User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
COVID-19 Is a Very Weird Virus
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
In the early days of the pandemic, before we really understood what COVID was, two specialties in the hospital had a foreboding sense that something was very strange about this virus. The first was the pulmonologists, who noticed the striking levels of hypoxemia — low oxygen in the blood — and the rapidity with which patients who had previously been stable would crash in the intensive care unit.
The second, and I mark myself among this group, were the nephrologists. The dialysis machines stopped working right. I remember rounding on patients in the hospital who were on dialysis for kidney failure in the setting of severe COVID infection and seeing clots forming on the dialysis filters. Some patients could barely get in a full treatment because the filters would clog so quickly.
We knew it was worse than flu because of the mortality rates, but these oddities made us realize that it was different too — not just a particularly nasty respiratory virus but one that had effects on the body that we hadn’t really seen before.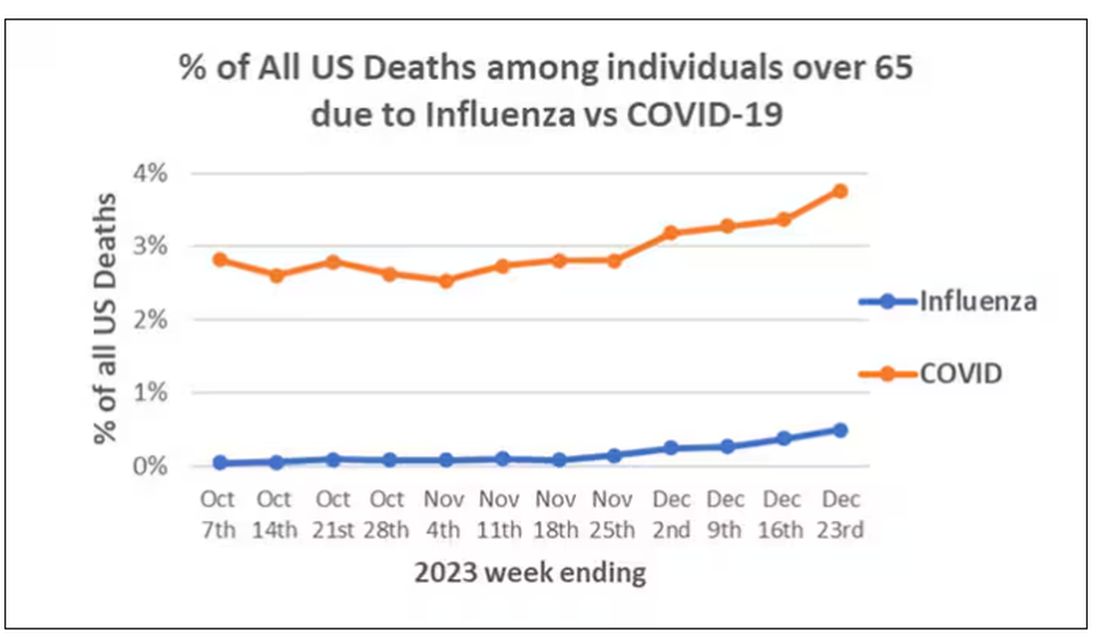
That’s why I’ve always been interested in studies that compare what happens to patients after COVID infection vs what happens to patients after other respiratory infections. This week, we’ll look at an intriguing study that suggests that COVID may lead to autoimmune diseases like rheumatoid arthritis, lupus, and vasculitis.
The study appears in the Annals of Internal Medicine and is made possible by the universal electronic health record systems of South Korea and Japan, who collaborated to create a truly staggering cohort of more than 20 million individuals living in those countries from 2020 to 2021.
The exposure of interest? COVID infection, experienced by just under 5% of that cohort over the study period. (Remember, there was a time when COVID infections were relatively controlled, particularly in some countries.)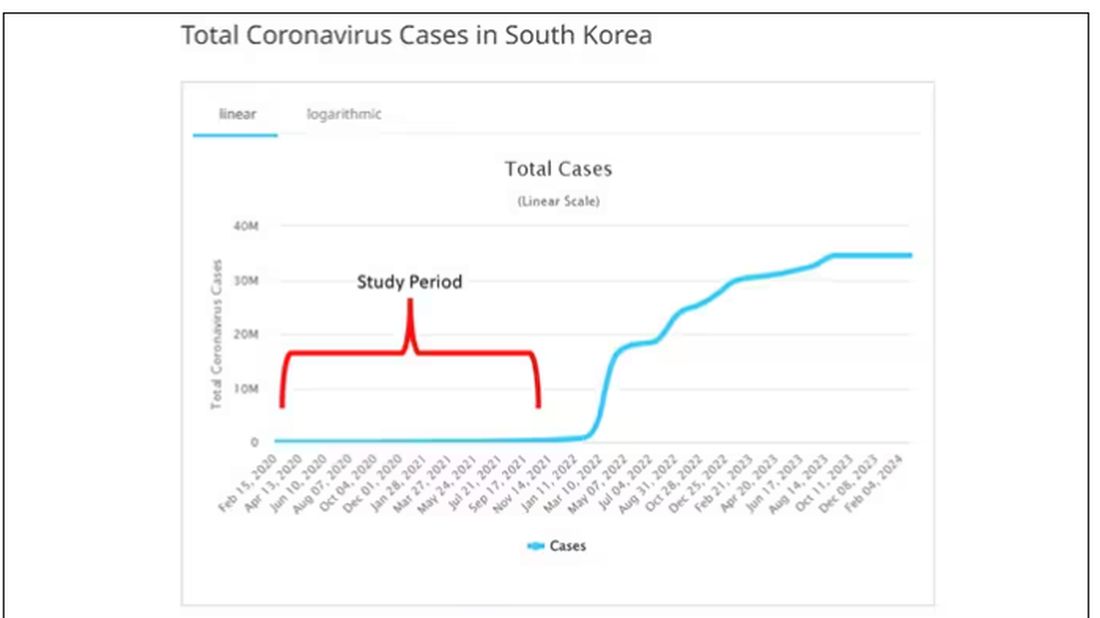
The researchers wanted to compare the risk for autoimmune disease among COVID-infected individuals against two control groups. The first control group was the general population. This is interesting but a difficult analysis, because people who become infected with COVID might be very different from the general population. The second control group was people infected with influenza. I like this a lot better; the risk factors for COVID and influenza are quite similar, and the fact that this group was diagnosed with flu means at least that they are getting medical care and are sort of “in the system,” so to speak.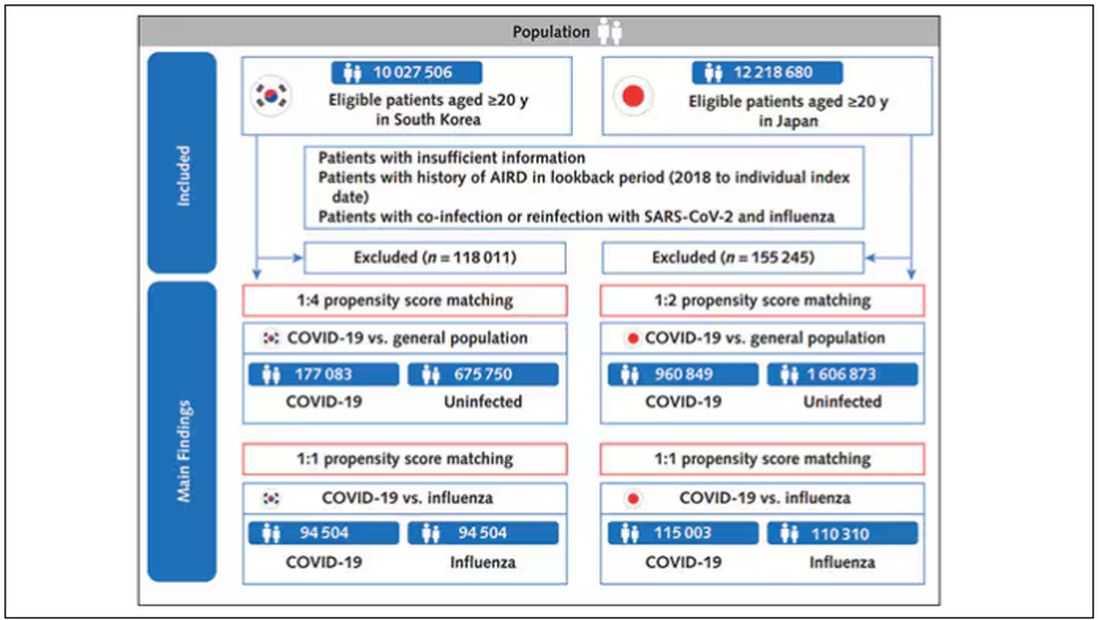
But it’s not enough to simply identify these folks and see who ends up with more autoimmune disease. The authors used propensity score matching to pair individuals infected with COVID with individuals from the control groups who were very similar to them. I’ve talked about this strategy before, but the basic idea is that you build a model predicting the likelihood of infection with COVID, based on a slew of factors — and the slew these authors used is pretty big, as shown below — and then stick people with similar risk for COVID together, with one member of the pair having had COVID and the other having eluded it (at least for the study period).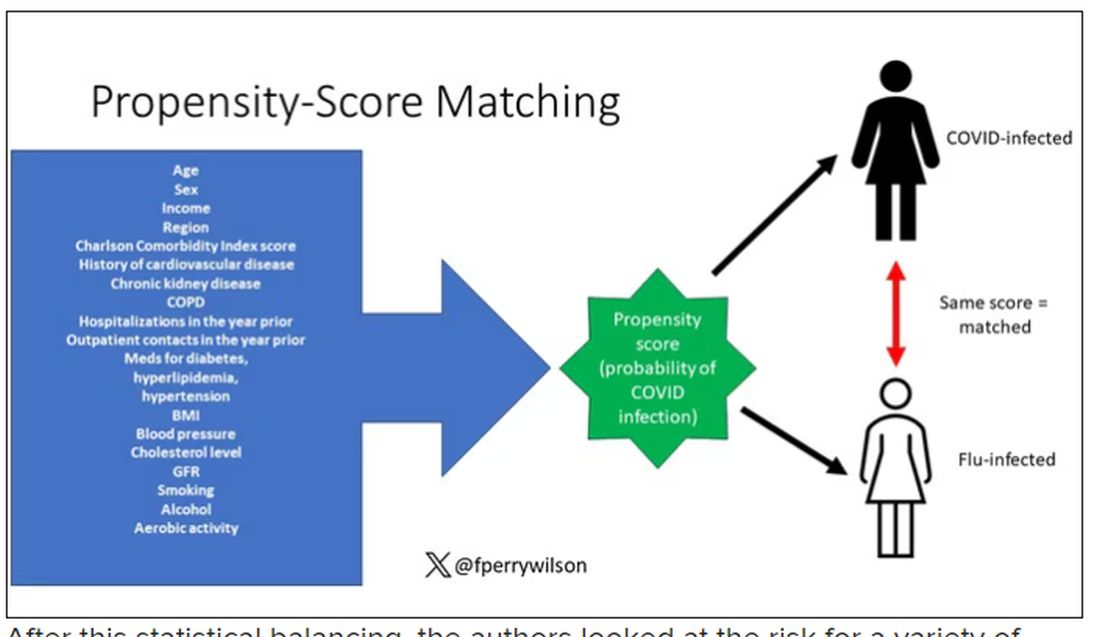
After this statistical balancing, the authors looked at the risk for a variety of autoimmune diseases.
Compared with those infected with flu, those infected with COVID were more likely to be diagnosed with any autoimmune condition, connective tissue disease, and, in Japan at least, inflammatory arthritis.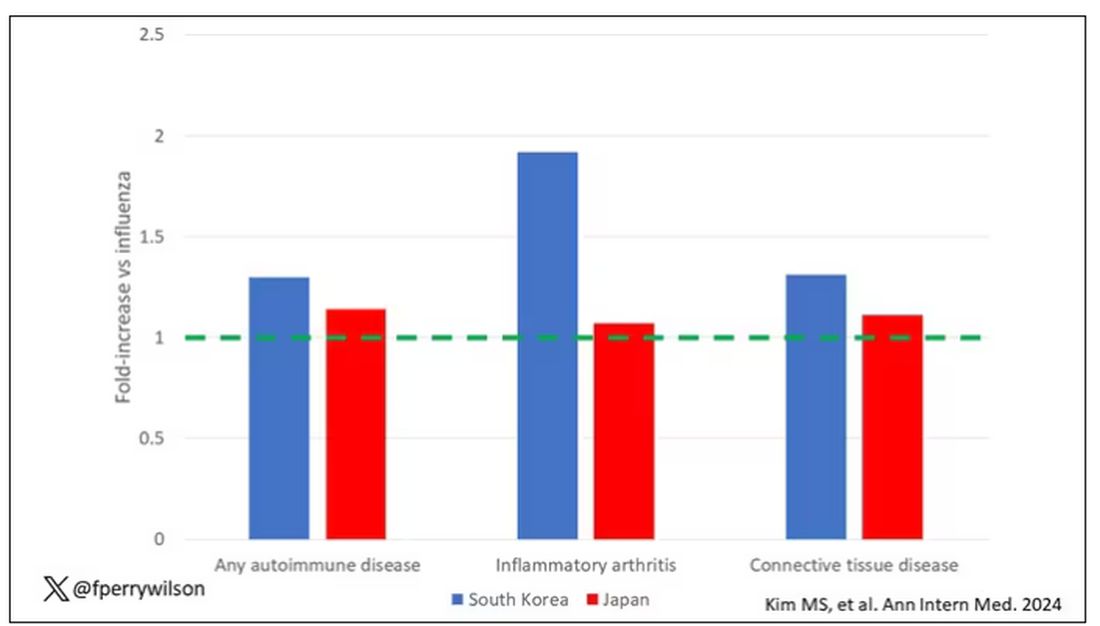
The authors acknowledge that being diagnosed with a disease might not be the same as actually having the disease, so in another analysis they looked only at people who received treatment for the autoimmune conditions, and the signals were even stronger in that group.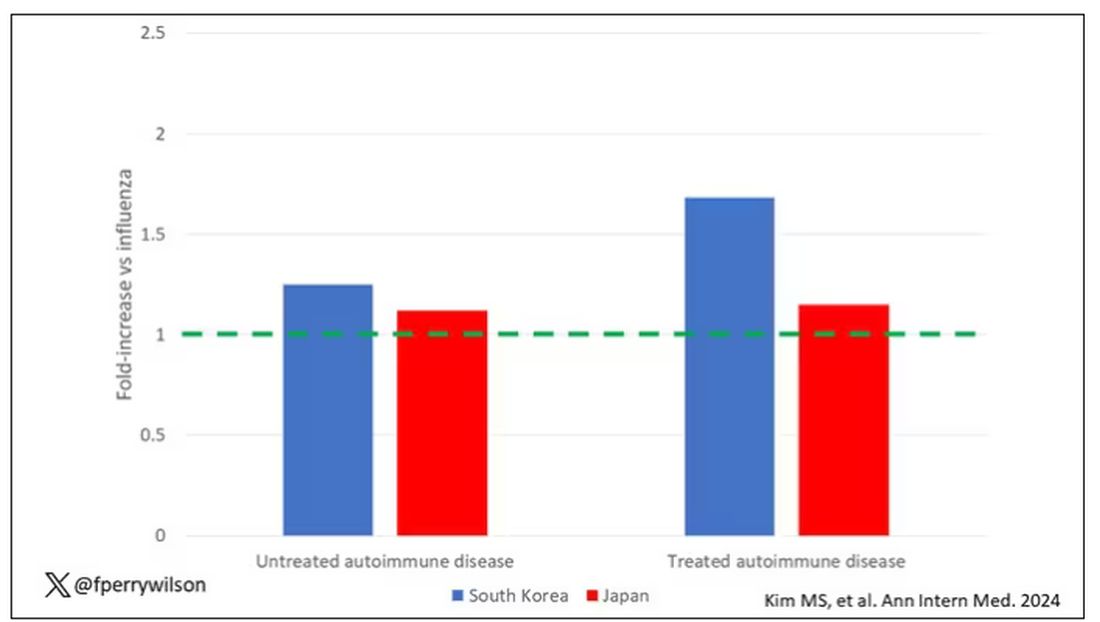
This risk seemed to be highest in the 6 months following the COVID infection, which makes sense biologically if we think that the infection is somehow screwing up the immune system.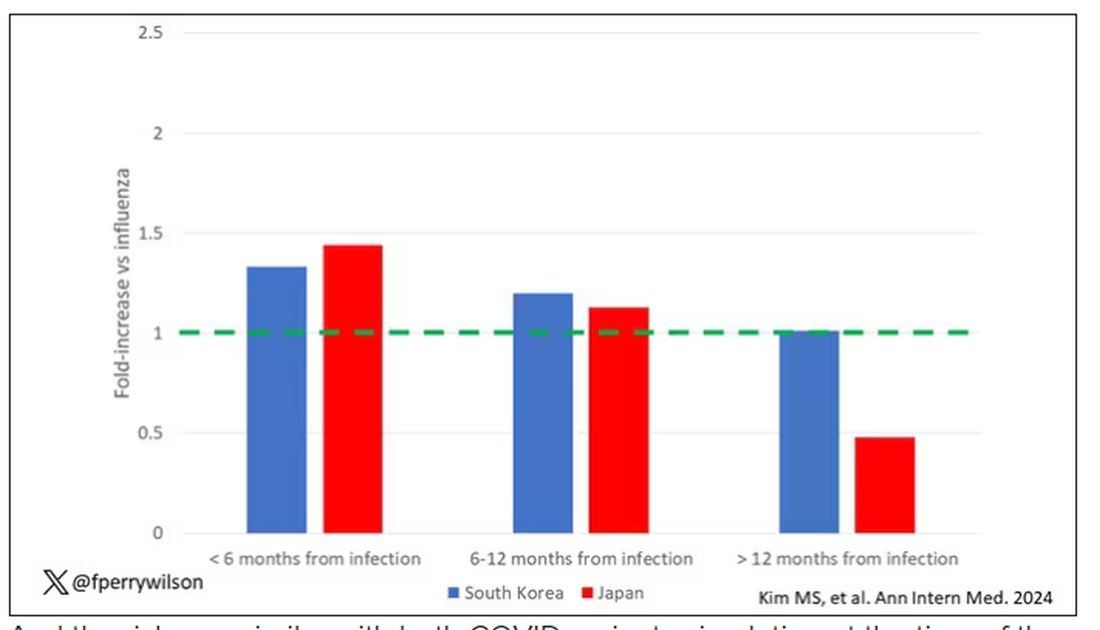
And the risk was similar with both COVID variants circulating at the time of the study.
The only factor that reduced the risk? You guessed it: vaccination. This is a particularly interesting finding because the exposure cohort was defined by having been infected with COVID. Therefore, the mechanism of protection is not prevention of infection; it’s something else. Perhaps vaccination helps to get the immune system in a state to respond to COVID infection more… appropriately?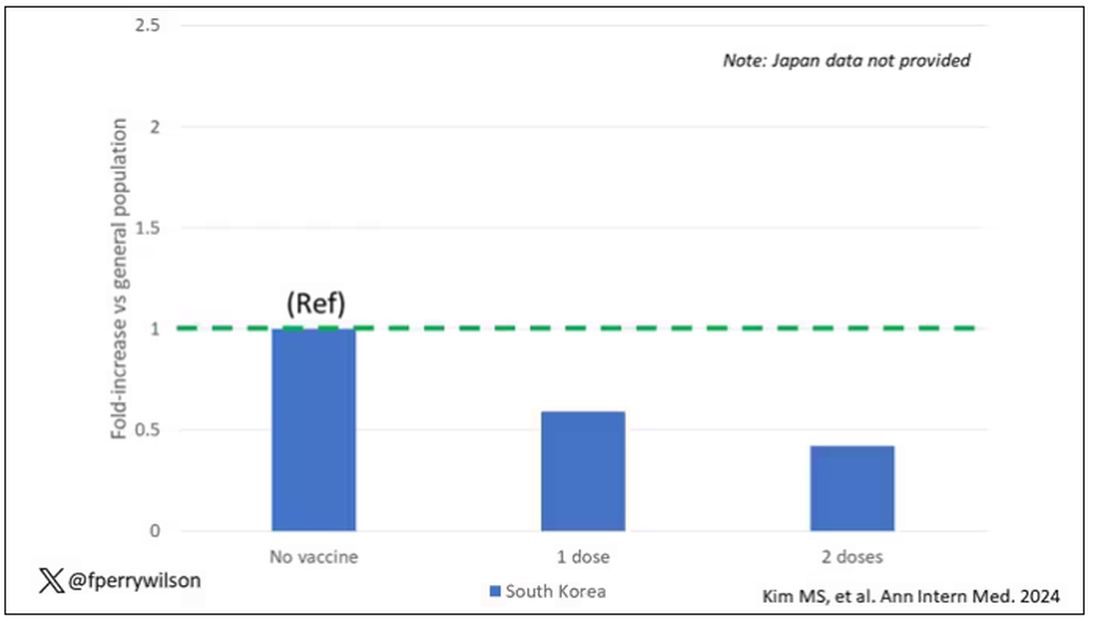
Yes, this study is observational. We can’t draw causal conclusions here. But it does reinforce my long-held belief that COVID is a weird virus, one with effects that are different from the respiratory viruses we are used to. I can’t say for certain whether COVID causes immune system dysfunction that puts someone at risk for autoimmunity — not from this study. But I can say it wouldn’t surprise me.
Dr. F. Perry Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
In the early days of the pandemic, before we really understood what COVID was, two specialties in the hospital had a foreboding sense that something was very strange about this virus. The first was the pulmonologists, who noticed the striking levels of hypoxemia — low oxygen in the blood — and the rapidity with which patients who had previously been stable would crash in the intensive care unit.
The second, and I mark myself among this group, were the nephrologists. The dialysis machines stopped working right. I remember rounding on patients in the hospital who were on dialysis for kidney failure in the setting of severe COVID infection and seeing clots forming on the dialysis filters. Some patients could barely get in a full treatment because the filters would clog so quickly.
We knew it was worse than flu because of the mortality rates, but these oddities made us realize that it was different too — not just a particularly nasty respiratory virus but one that had effects on the body that we hadn’t really seen before.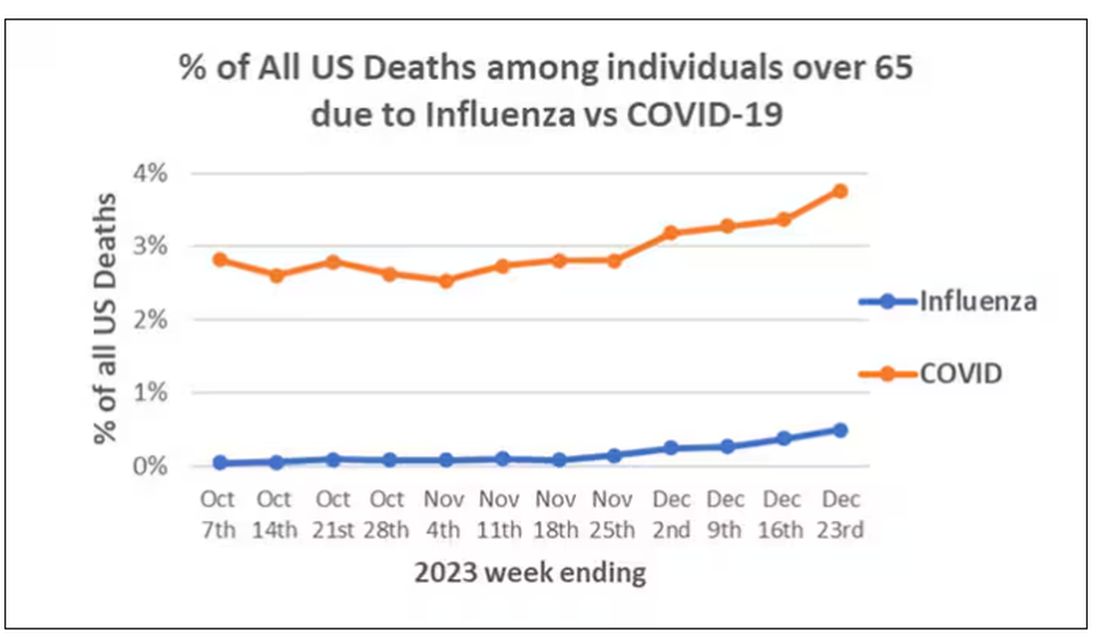
That’s why I’ve always been interested in studies that compare what happens to patients after COVID infection vs what happens to patients after other respiratory infections. This week, we’ll look at an intriguing study that suggests that COVID may lead to autoimmune diseases like rheumatoid arthritis, lupus, and vasculitis.
The study appears in the Annals of Internal Medicine and is made possible by the universal electronic health record systems of South Korea and Japan, who collaborated to create a truly staggering cohort of more than 20 million individuals living in those countries from 2020 to 2021.
The exposure of interest? COVID infection, experienced by just under 5% of that cohort over the study period. (Remember, there was a time when COVID infections were relatively controlled, particularly in some countries.)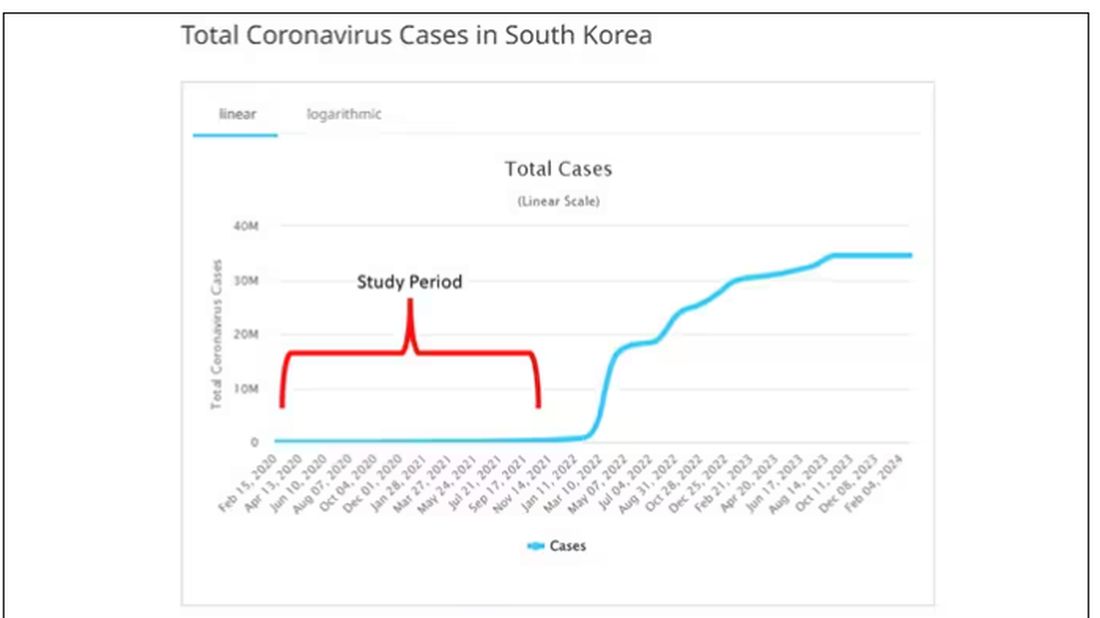
The researchers wanted to compare the risk for autoimmune disease among COVID-infected individuals against two control groups. The first control group was the general population. This is interesting but a difficult analysis, because people who become infected with COVID might be very different from the general population. The second control group was people infected with influenza. I like this a lot better; the risk factors for COVID and influenza are quite similar, and the fact that this group was diagnosed with flu means at least that they are getting medical care and are sort of “in the system,” so to speak.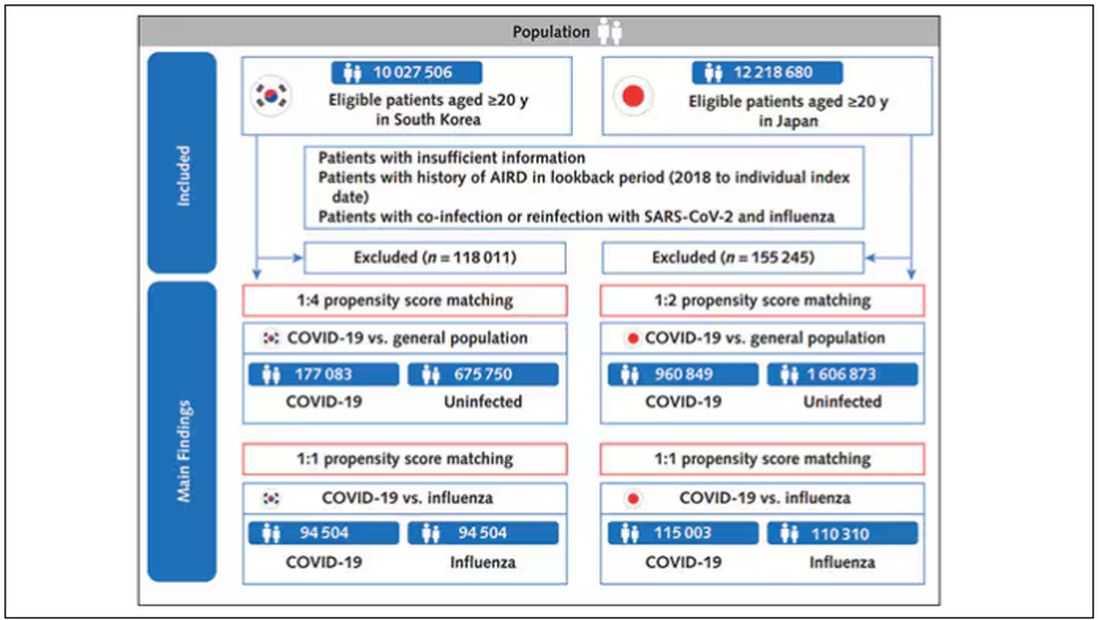
But it’s not enough to simply identify these folks and see who ends up with more autoimmune disease. The authors used propensity score matching to pair individuals infected with COVID with individuals from the control groups who were very similar to them. I’ve talked about this strategy before, but the basic idea is that you build a model predicting the likelihood of infection with COVID, based on a slew of factors — and the slew these authors used is pretty big, as shown below — and then stick people with similar risk for COVID together, with one member of the pair having had COVID and the other having eluded it (at least for the study period).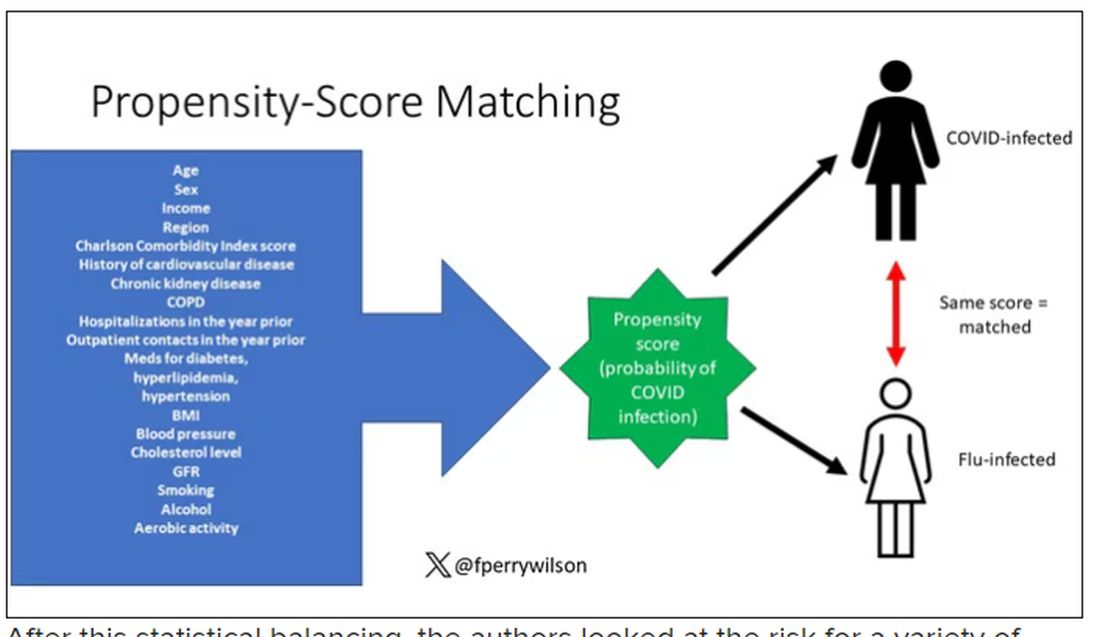
After this statistical balancing, the authors looked at the risk for a variety of autoimmune diseases.
Compared with those infected with flu, those infected with COVID were more likely to be diagnosed with any autoimmune condition, connective tissue disease, and, in Japan at least, inflammatory arthritis.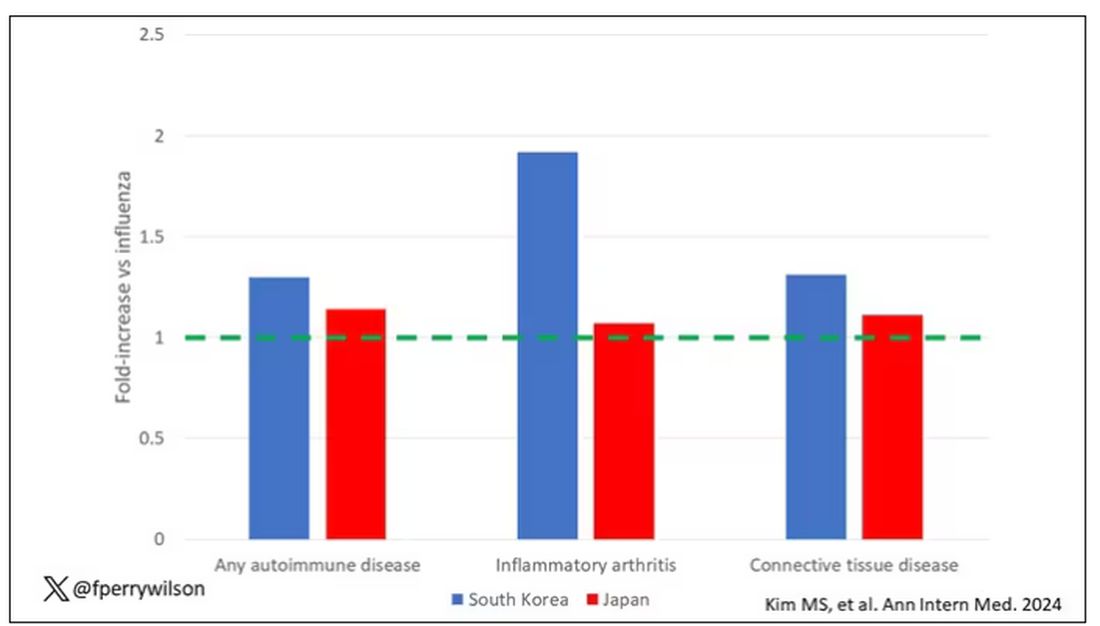
The authors acknowledge that being diagnosed with a disease might not be the same as actually having the disease, so in another analysis they looked only at people who received treatment for the autoimmune conditions, and the signals were even stronger in that group.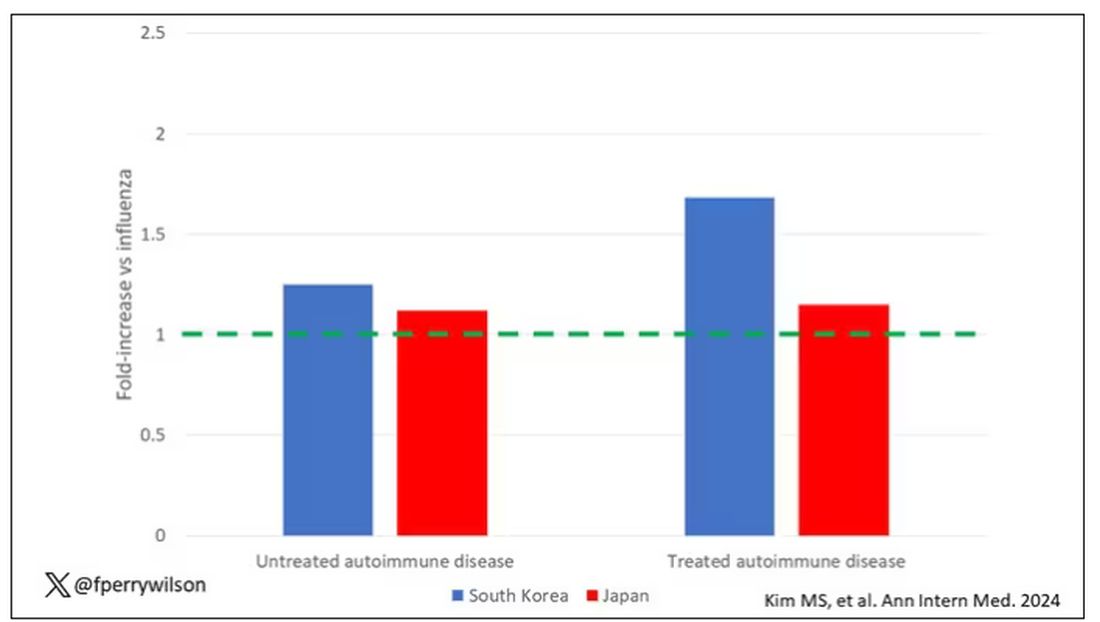
This risk seemed to be highest in the 6 months following the COVID infection, which makes sense biologically if we think that the infection is somehow screwing up the immune system.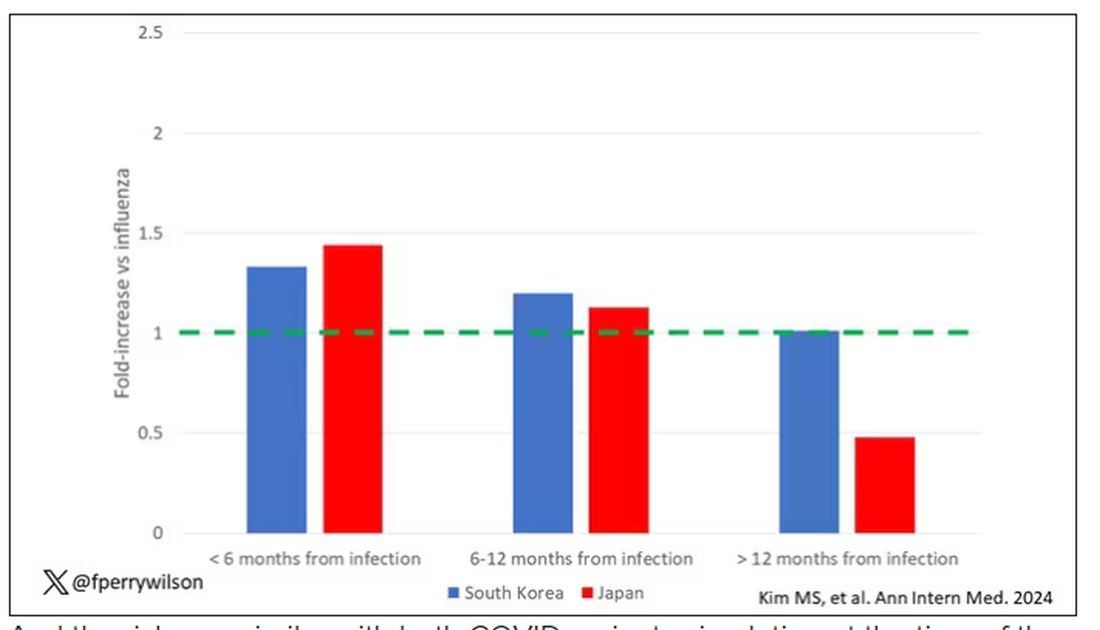
And the risk was similar with both COVID variants circulating at the time of the study.
The only factor that reduced the risk? You guessed it: vaccination. This is a particularly interesting finding because the exposure cohort was defined by having been infected with COVID. Therefore, the mechanism of protection is not prevention of infection; it’s something else. Perhaps vaccination helps to get the immune system in a state to respond to COVID infection more… appropriately?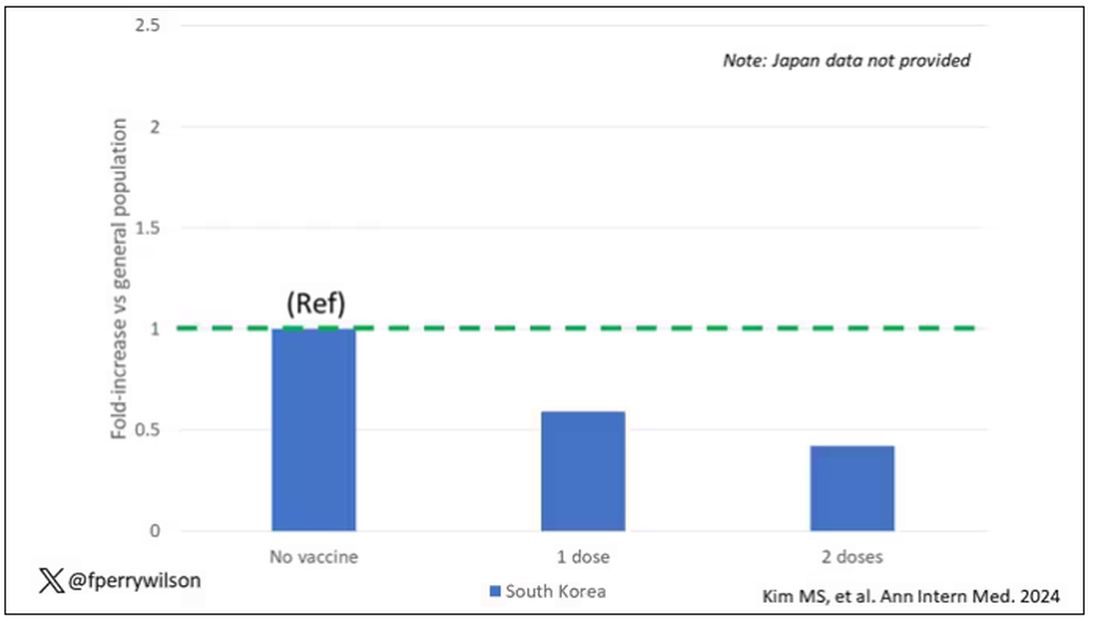
Yes, this study is observational. We can’t draw causal conclusions here. But it does reinforce my long-held belief that COVID is a weird virus, one with effects that are different from the respiratory viruses we are used to. I can’t say for certain whether COVID causes immune system dysfunction that puts someone at risk for autoimmunity — not from this study. But I can say it wouldn’t surprise me.
Dr. F. Perry Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
In the early days of the pandemic, before we really understood what COVID was, two specialties in the hospital had a foreboding sense that something was very strange about this virus. The first was the pulmonologists, who noticed the striking levels of hypoxemia — low oxygen in the blood — and the rapidity with which patients who had previously been stable would crash in the intensive care unit.
The second, and I mark myself among this group, were the nephrologists. The dialysis machines stopped working right. I remember rounding on patients in the hospital who were on dialysis for kidney failure in the setting of severe COVID infection and seeing clots forming on the dialysis filters. Some patients could barely get in a full treatment because the filters would clog so quickly.
We knew it was worse than flu because of the mortality rates, but these oddities made us realize that it was different too — not just a particularly nasty respiratory virus but one that had effects on the body that we hadn’t really seen before.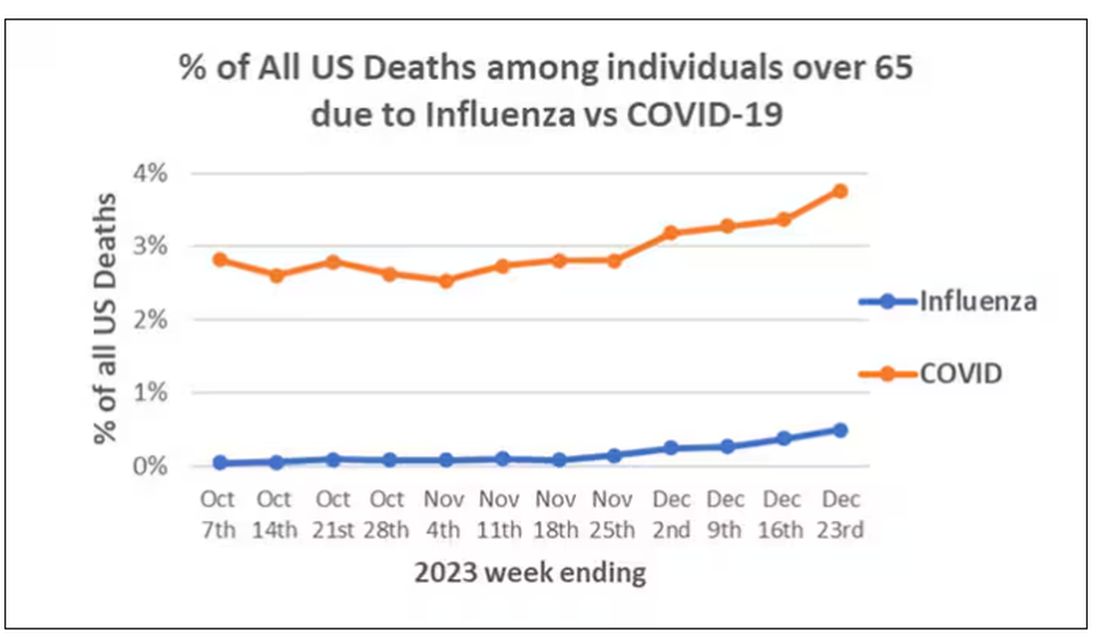
That’s why I’ve always been interested in studies that compare what happens to patients after COVID infection vs what happens to patients after other respiratory infections. This week, we’ll look at an intriguing study that suggests that COVID may lead to autoimmune diseases like rheumatoid arthritis, lupus, and vasculitis.
The study appears in the Annals of Internal Medicine and is made possible by the universal electronic health record systems of South Korea and Japan, who collaborated to create a truly staggering cohort of more than 20 million individuals living in those countries from 2020 to 2021.
The exposure of interest? COVID infection, experienced by just under 5% of that cohort over the study period. (Remember, there was a time when COVID infections were relatively controlled, particularly in some countries.)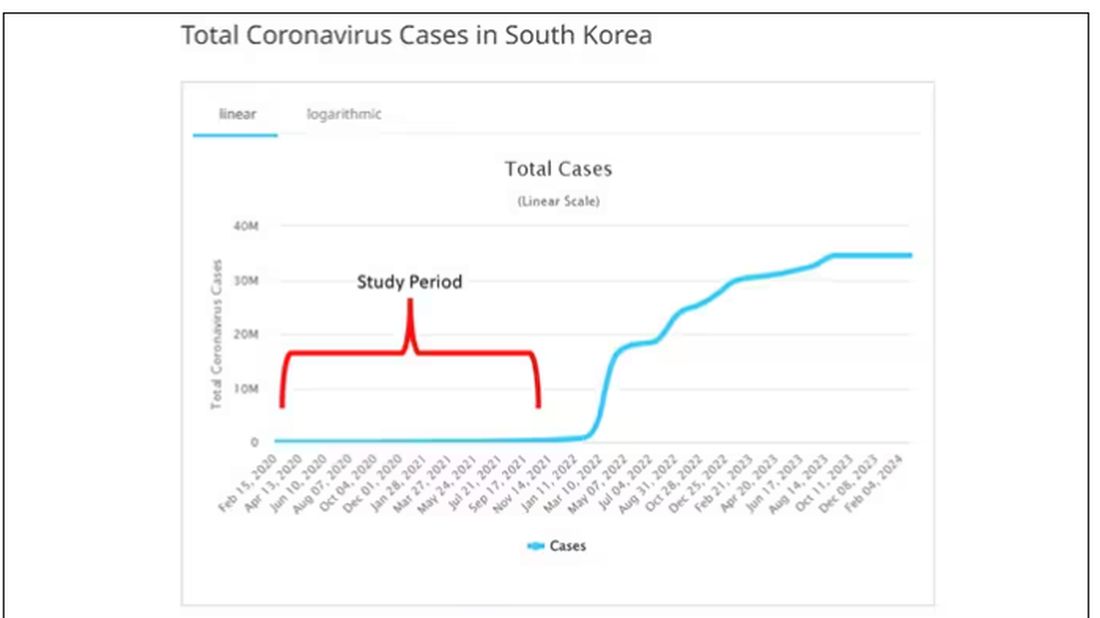
The researchers wanted to compare the risk for autoimmune disease among COVID-infected individuals against two control groups. The first control group was the general population. This is interesting but a difficult analysis, because people who become infected with COVID might be very different from the general population. The second control group was people infected with influenza. I like this a lot better; the risk factors for COVID and influenza are quite similar, and the fact that this group was diagnosed with flu means at least that they are getting medical care and are sort of “in the system,” so to speak.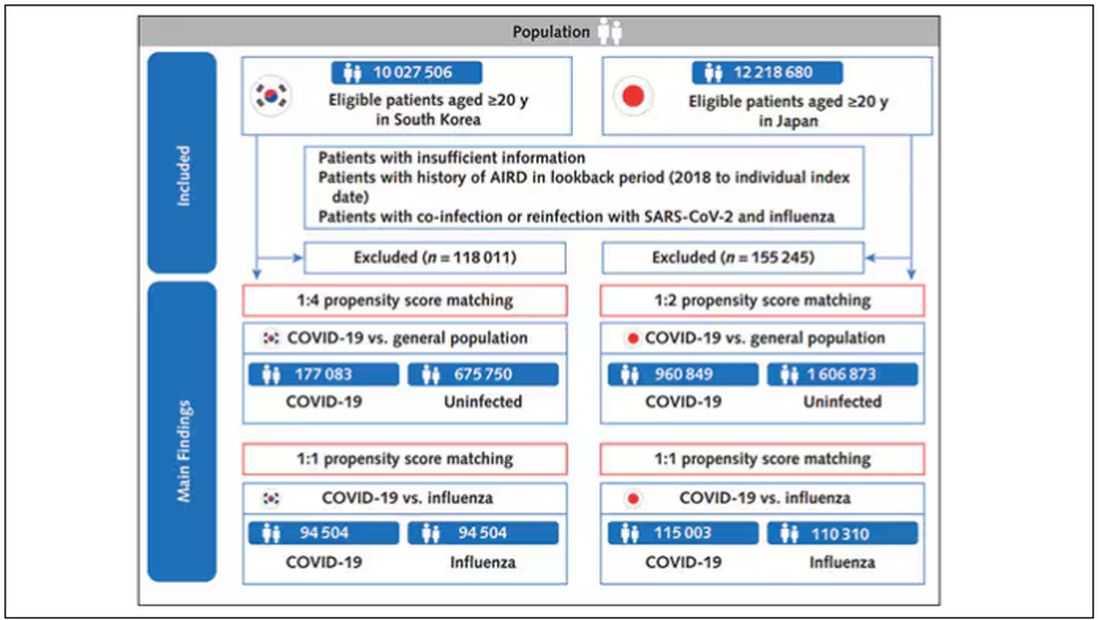
But it’s not enough to simply identify these folks and see who ends up with more autoimmune disease. The authors used propensity score matching to pair individuals infected with COVID with individuals from the control groups who were very similar to them. I’ve talked about this strategy before, but the basic idea is that you build a model predicting the likelihood of infection with COVID, based on a slew of factors — and the slew these authors used is pretty big, as shown below — and then stick people with similar risk for COVID together, with one member of the pair having had COVID and the other having eluded it (at least for the study period).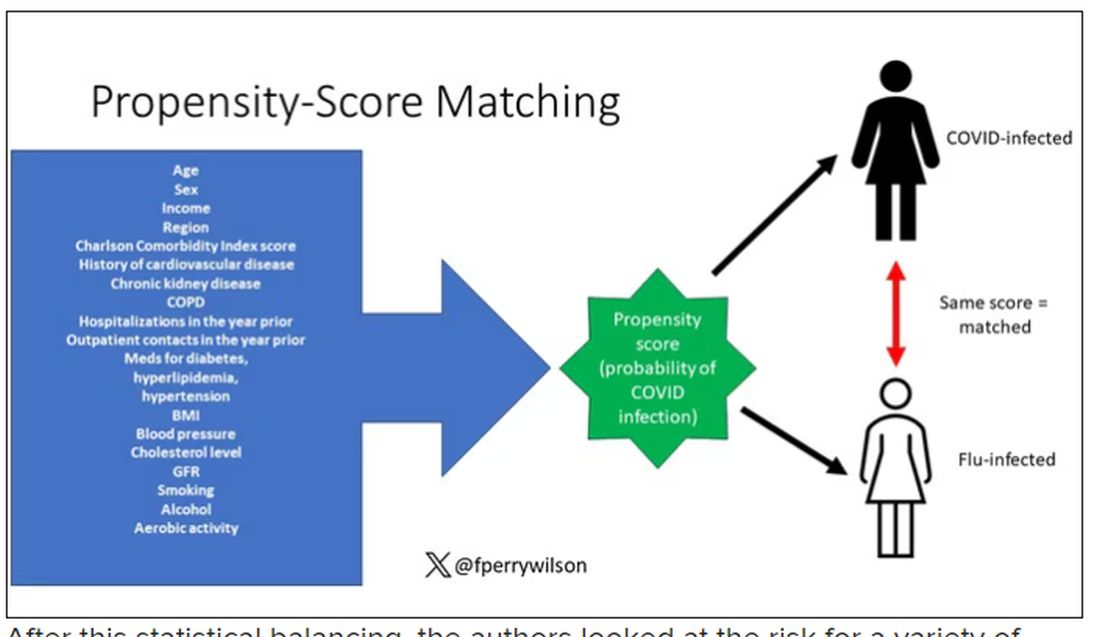
After this statistical balancing, the authors looked at the risk for a variety of autoimmune diseases.
Compared with those infected with flu, those infected with COVID were more likely to be diagnosed with any autoimmune condition, connective tissue disease, and, in Japan at least, inflammatory arthritis.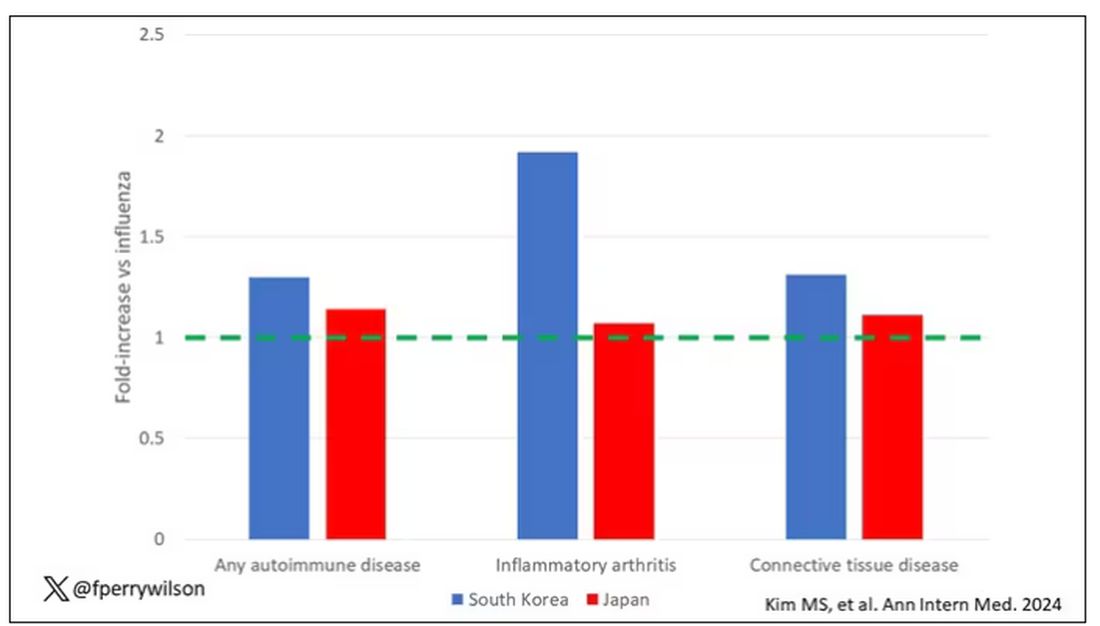
The authors acknowledge that being diagnosed with a disease might not be the same as actually having the disease, so in another analysis they looked only at people who received treatment for the autoimmune conditions, and the signals were even stronger in that group.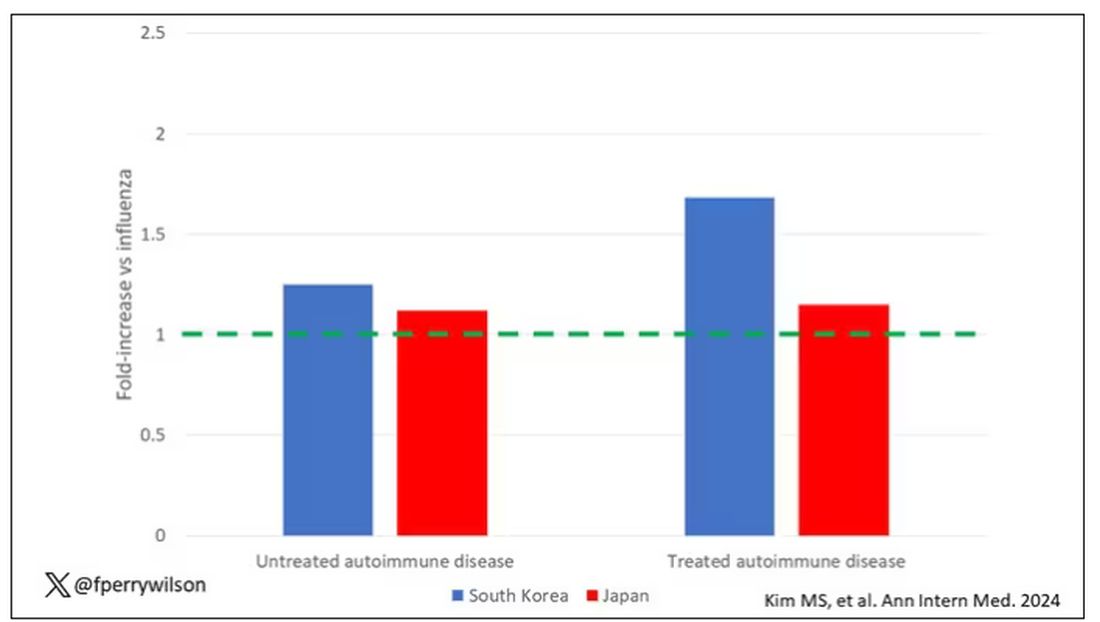
This risk seemed to be highest in the 6 months following the COVID infection, which makes sense biologically if we think that the infection is somehow screwing up the immune system.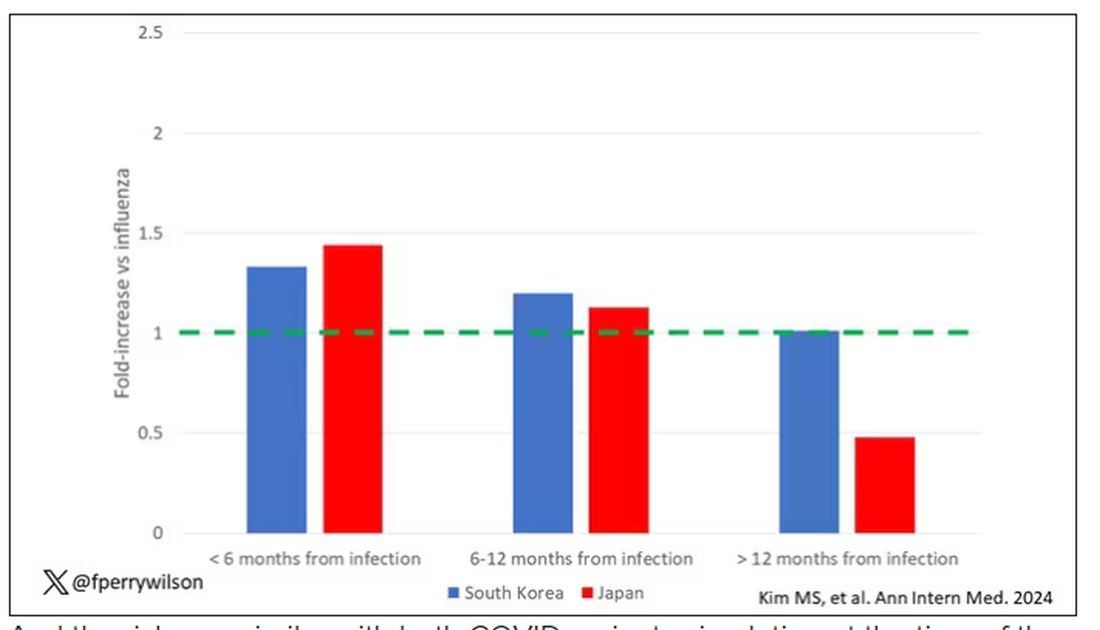
And the risk was similar with both COVID variants circulating at the time of the study.
The only factor that reduced the risk? You guessed it: vaccination. This is a particularly interesting finding because the exposure cohort was defined by having been infected with COVID. Therefore, the mechanism of protection is not prevention of infection; it’s something else. Perhaps vaccination helps to get the immune system in a state to respond to COVID infection more… appropriately?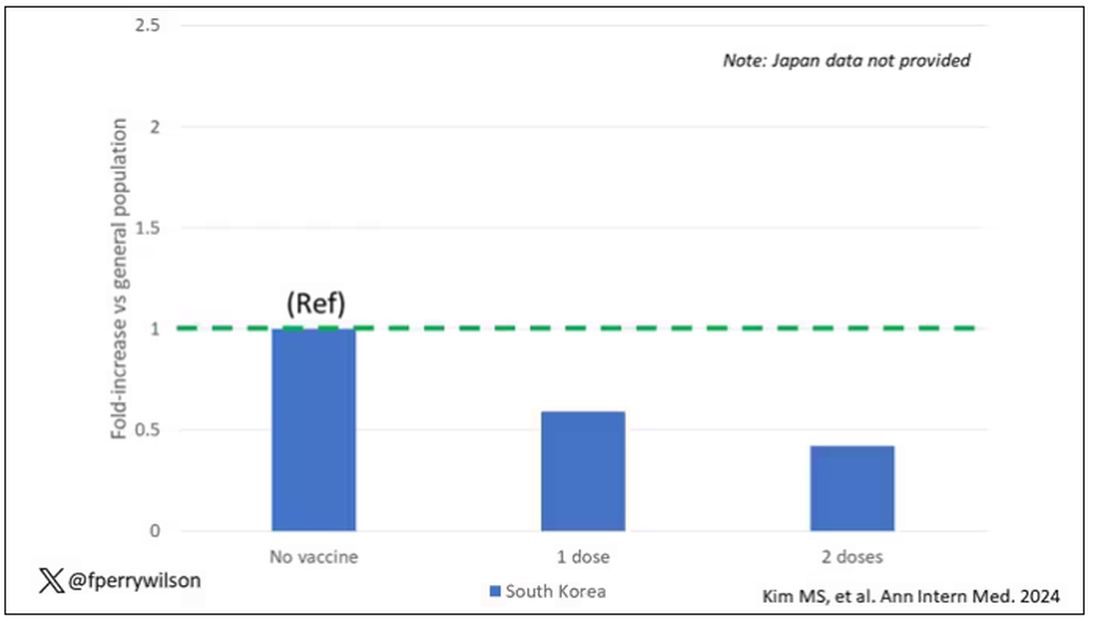
Yes, this study is observational. We can’t draw causal conclusions here. But it does reinforce my long-held belief that COVID is a weird virus, one with effects that are different from the respiratory viruses we are used to. I can’t say for certain whether COVID causes immune system dysfunction that puts someone at risk for autoimmunity — not from this study. But I can say it wouldn’t surprise me.
Dr. F. Perry Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
What’s Next for the World’s First HIV Vaccine?
When the world needed a COVID vaccine, leading HIV investigators answered the call to intervene in the coronavirus pandemic. Now, efforts to discover the world’s first HIV vaccine are revitalized.
“The body is capable of making antibodies to protect us from HIV,” says Yunda Huang, PhD, from the Fred Hutchinson Cancer Center in Seattle, Washington, who sat down with me before her talk today at the Conference on Retroviruses & Opportunistic Infections.
Dr. Huang spoke about the path forward for neutralizing antibody protection after the last attempt in a generation of HIV vaccine development ended in disappointment.
The past two decades marked the rise in HIV broadly neutralizing antibodies, with vaccine strategies to induce them. Promising advances include germline approaches, mRNA, and nanoparticle technologies.
The PrEP vaccine trial testing two experimental prevention regimens in Africa was stopped after investigators reported there is “little to no chance” the trial will show the vaccines are effective.
A Shape-Shifting Virus
HIV has been called the shape-shifting virus because it disguises itself so that even when people are able to make antibodies to it, the virus changes to escape.
But Dr. Huang and others are optimistic that an effective vaccine is still possible.
“We cannot and will not lose hope that the world will have an effective HIV vaccine that is accessible by all who need it, anywhere,” International AIDS Society (IAS) Executive Director Birgit Poniatowski said in a statement in December, when the trial was stopped.
HIV is a still persistent problem in the United States, according to the Centers for Disease Control and Prevention that reports it has affected an estimated 1.2 million people.
With new people infected every day around the globe, Dr. Huang says she feels a sense of urgency to help. “I think about all the people around the globe and the large number of young girls being hurt and I know our big pool of talent can intervene to change what we see happening.”
Dr. Huang says the clinical trial failures we’ve seen so far will help guide next steps in HIV research as much as successes typically do.
Advances in the Field
With significant advances in protein nanoparticle science, mRNA technology, adjuvant development, and B-cell and antibody analyses, a new wave of clinical trials are on the way.
And with so many new approaches in the works, the HIV Vaccine Trials Network is retooling how it operates to navigate a burgeoning field and identify the most promising regimens.
A new Discovery Medicine Program will help the network assess new vaccine candidates. It will also aim to rule out others earlier on.
For COVID-19 and the flu, multimeric nanoparticles are an important alternative under investigation that could also be adapted for HIV.
Dr. Huang says she is particularly excited to watch the progress in cocktails of combination monoclonals. “I’ve been working in this field for 20 years now and there is a misconception that with pre-exposure prophylaxis, our job is done, but HIV is so far from away from being solved.”
But you just never know, Dr. Huang says. With new research, “we could bump on something at any point that changes everything.”
A version of this article appeared on Medscape.com.
When the world needed a COVID vaccine, leading HIV investigators answered the call to intervene in the coronavirus pandemic. Now, efforts to discover the world’s first HIV vaccine are revitalized.
“The body is capable of making antibodies to protect us from HIV,” says Yunda Huang, PhD, from the Fred Hutchinson Cancer Center in Seattle, Washington, who sat down with me before her talk today at the Conference on Retroviruses & Opportunistic Infections.
Dr. Huang spoke about the path forward for neutralizing antibody protection after the last attempt in a generation of HIV vaccine development ended in disappointment.
The past two decades marked the rise in HIV broadly neutralizing antibodies, with vaccine strategies to induce them. Promising advances include germline approaches, mRNA, and nanoparticle technologies.
The PrEP vaccine trial testing two experimental prevention regimens in Africa was stopped after investigators reported there is “little to no chance” the trial will show the vaccines are effective.
A Shape-Shifting Virus
HIV has been called the shape-shifting virus because it disguises itself so that even when people are able to make antibodies to it, the virus changes to escape.
But Dr. Huang and others are optimistic that an effective vaccine is still possible.
“We cannot and will not lose hope that the world will have an effective HIV vaccine that is accessible by all who need it, anywhere,” International AIDS Society (IAS) Executive Director Birgit Poniatowski said in a statement in December, when the trial was stopped.
HIV is a still persistent problem in the United States, according to the Centers for Disease Control and Prevention that reports it has affected an estimated 1.2 million people.
With new people infected every day around the globe, Dr. Huang says she feels a sense of urgency to help. “I think about all the people around the globe and the large number of young girls being hurt and I know our big pool of talent can intervene to change what we see happening.”
Dr. Huang says the clinical trial failures we’ve seen so far will help guide next steps in HIV research as much as successes typically do.
Advances in the Field
With significant advances in protein nanoparticle science, mRNA technology, adjuvant development, and B-cell and antibody analyses, a new wave of clinical trials are on the way.
And with so many new approaches in the works, the HIV Vaccine Trials Network is retooling how it operates to navigate a burgeoning field and identify the most promising regimens.
A new Discovery Medicine Program will help the network assess new vaccine candidates. It will also aim to rule out others earlier on.
For COVID-19 and the flu, multimeric nanoparticles are an important alternative under investigation that could also be adapted for HIV.
Dr. Huang says she is particularly excited to watch the progress in cocktails of combination monoclonals. “I’ve been working in this field for 20 years now and there is a misconception that with pre-exposure prophylaxis, our job is done, but HIV is so far from away from being solved.”
But you just never know, Dr. Huang says. With new research, “we could bump on something at any point that changes everything.”
A version of this article appeared on Medscape.com.
When the world needed a COVID vaccine, leading HIV investigators answered the call to intervene in the coronavirus pandemic. Now, efforts to discover the world’s first HIV vaccine are revitalized.
“The body is capable of making antibodies to protect us from HIV,” says Yunda Huang, PhD, from the Fred Hutchinson Cancer Center in Seattle, Washington, who sat down with me before her talk today at the Conference on Retroviruses & Opportunistic Infections.
Dr. Huang spoke about the path forward for neutralizing antibody protection after the last attempt in a generation of HIV vaccine development ended in disappointment.
The past two decades marked the rise in HIV broadly neutralizing antibodies, with vaccine strategies to induce them. Promising advances include germline approaches, mRNA, and nanoparticle technologies.
The PrEP vaccine trial testing two experimental prevention regimens in Africa was stopped after investigators reported there is “little to no chance” the trial will show the vaccines are effective.
A Shape-Shifting Virus
HIV has been called the shape-shifting virus because it disguises itself so that even when people are able to make antibodies to it, the virus changes to escape.
But Dr. Huang and others are optimistic that an effective vaccine is still possible.
“We cannot and will not lose hope that the world will have an effective HIV vaccine that is accessible by all who need it, anywhere,” International AIDS Society (IAS) Executive Director Birgit Poniatowski said in a statement in December, when the trial was stopped.
HIV is a still persistent problem in the United States, according to the Centers for Disease Control and Prevention that reports it has affected an estimated 1.2 million people.
With new people infected every day around the globe, Dr. Huang says she feels a sense of urgency to help. “I think about all the people around the globe and the large number of young girls being hurt and I know our big pool of talent can intervene to change what we see happening.”
Dr. Huang says the clinical trial failures we’ve seen so far will help guide next steps in HIV research as much as successes typically do.
Advances in the Field
With significant advances in protein nanoparticle science, mRNA technology, adjuvant development, and B-cell and antibody analyses, a new wave of clinical trials are on the way.
And with so many new approaches in the works, the HIV Vaccine Trials Network is retooling how it operates to navigate a burgeoning field and identify the most promising regimens.
A new Discovery Medicine Program will help the network assess new vaccine candidates. It will also aim to rule out others earlier on.
For COVID-19 and the flu, multimeric nanoparticles are an important alternative under investigation that could also be adapted for HIV.
Dr. Huang says she is particularly excited to watch the progress in cocktails of combination monoclonals. “I’ve been working in this field for 20 years now and there is a misconception that with pre-exposure prophylaxis, our job is done, but HIV is so far from away from being solved.”
But you just never know, Dr. Huang says. With new research, “we could bump on something at any point that changes everything.”
A version of this article appeared on Medscape.com.
FROM CROI 2024
Doxy-PEP Cut STIs in San Francisco in Half
Syphilis and chlamydia infections were reduced by half among men who have sex with men and transgender women 1 year after San Francisco rolled out doxycycline postexposure prophylaxis (doxy-PEP), according to data presented at the Conference on Retroviruses and Opportunistic Infections (CROI) this week.
After a clinical trial showed that doxy-PEP taken after sex reduced the chance of acquiring syphilis, gonorrhea, and chlamydia by about two-thirds, the San Francisco Department of Public Health released the first guidelines in the country in October 2022.
So far, more than 3700 people in San Francisco have been prescribed doxy-PEP, reports Stephanie Cohen, MD, director of HIV and sexually transmitted infection (STI) prevention in the Disease Prevention and Control Branch of Public Health.
Dr. Cohen and her colleagues spent a year monitoring the uptake of doxy-PEP and used a computer model to predict what the rates of sexually transmitted infection would have been without doxy-PEP.
In November 2023, 13 months after the guidelines were introduced, they found that monthly chlamydia and early syphilis infections were 50% and 51% lower, respectively, than what was predicted by the model.
Fewer Infections
The drop in infections is having a tangible effect on patients in San Francisco, and many clinicians are noting that they are seeing far fewer positive tests. “The results that we’re seeing on a city-wide level are absolutely being experienced by individual providers and patients,” Dr. Cohen said.
However, the analysis showed no effect on rates of gonorrhea. It’s not clear why, although Dr. Cohen points out that doxy-PEP was less effective against gonorrhea in the clinical trial. And “there could be other factors in play,” she added. “Adherence might matter more, or it could be affected by the prevalence of tetracycline resistance in the community.”
With rates of STIs, particularly syphilis, quickly rising in recent years, healthcare providers have been scrambling to find effective interventions. So far, doxy-PEP has shown the most promise. “We’ve known for a while that all of the strategies we’ve been employing don’t seem to be working,” noted Chase Cannon, MD, an infectious disease specialist at the University of Washington in Seattle. “That’s why doxy-PEP is important. We haven’t had anything that can deflect the curve in a long time.”
What About the Side Effects?
Some concerns remain, however, about the widespread prophylactic use of antibiotics. There are no long-term safety data on the potential side effects of doxy-PEP, and there is still a lot of stigma around interventions that allow people to have sex the way they want, said Dr. Cannon.
But perhaps, the biggest concern is that doxy-PEP could contribute to antibiotic resistance. Those fears are not misplaced, Dr. Cannon added. The results of one study, presented in a poster at CROI, showed that stool samples from people prescribed doxy-PEP had elevated levels of bacterial genes that can confer resistance to tetracyclines, the class of antibiotics to which doxycycline belongs. There was no change in resistance to other classes of antibiotics and no difference in bacterial diversity over the 6 months of the study.
Dr. Cannon cautioned, however, that we can’t extrapolate these results to clinical outcomes. “We can look for signals [of resistance], but we don’t know if this means someone will fail therapy for chlamydia or syphilis,” he said.
There are still many challenges to overcome before doxy-PEP can be rolled out widely, Dr. Cohen explained. There is a lack of consensus among healthcare professionals about who should be offered doxy-PEP. The clinical trial results and the San Fransisco guidelines only apply to men who have sex with men and to transgender women.
Some clinicians argue that the intervention should be provided to a broader population, whereas others want to see more research to ensure that unnecessary antibiotic use is minimized.
So far just one study has tested doxy-PEP in another population — in women in Kenya — and it was found to not be effective. But the data suggest that adherence to the protocol was poor in that study, so the results may not be reliable, Dr. Cohen said.
“We need effective prevention tools for all genders, especially cis women who bear most of the morbidity,” she said. “It stands to reason that this should work for them, but without high-quality evidence, there is insufficient information to make a recommendation for cis women.”
The US Centers for Disease Control and Prevention is currently reviewing public and expert comments and refining final guidelines for release in the coming months, which should alleviate some of the uncertainty. “Many providers are waiting for that guidance before they will feel confident moving forward,” Dr. Cohen noted.
But despite the risks and uncertainty, doxy-PEP looks set to be a major part of the fight against STIs going forward. “Doxy-PEP is essential for us as a nation to be dealing with the syphilis epidemic,” Carl Dieffenbach, PhD, director of the Division of AIDS at the National Institute of Allergy and Infectious Disease, said in a video introduction to CROI.
A version of this article appeared on Medscape.com.
Syphilis and chlamydia infections were reduced by half among men who have sex with men and transgender women 1 year after San Francisco rolled out doxycycline postexposure prophylaxis (doxy-PEP), according to data presented at the Conference on Retroviruses and Opportunistic Infections (CROI) this week.
After a clinical trial showed that doxy-PEP taken after sex reduced the chance of acquiring syphilis, gonorrhea, and chlamydia by about two-thirds, the San Francisco Department of Public Health released the first guidelines in the country in October 2022.
So far, more than 3700 people in San Francisco have been prescribed doxy-PEP, reports Stephanie Cohen, MD, director of HIV and sexually transmitted infection (STI) prevention in the Disease Prevention and Control Branch of Public Health.
Dr. Cohen and her colleagues spent a year monitoring the uptake of doxy-PEP and used a computer model to predict what the rates of sexually transmitted infection would have been without doxy-PEP.
In November 2023, 13 months after the guidelines were introduced, they found that monthly chlamydia and early syphilis infections were 50% and 51% lower, respectively, than what was predicted by the model.
Fewer Infections
The drop in infections is having a tangible effect on patients in San Francisco, and many clinicians are noting that they are seeing far fewer positive tests. “The results that we’re seeing on a city-wide level are absolutely being experienced by individual providers and patients,” Dr. Cohen said.
However, the analysis showed no effect on rates of gonorrhea. It’s not clear why, although Dr. Cohen points out that doxy-PEP was less effective against gonorrhea in the clinical trial. And “there could be other factors in play,” she added. “Adherence might matter more, or it could be affected by the prevalence of tetracycline resistance in the community.”
With rates of STIs, particularly syphilis, quickly rising in recent years, healthcare providers have been scrambling to find effective interventions. So far, doxy-PEP has shown the most promise. “We’ve known for a while that all of the strategies we’ve been employing don’t seem to be working,” noted Chase Cannon, MD, an infectious disease specialist at the University of Washington in Seattle. “That’s why doxy-PEP is important. We haven’t had anything that can deflect the curve in a long time.”
What About the Side Effects?
Some concerns remain, however, about the widespread prophylactic use of antibiotics. There are no long-term safety data on the potential side effects of doxy-PEP, and there is still a lot of stigma around interventions that allow people to have sex the way they want, said Dr. Cannon.
But perhaps, the biggest concern is that doxy-PEP could contribute to antibiotic resistance. Those fears are not misplaced, Dr. Cannon added. The results of one study, presented in a poster at CROI, showed that stool samples from people prescribed doxy-PEP had elevated levels of bacterial genes that can confer resistance to tetracyclines, the class of antibiotics to which doxycycline belongs. There was no change in resistance to other classes of antibiotics and no difference in bacterial diversity over the 6 months of the study.
Dr. Cannon cautioned, however, that we can’t extrapolate these results to clinical outcomes. “We can look for signals [of resistance], but we don’t know if this means someone will fail therapy for chlamydia or syphilis,” he said.
There are still many challenges to overcome before doxy-PEP can be rolled out widely, Dr. Cohen explained. There is a lack of consensus among healthcare professionals about who should be offered doxy-PEP. The clinical trial results and the San Fransisco guidelines only apply to men who have sex with men and to transgender women.
Some clinicians argue that the intervention should be provided to a broader population, whereas others want to see more research to ensure that unnecessary antibiotic use is minimized.
So far just one study has tested doxy-PEP in another population — in women in Kenya — and it was found to not be effective. But the data suggest that adherence to the protocol was poor in that study, so the results may not be reliable, Dr. Cohen said.
“We need effective prevention tools for all genders, especially cis women who bear most of the morbidity,” she said. “It stands to reason that this should work for them, but without high-quality evidence, there is insufficient information to make a recommendation for cis women.”
The US Centers for Disease Control and Prevention is currently reviewing public and expert comments and refining final guidelines for release in the coming months, which should alleviate some of the uncertainty. “Many providers are waiting for that guidance before they will feel confident moving forward,” Dr. Cohen noted.
But despite the risks and uncertainty, doxy-PEP looks set to be a major part of the fight against STIs going forward. “Doxy-PEP is essential for us as a nation to be dealing with the syphilis epidemic,” Carl Dieffenbach, PhD, director of the Division of AIDS at the National Institute of Allergy and Infectious Disease, said in a video introduction to CROI.
A version of this article appeared on Medscape.com.
Syphilis and chlamydia infections were reduced by half among men who have sex with men and transgender women 1 year after San Francisco rolled out doxycycline postexposure prophylaxis (doxy-PEP), according to data presented at the Conference on Retroviruses and Opportunistic Infections (CROI) this week.
After a clinical trial showed that doxy-PEP taken after sex reduced the chance of acquiring syphilis, gonorrhea, and chlamydia by about two-thirds, the San Francisco Department of Public Health released the first guidelines in the country in October 2022.
So far, more than 3700 people in San Francisco have been prescribed doxy-PEP, reports Stephanie Cohen, MD, director of HIV and sexually transmitted infection (STI) prevention in the Disease Prevention and Control Branch of Public Health.
Dr. Cohen and her colleagues spent a year monitoring the uptake of doxy-PEP and used a computer model to predict what the rates of sexually transmitted infection would have been without doxy-PEP.
In November 2023, 13 months after the guidelines were introduced, they found that monthly chlamydia and early syphilis infections were 50% and 51% lower, respectively, than what was predicted by the model.
Fewer Infections
The drop in infections is having a tangible effect on patients in San Francisco, and many clinicians are noting that they are seeing far fewer positive tests. “The results that we’re seeing on a city-wide level are absolutely being experienced by individual providers and patients,” Dr. Cohen said.
However, the analysis showed no effect on rates of gonorrhea. It’s not clear why, although Dr. Cohen points out that doxy-PEP was less effective against gonorrhea in the clinical trial. And “there could be other factors in play,” she added. “Adherence might matter more, or it could be affected by the prevalence of tetracycline resistance in the community.”
With rates of STIs, particularly syphilis, quickly rising in recent years, healthcare providers have been scrambling to find effective interventions. So far, doxy-PEP has shown the most promise. “We’ve known for a while that all of the strategies we’ve been employing don’t seem to be working,” noted Chase Cannon, MD, an infectious disease specialist at the University of Washington in Seattle. “That’s why doxy-PEP is important. We haven’t had anything that can deflect the curve in a long time.”
What About the Side Effects?
Some concerns remain, however, about the widespread prophylactic use of antibiotics. There are no long-term safety data on the potential side effects of doxy-PEP, and there is still a lot of stigma around interventions that allow people to have sex the way they want, said Dr. Cannon.
But perhaps, the biggest concern is that doxy-PEP could contribute to antibiotic resistance. Those fears are not misplaced, Dr. Cannon added. The results of one study, presented in a poster at CROI, showed that stool samples from people prescribed doxy-PEP had elevated levels of bacterial genes that can confer resistance to tetracyclines, the class of antibiotics to which doxycycline belongs. There was no change in resistance to other classes of antibiotics and no difference in bacterial diversity over the 6 months of the study.
Dr. Cannon cautioned, however, that we can’t extrapolate these results to clinical outcomes. “We can look for signals [of resistance], but we don’t know if this means someone will fail therapy for chlamydia or syphilis,” he said.
There are still many challenges to overcome before doxy-PEP can be rolled out widely, Dr. Cohen explained. There is a lack of consensus among healthcare professionals about who should be offered doxy-PEP. The clinical trial results and the San Fransisco guidelines only apply to men who have sex with men and to transgender women.
Some clinicians argue that the intervention should be provided to a broader population, whereas others want to see more research to ensure that unnecessary antibiotic use is minimized.
So far just one study has tested doxy-PEP in another population — in women in Kenya — and it was found to not be effective. But the data suggest that adherence to the protocol was poor in that study, so the results may not be reliable, Dr. Cohen said.
“We need effective prevention tools for all genders, especially cis women who bear most of the morbidity,” she said. “It stands to reason that this should work for them, but without high-quality evidence, there is insufficient information to make a recommendation for cis women.”
The US Centers for Disease Control and Prevention is currently reviewing public and expert comments and refining final guidelines for release in the coming months, which should alleviate some of the uncertainty. “Many providers are waiting for that guidance before they will feel confident moving forward,” Dr. Cohen noted.
But despite the risks and uncertainty, doxy-PEP looks set to be a major part of the fight against STIs going forward. “Doxy-PEP is essential for us as a nation to be dealing with the syphilis epidemic,” Carl Dieffenbach, PhD, director of the Division of AIDS at the National Institute of Allergy and Infectious Disease, said in a video introduction to CROI.
A version of this article appeared on Medscape.com.
Hospital Mergers in 2024: Five Things to Know
Hospital mergers and acquisitions continue to garner intense scrutiny from lawmakers, with pressure likely to hold steady following the recent announcement of new antitrust guidelines and state and federal investigations into potential healthcare monopolies.
In December, the US Department of Justice (DOJ) and the Federal Trade Commission (FTC) released updated guidelines outlining the factors they consider when determining if a merger illegally monopolizes a local healthcare market or jeopardizes access to critical healthcare services.
Last week, the DOJ also announced a UnitedHealth Group antitrust probe, just months after the healthcare conglomerate’s workforce numbers indicated it is now affiliated with or employs 10% of the US physician workforce.
While the impact of the latest guidelines is yet to be seen, concerns over healthcare market consolidation are not new. Over the past two decades, mergers have attracted attention for contributing to a decline in independent hospitals, said Rachel M. Werner, MD, PhD, executive director of the Leonard Davis Institute of Health Economics at the University of Pennsylvania, Philadelphia, Pennsylvania.
“At this point, most hospitals are operating in a pretty concentrated market,” she said.
Here are five things to know about the current state of hospital mergers.
1. Record-Breaking Merger Enforcements
The DOJ and FTC reported the highest level of enforcement activity in over 20 years in fiscal year 2022 — the latest available data. Together, the agencies filed 50 merger enforcement actions and brought a record-breaking number of merger enforcement challenges, resulting in 11 approved actions, the restructuring or abandonment of seven mergers, and six business deals entering litigation.
Included in those statistics was a proposed merger between the two largest health systems in Rhode Island, Lifespan and Care New England Health System, which was abandoned after the FTC and the state Attorney General took steps to block it. the HCA branch in Utah Healthcare abandoned plans for to acquire five Salt Lake City area hospitals from competitor Steward Health Care System, as did RWJBarnabas Health after exploring a merger with Saint Peter's Healthcare System in New Jersey.
2. New Antitrust Guidelines Consider Labor Market
The new guidelines notably focus on labor competition, said Jody Boudreault, JD, attorney and chair of the Antitrust Life Sciences and Healthcare Group at Baker Botts law firm in Washington, DC. Health professionals typically have more employment opportunities in an urban area, unless hindered by restrictive noncompete agreements, and fewer options in rural settings.
In the Lifespan merger that fell through, Ms. Boudreault said that the newly created hospital system would have employed two thirds of Rhode Island's full-time nurses, limiting opportunities for local employment elsewhere.
“Going forward, I would expect federal authorities to review not only the competitive impact of the hospitals merging but also the competitive impact of the physician, and especially nursing, workforce,” she said.
FTC Chair Lina M. Khan noted similar labor market concerns.
In a statement to Congress, she said that hospital consolidation reduces options for employees, who fear “being blacklisted from further hiring in a system that controls many of the hospitals in the area” and “makes workers afraid to file complaints, organize their workplace, or leave before the end of a contract.”
3. Mergers Can Drive Care Costs Higher
When hospital markets become less competitive, the cost of care often increases. In Indiana, inpatient prices rose 13% in hospitals that merged. Another study found that prices at monopoly hospitals are 12% higher than in markets with four or more rivals. Even cross-market mergers, when hospitals in different geographic locations combine, can drive prices higher.
Dr. Werner told this news organization that more significant price hikes of 20-30% aren’t unheard of, with reimbursements by some commercial insurance companies rising as much as 50%. “That’s the direct price that the insurers pay, but the burden of those higher prices ultimately falls on patients through higher premiums,” she said.
Still, the American Hospital Association (AHA) says that mergers and acquisitions can significantly lower annual operating expenses per admission and reduce inpatient readmission rates and mortality measures. In comments to the FTC, the AHA stated that mergers could provide a lifeline for rural and community hospitals struggling with shrinking payer reimbursement and rising labor and supply costs. The business arrangements also could ensure these communities maintain continuity of care.
Although a cross-market merger may initially benefit cash-strapped rural hospitals, Dr. Werner urged caution.
“In the long run, it’s not clear that it is good for patients because we start to see decreased access to some types of service, like labor and delivery, which are services needed in rural markets,” she said.
4. Mergers to Watch in 2024
Ms. Boudreault, who represented RWJBarnabas in the abandoned Saint Peter’s transaction, says the courts widely accepted the old merger guidelines, and it will take time to see how the new measures are interpreted. “The guidelines don’t yet have the force of law, but they can be persuasive to a court.”
Looking ahead, she is watching how Steward Health Care navigates its impending financial collapse. The nation’s largest private for-profit health system was previously owned by private equity firm Cerberus Capital Management and includes nine Massachusetts hospitals plus entities in at least seven other states.
Ms. Boudreault also plans to monitor Jefferson Health’s intent to merge with Lehigh Valley Health Network. “It’s a pretty big deal because they would become a 30-hospital system,” said Ms. Boudreault. The newly formed network would become the largest employer in Philadelphia.
5. Merger and Acquisition Reversals Unlikely
Dr. Werner said that mergers and acquisitions are complicated business moves that are nearly impossible to undo once approved, so it makes sense for agencies to continue to evaluate them closely.
“The costs of healthcare are borne by us as a society,” she said. “We’re going to have to live with the ill effects of a consolidated market once we let hospitals merge, so they deserve additional scrutiny.”
A version of this article appeared on Medscape.com.
Hospital mergers and acquisitions continue to garner intense scrutiny from lawmakers, with pressure likely to hold steady following the recent announcement of new antitrust guidelines and state and federal investigations into potential healthcare monopolies.
In December, the US Department of Justice (DOJ) and the Federal Trade Commission (FTC) released updated guidelines outlining the factors they consider when determining if a merger illegally monopolizes a local healthcare market or jeopardizes access to critical healthcare services.
Last week, the DOJ also announced a UnitedHealth Group antitrust probe, just months after the healthcare conglomerate’s workforce numbers indicated it is now affiliated with or employs 10% of the US physician workforce.
While the impact of the latest guidelines is yet to be seen, concerns over healthcare market consolidation are not new. Over the past two decades, mergers have attracted attention for contributing to a decline in independent hospitals, said Rachel M. Werner, MD, PhD, executive director of the Leonard Davis Institute of Health Economics at the University of Pennsylvania, Philadelphia, Pennsylvania.
“At this point, most hospitals are operating in a pretty concentrated market,” she said.
Here are five things to know about the current state of hospital mergers.
1. Record-Breaking Merger Enforcements
The DOJ and FTC reported the highest level of enforcement activity in over 20 years in fiscal year 2022 — the latest available data. Together, the agencies filed 50 merger enforcement actions and brought a record-breaking number of merger enforcement challenges, resulting in 11 approved actions, the restructuring or abandonment of seven mergers, and six business deals entering litigation.
Included in those statistics was a proposed merger between the two largest health systems in Rhode Island, Lifespan and Care New England Health System, which was abandoned after the FTC and the state Attorney General took steps to block it. the HCA branch in Utah Healthcare abandoned plans for to acquire five Salt Lake City area hospitals from competitor Steward Health Care System, as did RWJBarnabas Health after exploring a merger with Saint Peter's Healthcare System in New Jersey.
2. New Antitrust Guidelines Consider Labor Market
The new guidelines notably focus on labor competition, said Jody Boudreault, JD, attorney and chair of the Antitrust Life Sciences and Healthcare Group at Baker Botts law firm in Washington, DC. Health professionals typically have more employment opportunities in an urban area, unless hindered by restrictive noncompete agreements, and fewer options in rural settings.
In the Lifespan merger that fell through, Ms. Boudreault said that the newly created hospital system would have employed two thirds of Rhode Island's full-time nurses, limiting opportunities for local employment elsewhere.
“Going forward, I would expect federal authorities to review not only the competitive impact of the hospitals merging but also the competitive impact of the physician, and especially nursing, workforce,” she said.
FTC Chair Lina M. Khan noted similar labor market concerns.
In a statement to Congress, she said that hospital consolidation reduces options for employees, who fear “being blacklisted from further hiring in a system that controls many of the hospitals in the area” and “makes workers afraid to file complaints, organize their workplace, or leave before the end of a contract.”
3. Mergers Can Drive Care Costs Higher
When hospital markets become less competitive, the cost of care often increases. In Indiana, inpatient prices rose 13% in hospitals that merged. Another study found that prices at monopoly hospitals are 12% higher than in markets with four or more rivals. Even cross-market mergers, when hospitals in different geographic locations combine, can drive prices higher.
Dr. Werner told this news organization that more significant price hikes of 20-30% aren’t unheard of, with reimbursements by some commercial insurance companies rising as much as 50%. “That’s the direct price that the insurers pay, but the burden of those higher prices ultimately falls on patients through higher premiums,” she said.
Still, the American Hospital Association (AHA) says that mergers and acquisitions can significantly lower annual operating expenses per admission and reduce inpatient readmission rates and mortality measures. In comments to the FTC, the AHA stated that mergers could provide a lifeline for rural and community hospitals struggling with shrinking payer reimbursement and rising labor and supply costs. The business arrangements also could ensure these communities maintain continuity of care.
Although a cross-market merger may initially benefit cash-strapped rural hospitals, Dr. Werner urged caution.
“In the long run, it’s not clear that it is good for patients because we start to see decreased access to some types of service, like labor and delivery, which are services needed in rural markets,” she said.
4. Mergers to Watch in 2024
Ms. Boudreault, who represented RWJBarnabas in the abandoned Saint Peter’s transaction, says the courts widely accepted the old merger guidelines, and it will take time to see how the new measures are interpreted. “The guidelines don’t yet have the force of law, but they can be persuasive to a court.”
Looking ahead, she is watching how Steward Health Care navigates its impending financial collapse. The nation’s largest private for-profit health system was previously owned by private equity firm Cerberus Capital Management and includes nine Massachusetts hospitals plus entities in at least seven other states.
Ms. Boudreault also plans to monitor Jefferson Health’s intent to merge with Lehigh Valley Health Network. “It’s a pretty big deal because they would become a 30-hospital system,” said Ms. Boudreault. The newly formed network would become the largest employer in Philadelphia.
5. Merger and Acquisition Reversals Unlikely
Dr. Werner said that mergers and acquisitions are complicated business moves that are nearly impossible to undo once approved, so it makes sense for agencies to continue to evaluate them closely.
“The costs of healthcare are borne by us as a society,” she said. “We’re going to have to live with the ill effects of a consolidated market once we let hospitals merge, so they deserve additional scrutiny.”
A version of this article appeared on Medscape.com.
Hospital mergers and acquisitions continue to garner intense scrutiny from lawmakers, with pressure likely to hold steady following the recent announcement of new antitrust guidelines and state and federal investigations into potential healthcare monopolies.
In December, the US Department of Justice (DOJ) and the Federal Trade Commission (FTC) released updated guidelines outlining the factors they consider when determining if a merger illegally monopolizes a local healthcare market or jeopardizes access to critical healthcare services.
Last week, the DOJ also announced a UnitedHealth Group antitrust probe, just months after the healthcare conglomerate’s workforce numbers indicated it is now affiliated with or employs 10% of the US physician workforce.
While the impact of the latest guidelines is yet to be seen, concerns over healthcare market consolidation are not new. Over the past two decades, mergers have attracted attention for contributing to a decline in independent hospitals, said Rachel M. Werner, MD, PhD, executive director of the Leonard Davis Institute of Health Economics at the University of Pennsylvania, Philadelphia, Pennsylvania.
“At this point, most hospitals are operating in a pretty concentrated market,” she said.
Here are five things to know about the current state of hospital mergers.
1. Record-Breaking Merger Enforcements
The DOJ and FTC reported the highest level of enforcement activity in over 20 years in fiscal year 2022 — the latest available data. Together, the agencies filed 50 merger enforcement actions and brought a record-breaking number of merger enforcement challenges, resulting in 11 approved actions, the restructuring or abandonment of seven mergers, and six business deals entering litigation.
Included in those statistics was a proposed merger between the two largest health systems in Rhode Island, Lifespan and Care New England Health System, which was abandoned after the FTC and the state Attorney General took steps to block it. the HCA branch in Utah Healthcare abandoned plans for to acquire five Salt Lake City area hospitals from competitor Steward Health Care System, as did RWJBarnabas Health after exploring a merger with Saint Peter's Healthcare System in New Jersey.
2. New Antitrust Guidelines Consider Labor Market
The new guidelines notably focus on labor competition, said Jody Boudreault, JD, attorney and chair of the Antitrust Life Sciences and Healthcare Group at Baker Botts law firm in Washington, DC. Health professionals typically have more employment opportunities in an urban area, unless hindered by restrictive noncompete agreements, and fewer options in rural settings.
In the Lifespan merger that fell through, Ms. Boudreault said that the newly created hospital system would have employed two thirds of Rhode Island's full-time nurses, limiting opportunities for local employment elsewhere.
“Going forward, I would expect federal authorities to review not only the competitive impact of the hospitals merging but also the competitive impact of the physician, and especially nursing, workforce,” she said.
FTC Chair Lina M. Khan noted similar labor market concerns.
In a statement to Congress, she said that hospital consolidation reduces options for employees, who fear “being blacklisted from further hiring in a system that controls many of the hospitals in the area” and “makes workers afraid to file complaints, organize their workplace, or leave before the end of a contract.”
3. Mergers Can Drive Care Costs Higher
When hospital markets become less competitive, the cost of care often increases. In Indiana, inpatient prices rose 13% in hospitals that merged. Another study found that prices at monopoly hospitals are 12% higher than in markets with four or more rivals. Even cross-market mergers, when hospitals in different geographic locations combine, can drive prices higher.
Dr. Werner told this news organization that more significant price hikes of 20-30% aren’t unheard of, with reimbursements by some commercial insurance companies rising as much as 50%. “That’s the direct price that the insurers pay, but the burden of those higher prices ultimately falls on patients through higher premiums,” she said.
Still, the American Hospital Association (AHA) says that mergers and acquisitions can significantly lower annual operating expenses per admission and reduce inpatient readmission rates and mortality measures. In comments to the FTC, the AHA stated that mergers could provide a lifeline for rural and community hospitals struggling with shrinking payer reimbursement and rising labor and supply costs. The business arrangements also could ensure these communities maintain continuity of care.
Although a cross-market merger may initially benefit cash-strapped rural hospitals, Dr. Werner urged caution.
“In the long run, it’s not clear that it is good for patients because we start to see decreased access to some types of service, like labor and delivery, which are services needed in rural markets,” she said.
4. Mergers to Watch in 2024
Ms. Boudreault, who represented RWJBarnabas in the abandoned Saint Peter’s transaction, says the courts widely accepted the old merger guidelines, and it will take time to see how the new measures are interpreted. “The guidelines don’t yet have the force of law, but they can be persuasive to a court.”
Looking ahead, she is watching how Steward Health Care navigates its impending financial collapse. The nation’s largest private for-profit health system was previously owned by private equity firm Cerberus Capital Management and includes nine Massachusetts hospitals plus entities in at least seven other states.
Ms. Boudreault also plans to monitor Jefferson Health’s intent to merge with Lehigh Valley Health Network. “It’s a pretty big deal because they would become a 30-hospital system,” said Ms. Boudreault. The newly formed network would become the largest employer in Philadelphia.
5. Merger and Acquisition Reversals Unlikely
Dr. Werner said that mergers and acquisitions are complicated business moves that are nearly impossible to undo once approved, so it makes sense for agencies to continue to evaluate them closely.
“The costs of healthcare are borne by us as a society,” she said. “We’re going to have to live with the ill effects of a consolidated market once we let hospitals merge, so they deserve additional scrutiny.”
A version of this article appeared on Medscape.com.
Midwife’s Fake Vaccinations Deserve Harsh Punishment: Ethicist
This transcript has been edited for clarity.
Hi. I’m Art Caplan, at the Division of Medical Ethics at New York University’s Grossman School of Medicine.
Very recently, a homeopathic midwife in New York was fined $300,000 for giving out phony injections for kids who were looking to get immunized in order to go to school. She gave pellets, which are sometimes called nosodes, I believe, with homeopathic ingredients, meaning next to nothing in them, and then basically certified that these children — and there were over 1500 of them — were compliant with New York State requirements to be vaccinated to go to school.
However, homeopathy is straight-up bunk. We have seen it again and again discredited as just something that doesn’t work. It has a tradition, but it’s basically nonsense. It certainly doesn’t work as a way to vaccinate anybody.
This midwife basically lied and gave phony certification to the parents of these kids. I’m not talking about the COVID-19 vaccine. I’m talking measles, mumps, rubella, flu, and polio — the childhood immunization schedule. For whatever reason, they put their faith in her and she went along with this fraud.
I think the fine is appropriate, but I think she should be penalized further. Why? When you send 1500 kids to school, mostly in Long Island, New York, but to schools all over the place, you are setting up conditions to bring back epidemic diseases like measles.
We’re already seeing measles outbreaks. At least five states have them. There’s a significant measles outbreak in Philadelphia. Although I can’t say for sure, I believe those outbreaks are directly linked to parents, post–COVID-19, becoming vaccine hesitant and either not vaccinating and lying or going to alternative practitioners like this midwife and claiming that they have been vaccinated.
You’re doing harm not only to the children who you allow to go to school under phony pretenses, but also you’re putting their classmates at risk. We all know that measles is very, very contagious. You’re risking the return of a disease that leads to hospitalization and sometimes even death. That is basically unconscionable.
I think her license should be taken away and she should not be practicing anymore. I believe that anyone who is involved in this kind of phony, dangerous, fraudulent practice ought to be severely punished.
Pre–COVID-19, we had just about gotten rid of measles and mumps. We didn’t see these diseases. Sometimes parents got a bit lazy in childhood vaccination basically because we had used immunization to get rid of the diseases.
Going to alternative healers and allowing people to get away with fraudulent nonsense risks bringing back disabling and deadly killers is not fair to you, me, and other people who are put at risk. It’s not fair to the kids who go to school with other kids who they think are vaccinated but aren’t.
I’m Art Caplan, at the Division of Medical Ethics at the New York University Grossman School of Medicine. Thanks for watching.
Arthur L. Caplan, PhD, has disclosed the following relevant financial relationships: Served as a director, officer, partner, employee, adviser, consultant, or trustee for Johnson & Johnson’s Panel for Compassionate Drug Use (unpaid position); serves as a contributing author and adviser for Medscape.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Hi. I’m Art Caplan, at the Division of Medical Ethics at New York University’s Grossman School of Medicine.
Very recently, a homeopathic midwife in New York was fined $300,000 for giving out phony injections for kids who were looking to get immunized in order to go to school. She gave pellets, which are sometimes called nosodes, I believe, with homeopathic ingredients, meaning next to nothing in them, and then basically certified that these children — and there were over 1500 of them — were compliant with New York State requirements to be vaccinated to go to school.
However, homeopathy is straight-up bunk. We have seen it again and again discredited as just something that doesn’t work. It has a tradition, but it’s basically nonsense. It certainly doesn’t work as a way to vaccinate anybody.
This midwife basically lied and gave phony certification to the parents of these kids. I’m not talking about the COVID-19 vaccine. I’m talking measles, mumps, rubella, flu, and polio — the childhood immunization schedule. For whatever reason, they put their faith in her and she went along with this fraud.
I think the fine is appropriate, but I think she should be penalized further. Why? When you send 1500 kids to school, mostly in Long Island, New York, but to schools all over the place, you are setting up conditions to bring back epidemic diseases like measles.
We’re already seeing measles outbreaks. At least five states have them. There’s a significant measles outbreak in Philadelphia. Although I can’t say for sure, I believe those outbreaks are directly linked to parents, post–COVID-19, becoming vaccine hesitant and either not vaccinating and lying or going to alternative practitioners like this midwife and claiming that they have been vaccinated.
You’re doing harm not only to the children who you allow to go to school under phony pretenses, but also you’re putting their classmates at risk. We all know that measles is very, very contagious. You’re risking the return of a disease that leads to hospitalization and sometimes even death. That is basically unconscionable.
I think her license should be taken away and she should not be practicing anymore. I believe that anyone who is involved in this kind of phony, dangerous, fraudulent practice ought to be severely punished.
Pre–COVID-19, we had just about gotten rid of measles and mumps. We didn’t see these diseases. Sometimes parents got a bit lazy in childhood vaccination basically because we had used immunization to get rid of the diseases.
Going to alternative healers and allowing people to get away with fraudulent nonsense risks bringing back disabling and deadly killers is not fair to you, me, and other people who are put at risk. It’s not fair to the kids who go to school with other kids who they think are vaccinated but aren’t.
I’m Art Caplan, at the Division of Medical Ethics at the New York University Grossman School of Medicine. Thanks for watching.
Arthur L. Caplan, PhD, has disclosed the following relevant financial relationships: Served as a director, officer, partner, employee, adviser, consultant, or trustee for Johnson & Johnson’s Panel for Compassionate Drug Use (unpaid position); serves as a contributing author and adviser for Medscape.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Hi. I’m Art Caplan, at the Division of Medical Ethics at New York University’s Grossman School of Medicine.
Very recently, a homeopathic midwife in New York was fined $300,000 for giving out phony injections for kids who were looking to get immunized in order to go to school. She gave pellets, which are sometimes called nosodes, I believe, with homeopathic ingredients, meaning next to nothing in them, and then basically certified that these children — and there were over 1500 of them — were compliant with New York State requirements to be vaccinated to go to school.
However, homeopathy is straight-up bunk. We have seen it again and again discredited as just something that doesn’t work. It has a tradition, but it’s basically nonsense. It certainly doesn’t work as a way to vaccinate anybody.
This midwife basically lied and gave phony certification to the parents of these kids. I’m not talking about the COVID-19 vaccine. I’m talking measles, mumps, rubella, flu, and polio — the childhood immunization schedule. For whatever reason, they put their faith in her and she went along with this fraud.
I think the fine is appropriate, but I think she should be penalized further. Why? When you send 1500 kids to school, mostly in Long Island, New York, but to schools all over the place, you are setting up conditions to bring back epidemic diseases like measles.
We’re already seeing measles outbreaks. At least five states have them. There’s a significant measles outbreak in Philadelphia. Although I can’t say for sure, I believe those outbreaks are directly linked to parents, post–COVID-19, becoming vaccine hesitant and either not vaccinating and lying or going to alternative practitioners like this midwife and claiming that they have been vaccinated.
You’re doing harm not only to the children who you allow to go to school under phony pretenses, but also you’re putting their classmates at risk. We all know that measles is very, very contagious. You’re risking the return of a disease that leads to hospitalization and sometimes even death. That is basically unconscionable.
I think her license should be taken away and she should not be practicing anymore. I believe that anyone who is involved in this kind of phony, dangerous, fraudulent practice ought to be severely punished.
Pre–COVID-19, we had just about gotten rid of measles and mumps. We didn’t see these diseases. Sometimes parents got a bit lazy in childhood vaccination basically because we had used immunization to get rid of the diseases.
Going to alternative healers and allowing people to get away with fraudulent nonsense risks bringing back disabling and deadly killers is not fair to you, me, and other people who are put at risk. It’s not fair to the kids who go to school with other kids who they think are vaccinated but aren’t.
I’m Art Caplan, at the Division of Medical Ethics at the New York University Grossman School of Medicine. Thanks for watching.
Arthur L. Caplan, PhD, has disclosed the following relevant financial relationships: Served as a director, officer, partner, employee, adviser, consultant, or trustee for Johnson & Johnson’s Panel for Compassionate Drug Use (unpaid position); serves as a contributing author and adviser for Medscape.
A version of this article appeared on Medscape.com.
Increased Risk of New Rheumatic Disease Follows COVID-19 Infection
The risk of developing a new autoimmune inflammatory rheumatic disease (AIRD) is greater following a COVID-19 infection than after an influenza infection or in the general population, according to a study published March 5 in Annals of Internal Medicine. More severe COVID-19 infections were linked to a greater risk of incident rheumatic disease, but vaccination appeared protective against development of a new AIRD.
“Importantly, this study shows the value of vaccination to prevent severe disease and these types of sequelae,” Anne Davidson, MBBS, a professor in the Institute of Molecular Medicine at The Feinstein Institutes for Medical Research in Manhasset, New York, who was not involved in the study, said in an interview.
Previous research had already identified the likelihood of an association between SARS-CoV-2 infection and subsequent development of a new AIRD. This new study, however, includes much larger cohorts from two different countries and relies on more robust methodology than previous studies, experts said.
“Unique steps were taken by the study authors to make sure that what they were looking at in terms of signal was most likely true,” Alfred Kim, MD, PhD, assistant professor of medicine in rheumatology at Washington University in St. Louis, who was not involved in the study, said in an interview. Dr. Davidson agreed, noting that these authors “were a bit more rigorous with ascertainment of the autoimmune diagnosis, using two codes and also checking that appropriate medications were administered.”
More Robust and Rigorous Research
Past cohort studies finding an increased risk of rheumatic disease after COVID-19 “based their findings solely on comparisons between infected and uninfected groups, which could be influenced by ascertainment bias due to disparities in care, differences in health-seeking tendencies, and inherent risks among the groups,” Min Seo Kim, MD, of the Broad Institute of MIT and Harvard, Cambridge, Massachusetts, and his colleagues reported. Their study, however, required at least two claims with codes for rheumatic disease and compared patients with COVID-19 to those with flu “to adjust for the potentially heightened detection of AIRD in SARS-CoV-2–infected persons owing to their interactions with the health care system.”
Dr. Alfred Kim said the fact that they used at least two claims codes “gives a little more credence that the patients were actually experiencing some sort of autoimmune inflammatory condition as opposed to a very transient issue post COVID that just went away on its own.”
He acknowledged that the previous research was reasonably strong, “especially in light of the fact that there has been so much work done on a molecular level demonstrating that COVID-19 is associated with a substantial increase in autoantibodies in a significant proportion of patients, so this always opened up the possibility that this could associate with some sort of autoimmune disease downstream.”
While the study is well done with a large population, “it still has limitations that might overestimate the effect,” Kevin W. Byram, MD, associate professor of medicine in rheumatology and immunology at Vanderbilt University Medical Center in Nashville, Tennessee, who was not involved in the study, said in an interview. “We certainly have seen individual cases of new rheumatic disease where COVID-19 infection is likely the trigger,” but the phenomenon is not new, he added.
“Many autoimmune diseases are spurred by a loss of tolerance that might be induced by a pathogen of some sort,” Dr. Byram said. “The study is right to point out different forms of bias that might be at play. One in particular that is important to consider in a study like this is the lack of case-level adjudication regarding the diagnosis of rheumatic disease” since the study relied on available ICD-10 codes and medication prescriptions.
The researchers used national claims data to compare risk of incident AIRD in 10,027,506 South Korean and 12,218,680 Japanese adults, aged 20 and older, at 1 month, 6 months, and 12 months after COVID-19 infection, influenza infection, or a matched index date for uninfected control participants. Only patients with at least two claims for AIRD were considered to have a new diagnosis.
Patients who had COVID-19 between January 2020 and December 2021, confirmed by PCR or antigen testing, were matched 1:1 with patients who had test-confirmed influenza during that time and 1:4 with uninfected control participants, whose index date was set to the infection date of their matched COVID-19 patient.
The propensity score matching was based on age, sex, household income, urban versus rural residence, and various clinical characteristics and history: body mass index; blood pressure; fasting blood glucose; glomerular filtration rate; smoking status; alcohol consumption; weekly aerobic physical activity; comorbidity index; hospitalizations and outpatient visits in the previous year; past use of diabetes, hyperlipidemia, or hypertension medication; and history of cardiovascular disease, chronic kidney disease, chronic obstructive pulmonary disease, or respiratory infectious disease.
Patients with a history of AIRD or with coinfection or reinfection of COVID-19 and influenza were excluded, as were patients diagnosed with rheumatic disease within a month of COVID-19 infection.
Risk Varied With Disease Severity and Vaccination Status
Among the Korean patients, 3.9% had a COVID-19 infection and 0.98% had an influenza infection. After matching, the comparison populations included 94,504 patients with COVID-19 versus 94,504 patients with flu, and 177,083 patients with COVID-19 versus 675,750 uninfected controls.
The risk of developing an AIRD at least 1 month after infection in South Korean patients with COVID-19 was 25% higher than in uninfected control participants (adjusted hazard ratio [aHR], 1.25; 95% CI, 1.18–1.31; P < .05) and 30% higher than in influenza patients (aHR, 1.3; 95% CI, 1.02–1.59; P < .05). Specifically, risk in South Korean patients with COVID-19 was significantly increased for connective tissue disease and both treated and untreated AIRD but not for inflammatory arthritis.
Among the Japanese patients, 8.2% had COVID-19 and 0.99% had flu, resulting in matched populations of 115,003 with COVID-19 versus 110,310 with flu, and 960,849 with COVID-19 versus 1,606,873 uninfected patients. The effect size was larger in Japanese patients, with a 79% increased risk for AIRD in patients with COVID-19, compared with the general population (aHR, 1.79; 95% CI, 1.77–1.82; P < .05) and a 14% increased risk, compared with patients with influenza infection (aHR, 1.14; 95% CI, 1.10–1.17; P < .05). In Japanese patients, risk was increased across all four categories, including a doubled risk for inflammatory arthritis (aHR, 2.02; 95% CI, 1.96–2.07; P < .05), compared with the general population.
The researchers had data only from the South Korean cohort to calculate risk based on vaccination status, SARS-CoV-2 variant (wild type versus Delta), and COVID-19 severity. Researchers determined a COVID-19 infection to be moderate-to-severe based on billing codes for ICU admission or requiring oxygen therapy, extracorporeal membrane oxygenation, renal replacement, or CPR.
Infection with both the original strain and the Delta variant were linked to similar increased risks for AIRD, but moderate to severe COVID-19 infections had greater risk of subsequent AIRD (aHR, 1.42; P < .05) than mild infections (aHR, 1.22; P < .05). Vaccination was linked to a lower risk of AIRD within the COVID-19 patient population: One dose was linked to a 41% reduced risk (HR, 0.59; P < .05) and two doses were linked to a 58% reduced risk (HR, 0.42; P < .05), regardless of the vaccine type, compared with unvaccinated patients with COVID-19. The apparent protective effect of vaccination was true only for patients with mild COVID-19, not those with moderate to severe infection.
“One has to wonder whether or not these people were at much higher risk of developing autoimmune disease that just got exposed because they got COVID, so that a fraction of these would have gotten an autoimmune disease downstream,” Dr. Alfred Kim said. Regardless, one clinical implication of the findings is the reduced risk in vaccinated patients, regardless of the vaccine type, given the fact that “mRNA vaccination in particular has not been associated with any autoantibody development,” he said.
Though the correlations in the study cannot translate to causation, several mechanisms might be at play in a viral infection contributing to autoimmune risk, Dr. Davidson said. Given that viral nucleic acids also recognize self-nucleic acids, “a large load of viral nucleic acid may break tolerance,” or “viral proteins could also mimic self-proteins,” she said. “In addition, tolerance may be broken by a highly inflammatory environment associated with the release of cytokines and other inflammatory mediators.”
The association between new-onset autoimmune disease and severe COVID-19 infection suggests multiple mechanisms may be involved in excess immune stimulation, Dr. Davidson said. But she added that it’s unclear how these findings, involving the original strain and Delta variant of SARS-CoV-2, might relate to currently circulating variants.
The research was funded by the National Research Foundation of Korea, the Korea Health Industry Development Institute, and the Ministry of Food and Drug Safety of the Republic of Korea. The authors reported no relevant financial relationships with industry. Dr. Alfred Kim has sponsored research agreements with AstraZeneca, Bristol-Myers Squibb, and Novartis; receives royalties from a patent with Kypha Inc.; and has done consulting or speaking for Amgen, ANI Pharmaceuticals, Aurinia Pharmaceuticals, Exagen Diagnostics, GlaxoSmithKline, Kypha, Miltenyi Biotech, Pfizer, Rheumatology & Arthritis Learning Network, Synthekine, Techtonic Therapeutics, and UpToDate. Dr. Byram reported consulting for TenSixteen Bio. Dr. Davidson had no disclosures.
The risk of developing a new autoimmune inflammatory rheumatic disease (AIRD) is greater following a COVID-19 infection than after an influenza infection or in the general population, according to a study published March 5 in Annals of Internal Medicine. More severe COVID-19 infections were linked to a greater risk of incident rheumatic disease, but vaccination appeared protective against development of a new AIRD.
“Importantly, this study shows the value of vaccination to prevent severe disease and these types of sequelae,” Anne Davidson, MBBS, a professor in the Institute of Molecular Medicine at The Feinstein Institutes for Medical Research in Manhasset, New York, who was not involved in the study, said in an interview.
Previous research had already identified the likelihood of an association between SARS-CoV-2 infection and subsequent development of a new AIRD. This new study, however, includes much larger cohorts from two different countries and relies on more robust methodology than previous studies, experts said.
“Unique steps were taken by the study authors to make sure that what they were looking at in terms of signal was most likely true,” Alfred Kim, MD, PhD, assistant professor of medicine in rheumatology at Washington University in St. Louis, who was not involved in the study, said in an interview. Dr. Davidson agreed, noting that these authors “were a bit more rigorous with ascertainment of the autoimmune diagnosis, using two codes and also checking that appropriate medications were administered.”
More Robust and Rigorous Research
Past cohort studies finding an increased risk of rheumatic disease after COVID-19 “based their findings solely on comparisons between infected and uninfected groups, which could be influenced by ascertainment bias due to disparities in care, differences in health-seeking tendencies, and inherent risks among the groups,” Min Seo Kim, MD, of the Broad Institute of MIT and Harvard, Cambridge, Massachusetts, and his colleagues reported. Their study, however, required at least two claims with codes for rheumatic disease and compared patients with COVID-19 to those with flu “to adjust for the potentially heightened detection of AIRD in SARS-CoV-2–infected persons owing to their interactions with the health care system.”
Dr. Alfred Kim said the fact that they used at least two claims codes “gives a little more credence that the patients were actually experiencing some sort of autoimmune inflammatory condition as opposed to a very transient issue post COVID that just went away on its own.”
He acknowledged that the previous research was reasonably strong, “especially in light of the fact that there has been so much work done on a molecular level demonstrating that COVID-19 is associated with a substantial increase in autoantibodies in a significant proportion of patients, so this always opened up the possibility that this could associate with some sort of autoimmune disease downstream.”
While the study is well done with a large population, “it still has limitations that might overestimate the effect,” Kevin W. Byram, MD, associate professor of medicine in rheumatology and immunology at Vanderbilt University Medical Center in Nashville, Tennessee, who was not involved in the study, said in an interview. “We certainly have seen individual cases of new rheumatic disease where COVID-19 infection is likely the trigger,” but the phenomenon is not new, he added.
“Many autoimmune diseases are spurred by a loss of tolerance that might be induced by a pathogen of some sort,” Dr. Byram said. “The study is right to point out different forms of bias that might be at play. One in particular that is important to consider in a study like this is the lack of case-level adjudication regarding the diagnosis of rheumatic disease” since the study relied on available ICD-10 codes and medication prescriptions.
The researchers used national claims data to compare risk of incident AIRD in 10,027,506 South Korean and 12,218,680 Japanese adults, aged 20 and older, at 1 month, 6 months, and 12 months after COVID-19 infection, influenza infection, or a matched index date for uninfected control participants. Only patients with at least two claims for AIRD were considered to have a new diagnosis.
Patients who had COVID-19 between January 2020 and December 2021, confirmed by PCR or antigen testing, were matched 1:1 with patients who had test-confirmed influenza during that time and 1:4 with uninfected control participants, whose index date was set to the infection date of their matched COVID-19 patient.
The propensity score matching was based on age, sex, household income, urban versus rural residence, and various clinical characteristics and history: body mass index; blood pressure; fasting blood glucose; glomerular filtration rate; smoking status; alcohol consumption; weekly aerobic physical activity; comorbidity index; hospitalizations and outpatient visits in the previous year; past use of diabetes, hyperlipidemia, or hypertension medication; and history of cardiovascular disease, chronic kidney disease, chronic obstructive pulmonary disease, or respiratory infectious disease.
Patients with a history of AIRD or with coinfection or reinfection of COVID-19 and influenza were excluded, as were patients diagnosed with rheumatic disease within a month of COVID-19 infection.
Risk Varied With Disease Severity and Vaccination Status
Among the Korean patients, 3.9% had a COVID-19 infection and 0.98% had an influenza infection. After matching, the comparison populations included 94,504 patients with COVID-19 versus 94,504 patients with flu, and 177,083 patients with COVID-19 versus 675,750 uninfected controls.
The risk of developing an AIRD at least 1 month after infection in South Korean patients with COVID-19 was 25% higher than in uninfected control participants (adjusted hazard ratio [aHR], 1.25; 95% CI, 1.18–1.31; P < .05) and 30% higher than in influenza patients (aHR, 1.3; 95% CI, 1.02–1.59; P < .05). Specifically, risk in South Korean patients with COVID-19 was significantly increased for connective tissue disease and both treated and untreated AIRD but not for inflammatory arthritis.
Among the Japanese patients, 8.2% had COVID-19 and 0.99% had flu, resulting in matched populations of 115,003 with COVID-19 versus 110,310 with flu, and 960,849 with COVID-19 versus 1,606,873 uninfected patients. The effect size was larger in Japanese patients, with a 79% increased risk for AIRD in patients with COVID-19, compared with the general population (aHR, 1.79; 95% CI, 1.77–1.82; P < .05) and a 14% increased risk, compared with patients with influenza infection (aHR, 1.14; 95% CI, 1.10–1.17; P < .05). In Japanese patients, risk was increased across all four categories, including a doubled risk for inflammatory arthritis (aHR, 2.02; 95% CI, 1.96–2.07; P < .05), compared with the general population.
The researchers had data only from the South Korean cohort to calculate risk based on vaccination status, SARS-CoV-2 variant (wild type versus Delta), and COVID-19 severity. Researchers determined a COVID-19 infection to be moderate-to-severe based on billing codes for ICU admission or requiring oxygen therapy, extracorporeal membrane oxygenation, renal replacement, or CPR.
Infection with both the original strain and the Delta variant were linked to similar increased risks for AIRD, but moderate to severe COVID-19 infections had greater risk of subsequent AIRD (aHR, 1.42; P < .05) than mild infections (aHR, 1.22; P < .05). Vaccination was linked to a lower risk of AIRD within the COVID-19 patient population: One dose was linked to a 41% reduced risk (HR, 0.59; P < .05) and two doses were linked to a 58% reduced risk (HR, 0.42; P < .05), regardless of the vaccine type, compared with unvaccinated patients with COVID-19. The apparent protective effect of vaccination was true only for patients with mild COVID-19, not those with moderate to severe infection.
“One has to wonder whether or not these people were at much higher risk of developing autoimmune disease that just got exposed because they got COVID, so that a fraction of these would have gotten an autoimmune disease downstream,” Dr. Alfred Kim said. Regardless, one clinical implication of the findings is the reduced risk in vaccinated patients, regardless of the vaccine type, given the fact that “mRNA vaccination in particular has not been associated with any autoantibody development,” he said.
Though the correlations in the study cannot translate to causation, several mechanisms might be at play in a viral infection contributing to autoimmune risk, Dr. Davidson said. Given that viral nucleic acids also recognize self-nucleic acids, “a large load of viral nucleic acid may break tolerance,” or “viral proteins could also mimic self-proteins,” she said. “In addition, tolerance may be broken by a highly inflammatory environment associated with the release of cytokines and other inflammatory mediators.”
The association between new-onset autoimmune disease and severe COVID-19 infection suggests multiple mechanisms may be involved in excess immune stimulation, Dr. Davidson said. But she added that it’s unclear how these findings, involving the original strain and Delta variant of SARS-CoV-2, might relate to currently circulating variants.
The research was funded by the National Research Foundation of Korea, the Korea Health Industry Development Institute, and the Ministry of Food and Drug Safety of the Republic of Korea. The authors reported no relevant financial relationships with industry. Dr. Alfred Kim has sponsored research agreements with AstraZeneca, Bristol-Myers Squibb, and Novartis; receives royalties from a patent with Kypha Inc.; and has done consulting or speaking for Amgen, ANI Pharmaceuticals, Aurinia Pharmaceuticals, Exagen Diagnostics, GlaxoSmithKline, Kypha, Miltenyi Biotech, Pfizer, Rheumatology & Arthritis Learning Network, Synthekine, Techtonic Therapeutics, and UpToDate. Dr. Byram reported consulting for TenSixteen Bio. Dr. Davidson had no disclosures.
The risk of developing a new autoimmune inflammatory rheumatic disease (AIRD) is greater following a COVID-19 infection than after an influenza infection or in the general population, according to a study published March 5 in Annals of Internal Medicine. More severe COVID-19 infections were linked to a greater risk of incident rheumatic disease, but vaccination appeared protective against development of a new AIRD.
“Importantly, this study shows the value of vaccination to prevent severe disease and these types of sequelae,” Anne Davidson, MBBS, a professor in the Institute of Molecular Medicine at The Feinstein Institutes for Medical Research in Manhasset, New York, who was not involved in the study, said in an interview.
Previous research had already identified the likelihood of an association between SARS-CoV-2 infection and subsequent development of a new AIRD. This new study, however, includes much larger cohorts from two different countries and relies on more robust methodology than previous studies, experts said.
“Unique steps were taken by the study authors to make sure that what they were looking at in terms of signal was most likely true,” Alfred Kim, MD, PhD, assistant professor of medicine in rheumatology at Washington University in St. Louis, who was not involved in the study, said in an interview. Dr. Davidson agreed, noting that these authors “were a bit more rigorous with ascertainment of the autoimmune diagnosis, using two codes and also checking that appropriate medications were administered.”
More Robust and Rigorous Research
Past cohort studies finding an increased risk of rheumatic disease after COVID-19 “based their findings solely on comparisons between infected and uninfected groups, which could be influenced by ascertainment bias due to disparities in care, differences in health-seeking tendencies, and inherent risks among the groups,” Min Seo Kim, MD, of the Broad Institute of MIT and Harvard, Cambridge, Massachusetts, and his colleagues reported. Their study, however, required at least two claims with codes for rheumatic disease and compared patients with COVID-19 to those with flu “to adjust for the potentially heightened detection of AIRD in SARS-CoV-2–infected persons owing to their interactions with the health care system.”
Dr. Alfred Kim said the fact that they used at least two claims codes “gives a little more credence that the patients were actually experiencing some sort of autoimmune inflammatory condition as opposed to a very transient issue post COVID that just went away on its own.”
He acknowledged that the previous research was reasonably strong, “especially in light of the fact that there has been so much work done on a molecular level demonstrating that COVID-19 is associated with a substantial increase in autoantibodies in a significant proportion of patients, so this always opened up the possibility that this could associate with some sort of autoimmune disease downstream.”
While the study is well done with a large population, “it still has limitations that might overestimate the effect,” Kevin W. Byram, MD, associate professor of medicine in rheumatology and immunology at Vanderbilt University Medical Center in Nashville, Tennessee, who was not involved in the study, said in an interview. “We certainly have seen individual cases of new rheumatic disease where COVID-19 infection is likely the trigger,” but the phenomenon is not new, he added.
“Many autoimmune diseases are spurred by a loss of tolerance that might be induced by a pathogen of some sort,” Dr. Byram said. “The study is right to point out different forms of bias that might be at play. One in particular that is important to consider in a study like this is the lack of case-level adjudication regarding the diagnosis of rheumatic disease” since the study relied on available ICD-10 codes and medication prescriptions.
The researchers used national claims data to compare risk of incident AIRD in 10,027,506 South Korean and 12,218,680 Japanese adults, aged 20 and older, at 1 month, 6 months, and 12 months after COVID-19 infection, influenza infection, or a matched index date for uninfected control participants. Only patients with at least two claims for AIRD were considered to have a new diagnosis.
Patients who had COVID-19 between January 2020 and December 2021, confirmed by PCR or antigen testing, were matched 1:1 with patients who had test-confirmed influenza during that time and 1:4 with uninfected control participants, whose index date was set to the infection date of their matched COVID-19 patient.
The propensity score matching was based on age, sex, household income, urban versus rural residence, and various clinical characteristics and history: body mass index; blood pressure; fasting blood glucose; glomerular filtration rate; smoking status; alcohol consumption; weekly aerobic physical activity; comorbidity index; hospitalizations and outpatient visits in the previous year; past use of diabetes, hyperlipidemia, or hypertension medication; and history of cardiovascular disease, chronic kidney disease, chronic obstructive pulmonary disease, or respiratory infectious disease.
Patients with a history of AIRD or with coinfection or reinfection of COVID-19 and influenza were excluded, as were patients diagnosed with rheumatic disease within a month of COVID-19 infection.
Risk Varied With Disease Severity and Vaccination Status
Among the Korean patients, 3.9% had a COVID-19 infection and 0.98% had an influenza infection. After matching, the comparison populations included 94,504 patients with COVID-19 versus 94,504 patients with flu, and 177,083 patients with COVID-19 versus 675,750 uninfected controls.
The risk of developing an AIRD at least 1 month after infection in South Korean patients with COVID-19 was 25% higher than in uninfected control participants (adjusted hazard ratio [aHR], 1.25; 95% CI, 1.18–1.31; P < .05) and 30% higher than in influenza patients (aHR, 1.3; 95% CI, 1.02–1.59; P < .05). Specifically, risk in South Korean patients with COVID-19 was significantly increased for connective tissue disease and both treated and untreated AIRD but not for inflammatory arthritis.
Among the Japanese patients, 8.2% had COVID-19 and 0.99% had flu, resulting in matched populations of 115,003 with COVID-19 versus 110,310 with flu, and 960,849 with COVID-19 versus 1,606,873 uninfected patients. The effect size was larger in Japanese patients, with a 79% increased risk for AIRD in patients with COVID-19, compared with the general population (aHR, 1.79; 95% CI, 1.77–1.82; P < .05) and a 14% increased risk, compared with patients with influenza infection (aHR, 1.14; 95% CI, 1.10–1.17; P < .05). In Japanese patients, risk was increased across all four categories, including a doubled risk for inflammatory arthritis (aHR, 2.02; 95% CI, 1.96–2.07; P < .05), compared with the general population.
The researchers had data only from the South Korean cohort to calculate risk based on vaccination status, SARS-CoV-2 variant (wild type versus Delta), and COVID-19 severity. Researchers determined a COVID-19 infection to be moderate-to-severe based on billing codes for ICU admission or requiring oxygen therapy, extracorporeal membrane oxygenation, renal replacement, or CPR.
Infection with both the original strain and the Delta variant were linked to similar increased risks for AIRD, but moderate to severe COVID-19 infections had greater risk of subsequent AIRD (aHR, 1.42; P < .05) than mild infections (aHR, 1.22; P < .05). Vaccination was linked to a lower risk of AIRD within the COVID-19 patient population: One dose was linked to a 41% reduced risk (HR, 0.59; P < .05) and two doses were linked to a 58% reduced risk (HR, 0.42; P < .05), regardless of the vaccine type, compared with unvaccinated patients with COVID-19. The apparent protective effect of vaccination was true only for patients with mild COVID-19, not those with moderate to severe infection.
“One has to wonder whether or not these people were at much higher risk of developing autoimmune disease that just got exposed because they got COVID, so that a fraction of these would have gotten an autoimmune disease downstream,” Dr. Alfred Kim said. Regardless, one clinical implication of the findings is the reduced risk in vaccinated patients, regardless of the vaccine type, given the fact that “mRNA vaccination in particular has not been associated with any autoantibody development,” he said.
Though the correlations in the study cannot translate to causation, several mechanisms might be at play in a viral infection contributing to autoimmune risk, Dr. Davidson said. Given that viral nucleic acids also recognize self-nucleic acids, “a large load of viral nucleic acid may break tolerance,” or “viral proteins could also mimic self-proteins,” she said. “In addition, tolerance may be broken by a highly inflammatory environment associated with the release of cytokines and other inflammatory mediators.”
The association between new-onset autoimmune disease and severe COVID-19 infection suggests multiple mechanisms may be involved in excess immune stimulation, Dr. Davidson said. But she added that it’s unclear how these findings, involving the original strain and Delta variant of SARS-CoV-2, might relate to currently circulating variants.
The research was funded by the National Research Foundation of Korea, the Korea Health Industry Development Institute, and the Ministry of Food and Drug Safety of the Republic of Korea. The authors reported no relevant financial relationships with industry. Dr. Alfred Kim has sponsored research agreements with AstraZeneca, Bristol-Myers Squibb, and Novartis; receives royalties from a patent with Kypha Inc.; and has done consulting or speaking for Amgen, ANI Pharmaceuticals, Aurinia Pharmaceuticals, Exagen Diagnostics, GlaxoSmithKline, Kypha, Miltenyi Biotech, Pfizer, Rheumatology & Arthritis Learning Network, Synthekine, Techtonic Therapeutics, and UpToDate. Dr. Byram reported consulting for TenSixteen Bio. Dr. Davidson had no disclosures.
FROM ANNALS OF INTERNAL MEDICINE
Oral Transmission of Chagas Disease Has Severe Effects
Thanks to decades of successful vector control strategies, vector-borne transmission of Chagas disease has significantly decreased in many regions. Oral ingestion of Trypanosoma cruzi through contaminated food and beverages, however, is increasing. Unlike vector transmission, oral transmission of Chagas disease entails high lethality in pediatric and adult populations.
“The oral transmission of Chagas disease is becoming a much more recognized route, and it is crucial to understand that people can die from this type of transmission,” Norman L. Beatty, MD, assistant professor of infectious diseases and global medicine at the University of Florida College of Medicine in Gainesville, Florida, told this news organization. Dr. Beatty is the lead author of a recent article on the subject.
In regions where the parasite circulates in the environment, people are consuming foods, fruit juices, and possibly wild animal meat that may be contaminated. “As we experience changes in our environment and in the way we consume food, it is crucial to consider how food preparation is carried out in areas where T cruzi transmission occurs in the environment,” said Dr. Beatty. “And as organic farming methods without insecticides become increasingly common, more research is needed in these areas, both in Latin America and in the United States, to understand if oral transmission of T cruzi is occurring.”
In the Amazon basin, foodborne transmission is already the leading cause of acute Chagas disease. It has been described in Argentina, Bolivia, Brazil, Colombia, Ecuador, French Guiana, and Venezuela.
Dr. Beatty’s colleagues recently treated a Brazilian patient at the hospital in Florida. “He came to our hospital very ill, with acute myocarditis after consuming contaminated açaí.” Clarifying that there is widespread awareness about oral transmission in Brazil, he stated, “We are concerned that it may not be recognized in other areas of Latin America.”
Mexico and regions of Central America have little to no information on oral transmission, but it is likely occurring, and cases may be going undetected in the region, said Dr. Beatty.
He investigated the issue in Colombia as part of an international collaboration involving the University of Antioquia, aiming to find ways to mitigate oral transmission and create a model that can be used throughout Latin America and the United States. For the Colombia study, they reviewed all cases reported to the Ministry of Health and Social Protection, and oral transmission turned out to be more common than the research group expected. “Still, I imagine that in certain areas with limited resources…there are many more cases that are not being reported.
“A myth I would like to dispel is that Chagas disease is not being transmitted in the United States,” Dr. Beatty added. He mentioned that at least 30 American states have vectors, and in Florida, it was documented that triatomines invaded homes and bit residents. In addition, 30% of these insects are infected with T cruzi. Research is underway to determine whether Floridians are becoming infected and if they are also at risk of contracting Chagas disease orally, said Dr. Beatty. “In the United States, we know very little about how many people are infected and what the infection routes are. Much more research is needed.”
Roberto Chuit, MD, PhD, a doctor in public health and an external consultant for the Pan American Health Organization (PAHO), agreed that this route of food contamination, which occurs because of vector-borne parasites, was until recently masked or hidden by the predominance of vector presence. Just as it began to gain importance as other transmission routes were controlled, “it now has extremely high importance in the Americas, as does vertical transmission,” he said.
In 2023, more than 50 years after the first description of oral transmission, the PAHO expert meeting proposed to alert health services and the broader community about the severity and potential lethality of oral Chagas disease outbreaks to elicit immediate responses and mitigation measures. The body also proposed conducting studies to provide detailed information on the contamination source and the wild vectors present in oral transmission foci.
Unique Clinical Manifestations
The exacerbated signs and symptoms of oral infection (see sidebar) are attributed to the high parasite loads in contaminated food and beverages. A single crushed triatomine along with a food or beverage harboring T cruzi can contain an estimated 600,000 metacyclic trypomastigotes, compared with 3000-4000 per µL when infection occurs by triatomine fecal matter. The robust systemic immune response observed in patients with acute oral Chagas disease is thought to result from more efficient transmission after penetration through the oral, pharyngeal, and gastric mucosae.
Seven Things to Know About Orally Transmitted Chagas Disease
1. It presents with exacerbated symptoms and rapid disease progression in immunocompetent individuals. This presentation is not common in vector-borne, congenital, or transfusion-related transmission. It can cause fulminant myocarditis and heart failure, meningoencephalitis, or potentially fatal shock due to parasitemia.
2. Most patients (71%-100%) with acute oral Chagas present with fever.
3. Electrocardiographic abnormalities, specifically ventricular depolarization alterations and pericardial involvement, are observed in most patients.
4. Facial edema, which typically affects the entire face and parts of the lips, is present in 57%-100% of patients with acute oral Chagas disease. In those with acute symptoms from vector transmission, unilateral periorbital swelling (Romaña’s sign) is more common.
5. Other notable systemic symptoms include edema of the lower extremities, myalgia, generalized lymphadenopathy, abdominal discomfort, dyspnea, vomiting, diarrhea, hepatomegaly, splenomegaly, headache, chest pain, cutaneous erythematous rash, jaundice, arthralgia, epistaxis, hematemesis, melena, and palpitations.
6. The incubation period after oral ingestion of products contaminated with Trypanosoma cruzi is approximately 3-22 days, in contrast to 4-15 days for vector-borne transmission and 8-160 days for transfusion and transplant-related transmission.
7. Patients need antiparasitic drugs immediately.
Thinking Epidemiologically
Dr. Chuit recalled that suspicion of food contamination should be based on epidemiology, especially in outbreaks affecting several people and in regions where Chagas vectors have been described. Sometimes, however, a single careless tourist consumes contaminated products.
“The difficulty is that many times it is not considered, and if it is not considered, the search for the parasite is not requested,” said Dr. Chuit. He added that it is common for the professional to consider Chagas disease only if viral and bacterial isolation tests are negative. Clinicians sometimes consider Chagas disease because the patient has not responded to regular treatments for other causes, such as antibiotics and hydration.
Epidemiology is important, especially when Chagas disease is diagnosed in groups or a family, because they are usually not isolated cases but outbreaks of 3-40 cases, according to Dr. Chuit. “Under these conditions, it must be quickly considered…that this parasite may be involved.”
One of the difficulties is that the source of these oral transmissions is not recognized most of the time. In general, the sources are usually foods that are more likely to be contaminated by insects or insect feces, such as orange juice or sugarcane. But in fact, any food or beverage left unattended could be contaminated by vectors or possible secretions from infected marsupial odoriferous glands.
An analysis of 32 outbreaks from 1965 to 2022 showed that the main foods involved in oral transmission were homemade fruit juices. But different vector species were identified, and the reservoirs were mainly dogs, rodents, and large American opossums (Didelphis).
The largest oral Chagas outbreak was linked to the consumption of contaminated guava juice in a primary school in Caracas, Venezuela. Nonindustrially produced açaí is a common source of orally acquired Chagas disease in Brazil. In Colombia, Chagas disease has been associated with the consumption of palm wine, sugar cane, and tangerine juice. Other oral transmission routes include consuming meat from wild animals and ingesting blood from infected armadillos, which is related to a traditional medicine practice.
Deadly Yet Easily Treatable
In the outbreak of 119 confirmed and suspected cases in Venezuela, 20.3% required hospitalization, and a 5-year-old child died of acute myocarditis. These percentages differ from those reported in vector transmission, which is asymptomatic in the acute phase for 95%-99% of cases or will only develop a mild febrile illness that resolves on its own.
“Not all cases will present as severe, because depending on the inoculum, there may be individuals with subclinical situations. But any food poisoning that occurs in endemic areas, where food is not properly controlled, and these street foods are associated with processes in jungle areas, raises the possibility that T cruzi is involved and should be considered as a differential diagnosis,» noted Dr. Chuit. “The treatment is highly effective, and people recover quickly.”
“The most important thing about oral transmission of Chagas is that someone infected in this way needs antiparasitic drugs immediately. We can cure them if we treat them immediately,” said Dr. Beatty, adding that treatment is sometimes delayed due to lack of access to appropriate antiparasitic drugs. “Here in the United States and in Latin America, it is quite common for healthcare professionals not to understand the differences between vector, vertical, and oral transmission. By not treating these patients, they become ill quickly.”
Dr. Beatty and Dr. Chuit declared no relevant financial conflicts of interest.
This story was translated from the Medscape Spanish edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Thanks to decades of successful vector control strategies, vector-borne transmission of Chagas disease has significantly decreased in many regions. Oral ingestion of Trypanosoma cruzi through contaminated food and beverages, however, is increasing. Unlike vector transmission, oral transmission of Chagas disease entails high lethality in pediatric and adult populations.
“The oral transmission of Chagas disease is becoming a much more recognized route, and it is crucial to understand that people can die from this type of transmission,” Norman L. Beatty, MD, assistant professor of infectious diseases and global medicine at the University of Florida College of Medicine in Gainesville, Florida, told this news organization. Dr. Beatty is the lead author of a recent article on the subject.
In regions where the parasite circulates in the environment, people are consuming foods, fruit juices, and possibly wild animal meat that may be contaminated. “As we experience changes in our environment and in the way we consume food, it is crucial to consider how food preparation is carried out in areas where T cruzi transmission occurs in the environment,” said Dr. Beatty. “And as organic farming methods without insecticides become increasingly common, more research is needed in these areas, both in Latin America and in the United States, to understand if oral transmission of T cruzi is occurring.”
In the Amazon basin, foodborne transmission is already the leading cause of acute Chagas disease. It has been described in Argentina, Bolivia, Brazil, Colombia, Ecuador, French Guiana, and Venezuela.
Dr. Beatty’s colleagues recently treated a Brazilian patient at the hospital in Florida. “He came to our hospital very ill, with acute myocarditis after consuming contaminated açaí.” Clarifying that there is widespread awareness about oral transmission in Brazil, he stated, “We are concerned that it may not be recognized in other areas of Latin America.”
Mexico and regions of Central America have little to no information on oral transmission, but it is likely occurring, and cases may be going undetected in the region, said Dr. Beatty.
He investigated the issue in Colombia as part of an international collaboration involving the University of Antioquia, aiming to find ways to mitigate oral transmission and create a model that can be used throughout Latin America and the United States. For the Colombia study, they reviewed all cases reported to the Ministry of Health and Social Protection, and oral transmission turned out to be more common than the research group expected. “Still, I imagine that in certain areas with limited resources…there are many more cases that are not being reported.
“A myth I would like to dispel is that Chagas disease is not being transmitted in the United States,” Dr. Beatty added. He mentioned that at least 30 American states have vectors, and in Florida, it was documented that triatomines invaded homes and bit residents. In addition, 30% of these insects are infected with T cruzi. Research is underway to determine whether Floridians are becoming infected and if they are also at risk of contracting Chagas disease orally, said Dr. Beatty. “In the United States, we know very little about how many people are infected and what the infection routes are. Much more research is needed.”
Roberto Chuit, MD, PhD, a doctor in public health and an external consultant for the Pan American Health Organization (PAHO), agreed that this route of food contamination, which occurs because of vector-borne parasites, was until recently masked or hidden by the predominance of vector presence. Just as it began to gain importance as other transmission routes were controlled, “it now has extremely high importance in the Americas, as does vertical transmission,” he said.
In 2023, more than 50 years after the first description of oral transmission, the PAHO expert meeting proposed to alert health services and the broader community about the severity and potential lethality of oral Chagas disease outbreaks to elicit immediate responses and mitigation measures. The body also proposed conducting studies to provide detailed information on the contamination source and the wild vectors present in oral transmission foci.
Unique Clinical Manifestations
The exacerbated signs and symptoms of oral infection (see sidebar) are attributed to the high parasite loads in contaminated food and beverages. A single crushed triatomine along with a food or beverage harboring T cruzi can contain an estimated 600,000 metacyclic trypomastigotes, compared with 3000-4000 per µL when infection occurs by triatomine fecal matter. The robust systemic immune response observed in patients with acute oral Chagas disease is thought to result from more efficient transmission after penetration through the oral, pharyngeal, and gastric mucosae.
Seven Things to Know About Orally Transmitted Chagas Disease
1. It presents with exacerbated symptoms and rapid disease progression in immunocompetent individuals. This presentation is not common in vector-borne, congenital, or transfusion-related transmission. It can cause fulminant myocarditis and heart failure, meningoencephalitis, or potentially fatal shock due to parasitemia.
2. Most patients (71%-100%) with acute oral Chagas present with fever.
3. Electrocardiographic abnormalities, specifically ventricular depolarization alterations and pericardial involvement, are observed in most patients.
4. Facial edema, which typically affects the entire face and parts of the lips, is present in 57%-100% of patients with acute oral Chagas disease. In those with acute symptoms from vector transmission, unilateral periorbital swelling (Romaña’s sign) is more common.
5. Other notable systemic symptoms include edema of the lower extremities, myalgia, generalized lymphadenopathy, abdominal discomfort, dyspnea, vomiting, diarrhea, hepatomegaly, splenomegaly, headache, chest pain, cutaneous erythematous rash, jaundice, arthralgia, epistaxis, hematemesis, melena, and palpitations.
6. The incubation period after oral ingestion of products contaminated with Trypanosoma cruzi is approximately 3-22 days, in contrast to 4-15 days for vector-borne transmission and 8-160 days for transfusion and transplant-related transmission.
7. Patients need antiparasitic drugs immediately.
Thinking Epidemiologically
Dr. Chuit recalled that suspicion of food contamination should be based on epidemiology, especially in outbreaks affecting several people and in regions where Chagas vectors have been described. Sometimes, however, a single careless tourist consumes contaminated products.
“The difficulty is that many times it is not considered, and if it is not considered, the search for the parasite is not requested,” said Dr. Chuit. He added that it is common for the professional to consider Chagas disease only if viral and bacterial isolation tests are negative. Clinicians sometimes consider Chagas disease because the patient has not responded to regular treatments for other causes, such as antibiotics and hydration.
Epidemiology is important, especially when Chagas disease is diagnosed in groups or a family, because they are usually not isolated cases but outbreaks of 3-40 cases, according to Dr. Chuit. “Under these conditions, it must be quickly considered…that this parasite may be involved.”
One of the difficulties is that the source of these oral transmissions is not recognized most of the time. In general, the sources are usually foods that are more likely to be contaminated by insects or insect feces, such as orange juice or sugarcane. But in fact, any food or beverage left unattended could be contaminated by vectors or possible secretions from infected marsupial odoriferous glands.
An analysis of 32 outbreaks from 1965 to 2022 showed that the main foods involved in oral transmission were homemade fruit juices. But different vector species were identified, and the reservoirs were mainly dogs, rodents, and large American opossums (Didelphis).
The largest oral Chagas outbreak was linked to the consumption of contaminated guava juice in a primary school in Caracas, Venezuela. Nonindustrially produced açaí is a common source of orally acquired Chagas disease in Brazil. In Colombia, Chagas disease has been associated with the consumption of palm wine, sugar cane, and tangerine juice. Other oral transmission routes include consuming meat from wild animals and ingesting blood from infected armadillos, which is related to a traditional medicine practice.
Deadly Yet Easily Treatable
In the outbreak of 119 confirmed and suspected cases in Venezuela, 20.3% required hospitalization, and a 5-year-old child died of acute myocarditis. These percentages differ from those reported in vector transmission, which is asymptomatic in the acute phase for 95%-99% of cases or will only develop a mild febrile illness that resolves on its own.
“Not all cases will present as severe, because depending on the inoculum, there may be individuals with subclinical situations. But any food poisoning that occurs in endemic areas, where food is not properly controlled, and these street foods are associated with processes in jungle areas, raises the possibility that T cruzi is involved and should be considered as a differential diagnosis,» noted Dr. Chuit. “The treatment is highly effective, and people recover quickly.”
“The most important thing about oral transmission of Chagas is that someone infected in this way needs antiparasitic drugs immediately. We can cure them if we treat them immediately,” said Dr. Beatty, adding that treatment is sometimes delayed due to lack of access to appropriate antiparasitic drugs. “Here in the United States and in Latin America, it is quite common for healthcare professionals not to understand the differences between vector, vertical, and oral transmission. By not treating these patients, they become ill quickly.”
Dr. Beatty and Dr. Chuit declared no relevant financial conflicts of interest.
This story was translated from the Medscape Spanish edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Thanks to decades of successful vector control strategies, vector-borne transmission of Chagas disease has significantly decreased in many regions. Oral ingestion of Trypanosoma cruzi through contaminated food and beverages, however, is increasing. Unlike vector transmission, oral transmission of Chagas disease entails high lethality in pediatric and adult populations.
“The oral transmission of Chagas disease is becoming a much more recognized route, and it is crucial to understand that people can die from this type of transmission,” Norman L. Beatty, MD, assistant professor of infectious diseases and global medicine at the University of Florida College of Medicine in Gainesville, Florida, told this news organization. Dr. Beatty is the lead author of a recent article on the subject.
In regions where the parasite circulates in the environment, people are consuming foods, fruit juices, and possibly wild animal meat that may be contaminated. “As we experience changes in our environment and in the way we consume food, it is crucial to consider how food preparation is carried out in areas where T cruzi transmission occurs in the environment,” said Dr. Beatty. “And as organic farming methods without insecticides become increasingly common, more research is needed in these areas, both in Latin America and in the United States, to understand if oral transmission of T cruzi is occurring.”
In the Amazon basin, foodborne transmission is already the leading cause of acute Chagas disease. It has been described in Argentina, Bolivia, Brazil, Colombia, Ecuador, French Guiana, and Venezuela.
Dr. Beatty’s colleagues recently treated a Brazilian patient at the hospital in Florida. “He came to our hospital very ill, with acute myocarditis after consuming contaminated açaí.” Clarifying that there is widespread awareness about oral transmission in Brazil, he stated, “We are concerned that it may not be recognized in other areas of Latin America.”
Mexico and regions of Central America have little to no information on oral transmission, but it is likely occurring, and cases may be going undetected in the region, said Dr. Beatty.
He investigated the issue in Colombia as part of an international collaboration involving the University of Antioquia, aiming to find ways to mitigate oral transmission and create a model that can be used throughout Latin America and the United States. For the Colombia study, they reviewed all cases reported to the Ministry of Health and Social Protection, and oral transmission turned out to be more common than the research group expected. “Still, I imagine that in certain areas with limited resources…there are many more cases that are not being reported.
“A myth I would like to dispel is that Chagas disease is not being transmitted in the United States,” Dr. Beatty added. He mentioned that at least 30 American states have vectors, and in Florida, it was documented that triatomines invaded homes and bit residents. In addition, 30% of these insects are infected with T cruzi. Research is underway to determine whether Floridians are becoming infected and if they are also at risk of contracting Chagas disease orally, said Dr. Beatty. “In the United States, we know very little about how many people are infected and what the infection routes are. Much more research is needed.”
Roberto Chuit, MD, PhD, a doctor in public health and an external consultant for the Pan American Health Organization (PAHO), agreed that this route of food contamination, which occurs because of vector-borne parasites, was until recently masked or hidden by the predominance of vector presence. Just as it began to gain importance as other transmission routes were controlled, “it now has extremely high importance in the Americas, as does vertical transmission,” he said.
In 2023, more than 50 years after the first description of oral transmission, the PAHO expert meeting proposed to alert health services and the broader community about the severity and potential lethality of oral Chagas disease outbreaks to elicit immediate responses and mitigation measures. The body also proposed conducting studies to provide detailed information on the contamination source and the wild vectors present in oral transmission foci.
Unique Clinical Manifestations
The exacerbated signs and symptoms of oral infection (see sidebar) are attributed to the high parasite loads in contaminated food and beverages. A single crushed triatomine along with a food or beverage harboring T cruzi can contain an estimated 600,000 metacyclic trypomastigotes, compared with 3000-4000 per µL when infection occurs by triatomine fecal matter. The robust systemic immune response observed in patients with acute oral Chagas disease is thought to result from more efficient transmission after penetration through the oral, pharyngeal, and gastric mucosae.
Seven Things to Know About Orally Transmitted Chagas Disease
1. It presents with exacerbated symptoms and rapid disease progression in immunocompetent individuals. This presentation is not common in vector-borne, congenital, or transfusion-related transmission. It can cause fulminant myocarditis and heart failure, meningoencephalitis, or potentially fatal shock due to parasitemia.
2. Most patients (71%-100%) with acute oral Chagas present with fever.
3. Electrocardiographic abnormalities, specifically ventricular depolarization alterations and pericardial involvement, are observed in most patients.
4. Facial edema, which typically affects the entire face and parts of the lips, is present in 57%-100% of patients with acute oral Chagas disease. In those with acute symptoms from vector transmission, unilateral periorbital swelling (Romaña’s sign) is more common.
5. Other notable systemic symptoms include edema of the lower extremities, myalgia, generalized lymphadenopathy, abdominal discomfort, dyspnea, vomiting, diarrhea, hepatomegaly, splenomegaly, headache, chest pain, cutaneous erythematous rash, jaundice, arthralgia, epistaxis, hematemesis, melena, and palpitations.
6. The incubation period after oral ingestion of products contaminated with Trypanosoma cruzi is approximately 3-22 days, in contrast to 4-15 days for vector-borne transmission and 8-160 days for transfusion and transplant-related transmission.
7. Patients need antiparasitic drugs immediately.
Thinking Epidemiologically
Dr. Chuit recalled that suspicion of food contamination should be based on epidemiology, especially in outbreaks affecting several people and in regions where Chagas vectors have been described. Sometimes, however, a single careless tourist consumes contaminated products.
“The difficulty is that many times it is not considered, and if it is not considered, the search for the parasite is not requested,” said Dr. Chuit. He added that it is common for the professional to consider Chagas disease only if viral and bacterial isolation tests are negative. Clinicians sometimes consider Chagas disease because the patient has not responded to regular treatments for other causes, such as antibiotics and hydration.
Epidemiology is important, especially when Chagas disease is diagnosed in groups or a family, because they are usually not isolated cases but outbreaks of 3-40 cases, according to Dr. Chuit. “Under these conditions, it must be quickly considered…that this parasite may be involved.”
One of the difficulties is that the source of these oral transmissions is not recognized most of the time. In general, the sources are usually foods that are more likely to be contaminated by insects or insect feces, such as orange juice or sugarcane. But in fact, any food or beverage left unattended could be contaminated by vectors or possible secretions from infected marsupial odoriferous glands.
An analysis of 32 outbreaks from 1965 to 2022 showed that the main foods involved in oral transmission were homemade fruit juices. But different vector species were identified, and the reservoirs were mainly dogs, rodents, and large American opossums (Didelphis).
The largest oral Chagas outbreak was linked to the consumption of contaminated guava juice in a primary school in Caracas, Venezuela. Nonindustrially produced açaí is a common source of orally acquired Chagas disease in Brazil. In Colombia, Chagas disease has been associated with the consumption of palm wine, sugar cane, and tangerine juice. Other oral transmission routes include consuming meat from wild animals and ingesting blood from infected armadillos, which is related to a traditional medicine practice.
Deadly Yet Easily Treatable
In the outbreak of 119 confirmed and suspected cases in Venezuela, 20.3% required hospitalization, and a 5-year-old child died of acute myocarditis. These percentages differ from those reported in vector transmission, which is asymptomatic in the acute phase for 95%-99% of cases or will only develop a mild febrile illness that resolves on its own.
“Not all cases will present as severe, because depending on the inoculum, there may be individuals with subclinical situations. But any food poisoning that occurs in endemic areas, where food is not properly controlled, and these street foods are associated with processes in jungle areas, raises the possibility that T cruzi is involved and should be considered as a differential diagnosis,» noted Dr. Chuit. “The treatment is highly effective, and people recover quickly.”
“The most important thing about oral transmission of Chagas is that someone infected in this way needs antiparasitic drugs immediately. We can cure them if we treat them immediately,” said Dr. Beatty, adding that treatment is sometimes delayed due to lack of access to appropriate antiparasitic drugs. “Here in the United States and in Latin America, it is quite common for healthcare professionals not to understand the differences between vector, vertical, and oral transmission. By not treating these patients, they become ill quickly.”
Dr. Beatty and Dr. Chuit declared no relevant financial conflicts of interest.
This story was translated from the Medscape Spanish edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
AAP Updates Guidance on Vaccine Communication and Hesitancy
The measles outbreak in Florida, occurring just as health officials announced an official end to Philadelphia’s measles outbreak and rising global cases, has cast attention once again on concerns about vaccine hesitancy. In the midst of Florida’s surgeon general avoiding measles vaccination recommendations for parents, the American Academy of Pediatrics has updated its clinical guidance on vaccine communication.
“Disruption to routine pediatric vaccination during the COVID-19 pandemic has left many children vulnerable to vaccine-preventable diseases and more locations susceptible to outbreaks in the United States and around the world,” Sean T. O’Leary, MD, MPH, a pediatric infectious diseases specialist and associate professor of pediatrics at the University of Colorado in Aurora, and his colleagues, wrote in the new report, published in the March issue of Pediatrics. “Geographic clustering of vaccine refusal further increases the risk of communicable disease outbreaks in certain communities even when vaccination rates at a state or national level remain high overall.”
The authors note that disease resurgence may bolster vaccine uptake, with media coverage of recent outbreaks linked to more pro-vaccine discussions and attitudes among parents. But the evidence on that remains inconclusive, and the authors point out the slow uptake in COVID-19 vaccination as parents navigate ongoing spread of both the disease and vaccine misinformation.
Conflicting Evidence on Postpandemic Attitudes
It remains unclear how parent attitudes toward vaccines have shifted, if at all, since the pandemic. A study published in Pediatrics from October 2023, which Dr. O’Leary also coauthored, analyzed data from an online survey of Colorado mothers between 2018 and 2021 and found no significant difference in vaccine hesitancy during the pandemic compared with pre-pandemic.
Among 3,553 respondents, 1 in 5 (20.4%) were vaccine hesitant overall. Though parents were twice as likely to feel uncertain in trusting vaccine information after the COVID-19 vaccines were authorized (adjusted odds ratio [aOR] 2.14), they were half as likely to be unsure about hesitancy toward childhood vaccines (aOR 0.48).
Another study in Pediatrics from October 2023 found that common concerns about COVID-19 vaccines among parents included infertility, long-term effects from the vaccines, and effects on preexisting medical conditions. But even then, participants in focus groups “expressed that they would listen to their doctor for information about COVID-19 vaccines,” wrote Aubree Honcoop, MPS, of the University of Nebraska Medical Center in Omaha, and her colleagues.
“I think what we’re seeing, very importantly, is that physicians seem to be the source people rely on,” said Walter Orenstein, MD, professor of medicine and associate director of the Emory Vaccine Center at Emory University in Atlanta. “But we need to give the physicians time and incentives to spend time with families,” such as a billing code for vaccine counseling, he said.
Dr. Orenstein was surprised to see the results from Colorado, but he noted they were from a small survey in a single state. He pointed to other findings, such as those from the University of Pennsylvania’s Annenberg Public Policy Center in November 2023, that found lower confidence overall among Americans toward vaccines.
Paul Offit, MD, director of the Vaccine Education Center and an attending infectious disease physician at Children’s Hospital of Philadelphia, where the city’s measles outbreak began, is similarly skeptical about the Colorado study’s findings that parent vaccine attitudes have changed little since the pandemic. At the AAP’s annual conference in October 2023, Dr. Offit asked pediatricians about their experiences while he signed books.
“I would ask, ‘So what’s it like out there? Are we winning or losing?’ ” he said. “I would say, to a person, everyone said they felt things were much worse now than they ever have been before.”
Clinical Guidance
The new report reviews previously published evidence on the spectrum of parental vaccine acceptance — from supporters and “go along to get along” parents to cautious acceptors and fence sitters to vaccine refusers — and the determinants that contribute to hesitancy. They also noted the social inequities that have played a role in vaccine uptake disparities.
“Distrust of health systems based on historic and ongoing discrimination and inequitable access to care are intertwined challenges that contribute to racial and ethnic disparities in vaccine uptake,” the authors wrote. “Although there has been progress in reducing racial, ethnic, and socioeconomic disparities in childhood vaccination coverage, the COVID-19 pandemic made clear how much work is yet to be done.”
The report also reviewed the societal, individual, payer and pediatric practice costs of vaccine refusal. The 1-year cost to taxpayers from the measles outbreak in New York City in 2018-2019, for example, was $8.4 million, excluding vaccination programs.
The report provides background information to equip pediatricians for conversations with parents about vaccines. Since safety is the top concern for vaccine hesitancy among parents, the authors advised pediatricians to be familiar with the process of vaccine testing, emergency use authorization, licensure, approval, recommendations, and safety monitoring, including the Vaccine Safety Datalink, the Vaccine Adverse Event Reporting System (VAERS), the FDA’s Biologics Effectiveness and Safety (BEST) system, and the CDC’s Clinical Immunization Safety Assessment Project (CISA).
“Because vaccines are generally given to healthy individuals to prevent disease, they are held to a higher safety standard than other medications,” the authors wrote before providing a summary of the process for physicians to reference. The report also includes information on vaccine ingredients and a chart of common misconceptions about vaccines with the corresponding facts.
Overcoming Hesitancy
Evidence-based strategies for increasing childhood vaccine uptake begin with a strong vaccine recommendation using a presumptive rather than participatory approach, the authors wrote. “A presumptive format is one in which the clinician asserts a position regarding vaccines using a closed-ended statement, such as ‘Sara is due for several vaccines today’ or ‘Well, we have to do some shots,’ ” the authors wrote. “This strategy is in contrast to a participatory format, in which an open-ended question is used to more explicitly invite the parent to voice an opinion, such as ‘How do you feel about vaccines today?’ ” The presumptive format and a strong recommendation are both associated with greater uptake, evidence shows.
For parents who express hesitancy, the authors provide a summary of additional evidence-based communication strategies, starting with motivational interviewing. Two other strategies they highlight include using language to re-emphasize the importance of adhering to the CDC recommended schedule — “He really needs these shots” — and bundling discussion of all recommended vaccines for a visit at once.
“Finally, clinicians can emphasize their own experiences when discussing the need for vaccination, including personal experience with vaccine-preventable diseases and the fact that they and their families are vaccinated because of their confidence in the safety and efficacy of the vaccines,” the authors wrote.
For families who refuse or delay vaccines, the authors reviewed the “ethical arguments both in favor of and against dismissal policies,” noting that nearly all pediatricians who report dismissing families who refuse vaccination are in private practice, since large systems are often unable to dismiss patients. They also point out that fewer pediatricians dismiss families for spreading out vaccines than outright refusing all vaccines.
”Dismissal of child patients of vaccine-refusing parents can be a difficult decision arrived at after considering multiple factors and documented attempts to counsel vaccine-refusing families,” they wrote. “However, if repeated attempts to help understand and address parental values and vaccine concerns fails to engender trust, move parents toward vaccine acceptance, or strengthen the therapeutic alliance, dismissal can be an acceptable option.”
Finally, the authors reminded pediatricians “that vaccine-hesitant parents are a heterogeneous group and that specific parental vaccine concerns need to be individually identified and addressed.” Working with families to discuss their questions and concerns is an opportunity to “build rapport and trust with a family,” they wrote, ”and, ultimately, protect their children from the scourge of vaccine-preventable diseases.”
The focus groups study was funded by the National Institutes of Health, and the authors reported having no disclosures. The Colorado attitudes study used no external funding, and the authors reported no disclosures. The new clinical report used no external funding, and the authors reported no disclosures. Dr. Orenstein is an uncompensated member of the Moderna Scientific Advisory Board. Dr. Offit codeveloped a licensed rotavirus vaccine, but he does not receive any royalties or own a patent for that.
The measles outbreak in Florida, occurring just as health officials announced an official end to Philadelphia’s measles outbreak and rising global cases, has cast attention once again on concerns about vaccine hesitancy. In the midst of Florida’s surgeon general avoiding measles vaccination recommendations for parents, the American Academy of Pediatrics has updated its clinical guidance on vaccine communication.
“Disruption to routine pediatric vaccination during the COVID-19 pandemic has left many children vulnerable to vaccine-preventable diseases and more locations susceptible to outbreaks in the United States and around the world,” Sean T. O’Leary, MD, MPH, a pediatric infectious diseases specialist and associate professor of pediatrics at the University of Colorado in Aurora, and his colleagues, wrote in the new report, published in the March issue of Pediatrics. “Geographic clustering of vaccine refusal further increases the risk of communicable disease outbreaks in certain communities even when vaccination rates at a state or national level remain high overall.”
The authors note that disease resurgence may bolster vaccine uptake, with media coverage of recent outbreaks linked to more pro-vaccine discussions and attitudes among parents. But the evidence on that remains inconclusive, and the authors point out the slow uptake in COVID-19 vaccination as parents navigate ongoing spread of both the disease and vaccine misinformation.
Conflicting Evidence on Postpandemic Attitudes
It remains unclear how parent attitudes toward vaccines have shifted, if at all, since the pandemic. A study published in Pediatrics from October 2023, which Dr. O’Leary also coauthored, analyzed data from an online survey of Colorado mothers between 2018 and 2021 and found no significant difference in vaccine hesitancy during the pandemic compared with pre-pandemic.
Among 3,553 respondents, 1 in 5 (20.4%) were vaccine hesitant overall. Though parents were twice as likely to feel uncertain in trusting vaccine information after the COVID-19 vaccines were authorized (adjusted odds ratio [aOR] 2.14), they were half as likely to be unsure about hesitancy toward childhood vaccines (aOR 0.48).
Another study in Pediatrics from October 2023 found that common concerns about COVID-19 vaccines among parents included infertility, long-term effects from the vaccines, and effects on preexisting medical conditions. But even then, participants in focus groups “expressed that they would listen to their doctor for information about COVID-19 vaccines,” wrote Aubree Honcoop, MPS, of the University of Nebraska Medical Center in Omaha, and her colleagues.
“I think what we’re seeing, very importantly, is that physicians seem to be the source people rely on,” said Walter Orenstein, MD, professor of medicine and associate director of the Emory Vaccine Center at Emory University in Atlanta. “But we need to give the physicians time and incentives to spend time with families,” such as a billing code for vaccine counseling, he said.
Dr. Orenstein was surprised to see the results from Colorado, but he noted they were from a small survey in a single state. He pointed to other findings, such as those from the University of Pennsylvania’s Annenberg Public Policy Center in November 2023, that found lower confidence overall among Americans toward vaccines.
Paul Offit, MD, director of the Vaccine Education Center and an attending infectious disease physician at Children’s Hospital of Philadelphia, where the city’s measles outbreak began, is similarly skeptical about the Colorado study’s findings that parent vaccine attitudes have changed little since the pandemic. At the AAP’s annual conference in October 2023, Dr. Offit asked pediatricians about their experiences while he signed books.
“I would ask, ‘So what’s it like out there? Are we winning or losing?’ ” he said. “I would say, to a person, everyone said they felt things were much worse now than they ever have been before.”
Clinical Guidance
The new report reviews previously published evidence on the spectrum of parental vaccine acceptance — from supporters and “go along to get along” parents to cautious acceptors and fence sitters to vaccine refusers — and the determinants that contribute to hesitancy. They also noted the social inequities that have played a role in vaccine uptake disparities.
“Distrust of health systems based on historic and ongoing discrimination and inequitable access to care are intertwined challenges that contribute to racial and ethnic disparities in vaccine uptake,” the authors wrote. “Although there has been progress in reducing racial, ethnic, and socioeconomic disparities in childhood vaccination coverage, the COVID-19 pandemic made clear how much work is yet to be done.”
The report also reviewed the societal, individual, payer and pediatric practice costs of vaccine refusal. The 1-year cost to taxpayers from the measles outbreak in New York City in 2018-2019, for example, was $8.4 million, excluding vaccination programs.
The report provides background information to equip pediatricians for conversations with parents about vaccines. Since safety is the top concern for vaccine hesitancy among parents, the authors advised pediatricians to be familiar with the process of vaccine testing, emergency use authorization, licensure, approval, recommendations, and safety monitoring, including the Vaccine Safety Datalink, the Vaccine Adverse Event Reporting System (VAERS), the FDA’s Biologics Effectiveness and Safety (BEST) system, and the CDC’s Clinical Immunization Safety Assessment Project (CISA).
“Because vaccines are generally given to healthy individuals to prevent disease, they are held to a higher safety standard than other medications,” the authors wrote before providing a summary of the process for physicians to reference. The report also includes information on vaccine ingredients and a chart of common misconceptions about vaccines with the corresponding facts.
Overcoming Hesitancy
Evidence-based strategies for increasing childhood vaccine uptake begin with a strong vaccine recommendation using a presumptive rather than participatory approach, the authors wrote. “A presumptive format is one in which the clinician asserts a position regarding vaccines using a closed-ended statement, such as ‘Sara is due for several vaccines today’ or ‘Well, we have to do some shots,’ ” the authors wrote. “This strategy is in contrast to a participatory format, in which an open-ended question is used to more explicitly invite the parent to voice an opinion, such as ‘How do you feel about vaccines today?’ ” The presumptive format and a strong recommendation are both associated with greater uptake, evidence shows.
For parents who express hesitancy, the authors provide a summary of additional evidence-based communication strategies, starting with motivational interviewing. Two other strategies they highlight include using language to re-emphasize the importance of adhering to the CDC recommended schedule — “He really needs these shots” — and bundling discussion of all recommended vaccines for a visit at once.
“Finally, clinicians can emphasize their own experiences when discussing the need for vaccination, including personal experience with vaccine-preventable diseases and the fact that they and their families are vaccinated because of their confidence in the safety and efficacy of the vaccines,” the authors wrote.
For families who refuse or delay vaccines, the authors reviewed the “ethical arguments both in favor of and against dismissal policies,” noting that nearly all pediatricians who report dismissing families who refuse vaccination are in private practice, since large systems are often unable to dismiss patients. They also point out that fewer pediatricians dismiss families for spreading out vaccines than outright refusing all vaccines.
”Dismissal of child patients of vaccine-refusing parents can be a difficult decision arrived at after considering multiple factors and documented attempts to counsel vaccine-refusing families,” they wrote. “However, if repeated attempts to help understand and address parental values and vaccine concerns fails to engender trust, move parents toward vaccine acceptance, or strengthen the therapeutic alliance, dismissal can be an acceptable option.”
Finally, the authors reminded pediatricians “that vaccine-hesitant parents are a heterogeneous group and that specific parental vaccine concerns need to be individually identified and addressed.” Working with families to discuss their questions and concerns is an opportunity to “build rapport and trust with a family,” they wrote, ”and, ultimately, protect their children from the scourge of vaccine-preventable diseases.”
The focus groups study was funded by the National Institutes of Health, and the authors reported having no disclosures. The Colorado attitudes study used no external funding, and the authors reported no disclosures. The new clinical report used no external funding, and the authors reported no disclosures. Dr. Orenstein is an uncompensated member of the Moderna Scientific Advisory Board. Dr. Offit codeveloped a licensed rotavirus vaccine, but he does not receive any royalties or own a patent for that.
The measles outbreak in Florida, occurring just as health officials announced an official end to Philadelphia’s measles outbreak and rising global cases, has cast attention once again on concerns about vaccine hesitancy. In the midst of Florida’s surgeon general avoiding measles vaccination recommendations for parents, the American Academy of Pediatrics has updated its clinical guidance on vaccine communication.
“Disruption to routine pediatric vaccination during the COVID-19 pandemic has left many children vulnerable to vaccine-preventable diseases and more locations susceptible to outbreaks in the United States and around the world,” Sean T. O’Leary, MD, MPH, a pediatric infectious diseases specialist and associate professor of pediatrics at the University of Colorado in Aurora, and his colleagues, wrote in the new report, published in the March issue of Pediatrics. “Geographic clustering of vaccine refusal further increases the risk of communicable disease outbreaks in certain communities even when vaccination rates at a state or national level remain high overall.”
The authors note that disease resurgence may bolster vaccine uptake, with media coverage of recent outbreaks linked to more pro-vaccine discussions and attitudes among parents. But the evidence on that remains inconclusive, and the authors point out the slow uptake in COVID-19 vaccination as parents navigate ongoing spread of both the disease and vaccine misinformation.
Conflicting Evidence on Postpandemic Attitudes
It remains unclear how parent attitudes toward vaccines have shifted, if at all, since the pandemic. A study published in Pediatrics from October 2023, which Dr. O’Leary also coauthored, analyzed data from an online survey of Colorado mothers between 2018 and 2021 and found no significant difference in vaccine hesitancy during the pandemic compared with pre-pandemic.
Among 3,553 respondents, 1 in 5 (20.4%) were vaccine hesitant overall. Though parents were twice as likely to feel uncertain in trusting vaccine information after the COVID-19 vaccines were authorized (adjusted odds ratio [aOR] 2.14), they were half as likely to be unsure about hesitancy toward childhood vaccines (aOR 0.48).
Another study in Pediatrics from October 2023 found that common concerns about COVID-19 vaccines among parents included infertility, long-term effects from the vaccines, and effects on preexisting medical conditions. But even then, participants in focus groups “expressed that they would listen to their doctor for information about COVID-19 vaccines,” wrote Aubree Honcoop, MPS, of the University of Nebraska Medical Center in Omaha, and her colleagues.
“I think what we’re seeing, very importantly, is that physicians seem to be the source people rely on,” said Walter Orenstein, MD, professor of medicine and associate director of the Emory Vaccine Center at Emory University in Atlanta. “But we need to give the physicians time and incentives to spend time with families,” such as a billing code for vaccine counseling, he said.
Dr. Orenstein was surprised to see the results from Colorado, but he noted they were from a small survey in a single state. He pointed to other findings, such as those from the University of Pennsylvania’s Annenberg Public Policy Center in November 2023, that found lower confidence overall among Americans toward vaccines.
Paul Offit, MD, director of the Vaccine Education Center and an attending infectious disease physician at Children’s Hospital of Philadelphia, where the city’s measles outbreak began, is similarly skeptical about the Colorado study’s findings that parent vaccine attitudes have changed little since the pandemic. At the AAP’s annual conference in October 2023, Dr. Offit asked pediatricians about their experiences while he signed books.
“I would ask, ‘So what’s it like out there? Are we winning or losing?’ ” he said. “I would say, to a person, everyone said they felt things were much worse now than they ever have been before.”
Clinical Guidance
The new report reviews previously published evidence on the spectrum of parental vaccine acceptance — from supporters and “go along to get along” parents to cautious acceptors and fence sitters to vaccine refusers — and the determinants that contribute to hesitancy. They also noted the social inequities that have played a role in vaccine uptake disparities.
“Distrust of health systems based on historic and ongoing discrimination and inequitable access to care are intertwined challenges that contribute to racial and ethnic disparities in vaccine uptake,” the authors wrote. “Although there has been progress in reducing racial, ethnic, and socioeconomic disparities in childhood vaccination coverage, the COVID-19 pandemic made clear how much work is yet to be done.”
The report also reviewed the societal, individual, payer and pediatric practice costs of vaccine refusal. The 1-year cost to taxpayers from the measles outbreak in New York City in 2018-2019, for example, was $8.4 million, excluding vaccination programs.
The report provides background information to equip pediatricians for conversations with parents about vaccines. Since safety is the top concern for vaccine hesitancy among parents, the authors advised pediatricians to be familiar with the process of vaccine testing, emergency use authorization, licensure, approval, recommendations, and safety monitoring, including the Vaccine Safety Datalink, the Vaccine Adverse Event Reporting System (VAERS), the FDA’s Biologics Effectiveness and Safety (BEST) system, and the CDC’s Clinical Immunization Safety Assessment Project (CISA).
“Because vaccines are generally given to healthy individuals to prevent disease, they are held to a higher safety standard than other medications,” the authors wrote before providing a summary of the process for physicians to reference. The report also includes information on vaccine ingredients and a chart of common misconceptions about vaccines with the corresponding facts.
Overcoming Hesitancy
Evidence-based strategies for increasing childhood vaccine uptake begin with a strong vaccine recommendation using a presumptive rather than participatory approach, the authors wrote. “A presumptive format is one in which the clinician asserts a position regarding vaccines using a closed-ended statement, such as ‘Sara is due for several vaccines today’ or ‘Well, we have to do some shots,’ ” the authors wrote. “This strategy is in contrast to a participatory format, in which an open-ended question is used to more explicitly invite the parent to voice an opinion, such as ‘How do you feel about vaccines today?’ ” The presumptive format and a strong recommendation are both associated with greater uptake, evidence shows.
For parents who express hesitancy, the authors provide a summary of additional evidence-based communication strategies, starting with motivational interviewing. Two other strategies they highlight include using language to re-emphasize the importance of adhering to the CDC recommended schedule — “He really needs these shots” — and bundling discussion of all recommended vaccines for a visit at once.
“Finally, clinicians can emphasize their own experiences when discussing the need for vaccination, including personal experience with vaccine-preventable diseases and the fact that they and their families are vaccinated because of their confidence in the safety and efficacy of the vaccines,” the authors wrote.
For families who refuse or delay vaccines, the authors reviewed the “ethical arguments both in favor of and against dismissal policies,” noting that nearly all pediatricians who report dismissing families who refuse vaccination are in private practice, since large systems are often unable to dismiss patients. They also point out that fewer pediatricians dismiss families for spreading out vaccines than outright refusing all vaccines.
”Dismissal of child patients of vaccine-refusing parents can be a difficult decision arrived at after considering multiple factors and documented attempts to counsel vaccine-refusing families,” they wrote. “However, if repeated attempts to help understand and address parental values and vaccine concerns fails to engender trust, move parents toward vaccine acceptance, or strengthen the therapeutic alliance, dismissal can be an acceptable option.”
Finally, the authors reminded pediatricians “that vaccine-hesitant parents are a heterogeneous group and that specific parental vaccine concerns need to be individually identified and addressed.” Working with families to discuss their questions and concerns is an opportunity to “build rapport and trust with a family,” they wrote, ”and, ultimately, protect their children from the scourge of vaccine-preventable diseases.”
The focus groups study was funded by the National Institutes of Health, and the authors reported having no disclosures. The Colorado attitudes study used no external funding, and the authors reported no disclosures. The new clinical report used no external funding, and the authors reported no disclosures. Dr. Orenstein is an uncompensated member of the Moderna Scientific Advisory Board. Dr. Offit codeveloped a licensed rotavirus vaccine, but he does not receive any royalties or own a patent for that.
FROM PEDIATRICS
Oral Herpes Tied to Double Dementia Risk in Older Adults
TOPLINE:
A history of herpes simplex virus (HSV) is associated with a more than doubling of the risk for dementia in older people, results of a prospective epidemiological study showed.
METHODOLOGY:
- The study included 1002 dementia-free 70-year-olds from the Prospective Investigation of Vasculature in Uppsala Seniors cohort who were assessed at baseline and at age 75 and 80 years and followed through medical records at age 85 years.
- Researchers collected and analyzed blood samples to detect anti-HSV and anti-HSV-1 immunoglobulin (Ig) G, anti-cytomegalovirus (CMV) IgG, anti-HSV IgM, and anti-HSV and anti-CMV IgG levels and apolipoprotein epsilon 4 (APOE 4) status of participants.
- Investigators collected information on anti-herpesvirus drug treatment and reviewed dementia diagnoses obtained from medical records to classify as established or probable dementia or Alzheimer’s disease (AD).
TAKEAWAY:
- 82% of participants were anti-HSV IgG carriers, of which 6% had received drug treatment for herpes virus, and 7% of participants developed all-cause dementia and 4% AD during the median 15-year follow up.
- In HSV and HSV-1 subsamples, treatment for herpes virus was not significantly associated with lower risks for AD (HR, 1.46, P = .532 and HR, 1.64; P = .419, respectively) or dementia (HR 1.70; P = .222 and HR, 1.60; P = .320, respectively).
- There was no significant interaction between anti-HSV IgG seroprevalence and APOE 4 with regard to dementia risk, likely due to underpowering, and there were no associations between anti-CMV IgG positivity or anti-HSV IgM positivity and AD or dementia.
IN PRACTICE:
“What’s special about this particular study is that the participants are roughly the same age, which makes the results even more reliable since age differences, which are otherwise linked to the development of dementia, cannot confuse the results,” lead author Erika Vestin, a medical student in the Department of Public Health and Caring Sciences, Clinical Geriatrics, Uppsala University, Sweden, said in a press release. Findings may drive dementia research further towards treating the illness at an early stage using common anti-herpes virus drugs, Ms. Vestin added.
SOURCE:
The study, with Ms. Vestin as lead author, was published online on February 14, 2024, in the Journal of Alzheimer’s Disease.
LIMITATIONS:
The study underrepresented people with diabetes, heart failure, and stroke and lacked information on treatment compliance, dosage, and length and number of prescriptions, which prevented analysis of dose dependency. Since dementia data collection relied on medical records, dementia cases may be underreported. Some cases of AD could have been misclassified as vascular dementia or other dementia.
DISCLOSURES:
The study was supported by the Gun and Bertil Stohne’s Foundation, Swedish Dementia Association, Swedish Society of Medicine, Märta Lundqvist Foundation, Thureus Foundation, Region Uppsala, Gamla Tjänarinnor Foundation, and Swedish Brain Foundation. The authors had no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
A history of herpes simplex virus (HSV) is associated with a more than doubling of the risk for dementia in older people, results of a prospective epidemiological study showed.
METHODOLOGY:
- The study included 1002 dementia-free 70-year-olds from the Prospective Investigation of Vasculature in Uppsala Seniors cohort who were assessed at baseline and at age 75 and 80 years and followed through medical records at age 85 years.
- Researchers collected and analyzed blood samples to detect anti-HSV and anti-HSV-1 immunoglobulin (Ig) G, anti-cytomegalovirus (CMV) IgG, anti-HSV IgM, and anti-HSV and anti-CMV IgG levels and apolipoprotein epsilon 4 (APOE 4) status of participants.
- Investigators collected information on anti-herpesvirus drug treatment and reviewed dementia diagnoses obtained from medical records to classify as established or probable dementia or Alzheimer’s disease (AD).
TAKEAWAY:
- 82% of participants were anti-HSV IgG carriers, of which 6% had received drug treatment for herpes virus, and 7% of participants developed all-cause dementia and 4% AD during the median 15-year follow up.
- In HSV and HSV-1 subsamples, treatment for herpes virus was not significantly associated with lower risks for AD (HR, 1.46, P = .532 and HR, 1.64; P = .419, respectively) or dementia (HR 1.70; P = .222 and HR, 1.60; P = .320, respectively).
- There was no significant interaction between anti-HSV IgG seroprevalence and APOE 4 with regard to dementia risk, likely due to underpowering, and there were no associations between anti-CMV IgG positivity or anti-HSV IgM positivity and AD or dementia.
IN PRACTICE:
“What’s special about this particular study is that the participants are roughly the same age, which makes the results even more reliable since age differences, which are otherwise linked to the development of dementia, cannot confuse the results,” lead author Erika Vestin, a medical student in the Department of Public Health and Caring Sciences, Clinical Geriatrics, Uppsala University, Sweden, said in a press release. Findings may drive dementia research further towards treating the illness at an early stage using common anti-herpes virus drugs, Ms. Vestin added.
SOURCE:
The study, with Ms. Vestin as lead author, was published online on February 14, 2024, in the Journal of Alzheimer’s Disease.
LIMITATIONS:
The study underrepresented people with diabetes, heart failure, and stroke and lacked information on treatment compliance, dosage, and length and number of prescriptions, which prevented analysis of dose dependency. Since dementia data collection relied on medical records, dementia cases may be underreported. Some cases of AD could have been misclassified as vascular dementia or other dementia.
DISCLOSURES:
The study was supported by the Gun and Bertil Stohne’s Foundation, Swedish Dementia Association, Swedish Society of Medicine, Märta Lundqvist Foundation, Thureus Foundation, Region Uppsala, Gamla Tjänarinnor Foundation, and Swedish Brain Foundation. The authors had no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
A history of herpes simplex virus (HSV) is associated with a more than doubling of the risk for dementia in older people, results of a prospective epidemiological study showed.
METHODOLOGY:
- The study included 1002 dementia-free 70-year-olds from the Prospective Investigation of Vasculature in Uppsala Seniors cohort who were assessed at baseline and at age 75 and 80 years and followed through medical records at age 85 years.
- Researchers collected and analyzed blood samples to detect anti-HSV and anti-HSV-1 immunoglobulin (Ig) G, anti-cytomegalovirus (CMV) IgG, anti-HSV IgM, and anti-HSV and anti-CMV IgG levels and apolipoprotein epsilon 4 (APOE 4) status of participants.
- Investigators collected information on anti-herpesvirus drug treatment and reviewed dementia diagnoses obtained from medical records to classify as established or probable dementia or Alzheimer’s disease (AD).
TAKEAWAY:
- 82% of participants were anti-HSV IgG carriers, of which 6% had received drug treatment for herpes virus, and 7% of participants developed all-cause dementia and 4% AD during the median 15-year follow up.
- In HSV and HSV-1 subsamples, treatment for herpes virus was not significantly associated with lower risks for AD (HR, 1.46, P = .532 and HR, 1.64; P = .419, respectively) or dementia (HR 1.70; P = .222 and HR, 1.60; P = .320, respectively).
- There was no significant interaction between anti-HSV IgG seroprevalence and APOE 4 with regard to dementia risk, likely due to underpowering, and there were no associations between anti-CMV IgG positivity or anti-HSV IgM positivity and AD or dementia.
IN PRACTICE:
“What’s special about this particular study is that the participants are roughly the same age, which makes the results even more reliable since age differences, which are otherwise linked to the development of dementia, cannot confuse the results,” lead author Erika Vestin, a medical student in the Department of Public Health and Caring Sciences, Clinical Geriatrics, Uppsala University, Sweden, said in a press release. Findings may drive dementia research further towards treating the illness at an early stage using common anti-herpes virus drugs, Ms. Vestin added.
SOURCE:
The study, with Ms. Vestin as lead author, was published online on February 14, 2024, in the Journal of Alzheimer’s Disease.
LIMITATIONS:
The study underrepresented people with diabetes, heart failure, and stroke and lacked information on treatment compliance, dosage, and length and number of prescriptions, which prevented analysis of dose dependency. Since dementia data collection relied on medical records, dementia cases may be underreported. Some cases of AD could have been misclassified as vascular dementia or other dementia.
DISCLOSURES:
The study was supported by the Gun and Bertil Stohne’s Foundation, Swedish Dementia Association, Swedish Society of Medicine, Märta Lundqvist Foundation, Thureus Foundation, Region Uppsala, Gamla Tjänarinnor Foundation, and Swedish Brain Foundation. The authors had no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
Do Kids With an October Birthday Have Protection From Flu?
TOPLINE:
A new study shows young children with October birthdays may have better protection against flu.
METHODOLOGY:
- Researchers analyzed data from the MarketScan Research Database between 2011 and 2018.
- They focused on 819,223 children aged 2-5 years who were vaccinated against influenza between August 1 and January 31 and whose birthdays fell during that window.
TAKEAWAY:
- Children born in October had the lowest rate of influenza diagnosis, with an average diagnosis rate of 2.7%, whereas those born in August had a diagnosis rate of 3%.
- Compared with children born in August, the adjusted odds ratio for influenza diagnosis in children born in October was 0.88 (95% CI, 0.85-0.92).
IN PRACTICE:
“The findings support current recommendations that children be vaccinated in October preceding a typical influenza season,” the authors of the study wrote.
SOURCE:
Anupam B. Jena, MD, PhD, with Harvard Medical School and Massachusetts General Hospital in Boston, Massachusetts, was the corresponding author on the study. The research was published online in BMJ .
LIMITATIONS:
The availability of the influenza vaccine and the peak of seasonal flu infections vary by year and region.
DISCLOSURES:
Researchers disclosed consulting fees from pharmaceutical and healthcare companies unrelated to the study.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article appeared on Medscape.com.
TOPLINE:
A new study shows young children with October birthdays may have better protection against flu.
METHODOLOGY:
- Researchers analyzed data from the MarketScan Research Database between 2011 and 2018.
- They focused on 819,223 children aged 2-5 years who were vaccinated against influenza between August 1 and January 31 and whose birthdays fell during that window.
TAKEAWAY:
- Children born in October had the lowest rate of influenza diagnosis, with an average diagnosis rate of 2.7%, whereas those born in August had a diagnosis rate of 3%.
- Compared with children born in August, the adjusted odds ratio for influenza diagnosis in children born in October was 0.88 (95% CI, 0.85-0.92).
IN PRACTICE:
“The findings support current recommendations that children be vaccinated in October preceding a typical influenza season,” the authors of the study wrote.
SOURCE:
Anupam B. Jena, MD, PhD, with Harvard Medical School and Massachusetts General Hospital in Boston, Massachusetts, was the corresponding author on the study. The research was published online in BMJ .
LIMITATIONS:
The availability of the influenza vaccine and the peak of seasonal flu infections vary by year and region.
DISCLOSURES:
Researchers disclosed consulting fees from pharmaceutical and healthcare companies unrelated to the study.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article appeared on Medscape.com.
TOPLINE:
A new study shows young children with October birthdays may have better protection against flu.
METHODOLOGY:
- Researchers analyzed data from the MarketScan Research Database between 2011 and 2018.
- They focused on 819,223 children aged 2-5 years who were vaccinated against influenza between August 1 and January 31 and whose birthdays fell during that window.
TAKEAWAY:
- Children born in October had the lowest rate of influenza diagnosis, with an average diagnosis rate of 2.7%, whereas those born in August had a diagnosis rate of 3%.
- Compared with children born in August, the adjusted odds ratio for influenza diagnosis in children born in October was 0.88 (95% CI, 0.85-0.92).
IN PRACTICE:
“The findings support current recommendations that children be vaccinated in October preceding a typical influenza season,” the authors of the study wrote.
SOURCE:
Anupam B. Jena, MD, PhD, with Harvard Medical School and Massachusetts General Hospital in Boston, Massachusetts, was the corresponding author on the study. The research was published online in BMJ .
LIMITATIONS:
The availability of the influenza vaccine and the peak of seasonal flu infections vary by year and region.
DISCLOSURES:
Researchers disclosed consulting fees from pharmaceutical and healthcare companies unrelated to the study.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article appeared on Medscape.com.