User login
American Academy of Pediatrics (AAP): 2013 National Conference and Exhibition
Smartphone technology could enable remote otitis media diagnosis
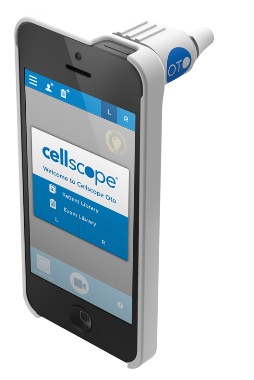
ORLANDO – A novel smartphone otoscope attachment provides clear, transmittable images of the ear drum or tympanic membrane, and could revolutionize the approach to diagnosing and managing ear infections, according to Dr. Kathryn Rappaport.
In a prospective study involving 63 children who presented to an emergency department between May and December 2012 with upper respiratory tract symptoms, the technology was as effective as a conventional otoscope, and was widely accepted by parents, Dr. Rappaport of Baylor College of Medicine, Houston, reported at the annual meeting of the American Academy of Pediatrics.
After receiving clinical care, each child in the study underwent bilateral otic videoscopy using both the smartphone otoscope (CellScope Oto) and a camera-fitted conventional otoscope. The procedures were performed in random order, said Dr. Rappaport, who was at Emory University in Atlanta when the study was conducted.
Of the children, who had a mean age of 2.9 years, 49 received a clinical diagnosis of acute otitis media by an ED practitioner. Based on independent scoring by four physicians who evaluated 31 CellScope Oto videos and 31 conventional otoscope videos from 26 subjects, there was no difference between the two technologies in either the diagnostic quality of the images or diagnosis confidence ratings.
Diagnosis and treatment decision making were similar with each device. Overall, the physician raters were in fair agreement regarding the clinical ED diagnosis of acute otitis media, while two of the raters had moderate to substantial agreement with the ED diagnosis and two had poor agreement with the ED diagnosis from images obtained via conventional otoscope, Dr. Rappaport said, noting that there was a significant correlation between antimicrobial use and image quality.
This indicated that higher-quality images were more likely to be associated with a definitive diagnosis, she said.
As for parent reactions to the use of the device, most (95%) responded favorably, stating that the CellScope Oto images improved their understanding of their child’s management. Also, 90% said they thought the technology would be easy to use, and they would feel comfortable using it remotely to transmit images to a provider.
The CellScope Oto has the potential to improve diagnosis and management, and to reduce costs associated with acute otitis media in children, Dr. Rappaport said.
The video images can provide a baseline, as well as ongoing documentation of a child’s condition. The video documentation could allow a child to be followed over a period of time – without the need for regular office visits – to help monitor for progression or resolution of middle ear effusion and to guide diagnosis and treatment decision making, she explained.
"Acute otitis media is the most common reason for antimicrobial prescriptions in children. In the future, we would like to study whether the ability to monitor for resolution of a patient’s middle ear effusion using digital imaging with the smartphone otoscope will lead to decreased antimicrobial prescriptions for acute otitis media in children," she said in an interview.
Dr. Rappaport reported having no relevant financial disclosures.
ORLANDO – A novel smartphone otoscope attachment provides clear, transmittable images of the ear drum or tympanic membrane, and could revolutionize the approach to diagnosing and managing ear infections, according to Dr. Kathryn Rappaport.
In a prospective study involving 63 children who presented to an emergency department between May and December 2012 with upper respiratory tract symptoms, the technology was as effective as a conventional otoscope, and was widely accepted by parents, Dr. Rappaport of Baylor College of Medicine, Houston, reported at the annual meeting of the American Academy of Pediatrics.
After receiving clinical care, each child in the study underwent bilateral otic videoscopy using both the smartphone otoscope (CellScope Oto) and a camera-fitted conventional otoscope. The procedures were performed in random order, said Dr. Rappaport, who was at Emory University in Atlanta when the study was conducted.
Of the children, who had a mean age of 2.9 years, 49 received a clinical diagnosis of acute otitis media by an ED practitioner. Based on independent scoring by four physicians who evaluated 31 CellScope Oto videos and 31 conventional otoscope videos from 26 subjects, there was no difference between the two technologies in either the diagnostic quality of the images or diagnosis confidence ratings.
Diagnosis and treatment decision making were similar with each device. Overall, the physician raters were in fair agreement regarding the clinical ED diagnosis of acute otitis media, while two of the raters had moderate to substantial agreement with the ED diagnosis and two had poor agreement with the ED diagnosis from images obtained via conventional otoscope, Dr. Rappaport said, noting that there was a significant correlation between antimicrobial use and image quality.
This indicated that higher-quality images were more likely to be associated with a definitive diagnosis, she said.
As for parent reactions to the use of the device, most (95%) responded favorably, stating that the CellScope Oto images improved their understanding of their child’s management. Also, 90% said they thought the technology would be easy to use, and they would feel comfortable using it remotely to transmit images to a provider.
The CellScope Oto has the potential to improve diagnosis and management, and to reduce costs associated with acute otitis media in children, Dr. Rappaport said.
The video images can provide a baseline, as well as ongoing documentation of a child’s condition. The video documentation could allow a child to be followed over a period of time – without the need for regular office visits – to help monitor for progression or resolution of middle ear effusion and to guide diagnosis and treatment decision making, she explained.
"Acute otitis media is the most common reason for antimicrobial prescriptions in children. In the future, we would like to study whether the ability to monitor for resolution of a patient’s middle ear effusion using digital imaging with the smartphone otoscope will lead to decreased antimicrobial prescriptions for acute otitis media in children," she said in an interview.
Dr. Rappaport reported having no relevant financial disclosures.
ORLANDO – A novel smartphone otoscope attachment provides clear, transmittable images of the ear drum or tympanic membrane, and could revolutionize the approach to diagnosing and managing ear infections, according to Dr. Kathryn Rappaport.
In a prospective study involving 63 children who presented to an emergency department between May and December 2012 with upper respiratory tract symptoms, the technology was as effective as a conventional otoscope, and was widely accepted by parents, Dr. Rappaport of Baylor College of Medicine, Houston, reported at the annual meeting of the American Academy of Pediatrics.
After receiving clinical care, each child in the study underwent bilateral otic videoscopy using both the smartphone otoscope (CellScope Oto) and a camera-fitted conventional otoscope. The procedures were performed in random order, said Dr. Rappaport, who was at Emory University in Atlanta when the study was conducted.
Of the children, who had a mean age of 2.9 years, 49 received a clinical diagnosis of acute otitis media by an ED practitioner. Based on independent scoring by four physicians who evaluated 31 CellScope Oto videos and 31 conventional otoscope videos from 26 subjects, there was no difference between the two technologies in either the diagnostic quality of the images or diagnosis confidence ratings.
Diagnosis and treatment decision making were similar with each device. Overall, the physician raters were in fair agreement regarding the clinical ED diagnosis of acute otitis media, while two of the raters had moderate to substantial agreement with the ED diagnosis and two had poor agreement with the ED diagnosis from images obtained via conventional otoscope, Dr. Rappaport said, noting that there was a significant correlation between antimicrobial use and image quality.
This indicated that higher-quality images were more likely to be associated with a definitive diagnosis, she said.
As for parent reactions to the use of the device, most (95%) responded favorably, stating that the CellScope Oto images improved their understanding of their child’s management. Also, 90% said they thought the technology would be easy to use, and they would feel comfortable using it remotely to transmit images to a provider.
The CellScope Oto has the potential to improve diagnosis and management, and to reduce costs associated with acute otitis media in children, Dr. Rappaport said.
The video images can provide a baseline, as well as ongoing documentation of a child’s condition. The video documentation could allow a child to be followed over a period of time – without the need for regular office visits – to help monitor for progression or resolution of middle ear effusion and to guide diagnosis and treatment decision making, she explained.
"Acute otitis media is the most common reason for antimicrobial prescriptions in children. In the future, we would like to study whether the ability to monitor for resolution of a patient’s middle ear effusion using digital imaging with the smartphone otoscope will lead to decreased antimicrobial prescriptions for acute otitis media in children," she said in an interview.
Dr. Rappaport reported having no relevant financial disclosures.
AT THE AAP NATIONAL CONFERENCE
Major finding: No difference was seen between the smartphone otoscope and a conventional otoscope in either the diagnostic quality of the images or diagnosis confidence ratings.
Data source: A prospective single-site study of 63 children.
Disclosures: Dr. Rappaport reported having no relevant financial disclosures.
Microarray is ‘go-to’ test for multiple congenital anomalies
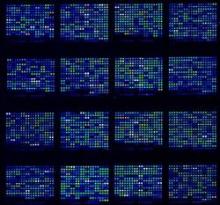
ORLANDO – Chromosomal microarray testing is ideal for narrowing down the diagnosis in most patients presenting with multiple congenital anomalies, according to Dr. Laurie Demmer.
"Microarray is the clinical geneticist’s favorite test right now. We order it every day – anytime we see somebody with multiple congenital anomalies, unless it’s obviously Down syndrome or another obvious syndrome," Dr. Demmer said during a "Genetic Testing Boot Camp" session at the annual meeting of the American Academy of Pediatrics.
For children presenting with a suspected syndrome, problems with growth, or a development or autism spectrum disorder, microarray is "really our go-to test right now," said Dr. Demmer, a pediatric clinical geneticist at Levine Children’s Hospital, Charlotte, N.C.
Also, if chromosomal testing demonstrates a certain karyotype, such as a translocation, then microarray testing is the best approach for determining if it is a balanced translocation. If a marker chromosome is detected, microarray will identify it.
Like karyotyping, which is often used when a chromosomal anomaly is suspected, microarray testing provides a look at the whole genome, but it is about 100 times more sensitive than a karyotype. It is high resolution like fluorescent in situ hybridization (FISH), which is a chromosomal testing method often used when a quicker answer is needed to help guide management.
Thus, microarray testing is "kind of the best of both worlds," Dr. Demmer said, adding that with microarray analysis, it is possible to look for small deletions and duplications on all the chromosomes within the whole genome.
At first, microarray testing was targeted; rather than looking at the whole genome, testing was performed to look for known syndromes such as 22q deletions and Williams syndrome and Smith-Magenis syndrome, for example. Expanding the view to the whole genome has allowed for diagnosis of new syndromes that were never known before.
"Every week I get one or two arrays back that are abnormal with a new deletion or duplication that I’d never seen or heard of before," she said, noting that a downside of this is that there’s no clear answer to what should be done with all of these "copy number variants." Currently they are being characterized in databases as a reference.
The latest generation of microarray testing (single nucleotide polymorphism, or SNP array) provides qualitative information not available with oligoarray testing.
"It allows us to tell the difference between chromosomes. ... It gives us the ability to tell if there is identity in the chromosomes," she said, explaining that this may mean identifying uniparental disomy (and likely Prader-Willi syndrome), consanguinity (and degree of relationship), and other circumstances associated with autosomal recessive disease.
A downside of microarray testing is that it only looks for deletions and duplications, and therefore does not detect balanced rearrangements. Thus a balanced translocation will not be detected on microarray testing, and an opportunity for genetic counseling could be missed.
Also, sometimes a copy number variant or deletion or duplication is found, and it is unclear how these should be interpreted.
A general rule of thumb, however, is that the bigger it is, the more likely it is to be significant, Dr. Demmer said, noting that in some of these cases, the parents are tested, and if a parent has the same copy number variant but is normal, the finding is usually a benign change.
Sometimes, however, a parent who has the copy number variant may be "on the spectrum somewhere, but not actually diagnosed, and they may have one of the changes associated with autism."
These cases require special care in interpretation, Dr. Demmer said. "If you’re going to send out for microarrays in your office and it comes back normal, that’s great, but if it comes back anything else, you may want to get a geneticist to help you," she said.
Similarly, unanticipated results – incidental findings – also occur, and these can be tricky to deal with. Examples include cases of unknown consanguinity and incest, she said.
Sometimes the incidental findings lead to improved outcomes. Dr. Demmer described one case involving an intellectually disabled 10-year-old girl who was incidentally found on microarray testing to be at genetic risk for familial adenomatous polyposis (FAP). A gastrointestinal examination showed that she already had thousands of polyps.
"So she has FAP, which we diagnosed by doing the microarray, and probably saved her life, because now we will treat her, and we’re going to prevent the colon cancer," she said.
Dr. Demmer reported having no disclosures.
ORLANDO – Chromosomal microarray testing is ideal for narrowing down the diagnosis in most patients presenting with multiple congenital anomalies, according to Dr. Laurie Demmer.
"Microarray is the clinical geneticist’s favorite test right now. We order it every day – anytime we see somebody with multiple congenital anomalies, unless it’s obviously Down syndrome or another obvious syndrome," Dr. Demmer said during a "Genetic Testing Boot Camp" session at the annual meeting of the American Academy of Pediatrics.
For children presenting with a suspected syndrome, problems with growth, or a development or autism spectrum disorder, microarray is "really our go-to test right now," said Dr. Demmer, a pediatric clinical geneticist at Levine Children’s Hospital, Charlotte, N.C.
Also, if chromosomal testing demonstrates a certain karyotype, such as a translocation, then microarray testing is the best approach for determining if it is a balanced translocation. If a marker chromosome is detected, microarray will identify it.
Like karyotyping, which is often used when a chromosomal anomaly is suspected, microarray testing provides a look at the whole genome, but it is about 100 times more sensitive than a karyotype. It is high resolution like fluorescent in situ hybridization (FISH), which is a chromosomal testing method often used when a quicker answer is needed to help guide management.
Thus, microarray testing is "kind of the best of both worlds," Dr. Demmer said, adding that with microarray analysis, it is possible to look for small deletions and duplications on all the chromosomes within the whole genome.
At first, microarray testing was targeted; rather than looking at the whole genome, testing was performed to look for known syndromes such as 22q deletions and Williams syndrome and Smith-Magenis syndrome, for example. Expanding the view to the whole genome has allowed for diagnosis of new syndromes that were never known before.
"Every week I get one or two arrays back that are abnormal with a new deletion or duplication that I’d never seen or heard of before," she said, noting that a downside of this is that there’s no clear answer to what should be done with all of these "copy number variants." Currently they are being characterized in databases as a reference.
The latest generation of microarray testing (single nucleotide polymorphism, or SNP array) provides qualitative information not available with oligoarray testing.
"It allows us to tell the difference between chromosomes. ... It gives us the ability to tell if there is identity in the chromosomes," she said, explaining that this may mean identifying uniparental disomy (and likely Prader-Willi syndrome), consanguinity (and degree of relationship), and other circumstances associated with autosomal recessive disease.
A downside of microarray testing is that it only looks for deletions and duplications, and therefore does not detect balanced rearrangements. Thus a balanced translocation will not be detected on microarray testing, and an opportunity for genetic counseling could be missed.
Also, sometimes a copy number variant or deletion or duplication is found, and it is unclear how these should be interpreted.
A general rule of thumb, however, is that the bigger it is, the more likely it is to be significant, Dr. Demmer said, noting that in some of these cases, the parents are tested, and if a parent has the same copy number variant but is normal, the finding is usually a benign change.
Sometimes, however, a parent who has the copy number variant may be "on the spectrum somewhere, but not actually diagnosed, and they may have one of the changes associated with autism."
These cases require special care in interpretation, Dr. Demmer said. "If you’re going to send out for microarrays in your office and it comes back normal, that’s great, but if it comes back anything else, you may want to get a geneticist to help you," she said.
Similarly, unanticipated results – incidental findings – also occur, and these can be tricky to deal with. Examples include cases of unknown consanguinity and incest, she said.
Sometimes the incidental findings lead to improved outcomes. Dr. Demmer described one case involving an intellectually disabled 10-year-old girl who was incidentally found on microarray testing to be at genetic risk for familial adenomatous polyposis (FAP). A gastrointestinal examination showed that she already had thousands of polyps.
"So she has FAP, which we diagnosed by doing the microarray, and probably saved her life, because now we will treat her, and we’re going to prevent the colon cancer," she said.
Dr. Demmer reported having no disclosures.
ORLANDO – Chromosomal microarray testing is ideal for narrowing down the diagnosis in most patients presenting with multiple congenital anomalies, according to Dr. Laurie Demmer.
"Microarray is the clinical geneticist’s favorite test right now. We order it every day – anytime we see somebody with multiple congenital anomalies, unless it’s obviously Down syndrome or another obvious syndrome," Dr. Demmer said during a "Genetic Testing Boot Camp" session at the annual meeting of the American Academy of Pediatrics.
For children presenting with a suspected syndrome, problems with growth, or a development or autism spectrum disorder, microarray is "really our go-to test right now," said Dr. Demmer, a pediatric clinical geneticist at Levine Children’s Hospital, Charlotte, N.C.
Also, if chromosomal testing demonstrates a certain karyotype, such as a translocation, then microarray testing is the best approach for determining if it is a balanced translocation. If a marker chromosome is detected, microarray will identify it.
Like karyotyping, which is often used when a chromosomal anomaly is suspected, microarray testing provides a look at the whole genome, but it is about 100 times more sensitive than a karyotype. It is high resolution like fluorescent in situ hybridization (FISH), which is a chromosomal testing method often used when a quicker answer is needed to help guide management.
Thus, microarray testing is "kind of the best of both worlds," Dr. Demmer said, adding that with microarray analysis, it is possible to look for small deletions and duplications on all the chromosomes within the whole genome.
At first, microarray testing was targeted; rather than looking at the whole genome, testing was performed to look for known syndromes such as 22q deletions and Williams syndrome and Smith-Magenis syndrome, for example. Expanding the view to the whole genome has allowed for diagnosis of new syndromes that were never known before.
"Every week I get one or two arrays back that are abnormal with a new deletion or duplication that I’d never seen or heard of before," she said, noting that a downside of this is that there’s no clear answer to what should be done with all of these "copy number variants." Currently they are being characterized in databases as a reference.
The latest generation of microarray testing (single nucleotide polymorphism, or SNP array) provides qualitative information not available with oligoarray testing.
"It allows us to tell the difference between chromosomes. ... It gives us the ability to tell if there is identity in the chromosomes," she said, explaining that this may mean identifying uniparental disomy (and likely Prader-Willi syndrome), consanguinity (and degree of relationship), and other circumstances associated with autosomal recessive disease.
A downside of microarray testing is that it only looks for deletions and duplications, and therefore does not detect balanced rearrangements. Thus a balanced translocation will not be detected on microarray testing, and an opportunity for genetic counseling could be missed.
Also, sometimes a copy number variant or deletion or duplication is found, and it is unclear how these should be interpreted.
A general rule of thumb, however, is that the bigger it is, the more likely it is to be significant, Dr. Demmer said, noting that in some of these cases, the parents are tested, and if a parent has the same copy number variant but is normal, the finding is usually a benign change.
Sometimes, however, a parent who has the copy number variant may be "on the spectrum somewhere, but not actually diagnosed, and they may have one of the changes associated with autism."
These cases require special care in interpretation, Dr. Demmer said. "If you’re going to send out for microarrays in your office and it comes back normal, that’s great, but if it comes back anything else, you may want to get a geneticist to help you," she said.
Similarly, unanticipated results – incidental findings – also occur, and these can be tricky to deal with. Examples include cases of unknown consanguinity and incest, she said.
Sometimes the incidental findings lead to improved outcomes. Dr. Demmer described one case involving an intellectually disabled 10-year-old girl who was incidentally found on microarray testing to be at genetic risk for familial adenomatous polyposis (FAP). A gastrointestinal examination showed that she already had thousands of polyps.
"So she has FAP, which we diagnosed by doing the microarray, and probably saved her life, because now we will treat her, and we’re going to prevent the colon cancer," she said.
Dr. Demmer reported having no disclosures.
EXPERT ANALYSIS FROM THE AAP NATIONAL CONFERENCE
Pediatric firearm injuries vary by age
ORLANDO – The majority of children and adolescents who presented with firearm-related injuries to an urban level 1 trauma center over a 6-year period were black males over age 14 years according to a retrospective review of patient records.
Furthermore, children aged 14 years and younger were more likely than were older children to be shot at home, Dr. Andrea C. Suen reported at the annual meeting of the American Academy of Pediatrics.
The findings, which also characterized other age-related injury patterns, injury sites, and methods of transportation to the hospital, provide important information that could help in the development of effective crime- and injury-prevention strategies, she said.
Of 456 patients aged 18 years and younger who presented to the trauma center between January 2005 and 2010, 78 were aged 14 years or younger and 378 were aged 15-18 years. Overall, 86% were male, and 80% were black, but these figures differed by age group; 72% and 89% of those 14 years and younger and those 15-18 years, respectively, were male, and 64% and 83% of those 14 years and younger and those 15-18 years, respectively, were black, said Dr. Suen, a third-year pediatric emergency medicine fellow at the University of Florida Health Science Center, Jacksonville.
Those aged 14 years and younger were almost four times more likely to be shot at home (odds ratio, 3.76), and were much more likely to arrive by ambulance than by private car or to walk in than those aged 15-18 years.
The most common injury sites among children under age 14 years were the extremities (51% of cases), the trunk (41%), the head (16%), and the neck (9%). Those aged 5-9 years had a greater than sixfold increase in the likelihood of multiple injury sites, compared with those aged 10-14 years (OR, 6.26), she said.
In both age groups, 7.1% of patients died as a result of their injury.
In nearly 70% of cases, the shooter was someone unknown to the patient, and in 64% of cases, the type of firearm was unknown.
The findings of this study illustrate important age-based differences in firearm injuries, and highlight a need for improved reporting in firearm-related incidents, according to primary author and investigator, Dr. Phyllis Hendry of the department of emergency medicine at the university, who noted that hospital and emergency medical services reports in this study often lacked important details – such as patient’s relationship to the shooter and type of gun used – necessary for development of effective prevention strategies.
In an interview, Dr. Hendry further noted that the findings underscore the need for pediatricians to address gun safety and precautions in the home, as firearm-related injuries in children and adolescents are an important cause of preventable injury and mortality.
Also, emergency physicians should consider making a referral to child protective services on pediatric firearm injuries to assess the safety of the home, she said. "In our study, only 13% of patients 0-14 years of age had child-protection referrals documented."
Dr. Suen and Dr. Hendry reported having no disclosures.
ORLANDO – The majority of children and adolescents who presented with firearm-related injuries to an urban level 1 trauma center over a 6-year period were black males over age 14 years according to a retrospective review of patient records.
Furthermore, children aged 14 years and younger were more likely than were older children to be shot at home, Dr. Andrea C. Suen reported at the annual meeting of the American Academy of Pediatrics.
The findings, which also characterized other age-related injury patterns, injury sites, and methods of transportation to the hospital, provide important information that could help in the development of effective crime- and injury-prevention strategies, she said.
Of 456 patients aged 18 years and younger who presented to the trauma center between January 2005 and 2010, 78 were aged 14 years or younger and 378 were aged 15-18 years. Overall, 86% were male, and 80% were black, but these figures differed by age group; 72% and 89% of those 14 years and younger and those 15-18 years, respectively, were male, and 64% and 83% of those 14 years and younger and those 15-18 years, respectively, were black, said Dr. Suen, a third-year pediatric emergency medicine fellow at the University of Florida Health Science Center, Jacksonville.
Those aged 14 years and younger were almost four times more likely to be shot at home (odds ratio, 3.76), and were much more likely to arrive by ambulance than by private car or to walk in than those aged 15-18 years.
The most common injury sites among children under age 14 years were the extremities (51% of cases), the trunk (41%), the head (16%), and the neck (9%). Those aged 5-9 years had a greater than sixfold increase in the likelihood of multiple injury sites, compared with those aged 10-14 years (OR, 6.26), she said.
In both age groups, 7.1% of patients died as a result of their injury.
In nearly 70% of cases, the shooter was someone unknown to the patient, and in 64% of cases, the type of firearm was unknown.
The findings of this study illustrate important age-based differences in firearm injuries, and highlight a need for improved reporting in firearm-related incidents, according to primary author and investigator, Dr. Phyllis Hendry of the department of emergency medicine at the university, who noted that hospital and emergency medical services reports in this study often lacked important details – such as patient’s relationship to the shooter and type of gun used – necessary for development of effective prevention strategies.
In an interview, Dr. Hendry further noted that the findings underscore the need for pediatricians to address gun safety and precautions in the home, as firearm-related injuries in children and adolescents are an important cause of preventable injury and mortality.
Also, emergency physicians should consider making a referral to child protective services on pediatric firearm injuries to assess the safety of the home, she said. "In our study, only 13% of patients 0-14 years of age had child-protection referrals documented."
Dr. Suen and Dr. Hendry reported having no disclosures.
ORLANDO – The majority of children and adolescents who presented with firearm-related injuries to an urban level 1 trauma center over a 6-year period were black males over age 14 years according to a retrospective review of patient records.
Furthermore, children aged 14 years and younger were more likely than were older children to be shot at home, Dr. Andrea C. Suen reported at the annual meeting of the American Academy of Pediatrics.
The findings, which also characterized other age-related injury patterns, injury sites, and methods of transportation to the hospital, provide important information that could help in the development of effective crime- and injury-prevention strategies, she said.
Of 456 patients aged 18 years and younger who presented to the trauma center between January 2005 and 2010, 78 were aged 14 years or younger and 378 were aged 15-18 years. Overall, 86% were male, and 80% were black, but these figures differed by age group; 72% and 89% of those 14 years and younger and those 15-18 years, respectively, were male, and 64% and 83% of those 14 years and younger and those 15-18 years, respectively, were black, said Dr. Suen, a third-year pediatric emergency medicine fellow at the University of Florida Health Science Center, Jacksonville.
Those aged 14 years and younger were almost four times more likely to be shot at home (odds ratio, 3.76), and were much more likely to arrive by ambulance than by private car or to walk in than those aged 15-18 years.
The most common injury sites among children under age 14 years were the extremities (51% of cases), the trunk (41%), the head (16%), and the neck (9%). Those aged 5-9 years had a greater than sixfold increase in the likelihood of multiple injury sites, compared with those aged 10-14 years (OR, 6.26), she said.
In both age groups, 7.1% of patients died as a result of their injury.
In nearly 70% of cases, the shooter was someone unknown to the patient, and in 64% of cases, the type of firearm was unknown.
The findings of this study illustrate important age-based differences in firearm injuries, and highlight a need for improved reporting in firearm-related incidents, according to primary author and investigator, Dr. Phyllis Hendry of the department of emergency medicine at the university, who noted that hospital and emergency medical services reports in this study often lacked important details – such as patient’s relationship to the shooter and type of gun used – necessary for development of effective prevention strategies.
In an interview, Dr. Hendry further noted that the findings underscore the need for pediatricians to address gun safety and precautions in the home, as firearm-related injuries in children and adolescents are an important cause of preventable injury and mortality.
Also, emergency physicians should consider making a referral to child protective services on pediatric firearm injuries to assess the safety of the home, she said. "In our study, only 13% of patients 0-14 years of age had child-protection referrals documented."
Dr. Suen and Dr. Hendry reported having no disclosures.
AT THE AAP NATIONAL CONFERENCE
Major finding: Children aged 14 years and under who experience firearm-related injury are more likely than are older children to be shot at home.
Data source: A retrospective review involving 456 patients.
Disclosures: Dr. Suen and Dr. Hendry reported having no disclosures.
Bicycle helmet use remains low, varies by ethnicity and socioeconomic status
ORLANDO – Only 11.3% of more than 1,200 children involved in bicycle-related accidents were wearing a helmet at the time of the accident, a study showed.
Children over age 12, and those of minority background and lower socioeconomic status, had the lowest rates of helmet use; thus the findings have implications for targeted education and prevention strategies, Dr. Veronica Sullins reported at the annual meeting of the American Academy of Pediatrics.
Of the 1,248 children from Los Angeles County who were included in the retrospective study of all injuries related to pediatric bicycle accidents between 2006 and 2011, most (85%) were boys. More than a third (35.2%) of white children wore helmets, but the rates were much lower for Asian (7.0%), black (6.0%), and Hispanic children (4.2%), said Dr. Sullins of the Harbor-UCLA Medical Center in Torrance, Calif.
This is despite laws mandating helmet use in Los Angeles County, Dr. Sullins noted.
The differences in helmet use also appeared to vary based on socioeconomic status; helmets were worn by 15.2% of those with private insurance, compared with 7.6% of those with public insurance, Dr. Sullins noted.
Children in the study had a median age of 13 years. Those over age 12 were less likely to wear helmets than were those aged 12 years or younger (odds ratio, 0.7).
Emergency surgery was required in 5.9% of the children, and only 34.1% returned to their preinjury status. Nine patients (0.7%) died as a result of their injuries; eight of those were not wearing a helmet.
The findings suggest that targeting low-income middle and high schools and minority communities with bicycle safety education and accident prevention strategies may help improve helmet use in children, Dr. Sullins said.
"We really need to focus our efforts and resources on education programs targeting the highest-risk groups. In Los Angeles County, these groups are middle and high school–aged children, minorities, and those of lower socioeconomic status," Dr. Sullins said in an interview.
According to the Centers for Disease Control and Prevention, an estimated 33 million children ride bicycles – for a total of 10 billion hours - each year, and nearly 400 children die as a result of bicycle crashes.
More than 150,000 emergency department visits each year are due to bicycle-related head injuries.
Helmet use has been shown to reduce bicycle-related head injuries by 80%; yet, as the results of this study and others show, the rate of helmet use remains low. The CDC reports that only 15% of adults and 19% of children wear helmets most or all of the time when riding a bicycle.
"We encourage other investigators to perform similar studies to identify [the highest-risk] groups specific to their regions or cities in order to more efficiently direct local injury prevention programs," Dr. Sullins said in the interview.
She reported having no relevant financial disclosures.
ORLANDO – Only 11.3% of more than 1,200 children involved in bicycle-related accidents were wearing a helmet at the time of the accident, a study showed.
Children over age 12, and those of minority background and lower socioeconomic status, had the lowest rates of helmet use; thus the findings have implications for targeted education and prevention strategies, Dr. Veronica Sullins reported at the annual meeting of the American Academy of Pediatrics.
Of the 1,248 children from Los Angeles County who were included in the retrospective study of all injuries related to pediatric bicycle accidents between 2006 and 2011, most (85%) were boys. More than a third (35.2%) of white children wore helmets, but the rates were much lower for Asian (7.0%), black (6.0%), and Hispanic children (4.2%), said Dr. Sullins of the Harbor-UCLA Medical Center in Torrance, Calif.
This is despite laws mandating helmet use in Los Angeles County, Dr. Sullins noted.
The differences in helmet use also appeared to vary based on socioeconomic status; helmets were worn by 15.2% of those with private insurance, compared with 7.6% of those with public insurance, Dr. Sullins noted.
Children in the study had a median age of 13 years. Those over age 12 were less likely to wear helmets than were those aged 12 years or younger (odds ratio, 0.7).
Emergency surgery was required in 5.9% of the children, and only 34.1% returned to their preinjury status. Nine patients (0.7%) died as a result of their injuries; eight of those were not wearing a helmet.
The findings suggest that targeting low-income middle and high schools and minority communities with bicycle safety education and accident prevention strategies may help improve helmet use in children, Dr. Sullins said.
"We really need to focus our efforts and resources on education programs targeting the highest-risk groups. In Los Angeles County, these groups are middle and high school–aged children, minorities, and those of lower socioeconomic status," Dr. Sullins said in an interview.
According to the Centers for Disease Control and Prevention, an estimated 33 million children ride bicycles – for a total of 10 billion hours - each year, and nearly 400 children die as a result of bicycle crashes.
More than 150,000 emergency department visits each year are due to bicycle-related head injuries.
Helmet use has been shown to reduce bicycle-related head injuries by 80%; yet, as the results of this study and others show, the rate of helmet use remains low. The CDC reports that only 15% of adults and 19% of children wear helmets most or all of the time when riding a bicycle.
"We encourage other investigators to perform similar studies to identify [the highest-risk] groups specific to their regions or cities in order to more efficiently direct local injury prevention programs," Dr. Sullins said in the interview.
She reported having no relevant financial disclosures.
ORLANDO – Only 11.3% of more than 1,200 children involved in bicycle-related accidents were wearing a helmet at the time of the accident, a study showed.
Children over age 12, and those of minority background and lower socioeconomic status, had the lowest rates of helmet use; thus the findings have implications for targeted education and prevention strategies, Dr. Veronica Sullins reported at the annual meeting of the American Academy of Pediatrics.
Of the 1,248 children from Los Angeles County who were included in the retrospective study of all injuries related to pediatric bicycle accidents between 2006 and 2011, most (85%) were boys. More than a third (35.2%) of white children wore helmets, but the rates were much lower for Asian (7.0%), black (6.0%), and Hispanic children (4.2%), said Dr. Sullins of the Harbor-UCLA Medical Center in Torrance, Calif.
This is despite laws mandating helmet use in Los Angeles County, Dr. Sullins noted.
The differences in helmet use also appeared to vary based on socioeconomic status; helmets were worn by 15.2% of those with private insurance, compared with 7.6% of those with public insurance, Dr. Sullins noted.
Children in the study had a median age of 13 years. Those over age 12 were less likely to wear helmets than were those aged 12 years or younger (odds ratio, 0.7).
Emergency surgery was required in 5.9% of the children, and only 34.1% returned to their preinjury status. Nine patients (0.7%) died as a result of their injuries; eight of those were not wearing a helmet.
The findings suggest that targeting low-income middle and high schools and minority communities with bicycle safety education and accident prevention strategies may help improve helmet use in children, Dr. Sullins said.
"We really need to focus our efforts and resources on education programs targeting the highest-risk groups. In Los Angeles County, these groups are middle and high school–aged children, minorities, and those of lower socioeconomic status," Dr. Sullins said in an interview.
According to the Centers for Disease Control and Prevention, an estimated 33 million children ride bicycles – for a total of 10 billion hours - each year, and nearly 400 children die as a result of bicycle crashes.
More than 150,000 emergency department visits each year are due to bicycle-related head injuries.
Helmet use has been shown to reduce bicycle-related head injuries by 80%; yet, as the results of this study and others show, the rate of helmet use remains low. The CDC reports that only 15% of adults and 19% of children wear helmets most or all of the time when riding a bicycle.
"We encourage other investigators to perform similar studies to identify [the highest-risk] groups specific to their regions or cities in order to more efficiently direct local injury prevention programs," Dr. Sullins said in the interview.
She reported having no relevant financial disclosures.
AT THE AAP NATIONAL CONFERENCE
Major finding: Only 11.3% of children injured in bicycle accidents were wearing a helmet (35.2%, 7.0%, 6.0%, and 4.2% of white, Asian, black, and Hispanic children, respectively).
Data source: A retrospective study of 1,248 cases of injury related to bicycle accidents during 2006-2011.
Disclosure: Dr. Sullins reported having no relevant financial disclosures.
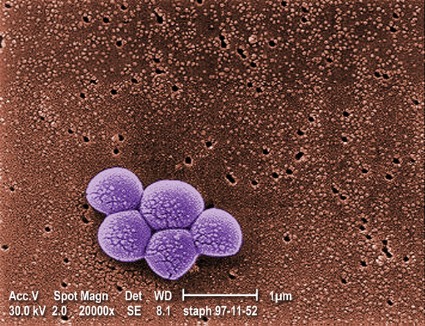
Increasing proportion of musculoskeletal infections involve MRSA
ORLANDO – The proportion of pediatric musculoskeletal infections involving methicillin-resistant Staphylococcus aureus vs. methicillin-sensitive S. aureus has increased dramatically over the past decade, according to a retrospective review of cases.
Between 2001 and 2010, 148 patients at the Children’s Hospital of Philadelphia presented with acute musculoskeletal S. aureus infection, and overall, 37 of those involved methicillin-resistant S. aureus (MRSA), Eric Sarkissian reported at the annual meeting of the American Academy of Pediatrics conference.
The proportion of musculoskeletal cases involving MRSA increased from 12% in 2001-2002 to about 35% in 2010, said Mr. Sarkissian, a 4th-year medical student at Drexel University, Philadelphia.
"Furthermore, we found that MRSA infections were associated with a significantly more complicated hospital stay," Mr. Sarkissian said.
MRSA and methicillin-sensitive S. aureus (MSSA) patients were undergoing magnetic resonance imaging at similar rates, but the average duration of hospitalization was longer for the MRSA patients (13 vs. 8 days), and more MRSA patients required multiple surgical procedures (38% vs. 15%), he said.
In addition, mean presenting C-reactive protein levels were higher in the MRSA vs. MSSA patients (14.7 mg/L vs. 9.8 mg/L), as were infection-related complications, including deep vein thrombosis, septic emboli, septic shock, recurrent infection, and/or avascular necrosis (22% vs. 6%).
MRSA patients also were more often admitted to the ICU for further treatment.
Patients included in this series – the largest known case series of children and adolescents presenting with culture-positive S. aureus osteomyelitis and/or septic arthritis – were consecutive patients with positive cultures of blood, bone, or joint aspirate. Those with postoperative and chronic infections were excluded in an effort to minimize bias caused by nosocomial infections, Mr. Sarkissian noted.
The findings support the ongoing concern that MRSA is evolving and becoming more virulent and invasive over time, compared with MSSA infections. In addition, the findings underscore the need for prompt recognition and aggressive treatment of MRSA musculoskeletal infections, as early recognition is paramount for avoiding sequelae and improving patient outcomes.
"A high index of suspicion is still necessary in the setting of musculoskeletal infections in pediatric patients. Multidisciplinary care provides the most successful opportunity for having improved patient outcomes, and this requires employing broad spectrum antibiotic coverage, using aggressive surgical management, and having an awareness of potential complications," Mr. Sarkissian said.
While clinical prediction models have been developed to help in detecting MRSA infections, outcomes using the models have varied geographically, suggesting that there are unknown regional differences among MRSA cases. It remains to be seen whether available models will be useful for identifying MRSA at presentation, he said.
Mr. Sarkissian reported having no disclosures.
ORLANDO – The proportion of pediatric musculoskeletal infections involving methicillin-resistant Staphylococcus aureus vs. methicillin-sensitive S. aureus has increased dramatically over the past decade, according to a retrospective review of cases.
Between 2001 and 2010, 148 patients at the Children’s Hospital of Philadelphia presented with acute musculoskeletal S. aureus infection, and overall, 37 of those involved methicillin-resistant S. aureus (MRSA), Eric Sarkissian reported at the annual meeting of the American Academy of Pediatrics conference.
The proportion of musculoskeletal cases involving MRSA increased from 12% in 2001-2002 to about 35% in 2010, said Mr. Sarkissian, a 4th-year medical student at Drexel University, Philadelphia.
"Furthermore, we found that MRSA infections were associated with a significantly more complicated hospital stay," Mr. Sarkissian said.
MRSA and methicillin-sensitive S. aureus (MSSA) patients were undergoing magnetic resonance imaging at similar rates, but the average duration of hospitalization was longer for the MRSA patients (13 vs. 8 days), and more MRSA patients required multiple surgical procedures (38% vs. 15%), he said.
In addition, mean presenting C-reactive protein levels were higher in the MRSA vs. MSSA patients (14.7 mg/L vs. 9.8 mg/L), as were infection-related complications, including deep vein thrombosis, septic emboli, septic shock, recurrent infection, and/or avascular necrosis (22% vs. 6%).
MRSA patients also were more often admitted to the ICU for further treatment.
Patients included in this series – the largest known case series of children and adolescents presenting with culture-positive S. aureus osteomyelitis and/or septic arthritis – were consecutive patients with positive cultures of blood, bone, or joint aspirate. Those with postoperative and chronic infections were excluded in an effort to minimize bias caused by nosocomial infections, Mr. Sarkissian noted.
The findings support the ongoing concern that MRSA is evolving and becoming more virulent and invasive over time, compared with MSSA infections. In addition, the findings underscore the need for prompt recognition and aggressive treatment of MRSA musculoskeletal infections, as early recognition is paramount for avoiding sequelae and improving patient outcomes.
"A high index of suspicion is still necessary in the setting of musculoskeletal infections in pediatric patients. Multidisciplinary care provides the most successful opportunity for having improved patient outcomes, and this requires employing broad spectrum antibiotic coverage, using aggressive surgical management, and having an awareness of potential complications," Mr. Sarkissian said.
While clinical prediction models have been developed to help in detecting MRSA infections, outcomes using the models have varied geographically, suggesting that there are unknown regional differences among MRSA cases. It remains to be seen whether available models will be useful for identifying MRSA at presentation, he said.
Mr. Sarkissian reported having no disclosures.
ORLANDO – The proportion of pediatric musculoskeletal infections involving methicillin-resistant Staphylococcus aureus vs. methicillin-sensitive S. aureus has increased dramatically over the past decade, according to a retrospective review of cases.
Between 2001 and 2010, 148 patients at the Children’s Hospital of Philadelphia presented with acute musculoskeletal S. aureus infection, and overall, 37 of those involved methicillin-resistant S. aureus (MRSA), Eric Sarkissian reported at the annual meeting of the American Academy of Pediatrics conference.
The proportion of musculoskeletal cases involving MRSA increased from 12% in 2001-2002 to about 35% in 2010, said Mr. Sarkissian, a 4th-year medical student at Drexel University, Philadelphia.
"Furthermore, we found that MRSA infections were associated with a significantly more complicated hospital stay," Mr. Sarkissian said.
MRSA and methicillin-sensitive S. aureus (MSSA) patients were undergoing magnetic resonance imaging at similar rates, but the average duration of hospitalization was longer for the MRSA patients (13 vs. 8 days), and more MRSA patients required multiple surgical procedures (38% vs. 15%), he said.
In addition, mean presenting C-reactive protein levels were higher in the MRSA vs. MSSA patients (14.7 mg/L vs. 9.8 mg/L), as were infection-related complications, including deep vein thrombosis, septic emboli, septic shock, recurrent infection, and/or avascular necrosis (22% vs. 6%).
MRSA patients also were more often admitted to the ICU for further treatment.
Patients included in this series – the largest known case series of children and adolescents presenting with culture-positive S. aureus osteomyelitis and/or septic arthritis – were consecutive patients with positive cultures of blood, bone, or joint aspirate. Those with postoperative and chronic infections were excluded in an effort to minimize bias caused by nosocomial infections, Mr. Sarkissian noted.
The findings support the ongoing concern that MRSA is evolving and becoming more virulent and invasive over time, compared with MSSA infections. In addition, the findings underscore the need for prompt recognition and aggressive treatment of MRSA musculoskeletal infections, as early recognition is paramount for avoiding sequelae and improving patient outcomes.
"A high index of suspicion is still necessary in the setting of musculoskeletal infections in pediatric patients. Multidisciplinary care provides the most successful opportunity for having improved patient outcomes, and this requires employing broad spectrum antibiotic coverage, using aggressive surgical management, and having an awareness of potential complications," Mr. Sarkissian said.
While clinical prediction models have been developed to help in detecting MRSA infections, outcomes using the models have varied geographically, suggesting that there are unknown regional differences among MRSA cases. It remains to be seen whether available models will be useful for identifying MRSA at presentation, he said.
Mr. Sarkissian reported having no disclosures.
AT THE AAP NATIONAL CONFERENCE
Major finding: The proportion of musculoskeletal infection cases involving MRSA vs. MSSA increased from 12% to 35% between 2001 and 2010.
Data source: A retrospective study of 148 consecutive cases.
Disclosures: Mr. Sarkissian reported having no disclosures.
Clinical report: Students may need school break after concussion
Patients who sustain a concussion need their physicians’ guidance in returning to school in a way that facilitates rather than hinders their recovery, and the American Academy of Pediatrics has issued a clinical report to help.
Most research on pediatric concussions has focused on returning the patient to sports or other physical activities, while data for managing the "return to learn" are sparse. Many published statements emphasize the need for "cognitive rest" – avoiding obvious potential cognitive stressors such as class work and homework – but fall short of identifying and dealing with the myriad other stimuli that can impede recovery or even worsen symptoms, reported Dr. Mark E. Halstead and his associates on the AAP Council on Sports Medicine and Fitness and the AAP Council on School Health (Pediatrics 2013;132:948-57).
An estimated 1.7 million traumatic brain injuries occur each year, many of them concussions. "Given that students typically appear well physically after a concussion, it may be difficult for educators, school administrators, and peers to fully understand the extent of deficits experienced by a student with a concussion." This, in turn, might make school officials reluctant to accept that they must make adjustments for such students.
Pediatricians are in an excellent position to inform these educators, as well as the patients themselves and their families, of the symptoms that might develop and the strategies to prevent or minimize cognitive stress during recovery, said Dr. Halstead, an orthopedic surgeon and sports medicine specialist at Washington University in St. Louis and Children’s Hospital of St. Louis, and his associates. Dr. Halstead also presented the clinical report Oct. 27 at the annual meeting of the American Academy of Pediatrics in Orlando.
The clinical report notes that most concussions resolve within 3 weeks of the injury, so most adjustments to the school environment can be made in the individual classroom setting without the need for a formalized written plan such as a 504 plan or individualized education plan. However, students who require longer-term recovery need more formalized accommodations and modifications.
The report lists typical signs and symptoms of concussion, along with adjustments that teachers and administrators can make to help the child returning to school.
Headache is the most frequent symptom and can recur throughout recovery. School personnel should be made aware that fluorescent lighting, loud noises, and even simply concentrating on a task can elicit headache in these patients, so they should be allowed to take breaks in a quiet area when needed.
Dizziness and lightheadedness also are common and can be provoked by standing quickly, walking in a crowd, or even just viewing motion on a screen or in person. Students with concussion should be allowed to close their eyes or put their heads down on the desk if necessary, and should be permitted to avoid crowded hallways and to move slowly from one place to another.
Common visual symptoms include light sensitivity and blurred or double vision. Students should be allowed to wear a hat with a brim or sunglasses, to turn off or dim room lights, to dim video screens, or to forgo movies or slide presentations. They should be excused if they have trouble reading or writing, or even paying attention to visual tasks.
Sensitivity to noise means that students with concussion might need to be excused from the lunchroom, recess, shop classes, music (band or choir) classes, activities in a gymnasium, and any other excessively noisy location, and should be permitted to use earplugs, Dr. Halstead and his associates said.
Students with concussion also have trouble with concentrating and remembering. Allowances should be made for a student’s difficulty absorbing new material and focusing in the classroom; in particular, testing, especially standardized testing, might need to be postponed until after the student has recovered from the concussion.
Finally, concussions often cause sleep disturbances that can lead to excessive fatigue, tardiness, falling asleep in class, and excessive absences from class. Students might require a late start to the school day or a shortened school day to allow them to rest.
This AAP clinical report was endorsed by the American Medical Society for Sports Medicine, the Brain Injury Association of America, the Canadian Paediatric Society, the National Association of School Nurses, the National Association of School Psychologists, and the National Federation of State High School Associations.
All clinical reports from the AAP expire automatically 5 years after publication unless "reaffirmed, revised, or retired at or before that time."
No conflicts of interest were reported.
This clinical report for the AAP is greatly needed, as the topic of return to learning (RTL) after concussion has been inadequately addressed. It is rare for school personnel and teachers to understand how concussion negatively impacts the injured student. This can cause a potential drop in grades and significant stress, which may delay recovery. Thankfully, many schools and athletic organizations have created plans to help injured athletes return to play, but now student-athletes will benefit from a complementary plan dedicated to returning to academics.
RTL is not a new topic for schools, as many have created plans for other conditions such as chronic illnesses or learning disorders. This report provides a framework that schools can use to create their own RTL plan.
The example put forth by Dr. Mark E. Halstead and his colleagues is a program that has been used successfully in several states. While the components of any good plan are similar, each school may tailor an RTL program to its unique academic needs.
Further research is still needed in order to help validate this program and to identify which academic adjustments are most beneficial to the concussed student-athlete.
Dr. Kevin D. Walter is associate professor of orthopedic surgery and pediatrics at the Medical College of Wisconsin in Milwaukee, and serves on the Institute of Medicine’s Committee on Sports-Related Concussions in Youth.
This clinical report for the AAP is greatly needed, as the topic of return to learning (RTL) after concussion has been inadequately addressed. It is rare for school personnel and teachers to understand how concussion negatively impacts the injured student. This can cause a potential drop in grades and significant stress, which may delay recovery. Thankfully, many schools and athletic organizations have created plans to help injured athletes return to play, but now student-athletes will benefit from a complementary plan dedicated to returning to academics.
RTL is not a new topic for schools, as many have created plans for other conditions such as chronic illnesses or learning disorders. This report provides a framework that schools can use to create their own RTL plan.
The example put forth by Dr. Mark E. Halstead and his colleagues is a program that has been used successfully in several states. While the components of any good plan are similar, each school may tailor an RTL program to its unique academic needs.
Further research is still needed in order to help validate this program and to identify which academic adjustments are most beneficial to the concussed student-athlete.
Dr. Kevin D. Walter is associate professor of orthopedic surgery and pediatrics at the Medical College of Wisconsin in Milwaukee, and serves on the Institute of Medicine’s Committee on Sports-Related Concussions in Youth.
This clinical report for the AAP is greatly needed, as the topic of return to learning (RTL) after concussion has been inadequately addressed. It is rare for school personnel and teachers to understand how concussion negatively impacts the injured student. This can cause a potential drop in grades and significant stress, which may delay recovery. Thankfully, many schools and athletic organizations have created plans to help injured athletes return to play, but now student-athletes will benefit from a complementary plan dedicated to returning to academics.
RTL is not a new topic for schools, as many have created plans for other conditions such as chronic illnesses or learning disorders. This report provides a framework that schools can use to create their own RTL plan.
The example put forth by Dr. Mark E. Halstead and his colleagues is a program that has been used successfully in several states. While the components of any good plan are similar, each school may tailor an RTL program to its unique academic needs.
Further research is still needed in order to help validate this program and to identify which academic adjustments are most beneficial to the concussed student-athlete.
Dr. Kevin D. Walter is associate professor of orthopedic surgery and pediatrics at the Medical College of Wisconsin in Milwaukee, and serves on the Institute of Medicine’s Committee on Sports-Related Concussions in Youth.
Patients who sustain a concussion need their physicians’ guidance in returning to school in a way that facilitates rather than hinders their recovery, and the American Academy of Pediatrics has issued a clinical report to help.
Most research on pediatric concussions has focused on returning the patient to sports or other physical activities, while data for managing the "return to learn" are sparse. Many published statements emphasize the need for "cognitive rest" – avoiding obvious potential cognitive stressors such as class work and homework – but fall short of identifying and dealing with the myriad other stimuli that can impede recovery or even worsen symptoms, reported Dr. Mark E. Halstead and his associates on the AAP Council on Sports Medicine and Fitness and the AAP Council on School Health (Pediatrics 2013;132:948-57).
An estimated 1.7 million traumatic brain injuries occur each year, many of them concussions. "Given that students typically appear well physically after a concussion, it may be difficult for educators, school administrators, and peers to fully understand the extent of deficits experienced by a student with a concussion." This, in turn, might make school officials reluctant to accept that they must make adjustments for such students.
Pediatricians are in an excellent position to inform these educators, as well as the patients themselves and their families, of the symptoms that might develop and the strategies to prevent or minimize cognitive stress during recovery, said Dr. Halstead, an orthopedic surgeon and sports medicine specialist at Washington University in St. Louis and Children’s Hospital of St. Louis, and his associates. Dr. Halstead also presented the clinical report Oct. 27 at the annual meeting of the American Academy of Pediatrics in Orlando.
The clinical report notes that most concussions resolve within 3 weeks of the injury, so most adjustments to the school environment can be made in the individual classroom setting without the need for a formalized written plan such as a 504 plan or individualized education plan. However, students who require longer-term recovery need more formalized accommodations and modifications.
The report lists typical signs and symptoms of concussion, along with adjustments that teachers and administrators can make to help the child returning to school.
Headache is the most frequent symptom and can recur throughout recovery. School personnel should be made aware that fluorescent lighting, loud noises, and even simply concentrating on a task can elicit headache in these patients, so they should be allowed to take breaks in a quiet area when needed.
Dizziness and lightheadedness also are common and can be provoked by standing quickly, walking in a crowd, or even just viewing motion on a screen or in person. Students with concussion should be allowed to close their eyes or put their heads down on the desk if necessary, and should be permitted to avoid crowded hallways and to move slowly from one place to another.
Common visual symptoms include light sensitivity and blurred or double vision. Students should be allowed to wear a hat with a brim or sunglasses, to turn off or dim room lights, to dim video screens, or to forgo movies or slide presentations. They should be excused if they have trouble reading or writing, or even paying attention to visual tasks.
Sensitivity to noise means that students with concussion might need to be excused from the lunchroom, recess, shop classes, music (band or choir) classes, activities in a gymnasium, and any other excessively noisy location, and should be permitted to use earplugs, Dr. Halstead and his associates said.
Students with concussion also have trouble with concentrating and remembering. Allowances should be made for a student’s difficulty absorbing new material and focusing in the classroom; in particular, testing, especially standardized testing, might need to be postponed until after the student has recovered from the concussion.
Finally, concussions often cause sleep disturbances that can lead to excessive fatigue, tardiness, falling asleep in class, and excessive absences from class. Students might require a late start to the school day or a shortened school day to allow them to rest.
This AAP clinical report was endorsed by the American Medical Society for Sports Medicine, the Brain Injury Association of America, the Canadian Paediatric Society, the National Association of School Nurses, the National Association of School Psychologists, and the National Federation of State High School Associations.
All clinical reports from the AAP expire automatically 5 years after publication unless "reaffirmed, revised, or retired at or before that time."
No conflicts of interest were reported.
Patients who sustain a concussion need their physicians’ guidance in returning to school in a way that facilitates rather than hinders their recovery, and the American Academy of Pediatrics has issued a clinical report to help.
Most research on pediatric concussions has focused on returning the patient to sports or other physical activities, while data for managing the "return to learn" are sparse. Many published statements emphasize the need for "cognitive rest" – avoiding obvious potential cognitive stressors such as class work and homework – but fall short of identifying and dealing with the myriad other stimuli that can impede recovery or even worsen symptoms, reported Dr. Mark E. Halstead and his associates on the AAP Council on Sports Medicine and Fitness and the AAP Council on School Health (Pediatrics 2013;132:948-57).
An estimated 1.7 million traumatic brain injuries occur each year, many of them concussions. "Given that students typically appear well physically after a concussion, it may be difficult for educators, school administrators, and peers to fully understand the extent of deficits experienced by a student with a concussion." This, in turn, might make school officials reluctant to accept that they must make adjustments for such students.
Pediatricians are in an excellent position to inform these educators, as well as the patients themselves and their families, of the symptoms that might develop and the strategies to prevent or minimize cognitive stress during recovery, said Dr. Halstead, an orthopedic surgeon and sports medicine specialist at Washington University in St. Louis and Children’s Hospital of St. Louis, and his associates. Dr. Halstead also presented the clinical report Oct. 27 at the annual meeting of the American Academy of Pediatrics in Orlando.
The clinical report notes that most concussions resolve within 3 weeks of the injury, so most adjustments to the school environment can be made in the individual classroom setting without the need for a formalized written plan such as a 504 plan or individualized education plan. However, students who require longer-term recovery need more formalized accommodations and modifications.
The report lists typical signs and symptoms of concussion, along with adjustments that teachers and administrators can make to help the child returning to school.
Headache is the most frequent symptom and can recur throughout recovery. School personnel should be made aware that fluorescent lighting, loud noises, and even simply concentrating on a task can elicit headache in these patients, so they should be allowed to take breaks in a quiet area when needed.
Dizziness and lightheadedness also are common and can be provoked by standing quickly, walking in a crowd, or even just viewing motion on a screen or in person. Students with concussion should be allowed to close their eyes or put their heads down on the desk if necessary, and should be permitted to avoid crowded hallways and to move slowly from one place to another.
Common visual symptoms include light sensitivity and blurred or double vision. Students should be allowed to wear a hat with a brim or sunglasses, to turn off or dim room lights, to dim video screens, or to forgo movies or slide presentations. They should be excused if they have trouble reading or writing, or even paying attention to visual tasks.
Sensitivity to noise means that students with concussion might need to be excused from the lunchroom, recess, shop classes, music (band or choir) classes, activities in a gymnasium, and any other excessively noisy location, and should be permitted to use earplugs, Dr. Halstead and his associates said.
Students with concussion also have trouble with concentrating and remembering. Allowances should be made for a student’s difficulty absorbing new material and focusing in the classroom; in particular, testing, especially standardized testing, might need to be postponed until after the student has recovered from the concussion.
Finally, concussions often cause sleep disturbances that can lead to excessive fatigue, tardiness, falling asleep in class, and excessive absences from class. Students might require a late start to the school day or a shortened school day to allow them to rest.
This AAP clinical report was endorsed by the American Medical Society for Sports Medicine, the Brain Injury Association of America, the Canadian Paediatric Society, the National Association of School Nurses, the National Association of School Psychologists, and the National Federation of State High School Associations.
All clinical reports from the AAP expire automatically 5 years after publication unless "reaffirmed, revised, or retired at or before that time."
No conflicts of interest were reported.
FROM PEDIATRICS
Major finding: Patients appear physically normal soon after sustaining a concussion, and the physician is in an excellent position to educate teachers, school officials, and parents about accommodations these patients might need when returning to school.
Data source: A clinical report aimed at helping physicians ease the transition back to a school environment for students who sustain concussions.
Disclosures: No conflicts of interest were reported.
Studies link maternal smoking with broad range of infant infections
ORLANDO – Maternal smoking has been associated with a number of serious respiratory and nonrespiratory infectious outcomes in infants, according to findings from two large case-control analyses.
Among 47,404 infants hospitalized for an infectious disease within 1 year of birth and 48,233 controls, and among 627 infants who died within 1 year of birth and 2,730 controls, maternal smoking was associated with both hospitalization because of to any infectious disease and mortality from any infectious disease (adjusted odds ratios, 1.52 and 1.51, respectively), Dr. Susanne Tanski of Dartmouth-Hitchcock Medical Center, Lebanon, N.H., reported at the annual meeting of the American Academy of Pediatrics.
Maternal smoking was associated with hospitalization due to a broad range of infectious diseases, including both respiratory and nonrespiratory diseases (adjusted OR, 1.69 and 1.27, respectively), said Dr. Tanski, who reported the findings of the subgroup analyses on behalf of lead study author Michael Metzger, Ph.D., and coauthor Dr. Abigail Halperin, both of the University of Washington, Seattle.
Stratification by birth weight and gestational age did not appreciably affect the findings with respect to morbidity risk in the infants of smoking mothers, which was found to be independent of both birth weight and gestational age. Mortality risk was found to be independent of gestational age, but the association among low birth weight infants was attenuated.
Even so, if an infant whose mother smoked was of normal weight and gestational age, exposure to maternal smoking appeared to carry an increased risk of infection as well as infectious disease mortality, Dr. Halperin said in an interview.
Included in the study were infants born in Washington from 1987 to 2004. The investigators reviewed linked birth certificate, death certificate, and hospital discharge records.
"We’ve known for a long time that babies born to mothers who smoke during pregnancy are at high risk for serious medical problems relating to low birth weight, premature delivery, and poor lung development, and while we have recognized respiratory infections as a common cause of these sometimes life-threatening infections, this study demonstrates that in utero exposure to smoke increases the risk of hospitalization and death from a much broader range of infections than previously documented," Dr. Halperin said.
She noted that the study was published earlier this year (Pediatr. Infect. Dis. 2013;32:e1-7 [doi:10.1097/INF.0b013e3182704bb5]) but received little notice. When the AAP invited her to submit an abstract for presentation at the conference, she said she was pleased to find that the paper was "selected for this honor."
"I’m very happy it’s receiving some attention now, because it is important to get this information out there so we can try to do something about it. We found that there was a dose-response effect related to number of cigarettes smoked per day, whereby smoking fewer cigarettes significantly lowered the risk for hospitalization," she said.
Thus, counseling pregnant women to reduce their smoking, even if they are not able to quit completely, may help reduce the impact of maternal smoking on infant outcomes, she said.
"Clinicians can help their patients stop smoking by providing nonjudgmental, positively framed advice to quit, and should strongly encourage pregnant women to quit smoking, both for their own health and for the health of their babies," she said, noting that women also should be counseled about the importance of protecting their children from secondhand smoke after birth, as secondhand smoke exposure increases the risk for many of the same infections seen in babies exposed in utero.
Evidence-based treatment, including counseling and approved cessation medication, should be offered to all patients who want to quit, regardless of whether or not they are pregnant, she added.
Dr. Tanski reported a having a patent pending and receiving royalties for a smoke sensor. Dr. Halperin and Mr. Metzger reported having no disclosures.
ORLANDO – Maternal smoking has been associated with a number of serious respiratory and nonrespiratory infectious outcomes in infants, according to findings from two large case-control analyses.
Among 47,404 infants hospitalized for an infectious disease within 1 year of birth and 48,233 controls, and among 627 infants who died within 1 year of birth and 2,730 controls, maternal smoking was associated with both hospitalization because of to any infectious disease and mortality from any infectious disease (adjusted odds ratios, 1.52 and 1.51, respectively), Dr. Susanne Tanski of Dartmouth-Hitchcock Medical Center, Lebanon, N.H., reported at the annual meeting of the American Academy of Pediatrics.
Maternal smoking was associated with hospitalization due to a broad range of infectious diseases, including both respiratory and nonrespiratory diseases (adjusted OR, 1.69 and 1.27, respectively), said Dr. Tanski, who reported the findings of the subgroup analyses on behalf of lead study author Michael Metzger, Ph.D., and coauthor Dr. Abigail Halperin, both of the University of Washington, Seattle.
Stratification by birth weight and gestational age did not appreciably affect the findings with respect to morbidity risk in the infants of smoking mothers, which was found to be independent of both birth weight and gestational age. Mortality risk was found to be independent of gestational age, but the association among low birth weight infants was attenuated.
Even so, if an infant whose mother smoked was of normal weight and gestational age, exposure to maternal smoking appeared to carry an increased risk of infection as well as infectious disease mortality, Dr. Halperin said in an interview.
Included in the study were infants born in Washington from 1987 to 2004. The investigators reviewed linked birth certificate, death certificate, and hospital discharge records.
"We’ve known for a long time that babies born to mothers who smoke during pregnancy are at high risk for serious medical problems relating to low birth weight, premature delivery, and poor lung development, and while we have recognized respiratory infections as a common cause of these sometimes life-threatening infections, this study demonstrates that in utero exposure to smoke increases the risk of hospitalization and death from a much broader range of infections than previously documented," Dr. Halperin said.
She noted that the study was published earlier this year (Pediatr. Infect. Dis. 2013;32:e1-7 [doi:10.1097/INF.0b013e3182704bb5]) but received little notice. When the AAP invited her to submit an abstract for presentation at the conference, she said she was pleased to find that the paper was "selected for this honor."
"I’m very happy it’s receiving some attention now, because it is important to get this information out there so we can try to do something about it. We found that there was a dose-response effect related to number of cigarettes smoked per day, whereby smoking fewer cigarettes significantly lowered the risk for hospitalization," she said.
Thus, counseling pregnant women to reduce their smoking, even if they are not able to quit completely, may help reduce the impact of maternal smoking on infant outcomes, she said.
"Clinicians can help their patients stop smoking by providing nonjudgmental, positively framed advice to quit, and should strongly encourage pregnant women to quit smoking, both for their own health and for the health of their babies," she said, noting that women also should be counseled about the importance of protecting their children from secondhand smoke after birth, as secondhand smoke exposure increases the risk for many of the same infections seen in babies exposed in utero.
Evidence-based treatment, including counseling and approved cessation medication, should be offered to all patients who want to quit, regardless of whether or not they are pregnant, she added.
Dr. Tanski reported a having a patent pending and receiving royalties for a smoke sensor. Dr. Halperin and Mr. Metzger reported having no disclosures.
ORLANDO – Maternal smoking has been associated with a number of serious respiratory and nonrespiratory infectious outcomes in infants, according to findings from two large case-control analyses.
Among 47,404 infants hospitalized for an infectious disease within 1 year of birth and 48,233 controls, and among 627 infants who died within 1 year of birth and 2,730 controls, maternal smoking was associated with both hospitalization because of to any infectious disease and mortality from any infectious disease (adjusted odds ratios, 1.52 and 1.51, respectively), Dr. Susanne Tanski of Dartmouth-Hitchcock Medical Center, Lebanon, N.H., reported at the annual meeting of the American Academy of Pediatrics.
Maternal smoking was associated with hospitalization due to a broad range of infectious diseases, including both respiratory and nonrespiratory diseases (adjusted OR, 1.69 and 1.27, respectively), said Dr. Tanski, who reported the findings of the subgroup analyses on behalf of lead study author Michael Metzger, Ph.D., and coauthor Dr. Abigail Halperin, both of the University of Washington, Seattle.
Stratification by birth weight and gestational age did not appreciably affect the findings with respect to morbidity risk in the infants of smoking mothers, which was found to be independent of both birth weight and gestational age. Mortality risk was found to be independent of gestational age, but the association among low birth weight infants was attenuated.
Even so, if an infant whose mother smoked was of normal weight and gestational age, exposure to maternal smoking appeared to carry an increased risk of infection as well as infectious disease mortality, Dr. Halperin said in an interview.
Included in the study were infants born in Washington from 1987 to 2004. The investigators reviewed linked birth certificate, death certificate, and hospital discharge records.
"We’ve known for a long time that babies born to mothers who smoke during pregnancy are at high risk for serious medical problems relating to low birth weight, premature delivery, and poor lung development, and while we have recognized respiratory infections as a common cause of these sometimes life-threatening infections, this study demonstrates that in utero exposure to smoke increases the risk of hospitalization and death from a much broader range of infections than previously documented," Dr. Halperin said.
She noted that the study was published earlier this year (Pediatr. Infect. Dis. 2013;32:e1-7 [doi:10.1097/INF.0b013e3182704bb5]) but received little notice. When the AAP invited her to submit an abstract for presentation at the conference, she said she was pleased to find that the paper was "selected for this honor."
"I’m very happy it’s receiving some attention now, because it is important to get this information out there so we can try to do something about it. We found that there was a dose-response effect related to number of cigarettes smoked per day, whereby smoking fewer cigarettes significantly lowered the risk for hospitalization," she said.
Thus, counseling pregnant women to reduce their smoking, even if they are not able to quit completely, may help reduce the impact of maternal smoking on infant outcomes, she said.
"Clinicians can help their patients stop smoking by providing nonjudgmental, positively framed advice to quit, and should strongly encourage pregnant women to quit smoking, both for their own health and for the health of their babies," she said, noting that women also should be counseled about the importance of protecting their children from secondhand smoke after birth, as secondhand smoke exposure increases the risk for many of the same infections seen in babies exposed in utero.
Evidence-based treatment, including counseling and approved cessation medication, should be offered to all patients who want to quit, regardless of whether or not they are pregnant, she added.
Dr. Tanski reported a having a patent pending and receiving royalties for a smoke sensor. Dr. Halperin and Mr. Metzger reported having no disclosures.
AT THE AAP NATIONAL CONFERENCE
Major finding: Maternal smoking was associated with both hospitalization due to any infectious disease and mortality due to any infectious disease (adjusted odds ratios, 1.52 and 1.51, respectively).
Data source: Two case-control analyses – one involving 47,404 infants hospitalized for an infectious disease within 1 year of birth and 48,233 controls and the other involving 627 infants who died within 1 year of birth and 2,730 controls.
Disclosures: Dr. Tanski reported having a patent pending and receiving royalties for a smoke sensor. Dr. Halperin and Dr. Metzger reported having no disclosures.
‘Supermagnet’ ingestion injuries remain a concern
ORLANDO – The popularity of powerful neodymium magnets has led to an increase in magnet ingestion–related injuries among young children, especially in recent years.
Of 2,700 ingestion injuries requiring admission or procedural intervention in children aged 0-18 years between April 1, 2001 and Dec. 21, 2012, 94 were ingestions of these "supermagnets," and, although the first such report was in 2004, a significant increase in both single and multiple magnet ingestion occurred over time. The largest increase involved multiple magnet ingestion in the last 3 years of the study, Dr. Daniel Rosenfield of the University of Toronto reported at the annual meeting of the American Academy of Pediatrics.
The ingestion of multiple magnets can be particularly dangerous, because the magnets – neodymium-iron-boron magnets that are 10-20 times stronger than traditional magnets – can link through loops of bowel and cause pressure necrosis.
"Without prompt recognition of multiple-magnet ingestion, bowel perforation, sepsis, and death can result," he said.
In fact, in this case series, 6 patients underwent surgical removal of the magnets and 10 underwent endoscopic removal. No deaths were reported, Dr. Rosenfield said.
The cases involved patients seen at the Hospital for Sick Children in Toronto. The patients ranged in age from 7 months to 13 years, with a mean age of 4.5 years. Most (65%) were boys.
Ingestion of up to 34 of the tiny magnets – which may look like candy to children – has been reported.
The findings confirm what physicians at the Hospital for Sick Children have suspected: that the ingestion of these dangerous toys has been increasing, with a spike in incidence over the past 3 years, Dr. Rosenfield said.
"What we’re seeing is really an epidemic driven by a new technology," he added.
Supermagnets came into the market in the early 2000s in toys, jewelry, and other novelty items, and they surged in popularity in the late 2000s when they were marketed in the form of novelty desk toys for adults. In the wake of several cases involving multiple magnet ingestion that resulted in a number of cases of pediatric bowel perforation, sepsis, and one death, the U.S. Consumer Product Safety Commission began work in 2012 to set industry safety standards and sought to remove certain supermagnet desk toys from the market. Canada also recently implemented a mandatory recall of some of the products and banned their sale, Dr. Rosenfield said.
He applauded the strong stance and action with respect to removing the products from the market but noted that the magnets can still be found in products sold before the recall, raising concerns that ingestion injuries will continue to occur.
Thus, clinicians should be aware of the risk of magnet ingestions and of the potential morbidity associated with ingestion, as well as with the appropriate management of patients who ingest the magnets. Furthermore, given data suggesting that many pediatricians are unaware of the dangers, health organizations should spread the word to physicians, parents, teachers, and the general public about the dangers to help assure that the magnets will be kept away from children, he said.
"These new magnets are vastly more powerful, smaller in size, and seem innocuous – parents just aren’t aware of the potential danger," he said.
Dr. Rosenfield reported having no disclosures.
ORLANDO – The popularity of powerful neodymium magnets has led to an increase in magnet ingestion–related injuries among young children, especially in recent years.
Of 2,700 ingestion injuries requiring admission or procedural intervention in children aged 0-18 years between April 1, 2001 and Dec. 21, 2012, 94 were ingestions of these "supermagnets," and, although the first such report was in 2004, a significant increase in both single and multiple magnet ingestion occurred over time. The largest increase involved multiple magnet ingestion in the last 3 years of the study, Dr. Daniel Rosenfield of the University of Toronto reported at the annual meeting of the American Academy of Pediatrics.
The ingestion of multiple magnets can be particularly dangerous, because the magnets – neodymium-iron-boron magnets that are 10-20 times stronger than traditional magnets – can link through loops of bowel and cause pressure necrosis.
"Without prompt recognition of multiple-magnet ingestion, bowel perforation, sepsis, and death can result," he said.
In fact, in this case series, 6 patients underwent surgical removal of the magnets and 10 underwent endoscopic removal. No deaths were reported, Dr. Rosenfield said.
The cases involved patients seen at the Hospital for Sick Children in Toronto. The patients ranged in age from 7 months to 13 years, with a mean age of 4.5 years. Most (65%) were boys.
Ingestion of up to 34 of the tiny magnets – which may look like candy to children – has been reported.
The findings confirm what physicians at the Hospital for Sick Children have suspected: that the ingestion of these dangerous toys has been increasing, with a spike in incidence over the past 3 years, Dr. Rosenfield said.
"What we’re seeing is really an epidemic driven by a new technology," he added.
Supermagnets came into the market in the early 2000s in toys, jewelry, and other novelty items, and they surged in popularity in the late 2000s when they were marketed in the form of novelty desk toys for adults. In the wake of several cases involving multiple magnet ingestion that resulted in a number of cases of pediatric bowel perforation, sepsis, and one death, the U.S. Consumer Product Safety Commission began work in 2012 to set industry safety standards and sought to remove certain supermagnet desk toys from the market. Canada also recently implemented a mandatory recall of some of the products and banned their sale, Dr. Rosenfield said.
He applauded the strong stance and action with respect to removing the products from the market but noted that the magnets can still be found in products sold before the recall, raising concerns that ingestion injuries will continue to occur.
Thus, clinicians should be aware of the risk of magnet ingestions and of the potential morbidity associated with ingestion, as well as with the appropriate management of patients who ingest the magnets. Furthermore, given data suggesting that many pediatricians are unaware of the dangers, health organizations should spread the word to physicians, parents, teachers, and the general public about the dangers to help assure that the magnets will be kept away from children, he said.
"These new magnets are vastly more powerful, smaller in size, and seem innocuous – parents just aren’t aware of the potential danger," he said.
Dr. Rosenfield reported having no disclosures.
ORLANDO – The popularity of powerful neodymium magnets has led to an increase in magnet ingestion–related injuries among young children, especially in recent years.
Of 2,700 ingestion injuries requiring admission or procedural intervention in children aged 0-18 years between April 1, 2001 and Dec. 21, 2012, 94 were ingestions of these "supermagnets," and, although the first such report was in 2004, a significant increase in both single and multiple magnet ingestion occurred over time. The largest increase involved multiple magnet ingestion in the last 3 years of the study, Dr. Daniel Rosenfield of the University of Toronto reported at the annual meeting of the American Academy of Pediatrics.
The ingestion of multiple magnets can be particularly dangerous, because the magnets – neodymium-iron-boron magnets that are 10-20 times stronger than traditional magnets – can link through loops of bowel and cause pressure necrosis.
"Without prompt recognition of multiple-magnet ingestion, bowel perforation, sepsis, and death can result," he said.
In fact, in this case series, 6 patients underwent surgical removal of the magnets and 10 underwent endoscopic removal. No deaths were reported, Dr. Rosenfield said.
The cases involved patients seen at the Hospital for Sick Children in Toronto. The patients ranged in age from 7 months to 13 years, with a mean age of 4.5 years. Most (65%) were boys.
Ingestion of up to 34 of the tiny magnets – which may look like candy to children – has been reported.
The findings confirm what physicians at the Hospital for Sick Children have suspected: that the ingestion of these dangerous toys has been increasing, with a spike in incidence over the past 3 years, Dr. Rosenfield said.
"What we’re seeing is really an epidemic driven by a new technology," he added.
Supermagnets came into the market in the early 2000s in toys, jewelry, and other novelty items, and they surged in popularity in the late 2000s when they were marketed in the form of novelty desk toys for adults. In the wake of several cases involving multiple magnet ingestion that resulted in a number of cases of pediatric bowel perforation, sepsis, and one death, the U.S. Consumer Product Safety Commission began work in 2012 to set industry safety standards and sought to remove certain supermagnet desk toys from the market. Canada also recently implemented a mandatory recall of some of the products and banned their sale, Dr. Rosenfield said.
He applauded the strong stance and action with respect to removing the products from the market but noted that the magnets can still be found in products sold before the recall, raising concerns that ingestion injuries will continue to occur.
Thus, clinicians should be aware of the risk of magnet ingestions and of the potential morbidity associated with ingestion, as well as with the appropriate management of patients who ingest the magnets. Furthermore, given data suggesting that many pediatricians are unaware of the dangers, health organizations should spread the word to physicians, parents, teachers, and the general public about the dangers to help assure that the magnets will be kept away from children, he said.
"These new magnets are vastly more powerful, smaller in size, and seem innocuous – parents just aren’t aware of the potential danger," he said.
Dr. Rosenfield reported having no disclosures.
AT THE AAP NATIONAL CONFERENCE
Major finding: A total of 94 cases of supermagnet ingestion occurred in children between April 1, 2001, and Dec. 21, 2012, at one institution.
Data source: A review of 2,700 ingestion injury cases.
Disclosures: Dr. Rosenfield reported having no disclosures.