User login
European cholesterol guidelines push LDL targets below 55 mg/dL
PARIS – The 2019 dyslipidemia management guidelines from the European Society of Cardiology set an LDL cholesterol target for very-high-risk people of less than 55 mg/dL (as well as at least a 50% cut from baseline), a class I recommendation. This marks the first time a cardiology society has either recommended a target goal for this measure below 70 mg/dL or endorsed treating patients to still-lower cholesterol once their level was already under 70 mg/dL.*
The guidelines went further by suggesting consideration of an even lower treatment target for LDL-cholesterol in very-high-risk, secondary prevention patients who have already had at least two atherosclerotic cardiovascular disease events during the past 2 years, a setting that could justify an LDL-cholesterol goal of less than 40 mg/dL (along with a cut from baseline of at least 50%), a class IIb recommendation that denotes a “may be considered,” endorsement.
“In all the trials, lower was better. There was no lower level of LDL cholesterol that’s been studied that was not better” for patient outcomes, Colin Baigent, BMBCH, said while presenting the new guideline at the annual congress of the European Society of Cardiology (ESC). “It’s very clear” that the full treatment benefit from lowering LDL-cholesterol extends to getting very-high risk patients below these levels, said Dr. Baigent, professor of cardiology at Oxford (England) University and one of three chairs of the ESC’s dyslipidemia guideline-writing panel.
While this change was seen as a notably aggressive goal and too fixed on a specific number by at least one author of the 2018 American Heart Association/American College of Cardiology cholesterol management guideline (J Am Coll Cardiol. 2019 Jun;73[24]:e285-e350), it was embraced by another U.S. expert not involved in writing the most recent U.S. recommendations.
“A goal for LDL-cholesterol of less than 55 mg/dL is reasonable; it’s well documented” by trial evidence “and I support it,” said Robert H. Eckel, MD, an endocrinologist and professor of medicine at the University of Colorado in Aurora. Dr. Eckel added that he “also supports” an LDL-cholesterol of less than 40 mg/dL in very-high-risk patients with a history of multiple events or with multiple residual risk factors, and he said he has applied this lower LDL-cholesterol goal in his practice for selected patients. But Dr. Eckel acknowledged in an interview that the evidence for it was less clear-cut than was the evidence behind a goal of less than 55 mg/dL. He also supported the concept of including a treatment goal in U.S. lipid recommendations, which in recent versions has been missing. “I fall back on a cholesterol goal for practical purposes” of making the success of cholesterol-lowering treatment easier to track.
The new ESC goal was characterized as “arbitrary” by Neil J. Stone, MD, vice-chair of the panel that wrote the 2018 AHA/ACC guideline, which relied on treating secondary-prevention patients at high risk to an LDL-cholesterol at least 50% less than before treatment, and recommended continued intensification for patients whose LDL-cholesterol level remained at or above 70 mg/dL.
“If the patient is at 58 mg/dL I’m not sure anyone can tell me what the difference is,” compared with reaching less than 55 mg/dL, Dr. Stone said in an interview. “I worry about focusing on a number and not on the concept that people at the very highest risk deserve the most intensive treatment; the Europeans agree, but they have a different way of looking at it. Despite this difference in approach, the new ESC guidelines and the 2018 U.S. guideline “are more similar than different,” stressed Dr. Stone, professor of medicine and preventive medicine at Northwestern University, Chicago.
However, other experts see an important difference in the risk faced by patients who reach the ESC’s recommended treatment goals and those who fall just short.
“It’s hard to lower an LDL-cholesterol that is already relatively low. People who are close to their cholesterol target need the most intensified treatment” to reach their goal, said Rory Collins, F.Med.Sci., professor of epidemiology at Oxford University. He was not on the ESC guidelines panel.
“It’s a mind shift that clinicians need to be most aggressive in treating patients with the highest risk” even when their LDL-cholesterol is low but not yet at the target level, Dr. Collins said during a discussion session at the congress.
The new ESC guidelines is about “both getting the LDL-cholesterol down to a certain level and also about achieving a big [at least 50%] change” from baseline. “I think the ESC guidelines make that crystal clear,” said Marc S. Sabatine, MD, professor of medicine at Harvard Medical School, Boston, and the sole American to participate in the ESC guidelines-writing panel.
The ESC also broke new ground by advocating an aggressive path toward achieving these LDL-cholesterol goals by elevating the newest and most potent class of approved LDL-cholesterol-lowering drugs, the PCSK9 (proprotein convertase subtilisin/kexin type 9) inhibitors, to a top-tier, class I recommendation (“is recommended”) for secondary prevention in very-high-risk patients not reaching their goal LDL-cholesterol level on a maximally tolerated statin plus ezetimibe. This recommendation to unequivocally add a PCSK9 inhibitor for this patient population contrasts with the 2018 AHA/ACC guideline that deemed adding a PCSK9 inhibitor a IIa recommendation (“is reasonable”).
A similar uptick in treatment aggressiveness appeared in the ESC’s recommendations for managing very-high-risk patients in a primary prevention setting, including those without familial hypercholesterolemia. For these people, the ESC panel, which worked in concert with the European Atherosclerosis Society, pegged adding a PCSK9 inhibitor as a IIb (“may be considered”) recommendation when these very-high-risk people fail to reach their LDL-cholesterol target on a maximally tolerated statin and ezetimibe. Once again, this opening to use a PCSK9 inhibitor contrasted with the 2018 U.S. guideline, which never mentioned an option of adding a PCSK9 inhibitor for primary prevention except when someone also has familial hypercholesterolemia and starts treatment with an LDL level of at least 190 mg/dL (a IIb recommendation). The new European guidelines proposed using a PCSK9 inhibitor as a second-line option to consider when needed for people whose very high risk derives primarily from older age and other factors such as smoking or hypertension that give them at least a 10% 10-year risk for cardiovascular death as estimated with the European-oriented SCORE risk calculator tables.
Updated SCORE risk designations appear in the new ESC dyslipidemia guidelines, and they show, for example, that in lower-risk European countries (mostly Western European nations) virtually all men who are at least 70 years old would fall into the very-high-risk category that makes them potential candidates for treatment with a PCSK9 inhibitor regardless of any other risk they may or may not have. In higher-risk (mostly Eastern European) countries this designation kicks in for most men once they reach the age of 65.
Several Congress attendees who came to a discussion session on the guidelines voiced concerns that the new revision will lead to substantially increased use of the these drugs and hence will significantly boost medical costs, because these drugs today are priced at about $6,000 annually to treat one patient. In response, members of the guideline-writing panel defended their decision as unavoidable given what’s been reported on the clinical impact of PCSK9 inhibitors when lowering LDL cholesterol and cutting atherosclerotic cardiovascular disease events.
“I commend the [ESC] guideline for focusing on the science and on what is best for patients. The U.S. guidelines conflated the science and the cost, and the recommendations got watered down by cost considerations,” said Dr. Sabatine, who has led several studies of PCSK9 inhibitors.
Dr. Baigent added that the panel “deliberated long and hard on cost, but we felt that we had to focus on the evidence. The cost will shift” in the future, he predicted.
Other U.S. physicians highlighted the need to take drug cost into account when writing public health policy documents such as lipid-management guidelines and questioned whether this more liberal use of PCSK9 inhibitors was justified.
“I think that in the absence of familial hypercholesterolemia you need to waffle around the edges to justify a PCSK9 inhibitor,” said Dr. Eckel. “The cost of PCSK9 inhibitors has come down, but at $6,000 per year you can’t ignore their cost.”
“In the U.S. we need to be mindful of the cost of treatment,” said Dr. Stone. “The ESC guidelines are probably more aggressive” than the 2018 U.S. guideline. “They use PCSK9 inhibitors perhaps more than we do; we [in the United States] prefer generic ezetimibe. A lot has to do with the definitions of risk. The European guidelines have a lot of risk definitions that differ” from the U.S. guideline, he said.
Members of the ESC guidelines panel acknowledged that the SCORE risk-assessment charts could overestimate risk in older people who need primary prevention treatment, as well as underestimate the risk in younger adults.
This inherent age bias in the SCORE risk tables make it “extremely important to contextualize” a person’s risk “by considering other risk factors,” advised Brian A. Ference, MD, an interventional cardiologist and professor at Cambridge (England) University who was a member of the ESC guidelines writing group.
The new ESC guidelines say that risk categorization “must be interpreted in light of the clinician’s knowledge and experience, and of the patient’s pretest likelihood” of cardiovascular disease.”
Dr. Baigent has received research funding from Boehringer Ingelheim, Novartis, and Pfizer. Dr. Eckel has been an expert witness on behalf of Sanofi/Regeneron. Dr. Sabatine and Dr. Ference have received honoraria and research funding from several companies including those that market lipid-lowering drugs. Dr. Stone and Dr. Collins had no disclosures.
*Correction, 9/20/19: A previous version of this article incorrectly stated that the ESC guidelines were the first by a medical society to recommend the lower cholesterol goals. The American Association of Clinical Endocrinologists included targets below 55 mg/dL in their 2017 dyslipidemia management guidelines.
SOURCE: Mach F et al. Eur Heart J. 2019 Aug 31. doi: 10.1093/eurheartj/ehz455.
The new ESC dyslipidemia guidelines recently presented at the society’s annual congress are a welcome addition to the lipid disorder treatment guidelines available to clinicians. These guidelines follow the groundbreaking recommendation in 2017 by AACE in their updated guidelines that introduced an LDL goal of <55 mg/dL in “extreme risk” patients. The ESC guidelines now also recommend an LDL goal of <55 mg/dL in “very-high-risk” patients but go further by also requiring a 50% reduction in LDL. Furthermore, they have established an LDL goal of <40 mg/dL in patients who experienced a second vascular event in the past 2 years while on maximally tolerated statin dose.
The ESC very-high-risk category shares many features with AACE’s extreme-risk category but is broader in that it includes patients without a clinical event who display unequivocal evidence of arteriosclerotic cardiovascular disease (ASCVD) on imaging and patients with severe chronic kidney disease (GFR <30 mL/min ) without known ASCVD. There are substantial differences between the ESC and AHA-ACC 2018 guidelines in the very-high-risk category. The AHA very-high-risk is directed toward secondary prevention only and requires two major ASCVD events or one major and at least two high-risk conditions. Moreover, elements of both major ASCVD events and high-risk conditions as well as the very-high-risk eligibility requirements could mean that some patients, who would clearly be classified by both ESC and AACE as candidates for an LDL goal of <55, may not qualify for threshold consideration for maximal LDL lowering below 70 mg/dL including the use of PCSK9 inhibitors. Relative to this point, the AHA-ACC guidelines do not classify past CABG or PCI as a major ASCVD event, nor is a TIA considered a major event or a high-risk condition.
For LDL, “lower is better” is supported by years of statin clinical trial evidence, along with the robust findings in the 2010 Cholesterol Trialists Collaboration. The goal of <55 mg/dL is supported by the IMPROVE-IT, FOURIER, and ODYSSEY trials. The ESC guidelines appropriately take this body of evidence and applies it to an aggressive treatment platform that, like AACE, sets clinically useful LDL goals for clinicians and patients. It takes early, aggressive LDL-lowering treatment to stay ahead of atherosclerotic plaque development in patients who are at very high or extreme risk. Following AACE’s lead, the ESC guidelines are the newest tool available to clinicians addressing this issue with the promise of further decreasing CVD events and extending lives.
Dr. Jellinger is a member of the editorial advisory board for Clinical Endocrinology News. He is professor of clinical medicine on the voluntary faculty at the University of Miami Miller School of Medicine and a practicing endocrinologist at The Center for Diabetes & Endocrine Care in Hollywood, Fla. He is past president of the American Association of Clinical Endocrinologists and the American College of Endocrinology and was chair of the writing committee for the 2017 AACE-ACE lipid guidelines.
The new ESC dyslipidemia guidelines recently presented at the society’s annual congress are a welcome addition to the lipid disorder treatment guidelines available to clinicians. These guidelines follow the groundbreaking recommendation in 2017 by AACE in their updated guidelines that introduced an LDL goal of <55 mg/dL in “extreme risk” patients. The ESC guidelines now also recommend an LDL goal of <55 mg/dL in “very-high-risk” patients but go further by also requiring a 50% reduction in LDL. Furthermore, they have established an LDL goal of <40 mg/dL in patients who experienced a second vascular event in the past 2 years while on maximally tolerated statin dose.
The ESC very-high-risk category shares many features with AACE’s extreme-risk category but is broader in that it includes patients without a clinical event who display unequivocal evidence of arteriosclerotic cardiovascular disease (ASCVD) on imaging and patients with severe chronic kidney disease (GFR <30 mL/min ) without known ASCVD. There are substantial differences between the ESC and AHA-ACC 2018 guidelines in the very-high-risk category. The AHA very-high-risk is directed toward secondary prevention only and requires two major ASCVD events or one major and at least two high-risk conditions. Moreover, elements of both major ASCVD events and high-risk conditions as well as the very-high-risk eligibility requirements could mean that some patients, who would clearly be classified by both ESC and AACE as candidates for an LDL goal of <55, may not qualify for threshold consideration for maximal LDL lowering below 70 mg/dL including the use of PCSK9 inhibitors. Relative to this point, the AHA-ACC guidelines do not classify past CABG or PCI as a major ASCVD event, nor is a TIA considered a major event or a high-risk condition.
For LDL, “lower is better” is supported by years of statin clinical trial evidence, along with the robust findings in the 2010 Cholesterol Trialists Collaboration. The goal of <55 mg/dL is supported by the IMPROVE-IT, FOURIER, and ODYSSEY trials. The ESC guidelines appropriately take this body of evidence and applies it to an aggressive treatment platform that, like AACE, sets clinically useful LDL goals for clinicians and patients. It takes early, aggressive LDL-lowering treatment to stay ahead of atherosclerotic plaque development in patients who are at very high or extreme risk. Following AACE’s lead, the ESC guidelines are the newest tool available to clinicians addressing this issue with the promise of further decreasing CVD events and extending lives.
Dr. Jellinger is a member of the editorial advisory board for Clinical Endocrinology News. He is professor of clinical medicine on the voluntary faculty at the University of Miami Miller School of Medicine and a practicing endocrinologist at The Center for Diabetes & Endocrine Care in Hollywood, Fla. He is past president of the American Association of Clinical Endocrinologists and the American College of Endocrinology and was chair of the writing committee for the 2017 AACE-ACE lipid guidelines.
The new ESC dyslipidemia guidelines recently presented at the society’s annual congress are a welcome addition to the lipid disorder treatment guidelines available to clinicians. These guidelines follow the groundbreaking recommendation in 2017 by AACE in their updated guidelines that introduced an LDL goal of <55 mg/dL in “extreme risk” patients. The ESC guidelines now also recommend an LDL goal of <55 mg/dL in “very-high-risk” patients but go further by also requiring a 50% reduction in LDL. Furthermore, they have established an LDL goal of <40 mg/dL in patients who experienced a second vascular event in the past 2 years while on maximally tolerated statin dose.
The ESC very-high-risk category shares many features with AACE’s extreme-risk category but is broader in that it includes patients without a clinical event who display unequivocal evidence of arteriosclerotic cardiovascular disease (ASCVD) on imaging and patients with severe chronic kidney disease (GFR <30 mL/min ) without known ASCVD. There are substantial differences between the ESC and AHA-ACC 2018 guidelines in the very-high-risk category. The AHA very-high-risk is directed toward secondary prevention only and requires two major ASCVD events or one major and at least two high-risk conditions. Moreover, elements of both major ASCVD events and high-risk conditions as well as the very-high-risk eligibility requirements could mean that some patients, who would clearly be classified by both ESC and AACE as candidates for an LDL goal of <55, may not qualify for threshold consideration for maximal LDL lowering below 70 mg/dL including the use of PCSK9 inhibitors. Relative to this point, the AHA-ACC guidelines do not classify past CABG or PCI as a major ASCVD event, nor is a TIA considered a major event or a high-risk condition.
For LDL, “lower is better” is supported by years of statin clinical trial evidence, along with the robust findings in the 2010 Cholesterol Trialists Collaboration. The goal of <55 mg/dL is supported by the IMPROVE-IT, FOURIER, and ODYSSEY trials. The ESC guidelines appropriately take this body of evidence and applies it to an aggressive treatment platform that, like AACE, sets clinically useful LDL goals for clinicians and patients. It takes early, aggressive LDL-lowering treatment to stay ahead of atherosclerotic plaque development in patients who are at very high or extreme risk. Following AACE’s lead, the ESC guidelines are the newest tool available to clinicians addressing this issue with the promise of further decreasing CVD events and extending lives.
Dr. Jellinger is a member of the editorial advisory board for Clinical Endocrinology News. He is professor of clinical medicine on the voluntary faculty at the University of Miami Miller School of Medicine and a practicing endocrinologist at The Center for Diabetes & Endocrine Care in Hollywood, Fla. He is past president of the American Association of Clinical Endocrinologists and the American College of Endocrinology and was chair of the writing committee for the 2017 AACE-ACE lipid guidelines.
PARIS – The 2019 dyslipidemia management guidelines from the European Society of Cardiology set an LDL cholesterol target for very-high-risk people of less than 55 mg/dL (as well as at least a 50% cut from baseline), a class I recommendation. This marks the first time a cardiology society has either recommended a target goal for this measure below 70 mg/dL or endorsed treating patients to still-lower cholesterol once their level was already under 70 mg/dL.*
The guidelines went further by suggesting consideration of an even lower treatment target for LDL-cholesterol in very-high-risk, secondary prevention patients who have already had at least two atherosclerotic cardiovascular disease events during the past 2 years, a setting that could justify an LDL-cholesterol goal of less than 40 mg/dL (along with a cut from baseline of at least 50%), a class IIb recommendation that denotes a “may be considered,” endorsement.
“In all the trials, lower was better. There was no lower level of LDL cholesterol that’s been studied that was not better” for patient outcomes, Colin Baigent, BMBCH, said while presenting the new guideline at the annual congress of the European Society of Cardiology (ESC). “It’s very clear” that the full treatment benefit from lowering LDL-cholesterol extends to getting very-high risk patients below these levels, said Dr. Baigent, professor of cardiology at Oxford (England) University and one of three chairs of the ESC’s dyslipidemia guideline-writing panel.
While this change was seen as a notably aggressive goal and too fixed on a specific number by at least one author of the 2018 American Heart Association/American College of Cardiology cholesterol management guideline (J Am Coll Cardiol. 2019 Jun;73[24]:e285-e350), it was embraced by another U.S. expert not involved in writing the most recent U.S. recommendations.
“A goal for LDL-cholesterol of less than 55 mg/dL is reasonable; it’s well documented” by trial evidence “and I support it,” said Robert H. Eckel, MD, an endocrinologist and professor of medicine at the University of Colorado in Aurora. Dr. Eckel added that he “also supports” an LDL-cholesterol of less than 40 mg/dL in very-high-risk patients with a history of multiple events or with multiple residual risk factors, and he said he has applied this lower LDL-cholesterol goal in his practice for selected patients. But Dr. Eckel acknowledged in an interview that the evidence for it was less clear-cut than was the evidence behind a goal of less than 55 mg/dL. He also supported the concept of including a treatment goal in U.S. lipid recommendations, which in recent versions has been missing. “I fall back on a cholesterol goal for practical purposes” of making the success of cholesterol-lowering treatment easier to track.
The new ESC goal was characterized as “arbitrary” by Neil J. Stone, MD, vice-chair of the panel that wrote the 2018 AHA/ACC guideline, which relied on treating secondary-prevention patients at high risk to an LDL-cholesterol at least 50% less than before treatment, and recommended continued intensification for patients whose LDL-cholesterol level remained at or above 70 mg/dL.
“If the patient is at 58 mg/dL I’m not sure anyone can tell me what the difference is,” compared with reaching less than 55 mg/dL, Dr. Stone said in an interview. “I worry about focusing on a number and not on the concept that people at the very highest risk deserve the most intensive treatment; the Europeans agree, but they have a different way of looking at it. Despite this difference in approach, the new ESC guidelines and the 2018 U.S. guideline “are more similar than different,” stressed Dr. Stone, professor of medicine and preventive medicine at Northwestern University, Chicago.
However, other experts see an important difference in the risk faced by patients who reach the ESC’s recommended treatment goals and those who fall just short.
“It’s hard to lower an LDL-cholesterol that is already relatively low. People who are close to their cholesterol target need the most intensified treatment” to reach their goal, said Rory Collins, F.Med.Sci., professor of epidemiology at Oxford University. He was not on the ESC guidelines panel.
“It’s a mind shift that clinicians need to be most aggressive in treating patients with the highest risk” even when their LDL-cholesterol is low but not yet at the target level, Dr. Collins said during a discussion session at the congress.
The new ESC guidelines is about “both getting the LDL-cholesterol down to a certain level and also about achieving a big [at least 50%] change” from baseline. “I think the ESC guidelines make that crystal clear,” said Marc S. Sabatine, MD, professor of medicine at Harvard Medical School, Boston, and the sole American to participate in the ESC guidelines-writing panel.
The ESC also broke new ground by advocating an aggressive path toward achieving these LDL-cholesterol goals by elevating the newest and most potent class of approved LDL-cholesterol-lowering drugs, the PCSK9 (proprotein convertase subtilisin/kexin type 9) inhibitors, to a top-tier, class I recommendation (“is recommended”) for secondary prevention in very-high-risk patients not reaching their goal LDL-cholesterol level on a maximally tolerated statin plus ezetimibe. This recommendation to unequivocally add a PCSK9 inhibitor for this patient population contrasts with the 2018 AHA/ACC guideline that deemed adding a PCSK9 inhibitor a IIa recommendation (“is reasonable”).
A similar uptick in treatment aggressiveness appeared in the ESC’s recommendations for managing very-high-risk patients in a primary prevention setting, including those without familial hypercholesterolemia. For these people, the ESC panel, which worked in concert with the European Atherosclerosis Society, pegged adding a PCSK9 inhibitor as a IIb (“may be considered”) recommendation when these very-high-risk people fail to reach their LDL-cholesterol target on a maximally tolerated statin and ezetimibe. Once again, this opening to use a PCSK9 inhibitor contrasted with the 2018 U.S. guideline, which never mentioned an option of adding a PCSK9 inhibitor for primary prevention except when someone also has familial hypercholesterolemia and starts treatment with an LDL level of at least 190 mg/dL (a IIb recommendation). The new European guidelines proposed using a PCSK9 inhibitor as a second-line option to consider when needed for people whose very high risk derives primarily from older age and other factors such as smoking or hypertension that give them at least a 10% 10-year risk for cardiovascular death as estimated with the European-oriented SCORE risk calculator tables.
Updated SCORE risk designations appear in the new ESC dyslipidemia guidelines, and they show, for example, that in lower-risk European countries (mostly Western European nations) virtually all men who are at least 70 years old would fall into the very-high-risk category that makes them potential candidates for treatment with a PCSK9 inhibitor regardless of any other risk they may or may not have. In higher-risk (mostly Eastern European) countries this designation kicks in for most men once they reach the age of 65.
Several Congress attendees who came to a discussion session on the guidelines voiced concerns that the new revision will lead to substantially increased use of the these drugs and hence will significantly boost medical costs, because these drugs today are priced at about $6,000 annually to treat one patient. In response, members of the guideline-writing panel defended their decision as unavoidable given what’s been reported on the clinical impact of PCSK9 inhibitors when lowering LDL cholesterol and cutting atherosclerotic cardiovascular disease events.
“I commend the [ESC] guideline for focusing on the science and on what is best for patients. The U.S. guidelines conflated the science and the cost, and the recommendations got watered down by cost considerations,” said Dr. Sabatine, who has led several studies of PCSK9 inhibitors.
Dr. Baigent added that the panel “deliberated long and hard on cost, but we felt that we had to focus on the evidence. The cost will shift” in the future, he predicted.
Other U.S. physicians highlighted the need to take drug cost into account when writing public health policy documents such as lipid-management guidelines and questioned whether this more liberal use of PCSK9 inhibitors was justified.
“I think that in the absence of familial hypercholesterolemia you need to waffle around the edges to justify a PCSK9 inhibitor,” said Dr. Eckel. “The cost of PCSK9 inhibitors has come down, but at $6,000 per year you can’t ignore their cost.”
“In the U.S. we need to be mindful of the cost of treatment,” said Dr. Stone. “The ESC guidelines are probably more aggressive” than the 2018 U.S. guideline. “They use PCSK9 inhibitors perhaps more than we do; we [in the United States] prefer generic ezetimibe. A lot has to do with the definitions of risk. The European guidelines have a lot of risk definitions that differ” from the U.S. guideline, he said.
Members of the ESC guidelines panel acknowledged that the SCORE risk-assessment charts could overestimate risk in older people who need primary prevention treatment, as well as underestimate the risk in younger adults.
This inherent age bias in the SCORE risk tables make it “extremely important to contextualize” a person’s risk “by considering other risk factors,” advised Brian A. Ference, MD, an interventional cardiologist and professor at Cambridge (England) University who was a member of the ESC guidelines writing group.
The new ESC guidelines say that risk categorization “must be interpreted in light of the clinician’s knowledge and experience, and of the patient’s pretest likelihood” of cardiovascular disease.”
Dr. Baigent has received research funding from Boehringer Ingelheim, Novartis, and Pfizer. Dr. Eckel has been an expert witness on behalf of Sanofi/Regeneron. Dr. Sabatine and Dr. Ference have received honoraria and research funding from several companies including those that market lipid-lowering drugs. Dr. Stone and Dr. Collins had no disclosures.
*Correction, 9/20/19: A previous version of this article incorrectly stated that the ESC guidelines were the first by a medical society to recommend the lower cholesterol goals. The American Association of Clinical Endocrinologists included targets below 55 mg/dL in their 2017 dyslipidemia management guidelines.
SOURCE: Mach F et al. Eur Heart J. 2019 Aug 31. doi: 10.1093/eurheartj/ehz455.
PARIS – The 2019 dyslipidemia management guidelines from the European Society of Cardiology set an LDL cholesterol target for very-high-risk people of less than 55 mg/dL (as well as at least a 50% cut from baseline), a class I recommendation. This marks the first time a cardiology society has either recommended a target goal for this measure below 70 mg/dL or endorsed treating patients to still-lower cholesterol once their level was already under 70 mg/dL.*
The guidelines went further by suggesting consideration of an even lower treatment target for LDL-cholesterol in very-high-risk, secondary prevention patients who have already had at least two atherosclerotic cardiovascular disease events during the past 2 years, a setting that could justify an LDL-cholesterol goal of less than 40 mg/dL (along with a cut from baseline of at least 50%), a class IIb recommendation that denotes a “may be considered,” endorsement.
“In all the trials, lower was better. There was no lower level of LDL cholesterol that’s been studied that was not better” for patient outcomes, Colin Baigent, BMBCH, said while presenting the new guideline at the annual congress of the European Society of Cardiology (ESC). “It’s very clear” that the full treatment benefit from lowering LDL-cholesterol extends to getting very-high risk patients below these levels, said Dr. Baigent, professor of cardiology at Oxford (England) University and one of three chairs of the ESC’s dyslipidemia guideline-writing panel.
While this change was seen as a notably aggressive goal and too fixed on a specific number by at least one author of the 2018 American Heart Association/American College of Cardiology cholesterol management guideline (J Am Coll Cardiol. 2019 Jun;73[24]:e285-e350), it was embraced by another U.S. expert not involved in writing the most recent U.S. recommendations.
“A goal for LDL-cholesterol of less than 55 mg/dL is reasonable; it’s well documented” by trial evidence “and I support it,” said Robert H. Eckel, MD, an endocrinologist and professor of medicine at the University of Colorado in Aurora. Dr. Eckel added that he “also supports” an LDL-cholesterol of less than 40 mg/dL in very-high-risk patients with a history of multiple events or with multiple residual risk factors, and he said he has applied this lower LDL-cholesterol goal in his practice for selected patients. But Dr. Eckel acknowledged in an interview that the evidence for it was less clear-cut than was the evidence behind a goal of less than 55 mg/dL. He also supported the concept of including a treatment goal in U.S. lipid recommendations, which in recent versions has been missing. “I fall back on a cholesterol goal for practical purposes” of making the success of cholesterol-lowering treatment easier to track.
The new ESC goal was characterized as “arbitrary” by Neil J. Stone, MD, vice-chair of the panel that wrote the 2018 AHA/ACC guideline, which relied on treating secondary-prevention patients at high risk to an LDL-cholesterol at least 50% less than before treatment, and recommended continued intensification for patients whose LDL-cholesterol level remained at or above 70 mg/dL.
“If the patient is at 58 mg/dL I’m not sure anyone can tell me what the difference is,” compared with reaching less than 55 mg/dL, Dr. Stone said in an interview. “I worry about focusing on a number and not on the concept that people at the very highest risk deserve the most intensive treatment; the Europeans agree, but they have a different way of looking at it. Despite this difference in approach, the new ESC guidelines and the 2018 U.S. guideline “are more similar than different,” stressed Dr. Stone, professor of medicine and preventive medicine at Northwestern University, Chicago.
However, other experts see an important difference in the risk faced by patients who reach the ESC’s recommended treatment goals and those who fall just short.
“It’s hard to lower an LDL-cholesterol that is already relatively low. People who are close to their cholesterol target need the most intensified treatment” to reach their goal, said Rory Collins, F.Med.Sci., professor of epidemiology at Oxford University. He was not on the ESC guidelines panel.
“It’s a mind shift that clinicians need to be most aggressive in treating patients with the highest risk” even when their LDL-cholesterol is low but not yet at the target level, Dr. Collins said during a discussion session at the congress.
The new ESC guidelines is about “both getting the LDL-cholesterol down to a certain level and also about achieving a big [at least 50%] change” from baseline. “I think the ESC guidelines make that crystal clear,” said Marc S. Sabatine, MD, professor of medicine at Harvard Medical School, Boston, and the sole American to participate in the ESC guidelines-writing panel.
The ESC also broke new ground by advocating an aggressive path toward achieving these LDL-cholesterol goals by elevating the newest and most potent class of approved LDL-cholesterol-lowering drugs, the PCSK9 (proprotein convertase subtilisin/kexin type 9) inhibitors, to a top-tier, class I recommendation (“is recommended”) for secondary prevention in very-high-risk patients not reaching their goal LDL-cholesterol level on a maximally tolerated statin plus ezetimibe. This recommendation to unequivocally add a PCSK9 inhibitor for this patient population contrasts with the 2018 AHA/ACC guideline that deemed adding a PCSK9 inhibitor a IIa recommendation (“is reasonable”).
A similar uptick in treatment aggressiveness appeared in the ESC’s recommendations for managing very-high-risk patients in a primary prevention setting, including those without familial hypercholesterolemia. For these people, the ESC panel, which worked in concert with the European Atherosclerosis Society, pegged adding a PCSK9 inhibitor as a IIb (“may be considered”) recommendation when these very-high-risk people fail to reach their LDL-cholesterol target on a maximally tolerated statin and ezetimibe. Once again, this opening to use a PCSK9 inhibitor contrasted with the 2018 U.S. guideline, which never mentioned an option of adding a PCSK9 inhibitor for primary prevention except when someone also has familial hypercholesterolemia and starts treatment with an LDL level of at least 190 mg/dL (a IIb recommendation). The new European guidelines proposed using a PCSK9 inhibitor as a second-line option to consider when needed for people whose very high risk derives primarily from older age and other factors such as smoking or hypertension that give them at least a 10% 10-year risk for cardiovascular death as estimated with the European-oriented SCORE risk calculator tables.
Updated SCORE risk designations appear in the new ESC dyslipidemia guidelines, and they show, for example, that in lower-risk European countries (mostly Western European nations) virtually all men who are at least 70 years old would fall into the very-high-risk category that makes them potential candidates for treatment with a PCSK9 inhibitor regardless of any other risk they may or may not have. In higher-risk (mostly Eastern European) countries this designation kicks in for most men once they reach the age of 65.
Several Congress attendees who came to a discussion session on the guidelines voiced concerns that the new revision will lead to substantially increased use of the these drugs and hence will significantly boost medical costs, because these drugs today are priced at about $6,000 annually to treat one patient. In response, members of the guideline-writing panel defended their decision as unavoidable given what’s been reported on the clinical impact of PCSK9 inhibitors when lowering LDL cholesterol and cutting atherosclerotic cardiovascular disease events.
“I commend the [ESC] guideline for focusing on the science and on what is best for patients. The U.S. guidelines conflated the science and the cost, and the recommendations got watered down by cost considerations,” said Dr. Sabatine, who has led several studies of PCSK9 inhibitors.
Dr. Baigent added that the panel “deliberated long and hard on cost, but we felt that we had to focus on the evidence. The cost will shift” in the future, he predicted.
Other U.S. physicians highlighted the need to take drug cost into account when writing public health policy documents such as lipid-management guidelines and questioned whether this more liberal use of PCSK9 inhibitors was justified.
“I think that in the absence of familial hypercholesterolemia you need to waffle around the edges to justify a PCSK9 inhibitor,” said Dr. Eckel. “The cost of PCSK9 inhibitors has come down, but at $6,000 per year you can’t ignore their cost.”
“In the U.S. we need to be mindful of the cost of treatment,” said Dr. Stone. “The ESC guidelines are probably more aggressive” than the 2018 U.S. guideline. “They use PCSK9 inhibitors perhaps more than we do; we [in the United States] prefer generic ezetimibe. A lot has to do with the definitions of risk. The European guidelines have a lot of risk definitions that differ” from the U.S. guideline, he said.
Members of the ESC guidelines panel acknowledged that the SCORE risk-assessment charts could overestimate risk in older people who need primary prevention treatment, as well as underestimate the risk in younger adults.
This inherent age bias in the SCORE risk tables make it “extremely important to contextualize” a person’s risk “by considering other risk factors,” advised Brian A. Ference, MD, an interventional cardiologist and professor at Cambridge (England) University who was a member of the ESC guidelines writing group.
The new ESC guidelines say that risk categorization “must be interpreted in light of the clinician’s knowledge and experience, and of the patient’s pretest likelihood” of cardiovascular disease.”
Dr. Baigent has received research funding from Boehringer Ingelheim, Novartis, and Pfizer. Dr. Eckel has been an expert witness on behalf of Sanofi/Regeneron. Dr. Sabatine and Dr. Ference have received honoraria and research funding from several companies including those that market lipid-lowering drugs. Dr. Stone and Dr. Collins had no disclosures.
*Correction, 9/20/19: A previous version of this article incorrectly stated that the ESC guidelines were the first by a medical society to recommend the lower cholesterol goals. The American Association of Clinical Endocrinologists included targets below 55 mg/dL in their 2017 dyslipidemia management guidelines.
SOURCE: Mach F et al. Eur Heart J. 2019 Aug 31. doi: 10.1093/eurheartj/ehz455.
REPORTING FROM THE ESC CONGRESS 2019
Survival at ‘overweight’ BMI surpasses ‘normal’
PARIS – Middle-aged adults with a body mass index of 25-29 kg/m2 had a significantly better adjusted survival during a median follow-up of nearly 10 years than did people with a “normal” body mass index of 20-24 kg/m2 in a worldwide study of more than 140,000. This finding suggests the current, widely accepted definition of normal body mass index is wrong.*
The new findings suggest that the current definition of a “healthy” body mass index (BMI) “should be re-evaluated,” Darryl P. Leong, MBBS, said at the annual Congress of the European Society of Cardiology. The analysis also identified a BMI specifically of 27 kg/m2 as associated with optimal survival among both women and men, “clearly outside the range of 20 to less than 25 kg/m2 that is considered normal,” said Dr. Leong, a cardiologist at McMaster University and the Population Health Research Institute, both in Hamilton, Ont.
Dr. Leong cited three potential explanations for why the new study identified optimal survival with a BMI of 25 to less than 30 kg/m2 among people who were 35-70 years old when they entered the study and were followed for a median of 9.5 years: The current study collected data and adjusted the results using a wider range of potential confounders than in prior studies, the data reflect the impact of contemporary interventions to reduce cardiovascular disease illness and death while past studies relied on data from earlier times when less cardiovascular disease protection occurred, and the current study included people from lower-income countries, although the finding is just as applicable to people who live in high-income countries, who were also included in the study population, noted Salim Yusuf, MBBS, principal investigator for the study.
A BMI of 20-24 kg/m2 “is actually low and harmful,” noted Dr. Yusuf in an interview. Despite recent data consistently showing better survival among people with a BMI of 25-29 kg/m2, panels that have recently written weight guidelines are “ossified” and “refuse to accept” the implications of these findings, said Dr. Yusuf, professor of medicine at McMaster and executive director of the Population Health Research Institute.
The results of the analyses that Dr. Leong reported also showed that BMI paled as a prognosticator for survival when compared with two other assessments of weight: waist/hip ratio, and even more powerful prognostically, a novel measure developed for this analysis that calculates the ratio of hand-grip strength/body weight. Waist/hip ratio adds the dimension of the location of body fat rather than just the amount, and the ratio of grip strength/body weight assesses the contribution of muscle mass to overall weight, noted Dr. Leong. He reported an optimal waist/hip ratio for survival of 0.83 in women and 0.93 in men, and an optimal strength/weight ratio of 0.42 in women and 0.50 in men. This means that a man whose hand-grip strength (measured in kg) is half of the person’s body weight has the best prospect for survival.
The study used data collected in PURE (Prospective Urban Rural Epidemiology Study) on 142,410 people aged 35-70 years from any one of four high-income countries, 12 middle-income countries, and five low-income countries. The study excluded people who had at baseline known coronary artery disease, stroke, heart failure, or cancer, and the adjusted analysis controlled for age, sex, region, education, activity, alcohol and tobacco use, and the baseline prevalence of hypertension and diabetes. During follow-up, 9,712 of these people died.
The researchers saw a nadir for mortality among people with a BMI of 25-29 kg/m2 for both cardiovascular and noncardiovascular deaths. In addition, the link between total mortality and BMI was strongest in the subgroup of people on one or more treatments aimed at preventing cardiovascular disease, while it essentially disappeared among people not receiving any cardiovascular disease preventive measures, highlighting that the relationship now identified depends on a context of overall cardiovascular disease risk reduction, Dr. Leong said. The results also showed a very clear, direct, linear relationship between higher BMI and both the incidence of diabetes and cardiovascular disease, as well as increased all-cause and noncardiovascular mortality among people with a BMI of less than 20 kg/m2.
Dr. Yusuf discussed the results of the analysis in a video interview.
The PURE study has received partial funding from unrestricted grants from several drug companies. Dr. Leong has been an advisor to Ferring Pharmaceuticals and has been a speaker on behalf of Janssen. Dr. Yusuf had no disclosures.
This story was updated 9/19/2019.
PARIS – Middle-aged adults with a body mass index of 25-29 kg/m2 had a significantly better adjusted survival during a median follow-up of nearly 10 years than did people with a “normal” body mass index of 20-24 kg/m2 in a worldwide study of more than 140,000. This finding suggests the current, widely accepted definition of normal body mass index is wrong.*
The new findings suggest that the current definition of a “healthy” body mass index (BMI) “should be re-evaluated,” Darryl P. Leong, MBBS, said at the annual Congress of the European Society of Cardiology. The analysis also identified a BMI specifically of 27 kg/m2 as associated with optimal survival among both women and men, “clearly outside the range of 20 to less than 25 kg/m2 that is considered normal,” said Dr. Leong, a cardiologist at McMaster University and the Population Health Research Institute, both in Hamilton, Ont.
Dr. Leong cited three potential explanations for why the new study identified optimal survival with a BMI of 25 to less than 30 kg/m2 among people who were 35-70 years old when they entered the study and were followed for a median of 9.5 years: The current study collected data and adjusted the results using a wider range of potential confounders than in prior studies, the data reflect the impact of contemporary interventions to reduce cardiovascular disease illness and death while past studies relied on data from earlier times when less cardiovascular disease protection occurred, and the current study included people from lower-income countries, although the finding is just as applicable to people who live in high-income countries, who were also included in the study population, noted Salim Yusuf, MBBS, principal investigator for the study.
A BMI of 20-24 kg/m2 “is actually low and harmful,” noted Dr. Yusuf in an interview. Despite recent data consistently showing better survival among people with a BMI of 25-29 kg/m2, panels that have recently written weight guidelines are “ossified” and “refuse to accept” the implications of these findings, said Dr. Yusuf, professor of medicine at McMaster and executive director of the Population Health Research Institute.
The results of the analyses that Dr. Leong reported also showed that BMI paled as a prognosticator for survival when compared with two other assessments of weight: waist/hip ratio, and even more powerful prognostically, a novel measure developed for this analysis that calculates the ratio of hand-grip strength/body weight. Waist/hip ratio adds the dimension of the location of body fat rather than just the amount, and the ratio of grip strength/body weight assesses the contribution of muscle mass to overall weight, noted Dr. Leong. He reported an optimal waist/hip ratio for survival of 0.83 in women and 0.93 in men, and an optimal strength/weight ratio of 0.42 in women and 0.50 in men. This means that a man whose hand-grip strength (measured in kg) is half of the person’s body weight has the best prospect for survival.
The study used data collected in PURE (Prospective Urban Rural Epidemiology Study) on 142,410 people aged 35-70 years from any one of four high-income countries, 12 middle-income countries, and five low-income countries. The study excluded people who had at baseline known coronary artery disease, stroke, heart failure, or cancer, and the adjusted analysis controlled for age, sex, region, education, activity, alcohol and tobacco use, and the baseline prevalence of hypertension and diabetes. During follow-up, 9,712 of these people died.
The researchers saw a nadir for mortality among people with a BMI of 25-29 kg/m2 for both cardiovascular and noncardiovascular deaths. In addition, the link between total mortality and BMI was strongest in the subgroup of people on one or more treatments aimed at preventing cardiovascular disease, while it essentially disappeared among people not receiving any cardiovascular disease preventive measures, highlighting that the relationship now identified depends on a context of overall cardiovascular disease risk reduction, Dr. Leong said. The results also showed a very clear, direct, linear relationship between higher BMI and both the incidence of diabetes and cardiovascular disease, as well as increased all-cause and noncardiovascular mortality among people with a BMI of less than 20 kg/m2.
Dr. Yusuf discussed the results of the analysis in a video interview.
The PURE study has received partial funding from unrestricted grants from several drug companies. Dr. Leong has been an advisor to Ferring Pharmaceuticals and has been a speaker on behalf of Janssen. Dr. Yusuf had no disclosures.
This story was updated 9/19/2019.
PARIS – Middle-aged adults with a body mass index of 25-29 kg/m2 had a significantly better adjusted survival during a median follow-up of nearly 10 years than did people with a “normal” body mass index of 20-24 kg/m2 in a worldwide study of more than 140,000. This finding suggests the current, widely accepted definition of normal body mass index is wrong.*
The new findings suggest that the current definition of a “healthy” body mass index (BMI) “should be re-evaluated,” Darryl P. Leong, MBBS, said at the annual Congress of the European Society of Cardiology. The analysis also identified a BMI specifically of 27 kg/m2 as associated with optimal survival among both women and men, “clearly outside the range of 20 to less than 25 kg/m2 that is considered normal,” said Dr. Leong, a cardiologist at McMaster University and the Population Health Research Institute, both in Hamilton, Ont.
Dr. Leong cited three potential explanations for why the new study identified optimal survival with a BMI of 25 to less than 30 kg/m2 among people who were 35-70 years old when they entered the study and were followed for a median of 9.5 years: The current study collected data and adjusted the results using a wider range of potential confounders than in prior studies, the data reflect the impact of contemporary interventions to reduce cardiovascular disease illness and death while past studies relied on data from earlier times when less cardiovascular disease protection occurred, and the current study included people from lower-income countries, although the finding is just as applicable to people who live in high-income countries, who were also included in the study population, noted Salim Yusuf, MBBS, principal investigator for the study.
A BMI of 20-24 kg/m2 “is actually low and harmful,” noted Dr. Yusuf in an interview. Despite recent data consistently showing better survival among people with a BMI of 25-29 kg/m2, panels that have recently written weight guidelines are “ossified” and “refuse to accept” the implications of these findings, said Dr. Yusuf, professor of medicine at McMaster and executive director of the Population Health Research Institute.
The results of the analyses that Dr. Leong reported also showed that BMI paled as a prognosticator for survival when compared with two other assessments of weight: waist/hip ratio, and even more powerful prognostically, a novel measure developed for this analysis that calculates the ratio of hand-grip strength/body weight. Waist/hip ratio adds the dimension of the location of body fat rather than just the amount, and the ratio of grip strength/body weight assesses the contribution of muscle mass to overall weight, noted Dr. Leong. He reported an optimal waist/hip ratio for survival of 0.83 in women and 0.93 in men, and an optimal strength/weight ratio of 0.42 in women and 0.50 in men. This means that a man whose hand-grip strength (measured in kg) is half of the person’s body weight has the best prospect for survival.
The study used data collected in PURE (Prospective Urban Rural Epidemiology Study) on 142,410 people aged 35-70 years from any one of four high-income countries, 12 middle-income countries, and five low-income countries. The study excluded people who had at baseline known coronary artery disease, stroke, heart failure, or cancer, and the adjusted analysis controlled for age, sex, region, education, activity, alcohol and tobacco use, and the baseline prevalence of hypertension and diabetes. During follow-up, 9,712 of these people died.
The researchers saw a nadir for mortality among people with a BMI of 25-29 kg/m2 for both cardiovascular and noncardiovascular deaths. In addition, the link between total mortality and BMI was strongest in the subgroup of people on one or more treatments aimed at preventing cardiovascular disease, while it essentially disappeared among people not receiving any cardiovascular disease preventive measures, highlighting that the relationship now identified depends on a context of overall cardiovascular disease risk reduction, Dr. Leong said. The results also showed a very clear, direct, linear relationship between higher BMI and both the incidence of diabetes and cardiovascular disease, as well as increased all-cause and noncardiovascular mortality among people with a BMI of less than 20 kg/m2.
Dr. Yusuf discussed the results of the analysis in a video interview.
The PURE study has received partial funding from unrestricted grants from several drug companies. Dr. Leong has been an advisor to Ferring Pharmaceuticals and has been a speaker on behalf of Janssen. Dr. Yusuf had no disclosures.
This story was updated 9/19/2019.
REPORTING FROM THE ESC CONGRESS 2019
siRNA drug safely halved LDL cholesterol in phase 3 ORION-11
PARIS – A small interfering RNA drug, inclisiran, safely halved LDL cholesterol levels in more than 800 patients in a phase 3, multicenter study, in a big step toward this drug coming onto the market and offering an alternative way to harness the potent cholesterol-lowering power of PCSK9 inhibition.
In the reported study – which enrolled patients with established cardiovascular disease, familial hypercholesterolemia, type 2 diabetes, or a high Framingham Risk Score – participants received inclisiran as a semiannual subcutaneous injection. The safe efficacy this produced showed the viability of a new way to deliver lipid-lowering therapy that guarantees compliance and is convenient for patients.
The prospect of lowering cholesterol with about the same potency as the monoclonal antibodies that block PCSK9 (proprotein convertase subtilisin/kexin type 9) activity but administered as a biannual injection “enables provider control over medication adherence, and may offer patients a meaningful new choice that is safe and convenient and has assured results,” Kausik K. Ray, MD, said at the annual congress of the European Society of Cardiology. The durable effect of the small interfering RNA (siRNA) agent “offers a huge advantage,” and “opens the field,” said Dr. Ray, a cardiologist and professor of public health at Imperial College, London.
He also highlighted the “excellent” safety profile seen in the 811 patients treated with inclisiran, compared with 804 patients in the study who received placebo. After four total injections of inclisiran spaced out over 450 days (about 15 months), the rate of treatment-emergent adverse events and serious events was virtually the same in the two treatment arms, and with no signal of inclisiran causing liver effects, renal or muscle injury, damage to blood components, or malignancy. The serial treatment with inclisiran that patients received – at baseline, 90, 270, and 450 days – produced no severe injection-site reactions, and transient mild or moderate injection-site reactions in just under 5% of patients.
Safety issues, such as more-severe injection-site reactions, thrombocytopenia, hepatotoxicity, and flu-like symptoms, plagued siRNA drugs during their earlier days of development, but more recently next-generation siRNA drugs with modified structures have produced much better safety performance, noted Richard C. Becker, MD, professor of medicine and director of the Heart, Lung, & Vascular Institute at the University of Cincinnati. The new-generation siRNAs such as inclisiran are “very well tolerated,” he said in an interview.
The Food and Drug Administration approved the first siRNA drug in August 2018, and in the year since then a few others have also come onto the U.S. market, Dr. Becker said.
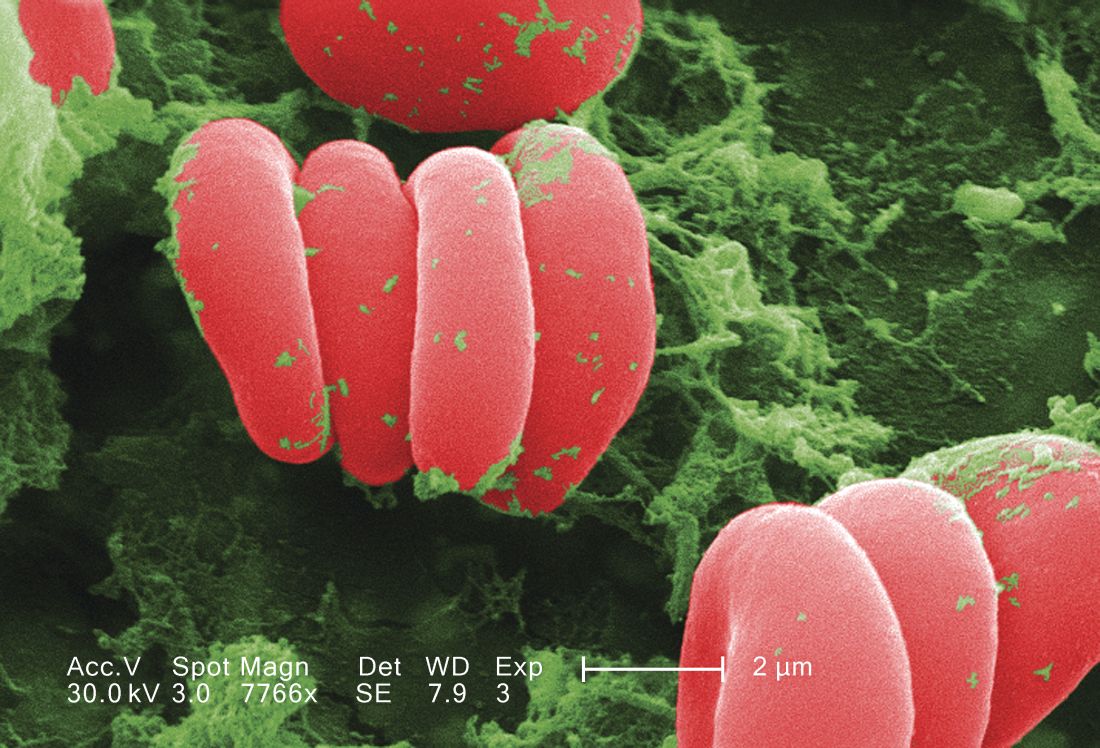
Like other siRNA drugs, the activity of inclisiran comes from a short RNA segment that is antisense to a particular messenger RNA (mRNA) target. In the case of inclisiran, the target is the mRNA for the PCSK9 enzyme produced in hepatocytes, and that decreases the number of LDL cholesterol receptors on the cell’s surface. When the antisense RNA molecule encounters a PCSK9 mRNA, the two bind and the mRNA is then degraded by a normal cell process. This cuts the cell’s production of the PCSK9 protein, resulting in more LDL cholesterol receptors on the cell’s surface that pull more LDL cholesterol from the blood. The blocking of PCSK9 activity by inclisiran is roughly equivalent to the action of the PCSK9 monoclonal antibodies that have now been on the U.S. market for a few years. Also like other siRNA drugs, the RNA of inclisiran is packaged so that, once injected into a patient, the RNA molecules travel to the liver and enter hepatocytes, where they exert their activity.
“No one has concerns about inclisiran being able to lower LDL [cholesterol], and there have been no safety signals. The data we have seen so far look very reassuring, and in particular has been very safe for the liver,” commented Marc S. Sabatine, MD, professor of medicine at Harvard Medical School, Boston, who has led several studies involving PCSK9-targeted drugs and is helping to run ORION-4, a 15,000-patient study of inclisiran designed to assess the drug’s effect on clinical events. Results from ORION-4 are not expected until about 2024.
“The PCSK9 inhibitors in general have been a huge advance for patients, and the more kinds of drugs we have to target PCSK9, the better,” he said in an interview.
The study reported by Dr. Ray, ORION-11, enrolled 1,617 patients with high atherosclerotic disease risk at 70 sites in six European countries and South Africa. The study’s primary efficacy endpoint was reduction from baseline in LDL cholesterol both at 510 days (about 17 months) after the first dose and also throughout the 15-month period that started 3 months after the first dose. The average reduction seen after 510 days was 54%, compared with baseline, and the time-averaged reduction during the 15-month window examined was 50%, Dr. Ray said. The results also showed a consistent reduction in LDL cholesterol in virtually every patient treated with inclisiran.
Two other phase 3 studies of inclisiran with similar design have been completed, and the results will come out before the end of 2019, according to a statement from the Medicines Company, which is developing the drug. The statement also said that the company plans to file their data with the FDA for marketing approval for inclisiran before the end of 2019. In the recent past, the FDA has approved drugs for the indication of lowering LDL cholesterol before evidence is available to prove that the agent has benefits for reducing clinical events.
Future studies of inclisiran will explore the efficacy of a single annual injection of the drug as an approach to primary prevention of cardiovascular disease, Dr. Ray said.
ORION-11 was sponsored by the Medicines Company. Dr. Ray is a consultant to it and to several other companies. Dr. Becker had no relevant disclosures. Dr. Sabatine has received research support from the Medicines Company and several other companies, and has received personal fees from Anthos Therapeutics, Bristol-Myers Squibb, CVS Caremark, Daiichi Sankyo, DalCor Pharmaceuticals, Dyrnamix, and Ionis.
PARIS – A small interfering RNA drug, inclisiran, safely halved LDL cholesterol levels in more than 800 patients in a phase 3, multicenter study, in a big step toward this drug coming onto the market and offering an alternative way to harness the potent cholesterol-lowering power of PCSK9 inhibition.
In the reported study – which enrolled patients with established cardiovascular disease, familial hypercholesterolemia, type 2 diabetes, or a high Framingham Risk Score – participants received inclisiran as a semiannual subcutaneous injection. The safe efficacy this produced showed the viability of a new way to deliver lipid-lowering therapy that guarantees compliance and is convenient for patients.
The prospect of lowering cholesterol with about the same potency as the monoclonal antibodies that block PCSK9 (proprotein convertase subtilisin/kexin type 9) activity but administered as a biannual injection “enables provider control over medication adherence, and may offer patients a meaningful new choice that is safe and convenient and has assured results,” Kausik K. Ray, MD, said at the annual congress of the European Society of Cardiology. The durable effect of the small interfering RNA (siRNA) agent “offers a huge advantage,” and “opens the field,” said Dr. Ray, a cardiologist and professor of public health at Imperial College, London.
He also highlighted the “excellent” safety profile seen in the 811 patients treated with inclisiran, compared with 804 patients in the study who received placebo. After four total injections of inclisiran spaced out over 450 days (about 15 months), the rate of treatment-emergent adverse events and serious events was virtually the same in the two treatment arms, and with no signal of inclisiran causing liver effects, renal or muscle injury, damage to blood components, or malignancy. The serial treatment with inclisiran that patients received – at baseline, 90, 270, and 450 days – produced no severe injection-site reactions, and transient mild or moderate injection-site reactions in just under 5% of patients.
Safety issues, such as more-severe injection-site reactions, thrombocytopenia, hepatotoxicity, and flu-like symptoms, plagued siRNA drugs during their earlier days of development, but more recently next-generation siRNA drugs with modified structures have produced much better safety performance, noted Richard C. Becker, MD, professor of medicine and director of the Heart, Lung, & Vascular Institute at the University of Cincinnati. The new-generation siRNAs such as inclisiran are “very well tolerated,” he said in an interview.
The Food and Drug Administration approved the first siRNA drug in August 2018, and in the year since then a few others have also come onto the U.S. market, Dr. Becker said.
Like other siRNA drugs, the activity of inclisiran comes from a short RNA segment that is antisense to a particular messenger RNA (mRNA) target. In the case of inclisiran, the target is the mRNA for the PCSK9 enzyme produced in hepatocytes, and that decreases the number of LDL cholesterol receptors on the cell’s surface. When the antisense RNA molecule encounters a PCSK9 mRNA, the two bind and the mRNA is then degraded by a normal cell process. This cuts the cell’s production of the PCSK9 protein, resulting in more LDL cholesterol receptors on the cell’s surface that pull more LDL cholesterol from the blood. The blocking of PCSK9 activity by inclisiran is roughly equivalent to the action of the PCSK9 monoclonal antibodies that have now been on the U.S. market for a few years. Also like other siRNA drugs, the RNA of inclisiran is packaged so that, once injected into a patient, the RNA molecules travel to the liver and enter hepatocytes, where they exert their activity.
“No one has concerns about inclisiran being able to lower LDL [cholesterol], and there have been no safety signals. The data we have seen so far look very reassuring, and in particular has been very safe for the liver,” commented Marc S. Sabatine, MD, professor of medicine at Harvard Medical School, Boston, who has led several studies involving PCSK9-targeted drugs and is helping to run ORION-4, a 15,000-patient study of inclisiran designed to assess the drug’s effect on clinical events. Results from ORION-4 are not expected until about 2024.
“The PCSK9 inhibitors in general have been a huge advance for patients, and the more kinds of drugs we have to target PCSK9, the better,” he said in an interview.
The study reported by Dr. Ray, ORION-11, enrolled 1,617 patients with high atherosclerotic disease risk at 70 sites in six European countries and South Africa. The study’s primary efficacy endpoint was reduction from baseline in LDL cholesterol both at 510 days (about 17 months) after the first dose and also throughout the 15-month period that started 3 months after the first dose. The average reduction seen after 510 days was 54%, compared with baseline, and the time-averaged reduction during the 15-month window examined was 50%, Dr. Ray said. The results also showed a consistent reduction in LDL cholesterol in virtually every patient treated with inclisiran.
Two other phase 3 studies of inclisiran with similar design have been completed, and the results will come out before the end of 2019, according to a statement from the Medicines Company, which is developing the drug. The statement also said that the company plans to file their data with the FDA for marketing approval for inclisiran before the end of 2019. In the recent past, the FDA has approved drugs for the indication of lowering LDL cholesterol before evidence is available to prove that the agent has benefits for reducing clinical events.
Future studies of inclisiran will explore the efficacy of a single annual injection of the drug as an approach to primary prevention of cardiovascular disease, Dr. Ray said.
ORION-11 was sponsored by the Medicines Company. Dr. Ray is a consultant to it and to several other companies. Dr. Becker had no relevant disclosures. Dr. Sabatine has received research support from the Medicines Company and several other companies, and has received personal fees from Anthos Therapeutics, Bristol-Myers Squibb, CVS Caremark, Daiichi Sankyo, DalCor Pharmaceuticals, Dyrnamix, and Ionis.
PARIS – A small interfering RNA drug, inclisiran, safely halved LDL cholesterol levels in more than 800 patients in a phase 3, multicenter study, in a big step toward this drug coming onto the market and offering an alternative way to harness the potent cholesterol-lowering power of PCSK9 inhibition.
In the reported study – which enrolled patients with established cardiovascular disease, familial hypercholesterolemia, type 2 diabetes, or a high Framingham Risk Score – participants received inclisiran as a semiannual subcutaneous injection. The safe efficacy this produced showed the viability of a new way to deliver lipid-lowering therapy that guarantees compliance and is convenient for patients.
The prospect of lowering cholesterol with about the same potency as the monoclonal antibodies that block PCSK9 (proprotein convertase subtilisin/kexin type 9) activity but administered as a biannual injection “enables provider control over medication adherence, and may offer patients a meaningful new choice that is safe and convenient and has assured results,” Kausik K. Ray, MD, said at the annual congress of the European Society of Cardiology. The durable effect of the small interfering RNA (siRNA) agent “offers a huge advantage,” and “opens the field,” said Dr. Ray, a cardiologist and professor of public health at Imperial College, London.
He also highlighted the “excellent” safety profile seen in the 811 patients treated with inclisiran, compared with 804 patients in the study who received placebo. After four total injections of inclisiran spaced out over 450 days (about 15 months), the rate of treatment-emergent adverse events and serious events was virtually the same in the two treatment arms, and with no signal of inclisiran causing liver effects, renal or muscle injury, damage to blood components, or malignancy. The serial treatment with inclisiran that patients received – at baseline, 90, 270, and 450 days – produced no severe injection-site reactions, and transient mild or moderate injection-site reactions in just under 5% of patients.
Safety issues, such as more-severe injection-site reactions, thrombocytopenia, hepatotoxicity, and flu-like symptoms, plagued siRNA drugs during their earlier days of development, but more recently next-generation siRNA drugs with modified structures have produced much better safety performance, noted Richard C. Becker, MD, professor of medicine and director of the Heart, Lung, & Vascular Institute at the University of Cincinnati. The new-generation siRNAs such as inclisiran are “very well tolerated,” he said in an interview.
The Food and Drug Administration approved the first siRNA drug in August 2018, and in the year since then a few others have also come onto the U.S. market, Dr. Becker said.
Like other siRNA drugs, the activity of inclisiran comes from a short RNA segment that is antisense to a particular messenger RNA (mRNA) target. In the case of inclisiran, the target is the mRNA for the PCSK9 enzyme produced in hepatocytes, and that decreases the number of LDL cholesterol receptors on the cell’s surface. When the antisense RNA molecule encounters a PCSK9 mRNA, the two bind and the mRNA is then degraded by a normal cell process. This cuts the cell’s production of the PCSK9 protein, resulting in more LDL cholesterol receptors on the cell’s surface that pull more LDL cholesterol from the blood. The blocking of PCSK9 activity by inclisiran is roughly equivalent to the action of the PCSK9 monoclonal antibodies that have now been on the U.S. market for a few years. Also like other siRNA drugs, the RNA of inclisiran is packaged so that, once injected into a patient, the RNA molecules travel to the liver and enter hepatocytes, where they exert their activity.
“No one has concerns about inclisiran being able to lower LDL [cholesterol], and there have been no safety signals. The data we have seen so far look very reassuring, and in particular has been very safe for the liver,” commented Marc S. Sabatine, MD, professor of medicine at Harvard Medical School, Boston, who has led several studies involving PCSK9-targeted drugs and is helping to run ORION-4, a 15,000-patient study of inclisiran designed to assess the drug’s effect on clinical events. Results from ORION-4 are not expected until about 2024.
“The PCSK9 inhibitors in general have been a huge advance for patients, and the more kinds of drugs we have to target PCSK9, the better,” he said in an interview.
The study reported by Dr. Ray, ORION-11, enrolled 1,617 patients with high atherosclerotic disease risk at 70 sites in six European countries and South Africa. The study’s primary efficacy endpoint was reduction from baseline in LDL cholesterol both at 510 days (about 17 months) after the first dose and also throughout the 15-month period that started 3 months after the first dose. The average reduction seen after 510 days was 54%, compared with baseline, and the time-averaged reduction during the 15-month window examined was 50%, Dr. Ray said. The results also showed a consistent reduction in LDL cholesterol in virtually every patient treated with inclisiran.
Two other phase 3 studies of inclisiran with similar design have been completed, and the results will come out before the end of 2019, according to a statement from the Medicines Company, which is developing the drug. The statement also said that the company plans to file their data with the FDA for marketing approval for inclisiran before the end of 2019. In the recent past, the FDA has approved drugs for the indication of lowering LDL cholesterol before evidence is available to prove that the agent has benefits for reducing clinical events.
Future studies of inclisiran will explore the efficacy of a single annual injection of the drug as an approach to primary prevention of cardiovascular disease, Dr. Ray said.
ORION-11 was sponsored by the Medicines Company. Dr. Ray is a consultant to it and to several other companies. Dr. Becker had no relevant disclosures. Dr. Sabatine has received research support from the Medicines Company and several other companies, and has received personal fees from Anthos Therapeutics, Bristol-Myers Squibb, CVS Caremark, Daiichi Sankyo, DalCor Pharmaceuticals, Dyrnamix, and Ionis.
REPORTING FROM THE ESC CONGRESS 2019
New hypertension cases halved with community-wide salt substitution
PARIS – In rural Peru, a comprehensive community-wide strategy to replace conventional table salt with a formulation that was 25% potassium chloride halved incident hypertension, also dropping blood pressure in participants with baseline hypertension.
The multifaceted intervention targeted six villages at the far north of Peru, replacing table salt with the lower-sodium substitute, J. Jaime Miranda, MD, PhD, said at a prevention-focused, late-breaking research session at the annual congress of the European Society of Cardiology. The 75/25 mixture had a palatable proportion of potassium, and was easily produced by combining table salt with potassium chloride crystals.
Dr. Miranda, director of the CRONICAS Center of Excellence at the Cayetano Heredia Peruvian University, Lima, and colleagues enrolled virtually all adult residents of the six villages in the study; patients who reported heart disease or chronic kidney disease were excluded.
“We wanted to achieve and shape a pragmatic study – and a pragmatic study that incorporates day-to-day behavior. We eat every day, but we think very little of our salt habits,” said Dr. Miranda in a video interview.
In all, 2,376 of 2,605 potential participants enrolled in the study, which used a stepped-wedge, cluster-randomized, controlled trial design. To track the primary outcome measures of systolic and diastolic BP, measurements were obtained every 5 months for a total of seven rounds of measurement, said Dr. Miranda.
Dr. Miranda said that the investigators borrowed principles from social marketing to ensure community-wide replacement of table salt with the low-sodium substitute. This meant that they branded and packaged the low-sodium salt and gave it to participants at no cost – but with a catch. To receive the low-sodium salt, participants had to turn in their table salt.
The effort was supported by promotional events and a trained “sales force” who brought messaging to families, restaurants, and key voices in the community. The attractively packaged replacement salt was distributed with a similarly branded shaker. “We wanted to guarantee the full replacement of salt in the entire village,” explained Dr. Miranda.
At the end of the study, individuals with hypertension saw a decrease in systolic BP of 1.92 mm Hg (95% confidence interval, –3.29 to –0.54).
New hypertension diagnoses, a secondary outcome measure, fell by 55% in participating villages; the hazard ratio for hypertension incidence was 0.45 (95% CI, 0.31-0.66) in a fully adjusted statistical model that accounted for clustering at the village level, as well as age, sex, education, wealth index, and body mass index, said Dr. Miranda.
Older village residents with hypertension saw greater BP reduction; for those aged at least 60 years, the mean reduction was 2.17 mm Hg (95% CI, –3.67 to –0.68).
The positive findings were met with broad applause during his presentation, a response that made his 15-hour trip from Lima to Paris worthwhile, said Dr. Miranda.
Adherence was assessed by obtaining 24-hour urine samples from a random sample of 100 participants before and after the study. “This was my biggest fear – that as soon as we left the door, people would go and throw it away,” said Dr. Miranda. Among these participants, excreted potassium rose, indicating adherence, but sodium stayed basically the same. Possible explanations included that individuals were adding table salt to their diets, or that other prepared foods or condiments contained high amounts of sodium.
The study shows the feasibility of a community-wide intervention that achieved the dual aims of population-wide reductions in BP and reduction in incident BP, and of achieving clinically meaningful benefits for the high-risk population, said Dr. Miranda. He remarked that the population was young overall, with a mean age of 43 years and a low mean baseline systolic BP of 113, making the modest population-wide reduction more notable.
“We wanted to shift the entire distribution of blood pressure in the village. And with that, we see gains not only in public health, but also effective improvements in blood pressure in those at high risk, particularly those who tend to have high blood pressure,” said Dr. Miranda.
Discussant Bruce Neal, MD, professor of medicine at the University of Sydney and senior director of the George Institute for Global Health in Newtown, Australia, congratulated Dr. Miranda and colleagues on accomplishing “a truly enormous project.” He began by noting that, though the reductions were modest, “the low starting blood pressures were almost certainly responsible for the magnitude of effect seen in this study.” He added that “this is nonetheless a worthwhile blood pressure reduction, particularly if it was sustained throughout life.”
Addressing the lack of decrease in excreted urine sodium, Dr. Neal noted that participants may have supplemented their diet with additional sodium by one means or another, “which might also have attenuated the blood pressure difference – but it could also reflect the challenges of measuring sodium and potassium effectively with 24-hour urine samples, which are difficult to collect.”
The lack of adverse effects was notable, said Dr. Neal. “When considering the use of salt substitute at the population level, the first question that arises is: ‘What about the risks of hyperkalemia?’
“I think those risks are probably greatly overstated,” he said, noting that only individuals with severe chronic kidney disease would likely be affected, and those individuals are already well versed on the importance of avoiding excess dietary potassium.
The study was funded by the National Institutes of Health through the Global Alliance for Chronic Disease program. Dr. Miranda reported that he had no conflicts of interest. Dr. Neal reported that he has financial relationships with Nu-Tec Salt and a Beijing-based salt manufacturer, related to research into salt substitutes.
PARIS – In rural Peru, a comprehensive community-wide strategy to replace conventional table salt with a formulation that was 25% potassium chloride halved incident hypertension, also dropping blood pressure in participants with baseline hypertension.
The multifaceted intervention targeted six villages at the far north of Peru, replacing table salt with the lower-sodium substitute, J. Jaime Miranda, MD, PhD, said at a prevention-focused, late-breaking research session at the annual congress of the European Society of Cardiology. The 75/25 mixture had a palatable proportion of potassium, and was easily produced by combining table salt with potassium chloride crystals.
Dr. Miranda, director of the CRONICAS Center of Excellence at the Cayetano Heredia Peruvian University, Lima, and colleagues enrolled virtually all adult residents of the six villages in the study; patients who reported heart disease or chronic kidney disease were excluded.
“We wanted to achieve and shape a pragmatic study – and a pragmatic study that incorporates day-to-day behavior. We eat every day, but we think very little of our salt habits,” said Dr. Miranda in a video interview.
In all, 2,376 of 2,605 potential participants enrolled in the study, which used a stepped-wedge, cluster-randomized, controlled trial design. To track the primary outcome measures of systolic and diastolic BP, measurements were obtained every 5 months for a total of seven rounds of measurement, said Dr. Miranda.
Dr. Miranda said that the investigators borrowed principles from social marketing to ensure community-wide replacement of table salt with the low-sodium substitute. This meant that they branded and packaged the low-sodium salt and gave it to participants at no cost – but with a catch. To receive the low-sodium salt, participants had to turn in their table salt.
The effort was supported by promotional events and a trained “sales force” who brought messaging to families, restaurants, and key voices in the community. The attractively packaged replacement salt was distributed with a similarly branded shaker. “We wanted to guarantee the full replacement of salt in the entire village,” explained Dr. Miranda.
At the end of the study, individuals with hypertension saw a decrease in systolic BP of 1.92 mm Hg (95% confidence interval, –3.29 to –0.54).
New hypertension diagnoses, a secondary outcome measure, fell by 55% in participating villages; the hazard ratio for hypertension incidence was 0.45 (95% CI, 0.31-0.66) in a fully adjusted statistical model that accounted for clustering at the village level, as well as age, sex, education, wealth index, and body mass index, said Dr. Miranda.
Older village residents with hypertension saw greater BP reduction; for those aged at least 60 years, the mean reduction was 2.17 mm Hg (95% CI, –3.67 to –0.68).
The positive findings were met with broad applause during his presentation, a response that made his 15-hour trip from Lima to Paris worthwhile, said Dr. Miranda.
Adherence was assessed by obtaining 24-hour urine samples from a random sample of 100 participants before and after the study. “This was my biggest fear – that as soon as we left the door, people would go and throw it away,” said Dr. Miranda. Among these participants, excreted potassium rose, indicating adherence, but sodium stayed basically the same. Possible explanations included that individuals were adding table salt to their diets, or that other prepared foods or condiments contained high amounts of sodium.
The study shows the feasibility of a community-wide intervention that achieved the dual aims of population-wide reductions in BP and reduction in incident BP, and of achieving clinically meaningful benefits for the high-risk population, said Dr. Miranda. He remarked that the population was young overall, with a mean age of 43 years and a low mean baseline systolic BP of 113, making the modest population-wide reduction more notable.
“We wanted to shift the entire distribution of blood pressure in the village. And with that, we see gains not only in public health, but also effective improvements in blood pressure in those at high risk, particularly those who tend to have high blood pressure,” said Dr. Miranda.
Discussant Bruce Neal, MD, professor of medicine at the University of Sydney and senior director of the George Institute for Global Health in Newtown, Australia, congratulated Dr. Miranda and colleagues on accomplishing “a truly enormous project.” He began by noting that, though the reductions were modest, “the low starting blood pressures were almost certainly responsible for the magnitude of effect seen in this study.” He added that “this is nonetheless a worthwhile blood pressure reduction, particularly if it was sustained throughout life.”
Addressing the lack of decrease in excreted urine sodium, Dr. Neal noted that participants may have supplemented their diet with additional sodium by one means or another, “which might also have attenuated the blood pressure difference – but it could also reflect the challenges of measuring sodium and potassium effectively with 24-hour urine samples, which are difficult to collect.”
The lack of adverse effects was notable, said Dr. Neal. “When considering the use of salt substitute at the population level, the first question that arises is: ‘What about the risks of hyperkalemia?’
“I think those risks are probably greatly overstated,” he said, noting that only individuals with severe chronic kidney disease would likely be affected, and those individuals are already well versed on the importance of avoiding excess dietary potassium.
The study was funded by the National Institutes of Health through the Global Alliance for Chronic Disease program. Dr. Miranda reported that he had no conflicts of interest. Dr. Neal reported that he has financial relationships with Nu-Tec Salt and a Beijing-based salt manufacturer, related to research into salt substitutes.
PARIS – In rural Peru, a comprehensive community-wide strategy to replace conventional table salt with a formulation that was 25% potassium chloride halved incident hypertension, also dropping blood pressure in participants with baseline hypertension.
The multifaceted intervention targeted six villages at the far north of Peru, replacing table salt with the lower-sodium substitute, J. Jaime Miranda, MD, PhD, said at a prevention-focused, late-breaking research session at the annual congress of the European Society of Cardiology. The 75/25 mixture had a palatable proportion of potassium, and was easily produced by combining table salt with potassium chloride crystals.
Dr. Miranda, director of the CRONICAS Center of Excellence at the Cayetano Heredia Peruvian University, Lima, and colleagues enrolled virtually all adult residents of the six villages in the study; patients who reported heart disease or chronic kidney disease were excluded.
“We wanted to achieve and shape a pragmatic study – and a pragmatic study that incorporates day-to-day behavior. We eat every day, but we think very little of our salt habits,” said Dr. Miranda in a video interview.
In all, 2,376 of 2,605 potential participants enrolled in the study, which used a stepped-wedge, cluster-randomized, controlled trial design. To track the primary outcome measures of systolic and diastolic BP, measurements were obtained every 5 months for a total of seven rounds of measurement, said Dr. Miranda.
Dr. Miranda said that the investigators borrowed principles from social marketing to ensure community-wide replacement of table salt with the low-sodium substitute. This meant that they branded and packaged the low-sodium salt and gave it to participants at no cost – but with a catch. To receive the low-sodium salt, participants had to turn in their table salt.
The effort was supported by promotional events and a trained “sales force” who brought messaging to families, restaurants, and key voices in the community. The attractively packaged replacement salt was distributed with a similarly branded shaker. “We wanted to guarantee the full replacement of salt in the entire village,” explained Dr. Miranda.
At the end of the study, individuals with hypertension saw a decrease in systolic BP of 1.92 mm Hg (95% confidence interval, –3.29 to –0.54).
New hypertension diagnoses, a secondary outcome measure, fell by 55% in participating villages; the hazard ratio for hypertension incidence was 0.45 (95% CI, 0.31-0.66) in a fully adjusted statistical model that accounted for clustering at the village level, as well as age, sex, education, wealth index, and body mass index, said Dr. Miranda.
Older village residents with hypertension saw greater BP reduction; for those aged at least 60 years, the mean reduction was 2.17 mm Hg (95% CI, –3.67 to –0.68).
The positive findings were met with broad applause during his presentation, a response that made his 15-hour trip from Lima to Paris worthwhile, said Dr. Miranda.
Adherence was assessed by obtaining 24-hour urine samples from a random sample of 100 participants before and after the study. “This was my biggest fear – that as soon as we left the door, people would go and throw it away,” said Dr. Miranda. Among these participants, excreted potassium rose, indicating adherence, but sodium stayed basically the same. Possible explanations included that individuals were adding table salt to their diets, or that other prepared foods or condiments contained high amounts of sodium.
The study shows the feasibility of a community-wide intervention that achieved the dual aims of population-wide reductions in BP and reduction in incident BP, and of achieving clinically meaningful benefits for the high-risk population, said Dr. Miranda. He remarked that the population was young overall, with a mean age of 43 years and a low mean baseline systolic BP of 113, making the modest population-wide reduction more notable.
“We wanted to shift the entire distribution of blood pressure in the village. And with that, we see gains not only in public health, but also effective improvements in blood pressure in those at high risk, particularly those who tend to have high blood pressure,” said Dr. Miranda.
Discussant Bruce Neal, MD, professor of medicine at the University of Sydney and senior director of the George Institute for Global Health in Newtown, Australia, congratulated Dr. Miranda and colleagues on accomplishing “a truly enormous project.” He began by noting that, though the reductions were modest, “the low starting blood pressures were almost certainly responsible for the magnitude of effect seen in this study.” He added that “this is nonetheless a worthwhile blood pressure reduction, particularly if it was sustained throughout life.”
Addressing the lack of decrease in excreted urine sodium, Dr. Neal noted that participants may have supplemented their diet with additional sodium by one means or another, “which might also have attenuated the blood pressure difference – but it could also reflect the challenges of measuring sodium and potassium effectively with 24-hour urine samples, which are difficult to collect.”
The lack of adverse effects was notable, said Dr. Neal. “When considering the use of salt substitute at the population level, the first question that arises is: ‘What about the risks of hyperkalemia?’
“I think those risks are probably greatly overstated,” he said, noting that only individuals with severe chronic kidney disease would likely be affected, and those individuals are already well versed on the importance of avoiding excess dietary potassium.
The study was funded by the National Institutes of Health through the Global Alliance for Chronic Disease program. Dr. Miranda reported that he had no conflicts of interest. Dr. Neal reported that he has financial relationships with Nu-Tec Salt and a Beijing-based salt manufacturer, related to research into salt substitutes.
REPORTING FROM THE ESC CONGRESS 2019
Genotyping for thrombosis control in PCI equal to standard therapy
Genotype-guided selection of oral P2Y 12 inhibitors for patients having percutaneous coronary intervention with stent implantation derives no clinical benefits overall when compared to standard treatment, according to results of the large, randomized POPular Genetics trial, although genotype guidance did result in lower rates of primary minor bleeding.
The study was presented at the annual congress of the European Society of Cardiology Study in Paris and published simultaneously in the New England Journal of Medicine.
POPular Genetics (CYP2C19 Genotype-Guided Antiplatelet Therapy in ST-Segment Elevation Myocardial Infarction Patients – Patient Outcome After Primary PCI) randomized 2,488 patients who had PCI to either P2Y12 inhibitor on the basis of early genetic testing for the CYP2C19 gene (1,242 patients) or standard treatment with either ticagrelor or prasugrel (1,246 patients) for 12 months. In the genotype-guided group, patients were assigned to one of two arms depending on results; carriers of CYP2C19*2 or CYP2C19*3 loss-of-function alleles received ticagrelor or prasugrel, and non-carriers receive clopidogrel. The study was conducted from Jun. 2011 to Apr. 2018.
Net adverse clinical events, which included any-cause death, myocardial infarction, stent thrombosis, stroke or major bleeding based on the Platelet Inhibition and Patient Outcomes (PLATO) criteria at 12 months were similar between both groups: 5.1% in the genotype-guided patients and 5.9% in the standard-treatment group (P less than .001), but rates of PLATO major or minor bleeding were 9.8% and 12.5%, respectively (P = .04).
When secondary outcomes were evaluated, no significant differences emerged between the two groups. Secondary outcomes included combined thrombotic outcomes (death from vascular causes, myocardial infarction, stent thrombosis or stroke; 2.7% for the genotype-guided group vs. 3.3% in the standard-treatment group), and PLATO major bleeding (2.3% in both groups). The difference in the primary bleeding outcomes between the groups was driven by a lower incidence of PLATO minor bleeding in the genotype-guided group, 7.6% vs. 10.5%.
The two takeaways from POPular Genetics, said Daniel M.F. Claassens, MD, and coauthors, are that giving clopidogrel to patients without a CYP2C19 loss-of-function allele did not elevate their risk of combined any-cause death and other adverse cardiac outcomes, including major bleeding, 12 months after PCI; and that giving clopidogrel to the genotype-guided group lowered the risk of minor bleeding.
Dr. Claassens and coauthors noted that since the Netherlands trial was designed in 2011, the development of newer-generation stents has considerably lowered rates of thrombotic events after acute coronary syndromes. “With the lower-than-anticipated incidence of the primary combined outcome in our trial, the prespecified noninferiority margin was wider relative to the incidence than originally expected,” they said. While the primary combined outcome was 21% higher than the incidence in the standard-treatment group at the upper end of the 95% confidence interval, the incidence was 11% higher in the standard-treatment group at the observed upper end of the 95% CI. This “gives stronger support to the conclusion that genotype-guided P2Y12 treatment is noninferior to standard treatment for the occurrence of thrombotic events,” Dr. Claassens and coauthors said.
The study report noted a number of limitations, including that more polymorphisms of the CyP2C19 gene may be linked to increased thrombotic or bleeding risk. “Therefore, our strategy based solely on the CYP2C19 genotype may not be the most useful strategy for some patients,” Dr. Claassens and coauthors said.
POPular Genetics received funding from the Netherlands Organization for Health Research and Development (ZonMw). Dr. Claassens receives grants from ZonMw and non-financial support from Spartan Biosciences.
SOURCE: Claassens DMF, et al. N Engl J. Med. Published online September 3, doi.org/10.1016/S0140-6736(19)31996-8.
Genotype-guided selection of oral P2Y 12 inhibitors for patients having percutaneous coronary intervention with stent implantation derives no clinical benefits overall when compared to standard treatment, according to results of the large, randomized POPular Genetics trial, although genotype guidance did result in lower rates of primary minor bleeding.
The study was presented at the annual congress of the European Society of Cardiology Study in Paris and published simultaneously in the New England Journal of Medicine.
POPular Genetics (CYP2C19 Genotype-Guided Antiplatelet Therapy in ST-Segment Elevation Myocardial Infarction Patients – Patient Outcome After Primary PCI) randomized 2,488 patients who had PCI to either P2Y12 inhibitor on the basis of early genetic testing for the CYP2C19 gene (1,242 patients) or standard treatment with either ticagrelor or prasugrel (1,246 patients) for 12 months. In the genotype-guided group, patients were assigned to one of two arms depending on results; carriers of CYP2C19*2 or CYP2C19*3 loss-of-function alleles received ticagrelor or prasugrel, and non-carriers receive clopidogrel. The study was conducted from Jun. 2011 to Apr. 2018.
Net adverse clinical events, which included any-cause death, myocardial infarction, stent thrombosis, stroke or major bleeding based on the Platelet Inhibition and Patient Outcomes (PLATO) criteria at 12 months were similar between both groups: 5.1% in the genotype-guided patients and 5.9% in the standard-treatment group (P less than .001), but rates of PLATO major or minor bleeding were 9.8% and 12.5%, respectively (P = .04).
When secondary outcomes were evaluated, no significant differences emerged between the two groups. Secondary outcomes included combined thrombotic outcomes (death from vascular causes, myocardial infarction, stent thrombosis or stroke; 2.7% for the genotype-guided group vs. 3.3% in the standard-treatment group), and PLATO major bleeding (2.3% in both groups). The difference in the primary bleeding outcomes between the groups was driven by a lower incidence of PLATO minor bleeding in the genotype-guided group, 7.6% vs. 10.5%.
The two takeaways from POPular Genetics, said Daniel M.F. Claassens, MD, and coauthors, are that giving clopidogrel to patients without a CYP2C19 loss-of-function allele did not elevate their risk of combined any-cause death and other adverse cardiac outcomes, including major bleeding, 12 months after PCI; and that giving clopidogrel to the genotype-guided group lowered the risk of minor bleeding.
Dr. Claassens and coauthors noted that since the Netherlands trial was designed in 2011, the development of newer-generation stents has considerably lowered rates of thrombotic events after acute coronary syndromes. “With the lower-than-anticipated incidence of the primary combined outcome in our trial, the prespecified noninferiority margin was wider relative to the incidence than originally expected,” they said. While the primary combined outcome was 21% higher than the incidence in the standard-treatment group at the upper end of the 95% confidence interval, the incidence was 11% higher in the standard-treatment group at the observed upper end of the 95% CI. This “gives stronger support to the conclusion that genotype-guided P2Y12 treatment is noninferior to standard treatment for the occurrence of thrombotic events,” Dr. Claassens and coauthors said.
The study report noted a number of limitations, including that more polymorphisms of the CyP2C19 gene may be linked to increased thrombotic or bleeding risk. “Therefore, our strategy based solely on the CYP2C19 genotype may not be the most useful strategy for some patients,” Dr. Claassens and coauthors said.
POPular Genetics received funding from the Netherlands Organization for Health Research and Development (ZonMw). Dr. Claassens receives grants from ZonMw and non-financial support from Spartan Biosciences.
SOURCE: Claassens DMF, et al. N Engl J. Med. Published online September 3, doi.org/10.1016/S0140-6736(19)31996-8.
Genotype-guided selection of oral P2Y 12 inhibitors for patients having percutaneous coronary intervention with stent implantation derives no clinical benefits overall when compared to standard treatment, according to results of the large, randomized POPular Genetics trial, although genotype guidance did result in lower rates of primary minor bleeding.
The study was presented at the annual congress of the European Society of Cardiology Study in Paris and published simultaneously in the New England Journal of Medicine.
POPular Genetics (CYP2C19 Genotype-Guided Antiplatelet Therapy in ST-Segment Elevation Myocardial Infarction Patients – Patient Outcome After Primary PCI) randomized 2,488 patients who had PCI to either P2Y12 inhibitor on the basis of early genetic testing for the CYP2C19 gene (1,242 patients) or standard treatment with either ticagrelor or prasugrel (1,246 patients) for 12 months. In the genotype-guided group, patients were assigned to one of two arms depending on results; carriers of CYP2C19*2 or CYP2C19*3 loss-of-function alleles received ticagrelor or prasugrel, and non-carriers receive clopidogrel. The study was conducted from Jun. 2011 to Apr. 2018.
Net adverse clinical events, which included any-cause death, myocardial infarction, stent thrombosis, stroke or major bleeding based on the Platelet Inhibition and Patient Outcomes (PLATO) criteria at 12 months were similar between both groups: 5.1% in the genotype-guided patients and 5.9% in the standard-treatment group (P less than .001), but rates of PLATO major or minor bleeding were 9.8% and 12.5%, respectively (P = .04).
When secondary outcomes were evaluated, no significant differences emerged between the two groups. Secondary outcomes included combined thrombotic outcomes (death from vascular causes, myocardial infarction, stent thrombosis or stroke; 2.7% for the genotype-guided group vs. 3.3% in the standard-treatment group), and PLATO major bleeding (2.3% in both groups). The difference in the primary bleeding outcomes between the groups was driven by a lower incidence of PLATO minor bleeding in the genotype-guided group, 7.6% vs. 10.5%.
The two takeaways from POPular Genetics, said Daniel M.F. Claassens, MD, and coauthors, are that giving clopidogrel to patients without a CYP2C19 loss-of-function allele did not elevate their risk of combined any-cause death and other adverse cardiac outcomes, including major bleeding, 12 months after PCI; and that giving clopidogrel to the genotype-guided group lowered the risk of minor bleeding.
Dr. Claassens and coauthors noted that since the Netherlands trial was designed in 2011, the development of newer-generation stents has considerably lowered rates of thrombotic events after acute coronary syndromes. “With the lower-than-anticipated incidence of the primary combined outcome in our trial, the prespecified noninferiority margin was wider relative to the incidence than originally expected,” they said. While the primary combined outcome was 21% higher than the incidence in the standard-treatment group at the upper end of the 95% confidence interval, the incidence was 11% higher in the standard-treatment group at the observed upper end of the 95% CI. This “gives stronger support to the conclusion that genotype-guided P2Y12 treatment is noninferior to standard treatment for the occurrence of thrombotic events,” Dr. Claassens and coauthors said.
The study report noted a number of limitations, including that more polymorphisms of the CyP2C19 gene may be linked to increased thrombotic or bleeding risk. “Therefore, our strategy based solely on the CYP2C19 genotype may not be the most useful strategy for some patients,” Dr. Claassens and coauthors said.
POPular Genetics received funding from the Netherlands Organization for Health Research and Development (ZonMw). Dr. Claassens receives grants from ZonMw and non-financial support from Spartan Biosciences.
SOURCE: Claassens DMF, et al. N Engl J. Med. Published online September 3, doi.org/10.1016/S0140-6736(19)31996-8.
AT THE ESC CONGRESS 2019
Key clinical point: Genotype-guided selection for oral P2Y12 inhibitors may benefit some patients.
Major finding: The genotype-guided group had primary bleeding rates of 9.8% vs. 12.5% for standard treatment.
Study details: POPular Genetics, an open-label blinded trial of 2,488 patients randomized to genotype-guided treatment or standard treatment after PCI, conducted from June 2011 through April 2018.
Disclosures: The study received funding from the Netherlands Organization for Health Research and Development (ZonMw). Dr. Claassens received grants from ZonMw and nonfinancial support from Spartan Biosciences.
Source: Claassens DMF, et al. N Engl J. Med. Published online September 3,doi.org/10.1016/S0140-6736(19)31996-8
In PAD, dropping statins ups death risk 43%
PARIS – , according to new research presented at the annual congress of the European Society of Cardiology.
Patients with peripheral manifestations of cardiovascular disease “are a population with an extremely high risk to suffer a heart attack or a stroke,” said Joern Dopheide, MD, during a press conference at the meeting. Despite the known benefits of statins, including the reduction of all-cause and cardiovascular death and the reduction of morbidity, adherence to guideline-directed statin therapy is far from optimal, said Dr. Dopheide of Bern (Switzerland) University Hospital.
Patients with peripheral artery disease (PAD) not taking statins had a mortality rate of 34%, more than three times that of patients adherent to an intensified statin regimen. More surprisingly, patients who had been on a statin and then stopped the medication also had a mortality rate of 33%, indistinguishable from those who had never been treated with a statin.
Although statin adherence is low in general, it’s especially low in patients with PAD, said Dr. Dopheide. Still, he said, “few systematic data exist on the prognostic value of statin adherence and the correlation between adherence and cardiovascular outcome in PAD patients.”
Accordingly, Dr. Dopheide and his coinvestigators sought to determine the association between statin adherence and survival in PAD patients. The researchers obtained baseline and follow-up data for a cohort of 691 symptomatic PAD patients seen at a single site, looking at statin dosage, LDL cholesterol levels, and survival.
The patients were followed for a period of 50 months. Dr. Dopheide said that “Over the time course, we were able to increase the statin adherence from about 73% to about 81%, and parallel to that, we were able to reduce the LDL cholesterol levels from about 97 to 83 mg/dL, and we were able to increase the intensity of patients on statin therapy.”
Dr. Dopheide said that he and his colleagues saw a dose-response effect, so that the biggest drop in cholesterol was seen in patients on high statin doses, on more potent statins, or both.
Intensity was increased in some cases by upping statin dose – the mean statin dose climbed from 50 to 58 mg daily during the study period. An alternative strategy was to switch to a more potent statin such as atorvastatin or rosuvastatin; sometimes both intensity and dose were boosted.
“We were able to see that patients who were always on their statin therapy had a pretty low mortality rate of about 20%,” a figure that was halved for patients on more intensive statin therapy, who had a mortality rate of 10% across the study period, said Dr. Dopheide. “Patients in whom we started a statin therapy still profited from it, and had only a 15% mortality,” he added.
Some of the most surprising – and disturbing – study findings involved those who reduced their statin dose: “When patients discontinued their usual dose and decreased it, they suffered an even higher mortality rate, of nearly 43%. So that was kind of surprising and shocking to us.”
Identifying these high-risk patients and keeping them adherent is a substantial clinical challenge, but an important goal, said Dr. Dopheide. “We know that patients with peripheral arterial disease are a little more underrepresented in daily practice; it’s hard to identify them, especially when they are asymptomatic,” he acknowledged. However, once a PAD patient is identified, “One should at least keep the patient on the statin dosage they have,” or initiate statins if needed.
Further, warned Dr. Dopheide, “One should never discontinue statin or decrease the dosage,” adding that PAD patients should be informed that they are at “very high risk for myocardial infarction or stroke.” These patients “should regard their statin therapy as one of the most important and life-saving medications they can take,” he said.
Dr. Dopheide reported no outside sources of funding and no conflicts of interest.
SOURCE: Dopheide, J., et al. ESC Congress 2019, Abstract P5363.
PARIS – , according to new research presented at the annual congress of the European Society of Cardiology.
Patients with peripheral manifestations of cardiovascular disease “are a population with an extremely high risk to suffer a heart attack or a stroke,” said Joern Dopheide, MD, during a press conference at the meeting. Despite the known benefits of statins, including the reduction of all-cause and cardiovascular death and the reduction of morbidity, adherence to guideline-directed statin therapy is far from optimal, said Dr. Dopheide of Bern (Switzerland) University Hospital.
Patients with peripheral artery disease (PAD) not taking statins had a mortality rate of 34%, more than three times that of patients adherent to an intensified statin regimen. More surprisingly, patients who had been on a statin and then stopped the medication also had a mortality rate of 33%, indistinguishable from those who had never been treated with a statin.
Although statin adherence is low in general, it’s especially low in patients with PAD, said Dr. Dopheide. Still, he said, “few systematic data exist on the prognostic value of statin adherence and the correlation between adherence and cardiovascular outcome in PAD patients.”
Accordingly, Dr. Dopheide and his coinvestigators sought to determine the association between statin adherence and survival in PAD patients. The researchers obtained baseline and follow-up data for a cohort of 691 symptomatic PAD patients seen at a single site, looking at statin dosage, LDL cholesterol levels, and survival.
The patients were followed for a period of 50 months. Dr. Dopheide said that “Over the time course, we were able to increase the statin adherence from about 73% to about 81%, and parallel to that, we were able to reduce the LDL cholesterol levels from about 97 to 83 mg/dL, and we were able to increase the intensity of patients on statin therapy.”
Dr. Dopheide said that he and his colleagues saw a dose-response effect, so that the biggest drop in cholesterol was seen in patients on high statin doses, on more potent statins, or both.
Intensity was increased in some cases by upping statin dose – the mean statin dose climbed from 50 to 58 mg daily during the study period. An alternative strategy was to switch to a more potent statin such as atorvastatin or rosuvastatin; sometimes both intensity and dose were boosted.
“We were able to see that patients who were always on their statin therapy had a pretty low mortality rate of about 20%,” a figure that was halved for patients on more intensive statin therapy, who had a mortality rate of 10% across the study period, said Dr. Dopheide. “Patients in whom we started a statin therapy still profited from it, and had only a 15% mortality,” he added.
Some of the most surprising – and disturbing – study findings involved those who reduced their statin dose: “When patients discontinued their usual dose and decreased it, they suffered an even higher mortality rate, of nearly 43%. So that was kind of surprising and shocking to us.”
Identifying these high-risk patients and keeping them adherent is a substantial clinical challenge, but an important goal, said Dr. Dopheide. “We know that patients with peripheral arterial disease are a little more underrepresented in daily practice; it’s hard to identify them, especially when they are asymptomatic,” he acknowledged. However, once a PAD patient is identified, “One should at least keep the patient on the statin dosage they have,” or initiate statins if needed.
Further, warned Dr. Dopheide, “One should never discontinue statin or decrease the dosage,” adding that PAD patients should be informed that they are at “very high risk for myocardial infarction or stroke.” These patients “should regard their statin therapy as one of the most important and life-saving medications they can take,” he said.
Dr. Dopheide reported no outside sources of funding and no conflicts of interest.
SOURCE: Dopheide, J., et al. ESC Congress 2019, Abstract P5363.
PARIS – , according to new research presented at the annual congress of the European Society of Cardiology.
Patients with peripheral manifestations of cardiovascular disease “are a population with an extremely high risk to suffer a heart attack or a stroke,” said Joern Dopheide, MD, during a press conference at the meeting. Despite the known benefits of statins, including the reduction of all-cause and cardiovascular death and the reduction of morbidity, adherence to guideline-directed statin therapy is far from optimal, said Dr. Dopheide of Bern (Switzerland) University Hospital.
Patients with peripheral artery disease (PAD) not taking statins had a mortality rate of 34%, more than three times that of patients adherent to an intensified statin regimen. More surprisingly, patients who had been on a statin and then stopped the medication also had a mortality rate of 33%, indistinguishable from those who had never been treated with a statin.
Although statin adherence is low in general, it’s especially low in patients with PAD, said Dr. Dopheide. Still, he said, “few systematic data exist on the prognostic value of statin adherence and the correlation between adherence and cardiovascular outcome in PAD patients.”
Accordingly, Dr. Dopheide and his coinvestigators sought to determine the association between statin adherence and survival in PAD patients. The researchers obtained baseline and follow-up data for a cohort of 691 symptomatic PAD patients seen at a single site, looking at statin dosage, LDL cholesterol levels, and survival.
The patients were followed for a period of 50 months. Dr. Dopheide said that “Over the time course, we were able to increase the statin adherence from about 73% to about 81%, and parallel to that, we were able to reduce the LDL cholesterol levels from about 97 to 83 mg/dL, and we were able to increase the intensity of patients on statin therapy.”
Dr. Dopheide said that he and his colleagues saw a dose-response effect, so that the biggest drop in cholesterol was seen in patients on high statin doses, on more potent statins, or both.
Intensity was increased in some cases by upping statin dose – the mean statin dose climbed from 50 to 58 mg daily during the study period. An alternative strategy was to switch to a more potent statin such as atorvastatin or rosuvastatin; sometimes both intensity and dose were boosted.
“We were able to see that patients who were always on their statin therapy had a pretty low mortality rate of about 20%,” a figure that was halved for patients on more intensive statin therapy, who had a mortality rate of 10% across the study period, said Dr. Dopheide. “Patients in whom we started a statin therapy still profited from it, and had only a 15% mortality,” he added.
Some of the most surprising – and disturbing – study findings involved those who reduced their statin dose: “When patients discontinued their usual dose and decreased it, they suffered an even higher mortality rate, of nearly 43%. So that was kind of surprising and shocking to us.”
Identifying these high-risk patients and keeping them adherent is a substantial clinical challenge, but an important goal, said Dr. Dopheide. “We know that patients with peripheral arterial disease are a little more underrepresented in daily practice; it’s hard to identify them, especially when they are asymptomatic,” he acknowledged. However, once a PAD patient is identified, “One should at least keep the patient on the statin dosage they have,” or initiate statins if needed.
Further, warned Dr. Dopheide, “One should never discontinue statin or decrease the dosage,” adding that PAD patients should be informed that they are at “very high risk for myocardial infarction or stroke.” These patients “should regard their statin therapy as one of the most important and life-saving medications they can take,” he said.
Dr. Dopheide reported no outside sources of funding and no conflicts of interest.
SOURCE: Dopheide, J., et al. ESC Congress 2019, Abstract P5363.
AT ESC CONGRESS 2019
DAPA-HF results transform dapagliflozin from antidiabetic to heart failure drug
PARIS – Treatment with the SGLT2 inhibitor dapagliflozin produced a statistically significant 27% drop in cardiovascular death or heart failure events in patients with existing heart failure with reduced ejection fraction and no diabetes, results that in a stroke changed the status of dapagliflozin from fundamentally a drug that treats diabetes to a drug that treats heart failure.

“Dapagliflozin offers a new approach to the treatment of heart failure with reduced ejection fraction” (HFrEF), John McMurray, MD, said at the annual congress of the European Society of Cardiology.
The results he reported from the DAPA-HF (Study to Evaluate the Effect of Dapagliflozin on the Incidence of Worsening Heart Failure or Cardiovascular Death in Patients With Chronic Heart Failure) trial showed statistically significant benefits when adding dapagliflozin to guideline-directed therapy for a list of outcomes that include a 17% drop in all-cause death compared with placebo, an 18% fall in cardiovascular death, and a 25% relative reduction in total heart failure hospitalizations plus cardiovascular deaths during a median follow-up of just over 18 months. The primary endpoint of the reduction in cardiovascular death, first heart failure hospitalization, or an urgent heart failure visit fell by 25% in the enrolled patients with diabetes (45% of the study population, all with type 2 diabetes), and by 27% in the remaining patients who had no diabetes, showing that the presence of diabetes had no impact on the heart failure benefit from dapagliflozin (Farxiga). The absolute reduction in the primary endpoint was about 5%, with a number needed to treat of 21 to prevent one primary endpoint during 18 months of treatment.
Dr. McMurray’s report of the primary endpoint as well as the finding that the drug was as effective in patients without diabetes as in those with diabetes were both met with loud applause by the packed congress audience.
The efficacy results also showed that 58% of patients on dapagliflozin had a clinically meaningful (5 point or greater) increase in their quality of life score on the Kansas City Cardiomyopathy Questionnaire after 8 months on treatment compared with a 51% rate in the placebo patients, a statistically significant difference.
The safety results showed no new signals for a drug that already has regulatory approval but was being used in a novel population. The rate of major hypoglycemia was virtually nonexistent, 0.2%, and identical in both treatment arms. All adverse events occurred at roughly equal rates in the dapagliflozin and placebo groups, with a 5% rate of adverse events leading to study discontinuation in both arms, and a serious adverse event rate of 38% in the dapaglifolzin patients and 42% in the placebo patients. The rate of worsening renal function was less than 2% in both arms and not statistically different.
“This is as close to a home run as you see in heart failure treatment,” commented Douglas L. Mann, MD, professor of medicine at Washington University, St. Louis, and a heart failure clinician and researcher.
DAPA-HF “is a landmark trial. It took a diabetes drug and used it in patients without diabetes, a concept that would have been considered outlandish 5 years ago. Scientifically it’s huge,” commented Deepak L. Bhatt, MD, professor of medicine at Harvard Medical School in Boston.
The DAPA-HF results were another step in the remarkable journey toward heart failure intervention taken by the SGLT2 (sodium glucose cotransport 2) inhibitor class of drugs that includes dapagliflozin as well as canagliflozin (Invokana) and empagliflozin(Jardiance), a path that began 4 years ago with the report of empagliflozin’s unexpected efficacy for reducing cardiovascular death and heart failure hospitalizations in a large cardiovascular-safety study, EMPA-REG OUTCOME (N Engl J Med. 2015 Nov 26;373[22]:2117-28). Subsequent reports showed similar effects benefiting heart failure and survival for canagliflozin and dapagliflozin, and now with DAPA-HF the evidence extended the benefit to heart failure patients regardless of whether they have diabetes. Additional studies now in progress are exploring the same question for empagliflozin and canagliflozin.
The results from DAPA-HF are likely a class effect for all these SGLT2 inhibitors, suggested Dr. McMurray in a video interview, a view shared by several other experts. He cautioned clinicians against using dapagliflozin to treat patients with heart failure with reduced ejection fraction (HFrEF) but without diabetes until this indication receives regulatory approval, and even then using dapagliflozin or other SGLT2 inhibitors this way may take some getting used to on the part of cardiologists and other clinicians.
“The results put dapagliflozin in the same league as [standard HFrEF drugs], but using it will require a shift in thinking. Most physicians will initially say “aren’t SGLT2 inhibitors used for treating diabetes?” Dr. Bhatt said.
“I’m sure most cardiologists are not familiar with the SGLT2 inhibitors; we’ll have to educate them,” conceded Dr. McMurray, professor of medical cardiology at the University of Glasgow. However, other aspects of dapagliflozin and this drug class in general may make the SGLT2 inhibitors particularly attractive and spur their use once labeling changes.
The adverse-event profile seen in DAPA-HF looked very “clean,” said Dr. Mann, especially compared with the other medical classes recommended in guidelines for patients with HFrEF: the angiotensin converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), beta-blockers, and mineralocorticoid-receptor antagonists such as spironolactone, and the angiotensin receptor-neprilysin inhibitor (ARNI) sacubitril-valsartan (Entresto). As used in DAPA-HF dapagliflozin also had the advantages of not needing dose titration or laboratory follow-up, as do several of these other drug classes.
“I think dapagliflozin will have a huge uptake [for treating HFrEF], because it will be easy for primary care physicians to prescribe. It will be easier to use than traditional heart failure medications.” Once approved for heart failure use, Dr. Mann predicted a standard dosing regimen for HFrEF patients of an ACE inhibitor, ARB or ARNI, a beta-blocker, a mineralocorticoid-receptor antagonist, and an SGLT2 inhibitor. He suggested that this large and cumbersome collection of medications could conceivably be simplified into a polypill.
He also saw a suggestion in the DAPA-HF results that combining dapagliflozin with the ARB valsartan might have similar efficacy to dapaglifozin plus sacubitril-valsartan, which might also help simplify heart failure treatment. In the trial, 11% of patients received sacubritril-valsartan, and the primary-endpoint reduction compared with placebo in this subgroup was 26%, compared with 25% for patients treated with an ACE inhibitor or ARB. Currently, labeling for sacubitril-valsartan calls for starting a patients on an ACE inhibitor or ARB, titrating them to a stable and effective dosage, and then stopping this regimen to switch to the ARNI. If dapagliflozin is also added, then a simpler approach would be to just start a patient on valsartan, optimize the dosage, and then start dapagliflozin and achieve the same benefit as from sacubitril-valsartan plus dapagliflozin. While an attractive scenario, it needs validation, Dr. Mann said in an interview.
One additional, notable finding from DAPA-HF was that the primary endpoint benefit appeared much stronger in patients with New York Heart Association class II heart failure at entry, two-thirds of the study population, compared with patients with class III or IV HFrEF. Compared with placebo the primary endpoint fell by 37% among the class II patients, a statistically significant difference, but by just 10% in the class III and IV patients, a reduction that was not significant compared with placebo. This too needs more study, commented Dr. Mann, as does the ways by which dapagliflozin and the other SGLT2 inhibitors benefit heart failure patients. Currently the ways by which dapagliflozin produced these results remain unknown.
DAPA-HF randomized a total of 4,744 patients at 410 sites in 20 countries. About 10% of enrolled patients were in the United States.
DAPA-HF was sponsored by AstraZeneca, the company that markets dapagliflozin (Farxiga). AstraZeneca paid Glasgow University to cover Dr. McMurray’s salary during the time he spent working as principal investigator of DAPA-HF. Dr. McMurray had no other relevant disclosures. Dr. Mann has been a consultant to Bristol-Myers Squibb, LivaNova, Novartis, and Tenaya Therapeutics. Dr. Bhatt has received research funding from AstraZeneca, and he has served as a consultant to or received research funding from several other companies.
PARIS – Treatment with the SGLT2 inhibitor dapagliflozin produced a statistically significant 27% drop in cardiovascular death or heart failure events in patients with existing heart failure with reduced ejection fraction and no diabetes, results that in a stroke changed the status of dapagliflozin from fundamentally a drug that treats diabetes to a drug that treats heart failure.

“Dapagliflozin offers a new approach to the treatment of heart failure with reduced ejection fraction” (HFrEF), John McMurray, MD, said at the annual congress of the European Society of Cardiology.
The results he reported from the DAPA-HF (Study to Evaluate the Effect of Dapagliflozin on the Incidence of Worsening Heart Failure or Cardiovascular Death in Patients With Chronic Heart Failure) trial showed statistically significant benefits when adding dapagliflozin to guideline-directed therapy for a list of outcomes that include a 17% drop in all-cause death compared with placebo, an 18% fall in cardiovascular death, and a 25% relative reduction in total heart failure hospitalizations plus cardiovascular deaths during a median follow-up of just over 18 months. The primary endpoint of the reduction in cardiovascular death, first heart failure hospitalization, or an urgent heart failure visit fell by 25% in the enrolled patients with diabetes (45% of the study population, all with type 2 diabetes), and by 27% in the remaining patients who had no diabetes, showing that the presence of diabetes had no impact on the heart failure benefit from dapagliflozin (Farxiga). The absolute reduction in the primary endpoint was about 5%, with a number needed to treat of 21 to prevent one primary endpoint during 18 months of treatment.
Dr. McMurray’s report of the primary endpoint as well as the finding that the drug was as effective in patients without diabetes as in those with diabetes were both met with loud applause by the packed congress audience.
The efficacy results also showed that 58% of patients on dapagliflozin had a clinically meaningful (5 point or greater) increase in their quality of life score on the Kansas City Cardiomyopathy Questionnaire after 8 months on treatment compared with a 51% rate in the placebo patients, a statistically significant difference.
The safety results showed no new signals for a drug that already has regulatory approval but was being used in a novel population. The rate of major hypoglycemia was virtually nonexistent, 0.2%, and identical in both treatment arms. All adverse events occurred at roughly equal rates in the dapagliflozin and placebo groups, with a 5% rate of adverse events leading to study discontinuation in both arms, and a serious adverse event rate of 38% in the dapaglifolzin patients and 42% in the placebo patients. The rate of worsening renal function was less than 2% in both arms and not statistically different.
“This is as close to a home run as you see in heart failure treatment,” commented Douglas L. Mann, MD, professor of medicine at Washington University, St. Louis, and a heart failure clinician and researcher.
DAPA-HF “is a landmark trial. It took a diabetes drug and used it in patients without diabetes, a concept that would have been considered outlandish 5 years ago. Scientifically it’s huge,” commented Deepak L. Bhatt, MD, professor of medicine at Harvard Medical School in Boston.
The DAPA-HF results were another step in the remarkable journey toward heart failure intervention taken by the SGLT2 (sodium glucose cotransport 2) inhibitor class of drugs that includes dapagliflozin as well as canagliflozin (Invokana) and empagliflozin(Jardiance), a path that began 4 years ago with the report of empagliflozin’s unexpected efficacy for reducing cardiovascular death and heart failure hospitalizations in a large cardiovascular-safety study, EMPA-REG OUTCOME (N Engl J Med. 2015 Nov 26;373[22]:2117-28). Subsequent reports showed similar effects benefiting heart failure and survival for canagliflozin and dapagliflozin, and now with DAPA-HF the evidence extended the benefit to heart failure patients regardless of whether they have diabetes. Additional studies now in progress are exploring the same question for empagliflozin and canagliflozin.
The results from DAPA-HF are likely a class effect for all these SGLT2 inhibitors, suggested Dr. McMurray in a video interview, a view shared by several other experts. He cautioned clinicians against using dapagliflozin to treat patients with heart failure with reduced ejection fraction (HFrEF) but without diabetes until this indication receives regulatory approval, and even then using dapagliflozin or other SGLT2 inhibitors this way may take some getting used to on the part of cardiologists and other clinicians.
“The results put dapagliflozin in the same league as [standard HFrEF drugs], but using it will require a shift in thinking. Most physicians will initially say “aren’t SGLT2 inhibitors used for treating diabetes?” Dr. Bhatt said.
“I’m sure most cardiologists are not familiar with the SGLT2 inhibitors; we’ll have to educate them,” conceded Dr. McMurray, professor of medical cardiology at the University of Glasgow. However, other aspects of dapagliflozin and this drug class in general may make the SGLT2 inhibitors particularly attractive and spur their use once labeling changes.
The adverse-event profile seen in DAPA-HF looked very “clean,” said Dr. Mann, especially compared with the other medical classes recommended in guidelines for patients with HFrEF: the angiotensin converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), beta-blockers, and mineralocorticoid-receptor antagonists such as spironolactone, and the angiotensin receptor-neprilysin inhibitor (ARNI) sacubitril-valsartan (Entresto). As used in DAPA-HF dapagliflozin also had the advantages of not needing dose titration or laboratory follow-up, as do several of these other drug classes.
“I think dapagliflozin will have a huge uptake [for treating HFrEF], because it will be easy for primary care physicians to prescribe. It will be easier to use than traditional heart failure medications.” Once approved for heart failure use, Dr. Mann predicted a standard dosing regimen for HFrEF patients of an ACE inhibitor, ARB or ARNI, a beta-blocker, a mineralocorticoid-receptor antagonist, and an SGLT2 inhibitor. He suggested that this large and cumbersome collection of medications could conceivably be simplified into a polypill.
He also saw a suggestion in the DAPA-HF results that combining dapagliflozin with the ARB valsartan might have similar efficacy to dapaglifozin plus sacubitril-valsartan, which might also help simplify heart failure treatment. In the trial, 11% of patients received sacubritril-valsartan, and the primary-endpoint reduction compared with placebo in this subgroup was 26%, compared with 25% for patients treated with an ACE inhibitor or ARB. Currently, labeling for sacubitril-valsartan calls for starting a patients on an ACE inhibitor or ARB, titrating them to a stable and effective dosage, and then stopping this regimen to switch to the ARNI. If dapagliflozin is also added, then a simpler approach would be to just start a patient on valsartan, optimize the dosage, and then start dapagliflozin and achieve the same benefit as from sacubitril-valsartan plus dapagliflozin. While an attractive scenario, it needs validation, Dr. Mann said in an interview.
One additional, notable finding from DAPA-HF was that the primary endpoint benefit appeared much stronger in patients with New York Heart Association class II heart failure at entry, two-thirds of the study population, compared with patients with class III or IV HFrEF. Compared with placebo the primary endpoint fell by 37% among the class II patients, a statistically significant difference, but by just 10% in the class III and IV patients, a reduction that was not significant compared with placebo. This too needs more study, commented Dr. Mann, as does the ways by which dapagliflozin and the other SGLT2 inhibitors benefit heart failure patients. Currently the ways by which dapagliflozin produced these results remain unknown.
DAPA-HF randomized a total of 4,744 patients at 410 sites in 20 countries. About 10% of enrolled patients were in the United States.
DAPA-HF was sponsored by AstraZeneca, the company that markets dapagliflozin (Farxiga). AstraZeneca paid Glasgow University to cover Dr. McMurray’s salary during the time he spent working as principal investigator of DAPA-HF. Dr. McMurray had no other relevant disclosures. Dr. Mann has been a consultant to Bristol-Myers Squibb, LivaNova, Novartis, and Tenaya Therapeutics. Dr. Bhatt has received research funding from AstraZeneca, and he has served as a consultant to or received research funding from several other companies.
PARIS – Treatment with the SGLT2 inhibitor dapagliflozin produced a statistically significant 27% drop in cardiovascular death or heart failure events in patients with existing heart failure with reduced ejection fraction and no diabetes, results that in a stroke changed the status of dapagliflozin from fundamentally a drug that treats diabetes to a drug that treats heart failure.

“Dapagliflozin offers a new approach to the treatment of heart failure with reduced ejection fraction” (HFrEF), John McMurray, MD, said at the annual congress of the European Society of Cardiology.
The results he reported from the DAPA-HF (Study to Evaluate the Effect of Dapagliflozin on the Incidence of Worsening Heart Failure or Cardiovascular Death in Patients With Chronic Heart Failure) trial showed statistically significant benefits when adding dapagliflozin to guideline-directed therapy for a list of outcomes that include a 17% drop in all-cause death compared with placebo, an 18% fall in cardiovascular death, and a 25% relative reduction in total heart failure hospitalizations plus cardiovascular deaths during a median follow-up of just over 18 months. The primary endpoint of the reduction in cardiovascular death, first heart failure hospitalization, or an urgent heart failure visit fell by 25% in the enrolled patients with diabetes (45% of the study population, all with type 2 diabetes), and by 27% in the remaining patients who had no diabetes, showing that the presence of diabetes had no impact on the heart failure benefit from dapagliflozin (Farxiga). The absolute reduction in the primary endpoint was about 5%, with a number needed to treat of 21 to prevent one primary endpoint during 18 months of treatment.
Dr. McMurray’s report of the primary endpoint as well as the finding that the drug was as effective in patients without diabetes as in those with diabetes were both met with loud applause by the packed congress audience.
The efficacy results also showed that 58% of patients on dapagliflozin had a clinically meaningful (5 point or greater) increase in their quality of life score on the Kansas City Cardiomyopathy Questionnaire after 8 months on treatment compared with a 51% rate in the placebo patients, a statistically significant difference.
The safety results showed no new signals for a drug that already has regulatory approval but was being used in a novel population. The rate of major hypoglycemia was virtually nonexistent, 0.2%, and identical in both treatment arms. All adverse events occurred at roughly equal rates in the dapagliflozin and placebo groups, with a 5% rate of adverse events leading to study discontinuation in both arms, and a serious adverse event rate of 38% in the dapaglifolzin patients and 42% in the placebo patients. The rate of worsening renal function was less than 2% in both arms and not statistically different.
“This is as close to a home run as you see in heart failure treatment,” commented Douglas L. Mann, MD, professor of medicine at Washington University, St. Louis, and a heart failure clinician and researcher.
DAPA-HF “is a landmark trial. It took a diabetes drug and used it in patients without diabetes, a concept that would have been considered outlandish 5 years ago. Scientifically it’s huge,” commented Deepak L. Bhatt, MD, professor of medicine at Harvard Medical School in Boston.
The DAPA-HF results were another step in the remarkable journey toward heart failure intervention taken by the SGLT2 (sodium glucose cotransport 2) inhibitor class of drugs that includes dapagliflozin as well as canagliflozin (Invokana) and empagliflozin(Jardiance), a path that began 4 years ago with the report of empagliflozin’s unexpected efficacy for reducing cardiovascular death and heart failure hospitalizations in a large cardiovascular-safety study, EMPA-REG OUTCOME (N Engl J Med. 2015 Nov 26;373[22]:2117-28). Subsequent reports showed similar effects benefiting heart failure and survival for canagliflozin and dapagliflozin, and now with DAPA-HF the evidence extended the benefit to heart failure patients regardless of whether they have diabetes. Additional studies now in progress are exploring the same question for empagliflozin and canagliflozin.
The results from DAPA-HF are likely a class effect for all these SGLT2 inhibitors, suggested Dr. McMurray in a video interview, a view shared by several other experts. He cautioned clinicians against using dapagliflozin to treat patients with heart failure with reduced ejection fraction (HFrEF) but without diabetes until this indication receives regulatory approval, and even then using dapagliflozin or other SGLT2 inhibitors this way may take some getting used to on the part of cardiologists and other clinicians.
“The results put dapagliflozin in the same league as [standard HFrEF drugs], but using it will require a shift in thinking. Most physicians will initially say “aren’t SGLT2 inhibitors used for treating diabetes?” Dr. Bhatt said.
“I’m sure most cardiologists are not familiar with the SGLT2 inhibitors; we’ll have to educate them,” conceded Dr. McMurray, professor of medical cardiology at the University of Glasgow. However, other aspects of dapagliflozin and this drug class in general may make the SGLT2 inhibitors particularly attractive and spur their use once labeling changes.
The adverse-event profile seen in DAPA-HF looked very “clean,” said Dr. Mann, especially compared with the other medical classes recommended in guidelines for patients with HFrEF: the angiotensin converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), beta-blockers, and mineralocorticoid-receptor antagonists such as spironolactone, and the angiotensin receptor-neprilysin inhibitor (ARNI) sacubitril-valsartan (Entresto). As used in DAPA-HF dapagliflozin also had the advantages of not needing dose titration or laboratory follow-up, as do several of these other drug classes.
“I think dapagliflozin will have a huge uptake [for treating HFrEF], because it will be easy for primary care physicians to prescribe. It will be easier to use than traditional heart failure medications.” Once approved for heart failure use, Dr. Mann predicted a standard dosing regimen for HFrEF patients of an ACE inhibitor, ARB or ARNI, a beta-blocker, a mineralocorticoid-receptor antagonist, and an SGLT2 inhibitor. He suggested that this large and cumbersome collection of medications could conceivably be simplified into a polypill.
He also saw a suggestion in the DAPA-HF results that combining dapagliflozin with the ARB valsartan might have similar efficacy to dapaglifozin plus sacubitril-valsartan, which might also help simplify heart failure treatment. In the trial, 11% of patients received sacubritril-valsartan, and the primary-endpoint reduction compared with placebo in this subgroup was 26%, compared with 25% for patients treated with an ACE inhibitor or ARB. Currently, labeling for sacubitril-valsartan calls for starting a patients on an ACE inhibitor or ARB, titrating them to a stable and effective dosage, and then stopping this regimen to switch to the ARNI. If dapagliflozin is also added, then a simpler approach would be to just start a patient on valsartan, optimize the dosage, and then start dapagliflozin and achieve the same benefit as from sacubitril-valsartan plus dapagliflozin. While an attractive scenario, it needs validation, Dr. Mann said in an interview.
One additional, notable finding from DAPA-HF was that the primary endpoint benefit appeared much stronger in patients with New York Heart Association class II heart failure at entry, two-thirds of the study population, compared with patients with class III or IV HFrEF. Compared with placebo the primary endpoint fell by 37% among the class II patients, a statistically significant difference, but by just 10% in the class III and IV patients, a reduction that was not significant compared with placebo. This too needs more study, commented Dr. Mann, as does the ways by which dapagliflozin and the other SGLT2 inhibitors benefit heart failure patients. Currently the ways by which dapagliflozin produced these results remain unknown.
DAPA-HF randomized a total of 4,744 patients at 410 sites in 20 countries. About 10% of enrolled patients were in the United States.
DAPA-HF was sponsored by AstraZeneca, the company that markets dapagliflozin (Farxiga). AstraZeneca paid Glasgow University to cover Dr. McMurray’s salary during the time he spent working as principal investigator of DAPA-HF. Dr. McMurray had no other relevant disclosures. Dr. Mann has been a consultant to Bristol-Myers Squibb, LivaNova, Novartis, and Tenaya Therapeutics. Dr. Bhatt has received research funding from AstraZeneca, and he has served as a consultant to or received research funding from several other companies.
REPORTING FROM THE ESC CONGRESS 2019
Key clinical point: Dapagliflozin produced multiple, statistically significant benefits in heart failure patients on top of guideline-directed therapy.
Major finding: The study’s primary endpoint fell by a statistically significant 27% with dapagliflozin compared with placebo in patients without diabetes.
Study details: DAPA-HF, a multinational study with 4,744 patients at 410 sites.
Disclosures: DAPA-HF was sponsored by AstraZeneca, the company that markets dapagliflozin (Farxiga). AstraZeneca paid Glasgow University to cover Dr. McMurray’s salary during the time he spent working as principal investigator of DAPA-HF.
Community intervention curbs CV disease in hypertensive adults
A community-based care model to control hypertension led by nonphysician health care workers significantly reduced cardiovascular disease risk over 12 months, data from a cluster-controlled randomized study has shown.
Hypertension remains the most common risk factor for cardiovascular disease, but fewer than 20% of individuals with hypertension have their blood pressure controlled, wrote Jon-David Schwalm, MD, of McMaster University in Hamilton, Ont., and colleagues. To help control hypertension in underserved populations, the researchers tested a care model involving nonphysician health workers (NPHWs), primary care physicians, and family members.
The HOPE4 study, presented at the annual congress of the European Society of Cardiology and published simultaneously in the Lancet, included 1,371 adults aged 50 years and older with new or poorly controlled hypertension from 30 communities in Colombia and Malaysia. Sixteen communities were randomized to usual care and 14 to an intervention. The intervention included community screening and treatment of cardiovascular disease risk factors by NPHWs, free medications recommended by NPHWs under physician supervision, and family support for treatment adherence.
After 12 months, the Framingham Risk Scores for 10-year cardiovascular disease risk were significantly lower in the intervention group, compared with the control group (–11.17% vs. –6.40%). In addition, the intervention group showed a significant 11.45 mm Hg greater reduction in systolic blood pressure and a significant 0.41 mmol/L reduction in LDL cholesterol, compared with controls (P less than .0001 for both measures).
Baseline characteristics were similar between the two groups. Approximately 74% of the participants had a history of poorly controlled hypertension, while the remaining patients had new hypertension diagnoses.
“NPHWs were found to be consistently accurate in their ability to identify cardiovascular risk (patient identified by NPHWs as having poorly controlled blood pressure and medication was indicated) and recommend appropriate therapies (antihypertensives and statin as per the study algorithm) when compared with the assessment by local primary care physicians,” the researchers wrote. The study shows how effectively NPHWs can help reduce cardiovascular disease risk at the community level with proper training, effective community outreach, and task sharing with physicians and family members, they noted.
The findings were limited by the inability to assess the safety of specific medications, but no differences in adverse events were reported between the intervention and control groups. Other limitations included the screening of controls for cardiovascular disease risk at baseline, which meant that controls may have modified their behavior as a result, the researchers noted. In addition, the study was not blinded and surrogate outcomes were used because of the short study duration and relatively small sample size, they said.
However, the results support the use of a comprehensive, NPHW-led model, and “the HOPE 4 strategy could help to attain the UN General Assembly Action Plan for a one-third reduction in premature mortality from cardiovascular disease” by 2030, the researchers concluded.
The study was supported by the Canadian Institutes of Health Research; Grand Challenges Canada; Ontario SPOR Support Unit and the Ontario Ministry of Health and Long-Term Care; Boehringer Ingelheim; Department of Management of Non-Communicable Diseases, World Health Organization; and the Population Health Research Institute. Lead author Dr. Schwalm and several coauthors disclosed grants to their institutions for this study from the Canadian Institutes of Health Research, Ontario Ministry of Health and Long-Term Care, Boehringer Ingelheim, and the Department of Management of Non-Communicable Diseases, WHO.
SOURCE: Schwalm J-D et al. Lancet. 2019 Sept 2. doi: http://dx.doi.org/10.1016/ S0140-6736(19)31949-X.
A community-based care model to control hypertension led by nonphysician health care workers significantly reduced cardiovascular disease risk over 12 months, data from a cluster-controlled randomized study has shown.
Hypertension remains the most common risk factor for cardiovascular disease, but fewer than 20% of individuals with hypertension have their blood pressure controlled, wrote Jon-David Schwalm, MD, of McMaster University in Hamilton, Ont., and colleagues. To help control hypertension in underserved populations, the researchers tested a care model involving nonphysician health workers (NPHWs), primary care physicians, and family members.
The HOPE4 study, presented at the annual congress of the European Society of Cardiology and published simultaneously in the Lancet, included 1,371 adults aged 50 years and older with new or poorly controlled hypertension from 30 communities in Colombia and Malaysia. Sixteen communities were randomized to usual care and 14 to an intervention. The intervention included community screening and treatment of cardiovascular disease risk factors by NPHWs, free medications recommended by NPHWs under physician supervision, and family support for treatment adherence.
After 12 months, the Framingham Risk Scores for 10-year cardiovascular disease risk were significantly lower in the intervention group, compared with the control group (–11.17% vs. –6.40%). In addition, the intervention group showed a significant 11.45 mm Hg greater reduction in systolic blood pressure and a significant 0.41 mmol/L reduction in LDL cholesterol, compared with controls (P less than .0001 for both measures).
Baseline characteristics were similar between the two groups. Approximately 74% of the participants had a history of poorly controlled hypertension, while the remaining patients had new hypertension diagnoses.
“NPHWs were found to be consistently accurate in their ability to identify cardiovascular risk (patient identified by NPHWs as having poorly controlled blood pressure and medication was indicated) and recommend appropriate therapies (antihypertensives and statin as per the study algorithm) when compared with the assessment by local primary care physicians,” the researchers wrote. The study shows how effectively NPHWs can help reduce cardiovascular disease risk at the community level with proper training, effective community outreach, and task sharing with physicians and family members, they noted.
The findings were limited by the inability to assess the safety of specific medications, but no differences in adverse events were reported between the intervention and control groups. Other limitations included the screening of controls for cardiovascular disease risk at baseline, which meant that controls may have modified their behavior as a result, the researchers noted. In addition, the study was not blinded and surrogate outcomes were used because of the short study duration and relatively small sample size, they said.
However, the results support the use of a comprehensive, NPHW-led model, and “the HOPE 4 strategy could help to attain the UN General Assembly Action Plan for a one-third reduction in premature mortality from cardiovascular disease” by 2030, the researchers concluded.
The study was supported by the Canadian Institutes of Health Research; Grand Challenges Canada; Ontario SPOR Support Unit and the Ontario Ministry of Health and Long-Term Care; Boehringer Ingelheim; Department of Management of Non-Communicable Diseases, World Health Organization; and the Population Health Research Institute. Lead author Dr. Schwalm and several coauthors disclosed grants to their institutions for this study from the Canadian Institutes of Health Research, Ontario Ministry of Health and Long-Term Care, Boehringer Ingelheim, and the Department of Management of Non-Communicable Diseases, WHO.
SOURCE: Schwalm J-D et al. Lancet. 2019 Sept 2. doi: http://dx.doi.org/10.1016/ S0140-6736(19)31949-X.
A community-based care model to control hypertension led by nonphysician health care workers significantly reduced cardiovascular disease risk over 12 months, data from a cluster-controlled randomized study has shown.
Hypertension remains the most common risk factor for cardiovascular disease, but fewer than 20% of individuals with hypertension have their blood pressure controlled, wrote Jon-David Schwalm, MD, of McMaster University in Hamilton, Ont., and colleagues. To help control hypertension in underserved populations, the researchers tested a care model involving nonphysician health workers (NPHWs), primary care physicians, and family members.
The HOPE4 study, presented at the annual congress of the European Society of Cardiology and published simultaneously in the Lancet, included 1,371 adults aged 50 years and older with new or poorly controlled hypertension from 30 communities in Colombia and Malaysia. Sixteen communities were randomized to usual care and 14 to an intervention. The intervention included community screening and treatment of cardiovascular disease risk factors by NPHWs, free medications recommended by NPHWs under physician supervision, and family support for treatment adherence.
After 12 months, the Framingham Risk Scores for 10-year cardiovascular disease risk were significantly lower in the intervention group, compared with the control group (–11.17% vs. –6.40%). In addition, the intervention group showed a significant 11.45 mm Hg greater reduction in systolic blood pressure and a significant 0.41 mmol/L reduction in LDL cholesterol, compared with controls (P less than .0001 for both measures).
Baseline characteristics were similar between the two groups. Approximately 74% of the participants had a history of poorly controlled hypertension, while the remaining patients had new hypertension diagnoses.
“NPHWs were found to be consistently accurate in their ability to identify cardiovascular risk (patient identified by NPHWs as having poorly controlled blood pressure and medication was indicated) and recommend appropriate therapies (antihypertensives and statin as per the study algorithm) when compared with the assessment by local primary care physicians,” the researchers wrote. The study shows how effectively NPHWs can help reduce cardiovascular disease risk at the community level with proper training, effective community outreach, and task sharing with physicians and family members, they noted.
The findings were limited by the inability to assess the safety of specific medications, but no differences in adverse events were reported between the intervention and control groups. Other limitations included the screening of controls for cardiovascular disease risk at baseline, which meant that controls may have modified their behavior as a result, the researchers noted. In addition, the study was not blinded and surrogate outcomes were used because of the short study duration and relatively small sample size, they said.
However, the results support the use of a comprehensive, NPHW-led model, and “the HOPE 4 strategy could help to attain the UN General Assembly Action Plan for a one-third reduction in premature mortality from cardiovascular disease” by 2030, the researchers concluded.
The study was supported by the Canadian Institutes of Health Research; Grand Challenges Canada; Ontario SPOR Support Unit and the Ontario Ministry of Health and Long-Term Care; Boehringer Ingelheim; Department of Management of Non-Communicable Diseases, World Health Organization; and the Population Health Research Institute. Lead author Dr. Schwalm and several coauthors disclosed grants to their institutions for this study from the Canadian Institutes of Health Research, Ontario Ministry of Health and Long-Term Care, Boehringer Ingelheim, and the Department of Management of Non-Communicable Diseases, WHO.
SOURCE: Schwalm J-D et al. Lancet. 2019 Sept 2. doi: http://dx.doi.org/10.1016/ S0140-6736(19)31949-X.
AT THE ESC CONGRESS 2019
Key clinical point: A community-based model for managing hypertension significantly improved blood pressure and reduced cardiovascular disease risk in adults with hypertension.
Major finding: Framingham Risk Scores decreased by –11.17% in the intervention group vs. –6.40% in the control group (P less than ·0001).
Study details: The data come from a community-based, randomized, controlled trial of 1,371 adults with new or poorly controlled hypertension.
Disclosures: The study was supported by the Canadian Institutes of Health Research: Grand Challenges Canada: Ontario SPOR Support Unit and the Ontario Ministry of Health and Long-Term Care; Boehringer Ingelheim; Department of Management of Non-Communicable Diseases, WHO; and Population Health Research Institute. Lead author Dr. Schwalm and several coauthors disclosed grants to their institutions for this study from the Canadian Institutes of Health Research, Ontario Ministry of Health and Long-Term Care, Boehringer Ingelheim, and the Department of Management of Non-Communicable Diseases, WHO.
Source: Schwalm J-D et al. Lancet. 2019 Sept 2. doi: http://dx.doi.org/10.1016/ S0140-6736(19)31949-X.
Sacubitril-valsartan effect on aortic stiffness minimal
PARIS –A study of the angiotensin receptor-neprilysin inhibitor sacubitril-valsartan supports updated guidelines that encourage ARNI substitution for traditional therapies in lower-risk heart failure patients, although the study found , according results reported here at the annual congress of the European Society of Cardiology. The study was published simultaneously in JAMA.
“The study findings may provide insight into mechanisms underlying the effects of sacubitril-valsartan in heart failure and reduced ejection fraction,” lead author Akshay S. Desai, MD, of Brigham and Women’s Hospital, Boston, and co-authors wrote.
The study set out to determine the pathophysiologic mechanisms behind the clinical effects of sacubitril-valsartan, compared with enalapril in patients with heart failure and reduced ejection fraction (HFrEF). The EVALUATE-HF trial evaluated 464 patients age 50 years and older with multiple cardiovascular symptoms, including chronic heart failure with ejection fraction of less than 40%. Aortic characteristic impedance, a measure of central aortic stiffness, was evaluated with two-dimensional echocardiography at screening, then at four, 12 and 24 weeks. The primary endpoint was change in aortic characteristic impedance between the two treatment groups at 12 weeks.
Aortic characteristic impedance at baseline to 12 weeks decreased from 223.8 to 218.9 dyne x s/cm 5 in the sacubitril-valsartan treatment group and increased from 213.2 to 214.4 dyne x s/cm 5 in the enalapril group. “There was no statistically significant difference between groups in the change from baseline,” the investigators wrote. The between-group difference factored out to -2.2 dyne x s/cm 5 , ranging from -17.6 to 13.2 dyne x s/cm 5 . This was despite a reduction in brachial systolic blood pressure (6.5 and 1.6 mm Hg) and central systolic blood pressure (4.9 and 2.3 mm Hg), respectively.
The sacubitril-valsartan group showed greater reductions in left ventricular end-diastolic volume index, left ventricular end-systolic volume index, left atrial volume index and mitral E/e ′ ratio. “Although ejection fraction increased modestly by 1.9% in the sacubitril-valsartan group and by 1.3% in the enalapril group, we observed no significant between-group differences in change from baseline to 12 weeks in left ventricular ejection fraction or in other measured parameters,” the investigators wrote. Those other parameters include global longitudinal strain, mitral e ′ velocity or arterial elastance:ventricular elastance ratio. Rates of hypertension, hyperkalemia, and worsening renal function were similar in both groups.
Another secondary outcome was change from baseline in the overall 12-item Kansas City Cardiomyopathy Questionnaire (KCCQ). A post-hoc analysis evaluated patients who achieved a statistically significant 5-points-or-greater change in KCCQ score, finding the score improved by 8.9 points in the sacubitril-valsartan group and 4.3 points in the enalapril group, a difference wider than 8-month results from the PARADIGM-HF trial ( Circ Heart Fail. 2017;10:e003430). “These data suggest that clinical benefits of sacubitril-valsartan compared with enalapril in patients with HFrEF are likely unrelated to changes in central aortic stiffness or pulsatile load, despite favorable effects of neprilysin inhibition on myocardial remodeling and wall stress,” the investigators wrote.
The data support the current guidelines for substituting ARNI for angiotensin-converting enzyme (ACE) inhibitors/angiotensin receptor blockers therapy, “even in the face of apparent clinical stability,” Dr. Desai and co-authors said. In an invited commentary, Mark H. Drazner, MD , of Texas Southwestern Medical Center in Dallas, said the EVALUATE-HF trial, along with the observational PROVE-HF trial data also reported at the ESC meeting (JAMA. 2019 Sept 2. doi:10.1001/jama.2019.12821), “strongly suggest” ARNI therapy can promote cardiac reverse remodeling in patients with HFrEF. “As with beta-blockers and ACE inhibitors, it thus appears that the benefits of ARNI therapy on clinical outcomes in patients with HFrEF are mediated, at least in part, by their favorable effects on the adverse cardiac remodeling that characterizes the condition,” Dr. Desai and co-authors wrote.
The EVALUATE-HF trial was sponsored by Novartis. Dr. Desai disclosed financial relationships with Alnylam, AstraZeneca, Novartis, Abbott, Biofourmis, Boehringer Ingelheim, Boston Scientific, DalCor Pharma and Regeneron. Dr. Drazner has no financial relationships to disclose.
SOURCE: Desai AS et al. JAMA. 2019 Sept 2. doi:10.1001/jama.2019.12843.
PARIS –A study of the angiotensin receptor-neprilysin inhibitor sacubitril-valsartan supports updated guidelines that encourage ARNI substitution for traditional therapies in lower-risk heart failure patients, although the study found , according results reported here at the annual congress of the European Society of Cardiology. The study was published simultaneously in JAMA.
“The study findings may provide insight into mechanisms underlying the effects of sacubitril-valsartan in heart failure and reduced ejection fraction,” lead author Akshay S. Desai, MD, of Brigham and Women’s Hospital, Boston, and co-authors wrote.
The study set out to determine the pathophysiologic mechanisms behind the clinical effects of sacubitril-valsartan, compared with enalapril in patients with heart failure and reduced ejection fraction (HFrEF). The EVALUATE-HF trial evaluated 464 patients age 50 years and older with multiple cardiovascular symptoms, including chronic heart failure with ejection fraction of less than 40%. Aortic characteristic impedance, a measure of central aortic stiffness, was evaluated with two-dimensional echocardiography at screening, then at four, 12 and 24 weeks. The primary endpoint was change in aortic characteristic impedance between the two treatment groups at 12 weeks.
Aortic characteristic impedance at baseline to 12 weeks decreased from 223.8 to 218.9 dyne x s/cm 5 in the sacubitril-valsartan treatment group and increased from 213.2 to 214.4 dyne x s/cm 5 in the enalapril group. “There was no statistically significant difference between groups in the change from baseline,” the investigators wrote. The between-group difference factored out to -2.2 dyne x s/cm 5 , ranging from -17.6 to 13.2 dyne x s/cm 5 . This was despite a reduction in brachial systolic blood pressure (6.5 and 1.6 mm Hg) and central systolic blood pressure (4.9 and 2.3 mm Hg), respectively.
The sacubitril-valsartan group showed greater reductions in left ventricular end-diastolic volume index, left ventricular end-systolic volume index, left atrial volume index and mitral E/e ′ ratio. “Although ejection fraction increased modestly by 1.9% in the sacubitril-valsartan group and by 1.3% in the enalapril group, we observed no significant between-group differences in change from baseline to 12 weeks in left ventricular ejection fraction or in other measured parameters,” the investigators wrote. Those other parameters include global longitudinal strain, mitral e ′ velocity or arterial elastance:ventricular elastance ratio. Rates of hypertension, hyperkalemia, and worsening renal function were similar in both groups.
Another secondary outcome was change from baseline in the overall 12-item Kansas City Cardiomyopathy Questionnaire (KCCQ). A post-hoc analysis evaluated patients who achieved a statistically significant 5-points-or-greater change in KCCQ score, finding the score improved by 8.9 points in the sacubitril-valsartan group and 4.3 points in the enalapril group, a difference wider than 8-month results from the PARADIGM-HF trial ( Circ Heart Fail. 2017;10:e003430). “These data suggest that clinical benefits of sacubitril-valsartan compared with enalapril in patients with HFrEF are likely unrelated to changes in central aortic stiffness or pulsatile load, despite favorable effects of neprilysin inhibition on myocardial remodeling and wall stress,” the investigators wrote.
The data support the current guidelines for substituting ARNI for angiotensin-converting enzyme (ACE) inhibitors/angiotensin receptor blockers therapy, “even in the face of apparent clinical stability,” Dr. Desai and co-authors said. In an invited commentary, Mark H. Drazner, MD , of Texas Southwestern Medical Center in Dallas, said the EVALUATE-HF trial, along with the observational PROVE-HF trial data also reported at the ESC meeting (JAMA. 2019 Sept 2. doi:10.1001/jama.2019.12821), “strongly suggest” ARNI therapy can promote cardiac reverse remodeling in patients with HFrEF. “As with beta-blockers and ACE inhibitors, it thus appears that the benefits of ARNI therapy on clinical outcomes in patients with HFrEF are mediated, at least in part, by their favorable effects on the adverse cardiac remodeling that characterizes the condition,” Dr. Desai and co-authors wrote.
The EVALUATE-HF trial was sponsored by Novartis. Dr. Desai disclosed financial relationships with Alnylam, AstraZeneca, Novartis, Abbott, Biofourmis, Boehringer Ingelheim, Boston Scientific, DalCor Pharma and Regeneron. Dr. Drazner has no financial relationships to disclose.
SOURCE: Desai AS et al. JAMA. 2019 Sept 2. doi:10.1001/jama.2019.12843.
PARIS –A study of the angiotensin receptor-neprilysin inhibitor sacubitril-valsartan supports updated guidelines that encourage ARNI substitution for traditional therapies in lower-risk heart failure patients, although the study found , according results reported here at the annual congress of the European Society of Cardiology. The study was published simultaneously in JAMA.
“The study findings may provide insight into mechanisms underlying the effects of sacubitril-valsartan in heart failure and reduced ejection fraction,” lead author Akshay S. Desai, MD, of Brigham and Women’s Hospital, Boston, and co-authors wrote.
The study set out to determine the pathophysiologic mechanisms behind the clinical effects of sacubitril-valsartan, compared with enalapril in patients with heart failure and reduced ejection fraction (HFrEF). The EVALUATE-HF trial evaluated 464 patients age 50 years and older with multiple cardiovascular symptoms, including chronic heart failure with ejection fraction of less than 40%. Aortic characteristic impedance, a measure of central aortic stiffness, was evaluated with two-dimensional echocardiography at screening, then at four, 12 and 24 weeks. The primary endpoint was change in aortic characteristic impedance between the two treatment groups at 12 weeks.
Aortic characteristic impedance at baseline to 12 weeks decreased from 223.8 to 218.9 dyne x s/cm 5 in the sacubitril-valsartan treatment group and increased from 213.2 to 214.4 dyne x s/cm 5 in the enalapril group. “There was no statistically significant difference between groups in the change from baseline,” the investigators wrote. The between-group difference factored out to -2.2 dyne x s/cm 5 , ranging from -17.6 to 13.2 dyne x s/cm 5 . This was despite a reduction in brachial systolic blood pressure (6.5 and 1.6 mm Hg) and central systolic blood pressure (4.9 and 2.3 mm Hg), respectively.
The sacubitril-valsartan group showed greater reductions in left ventricular end-diastolic volume index, left ventricular end-systolic volume index, left atrial volume index and mitral E/e ′ ratio. “Although ejection fraction increased modestly by 1.9% in the sacubitril-valsartan group and by 1.3% in the enalapril group, we observed no significant between-group differences in change from baseline to 12 weeks in left ventricular ejection fraction or in other measured parameters,” the investigators wrote. Those other parameters include global longitudinal strain, mitral e ′ velocity or arterial elastance:ventricular elastance ratio. Rates of hypertension, hyperkalemia, and worsening renal function were similar in both groups.
Another secondary outcome was change from baseline in the overall 12-item Kansas City Cardiomyopathy Questionnaire (KCCQ). A post-hoc analysis evaluated patients who achieved a statistically significant 5-points-or-greater change in KCCQ score, finding the score improved by 8.9 points in the sacubitril-valsartan group and 4.3 points in the enalapril group, a difference wider than 8-month results from the PARADIGM-HF trial ( Circ Heart Fail. 2017;10:e003430). “These data suggest that clinical benefits of sacubitril-valsartan compared with enalapril in patients with HFrEF are likely unrelated to changes in central aortic stiffness or pulsatile load, despite favorable effects of neprilysin inhibition on myocardial remodeling and wall stress,” the investigators wrote.
The data support the current guidelines for substituting ARNI for angiotensin-converting enzyme (ACE) inhibitors/angiotensin receptor blockers therapy, “even in the face of apparent clinical stability,” Dr. Desai and co-authors said. In an invited commentary, Mark H. Drazner, MD , of Texas Southwestern Medical Center in Dallas, said the EVALUATE-HF trial, along with the observational PROVE-HF trial data also reported at the ESC meeting (JAMA. 2019 Sept 2. doi:10.1001/jama.2019.12821), “strongly suggest” ARNI therapy can promote cardiac reverse remodeling in patients with HFrEF. “As with beta-blockers and ACE inhibitors, it thus appears that the benefits of ARNI therapy on clinical outcomes in patients with HFrEF are mediated, at least in part, by their favorable effects on the adverse cardiac remodeling that characterizes the condition,” Dr. Desai and co-authors wrote.
The EVALUATE-HF trial was sponsored by Novartis. Dr. Desai disclosed financial relationships with Alnylam, AstraZeneca, Novartis, Abbott, Biofourmis, Boehringer Ingelheim, Boston Scientific, DalCor Pharma and Regeneron. Dr. Drazner has no financial relationships to disclose.
SOURCE: Desai AS et al. JAMA. 2019 Sept 2. doi:10.1001/jama.2019.12843.
AT THE ESC CONGRESS 2019
Key clinical point: Sacubitril-valsartan does not significantly reduce aortic stiffness, compared with enalapril.
Major finding: The difference in aortic characteristic impedance was -2.2 dyne x s/cm5 between treatment groups.
Study details: EVALUATE-HF is a randomized, double-blind clinical trial of 464 participants with heart failure and ejection fraction of less than 40%.
Disclosures: The study was sponsored by Novartis. Dr. Desai disclosed financial relationships with Alnylam, AstraZeneca, Novartis, Abbott, Biofourmis, Boehringer Ingelheim, Boston Scientific, DalCor Pharma and Regeneron.
Source: Desai AS, et al. JAMA. 2019 Sept 2. doi:10.1001/jama.2019.12843
Weight loss surgery linked to lower CV event risk in diabetes
, compared with nonsurgical management, according to data presented at the annual congress of the European Society of Cardiology.
The retrospective cohort study, simultaneously published in JAMA, looked at outcomes in 13,722 individuals with type 2 diabetes and obesity, 2,287 of whom underwent metabolic surgery and the rest of the matched cohort receiving usual care.
At 8 years of follow-up, the cumulative incidence of the primary endpoint – a composite of first occurrence of all-cause mortality, coronary artery events, cerebrovascular events, heart failure, nephropathy, and atrial fibrillation – was 30.8% in the weight loss–surgery group and 47.7% in the nonsurgical-control group, representing a 39% lower risk with weight loss surgery (P less than .001).
The analysis failed to find any interaction with sex, age, body mass index (BMI), HbA1c level, estimated glomerular filtration rate, or use of insulin, sulfonylureas, or lipid-lowering medications.
Metabolic surgery was also associated with a significantly lower cumulative incidence of myocardial infarction, ischemic stroke and mortality than usual care (17% vs. 27.6%).
In particular, researchers saw a significant 41% reduction in the risk of death at eight years in the surgical group compared to usual care (10% vs. 17.8%), a 62% reduction in the risk of heart failure, a 31% reduction in the risk of coronary artery disease, and a 60% reduction in nephropathy risk. Metabolic surgery was also associated with a 33% reduction in cerebrovascular disease risk, and a 22% lower risk of atrial fibrillation.
In the group that underwent metabolic surgery, mean bodyweight at 8 years was reduced by 29.1 kg, compared with 8.7 kg in the control group. At baseline, 75% of the metabolic surgery group had a BMI of 40 kg/m2 or above, 20% had a BMI between 35-39.9, and 5% had a BMI between 30-34.9.
The surgery was also associated with significantly greater reductions in HbA1c, and in the use of noninsulin diabetes medications, insulin, antihypertensive medications, lipid-lowering therapies, and aspirin.
The most common surgical weight loss procedure was Roux-en-Y gastric bypass (63%), followed by sleeve gastrectomy (32%), and adjustable gastric banding (5%). Five patients underwent duodenal switch.
In the 90 days after surgery, 3% of patients experienced bleeding that required transfusion, 2.5% experienced pulmonary adverse events, 1% experienced venous thromboembolism, 0.7% experienced cardiac events, and 0.2% experienced renal failure that required dialysis. There were also 15 deaths (0.7%) in the surgical group, and 4.8% of patients required abdominal surgical intervention.
“We speculate that the lower rate of [major adverse cardiovascular events] after metabolic surgery observed in this study may be related to substantial and sustained weight loss with subsequent improvement in metabolic, structural, hemodynamic, and neurohormonal abnormalities,” wrote Ali Aminian, MD, of the Bariatric and Metabolic Institute at the Cleveland Clinic, and coauthors.
“Although large and sustained surgically induced weight loss has profound physiologic effects, a growing body of evidence indicates that some of the beneficial metabolic and neurohormonal changes that occur after metabolic surgical procedures are related to anatomical changes in the gastrointestinal tract that are partially independent of weight loss,” they wrote.
The authors, however, were also keen to point out that their study was observational, and should therefore be considered “hypothesis generating.” While the two study groups were matched on 37 baseline covariates, those in the surgical group did have a higher body weight, higher BMI, higher rates of dyslipidemia, and higher rates of hypertension.
“The findings from this observational study must be confirmed in randomized clinical trials,” they noted.
The study was partly funded by Medtronic, and one author was supported by the National Institute of Diabetes and Digestive and Kidney Diseases. Five authors declared funding and support from private industry, including from Medtronic, and one author declared institutional grants.
SOURCE: Aminian A et al. JAMA 2019, Sept 2. DOI: 10.1001/jama.2019.14231.
Despite a focus on reducing macrovascular events in individuals with type 2 diabetes, none of the major randomized controlled trials of glucose-lowering interventions that support current treatment guidelines have achieved this outcome. This study of bariatric surgery in obese patients with diabetes, however, does show reductions in major adverse cardiovascular events, although these outcomes should be interpreted with caution because of their observational nature and imprecise matching of the study groups.
Despite this, the many known benefits associated with bariatric surgery–induced weight loss suggest that for carefully selected, motivated patients with obesity and type 2 diabetes – who have been unable to lose weight by other means – this could be the preferred treatment option.
Dr. Edward H. Livingston is the deputy editor of JAMA and with the department of surgery at the University of California, Los Angeles. These comments are adapted from an accompanying editorial (JAMA 2019, Sept 2. DOI:10.1001/jama.2019.14577). No conflicts of interest were declared.
Despite a focus on reducing macrovascular events in individuals with type 2 diabetes, none of the major randomized controlled trials of glucose-lowering interventions that support current treatment guidelines have achieved this outcome. This study of bariatric surgery in obese patients with diabetes, however, does show reductions in major adverse cardiovascular events, although these outcomes should be interpreted with caution because of their observational nature and imprecise matching of the study groups.
Despite this, the many known benefits associated with bariatric surgery–induced weight loss suggest that for carefully selected, motivated patients with obesity and type 2 diabetes – who have been unable to lose weight by other means – this could be the preferred treatment option.
Dr. Edward H. Livingston is the deputy editor of JAMA and with the department of surgery at the University of California, Los Angeles. These comments are adapted from an accompanying editorial (JAMA 2019, Sept 2. DOI:10.1001/jama.2019.14577). No conflicts of interest were declared.
Despite a focus on reducing macrovascular events in individuals with type 2 diabetes, none of the major randomized controlled trials of glucose-lowering interventions that support current treatment guidelines have achieved this outcome. This study of bariatric surgery in obese patients with diabetes, however, does show reductions in major adverse cardiovascular events, although these outcomes should be interpreted with caution because of their observational nature and imprecise matching of the study groups.
Despite this, the many known benefits associated with bariatric surgery–induced weight loss suggest that for carefully selected, motivated patients with obesity and type 2 diabetes – who have been unable to lose weight by other means – this could be the preferred treatment option.
Dr. Edward H. Livingston is the deputy editor of JAMA and with the department of surgery at the University of California, Los Angeles. These comments are adapted from an accompanying editorial (JAMA 2019, Sept 2. DOI:10.1001/jama.2019.14577). No conflicts of interest were declared.
, compared with nonsurgical management, according to data presented at the annual congress of the European Society of Cardiology.
The retrospective cohort study, simultaneously published in JAMA, looked at outcomes in 13,722 individuals with type 2 diabetes and obesity, 2,287 of whom underwent metabolic surgery and the rest of the matched cohort receiving usual care.
At 8 years of follow-up, the cumulative incidence of the primary endpoint – a composite of first occurrence of all-cause mortality, coronary artery events, cerebrovascular events, heart failure, nephropathy, and atrial fibrillation – was 30.8% in the weight loss–surgery group and 47.7% in the nonsurgical-control group, representing a 39% lower risk with weight loss surgery (P less than .001).
The analysis failed to find any interaction with sex, age, body mass index (BMI), HbA1c level, estimated glomerular filtration rate, or use of insulin, sulfonylureas, or lipid-lowering medications.
Metabolic surgery was also associated with a significantly lower cumulative incidence of myocardial infarction, ischemic stroke and mortality than usual care (17% vs. 27.6%).
In particular, researchers saw a significant 41% reduction in the risk of death at eight years in the surgical group compared to usual care (10% vs. 17.8%), a 62% reduction in the risk of heart failure, a 31% reduction in the risk of coronary artery disease, and a 60% reduction in nephropathy risk. Metabolic surgery was also associated with a 33% reduction in cerebrovascular disease risk, and a 22% lower risk of atrial fibrillation.
In the group that underwent metabolic surgery, mean bodyweight at 8 years was reduced by 29.1 kg, compared with 8.7 kg in the control group. At baseline, 75% of the metabolic surgery group had a BMI of 40 kg/m2 or above, 20% had a BMI between 35-39.9, and 5% had a BMI between 30-34.9.
The surgery was also associated with significantly greater reductions in HbA1c, and in the use of noninsulin diabetes medications, insulin, antihypertensive medications, lipid-lowering therapies, and aspirin.
The most common surgical weight loss procedure was Roux-en-Y gastric bypass (63%), followed by sleeve gastrectomy (32%), and adjustable gastric banding (5%). Five patients underwent duodenal switch.
In the 90 days after surgery, 3% of patients experienced bleeding that required transfusion, 2.5% experienced pulmonary adverse events, 1% experienced venous thromboembolism, 0.7% experienced cardiac events, and 0.2% experienced renal failure that required dialysis. There were also 15 deaths (0.7%) in the surgical group, and 4.8% of patients required abdominal surgical intervention.
“We speculate that the lower rate of [major adverse cardiovascular events] after metabolic surgery observed in this study may be related to substantial and sustained weight loss with subsequent improvement in metabolic, structural, hemodynamic, and neurohormonal abnormalities,” wrote Ali Aminian, MD, of the Bariatric and Metabolic Institute at the Cleveland Clinic, and coauthors.
“Although large and sustained surgically induced weight loss has profound physiologic effects, a growing body of evidence indicates that some of the beneficial metabolic and neurohormonal changes that occur after metabolic surgical procedures are related to anatomical changes in the gastrointestinal tract that are partially independent of weight loss,” they wrote.
The authors, however, were also keen to point out that their study was observational, and should therefore be considered “hypothesis generating.” While the two study groups were matched on 37 baseline covariates, those in the surgical group did have a higher body weight, higher BMI, higher rates of dyslipidemia, and higher rates of hypertension.
“The findings from this observational study must be confirmed in randomized clinical trials,” they noted.
The study was partly funded by Medtronic, and one author was supported by the National Institute of Diabetes and Digestive and Kidney Diseases. Five authors declared funding and support from private industry, including from Medtronic, and one author declared institutional grants.
SOURCE: Aminian A et al. JAMA 2019, Sept 2. DOI: 10.1001/jama.2019.14231.
, compared with nonsurgical management, according to data presented at the annual congress of the European Society of Cardiology.
The retrospective cohort study, simultaneously published in JAMA, looked at outcomes in 13,722 individuals with type 2 diabetes and obesity, 2,287 of whom underwent metabolic surgery and the rest of the matched cohort receiving usual care.
At 8 years of follow-up, the cumulative incidence of the primary endpoint – a composite of first occurrence of all-cause mortality, coronary artery events, cerebrovascular events, heart failure, nephropathy, and atrial fibrillation – was 30.8% in the weight loss–surgery group and 47.7% in the nonsurgical-control group, representing a 39% lower risk with weight loss surgery (P less than .001).
The analysis failed to find any interaction with sex, age, body mass index (BMI), HbA1c level, estimated glomerular filtration rate, or use of insulin, sulfonylureas, or lipid-lowering medications.
Metabolic surgery was also associated with a significantly lower cumulative incidence of myocardial infarction, ischemic stroke and mortality than usual care (17% vs. 27.6%).
In particular, researchers saw a significant 41% reduction in the risk of death at eight years in the surgical group compared to usual care (10% vs. 17.8%), a 62% reduction in the risk of heart failure, a 31% reduction in the risk of coronary artery disease, and a 60% reduction in nephropathy risk. Metabolic surgery was also associated with a 33% reduction in cerebrovascular disease risk, and a 22% lower risk of atrial fibrillation.
In the group that underwent metabolic surgery, mean bodyweight at 8 years was reduced by 29.1 kg, compared with 8.7 kg in the control group. At baseline, 75% of the metabolic surgery group had a BMI of 40 kg/m2 or above, 20% had a BMI between 35-39.9, and 5% had a BMI between 30-34.9.
The surgery was also associated with significantly greater reductions in HbA1c, and in the use of noninsulin diabetes medications, insulin, antihypertensive medications, lipid-lowering therapies, and aspirin.
The most common surgical weight loss procedure was Roux-en-Y gastric bypass (63%), followed by sleeve gastrectomy (32%), and adjustable gastric banding (5%). Five patients underwent duodenal switch.
In the 90 days after surgery, 3% of patients experienced bleeding that required transfusion, 2.5% experienced pulmonary adverse events, 1% experienced venous thromboembolism, 0.7% experienced cardiac events, and 0.2% experienced renal failure that required dialysis. There were also 15 deaths (0.7%) in the surgical group, and 4.8% of patients required abdominal surgical intervention.
“We speculate that the lower rate of [major adverse cardiovascular events] after metabolic surgery observed in this study may be related to substantial and sustained weight loss with subsequent improvement in metabolic, structural, hemodynamic, and neurohormonal abnormalities,” wrote Ali Aminian, MD, of the Bariatric and Metabolic Institute at the Cleveland Clinic, and coauthors.
“Although large and sustained surgically induced weight loss has profound physiologic effects, a growing body of evidence indicates that some of the beneficial metabolic and neurohormonal changes that occur after metabolic surgical procedures are related to anatomical changes in the gastrointestinal tract that are partially independent of weight loss,” they wrote.
The authors, however, were also keen to point out that their study was observational, and should therefore be considered “hypothesis generating.” While the two study groups were matched on 37 baseline covariates, those in the surgical group did have a higher body weight, higher BMI, higher rates of dyslipidemia, and higher rates of hypertension.
“The findings from this observational study must be confirmed in randomized clinical trials,” they noted.
The study was partly funded by Medtronic, and one author was supported by the National Institute of Diabetes and Digestive and Kidney Diseases. Five authors declared funding and support from private industry, including from Medtronic, and one author declared institutional grants.
SOURCE: Aminian A et al. JAMA 2019, Sept 2. DOI: 10.1001/jama.2019.14231.
AT THE ESC CONGRESS 2019
Key clinical point: Bariatric surgery may reduce the risk of cardiovascular events in people with type 2 diabetes.
Major finding: Bariatric surgery is associated with a 39% reduction in risk of major cardiovascular events.
Study details: Retrospective cohort study in 13,722 individuals with type 2 diabetes and obesity.
Disclosures: The study was partly funded by Medtronic, and one author was supported by the National Institute of Diabetes and Digestive and Kidney Diseases. Five authors declared funding and support from private industry, including from Medtronic, and one author declared institutional grants.
Source: Aminian A et al. JAMA 2019, September 2. DOI: 10.1001/jama.2019.14231.