User login
Extended-release granisetron superior antiemetic for cisplatin chemotherapy
SAN DIEGO – An investigational extended-release formulation of granisetron outperformed ondansetron as a component of triple-drug antiemetic therapy for patients on cisplatin-based highly emetogenic chemotherapy, Dr. Lee Schwartzberg reported at the annual meeting of the Society of Gynecologic Oncology.
He presented a post hoc subgroup analysis drawn from the previously reported pivotal phase III 942-patient MAGIC trial of extended-release granisetron (Sustol), formerly known as APF530, versus ondansetron (Zofran) as part of the triple-drug antiemetic regimen recommended in National Community Cancer Network guidelines for the prevention of chemotherapy-induced nausea and vomiting (CINV) in patients on highly emetogenic chemotherapy .
Dr. Schwartzberg and coinvestigators focused on the 251 MAGIC participants on high-dose cisplatin-based chemotherapy. The reason? Few studies have examined the management of CINV in patients on platinum-based regimens, commonly used in treating gynecologic cancers, explained Dr. Schwartzberg, medical director of the West Clinic in Memphis.
Sustol consists of 2% granisetron in a proprietary slow-release vehicle. A single 500-mg subcutaneous dose containing 10 mg of granisetron maintains therapeutic blood levels of granisetron for 5 days or longer. These pharmacokinetics make APF530 an attractive strategy for preventing both acute and delayed chemotherapy-induced nausea and vomiting. The delayed phase, which affects many cancer patients 2-5 days following administration of chemotherapy, has traditionally been a particularly difficult management challenge.
National Community Cancer Network guidelines recommend that patients on highly emetogenic chemotherapy receive a potent three-drug antiemetic regimen consisting of a 5-hydroxytryptoamine-3 receptor antagonist – ondansetron and granisetron fall within this class – along with a neurokinin-1 receptor antagonist and dexamethasone.
MAGIC was a double-blind, prospective, multicenter trial in which 942 patients on highly emetogenic chemotherapy received either 500 mg of subcutaneous extended-release granisetron or intravenous ondansetron at 0.15 mg/kg. In addition, all participants concomitantly got 150 mg of the neurokinin-1 receptor antagonist fosaprepitant (Emend) plus 12 mg of IV dexamethasone on day 1, followed by 8 mg of oral dexamethasone once on day 2 and 8 mg twice daily on days 3 and 4.
In the overall trial, extended-release granisetron significantly outperformed ondansetron. The primary endpoint – complete response defined as no emesis and no use of rescue medication for CINV during the delayed phase – was achieved in 64.7% of the Sustol group, compared with 56.6% on ondansetron.
Results in Dr. Schwartzberg’s post hoc analysis confined to the 251 randomized patients on high-dose cisplatin-based chemotherapy paralleled those in the overall trial: a 64.8% complete response rate in the delayed phase in the granisetron group versus 56.3% with ondansetron. That absolute 8.5% difference favoring the investigational agent translates to a number needed to treat (NNT) of 12.
In the 112 women on highly emetogenic cisplatin-based chemotherapy, the complete response rates in the delayed phase were 61.6% with extended-release granisetron and 53.2% with ondansetron, for an absolute 10.3% difference and an NNT of 10.
Heron Therapeutics, which is developing extended-release granisetron, is awaiting word from the Food and Drug Administration regarding the company’s application for marketing approval.
The MAGIC trial was sponsored by Heron Therapeutics. Dr. Schwartzberg is a consultant to the company.
SAN DIEGO – An investigational extended-release formulation of granisetron outperformed ondansetron as a component of triple-drug antiemetic therapy for patients on cisplatin-based highly emetogenic chemotherapy, Dr. Lee Schwartzberg reported at the annual meeting of the Society of Gynecologic Oncology.
He presented a post hoc subgroup analysis drawn from the previously reported pivotal phase III 942-patient MAGIC trial of extended-release granisetron (Sustol), formerly known as APF530, versus ondansetron (Zofran) as part of the triple-drug antiemetic regimen recommended in National Community Cancer Network guidelines for the prevention of chemotherapy-induced nausea and vomiting (CINV) in patients on highly emetogenic chemotherapy .
Dr. Schwartzberg and coinvestigators focused on the 251 MAGIC participants on high-dose cisplatin-based chemotherapy. The reason? Few studies have examined the management of CINV in patients on platinum-based regimens, commonly used in treating gynecologic cancers, explained Dr. Schwartzberg, medical director of the West Clinic in Memphis.
Sustol consists of 2% granisetron in a proprietary slow-release vehicle. A single 500-mg subcutaneous dose containing 10 mg of granisetron maintains therapeutic blood levels of granisetron for 5 days or longer. These pharmacokinetics make APF530 an attractive strategy for preventing both acute and delayed chemotherapy-induced nausea and vomiting. The delayed phase, which affects many cancer patients 2-5 days following administration of chemotherapy, has traditionally been a particularly difficult management challenge.
National Community Cancer Network guidelines recommend that patients on highly emetogenic chemotherapy receive a potent three-drug antiemetic regimen consisting of a 5-hydroxytryptoamine-3 receptor antagonist – ondansetron and granisetron fall within this class – along with a neurokinin-1 receptor antagonist and dexamethasone.
MAGIC was a double-blind, prospective, multicenter trial in which 942 patients on highly emetogenic chemotherapy received either 500 mg of subcutaneous extended-release granisetron or intravenous ondansetron at 0.15 mg/kg. In addition, all participants concomitantly got 150 mg of the neurokinin-1 receptor antagonist fosaprepitant (Emend) plus 12 mg of IV dexamethasone on day 1, followed by 8 mg of oral dexamethasone once on day 2 and 8 mg twice daily on days 3 and 4.
In the overall trial, extended-release granisetron significantly outperformed ondansetron. The primary endpoint – complete response defined as no emesis and no use of rescue medication for CINV during the delayed phase – was achieved in 64.7% of the Sustol group, compared with 56.6% on ondansetron.
Results in Dr. Schwartzberg’s post hoc analysis confined to the 251 randomized patients on high-dose cisplatin-based chemotherapy paralleled those in the overall trial: a 64.8% complete response rate in the delayed phase in the granisetron group versus 56.3% with ondansetron. That absolute 8.5% difference favoring the investigational agent translates to a number needed to treat (NNT) of 12.
In the 112 women on highly emetogenic cisplatin-based chemotherapy, the complete response rates in the delayed phase were 61.6% with extended-release granisetron and 53.2% with ondansetron, for an absolute 10.3% difference and an NNT of 10.
Heron Therapeutics, which is developing extended-release granisetron, is awaiting word from the Food and Drug Administration regarding the company’s application for marketing approval.
The MAGIC trial was sponsored by Heron Therapeutics. Dr. Schwartzberg is a consultant to the company.
SAN DIEGO – An investigational extended-release formulation of granisetron outperformed ondansetron as a component of triple-drug antiemetic therapy for patients on cisplatin-based highly emetogenic chemotherapy, Dr. Lee Schwartzberg reported at the annual meeting of the Society of Gynecologic Oncology.
He presented a post hoc subgroup analysis drawn from the previously reported pivotal phase III 942-patient MAGIC trial of extended-release granisetron (Sustol), formerly known as APF530, versus ondansetron (Zofran) as part of the triple-drug antiemetic regimen recommended in National Community Cancer Network guidelines for the prevention of chemotherapy-induced nausea and vomiting (CINV) in patients on highly emetogenic chemotherapy .
Dr. Schwartzberg and coinvestigators focused on the 251 MAGIC participants on high-dose cisplatin-based chemotherapy. The reason? Few studies have examined the management of CINV in patients on platinum-based regimens, commonly used in treating gynecologic cancers, explained Dr. Schwartzberg, medical director of the West Clinic in Memphis.
Sustol consists of 2% granisetron in a proprietary slow-release vehicle. A single 500-mg subcutaneous dose containing 10 mg of granisetron maintains therapeutic blood levels of granisetron for 5 days or longer. These pharmacokinetics make APF530 an attractive strategy for preventing both acute and delayed chemotherapy-induced nausea and vomiting. The delayed phase, which affects many cancer patients 2-5 days following administration of chemotherapy, has traditionally been a particularly difficult management challenge.
National Community Cancer Network guidelines recommend that patients on highly emetogenic chemotherapy receive a potent three-drug antiemetic regimen consisting of a 5-hydroxytryptoamine-3 receptor antagonist – ondansetron and granisetron fall within this class – along with a neurokinin-1 receptor antagonist and dexamethasone.
MAGIC was a double-blind, prospective, multicenter trial in which 942 patients on highly emetogenic chemotherapy received either 500 mg of subcutaneous extended-release granisetron or intravenous ondansetron at 0.15 mg/kg. In addition, all participants concomitantly got 150 mg of the neurokinin-1 receptor antagonist fosaprepitant (Emend) plus 12 mg of IV dexamethasone on day 1, followed by 8 mg of oral dexamethasone once on day 2 and 8 mg twice daily on days 3 and 4.
In the overall trial, extended-release granisetron significantly outperformed ondansetron. The primary endpoint – complete response defined as no emesis and no use of rescue medication for CINV during the delayed phase – was achieved in 64.7% of the Sustol group, compared with 56.6% on ondansetron.
Results in Dr. Schwartzberg’s post hoc analysis confined to the 251 randomized patients on high-dose cisplatin-based chemotherapy paralleled those in the overall trial: a 64.8% complete response rate in the delayed phase in the granisetron group versus 56.3% with ondansetron. That absolute 8.5% difference favoring the investigational agent translates to a number needed to treat (NNT) of 12.
In the 112 women on highly emetogenic cisplatin-based chemotherapy, the complete response rates in the delayed phase were 61.6% with extended-release granisetron and 53.2% with ondansetron, for an absolute 10.3% difference and an NNT of 10.
Heron Therapeutics, which is developing extended-release granisetron, is awaiting word from the Food and Drug Administration regarding the company’s application for marketing approval.
The MAGIC trial was sponsored by Heron Therapeutics. Dr. Schwartzberg is a consultant to the company.
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: Investigational agent outperforms ondansetron during delayed phase of highly emetogenic cisplatin-based chemotherapy-induced nausea and vomiting.
Major finding: Complete response rate during delayed phase was 64.8% when triple antiemetic therapy included extended-release granisetron and 56.3% when the regimen included ondansetron.
Data source: This post hoc subgroup analysis of the 942-patient pivotal phase III MAGIC trial focused specifically on the 251 participants on highly emetogenic cisplatin-based chemotherapy.
Disclosures: The study presenter reported serving as a consultant to Heron Therapeutics, which sponsored the MAGIC trial.
Women with ovarian cancer wait over a month to start treatment
SAN DIEGO – Women diagnosed with ovarian cancer waited about 38 days, on average, from the initial concerning imaging test to initiation of treatment, according to a study analyzing health care transit times at a single community hospital.
“Ovarian cancer is such a hard disease to diagnose early,” Christopher J. LaFargue, MD, lead study author, said in an interview at the annual meeting of the Society of Gynecologic Oncology. “Once it’s diagnosed, it’s imperative that women get in to see the gynecologic oncologist [and] make sure their treatment care isn’t lagged for any reason.”
In an effort to characterize the length of time between critical points in the care of women with ovarian cancer and determine the impact of patient demographics, Dr. LaFargue and his associates retrospectively evaluated the medical records of 45 women who were diagnosed with ovarian cancer at Long Beach (Calif.) Memorial Medical Center between January 2012 and May 2015.
They examined patient demographics, including preoperative CA-125. Time points of interest were first concerning imaging test, first gynecologic oncology appointment, initiation of treatment, and adjuvant therapy. They used univariate analyses to determine associations between specific patient demographics and the time intervals of interest.
Dr. LaFargue, a resident in the department of obstetrics and gynecology at the University of California, Irvine, reported that the mean age of patients was 61 years, and the mean driving distance to the hospital from the patients’ home was 11 miles. More than half of the patients were white (58%) and 62% of patients were diagnosed with stage III or IV disease. Preoperative CA-125 exceeded 200 U/mL in 62% of patients. Medicare enrollees with supplemental insurance made up less than half of the group (44%).
The researchers found that the average time from initial concerning imaging to start of treatment was about 38 days. The average time from initial imaging to the first office visit with a gynecologic oncologist was about 18 days. The time from that appointment to initial treatment was 19 days, on average. The time from the start of neoadjuvant chemotherapy to interval cytoreductive surgery was 103 days, on average.
The only factor that significantly impacted transit time was a patient’s CA-125 level. Those who had a level of 200 U/mL or greater were more likely to receive surgery or treatment quicker, compared with those who had a CA-125 level less than 200 U/mL. No other statistically significant associations between patient demographics and length of time intervals were observed.
“It would have been nice to have seen a correlation with insurance status,” Dr. LaFargue said. “That’s kind of what we were hoping for, because then you can make an argument with insurance payers that patients who have Medicare aren’t getting treated as quickly as those who have a PPO, for example.”
He acknowledged certain limitations of the study, including its small sample size, lack of outcomes data, and the fact that it was conducted in a community hospital setting.
Dr. LaFargue reported having no financial disclosures.
SAN DIEGO – Women diagnosed with ovarian cancer waited about 38 days, on average, from the initial concerning imaging test to initiation of treatment, according to a study analyzing health care transit times at a single community hospital.
“Ovarian cancer is such a hard disease to diagnose early,” Christopher J. LaFargue, MD, lead study author, said in an interview at the annual meeting of the Society of Gynecologic Oncology. “Once it’s diagnosed, it’s imperative that women get in to see the gynecologic oncologist [and] make sure their treatment care isn’t lagged for any reason.”
In an effort to characterize the length of time between critical points in the care of women with ovarian cancer and determine the impact of patient demographics, Dr. LaFargue and his associates retrospectively evaluated the medical records of 45 women who were diagnosed with ovarian cancer at Long Beach (Calif.) Memorial Medical Center between January 2012 and May 2015.
They examined patient demographics, including preoperative CA-125. Time points of interest were first concerning imaging test, first gynecologic oncology appointment, initiation of treatment, and adjuvant therapy. They used univariate analyses to determine associations between specific patient demographics and the time intervals of interest.
Dr. LaFargue, a resident in the department of obstetrics and gynecology at the University of California, Irvine, reported that the mean age of patients was 61 years, and the mean driving distance to the hospital from the patients’ home was 11 miles. More than half of the patients were white (58%) and 62% of patients were diagnosed with stage III or IV disease. Preoperative CA-125 exceeded 200 U/mL in 62% of patients. Medicare enrollees with supplemental insurance made up less than half of the group (44%).
The researchers found that the average time from initial concerning imaging to start of treatment was about 38 days. The average time from initial imaging to the first office visit with a gynecologic oncologist was about 18 days. The time from that appointment to initial treatment was 19 days, on average. The time from the start of neoadjuvant chemotherapy to interval cytoreductive surgery was 103 days, on average.
The only factor that significantly impacted transit time was a patient’s CA-125 level. Those who had a level of 200 U/mL or greater were more likely to receive surgery or treatment quicker, compared with those who had a CA-125 level less than 200 U/mL. No other statistically significant associations between patient demographics and length of time intervals were observed.
“It would have been nice to have seen a correlation with insurance status,” Dr. LaFargue said. “That’s kind of what we were hoping for, because then you can make an argument with insurance payers that patients who have Medicare aren’t getting treated as quickly as those who have a PPO, for example.”
He acknowledged certain limitations of the study, including its small sample size, lack of outcomes data, and the fact that it was conducted in a community hospital setting.
Dr. LaFargue reported having no financial disclosures.
SAN DIEGO – Women diagnosed with ovarian cancer waited about 38 days, on average, from the initial concerning imaging test to initiation of treatment, according to a study analyzing health care transit times at a single community hospital.
“Ovarian cancer is such a hard disease to diagnose early,” Christopher J. LaFargue, MD, lead study author, said in an interview at the annual meeting of the Society of Gynecologic Oncology. “Once it’s diagnosed, it’s imperative that women get in to see the gynecologic oncologist [and] make sure their treatment care isn’t lagged for any reason.”
In an effort to characterize the length of time between critical points in the care of women with ovarian cancer and determine the impact of patient demographics, Dr. LaFargue and his associates retrospectively evaluated the medical records of 45 women who were diagnosed with ovarian cancer at Long Beach (Calif.) Memorial Medical Center between January 2012 and May 2015.
They examined patient demographics, including preoperative CA-125. Time points of interest were first concerning imaging test, first gynecologic oncology appointment, initiation of treatment, and adjuvant therapy. They used univariate analyses to determine associations between specific patient demographics and the time intervals of interest.
Dr. LaFargue, a resident in the department of obstetrics and gynecology at the University of California, Irvine, reported that the mean age of patients was 61 years, and the mean driving distance to the hospital from the patients’ home was 11 miles. More than half of the patients were white (58%) and 62% of patients were diagnosed with stage III or IV disease. Preoperative CA-125 exceeded 200 U/mL in 62% of patients. Medicare enrollees with supplemental insurance made up less than half of the group (44%).
The researchers found that the average time from initial concerning imaging to start of treatment was about 38 days. The average time from initial imaging to the first office visit with a gynecologic oncologist was about 18 days. The time from that appointment to initial treatment was 19 days, on average. The time from the start of neoadjuvant chemotherapy to interval cytoreductive surgery was 103 days, on average.
The only factor that significantly impacted transit time was a patient’s CA-125 level. Those who had a level of 200 U/mL or greater were more likely to receive surgery or treatment quicker, compared with those who had a CA-125 level less than 200 U/mL. No other statistically significant associations between patient demographics and length of time intervals were observed.
“It would have been nice to have seen a correlation with insurance status,” Dr. LaFargue said. “That’s kind of what we were hoping for, because then you can make an argument with insurance payers that patients who have Medicare aren’t getting treated as quickly as those who have a PPO, for example.”
He acknowledged certain limitations of the study, including its small sample size, lack of outcomes data, and the fact that it was conducted in a community hospital setting.
Dr. LaFargue reported having no financial disclosures.
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: Initiation of treatment for ovarian cancer following the first concerning imaging test took an average of about 38 days.
Major finding: The average time from the initial imaging test to the first visit with a gynecologic oncologist was about 18 days.
Data source: A retrospective evaluation of 45 women who were diagnosed with ovarian cancer between January 2012 and May 2015 at a community hospital.
Disclosures: Dr. LaFargue reported having no financial disclosures.
Symptoms linger after ‘successful’ gyn. cancer therapy
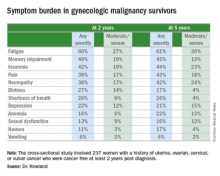
SAN DIEGO – Fully half of gynecologic cancer survivors who are done with treatment and cancer free nonetheless report having moderate to severe symptoms 2 and even 5 years after diagnosis, Dr. Michelle Rowland reported at the annual meeting of the Society of Gynecologic Oncology.
The most common symptoms in her cross-sectional study of 237 women with a history of uterine, ovarian, cervical, or vulvar cancer who were cancer free and at least 2 years post diagnosis were fatigue, insomnia, pain, memory impairment, and neuropathy, according to Dr. Rowland, a gynecologic oncology fellow at the University of Oklahoma in Oklahoma City.
She found the high prevalence of fatigue in gynecologic cancer survivors so distant from treatment particularly unexpected.
“The fact that 60% of women report some degree of fatigue 2 and 5 years out from their gynecologic cancer diagnosis was surprising to me,” she said in an interview. “Fatigue is something we usually think of as being related either to the treatment that they’re getting or to the cancer itself. But these women don’t have cancer anymore and are not being treated.”
The cross-sectional study included 237 patients who completed a self-assessment symptom questionnaire during a university outpatient gynecologic oncology clinic for ongoing routine disease surveillance. All were believed to be cancer free and none were receiving treatment 2 or more years post diagnosis. Seventy-seven of the women were 5 or more years out from diagnosis. The prevalence and self-rated severity of symptoms on a 0-10 scale were similar in the 2- and 5-year survivor groups.
One-quarter of the 2-year survivors reported having three or more moderate to severe symptoms as defined by a rating of 4-10. So did 29% of the 5-year survivors.
Three-quarters of women reported having one or more symptom.
In an effort to identify predictors of high symptom burden, Dr. Rowland and coinvestigators conducted a multivariate logistic regression analysis controlling for tumor stage, disease, site, race, and all forms of cancer therapy received. Prior chemotherapy proved to be an independent risk factor for high symptom burden at 2 years, while prior radiation therapy predicted high symptom burden at 5 or more years. Of note, cancer type was not predictive.
Roughly 40% of subjects reported currently being on medications for chronic pain, 11% were taking antianxiety drugs, and a similar proportion were using sleep aids.
Dr. Rowland concluded that long-term follow-up of gynecologic cancer survivors should include a symptom assessment. Survivor clinics, which are becoming increasingly common, offer a way to specifically address ongoing symptoms.
She reported having no financial conflicts regarding her study.
SAN DIEGO – Fully half of gynecologic cancer survivors who are done with treatment and cancer free nonetheless report having moderate to severe symptoms 2 and even 5 years after diagnosis, Dr. Michelle Rowland reported at the annual meeting of the Society of Gynecologic Oncology.
The most common symptoms in her cross-sectional study of 237 women with a history of uterine, ovarian, cervical, or vulvar cancer who were cancer free and at least 2 years post diagnosis were fatigue, insomnia, pain, memory impairment, and neuropathy, according to Dr. Rowland, a gynecologic oncology fellow at the University of Oklahoma in Oklahoma City.
She found the high prevalence of fatigue in gynecologic cancer survivors so distant from treatment particularly unexpected.
“The fact that 60% of women report some degree of fatigue 2 and 5 years out from their gynecologic cancer diagnosis was surprising to me,” she said in an interview. “Fatigue is something we usually think of as being related either to the treatment that they’re getting or to the cancer itself. But these women don’t have cancer anymore and are not being treated.”
The cross-sectional study included 237 patients who completed a self-assessment symptom questionnaire during a university outpatient gynecologic oncology clinic for ongoing routine disease surveillance. All were believed to be cancer free and none were receiving treatment 2 or more years post diagnosis. Seventy-seven of the women were 5 or more years out from diagnosis. The prevalence and self-rated severity of symptoms on a 0-10 scale were similar in the 2- and 5-year survivor groups.
One-quarter of the 2-year survivors reported having three or more moderate to severe symptoms as defined by a rating of 4-10. So did 29% of the 5-year survivors.
Three-quarters of women reported having one or more symptom.
In an effort to identify predictors of high symptom burden, Dr. Rowland and coinvestigators conducted a multivariate logistic regression analysis controlling for tumor stage, disease, site, race, and all forms of cancer therapy received. Prior chemotherapy proved to be an independent risk factor for high symptom burden at 2 years, while prior radiation therapy predicted high symptom burden at 5 or more years. Of note, cancer type was not predictive.
Roughly 40% of subjects reported currently being on medications for chronic pain, 11% were taking antianxiety drugs, and a similar proportion were using sleep aids.
Dr. Rowland concluded that long-term follow-up of gynecologic cancer survivors should include a symptom assessment. Survivor clinics, which are becoming increasingly common, offer a way to specifically address ongoing symptoms.
She reported having no financial conflicts regarding her study.
SAN DIEGO – Fully half of gynecologic cancer survivors who are done with treatment and cancer free nonetheless report having moderate to severe symptoms 2 and even 5 years after diagnosis, Dr. Michelle Rowland reported at the annual meeting of the Society of Gynecologic Oncology.
The most common symptoms in her cross-sectional study of 237 women with a history of uterine, ovarian, cervical, or vulvar cancer who were cancer free and at least 2 years post diagnosis were fatigue, insomnia, pain, memory impairment, and neuropathy, according to Dr. Rowland, a gynecologic oncology fellow at the University of Oklahoma in Oklahoma City.
She found the high prevalence of fatigue in gynecologic cancer survivors so distant from treatment particularly unexpected.
“The fact that 60% of women report some degree of fatigue 2 and 5 years out from their gynecologic cancer diagnosis was surprising to me,” she said in an interview. “Fatigue is something we usually think of as being related either to the treatment that they’re getting or to the cancer itself. But these women don’t have cancer anymore and are not being treated.”
The cross-sectional study included 237 patients who completed a self-assessment symptom questionnaire during a university outpatient gynecologic oncology clinic for ongoing routine disease surveillance. All were believed to be cancer free and none were receiving treatment 2 or more years post diagnosis. Seventy-seven of the women were 5 or more years out from diagnosis. The prevalence and self-rated severity of symptoms on a 0-10 scale were similar in the 2- and 5-year survivor groups.
One-quarter of the 2-year survivors reported having three or more moderate to severe symptoms as defined by a rating of 4-10. So did 29% of the 5-year survivors.
Three-quarters of women reported having one or more symptom.
In an effort to identify predictors of high symptom burden, Dr. Rowland and coinvestigators conducted a multivariate logistic regression analysis controlling for tumor stage, disease, site, race, and all forms of cancer therapy received. Prior chemotherapy proved to be an independent risk factor for high symptom burden at 2 years, while prior radiation therapy predicted high symptom burden at 5 or more years. Of note, cancer type was not predictive.
Roughly 40% of subjects reported currently being on medications for chronic pain, 11% were taking antianxiety drugs, and a similar proportion were using sleep aids.
Dr. Rowland concluded that long-term follow-up of gynecologic cancer survivors should include a symptom assessment. Survivor clinics, which are becoming increasingly common, offer a way to specifically address ongoing symptoms.
She reported having no financial conflicts regarding her study.
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: Long-term follow-up of gynecologic cancer survivors should include assessment of cancer- or treatment-related symptoms.
Major finding: One-quarter of cancer-free patients reported three or more lingering symptoms of moderate to severe intensity 2 years after diagnosis.
Data source: This cross-sectional study utilized a structured questionnaire to evaluate the types and severity of symptoms present in 237 former gynecologic cancer patients who were off treatment and cancer free at least 2 years after diagnosis.
Disclosures: The study presenter reported having no financial conflicts of interest.
Statins improve ovarian cancer survival
SAN DIEGO – Statin therapy was independently associated with a substantial survival benefit in women with ovarian cancer in an analysis of the linked Surveillance, Epidemiology and End Results and Medicare databases.
“This is the largest series ever reported supporting the anticancer effect of statin therapy on epithelial ovarian cancer with a concomitant improvement in overall survival. A prospective study in ovarian cancer patients is warranted. Identification of biomarkers that may predict response to statins would help further select patient populations and guide therapy,” Dr. Tilley Jenkins Vogel said in presenting the study results at the annual meeting of the Society of Gynecologic Oncology.
She and her coinvestigators at Cedars-Sinai Medical Center in Los Angeles identified 1,510 women in the SEER registry who were diagnosed with epithelial ovarian cancer during 2007-2009, underwent primary surgical resection, and survived for at least 60 days post surgery. Forty-nine percent were stage III, 25% stage IV. Forty-two percent of the women were on a statin.
Mean overall survival in the statin users was 32.2 months compared to 28.7 months in nonusers. In the stage III cohort, mean overall survival in statin users versus nonusers was 31.7 and 25.9 months.
In a multivariate analysis adjusted for potential confounders of age, race, heart disease and other comorbid conditions prior to cancer diagnosis, and the use of platinum-based chemotherapy, statin therapy was independently associated with a 34% reduction in the risk of mortality. In women whose ovarian cancer histology was serous, statin use was associated with a 31% reduction in death; in those with a nonserous histology, it was a 48% reduction, Dr. Vogel continued.
Diving deeper into the dataset, she found that the overall survival benefit was present only in the 89% of statin users who were on lipophilic statins, such as atorvastatin or simvastatin. This is consistent with other investigators’ reports that the noncardiovascular benefits of statin therapy are largely restricted to the lipophilic class of the LDL-lowering agents.
An anti–ovarian cancer benefit for statin therapy appears to have biologic plausibility, according to Dr. Vogel. She and her coworkers have previously shown synergistic cytotoxicity in vitro when statins are administered concurrently with platinum chemotherapy.
“This effect is believed to be mediated by greater inhibition of cell proliferation, increased apoptosis, and modification of proteins in the RAS pathway,” she said.
Rapidly growing cells, such as cancer cells, require cholesterol to synthesize cell membrane. It’s hypothesized that one mechanism for statins’ anticancer effect is that by reducing intracellular cholesterol levels the drugs interfere with this process, Dr. Vogel noted.
She reported having no financial conflicts regarding this study, conducted without commercial support.
SAN DIEGO – Statin therapy was independently associated with a substantial survival benefit in women with ovarian cancer in an analysis of the linked Surveillance, Epidemiology and End Results and Medicare databases.
“This is the largest series ever reported supporting the anticancer effect of statin therapy on epithelial ovarian cancer with a concomitant improvement in overall survival. A prospective study in ovarian cancer patients is warranted. Identification of biomarkers that may predict response to statins would help further select patient populations and guide therapy,” Dr. Tilley Jenkins Vogel said in presenting the study results at the annual meeting of the Society of Gynecologic Oncology.
She and her coinvestigators at Cedars-Sinai Medical Center in Los Angeles identified 1,510 women in the SEER registry who were diagnosed with epithelial ovarian cancer during 2007-2009, underwent primary surgical resection, and survived for at least 60 days post surgery. Forty-nine percent were stage III, 25% stage IV. Forty-two percent of the women were on a statin.
Mean overall survival in the statin users was 32.2 months compared to 28.7 months in nonusers. In the stage III cohort, mean overall survival in statin users versus nonusers was 31.7 and 25.9 months.
In a multivariate analysis adjusted for potential confounders of age, race, heart disease and other comorbid conditions prior to cancer diagnosis, and the use of platinum-based chemotherapy, statin therapy was independently associated with a 34% reduction in the risk of mortality. In women whose ovarian cancer histology was serous, statin use was associated with a 31% reduction in death; in those with a nonserous histology, it was a 48% reduction, Dr. Vogel continued.
Diving deeper into the dataset, she found that the overall survival benefit was present only in the 89% of statin users who were on lipophilic statins, such as atorvastatin or simvastatin. This is consistent with other investigators’ reports that the noncardiovascular benefits of statin therapy are largely restricted to the lipophilic class of the LDL-lowering agents.
An anti–ovarian cancer benefit for statin therapy appears to have biologic plausibility, according to Dr. Vogel. She and her coworkers have previously shown synergistic cytotoxicity in vitro when statins are administered concurrently with platinum chemotherapy.
“This effect is believed to be mediated by greater inhibition of cell proliferation, increased apoptosis, and modification of proteins in the RAS pathway,” she said.
Rapidly growing cells, such as cancer cells, require cholesterol to synthesize cell membrane. It’s hypothesized that one mechanism for statins’ anticancer effect is that by reducing intracellular cholesterol levels the drugs interfere with this process, Dr. Vogel noted.
She reported having no financial conflicts regarding this study, conducted without commercial support.
SAN DIEGO – Statin therapy was independently associated with a substantial survival benefit in women with ovarian cancer in an analysis of the linked Surveillance, Epidemiology and End Results and Medicare databases.
“This is the largest series ever reported supporting the anticancer effect of statin therapy on epithelial ovarian cancer with a concomitant improvement in overall survival. A prospective study in ovarian cancer patients is warranted. Identification of biomarkers that may predict response to statins would help further select patient populations and guide therapy,” Dr. Tilley Jenkins Vogel said in presenting the study results at the annual meeting of the Society of Gynecologic Oncology.
She and her coinvestigators at Cedars-Sinai Medical Center in Los Angeles identified 1,510 women in the SEER registry who were diagnosed with epithelial ovarian cancer during 2007-2009, underwent primary surgical resection, and survived for at least 60 days post surgery. Forty-nine percent were stage III, 25% stage IV. Forty-two percent of the women were on a statin.
Mean overall survival in the statin users was 32.2 months compared to 28.7 months in nonusers. In the stage III cohort, mean overall survival in statin users versus nonusers was 31.7 and 25.9 months.
In a multivariate analysis adjusted for potential confounders of age, race, heart disease and other comorbid conditions prior to cancer diagnosis, and the use of platinum-based chemotherapy, statin therapy was independently associated with a 34% reduction in the risk of mortality. In women whose ovarian cancer histology was serous, statin use was associated with a 31% reduction in death; in those with a nonserous histology, it was a 48% reduction, Dr. Vogel continued.
Diving deeper into the dataset, she found that the overall survival benefit was present only in the 89% of statin users who were on lipophilic statins, such as atorvastatin or simvastatin. This is consistent with other investigators’ reports that the noncardiovascular benefits of statin therapy are largely restricted to the lipophilic class of the LDL-lowering agents.
An anti–ovarian cancer benefit for statin therapy appears to have biologic plausibility, according to Dr. Vogel. She and her coworkers have previously shown synergistic cytotoxicity in vitro when statins are administered concurrently with platinum chemotherapy.
“This effect is believed to be mediated by greater inhibition of cell proliferation, increased apoptosis, and modification of proteins in the RAS pathway,” she said.
Rapidly growing cells, such as cancer cells, require cholesterol to synthesize cell membrane. It’s hypothesized that one mechanism for statins’ anticancer effect is that by reducing intracellular cholesterol levels the drugs interfere with this process, Dr. Vogel noted.
She reported having no financial conflicts regarding this study, conducted without commercial support.
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: The risk of all-cause mortality in ovarian cancer patients on statin therapy was reduced by one-third.
Major finding: Mean survival in a large cohort of women with stage III ovarian cancer was 5.8 months longer among those on statin therapy.
Data source: A retrospective study of 1,510 women diagnosed with epithelial ovarian cancer during 2007-2009.
Disclosures: Dr. Vogel reported having no financial conflicts regarding this study, conducted without commercial support.
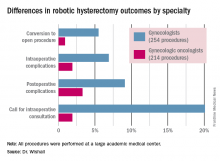
Gyn. oncologists are in demand for robotic hysterectomy
SAN DIEGO – The demand for gynecologic oncologists to perform robotic hysterectomies – even for benign indications – has increased to the point that additional fellowship training spots will be necessary to meet the need, Dr. Kayla M. Wishall said at the annual meeting of the Society of Gynecologic Oncology.
More and more patients want their hysterectomies performed robotically. They find the high-quality optics and minimally invasive nature of the robotic procedure appealing – smaller incisions, less blood loss, shorter hospital stay, and faster recovery. And gynecologic oncologists are getting an increasing number of referrals because of their special expertise in robotic surgery and extensive experience with higher-risk patients, explained Dr. Wishall, a gynecologic oncologist at Hahnemann University Hospital/Drexel University in Philadelphia.
“This trend will likely tax the limited resources of gynecologic oncologists,” she added.
Another possible reason for the growing demand for gynecologic oncologist–performed robotic hysterectomies is that these subspecialists achieve better outcomes than gynecologists who do robotic hysterectomies, at least according to the findings of a retrospective study performed by Dr. Wishall, which included all of the 468 robotic hysterectomies performed at a large academic medical center in a recent 5-year period.
Gynecologic oncologists performed 64 (16.5%) of the 387 robotic hysterectomies done for benign indications. All told, gynecologists did 254 of the robotic hysterectomies; gynecologic oncologists performed 214.
Even though patients referred to gynecologic oncologists for these procedures were older, heavier, more likely to have had previous abdominal surgery, more often members of racial minorities, and had a higher prevalence of cardiac comorbidities, they experienced significantly fewer intra- and postoperative complications than patients whose robotic hysterectomies were performed by gynecologists, Dr. Wishall reported.
The combined intraoperative and postoperative complication rate for robotic hysterectomies performed by gynecologic oncologists was 5.2%, compared with 16% for gynecologists. But the rate of cardiac comorbidities, for instance, was 36.4% among patients seeing gynecologic oncologists, compared with 23.6% among those seeing gynecologists.
Moreover, gynecologists were about 10-fold more likely than gynecologic oncologists to call for an intraoperative consultation and sixfold more likely to convert their robotic hysterectomy to an open procedure. Their average operating room time was about 40% longer (244 minutes versus 171 minutes), too, in this single-center experience.
Dr. Wishall reported having no financial conflicts related to her study, which was conducted free of commercial support.
I read this article initially with amusement and then with outrage and disdain. This article summarizes the single-site, retrospective study by Dr. Kayla Wishall at the annual meeting of the Society of Gynecologic Oncology. Not only is this nonscience, but nonsensical science. As a single center retrospective study, conclusions must be suspect.

|
Dr. Charles E. Miller |
The comparison numbers of the two groups are small. While confounders would appear to be greater in the oncology group, we know nothing about the difficulty of the surgeries themselves – size of uterus, adnexal disease, endometriosis, pelvic adhesions, etc. Oftentimes, gynecologic oncologists dealing with endometrial carcinoma are going to face a less difficult challenge than a generalist dealing with an 18-weeks–size uterus in a woman who has undergone three prior C-sections, an open myomectomy, or stage IV endometriosis.
We are also not privy to the experience of the surgeons involved; that is, the number of procedures performed by each surgeon in the compared groups. It is certainly well known that complications decrease with surgeon experience. In a multicenter analysis by Peter Lim et al., looking at robotic assisted hysterectomies performed by high-volume surgeons (60 or more prior procedures), the intraoperative complication rate was only 0.7% and the postoperative complication rate 6.3% (Int J Gynaecol Obstet. 2016 Jun;133[3]:359-64).
As a benign gynecologist who has been performing minimally invasive gynecologic surgery for 30 years and more recently, robotic surgery, I am shocked with the tenor of this study, as it would imply that unless someone is boarded in gynecologic oncology, he or she should not be performing robotic hysterectomies.
I would advise Dr. Wishall to reevaluate her surgeon population and look at the impact of experience as well as procedure difficultly. I am absolutely sure that she will find that many of the surgeons with excellent outcomes will be generalists, who are well experienced in robotic hysterectomy.
Dr. Charles E. Miller is a clinical associate professor at the University of Illinois at Chicago, and a reproductive endocrinologist and minimally invasive gynecologic surgeon in private practice in Naperville and Schaumburg, Ill. He reported having no financial disclosures relevant to this article.
I read this article initially with amusement and then with outrage and disdain. This article summarizes the single-site, retrospective study by Dr. Kayla Wishall at the annual meeting of the Society of Gynecologic Oncology. Not only is this nonscience, but nonsensical science. As a single center retrospective study, conclusions must be suspect.

|
Dr. Charles E. Miller |
The comparison numbers of the two groups are small. While confounders would appear to be greater in the oncology group, we know nothing about the difficulty of the surgeries themselves – size of uterus, adnexal disease, endometriosis, pelvic adhesions, etc. Oftentimes, gynecologic oncologists dealing with endometrial carcinoma are going to face a less difficult challenge than a generalist dealing with an 18-weeks–size uterus in a woman who has undergone three prior C-sections, an open myomectomy, or stage IV endometriosis.
We are also not privy to the experience of the surgeons involved; that is, the number of procedures performed by each surgeon in the compared groups. It is certainly well known that complications decrease with surgeon experience. In a multicenter analysis by Peter Lim et al., looking at robotic assisted hysterectomies performed by high-volume surgeons (60 or more prior procedures), the intraoperative complication rate was only 0.7% and the postoperative complication rate 6.3% (Int J Gynaecol Obstet. 2016 Jun;133[3]:359-64).
As a benign gynecologist who has been performing minimally invasive gynecologic surgery for 30 years and more recently, robotic surgery, I am shocked with the tenor of this study, as it would imply that unless someone is boarded in gynecologic oncology, he or she should not be performing robotic hysterectomies.
I would advise Dr. Wishall to reevaluate her surgeon population and look at the impact of experience as well as procedure difficultly. I am absolutely sure that she will find that many of the surgeons with excellent outcomes will be generalists, who are well experienced in robotic hysterectomy.
Dr. Charles E. Miller is a clinical associate professor at the University of Illinois at Chicago, and a reproductive endocrinologist and minimally invasive gynecologic surgeon in private practice in Naperville and Schaumburg, Ill. He reported having no financial disclosures relevant to this article.
I read this article initially with amusement and then with outrage and disdain. This article summarizes the single-site, retrospective study by Dr. Kayla Wishall at the annual meeting of the Society of Gynecologic Oncology. Not only is this nonscience, but nonsensical science. As a single center retrospective study, conclusions must be suspect.

|
Dr. Charles E. Miller |
The comparison numbers of the two groups are small. While confounders would appear to be greater in the oncology group, we know nothing about the difficulty of the surgeries themselves – size of uterus, adnexal disease, endometriosis, pelvic adhesions, etc. Oftentimes, gynecologic oncologists dealing with endometrial carcinoma are going to face a less difficult challenge than a generalist dealing with an 18-weeks–size uterus in a woman who has undergone three prior C-sections, an open myomectomy, or stage IV endometriosis.
We are also not privy to the experience of the surgeons involved; that is, the number of procedures performed by each surgeon in the compared groups. It is certainly well known that complications decrease with surgeon experience. In a multicenter analysis by Peter Lim et al., looking at robotic assisted hysterectomies performed by high-volume surgeons (60 or more prior procedures), the intraoperative complication rate was only 0.7% and the postoperative complication rate 6.3% (Int J Gynaecol Obstet. 2016 Jun;133[3]:359-64).
As a benign gynecologist who has been performing minimally invasive gynecologic surgery for 30 years and more recently, robotic surgery, I am shocked with the tenor of this study, as it would imply that unless someone is boarded in gynecologic oncology, he or she should not be performing robotic hysterectomies.
I would advise Dr. Wishall to reevaluate her surgeon population and look at the impact of experience as well as procedure difficultly. I am absolutely sure that she will find that many of the surgeons with excellent outcomes will be generalists, who are well experienced in robotic hysterectomy.
Dr. Charles E. Miller is a clinical associate professor at the University of Illinois at Chicago, and a reproductive endocrinologist and minimally invasive gynecologic surgeon in private practice in Naperville and Schaumburg, Ill. He reported having no financial disclosures relevant to this article.
SAN DIEGO – The demand for gynecologic oncologists to perform robotic hysterectomies – even for benign indications – has increased to the point that additional fellowship training spots will be necessary to meet the need, Dr. Kayla M. Wishall said at the annual meeting of the Society of Gynecologic Oncology.
More and more patients want their hysterectomies performed robotically. They find the high-quality optics and minimally invasive nature of the robotic procedure appealing – smaller incisions, less blood loss, shorter hospital stay, and faster recovery. And gynecologic oncologists are getting an increasing number of referrals because of their special expertise in robotic surgery and extensive experience with higher-risk patients, explained Dr. Wishall, a gynecologic oncologist at Hahnemann University Hospital/Drexel University in Philadelphia.
“This trend will likely tax the limited resources of gynecologic oncologists,” she added.
Another possible reason for the growing demand for gynecologic oncologist–performed robotic hysterectomies is that these subspecialists achieve better outcomes than gynecologists who do robotic hysterectomies, at least according to the findings of a retrospective study performed by Dr. Wishall, which included all of the 468 robotic hysterectomies performed at a large academic medical center in a recent 5-year period.
Gynecologic oncologists performed 64 (16.5%) of the 387 robotic hysterectomies done for benign indications. All told, gynecologists did 254 of the robotic hysterectomies; gynecologic oncologists performed 214.
Even though patients referred to gynecologic oncologists for these procedures were older, heavier, more likely to have had previous abdominal surgery, more often members of racial minorities, and had a higher prevalence of cardiac comorbidities, they experienced significantly fewer intra- and postoperative complications than patients whose robotic hysterectomies were performed by gynecologists, Dr. Wishall reported.
The combined intraoperative and postoperative complication rate for robotic hysterectomies performed by gynecologic oncologists was 5.2%, compared with 16% for gynecologists. But the rate of cardiac comorbidities, for instance, was 36.4% among patients seeing gynecologic oncologists, compared with 23.6% among those seeing gynecologists.
Moreover, gynecologists were about 10-fold more likely than gynecologic oncologists to call for an intraoperative consultation and sixfold more likely to convert their robotic hysterectomy to an open procedure. Their average operating room time was about 40% longer (244 minutes versus 171 minutes), too, in this single-center experience.
Dr. Wishall reported having no financial conflicts related to her study, which was conducted free of commercial support.
SAN DIEGO – The demand for gynecologic oncologists to perform robotic hysterectomies – even for benign indications – has increased to the point that additional fellowship training spots will be necessary to meet the need, Dr. Kayla M. Wishall said at the annual meeting of the Society of Gynecologic Oncology.
More and more patients want their hysterectomies performed robotically. They find the high-quality optics and minimally invasive nature of the robotic procedure appealing – smaller incisions, less blood loss, shorter hospital stay, and faster recovery. And gynecologic oncologists are getting an increasing number of referrals because of their special expertise in robotic surgery and extensive experience with higher-risk patients, explained Dr. Wishall, a gynecologic oncologist at Hahnemann University Hospital/Drexel University in Philadelphia.
“This trend will likely tax the limited resources of gynecologic oncologists,” she added.
Another possible reason for the growing demand for gynecologic oncologist–performed robotic hysterectomies is that these subspecialists achieve better outcomes than gynecologists who do robotic hysterectomies, at least according to the findings of a retrospective study performed by Dr. Wishall, which included all of the 468 robotic hysterectomies performed at a large academic medical center in a recent 5-year period.
Gynecologic oncologists performed 64 (16.5%) of the 387 robotic hysterectomies done for benign indications. All told, gynecologists did 254 of the robotic hysterectomies; gynecologic oncologists performed 214.
Even though patients referred to gynecologic oncologists for these procedures were older, heavier, more likely to have had previous abdominal surgery, more often members of racial minorities, and had a higher prevalence of cardiac comorbidities, they experienced significantly fewer intra- and postoperative complications than patients whose robotic hysterectomies were performed by gynecologists, Dr. Wishall reported.
The combined intraoperative and postoperative complication rate for robotic hysterectomies performed by gynecologic oncologists was 5.2%, compared with 16% for gynecologists. But the rate of cardiac comorbidities, for instance, was 36.4% among patients seeing gynecologic oncologists, compared with 23.6% among those seeing gynecologists.
Moreover, gynecologists were about 10-fold more likely than gynecologic oncologists to call for an intraoperative consultation and sixfold more likely to convert their robotic hysterectomy to an open procedure. Their average operating room time was about 40% longer (244 minutes versus 171 minutes), too, in this single-center experience.
Dr. Wishall reported having no financial conflicts related to her study, which was conducted free of commercial support.
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: Gynecologic oncologists achieved better robotic hysterectomy outcomes than gynecologists despite challenging referrals.
Major finding: The combined intraoperative and postoperative complication rate for robotic hysterectomies performed by gynecologic oncologists was 5.2%, compared with 16% for gynecologists.
Data source: A retrospective observational study conducted at a single center included 254 women whose robotic hysterectomies were performed by gynecologists and 214 done by gynecologic oncologists.
Disclosures: Dr. Wishall reported having no financial conflicts related to the study, which was conducted free of commercial support.
Few locally advanced cervical cancer patients get guideline-directed therapies
SAN DIEGO – Failure to adhere to category 1 National Comprehensive Cancer Network guidelines for the management of locally advanced stage IIB-IVA cervical cancer is rampant – and it’s associated with significantly reduced survival, Dr. Jennifer L. Brown reported at the annual meeting of the Society of Gynecologic Oncology.
“Our study demonstrates opportunities to improve quality of care for women with locally advanced cervical cancer,” said Dr. Brown, a gynecologic oncologist at Fox Chase Cancer Center in Philadelphia.
She and her coinvestigators analyzed the American College of Surgeons/American Cancer Society National Cancer Data Base registry for 2002-2012 and identified 24,952 women treated for stage IIB-IVA cervical cancer. The investigators’ interest was in examining patterns of adherence to category 1 National Comprehensive Cancer Network (NCCN) guidelines in this population, and how adherence rates changed during the decade-long study period.
The key category 1 guidelines recommend concurrent radiation and cisplatin-based chemotherapy followed by brachytherapy for the primary treatment of locally advanced cervical cancer. Moreover, prior to initiating this therapy, pelvic and para-aortic lymph node involvement should be assessed with imaging or surgical staging in order to guide the appropriate radiotherapy dose.
Overall, according to Dr. Brown, only 5,935 women (23.8%) were treated in accordance with the NCCN guidelines recommending concurrent radiation and cisplatin-based chemotherapy followed by brachytherapy. Their median survival was 99.8 months, compared with 52.5 months for patients who didn’t receive category 1 treatment.
Similarly, a mere 23.5% of patients with locally advanced cervical cancer underwent pretreatment lymph node assessment. Those who did had a huge advantage in subsequent median survival: 123.2 months, compared with 48.6 months in those who didn’t undergo pretreatment lymph node staging, she continued.
Also, survival was significantly better among patients whose primary therapy was completed in 8 weeks or less: a median survival of 115.4 versus 82.3 months.
Nonadherence to the category 1 guidelines was disturbingly more common for African Americans, Hispanics, women over age 70, and those who were low income or had a low education level.
Compliance with the NCCN treatment guidelines improved over the study period, from roughly 19% in 2002 to 26% by 2012. However, adherence to the pretreatment lymph node assessment recommendations actually declined over time.
Dr. Brown found marked regional variation in adherence to the NCCN guidelines. It was greatest in the Rocky Mountain region and lowest in Kentucky, Tennessee, Mississippi, and Alabama.
She reported having no relevant financial conflicts.
SAN DIEGO – Failure to adhere to category 1 National Comprehensive Cancer Network guidelines for the management of locally advanced stage IIB-IVA cervical cancer is rampant – and it’s associated with significantly reduced survival, Dr. Jennifer L. Brown reported at the annual meeting of the Society of Gynecologic Oncology.
“Our study demonstrates opportunities to improve quality of care for women with locally advanced cervical cancer,” said Dr. Brown, a gynecologic oncologist at Fox Chase Cancer Center in Philadelphia.
She and her coinvestigators analyzed the American College of Surgeons/American Cancer Society National Cancer Data Base registry for 2002-2012 and identified 24,952 women treated for stage IIB-IVA cervical cancer. The investigators’ interest was in examining patterns of adherence to category 1 National Comprehensive Cancer Network (NCCN) guidelines in this population, and how adherence rates changed during the decade-long study period.
The key category 1 guidelines recommend concurrent radiation and cisplatin-based chemotherapy followed by brachytherapy for the primary treatment of locally advanced cervical cancer. Moreover, prior to initiating this therapy, pelvic and para-aortic lymph node involvement should be assessed with imaging or surgical staging in order to guide the appropriate radiotherapy dose.
Overall, according to Dr. Brown, only 5,935 women (23.8%) were treated in accordance with the NCCN guidelines recommending concurrent radiation and cisplatin-based chemotherapy followed by brachytherapy. Their median survival was 99.8 months, compared with 52.5 months for patients who didn’t receive category 1 treatment.
Similarly, a mere 23.5% of patients with locally advanced cervical cancer underwent pretreatment lymph node assessment. Those who did had a huge advantage in subsequent median survival: 123.2 months, compared with 48.6 months in those who didn’t undergo pretreatment lymph node staging, she continued.
Also, survival was significantly better among patients whose primary therapy was completed in 8 weeks or less: a median survival of 115.4 versus 82.3 months.
Nonadherence to the category 1 guidelines was disturbingly more common for African Americans, Hispanics, women over age 70, and those who were low income or had a low education level.
Compliance with the NCCN treatment guidelines improved over the study period, from roughly 19% in 2002 to 26% by 2012. However, adherence to the pretreatment lymph node assessment recommendations actually declined over time.
Dr. Brown found marked regional variation in adherence to the NCCN guidelines. It was greatest in the Rocky Mountain region and lowest in Kentucky, Tennessee, Mississippi, and Alabama.
She reported having no relevant financial conflicts.
SAN DIEGO – Failure to adhere to category 1 National Comprehensive Cancer Network guidelines for the management of locally advanced stage IIB-IVA cervical cancer is rampant – and it’s associated with significantly reduced survival, Dr. Jennifer L. Brown reported at the annual meeting of the Society of Gynecologic Oncology.
“Our study demonstrates opportunities to improve quality of care for women with locally advanced cervical cancer,” said Dr. Brown, a gynecologic oncologist at Fox Chase Cancer Center in Philadelphia.
She and her coinvestigators analyzed the American College of Surgeons/American Cancer Society National Cancer Data Base registry for 2002-2012 and identified 24,952 women treated for stage IIB-IVA cervical cancer. The investigators’ interest was in examining patterns of adherence to category 1 National Comprehensive Cancer Network (NCCN) guidelines in this population, and how adherence rates changed during the decade-long study period.
The key category 1 guidelines recommend concurrent radiation and cisplatin-based chemotherapy followed by brachytherapy for the primary treatment of locally advanced cervical cancer. Moreover, prior to initiating this therapy, pelvic and para-aortic lymph node involvement should be assessed with imaging or surgical staging in order to guide the appropriate radiotherapy dose.
Overall, according to Dr. Brown, only 5,935 women (23.8%) were treated in accordance with the NCCN guidelines recommending concurrent radiation and cisplatin-based chemotherapy followed by brachytherapy. Their median survival was 99.8 months, compared with 52.5 months for patients who didn’t receive category 1 treatment.
Similarly, a mere 23.5% of patients with locally advanced cervical cancer underwent pretreatment lymph node assessment. Those who did had a huge advantage in subsequent median survival: 123.2 months, compared with 48.6 months in those who didn’t undergo pretreatment lymph node staging, she continued.
Also, survival was significantly better among patients whose primary therapy was completed in 8 weeks or less: a median survival of 115.4 versus 82.3 months.
Nonadherence to the category 1 guidelines was disturbingly more common for African Americans, Hispanics, women over age 70, and those who were low income or had a low education level.
Compliance with the NCCN treatment guidelines improved over the study period, from roughly 19% in 2002 to 26% by 2012. However, adherence to the pretreatment lymph node assessment recommendations actually declined over time.
Dr. Brown found marked regional variation in adherence to the NCCN guidelines. It was greatest in the Rocky Mountain region and lowest in Kentucky, Tennessee, Mississippi, and Alabama.
She reported having no relevant financial conflicts.
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: Only about one in four women with locally advanced cervical cancer receive guideline-recommended treatment.
Major finding: Median survival was 99.8 months among the 23.8% of women whose locally advanced cervical cancer was treated in accord with category 1 NCCN guidelines, compared with 52.5 months when it was not.
Data source: A retrospective study of the National Cancer Data Base including nearly 25,000 women treated for stage IIB-IVA cervical cancer.
Disclosures: The presenter reported having no relevant financial conflicts.
Primary care residents’ approaches to HPV vaccine vary by specialty
SAN DIEGO – Among U.S. resident trainees in the primary care specialties, ob.gyn. and internal medicine resident physicians are the clear laggards when it comes to counseling appropriate candidates to receive the human papillomavirus (HPV) vaccine, Dr. Tiffany Zigras reported at the annual meeting of the Society of Gynecologic Oncology.
Pediatric residents led the way in self-reported “always” counseling eligible patients to receive the three-dose HPV vaccine series in her national survey, with family medicine residents in firm command of second place.
Although the HPV vaccine was approved by the Food and Drug Administration in 2006, uptake remains low. A 2014 report based upon National Health Interview Survey data concluded only 13.6% of U.S. women ages 18-26 had received all three doses of the vaccine. A national Status of Cancer report concluded that only 32% of females ages 13-17 years had been vaccinated; in the uninsured population this rate fell to a mere 14.1% (Am J Public Health. 2014 May;104(5):946-53), noted Dr. Zigras of Bridgeport (Conn.) Hospital/Yale New Haven Health.
Since physician recommendation is known to play a key role in vaccine uptake and the approach taken by primary care residents hadn’t previously been studied, Dr. Zigras and her coinvestigators created a 37-item electronic survey and sent it to residency program directors in the various primary care disciplines with a request that they share the web link with their trainees.
The survey was completed by 1,549 resident physicians. Fully 82% of the pediatric residents indicated that they “always” recommend the HPV vaccine as an important means of cancer prevention. So did 64% of family medicine residents, 39% of ob.gyn. residents, and 28% of internal medicine residents.
Overall, female primary care residents were three times more likely than their male counterparts to always recommend the HPV vaccine to their eligible patients.
Primary care residents cited parental disapproval as a major reason for vaccine refusal in 49% of cases, fear of vaccines in general as an insurmountable issue in 34%, and fear of needles as a significant factor in 14%.
Whether or not respondent residents had received education about the vaccine during medical school had no bearing on their current self-described rate of HPV vaccine recommendation. However, residents who reported receiving education about the risks, benefits, and value of the vaccine during their residency training were significantly more likely to always recommend it for eligible patients.
“Residents have a unique opportunity to capture a subset of patients who may otherwise not have an opportunity to receive the HPV vaccine,” Dr. Zigras observed. “Education about the HPV vaccine in resident curriculum is critical to improve the uptake of the HPV vaccine in the United States.”
She reported no financial conflicts with regard to her study.
SAN DIEGO – Among U.S. resident trainees in the primary care specialties, ob.gyn. and internal medicine resident physicians are the clear laggards when it comes to counseling appropriate candidates to receive the human papillomavirus (HPV) vaccine, Dr. Tiffany Zigras reported at the annual meeting of the Society of Gynecologic Oncology.
Pediatric residents led the way in self-reported “always” counseling eligible patients to receive the three-dose HPV vaccine series in her national survey, with family medicine residents in firm command of second place.
Although the HPV vaccine was approved by the Food and Drug Administration in 2006, uptake remains low. A 2014 report based upon National Health Interview Survey data concluded only 13.6% of U.S. women ages 18-26 had received all three doses of the vaccine. A national Status of Cancer report concluded that only 32% of females ages 13-17 years had been vaccinated; in the uninsured population this rate fell to a mere 14.1% (Am J Public Health. 2014 May;104(5):946-53), noted Dr. Zigras of Bridgeport (Conn.) Hospital/Yale New Haven Health.
Since physician recommendation is known to play a key role in vaccine uptake and the approach taken by primary care residents hadn’t previously been studied, Dr. Zigras and her coinvestigators created a 37-item electronic survey and sent it to residency program directors in the various primary care disciplines with a request that they share the web link with their trainees.
The survey was completed by 1,549 resident physicians. Fully 82% of the pediatric residents indicated that they “always” recommend the HPV vaccine as an important means of cancer prevention. So did 64% of family medicine residents, 39% of ob.gyn. residents, and 28% of internal medicine residents.
Overall, female primary care residents were three times more likely than their male counterparts to always recommend the HPV vaccine to their eligible patients.
Primary care residents cited parental disapproval as a major reason for vaccine refusal in 49% of cases, fear of vaccines in general as an insurmountable issue in 34%, and fear of needles as a significant factor in 14%.
Whether or not respondent residents had received education about the vaccine during medical school had no bearing on their current self-described rate of HPV vaccine recommendation. However, residents who reported receiving education about the risks, benefits, and value of the vaccine during their residency training were significantly more likely to always recommend it for eligible patients.
“Residents have a unique opportunity to capture a subset of patients who may otherwise not have an opportunity to receive the HPV vaccine,” Dr. Zigras observed. “Education about the HPV vaccine in resident curriculum is critical to improve the uptake of the HPV vaccine in the United States.”
She reported no financial conflicts with regard to her study.
SAN DIEGO – Among U.S. resident trainees in the primary care specialties, ob.gyn. and internal medicine resident physicians are the clear laggards when it comes to counseling appropriate candidates to receive the human papillomavirus (HPV) vaccine, Dr. Tiffany Zigras reported at the annual meeting of the Society of Gynecologic Oncology.
Pediatric residents led the way in self-reported “always” counseling eligible patients to receive the three-dose HPV vaccine series in her national survey, with family medicine residents in firm command of second place.
Although the HPV vaccine was approved by the Food and Drug Administration in 2006, uptake remains low. A 2014 report based upon National Health Interview Survey data concluded only 13.6% of U.S. women ages 18-26 had received all three doses of the vaccine. A national Status of Cancer report concluded that only 32% of females ages 13-17 years had been vaccinated; in the uninsured population this rate fell to a mere 14.1% (Am J Public Health. 2014 May;104(5):946-53), noted Dr. Zigras of Bridgeport (Conn.) Hospital/Yale New Haven Health.
Since physician recommendation is known to play a key role in vaccine uptake and the approach taken by primary care residents hadn’t previously been studied, Dr. Zigras and her coinvestigators created a 37-item electronic survey and sent it to residency program directors in the various primary care disciplines with a request that they share the web link with their trainees.
The survey was completed by 1,549 resident physicians. Fully 82% of the pediatric residents indicated that they “always” recommend the HPV vaccine as an important means of cancer prevention. So did 64% of family medicine residents, 39% of ob.gyn. residents, and 28% of internal medicine residents.
Overall, female primary care residents were three times more likely than their male counterparts to always recommend the HPV vaccine to their eligible patients.
Primary care residents cited parental disapproval as a major reason for vaccine refusal in 49% of cases, fear of vaccines in general as an insurmountable issue in 34%, and fear of needles as a significant factor in 14%.
Whether or not respondent residents had received education about the vaccine during medical school had no bearing on their current self-described rate of HPV vaccine recommendation. However, residents who reported receiving education about the risks, benefits, and value of the vaccine during their residency training were significantly more likely to always recommend it for eligible patients.
“Residents have a unique opportunity to capture a subset of patients who may otherwise not have an opportunity to receive the HPV vaccine,” Dr. Zigras observed. “Education about the HPV vaccine in resident curriculum is critical to improve the uptake of the HPV vaccine in the United States.”
She reported no financial conflicts with regard to her study.
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Primary care residents’ approach to HPV vaccine vary by specialty
SAN DIEGO – Among U.S. resident trainees in the primary care specialties, ob.gyn. and internal medicine resident physicians are the clear laggards when it comes to counseling appropriate candidates to receive the human papillomavirus (HPV) vaccine, Dr. Tiffany Zigras reported at the annual meeting of the Society of Gynecologic Oncology.
Pediatric residents led the way in self-reported “always” counseling eligible patients to receive the three-dose HPV vaccine series in her national survey, with family medicine residents in firm command of second place.
Although the HPV vaccine was approved by the Food and Drug Administration in 2006, uptake remains low. A 2014 report based upon National Health Interview Survey data concluded only 13.6% of U.S. women ages 18-26 had received all three doses of the vaccine. A national Status of Cancer report concluded that only 32% of females ages 13-17 years had been vaccinated; in the uninsured population this rate fell to a mere 14.1% (Am J Public Health. 2014 May;104(5):946-53), noted Dr. Zigras of Bridgeport (Conn.) Hospital/Yale New Haven Health.
Since physician recommendation is known to play a key role in vaccine uptake and the approach taken by primary care residents hadn’t previously been studied, Dr. Zigras and her coinvestigators created a 37-item electronic survey and sent it to residency program directors in the various primary care disciplines with a request that they share the web link with their trainees.
The survey was completed by 1,549 resident physicians. Fully 82% of the pediatric residents indicated that they “always” recommend the HPV vaccine as an important means of cancer prevention. So did 64% of family medicine residents, 39% of ob.gyn. residents, and 28% of internal medicine residents.
Overall, female primary care residents were three times more likely than their male counterparts to always recommend the HPV vaccine to their eligible patients.
Primary care residents cited parental disapproval as a major reason for vaccine refusal in 49% of cases, fear of vaccines in general as an insurmountable issue in 34%, and fear of needles as a significant factor in 14%.
Whether or not respondent residents had received education about the vaccine during medical school had no bearing on their current self-described rate of HPV vaccine recommendation. However, residents who reported receiving education about the risks, benefits, and value of the vaccine during their residency training were significantly more likely to always recommend it for eligible patients.
“Residents have a unique opportunity to capture a subset of patients who may otherwise not have an opportunity to receive the HPV vaccine,” Dr. Zigras observed. “Education about the HPV vaccine in resident curriculum is critical to improve the uptake of the HPV vaccine in the United States.”
She reported no financial conflicts with regard to her study.
SAN DIEGO – Among U.S. resident trainees in the primary care specialties, ob.gyn. and internal medicine resident physicians are the clear laggards when it comes to counseling appropriate candidates to receive the human papillomavirus (HPV) vaccine, Dr. Tiffany Zigras reported at the annual meeting of the Society of Gynecologic Oncology.
Pediatric residents led the way in self-reported “always” counseling eligible patients to receive the three-dose HPV vaccine series in her national survey, with family medicine residents in firm command of second place.
Although the HPV vaccine was approved by the Food and Drug Administration in 2006, uptake remains low. A 2014 report based upon National Health Interview Survey data concluded only 13.6% of U.S. women ages 18-26 had received all three doses of the vaccine. A national Status of Cancer report concluded that only 32% of females ages 13-17 years had been vaccinated; in the uninsured population this rate fell to a mere 14.1% (Am J Public Health. 2014 May;104(5):946-53), noted Dr. Zigras of Bridgeport (Conn.) Hospital/Yale New Haven Health.
Since physician recommendation is known to play a key role in vaccine uptake and the approach taken by primary care residents hadn’t previously been studied, Dr. Zigras and her coinvestigators created a 37-item electronic survey and sent it to residency program directors in the various primary care disciplines with a request that they share the web link with their trainees.
The survey was completed by 1,549 resident physicians. Fully 82% of the pediatric residents indicated that they “always” recommend the HPV vaccine as an important means of cancer prevention. So did 64% of family medicine residents, 39% of ob.gyn. residents, and 28% of internal medicine residents.
Overall, female primary care residents were three times more likely than their male counterparts to always recommend the HPV vaccine to their eligible patients.
Primary care residents cited parental disapproval as a major reason for vaccine refusal in 49% of cases, fear of vaccines in general as an insurmountable issue in 34%, and fear of needles as a significant factor in 14%.
Whether or not respondent residents had received education about the vaccine during medical school had no bearing on their current self-described rate of HPV vaccine recommendation. However, residents who reported receiving education about the risks, benefits, and value of the vaccine during their residency training were significantly more likely to always recommend it for eligible patients.
“Residents have a unique opportunity to capture a subset of patients who may otherwise not have an opportunity to receive the HPV vaccine,” Dr. Zigras observed. “Education about the HPV vaccine in resident curriculum is critical to improve the uptake of the HPV vaccine in the United States.”
She reported no financial conflicts with regard to her study.
SAN DIEGO – Among U.S. resident trainees in the primary care specialties, ob.gyn. and internal medicine resident physicians are the clear laggards when it comes to counseling appropriate candidates to receive the human papillomavirus (HPV) vaccine, Dr. Tiffany Zigras reported at the annual meeting of the Society of Gynecologic Oncology.
Pediatric residents led the way in self-reported “always” counseling eligible patients to receive the three-dose HPV vaccine series in her national survey, with family medicine residents in firm command of second place.
Although the HPV vaccine was approved by the Food and Drug Administration in 2006, uptake remains low. A 2014 report based upon National Health Interview Survey data concluded only 13.6% of U.S. women ages 18-26 had received all three doses of the vaccine. A national Status of Cancer report concluded that only 32% of females ages 13-17 years had been vaccinated; in the uninsured population this rate fell to a mere 14.1% (Am J Public Health. 2014 May;104(5):946-53), noted Dr. Zigras of Bridgeport (Conn.) Hospital/Yale New Haven Health.
Since physician recommendation is known to play a key role in vaccine uptake and the approach taken by primary care residents hadn’t previously been studied, Dr. Zigras and her coinvestigators created a 37-item electronic survey and sent it to residency program directors in the various primary care disciplines with a request that they share the web link with their trainees.
The survey was completed by 1,549 resident physicians. Fully 82% of the pediatric residents indicated that they “always” recommend the HPV vaccine as an important means of cancer prevention. So did 64% of family medicine residents, 39% of ob.gyn. residents, and 28% of internal medicine residents.
Overall, female primary care residents were three times more likely than their male counterparts to always recommend the HPV vaccine to their eligible patients.
Primary care residents cited parental disapproval as a major reason for vaccine refusal in 49% of cases, fear of vaccines in general as an insurmountable issue in 34%, and fear of needles as a significant factor in 14%.
Whether or not respondent residents had received education about the vaccine during medical school had no bearing on their current self-described rate of HPV vaccine recommendation. However, residents who reported receiving education about the risks, benefits, and value of the vaccine during their residency training were significantly more likely to always recommend it for eligible patients.
“Residents have a unique opportunity to capture a subset of patients who may otherwise not have an opportunity to receive the HPV vaccine,” Dr. Zigras observed. “Education about the HPV vaccine in resident curriculum is critical to improve the uptake of the HPV vaccine in the United States.”
She reported no financial conflicts with regard to her study.
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: Nationally, pediatric and family medicine residents are tops among primary care trainees in terms of consistently recommending the HPV vaccine for eligible patients.
Major finding: Of pediatric residents, 82% report “always” recommending the HPV vaccine to appropriate candidates, compared with just 28% of internal medicine residents.
Data source: This 37-item electronic survey was completed by nearly 1,600 U.S. primary care resident physicians.
Disclosures: The study presenter reported having no financial conflicts of interest.
Bone Marrow Transplant Cures Severe HPV Disease in GATA2 Immunodeficiency
SAN DIEGO – When genital warts return again and again in women no matter what’s tried, it’s time to think of GATA2 immunodeficiency, according to investigators from the National Institutes of Health, in Bethesda, Md.
A bone marrow transplant may prove curative, ending the cycle of vulvectomies and other surgeries, they said at the annual meeting of the Society of Gynecologic Oncology.
Surgery, at least before transplant, isn’t the answer because “the lesions are going to come right back.” When HPV is severe and persistent, “consider referral to an infectious disease immunologist who can work women up for GATA2 mutations, or you can just contact the NIH. Bone marrow transplantation is the only known curative treatment for HPV disease in GATA2 deficiency,” said lead investigator Ehren Dancy, a medical student in the Medical Research Scholars Program at the NIH.GATA2 [GATA binding protein 2] is a transcription factor key to the development and maintenance of hematopoiesis. Mutations in the GATA2 gene lead to a primary immunodeficiency marked by progressive monocytopenia, and B-cell and natural killer cell lymphopenia. Since 2011, GATA2 mutations have been linked to an ever increasing range of serious medical problems, including severe, persistent, and multifocal human papillomavirus (HPV) infections in women.
While 70% of healthy women clear HPV in 1 year, and more than 90% in 2 years, that wasn’t the case with the 35 women with GATA2 mutations at NIH. Twenty-seven (77%) reported abnormal Pap smears and/or genital and perigenital warts, generally diagnosed in the early to mid-20s. Twenty-one (78%) cases recurred despite treatment. About half the women had five or more surgeries, including cone biopsy, laser ablation, and vulvectomy. Seven women were diagnosed with HPV genital cancer before the age of 41; one has died.
Ten women have had bone marrow transplants, with a median follow-up of 16 months. HPV resolved in four and significantly improved in six. None of the patients in the review “demonstrated long-term HPV treatment response without bone marrow transplantation,” the investigators said.
Natural killer and monocyte cell counts were far below normal at the time of transplant.
SAN DIEGO – When genital warts return again and again in women no matter what’s tried, it’s time to think of GATA2 immunodeficiency, according to investigators from the National Institutes of Health, in Bethesda, Md.
A bone marrow transplant may prove curative, ending the cycle of vulvectomies and other surgeries, they said at the annual meeting of the Society of Gynecologic Oncology.
Surgery, at least before transplant, isn’t the answer because “the lesions are going to come right back.” When HPV is severe and persistent, “consider referral to an infectious disease immunologist who can work women up for GATA2 mutations, or you can just contact the NIH. Bone marrow transplantation is the only known curative treatment for HPV disease in GATA2 deficiency,” said lead investigator Ehren Dancy, a medical student in the Medical Research Scholars Program at the NIH.GATA2 [GATA binding protein 2] is a transcription factor key to the development and maintenance of hematopoiesis. Mutations in the GATA2 gene lead to a primary immunodeficiency marked by progressive monocytopenia, and B-cell and natural killer cell lymphopenia. Since 2011, GATA2 mutations have been linked to an ever increasing range of serious medical problems, including severe, persistent, and multifocal human papillomavirus (HPV) infections in women.
While 70% of healthy women clear HPV in 1 year, and more than 90% in 2 years, that wasn’t the case with the 35 women with GATA2 mutations at NIH. Twenty-seven (77%) reported abnormal Pap smears and/or genital and perigenital warts, generally diagnosed in the early to mid-20s. Twenty-one (78%) cases recurred despite treatment. About half the women had five or more surgeries, including cone biopsy, laser ablation, and vulvectomy. Seven women were diagnosed with HPV genital cancer before the age of 41; one has died.
Ten women have had bone marrow transplants, with a median follow-up of 16 months. HPV resolved in four and significantly improved in six. None of the patients in the review “demonstrated long-term HPV treatment response without bone marrow transplantation,” the investigators said.
Natural killer and monocyte cell counts were far below normal at the time of transplant.
SAN DIEGO – When genital warts return again and again in women no matter what’s tried, it’s time to think of GATA2 immunodeficiency, according to investigators from the National Institutes of Health, in Bethesda, Md.
A bone marrow transplant may prove curative, ending the cycle of vulvectomies and other surgeries, they said at the annual meeting of the Society of Gynecologic Oncology.
Surgery, at least before transplant, isn’t the answer because “the lesions are going to come right back.” When HPV is severe and persistent, “consider referral to an infectious disease immunologist who can work women up for GATA2 mutations, or you can just contact the NIH. Bone marrow transplantation is the only known curative treatment for HPV disease in GATA2 deficiency,” said lead investigator Ehren Dancy, a medical student in the Medical Research Scholars Program at the NIH.GATA2 [GATA binding protein 2] is a transcription factor key to the development and maintenance of hematopoiesis. Mutations in the GATA2 gene lead to a primary immunodeficiency marked by progressive monocytopenia, and B-cell and natural killer cell lymphopenia. Since 2011, GATA2 mutations have been linked to an ever increasing range of serious medical problems, including severe, persistent, and multifocal human papillomavirus (HPV) infections in women.
While 70% of healthy women clear HPV in 1 year, and more than 90% in 2 years, that wasn’t the case with the 35 women with GATA2 mutations at NIH. Twenty-seven (77%) reported abnormal Pap smears and/or genital and perigenital warts, generally diagnosed in the early to mid-20s. Twenty-one (78%) cases recurred despite treatment. About half the women had five or more surgeries, including cone biopsy, laser ablation, and vulvectomy. Seven women were diagnosed with HPV genital cancer before the age of 41; one has died.
Ten women have had bone marrow transplants, with a median follow-up of 16 months. HPV resolved in four and significantly improved in six. None of the patients in the review “demonstrated long-term HPV treatment response without bone marrow transplantation,” the investigators said.
Natural killer and monocyte cell counts were far below normal at the time of transplant.
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Bone marrow transplant cures severe HPV disease in GATA2 immunodeficiency
SAN DIEGO – When genital warts return again and again in women no matter what’s tried, it’s time to think of GATA2 immunodeficiency, according to investigators from the National Institutes of Health, in Bethesda, Md.
A bone marrow transplant may prove curative, ending the cycle of vulvectomies and other surgeries, they said at the annual meeting of the Society of Gynecologic Oncology.
Surgery, at least before transplant, isn’t the answer because “the lesions are going to come right back.” When HPV is severe and persistent, “consider referral to an infectious disease immunologist who can work women up for GATA2 mutations, or you can just contact the NIH. Bone marrow transplantation is the only known curative treatment for HPV disease in GATA2 deficiency,” said lead investigator Ehren Dancy, a medical student in the Medical Research Scholars Program at the NIH.GATA2 [GATA binding protein 2] is a transcription factor key to the development and maintenance of hematopoiesis. Mutations in the GATA2 gene lead to a primary immunodeficiency marked by progressive monocytopenia, and B-cell and natural killer cell lymphopenia. Since 2011, GATA2 mutations have been linked to an ever increasing range of serious medical problems, including severe, persistent, and multifocal human papillomavirus (HPV) infections in women.
While 70% of healthy women clear HPV in 1 year, and more than 90% in 2 years, that wasn’t the case with the 35 women with GATA2 mutations at NIH. Twenty-seven (77%) reported abnormal Pap smears and/or genital and perigenital warts, generally diagnosed in the early to mid-20s. Twenty-one (78%) cases recurred despite treatment. About half the women had five or more surgeries, including cone biopsy, laser ablation, and vulvectomy. Seven women were diagnosed with HPV genital cancer before the age of 41; one has died.
Ten women have had bone marrow transplants, with a median follow-up of 16 months. HPV resolved in four and significantly improved in six. None of the patients in the review “demonstrated long-term HPV treatment response without bone marrow transplantation,” the investigators said.
Natural killer and monocyte cell counts were far below normal at the time of transplant.
SAN DIEGO – When genital warts return again and again in women no matter what’s tried, it’s time to think of GATA2 immunodeficiency, according to investigators from the National Institutes of Health, in Bethesda, Md.
A bone marrow transplant may prove curative, ending the cycle of vulvectomies and other surgeries, they said at the annual meeting of the Society of Gynecologic Oncology.
Surgery, at least before transplant, isn’t the answer because “the lesions are going to come right back.” When HPV is severe and persistent, “consider referral to an infectious disease immunologist who can work women up for GATA2 mutations, or you can just contact the NIH. Bone marrow transplantation is the only known curative treatment for HPV disease in GATA2 deficiency,” said lead investigator Ehren Dancy, a medical student in the Medical Research Scholars Program at the NIH.GATA2 [GATA binding protein 2] is a transcription factor key to the development and maintenance of hematopoiesis. Mutations in the GATA2 gene lead to a primary immunodeficiency marked by progressive monocytopenia, and B-cell and natural killer cell lymphopenia. Since 2011, GATA2 mutations have been linked to an ever increasing range of serious medical problems, including severe, persistent, and multifocal human papillomavirus (HPV) infections in women.
While 70% of healthy women clear HPV in 1 year, and more than 90% in 2 years, that wasn’t the case with the 35 women with GATA2 mutations at NIH. Twenty-seven (77%) reported abnormal Pap smears and/or genital and perigenital warts, generally diagnosed in the early to mid-20s. Twenty-one (78%) cases recurred despite treatment. About half the women had five or more surgeries, including cone biopsy, laser ablation, and vulvectomy. Seven women were diagnosed with HPV genital cancer before the age of 41; one has died.
Ten women have had bone marrow transplants, with a median follow-up of 16 months. HPV resolved in four and significantly improved in six. None of the patients in the review “demonstrated long-term HPV treatment response without bone marrow transplantation,” the investigators said.
Natural killer and monocyte cell counts were far below normal at the time of transplant.
SAN DIEGO – When genital warts return again and again in women no matter what’s tried, it’s time to think of GATA2 immunodeficiency, according to investigators from the National Institutes of Health, in Bethesda, Md.
A bone marrow transplant may prove curative, ending the cycle of vulvectomies and other surgeries, they said at the annual meeting of the Society of Gynecologic Oncology.
Surgery, at least before transplant, isn’t the answer because “the lesions are going to come right back.” When HPV is severe and persistent, “consider referral to an infectious disease immunologist who can work women up for GATA2 mutations, or you can just contact the NIH. Bone marrow transplantation is the only known curative treatment for HPV disease in GATA2 deficiency,” said lead investigator Ehren Dancy, a medical student in the Medical Research Scholars Program at the NIH.GATA2 [GATA binding protein 2] is a transcription factor key to the development and maintenance of hematopoiesis. Mutations in the GATA2 gene lead to a primary immunodeficiency marked by progressive monocytopenia, and B-cell and natural killer cell lymphopenia. Since 2011, GATA2 mutations have been linked to an ever increasing range of serious medical problems, including severe, persistent, and multifocal human papillomavirus (HPV) infections in women.
While 70% of healthy women clear HPV in 1 year, and more than 90% in 2 years, that wasn’t the case with the 35 women with GATA2 mutations at NIH. Twenty-seven (77%) reported abnormal Pap smears and/or genital and perigenital warts, generally diagnosed in the early to mid-20s. Twenty-one (78%) cases recurred despite treatment. About half the women had five or more surgeries, including cone biopsy, laser ablation, and vulvectomy. Seven women were diagnosed with HPV genital cancer before the age of 41; one has died.
Ten women have had bone marrow transplants, with a median follow-up of 16 months. HPV resolved in four and significantly improved in six. None of the patients in the review “demonstrated long-term HPV treatment response without bone marrow transplantation,” the investigators said.
Natural killer and monocyte cell counts were far below normal at the time of transplant.
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: Refer women with severe, refractory HPV disease for genetic work-up and possible bone marrow transplant.
Major finding: Twenty-seven (77%) of GATA2 deficient women reported abnormal Pap smears and/or genital and perigenital warts, generally diagnosed in the early to mid-20s.
Data source: Review of 35 women with GATA2 mutations.
Disclosures: There was no outside funding for the work. The presenter had no disclosures.