User login
ID Practitioner is an independent news source that provides infectious disease specialists with timely and relevant news and commentary about clinical developments and the impact of health care policy on the infectious disease specialist’s practice. Specialty focus topics include antimicrobial resistance, emerging infections, global ID, hepatitis, HIV, hospital-acquired infections, immunizations and vaccines, influenza, mycoses, pediatric infections, and STIs. Infectious Diseases News is owned by Frontline Medical Communications.
sofosbuvir
ritonavir with dasabuvir
discount
support path
program
ritonavir
greedy
ledipasvir
assistance
viekira pak
vpak
advocacy
needy
protest
abbvie
paritaprevir
ombitasvir
direct-acting antivirals
dasabuvir
gilead
fake-ovir
support
v pak
oasis
harvoni
section[contains(@class, 'footer-nav-section-wrapper')]
div[contains(@class, 'pane-pub-article-idp')]
div[contains(@class, 'pane-medstat-latest-articles-articles-section')]
div[contains(@class, 'pane-pub-home-idp')]
div[contains(@class, 'pane-pub-topic-idp')]
Creatine may improve key long COVID symptoms: Small study
Taking creatine as a supplement for 6 months appears to significantly improve clinical features of post–COVID-19 fatigue syndrome (PVFS or long COVID), a small randomized, placebo-controlled, double-blinded study suggests.
Researchers, led by Jelena Slankamenac, with Applied Bioenergetics Lab, Faculty of Sport and PE, University of Novi Sad, Serbia, published their findings in Food, Science & Nutrition .
“This is the first human study known to the authors that evaluated the efficacy and safety of supplemental creatine for fatigue, tissue bioenergetics, and patient-reported outcomes in patients with post–COVID-19 fatigue syndrome,” the authors write.
They say the findings may be attributed to creatine’s “energy-replenishing and neuroprotective activity.”
Significant reductions in symptoms
Researchers randomized the 12 participants into two groups of 6 each. The creatine group received 4 g creatine monohydrate per day, while the placebo group received the same amount of inulin.
At 3 months, dietary creatine supplements produced a significant reduction in fatigue, compared with baseline values ( P = .04) and significantly improved scores for several long COVID–related symptoms, including loss of taste, breathing difficulties, body aches, headache, and difficulties concentrating) ( P < .05), the researchers report.
Intervention effect sizes were assessed by Cohen statistics, with a d of at least 0.8 indicating a large effect.
Among highlights of the results were that patients reported a significant 77.8% drop in scores for concentration difficulties at the 3-month follow-up (Cohen’s effect, d = 1.19) and no concentration difficulties at the 6-month follow-up (Cohen’s effect, d = 2.46).
Total creatine levels increased in several locations across the brain (as much as 33% for right parietal white matter). No changes in tissue creatine levels were found in the placebo group during the trial.
“Since PVFS is characterized by impaired tissue bioenergetics ..., supplemental creatine might be an effective dietary intervention to uphold brain creatine in post–COVID-19 fatigue syndrome,” the authors write.
The authors add that creatine supplements for long COVID patients could benefit organs beyond the brain as participants saw “a significant drop in lung and body pain after the intervention.”
Unanswered questions
Some experts said the results should be interpreted with caution.
“This research paper is very interesting,” says Nisha Viswanathan, MD, director of the long COVID program at University of California, Los Angeles, “but the limited number of patients makes the results difficult to generalize.”
Dr. Viswanathan, who was not part of the study, pointed out that the patients included in this study had a recent COVID infection (under 3 months).
“Acute COVID infection can take up to 3 months to resolve,” she says. “We define patients with long COVID as those with symptoms lasting greater than 3 months. Therefore, these patients could have had improvements in their fatigue due to the natural course of the illness rather than creatine supplementation.”
Alba Azola, MD, assistant professor in the department of physical medicine and rehabilitation at Johns Hopkins University, Baltimore, said she also was troubled by the window of 3 months for recent COVID infection.
She said she would like to see results for patients who have ongoing symptoms for at least 6 months after infection, especially given creatine supplements’ history in research.
Creatine supplements for other conditions, such as fibromyalgia and chronic fatigue syndrome, have been tested for nearly 2 decades, she pointed out, with conflicting findings, something the authors acknowledge in the paper.
“I think it’s premature to say (creatine) is the key,” she says. She added that the small sample size is important to consider given the heterogeneity of patients with long COVID.
That said, Dr. Azola says, she applauds all efforts to find treatments for long COVID, especially randomized, controlled studies like this one.
No major side effects
No major side effects were reported for either intervention, except for transient mild nausea reported by one patient after taking creatine.
Compliance with the intervention was 90.6% ± 3.5% in the creatine group and 95.3% ± 5.0% in the control group (P = .04).
Participants were eligible for inclusion if they were 18-65 years old, had a positive COVID test within the last 3 months (documented by a valid polymerase chain reaction [PCR] or antigen test performed in a COVID-19–certified lab); had moderate to severe fatigue; and at least one additional COVID-related symptom, including loss of taste or smell, breathing trouble, lung pain, body aches, headaches, or difficulties concentrating.
The authors acknowledge that they selected a sample of young to middle-aged adults experiencing moderate long COVID symptoms, and it’s unknown whether creatine is equally effective in other PVFS populations, such as elderly people, children, or patients with less or more severe disease.
Senior author Dr. Sergei Ostojic serves as a member of the Scientific Advisory Board on creatine in health and medicine (AlzChem LLC). He co-owns a patent for “Supplements Based on Liquid Creatine” at the European Patent Office. He has received research support related to creatine during the past 36 months from the Serbian Ministry of Education, Science, and Technological Development; Provincial Secretariat for Higher Education and Scientific Research; Alzchem GmbH; ThermoLife International; and Hueston Hennigan LLP. He does not own stocks and shares in any organization. Other authors declare no known relevant financial interests. Dr. Viswanathan and Dr. Azola report no relevant financial relationships.
Taking creatine as a supplement for 6 months appears to significantly improve clinical features of post–COVID-19 fatigue syndrome (PVFS or long COVID), a small randomized, placebo-controlled, double-blinded study suggests.
Researchers, led by Jelena Slankamenac, with Applied Bioenergetics Lab, Faculty of Sport and PE, University of Novi Sad, Serbia, published their findings in Food, Science & Nutrition .
“This is the first human study known to the authors that evaluated the efficacy and safety of supplemental creatine for fatigue, tissue bioenergetics, and patient-reported outcomes in patients with post–COVID-19 fatigue syndrome,” the authors write.
They say the findings may be attributed to creatine’s “energy-replenishing and neuroprotective activity.”
Significant reductions in symptoms
Researchers randomized the 12 participants into two groups of 6 each. The creatine group received 4 g creatine monohydrate per day, while the placebo group received the same amount of inulin.
At 3 months, dietary creatine supplements produced a significant reduction in fatigue, compared with baseline values ( P = .04) and significantly improved scores for several long COVID–related symptoms, including loss of taste, breathing difficulties, body aches, headache, and difficulties concentrating) ( P < .05), the researchers report.
Intervention effect sizes were assessed by Cohen statistics, with a d of at least 0.8 indicating a large effect.
Among highlights of the results were that patients reported a significant 77.8% drop in scores for concentration difficulties at the 3-month follow-up (Cohen’s effect, d = 1.19) and no concentration difficulties at the 6-month follow-up (Cohen’s effect, d = 2.46).
Total creatine levels increased in several locations across the brain (as much as 33% for right parietal white matter). No changes in tissue creatine levels were found in the placebo group during the trial.
“Since PVFS is characterized by impaired tissue bioenergetics ..., supplemental creatine might be an effective dietary intervention to uphold brain creatine in post–COVID-19 fatigue syndrome,” the authors write.
The authors add that creatine supplements for long COVID patients could benefit organs beyond the brain as participants saw “a significant drop in lung and body pain after the intervention.”
Unanswered questions
Some experts said the results should be interpreted with caution.
“This research paper is very interesting,” says Nisha Viswanathan, MD, director of the long COVID program at University of California, Los Angeles, “but the limited number of patients makes the results difficult to generalize.”
Dr. Viswanathan, who was not part of the study, pointed out that the patients included in this study had a recent COVID infection (under 3 months).
“Acute COVID infection can take up to 3 months to resolve,” she says. “We define patients with long COVID as those with symptoms lasting greater than 3 months. Therefore, these patients could have had improvements in their fatigue due to the natural course of the illness rather than creatine supplementation.”
Alba Azola, MD, assistant professor in the department of physical medicine and rehabilitation at Johns Hopkins University, Baltimore, said she also was troubled by the window of 3 months for recent COVID infection.
She said she would like to see results for patients who have ongoing symptoms for at least 6 months after infection, especially given creatine supplements’ history in research.
Creatine supplements for other conditions, such as fibromyalgia and chronic fatigue syndrome, have been tested for nearly 2 decades, she pointed out, with conflicting findings, something the authors acknowledge in the paper.
“I think it’s premature to say (creatine) is the key,” she says. She added that the small sample size is important to consider given the heterogeneity of patients with long COVID.
That said, Dr. Azola says, she applauds all efforts to find treatments for long COVID, especially randomized, controlled studies like this one.
No major side effects
No major side effects were reported for either intervention, except for transient mild nausea reported by one patient after taking creatine.
Compliance with the intervention was 90.6% ± 3.5% in the creatine group and 95.3% ± 5.0% in the control group (P = .04).
Participants were eligible for inclusion if they were 18-65 years old, had a positive COVID test within the last 3 months (documented by a valid polymerase chain reaction [PCR] or antigen test performed in a COVID-19–certified lab); had moderate to severe fatigue; and at least one additional COVID-related symptom, including loss of taste or smell, breathing trouble, lung pain, body aches, headaches, or difficulties concentrating.
The authors acknowledge that they selected a sample of young to middle-aged adults experiencing moderate long COVID symptoms, and it’s unknown whether creatine is equally effective in other PVFS populations, such as elderly people, children, or patients with less or more severe disease.
Senior author Dr. Sergei Ostojic serves as a member of the Scientific Advisory Board on creatine in health and medicine (AlzChem LLC). He co-owns a patent for “Supplements Based on Liquid Creatine” at the European Patent Office. He has received research support related to creatine during the past 36 months from the Serbian Ministry of Education, Science, and Technological Development; Provincial Secretariat for Higher Education and Scientific Research; Alzchem GmbH; ThermoLife International; and Hueston Hennigan LLP. He does not own stocks and shares in any organization. Other authors declare no known relevant financial interests. Dr. Viswanathan and Dr. Azola report no relevant financial relationships.
Taking creatine as a supplement for 6 months appears to significantly improve clinical features of post–COVID-19 fatigue syndrome (PVFS or long COVID), a small randomized, placebo-controlled, double-blinded study suggests.
Researchers, led by Jelena Slankamenac, with Applied Bioenergetics Lab, Faculty of Sport and PE, University of Novi Sad, Serbia, published their findings in Food, Science & Nutrition .
“This is the first human study known to the authors that evaluated the efficacy and safety of supplemental creatine for fatigue, tissue bioenergetics, and patient-reported outcomes in patients with post–COVID-19 fatigue syndrome,” the authors write.
They say the findings may be attributed to creatine’s “energy-replenishing and neuroprotective activity.”
Significant reductions in symptoms
Researchers randomized the 12 participants into two groups of 6 each. The creatine group received 4 g creatine monohydrate per day, while the placebo group received the same amount of inulin.
At 3 months, dietary creatine supplements produced a significant reduction in fatigue, compared with baseline values ( P = .04) and significantly improved scores for several long COVID–related symptoms, including loss of taste, breathing difficulties, body aches, headache, and difficulties concentrating) ( P < .05), the researchers report.
Intervention effect sizes were assessed by Cohen statistics, with a d of at least 0.8 indicating a large effect.
Among highlights of the results were that patients reported a significant 77.8% drop in scores for concentration difficulties at the 3-month follow-up (Cohen’s effect, d = 1.19) and no concentration difficulties at the 6-month follow-up (Cohen’s effect, d = 2.46).
Total creatine levels increased in several locations across the brain (as much as 33% for right parietal white matter). No changes in tissue creatine levels were found in the placebo group during the trial.
“Since PVFS is characterized by impaired tissue bioenergetics ..., supplemental creatine might be an effective dietary intervention to uphold brain creatine in post–COVID-19 fatigue syndrome,” the authors write.
The authors add that creatine supplements for long COVID patients could benefit organs beyond the brain as participants saw “a significant drop in lung and body pain after the intervention.”
Unanswered questions
Some experts said the results should be interpreted with caution.
“This research paper is very interesting,” says Nisha Viswanathan, MD, director of the long COVID program at University of California, Los Angeles, “but the limited number of patients makes the results difficult to generalize.”
Dr. Viswanathan, who was not part of the study, pointed out that the patients included in this study had a recent COVID infection (under 3 months).
“Acute COVID infection can take up to 3 months to resolve,” she says. “We define patients with long COVID as those with symptoms lasting greater than 3 months. Therefore, these patients could have had improvements in their fatigue due to the natural course of the illness rather than creatine supplementation.”
Alba Azola, MD, assistant professor in the department of physical medicine and rehabilitation at Johns Hopkins University, Baltimore, said she also was troubled by the window of 3 months for recent COVID infection.
She said she would like to see results for patients who have ongoing symptoms for at least 6 months after infection, especially given creatine supplements’ history in research.
Creatine supplements for other conditions, such as fibromyalgia and chronic fatigue syndrome, have been tested for nearly 2 decades, she pointed out, with conflicting findings, something the authors acknowledge in the paper.
“I think it’s premature to say (creatine) is the key,” she says. She added that the small sample size is important to consider given the heterogeneity of patients with long COVID.
That said, Dr. Azola says, she applauds all efforts to find treatments for long COVID, especially randomized, controlled studies like this one.
No major side effects
No major side effects were reported for either intervention, except for transient mild nausea reported by one patient after taking creatine.
Compliance with the intervention was 90.6% ± 3.5% in the creatine group and 95.3% ± 5.0% in the control group (P = .04).
Participants were eligible for inclusion if they were 18-65 years old, had a positive COVID test within the last 3 months (documented by a valid polymerase chain reaction [PCR] or antigen test performed in a COVID-19–certified lab); had moderate to severe fatigue; and at least one additional COVID-related symptom, including loss of taste or smell, breathing trouble, lung pain, body aches, headaches, or difficulties concentrating.
The authors acknowledge that they selected a sample of young to middle-aged adults experiencing moderate long COVID symptoms, and it’s unknown whether creatine is equally effective in other PVFS populations, such as elderly people, children, or patients with less or more severe disease.
Senior author Dr. Sergei Ostojic serves as a member of the Scientific Advisory Board on creatine in health and medicine (AlzChem LLC). He co-owns a patent for “Supplements Based on Liquid Creatine” at the European Patent Office. He has received research support related to creatine during the past 36 months from the Serbian Ministry of Education, Science, and Technological Development; Provincial Secretariat for Higher Education and Scientific Research; Alzchem GmbH; ThermoLife International; and Hueston Hennigan LLP. He does not own stocks and shares in any organization. Other authors declare no known relevant financial interests. Dr. Viswanathan and Dr. Azola report no relevant financial relationships.
FROM FOOD, SCIENCE & NUTRITION
Primary care clinicians should spearhead HIV prevention
HIV continues to be a significant public health concern in the United States, with an estimated 1.2 million people currently living with the virus and more than 30,000 new diagnoses in 2020 alone.
Primary care clinicians can help decrease rates of HIV infection by prescribing pre-exposure prophylaxis to people who are sexually active.
But many do not.
“In medical school, we don’t spend much time discussing sexuality, sexual behavior, sexually transmitted infections, and such, so providers may feel uncomfortable asking what kind of sex their patient is having and with whom, whether they use a condom, and other basics,” said Matthew M. Hamill, MBChB, PhD, MPH, a specialist in sexually transmitted diseases at Johns Hopkins Medicine, Baltimore.
PrEP (pre-exposure prophylaxis) is an antiviral medication that cuts the risk of contracting HIV through sex by around 99% when taken as prescribed, according to the Centers for Disease Control and Prevention.
“Many people who would benefit from PrEP are not receiving this highly effective medication,” said John B. Wong, MD, a primary care internist and professor of medicine at Tufts University, Boston. The gap is particularly acute among Black, Hispanic, and Latino people, who are significantly more likely to be diagnosed with HIV but are much less likely than Whites to receive PrEP, he said.
Dr. Wong, a member of the U.S. Preventive Services Task Force, helped write the group’s new PrEP recommendations. Published in August, the guidelines call for clinicians to prescribe the drugs to adolescents and adults who do not have HIV but are at an increased risk for infection.
“Primary care physicians are ideally positioned to prescribe PrEP for their patients because they have longitudinal relationships: They get to know their patients, and hopefully their patients feel comfortable talking with them about their sexual health,” said Brandon Pollak, MD, a primary care physician and HIV specialist at the Ohio State University College of Medicine, Columbus.
Dr. Pollak, who was not involved with the USPSTF recommendations, cares for patients who are heterosexual and living with HIV.
Clinicians should consider PrEP for all patients who have sex with someone who has HIV, do not use condoms, or have had a sexually transmitted infection within the previous 6 months. Men who have sex with men, transgender women who have sex with men, people who inject illicit drugs or engage in transactional sex, and Black, Hispanic, and Latino individuals also are at increased risk for the infection.
“The vast majority of patients on PrEP in any form sail through with no problems; they have regular lab work and can follow up in person or by telemedicine,” Dr. Hamill said. “They tend to be young, fit people without complicated medical histories, and the medications are very well-tolerated, particularly if people expect some short-term side effects.”
What you need to know when prescribing PrEP
Prescribing PrEP is similar in complexity to prescribing hypertension or diabetes medications, Dr. Hamill said.
Because taking the medications while already infected with the virus can lead to the emergence of drug-resistant HIV, patients must have a negative HIV test before starting PrEP. In addition, the USPSTF recommends testing for other sexually transmitted infections and for pregnancy, if appropriate. The task force also recommends conducting kidney function and hepatitis B tests, and a lipid profile before starting specific types of PrEP.
HIV screening is also recommended at 3-month intervals.
“Providers may order labs done at 3- to 4-month intervals but only see patients in clinic once or twice per year, depending on patient needs and risk behaviors,” said Jill S. Blumenthal, MD, associate professor of medicine at UC San Diego Health.
Clinicians should consider medication adherence and whether a patient is likely to take a pill once a day or could benefit from receiving an injection every 2 months. Patients may experience side effects such as diarrhea or headache with oral PrEP or soreness at the injection site. In rare cases, some of the drugs may cause kidney toxicity or bone mineral loss, according to Dr. Hamill.
Three similarly effective forms of PrEP approved by the U.S. Food and Drug Administration enable clinicians to tailor the medications to the specific needs and preferences of each patient. Truvada (emtricitabine and tenofovir disoproxil fumarate) and Descovy (emtricitabine and tenofovir alafenamide) are both daily tablets, although the latter is not advised for people assigned female sex at birth who have receptive vaginal sex. Apretude (cabotegravir), an injectable agent, is not recommended for people who inject illegal drugs.
Patients with renal or bone disease are not good candidates for Truvada.
“Truvada can decrease bone density, so for someone with osteoporosis, you might choose Descovy or Apretude,” Dr. Pollak said. “For someone with chronic kidney disease, consider Descovy or Apretude. “If a patient has hepatitis B, Truvada or Descovy are appropriate, because hepatitis B is treatable.”
Patients taking an injectable PrEP may need more attention, because the concentration of the medication in the body decreases slowly and may linger for many months at low levels that don’t prevent HIV, according to Dr. Hamill. Someone who acquires HIV during that “tail” period might develop resistance to PrEP.
New research also showed that Descovy users were at elevated risk of developing hypertension and statin initiation, especially among those over age 40 years.
Primary care physicians may want to consult with renal specialists about medication safety in patients with severe kidney disease or with rheumatologists or endocrinologists about metabolic bone disease concerns, Dr. Hamill said.
Meanwhile, if a person begins a monogamous relationship and their risk for HIV drops, “it’s fine to stop taking PrEP tablets,” Dr. Pollak said. “I would still recommend routine HIV screening every 6 or 12 months or however often, depending on other risk factors.”
Caring for these patients entails ensuring labs are completed, monitoring adherence, ordering refills, and scheduling regular follow-up visits.
“For the vast majority of patients, the primary care physician is perfectly equipped for their care through the entire PrEP journey, from discussion and initiation to provision of PrEP,” and most cases do not require specialist care, Dr. Hamill said.
However, “if PrEP fails, which is exceedingly rare, primary care physicians should refer patients immediately, preferably with a warm handoff, for linkage to HIV care,” Dr. Blumenthal said.
Talking about PrEP opens the door to conversations with patients about sexual health and broader health issues, Dr. Hamill said. Although these may not come naturally to primary care clinicians, training is available. The National Network of STD Clinical Prevention Training Centers, funded by the CDC, trains providers on how to overcome their anxiety and have open, inclusive conversations about sexuality and sexual behaviors with transgender and gender-diverse, nonbinary people.
“People worry about saying the wrong thing, about causing offense,” Dr. Hamill said. “But once you get comfortable discussing sexuality, you may open conversations around other health issues.”
Barriers for patients
The task force identified several barriers to PrEP access for patients because of lack of trusting relationships with health care, the effects of structural racism on health disparities, and persistent biases within the health care system.
Racial and ethnic disparities in HIV incidence persist, with 42% of new diagnoses occurring among Black people, 27% among Hispanic or Latino people, and 26% among White people in 2020.
Rates of PrEP usage for a year or longer are also low. Sometimes the patient no longer needs PrEP, but barriers often involve the costs of taking time off from work and arranging transportation to clinic visits.
Although nearly all insurance plans and state Medicaid programs cover PrEP, if a patient does not have coverage, the drugs and required tests and office visits can be expensive.
“One of the biggest barriers for all providers is navigating our complicated health system and drug assistance programs,” said Mehri S. McKellar, MD, associate professor of medicine at Duke University School of Medicine, Durham, N.C.
But lower-cost FDA-approved generic emtricitabine/tenofovir disoproxil fumarate is now available, and clinicians can direct patients to programs that help provide the medications at low or no cost.
“Providing PrEP care is straightforward, beneficial, and satisfying,” Dr. Hamill said. “You help people protect themselves from a life-changing diagnosis, and the health system doesn’t need to pay the cost of treating HIV. Everyone wins.”
Dr. Hamill, Dr. McKellar, Dr. Pollak, and Dr. Wong have reported no relevant financial relationships. Dr. Blumenthal has reported a financial relationship with Gilead Sciences.
A version of this article appeared on Medscape.com.
HIV continues to be a significant public health concern in the United States, with an estimated 1.2 million people currently living with the virus and more than 30,000 new diagnoses in 2020 alone.
Primary care clinicians can help decrease rates of HIV infection by prescribing pre-exposure prophylaxis to people who are sexually active.
But many do not.
“In medical school, we don’t spend much time discussing sexuality, sexual behavior, sexually transmitted infections, and such, so providers may feel uncomfortable asking what kind of sex their patient is having and with whom, whether they use a condom, and other basics,” said Matthew M. Hamill, MBChB, PhD, MPH, a specialist in sexually transmitted diseases at Johns Hopkins Medicine, Baltimore.
PrEP (pre-exposure prophylaxis) is an antiviral medication that cuts the risk of contracting HIV through sex by around 99% when taken as prescribed, according to the Centers for Disease Control and Prevention.
“Many people who would benefit from PrEP are not receiving this highly effective medication,” said John B. Wong, MD, a primary care internist and professor of medicine at Tufts University, Boston. The gap is particularly acute among Black, Hispanic, and Latino people, who are significantly more likely to be diagnosed with HIV but are much less likely than Whites to receive PrEP, he said.
Dr. Wong, a member of the U.S. Preventive Services Task Force, helped write the group’s new PrEP recommendations. Published in August, the guidelines call for clinicians to prescribe the drugs to adolescents and adults who do not have HIV but are at an increased risk for infection.
“Primary care physicians are ideally positioned to prescribe PrEP for their patients because they have longitudinal relationships: They get to know their patients, and hopefully their patients feel comfortable talking with them about their sexual health,” said Brandon Pollak, MD, a primary care physician and HIV specialist at the Ohio State University College of Medicine, Columbus.
Dr. Pollak, who was not involved with the USPSTF recommendations, cares for patients who are heterosexual and living with HIV.
Clinicians should consider PrEP for all patients who have sex with someone who has HIV, do not use condoms, or have had a sexually transmitted infection within the previous 6 months. Men who have sex with men, transgender women who have sex with men, people who inject illicit drugs or engage in transactional sex, and Black, Hispanic, and Latino individuals also are at increased risk for the infection.
“The vast majority of patients on PrEP in any form sail through with no problems; they have regular lab work and can follow up in person or by telemedicine,” Dr. Hamill said. “They tend to be young, fit people without complicated medical histories, and the medications are very well-tolerated, particularly if people expect some short-term side effects.”
What you need to know when prescribing PrEP
Prescribing PrEP is similar in complexity to prescribing hypertension or diabetes medications, Dr. Hamill said.
Because taking the medications while already infected with the virus can lead to the emergence of drug-resistant HIV, patients must have a negative HIV test before starting PrEP. In addition, the USPSTF recommends testing for other sexually transmitted infections and for pregnancy, if appropriate. The task force also recommends conducting kidney function and hepatitis B tests, and a lipid profile before starting specific types of PrEP.
HIV screening is also recommended at 3-month intervals.
“Providers may order labs done at 3- to 4-month intervals but only see patients in clinic once or twice per year, depending on patient needs and risk behaviors,” said Jill S. Blumenthal, MD, associate professor of medicine at UC San Diego Health.
Clinicians should consider medication adherence and whether a patient is likely to take a pill once a day or could benefit from receiving an injection every 2 months. Patients may experience side effects such as diarrhea or headache with oral PrEP or soreness at the injection site. In rare cases, some of the drugs may cause kidney toxicity or bone mineral loss, according to Dr. Hamill.
Three similarly effective forms of PrEP approved by the U.S. Food and Drug Administration enable clinicians to tailor the medications to the specific needs and preferences of each patient. Truvada (emtricitabine and tenofovir disoproxil fumarate) and Descovy (emtricitabine and tenofovir alafenamide) are both daily tablets, although the latter is not advised for people assigned female sex at birth who have receptive vaginal sex. Apretude (cabotegravir), an injectable agent, is not recommended for people who inject illegal drugs.
Patients with renal or bone disease are not good candidates for Truvada.
“Truvada can decrease bone density, so for someone with osteoporosis, you might choose Descovy or Apretude,” Dr. Pollak said. “For someone with chronic kidney disease, consider Descovy or Apretude. “If a patient has hepatitis B, Truvada or Descovy are appropriate, because hepatitis B is treatable.”
Patients taking an injectable PrEP may need more attention, because the concentration of the medication in the body decreases slowly and may linger for many months at low levels that don’t prevent HIV, according to Dr. Hamill. Someone who acquires HIV during that “tail” period might develop resistance to PrEP.
New research also showed that Descovy users were at elevated risk of developing hypertension and statin initiation, especially among those over age 40 years.
Primary care physicians may want to consult with renal specialists about medication safety in patients with severe kidney disease or with rheumatologists or endocrinologists about metabolic bone disease concerns, Dr. Hamill said.
Meanwhile, if a person begins a monogamous relationship and their risk for HIV drops, “it’s fine to stop taking PrEP tablets,” Dr. Pollak said. “I would still recommend routine HIV screening every 6 or 12 months or however often, depending on other risk factors.”
Caring for these patients entails ensuring labs are completed, monitoring adherence, ordering refills, and scheduling regular follow-up visits.
“For the vast majority of patients, the primary care physician is perfectly equipped for their care through the entire PrEP journey, from discussion and initiation to provision of PrEP,” and most cases do not require specialist care, Dr. Hamill said.
However, “if PrEP fails, which is exceedingly rare, primary care physicians should refer patients immediately, preferably with a warm handoff, for linkage to HIV care,” Dr. Blumenthal said.
Talking about PrEP opens the door to conversations with patients about sexual health and broader health issues, Dr. Hamill said. Although these may not come naturally to primary care clinicians, training is available. The National Network of STD Clinical Prevention Training Centers, funded by the CDC, trains providers on how to overcome their anxiety and have open, inclusive conversations about sexuality and sexual behaviors with transgender and gender-diverse, nonbinary people.
“People worry about saying the wrong thing, about causing offense,” Dr. Hamill said. “But once you get comfortable discussing sexuality, you may open conversations around other health issues.”
Barriers for patients
The task force identified several barriers to PrEP access for patients because of lack of trusting relationships with health care, the effects of structural racism on health disparities, and persistent biases within the health care system.
Racial and ethnic disparities in HIV incidence persist, with 42% of new diagnoses occurring among Black people, 27% among Hispanic or Latino people, and 26% among White people in 2020.
Rates of PrEP usage for a year or longer are also low. Sometimes the patient no longer needs PrEP, but barriers often involve the costs of taking time off from work and arranging transportation to clinic visits.
Although nearly all insurance plans and state Medicaid programs cover PrEP, if a patient does not have coverage, the drugs and required tests and office visits can be expensive.
“One of the biggest barriers for all providers is navigating our complicated health system and drug assistance programs,” said Mehri S. McKellar, MD, associate professor of medicine at Duke University School of Medicine, Durham, N.C.
But lower-cost FDA-approved generic emtricitabine/tenofovir disoproxil fumarate is now available, and clinicians can direct patients to programs that help provide the medications at low or no cost.
“Providing PrEP care is straightforward, beneficial, and satisfying,” Dr. Hamill said. “You help people protect themselves from a life-changing diagnosis, and the health system doesn’t need to pay the cost of treating HIV. Everyone wins.”
Dr. Hamill, Dr. McKellar, Dr. Pollak, and Dr. Wong have reported no relevant financial relationships. Dr. Blumenthal has reported a financial relationship with Gilead Sciences.
A version of this article appeared on Medscape.com.
HIV continues to be a significant public health concern in the United States, with an estimated 1.2 million people currently living with the virus and more than 30,000 new diagnoses in 2020 alone.
Primary care clinicians can help decrease rates of HIV infection by prescribing pre-exposure prophylaxis to people who are sexually active.
But many do not.
“In medical school, we don’t spend much time discussing sexuality, sexual behavior, sexually transmitted infections, and such, so providers may feel uncomfortable asking what kind of sex their patient is having and with whom, whether they use a condom, and other basics,” said Matthew M. Hamill, MBChB, PhD, MPH, a specialist in sexually transmitted diseases at Johns Hopkins Medicine, Baltimore.
PrEP (pre-exposure prophylaxis) is an antiviral medication that cuts the risk of contracting HIV through sex by around 99% when taken as prescribed, according to the Centers for Disease Control and Prevention.
“Many people who would benefit from PrEP are not receiving this highly effective medication,” said John B. Wong, MD, a primary care internist and professor of medicine at Tufts University, Boston. The gap is particularly acute among Black, Hispanic, and Latino people, who are significantly more likely to be diagnosed with HIV but are much less likely than Whites to receive PrEP, he said.
Dr. Wong, a member of the U.S. Preventive Services Task Force, helped write the group’s new PrEP recommendations. Published in August, the guidelines call for clinicians to prescribe the drugs to adolescents and adults who do not have HIV but are at an increased risk for infection.
“Primary care physicians are ideally positioned to prescribe PrEP for their patients because they have longitudinal relationships: They get to know their patients, and hopefully their patients feel comfortable talking with them about their sexual health,” said Brandon Pollak, MD, a primary care physician and HIV specialist at the Ohio State University College of Medicine, Columbus.
Dr. Pollak, who was not involved with the USPSTF recommendations, cares for patients who are heterosexual and living with HIV.
Clinicians should consider PrEP for all patients who have sex with someone who has HIV, do not use condoms, or have had a sexually transmitted infection within the previous 6 months. Men who have sex with men, transgender women who have sex with men, people who inject illicit drugs or engage in transactional sex, and Black, Hispanic, and Latino individuals also are at increased risk for the infection.
“The vast majority of patients on PrEP in any form sail through with no problems; they have regular lab work and can follow up in person or by telemedicine,” Dr. Hamill said. “They tend to be young, fit people without complicated medical histories, and the medications are very well-tolerated, particularly if people expect some short-term side effects.”
What you need to know when prescribing PrEP
Prescribing PrEP is similar in complexity to prescribing hypertension or diabetes medications, Dr. Hamill said.
Because taking the medications while already infected with the virus can lead to the emergence of drug-resistant HIV, patients must have a negative HIV test before starting PrEP. In addition, the USPSTF recommends testing for other sexually transmitted infections and for pregnancy, if appropriate. The task force also recommends conducting kidney function and hepatitis B tests, and a lipid profile before starting specific types of PrEP.
HIV screening is also recommended at 3-month intervals.
“Providers may order labs done at 3- to 4-month intervals but only see patients in clinic once or twice per year, depending on patient needs and risk behaviors,” said Jill S. Blumenthal, MD, associate professor of medicine at UC San Diego Health.
Clinicians should consider medication adherence and whether a patient is likely to take a pill once a day or could benefit from receiving an injection every 2 months. Patients may experience side effects such as diarrhea or headache with oral PrEP or soreness at the injection site. In rare cases, some of the drugs may cause kidney toxicity or bone mineral loss, according to Dr. Hamill.
Three similarly effective forms of PrEP approved by the U.S. Food and Drug Administration enable clinicians to tailor the medications to the specific needs and preferences of each patient. Truvada (emtricitabine and tenofovir disoproxil fumarate) and Descovy (emtricitabine and tenofovir alafenamide) are both daily tablets, although the latter is not advised for people assigned female sex at birth who have receptive vaginal sex. Apretude (cabotegravir), an injectable agent, is not recommended for people who inject illegal drugs.
Patients with renal or bone disease are not good candidates for Truvada.
“Truvada can decrease bone density, so for someone with osteoporosis, you might choose Descovy or Apretude,” Dr. Pollak said. “For someone with chronic kidney disease, consider Descovy or Apretude. “If a patient has hepatitis B, Truvada or Descovy are appropriate, because hepatitis B is treatable.”
Patients taking an injectable PrEP may need more attention, because the concentration of the medication in the body decreases slowly and may linger for many months at low levels that don’t prevent HIV, according to Dr. Hamill. Someone who acquires HIV during that “tail” period might develop resistance to PrEP.
New research also showed that Descovy users were at elevated risk of developing hypertension and statin initiation, especially among those over age 40 years.
Primary care physicians may want to consult with renal specialists about medication safety in patients with severe kidney disease or with rheumatologists or endocrinologists about metabolic bone disease concerns, Dr. Hamill said.
Meanwhile, if a person begins a monogamous relationship and their risk for HIV drops, “it’s fine to stop taking PrEP tablets,” Dr. Pollak said. “I would still recommend routine HIV screening every 6 or 12 months or however often, depending on other risk factors.”
Caring for these patients entails ensuring labs are completed, monitoring adherence, ordering refills, and scheduling regular follow-up visits.
“For the vast majority of patients, the primary care physician is perfectly equipped for their care through the entire PrEP journey, from discussion and initiation to provision of PrEP,” and most cases do not require specialist care, Dr. Hamill said.
However, “if PrEP fails, which is exceedingly rare, primary care physicians should refer patients immediately, preferably with a warm handoff, for linkage to HIV care,” Dr. Blumenthal said.
Talking about PrEP opens the door to conversations with patients about sexual health and broader health issues, Dr. Hamill said. Although these may not come naturally to primary care clinicians, training is available. The National Network of STD Clinical Prevention Training Centers, funded by the CDC, trains providers on how to overcome their anxiety and have open, inclusive conversations about sexuality and sexual behaviors with transgender and gender-diverse, nonbinary people.
“People worry about saying the wrong thing, about causing offense,” Dr. Hamill said. “But once you get comfortable discussing sexuality, you may open conversations around other health issues.”
Barriers for patients
The task force identified several barriers to PrEP access for patients because of lack of trusting relationships with health care, the effects of structural racism on health disparities, and persistent biases within the health care system.
Racial and ethnic disparities in HIV incidence persist, with 42% of new diagnoses occurring among Black people, 27% among Hispanic or Latino people, and 26% among White people in 2020.
Rates of PrEP usage for a year or longer are also low. Sometimes the patient no longer needs PrEP, but barriers often involve the costs of taking time off from work and arranging transportation to clinic visits.
Although nearly all insurance plans and state Medicaid programs cover PrEP, if a patient does not have coverage, the drugs and required tests and office visits can be expensive.
“One of the biggest barriers for all providers is navigating our complicated health system and drug assistance programs,” said Mehri S. McKellar, MD, associate professor of medicine at Duke University School of Medicine, Durham, N.C.
But lower-cost FDA-approved generic emtricitabine/tenofovir disoproxil fumarate is now available, and clinicians can direct patients to programs that help provide the medications at low or no cost.
“Providing PrEP care is straightforward, beneficial, and satisfying,” Dr. Hamill said. “You help people protect themselves from a life-changing diagnosis, and the health system doesn’t need to pay the cost of treating HIV. Everyone wins.”
Dr. Hamill, Dr. McKellar, Dr. Pollak, and Dr. Wong have reported no relevant financial relationships. Dr. Blumenthal has reported a financial relationship with Gilead Sciences.
A version of this article appeared on Medscape.com.
Paxlovid and Lagevrio benefit COVID outpatients in Omicron era
The American College of Physicians has issued an updated version of its living, rapid practice point guideline on the best treatment options for outpatients with confirmed COVID-19 in the era of the dominant Omicron variant of SARS-CoV-2. The recommendations in version 2 apply to persons presenting with mild to moderate infection and symptom onset in the past 5 days who are at high risk for progression to severe disease and potential hospitalization or death.
Version 1 appeared in late 2022.
While outpatient management is appropriate for most patients, treatment should be personalized and based on careful risk stratification and informed decision-making, said the guideline authors, led by Amir Qaseem, MD, PhD, MHA, vice president of clinical policy and the Center for Evidence Reviews at the ACP in Philadelphia.
Practice points
- Consider the oral antivirals nirmatrelvir-ritonavir (Paxlovid) or molnupiravir (Lagevrio) for symptomatic outpatients with confirmed mild to moderate COVID-19 who are within 5 days of the onset of symptoms and at high risk for progressing to severe disease.
New evidence for the Omicron variant suggests a possible net benefit of the antiviral molnupiravir versus standard or no treatment in terms of reducing recovery time if treatment is initiated within 5 days of symptom onset. Nirmatrelvir-ritonavir was associated with reductions in COVID-19 hospitalization and all-cause mortality.
“The practice points only address [whether] treatments work compared to placebo, no treatment, or usual care,” cautioned Linda L. Humphrey, MD, MPH, MACP, chair of the ACP’s Population Health and Medical Science Committee and a professor of medicine at Oregon Health and Science University VA Portland Health Care System. The ACP continues to monitor the evidence. “Once enough evidence has emerged, it will be possible to compare treatments to each other. Until that time we are unable to determine if there is an advantage to using one treatment over another.”
- Do not use the antiparasitic ivermectin (Stromectol) or the monoclonal antibody sotrovimab (Xevudy) to treat this patient population. “It is not expected to be effective against the Omicron variant,” Dr. Humphrey said.
There was no evidence to support the use of medications such as corticosteroids, antibiotics, antihistamines, SSRIs, and multiple other agents.
“The guideline is not a departure from previous knowledge and reflects what appears in other guidelines and is already being done generally in practice,” said Mirella Salvatore, MD, an associate professor of medicine and population health sciences at Weill Cornell Medicine, New York, who was not involved in the ACP statement. It is therefore unlikely the recommendations will trigger controversy or negative feedback, added Dr. Salvatore, who is also a spokesperson for the Infectious Diseases Society of America. “We believe that our evidence-based approach, which considers the balance of benefits and harms of various treatments, will be embraced by the physician community,” Dr. Humphrey said.
The updated recommendations are based on new data from the evidence review of multiple treatments, which concluded that both nirmatrelvir-ritonavir and molnupiravir likely improve outcomes for outpatients with mild to moderate COVID-19. The review was conducted after the emergence of the Omicron variant by the ACP Center for Evidence Reviews at Cochrane Austria/University for Continuing Education Krems (Austria).
Review details
Inclusion criteria were modified to focus on the Omicron variant by limiting eligible studies to only those enrolling patients on or after Nov. 26, 2021. The investigators included two randomized controlled trials and six retrospective cohort studies and ranked quality of evidence for the effectiveness of the following treatments, compared with usual care or no treatment: azithromycin, camostat mesylate, chloroquine-hydroxychloroquine, chlorpheniramine, colchicine, convalescent plasma, corticosteroids, ensitrelvir, favipiravir, fluvoxamine, ivermectin, lopinavir-ritonavir, molnupiravir, neutralizing monoclonal antibodies, metformin, niclosamide, nitazoxanide, nirmatrelvir-ritonavir, and remdesivir.
It compared results for all-cause and COVID-specific mortality, recovery, time to recovery, COVID hospitalization, and adverse and serious adverse events.
Nirmatrelvir-ritonavir was associated with a reduction in hospitalization caused by COVID-19 of 0.7% versus 1.2% (moderate certainty of evidence [COE]) and a reduction in all-cause mortality of less than 0.1% versus 0.2% (moderate COE).
Molnupiravir led to a higher recovery rate of 31.8% versus 22.6% (moderate COE) and a reduced time to recovery of 9 versus 15 median days (moderate COE). It had no effect, however, on all-cause mortality: 0.02% versus 0.04% (moderate COE). Nor did it affect the incidence of serious adverse events: 0.4% versus 0.3% (moderate COE).
“There have been no head-to-head comparative studies of these two treatments, but nirmatrelvir-ritonavir appears to be the preferred treatment,” Dr. Salvatore said. She noted that molnupiravir cannot be used in pregnant women or young persons under age 18, while nirmatrelvir-ritonavir carries the risk of drug interactions. Viral rebound and recurrence of symptoms have been reported in some patients receiving nirmatrelvir-ritonavir.
In other review findings, ivermectin had no effect on time to recovery (moderate COE) and adverse events versus placebo (low COE). Sotrovimab resulted in no difference in all-cause mortality, compared with no treatment (low COE). There were no eligible studies for all of the other treatments of interest nor were there any that specifically evaluated the benefits and harms of treatments for the Omicron variant.
The panel pointed to the need for more evaluation of the efficacy, effectiveness, and comparative effectiveness, as well as harms of pharmacologic and biologic treatments of COVID-19 in the outpatient setting, particularly in the context of changing dominant SARS-CoV-2 variants and subvariants.
Another area requiring further research is the effectiveness of retreatment in patients with previous COVID-19 infection. Subgroup analyses are also needed to assess whether the efficacy and effectiveness of outpatient treatments vary by age, sex, socioeconomic status, and comorbid conditions – or by SARS-CoV-2 variant, immunity status (prior SARS-CoV-2 infection, vaccination status, or time since infection or vaccination), symptom duration, or disease severity.
Dr. Salvatore agreed that more research is needed in special convalescent groups. “For instance, those with cancer who are immunocompromised may need longer treatment and adjunctive treatment with convalescent plasma. But is difficult to find a large enough study with 5,000 immunocompromised patients.”
Financial support for the development of the practice points came exclusively from the ACP operating budget. The evidence review was funded by the ACP. The authors disclosed no relevant high-level competing interests with regard to this guidance, although several authors reported intellectual interests in various areas of research. Dr. Salvatore disclosed no conflicts of interest relevant to her comments but is engaged in influenza research for Genentech.
The American College of Physicians has issued an updated version of its living, rapid practice point guideline on the best treatment options for outpatients with confirmed COVID-19 in the era of the dominant Omicron variant of SARS-CoV-2. The recommendations in version 2 apply to persons presenting with mild to moderate infection and symptom onset in the past 5 days who are at high risk for progression to severe disease and potential hospitalization or death.
Version 1 appeared in late 2022.
While outpatient management is appropriate for most patients, treatment should be personalized and based on careful risk stratification and informed decision-making, said the guideline authors, led by Amir Qaseem, MD, PhD, MHA, vice president of clinical policy and the Center for Evidence Reviews at the ACP in Philadelphia.
Practice points
- Consider the oral antivirals nirmatrelvir-ritonavir (Paxlovid) or molnupiravir (Lagevrio) for symptomatic outpatients with confirmed mild to moderate COVID-19 who are within 5 days of the onset of symptoms and at high risk for progressing to severe disease.
New evidence for the Omicron variant suggests a possible net benefit of the antiviral molnupiravir versus standard or no treatment in terms of reducing recovery time if treatment is initiated within 5 days of symptom onset. Nirmatrelvir-ritonavir was associated with reductions in COVID-19 hospitalization and all-cause mortality.
“The practice points only address [whether] treatments work compared to placebo, no treatment, or usual care,” cautioned Linda L. Humphrey, MD, MPH, MACP, chair of the ACP’s Population Health and Medical Science Committee and a professor of medicine at Oregon Health and Science University VA Portland Health Care System. The ACP continues to monitor the evidence. “Once enough evidence has emerged, it will be possible to compare treatments to each other. Until that time we are unable to determine if there is an advantage to using one treatment over another.”
- Do not use the antiparasitic ivermectin (Stromectol) or the monoclonal antibody sotrovimab (Xevudy) to treat this patient population. “It is not expected to be effective against the Omicron variant,” Dr. Humphrey said.
There was no evidence to support the use of medications such as corticosteroids, antibiotics, antihistamines, SSRIs, and multiple other agents.
“The guideline is not a departure from previous knowledge and reflects what appears in other guidelines and is already being done generally in practice,” said Mirella Salvatore, MD, an associate professor of medicine and population health sciences at Weill Cornell Medicine, New York, who was not involved in the ACP statement. It is therefore unlikely the recommendations will trigger controversy or negative feedback, added Dr. Salvatore, who is also a spokesperson for the Infectious Diseases Society of America. “We believe that our evidence-based approach, which considers the balance of benefits and harms of various treatments, will be embraced by the physician community,” Dr. Humphrey said.
The updated recommendations are based on new data from the evidence review of multiple treatments, which concluded that both nirmatrelvir-ritonavir and molnupiravir likely improve outcomes for outpatients with mild to moderate COVID-19. The review was conducted after the emergence of the Omicron variant by the ACP Center for Evidence Reviews at Cochrane Austria/University for Continuing Education Krems (Austria).
Review details
Inclusion criteria were modified to focus on the Omicron variant by limiting eligible studies to only those enrolling patients on or after Nov. 26, 2021. The investigators included two randomized controlled trials and six retrospective cohort studies and ranked quality of evidence for the effectiveness of the following treatments, compared with usual care or no treatment: azithromycin, camostat mesylate, chloroquine-hydroxychloroquine, chlorpheniramine, colchicine, convalescent plasma, corticosteroids, ensitrelvir, favipiravir, fluvoxamine, ivermectin, lopinavir-ritonavir, molnupiravir, neutralizing monoclonal antibodies, metformin, niclosamide, nitazoxanide, nirmatrelvir-ritonavir, and remdesivir.
It compared results for all-cause and COVID-specific mortality, recovery, time to recovery, COVID hospitalization, and adverse and serious adverse events.
Nirmatrelvir-ritonavir was associated with a reduction in hospitalization caused by COVID-19 of 0.7% versus 1.2% (moderate certainty of evidence [COE]) and a reduction in all-cause mortality of less than 0.1% versus 0.2% (moderate COE).
Molnupiravir led to a higher recovery rate of 31.8% versus 22.6% (moderate COE) and a reduced time to recovery of 9 versus 15 median days (moderate COE). It had no effect, however, on all-cause mortality: 0.02% versus 0.04% (moderate COE). Nor did it affect the incidence of serious adverse events: 0.4% versus 0.3% (moderate COE).
“There have been no head-to-head comparative studies of these two treatments, but nirmatrelvir-ritonavir appears to be the preferred treatment,” Dr. Salvatore said. She noted that molnupiravir cannot be used in pregnant women or young persons under age 18, while nirmatrelvir-ritonavir carries the risk of drug interactions. Viral rebound and recurrence of symptoms have been reported in some patients receiving nirmatrelvir-ritonavir.
In other review findings, ivermectin had no effect on time to recovery (moderate COE) and adverse events versus placebo (low COE). Sotrovimab resulted in no difference in all-cause mortality, compared with no treatment (low COE). There were no eligible studies for all of the other treatments of interest nor were there any that specifically evaluated the benefits and harms of treatments for the Omicron variant.
The panel pointed to the need for more evaluation of the efficacy, effectiveness, and comparative effectiveness, as well as harms of pharmacologic and biologic treatments of COVID-19 in the outpatient setting, particularly in the context of changing dominant SARS-CoV-2 variants and subvariants.
Another area requiring further research is the effectiveness of retreatment in patients with previous COVID-19 infection. Subgroup analyses are also needed to assess whether the efficacy and effectiveness of outpatient treatments vary by age, sex, socioeconomic status, and comorbid conditions – or by SARS-CoV-2 variant, immunity status (prior SARS-CoV-2 infection, vaccination status, or time since infection or vaccination), symptom duration, or disease severity.
Dr. Salvatore agreed that more research is needed in special convalescent groups. “For instance, those with cancer who are immunocompromised may need longer treatment and adjunctive treatment with convalescent plasma. But is difficult to find a large enough study with 5,000 immunocompromised patients.”
Financial support for the development of the practice points came exclusively from the ACP operating budget. The evidence review was funded by the ACP. The authors disclosed no relevant high-level competing interests with regard to this guidance, although several authors reported intellectual interests in various areas of research. Dr. Salvatore disclosed no conflicts of interest relevant to her comments but is engaged in influenza research for Genentech.
The American College of Physicians has issued an updated version of its living, rapid practice point guideline on the best treatment options for outpatients with confirmed COVID-19 in the era of the dominant Omicron variant of SARS-CoV-2. The recommendations in version 2 apply to persons presenting with mild to moderate infection and symptom onset in the past 5 days who are at high risk for progression to severe disease and potential hospitalization or death.
Version 1 appeared in late 2022.
While outpatient management is appropriate for most patients, treatment should be personalized and based on careful risk stratification and informed decision-making, said the guideline authors, led by Amir Qaseem, MD, PhD, MHA, vice president of clinical policy and the Center for Evidence Reviews at the ACP in Philadelphia.
Practice points
- Consider the oral antivirals nirmatrelvir-ritonavir (Paxlovid) or molnupiravir (Lagevrio) for symptomatic outpatients with confirmed mild to moderate COVID-19 who are within 5 days of the onset of symptoms and at high risk for progressing to severe disease.
New evidence for the Omicron variant suggests a possible net benefit of the antiviral molnupiravir versus standard or no treatment in terms of reducing recovery time if treatment is initiated within 5 days of symptom onset. Nirmatrelvir-ritonavir was associated with reductions in COVID-19 hospitalization and all-cause mortality.
“The practice points only address [whether] treatments work compared to placebo, no treatment, or usual care,” cautioned Linda L. Humphrey, MD, MPH, MACP, chair of the ACP’s Population Health and Medical Science Committee and a professor of medicine at Oregon Health and Science University VA Portland Health Care System. The ACP continues to monitor the evidence. “Once enough evidence has emerged, it will be possible to compare treatments to each other. Until that time we are unable to determine if there is an advantage to using one treatment over another.”
- Do not use the antiparasitic ivermectin (Stromectol) or the monoclonal antibody sotrovimab (Xevudy) to treat this patient population. “It is not expected to be effective against the Omicron variant,” Dr. Humphrey said.
There was no evidence to support the use of medications such as corticosteroids, antibiotics, antihistamines, SSRIs, and multiple other agents.
“The guideline is not a departure from previous knowledge and reflects what appears in other guidelines and is already being done generally in practice,” said Mirella Salvatore, MD, an associate professor of medicine and population health sciences at Weill Cornell Medicine, New York, who was not involved in the ACP statement. It is therefore unlikely the recommendations will trigger controversy or negative feedback, added Dr. Salvatore, who is also a spokesperson for the Infectious Diseases Society of America. “We believe that our evidence-based approach, which considers the balance of benefits and harms of various treatments, will be embraced by the physician community,” Dr. Humphrey said.
The updated recommendations are based on new data from the evidence review of multiple treatments, which concluded that both nirmatrelvir-ritonavir and molnupiravir likely improve outcomes for outpatients with mild to moderate COVID-19. The review was conducted after the emergence of the Omicron variant by the ACP Center for Evidence Reviews at Cochrane Austria/University for Continuing Education Krems (Austria).
Review details
Inclusion criteria were modified to focus on the Omicron variant by limiting eligible studies to only those enrolling patients on or after Nov. 26, 2021. The investigators included two randomized controlled trials and six retrospective cohort studies and ranked quality of evidence for the effectiveness of the following treatments, compared with usual care or no treatment: azithromycin, camostat mesylate, chloroquine-hydroxychloroquine, chlorpheniramine, colchicine, convalescent plasma, corticosteroids, ensitrelvir, favipiravir, fluvoxamine, ivermectin, lopinavir-ritonavir, molnupiravir, neutralizing monoclonal antibodies, metformin, niclosamide, nitazoxanide, nirmatrelvir-ritonavir, and remdesivir.
It compared results for all-cause and COVID-specific mortality, recovery, time to recovery, COVID hospitalization, and adverse and serious adverse events.
Nirmatrelvir-ritonavir was associated with a reduction in hospitalization caused by COVID-19 of 0.7% versus 1.2% (moderate certainty of evidence [COE]) and a reduction in all-cause mortality of less than 0.1% versus 0.2% (moderate COE).
Molnupiravir led to a higher recovery rate of 31.8% versus 22.6% (moderate COE) and a reduced time to recovery of 9 versus 15 median days (moderate COE). It had no effect, however, on all-cause mortality: 0.02% versus 0.04% (moderate COE). Nor did it affect the incidence of serious adverse events: 0.4% versus 0.3% (moderate COE).
“There have been no head-to-head comparative studies of these two treatments, but nirmatrelvir-ritonavir appears to be the preferred treatment,” Dr. Salvatore said. She noted that molnupiravir cannot be used in pregnant women or young persons under age 18, while nirmatrelvir-ritonavir carries the risk of drug interactions. Viral rebound and recurrence of symptoms have been reported in some patients receiving nirmatrelvir-ritonavir.
In other review findings, ivermectin had no effect on time to recovery (moderate COE) and adverse events versus placebo (low COE). Sotrovimab resulted in no difference in all-cause mortality, compared with no treatment (low COE). There were no eligible studies for all of the other treatments of interest nor were there any that specifically evaluated the benefits and harms of treatments for the Omicron variant.
The panel pointed to the need for more evaluation of the efficacy, effectiveness, and comparative effectiveness, as well as harms of pharmacologic and biologic treatments of COVID-19 in the outpatient setting, particularly in the context of changing dominant SARS-CoV-2 variants and subvariants.
Another area requiring further research is the effectiveness of retreatment in patients with previous COVID-19 infection. Subgroup analyses are also needed to assess whether the efficacy and effectiveness of outpatient treatments vary by age, sex, socioeconomic status, and comorbid conditions – or by SARS-CoV-2 variant, immunity status (prior SARS-CoV-2 infection, vaccination status, or time since infection or vaccination), symptom duration, or disease severity.
Dr. Salvatore agreed that more research is needed in special convalescent groups. “For instance, those with cancer who are immunocompromised may need longer treatment and adjunctive treatment with convalescent plasma. But is difficult to find a large enough study with 5,000 immunocompromised patients.”
Financial support for the development of the practice points came exclusively from the ACP operating budget. The evidence review was funded by the ACP. The authors disclosed no relevant high-level competing interests with regard to this guidance, although several authors reported intellectual interests in various areas of research. Dr. Salvatore disclosed no conflicts of interest relevant to her comments but is engaged in influenza research for Genentech.
FROM ANNALS OF INTERNAL MEDICINE
New COVID vaccines force bivalents out
COVID vaccines will have a new formulation in 2023, according to a decision announced by the U.S. Food and Drug Administration, that will focus efforts on circulating variants. The move pushes last year’s bivalent vaccines out of circulation because they will no longer be authorized for use in the United States.
The updated mRNA vaccines for 2023-2024 are being revised to include a single component that corresponds to the Omicron variant XBB.1.5. Like the bivalents offered before, the new monovalents are being manufactured by Moderna and Pfizer.
The new vaccines are authorized for use in individuals age 6 months and older. And the new options are being developed using a similar process as previous formulations, according to the FDA.
Targeting circulating variants
In recent studies, regulators point out the extent of neutralization observed by the updated vaccines against currently circulating viral variants causing COVID-19, including EG.5, BA.2.86, appears to be of a similar magnitude to the extent of neutralization observed with previous versions of the vaccines against corresponding prior variants.
“This suggests that the vaccines are a good match for protecting against the currently circulating COVID-19 variants,” according to the report.
Hundreds of millions of people in the United States have already received previously approved mRNA COVID vaccines, according to regulators who say the benefit-to-risk profile is well understood as they move forward with new formulations.
“Vaccination remains critical to public health and continued protection against serious consequences of COVID-19, including hospitalization and death,” Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, said in a statement. “The public can be assured that these updated vaccines have met the agency’s rigorous scientific standards for safety, effectiveness, and manufacturing quality. We very much encourage those who are eligible to consider getting vaccinated.”
Timing the effort
On Sept. 12 the U.S. Centers for Disease Control and Prevention recommended that everyone 6 months and older get an updated COVID-19 vaccine. Updated vaccines from Pfizer-BioNTech and Moderna will be available later this week, according to the agency.
This article was updated 9/14/23.
A version of this article appeared on Medscape.com.
COVID vaccines will have a new formulation in 2023, according to a decision announced by the U.S. Food and Drug Administration, that will focus efforts on circulating variants. The move pushes last year’s bivalent vaccines out of circulation because they will no longer be authorized for use in the United States.
The updated mRNA vaccines for 2023-2024 are being revised to include a single component that corresponds to the Omicron variant XBB.1.5. Like the bivalents offered before, the new monovalents are being manufactured by Moderna and Pfizer.
The new vaccines are authorized for use in individuals age 6 months and older. And the new options are being developed using a similar process as previous formulations, according to the FDA.
Targeting circulating variants
In recent studies, regulators point out the extent of neutralization observed by the updated vaccines against currently circulating viral variants causing COVID-19, including EG.5, BA.2.86, appears to be of a similar magnitude to the extent of neutralization observed with previous versions of the vaccines against corresponding prior variants.
“This suggests that the vaccines are a good match for protecting against the currently circulating COVID-19 variants,” according to the report.
Hundreds of millions of people in the United States have already received previously approved mRNA COVID vaccines, according to regulators who say the benefit-to-risk profile is well understood as they move forward with new formulations.
“Vaccination remains critical to public health and continued protection against serious consequences of COVID-19, including hospitalization and death,” Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, said in a statement. “The public can be assured that these updated vaccines have met the agency’s rigorous scientific standards for safety, effectiveness, and manufacturing quality. We very much encourage those who are eligible to consider getting vaccinated.”
Timing the effort
On Sept. 12 the U.S. Centers for Disease Control and Prevention recommended that everyone 6 months and older get an updated COVID-19 vaccine. Updated vaccines from Pfizer-BioNTech and Moderna will be available later this week, according to the agency.
This article was updated 9/14/23.
A version of this article appeared on Medscape.com.
COVID vaccines will have a new formulation in 2023, according to a decision announced by the U.S. Food and Drug Administration, that will focus efforts on circulating variants. The move pushes last year’s bivalent vaccines out of circulation because they will no longer be authorized for use in the United States.
The updated mRNA vaccines for 2023-2024 are being revised to include a single component that corresponds to the Omicron variant XBB.1.5. Like the bivalents offered before, the new monovalents are being manufactured by Moderna and Pfizer.
The new vaccines are authorized for use in individuals age 6 months and older. And the new options are being developed using a similar process as previous formulations, according to the FDA.
Targeting circulating variants
In recent studies, regulators point out the extent of neutralization observed by the updated vaccines against currently circulating viral variants causing COVID-19, including EG.5, BA.2.86, appears to be of a similar magnitude to the extent of neutralization observed with previous versions of the vaccines against corresponding prior variants.
“This suggests that the vaccines are a good match for protecting against the currently circulating COVID-19 variants,” according to the report.
Hundreds of millions of people in the United States have already received previously approved mRNA COVID vaccines, according to regulators who say the benefit-to-risk profile is well understood as they move forward with new formulations.
“Vaccination remains critical to public health and continued protection against serious consequences of COVID-19, including hospitalization and death,” Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, said in a statement. “The public can be assured that these updated vaccines have met the agency’s rigorous scientific standards for safety, effectiveness, and manufacturing quality. We very much encourage those who are eligible to consider getting vaccinated.”
Timing the effort
On Sept. 12 the U.S. Centers for Disease Control and Prevention recommended that everyone 6 months and older get an updated COVID-19 vaccine. Updated vaccines from Pfizer-BioNTech and Moderna will be available later this week, according to the agency.
This article was updated 9/14/23.
A version of this article appeared on Medscape.com.
RSV season has started, and this year could be different
The Centers for Disease Control and Prevention issued a national alert to health officials Sept. 5, urging them to offer new medicines that can prevent severe cases of the respiratory virus in very young children and in older people. Those two groups are at the highest risk of potentially deadly complications from RSV.
Typically, the CDC considers the start of RSV season to occur when the rate of positive tests for the virus goes above 3% for 2 consecutive weeks. In Florida, the rate has been around 5% in recent weeks, and in Georgia, there has been an increase in RSV-related hospitalizations. Most of the hospitalizations in Georgia have been among infants less than a year old.
“Historically, such regional increases have predicted the beginning of RSV season nationally, with increased RSV activity spreading north and west over the following 2-3 months,” the CDC said.
Most children have been infected with RSV by the time they are 2 years old. Historically, up to 80,000 children under 5 years old are hospitalized annually because of the virus, and between 100 and 300 die from complications each year.
Those figures could be drastically different this year because new preventive treatments are available.
The CDC recommends that all children under 8 months old receive the newly approved monoclonal antibody treatment nirsevimab (Beyfortus). Children up to 19 months old at high risk of severe complications from RSV are also eligible for the single-dose shot. In clinical trials, the treatment was 80% effective at preventing RSV infections from becoming so severe that children had to be hospitalized. The protection lasted about 5 months.
Older people are also at a heightened risk of severe illness from RSV, and two new vaccines are available this season. The vaccines are called Arexvy and Abrysvo, and the single-dose shots are approved for people ages 60 years and older. They are more than 80% effective at making severe lower respiratory complications less likely.
Last year’s RSV season started during the summer and peaked in October and November, which was earlier than usual. There’s no indication yet of when RSV season may peak this year. Last year and throughout the pandemic, RSV held its historical pattern of starting in Florida.
A version of this article appeared on WebMD.com.
The Centers for Disease Control and Prevention issued a national alert to health officials Sept. 5, urging them to offer new medicines that can prevent severe cases of the respiratory virus in very young children and in older people. Those two groups are at the highest risk of potentially deadly complications from RSV.
Typically, the CDC considers the start of RSV season to occur when the rate of positive tests for the virus goes above 3% for 2 consecutive weeks. In Florida, the rate has been around 5% in recent weeks, and in Georgia, there has been an increase in RSV-related hospitalizations. Most of the hospitalizations in Georgia have been among infants less than a year old.
“Historically, such regional increases have predicted the beginning of RSV season nationally, with increased RSV activity spreading north and west over the following 2-3 months,” the CDC said.
Most children have been infected with RSV by the time they are 2 years old. Historically, up to 80,000 children under 5 years old are hospitalized annually because of the virus, and between 100 and 300 die from complications each year.
Those figures could be drastically different this year because new preventive treatments are available.
The CDC recommends that all children under 8 months old receive the newly approved monoclonal antibody treatment nirsevimab (Beyfortus). Children up to 19 months old at high risk of severe complications from RSV are also eligible for the single-dose shot. In clinical trials, the treatment was 80% effective at preventing RSV infections from becoming so severe that children had to be hospitalized. The protection lasted about 5 months.
Older people are also at a heightened risk of severe illness from RSV, and two new vaccines are available this season. The vaccines are called Arexvy and Abrysvo, and the single-dose shots are approved for people ages 60 years and older. They are more than 80% effective at making severe lower respiratory complications less likely.
Last year’s RSV season started during the summer and peaked in October and November, which was earlier than usual. There’s no indication yet of when RSV season may peak this year. Last year and throughout the pandemic, RSV held its historical pattern of starting in Florida.
A version of this article appeared on WebMD.com.
The Centers for Disease Control and Prevention issued a national alert to health officials Sept. 5, urging them to offer new medicines that can prevent severe cases of the respiratory virus in very young children and in older people. Those two groups are at the highest risk of potentially deadly complications from RSV.
Typically, the CDC considers the start of RSV season to occur when the rate of positive tests for the virus goes above 3% for 2 consecutive weeks. In Florida, the rate has been around 5% in recent weeks, and in Georgia, there has been an increase in RSV-related hospitalizations. Most of the hospitalizations in Georgia have been among infants less than a year old.
“Historically, such regional increases have predicted the beginning of RSV season nationally, with increased RSV activity spreading north and west over the following 2-3 months,” the CDC said.
Most children have been infected with RSV by the time they are 2 years old. Historically, up to 80,000 children under 5 years old are hospitalized annually because of the virus, and between 100 and 300 die from complications each year.
Those figures could be drastically different this year because new preventive treatments are available.
The CDC recommends that all children under 8 months old receive the newly approved monoclonal antibody treatment nirsevimab (Beyfortus). Children up to 19 months old at high risk of severe complications from RSV are also eligible for the single-dose shot. In clinical trials, the treatment was 80% effective at preventing RSV infections from becoming so severe that children had to be hospitalized. The protection lasted about 5 months.
Older people are also at a heightened risk of severe illness from RSV, and two new vaccines are available this season. The vaccines are called Arexvy and Abrysvo, and the single-dose shots are approved for people ages 60 years and older. They are more than 80% effective at making severe lower respiratory complications less likely.
Last year’s RSV season started during the summer and peaked in October and November, which was earlier than usual. There’s no indication yet of when RSV season may peak this year. Last year and throughout the pandemic, RSV held its historical pattern of starting in Florida.
A version of this article appeared on WebMD.com.
New Moderna vaccine to work against recent COVID variant
“The company said its shot generated an 8.7-fold increase in neutralizing antibodies in humans against BA.2.86, which is being tracked by the World Health Organization and the U.S. Centers for Disease Control and Prevention,” Reuters reported.
“We think this is news people will want to hear as they prepare to go out and get their fall boosters,” Jacqueline Miller, Moderna head of infectious diseases, told the news agency.
The CDC said that the BA.2.86 variant might be more likely to infect people who have already had COVID or previous vaccinations. BA.2.86 is an Omicron variant. It has undergone more mutations than XBB.1.5, which has dominated most of this year and was the intended target of the updated shots.
BA.2.86 does not have a strong presence in the United States yet. However, officials are concerned about its high number of mutations, NBC News reported.
The FDA is expected to approve the new Moderna shot by early October.
Pfizer told NBC that its updated booster also generated a strong antibody response against Omicron variants, including BA.2.86.
COVID-19 cases and hospitalizations have been increasing in the U.S. because of the rise of several variants.
Experts told Reuters that BA.2.86 probably won’t cause a wave of severe disease and death because immunity has been built up around the world through previous infections and mass vaccinations.
A version of this article appeared on WebMD.com.
“The company said its shot generated an 8.7-fold increase in neutralizing antibodies in humans against BA.2.86, which is being tracked by the World Health Organization and the U.S. Centers for Disease Control and Prevention,” Reuters reported.
“We think this is news people will want to hear as they prepare to go out and get their fall boosters,” Jacqueline Miller, Moderna head of infectious diseases, told the news agency.
The CDC said that the BA.2.86 variant might be more likely to infect people who have already had COVID or previous vaccinations. BA.2.86 is an Omicron variant. It has undergone more mutations than XBB.1.5, which has dominated most of this year and was the intended target of the updated shots.
BA.2.86 does not have a strong presence in the United States yet. However, officials are concerned about its high number of mutations, NBC News reported.
The FDA is expected to approve the new Moderna shot by early October.
Pfizer told NBC that its updated booster also generated a strong antibody response against Omicron variants, including BA.2.86.
COVID-19 cases and hospitalizations have been increasing in the U.S. because of the rise of several variants.
Experts told Reuters that BA.2.86 probably won’t cause a wave of severe disease and death because immunity has been built up around the world through previous infections and mass vaccinations.
A version of this article appeared on WebMD.com.
“The company said its shot generated an 8.7-fold increase in neutralizing antibodies in humans against BA.2.86, which is being tracked by the World Health Organization and the U.S. Centers for Disease Control and Prevention,” Reuters reported.
“We think this is news people will want to hear as they prepare to go out and get their fall boosters,” Jacqueline Miller, Moderna head of infectious diseases, told the news agency.
The CDC said that the BA.2.86 variant might be more likely to infect people who have already had COVID or previous vaccinations. BA.2.86 is an Omicron variant. It has undergone more mutations than XBB.1.5, which has dominated most of this year and was the intended target of the updated shots.
BA.2.86 does not have a strong presence in the United States yet. However, officials are concerned about its high number of mutations, NBC News reported.
The FDA is expected to approve the new Moderna shot by early October.
Pfizer told NBC that its updated booster also generated a strong antibody response against Omicron variants, including BA.2.86.
COVID-19 cases and hospitalizations have been increasing in the U.S. because of the rise of several variants.
Experts told Reuters that BA.2.86 probably won’t cause a wave of severe disease and death because immunity has been built up around the world through previous infections and mass vaccinations.
A version of this article appeared on WebMD.com.
No benefit of anti-inflammatory strategy in acute myocarditis
AMSTERDAM – A short course of the interleukin-1 receptor antagonist, anakinra, appeared safe but did not reduce complications of acute myocarditis in the ARAMIS trial.
The trial was presented at the annual congress of the European Society of Cardiology.
Lead investigator, Mathieu Kerneis, MD, Pitie Salpetriere APHP University Hospital, Paris, said this was the largest randomized controlled trial of patients with acute myocarditis and probably the first ever study in the acute setting of myocarditis patients diagnosed with cardiac magnetic resonance (CMR) imaging, not on biopsy, who are mostly at low risk for events.
He suggested that one of the reasons for the neutral result could have been the low-risk population involved and the low complication rate. “We enrolled an all-comer acute myocarditis population diagnosed with CMR, who were mostly at a low risk of complications,” he noted.
“I don’t think the story of anti-inflammatory drugs in acute myocarditis is over. This is just the beginning. This was the first trial, and it was just a phase 2 trial. We need further randomized trials to explore the potential benefit of an anti-inflammatory strategy in acute myocarditis patients at higher risk of complications. In addition, larger studies are needed to evaluate prolonged anti-inflammatory strategies in acute myocarditis patients at low-to-moderate risk of complications,” Dr. Kerneis concluded.
“It is very challenging to do a trial in high-risk patients with myocarditis as these patients are quite rare,” he added.
Inflammation of the myocardium
Dr. Kerneis explained that acute myocarditis is an inflammation of the myocardium that can cause permanent damage to the heart muscle and lead to myocardial infarction, stroke, heart failure, arrhythmias, and death. The condition can occur in individuals of all ages but is most frequent in young people. There is no specific treatment, but patients are generally treated with beta-blockers, angiotensin-converting enzyme (ACE) inhibitors, and sometimes steroids.
Anakinra is an interleukin-1 receptor antagonist that works by targeting the interleukin-1β innate immune pathway. Anakinra is used for the treatment of rheumatoid arthritis and has shown efficacy in pericarditis. Dr. Kerneis noted that there have been several case reports of successful treatment with anakinra in acute myocarditis.
The ARAMIS trial – conducted at six academic centers in France – was the first randomized study to evaluate inhibition of the interleukin-1β innate immune pathway in myocarditis patients. The trial enrolled 120 hospitalized, symptomatic patients with chest pain, increased cardiac troponin, and acute myocarditis diagnosed using CMR. More than half had had a recent bacterial or viral infection.
Patients were randomized within 72 hours of hospital admission to a daily subcutaneous dose of anakinra 100 mg or placebo until hospital discharge. Patients in both groups received standard-of-care treatments, including an ACE inhibitor, for at least 1 month. Consistent with prior data, the median age of participants was 28 years and 90% were men.
The primary endpoint was the number of days free of myocarditis complications (heart failure requiring hospitalization, chest pain requiring medication, left ventricular ejection fraction less than 50%, and ventricular arrhythmias) within 28 days postdischarge.
There was no significant difference in this endpoint between the two arms, with a median of 30 days for anakinra versus 31 days for placebo.
Overall, the rate of the composite endpoint of myocarditis complications occurred in 13.7% of patients, and there was a numerical reduction in the number of patients with these myocarditis complications with anakinra – 6 patients (10.5%) in the anakinra group versus 10 patients (16.5%) in the placebo group (odds ratio, 0.59; 95% confidence interval, 0.19-1.78). This was driven by fewer patients with chest pain requiring new medication (two patients versus six patients).
The safety endpoint was the number of serious adverse events within 28 days postdischarge. This endpoint occurred in seven patients (12.1%) in the anakinra arm and six patients (10.2%) in the placebo arm, with no significant difference between groups. Cases of severe infection within 28 days postdischarge were reported in both arms.
Low-risk population
Designated discussant of the study at the ESC Hotline session, Enrico Ammirati, MD, PhD, University of Milano-Bicocca, Monza, Italy, said that patients involved in ARAMIS fit the profile of acute myocarditis and that the CMR diagnosis was positive in all the patients enrolled.
Dr. Ammirati agreed with Dr. Kerneis that the neutral results of the study were probably caused by the low-risk population. “If we look at retrospective registries, at 30 days there are zero cardiac deaths or heart transplants at 30 days in patients with a low-risk presentation.
“The ARAMIS trial has shown the feasibility of conducting studies in the setting of acute myocarditis, and even if the primary endpoint was neutral, some important data are still missing, such as change in ejection fraction and troponin levels,” he noted.
“In terms of future perspective, we are moving to assessing efficacy of anakinra or other immunosuppressive drugs from acute low risk patients to higher risk patients with heart failure and severe dysfunction,” he said.
Dr. Ammirati is the lead investigator of another ongoing study in such a higher-risk population; the MYTHS trial is investigating the use of intravenous steroids in patients with suspected acute myocarditis complicated by acute heart failure or cardiogenic shock, and an ejection fraction below 41%.
“So, we will have more results on the best treatment in this higher risk group of patients,” he concluded.
The ARAMIS trial was an academic study funded by the French Health Ministry and coordinated by the ACTION Group. Dr. Kerneis reports having received consulting fees from Kiniksa, Sanofi, and Bayer, and holds a patent for use of abatacept in immune checkpoint inhibitor (ICI)–induced myocarditis.
A version of this article first appeared on Medscape.com.
AMSTERDAM – A short course of the interleukin-1 receptor antagonist, anakinra, appeared safe but did not reduce complications of acute myocarditis in the ARAMIS trial.
The trial was presented at the annual congress of the European Society of Cardiology.
Lead investigator, Mathieu Kerneis, MD, Pitie Salpetriere APHP University Hospital, Paris, said this was the largest randomized controlled trial of patients with acute myocarditis and probably the first ever study in the acute setting of myocarditis patients diagnosed with cardiac magnetic resonance (CMR) imaging, not on biopsy, who are mostly at low risk for events.
He suggested that one of the reasons for the neutral result could have been the low-risk population involved and the low complication rate. “We enrolled an all-comer acute myocarditis population diagnosed with CMR, who were mostly at a low risk of complications,” he noted.
“I don’t think the story of anti-inflammatory drugs in acute myocarditis is over. This is just the beginning. This was the first trial, and it was just a phase 2 trial. We need further randomized trials to explore the potential benefit of an anti-inflammatory strategy in acute myocarditis patients at higher risk of complications. In addition, larger studies are needed to evaluate prolonged anti-inflammatory strategies in acute myocarditis patients at low-to-moderate risk of complications,” Dr. Kerneis concluded.
“It is very challenging to do a trial in high-risk patients with myocarditis as these patients are quite rare,” he added.
Inflammation of the myocardium
Dr. Kerneis explained that acute myocarditis is an inflammation of the myocardium that can cause permanent damage to the heart muscle and lead to myocardial infarction, stroke, heart failure, arrhythmias, and death. The condition can occur in individuals of all ages but is most frequent in young people. There is no specific treatment, but patients are generally treated with beta-blockers, angiotensin-converting enzyme (ACE) inhibitors, and sometimes steroids.
Anakinra is an interleukin-1 receptor antagonist that works by targeting the interleukin-1β innate immune pathway. Anakinra is used for the treatment of rheumatoid arthritis and has shown efficacy in pericarditis. Dr. Kerneis noted that there have been several case reports of successful treatment with anakinra in acute myocarditis.
The ARAMIS trial – conducted at six academic centers in France – was the first randomized study to evaluate inhibition of the interleukin-1β innate immune pathway in myocarditis patients. The trial enrolled 120 hospitalized, symptomatic patients with chest pain, increased cardiac troponin, and acute myocarditis diagnosed using CMR. More than half had had a recent bacterial or viral infection.
Patients were randomized within 72 hours of hospital admission to a daily subcutaneous dose of anakinra 100 mg or placebo until hospital discharge. Patients in both groups received standard-of-care treatments, including an ACE inhibitor, for at least 1 month. Consistent with prior data, the median age of participants was 28 years and 90% were men.
The primary endpoint was the number of days free of myocarditis complications (heart failure requiring hospitalization, chest pain requiring medication, left ventricular ejection fraction less than 50%, and ventricular arrhythmias) within 28 days postdischarge.
There was no significant difference in this endpoint between the two arms, with a median of 30 days for anakinra versus 31 days for placebo.
Overall, the rate of the composite endpoint of myocarditis complications occurred in 13.7% of patients, and there was a numerical reduction in the number of patients with these myocarditis complications with anakinra – 6 patients (10.5%) in the anakinra group versus 10 patients (16.5%) in the placebo group (odds ratio, 0.59; 95% confidence interval, 0.19-1.78). This was driven by fewer patients with chest pain requiring new medication (two patients versus six patients).
The safety endpoint was the number of serious adverse events within 28 days postdischarge. This endpoint occurred in seven patients (12.1%) in the anakinra arm and six patients (10.2%) in the placebo arm, with no significant difference between groups. Cases of severe infection within 28 days postdischarge were reported in both arms.
Low-risk population
Designated discussant of the study at the ESC Hotline session, Enrico Ammirati, MD, PhD, University of Milano-Bicocca, Monza, Italy, said that patients involved in ARAMIS fit the profile of acute myocarditis and that the CMR diagnosis was positive in all the patients enrolled.
Dr. Ammirati agreed with Dr. Kerneis that the neutral results of the study were probably caused by the low-risk population. “If we look at retrospective registries, at 30 days there are zero cardiac deaths or heart transplants at 30 days in patients with a low-risk presentation.
“The ARAMIS trial has shown the feasibility of conducting studies in the setting of acute myocarditis, and even if the primary endpoint was neutral, some important data are still missing, such as change in ejection fraction and troponin levels,” he noted.
“In terms of future perspective, we are moving to assessing efficacy of anakinra or other immunosuppressive drugs from acute low risk patients to higher risk patients with heart failure and severe dysfunction,” he said.
Dr. Ammirati is the lead investigator of another ongoing study in such a higher-risk population; the MYTHS trial is investigating the use of intravenous steroids in patients with suspected acute myocarditis complicated by acute heart failure or cardiogenic shock, and an ejection fraction below 41%.
“So, we will have more results on the best treatment in this higher risk group of patients,” he concluded.
The ARAMIS trial was an academic study funded by the French Health Ministry and coordinated by the ACTION Group. Dr. Kerneis reports having received consulting fees from Kiniksa, Sanofi, and Bayer, and holds a patent for use of abatacept in immune checkpoint inhibitor (ICI)–induced myocarditis.
A version of this article first appeared on Medscape.com.
AMSTERDAM – A short course of the interleukin-1 receptor antagonist, anakinra, appeared safe but did not reduce complications of acute myocarditis in the ARAMIS trial.
The trial was presented at the annual congress of the European Society of Cardiology.
Lead investigator, Mathieu Kerneis, MD, Pitie Salpetriere APHP University Hospital, Paris, said this was the largest randomized controlled trial of patients with acute myocarditis and probably the first ever study in the acute setting of myocarditis patients diagnosed with cardiac magnetic resonance (CMR) imaging, not on biopsy, who are mostly at low risk for events.
He suggested that one of the reasons for the neutral result could have been the low-risk population involved and the low complication rate. “We enrolled an all-comer acute myocarditis population diagnosed with CMR, who were mostly at a low risk of complications,” he noted.
“I don’t think the story of anti-inflammatory drugs in acute myocarditis is over. This is just the beginning. This was the first trial, and it was just a phase 2 trial. We need further randomized trials to explore the potential benefit of an anti-inflammatory strategy in acute myocarditis patients at higher risk of complications. In addition, larger studies are needed to evaluate prolonged anti-inflammatory strategies in acute myocarditis patients at low-to-moderate risk of complications,” Dr. Kerneis concluded.
“It is very challenging to do a trial in high-risk patients with myocarditis as these patients are quite rare,” he added.
Inflammation of the myocardium
Dr. Kerneis explained that acute myocarditis is an inflammation of the myocardium that can cause permanent damage to the heart muscle and lead to myocardial infarction, stroke, heart failure, arrhythmias, and death. The condition can occur in individuals of all ages but is most frequent in young people. There is no specific treatment, but patients are generally treated with beta-blockers, angiotensin-converting enzyme (ACE) inhibitors, and sometimes steroids.
Anakinra is an interleukin-1 receptor antagonist that works by targeting the interleukin-1β innate immune pathway. Anakinra is used for the treatment of rheumatoid arthritis and has shown efficacy in pericarditis. Dr. Kerneis noted that there have been several case reports of successful treatment with anakinra in acute myocarditis.
The ARAMIS trial – conducted at six academic centers in France – was the first randomized study to evaluate inhibition of the interleukin-1β innate immune pathway in myocarditis patients. The trial enrolled 120 hospitalized, symptomatic patients with chest pain, increased cardiac troponin, and acute myocarditis diagnosed using CMR. More than half had had a recent bacterial or viral infection.
Patients were randomized within 72 hours of hospital admission to a daily subcutaneous dose of anakinra 100 mg or placebo until hospital discharge. Patients in both groups received standard-of-care treatments, including an ACE inhibitor, for at least 1 month. Consistent with prior data, the median age of participants was 28 years and 90% were men.
The primary endpoint was the number of days free of myocarditis complications (heart failure requiring hospitalization, chest pain requiring medication, left ventricular ejection fraction less than 50%, and ventricular arrhythmias) within 28 days postdischarge.
There was no significant difference in this endpoint between the two arms, with a median of 30 days for anakinra versus 31 days for placebo.
Overall, the rate of the composite endpoint of myocarditis complications occurred in 13.7% of patients, and there was a numerical reduction in the number of patients with these myocarditis complications with anakinra – 6 patients (10.5%) in the anakinra group versus 10 patients (16.5%) in the placebo group (odds ratio, 0.59; 95% confidence interval, 0.19-1.78). This was driven by fewer patients with chest pain requiring new medication (two patients versus six patients).
The safety endpoint was the number of serious adverse events within 28 days postdischarge. This endpoint occurred in seven patients (12.1%) in the anakinra arm and six patients (10.2%) in the placebo arm, with no significant difference between groups. Cases of severe infection within 28 days postdischarge were reported in both arms.
Low-risk population
Designated discussant of the study at the ESC Hotline session, Enrico Ammirati, MD, PhD, University of Milano-Bicocca, Monza, Italy, said that patients involved in ARAMIS fit the profile of acute myocarditis and that the CMR diagnosis was positive in all the patients enrolled.
Dr. Ammirati agreed with Dr. Kerneis that the neutral results of the study were probably caused by the low-risk population. “If we look at retrospective registries, at 30 days there are zero cardiac deaths or heart transplants at 30 days in patients with a low-risk presentation.
“The ARAMIS trial has shown the feasibility of conducting studies in the setting of acute myocarditis, and even if the primary endpoint was neutral, some important data are still missing, such as change in ejection fraction and troponin levels,” he noted.
“In terms of future perspective, we are moving to assessing efficacy of anakinra or other immunosuppressive drugs from acute low risk patients to higher risk patients with heart failure and severe dysfunction,” he said.
Dr. Ammirati is the lead investigator of another ongoing study in such a higher-risk population; the MYTHS trial is investigating the use of intravenous steroids in patients with suspected acute myocarditis complicated by acute heart failure or cardiogenic shock, and an ejection fraction below 41%.
“So, we will have more results on the best treatment in this higher risk group of patients,” he concluded.
The ARAMIS trial was an academic study funded by the French Health Ministry and coordinated by the ACTION Group. Dr. Kerneis reports having received consulting fees from Kiniksa, Sanofi, and Bayer, and holds a patent for use of abatacept in immune checkpoint inhibitor (ICI)–induced myocarditis.
A version of this article first appeared on Medscape.com.
AT ESC CONGRESS 2023
The new normal in body temperature
This transcript has been edited for clarity.
Every branch of science has its constants. Physics has the speed of light, the gravitational constant, the Planck constant. Chemistry gives us Avogadro’s number, Faraday’s constant, the charge of an electron. Medicine isn’t quite as reliable as physics when it comes to these things, but insofar as there are any constants in medicine, might I suggest normal body temperature: 37° Celsius, 98.6° Fahrenheit.
Sure, serum sodium may be less variable and lactate concentration more clinically relevant, but even my 7-year-old knows that normal body temperature is 98.6°.
Except, as it turns out, 98.6° isn’t normal at all.
How did we arrive at 37.0° C for normal body temperature? We got it from this guy – German physician Carl Reinhold August Wunderlich, who, in addition to looking eerily like Luciano Pavarotti, was the first to realize that fever was not itself a disease but a symptom of one.
In 1851, Dr. Wunderlich released his measurements of more than 1 million body temperatures taken from 25,000 Germans – a painstaking process at the time, which employed a foot-long thermometer and took 20 minutes to obtain a measurement.
The average temperature measured, of course, was 37° C.
We’re more than 150 years post-Wunderlich right now, and the average person in the United States might be quite a bit different from the average German in 1850. Moreover, we can do a lot better than just measuring a ton of people and taking the average, because we have statistics. The problem with measuring a bunch of people and taking the average temperature as normal is that you can’t be sure that the people you are measuring are normal. There are obvious causes of elevated temperature that you could exclude. Let’s not take people with a respiratory infection or who are taking Tylenol, for example. But as highlighted in this paper in JAMA Internal Medicine, we can do a lot better than that.
The study leverages the fact that body temperature is typically measured during all medical office visits and recorded in the ever-present electronic medical record.
Researchers from Stanford identified 724,199 patient encounters with outpatient temperature data. They excluded extreme temperatures – less than 34° C or greater than 40° C – excluded patients under 20 or above 80 years, and excluded those with extremes of height, weight, or body mass index.
You end up with a distribution like this. Note that the peak is clearly lower than 37° C.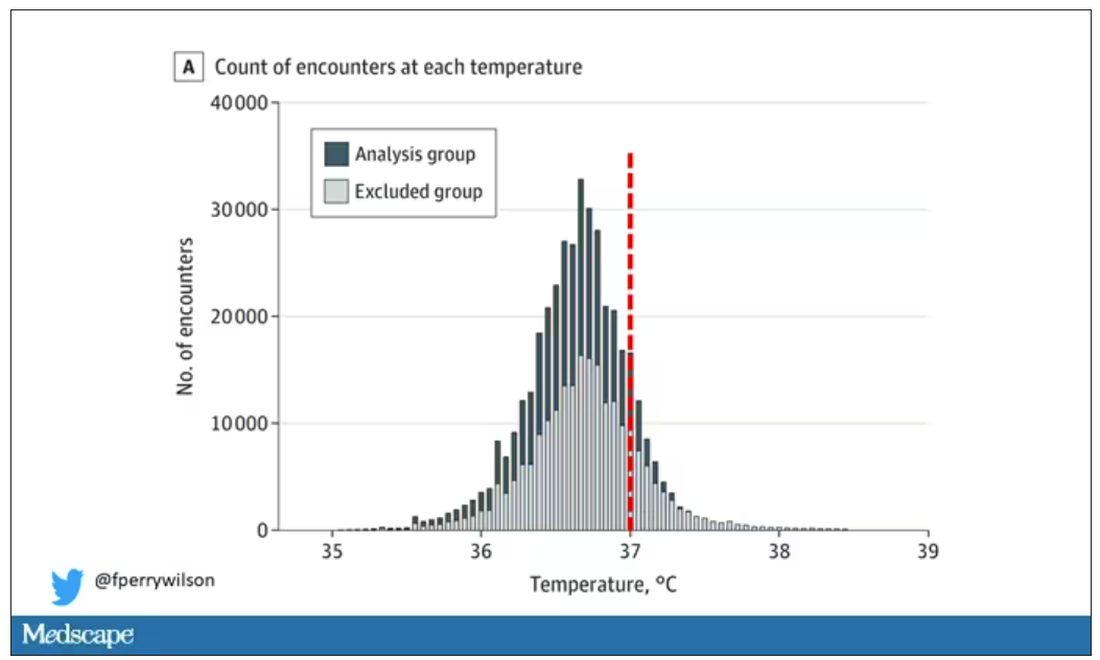
But we’re still not at “normal.” Some people would be seeing their doctor for conditions that affect body temperature, such as infection. You could use diagnosis codes to flag these individuals and drop them, but that feels a bit arbitrary.
I really love how the researchers used data to fix this problem. They used a technique called LIMIT (Laboratory Information Mining for Individualized Thresholds). It works like this:
Take all the temperature measurements and then identify the outliers – the very tails of the distribution.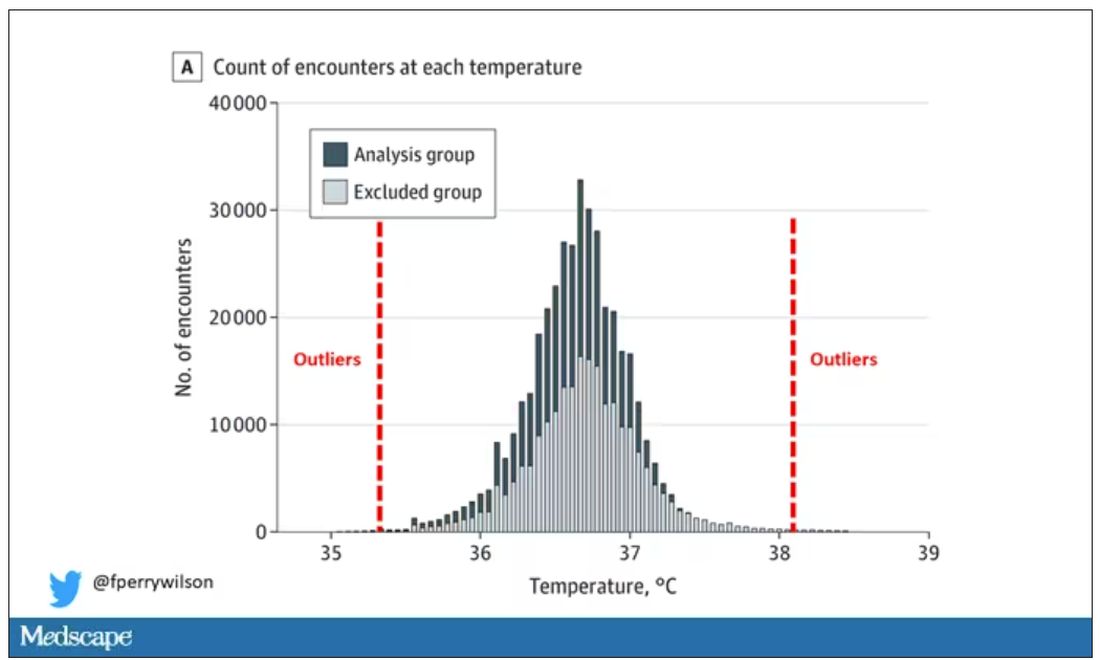
Look at all the diagnosis codes in those distributions. Determine which diagnosis codes are overrepresented in those distributions. Now you have a data-driven way to say that yes, these diagnoses are associated with weird temperatures. Next, eliminate everyone with those diagnoses from the dataset. What you are left with is a normal population, or at least a population that doesn’t have a condition that seems to meaningfully affect temperature.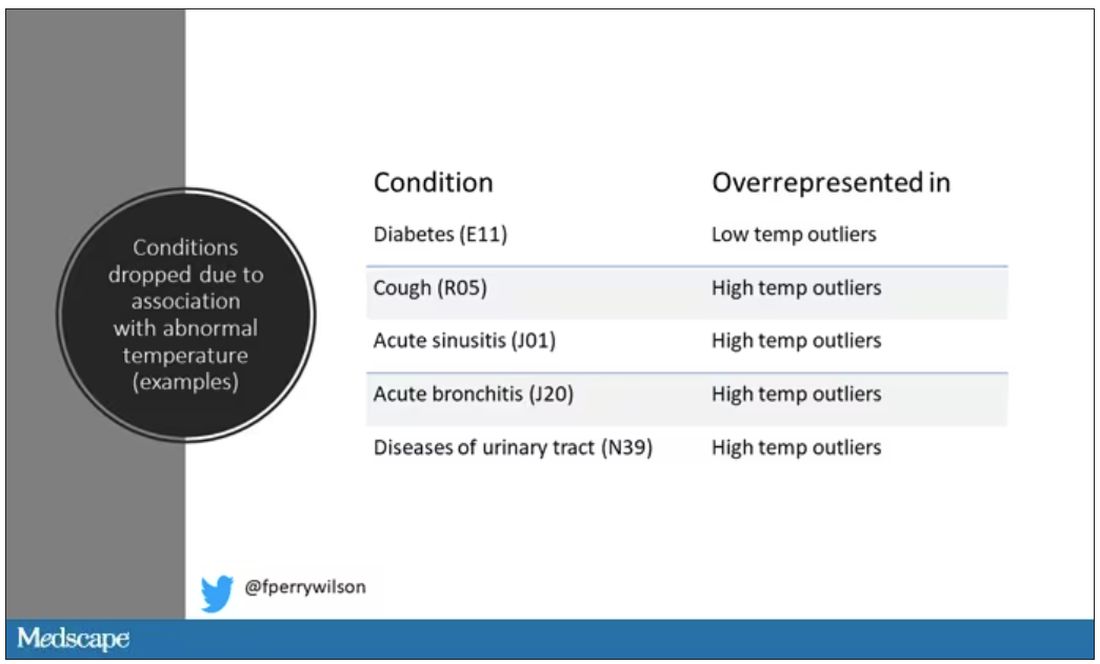
So, who was dropped? Well, a lot of people, actually. It turned out that diabetes was way overrepresented in the outlier group. Although 9.2% of the population had diabetes, 26% of people with very low temperatures did, so everyone with diabetes is removed from the dataset. While 5% of the population had a cough at their encounter, 7% of the people with very high temperature and 7% of the people with very low temperature had a cough, so everyone with cough gets thrown out.
The algorithm excluded people on antibiotics or who had sinusitis, urinary tract infections, pneumonia, and, yes, a diagnosis of “fever.” The list makes sense, which is always nice when you have a purely algorithmic classification system.
What do we have left? What is the real normal temperature? Ready?
It’s 36.64° C, or about 98.0° F.
Of course, normal temperature varied depending on the time of day it was measured – higher in the afternoon.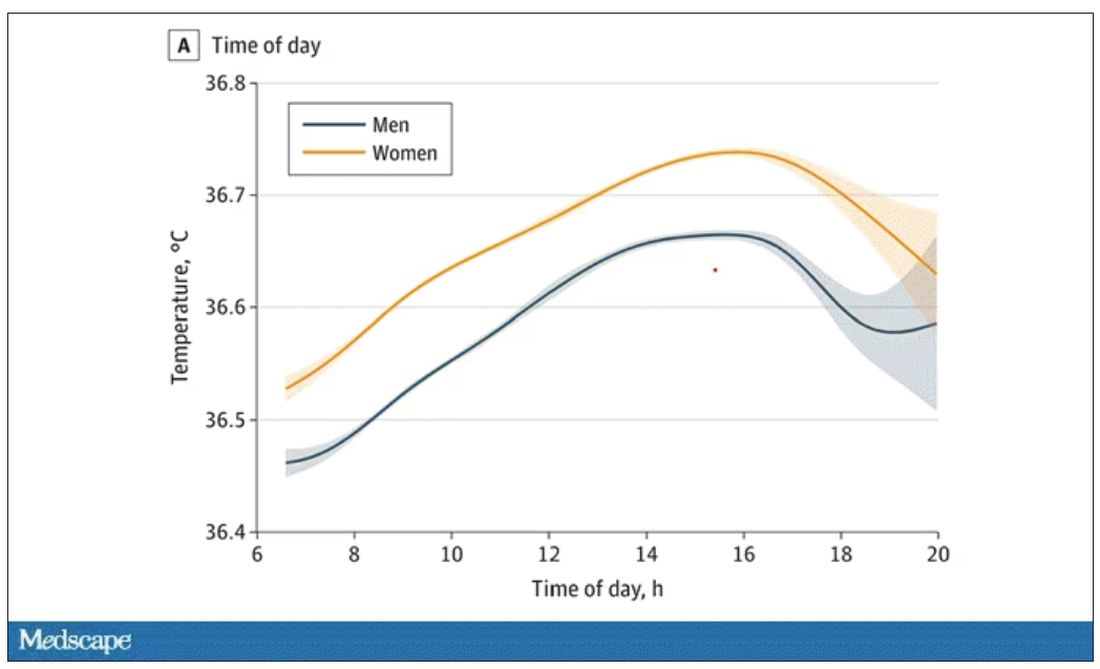
The normal temperature in women tended to be higher than in men. The normal temperature declined with age as well.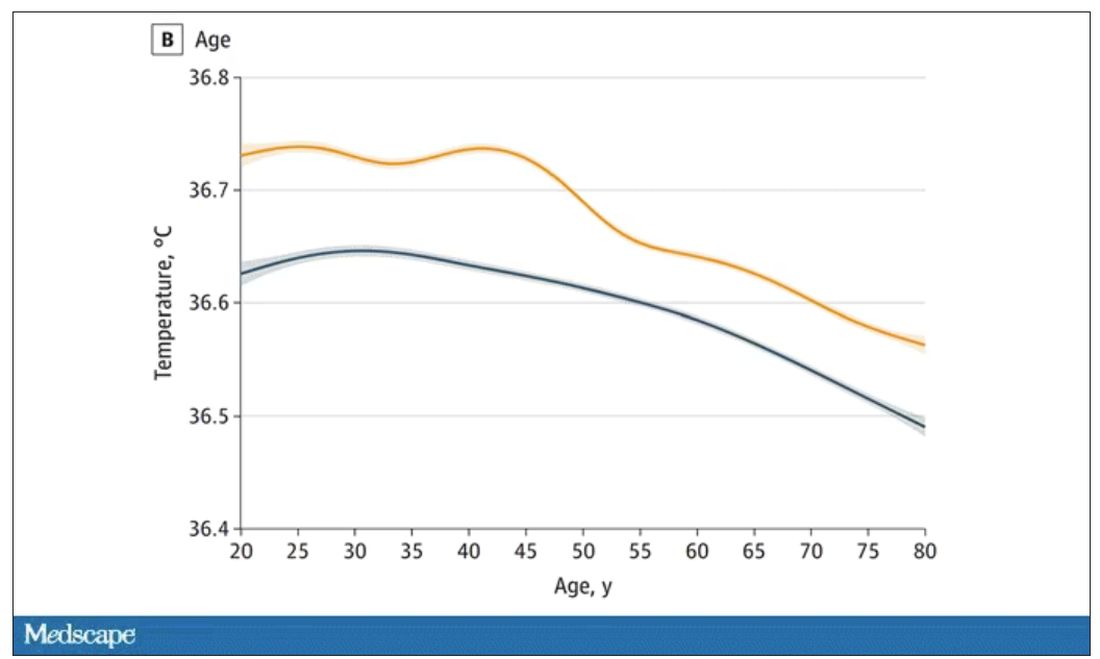
In fact, the researchers built a nice online calculator where you can enter your own, or your patient’s, parameters and calculate a normal body temperature for them. Here’s mine. My normal temperature at around 2 p.m. should be 36.7° C.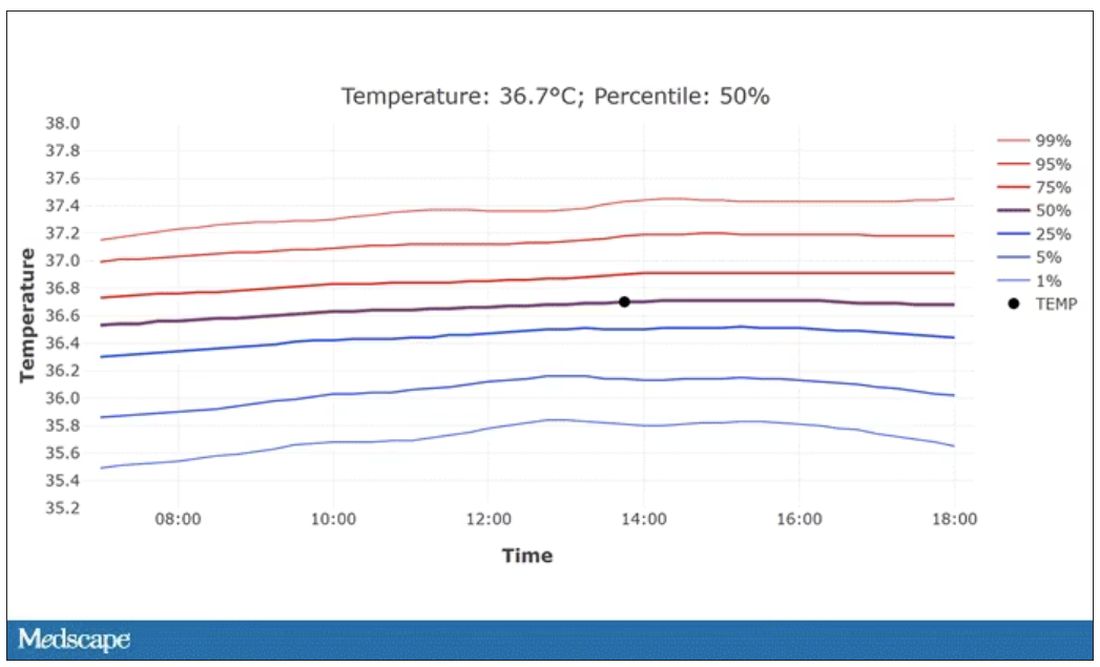
So, we’re all more cold-blooded than we thought. Is this just because of better methods? Maybe. But studies have actually shown that body temperature may be decreasing over time in humans, possibly because of the lower levels of inflammation we face in modern life (thanks to improvements in hygiene and antibiotics).
Of course, I’m sure some of you are asking yourselves whether any of this really matters. Is 37° C close enough?
Sure, this may be sort of puttering around the edges of physical diagnosis, but I think the methodology is really interesting and can obviously be applied to other broadly collected data points. But these data show us that thin, older individuals really do run cooler, and that we may need to pay more attention to a low-grade fever in that population than we otherwise would.
In any case, it’s time for a little re-education. If someone asks you what normal body temperature is, just say 36.6° C, 98.0° F. For his work in this area, I suggest we call it Wunderlich’s constant.
Dr. Wilson is associate professor of medicine and public health at Yale University, New Haven, Conn., and director of Yale’s Clinical and Translational Research Accelerator. He has no disclosures.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Every branch of science has its constants. Physics has the speed of light, the gravitational constant, the Planck constant. Chemistry gives us Avogadro’s number, Faraday’s constant, the charge of an electron. Medicine isn’t quite as reliable as physics when it comes to these things, but insofar as there are any constants in medicine, might I suggest normal body temperature: 37° Celsius, 98.6° Fahrenheit.
Sure, serum sodium may be less variable and lactate concentration more clinically relevant, but even my 7-year-old knows that normal body temperature is 98.6°.
Except, as it turns out, 98.6° isn’t normal at all.
How did we arrive at 37.0° C for normal body temperature? We got it from this guy – German physician Carl Reinhold August Wunderlich, who, in addition to looking eerily like Luciano Pavarotti, was the first to realize that fever was not itself a disease but a symptom of one.
In 1851, Dr. Wunderlich released his measurements of more than 1 million body temperatures taken from 25,000 Germans – a painstaking process at the time, which employed a foot-long thermometer and took 20 minutes to obtain a measurement.
The average temperature measured, of course, was 37° C.
We’re more than 150 years post-Wunderlich right now, and the average person in the United States might be quite a bit different from the average German in 1850. Moreover, we can do a lot better than just measuring a ton of people and taking the average, because we have statistics. The problem with measuring a bunch of people and taking the average temperature as normal is that you can’t be sure that the people you are measuring are normal. There are obvious causes of elevated temperature that you could exclude. Let’s not take people with a respiratory infection or who are taking Tylenol, for example. But as highlighted in this paper in JAMA Internal Medicine, we can do a lot better than that.
The study leverages the fact that body temperature is typically measured during all medical office visits and recorded in the ever-present electronic medical record.
Researchers from Stanford identified 724,199 patient encounters with outpatient temperature data. They excluded extreme temperatures – less than 34° C or greater than 40° C – excluded patients under 20 or above 80 years, and excluded those with extremes of height, weight, or body mass index.
You end up with a distribution like this. Note that the peak is clearly lower than 37° C.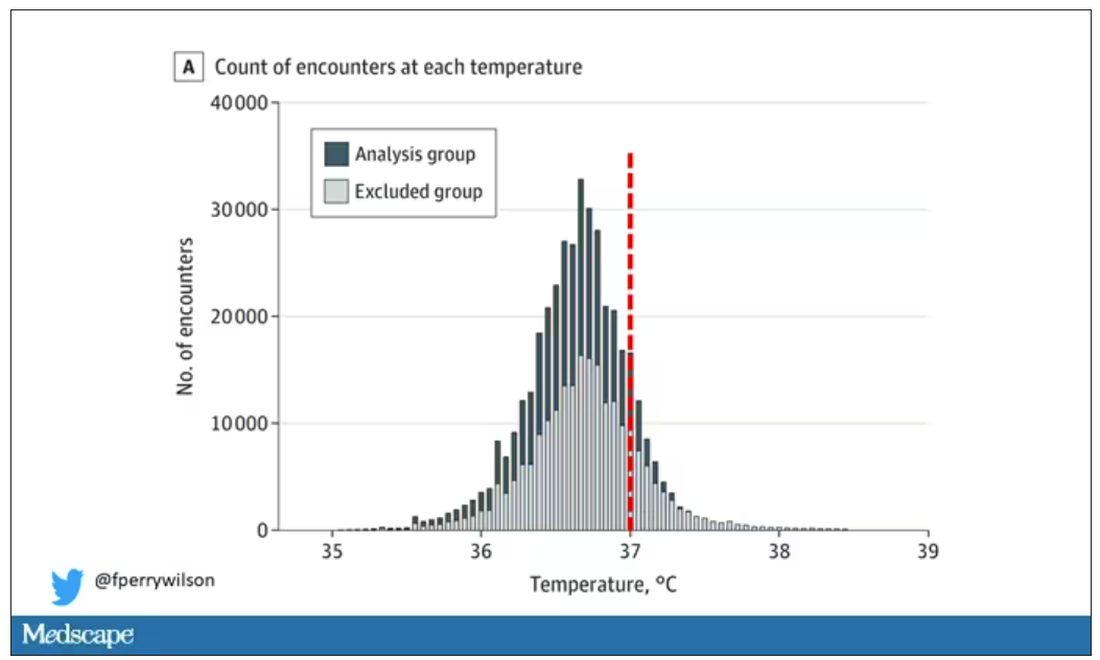
But we’re still not at “normal.” Some people would be seeing their doctor for conditions that affect body temperature, such as infection. You could use diagnosis codes to flag these individuals and drop them, but that feels a bit arbitrary.
I really love how the researchers used data to fix this problem. They used a technique called LIMIT (Laboratory Information Mining for Individualized Thresholds). It works like this:
Take all the temperature measurements and then identify the outliers – the very tails of the distribution.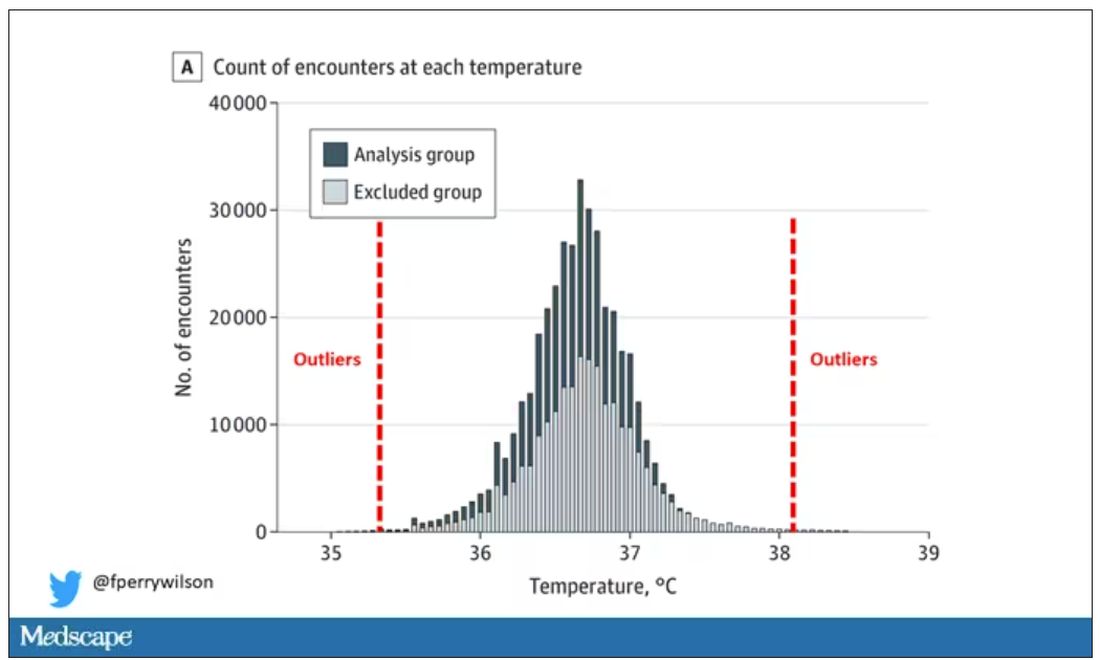
Look at all the diagnosis codes in those distributions. Determine which diagnosis codes are overrepresented in those distributions. Now you have a data-driven way to say that yes, these diagnoses are associated with weird temperatures. Next, eliminate everyone with those diagnoses from the dataset. What you are left with is a normal population, or at least a population that doesn’t have a condition that seems to meaningfully affect temperature.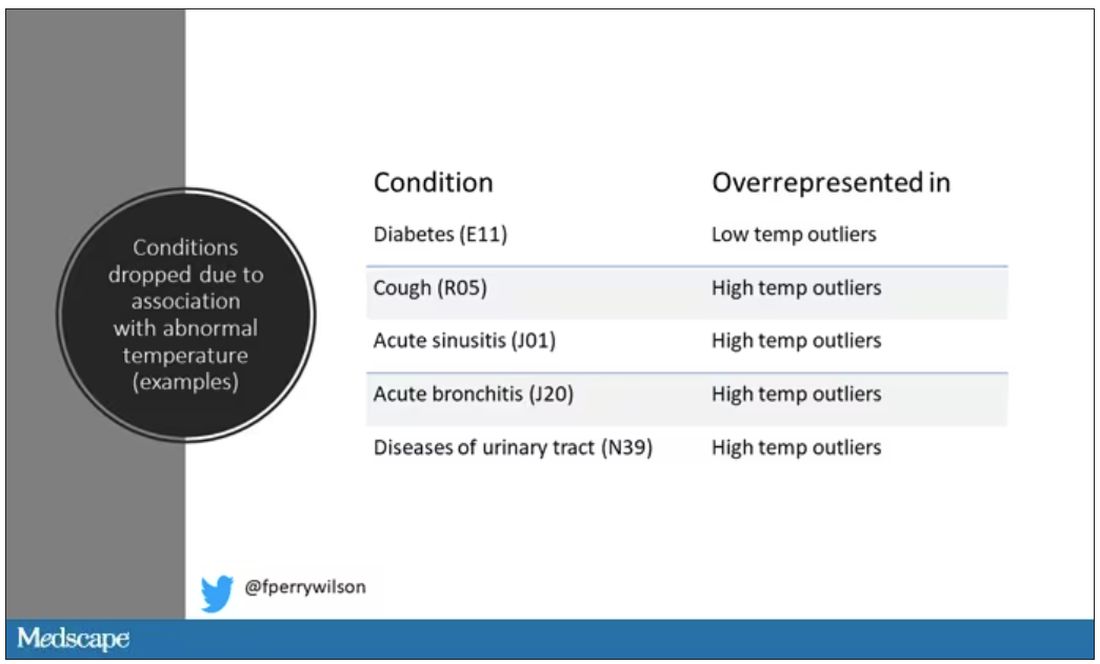
So, who was dropped? Well, a lot of people, actually. It turned out that diabetes was way overrepresented in the outlier group. Although 9.2% of the population had diabetes, 26% of people with very low temperatures did, so everyone with diabetes is removed from the dataset. While 5% of the population had a cough at their encounter, 7% of the people with very high temperature and 7% of the people with very low temperature had a cough, so everyone with cough gets thrown out.
The algorithm excluded people on antibiotics or who had sinusitis, urinary tract infections, pneumonia, and, yes, a diagnosis of “fever.” The list makes sense, which is always nice when you have a purely algorithmic classification system.
What do we have left? What is the real normal temperature? Ready?
It’s 36.64° C, or about 98.0° F.
Of course, normal temperature varied depending on the time of day it was measured – higher in the afternoon.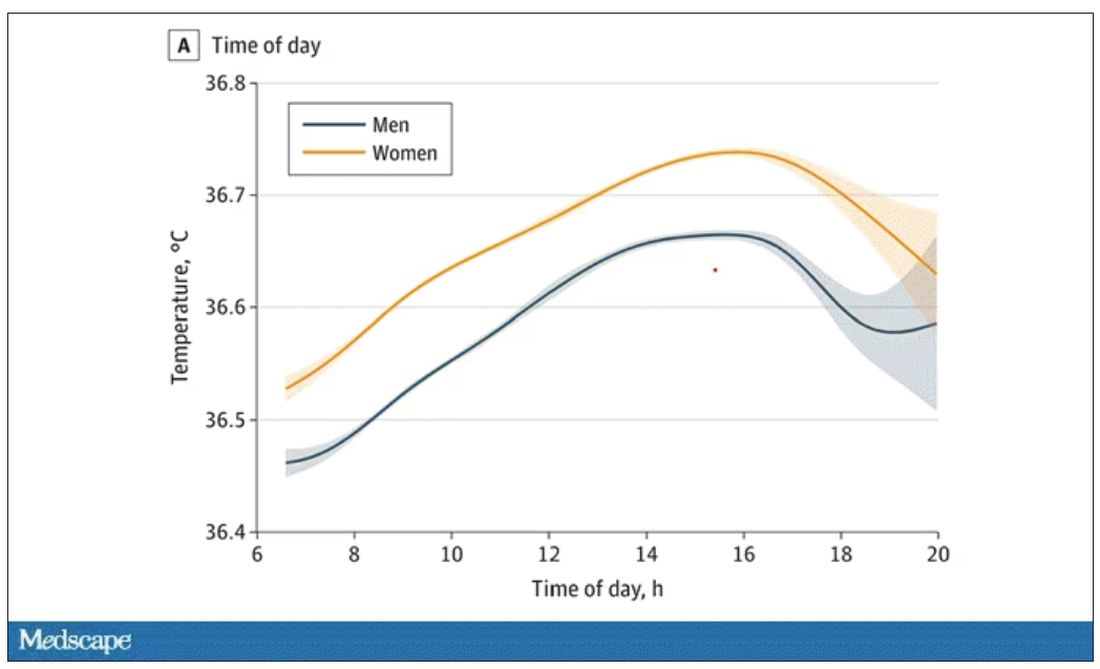
The normal temperature in women tended to be higher than in men. The normal temperature declined with age as well.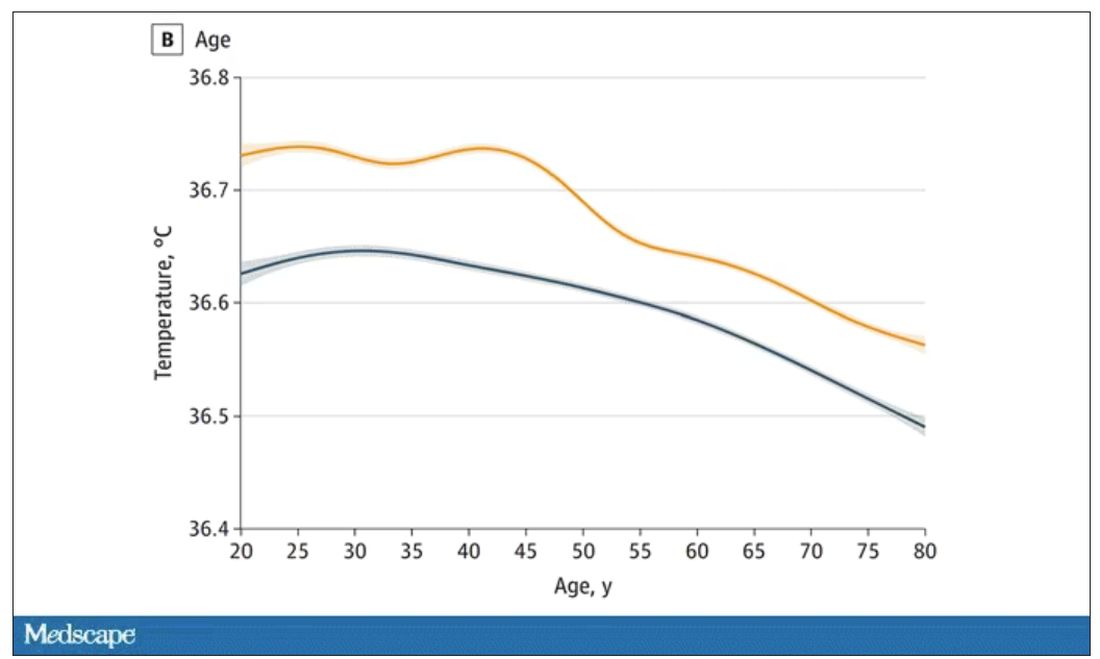
In fact, the researchers built a nice online calculator where you can enter your own, or your patient’s, parameters and calculate a normal body temperature for them. Here’s mine. My normal temperature at around 2 p.m. should be 36.7° C.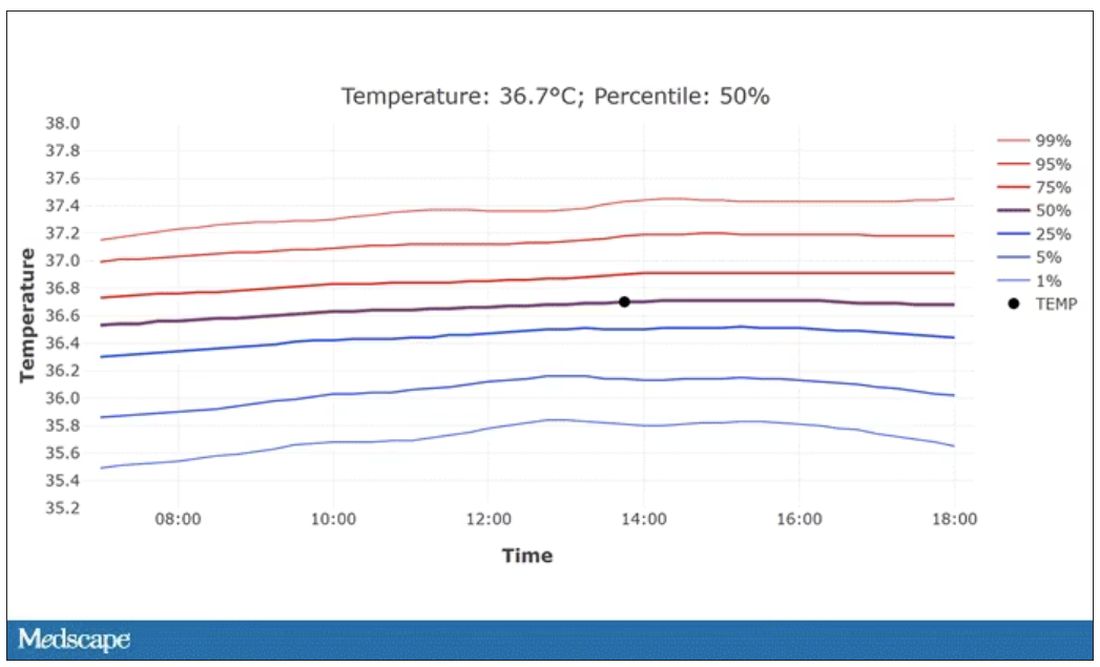
So, we’re all more cold-blooded than we thought. Is this just because of better methods? Maybe. But studies have actually shown that body temperature may be decreasing over time in humans, possibly because of the lower levels of inflammation we face in modern life (thanks to improvements in hygiene and antibiotics).
Of course, I’m sure some of you are asking yourselves whether any of this really matters. Is 37° C close enough?
Sure, this may be sort of puttering around the edges of physical diagnosis, but I think the methodology is really interesting and can obviously be applied to other broadly collected data points. But these data show us that thin, older individuals really do run cooler, and that we may need to pay more attention to a low-grade fever in that population than we otherwise would.
In any case, it’s time for a little re-education. If someone asks you what normal body temperature is, just say 36.6° C, 98.0° F. For his work in this area, I suggest we call it Wunderlich’s constant.
Dr. Wilson is associate professor of medicine and public health at Yale University, New Haven, Conn., and director of Yale’s Clinical and Translational Research Accelerator. He has no disclosures.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Every branch of science has its constants. Physics has the speed of light, the gravitational constant, the Planck constant. Chemistry gives us Avogadro’s number, Faraday’s constant, the charge of an electron. Medicine isn’t quite as reliable as physics when it comes to these things, but insofar as there are any constants in medicine, might I suggest normal body temperature: 37° Celsius, 98.6° Fahrenheit.
Sure, serum sodium may be less variable and lactate concentration more clinically relevant, but even my 7-year-old knows that normal body temperature is 98.6°.
Except, as it turns out, 98.6° isn’t normal at all.
How did we arrive at 37.0° C for normal body temperature? We got it from this guy – German physician Carl Reinhold August Wunderlich, who, in addition to looking eerily like Luciano Pavarotti, was the first to realize that fever was not itself a disease but a symptom of one.
In 1851, Dr. Wunderlich released his measurements of more than 1 million body temperatures taken from 25,000 Germans – a painstaking process at the time, which employed a foot-long thermometer and took 20 minutes to obtain a measurement.
The average temperature measured, of course, was 37° C.
We’re more than 150 years post-Wunderlich right now, and the average person in the United States might be quite a bit different from the average German in 1850. Moreover, we can do a lot better than just measuring a ton of people and taking the average, because we have statistics. The problem with measuring a bunch of people and taking the average temperature as normal is that you can’t be sure that the people you are measuring are normal. There are obvious causes of elevated temperature that you could exclude. Let’s not take people with a respiratory infection or who are taking Tylenol, for example. But as highlighted in this paper in JAMA Internal Medicine, we can do a lot better than that.
The study leverages the fact that body temperature is typically measured during all medical office visits and recorded in the ever-present electronic medical record.
Researchers from Stanford identified 724,199 patient encounters with outpatient temperature data. They excluded extreme temperatures – less than 34° C or greater than 40° C – excluded patients under 20 or above 80 years, and excluded those with extremes of height, weight, or body mass index.
You end up with a distribution like this. Note that the peak is clearly lower than 37° C.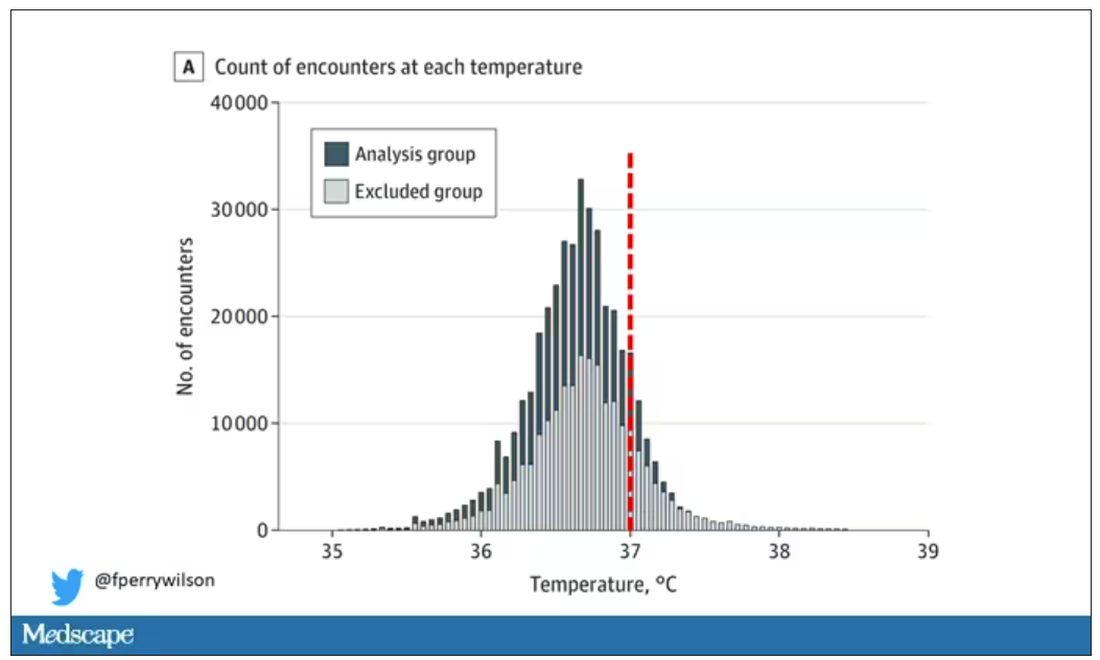
But we’re still not at “normal.” Some people would be seeing their doctor for conditions that affect body temperature, such as infection. You could use diagnosis codes to flag these individuals and drop them, but that feels a bit arbitrary.
I really love how the researchers used data to fix this problem. They used a technique called LIMIT (Laboratory Information Mining for Individualized Thresholds). It works like this:
Take all the temperature measurements and then identify the outliers – the very tails of the distribution.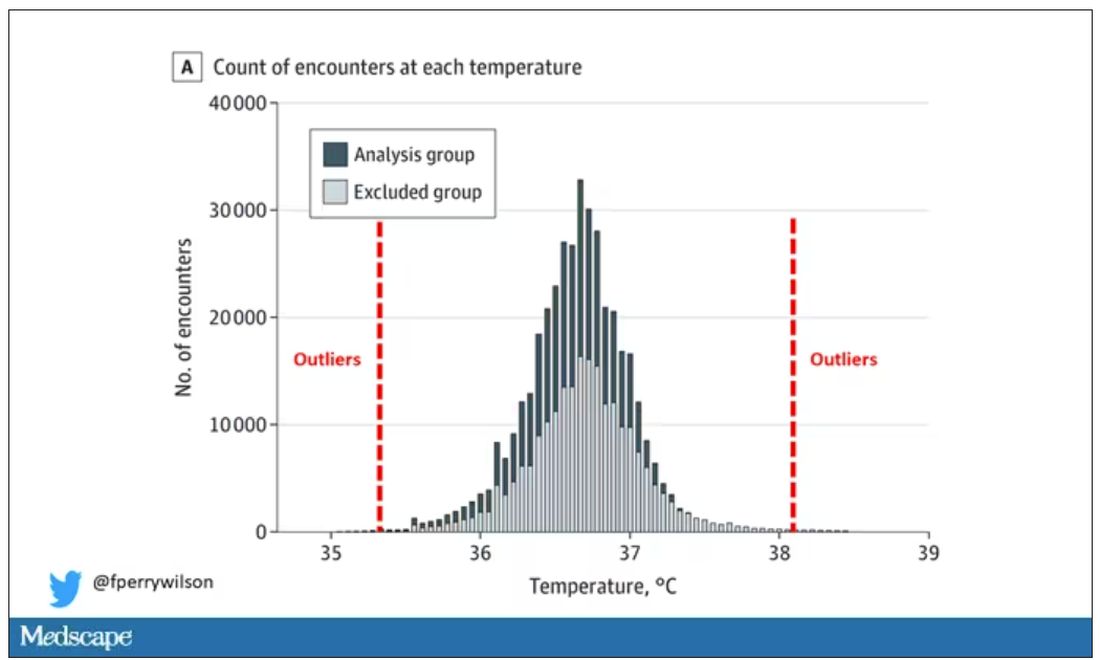
Look at all the diagnosis codes in those distributions. Determine which diagnosis codes are overrepresented in those distributions. Now you have a data-driven way to say that yes, these diagnoses are associated with weird temperatures. Next, eliminate everyone with those diagnoses from the dataset. What you are left with is a normal population, or at least a population that doesn’t have a condition that seems to meaningfully affect temperature.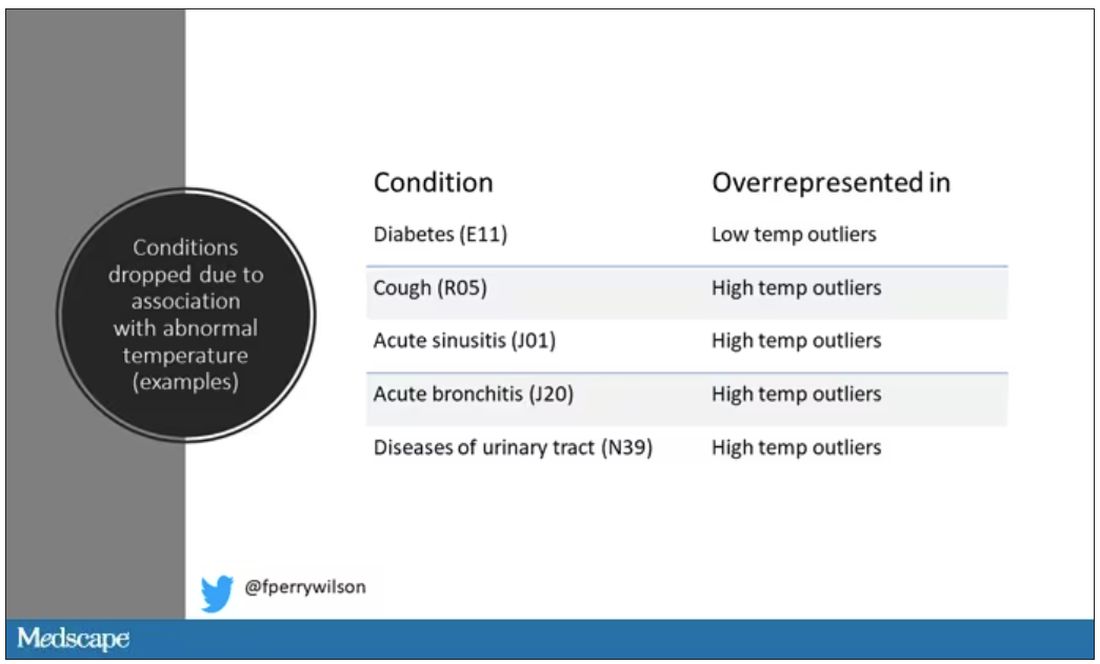
So, who was dropped? Well, a lot of people, actually. It turned out that diabetes was way overrepresented in the outlier group. Although 9.2% of the population had diabetes, 26% of people with very low temperatures did, so everyone with diabetes is removed from the dataset. While 5% of the population had a cough at their encounter, 7% of the people with very high temperature and 7% of the people with very low temperature had a cough, so everyone with cough gets thrown out.
The algorithm excluded people on antibiotics or who had sinusitis, urinary tract infections, pneumonia, and, yes, a diagnosis of “fever.” The list makes sense, which is always nice when you have a purely algorithmic classification system.
What do we have left? What is the real normal temperature? Ready?
It’s 36.64° C, or about 98.0° F.
Of course, normal temperature varied depending on the time of day it was measured – higher in the afternoon.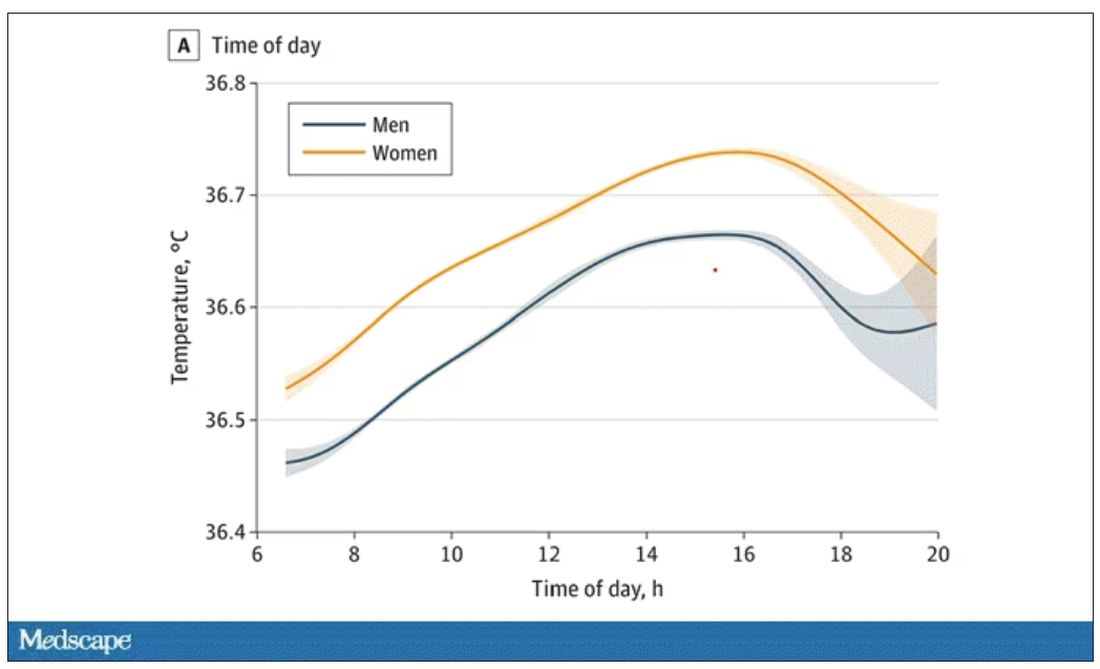
The normal temperature in women tended to be higher than in men. The normal temperature declined with age as well.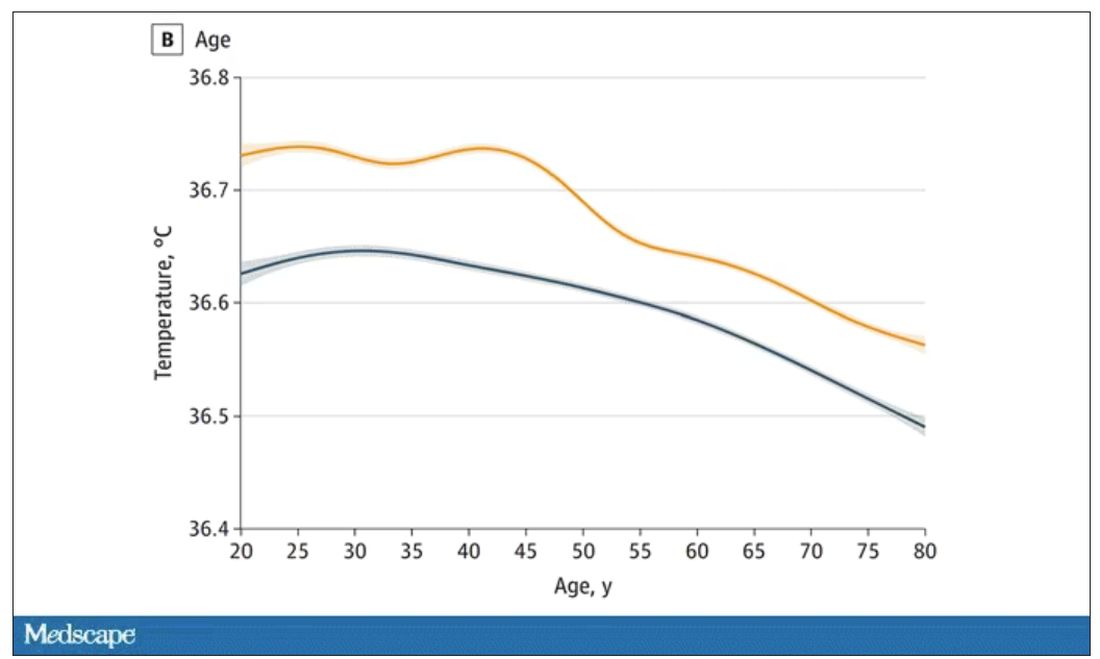
In fact, the researchers built a nice online calculator where you can enter your own, or your patient’s, parameters and calculate a normal body temperature for them. Here’s mine. My normal temperature at around 2 p.m. should be 36.7° C.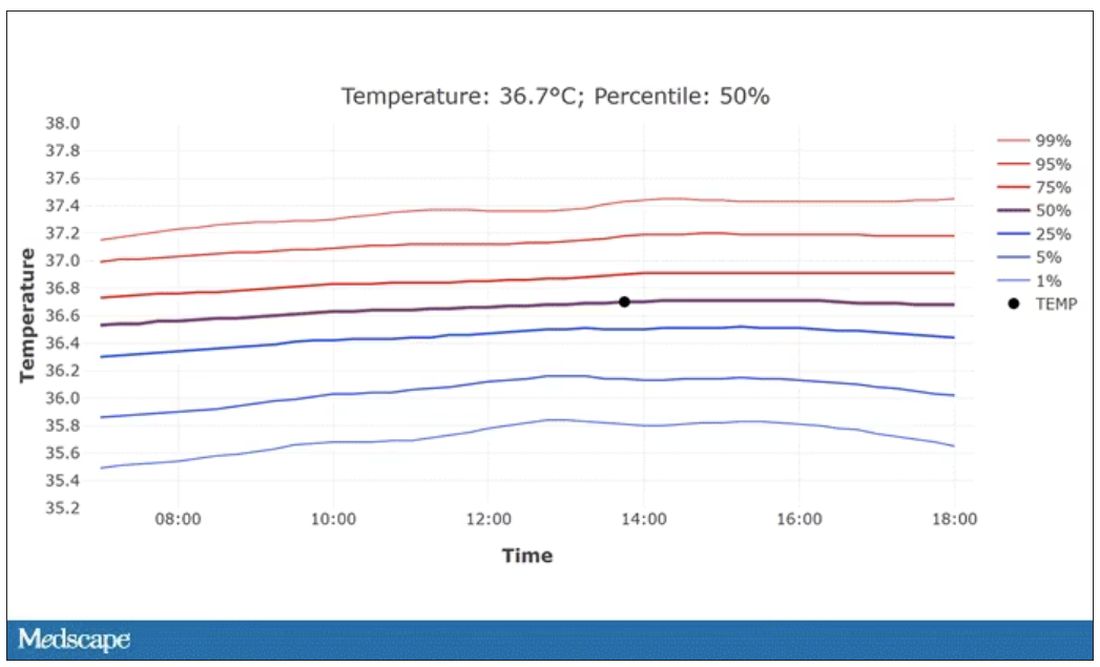
So, we’re all more cold-blooded than we thought. Is this just because of better methods? Maybe. But studies have actually shown that body temperature may be decreasing over time in humans, possibly because of the lower levels of inflammation we face in modern life (thanks to improvements in hygiene and antibiotics).
Of course, I’m sure some of you are asking yourselves whether any of this really matters. Is 37° C close enough?
Sure, this may be sort of puttering around the edges of physical diagnosis, but I think the methodology is really interesting and can obviously be applied to other broadly collected data points. But these data show us that thin, older individuals really do run cooler, and that we may need to pay more attention to a low-grade fever in that population than we otherwise would.
In any case, it’s time for a little re-education. If someone asks you what normal body temperature is, just say 36.6° C, 98.0° F. For his work in this area, I suggest we call it Wunderlich’s constant.
Dr. Wilson is associate professor of medicine and public health at Yale University, New Haven, Conn., and director of Yale’s Clinical and Translational Research Accelerator. He has no disclosures.
A version of this article appeared on Medscape.com.
New AI-enhanced bandages poised to transform wound treatment
You cut yourself. You put on a bandage. In a week or so, your wound heals.
Most people take this routine for granted. But for the more than 8.2 million Americans who have chronic wounds, it’s not so simple.
Traumatic injuries, post-surgical complications, advanced age, and chronic illnesses like diabetes and vascular disease can all disrupt the delicate healing process, leading to wounds that last months or years.
Left untreated, about 30% led to amputation. And recent studies show the risk of dying from a chronic wound complication within 5 years rivals that of most cancers.
Yet until recently, medical technology had not kept up with what experts say is a snowballing threat to public health.
“Wound care – even with all of the billions of products that are sold – still exists on kind of a medieval level,” said Geoffrey Gurtner, MD, chair of the department of surgery and professor of biomedical engineering at the University of Arizona College of Medicine. “We’re still putting on poultices and salves ... and when it comes to diagnosing infection, it’s really an art. I think we can do better.”
Old-school bandage meets AI
Dr. Gurtner is among dozens of clinicians and researchers reimagining the humble bandage, combining cutting-edge materials science with artificial intelligence and patient data to develop “smart bandages” that do far more than shield a wound.
Someday soon, these paper-thin bandages embedded with miniaturized electronics could monitor the healing process in real time, alerting the patient – or a doctor – when things go wrong. With the press of a smartphone button, that bandage could deliver medicine to fight an infection or an electrical pulse to stimulate healing.
Some “closed-loop” designs need no prompting, instead monitoring the wound and automatically giving it what it needs.
Others in development could halt a battlefield wound from hemorrhaging or kick-start healing in a blast wound, preventing longer-term disability.
The same technologies could – if the price is right – speed up healing and reduce scarring in minor cuts and scrapes, too, said Dr. Gurtner.
And unlike many cutting-edge medical innovations, these next-generation bandages could be made relatively cheaply and benefit some of the most vulnerable populations, including older adults, people with low incomes, and those in developing countries.
They could also save the health care system money, as the U.S. spends more than $28 billion annually treating chronic wounds.
“This is a condition that many patients find shameful and embarrassing, so there hasn’t been a lot of advocacy,” said Dr. Gurtner, outgoing board president of the Wound Healing Society. “It’s a relatively ignored problem afflicting an underserved population that has a huge cost. It’s a perfect storm.”
How wounds heal, or don’t
Wound healing is one of the most complex processes of the human body.
First platelets rush to the injury, prompting blood to clot. Then immune cells emit compounds called inflammatory cytokines, helping to fight off pathogens and keep infection at bay. Other compounds, including nitric oxide, spark the growth of new blood vessels and collagen to rebuild skin and connective tissue. As inflammation slows and stops, the flesh continues to reform.
But some conditions can stall the process, often in the inflammatory stage.
In people with diabetes, high glucose levels and poor circulation tend to sabotage the process. And people with nerve damage from spinal cord injuries, diabetes, or other ailments may not be able to feel it when a wound is getting worse or reinjured.
“We end up with patients going months with open wounds that are festering and infected,” said Roslyn Rivkah Isseroff, MD, professor of dermatology at the University of California Davis and head of the VA Northern California Health Care System’s wound healing clinic. “The patients are upset with the smell. These open ulcers put the patient at risk for systemic infection, like sepsis.” It can impact mental health, draining the patient’s ability to care for their wound.
“We see them once a week and send them home and say change your dressing every day, and they say, ‘I can barely move. I can’t do this,’ ” said Dr. Isseroff.
Checking for infection means removing bandages and culturing the wound. That can be painful, and results take time.
A lot can happen to a wound in a week.
“Sometimes, they come back and it’s a disaster, and they have to be admitted to the ER or even get an amputation,” Dr. Gurtner said.
People who are housing insecure or lack access to health care are even more vulnerable to complications.
“If you had the ability to say ‘there is something bad happening,’ you could do a lot to prevent this cascade and downward spiral.”
Bandages 2.0
In 2019, the Defense Advanced Research Projects Agency, the research arm of the Department of Defense, launched the Bioelectronics for Tissue Regeneration program to encourage scientists to develop a “closed-loop” bandage capable of both monitoring and hastening healing.
Tens of millions in funding has kick-started a flood of innovation since.
“It’s kind of a race to the finish,” said Marco Rolandi, PhD, associate professor of electrical and computer engineering at the University of California Santa Cruz and the principal investigator for a team including engineers, medical doctors, and computer scientists from UC Santa Cruz, UC Davis, and Tufts. “I’ve been amazed and impressed at all the work coming out.”
His team’s goal is to cut healing time in half by using (a) real-time monitoring of how a wound is healing – using indicators like temperature, pH level, oxygen, moisture, glucose, electrical activity, and certain proteins, and (b) appropriate stimulation.
“Every wound is different, so there is no one solution,” said Dr. Isseroff, the team’s clinical lead. “The idea is that it will be able to sense different parameters unique to the wound, use AI to figure out what stage it is in, and provide the right stimulus to kick it out of that stalled stage.”
The team has developed a proof-of-concept prototype: a bandage embedded with a tiny camera that takes pictures and transmits them to a computer algorithm to assess the wound’s progress. Miniaturized battery-powered actuators, or motors, automatically deliver medication.
Phase I trials in rodents went well, Dr. Rolandi said. The team is now testing the bandage on pigs.
Across the globe, other promising developments are underway.
In a scientific paper published in May, researchers at the University of Glasgow described a new “low-cost, environmentally friendly” bandage embedded with light-emitting diodes that use ultraviolet light to kill bacteria – no antibiotics needed. The fabric is stitched with a slim, flexible coil that powers the lights without a battery using wireless power transfer. In lab studies, it eradicated gram-negative bacteria (some of the nastiest bugs) in 6 hours.
Also in May, in the journal Bioactive Materials, a Penn State team detailed a bandage with medicine-injecting microneedles that can halt bleeding immediately after injury. In lab and animal tests, it reduced clotting time from 11.5 minutes to 1.3 minutes and bleeding by 90%.
“With hemorrhaging injuries, it is often the loss of blood – not the injury itself – that causes death,” said study author Amir Sheikhi, PhD, assistant professor of chemical and biomedical engineering at Penn State. “Those 10 minutes could be the difference between life and death.”
Another smart bandage, developed at Northwestern University, Chicago, harmlessly dissolves – electrodes and all – into the body after it is no longer needed, eliminating what can be a painful removal.
Guillermo Ameer, DSc, a study author reporting on the technology in Science Advances, hopes it could be made cheaply and used in developing countries.
“We’d like to create something that you could use in your home, even in a very remote village,” said Dr. Ameer, professor of biomedical engineering at Northwestern.
Timeline for clinical use
These are early days for the smart bandage, scientists say. Most studies have been in rodents and more work is needed to develop human-scale bandages, reduce cost, solve long-term data storage, and ensure material adheres well without irritating the skin.
But Dr. Gurtner is hopeful that some iteration could be used in clinical practice within a few years.
In May, he and colleagues at Stanford (Calif.) University published a paper in Nature Biotechnology describing their smart bandage. It includes a microcontroller unit, a radio antenna, biosensors, and an electrical stimulator all affixed to a rubbery, skin-like polymer (or hydrogel) about the thickness of a single coat of latex paint.
The bandage senses changes in temperature and electrical conductivity as the wound heals, and it gives electrical stimulation to accelerate that healing.
Animals treated with the bandage healed 25% faster, with 50% less scarring.
Electrical currents are already used for wound healing in clinical practice, Dr. Gurtner said. Because the stimulus is already approved and the cost to make the bandage could be low (as little as $10 to $50), he believes it could be ushered through the approval processes relatively quickly.
“Is this the ultimate embodiment of all the bells and whistles that are possible in a smart bandage? No. Not yet,” he said. “But we think it will help people. And right now, that’s good enough.”
A version of this article appeared on WebMD.com.
You cut yourself. You put on a bandage. In a week or so, your wound heals.
Most people take this routine for granted. But for the more than 8.2 million Americans who have chronic wounds, it’s not so simple.
Traumatic injuries, post-surgical complications, advanced age, and chronic illnesses like diabetes and vascular disease can all disrupt the delicate healing process, leading to wounds that last months or years.
Left untreated, about 30% led to amputation. And recent studies show the risk of dying from a chronic wound complication within 5 years rivals that of most cancers.
Yet until recently, medical technology had not kept up with what experts say is a snowballing threat to public health.
“Wound care – even with all of the billions of products that are sold – still exists on kind of a medieval level,” said Geoffrey Gurtner, MD, chair of the department of surgery and professor of biomedical engineering at the University of Arizona College of Medicine. “We’re still putting on poultices and salves ... and when it comes to diagnosing infection, it’s really an art. I think we can do better.”
Old-school bandage meets AI
Dr. Gurtner is among dozens of clinicians and researchers reimagining the humble bandage, combining cutting-edge materials science with artificial intelligence and patient data to develop “smart bandages” that do far more than shield a wound.
Someday soon, these paper-thin bandages embedded with miniaturized electronics could monitor the healing process in real time, alerting the patient – or a doctor – when things go wrong. With the press of a smartphone button, that bandage could deliver medicine to fight an infection or an electrical pulse to stimulate healing.
Some “closed-loop” designs need no prompting, instead monitoring the wound and automatically giving it what it needs.
Others in development could halt a battlefield wound from hemorrhaging or kick-start healing in a blast wound, preventing longer-term disability.
The same technologies could – if the price is right – speed up healing and reduce scarring in minor cuts and scrapes, too, said Dr. Gurtner.
And unlike many cutting-edge medical innovations, these next-generation bandages could be made relatively cheaply and benefit some of the most vulnerable populations, including older adults, people with low incomes, and those in developing countries.
They could also save the health care system money, as the U.S. spends more than $28 billion annually treating chronic wounds.
“This is a condition that many patients find shameful and embarrassing, so there hasn’t been a lot of advocacy,” said Dr. Gurtner, outgoing board president of the Wound Healing Society. “It’s a relatively ignored problem afflicting an underserved population that has a huge cost. It’s a perfect storm.”
How wounds heal, or don’t
Wound healing is one of the most complex processes of the human body.
First platelets rush to the injury, prompting blood to clot. Then immune cells emit compounds called inflammatory cytokines, helping to fight off pathogens and keep infection at bay. Other compounds, including nitric oxide, spark the growth of new blood vessels and collagen to rebuild skin and connective tissue. As inflammation slows and stops, the flesh continues to reform.
But some conditions can stall the process, often in the inflammatory stage.
In people with diabetes, high glucose levels and poor circulation tend to sabotage the process. And people with nerve damage from spinal cord injuries, diabetes, or other ailments may not be able to feel it when a wound is getting worse or reinjured.
“We end up with patients going months with open wounds that are festering and infected,” said Roslyn Rivkah Isseroff, MD, professor of dermatology at the University of California Davis and head of the VA Northern California Health Care System’s wound healing clinic. “The patients are upset with the smell. These open ulcers put the patient at risk for systemic infection, like sepsis.” It can impact mental health, draining the patient’s ability to care for their wound.
“We see them once a week and send them home and say change your dressing every day, and they say, ‘I can barely move. I can’t do this,’ ” said Dr. Isseroff.
Checking for infection means removing bandages and culturing the wound. That can be painful, and results take time.
A lot can happen to a wound in a week.
“Sometimes, they come back and it’s a disaster, and they have to be admitted to the ER or even get an amputation,” Dr. Gurtner said.
People who are housing insecure or lack access to health care are even more vulnerable to complications.
“If you had the ability to say ‘there is something bad happening,’ you could do a lot to prevent this cascade and downward spiral.”
Bandages 2.0
In 2019, the Defense Advanced Research Projects Agency, the research arm of the Department of Defense, launched the Bioelectronics for Tissue Regeneration program to encourage scientists to develop a “closed-loop” bandage capable of both monitoring and hastening healing.
Tens of millions in funding has kick-started a flood of innovation since.
“It’s kind of a race to the finish,” said Marco Rolandi, PhD, associate professor of electrical and computer engineering at the University of California Santa Cruz and the principal investigator for a team including engineers, medical doctors, and computer scientists from UC Santa Cruz, UC Davis, and Tufts. “I’ve been amazed and impressed at all the work coming out.”
His team’s goal is to cut healing time in half by using (a) real-time monitoring of how a wound is healing – using indicators like temperature, pH level, oxygen, moisture, glucose, electrical activity, and certain proteins, and (b) appropriate stimulation.
“Every wound is different, so there is no one solution,” said Dr. Isseroff, the team’s clinical lead. “The idea is that it will be able to sense different parameters unique to the wound, use AI to figure out what stage it is in, and provide the right stimulus to kick it out of that stalled stage.”
The team has developed a proof-of-concept prototype: a bandage embedded with a tiny camera that takes pictures and transmits them to a computer algorithm to assess the wound’s progress. Miniaturized battery-powered actuators, or motors, automatically deliver medication.
Phase I trials in rodents went well, Dr. Rolandi said. The team is now testing the bandage on pigs.
Across the globe, other promising developments are underway.
In a scientific paper published in May, researchers at the University of Glasgow described a new “low-cost, environmentally friendly” bandage embedded with light-emitting diodes that use ultraviolet light to kill bacteria – no antibiotics needed. The fabric is stitched with a slim, flexible coil that powers the lights without a battery using wireless power transfer. In lab studies, it eradicated gram-negative bacteria (some of the nastiest bugs) in 6 hours.
Also in May, in the journal Bioactive Materials, a Penn State team detailed a bandage with medicine-injecting microneedles that can halt bleeding immediately after injury. In lab and animal tests, it reduced clotting time from 11.5 minutes to 1.3 minutes and bleeding by 90%.
“With hemorrhaging injuries, it is often the loss of blood – not the injury itself – that causes death,” said study author Amir Sheikhi, PhD, assistant professor of chemical and biomedical engineering at Penn State. “Those 10 minutes could be the difference between life and death.”
Another smart bandage, developed at Northwestern University, Chicago, harmlessly dissolves – electrodes and all – into the body after it is no longer needed, eliminating what can be a painful removal.
Guillermo Ameer, DSc, a study author reporting on the technology in Science Advances, hopes it could be made cheaply and used in developing countries.
“We’d like to create something that you could use in your home, even in a very remote village,” said Dr. Ameer, professor of biomedical engineering at Northwestern.
Timeline for clinical use
These are early days for the smart bandage, scientists say. Most studies have been in rodents and more work is needed to develop human-scale bandages, reduce cost, solve long-term data storage, and ensure material adheres well without irritating the skin.
But Dr. Gurtner is hopeful that some iteration could be used in clinical practice within a few years.
In May, he and colleagues at Stanford (Calif.) University published a paper in Nature Biotechnology describing their smart bandage. It includes a microcontroller unit, a radio antenna, biosensors, and an electrical stimulator all affixed to a rubbery, skin-like polymer (or hydrogel) about the thickness of a single coat of latex paint.
The bandage senses changes in temperature and electrical conductivity as the wound heals, and it gives electrical stimulation to accelerate that healing.
Animals treated with the bandage healed 25% faster, with 50% less scarring.
Electrical currents are already used for wound healing in clinical practice, Dr. Gurtner said. Because the stimulus is already approved and the cost to make the bandage could be low (as little as $10 to $50), he believes it could be ushered through the approval processes relatively quickly.
“Is this the ultimate embodiment of all the bells and whistles that are possible in a smart bandage? No. Not yet,” he said. “But we think it will help people. And right now, that’s good enough.”
A version of this article appeared on WebMD.com.
You cut yourself. You put on a bandage. In a week or so, your wound heals.
Most people take this routine for granted. But for the more than 8.2 million Americans who have chronic wounds, it’s not so simple.
Traumatic injuries, post-surgical complications, advanced age, and chronic illnesses like diabetes and vascular disease can all disrupt the delicate healing process, leading to wounds that last months or years.
Left untreated, about 30% led to amputation. And recent studies show the risk of dying from a chronic wound complication within 5 years rivals that of most cancers.
Yet until recently, medical technology had not kept up with what experts say is a snowballing threat to public health.
“Wound care – even with all of the billions of products that are sold – still exists on kind of a medieval level,” said Geoffrey Gurtner, MD, chair of the department of surgery and professor of biomedical engineering at the University of Arizona College of Medicine. “We’re still putting on poultices and salves ... and when it comes to diagnosing infection, it’s really an art. I think we can do better.”
Old-school bandage meets AI
Dr. Gurtner is among dozens of clinicians and researchers reimagining the humble bandage, combining cutting-edge materials science with artificial intelligence and patient data to develop “smart bandages” that do far more than shield a wound.
Someday soon, these paper-thin bandages embedded with miniaturized electronics could monitor the healing process in real time, alerting the patient – or a doctor – when things go wrong. With the press of a smartphone button, that bandage could deliver medicine to fight an infection or an electrical pulse to stimulate healing.
Some “closed-loop” designs need no prompting, instead monitoring the wound and automatically giving it what it needs.
Others in development could halt a battlefield wound from hemorrhaging or kick-start healing in a blast wound, preventing longer-term disability.
The same technologies could – if the price is right – speed up healing and reduce scarring in minor cuts and scrapes, too, said Dr. Gurtner.
And unlike many cutting-edge medical innovations, these next-generation bandages could be made relatively cheaply and benefit some of the most vulnerable populations, including older adults, people with low incomes, and those in developing countries.
They could also save the health care system money, as the U.S. spends more than $28 billion annually treating chronic wounds.
“This is a condition that many patients find shameful and embarrassing, so there hasn’t been a lot of advocacy,” said Dr. Gurtner, outgoing board president of the Wound Healing Society. “It’s a relatively ignored problem afflicting an underserved population that has a huge cost. It’s a perfect storm.”
How wounds heal, or don’t
Wound healing is one of the most complex processes of the human body.
First platelets rush to the injury, prompting blood to clot. Then immune cells emit compounds called inflammatory cytokines, helping to fight off pathogens and keep infection at bay. Other compounds, including nitric oxide, spark the growth of new blood vessels and collagen to rebuild skin and connective tissue. As inflammation slows and stops, the flesh continues to reform.
But some conditions can stall the process, often in the inflammatory stage.
In people with diabetes, high glucose levels and poor circulation tend to sabotage the process. And people with nerve damage from spinal cord injuries, diabetes, or other ailments may not be able to feel it when a wound is getting worse or reinjured.
“We end up with patients going months with open wounds that are festering and infected,” said Roslyn Rivkah Isseroff, MD, professor of dermatology at the University of California Davis and head of the VA Northern California Health Care System’s wound healing clinic. “The patients are upset with the smell. These open ulcers put the patient at risk for systemic infection, like sepsis.” It can impact mental health, draining the patient’s ability to care for their wound.
“We see them once a week and send them home and say change your dressing every day, and they say, ‘I can barely move. I can’t do this,’ ” said Dr. Isseroff.
Checking for infection means removing bandages and culturing the wound. That can be painful, and results take time.
A lot can happen to a wound in a week.
“Sometimes, they come back and it’s a disaster, and they have to be admitted to the ER or even get an amputation,” Dr. Gurtner said.
People who are housing insecure or lack access to health care are even more vulnerable to complications.
“If you had the ability to say ‘there is something bad happening,’ you could do a lot to prevent this cascade and downward spiral.”
Bandages 2.0
In 2019, the Defense Advanced Research Projects Agency, the research arm of the Department of Defense, launched the Bioelectronics for Tissue Regeneration program to encourage scientists to develop a “closed-loop” bandage capable of both monitoring and hastening healing.
Tens of millions in funding has kick-started a flood of innovation since.
“It’s kind of a race to the finish,” said Marco Rolandi, PhD, associate professor of electrical and computer engineering at the University of California Santa Cruz and the principal investigator for a team including engineers, medical doctors, and computer scientists from UC Santa Cruz, UC Davis, and Tufts. “I’ve been amazed and impressed at all the work coming out.”
His team’s goal is to cut healing time in half by using (a) real-time monitoring of how a wound is healing – using indicators like temperature, pH level, oxygen, moisture, glucose, electrical activity, and certain proteins, and (b) appropriate stimulation.
“Every wound is different, so there is no one solution,” said Dr. Isseroff, the team’s clinical lead. “The idea is that it will be able to sense different parameters unique to the wound, use AI to figure out what stage it is in, and provide the right stimulus to kick it out of that stalled stage.”
The team has developed a proof-of-concept prototype: a bandage embedded with a tiny camera that takes pictures and transmits them to a computer algorithm to assess the wound’s progress. Miniaturized battery-powered actuators, or motors, automatically deliver medication.
Phase I trials in rodents went well, Dr. Rolandi said. The team is now testing the bandage on pigs.
Across the globe, other promising developments are underway.
In a scientific paper published in May, researchers at the University of Glasgow described a new “low-cost, environmentally friendly” bandage embedded with light-emitting diodes that use ultraviolet light to kill bacteria – no antibiotics needed. The fabric is stitched with a slim, flexible coil that powers the lights without a battery using wireless power transfer. In lab studies, it eradicated gram-negative bacteria (some of the nastiest bugs) in 6 hours.
Also in May, in the journal Bioactive Materials, a Penn State team detailed a bandage with medicine-injecting microneedles that can halt bleeding immediately after injury. In lab and animal tests, it reduced clotting time from 11.5 minutes to 1.3 minutes and bleeding by 90%.
“With hemorrhaging injuries, it is often the loss of blood – not the injury itself – that causes death,” said study author Amir Sheikhi, PhD, assistant professor of chemical and biomedical engineering at Penn State. “Those 10 minutes could be the difference between life and death.”
Another smart bandage, developed at Northwestern University, Chicago, harmlessly dissolves – electrodes and all – into the body after it is no longer needed, eliminating what can be a painful removal.
Guillermo Ameer, DSc, a study author reporting on the technology in Science Advances, hopes it could be made cheaply and used in developing countries.
“We’d like to create something that you could use in your home, even in a very remote village,” said Dr. Ameer, professor of biomedical engineering at Northwestern.
Timeline for clinical use
These are early days for the smart bandage, scientists say. Most studies have been in rodents and more work is needed to develop human-scale bandages, reduce cost, solve long-term data storage, and ensure material adheres well without irritating the skin.
But Dr. Gurtner is hopeful that some iteration could be used in clinical practice within a few years.
In May, he and colleagues at Stanford (Calif.) University published a paper in Nature Biotechnology describing their smart bandage. It includes a microcontroller unit, a radio antenna, biosensors, and an electrical stimulator all affixed to a rubbery, skin-like polymer (or hydrogel) about the thickness of a single coat of latex paint.
The bandage senses changes in temperature and electrical conductivity as the wound heals, and it gives electrical stimulation to accelerate that healing.
Animals treated with the bandage healed 25% faster, with 50% less scarring.
Electrical currents are already used for wound healing in clinical practice, Dr. Gurtner said. Because the stimulus is already approved and the cost to make the bandage could be low (as little as $10 to $50), he believes it could be ushered through the approval processes relatively quickly.
“Is this the ultimate embodiment of all the bells and whistles that are possible in a smart bandage? No. Not yet,” he said. “But we think it will help people. And right now, that’s good enough.”
A version of this article appeared on WebMD.com.
‘Missed opportunities’ for accurate diagnosing of women with vaginitis
Although the standard of care of diagnosing vaginitis is clinical evaluation, many practices do not perform accurate and comprehensive clinical examinations for a variety for reasons, and the Centers for Disease Control and Prevention currently recommends molecular testing, wrote Casey N. Pinto, PhD, of Penn State University, Hershey, and colleagues. The CDC also recommends testing women with vaginitis for Chlamydia trachomatis (CT) and Neissaria gonorrhoeae (NG) given the high rate of coinfections between vaginitis and these sexually transmitted infections, but data on cotesting in clinical practice are limited, they said.
In a study published in Sexually Transmitted Diseases, the researchers reviewed data from a commercial administrative claims database for 1,359,289 women aged 18-50 years who were diagnosed with vaginitis between 2012 and 2017.
The women were categorized into groups based on type of vaginitis diagnosis: nucleic amplification test (NAAT), DNA probe test, traditional lab test, and those diagnosed clinically at an index visit but with no CPT code for further testing.
Overall, nearly half of the women (49.2%) had no CPT code for further vaginitis testing beyond clinical diagnosis. Of those with CPT codes for testing, 50.9% underwent traditional point-of-care testing, wet mount, or culture, 23.5% had a DNA probe, and 20.6% had NAAT testing.
Approximately one-third (34%) of women were cotested for CT/NG. Testing rates varied widely across the type of vaginitis test, from 70.8% of women who received NAAT to 22.8% of women with no CPT code. In multivariate analysis including age, region, and the Charlson Comorbidity Index (CCI), those tested with NAAT were eight times more likely to be cotested for CT/NG than those with no CPT code (odds ratio, 8.77; P < .0001).
Women who received a traditional test or DNA probe test for vaginitis also were more likely to have CT/NG testing than women with no CPT code, but only 1.8-2.5 times as likely.
“Our data suggest that most clinicians are not engaging the standard of care for testing and diagnosing vaginitis, or not engaging in comprehensive care by cotesting for vaginitis and CT/NG when patients may be at risk, resulting in missed opportunities for accurate diagnosis and potential associated coinfections,” the researchers wrote in their discussion. The higher rates for CT/NG testing among women receiving either NAAT or DNA probe vaginitis testing could be attributed to bundled testing, they noted, and the lower rate of CT/NG testing for patients with no CPT code could stem from limited access to microscopy or clinician preference for clinical diagnosis only, they said.
The findings were limited by several factors, including the lack of data on testing and diagnoses prior to the study period and not billed to insurance, and by the inability to account for variables including race, ethnicity, and socioeconomic status, the researchers noted.
However, the results highlight the need for more comprehensive care in vaginitis testing to take advantage of opportunities to identify CT or NG in women diagnosed with vaginitis, they concluded.
The study was supported by Becton, Dickinson and Company. Lead author Dr. Pinto disclosed consulting for Becton, Dickinson and Company, and receiving an honorarium from Roche.
Although the standard of care of diagnosing vaginitis is clinical evaluation, many practices do not perform accurate and comprehensive clinical examinations for a variety for reasons, and the Centers for Disease Control and Prevention currently recommends molecular testing, wrote Casey N. Pinto, PhD, of Penn State University, Hershey, and colleagues. The CDC also recommends testing women with vaginitis for Chlamydia trachomatis (CT) and Neissaria gonorrhoeae (NG) given the high rate of coinfections between vaginitis and these sexually transmitted infections, but data on cotesting in clinical practice are limited, they said.
In a study published in Sexually Transmitted Diseases, the researchers reviewed data from a commercial administrative claims database for 1,359,289 women aged 18-50 years who were diagnosed with vaginitis between 2012 and 2017.
The women were categorized into groups based on type of vaginitis diagnosis: nucleic amplification test (NAAT), DNA probe test, traditional lab test, and those diagnosed clinically at an index visit but with no CPT code for further testing.
Overall, nearly half of the women (49.2%) had no CPT code for further vaginitis testing beyond clinical diagnosis. Of those with CPT codes for testing, 50.9% underwent traditional point-of-care testing, wet mount, or culture, 23.5% had a DNA probe, and 20.6% had NAAT testing.
Approximately one-third (34%) of women were cotested for CT/NG. Testing rates varied widely across the type of vaginitis test, from 70.8% of women who received NAAT to 22.8% of women with no CPT code. In multivariate analysis including age, region, and the Charlson Comorbidity Index (CCI), those tested with NAAT were eight times more likely to be cotested for CT/NG than those with no CPT code (odds ratio, 8.77; P < .0001).
Women who received a traditional test or DNA probe test for vaginitis also were more likely to have CT/NG testing than women with no CPT code, but only 1.8-2.5 times as likely.
“Our data suggest that most clinicians are not engaging the standard of care for testing and diagnosing vaginitis, or not engaging in comprehensive care by cotesting for vaginitis and CT/NG when patients may be at risk, resulting in missed opportunities for accurate diagnosis and potential associated coinfections,” the researchers wrote in their discussion. The higher rates for CT/NG testing among women receiving either NAAT or DNA probe vaginitis testing could be attributed to bundled testing, they noted, and the lower rate of CT/NG testing for patients with no CPT code could stem from limited access to microscopy or clinician preference for clinical diagnosis only, they said.
The findings were limited by several factors, including the lack of data on testing and diagnoses prior to the study period and not billed to insurance, and by the inability to account for variables including race, ethnicity, and socioeconomic status, the researchers noted.
However, the results highlight the need for more comprehensive care in vaginitis testing to take advantage of opportunities to identify CT or NG in women diagnosed with vaginitis, they concluded.
The study was supported by Becton, Dickinson and Company. Lead author Dr. Pinto disclosed consulting for Becton, Dickinson and Company, and receiving an honorarium from Roche.
Although the standard of care of diagnosing vaginitis is clinical evaluation, many practices do not perform accurate and comprehensive clinical examinations for a variety for reasons, and the Centers for Disease Control and Prevention currently recommends molecular testing, wrote Casey N. Pinto, PhD, of Penn State University, Hershey, and colleagues. The CDC also recommends testing women with vaginitis for Chlamydia trachomatis (CT) and Neissaria gonorrhoeae (NG) given the high rate of coinfections between vaginitis and these sexually transmitted infections, but data on cotesting in clinical practice are limited, they said.
In a study published in Sexually Transmitted Diseases, the researchers reviewed data from a commercial administrative claims database for 1,359,289 women aged 18-50 years who were diagnosed with vaginitis between 2012 and 2017.
The women were categorized into groups based on type of vaginitis diagnosis: nucleic amplification test (NAAT), DNA probe test, traditional lab test, and those diagnosed clinically at an index visit but with no CPT code for further testing.
Overall, nearly half of the women (49.2%) had no CPT code for further vaginitis testing beyond clinical diagnosis. Of those with CPT codes for testing, 50.9% underwent traditional point-of-care testing, wet mount, or culture, 23.5% had a DNA probe, and 20.6% had NAAT testing.
Approximately one-third (34%) of women were cotested for CT/NG. Testing rates varied widely across the type of vaginitis test, from 70.8% of women who received NAAT to 22.8% of women with no CPT code. In multivariate analysis including age, region, and the Charlson Comorbidity Index (CCI), those tested with NAAT were eight times more likely to be cotested for CT/NG than those with no CPT code (odds ratio, 8.77; P < .0001).
Women who received a traditional test or DNA probe test for vaginitis also were more likely to have CT/NG testing than women with no CPT code, but only 1.8-2.5 times as likely.
“Our data suggest that most clinicians are not engaging the standard of care for testing and diagnosing vaginitis, or not engaging in comprehensive care by cotesting for vaginitis and CT/NG when patients may be at risk, resulting in missed opportunities for accurate diagnosis and potential associated coinfections,” the researchers wrote in their discussion. The higher rates for CT/NG testing among women receiving either NAAT or DNA probe vaginitis testing could be attributed to bundled testing, they noted, and the lower rate of CT/NG testing for patients with no CPT code could stem from limited access to microscopy or clinician preference for clinical diagnosis only, they said.
The findings were limited by several factors, including the lack of data on testing and diagnoses prior to the study period and not billed to insurance, and by the inability to account for variables including race, ethnicity, and socioeconomic status, the researchers noted.
However, the results highlight the need for more comprehensive care in vaginitis testing to take advantage of opportunities to identify CT or NG in women diagnosed with vaginitis, they concluded.
The study was supported by Becton, Dickinson and Company. Lead author Dr. Pinto disclosed consulting for Becton, Dickinson and Company, and receiving an honorarium from Roche.
FROM SEXUALLY TRANSMITTED DISEASES

