User login
Fix the gums, save the heart?
SAN DIEGO – Successful treatment of periodontal disease appears to slow progression of subclinical cardiovascular disease, Anders Holmlund, D.D.S., reported at the annual meeting of the American College of Cardiology.
Previous studies have described an association between periodontal disease and increased risk of cardiovascular disease. This new Swedish observational study breaks fresh ground in showing for the first time that among patients who seek treatment for periodontal disease, treatment responders have an adjusted 28% lower risk of future fatal or nonfatal MI, stroke, or heart failure than that of nonresponders, according to Dr. Holmlund of Uppsala (Sweden) University.
He reported on 5,298 individuals with periodontal disease who were referred to a specialized university periodontal clinic for treatment. Twenty percent were classified as treatment nonresponders, meaning that 1 year after beginning active treatment, more than 20% of their initial problem gum pockets remained at least 5 mm deep and at least one in five of their pockets exhibited bleeding upon probing.
Analysis of Swedish comprehensive national registries showed that during a median of 16.8 years of follow-up, the incidence of new-onset cardiovascular disease was 21.6% in the periodontal treatment nonresponders, compared with 16.3% in responders.
Upon adjustment for patient demographics, smoking, education level, baseline number of teeth, number of pockets 5 mm deep or more, and bleeding upon probing, the treatment responders had a 28% lower risk of fatal or nonfatal MI, stroke, or heart failure.
Dr. Holmlund reported having no financial conflicts regarding this study, which was funded by governmental and university research grants.
SAN DIEGO – Successful treatment of periodontal disease appears to slow progression of subclinical cardiovascular disease, Anders Holmlund, D.D.S., reported at the annual meeting of the American College of Cardiology.
Previous studies have described an association between periodontal disease and increased risk of cardiovascular disease. This new Swedish observational study breaks fresh ground in showing for the first time that among patients who seek treatment for periodontal disease, treatment responders have an adjusted 28% lower risk of future fatal or nonfatal MI, stroke, or heart failure than that of nonresponders, according to Dr. Holmlund of Uppsala (Sweden) University.
He reported on 5,298 individuals with periodontal disease who were referred to a specialized university periodontal clinic for treatment. Twenty percent were classified as treatment nonresponders, meaning that 1 year after beginning active treatment, more than 20% of their initial problem gum pockets remained at least 5 mm deep and at least one in five of their pockets exhibited bleeding upon probing.
Analysis of Swedish comprehensive national registries showed that during a median of 16.8 years of follow-up, the incidence of new-onset cardiovascular disease was 21.6% in the periodontal treatment nonresponders, compared with 16.3% in responders.
Upon adjustment for patient demographics, smoking, education level, baseline number of teeth, number of pockets 5 mm deep or more, and bleeding upon probing, the treatment responders had a 28% lower risk of fatal or nonfatal MI, stroke, or heart failure.
Dr. Holmlund reported having no financial conflicts regarding this study, which was funded by governmental and university research grants.
SAN DIEGO – Successful treatment of periodontal disease appears to slow progression of subclinical cardiovascular disease, Anders Holmlund, D.D.S., reported at the annual meeting of the American College of Cardiology.
Previous studies have described an association between periodontal disease and increased risk of cardiovascular disease. This new Swedish observational study breaks fresh ground in showing for the first time that among patients who seek treatment for periodontal disease, treatment responders have an adjusted 28% lower risk of future fatal or nonfatal MI, stroke, or heart failure than that of nonresponders, according to Dr. Holmlund of Uppsala (Sweden) University.
He reported on 5,298 individuals with periodontal disease who were referred to a specialized university periodontal clinic for treatment. Twenty percent were classified as treatment nonresponders, meaning that 1 year after beginning active treatment, more than 20% of their initial problem gum pockets remained at least 5 mm deep and at least one in five of their pockets exhibited bleeding upon probing.
Analysis of Swedish comprehensive national registries showed that during a median of 16.8 years of follow-up, the incidence of new-onset cardiovascular disease was 21.6% in the periodontal treatment nonresponders, compared with 16.3% in responders.
Upon adjustment for patient demographics, smoking, education level, baseline number of teeth, number of pockets 5 mm deep or more, and bleeding upon probing, the treatment responders had a 28% lower risk of fatal or nonfatal MI, stroke, or heart failure.
Dr. Holmlund reported having no financial conflicts regarding this study, which was funded by governmental and university research grants.
AT ACC 15
Key clinical point: Successful treatment of periodontal disease may reduce the risk of future cardiovascular disease.
Major finding: During nearly 90,000 patient-years of follow-up of individuals who were treated in a specialized periodontal clinic, those whose gum disease responded to therapy had a 28% lower risk of developing cardiovascular disease.
Data source: An observational study of 5,298 Swedes treated for periodontal disease and followed for a median of 16.8 years.
Disclosures: The presenter reported having no financial conflicts regarding this study, which was funded by governmental and university research grants.
Novel agent fails to reduce infarct size, but may cut heart failure, protect kidneys
SAN DIEGO– Bendavia, a novel agent designed to prevent reperfusion injury by improving myocardial energetics, failed to reduce infarct size in ST-elevation MI patients in a phase II randomized trial.
Despite this disappointing result on the primary study endpoint, there was a silver lining. The study, known as the EMBRACE STEMI trial, generated two provocative findings in exploratory, hypothesis-generating secondary analyses: Bendavia appeared to reduce new-onset symptomatic heart failure early on after percutaneous coronary intervention, and the drug also had an apparent renal protective effect, Dr. C. Michael Gibson reported at the annual meeting of the American College of Cardiology.
These two potentially important findings are being studied more fully in three ongoing prospective, randomized, double-blind, placebo-controlled trials, added Dr. Gibson, professor of medicine at Harvard Medical School, Boston, and chairman of EMBRACE STEMI (Evaluation of Myocardial Effects of Bendavia for Reducing Reperfusion Injury in Patients With Acute Coronary Events).
As for the negative result in terms of the primary study hypothesis that Bendavia would reduce infarct size by preventing reperfusion injury in patients undergoing PCI for large STEMIs, as it had done successfully in animal models, the cardiologist said all indications are that the investigators targeted the right patients at the right time with the right dose of the medication.
“I think we conducted the experiment in such a way that if there was a ‘there’ there, we were going to see it,” Dr. Gibson said.
EMBRACE STEMI included 118 patients with large, first-time, anterior MIs featuring proximal or mid-left anterior descending coronary artery lesions. To be eligible for the study, patients had to arrive at the catheterization lab with a closed artery within 4 hours after symptom onset. They were then randomized in double-blind fashion to intravenous Bendavia at 0.05 mg/kg per hour for 1 hour beginning 15 minutes before PCI or to an equal volume of placebo.
The study, conducted by the PERFUSE study group at 24 sites in the United States and three European countries, was planned to be considerably larger, but to the surprise of investigators, 40% of patients arrived at the cath lab with an open artery.
“This is higher than the historical figure of 20%,” Dr. Gibson noted. “I think this is one of the notable findings in this study: Whether due to earlier presentation or better pharmacotherapy, it’s tougher to locate people with closed arteries for these kinds of studies in 2015.”
Bendavia did not significantly reduce infarct size as measured by the areas under the curve for creatine kinase MB (CK-MB) or troponin I over the initial 72 hours after PCI. Moreover, cardiac MRIs obtained at 4 and 30 days post PCI showed no significant difference between the Bendavia and placebo groups in infarct volume, left ventricular mass, edema volume, or left ventricular ejection fraction. Rates of ST-segment resolution immediately and 24 hours post PCI did not differ between the two groups, either. Nor did TIMI flow grade, frame count, or myocardial perfusion grade. Also, 30-day and 6-month rates of the composite clinical endpoint of death, new-onset heart failure beginning more than 24 hours post PCI, and heart failure rehospitalization did not differ in the Bendavia and control groups.
However, the incidence of new-onset heart failure within the first 8 hours post PCI was 8.6% in the Bendavia group compared with 18.3% in controls. This finding has prompted the two ongoing randomized trials where Bendavia is being tested in higher doses in patients with stable heart failure with reduced ejection fraction.
Bendavia is a peptide targeting the mitochondria, where it binds with cardiolipin and preserves the integrity of the electron transport system. In animal models of heart failure, it improves left ventricular function.
“It’s not an inotrope. It doesn’t change heart rate or blood pressure. Rather than increasing demands on the heart, it offers a supply side solution in improving myocardial energetics,” Dr. Gibson explained.
Bendavia was associated with renal preservation as reflected in a significantly smaller increase in creatinine level in the first 12 hours post PCI: 1.0 mcmol/L compared with 3.7 mcmol/L in controls.
This finding piqued the interest of discussant Dr. James B. McClurken, professor and vice chair of surgery at Temple University in Philadelphia.
“The renal protective findings have widespread potential application, including for coronary artery bypass surgery patients. What are your thoughts about the mechanism?” he asked.
Dr. Gibson replied that a small study done at the Mayo Clinic suggests a biologically plausible mechanism: Bendavia dramatically improved kidney hypoxia secondary to ischemia and the dye load entailed in longer PCI procedures.
Dr. Gibson reported receiving a research grant from Stealth BioTherapeutics to conduct the EMBRACE STEMI trial. He serves as a consultant to numerous pharmaceutical and medical device companies.
SAN DIEGO– Bendavia, a novel agent designed to prevent reperfusion injury by improving myocardial energetics, failed to reduce infarct size in ST-elevation MI patients in a phase II randomized trial.
Despite this disappointing result on the primary study endpoint, there was a silver lining. The study, known as the EMBRACE STEMI trial, generated two provocative findings in exploratory, hypothesis-generating secondary analyses: Bendavia appeared to reduce new-onset symptomatic heart failure early on after percutaneous coronary intervention, and the drug also had an apparent renal protective effect, Dr. C. Michael Gibson reported at the annual meeting of the American College of Cardiology.
These two potentially important findings are being studied more fully in three ongoing prospective, randomized, double-blind, placebo-controlled trials, added Dr. Gibson, professor of medicine at Harvard Medical School, Boston, and chairman of EMBRACE STEMI (Evaluation of Myocardial Effects of Bendavia for Reducing Reperfusion Injury in Patients With Acute Coronary Events).
As for the negative result in terms of the primary study hypothesis that Bendavia would reduce infarct size by preventing reperfusion injury in patients undergoing PCI for large STEMIs, as it had done successfully in animal models, the cardiologist said all indications are that the investigators targeted the right patients at the right time with the right dose of the medication.
“I think we conducted the experiment in such a way that if there was a ‘there’ there, we were going to see it,” Dr. Gibson said.
EMBRACE STEMI included 118 patients with large, first-time, anterior MIs featuring proximal or mid-left anterior descending coronary artery lesions. To be eligible for the study, patients had to arrive at the catheterization lab with a closed artery within 4 hours after symptom onset. They were then randomized in double-blind fashion to intravenous Bendavia at 0.05 mg/kg per hour for 1 hour beginning 15 minutes before PCI or to an equal volume of placebo.
The study, conducted by the PERFUSE study group at 24 sites in the United States and three European countries, was planned to be considerably larger, but to the surprise of investigators, 40% of patients arrived at the cath lab with an open artery.
“This is higher than the historical figure of 20%,” Dr. Gibson noted. “I think this is one of the notable findings in this study: Whether due to earlier presentation or better pharmacotherapy, it’s tougher to locate people with closed arteries for these kinds of studies in 2015.”
Bendavia did not significantly reduce infarct size as measured by the areas under the curve for creatine kinase MB (CK-MB) or troponin I over the initial 72 hours after PCI. Moreover, cardiac MRIs obtained at 4 and 30 days post PCI showed no significant difference between the Bendavia and placebo groups in infarct volume, left ventricular mass, edema volume, or left ventricular ejection fraction. Rates of ST-segment resolution immediately and 24 hours post PCI did not differ between the two groups, either. Nor did TIMI flow grade, frame count, or myocardial perfusion grade. Also, 30-day and 6-month rates of the composite clinical endpoint of death, new-onset heart failure beginning more than 24 hours post PCI, and heart failure rehospitalization did not differ in the Bendavia and control groups.
However, the incidence of new-onset heart failure within the first 8 hours post PCI was 8.6% in the Bendavia group compared with 18.3% in controls. This finding has prompted the two ongoing randomized trials where Bendavia is being tested in higher doses in patients with stable heart failure with reduced ejection fraction.
Bendavia is a peptide targeting the mitochondria, where it binds with cardiolipin and preserves the integrity of the electron transport system. In animal models of heart failure, it improves left ventricular function.
“It’s not an inotrope. It doesn’t change heart rate or blood pressure. Rather than increasing demands on the heart, it offers a supply side solution in improving myocardial energetics,” Dr. Gibson explained.
Bendavia was associated with renal preservation as reflected in a significantly smaller increase in creatinine level in the first 12 hours post PCI: 1.0 mcmol/L compared with 3.7 mcmol/L in controls.
This finding piqued the interest of discussant Dr. James B. McClurken, professor and vice chair of surgery at Temple University in Philadelphia.
“The renal protective findings have widespread potential application, including for coronary artery bypass surgery patients. What are your thoughts about the mechanism?” he asked.
Dr. Gibson replied that a small study done at the Mayo Clinic suggests a biologically plausible mechanism: Bendavia dramatically improved kidney hypoxia secondary to ischemia and the dye load entailed in longer PCI procedures.
Dr. Gibson reported receiving a research grant from Stealth BioTherapeutics to conduct the EMBRACE STEMI trial. He serves as a consultant to numerous pharmaceutical and medical device companies.
SAN DIEGO– Bendavia, a novel agent designed to prevent reperfusion injury by improving myocardial energetics, failed to reduce infarct size in ST-elevation MI patients in a phase II randomized trial.
Despite this disappointing result on the primary study endpoint, there was a silver lining. The study, known as the EMBRACE STEMI trial, generated two provocative findings in exploratory, hypothesis-generating secondary analyses: Bendavia appeared to reduce new-onset symptomatic heart failure early on after percutaneous coronary intervention, and the drug also had an apparent renal protective effect, Dr. C. Michael Gibson reported at the annual meeting of the American College of Cardiology.
These two potentially important findings are being studied more fully in three ongoing prospective, randomized, double-blind, placebo-controlled trials, added Dr. Gibson, professor of medicine at Harvard Medical School, Boston, and chairman of EMBRACE STEMI (Evaluation of Myocardial Effects of Bendavia for Reducing Reperfusion Injury in Patients With Acute Coronary Events).
As for the negative result in terms of the primary study hypothesis that Bendavia would reduce infarct size by preventing reperfusion injury in patients undergoing PCI for large STEMIs, as it had done successfully in animal models, the cardiologist said all indications are that the investigators targeted the right patients at the right time with the right dose of the medication.
“I think we conducted the experiment in such a way that if there was a ‘there’ there, we were going to see it,” Dr. Gibson said.
EMBRACE STEMI included 118 patients with large, first-time, anterior MIs featuring proximal or mid-left anterior descending coronary artery lesions. To be eligible for the study, patients had to arrive at the catheterization lab with a closed artery within 4 hours after symptom onset. They were then randomized in double-blind fashion to intravenous Bendavia at 0.05 mg/kg per hour for 1 hour beginning 15 minutes before PCI or to an equal volume of placebo.
The study, conducted by the PERFUSE study group at 24 sites in the United States and three European countries, was planned to be considerably larger, but to the surprise of investigators, 40% of patients arrived at the cath lab with an open artery.
“This is higher than the historical figure of 20%,” Dr. Gibson noted. “I think this is one of the notable findings in this study: Whether due to earlier presentation or better pharmacotherapy, it’s tougher to locate people with closed arteries for these kinds of studies in 2015.”
Bendavia did not significantly reduce infarct size as measured by the areas under the curve for creatine kinase MB (CK-MB) or troponin I over the initial 72 hours after PCI. Moreover, cardiac MRIs obtained at 4 and 30 days post PCI showed no significant difference between the Bendavia and placebo groups in infarct volume, left ventricular mass, edema volume, or left ventricular ejection fraction. Rates of ST-segment resolution immediately and 24 hours post PCI did not differ between the two groups, either. Nor did TIMI flow grade, frame count, or myocardial perfusion grade. Also, 30-day and 6-month rates of the composite clinical endpoint of death, new-onset heart failure beginning more than 24 hours post PCI, and heart failure rehospitalization did not differ in the Bendavia and control groups.
However, the incidence of new-onset heart failure within the first 8 hours post PCI was 8.6% in the Bendavia group compared with 18.3% in controls. This finding has prompted the two ongoing randomized trials where Bendavia is being tested in higher doses in patients with stable heart failure with reduced ejection fraction.
Bendavia is a peptide targeting the mitochondria, where it binds with cardiolipin and preserves the integrity of the electron transport system. In animal models of heart failure, it improves left ventricular function.
“It’s not an inotrope. It doesn’t change heart rate or blood pressure. Rather than increasing demands on the heart, it offers a supply side solution in improving myocardial energetics,” Dr. Gibson explained.
Bendavia was associated with renal preservation as reflected in a significantly smaller increase in creatinine level in the first 12 hours post PCI: 1.0 mcmol/L compared with 3.7 mcmol/L in controls.
This finding piqued the interest of discussant Dr. James B. McClurken, professor and vice chair of surgery at Temple University in Philadelphia.
“The renal protective findings have widespread potential application, including for coronary artery bypass surgery patients. What are your thoughts about the mechanism?” he asked.
Dr. Gibson replied that a small study done at the Mayo Clinic suggests a biologically plausible mechanism: Bendavia dramatically improved kidney hypoxia secondary to ischemia and the dye load entailed in longer PCI procedures.
Dr. Gibson reported receiving a research grant from Stealth BioTherapeutics to conduct the EMBRACE STEMI trial. He serves as a consultant to numerous pharmaceutical and medical device companies.
AT ACC 15
Key clinical point: A novel agent that boosts mitochondrial energy did not prevent irreversible reperfusion injury in MI patients undergoing percutaneous coronary intervention.
Major finding: The geometric mean of the area under the curve for serum CK-MB over the first 72 hours post-PCI was 5,570 ng/mL with Bendavia and similar at 5,785 ng/mL with placebo.
Data source: EMBRACE STEMI, a four-country, 24-site, randomized, double-blind, placebo-controlled phase II study conducted in 118 patients who presented with large ST-elevation MIs.
Disclosures: EMBRACE STEMI was funded by Stealth BioTherapeutics. The presenter received a research grant as study chairman.
VIDEO: Data support switching to transradial PCI access
SAN DIEGO – Cardiologists should switch from transfemoral to transradial access in acute coronary syndrome patients undergoing percutaneous coronary intervention, given the reduced mortality rates associated with the transradial approach in the MATRIX study and other studies, Dr. Cindy L. Grines said at the annual meeting of the American College of Cardiology.
Because U.S. interventionalists are “under the clock” when treating patients with ST-elevation myocardial infarction, “many physicians have been unwilling to risk having a difficult transradial case that would take too much time,” explained Dr. Grines, an interventional cardiologist at the Detroit Medical Center.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
For that and other reasons, American interventionalists have been “slow adopters” of the transradial approach, currently using it for about 20% of PCIs, compared with a worldwide rate of about 70%.
It may take instituting incentives to get U.S. cardiologists to change their practice, Dr. Grines suggested in an interview. That could involve increased reimbursement for PCIs done transradially, an increased allowance on acceptable door-to-balloon times for STEMI patients treated transradially, or imposition of new standards for quality assurance that mandate use of transradial in a certain percentage of PCI cases, she said.
The MATRIX study included a second, independent, prespecified analysis that compared outcomes in patients randomized to treatment with two different antithrombin drugs, either bivalirudin (Angiomax) or unfractionated heparin.
That part of the study showed that while treatment with either of the two drugs resulted in no statistically significant difference in the study’s two primary endpoints, treatment with bivalirudin led to statistically significant reductions in all-cause death and cardiovascular death, as well as in major bleeding events, compared with patients treated with unfractionated heparin (Lancet 2015 [doi:10.1016/S0140-6736(15)60292-6]).
Although bivalirudin has generally been the more commonly used antithrombin drug in this clinical setting by U.S. interventionalists in recent years, results reported last year from the HEAT-PCI trial (Lancet 2014;384:1849-58) that showed better outcomes with unfractionated heparin have led to reduced use of bivalirudin, Dr. Grines said.
The new results from MATRIX coupled with results from other trials that compared those drugs can make clinicians “more confident about the benefit of bivalirudin,” she said.
Dr. Grines has been a consultant to and received honoraria from the Medicines Company, which markets Angiomax, and from Abbott Vascular, Merck, and the Volcano Group.
On Twitter @mitchelzoler
SAN DIEGO – Cardiologists should switch from transfemoral to transradial access in acute coronary syndrome patients undergoing percutaneous coronary intervention, given the reduced mortality rates associated with the transradial approach in the MATRIX study and other studies, Dr. Cindy L. Grines said at the annual meeting of the American College of Cardiology.
Because U.S. interventionalists are “under the clock” when treating patients with ST-elevation myocardial infarction, “many physicians have been unwilling to risk having a difficult transradial case that would take too much time,” explained Dr. Grines, an interventional cardiologist at the Detroit Medical Center.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
For that and other reasons, American interventionalists have been “slow adopters” of the transradial approach, currently using it for about 20% of PCIs, compared with a worldwide rate of about 70%.
It may take instituting incentives to get U.S. cardiologists to change their practice, Dr. Grines suggested in an interview. That could involve increased reimbursement for PCIs done transradially, an increased allowance on acceptable door-to-balloon times for STEMI patients treated transradially, or imposition of new standards for quality assurance that mandate use of transradial in a certain percentage of PCI cases, she said.
The MATRIX study included a second, independent, prespecified analysis that compared outcomes in patients randomized to treatment with two different antithrombin drugs, either bivalirudin (Angiomax) or unfractionated heparin.
That part of the study showed that while treatment with either of the two drugs resulted in no statistically significant difference in the study’s two primary endpoints, treatment with bivalirudin led to statistically significant reductions in all-cause death and cardiovascular death, as well as in major bleeding events, compared with patients treated with unfractionated heparin (Lancet 2015 [doi:10.1016/S0140-6736(15)60292-6]).
Although bivalirudin has generally been the more commonly used antithrombin drug in this clinical setting by U.S. interventionalists in recent years, results reported last year from the HEAT-PCI trial (Lancet 2014;384:1849-58) that showed better outcomes with unfractionated heparin have led to reduced use of bivalirudin, Dr. Grines said.
The new results from MATRIX coupled with results from other trials that compared those drugs can make clinicians “more confident about the benefit of bivalirudin,” she said.
Dr. Grines has been a consultant to and received honoraria from the Medicines Company, which markets Angiomax, and from Abbott Vascular, Merck, and the Volcano Group.
On Twitter @mitchelzoler
SAN DIEGO – Cardiologists should switch from transfemoral to transradial access in acute coronary syndrome patients undergoing percutaneous coronary intervention, given the reduced mortality rates associated with the transradial approach in the MATRIX study and other studies, Dr. Cindy L. Grines said at the annual meeting of the American College of Cardiology.
Because U.S. interventionalists are “under the clock” when treating patients with ST-elevation myocardial infarction, “many physicians have been unwilling to risk having a difficult transradial case that would take too much time,” explained Dr. Grines, an interventional cardiologist at the Detroit Medical Center.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
For that and other reasons, American interventionalists have been “slow adopters” of the transradial approach, currently using it for about 20% of PCIs, compared with a worldwide rate of about 70%.
It may take instituting incentives to get U.S. cardiologists to change their practice, Dr. Grines suggested in an interview. That could involve increased reimbursement for PCIs done transradially, an increased allowance on acceptable door-to-balloon times for STEMI patients treated transradially, or imposition of new standards for quality assurance that mandate use of transradial in a certain percentage of PCI cases, she said.
The MATRIX study included a second, independent, prespecified analysis that compared outcomes in patients randomized to treatment with two different antithrombin drugs, either bivalirudin (Angiomax) or unfractionated heparin.
That part of the study showed that while treatment with either of the two drugs resulted in no statistically significant difference in the study’s two primary endpoints, treatment with bivalirudin led to statistically significant reductions in all-cause death and cardiovascular death, as well as in major bleeding events, compared with patients treated with unfractionated heparin (Lancet 2015 [doi:10.1016/S0140-6736(15)60292-6]).
Although bivalirudin has generally been the more commonly used antithrombin drug in this clinical setting by U.S. interventionalists in recent years, results reported last year from the HEAT-PCI trial (Lancet 2014;384:1849-58) that showed better outcomes with unfractionated heparin have led to reduced use of bivalirudin, Dr. Grines said.
The new results from MATRIX coupled with results from other trials that compared those drugs can make clinicians “more confident about the benefit of bivalirudin,” she said.
Dr. Grines has been a consultant to and received honoraria from the Medicines Company, which markets Angiomax, and from Abbott Vascular, Merck, and the Volcano Group.
On Twitter @mitchelzoler
EXPERT ANALYSIS FROM ACC 15
Ablation cuts AF recurrence 2.5-fold vs. amiodarone in heart failure
SAN DIEGO – Catheter ablation proved superior to amiodarone for treatment of persistent atrial fibrillation in patients with systolic heart failure in the randomized AATAC-AF trial.
The rate of the primary study endpoint – freedom from recurrent AF through 26 months of prospective follow-up– was 70% in the catheter ablation group, twice the 34% rate with amiodarone, Dr. Luigi Di Biase reported at the annual meeting of the American College of Cardiology. After covariate adjustment, the investigators found that recurrence was 2.5 times more likely in the patients treated with amiodarone.
But he added a major caveat: pulmonary vein antrum isolation (PVI) alone was no better than the antiarrhythmic drug. The high overall treatment success rate seen with catheter ablation in the trial was achieved by operators who performed PVI plus some additional form of ablation of their own choosing, such as elimination of non–pulmonary vein triggers, ablation of complex fractionated electrograms, and/or additional linear ablation lesions, according to Dr. Di Biase, head of electrophysiology at the Albert Einstein College of Medicine, New York.
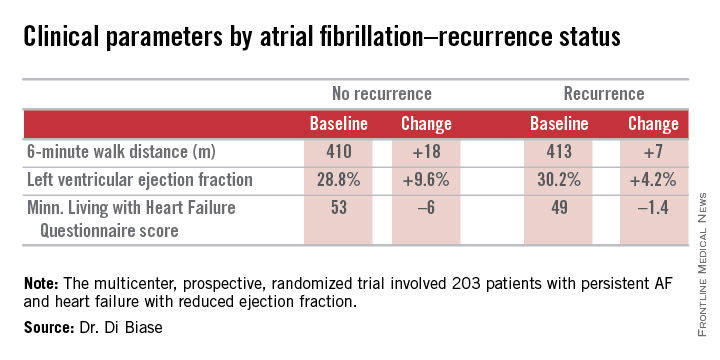
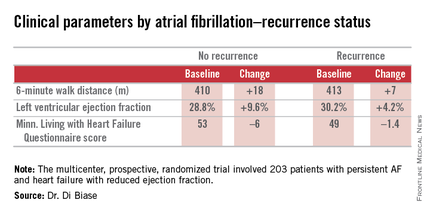
AATAC-AF (Ablation versus Amiodarone for Treatment of Atrial Fibrillation in Patients with Congestive Heart Failure and an Implanted ICD/CRTD) was a multicenter, prospective, randomized trial involving 203 patients with persistent AF and heart failure with reduced ejection fraction. Patients randomized to ablation had to receive PVI at a minimum; operators could perform additional ablation according to their preference. Twenty percent of patients randomized to ablation received PVI alone; 80% underwent additional posterior wall and non–pulmonary vein trigger ablation. The 26-month rate of freedom from recurrence of AF was 36% in patients who received PVI alone and 79% in those who underwent more extensive ablations. A particular strength of the AATAC study was that all participants had an implantable cardioverter-defibrillator and/or cardiac resynchronization therapy device, permitting detection of AF with a much higher degree of accuracy than possible in most AF ablation trials.
Any recurrent AF episodes during the first 3 months of follow-up were excluded from the analysis, regardless of whether patients were in the ablation or amiodarone arms, in accord with the 3-month blanking period that’s standard among electrophysiologists. Patients averaged 1.4 ablation sessions during the first 3 months of the trial.
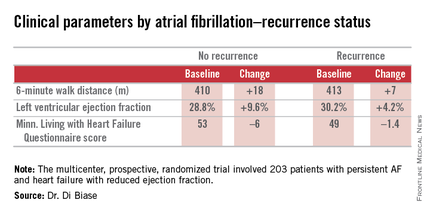
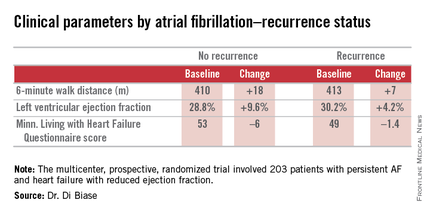
Regardless of treatment, patients in whom AF did not recur showed significantly greater improvement in left ventricular ejection fraction, exercise capacity, and heart failure–related quality of life.
In addition, all-cause mortality during follow-up was significantly lower in the ablation group: 8%, compared with 18% in patients assigned to amiodarone. Moreover, the rate of hospitalization for arrhythmia or worsening heart failure was 31% in the ablation group versus 57% in patients on amiodarone. The economic implications of this sharp reduction in hospitalizations will be the subject of further study, according to Dr. Di Biase.
Also noteworthy was the finding that seven patients had to discontinue amiodarone due to serious side effects: four because of thyroid toxicity, two for pulmonary toxicity, and one owing to hepatic dysfunction, he continued.
Discussant Dr. Richard I. Fogel, current president of the Heart Rhythm Society, commented that “the 70% arrhythmia-free follow-up was a little surprising to me.”
“That seems a little bit high, particularly in a group with persistent atrial fibrillation,” observed Dr. Fogel, who is chief executive officer at St. Vincent Medical Group, Indianapolis.
Dr. Di Biase attributed the high success rate to two factors: One, only highly experienced operators participated in AATAC, and two, most of them weren’t content to stick to PVI alone.
“If you try to do a more extensive procedure addressing non–pulmonary vein triggers in other areas in the left atrium, the success rate is increased by far,” the electrophysiologist said.
As for a possible mechanism for the mortality benefit seen with ablation, “several studies have shown that in a population with heart failure with reduced ejection fraction, atrial fibrillation is an independent predictor of mortality,” Dr. Di Biase said. “So I believe that staying in sinus rhythm may have affected the long-term mortality. If you have a treatment that reduces the amount of time in atrial fibrillation, you may reduce mortality.”
While catheter ablation is an increasingly popular treatment strategy in patients with drug-refractory paroxysmal AF, it has been understudied in the setting of AF and comorbid heart failure. These two conditions are commonly coexistent, and they feed on each other in a destructive way: AF worsens heart failure, and heart failure tends to make AF worse.
AATAC was funded by the participating investigators and institutions without external financial support. Dr. Di Biase reported serving as a consultant to Biosense Webster and St. Jude Medical and serving as a paid speaker for Atricure, Biotronik, Medtronic, Boston Scientific, and Epi EP.
SAN DIEGO – Catheter ablation proved superior to amiodarone for treatment of persistent atrial fibrillation in patients with systolic heart failure in the randomized AATAC-AF trial.
The rate of the primary study endpoint – freedom from recurrent AF through 26 months of prospective follow-up– was 70% in the catheter ablation group, twice the 34% rate with amiodarone, Dr. Luigi Di Biase reported at the annual meeting of the American College of Cardiology. After covariate adjustment, the investigators found that recurrence was 2.5 times more likely in the patients treated with amiodarone.
But he added a major caveat: pulmonary vein antrum isolation (PVI) alone was no better than the antiarrhythmic drug. The high overall treatment success rate seen with catheter ablation in the trial was achieved by operators who performed PVI plus some additional form of ablation of their own choosing, such as elimination of non–pulmonary vein triggers, ablation of complex fractionated electrograms, and/or additional linear ablation lesions, according to Dr. Di Biase, head of electrophysiology at the Albert Einstein College of Medicine, New York.
AATAC-AF (Ablation versus Amiodarone for Treatment of Atrial Fibrillation in Patients with Congestive Heart Failure and an Implanted ICD/CRTD) was a multicenter, prospective, randomized trial involving 203 patients with persistent AF and heart failure with reduced ejection fraction. Patients randomized to ablation had to receive PVI at a minimum; operators could perform additional ablation according to their preference. Twenty percent of patients randomized to ablation received PVI alone; 80% underwent additional posterior wall and non–pulmonary vein trigger ablation. The 26-month rate of freedom from recurrence of AF was 36% in patients who received PVI alone and 79% in those who underwent more extensive ablations. A particular strength of the AATAC study was that all participants had an implantable cardioverter-defibrillator and/or cardiac resynchronization therapy device, permitting detection of AF with a much higher degree of accuracy than possible in most AF ablation trials.
Any recurrent AF episodes during the first 3 months of follow-up were excluded from the analysis, regardless of whether patients were in the ablation or amiodarone arms, in accord with the 3-month blanking period that’s standard among electrophysiologists. Patients averaged 1.4 ablation sessions during the first 3 months of the trial.
Regardless of treatment, patients in whom AF did not recur showed significantly greater improvement in left ventricular ejection fraction, exercise capacity, and heart failure–related quality of life.
In addition, all-cause mortality during follow-up was significantly lower in the ablation group: 8%, compared with 18% in patients assigned to amiodarone. Moreover, the rate of hospitalization for arrhythmia or worsening heart failure was 31% in the ablation group versus 57% in patients on amiodarone. The economic implications of this sharp reduction in hospitalizations will be the subject of further study, according to Dr. Di Biase.
Also noteworthy was the finding that seven patients had to discontinue amiodarone due to serious side effects: four because of thyroid toxicity, two for pulmonary toxicity, and one owing to hepatic dysfunction, he continued.
Discussant Dr. Richard I. Fogel, current president of the Heart Rhythm Society, commented that “the 70% arrhythmia-free follow-up was a little surprising to me.”
“That seems a little bit high, particularly in a group with persistent atrial fibrillation,” observed Dr. Fogel, who is chief executive officer at St. Vincent Medical Group, Indianapolis.
Dr. Di Biase attributed the high success rate to two factors: One, only highly experienced operators participated in AATAC, and two, most of them weren’t content to stick to PVI alone.
“If you try to do a more extensive procedure addressing non–pulmonary vein triggers in other areas in the left atrium, the success rate is increased by far,” the electrophysiologist said.
As for a possible mechanism for the mortality benefit seen with ablation, “several studies have shown that in a population with heart failure with reduced ejection fraction, atrial fibrillation is an independent predictor of mortality,” Dr. Di Biase said. “So I believe that staying in sinus rhythm may have affected the long-term mortality. If you have a treatment that reduces the amount of time in atrial fibrillation, you may reduce mortality.”
While catheter ablation is an increasingly popular treatment strategy in patients with drug-refractory paroxysmal AF, it has been understudied in the setting of AF and comorbid heart failure. These two conditions are commonly coexistent, and they feed on each other in a destructive way: AF worsens heart failure, and heart failure tends to make AF worse.
AATAC was funded by the participating investigators and institutions without external financial support. Dr. Di Biase reported serving as a consultant to Biosense Webster and St. Jude Medical and serving as a paid speaker for Atricure, Biotronik, Medtronic, Boston Scientific, and Epi EP.
SAN DIEGO – Catheter ablation proved superior to amiodarone for treatment of persistent atrial fibrillation in patients with systolic heart failure in the randomized AATAC-AF trial.
The rate of the primary study endpoint – freedom from recurrent AF through 26 months of prospective follow-up– was 70% in the catheter ablation group, twice the 34% rate with amiodarone, Dr. Luigi Di Biase reported at the annual meeting of the American College of Cardiology. After covariate adjustment, the investigators found that recurrence was 2.5 times more likely in the patients treated with amiodarone.
But he added a major caveat: pulmonary vein antrum isolation (PVI) alone was no better than the antiarrhythmic drug. The high overall treatment success rate seen with catheter ablation in the trial was achieved by operators who performed PVI plus some additional form of ablation of their own choosing, such as elimination of non–pulmonary vein triggers, ablation of complex fractionated electrograms, and/or additional linear ablation lesions, according to Dr. Di Biase, head of electrophysiology at the Albert Einstein College of Medicine, New York.
AATAC-AF (Ablation versus Amiodarone for Treatment of Atrial Fibrillation in Patients with Congestive Heart Failure and an Implanted ICD/CRTD) was a multicenter, prospective, randomized trial involving 203 patients with persistent AF and heart failure with reduced ejection fraction. Patients randomized to ablation had to receive PVI at a minimum; operators could perform additional ablation according to their preference. Twenty percent of patients randomized to ablation received PVI alone; 80% underwent additional posterior wall and non–pulmonary vein trigger ablation. The 26-month rate of freedom from recurrence of AF was 36% in patients who received PVI alone and 79% in those who underwent more extensive ablations. A particular strength of the AATAC study was that all participants had an implantable cardioverter-defibrillator and/or cardiac resynchronization therapy device, permitting detection of AF with a much higher degree of accuracy than possible in most AF ablation trials.
Any recurrent AF episodes during the first 3 months of follow-up were excluded from the analysis, regardless of whether patients were in the ablation or amiodarone arms, in accord with the 3-month blanking period that’s standard among electrophysiologists. Patients averaged 1.4 ablation sessions during the first 3 months of the trial.
Regardless of treatment, patients in whom AF did not recur showed significantly greater improvement in left ventricular ejection fraction, exercise capacity, and heart failure–related quality of life.
In addition, all-cause mortality during follow-up was significantly lower in the ablation group: 8%, compared with 18% in patients assigned to amiodarone. Moreover, the rate of hospitalization for arrhythmia or worsening heart failure was 31% in the ablation group versus 57% in patients on amiodarone. The economic implications of this sharp reduction in hospitalizations will be the subject of further study, according to Dr. Di Biase.
Also noteworthy was the finding that seven patients had to discontinue amiodarone due to serious side effects: four because of thyroid toxicity, two for pulmonary toxicity, and one owing to hepatic dysfunction, he continued.
Discussant Dr. Richard I. Fogel, current president of the Heart Rhythm Society, commented that “the 70% arrhythmia-free follow-up was a little surprising to me.”
“That seems a little bit high, particularly in a group with persistent atrial fibrillation,” observed Dr. Fogel, who is chief executive officer at St. Vincent Medical Group, Indianapolis.
Dr. Di Biase attributed the high success rate to two factors: One, only highly experienced operators participated in AATAC, and two, most of them weren’t content to stick to PVI alone.
“If you try to do a more extensive procedure addressing non–pulmonary vein triggers in other areas in the left atrium, the success rate is increased by far,” the electrophysiologist said.
As for a possible mechanism for the mortality benefit seen with ablation, “several studies have shown that in a population with heart failure with reduced ejection fraction, atrial fibrillation is an independent predictor of mortality,” Dr. Di Biase said. “So I believe that staying in sinus rhythm may have affected the long-term mortality. If you have a treatment that reduces the amount of time in atrial fibrillation, you may reduce mortality.”
While catheter ablation is an increasingly popular treatment strategy in patients with drug-refractory paroxysmal AF, it has been understudied in the setting of AF and comorbid heart failure. These two conditions are commonly coexistent, and they feed on each other in a destructive way: AF worsens heart failure, and heart failure tends to make AF worse.
AATAC was funded by the participating investigators and institutions without external financial support. Dr. Di Biase reported serving as a consultant to Biosense Webster and St. Jude Medical and serving as a paid speaker for Atricure, Biotronik, Medtronic, Boston Scientific, and Epi EP.
AT ACC 15
Key clinical point: Catheter ablation is hands down more effective than amiodarone for the treatment of persistent atrial fibrillation in patients with systolic heart failure.
Major finding: The rate of freedom from recurrent atrial fibrillation during 26 months of follow-up was 70% in patients randomized to catheter ablation, compared with 34% in those assigned to amiodarone.
Data source: The AATAC-AF study was a multicenter, randomized, prospective clinical trial inc 203 patients.
Disclosures: The trial was funded by the participating investigators and institutions without commercial support. Dr. Di Biase reported serving as a consultant to Biosense Webster and St. Jude Medical and serving as a paid speaker for Atricure, Biotronik, Medtronic, Boston Scientific, and Epi EP.
U.S. lagging on transradial PCI endangers patients
Why are American cardiologists so far behind the worldwide curve in performing percutaneous coronary interventions by the radial-artery route?
The degree to which ACS patients suffer needlessly when they undergo percutaneous coronary intervention (PCI) via their femoral artery and not with transradial access was finally, definitively demonstrated in results from the MATRIX Access trial, presented earlier this week at the annual meeting of the American College of Cardiology. The MATRIX results showed in more than 8,000 patients that using a transradial approach for PCI was linked with a statistically significant improvement in 30-day patient survival, a 0.6% absolute difference. For every 167 patients treated by the transradial route, an additional patient lived, compared with similar patients treated with transfemoral access.
The radial approach also cut serious access-site bleeding episodes by an absolute 0.7%, and it was this difference that appeared to mainly drive the difference in patient survival. As study discussant Dr. Roxana Mehran declared from the dais following the MATRIX report, “Bleeding matters! Here is where it’s been proven.”
Results from a second, unrelated trial reported at the meeting, TOTAL, showed that during 2010-2014, in more than 10,000 patients with ST-elevation myocardial infarction treated by PCI in 20 different countries, 68% of patients underwent their procedure via a transradial route.
In contrast, cardiologists I spoke with at the meeting said that recent estimates of PCI use by U.S. interventionalists indicated that they perform roughly 20% of PCIs transradially. That level substantially jumped over the past decade; 10 years ago U.S. transradial use stood at about 3% of all PCIs, my sources said. But 20% still lags woefully behind a worldwide rate of 68%, especially when access site can make a life-or-death difference.
Interventionalists at the meeting also told me some reasons why transfemoral access remains favored. First, it’s the approach many operators first trained in, so they are more familiar and comfortable with it. Second, transradial PCI can take longer, result in higher radiation exposure, and in some patients it’s simply impossible, which means crossover to transfemoral anyway. Finally, transfemoral PCI is just plain easier, they said.
Most of these reasons fall flat when contrasted with causing significantly fewer serious bleeds and improved survival. Of course, when transradial proves impossible there is no choice other than going with transfemoral, but as proponents of transradial said at the meeting, it is a matter of making transradial the initial, default strategy and only resorting to transfemoral when absolutely necessary.
The MATRIX results had another very important finding: To get the best outcomes, centers that offer PCI to acute coronary syndrome patients can’t simply dabble with the transradial approach; they need to be all in. A subanalysis of the MATRIX mortality benefit for transradial procedures showed a striking and statistically significant link between operator commitment to the transradial approach and the ability to give patients a mortality benefit by using the transradial approach. This analysis subdivided the patients into three categories depending on the frequency at which the center where they were treated performed transradial PCI. The three subgroups were centers that did 64% or fewer of their cases transradially, centers that did 65%-79% of their patients transradially, and centers that did 80% or more of their cases via the radial artery.
The data showed that patients treated at centers that used the transradial approach in no more than 64% of their cases actually had a small trend toward better 30-day survival rates when they underwent a transfemoral procedure, although it was not a statistically significant difference. Among the subgroup of patients treated at centers that fell into the middle range of transradial use in everyday practice there was a trend toward better survival with transradial treatment, compared with transfemoral, but again not a statistically significant difference.
It was only among the patients treated at centers that used transradial access nearly all the time, for 80% or more of cases, where transradial use made a statistically significant difference in survival. In this subgroup, patients treated transradially had a 52% relative survival advantage compared with similar patients treated at the same center but via a transfemoral approach.
In other words, when a center in the MATRIX trial did at least 80% of cases with the transradial approach, the patients treated there that way had less than half the 30-day mortality rate, compared with similar patients treated at the same center but by PCI that used a transfemoral approach.
Choosing the PCI access site has moved beyond physician preference and convenience. It’s a matter of patient well-being.
On Twitter @mitchelzoler
Why are American cardiologists so far behind the worldwide curve in performing percutaneous coronary interventions by the radial-artery route?
The degree to which ACS patients suffer needlessly when they undergo percutaneous coronary intervention (PCI) via their femoral artery and not with transradial access was finally, definitively demonstrated in results from the MATRIX Access trial, presented earlier this week at the annual meeting of the American College of Cardiology. The MATRIX results showed in more than 8,000 patients that using a transradial approach for PCI was linked with a statistically significant improvement in 30-day patient survival, a 0.6% absolute difference. For every 167 patients treated by the transradial route, an additional patient lived, compared with similar patients treated with transfemoral access.
The radial approach also cut serious access-site bleeding episodes by an absolute 0.7%, and it was this difference that appeared to mainly drive the difference in patient survival. As study discussant Dr. Roxana Mehran declared from the dais following the MATRIX report, “Bleeding matters! Here is where it’s been proven.”
Results from a second, unrelated trial reported at the meeting, TOTAL, showed that during 2010-2014, in more than 10,000 patients with ST-elevation myocardial infarction treated by PCI in 20 different countries, 68% of patients underwent their procedure via a transradial route.
In contrast, cardiologists I spoke with at the meeting said that recent estimates of PCI use by U.S. interventionalists indicated that they perform roughly 20% of PCIs transradially. That level substantially jumped over the past decade; 10 years ago U.S. transradial use stood at about 3% of all PCIs, my sources said. But 20% still lags woefully behind a worldwide rate of 68%, especially when access site can make a life-or-death difference.
Interventionalists at the meeting also told me some reasons why transfemoral access remains favored. First, it’s the approach many operators first trained in, so they are more familiar and comfortable with it. Second, transradial PCI can take longer, result in higher radiation exposure, and in some patients it’s simply impossible, which means crossover to transfemoral anyway. Finally, transfemoral PCI is just plain easier, they said.
Most of these reasons fall flat when contrasted with causing significantly fewer serious bleeds and improved survival. Of course, when transradial proves impossible there is no choice other than going with transfemoral, but as proponents of transradial said at the meeting, it is a matter of making transradial the initial, default strategy and only resorting to transfemoral when absolutely necessary.
The MATRIX results had another very important finding: To get the best outcomes, centers that offer PCI to acute coronary syndrome patients can’t simply dabble with the transradial approach; they need to be all in. A subanalysis of the MATRIX mortality benefit for transradial procedures showed a striking and statistically significant link between operator commitment to the transradial approach and the ability to give patients a mortality benefit by using the transradial approach. This analysis subdivided the patients into three categories depending on the frequency at which the center where they were treated performed transradial PCI. The three subgroups were centers that did 64% or fewer of their cases transradially, centers that did 65%-79% of their patients transradially, and centers that did 80% or more of their cases via the radial artery.
The data showed that patients treated at centers that used the transradial approach in no more than 64% of their cases actually had a small trend toward better 30-day survival rates when they underwent a transfemoral procedure, although it was not a statistically significant difference. Among the subgroup of patients treated at centers that fell into the middle range of transradial use in everyday practice there was a trend toward better survival with transradial treatment, compared with transfemoral, but again not a statistically significant difference.
It was only among the patients treated at centers that used transradial access nearly all the time, for 80% or more of cases, where transradial use made a statistically significant difference in survival. In this subgroup, patients treated transradially had a 52% relative survival advantage compared with similar patients treated at the same center but via a transfemoral approach.
In other words, when a center in the MATRIX trial did at least 80% of cases with the transradial approach, the patients treated there that way had less than half the 30-day mortality rate, compared with similar patients treated at the same center but by PCI that used a transfemoral approach.
Choosing the PCI access site has moved beyond physician preference and convenience. It’s a matter of patient well-being.
On Twitter @mitchelzoler
Why are American cardiologists so far behind the worldwide curve in performing percutaneous coronary interventions by the radial-artery route?
The degree to which ACS patients suffer needlessly when they undergo percutaneous coronary intervention (PCI) via their femoral artery and not with transradial access was finally, definitively demonstrated in results from the MATRIX Access trial, presented earlier this week at the annual meeting of the American College of Cardiology. The MATRIX results showed in more than 8,000 patients that using a transradial approach for PCI was linked with a statistically significant improvement in 30-day patient survival, a 0.6% absolute difference. For every 167 patients treated by the transradial route, an additional patient lived, compared with similar patients treated with transfemoral access.
The radial approach also cut serious access-site bleeding episodes by an absolute 0.7%, and it was this difference that appeared to mainly drive the difference in patient survival. As study discussant Dr. Roxana Mehran declared from the dais following the MATRIX report, “Bleeding matters! Here is where it’s been proven.”
Results from a second, unrelated trial reported at the meeting, TOTAL, showed that during 2010-2014, in more than 10,000 patients with ST-elevation myocardial infarction treated by PCI in 20 different countries, 68% of patients underwent their procedure via a transradial route.
In contrast, cardiologists I spoke with at the meeting said that recent estimates of PCI use by U.S. interventionalists indicated that they perform roughly 20% of PCIs transradially. That level substantially jumped over the past decade; 10 years ago U.S. transradial use stood at about 3% of all PCIs, my sources said. But 20% still lags woefully behind a worldwide rate of 68%, especially when access site can make a life-or-death difference.
Interventionalists at the meeting also told me some reasons why transfemoral access remains favored. First, it’s the approach many operators first trained in, so they are more familiar and comfortable with it. Second, transradial PCI can take longer, result in higher radiation exposure, and in some patients it’s simply impossible, which means crossover to transfemoral anyway. Finally, transfemoral PCI is just plain easier, they said.
Most of these reasons fall flat when contrasted with causing significantly fewer serious bleeds and improved survival. Of course, when transradial proves impossible there is no choice other than going with transfemoral, but as proponents of transradial said at the meeting, it is a matter of making transradial the initial, default strategy and only resorting to transfemoral when absolutely necessary.
The MATRIX results had another very important finding: To get the best outcomes, centers that offer PCI to acute coronary syndrome patients can’t simply dabble with the transradial approach; they need to be all in. A subanalysis of the MATRIX mortality benefit for transradial procedures showed a striking and statistically significant link between operator commitment to the transradial approach and the ability to give patients a mortality benefit by using the transradial approach. This analysis subdivided the patients into three categories depending on the frequency at which the center where they were treated performed transradial PCI. The three subgroups were centers that did 64% or fewer of their cases transradially, centers that did 65%-79% of their patients transradially, and centers that did 80% or more of their cases via the radial artery.
The data showed that patients treated at centers that used the transradial approach in no more than 64% of their cases actually had a small trend toward better 30-day survival rates when they underwent a transfemoral procedure, although it was not a statistically significant difference. Among the subgroup of patients treated at centers that fell into the middle range of transradial use in everyday practice there was a trend toward better survival with transradial treatment, compared with transfemoral, but again not a statistically significant difference.
It was only among the patients treated at centers that used transradial access nearly all the time, for 80% or more of cases, where transradial use made a statistically significant difference in survival. In this subgroup, patients treated transradially had a 52% relative survival advantage compared with similar patients treated at the same center but via a transfemoral approach.
In other words, when a center in the MATRIX trial did at least 80% of cases with the transradial approach, the patients treated there that way had less than half the 30-day mortality rate, compared with similar patients treated at the same center but by PCI that used a transfemoral approach.
Choosing the PCI access site has moved beyond physician preference and convenience. It’s a matter of patient well-being.
On Twitter @mitchelzoler
Transradial PCI outperforms transfemoral for acute coronary syndromes
SAN DIEGO – The unshakable grip that transfemoral access has held on coronary artery catheterization for the U.S. practice of interventional cardiology may finally loosen with results from an 8,000-patient, multinational controlled trial.
MATRIX showed that transradial access for coronary catheterization of patients with acute coronary syndrome (ACS) produced significantly fewer access-site bleeding events and significantly improved patient survival, compared with transfemoral access.
“Our results, in conjunction with the updated meta-analysis, suggest that the radial approach should become the default access for patients with acute coronary syndrome undergoing invasive management,” Dr. Marco Valgimigli said at the annual meeting of the American College of Cardiology. “Access site does matter, and a reduction in access-site bleeding complications seems to translate into a mortality benefit,” said Dr. Valgimigli, an interventional cardiologist at Erasmus University Medical Center in Rotterdam, the Netherlands.
The MATRIX (Minimizing Adverse Haemorrhagic Events by Transradial Access Site and Systemic Implementation of Angiox) trial enrolled 8,404 ACS patients at 78 sites in four European countries: Italy, Spain, Sweden, and the Netherlands. The study randomized patients undergoing percutaneous coronary intervention (PCI) to catheterization via either the patient’s radial or femoral artery. After 30 days, the combined rate of death, myocardial infarction, stroke, and major bleeding was reduced by an absolute rate of 1.9% among the patients treated with transradial access, a 17% relative risk reduction that was statistically significant for one of the study’s two primary endpoints.
This outcome difference seemed driven primarily by significant reductions in major bleeds and specifically major access-site bleeds, and this led to a statistically significant reduction in all-cause death by 0.6%, a 28% relative risk reduction in 30-day mortality tied to transradial access, Dr. Valgimigli said.
“I think this will be the study that helps change guidelines, to make radial artery access the default approach,” commented Dr. Sanjit S. Jolly, an interventional cardiologist at McMaster University in Hamilton, Ont.
“The United States is very behind in the use of transradial access; it’s used in about 20% of coronary PCIs,” noted Dr. Cindy L. Grines, an interventional cardiologist at the Detroit Medical Center. “We need to make a concerted effort in the United States to retrain practitioners to do transradial procedures. This approach is initially more time consuming, involves more radiation exposure, and can be frustrating, so we probably need to incentivize physicians by increasing their reimbursement for transradial PCIs and by making it part of quality assurance programs. Unless we do something like that, transradial use may not change,” Dr. Grines said in an interview.
The significant superiority of transradial over transfemoral access for both patient survival and for one of the study’s primary endpoints contrasted with the neutral result seen in an earlier major study that compared the two access approaches, RIVAL (Radial Versus Femoral Access for Coronary Angiography and Intervention in Patients With Acute Coronary Syndromes; Lancet 2011;377:1409-20).
Dr. Valgimigli also reported results from a meta-analysis that combined the MATRIX and RIVAL results as well as data from a few additional much smaller trials. This combined analysis, which involved a total of more than 19,000 ACS patients randomized to PCI via one of the two access sites, further confirmed that transradial catheterization linked with statistically significant reductions in death, in major bleeds not associated with coronary artery surgery, and in the combined endpoint of death, myocardial infarction, and stroke, he said. Concurrent with his report at the meeting, the MATRIX results as well as the updated meta-analysis results, appeared in an article published online (Lancet 2015 [doi:10.1016/S0140-6736(15)60292-6]).
The MATRIX study used only highly experienced interventionalists who had extensive familiarity with performing PCI using both types of access. They successfully used transradial access in 94% of patients randomized to that approach, but in the other 6% technical difficulties resulted in a crossover to the transfemoral route. Among patients randomized to transfemoral access, 2% required crossover to a transradial procedure.
MATRIX was an investigator-initiated study that received grant support from Terumo and the Medicines Co. Dr. Valgimigli had no relevant financial disclosures. Dr. Jolly has been a consultant to AstraZeneca, has been a speaker on behalf of St. Jude, and has received research grants from Medtronic. Dr. Grines has been a consultant to and received honoraria from Abbott Vascular, the Medicines Co., Merck, and the Volcano Group.
[email protected]
On Twitter @mitchelzoler
U.S. interventionalists have lagged in adopting transradial access for percutaneous coronary interventions. I reviewed the status within the past year and found that about 17% of all U.S. percutaneous coronary interventions were done by transradial access, and this level jibes with recent results from a survey of U.S. interventionalists.

|
Dr. David E. Kandzari |
American use of transradial access grew markedly over the last decade. Ten years ago, the rate stood at about 3%. But it remains well behind most other countries. Results reported at the ACC meeting from another large international study of coronary interventions in ST-elevation myocardial infarction patients showed a 68% worldwide rate of transradial access (N. Engl. J. Med. 2015 [doi:10.1056/NEJMoa1415098])
I believe that the MATRIX results will help further fuel change in U.S. practice. Soon, quality assurance programs at many U.S. hospitals may incorporate transradial access as a performance measure.
The accumulated evidence, now including the MATRIX results, supports transradial access as the default approach for vascular access during coronary procedures. However, in some patients transradial access is impossible, especially in some women, in the elderly, and in patients with a high body mass index.
Dr. David E. Kandzari, director of interventional cardiology at the Piedmont Heart Institute in Atlanta, made these comments in an interview. He has been a consultant to Medtronic and Boston Scientific and has received research support from Abbott Vascular, Biotronik, Boston Scientific, and Medtronic.
U.S. interventionalists have lagged in adopting transradial access for percutaneous coronary interventions. I reviewed the status within the past year and found that about 17% of all U.S. percutaneous coronary interventions were done by transradial access, and this level jibes with recent results from a survey of U.S. interventionalists.

|
Dr. David E. Kandzari |
American use of transradial access grew markedly over the last decade. Ten years ago, the rate stood at about 3%. But it remains well behind most other countries. Results reported at the ACC meeting from another large international study of coronary interventions in ST-elevation myocardial infarction patients showed a 68% worldwide rate of transradial access (N. Engl. J. Med. 2015 [doi:10.1056/NEJMoa1415098])
I believe that the MATRIX results will help further fuel change in U.S. practice. Soon, quality assurance programs at many U.S. hospitals may incorporate transradial access as a performance measure.
The accumulated evidence, now including the MATRIX results, supports transradial access as the default approach for vascular access during coronary procedures. However, in some patients transradial access is impossible, especially in some women, in the elderly, and in patients with a high body mass index.
Dr. David E. Kandzari, director of interventional cardiology at the Piedmont Heart Institute in Atlanta, made these comments in an interview. He has been a consultant to Medtronic and Boston Scientific and has received research support from Abbott Vascular, Biotronik, Boston Scientific, and Medtronic.
U.S. interventionalists have lagged in adopting transradial access for percutaneous coronary interventions. I reviewed the status within the past year and found that about 17% of all U.S. percutaneous coronary interventions were done by transradial access, and this level jibes with recent results from a survey of U.S. interventionalists.

|
Dr. David E. Kandzari |
American use of transradial access grew markedly over the last decade. Ten years ago, the rate stood at about 3%. But it remains well behind most other countries. Results reported at the ACC meeting from another large international study of coronary interventions in ST-elevation myocardial infarction patients showed a 68% worldwide rate of transradial access (N. Engl. J. Med. 2015 [doi:10.1056/NEJMoa1415098])
I believe that the MATRIX results will help further fuel change in U.S. practice. Soon, quality assurance programs at many U.S. hospitals may incorporate transradial access as a performance measure.
The accumulated evidence, now including the MATRIX results, supports transradial access as the default approach for vascular access during coronary procedures. However, in some patients transradial access is impossible, especially in some women, in the elderly, and in patients with a high body mass index.
Dr. David E. Kandzari, director of interventional cardiology at the Piedmont Heart Institute in Atlanta, made these comments in an interview. He has been a consultant to Medtronic and Boston Scientific and has received research support from Abbott Vascular, Biotronik, Boston Scientific, and Medtronic.
SAN DIEGO – The unshakable grip that transfemoral access has held on coronary artery catheterization for the U.S. practice of interventional cardiology may finally loosen with results from an 8,000-patient, multinational controlled trial.
MATRIX showed that transradial access for coronary catheterization of patients with acute coronary syndrome (ACS) produced significantly fewer access-site bleeding events and significantly improved patient survival, compared with transfemoral access.
“Our results, in conjunction with the updated meta-analysis, suggest that the radial approach should become the default access for patients with acute coronary syndrome undergoing invasive management,” Dr. Marco Valgimigli said at the annual meeting of the American College of Cardiology. “Access site does matter, and a reduction in access-site bleeding complications seems to translate into a mortality benefit,” said Dr. Valgimigli, an interventional cardiologist at Erasmus University Medical Center in Rotterdam, the Netherlands.
The MATRIX (Minimizing Adverse Haemorrhagic Events by Transradial Access Site and Systemic Implementation of Angiox) trial enrolled 8,404 ACS patients at 78 sites in four European countries: Italy, Spain, Sweden, and the Netherlands. The study randomized patients undergoing percutaneous coronary intervention (PCI) to catheterization via either the patient’s radial or femoral artery. After 30 days, the combined rate of death, myocardial infarction, stroke, and major bleeding was reduced by an absolute rate of 1.9% among the patients treated with transradial access, a 17% relative risk reduction that was statistically significant for one of the study’s two primary endpoints.
This outcome difference seemed driven primarily by significant reductions in major bleeds and specifically major access-site bleeds, and this led to a statistically significant reduction in all-cause death by 0.6%, a 28% relative risk reduction in 30-day mortality tied to transradial access, Dr. Valgimigli said.
“I think this will be the study that helps change guidelines, to make radial artery access the default approach,” commented Dr. Sanjit S. Jolly, an interventional cardiologist at McMaster University in Hamilton, Ont.
“The United States is very behind in the use of transradial access; it’s used in about 20% of coronary PCIs,” noted Dr. Cindy L. Grines, an interventional cardiologist at the Detroit Medical Center. “We need to make a concerted effort in the United States to retrain practitioners to do transradial procedures. This approach is initially more time consuming, involves more radiation exposure, and can be frustrating, so we probably need to incentivize physicians by increasing their reimbursement for transradial PCIs and by making it part of quality assurance programs. Unless we do something like that, transradial use may not change,” Dr. Grines said in an interview.
The significant superiority of transradial over transfemoral access for both patient survival and for one of the study’s primary endpoints contrasted with the neutral result seen in an earlier major study that compared the two access approaches, RIVAL (Radial Versus Femoral Access for Coronary Angiography and Intervention in Patients With Acute Coronary Syndromes; Lancet 2011;377:1409-20).
Dr. Valgimigli also reported results from a meta-analysis that combined the MATRIX and RIVAL results as well as data from a few additional much smaller trials. This combined analysis, which involved a total of more than 19,000 ACS patients randomized to PCI via one of the two access sites, further confirmed that transradial catheterization linked with statistically significant reductions in death, in major bleeds not associated with coronary artery surgery, and in the combined endpoint of death, myocardial infarction, and stroke, he said. Concurrent with his report at the meeting, the MATRIX results as well as the updated meta-analysis results, appeared in an article published online (Lancet 2015 [doi:10.1016/S0140-6736(15)60292-6]).
The MATRIX study used only highly experienced interventionalists who had extensive familiarity with performing PCI using both types of access. They successfully used transradial access in 94% of patients randomized to that approach, but in the other 6% technical difficulties resulted in a crossover to the transfemoral route. Among patients randomized to transfemoral access, 2% required crossover to a transradial procedure.
MATRIX was an investigator-initiated study that received grant support from Terumo and the Medicines Co. Dr. Valgimigli had no relevant financial disclosures. Dr. Jolly has been a consultant to AstraZeneca, has been a speaker on behalf of St. Jude, and has received research grants from Medtronic. Dr. Grines has been a consultant to and received honoraria from Abbott Vascular, the Medicines Co., Merck, and the Volcano Group.
[email protected]
On Twitter @mitchelzoler
SAN DIEGO – The unshakable grip that transfemoral access has held on coronary artery catheterization for the U.S. practice of interventional cardiology may finally loosen with results from an 8,000-patient, multinational controlled trial.
MATRIX showed that transradial access for coronary catheterization of patients with acute coronary syndrome (ACS) produced significantly fewer access-site bleeding events and significantly improved patient survival, compared with transfemoral access.
“Our results, in conjunction with the updated meta-analysis, suggest that the radial approach should become the default access for patients with acute coronary syndrome undergoing invasive management,” Dr. Marco Valgimigli said at the annual meeting of the American College of Cardiology. “Access site does matter, and a reduction in access-site bleeding complications seems to translate into a mortality benefit,” said Dr. Valgimigli, an interventional cardiologist at Erasmus University Medical Center in Rotterdam, the Netherlands.
The MATRIX (Minimizing Adverse Haemorrhagic Events by Transradial Access Site and Systemic Implementation of Angiox) trial enrolled 8,404 ACS patients at 78 sites in four European countries: Italy, Spain, Sweden, and the Netherlands. The study randomized patients undergoing percutaneous coronary intervention (PCI) to catheterization via either the patient’s radial or femoral artery. After 30 days, the combined rate of death, myocardial infarction, stroke, and major bleeding was reduced by an absolute rate of 1.9% among the patients treated with transradial access, a 17% relative risk reduction that was statistically significant for one of the study’s two primary endpoints.
This outcome difference seemed driven primarily by significant reductions in major bleeds and specifically major access-site bleeds, and this led to a statistically significant reduction in all-cause death by 0.6%, a 28% relative risk reduction in 30-day mortality tied to transradial access, Dr. Valgimigli said.
“I think this will be the study that helps change guidelines, to make radial artery access the default approach,” commented Dr. Sanjit S. Jolly, an interventional cardiologist at McMaster University in Hamilton, Ont.
“The United States is very behind in the use of transradial access; it’s used in about 20% of coronary PCIs,” noted Dr. Cindy L. Grines, an interventional cardiologist at the Detroit Medical Center. “We need to make a concerted effort in the United States to retrain practitioners to do transradial procedures. This approach is initially more time consuming, involves more radiation exposure, and can be frustrating, so we probably need to incentivize physicians by increasing their reimbursement for transradial PCIs and by making it part of quality assurance programs. Unless we do something like that, transradial use may not change,” Dr. Grines said in an interview.
The significant superiority of transradial over transfemoral access for both patient survival and for one of the study’s primary endpoints contrasted with the neutral result seen in an earlier major study that compared the two access approaches, RIVAL (Radial Versus Femoral Access for Coronary Angiography and Intervention in Patients With Acute Coronary Syndromes; Lancet 2011;377:1409-20).
Dr. Valgimigli also reported results from a meta-analysis that combined the MATRIX and RIVAL results as well as data from a few additional much smaller trials. This combined analysis, which involved a total of more than 19,000 ACS patients randomized to PCI via one of the two access sites, further confirmed that transradial catheterization linked with statistically significant reductions in death, in major bleeds not associated with coronary artery surgery, and in the combined endpoint of death, myocardial infarction, and stroke, he said. Concurrent with his report at the meeting, the MATRIX results as well as the updated meta-analysis results, appeared in an article published online (Lancet 2015 [doi:10.1016/S0140-6736(15)60292-6]).
The MATRIX study used only highly experienced interventionalists who had extensive familiarity with performing PCI using both types of access. They successfully used transradial access in 94% of patients randomized to that approach, but in the other 6% technical difficulties resulted in a crossover to the transfemoral route. Among patients randomized to transfemoral access, 2% required crossover to a transradial procedure.
MATRIX was an investigator-initiated study that received grant support from Terumo and the Medicines Co. Dr. Valgimigli had no relevant financial disclosures. Dr. Jolly has been a consultant to AstraZeneca, has been a speaker on behalf of St. Jude, and has received research grants from Medtronic. Dr. Grines has been a consultant to and received honoraria from Abbott Vascular, the Medicines Co., Merck, and the Volcano Group.
[email protected]
On Twitter @mitchelzoler
AT ACC 15
Key clinical point: ACS patients randomized to transradial access for PCI had significantly better survival at 30 days, compared with those treated via the transfemoral route.
Major finding: Thirty-day all-cause death occurred in 0.6% fewer patients using transradial access, a 28% relative risk reduction.
Data source: MATRIX, a multicenter, randomized controlled trial with 8,404 patients.
Disclosures: MATRIX was an investigator-initiated study that received grant support from Terumo and the Medicines Co. Dr. Valgimigli had no relevant financial disclosures. Dr. Jolly has been a consultant to AstraZeneca, has been a speaker on behalf of St. Jude, and has received research grants from Medtronic. Dr. Grines has been a consultant to and received honoraria from Abbott Vascular, the Medicines Co., Merck, and the Volcano Group.
Baroreflex activation therapy improves heart failure symptoms
SAN DIEGO– Baroreflex activation therapy showed promise as an important new device therapy for patients with New York Heart Association Class III heart failure, according to researchers.
In a preliminary randomized trial, the investigational therapy demonstrated safety comparable to that of established device therapies for heart failure. And it significantly improved functional status, exercise capacity, and quality of life while reducing levels of the biomarker N-terminal pro-brain natriuretic peptide (NT-proBNP) and days-in-hospital for worsening heart failure, Dr. William T. Abraham said at the annual meeting of the American College of Cardiology.
“The trial showed important results,” he said. “If these observations are confirmed in larger studies, baroreflex activation therapy may offer a new addition for the treatment of advanced heart failure patients with a reduced left ventricular ejection fraction.”
Novel therapies for patients with NYHA class III heart failure with a reduced ejection fraction (HFrEF) are sorely needed, he added, as 25%-35% of patients with HFrEF remain in NYHA class III despite current drug and device therapies. These patients are moderately symptomatic, meaning they are sick enough that their quality of life is sharply diminished, but not sufficiently ill to qualify for advanced heart therapies, such as cardiac transplantation or a left ventricular assist device.
Dr. Abraham presented the findings of a multinational, prospective, randomized, 6-month, controlled trial involving 140 NYHA class III HFrEF patients in the United States, Canada, Germany, and France. They were randomized to optimal guideline-directed medical therapy alone or in conjunction with baroreflex activation therapy (BAT), a form of neuromodulatory therapy involving electrical stimulation of the carotid baroreflex baroreceptor delivered by an implanted device similar to a pacemaker.
Progressive heart failure is characterized by increased sympathetic and reduced parasympathetic nerve activity. BAT addresses both abnormalities.
“This form of neuromodulation differs from other forms of neuromodulation in that it does not target a peripheral efferent nerve, but rather it targets the carotid baroreceptor. It targets afferent signals to the brain, which then produce an integrated autonomic nervous system response resulting in inhibition of sympathetic activity and enhancement of parasympathetic activity. So this is a physiologic form of autonomic rebalancing that is mediated via the CNS,” explained Dr. Abraham, professor of medicine and director of the division of cardiovascular medicine at Ohio State University, Columbus.
The primary safety endpoint was freedom from system- and procedure-related major adverse neurologic and cardiovascular events at 6 months. The rate was 97.2%. There were no deaths, and complications – all of which occurred within the first 7 days – were few and short lived, with rates similar to those seen with implantable cardioverter-defibrillators (ICDs) and cardiac resynchronization therapy (CRT). The BAT device, known as the CVRx Barostim neo, did not interact with the ICDs and CRT devices present in a large number of participants. No hypotension occurred in this normotensive HFrEF population.
To place the efficacy outcomes in perspective, Dr. Abraham continued, it’s worth noting that the average 19.5-point between-group difference favoring BAT in scores on the Minnesota Living with Heart Failure Quality of Life Questionnaire (MLHFQ) at 6 months compared to a baseline of 45 points dwarfs the benefits obtainable with standard therapies.
“Please remember that our best drug therapies for HFrEF – ACE inhibitors and beta blockers– improve the MLHFQ score by 4 or 5 points, and cardiac resynchronization therapy improves that score by an average of 9 or 10 points,” he said. From a baseline of 300 meters, the 6-minute hall walk distance improved by 58 meters more in the BAT group than in controls. By comparison, CRT improves the distance walked in 6 minutes by about 30 meters.
“The magnitude of benefit of BAT exceeds that seen with standard therapies, it was seen on top of those standard therapies, and it certainly falls into a range that would be considered clinically meaningful,” the cardiologist asserted.
Left ventricular ejection fraction improved in the BAT group by an average of 2.4% from a baseline of 24% while decreasing by 0.1% in controls. The between-group difference in NT-proBNP at 6 months was 342 pg/mL in favor of the BAT group, starting from a baseline level of roughly 1,300 pg/mL.
The BAT group averaged 6.95 hospital days per year for worsening heart failure during the 6 months prior to enrollment and 0.67 days per year in the 6 months following device activation, for an adjusted 82% relative risk reduction. In contrast, hospital days for heart failure remained steady in controls. The possibility of a new treatment that reduces heart failure hospitalizations is of particular interest in light of the enormous financial burden such hospitalizations currently place upon the Medicare system.
Simultaneously with Dr. Abraham’s presentation at ACC 15, the study manuscript was published online (JACC: Heart Failure 2015 [doi: 10.1016/j.jchf.2015.02.006]).
Dr. Abraham is a consultant to CVRx (which funded the study), as well as Novartis, St. Jude Medical, CardioMEMS, and Abbott Vascular.
SAN DIEGO– Baroreflex activation therapy showed promise as an important new device therapy for patients with New York Heart Association Class III heart failure, according to researchers.
In a preliminary randomized trial, the investigational therapy demonstrated safety comparable to that of established device therapies for heart failure. And it significantly improved functional status, exercise capacity, and quality of life while reducing levels of the biomarker N-terminal pro-brain natriuretic peptide (NT-proBNP) and days-in-hospital for worsening heart failure, Dr. William T. Abraham said at the annual meeting of the American College of Cardiology.
“The trial showed important results,” he said. “If these observations are confirmed in larger studies, baroreflex activation therapy may offer a new addition for the treatment of advanced heart failure patients with a reduced left ventricular ejection fraction.”
Novel therapies for patients with NYHA class III heart failure with a reduced ejection fraction (HFrEF) are sorely needed, he added, as 25%-35% of patients with HFrEF remain in NYHA class III despite current drug and device therapies. These patients are moderately symptomatic, meaning they are sick enough that their quality of life is sharply diminished, but not sufficiently ill to qualify for advanced heart therapies, such as cardiac transplantation or a left ventricular assist device.
Dr. Abraham presented the findings of a multinational, prospective, randomized, 6-month, controlled trial involving 140 NYHA class III HFrEF patients in the United States, Canada, Germany, and France. They were randomized to optimal guideline-directed medical therapy alone or in conjunction with baroreflex activation therapy (BAT), a form of neuromodulatory therapy involving electrical stimulation of the carotid baroreflex baroreceptor delivered by an implanted device similar to a pacemaker.
Progressive heart failure is characterized by increased sympathetic and reduced parasympathetic nerve activity. BAT addresses both abnormalities.
“This form of neuromodulation differs from other forms of neuromodulation in that it does not target a peripheral efferent nerve, but rather it targets the carotid baroreceptor. It targets afferent signals to the brain, which then produce an integrated autonomic nervous system response resulting in inhibition of sympathetic activity and enhancement of parasympathetic activity. So this is a physiologic form of autonomic rebalancing that is mediated via the CNS,” explained Dr. Abraham, professor of medicine and director of the division of cardiovascular medicine at Ohio State University, Columbus.
The primary safety endpoint was freedom from system- and procedure-related major adverse neurologic and cardiovascular events at 6 months. The rate was 97.2%. There were no deaths, and complications – all of which occurred within the first 7 days – were few and short lived, with rates similar to those seen with implantable cardioverter-defibrillators (ICDs) and cardiac resynchronization therapy (CRT). The BAT device, known as the CVRx Barostim neo, did not interact with the ICDs and CRT devices present in a large number of participants. No hypotension occurred in this normotensive HFrEF population.
To place the efficacy outcomes in perspective, Dr. Abraham continued, it’s worth noting that the average 19.5-point between-group difference favoring BAT in scores on the Minnesota Living with Heart Failure Quality of Life Questionnaire (MLHFQ) at 6 months compared to a baseline of 45 points dwarfs the benefits obtainable with standard therapies.
“Please remember that our best drug therapies for HFrEF – ACE inhibitors and beta blockers– improve the MLHFQ score by 4 or 5 points, and cardiac resynchronization therapy improves that score by an average of 9 or 10 points,” he said. From a baseline of 300 meters, the 6-minute hall walk distance improved by 58 meters more in the BAT group than in controls. By comparison, CRT improves the distance walked in 6 minutes by about 30 meters.
“The magnitude of benefit of BAT exceeds that seen with standard therapies, it was seen on top of those standard therapies, and it certainly falls into a range that would be considered clinically meaningful,” the cardiologist asserted.
Left ventricular ejection fraction improved in the BAT group by an average of 2.4% from a baseline of 24% while decreasing by 0.1% in controls. The between-group difference in NT-proBNP at 6 months was 342 pg/mL in favor of the BAT group, starting from a baseline level of roughly 1,300 pg/mL.
The BAT group averaged 6.95 hospital days per year for worsening heart failure during the 6 months prior to enrollment and 0.67 days per year in the 6 months following device activation, for an adjusted 82% relative risk reduction. In contrast, hospital days for heart failure remained steady in controls. The possibility of a new treatment that reduces heart failure hospitalizations is of particular interest in light of the enormous financial burden such hospitalizations currently place upon the Medicare system.
Simultaneously with Dr. Abraham’s presentation at ACC 15, the study manuscript was published online (JACC: Heart Failure 2015 [doi: 10.1016/j.jchf.2015.02.006]).
Dr. Abraham is a consultant to CVRx (which funded the study), as well as Novartis, St. Jude Medical, CardioMEMS, and Abbott Vascular.
SAN DIEGO– Baroreflex activation therapy showed promise as an important new device therapy for patients with New York Heart Association Class III heart failure, according to researchers.
In a preliminary randomized trial, the investigational therapy demonstrated safety comparable to that of established device therapies for heart failure. And it significantly improved functional status, exercise capacity, and quality of life while reducing levels of the biomarker N-terminal pro-brain natriuretic peptide (NT-proBNP) and days-in-hospital for worsening heart failure, Dr. William T. Abraham said at the annual meeting of the American College of Cardiology.
“The trial showed important results,” he said. “If these observations are confirmed in larger studies, baroreflex activation therapy may offer a new addition for the treatment of advanced heart failure patients with a reduced left ventricular ejection fraction.”
Novel therapies for patients with NYHA class III heart failure with a reduced ejection fraction (HFrEF) are sorely needed, he added, as 25%-35% of patients with HFrEF remain in NYHA class III despite current drug and device therapies. These patients are moderately symptomatic, meaning they are sick enough that their quality of life is sharply diminished, but not sufficiently ill to qualify for advanced heart therapies, such as cardiac transplantation or a left ventricular assist device.
Dr. Abraham presented the findings of a multinational, prospective, randomized, 6-month, controlled trial involving 140 NYHA class III HFrEF patients in the United States, Canada, Germany, and France. They were randomized to optimal guideline-directed medical therapy alone or in conjunction with baroreflex activation therapy (BAT), a form of neuromodulatory therapy involving electrical stimulation of the carotid baroreflex baroreceptor delivered by an implanted device similar to a pacemaker.
Progressive heart failure is characterized by increased sympathetic and reduced parasympathetic nerve activity. BAT addresses both abnormalities.
“This form of neuromodulation differs from other forms of neuromodulation in that it does not target a peripheral efferent nerve, but rather it targets the carotid baroreceptor. It targets afferent signals to the brain, which then produce an integrated autonomic nervous system response resulting in inhibition of sympathetic activity and enhancement of parasympathetic activity. So this is a physiologic form of autonomic rebalancing that is mediated via the CNS,” explained Dr. Abraham, professor of medicine and director of the division of cardiovascular medicine at Ohio State University, Columbus.
The primary safety endpoint was freedom from system- and procedure-related major adverse neurologic and cardiovascular events at 6 months. The rate was 97.2%. There were no deaths, and complications – all of which occurred within the first 7 days – were few and short lived, with rates similar to those seen with implantable cardioverter-defibrillators (ICDs) and cardiac resynchronization therapy (CRT). The BAT device, known as the CVRx Barostim neo, did not interact with the ICDs and CRT devices present in a large number of participants. No hypotension occurred in this normotensive HFrEF population.
To place the efficacy outcomes in perspective, Dr. Abraham continued, it’s worth noting that the average 19.5-point between-group difference favoring BAT in scores on the Minnesota Living with Heart Failure Quality of Life Questionnaire (MLHFQ) at 6 months compared to a baseline of 45 points dwarfs the benefits obtainable with standard therapies.
“Please remember that our best drug therapies for HFrEF – ACE inhibitors and beta blockers– improve the MLHFQ score by 4 or 5 points, and cardiac resynchronization therapy improves that score by an average of 9 or 10 points,” he said. From a baseline of 300 meters, the 6-minute hall walk distance improved by 58 meters more in the BAT group than in controls. By comparison, CRT improves the distance walked in 6 minutes by about 30 meters.
“The magnitude of benefit of BAT exceeds that seen with standard therapies, it was seen on top of those standard therapies, and it certainly falls into a range that would be considered clinically meaningful,” the cardiologist asserted.
Left ventricular ejection fraction improved in the BAT group by an average of 2.4% from a baseline of 24% while decreasing by 0.1% in controls. The between-group difference in NT-proBNP at 6 months was 342 pg/mL in favor of the BAT group, starting from a baseline level of roughly 1,300 pg/mL.
The BAT group averaged 6.95 hospital days per year for worsening heart failure during the 6 months prior to enrollment and 0.67 days per year in the 6 months following device activation, for an adjusted 82% relative risk reduction. In contrast, hospital days for heart failure remained steady in controls. The possibility of a new treatment that reduces heart failure hospitalizations is of particular interest in light of the enormous financial burden such hospitalizations currently place upon the Medicare system.
Simultaneously with Dr. Abraham’s presentation at ACC 15, the study manuscript was published online (JACC: Heart Failure 2015 [doi: 10.1016/j.jchf.2015.02.006]).
Dr. Abraham is a consultant to CVRx (which funded the study), as well as Novartis, St. Jude Medical, CardioMEMS, and Abbott Vascular.
AT ACC 15
Key clinical point: Baroreflex activation therapy is safe and improves multiple aspects of NYHA class III heart failure with reduced ejection fraction.
Major finding: Fifty-five percent of patients assigned to baroreflex activation therapy plus optimal guideline-directed medical therapy showed at least a one-class-rank improvement at 6 months of follow-up, compared with 24% of controls on optimal medical therapy alone.
Data source: A multinational, prospective, randomized, 6-month, controlled clinical trial of 140 patients with NYHA class III HFrEF.
Disclosures: Dr. Abraham is a consultant to CVRx (which funded the study), as well as Novartis, St. Jude Medical, CardioMEMS, and Abbott Vascular.
VIDEO: Long-term PARTNER 1 data tip scales toward TAVR
SAN DIEGO – The 5-year results of the PARTNER 1 trial in presented at the annual meeting of the American College of Cardiology were reassuring for clinicians treating patients with severe aortic stenosis at high risk for surgery, said to Dr. Jeffrey J. Popma of Beth Israel DeaconessMedical Center, Boston, in a video interview. The data showed comparable mortality between transcatheter aortic valve replacement (TAVR) and surgical aortic valve replacement (SAVR), as well as long-term durability of the SAPIEN transcatheter valve, he said.
With these similar outcome results, Dr. Popma asks, can the less-invasive TAVR procedure be considered the preferred treatment over SAVR in these very-sick patients?
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN DIEGO – The 5-year results of the PARTNER 1 trial in presented at the annual meeting of the American College of Cardiology were reassuring for clinicians treating patients with severe aortic stenosis at high risk for surgery, said to Dr. Jeffrey J. Popma of Beth Israel DeaconessMedical Center, Boston, in a video interview. The data showed comparable mortality between transcatheter aortic valve replacement (TAVR) and surgical aortic valve replacement (SAVR), as well as long-term durability of the SAPIEN transcatheter valve, he said.
With these similar outcome results, Dr. Popma asks, can the less-invasive TAVR procedure be considered the preferred treatment over SAVR in these very-sick patients?
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN DIEGO – The 5-year results of the PARTNER 1 trial in presented at the annual meeting of the American College of Cardiology were reassuring for clinicians treating patients with severe aortic stenosis at high risk for surgery, said to Dr. Jeffrey J. Popma of Beth Israel DeaconessMedical Center, Boston, in a video interview. The data showed comparable mortality between transcatheter aortic valve replacement (TAVR) and surgical aortic valve replacement (SAVR), as well as long-term durability of the SAPIEN transcatheter valve, he said.
With these similar outcome results, Dr. Popma asks, can the less-invasive TAVR procedure be considered the preferred treatment over SAVR in these very-sick patients?
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ACC 15
VIDEO: SAPIEN and CoreValve provide complementary TAVR options
SAN DIEGO – Long-term outcome results from the trials that compared the first-generation SAPIEN system and the CoreValve system for transcatheter aortic valve replacement (TAVR) have shown that both devices had excellent performance, compared with surgical aortic valve replacement.
The SAPIEN system continued to show similar performance, compared with surgery after 5-year follow-up, and the CoreValve showed even better superiority to surgery after 2 years, compared with first-year results.
But the performance of the two systems for TAVR should not be interpreted to suggest that CoreValve outperforms the SAPIEN system, cautioned Dr. Stephen Ramee during an interview at the annual meeting of the American College of Cardiology.
The CoreValve study began 4 years after the PARTNER trial that studied the SAPIEN valve, and during that intervening period, the cardiologists and cardiac surgeons who collaborate on TAVR learned important lessons on how to better select patients and how to avoid other risks during the procedure, said Dr. Ramee, an interventional cardiologist and director of the John Ochsner Heart and Vascular Institute in New Orleans.
As a consequence, the SAPIEN valve (currently the XT system) remains a very viable option, and Dr. Ramee said he generally used the SAPIEN XT system for about 60% of his cases. The major patient group best suited for CoreValve TAVR are patients with a highly calcified aortic-valve annulus, which is better suited to the self-expanding CoreValve because of a reduced risk for rupture of the annulus during balloon expansion with the SAPIEN valve.
Dr. Ramee has received honoraria from Edwards and Medtronic, the companies that respectively market the SAPIEN and CoreValve systems. He also has a financial interest in several companies developing new TAVR devices.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter mitchelzoler
SAN DIEGO – Long-term outcome results from the trials that compared the first-generation SAPIEN system and the CoreValve system for transcatheter aortic valve replacement (TAVR) have shown that both devices had excellent performance, compared with surgical aortic valve replacement.
The SAPIEN system continued to show similar performance, compared with surgery after 5-year follow-up, and the CoreValve showed even better superiority to surgery after 2 years, compared with first-year results.
But the performance of the two systems for TAVR should not be interpreted to suggest that CoreValve outperforms the SAPIEN system, cautioned Dr. Stephen Ramee during an interview at the annual meeting of the American College of Cardiology.
The CoreValve study began 4 years after the PARTNER trial that studied the SAPIEN valve, and during that intervening period, the cardiologists and cardiac surgeons who collaborate on TAVR learned important lessons on how to better select patients and how to avoid other risks during the procedure, said Dr. Ramee, an interventional cardiologist and director of the John Ochsner Heart and Vascular Institute in New Orleans.
As a consequence, the SAPIEN valve (currently the XT system) remains a very viable option, and Dr. Ramee said he generally used the SAPIEN XT system for about 60% of his cases. The major patient group best suited for CoreValve TAVR are patients with a highly calcified aortic-valve annulus, which is better suited to the self-expanding CoreValve because of a reduced risk for rupture of the annulus during balloon expansion with the SAPIEN valve.
Dr. Ramee has received honoraria from Edwards and Medtronic, the companies that respectively market the SAPIEN and CoreValve systems. He also has a financial interest in several companies developing new TAVR devices.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter mitchelzoler
SAN DIEGO – Long-term outcome results from the trials that compared the first-generation SAPIEN system and the CoreValve system for transcatheter aortic valve replacement (TAVR) have shown that both devices had excellent performance, compared with surgical aortic valve replacement.
The SAPIEN system continued to show similar performance, compared with surgery after 5-year follow-up, and the CoreValve showed even better superiority to surgery after 2 years, compared with first-year results.
But the performance of the two systems for TAVR should not be interpreted to suggest that CoreValve outperforms the SAPIEN system, cautioned Dr. Stephen Ramee during an interview at the annual meeting of the American College of Cardiology.
The CoreValve study began 4 years after the PARTNER trial that studied the SAPIEN valve, and during that intervening period, the cardiologists and cardiac surgeons who collaborate on TAVR learned important lessons on how to better select patients and how to avoid other risks during the procedure, said Dr. Ramee, an interventional cardiologist and director of the John Ochsner Heart and Vascular Institute in New Orleans.
As a consequence, the SAPIEN valve (currently the XT system) remains a very viable option, and Dr. Ramee said he generally used the SAPIEN XT system for about 60% of his cases. The major patient group best suited for CoreValve TAVR are patients with a highly calcified aortic-valve annulus, which is better suited to the self-expanding CoreValve because of a reduced risk for rupture of the annulus during balloon expansion with the SAPIEN valve.
Dr. Ramee has received honoraria from Edwards and Medtronic, the companies that respectively market the SAPIEN and CoreValve systems. He also has a financial interest in several companies developing new TAVR devices.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter mitchelzoler
EXPERT ANALYSIS FROM ACC 15
Everolimus-eluting stents linked to higher MI risk than CABG
Percutaneous coronary intervention with second-generation everolimus-eluting stents is associated with a similar risk of death but a higher risk of myocardial infarction and repeat revascularization than is coronary-artery bypass grafting.
An observational registry study of 34,819 patients with multivessel coronary artery disease who underwent one or the other procedure showed a similar risk of death at a mean follow-up of 2.9 years between patients who underwent PCI with everolimus-eluting stents and those who underwent CABG (3.1% and 2.9% per year, hazard ratio, 1.04; P = .50).
However, those in the percutaneous coronary intervention (PCI) group had a 51% greater risk of MI (95% confidence interval, 1.29-1.77; P < .001).
This increase in risk was significant only in patients who had incomplete revascularization and not in those with complete revascularization. In addition, the increase in risk largely was tied to spontaneous myocardial infarction, according to the findings.
“Randomized trials comparing PCI with CABG have not been typically powered to evaluate differences in the rates of myocardial infarction, stroke, and death from any cause; instead, they have been based on composite outcomes that include repeat revascularization,” wrote Dr. Sripal Bangalore of the cardiovascular clinical research center at the New York University, and his coauthors.
Patients undergoing PCI with everolimus-eluting stents also had a greater than twofold increase in the risk of repeat revascularization (hazard ratio, 2.35; 95% CI, 2.14-2.58; P < .001), but particularly in patients with three-vessel as opposed to two-vessel disease.
However, those in the PCI group also had a 58% lower risk of stroke than did those in the CABG group (95% CI, 0.50-0.76; P < .001), which was driven largely by a reduced risk in the first 30 days after the procedure (N. Engl. J. Med. 2015 March 16 [doi:10.1056/NEJMoa1412168]).
In the short term – in the hospital or within 30 days of the procedure – patients who underwent PCI showed significantly lower risk of death and stroke but no significant differences in MI risk.
“Thus, the choice between CABG and PCI with everolimus-eluting stents may depend on whether complete revascularization can be achieved with PCI,” the authors wrote. “If the answer is yes, the choice between PCI and CABG should be made on the basis of weighing the short-term risk of death and stroke against the long-term risk of revascularization with PCI.”
The authors acknowledged limitations of the study. It was a nonrandomized, observational trial; it did not examine variables such as smoking and other comorbidities; and it did not capture other neurologic events, such as transient ischemic attack.
The study was supported by Abbott Vascular. Dr. Bangalore has received consultant fees or honoraria from Abbott Vascular, Boehringer Ingelheim, Daiichi Sankyo, Gilead Sciences, Pfizer, and Unique Pharmaceuticals.
CABG previously has been shown to be associated with fewer repeat vascularizations than has PCI, but questions have been raised about incremental improvements in stent technology that might narrow this gap.

|
Dr. Robert A. Harrington |
However, data from this and the BEST study show there are clearly trade-offs between the two revascularization strategies that need to be discussed with patients as part of the shared decision-making process.
The early risk of stroke with CABG may be unacceptable to some, while others may want to avoid the risk of a later myocardial infarction or repeat procedure associated with PCI.
Dr. Robert A. Harrington is Arthur L. Bloomfield Professor of Medicine at Stanford (Calif.) University. These comments are taken from an editorial (N. Engl. J. Med. 2015 March 16 [doi:10.1056/NEJMe1501045]) accompanying this and the BEST study, which was also presented at the annual meeting of the American College of Cardiology in San Diego (N. Engl. J. Med. 2015 March 15 [doi:10.1056/NEJMoa1415447]). Dr. Harrington has received consultant fees and/or research grants from numerous pharmaceutical and device companies, including Amgen, Medtronic, Merck, Novartis, GlaxoSmithKline, and the Medicines Company. He is a principal or has ownership interest in Element Science and MyoKardia.
CABG previously has been shown to be associated with fewer repeat vascularizations than has PCI, but questions have been raised about incremental improvements in stent technology that might narrow this gap.

|
Dr. Robert A. Harrington |
However, data from this and the BEST study show there are clearly trade-offs between the two revascularization strategies that need to be discussed with patients as part of the shared decision-making process.
The early risk of stroke with CABG may be unacceptable to some, while others may want to avoid the risk of a later myocardial infarction or repeat procedure associated with PCI.
Dr. Robert A. Harrington is Arthur L. Bloomfield Professor of Medicine at Stanford (Calif.) University. These comments are taken from an editorial (N. Engl. J. Med. 2015 March 16 [doi:10.1056/NEJMe1501045]) accompanying this and the BEST study, which was also presented at the annual meeting of the American College of Cardiology in San Diego (N. Engl. J. Med. 2015 March 15 [doi:10.1056/NEJMoa1415447]). Dr. Harrington has received consultant fees and/or research grants from numerous pharmaceutical and device companies, including Amgen, Medtronic, Merck, Novartis, GlaxoSmithKline, and the Medicines Company. He is a principal or has ownership interest in Element Science and MyoKardia.
CABG previously has been shown to be associated with fewer repeat vascularizations than has PCI, but questions have been raised about incremental improvements in stent technology that might narrow this gap.

|
Dr. Robert A. Harrington |
However, data from this and the BEST study show there are clearly trade-offs between the two revascularization strategies that need to be discussed with patients as part of the shared decision-making process.
The early risk of stroke with CABG may be unacceptable to some, while others may want to avoid the risk of a later myocardial infarction or repeat procedure associated with PCI.
Dr. Robert A. Harrington is Arthur L. Bloomfield Professor of Medicine at Stanford (Calif.) University. These comments are taken from an editorial (N. Engl. J. Med. 2015 March 16 [doi:10.1056/NEJMe1501045]) accompanying this and the BEST study, which was also presented at the annual meeting of the American College of Cardiology in San Diego (N. Engl. J. Med. 2015 March 15 [doi:10.1056/NEJMoa1415447]). Dr. Harrington has received consultant fees and/or research grants from numerous pharmaceutical and device companies, including Amgen, Medtronic, Merck, Novartis, GlaxoSmithKline, and the Medicines Company. He is a principal or has ownership interest in Element Science and MyoKardia.
Percutaneous coronary intervention with second-generation everolimus-eluting stents is associated with a similar risk of death but a higher risk of myocardial infarction and repeat revascularization than is coronary-artery bypass grafting.
An observational registry study of 34,819 patients with multivessel coronary artery disease who underwent one or the other procedure showed a similar risk of death at a mean follow-up of 2.9 years between patients who underwent PCI with everolimus-eluting stents and those who underwent CABG (3.1% and 2.9% per year, hazard ratio, 1.04; P = .50).
However, those in the percutaneous coronary intervention (PCI) group had a 51% greater risk of MI (95% confidence interval, 1.29-1.77; P < .001).
This increase in risk was significant only in patients who had incomplete revascularization and not in those with complete revascularization. In addition, the increase in risk largely was tied to spontaneous myocardial infarction, according to the findings.
“Randomized trials comparing PCI with CABG have not been typically powered to evaluate differences in the rates of myocardial infarction, stroke, and death from any cause; instead, they have been based on composite outcomes that include repeat revascularization,” wrote Dr. Sripal Bangalore of the cardiovascular clinical research center at the New York University, and his coauthors.
Patients undergoing PCI with everolimus-eluting stents also had a greater than twofold increase in the risk of repeat revascularization (hazard ratio, 2.35; 95% CI, 2.14-2.58; P < .001), but particularly in patients with three-vessel as opposed to two-vessel disease.
However, those in the PCI group also had a 58% lower risk of stroke than did those in the CABG group (95% CI, 0.50-0.76; P < .001), which was driven largely by a reduced risk in the first 30 days after the procedure (N. Engl. J. Med. 2015 March 16 [doi:10.1056/NEJMoa1412168]).
In the short term – in the hospital or within 30 days of the procedure – patients who underwent PCI showed significantly lower risk of death and stroke but no significant differences in MI risk.
“Thus, the choice between CABG and PCI with everolimus-eluting stents may depend on whether complete revascularization can be achieved with PCI,” the authors wrote. “If the answer is yes, the choice between PCI and CABG should be made on the basis of weighing the short-term risk of death and stroke against the long-term risk of revascularization with PCI.”
The authors acknowledged limitations of the study. It was a nonrandomized, observational trial; it did not examine variables such as smoking and other comorbidities; and it did not capture other neurologic events, such as transient ischemic attack.
The study was supported by Abbott Vascular. Dr. Bangalore has received consultant fees or honoraria from Abbott Vascular, Boehringer Ingelheim, Daiichi Sankyo, Gilead Sciences, Pfizer, and Unique Pharmaceuticals.
Percutaneous coronary intervention with second-generation everolimus-eluting stents is associated with a similar risk of death but a higher risk of myocardial infarction and repeat revascularization than is coronary-artery bypass grafting.
An observational registry study of 34,819 patients with multivessel coronary artery disease who underwent one or the other procedure showed a similar risk of death at a mean follow-up of 2.9 years between patients who underwent PCI with everolimus-eluting stents and those who underwent CABG (3.1% and 2.9% per year, hazard ratio, 1.04; P = .50).
However, those in the percutaneous coronary intervention (PCI) group had a 51% greater risk of MI (95% confidence interval, 1.29-1.77; P < .001).
This increase in risk was significant only in patients who had incomplete revascularization and not in those with complete revascularization. In addition, the increase in risk largely was tied to spontaneous myocardial infarction, according to the findings.
“Randomized trials comparing PCI with CABG have not been typically powered to evaluate differences in the rates of myocardial infarction, stroke, and death from any cause; instead, they have been based on composite outcomes that include repeat revascularization,” wrote Dr. Sripal Bangalore of the cardiovascular clinical research center at the New York University, and his coauthors.
Patients undergoing PCI with everolimus-eluting stents also had a greater than twofold increase in the risk of repeat revascularization (hazard ratio, 2.35; 95% CI, 2.14-2.58; P < .001), but particularly in patients with three-vessel as opposed to two-vessel disease.
However, those in the PCI group also had a 58% lower risk of stroke than did those in the CABG group (95% CI, 0.50-0.76; P < .001), which was driven largely by a reduced risk in the first 30 days after the procedure (N. Engl. J. Med. 2015 March 16 [doi:10.1056/NEJMoa1412168]).
In the short term – in the hospital or within 30 days of the procedure – patients who underwent PCI showed significantly lower risk of death and stroke but no significant differences in MI risk.
“Thus, the choice between CABG and PCI with everolimus-eluting stents may depend on whether complete revascularization can be achieved with PCI,” the authors wrote. “If the answer is yes, the choice between PCI and CABG should be made on the basis of weighing the short-term risk of death and stroke against the long-term risk of revascularization with PCI.”
The authors acknowledged limitations of the study. It was a nonrandomized, observational trial; it did not examine variables such as smoking and other comorbidities; and it did not capture other neurologic events, such as transient ischemic attack.
The study was supported by Abbott Vascular. Dr. Bangalore has received consultant fees or honoraria from Abbott Vascular, Boehringer Ingelheim, Daiichi Sankyo, Gilead Sciences, Pfizer, and Unique Pharmaceuticals.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: PCI with second-generation everolimus-eluting stents is associated with a similar risk of death but a higher risk of MI and repeat revascularization than does CABG.
Major finding: PCI was associated with a 51% greater risk of MI at 2.9 years of follow-up, compared with CABG.
Data source: An observational registry study of 34,819 patients with multivessel coronary artery disease.
Disclosures: The study was supported by Abbott Vascular. Dr. Bangalore has received consultant fees or honoraria from Abbott Vascular, Boehringer Ingelheim, Daiichi Sankyo, Gilead Sciences, Pfizer, and Unique Pharmaceuticals.