User login
Make assessment of immunization status of older adults routine
ATLANTA – In the opinion of John M. Kelso, MD, assessment of immunization status in older adults should be a routine part of all visits.
“Don’t assume that your patients are getting their vaccines someplace else,” he said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. “We should be taking advantage of the fact that these patients are in our offices.”
Inactivated influenza vaccine (IIV3)
For adults aged 65 and older, the high-dose, trivalent version of the flu vaccine (60 micrograms of hemagglutinin per strain, or IIV3-HD) may be preferable to the standard dose of 15 micrograms of hemagglutinin per strain (IIV3-SD). A study of nearly 32,000 patients found that IIV3-HD induced significantly higher antibody responses and provided better protection against laboratory-confirmed influenza, compared with IIV3-SD (N Engl J Med. 2014;371:635-45). The relative efficacy of high dose vs. standard dose was 24.2%. “That means that one-quarter of all breakthrough influenza illnesses could be prevented if IIV3HD were used instead of IIV3-SD,” Dr. Kelso said.
Another approach is to use an adjuvanted influenza vaccine, which contains the standard 15 micrograms of influenza antigen but the adjuvant is MF59, a squalene-based oil-in-water emulsion. One small study of 282 patients aged 65 and older showed the adjuvanted vaccine to be more effective than the unadjuvanted vaccine (Vaccine. 2013;51:1622-8).
The Centers for Disease Control and Prevention does not express a preference for the high-dose or adjuvanted vaccine, but rather stresses the importance of influenza vaccination with whatever age-appropriate IIV formulation is available at the time of the patient’s visit.
The 13-valent pneumococcal conjugate vaccine (PCV13) and the 23-valent pneumococcal polysaccharide vaccine (PPSV23)
All adults who turn 65 years of age should receive the PCV13, followed 1 year later by the PPSV23. For those who already received the PPSV23 after age 65 years of age, they should receive the PCV13 at least 1 year later. “The real bulk of hospitalizations and fatalities from invasive pneumococcal disease are happening to people over 65 year of age,” said Dr. Kelso, who is also a clinical professor of pediatrics and internal medicine at the University of California, San Diego “So there’s a real need here for vaccination.”
Tdap
This should be administered to all adolescents and adults regardless of interval since their last tetanus-diphtheria vaccine. “This includes those age 65 years of age and older in whom the vaccine has been found to be equally safe and immunogenic,” Dr. Kelso said. “This is important not only to prevent pertussis in older adults, but also to prevent them from spreading the disease to infants where it can be fatal.”
Zoster vaccine
One in three adults will develop zoster during their lifetime, he said, and one million episodes occur in the United States each year. Common complications include postherpetic neuralgia and eye involvement that can result in loss of vision. The CDC recommends routine vaccination of all immunocompetent persons over age 60 with one dose of zoster vaccine. “Persons who report a previous episode of zoster can be vaccinated but it is not indicated to treat acute zoster, to prevent persons with acute zoster from developing postherpetic neuralgia, or to treat ongoing postherpetic neuralgia,” Dr. Kelso said.
He reported having no relevant financial disclosures.
ATLANTA – In the opinion of John M. Kelso, MD, assessment of immunization status in older adults should be a routine part of all visits.
“Don’t assume that your patients are getting their vaccines someplace else,” he said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. “We should be taking advantage of the fact that these patients are in our offices.”
Inactivated influenza vaccine (IIV3)
For adults aged 65 and older, the high-dose, trivalent version of the flu vaccine (60 micrograms of hemagglutinin per strain, or IIV3-HD) may be preferable to the standard dose of 15 micrograms of hemagglutinin per strain (IIV3-SD). A study of nearly 32,000 patients found that IIV3-HD induced significantly higher antibody responses and provided better protection against laboratory-confirmed influenza, compared with IIV3-SD (N Engl J Med. 2014;371:635-45). The relative efficacy of high dose vs. standard dose was 24.2%. “That means that one-quarter of all breakthrough influenza illnesses could be prevented if IIV3HD were used instead of IIV3-SD,” Dr. Kelso said.
Another approach is to use an adjuvanted influenza vaccine, which contains the standard 15 micrograms of influenza antigen but the adjuvant is MF59, a squalene-based oil-in-water emulsion. One small study of 282 patients aged 65 and older showed the adjuvanted vaccine to be more effective than the unadjuvanted vaccine (Vaccine. 2013;51:1622-8).
The Centers for Disease Control and Prevention does not express a preference for the high-dose or adjuvanted vaccine, but rather stresses the importance of influenza vaccination with whatever age-appropriate IIV formulation is available at the time of the patient’s visit.
The 13-valent pneumococcal conjugate vaccine (PCV13) and the 23-valent pneumococcal polysaccharide vaccine (PPSV23)
All adults who turn 65 years of age should receive the PCV13, followed 1 year later by the PPSV23. For those who already received the PPSV23 after age 65 years of age, they should receive the PCV13 at least 1 year later. “The real bulk of hospitalizations and fatalities from invasive pneumococcal disease are happening to people over 65 year of age,” said Dr. Kelso, who is also a clinical professor of pediatrics and internal medicine at the University of California, San Diego “So there’s a real need here for vaccination.”
Tdap
This should be administered to all adolescents and adults regardless of interval since their last tetanus-diphtheria vaccine. “This includes those age 65 years of age and older in whom the vaccine has been found to be equally safe and immunogenic,” Dr. Kelso said. “This is important not only to prevent pertussis in older adults, but also to prevent them from spreading the disease to infants where it can be fatal.”
Zoster vaccine
One in three adults will develop zoster during their lifetime, he said, and one million episodes occur in the United States each year. Common complications include postherpetic neuralgia and eye involvement that can result in loss of vision. The CDC recommends routine vaccination of all immunocompetent persons over age 60 with one dose of zoster vaccine. “Persons who report a previous episode of zoster can be vaccinated but it is not indicated to treat acute zoster, to prevent persons with acute zoster from developing postherpetic neuralgia, or to treat ongoing postherpetic neuralgia,” Dr. Kelso said.
He reported having no relevant financial disclosures.
ATLANTA – In the opinion of John M. Kelso, MD, assessment of immunization status in older adults should be a routine part of all visits.
“Don’t assume that your patients are getting their vaccines someplace else,” he said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. “We should be taking advantage of the fact that these patients are in our offices.”
Inactivated influenza vaccine (IIV3)
For adults aged 65 and older, the high-dose, trivalent version of the flu vaccine (60 micrograms of hemagglutinin per strain, or IIV3-HD) may be preferable to the standard dose of 15 micrograms of hemagglutinin per strain (IIV3-SD). A study of nearly 32,000 patients found that IIV3-HD induced significantly higher antibody responses and provided better protection against laboratory-confirmed influenza, compared with IIV3-SD (N Engl J Med. 2014;371:635-45). The relative efficacy of high dose vs. standard dose was 24.2%. “That means that one-quarter of all breakthrough influenza illnesses could be prevented if IIV3HD were used instead of IIV3-SD,” Dr. Kelso said.
Another approach is to use an adjuvanted influenza vaccine, which contains the standard 15 micrograms of influenza antigen but the adjuvant is MF59, a squalene-based oil-in-water emulsion. One small study of 282 patients aged 65 and older showed the adjuvanted vaccine to be more effective than the unadjuvanted vaccine (Vaccine. 2013;51:1622-8).
The Centers for Disease Control and Prevention does not express a preference for the high-dose or adjuvanted vaccine, but rather stresses the importance of influenza vaccination with whatever age-appropriate IIV formulation is available at the time of the patient’s visit.
The 13-valent pneumococcal conjugate vaccine (PCV13) and the 23-valent pneumococcal polysaccharide vaccine (PPSV23)
All adults who turn 65 years of age should receive the PCV13, followed 1 year later by the PPSV23. For those who already received the PPSV23 after age 65 years of age, they should receive the PCV13 at least 1 year later. “The real bulk of hospitalizations and fatalities from invasive pneumococcal disease are happening to people over 65 year of age,” said Dr. Kelso, who is also a clinical professor of pediatrics and internal medicine at the University of California, San Diego “So there’s a real need here for vaccination.”
Tdap
This should be administered to all adolescents and adults regardless of interval since their last tetanus-diphtheria vaccine. “This includes those age 65 years of age and older in whom the vaccine has been found to be equally safe and immunogenic,” Dr. Kelso said. “This is important not only to prevent pertussis in older adults, but also to prevent them from spreading the disease to infants where it can be fatal.”
Zoster vaccine
One in three adults will develop zoster during their lifetime, he said, and one million episodes occur in the United States each year. Common complications include postherpetic neuralgia and eye involvement that can result in loss of vision. The CDC recommends routine vaccination of all immunocompetent persons over age 60 with one dose of zoster vaccine. “Persons who report a previous episode of zoster can be vaccinated but it is not indicated to treat acute zoster, to prevent persons with acute zoster from developing postherpetic neuralgia, or to treat ongoing postherpetic neuralgia,” Dr. Kelso said.
He reported having no relevant financial disclosures.
EXPERT ANALYSIS AT THE 2017 AAAAI ANNUAL MEETING
Many patients’ severe asthma remains uncontrolled
ATLANTA – More than half of patients severe asthma have disease that remains uncontrolled at their index date of treatment, and 39% remained uncontrolled at 12 months of follow-up, results from a large single specialty practice study showed.
“Severe asthma accounts for only 5%-10% of all asthma [in] patients but at least half of the health care costs, and it’s a significant burden to those who suffer from it,” study author Brian D. Stone, MD, said in an interview at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
The mean age of patients was 44.4 years, 67% were female, 78% were white, 77% had concomitant rhinitis, 21% had sinusitis, and 44% had allergic sensitivities. The mean baseline prebronchodilation FEV1 and FEV1% predicted were 2.45 L and 79.7%, respectively. The mean baseline ACT score was 17, with 61% of patients having ACT scores of 19 or lower, indicating poor symptom control.
Using National Asthma Education and Prevention Program criteria, the researchers found that 52% of patients had uncontrolled asthma at the index date and 39% remained uncontrolled at 12 months of follow-up. In an effort to better manage their severe asthma, more than one-third of patients on Step 4 therapy and 60% of patients on Step 5 therapy changed their asthma controller medications during follow-up.
“As an asthma specialist, I hoped that more [of these patients] would have come under control. These are the most difficult patients to treat,” said Dr. Stone, who practices at Allergy Partners of San Diego. “It’s a population that deserves special attention, and interventions are probably going to be on multiple levels, depending on what type of severe persistent asthma they have. More therapies are needed.”
He acknowledged certain limitations of the study, including the fact that patients were treated by specialists in allergy, asthma, and immunology and, therefore, may not represent the general population with asthma.
The study was supported by AstraZeneca. Dr. Stone reported having no relevant financial disclosures.
ATLANTA – More than half of patients severe asthma have disease that remains uncontrolled at their index date of treatment, and 39% remained uncontrolled at 12 months of follow-up, results from a large single specialty practice study showed.
“Severe asthma accounts for only 5%-10% of all asthma [in] patients but at least half of the health care costs, and it’s a significant burden to those who suffer from it,” study author Brian D. Stone, MD, said in an interview at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
The mean age of patients was 44.4 years, 67% were female, 78% were white, 77% had concomitant rhinitis, 21% had sinusitis, and 44% had allergic sensitivities. The mean baseline prebronchodilation FEV1 and FEV1% predicted were 2.45 L and 79.7%, respectively. The mean baseline ACT score was 17, with 61% of patients having ACT scores of 19 or lower, indicating poor symptom control.
Using National Asthma Education and Prevention Program criteria, the researchers found that 52% of patients had uncontrolled asthma at the index date and 39% remained uncontrolled at 12 months of follow-up. In an effort to better manage their severe asthma, more than one-third of patients on Step 4 therapy and 60% of patients on Step 5 therapy changed their asthma controller medications during follow-up.
“As an asthma specialist, I hoped that more [of these patients] would have come under control. These are the most difficult patients to treat,” said Dr. Stone, who practices at Allergy Partners of San Diego. “It’s a population that deserves special attention, and interventions are probably going to be on multiple levels, depending on what type of severe persistent asthma they have. More therapies are needed.”
He acknowledged certain limitations of the study, including the fact that patients were treated by specialists in allergy, asthma, and immunology and, therefore, may not represent the general population with asthma.
The study was supported by AstraZeneca. Dr. Stone reported having no relevant financial disclosures.
ATLANTA – More than half of patients severe asthma have disease that remains uncontrolled at their index date of treatment, and 39% remained uncontrolled at 12 months of follow-up, results from a large single specialty practice study showed.
“Severe asthma accounts for only 5%-10% of all asthma [in] patients but at least half of the health care costs, and it’s a significant burden to those who suffer from it,” study author Brian D. Stone, MD, said in an interview at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
The mean age of patients was 44.4 years, 67% were female, 78% were white, 77% had concomitant rhinitis, 21% had sinusitis, and 44% had allergic sensitivities. The mean baseline prebronchodilation FEV1 and FEV1% predicted were 2.45 L and 79.7%, respectively. The mean baseline ACT score was 17, with 61% of patients having ACT scores of 19 or lower, indicating poor symptom control.
Using National Asthma Education and Prevention Program criteria, the researchers found that 52% of patients had uncontrolled asthma at the index date and 39% remained uncontrolled at 12 months of follow-up. In an effort to better manage their severe asthma, more than one-third of patients on Step 4 therapy and 60% of patients on Step 5 therapy changed their asthma controller medications during follow-up.
“As an asthma specialist, I hoped that more [of these patients] would have come under control. These are the most difficult patients to treat,” said Dr. Stone, who practices at Allergy Partners of San Diego. “It’s a population that deserves special attention, and interventions are probably going to be on multiple levels, depending on what type of severe persistent asthma they have. More therapies are needed.”
He acknowledged certain limitations of the study, including the fact that patients were treated by specialists in allergy, asthma, and immunology and, therefore, may not represent the general population with asthma.
The study was supported by AstraZeneca. Dr. Stone reported having no relevant financial disclosures.
AT THE 2017 AAAAI ANNUAL MEETING
Key clinical point:
Major finding: More than half of patients with severe asthma (52%) had uncontrolled disease at the index date of treatment, and 39% remained uncontrolled at 12 months of follow-up.
Data source: A retrospective review of 12,922 patients aged 12 years and older with severe asthma who were treated between Jan. 1, 2010, and April 30, 2016.
Disclosures: The study was supported by AstraZeneca. Dr. Stone reported no relevant financial disclosures.
What happens when a baked egg oral challenge is negative?
ATLANTA – The majority of patients who had cooked egg exposure following a negative physician-supervised baked egg oral challenge are tolerating cooked egg, according to a retrospective study.
However, no correlation between results and development of tolerance was identified with skin prick testing or serum IgE testing.
To find out, Dr. Peng, a second-year fellow in the department of pediatrics at the University of California, Los Angeles, and her associates identified 22 patients who underwent negative physician-supervised baked egg oral challenges from July 2011 until June 2016. They reviewed medical charts to obtain data on age, clinical history, skin prick test results, and results of serum IgE testing to egg and its components. Next, the researchers contacted patients and their families and invited them to participate in a telephone survey about patterns of baked, cooked, and raw egg exposure and associated reactions, following their negative baked challenge. The patients ranged in age from 10 months to 44 years and their mean age was 7 years.
Dr. Peng presented results from 18 of the 22 patients who were successfully contacted. A mean of 26 months had passed since their baked egg oral challenge. Of these patients, 17 (94%) have had continued exposure to egg while 15 (83%) have shown tolerance to cooked egg. The researchers observed variable patterns of baked egg intake following the negative physician-supervised baked egg challenge. “Some patients are able to tolerate cooked egg rapidly but are not interested in continuing frequent consumption,” Dr. Peng said. “They may say, ‘My 3-year-old doesn’t like scrambled eggs, so I’m not going to keep pushing them.’ They’re not considering themselves egg allergic so their quality of life is much better. I understand that tolerating baked egg is a big deal, as an allergist I want to see them do more, such as tolerating cooked egg.”
When patients were asked about adverse reactions to egg consumption, three (17%) described gastrointestinal symptoms, five (28%) described cutaneous symptoms, and three (17%) described respiratory reactions. Dr. Peng noted that of the three patients who have not achieved tolerance to cooked egg, one patient reported mild reaction to baked egg 2 weeks after the baked egg challenge, while the other two continue to have baked egg exposure but have not yet introduced cooked egg into their diets. “I hope that most pediatricians and family practice physicians consider referral to an allergist if they’re not comfortable introducing a baked egg oral challenge.”
The researchers could not identify any correlation between skin prick or serum IgE test results and development of tolerance to cooked egg. “Data in the literature suggests that serum testing is predictive [of tolerance], but it’s not 100%,” Dr. Peng said.
She reported having no relevant financial disclosures.
ATLANTA – The majority of patients who had cooked egg exposure following a negative physician-supervised baked egg oral challenge are tolerating cooked egg, according to a retrospective study.
However, no correlation between results and development of tolerance was identified with skin prick testing or serum IgE testing.
To find out, Dr. Peng, a second-year fellow in the department of pediatrics at the University of California, Los Angeles, and her associates identified 22 patients who underwent negative physician-supervised baked egg oral challenges from July 2011 until June 2016. They reviewed medical charts to obtain data on age, clinical history, skin prick test results, and results of serum IgE testing to egg and its components. Next, the researchers contacted patients and their families and invited them to participate in a telephone survey about patterns of baked, cooked, and raw egg exposure and associated reactions, following their negative baked challenge. The patients ranged in age from 10 months to 44 years and their mean age was 7 years.
Dr. Peng presented results from 18 of the 22 patients who were successfully contacted. A mean of 26 months had passed since their baked egg oral challenge. Of these patients, 17 (94%) have had continued exposure to egg while 15 (83%) have shown tolerance to cooked egg. The researchers observed variable patterns of baked egg intake following the negative physician-supervised baked egg challenge. “Some patients are able to tolerate cooked egg rapidly but are not interested in continuing frequent consumption,” Dr. Peng said. “They may say, ‘My 3-year-old doesn’t like scrambled eggs, so I’m not going to keep pushing them.’ They’re not considering themselves egg allergic so their quality of life is much better. I understand that tolerating baked egg is a big deal, as an allergist I want to see them do more, such as tolerating cooked egg.”
When patients were asked about adverse reactions to egg consumption, three (17%) described gastrointestinal symptoms, five (28%) described cutaneous symptoms, and three (17%) described respiratory reactions. Dr. Peng noted that of the three patients who have not achieved tolerance to cooked egg, one patient reported mild reaction to baked egg 2 weeks after the baked egg challenge, while the other two continue to have baked egg exposure but have not yet introduced cooked egg into their diets. “I hope that most pediatricians and family practice physicians consider referral to an allergist if they’re not comfortable introducing a baked egg oral challenge.”
The researchers could not identify any correlation between skin prick or serum IgE test results and development of tolerance to cooked egg. “Data in the literature suggests that serum testing is predictive [of tolerance], but it’s not 100%,” Dr. Peng said.
She reported having no relevant financial disclosures.
ATLANTA – The majority of patients who had cooked egg exposure following a negative physician-supervised baked egg oral challenge are tolerating cooked egg, according to a retrospective study.
However, no correlation between results and development of tolerance was identified with skin prick testing or serum IgE testing.
To find out, Dr. Peng, a second-year fellow in the department of pediatrics at the University of California, Los Angeles, and her associates identified 22 patients who underwent negative physician-supervised baked egg oral challenges from July 2011 until June 2016. They reviewed medical charts to obtain data on age, clinical history, skin prick test results, and results of serum IgE testing to egg and its components. Next, the researchers contacted patients and their families and invited them to participate in a telephone survey about patterns of baked, cooked, and raw egg exposure and associated reactions, following their negative baked challenge. The patients ranged in age from 10 months to 44 years and their mean age was 7 years.
Dr. Peng presented results from 18 of the 22 patients who were successfully contacted. A mean of 26 months had passed since their baked egg oral challenge. Of these patients, 17 (94%) have had continued exposure to egg while 15 (83%) have shown tolerance to cooked egg. The researchers observed variable patterns of baked egg intake following the negative physician-supervised baked egg challenge. “Some patients are able to tolerate cooked egg rapidly but are not interested in continuing frequent consumption,” Dr. Peng said. “They may say, ‘My 3-year-old doesn’t like scrambled eggs, so I’m not going to keep pushing them.’ They’re not considering themselves egg allergic so their quality of life is much better. I understand that tolerating baked egg is a big deal, as an allergist I want to see them do more, such as tolerating cooked egg.”
When patients were asked about adverse reactions to egg consumption, three (17%) described gastrointestinal symptoms, five (28%) described cutaneous symptoms, and three (17%) described respiratory reactions. Dr. Peng noted that of the three patients who have not achieved tolerance to cooked egg, one patient reported mild reaction to baked egg 2 weeks after the baked egg challenge, while the other two continue to have baked egg exposure but have not yet introduced cooked egg into their diets. “I hope that most pediatricians and family practice physicians consider referral to an allergist if they’re not comfortable introducing a baked egg oral challenge.”
The researchers could not identify any correlation between skin prick or serum IgE test results and development of tolerance to cooked egg. “Data in the literature suggests that serum testing is predictive [of tolerance], but it’s not 100%,” Dr. Peng said.
She reported having no relevant financial disclosures.
AT THE 2017 AAAAI ANNUAL MEETING
Key clinical point:
Major finding: Following a negative physician-supervised baked egg oral challenge 94% of patients have had continued exposure to egg while 83% have shown tolerance to cooked egg.
Data source: A retrospective review of 22 patients who underwent a physician-supervised negative oral baked egg challenge.
Disclosures: Dr. Peng reported having no relevant financial disclosures.
Omalizumab may help chronic rhinosinusitis symptoms
ATLANTA – Patients with severe and recalcitrant chronic rhinosinusitis who were treated with omalizumab reported improvement in symptoms, compared with controls, results from a small single-center study suggested.
A recombinant DNA-derived humanized monoclonal antibody that binds to human IgE, omalizumab is approved for use in patients 12 years or older with moderate to severe persistent asthma and inadequately controlled symptoms with inhaled corticosteroids. Two small randomized controlled trials (J Allergy Clin Immunol. 2013;131[1]:110-6 and Rhinology 2010;48[3]:318-24) have shown that omalizumab reduces polyp size and improves sinus inflammation, Shaun J. Kilty, MD, said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
For the current study, Dr. Kilty and his associates evaluated the clinical effect of omalizumab on sinus symptom and disease control in 25 patients with recalcitrant chronic rhinosinusitis (CRS) who were receiving anti-IgE therapy as part of their asthma treatment. Five control patients were included. The researchers used a visual analog scale to measure changes over time among study participants in overall CRS symptoms and major CRS symptoms, including facial pain, nasal obstruction, rhinorrhea, and olfaction. The mean age of the patients was 50 years and 49 years in the omalizumab and control groups, respectively. The mean duration of treatment was 19 months, and most had nasal polyps (76% in the omalizumab group and 80% in the control group).
Dr. Kilty reported that among patients in the omalizumab treatment group, overall symptoms improved by 70%. The individual symptom that improved the most was facial pain (79%), followed by nasal obstruction (70%), rhinorrhea (56%), and olfaction (56%). Among the control group, overall symptoms improved by 17%. Rhinorrhea improved by 16% and nasal obstruction by 15%, but no improvements in facial pain or in olfaction were observed. Symptom improvement was significantly higher for omalizumab-treated patients in every category (P less than .05).
A subset analysis of eight patients in the treatment group and three in the control group who had aspirin-exacerbated respiratory disease (AERD) revealed significant differences between groups for nasal obstruction (P = .05) and olfaction (P = .03), but not for rhinorrhea and overall symptom improvement (P = .5 and P = .1, respectively). “Within the group treated with omalizumab, there were no significant differences in any of the categories when comparing patients with CRS with nasal polyps to those with AERD,” the researchers wrote in their abstract.
“I think there’s a strong enough signal to indicate that this biologic therapy does work in patients with chronic sinusitis with polyps,” Dr. Kilty said. “I think it needs to be better determined exactly what patient cohort is best to use it, and similarly better-structured randomized trials are needed to evaluate the effect of this biologic.”
He reported having no relevant financial disclosures.
ATLANTA – Patients with severe and recalcitrant chronic rhinosinusitis who were treated with omalizumab reported improvement in symptoms, compared with controls, results from a small single-center study suggested.
A recombinant DNA-derived humanized monoclonal antibody that binds to human IgE, omalizumab is approved for use in patients 12 years or older with moderate to severe persistent asthma and inadequately controlled symptoms with inhaled corticosteroids. Two small randomized controlled trials (J Allergy Clin Immunol. 2013;131[1]:110-6 and Rhinology 2010;48[3]:318-24) have shown that omalizumab reduces polyp size and improves sinus inflammation, Shaun J. Kilty, MD, said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
For the current study, Dr. Kilty and his associates evaluated the clinical effect of omalizumab on sinus symptom and disease control in 25 patients with recalcitrant chronic rhinosinusitis (CRS) who were receiving anti-IgE therapy as part of their asthma treatment. Five control patients were included. The researchers used a visual analog scale to measure changes over time among study participants in overall CRS symptoms and major CRS symptoms, including facial pain, nasal obstruction, rhinorrhea, and olfaction. The mean age of the patients was 50 years and 49 years in the omalizumab and control groups, respectively. The mean duration of treatment was 19 months, and most had nasal polyps (76% in the omalizumab group and 80% in the control group).
Dr. Kilty reported that among patients in the omalizumab treatment group, overall symptoms improved by 70%. The individual symptom that improved the most was facial pain (79%), followed by nasal obstruction (70%), rhinorrhea (56%), and olfaction (56%). Among the control group, overall symptoms improved by 17%. Rhinorrhea improved by 16% and nasal obstruction by 15%, but no improvements in facial pain or in olfaction were observed. Symptom improvement was significantly higher for omalizumab-treated patients in every category (P less than .05).
A subset analysis of eight patients in the treatment group and three in the control group who had aspirin-exacerbated respiratory disease (AERD) revealed significant differences between groups for nasal obstruction (P = .05) and olfaction (P = .03), but not for rhinorrhea and overall symptom improvement (P = .5 and P = .1, respectively). “Within the group treated with omalizumab, there were no significant differences in any of the categories when comparing patients with CRS with nasal polyps to those with AERD,” the researchers wrote in their abstract.
“I think there’s a strong enough signal to indicate that this biologic therapy does work in patients with chronic sinusitis with polyps,” Dr. Kilty said. “I think it needs to be better determined exactly what patient cohort is best to use it, and similarly better-structured randomized trials are needed to evaluate the effect of this biologic.”
He reported having no relevant financial disclosures.
ATLANTA – Patients with severe and recalcitrant chronic rhinosinusitis who were treated with omalizumab reported improvement in symptoms, compared with controls, results from a small single-center study suggested.
A recombinant DNA-derived humanized monoclonal antibody that binds to human IgE, omalizumab is approved for use in patients 12 years or older with moderate to severe persistent asthma and inadequately controlled symptoms with inhaled corticosteroids. Two small randomized controlled trials (J Allergy Clin Immunol. 2013;131[1]:110-6 and Rhinology 2010;48[3]:318-24) have shown that omalizumab reduces polyp size and improves sinus inflammation, Shaun J. Kilty, MD, said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
For the current study, Dr. Kilty and his associates evaluated the clinical effect of omalizumab on sinus symptom and disease control in 25 patients with recalcitrant chronic rhinosinusitis (CRS) who were receiving anti-IgE therapy as part of their asthma treatment. Five control patients were included. The researchers used a visual analog scale to measure changes over time among study participants in overall CRS symptoms and major CRS symptoms, including facial pain, nasal obstruction, rhinorrhea, and olfaction. The mean age of the patients was 50 years and 49 years in the omalizumab and control groups, respectively. The mean duration of treatment was 19 months, and most had nasal polyps (76% in the omalizumab group and 80% in the control group).
Dr. Kilty reported that among patients in the omalizumab treatment group, overall symptoms improved by 70%. The individual symptom that improved the most was facial pain (79%), followed by nasal obstruction (70%), rhinorrhea (56%), and olfaction (56%). Among the control group, overall symptoms improved by 17%. Rhinorrhea improved by 16% and nasal obstruction by 15%, but no improvements in facial pain or in olfaction were observed. Symptom improvement was significantly higher for omalizumab-treated patients in every category (P less than .05).
A subset analysis of eight patients in the treatment group and three in the control group who had aspirin-exacerbated respiratory disease (AERD) revealed significant differences between groups for nasal obstruction (P = .05) and olfaction (P = .03), but not for rhinorrhea and overall symptom improvement (P = .5 and P = .1, respectively). “Within the group treated with omalizumab, there were no significant differences in any of the categories when comparing patients with CRS with nasal polyps to those with AERD,” the researchers wrote in their abstract.
“I think there’s a strong enough signal to indicate that this biologic therapy does work in patients with chronic sinusitis with polyps,” Dr. Kilty said. “I think it needs to be better determined exactly what patient cohort is best to use it, and similarly better-structured randomized trials are needed to evaluate the effect of this biologic.”
He reported having no relevant financial disclosures.
AT 2017 AAAAI ANNUAL MEETING
Key clinical point: In patients with severe chronic rhinosinusitis, omalizumab treatment provided significant improvement in every major clinical symptom of the condition.
Major finding: Among patients in the omalizumab treatment group, overall symptoms improved by 70%.
Data source: A study that evaluated the clinical effect of omalizumab in 25 patients with recalcitrant chronic rhinosinusitis who were receiving anti-IgE therapy as part of their asthma treatment and 5 control patients.
Disclosures: Dr. Kilty reported having no relevant financial disclosures.
A history of asthma exacerbations predicts future exacerbations
ATLANTA – Asthma exacerbations are common, severe events that can be life-threatening and can accelerate loss of lung function. That’s why it’s important to flag high-risk patients in your clinical practice, Nizar N. Jarjour, MD, said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
Each year in the United States there are 15 million clinic visits, 2 million ED visits, and 500,000 hospitalizations for severe asthma exacerbations. “These exacerbations cause a high cost on the health care system, they lead to loss of work or school, and they’re a burden to patients and certainly to their families,” said Dr. Jarjour, professor of medicine and division head of allergy, pulmonary and critical care at the University of Wisconsin, Madison.
Factors implicated in asthma exacerbation include air pollution, cigarette smoke, occupational exposure, stress, and allergen exposure, but 50%-85% of cases are related to viral upper respiratory infections. “Any respiratory pathogen can precipitate attacks, but rhinoviruses are the most common,” he said. “Seasonal viral [upper respiratory infections] correlate with hospital admissions for asthma, and peak in spring and fall.”
Purported ways that a viral upper respiratory infection can lead to asthma exacerbation include enhanced airway responsiveness, increased eosinophilic airway inflammation in response to antigen, enhanced lower airway neutrophilic inflammation, and direct infection of the lower airway. “There are is an accentuated eosinophilic inflammation in response to allergen challenge when somebody has a cold,” Dr. Jarjour explained. “But the viral infection can actually directly lead to eosinophilic inflammation, perhaps through TSLP [thymic stromal lymphopoietin], interleukin (IL)-25, and IL-33 simulating the ILC2 (type 2 innate lymphoid cells). So there are both accentuating response to allergens as well as direct enhancement of eosinophilic inflammation following viral infection.”
One study that examined airway lavage following experimental infection found that patients had increased numbers of neutrophils in their airway sample (J Allergy Clin Immunol. 2000;105:1169-77). This means that asthma exacerbation triggers neutrophilic inflammation, which relates to the induction of cytokines and chemokines in the upper airway. “We have also demonstrated increased circulation of G-CSF [granulocyte–colony stimulating factor] and nasal IL-8 in the upper airway related to increased neutrophil recruitment,” Dr. Jarjour said.
Host factors associated with asthma exacerbations include altered innate immune response in the form of a defect in production of antiviral cytokines in response to viral infection, and a greater T helper (Th)2/Th1 ratio. Other factors include eosinophilic inflammation and greater levels of specific IgE to dust mite. Baseline data from 709 patients enrolled in the National Heart, Lung, and Blood Institute Severe Asthma Research Program III (SARP-3) showed that three top risk factors for asthma exacerbations are gastroesophageal reflux disease (relative risk (RR) 1.6), greater blood eosinophil count (RR 1.6), and obesity (RR 1.2) (Am J Resp Care Med. 2017; 195:302-13).
Risk factors for exacerbation noted in various epidemiological studies include African American and Hispanic races, poor access to medical care, inadequate chronic control, smoking, allergen sensitivity to cats and dogs, gastroesophageal reflux disease, high body mass index, sinusitis, and uncontrolled eosinophilic inflammation. Key findings from a follow-up study of SARP-3 patients include the fact that the absence of exacerbations on a 12-month recall predicted future stability.
“More importantly, participants with severe disease and two or more exacerbations at baseline had a 75% chance of having an exacerbation in the following year,” Dr. Jarjour said. “This is a call for us to pay more close attention to these patients and is an important fact to keep in mind when designing clinical trials. A history of exacerbations is the best predictor of future exacerbation.”
Dr. Jarjour disclosed that he has received research funding from the National Heart, Lung, and Blood Institute and consulting fees from AstraZeneca and Teva Pharmaceutical. He is a member of the American Board of Internal Medicine–Pulmonary Exam Subcommittee.
ATLANTA – Asthma exacerbations are common, severe events that can be life-threatening and can accelerate loss of lung function. That’s why it’s important to flag high-risk patients in your clinical practice, Nizar N. Jarjour, MD, said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
Each year in the United States there are 15 million clinic visits, 2 million ED visits, and 500,000 hospitalizations for severe asthma exacerbations. “These exacerbations cause a high cost on the health care system, they lead to loss of work or school, and they’re a burden to patients and certainly to their families,” said Dr. Jarjour, professor of medicine and division head of allergy, pulmonary and critical care at the University of Wisconsin, Madison.
Factors implicated in asthma exacerbation include air pollution, cigarette smoke, occupational exposure, stress, and allergen exposure, but 50%-85% of cases are related to viral upper respiratory infections. “Any respiratory pathogen can precipitate attacks, but rhinoviruses are the most common,” he said. “Seasonal viral [upper respiratory infections] correlate with hospital admissions for asthma, and peak in spring and fall.”
Purported ways that a viral upper respiratory infection can lead to asthma exacerbation include enhanced airway responsiveness, increased eosinophilic airway inflammation in response to antigen, enhanced lower airway neutrophilic inflammation, and direct infection of the lower airway. “There are is an accentuated eosinophilic inflammation in response to allergen challenge when somebody has a cold,” Dr. Jarjour explained. “But the viral infection can actually directly lead to eosinophilic inflammation, perhaps through TSLP [thymic stromal lymphopoietin], interleukin (IL)-25, and IL-33 simulating the ILC2 (type 2 innate lymphoid cells). So there are both accentuating response to allergens as well as direct enhancement of eosinophilic inflammation following viral infection.”
One study that examined airway lavage following experimental infection found that patients had increased numbers of neutrophils in their airway sample (J Allergy Clin Immunol. 2000;105:1169-77). This means that asthma exacerbation triggers neutrophilic inflammation, which relates to the induction of cytokines and chemokines in the upper airway. “We have also demonstrated increased circulation of G-CSF [granulocyte–colony stimulating factor] and nasal IL-8 in the upper airway related to increased neutrophil recruitment,” Dr. Jarjour said.
Host factors associated with asthma exacerbations include altered innate immune response in the form of a defect in production of antiviral cytokines in response to viral infection, and a greater T helper (Th)2/Th1 ratio. Other factors include eosinophilic inflammation and greater levels of specific IgE to dust mite. Baseline data from 709 patients enrolled in the National Heart, Lung, and Blood Institute Severe Asthma Research Program III (SARP-3) showed that three top risk factors for asthma exacerbations are gastroesophageal reflux disease (relative risk (RR) 1.6), greater blood eosinophil count (RR 1.6), and obesity (RR 1.2) (Am J Resp Care Med. 2017; 195:302-13).
Risk factors for exacerbation noted in various epidemiological studies include African American and Hispanic races, poor access to medical care, inadequate chronic control, smoking, allergen sensitivity to cats and dogs, gastroesophageal reflux disease, high body mass index, sinusitis, and uncontrolled eosinophilic inflammation. Key findings from a follow-up study of SARP-3 patients include the fact that the absence of exacerbations on a 12-month recall predicted future stability.
“More importantly, participants with severe disease and two or more exacerbations at baseline had a 75% chance of having an exacerbation in the following year,” Dr. Jarjour said. “This is a call for us to pay more close attention to these patients and is an important fact to keep in mind when designing clinical trials. A history of exacerbations is the best predictor of future exacerbation.”
Dr. Jarjour disclosed that he has received research funding from the National Heart, Lung, and Blood Institute and consulting fees from AstraZeneca and Teva Pharmaceutical. He is a member of the American Board of Internal Medicine–Pulmonary Exam Subcommittee.
ATLANTA – Asthma exacerbations are common, severe events that can be life-threatening and can accelerate loss of lung function. That’s why it’s important to flag high-risk patients in your clinical practice, Nizar N. Jarjour, MD, said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
Each year in the United States there are 15 million clinic visits, 2 million ED visits, and 500,000 hospitalizations for severe asthma exacerbations. “These exacerbations cause a high cost on the health care system, they lead to loss of work or school, and they’re a burden to patients and certainly to their families,” said Dr. Jarjour, professor of medicine and division head of allergy, pulmonary and critical care at the University of Wisconsin, Madison.
Factors implicated in asthma exacerbation include air pollution, cigarette smoke, occupational exposure, stress, and allergen exposure, but 50%-85% of cases are related to viral upper respiratory infections. “Any respiratory pathogen can precipitate attacks, but rhinoviruses are the most common,” he said. “Seasonal viral [upper respiratory infections] correlate with hospital admissions for asthma, and peak in spring and fall.”
Purported ways that a viral upper respiratory infection can lead to asthma exacerbation include enhanced airway responsiveness, increased eosinophilic airway inflammation in response to antigen, enhanced lower airway neutrophilic inflammation, and direct infection of the lower airway. “There are is an accentuated eosinophilic inflammation in response to allergen challenge when somebody has a cold,” Dr. Jarjour explained. “But the viral infection can actually directly lead to eosinophilic inflammation, perhaps through TSLP [thymic stromal lymphopoietin], interleukin (IL)-25, and IL-33 simulating the ILC2 (type 2 innate lymphoid cells). So there are both accentuating response to allergens as well as direct enhancement of eosinophilic inflammation following viral infection.”
One study that examined airway lavage following experimental infection found that patients had increased numbers of neutrophils in their airway sample (J Allergy Clin Immunol. 2000;105:1169-77). This means that asthma exacerbation triggers neutrophilic inflammation, which relates to the induction of cytokines and chemokines in the upper airway. “We have also demonstrated increased circulation of G-CSF [granulocyte–colony stimulating factor] and nasal IL-8 in the upper airway related to increased neutrophil recruitment,” Dr. Jarjour said.
Host factors associated with asthma exacerbations include altered innate immune response in the form of a defect in production of antiviral cytokines in response to viral infection, and a greater T helper (Th)2/Th1 ratio. Other factors include eosinophilic inflammation and greater levels of specific IgE to dust mite. Baseline data from 709 patients enrolled in the National Heart, Lung, and Blood Institute Severe Asthma Research Program III (SARP-3) showed that three top risk factors for asthma exacerbations are gastroesophageal reflux disease (relative risk (RR) 1.6), greater blood eosinophil count (RR 1.6), and obesity (RR 1.2) (Am J Resp Care Med. 2017; 195:302-13).
Risk factors for exacerbation noted in various epidemiological studies include African American and Hispanic races, poor access to medical care, inadequate chronic control, smoking, allergen sensitivity to cats and dogs, gastroesophageal reflux disease, high body mass index, sinusitis, and uncontrolled eosinophilic inflammation. Key findings from a follow-up study of SARP-3 patients include the fact that the absence of exacerbations on a 12-month recall predicted future stability.
“More importantly, participants with severe disease and two or more exacerbations at baseline had a 75% chance of having an exacerbation in the following year,” Dr. Jarjour said. “This is a call for us to pay more close attention to these patients and is an important fact to keep in mind when designing clinical trials. A history of exacerbations is the best predictor of future exacerbation.”
Dr. Jarjour disclosed that he has received research funding from the National Heart, Lung, and Blood Institute and consulting fees from AstraZeneca and Teva Pharmaceutical. He is a member of the American Board of Internal Medicine–Pulmonary Exam Subcommittee.
One peanut daily might maintain childhood immunotherapy gains
ATLANTA – One year or more after peanut immunotherapy, 27 of 33 (82%) children were eating peanuts regularly, most without problems, in a survey from the Children’s Hospital of Philadelphia.
The finding speaks to the durability of peanut immunotherapy, something that’s been a concern for physicians and families. It suggests that peanut immunotherapy might give children long-term protection from accidental exposure, so long as they continue to eat a small amount of peanut almost every day after desensitization.
She and her team surveyed the families of 15 children who completed a trial of epicutaneous peanut immunotherapy (EPIT) and 9 who completed a trial of oral immunotherapy (OIT) about a year after the studies ended. They also surveyed families of nine children about 2 years after they completed a trial of OIT plus omalizumab (Xolair) for peanut allergy. The investigators and families chose maintenance doses based on results from the final peanut challenges, and children were warned against running around within 2 hours of their dose, to prevent exercised-induced reactions.
The point of using omalizumab in the one trial was to see if it helped children ramp up immunotherapy more quickly and tolerate higher final peanut doses. It did, and the nine omalizumab children were on the highest maintenance doses of peanut at 2-year follow-up, with almost all of them consuming an average of at least one peanut a day. Perhaps because of that, three of the four anaphylactic reactions were in the omalizumab group.
The fourth reaction was in a child who completed the OIT trial. There was no anaphylaxis in EPIT children. About 60% in both groups reported eating an average of at least a peanut a day at 1-year follow-up.
About three-quarters of the children ate peanut-containing candy to get their maintenance dose. Others ate peanuts or peanut butter or sprinkled peanut flour on their food. Just six children, all from the EPIT cohort, said they liked the taste of peanuts.
Meanwhile, 6 of the 33 children (18%) – 1 in the omalizumab group, 3 in the EPIT arm, and 2 in the OIT group – refused to eat peanuts after their immunotherapy trials.
Posttrial peanut dosing ranged from once a month to daily, and the majority of subjects ate peanut about five times per week. All of the anaphylaxis children recovered without incident and resumed peanut maintenance. A couple of the children in the EPIT group had an itch in their throat when they switched to eating peanuts, but it resolved on its own. One child in the omalizumab group and one in the OIT group reported gastrointestinal symptoms with maintenance dosing.
The original trials funded the follow-up. Ms. Ott Lewis had no relevant financial disclosures.
ATLANTA – One year or more after peanut immunotherapy, 27 of 33 (82%) children were eating peanuts regularly, most without problems, in a survey from the Children’s Hospital of Philadelphia.
The finding speaks to the durability of peanut immunotherapy, something that’s been a concern for physicians and families. It suggests that peanut immunotherapy might give children long-term protection from accidental exposure, so long as they continue to eat a small amount of peanut almost every day after desensitization.
She and her team surveyed the families of 15 children who completed a trial of epicutaneous peanut immunotherapy (EPIT) and 9 who completed a trial of oral immunotherapy (OIT) about a year after the studies ended. They also surveyed families of nine children about 2 years after they completed a trial of OIT plus omalizumab (Xolair) for peanut allergy. The investigators and families chose maintenance doses based on results from the final peanut challenges, and children were warned against running around within 2 hours of their dose, to prevent exercised-induced reactions.
The point of using omalizumab in the one trial was to see if it helped children ramp up immunotherapy more quickly and tolerate higher final peanut doses. It did, and the nine omalizumab children were on the highest maintenance doses of peanut at 2-year follow-up, with almost all of them consuming an average of at least one peanut a day. Perhaps because of that, three of the four anaphylactic reactions were in the omalizumab group.
The fourth reaction was in a child who completed the OIT trial. There was no anaphylaxis in EPIT children. About 60% in both groups reported eating an average of at least a peanut a day at 1-year follow-up.
About three-quarters of the children ate peanut-containing candy to get their maintenance dose. Others ate peanuts or peanut butter or sprinkled peanut flour on their food. Just six children, all from the EPIT cohort, said they liked the taste of peanuts.
Meanwhile, 6 of the 33 children (18%) – 1 in the omalizumab group, 3 in the EPIT arm, and 2 in the OIT group – refused to eat peanuts after their immunotherapy trials.
Posttrial peanut dosing ranged from once a month to daily, and the majority of subjects ate peanut about five times per week. All of the anaphylaxis children recovered without incident and resumed peanut maintenance. A couple of the children in the EPIT group had an itch in their throat when they switched to eating peanuts, but it resolved on its own. One child in the omalizumab group and one in the OIT group reported gastrointestinal symptoms with maintenance dosing.
The original trials funded the follow-up. Ms. Ott Lewis had no relevant financial disclosures.
ATLANTA – One year or more after peanut immunotherapy, 27 of 33 (82%) children were eating peanuts regularly, most without problems, in a survey from the Children’s Hospital of Philadelphia.
The finding speaks to the durability of peanut immunotherapy, something that’s been a concern for physicians and families. It suggests that peanut immunotherapy might give children long-term protection from accidental exposure, so long as they continue to eat a small amount of peanut almost every day after desensitization.
She and her team surveyed the families of 15 children who completed a trial of epicutaneous peanut immunotherapy (EPIT) and 9 who completed a trial of oral immunotherapy (OIT) about a year after the studies ended. They also surveyed families of nine children about 2 years after they completed a trial of OIT plus omalizumab (Xolair) for peanut allergy. The investigators and families chose maintenance doses based on results from the final peanut challenges, and children were warned against running around within 2 hours of their dose, to prevent exercised-induced reactions.
The point of using omalizumab in the one trial was to see if it helped children ramp up immunotherapy more quickly and tolerate higher final peanut doses. It did, and the nine omalizumab children were on the highest maintenance doses of peanut at 2-year follow-up, with almost all of them consuming an average of at least one peanut a day. Perhaps because of that, three of the four anaphylactic reactions were in the omalizumab group.
The fourth reaction was in a child who completed the OIT trial. There was no anaphylaxis in EPIT children. About 60% in both groups reported eating an average of at least a peanut a day at 1-year follow-up.
About three-quarters of the children ate peanut-containing candy to get their maintenance dose. Others ate peanuts or peanut butter or sprinkled peanut flour on their food. Just six children, all from the EPIT cohort, said they liked the taste of peanuts.
Meanwhile, 6 of the 33 children (18%) – 1 in the omalizumab group, 3 in the EPIT arm, and 2 in the OIT group – refused to eat peanuts after their immunotherapy trials.
Posttrial peanut dosing ranged from once a month to daily, and the majority of subjects ate peanut about five times per week. All of the anaphylaxis children recovered without incident and resumed peanut maintenance. A couple of the children in the EPIT group had an itch in their throat when they switched to eating peanuts, but it resolved on its own. One child in the omalizumab group and one in the OIT group reported gastrointestinal symptoms with maintenance dosing.
The original trials funded the follow-up. Ms. Ott Lewis had no relevant financial disclosures.
Key clinical point: Eating more than that might increase the risk of reaction.
Major finding: There were four anaphylactic reactions, three of which were among children on the highest maintenance doses.
Data source: Follow-up surveys a year or more after peanut desensitization trials in 33 children.
Disclosures: The original trials funded the follow-up. The lead investigator had no relevant financial disclosures.
Survey eyes trends in care of severe pediatric asthma
ATLANTA – The treatment of pediatric severe acute asthma has changed over the past 21 years, but interspecialty differences in the management of these patients persist, results from a national survey suggest.
“I think it’s good for every ER and ICU department to have a conversation with providers about what to do when these kinds of patients come in,” lead study author Roua Azmeh, MD, said in an interview at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. “A lot of ERs are establishing protocols. I think that’s going to be the wave of the future.”
The National Heart, Blood, and Lung Institute Asthma Guidelines, first published in 1991, were most recently revised in 2007. In an effort to observe changes in asthma management in pediatric EDs and ICUs over the past 21 years, and to compare common management strategies, Dr. Azmeh and her associates distributed a 16-question online survey to 144 current program directors of U.S. training programs in pediatric emergency medicine and pediatric critical care. Results were compared to a similar survey that was sent by snail mail to program directors of U.S. training programs in pediatric emergency medicine and pediatric critical care in 1995.
Dr. Azmeh, a fellow in allergy and immunology at the Saint Louis University, reported results from 62 respondents who completed the 2016 questionnaire (43%). For initial management of pediatric acute severe asthma, a greater proportion of program directors in pediatric critical care reported using parenteral corticosteroids, compared with their counterparts in pediatric emergency medicine (85% vs. 32%, respectively; P less than .0001), as well as continuous beta 2-agonists (73% vs. 56%; P less than .05). A majority of overall respondents (98%) did not use theophylline for initial management, but more program directors in pediatric critical care reported using it for treatment failure, compared with their counterparts in pediatric emergency medicine (56% vs. 20%, respectively; P less than .0071). There was a trend among all respondents for more use of heliox for treatment failure than for initial management (13% vs. 6%).
When the researchers compared current survey responses to responses from the 1995 survey, they observed that program training directors across both specialties increased the use of nebulized ipratropium bromide in initial management and treatment failure (17% vs. 69%; P less than .0001 and 33% vs. 42%; P less than .05) and decreased use of theophylline for initial management of severe acute asthma (17% vs. 3%; P less than .05). However, theophylline is still used in treatment failure.
Among respondents to the 2016 survey, program directors in pediatric emergency medicine were less likely than were those in pediatric critical care to use continuous nebulized beta-2 agonists for initial management or to add parenteral selective beta-2 agonists (56% vs. 73% and 12% vs. 21%, respectively; P less than .05). They also were less likely to use theophylline in treatment failure (20% vs. 56%; P less than .05).
Dr. Azmeh reported having no relevant financial disclosures.
Surveys are interesting to establish a trend for what residents and fellows are being taught in emergency rooms and critical care units. The parenteral steroid use difference for the two groups in 2016 may be related to the fact that the emergency room hasn’t decide
Surveys are interesting to establish a trend for what residents and fellows are being taught in emergency rooms and critical care units. The parenteral steroid use difference for the two groups in 2016 may be related to the fact that the emergency room hasn’t decide
Surveys are interesting to establish a trend for what residents and fellows are being taught in emergency rooms and critical care units. The parenteral steroid use difference for the two groups in 2016 may be related to the fact that the emergency room hasn’t decide
ATLANTA – The treatment of pediatric severe acute asthma has changed over the past 21 years, but interspecialty differences in the management of these patients persist, results from a national survey suggest.
“I think it’s good for every ER and ICU department to have a conversation with providers about what to do when these kinds of patients come in,” lead study author Roua Azmeh, MD, said in an interview at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. “A lot of ERs are establishing protocols. I think that’s going to be the wave of the future.”
The National Heart, Blood, and Lung Institute Asthma Guidelines, first published in 1991, were most recently revised in 2007. In an effort to observe changes in asthma management in pediatric EDs and ICUs over the past 21 years, and to compare common management strategies, Dr. Azmeh and her associates distributed a 16-question online survey to 144 current program directors of U.S. training programs in pediatric emergency medicine and pediatric critical care. Results were compared to a similar survey that was sent by snail mail to program directors of U.S. training programs in pediatric emergency medicine and pediatric critical care in 1995.
Dr. Azmeh, a fellow in allergy and immunology at the Saint Louis University, reported results from 62 respondents who completed the 2016 questionnaire (43%). For initial management of pediatric acute severe asthma, a greater proportion of program directors in pediatric critical care reported using parenteral corticosteroids, compared with their counterparts in pediatric emergency medicine (85% vs. 32%, respectively; P less than .0001), as well as continuous beta 2-agonists (73% vs. 56%; P less than .05). A majority of overall respondents (98%) did not use theophylline for initial management, but more program directors in pediatric critical care reported using it for treatment failure, compared with their counterparts in pediatric emergency medicine (56% vs. 20%, respectively; P less than .0071). There was a trend among all respondents for more use of heliox for treatment failure than for initial management (13% vs. 6%).
When the researchers compared current survey responses to responses from the 1995 survey, they observed that program training directors across both specialties increased the use of nebulized ipratropium bromide in initial management and treatment failure (17% vs. 69%; P less than .0001 and 33% vs. 42%; P less than .05) and decreased use of theophylline for initial management of severe acute asthma (17% vs. 3%; P less than .05). However, theophylline is still used in treatment failure.
Among respondents to the 2016 survey, program directors in pediatric emergency medicine were less likely than were those in pediatric critical care to use continuous nebulized beta-2 agonists for initial management or to add parenteral selective beta-2 agonists (56% vs. 73% and 12% vs. 21%, respectively; P less than .05). They also were less likely to use theophylline in treatment failure (20% vs. 56%; P less than .05).
Dr. Azmeh reported having no relevant financial disclosures.
ATLANTA – The treatment of pediatric severe acute asthma has changed over the past 21 years, but interspecialty differences in the management of these patients persist, results from a national survey suggest.
“I think it’s good for every ER and ICU department to have a conversation with providers about what to do when these kinds of patients come in,” lead study author Roua Azmeh, MD, said in an interview at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. “A lot of ERs are establishing protocols. I think that’s going to be the wave of the future.”
The National Heart, Blood, and Lung Institute Asthma Guidelines, first published in 1991, were most recently revised in 2007. In an effort to observe changes in asthma management in pediatric EDs and ICUs over the past 21 years, and to compare common management strategies, Dr. Azmeh and her associates distributed a 16-question online survey to 144 current program directors of U.S. training programs in pediatric emergency medicine and pediatric critical care. Results were compared to a similar survey that was sent by snail mail to program directors of U.S. training programs in pediatric emergency medicine and pediatric critical care in 1995.
Dr. Azmeh, a fellow in allergy and immunology at the Saint Louis University, reported results from 62 respondents who completed the 2016 questionnaire (43%). For initial management of pediatric acute severe asthma, a greater proportion of program directors in pediatric critical care reported using parenteral corticosteroids, compared with their counterparts in pediatric emergency medicine (85% vs. 32%, respectively; P less than .0001), as well as continuous beta 2-agonists (73% vs. 56%; P less than .05). A majority of overall respondents (98%) did not use theophylline for initial management, but more program directors in pediatric critical care reported using it for treatment failure, compared with their counterparts in pediatric emergency medicine (56% vs. 20%, respectively; P less than .0071). There was a trend among all respondents for more use of heliox for treatment failure than for initial management (13% vs. 6%).
When the researchers compared current survey responses to responses from the 1995 survey, they observed that program training directors across both specialties increased the use of nebulized ipratropium bromide in initial management and treatment failure (17% vs. 69%; P less than .0001 and 33% vs. 42%; P less than .05) and decreased use of theophylline for initial management of severe acute asthma (17% vs. 3%; P less than .05). However, theophylline is still used in treatment failure.
Among respondents to the 2016 survey, program directors in pediatric emergency medicine were less likely than were those in pediatric critical care to use continuous nebulized beta-2 agonists for initial management or to add parenteral selective beta-2 agonists (56% vs. 73% and 12% vs. 21%, respectively; P less than .05). They also were less likely to use theophylline in treatment failure (20% vs. 56%; P less than .05).
Dr. Azmeh reported having no relevant financial disclosures.
Key clinical point:
Major finding: For initial management of pediatric acute severe asthma, a greater proportion of program directors in pediatric critical care reported using parenteral corticosteroids, compared with their counterparts in pediatric emergency medicine (85% vs. 32%, respectively; P less than .0001).
Data source: Results from a 16-question online survey sent to 144 current program directors of U.S. training programs in pediatric emergency medicine and pediatric critical care.
Disclosures: Dr. Azmeh reported having no relevant financial disclosures.
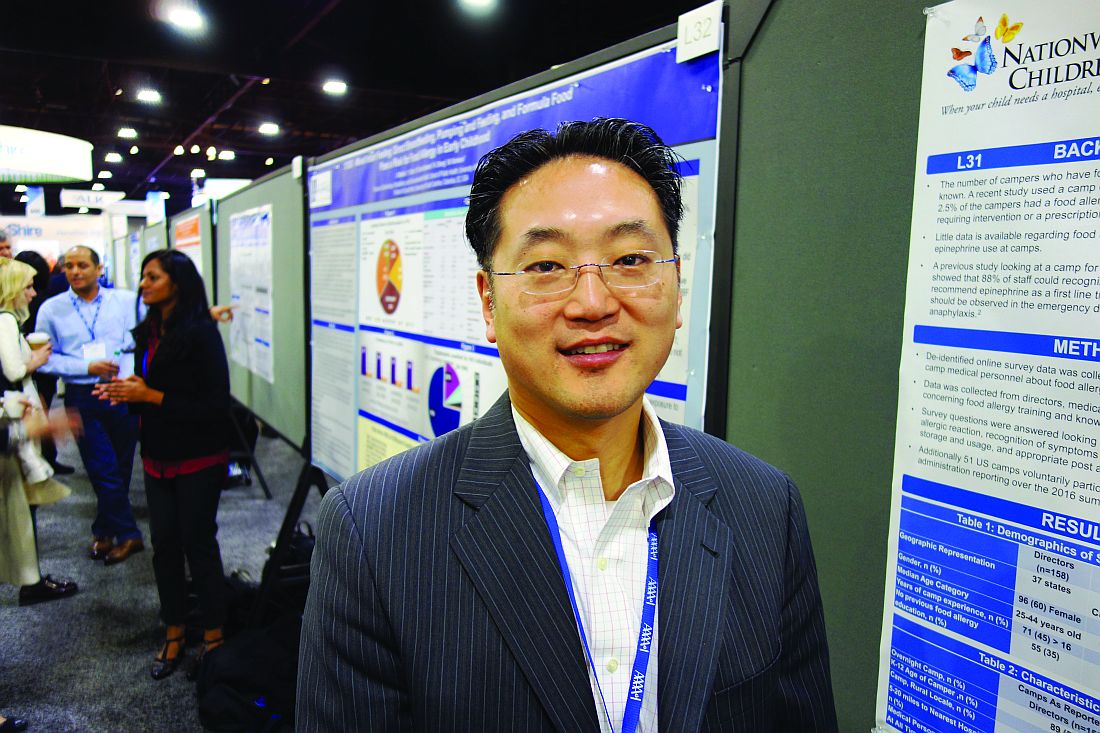
Summer camps need help managing childhood anaphylaxis
ATLANTA – Summer camp personnel need a refresher course on the recognition, treatment, and prevention of allergic reactions in children, according to an online survey of camps in almost 40 U.S. states and Canadian provinces.
There’s a lot of data about how schools handle allergies but almost nothing about summer camps. To fill the gap, the investigators sent surveys across North America to 158 camp directors, 141 camp medical personnel – mostly registered nurses – and 198 camp staffers. Most of the camps were traditional rural affairs where children stay for several weeks, but there were also suburban and city day camps.
The results weren’t good. About a third of directors and staff, and almost 20% of medical personnel, said they had no education on food allergies. Less than 40% had a good understanding of the different ways that anaphylaxis can present. Less than 80% of camp directors and medical personnel and less than 50% of staff knew the right sequence for anaphylaxis treatment – epinephrine first, followed by a 911 call, and then a call to parents. Many respondents didn’t know the correct injection site for epinephrine.
They also were confused about hand sanitizers versus soap and water. Many mistakenly thought that sanitizers were as good as washing for removing allergens. “Their knowledge about how to clean tables and clean hands of food allergens was limited,” said lead investigator Margaret T. Redmond, MD, an allergist at Nationwide Children’s Hospital in Columbus, Ohio.
It all points to the need for education. “We were surprised at the poor recognition of anaphylactic symptoms. We are trying to identify the weaknesses in camps for targeted interventions. We know from the school data that, with education, people can change,” Dr. Redmond said.
During the 2016 summer session, 51 camps agreed to report epinephrine. Most were rural, with an average of 150 campers per day staying a median of 51 days. There were 12 epinephrine shots over that time, about half for peanut reactions and the rest for bee, wasp, and fire ant stings. None of the children died.
“Families that have kids with food allergies should reach out to camps about their policies and make sure they have epinephrine available at all times and that they have food allergy action plans” that staff know about, Dr. Redmond said.
The work was funded by Mylan and kaleo, both makers of epinephrine autoinjectors. Dr. Lee and Dr. Redmond had no relevant financial disclosures.
ATLANTA – Summer camp personnel need a refresher course on the recognition, treatment, and prevention of allergic reactions in children, according to an online survey of camps in almost 40 U.S. states and Canadian provinces.
There’s a lot of data about how schools handle allergies but almost nothing about summer camps. To fill the gap, the investigators sent surveys across North America to 158 camp directors, 141 camp medical personnel – mostly registered nurses – and 198 camp staffers. Most of the camps were traditional rural affairs where children stay for several weeks, but there were also suburban and city day camps.
The results weren’t good. About a third of directors and staff, and almost 20% of medical personnel, said they had no education on food allergies. Less than 40% had a good understanding of the different ways that anaphylaxis can present. Less than 80% of camp directors and medical personnel and less than 50% of staff knew the right sequence for anaphylaxis treatment – epinephrine first, followed by a 911 call, and then a call to parents. Many respondents didn’t know the correct injection site for epinephrine.
They also were confused about hand sanitizers versus soap and water. Many mistakenly thought that sanitizers were as good as washing for removing allergens. “Their knowledge about how to clean tables and clean hands of food allergens was limited,” said lead investigator Margaret T. Redmond, MD, an allergist at Nationwide Children’s Hospital in Columbus, Ohio.
It all points to the need for education. “We were surprised at the poor recognition of anaphylactic symptoms. We are trying to identify the weaknesses in camps for targeted interventions. We know from the school data that, with education, people can change,” Dr. Redmond said.
During the 2016 summer session, 51 camps agreed to report epinephrine. Most were rural, with an average of 150 campers per day staying a median of 51 days. There were 12 epinephrine shots over that time, about half for peanut reactions and the rest for bee, wasp, and fire ant stings. None of the children died.
“Families that have kids with food allergies should reach out to camps about their policies and make sure they have epinephrine available at all times and that they have food allergy action plans” that staff know about, Dr. Redmond said.
The work was funded by Mylan and kaleo, both makers of epinephrine autoinjectors. Dr. Lee and Dr. Redmond had no relevant financial disclosures.
ATLANTA – Summer camp personnel need a refresher course on the recognition, treatment, and prevention of allergic reactions in children, according to an online survey of camps in almost 40 U.S. states and Canadian provinces.
There’s a lot of data about how schools handle allergies but almost nothing about summer camps. To fill the gap, the investigators sent surveys across North America to 158 camp directors, 141 camp medical personnel – mostly registered nurses – and 198 camp staffers. Most of the camps were traditional rural affairs where children stay for several weeks, but there were also suburban and city day camps.
The results weren’t good. About a third of directors and staff, and almost 20% of medical personnel, said they had no education on food allergies. Less than 40% had a good understanding of the different ways that anaphylaxis can present. Less than 80% of camp directors and medical personnel and less than 50% of staff knew the right sequence for anaphylaxis treatment – epinephrine first, followed by a 911 call, and then a call to parents. Many respondents didn’t know the correct injection site for epinephrine.
They also were confused about hand sanitizers versus soap and water. Many mistakenly thought that sanitizers were as good as washing for removing allergens. “Their knowledge about how to clean tables and clean hands of food allergens was limited,” said lead investigator Margaret T. Redmond, MD, an allergist at Nationwide Children’s Hospital in Columbus, Ohio.
It all points to the need for education. “We were surprised at the poor recognition of anaphylactic symptoms. We are trying to identify the weaknesses in camps for targeted interventions. We know from the school data that, with education, people can change,” Dr. Redmond said.
During the 2016 summer session, 51 camps agreed to report epinephrine. Most were rural, with an average of 150 campers per day staying a median of 51 days. There were 12 epinephrine shots over that time, about half for peanut reactions and the rest for bee, wasp, and fire ant stings. None of the children died.
“Families that have kids with food allergies should reach out to camps about their policies and make sure they have epinephrine available at all times and that they have food allergy action plans” that staff know about, Dr. Redmond said.
The work was funded by Mylan and kaleo, both makers of epinephrine autoinjectors. Dr. Lee and Dr. Redmond had no relevant financial disclosures.
AT AAAAI 2017 ANNUAL MEETING
Key clinical point:
Major finding: About a third of directors and camp staff and almost 20% of medical personnel (mostly registered nurses) said they had no previous education on food allergies.
Data source: An online survey of camps in almost 40 U.S. states and Canadian provinces, including almost 500 personnel.
Disclosures: The work was funded by Mylan and kaleo, both makers of epinephrine autoinjectors. Dr. Lee and Dr. Redmond had no relevant financial disclosures.
The many faces of formaldehyde contact allergy
ATLANTA – Formaldehyde has various clinical presentations and variable thresholds to trigger allergic contact dermatitis, so it requires a high index of suspicion, according to Salma de la Feld, MD.
It may present as irritant contact dermatitis, allergic contact dermatitis (especially to the hands and face), airborne allergic contact dermatitis, or systemic allergic contact dermatitis (to aspartame).
From most-releasing to least-releasing, these chemicals include quaternium-15, diazolidinyl urea, DMDM hydantoin, imidazolidinyl urea, and bronopol. Exposure can come from personal care products, prescription topical steroids and acne creams, Brazilian hair keratin, cigarettes, and textiles made of blended fabrics, as well as occupations such as a leather handler, surgical nurse, pathology lab worker, and hairdresser.
“Patients can be allergic to either the formaldehyde that [a product] releases or the non–formaldehyde component or both,” said Dr. de la Feld, who is a dermatologist at Emory University, Atlanta.
Recent studies suggest that the formaldehyde allergen should be tested at 2% instead of at 1%. “You do get a few more irritant reactions [with this approach], but you’re also going to catch more people who have a true positive reaction,” she said. “If you see a borderline papule with a little pink, that might be an irritant. You want to test for the formaldehyde releasers. When you do have a positive reaction, you want to have a high index of suspicion. Patients have to be strict in what personal care products they’re using. Some people might be able to tolerate a low concentration of formaldehyde in some products and that magic number differs between patients.”
From a treatment standpoint, Dr. de la Feld advises patients to avoid all formaldehyde releasers and to wear 100% fabrics in an effort to steer clear of textile exposure. “I like to have people be really strict [in their avoidance] when they’re first starting out,” she said. “They don’t like it, but I’ll say, ‘You’re so itchy. Let’s start really strict to get you clear and better.’ Once they’re better and there’s that one moisturizing cream that they really love, then [you] can do a repeat open application test. If nothing happens, it’s probably safe. If [they] start getting red and itchy there, [they] should probably throw away that moisturizer.”
Fragrance
Fragrance, which was named Allergen of the Year in 2007, is another common contact allergen. An estimated 4%-11% of the worldwide population is allergic to fragrance mix, while 1.6%-10.8% is allergic to balsam of Peru. T.R.U.E. tests for the allergen often yield false-negative results. Clinicians who fail to test for fragrance mix 2 will miss about one-third of fragrance allergic contact dermatitis diagnoses. “If the distribution is scattered, you want to be suspicious for fragrance allergy,” Dr. de la Feld said. “Sometimes patients get exposed inadvertently by their significant other or by a family member who is spraying a fragrant product.” Treatment is avoidance. “You want to tell patients to look for products labeled as fragrance free,” she said. “ ‘Unscented’ does not count. When patients tell you that they’re not using any perfume, you want to ask them if they’ve put any on their clothes.”
Systemic contact dermatitis
Dr. de la Feld finished her presentation by discussing systemic contact dermatitis, which she defined as a rash from systemic exposure to an allergen in someone who was previously sensitized. Alternative names for the condition include endogenous contact eczema, systemically-induced contact dermatitis, and internal-external contact-type hypersensitivity. She acknowledged that not all dermatologists believe systemic contact dermatitis to be a true clinical condition, but she does.
“It’s most classically and commonly reported with nickel and balsam of Peru and more slowly with some other allergens,” she said. “It can have multiple clinical presentations, and it’s not always widespread.” The three most common presentations are dyshidrotic hand eczema, sites of prior contact dermatitis (from contact or patch test), and anogenital and/or flexural areas (Baboon syndrome). There are other reports of systemic contact dermatitis presenting as disseminated patchy dermatitis, generalized erythroderma, cheilitis, and lichen planus of the lip.
Dr. de la Feld reported having no relevant financial disclosures.
Correction, 3/28/17: In an earlier version of this article Dr. de la Feld's name was misstated in the photo caption.
ATLANTA – Formaldehyde has various clinical presentations and variable thresholds to trigger allergic contact dermatitis, so it requires a high index of suspicion, according to Salma de la Feld, MD.
It may present as irritant contact dermatitis, allergic contact dermatitis (especially to the hands and face), airborne allergic contact dermatitis, or systemic allergic contact dermatitis (to aspartame).
From most-releasing to least-releasing, these chemicals include quaternium-15, diazolidinyl urea, DMDM hydantoin, imidazolidinyl urea, and bronopol. Exposure can come from personal care products, prescription topical steroids and acne creams, Brazilian hair keratin, cigarettes, and textiles made of blended fabrics, as well as occupations such as a leather handler, surgical nurse, pathology lab worker, and hairdresser.
“Patients can be allergic to either the formaldehyde that [a product] releases or the non–formaldehyde component or both,” said Dr. de la Feld, who is a dermatologist at Emory University, Atlanta.
Recent studies suggest that the formaldehyde allergen should be tested at 2% instead of at 1%. “You do get a few more irritant reactions [with this approach], but you’re also going to catch more people who have a true positive reaction,” she said. “If you see a borderline papule with a little pink, that might be an irritant. You want to test for the formaldehyde releasers. When you do have a positive reaction, you want to have a high index of suspicion. Patients have to be strict in what personal care products they’re using. Some people might be able to tolerate a low concentration of formaldehyde in some products and that magic number differs between patients.”
From a treatment standpoint, Dr. de la Feld advises patients to avoid all formaldehyde releasers and to wear 100% fabrics in an effort to steer clear of textile exposure. “I like to have people be really strict [in their avoidance] when they’re first starting out,” she said. “They don’t like it, but I’ll say, ‘You’re so itchy. Let’s start really strict to get you clear and better.’ Once they’re better and there’s that one moisturizing cream that they really love, then [you] can do a repeat open application test. If nothing happens, it’s probably safe. If [they] start getting red and itchy there, [they] should probably throw away that moisturizer.”
Fragrance
Fragrance, which was named Allergen of the Year in 2007, is another common contact allergen. An estimated 4%-11% of the worldwide population is allergic to fragrance mix, while 1.6%-10.8% is allergic to balsam of Peru. T.R.U.E. tests for the allergen often yield false-negative results. Clinicians who fail to test for fragrance mix 2 will miss about one-third of fragrance allergic contact dermatitis diagnoses. “If the distribution is scattered, you want to be suspicious for fragrance allergy,” Dr. de la Feld said. “Sometimes patients get exposed inadvertently by their significant other or by a family member who is spraying a fragrant product.” Treatment is avoidance. “You want to tell patients to look for products labeled as fragrance free,” she said. “ ‘Unscented’ does not count. When patients tell you that they’re not using any perfume, you want to ask them if they’ve put any on their clothes.”
Systemic contact dermatitis
Dr. de la Feld finished her presentation by discussing systemic contact dermatitis, which she defined as a rash from systemic exposure to an allergen in someone who was previously sensitized. Alternative names for the condition include endogenous contact eczema, systemically-induced contact dermatitis, and internal-external contact-type hypersensitivity. She acknowledged that not all dermatologists believe systemic contact dermatitis to be a true clinical condition, but she does.
“It’s most classically and commonly reported with nickel and balsam of Peru and more slowly with some other allergens,” she said. “It can have multiple clinical presentations, and it’s not always widespread.” The three most common presentations are dyshidrotic hand eczema, sites of prior contact dermatitis (from contact or patch test), and anogenital and/or flexural areas (Baboon syndrome). There are other reports of systemic contact dermatitis presenting as disseminated patchy dermatitis, generalized erythroderma, cheilitis, and lichen planus of the lip.
Dr. de la Feld reported having no relevant financial disclosures.
Correction, 3/28/17: In an earlier version of this article Dr. de la Feld's name was misstated in the photo caption.
ATLANTA – Formaldehyde has various clinical presentations and variable thresholds to trigger allergic contact dermatitis, so it requires a high index of suspicion, according to Salma de la Feld, MD.
It may present as irritant contact dermatitis, allergic contact dermatitis (especially to the hands and face), airborne allergic contact dermatitis, or systemic allergic contact dermatitis (to aspartame).
From most-releasing to least-releasing, these chemicals include quaternium-15, diazolidinyl urea, DMDM hydantoin, imidazolidinyl urea, and bronopol. Exposure can come from personal care products, prescription topical steroids and acne creams, Brazilian hair keratin, cigarettes, and textiles made of blended fabrics, as well as occupations such as a leather handler, surgical nurse, pathology lab worker, and hairdresser.
“Patients can be allergic to either the formaldehyde that [a product] releases or the non–formaldehyde component or both,” said Dr. de la Feld, who is a dermatologist at Emory University, Atlanta.
Recent studies suggest that the formaldehyde allergen should be tested at 2% instead of at 1%. “You do get a few more irritant reactions [with this approach], but you’re also going to catch more people who have a true positive reaction,” she said. “If you see a borderline papule with a little pink, that might be an irritant. You want to test for the formaldehyde releasers. When you do have a positive reaction, you want to have a high index of suspicion. Patients have to be strict in what personal care products they’re using. Some people might be able to tolerate a low concentration of formaldehyde in some products and that magic number differs between patients.”
From a treatment standpoint, Dr. de la Feld advises patients to avoid all formaldehyde releasers and to wear 100% fabrics in an effort to steer clear of textile exposure. “I like to have people be really strict [in their avoidance] when they’re first starting out,” she said. “They don’t like it, but I’ll say, ‘You’re so itchy. Let’s start really strict to get you clear and better.’ Once they’re better and there’s that one moisturizing cream that they really love, then [you] can do a repeat open application test. If nothing happens, it’s probably safe. If [they] start getting red and itchy there, [they] should probably throw away that moisturizer.”
Fragrance
Fragrance, which was named Allergen of the Year in 2007, is another common contact allergen. An estimated 4%-11% of the worldwide population is allergic to fragrance mix, while 1.6%-10.8% is allergic to balsam of Peru. T.R.U.E. tests for the allergen often yield false-negative results. Clinicians who fail to test for fragrance mix 2 will miss about one-third of fragrance allergic contact dermatitis diagnoses. “If the distribution is scattered, you want to be suspicious for fragrance allergy,” Dr. de la Feld said. “Sometimes patients get exposed inadvertently by their significant other or by a family member who is spraying a fragrant product.” Treatment is avoidance. “You want to tell patients to look for products labeled as fragrance free,” she said. “ ‘Unscented’ does not count. When patients tell you that they’re not using any perfume, you want to ask them if they’ve put any on their clothes.”
Systemic contact dermatitis
Dr. de la Feld finished her presentation by discussing systemic contact dermatitis, which she defined as a rash from systemic exposure to an allergen in someone who was previously sensitized. Alternative names for the condition include endogenous contact eczema, systemically-induced contact dermatitis, and internal-external contact-type hypersensitivity. She acknowledged that not all dermatologists believe systemic contact dermatitis to be a true clinical condition, but she does.
“It’s most classically and commonly reported with nickel and balsam of Peru and more slowly with some other allergens,” she said. “It can have multiple clinical presentations, and it’s not always widespread.” The three most common presentations are dyshidrotic hand eczema, sites of prior contact dermatitis (from contact or patch test), and anogenital and/or flexural areas (Baboon syndrome). There are other reports of systemic contact dermatitis presenting as disseminated patchy dermatitis, generalized erythroderma, cheilitis, and lichen planus of the lip.
Dr. de la Feld reported having no relevant financial disclosures.
Correction, 3/28/17: In an earlier version of this article Dr. de la Feld's name was misstated in the photo caption.
EXPERT ANALYSIS AT THE 2017 AAAAI ANNUAL MEETING
Failed ear tubes and antibiotics? Think eosinophilic otitis media
ATLANTA – By the time adults with severe, chronic ear pain end up at the Mayo Clinic in Rochester, Minn., it’s not uncommon for them to have failed antibiotics and gone through a dozen or more sets of ear tubes that didn’t work, followed by surgery – mastoidectomy – to no avail.
“When they get to us, they are struggling. It’s miserable,” said allergist Erin Willits, MD, of Mayo’s division of allergy and immunology inRochester, Minn.
Dr. Willits and her colleagues described the first cohort ever assembled in the United States at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. Most of the research into EOM has been done in Japan, but Mayo has recognized the problem and ENT doctors and allergists there are working together to identify and treat patients. So far, interferon injections seem to be the best option.
The common denominator in all 32 patients was a history of asthma and nasal polyps. Perhaps in EOM, eosinophilic lung and sinus inflammation extends to the eustachian tubes, but that’s not clear yet. Some of the patients also had polyps in their ear canals, and 13 (41%) had a convincing history of aspirin sensitivity. They also had viscous middle-ear effusions, which is why ear tubes don’t help.
In short, the researchers found that a history of asthma and nasal polyps should trigger investigation for EOM in adults with chronic, refractory ear pain.
Of 25 patients, 19 (76%) also had ear disease on CT scan, most commonly inner ear or mastoid opacification. Eighteen patients tested had eosinophilic cationic protein levels above 1,000 ng/mL in their middle-ear effusions, which is high, and 12 out of 30 (40%) were markedly eosinophilic on CBC. The average age of EOM onset was 55.5 years. There were 17 women and 15 men in the cohort.
There was some degree of bilateral hearing loss in nearly every patient, generally a mix of conductive and sensorineural deficits.
“A lot of them start off with conductive hearing loss and progress to sensorineural hearing loss, which can be permanent,” Dr. Willits said. “That’s the biggest thing I want people to recognize: If you start to work with an ENT to try to [identify and] treat these patients, you hopefully can prevent hearing loss.”
Many patients have a robust response to pegylated interferon-alpha. “It kind of dries up their ears, and they feel better,” Dr. Willits noted. Usually it’s given every 2-4 weeks, but some patients can get away with every 6 weeks and lower doses. The side effects are rough, however, and symptoms come back if it’s stopped. It’s also hard to get insurance companies to cover it for EOM (Laryngoscope. 2016 Sep 26. doi: 10.1002/lary.26303).
“It’s not a great treatment, but it’s about all we have,” she said. Omalizumab (Xolair) “has been tried, but it doesn’t help a lot of patients. We are hopeful some of these newer biologics” – such as dupilumab or mepolizumab (Nucala) – “will give these patients relief.”
Dr. Willits had no relevant disclosures.
ATLANTA – By the time adults with severe, chronic ear pain end up at the Mayo Clinic in Rochester, Minn., it’s not uncommon for them to have failed antibiotics and gone through a dozen or more sets of ear tubes that didn’t work, followed by surgery – mastoidectomy – to no avail.
“When they get to us, they are struggling. It’s miserable,” said allergist Erin Willits, MD, of Mayo’s division of allergy and immunology inRochester, Minn.
Dr. Willits and her colleagues described the first cohort ever assembled in the United States at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. Most of the research into EOM has been done in Japan, but Mayo has recognized the problem and ENT doctors and allergists there are working together to identify and treat patients. So far, interferon injections seem to be the best option.
The common denominator in all 32 patients was a history of asthma and nasal polyps. Perhaps in EOM, eosinophilic lung and sinus inflammation extends to the eustachian tubes, but that’s not clear yet. Some of the patients also had polyps in their ear canals, and 13 (41%) had a convincing history of aspirin sensitivity. They also had viscous middle-ear effusions, which is why ear tubes don’t help.
In short, the researchers found that a history of asthma and nasal polyps should trigger investigation for EOM in adults with chronic, refractory ear pain.
Of 25 patients, 19 (76%) also had ear disease on CT scan, most commonly inner ear or mastoid opacification. Eighteen patients tested had eosinophilic cationic protein levels above 1,000 ng/mL in their middle-ear effusions, which is high, and 12 out of 30 (40%) were markedly eosinophilic on CBC. The average age of EOM onset was 55.5 years. There were 17 women and 15 men in the cohort.
There was some degree of bilateral hearing loss in nearly every patient, generally a mix of conductive and sensorineural deficits.
“A lot of them start off with conductive hearing loss and progress to sensorineural hearing loss, which can be permanent,” Dr. Willits said. “That’s the biggest thing I want people to recognize: If you start to work with an ENT to try to [identify and] treat these patients, you hopefully can prevent hearing loss.”
Many patients have a robust response to pegylated interferon-alpha. “It kind of dries up their ears, and they feel better,” Dr. Willits noted. Usually it’s given every 2-4 weeks, but some patients can get away with every 6 weeks and lower doses. The side effects are rough, however, and symptoms come back if it’s stopped. It’s also hard to get insurance companies to cover it for EOM (Laryngoscope. 2016 Sep 26. doi: 10.1002/lary.26303).
“It’s not a great treatment, but it’s about all we have,” she said. Omalizumab (Xolair) “has been tried, but it doesn’t help a lot of patients. We are hopeful some of these newer biologics” – such as dupilumab or mepolizumab (Nucala) – “will give these patients relief.”
Dr. Willits had no relevant disclosures.
ATLANTA – By the time adults with severe, chronic ear pain end up at the Mayo Clinic in Rochester, Minn., it’s not uncommon for them to have failed antibiotics and gone through a dozen or more sets of ear tubes that didn’t work, followed by surgery – mastoidectomy – to no avail.
“When they get to us, they are struggling. It’s miserable,” said allergist Erin Willits, MD, of Mayo’s division of allergy and immunology inRochester, Minn.
Dr. Willits and her colleagues described the first cohort ever assembled in the United States at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. Most of the research into EOM has been done in Japan, but Mayo has recognized the problem and ENT doctors and allergists there are working together to identify and treat patients. So far, interferon injections seem to be the best option.
The common denominator in all 32 patients was a history of asthma and nasal polyps. Perhaps in EOM, eosinophilic lung and sinus inflammation extends to the eustachian tubes, but that’s not clear yet. Some of the patients also had polyps in their ear canals, and 13 (41%) had a convincing history of aspirin sensitivity. They also had viscous middle-ear effusions, which is why ear tubes don’t help.
In short, the researchers found that a history of asthma and nasal polyps should trigger investigation for EOM in adults with chronic, refractory ear pain.
Of 25 patients, 19 (76%) also had ear disease on CT scan, most commonly inner ear or mastoid opacification. Eighteen patients tested had eosinophilic cationic protein levels above 1,000 ng/mL in their middle-ear effusions, which is high, and 12 out of 30 (40%) were markedly eosinophilic on CBC. The average age of EOM onset was 55.5 years. There were 17 women and 15 men in the cohort.
There was some degree of bilateral hearing loss in nearly every patient, generally a mix of conductive and sensorineural deficits.
“A lot of them start off with conductive hearing loss and progress to sensorineural hearing loss, which can be permanent,” Dr. Willits said. “That’s the biggest thing I want people to recognize: If you start to work with an ENT to try to [identify and] treat these patients, you hopefully can prevent hearing loss.”
Many patients have a robust response to pegylated interferon-alpha. “It kind of dries up their ears, and they feel better,” Dr. Willits noted. Usually it’s given every 2-4 weeks, but some patients can get away with every 6 weeks and lower doses. The side effects are rough, however, and symptoms come back if it’s stopped. It’s also hard to get insurance companies to cover it for EOM (Laryngoscope. 2016 Sep 26. doi: 10.1002/lary.26303).
“It’s not a great treatment, but it’s about all we have,” she said. Omalizumab (Xolair) “has been tried, but it doesn’t help a lot of patients. We are hopeful some of these newer biologics” – such as dupilumab or mepolizumab (Nucala) – “will give these patients relief.”
Dr. Willits had no relevant disclosures.
AT 2017 AAAAI ANNUAL MEETING
Key clinical point:
Major finding: Each of the 32 patients in the cohort had a history of both.
Data source: The first EOM cohort ever described in the United States.
Disclosures: Dr. Willits had no disclosures.