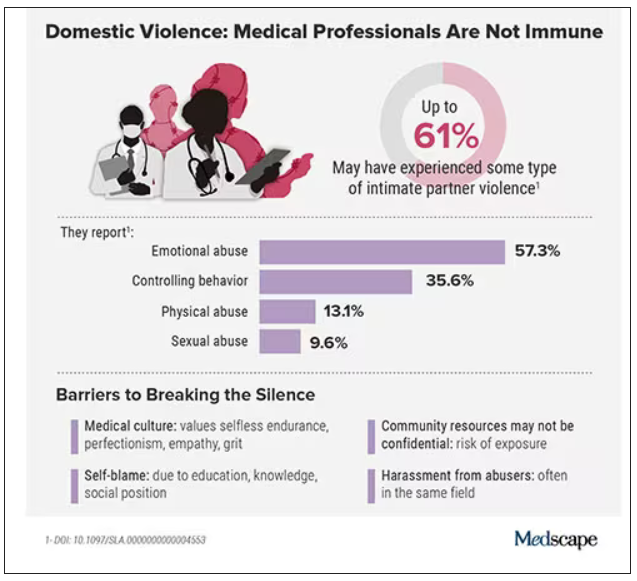
While the vast majority have stayed silent, those who have spoken out say there’s a need for targeted interventions to educate medical professionals as well as more supportive policies throughout the health care system.
Are health care workers more at risk?
Although more studies are needed, research indicates health care workers experience domestic violence at rates comparable to those of other populations, whereas some data suggest rates may be higher.
In the United States, more than one in three women and one in four men experience some form of intimate partner violence in their lifetime. Similarly, a 2020 study found that 24% of 400 physicians responding to a survey reported a history of domestic violence, with 15% reporting verbal abuse, 8% reporting physical violence, 4% reporting sexual abuse, and 4% reporting stalking.
Meanwhile, in an anonymous survey completed by 882 practicing surgeons and trainees in the United States from late 2018 to early 2019, more than 60% reported experiencing some type of intimate partner violence, most commonly emotional abuse.
Recent studies in the United Kingdom, Australia, and elsewhere show that significant numbers of medical professionals are fighting this battle. A 2019 study of more than 2,000 nurses, midwives, and health care assistants in the United Kingdom found that nurses were three times more likely to experience domestic violence than the average person.
What would help solve this problem: More study of health care worker-survivors as a unique group with unique risk factors. In general, domestic violence is most prevalent among women and people in marginalized groups. But young adults, such as medical students and trainees, can face an increased risk due to economic strain. Major life changes, such as relocating for residency, can also drive up stress and fray social connections, further isolating victims.
Why it’s so much harder for medical professionals to reveal abuse
For medical professionals accustomed to being strong and forging on, identifying as a victim of abuse can seem like a personal contradiction. It can feel easier to separate their personal and professional lives rather than face a complex reality.
In a personal essay on KevinMD.com, medical student Chloe N. L. Lee describes this emotional turmoil. “As an aspiring psychiatrist, I questioned my character judgment (how did I end up with a misogynistic abuser?) and wondered if I ought to have known better. I worried that my colleagues would deem me unfit to care for patients. And I thought that this was not supposed to happen to women like me,” Ms. Lee writes.
Kimberly, a licensed therapist, experienced a similar pattern of self-blame when her partner began exhibiting violent behavior. “For a long time, I felt guilty because I said to myself, You’re a therapist. You’re supposed to know this,” she recalls. At the same time, she felt driven to help him and sought couples therapy as his violence escalated.
Whitney, a pharmacist, recognized the “hallmarks” of abuse in her relationship, but she coped by compartmentalizing. Whitney says she was vulnerable to her abuser as a young college student who struggled financially. As he showered her with gifts, she found herself waving away red flags like aggressiveness or overprotectiveness.
After Whitney graduated, her partner’s emotional manipulation escalated into frequent physical assaults. When he gave her a black eye, she could not bring herself to go into work. She quit her job without notice. Despite a spotless record, none of her coworkers ever reached out to investigate her sudden departure.
It would take 8 years for Whitney to acknowledge the abuse and seize a moment to escape. She fled with just her purse and started over in a new city, rebuilding her life in the midst of harassment and threats from her ex. She says she’s grateful to be alive.
An imperfect system doesn’t help
Health care workers rarely ask for support or disclose abuse at work. Some have cited stigma, a lack of confidentiality (especially when the abuser is also in health care), fears about colleagues’ judgment, and a culture that doesn’t prioritize self-care.
Sometimes policies get in the way: In a 2021 qualitative study of interviews with 21 female physician-survivors in the United Kingdom, many said that despite the intense stress of abuse and recovery, they were unable to take any time off.
Of 180 UK-based midwife-survivors interviewed in a 2018 study, only 60 sought support at work and 30 received it. Many said their supervisors pressured them to report the abuse and get back to work, called social services behind their back, or reported them to their professional regulator. “I was treated like the perpetrator,” one said. Barbara Hernandez, PhD, a researcher who studies physician-survivors and director of physician vitality at Loma Linda University in southern California, says workplace violence and mistreatment from patients or colleagues – and a poor institutional response – can make those in health care feel like they have to “shut up and put up,” priming them to also tolerate abuse at home.
When survivors do reach out, there can be a disconnect between the resources they need and those they’re offered, Dr. Hernandez adds. In a recent survey of 400 physicians she conducted, respondents typically said they would advise a physician-survivor to “get to a shelter quickly.” But when roles were reversed, they admitted going to a shelter was the least feasible option. Support groups can also be problematic in smaller communities where physicians might be recognized or see their own patients.
Complicating matters further, the violence often comes from within the medical community. This can lead to particularly malicious abuse tactics like sending false accusations to a victim’s regulatory college or board; prolonged court and custody battles to drain them of all resources and their ability to hold a job; or even sabotage, harassment, or violence at work. The sheen of the abuser’s public persona, on the other hand, can guard them from any accountability.
For example, one physician-survivor said her ex-partner, a psychiatrist, coerced her into believing she was mentally ill, claimed she was “psychotic” in order to take back their children after she left, and had numerous colleagues serve as character witnesses in court for him, “saying he couldn’t have done any of these things, how great he is, and what a wonderful father he is.”
Slow progress is still progress
After Sherilyn M. Gordon-Burroughs, MD, a Texas-based transplant surgeon, mother, and educator, was killed by her husband in a murder-suicide in 2017, her friends Barbara Lee Bass, MD, president of the American College of Surgeons, and Patricia L. Turner, MD, were spurred into action. Together, they founded the ACS Intimate Partner Violence Task Force. Their mission is to educate surgeons to identify the signs of intimate partner violence (IPV) in themselves and their colleagues and connect them with resources.
“There is a concerted effort to close that gap,” says D’Andrea K. Joseph, MD, cochair of the task force and chief of trauma and acute care surgery at NYU Langone in New York. In the future, Dr. Joseph predicts, “making this a part of the curriculum, that it’s standardized for residents and trainees, that there is a safe place for victims ... and that we can band together and really recognize and assist our colleagues who are in trouble.”
Resources created by the ACS IPV task force, such as the toolkit and curriculum, provide a model for other health care leaders. But there have been few similar initiatives aimed at increasing IPV intervention within the medical system.
What you can do in your workplace
In her essay, Ms. Lee explains that a major turning point came when a physician friend explicitly asked if she was experiencing abuse. He then gently confirmed she was, and asked without judgment how he could support her, an approach that mirrors advice from the National Domestic Violence Hotline.
“Having a physician validate that this was, indeed, an abusive situation helped enormously ... I believe it may have saved my life,” she writes.
That validation can be crucial, and Dr. Abadilla urges other physicians to regularly check in with colleagues, especially those who seem particularly positive with a go-getter attitude and yet may not seem themselves. That was how she presented when she was struggling the most.
Supporting systemic changes within your organization and beyond is also important. The authors of the 2022 meta-analysis stress the need for domestic violence training, legislative changes, paid leave, and union support.
Finding strength in recovery
Over a decade after escaping her abuser, Whitney says she’s only just begun to share her experience, but what she’s learned has made her a better pharmacist. She says she’s more attuned to subtle signs something could be off with patients and coworkers. When someone makes comments about feeling anxious or that they can’t do anything right, it’s important to ask why, she says.
Recently, Kimberly has opened up to her mentor and other therapists, many of whom have shared that they’re also survivors.
“The last thing I said to [my abuser] is you think you’ve won and you’re hurting me, but what you’ve done to me – I’m going to utilize this and I’m going to help other people,” Kimberly says. “This pain that I have will go away, and I’m going to save the lives of others.”
A version of this article first appeared on Medscape.com.
To protect survivors’ identities, some names have been changed or shortened.
Natasha Abadilla, MD, met the man who would become her abuser while working abroad for a public health nonprofit. When he began emotionally and physically abusing her, she did everything she could to hide it.
“My coworkers knew nothing of the abuse. I became an expert in applying makeup to hide the bruises,” recalls Dr. Abadilla, now a second-year resident and pediatric neurologist at Lucile Packard Children’s Hospital at Stanford.
Dr. Abadilla says she strongly identifies as a hard worker and – to this day – hopes her work did not falter despite her partner’s constant drain on her. But the impact of the abuse continued to affect her for years. Like many survivors of domestic violence, she struggled with PTSD and depression.
Health care workers are often the first point of contact for survivors of domestic violence. Experts and advocates continue to push for more training for clinicians to identify and respond to signs among their patients. Often missing from this conversation is the reality that those tasked with screening can also be victims of intimate partner violence themselves.
What’s more: The very strengths that medical professionals often pride themselves on – perfectionism, empathy, grit – can make it harder for them to identify abuse in their own relationships and push through humiliation and shame to seek help.
Dr. Abadilla is exceptional among survivors in the medical field. Rather than keep her experience quiet, she has shared it publicly.
Awareness, she believes, can save lives.
An understudied problem in an underserved group
The majority of research on health care workers in this area has focused on workplace violence, which 62% experience worldwide. But intimate partner violence remains understudied and underdiscussed. Some medical professionals are even saddled with a “double burden,” facing trauma at work and at home, note the authors of a 2022 meta-analysis published in the journal Trauma, Violence, & Abuse.
The problem has had dire consequences. In recent years, many health care workers have been killed by their abusers:
- In 2016, Casey M. Drawert, MD, a Texas-based critical care anesthesiologist, was fatally shot by her husband in a murder-suicide.
- In 2018, Tamara O’Neal, MD, an ER physician, and Dayna Less, a first-year pharmacy resident, were killed by Dr. O’Neal’s ex-fiancé at Mercy Hospital in Chicago.
- In 2019, Sarah Hawley, MD, a first-year University of Utah resident, was fatally shot by her boyfriend in a murder-suicide.
- In 2021, Moria Kinsey, a nurse practitioner in Tahlequah, Okla., was murdered by a physician.
- In July of 2023, Gwendolyn Lavonne Riddick, DO, an ob.gyn. in North Carolina, was fatally shot by the father of her 3-year-old son.
There are others.
In the wake of these tragedies, calls for health care workers to screen each other as well as patients have grown. But for an untold number of survivors, breaking the silence is still not possible due to concerns about their reputation, professional consequences, the threat of harassment from abusers who are often in the same field, a medical culture of selfless endurance, and a lack of appropriate resources.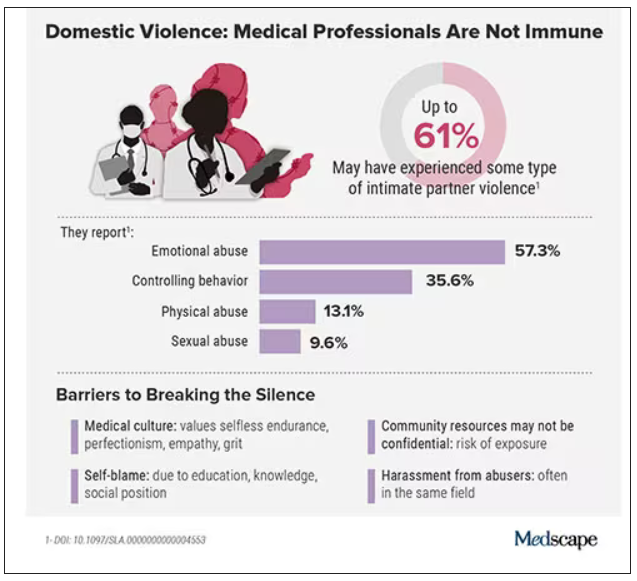
While the vast majority have stayed silent, those who have spoken out say there’s a need for targeted interventions to educate medical professionals as well as more supportive policies throughout the health care system.
Are health care workers more at risk?
Although more studies are needed, research indicates health care workers experience domestic violence at rates comparable to those of other populations, whereas some data suggest rates may be higher.
In the United States, more than one in three women and one in four men experience some form of intimate partner violence in their lifetime. Similarly, a 2020 study found that 24% of 400 physicians responding to a survey reported a history of domestic violence, with 15% reporting verbal abuse, 8% reporting physical violence, 4% reporting sexual abuse, and 4% reporting stalking.
Meanwhile, in an anonymous survey completed by 882 practicing surgeons and trainees in the United States from late 2018 to early 2019, more than 60% reported experiencing some type of intimate partner violence, most commonly emotional abuse.
Recent studies in the United Kingdom, Australia, and elsewhere show that significant numbers of medical professionals are fighting this battle. A 2019 study of more than 2,000 nurses, midwives, and health care assistants in the United Kingdom found that nurses were three times more likely to experience domestic violence than the average person.
What would help solve this problem: More study of health care worker-survivors as a unique group with unique risk factors. In general, domestic violence is most prevalent among women and people in marginalized groups. But young adults, such as medical students and trainees, can face an increased risk due to economic strain. Major life changes, such as relocating for residency, can also drive up stress and fray social connections, further isolating victims.
Why it’s so much harder for medical professionals to reveal abuse
For medical professionals accustomed to being strong and forging on, identifying as a victim of abuse can seem like a personal contradiction. It can feel easier to separate their personal and professional lives rather than face a complex reality.
In a personal essay on KevinMD.com, medical student Chloe N. L. Lee describes this emotional turmoil. “As an aspiring psychiatrist, I questioned my character judgment (how did I end up with a misogynistic abuser?) and wondered if I ought to have known better. I worried that my colleagues would deem me unfit to care for patients. And I thought that this was not supposed to happen to women like me,” Ms. Lee writes.
Kimberly, a licensed therapist, experienced a similar pattern of self-blame when her partner began exhibiting violent behavior. “For a long time, I felt guilty because I said to myself, You’re a therapist. You’re supposed to know this,” she recalls. At the same time, she felt driven to help him and sought couples therapy as his violence escalated.
Whitney, a pharmacist, recognized the “hallmarks” of abuse in her relationship, but she coped by compartmentalizing. Whitney says she was vulnerable to her abuser as a young college student who struggled financially. As he showered her with gifts, she found herself waving away red flags like aggressiveness or overprotectiveness.
After Whitney graduated, her partner’s emotional manipulation escalated into frequent physical assaults. When he gave her a black eye, she could not bring herself to go into work. She quit her job without notice. Despite a spotless record, none of her coworkers ever reached out to investigate her sudden departure.
It would take 8 years for Whitney to acknowledge the abuse and seize a moment to escape. She fled with just her purse and started over in a new city, rebuilding her life in the midst of harassment and threats from her ex. She says she’s grateful to be alive.
An imperfect system doesn’t help
Health care workers rarely ask for support or disclose abuse at work. Some have cited stigma, a lack of confidentiality (especially when the abuser is also in health care), fears about colleagues’ judgment, and a culture that doesn’t prioritize self-care.
Sometimes policies get in the way: In a 2021 qualitative study of interviews with 21 female physician-survivors in the United Kingdom, many said that despite the intense stress of abuse and recovery, they were unable to take any time off.
Of 180 UK-based midwife-survivors interviewed in a 2018 study, only 60 sought support at work and 30 received it. Many said their supervisors pressured them to report the abuse and get back to work, called social services behind their back, or reported them to their professional regulator. “I was treated like the perpetrator,” one said. Barbara Hernandez, PhD, a researcher who studies physician-survivors and director of physician vitality at Loma Linda University in southern California, says workplace violence and mistreatment from patients or colleagues – and a poor institutional response – can make those in health care feel like they have to “shut up and put up,” priming them to also tolerate abuse at home.
When survivors do reach out, there can be a disconnect between the resources they need and those they’re offered, Dr. Hernandez adds. In a recent survey of 400 physicians she conducted, respondents typically said they would advise a physician-survivor to “get to a shelter quickly.” But when roles were reversed, they admitted going to a shelter was the least feasible option. Support groups can also be problematic in smaller communities where physicians might be recognized or see their own patients.
Complicating matters further, the violence often comes from within the medical community. This can lead to particularly malicious abuse tactics like sending false accusations to a victim’s regulatory college or board; prolonged court and custody battles to drain them of all resources and their ability to hold a job; or even sabotage, harassment, or violence at work. The sheen of the abuser’s public persona, on the other hand, can guard them from any accountability.
For example, one physician-survivor said her ex-partner, a psychiatrist, coerced her into believing she was mentally ill, claimed she was “psychotic” in order to take back their children after she left, and had numerous colleagues serve as character witnesses in court for him, “saying he couldn’t have done any of these things, how great he is, and what a wonderful father he is.”
Slow progress is still progress
After Sherilyn M. Gordon-Burroughs, MD, a Texas-based transplant surgeon, mother, and educator, was killed by her husband in a murder-suicide in 2017, her friends Barbara Lee Bass, MD, president of the American College of Surgeons, and Patricia L. Turner, MD, were spurred into action. Together, they founded the ACS Intimate Partner Violence Task Force. Their mission is to educate surgeons to identify the signs of intimate partner violence (IPV) in themselves and their colleagues and connect them with resources.
“There is a concerted effort to close that gap,” says D’Andrea K. Joseph, MD, cochair of the task force and chief of trauma and acute care surgery at NYU Langone in New York. In the future, Dr. Joseph predicts, “making this a part of the curriculum, that it’s standardized for residents and trainees, that there is a safe place for victims ... and that we can band together and really recognize and assist our colleagues who are in trouble.”
Resources created by the ACS IPV task force, such as the toolkit and curriculum, provide a model for other health care leaders. But there have been few similar initiatives aimed at increasing IPV intervention within the medical system.
What you can do in your workplace
In her essay, Ms. Lee explains that a major turning point came when a physician friend explicitly asked if she was experiencing abuse. He then gently confirmed she was, and asked without judgment how he could support her, an approach that mirrors advice from the National Domestic Violence Hotline.
“Having a physician validate that this was, indeed, an abusive situation helped enormously ... I believe it may have saved my life,” she writes.
That validation can be crucial, and Dr. Abadilla urges other physicians to regularly check in with colleagues, especially those who seem particularly positive with a go-getter attitude and yet may not seem themselves. That was how she presented when she was struggling the most.
Supporting systemic changes within your organization and beyond is also important. The authors of the 2022 meta-analysis stress the need for domestic violence training, legislative changes, paid leave, and union support.
Finding strength in recovery
Over a decade after escaping her abuser, Whitney says she’s only just begun to share her experience, but what she’s learned has made her a better pharmacist. She says she’s more attuned to subtle signs something could be off with patients and coworkers. When someone makes comments about feeling anxious or that they can’t do anything right, it’s important to ask why, she says.
Recently, Kimberly has opened up to her mentor and other therapists, many of whom have shared that they’re also survivors.
“The last thing I said to [my abuser] is you think you’ve won and you’re hurting me, but what you’ve done to me – I’m going to utilize this and I’m going to help other people,” Kimberly says. “This pain that I have will go away, and I’m going to save the lives of others.”
A version of this article first appeared on Medscape.com.
To protect survivors’ identities, some names have been changed or shortened.
Natasha Abadilla, MD, met the man who would become her abuser while working abroad for a public health nonprofit. When he began emotionally and physically abusing her, she did everything she could to hide it.
“My coworkers knew nothing of the abuse. I became an expert in applying makeup to hide the bruises,” recalls Dr. Abadilla, now a second-year resident and pediatric neurologist at Lucile Packard Children’s Hospital at Stanford.
Dr. Abadilla says she strongly identifies as a hard worker and – to this day – hopes her work did not falter despite her partner’s constant drain on her. But the impact of the abuse continued to affect her for years. Like many survivors of domestic violence, she struggled with PTSD and depression.
Health care workers are often the first point of contact for survivors of domestic violence. Experts and advocates continue to push for more training for clinicians to identify and respond to signs among their patients. Often missing from this conversation is the reality that those tasked with screening can also be victims of intimate partner violence themselves.
What’s more: The very strengths that medical professionals often pride themselves on – perfectionism, empathy, grit – can make it harder for them to identify abuse in their own relationships and push through humiliation and shame to seek help.
Dr. Abadilla is exceptional among survivors in the medical field. Rather than keep her experience quiet, she has shared it publicly.
Awareness, she believes, can save lives.
An understudied problem in an underserved group
The majority of research on health care workers in this area has focused on workplace violence, which 62% experience worldwide. But intimate partner violence remains understudied and underdiscussed. Some medical professionals are even saddled with a “double burden,” facing trauma at work and at home, note the authors of a 2022 meta-analysis published in the journal Trauma, Violence, & Abuse.
The problem has had dire consequences. In recent years, many health care workers have been killed by their abusers:
- In 2016, Casey M. Drawert, MD, a Texas-based critical care anesthesiologist, was fatally shot by her husband in a murder-suicide.
- In 2018, Tamara O’Neal, MD, an ER physician, and Dayna Less, a first-year pharmacy resident, were killed by Dr. O’Neal’s ex-fiancé at Mercy Hospital in Chicago.
- In 2019, Sarah Hawley, MD, a first-year University of Utah resident, was fatally shot by her boyfriend in a murder-suicide.
- In 2021, Moria Kinsey, a nurse practitioner in Tahlequah, Okla., was murdered by a physician.
- In July of 2023, Gwendolyn Lavonne Riddick, DO, an ob.gyn. in North Carolina, was fatally shot by the father of her 3-year-old son.
There are others.
In the wake of these tragedies, calls for health care workers to screen each other as well as patients have grown. But for an untold number of survivors, breaking the silence is still not possible due to concerns about their reputation, professional consequences, the threat of harassment from abusers who are often in the same field, a medical culture of selfless endurance, and a lack of appropriate resources.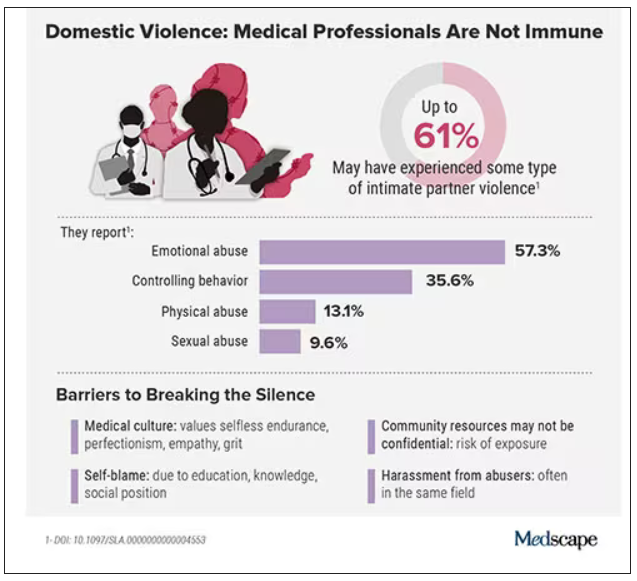
While the vast majority have stayed silent, those who have spoken out say there’s a need for targeted interventions to educate medical professionals as well as more supportive policies throughout the health care system.
Are health care workers more at risk?
Although more studies are needed, research indicates health care workers experience domestic violence at rates comparable to those of other populations, whereas some data suggest rates may be higher.
In the United States, more than one in three women and one in four men experience some form of intimate partner violence in their lifetime. Similarly, a 2020 study found that 24% of 400 physicians responding to a survey reported a history of domestic violence, with 15% reporting verbal abuse, 8% reporting physical violence, 4% reporting sexual abuse, and 4% reporting stalking.
Meanwhile, in an anonymous survey completed by 882 practicing surgeons and trainees in the United States from late 2018 to early 2019, more than 60% reported experiencing some type of intimate partner violence, most commonly emotional abuse.
Recent studies in the United Kingdom, Australia, and elsewhere show that significant numbers of medical professionals are fighting this battle. A 2019 study of more than 2,000 nurses, midwives, and health care assistants in the United Kingdom found that nurses were three times more likely to experience domestic violence than the average person.
What would help solve this problem: More study of health care worker-survivors as a unique group with unique risk factors. In general, domestic violence is most prevalent among women and people in marginalized groups. But young adults, such as medical students and trainees, can face an increased risk due to economic strain. Major life changes, such as relocating for residency, can also drive up stress and fray social connections, further isolating victims.
Why it’s so much harder for medical professionals to reveal abuse
For medical professionals accustomed to being strong and forging on, identifying as a victim of abuse can seem like a personal contradiction. It can feel easier to separate their personal and professional lives rather than face a complex reality.
In a personal essay on KevinMD.com, medical student Chloe N. L. Lee describes this emotional turmoil. “As an aspiring psychiatrist, I questioned my character judgment (how did I end up with a misogynistic abuser?) and wondered if I ought to have known better. I worried that my colleagues would deem me unfit to care for patients. And I thought that this was not supposed to happen to women like me,” Ms. Lee writes.
Kimberly, a licensed therapist, experienced a similar pattern of self-blame when her partner began exhibiting violent behavior. “For a long time, I felt guilty because I said to myself, You’re a therapist. You’re supposed to know this,” she recalls. At the same time, she felt driven to help him and sought couples therapy as his violence escalated.
Whitney, a pharmacist, recognized the “hallmarks” of abuse in her relationship, but she coped by compartmentalizing. Whitney says she was vulnerable to her abuser as a young college student who struggled financially. As he showered her with gifts, she found herself waving away red flags like aggressiveness or overprotectiveness.
After Whitney graduated, her partner’s emotional manipulation escalated into frequent physical assaults. When he gave her a black eye, she could not bring herself to go into work. She quit her job without notice. Despite a spotless record, none of her coworkers ever reached out to investigate her sudden departure.
It would take 8 years for Whitney to acknowledge the abuse and seize a moment to escape. She fled with just her purse and started over in a new city, rebuilding her life in the midst of harassment and threats from her ex. She says she’s grateful to be alive.
An imperfect system doesn’t help
Health care workers rarely ask for support or disclose abuse at work. Some have cited stigma, a lack of confidentiality (especially when the abuser is also in health care), fears about colleagues’ judgment, and a culture that doesn’t prioritize self-care.
Sometimes policies get in the way: In a 2021 qualitative study of interviews with 21 female physician-survivors in the United Kingdom, many said that despite the intense stress of abuse and recovery, they were unable to take any time off.
Of 180 UK-based midwife-survivors interviewed in a 2018 study, only 60 sought support at work and 30 received it. Many said their supervisors pressured them to report the abuse and get back to work, called social services behind their back, or reported them to their professional regulator. “I was treated like the perpetrator,” one said. Barbara Hernandez, PhD, a researcher who studies physician-survivors and director of physician vitality at Loma Linda University in southern California, says workplace violence and mistreatment from patients or colleagues – and a poor institutional response – can make those in health care feel like they have to “shut up and put up,” priming them to also tolerate abuse at home.
When survivors do reach out, there can be a disconnect between the resources they need and those they’re offered, Dr. Hernandez adds. In a recent survey of 400 physicians she conducted, respondents typically said they would advise a physician-survivor to “get to a shelter quickly.” But when roles were reversed, they admitted going to a shelter was the least feasible option. Support groups can also be problematic in smaller communities where physicians might be recognized or see their own patients.
Complicating matters further, the violence often comes from within the medical community. This can lead to particularly malicious abuse tactics like sending false accusations to a victim’s regulatory college or board; prolonged court and custody battles to drain them of all resources and their ability to hold a job; or even sabotage, harassment, or violence at work. The sheen of the abuser’s public persona, on the other hand, can guard them from any accountability.
For example, one physician-survivor said her ex-partner, a psychiatrist, coerced her into believing she was mentally ill, claimed she was “psychotic” in order to take back their children after she left, and had numerous colleagues serve as character witnesses in court for him, “saying he couldn’t have done any of these things, how great he is, and what a wonderful father he is.”
Slow progress is still progress
After Sherilyn M. Gordon-Burroughs, MD, a Texas-based transplant surgeon, mother, and educator, was killed by her husband in a murder-suicide in 2017, her friends Barbara Lee Bass, MD, president of the American College of Surgeons, and Patricia L. Turner, MD, were spurred into action. Together, they founded the ACS Intimate Partner Violence Task Force. Their mission is to educate surgeons to identify the signs of intimate partner violence (IPV) in themselves and their colleagues and connect them with resources.
“There is a concerted effort to close that gap,” says D’Andrea K. Joseph, MD, cochair of the task force and chief of trauma and acute care surgery at NYU Langone in New York. In the future, Dr. Joseph predicts, “making this a part of the curriculum, that it’s standardized for residents and trainees, that there is a safe place for victims ... and that we can band together and really recognize and assist our colleagues who are in trouble.”
Resources created by the ACS IPV task force, such as the toolkit and curriculum, provide a model for other health care leaders. But there have been few similar initiatives aimed at increasing IPV intervention within the medical system.
What you can do in your workplace
In her essay, Ms. Lee explains that a major turning point came when a physician friend explicitly asked if she was experiencing abuse. He then gently confirmed she was, and asked without judgment how he could support her, an approach that mirrors advice from the National Domestic Violence Hotline.
“Having a physician validate that this was, indeed, an abusive situation helped enormously ... I believe it may have saved my life,” she writes.
That validation can be crucial, and Dr. Abadilla urges other physicians to regularly check in with colleagues, especially those who seem particularly positive with a go-getter attitude and yet may not seem themselves. That was how she presented when she was struggling the most.
Supporting systemic changes within your organization and beyond is also important. The authors of the 2022 meta-analysis stress the need for domestic violence training, legislative changes, paid leave, and union support.
Finding strength in recovery
Over a decade after escaping her abuser, Whitney says she’s only just begun to share her experience, but what she’s learned has made her a better pharmacist. She says she’s more attuned to subtle signs something could be off with patients and coworkers. When someone makes comments about feeling anxious or that they can’t do anything right, it’s important to ask why, she says.
Recently, Kimberly has opened up to her mentor and other therapists, many of whom have shared that they’re also survivors.
“The last thing I said to [my abuser] is you think you’ve won and you’re hurting me, but what you’ve done to me – I’m going to utilize this and I’m going to help other people,” Kimberly says. “This pain that I have will go away, and I’m going to save the lives of others.”
A version of this article first appeared on Medscape.com.
One in five doctors with long COVID can no longer work: Survey
Crippling symptoms, lost careers, and eroded incomes: This is the harsh reality for doctors suffering with long COVID, according to the first major survey of physicians with the condition.
The survey, conducted by the British Medical Association and the Long COVID Doctors for Action support group, sheds light on the lingering effects of long COVID on more than 600 chronically ill and disabled doctors with the condition. It also spotlights what they describe as a lack of medical and financial support from their government and employers at the National Health Service.
“We feel betrayed and abandoned,” said Kelly Fearnley, MBChB, chair and cofounder of Long COVID Doctors for Action. “At a time of national crisis, when health care workers were asked to step up, we did. When the nation needed us, we stepped up. We put our lives on the line. We put our families’ lives on the line. And now that we are injured after knowingly being unprotected and deliberately and repeatedly exposed to a level 3 biohazard, we now find ourselves in this position.”
Dr. Fearnley fell ill while working in a hospital’s COVID ward in November 2020. She is one of an estimated 2 million people in the United Kingdom – including thousands of NHS employees – with long COVID. She hasn’t been able to return to work in nearly 3 years.
Long COVID affects more than 65 million people worldwide. It is estimated that 1 in 10 people infected with the virus develop long-term symptoms. In the United Kingdom, health care and social care workers are seven times more likely to have had severe COVID-19 than other types of employees.
Doctors responding to the BMA survey reported a wide range of long COVID symptoms, including fatigue, headaches, muscular pain, nerve damage, joint pain, and respiratory problems.
Among the survey’s key findings, 60% of doctors said long COVID has affected their ability to carry out day-to-day tasks on a regular basis. Almost one in five (18%) said they were no longer able to work, while fewer than one in three (31%) were working full time. This compares with more than half (57%) of respondents working full time before the onset of their COVID illness – a decline of 46%.
Nearly half (48%) of respondents said they have experienced some form of loss of earnings as a result of long COVID, and almost half of the doctors were never referred to an NHS long COVID clinic. The survey included the following first-person accounts from doctors living with the condition.
- One doctor said: “I nearly lost my life, my home, my partner and my career. I have received little support to help keep these. The impact on my mental health nearly cost [me] my life again.”
- A senior consulting physician commented: “Life is absolutely miserable. Every day is a struggle. I wake up exhausted, the insomnia and night terrors are horrendous as I live through my worst fears every night. Any activity such as eating meals, washing, etc., will mean I have to go to bed for a few hours. I am unable to look after myself or my child, exercise or maintain social relationships. I have no financial security. Long COVID has totally destroyed my life.”
- A salaried general practitioner said: “I can no longer work, finances are ruined. I didn’t have employment protection so am now unemployed and penniless.”
Calls for action from the BMA include the following:
- Financial support for doctors and health care staff with long COVID.
- The recognition of long COVID as an occupational disease among health care workers, along with a definition of the condition that covers all of the debilitating disease’s symptoms.
- Improved access to physical and mental health services to help comprehensive assessment, investigations, and treatment.
- Greater workplace protection for health care staff who risk their lives for others.
- Better support for long COVID sufferers to return to work safely if they can, including a flexible approach to the use of workplace adjustments.
“One would think, given the circumstances under which we fell ill and current workforce shortages, NHS employers would be eager to do everything to facilitate the return to work of people with long COVID,” said Dr. Fearnley. “However, NHS employers are legally required to implement only ‘reasonable adjustments,’ and so things such as extended phased return or adjustments to shift patterns are not always being facilitated. Instead, an increasing number of employers are choosing to terminate contracts.”
Raymond Agius, the BMA’s occupational medicine committee cochair, also put the blame on inadequate safety measures for doctors. Those inadequate measures persist to this day, inasmuch as U.K. hospitals have dropped masking requirements.
“During the COVID-19 pandemic, doctors were left exposed and unprotected at work,” he said in a BMA press release. “They often did not have access to the right PPE. ... Too many risk assessments of workplaces and especially of vulnerable doctors were not undertaken.”
A small minority of doctors who were surveyed said they had access to respiratory protective equipment about the time they contracted COVID-19. Only 11% had access to an FFP2 respirator (the equivalent of an N95 mask); 16% had an FFP3 respirator (the equivalent of an N99 mask).
To date, the British government hasn’t issued much of a response to the survey, saying only that it has invested more than ₤50 million to better understand long COVID.
A version of this article first appeared on Medscape.com.
Crippling symptoms, lost careers, and eroded incomes: This is the harsh reality for doctors suffering with long COVID, according to the first major survey of physicians with the condition.
The survey, conducted by the British Medical Association and the Long COVID Doctors for Action support group, sheds light on the lingering effects of long COVID on more than 600 chronically ill and disabled doctors with the condition. It also spotlights what they describe as a lack of medical and financial support from their government and employers at the National Health Service.
“We feel betrayed and abandoned,” said Kelly Fearnley, MBChB, chair and cofounder of Long COVID Doctors for Action. “At a time of national crisis, when health care workers were asked to step up, we did. When the nation needed us, we stepped up. We put our lives on the line. We put our families’ lives on the line. And now that we are injured after knowingly being unprotected and deliberately and repeatedly exposed to a level 3 biohazard, we now find ourselves in this position.”
Dr. Fearnley fell ill while working in a hospital’s COVID ward in November 2020. She is one of an estimated 2 million people in the United Kingdom – including thousands of NHS employees – with long COVID. She hasn’t been able to return to work in nearly 3 years.
Long COVID affects more than 65 million people worldwide. It is estimated that 1 in 10 people infected with the virus develop long-term symptoms. In the United Kingdom, health care and social care workers are seven times more likely to have had severe COVID-19 than other types of employees.
Doctors responding to the BMA survey reported a wide range of long COVID symptoms, including fatigue, headaches, muscular pain, nerve damage, joint pain, and respiratory problems.
Among the survey’s key findings, 60% of doctors said long COVID has affected their ability to carry out day-to-day tasks on a regular basis. Almost one in five (18%) said they were no longer able to work, while fewer than one in three (31%) were working full time. This compares with more than half (57%) of respondents working full time before the onset of their COVID illness – a decline of 46%.
Nearly half (48%) of respondents said they have experienced some form of loss of earnings as a result of long COVID, and almost half of the doctors were never referred to an NHS long COVID clinic. The survey included the following first-person accounts from doctors living with the condition.
- One doctor said: “I nearly lost my life, my home, my partner and my career. I have received little support to help keep these. The impact on my mental health nearly cost [me] my life again.”
- A senior consulting physician commented: “Life is absolutely miserable. Every day is a struggle. I wake up exhausted, the insomnia and night terrors are horrendous as I live through my worst fears every night. Any activity such as eating meals, washing, etc., will mean I have to go to bed for a few hours. I am unable to look after myself or my child, exercise or maintain social relationships. I have no financial security. Long COVID has totally destroyed my life.”
- A salaried general practitioner said: “I can no longer work, finances are ruined. I didn’t have employment protection so am now unemployed and penniless.”
Calls for action from the BMA include the following:
- Financial support for doctors and health care staff with long COVID.
- The recognition of long COVID as an occupational disease among health care workers, along with a definition of the condition that covers all of the debilitating disease’s symptoms.
- Improved access to physical and mental health services to help comprehensive assessment, investigations, and treatment.
- Greater workplace protection for health care staff who risk their lives for others.
- Better support for long COVID sufferers to return to work safely if they can, including a flexible approach to the use of workplace adjustments.
“One would think, given the circumstances under which we fell ill and current workforce shortages, NHS employers would be eager to do everything to facilitate the return to work of people with long COVID,” said Dr. Fearnley. “However, NHS employers are legally required to implement only ‘reasonable adjustments,’ and so things such as extended phased return or adjustments to shift patterns are not always being facilitated. Instead, an increasing number of employers are choosing to terminate contracts.”
Raymond Agius, the BMA’s occupational medicine committee cochair, also put the blame on inadequate safety measures for doctors. Those inadequate measures persist to this day, inasmuch as U.K. hospitals have dropped masking requirements.
“During the COVID-19 pandemic, doctors were left exposed and unprotected at work,” he said in a BMA press release. “They often did not have access to the right PPE. ... Too many risk assessments of workplaces and especially of vulnerable doctors were not undertaken.”
A small minority of doctors who were surveyed said they had access to respiratory protective equipment about the time they contracted COVID-19. Only 11% had access to an FFP2 respirator (the equivalent of an N95 mask); 16% had an FFP3 respirator (the equivalent of an N99 mask).
To date, the British government hasn’t issued much of a response to the survey, saying only that it has invested more than ₤50 million to better understand long COVID.
A version of this article first appeared on Medscape.com.
Crippling symptoms, lost careers, and eroded incomes: This is the harsh reality for doctors suffering with long COVID, according to the first major survey of physicians with the condition.
The survey, conducted by the British Medical Association and the Long COVID Doctors for Action support group, sheds light on the lingering effects of long COVID on more than 600 chronically ill and disabled doctors with the condition. It also spotlights what they describe as a lack of medical and financial support from their government and employers at the National Health Service.
“We feel betrayed and abandoned,” said Kelly Fearnley, MBChB, chair and cofounder of Long COVID Doctors for Action. “At a time of national crisis, when health care workers were asked to step up, we did. When the nation needed us, we stepped up. We put our lives on the line. We put our families’ lives on the line. And now that we are injured after knowingly being unprotected and deliberately and repeatedly exposed to a level 3 biohazard, we now find ourselves in this position.”
Dr. Fearnley fell ill while working in a hospital’s COVID ward in November 2020. She is one of an estimated 2 million people in the United Kingdom – including thousands of NHS employees – with long COVID. She hasn’t been able to return to work in nearly 3 years.
Long COVID affects more than 65 million people worldwide. It is estimated that 1 in 10 people infected with the virus develop long-term symptoms. In the United Kingdom, health care and social care workers are seven times more likely to have had severe COVID-19 than other types of employees.
Doctors responding to the BMA survey reported a wide range of long COVID symptoms, including fatigue, headaches, muscular pain, nerve damage, joint pain, and respiratory problems.
Among the survey’s key findings, 60% of doctors said long COVID has affected their ability to carry out day-to-day tasks on a regular basis. Almost one in five (18%) said they were no longer able to work, while fewer than one in three (31%) were working full time. This compares with more than half (57%) of respondents working full time before the onset of their COVID illness – a decline of 46%.
Nearly half (48%) of respondents said they have experienced some form of loss of earnings as a result of long COVID, and almost half of the doctors were never referred to an NHS long COVID clinic. The survey included the following first-person accounts from doctors living with the condition.
- One doctor said: “I nearly lost my life, my home, my partner and my career. I have received little support to help keep these. The impact on my mental health nearly cost [me] my life again.”
- A senior consulting physician commented: “Life is absolutely miserable. Every day is a struggle. I wake up exhausted, the insomnia and night terrors are horrendous as I live through my worst fears every night. Any activity such as eating meals, washing, etc., will mean I have to go to bed for a few hours. I am unable to look after myself or my child, exercise or maintain social relationships. I have no financial security. Long COVID has totally destroyed my life.”
- A salaried general practitioner said: “I can no longer work, finances are ruined. I didn’t have employment protection so am now unemployed and penniless.”
Calls for action from the BMA include the following:
- Financial support for doctors and health care staff with long COVID.
- The recognition of long COVID as an occupational disease among health care workers, along with a definition of the condition that covers all of the debilitating disease’s symptoms.
- Improved access to physical and mental health services to help comprehensive assessment, investigations, and treatment.
- Greater workplace protection for health care staff who risk their lives for others.
- Better support for long COVID sufferers to return to work safely if they can, including a flexible approach to the use of workplace adjustments.
“One would think, given the circumstances under which we fell ill and current workforce shortages, NHS employers would be eager to do everything to facilitate the return to work of people with long COVID,” said Dr. Fearnley. “However, NHS employers are legally required to implement only ‘reasonable adjustments,’ and so things such as extended phased return or adjustments to shift patterns are not always being facilitated. Instead, an increasing number of employers are choosing to terminate contracts.”
Raymond Agius, the BMA’s occupational medicine committee cochair, also put the blame on inadequate safety measures for doctors. Those inadequate measures persist to this day, inasmuch as U.K. hospitals have dropped masking requirements.
“During the COVID-19 pandemic, doctors were left exposed and unprotected at work,” he said in a BMA press release. “They often did not have access to the right PPE. ... Too many risk assessments of workplaces and especially of vulnerable doctors were not undertaken.”
A small minority of doctors who were surveyed said they had access to respiratory protective equipment about the time they contracted COVID-19. Only 11% had access to an FFP2 respirator (the equivalent of an N95 mask); 16% had an FFP3 respirator (the equivalent of an N99 mask).
To date, the British government hasn’t issued much of a response to the survey, saying only that it has invested more than ₤50 million to better understand long COVID.
A version of this article first appeared on Medscape.com.
Resident creates AI alternative to U.S. News med school ranking
For decades, pre-med students depended on the annual medical school rankings by U.S. News and World Report to decide where to apply for physician education. But after several prominent med schools pulled out of the rankings, one resident began experimenting with artificial intelligence (AI) to create an alternative.
Brandon Turner MD, MSc, a radiation oncology resident at Massachusetts General Hospital in Boston, developed a free do-it-yourself tool using AI that allows prospective students to rank medical schools based on considerations that are most important to them. His research was published online in JAMA Network Open.
“One of the flaws with conventional ranking systems is that the metrics used in these tools are weighted based on the preferences and views of the people who developed these rankings, but those may not work for everyone,” Dr. Turner told this news organization.
He explained that there are different types of metrics used in the U.S. News ranking: one for research and the other for primary care. “The research rankings carry the most prestige and are the ones that most people know about,” he explained. These metrics take into account factors such as how many grant dollars the medical school receives and the average size of those grants per faculty member, Dr. Turner said.
Admission metrics are also included – for example, the median grade point average or MCAT scores of students who have been accepted. “These don’t tell you anything about the research output of the school, only about how selective the school is,” he said.
Primary care metrics might focus on how many graduates of a given school go into primary care, or how other schools rate the quality of primary care training at a given school – a process called peer assessment, Dr. Turner said.
But even though these might be helpful, students may be more interested in the cost of attendance, average debt, representation of minorities, and how many graduates pass their boards, he said. “U.S. News metrics don’t capture these things, but I included them in my algorithm.”
A U.S. News spokesperson said that the publication continues to help students and their families make decisions about their future education. The spokesperson cited U.S. News’ explanation of how it calculates its rankings. “A school’s overall Best Medical Schools rank should be one consideration and not the lone determinant in where a student applies and accepts,” the article states.
Dr. Turner agreed ranking systems are a good starting point when researching med schools, “but the values reflected in the ranking may not reflect an individual’s goals.”
Tyra-Lee Brett, a premed student at the University of South Florida, Tampa, believes an additional tool for students to evaluate medical schools is needed – and she could potentially see herself using Dr. Turner’s creation.
Still, Ms. Brett, a premed trustee of the American Medical Student Association, doesn’t regard any ranking tool as the “be all and end all.” Rather, she feels that the most effective tool would be based on students’ lived experiences. The AMSA is developing a scorecard in which students grade schools based on their opinions about such issues as housing, family planning, and environmental health, she said.
No prior judgments
To develop his algorithm, Dr. Turner used a branch of AI called “unsupervised learning.” It doesn’t make a prior judgment about what the data should look like, Dr. Turner explained.
“You’re just analyzing natural trends within the data.”
The algorithm tries to find and discover clusters or patterns within the data. “It’s like saying to the algorithm: ‘I want you to tell me what schools you think should be grouped together based on the data I feed you,’ which is the data that the user selects based on his or her personal preferences.”
U.S. News has been transparent about the metrics it uses, Dr. Turner notes. “When I started looking into how rankings are developed, I saw that there was transparency, and the reasoning for choosing the metrics used to develop the ranking was pretty sound,” he said.
“But I didn’t see any justification as to why they chose the particular metrics and weighted them in the way that they did.”
Dr. Turner extracted data from the 2023 U.S. News report, which ranked 109 allopathic medical schools, and applied several scenarios to the results to create his alternative ranking system.
In one scenario, he used the same research metrics used by U.S. News, such as a peer research assessment, median federal research activity per full-time faculty member, median GPA, median MCAT, acceptance rate, and faculty-student ratio.
In another scenario, he included four additional metrics: debt, in-state cost of attendance, USMLE Step 1 passing rate, and percentage of underrepresented students with minority race or ethnicity at the school.
For example, a user can rank the importance of the diversity of the class, amount of debt students expect to incur, and amount of research funding the medical school receives. After selecting those factors, the tool generates tiered results displayed in a circle, a shape chosen to avoid the appearance of the hierarchy associated with traditional rankings, Dr. Turner said.
“A prospective student might not care about acceptance rates and MCAT scores, and instead cares about diversity and debt,” Dr. Turner said. He looks forward to extending this approach to the ranking of colleges as well.
‘Imperfect measures’
“The model and interesting online tool that Dr. Turner created allows a premed [student] to generate custom rankings that are in line with their own priorities,” said Christopher Worsham, MD, MPH, a critical care physician in Mass General’s division of pulmonary and critical care medicine.
But Dr. Worsham, also a teaching associate at Harvard Medical School’s department of health care policy, expressed concern that factors figuring into the rankings by U.S. News and Dr. Turner’s alternative “are imperfect measures of medical school quality.”
For example, a student interested in research might favor federal research funding in their customized rankings with Dr. Turner’s model. “But higher research funding doesn’t necessarily translate into a better education for students, particularly when differentiating between two major research systems,” Dr. Worsham noted.
Dr. Worsham added that neither ranking system accurately predicts the quality of doctors graduating from the schools. Instead, he’d like to see ranking systems based on which schools’ graduates deliver the best patient outcomes, whether that’s through direct patient care, impactful research, or leadership within the health care system.
Michael Sauder, PhD, professor of sociology at the University of Iowa, Iowa City, said the model could offer a valuable alternative to the U.S. News ranking system. It might help users develop their own criteria for determining the ranking of medical schools, which is a big improvement over a “one-size-fits-all” approach, Dr. Sauder said.
And Hanna Stotland, an admission consultant based in Chicago, noted that most students rely on rankings because they “don’t have the luxury of advisers who know the ins and outs of different medical schools.” Given the role that rankings play, Ms. Stotland expects that every new ranking tool will have some influence on students.
This tool in particular “has the potential to be useful for students who have identified values they want their medical school to share.” For example, students who care about racial diversity “could use it to easily identify schools that are successful on that metric,” Ms. Stotland said.
Sujay Ratna, a 2nd-year med student at Icahn School of Medicine at Mount Sinai in New York, said he considered the U.S. News ranking his “go-to tool” when he was applying to med school.
But after reading Dr. Turner’s article, the AMSA membership vice president tried the algorithm. “I definitely would have used it had it existed when I was thinking of what schools to apply to and what [schools] to attend.”
The study had no specific funding. Dr. Turner, Dr. Worsham, Dr. Sauder, Ms. Stotland, Ms. Brett, and Mr. Ratna report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
For decades, pre-med students depended on the annual medical school rankings by U.S. News and World Report to decide where to apply for physician education. But after several prominent med schools pulled out of the rankings, one resident began experimenting with artificial intelligence (AI) to create an alternative.
Brandon Turner MD, MSc, a radiation oncology resident at Massachusetts General Hospital in Boston, developed a free do-it-yourself tool using AI that allows prospective students to rank medical schools based on considerations that are most important to them. His research was published online in JAMA Network Open.
“One of the flaws with conventional ranking systems is that the metrics used in these tools are weighted based on the preferences and views of the people who developed these rankings, but those may not work for everyone,” Dr. Turner told this news organization.
He explained that there are different types of metrics used in the U.S. News ranking: one for research and the other for primary care. “The research rankings carry the most prestige and are the ones that most people know about,” he explained. These metrics take into account factors such as how many grant dollars the medical school receives and the average size of those grants per faculty member, Dr. Turner said.
Admission metrics are also included – for example, the median grade point average or MCAT scores of students who have been accepted. “These don’t tell you anything about the research output of the school, only about how selective the school is,” he said.
Primary care metrics might focus on how many graduates of a given school go into primary care, or how other schools rate the quality of primary care training at a given school – a process called peer assessment, Dr. Turner said.
But even though these might be helpful, students may be more interested in the cost of attendance, average debt, representation of minorities, and how many graduates pass their boards, he said. “U.S. News metrics don’t capture these things, but I included them in my algorithm.”
A U.S. News spokesperson said that the publication continues to help students and their families make decisions about their future education. The spokesperson cited U.S. News’ explanation of how it calculates its rankings. “A school’s overall Best Medical Schools rank should be one consideration and not the lone determinant in where a student applies and accepts,” the article states.
Dr. Turner agreed ranking systems are a good starting point when researching med schools, “but the values reflected in the ranking may not reflect an individual’s goals.”
Tyra-Lee Brett, a premed student at the University of South Florida, Tampa, believes an additional tool for students to evaluate medical schools is needed – and she could potentially see herself using Dr. Turner’s creation.
Still, Ms. Brett, a premed trustee of the American Medical Student Association, doesn’t regard any ranking tool as the “be all and end all.” Rather, she feels that the most effective tool would be based on students’ lived experiences. The AMSA is developing a scorecard in which students grade schools based on their opinions about such issues as housing, family planning, and environmental health, she said.
No prior judgments
To develop his algorithm, Dr. Turner used a branch of AI called “unsupervised learning.” It doesn’t make a prior judgment about what the data should look like, Dr. Turner explained.
“You’re just analyzing natural trends within the data.”
The algorithm tries to find and discover clusters or patterns within the data. “It’s like saying to the algorithm: ‘I want you to tell me what schools you think should be grouped together based on the data I feed you,’ which is the data that the user selects based on his or her personal preferences.”
U.S. News has been transparent about the metrics it uses, Dr. Turner notes. “When I started looking into how rankings are developed, I saw that there was transparency, and the reasoning for choosing the metrics used to develop the ranking was pretty sound,” he said.
“But I didn’t see any justification as to why they chose the particular metrics and weighted them in the way that they did.”
Dr. Turner extracted data from the 2023 U.S. News report, which ranked 109 allopathic medical schools, and applied several scenarios to the results to create his alternative ranking system.
In one scenario, he used the same research metrics used by U.S. News, such as a peer research assessment, median federal research activity per full-time faculty member, median GPA, median MCAT, acceptance rate, and faculty-student ratio.
In another scenario, he included four additional metrics: debt, in-state cost of attendance, USMLE Step 1 passing rate, and percentage of underrepresented students with minority race or ethnicity at the school.
For example, a user can rank the importance of the diversity of the class, amount of debt students expect to incur, and amount of research funding the medical school receives. After selecting those factors, the tool generates tiered results displayed in a circle, a shape chosen to avoid the appearance of the hierarchy associated with traditional rankings, Dr. Turner said.
“A prospective student might not care about acceptance rates and MCAT scores, and instead cares about diversity and debt,” Dr. Turner said. He looks forward to extending this approach to the ranking of colleges as well.
‘Imperfect measures’
“The model and interesting online tool that Dr. Turner created allows a premed [student] to generate custom rankings that are in line with their own priorities,” said Christopher Worsham, MD, MPH, a critical care physician in Mass General’s division of pulmonary and critical care medicine.
But Dr. Worsham, also a teaching associate at Harvard Medical School’s department of health care policy, expressed concern that factors figuring into the rankings by U.S. News and Dr. Turner’s alternative “are imperfect measures of medical school quality.”
For example, a student interested in research might favor federal research funding in their customized rankings with Dr. Turner’s model. “But higher research funding doesn’t necessarily translate into a better education for students, particularly when differentiating between two major research systems,” Dr. Worsham noted.
Dr. Worsham added that neither ranking system accurately predicts the quality of doctors graduating from the schools. Instead, he’d like to see ranking systems based on which schools’ graduates deliver the best patient outcomes, whether that’s through direct patient care, impactful research, or leadership within the health care system.
Michael Sauder, PhD, professor of sociology at the University of Iowa, Iowa City, said the model could offer a valuable alternative to the U.S. News ranking system. It might help users develop their own criteria for determining the ranking of medical schools, which is a big improvement over a “one-size-fits-all” approach, Dr. Sauder said.
And Hanna Stotland, an admission consultant based in Chicago, noted that most students rely on rankings because they “don’t have the luxury of advisers who know the ins and outs of different medical schools.” Given the role that rankings play, Ms. Stotland expects that every new ranking tool will have some influence on students.
This tool in particular “has the potential to be useful for students who have identified values they want their medical school to share.” For example, students who care about racial diversity “could use it to easily identify schools that are successful on that metric,” Ms. Stotland said.
Sujay Ratna, a 2nd-year med student at Icahn School of Medicine at Mount Sinai in New York, said he considered the U.S. News ranking his “go-to tool” when he was applying to med school.
But after reading Dr. Turner’s article, the AMSA membership vice president tried the algorithm. “I definitely would have used it had it existed when I was thinking of what schools to apply to and what [schools] to attend.”
The study had no specific funding. Dr. Turner, Dr. Worsham, Dr. Sauder, Ms. Stotland, Ms. Brett, and Mr. Ratna report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
For decades, pre-med students depended on the annual medical school rankings by U.S. News and World Report to decide where to apply for physician education. But after several prominent med schools pulled out of the rankings, one resident began experimenting with artificial intelligence (AI) to create an alternative.
Brandon Turner MD, MSc, a radiation oncology resident at Massachusetts General Hospital in Boston, developed a free do-it-yourself tool using AI that allows prospective students to rank medical schools based on considerations that are most important to them. His research was published online in JAMA Network Open.
“One of the flaws with conventional ranking systems is that the metrics used in these tools are weighted based on the preferences and views of the people who developed these rankings, but those may not work for everyone,” Dr. Turner told this news organization.
He explained that there are different types of metrics used in the U.S. News ranking: one for research and the other for primary care. “The research rankings carry the most prestige and are the ones that most people know about,” he explained. These metrics take into account factors such as how many grant dollars the medical school receives and the average size of those grants per faculty member, Dr. Turner said.
Admission metrics are also included – for example, the median grade point average or MCAT scores of students who have been accepted. “These don’t tell you anything about the research output of the school, only about how selective the school is,” he said.
Primary care metrics might focus on how many graduates of a given school go into primary care, or how other schools rate the quality of primary care training at a given school – a process called peer assessment, Dr. Turner said.
But even though these might be helpful, students may be more interested in the cost of attendance, average debt, representation of minorities, and how many graduates pass their boards, he said. “U.S. News metrics don’t capture these things, but I included them in my algorithm.”
A U.S. News spokesperson said that the publication continues to help students and their families make decisions about their future education. The spokesperson cited U.S. News’ explanation of how it calculates its rankings. “A school’s overall Best Medical Schools rank should be one consideration and not the lone determinant in where a student applies and accepts,” the article states.
Dr. Turner agreed ranking systems are a good starting point when researching med schools, “but the values reflected in the ranking may not reflect an individual’s goals.”
Tyra-Lee Brett, a premed student at the University of South Florida, Tampa, believes an additional tool for students to evaluate medical schools is needed – and she could potentially see herself using Dr. Turner’s creation.
Still, Ms. Brett, a premed trustee of the American Medical Student Association, doesn’t regard any ranking tool as the “be all and end all.” Rather, she feels that the most effective tool would be based on students’ lived experiences. The AMSA is developing a scorecard in which students grade schools based on their opinions about such issues as housing, family planning, and environmental health, she said.
No prior judgments
To develop his algorithm, Dr. Turner used a branch of AI called “unsupervised learning.” It doesn’t make a prior judgment about what the data should look like, Dr. Turner explained.
“You’re just analyzing natural trends within the data.”
The algorithm tries to find and discover clusters or patterns within the data. “It’s like saying to the algorithm: ‘I want you to tell me what schools you think should be grouped together based on the data I feed you,’ which is the data that the user selects based on his or her personal preferences.”
U.S. News has been transparent about the metrics it uses, Dr. Turner notes. “When I started looking into how rankings are developed, I saw that there was transparency, and the reasoning for choosing the metrics used to develop the ranking was pretty sound,” he said.
“But I didn’t see any justification as to why they chose the particular metrics and weighted them in the way that they did.”
Dr. Turner extracted data from the 2023 U.S. News report, which ranked 109 allopathic medical schools, and applied several scenarios to the results to create his alternative ranking system.
In one scenario, he used the same research metrics used by U.S. News, such as a peer research assessment, median federal research activity per full-time faculty member, median GPA, median MCAT, acceptance rate, and faculty-student ratio.
In another scenario, he included four additional metrics: debt, in-state cost of attendance, USMLE Step 1 passing rate, and percentage of underrepresented students with minority race or ethnicity at the school.
For example, a user can rank the importance of the diversity of the class, amount of debt students expect to incur, and amount of research funding the medical school receives. After selecting those factors, the tool generates tiered results displayed in a circle, a shape chosen to avoid the appearance of the hierarchy associated with traditional rankings, Dr. Turner said.
“A prospective student might not care about acceptance rates and MCAT scores, and instead cares about diversity and debt,” Dr. Turner said. He looks forward to extending this approach to the ranking of colleges as well.
‘Imperfect measures’
“The model and interesting online tool that Dr. Turner created allows a premed [student] to generate custom rankings that are in line with their own priorities,” said Christopher Worsham, MD, MPH, a critical care physician in Mass General’s division of pulmonary and critical care medicine.
But Dr. Worsham, also a teaching associate at Harvard Medical School’s department of health care policy, expressed concern that factors figuring into the rankings by U.S. News and Dr. Turner’s alternative “are imperfect measures of medical school quality.”
For example, a student interested in research might favor federal research funding in their customized rankings with Dr. Turner’s model. “But higher research funding doesn’t necessarily translate into a better education for students, particularly when differentiating between two major research systems,” Dr. Worsham noted.
Dr. Worsham added that neither ranking system accurately predicts the quality of doctors graduating from the schools. Instead, he’d like to see ranking systems based on which schools’ graduates deliver the best patient outcomes, whether that’s through direct patient care, impactful research, or leadership within the health care system.
Michael Sauder, PhD, professor of sociology at the University of Iowa, Iowa City, said the model could offer a valuable alternative to the U.S. News ranking system. It might help users develop their own criteria for determining the ranking of medical schools, which is a big improvement over a “one-size-fits-all” approach, Dr. Sauder said.
And Hanna Stotland, an admission consultant based in Chicago, noted that most students rely on rankings because they “don’t have the luxury of advisers who know the ins and outs of different medical schools.” Given the role that rankings play, Ms. Stotland expects that every new ranking tool will have some influence on students.
This tool in particular “has the potential to be useful for students who have identified values they want their medical school to share.” For example, students who care about racial diversity “could use it to easily identify schools that are successful on that metric,” Ms. Stotland said.
Sujay Ratna, a 2nd-year med student at Icahn School of Medicine at Mount Sinai in New York, said he considered the U.S. News ranking his “go-to tool” when he was applying to med school.
But after reading Dr. Turner’s article, the AMSA membership vice president tried the algorithm. “I definitely would have used it had it existed when I was thinking of what schools to apply to and what [schools] to attend.”
The study had no specific funding. Dr. Turner, Dr. Worsham, Dr. Sauder, Ms. Stotland, Ms. Brett, and Mr. Ratna report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Q&A: What to know about the new BA 2.86 COVID variant
The Centers for Disease Control and Prevention and the World Health Organization have dubbed the BA 2.86 variant of COVID-19 as a variant to watch.
So far, only 26 cases of “Pirola,” as the new variant is being called, have been identified: 10 in Denmark, four each in Sweden and the United States, three in South Africa, two in Portugal, and one each the United Kingdom, Israel, and Canada. BA 2.86 is a subvariant of Omicron, but according to reports from the CDC, the strain has many more mutations than the ones that came before it.
With so many facts still unknown about this new variant, this news organization asked experts what people need to be aware of as it continues to spread.
What is unique about the BA 2.86 variant?
“It is unique in that it has more than three mutations on the spike protein,” said Purvi S. Parikh, MD, an infectious disease expert at New York University’s Langone Health. The virus uses the spike proteins to enter our cells.
This “may mean it will be more transmissible, cause more severe disease, and/or our vaccines and treatments may not work as well, as compared to other variants,” she said.
What do we need to watch with BA 2.86 going forward?
“We don’t know if this variant will be associated with a change in the disease severity. We currently see increased numbers of cases in general, even though we don’t yet see the BA.2.86 in our system,” said Heba Mostafa, PhD, director of the molecular virology laboratory at Johns Hopkins Hospital in Baltimore.
“It is important to monitor BA.2.86 (and other variants) and understand how its evolution impacts the number of cases and disease outcomes,” she said. “We should all be aware of the current increase in cases, though, and try to get tested and be treated as soon as possible, as antivirals should be effective against the circulating variants.”
What should doctors know?
Dr. Parikh said doctors should generally expect more COVID cases in their clinics and make sure to screen patients even if their symptoms are mild.
“We have tools that can be used – antivirals like Paxlovid are still efficacious with current dominant strains such as EG.5,” she said. “And encourage your patients to get their boosters, mask, wash hands, and social distance.”
How well can our vaccines fight BA 2.86?
“Vaccine coverage for the BA.2.86 is an area of uncertainty right now,” said Dr. Mostafa.
In its report, the CDC said scientists are still figuring out how well the updated COVID vaccine works. It’s expected to be available in the fall, and for now, they believe the new shot will still make infections less severe, new variants and all.
Prior vaccinations and infections have created antibodies in many people, and that will likely provide some protection, Dr. Mostafa said. “When we experienced the Omicron wave in December 2021, even though the variant was distant from what circulated before its emergence and was associated with a very large increase in the number of cases, vaccinations were still protective against severe disease.”
What is the most important thing to keep track of when it comes to this variant?
According to Dr. Parikh, “it’s most important to monitor how transmissible [BA 2.86] is, how severe it is, and if our current treatments and vaccines work.”
Dr. Mostafa said how well the new variants escape existing antibody protection should also be studied and watched closely.
What does this stage of the virus mutation tell us about where we are in the pandemic?
The history of the coronavirus over the past few years shows that variants with many changes evolve and can spread very quickly, Dr. Mostafa said. “Now that the virus is endemic, it is essential to monitor, update vaccinations if necessary, diagnose, treat, and implement infection control measures when necessary.”
With the limited data we have so far, experts seem to agree that while the variant’s makeup raises some red flags, it is too soon to jump to any conclusions about how easy it is to catch it and the ways it may change how the virus impacts those who contract it.
A version of this article first appeared on WebMD.com.
The Centers for Disease Control and Prevention and the World Health Organization have dubbed the BA 2.86 variant of COVID-19 as a variant to watch.
So far, only 26 cases of “Pirola,” as the new variant is being called, have been identified: 10 in Denmark, four each in Sweden and the United States, three in South Africa, two in Portugal, and one each the United Kingdom, Israel, and Canada. BA 2.86 is a subvariant of Omicron, but according to reports from the CDC, the strain has many more mutations than the ones that came before it.
With so many facts still unknown about this new variant, this news organization asked experts what people need to be aware of as it continues to spread.
What is unique about the BA 2.86 variant?
“It is unique in that it has more than three mutations on the spike protein,” said Purvi S. Parikh, MD, an infectious disease expert at New York University’s Langone Health. The virus uses the spike proteins to enter our cells.
This “may mean it will be more transmissible, cause more severe disease, and/or our vaccines and treatments may not work as well, as compared to other variants,” she said.
What do we need to watch with BA 2.86 going forward?
“We don’t know if this variant will be associated with a change in the disease severity. We currently see increased numbers of cases in general, even though we don’t yet see the BA.2.86 in our system,” said Heba Mostafa, PhD, director of the molecular virology laboratory at Johns Hopkins Hospital in Baltimore.
“It is important to monitor BA.2.86 (and other variants) and understand how its evolution impacts the number of cases and disease outcomes,” she said. “We should all be aware of the current increase in cases, though, and try to get tested and be treated as soon as possible, as antivirals should be effective against the circulating variants.”
What should doctors know?
Dr. Parikh said doctors should generally expect more COVID cases in their clinics and make sure to screen patients even if their symptoms are mild.
“We have tools that can be used – antivirals like Paxlovid are still efficacious with current dominant strains such as EG.5,” she said. “And encourage your patients to get their boosters, mask, wash hands, and social distance.”
How well can our vaccines fight BA 2.86?
“Vaccine coverage for the BA.2.86 is an area of uncertainty right now,” said Dr. Mostafa.
In its report, the CDC said scientists are still figuring out how well the updated COVID vaccine works. It’s expected to be available in the fall, and for now, they believe the new shot will still make infections less severe, new variants and all.
Prior vaccinations and infections have created antibodies in many people, and that will likely provide some protection, Dr. Mostafa said. “When we experienced the Omicron wave in December 2021, even though the variant was distant from what circulated before its emergence and was associated with a very large increase in the number of cases, vaccinations were still protective against severe disease.”
What is the most important thing to keep track of when it comes to this variant?
According to Dr. Parikh, “it’s most important to monitor how transmissible [BA 2.86] is, how severe it is, and if our current treatments and vaccines work.”
Dr. Mostafa said how well the new variants escape existing antibody protection should also be studied and watched closely.
What does this stage of the virus mutation tell us about where we are in the pandemic?
The history of the coronavirus over the past few years shows that variants with many changes evolve and can spread very quickly, Dr. Mostafa said. “Now that the virus is endemic, it is essential to monitor, update vaccinations if necessary, diagnose, treat, and implement infection control measures when necessary.”
With the limited data we have so far, experts seem to agree that while the variant’s makeup raises some red flags, it is too soon to jump to any conclusions about how easy it is to catch it and the ways it may change how the virus impacts those who contract it.
A version of this article first appeared on WebMD.com.
The Centers for Disease Control and Prevention and the World Health Organization have dubbed the BA 2.86 variant of COVID-19 as a variant to watch.
So far, only 26 cases of “Pirola,” as the new variant is being called, have been identified: 10 in Denmark, four each in Sweden and the United States, three in South Africa, two in Portugal, and one each the United Kingdom, Israel, and Canada. BA 2.86 is a subvariant of Omicron, but according to reports from the CDC, the strain has many more mutations than the ones that came before it.
With so many facts still unknown about this new variant, this news organization asked experts what people need to be aware of as it continues to spread.
What is unique about the BA 2.86 variant?
“It is unique in that it has more than three mutations on the spike protein,” said Purvi S. Parikh, MD, an infectious disease expert at New York University’s Langone Health. The virus uses the spike proteins to enter our cells.
This “may mean it will be more transmissible, cause more severe disease, and/or our vaccines and treatments may not work as well, as compared to other variants,” she said.
What do we need to watch with BA 2.86 going forward?
“We don’t know if this variant will be associated with a change in the disease severity. We currently see increased numbers of cases in general, even though we don’t yet see the BA.2.86 in our system,” said Heba Mostafa, PhD, director of the molecular virology laboratory at Johns Hopkins Hospital in Baltimore.
“It is important to monitor BA.2.86 (and other variants) and understand how its evolution impacts the number of cases and disease outcomes,” she said. “We should all be aware of the current increase in cases, though, and try to get tested and be treated as soon as possible, as antivirals should be effective against the circulating variants.”
What should doctors know?
Dr. Parikh said doctors should generally expect more COVID cases in their clinics and make sure to screen patients even if their symptoms are mild.
“We have tools that can be used – antivirals like Paxlovid are still efficacious with current dominant strains such as EG.5,” she said. “And encourage your patients to get their boosters, mask, wash hands, and social distance.”
How well can our vaccines fight BA 2.86?
“Vaccine coverage for the BA.2.86 is an area of uncertainty right now,” said Dr. Mostafa.
In its report, the CDC said scientists are still figuring out how well the updated COVID vaccine works. It’s expected to be available in the fall, and for now, they believe the new shot will still make infections less severe, new variants and all.
Prior vaccinations and infections have created antibodies in many people, and that will likely provide some protection, Dr. Mostafa said. “When we experienced the Omicron wave in December 2021, even though the variant was distant from what circulated before its emergence and was associated with a very large increase in the number of cases, vaccinations were still protective against severe disease.”
What is the most important thing to keep track of when it comes to this variant?
According to Dr. Parikh, “it’s most important to monitor how transmissible [BA 2.86] is, how severe it is, and if our current treatments and vaccines work.”
Dr. Mostafa said how well the new variants escape existing antibody protection should also be studied and watched closely.
What does this stage of the virus mutation tell us about where we are in the pandemic?
The history of the coronavirus over the past few years shows that variants with many changes evolve and can spread very quickly, Dr. Mostafa said. “Now that the virus is endemic, it is essential to monitor, update vaccinations if necessary, diagnose, treat, and implement infection control measures when necessary.”
With the limited data we have so far, experts seem to agree that while the variant’s makeup raises some red flags, it is too soon to jump to any conclusions about how easy it is to catch it and the ways it may change how the virus impacts those who contract it.
A version of this article first appeared on WebMD.com.
One in five men carries high-risk HPV in international study
Findings from a meta-analysis of 65 studies conducted in 35 countries indicate that These estimates provide further weight to arguments in favor of vaccinating boys against HPV to prevent certain types of cancer.
“Our results support that sexually active men, regardless of age, are an important reservoir of HPV genital infection,” wrote the authors in The Lancet Global Health . “These estimates emphasize the importance of incorporating men into comprehensive HPV prevention strategies to reduce HPV-related morbidity and mortality in men and ultimately achieve elimination of cervical cancer and other HPV-related diseases.”
Literature review
HPV infection is the most common sexually transmitted viral infection worldwide. More than 200 HPV types can be transmitted sexually, and at least 12 types are oncogenic. Previous studies have shown that most sexually active men and women acquire at least one genital HPV infection during their lifetime.
Although most HPV infections are asymptomatic, they can lead to cancer. Indeed, HPV is involved in the development of cervical, vulval, and vaginal cancers, as well as oropharyngeal and anal cancers, which also affect the male population. More than 25% of cancers caused by HPV occur in men.
Despite these observations, fewer epidemiologic studies have assessed HPV infection in men than in women. To determine the prevalence of HPV infection in the male population, Laia Bruni, MD, MPH, PhD, an epidemiologist at the Catalan Institute of Oncology in Barcelona, and her colleagues collated data from 65 studies conducted in 35 countries pertaining to males older than 15 years.
In this literature review, the researchers selected studies that reported infection rates in males without HPV-related symptoms. Studies conducted exclusively in populations that were considered at increased risk for sexually transmitted infections (STIs) were excluded. Overall, the analysis included close to 45,000 men.
Prevalent HPV genotype
Testing for HPV was conducted on samples collected from the anus and genitals. The results show a global pooled prevalence of HPV infection in males older than 15 years of 31% for any HPV and 21% for HR-HPV. One of these viruses, HPV-16, was the most prevalent HPV genotype (5% prevalence).
HPV prevalence was highest among young adults. It stabilized and decreased from age 50 years. Between ages 25 and 29 years, 35% of men are infected with HPV. It should be noted that prevalence is already high in the youngest group, reaching 28% in males between the ages of 15 and 19 years. The variations are similar for HR-HPV infections.
This age-related change is different from rates in women. Among the female population, HPV prevalence peaks soon after first sexual activity and declines with age, with a slight rebound after ages 50–55 years (i.e., often after or around the time of menopause), wrote the researchers.
The results also show country- and region-based disparities. The pooled prevalence for any HPV was highest in Sub-Saharan Africa (37%), followed by Europe and Northern America (36%). The lowest prevalence was in East and Southeast Asia (15%). Here again, the trends are similar with high-risk HPV.
Preventive measures
“Our study draws attention to the high prevalence, ranging from 20% to 30% for HR-HPV in men across most regions, and the need for strengthening HPV prevention within overall STI control efforts,” wrote the authors.
“Future epidemiological studies are needed to monitor trends in prevalence in men, especially considering the roll-out of HPV vaccination in girls and young women and that many countries are beginning to vaccinate boys.”
In France, the HPV vaccination program was extended in 2021 to include all boys between the ages of 11 and 14 years (two-dose schedule), with a catch-up course in males up to age 19 years (three-dose schedule). This is the same vaccine program as for girls. It is also recommended for men up to age 26 years who have sex with other men.
The 2023 return to school will see the launch of a general vaccination campaign aimed at seventh-grade students, both boys and girls, with parental consent, to increase vaccine coverage. In 2021, vaccine uptake was 43.6% in girls between the ages of 15 and 18 years and scarcely 6% in boys, according to Public Health France.
Two vaccines are in use: the bivalent Cervarix vaccine, which is effective against HPV-16 and HPV-18, and the nonavalent Gardasil 9, which is effective against types 16, 18, 31, 33, 45, 52, and 58. Both provide protection against HPV-16, the type most common in men, which is responsible for more than half of cases of cervical cancer.
This article was translated from the Medscape French Edition. A version appeared on Medscape.com.
Findings from a meta-analysis of 65 studies conducted in 35 countries indicate that These estimates provide further weight to arguments in favor of vaccinating boys against HPV to prevent certain types of cancer.
“Our results support that sexually active men, regardless of age, are an important reservoir of HPV genital infection,” wrote the authors in The Lancet Global Health . “These estimates emphasize the importance of incorporating men into comprehensive HPV prevention strategies to reduce HPV-related morbidity and mortality in men and ultimately achieve elimination of cervical cancer and other HPV-related diseases.”
Literature review
HPV infection is the most common sexually transmitted viral infection worldwide. More than 200 HPV types can be transmitted sexually, and at least 12 types are oncogenic. Previous studies have shown that most sexually active men and women acquire at least one genital HPV infection during their lifetime.
Although most HPV infections are asymptomatic, they can lead to cancer. Indeed, HPV is involved in the development of cervical, vulval, and vaginal cancers, as well as oropharyngeal and anal cancers, which also affect the male population. More than 25% of cancers caused by HPV occur in men.
Despite these observations, fewer epidemiologic studies have assessed HPV infection in men than in women. To determine the prevalence of HPV infection in the male population, Laia Bruni, MD, MPH, PhD, an epidemiologist at the Catalan Institute of Oncology in Barcelona, and her colleagues collated data from 65 studies conducted in 35 countries pertaining to males older than 15 years.
In this literature review, the researchers selected studies that reported infection rates in males without HPV-related symptoms. Studies conducted exclusively in populations that were considered at increased risk for sexually transmitted infections (STIs) were excluded. Overall, the analysis included close to 45,000 men.
Prevalent HPV genotype
Testing for HPV was conducted on samples collected from the anus and genitals. The results show a global pooled prevalence of HPV infection in males older than 15 years of 31% for any HPV and 21% for HR-HPV. One of these viruses, HPV-16, was the most prevalent HPV genotype (5% prevalence).
HPV prevalence was highest among young adults. It stabilized and decreased from age 50 years. Between ages 25 and 29 years, 35% of men are infected with HPV. It should be noted that prevalence is already high in the youngest group, reaching 28% in males between the ages of 15 and 19 years. The variations are similar for HR-HPV infections.
This age-related change is different from rates in women. Among the female population, HPV prevalence peaks soon after first sexual activity and declines with age, with a slight rebound after ages 50–55 years (i.e., often after or around the time of menopause), wrote the researchers.
The results also show country- and region-based disparities. The pooled prevalence for any HPV was highest in Sub-Saharan Africa (37%), followed by Europe and Northern America (36%). The lowest prevalence was in East and Southeast Asia (15%). Here again, the trends are similar with high-risk HPV.
Preventive measures
“Our study draws attention to the high prevalence, ranging from 20% to 30% for HR-HPV in men across most regions, and the need for strengthening HPV prevention within overall STI control efforts,” wrote the authors.
“Future epidemiological studies are needed to monitor trends in prevalence in men, especially considering the roll-out of HPV vaccination in girls and young women and that many countries are beginning to vaccinate boys.”
In France, the HPV vaccination program was extended in 2021 to include all boys between the ages of 11 and 14 years (two-dose schedule), with a catch-up course in males up to age 19 years (three-dose schedule). This is the same vaccine program as for girls. It is also recommended for men up to age 26 years who have sex with other men.
The 2023 return to school will see the launch of a general vaccination campaign aimed at seventh-grade students, both boys and girls, with parental consent, to increase vaccine coverage. In 2021, vaccine uptake was 43.6% in girls between the ages of 15 and 18 years and scarcely 6% in boys, according to Public Health France.
Two vaccines are in use: the bivalent Cervarix vaccine, which is effective against HPV-16 and HPV-18, and the nonavalent Gardasil 9, which is effective against types 16, 18, 31, 33, 45, 52, and 58. Both provide protection against HPV-16, the type most common in men, which is responsible for more than half of cases of cervical cancer.
This article was translated from the Medscape French Edition. A version appeared on Medscape.com.
Findings from a meta-analysis of 65 studies conducted in 35 countries indicate that These estimates provide further weight to arguments in favor of vaccinating boys against HPV to prevent certain types of cancer.
“Our results support that sexually active men, regardless of age, are an important reservoir of HPV genital infection,” wrote the authors in The Lancet Global Health . “These estimates emphasize the importance of incorporating men into comprehensive HPV prevention strategies to reduce HPV-related morbidity and mortality in men and ultimately achieve elimination of cervical cancer and other HPV-related diseases.”
Literature review
HPV infection is the most common sexually transmitted viral infection worldwide. More than 200 HPV types can be transmitted sexually, and at least 12 types are oncogenic. Previous studies have shown that most sexually active men and women acquire at least one genital HPV infection during their lifetime.
Although most HPV infections are asymptomatic, they can lead to cancer. Indeed, HPV is involved in the development of cervical, vulval, and vaginal cancers, as well as oropharyngeal and anal cancers, which also affect the male population. More than 25% of cancers caused by HPV occur in men.
Despite these observations, fewer epidemiologic studies have assessed HPV infection in men than in women. To determine the prevalence of HPV infection in the male population, Laia Bruni, MD, MPH, PhD, an epidemiologist at the Catalan Institute of Oncology in Barcelona, and her colleagues collated data from 65 studies conducted in 35 countries pertaining to males older than 15 years.
In this literature review, the researchers selected studies that reported infection rates in males without HPV-related symptoms. Studies conducted exclusively in populations that were considered at increased risk for sexually transmitted infections (STIs) were excluded. Overall, the analysis included close to 45,000 men.
Prevalent HPV genotype
Testing for HPV was conducted on samples collected from the anus and genitals. The results show a global pooled prevalence of HPV infection in males older than 15 years of 31% for any HPV and 21% for HR-HPV. One of these viruses, HPV-16, was the most prevalent HPV genotype (5% prevalence).
HPV prevalence was highest among young adults. It stabilized and decreased from age 50 years. Between ages 25 and 29 years, 35% of men are infected with HPV. It should be noted that prevalence is already high in the youngest group, reaching 28% in males between the ages of 15 and 19 years. The variations are similar for HR-HPV infections.
This age-related change is different from rates in women. Among the female population, HPV prevalence peaks soon after first sexual activity and declines with age, with a slight rebound after ages 50–55 years (i.e., often after or around the time of menopause), wrote the researchers.
The results also show country- and region-based disparities. The pooled prevalence for any HPV was highest in Sub-Saharan Africa (37%), followed by Europe and Northern America (36%). The lowest prevalence was in East and Southeast Asia (15%). Here again, the trends are similar with high-risk HPV.
Preventive measures
“Our study draws attention to the high prevalence, ranging from 20% to 30% for HR-HPV in men across most regions, and the need for strengthening HPV prevention within overall STI control efforts,” wrote the authors.
“Future epidemiological studies are needed to monitor trends in prevalence in men, especially considering the roll-out of HPV vaccination in girls and young women and that many countries are beginning to vaccinate boys.”
In France, the HPV vaccination program was extended in 2021 to include all boys between the ages of 11 and 14 years (two-dose schedule), with a catch-up course in males up to age 19 years (three-dose schedule). This is the same vaccine program as for girls. It is also recommended for men up to age 26 years who have sex with other men.
The 2023 return to school will see the launch of a general vaccination campaign aimed at seventh-grade students, both boys and girls, with parental consent, to increase vaccine coverage. In 2021, vaccine uptake was 43.6% in girls between the ages of 15 and 18 years and scarcely 6% in boys, according to Public Health France.
Two vaccines are in use: the bivalent Cervarix vaccine, which is effective against HPV-16 and HPV-18, and the nonavalent Gardasil 9, which is effective against types 16, 18, 31, 33, 45, 52, and 58. Both provide protection against HPV-16, the type most common in men, which is responsible for more than half of cases of cervical cancer.
This article was translated from the Medscape French Edition. A version appeared on Medscape.com.
FROM THE LANCET GLOBAL HEALTH
How to optimize in-hospital antimicrobial prescribing?
Variability in antimicrobial prescribing among hospital-based physicians is not associated with patient characteristics or clinical outcomes, data suggest. The lowest level of such prescribing within each hospital could be considered a target for antimicrobial stewardship, according to the researchers.
In a multicenter study of 124 physicians responsible for more than 124,000 hospitalized patients, the difference in mean prescribing between the highest and lowest quartiles of prescription volume was 15.8 days of treatment per 100 patient-days.
Baseline patient characteristics were similar across the quartiles, and there were no differences in patient outcomes, including in-hospital deaths, hospital length of stay, intensive care unit transfer, and hospital readmission.
Although the investigators expected variation in prescribing, “what surprised us most was the limited association with any differences in clinical outcomes, particularly when it came to the amount of antimicrobials used,” study author Mark T. McIntyre, PharmD, pharmacotherapy specialist at the Sinai Health System in Toronto, told this news organization.
“Importantly, this is not a study that defines quality of care,” he said. “We looked at natural variation in practice and association with outcomes. So, I don’t want clinicians to think, ‘Well, I’m high, therefore I’m bad,’ or, ‘I’m low, therefore I’m good.’
“This is an early explanatory analysis that asks whether this is an opportunity to optimize prescribing in ways we hadn’t thought of before,” he said. “Now that we don’t have an association with higher or lower prescribing and outcomes, we can look at what else is driving that antimicrobial prescribing and what we can do about it. Comfort level, risk tolerance, and social, cultural, and contextual factors all likely play a role.”
The study was published online in the Canadian Medical Association Journal.
Antimicrobial reductions possible
The investigators conducted a retrospective cohort study using the General Medicine Inpatient Initiative database to assess physician-level volume and spectrum of antimicrobial prescribing in adult general medical wards. Four academic hospitals in Toronto were evaluated for the period 2010 to 2019.
The investigators stratified physicians into quartiles by hospital site on the basis of volume of antimicrobial prescribing (specifically, days of therapy per 100 patient-days and antimicrobial-free days) and antibacterial spectrum (modified spectrum score, which assigns a value to each antibacterial agent on the basis of its breadth of coverage).
They also examined potential differences between physician quartiles in patient characteristics, such as age, sex, the Laboratory-Based Acute Physiology Score, discharge diagnosis, and the Charlson Comorbidity Index.
Multilevel modeling allowed the investigators to evaluate the association between clinical outcomes and antimicrobial volume and spectrum.
The primary measure was days of therapy per 100 patient-days.
As noted, the cohort included 124 physicians who were responsible for 124,158 hospital admissions. The median physician-level volume of antimicrobial prescribing was 56.1 days of therapy per 100 patient-days. Patient characteristics were balanced across the quartiles of physician prescribing.
The difference in mean prescribing between physician quartile 4 and quartile 1 was 15.8 days of therapy per 100 patient-days, meaning the median physician in quartile 4 prescribed antimicrobials at a volume that was 30% higher than that of the median physician in quartile 1.
No significant differences were noted for any clinical outcome with regard to quartile of days of therapy, antimicrobial-free days, or modified spectrum score after adjustment for patient-level characteristics.
In addition, no significant differences in the case mix between quartile 4 and quartile 1 were found when the cohort was restricted to patients admitted and discharged by the same most responsible person, nor were differences found in an analysis that was restricted to those without a discharge diagnosis code of palliative care.
In-hospital mortality was higher among patients cared for by prescribers with higher modified spectrum scores (odds ratio, 1.13). “We still can’t fully explain this finding,” Dr. McIntyre acknowledged. “We only saw that in our primary analysis. When we did several sensitivity analyses, that finding didn’t appear.”
The authors concluded, “Ultimately, without discernible benefit in outcomes of patients of physicians who prescribe more frequently, less antimicrobial exposure may be possible, leading to lower risk of antimicrobial resistance.”
Decision-making support
Commenting on the study, Lawrence I. Kaplan, MD, section chief of general internal medicine and associate dean for interprofessional education at the Lewis Katz School of Medicine at Temple University in Philadelphia, said, “Trying to get to the lowest quartile would be a goal, and given that physician characteristics are involved, I think there needs to be much better training in clinical management decision-making: how you come about making a decision based on a diagnosis for a particular patient, in or out of the hospital.” Dr. Kaplan was not involved in the research.
“Clinical decision-making tools that can be plugged into the electronic health record can help,” he suggested. “The tools basically ask if a patient meets certain criteria and then might give a prompt that says, for example, ‘These symptoms are not consistent with bacterial sinusitis. The patient should be treated with decongestants, nasal steroids, et cetera, because antibiotics aren’t appropriate.’
“It’s a bit like checkbox medicine, which a lot of physicians bridle at,” he said. “But if it’s really based on evidence, I think that’s an appropriate use of evidence-based medicine.”
Dr. Kaplan said that more research is needed into the best way to get a physician or any provider to step back and say, “Is this the right decision?” or, “I’m doing this but I’m really on shaky ground. What am I missing?’” He noted that the Society for Medical Decision Making publishes research and resources in this area.
“I love the fact that the paper was authored by an interdisciplinary group,” Dr. Kaplan added. “A pharmacist embedded in the team can, for example, help with treatment decision-making and point out potential drug interactions that prescribers might not be aware of.
“We need to stop practicing medicine siloed, which is what we do a lot of ways, both in the hospital and out of the hospital, because it’s the path of least resistance,” Dr. Kaplan added. “But when we can say, ‘Hey, I have a question about this,’ be it to a computer or a colleague, I would argue that we come up with better care.”
No funding was provided for the study. Dr. McIntyre and Dr. Kaplan have disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Variability in antimicrobial prescribing among hospital-based physicians is not associated with patient characteristics or clinical outcomes, data suggest. The lowest level of such prescribing within each hospital could be considered a target for antimicrobial stewardship, according to the researchers.
In a multicenter study of 124 physicians responsible for more than 124,000 hospitalized patients, the difference in mean prescribing between the highest and lowest quartiles of prescription volume was 15.8 days of treatment per 100 patient-days.
Baseline patient characteristics were similar across the quartiles, and there were no differences in patient outcomes, including in-hospital deaths, hospital length of stay, intensive care unit transfer, and hospital readmission.
Although the investigators expected variation in prescribing, “what surprised us most was the limited association with any differences in clinical outcomes, particularly when it came to the amount of antimicrobials used,” study author Mark T. McIntyre, PharmD, pharmacotherapy specialist at the Sinai Health System in Toronto, told this news organization.
“Importantly, this is not a study that defines quality of care,” he said. “We looked at natural variation in practice and association with outcomes. So, I don’t want clinicians to think, ‘Well, I’m high, therefore I’m bad,’ or, ‘I’m low, therefore I’m good.’
“This is an early explanatory analysis that asks whether this is an opportunity to optimize prescribing in ways we hadn’t thought of before,” he said. “Now that we don’t have an association with higher or lower prescribing and outcomes, we can look at what else is driving that antimicrobial prescribing and what we can do about it. Comfort level, risk tolerance, and social, cultural, and contextual factors all likely play a role.”
The study was published online in the Canadian Medical Association Journal.
Antimicrobial reductions possible
The investigators conducted a retrospective cohort study using the General Medicine Inpatient Initiative database to assess physician-level volume and spectrum of antimicrobial prescribing in adult general medical wards. Four academic hospitals in Toronto were evaluated for the period 2010 to 2019.
The investigators stratified physicians into quartiles by hospital site on the basis of volume of antimicrobial prescribing (specifically, days of therapy per 100 patient-days and antimicrobial-free days) and antibacterial spectrum (modified spectrum score, which assigns a value to each antibacterial agent on the basis of its breadth of coverage).
They also examined potential differences between physician quartiles in patient characteristics, such as age, sex, the Laboratory-Based Acute Physiology Score, discharge diagnosis, and the Charlson Comorbidity Index.
Multilevel modeling allowed the investigators to evaluate the association between clinical outcomes and antimicrobial volume and spectrum.
The primary measure was days of therapy per 100 patient-days.
As noted, the cohort included 124 physicians who were responsible for 124,158 hospital admissions. The median physician-level volume of antimicrobial prescribing was 56.1 days of therapy per 100 patient-days. Patient characteristics were balanced across the quartiles of physician prescribing.
The difference in mean prescribing between physician quartile 4 and quartile 1 was 15.8 days of therapy per 100 patient-days, meaning the median physician in quartile 4 prescribed antimicrobials at a volume that was 30% higher than that of the median physician in quartile 1.
No significant differences were noted for any clinical outcome with regard to quartile of days of therapy, antimicrobial-free days, or modified spectrum score after adjustment for patient-level characteristics.
In addition, no significant differences in the case mix between quartile 4 and quartile 1 were found when the cohort was restricted to patients admitted and discharged by the same most responsible person, nor were differences found in an analysis that was restricted to those without a discharge diagnosis code of palliative care.
In-hospital mortality was higher among patients cared for by prescribers with higher modified spectrum scores (odds ratio, 1.13). “We still can’t fully explain this finding,” Dr. McIntyre acknowledged. “We only saw that in our primary analysis. When we did several sensitivity analyses, that finding didn’t appear.”
The authors concluded, “Ultimately, without discernible benefit in outcomes of patients of physicians who prescribe more frequently, less antimicrobial exposure may be possible, leading to lower risk of antimicrobial resistance.”
Decision-making support
Commenting on the study, Lawrence I. Kaplan, MD, section chief of general internal medicine and associate dean for interprofessional education at the Lewis Katz School of Medicine at Temple University in Philadelphia, said, “Trying to get to the lowest quartile would be a goal, and given that physician characteristics are involved, I think there needs to be much better training in clinical management decision-making: how you come about making a decision based on a diagnosis for a particular patient, in or out of the hospital.” Dr. Kaplan was not involved in the research.
“Clinical decision-making tools that can be plugged into the electronic health record can help,” he suggested. “The tools basically ask if a patient meets certain criteria and then might give a prompt that says, for example, ‘These symptoms are not consistent with bacterial sinusitis. The patient should be treated with decongestants, nasal steroids, et cetera, because antibiotics aren’t appropriate.’
“It’s a bit like checkbox medicine, which a lot of physicians bridle at,” he said. “But if it’s really based on evidence, I think that’s an appropriate use of evidence-based medicine.”
Dr. Kaplan said that more research is needed into the best way to get a physician or any provider to step back and say, “Is this the right decision?” or, “I’m doing this but I’m really on shaky ground. What am I missing?’” He noted that the Society for Medical Decision Making publishes research and resources in this area.
“I love the fact that the paper was authored by an interdisciplinary group,” Dr. Kaplan added. “A pharmacist embedded in the team can, for example, help with treatment decision-making and point out potential drug interactions that prescribers might not be aware of.
“We need to stop practicing medicine siloed, which is what we do a lot of ways, both in the hospital and out of the hospital, because it’s the path of least resistance,” Dr. Kaplan added. “But when we can say, ‘Hey, I have a question about this,’ be it to a computer or a colleague, I would argue that we come up with better care.”
No funding was provided for the study. Dr. McIntyre and Dr. Kaplan have disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Variability in antimicrobial prescribing among hospital-based physicians is not associated with patient characteristics or clinical outcomes, data suggest. The lowest level of such prescribing within each hospital could be considered a target for antimicrobial stewardship, according to the researchers.
In a multicenter study of 124 physicians responsible for more than 124,000 hospitalized patients, the difference in mean prescribing between the highest and lowest quartiles of prescription volume was 15.8 days of treatment per 100 patient-days.
Baseline patient characteristics were similar across the quartiles, and there were no differences in patient outcomes, including in-hospital deaths, hospital length of stay, intensive care unit transfer, and hospital readmission.
Although the investigators expected variation in prescribing, “what surprised us most was the limited association with any differences in clinical outcomes, particularly when it came to the amount of antimicrobials used,” study author Mark T. McIntyre, PharmD, pharmacotherapy specialist at the Sinai Health System in Toronto, told this news organization.
“Importantly, this is not a study that defines quality of care,” he said. “We looked at natural variation in practice and association with outcomes. So, I don’t want clinicians to think, ‘Well, I’m high, therefore I’m bad,’ or, ‘I’m low, therefore I’m good.’
“This is an early explanatory analysis that asks whether this is an opportunity to optimize prescribing in ways we hadn’t thought of before,” he said. “Now that we don’t have an association with higher or lower prescribing and outcomes, we can look at what else is driving that antimicrobial prescribing and what we can do about it. Comfort level, risk tolerance, and social, cultural, and contextual factors all likely play a role.”
The study was published online in the Canadian Medical Association Journal.
Antimicrobial reductions possible
The investigators conducted a retrospective cohort study using the General Medicine Inpatient Initiative database to assess physician-level volume and spectrum of antimicrobial prescribing in adult general medical wards. Four academic hospitals in Toronto were evaluated for the period 2010 to 2019.
The investigators stratified physicians into quartiles by hospital site on the basis of volume of antimicrobial prescribing (specifically, days of therapy per 100 patient-days and antimicrobial-free days) and antibacterial spectrum (modified spectrum score, which assigns a value to each antibacterial agent on the basis of its breadth of coverage).
They also examined potential differences between physician quartiles in patient characteristics, such as age, sex, the Laboratory-Based Acute Physiology Score, discharge diagnosis, and the Charlson Comorbidity Index.
Multilevel modeling allowed the investigators to evaluate the association between clinical outcomes and antimicrobial volume and spectrum.
The primary measure was days of therapy per 100 patient-days.
As noted, the cohort included 124 physicians who were responsible for 124,158 hospital admissions. The median physician-level volume of antimicrobial prescribing was 56.1 days of therapy per 100 patient-days. Patient characteristics were balanced across the quartiles of physician prescribing.
The difference in mean prescribing between physician quartile 4 and quartile 1 was 15.8 days of therapy per 100 patient-days, meaning the median physician in quartile 4 prescribed antimicrobials at a volume that was 30% higher than that of the median physician in quartile 1.
No significant differences were noted for any clinical outcome with regard to quartile of days of therapy, antimicrobial-free days, or modified spectrum score after adjustment for patient-level characteristics.
In addition, no significant differences in the case mix between quartile 4 and quartile 1 were found when the cohort was restricted to patients admitted and discharged by the same most responsible person, nor were differences found in an analysis that was restricted to those without a discharge diagnosis code of palliative care.
In-hospital mortality was higher among patients cared for by prescribers with higher modified spectrum scores (odds ratio, 1.13). “We still can’t fully explain this finding,” Dr. McIntyre acknowledged. “We only saw that in our primary analysis. When we did several sensitivity analyses, that finding didn’t appear.”
The authors concluded, “Ultimately, without discernible benefit in outcomes of patients of physicians who prescribe more frequently, less antimicrobial exposure may be possible, leading to lower risk of antimicrobial resistance.”
Decision-making support
Commenting on the study, Lawrence I. Kaplan, MD, section chief of general internal medicine and associate dean for interprofessional education at the Lewis Katz School of Medicine at Temple University in Philadelphia, said, “Trying to get to the lowest quartile would be a goal, and given that physician characteristics are involved, I think there needs to be much better training in clinical management decision-making: how you come about making a decision based on a diagnosis for a particular patient, in or out of the hospital.” Dr. Kaplan was not involved in the research.
“Clinical decision-making tools that can be plugged into the electronic health record can help,” he suggested. “The tools basically ask if a patient meets certain criteria and then might give a prompt that says, for example, ‘These symptoms are not consistent with bacterial sinusitis. The patient should be treated with decongestants, nasal steroids, et cetera, because antibiotics aren’t appropriate.’
“It’s a bit like checkbox medicine, which a lot of physicians bridle at,” he said. “But if it’s really based on evidence, I think that’s an appropriate use of evidence-based medicine.”
Dr. Kaplan said that more research is needed into the best way to get a physician or any provider to step back and say, “Is this the right decision?” or, “I’m doing this but I’m really on shaky ground. What am I missing?’” He noted that the Society for Medical Decision Making publishes research and resources in this area.
“I love the fact that the paper was authored by an interdisciplinary group,” Dr. Kaplan added. “A pharmacist embedded in the team can, for example, help with treatment decision-making and point out potential drug interactions that prescribers might not be aware of.
“We need to stop practicing medicine siloed, which is what we do a lot of ways, both in the hospital and out of the hospital, because it’s the path of least resistance,” Dr. Kaplan added. “But when we can say, ‘Hey, I have a question about this,’ be it to a computer or a colleague, I would argue that we come up with better care.”
No funding was provided for the study. Dr. McIntyre and Dr. Kaplan have disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Making one key connection may increase HPV vax uptake
The understanding that human papillomavirus (HPV) causes oropharyngeal squamous cell carcinoma (OPSCC) has been linked with increased likelihood of adults having been vaccinated for HPV, new research indicates.
In a study published online in JAMA Otolaryngology–Head and Neck Surgery, most of the 288 adults surveyed with validated questions were not aware that HPV causes OPSCC and had not been told of the relationship by their health care provider.
Researchers found that when participants knew about the relationship between HPV infection and OPSCC they were more than three times as likely to be vaccinated (odds ratio, 3.7; 95% confidence interval, 1.8-7.6) as those without the knowledge.
The survey was paired with a novel point-of-care adult vaccination program within an otolaryngology clinic.
“Targeted education aimed at unvaccinated adults establishing the relationship between HPV infection and OPSCC, paired with point-of-care vaccination, may be an innovative strategy for increasing HPV vaccination rates in adults,” write the authors, led by Jacob C. Bloom, MD, with the department of otolaryngology–head and neck surgery at Boston Medical Center.
Current HPV vaccination recommendations include three parts:
- Routine vaccination at age 11 or 12 years
- Catch-up vaccination at ages 13-26 years if not adequately vaccinated
- Shared clinical decision-making in adults aged 27-45 years if the vaccine series has not been completed.
Despite proven efficacy and safety of the HPV vaccine, vaccination rates are low for adults. Although 75% of adolescents aged 13-17 years have initiated the HPV vaccine, recent studies show only 16% of U.S. men aged 18-21 years have received at least 1 dose of the HPV vaccine, the authors write.
Christiana Zhang, MD, with the division of internal medicine at Johns Hopkins University in Baltimore, who was not part of the study, said she was not surprised by the lack of knowledge about the HPV-OPSCC link.
Patients are often counseled on the relationship between HPV and genital warts or anogenital cancers like cervical cancer, she says, but there is less patient education surrounding the relationship between HPV and oropharyngeal cancers.
She says she does counsel patients on the link with OPSCC, but not all providers do and provider knowledge in general surrounding HPV is low.
“Research has shown that knowledge and confidence among health care providers surrounding HPV vaccination is generally low, and this corresponds with a low vaccination recommendation rate,” she says.
She adds, “Patient education on HPV infection and its relationship with OPSCC, paired with point-of-care vaccination for qualifying patients, is a great approach.”
But the education needs to go beyond patients, she says.
“Given the important role that health care providers play in vaccine uptake, I think further efforts are needed to educate providers on HPV vaccination as well,” she says.
The study included patients aged 18-45 years who sought routine outpatient care at the otolaryngology clinic at Boston Medical Center from Sept. 1, 2020, to May 19, 2021.
Limitations of this study include studying a population from a single otolaryngology clinic in an urban, academic medical center. The population was more racially and ethnically diverse than the U.S. population with 60.3% identifying as racial and ethnic minorities. Gender and educational levels were also not reflective of U.S. demographics as half (50.8%) of the participants had a college degree or higher and 58.3% were women.
Dr. Bloom reports grants from the American Head and Neck Cancer Society during the conduct of the study. Coauthor Dr. Faden reports personal fees from Merck, Neotic, Focus, BMS, Chrystalis Biomedical Advisors, and Guidepoint; receiving nonfinancial support from BostonGene and Predicine; and receiving grants from Calico outside the submitted work. Dr. Zhang reports no relevant financial relationships.
The understanding that human papillomavirus (HPV) causes oropharyngeal squamous cell carcinoma (OPSCC) has been linked with increased likelihood of adults having been vaccinated for HPV, new research indicates.
In a study published online in JAMA Otolaryngology–Head and Neck Surgery, most of the 288 adults surveyed with validated questions were not aware that HPV causes OPSCC and had not been told of the relationship by their health care provider.
Researchers found that when participants knew about the relationship between HPV infection and OPSCC they were more than three times as likely to be vaccinated (odds ratio, 3.7; 95% confidence interval, 1.8-7.6) as those without the knowledge.
The survey was paired with a novel point-of-care adult vaccination program within an otolaryngology clinic.
“Targeted education aimed at unvaccinated adults establishing the relationship between HPV infection and OPSCC, paired with point-of-care vaccination, may be an innovative strategy for increasing HPV vaccination rates in adults,” write the authors, led by Jacob C. Bloom, MD, with the department of otolaryngology–head and neck surgery at Boston Medical Center.
Current HPV vaccination recommendations include three parts:
- Routine vaccination at age 11 or 12 years
- Catch-up vaccination at ages 13-26 years if not adequately vaccinated
- Shared clinical decision-making in adults aged 27-45 years if the vaccine series has not been completed.
Despite proven efficacy and safety of the HPV vaccine, vaccination rates are low for adults. Although 75% of adolescents aged 13-17 years have initiated the HPV vaccine, recent studies show only 16% of U.S. men aged 18-21 years have received at least 1 dose of the HPV vaccine, the authors write.
Christiana Zhang, MD, with the division of internal medicine at Johns Hopkins University in Baltimore, who was not part of the study, said she was not surprised by the lack of knowledge about the HPV-OPSCC link.
Patients are often counseled on the relationship between HPV and genital warts or anogenital cancers like cervical cancer, she says, but there is less patient education surrounding the relationship between HPV and oropharyngeal cancers.
She says she does counsel patients on the link with OPSCC, but not all providers do and provider knowledge in general surrounding HPV is low.
“Research has shown that knowledge and confidence among health care providers surrounding HPV vaccination is generally low, and this corresponds with a low vaccination recommendation rate,” she says.
She adds, “Patient education on HPV infection and its relationship with OPSCC, paired with point-of-care vaccination for qualifying patients, is a great approach.”
But the education needs to go beyond patients, she says.
“Given the important role that health care providers play in vaccine uptake, I think further efforts are needed to educate providers on HPV vaccination as well,” she says.
The study included patients aged 18-45 years who sought routine outpatient care at the otolaryngology clinic at Boston Medical Center from Sept. 1, 2020, to May 19, 2021.
Limitations of this study include studying a population from a single otolaryngology clinic in an urban, academic medical center. The population was more racially and ethnically diverse than the U.S. population with 60.3% identifying as racial and ethnic minorities. Gender and educational levels were also not reflective of U.S. demographics as half (50.8%) of the participants had a college degree or higher and 58.3% were women.
Dr. Bloom reports grants from the American Head and Neck Cancer Society during the conduct of the study. Coauthor Dr. Faden reports personal fees from Merck, Neotic, Focus, BMS, Chrystalis Biomedical Advisors, and Guidepoint; receiving nonfinancial support from BostonGene and Predicine; and receiving grants from Calico outside the submitted work. Dr. Zhang reports no relevant financial relationships.
The understanding that human papillomavirus (HPV) causes oropharyngeal squamous cell carcinoma (OPSCC) has been linked with increased likelihood of adults having been vaccinated for HPV, new research indicates.
In a study published online in JAMA Otolaryngology–Head and Neck Surgery, most of the 288 adults surveyed with validated questions were not aware that HPV causes OPSCC and had not been told of the relationship by their health care provider.
Researchers found that when participants knew about the relationship between HPV infection and OPSCC they were more than three times as likely to be vaccinated (odds ratio, 3.7; 95% confidence interval, 1.8-7.6) as those without the knowledge.
The survey was paired with a novel point-of-care adult vaccination program within an otolaryngology clinic.
“Targeted education aimed at unvaccinated adults establishing the relationship between HPV infection and OPSCC, paired with point-of-care vaccination, may be an innovative strategy for increasing HPV vaccination rates in adults,” write the authors, led by Jacob C. Bloom, MD, with the department of otolaryngology–head and neck surgery at Boston Medical Center.
Current HPV vaccination recommendations include three parts:
- Routine vaccination at age 11 or 12 years
- Catch-up vaccination at ages 13-26 years if not adequately vaccinated
- Shared clinical decision-making in adults aged 27-45 years if the vaccine series has not been completed.
Despite proven efficacy and safety of the HPV vaccine, vaccination rates are low for adults. Although 75% of adolescents aged 13-17 years have initiated the HPV vaccine, recent studies show only 16% of U.S. men aged 18-21 years have received at least 1 dose of the HPV vaccine, the authors write.
Christiana Zhang, MD, with the division of internal medicine at Johns Hopkins University in Baltimore, who was not part of the study, said she was not surprised by the lack of knowledge about the HPV-OPSCC link.
Patients are often counseled on the relationship between HPV and genital warts or anogenital cancers like cervical cancer, she says, but there is less patient education surrounding the relationship between HPV and oropharyngeal cancers.
She says she does counsel patients on the link with OPSCC, but not all providers do and provider knowledge in general surrounding HPV is low.
“Research has shown that knowledge and confidence among health care providers surrounding HPV vaccination is generally low, and this corresponds with a low vaccination recommendation rate,” she says.
She adds, “Patient education on HPV infection and its relationship with OPSCC, paired with point-of-care vaccination for qualifying patients, is a great approach.”
But the education needs to go beyond patients, she says.
“Given the important role that health care providers play in vaccine uptake, I think further efforts are needed to educate providers on HPV vaccination as well,” she says.
The study included patients aged 18-45 years who sought routine outpatient care at the otolaryngology clinic at Boston Medical Center from Sept. 1, 2020, to May 19, 2021.
Limitations of this study include studying a population from a single otolaryngology clinic in an urban, academic medical center. The population was more racially and ethnically diverse than the U.S. population with 60.3% identifying as racial and ethnic minorities. Gender and educational levels were also not reflective of U.S. demographics as half (50.8%) of the participants had a college degree or higher and 58.3% were women.
Dr. Bloom reports grants from the American Head and Neck Cancer Society during the conduct of the study. Coauthor Dr. Faden reports personal fees from Merck, Neotic, Focus, BMS, Chrystalis Biomedical Advisors, and Guidepoint; receiving nonfinancial support from BostonGene and Predicine; and receiving grants from Calico outside the submitted work. Dr. Zhang reports no relevant financial relationships.
FROM JAMA OTOLARYNGOLOGY–HEAD AND NECK SURGERY
New RSV shot is a monoclonal antibody, not a vaccine
For the first time in the fall of 2023, families will be offered season-long protection for infants and some children against respiratory syncytial virus (RSV).
The Food and Drug Administration in July approved a prevention called nirsevimab (Beyfortus, AstraZeneca/Sanofi) and it is expected to be widely rolled out in the coming weeks as the RSV season begins.
And monoclonal antibodies are often used for treatment rather than prevention.
Adding to potential confusion is the fact the Centers for Disease Control and Prevention has included nirsevimab in the Vaccines for Children program, which covers the costs for uninsured kids and makes it more accessible.
Nirsevimab is approved for infants (up to 8 months old) born during or entering their first RSV season, and in children up to 2 years of age who are still vulnerable to severe RSV through their second season.
It’s recommended that all infants get one injection in their first 8 months for prevention instead of the previous monthly shots used to help prevent kids at high risk from getting severe RSV.
If monoclonal antibodies can be used for preventing disease in infants, could they become a viable vaccine alternative for adults?
Specialists say no.
That’s partly because of the difference in body size. Although an injection is an option for a newborn, pediatricians suggest, it would take far too much of the treatment to work as a shot for adults.
Ruth Karron, MD, an expert in pediatric infectious diseases at Johns Hopkins Medicine, Baltimore, said that, while vaccines come in small amounts and activate immune cells, monoclonal antibodies are more like a drug, with the dose based on weight.
“You’d have to give it intravenously,” for larger doses, she explained, which has never been studied before and would also be very expensive. “It really couldn’t be an option for adults.”
What’s the difference between vaccines and antibodies?
Monoclonal antibodies are proteins made in a lab to mimic the immune system’s ability to fight pathogens such as viruses.
Dr. Karron explained that a wide variety of monoclonal antibodies have long been used to treat diseases such as cancers and autoimmune disease. In recent years, the antibodies have been used to treat COVID.
Monoclonal antibodies have also been used to treat RSV in children, but the effects don’t last long – they confer passive immunity and “when it’s gone, it’s gone,” Dr. Karron said.
That means kids at high risk for severe RSV have had to get monthly injections.
But with nirsevimab, the mutated antibodies stay in circulation longer so they can last 5 or 6 months, enough to cover the RSV season, Dr. Karron explained. “It’s highly, highly effective.”
Vaccines train the body
“The idea with vaccines is that you engage the individual’s immune system. You teach it to make antibodies,” Dr. Karron said. Conversely, “you give an antibody and it’s good for as long as the antibody lasts. It’s not teaching your body anything.”
Frank Esper, MD, a pediatric infectious disease specialist at Cleveland Clinic Children’s Hospital, said monoclonal antibody protection for RSV is particularly welcome. “We’ve been trying to make an RSV vaccine since the 1960s and have done nothing but fail miserably.”
“The best thing is always a vaccine,” Dr. Esper said, explaining that vaccines teach the body to make its own antibodies and confer long-term protection and are “probably more efficacious than anything that’s ever manmade.
“But since we’ve really not done very well for pediatric RSV vaccines, nirsevimab is certainly something I’m looking forward to,” he said.
Fast-acting monoclonal antibodies
An advantage for monoclonal antibodies is that they start working almost immediately.
Children can get sick with RSV in the first few months of life so the speed of the monoclonal antibodies to begin protection is important, Dr. Esper said, adding that RSV “is the worst during the first year of life.”
The peak age for babies getting infected enough to require hospitalization is about 2 months, he said.
By 14 months, he said, kids’ immune systems and airways have matured enough “that it’s not nearly as bad.”
To get protection from a vaccine, he added, “usually takes 2-4 weeks from the time you get your shot to the time you see some benefit. With an antibody, you’re bypassing the processing that the body has to do, and it goes straight to ‘protection’ mode,” Dr. Esper said. “You get protected pretty much as soon as you get the antibody.”
A version of this article first appeared on Medscape.com.
For the first time in the fall of 2023, families will be offered season-long protection for infants and some children against respiratory syncytial virus (RSV).
The Food and Drug Administration in July approved a prevention called nirsevimab (Beyfortus, AstraZeneca/Sanofi) and it is expected to be widely rolled out in the coming weeks as the RSV season begins.
And monoclonal antibodies are often used for treatment rather than prevention.
Adding to potential confusion is the fact the Centers for Disease Control and Prevention has included nirsevimab in the Vaccines for Children program, which covers the costs for uninsured kids and makes it more accessible.
Nirsevimab is approved for infants (up to 8 months old) born during or entering their first RSV season, and in children up to 2 years of age who are still vulnerable to severe RSV through their second season.
It’s recommended that all infants get one injection in their first 8 months for prevention instead of the previous monthly shots used to help prevent kids at high risk from getting severe RSV.
If monoclonal antibodies can be used for preventing disease in infants, could they become a viable vaccine alternative for adults?
Specialists say no.
That’s partly because of the difference in body size. Although an injection is an option for a newborn, pediatricians suggest, it would take far too much of the treatment to work as a shot for adults.
Ruth Karron, MD, an expert in pediatric infectious diseases at Johns Hopkins Medicine, Baltimore, said that, while vaccines come in small amounts and activate immune cells, monoclonal antibodies are more like a drug, with the dose based on weight.
“You’d have to give it intravenously,” for larger doses, she explained, which has never been studied before and would also be very expensive. “It really couldn’t be an option for adults.”
What’s the difference between vaccines and antibodies?
Monoclonal antibodies are proteins made in a lab to mimic the immune system’s ability to fight pathogens such as viruses.
Dr. Karron explained that a wide variety of monoclonal antibodies have long been used to treat diseases such as cancers and autoimmune disease. In recent years, the antibodies have been used to treat COVID.
Monoclonal antibodies have also been used to treat RSV in children, but the effects don’t last long – they confer passive immunity and “when it’s gone, it’s gone,” Dr. Karron said.
That means kids at high risk for severe RSV have had to get monthly injections.
But with nirsevimab, the mutated antibodies stay in circulation longer so they can last 5 or 6 months, enough to cover the RSV season, Dr. Karron explained. “It’s highly, highly effective.”
Vaccines train the body
“The idea with vaccines is that you engage the individual’s immune system. You teach it to make antibodies,” Dr. Karron said. Conversely, “you give an antibody and it’s good for as long as the antibody lasts. It’s not teaching your body anything.”
Frank Esper, MD, a pediatric infectious disease specialist at Cleveland Clinic Children’s Hospital, said monoclonal antibody protection for RSV is particularly welcome. “We’ve been trying to make an RSV vaccine since the 1960s and have done nothing but fail miserably.”
“The best thing is always a vaccine,” Dr. Esper said, explaining that vaccines teach the body to make its own antibodies and confer long-term protection and are “probably more efficacious than anything that’s ever manmade.
“But since we’ve really not done very well for pediatric RSV vaccines, nirsevimab is certainly something I’m looking forward to,” he said.
Fast-acting monoclonal antibodies
An advantage for monoclonal antibodies is that they start working almost immediately.
Children can get sick with RSV in the first few months of life so the speed of the monoclonal antibodies to begin protection is important, Dr. Esper said, adding that RSV “is the worst during the first year of life.”
The peak age for babies getting infected enough to require hospitalization is about 2 months, he said.
By 14 months, he said, kids’ immune systems and airways have matured enough “that it’s not nearly as bad.”
To get protection from a vaccine, he added, “usually takes 2-4 weeks from the time you get your shot to the time you see some benefit. With an antibody, you’re bypassing the processing that the body has to do, and it goes straight to ‘protection’ mode,” Dr. Esper said. “You get protected pretty much as soon as you get the antibody.”
A version of this article first appeared on Medscape.com.
For the first time in the fall of 2023, families will be offered season-long protection for infants and some children against respiratory syncytial virus (RSV).
The Food and Drug Administration in July approved a prevention called nirsevimab (Beyfortus, AstraZeneca/Sanofi) and it is expected to be widely rolled out in the coming weeks as the RSV season begins.
And monoclonal antibodies are often used for treatment rather than prevention.
Adding to potential confusion is the fact the Centers for Disease Control and Prevention has included nirsevimab in the Vaccines for Children program, which covers the costs for uninsured kids and makes it more accessible.
Nirsevimab is approved for infants (up to 8 months old) born during or entering their first RSV season, and in children up to 2 years of age who are still vulnerable to severe RSV through their second season.
It’s recommended that all infants get one injection in their first 8 months for prevention instead of the previous monthly shots used to help prevent kids at high risk from getting severe RSV.
If monoclonal antibodies can be used for preventing disease in infants, could they become a viable vaccine alternative for adults?
Specialists say no.
That’s partly because of the difference in body size. Although an injection is an option for a newborn, pediatricians suggest, it would take far too much of the treatment to work as a shot for adults.
Ruth Karron, MD, an expert in pediatric infectious diseases at Johns Hopkins Medicine, Baltimore, said that, while vaccines come in small amounts and activate immune cells, monoclonal antibodies are more like a drug, with the dose based on weight.
“You’d have to give it intravenously,” for larger doses, she explained, which has never been studied before and would also be very expensive. “It really couldn’t be an option for adults.”
What’s the difference between vaccines and antibodies?
Monoclonal antibodies are proteins made in a lab to mimic the immune system’s ability to fight pathogens such as viruses.
Dr. Karron explained that a wide variety of monoclonal antibodies have long been used to treat diseases such as cancers and autoimmune disease. In recent years, the antibodies have been used to treat COVID.
Monoclonal antibodies have also been used to treat RSV in children, but the effects don’t last long – they confer passive immunity and “when it’s gone, it’s gone,” Dr. Karron said.
That means kids at high risk for severe RSV have had to get monthly injections.
But with nirsevimab, the mutated antibodies stay in circulation longer so they can last 5 or 6 months, enough to cover the RSV season, Dr. Karron explained. “It’s highly, highly effective.”
Vaccines train the body
“The idea with vaccines is that you engage the individual’s immune system. You teach it to make antibodies,” Dr. Karron said. Conversely, “you give an antibody and it’s good for as long as the antibody lasts. It’s not teaching your body anything.”
Frank Esper, MD, a pediatric infectious disease specialist at Cleveland Clinic Children’s Hospital, said monoclonal antibody protection for RSV is particularly welcome. “We’ve been trying to make an RSV vaccine since the 1960s and have done nothing but fail miserably.”
“The best thing is always a vaccine,” Dr. Esper said, explaining that vaccines teach the body to make its own antibodies and confer long-term protection and are “probably more efficacious than anything that’s ever manmade.
“But since we’ve really not done very well for pediatric RSV vaccines, nirsevimab is certainly something I’m looking forward to,” he said.
Fast-acting monoclonal antibodies
An advantage for monoclonal antibodies is that they start working almost immediately.
Children can get sick with RSV in the first few months of life so the speed of the monoclonal antibodies to begin protection is important, Dr. Esper said, adding that RSV “is the worst during the first year of life.”
The peak age for babies getting infected enough to require hospitalization is about 2 months, he said.
By 14 months, he said, kids’ immune systems and airways have matured enough “that it’s not nearly as bad.”
To get protection from a vaccine, he added, “usually takes 2-4 weeks from the time you get your shot to the time you see some benefit. With an antibody, you’re bypassing the processing that the body has to do, and it goes straight to ‘protection’ mode,” Dr. Esper said. “You get protected pretty much as soon as you get the antibody.”
A version of this article first appeared on Medscape.com.