User login
Orlando Dermatology Aesthetic and Clinical (ODAC) Conference
Simple early interventions enhance dermatologic care across the lifespan
ORLANDO – Generational dermatology can be conceptualized by looking at patients now in their 50s, 60s, and 70s and thinking about what aspects of aging could have been targeted 20 years ago had currently available tools been available then, according to Dr. Wendy E. Roberts.
“What interventions would we select for our patients, and what tools do we have that we did not have then?” said Dr. Roberts of Rancho Mirage, Calif.
One area for intervention that stands out is integumentary system collapse, with such features as stress tears, purpura, and photodamage, she said, noting that these aren’t things that happen overnight. Preventive measures, beginning with a focus on the skin barrier, can go a long way toward preventing this type of organ damage.
“Skin barrier has been upgraded to a major feature of a variety of common disease states, so I encourage everyone to start your therapeutic plan by assessing this skin care component – assessing the integrity of the skin,” she said, explaining that entities including xerosis, pruritus, purpura, and rosacea share a common factor: skin barrier abnormalities.
Understanding what is normal, what indicates injury, and what is considered progressive pathology with respect to skin barrier is important.
Consider xerosis, for example.
For a long time, the condition was relegated to “just dry skin.” But xerosis is the No. 1 aging skin issue for both men and women, she noted.
Further, it contributes to other important skin pathology, including pruritus, lichen simplex chronicus, and foot fissures.
“This happens because over the course of our lifetime, we have decreasing epidermal keratinocyte transit time,” she explained.
Of note, foot ulcers are a billion dollar burden on the American health care system, and a major contributing factor – accounting for about 70% of foot ulcers – is hyperkeratosis, she said, adding that “there’s something to be said about foot care and moisturization.”
“I always recommend this in my evolving aging patients. It’s something we really need to think about, and we can’t wait to think about it in the 7th decade,” she said referring to moisturization and good skin care habits.
Moisturization is the key, and it involves the use of protectants that produce an additional barrier to water loss, hydration with moisturizers that decrease transepidermal water loss and restore water to the epidermis, and emollients that intercalate and form a nice skin barrier. Using all three is advisable, as each has a specific function, she said.
Other pearls for xerosis management include a review of all possible contributors: photodamage, menopausal status, hormonal status, comorbidities, thyroid status, and emerging medication issues. Statins and systemic retinoids, in particular, can contribute.
Climate and living environment also should be considered, as cold (and use of heating units), high altitude, and desert areas can increase the risk of xerosis.
Advise patients with xerosis to avoid prolonged contact with hot water and with detergent cleansers (in lieu of moisturizing cleansers), and recommend twice daily application of cream- or oil-based vehicles rather than lotions. Supplements, including omega-3s, vitamin A, vitamin B, and primrose may also provide some benefit, she said.
Among the other tools that Dr. Roberts recommended for use earlier in life to help improve outcomes across the lifespan are imaging technologies and full-body skin exams.
Visual interactive systems that can bring patients awareness regarding the aging process, and imaging of pigmented lesions via dermoscopy that can help track changes over time are examples of imaging modalities that can be used. Programs exist that allow patients to log in to a program from home and view the images of their skin online.
Examples include Touch MD by Alphaeon, MelaFind by MELA Sciences, and Visia by Canfield Scientific which can be useful not only for cosmetic dermatology, but also for medical dermatology, she said.
“These tools aren’t just research tools; these tools really help communicate the attributes of all aspects of aging skin and can be very beneficial,” she said.
Such images can be useful in children as well, as they can show the early effects of photodamage and encourage parents to begin sun protection efforts early.
Full-body skin exams are a must, because the most deadly skin cancers occur most often on typically covered sites. Such exams also can be used as a tool to discuss medical, cosmetic, and oncologic issues that are important throughout the aging process, she said.
Dr. Roberts reported that she is a speaker or consultant for, and/or has received honoraria from Allergan, Colorescience, L’Oreal, La Roche-Posay, NeoStrata, SkinMedica, Theraplex, and Top MD Skincare.
ORLANDO – Generational dermatology can be conceptualized by looking at patients now in their 50s, 60s, and 70s and thinking about what aspects of aging could have been targeted 20 years ago had currently available tools been available then, according to Dr. Wendy E. Roberts.
“What interventions would we select for our patients, and what tools do we have that we did not have then?” said Dr. Roberts of Rancho Mirage, Calif.
One area for intervention that stands out is integumentary system collapse, with such features as stress tears, purpura, and photodamage, she said, noting that these aren’t things that happen overnight. Preventive measures, beginning with a focus on the skin barrier, can go a long way toward preventing this type of organ damage.
“Skin barrier has been upgraded to a major feature of a variety of common disease states, so I encourage everyone to start your therapeutic plan by assessing this skin care component – assessing the integrity of the skin,” she said, explaining that entities including xerosis, pruritus, purpura, and rosacea share a common factor: skin barrier abnormalities.
Understanding what is normal, what indicates injury, and what is considered progressive pathology with respect to skin barrier is important.
Consider xerosis, for example.
For a long time, the condition was relegated to “just dry skin.” But xerosis is the No. 1 aging skin issue for both men and women, she noted.
Further, it contributes to other important skin pathology, including pruritus, lichen simplex chronicus, and foot fissures.
“This happens because over the course of our lifetime, we have decreasing epidermal keratinocyte transit time,” she explained.
Of note, foot ulcers are a billion dollar burden on the American health care system, and a major contributing factor – accounting for about 70% of foot ulcers – is hyperkeratosis, she said, adding that “there’s something to be said about foot care and moisturization.”
“I always recommend this in my evolving aging patients. It’s something we really need to think about, and we can’t wait to think about it in the 7th decade,” she said referring to moisturization and good skin care habits.
Moisturization is the key, and it involves the use of protectants that produce an additional barrier to water loss, hydration with moisturizers that decrease transepidermal water loss and restore water to the epidermis, and emollients that intercalate and form a nice skin barrier. Using all three is advisable, as each has a specific function, she said.
Other pearls for xerosis management include a review of all possible contributors: photodamage, menopausal status, hormonal status, comorbidities, thyroid status, and emerging medication issues. Statins and systemic retinoids, in particular, can contribute.
Climate and living environment also should be considered, as cold (and use of heating units), high altitude, and desert areas can increase the risk of xerosis.
Advise patients with xerosis to avoid prolonged contact with hot water and with detergent cleansers (in lieu of moisturizing cleansers), and recommend twice daily application of cream- or oil-based vehicles rather than lotions. Supplements, including omega-3s, vitamin A, vitamin B, and primrose may also provide some benefit, she said.
Among the other tools that Dr. Roberts recommended for use earlier in life to help improve outcomes across the lifespan are imaging technologies and full-body skin exams.
Visual interactive systems that can bring patients awareness regarding the aging process, and imaging of pigmented lesions via dermoscopy that can help track changes over time are examples of imaging modalities that can be used. Programs exist that allow patients to log in to a program from home and view the images of their skin online.
Examples include Touch MD by Alphaeon, MelaFind by MELA Sciences, and Visia by Canfield Scientific which can be useful not only for cosmetic dermatology, but also for medical dermatology, she said.
“These tools aren’t just research tools; these tools really help communicate the attributes of all aspects of aging skin and can be very beneficial,” she said.
Such images can be useful in children as well, as they can show the early effects of photodamage and encourage parents to begin sun protection efforts early.
Full-body skin exams are a must, because the most deadly skin cancers occur most often on typically covered sites. Such exams also can be used as a tool to discuss medical, cosmetic, and oncologic issues that are important throughout the aging process, she said.
Dr. Roberts reported that she is a speaker or consultant for, and/or has received honoraria from Allergan, Colorescience, L’Oreal, La Roche-Posay, NeoStrata, SkinMedica, Theraplex, and Top MD Skincare.
ORLANDO – Generational dermatology can be conceptualized by looking at patients now in their 50s, 60s, and 70s and thinking about what aspects of aging could have been targeted 20 years ago had currently available tools been available then, according to Dr. Wendy E. Roberts.
“What interventions would we select for our patients, and what tools do we have that we did not have then?” said Dr. Roberts of Rancho Mirage, Calif.
One area for intervention that stands out is integumentary system collapse, with such features as stress tears, purpura, and photodamage, she said, noting that these aren’t things that happen overnight. Preventive measures, beginning with a focus on the skin barrier, can go a long way toward preventing this type of organ damage.
“Skin barrier has been upgraded to a major feature of a variety of common disease states, so I encourage everyone to start your therapeutic plan by assessing this skin care component – assessing the integrity of the skin,” she said, explaining that entities including xerosis, pruritus, purpura, and rosacea share a common factor: skin barrier abnormalities.
Understanding what is normal, what indicates injury, and what is considered progressive pathology with respect to skin barrier is important.
Consider xerosis, for example.
For a long time, the condition was relegated to “just dry skin.” But xerosis is the No. 1 aging skin issue for both men and women, she noted.
Further, it contributes to other important skin pathology, including pruritus, lichen simplex chronicus, and foot fissures.
“This happens because over the course of our lifetime, we have decreasing epidermal keratinocyte transit time,” she explained.
Of note, foot ulcers are a billion dollar burden on the American health care system, and a major contributing factor – accounting for about 70% of foot ulcers – is hyperkeratosis, she said, adding that “there’s something to be said about foot care and moisturization.”
“I always recommend this in my evolving aging patients. It’s something we really need to think about, and we can’t wait to think about it in the 7th decade,” she said referring to moisturization and good skin care habits.
Moisturization is the key, and it involves the use of protectants that produce an additional barrier to water loss, hydration with moisturizers that decrease transepidermal water loss and restore water to the epidermis, and emollients that intercalate and form a nice skin barrier. Using all three is advisable, as each has a specific function, she said.
Other pearls for xerosis management include a review of all possible contributors: photodamage, menopausal status, hormonal status, comorbidities, thyroid status, and emerging medication issues. Statins and systemic retinoids, in particular, can contribute.
Climate and living environment also should be considered, as cold (and use of heating units), high altitude, and desert areas can increase the risk of xerosis.
Advise patients with xerosis to avoid prolonged contact with hot water and with detergent cleansers (in lieu of moisturizing cleansers), and recommend twice daily application of cream- or oil-based vehicles rather than lotions. Supplements, including omega-3s, vitamin A, vitamin B, and primrose may also provide some benefit, she said.
Among the other tools that Dr. Roberts recommended for use earlier in life to help improve outcomes across the lifespan are imaging technologies and full-body skin exams.
Visual interactive systems that can bring patients awareness regarding the aging process, and imaging of pigmented lesions via dermoscopy that can help track changes over time are examples of imaging modalities that can be used. Programs exist that allow patients to log in to a program from home and view the images of their skin online.
Examples include Touch MD by Alphaeon, MelaFind by MELA Sciences, and Visia by Canfield Scientific which can be useful not only for cosmetic dermatology, but also for medical dermatology, she said.
“These tools aren’t just research tools; these tools really help communicate the attributes of all aspects of aging skin and can be very beneficial,” she said.
Such images can be useful in children as well, as they can show the early effects of photodamage and encourage parents to begin sun protection efforts early.
Full-body skin exams are a must, because the most deadly skin cancers occur most often on typically covered sites. Such exams also can be used as a tool to discuss medical, cosmetic, and oncologic issues that are important throughout the aging process, she said.
Dr. Roberts reported that she is a speaker or consultant for, and/or has received honoraria from Allergan, Colorescience, L’Oreal, La Roche-Posay, NeoStrata, SkinMedica, Theraplex, and Top MD Skincare.
EXPERT ANALYSIS FROM THE ODAC CONFERENCE
New and existing hyperhidrosis treatments offer improved quality of life
ORLANDO – About 8 million people in the United States are diagnosed with hyperhidrosis, including about 1.6% of adolescents and 0.6% of prepubertal children.
Strikingly, about 70% of patients with symptoms of hyperhidrosis do not consult a physician about their symptoms, but it is likely they are well aware that something isn’t right; patients with hyperhidrosis sweat at a rate that is about four to five times greater than that in healthy controls, according to Dr. Adam Friedman.
Hyperhidrosis peaks between the ages of 18 and 54 years – the prime college and working years – so the impact on day-to-day activities can be substantial, if not disabling. In fact, patients rate the effects of hyperhidrosis on quality of life as greater than those associated with psoriasis and eczema. Similarly, school-age children can be dramatically affected by the condition, as handwriting, keeping papers and keyboards dry, sports activities, and use of handheld electronics pose specific challenges, Dr. Friedman said at the Orlando Dermatology Aesthetic and Clinical conference.
Patients may have general or focal hyperhidrosis. General hyperhidrosis can be secondary to any number of substances or conditions, including drugs, toxins, substance use, cardiovascular disorders, respiratory failure, infections, malignancies, or endocrine/metabolic disorders. Focal hyperhidrosis may be primary idiopathic, associated with neuropathies, or secondary to spinal disease or injury.
There is no known etiology, but genetics may play a role; 65% of patients in one study reported a family history of the condition.
When evaluating patients, begin with a review of systems, especially if there is concern that the hyperhidrosis is secondary to another condition. Ask about age of onset, location (about half of all patients have axillary hyperhidrosis), triggers, and symptoms. Perform a physical exam, looking for any anatomical abnormalities, as postsurgical anatomic abnormalities are a major cause of focal hyperhidrosis, and be sure to ask patients about the extent of their symptoms and the effects of the disease on their daily activities, advised Dr. Friedman, director of dermatologic research at the Albert Einstein College of Medicine, New York.
In terms of laboratory evaluation, gravimetric testing is “the golden tool” for research, but a starch iodine test to define the extent and areas of disease is the best clinical tool, he said.
A primary hyperhidrosis diagnosis requires that the patients have focal, visible, excessive sweating of 6 months duration with no apparent cause, and two of the following: bilateral and symmetric sweating, impairment of daily activities, at least one episode per week, onset of less than 25 years, positive family history, and cessation during sleep.
Noninvasive treatment options include topical antiperspirants and other topical agents, systemic medications, and iontophoresis, and minimally invasive options include botulinum toxin injections and energy-based treatments.
The standard, first-line, go-to topical treatment is aluminum salts, which come in a variety of formulations. The concentration used depends on the area affected. For example, 10%-25% can be used for the axillae, and 30%-40% can be used for the palms and soles.
Over-the-counter clinical strength products also are available and are formulated to cause less skin irritation.
Optimal use of topical treatments requires that the product remain on the skin for 6-8 hours. Overnight application is ideal, because patients typically don’t sweat at night, Dr. Friedman said, adding that the medication should be washed off before daytime sweating begins.
Nonmedicated deodorant can be used in the morning after bathing.
Dr. Friedman also recommended waiting 24-48 hours after shaving to apply topical medications, and he noted that patients should be advised to wear white or light-colored clothing, as aluminum salts will stain.
Additionally, prewashing the area to be treated is not advisable, as this introduces moisture, which can form hydrochloric acid when combined with the aluminum chloride. If irritation does occur, treat with low-potency topical steroids.
Pediatric use of topical treatments has not been specifically studied, but treatment is generally the same as in older patients. However, compliance can be a problem.
“I usually recommend application every night for the first month under occlusion with a tight-fitting white T-shirt, and then three times per week thereafter,” he said.
Noninvasive treatments are pretty simple, but require educating the patients to ensure correct use, he noted.
Keep in mind that many insurance companies consider other treatments, including iontophoresis and onabotulinumtoxinA to be medically necessary only when topical aluminum chloride or other extra-strength antiperspirants are ineffective or result in a severe rash, he added.
As for systemic agents, none have been specifically tested for hyperhidrosis in clinical trials, so use is off-label and based on case reports or small case series. Anticholinergics, including glycopyrrolate and oxybutynin, have been used with some success.
“I actually prefer glycopyrrolate, because it does not cross the blood-brain barrier, so it is associated with fewer overall systemic and neurologic side effects,” Dr. Friedman said, noting that he starts with 1 mg twice daily, titrated slowly up to a maximum of 6 mg daily.
An oral solution is available, which is useful for treating children, he said, noting that data suggest anticholinergics can be very effective in children. In one recent study, 90% of 31 children treated with an average dose of 2 mg per day of glycopyrrolate experienced improvement (J. Am. Acad. Dermatol. 2012;67:918-23). In a review of 59 children treated with oxybutynin for palmar-plantar hyperhidrosis titrated up to 5 mg twice daily, 90% experienced improvement (Pediatr. Dermatol. 2014 Dec. 10 [doi:10.1111/pde.12385]). Central nervous system side effects were more common in the latter study, however.
The downside of using anticholinergics is the need for long-term therapy and the long list of possible side effects, including dry mouth, dry eyes, constipation, blurred vision, and urinary retention – among many others, he said.
For patients with hyperhidrosis due to social phobia and performance anxiety, consider using beta-blockers. Give 10-20 mg about an hour before performance, or 5 mg in those with low blood pressure, slow baseline heart rate, or very small body mass index. A trial run at home before a performance is advisable. A number of contraindications to beta-blocker use exist, including bradycardia, atrioventricular block, and asthma, just to name a few, Dr. Friedman said.
Minimally invasive treatment options include botulinum toxin injections and energy based treatments.
Botulinum toxin injections last 3-7 months and are quite effective, with 90% of patients reporting improvement, but they can be painful and are expensive at $1,400-$1,600 per treatment.
Among new and emerging treatments that show promise are MiraDry, a microwave energy technology approved in 2011 for axillary hyperhidrosis, and topical botulinum toxin, delivered without needles thanks to nanotechnology.
The latter is currently under development by at least two companies, and trials are underway. Early data suggest treatment reduces sweating by 40%, Dr. Friedman said.
Dr. Friedman reported having no relevant financial disclosures.
ORLANDO – About 8 million people in the United States are diagnosed with hyperhidrosis, including about 1.6% of adolescents and 0.6% of prepubertal children.
Strikingly, about 70% of patients with symptoms of hyperhidrosis do not consult a physician about their symptoms, but it is likely they are well aware that something isn’t right; patients with hyperhidrosis sweat at a rate that is about four to five times greater than that in healthy controls, according to Dr. Adam Friedman.
Hyperhidrosis peaks between the ages of 18 and 54 years – the prime college and working years – so the impact on day-to-day activities can be substantial, if not disabling. In fact, patients rate the effects of hyperhidrosis on quality of life as greater than those associated with psoriasis and eczema. Similarly, school-age children can be dramatically affected by the condition, as handwriting, keeping papers and keyboards dry, sports activities, and use of handheld electronics pose specific challenges, Dr. Friedman said at the Orlando Dermatology Aesthetic and Clinical conference.
Patients may have general or focal hyperhidrosis. General hyperhidrosis can be secondary to any number of substances or conditions, including drugs, toxins, substance use, cardiovascular disorders, respiratory failure, infections, malignancies, or endocrine/metabolic disorders. Focal hyperhidrosis may be primary idiopathic, associated with neuropathies, or secondary to spinal disease or injury.
There is no known etiology, but genetics may play a role; 65% of patients in one study reported a family history of the condition.
When evaluating patients, begin with a review of systems, especially if there is concern that the hyperhidrosis is secondary to another condition. Ask about age of onset, location (about half of all patients have axillary hyperhidrosis), triggers, and symptoms. Perform a physical exam, looking for any anatomical abnormalities, as postsurgical anatomic abnormalities are a major cause of focal hyperhidrosis, and be sure to ask patients about the extent of their symptoms and the effects of the disease on their daily activities, advised Dr. Friedman, director of dermatologic research at the Albert Einstein College of Medicine, New York.
In terms of laboratory evaluation, gravimetric testing is “the golden tool” for research, but a starch iodine test to define the extent and areas of disease is the best clinical tool, he said.
A primary hyperhidrosis diagnosis requires that the patients have focal, visible, excessive sweating of 6 months duration with no apparent cause, and two of the following: bilateral and symmetric sweating, impairment of daily activities, at least one episode per week, onset of less than 25 years, positive family history, and cessation during sleep.
Noninvasive treatment options include topical antiperspirants and other topical agents, systemic medications, and iontophoresis, and minimally invasive options include botulinum toxin injections and energy-based treatments.
The standard, first-line, go-to topical treatment is aluminum salts, which come in a variety of formulations. The concentration used depends on the area affected. For example, 10%-25% can be used for the axillae, and 30%-40% can be used for the palms and soles.
Over-the-counter clinical strength products also are available and are formulated to cause less skin irritation.
Optimal use of topical treatments requires that the product remain on the skin for 6-8 hours. Overnight application is ideal, because patients typically don’t sweat at night, Dr. Friedman said, adding that the medication should be washed off before daytime sweating begins.
Nonmedicated deodorant can be used in the morning after bathing.
Dr. Friedman also recommended waiting 24-48 hours after shaving to apply topical medications, and he noted that patients should be advised to wear white or light-colored clothing, as aluminum salts will stain.
Additionally, prewashing the area to be treated is not advisable, as this introduces moisture, which can form hydrochloric acid when combined with the aluminum chloride. If irritation does occur, treat with low-potency topical steroids.
Pediatric use of topical treatments has not been specifically studied, but treatment is generally the same as in older patients. However, compliance can be a problem.
“I usually recommend application every night for the first month under occlusion with a tight-fitting white T-shirt, and then three times per week thereafter,” he said.
Noninvasive treatments are pretty simple, but require educating the patients to ensure correct use, he noted.
Keep in mind that many insurance companies consider other treatments, including iontophoresis and onabotulinumtoxinA to be medically necessary only when topical aluminum chloride or other extra-strength antiperspirants are ineffective or result in a severe rash, he added.
As for systemic agents, none have been specifically tested for hyperhidrosis in clinical trials, so use is off-label and based on case reports or small case series. Anticholinergics, including glycopyrrolate and oxybutynin, have been used with some success.
“I actually prefer glycopyrrolate, because it does not cross the blood-brain barrier, so it is associated with fewer overall systemic and neurologic side effects,” Dr. Friedman said, noting that he starts with 1 mg twice daily, titrated slowly up to a maximum of 6 mg daily.
An oral solution is available, which is useful for treating children, he said, noting that data suggest anticholinergics can be very effective in children. In one recent study, 90% of 31 children treated with an average dose of 2 mg per day of glycopyrrolate experienced improvement (J. Am. Acad. Dermatol. 2012;67:918-23). In a review of 59 children treated with oxybutynin for palmar-plantar hyperhidrosis titrated up to 5 mg twice daily, 90% experienced improvement (Pediatr. Dermatol. 2014 Dec. 10 [doi:10.1111/pde.12385]). Central nervous system side effects were more common in the latter study, however.
The downside of using anticholinergics is the need for long-term therapy and the long list of possible side effects, including dry mouth, dry eyes, constipation, blurred vision, and urinary retention – among many others, he said.
For patients with hyperhidrosis due to social phobia and performance anxiety, consider using beta-blockers. Give 10-20 mg about an hour before performance, or 5 mg in those with low blood pressure, slow baseline heart rate, or very small body mass index. A trial run at home before a performance is advisable. A number of contraindications to beta-blocker use exist, including bradycardia, atrioventricular block, and asthma, just to name a few, Dr. Friedman said.
Minimally invasive treatment options include botulinum toxin injections and energy based treatments.
Botulinum toxin injections last 3-7 months and are quite effective, with 90% of patients reporting improvement, but they can be painful and are expensive at $1,400-$1,600 per treatment.
Among new and emerging treatments that show promise are MiraDry, a microwave energy technology approved in 2011 for axillary hyperhidrosis, and topical botulinum toxin, delivered without needles thanks to nanotechnology.
The latter is currently under development by at least two companies, and trials are underway. Early data suggest treatment reduces sweating by 40%, Dr. Friedman said.
Dr. Friedman reported having no relevant financial disclosures.
ORLANDO – About 8 million people in the United States are diagnosed with hyperhidrosis, including about 1.6% of adolescents and 0.6% of prepubertal children.
Strikingly, about 70% of patients with symptoms of hyperhidrosis do not consult a physician about their symptoms, but it is likely they are well aware that something isn’t right; patients with hyperhidrosis sweat at a rate that is about four to five times greater than that in healthy controls, according to Dr. Adam Friedman.
Hyperhidrosis peaks between the ages of 18 and 54 years – the prime college and working years – so the impact on day-to-day activities can be substantial, if not disabling. In fact, patients rate the effects of hyperhidrosis on quality of life as greater than those associated with psoriasis and eczema. Similarly, school-age children can be dramatically affected by the condition, as handwriting, keeping papers and keyboards dry, sports activities, and use of handheld electronics pose specific challenges, Dr. Friedman said at the Orlando Dermatology Aesthetic and Clinical conference.
Patients may have general or focal hyperhidrosis. General hyperhidrosis can be secondary to any number of substances or conditions, including drugs, toxins, substance use, cardiovascular disorders, respiratory failure, infections, malignancies, or endocrine/metabolic disorders. Focal hyperhidrosis may be primary idiopathic, associated with neuropathies, or secondary to spinal disease or injury.
There is no known etiology, but genetics may play a role; 65% of patients in one study reported a family history of the condition.
When evaluating patients, begin with a review of systems, especially if there is concern that the hyperhidrosis is secondary to another condition. Ask about age of onset, location (about half of all patients have axillary hyperhidrosis), triggers, and symptoms. Perform a physical exam, looking for any anatomical abnormalities, as postsurgical anatomic abnormalities are a major cause of focal hyperhidrosis, and be sure to ask patients about the extent of their symptoms and the effects of the disease on their daily activities, advised Dr. Friedman, director of dermatologic research at the Albert Einstein College of Medicine, New York.
In terms of laboratory evaluation, gravimetric testing is “the golden tool” for research, but a starch iodine test to define the extent and areas of disease is the best clinical tool, he said.
A primary hyperhidrosis diagnosis requires that the patients have focal, visible, excessive sweating of 6 months duration with no apparent cause, and two of the following: bilateral and symmetric sweating, impairment of daily activities, at least one episode per week, onset of less than 25 years, positive family history, and cessation during sleep.
Noninvasive treatment options include topical antiperspirants and other topical agents, systemic medications, and iontophoresis, and minimally invasive options include botulinum toxin injections and energy-based treatments.
The standard, first-line, go-to topical treatment is aluminum salts, which come in a variety of formulations. The concentration used depends on the area affected. For example, 10%-25% can be used for the axillae, and 30%-40% can be used for the palms and soles.
Over-the-counter clinical strength products also are available and are formulated to cause less skin irritation.
Optimal use of topical treatments requires that the product remain on the skin for 6-8 hours. Overnight application is ideal, because patients typically don’t sweat at night, Dr. Friedman said, adding that the medication should be washed off before daytime sweating begins.
Nonmedicated deodorant can be used in the morning after bathing.
Dr. Friedman also recommended waiting 24-48 hours after shaving to apply topical medications, and he noted that patients should be advised to wear white or light-colored clothing, as aluminum salts will stain.
Additionally, prewashing the area to be treated is not advisable, as this introduces moisture, which can form hydrochloric acid when combined with the aluminum chloride. If irritation does occur, treat with low-potency topical steroids.
Pediatric use of topical treatments has not been specifically studied, but treatment is generally the same as in older patients. However, compliance can be a problem.
“I usually recommend application every night for the first month under occlusion with a tight-fitting white T-shirt, and then three times per week thereafter,” he said.
Noninvasive treatments are pretty simple, but require educating the patients to ensure correct use, he noted.
Keep in mind that many insurance companies consider other treatments, including iontophoresis and onabotulinumtoxinA to be medically necessary only when topical aluminum chloride or other extra-strength antiperspirants are ineffective or result in a severe rash, he added.
As for systemic agents, none have been specifically tested for hyperhidrosis in clinical trials, so use is off-label and based on case reports or small case series. Anticholinergics, including glycopyrrolate and oxybutynin, have been used with some success.
“I actually prefer glycopyrrolate, because it does not cross the blood-brain barrier, so it is associated with fewer overall systemic and neurologic side effects,” Dr. Friedman said, noting that he starts with 1 mg twice daily, titrated slowly up to a maximum of 6 mg daily.
An oral solution is available, which is useful for treating children, he said, noting that data suggest anticholinergics can be very effective in children. In one recent study, 90% of 31 children treated with an average dose of 2 mg per day of glycopyrrolate experienced improvement (J. Am. Acad. Dermatol. 2012;67:918-23). In a review of 59 children treated with oxybutynin for palmar-plantar hyperhidrosis titrated up to 5 mg twice daily, 90% experienced improvement (Pediatr. Dermatol. 2014 Dec. 10 [doi:10.1111/pde.12385]). Central nervous system side effects were more common in the latter study, however.
The downside of using anticholinergics is the need for long-term therapy and the long list of possible side effects, including dry mouth, dry eyes, constipation, blurred vision, and urinary retention – among many others, he said.
For patients with hyperhidrosis due to social phobia and performance anxiety, consider using beta-blockers. Give 10-20 mg about an hour before performance, or 5 mg in those with low blood pressure, slow baseline heart rate, or very small body mass index. A trial run at home before a performance is advisable. A number of contraindications to beta-blocker use exist, including bradycardia, atrioventricular block, and asthma, just to name a few, Dr. Friedman said.
Minimally invasive treatment options include botulinum toxin injections and energy based treatments.
Botulinum toxin injections last 3-7 months and are quite effective, with 90% of patients reporting improvement, but they can be painful and are expensive at $1,400-$1,600 per treatment.
Among new and emerging treatments that show promise are MiraDry, a microwave energy technology approved in 2011 for axillary hyperhidrosis, and topical botulinum toxin, delivered without needles thanks to nanotechnology.
The latter is currently under development by at least two companies, and trials are underway. Early data suggest treatment reduces sweating by 40%, Dr. Friedman said.
Dr. Friedman reported having no relevant financial disclosures.
EXPERT ANALYSIS FROM THE ODAC CONFERENCE
Detailed history, nonsedating antihistamines improve management of pediatric urticaria
ORLANDO – Acute urticaria in children is most often caused by infection, food, or medication, and a detailed history is imperative for improving the likelihood of identifying the culprit, according to Dr. Adam Friedman.
Mycoplasma is a particularly common infectious cause in children, but adenovirus, enterovirus, rotavirus, respiratory syncytial virus, Epstein-Barr virus, and cytomegalovirus also have been implicated in urticaria cases, Dr. Friedman, director of dermatologic research at the Albert Einstein College of Medicine, New York, said at the Orlando Dermatology Aesthetic and Clinical Conference.
With respect to foods, ask about intake of milk, eggs, peanuts, wheat, and soy. When it comes to prescription medications, antibiotics are an especially common cause.
“Nonsteroidal anti-inflammatory drugs are also a very important one. If you have a patient with a history of urticaria or a pediatric patient who has a history of urticaria of the mucosa, definitely educate the parents not to give them NSAIDs,” Dr. Friedman said.
Nonimmunologic direct mast cell activation also can be a source of acute urticaria, resulting from exposure to numerous products. These include, but are not limited to, polymyxin B, radiocontrast media, opiates, muscle relaxants, salicylates, and NSAIDs, all of which can “potentially induce urticaria in almost anyone,” he said.
Identifying the cause is more likely in acute case than in chronic cases, for which the etiology is unknown about 70% of time. Regardless, the good news is that about two-thirds of cases are self-limiting; it’s the other third that poses the greatest challenge, he said.
The best bet for nailing down a diagnosis and identifying the cause is an extensive history and physical evaluation.
“Ask a million and one questions to really get to the root of it. In some cases, chronic urticaria is really a diagnosis of exclusion,” he said.
Asking the patient to keep a diary to help identify any unusual exposures just prior to the episode, and having the patient or parent take pictures of the skin are shortcuts that can help.
Extensive laboratory testing is rarely helpful, but certain tests may be warranted. New European guidelines call for erythrocyte sedimentation rate/C-reactive protein and blood differential testing for chronic spontaneous urticaria, but others – like liver function tests, hepatitis B, antinuclear antibody, stool, urinalysis, thyroid function, and antithyroid antibodies – should be directed by the history. A complement panel may be useful in cases involving angioedema, and allergy skin testing may be warranted if a specific trigger can be implicated, but “don’t just order for the sake of ordering,” he said.
Biopsies are not typically useful except in suspected neutrophilic urticaria, which may indicate an association with autoimmune disease, as well as offer some insight into whether dapsone treatment would be helpful over other third-line therapies. Persistent cases of urticaria (lasting over 24-48 hours in one location) may suggest urticarial vasculitis, which would warrant a biopsy.
The therapeutic approach to urticaria involves educating patients about avoiding triggers and identifying and addressing underlying conditions, and using medications that address the pathophysiology of the disease (mast cells, histamine, etc).
In children, the guidelines are generally similar to those in adults, but there is a real push to avoid systemic steroids, Dr. Friedman said, noting that the only time he uses systemic steroids is as a bridge to get to the point where other therapies are beginning to take effect.
Other key concepts for managing urticaria in children, as published in 2013 (Acta. Derm. Venereol. 2013;93:500-8), include using second-generation histamine1 antihistamines for symptom relief, avoiding first-generation H1 antihistamines (due mainly to sedation), and using other therapeutic interventions only after carefully weighing risks and benefits, as evidence in children is lacking.
Nonsedating antihistamines are preferable, as sending kids to school on sedating medications can impact learning as well as social interaction, ultimately resulting in developmental delay.
Keep in mind that standard doses of such medications often are inadequate, and it is acceptable to work up to four times the dose, even in children, he said.
Triple-drug therapy, including H1 and H2 antagonists plus leukotriene blockers may be necessary.
“This is a very complicated and still important disease. The key is history – sometimes – and climbing the therapeutic ladder. These patients are really uncomfortable, and they will love you if you get this disease under control,” Dr. Friedman said.
One thing that might provide some comfort to the patients and their parents is the fact that urticaria in children does seem to have a point of remission. Parents often fear that their children will be plagued with urticaria for life, but a recent study of 92 patients showed that the remission rates at 1, 3, and 5 years were 18.5%, 54%, and 67.7% (J. Am. Acad. Dermatol. 2014;71:663-8).
The median duration of chronic urticaria was 4.3 years.
“That doesn’t sound great, but in considering one’s entire lifetime, it keeps things in perspective,” he said.
Dr. Friedman reported having no relevant disclosures.
ORLANDO – Acute urticaria in children is most often caused by infection, food, or medication, and a detailed history is imperative for improving the likelihood of identifying the culprit, according to Dr. Adam Friedman.
Mycoplasma is a particularly common infectious cause in children, but adenovirus, enterovirus, rotavirus, respiratory syncytial virus, Epstein-Barr virus, and cytomegalovirus also have been implicated in urticaria cases, Dr. Friedman, director of dermatologic research at the Albert Einstein College of Medicine, New York, said at the Orlando Dermatology Aesthetic and Clinical Conference.
With respect to foods, ask about intake of milk, eggs, peanuts, wheat, and soy. When it comes to prescription medications, antibiotics are an especially common cause.
“Nonsteroidal anti-inflammatory drugs are also a very important one. If you have a patient with a history of urticaria or a pediatric patient who has a history of urticaria of the mucosa, definitely educate the parents not to give them NSAIDs,” Dr. Friedman said.
Nonimmunologic direct mast cell activation also can be a source of acute urticaria, resulting from exposure to numerous products. These include, but are not limited to, polymyxin B, radiocontrast media, opiates, muscle relaxants, salicylates, and NSAIDs, all of which can “potentially induce urticaria in almost anyone,” he said.
Identifying the cause is more likely in acute case than in chronic cases, for which the etiology is unknown about 70% of time. Regardless, the good news is that about two-thirds of cases are self-limiting; it’s the other third that poses the greatest challenge, he said.
The best bet for nailing down a diagnosis and identifying the cause is an extensive history and physical evaluation.
“Ask a million and one questions to really get to the root of it. In some cases, chronic urticaria is really a diagnosis of exclusion,” he said.
Asking the patient to keep a diary to help identify any unusual exposures just prior to the episode, and having the patient or parent take pictures of the skin are shortcuts that can help.
Extensive laboratory testing is rarely helpful, but certain tests may be warranted. New European guidelines call for erythrocyte sedimentation rate/C-reactive protein and blood differential testing for chronic spontaneous urticaria, but others – like liver function tests, hepatitis B, antinuclear antibody, stool, urinalysis, thyroid function, and antithyroid antibodies – should be directed by the history. A complement panel may be useful in cases involving angioedema, and allergy skin testing may be warranted if a specific trigger can be implicated, but “don’t just order for the sake of ordering,” he said.
Biopsies are not typically useful except in suspected neutrophilic urticaria, which may indicate an association with autoimmune disease, as well as offer some insight into whether dapsone treatment would be helpful over other third-line therapies. Persistent cases of urticaria (lasting over 24-48 hours in one location) may suggest urticarial vasculitis, which would warrant a biopsy.
The therapeutic approach to urticaria involves educating patients about avoiding triggers and identifying and addressing underlying conditions, and using medications that address the pathophysiology of the disease (mast cells, histamine, etc).
In children, the guidelines are generally similar to those in adults, but there is a real push to avoid systemic steroids, Dr. Friedman said, noting that the only time he uses systemic steroids is as a bridge to get to the point where other therapies are beginning to take effect.
Other key concepts for managing urticaria in children, as published in 2013 (Acta. Derm. Venereol. 2013;93:500-8), include using second-generation histamine1 antihistamines for symptom relief, avoiding first-generation H1 antihistamines (due mainly to sedation), and using other therapeutic interventions only after carefully weighing risks and benefits, as evidence in children is lacking.
Nonsedating antihistamines are preferable, as sending kids to school on sedating medications can impact learning as well as social interaction, ultimately resulting in developmental delay.
Keep in mind that standard doses of such medications often are inadequate, and it is acceptable to work up to four times the dose, even in children, he said.
Triple-drug therapy, including H1 and H2 antagonists plus leukotriene blockers may be necessary.
“This is a very complicated and still important disease. The key is history – sometimes – and climbing the therapeutic ladder. These patients are really uncomfortable, and they will love you if you get this disease under control,” Dr. Friedman said.
One thing that might provide some comfort to the patients and their parents is the fact that urticaria in children does seem to have a point of remission. Parents often fear that their children will be plagued with urticaria for life, but a recent study of 92 patients showed that the remission rates at 1, 3, and 5 years were 18.5%, 54%, and 67.7% (J. Am. Acad. Dermatol. 2014;71:663-8).
The median duration of chronic urticaria was 4.3 years.
“That doesn’t sound great, but in considering one’s entire lifetime, it keeps things in perspective,” he said.
Dr. Friedman reported having no relevant disclosures.
ORLANDO – Acute urticaria in children is most often caused by infection, food, or medication, and a detailed history is imperative for improving the likelihood of identifying the culprit, according to Dr. Adam Friedman.
Mycoplasma is a particularly common infectious cause in children, but adenovirus, enterovirus, rotavirus, respiratory syncytial virus, Epstein-Barr virus, and cytomegalovirus also have been implicated in urticaria cases, Dr. Friedman, director of dermatologic research at the Albert Einstein College of Medicine, New York, said at the Orlando Dermatology Aesthetic and Clinical Conference.
With respect to foods, ask about intake of milk, eggs, peanuts, wheat, and soy. When it comes to prescription medications, antibiotics are an especially common cause.
“Nonsteroidal anti-inflammatory drugs are also a very important one. If you have a patient with a history of urticaria or a pediatric patient who has a history of urticaria of the mucosa, definitely educate the parents not to give them NSAIDs,” Dr. Friedman said.
Nonimmunologic direct mast cell activation also can be a source of acute urticaria, resulting from exposure to numerous products. These include, but are not limited to, polymyxin B, radiocontrast media, opiates, muscle relaxants, salicylates, and NSAIDs, all of which can “potentially induce urticaria in almost anyone,” he said.
Identifying the cause is more likely in acute case than in chronic cases, for which the etiology is unknown about 70% of time. Regardless, the good news is that about two-thirds of cases are self-limiting; it’s the other third that poses the greatest challenge, he said.
The best bet for nailing down a diagnosis and identifying the cause is an extensive history and physical evaluation.
“Ask a million and one questions to really get to the root of it. In some cases, chronic urticaria is really a diagnosis of exclusion,” he said.
Asking the patient to keep a diary to help identify any unusual exposures just prior to the episode, and having the patient or parent take pictures of the skin are shortcuts that can help.
Extensive laboratory testing is rarely helpful, but certain tests may be warranted. New European guidelines call for erythrocyte sedimentation rate/C-reactive protein and blood differential testing for chronic spontaneous urticaria, but others – like liver function tests, hepatitis B, antinuclear antibody, stool, urinalysis, thyroid function, and antithyroid antibodies – should be directed by the history. A complement panel may be useful in cases involving angioedema, and allergy skin testing may be warranted if a specific trigger can be implicated, but “don’t just order for the sake of ordering,” he said.
Biopsies are not typically useful except in suspected neutrophilic urticaria, which may indicate an association with autoimmune disease, as well as offer some insight into whether dapsone treatment would be helpful over other third-line therapies. Persistent cases of urticaria (lasting over 24-48 hours in one location) may suggest urticarial vasculitis, which would warrant a biopsy.
The therapeutic approach to urticaria involves educating patients about avoiding triggers and identifying and addressing underlying conditions, and using medications that address the pathophysiology of the disease (mast cells, histamine, etc).
In children, the guidelines are generally similar to those in adults, but there is a real push to avoid systemic steroids, Dr. Friedman said, noting that the only time he uses systemic steroids is as a bridge to get to the point where other therapies are beginning to take effect.
Other key concepts for managing urticaria in children, as published in 2013 (Acta. Derm. Venereol. 2013;93:500-8), include using second-generation histamine1 antihistamines for symptom relief, avoiding first-generation H1 antihistamines (due mainly to sedation), and using other therapeutic interventions only after carefully weighing risks and benefits, as evidence in children is lacking.
Nonsedating antihistamines are preferable, as sending kids to school on sedating medications can impact learning as well as social interaction, ultimately resulting in developmental delay.
Keep in mind that standard doses of such medications often are inadequate, and it is acceptable to work up to four times the dose, even in children, he said.
Triple-drug therapy, including H1 and H2 antagonists plus leukotriene blockers may be necessary.
“This is a very complicated and still important disease. The key is history – sometimes – and climbing the therapeutic ladder. These patients are really uncomfortable, and they will love you if you get this disease under control,” Dr. Friedman said.
One thing that might provide some comfort to the patients and their parents is the fact that urticaria in children does seem to have a point of remission. Parents often fear that their children will be plagued with urticaria for life, but a recent study of 92 patients showed that the remission rates at 1, 3, and 5 years were 18.5%, 54%, and 67.7% (J. Am. Acad. Dermatol. 2014;71:663-8).
The median duration of chronic urticaria was 4.3 years.
“That doesn’t sound great, but in considering one’s entire lifetime, it keeps things in perspective,” he said.
Dr. Friedman reported having no relevant disclosures.
EXPERT ANALYSIS FROM THE ODAC CONFERENCE
Survey: Psoriasis/Psoriatic Arthritis Undertreated
ORLANDO – Patients with psoriasis and psoriatic arthritis have a high level of dissatisfaction with current treatment options and have numerous unmet health care needs, according to the U.S. findings from the Multinational Assessment of Psoriasis and Psoriatic Arthritis (MAPP) survey.
Of 1,005 U.S. adults who participated in the population-based telephone survey, 735 had psoriasis diagnosed by a health care provider, and 270 had psoriatic arthritis diagnosed – with or without a diagnosis of psoriasis. Half of those surveyed reported dissatisfaction with available oral and biologic therapies, Dr. Mark Lebwohl of Mount Sinai Hospital, New York, and his colleagues reported in a poster at the Orlando Dermatology Aesthetic and Clinical Conference.
Most respondents with psoriasis reported moderate symptoms (40%), with about 30% each reporting mild or severe symptoms. Itching was the most bothersome symptom, occurring in about 42% of patients, followed by flaking (26%) and scales (22%). Itching was the greatest contributor to estimates of disease severity.
Psoriatic arthritis patients were more likely to report severe symptoms (56%), while 12% reported mild symptoms, and about a third reported moderate symptoms. Itching was the most bothersome symptom among these patients, followed by pain (21%) and flaking (19%). Pain and joint swelling were the greatest contributors to estimates of disease severity in this group, the investigators said.
The majority of respondents (57%) had seen a doctor in the past year. For psoriasis patients, that doctor was most often a dermatologist (57%), while psoriatic arthritis patients most often saw a rheumatologist (38%).
A third of patients most often saw a primary care physician.
The main reasons cited for not having seen a doctor in the past year were having mild or no symptoms, and a feeling that a health care provider would be unable to help.
Of concern, patterns reported by the patients indicated widespread undertreatment of psoriasis and psoriatic arthritis, they said.
More than one in five psoriasis patients (22%) reported no treatment at the time of the survey, and although most described their disease as moderate or severe, only 23% reported ever discussing the use of conventional oral or biologic therapies with their health care providers, and only 9% were currently receiving systemic therapy; most were using prescription topical therapy.
Psoriatic arthritis patients were much more likely than were psoriasis patients to have ever used a conventional oral or biologic therapy, but only 50% were receiving systemic therapy, while 26% reported use of biologic therapy and 24% reported use of an oral therapy.
Methotrexate was the conventional oral therapy used most often (68% of the time), followed by cyclosporine and acitretin (in 14% and 12% of patients, respectively), and etanercept was the biologic therapy used most often (56%) followed by adalimumab (used by 48%).
The most common reasons for discontinuing treatment were concerns about safety, issues with tolerability, and lack or loss of effectiveness. The greatest contributors to treatment burden among those using conventional oral therapies were side effects and the need for laboratory monitoring, and the greatest contributors among those using biologics were concerns about long-term safety, anxiety or fear, pain, and inconvenience associated with self injection.
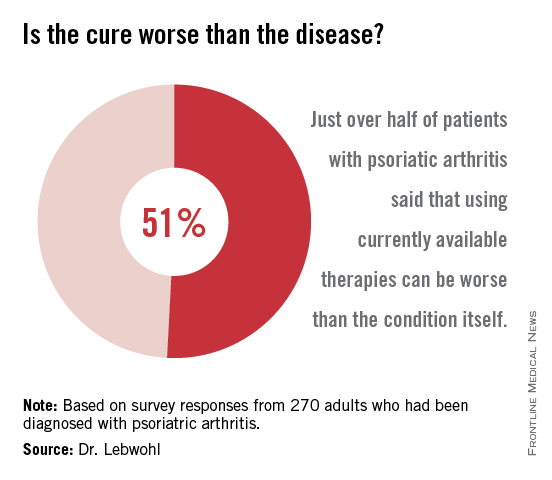
More than half of all respondents with psoriatic arthritis (51%) agreed that using currently available therapies can be worse than the condition itself, and 88% said better therapies are needed.
These results underscore the need for improved screening, as many patients with joint symptoms had not been diagnosed with psoriatic arthritis. They also demonstrate a need for improved assessment of disease severity; pruritus – which was reported as the most bothersome symptom – “is not included in most assessment tools,” the investigators noted.
Further, the results highlight the need for a higher level of treatment in many patients, they said, explaining that survey responses indicated substantial undertreatment in numerous cases. Many patients were receiving no treatment or only topical treatment, and many who were experiencing symptoms were not currently seeking care from a health care provider.
The MAPP survey is the first large-scale, multinational, population-based survey of psoriasis and psoriatic arthritis patients. The survey included 3,426 patients and 781 physicians in North America and Europe. The U.S. findings, which indicate little systematic implementation of treatment algorithms as well as widespread undertreatment, are particularly important given that psoriasis affects 3.2% of adults in the United States, and that 30% of those patients have psoriatic arthritis, the researchers noted.
Most of these patients report that their condition affects their emotional well-being, their quality of life, and their daily activities, they noted.
“These findings deserve attention and action to improve the care and lives of patients with psoriasis and psoriatic arthritis,” they concluded.
The survey was sponsored by Celgene, which markets apremilast (Otezla). Dr. Lebwohl disclosed ties to numerous pharmaceutical companies, including several that market drugs for psoriasis and psoriatic arthritis.
ORLANDO – Patients with psoriasis and psoriatic arthritis have a high level of dissatisfaction with current treatment options and have numerous unmet health care needs, according to the U.S. findings from the Multinational Assessment of Psoriasis and Psoriatic Arthritis (MAPP) survey.
Of 1,005 U.S. adults who participated in the population-based telephone survey, 735 had psoriasis diagnosed by a health care provider, and 270 had psoriatic arthritis diagnosed – with or without a diagnosis of psoriasis. Half of those surveyed reported dissatisfaction with available oral and biologic therapies, Dr. Mark Lebwohl of Mount Sinai Hospital, New York, and his colleagues reported in a poster at the Orlando Dermatology Aesthetic and Clinical Conference.
Most respondents with psoriasis reported moderate symptoms (40%), with about 30% each reporting mild or severe symptoms. Itching was the most bothersome symptom, occurring in about 42% of patients, followed by flaking (26%) and scales (22%). Itching was the greatest contributor to estimates of disease severity.
Psoriatic arthritis patients were more likely to report severe symptoms (56%), while 12% reported mild symptoms, and about a third reported moderate symptoms. Itching was the most bothersome symptom among these patients, followed by pain (21%) and flaking (19%). Pain and joint swelling were the greatest contributors to estimates of disease severity in this group, the investigators said.
The majority of respondents (57%) had seen a doctor in the past year. For psoriasis patients, that doctor was most often a dermatologist (57%), while psoriatic arthritis patients most often saw a rheumatologist (38%).
A third of patients most often saw a primary care physician.
The main reasons cited for not having seen a doctor in the past year were having mild or no symptoms, and a feeling that a health care provider would be unable to help.
Of concern, patterns reported by the patients indicated widespread undertreatment of psoriasis and psoriatic arthritis, they said.
More than one in five psoriasis patients (22%) reported no treatment at the time of the survey, and although most described their disease as moderate or severe, only 23% reported ever discussing the use of conventional oral or biologic therapies with their health care providers, and only 9% were currently receiving systemic therapy; most were using prescription topical therapy.
Psoriatic arthritis patients were much more likely than were psoriasis patients to have ever used a conventional oral or biologic therapy, but only 50% were receiving systemic therapy, while 26% reported use of biologic therapy and 24% reported use of an oral therapy.
Methotrexate was the conventional oral therapy used most often (68% of the time), followed by cyclosporine and acitretin (in 14% and 12% of patients, respectively), and etanercept was the biologic therapy used most often (56%) followed by adalimumab (used by 48%).
The most common reasons for discontinuing treatment were concerns about safety, issues with tolerability, and lack or loss of effectiveness. The greatest contributors to treatment burden among those using conventional oral therapies were side effects and the need for laboratory monitoring, and the greatest contributors among those using biologics were concerns about long-term safety, anxiety or fear, pain, and inconvenience associated with self injection.
More than half of all respondents with psoriatic arthritis (51%) agreed that using currently available therapies can be worse than the condition itself, and 88% said better therapies are needed.
These results underscore the need for improved screening, as many patients with joint symptoms had not been diagnosed with psoriatic arthritis. They also demonstrate a need for improved assessment of disease severity; pruritus – which was reported as the most bothersome symptom – “is not included in most assessment tools,” the investigators noted.
Further, the results highlight the need for a higher level of treatment in many patients, they said, explaining that survey responses indicated substantial undertreatment in numerous cases. Many patients were receiving no treatment or only topical treatment, and many who were experiencing symptoms were not currently seeking care from a health care provider.
The MAPP survey is the first large-scale, multinational, population-based survey of psoriasis and psoriatic arthritis patients. The survey included 3,426 patients and 781 physicians in North America and Europe. The U.S. findings, which indicate little systematic implementation of treatment algorithms as well as widespread undertreatment, are particularly important given that psoriasis affects 3.2% of adults in the United States, and that 30% of those patients have psoriatic arthritis, the researchers noted.
Most of these patients report that their condition affects their emotional well-being, their quality of life, and their daily activities, they noted.
“These findings deserve attention and action to improve the care and lives of patients with psoriasis and psoriatic arthritis,” they concluded.
The survey was sponsored by Celgene, which markets apremilast (Otezla). Dr. Lebwohl disclosed ties to numerous pharmaceutical companies, including several that market drugs for psoriasis and psoriatic arthritis.
ORLANDO – Patients with psoriasis and psoriatic arthritis have a high level of dissatisfaction with current treatment options and have numerous unmet health care needs, according to the U.S. findings from the Multinational Assessment of Psoriasis and Psoriatic Arthritis (MAPP) survey.
Of 1,005 U.S. adults who participated in the population-based telephone survey, 735 had psoriasis diagnosed by a health care provider, and 270 had psoriatic arthritis diagnosed – with or without a diagnosis of psoriasis. Half of those surveyed reported dissatisfaction with available oral and biologic therapies, Dr. Mark Lebwohl of Mount Sinai Hospital, New York, and his colleagues reported in a poster at the Orlando Dermatology Aesthetic and Clinical Conference.
Most respondents with psoriasis reported moderate symptoms (40%), with about 30% each reporting mild or severe symptoms. Itching was the most bothersome symptom, occurring in about 42% of patients, followed by flaking (26%) and scales (22%). Itching was the greatest contributor to estimates of disease severity.
Psoriatic arthritis patients were more likely to report severe symptoms (56%), while 12% reported mild symptoms, and about a third reported moderate symptoms. Itching was the most bothersome symptom among these patients, followed by pain (21%) and flaking (19%). Pain and joint swelling were the greatest contributors to estimates of disease severity in this group, the investigators said.
The majority of respondents (57%) had seen a doctor in the past year. For psoriasis patients, that doctor was most often a dermatologist (57%), while psoriatic arthritis patients most often saw a rheumatologist (38%).
A third of patients most often saw a primary care physician.
The main reasons cited for not having seen a doctor in the past year were having mild or no symptoms, and a feeling that a health care provider would be unable to help.
Of concern, patterns reported by the patients indicated widespread undertreatment of psoriasis and psoriatic arthritis, they said.
More than one in five psoriasis patients (22%) reported no treatment at the time of the survey, and although most described their disease as moderate or severe, only 23% reported ever discussing the use of conventional oral or biologic therapies with their health care providers, and only 9% were currently receiving systemic therapy; most were using prescription topical therapy.
Psoriatic arthritis patients were much more likely than were psoriasis patients to have ever used a conventional oral or biologic therapy, but only 50% were receiving systemic therapy, while 26% reported use of biologic therapy and 24% reported use of an oral therapy.
Methotrexate was the conventional oral therapy used most often (68% of the time), followed by cyclosporine and acitretin (in 14% and 12% of patients, respectively), and etanercept was the biologic therapy used most often (56%) followed by adalimumab (used by 48%).
The most common reasons for discontinuing treatment were concerns about safety, issues with tolerability, and lack or loss of effectiveness. The greatest contributors to treatment burden among those using conventional oral therapies were side effects and the need for laboratory monitoring, and the greatest contributors among those using biologics were concerns about long-term safety, anxiety or fear, pain, and inconvenience associated with self injection.
More than half of all respondents with psoriatic arthritis (51%) agreed that using currently available therapies can be worse than the condition itself, and 88% said better therapies are needed.
These results underscore the need for improved screening, as many patients with joint symptoms had not been diagnosed with psoriatic arthritis. They also demonstrate a need for improved assessment of disease severity; pruritus – which was reported as the most bothersome symptom – “is not included in most assessment tools,” the investigators noted.
Further, the results highlight the need for a higher level of treatment in many patients, they said, explaining that survey responses indicated substantial undertreatment in numerous cases. Many patients were receiving no treatment or only topical treatment, and many who were experiencing symptoms were not currently seeking care from a health care provider.
The MAPP survey is the first large-scale, multinational, population-based survey of psoriasis and psoriatic arthritis patients. The survey included 3,426 patients and 781 physicians in North America and Europe. The U.S. findings, which indicate little systematic implementation of treatment algorithms as well as widespread undertreatment, are particularly important given that psoriasis affects 3.2% of adults in the United States, and that 30% of those patients have psoriatic arthritis, the researchers noted.
Most of these patients report that their condition affects their emotional well-being, their quality of life, and their daily activities, they noted.
“These findings deserve attention and action to improve the care and lives of patients with psoriasis and psoriatic arthritis,” they concluded.
The survey was sponsored by Celgene, which markets apremilast (Otezla). Dr. Lebwohl disclosed ties to numerous pharmaceutical companies, including several that market drugs for psoriasis and psoriatic arthritis.
AT THE ODAC CONFERENCE
Survey: Psoriasis/psoriatic arthritis undertreated
ORLANDO – Patients with psoriasis and psoriatic arthritis have a high level of dissatisfaction with current treatment options and have numerous unmet health care needs, according to the U.S. findings from the Multinational Assessment of Psoriasis and Psoriatic Arthritis (MAPP) survey.
Of 1,005 U.S. adults who participated in the population-based telephone survey, 735 had psoriasis diagnosed by a health care provider, and 270 had psoriatic arthritis diagnosed – with or without a diagnosis of psoriasis. Half of those surveyed reported dissatisfaction with available oral and biologic therapies, Dr. Mark Lebwohl of Mount Sinai Hospital, New York, and his colleagues reported in a poster at the Orlando Dermatology Aesthetic and Clinical Conference.
Most respondents with psoriasis reported moderate symptoms (40%), with about 30% each reporting mild or severe symptoms. Itching was the most bothersome symptom, occurring in about 42% of patients, followed by flaking (26%) and scales (22%). Itching was the greatest contributor to estimates of disease severity.
Psoriatic arthritis patients were more likely to report severe symptoms (56%), while 12% reported mild symptoms, and about a third reported moderate symptoms. Itching was the most bothersome symptom among these patients, followed by pain (21%) and flaking (19%). Pain and joint swelling were the greatest contributors to estimates of disease severity in this group, the investigators said.
The majority of respondents (57%) had seen a doctor in the past year. For psoriasis patients, that doctor was most often a dermatologist (57%), while psoriatic arthritis patients most often saw a rheumatologist (38%).
A third of patients most often saw a primary care physician.
The main reasons cited for not having seen a doctor in the past year were having mild or no symptoms, and a feeling that a health care provider would be unable to help.
Of concern, patterns reported by the patients indicated widespread undertreatment of psoriasis and psoriatic arthritis, they said.
More than one in five psoriasis patients (22%) reported no treatment at the time of the survey, and although most described their disease as moderate or severe, only 23% reported ever discussing the use of conventional oral or biologic therapies with their health care providers, and only 9% were currently receiving systemic therapy; most were using prescription topical therapy.
Psoriatic arthritis patients were much more likely than were psoriasis patients to have ever used a conventional oral or biologic therapy, but only 50% were receiving systemic therapy, while 26% reported use of biologic therapy and 24% reported use of an oral therapy.
Methotrexate was the conventional oral therapy used most often (68% of the time), followed by cyclosporine and acitretin (in 14% and 12% of patients, respectively), and etanercept was the biologic therapy used most often (56%) followed by adalimumab (used by 48%).
The most common reasons for discontinuing treatment were concerns about safety, issues with tolerability, and lack or loss of effectiveness. The greatest contributors to treatment burden among those using conventional oral therapies were side effects and the need for laboratory monitoring, and the greatest contributors among those using biologics were concerns about long-term safety, anxiety or fear, pain, and inconvenience associated with self injection.
More than half of all respondents with psoriatic arthritis (51%) agreed that using currently available therapies can be worse than the condition itself, and 88% said better therapies are needed.
These results underscore the need for improved screening, as many patients with joint symptoms had not been diagnosed with psoriatic arthritis. They also demonstrate a need for improved assessment of disease severity; pruritus – which was reported as the most bothersome symptom – “is not included in most assessment tools,” the investigators noted.
Further, the results highlight the need for a higher level of treatment in many patients, they said, explaining that survey responses indicated substantial undertreatment in numerous cases. Many patients were receiving no treatment or only topical treatment, and many who were experiencing symptoms were not currently seeking care from a health care provider.
The MAPP survey is the first large-scale, multinational, population-based survey of psoriasis and psoriatic arthritis patients. The survey included 3,426 patients and 781 physicians in North America and Europe. The U.S. findings, which indicate little systematic implementation of treatment algorithms as well as widespread undertreatment, are particularly important given that psoriasis affects 3.2% of adults in the United States, and that 30% of those patients have psoriatic arthritis, the researchers noted.
Most of these patients report that their condition affects their emotional well-being, their quality of life, and their daily activities, they noted.
“These findings deserve attention and action to improve the care and lives of patients with psoriasis and psoriatic arthritis,” they concluded.
The survey was sponsored by Celgene, which markets apremilast (Otezla). Dr. Lebwohl disclosed ties to numerous pharmaceutical companies, including several that market drugs for psoriasis and psoriatic arthritis.
ORLANDO – Patients with psoriasis and psoriatic arthritis have a high level of dissatisfaction with current treatment options and have numerous unmet health care needs, according to the U.S. findings from the Multinational Assessment of Psoriasis and Psoriatic Arthritis (MAPP) survey.
Of 1,005 U.S. adults who participated in the population-based telephone survey, 735 had psoriasis diagnosed by a health care provider, and 270 had psoriatic arthritis diagnosed – with or without a diagnosis of psoriasis. Half of those surveyed reported dissatisfaction with available oral and biologic therapies, Dr. Mark Lebwohl of Mount Sinai Hospital, New York, and his colleagues reported in a poster at the Orlando Dermatology Aesthetic and Clinical Conference.
Most respondents with psoriasis reported moderate symptoms (40%), with about 30% each reporting mild or severe symptoms. Itching was the most bothersome symptom, occurring in about 42% of patients, followed by flaking (26%) and scales (22%). Itching was the greatest contributor to estimates of disease severity.
Psoriatic arthritis patients were more likely to report severe symptoms (56%), while 12% reported mild symptoms, and about a third reported moderate symptoms. Itching was the most bothersome symptom among these patients, followed by pain (21%) and flaking (19%). Pain and joint swelling were the greatest contributors to estimates of disease severity in this group, the investigators said.
The majority of respondents (57%) had seen a doctor in the past year. For psoriasis patients, that doctor was most often a dermatologist (57%), while psoriatic arthritis patients most often saw a rheumatologist (38%).
A third of patients most often saw a primary care physician.
The main reasons cited for not having seen a doctor in the past year were having mild or no symptoms, and a feeling that a health care provider would be unable to help.
Of concern, patterns reported by the patients indicated widespread undertreatment of psoriasis and psoriatic arthritis, they said.
More than one in five psoriasis patients (22%) reported no treatment at the time of the survey, and although most described their disease as moderate or severe, only 23% reported ever discussing the use of conventional oral or biologic therapies with their health care providers, and only 9% were currently receiving systemic therapy; most were using prescription topical therapy.
Psoriatic arthritis patients were much more likely than were psoriasis patients to have ever used a conventional oral or biologic therapy, but only 50% were receiving systemic therapy, while 26% reported use of biologic therapy and 24% reported use of an oral therapy.
Methotrexate was the conventional oral therapy used most often (68% of the time), followed by cyclosporine and acitretin (in 14% and 12% of patients, respectively), and etanercept was the biologic therapy used most often (56%) followed by adalimumab (used by 48%).
The most common reasons for discontinuing treatment were concerns about safety, issues with tolerability, and lack or loss of effectiveness. The greatest contributors to treatment burden among those using conventional oral therapies were side effects and the need for laboratory monitoring, and the greatest contributors among those using biologics were concerns about long-term safety, anxiety or fear, pain, and inconvenience associated with self injection.
More than half of all respondents with psoriatic arthritis (51%) agreed that using currently available therapies can be worse than the condition itself, and 88% said better therapies are needed.
These results underscore the need for improved screening, as many patients with joint symptoms had not been diagnosed with psoriatic arthritis. They also demonstrate a need for improved assessment of disease severity; pruritus – which was reported as the most bothersome symptom – “is not included in most assessment tools,” the investigators noted.
Further, the results highlight the need for a higher level of treatment in many patients, they said, explaining that survey responses indicated substantial undertreatment in numerous cases. Many patients were receiving no treatment or only topical treatment, and many who were experiencing symptoms were not currently seeking care from a health care provider.
The MAPP survey is the first large-scale, multinational, population-based survey of psoriasis and psoriatic arthritis patients. The survey included 3,426 patients and 781 physicians in North America and Europe. The U.S. findings, which indicate little systematic implementation of treatment algorithms as well as widespread undertreatment, are particularly important given that psoriasis affects 3.2% of adults in the United States, and that 30% of those patients have psoriatic arthritis, the researchers noted.
Most of these patients report that their condition affects their emotional well-being, their quality of life, and their daily activities, they noted.
“These findings deserve attention and action to improve the care and lives of patients with psoriasis and psoriatic arthritis,” they concluded.
The survey was sponsored by Celgene, which markets apremilast (Otezla). Dr. Lebwohl disclosed ties to numerous pharmaceutical companies, including several that market drugs for psoriasis and psoriatic arthritis.
ORLANDO – Patients with psoriasis and psoriatic arthritis have a high level of dissatisfaction with current treatment options and have numerous unmet health care needs, according to the U.S. findings from the Multinational Assessment of Psoriasis and Psoriatic Arthritis (MAPP) survey.
Of 1,005 U.S. adults who participated in the population-based telephone survey, 735 had psoriasis diagnosed by a health care provider, and 270 had psoriatic arthritis diagnosed – with or without a diagnosis of psoriasis. Half of those surveyed reported dissatisfaction with available oral and biologic therapies, Dr. Mark Lebwohl of Mount Sinai Hospital, New York, and his colleagues reported in a poster at the Orlando Dermatology Aesthetic and Clinical Conference.
Most respondents with psoriasis reported moderate symptoms (40%), with about 30% each reporting mild or severe symptoms. Itching was the most bothersome symptom, occurring in about 42% of patients, followed by flaking (26%) and scales (22%). Itching was the greatest contributor to estimates of disease severity.
Psoriatic arthritis patients were more likely to report severe symptoms (56%), while 12% reported mild symptoms, and about a third reported moderate symptoms. Itching was the most bothersome symptom among these patients, followed by pain (21%) and flaking (19%). Pain and joint swelling were the greatest contributors to estimates of disease severity in this group, the investigators said.
The majority of respondents (57%) had seen a doctor in the past year. For psoriasis patients, that doctor was most often a dermatologist (57%), while psoriatic arthritis patients most often saw a rheumatologist (38%).
A third of patients most often saw a primary care physician.
The main reasons cited for not having seen a doctor in the past year were having mild or no symptoms, and a feeling that a health care provider would be unable to help.
Of concern, patterns reported by the patients indicated widespread undertreatment of psoriasis and psoriatic arthritis, they said.
More than one in five psoriasis patients (22%) reported no treatment at the time of the survey, and although most described their disease as moderate or severe, only 23% reported ever discussing the use of conventional oral or biologic therapies with their health care providers, and only 9% were currently receiving systemic therapy; most were using prescription topical therapy.
Psoriatic arthritis patients were much more likely than were psoriasis patients to have ever used a conventional oral or biologic therapy, but only 50% were receiving systemic therapy, while 26% reported use of biologic therapy and 24% reported use of an oral therapy.
Methotrexate was the conventional oral therapy used most often (68% of the time), followed by cyclosporine and acitretin (in 14% and 12% of patients, respectively), and etanercept was the biologic therapy used most often (56%) followed by adalimumab (used by 48%).
The most common reasons for discontinuing treatment were concerns about safety, issues with tolerability, and lack or loss of effectiveness. The greatest contributors to treatment burden among those using conventional oral therapies were side effects and the need for laboratory monitoring, and the greatest contributors among those using biologics were concerns about long-term safety, anxiety or fear, pain, and inconvenience associated with self injection.
More than half of all respondents with psoriatic arthritis (51%) agreed that using currently available therapies can be worse than the condition itself, and 88% said better therapies are needed.
These results underscore the need for improved screening, as many patients with joint symptoms had not been diagnosed with psoriatic arthritis. They also demonstrate a need for improved assessment of disease severity; pruritus – which was reported as the most bothersome symptom – “is not included in most assessment tools,” the investigators noted.
Further, the results highlight the need for a higher level of treatment in many patients, they said, explaining that survey responses indicated substantial undertreatment in numerous cases. Many patients were receiving no treatment or only topical treatment, and many who were experiencing symptoms were not currently seeking care from a health care provider.
The MAPP survey is the first large-scale, multinational, population-based survey of psoriasis and psoriatic arthritis patients. The survey included 3,426 patients and 781 physicians in North America and Europe. The U.S. findings, which indicate little systematic implementation of treatment algorithms as well as widespread undertreatment, are particularly important given that psoriasis affects 3.2% of adults in the United States, and that 30% of those patients have psoriatic arthritis, the researchers noted.
Most of these patients report that their condition affects their emotional well-being, their quality of life, and their daily activities, they noted.
“These findings deserve attention and action to improve the care and lives of patients with psoriasis and psoriatic arthritis,” they concluded.
The survey was sponsored by Celgene, which markets apremilast (Otezla). Dr. Lebwohl disclosed ties to numerous pharmaceutical companies, including several that market drugs for psoriasis and psoriatic arthritis.
AT THE ODAC CONFERENCE
Key clinical point: Psoriasis and psoriatic arthritis treatment algorithms are underused, and patients are often undertreated.
Major finding: Among survey respondents, 22% were on no treatment, and 23% reported ever discussing conventional oral or biologic therapies with a health care provider.
Data source: A telephone survey (MAPP) of 735 psoriasis and 270 psoriatic arthritis patients.
Disclosures: The survey was sponsored by Celgene, which markets apremilast (Otezla). Dr. Lebwohl disclosed ties to numerous pharmaceutical companies, including several that market drugs for psoriasis and psoriatic arthritis.
Subungual Exostosis Masquerades as Nail Fungus
ORLANDO – In a patient presenting with a tender, firm lesion under the nail, think subungual exostosis, Dr. Phoebe Rich advised.
Subungual exostosis is a benign bony growth that can cause discomfort by pressing up from the nail bed. It can be mistaken for onychomycosis, but keep in mind that only 50% of those presenting with nail disorders will have onychomycosis, so it is important to consider other diagnoses, Dr. Rich, director of the Nail Disorder Center at Oregon Health and Science University, Portland, said at the Orlando Dermatology Aesthetic and Clinical Conference.
She described a teenager who presented with a growth under her nail, which the patient thought was nail fungus. The lesion developed after an injury experienced during a touch football game 2 months earlier.
An X-ray will aid in the diagnosis of such lesions, Dr. Rich said.
“You want to know that’s what it is … because you don’t want to just cut into it for a biopsy if you don’t know that it’s bone,” she said.
The diagnosis can be confirmed by removing the nail to take a look at the tumor.
“They are pretty characteristic. They are a bony growth. They’re actually composed of bone with a fibro-cartilaginous cap,” she said noting that tenderness is an important clue to the diagnosis.
Subungual exostosis occurs more often in toes than fingers, more often in girls than boys, and more often in children and young adults than older individuals, Dr. Rich noted.
Surgical removal is typically successful; the recurrence rate is about 10%, and recurrence is more common in children.
Presentation varies; some lesions can be quite obvious, with the growth protruding from under the nail, while others are more subtle. Dr. Rich described one young college student who presented with slight white spotting of the nail, and slight onycholysis. The patient had tenderness of the nail area when pressed, and the tumor peeked out from under the nail.
“If you see something like this, get an X-ray,” she said, adding: “You can be a hero and make the diagnosis. Don’t just treat it as though it’s a fungus.”
“If you’re very comfortable and expert at nails, great. Otherwise, make the diagnosis and send them to someone else, but you can really help these patients a lot,” she said.
Dr. Rich has participated in clinical trials with companies with antifungal/onychomycosis drugs, including Anacor, Merz, and Valeant.
ORLANDO – In a patient presenting with a tender, firm lesion under the nail, think subungual exostosis, Dr. Phoebe Rich advised.
Subungual exostosis is a benign bony growth that can cause discomfort by pressing up from the nail bed. It can be mistaken for onychomycosis, but keep in mind that only 50% of those presenting with nail disorders will have onychomycosis, so it is important to consider other diagnoses, Dr. Rich, director of the Nail Disorder Center at Oregon Health and Science University, Portland, said at the Orlando Dermatology Aesthetic and Clinical Conference.
She described a teenager who presented with a growth under her nail, which the patient thought was nail fungus. The lesion developed after an injury experienced during a touch football game 2 months earlier.
An X-ray will aid in the diagnosis of such lesions, Dr. Rich said.
“You want to know that’s what it is … because you don’t want to just cut into it for a biopsy if you don’t know that it’s bone,” she said.
The diagnosis can be confirmed by removing the nail to take a look at the tumor.
“They are pretty characteristic. They are a bony growth. They’re actually composed of bone with a fibro-cartilaginous cap,” she said noting that tenderness is an important clue to the diagnosis.
Subungual exostosis occurs more often in toes than fingers, more often in girls than boys, and more often in children and young adults than older individuals, Dr. Rich noted.
Surgical removal is typically successful; the recurrence rate is about 10%, and recurrence is more common in children.
Presentation varies; some lesions can be quite obvious, with the growth protruding from under the nail, while others are more subtle. Dr. Rich described one young college student who presented with slight white spotting of the nail, and slight onycholysis. The patient had tenderness of the nail area when pressed, and the tumor peeked out from under the nail.
“If you see something like this, get an X-ray,” she said, adding: “You can be a hero and make the diagnosis. Don’t just treat it as though it’s a fungus.”
“If you’re very comfortable and expert at nails, great. Otherwise, make the diagnosis and send them to someone else, but you can really help these patients a lot,” she said.
Dr. Rich has participated in clinical trials with companies with antifungal/onychomycosis drugs, including Anacor, Merz, and Valeant.
ORLANDO – In a patient presenting with a tender, firm lesion under the nail, think subungual exostosis, Dr. Phoebe Rich advised.
Subungual exostosis is a benign bony growth that can cause discomfort by pressing up from the nail bed. It can be mistaken for onychomycosis, but keep in mind that only 50% of those presenting with nail disorders will have onychomycosis, so it is important to consider other diagnoses, Dr. Rich, director of the Nail Disorder Center at Oregon Health and Science University, Portland, said at the Orlando Dermatology Aesthetic and Clinical Conference.
She described a teenager who presented with a growth under her nail, which the patient thought was nail fungus. The lesion developed after an injury experienced during a touch football game 2 months earlier.
An X-ray will aid in the diagnosis of such lesions, Dr. Rich said.
“You want to know that’s what it is … because you don’t want to just cut into it for a biopsy if you don’t know that it’s bone,” she said.
The diagnosis can be confirmed by removing the nail to take a look at the tumor.
“They are pretty characteristic. They are a bony growth. They’re actually composed of bone with a fibro-cartilaginous cap,” she said noting that tenderness is an important clue to the diagnosis.
Subungual exostosis occurs more often in toes than fingers, more often in girls than boys, and more often in children and young adults than older individuals, Dr. Rich noted.
Surgical removal is typically successful; the recurrence rate is about 10%, and recurrence is more common in children.
Presentation varies; some lesions can be quite obvious, with the growth protruding from under the nail, while others are more subtle. Dr. Rich described one young college student who presented with slight white spotting of the nail, and slight onycholysis. The patient had tenderness of the nail area when pressed, and the tumor peeked out from under the nail.
“If you see something like this, get an X-ray,” she said, adding: “You can be a hero and make the diagnosis. Don’t just treat it as though it’s a fungus.”
“If you’re very comfortable and expert at nails, great. Otherwise, make the diagnosis and send them to someone else, but you can really help these patients a lot,” she said.
Dr. Rich has participated in clinical trials with companies with antifungal/onychomycosis drugs, including Anacor, Merz, and Valeant.
EXPERT ANALYSIS AT THE ODAC CONFERENCE
Subungual exostosis masquerades as nail fungus
ORLANDO – In a patient presenting with a tender, firm lesion under the nail, think subungual exostosis, Dr. Phoebe Rich advised.
Subungual exostosis is a benign bony growth that can cause discomfort by pressing up from the nail bed. It can be mistaken for onychomycosis, but keep in mind that only 50% of those presenting with nail disorders will have onychomycosis, so it is important to consider other diagnoses, Dr. Rich, director of the Nail Disorder Center at Oregon Health and Science University, Portland, said at the Orlando Dermatology Aesthetic and Clinical Conference.
She described a teenager who presented with a growth under her nail, which the patient thought was nail fungus. The lesion developed after an injury experienced during a touch football game 2 months earlier.
An X-ray will aid in the diagnosis of such lesions, Dr. Rich said.
“You want to know that’s what it is … because you don’t want to just cut into it for a biopsy if you don’t know that it’s bone,” she said.
The diagnosis can be confirmed by removing the nail to take a look at the tumor.
“They are pretty characteristic. They are a bony growth. They’re actually composed of bone with a fibro-cartilaginous cap,” she said noting that tenderness is an important clue to the diagnosis.
Subungual exostosis occurs more often in toes than fingers, more often in girls than boys, and more often in children and young adults than older individuals, Dr. Rich noted.
Surgical removal is typically successful; the recurrence rate is about 10%, and recurrence is more common in children.
Presentation varies; some lesions can be quite obvious, with the growth protruding from under the nail, while others are more subtle. Dr. Rich described one young college student who presented with slight white spotting of the nail, and slight onycholysis. The patient had tenderness of the nail area when pressed, and the tumor peeked out from under the nail.
“If you see something like this, get an X-ray,” she said, adding: “You can be a hero and make the diagnosis. Don’t just treat it as though it’s a fungus.”
“If you’re very comfortable and expert at nails, great. Otherwise, make the diagnosis and send them to someone else, but you can really help these patients a lot,” she said.
Dr. Rich has participated in clinical trials with companies with antifungal/onychomycosis drugs, including Anacor, Merz, and Valeant.
ORLANDO – In a patient presenting with a tender, firm lesion under the nail, think subungual exostosis, Dr. Phoebe Rich advised.
Subungual exostosis is a benign bony growth that can cause discomfort by pressing up from the nail bed. It can be mistaken for onychomycosis, but keep in mind that only 50% of those presenting with nail disorders will have onychomycosis, so it is important to consider other diagnoses, Dr. Rich, director of the Nail Disorder Center at Oregon Health and Science University, Portland, said at the Orlando Dermatology Aesthetic and Clinical Conference.
She described a teenager who presented with a growth under her nail, which the patient thought was nail fungus. The lesion developed after an injury experienced during a touch football game 2 months earlier.
An X-ray will aid in the diagnosis of such lesions, Dr. Rich said.
“You want to know that’s what it is … because you don’t want to just cut into it for a biopsy if you don’t know that it’s bone,” she said.
The diagnosis can be confirmed by removing the nail to take a look at the tumor.
“They are pretty characteristic. They are a bony growth. They’re actually composed of bone with a fibro-cartilaginous cap,” she said noting that tenderness is an important clue to the diagnosis.
Subungual exostosis occurs more often in toes than fingers, more often in girls than boys, and more often in children and young adults than older individuals, Dr. Rich noted.
Surgical removal is typically successful; the recurrence rate is about 10%, and recurrence is more common in children.
Presentation varies; some lesions can be quite obvious, with the growth protruding from under the nail, while others are more subtle. Dr. Rich described one young college student who presented with slight white spotting of the nail, and slight onycholysis. The patient had tenderness of the nail area when pressed, and the tumor peeked out from under the nail.
“If you see something like this, get an X-ray,” she said, adding: “You can be a hero and make the diagnosis. Don’t just treat it as though it’s a fungus.”
“If you’re very comfortable and expert at nails, great. Otherwise, make the diagnosis and send them to someone else, but you can really help these patients a lot,” she said.
Dr. Rich has participated in clinical trials with companies with antifungal/onychomycosis drugs, including Anacor, Merz, and Valeant.
ORLANDO – In a patient presenting with a tender, firm lesion under the nail, think subungual exostosis, Dr. Phoebe Rich advised.
Subungual exostosis is a benign bony growth that can cause discomfort by pressing up from the nail bed. It can be mistaken for onychomycosis, but keep in mind that only 50% of those presenting with nail disorders will have onychomycosis, so it is important to consider other diagnoses, Dr. Rich, director of the Nail Disorder Center at Oregon Health and Science University, Portland, said at the Orlando Dermatology Aesthetic and Clinical Conference.
She described a teenager who presented with a growth under her nail, which the patient thought was nail fungus. The lesion developed after an injury experienced during a touch football game 2 months earlier.
An X-ray will aid in the diagnosis of such lesions, Dr. Rich said.
“You want to know that’s what it is … because you don’t want to just cut into it for a biopsy if you don’t know that it’s bone,” she said.
The diagnosis can be confirmed by removing the nail to take a look at the tumor.
“They are pretty characteristic. They are a bony growth. They’re actually composed of bone with a fibro-cartilaginous cap,” she said noting that tenderness is an important clue to the diagnosis.
Subungual exostosis occurs more often in toes than fingers, more often in girls than boys, and more often in children and young adults than older individuals, Dr. Rich noted.
Surgical removal is typically successful; the recurrence rate is about 10%, and recurrence is more common in children.
Presentation varies; some lesions can be quite obvious, with the growth protruding from under the nail, while others are more subtle. Dr. Rich described one young college student who presented with slight white spotting of the nail, and slight onycholysis. The patient had tenderness of the nail area when pressed, and the tumor peeked out from under the nail.
“If you see something like this, get an X-ray,” she said, adding: “You can be a hero and make the diagnosis. Don’t just treat it as though it’s a fungus.”
“If you’re very comfortable and expert at nails, great. Otherwise, make the diagnosis and send them to someone else, but you can really help these patients a lot,” she said.
Dr. Rich has participated in clinical trials with companies with antifungal/onychomycosis drugs, including Anacor, Merz, and Valeant.
EXPERT ANALYSIS AT THE ODAC CONFERENCE
Corticosteroid spray quickly, safely relieves psoriasis scaling
ORLANDO – A topical corticosteroid spray quickly and effectively reduced scaling in patients with plaque psoriasis, according to pooled phase III study results.
After 1 week of twice daily application of 0.25% Topicort spray (TaroPharma, Hawthorne, N.Y.), scaling was clear or almost clear in 29% of 120 treated patients, and was mild in an additional 40% of patients. At 4 weeks, scaling was clear or almost clear in 61% of patients, and mild in an additional 23%, Dr. Brian Keegan of East Windsor, N.J., reported in a poster at the Orlando Dermatology Aesthetic and Clinical Conference.
Additionally, 70% of patients experienced global improvement in psoriasis after 4 weeks of treatment; psoriasis was clear or almost clear in 42% of patients, and mild in 28%, Dr. Keegan said.
Study participants were adults with 10%-86% of body area affected by plaque psoriasis. Most of the patients (58%) were aged 41-to-64 years with a mean affected body surface area of 17%. Most had moderate scaling, but about a third of patients had severe or very severe scaling.
They applied Topicort 0.25% spray twice daily for 4 weeks.
The only adverse events that occurred in more than 1% of patients were dryness, irritation, and pruritus at the application site, which each occurred in 2%-3% of patients.
Treatment with Topicort – a class 1 super-potent corticosteroid indicated for up to 4 weeks of treatment of plaque psoriasis – quickly and safely relieved scaling in the majority of patients treated, Dr. Keegan concluded, noting that the findings are important given that scaling is very common among patients with plaque psoriasis, many of whom find it to be bothersome.
In fact, 94% of more than 17,000 participants in a National Psoriasis Foundation survey reported being bothered by scaling, he noted.
This study was sponsored by TaroPharma.
ORLANDO – A topical corticosteroid spray quickly and effectively reduced scaling in patients with plaque psoriasis, according to pooled phase III study results.
After 1 week of twice daily application of 0.25% Topicort spray (TaroPharma, Hawthorne, N.Y.), scaling was clear or almost clear in 29% of 120 treated patients, and was mild in an additional 40% of patients. At 4 weeks, scaling was clear or almost clear in 61% of patients, and mild in an additional 23%, Dr. Brian Keegan of East Windsor, N.J., reported in a poster at the Orlando Dermatology Aesthetic and Clinical Conference.
Additionally, 70% of patients experienced global improvement in psoriasis after 4 weeks of treatment; psoriasis was clear or almost clear in 42% of patients, and mild in 28%, Dr. Keegan said.
Study participants were adults with 10%-86% of body area affected by plaque psoriasis. Most of the patients (58%) were aged 41-to-64 years with a mean affected body surface area of 17%. Most had moderate scaling, but about a third of patients had severe or very severe scaling.
They applied Topicort 0.25% spray twice daily for 4 weeks.
The only adverse events that occurred in more than 1% of patients were dryness, irritation, and pruritus at the application site, which each occurred in 2%-3% of patients.
Treatment with Topicort – a class 1 super-potent corticosteroid indicated for up to 4 weeks of treatment of plaque psoriasis – quickly and safely relieved scaling in the majority of patients treated, Dr. Keegan concluded, noting that the findings are important given that scaling is very common among patients with plaque psoriasis, many of whom find it to be bothersome.
In fact, 94% of more than 17,000 participants in a National Psoriasis Foundation survey reported being bothered by scaling, he noted.
This study was sponsored by TaroPharma.
ORLANDO – A topical corticosteroid spray quickly and effectively reduced scaling in patients with plaque psoriasis, according to pooled phase III study results.
After 1 week of twice daily application of 0.25% Topicort spray (TaroPharma, Hawthorne, N.Y.), scaling was clear or almost clear in 29% of 120 treated patients, and was mild in an additional 40% of patients. At 4 weeks, scaling was clear or almost clear in 61% of patients, and mild in an additional 23%, Dr. Brian Keegan of East Windsor, N.J., reported in a poster at the Orlando Dermatology Aesthetic and Clinical Conference.
Additionally, 70% of patients experienced global improvement in psoriasis after 4 weeks of treatment; psoriasis was clear or almost clear in 42% of patients, and mild in 28%, Dr. Keegan said.
Study participants were adults with 10%-86% of body area affected by plaque psoriasis. Most of the patients (58%) were aged 41-to-64 years with a mean affected body surface area of 17%. Most had moderate scaling, but about a third of patients had severe or very severe scaling.
They applied Topicort 0.25% spray twice daily for 4 weeks.
The only adverse events that occurred in more than 1% of patients were dryness, irritation, and pruritus at the application site, which each occurred in 2%-3% of patients.
Treatment with Topicort – a class 1 super-potent corticosteroid indicated for up to 4 weeks of treatment of plaque psoriasis – quickly and safely relieved scaling in the majority of patients treated, Dr. Keegan concluded, noting that the findings are important given that scaling is very common among patients with plaque psoriasis, many of whom find it to be bothersome.
In fact, 94% of more than 17,000 participants in a National Psoriasis Foundation survey reported being bothered by scaling, he noted.
This study was sponsored by TaroPharma.
AT THE ODAC CONFERENCE
Key clinical point: Psoriasis patients with scaling are likely to respond to corticosteroid spray treatment.
Major finding: At 4 weeks, scaling was clear, almost clear, or mild in 84% of patients.
Data source: An analysis of pooled phase III trial data for 120 patients.
Disclosures: This study was sponsored by TaroPharma.
Wrinkle filler also works for acne scars
ORLANDO – A non-resorbable wrinkle filler proved highly effective and durable for the treatment of atrophic acne scars in a randomized, controlled, multicenter study.
At 1 month after treatment with polymethylmethacrylate-collagen, or PMMA-collagen (Artefill, Suneva Medical, Inc.), nearly 70% of 97 subjects showed at least a 2-point improvement on the validated 4-point Acne Scar Rating Scale, compared with about 40% of 50 control subjects injected with saline. At 6 months, the response rate remained above 60% in the PMMA-collagen group, but dropped closer to 30% among those in the control group, Dr. James M. Spencer of Mount Sinai School of Medicine, New York reported in a poster at the Orlando Dermatology Aesthetic and Clinical Conference.
The control group subjects were then crossed over to the treatment group, and, at 12 months, the response rates were about 70% and nearly 60% in the treatment and control groups, respectively, he said.
Similarly, both Physician and Subject Global Aesthetic Improvement Scale (PGAIS/SGAIS) scores diverged during a 6-month evaluator-blinded phase of the study, then converged after crossover by the control group subjects. For example, the percentage of treatment and control group subjects with improvement at 1 month and 6 months according to the 5-point PGAIS was about 90% vs. less than 65%, and about 80% vs. about 30%, respectively. More than 90% in both groups showed improvement at 12 months, after control group crossover.
Additionally, subject satisfaction at 1 and 6 months in the treatment and control groups based on assessment of scar correction using Patient Satisfaction Scale scores was above 80% vs. about 60%, and about 80% vs. about 50%, respectively. Satisfaction in both groups was between 80% and 90% at 12 months, after control group crossover.
Study subjects, who had a mean age of 44 years, were enrolled from 10 U.S. centers and were treated during one injection session. An additional touch-up injection was allowed as needed. A total of 1,292 scars were treated in the 97 treatment group subjects, and 424 were treated in the 50 control group subjects. Participants were evaluated by blinded assessors at 2 weeks and 1, 3, and 6 months, after which control group subjects were treated with PMMA-collagen. Assessments were made in open-label fashion at 9 and 12 months. Most subjects (61%) were women, and 20% had Fitzpatrick skin types 5 or 6.
During the blinded portion of the study, six treatment-related adverse events were reported among treatment group subjects, and two were reported among control group subjects. None of the subjects experienced granulomas, changes in pigmentation, or hypertrophic scarring.
This study is the first randomized, blinded study of PMMA-collagen for treating acne scars, Dr. Spencer noted, adding that the findings demonstrate the efficacy and safety of PMMA-collagen for this purpose.
“The improvement is durable, lasting for 12 months,” he wrote, noting that the filler is easily administered and requires minimal training in those who are familiar with dermal fillers.
“PMMA-collagen works very well on deep, severe acne scars, and should also work very well on shallow scars,” he said.
The product may enable practitioners to effectively treat acne scarring without a large capital equipment expenditure and without the risks associated with resurfacing procedures,” he said.
This study was sponsored by Suneva Medical, Inc.
ORLANDO – A non-resorbable wrinkle filler proved highly effective and durable for the treatment of atrophic acne scars in a randomized, controlled, multicenter study.
At 1 month after treatment with polymethylmethacrylate-collagen, or PMMA-collagen (Artefill, Suneva Medical, Inc.), nearly 70% of 97 subjects showed at least a 2-point improvement on the validated 4-point Acne Scar Rating Scale, compared with about 40% of 50 control subjects injected with saline. At 6 months, the response rate remained above 60% in the PMMA-collagen group, but dropped closer to 30% among those in the control group, Dr. James M. Spencer of Mount Sinai School of Medicine, New York reported in a poster at the Orlando Dermatology Aesthetic and Clinical Conference.
The control group subjects were then crossed over to the treatment group, and, at 12 months, the response rates were about 70% and nearly 60% in the treatment and control groups, respectively, he said.
Similarly, both Physician and Subject Global Aesthetic Improvement Scale (PGAIS/SGAIS) scores diverged during a 6-month evaluator-blinded phase of the study, then converged after crossover by the control group subjects. For example, the percentage of treatment and control group subjects with improvement at 1 month and 6 months according to the 5-point PGAIS was about 90% vs. less than 65%, and about 80% vs. about 30%, respectively. More than 90% in both groups showed improvement at 12 months, after control group crossover.
Additionally, subject satisfaction at 1 and 6 months in the treatment and control groups based on assessment of scar correction using Patient Satisfaction Scale scores was above 80% vs. about 60%, and about 80% vs. about 50%, respectively. Satisfaction in both groups was between 80% and 90% at 12 months, after control group crossover.
Study subjects, who had a mean age of 44 years, were enrolled from 10 U.S. centers and were treated during one injection session. An additional touch-up injection was allowed as needed. A total of 1,292 scars were treated in the 97 treatment group subjects, and 424 were treated in the 50 control group subjects. Participants were evaluated by blinded assessors at 2 weeks and 1, 3, and 6 months, after which control group subjects were treated with PMMA-collagen. Assessments were made in open-label fashion at 9 and 12 months. Most subjects (61%) were women, and 20% had Fitzpatrick skin types 5 or 6.
During the blinded portion of the study, six treatment-related adverse events were reported among treatment group subjects, and two were reported among control group subjects. None of the subjects experienced granulomas, changes in pigmentation, or hypertrophic scarring.
This study is the first randomized, blinded study of PMMA-collagen for treating acne scars, Dr. Spencer noted, adding that the findings demonstrate the efficacy and safety of PMMA-collagen for this purpose.
“The improvement is durable, lasting for 12 months,” he wrote, noting that the filler is easily administered and requires minimal training in those who are familiar with dermal fillers.
“PMMA-collagen works very well on deep, severe acne scars, and should also work very well on shallow scars,” he said.
The product may enable practitioners to effectively treat acne scarring without a large capital equipment expenditure and without the risks associated with resurfacing procedures,” he said.
This study was sponsored by Suneva Medical, Inc.
ORLANDO – A non-resorbable wrinkle filler proved highly effective and durable for the treatment of atrophic acne scars in a randomized, controlled, multicenter study.
At 1 month after treatment with polymethylmethacrylate-collagen, or PMMA-collagen (Artefill, Suneva Medical, Inc.), nearly 70% of 97 subjects showed at least a 2-point improvement on the validated 4-point Acne Scar Rating Scale, compared with about 40% of 50 control subjects injected with saline. At 6 months, the response rate remained above 60% in the PMMA-collagen group, but dropped closer to 30% among those in the control group, Dr. James M. Spencer of Mount Sinai School of Medicine, New York reported in a poster at the Orlando Dermatology Aesthetic and Clinical Conference.
The control group subjects were then crossed over to the treatment group, and, at 12 months, the response rates were about 70% and nearly 60% in the treatment and control groups, respectively, he said.
Similarly, both Physician and Subject Global Aesthetic Improvement Scale (PGAIS/SGAIS) scores diverged during a 6-month evaluator-blinded phase of the study, then converged after crossover by the control group subjects. For example, the percentage of treatment and control group subjects with improvement at 1 month and 6 months according to the 5-point PGAIS was about 90% vs. less than 65%, and about 80% vs. about 30%, respectively. More than 90% in both groups showed improvement at 12 months, after control group crossover.
Additionally, subject satisfaction at 1 and 6 months in the treatment and control groups based on assessment of scar correction using Patient Satisfaction Scale scores was above 80% vs. about 60%, and about 80% vs. about 50%, respectively. Satisfaction in both groups was between 80% and 90% at 12 months, after control group crossover.
Study subjects, who had a mean age of 44 years, were enrolled from 10 U.S. centers and were treated during one injection session. An additional touch-up injection was allowed as needed. A total of 1,292 scars were treated in the 97 treatment group subjects, and 424 were treated in the 50 control group subjects. Participants were evaluated by blinded assessors at 2 weeks and 1, 3, and 6 months, after which control group subjects were treated with PMMA-collagen. Assessments were made in open-label fashion at 9 and 12 months. Most subjects (61%) were women, and 20% had Fitzpatrick skin types 5 or 6.
During the blinded portion of the study, six treatment-related adverse events were reported among treatment group subjects, and two were reported among control group subjects. None of the subjects experienced granulomas, changes in pigmentation, or hypertrophic scarring.
This study is the first randomized, blinded study of PMMA-collagen for treating acne scars, Dr. Spencer noted, adding that the findings demonstrate the efficacy and safety of PMMA-collagen for this purpose.
“The improvement is durable, lasting for 12 months,” he wrote, noting that the filler is easily administered and requires minimal training in those who are familiar with dermal fillers.
“PMMA-collagen works very well on deep, severe acne scars, and should also work very well on shallow scars,” he said.
The product may enable practitioners to effectively treat acne scarring without a large capital equipment expenditure and without the risks associated with resurfacing procedures,” he said.
This study was sponsored by Suneva Medical, Inc.
AT THE ODAC CONFERENCE
Key clinical point: PMMA-collagen is safe, effective, and practical for treating atrophic acne scars.
Major finding: Nearly 70% of treated subjects vs. 40% of controls showed at least a 2-point improvement on the Acne Scar Rating Scale
Data source: A randomized, controlled, multicenter study of 147 subjects.
Disclosures: This study was sponsored by Suneva Medical, Inc.
Combined OTC, prescription acne regimen satisfied young patients
ORLANDO – A three-component combined over-the-counter and prescription skin care regimen was safe, effective, well tolerated, and well liked by acne vulgaris patients aged 12 years and older in an open-label multicenter study.
Of 81 participants with a mean age of 19 years, mild or moderate facial acne vulgaris, and mean acne vulgaris duration of 4.4 years, 89.2% agreed or strongly agreed that they liked the regimen, 87.9% reported overall satisfaction, and 87.9% said they would recommend the regimen to others.
Nearly all participants (95.9%) said the regimen was easy to use, 73% reported improved skin texture, and 70.3% said the regimen met their needs, Dr. Michael H. Gold of Nashville, Tenn., reported in a poster at the Orlando Dermatology Aesthetic and Clinical Conference.
Treatment involved once-daily application of a prescription topical gel containing adapalene 1% and benzoyl peroxide 2.5%, as well as the use of two over-the-counter products designed for acne-prone skin: a foaming cleanser used twice daily and a moisturizer with broad spectrum SPF 30 sunscreen used once daily. Treatment continued for 8 weeks.
In addition to the subjective patient satisfaction questionnaire, subjects were assessed based on total inflammatory and noninflammatory lesion counts; photographic evaluation of skin shininess, texture, and presence of Propionibacterium acnes; cutaneous tolerability scores for stinging, burning, erythema, scaling, and dryness; and adverse events.
The therapeutic effect was evident in most patients at 2 weeks, with a reduction in the number of lesions. After 8 weeks, total inflammatory and noninflammatory lesion counts were significantly reduced, compared with baseline. Skin shininess and P. acnes also were significantly reduced by 8 weeks, Dr. Gold noted.
Most patients had no cutaneous irritation; the proportion of patients experiencing irritation was smaller than in prior phase II and III studies that evaluated benzoyl peroxide once-daily gel with or without moisturizer. Of 553 patients from those prior studies, 4% and 1% reported moderate and severe erythema, respectively, compared with 1% and 0% of the patients in the current study. In addition 3% and 1% of patients in earlier phase II and III studies, respectively, reported moderate or severe stinging/burning, compared with none of the patients in the current study.
A total of 18 adverse events were reported by 13 patients in the current study, and 17 events were considered to be related to the skin care regimen. None of the affected patients discontinued the regimen, and none of the patients reported serious adverse events.
Of note, 70% of patients agreed or strongly agreed that a sunscreen made for acne-prone skin was important to them, Dr. Gold said.
He and his colleagues concluded that a complete three-component, acne-specific regimen designed to clean, moisturize, medicate, and photoprotect is important for optimizing patient outcomes, and that the regimen used in this study was associated with good outcomes and high levels of patient satisfaction.
This study was funded by Galderma Laboratories.
ORLANDO – A three-component combined over-the-counter and prescription skin care regimen was safe, effective, well tolerated, and well liked by acne vulgaris patients aged 12 years and older in an open-label multicenter study.
Of 81 participants with a mean age of 19 years, mild or moderate facial acne vulgaris, and mean acne vulgaris duration of 4.4 years, 89.2% agreed or strongly agreed that they liked the regimen, 87.9% reported overall satisfaction, and 87.9% said they would recommend the regimen to others.
Nearly all participants (95.9%) said the regimen was easy to use, 73% reported improved skin texture, and 70.3% said the regimen met their needs, Dr. Michael H. Gold of Nashville, Tenn., reported in a poster at the Orlando Dermatology Aesthetic and Clinical Conference.
Treatment involved once-daily application of a prescription topical gel containing adapalene 1% and benzoyl peroxide 2.5%, as well as the use of two over-the-counter products designed for acne-prone skin: a foaming cleanser used twice daily and a moisturizer with broad spectrum SPF 30 sunscreen used once daily. Treatment continued for 8 weeks.
In addition to the subjective patient satisfaction questionnaire, subjects were assessed based on total inflammatory and noninflammatory lesion counts; photographic evaluation of skin shininess, texture, and presence of Propionibacterium acnes; cutaneous tolerability scores for stinging, burning, erythema, scaling, and dryness; and adverse events.
The therapeutic effect was evident in most patients at 2 weeks, with a reduction in the number of lesions. After 8 weeks, total inflammatory and noninflammatory lesion counts were significantly reduced, compared with baseline. Skin shininess and P. acnes also were significantly reduced by 8 weeks, Dr. Gold noted.
Most patients had no cutaneous irritation; the proportion of patients experiencing irritation was smaller than in prior phase II and III studies that evaluated benzoyl peroxide once-daily gel with or without moisturizer. Of 553 patients from those prior studies, 4% and 1% reported moderate and severe erythema, respectively, compared with 1% and 0% of the patients in the current study. In addition 3% and 1% of patients in earlier phase II and III studies, respectively, reported moderate or severe stinging/burning, compared with none of the patients in the current study.
A total of 18 adverse events were reported by 13 patients in the current study, and 17 events were considered to be related to the skin care regimen. None of the affected patients discontinued the regimen, and none of the patients reported serious adverse events.
Of note, 70% of patients agreed or strongly agreed that a sunscreen made for acne-prone skin was important to them, Dr. Gold said.
He and his colleagues concluded that a complete three-component, acne-specific regimen designed to clean, moisturize, medicate, and photoprotect is important for optimizing patient outcomes, and that the regimen used in this study was associated with good outcomes and high levels of patient satisfaction.
This study was funded by Galderma Laboratories.
ORLANDO – A three-component combined over-the-counter and prescription skin care regimen was safe, effective, well tolerated, and well liked by acne vulgaris patients aged 12 years and older in an open-label multicenter study.
Of 81 participants with a mean age of 19 years, mild or moderate facial acne vulgaris, and mean acne vulgaris duration of 4.4 years, 89.2% agreed or strongly agreed that they liked the regimen, 87.9% reported overall satisfaction, and 87.9% said they would recommend the regimen to others.
Nearly all participants (95.9%) said the regimen was easy to use, 73% reported improved skin texture, and 70.3% said the regimen met their needs, Dr. Michael H. Gold of Nashville, Tenn., reported in a poster at the Orlando Dermatology Aesthetic and Clinical Conference.
Treatment involved once-daily application of a prescription topical gel containing adapalene 1% and benzoyl peroxide 2.5%, as well as the use of two over-the-counter products designed for acne-prone skin: a foaming cleanser used twice daily and a moisturizer with broad spectrum SPF 30 sunscreen used once daily. Treatment continued for 8 weeks.
In addition to the subjective patient satisfaction questionnaire, subjects were assessed based on total inflammatory and noninflammatory lesion counts; photographic evaluation of skin shininess, texture, and presence of Propionibacterium acnes; cutaneous tolerability scores for stinging, burning, erythema, scaling, and dryness; and adverse events.
The therapeutic effect was evident in most patients at 2 weeks, with a reduction in the number of lesions. After 8 weeks, total inflammatory and noninflammatory lesion counts were significantly reduced, compared with baseline. Skin shininess and P. acnes also were significantly reduced by 8 weeks, Dr. Gold noted.
Most patients had no cutaneous irritation; the proportion of patients experiencing irritation was smaller than in prior phase II and III studies that evaluated benzoyl peroxide once-daily gel with or without moisturizer. Of 553 patients from those prior studies, 4% and 1% reported moderate and severe erythema, respectively, compared with 1% and 0% of the patients in the current study. In addition 3% and 1% of patients in earlier phase II and III studies, respectively, reported moderate or severe stinging/burning, compared with none of the patients in the current study.
A total of 18 adverse events were reported by 13 patients in the current study, and 17 events were considered to be related to the skin care regimen. None of the affected patients discontinued the regimen, and none of the patients reported serious adverse events.
Of note, 70% of patients agreed or strongly agreed that a sunscreen made for acne-prone skin was important to them, Dr. Gold said.
He and his colleagues concluded that a complete three-component, acne-specific regimen designed to clean, moisturize, medicate, and photoprotect is important for optimizing patient outcomes, and that the regimen used in this study was associated with good outcomes and high levels of patient satisfaction.
This study was funded by Galderma Laboratories.
AT THE ODAC CONFERENCE
Key clinical point: Children and young adults with acne vulgaris adhered to a three-part skin care regimen involving prescription and OTC products.
Major finding: 87.9% of patients reported overall satisfaction.
Data source: An open-label, multicenter study.
Disclosures: The study was funded by Galderma Laboratories.