User login
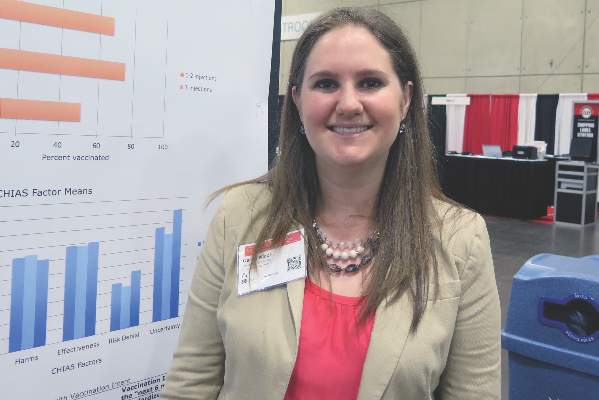
College students report perceived barriers to HPV vaccine
SAN DIEGO – College-aged men and women had positive attitudes toward human papillomavirus vaccination, yet perceived cost and access barriers factored into their decision to receive the vaccine, results from a large survey found.
“The people reporting the higher barrier scores were the same ones who had the highest intent to receive the vaccine,” Dr. Casey Nicol, lead study author, said in an interview at the annual meeting of the Society of Gynecologic Oncology. “It’s a shame, because these are people who want it, and there are ways for them to get vaccinated; they just don’t know about them. I think there’s a big opportunity for education and public health outreach.”
Dr. Nicol and her associates sent an online survey to a random sample of 3,000 students at the University of Virginia, Charlottesville, who were between 18 and 26 years old. The survey included questions about their human papillomavirus (HPV) vaccination status and intention as well as 17 items from the modified Carolina HPV Immunization Attitudes and Beliefs Scale (CHIAS).
“A lot of the previous research I could find focused more on parental attitudes about HPV vaccination rather than adolescent and young adult attitudes,” said Dr. Nicol, who is a resident in the department of obstetrics and gynecology at the University of Virginia.
Of the 3,000 surveys sent, 776 were completed and used in the final analysis, for a response rate of 26%. More than two-thirds of the respondents (70%) were women, and their mean age was 20 years. In all, 67% of students reported having received at least one HPV vaccination, and the proportion was higher for women, compared with men (75% vs. 51%, respectively).
“In our college population we found that the vaccination rates were not as bad as we expected,” Dr. Nicol said. “It was about double the national average for our women and about 20 times the national average for our men.”
No sex differences were observed in responses to 14 of the 17 CHIAS items, and CHIAS factor means for men and women did not differ for any of the five factor groupings, which included barriers, harms, effectiveness, risk denial, and uncertainty.
Dr. Nicol reported that the barriers score was the factor most strongly associated with vaccination intent “today.” It was also strongly associated with vaccination intent for “the next 6 months” (P = .001).
Items in the barriers factor category included the following:
• “It would be hard to find a provider or clinic that would be easy to get to for getting vaccinated against HPV.”
• “It would be hard to find a provider or clinic where I could afford the HPV vaccine.”
• “It would be hard to find a provider or clinic that has the HPV vaccine available.”
• “It would be hard to find a provider or clinic where I don’t have to wait a long time to get an appointment to get vaccinated.”
Dr. Nicol said that the findings underscore the importance of decreasing cost and access barriers in order to improve HPV vaccination rates among young adults.
“If you don’t offer the HPV vaccine at your office, at least provide your patients with” cost information and the “location of the clinics that do have it available,” she advised. “It seems like that would increase the prevalence of more students getting vaccinated.”
Dr. Nicol reported having no relevant financial disclosures.
SAN DIEGO – College-aged men and women had positive attitudes toward human papillomavirus vaccination, yet perceived cost and access barriers factored into their decision to receive the vaccine, results from a large survey found.
“The people reporting the higher barrier scores were the same ones who had the highest intent to receive the vaccine,” Dr. Casey Nicol, lead study author, said in an interview at the annual meeting of the Society of Gynecologic Oncology. “It’s a shame, because these are people who want it, and there are ways for them to get vaccinated; they just don’t know about them. I think there’s a big opportunity for education and public health outreach.”
Dr. Nicol and her associates sent an online survey to a random sample of 3,000 students at the University of Virginia, Charlottesville, who were between 18 and 26 years old. The survey included questions about their human papillomavirus (HPV) vaccination status and intention as well as 17 items from the modified Carolina HPV Immunization Attitudes and Beliefs Scale (CHIAS).
“A lot of the previous research I could find focused more on parental attitudes about HPV vaccination rather than adolescent and young adult attitudes,” said Dr. Nicol, who is a resident in the department of obstetrics and gynecology at the University of Virginia.
Of the 3,000 surveys sent, 776 were completed and used in the final analysis, for a response rate of 26%. More than two-thirds of the respondents (70%) were women, and their mean age was 20 years. In all, 67% of students reported having received at least one HPV vaccination, and the proportion was higher for women, compared with men (75% vs. 51%, respectively).
“In our college population we found that the vaccination rates were not as bad as we expected,” Dr. Nicol said. “It was about double the national average for our women and about 20 times the national average for our men.”
No sex differences were observed in responses to 14 of the 17 CHIAS items, and CHIAS factor means for men and women did not differ for any of the five factor groupings, which included barriers, harms, effectiveness, risk denial, and uncertainty.
Dr. Nicol reported that the barriers score was the factor most strongly associated with vaccination intent “today.” It was also strongly associated with vaccination intent for “the next 6 months” (P = .001).
Items in the barriers factor category included the following:
• “It would be hard to find a provider or clinic that would be easy to get to for getting vaccinated against HPV.”
• “It would be hard to find a provider or clinic where I could afford the HPV vaccine.”
• “It would be hard to find a provider or clinic that has the HPV vaccine available.”
• “It would be hard to find a provider or clinic where I don’t have to wait a long time to get an appointment to get vaccinated.”
Dr. Nicol said that the findings underscore the importance of decreasing cost and access barriers in order to improve HPV vaccination rates among young adults.
“If you don’t offer the HPV vaccine at your office, at least provide your patients with” cost information and the “location of the clinics that do have it available,” she advised. “It seems like that would increase the prevalence of more students getting vaccinated.”
Dr. Nicol reported having no relevant financial disclosures.
SAN DIEGO – College-aged men and women had positive attitudes toward human papillomavirus vaccination, yet perceived cost and access barriers factored into their decision to receive the vaccine, results from a large survey found.
“The people reporting the higher barrier scores were the same ones who had the highest intent to receive the vaccine,” Dr. Casey Nicol, lead study author, said in an interview at the annual meeting of the Society of Gynecologic Oncology. “It’s a shame, because these are people who want it, and there are ways for them to get vaccinated; they just don’t know about them. I think there’s a big opportunity for education and public health outreach.”
Dr. Nicol and her associates sent an online survey to a random sample of 3,000 students at the University of Virginia, Charlottesville, who were between 18 and 26 years old. The survey included questions about their human papillomavirus (HPV) vaccination status and intention as well as 17 items from the modified Carolina HPV Immunization Attitudes and Beliefs Scale (CHIAS).
“A lot of the previous research I could find focused more on parental attitudes about HPV vaccination rather than adolescent and young adult attitudes,” said Dr. Nicol, who is a resident in the department of obstetrics and gynecology at the University of Virginia.
Of the 3,000 surveys sent, 776 were completed and used in the final analysis, for a response rate of 26%. More than two-thirds of the respondents (70%) were women, and their mean age was 20 years. In all, 67% of students reported having received at least one HPV vaccination, and the proportion was higher for women, compared with men (75% vs. 51%, respectively).
“In our college population we found that the vaccination rates were not as bad as we expected,” Dr. Nicol said. “It was about double the national average for our women and about 20 times the national average for our men.”
No sex differences were observed in responses to 14 of the 17 CHIAS items, and CHIAS factor means for men and women did not differ for any of the five factor groupings, which included barriers, harms, effectiveness, risk denial, and uncertainty.
Dr. Nicol reported that the barriers score was the factor most strongly associated with vaccination intent “today.” It was also strongly associated with vaccination intent for “the next 6 months” (P = .001).
Items in the barriers factor category included the following:
• “It would be hard to find a provider or clinic that would be easy to get to for getting vaccinated against HPV.”
• “It would be hard to find a provider or clinic where I could afford the HPV vaccine.”
• “It would be hard to find a provider or clinic that has the HPV vaccine available.”
• “It would be hard to find a provider or clinic where I don’t have to wait a long time to get an appointment to get vaccinated.”
Dr. Nicol said that the findings underscore the importance of decreasing cost and access barriers in order to improve HPV vaccination rates among young adults.
“If you don’t offer the HPV vaccine at your office, at least provide your patients with” cost information and the “location of the clinics that do have it available,” she advised. “It seems like that would increase the prevalence of more students getting vaccinated.”
Dr. Nicol reported having no relevant financial disclosures.
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: The rate of HPV vaccination among college students was higher than expected.
Major finding: In all, 67% of students reported having received at least one HPV vaccination, and the proportion was higher for women, compared with men (75% vs. 51%, respectively).
Data source: An online survey of 3,000 students at the University of Virginia, Charlottesville, who were between 18 and 26 years old.
Disclosures:Dr. Nicol reported having no relevant financial disclosures.
Gynecologic oncologists often missing from pediatric pelvic evaluations
SAN DIEGO – Young women and girls with gynecologic malignancies more often present with pain and masses greater than 5 cm in size, compared with their counterparts who have benign disease. Additionally, gynecologic oncologists are inconsistently involved in the management of this patient population.
Those are key findings from a study that set out to compare the clinical presentation and surgical outcomes of women and girls younger than 21 years old who had a pelvic mass.
“If something is suspicious, it’s not a bad idea to get your colleagues who specialize in gynecologic cancer involved sooner rather than later,” Dr. Teuta Shemshedini, the lead study author, said in an interview at the annual meeting of the Society of Gynecologic Oncology. Clinicians who specialize in gynecologic oncology “were often talked to either intraoperatively or postoperatively, so we were kind of working backwards when we could have sat with patients and the families before the surgery and worked forward.”
Dr. Shemshedini, who is a fourth-year resident in the department of obstetrics and gynecology at Westchester Medical Center, Valhalla, N.Y., and her associates reviewed medical records of all women and girls younger than 21 years old who underwent primary surgery for a pelvic mass at the medical center from 2010 to 2015.
Of the 138 patients evaluated, 77 were included in the final analysis: 57 who had benign disease and 20 who had malignant disease. The mean age of the patients was 13.5 years and the mean adnexal mass size was 9.8 cm in the benign group, compared with 15.5 cm in the malignant group (P = .005). The most common presentation was pain, which occurred in 75% of all cases.
Gynecologic oncologists were consulted on 10 cases (13%), with six of the 10 consults (60%) requested by pediatric gynecologists. However, only two of eight (25%) were preoperative consults in malignant cases.
The researchers also observed that tumors greater than 10 cm in size were found in 75% of malignancies, and all tumors 5 cm or smaller were benign (14%). Clinicians did not use tumor markers in 29% of the entire study group, even though tumor markers were elevated in 70% of the malignant cases.
Laparoscopic surgery was performed in 35 patients (45%), with a majority of cases being benign. The most common benign tumors were mature teratomas (70%). The most common malignant tumors were borderline ovarian tumors (35%), followed by immature teratomas (20%), and mixed germ cell tumors (20%). More than half of malignant tumors (55%) were stage I.
“The most surprising part was that we weren’t getting gynecologic oncology involved soon enough,” Dr. Shemshedini said. “I think most people are very surprised when a mass comes back as cancer in kids, especially ovarian cancer. In adults we see epithelial cancer most commonly, while in kids it’s more of the germ cell tumors. Those are rare.”
Dr. Shemshedini reported having no financial disclosures.
SAN DIEGO – Young women and girls with gynecologic malignancies more often present with pain and masses greater than 5 cm in size, compared with their counterparts who have benign disease. Additionally, gynecologic oncologists are inconsistently involved in the management of this patient population.
Those are key findings from a study that set out to compare the clinical presentation and surgical outcomes of women and girls younger than 21 years old who had a pelvic mass.
“If something is suspicious, it’s not a bad idea to get your colleagues who specialize in gynecologic cancer involved sooner rather than later,” Dr. Teuta Shemshedini, the lead study author, said in an interview at the annual meeting of the Society of Gynecologic Oncology. Clinicians who specialize in gynecologic oncology “were often talked to either intraoperatively or postoperatively, so we were kind of working backwards when we could have sat with patients and the families before the surgery and worked forward.”
Dr. Shemshedini, who is a fourth-year resident in the department of obstetrics and gynecology at Westchester Medical Center, Valhalla, N.Y., and her associates reviewed medical records of all women and girls younger than 21 years old who underwent primary surgery for a pelvic mass at the medical center from 2010 to 2015.
Of the 138 patients evaluated, 77 were included in the final analysis: 57 who had benign disease and 20 who had malignant disease. The mean age of the patients was 13.5 years and the mean adnexal mass size was 9.8 cm in the benign group, compared with 15.5 cm in the malignant group (P = .005). The most common presentation was pain, which occurred in 75% of all cases.
Gynecologic oncologists were consulted on 10 cases (13%), with six of the 10 consults (60%) requested by pediatric gynecologists. However, only two of eight (25%) were preoperative consults in malignant cases.
The researchers also observed that tumors greater than 10 cm in size were found in 75% of malignancies, and all tumors 5 cm or smaller were benign (14%). Clinicians did not use tumor markers in 29% of the entire study group, even though tumor markers were elevated in 70% of the malignant cases.
Laparoscopic surgery was performed in 35 patients (45%), with a majority of cases being benign. The most common benign tumors were mature teratomas (70%). The most common malignant tumors were borderline ovarian tumors (35%), followed by immature teratomas (20%), and mixed germ cell tumors (20%). More than half of malignant tumors (55%) were stage I.
“The most surprising part was that we weren’t getting gynecologic oncology involved soon enough,” Dr. Shemshedini said. “I think most people are very surprised when a mass comes back as cancer in kids, especially ovarian cancer. In adults we see epithelial cancer most commonly, while in kids it’s more of the germ cell tumors. Those are rare.”
Dr. Shemshedini reported having no financial disclosures.
SAN DIEGO – Young women and girls with gynecologic malignancies more often present with pain and masses greater than 5 cm in size, compared with their counterparts who have benign disease. Additionally, gynecologic oncologists are inconsistently involved in the management of this patient population.
Those are key findings from a study that set out to compare the clinical presentation and surgical outcomes of women and girls younger than 21 years old who had a pelvic mass.
“If something is suspicious, it’s not a bad idea to get your colleagues who specialize in gynecologic cancer involved sooner rather than later,” Dr. Teuta Shemshedini, the lead study author, said in an interview at the annual meeting of the Society of Gynecologic Oncology. Clinicians who specialize in gynecologic oncology “were often talked to either intraoperatively or postoperatively, so we were kind of working backwards when we could have sat with patients and the families before the surgery and worked forward.”
Dr. Shemshedini, who is a fourth-year resident in the department of obstetrics and gynecology at Westchester Medical Center, Valhalla, N.Y., and her associates reviewed medical records of all women and girls younger than 21 years old who underwent primary surgery for a pelvic mass at the medical center from 2010 to 2015.
Of the 138 patients evaluated, 77 were included in the final analysis: 57 who had benign disease and 20 who had malignant disease. The mean age of the patients was 13.5 years and the mean adnexal mass size was 9.8 cm in the benign group, compared with 15.5 cm in the malignant group (P = .005). The most common presentation was pain, which occurred in 75% of all cases.
Gynecologic oncologists were consulted on 10 cases (13%), with six of the 10 consults (60%) requested by pediatric gynecologists. However, only two of eight (25%) were preoperative consults in malignant cases.
The researchers also observed that tumors greater than 10 cm in size were found in 75% of malignancies, and all tumors 5 cm or smaller were benign (14%). Clinicians did not use tumor markers in 29% of the entire study group, even though tumor markers were elevated in 70% of the malignant cases.
Laparoscopic surgery was performed in 35 patients (45%), with a majority of cases being benign. The most common benign tumors were mature teratomas (70%). The most common malignant tumors were borderline ovarian tumors (35%), followed by immature teratomas (20%), and mixed germ cell tumors (20%). More than half of malignant tumors (55%) were stage I.
“The most surprising part was that we weren’t getting gynecologic oncology involved soon enough,” Dr. Shemshedini said. “I think most people are very surprised when a mass comes back as cancer in kids, especially ovarian cancer. In adults we see epithelial cancer most commonly, while in kids it’s more of the germ cell tumors. Those are rare.”
Dr. Shemshedini reported having no financial disclosures.
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: Among young women and girls with pelvic malignancies, the mass is often greater than 5 cm in size.
Major finding: The mean adnexal mass size was 9.8 cm in the benign group, compared with 15.5 cm in the malignant group (P =.005).
Data source: A review of medical records from 77 women and girls younger than 21 years old who underwent primary surgery for a pelvic mass from 2010 to 2015.
Disclosures: Dr. Shemshedini reported having no financial disclosures.
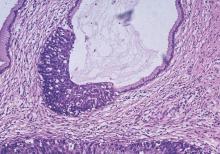
Early biopsy predicts levonorgestrel IUD response in endometrial cancer
SAN DIEGO – Endometrial pathology findings at 3 months predicted response to levonorgestrel-releasing IUD treatment for complex atypical hyperplasia or grade 1 endometrial cancer at the MD Anderson Cancer Center in Houston.
Twenty-nine of 32 women (91%) who responded by 12 months showed stromal, glandular, or other endometrial changes indicating an effect at 3 months, vs. only 3 of 9 nonresponders (33%) (P less than .001). There were no differences in responders versus nonresponders in median age (47 vs. 56 years, P = .2) or body mass index (45 vs. 55 kg/m2, P = .16).
The finding addresses an “unmet need” for markers of response to levonorgestrel-releasing IUD therapy. “You can look at [early] pathology” and have an idea how patients will do, Dr. Shannon Westin, a study investigator who is with the department of gynecologic oncology at MD Anderson, said at the annual meeting of the Society of Gynecologic Oncology.
Twenty-seven of 29 women (93%) with complex atypical hyperplasia (CAH) responded completely to the IUD, meaning they had normal endometrium or hyperplasia without atypia at 12 months. The response rate for endometrial cancer was 67%; 7 of 12 women had a complete response, and an 8th was diagnosed at 12 months with CAH, indicating a partial response. The rest of the patients remained stable or progressed.
Endometrial biopsies were performed every 3 months; the team also did molecular testing on tumors from 20 patients. Baseline protein Ki67 – a marker of proliferation – was significantly higher in nonresponders. Expression of several estrogen-induced genes was higher in responders.
Patients opted for the IUD to retain fertility or because obesity or comorbidities precluded surgery. Exclusion criteria included prior treatment for CAH or endometrial cancer, evidence of extrauterine spread, or levonorgestrel IUD contraindications, such as uterine infection.
Adverse events – primarily irregular bleeding and cramping – were mild and tended to resolve by 12 months. Treatment had little effect on measures of social, mental, and physical function. About half of the patients were white, a third were Hispanic, and most of the remaining patients were black.
There was no external funding for the work. Dr. Westin is a consultant for AstraZeneca, Medivation, Roche, Ovation, and Vermillion, and reported receiving research funding from AstraZeneca, Critical Outcomes Technologies, and Novartis.
SAN DIEGO – Endometrial pathology findings at 3 months predicted response to levonorgestrel-releasing IUD treatment for complex atypical hyperplasia or grade 1 endometrial cancer at the MD Anderson Cancer Center in Houston.
Twenty-nine of 32 women (91%) who responded by 12 months showed stromal, glandular, or other endometrial changes indicating an effect at 3 months, vs. only 3 of 9 nonresponders (33%) (P less than .001). There were no differences in responders versus nonresponders in median age (47 vs. 56 years, P = .2) or body mass index (45 vs. 55 kg/m2, P = .16).
The finding addresses an “unmet need” for markers of response to levonorgestrel-releasing IUD therapy. “You can look at [early] pathology” and have an idea how patients will do, Dr. Shannon Westin, a study investigator who is with the department of gynecologic oncology at MD Anderson, said at the annual meeting of the Society of Gynecologic Oncology.
Twenty-seven of 29 women (93%) with complex atypical hyperplasia (CAH) responded completely to the IUD, meaning they had normal endometrium or hyperplasia without atypia at 12 months. The response rate for endometrial cancer was 67%; 7 of 12 women had a complete response, and an 8th was diagnosed at 12 months with CAH, indicating a partial response. The rest of the patients remained stable or progressed.
Endometrial biopsies were performed every 3 months; the team also did molecular testing on tumors from 20 patients. Baseline protein Ki67 – a marker of proliferation – was significantly higher in nonresponders. Expression of several estrogen-induced genes was higher in responders.
Patients opted for the IUD to retain fertility or because obesity or comorbidities precluded surgery. Exclusion criteria included prior treatment for CAH or endometrial cancer, evidence of extrauterine spread, or levonorgestrel IUD contraindications, such as uterine infection.
Adverse events – primarily irregular bleeding and cramping – were mild and tended to resolve by 12 months. Treatment had little effect on measures of social, mental, and physical function. About half of the patients were white, a third were Hispanic, and most of the remaining patients were black.
There was no external funding for the work. Dr. Westin is a consultant for AstraZeneca, Medivation, Roche, Ovation, and Vermillion, and reported receiving research funding from AstraZeneca, Critical Outcomes Technologies, and Novartis.
SAN DIEGO – Endometrial pathology findings at 3 months predicted response to levonorgestrel-releasing IUD treatment for complex atypical hyperplasia or grade 1 endometrial cancer at the MD Anderson Cancer Center in Houston.
Twenty-nine of 32 women (91%) who responded by 12 months showed stromal, glandular, or other endometrial changes indicating an effect at 3 months, vs. only 3 of 9 nonresponders (33%) (P less than .001). There were no differences in responders versus nonresponders in median age (47 vs. 56 years, P = .2) or body mass index (45 vs. 55 kg/m2, P = .16).
The finding addresses an “unmet need” for markers of response to levonorgestrel-releasing IUD therapy. “You can look at [early] pathology” and have an idea how patients will do, Dr. Shannon Westin, a study investigator who is with the department of gynecologic oncology at MD Anderson, said at the annual meeting of the Society of Gynecologic Oncology.
Twenty-seven of 29 women (93%) with complex atypical hyperplasia (CAH) responded completely to the IUD, meaning they had normal endometrium or hyperplasia without atypia at 12 months. The response rate for endometrial cancer was 67%; 7 of 12 women had a complete response, and an 8th was diagnosed at 12 months with CAH, indicating a partial response. The rest of the patients remained stable or progressed.
Endometrial biopsies were performed every 3 months; the team also did molecular testing on tumors from 20 patients. Baseline protein Ki67 – a marker of proliferation – was significantly higher in nonresponders. Expression of several estrogen-induced genes was higher in responders.
Patients opted for the IUD to retain fertility or because obesity or comorbidities precluded surgery. Exclusion criteria included prior treatment for CAH or endometrial cancer, evidence of extrauterine spread, or levonorgestrel IUD contraindications, such as uterine infection.
Adverse events – primarily irregular bleeding and cramping – were mild and tended to resolve by 12 months. Treatment had little effect on measures of social, mental, and physical function. About half of the patients were white, a third were Hispanic, and most of the remaining patients were black.
There was no external funding for the work. Dr. Westin is a consultant for AstraZeneca, Medivation, Roche, Ovation, and Vermillion, and reported receiving research funding from AstraZeneca, Critical Outcomes Technologies, and Novartis.
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: Pathology and molecular findings identify good candidates for levonorgestrel IUD therapy.
Major finding: Twenty-nine of 32 women (91%) who responded by 12 months showed stromal, glandular, or other endometrial changes indicating an effect at 3 months, versus only 3 of 9 nonresponders (33%) (P less than .001).
Data source: A prospective investigation of 41 women.
Disclosures: There was no external funding for the work. Dr. Westin is a consultant for and receives research funding from AstraZeneca and several other companies.
Study ranks risk factors for cervical cancer recurrence
SAN DIEGO – Among patients with stage IB cervical cancer, deep stromal invasion and large tumor size are the two biggest factors associated with increased risk of recurrence. Higher risk-weighted surgical-pathological scores were also associated with decreased benefit of concurrent chemoradiotherapy after surgery.
Those are key findings from a Gynecologic Oncology Group (GOG) ancillary data analysis reported by Dr. Koji Matsuo at the annual meeting of the Society of Gynecologic Oncology.
“Surgery remains the mainstay of treatment for early-stage cervical cancer,” Dr. Matsuo, assistant director of the gynecologic oncology clinic at the University of Southern California, Los Angeles, said in an interview prior to the meeting. “Surgical specimen is useful to identify certain types of factors that can benefit from postoperative adjuvant therapy with concurrent chemoradiotherapy. Traditionally, tumor factors are grouped into high, intermediate, and low risk. Tumors often exhibit multiple risk factors and magnitude of significance for survival may differ across the tumor factors. In this study, we examined the effects of combination of multiple risk factors by weighing magnitude of significance for recurrence.”
The researchers analyzed data from 1,538 stage IB cervical cancer patients who underwent primary radical hysterectomy and pelvic lymphadenectomy. They used a multivariate model to examine hazard ratios associated with disease-free survival (DFS) for seven surgical-pathological risk factors: nodal metastasis, parametrial involvement, surgical margin, lymphovascular space invasion (LVSI), deep stromal invasion, large tumor, and histology. Next, they used a risk-weighted surgical-pathological score (a sum of HR scores) to determine DFS and compared it to a traditional risk factor model.
The median age of patients in the study was 41 years, the median follow-up time was 84 months, the recurrence rate was 26%, and the mortality rate was 27%.
Dr. Matsuo reported that based on the risk-weighted surgical-pathological score model, factors associated with the highest risk of recurrence were deep stromal invasion (HR 1.85), large tumor size (HR 1.81), parametrial involvement (HR 1.73), LVSI (HR 1.37), histology (HR 1.30), and nodal metastasis (HR 1.29; P less than .05 for all).
The 5-year DFS rates based on risk-weighted scores were 85.6% for score 0, 89.1% for the first quartile, 79.6% for the second quartile, 69.3% for the third quartile, and 50.2% for fourth quartile (P less than .001). A fourth-quartile score in the risk-weighted model had a significantly lower 5-year DFS rate, compared with the traditional risk factor model high-risk group (50.2% vs. 60.9%; P less than .001).
Dr. Matsuo and his associates also found that higher risk-weighted surgical-pathological scores were associated with decreased benefit of concurrent chemoradiotherapy after surgery.
“That has been the mainstay of postoperative treatment in adjuvant therapy for a group of cervical cancer with high risk of recurrence,” he said. “It is beneficial to be aware that each tumor factor has a different risk for recurrence and tumors may exhibit multiple risk factors that can be associated with decreased benefit of concurrent chemoradiotherapy after surgical treatment.”
He acknowledged certain limitations of the study, including the lack of information regarding the site of recurrence.
Dr. Matsuo reported having no financial disclosures.
SAN DIEGO – Among patients with stage IB cervical cancer, deep stromal invasion and large tumor size are the two biggest factors associated with increased risk of recurrence. Higher risk-weighted surgical-pathological scores were also associated with decreased benefit of concurrent chemoradiotherapy after surgery.
Those are key findings from a Gynecologic Oncology Group (GOG) ancillary data analysis reported by Dr. Koji Matsuo at the annual meeting of the Society of Gynecologic Oncology.
“Surgery remains the mainstay of treatment for early-stage cervical cancer,” Dr. Matsuo, assistant director of the gynecologic oncology clinic at the University of Southern California, Los Angeles, said in an interview prior to the meeting. “Surgical specimen is useful to identify certain types of factors that can benefit from postoperative adjuvant therapy with concurrent chemoradiotherapy. Traditionally, tumor factors are grouped into high, intermediate, and low risk. Tumors often exhibit multiple risk factors and magnitude of significance for survival may differ across the tumor factors. In this study, we examined the effects of combination of multiple risk factors by weighing magnitude of significance for recurrence.”
The researchers analyzed data from 1,538 stage IB cervical cancer patients who underwent primary radical hysterectomy and pelvic lymphadenectomy. They used a multivariate model to examine hazard ratios associated with disease-free survival (DFS) for seven surgical-pathological risk factors: nodal metastasis, parametrial involvement, surgical margin, lymphovascular space invasion (LVSI), deep stromal invasion, large tumor, and histology. Next, they used a risk-weighted surgical-pathological score (a sum of HR scores) to determine DFS and compared it to a traditional risk factor model.
The median age of patients in the study was 41 years, the median follow-up time was 84 months, the recurrence rate was 26%, and the mortality rate was 27%.
Dr. Matsuo reported that based on the risk-weighted surgical-pathological score model, factors associated with the highest risk of recurrence were deep stromal invasion (HR 1.85), large tumor size (HR 1.81), parametrial involvement (HR 1.73), LVSI (HR 1.37), histology (HR 1.30), and nodal metastasis (HR 1.29; P less than .05 for all).
The 5-year DFS rates based on risk-weighted scores were 85.6% for score 0, 89.1% for the first quartile, 79.6% for the second quartile, 69.3% for the third quartile, and 50.2% for fourth quartile (P less than .001). A fourth-quartile score in the risk-weighted model had a significantly lower 5-year DFS rate, compared with the traditional risk factor model high-risk group (50.2% vs. 60.9%; P less than .001).
Dr. Matsuo and his associates also found that higher risk-weighted surgical-pathological scores were associated with decreased benefit of concurrent chemoradiotherapy after surgery.
“That has been the mainstay of postoperative treatment in adjuvant therapy for a group of cervical cancer with high risk of recurrence,” he said. “It is beneficial to be aware that each tumor factor has a different risk for recurrence and tumors may exhibit multiple risk factors that can be associated with decreased benefit of concurrent chemoradiotherapy after surgical treatment.”
He acknowledged certain limitations of the study, including the lack of information regarding the site of recurrence.
Dr. Matsuo reported having no financial disclosures.
SAN DIEGO – Among patients with stage IB cervical cancer, deep stromal invasion and large tumor size are the two biggest factors associated with increased risk of recurrence. Higher risk-weighted surgical-pathological scores were also associated with decreased benefit of concurrent chemoradiotherapy after surgery.
Those are key findings from a Gynecologic Oncology Group (GOG) ancillary data analysis reported by Dr. Koji Matsuo at the annual meeting of the Society of Gynecologic Oncology.
“Surgery remains the mainstay of treatment for early-stage cervical cancer,” Dr. Matsuo, assistant director of the gynecologic oncology clinic at the University of Southern California, Los Angeles, said in an interview prior to the meeting. “Surgical specimen is useful to identify certain types of factors that can benefit from postoperative adjuvant therapy with concurrent chemoradiotherapy. Traditionally, tumor factors are grouped into high, intermediate, and low risk. Tumors often exhibit multiple risk factors and magnitude of significance for survival may differ across the tumor factors. In this study, we examined the effects of combination of multiple risk factors by weighing magnitude of significance for recurrence.”
The researchers analyzed data from 1,538 stage IB cervical cancer patients who underwent primary radical hysterectomy and pelvic lymphadenectomy. They used a multivariate model to examine hazard ratios associated with disease-free survival (DFS) for seven surgical-pathological risk factors: nodal metastasis, parametrial involvement, surgical margin, lymphovascular space invasion (LVSI), deep stromal invasion, large tumor, and histology. Next, they used a risk-weighted surgical-pathological score (a sum of HR scores) to determine DFS and compared it to a traditional risk factor model.
The median age of patients in the study was 41 years, the median follow-up time was 84 months, the recurrence rate was 26%, and the mortality rate was 27%.
Dr. Matsuo reported that based on the risk-weighted surgical-pathological score model, factors associated with the highest risk of recurrence were deep stromal invasion (HR 1.85), large tumor size (HR 1.81), parametrial involvement (HR 1.73), LVSI (HR 1.37), histology (HR 1.30), and nodal metastasis (HR 1.29; P less than .05 for all).
The 5-year DFS rates based on risk-weighted scores were 85.6% for score 0, 89.1% for the first quartile, 79.6% for the second quartile, 69.3% for the third quartile, and 50.2% for fourth quartile (P less than .001). A fourth-quartile score in the risk-weighted model had a significantly lower 5-year DFS rate, compared with the traditional risk factor model high-risk group (50.2% vs. 60.9%; P less than .001).
Dr. Matsuo and his associates also found that higher risk-weighted surgical-pathological scores were associated with decreased benefit of concurrent chemoradiotherapy after surgery.
“That has been the mainstay of postoperative treatment in adjuvant therapy for a group of cervical cancer with high risk of recurrence,” he said. “It is beneficial to be aware that each tumor factor has a different risk for recurrence and tumors may exhibit multiple risk factors that can be associated with decreased benefit of concurrent chemoradiotherapy after surgical treatment.”
He acknowledged certain limitations of the study, including the lack of information regarding the site of recurrence.
Dr. Matsuo reported having no financial disclosures.
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: Deep stromal invasion and large tumor size are two risk factors associated with increased risk of stage IB cervical cancer recurrence.
Major finding: A risk-weighted model for determining recurrence of cervical cancer had a significantly lower 5-year disease-free survival rate, compared with the traditional high-risk group (50.2% vs. 60.9%; P less than .001).
Data source: An ancillary analysis of Gynecologic Oncology Group data from 1,538 stage IB cervical cancer patients who underwent primary radical hysterectomy and pelvic lymphadenectomy.
Disclosures: Dr. Matsuo reported having no financial disclosures.
Younger age at diagnosis worsens cervical cancer prognosis
SAN DIEGO – Being diagnosed with cervical cancer before the age of 40 was independently associated with worse overall survival, results from a single-center study demonstrated.
“While there exist certain conventional prognostic factors in cervical cancer survival, such as stage of disease, size of tumor, lymph node status, and tumor differentiation, the effect of age on cervical cancer is not well delineated,” researchers led by Dr. Erica L. Stockwell wrote in a poster abstract presented at the annual meeting of Society of Gynecologic Oncology. “There are conflicting reports of the effect that age has on survival with cervical cancer. There are studies that report both improved and worsened prognosis based on age.”
Dr. Stockwell, of the department of obstetrics, gynecology, and women’s health at the University of Minnesota, Minneapolis, and her associates retrospectively reviewed the charts of 447 women diagnosed with cervical cancer at the university from Jan. 1, 2003, to Dec. 31, 2012. They compared women younger than 40 years of age with those age 40 years and older for comorbidities, histology, disease stage, and treatment, and used Cox regression models to conduct univariate analysis of potential factors associated with overall survival.
The median age of patients at diagnosis was 49 years, 71% had stage I or II disease, and 72% had squamous cell histology.
Compared with older women, younger women were significantly less likely to have advanced stage disease and were therefore more likely to receive surgery, as well as less likely to undergo definitive radiation therapy (P less than .0001 for both associations). Univariate analysis revealed no significant association between age and overall survival. However, advanced stage disease, rare histology, and treatment with radiation were associated with significantly poorer overall survival.
The researchers also found that cancer history, advanced stage disease, adenocarcinoma histology, and treatment with either surgery or radiation alone, compared with surgery plus radiation, remained significantly associated with poorer overall survival following adjustment for potential confounders. After Dr. Stockwell and her associates adjusted for race, presence of diabetes, hypertension, history of other cancer, disease stage, histology, and treatment, younger age at diagnosis was significantly associated with poorer overall survival (odds ratio 1.90; P = .04).
“Further investigation into tumor characteristics of young women to determine why stage for stage they had a more virulent course is warranted,” the researchers concluded.
They reported having no financial disclosures.
SAN DIEGO – Being diagnosed with cervical cancer before the age of 40 was independently associated with worse overall survival, results from a single-center study demonstrated.
“While there exist certain conventional prognostic factors in cervical cancer survival, such as stage of disease, size of tumor, lymph node status, and tumor differentiation, the effect of age on cervical cancer is not well delineated,” researchers led by Dr. Erica L. Stockwell wrote in a poster abstract presented at the annual meeting of Society of Gynecologic Oncology. “There are conflicting reports of the effect that age has on survival with cervical cancer. There are studies that report both improved and worsened prognosis based on age.”
Dr. Stockwell, of the department of obstetrics, gynecology, and women’s health at the University of Minnesota, Minneapolis, and her associates retrospectively reviewed the charts of 447 women diagnosed with cervical cancer at the university from Jan. 1, 2003, to Dec. 31, 2012. They compared women younger than 40 years of age with those age 40 years and older for comorbidities, histology, disease stage, and treatment, and used Cox regression models to conduct univariate analysis of potential factors associated with overall survival.
The median age of patients at diagnosis was 49 years, 71% had stage I or II disease, and 72% had squamous cell histology.
Compared with older women, younger women were significantly less likely to have advanced stage disease and were therefore more likely to receive surgery, as well as less likely to undergo definitive radiation therapy (P less than .0001 for both associations). Univariate analysis revealed no significant association between age and overall survival. However, advanced stage disease, rare histology, and treatment with radiation were associated with significantly poorer overall survival.
The researchers also found that cancer history, advanced stage disease, adenocarcinoma histology, and treatment with either surgery or radiation alone, compared with surgery plus radiation, remained significantly associated with poorer overall survival following adjustment for potential confounders. After Dr. Stockwell and her associates adjusted for race, presence of diabetes, hypertension, history of other cancer, disease stage, histology, and treatment, younger age at diagnosis was significantly associated with poorer overall survival (odds ratio 1.90; P = .04).
“Further investigation into tumor characteristics of young women to determine why stage for stage they had a more virulent course is warranted,” the researchers concluded.
They reported having no financial disclosures.
SAN DIEGO – Being diagnosed with cervical cancer before the age of 40 was independently associated with worse overall survival, results from a single-center study demonstrated.
“While there exist certain conventional prognostic factors in cervical cancer survival, such as stage of disease, size of tumor, lymph node status, and tumor differentiation, the effect of age on cervical cancer is not well delineated,” researchers led by Dr. Erica L. Stockwell wrote in a poster abstract presented at the annual meeting of Society of Gynecologic Oncology. “There are conflicting reports of the effect that age has on survival with cervical cancer. There are studies that report both improved and worsened prognosis based on age.”
Dr. Stockwell, of the department of obstetrics, gynecology, and women’s health at the University of Minnesota, Minneapolis, and her associates retrospectively reviewed the charts of 447 women diagnosed with cervical cancer at the university from Jan. 1, 2003, to Dec. 31, 2012. They compared women younger than 40 years of age with those age 40 years and older for comorbidities, histology, disease stage, and treatment, and used Cox regression models to conduct univariate analysis of potential factors associated with overall survival.
The median age of patients at diagnosis was 49 years, 71% had stage I or II disease, and 72% had squamous cell histology.
Compared with older women, younger women were significantly less likely to have advanced stage disease and were therefore more likely to receive surgery, as well as less likely to undergo definitive radiation therapy (P less than .0001 for both associations). Univariate analysis revealed no significant association between age and overall survival. However, advanced stage disease, rare histology, and treatment with radiation were associated with significantly poorer overall survival.
The researchers also found that cancer history, advanced stage disease, adenocarcinoma histology, and treatment with either surgery or radiation alone, compared with surgery plus radiation, remained significantly associated with poorer overall survival following adjustment for potential confounders. After Dr. Stockwell and her associates adjusted for race, presence of diabetes, hypertension, history of other cancer, disease stage, histology, and treatment, younger age at diagnosis was significantly associated with poorer overall survival (odds ratio 1.90; P = .04).
“Further investigation into tumor characteristics of young women to determine why stage for stage they had a more virulent course is warranted,” the researchers concluded.
They reported having no financial disclosures.
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: Being younger than age 40 at diagnosis of cervical cancer was associated with poorer overall survival.
Major finding: After adjustment for race, presence of diabetes, hypertension, history of other cancer, disease stage, histology, and treatment, being younger than 40 years old at diagnosis of cervical cancer was significantly associated with poorer overall survival (odds ratio 1.90; P = .04).
Data source: A retrospective review of 447 women diagnosed with cervical cancer from Jan. 1, 2003, to Dec. 31, 2012.
Disclosures: The researchers reported having no financial disclosures.
Skip lymphadenectomy if SLN mapping finds low-grade endometrial cancer
SAN DIEGO – Lymphadenectomy is unnecessary if sentinel lymph node mapping successfully stages low-grade endometrial cancer, according to researchers from Johns Hopkins University in Baltimore.
Lymphadenectomy guided by frozen section remains common in the United States. But the Johns Hopkins research team found that using sentinel lymph node (SLN) mapping and biopsy instead cuts the rate of lymphadenectomy by 76%, without reducing the detection of lymphatic metastases.
It’s an important finding for cancer patients likely to survive their diagnosis. “We see low-grade patients in the clinic” who’ve had unnecessary lymphadenectomies, “and they are in terrible shape,” said investigator Dr. Abdulrahman Sinno, a gynecologic oncology fellow at Johns Hopkins. Up to half “have horrible side effects,” including crippling lymphedema and pain.
SLN mapping is “an alternative that gives us the information we need for nodal assessment without putting patients at risk. You’ll know if patients have metastases or not. If they fail to map, you do a frozen section, and if you have high-risk features, a lymphadenectomy only on [the side] that didn’t map,” Dr. Sinno said at the annual meeting of the Society of Gynecologic Oncology.
For the past several years, physicians at Johns Hopkins has been doing both SLN mapping for low-grade endometrial cancer as well as frozen sections to decide the need for lymphadenectomy. Using both approaches allowed the investigators to review how patients would have fared if they had gotten only one.
“[We could] safely study the utility of SLN mapping while maintaining the historical standard of using frozen sections to direct the need for lymphadenectomy,” Dr. Sinno said.
SLN mapping outperformed frozen section. Among 114 women, most with grade 1 disease but some with grade 2 or complex atypical hyperplasia, 8 had lymph node metastases. Mapping identified every one, five by standard hematoxylin-eosin staining, and three by ultrastaging. Frozen-section guided lymphadenectomy missed three.
Eighty four (37%) of the 224 hemi-pelvises in the study had lymphadenectomies based on worrisome frozen-section findings. If SLN mapping had been relied on to make the call, lymphadenectomies would have been performed in 20 (9%), a statistically significant difference (P = 0.004).
“Strategies that rely exclusively on uterine frozen section result in significant overtreatment. In the absence of a therapeutic benefit to lymphadenectomy, we believe” this is “unjustifiable when an alternative exists.” At Johns Hopkins these days, “if you map, you’re done,” Dr. Sinno said.
Almost two-thirds of the women had grade 1 endometrial cancer on preoperative histopathology, and about the same number on final pathology. Bilateral SLN mapping was successful in 71 cases (62%) and unilateral mapping in 27 cases (24%). At least one SLN was detected in 98 women (86%).
There were six recurrences after a median follow-up of 15 months. Four were in women who had full pelvic and periaortic lymphadenectomies that were negative. There was also a port site recurrence and a recurrence in an outlying patient with advanced disease. Overall, “recurrence was independent of whether sentinel nodes were applied,” Dr. Sinno said.
Women in the study were a median of 60 years old, with a median body mass index of 33.3 kg/m2.
Dr. Sinno reported having no relevant financial disclosures.
SAN DIEGO – Lymphadenectomy is unnecessary if sentinel lymph node mapping successfully stages low-grade endometrial cancer, according to researchers from Johns Hopkins University in Baltimore.
Lymphadenectomy guided by frozen section remains common in the United States. But the Johns Hopkins research team found that using sentinel lymph node (SLN) mapping and biopsy instead cuts the rate of lymphadenectomy by 76%, without reducing the detection of lymphatic metastases.
It’s an important finding for cancer patients likely to survive their diagnosis. “We see low-grade patients in the clinic” who’ve had unnecessary lymphadenectomies, “and they are in terrible shape,” said investigator Dr. Abdulrahman Sinno, a gynecologic oncology fellow at Johns Hopkins. Up to half “have horrible side effects,” including crippling lymphedema and pain.
SLN mapping is “an alternative that gives us the information we need for nodal assessment without putting patients at risk. You’ll know if patients have metastases or not. If they fail to map, you do a frozen section, and if you have high-risk features, a lymphadenectomy only on [the side] that didn’t map,” Dr. Sinno said at the annual meeting of the Society of Gynecologic Oncology.
For the past several years, physicians at Johns Hopkins has been doing both SLN mapping for low-grade endometrial cancer as well as frozen sections to decide the need for lymphadenectomy. Using both approaches allowed the investigators to review how patients would have fared if they had gotten only one.
“[We could] safely study the utility of SLN mapping while maintaining the historical standard of using frozen sections to direct the need for lymphadenectomy,” Dr. Sinno said.
SLN mapping outperformed frozen section. Among 114 women, most with grade 1 disease but some with grade 2 or complex atypical hyperplasia, 8 had lymph node metastases. Mapping identified every one, five by standard hematoxylin-eosin staining, and three by ultrastaging. Frozen-section guided lymphadenectomy missed three.
Eighty four (37%) of the 224 hemi-pelvises in the study had lymphadenectomies based on worrisome frozen-section findings. If SLN mapping had been relied on to make the call, lymphadenectomies would have been performed in 20 (9%), a statistically significant difference (P = 0.004).
“Strategies that rely exclusively on uterine frozen section result in significant overtreatment. In the absence of a therapeutic benefit to lymphadenectomy, we believe” this is “unjustifiable when an alternative exists.” At Johns Hopkins these days, “if you map, you’re done,” Dr. Sinno said.
Almost two-thirds of the women had grade 1 endometrial cancer on preoperative histopathology, and about the same number on final pathology. Bilateral SLN mapping was successful in 71 cases (62%) and unilateral mapping in 27 cases (24%). At least one SLN was detected in 98 women (86%).
There were six recurrences after a median follow-up of 15 months. Four were in women who had full pelvic and periaortic lymphadenectomies that were negative. There was also a port site recurrence and a recurrence in an outlying patient with advanced disease. Overall, “recurrence was independent of whether sentinel nodes were applied,” Dr. Sinno said.
Women in the study were a median of 60 years old, with a median body mass index of 33.3 kg/m2.
Dr. Sinno reported having no relevant financial disclosures.
SAN DIEGO – Lymphadenectomy is unnecessary if sentinel lymph node mapping successfully stages low-grade endometrial cancer, according to researchers from Johns Hopkins University in Baltimore.
Lymphadenectomy guided by frozen section remains common in the United States. But the Johns Hopkins research team found that using sentinel lymph node (SLN) mapping and biopsy instead cuts the rate of lymphadenectomy by 76%, without reducing the detection of lymphatic metastases.
It’s an important finding for cancer patients likely to survive their diagnosis. “We see low-grade patients in the clinic” who’ve had unnecessary lymphadenectomies, “and they are in terrible shape,” said investigator Dr. Abdulrahman Sinno, a gynecologic oncology fellow at Johns Hopkins. Up to half “have horrible side effects,” including crippling lymphedema and pain.
SLN mapping is “an alternative that gives us the information we need for nodal assessment without putting patients at risk. You’ll know if patients have metastases or not. If they fail to map, you do a frozen section, and if you have high-risk features, a lymphadenectomy only on [the side] that didn’t map,” Dr. Sinno said at the annual meeting of the Society of Gynecologic Oncology.
For the past several years, physicians at Johns Hopkins has been doing both SLN mapping for low-grade endometrial cancer as well as frozen sections to decide the need for lymphadenectomy. Using both approaches allowed the investigators to review how patients would have fared if they had gotten only one.
“[We could] safely study the utility of SLN mapping while maintaining the historical standard of using frozen sections to direct the need for lymphadenectomy,” Dr. Sinno said.
SLN mapping outperformed frozen section. Among 114 women, most with grade 1 disease but some with grade 2 or complex atypical hyperplasia, 8 had lymph node metastases. Mapping identified every one, five by standard hematoxylin-eosin staining, and three by ultrastaging. Frozen-section guided lymphadenectomy missed three.
Eighty four (37%) of the 224 hemi-pelvises in the study had lymphadenectomies based on worrisome frozen-section findings. If SLN mapping had been relied on to make the call, lymphadenectomies would have been performed in 20 (9%), a statistically significant difference (P = 0.004).
“Strategies that rely exclusively on uterine frozen section result in significant overtreatment. In the absence of a therapeutic benefit to lymphadenectomy, we believe” this is “unjustifiable when an alternative exists.” At Johns Hopkins these days, “if you map, you’re done,” Dr. Sinno said.
Almost two-thirds of the women had grade 1 endometrial cancer on preoperative histopathology, and about the same number on final pathology. Bilateral SLN mapping was successful in 71 cases (62%) and unilateral mapping in 27 cases (24%). At least one SLN was detected in 98 women (86%).
There were six recurrences after a median follow-up of 15 months. Four were in women who had full pelvic and periaortic lymphadenectomies that were negative. There was also a port site recurrence and a recurrence in an outlying patient with advanced disease. Overall, “recurrence was independent of whether sentinel nodes were applied,” Dr. Sinno said.
Women in the study were a median of 60 years old, with a median body mass index of 33.3 kg/m2.
Dr. Sinno reported having no relevant financial disclosures.
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: Successful sentinel lymph node mapping gives all the information needed for nodal assessment.
Major finding: Sentinel lymph node mapping identified all eight nodal metastases; frozen-section guided lymphadenectomy missed three.
Data source: A review of 114 cases at Johns Hopkins University.
Disclosures: Dr. Sinno reported having no relevant financial disclosures.
Nodal SUVmax on imaging may be prognostic biomarker in advanced cervical cancer
SAN DIEGO – Primary tumor metabolic parameters were not significant prognostic factors for tumor recurrence in patients with regional lymph node–involved, locally advanced cervical cancer, but nodal maximum standardized uptake value from advanced pretreatment imaging was, according to results from a South Korean study.
At the annual meeting of the Society of Gynecologic Oncology, Dr. Gun Oh Chong said that negative prognostic factors of locally advanced cervical cancer treated with computer-controlled radiation therapy (CCRT) include advanced FIGO stage, large tumor size, and the presence of lymph node metastasis. Pretreatment 18fluorodeoxyglucose positron emission tomography/computed tomography (FDG-PET/CT) is widely used to detect lymph node involvement, distant metastasis, and recurrent disease, “but the degree of F-18 FDG uptake in regional lymph nodes has not been fully investigated,” said Dr. Chong of the gynecologic cancer center at Kyungpook National University Medical Center, Daegu, South Korea. “There is no comparison study on the prognostic value of F-18 FDG uptake in primary tumor and regional lymph node in patients who had regional lymph node involvement.”
In an effort to compare the prognostic value of primary tumor and regional lymph node metabolic parameters for predicting tumor recurrence and to identify the most powerful biological marker predictive of tumor recurrence measured by pretreatment FDG-PET/CT, the researchers evaluated 56 patients with cervical cancer who had pelvic and/or para-aortic lymph node metastasis.
Metabolic parameters studied included the maximum standardized uptake value (SUVmax), the metabolic tumor volume (MTV), and total lesion glycolysis (TLG) of the primary tumors and lymph nodes, which were measured with pretreatment FDG-PET/CT. They used the clinical metabolic parameters to perform univariate and multivariate analyses for disease-free survival.
The mean age of patients was 52 years and the majority (79%) had stage IIB disease. Dr. Chong reported that no differences in disease-free survival were observed according to the metabolic parameters in the primary tumors. However, disease-free survival was significantly longer in patients with low values of nodal metabolic parameters than in those with high values of nodal metabolic parameters.
On univariate analysis, the nodal metabolic parameters SUVmax, MTV, and TLG were significantly associated with disease-free survival, as were para-aortic lymph node metastasis, and posttreatment response. On multivariate analysis only two variables were significant determinants of disease-free survival: nodal SUVmax (4.7 or higher vs. 4.7 or lower; hazard ratio, 4.15; P = .041) and posttreatment response (partial response or progressive disease vs. complete response; HR, 7.16; P = .007). Only nodal SUVmax was an independent pretreatment prognostic factor for DFS, and the optimal cutoff for nodal SUVmax to predict progression was 4.7.
Dr. Chong reported having no financial disclosures.
SAN DIEGO – Primary tumor metabolic parameters were not significant prognostic factors for tumor recurrence in patients with regional lymph node–involved, locally advanced cervical cancer, but nodal maximum standardized uptake value from advanced pretreatment imaging was, according to results from a South Korean study.
At the annual meeting of the Society of Gynecologic Oncology, Dr. Gun Oh Chong said that negative prognostic factors of locally advanced cervical cancer treated with computer-controlled radiation therapy (CCRT) include advanced FIGO stage, large tumor size, and the presence of lymph node metastasis. Pretreatment 18fluorodeoxyglucose positron emission tomography/computed tomography (FDG-PET/CT) is widely used to detect lymph node involvement, distant metastasis, and recurrent disease, “but the degree of F-18 FDG uptake in regional lymph nodes has not been fully investigated,” said Dr. Chong of the gynecologic cancer center at Kyungpook National University Medical Center, Daegu, South Korea. “There is no comparison study on the prognostic value of F-18 FDG uptake in primary tumor and regional lymph node in patients who had regional lymph node involvement.”
In an effort to compare the prognostic value of primary tumor and regional lymph node metabolic parameters for predicting tumor recurrence and to identify the most powerful biological marker predictive of tumor recurrence measured by pretreatment FDG-PET/CT, the researchers evaluated 56 patients with cervical cancer who had pelvic and/or para-aortic lymph node metastasis.
Metabolic parameters studied included the maximum standardized uptake value (SUVmax), the metabolic tumor volume (MTV), and total lesion glycolysis (TLG) of the primary tumors and lymph nodes, which were measured with pretreatment FDG-PET/CT. They used the clinical metabolic parameters to perform univariate and multivariate analyses for disease-free survival.
The mean age of patients was 52 years and the majority (79%) had stage IIB disease. Dr. Chong reported that no differences in disease-free survival were observed according to the metabolic parameters in the primary tumors. However, disease-free survival was significantly longer in patients with low values of nodal metabolic parameters than in those with high values of nodal metabolic parameters.
On univariate analysis, the nodal metabolic parameters SUVmax, MTV, and TLG were significantly associated with disease-free survival, as were para-aortic lymph node metastasis, and posttreatment response. On multivariate analysis only two variables were significant determinants of disease-free survival: nodal SUVmax (4.7 or higher vs. 4.7 or lower; hazard ratio, 4.15; P = .041) and posttreatment response (partial response or progressive disease vs. complete response; HR, 7.16; P = .007). Only nodal SUVmax was an independent pretreatment prognostic factor for DFS, and the optimal cutoff for nodal SUVmax to predict progression was 4.7.
Dr. Chong reported having no financial disclosures.
SAN DIEGO – Primary tumor metabolic parameters were not significant prognostic factors for tumor recurrence in patients with regional lymph node–involved, locally advanced cervical cancer, but nodal maximum standardized uptake value from advanced pretreatment imaging was, according to results from a South Korean study.
At the annual meeting of the Society of Gynecologic Oncology, Dr. Gun Oh Chong said that negative prognostic factors of locally advanced cervical cancer treated with computer-controlled radiation therapy (CCRT) include advanced FIGO stage, large tumor size, and the presence of lymph node metastasis. Pretreatment 18fluorodeoxyglucose positron emission tomography/computed tomography (FDG-PET/CT) is widely used to detect lymph node involvement, distant metastasis, and recurrent disease, “but the degree of F-18 FDG uptake in regional lymph nodes has not been fully investigated,” said Dr. Chong of the gynecologic cancer center at Kyungpook National University Medical Center, Daegu, South Korea. “There is no comparison study on the prognostic value of F-18 FDG uptake in primary tumor and regional lymph node in patients who had regional lymph node involvement.”
In an effort to compare the prognostic value of primary tumor and regional lymph node metabolic parameters for predicting tumor recurrence and to identify the most powerful biological marker predictive of tumor recurrence measured by pretreatment FDG-PET/CT, the researchers evaluated 56 patients with cervical cancer who had pelvic and/or para-aortic lymph node metastasis.
Metabolic parameters studied included the maximum standardized uptake value (SUVmax), the metabolic tumor volume (MTV), and total lesion glycolysis (TLG) of the primary tumors and lymph nodes, which were measured with pretreatment FDG-PET/CT. They used the clinical metabolic parameters to perform univariate and multivariate analyses for disease-free survival.
The mean age of patients was 52 years and the majority (79%) had stage IIB disease. Dr. Chong reported that no differences in disease-free survival were observed according to the metabolic parameters in the primary tumors. However, disease-free survival was significantly longer in patients with low values of nodal metabolic parameters than in those with high values of nodal metabolic parameters.
On univariate analysis, the nodal metabolic parameters SUVmax, MTV, and TLG were significantly associated with disease-free survival, as were para-aortic lymph node metastasis, and posttreatment response. On multivariate analysis only two variables were significant determinants of disease-free survival: nodal SUVmax (4.7 or higher vs. 4.7 or lower; hazard ratio, 4.15; P = .041) and posttreatment response (partial response or progressive disease vs. complete response; HR, 7.16; P = .007). Only nodal SUVmax was an independent pretreatment prognostic factor for DFS, and the optimal cutoff for nodal SUVmax to predict progression was 4.7.
Dr. Chong reported having no financial disclosures.
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: Nodal SUVmax on advanced imaging may be a prognostic biomarker to predict recurrence in patients with locally advanced cervical cancer.
Major finding: On multivariate analysis, only two variables were significant determinants of disease-free survival: nodal SUVmax (4.7 or higher vs. 4.7 or lower; HR, 4.15; P = .041) and posttreatment response (partial response or progressive disease vs. complete response; HR, 7.16; P = .007).
Data source: A study of 56 patients with cervical cancer who had pelvic and/or para-aortic lymph node metastasis.
Disclosures: Dr. Chong reported having no financial disclosures.
Gynecologic cancer patients underutilize advance care directives
SAN DIEGO – Fewer than half of gynecologic oncology patients surveyed at a major cancer center had completed advance care directives regarding their preferences for end-of-life care, and most of those who did had no copy of the documents in their medical records, Dr. Alaina J. Brown reported at the annual meeting of the Society of Gynecologic Oncology.
“These findings indicate there is room to improve advance directive planning documentation in our patient population,” said Dr. Brown, a fellow in gynecologic oncology and reproductive medicine at the University of Texas MD Anderson Cancer Center in Houston.
“Providers must identify and address barriers to advance care planning documentation in order to assist patients in achieving their end-of-life care goals ... I think we need to focus on educating ourselves and becoming proactive about trying to have these conversations earlier in treatment instead of when a patient is quite ill and we know that they’re going to pass away within the next week or so,” she added.
One barrier has recently been overcome by Medicare’s new policy – effective beginning this past January – of providing reimbursement for advance care planning as a separate and billable service.
In addition, Dr. Brown’s survey of 110 gynecologic oncology patients identified two significant psychological barriers to advance care planning: high levels of death anxiety and a feeling of distress that symptoms and/or treatment side effects are interfering with daily activities and relationships.
The survey showed that while 75% of the patients were familiar with advance care directives such as a living will or medical power of attorney, only 49% of subjects had actually completed those documents, and a mere 18% had a copy of an advance care directive in their medical record.
Half of the subjects had recurrent cancer, the rest were visiting the gynecologic oncology service for active surveillance. Only a minority of those with recurrent cancer had completed advance care directives.
Study participants completed two validated, self-administered questionnaire surveys: the 19-item MD Anderson Symptom Inventory (MDASI), which assesses patient-reported disease symptoms and treatment side effects during the previous 24 hours, and the 15-item Templer’s Death Anxiety Scale.
The mean MDASI Interference score, a measure of overall symptom distress and the impact of symptoms on daily life, was significantly higher in gynecologic oncology patients who hadn’t completed advance directives than in those who had. Similarly, patients who hadn’t completed advance directives scored significantly higher on the death anxiety metric.
“Patients with recurrent disease and those with increased disease symptom burden and death anxiety should be targeted for advance care planning discussions, as they may be less likely to engage in advance care planning activities,” Dr. Brown concluded.
She noted that prior research in other medical fields has shown that holding early planning discussions about end-of-life issues improves the likelihood that a patient’s final wishes will be honored, reduces utilization of hospital resources at the end of life, and reduces distress among the patient and family members. It’s important for gynecologic oncologists to step forward in this area because they are in a unique position: they often manage a cancer patient’s surgical care as well as chemotherapy and then later assist in the transition to end of life, she added.
At the conference session on palliative care where Dr. Brown presented her findings, audience members said the 49% completion rate for advance care directives that she found in her study was actually quite impressive; at many gynecologic oncology services the rates are in the 20%-25% range. The audience consensus was that much of the blame for the low rates of advance care planning documentation in their field belongs on the shoulders of gynecologic oncologists themselves.
“I would say that it’s entirely our fault,” declared session codirector Dr. Stephanie Blank of New York University.
Dr. Brown said as a result of her survey findings, she and her colleagues are working to change the institutional practice at MD Anderson such that completion of advance care directive planning directives with documentation in the medical record becomes a quality-of-care goal within the first few patient visits.
“In the past we had a social worker come to those patients who checked off a box on a form in the waiting room; now we’re trying to be more proactive about having a provider engage the patients early on,” she explained.
She reported having no financial conflicts of interest regarding her study.
SAN DIEGO – Fewer than half of gynecologic oncology patients surveyed at a major cancer center had completed advance care directives regarding their preferences for end-of-life care, and most of those who did had no copy of the documents in their medical records, Dr. Alaina J. Brown reported at the annual meeting of the Society of Gynecologic Oncology.
“These findings indicate there is room to improve advance directive planning documentation in our patient population,” said Dr. Brown, a fellow in gynecologic oncology and reproductive medicine at the University of Texas MD Anderson Cancer Center in Houston.
“Providers must identify and address barriers to advance care planning documentation in order to assist patients in achieving their end-of-life care goals ... I think we need to focus on educating ourselves and becoming proactive about trying to have these conversations earlier in treatment instead of when a patient is quite ill and we know that they’re going to pass away within the next week or so,” she added.
One barrier has recently been overcome by Medicare’s new policy – effective beginning this past January – of providing reimbursement for advance care planning as a separate and billable service.
In addition, Dr. Brown’s survey of 110 gynecologic oncology patients identified two significant psychological barriers to advance care planning: high levels of death anxiety and a feeling of distress that symptoms and/or treatment side effects are interfering with daily activities and relationships.
The survey showed that while 75% of the patients were familiar with advance care directives such as a living will or medical power of attorney, only 49% of subjects had actually completed those documents, and a mere 18% had a copy of an advance care directive in their medical record.
Half of the subjects had recurrent cancer, the rest were visiting the gynecologic oncology service for active surveillance. Only a minority of those with recurrent cancer had completed advance care directives.
Study participants completed two validated, self-administered questionnaire surveys: the 19-item MD Anderson Symptom Inventory (MDASI), which assesses patient-reported disease symptoms and treatment side effects during the previous 24 hours, and the 15-item Templer’s Death Anxiety Scale.
The mean MDASI Interference score, a measure of overall symptom distress and the impact of symptoms on daily life, was significantly higher in gynecologic oncology patients who hadn’t completed advance directives than in those who had. Similarly, patients who hadn’t completed advance directives scored significantly higher on the death anxiety metric.
“Patients with recurrent disease and those with increased disease symptom burden and death anxiety should be targeted for advance care planning discussions, as they may be less likely to engage in advance care planning activities,” Dr. Brown concluded.
She noted that prior research in other medical fields has shown that holding early planning discussions about end-of-life issues improves the likelihood that a patient’s final wishes will be honored, reduces utilization of hospital resources at the end of life, and reduces distress among the patient and family members. It’s important for gynecologic oncologists to step forward in this area because they are in a unique position: they often manage a cancer patient’s surgical care as well as chemotherapy and then later assist in the transition to end of life, she added.
At the conference session on palliative care where Dr. Brown presented her findings, audience members said the 49% completion rate for advance care directives that she found in her study was actually quite impressive; at many gynecologic oncology services the rates are in the 20%-25% range. The audience consensus was that much of the blame for the low rates of advance care planning documentation in their field belongs on the shoulders of gynecologic oncologists themselves.
“I would say that it’s entirely our fault,” declared session codirector Dr. Stephanie Blank of New York University.
Dr. Brown said as a result of her survey findings, she and her colleagues are working to change the institutional practice at MD Anderson such that completion of advance care directive planning directives with documentation in the medical record becomes a quality-of-care goal within the first few patient visits.
“In the past we had a social worker come to those patients who checked off a box on a form in the waiting room; now we’re trying to be more proactive about having a provider engage the patients early on,” she explained.
She reported having no financial conflicts of interest regarding her study.
SAN DIEGO – Fewer than half of gynecologic oncology patients surveyed at a major cancer center had completed advance care directives regarding their preferences for end-of-life care, and most of those who did had no copy of the documents in their medical records, Dr. Alaina J. Brown reported at the annual meeting of the Society of Gynecologic Oncology.
“These findings indicate there is room to improve advance directive planning documentation in our patient population,” said Dr. Brown, a fellow in gynecologic oncology and reproductive medicine at the University of Texas MD Anderson Cancer Center in Houston.
“Providers must identify and address barriers to advance care planning documentation in order to assist patients in achieving their end-of-life care goals ... I think we need to focus on educating ourselves and becoming proactive about trying to have these conversations earlier in treatment instead of when a patient is quite ill and we know that they’re going to pass away within the next week or so,” she added.
One barrier has recently been overcome by Medicare’s new policy – effective beginning this past January – of providing reimbursement for advance care planning as a separate and billable service.
In addition, Dr. Brown’s survey of 110 gynecologic oncology patients identified two significant psychological barriers to advance care planning: high levels of death anxiety and a feeling of distress that symptoms and/or treatment side effects are interfering with daily activities and relationships.
The survey showed that while 75% of the patients were familiar with advance care directives such as a living will or medical power of attorney, only 49% of subjects had actually completed those documents, and a mere 18% had a copy of an advance care directive in their medical record.
Half of the subjects had recurrent cancer, the rest were visiting the gynecologic oncology service for active surveillance. Only a minority of those with recurrent cancer had completed advance care directives.
Study participants completed two validated, self-administered questionnaire surveys: the 19-item MD Anderson Symptom Inventory (MDASI), which assesses patient-reported disease symptoms and treatment side effects during the previous 24 hours, and the 15-item Templer’s Death Anxiety Scale.
The mean MDASI Interference score, a measure of overall symptom distress and the impact of symptoms on daily life, was significantly higher in gynecologic oncology patients who hadn’t completed advance directives than in those who had. Similarly, patients who hadn’t completed advance directives scored significantly higher on the death anxiety metric.
“Patients with recurrent disease and those with increased disease symptom burden and death anxiety should be targeted for advance care planning discussions, as they may be less likely to engage in advance care planning activities,” Dr. Brown concluded.
She noted that prior research in other medical fields has shown that holding early planning discussions about end-of-life issues improves the likelihood that a patient’s final wishes will be honored, reduces utilization of hospital resources at the end of life, and reduces distress among the patient and family members. It’s important for gynecologic oncologists to step forward in this area because they are in a unique position: they often manage a cancer patient’s surgical care as well as chemotherapy and then later assist in the transition to end of life, she added.
At the conference session on palliative care where Dr. Brown presented her findings, audience members said the 49% completion rate for advance care directives that she found in her study was actually quite impressive; at many gynecologic oncology services the rates are in the 20%-25% range. The audience consensus was that much of the blame for the low rates of advance care planning documentation in their field belongs on the shoulders of gynecologic oncologists themselves.
“I would say that it’s entirely our fault,” declared session codirector Dr. Stephanie Blank of New York University.
Dr. Brown said as a result of her survey findings, she and her colleagues are working to change the institutional practice at MD Anderson such that completion of advance care directive planning directives with documentation in the medical record becomes a quality-of-care goal within the first few patient visits.
“In the past we had a social worker come to those patients who checked off a box on a form in the waiting room; now we’re trying to be more proactive about having a provider engage the patients early on,” she explained.
She reported having no financial conflicts of interest regarding her study.
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: Gynecologic oncologists aren’t doing well at helping their patients create advance care directives in a timely way.
Major finding: Fewer than one in five gynecologic oncology patients surveyed had an advance care directive included in the medical chart.
Data source: Survey of 110 gynecologic oncology patients at a major cancer center to examine the relationship between completion of advance care directives and patients’ levels of death anxiety and symptom burden.
Disclosures: The presenter reported having no financial conflicts regarding her study, which was conducted free of commercial support.
Observation might be best in advanced-stage, low-grade ovarian CA
SAN DIEGO – Surgery, chemotherapy, and radiation do not prolong survival in advanced-stage but low-grade papillary serous ovarian cancer, according to a review of 1,159 low-grade cases in the National Cancer Data Base.
“All you are doing is exposing patients to the toxicity without any benefit. You [should] think really hard about whether or not to give [low-grade] patients radiation or chemotherapy, instead of just following them,” said investigator Dr. Allison Gockley, an ob.gyn. at Brigham and Women’s Hospital and Massachusetts General Hospital in Boston.
Seventy-four percent of the women received platinum-based chemotherapy, but it made no difference in survival (hazard ratio, 0.94; 95% CI, 0.75 -1.19); likewise, radiation made no difference in the seven women (0.6%) who received it.
Lymphadenectomy was the only thing associated with improved survival (HR, 0.5; 95% CI, 0.4-0.7). Dr. Gockley said she suspects it was a marker for careful surgery, but even surgery didn’t improve survival in low-grade cases (HR, 0.93; 95% CI, 0.51-1.70), although most patients had an operation.
The percentages of women who had surgery, chemotherapy, and radiation were almost identical among the 24,073 advanced-stage, high-grade cases also considered in the review, except that low-grade patients were more likely to get radiation. The approaches help high-grade cases, but “it feels very unsatisfying to me to treat low-grade” patients the same way when “they obviously have” different tumor biology, Dr. Gockley said at the annual meeting of the Society of Gynecologic Oncology.
She said she’s found similar issues with early-stage uterine clear cell carcinoma. The problem is that there just aren’t much data to guide treatment in less-dangerous gynecologic cancers, so patients end up being treated like they have advanced disease. “We need to step up and focus [study] on patients with these tumors so we can have specific treatments. For a lot of these rare tumors” – advanced-stage, low-grade disease represents about 5% of ovarian cancer – “these patients would probably do better if we had supertargeted chemotherapy,” she said.
In the absence of evidence, some patients opt for aggressive treatment “because it makes them feel that they can do something to control their disease.” As for doctors, “I’ve been in rooms where it’s very highly advocated, and others where physicians are more hesitant. What happens in the end is very much about how doctors [frame] the discussion,” Dr. Gockley said.
Her institutions follow national trends; very few patients get radiation, but most get chemotherapy, sometimes three cycles instead of six, or in low dose.
She and her colleagues looked into the issue because “we’ve seen a bunch of patients on our services recently who have low-grade, advanced-stage” ovarian cancer. The investigators wanted to know how other institutions handle the situation.
Most of the low-grade patients had stage III disease, and the rest had stage IV. Their mean age at diagnosis was 54 years, 9 years earlier than for high-grade diagnoses. About half of stage III patients were alive at 10 years, vs. about 20% of stage IV patients. As expected, high-grade patients died sooner.
SAN DIEGO – Surgery, chemotherapy, and radiation do not prolong survival in advanced-stage but low-grade papillary serous ovarian cancer, according to a review of 1,159 low-grade cases in the National Cancer Data Base.
“All you are doing is exposing patients to the toxicity without any benefit. You [should] think really hard about whether or not to give [low-grade] patients radiation or chemotherapy, instead of just following them,” said investigator Dr. Allison Gockley, an ob.gyn. at Brigham and Women’s Hospital and Massachusetts General Hospital in Boston.
Seventy-four percent of the women received platinum-based chemotherapy, but it made no difference in survival (hazard ratio, 0.94; 95% CI, 0.75 -1.19); likewise, radiation made no difference in the seven women (0.6%) who received it.
Lymphadenectomy was the only thing associated with improved survival (HR, 0.5; 95% CI, 0.4-0.7). Dr. Gockley said she suspects it was a marker for careful surgery, but even surgery didn’t improve survival in low-grade cases (HR, 0.93; 95% CI, 0.51-1.70), although most patients had an operation.
The percentages of women who had surgery, chemotherapy, and radiation were almost identical among the 24,073 advanced-stage, high-grade cases also considered in the review, except that low-grade patients were more likely to get radiation. The approaches help high-grade cases, but “it feels very unsatisfying to me to treat low-grade” patients the same way when “they obviously have” different tumor biology, Dr. Gockley said at the annual meeting of the Society of Gynecologic Oncology.
She said she’s found similar issues with early-stage uterine clear cell carcinoma. The problem is that there just aren’t much data to guide treatment in less-dangerous gynecologic cancers, so patients end up being treated like they have advanced disease. “We need to step up and focus [study] on patients with these tumors so we can have specific treatments. For a lot of these rare tumors” – advanced-stage, low-grade disease represents about 5% of ovarian cancer – “these patients would probably do better if we had supertargeted chemotherapy,” she said.
In the absence of evidence, some patients opt for aggressive treatment “because it makes them feel that they can do something to control their disease.” As for doctors, “I’ve been in rooms where it’s very highly advocated, and others where physicians are more hesitant. What happens in the end is very much about how doctors [frame] the discussion,” Dr. Gockley said.
Her institutions follow national trends; very few patients get radiation, but most get chemotherapy, sometimes three cycles instead of six, or in low dose.
She and her colleagues looked into the issue because “we’ve seen a bunch of patients on our services recently who have low-grade, advanced-stage” ovarian cancer. The investigators wanted to know how other institutions handle the situation.
Most of the low-grade patients had stage III disease, and the rest had stage IV. Their mean age at diagnosis was 54 years, 9 years earlier than for high-grade diagnoses. About half of stage III patients were alive at 10 years, vs. about 20% of stage IV patients. As expected, high-grade patients died sooner.
SAN DIEGO – Surgery, chemotherapy, and radiation do not prolong survival in advanced-stage but low-grade papillary serous ovarian cancer, according to a review of 1,159 low-grade cases in the National Cancer Data Base.
“All you are doing is exposing patients to the toxicity without any benefit. You [should] think really hard about whether or not to give [low-grade] patients radiation or chemotherapy, instead of just following them,” said investigator Dr. Allison Gockley, an ob.gyn. at Brigham and Women’s Hospital and Massachusetts General Hospital in Boston.
Seventy-four percent of the women received platinum-based chemotherapy, but it made no difference in survival (hazard ratio, 0.94; 95% CI, 0.75 -1.19); likewise, radiation made no difference in the seven women (0.6%) who received it.
Lymphadenectomy was the only thing associated with improved survival (HR, 0.5; 95% CI, 0.4-0.7). Dr. Gockley said she suspects it was a marker for careful surgery, but even surgery didn’t improve survival in low-grade cases (HR, 0.93; 95% CI, 0.51-1.70), although most patients had an operation.
The percentages of women who had surgery, chemotherapy, and radiation were almost identical among the 24,073 advanced-stage, high-grade cases also considered in the review, except that low-grade patients were more likely to get radiation. The approaches help high-grade cases, but “it feels very unsatisfying to me to treat low-grade” patients the same way when “they obviously have” different tumor biology, Dr. Gockley said at the annual meeting of the Society of Gynecologic Oncology.
She said she’s found similar issues with early-stage uterine clear cell carcinoma. The problem is that there just aren’t much data to guide treatment in less-dangerous gynecologic cancers, so patients end up being treated like they have advanced disease. “We need to step up and focus [study] on patients with these tumors so we can have specific treatments. For a lot of these rare tumors” – advanced-stage, low-grade disease represents about 5% of ovarian cancer – “these patients would probably do better if we had supertargeted chemotherapy,” she said.
In the absence of evidence, some patients opt for aggressive treatment “because it makes them feel that they can do something to control their disease.” As for doctors, “I’ve been in rooms where it’s very highly advocated, and others where physicians are more hesitant. What happens in the end is very much about how doctors [frame] the discussion,” Dr. Gockley said.
Her institutions follow national trends; very few patients get radiation, but most get chemotherapy, sometimes three cycles instead of six, or in low dose.
She and her colleagues looked into the issue because “we’ve seen a bunch of patients on our services recently who have low-grade, advanced-stage” ovarian cancer. The investigators wanted to know how other institutions handle the situation.
Most of the low-grade patients had stage III disease, and the rest had stage IV. Their mean age at diagnosis was 54 years, 9 years earlier than for high-grade diagnoses. About half of stage III patients were alive at 10 years, vs. about 20% of stage IV patients. As expected, high-grade patients died sooner.
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: Low-grade ovarian cancer is overtreated.
Major finding: Seventy-four percent of the women received platinum-based chemotherapy, but it made no difference in survival (HR, 0.94; 95% CI, 0.75-1.19).
Data source: A review of more than 25,000 ovarian cancer cases in the National Cancer Data Base.
Disclosures: The presenter had no disclosures, and there was no outside funding for the work.
Aspirin may improve survival in endometrial cancer
SAN DIEGO – Endometrial cancer patients who regularly took low-dose aspirin experienced markedly better 5-year disease-free and overall survival compared to nonusers in an observational study, Dr. Koji Matsuo reported at the annual meeting of the Society of Gynecologic Oncology.
This apparent survival-prolonging effect of aspirin was greatest in women who were obese, less than 60 years old, had type 1 endometrial cancer, and/or received postoperative whole pelvic radiotherapy. In fact, the benefits achieved statistical significance only in patients who fit into one or more of these subgroups, added Dr. Matsuo of the University of Southern California, Los Angeles.
He presented a multicenter retrospective study of 1,687 patients with surgically staged endometrial cancer, 158 of whom were regular users of low-dose aspirin for various reasons, mainly cardioprotection.
The 5-year disease-free survival rates in aspirin users and nonusers were 90.6% and 80.9%, respectively. The 5-year overall survival rates were 96.4%, compared with 87.3%. Aspirin users had a higher cardiovascular risk profile. Their mean BMI was 36.7 kg/m2, versus 29.6 kg/m2 for nonusers. Moreover, aspirin users were also significantly more likely to have hypertension, diabetes, and hypercholesterolemia, and to be taking medications to manage those conditions.
In a multivariate analysis controlled for age, ethnicity, obesity, medications, tumor grade, stage, and histology, as well as the use of postoperative radiation therapy or chemotherapy, the adjusted 5-year risk of disease progression was 54% lower among aspirin users than in nonusers. The risk of all-cause mortality was reduced by 77%, according to Dr. Matsuo.
Aspirin’s mechanism of anti-oncogenic benefit in the setting of endometrial cancer is believed to involve its ability to inhibit COX-2, thereby curbing the chronic inflammation that figures prominently in the disease. Dr. Matsuo called attention to a recent retrospective cohort study by investigators at Montefiore Medical Center in New York. In that study, concomitant use of aspirin and a statin by endometrial cancer patients was associated with a robust 75% reduction in the risk of cancer-specific mortality, compared with women on neither (Obstet Gynecol. 2015 Jul;126[1]:144-50).
On the separate issue of whether aspirin is also useful for prevention of endometrial cancer, Dr. Matsuo noted that a recent Danish meta-analysis demonstrated a significantly reduced risk of developing the malignancy in regular users of aspirin, particularly if obese. The relative risk reduction in obese aspirin users, compared with nonusers, amounted to 44% in case-control studies and 20% in cohort studies (Gynecol Oncol. 2016 Feb;140[2]:352-8).
Discussant Dr. Kala Visvanathan commented that while the usual caveats about nonrandomized studies such as Dr. Matsuo’s apply – they must be considered hypothesis-generating rather than definitive because of the possibility of unrecognized confounders – repurposing an old drug such as aspirin as a treatment for cancer has enormous appeal.
The safety profiles and drug interactions of older medications such as aspirin, statins, and metformin are well established. And the ability to use an inexpensive older drug to simultaneously prevent or treat multiple common and serious diseases is a tantalizing prospect, observed Dr. Visvanathan, professor of epidemiology and oncology at Johns Hopkins University, Baltimore.
SAN DIEGO – Endometrial cancer patients who regularly took low-dose aspirin experienced markedly better 5-year disease-free and overall survival compared to nonusers in an observational study, Dr. Koji Matsuo reported at the annual meeting of the Society of Gynecologic Oncology.
This apparent survival-prolonging effect of aspirin was greatest in women who were obese, less than 60 years old, had type 1 endometrial cancer, and/or received postoperative whole pelvic radiotherapy. In fact, the benefits achieved statistical significance only in patients who fit into one or more of these subgroups, added Dr. Matsuo of the University of Southern California, Los Angeles.
He presented a multicenter retrospective study of 1,687 patients with surgically staged endometrial cancer, 158 of whom were regular users of low-dose aspirin for various reasons, mainly cardioprotection.
The 5-year disease-free survival rates in aspirin users and nonusers were 90.6% and 80.9%, respectively. The 5-year overall survival rates were 96.4%, compared with 87.3%. Aspirin users had a higher cardiovascular risk profile. Their mean BMI was 36.7 kg/m2, versus 29.6 kg/m2 for nonusers. Moreover, aspirin users were also significantly more likely to have hypertension, diabetes, and hypercholesterolemia, and to be taking medications to manage those conditions.
In a multivariate analysis controlled for age, ethnicity, obesity, medications, tumor grade, stage, and histology, as well as the use of postoperative radiation therapy or chemotherapy, the adjusted 5-year risk of disease progression was 54% lower among aspirin users than in nonusers. The risk of all-cause mortality was reduced by 77%, according to Dr. Matsuo.
Aspirin’s mechanism of anti-oncogenic benefit in the setting of endometrial cancer is believed to involve its ability to inhibit COX-2, thereby curbing the chronic inflammation that figures prominently in the disease. Dr. Matsuo called attention to a recent retrospective cohort study by investigators at Montefiore Medical Center in New York. In that study, concomitant use of aspirin and a statin by endometrial cancer patients was associated with a robust 75% reduction in the risk of cancer-specific mortality, compared with women on neither (Obstet Gynecol. 2015 Jul;126[1]:144-50).
On the separate issue of whether aspirin is also useful for prevention of endometrial cancer, Dr. Matsuo noted that a recent Danish meta-analysis demonstrated a significantly reduced risk of developing the malignancy in regular users of aspirin, particularly if obese. The relative risk reduction in obese aspirin users, compared with nonusers, amounted to 44% in case-control studies and 20% in cohort studies (Gynecol Oncol. 2016 Feb;140[2]:352-8).
Discussant Dr. Kala Visvanathan commented that while the usual caveats about nonrandomized studies such as Dr. Matsuo’s apply – they must be considered hypothesis-generating rather than definitive because of the possibility of unrecognized confounders – repurposing an old drug such as aspirin as a treatment for cancer has enormous appeal.
The safety profiles and drug interactions of older medications such as aspirin, statins, and metformin are well established. And the ability to use an inexpensive older drug to simultaneously prevent or treat multiple common and serious diseases is a tantalizing prospect, observed Dr. Visvanathan, professor of epidemiology and oncology at Johns Hopkins University, Baltimore.
SAN DIEGO – Endometrial cancer patients who regularly took low-dose aspirin experienced markedly better 5-year disease-free and overall survival compared to nonusers in an observational study, Dr. Koji Matsuo reported at the annual meeting of the Society of Gynecologic Oncology.
This apparent survival-prolonging effect of aspirin was greatest in women who were obese, less than 60 years old, had type 1 endometrial cancer, and/or received postoperative whole pelvic radiotherapy. In fact, the benefits achieved statistical significance only in patients who fit into one or more of these subgroups, added Dr. Matsuo of the University of Southern California, Los Angeles.
He presented a multicenter retrospective study of 1,687 patients with surgically staged endometrial cancer, 158 of whom were regular users of low-dose aspirin for various reasons, mainly cardioprotection.
The 5-year disease-free survival rates in aspirin users and nonusers were 90.6% and 80.9%, respectively. The 5-year overall survival rates were 96.4%, compared with 87.3%. Aspirin users had a higher cardiovascular risk profile. Their mean BMI was 36.7 kg/m2, versus 29.6 kg/m2 for nonusers. Moreover, aspirin users were also significantly more likely to have hypertension, diabetes, and hypercholesterolemia, and to be taking medications to manage those conditions.
In a multivariate analysis controlled for age, ethnicity, obesity, medications, tumor grade, stage, and histology, as well as the use of postoperative radiation therapy or chemotherapy, the adjusted 5-year risk of disease progression was 54% lower among aspirin users than in nonusers. The risk of all-cause mortality was reduced by 77%, according to Dr. Matsuo.
Aspirin’s mechanism of anti-oncogenic benefit in the setting of endometrial cancer is believed to involve its ability to inhibit COX-2, thereby curbing the chronic inflammation that figures prominently in the disease. Dr. Matsuo called attention to a recent retrospective cohort study by investigators at Montefiore Medical Center in New York. In that study, concomitant use of aspirin and a statin by endometrial cancer patients was associated with a robust 75% reduction in the risk of cancer-specific mortality, compared with women on neither (Obstet Gynecol. 2015 Jul;126[1]:144-50).
On the separate issue of whether aspirin is also useful for prevention of endometrial cancer, Dr. Matsuo noted that a recent Danish meta-analysis demonstrated a significantly reduced risk of developing the malignancy in regular users of aspirin, particularly if obese. The relative risk reduction in obese aspirin users, compared with nonusers, amounted to 44% in case-control studies and 20% in cohort studies (Gynecol Oncol. 2016 Feb;140[2]:352-8).
Discussant Dr. Kala Visvanathan commented that while the usual caveats about nonrandomized studies such as Dr. Matsuo’s apply – they must be considered hypothesis-generating rather than definitive because of the possibility of unrecognized confounders – repurposing an old drug such as aspirin as a treatment for cancer has enormous appeal.
The safety profiles and drug interactions of older medications such as aspirin, statins, and metformin are well established. And the ability to use an inexpensive older drug to simultaneously prevent or treat multiple common and serious diseases is a tantalizing prospect, observed Dr. Visvanathan, professor of epidemiology and oncology at Johns Hopkins University, Baltimore.
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: Low-dose aspirin may protect against progression of endometrial cancer.
Major finding: The 5-year disease-free survival rate in endometrial cancer patients who regularly used low-dose aspirin was 90.6%, compared with 80.9% in nonusers.
Data source: This was a multicenter retrospective study of 1,687 women with endometrial cancer.
Disclosures: The presenter reported having no financial conflicts regarding this study, conducted without commercial support.