User login
Radiological Society of North America (RSNA): Annual Meeting
Energy drinks amped up left ventricular contractility
CHICAGO – Consumption of an energy drink containing caffeine and taurine slightly, but significantly, altered left ventricular contractility in healthy volunteers, while consuming the same amount of caffeine alone did not lead to an alteration in contractility in a prospective study.
"A possible explanation for this finding could be the presence of taurine, which has been shown to increase the release of calcium in muscles," Dr. Jonas Dörner reported at the annual meeting of the Radiological Society of North America.
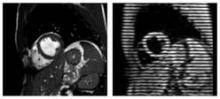
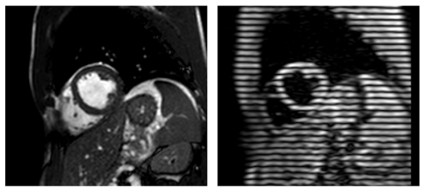
He and his colleagues performed cardiac magnetic resonance imaging (MRI) in 31 volunteers before and 1 hour after consumption of an energy drink containing caffeine (32 mg/100 mL) and taurine (400 mg/100 mL). The average patient age was 27.7 years.
Postconsumption images revealed that mean peak strain increased 7% from baseline (–22.84 vs. –24.35; P < .0001) and peak systolic strain rate – a measure of deformation with respect to time – increased by 6% (–1.19 vs –1.26; P = .0032), reported Dr. Dörner, with the University of Bonn, Germany.
The investigators did not find any significant changes in heart rate, systolic blood pressure, or left ventricular (LV) ejection fraction. LV end-diastolic volume and LV stroke volume increased significantly by 2% and 4%, respectively.
The same imaging protocol was repeated on a different day in 10 patients after consumption of caffeine only. No significant differences were seen in mean peak strain (–22.99 vs. –23.20) or mean peak systolic strain rate (–1.15 vs. –1.16) with caffeine alone, although diastolic blood pressure was significantly elevated and LV end-diastolic volume significantly decreased, Dr. Dörner said.
The current study took advantage of an MRI technique called complementary spatial modulation of magnetization (CSPAMM) for LV myocardial tagging. The technique is more exact than traditional ultrasound or speckle tracking and is able to measure very small differences in strain, he explained in an interview.
Although the differences in strain in the study were "subtle," the findings need to be taken into perspective because younger patients often consume higher doses of caffeine and taurine via energy drinks. According to the Food and Drug Administration, caffeinated sodas cannot contain more than 71 mg of caffeine per 12 fluid ounces (approximately 20 mg/100 mL), but energy drinks often contain three times that amount, he noted.
More than 500 brands of energy drinks are available worldwide, and 30%-50% are consumed by children, teenagers, and young adults. A report by the European Food Safety Authority found no adverse effects for up to 1 g of taurine per kilogram of body weight per day.
Further studies are needed to evaluate the effect of long-term energy drink consumption and the effect of these drinks on patients with heart disease and in combination with alcohol, Dr. Dörner said.
Dr. Dörner reported having no financial disclosures; a coauthor reported consulting for Medtronic.
Dr. Marcos I. Restrepo, FCCP, comments: This series of observations calls into attention the possible risks of the multiple energy drinks (and its contents) available in the market. The worry that high levels of caffeine and taurine found in energy drinks affect contractility in healthy volunteers should raise concerns in patients with comorbid conditions or unidentified heart problems. In addition, regular consumers of energy drinks may worry about potential heart problems, if the consumption occurs repetitively and for longer periods. There is hope that regulatory agencies consider these findings and promote more studies to address the possible risks related to ingestion of energy drinks.
Dr. Marcos I. Restrepo, FCCP, comments: This series of observations calls into attention the possible risks of the multiple energy drinks (and its contents) available in the market. The worry that high levels of caffeine and taurine found in energy drinks affect contractility in healthy volunteers should raise concerns in patients with comorbid conditions or unidentified heart problems. In addition, regular consumers of energy drinks may worry about potential heart problems, if the consumption occurs repetitively and for longer periods. There is hope that regulatory agencies consider these findings and promote more studies to address the possible risks related to ingestion of energy drinks.
Dr. Marcos I. Restrepo, FCCP, comments: This series of observations calls into attention the possible risks of the multiple energy drinks (and its contents) available in the market. The worry that high levels of caffeine and taurine found in energy drinks affect contractility in healthy volunteers should raise concerns in patients with comorbid conditions or unidentified heart problems. In addition, regular consumers of energy drinks may worry about potential heart problems, if the consumption occurs repetitively and for longer periods. There is hope that regulatory agencies consider these findings and promote more studies to address the possible risks related to ingestion of energy drinks.
CHICAGO – Consumption of an energy drink containing caffeine and taurine slightly, but significantly, altered left ventricular contractility in healthy volunteers, while consuming the same amount of caffeine alone did not lead to an alteration in contractility in a prospective study.
"A possible explanation for this finding could be the presence of taurine, which has been shown to increase the release of calcium in muscles," Dr. Jonas Dörner reported at the annual meeting of the Radiological Society of North America.
He and his colleagues performed cardiac magnetic resonance imaging (MRI) in 31 volunteers before and 1 hour after consumption of an energy drink containing caffeine (32 mg/100 mL) and taurine (400 mg/100 mL). The average patient age was 27.7 years.
Postconsumption images revealed that mean peak strain increased 7% from baseline (–22.84 vs. –24.35; P < .0001) and peak systolic strain rate – a measure of deformation with respect to time – increased by 6% (–1.19 vs –1.26; P = .0032), reported Dr. Dörner, with the University of Bonn, Germany.
The investigators did not find any significant changes in heart rate, systolic blood pressure, or left ventricular (LV) ejection fraction. LV end-diastolic volume and LV stroke volume increased significantly by 2% and 4%, respectively.
The same imaging protocol was repeated on a different day in 10 patients after consumption of caffeine only. No significant differences were seen in mean peak strain (–22.99 vs. –23.20) or mean peak systolic strain rate (–1.15 vs. –1.16) with caffeine alone, although diastolic blood pressure was significantly elevated and LV end-diastolic volume significantly decreased, Dr. Dörner said.
The current study took advantage of an MRI technique called complementary spatial modulation of magnetization (CSPAMM) for LV myocardial tagging. The technique is more exact than traditional ultrasound or speckle tracking and is able to measure very small differences in strain, he explained in an interview.
Although the differences in strain in the study were "subtle," the findings need to be taken into perspective because younger patients often consume higher doses of caffeine and taurine via energy drinks. According to the Food and Drug Administration, caffeinated sodas cannot contain more than 71 mg of caffeine per 12 fluid ounces (approximately 20 mg/100 mL), but energy drinks often contain three times that amount, he noted.
More than 500 brands of energy drinks are available worldwide, and 30%-50% are consumed by children, teenagers, and young adults. A report by the European Food Safety Authority found no adverse effects for up to 1 g of taurine per kilogram of body weight per day.
Further studies are needed to evaluate the effect of long-term energy drink consumption and the effect of these drinks on patients with heart disease and in combination with alcohol, Dr. Dörner said.
Dr. Dörner reported having no financial disclosures; a coauthor reported consulting for Medtronic.
CHICAGO – Consumption of an energy drink containing caffeine and taurine slightly, but significantly, altered left ventricular contractility in healthy volunteers, while consuming the same amount of caffeine alone did not lead to an alteration in contractility in a prospective study.
"A possible explanation for this finding could be the presence of taurine, which has been shown to increase the release of calcium in muscles," Dr. Jonas Dörner reported at the annual meeting of the Radiological Society of North America.
He and his colleagues performed cardiac magnetic resonance imaging (MRI) in 31 volunteers before and 1 hour after consumption of an energy drink containing caffeine (32 mg/100 mL) and taurine (400 mg/100 mL). The average patient age was 27.7 years.
Postconsumption images revealed that mean peak strain increased 7% from baseline (–22.84 vs. –24.35; P < .0001) and peak systolic strain rate – a measure of deformation with respect to time – increased by 6% (–1.19 vs –1.26; P = .0032), reported Dr. Dörner, with the University of Bonn, Germany.
The investigators did not find any significant changes in heart rate, systolic blood pressure, or left ventricular (LV) ejection fraction. LV end-diastolic volume and LV stroke volume increased significantly by 2% and 4%, respectively.
The same imaging protocol was repeated on a different day in 10 patients after consumption of caffeine only. No significant differences were seen in mean peak strain (–22.99 vs. –23.20) or mean peak systolic strain rate (–1.15 vs. –1.16) with caffeine alone, although diastolic blood pressure was significantly elevated and LV end-diastolic volume significantly decreased, Dr. Dörner said.
The current study took advantage of an MRI technique called complementary spatial modulation of magnetization (CSPAMM) for LV myocardial tagging. The technique is more exact than traditional ultrasound or speckle tracking and is able to measure very small differences in strain, he explained in an interview.
Although the differences in strain in the study were "subtle," the findings need to be taken into perspective because younger patients often consume higher doses of caffeine and taurine via energy drinks. According to the Food and Drug Administration, caffeinated sodas cannot contain more than 71 mg of caffeine per 12 fluid ounces (approximately 20 mg/100 mL), but energy drinks often contain three times that amount, he noted.
More than 500 brands of energy drinks are available worldwide, and 30%-50% are consumed by children, teenagers, and young adults. A report by the European Food Safety Authority found no adverse effects for up to 1 g of taurine per kilogram of body weight per day.
Further studies are needed to evaluate the effect of long-term energy drink consumption and the effect of these drinks on patients with heart disease and in combination with alcohol, Dr. Dörner said.
Dr. Dörner reported having no financial disclosures; a coauthor reported consulting for Medtronic.
Major finding: One hour after consumption of an energy drink containing caffeine and taurine, mean peak strain increased 7% from baseline and peak systolic strain rate increased 6%.
Data source: A prospective study of 31 healthy volunteers.
Disclosures: Dr. Dörner reported having no financial disclosures; a coauthor reported consulting for Medtronic.
Cardiac CT angiography feasible at ultralow radiation doses
CHICAGO – Coronary computed tomography angiography with diagnostic image quality is feasible at an ultralow radiation dose of 0.2 millisievert using model-based iterative reconstruction.
This represents roughly an 80% reduction in radiation dose compared with standard coronary CT angiography, Dr. Julia Stehli said at the annual meeting of the Radiological Society of North America.
Increasing concerns about radiation exposure have prompted the use of prospective ECG triggering to reduce radiation doses from 20 mSv to 2 mSv or less. Several vendors also have developed new raw-data–based iterative reconstruction algorithms to further reduce radiation doses, but the trade-off can be increased image noise.
The model-based iterative reconstruction (MIBR) algorithm (GE Healthcare), however, has shown promising results for noise reduction, said Dr. Stehli of University Hospital Zurich. The technology, known as Veo, is already in use in the United States, Europe, and Asia for abdominal CT scans but is not yet commercially available for cardiac scans because of the added complexity of ECG triggering.
Dr. Stehli reported on the hospital’s first clinical experience with MIBR in 25 consecutive prospectively enrolled patients with suspected coronary artery disease who underwent standard low-dose coronary CT angiography (CCTA) and same-day ultralow-dose CCTA on a 64-slice CT scanner with prospective ECG triggering. Tube voltage and current were adapted to body mass index, which covered a wide range from 18.4 kg/m2 to 40.2 kg/m2. Contrast media volume and flow rate were adapted to body surface area. Intravenous beta-blockers were used prior to CCTA in 20 patients.
Standard CCTA was reconstructed using 30% of adaptive statistical iterative reconstruction (ASIR) according to usual hospital practice, while the ultralow-dose images were sent to the vendor for reconstruction with MIBR.
The effective radiation dose was 1.3 mSv with standard CCTA and 0.2 mSv in the ultralow-dose CCTA group (P less than .001), which is in the range reported for a postero-anterior and lateral chest X-ray, Dr. Stehli said.
A total of 100 vessels and 330 coronary artery segments were semiquantitatively assessed by two blinded, independent readers using a 4-point Likert scale, with 1 being nondiagnostic, 2 good, 3 adequate, and 4 excellent. The Kappa value for interobserver agreement of image quality was 0.8.
The average image quality score per segment was 3.3 with standard CCTA vs. 3.4 with ultralow-dose MBIR (P less than .05), she said.
Diagnostic image quality (score 2-4) was found in 319 segments (97%) and 317 segments (96%), respectively.
"These numbers are quite revolutionary," session comoderator Dr. Konstantin Nikolaou, professor of radiology at the University of Munich, said in an interview. "We’ve heard about 1.0 [mSv], so 0.2 [mSv] is great."
Still, more details are needed on exactly how the protocol works and the need to send images to the vendor for MBIR reconstruction, he said.
During a discussion of the results, Dr. Stehli said that reconstruction by the vendor typically took about 15 minutes, but Dr. Nikolau said that "it’s hard to say if that is feasible in routine clinical practice."
The ultimate test for the ultralow-dose protocol will be the clinical outcomes data, expected to be reported in 2014.
"If that proves to be robust and works in many patients and rates a good diagnostic accuracy, it would be great," Dr. Nikolau said.
The investigators would not release details on the clinical outcomes but said sensitivity and specificity for the new protocol are good.
"We believe this will have clinical applications in the near future," Dr. Stehli said in an interview.
Most patients in the study presented with chest pain (72%), and 56% were smokers, 44% had arterial hypertension, and 36% had a family history of cardiovascular disease. Their mean age was 58 years.
Dr. Stehli and her associates reported having no financial disclosures.
CHICAGO – Coronary computed tomography angiography with diagnostic image quality is feasible at an ultralow radiation dose of 0.2 millisievert using model-based iterative reconstruction.
This represents roughly an 80% reduction in radiation dose compared with standard coronary CT angiography, Dr. Julia Stehli said at the annual meeting of the Radiological Society of North America.
Increasing concerns about radiation exposure have prompted the use of prospective ECG triggering to reduce radiation doses from 20 mSv to 2 mSv or less. Several vendors also have developed new raw-data–based iterative reconstruction algorithms to further reduce radiation doses, but the trade-off can be increased image noise.
The model-based iterative reconstruction (MIBR) algorithm (GE Healthcare), however, has shown promising results for noise reduction, said Dr. Stehli of University Hospital Zurich. The technology, known as Veo, is already in use in the United States, Europe, and Asia for abdominal CT scans but is not yet commercially available for cardiac scans because of the added complexity of ECG triggering.
Dr. Stehli reported on the hospital’s first clinical experience with MIBR in 25 consecutive prospectively enrolled patients with suspected coronary artery disease who underwent standard low-dose coronary CT angiography (CCTA) and same-day ultralow-dose CCTA on a 64-slice CT scanner with prospective ECG triggering. Tube voltage and current were adapted to body mass index, which covered a wide range from 18.4 kg/m2 to 40.2 kg/m2. Contrast media volume and flow rate were adapted to body surface area. Intravenous beta-blockers were used prior to CCTA in 20 patients.
Standard CCTA was reconstructed using 30% of adaptive statistical iterative reconstruction (ASIR) according to usual hospital practice, while the ultralow-dose images were sent to the vendor for reconstruction with MIBR.
The effective radiation dose was 1.3 mSv with standard CCTA and 0.2 mSv in the ultralow-dose CCTA group (P less than .001), which is in the range reported for a postero-anterior and lateral chest X-ray, Dr. Stehli said.
A total of 100 vessels and 330 coronary artery segments were semiquantitatively assessed by two blinded, independent readers using a 4-point Likert scale, with 1 being nondiagnostic, 2 good, 3 adequate, and 4 excellent. The Kappa value for interobserver agreement of image quality was 0.8.
The average image quality score per segment was 3.3 with standard CCTA vs. 3.4 with ultralow-dose MBIR (P less than .05), she said.
Diagnostic image quality (score 2-4) was found in 319 segments (97%) and 317 segments (96%), respectively.
"These numbers are quite revolutionary," session comoderator Dr. Konstantin Nikolaou, professor of radiology at the University of Munich, said in an interview. "We’ve heard about 1.0 [mSv], so 0.2 [mSv] is great."
Still, more details are needed on exactly how the protocol works and the need to send images to the vendor for MBIR reconstruction, he said.
During a discussion of the results, Dr. Stehli said that reconstruction by the vendor typically took about 15 minutes, but Dr. Nikolau said that "it’s hard to say if that is feasible in routine clinical practice."
The ultimate test for the ultralow-dose protocol will be the clinical outcomes data, expected to be reported in 2014.
"If that proves to be robust and works in many patients and rates a good diagnostic accuracy, it would be great," Dr. Nikolau said.
The investigators would not release details on the clinical outcomes but said sensitivity and specificity for the new protocol are good.
"We believe this will have clinical applications in the near future," Dr. Stehli said in an interview.
Most patients in the study presented with chest pain (72%), and 56% were smokers, 44% had arterial hypertension, and 36% had a family history of cardiovascular disease. Their mean age was 58 years.
Dr. Stehli and her associates reported having no financial disclosures.
CHICAGO – Coronary computed tomography angiography with diagnostic image quality is feasible at an ultralow radiation dose of 0.2 millisievert using model-based iterative reconstruction.
This represents roughly an 80% reduction in radiation dose compared with standard coronary CT angiography, Dr. Julia Stehli said at the annual meeting of the Radiological Society of North America.
Increasing concerns about radiation exposure have prompted the use of prospective ECG triggering to reduce radiation doses from 20 mSv to 2 mSv or less. Several vendors also have developed new raw-data–based iterative reconstruction algorithms to further reduce radiation doses, but the trade-off can be increased image noise.
The model-based iterative reconstruction (MIBR) algorithm (GE Healthcare), however, has shown promising results for noise reduction, said Dr. Stehli of University Hospital Zurich. The technology, known as Veo, is already in use in the United States, Europe, and Asia for abdominal CT scans but is not yet commercially available for cardiac scans because of the added complexity of ECG triggering.
Dr. Stehli reported on the hospital’s first clinical experience with MIBR in 25 consecutive prospectively enrolled patients with suspected coronary artery disease who underwent standard low-dose coronary CT angiography (CCTA) and same-day ultralow-dose CCTA on a 64-slice CT scanner with prospective ECG triggering. Tube voltage and current were adapted to body mass index, which covered a wide range from 18.4 kg/m2 to 40.2 kg/m2. Contrast media volume and flow rate were adapted to body surface area. Intravenous beta-blockers were used prior to CCTA in 20 patients.
Standard CCTA was reconstructed using 30% of adaptive statistical iterative reconstruction (ASIR) according to usual hospital practice, while the ultralow-dose images were sent to the vendor for reconstruction with MIBR.
The effective radiation dose was 1.3 mSv with standard CCTA and 0.2 mSv in the ultralow-dose CCTA group (P less than .001), which is in the range reported for a postero-anterior and lateral chest X-ray, Dr. Stehli said.
A total of 100 vessels and 330 coronary artery segments were semiquantitatively assessed by two blinded, independent readers using a 4-point Likert scale, with 1 being nondiagnostic, 2 good, 3 adequate, and 4 excellent. The Kappa value for interobserver agreement of image quality was 0.8.
The average image quality score per segment was 3.3 with standard CCTA vs. 3.4 with ultralow-dose MBIR (P less than .05), she said.
Diagnostic image quality (score 2-4) was found in 319 segments (97%) and 317 segments (96%), respectively.
"These numbers are quite revolutionary," session comoderator Dr. Konstantin Nikolaou, professor of radiology at the University of Munich, said in an interview. "We’ve heard about 1.0 [mSv], so 0.2 [mSv] is great."
Still, more details are needed on exactly how the protocol works and the need to send images to the vendor for MBIR reconstruction, he said.
During a discussion of the results, Dr. Stehli said that reconstruction by the vendor typically took about 15 minutes, but Dr. Nikolau said that "it’s hard to say if that is feasible in routine clinical practice."
The ultimate test for the ultralow-dose protocol will be the clinical outcomes data, expected to be reported in 2014.
"If that proves to be robust and works in many patients and rates a good diagnostic accuracy, it would be great," Dr. Nikolau said.
The investigators would not release details on the clinical outcomes but said sensitivity and specificity for the new protocol are good.
"We believe this will have clinical applications in the near future," Dr. Stehli said in an interview.
Most patients in the study presented with chest pain (72%), and 56% were smokers, 44% had arterial hypertension, and 36% had a family history of cardiovascular disease. Their mean age was 58 years.
Dr. Stehli and her associates reported having no financial disclosures.
AT RSNA 2013
Major finding: The effective radiation dose was 1.3 mSv with standard CCTA and 0.2 mSv in the ultralow-dose CCTA group (P less than .001).
Data source: A prospective study of 25 patients with suspected coronary artery disease.
Disclosures: Dr. Stehli and her coauthors reported having no financial disclosures.
Mild coronary artery disease is gender blind
CHICAGO – Men and women may not really be all that different when it comes to mild coronary artery disease.
A prospective, multinational registry analysis found that 1.2% of women and 1.1% of men with mild, nonobstructive coronary artery disease on coronary CT angiography experience a major adverse cardiovascular event, either heart attack or death, each year.
For those free of coronary artery disease (CAD), the event rate was 0.3% for both sexes, Dr. Jonathon A. Leipsic reported at the annual meeting of the Radiological Society of North America.
Women’s heart disease is typically viewed as different from men’s heart disease, in part because of women’s unique presenting symptomatology. Studies such as the Women’s Health Initiative have also reported that women with nonspecific or atypical chest pain have a twofold greater risk for nonfatal MI.
Importantly, all prior data has been reliant on invasive coronary angiography for anatomical coronary assessment, observed Dr. Leipsic, codirector of advanced cardiac imaging, Providence Health Care Heart Center at St. Paul’s Hospital, Vancouver, B.C.
The current analysis, however, used data from the prospective CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter) registry, which tracks roughly 28,000 individuals in North America, Europe, and Asia who have undergone coronary CT angiography.
The results represent a major shift in thinking, Dr. Leipsic said in an interview.
"What we realize is that CT identifies mild disease in the wall in a way that the invasive angiogram does not," he said. "So suddenly, when you say you have a normal invasive angiogram, there may still be mild disease in the arteries, whereas when you have a normal CT in a woman, our data would suggest that those women do very well, even if they have symptoms."
Dr. Leipsic and his associates identified 18,158 patients in the CONFIRM registry with no disease or mild CAD with less than 50% stenosis. Propensity matching for risk factors, chest pain, and extent of disease left 11,462 patients.
Their average age was 55 years, 34% were asymptomatic, 45% had hypertension, 12% were diabetic, and 18% were current smokers.
Of these, 37 had an MI; 120 died; and 7 had an MI and died (1.4%).
The annual major adverse cardiovascular event (MACE) rate was 0.6% overall, and was significantly different between patients with a normal CT and those with nonobstructive disease (0.3% vs. 1.1%), Dr. Leipsic said.
"This mild disease we see on CT is not just incidental," he said during a press briefing at the meeting. "It actually identifies patients who are at increased risk of having a heart attack and dying, with an increased risk of 1.84 for the overall cohort (P = .001)."
Notably, 3-year MACE-free survival was similar among men and women without coronary plaque on CT as well as those with non-obstructive disease.
Dr. Leipsic commented that detractors of the data have argued that the analysis failed to focus on women at the greatest risk – those with atypical symptoms. A further sub-analysis, however, based on the presence or absence of symptoms and the type of symptoms (nonanginal chest pain, atypical angina, and typical angina), once again "found that men and women behave similarly," he said.
Event rates were lower in men and women with normal CT scans and elevated in both sexes in the setting of nonobstructive disease, "regardless of the nature of chest pain and even in the absence of chest pain," he noted.
Press briefing moderator Dr. Candice Johnstone of the Medical College of Wisconsin, Milwaukee, said in an interview, "Observational studies have limits, but at the same time, I think it may be a paradigm shift, in that it may be a new tool in our toolbox for people at lower risk of heart disease to avoid an invasive procedure."
Dr. Leipsic reported financial relationships with several entities including GE Healthcare, HeartFlow, Edwards LifeSciences, and TC3.
CHICAGO – Men and women may not really be all that different when it comes to mild coronary artery disease.
A prospective, multinational registry analysis found that 1.2% of women and 1.1% of men with mild, nonobstructive coronary artery disease on coronary CT angiography experience a major adverse cardiovascular event, either heart attack or death, each year.
For those free of coronary artery disease (CAD), the event rate was 0.3% for both sexes, Dr. Jonathon A. Leipsic reported at the annual meeting of the Radiological Society of North America.
Women’s heart disease is typically viewed as different from men’s heart disease, in part because of women’s unique presenting symptomatology. Studies such as the Women’s Health Initiative have also reported that women with nonspecific or atypical chest pain have a twofold greater risk for nonfatal MI.
Importantly, all prior data has been reliant on invasive coronary angiography for anatomical coronary assessment, observed Dr. Leipsic, codirector of advanced cardiac imaging, Providence Health Care Heart Center at St. Paul’s Hospital, Vancouver, B.C.
The current analysis, however, used data from the prospective CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter) registry, which tracks roughly 28,000 individuals in North America, Europe, and Asia who have undergone coronary CT angiography.
The results represent a major shift in thinking, Dr. Leipsic said in an interview.
"What we realize is that CT identifies mild disease in the wall in a way that the invasive angiogram does not," he said. "So suddenly, when you say you have a normal invasive angiogram, there may still be mild disease in the arteries, whereas when you have a normal CT in a woman, our data would suggest that those women do very well, even if they have symptoms."
Dr. Leipsic and his associates identified 18,158 patients in the CONFIRM registry with no disease or mild CAD with less than 50% stenosis. Propensity matching for risk factors, chest pain, and extent of disease left 11,462 patients.
Their average age was 55 years, 34% were asymptomatic, 45% had hypertension, 12% were diabetic, and 18% were current smokers.
Of these, 37 had an MI; 120 died; and 7 had an MI and died (1.4%).
The annual major adverse cardiovascular event (MACE) rate was 0.6% overall, and was significantly different between patients with a normal CT and those with nonobstructive disease (0.3% vs. 1.1%), Dr. Leipsic said.
"This mild disease we see on CT is not just incidental," he said during a press briefing at the meeting. "It actually identifies patients who are at increased risk of having a heart attack and dying, with an increased risk of 1.84 for the overall cohort (P = .001)."
Notably, 3-year MACE-free survival was similar among men and women without coronary plaque on CT as well as those with non-obstructive disease.
Dr. Leipsic commented that detractors of the data have argued that the analysis failed to focus on women at the greatest risk – those with atypical symptoms. A further sub-analysis, however, based on the presence or absence of symptoms and the type of symptoms (nonanginal chest pain, atypical angina, and typical angina), once again "found that men and women behave similarly," he said.
Event rates were lower in men and women with normal CT scans and elevated in both sexes in the setting of nonobstructive disease, "regardless of the nature of chest pain and even in the absence of chest pain," he noted.
Press briefing moderator Dr. Candice Johnstone of the Medical College of Wisconsin, Milwaukee, said in an interview, "Observational studies have limits, but at the same time, I think it may be a paradigm shift, in that it may be a new tool in our toolbox for people at lower risk of heart disease to avoid an invasive procedure."
Dr. Leipsic reported financial relationships with several entities including GE Healthcare, HeartFlow, Edwards LifeSciences, and TC3.
CHICAGO – Men and women may not really be all that different when it comes to mild coronary artery disease.
A prospective, multinational registry analysis found that 1.2% of women and 1.1% of men with mild, nonobstructive coronary artery disease on coronary CT angiography experience a major adverse cardiovascular event, either heart attack or death, each year.
For those free of coronary artery disease (CAD), the event rate was 0.3% for both sexes, Dr. Jonathon A. Leipsic reported at the annual meeting of the Radiological Society of North America.
Women’s heart disease is typically viewed as different from men’s heart disease, in part because of women’s unique presenting symptomatology. Studies such as the Women’s Health Initiative have also reported that women with nonspecific or atypical chest pain have a twofold greater risk for nonfatal MI.
Importantly, all prior data has been reliant on invasive coronary angiography for anatomical coronary assessment, observed Dr. Leipsic, codirector of advanced cardiac imaging, Providence Health Care Heart Center at St. Paul’s Hospital, Vancouver, B.C.
The current analysis, however, used data from the prospective CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter) registry, which tracks roughly 28,000 individuals in North America, Europe, and Asia who have undergone coronary CT angiography.
The results represent a major shift in thinking, Dr. Leipsic said in an interview.
"What we realize is that CT identifies mild disease in the wall in a way that the invasive angiogram does not," he said. "So suddenly, when you say you have a normal invasive angiogram, there may still be mild disease in the arteries, whereas when you have a normal CT in a woman, our data would suggest that those women do very well, even if they have symptoms."
Dr. Leipsic and his associates identified 18,158 patients in the CONFIRM registry with no disease or mild CAD with less than 50% stenosis. Propensity matching for risk factors, chest pain, and extent of disease left 11,462 patients.
Their average age was 55 years, 34% were asymptomatic, 45% had hypertension, 12% were diabetic, and 18% were current smokers.
Of these, 37 had an MI; 120 died; and 7 had an MI and died (1.4%).
The annual major adverse cardiovascular event (MACE) rate was 0.6% overall, and was significantly different between patients with a normal CT and those with nonobstructive disease (0.3% vs. 1.1%), Dr. Leipsic said.
"This mild disease we see on CT is not just incidental," he said during a press briefing at the meeting. "It actually identifies patients who are at increased risk of having a heart attack and dying, with an increased risk of 1.84 for the overall cohort (P = .001)."
Notably, 3-year MACE-free survival was similar among men and women without coronary plaque on CT as well as those with non-obstructive disease.
Dr. Leipsic commented that detractors of the data have argued that the analysis failed to focus on women at the greatest risk – those with atypical symptoms. A further sub-analysis, however, based on the presence or absence of symptoms and the type of symptoms (nonanginal chest pain, atypical angina, and typical angina), once again "found that men and women behave similarly," he said.
Event rates were lower in men and women with normal CT scans and elevated in both sexes in the setting of nonobstructive disease, "regardless of the nature of chest pain and even in the absence of chest pain," he noted.
Press briefing moderator Dr. Candice Johnstone of the Medical College of Wisconsin, Milwaukee, said in an interview, "Observational studies have limits, but at the same time, I think it may be a paradigm shift, in that it may be a new tool in our toolbox for people at lower risk of heart disease to avoid an invasive procedure."
Dr. Leipsic reported financial relationships with several entities including GE Healthcare, HeartFlow, Edwards LifeSciences, and TC3.
AT RSNA 2013
Major finding: In patients with mild, nonobstructive coronary disease, the annual MACE rate was 1.2% in women and 1.1% in men (P = .95).
Data source: An observational registry study in 11,462 patients with no disease or mild coronary disease with less than 50% stenosis.
Disclosures: Dr. Leipsic reported financial relationships with several entities including GE Healthcare, HeartFlow, Edwards LifeSciences, and TC3.
Breast tomosynthesis moving beyond clinical trials
CHICAGO – Screening all-comers with three-dimensional mammography increased breast cancer detection by 22.7% and reduced recall rates by 15.6% in a large observational study.
Although a 3D digital breast tomosynthesis (DBT) system was approved for breast cancer screening and diagnosis in the United States in 2011, DBT is typically a supplemental screening tool to standard 2D digital mammography.
In November 2011, however, the Hospital of the University of Pennsylvania, Philadelphia, took the plunge and began using DBT for every breast screening patient, regardless of age, cancer risk, breast density, or ability to pay.
Over a 17-month-period, DBT detected 82 cancers in 15,632 women, or 5.25 cancers per 1,000 cases, Dr. Emily F. Conant reported at the annual meeting of the Radiological Society of North America.
This compares with 46 cancers, or 4.28 cancers per 1,000 cases, detected with conventional mammography in 10,752 women in the 12 months prior to the switch.
The difference in cancer detection rates between 2D and 3D mammography did not reach statistical significance (P = .226), probably because of the small number of cases, Dr. Conant, a radiology professor at the hospital, said at a press briefing.
Compared with conventional mammography, however, DBT significantly improved the proportion of positive screening mammograms from which cancer was diagnosed by 45% (P = .036) and increased the detection of deadly invasive cancers by a nonsignificant 31%.
When asked whether the study showed that invasive lobular cancer can be better detected with DBT, Dr. Conant replied, "Yes. Those were the most remarkable cases, because those tumors tend to be large at presentation and notoriously difficult to detect because they don’t often form the mass that an invasive ductal carcinoma does."
Press briefing moderator Dr. Debra L. Somers Copit, chief of mammography and director of the Gershon-Cohen Breast Clinic at Einstein Medical Center, Philadelphia, described the improvements in cancer detection in the real-world cohort as "groundbreaking work for this modality that we hope will pan out across multiple institutions."
Reimbursement is problematic, however, as insurers will only pay for 2D mammography images taken as part of a tomosynthesis screening exam, she said in an interview.
Still, she personally believes tomosynthesis should now be the standard of care, adding, "I can’t imagine reading a mammogram without it."
Results from the current study are comparable with data reported recently from trials in the United States (Radiology 2013;269:694-700) and Norway (Eur. Radiol. 2013;23:2061-71) that paired 2D imaging with 3D tomosynthesis, Dr. Conant observed.
When the investigators looked at the independent risk factor of breast density, DBT also did a better job of detecting cancer than conventional mammography in fatty, scattered, heterogeneous, and extremely dense breasts, and it improved recall rates for all categories except extremely dense breasts, she said.
Overall, DBT significantly reduced the proportion of women recalled for additional imaging from 10.39% to 8.77% (P = .001).
DBT is an exciting improvement over 2D mammography and more economical than breast screening with magnetic resonance imaging, but it is "not the solution to everything," Dr. Conant said. The radiation dose for the average breast is within safety limits, but twice that of a regular mammogram.
"The cost to the patient is not monetary at our site; it may be at other sites," she said. "I think right now the dose is the biggest cost."
The May 2013 approval of Hologic’s C-View 2D imaging software, which eliminates the need for additional 2D exposures by generating 2D images from 3D tomosynthesis data, might address this, Dr. Conant added.
Dr. Conant reported consulting for Hologic. Her coauthors reported no financial disclosures. Dr. Copit is on Hologic’s scientific advisory board.
CHICAGO – Screening all-comers with three-dimensional mammography increased breast cancer detection by 22.7% and reduced recall rates by 15.6% in a large observational study.
Although a 3D digital breast tomosynthesis (DBT) system was approved for breast cancer screening and diagnosis in the United States in 2011, DBT is typically a supplemental screening tool to standard 2D digital mammography.
In November 2011, however, the Hospital of the University of Pennsylvania, Philadelphia, took the plunge and began using DBT for every breast screening patient, regardless of age, cancer risk, breast density, or ability to pay.
Over a 17-month-period, DBT detected 82 cancers in 15,632 women, or 5.25 cancers per 1,000 cases, Dr. Emily F. Conant reported at the annual meeting of the Radiological Society of North America.
This compares with 46 cancers, or 4.28 cancers per 1,000 cases, detected with conventional mammography in 10,752 women in the 12 months prior to the switch.
The difference in cancer detection rates between 2D and 3D mammography did not reach statistical significance (P = .226), probably because of the small number of cases, Dr. Conant, a radiology professor at the hospital, said at a press briefing.
Compared with conventional mammography, however, DBT significantly improved the proportion of positive screening mammograms from which cancer was diagnosed by 45% (P = .036) and increased the detection of deadly invasive cancers by a nonsignificant 31%.
When asked whether the study showed that invasive lobular cancer can be better detected with DBT, Dr. Conant replied, "Yes. Those were the most remarkable cases, because those tumors tend to be large at presentation and notoriously difficult to detect because they don’t often form the mass that an invasive ductal carcinoma does."
Press briefing moderator Dr. Debra L. Somers Copit, chief of mammography and director of the Gershon-Cohen Breast Clinic at Einstein Medical Center, Philadelphia, described the improvements in cancer detection in the real-world cohort as "groundbreaking work for this modality that we hope will pan out across multiple institutions."
Reimbursement is problematic, however, as insurers will only pay for 2D mammography images taken as part of a tomosynthesis screening exam, she said in an interview.
Still, she personally believes tomosynthesis should now be the standard of care, adding, "I can’t imagine reading a mammogram without it."
Results from the current study are comparable with data reported recently from trials in the United States (Radiology 2013;269:694-700) and Norway (Eur. Radiol. 2013;23:2061-71) that paired 2D imaging with 3D tomosynthesis, Dr. Conant observed.
When the investigators looked at the independent risk factor of breast density, DBT also did a better job of detecting cancer than conventional mammography in fatty, scattered, heterogeneous, and extremely dense breasts, and it improved recall rates for all categories except extremely dense breasts, she said.
Overall, DBT significantly reduced the proportion of women recalled for additional imaging from 10.39% to 8.77% (P = .001).
DBT is an exciting improvement over 2D mammography and more economical than breast screening with magnetic resonance imaging, but it is "not the solution to everything," Dr. Conant said. The radiation dose for the average breast is within safety limits, but twice that of a regular mammogram.
"The cost to the patient is not monetary at our site; it may be at other sites," she said. "I think right now the dose is the biggest cost."
The May 2013 approval of Hologic’s C-View 2D imaging software, which eliminates the need for additional 2D exposures by generating 2D images from 3D tomosynthesis data, might address this, Dr. Conant added.
Dr. Conant reported consulting for Hologic. Her coauthors reported no financial disclosures. Dr. Copit is on Hologic’s scientific advisory board.
CHICAGO – Screening all-comers with three-dimensional mammography increased breast cancer detection by 22.7% and reduced recall rates by 15.6% in a large observational study.
Although a 3D digital breast tomosynthesis (DBT) system was approved for breast cancer screening and diagnosis in the United States in 2011, DBT is typically a supplemental screening tool to standard 2D digital mammography.
In November 2011, however, the Hospital of the University of Pennsylvania, Philadelphia, took the plunge and began using DBT for every breast screening patient, regardless of age, cancer risk, breast density, or ability to pay.
Over a 17-month-period, DBT detected 82 cancers in 15,632 women, or 5.25 cancers per 1,000 cases, Dr. Emily F. Conant reported at the annual meeting of the Radiological Society of North America.
This compares with 46 cancers, or 4.28 cancers per 1,000 cases, detected with conventional mammography in 10,752 women in the 12 months prior to the switch.
The difference in cancer detection rates between 2D and 3D mammography did not reach statistical significance (P = .226), probably because of the small number of cases, Dr. Conant, a radiology professor at the hospital, said at a press briefing.
Compared with conventional mammography, however, DBT significantly improved the proportion of positive screening mammograms from which cancer was diagnosed by 45% (P = .036) and increased the detection of deadly invasive cancers by a nonsignificant 31%.
When asked whether the study showed that invasive lobular cancer can be better detected with DBT, Dr. Conant replied, "Yes. Those were the most remarkable cases, because those tumors tend to be large at presentation and notoriously difficult to detect because they don’t often form the mass that an invasive ductal carcinoma does."
Press briefing moderator Dr. Debra L. Somers Copit, chief of mammography and director of the Gershon-Cohen Breast Clinic at Einstein Medical Center, Philadelphia, described the improvements in cancer detection in the real-world cohort as "groundbreaking work for this modality that we hope will pan out across multiple institutions."
Reimbursement is problematic, however, as insurers will only pay for 2D mammography images taken as part of a tomosynthesis screening exam, she said in an interview.
Still, she personally believes tomosynthesis should now be the standard of care, adding, "I can’t imagine reading a mammogram without it."
Results from the current study are comparable with data reported recently from trials in the United States (Radiology 2013;269:694-700) and Norway (Eur. Radiol. 2013;23:2061-71) that paired 2D imaging with 3D tomosynthesis, Dr. Conant observed.
When the investigators looked at the independent risk factor of breast density, DBT also did a better job of detecting cancer than conventional mammography in fatty, scattered, heterogeneous, and extremely dense breasts, and it improved recall rates for all categories except extremely dense breasts, she said.
Overall, DBT significantly reduced the proportion of women recalled for additional imaging from 10.39% to 8.77% (P = .001).
DBT is an exciting improvement over 2D mammography and more economical than breast screening with magnetic resonance imaging, but it is "not the solution to everything," Dr. Conant said. The radiation dose for the average breast is within safety limits, but twice that of a regular mammogram.
"The cost to the patient is not monetary at our site; it may be at other sites," she said. "I think right now the dose is the biggest cost."
The May 2013 approval of Hologic’s C-View 2D imaging software, which eliminates the need for additional 2D exposures by generating 2D images from 3D tomosynthesis data, might address this, Dr. Conant added.
Dr. Conant reported consulting for Hologic. Her coauthors reported no financial disclosures. Dr. Copit is on Hologic’s scientific advisory board.
AT RSNA 2013
Major finding: Digital breast tomosynthesis detected 5.25 cancers per 1,000 cases over a 17-month period, compared with 4.28 cancers per 1,000 cases over 12 months with conventional mammography.
Data source: An observational study of 15,632 women screened using DBT and 10,752 women using 2-D digital mammography at the Hospital of the University of Pennsylvania.
Disclosures: Dr. Conant reported consulting for Hologic Inc. Her coauthors reported no financial disclosures. Dr. Copit is on Hologic’s scientific advisory board.
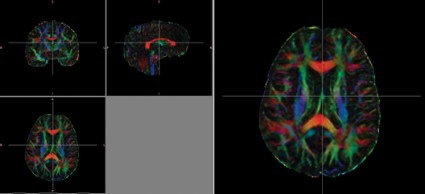
DTI detects long-term axonal injury in veterans with TBI
CHICAGO – Diffusion tensor imaging identified axonal damage in veterans more than 4 years after a blast-related traumatic brain injury in a phase I/II study.
None of the veterans had abnormalities on conventional CT or MRI, Thomas M. Malone reported at the annual meeting of the Radiological Society of North America.
Prior studies have shown that diffusion tensor imaging (DTI) identified white matter injuries in the middle cerebellar peduncles, cingulum bundles, and right orbitofrontal region of asymptomatic veterans with mild TBI less than 90 days post injury (N. Engl. J. Med. 2011;364:2091-100).
However, another study showed that the correlation between DTI findings and neuropsychological symptoms in the acute phase was inconsistent at 2.5 years (J. Neurotrauma 2010;27:683-94).
In the phase I portion of the current study, 10 veterans with blast-related mild TBI were evaluated at an average of 51.3 months after injury, along with 10 healthy controls.
Despite having normal findings on CT and MR imaging, veterans had significantly higher average DTI-derived fractional anisotropy (FA) values than did controls in the right posterior limb of the internal capsule (0.739 vs. 0.706; P less than .05) and left posterior limb of the internal capsule (0.777 vs. 0.716; P less than .05). FA values were similar between groups in the anterior limbs of the internal capsule and genu and splenium of the corpus callosum. These higher FA values differ from results found in DTI studies conducted during the acute phase of blast-related mild TBI, said Mr. Malone of St. Louis University.
Overall, veterans scored significantly lower than did controls on the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS), immediate memory index (81.6 vs. 99.8; P less than .01), visual-constructional index (82.9 vs. 100.2; P less than .05), and delayed memory index (81.5 vs. 97.4; P less than .05).
Significant correlations were found between internal capsule FA values and neuropsychological tests measuring attention, memory, and motor functioning, including the RBANS and grooved pegboard test, Mr. Malone said.
For the phase II portion of the study, the investigators increased the cohort to 21 mild TBI and 8 moderate TBI veterans and 19 healthy controls, and removed outliers with FA values more than 2 standard deviations above or below the mean.
In this analysis, average FA values were significantly lower in the splenium of the corpus callosum among veterans than in controls (0.777 vs. 0.79; P less than .05).
"Decreased FA values among the TBI group are perhaps indicative of fiber damage and may explain the chronic deficits observed in mild blast injuries," Mr. Malone said.
Recovery from long-term axonal injury is possible, but the brain has somewhat limited capabilities in repairing itself, said senior author Dr. Richard Bucholz, professor and vice chair of neurosurgery at St. Louis University.
"My general feeling is if it doesn’t repair at 51 months, it probably never repairs," he said in an interview.
Although DTI findings of long-term axonal injury have important implications in terms of rehabilitation and continued problems associated with TBI injuries, both men urged caution in interpreting the results.
"I wouldn’t want to sell this as a diagnostic test," Mr. Malone said in a press briefing. "These were between-group differences."
Future studies will require larger numbers of veterans and the use of more robust preprocessing software such as Tortoise from the National Institutes of Health, automated segmentation, and voxel-based morphometry analysis.
Mr. Malone and his coauthors reported having no relevant financial disclosures.
CHICAGO – Diffusion tensor imaging identified axonal damage in veterans more than 4 years after a blast-related traumatic brain injury in a phase I/II study.
None of the veterans had abnormalities on conventional CT or MRI, Thomas M. Malone reported at the annual meeting of the Radiological Society of North America.
Prior studies have shown that diffusion tensor imaging (DTI) identified white matter injuries in the middle cerebellar peduncles, cingulum bundles, and right orbitofrontal region of asymptomatic veterans with mild TBI less than 90 days post injury (N. Engl. J. Med. 2011;364:2091-100).
However, another study showed that the correlation between DTI findings and neuropsychological symptoms in the acute phase was inconsistent at 2.5 years (J. Neurotrauma 2010;27:683-94).
In the phase I portion of the current study, 10 veterans with blast-related mild TBI were evaluated at an average of 51.3 months after injury, along with 10 healthy controls.
Despite having normal findings on CT and MR imaging, veterans had significantly higher average DTI-derived fractional anisotropy (FA) values than did controls in the right posterior limb of the internal capsule (0.739 vs. 0.706; P less than .05) and left posterior limb of the internal capsule (0.777 vs. 0.716; P less than .05). FA values were similar between groups in the anterior limbs of the internal capsule and genu and splenium of the corpus callosum. These higher FA values differ from results found in DTI studies conducted during the acute phase of blast-related mild TBI, said Mr. Malone of St. Louis University.
Overall, veterans scored significantly lower than did controls on the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS), immediate memory index (81.6 vs. 99.8; P less than .01), visual-constructional index (82.9 vs. 100.2; P less than .05), and delayed memory index (81.5 vs. 97.4; P less than .05).
Significant correlations were found between internal capsule FA values and neuropsychological tests measuring attention, memory, and motor functioning, including the RBANS and grooved pegboard test, Mr. Malone said.
For the phase II portion of the study, the investigators increased the cohort to 21 mild TBI and 8 moderate TBI veterans and 19 healthy controls, and removed outliers with FA values more than 2 standard deviations above or below the mean.
In this analysis, average FA values were significantly lower in the splenium of the corpus callosum among veterans than in controls (0.777 vs. 0.79; P less than .05).
"Decreased FA values among the TBI group are perhaps indicative of fiber damage and may explain the chronic deficits observed in mild blast injuries," Mr. Malone said.
Recovery from long-term axonal injury is possible, but the brain has somewhat limited capabilities in repairing itself, said senior author Dr. Richard Bucholz, professor and vice chair of neurosurgery at St. Louis University.
"My general feeling is if it doesn’t repair at 51 months, it probably never repairs," he said in an interview.
Although DTI findings of long-term axonal injury have important implications in terms of rehabilitation and continued problems associated with TBI injuries, both men urged caution in interpreting the results.
"I wouldn’t want to sell this as a diagnostic test," Mr. Malone said in a press briefing. "These were between-group differences."
Future studies will require larger numbers of veterans and the use of more robust preprocessing software such as Tortoise from the National Institutes of Health, automated segmentation, and voxel-based morphometry analysis.
Mr. Malone and his coauthors reported having no relevant financial disclosures.
CHICAGO – Diffusion tensor imaging identified axonal damage in veterans more than 4 years after a blast-related traumatic brain injury in a phase I/II study.
None of the veterans had abnormalities on conventional CT or MRI, Thomas M. Malone reported at the annual meeting of the Radiological Society of North America.
Prior studies have shown that diffusion tensor imaging (DTI) identified white matter injuries in the middle cerebellar peduncles, cingulum bundles, and right orbitofrontal region of asymptomatic veterans with mild TBI less than 90 days post injury (N. Engl. J. Med. 2011;364:2091-100).
However, another study showed that the correlation between DTI findings and neuropsychological symptoms in the acute phase was inconsistent at 2.5 years (J. Neurotrauma 2010;27:683-94).
In the phase I portion of the current study, 10 veterans with blast-related mild TBI were evaluated at an average of 51.3 months after injury, along with 10 healthy controls.
Despite having normal findings on CT and MR imaging, veterans had significantly higher average DTI-derived fractional anisotropy (FA) values than did controls in the right posterior limb of the internal capsule (0.739 vs. 0.706; P less than .05) and left posterior limb of the internal capsule (0.777 vs. 0.716; P less than .05). FA values were similar between groups in the anterior limbs of the internal capsule and genu and splenium of the corpus callosum. These higher FA values differ from results found in DTI studies conducted during the acute phase of blast-related mild TBI, said Mr. Malone of St. Louis University.
Overall, veterans scored significantly lower than did controls on the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS), immediate memory index (81.6 vs. 99.8; P less than .01), visual-constructional index (82.9 vs. 100.2; P less than .05), and delayed memory index (81.5 vs. 97.4; P less than .05).
Significant correlations were found between internal capsule FA values and neuropsychological tests measuring attention, memory, and motor functioning, including the RBANS and grooved pegboard test, Mr. Malone said.
For the phase II portion of the study, the investigators increased the cohort to 21 mild TBI and 8 moderate TBI veterans and 19 healthy controls, and removed outliers with FA values more than 2 standard deviations above or below the mean.
In this analysis, average FA values were significantly lower in the splenium of the corpus callosum among veterans than in controls (0.777 vs. 0.79; P less than .05).
"Decreased FA values among the TBI group are perhaps indicative of fiber damage and may explain the chronic deficits observed in mild blast injuries," Mr. Malone said.
Recovery from long-term axonal injury is possible, but the brain has somewhat limited capabilities in repairing itself, said senior author Dr. Richard Bucholz, professor and vice chair of neurosurgery at St. Louis University.
"My general feeling is if it doesn’t repair at 51 months, it probably never repairs," he said in an interview.
Although DTI findings of long-term axonal injury have important implications in terms of rehabilitation and continued problems associated with TBI injuries, both men urged caution in interpreting the results.
"I wouldn’t want to sell this as a diagnostic test," Mr. Malone said in a press briefing. "These were between-group differences."
Future studies will require larger numbers of veterans and the use of more robust preprocessing software such as Tortoise from the National Institutes of Health, automated segmentation, and voxel-based morphometry analysis.
Mr. Malone and his coauthors reported having no relevant financial disclosures.
AT RSNA 2013
Major finding: Veterans had significantly higher average diffusion tensor imaging–derived fractional anisotropy values than did healthy controls in the right posterior limb of the internal capsule (0.739 vs. 0.706; P less than .05) and left posterior limb of the internal capsule (0.777 vs. 0.716; P less than .05)
Data source: A retrospective phase I/II study in 39 veterans with traumatic brain injury and 29 healthy controls.
Disclosures: Mr. Malone and his coauthors reported having no relevant financial disclosures.
Energy drinks amp up heart contractility
CHICAGO – Consumption of an energy drink containing caffeine and taurine slightly, but significantly, altered left ventricular contractility in healthy volunteers, while consuming the same amount of caffeine alone did not lead to an alteration in contractility in a prospective study.
"A possible explanation for this finding could be the presence of taurine, which has been shown to increase the release of calcium in muscles," Dr. Jonas Dörner reported at the annual meeting of the Radiological Society of North America.
Cardiac magnetic resonance imaging (MRI) was performed in 31 volunteers before and 1 hour after consuming an energy drink containing caffeine (32 mg/100 mL) and taurine (400 mg/100 mL). The average patient age was 27.7 years.
Postconsumption images revealed that mean peak strain increased 7% from baseline (–22.84 vs. –24.35; P < .0001) and peak systolic strain rate – a measure of deformation with respect to time– increased by 6% (–1.19 to –1.26; P = .0032), said Dr. Dörner, with the University of Bonn, Germany.
No significant changes were found in heart rate, systolic blood pressure, or left ventricular (LV) ejection fraction. LV end-diastolic volume and LV stroke volume increased significantly by 2% and 4%, respectively.
The same imaging protocol was repeated on a different day in 10 patients after consumption of caffeine only. No significant differences were seen in mean peak strain (–22.99 vs. –23.20) or mean peak systolic strain rate (–1.15 vs. –1.16) with caffeine alone, although diastolic blood pressure was significantly elevated and LV end-diastolic volume significantly decreased, Dr. Dörner said.
The current study took advantage of an MRI technique called complementary spatial modulation of magnetization (CSPAMM) for LV myocardial tagging. The technique is more exact than traditional ultrasound or speckle tracking and is able to measure very small differences in strain, he explained in an interview.
Although the differences in strain in the study were "subtle," the findings need to be taken into perspective because younger patients often consume higher doses of caffeine and taurine via energy drinks. According to the Food and Drug Administration, caffeinated sodas cannot contain more than 71 mg of caffeine per 12 fluid ounces (approximately 20 mg/100 mL), but energy drinks often contain three times that amount, he noted.
More than 500 brands of energy drinks are available worldwide, and 30%-50% are consumed by children, teenagers, and young adults. A report by the European Food Safety Authority found no adverse effects for up to 1 g of taurine per kilogram of body weight per day.
Further studies are needed to evaluate the effect of long-term energy drink consumption and the effect of these drinks on patients with heart disease and in combination with alcohol, Dr. Dörner said.
Dr. Dörner reported having no financial disclosures; a coauthor reported consulting for Medtronic.
CHICAGO – Consumption of an energy drink containing caffeine and taurine slightly, but significantly, altered left ventricular contractility in healthy volunteers, while consuming the same amount of caffeine alone did not lead to an alteration in contractility in a prospective study.
"A possible explanation for this finding could be the presence of taurine, which has been shown to increase the release of calcium in muscles," Dr. Jonas Dörner reported at the annual meeting of the Radiological Society of North America.
Cardiac magnetic resonance imaging (MRI) was performed in 31 volunteers before and 1 hour after consuming an energy drink containing caffeine (32 mg/100 mL) and taurine (400 mg/100 mL). The average patient age was 27.7 years.
Postconsumption images revealed that mean peak strain increased 7% from baseline (–22.84 vs. –24.35; P < .0001) and peak systolic strain rate – a measure of deformation with respect to time– increased by 6% (–1.19 to –1.26; P = .0032), said Dr. Dörner, with the University of Bonn, Germany.
No significant changes were found in heart rate, systolic blood pressure, or left ventricular (LV) ejection fraction. LV end-diastolic volume and LV stroke volume increased significantly by 2% and 4%, respectively.
The same imaging protocol was repeated on a different day in 10 patients after consumption of caffeine only. No significant differences were seen in mean peak strain (–22.99 vs. –23.20) or mean peak systolic strain rate (–1.15 vs. –1.16) with caffeine alone, although diastolic blood pressure was significantly elevated and LV end-diastolic volume significantly decreased, Dr. Dörner said.
The current study took advantage of an MRI technique called complementary spatial modulation of magnetization (CSPAMM) for LV myocardial tagging. The technique is more exact than traditional ultrasound or speckle tracking and is able to measure very small differences in strain, he explained in an interview.
Although the differences in strain in the study were "subtle," the findings need to be taken into perspective because younger patients often consume higher doses of caffeine and taurine via energy drinks. According to the Food and Drug Administration, caffeinated sodas cannot contain more than 71 mg of caffeine per 12 fluid ounces (approximately 20 mg/100 mL), but energy drinks often contain three times that amount, he noted.
More than 500 brands of energy drinks are available worldwide, and 30%-50% are consumed by children, teenagers, and young adults. A report by the European Food Safety Authority found no adverse effects for up to 1 g of taurine per kilogram of body weight per day.
Further studies are needed to evaluate the effect of long-term energy drink consumption and the effect of these drinks on patients with heart disease and in combination with alcohol, Dr. Dörner said.
Dr. Dörner reported having no financial disclosures; a coauthor reported consulting for Medtronic.
CHICAGO – Consumption of an energy drink containing caffeine and taurine slightly, but significantly, altered left ventricular contractility in healthy volunteers, while consuming the same amount of caffeine alone did not lead to an alteration in contractility in a prospective study.
"A possible explanation for this finding could be the presence of taurine, which has been shown to increase the release of calcium in muscles," Dr. Jonas Dörner reported at the annual meeting of the Radiological Society of North America.
Cardiac magnetic resonance imaging (MRI) was performed in 31 volunteers before and 1 hour after consuming an energy drink containing caffeine (32 mg/100 mL) and taurine (400 mg/100 mL). The average patient age was 27.7 years.
Postconsumption images revealed that mean peak strain increased 7% from baseline (–22.84 vs. –24.35; P < .0001) and peak systolic strain rate – a measure of deformation with respect to time– increased by 6% (–1.19 to –1.26; P = .0032), said Dr. Dörner, with the University of Bonn, Germany.
No significant changes were found in heart rate, systolic blood pressure, or left ventricular (LV) ejection fraction. LV end-diastolic volume and LV stroke volume increased significantly by 2% and 4%, respectively.
The same imaging protocol was repeated on a different day in 10 patients after consumption of caffeine only. No significant differences were seen in mean peak strain (–22.99 vs. –23.20) or mean peak systolic strain rate (–1.15 vs. –1.16) with caffeine alone, although diastolic blood pressure was significantly elevated and LV end-diastolic volume significantly decreased, Dr. Dörner said.
The current study took advantage of an MRI technique called complementary spatial modulation of magnetization (CSPAMM) for LV myocardial tagging. The technique is more exact than traditional ultrasound or speckle tracking and is able to measure very small differences in strain, he explained in an interview.
Although the differences in strain in the study were "subtle," the findings need to be taken into perspective because younger patients often consume higher doses of caffeine and taurine via energy drinks. According to the Food and Drug Administration, caffeinated sodas cannot contain more than 71 mg of caffeine per 12 fluid ounces (approximately 20 mg/100 mL), but energy drinks often contain three times that amount, he noted.
More than 500 brands of energy drinks are available worldwide, and 30%-50% are consumed by children, teenagers, and young adults. A report by the European Food Safety Authority found no adverse effects for up to 1 g of taurine per kilogram of body weight per day.
Further studies are needed to evaluate the effect of long-term energy drink consumption and the effect of these drinks on patients with heart disease and in combination with alcohol, Dr. Dörner said.
Dr. Dörner reported having no financial disclosures; a coauthor reported consulting for Medtronic.
AT RSNA 2013
Major finding: One hour after consumption of an energy drink containing caffeine and taurine, mean peak strain increased 7% from baseline and peak systolic strain rate increased 6%.
Data source: A prospective study of 31 healthy volunteers.
Disclosures: Dr. Dörner reported having no financial disclosures; a coauthor reported consulting for Medtronic.