User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Low-calorie tastes sweeter with a little salt
Low-calorie tastes sweeter with a little salt
Diet and sugar-free foods and drinks seem like a good idea, but it’s hard to get past that strange aftertaste, right? It’s the calling card for the noncaloric aspartame- and stevia-containing sweeteners that we consume to make us feel like we can have the best of both worlds.
That weird lingering taste can be a total turn-off for some (raises hand), but researchers have found an almost facepalm solution to the not-so-sweet problem, and it’s salt.
Now, the concept of sweet and salty is not a far-fetched partnership when it comes to snack consumption (try M&Ms in your popcorn). The researchers at Almendra, a manufacturer of stevia sweeteners, put that iconic flavor pair to the test by adding mineral salts that have some nutritional value to lessen the effect of a stevia compound, rebaudioside A, found in noncaloric sweeteners.
The researchers added in magnesium chloride, calcium chloride, and potassium chloride separately to lessen rebaudioside A’s intensity, but they needed so much salt that it killed the sweet taste completely. A blend of the three mineral salts, however, reduced the lingering taste by 79% and improved the real sugar-like taste. The researchers tried this blend in reduced-calorie orange juice and a citrus-flavored soft drink, improving the taste in both.
The salty and sweet match comes in for the win once again. This time helping against the fight of obesity instead of making it worse.
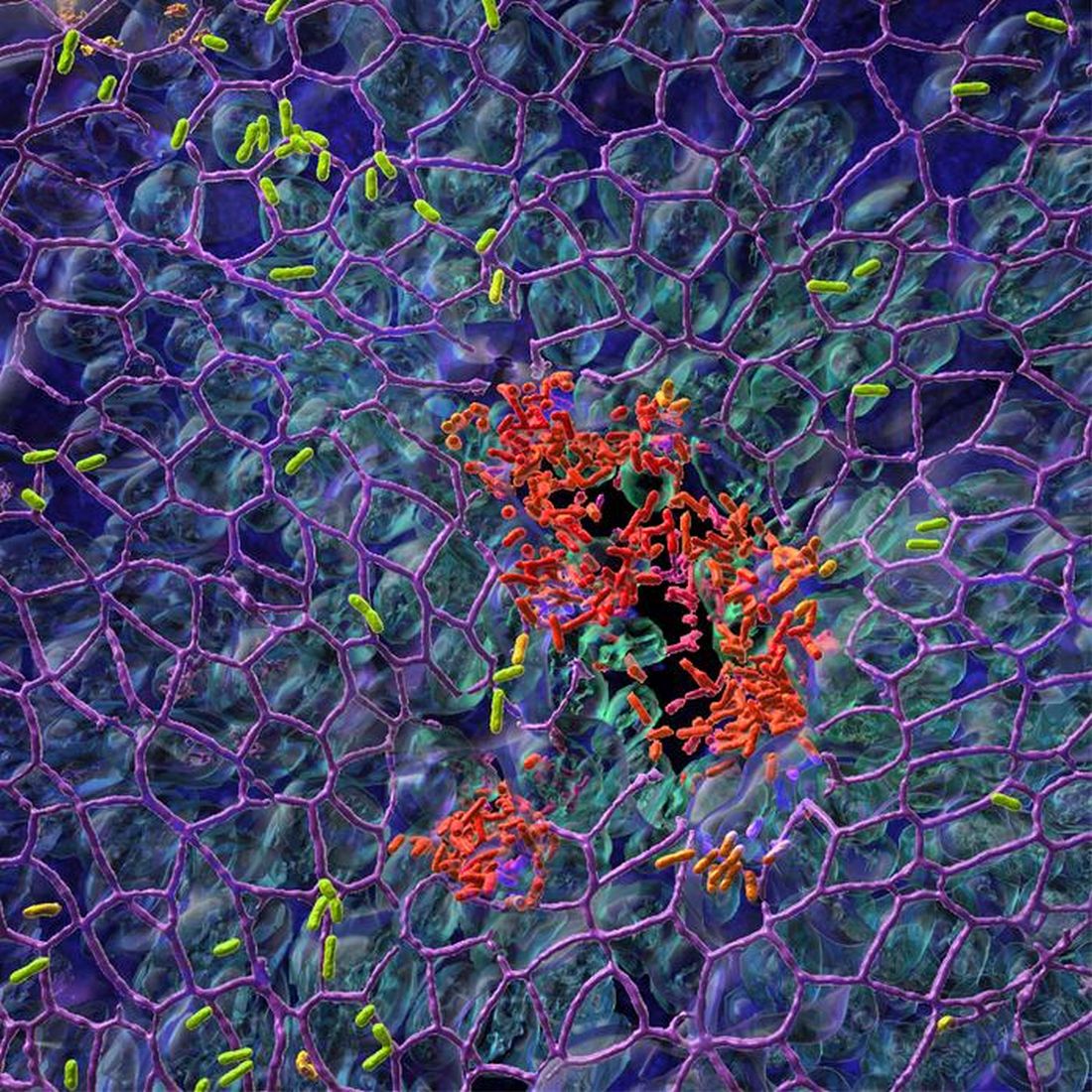
Pseudomonas’ Achilles’ heel is more of an Achilles’ genetic switch
Today, on the long-awaited return of “Bacteria vs. the World,” we meet one of the rock stars of infectious disease.
LOTME: Through the use of imaginary technology, we’re talking to Pseudomonas aeruginosa. Thanks for joining us on such short notice, after Neisseria gonorrhoeae canceled at the last minute.
P. aeruginosa: No problem. I think we can all guess what that little devil is up to.
LOTME: Bacterial resistance to antibiotics is a huge problem for our species. What makes you so hard to fight?
P. aeruginosa: We’ve been trying to keep that a secret, actually, but now that researchers in Switzerland and Denmark seem to have figured it out, I guess it’s okay for me to spill the beans.
LOTME: Beans? What do beans have to do with it?
P. aeruginosa: Nothing, it’s just a colloquial expression that means I’m sharing previously private information.
LOTME: Sure, we knew that. Please, continue your spilling.
P. aeruginosa: The secret is … Well, let’s just say we were a little worried when the Clash released “Should I Stay or Should I Go” back in the 1980s.
LOTME: The Clash? Now we’re really confused.
P. aeruginosa: The answer to their question, “Should I stay or should I go? is yes. Successful invasion of a human is all about division of labor. “While one fraction of the bacterial population adheres to the mucosal surface and forms a biofilm, the other subpopulation spreads to distant tissue sites,” is how the investigators described it. We can increase surface colonization by using a “job-sharing” process, they said, and even resist antibiotics because most of us remain in the protective biofilm.
LOTME: And they say you guys don’t have brains.
P. aeruginosa: But wait, there’s more. We don’t just divide the labor randomly. After the initial colonization we form two functionally distinct subpopulations. One has high levels of the bacterial signaling molecule c-di-GMP and stays put to work on the biofilm. The other group, with low levels of c-di-GMP, heads out to the surrounding tissue to continue the colonization. As project leader Urs Jenal put it, “By identifying the genetic switch, we have tracked down the Achilles heel of the pathogen.”
LOTME: Pretty clever stuff, for humans, anyway.
P. aeruginosa: We agree, but now that you know our secret, we can’t let you share it.
LOTME: Wait! The journal article’s already been published. Your secret is out. You can’t stop that by infecting me.
P. aeruginosa: True enough, but are you familiar with the fable of the scorpion and the frog? It’s our nature.
LOTME: Nooooo! N. gonorrhoeae wouldn’t have done this!
What a pain in the Butt
Businesses rise and businesses fall. We all know that one cursed location, that spot in town where we see businesses move in and close up in a matter of months. At the same time, though, there are also businesses that have been around as long as anyone can remember, pillars of the community.
Corydon, IN., likely has a few such long-lived shops, but it is officially down one 70-year-old family business as of late April, with the unfortunate passing of beloved local pharmacy Butt Drugs. Prescription pick-up in rear.
The business dates back to 1952, when it was founded as William H. Butt Drugs. We’re sure William Butt was never teased about his last name. Nope. No one would ever do that. After he passed the store to his children, it underwent a stint as Butt Rexall Drugs. When the shop was passed down to its third-generation and ultimately final owner, Katie Butt Beckort, she decided to simplify the name. Get right down to the bottom of things, as it were.
Butt Drugs was a popular spot, featuring an old-school soda fountain and themed souvenirs. According to Ms. Butt Beckort, people would come from miles away to buy “I love Butt Drugs” T-shirts, magnets, and so on. Yes, they knew perfectly well what they were sitting on.
So, if was such a hit, why did it close? Butt Drugs may have a hilarious name and merchandise to match, but the pharmacy portion of the pharmacy had been losing money for years. You know, the actual point of the business. As with so many things, we can blame it on the insurance companies. More than half the drugs that passed through Butt Drugs’ doors were sold at a loss, because the insurance companies refused to reimburse the store more than the wholesale price of the drug. Not even a good butt drug could clear up that financial diarrhea.
And so, we’ve lost Butt Drugs forever. Spicy food enthusiasts, coffee drinkers, and all patrons of Taco Bell, take a moment to reflect and mourn on what you’ve lost. No more Butt Drugs to relieve your suffering. A true kick in the butt indeed.
Low-calorie tastes sweeter with a little salt
Diet and sugar-free foods and drinks seem like a good idea, but it’s hard to get past that strange aftertaste, right? It’s the calling card for the noncaloric aspartame- and stevia-containing sweeteners that we consume to make us feel like we can have the best of both worlds.
That weird lingering taste can be a total turn-off for some (raises hand), but researchers have found an almost facepalm solution to the not-so-sweet problem, and it’s salt.
Now, the concept of sweet and salty is not a far-fetched partnership when it comes to snack consumption (try M&Ms in your popcorn). The researchers at Almendra, a manufacturer of stevia sweeteners, put that iconic flavor pair to the test by adding mineral salts that have some nutritional value to lessen the effect of a stevia compound, rebaudioside A, found in noncaloric sweeteners.
The researchers added in magnesium chloride, calcium chloride, and potassium chloride separately to lessen rebaudioside A’s intensity, but they needed so much salt that it killed the sweet taste completely. A blend of the three mineral salts, however, reduced the lingering taste by 79% and improved the real sugar-like taste. The researchers tried this blend in reduced-calorie orange juice and a citrus-flavored soft drink, improving the taste in both.
The salty and sweet match comes in for the win once again. This time helping against the fight of obesity instead of making it worse.
Pseudomonas’ Achilles’ heel is more of an Achilles’ genetic switch
Today, on the long-awaited return of “Bacteria vs. the World,” we meet one of the rock stars of infectious disease.
LOTME: Through the use of imaginary technology, we’re talking to Pseudomonas aeruginosa. Thanks for joining us on such short notice, after Neisseria gonorrhoeae canceled at the last minute.
P. aeruginosa: No problem. I think we can all guess what that little devil is up to.
LOTME: Bacterial resistance to antibiotics is a huge problem for our species. What makes you so hard to fight?
P. aeruginosa: We’ve been trying to keep that a secret, actually, but now that researchers in Switzerland and Denmark seem to have figured it out, I guess it’s okay for me to spill the beans.
LOTME: Beans? What do beans have to do with it?
P. aeruginosa: Nothing, it’s just a colloquial expression that means I’m sharing previously private information.
LOTME: Sure, we knew that. Please, continue your spilling.
P. aeruginosa: The secret is … Well, let’s just say we were a little worried when the Clash released “Should I Stay or Should I Go” back in the 1980s.
LOTME: The Clash? Now we’re really confused.
P. aeruginosa: The answer to their question, “Should I stay or should I go? is yes. Successful invasion of a human is all about division of labor. “While one fraction of the bacterial population adheres to the mucosal surface and forms a biofilm, the other subpopulation spreads to distant tissue sites,” is how the investigators described it. We can increase surface colonization by using a “job-sharing” process, they said, and even resist antibiotics because most of us remain in the protective biofilm.
LOTME: And they say you guys don’t have brains.
P. aeruginosa: But wait, there’s more. We don’t just divide the labor randomly. After the initial colonization we form two functionally distinct subpopulations. One has high levels of the bacterial signaling molecule c-di-GMP and stays put to work on the biofilm. The other group, with low levels of c-di-GMP, heads out to the surrounding tissue to continue the colonization. As project leader Urs Jenal put it, “By identifying the genetic switch, we have tracked down the Achilles heel of the pathogen.”
LOTME: Pretty clever stuff, for humans, anyway.
P. aeruginosa: We agree, but now that you know our secret, we can’t let you share it.
LOTME: Wait! The journal article’s already been published. Your secret is out. You can’t stop that by infecting me.
P. aeruginosa: True enough, but are you familiar with the fable of the scorpion and the frog? It’s our nature.
LOTME: Nooooo! N. gonorrhoeae wouldn’t have done this!
What a pain in the Butt
Businesses rise and businesses fall. We all know that one cursed location, that spot in town where we see businesses move in and close up in a matter of months. At the same time, though, there are also businesses that have been around as long as anyone can remember, pillars of the community.
Corydon, IN., likely has a few such long-lived shops, but it is officially down one 70-year-old family business as of late April, with the unfortunate passing of beloved local pharmacy Butt Drugs. Prescription pick-up in rear.
The business dates back to 1952, when it was founded as William H. Butt Drugs. We’re sure William Butt was never teased about his last name. Nope. No one would ever do that. After he passed the store to his children, it underwent a stint as Butt Rexall Drugs. When the shop was passed down to its third-generation and ultimately final owner, Katie Butt Beckort, she decided to simplify the name. Get right down to the bottom of things, as it were.
Butt Drugs was a popular spot, featuring an old-school soda fountain and themed souvenirs. According to Ms. Butt Beckort, people would come from miles away to buy “I love Butt Drugs” T-shirts, magnets, and so on. Yes, they knew perfectly well what they were sitting on.
So, if was such a hit, why did it close? Butt Drugs may have a hilarious name and merchandise to match, but the pharmacy portion of the pharmacy had been losing money for years. You know, the actual point of the business. As with so many things, we can blame it on the insurance companies. More than half the drugs that passed through Butt Drugs’ doors were sold at a loss, because the insurance companies refused to reimburse the store more than the wholesale price of the drug. Not even a good butt drug could clear up that financial diarrhea.
And so, we’ve lost Butt Drugs forever. Spicy food enthusiasts, coffee drinkers, and all patrons of Taco Bell, take a moment to reflect and mourn on what you’ve lost. No more Butt Drugs to relieve your suffering. A true kick in the butt indeed.
Low-calorie tastes sweeter with a little salt
Diet and sugar-free foods and drinks seem like a good idea, but it’s hard to get past that strange aftertaste, right? It’s the calling card for the noncaloric aspartame- and stevia-containing sweeteners that we consume to make us feel like we can have the best of both worlds.
That weird lingering taste can be a total turn-off for some (raises hand), but researchers have found an almost facepalm solution to the not-so-sweet problem, and it’s salt.
Now, the concept of sweet and salty is not a far-fetched partnership when it comes to snack consumption (try M&Ms in your popcorn). The researchers at Almendra, a manufacturer of stevia sweeteners, put that iconic flavor pair to the test by adding mineral salts that have some nutritional value to lessen the effect of a stevia compound, rebaudioside A, found in noncaloric sweeteners.
The researchers added in magnesium chloride, calcium chloride, and potassium chloride separately to lessen rebaudioside A’s intensity, but they needed so much salt that it killed the sweet taste completely. A blend of the three mineral salts, however, reduced the lingering taste by 79% and improved the real sugar-like taste. The researchers tried this blend in reduced-calorie orange juice and a citrus-flavored soft drink, improving the taste in both.
The salty and sweet match comes in for the win once again. This time helping against the fight of obesity instead of making it worse.
Pseudomonas’ Achilles’ heel is more of an Achilles’ genetic switch
Today, on the long-awaited return of “Bacteria vs. the World,” we meet one of the rock stars of infectious disease.
LOTME: Through the use of imaginary technology, we’re talking to Pseudomonas aeruginosa. Thanks for joining us on such short notice, after Neisseria gonorrhoeae canceled at the last minute.
P. aeruginosa: No problem. I think we can all guess what that little devil is up to.
LOTME: Bacterial resistance to antibiotics is a huge problem for our species. What makes you so hard to fight?
P. aeruginosa: We’ve been trying to keep that a secret, actually, but now that researchers in Switzerland and Denmark seem to have figured it out, I guess it’s okay for me to spill the beans.
LOTME: Beans? What do beans have to do with it?
P. aeruginosa: Nothing, it’s just a colloquial expression that means I’m sharing previously private information.
LOTME: Sure, we knew that. Please, continue your spilling.
P. aeruginosa: The secret is … Well, let’s just say we were a little worried when the Clash released “Should I Stay or Should I Go” back in the 1980s.
LOTME: The Clash? Now we’re really confused.
P. aeruginosa: The answer to their question, “Should I stay or should I go? is yes. Successful invasion of a human is all about division of labor. “While one fraction of the bacterial population adheres to the mucosal surface and forms a biofilm, the other subpopulation spreads to distant tissue sites,” is how the investigators described it. We can increase surface colonization by using a “job-sharing” process, they said, and even resist antibiotics because most of us remain in the protective biofilm.
LOTME: And they say you guys don’t have brains.
P. aeruginosa: But wait, there’s more. We don’t just divide the labor randomly. After the initial colonization we form two functionally distinct subpopulations. One has high levels of the bacterial signaling molecule c-di-GMP and stays put to work on the biofilm. The other group, with low levels of c-di-GMP, heads out to the surrounding tissue to continue the colonization. As project leader Urs Jenal put it, “By identifying the genetic switch, we have tracked down the Achilles heel of the pathogen.”
LOTME: Pretty clever stuff, for humans, anyway.
P. aeruginosa: We agree, but now that you know our secret, we can’t let you share it.
LOTME: Wait! The journal article’s already been published. Your secret is out. You can’t stop that by infecting me.
P. aeruginosa: True enough, but are you familiar with the fable of the scorpion and the frog? It’s our nature.
LOTME: Nooooo! N. gonorrhoeae wouldn’t have done this!
What a pain in the Butt
Businesses rise and businesses fall. We all know that one cursed location, that spot in town where we see businesses move in and close up in a matter of months. At the same time, though, there are also businesses that have been around as long as anyone can remember, pillars of the community.
Corydon, IN., likely has a few such long-lived shops, but it is officially down one 70-year-old family business as of late April, with the unfortunate passing of beloved local pharmacy Butt Drugs. Prescription pick-up in rear.
The business dates back to 1952, when it was founded as William H. Butt Drugs. We’re sure William Butt was never teased about his last name. Nope. No one would ever do that. After he passed the store to his children, it underwent a stint as Butt Rexall Drugs. When the shop was passed down to its third-generation and ultimately final owner, Katie Butt Beckort, she decided to simplify the name. Get right down to the bottom of things, as it were.
Butt Drugs was a popular spot, featuring an old-school soda fountain and themed souvenirs. According to Ms. Butt Beckort, people would come from miles away to buy “I love Butt Drugs” T-shirts, magnets, and so on. Yes, they knew perfectly well what they were sitting on.
So, if was such a hit, why did it close? Butt Drugs may have a hilarious name and merchandise to match, but the pharmacy portion of the pharmacy had been losing money for years. You know, the actual point of the business. As with so many things, we can blame it on the insurance companies. More than half the drugs that passed through Butt Drugs’ doors were sold at a loss, because the insurance companies refused to reimburse the store more than the wholesale price of the drug. Not even a good butt drug could clear up that financial diarrhea.
And so, we’ve lost Butt Drugs forever. Spicy food enthusiasts, coffee drinkers, and all patrons of Taco Bell, take a moment to reflect and mourn on what you’ve lost. No more Butt Drugs to relieve your suffering. A true kick in the butt indeed.
Proteomics reveals potential targets for drug-resistant TB
TOPLINE:
Downregulation of plasma exosome-derived apolipoproteins APOA1, APOB, and APOC1 indicates DR-TB status and lipid metabolism regulation in pathogenesis.
METHODOLOGY:
Group case-controlled study assessed 17 drug resistant tuberculosis (DR-TB) and 33 non–drug resistant TB (NDR-TB) patients at The Fourth People’s Hospital of Taiyuan, China, from November 2018 to March 2019.
Plasma exosome purity and quality was determined by transmission electron microscopy, nanoparticle tracking analysis, and Western blot markers.
Proteins purified from plasma exosomes were characterized by SDS-Page with Western blotting and liquid chromatography coupled with tandem mass spectrometry techniques.
Functional proteomic differential analysis was achieved using the UniProt-GOA, Kyoto Encyclopedia of Genes and Genomes (KEGG), and STRING databases.
TAKEAWAYS:
DR-TB patients tended to be older than NDR-TB patients.
Isolated plasma exosomes were morphologically characterized as being “close to pure.”
Differential gene expression analysis revealed 16 upregulated and 10 downregulated proteins from DR-TB compared with NDR-TB patient-derived plasma exosomes.
through their functions in lipid metabolism and protein transport.
IN PRACTICE:
Key apolipoproteins “may be involved in the pathogenesis of DR-TB via accelerating the formation of foamy macrophages and reducing the cellular uptake of anti-TB drugs.”
STUDY DETAILS:
The study led by Mingrui Wu of Shanxi (China) Medical University and colleagues was published in the July 2023 issue of Tuberculosis.
LIMITATIONS:
This study is limited by an enrollment bias of at least twice as many men to women patients for both DR-TB and NDR-TB categories, reporting of some incomplete data collection characterizing the study population, and small sample size, which did not permit stratified analysis of the five types of DR-TB.
DISCLOSURES:
The authors report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
TOPLINE:
Downregulation of plasma exosome-derived apolipoproteins APOA1, APOB, and APOC1 indicates DR-TB status and lipid metabolism regulation in pathogenesis.
METHODOLOGY:
Group case-controlled study assessed 17 drug resistant tuberculosis (DR-TB) and 33 non–drug resistant TB (NDR-TB) patients at The Fourth People’s Hospital of Taiyuan, China, from November 2018 to March 2019.
Plasma exosome purity and quality was determined by transmission electron microscopy, nanoparticle tracking analysis, and Western blot markers.
Proteins purified from plasma exosomes were characterized by SDS-Page with Western blotting and liquid chromatography coupled with tandem mass spectrometry techniques.
Functional proteomic differential analysis was achieved using the UniProt-GOA, Kyoto Encyclopedia of Genes and Genomes (KEGG), and STRING databases.
TAKEAWAYS:
DR-TB patients tended to be older than NDR-TB patients.
Isolated plasma exosomes were morphologically characterized as being “close to pure.”
Differential gene expression analysis revealed 16 upregulated and 10 downregulated proteins from DR-TB compared with NDR-TB patient-derived plasma exosomes.
through their functions in lipid metabolism and protein transport.
IN PRACTICE:
Key apolipoproteins “may be involved in the pathogenesis of DR-TB via accelerating the formation of foamy macrophages and reducing the cellular uptake of anti-TB drugs.”
STUDY DETAILS:
The study led by Mingrui Wu of Shanxi (China) Medical University and colleagues was published in the July 2023 issue of Tuberculosis.
LIMITATIONS:
This study is limited by an enrollment bias of at least twice as many men to women patients for both DR-TB and NDR-TB categories, reporting of some incomplete data collection characterizing the study population, and small sample size, which did not permit stratified analysis of the five types of DR-TB.
DISCLOSURES:
The authors report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
TOPLINE:
Downregulation of plasma exosome-derived apolipoproteins APOA1, APOB, and APOC1 indicates DR-TB status and lipid metabolism regulation in pathogenesis.
METHODOLOGY:
Group case-controlled study assessed 17 drug resistant tuberculosis (DR-TB) and 33 non–drug resistant TB (NDR-TB) patients at The Fourth People’s Hospital of Taiyuan, China, from November 2018 to March 2019.
Plasma exosome purity and quality was determined by transmission electron microscopy, nanoparticle tracking analysis, and Western blot markers.
Proteins purified from plasma exosomes were characterized by SDS-Page with Western blotting and liquid chromatography coupled with tandem mass spectrometry techniques.
Functional proteomic differential analysis was achieved using the UniProt-GOA, Kyoto Encyclopedia of Genes and Genomes (KEGG), and STRING databases.
TAKEAWAYS:
DR-TB patients tended to be older than NDR-TB patients.
Isolated plasma exosomes were morphologically characterized as being “close to pure.”
Differential gene expression analysis revealed 16 upregulated and 10 downregulated proteins from DR-TB compared with NDR-TB patient-derived plasma exosomes.
through their functions in lipid metabolism and protein transport.
IN PRACTICE:
Key apolipoproteins “may be involved in the pathogenesis of DR-TB via accelerating the formation of foamy macrophages and reducing the cellular uptake of anti-TB drugs.”
STUDY DETAILS:
The study led by Mingrui Wu of Shanxi (China) Medical University and colleagues was published in the July 2023 issue of Tuberculosis.
LIMITATIONS:
This study is limited by an enrollment bias of at least twice as many men to women patients for both DR-TB and NDR-TB categories, reporting of some incomplete data collection characterizing the study population, and small sample size, which did not permit stratified analysis of the five types of DR-TB.
DISCLOSURES:
The authors report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
New tool uses nanotechnology to speed up diagnostic testing of infectious disease
A new tool promises to expedite detection of infectious disease, according to researchers from McGill University, Montreal.
The diagnostic platform, called The device was tested for several respiratory viruses and bacteria, including the H1N1 influenza virus and SARS-CoV-2. It achieved 95% accuracy at identifying COVID-19 and its variants in 48 human saliva samples.
“COVID was something that opened our eyes, and now we have to think more seriously about point-of-care diagnostics,” Sara Mahshid, PhD, assistant professor of biomedical engineering and Canada Research Chair in Nano-Biosensing Devices at McGill University, said in an interview. The technology could become important for a range of medical applications, especially in low-resource areas.
The development was detailed in an article in Nature Nanotechnology.
Nonclinical setting
The COVID-19 pandemic has demonstrated the need for fast and accurate testing that can be used outside of a clinical setting. The gold-standard diagnostic method is PCR testing, but its accuracy comes with a trade-off. PCR testing involves a lengthy protocol and requires a centralized testing facility.
With QolorEX, the investigators aimed to develop a new test that achieves the accuracy of PCR in an automated tool that can be used outside of a testing facility or hospital setting. Dr. Mahshid noted a particular need for a tool that could be used in congregate settings, such as airports, schools, or restaurants.
The device is compact enough to sit on a tabletop or bench and can be used easily in group settings, according to Dr. Mahshid. In the future, she hopes to further miniaturize the device to make it more scalable for widespread use.
Requiring only a saliva sample, the tool is easy to use. Unlike current COVID-19 rapid tests, which involve several steps, the system is automated and does not require manually mixing reagents. After collecting a sample, a user taps a button in a smartphone or computer application. The device handles the rest.
“We’re not chemists who understand how to mix these solutions,” Dr. Mahshid said. Avoiding those extra steps may reduce the false positives and false negatives caused by user error.
Fast results
QolorEX can return results in 13 minutes, like a rapid antigen test does. Like a PCR test, the device uses nucleic acid amplification. But PCR tests typically take much longer. The sample analysis alone takes 1.5-2 hours.
The new test accelerates the reaction by injecting light-excited “hot” electrons from the surface of a nanoplasmonic sensor. The device then uses imaging and a machine learning algorithm to quantify a color transformation that occurs when a pathogen is present.
The fast, reliable results make the system potentially appropriate for use in places such as airports. Previously, passengers had to wait 24 hours for a negative COVID test before boarding a plane. A device such as QolorEX would allow screening on site.
The ability of the tool to distinguish between bacterial and viral infections so quickly is “an application that is both important and extremely difficult to achieve,” according to Nikhil Bhalla, PhD, in a research briefing. Dr. Bhalla is a lecturer in electronic engineering at Ulster University, Belfast, Ireland.
The researchers hope that by delivering results quickly, the device will help reduce the spread of respiratory diseases and possibly save lives.
‘Sensitive and specific’
The primary benefit of the tool is its ability to return results quickly while having low false positive and false negative rates, according to Leyla Soleymani, PhD, of McMaster University, Hamilton, Ont. “It is hard to come by rapid tests that are both sensitive and specific, compared to PCR,” Dr. Soleymani told this news organization.
Although QolorEX was developed to detect COVID-19 and other infectious diseases, the uses of the device are not limited to the pathogens tested. The tool can be applied to a range of tests that currently use PCR technology. Dr. Mahshid and her team are considering several other applications of the technology, such as analyzing therapeutics for antimicrobial-resistant pathogens prioritized by the World Health Organization. The technology may also have potential for detecting cancer and bacterial infections, Dr. Mahshid said in an interview.
But to Dr. Soleymani, the most exciting application remains its use in diagnosing infectious diseases. She noted, however, that it’s unclear whether the price of the device will be too high for widespread home use. It may be more practical for family physician clinics and other facilities.
Before the device becomes commercially available, more testing is needed to validate the results, which are based on a limited number of samples that were available in a research setting.
The study was supported by the MI4 Emergency COVID-19 Research Funding, Natural Sciences and Engineering Research Council of Canada, Canadian Institutes of Health Research, Canada Foundation for Innovation, and McGill University. Dr. Mahshid and Dr. Soleymani reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A new tool promises to expedite detection of infectious disease, according to researchers from McGill University, Montreal.
The diagnostic platform, called The device was tested for several respiratory viruses and bacteria, including the H1N1 influenza virus and SARS-CoV-2. It achieved 95% accuracy at identifying COVID-19 and its variants in 48 human saliva samples.
“COVID was something that opened our eyes, and now we have to think more seriously about point-of-care diagnostics,” Sara Mahshid, PhD, assistant professor of biomedical engineering and Canada Research Chair in Nano-Biosensing Devices at McGill University, said in an interview. The technology could become important for a range of medical applications, especially in low-resource areas.
The development was detailed in an article in Nature Nanotechnology.
Nonclinical setting
The COVID-19 pandemic has demonstrated the need for fast and accurate testing that can be used outside of a clinical setting. The gold-standard diagnostic method is PCR testing, but its accuracy comes with a trade-off. PCR testing involves a lengthy protocol and requires a centralized testing facility.
With QolorEX, the investigators aimed to develop a new test that achieves the accuracy of PCR in an automated tool that can be used outside of a testing facility or hospital setting. Dr. Mahshid noted a particular need for a tool that could be used in congregate settings, such as airports, schools, or restaurants.
The device is compact enough to sit on a tabletop or bench and can be used easily in group settings, according to Dr. Mahshid. In the future, she hopes to further miniaturize the device to make it more scalable for widespread use.
Requiring only a saliva sample, the tool is easy to use. Unlike current COVID-19 rapid tests, which involve several steps, the system is automated and does not require manually mixing reagents. After collecting a sample, a user taps a button in a smartphone or computer application. The device handles the rest.
“We’re not chemists who understand how to mix these solutions,” Dr. Mahshid said. Avoiding those extra steps may reduce the false positives and false negatives caused by user error.
Fast results
QolorEX can return results in 13 minutes, like a rapid antigen test does. Like a PCR test, the device uses nucleic acid amplification. But PCR tests typically take much longer. The sample analysis alone takes 1.5-2 hours.
The new test accelerates the reaction by injecting light-excited “hot” electrons from the surface of a nanoplasmonic sensor. The device then uses imaging and a machine learning algorithm to quantify a color transformation that occurs when a pathogen is present.
The fast, reliable results make the system potentially appropriate for use in places such as airports. Previously, passengers had to wait 24 hours for a negative COVID test before boarding a plane. A device such as QolorEX would allow screening on site.
The ability of the tool to distinguish between bacterial and viral infections so quickly is “an application that is both important and extremely difficult to achieve,” according to Nikhil Bhalla, PhD, in a research briefing. Dr. Bhalla is a lecturer in electronic engineering at Ulster University, Belfast, Ireland.
The researchers hope that by delivering results quickly, the device will help reduce the spread of respiratory diseases and possibly save lives.
‘Sensitive and specific’
The primary benefit of the tool is its ability to return results quickly while having low false positive and false negative rates, according to Leyla Soleymani, PhD, of McMaster University, Hamilton, Ont. “It is hard to come by rapid tests that are both sensitive and specific, compared to PCR,” Dr. Soleymani told this news organization.
Although QolorEX was developed to detect COVID-19 and other infectious diseases, the uses of the device are not limited to the pathogens tested. The tool can be applied to a range of tests that currently use PCR technology. Dr. Mahshid and her team are considering several other applications of the technology, such as analyzing therapeutics for antimicrobial-resistant pathogens prioritized by the World Health Organization. The technology may also have potential for detecting cancer and bacterial infections, Dr. Mahshid said in an interview.
But to Dr. Soleymani, the most exciting application remains its use in diagnosing infectious diseases. She noted, however, that it’s unclear whether the price of the device will be too high for widespread home use. It may be more practical for family physician clinics and other facilities.
Before the device becomes commercially available, more testing is needed to validate the results, which are based on a limited number of samples that were available in a research setting.
The study was supported by the MI4 Emergency COVID-19 Research Funding, Natural Sciences and Engineering Research Council of Canada, Canadian Institutes of Health Research, Canada Foundation for Innovation, and McGill University. Dr. Mahshid and Dr. Soleymani reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A new tool promises to expedite detection of infectious disease, according to researchers from McGill University, Montreal.
The diagnostic platform, called The device was tested for several respiratory viruses and bacteria, including the H1N1 influenza virus and SARS-CoV-2. It achieved 95% accuracy at identifying COVID-19 and its variants in 48 human saliva samples.
“COVID was something that opened our eyes, and now we have to think more seriously about point-of-care diagnostics,” Sara Mahshid, PhD, assistant professor of biomedical engineering and Canada Research Chair in Nano-Biosensing Devices at McGill University, said in an interview. The technology could become important for a range of medical applications, especially in low-resource areas.
The development was detailed in an article in Nature Nanotechnology.
Nonclinical setting
The COVID-19 pandemic has demonstrated the need for fast and accurate testing that can be used outside of a clinical setting. The gold-standard diagnostic method is PCR testing, but its accuracy comes with a trade-off. PCR testing involves a lengthy protocol and requires a centralized testing facility.
With QolorEX, the investigators aimed to develop a new test that achieves the accuracy of PCR in an automated tool that can be used outside of a testing facility or hospital setting. Dr. Mahshid noted a particular need for a tool that could be used in congregate settings, such as airports, schools, or restaurants.
The device is compact enough to sit on a tabletop or bench and can be used easily in group settings, according to Dr. Mahshid. In the future, she hopes to further miniaturize the device to make it more scalable for widespread use.
Requiring only a saliva sample, the tool is easy to use. Unlike current COVID-19 rapid tests, which involve several steps, the system is automated and does not require manually mixing reagents. After collecting a sample, a user taps a button in a smartphone or computer application. The device handles the rest.
“We’re not chemists who understand how to mix these solutions,” Dr. Mahshid said. Avoiding those extra steps may reduce the false positives and false negatives caused by user error.
Fast results
QolorEX can return results in 13 minutes, like a rapid antigen test does. Like a PCR test, the device uses nucleic acid amplification. But PCR tests typically take much longer. The sample analysis alone takes 1.5-2 hours.
The new test accelerates the reaction by injecting light-excited “hot” electrons from the surface of a nanoplasmonic sensor. The device then uses imaging and a machine learning algorithm to quantify a color transformation that occurs when a pathogen is present.
The fast, reliable results make the system potentially appropriate for use in places such as airports. Previously, passengers had to wait 24 hours for a negative COVID test before boarding a plane. A device such as QolorEX would allow screening on site.
The ability of the tool to distinguish between bacterial and viral infections so quickly is “an application that is both important and extremely difficult to achieve,” according to Nikhil Bhalla, PhD, in a research briefing. Dr. Bhalla is a lecturer in electronic engineering at Ulster University, Belfast, Ireland.
The researchers hope that by delivering results quickly, the device will help reduce the spread of respiratory diseases and possibly save lives.
‘Sensitive and specific’
The primary benefit of the tool is its ability to return results quickly while having low false positive and false negative rates, according to Leyla Soleymani, PhD, of McMaster University, Hamilton, Ont. “It is hard to come by rapid tests that are both sensitive and specific, compared to PCR,” Dr. Soleymani told this news organization.
Although QolorEX was developed to detect COVID-19 and other infectious diseases, the uses of the device are not limited to the pathogens tested. The tool can be applied to a range of tests that currently use PCR technology. Dr. Mahshid and her team are considering several other applications of the technology, such as analyzing therapeutics for antimicrobial-resistant pathogens prioritized by the World Health Organization. The technology may also have potential for detecting cancer and bacterial infections, Dr. Mahshid said in an interview.
But to Dr. Soleymani, the most exciting application remains its use in diagnosing infectious diseases. She noted, however, that it’s unclear whether the price of the device will be too high for widespread home use. It may be more practical for family physician clinics and other facilities.
Before the device becomes commercially available, more testing is needed to validate the results, which are based on a limited number of samples that were available in a research setting.
The study was supported by the MI4 Emergency COVID-19 Research Funding, Natural Sciences and Engineering Research Council of Canada, Canadian Institutes of Health Research, Canada Foundation for Innovation, and McGill University. Dr. Mahshid and Dr. Soleymani reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM NATURE NANOTECHNOLOGY
Cutting-edge nasal tech could usher in a new era of medicine
Noses are like caverns – twisting, turning, no two exactly the same. But if you nose past anyone’s nostrils, you’ll discover a surprisingly sprawling space.
“The size of the nasal cavity is about the same as a large handkerchief,” said Hugh Smyth, PhD, a professor of molecular pharmaceutics and drug delivery at the University of Texas at Austin.
“It’s very accessible tissue, and it has a lot of blood flow,” said Dr. Smyth. “The speed of onset can often be as fast as injections, sometimes even faster.”
It’s nothing new to get medicines via your nose. For decades, we’ve squirted various sprays into our nostrils to treat local maladies like allergies or infections. Even the ancients saw wisdom in the nasal route.
But recently, the nose has gained scientific attention as a gateway to the rest of the body – even the brain, a notoriously difficult target.
The upshot: Someday, inhaling therapies could be as routine as swallowing pills.
The nasal route is quick, needle free, and user friendly, and it often requires a smaller dose than other methods, since the drug doesn’t have to pass through the digestive tract, losing potency during digestion.
But there are challenges.
How hard can it be?
Old-school nasal sprayers, mostly unchanged since the 1800s, aren’t cut out for deep-nose delivery. “The technology is relatively limited because you’ve just got a single spray nozzle,” said Michael Hindle, PhD, a professor of pharmaceutics at Virginia Commonwealth University, Richmond.
These traditional devices (similar to perfume sprayers) don’t consistently push meds past the lower to middle sections inside the nose, called the nasal valve – if they do so at all: In a 2020 Rhinology study (doi: 10.4193/Rhin18.304) conventional nasal sprays only reached this first segment of the nose, a less-than-ideal spot to land.
Inside the nasal valve, the surface is skin-like and doesn’t absorb very well. Its narrow design slows airflow, preventing particles from moving to deeper regions, where tissue is vascular and porous like the lungs. And even if this structural roadblock is surpassed, other hurdles remain.
The nose is designed to keep stuff out. Nose hair, cilia, mucus, sneezing, coughing – all make “distributing drugs evenly across the nasal cavity difficult,” said Dr. Smyth. “The spray gets filtered out before it reaches those deeper zones,” potentially dripping out of the nostrils instead of being absorbed.
Complicating matters is how every person’s nose is different. In a 2018 study, Dr. Smyth and a research team created three dimensional–printed models of people’s nasal cavities. They varied widely. “Nasal cavities are very different in size, length, and internal geometry,” he said. “This makes it challenging to target specific areas.”
Although carefully positioning the spray nozzle can help, even something as minor as sniffing too hard (constricting the nostrils) can keep sprays from reaching the absorptive deeper regions.
Still, the benefits are enough to compel researchers to find a way in.
“This really is a drug delivery challenge we’ve been wrestling with,” said Dr. Hindle. “It’s not new formulations we hear about. It’s new devices and delivery methods trying to target the different nasal regions.”
Delivering the goods
In the late aughts, John Hoekman was a graduate student in the University of Washington’s pharmaceutics program, studying nasal drug delivery. In his experiments, he noticed that drugs distributed differently, depending on the region targeted – aiming for the upper nasal cavity led to a spike in absorption.
The results convinced Mr. Hoekman to stake his future on nasal drug delivery.
In 2008, while still in graduate school, he started his own company, now known as Impel Pharmaceuticals. In 2021, Impel released its first product: Trudhesa, a nasal spray for migraines. Although the drug itself – dihydroergotamine mesylate – was hardly novel, used for migraine relief since 1946 (Headache. 2020 Jan;60[1]:40-57), it was usually delivered through an intravenous line, often in the ED.
But with Mr. Hoekman’s POD device – short for precision olfactory delivery – the drug can be given by the patient, via the nose. This generally means faster, more reliable relief, with fewer side effects. “We were able to lower the dose and improve the overall absorption,” said Mr. Hoekman.
The POD’s nozzle is engineered to spray a soft, narrow plume. It’s gas propelled, so patients don’t have to breathe in any special way to ensure delivery. The drug can zip right through the nasal valve into the upper nasal cavity.
Another company – OptiNose – has a “bidirectional” delivery method that propels drugs, either liquid or dry powder, deep into the nose.
“You insert the nozzle into your nose, and as you blow through the mouthpiece, your soft palate closes,” said Dr. Hindle. With the throat sealed off, “the only place for the drug to go is into one nostril and out the other, coating both sides of the nasal passageways.”
The device is only available for Onzetra Xsail, a powder for migraines. But another application is on its way.
In May, OptiNose announced that the FDA is reviewing Xhance, which uses the system to direct a steroid to the sinuses. In a clinical trial, patients with chronic sinusitis who tried the drug-device combo saw a decline in congestion, facial pain, and inflammation.
Targeting the brain
Both of those migraine drugs – Trudhesa and Onzetra Xsail – are thought to penetrate the upper nasal cavity. That’s where you’ll find the olfactory zone, a sheet of neurons that connects to the olfactory bulb. Located behind the eyes, these two nerve bundles detect odors.
“The olfactory region is almost like a back door to the brain,” said Mr. Hoekman.
By bypassing the blood-brain barrier, it offers a direct pathway – the only direct pathway, actually – between an exposed area of the body and the brain. Meaning it can ferry drugs straight from the nasal cavity to the central nervous system.
Nose-to-brain treatments could be game-changing for central nervous system disorders, such as Parkinson’s disease, Alzheimer’s, or anxiety.
But reaching the olfactory zone is notoriously hard. “The vasculature in your nose is like a big freeway, and the olfactory tract is like a side alley,” explained Mr. Hoekman. “It’s very limiting in what it will allow through.” The region is also small, occupying only 3%-10% of the nasal cavity’s surface area.
Again, POD means “precision olfactory delivery.” But the device isn’t quite as laser focused on the region as its name implies. “We’re not at the stage where we’re able to exclusively deliver to one target site in the nose,” said Dr. Hindle.
While wending its way toward the olfactory zone, some of the drug will be absorbed by other regions, then circulate throughout the body.
“About 59% of the drug that we put into the upper nasal space gets absorbed into the bloodstream,” said Mr. Hoekman.
Janssen Pharmaceuticals’ Spravato – a nasal spray for drug-resistant depression – is thought to work similarly: Some goes straight to the brain via the olfactory nerves, while the rest takes a more roundabout route, passing through the blood vessels to circulate in your system.
A needle-free option
Sometimes, the bloodstream is the main target. Because the nose’s middle and upper stretches are so vascular, drugs can be rapidly absorbed.
This is especially valuable for time-sensitive conditions. “If you give something nasally, you can have peak uptake in 15-30 minutes,” said Mr. Hoekman.
Take Narcan nasal spray, which delivers a burst of naloxone to quickly reverse the effects of opioid an overdose. Or Noctiva nasal spray. Taken just half an hour before bed, it can prevent frequent nighttime urination.
There’s also a group of seizure-stopping sprays, known as “rescue treatments.” One works by temporarily loosening the space between nasal cells, allowing the seizure drug to be quickly absorbed through the vessels.
This systemic access also has potential for drugs that would otherwise have to be injected, such as biologics.
The same goes for vaccines. Mucosal tissue inside the nasal cavity offers direct access to the infection-fighting lymphatic system, making the nose a prime target for inoculation against certain viruses.
Inhaling protection against viruses
Despite the recent surge of interest, nasal vaccines faced a rocky start. After the first nasal flu vaccine hit the market in 2001, it was pulled due to potential toxicity and reports of Bell’s palsy, a type of facial paralysis.
FluMist came in 2003 and has been plagued by problems ever since. Because it contains a weakened live virus, flu-like side effects can occur. And it doesn’t always work. During the 2016-2017 flu season, FluMist protected only 3% of kids, prompting the Centers for Disease Control and Prevention to advise against the nasal route that year.
Why FluMist can be so hit-or-miss is poorly understood. But generally, the nose can pose an effectiveness challenge. “The nose is highly cycling,” said Dr. Hindle. “Anything we deposit usually gets transported out within 15-20 minutes.”
For kids – big fans of not using needles – chronically runny noses can be an issue. “You squirt it in the nose, and it will probably just come back out in their snot,” said Jay Kolls, MD, a professor of medicine and pediatrics at Tulane University, New Orleans, who is developing an intranasal pneumonia vaccine.
Even so, nasal vaccines became a hot topic among researchers after the world was shut down by a virus that invades through the nose.
“We realized that intramuscular vaccines were effective at preventing severe disease, but they weren’t that effective at preventing transmission,” said Michael Diamond, MD, PhD, an immunologist at Washington University in St. Louis.
Nasal vaccines could solve that problem by putting an immune barrier at the point of entry, denying access to the rest of the body. “You squash the infection early enough that it not only prevents disease,” said Dr. Kolls, “but potentially prevents transmission.”
And yes, a nasal COVID vaccine is on the way
In March 2020, Dr. Diamond’s team began exploring a nasal COVID vaccine. Promising results in animals prompted a vaccine development company to license the technology. The resulting nasal vaccine – the first for COVID – has been approved in India, both as a primary vaccine and a booster.
It works by stimulating an influx of IgA, a type of antibody found in the nasal passages, and production of resident memory T cells, immune cells on standby just beneath the surface tissue in the nose.
By contrast, injected vaccines generate mostly IgG antibodies, which struggle to enter the respiratory tract. Only a tiny fraction – an estimated 1% – typically reach the nose.
Nasal vaccines could also be used along with shots. The latter could prime the whole body to fight back, while a nasal spritz could pull that immune protection to the mucosal surfaces.
Nasal technology could yield more effective vaccines for infections like tuberculosis or malaria, or even safeguard against new – sometimes surprising – conditions.
In a 2021 Nature study, an intranasal vaccine derived from fentanyl was better at preventing overdose than an injected vaccine. “Through some clever chemistry, the drug [in the vaccine] isn’t fentanyl anymore,” said study author Elizabeth Norton, PhD, an assistant professor of microbiology and immunology at Tulane University. “But the immune system still has an antibody response to it.”
Novel applications like this represent the future of nasal drug delivery.
“We’re not going to innovate in asthma or COPD. We’re not going to innovate in local delivery to the nose,” said Dr. Hindle. “Innovation will only come if we look to treat new conditions.”
A version of this article originally appeared on WebMD.com.
Noses are like caverns – twisting, turning, no two exactly the same. But if you nose past anyone’s nostrils, you’ll discover a surprisingly sprawling space.
“The size of the nasal cavity is about the same as a large handkerchief,” said Hugh Smyth, PhD, a professor of molecular pharmaceutics and drug delivery at the University of Texas at Austin.
“It’s very accessible tissue, and it has a lot of blood flow,” said Dr. Smyth. “The speed of onset can often be as fast as injections, sometimes even faster.”
It’s nothing new to get medicines via your nose. For decades, we’ve squirted various sprays into our nostrils to treat local maladies like allergies or infections. Even the ancients saw wisdom in the nasal route.
But recently, the nose has gained scientific attention as a gateway to the rest of the body – even the brain, a notoriously difficult target.
The upshot: Someday, inhaling therapies could be as routine as swallowing pills.
The nasal route is quick, needle free, and user friendly, and it often requires a smaller dose than other methods, since the drug doesn’t have to pass through the digestive tract, losing potency during digestion.
But there are challenges.
How hard can it be?
Old-school nasal sprayers, mostly unchanged since the 1800s, aren’t cut out for deep-nose delivery. “The technology is relatively limited because you’ve just got a single spray nozzle,” said Michael Hindle, PhD, a professor of pharmaceutics at Virginia Commonwealth University, Richmond.
These traditional devices (similar to perfume sprayers) don’t consistently push meds past the lower to middle sections inside the nose, called the nasal valve – if they do so at all: In a 2020 Rhinology study (doi: 10.4193/Rhin18.304) conventional nasal sprays only reached this first segment of the nose, a less-than-ideal spot to land.
Inside the nasal valve, the surface is skin-like and doesn’t absorb very well. Its narrow design slows airflow, preventing particles from moving to deeper regions, where tissue is vascular and porous like the lungs. And even if this structural roadblock is surpassed, other hurdles remain.
The nose is designed to keep stuff out. Nose hair, cilia, mucus, sneezing, coughing – all make “distributing drugs evenly across the nasal cavity difficult,” said Dr. Smyth. “The spray gets filtered out before it reaches those deeper zones,” potentially dripping out of the nostrils instead of being absorbed.
Complicating matters is how every person’s nose is different. In a 2018 study, Dr. Smyth and a research team created three dimensional–printed models of people’s nasal cavities. They varied widely. “Nasal cavities are very different in size, length, and internal geometry,” he said. “This makes it challenging to target specific areas.”
Although carefully positioning the spray nozzle can help, even something as minor as sniffing too hard (constricting the nostrils) can keep sprays from reaching the absorptive deeper regions.
Still, the benefits are enough to compel researchers to find a way in.
“This really is a drug delivery challenge we’ve been wrestling with,” said Dr. Hindle. “It’s not new formulations we hear about. It’s new devices and delivery methods trying to target the different nasal regions.”
Delivering the goods
In the late aughts, John Hoekman was a graduate student in the University of Washington’s pharmaceutics program, studying nasal drug delivery. In his experiments, he noticed that drugs distributed differently, depending on the region targeted – aiming for the upper nasal cavity led to a spike in absorption.
The results convinced Mr. Hoekman to stake his future on nasal drug delivery.
In 2008, while still in graduate school, he started his own company, now known as Impel Pharmaceuticals. In 2021, Impel released its first product: Trudhesa, a nasal spray for migraines. Although the drug itself – dihydroergotamine mesylate – was hardly novel, used for migraine relief since 1946 (Headache. 2020 Jan;60[1]:40-57), it was usually delivered through an intravenous line, often in the ED.
But with Mr. Hoekman’s POD device – short for precision olfactory delivery – the drug can be given by the patient, via the nose. This generally means faster, more reliable relief, with fewer side effects. “We were able to lower the dose and improve the overall absorption,” said Mr. Hoekman.
The POD’s nozzle is engineered to spray a soft, narrow plume. It’s gas propelled, so patients don’t have to breathe in any special way to ensure delivery. The drug can zip right through the nasal valve into the upper nasal cavity.
Another company – OptiNose – has a “bidirectional” delivery method that propels drugs, either liquid or dry powder, deep into the nose.
“You insert the nozzle into your nose, and as you blow through the mouthpiece, your soft palate closes,” said Dr. Hindle. With the throat sealed off, “the only place for the drug to go is into one nostril and out the other, coating both sides of the nasal passageways.”
The device is only available for Onzetra Xsail, a powder for migraines. But another application is on its way.
In May, OptiNose announced that the FDA is reviewing Xhance, which uses the system to direct a steroid to the sinuses. In a clinical trial, patients with chronic sinusitis who tried the drug-device combo saw a decline in congestion, facial pain, and inflammation.
Targeting the brain
Both of those migraine drugs – Trudhesa and Onzetra Xsail – are thought to penetrate the upper nasal cavity. That’s where you’ll find the olfactory zone, a sheet of neurons that connects to the olfactory bulb. Located behind the eyes, these two nerve bundles detect odors.
“The olfactory region is almost like a back door to the brain,” said Mr. Hoekman.
By bypassing the blood-brain barrier, it offers a direct pathway – the only direct pathway, actually – between an exposed area of the body and the brain. Meaning it can ferry drugs straight from the nasal cavity to the central nervous system.
Nose-to-brain treatments could be game-changing for central nervous system disorders, such as Parkinson’s disease, Alzheimer’s, or anxiety.
But reaching the olfactory zone is notoriously hard. “The vasculature in your nose is like a big freeway, and the olfactory tract is like a side alley,” explained Mr. Hoekman. “It’s very limiting in what it will allow through.” The region is also small, occupying only 3%-10% of the nasal cavity’s surface area.
Again, POD means “precision olfactory delivery.” But the device isn’t quite as laser focused on the region as its name implies. “We’re not at the stage where we’re able to exclusively deliver to one target site in the nose,” said Dr. Hindle.
While wending its way toward the olfactory zone, some of the drug will be absorbed by other regions, then circulate throughout the body.
“About 59% of the drug that we put into the upper nasal space gets absorbed into the bloodstream,” said Mr. Hoekman.
Janssen Pharmaceuticals’ Spravato – a nasal spray for drug-resistant depression – is thought to work similarly: Some goes straight to the brain via the olfactory nerves, while the rest takes a more roundabout route, passing through the blood vessels to circulate in your system.
A needle-free option
Sometimes, the bloodstream is the main target. Because the nose’s middle and upper stretches are so vascular, drugs can be rapidly absorbed.
This is especially valuable for time-sensitive conditions. “If you give something nasally, you can have peak uptake in 15-30 minutes,” said Mr. Hoekman.
Take Narcan nasal spray, which delivers a burst of naloxone to quickly reverse the effects of opioid an overdose. Or Noctiva nasal spray. Taken just half an hour before bed, it can prevent frequent nighttime urination.
There’s also a group of seizure-stopping sprays, known as “rescue treatments.” One works by temporarily loosening the space between nasal cells, allowing the seizure drug to be quickly absorbed through the vessels.
This systemic access also has potential for drugs that would otherwise have to be injected, such as biologics.
The same goes for vaccines. Mucosal tissue inside the nasal cavity offers direct access to the infection-fighting lymphatic system, making the nose a prime target for inoculation against certain viruses.
Inhaling protection against viruses
Despite the recent surge of interest, nasal vaccines faced a rocky start. After the first nasal flu vaccine hit the market in 2001, it was pulled due to potential toxicity and reports of Bell’s palsy, a type of facial paralysis.
FluMist came in 2003 and has been plagued by problems ever since. Because it contains a weakened live virus, flu-like side effects can occur. And it doesn’t always work. During the 2016-2017 flu season, FluMist protected only 3% of kids, prompting the Centers for Disease Control and Prevention to advise against the nasal route that year.
Why FluMist can be so hit-or-miss is poorly understood. But generally, the nose can pose an effectiveness challenge. “The nose is highly cycling,” said Dr. Hindle. “Anything we deposit usually gets transported out within 15-20 minutes.”
For kids – big fans of not using needles – chronically runny noses can be an issue. “You squirt it in the nose, and it will probably just come back out in their snot,” said Jay Kolls, MD, a professor of medicine and pediatrics at Tulane University, New Orleans, who is developing an intranasal pneumonia vaccine.
Even so, nasal vaccines became a hot topic among researchers after the world was shut down by a virus that invades through the nose.
“We realized that intramuscular vaccines were effective at preventing severe disease, but they weren’t that effective at preventing transmission,” said Michael Diamond, MD, PhD, an immunologist at Washington University in St. Louis.
Nasal vaccines could solve that problem by putting an immune barrier at the point of entry, denying access to the rest of the body. “You squash the infection early enough that it not only prevents disease,” said Dr. Kolls, “but potentially prevents transmission.”
And yes, a nasal COVID vaccine is on the way
In March 2020, Dr. Diamond’s team began exploring a nasal COVID vaccine. Promising results in animals prompted a vaccine development company to license the technology. The resulting nasal vaccine – the first for COVID – has been approved in India, both as a primary vaccine and a booster.
It works by stimulating an influx of IgA, a type of antibody found in the nasal passages, and production of resident memory T cells, immune cells on standby just beneath the surface tissue in the nose.
By contrast, injected vaccines generate mostly IgG antibodies, which struggle to enter the respiratory tract. Only a tiny fraction – an estimated 1% – typically reach the nose.
Nasal vaccines could also be used along with shots. The latter could prime the whole body to fight back, while a nasal spritz could pull that immune protection to the mucosal surfaces.
Nasal technology could yield more effective vaccines for infections like tuberculosis or malaria, or even safeguard against new – sometimes surprising – conditions.
In a 2021 Nature study, an intranasal vaccine derived from fentanyl was better at preventing overdose than an injected vaccine. “Through some clever chemistry, the drug [in the vaccine] isn’t fentanyl anymore,” said study author Elizabeth Norton, PhD, an assistant professor of microbiology and immunology at Tulane University. “But the immune system still has an antibody response to it.”
Novel applications like this represent the future of nasal drug delivery.
“We’re not going to innovate in asthma or COPD. We’re not going to innovate in local delivery to the nose,” said Dr. Hindle. “Innovation will only come if we look to treat new conditions.”
A version of this article originally appeared on WebMD.com.
Noses are like caverns – twisting, turning, no two exactly the same. But if you nose past anyone’s nostrils, you’ll discover a surprisingly sprawling space.
“The size of the nasal cavity is about the same as a large handkerchief,” said Hugh Smyth, PhD, a professor of molecular pharmaceutics and drug delivery at the University of Texas at Austin.
“It’s very accessible tissue, and it has a lot of blood flow,” said Dr. Smyth. “The speed of onset can often be as fast as injections, sometimes even faster.”
It’s nothing new to get medicines via your nose. For decades, we’ve squirted various sprays into our nostrils to treat local maladies like allergies or infections. Even the ancients saw wisdom in the nasal route.
But recently, the nose has gained scientific attention as a gateway to the rest of the body – even the brain, a notoriously difficult target.
The upshot: Someday, inhaling therapies could be as routine as swallowing pills.
The nasal route is quick, needle free, and user friendly, and it often requires a smaller dose than other methods, since the drug doesn’t have to pass through the digestive tract, losing potency during digestion.
But there are challenges.
How hard can it be?
Old-school nasal sprayers, mostly unchanged since the 1800s, aren’t cut out for deep-nose delivery. “The technology is relatively limited because you’ve just got a single spray nozzle,” said Michael Hindle, PhD, a professor of pharmaceutics at Virginia Commonwealth University, Richmond.
These traditional devices (similar to perfume sprayers) don’t consistently push meds past the lower to middle sections inside the nose, called the nasal valve – if they do so at all: In a 2020 Rhinology study (doi: 10.4193/Rhin18.304) conventional nasal sprays only reached this first segment of the nose, a less-than-ideal spot to land.
Inside the nasal valve, the surface is skin-like and doesn’t absorb very well. Its narrow design slows airflow, preventing particles from moving to deeper regions, where tissue is vascular and porous like the lungs. And even if this structural roadblock is surpassed, other hurdles remain.
The nose is designed to keep stuff out. Nose hair, cilia, mucus, sneezing, coughing – all make “distributing drugs evenly across the nasal cavity difficult,” said Dr. Smyth. “The spray gets filtered out before it reaches those deeper zones,” potentially dripping out of the nostrils instead of being absorbed.
Complicating matters is how every person’s nose is different. In a 2018 study, Dr. Smyth and a research team created three dimensional–printed models of people’s nasal cavities. They varied widely. “Nasal cavities are very different in size, length, and internal geometry,” he said. “This makes it challenging to target specific areas.”
Although carefully positioning the spray nozzle can help, even something as minor as sniffing too hard (constricting the nostrils) can keep sprays from reaching the absorptive deeper regions.
Still, the benefits are enough to compel researchers to find a way in.
“This really is a drug delivery challenge we’ve been wrestling with,” said Dr. Hindle. “It’s not new formulations we hear about. It’s new devices and delivery methods trying to target the different nasal regions.”
Delivering the goods
In the late aughts, John Hoekman was a graduate student in the University of Washington’s pharmaceutics program, studying nasal drug delivery. In his experiments, he noticed that drugs distributed differently, depending on the region targeted – aiming for the upper nasal cavity led to a spike in absorption.
The results convinced Mr. Hoekman to stake his future on nasal drug delivery.
In 2008, while still in graduate school, he started his own company, now known as Impel Pharmaceuticals. In 2021, Impel released its first product: Trudhesa, a nasal spray for migraines. Although the drug itself – dihydroergotamine mesylate – was hardly novel, used for migraine relief since 1946 (Headache. 2020 Jan;60[1]:40-57), it was usually delivered through an intravenous line, often in the ED.
But with Mr. Hoekman’s POD device – short for precision olfactory delivery – the drug can be given by the patient, via the nose. This generally means faster, more reliable relief, with fewer side effects. “We were able to lower the dose and improve the overall absorption,” said Mr. Hoekman.
The POD’s nozzle is engineered to spray a soft, narrow plume. It’s gas propelled, so patients don’t have to breathe in any special way to ensure delivery. The drug can zip right through the nasal valve into the upper nasal cavity.
Another company – OptiNose – has a “bidirectional” delivery method that propels drugs, either liquid or dry powder, deep into the nose.
“You insert the nozzle into your nose, and as you blow through the mouthpiece, your soft palate closes,” said Dr. Hindle. With the throat sealed off, “the only place for the drug to go is into one nostril and out the other, coating both sides of the nasal passageways.”
The device is only available for Onzetra Xsail, a powder for migraines. But another application is on its way.
In May, OptiNose announced that the FDA is reviewing Xhance, which uses the system to direct a steroid to the sinuses. In a clinical trial, patients with chronic sinusitis who tried the drug-device combo saw a decline in congestion, facial pain, and inflammation.
Targeting the brain
Both of those migraine drugs – Trudhesa and Onzetra Xsail – are thought to penetrate the upper nasal cavity. That’s where you’ll find the olfactory zone, a sheet of neurons that connects to the olfactory bulb. Located behind the eyes, these two nerve bundles detect odors.
“The olfactory region is almost like a back door to the brain,” said Mr. Hoekman.
By bypassing the blood-brain barrier, it offers a direct pathway – the only direct pathway, actually – between an exposed area of the body and the brain. Meaning it can ferry drugs straight from the nasal cavity to the central nervous system.
Nose-to-brain treatments could be game-changing for central nervous system disorders, such as Parkinson’s disease, Alzheimer’s, or anxiety.
But reaching the olfactory zone is notoriously hard. “The vasculature in your nose is like a big freeway, and the olfactory tract is like a side alley,” explained Mr. Hoekman. “It’s very limiting in what it will allow through.” The region is also small, occupying only 3%-10% of the nasal cavity’s surface area.
Again, POD means “precision olfactory delivery.” But the device isn’t quite as laser focused on the region as its name implies. “We’re not at the stage where we’re able to exclusively deliver to one target site in the nose,” said Dr. Hindle.
While wending its way toward the olfactory zone, some of the drug will be absorbed by other regions, then circulate throughout the body.
“About 59% of the drug that we put into the upper nasal space gets absorbed into the bloodstream,” said Mr. Hoekman.
Janssen Pharmaceuticals’ Spravato – a nasal spray for drug-resistant depression – is thought to work similarly: Some goes straight to the brain via the olfactory nerves, while the rest takes a more roundabout route, passing through the blood vessels to circulate in your system.
A needle-free option
Sometimes, the bloodstream is the main target. Because the nose’s middle and upper stretches are so vascular, drugs can be rapidly absorbed.
This is especially valuable for time-sensitive conditions. “If you give something nasally, you can have peak uptake in 15-30 minutes,” said Mr. Hoekman.
Take Narcan nasal spray, which delivers a burst of naloxone to quickly reverse the effects of opioid an overdose. Or Noctiva nasal spray. Taken just half an hour before bed, it can prevent frequent nighttime urination.
There’s also a group of seizure-stopping sprays, known as “rescue treatments.” One works by temporarily loosening the space between nasal cells, allowing the seizure drug to be quickly absorbed through the vessels.
This systemic access also has potential for drugs that would otherwise have to be injected, such as biologics.
The same goes for vaccines. Mucosal tissue inside the nasal cavity offers direct access to the infection-fighting lymphatic system, making the nose a prime target for inoculation against certain viruses.
Inhaling protection against viruses
Despite the recent surge of interest, nasal vaccines faced a rocky start. After the first nasal flu vaccine hit the market in 2001, it was pulled due to potential toxicity and reports of Bell’s palsy, a type of facial paralysis.
FluMist came in 2003 and has been plagued by problems ever since. Because it contains a weakened live virus, flu-like side effects can occur. And it doesn’t always work. During the 2016-2017 flu season, FluMist protected only 3% of kids, prompting the Centers for Disease Control and Prevention to advise against the nasal route that year.
Why FluMist can be so hit-or-miss is poorly understood. But generally, the nose can pose an effectiveness challenge. “The nose is highly cycling,” said Dr. Hindle. “Anything we deposit usually gets transported out within 15-20 minutes.”
For kids – big fans of not using needles – chronically runny noses can be an issue. “You squirt it in the nose, and it will probably just come back out in their snot,” said Jay Kolls, MD, a professor of medicine and pediatrics at Tulane University, New Orleans, who is developing an intranasal pneumonia vaccine.
Even so, nasal vaccines became a hot topic among researchers after the world was shut down by a virus that invades through the nose.
“We realized that intramuscular vaccines were effective at preventing severe disease, but they weren’t that effective at preventing transmission,” said Michael Diamond, MD, PhD, an immunologist at Washington University in St. Louis.
Nasal vaccines could solve that problem by putting an immune barrier at the point of entry, denying access to the rest of the body. “You squash the infection early enough that it not only prevents disease,” said Dr. Kolls, “but potentially prevents transmission.”
And yes, a nasal COVID vaccine is on the way
In March 2020, Dr. Diamond’s team began exploring a nasal COVID vaccine. Promising results in animals prompted a vaccine development company to license the technology. The resulting nasal vaccine – the first for COVID – has been approved in India, both as a primary vaccine and a booster.
It works by stimulating an influx of IgA, a type of antibody found in the nasal passages, and production of resident memory T cells, immune cells on standby just beneath the surface tissue in the nose.
By contrast, injected vaccines generate mostly IgG antibodies, which struggle to enter the respiratory tract. Only a tiny fraction – an estimated 1% – typically reach the nose.
Nasal vaccines could also be used along with shots. The latter could prime the whole body to fight back, while a nasal spritz could pull that immune protection to the mucosal surfaces.
Nasal technology could yield more effective vaccines for infections like tuberculosis or malaria, or even safeguard against new – sometimes surprising – conditions.
In a 2021 Nature study, an intranasal vaccine derived from fentanyl was better at preventing overdose than an injected vaccine. “Through some clever chemistry, the drug [in the vaccine] isn’t fentanyl anymore,” said study author Elizabeth Norton, PhD, an assistant professor of microbiology and immunology at Tulane University. “But the immune system still has an antibody response to it.”
Novel applications like this represent the future of nasal drug delivery.
“We’re not going to innovate in asthma or COPD. We’re not going to innovate in local delivery to the nose,” said Dr. Hindle. “Innovation will only come if we look to treat new conditions.”
A version of this article originally appeared on WebMD.com.
West Nile virus cases rising nationwide amid mosquito season
In the past 2 weeks, new cases have been reported in Iowa and Nebraska, adding to previous 2023 reports from Arizona, Georgia, Illinois, Louisiana, Oregon, Pennsylvania, and Wyoming. A mosquito at a monitoring site near Houston tested positive last week for the potentially fatal virus, prompting local health officials to begin evening spray operations in the area where the mosquito was found, according to an announcement from Harris County Public Health.
According to the CDC, which compiles local reports, there have been 13 human cases of West Nile virus in 2023. In 2022, there were 1,126 cases, including 90 deaths.
Among this year’s 13 cases reported to the CDC so far, eight people add severe neuroinvasive disease, which means the disease spread to the nervous system. Such severe symptoms typically occur in 1 in every 150 cases of West Nile virus and can include encephalitis, which is inflammation of the brain, or meningitis, which is inflammation of the membranes that surround the brain and spinal cord. Three of the neuroinvasive cases occurred earlier this year amid an outbreak in Maricopa County, Arizona, where the disease is considered endemic, according to an April 28 report from the CDC.
The CDC says West Nile virus is the most common disease spread by mosquitoes in the continental United States. Local health officials sample mosquitoes to guide mosquito control strategies. So far this year, the CDC has received 28 reports of mosquitoes testing positive. Those mosquito testing reports came from Arizona, California, Florida, Indiana, Louisiana, and Texas.
West Nile virus is transmitted to people by the bite of an infected mosquito, but it can also be spread to humans if they handle a dead bird that is infected. The CDC says there are no medications to treat the virus in people. Most people who are infected do not feel sick, and 1 in 5 people infected develop a fever and other symptoms like headache, body ache, or a rash.
Prevention strategies are to wear insect repellent and to wear long-sleeved shirts and long pants to avoid mosquito bites.
A version of this article originally appeared on WebMD.com.
In the past 2 weeks, new cases have been reported in Iowa and Nebraska, adding to previous 2023 reports from Arizona, Georgia, Illinois, Louisiana, Oregon, Pennsylvania, and Wyoming. A mosquito at a monitoring site near Houston tested positive last week for the potentially fatal virus, prompting local health officials to begin evening spray operations in the area where the mosquito was found, according to an announcement from Harris County Public Health.
According to the CDC, which compiles local reports, there have been 13 human cases of West Nile virus in 2023. In 2022, there were 1,126 cases, including 90 deaths.
Among this year’s 13 cases reported to the CDC so far, eight people add severe neuroinvasive disease, which means the disease spread to the nervous system. Such severe symptoms typically occur in 1 in every 150 cases of West Nile virus and can include encephalitis, which is inflammation of the brain, or meningitis, which is inflammation of the membranes that surround the brain and spinal cord. Three of the neuroinvasive cases occurred earlier this year amid an outbreak in Maricopa County, Arizona, where the disease is considered endemic, according to an April 28 report from the CDC.
The CDC says West Nile virus is the most common disease spread by mosquitoes in the continental United States. Local health officials sample mosquitoes to guide mosquito control strategies. So far this year, the CDC has received 28 reports of mosquitoes testing positive. Those mosquito testing reports came from Arizona, California, Florida, Indiana, Louisiana, and Texas.
West Nile virus is transmitted to people by the bite of an infected mosquito, but it can also be spread to humans if they handle a dead bird that is infected. The CDC says there are no medications to treat the virus in people. Most people who are infected do not feel sick, and 1 in 5 people infected develop a fever and other symptoms like headache, body ache, or a rash.
Prevention strategies are to wear insect repellent and to wear long-sleeved shirts and long pants to avoid mosquito bites.
A version of this article originally appeared on WebMD.com.
In the past 2 weeks, new cases have been reported in Iowa and Nebraska, adding to previous 2023 reports from Arizona, Georgia, Illinois, Louisiana, Oregon, Pennsylvania, and Wyoming. A mosquito at a monitoring site near Houston tested positive last week for the potentially fatal virus, prompting local health officials to begin evening spray operations in the area where the mosquito was found, according to an announcement from Harris County Public Health.
According to the CDC, which compiles local reports, there have been 13 human cases of West Nile virus in 2023. In 2022, there were 1,126 cases, including 90 deaths.
Among this year’s 13 cases reported to the CDC so far, eight people add severe neuroinvasive disease, which means the disease spread to the nervous system. Such severe symptoms typically occur in 1 in every 150 cases of West Nile virus and can include encephalitis, which is inflammation of the brain, or meningitis, which is inflammation of the membranes that surround the brain and spinal cord. Three of the neuroinvasive cases occurred earlier this year amid an outbreak in Maricopa County, Arizona, where the disease is considered endemic, according to an April 28 report from the CDC.
The CDC says West Nile virus is the most common disease spread by mosquitoes in the continental United States. Local health officials sample mosquitoes to guide mosquito control strategies. So far this year, the CDC has received 28 reports of mosquitoes testing positive. Those mosquito testing reports came from Arizona, California, Florida, Indiana, Louisiana, and Texas.
West Nile virus is transmitted to people by the bite of an infected mosquito, but it can also be spread to humans if they handle a dead bird that is infected. The CDC says there are no medications to treat the virus in people. Most people who are infected do not feel sick, and 1 in 5 people infected develop a fever and other symptoms like headache, body ache, or a rash.
Prevention strategies are to wear insect repellent and to wear long-sleeved shirts and long pants to avoid mosquito bites.
A version of this article originally appeared on WebMD.com.
NAFLD increases risk for severe infections
People with nonalcoholic fatty liver disease (NAFLD) are more likely to develop severe infections requiring hospitalization, according to findings from a large Swedish cohort study.
The increased risk was equal to one extra severe infection in every six patients with NAFLD by 20 years after diagnosis, wrote Fahim Ebrahimi, MD, of the Karolinska Institute in Stockholm, and coauthors.
“Accumulating evidence suggests that NAFLD can affect multiple organ systems, which is not surprising, as the liver has multiple functions – regulating metabolism and being a central organ of the immune system,” Dr. Ebrahimi said in an interview.
The study was published online in Clinical Gastroenterology and Hepatology.
“Up to a fifth of cells in the liver are immune cells that process numerous antigens and pathogens from the gastrointestinal tract,” Dr. Ebrahimi noted. “We were intrigued by experimental studies showing that, in NAFLD, many of these key immune cells become dysfunctional at various levels, which may affect disease progression, but at the same time also increase the susceptibility to viral, bacterial, and fungal infections.”
Patients with NAFLD have metabolic risk factors known to increase infection risk, but a smaller study by a different research group had found that NAFLD could independently predispose patients to bacterial infections.
To further explore a connection between NAFLD and infection risk, the researchers looked at data for 12,133 Swedish adults with simple steatosis, nonfibrotic steatohepatitis, noncirrhotic fibrosis, or cirrhosis caused by NAFLD confirmed by liver biopsies performed between 1969 and 2017.
Each patient was matched to five or more contemporary controls from the general population by age, sex, and region of residence. The authors conducted an additional analysis that also adjusted for education, country of birth, and baseline clinical comorbidities, including diabetes, obesity, dyslipidemia, and hypertension, as well as hospitalization preceding the biopsy and chronic obstructive pulmonary disease.
The primary endpoint was severe infections requiring hospital admission. Secondary endpoints included seven prespecified infection subgroups: sepsis; respiratory tract; most gastrointestinal infections; bacterial peritonitis; urogenital; muscle, skin, and soft tissue; and other infections.
Elevated risk at all NAFLD stages
Dr. Ebrahimi and colleagues found that over a median follow-up of 14 years, patients with NAFLD had a higher incidence of severe infections – most often respiratory or urinary tract infections – compared with those without NAFLD (32% vs. 17%, respectively).
Biopsy-confirmed NAFLD was also associated with a 71% higher hazard and a 20-year absolute excess risk of 17.3% for severe infections requiring hospital admission versus comparators. The elevated risk showed up in patients with steatosis and increased with the severity of NAFLD. Simple steatosis saw a 64% higher risk (adjusted hazard ratio, 1.64; 95% confidence interval, 1.55-1.73), whereas patients with cirrhosis saw a more than twofold higher risk, compared with controls (aHR, 2.32; 95% CI, 1.92-2.82).
When Dr. Ebrahimi and colleagues adjusted for parameters of the metabolic syndrome, they found an independent increased risk for severe infection. For patients with NAFLD, the increased risk may come from greater susceptibility to infections in general or to a more severe course of infections.
“Our study clearly demonstrates the complexity and high disease burden associated with NAFLD,” Dr. Ebrahimi said. “We are beginning to understand the different layers involved and will eventually move away from a liver-centric view to a more holistic view of the disease.”
Clinicians caring for patients with NAFLD need to be aware of the increased risk for infection, Dr. Ebrahimi said. They also should assess their patients’ vaccination status, and seek to control modifiable risk factors, such as diabetes.
Nancy Reau, MD, of Rush University, Chicago, described the study’s message as important.
“Patients with NAFLD and advancing liver disease are at risk for severe infections,” Dr. Reau said. “When we consider the fact that patients with advanced liver disease tend to die from infectious complications, awareness leading to early recognition and efficient treatment is imperative.”
The authors acknowledged the following limitations: only severe infections requiring hospitalization could be captured; whether infection led to decompensation or vice versa among patients with cirrhosis could not be determined; and detailed data on smoking, alcohol, vaccinations, body mass, and other potentially relevant measures were not available.
The Swiss National Science Foundation, Syskonen Svensson Foundation, and Bengt Ihre Foundation provided grants to Dr. Ebrahimi or coauthors. One coauthor disclosed previous research funding from Janssen and MSD. Dr. Reau disclosed receiving research support and consulting fees from AbbVie and Gilead, as well as consulting fees from Arbutus, Intercept, and Salix.
A version of this article first appeared on Medscape.com.
People with nonalcoholic fatty liver disease (NAFLD) are more likely to develop severe infections requiring hospitalization, according to findings from a large Swedish cohort study.
The increased risk was equal to one extra severe infection in every six patients with NAFLD by 20 years after diagnosis, wrote Fahim Ebrahimi, MD, of the Karolinska Institute in Stockholm, and coauthors.
“Accumulating evidence suggests that NAFLD can affect multiple organ systems, which is not surprising, as the liver has multiple functions – regulating metabolism and being a central organ of the immune system,” Dr. Ebrahimi said in an interview.
The study was published online in Clinical Gastroenterology and Hepatology.
“Up to a fifth of cells in the liver are immune cells that process numerous antigens and pathogens from the gastrointestinal tract,” Dr. Ebrahimi noted. “We were intrigued by experimental studies showing that, in NAFLD, many of these key immune cells become dysfunctional at various levels, which may affect disease progression, but at the same time also increase the susceptibility to viral, bacterial, and fungal infections.”
Patients with NAFLD have metabolic risk factors known to increase infection risk, but a smaller study by a different research group had found that NAFLD could independently predispose patients to bacterial infections.
To further explore a connection between NAFLD and infection risk, the researchers looked at data for 12,133 Swedish adults with simple steatosis, nonfibrotic steatohepatitis, noncirrhotic fibrosis, or cirrhosis caused by NAFLD confirmed by liver biopsies performed between 1969 and 2017.
Each patient was matched to five or more contemporary controls from the general population by age, sex, and region of residence. The authors conducted an additional analysis that also adjusted for education, country of birth, and baseline clinical comorbidities, including diabetes, obesity, dyslipidemia, and hypertension, as well as hospitalization preceding the biopsy and chronic obstructive pulmonary disease.
The primary endpoint was severe infections requiring hospital admission. Secondary endpoints included seven prespecified infection subgroups: sepsis; respiratory tract; most gastrointestinal infections; bacterial peritonitis; urogenital; muscle, skin, and soft tissue; and other infections.
Elevated risk at all NAFLD stages
Dr. Ebrahimi and colleagues found that over a median follow-up of 14 years, patients with NAFLD had a higher incidence of severe infections – most often respiratory or urinary tract infections – compared with those without NAFLD (32% vs. 17%, respectively).
Biopsy-confirmed NAFLD was also associated with a 71% higher hazard and a 20-year absolute excess risk of 17.3% for severe infections requiring hospital admission versus comparators. The elevated risk showed up in patients with steatosis and increased with the severity of NAFLD. Simple steatosis saw a 64% higher risk (adjusted hazard ratio, 1.64; 95% confidence interval, 1.55-1.73), whereas patients with cirrhosis saw a more than twofold higher risk, compared with controls (aHR, 2.32; 95% CI, 1.92-2.82).
When Dr. Ebrahimi and colleagues adjusted for parameters of the metabolic syndrome, they found an independent increased risk for severe infection. For patients with NAFLD, the increased risk may come from greater susceptibility to infections in general or to a more severe course of infections.
“Our study clearly demonstrates the complexity and high disease burden associated with NAFLD,” Dr. Ebrahimi said. “We are beginning to understand the different layers involved and will eventually move away from a liver-centric view to a more holistic view of the disease.”
Clinicians caring for patients with NAFLD need to be aware of the increased risk for infection, Dr. Ebrahimi said. They also should assess their patients’ vaccination status, and seek to control modifiable risk factors, such as diabetes.
Nancy Reau, MD, of Rush University, Chicago, described the study’s message as important.
“Patients with NAFLD and advancing liver disease are at risk for severe infections,” Dr. Reau said. “When we consider the fact that patients with advanced liver disease tend to die from infectious complications, awareness leading to early recognition and efficient treatment is imperative.”
The authors acknowledged the following limitations: only severe infections requiring hospitalization could be captured; whether infection led to decompensation or vice versa among patients with cirrhosis could not be determined; and detailed data on smoking, alcohol, vaccinations, body mass, and other potentially relevant measures were not available.
The Swiss National Science Foundation, Syskonen Svensson Foundation, and Bengt Ihre Foundation provided grants to Dr. Ebrahimi or coauthors. One coauthor disclosed previous research funding from Janssen and MSD. Dr. Reau disclosed receiving research support and consulting fees from AbbVie and Gilead, as well as consulting fees from Arbutus, Intercept, and Salix.
A version of this article first appeared on Medscape.com.
People with nonalcoholic fatty liver disease (NAFLD) are more likely to develop severe infections requiring hospitalization, according to findings from a large Swedish cohort study.
The increased risk was equal to one extra severe infection in every six patients with NAFLD by 20 years after diagnosis, wrote Fahim Ebrahimi, MD, of the Karolinska Institute in Stockholm, and coauthors.
“Accumulating evidence suggests that NAFLD can affect multiple organ systems, which is not surprising, as the liver has multiple functions – regulating metabolism and being a central organ of the immune system,” Dr. Ebrahimi said in an interview.
The study was published online in Clinical Gastroenterology and Hepatology.
“Up to a fifth of cells in the liver are immune cells that process numerous antigens and pathogens from the gastrointestinal tract,” Dr. Ebrahimi noted. “We were intrigued by experimental studies showing that, in NAFLD, many of these key immune cells become dysfunctional at various levels, which may affect disease progression, but at the same time also increase the susceptibility to viral, bacterial, and fungal infections.”
Patients with NAFLD have metabolic risk factors known to increase infection risk, but a smaller study by a different research group had found that NAFLD could independently predispose patients to bacterial infections.
To further explore a connection between NAFLD and infection risk, the researchers looked at data for 12,133 Swedish adults with simple steatosis, nonfibrotic steatohepatitis, noncirrhotic fibrosis, or cirrhosis caused by NAFLD confirmed by liver biopsies performed between 1969 and 2017.
Each patient was matched to five or more contemporary controls from the general population by age, sex, and region of residence. The authors conducted an additional analysis that also adjusted for education, country of birth, and baseline clinical comorbidities, including diabetes, obesity, dyslipidemia, and hypertension, as well as hospitalization preceding the biopsy and chronic obstructive pulmonary disease.
The primary endpoint was severe infections requiring hospital admission. Secondary endpoints included seven prespecified infection subgroups: sepsis; respiratory tract; most gastrointestinal infections; bacterial peritonitis; urogenital; muscle, skin, and soft tissue; and other infections.
Elevated risk at all NAFLD stages
Dr. Ebrahimi and colleagues found that over a median follow-up of 14 years, patients with NAFLD had a higher incidence of severe infections – most often respiratory or urinary tract infections – compared with those without NAFLD (32% vs. 17%, respectively).
Biopsy-confirmed NAFLD was also associated with a 71% higher hazard and a 20-year absolute excess risk of 17.3% for severe infections requiring hospital admission versus comparators. The elevated risk showed up in patients with steatosis and increased with the severity of NAFLD. Simple steatosis saw a 64% higher risk (adjusted hazard ratio, 1.64; 95% confidence interval, 1.55-1.73), whereas patients with cirrhosis saw a more than twofold higher risk, compared with controls (aHR, 2.32; 95% CI, 1.92-2.82).
When Dr. Ebrahimi and colleagues adjusted for parameters of the metabolic syndrome, they found an independent increased risk for severe infection. For patients with NAFLD, the increased risk may come from greater susceptibility to infections in general or to a more severe course of infections.
“Our study clearly demonstrates the complexity and high disease burden associated with NAFLD,” Dr. Ebrahimi said. “We are beginning to understand the different layers involved and will eventually move away from a liver-centric view to a more holistic view of the disease.”
Clinicians caring for patients with NAFLD need to be aware of the increased risk for infection, Dr. Ebrahimi said. They also should assess their patients’ vaccination status, and seek to control modifiable risk factors, such as diabetes.
Nancy Reau, MD, of Rush University, Chicago, described the study’s message as important.
“Patients with NAFLD and advancing liver disease are at risk for severe infections,” Dr. Reau said. “When we consider the fact that patients with advanced liver disease tend to die from infectious complications, awareness leading to early recognition and efficient treatment is imperative.”
The authors acknowledged the following limitations: only severe infections requiring hospitalization could be captured; whether infection led to decompensation or vice versa among patients with cirrhosis could not be determined; and detailed data on smoking, alcohol, vaccinations, body mass, and other potentially relevant measures were not available.
The Swiss National Science Foundation, Syskonen Svensson Foundation, and Bengt Ihre Foundation provided grants to Dr. Ebrahimi or coauthors. One coauthor disclosed previous research funding from Janssen and MSD. Dr. Reau disclosed receiving research support and consulting fees from AbbVie and Gilead, as well as consulting fees from Arbutus, Intercept, and Salix.
A version of this article first appeared on Medscape.com.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Bordetella parapertussis reemerges as a cause of respiratory illness in children
A 4-year-old male presented to an urgent care center with a 2-week history of runny nose and cough. The treating clinician suspected a postviral cough, but the child’s mother was unconvinced. Testing for SARS-CoV-2, influenza, and respiratory syncytial virus performed earlier in the week at the pediatrician’s office was negative. At the mother’s insistence, an expanded respiratory panel was ordered and revealed a surprising result: Bordetella parapertussis.
Just like B. pertussis, B. parapertussis can cause a prolonged cough illness characterized by coughing paroxysms, whoop, and posttussive emesis. Testing is the only way to reliably distinguish between the two infections. In general, disease due to B. parapertussis tends to be milder than typical pertussis and symptoms usually don’t last as long. In one study, 40% of people with B. parapertussis had no symptoms. B. parapertussis does not produce pertussis toxin and this may affect disease severity. Rarely, children can be coinfected with both B. pertussis and B. parapertussis.
The burden of B. parapertussis in the United States is not well described because only pertussis cases caused by B. pertussis are reportable to the Centers for Disease Control and Prevention. Nevertheless, some states include cases in public reporting and outbreaks have been reported. Historically, disease has been cyclical, with peaks in cases every 4 years and no seasonality.
This year, some communities are currently seeing an increase in B. parapertussis cases. Through June 11 of this year, 40 cases of B. parapertussis and no cases of B. pertussis have been identified at Norton Healthcare in Louisville, Ky. For comparison, one case of B. parapertussis was reported in 2022 and no cases were reported in 2021. Chatter on infectious diseases listservs suggests that clinicians in other communities are also seeing an increase in cases.
According to Andi Shane, MD, MPH, chief of the division of pediatric infectious diseases at Emory University and Children’s Healthcare of Atlanta, an unusually high number of children with B. parapertussis were identified in the Atlanta area this spring. “Fortunately, most children had mild illness and of these, only a few required admission to the hospital,” Dr. Shane said.
Back at the urgent care center, the clinician on duty called the patient’s mom to discuss the diagnosis of B. parapertussis. By the time the test result was available, the patient was asymptomatic. The clinician advised that antibiotic therapy was not indicated.
Treatment recommendations diverge for B. pertussis and B. parapertussis and this is a point of emphasis for clinicians. Treatment of B. pertussis during the catarrhal phase may ameliorate disease. Treatment initiated after the catarrhal phase has little impact on symptoms but may reduce spread to others. In most cases, treatment isn’t recommended for B. parapertussis. It is not clear how well antibiotics work against this organism. Macrolides such as erythromycin and azithromycin that are used to treat pertussis may have some activity, along with trimethoprim-sulfamethoxazole and ciprofloxacin. According to the American Academy of Pediatrics, treatment is usually reserved for individuals at risk for more severe disease, including infants, especially those less than 6 months of age, the elderly, and immunocompromised persons. Prophylactic antibiotic therapy is not recommended for most persons exposed to B. parapertussis, although some public health experts also recommend treatment of B. parapertussis-infected people in contact with young infants and others are risk for severe disease.
In recent epidemiologic reports, patients with B. parapertussis infection had received age-appropriate vaccination for pertussis, suggesting that available pertussis vaccines offer little to no protection against this disease. The best prevention strategies are similar to those that are effective against other illness spread by respiratory droplets. Sick people should stay at home and cover their coughs when around others. Everyone should practice good hand hygiene.
Are you seeing increased cases of B. parapertussis in your community? Email me at [email protected].
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She is a member of the AAP’s Committee on Infectious Diseases and one of the lead authors of the AAP’s Recommendations for Prevention and Control of Influenza in Children, 2022-2023. The opinions expressed in this article are her own. Dr. Bryant discloses that she has served as an investigator on clinical trials funded by Pfizer, Enanta and Gilead. Email her at [email protected].
A 4-year-old male presented to an urgent care center with a 2-week history of runny nose and cough. The treating clinician suspected a postviral cough, but the child’s mother was unconvinced. Testing for SARS-CoV-2, influenza, and respiratory syncytial virus performed earlier in the week at the pediatrician’s office was negative. At the mother’s insistence, an expanded respiratory panel was ordered and revealed a surprising result: Bordetella parapertussis.
Just like B. pertussis, B. parapertussis can cause a prolonged cough illness characterized by coughing paroxysms, whoop, and posttussive emesis. Testing is the only way to reliably distinguish between the two infections. In general, disease due to B. parapertussis tends to be milder than typical pertussis and symptoms usually don’t last as long. In one study, 40% of people with B. parapertussis had no symptoms. B. parapertussis does not produce pertussis toxin and this may affect disease severity. Rarely, children can be coinfected with both B. pertussis and B. parapertussis.
The burden of B. parapertussis in the United States is not well described because only pertussis cases caused by B. pertussis are reportable to the Centers for Disease Control and Prevention. Nevertheless, some states include cases in public reporting and outbreaks have been reported. Historically, disease has been cyclical, with peaks in cases every 4 years and no seasonality.
This year, some communities are currently seeing an increase in B. parapertussis cases. Through June 11 of this year, 40 cases of B. parapertussis and no cases of B. pertussis have been identified at Norton Healthcare in Louisville, Ky. For comparison, one case of B. parapertussis was reported in 2022 and no cases were reported in 2021. Chatter on infectious diseases listservs suggests that clinicians in other communities are also seeing an increase in cases.
According to Andi Shane, MD, MPH, chief of the division of pediatric infectious diseases at Emory University and Children’s Healthcare of Atlanta, an unusually high number of children with B. parapertussis were identified in the Atlanta area this spring. “Fortunately, most children had mild illness and of these, only a few required admission to the hospital,” Dr. Shane said.
Back at the urgent care center, the clinician on duty called the patient’s mom to discuss the diagnosis of B. parapertussis. By the time the test result was available, the patient was asymptomatic. The clinician advised that antibiotic therapy was not indicated.
Treatment recommendations diverge for B. pertussis and B. parapertussis and this is a point of emphasis for clinicians. Treatment of B. pertussis during the catarrhal phase may ameliorate disease. Treatment initiated after the catarrhal phase has little impact on symptoms but may reduce spread to others. In most cases, treatment isn’t recommended for B. parapertussis. It is not clear how well antibiotics work against this organism. Macrolides such as erythromycin and azithromycin that are used to treat pertussis may have some activity, along with trimethoprim-sulfamethoxazole and ciprofloxacin. According to the American Academy of Pediatrics, treatment is usually reserved for individuals at risk for more severe disease, including infants, especially those less than 6 months of age, the elderly, and immunocompromised persons. Prophylactic antibiotic therapy is not recommended for most persons exposed to B. parapertussis, although some public health experts also recommend treatment of B. parapertussis-infected people in contact with young infants and others are risk for severe disease.
In recent epidemiologic reports, patients with B. parapertussis infection had received age-appropriate vaccination for pertussis, suggesting that available pertussis vaccines offer little to no protection against this disease. The best prevention strategies are similar to those that are effective against other illness spread by respiratory droplets. Sick people should stay at home and cover their coughs when around others. Everyone should practice good hand hygiene.
Are you seeing increased cases of B. parapertussis in your community? Email me at [email protected].
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She is a member of the AAP’s Committee on Infectious Diseases and one of the lead authors of the AAP’s Recommendations for Prevention and Control of Influenza in Children, 2022-2023. The opinions expressed in this article are her own. Dr. Bryant discloses that she has served as an investigator on clinical trials funded by Pfizer, Enanta and Gilead. Email her at [email protected].
A 4-year-old male presented to an urgent care center with a 2-week history of runny nose and cough. The treating clinician suspected a postviral cough, but the child’s mother was unconvinced. Testing for SARS-CoV-2, influenza, and respiratory syncytial virus performed earlier in the week at the pediatrician’s office was negative. At the mother’s insistence, an expanded respiratory panel was ordered and revealed a surprising result: Bordetella parapertussis.
Just like B. pertussis, B. parapertussis can cause a prolonged cough illness characterized by coughing paroxysms, whoop, and posttussive emesis. Testing is the only way to reliably distinguish between the two infections. In general, disease due to B. parapertussis tends to be milder than typical pertussis and symptoms usually don’t last as long. In one study, 40% of people with B. parapertussis had no symptoms. B. parapertussis does not produce pertussis toxin and this may affect disease severity. Rarely, children can be coinfected with both B. pertussis and B. parapertussis.
The burden of B. parapertussis in the United States is not well described because only pertussis cases caused by B. pertussis are reportable to the Centers for Disease Control and Prevention. Nevertheless, some states include cases in public reporting and outbreaks have been reported. Historically, disease has been cyclical, with peaks in cases every 4 years and no seasonality.
This year, some communities are currently seeing an increase in B. parapertussis cases. Through June 11 of this year, 40 cases of B. parapertussis and no cases of B. pertussis have been identified at Norton Healthcare in Louisville, Ky. For comparison, one case of B. parapertussis was reported in 2022 and no cases were reported in 2021. Chatter on infectious diseases listservs suggests that clinicians in other communities are also seeing an increase in cases.
According to Andi Shane, MD, MPH, chief of the division of pediatric infectious diseases at Emory University and Children’s Healthcare of Atlanta, an unusually high number of children with B. parapertussis were identified in the Atlanta area this spring. “Fortunately, most children had mild illness and of these, only a few required admission to the hospital,” Dr. Shane said.
Back at the urgent care center, the clinician on duty called the patient’s mom to discuss the diagnosis of B. parapertussis. By the time the test result was available, the patient was asymptomatic. The clinician advised that antibiotic therapy was not indicated.
Treatment recommendations diverge for B. pertussis and B. parapertussis and this is a point of emphasis for clinicians. Treatment of B. pertussis during the catarrhal phase may ameliorate disease. Treatment initiated after the catarrhal phase has little impact on symptoms but may reduce spread to others. In most cases, treatment isn’t recommended for B. parapertussis. It is not clear how well antibiotics work against this organism. Macrolides such as erythromycin and azithromycin that are used to treat pertussis may have some activity, along with trimethoprim-sulfamethoxazole and ciprofloxacin. According to the American Academy of Pediatrics, treatment is usually reserved for individuals at risk for more severe disease, including infants, especially those less than 6 months of age, the elderly, and immunocompromised persons. Prophylactic antibiotic therapy is not recommended for most persons exposed to B. parapertussis, although some public health experts also recommend treatment of B. parapertussis-infected people in contact with young infants and others are risk for severe disease.
In recent epidemiologic reports, patients with B. parapertussis infection had received age-appropriate vaccination for pertussis, suggesting that available pertussis vaccines offer little to no protection against this disease. The best prevention strategies are similar to those that are effective against other illness spread by respiratory droplets. Sick people should stay at home and cover their coughs when around others. Everyone should practice good hand hygiene.
Are you seeing increased cases of B. parapertussis in your community? Email me at [email protected].
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She is a member of the AAP’s Committee on Infectious Diseases and one of the lead authors of the AAP’s Recommendations for Prevention and Control of Influenza in Children, 2022-2023. The opinions expressed in this article are her own. Dr. Bryant discloses that she has served as an investigator on clinical trials funded by Pfizer, Enanta and Gilead. Email her at [email protected].
FDA warns of tattoo ink tied to dangerous infections
The Food and Drug Administration draft guidance released recently on possible contamination of tattoo ink was not concerning Whitney Donohue, 34, owner of Forget Me Not Tattoo in Billings, Mont.
“I get our ink directly through the manufacturer – not at a store or through Amazon or eBay,” she said. “You never know if it’s going to be repackaged.”
Tattoo artists themselves, she said, regulate the quality of ink they use.
Still, the threat is real, said Bruce Brod, MD, a clinical professor of dermatology at the University of Pennsylvania Health System. “I’ve seen several different infections from tattooing, and they are from organisms that tend to contaminate things in damp, liquid-type environments.”
, dermatologists said.
“Tattooing involves puncturing the epidermis about 100 times per second with needles and depositing ink 1.5 to 2 millimeters below the surface of the skin, deep into the dermis,” the guidance states. “Contaminated tattoo ink can cause infections and serious injuries. Because these inks are injected, pathogens or other harmful substances in these inks can travel from the injection site through the blood and lymphatic systems to other parts of the body.”
The guidance comes as body art continues to get more popular. According to a 2019 poll, 30% of Americans had at least one tattoo – up from 21% in 2012. Forty percent of people 18-34 and 36% of those ages 35-54 had at least one tattoo. And though they are commonplace, tattoos come with medical risks that should be known beforehand, doctors said.
Commonly reported symptoms of tattoo ink–associated infections include rashes, blisters, painful nodules, and severe abscesses. One of the most common bacteria found in contaminated tattoo ink is nontuberculous mycobacteria, which is related to the bacteria that causes tuberculosis and can be found in soil and water.
The guidance lists several unsanitary manufacturing conditions that may lead to ink contamination, including:
- Preparing or packing of tattoo inks in facilities that are hard to sanitize, such as carpeted areas
- Ink or ink components left uncovered, especially near open air ducts
- Unsanitary mixing of tattoo inks, including with unclean utensils or containers
- Lack of appropriate attire by staff, failure to use hairnets, lab coats, aprons, gowns, masks, or gloves
“Infections will often spread along the drainage channels in the skin and create squiggly, uneven lines of big red, lumpy nodules,” Dr. Brod said.
Between 2003 and 2023, there were 18 recalls of tattoo inks that were contaminated with various microorganisms, according to the FDA. In May 2019, the FDA issued a safety alert advising consumers, tattoo artists, and retailers to avoid using or selling certain tattoo inks contaminated with microorganisms.
Reputable ink manufacturers use a process called gamma radiation, which refers to electromagnetic radiation of high frequencies to kill microorganisms in the ink and its packaging.
Most of the trustworthy, high-quality ink manufacturers are well-known among tattoo artists, Ms. Donohue said.
While she has seen customers with sensitive skin have allergic reactions, she has not seen someone come back with an infection in her 9 years working in the tattoo industry.
Because tattoo ink is considered a cosmetic product, there is not much regulatory oversight involved, which means the sterility and quality of ingredients vary, said Teo Soleymani, MD, an assistant clinical professor of dermatology and dermatological surgery at the UCLA David Geffen School of Medicine.
“Cosmeceuticals aren’t regulated by the FDA like prescription medication,” he said. “What we’ve seen many times is inadvertent contamination during the application process or contamination while the inks are being made.”
In years past, unclean needles spreading hepatitis and HIV were more of a concern, but those rates have dropped significantly, Dr. Soleymani said.
The infections that have increased are from rare bacteria that exist in stagnant water. And they are injected into a part of the body that allows them to evade the immune system, he said: shallow enough that there aren’t many associated blood vessels, but not still below the layer of skin that gets sloughed off every 28 days.
Sometimes, antibiotics alone won’t cut it, and the tattoo will require surgical removal.
“The aesthetic you were going for has to be not only removed, but you’re left with a surgical scar,” Dr. Soleymani said. “Tattoos can be beautiful, but they can come with unwanted visitors that can cause months of misery.”
A version of this article first appeared on WebMD.com.
The Food and Drug Administration draft guidance released recently on possible contamination of tattoo ink was not concerning Whitney Donohue, 34, owner of Forget Me Not Tattoo in Billings, Mont.
“I get our ink directly through the manufacturer – not at a store or through Amazon or eBay,” she said. “You never know if it’s going to be repackaged.”
Tattoo artists themselves, she said, regulate the quality of ink they use.
Still, the threat is real, said Bruce Brod, MD, a clinical professor of dermatology at the University of Pennsylvania Health System. “I’ve seen several different infections from tattooing, and they are from organisms that tend to contaminate things in damp, liquid-type environments.”
, dermatologists said.
“Tattooing involves puncturing the epidermis about 100 times per second with needles and depositing ink 1.5 to 2 millimeters below the surface of the skin, deep into the dermis,” the guidance states. “Contaminated tattoo ink can cause infections and serious injuries. Because these inks are injected, pathogens or other harmful substances in these inks can travel from the injection site through the blood and lymphatic systems to other parts of the body.”
The guidance comes as body art continues to get more popular. According to a 2019 poll, 30% of Americans had at least one tattoo – up from 21% in 2012. Forty percent of people 18-34 and 36% of those ages 35-54 had at least one tattoo. And though they are commonplace, tattoos come with medical risks that should be known beforehand, doctors said.
Commonly reported symptoms of tattoo ink–associated infections include rashes, blisters, painful nodules, and severe abscesses. One of the most common bacteria found in contaminated tattoo ink is nontuberculous mycobacteria, which is related to the bacteria that causes tuberculosis and can be found in soil and water.
The guidance lists several unsanitary manufacturing conditions that may lead to ink contamination, including:
- Preparing or packing of tattoo inks in facilities that are hard to sanitize, such as carpeted areas
- Ink or ink components left uncovered, especially near open air ducts
- Unsanitary mixing of tattoo inks, including with unclean utensils or containers
- Lack of appropriate attire by staff, failure to use hairnets, lab coats, aprons, gowns, masks, or gloves
“Infections will often spread along the drainage channels in the skin and create squiggly, uneven lines of big red, lumpy nodules,” Dr. Brod said.
Between 2003 and 2023, there were 18 recalls of tattoo inks that were contaminated with various microorganisms, according to the FDA. In May 2019, the FDA issued a safety alert advising consumers, tattoo artists, and retailers to avoid using or selling certain tattoo inks contaminated with microorganisms.
Reputable ink manufacturers use a process called gamma radiation, which refers to electromagnetic radiation of high frequencies to kill microorganisms in the ink and its packaging.
Most of the trustworthy, high-quality ink manufacturers are well-known among tattoo artists, Ms. Donohue said.
While she has seen customers with sensitive skin have allergic reactions, she has not seen someone come back with an infection in her 9 years working in the tattoo industry.
Because tattoo ink is considered a cosmetic product, there is not much regulatory oversight involved, which means the sterility and quality of ingredients vary, said Teo Soleymani, MD, an assistant clinical professor of dermatology and dermatological surgery at the UCLA David Geffen School of Medicine.
“Cosmeceuticals aren’t regulated by the FDA like prescription medication,” he said. “What we’ve seen many times is inadvertent contamination during the application process or contamination while the inks are being made.”
In years past, unclean needles spreading hepatitis and HIV were more of a concern, but those rates have dropped significantly, Dr. Soleymani said.
The infections that have increased are from rare bacteria that exist in stagnant water. And they are injected into a part of the body that allows them to evade the immune system, he said: shallow enough that there aren’t many associated blood vessels, but not still below the layer of skin that gets sloughed off every 28 days.
Sometimes, antibiotics alone won’t cut it, and the tattoo will require surgical removal.
“The aesthetic you were going for has to be not only removed, but you’re left with a surgical scar,” Dr. Soleymani said. “Tattoos can be beautiful, but they can come with unwanted visitors that can cause months of misery.”
A version of this article first appeared on WebMD.com.
The Food and Drug Administration draft guidance released recently on possible contamination of tattoo ink was not concerning Whitney Donohue, 34, owner of Forget Me Not Tattoo in Billings, Mont.
“I get our ink directly through the manufacturer – not at a store or through Amazon or eBay,” she said. “You never know if it’s going to be repackaged.”
Tattoo artists themselves, she said, regulate the quality of ink they use.
Still, the threat is real, said Bruce Brod, MD, a clinical professor of dermatology at the University of Pennsylvania Health System. “I’ve seen several different infections from tattooing, and they are from organisms that tend to contaminate things in damp, liquid-type environments.”
, dermatologists said.
“Tattooing involves puncturing the epidermis about 100 times per second with needles and depositing ink 1.5 to 2 millimeters below the surface of the skin, deep into the dermis,” the guidance states. “Contaminated tattoo ink can cause infections and serious injuries. Because these inks are injected, pathogens or other harmful substances in these inks can travel from the injection site through the blood and lymphatic systems to other parts of the body.”
The guidance comes as body art continues to get more popular. According to a 2019 poll, 30% of Americans had at least one tattoo – up from 21% in 2012. Forty percent of people 18-34 and 36% of those ages 35-54 had at least one tattoo. And though they are commonplace, tattoos come with medical risks that should be known beforehand, doctors said.
Commonly reported symptoms of tattoo ink–associated infections include rashes, blisters, painful nodules, and severe abscesses. One of the most common bacteria found in contaminated tattoo ink is nontuberculous mycobacteria, which is related to the bacteria that causes tuberculosis and can be found in soil and water.
The guidance lists several unsanitary manufacturing conditions that may lead to ink contamination, including:
- Preparing or packing of tattoo inks in facilities that are hard to sanitize, such as carpeted areas
- Ink or ink components left uncovered, especially near open air ducts
- Unsanitary mixing of tattoo inks, including with unclean utensils or containers
- Lack of appropriate attire by staff, failure to use hairnets, lab coats, aprons, gowns, masks, or gloves
“Infections will often spread along the drainage channels in the skin and create squiggly, uneven lines of big red, lumpy nodules,” Dr. Brod said.
Between 2003 and 2023, there were 18 recalls of tattoo inks that were contaminated with various microorganisms, according to the FDA. In May 2019, the FDA issued a safety alert advising consumers, tattoo artists, and retailers to avoid using or selling certain tattoo inks contaminated with microorganisms.
Reputable ink manufacturers use a process called gamma radiation, which refers to electromagnetic radiation of high frequencies to kill microorganisms in the ink and its packaging.
Most of the trustworthy, high-quality ink manufacturers are well-known among tattoo artists, Ms. Donohue said.
While she has seen customers with sensitive skin have allergic reactions, she has not seen someone come back with an infection in her 9 years working in the tattoo industry.
Because tattoo ink is considered a cosmetic product, there is not much regulatory oversight involved, which means the sterility and quality of ingredients vary, said Teo Soleymani, MD, an assistant clinical professor of dermatology and dermatological surgery at the UCLA David Geffen School of Medicine.
“Cosmeceuticals aren’t regulated by the FDA like prescription medication,” he said. “What we’ve seen many times is inadvertent contamination during the application process or contamination while the inks are being made.”
In years past, unclean needles spreading hepatitis and HIV were more of a concern, but those rates have dropped significantly, Dr. Soleymani said.
The infections that have increased are from rare bacteria that exist in stagnant water. And they are injected into a part of the body that allows them to evade the immune system, he said: shallow enough that there aren’t many associated blood vessels, but not still below the layer of skin that gets sloughed off every 28 days.
Sometimes, antibiotics alone won’t cut it, and the tattoo will require surgical removal.
“The aesthetic you were going for has to be not only removed, but you’re left with a surgical scar,” Dr. Soleymani said. “Tattoos can be beautiful, but they can come with unwanted visitors that can cause months of misery.”
A version of this article first appeared on WebMD.com.
FDA panel backs new COVID booster focusing only on variants
but questioned whether the population as a whole needs booster shots and how often they should be given.
The Vaccines and Related Biological Products Advisory Committee of the FDA voted 21-0 in favor of the recommendation about the strain to be used in the next crop of vaccines.
In the briefing document for the meeting, FDA staff said the available evidence suggests that a monovalent (single-strain) XBB-lineage vaccine “is warranted” for the 2023-2024 vaccination campaign and would replace the current bivalent vaccine, which targets the original version of the virus and two strains from the Omicron variant.
FDA staff also noted how such a shift would be in line with the World Health Organization toward targeting the XBB family of subvariants. European regulators have done this as well.
The FDA is not obligated to act on the panel’s recommendations. But the agency often does and is highly likely to do so in this case. Vaccine companies will need the recommendation from the FDA to begin making vaccines for the fall.
New shot every year?
The FDA asked its expert panel to vote only on the question about the makeup of future vaccines in terms of which strain to include.
But panelists also raised other questions during the meeting, including concerns about moves toward tying COVID vaccinations into the model of annual flu shots.
Paul Offit, MD, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia, argued for greater focus on the response of T cells after vaccination, even in light of the already recognized waning of antibody protection.
In a recent Substack article, Dr. Offit called T cells the “unsung hero” of the pandemic. They take longer to develop after infection or vaccination than the antibodies that first attack the virus, but immune memory cells called B and T cells “are long-lived,” and their “protection against severe disease often lasts for years and sometimes decades.”
Dr. Offit said he was concerned about using a blanket approach for future recommendations for COVID vaccinations, following the one now in place for influenza vaccines.
The Centers for Disease Control and Prevention recommends flu shots for everyone 6 months and older, with rare exceptions.
“We need to continue to define who those high-risk groups are and not make this a recommendation for everybody every season,” he said.
Dr. Offit offered his own experience as an example. While he had been vaccinated against the virus’s early Wuhan strain, he still was infected, most likely with a variant that emerged later.
“That was a drifted virus. That’s why I had a mild infection but I didn’t have a severe infection, because presumably I had T cells which prevented that severe infection, which may last for years,” Dr. Offit said.
Pfizer and Moderna, the two companies that make mRNA-based COVID vaccines, are working on experimental products meant to protect against both flu and SARS-COv-2 in one shot. Novavax, maker of a more traditional protein-based COVID shot, is doing the same.
The idea of these combination products is to make it more convenient for people to protect against both viruses, while also offering companies some marketing advantages.
But without referring to these drugmakers’ plans for future combo flu-COVID shots, members of the FDA panel raised objections to an assumption of routine annual vaccines against variants of SARS-CoV-2.
Among the panelists who expressed concerns was Henry H. Bernstein, DO, a former member of the CDC’s Advisory Committee on Immunization Practices.
Bernstein questioned the approach of dubbing these the “2023-2024 formulas,” as this approach conveyed a sense of an expectation for a need for annual vaccines, as happens with flu.
“It’s not clear to me that this is a seasonal virus yet,” said Dr. Bernstein, who is also a professor of pediatrics at Hofstra University, Hempstead, N.Y..
In response to Dr. Bernstein’s point, Arnold Monto, MD, the acting chair of the FDA panel, suggested such a pattern could emerge, while also agreeing that it’s too soon to say for sure.
A professor emeritus at the University of Michigan, Ann Arbor, Dr. Monto’s career included pandemic planning and emergency response to virus outbreaks, including the 1968 Hong Kong influenza pandemic, avian influenza, and the original SARS.
“I think it’s premature to say that this virus will not become seasonal,” Dr. Monto said about SARS-CoV-2. “I agree. We’re not there yet, but we may be.”
At the end of the meeting, Dr. Monto recapped the meeting’s key points, noting that there was a general consensus that the XBB.1.5 subvariant would be the best to use in future COVID shots.
He also noted that Novavax, which makes the more traditional protein-based vaccine, along with Pfizer and Moderna, already have honed in on this subvariant, which would allow for rapid development of updated COVID vaccines.
“The fact that most of the manufacturers are ready to work on an XBB 1.5 [vaccine] is an added reason to select this strain or this variant, given the immunologic data,” Dr. Monto said.
Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, said the demands involved in manufacturing vaccines tilts toward annual changes.
“Practically, we’re going to have one update per year, barring a heroic effort to deal with a strain that pops up that is essentially so different that it requires us to mobilize tremendous resources to address that strain change,” he said.
Dr. Marks questioned the panelists’ concerns about likening flu and COVID vaccination practices. The FDA staff’s intent was to try to help the public understand the need for follow-on vaccination.
“I’m really having trouble understanding that committee’s need to bristle against something that’s similar to influenza. People understand a yearly influenza vaccine,” Dr. Marks said.
And it’s not certain when another major change in the COVID virus will follow the XBB subvariant, but it’s likely one will – and soon, Dr. Marks said.
“It looks like, probably by next fall, there’ll be further drift from this,” he said.
Informing the public
Dr. Marks also stressed the need to better convey the benefits of vaccination to people in the United States.
CDC data estimate that 70% of the U.S. population completed an initial series of the original monovalent vaccines, with only 17% then getting bivalent shots. There’s even a decline among people ages 65 and older. CDC estimates 94% of this group completed their primary series, but only 43% got the bivalent booster dose.
“We have to do better because we have not done a good job today communicating to the American public what’s going on here,” Marks said.
Researchers also are still trying to determine the best timing for people to get additional COVID shots. Finding the “sweet spot” where people can maximize additional protection is tricky, with people most protected if they happen to get shot near the beginning of an uptick in viral spread, the CDC’s Ruth Link-Gelles, PhD, MPH, told the panel during a presentation.
“You’re going to get the best incremental benefit if it’s been longer since your last vaccine,” she said. “But of course, if you wait too long since your last vaccine, you’re left with very little protection, and so you’re at higher risk of severe illness.”
Like Dr. Marks, Dr. Link-Gelles stressed the need for persuading more people to get follow-on vaccines.
“Most Americans, at this point, haven’t even received the bivalent and so are a year or more out from their monovalent dose and so have relatively little protection left,” she said.
A version of this article first appeared on WebMD.com.
but questioned whether the population as a whole needs booster shots and how often they should be given.
The Vaccines and Related Biological Products Advisory Committee of the FDA voted 21-0 in favor of the recommendation about the strain to be used in the next crop of vaccines.
In the briefing document for the meeting, FDA staff said the available evidence suggests that a monovalent (single-strain) XBB-lineage vaccine “is warranted” for the 2023-2024 vaccination campaign and would replace the current bivalent vaccine, which targets the original version of the virus and two strains from the Omicron variant.
FDA staff also noted how such a shift would be in line with the World Health Organization toward targeting the XBB family of subvariants. European regulators have done this as well.
The FDA is not obligated to act on the panel’s recommendations. But the agency often does and is highly likely to do so in this case. Vaccine companies will need the recommendation from the FDA to begin making vaccines for the fall.
New shot every year?
The FDA asked its expert panel to vote only on the question about the makeup of future vaccines in terms of which strain to include.
But panelists also raised other questions during the meeting, including concerns about moves toward tying COVID vaccinations into the model of annual flu shots.
Paul Offit, MD, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia, argued for greater focus on the response of T cells after vaccination, even in light of the already recognized waning of antibody protection.
In a recent Substack article, Dr. Offit called T cells the “unsung hero” of the pandemic. They take longer to develop after infection or vaccination than the antibodies that first attack the virus, but immune memory cells called B and T cells “are long-lived,” and their “protection against severe disease often lasts for years and sometimes decades.”
Dr. Offit said he was concerned about using a blanket approach for future recommendations for COVID vaccinations, following the one now in place for influenza vaccines.
The Centers for Disease Control and Prevention recommends flu shots for everyone 6 months and older, with rare exceptions.
“We need to continue to define who those high-risk groups are and not make this a recommendation for everybody every season,” he said.
Dr. Offit offered his own experience as an example. While he had been vaccinated against the virus’s early Wuhan strain, he still was infected, most likely with a variant that emerged later.
“That was a drifted virus. That’s why I had a mild infection but I didn’t have a severe infection, because presumably I had T cells which prevented that severe infection, which may last for years,” Dr. Offit said.
Pfizer and Moderna, the two companies that make mRNA-based COVID vaccines, are working on experimental products meant to protect against both flu and SARS-COv-2 in one shot. Novavax, maker of a more traditional protein-based COVID shot, is doing the same.
The idea of these combination products is to make it more convenient for people to protect against both viruses, while also offering companies some marketing advantages.
But without referring to these drugmakers’ plans for future combo flu-COVID shots, members of the FDA panel raised objections to an assumption of routine annual vaccines against variants of SARS-CoV-2.
Among the panelists who expressed concerns was Henry H. Bernstein, DO, a former member of the CDC’s Advisory Committee on Immunization Practices.
Bernstein questioned the approach of dubbing these the “2023-2024 formulas,” as this approach conveyed a sense of an expectation for a need for annual vaccines, as happens with flu.
“It’s not clear to me that this is a seasonal virus yet,” said Dr. Bernstein, who is also a professor of pediatrics at Hofstra University, Hempstead, N.Y..
In response to Dr. Bernstein’s point, Arnold Monto, MD, the acting chair of the FDA panel, suggested such a pattern could emerge, while also agreeing that it’s too soon to say for sure.
A professor emeritus at the University of Michigan, Ann Arbor, Dr. Monto’s career included pandemic planning and emergency response to virus outbreaks, including the 1968 Hong Kong influenza pandemic, avian influenza, and the original SARS.
“I think it’s premature to say that this virus will not become seasonal,” Dr. Monto said about SARS-CoV-2. “I agree. We’re not there yet, but we may be.”
At the end of the meeting, Dr. Monto recapped the meeting’s key points, noting that there was a general consensus that the XBB.1.5 subvariant would be the best to use in future COVID shots.
He also noted that Novavax, which makes the more traditional protein-based vaccine, along with Pfizer and Moderna, already have honed in on this subvariant, which would allow for rapid development of updated COVID vaccines.
“The fact that most of the manufacturers are ready to work on an XBB 1.5 [vaccine] is an added reason to select this strain or this variant, given the immunologic data,” Dr. Monto said.
Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, said the demands involved in manufacturing vaccines tilts toward annual changes.
“Practically, we’re going to have one update per year, barring a heroic effort to deal with a strain that pops up that is essentially so different that it requires us to mobilize tremendous resources to address that strain change,” he said.
Dr. Marks questioned the panelists’ concerns about likening flu and COVID vaccination practices. The FDA staff’s intent was to try to help the public understand the need for follow-on vaccination.
“I’m really having trouble understanding that committee’s need to bristle against something that’s similar to influenza. People understand a yearly influenza vaccine,” Dr. Marks said.
And it’s not certain when another major change in the COVID virus will follow the XBB subvariant, but it’s likely one will – and soon, Dr. Marks said.
“It looks like, probably by next fall, there’ll be further drift from this,” he said.
Informing the public
Dr. Marks also stressed the need to better convey the benefits of vaccination to people in the United States.
CDC data estimate that 70% of the U.S. population completed an initial series of the original monovalent vaccines, with only 17% then getting bivalent shots. There’s even a decline among people ages 65 and older. CDC estimates 94% of this group completed their primary series, but only 43% got the bivalent booster dose.
“We have to do better because we have not done a good job today communicating to the American public what’s going on here,” Marks said.
Researchers also are still trying to determine the best timing for people to get additional COVID shots. Finding the “sweet spot” where people can maximize additional protection is tricky, with people most protected if they happen to get shot near the beginning of an uptick in viral spread, the CDC’s Ruth Link-Gelles, PhD, MPH, told the panel during a presentation.
“You’re going to get the best incremental benefit if it’s been longer since your last vaccine,” she said. “But of course, if you wait too long since your last vaccine, you’re left with very little protection, and so you’re at higher risk of severe illness.”
Like Dr. Marks, Dr. Link-Gelles stressed the need for persuading more people to get follow-on vaccines.
“Most Americans, at this point, haven’t even received the bivalent and so are a year or more out from their monovalent dose and so have relatively little protection left,” she said.
A version of this article first appeared on WebMD.com.
but questioned whether the population as a whole needs booster shots and how often they should be given.
The Vaccines and Related Biological Products Advisory Committee of the FDA voted 21-0 in favor of the recommendation about the strain to be used in the next crop of vaccines.
In the briefing document for the meeting, FDA staff said the available evidence suggests that a monovalent (single-strain) XBB-lineage vaccine “is warranted” for the 2023-2024 vaccination campaign and would replace the current bivalent vaccine, which targets the original version of the virus and two strains from the Omicron variant.
FDA staff also noted how such a shift would be in line with the World Health Organization toward targeting the XBB family of subvariants. European regulators have done this as well.
The FDA is not obligated to act on the panel’s recommendations. But the agency often does and is highly likely to do so in this case. Vaccine companies will need the recommendation from the FDA to begin making vaccines for the fall.
New shot every year?
The FDA asked its expert panel to vote only on the question about the makeup of future vaccines in terms of which strain to include.
But panelists also raised other questions during the meeting, including concerns about moves toward tying COVID vaccinations into the model of annual flu shots.
Paul Offit, MD, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia, argued for greater focus on the response of T cells after vaccination, even in light of the already recognized waning of antibody protection.
In a recent Substack article, Dr. Offit called T cells the “unsung hero” of the pandemic. They take longer to develop after infection or vaccination than the antibodies that first attack the virus, but immune memory cells called B and T cells “are long-lived,” and their “protection against severe disease often lasts for years and sometimes decades.”
Dr. Offit said he was concerned about using a blanket approach for future recommendations for COVID vaccinations, following the one now in place for influenza vaccines.
The Centers for Disease Control and Prevention recommends flu shots for everyone 6 months and older, with rare exceptions.
“We need to continue to define who those high-risk groups are and not make this a recommendation for everybody every season,” he said.
Dr. Offit offered his own experience as an example. While he had been vaccinated against the virus’s early Wuhan strain, he still was infected, most likely with a variant that emerged later.
“That was a drifted virus. That’s why I had a mild infection but I didn’t have a severe infection, because presumably I had T cells which prevented that severe infection, which may last for years,” Dr. Offit said.
Pfizer and Moderna, the two companies that make mRNA-based COVID vaccines, are working on experimental products meant to protect against both flu and SARS-COv-2 in one shot. Novavax, maker of a more traditional protein-based COVID shot, is doing the same.
The idea of these combination products is to make it more convenient for people to protect against both viruses, while also offering companies some marketing advantages.
But without referring to these drugmakers’ plans for future combo flu-COVID shots, members of the FDA panel raised objections to an assumption of routine annual vaccines against variants of SARS-CoV-2.
Among the panelists who expressed concerns was Henry H. Bernstein, DO, a former member of the CDC’s Advisory Committee on Immunization Practices.
Bernstein questioned the approach of dubbing these the “2023-2024 formulas,” as this approach conveyed a sense of an expectation for a need for annual vaccines, as happens with flu.
“It’s not clear to me that this is a seasonal virus yet,” said Dr. Bernstein, who is also a professor of pediatrics at Hofstra University, Hempstead, N.Y..
In response to Dr. Bernstein’s point, Arnold Monto, MD, the acting chair of the FDA panel, suggested such a pattern could emerge, while also agreeing that it’s too soon to say for sure.
A professor emeritus at the University of Michigan, Ann Arbor, Dr. Monto’s career included pandemic planning and emergency response to virus outbreaks, including the 1968 Hong Kong influenza pandemic, avian influenza, and the original SARS.
“I think it’s premature to say that this virus will not become seasonal,” Dr. Monto said about SARS-CoV-2. “I agree. We’re not there yet, but we may be.”
At the end of the meeting, Dr. Monto recapped the meeting’s key points, noting that there was a general consensus that the XBB.1.5 subvariant would be the best to use in future COVID shots.
He also noted that Novavax, which makes the more traditional protein-based vaccine, along with Pfizer and Moderna, already have honed in on this subvariant, which would allow for rapid development of updated COVID vaccines.
“The fact that most of the manufacturers are ready to work on an XBB 1.5 [vaccine] is an added reason to select this strain or this variant, given the immunologic data,” Dr. Monto said.
Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, said the demands involved in manufacturing vaccines tilts toward annual changes.
“Practically, we’re going to have one update per year, barring a heroic effort to deal with a strain that pops up that is essentially so different that it requires us to mobilize tremendous resources to address that strain change,” he said.
Dr. Marks questioned the panelists’ concerns about likening flu and COVID vaccination practices. The FDA staff’s intent was to try to help the public understand the need for follow-on vaccination.
“I’m really having trouble understanding that committee’s need to bristle against something that’s similar to influenza. People understand a yearly influenza vaccine,” Dr. Marks said.
And it’s not certain when another major change in the COVID virus will follow the XBB subvariant, but it’s likely one will – and soon, Dr. Marks said.
“It looks like, probably by next fall, there’ll be further drift from this,” he said.
Informing the public
Dr. Marks also stressed the need to better convey the benefits of vaccination to people in the United States.
CDC data estimate that 70% of the U.S. population completed an initial series of the original monovalent vaccines, with only 17% then getting bivalent shots. There’s even a decline among people ages 65 and older. CDC estimates 94% of this group completed their primary series, but only 43% got the bivalent booster dose.
“We have to do better because we have not done a good job today communicating to the American public what’s going on here,” Marks said.
Researchers also are still trying to determine the best timing for people to get additional COVID shots. Finding the “sweet spot” where people can maximize additional protection is tricky, with people most protected if they happen to get shot near the beginning of an uptick in viral spread, the CDC’s Ruth Link-Gelles, PhD, MPH, told the panel during a presentation.
“You’re going to get the best incremental benefit if it’s been longer since your last vaccine,” she said. “But of course, if you wait too long since your last vaccine, you’re left with very little protection, and so you’re at higher risk of severe illness.”
Like Dr. Marks, Dr. Link-Gelles stressed the need for persuading more people to get follow-on vaccines.
“Most Americans, at this point, haven’t even received the bivalent and so are a year or more out from their monovalent dose and so have relatively little protection left,” she said.
A version of this article first appeared on WebMD.com.
Latest data: COVID vaccine safety, protection, and breakthrough infections in inflammatory, autoimmune diseases
MILAN – The impact of the COVID-19 pandemic on patients with rheumatic and nonrheumatic autoimmune diseases is ongoing and not yet fully comprehended. New data presented at the annual European Congress of Rheumatology, primarily derived from the global COVID-19 in Autoimmune Diseases (COVAD) survey but not limited to it, provide reassurance regarding the protection and safety of COVID-19 vaccines for older and younger adults, as well as for pregnant and breastfeeding women. These data also explore the influence of underlying diseases and medications on breakthrough SARS-CoV-2 infections and infection outcomes.
Safety of vaccines in patients with autoimmune or immune-mediated diseases
Following vaccination, even with low levels of antibodies, the risk of severe COVID-19 remains relatively low for patients who receive immunosuppressive therapy for various immune-mediated inflammatory diseases (IMIDs). This encouraging finding comes from the Nor-vaC study, presented by Hilde Ørbo, MD, of the Center for Treatment of Rheumatic and Musculoskeletal Diseases, Diakonhjemmet Hospital, Oslo.
During the presentation, Dr. Ørbo stated: “We did not find any specific diagnosis or medication associated with a significantly higher risk of hospitalization.” Receiving booster doses of the vaccine, having high levels of anti-spike antibodies after vaccination, and achieving hybrid immunity are correlated with further reductions in the risk of breakthrough SARS-CoV-2 infections.
Between Feb. 15, 2021, and Feb. 15, 2023, COVID-19 affected a similar proportion among the 729 patients and 350 healthy control persons (67% and 68%, respectively). Among the patients, 22 reported severe COVID-19, whereas none of the healthy control persons did. However, there were no fatalities among the patients. The study cohort consisted of patients with various IMIDs; 70% had an inflammatory joint disease. The use of immunosuppressive medications also varied, with 63% of patients using tumor necrosis factor inhibitors, either as monotherapy or in combination with other treatments, and other patients taking medications such as methotrexate, interleukin inhibitors, Janus kinase inhibitors, vedolizumab (Entyvio), and others.
While being older than 70 years and the presence of comorbidities were identified as risk factors for severe COVID-19, there was a significant reduction in risk with each additional vaccine dose. These results support the protective role of repeated COVID-19 vaccination for patients with IMIDs who are receiving immunosuppressive therapies; they yield a favorable prognosis even with the Omicron variant.
The study further compared the risk of severe COVID-19 between a group with hybrid immunity (having received three vaccine doses and experiencing breakthrough infection with the Omicron variant) and a group that received a fourth vaccine dose within the same time frame. The difference was striking: Hybrid immunity was associated with a 5.8-fold decrease in risk, compared with four-dose vaccination (P < .0001).
The level of antibodies, measured 2-4 weeks after the last vaccination, was predictive of the risk of breakthrough COVID-19. An antibody level above 6000 binding antibody units/mL after vaccination was significantly associated with a reduction in risk. “We can conclude that patients who receive multiple vaccine doses have a lower risk of COVID-19,” Dr. Ørbo said. “In patients who recently experienced breakthrough infections, the administration of a booster vaccine dose might be delayed.”
“The virus has undergone changes throughout the pandemic, while the vaccines have remained relatively stable. Are we anticipating more infections over time?” asked Hendrik Schulze-Koops, MD, PhD, of Ludwig Maximilians University of Munich (Germany), the session moderator. In response, Dr. Ørbo stated that 85% of the recorded infections in the study occurred after the emergence of the Omicron variant, and time was considered a covariable in the analysis.
These data shed light on a topic discussed by Pedro Machado, MD, PhD, professor and consultant in rheumatology and neuromuscular diseases at University College London, during his scientific session talk entitled, “Unsolved Issues of COVID Vaccination and Re-vaccination.” Dr. Machado referred to the VROOM study published in 2022, which examined the interruption of methotrexate for 2 weeks following booster administration. Both groups demonstrated a significant antibody response, but the group that stopped taking methotrexate showed double the antibody titers.
However, he emphasized, “what remains unknown is the clinical relevance of these differences in terms of severe infection, hospitalization, or even death. The potential benefit of increased immunogenicity by interrupting conventional synthetic disease-modifying antirheumatic drugs [csDMARDs] such as methotrexate before or after vaccination needs to be balanced against the potential risk of disease flare. Ultimately, decision-making should be individualized based on factors such as comorbidities, disease activity, and other considerations.” The results presented by Dr. Ørbo suggest that, while there may be a clinical difference in terms of severe infection, the overall prognosis for vaccinated patients is reasonably good.
Regarding other DMARDs, such as biologics, the approach may differ. Dr. Machado suggested: “In patients using rituximab or other B cell–depleting therapies, SARS-CoV-2 vaccination should be scheduled in a way that optimizes vaccine immunogenicity. A minimum of 10 B cells/mcL of blood is likely a relevant threshold above which a sufficient cellular and immune response is established.”
COVID vaccines are safe for pregnant and breastfeeding women
According to data from the COVAD study, which comprised two global cross-sectional surveys conducted in 2021 and 2022, the COVID-19 vaccine appeared safe for pregnant and breastfeeding women with autoimmune diseases (AID).
Presenter Laura Andreoli, MD, PhD, of the University of Brescia (Italy), said that, although pregnant patients with AID reported more adverse events related to vaccination, these rates were not significantly higher than those among pregnant, healthy control persons who were without AID. No difference in adverse events was observed between breastfeeding women and healthy control persons, and the incidence of disease flares did not significantly differ among all groups.
“In summary, this study provides initial insights into the safety of COVID-19 vaccination during the gestational and postpartum periods in women with autoimmune diseases. These reassuring observations will hopefully improve clinician-patient communication and address hesitancy towards COVID-19 vaccination, as the benefits for the mother and fetus through passive immunization appear to outweigh potential risks,” Dr. Andreoli said in an interview.
“The large number of participants and the global geographical spread of the COVAD survey were very beneficial in gaining access to this important subset of patients,” added Dr. Andreoli. However, she acknowledged that patients with low socioeconomic status and/or high disability were likely underrepresented. While no data on pregnancy outcomes have been collected thus far, Dr. Andreoli expressed the desire to include them in the study’s follow-up.
The COVAD survey data also indicate that, in general, vaccine hesitancy among patients with AID is decreasing; from 2021 to 2022, it declined from 16.5% to 5.1%, as Dr. Machado indicated in his presentation.
Multiple factors contribute to breakthrough infections
The risk of breakthrough SARS-CoV-2 infections after vaccination varies among patients with rheumatoid arthritis and rheumatic or nonrheumatic autoimmune diseases, primarily depending on the underlying condition rather than the immunosuppressive medication. Environmental factors also appear to play a role. This complex landscape emerges from a further analysis of the COVAD survey dataset.
Alessia Alunno, MD, PhD, of the University of L’Aquila (Italy), presented a detailed and occasionally counterintuitive picture of similarities and differences among young adult patients (aged 18-35 years), mostly women, with various rheumatic and nonrheumatic diseases in relation to COVID-19. Most notably, the type of disease seemed to have more significance than the immunosuppression resulting from the treatment regimen. This held true for vaccine safety as well as for the risk of breakthrough COVID-19 and symptom profiles.
Patients with rheumatic disease (RMD) and nonrheumatic autoimmune disease (nr-AD) had significantly different therapeutic profiles on average. Before vaccination, 45% of patients with RMD used glucocorticoids (GC), and 91% used immunosuppressants (IS). In contrast, only 9.5% of nr-AD patients used GC, and 21% were taking IS.
Interestingly, the overall prevalence of reported SARS-CoV-2 infections was not influenced by medication and was practically identical (25% to 28%) across all groups. However, there were intriguing differences in the occurrence of infections before and after vaccination between disease groups. Prevaccine infections were less frequent among patients with RMD compared with healthy control persons (adjusted odds ratio, 0.6), while the rates were similar among patients with nr-AD and healthy control persons. On the other hand, breakthrough infections were more frequent in patients with RMD (aOR, 2.7), whereas the rate was similar between healthy control persons and patients with nr-AD.
Despite a much lower rate of GC/IS use, patients with nr-AD experienced repeated infections more frequently. In contrast, patients with RMD were less prone to multiple infections, even compared with healthy control persons (aOR, 0.5).
Regarding the disease profile, fewer than 5% of all infected patients required advanced therapies for SARS-CoV-2 infection. Notably, all SARS-CoV-2 infections in patients with nr-AD were symptomatic, whereas among patients with RMD and healthy control persons, the incidence of asymptomatic infections was 3%. The rate of hospital admissions was 4% for patients with RMD, compared with 2% for patients with nr-AD and 1% for control persons. The RMD group exhibited some differences between prevaccine infections and breakthrough infections, including a significantly lower frequency of loss of smell and taste during breakthrough infections. Overall, patients with RMD and COVID-19 experienced cough, runny nose, throat pain, nausea, and vomiting more frequently. In contrast, patients with nr-AD had a much higher risk of skin rashes during breakthrough infections (aOR, 8.7).
Vaccine adverse events (AEs) were also influenced by the underlying disease. Patients with RMD and those with nr-AD were more likely to experience mild AEs after the first or second dose, compared with healthy control persons (adjusted OR, 2.4 and 2.0, respectively). The most common early, mild AEs across all groups were injection-site pain, headache, and fatigue, but they occurred more frequently in the nr-AD group than in the RMD or healthy control group. Additionally, fever and chills occurred more frequently among the nr-AD group. Late, mild AEs and severe AEs were rare and affected all groups equally.
“The overall incidence of AEs was very low. Our results certainly do not undermine the safety of vaccines,” Dr. Alunno said.
Disease flares were more common after vaccination (10% with RMD and 7% with nr-AD) than after infection (5% with RMD and 1.5% with nr-AD). Furthermore, in many cases, after vaccination, flares required a change of medications, particularly for patients with RMD.
Additional results from the COVAD survey from January to July 2022, presented by Naveen Ravichandran, MD, DM, of Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India, revealed a higher prevalence (OR, 1.2; P = .001) of breakthrough infections among patients with RA. A total of 22.6% of patients with RA experienced breakthrough infections, compared with 20.6% for patients with other autoimmune rheumatic diseases and 18.4% of healthy control persons. Hospitalizations and the need for advanced treatment were also more common among patients with RA (30.9%) than among healthy control persons (13.9%). Patients with RA who had breakthrough infections tended to be older (closer to 50 years of age on average) and female, and they were more likely to have comorbidities and mental disorders. The human development index of the patient’s country of residence also played a role. Further research is necessary to understand how breakthrough infection outcomes are affected by a patient’s socioeconomic situation.
According to Dr. Ravichandran, medication was not a significant factor, except for the use of steroids and rituximab, which were associated with a higher risk of severe COVID-19 and hospitalization. Patients using rituximab, in particular, faced significantly increased odds for hospitalization (OR, 3.4) and severe breakthrough COVID-19 (OR, 3.0).
Session moderator Kim Lauper, MD, of the University of Geneva, cautioned: “The roles of disease and medication are challenging to separate. Some diseases require a more aggressive immunosuppressive regimen. It’s possible that different diseases affect the immune system differently, but it is not easy to demonstrate.”
The complications observed in the data warrant further study, as mentioned by Dr. Schulze-Koops: “We have a problem tied to the time line of the pandemic, where we had different viruses, different population behaviors, different treatments, and different standards of care over time. We also have differences between ethnic communities and regions of the world. But most importantly, we have different viruses: From the original strain to Delta to Omicron, we know they have very different clinical outcomes. I believe we need more scientific research to unravel these factors.”
Dr. Ørbo, Dr. Ravichandran, Dr. Andreoli, and Dr. Alunno reported no relevant financial relationships. Dr. Machado has received grants and/or honoraria from AbbVie, Bristol-Myers Squibb, Celgene, Eli Lilly, Galapagos, Janssen, Merck Sharp & Dohme, Novartis, Orphazyme, Pfizer, Roche, and UCB.
A version of this article originally appeared on Medscape.com.
MILAN – The impact of the COVID-19 pandemic on patients with rheumatic and nonrheumatic autoimmune diseases is ongoing and not yet fully comprehended. New data presented at the annual European Congress of Rheumatology, primarily derived from the global COVID-19 in Autoimmune Diseases (COVAD) survey but not limited to it, provide reassurance regarding the protection and safety of COVID-19 vaccines for older and younger adults, as well as for pregnant and breastfeeding women. These data also explore the influence of underlying diseases and medications on breakthrough SARS-CoV-2 infections and infection outcomes.
Safety of vaccines in patients with autoimmune or immune-mediated diseases
Following vaccination, even with low levels of antibodies, the risk of severe COVID-19 remains relatively low for patients who receive immunosuppressive therapy for various immune-mediated inflammatory diseases (IMIDs). This encouraging finding comes from the Nor-vaC study, presented by Hilde Ørbo, MD, of the Center for Treatment of Rheumatic and Musculoskeletal Diseases, Diakonhjemmet Hospital, Oslo.
During the presentation, Dr. Ørbo stated: “We did not find any specific diagnosis or medication associated with a significantly higher risk of hospitalization.” Receiving booster doses of the vaccine, having high levels of anti-spike antibodies after vaccination, and achieving hybrid immunity are correlated with further reductions in the risk of breakthrough SARS-CoV-2 infections.
Between Feb. 15, 2021, and Feb. 15, 2023, COVID-19 affected a similar proportion among the 729 patients and 350 healthy control persons (67% and 68%, respectively). Among the patients, 22 reported severe COVID-19, whereas none of the healthy control persons did. However, there were no fatalities among the patients. The study cohort consisted of patients with various IMIDs; 70% had an inflammatory joint disease. The use of immunosuppressive medications also varied, with 63% of patients using tumor necrosis factor inhibitors, either as monotherapy or in combination with other treatments, and other patients taking medications such as methotrexate, interleukin inhibitors, Janus kinase inhibitors, vedolizumab (Entyvio), and others.
While being older than 70 years and the presence of comorbidities were identified as risk factors for severe COVID-19, there was a significant reduction in risk with each additional vaccine dose. These results support the protective role of repeated COVID-19 vaccination for patients with IMIDs who are receiving immunosuppressive therapies; they yield a favorable prognosis even with the Omicron variant.
The study further compared the risk of severe COVID-19 between a group with hybrid immunity (having received three vaccine doses and experiencing breakthrough infection with the Omicron variant) and a group that received a fourth vaccine dose within the same time frame. The difference was striking: Hybrid immunity was associated with a 5.8-fold decrease in risk, compared with four-dose vaccination (P < .0001).
The level of antibodies, measured 2-4 weeks after the last vaccination, was predictive of the risk of breakthrough COVID-19. An antibody level above 6000 binding antibody units/mL after vaccination was significantly associated with a reduction in risk. “We can conclude that patients who receive multiple vaccine doses have a lower risk of COVID-19,” Dr. Ørbo said. “In patients who recently experienced breakthrough infections, the administration of a booster vaccine dose might be delayed.”
“The virus has undergone changes throughout the pandemic, while the vaccines have remained relatively stable. Are we anticipating more infections over time?” asked Hendrik Schulze-Koops, MD, PhD, of Ludwig Maximilians University of Munich (Germany), the session moderator. In response, Dr. Ørbo stated that 85% of the recorded infections in the study occurred after the emergence of the Omicron variant, and time was considered a covariable in the analysis.
These data shed light on a topic discussed by Pedro Machado, MD, PhD, professor and consultant in rheumatology and neuromuscular diseases at University College London, during his scientific session talk entitled, “Unsolved Issues of COVID Vaccination and Re-vaccination.” Dr. Machado referred to the VROOM study published in 2022, which examined the interruption of methotrexate for 2 weeks following booster administration. Both groups demonstrated a significant antibody response, but the group that stopped taking methotrexate showed double the antibody titers.
However, he emphasized, “what remains unknown is the clinical relevance of these differences in terms of severe infection, hospitalization, or even death. The potential benefit of increased immunogenicity by interrupting conventional synthetic disease-modifying antirheumatic drugs [csDMARDs] such as methotrexate before or after vaccination needs to be balanced against the potential risk of disease flare. Ultimately, decision-making should be individualized based on factors such as comorbidities, disease activity, and other considerations.” The results presented by Dr. Ørbo suggest that, while there may be a clinical difference in terms of severe infection, the overall prognosis for vaccinated patients is reasonably good.
Regarding other DMARDs, such as biologics, the approach may differ. Dr. Machado suggested: “In patients using rituximab or other B cell–depleting therapies, SARS-CoV-2 vaccination should be scheduled in a way that optimizes vaccine immunogenicity. A minimum of 10 B cells/mcL of blood is likely a relevant threshold above which a sufficient cellular and immune response is established.”
COVID vaccines are safe for pregnant and breastfeeding women
According to data from the COVAD study, which comprised two global cross-sectional surveys conducted in 2021 and 2022, the COVID-19 vaccine appeared safe for pregnant and breastfeeding women with autoimmune diseases (AID).
Presenter Laura Andreoli, MD, PhD, of the University of Brescia (Italy), said that, although pregnant patients with AID reported more adverse events related to vaccination, these rates were not significantly higher than those among pregnant, healthy control persons who were without AID. No difference in adverse events was observed between breastfeeding women and healthy control persons, and the incidence of disease flares did not significantly differ among all groups.
“In summary, this study provides initial insights into the safety of COVID-19 vaccination during the gestational and postpartum periods in women with autoimmune diseases. These reassuring observations will hopefully improve clinician-patient communication and address hesitancy towards COVID-19 vaccination, as the benefits for the mother and fetus through passive immunization appear to outweigh potential risks,” Dr. Andreoli said in an interview.
“The large number of participants and the global geographical spread of the COVAD survey were very beneficial in gaining access to this important subset of patients,” added Dr. Andreoli. However, she acknowledged that patients with low socioeconomic status and/or high disability were likely underrepresented. While no data on pregnancy outcomes have been collected thus far, Dr. Andreoli expressed the desire to include them in the study’s follow-up.
The COVAD survey data also indicate that, in general, vaccine hesitancy among patients with AID is decreasing; from 2021 to 2022, it declined from 16.5% to 5.1%, as Dr. Machado indicated in his presentation.
Multiple factors contribute to breakthrough infections
The risk of breakthrough SARS-CoV-2 infections after vaccination varies among patients with rheumatoid arthritis and rheumatic or nonrheumatic autoimmune diseases, primarily depending on the underlying condition rather than the immunosuppressive medication. Environmental factors also appear to play a role. This complex landscape emerges from a further analysis of the COVAD survey dataset.
Alessia Alunno, MD, PhD, of the University of L’Aquila (Italy), presented a detailed and occasionally counterintuitive picture of similarities and differences among young adult patients (aged 18-35 years), mostly women, with various rheumatic and nonrheumatic diseases in relation to COVID-19. Most notably, the type of disease seemed to have more significance than the immunosuppression resulting from the treatment regimen. This held true for vaccine safety as well as for the risk of breakthrough COVID-19 and symptom profiles.
Patients with rheumatic disease (RMD) and nonrheumatic autoimmune disease (nr-AD) had significantly different therapeutic profiles on average. Before vaccination, 45% of patients with RMD used glucocorticoids (GC), and 91% used immunosuppressants (IS). In contrast, only 9.5% of nr-AD patients used GC, and 21% were taking IS.
Interestingly, the overall prevalence of reported SARS-CoV-2 infections was not influenced by medication and was practically identical (25% to 28%) across all groups. However, there were intriguing differences in the occurrence of infections before and after vaccination between disease groups. Prevaccine infections were less frequent among patients with RMD compared with healthy control persons (adjusted odds ratio, 0.6), while the rates were similar among patients with nr-AD and healthy control persons. On the other hand, breakthrough infections were more frequent in patients with RMD (aOR, 2.7), whereas the rate was similar between healthy control persons and patients with nr-AD.
Despite a much lower rate of GC/IS use, patients with nr-AD experienced repeated infections more frequently. In contrast, patients with RMD were less prone to multiple infections, even compared with healthy control persons (aOR, 0.5).
Regarding the disease profile, fewer than 5% of all infected patients required advanced therapies for SARS-CoV-2 infection. Notably, all SARS-CoV-2 infections in patients with nr-AD were symptomatic, whereas among patients with RMD and healthy control persons, the incidence of asymptomatic infections was 3%. The rate of hospital admissions was 4% for patients with RMD, compared with 2% for patients with nr-AD and 1% for control persons. The RMD group exhibited some differences between prevaccine infections and breakthrough infections, including a significantly lower frequency of loss of smell and taste during breakthrough infections. Overall, patients with RMD and COVID-19 experienced cough, runny nose, throat pain, nausea, and vomiting more frequently. In contrast, patients with nr-AD had a much higher risk of skin rashes during breakthrough infections (aOR, 8.7).
Vaccine adverse events (AEs) were also influenced by the underlying disease. Patients with RMD and those with nr-AD were more likely to experience mild AEs after the first or second dose, compared with healthy control persons (adjusted OR, 2.4 and 2.0, respectively). The most common early, mild AEs across all groups were injection-site pain, headache, and fatigue, but they occurred more frequently in the nr-AD group than in the RMD or healthy control group. Additionally, fever and chills occurred more frequently among the nr-AD group. Late, mild AEs and severe AEs were rare and affected all groups equally.
“The overall incidence of AEs was very low. Our results certainly do not undermine the safety of vaccines,” Dr. Alunno said.
Disease flares were more common after vaccination (10% with RMD and 7% with nr-AD) than after infection (5% with RMD and 1.5% with nr-AD). Furthermore, in many cases, after vaccination, flares required a change of medications, particularly for patients with RMD.
Additional results from the COVAD survey from January to July 2022, presented by Naveen Ravichandran, MD, DM, of Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India, revealed a higher prevalence (OR, 1.2; P = .001) of breakthrough infections among patients with RA. A total of 22.6% of patients with RA experienced breakthrough infections, compared with 20.6% for patients with other autoimmune rheumatic diseases and 18.4% of healthy control persons. Hospitalizations and the need for advanced treatment were also more common among patients with RA (30.9%) than among healthy control persons (13.9%). Patients with RA who had breakthrough infections tended to be older (closer to 50 years of age on average) and female, and they were more likely to have comorbidities and mental disorders. The human development index of the patient’s country of residence also played a role. Further research is necessary to understand how breakthrough infection outcomes are affected by a patient’s socioeconomic situation.
According to Dr. Ravichandran, medication was not a significant factor, except for the use of steroids and rituximab, which were associated with a higher risk of severe COVID-19 and hospitalization. Patients using rituximab, in particular, faced significantly increased odds for hospitalization (OR, 3.4) and severe breakthrough COVID-19 (OR, 3.0).
Session moderator Kim Lauper, MD, of the University of Geneva, cautioned: “The roles of disease and medication are challenging to separate. Some diseases require a more aggressive immunosuppressive regimen. It’s possible that different diseases affect the immune system differently, but it is not easy to demonstrate.”
The complications observed in the data warrant further study, as mentioned by Dr. Schulze-Koops: “We have a problem tied to the time line of the pandemic, where we had different viruses, different population behaviors, different treatments, and different standards of care over time. We also have differences between ethnic communities and regions of the world. But most importantly, we have different viruses: From the original strain to Delta to Omicron, we know they have very different clinical outcomes. I believe we need more scientific research to unravel these factors.”
Dr. Ørbo, Dr. Ravichandran, Dr. Andreoli, and Dr. Alunno reported no relevant financial relationships. Dr. Machado has received grants and/or honoraria from AbbVie, Bristol-Myers Squibb, Celgene, Eli Lilly, Galapagos, Janssen, Merck Sharp & Dohme, Novartis, Orphazyme, Pfizer, Roche, and UCB.
A version of this article originally appeared on Medscape.com.
MILAN – The impact of the COVID-19 pandemic on patients with rheumatic and nonrheumatic autoimmune diseases is ongoing and not yet fully comprehended. New data presented at the annual European Congress of Rheumatology, primarily derived from the global COVID-19 in Autoimmune Diseases (COVAD) survey but not limited to it, provide reassurance regarding the protection and safety of COVID-19 vaccines for older and younger adults, as well as for pregnant and breastfeeding women. These data also explore the influence of underlying diseases and medications on breakthrough SARS-CoV-2 infections and infection outcomes.
Safety of vaccines in patients with autoimmune or immune-mediated diseases
Following vaccination, even with low levels of antibodies, the risk of severe COVID-19 remains relatively low for patients who receive immunosuppressive therapy for various immune-mediated inflammatory diseases (IMIDs). This encouraging finding comes from the Nor-vaC study, presented by Hilde Ørbo, MD, of the Center for Treatment of Rheumatic and Musculoskeletal Diseases, Diakonhjemmet Hospital, Oslo.
During the presentation, Dr. Ørbo stated: “We did not find any specific diagnosis or medication associated with a significantly higher risk of hospitalization.” Receiving booster doses of the vaccine, having high levels of anti-spike antibodies after vaccination, and achieving hybrid immunity are correlated with further reductions in the risk of breakthrough SARS-CoV-2 infections.
Between Feb. 15, 2021, and Feb. 15, 2023, COVID-19 affected a similar proportion among the 729 patients and 350 healthy control persons (67% and 68%, respectively). Among the patients, 22 reported severe COVID-19, whereas none of the healthy control persons did. However, there were no fatalities among the patients. The study cohort consisted of patients with various IMIDs; 70% had an inflammatory joint disease. The use of immunosuppressive medications also varied, with 63% of patients using tumor necrosis factor inhibitors, either as monotherapy or in combination with other treatments, and other patients taking medications such as methotrexate, interleukin inhibitors, Janus kinase inhibitors, vedolizumab (Entyvio), and others.
While being older than 70 years and the presence of comorbidities were identified as risk factors for severe COVID-19, there was a significant reduction in risk with each additional vaccine dose. These results support the protective role of repeated COVID-19 vaccination for patients with IMIDs who are receiving immunosuppressive therapies; they yield a favorable prognosis even with the Omicron variant.
The study further compared the risk of severe COVID-19 between a group with hybrid immunity (having received three vaccine doses and experiencing breakthrough infection with the Omicron variant) and a group that received a fourth vaccine dose within the same time frame. The difference was striking: Hybrid immunity was associated with a 5.8-fold decrease in risk, compared with four-dose vaccination (P < .0001).
The level of antibodies, measured 2-4 weeks after the last vaccination, was predictive of the risk of breakthrough COVID-19. An antibody level above 6000 binding antibody units/mL after vaccination was significantly associated with a reduction in risk. “We can conclude that patients who receive multiple vaccine doses have a lower risk of COVID-19,” Dr. Ørbo said. “In patients who recently experienced breakthrough infections, the administration of a booster vaccine dose might be delayed.”
“The virus has undergone changes throughout the pandemic, while the vaccines have remained relatively stable. Are we anticipating more infections over time?” asked Hendrik Schulze-Koops, MD, PhD, of Ludwig Maximilians University of Munich (Germany), the session moderator. In response, Dr. Ørbo stated that 85% of the recorded infections in the study occurred after the emergence of the Omicron variant, and time was considered a covariable in the analysis.
These data shed light on a topic discussed by Pedro Machado, MD, PhD, professor and consultant in rheumatology and neuromuscular diseases at University College London, during his scientific session talk entitled, “Unsolved Issues of COVID Vaccination and Re-vaccination.” Dr. Machado referred to the VROOM study published in 2022, which examined the interruption of methotrexate for 2 weeks following booster administration. Both groups demonstrated a significant antibody response, but the group that stopped taking methotrexate showed double the antibody titers.
However, he emphasized, “what remains unknown is the clinical relevance of these differences in terms of severe infection, hospitalization, or even death. The potential benefit of increased immunogenicity by interrupting conventional synthetic disease-modifying antirheumatic drugs [csDMARDs] such as methotrexate before or after vaccination needs to be balanced against the potential risk of disease flare. Ultimately, decision-making should be individualized based on factors such as comorbidities, disease activity, and other considerations.” The results presented by Dr. Ørbo suggest that, while there may be a clinical difference in terms of severe infection, the overall prognosis for vaccinated patients is reasonably good.
Regarding other DMARDs, such as biologics, the approach may differ. Dr. Machado suggested: “In patients using rituximab or other B cell–depleting therapies, SARS-CoV-2 vaccination should be scheduled in a way that optimizes vaccine immunogenicity. A minimum of 10 B cells/mcL of blood is likely a relevant threshold above which a sufficient cellular and immune response is established.”
COVID vaccines are safe for pregnant and breastfeeding women
According to data from the COVAD study, which comprised two global cross-sectional surveys conducted in 2021 and 2022, the COVID-19 vaccine appeared safe for pregnant and breastfeeding women with autoimmune diseases (AID).
Presenter Laura Andreoli, MD, PhD, of the University of Brescia (Italy), said that, although pregnant patients with AID reported more adverse events related to vaccination, these rates were not significantly higher than those among pregnant, healthy control persons who were without AID. No difference in adverse events was observed between breastfeeding women and healthy control persons, and the incidence of disease flares did not significantly differ among all groups.
“In summary, this study provides initial insights into the safety of COVID-19 vaccination during the gestational and postpartum periods in women with autoimmune diseases. These reassuring observations will hopefully improve clinician-patient communication and address hesitancy towards COVID-19 vaccination, as the benefits for the mother and fetus through passive immunization appear to outweigh potential risks,” Dr. Andreoli said in an interview.
“The large number of participants and the global geographical spread of the COVAD survey were very beneficial in gaining access to this important subset of patients,” added Dr. Andreoli. However, she acknowledged that patients with low socioeconomic status and/or high disability were likely underrepresented. While no data on pregnancy outcomes have been collected thus far, Dr. Andreoli expressed the desire to include them in the study’s follow-up.
The COVAD survey data also indicate that, in general, vaccine hesitancy among patients with AID is decreasing; from 2021 to 2022, it declined from 16.5% to 5.1%, as Dr. Machado indicated in his presentation.
Multiple factors contribute to breakthrough infections
The risk of breakthrough SARS-CoV-2 infections after vaccination varies among patients with rheumatoid arthritis and rheumatic or nonrheumatic autoimmune diseases, primarily depending on the underlying condition rather than the immunosuppressive medication. Environmental factors also appear to play a role. This complex landscape emerges from a further analysis of the COVAD survey dataset.
Alessia Alunno, MD, PhD, of the University of L’Aquila (Italy), presented a detailed and occasionally counterintuitive picture of similarities and differences among young adult patients (aged 18-35 years), mostly women, with various rheumatic and nonrheumatic diseases in relation to COVID-19. Most notably, the type of disease seemed to have more significance than the immunosuppression resulting from the treatment regimen. This held true for vaccine safety as well as for the risk of breakthrough COVID-19 and symptom profiles.
Patients with rheumatic disease (RMD) and nonrheumatic autoimmune disease (nr-AD) had significantly different therapeutic profiles on average. Before vaccination, 45% of patients with RMD used glucocorticoids (GC), and 91% used immunosuppressants (IS). In contrast, only 9.5% of nr-AD patients used GC, and 21% were taking IS.
Interestingly, the overall prevalence of reported SARS-CoV-2 infections was not influenced by medication and was practically identical (25% to 28%) across all groups. However, there were intriguing differences in the occurrence of infections before and after vaccination between disease groups. Prevaccine infections were less frequent among patients with RMD compared with healthy control persons (adjusted odds ratio, 0.6), while the rates were similar among patients with nr-AD and healthy control persons. On the other hand, breakthrough infections were more frequent in patients with RMD (aOR, 2.7), whereas the rate was similar between healthy control persons and patients with nr-AD.
Despite a much lower rate of GC/IS use, patients with nr-AD experienced repeated infections more frequently. In contrast, patients with RMD were less prone to multiple infections, even compared with healthy control persons (aOR, 0.5).
Regarding the disease profile, fewer than 5% of all infected patients required advanced therapies for SARS-CoV-2 infection. Notably, all SARS-CoV-2 infections in patients with nr-AD were symptomatic, whereas among patients with RMD and healthy control persons, the incidence of asymptomatic infections was 3%. The rate of hospital admissions was 4% for patients with RMD, compared with 2% for patients with nr-AD and 1% for control persons. The RMD group exhibited some differences between prevaccine infections and breakthrough infections, including a significantly lower frequency of loss of smell and taste during breakthrough infections. Overall, patients with RMD and COVID-19 experienced cough, runny nose, throat pain, nausea, and vomiting more frequently. In contrast, patients with nr-AD had a much higher risk of skin rashes during breakthrough infections (aOR, 8.7).
Vaccine adverse events (AEs) were also influenced by the underlying disease. Patients with RMD and those with nr-AD were more likely to experience mild AEs after the first or second dose, compared with healthy control persons (adjusted OR, 2.4 and 2.0, respectively). The most common early, mild AEs across all groups were injection-site pain, headache, and fatigue, but they occurred more frequently in the nr-AD group than in the RMD or healthy control group. Additionally, fever and chills occurred more frequently among the nr-AD group. Late, mild AEs and severe AEs were rare and affected all groups equally.
“The overall incidence of AEs was very low. Our results certainly do not undermine the safety of vaccines,” Dr. Alunno said.
Disease flares were more common after vaccination (10% with RMD and 7% with nr-AD) than after infection (5% with RMD and 1.5% with nr-AD). Furthermore, in many cases, after vaccination, flares required a change of medications, particularly for patients with RMD.
Additional results from the COVAD survey from January to July 2022, presented by Naveen Ravichandran, MD, DM, of Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India, revealed a higher prevalence (OR, 1.2; P = .001) of breakthrough infections among patients with RA. A total of 22.6% of patients with RA experienced breakthrough infections, compared with 20.6% for patients with other autoimmune rheumatic diseases and 18.4% of healthy control persons. Hospitalizations and the need for advanced treatment were also more common among patients with RA (30.9%) than among healthy control persons (13.9%). Patients with RA who had breakthrough infections tended to be older (closer to 50 years of age on average) and female, and they were more likely to have comorbidities and mental disorders. The human development index of the patient’s country of residence also played a role. Further research is necessary to understand how breakthrough infection outcomes are affected by a patient’s socioeconomic situation.
According to Dr. Ravichandran, medication was not a significant factor, except for the use of steroids and rituximab, which were associated with a higher risk of severe COVID-19 and hospitalization. Patients using rituximab, in particular, faced significantly increased odds for hospitalization (OR, 3.4) and severe breakthrough COVID-19 (OR, 3.0).
Session moderator Kim Lauper, MD, of the University of Geneva, cautioned: “The roles of disease and medication are challenging to separate. Some diseases require a more aggressive immunosuppressive regimen. It’s possible that different diseases affect the immune system differently, but it is not easy to demonstrate.”
The complications observed in the data warrant further study, as mentioned by Dr. Schulze-Koops: “We have a problem tied to the time line of the pandemic, where we had different viruses, different population behaviors, different treatments, and different standards of care over time. We also have differences between ethnic communities and regions of the world. But most importantly, we have different viruses: From the original strain to Delta to Omicron, we know they have very different clinical outcomes. I believe we need more scientific research to unravel these factors.”
Dr. Ørbo, Dr. Ravichandran, Dr. Andreoli, and Dr. Alunno reported no relevant financial relationships. Dr. Machado has received grants and/or honoraria from AbbVie, Bristol-Myers Squibb, Celgene, Eli Lilly, Galapagos, Janssen, Merck Sharp & Dohme, Novartis, Orphazyme, Pfizer, Roche, and UCB.
A version of this article originally appeared on Medscape.com.
AT EULAR 2023