User login
Interscience Conference on Antimicrobial Agents & Chemotherapy (ICAAC)/ International Congress of Chemotherapy (ICC)
Diabetic foot ulcer: Early closure optimal
SAN DIEGO – Early wound closure prior to hospital discharge after surgical debridement of infected diabetic foot ulcers yields higher ulcer healing rates and a shorter time to healing, compared with various nonclosure wound management methods, according to a propensity-matched study.
How best to manage the open wound following nonamputative surgery of infected diabetic foot ulcers has been controversial. But early wound closure during the index hospitalization was the clear winner in this comparative study, according to Dr. Shey-Ying Chen who presented the research at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
He presented a retrospective comparison between 179 diabetic foot ulcer (DFU) patients with early wound closure after surgical debridement and an equal number of matched controls treated with various nonclosure techniques, including negative pressure wound therapy and the repeated application of moist dressings.
The two study groups were matched first on the basis of DFU location – toe, forefoot, midfoot, or rear foot – and then further propensity matched based on demographics, comorbid conditions, the presence of neuropathy, ulcer status by Wagner classification, infection severity, revascularization procedures, and other variables.
During 1 year of follow-up post discharge, ulcer healing occurred in 75% of the early wound closure group, compared with 66% of the nonclosure patients. Readmission for further treatment of the index ulcer occurred in 33% of the early closure group and 53% of the nonclosure group.
Other outcomes were also superior in the early wound closure group, noted Dr. Chen of Beth Israel Deaconess Medical Center, Boston.
Two independent predictors of DFU healing during the follow-up period emerged from a Cox regression analysis: early wound closure, with an adjusted odds ratio of 1.63, and acute as opposed to chronic DFU, with an OR of 1.35.
Ulcer healing was significantly less likely in those patients who had peripheral vascular disease, with an OR of 0.62; or neuropathy, with an OR of 0.53; and methicillin-resistant Staphylococcus aureus wound infection, with an OR of 0.59, Dr. Chen continued.
Underscoring the longer-term difficulties faced by patients with DFUs, it’s noteworthy that 11.5% of patients in both study arms underwent new amputations during the year of follow-up.
Moreover, a new diagnosis of osteomyelitis was made in 20% of the early wound closure group and 26% of the nonclosure group, a nonsignificant difference.
Dr. Adolf W. Karchmer, Dr. Chen’s senior coinvestigator, said the outcome data are too new to be able to gauge how vascular, orthopedic, and podiatric surgeons will react.
The investigators reported that they had no financial conflicts with regard to this study, which was conducted without commercial sponsorship.
With increasing prevalence of diabetes in the population, diabetic foot ulcers and infections present a significant clinical problem. Infected diabetic foot ulcers usually require an initial debridement of infected and necrotic tissue but there are many options for subsequent wound management.These included secondary wound closure, if possible, or use of adjunctive techniques for wound care, including negative pressure wound therapy, hyperbaric oxygen and a variety of wound care products designed for optimal healing.
Dr. Chen and his colleagues report their retrospective experience in 179 patients treated with early wound closure and compare outcomes with an equal number of matched controls treated with various nonclosure techniques such as negative pressure wound therapy and repeated applications of moist dressings. They found improved outcomes with the early closure group when analyzed for ulcer healing, readmission, and other outcome assessments. Specific times for healing after surgical debridement were an average of 105 days in the early wound closure group versus 136 days in those wounds managed with nonclosure techniques. As would be predicted, peripheral vascular disease and methicillin-resistant Staphylococcus aureus wound infections were found to adversely affect wound healing in both groups.
It is unclear in this report how many of the wounds were not amenable to early closure or what specific wound care regimen was used in the patients treated with continued wound care only. In addition, although it is stated that peripheral vascular disease adversely affected wound healing, it is not clear if these patients underwent revascularization as part of their comprehensive management.
Finally, Dr. Adolf W. Karchmer, the senior co-investigator in the trial, states that these data are too new to assess how other specialists will react. Clearly wound care and diabetic foot care should involve a multidisciplinary approach including wound care specialists as well as vascular surgeons, podiatrists, orthopedic surgeons, infectious disease specialists, and others. Observations and studies such as this are important to advance the science and specialty of wound care and continued data collection will help to optimize patient outcomes.
Dr. Larry Scher is a professor of clinical surgery and attending vascular surgeon at Montefiore Medical Center/Albert Einstein College of Medicine, Bronx, N.Y. He is also an associate medical editor for Vascular Specialist.
With increasing prevalence of diabetes in the population, diabetic foot ulcers and infections present a significant clinical problem. Infected diabetic foot ulcers usually require an initial debridement of infected and necrotic tissue but there are many options for subsequent wound management.These included secondary wound closure, if possible, or use of adjunctive techniques for wound care, including negative pressure wound therapy, hyperbaric oxygen and a variety of wound care products designed for optimal healing.
Dr. Chen and his colleagues report their retrospective experience in 179 patients treated with early wound closure and compare outcomes with an equal number of matched controls treated with various nonclosure techniques such as negative pressure wound therapy and repeated applications of moist dressings. They found improved outcomes with the early closure group when analyzed for ulcer healing, readmission, and other outcome assessments. Specific times for healing after surgical debridement were an average of 105 days in the early wound closure group versus 136 days in those wounds managed with nonclosure techniques. As would be predicted, peripheral vascular disease and methicillin-resistant Staphylococcus aureus wound infections were found to adversely affect wound healing in both groups.
It is unclear in this report how many of the wounds were not amenable to early closure or what specific wound care regimen was used in the patients treated with continued wound care only. In addition, although it is stated that peripheral vascular disease adversely affected wound healing, it is not clear if these patients underwent revascularization as part of their comprehensive management.
Finally, Dr. Adolf W. Karchmer, the senior co-investigator in the trial, states that these data are too new to assess how other specialists will react. Clearly wound care and diabetic foot care should involve a multidisciplinary approach including wound care specialists as well as vascular surgeons, podiatrists, orthopedic surgeons, infectious disease specialists, and others. Observations and studies such as this are important to advance the science and specialty of wound care and continued data collection will help to optimize patient outcomes.
Dr. Larry Scher is a professor of clinical surgery and attending vascular surgeon at Montefiore Medical Center/Albert Einstein College of Medicine, Bronx, N.Y. He is also an associate medical editor for Vascular Specialist.
With increasing prevalence of diabetes in the population, diabetic foot ulcers and infections present a significant clinical problem. Infected diabetic foot ulcers usually require an initial debridement of infected and necrotic tissue but there are many options for subsequent wound management.These included secondary wound closure, if possible, or use of adjunctive techniques for wound care, including negative pressure wound therapy, hyperbaric oxygen and a variety of wound care products designed for optimal healing.
Dr. Chen and his colleagues report their retrospective experience in 179 patients treated with early wound closure and compare outcomes with an equal number of matched controls treated with various nonclosure techniques such as negative pressure wound therapy and repeated applications of moist dressings. They found improved outcomes with the early closure group when analyzed for ulcer healing, readmission, and other outcome assessments. Specific times for healing after surgical debridement were an average of 105 days in the early wound closure group versus 136 days in those wounds managed with nonclosure techniques. As would be predicted, peripheral vascular disease and methicillin-resistant Staphylococcus aureus wound infections were found to adversely affect wound healing in both groups.
It is unclear in this report how many of the wounds were not amenable to early closure or what specific wound care regimen was used in the patients treated with continued wound care only. In addition, although it is stated that peripheral vascular disease adversely affected wound healing, it is not clear if these patients underwent revascularization as part of their comprehensive management.
Finally, Dr. Adolf W. Karchmer, the senior co-investigator in the trial, states that these data are too new to assess how other specialists will react. Clearly wound care and diabetic foot care should involve a multidisciplinary approach including wound care specialists as well as vascular surgeons, podiatrists, orthopedic surgeons, infectious disease specialists, and others. Observations and studies such as this are important to advance the science and specialty of wound care and continued data collection will help to optimize patient outcomes.
Dr. Larry Scher is a professor of clinical surgery and attending vascular surgeon at Montefiore Medical Center/Albert Einstein College of Medicine, Bronx, N.Y. He is also an associate medical editor for Vascular Specialist.
SAN DIEGO – Early wound closure prior to hospital discharge after surgical debridement of infected diabetic foot ulcers yields higher ulcer healing rates and a shorter time to healing, compared with various nonclosure wound management methods, according to a propensity-matched study.
How best to manage the open wound following nonamputative surgery of infected diabetic foot ulcers has been controversial. But early wound closure during the index hospitalization was the clear winner in this comparative study, according to Dr. Shey-Ying Chen who presented the research at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
He presented a retrospective comparison between 179 diabetic foot ulcer (DFU) patients with early wound closure after surgical debridement and an equal number of matched controls treated with various nonclosure techniques, including negative pressure wound therapy and the repeated application of moist dressings.
The two study groups were matched first on the basis of DFU location – toe, forefoot, midfoot, or rear foot – and then further propensity matched based on demographics, comorbid conditions, the presence of neuropathy, ulcer status by Wagner classification, infection severity, revascularization procedures, and other variables.
During 1 year of follow-up post discharge, ulcer healing occurred in 75% of the early wound closure group, compared with 66% of the nonclosure patients. Readmission for further treatment of the index ulcer occurred in 33% of the early closure group and 53% of the nonclosure group.
Other outcomes were also superior in the early wound closure group, noted Dr. Chen of Beth Israel Deaconess Medical Center, Boston.
Two independent predictors of DFU healing during the follow-up period emerged from a Cox regression analysis: early wound closure, with an adjusted odds ratio of 1.63, and acute as opposed to chronic DFU, with an OR of 1.35.
Ulcer healing was significantly less likely in those patients who had peripheral vascular disease, with an OR of 0.62; or neuropathy, with an OR of 0.53; and methicillin-resistant Staphylococcus aureus wound infection, with an OR of 0.59, Dr. Chen continued.
Underscoring the longer-term difficulties faced by patients with DFUs, it’s noteworthy that 11.5% of patients in both study arms underwent new amputations during the year of follow-up.
Moreover, a new diagnosis of osteomyelitis was made in 20% of the early wound closure group and 26% of the nonclosure group, a nonsignificant difference.
Dr. Adolf W. Karchmer, Dr. Chen’s senior coinvestigator, said the outcome data are too new to be able to gauge how vascular, orthopedic, and podiatric surgeons will react.
The investigators reported that they had no financial conflicts with regard to this study, which was conducted without commercial sponsorship.
SAN DIEGO – Early wound closure prior to hospital discharge after surgical debridement of infected diabetic foot ulcers yields higher ulcer healing rates and a shorter time to healing, compared with various nonclosure wound management methods, according to a propensity-matched study.
How best to manage the open wound following nonamputative surgery of infected diabetic foot ulcers has been controversial. But early wound closure during the index hospitalization was the clear winner in this comparative study, according to Dr. Shey-Ying Chen who presented the research at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
He presented a retrospective comparison between 179 diabetic foot ulcer (DFU) patients with early wound closure after surgical debridement and an equal number of matched controls treated with various nonclosure techniques, including negative pressure wound therapy and the repeated application of moist dressings.
The two study groups were matched first on the basis of DFU location – toe, forefoot, midfoot, or rear foot – and then further propensity matched based on demographics, comorbid conditions, the presence of neuropathy, ulcer status by Wagner classification, infection severity, revascularization procedures, and other variables.
During 1 year of follow-up post discharge, ulcer healing occurred in 75% of the early wound closure group, compared with 66% of the nonclosure patients. Readmission for further treatment of the index ulcer occurred in 33% of the early closure group and 53% of the nonclosure group.
Other outcomes were also superior in the early wound closure group, noted Dr. Chen of Beth Israel Deaconess Medical Center, Boston.
Two independent predictors of DFU healing during the follow-up period emerged from a Cox regression analysis: early wound closure, with an adjusted odds ratio of 1.63, and acute as opposed to chronic DFU, with an OR of 1.35.
Ulcer healing was significantly less likely in those patients who had peripheral vascular disease, with an OR of 0.62; or neuropathy, with an OR of 0.53; and methicillin-resistant Staphylococcus aureus wound infection, with an OR of 0.59, Dr. Chen continued.
Underscoring the longer-term difficulties faced by patients with DFUs, it’s noteworthy that 11.5% of patients in both study arms underwent new amputations during the year of follow-up.
Moreover, a new diagnosis of osteomyelitis was made in 20% of the early wound closure group and 26% of the nonclosure group, a nonsignificant difference.
Dr. Adolf W. Karchmer, Dr. Chen’s senior coinvestigator, said the outcome data are too new to be able to gauge how vascular, orthopedic, and podiatric surgeons will react.
The investigators reported that they had no financial conflicts with regard to this study, which was conducted without commercial sponsorship.
Resistant gonorrhea rates high in China, raise concerns in U.S.
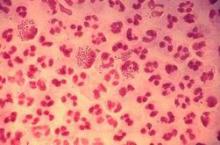
SAN DIEGO – Experts in the field of Neisseria gonorrhoeae antimicrobial resistance are warily watching developments in China, where rates of nonsusceptibility to ceftriaxone are reportedly shooting through the roof.
In the United States at present, gonococcal resistance to ceftriaxone is exceedingly rare: well under 1% of isolates have elevated minimum inhibitory concentrations (MICs) to this cornerstone of empiric therapy. In Europe, the rate is about 3%. What’s really disturbing is that recent data from the World Health Organization Gonococcal Antimicrobial Surveillance Program indicate ceftriaxone nonsusceptibility rates in China are in the 20%-30%-plus range, Dr. Joseph Duncan said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
“This is very concerning for the potential spread of this type of resistance across the world at some point. It’s just ready to explode,” observed Dr. Duncan of the University of North Carolina, Chapel Hill.
Anytime gonococcal resistance rates to a drug reach about 5%, it spells trouble.
“Gonorrhea treatment is often syndromic. An isolated swab is taken, identified by Gram stain, you give them empiric therapy, and the patients walk out of the clinic and never come back. So you don’t want to have a 5% failure rate for your initial therapy,” he explained.
Neisseria gonorrhoeae has acquired resistance to virtually every antibiotic ever used to treat the infection. Treatment options are running out, which is why the Centers for Disease Control and Prevention has designated gonorrhea as an immediate public health threat requiring urgent and aggressive action.
The 2015 CDC Sexually Transmitted Disease Treatment Guidelines recommend only one front-line treatment for gonorrhea: dual therapy with ceftriaxone at 250 mg IM in a single dose plus azithromycin 1 g orally, also in a single dose. Given N. gonorrhoeae’s adaptability, experts believe that’s not a long-term solution.
After all, 5%-10% of gonococcal isolates in Europe and China are azithromycin-resistant, and while CDC surveillance data showed less than 1% of strains in the United States were azithromycin-resistant through 2013, preliminary data for 2014 show a concerning jump to 2.5%, according to Dr. Duncan’s fellow panelist Dr. Kimberly Workowski, professor of medicine at Emory University in Atlanta and lead author of the 2015 CDC STD guidelines.
Dr. Duncan described the state of the ongoing aggressive multipronged attempts to combat antimicrobial resistance in N. gonorrhoeae. This effort includes new antibiotics in the developmental pipeline, attempts to repurpose existing antibiotics, rapid point-of-care antibiotic susceptibility tests, and vaccine development.
He also highlighted the factors that have led to the bug’s capacity to acquire resistance to so many antibiotics having different mechanisms of action. One key factor is the organism’s sheer competence as expressed in genetic lability.
“This bacteria is continually sampling DNA from the environment. The organisms are constantly swapping genes and DNA segments with commensal Neisseria species. In fact, even human DNA sequences have been found inside the gonococcal genome,” Dr. Duncan said.
While high-level antibiotic resistance can be acquired in a single dramatic step, it can also come about through multiple smaller steps, each one yielding only low-level resistance. “This allows for the sort of creeping [minimum inhibitory concentration] that we’ve seen with the gonococcus, particularly with the extended-spectrum cephalosporin antibiotics,” Dr. Duncan continued.
Also, it’s apparent that even in the absence of antibiotics, other pressures can select for antibiotic-resistant strains. Dr. Duncan credited one of his mentors, William M. Shafer, Ph.D., of Emory University, with developing the hypothesis that fecal lipids might be an important driver of increased resistance rates. Supporting this hypothesis, he noted, is the finding in multiple studies that rectal gonococcal isolates consistently have a somewhat higher prevalence of resistance than those obtained from other sites.
Turning to the effort to curb antibiotic resistance, Dr. Duncan said the drug farthest along in the pipeline is solithromycin, a novel macrolide being developed by Cempra Pharmaceuticals in both oral and IV formulations. Solithromycin, a first-in-class fluoroketolide, is active against a broad range of Gram-positive organisms, among them Legionella, Chlamydia, Mycoplasma, and Ureaplasma, including macrolide-resistant strains. Its ability to bind to three ribosomal sites is thought to minimize development of resistance.
Two positive phase 3 clinical trials of solithromycin have been completed in patients with community-acquired bacterial pneumonia. A phase 3 trial in gonorrhea is ongoing after a positive phase 2 study.
Two bacterial topoisomerase inhibitors are in soon-to-be-completed phase 2 studies.
Delafloxacin, a new fluoroquinolone, was in a phase 3 clinical trial for gonorrhea that was terminated early due to ineffectiveness.
There is considerable interest in bringing back single-dose IM gentamicin (Garamycin) for the treatment of gonorrhea. A systematic review of five studies (Syst Rev. 2014 Sep 19;3:104. doi: 10.1186/2046-4053-3-104) reported cure rates that were mostly in the 90% range, but “not quite high enough to say you’d want to go to gentamicin as your front-line therapy,” in Dr. Duncan’s opinion.
Dr. Workowski noted that the National Institutes of Health is interested in trying to resurrect cefixime (Suprax) for gonorrhea after the CDC guidelines demoted it several years ago. An ongoing clinical trial is examining the impact of increasing the dose and duration of therapy.
Public health officials are also interested in spectinomycin, an antibiotic not currently available in the United States, which has achieved high cure rates as single-dose therapy in several foreign studies.
Dr. Duncan noted that a randomized trial of gentamicin plus azithromycin or gemifloxacin (Factive) plus azithromycin reported cure rates of 100% and 99.5%, respectively (Clin Infect Dis. 2014 Oct 15;59(8):1083-91). He found the study less than convincing, however: “These strains were almost all susceptibile to azithromycin, so you can’t actually say that gentamicin or gemifloxacin added a lot,” he said.
A number of researchers are working on rapid tests for susceptibility of a particular gonococcal strain so physicians could choose an effective antimicrobial for an individual patient right from the start.
“These are all in the developmental phase. It’s going to be difficult, because there are so many different mechanisms for resistance,” he said.
Similarly, vaccine development in the gonococcal field is a great challenge. The microorganism’s multiple mechanisms of immune evasion make it tough to identify correlates of protection, Dr. Duncan continued.
“Epidemiologic studies suggest there is not efficient development of natural immunity. Folks who get gonorrhea and then come back with reinfection often have the exact same strain,” he noted.
Dr. Duncan’s research is funded by the National Institutes of Health and the Burroughs Wellcome Fund. He reported having no financial conflicts of interest.
SAN DIEGO – Experts in the field of Neisseria gonorrhoeae antimicrobial resistance are warily watching developments in China, where rates of nonsusceptibility to ceftriaxone are reportedly shooting through the roof.
In the United States at present, gonococcal resistance to ceftriaxone is exceedingly rare: well under 1% of isolates have elevated minimum inhibitory concentrations (MICs) to this cornerstone of empiric therapy. In Europe, the rate is about 3%. What’s really disturbing is that recent data from the World Health Organization Gonococcal Antimicrobial Surveillance Program indicate ceftriaxone nonsusceptibility rates in China are in the 20%-30%-plus range, Dr. Joseph Duncan said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
“This is very concerning for the potential spread of this type of resistance across the world at some point. It’s just ready to explode,” observed Dr. Duncan of the University of North Carolina, Chapel Hill.
Anytime gonococcal resistance rates to a drug reach about 5%, it spells trouble.
“Gonorrhea treatment is often syndromic. An isolated swab is taken, identified by Gram stain, you give them empiric therapy, and the patients walk out of the clinic and never come back. So you don’t want to have a 5% failure rate for your initial therapy,” he explained.
Neisseria gonorrhoeae has acquired resistance to virtually every antibiotic ever used to treat the infection. Treatment options are running out, which is why the Centers for Disease Control and Prevention has designated gonorrhea as an immediate public health threat requiring urgent and aggressive action.
The 2015 CDC Sexually Transmitted Disease Treatment Guidelines recommend only one front-line treatment for gonorrhea: dual therapy with ceftriaxone at 250 mg IM in a single dose plus azithromycin 1 g orally, also in a single dose. Given N. gonorrhoeae’s adaptability, experts believe that’s not a long-term solution.
After all, 5%-10% of gonococcal isolates in Europe and China are azithromycin-resistant, and while CDC surveillance data showed less than 1% of strains in the United States were azithromycin-resistant through 2013, preliminary data for 2014 show a concerning jump to 2.5%, according to Dr. Duncan’s fellow panelist Dr. Kimberly Workowski, professor of medicine at Emory University in Atlanta and lead author of the 2015 CDC STD guidelines.
Dr. Duncan described the state of the ongoing aggressive multipronged attempts to combat antimicrobial resistance in N. gonorrhoeae. This effort includes new antibiotics in the developmental pipeline, attempts to repurpose existing antibiotics, rapid point-of-care antibiotic susceptibility tests, and vaccine development.
He also highlighted the factors that have led to the bug’s capacity to acquire resistance to so many antibiotics having different mechanisms of action. One key factor is the organism’s sheer competence as expressed in genetic lability.
“This bacteria is continually sampling DNA from the environment. The organisms are constantly swapping genes and DNA segments with commensal Neisseria species. In fact, even human DNA sequences have been found inside the gonococcal genome,” Dr. Duncan said.
While high-level antibiotic resistance can be acquired in a single dramatic step, it can also come about through multiple smaller steps, each one yielding only low-level resistance. “This allows for the sort of creeping [minimum inhibitory concentration] that we’ve seen with the gonococcus, particularly with the extended-spectrum cephalosporin antibiotics,” Dr. Duncan continued.
Also, it’s apparent that even in the absence of antibiotics, other pressures can select for antibiotic-resistant strains. Dr. Duncan credited one of his mentors, William M. Shafer, Ph.D., of Emory University, with developing the hypothesis that fecal lipids might be an important driver of increased resistance rates. Supporting this hypothesis, he noted, is the finding in multiple studies that rectal gonococcal isolates consistently have a somewhat higher prevalence of resistance than those obtained from other sites.
Turning to the effort to curb antibiotic resistance, Dr. Duncan said the drug farthest along in the pipeline is solithromycin, a novel macrolide being developed by Cempra Pharmaceuticals in both oral and IV formulations. Solithromycin, a first-in-class fluoroketolide, is active against a broad range of Gram-positive organisms, among them Legionella, Chlamydia, Mycoplasma, and Ureaplasma, including macrolide-resistant strains. Its ability to bind to three ribosomal sites is thought to minimize development of resistance.
Two positive phase 3 clinical trials of solithromycin have been completed in patients with community-acquired bacterial pneumonia. A phase 3 trial in gonorrhea is ongoing after a positive phase 2 study.
Two bacterial topoisomerase inhibitors are in soon-to-be-completed phase 2 studies.
Delafloxacin, a new fluoroquinolone, was in a phase 3 clinical trial for gonorrhea that was terminated early due to ineffectiveness.
There is considerable interest in bringing back single-dose IM gentamicin (Garamycin) for the treatment of gonorrhea. A systematic review of five studies (Syst Rev. 2014 Sep 19;3:104. doi: 10.1186/2046-4053-3-104) reported cure rates that were mostly in the 90% range, but “not quite high enough to say you’d want to go to gentamicin as your front-line therapy,” in Dr. Duncan’s opinion.
Dr. Workowski noted that the National Institutes of Health is interested in trying to resurrect cefixime (Suprax) for gonorrhea after the CDC guidelines demoted it several years ago. An ongoing clinical trial is examining the impact of increasing the dose and duration of therapy.
Public health officials are also interested in spectinomycin, an antibiotic not currently available in the United States, which has achieved high cure rates as single-dose therapy in several foreign studies.
Dr. Duncan noted that a randomized trial of gentamicin plus azithromycin or gemifloxacin (Factive) plus azithromycin reported cure rates of 100% and 99.5%, respectively (Clin Infect Dis. 2014 Oct 15;59(8):1083-91). He found the study less than convincing, however: “These strains were almost all susceptibile to azithromycin, so you can’t actually say that gentamicin or gemifloxacin added a lot,” he said.
A number of researchers are working on rapid tests for susceptibility of a particular gonococcal strain so physicians could choose an effective antimicrobial for an individual patient right from the start.
“These are all in the developmental phase. It’s going to be difficult, because there are so many different mechanisms for resistance,” he said.
Similarly, vaccine development in the gonococcal field is a great challenge. The microorganism’s multiple mechanisms of immune evasion make it tough to identify correlates of protection, Dr. Duncan continued.
“Epidemiologic studies suggest there is not efficient development of natural immunity. Folks who get gonorrhea and then come back with reinfection often have the exact same strain,” he noted.
Dr. Duncan’s research is funded by the National Institutes of Health and the Burroughs Wellcome Fund. He reported having no financial conflicts of interest.
SAN DIEGO – Experts in the field of Neisseria gonorrhoeae antimicrobial resistance are warily watching developments in China, where rates of nonsusceptibility to ceftriaxone are reportedly shooting through the roof.
In the United States at present, gonococcal resistance to ceftriaxone is exceedingly rare: well under 1% of isolates have elevated minimum inhibitory concentrations (MICs) to this cornerstone of empiric therapy. In Europe, the rate is about 3%. What’s really disturbing is that recent data from the World Health Organization Gonococcal Antimicrobial Surveillance Program indicate ceftriaxone nonsusceptibility rates in China are in the 20%-30%-plus range, Dr. Joseph Duncan said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
“This is very concerning for the potential spread of this type of resistance across the world at some point. It’s just ready to explode,” observed Dr. Duncan of the University of North Carolina, Chapel Hill.
Anytime gonococcal resistance rates to a drug reach about 5%, it spells trouble.
“Gonorrhea treatment is often syndromic. An isolated swab is taken, identified by Gram stain, you give them empiric therapy, and the patients walk out of the clinic and never come back. So you don’t want to have a 5% failure rate for your initial therapy,” he explained.
Neisseria gonorrhoeae has acquired resistance to virtually every antibiotic ever used to treat the infection. Treatment options are running out, which is why the Centers for Disease Control and Prevention has designated gonorrhea as an immediate public health threat requiring urgent and aggressive action.
The 2015 CDC Sexually Transmitted Disease Treatment Guidelines recommend only one front-line treatment for gonorrhea: dual therapy with ceftriaxone at 250 mg IM in a single dose plus azithromycin 1 g orally, also in a single dose. Given N. gonorrhoeae’s adaptability, experts believe that’s not a long-term solution.
After all, 5%-10% of gonococcal isolates in Europe and China are azithromycin-resistant, and while CDC surveillance data showed less than 1% of strains in the United States were azithromycin-resistant through 2013, preliminary data for 2014 show a concerning jump to 2.5%, according to Dr. Duncan’s fellow panelist Dr. Kimberly Workowski, professor of medicine at Emory University in Atlanta and lead author of the 2015 CDC STD guidelines.
Dr. Duncan described the state of the ongoing aggressive multipronged attempts to combat antimicrobial resistance in N. gonorrhoeae. This effort includes new antibiotics in the developmental pipeline, attempts to repurpose existing antibiotics, rapid point-of-care antibiotic susceptibility tests, and vaccine development.
He also highlighted the factors that have led to the bug’s capacity to acquire resistance to so many antibiotics having different mechanisms of action. One key factor is the organism’s sheer competence as expressed in genetic lability.
“This bacteria is continually sampling DNA from the environment. The organisms are constantly swapping genes and DNA segments with commensal Neisseria species. In fact, even human DNA sequences have been found inside the gonococcal genome,” Dr. Duncan said.
While high-level antibiotic resistance can be acquired in a single dramatic step, it can also come about through multiple smaller steps, each one yielding only low-level resistance. “This allows for the sort of creeping [minimum inhibitory concentration] that we’ve seen with the gonococcus, particularly with the extended-spectrum cephalosporin antibiotics,” Dr. Duncan continued.
Also, it’s apparent that even in the absence of antibiotics, other pressures can select for antibiotic-resistant strains. Dr. Duncan credited one of his mentors, William M. Shafer, Ph.D., of Emory University, with developing the hypothesis that fecal lipids might be an important driver of increased resistance rates. Supporting this hypothesis, he noted, is the finding in multiple studies that rectal gonococcal isolates consistently have a somewhat higher prevalence of resistance than those obtained from other sites.
Turning to the effort to curb antibiotic resistance, Dr. Duncan said the drug farthest along in the pipeline is solithromycin, a novel macrolide being developed by Cempra Pharmaceuticals in both oral and IV formulations. Solithromycin, a first-in-class fluoroketolide, is active against a broad range of Gram-positive organisms, among them Legionella, Chlamydia, Mycoplasma, and Ureaplasma, including macrolide-resistant strains. Its ability to bind to three ribosomal sites is thought to minimize development of resistance.
Two positive phase 3 clinical trials of solithromycin have been completed in patients with community-acquired bacterial pneumonia. A phase 3 trial in gonorrhea is ongoing after a positive phase 2 study.
Two bacterial topoisomerase inhibitors are in soon-to-be-completed phase 2 studies.
Delafloxacin, a new fluoroquinolone, was in a phase 3 clinical trial for gonorrhea that was terminated early due to ineffectiveness.
There is considerable interest in bringing back single-dose IM gentamicin (Garamycin) for the treatment of gonorrhea. A systematic review of five studies (Syst Rev. 2014 Sep 19;3:104. doi: 10.1186/2046-4053-3-104) reported cure rates that were mostly in the 90% range, but “not quite high enough to say you’d want to go to gentamicin as your front-line therapy,” in Dr. Duncan’s opinion.
Dr. Workowski noted that the National Institutes of Health is interested in trying to resurrect cefixime (Suprax) for gonorrhea after the CDC guidelines demoted it several years ago. An ongoing clinical trial is examining the impact of increasing the dose and duration of therapy.
Public health officials are also interested in spectinomycin, an antibiotic not currently available in the United States, which has achieved high cure rates as single-dose therapy in several foreign studies.
Dr. Duncan noted that a randomized trial of gentamicin plus azithromycin or gemifloxacin (Factive) plus azithromycin reported cure rates of 100% and 99.5%, respectively (Clin Infect Dis. 2014 Oct 15;59(8):1083-91). He found the study less than convincing, however: “These strains were almost all susceptibile to azithromycin, so you can’t actually say that gentamicin or gemifloxacin added a lot,” he said.
A number of researchers are working on rapid tests for susceptibility of a particular gonococcal strain so physicians could choose an effective antimicrobial for an individual patient right from the start.
“These are all in the developmental phase. It’s going to be difficult, because there are so many different mechanisms for resistance,” he said.
Similarly, vaccine development in the gonococcal field is a great challenge. The microorganism’s multiple mechanisms of immune evasion make it tough to identify correlates of protection, Dr. Duncan continued.
“Epidemiologic studies suggest there is not efficient development of natural immunity. Folks who get gonorrhea and then come back with reinfection often have the exact same strain,” he noted.
Dr. Duncan’s research is funded by the National Institutes of Health and the Burroughs Wellcome Fund. He reported having no financial conflicts of interest.
EXPERT ANALYSIS FROM ICAAC 2015
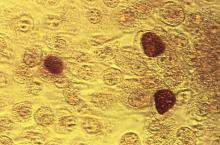
Answers elusive in quest for better chlamydia treatment
SAN DIEGO – The hottest topic today in the treatment of sexually transmitted diseases caused by Chlamydia trachomatis is the unresolved question of whether azithromycin is still as effective as doxycycline, the other current guideline-recommended, first-line therapy, Dr. Kimberly Workowski said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
“This is important, because doxycycline is administered twice a day for 7 days, and azithromycin is given as a single pill suitable for directly observed therapy,” noted Dr. Workowski, professor of medicine at Emory University in Atlanta and lead author of the 2015 Centers for Disease Control and Prevention STD treatment guidelines.
Several recent retrospective case series have suggested azithromycin is less effective, with the biggest efficacy gap being seen in rectal C. trachomatis infections. These nonrandomized studies were further supported by an Australian meta-analysis of six randomized, controlled trials comparing the two antibiotics for the treatment of genital chlamydia. The investigators found roughly 3% greater efficacy for doxycycline, compared with azithromycin, for urogenital chlamydia, and a 7% advantage for doxycycline in treating symptomatic urethral infection in men.
However, the investigators were quick to add the caveat that “the quality of the evidence varies considerably” (Clin Infect Dis. 2014 Jul 15;59(2):193-205).
There’s a pressing need for better data. Dr. Workowski and her colleagues on the STD guidelines panel are eagerly awaiting the results of a well-structured randomized trial led by Dr. William M. Geisler, professor of medicine at the University of Alabama, Birmingham. The investigators randomized more than 300 chlamydia-infected male and female inmates in youth correctional facilities to guideline-recommended azithromycin at 1 g orally in a single dose or oral doxycycline at 100 mg twice daily for 7 days. The results, which are anticipated soon, should influence clinical practice, Dr. Workowski said.
“There is something going on here that we’re trying to understand. It may have something to do with organism load,” according to Dr. Workowski.
Here’s what else is new in chlamydia:
•Pregnancy: For treatment of chlamydia in pregnancy, amoxicillin at 500 mg orally t.i.d. for 7 days has been demoted from a first-line recommended therapy to alternative-regimen status. Now, the sole recommended first-line treatment in pregnancy is oral azithromycin at 1 g orally in a single dose.
“We did this based on in vitro studies showing Chlamydia trachomatis is not well-killed by amoxicillin. Instead, the drug induces persistent viable noninfectious forms which can sometimes reactivate,” Dr. Workowski explained.
•Delayed-release doxycycline: This FDA-approved drug, known as Doryx, administered as a 200-mg tablet once daily for 7 days, “might be an alternative” to the standard generic doxycycline regimen of 100 mg twice daily for 7 days, according to the current Centers for Disease Control and Prevention guidelines. In a randomized, double-blind trial, the new agent was as effective as twice-daily generic doxycycline in men and women with urogenital C. trachomatis infection, and it had fewer gastrointestinal side effects. Doryx is costlier than the twice-daily alternatives.
• Lymphogranuloma venereum: The current guidelines repeat a point made in previous editions, but one Dr. Workowski believes remains underappreciated and thus worthy of emphasis: Rectal exposure to C. trachomatis serovars L1, L2, and L3 in men who have sex with men or in women who have rectal sex can cause lymphogranuloma venereum, which takes the form of proctocolitis mimicking inflammatory bowel disease.
At the time of the initial visit, before results of diagnostic tests for chlamydia are available, patients suspected of having lymphogranuloma venereum should be started presumptively on the recommended regimen for this STD, which is oral doxycycline at 100 mg b.i.d. for 21 days.
“If you also see painful ulcers or, on anoscopy, mucosal ulcers, you should also treat empirically for herpes simplex until your culture results come back,” she added.
Dr. Workowski reported having no financial conflicts of interest.
SAN DIEGO – The hottest topic today in the treatment of sexually transmitted diseases caused by Chlamydia trachomatis is the unresolved question of whether azithromycin is still as effective as doxycycline, the other current guideline-recommended, first-line therapy, Dr. Kimberly Workowski said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
“This is important, because doxycycline is administered twice a day for 7 days, and azithromycin is given as a single pill suitable for directly observed therapy,” noted Dr. Workowski, professor of medicine at Emory University in Atlanta and lead author of the 2015 Centers for Disease Control and Prevention STD treatment guidelines.
Several recent retrospective case series have suggested azithromycin is less effective, with the biggest efficacy gap being seen in rectal C. trachomatis infections. These nonrandomized studies were further supported by an Australian meta-analysis of six randomized, controlled trials comparing the two antibiotics for the treatment of genital chlamydia. The investigators found roughly 3% greater efficacy for doxycycline, compared with azithromycin, for urogenital chlamydia, and a 7% advantage for doxycycline in treating symptomatic urethral infection in men.
However, the investigators were quick to add the caveat that “the quality of the evidence varies considerably” (Clin Infect Dis. 2014 Jul 15;59(2):193-205).
There’s a pressing need for better data. Dr. Workowski and her colleagues on the STD guidelines panel are eagerly awaiting the results of a well-structured randomized trial led by Dr. William M. Geisler, professor of medicine at the University of Alabama, Birmingham. The investigators randomized more than 300 chlamydia-infected male and female inmates in youth correctional facilities to guideline-recommended azithromycin at 1 g orally in a single dose or oral doxycycline at 100 mg twice daily for 7 days. The results, which are anticipated soon, should influence clinical practice, Dr. Workowski said.
“There is something going on here that we’re trying to understand. It may have something to do with organism load,” according to Dr. Workowski.
Here’s what else is new in chlamydia:
•Pregnancy: For treatment of chlamydia in pregnancy, amoxicillin at 500 mg orally t.i.d. for 7 days has been demoted from a first-line recommended therapy to alternative-regimen status. Now, the sole recommended first-line treatment in pregnancy is oral azithromycin at 1 g orally in a single dose.
“We did this based on in vitro studies showing Chlamydia trachomatis is not well-killed by amoxicillin. Instead, the drug induces persistent viable noninfectious forms which can sometimes reactivate,” Dr. Workowski explained.
•Delayed-release doxycycline: This FDA-approved drug, known as Doryx, administered as a 200-mg tablet once daily for 7 days, “might be an alternative” to the standard generic doxycycline regimen of 100 mg twice daily for 7 days, according to the current Centers for Disease Control and Prevention guidelines. In a randomized, double-blind trial, the new agent was as effective as twice-daily generic doxycycline in men and women with urogenital C. trachomatis infection, and it had fewer gastrointestinal side effects. Doryx is costlier than the twice-daily alternatives.
• Lymphogranuloma venereum: The current guidelines repeat a point made in previous editions, but one Dr. Workowski believes remains underappreciated and thus worthy of emphasis: Rectal exposure to C. trachomatis serovars L1, L2, and L3 in men who have sex with men or in women who have rectal sex can cause lymphogranuloma venereum, which takes the form of proctocolitis mimicking inflammatory bowel disease.
At the time of the initial visit, before results of diagnostic tests for chlamydia are available, patients suspected of having lymphogranuloma venereum should be started presumptively on the recommended regimen for this STD, which is oral doxycycline at 100 mg b.i.d. for 21 days.
“If you also see painful ulcers or, on anoscopy, mucosal ulcers, you should also treat empirically for herpes simplex until your culture results come back,” she added.
Dr. Workowski reported having no financial conflicts of interest.
SAN DIEGO – The hottest topic today in the treatment of sexually transmitted diseases caused by Chlamydia trachomatis is the unresolved question of whether azithromycin is still as effective as doxycycline, the other current guideline-recommended, first-line therapy, Dr. Kimberly Workowski said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
“This is important, because doxycycline is administered twice a day for 7 days, and azithromycin is given as a single pill suitable for directly observed therapy,” noted Dr. Workowski, professor of medicine at Emory University in Atlanta and lead author of the 2015 Centers for Disease Control and Prevention STD treatment guidelines.
Several recent retrospective case series have suggested azithromycin is less effective, with the biggest efficacy gap being seen in rectal C. trachomatis infections. These nonrandomized studies were further supported by an Australian meta-analysis of six randomized, controlled trials comparing the two antibiotics for the treatment of genital chlamydia. The investigators found roughly 3% greater efficacy for doxycycline, compared with azithromycin, for urogenital chlamydia, and a 7% advantage for doxycycline in treating symptomatic urethral infection in men.
However, the investigators were quick to add the caveat that “the quality of the evidence varies considerably” (Clin Infect Dis. 2014 Jul 15;59(2):193-205).
There’s a pressing need for better data. Dr. Workowski and her colleagues on the STD guidelines panel are eagerly awaiting the results of a well-structured randomized trial led by Dr. William M. Geisler, professor of medicine at the University of Alabama, Birmingham. The investigators randomized more than 300 chlamydia-infected male and female inmates in youth correctional facilities to guideline-recommended azithromycin at 1 g orally in a single dose or oral doxycycline at 100 mg twice daily for 7 days. The results, which are anticipated soon, should influence clinical practice, Dr. Workowski said.
“There is something going on here that we’re trying to understand. It may have something to do with organism load,” according to Dr. Workowski.
Here’s what else is new in chlamydia:
•Pregnancy: For treatment of chlamydia in pregnancy, amoxicillin at 500 mg orally t.i.d. for 7 days has been demoted from a first-line recommended therapy to alternative-regimen status. Now, the sole recommended first-line treatment in pregnancy is oral azithromycin at 1 g orally in a single dose.
“We did this based on in vitro studies showing Chlamydia trachomatis is not well-killed by amoxicillin. Instead, the drug induces persistent viable noninfectious forms which can sometimes reactivate,” Dr. Workowski explained.
•Delayed-release doxycycline: This FDA-approved drug, known as Doryx, administered as a 200-mg tablet once daily for 7 days, “might be an alternative” to the standard generic doxycycline regimen of 100 mg twice daily for 7 days, according to the current Centers for Disease Control and Prevention guidelines. In a randomized, double-blind trial, the new agent was as effective as twice-daily generic doxycycline in men and women with urogenital C. trachomatis infection, and it had fewer gastrointestinal side effects. Doryx is costlier than the twice-daily alternatives.
• Lymphogranuloma venereum: The current guidelines repeat a point made in previous editions, but one Dr. Workowski believes remains underappreciated and thus worthy of emphasis: Rectal exposure to C. trachomatis serovars L1, L2, and L3 in men who have sex with men or in women who have rectal sex can cause lymphogranuloma venereum, which takes the form of proctocolitis mimicking inflammatory bowel disease.
At the time of the initial visit, before results of diagnostic tests for chlamydia are available, patients suspected of having lymphogranuloma venereum should be started presumptively on the recommended regimen for this STD, which is oral doxycycline at 100 mg b.i.d. for 21 days.
“If you also see painful ulcers or, on anoscopy, mucosal ulcers, you should also treat empirically for herpes simplex until your culture results come back,” she added.
Dr. Workowski reported having no financial conflicts of interest.
EXPERT ANALYSIS FROM ICAAC 2015
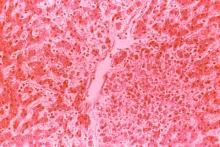
Dengue disease is here and U.S. physicians need to get to know it
SAN DIEGO – With dengue disease now knocking on the door of the United States, it’s a good time for American physicians to get up to speed regarding the most rapidly spreading mosquito-borne viral disease in the world.
That’s a particularly sound idea if they – or their patients – plan to visit anywhere in the Caribbean, Central America, Brazil, East Asia, or large swathes of Africa, where the disease is a major and rapidly growing public health problem. The World Health Organization estimates 3.6 billion people worldwide are at risk for dengue disease, with up to 100 million symptomatic infections occurring annually, 250,000-500,000 cases of severe dengue, and 21,000 deaths due to the disease. There have been recent outbreaks in South Florida, Texas, and Hawaii, Dr. Federico Narvaez noted at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
The most important thing for clinicians to know about dengue disease is how to identify the subset of up to 10% of symptomatic dengue patients who – absent appropriate intervention – will progress to severe disease marked by pronounced plasma leakage leading to shock, respiratory failure, severe hemorrhage, and/or organ failure, he stressed. This is a disease that can cause death within the space of 24-48 hours in a person who was healthy just a few days before. And there are a handful of warning signs that predictably occur on day 3 or 4 of the illness, when the initial high fever comes down, before things take a dramatic turn for the worse.
“Timely diagnosis improves prognosis. If properly managed, the case fatality rate of severe dengue is less than 1%,” said Dr. Narvaez of the National Pediatric Reference Hospital and the Nicaragua Ministry of Health in Managua.
The traditional WHO classification for dengue into self-limited dengue fever, dengue hemorrhagic fever, and dengue shock syndrome was replaced in 2009 by a system that Dr. Narvaez and other experts consider a big step forward in guiding clinical management. Under the revised WHO classification, dengue disease is divided into dengue without warning signs, dengue with warning signs, and severe dengue.
In a study of 544 laboratory-confirmed cases of pediatric dengue in Managua, Dr. Narvaez and coinvestigators compared the former and revised WHO classifications and demonstrated that the 2009 revised system boosted the positive predictive value for need for inpatient care from 43% to 67% (PLoS Negl Trop Dis. 2011 Nov;5[11]:e1397. doi: 10.1371/journal.pntd.0001397. Epub 2011 Nov 8).
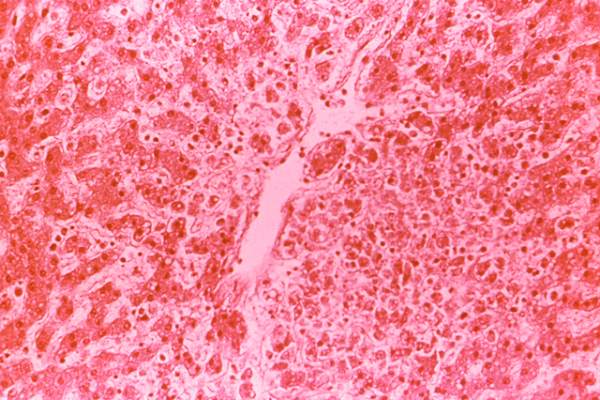
Some key points about dengue disease: It has two distinct mosquito vectors, Aedis aegypti and A. albonictus. There are four cocirculating serotypes; infection with one doesn’t protect against infection with the others. Three-quarters of infections are asymptomatic. Symptomatic infections follow a three-stage course: the febrile, critical, and recovery phases. And the primary pathophysiology of dengue disease is plasma leakage.
The febrile phase is marked by abrupt onset of high fever plus various combinations of severe headache, facial flushing, a transient macular or maculopapular rash, retro-orbital pain, and/or the intense arthralgias/myalgias which have led to dengue being known as ‘breakbone fever.’
The critical phase begins around the time of defervescence. This is when clinically significant plasma leakage can occur, with resultant compensated or decompensated shock and other severe complications. The critical phase is the time for vigilance regarding the appearance of the 2009 WHO warning signs of increased risk for shock: abdominal pain, an abrupt rise in hematocrit concurrent with a rapid drop in platelets, mucosal bleeding, development of ascites or other clinically apparent fluid accumulation, liver enlargement of more than 2 cm, persistent vomiting, and restlessness/lethargy.
In a soon-to-be-published study of 812 Nicaraguan dengue patients, 220 of whom developed shock, Dr. Narvaez and coworkers found that the presence of any of the warning signs except persistent vomiting was associated with significantly increased likelihood of subsequent shock, with the magnitude of increased risk ranging from 1.31 to 2.3. Moreover, other studies have demonstrated that by acting upon these warning signs by means of cautious administration of intravenous fluids and other supportive measures, the risk of developing shock is reduced.
The WHO warning signs are particularly valuable in the often resource-poor countries where dengue is most common. In such settings most front-line primary care physicians lack ready access to ultrasound imaging of the gallbladder looking for evidence of wall thickening. A thickened gallbladder wall is an expression of subclinical plasma leakage, which has been shown in multiple studies to be even better at identifying patients at risk for severe dengue than the WHO warning signs.
For example, a prospective hospital-based study in which Dutch and Indonesian investigators utilized serial daily bedside ultrasonography with a hand-held imaging device found that gallbladder wall edema at enrollment had a 35% positive predictive value and a 90% negative predictive value for subsequent severe dengue (PLoS Negl Trop Dis. 2013 Jun 13;7[6]:e2277. doi: 10.1371/journal.pntd.0002277).
The critical phase typically lasts from day 3 or 4 through day 6 of the illness. This is followed by the recovery phase, marked by reabsorption of extravasated fluid over the course of 48-72 hours, increased diuresis, and stabilization of hemodynamic status. The appearance of a highly pruritic and erythematous rash with small islands of normal skin is another common finding that indicates the patient’s condition will continue to improve. A temporary bradycardia is also quite common during the recovery phase, according to Dr. Narvaez.
He reported having no financial conflicts of interest regarding his presentation.
SAN DIEGO – With dengue disease now knocking on the door of the United States, it’s a good time for American physicians to get up to speed regarding the most rapidly spreading mosquito-borne viral disease in the world.
That’s a particularly sound idea if they – or their patients – plan to visit anywhere in the Caribbean, Central America, Brazil, East Asia, or large swathes of Africa, where the disease is a major and rapidly growing public health problem. The World Health Organization estimates 3.6 billion people worldwide are at risk for dengue disease, with up to 100 million symptomatic infections occurring annually, 250,000-500,000 cases of severe dengue, and 21,000 deaths due to the disease. There have been recent outbreaks in South Florida, Texas, and Hawaii, Dr. Federico Narvaez noted at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
The most important thing for clinicians to know about dengue disease is how to identify the subset of up to 10% of symptomatic dengue patients who – absent appropriate intervention – will progress to severe disease marked by pronounced plasma leakage leading to shock, respiratory failure, severe hemorrhage, and/or organ failure, he stressed. This is a disease that can cause death within the space of 24-48 hours in a person who was healthy just a few days before. And there are a handful of warning signs that predictably occur on day 3 or 4 of the illness, when the initial high fever comes down, before things take a dramatic turn for the worse.
“Timely diagnosis improves prognosis. If properly managed, the case fatality rate of severe dengue is less than 1%,” said Dr. Narvaez of the National Pediatric Reference Hospital and the Nicaragua Ministry of Health in Managua.
The traditional WHO classification for dengue into self-limited dengue fever, dengue hemorrhagic fever, and dengue shock syndrome was replaced in 2009 by a system that Dr. Narvaez and other experts consider a big step forward in guiding clinical management. Under the revised WHO classification, dengue disease is divided into dengue without warning signs, dengue with warning signs, and severe dengue.
In a study of 544 laboratory-confirmed cases of pediatric dengue in Managua, Dr. Narvaez and coinvestigators compared the former and revised WHO classifications and demonstrated that the 2009 revised system boosted the positive predictive value for need for inpatient care from 43% to 67% (PLoS Negl Trop Dis. 2011 Nov;5[11]:e1397. doi: 10.1371/journal.pntd.0001397. Epub 2011 Nov 8).
Some key points about dengue disease: It has two distinct mosquito vectors, Aedis aegypti and A. albonictus. There are four cocirculating serotypes; infection with one doesn’t protect against infection with the others. Three-quarters of infections are asymptomatic. Symptomatic infections follow a three-stage course: the febrile, critical, and recovery phases. And the primary pathophysiology of dengue disease is plasma leakage.
The febrile phase is marked by abrupt onset of high fever plus various combinations of severe headache, facial flushing, a transient macular or maculopapular rash, retro-orbital pain, and/or the intense arthralgias/myalgias which have led to dengue being known as ‘breakbone fever.’
The critical phase begins around the time of defervescence. This is when clinically significant plasma leakage can occur, with resultant compensated or decompensated shock and other severe complications. The critical phase is the time for vigilance regarding the appearance of the 2009 WHO warning signs of increased risk for shock: abdominal pain, an abrupt rise in hematocrit concurrent with a rapid drop in platelets, mucosal bleeding, development of ascites or other clinically apparent fluid accumulation, liver enlargement of more than 2 cm, persistent vomiting, and restlessness/lethargy.
In a soon-to-be-published study of 812 Nicaraguan dengue patients, 220 of whom developed shock, Dr. Narvaez and coworkers found that the presence of any of the warning signs except persistent vomiting was associated with significantly increased likelihood of subsequent shock, with the magnitude of increased risk ranging from 1.31 to 2.3. Moreover, other studies have demonstrated that by acting upon these warning signs by means of cautious administration of intravenous fluids and other supportive measures, the risk of developing shock is reduced.
The WHO warning signs are particularly valuable in the often resource-poor countries where dengue is most common. In such settings most front-line primary care physicians lack ready access to ultrasound imaging of the gallbladder looking for evidence of wall thickening. A thickened gallbladder wall is an expression of subclinical plasma leakage, which has been shown in multiple studies to be even better at identifying patients at risk for severe dengue than the WHO warning signs.
For example, a prospective hospital-based study in which Dutch and Indonesian investigators utilized serial daily bedside ultrasonography with a hand-held imaging device found that gallbladder wall edema at enrollment had a 35% positive predictive value and a 90% negative predictive value for subsequent severe dengue (PLoS Negl Trop Dis. 2013 Jun 13;7[6]:e2277. doi: 10.1371/journal.pntd.0002277).
The critical phase typically lasts from day 3 or 4 through day 6 of the illness. This is followed by the recovery phase, marked by reabsorption of extravasated fluid over the course of 48-72 hours, increased diuresis, and stabilization of hemodynamic status. The appearance of a highly pruritic and erythematous rash with small islands of normal skin is another common finding that indicates the patient’s condition will continue to improve. A temporary bradycardia is also quite common during the recovery phase, according to Dr. Narvaez.
He reported having no financial conflicts of interest regarding his presentation.
SAN DIEGO – With dengue disease now knocking on the door of the United States, it’s a good time for American physicians to get up to speed regarding the most rapidly spreading mosquito-borne viral disease in the world.
That’s a particularly sound idea if they – or their patients – plan to visit anywhere in the Caribbean, Central America, Brazil, East Asia, or large swathes of Africa, where the disease is a major and rapidly growing public health problem. The World Health Organization estimates 3.6 billion people worldwide are at risk for dengue disease, with up to 100 million symptomatic infections occurring annually, 250,000-500,000 cases of severe dengue, and 21,000 deaths due to the disease. There have been recent outbreaks in South Florida, Texas, and Hawaii, Dr. Federico Narvaez noted at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
The most important thing for clinicians to know about dengue disease is how to identify the subset of up to 10% of symptomatic dengue patients who – absent appropriate intervention – will progress to severe disease marked by pronounced plasma leakage leading to shock, respiratory failure, severe hemorrhage, and/or organ failure, he stressed. This is a disease that can cause death within the space of 24-48 hours in a person who was healthy just a few days before. And there are a handful of warning signs that predictably occur on day 3 or 4 of the illness, when the initial high fever comes down, before things take a dramatic turn for the worse.
“Timely diagnosis improves prognosis. If properly managed, the case fatality rate of severe dengue is less than 1%,” said Dr. Narvaez of the National Pediatric Reference Hospital and the Nicaragua Ministry of Health in Managua.
The traditional WHO classification for dengue into self-limited dengue fever, dengue hemorrhagic fever, and dengue shock syndrome was replaced in 2009 by a system that Dr. Narvaez and other experts consider a big step forward in guiding clinical management. Under the revised WHO classification, dengue disease is divided into dengue without warning signs, dengue with warning signs, and severe dengue.
In a study of 544 laboratory-confirmed cases of pediatric dengue in Managua, Dr. Narvaez and coinvestigators compared the former and revised WHO classifications and demonstrated that the 2009 revised system boosted the positive predictive value for need for inpatient care from 43% to 67% (PLoS Negl Trop Dis. 2011 Nov;5[11]:e1397. doi: 10.1371/journal.pntd.0001397. Epub 2011 Nov 8).
Some key points about dengue disease: It has two distinct mosquito vectors, Aedis aegypti and A. albonictus. There are four cocirculating serotypes; infection with one doesn’t protect against infection with the others. Three-quarters of infections are asymptomatic. Symptomatic infections follow a three-stage course: the febrile, critical, and recovery phases. And the primary pathophysiology of dengue disease is plasma leakage.
The febrile phase is marked by abrupt onset of high fever plus various combinations of severe headache, facial flushing, a transient macular or maculopapular rash, retro-orbital pain, and/or the intense arthralgias/myalgias which have led to dengue being known as ‘breakbone fever.’
The critical phase begins around the time of defervescence. This is when clinically significant plasma leakage can occur, with resultant compensated or decompensated shock and other severe complications. The critical phase is the time for vigilance regarding the appearance of the 2009 WHO warning signs of increased risk for shock: abdominal pain, an abrupt rise in hematocrit concurrent with a rapid drop in platelets, mucosal bleeding, development of ascites or other clinically apparent fluid accumulation, liver enlargement of more than 2 cm, persistent vomiting, and restlessness/lethargy.
In a soon-to-be-published study of 812 Nicaraguan dengue patients, 220 of whom developed shock, Dr. Narvaez and coworkers found that the presence of any of the warning signs except persistent vomiting was associated with significantly increased likelihood of subsequent shock, with the magnitude of increased risk ranging from 1.31 to 2.3. Moreover, other studies have demonstrated that by acting upon these warning signs by means of cautious administration of intravenous fluids and other supportive measures, the risk of developing shock is reduced.
The WHO warning signs are particularly valuable in the often resource-poor countries where dengue is most common. In such settings most front-line primary care physicians lack ready access to ultrasound imaging of the gallbladder looking for evidence of wall thickening. A thickened gallbladder wall is an expression of subclinical plasma leakage, which has been shown in multiple studies to be even better at identifying patients at risk for severe dengue than the WHO warning signs.
For example, a prospective hospital-based study in which Dutch and Indonesian investigators utilized serial daily bedside ultrasonography with a hand-held imaging device found that gallbladder wall edema at enrollment had a 35% positive predictive value and a 90% negative predictive value for subsequent severe dengue (PLoS Negl Trop Dis. 2013 Jun 13;7[6]:e2277. doi: 10.1371/journal.pntd.0002277).
The critical phase typically lasts from day 3 or 4 through day 6 of the illness. This is followed by the recovery phase, marked by reabsorption of extravasated fluid over the course of 48-72 hours, increased diuresis, and stabilization of hemodynamic status. The appearance of a highly pruritic and erythematous rash with small islands of normal skin is another common finding that indicates the patient’s condition will continue to improve. A temporary bradycardia is also quite common during the recovery phase, according to Dr. Narvaez.
He reported having no financial conflicts of interest regarding his presentation.
EXPERT ANALYSIS FROM ICAAC 2015
Promising nonvaccine approaches to controlling dengue
SAN DIEGO – In the aftermath of the latest somewhat disappointing report on the effort to develop a dengue vaccine, novel nonvaccine approaches aimed at curbing this rapidly growing public health problem are drawing renewed attention, Eva Harris, Ph.D., declared at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
These promising nonvaccine tools fall into several categories: vector control using genetically modified mosquitoes, development of new and better insecticides, and communitywide nonpesticide-based source reduction programs, explained Dr. Harris, professor of infectious diseases and vaccinology and director of the Center for Global Public Health at the University of California, Berkeley.
Many dengue experts, Dr. Harris among them, were disappointed in the recently reported long-term results of several large clinical trials of the candidate dengue vaccine furthest along in the developmental pipeline. The Sanofi Pasteur vaccine, known as CYD-TDV, is due for review and potential registration by the World Health Organization next year. The latest results show favorable safety but suboptimal efficacy. On the plus side, the data showed that children aged 9-16 years continued to benefit 3-4 years after vaccination. There was, however, a disturbing finding: children younger than 9 years of age at vaccination had an increased risk of hospitalization for dengue when they were naturally infected in the third year following vaccination (N Engl J Med. 2015;373[13]:1195-206).
In an accompanying editorial titled “A Candidate Dengue Vaccine Walks a Tightrope,” Dr. Cameron P. Simmons called the latter finding “a particularly unwelcome outcome” that, if not due to chance, raises the possibility that immunization of young children elicits only transient antibody-mediated immunity. As their antibody titers wane over time, these vaccinated children may, through sensitization, be predisposed to clinical dengue infections that are sufficiently serious to warrant hospitalization. It’s possible, but unproved, that booster doses of the vaccine might circumvent this problem, he added.
“The bumpy road to a vaccine-based solution for dengue continues,” observed Dr. Simmons of the University of Melbourne (N Engl J Med. 2015;373[13]:1263-4).
Dr. Harris noted that two other vaccines, one sponsored by the National Institutes of Health and the other by Takeda, are due to start large, long-term phase-III clinical trials in the next few months. And Merck and GlaxoSmithKline have next-generation vaccines in phase-I studies. But possible consideration of any of these vaccines for regulatory approval is a long ways off, and her focus at ICAAC 2015 was on nonvaccine solutions.
She and her coinvestigators recently published positive results of their landmark randomized controlled trial of a pesticide-free, community-based mobilization program for dengue prevention known as the Camino Verde, or Green Way (BMJ. 2015;351:h3267).
The impetus for this program was recognition of the shortcomings of current dengue control efforts, which rely heavily upon massive use of the organophosphate pesticide temephos (Abate) in household water containers where the mosquito vectors breed. The pesticide program hasn’t prevented ongoing rapid growth of the dengue pandemic. Moreover, the associated human toxicity and negative environmental effects are a mounting concern.
Camino Verde is a nonchemical alternative approach in which facilitators run intervention design groups in neighborhoods to inform community leaders and other residents about the scope of their local dengue mosquito problem based upon entomologic survey results and then help develop consensus regarding community-specific programs for chemical-free prevention of mosquito reproduction. Popular options included introduction of fish into water storage containers, cleanup campaigns targeting abandoned tires and other standing-water sources, and scrubbing and covering water tanks. Allowing each participating site to select its own interventions encouraged strong community support, Dr. Harris explained.
The prospective Camino Verde study involved nearly 19,000 households with more than 85,000 residents in Nicaragua and Mexico. Clusters of households were randomized to continuation of the temephos-based, government-run dengue control program with or without adding on the Camino Verde intervention.
Among the key findings: There was a 30% lower risk of serologic infection with dengue virus among children from intervention sites, as well as a 25% reduction in dengue illness among people of all ages. The numbers needed to treat were 30 for a reduced risk of infection in children and 71 for a lower risk of illness. Investigators also documented a 44% reduction in houses containing Aedes aegypti larvae or pupae in Camino Verde–participating sites, compared with control communities.
This study provides the first-ever solid serologic evidence that a pesticide-free community mobilization effort has a positive impact on dengue infection. The logical next step is for governments in dengue-endemic countries to adopt such an approach, she said.
At least three different strategies of genetic modification of dengue-vector mosquitoes are being pursued in an effort to reduce dengue transmission. All show promise as partial solutions, in Dr. Harris’ view.
Release of sterile transgenic A. aegypti males over the course of a year in a Brazilian suburb resulted in a 95% reduction in the size of the local A. aegypti population, compared with an adjacent control area (PLoS Negl Trop Dis. 2015;9[7]:e0003864). Investigators at Colorado State University in Fort Collins have developed a transgenic strain of A. aegypti males carrying a dominant lethal gene resulting in next-generation flightless females that can’t mate or avoid predators (Proc Natl Acad Sci U S A. 2011;108[12]:4772-5).
In another approach, an international collaborative group has performed field-release trials of A. aegypti mosquitoes deliberately infected with a strain of the intracellular bacterium Wolbachia, which renders the insects resistant to dengue virus infection. The group’s mathematical modeling suggested widespread adoption of this approach would reduce dengue virus transmission by 66%-75%. The investigators predicted this would be sufficient to eliminate dengue in low- or moderate-transmission areas but probably wouldn’t accomplish complete control in the highest-risk areas (Sci Transl Med. 2015;7[279]:279ra37).
Dr. Harris reported that the Camino Verde trial was funded by the UBS Optimus Foundation. She reported having no financial conflicts of interest.
SAN DIEGO – In the aftermath of the latest somewhat disappointing report on the effort to develop a dengue vaccine, novel nonvaccine approaches aimed at curbing this rapidly growing public health problem are drawing renewed attention, Eva Harris, Ph.D., declared at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
These promising nonvaccine tools fall into several categories: vector control using genetically modified mosquitoes, development of new and better insecticides, and communitywide nonpesticide-based source reduction programs, explained Dr. Harris, professor of infectious diseases and vaccinology and director of the Center for Global Public Health at the University of California, Berkeley.
Many dengue experts, Dr. Harris among them, were disappointed in the recently reported long-term results of several large clinical trials of the candidate dengue vaccine furthest along in the developmental pipeline. The Sanofi Pasteur vaccine, known as CYD-TDV, is due for review and potential registration by the World Health Organization next year. The latest results show favorable safety but suboptimal efficacy. On the plus side, the data showed that children aged 9-16 years continued to benefit 3-4 years after vaccination. There was, however, a disturbing finding: children younger than 9 years of age at vaccination had an increased risk of hospitalization for dengue when they were naturally infected in the third year following vaccination (N Engl J Med. 2015;373[13]:1195-206).
In an accompanying editorial titled “A Candidate Dengue Vaccine Walks a Tightrope,” Dr. Cameron P. Simmons called the latter finding “a particularly unwelcome outcome” that, if not due to chance, raises the possibility that immunization of young children elicits only transient antibody-mediated immunity. As their antibody titers wane over time, these vaccinated children may, through sensitization, be predisposed to clinical dengue infections that are sufficiently serious to warrant hospitalization. It’s possible, but unproved, that booster doses of the vaccine might circumvent this problem, he added.
“The bumpy road to a vaccine-based solution for dengue continues,” observed Dr. Simmons of the University of Melbourne (N Engl J Med. 2015;373[13]:1263-4).
Dr. Harris noted that two other vaccines, one sponsored by the National Institutes of Health and the other by Takeda, are due to start large, long-term phase-III clinical trials in the next few months. And Merck and GlaxoSmithKline have next-generation vaccines in phase-I studies. But possible consideration of any of these vaccines for regulatory approval is a long ways off, and her focus at ICAAC 2015 was on nonvaccine solutions.
She and her coinvestigators recently published positive results of their landmark randomized controlled trial of a pesticide-free, community-based mobilization program for dengue prevention known as the Camino Verde, or Green Way (BMJ. 2015;351:h3267).
The impetus for this program was recognition of the shortcomings of current dengue control efforts, which rely heavily upon massive use of the organophosphate pesticide temephos (Abate) in household water containers where the mosquito vectors breed. The pesticide program hasn’t prevented ongoing rapid growth of the dengue pandemic. Moreover, the associated human toxicity and negative environmental effects are a mounting concern.
Camino Verde is a nonchemical alternative approach in which facilitators run intervention design groups in neighborhoods to inform community leaders and other residents about the scope of their local dengue mosquito problem based upon entomologic survey results and then help develop consensus regarding community-specific programs for chemical-free prevention of mosquito reproduction. Popular options included introduction of fish into water storage containers, cleanup campaigns targeting abandoned tires and other standing-water sources, and scrubbing and covering water tanks. Allowing each participating site to select its own interventions encouraged strong community support, Dr. Harris explained.
The prospective Camino Verde study involved nearly 19,000 households with more than 85,000 residents in Nicaragua and Mexico. Clusters of households were randomized to continuation of the temephos-based, government-run dengue control program with or without adding on the Camino Verde intervention.
Among the key findings: There was a 30% lower risk of serologic infection with dengue virus among children from intervention sites, as well as a 25% reduction in dengue illness among people of all ages. The numbers needed to treat were 30 for a reduced risk of infection in children and 71 for a lower risk of illness. Investigators also documented a 44% reduction in houses containing Aedes aegypti larvae or pupae in Camino Verde–participating sites, compared with control communities.
This study provides the first-ever solid serologic evidence that a pesticide-free community mobilization effort has a positive impact on dengue infection. The logical next step is for governments in dengue-endemic countries to adopt such an approach, she said.
At least three different strategies of genetic modification of dengue-vector mosquitoes are being pursued in an effort to reduce dengue transmission. All show promise as partial solutions, in Dr. Harris’ view.
Release of sterile transgenic A. aegypti males over the course of a year in a Brazilian suburb resulted in a 95% reduction in the size of the local A. aegypti population, compared with an adjacent control area (PLoS Negl Trop Dis. 2015;9[7]:e0003864). Investigators at Colorado State University in Fort Collins have developed a transgenic strain of A. aegypti males carrying a dominant lethal gene resulting in next-generation flightless females that can’t mate or avoid predators (Proc Natl Acad Sci U S A. 2011;108[12]:4772-5).
In another approach, an international collaborative group has performed field-release trials of A. aegypti mosquitoes deliberately infected with a strain of the intracellular bacterium Wolbachia, which renders the insects resistant to dengue virus infection. The group’s mathematical modeling suggested widespread adoption of this approach would reduce dengue virus transmission by 66%-75%. The investigators predicted this would be sufficient to eliminate dengue in low- or moderate-transmission areas but probably wouldn’t accomplish complete control in the highest-risk areas (Sci Transl Med. 2015;7[279]:279ra37).
Dr. Harris reported that the Camino Verde trial was funded by the UBS Optimus Foundation. She reported having no financial conflicts of interest.
SAN DIEGO – In the aftermath of the latest somewhat disappointing report on the effort to develop a dengue vaccine, novel nonvaccine approaches aimed at curbing this rapidly growing public health problem are drawing renewed attention, Eva Harris, Ph.D., declared at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
These promising nonvaccine tools fall into several categories: vector control using genetically modified mosquitoes, development of new and better insecticides, and communitywide nonpesticide-based source reduction programs, explained Dr. Harris, professor of infectious diseases and vaccinology and director of the Center for Global Public Health at the University of California, Berkeley.
Many dengue experts, Dr. Harris among them, were disappointed in the recently reported long-term results of several large clinical trials of the candidate dengue vaccine furthest along in the developmental pipeline. The Sanofi Pasteur vaccine, known as CYD-TDV, is due for review and potential registration by the World Health Organization next year. The latest results show favorable safety but suboptimal efficacy. On the plus side, the data showed that children aged 9-16 years continued to benefit 3-4 years after vaccination. There was, however, a disturbing finding: children younger than 9 years of age at vaccination had an increased risk of hospitalization for dengue when they were naturally infected in the third year following vaccination (N Engl J Med. 2015;373[13]:1195-206).
In an accompanying editorial titled “A Candidate Dengue Vaccine Walks a Tightrope,” Dr. Cameron P. Simmons called the latter finding “a particularly unwelcome outcome” that, if not due to chance, raises the possibility that immunization of young children elicits only transient antibody-mediated immunity. As their antibody titers wane over time, these vaccinated children may, through sensitization, be predisposed to clinical dengue infections that are sufficiently serious to warrant hospitalization. It’s possible, but unproved, that booster doses of the vaccine might circumvent this problem, he added.
“The bumpy road to a vaccine-based solution for dengue continues,” observed Dr. Simmons of the University of Melbourne (N Engl J Med. 2015;373[13]:1263-4).
Dr. Harris noted that two other vaccines, one sponsored by the National Institutes of Health and the other by Takeda, are due to start large, long-term phase-III clinical trials in the next few months. And Merck and GlaxoSmithKline have next-generation vaccines in phase-I studies. But possible consideration of any of these vaccines for regulatory approval is a long ways off, and her focus at ICAAC 2015 was on nonvaccine solutions.
She and her coinvestigators recently published positive results of their landmark randomized controlled trial of a pesticide-free, community-based mobilization program for dengue prevention known as the Camino Verde, or Green Way (BMJ. 2015;351:h3267).
The impetus for this program was recognition of the shortcomings of current dengue control efforts, which rely heavily upon massive use of the organophosphate pesticide temephos (Abate) in household water containers where the mosquito vectors breed. The pesticide program hasn’t prevented ongoing rapid growth of the dengue pandemic. Moreover, the associated human toxicity and negative environmental effects are a mounting concern.
Camino Verde is a nonchemical alternative approach in which facilitators run intervention design groups in neighborhoods to inform community leaders and other residents about the scope of their local dengue mosquito problem based upon entomologic survey results and then help develop consensus regarding community-specific programs for chemical-free prevention of mosquito reproduction. Popular options included introduction of fish into water storage containers, cleanup campaigns targeting abandoned tires and other standing-water sources, and scrubbing and covering water tanks. Allowing each participating site to select its own interventions encouraged strong community support, Dr. Harris explained.
The prospective Camino Verde study involved nearly 19,000 households with more than 85,000 residents in Nicaragua and Mexico. Clusters of households were randomized to continuation of the temephos-based, government-run dengue control program with or without adding on the Camino Verde intervention.
Among the key findings: There was a 30% lower risk of serologic infection with dengue virus among children from intervention sites, as well as a 25% reduction in dengue illness among people of all ages. The numbers needed to treat were 30 for a reduced risk of infection in children and 71 for a lower risk of illness. Investigators also documented a 44% reduction in houses containing Aedes aegypti larvae or pupae in Camino Verde–participating sites, compared with control communities.
This study provides the first-ever solid serologic evidence that a pesticide-free community mobilization effort has a positive impact on dengue infection. The logical next step is for governments in dengue-endemic countries to adopt such an approach, she said.
At least three different strategies of genetic modification of dengue-vector mosquitoes are being pursued in an effort to reduce dengue transmission. All show promise as partial solutions, in Dr. Harris’ view.
Release of sterile transgenic A. aegypti males over the course of a year in a Brazilian suburb resulted in a 95% reduction in the size of the local A. aegypti population, compared with an adjacent control area (PLoS Negl Trop Dis. 2015;9[7]:e0003864). Investigators at Colorado State University in Fort Collins have developed a transgenic strain of A. aegypti males carrying a dominant lethal gene resulting in next-generation flightless females that can’t mate or avoid predators (Proc Natl Acad Sci U S A. 2011;108[12]:4772-5).
In another approach, an international collaborative group has performed field-release trials of A. aegypti mosquitoes deliberately infected with a strain of the intracellular bacterium Wolbachia, which renders the insects resistant to dengue virus infection. The group’s mathematical modeling suggested widespread adoption of this approach would reduce dengue virus transmission by 66%-75%. The investigators predicted this would be sufficient to eliminate dengue in low- or moderate-transmission areas but probably wouldn’t accomplish complete control in the highest-risk areas (Sci Transl Med. 2015;7[279]:279ra37).
Dr. Harris reported that the Camino Verde trial was funded by the UBS Optimus Foundation. She reported having no financial conflicts of interest.
EXPERT ANALYSIS FROM ICAAC 2015
Big declines seen in aspergillosis mortality
SAN DIEGO – In-hospital mortality in patients with aspergillosis plummeted nationally, according to data from 2001-2011, with the biggest improvement seen in immunocompromised patients traditionally considered at high mortality risk, Dr. Masako Mizusawa reported at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
The decline in in-hospital mortality wasn’t linear. Rather, it followed a stepwise pattern, and those steps occurred in association with three major advances during the study years: Food and Drug Administration approval of voriconazole in 2002, the FDA’s 2003 approval of the galactomannan serologic assay allowing for speedier diagnosis of aspergillosis, and the 2008 Infectious Diseases Society of America clinical practice guidelines on the treatment of aspergillosis (Clin Infect Dis. 2008 Feb 1;46[3]:327-60).
“This was an observational study and we can’t actually say that these events are causative. But just looking at the time relationship, it certainly looks plausible,” Dr. Mizusawa said.
In addition, the median hospital length of stay decreased from 9 to 7 days in patients with this potentially life-threatening infection, noted Dr. Mizusawa of Tufts Medical Center, Boston.
She presented what she believes is the largest U.S. longitudinal study of hospital care for aspergillosis. The retrospective study used nationally representative data from the Agency for Healthcare Research and Quality’s Healthcare Utilization and Cost Project–Nationwide Inpatient Sample.
Dr. Mizusawa and coinvestigators defined aspergillosis patients as being at high mortality risk if they had established risk factors indicative of immunocompromise, including hematologic malignancy, neutropenia, recent stem cell or solid organ transplantation, HIV, or rheumatologic disease. Patients at lower mortality risk included those with asthma, COPD, diabetes, malnutrition, pulmonary tuberculosis, or non-TB mycobacterial infection.
The proportion of patients who were high risk climbed over the years, from 41% among the 892 patients with aspergillosis-related hospitalization in the 2001 sample to 50% among 1,420 patients in 2011. Yet in-hospital mortality in high-risk patients fell from 26.4% in 2001 to 9.1% in 2011. Meanwhile, the mortality rate in lower-risk patients improved from 14.6% to 6.6%. The overall in-hospital mortality rate went from 18.8% to 7.7%.
Of note, the proportion of aspergillosis patients with renal failure jumped from 9.8% in 2001 to 21.5% in 2011, even though the treatments for aspergillosis are relatively non-nephrotoxic, with the exception of amphotericin B. The outlook for these patients has improved greatly: In-hospital mortality for aspergillosis patients in renal failure went from 40.2% in 2001 to 16.1% in 2011.
While in-hospital mortality and length of stay were decreasing during the study years, total hospital charges for patients with aspergillosis were going up: from a median of $29,998 in 2001 to $44,888 in 2001 dollars a decade later. This cost-of-care increase was confined to patients at lower baseline risk or with no risk factors. Somewhat surprisingly, the high-risk group didn’t have a significant increase in hospital charges over the 10-year period.
“Maybe we’re just doing a better job of treating them, so they may not necessarily have to use a lot of resources,” Dr. Mizusawa offered as explanation.
She reported having no financial conflicts regarding this unfunded study.
SAN DIEGO – In-hospital mortality in patients with aspergillosis plummeted nationally, according to data from 2001-2011, with the biggest improvement seen in immunocompromised patients traditionally considered at high mortality risk, Dr. Masako Mizusawa reported at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
The decline in in-hospital mortality wasn’t linear. Rather, it followed a stepwise pattern, and those steps occurred in association with three major advances during the study years: Food and Drug Administration approval of voriconazole in 2002, the FDA’s 2003 approval of the galactomannan serologic assay allowing for speedier diagnosis of aspergillosis, and the 2008 Infectious Diseases Society of America clinical practice guidelines on the treatment of aspergillosis (Clin Infect Dis. 2008 Feb 1;46[3]:327-60).
“This was an observational study and we can’t actually say that these events are causative. But just looking at the time relationship, it certainly looks plausible,” Dr. Mizusawa said.
In addition, the median hospital length of stay decreased from 9 to 7 days in patients with this potentially life-threatening infection, noted Dr. Mizusawa of Tufts Medical Center, Boston.
She presented what she believes is the largest U.S. longitudinal study of hospital care for aspergillosis. The retrospective study used nationally representative data from the Agency for Healthcare Research and Quality’s Healthcare Utilization and Cost Project–Nationwide Inpatient Sample.
Dr. Mizusawa and coinvestigators defined aspergillosis patients as being at high mortality risk if they had established risk factors indicative of immunocompromise, including hematologic malignancy, neutropenia, recent stem cell or solid organ transplantation, HIV, or rheumatologic disease. Patients at lower mortality risk included those with asthma, COPD, diabetes, malnutrition, pulmonary tuberculosis, or non-TB mycobacterial infection.
The proportion of patients who were high risk climbed over the years, from 41% among the 892 patients with aspergillosis-related hospitalization in the 2001 sample to 50% among 1,420 patients in 2011. Yet in-hospital mortality in high-risk patients fell from 26.4% in 2001 to 9.1% in 2011. Meanwhile, the mortality rate in lower-risk patients improved from 14.6% to 6.6%. The overall in-hospital mortality rate went from 18.8% to 7.7%.
Of note, the proportion of aspergillosis patients with renal failure jumped from 9.8% in 2001 to 21.5% in 2011, even though the treatments for aspergillosis are relatively non-nephrotoxic, with the exception of amphotericin B. The outlook for these patients has improved greatly: In-hospital mortality for aspergillosis patients in renal failure went from 40.2% in 2001 to 16.1% in 2011.
While in-hospital mortality and length of stay were decreasing during the study years, total hospital charges for patients with aspergillosis were going up: from a median of $29,998 in 2001 to $44,888 in 2001 dollars a decade later. This cost-of-care increase was confined to patients at lower baseline risk or with no risk factors. Somewhat surprisingly, the high-risk group didn’t have a significant increase in hospital charges over the 10-year period.
“Maybe we’re just doing a better job of treating them, so they may not necessarily have to use a lot of resources,” Dr. Mizusawa offered as explanation.
She reported having no financial conflicts regarding this unfunded study.
SAN DIEGO – In-hospital mortality in patients with aspergillosis plummeted nationally, according to data from 2001-2011, with the biggest improvement seen in immunocompromised patients traditionally considered at high mortality risk, Dr. Masako Mizusawa reported at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
The decline in in-hospital mortality wasn’t linear. Rather, it followed a stepwise pattern, and those steps occurred in association with three major advances during the study years: Food and Drug Administration approval of voriconazole in 2002, the FDA’s 2003 approval of the galactomannan serologic assay allowing for speedier diagnosis of aspergillosis, and the 2008 Infectious Diseases Society of America clinical practice guidelines on the treatment of aspergillosis (Clin Infect Dis. 2008 Feb 1;46[3]:327-60).
“This was an observational study and we can’t actually say that these events are causative. But just looking at the time relationship, it certainly looks plausible,” Dr. Mizusawa said.
In addition, the median hospital length of stay decreased from 9 to 7 days in patients with this potentially life-threatening infection, noted Dr. Mizusawa of Tufts Medical Center, Boston.
She presented what she believes is the largest U.S. longitudinal study of hospital care for aspergillosis. The retrospective study used nationally representative data from the Agency for Healthcare Research and Quality’s Healthcare Utilization and Cost Project–Nationwide Inpatient Sample.
Dr. Mizusawa and coinvestigators defined aspergillosis patients as being at high mortality risk if they had established risk factors indicative of immunocompromise, including hematologic malignancy, neutropenia, recent stem cell or solid organ transplantation, HIV, or rheumatologic disease. Patients at lower mortality risk included those with asthma, COPD, diabetes, malnutrition, pulmonary tuberculosis, or non-TB mycobacterial infection.
The proportion of patients who were high risk climbed over the years, from 41% among the 892 patients with aspergillosis-related hospitalization in the 2001 sample to 50% among 1,420 patients in 2011. Yet in-hospital mortality in high-risk patients fell from 26.4% in 2001 to 9.1% in 2011. Meanwhile, the mortality rate in lower-risk patients improved from 14.6% to 6.6%. The overall in-hospital mortality rate went from 18.8% to 7.7%.
Of note, the proportion of aspergillosis patients with renal failure jumped from 9.8% in 2001 to 21.5% in 2011, even though the treatments for aspergillosis are relatively non-nephrotoxic, with the exception of amphotericin B. The outlook for these patients has improved greatly: In-hospital mortality for aspergillosis patients in renal failure went from 40.2% in 2001 to 16.1% in 2011.
While in-hospital mortality and length of stay were decreasing during the study years, total hospital charges for patients with aspergillosis were going up: from a median of $29,998 in 2001 to $44,888 in 2001 dollars a decade later. This cost-of-care increase was confined to patients at lower baseline risk or with no risk factors. Somewhat surprisingly, the high-risk group didn’t have a significant increase in hospital charges over the 10-year period.
“Maybe we’re just doing a better job of treating them, so they may not necessarily have to use a lot of resources,” Dr. Mizusawa offered as explanation.
She reported having no financial conflicts regarding this unfunded study.
AT ICAAC 2015
Key clinical point: In-hospital mortality has more than halved for patients with aspergillosis-related hospitalization during a recent 10-year period.
Major finding: In-hospital mortality among patients with an aspergillosis-related hospitalization fell nationally from 18.8% in 2001 to 7.7% in 2011, with the biggest drop occurring in those at high risk.
Data source: A retrospective study of nationally representative data from the Healthcare Utilization and Cost Project–Nationwide Inpatient Sample for 2001-2011.
Disclosures: The presenter reported having no financial conflicts regarding this unfunded study.
Old drug is new treatment for chronic prostatitis
SAN DIEGO – Oral fosfomycin, a drug used for more than 4 decades to treat urinary tract infections in women, has gained a new life as a promising treatment for chronic prostatitis.
In the largest patient series reported to date, a 6-week course of fosfomycin resulted in an 85% clinical cure rate in 20 men with chronic prostatitis due to multidrug-resistant pathogens, Dr. Ilias Karaiskos reported at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
This is a most welcome development because chronic prostatitis is a common condition and Escherichia coli – the number-one pathogen – is becoming increasingly resistant to fluoroquinolones, long considered the first-line therapy. The quinolone resistance issue is of particular concern because most other antibiotics lack the pharmacokinetics required to penetrate the prostate gland, explained Dr. Karaiskos of Hygeia General Hospital in Athens.
A recent study by other investigators showing that fosfomycin penetrates the prostate and achieves potentially therapeutic levels (Clin Infect Dis. 2014 Feb;58[4]:e101-5) inspired Dr. Karaiskos and coworkers to conduct their open 20-patient trial. Participants averaged 2.25 prior episodes of prostatitis.
Urine cultures showed that the most common pathogen was indeed E. coli, and that 15 of the 20 strains were resistant to fluoroquinolones. Most strains were also resistant to minocycline and trimethoprim-sulfamethoxazole. However, all strains were sensitive to fosfomycin (Monurol).
Dosing of fosfomycin in the study was 3 g once daily for the first week, then 3 g every 48 hours for the next 5 weeks.
Seventeen of 20 patients experienced clinical cure, defined as resolution of all symptoms plus absence of any evidence of inflammation upon follow-up imaging of the prostate by transrectal ultrasound or MRI upon treatment completion after 6 weeks of fosfomycin. Two patients failed to respond, and one discontinued treatment due to diarrhea.
Diarrhea was the most common treatment-emergent adverse event, affecting 5 of 20 patients. In most instances, diarrhea subsided when the dosing intervals were extended.
Further studies are needed to clarify the best fosfomycin dosing regimen for chronic prostatitis, Dr. Karaiskos said. For uncomplicated urinary tract infections the drug is typically given in a single megadose.
Dr. Karaiskos reported having no financial conflicts regarding this study, conducted free of commercial support.
SAN DIEGO – Oral fosfomycin, a drug used for more than 4 decades to treat urinary tract infections in women, has gained a new life as a promising treatment for chronic prostatitis.
In the largest patient series reported to date, a 6-week course of fosfomycin resulted in an 85% clinical cure rate in 20 men with chronic prostatitis due to multidrug-resistant pathogens, Dr. Ilias Karaiskos reported at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
This is a most welcome development because chronic prostatitis is a common condition and Escherichia coli – the number-one pathogen – is becoming increasingly resistant to fluoroquinolones, long considered the first-line therapy. The quinolone resistance issue is of particular concern because most other antibiotics lack the pharmacokinetics required to penetrate the prostate gland, explained Dr. Karaiskos of Hygeia General Hospital in Athens.
A recent study by other investigators showing that fosfomycin penetrates the prostate and achieves potentially therapeutic levels (Clin Infect Dis. 2014 Feb;58[4]:e101-5) inspired Dr. Karaiskos and coworkers to conduct their open 20-patient trial. Participants averaged 2.25 prior episodes of prostatitis.
Urine cultures showed that the most common pathogen was indeed E. coli, and that 15 of the 20 strains were resistant to fluoroquinolones. Most strains were also resistant to minocycline and trimethoprim-sulfamethoxazole. However, all strains were sensitive to fosfomycin (Monurol).
Dosing of fosfomycin in the study was 3 g once daily for the first week, then 3 g every 48 hours for the next 5 weeks.
Seventeen of 20 patients experienced clinical cure, defined as resolution of all symptoms plus absence of any evidence of inflammation upon follow-up imaging of the prostate by transrectal ultrasound or MRI upon treatment completion after 6 weeks of fosfomycin. Two patients failed to respond, and one discontinued treatment due to diarrhea.
Diarrhea was the most common treatment-emergent adverse event, affecting 5 of 20 patients. In most instances, diarrhea subsided when the dosing intervals were extended.
Further studies are needed to clarify the best fosfomycin dosing regimen for chronic prostatitis, Dr. Karaiskos said. For uncomplicated urinary tract infections the drug is typically given in a single megadose.
Dr. Karaiskos reported having no financial conflicts regarding this study, conducted free of commercial support.
SAN DIEGO – Oral fosfomycin, a drug used for more than 4 decades to treat urinary tract infections in women, has gained a new life as a promising treatment for chronic prostatitis.
In the largest patient series reported to date, a 6-week course of fosfomycin resulted in an 85% clinical cure rate in 20 men with chronic prostatitis due to multidrug-resistant pathogens, Dr. Ilias Karaiskos reported at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
This is a most welcome development because chronic prostatitis is a common condition and Escherichia coli – the number-one pathogen – is becoming increasingly resistant to fluoroquinolones, long considered the first-line therapy. The quinolone resistance issue is of particular concern because most other antibiotics lack the pharmacokinetics required to penetrate the prostate gland, explained Dr. Karaiskos of Hygeia General Hospital in Athens.
A recent study by other investigators showing that fosfomycin penetrates the prostate and achieves potentially therapeutic levels (Clin Infect Dis. 2014 Feb;58[4]:e101-5) inspired Dr. Karaiskos and coworkers to conduct their open 20-patient trial. Participants averaged 2.25 prior episodes of prostatitis.
Urine cultures showed that the most common pathogen was indeed E. coli, and that 15 of the 20 strains were resistant to fluoroquinolones. Most strains were also resistant to minocycline and trimethoprim-sulfamethoxazole. However, all strains were sensitive to fosfomycin (Monurol).
Dosing of fosfomycin in the study was 3 g once daily for the first week, then 3 g every 48 hours for the next 5 weeks.
Seventeen of 20 patients experienced clinical cure, defined as resolution of all symptoms plus absence of any evidence of inflammation upon follow-up imaging of the prostate by transrectal ultrasound or MRI upon treatment completion after 6 weeks of fosfomycin. Two patients failed to respond, and one discontinued treatment due to diarrhea.
Diarrhea was the most common treatment-emergent adverse event, affecting 5 of 20 patients. In most instances, diarrhea subsided when the dosing intervals were extended.
Further studies are needed to clarify the best fosfomycin dosing regimen for chronic prostatitis, Dr. Karaiskos said. For uncomplicated urinary tract infections the drug is typically given in a single megadose.
Dr. Karaiskos reported having no financial conflicts regarding this study, conducted free of commercial support.
AT ICAAC 2015
Key clinical point: Oral fosfomycin is an effective alternative to fluoroquinolones in chronic prostatitis patients.
Major finding: Six weeks of oral fosfomycin resulted in an 85% clinical cure rate in 20 men with multidrug-resistant chronic prostatitis.
Data source: This was an open-label, uncontrolled study.
Disclosures: The presenter reported having no financial conflicts regarding the study, conducted free of commercial support.
Results mixed in hospital efforts to tackle antimicrobial resistance
SAN DIEGO – Canadian hospitals are making progress in reducing the rates of methicillin-resistant Staphylococcus aureus, but the rates of antimicrobial resistance in Canadian hospitals increased significantly for extended-spectrum beta-lactamase–producing Escherichia coli and Klebsiella pneumoniae, as well as vancomycin-resistant enterococci.
Those are among the key findings from a large national analysis known as CANWARD that were presented at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. “What it’s telling us is that some of the things that we’re doing on the antimicrobial resistance side are working,” lead study author George G. Zhanel, Pharm.D., professor of microbiology and infectious diseases at the University of Manitoba, Winnipeg, said in an interview. “But it also tells us that some of these pathogens like [vancomycin-resistant enterococci] and [extended-spectrum beta-lactamase]–producing E. coli continue to go up. So there is some good news and some bad news, but it tells us that it’s not all just doom and gloom. Some progress has been made, but there’s still a long way to go.”
Conducted annually, CANWARD is a national health surveillance study that assesses pathogens causing infections in Canadian hospitals and their patterns of antimicrobial resistance. For the current analysis, Dr. Zhanel and his associates collected 36,607 isolates from patients in tertiary care hospitals in Canada from January 2007 to December 2014. They used Clinical and Laboratory Standards Institute broth microdilution methods to perform antimicrobial susceptibility testing on more than 45 marketed and investigational agents.
Slightly more than half of the patients (55%) were male, and 87% were over age 18. The most common pathogens were E. coli (19.7%), methicillin-susceptible Staphylococcus aureus (MSSA; 16.4%), Pseudomonas aeruginosa (8.7%), S. pneumoniae (6.5%), K. pneumoniae (6.1%), methicillin-resistant S. aureus (MRSA; 4.7%), Enterococcus species (4.0%), and Hemophilus influenzae (4.0%). Susceptibility rates for E. coli were 99.9% for meropenem and tigecycline, 99.7% for ertapenem, 97.7% for piperacillin/tazobactam, 92.5% for ceftriaxone, 90.4% for gentamicin, 77.2% for ciprofloxacin, and 73.0% for trimethoprim and sulfamethoxazole. Susceptibility rates for P. aeruginosa were 94.2% for colistin, 84.3% for piperacillin/tazobactam, 83.3% for ceftazidime, 81.2% for meropenem, 77.6% for gentamicin, and 74.1% for ciprofloxacin. Susceptibility rates for MRSA were 100% for linezolid and telavancin, 99.9% for daptomycin, 99.4% for tigecycline, 99.1% for vancomycin, and 93.3% for trimethoprim and sulfamethoxazole. The rates of resistant organisms between 2007 and 2014 increased significantly for extended-spectrum beta-lactamase–producing E. coli (from 3.4% to 11.6%) and K. pneumoniae (from 1.5% to 6.5%), as well as vancomycin-resistant enterococci (from 1.8% to 7.0%), while rates of MRSA significantly declined (from 26.1% to 20.2%).
“The biggest surprise to me is that the hospital-acquired genotype of MRSA is going down,” Dr. Zhanel commented. “The community-acquired genotype is still going up, but the hospital-acquired [genotype] has plummeted in hospitals.”
He noted that CANWARD data suggest that antimicrobial resistance “is not confined to one part of the hospital. We have resistance happening in medical wards, ICUs, and hospital emergency rooms. We consistently find that resistance is highest in the ICU and by far the lowest in the ER. With clinics we find that it’s a variable scenario.”
The study was supported in part by Abbott, Achaogen, Affinium, Astellas, Astra Zeneca, Bayer, Cerexa/Forest, Cubist, Galderma Laboratories, Merck, Paladin Labs, Pfizer/Wyeth, Sunovion, and the Medicines Co. The researchers reported having no relevant financial disclosures.
SAN DIEGO – Canadian hospitals are making progress in reducing the rates of methicillin-resistant Staphylococcus aureus, but the rates of antimicrobial resistance in Canadian hospitals increased significantly for extended-spectrum beta-lactamase–producing Escherichia coli and Klebsiella pneumoniae, as well as vancomycin-resistant enterococci.
Those are among the key findings from a large national analysis known as CANWARD that were presented at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. “What it’s telling us is that some of the things that we’re doing on the antimicrobial resistance side are working,” lead study author George G. Zhanel, Pharm.D., professor of microbiology and infectious diseases at the University of Manitoba, Winnipeg, said in an interview. “But it also tells us that some of these pathogens like [vancomycin-resistant enterococci] and [extended-spectrum beta-lactamase]–producing E. coli continue to go up. So there is some good news and some bad news, but it tells us that it’s not all just doom and gloom. Some progress has been made, but there’s still a long way to go.”
Conducted annually, CANWARD is a national health surveillance study that assesses pathogens causing infections in Canadian hospitals and their patterns of antimicrobial resistance. For the current analysis, Dr. Zhanel and his associates collected 36,607 isolates from patients in tertiary care hospitals in Canada from January 2007 to December 2014. They used Clinical and Laboratory Standards Institute broth microdilution methods to perform antimicrobial susceptibility testing on more than 45 marketed and investigational agents.
Slightly more than half of the patients (55%) were male, and 87% were over age 18. The most common pathogens were E. coli (19.7%), methicillin-susceptible Staphylococcus aureus (MSSA; 16.4%), Pseudomonas aeruginosa (8.7%), S. pneumoniae (6.5%), K. pneumoniae (6.1%), methicillin-resistant S. aureus (MRSA; 4.7%), Enterococcus species (4.0%), and Hemophilus influenzae (4.0%). Susceptibility rates for E. coli were 99.9% for meropenem and tigecycline, 99.7% for ertapenem, 97.7% for piperacillin/tazobactam, 92.5% for ceftriaxone, 90.4% for gentamicin, 77.2% for ciprofloxacin, and 73.0% for trimethoprim and sulfamethoxazole. Susceptibility rates for P. aeruginosa were 94.2% for colistin, 84.3% for piperacillin/tazobactam, 83.3% for ceftazidime, 81.2% for meropenem, 77.6% for gentamicin, and 74.1% for ciprofloxacin. Susceptibility rates for MRSA were 100% for linezolid and telavancin, 99.9% for daptomycin, 99.4% for tigecycline, 99.1% for vancomycin, and 93.3% for trimethoprim and sulfamethoxazole. The rates of resistant organisms between 2007 and 2014 increased significantly for extended-spectrum beta-lactamase–producing E. coli (from 3.4% to 11.6%) and K. pneumoniae (from 1.5% to 6.5%), as well as vancomycin-resistant enterococci (from 1.8% to 7.0%), while rates of MRSA significantly declined (from 26.1% to 20.2%).
“The biggest surprise to me is that the hospital-acquired genotype of MRSA is going down,” Dr. Zhanel commented. “The community-acquired genotype is still going up, but the hospital-acquired [genotype] has plummeted in hospitals.”
He noted that CANWARD data suggest that antimicrobial resistance “is not confined to one part of the hospital. We have resistance happening in medical wards, ICUs, and hospital emergency rooms. We consistently find that resistance is highest in the ICU and by far the lowest in the ER. With clinics we find that it’s a variable scenario.”
The study was supported in part by Abbott, Achaogen, Affinium, Astellas, Astra Zeneca, Bayer, Cerexa/Forest, Cubist, Galderma Laboratories, Merck, Paladin Labs, Pfizer/Wyeth, Sunovion, and the Medicines Co. The researchers reported having no relevant financial disclosures.
SAN DIEGO – Canadian hospitals are making progress in reducing the rates of methicillin-resistant Staphylococcus aureus, but the rates of antimicrobial resistance in Canadian hospitals increased significantly for extended-spectrum beta-lactamase–producing Escherichia coli and Klebsiella pneumoniae, as well as vancomycin-resistant enterococci.
Those are among the key findings from a large national analysis known as CANWARD that were presented at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. “What it’s telling us is that some of the things that we’re doing on the antimicrobial resistance side are working,” lead study author George G. Zhanel, Pharm.D., professor of microbiology and infectious diseases at the University of Manitoba, Winnipeg, said in an interview. “But it also tells us that some of these pathogens like [vancomycin-resistant enterococci] and [extended-spectrum beta-lactamase]–producing E. coli continue to go up. So there is some good news and some bad news, but it tells us that it’s not all just doom and gloom. Some progress has been made, but there’s still a long way to go.”
Conducted annually, CANWARD is a national health surveillance study that assesses pathogens causing infections in Canadian hospitals and their patterns of antimicrobial resistance. For the current analysis, Dr. Zhanel and his associates collected 36,607 isolates from patients in tertiary care hospitals in Canada from January 2007 to December 2014. They used Clinical and Laboratory Standards Institute broth microdilution methods to perform antimicrobial susceptibility testing on more than 45 marketed and investigational agents.
Slightly more than half of the patients (55%) were male, and 87% were over age 18. The most common pathogens were E. coli (19.7%), methicillin-susceptible Staphylococcus aureus (MSSA; 16.4%), Pseudomonas aeruginosa (8.7%), S. pneumoniae (6.5%), K. pneumoniae (6.1%), methicillin-resistant S. aureus (MRSA; 4.7%), Enterococcus species (4.0%), and Hemophilus influenzae (4.0%). Susceptibility rates for E. coli were 99.9% for meropenem and tigecycline, 99.7% for ertapenem, 97.7% for piperacillin/tazobactam, 92.5% for ceftriaxone, 90.4% for gentamicin, 77.2% for ciprofloxacin, and 73.0% for trimethoprim and sulfamethoxazole. Susceptibility rates for P. aeruginosa were 94.2% for colistin, 84.3% for piperacillin/tazobactam, 83.3% for ceftazidime, 81.2% for meropenem, 77.6% for gentamicin, and 74.1% for ciprofloxacin. Susceptibility rates for MRSA were 100% for linezolid and telavancin, 99.9% for daptomycin, 99.4% for tigecycline, 99.1% for vancomycin, and 93.3% for trimethoprim and sulfamethoxazole. The rates of resistant organisms between 2007 and 2014 increased significantly for extended-spectrum beta-lactamase–producing E. coli (from 3.4% to 11.6%) and K. pneumoniae (from 1.5% to 6.5%), as well as vancomycin-resistant enterococci (from 1.8% to 7.0%), while rates of MRSA significantly declined (from 26.1% to 20.2%).
“The biggest surprise to me is that the hospital-acquired genotype of MRSA is going down,” Dr. Zhanel commented. “The community-acquired genotype is still going up, but the hospital-acquired [genotype] has plummeted in hospitals.”
He noted that CANWARD data suggest that antimicrobial resistance “is not confined to one part of the hospital. We have resistance happening in medical wards, ICUs, and hospital emergency rooms. We consistently find that resistance is highest in the ICU and by far the lowest in the ER. With clinics we find that it’s a variable scenario.”
The study was supported in part by Abbott, Achaogen, Affinium, Astellas, Astra Zeneca, Bayer, Cerexa/Forest, Cubist, Galderma Laboratories, Merck, Paladin Labs, Pfizer/Wyeth, Sunovion, and the Medicines Co. The researchers reported having no relevant financial disclosures.
AT ICAAC 2015
Key clinical point: In Canadian hospitals, the rate of resistant organisms have increased significantly for E. coli and other pathogens but have decreased for MRSA.
Major finding: Rates of resistant organisms between 2007 and 2014 increased significantly for extended-spectrum beta-lactamase–producing E. coli (from 3.4% to 11.6%) and K. pneumoniae (from 1.5% to 6.5%), as well as vancomycin-resistant enterococci (from 1.8% to 7.0%), while rates of MRSA significantly declined (from 26.1% to 20.2%).
Data source: A lab analysis of 36,607 isolates from patients in tertiary care hospitals in Canada from January 2007 to December 2014.
Disclosures: The study was supported in part by Abbott, Achaogen, Affinium, Astellas, Astra Zeneca, Bayer, Cerexa/Forest, Cubist, Galderma Laboratories, Merck, Paladin Labs, Pfizer/Wyeth, Sunovion, and the Medicines Co. The researchers reported having no relevant financial disclosures.
Peramivir effective against most flu viruses circulating globally
SAN DIEGO – The neuraminidase inhibitor peramivir inhibited about 99% of seasonal influenza A and B viruses circulating globally during the 2013-2014 and 2014-2015 influenza seasons, a large analysis demonstrated.
“The frequency of H1N1pdm09 viruses carrying neuraminidase (NA) H275Y remained low during both seasons; this mutation confers resistance to oseltamivir and peramivir,” said Margaret Okomo-Adhiambo, Ph.D., at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. In addition, “a small proportion of viruses contained other neuraminidase changes that affect binding of peramivir to viral enzymes and may decrease virus susceptibility. These changes need to be closely monitored.”
Approved by the FDA in December of 2014, peramivir (Rapivab) is the only antiviral agent for influenza treatment to come to market in nearly 20 years. Approved for intravenous administration as a single dose, it is indicated for adults with acute uncomplicated influenza who may have trouble taking orally administered or inhaled neuraminidase (NA) inhibitors. Other NA inhibitors approved by the FDA for influenza infection include oseltamivir, which is orally administered, and zanamivir, which is inhaled.
For the current analysis, Dr. Okomo-Adhiambo of the influenza division at the Centers for Disease Control and Prevention, Atlanta, and her associates tested influenza virus susceptibility to peramivir during the 2013-2014 and 2014-2015 influenza seasons as part of the World Health Organization Global Influenza Surveillance and Response System. A total of 8,426 viruses were tested, 75% of which were circulating in the United States.
Dr. Okomo-Adhiambo reported that during the 2013-2014 and 2014-2015 influenza seasons, about 99% of influenza type A and B viruses were inhibited by peramivir, except for a few viruses belonging to subtype A(H1N1)pdm09 (1.5%), subtype A(H3N2) (0.2%), and type B (0.4%). In addition, NA activity of type A viruses was five to six times more sensitive to inhibition by peramivir, compared with type B NA.
She concluded her presentation by noting that studies “are needed to establish molecular markers of clinically relevant resistance to peramivir.”
The researchers reported having no financial disclosures.
SAN DIEGO – The neuraminidase inhibitor peramivir inhibited about 99% of seasonal influenza A and B viruses circulating globally during the 2013-2014 and 2014-2015 influenza seasons, a large analysis demonstrated.
“The frequency of H1N1pdm09 viruses carrying neuraminidase (NA) H275Y remained low during both seasons; this mutation confers resistance to oseltamivir and peramivir,” said Margaret Okomo-Adhiambo, Ph.D., at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. In addition, “a small proportion of viruses contained other neuraminidase changes that affect binding of peramivir to viral enzymes and may decrease virus susceptibility. These changes need to be closely monitored.”
Approved by the FDA in December of 2014, peramivir (Rapivab) is the only antiviral agent for influenza treatment to come to market in nearly 20 years. Approved for intravenous administration as a single dose, it is indicated for adults with acute uncomplicated influenza who may have trouble taking orally administered or inhaled neuraminidase (NA) inhibitors. Other NA inhibitors approved by the FDA for influenza infection include oseltamivir, which is orally administered, and zanamivir, which is inhaled.
For the current analysis, Dr. Okomo-Adhiambo of the influenza division at the Centers for Disease Control and Prevention, Atlanta, and her associates tested influenza virus susceptibility to peramivir during the 2013-2014 and 2014-2015 influenza seasons as part of the World Health Organization Global Influenza Surveillance and Response System. A total of 8,426 viruses were tested, 75% of which were circulating in the United States.
Dr. Okomo-Adhiambo reported that during the 2013-2014 and 2014-2015 influenza seasons, about 99% of influenza type A and B viruses were inhibited by peramivir, except for a few viruses belonging to subtype A(H1N1)pdm09 (1.5%), subtype A(H3N2) (0.2%), and type B (0.4%). In addition, NA activity of type A viruses was five to six times more sensitive to inhibition by peramivir, compared with type B NA.
She concluded her presentation by noting that studies “are needed to establish molecular markers of clinically relevant resistance to peramivir.”
The researchers reported having no financial disclosures.
SAN DIEGO – The neuraminidase inhibitor peramivir inhibited about 99% of seasonal influenza A and B viruses circulating globally during the 2013-2014 and 2014-2015 influenza seasons, a large analysis demonstrated.
“The frequency of H1N1pdm09 viruses carrying neuraminidase (NA) H275Y remained low during both seasons; this mutation confers resistance to oseltamivir and peramivir,” said Margaret Okomo-Adhiambo, Ph.D., at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. In addition, “a small proportion of viruses contained other neuraminidase changes that affect binding of peramivir to viral enzymes and may decrease virus susceptibility. These changes need to be closely monitored.”
Approved by the FDA in December of 2014, peramivir (Rapivab) is the only antiviral agent for influenza treatment to come to market in nearly 20 years. Approved for intravenous administration as a single dose, it is indicated for adults with acute uncomplicated influenza who may have trouble taking orally administered or inhaled neuraminidase (NA) inhibitors. Other NA inhibitors approved by the FDA for influenza infection include oseltamivir, which is orally administered, and zanamivir, which is inhaled.
For the current analysis, Dr. Okomo-Adhiambo of the influenza division at the Centers for Disease Control and Prevention, Atlanta, and her associates tested influenza virus susceptibility to peramivir during the 2013-2014 and 2014-2015 influenza seasons as part of the World Health Organization Global Influenza Surveillance and Response System. A total of 8,426 viruses were tested, 75% of which were circulating in the United States.
Dr. Okomo-Adhiambo reported that during the 2013-2014 and 2014-2015 influenza seasons, about 99% of influenza type A and B viruses were inhibited by peramivir, except for a few viruses belonging to subtype A(H1N1)pdm09 (1.5%), subtype A(H3N2) (0.2%), and type B (0.4%). In addition, NA activity of type A viruses was five to six times more sensitive to inhibition by peramivir, compared with type B NA.
She concluded her presentation by noting that studies “are needed to establish molecular markers of clinically relevant resistance to peramivir.”
The researchers reported having no financial disclosures.
AT ICAAC 2015
Key clinical point: Peramivir is potently effective against seasonal influenza viruses circulating globally.
Major finding: During the 2013-2014 and 2014-2015 influenza seasons, about 99% of influenza type A and B viruses were inhibited by peramivir.
Data source: An analysis of 8,426 influenza viruses that were tested during the 2013-2014 and 2014-2015 influenza seasons as part of the World Health Organization Global Influenza Surveillance and Response System.
Disclosures: The researchers reporting having no financial disclosures.
Simple breath test effectively detected TB
SAN DIEGO – Researchers in England used a novel gas analysis technique to detect tuberculosis in the breath, with a sensitivity of 93% and a specificity of 94%.
“Clearly these are promising results,” Dr. Amandip Sahota said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. “What interested me the most is that we were able to detect a significant difference in chemicals in both pulmonary and extra-pulmonary TB, which did indicate to us that the disease does not need to be limited to the lungs to be detectable in the breath.”
According to the latest data from the World Health Organization, there were 9 million active TB cases and 1.5 million deaths from the disease in 2013. Of these deaths, 80,000 were in children.
“TB remains a diagnostic challenge well into the 21st Century,” said Dr. Sahota, a consultant physician in infectious diseases at University Hospitals of Leicester, England. “We are still heavily reliant on the standard culture, which is both slow and resource-intensive throughout the world. Despite the advent of TB-PCR, we are still far away from a diagnostic test which is both available at point of care, at low cost, and is available throughout the world.”
In a study he conducted during his time as a research fellow at the University Hospitals of Coventry, in association with colleagues at the University of Warwick, Dr. Sahota and his associates used a field asymmetric ion mobility spectrometry device to collect samples of exhaled breath from 25 patients with suspected pulmonary or extra-pulmonary TB over a period of 6 months, before or within 1 week of treatment. For comparison, exhaled breath from 19 healthy controls was also obtained.
While ion mobility spectrometry has been used for years by the military and the security industry to detect explosives, for example, the technology has more recently been used to help diagnose medical conditions ranging from cancers to infections.
“Breath testing for TB is not new, but what is very exciting is the advent of newer gas sensor technologies which are being developed in line with a clinical need,” Dr. Sahota explained. “The point of interest here is volatile organic compounds: chemicals which are gaseous at ambient temperatures, often produce odors, and are endogenous products of metabolism in both health and disease states. So testing for breath can be quick, easy, and noninvasive. Clearly there’s plenty of sample. It’s rapid, and it allows access to chemicals in the blood, which are visible in the breath through ventilator processes.”
Patients in the study, which is believed to be the first of its kind, breathed into a 3L Tedlar air sample bag and the samples were tested within 2 hours with a portable field asymmetric ion mobility spectrometry device made by Oxford Immunotec, Inc. After measuring the ionic mobility of volatile organic compounds in the headspace, the researchers determined that the test was highly effective in detecting TB in the breath, with a sensitivity of 93% and a specificity of 94%.
“Clearly this is a small study and we do need to repeat this in a larger cohort to validate it further,” Dr. Sahota said. “We also need to investigate potential confounders such as other comorbidities and medications. Ideally, we’d like to use a smaller, more portable instrument which is ideally hand-held, so we’re exploring commercial partnerships.”
The study was funded by the Medical Research Council. The researchers reported having no financial disclosures.
*This story was updated on 10/5/2015.
SAN DIEGO – Researchers in England used a novel gas analysis technique to detect tuberculosis in the breath, with a sensitivity of 93% and a specificity of 94%.
“Clearly these are promising results,” Dr. Amandip Sahota said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. “What interested me the most is that we were able to detect a significant difference in chemicals in both pulmonary and extra-pulmonary TB, which did indicate to us that the disease does not need to be limited to the lungs to be detectable in the breath.”
According to the latest data from the World Health Organization, there were 9 million active TB cases and 1.5 million deaths from the disease in 2013. Of these deaths, 80,000 were in children.
“TB remains a diagnostic challenge well into the 21st Century,” said Dr. Sahota, a consultant physician in infectious diseases at University Hospitals of Leicester, England. “We are still heavily reliant on the standard culture, which is both slow and resource-intensive throughout the world. Despite the advent of TB-PCR, we are still far away from a diagnostic test which is both available at point of care, at low cost, and is available throughout the world.”
In a study he conducted during his time as a research fellow at the University Hospitals of Coventry, in association with colleagues at the University of Warwick, Dr. Sahota and his associates used a field asymmetric ion mobility spectrometry device to collect samples of exhaled breath from 25 patients with suspected pulmonary or extra-pulmonary TB over a period of 6 months, before or within 1 week of treatment. For comparison, exhaled breath from 19 healthy controls was also obtained.
While ion mobility spectrometry has been used for years by the military and the security industry to detect explosives, for example, the technology has more recently been used to help diagnose medical conditions ranging from cancers to infections.
“Breath testing for TB is not new, but what is very exciting is the advent of newer gas sensor technologies which are being developed in line with a clinical need,” Dr. Sahota explained. “The point of interest here is volatile organic compounds: chemicals which are gaseous at ambient temperatures, often produce odors, and are endogenous products of metabolism in both health and disease states. So testing for breath can be quick, easy, and noninvasive. Clearly there’s plenty of sample. It’s rapid, and it allows access to chemicals in the blood, which are visible in the breath through ventilator processes.”
Patients in the study, which is believed to be the first of its kind, breathed into a 3L Tedlar air sample bag and the samples were tested within 2 hours with a portable field asymmetric ion mobility spectrometry device made by Oxford Immunotec, Inc. After measuring the ionic mobility of volatile organic compounds in the headspace, the researchers determined that the test was highly effective in detecting TB in the breath, with a sensitivity of 93% and a specificity of 94%.
“Clearly this is a small study and we do need to repeat this in a larger cohort to validate it further,” Dr. Sahota said. “We also need to investigate potential confounders such as other comorbidities and medications. Ideally, we’d like to use a smaller, more portable instrument which is ideally hand-held, so we’re exploring commercial partnerships.”
The study was funded by the Medical Research Council. The researchers reported having no financial disclosures.
*This story was updated on 10/5/2015.
SAN DIEGO – Researchers in England used a novel gas analysis technique to detect tuberculosis in the breath, with a sensitivity of 93% and a specificity of 94%.
“Clearly these are promising results,” Dr. Amandip Sahota said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. “What interested me the most is that we were able to detect a significant difference in chemicals in both pulmonary and extra-pulmonary TB, which did indicate to us that the disease does not need to be limited to the lungs to be detectable in the breath.”
According to the latest data from the World Health Organization, there were 9 million active TB cases and 1.5 million deaths from the disease in 2013. Of these deaths, 80,000 were in children.
“TB remains a diagnostic challenge well into the 21st Century,” said Dr. Sahota, a consultant physician in infectious diseases at University Hospitals of Leicester, England. “We are still heavily reliant on the standard culture, which is both slow and resource-intensive throughout the world. Despite the advent of TB-PCR, we are still far away from a diagnostic test which is both available at point of care, at low cost, and is available throughout the world.”
In a study he conducted during his time as a research fellow at the University Hospitals of Coventry, in association with colleagues at the University of Warwick, Dr. Sahota and his associates used a field asymmetric ion mobility spectrometry device to collect samples of exhaled breath from 25 patients with suspected pulmonary or extra-pulmonary TB over a period of 6 months, before or within 1 week of treatment. For comparison, exhaled breath from 19 healthy controls was also obtained.
While ion mobility spectrometry has been used for years by the military and the security industry to detect explosives, for example, the technology has more recently been used to help diagnose medical conditions ranging from cancers to infections.
“Breath testing for TB is not new, but what is very exciting is the advent of newer gas sensor technologies which are being developed in line with a clinical need,” Dr. Sahota explained. “The point of interest here is volatile organic compounds: chemicals which are gaseous at ambient temperatures, often produce odors, and are endogenous products of metabolism in both health and disease states. So testing for breath can be quick, easy, and noninvasive. Clearly there’s plenty of sample. It’s rapid, and it allows access to chemicals in the blood, which are visible in the breath through ventilator processes.”
Patients in the study, which is believed to be the first of its kind, breathed into a 3L Tedlar air sample bag and the samples were tested within 2 hours with a portable field asymmetric ion mobility spectrometry device made by Oxford Immunotec, Inc. After measuring the ionic mobility of volatile organic compounds in the headspace, the researchers determined that the test was highly effective in detecting TB in the breath, with a sensitivity of 93% and a specificity of 94%.
“Clearly this is a small study and we do need to repeat this in a larger cohort to validate it further,” Dr. Sahota said. “We also need to investigate potential confounders such as other comorbidities and medications. Ideally, we’d like to use a smaller, more portable instrument which is ideally hand-held, so we’re exploring commercial partnerships.”
The study was funded by the Medical Research Council. The researchers reported having no financial disclosures.
*This story was updated on 10/5/2015.
AT ICAAC 2015
Key clinical point: A quick breath test was highly effective in detecting tuberculosis.
Major finding: Using field asymmetric ion mobility spectrometry to detect tuberculosis had a sensitivity of 93% and a specificity of 94%.
Data source: An analysis of volatile active compounds in samples of exhaled breath from 25 patients with suspected pulmonary or extra-pulmonary TB over a period of 6 months.
Disclosures: The study was funded by the Medical Research Council. The researchers reported having no financial disclosures.