User login
Shining a light on nonplaque psoriasis
MIAMI – People with nonplaque psoriasis could soon have their day. Some patients with nail, inverse, and genital psoriasis, for example, fail to meet traditional criteria for moderate to severe disease and therefore do not meet label indications for treatment.
That could soon change if dermatologist Abrar A. Qureshi, MD, and rheumatologist-dermatologist Joseph F. Merola, MD, have their way, according to their dual presentation at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
“What we’re trying to do really is go into redefining moderate to severe psoriasis. The current definition is moderate to severe plaque psoriasis,” said Dr. Qureshi, chief of dermatology at Rhode Island Hospital in Providence. “If you look at all the labels out there, it’s plaque disease.”
However, “psoriasis is poly phenotype,” Dr. Qureshi said. “This paradigm needs to change in the next few years to redefine what moderate to severe psoriasis is.” A patient with limited, nonplaque psoriasis on their elbows, one knee, or who presents only with perianal disease, for example, might not meet the traditional definition of moderate to severe psoriasis. Another patient might just have scalp disease or inverse psoriasis on a limited body area.
Currently, the Psoriasis Area and Severity Index (PASI), Physician Global Assessment (PGA) and Body Surface Area (BSA) assessments classify mild, moderate, and severe psoriasis, “with the majority of people out there in the world with mild psoriasis,” Dr. Qureshi said. A new measure called the Comprehensive Assessment of the Psoriasis Patient (CAPP) “captures more people with moderate to severe disease.”
CAPP includes a measure of plaque disease, palmoplantar, nail, scale, inverse, and genital psoriasis. “Where PASI fails, we hope the CAPP meets this unmet need,” said Dr. Merola, codirector of the Center for Skin and Related Musculoskeletal Diseases, a combined clinic at Brigham and Women’s Hospital in Boston. The two highest phenotypic scores are added to the plaque score for a final CAPP score. “It’s easy to use.”
A newly announced genital psoriasis component of CAPP measures any suprapubic, perineal, and genital involvement. Thickness, scale, and severity are included in CAPP, as well as secondary skin changes like fissuring or erosion. Then the score is equally weighted with the patient reported outcomes of pain and effect on intimacy rated on a simple visual analog scale.
Dr. Merola, Dr. Qureshi, and their colleagues collaborated on a study looking at the prevalence of nonplaque psoriasis among almost 4,000 patients (Clin Exp Dermatol. 2016;41:486-9).
“It surprised us to see such a high prevalence of inverse disease, almost 24%,” Dr. Merola said. “Many of these patients have two nonplaque phenotypes. It’s also important because it seems like there is an increased psoriatic arthritis risk.”
“The nail story and the scalp story have been out there a while, but looking at inverse disease there was a fairly high hazard ratio [2.07] for development of psoriatic arthritis.”
Proposing a polyphenotype psoriasis clinical trial
“I will end with a recommendation for a polyphenotype psoriasis clinical trial, to be really controversial,” Dr. Qureshi said. “We want to capture only the people who qualify as moderate to severe with the new measure and look at them before and after therapy.” He added participants would be “people out there in clinic who are currently not receiving treatment.”
During the Q&A, a meeting attendee asked if the investigators could recruit enough patients with nonplaque psoriasis. “We think it’s about 15%-23%,” Dr. Qureshi said. “The only type we cannot capture well is the palmoplantar phenotype because of its really low prevalence.”
MIAMI – People with nonplaque psoriasis could soon have their day. Some patients with nail, inverse, and genital psoriasis, for example, fail to meet traditional criteria for moderate to severe disease and therefore do not meet label indications for treatment.
That could soon change if dermatologist Abrar A. Qureshi, MD, and rheumatologist-dermatologist Joseph F. Merola, MD, have their way, according to their dual presentation at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
“What we’re trying to do really is go into redefining moderate to severe psoriasis. The current definition is moderate to severe plaque psoriasis,” said Dr. Qureshi, chief of dermatology at Rhode Island Hospital in Providence. “If you look at all the labels out there, it’s plaque disease.”
However, “psoriasis is poly phenotype,” Dr. Qureshi said. “This paradigm needs to change in the next few years to redefine what moderate to severe psoriasis is.” A patient with limited, nonplaque psoriasis on their elbows, one knee, or who presents only with perianal disease, for example, might not meet the traditional definition of moderate to severe psoriasis. Another patient might just have scalp disease or inverse psoriasis on a limited body area.
Currently, the Psoriasis Area and Severity Index (PASI), Physician Global Assessment (PGA) and Body Surface Area (BSA) assessments classify mild, moderate, and severe psoriasis, “with the majority of people out there in the world with mild psoriasis,” Dr. Qureshi said. A new measure called the Comprehensive Assessment of the Psoriasis Patient (CAPP) “captures more people with moderate to severe disease.”
CAPP includes a measure of plaque disease, palmoplantar, nail, scale, inverse, and genital psoriasis. “Where PASI fails, we hope the CAPP meets this unmet need,” said Dr. Merola, codirector of the Center for Skin and Related Musculoskeletal Diseases, a combined clinic at Brigham and Women’s Hospital in Boston. The two highest phenotypic scores are added to the plaque score for a final CAPP score. “It’s easy to use.”
A newly announced genital psoriasis component of CAPP measures any suprapubic, perineal, and genital involvement. Thickness, scale, and severity are included in CAPP, as well as secondary skin changes like fissuring or erosion. Then the score is equally weighted with the patient reported outcomes of pain and effect on intimacy rated on a simple visual analog scale.
Dr. Merola, Dr. Qureshi, and their colleagues collaborated on a study looking at the prevalence of nonplaque psoriasis among almost 4,000 patients (Clin Exp Dermatol. 2016;41:486-9).
“It surprised us to see such a high prevalence of inverse disease, almost 24%,” Dr. Merola said. “Many of these patients have two nonplaque phenotypes. It’s also important because it seems like there is an increased psoriatic arthritis risk.”
“The nail story and the scalp story have been out there a while, but looking at inverse disease there was a fairly high hazard ratio [2.07] for development of psoriatic arthritis.”
Proposing a polyphenotype psoriasis clinical trial
“I will end with a recommendation for a polyphenotype psoriasis clinical trial, to be really controversial,” Dr. Qureshi said. “We want to capture only the people who qualify as moderate to severe with the new measure and look at them before and after therapy.” He added participants would be “people out there in clinic who are currently not receiving treatment.”
During the Q&A, a meeting attendee asked if the investigators could recruit enough patients with nonplaque psoriasis. “We think it’s about 15%-23%,” Dr. Qureshi said. “The only type we cannot capture well is the palmoplantar phenotype because of its really low prevalence.”
MIAMI – People with nonplaque psoriasis could soon have their day. Some patients with nail, inverse, and genital psoriasis, for example, fail to meet traditional criteria for moderate to severe disease and therefore do not meet label indications for treatment.
That could soon change if dermatologist Abrar A. Qureshi, MD, and rheumatologist-dermatologist Joseph F. Merola, MD, have their way, according to their dual presentation at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
“What we’re trying to do really is go into redefining moderate to severe psoriasis. The current definition is moderate to severe plaque psoriasis,” said Dr. Qureshi, chief of dermatology at Rhode Island Hospital in Providence. “If you look at all the labels out there, it’s plaque disease.”
However, “psoriasis is poly phenotype,” Dr. Qureshi said. “This paradigm needs to change in the next few years to redefine what moderate to severe psoriasis is.” A patient with limited, nonplaque psoriasis on their elbows, one knee, or who presents only with perianal disease, for example, might not meet the traditional definition of moderate to severe psoriasis. Another patient might just have scalp disease or inverse psoriasis on a limited body area.
Currently, the Psoriasis Area and Severity Index (PASI), Physician Global Assessment (PGA) and Body Surface Area (BSA) assessments classify mild, moderate, and severe psoriasis, “with the majority of people out there in the world with mild psoriasis,” Dr. Qureshi said. A new measure called the Comprehensive Assessment of the Psoriasis Patient (CAPP) “captures more people with moderate to severe disease.”
CAPP includes a measure of plaque disease, palmoplantar, nail, scale, inverse, and genital psoriasis. “Where PASI fails, we hope the CAPP meets this unmet need,” said Dr. Merola, codirector of the Center for Skin and Related Musculoskeletal Diseases, a combined clinic at Brigham and Women’s Hospital in Boston. The two highest phenotypic scores are added to the plaque score for a final CAPP score. “It’s easy to use.”
A newly announced genital psoriasis component of CAPP measures any suprapubic, perineal, and genital involvement. Thickness, scale, and severity are included in CAPP, as well as secondary skin changes like fissuring or erosion. Then the score is equally weighted with the patient reported outcomes of pain and effect on intimacy rated on a simple visual analog scale.
Dr. Merola, Dr. Qureshi, and their colleagues collaborated on a study looking at the prevalence of nonplaque psoriasis among almost 4,000 patients (Clin Exp Dermatol. 2016;41:486-9).
“It surprised us to see such a high prevalence of inverse disease, almost 24%,” Dr. Merola said. “Many of these patients have two nonplaque phenotypes. It’s also important because it seems like there is an increased psoriatic arthritis risk.”
“The nail story and the scalp story have been out there a while, but looking at inverse disease there was a fairly high hazard ratio [2.07] for development of psoriatic arthritis.”
Proposing a polyphenotype psoriasis clinical trial
“I will end with a recommendation for a polyphenotype psoriasis clinical trial, to be really controversial,” Dr. Qureshi said. “We want to capture only the people who qualify as moderate to severe with the new measure and look at them before and after therapy.” He added participants would be “people out there in clinic who are currently not receiving treatment.”
During the Q&A, a meeting attendee asked if the investigators could recruit enough patients with nonplaque psoriasis. “We think it’s about 15%-23%,” Dr. Qureshi said. “The only type we cannot capture well is the palmoplantar phenotype because of its really low prevalence.”
AT 2016 GRAPPA ANNUAL MEETING
Key clinical point: The Comprehensive Assessment of the Psoriasis Patient measure could expand the number of patients with moderate to severe disease.
Major finding: Up to 24% of psoriasis patients can present with nonplaque psoriasis.
Data source: A study looking at the prevalence of nonplaque psoriasis among almost 4,000 patients.
Disclosures: Dr. Qureshi and Dr. Merola had no relevant disclosures.
Psoriasis symptom measure could help rheumatologists assess severity
MIAMI – The Psoriasis Symptom Inventory measure could help rheumatologists more easily gauge the severity of moderate to severe psoriasis. The eight-item tool in development correlates well with the Psoriasis Area and Severity Index and is easier to use in rheumatology settings, according to a presentation at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
“One of the ways it can be useful is in a rheumatology setting [to gauge psoriasis severity] when you’re looking at psoriatic arthritis patients,” said Philip J. Mease, MD. But “you might ask: Why is this of utility when we have an actual physical examination score like the PASI [Psoriasis Area and Severity Index] score?”
“Arguably, rheumatologists really don’t do PASI scores at all, practically speaking. If they do them, the quality of the evaluation is more questionable than [when] done by a dermatologist,” Dr. Mease said at the meeting.
The Psoriasis Symptom Inventory (PSI) focuses on redness, scaling, burning, stinging, peeling, flaking, and pain of skin lesions. The instrument was “rigorously developed by a team at Amgen that worked on it with patient groups and others to come up with a patient-reported outcome [tool],” said Dr. Mease, a rheumatologist at the Swedish Medical Center in Seattle. The first question, for example, is: “During the last 24 hours, how severe was the itch from your psoriasis?” Responses range from “not at all” to “very severe.”
Other researchers compared the PSI to PASI to assess symptom severity and clinical status changes, and the PSI “correlates very well,” Dr. Mease said (J Dermatolog Treat. 2014 Feb;25[1]:8-14). In addition, others have validated the PSI in both psoriasis and psoriatic arthritis and suggest a role in research (J Dermatolog Treat. 2013 Aug;24[4]:255-60).
“In a registry or clinical trial setting, this would be a very simple, eight-question patient-reported outcome that … could be employed as a potential substitute for the PASI where it may not be practical,” Dr. Mease said. The PSI can be adjusted to ask about symptoms over the previous 24 hours or past 7 days.
A current limitation is that “we don’t know how this instrument performs in patients with low body surface area psoriasis,” Dr. Mease said. Typically, psoriasis studies enroll participants with at least 10% body surface area involvement. During the Q&A, an attendee pointed out that even less than 3% body surface area psoriasis is relevant in clinical practice. Dr. Mease agreed, and said a future registry study could validate the PSI in this patient population. “There are discussions now with Amgen to possibly use the PSI in the CORRONA registry of psoriatic patients,” he said. “Because of its rigorous development and high psychometric properties, it would be great if it could be used more broadly. I know there are discussions going on in that regard.”
Amgen is evaluating responder definitions for the PSI that correlate with PASI-50, –75 and –90 responses. The firm is also looking at ways to share the PSI instrument with clinicians and researchers. Brian Ortmeier, executive director at Amgen in Los Angeles and one of the developers of PSI, said at the GRAPPA meeting, “Our intent is get the PSI out into the public domain as a disease management tool.”
Dr. Mease is a consultant to and speaker for Amgen and receives research support from the company.
MIAMI – The Psoriasis Symptom Inventory measure could help rheumatologists more easily gauge the severity of moderate to severe psoriasis. The eight-item tool in development correlates well with the Psoriasis Area and Severity Index and is easier to use in rheumatology settings, according to a presentation at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
“One of the ways it can be useful is in a rheumatology setting [to gauge psoriasis severity] when you’re looking at psoriatic arthritis patients,” said Philip J. Mease, MD. But “you might ask: Why is this of utility when we have an actual physical examination score like the PASI [Psoriasis Area and Severity Index] score?”
“Arguably, rheumatologists really don’t do PASI scores at all, practically speaking. If they do them, the quality of the evaluation is more questionable than [when] done by a dermatologist,” Dr. Mease said at the meeting.
The Psoriasis Symptom Inventory (PSI) focuses on redness, scaling, burning, stinging, peeling, flaking, and pain of skin lesions. The instrument was “rigorously developed by a team at Amgen that worked on it with patient groups and others to come up with a patient-reported outcome [tool],” said Dr. Mease, a rheumatologist at the Swedish Medical Center in Seattle. The first question, for example, is: “During the last 24 hours, how severe was the itch from your psoriasis?” Responses range from “not at all” to “very severe.”
Other researchers compared the PSI to PASI to assess symptom severity and clinical status changes, and the PSI “correlates very well,” Dr. Mease said (J Dermatolog Treat. 2014 Feb;25[1]:8-14). In addition, others have validated the PSI in both psoriasis and psoriatic arthritis and suggest a role in research (J Dermatolog Treat. 2013 Aug;24[4]:255-60).
“In a registry or clinical trial setting, this would be a very simple, eight-question patient-reported outcome that … could be employed as a potential substitute for the PASI where it may not be practical,” Dr. Mease said. The PSI can be adjusted to ask about symptoms over the previous 24 hours or past 7 days.
A current limitation is that “we don’t know how this instrument performs in patients with low body surface area psoriasis,” Dr. Mease said. Typically, psoriasis studies enroll participants with at least 10% body surface area involvement. During the Q&A, an attendee pointed out that even less than 3% body surface area psoriasis is relevant in clinical practice. Dr. Mease agreed, and said a future registry study could validate the PSI in this patient population. “There are discussions now with Amgen to possibly use the PSI in the CORRONA registry of psoriatic patients,” he said. “Because of its rigorous development and high psychometric properties, it would be great if it could be used more broadly. I know there are discussions going on in that regard.”
Amgen is evaluating responder definitions for the PSI that correlate with PASI-50, –75 and –90 responses. The firm is also looking at ways to share the PSI instrument with clinicians and researchers. Brian Ortmeier, executive director at Amgen in Los Angeles and one of the developers of PSI, said at the GRAPPA meeting, “Our intent is get the PSI out into the public domain as a disease management tool.”
Dr. Mease is a consultant to and speaker for Amgen and receives research support from the company.
MIAMI – The Psoriasis Symptom Inventory measure could help rheumatologists more easily gauge the severity of moderate to severe psoriasis. The eight-item tool in development correlates well with the Psoriasis Area and Severity Index and is easier to use in rheumatology settings, according to a presentation at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
“One of the ways it can be useful is in a rheumatology setting [to gauge psoriasis severity] when you’re looking at psoriatic arthritis patients,” said Philip J. Mease, MD. But “you might ask: Why is this of utility when we have an actual physical examination score like the PASI [Psoriasis Area and Severity Index] score?”
“Arguably, rheumatologists really don’t do PASI scores at all, practically speaking. If they do them, the quality of the evaluation is more questionable than [when] done by a dermatologist,” Dr. Mease said at the meeting.
The Psoriasis Symptom Inventory (PSI) focuses on redness, scaling, burning, stinging, peeling, flaking, and pain of skin lesions. The instrument was “rigorously developed by a team at Amgen that worked on it with patient groups and others to come up with a patient-reported outcome [tool],” said Dr. Mease, a rheumatologist at the Swedish Medical Center in Seattle. The first question, for example, is: “During the last 24 hours, how severe was the itch from your psoriasis?” Responses range from “not at all” to “very severe.”
Other researchers compared the PSI to PASI to assess symptom severity and clinical status changes, and the PSI “correlates very well,” Dr. Mease said (J Dermatolog Treat. 2014 Feb;25[1]:8-14). In addition, others have validated the PSI in both psoriasis and psoriatic arthritis and suggest a role in research (J Dermatolog Treat. 2013 Aug;24[4]:255-60).
“In a registry or clinical trial setting, this would be a very simple, eight-question patient-reported outcome that … could be employed as a potential substitute for the PASI where it may not be practical,” Dr. Mease said. The PSI can be adjusted to ask about symptoms over the previous 24 hours or past 7 days.
A current limitation is that “we don’t know how this instrument performs in patients with low body surface area psoriasis,” Dr. Mease said. Typically, psoriasis studies enroll participants with at least 10% body surface area involvement. During the Q&A, an attendee pointed out that even less than 3% body surface area psoriasis is relevant in clinical practice. Dr. Mease agreed, and said a future registry study could validate the PSI in this patient population. “There are discussions now with Amgen to possibly use the PSI in the CORRONA registry of psoriatic patients,” he said. “Because of its rigorous development and high psychometric properties, it would be great if it could be used more broadly. I know there are discussions going on in that regard.”
Amgen is evaluating responder definitions for the PSI that correlate with PASI-50, –75 and –90 responses. The firm is also looking at ways to share the PSI instrument with clinicians and researchers. Brian Ortmeier, executive director at Amgen in Los Angeles and one of the developers of PSI, said at the GRAPPA meeting, “Our intent is get the PSI out into the public domain as a disease management tool.”
Dr. Mease is a consultant to and speaker for Amgen and receives research support from the company.
EXPERT ANALYSIS FROM 2016 GRAPPA ANNUAL MEETING
Skin microbiome may differ in unique ways in psoriatic arthritis, psoriasis patients
MIAMI – As patients with psoriasis develop psoriatic arthritis, the abundance of particular genera in the skin microbiome decreases, according to a preliminary study characterizing cutaneous microbiota in these populations.
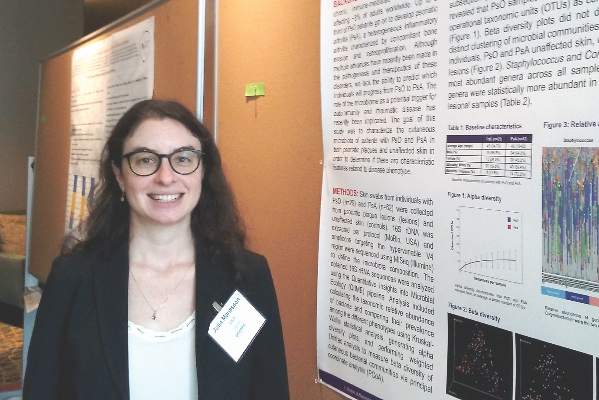
“The big overall message is there might be a decrease in microbiota diversity as you progress through the disease spectrum,” Julia Manasson, MD, a fellow in the division of rheumatology at New York University said. “This is the first study characterizing the cutaneous microbial compositions of subjects with psoriasis and psoriatic arthritis in both psoriatic lesions and unaffected skin.”
A previous study that revealed changes in gut microbiome between psoriasis and psoriatic arthritis patient stool samples (Arthritis Rheumatol. 2015;67:128-39) prompted the current research, which is “trying to see if the skin has a similar manifestation,” Dr. Manasson said during an oral presentation of her poster at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
“The microbiome has been implicated as a potential trigger for inflammation and autoimmune disease,” Dr. Manasson noted.
To investigate a potential role of the skin microbiome, the investigators swabbed lesions and unaffected skin (on a contralateral site) in 29 people with psoriasis and 62 others with psoriatic arthritis. They extracted, amplified, and sequenced DNA from the samples. No participants in the study were on treatment with biologics, disease-modifying antirheumatic drugs, or steroids at the time of assessment. The psoriasis group was 66% men and had an average age of 45 years; the psoriatic arthritis group was 55% men and the average age was 42.
Dr. Manasson and her colleagues calculated the taxonomic relative abundance and contrasted their prevalence among the four skin phenotypes examined: lesions and unaffected skin of psoriasis patients and lesions and unaffected skin of psoriatic arthritis patients. Alpha diversity plots revealed a similar number of operational taxonomic units (OTUs) between psoriasis and psoriatic arthritis samples. Beta diversity analysis showed no distinct clustering or significant difference in microbiota communities among different phenotypes.
“We saw more of a decrease in nonlesional skin and across clinical severity, too,” Dr. Manasson said. “Globally, we didn’t see significant differences [in microbiota present].”
Staphylococcus and Corynebacterium were the predominant bacteria in all samples, but there were also specific genera that were less common in psoriatic arthritis patients and in lesional skin. These less abundant genera included unclassified Bradyrhizobiaceae, Rahnella, unclassified Prevotellaceae, and Parvibaculum.
“It looks like you had some differences between lesion and nonlesional skin,” Alice Gottlieb, MD, chair and dermatologist in chief at Tufts Medical Center in Boston. “In psoriasis, the barrier function is not normal. You may want to look at atopic dermatitis where you clearly have altered barrier function.”
Dr. Manasson said they used a skin swab, so they did not assess barrier function.
“The nonlesional skin may be more interesting to look at,” Dr. Gottlieb added. “If you see a difference in nonlesional skin, it could be more [conclusive].”
Microbiome stability often changes in individuals from week to week, commented Philip Helliwell, DM, PhD, a rheumatologist at the University of Leeds in England and president of GRAPPA. Dr. Manasson said she could assess variability over time in the future. She also would like to evaluate how therapies, including antibiotics, alter the skin microbiome.
Lack of a healthy control group is a potential limitation of the study. Some unanswered questions remain, Dr. Manasson said, such as what are the regional differences in skin microbiota, for example, between a patient’s scalp and forearm? She added, “The most interesting question is what does this actually mean? What are the downstream effects?”
If a decrease in skin microbiome flora diversity is verified in future research as a sign that a patient with psoriasis is at elevated risk for developing psoriatic arthritis, it could help physicians predict who will progress. Currently, about 30% of psoriatic patients go on to develop joint disease, but methods to identify this subpopulation remain elusive.
Dr. Manasson, Dr. Gottlieb, and Dr. Helliwell had no relevant financial disclosures.
MIAMI – As patients with psoriasis develop psoriatic arthritis, the abundance of particular genera in the skin microbiome decreases, according to a preliminary study characterizing cutaneous microbiota in these populations.
“The big overall message is there might be a decrease in microbiota diversity as you progress through the disease spectrum,” Julia Manasson, MD, a fellow in the division of rheumatology at New York University said. “This is the first study characterizing the cutaneous microbial compositions of subjects with psoriasis and psoriatic arthritis in both psoriatic lesions and unaffected skin.”
A previous study that revealed changes in gut microbiome between psoriasis and psoriatic arthritis patient stool samples (Arthritis Rheumatol. 2015;67:128-39) prompted the current research, which is “trying to see if the skin has a similar manifestation,” Dr. Manasson said during an oral presentation of her poster at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
“The microbiome has been implicated as a potential trigger for inflammation and autoimmune disease,” Dr. Manasson noted.
To investigate a potential role of the skin microbiome, the investigators swabbed lesions and unaffected skin (on a contralateral site) in 29 people with psoriasis and 62 others with psoriatic arthritis. They extracted, amplified, and sequenced DNA from the samples. No participants in the study were on treatment with biologics, disease-modifying antirheumatic drugs, or steroids at the time of assessment. The psoriasis group was 66% men and had an average age of 45 years; the psoriatic arthritis group was 55% men and the average age was 42.
Dr. Manasson and her colleagues calculated the taxonomic relative abundance and contrasted their prevalence among the four skin phenotypes examined: lesions and unaffected skin of psoriasis patients and lesions and unaffected skin of psoriatic arthritis patients. Alpha diversity plots revealed a similar number of operational taxonomic units (OTUs) between psoriasis and psoriatic arthritis samples. Beta diversity analysis showed no distinct clustering or significant difference in microbiota communities among different phenotypes.
“We saw more of a decrease in nonlesional skin and across clinical severity, too,” Dr. Manasson said. “Globally, we didn’t see significant differences [in microbiota present].”
Staphylococcus and Corynebacterium were the predominant bacteria in all samples, but there were also specific genera that were less common in psoriatic arthritis patients and in lesional skin. These less abundant genera included unclassified Bradyrhizobiaceae, Rahnella, unclassified Prevotellaceae, and Parvibaculum.
“It looks like you had some differences between lesion and nonlesional skin,” Alice Gottlieb, MD, chair and dermatologist in chief at Tufts Medical Center in Boston. “In psoriasis, the barrier function is not normal. You may want to look at atopic dermatitis where you clearly have altered barrier function.”
Dr. Manasson said they used a skin swab, so they did not assess barrier function.
“The nonlesional skin may be more interesting to look at,” Dr. Gottlieb added. “If you see a difference in nonlesional skin, it could be more [conclusive].”
Microbiome stability often changes in individuals from week to week, commented Philip Helliwell, DM, PhD, a rheumatologist at the University of Leeds in England and president of GRAPPA. Dr. Manasson said she could assess variability over time in the future. She also would like to evaluate how therapies, including antibiotics, alter the skin microbiome.
Lack of a healthy control group is a potential limitation of the study. Some unanswered questions remain, Dr. Manasson said, such as what are the regional differences in skin microbiota, for example, between a patient’s scalp and forearm? She added, “The most interesting question is what does this actually mean? What are the downstream effects?”
If a decrease in skin microbiome flora diversity is verified in future research as a sign that a patient with psoriasis is at elevated risk for developing psoriatic arthritis, it could help physicians predict who will progress. Currently, about 30% of psoriatic patients go on to develop joint disease, but methods to identify this subpopulation remain elusive.
Dr. Manasson, Dr. Gottlieb, and Dr. Helliwell had no relevant financial disclosures.
MIAMI – As patients with psoriasis develop psoriatic arthritis, the abundance of particular genera in the skin microbiome decreases, according to a preliminary study characterizing cutaneous microbiota in these populations.
“The big overall message is there might be a decrease in microbiota diversity as you progress through the disease spectrum,” Julia Manasson, MD, a fellow in the division of rheumatology at New York University said. “This is the first study characterizing the cutaneous microbial compositions of subjects with psoriasis and psoriatic arthritis in both psoriatic lesions and unaffected skin.”
A previous study that revealed changes in gut microbiome between psoriasis and psoriatic arthritis patient stool samples (Arthritis Rheumatol. 2015;67:128-39) prompted the current research, which is “trying to see if the skin has a similar manifestation,” Dr. Manasson said during an oral presentation of her poster at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
“The microbiome has been implicated as a potential trigger for inflammation and autoimmune disease,” Dr. Manasson noted.
To investigate a potential role of the skin microbiome, the investigators swabbed lesions and unaffected skin (on a contralateral site) in 29 people with psoriasis and 62 others with psoriatic arthritis. They extracted, amplified, and sequenced DNA from the samples. No participants in the study were on treatment with biologics, disease-modifying antirheumatic drugs, or steroids at the time of assessment. The psoriasis group was 66% men and had an average age of 45 years; the psoriatic arthritis group was 55% men and the average age was 42.
Dr. Manasson and her colleagues calculated the taxonomic relative abundance and contrasted their prevalence among the four skin phenotypes examined: lesions and unaffected skin of psoriasis patients and lesions and unaffected skin of psoriatic arthritis patients. Alpha diversity plots revealed a similar number of operational taxonomic units (OTUs) between psoriasis and psoriatic arthritis samples. Beta diversity analysis showed no distinct clustering or significant difference in microbiota communities among different phenotypes.
“We saw more of a decrease in nonlesional skin and across clinical severity, too,” Dr. Manasson said. “Globally, we didn’t see significant differences [in microbiota present].”
Staphylococcus and Corynebacterium were the predominant bacteria in all samples, but there were also specific genera that were less common in psoriatic arthritis patients and in lesional skin. These less abundant genera included unclassified Bradyrhizobiaceae, Rahnella, unclassified Prevotellaceae, and Parvibaculum.
“It looks like you had some differences between lesion and nonlesional skin,” Alice Gottlieb, MD, chair and dermatologist in chief at Tufts Medical Center in Boston. “In psoriasis, the barrier function is not normal. You may want to look at atopic dermatitis where you clearly have altered barrier function.”
Dr. Manasson said they used a skin swab, so they did not assess barrier function.
“The nonlesional skin may be more interesting to look at,” Dr. Gottlieb added. “If you see a difference in nonlesional skin, it could be more [conclusive].”
Microbiome stability often changes in individuals from week to week, commented Philip Helliwell, DM, PhD, a rheumatologist at the University of Leeds in England and president of GRAPPA. Dr. Manasson said she could assess variability over time in the future. She also would like to evaluate how therapies, including antibiotics, alter the skin microbiome.
Lack of a healthy control group is a potential limitation of the study. Some unanswered questions remain, Dr. Manasson said, such as what are the regional differences in skin microbiota, for example, between a patient’s scalp and forearm? She added, “The most interesting question is what does this actually mean? What are the downstream effects?”
If a decrease in skin microbiome flora diversity is verified in future research as a sign that a patient with psoriasis is at elevated risk for developing psoriatic arthritis, it could help physicians predict who will progress. Currently, about 30% of psoriatic patients go on to develop joint disease, but methods to identify this subpopulation remain elusive.
Dr. Manasson, Dr. Gottlieb, and Dr. Helliwell had no relevant financial disclosures.
AT 2016 GRAPPA ANNUAL MEETING
Key clinical point:Changes in skin microbiome diversity in patients with psoriasis might someday help to predict progression to psoriatic arthritis.
Major finding: The abundance of specific genera was decreased in psoriatic arthritis patients and in their lesional skin relative to patients with psoriasis only.
Data source: Comparison of 29 people with psoriasis versus 62 with psoriatic arthritis.
Disclosures: Dr. Manasson, Dr. Gottlieb, and Dr. Helliwell had no relevant disclosures.
Ultrasound’s role in detecting enthesitis in psoriatic arthritis remains debatable
MIAMI – Ultrasound-detected enthesitis was associated with both destructive and bone formation lesions on radiography of peripheral and axial joints in a study of 222 patients with psoriatic arthritis. But its lack of correlation to clinically detected enthesitis in this study and in others has made its clinical usefulness somewhat controversial.
“This is not first time we see this result in the literature,” Ari Polachek, MD, said when presenting the research at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA). The findings suggest ultrasound reveals something different than a physical examination does, and because it’s more sensitive and specific, ultrasound is more accurate, he said.
Diagnostic disagreement
Some differing opinions arose during a discussion after Dr. Polachek’s presentation. “When you look at the enthesitis measures [with ultrasound] ... you don’t necessarily measure the same enthesitis points you measure in clinical practice,” said Dafna D. Gladman, MD, a senior scientist at Toronto Western Hospital’s Krembil Research Institute and a rheumatologist at the University of Toronto. “We have to be careful. I don’t think we should immediately cancel the relationship between the ultrasound and clinical exam.”
“Well, I disagree entirely,” said Philip Helliwell, DM, PhD, senior lecturer in rheumatology at the University of Leeds, England, and president of GRAPPA. “We have looked at the Leeds [Enthesitis Index] with ultrasound and MRI and found no significant relationship at all.” Although Dr. Helliwell said there is a possible role for ultrasound to detect enthesitis in the Achilles, “We are fooling ourselves if we are measuring enthesitis as a pathologic entity. I don’t really know what we’re measuring when we do these scores.”
“My message is you do not need to scan every patient,” Dr. Polachek said in an interview. If a physician remains unsure about the physical exam results, it can be useful. Dr. Polachek, who completed his medical training in Israel, added: “In Israel, we say that ultrasound is ‘the final judge.’ ”
Association with radiographic joint findings
The investigators achieved their study aim: demonstrating that the severity of sonographic enthesitis is a marker of radiographic peripheral and axial joint damage in psoriatic arthritis. They found an association for both destructive and bone formation lesions.
“These findings highlight the potential role of enthesitis in the pathogenesis of articular damage in psoriatic arthritis,” said Dr. Polachek, clinical and research fellow at the University of Toronto.
The researchers assessed 12 entheseal sites with ultrasound. They used the Madrid Sonography Enthesitis Index scoring system (MASEI) to determine the global extent of enthesitis in each patient. In addition, they used the modified Steinbrocker score to assess peripheral joint damage, and the modified Stoke Ankylosing Spondylitis Spine Score (mSASSS) to assess spinal damage. Patients also underwent a clinical exam and were asked about their medical history.
Multivariate analysis revealed a significant association between higher MASEI score and joint ankylosis (odds ratio, 2.09; P = .0001) and arthritis mutilans (OR, 1.73; P = .005). The total MASEI score was associated with the modified Steinbrocker score (OR, 9.3; P less than .0001) in a logistic regression analysis; total MASEI also significantly correlated with the mSASSS measure of spinal damage (OR, 1.55; P less than .0001) in a linear regression analysis.
Participants had a mean age of 56 years and a 17-year mean duration of psoriatic arthritis. They presented with a mean of 2.4 tender joints and 1.1 swollen joints. At study entry, their mean scores were 15.6 on MASEI, 18.1 on modified Steinbrocker, and 1.72 on mSASSS.
The strengths of the study included a large number of participants and control of multiple possible confounders (age, sex, body mass index, duration of psoriatic arthritis, and use of disease-modifying antirheumatic drugs and biologics). It is limited by its cross-sectional design, which rules out inferences of causality.
Clinical confirmation
“Traditionally, patients came in with a tender joint, and we might not see anything. Now I can put the sensor down and say they have inflammation,” Dr. Polachek said. In such cases, he may suggest more aggressive treatment. However, if an asymptomatic patient has ultrasound findings, “right now the recommendation is not to do anything. Otherwise, it could be overtreatment.”
“This is the future,” Dr. Polachek said. “I started doing ultrasound myself – it’s a game changer.”
Dr. Polachek has received funding from Janssen and the Krembil Research Institute.
MIAMI – Ultrasound-detected enthesitis was associated with both destructive and bone formation lesions on radiography of peripheral and axial joints in a study of 222 patients with psoriatic arthritis. But its lack of correlation to clinically detected enthesitis in this study and in others has made its clinical usefulness somewhat controversial.
“This is not first time we see this result in the literature,” Ari Polachek, MD, said when presenting the research at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA). The findings suggest ultrasound reveals something different than a physical examination does, and because it’s more sensitive and specific, ultrasound is more accurate, he said.
Diagnostic disagreement
Some differing opinions arose during a discussion after Dr. Polachek’s presentation. “When you look at the enthesitis measures [with ultrasound] ... you don’t necessarily measure the same enthesitis points you measure in clinical practice,” said Dafna D. Gladman, MD, a senior scientist at Toronto Western Hospital’s Krembil Research Institute and a rheumatologist at the University of Toronto. “We have to be careful. I don’t think we should immediately cancel the relationship between the ultrasound and clinical exam.”
“Well, I disagree entirely,” said Philip Helliwell, DM, PhD, senior lecturer in rheumatology at the University of Leeds, England, and president of GRAPPA. “We have looked at the Leeds [Enthesitis Index] with ultrasound and MRI and found no significant relationship at all.” Although Dr. Helliwell said there is a possible role for ultrasound to detect enthesitis in the Achilles, “We are fooling ourselves if we are measuring enthesitis as a pathologic entity. I don’t really know what we’re measuring when we do these scores.”
“My message is you do not need to scan every patient,” Dr. Polachek said in an interview. If a physician remains unsure about the physical exam results, it can be useful. Dr. Polachek, who completed his medical training in Israel, added: “In Israel, we say that ultrasound is ‘the final judge.’ ”
Association with radiographic joint findings
The investigators achieved their study aim: demonstrating that the severity of sonographic enthesitis is a marker of radiographic peripheral and axial joint damage in psoriatic arthritis. They found an association for both destructive and bone formation lesions.
“These findings highlight the potential role of enthesitis in the pathogenesis of articular damage in psoriatic arthritis,” said Dr. Polachek, clinical and research fellow at the University of Toronto.
The researchers assessed 12 entheseal sites with ultrasound. They used the Madrid Sonography Enthesitis Index scoring system (MASEI) to determine the global extent of enthesitis in each patient. In addition, they used the modified Steinbrocker score to assess peripheral joint damage, and the modified Stoke Ankylosing Spondylitis Spine Score (mSASSS) to assess spinal damage. Patients also underwent a clinical exam and were asked about their medical history.
Multivariate analysis revealed a significant association between higher MASEI score and joint ankylosis (odds ratio, 2.09; P = .0001) and arthritis mutilans (OR, 1.73; P = .005). The total MASEI score was associated with the modified Steinbrocker score (OR, 9.3; P less than .0001) in a logistic regression analysis; total MASEI also significantly correlated with the mSASSS measure of spinal damage (OR, 1.55; P less than .0001) in a linear regression analysis.
Participants had a mean age of 56 years and a 17-year mean duration of psoriatic arthritis. They presented with a mean of 2.4 tender joints and 1.1 swollen joints. At study entry, their mean scores were 15.6 on MASEI, 18.1 on modified Steinbrocker, and 1.72 on mSASSS.
The strengths of the study included a large number of participants and control of multiple possible confounders (age, sex, body mass index, duration of psoriatic arthritis, and use of disease-modifying antirheumatic drugs and biologics). It is limited by its cross-sectional design, which rules out inferences of causality.
Clinical confirmation
“Traditionally, patients came in with a tender joint, and we might not see anything. Now I can put the sensor down and say they have inflammation,” Dr. Polachek said. In such cases, he may suggest more aggressive treatment. However, if an asymptomatic patient has ultrasound findings, “right now the recommendation is not to do anything. Otherwise, it could be overtreatment.”
“This is the future,” Dr. Polachek said. “I started doing ultrasound myself – it’s a game changer.”
Dr. Polachek has received funding from Janssen and the Krembil Research Institute.
MIAMI – Ultrasound-detected enthesitis was associated with both destructive and bone formation lesions on radiography of peripheral and axial joints in a study of 222 patients with psoriatic arthritis. But its lack of correlation to clinically detected enthesitis in this study and in others has made its clinical usefulness somewhat controversial.
“This is not first time we see this result in the literature,” Ari Polachek, MD, said when presenting the research at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA). The findings suggest ultrasound reveals something different than a physical examination does, and because it’s more sensitive and specific, ultrasound is more accurate, he said.
Diagnostic disagreement
Some differing opinions arose during a discussion after Dr. Polachek’s presentation. “When you look at the enthesitis measures [with ultrasound] ... you don’t necessarily measure the same enthesitis points you measure in clinical practice,” said Dafna D. Gladman, MD, a senior scientist at Toronto Western Hospital’s Krembil Research Institute and a rheumatologist at the University of Toronto. “We have to be careful. I don’t think we should immediately cancel the relationship between the ultrasound and clinical exam.”
“Well, I disagree entirely,” said Philip Helliwell, DM, PhD, senior lecturer in rheumatology at the University of Leeds, England, and president of GRAPPA. “We have looked at the Leeds [Enthesitis Index] with ultrasound and MRI and found no significant relationship at all.” Although Dr. Helliwell said there is a possible role for ultrasound to detect enthesitis in the Achilles, “We are fooling ourselves if we are measuring enthesitis as a pathologic entity. I don’t really know what we’re measuring when we do these scores.”
“My message is you do not need to scan every patient,” Dr. Polachek said in an interview. If a physician remains unsure about the physical exam results, it can be useful. Dr. Polachek, who completed his medical training in Israel, added: “In Israel, we say that ultrasound is ‘the final judge.’ ”
Association with radiographic joint findings
The investigators achieved their study aim: demonstrating that the severity of sonographic enthesitis is a marker of radiographic peripheral and axial joint damage in psoriatic arthritis. They found an association for both destructive and bone formation lesions.
“These findings highlight the potential role of enthesitis in the pathogenesis of articular damage in psoriatic arthritis,” said Dr. Polachek, clinical and research fellow at the University of Toronto.
The researchers assessed 12 entheseal sites with ultrasound. They used the Madrid Sonography Enthesitis Index scoring system (MASEI) to determine the global extent of enthesitis in each patient. In addition, they used the modified Steinbrocker score to assess peripheral joint damage, and the modified Stoke Ankylosing Spondylitis Spine Score (mSASSS) to assess spinal damage. Patients also underwent a clinical exam and were asked about their medical history.
Multivariate analysis revealed a significant association between higher MASEI score and joint ankylosis (odds ratio, 2.09; P = .0001) and arthritis mutilans (OR, 1.73; P = .005). The total MASEI score was associated with the modified Steinbrocker score (OR, 9.3; P less than .0001) in a logistic regression analysis; total MASEI also significantly correlated with the mSASSS measure of spinal damage (OR, 1.55; P less than .0001) in a linear regression analysis.
Participants had a mean age of 56 years and a 17-year mean duration of psoriatic arthritis. They presented with a mean of 2.4 tender joints and 1.1 swollen joints. At study entry, their mean scores were 15.6 on MASEI, 18.1 on modified Steinbrocker, and 1.72 on mSASSS.
The strengths of the study included a large number of participants and control of multiple possible confounders (age, sex, body mass index, duration of psoriatic arthritis, and use of disease-modifying antirheumatic drugs and biologics). It is limited by its cross-sectional design, which rules out inferences of causality.
Clinical confirmation
“Traditionally, patients came in with a tender joint, and we might not see anything. Now I can put the sensor down and say they have inflammation,” Dr. Polachek said. In such cases, he may suggest more aggressive treatment. However, if an asymptomatic patient has ultrasound findings, “right now the recommendation is not to do anything. Otherwise, it could be overtreatment.”
“This is the future,” Dr. Polachek said. “I started doing ultrasound myself – it’s a game changer.”
Dr. Polachek has received funding from Janssen and the Krembil Research Institute.
AT 2016 GRAPPA
Key clinical point: Ultrasound can diagnose enthesitis in psoriatic arthritis, but findings differ from physical exam.
Major finding: Multivariate analysis revealed a significant association between higher MASEI score and joint ankylosis (OR, 2.09; P = .0001) and arthritis mutilans (OR, 1.73; P = .005).
Data source: Cross-sectional study of 222 patients with psoriatic arthritis.
Disclosures: Dr. Polachek has received funding from Janssen and the Krembil Research Institute.
Psoriatic flare assessment tool in validation stage
MIAMI – Reaching a consensus on measurement and assessment of flare in psoriatic arthritis remains challenging, especially with no widely accepted definition and differing opinions among patients and physicians. But getting standard evaluation of flare under control is critical for both clinical and research outcomes.
Through a series of patient interviews, physician surveys, and lessons learned in rheumatoid arthritis, the GRAPPA Flare Project is close to a validated flare instrument. A 10-question flare assessment tool is now in the final validation stage, according to a presentation at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
“Flare is a clearly personal experience and varies from patient to patient. It’s clear that physicians and patients have clearly different ideas of what flare is. Bringing those two worlds together was a challenge,” Philip Helliwell, MD, of Leeds (England) University and GRAPPA president, said at the meeting.
“Some societies – I’m not going to mention any names – have gone down the route of a definition of flare linked to disease activity measures. We have not done this,” Dr. Helliwell said.
Instead, the Flare Project is taking a patient-driven and physician-reviewed approach. Investigators cast a wide net, identifying 79 factors important to patients in six major domains: skin, joint, emotional, participation, fatigue, and unclassified. The results were published in 2015 (Rheumatology [Oxford]. 2015 Aug;54[8]:1448-53). Through a Delphi survey, physicians reviewed these considerations. Then GRAPPA identified items important to both patients and physicians and developed a preliminary flare instrument.
Unlike most assessment tools for psoriatic disease, the new instrument includes patient-reported emotional well-being. Niti Goel, MD, of Duke University, Durham, N.C., said that physicians do not always ask patients about the psychological impact of their disease, so the tool “could provide additional information.”
Another goal of the project is to provide standard answers to some of the common questions related to psoriatic arthritis, including: What exactly is a flare? Does the definition truly capture the worsening of disease? Are there different types of flares? Is flare different if you start from a point of high disease activity? What self-management and other interventions are effective for flare?
GRAPPA adopted a definition of flare developed from rheumatoid arthritis, stating that flare is any worsening of disease activity that would, if persistent, in most cases lead to initiation or change of therapy (J Rheumatol. 2009 Oct;36[10]:2335-41).
“It took [them] some time to get to that definition,” Dr. Helliwell said. “We know from rheumatoid arthritis that there is a lot more to a flare than joint swelling and pain.”
The GRAPPA flare tool is now in the validation stage, Dr. Helliwell said, and will be tested in several studies, including a prospective multicenter study where the 10-item questionnaire will be administered to patients.
A meeting attendee commented that the patient and physician global scales are sufficient and asked: “Is there really a need for a flare instrument?”
“I accept what you are saying, but I would also retort that knowledge is power, and the more information we get, the more we know about what we are doing,” Dr. Helliwell said. “We are going to collect all our information – physician global, patient global, composite disease measures – everything within that study.”
Dr. Helliwell and Dr. Goel reported having no relevant financial disclosures.
MIAMI – Reaching a consensus on measurement and assessment of flare in psoriatic arthritis remains challenging, especially with no widely accepted definition and differing opinions among patients and physicians. But getting standard evaluation of flare under control is critical for both clinical and research outcomes.
Through a series of patient interviews, physician surveys, and lessons learned in rheumatoid arthritis, the GRAPPA Flare Project is close to a validated flare instrument. A 10-question flare assessment tool is now in the final validation stage, according to a presentation at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
“Flare is a clearly personal experience and varies from patient to patient. It’s clear that physicians and patients have clearly different ideas of what flare is. Bringing those two worlds together was a challenge,” Philip Helliwell, MD, of Leeds (England) University and GRAPPA president, said at the meeting.
“Some societies – I’m not going to mention any names – have gone down the route of a definition of flare linked to disease activity measures. We have not done this,” Dr. Helliwell said.
Instead, the Flare Project is taking a patient-driven and physician-reviewed approach. Investigators cast a wide net, identifying 79 factors important to patients in six major domains: skin, joint, emotional, participation, fatigue, and unclassified. The results were published in 2015 (Rheumatology [Oxford]. 2015 Aug;54[8]:1448-53). Through a Delphi survey, physicians reviewed these considerations. Then GRAPPA identified items important to both patients and physicians and developed a preliminary flare instrument.
Unlike most assessment tools for psoriatic disease, the new instrument includes patient-reported emotional well-being. Niti Goel, MD, of Duke University, Durham, N.C., said that physicians do not always ask patients about the psychological impact of their disease, so the tool “could provide additional information.”
Another goal of the project is to provide standard answers to some of the common questions related to psoriatic arthritis, including: What exactly is a flare? Does the definition truly capture the worsening of disease? Are there different types of flares? Is flare different if you start from a point of high disease activity? What self-management and other interventions are effective for flare?
GRAPPA adopted a definition of flare developed from rheumatoid arthritis, stating that flare is any worsening of disease activity that would, if persistent, in most cases lead to initiation or change of therapy (J Rheumatol. 2009 Oct;36[10]:2335-41).
“It took [them] some time to get to that definition,” Dr. Helliwell said. “We know from rheumatoid arthritis that there is a lot more to a flare than joint swelling and pain.”
The GRAPPA flare tool is now in the validation stage, Dr. Helliwell said, and will be tested in several studies, including a prospective multicenter study where the 10-item questionnaire will be administered to patients.
A meeting attendee commented that the patient and physician global scales are sufficient and asked: “Is there really a need for a flare instrument?”
“I accept what you are saying, but I would also retort that knowledge is power, and the more information we get, the more we know about what we are doing,” Dr. Helliwell said. “We are going to collect all our information – physician global, patient global, composite disease measures – everything within that study.”
Dr. Helliwell and Dr. Goel reported having no relevant financial disclosures.
MIAMI – Reaching a consensus on measurement and assessment of flare in psoriatic arthritis remains challenging, especially with no widely accepted definition and differing opinions among patients and physicians. But getting standard evaluation of flare under control is critical for both clinical and research outcomes.
Through a series of patient interviews, physician surveys, and lessons learned in rheumatoid arthritis, the GRAPPA Flare Project is close to a validated flare instrument. A 10-question flare assessment tool is now in the final validation stage, according to a presentation at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
“Flare is a clearly personal experience and varies from patient to patient. It’s clear that physicians and patients have clearly different ideas of what flare is. Bringing those two worlds together was a challenge,” Philip Helliwell, MD, of Leeds (England) University and GRAPPA president, said at the meeting.
“Some societies – I’m not going to mention any names – have gone down the route of a definition of flare linked to disease activity measures. We have not done this,” Dr. Helliwell said.
Instead, the Flare Project is taking a patient-driven and physician-reviewed approach. Investigators cast a wide net, identifying 79 factors important to patients in six major domains: skin, joint, emotional, participation, fatigue, and unclassified. The results were published in 2015 (Rheumatology [Oxford]. 2015 Aug;54[8]:1448-53). Through a Delphi survey, physicians reviewed these considerations. Then GRAPPA identified items important to both patients and physicians and developed a preliminary flare instrument.
Unlike most assessment tools for psoriatic disease, the new instrument includes patient-reported emotional well-being. Niti Goel, MD, of Duke University, Durham, N.C., said that physicians do not always ask patients about the psychological impact of their disease, so the tool “could provide additional information.”
Another goal of the project is to provide standard answers to some of the common questions related to psoriatic arthritis, including: What exactly is a flare? Does the definition truly capture the worsening of disease? Are there different types of flares? Is flare different if you start from a point of high disease activity? What self-management and other interventions are effective for flare?
GRAPPA adopted a definition of flare developed from rheumatoid arthritis, stating that flare is any worsening of disease activity that would, if persistent, in most cases lead to initiation or change of therapy (J Rheumatol. 2009 Oct;36[10]:2335-41).
“It took [them] some time to get to that definition,” Dr. Helliwell said. “We know from rheumatoid arthritis that there is a lot more to a flare than joint swelling and pain.”
The GRAPPA flare tool is now in the validation stage, Dr. Helliwell said, and will be tested in several studies, including a prospective multicenter study where the 10-item questionnaire will be administered to patients.
A meeting attendee commented that the patient and physician global scales are sufficient and asked: “Is there really a need for a flare instrument?”
“I accept what you are saying, but I would also retort that knowledge is power, and the more information we get, the more we know about what we are doing,” Dr. Helliwell said. “We are going to collect all our information – physician global, patient global, composite disease measures – everything within that study.”
Dr. Helliwell and Dr. Goel reported having no relevant financial disclosures.
EXPERT ANALYSIS FROM 2016 GRAPPA ANNUAL MEETING
Psoriatic Arthritis Patients Face More Endocrine Comorbidities
MIAMI – Diabetes mellitus, hypothyroidism, Cushing’s disease, and osteoporosis occur more frequently in people with psoriatic arthritis than in controls, a large cohort study reveals. Prevalence of these endocrine conditions was greater in a group of 3,161 patients with psoriatic arthritis, compared with 31,610 matched controls.
“We recommend that physicians should be aware of comorbid associations to provide comprehensive medical care to patients with psoriatic arthritis,” said Amir Haddad, MD, of the department of rheumatology at Carmel Medical Center in Haifa, Israel.
Dr. Haddad and his colleagues, however, found no significant differences in the prevalence of hyperthyroidism, hypo- and hyperparathyroidism, hyperprolactinemia, Addison’s disease, diabetes insipidus, pituitary adenoma, or acromegaly between groups in this retrospective, cross-sectional study.
They identified 1,474 men and 1,687 women diagnosed with psoriatic disease from 2000 to 2013 using the Clalit health services database in Israel. This group was a mean of 58 years old and 53% were women. Each patient was matched with 10 age- and gender-matched controls without psoriatic disease for the study.
“This is, to our knowledge, one of the largest real-life cohorts of psoriatic patient registries,” Dr. Haddad said at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA).
In the psoriatic arthritis group versus controls, diabetes mellitus prevalence was 27.9% vs. 20.7%; for hypothyroidism it was 12.7% vs. 8.6%; and for Cushing’s disease it was 0.3% vs. 0.1%. All these differences were statically significant (P less than 0.0001). Osteoporosis prevalence also differed significantly between the psoriatic arthritis and control groups: 13.2% vs. 9.1% (P less than 0.001).
Greater awareness of nonskin and nonjoint comorbidities is important, Dr. Haddad said, because it can influence choice of therapy and management of patients with psoriatic arthritis.
The investigators also conducted univariate and multivariate regression analyses. Compared with controls, the results suggest psoriatic arthritis patients have a higher risk for diabetes mellitus (odds ratio, 1.48), hypothyroidism (OR, 1.56), and osteoporosis (OR, 1.52). The risk for Cushing’s disease was notably higher (OR, 5.31) in the univariate analysis.
Risks for these endocrine conditions remained higher for the psoriatic arthritis patients in a multivariate regression analysis as well. For example, risk for diabetes mellitus (OR, 1.30) remained after adjusting for age, gender, smoking, obesity, and steroid use. Risk of hypothyroidism (OR, 1.61) remained after adjusting for age and gender; risk of osteoporosis (OR, 1.50) after adjusting for age, gender, steroid use, and smoking; and risk of Cushing’s disease (OR, 3.79) after adjustment for age, gender, and steroid use.
The large, population-based cohort is a strength of the study. “We are now going back to see how many of these patients were seen by rheumatologists,” Dr. Haddad said. A lack of association with disease burden is a potential limitation, he added.
Thirty percent of patients were treated with biologics and about 67% with steroids. “That number treated with steroids seems high,” a meeting attendee commented. Dr. Haddad explained that it is the percentage ever treated with steroids, not necessarily currently on steroids.
In a separate session at the GRAPPA meeting addressing psoriatic disease treatment recommendations, an attendee asked about specific recommendations for comorbidities. For now, GRAPPA plans to include comorbidities within its overall recommendations, as it did in its most recent update, released in January 2016. A limited amount of data is a primary reason.
“As the evidence on comorbidities gets better, we may someday have separate recommendations for comorbidities,” said Laura Coates, MD, a clinical lecturer in rheumatology at the University of Leeds (England).
“The comorbidities are very important,” said Arthur F. Kavanaugh, MD, professor of medicine at the University of California, San Diego. “That’s trickier and deals with the international nature of GRAPPA. It’s hard to say, ‘Go see this specialist,’ because that might not be standard of care in that country.”
Dr. Haddad, Dr. Coates, and Dr. Kavanaugh reported having no relevant financial disclosures.
MIAMI – Diabetes mellitus, hypothyroidism, Cushing’s disease, and osteoporosis occur more frequently in people with psoriatic arthritis than in controls, a large cohort study reveals. Prevalence of these endocrine conditions was greater in a group of 3,161 patients with psoriatic arthritis, compared with 31,610 matched controls.
“We recommend that physicians should be aware of comorbid associations to provide comprehensive medical care to patients with psoriatic arthritis,” said Amir Haddad, MD, of the department of rheumatology at Carmel Medical Center in Haifa, Israel.
Dr. Haddad and his colleagues, however, found no significant differences in the prevalence of hyperthyroidism, hypo- and hyperparathyroidism, hyperprolactinemia, Addison’s disease, diabetes insipidus, pituitary adenoma, or acromegaly between groups in this retrospective, cross-sectional study.
They identified 1,474 men and 1,687 women diagnosed with psoriatic disease from 2000 to 2013 using the Clalit health services database in Israel. This group was a mean of 58 years old and 53% were women. Each patient was matched with 10 age- and gender-matched controls without psoriatic disease for the study.
“This is, to our knowledge, one of the largest real-life cohorts of psoriatic patient registries,” Dr. Haddad said at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA).
In the psoriatic arthritis group versus controls, diabetes mellitus prevalence was 27.9% vs. 20.7%; for hypothyroidism it was 12.7% vs. 8.6%; and for Cushing’s disease it was 0.3% vs. 0.1%. All these differences were statically significant (P less than 0.0001). Osteoporosis prevalence also differed significantly between the psoriatic arthritis and control groups: 13.2% vs. 9.1% (P less than 0.001).
Greater awareness of nonskin and nonjoint comorbidities is important, Dr. Haddad said, because it can influence choice of therapy and management of patients with psoriatic arthritis.
The investigators also conducted univariate and multivariate regression analyses. Compared with controls, the results suggest psoriatic arthritis patients have a higher risk for diabetes mellitus (odds ratio, 1.48), hypothyroidism (OR, 1.56), and osteoporosis (OR, 1.52). The risk for Cushing’s disease was notably higher (OR, 5.31) in the univariate analysis.
Risks for these endocrine conditions remained higher for the psoriatic arthritis patients in a multivariate regression analysis as well. For example, risk for diabetes mellitus (OR, 1.30) remained after adjusting for age, gender, smoking, obesity, and steroid use. Risk of hypothyroidism (OR, 1.61) remained after adjusting for age and gender; risk of osteoporosis (OR, 1.50) after adjusting for age, gender, steroid use, and smoking; and risk of Cushing’s disease (OR, 3.79) after adjustment for age, gender, and steroid use.
The large, population-based cohort is a strength of the study. “We are now going back to see how many of these patients were seen by rheumatologists,” Dr. Haddad said. A lack of association with disease burden is a potential limitation, he added.
Thirty percent of patients were treated with biologics and about 67% with steroids. “That number treated with steroids seems high,” a meeting attendee commented. Dr. Haddad explained that it is the percentage ever treated with steroids, not necessarily currently on steroids.
In a separate session at the GRAPPA meeting addressing psoriatic disease treatment recommendations, an attendee asked about specific recommendations for comorbidities. For now, GRAPPA plans to include comorbidities within its overall recommendations, as it did in its most recent update, released in January 2016. A limited amount of data is a primary reason.
“As the evidence on comorbidities gets better, we may someday have separate recommendations for comorbidities,” said Laura Coates, MD, a clinical lecturer in rheumatology at the University of Leeds (England).
“The comorbidities are very important,” said Arthur F. Kavanaugh, MD, professor of medicine at the University of California, San Diego. “That’s trickier and deals with the international nature of GRAPPA. It’s hard to say, ‘Go see this specialist,’ because that might not be standard of care in that country.”
Dr. Haddad, Dr. Coates, and Dr. Kavanaugh reported having no relevant financial disclosures.
MIAMI – Diabetes mellitus, hypothyroidism, Cushing’s disease, and osteoporosis occur more frequently in people with psoriatic arthritis than in controls, a large cohort study reveals. Prevalence of these endocrine conditions was greater in a group of 3,161 patients with psoriatic arthritis, compared with 31,610 matched controls.
“We recommend that physicians should be aware of comorbid associations to provide comprehensive medical care to patients with psoriatic arthritis,” said Amir Haddad, MD, of the department of rheumatology at Carmel Medical Center in Haifa, Israel.
Dr. Haddad and his colleagues, however, found no significant differences in the prevalence of hyperthyroidism, hypo- and hyperparathyroidism, hyperprolactinemia, Addison’s disease, diabetes insipidus, pituitary adenoma, or acromegaly between groups in this retrospective, cross-sectional study.
They identified 1,474 men and 1,687 women diagnosed with psoriatic disease from 2000 to 2013 using the Clalit health services database in Israel. This group was a mean of 58 years old and 53% were women. Each patient was matched with 10 age- and gender-matched controls without psoriatic disease for the study.
“This is, to our knowledge, one of the largest real-life cohorts of psoriatic patient registries,” Dr. Haddad said at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA).
In the psoriatic arthritis group versus controls, diabetes mellitus prevalence was 27.9% vs. 20.7%; for hypothyroidism it was 12.7% vs. 8.6%; and for Cushing’s disease it was 0.3% vs. 0.1%. All these differences were statically significant (P less than 0.0001). Osteoporosis prevalence also differed significantly between the psoriatic arthritis and control groups: 13.2% vs. 9.1% (P less than 0.001).
Greater awareness of nonskin and nonjoint comorbidities is important, Dr. Haddad said, because it can influence choice of therapy and management of patients with psoriatic arthritis.
The investigators also conducted univariate and multivariate regression analyses. Compared with controls, the results suggest psoriatic arthritis patients have a higher risk for diabetes mellitus (odds ratio, 1.48), hypothyroidism (OR, 1.56), and osteoporosis (OR, 1.52). The risk for Cushing’s disease was notably higher (OR, 5.31) in the univariate analysis.
Risks for these endocrine conditions remained higher for the psoriatic arthritis patients in a multivariate regression analysis as well. For example, risk for diabetes mellitus (OR, 1.30) remained after adjusting for age, gender, smoking, obesity, and steroid use. Risk of hypothyroidism (OR, 1.61) remained after adjusting for age and gender; risk of osteoporosis (OR, 1.50) after adjusting for age, gender, steroid use, and smoking; and risk of Cushing’s disease (OR, 3.79) after adjustment for age, gender, and steroid use.
The large, population-based cohort is a strength of the study. “We are now going back to see how many of these patients were seen by rheumatologists,” Dr. Haddad said. A lack of association with disease burden is a potential limitation, he added.
Thirty percent of patients were treated with biologics and about 67% with steroids. “That number treated with steroids seems high,” a meeting attendee commented. Dr. Haddad explained that it is the percentage ever treated with steroids, not necessarily currently on steroids.
In a separate session at the GRAPPA meeting addressing psoriatic disease treatment recommendations, an attendee asked about specific recommendations for comorbidities. For now, GRAPPA plans to include comorbidities within its overall recommendations, as it did in its most recent update, released in January 2016. A limited amount of data is a primary reason.
“As the evidence on comorbidities gets better, we may someday have separate recommendations for comorbidities,” said Laura Coates, MD, a clinical lecturer in rheumatology at the University of Leeds (England).
“The comorbidities are very important,” said Arthur F. Kavanaugh, MD, professor of medicine at the University of California, San Diego. “That’s trickier and deals with the international nature of GRAPPA. It’s hard to say, ‘Go see this specialist,’ because that might not be standard of care in that country.”
Dr. Haddad, Dr. Coates, and Dr. Kavanaugh reported having no relevant financial disclosures.
AT 2016 GRAPPA ANNUAL MEETING
Psoriatic arthritis patients face more endocrine comorbidities
MIAMI – Diabetes mellitus, hypothyroidism, Cushing’s disease, and osteoporosis occur more frequently in people with psoriatic arthritis than in controls, a large cohort study reveals. Prevalence of these endocrine conditions was greater in a group of 3,161 patients with psoriatic arthritis, compared with 31,610 matched controls.
“We recommend that physicians should be aware of comorbid associations to provide comprehensive medical care to patients with psoriatic arthritis,” said Amir Haddad, MD, of the department of rheumatology at Carmel Medical Center in Haifa, Israel.
Dr. Haddad and his colleagues, however, found no significant differences in the prevalence of hyperthyroidism, hypo- and hyperparathyroidism, hyperprolactinemia, Addison’s disease, diabetes insipidus, pituitary adenoma, or acromegaly between groups in this retrospective, cross-sectional study.
They identified 1,474 men and 1,687 women diagnosed with psoriatic disease from 2000 to 2013 using the Clalit health services database in Israel. This group was a mean of 58 years old and 53% were women. Each patient was matched with 10 age- and gender-matched controls without psoriatic disease for the study.
“This is, to our knowledge, one of the largest real-life cohorts of psoriatic patient registries,” Dr. Haddad said at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA).
In the psoriatic arthritis group versus controls, diabetes mellitus prevalence was 27.9% vs. 20.7%; for hypothyroidism it was 12.7% vs. 8.6%; and for Cushing’s disease it was 0.3% vs. 0.1%. All these differences were statically significant (P less than 0.0001). Osteoporosis prevalence also differed significantly between the psoriatic arthritis and control groups: 13.2% vs. 9.1% (P less than 0.001).
Greater awareness of nonskin and nonjoint comorbidities is important, Dr. Haddad said, because it can influence choice of therapy and management of patients with psoriatic arthritis.
The investigators also conducted univariate and multivariate regression analyses. Compared with controls, the results suggest psoriatic arthritis patients have a higher risk for diabetes mellitus (odds ratio, 1.48), hypothyroidism (OR, 1.56), and osteoporosis (OR, 1.52). The risk for Cushing’s disease was notably higher (OR, 5.31) in the univariate analysis.
Risks for these endocrine conditions remained higher for the psoriatic arthritis patients in a multivariate regression analysis as well. For example, risk for diabetes mellitus (OR, 1.30) remained after adjusting for age, gender, smoking, obesity, and steroid use. Risk of hypothyroidism (OR, 1.61) remained after adjusting for age and gender; risk of osteoporosis (OR, 1.50) after adjusting for age, gender, steroid use, and smoking; and risk of Cushing’s disease (OR, 3.79) after adjustment for age, gender, and steroid use.
The large, population-based cohort is a strength of the study. “We are now going back to see how many of these patients were seen by rheumatologists,” Dr. Haddad said. A lack of association with disease burden is a potential limitation, he added.
Thirty percent of patients were treated with biologics and about 67% with steroids. “That number treated with steroids seems high,” a meeting attendee commented. Dr. Haddad explained that it is the percentage ever treated with steroids, not necessarily currently on steroids.
In a separate session at the GRAPPA meeting addressing psoriatic disease treatment recommendations, an attendee asked about specific recommendations for comorbidities. For now, GRAPPA plans to include comorbidities within its overall recommendations, as it did in its most recent update, released in January 2016. A limited amount of data is a primary reason.
“As the evidence on comorbidities gets better, we may someday have separate recommendations for comorbidities,” said Laura Coates, MD, a clinical lecturer in rheumatology at the University of Leeds (England).
“The comorbidities are very important,” said Arthur F. Kavanaugh, MD, professor of medicine at the University of California, San Diego. “That’s trickier and deals with the international nature of GRAPPA. It’s hard to say, ‘Go see this specialist,’ because that might not be standard of care in that country.”
Dr. Haddad, Dr. Coates, and Dr. Kavanaugh reported having no relevant financial disclosures.
MIAMI – Diabetes mellitus, hypothyroidism, Cushing’s disease, and osteoporosis occur more frequently in people with psoriatic arthritis than in controls, a large cohort study reveals. Prevalence of these endocrine conditions was greater in a group of 3,161 patients with psoriatic arthritis, compared with 31,610 matched controls.
“We recommend that physicians should be aware of comorbid associations to provide comprehensive medical care to patients with psoriatic arthritis,” said Amir Haddad, MD, of the department of rheumatology at Carmel Medical Center in Haifa, Israel.
Dr. Haddad and his colleagues, however, found no significant differences in the prevalence of hyperthyroidism, hypo- and hyperparathyroidism, hyperprolactinemia, Addison’s disease, diabetes insipidus, pituitary adenoma, or acromegaly between groups in this retrospective, cross-sectional study.
They identified 1,474 men and 1,687 women diagnosed with psoriatic disease from 2000 to 2013 using the Clalit health services database in Israel. This group was a mean of 58 years old and 53% were women. Each patient was matched with 10 age- and gender-matched controls without psoriatic disease for the study.
“This is, to our knowledge, one of the largest real-life cohorts of psoriatic patient registries,” Dr. Haddad said at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA).
In the psoriatic arthritis group versus controls, diabetes mellitus prevalence was 27.9% vs. 20.7%; for hypothyroidism it was 12.7% vs. 8.6%; and for Cushing’s disease it was 0.3% vs. 0.1%. All these differences were statically significant (P less than 0.0001). Osteoporosis prevalence also differed significantly between the psoriatic arthritis and control groups: 13.2% vs. 9.1% (P less than 0.001).
Greater awareness of nonskin and nonjoint comorbidities is important, Dr. Haddad said, because it can influence choice of therapy and management of patients with psoriatic arthritis.
The investigators also conducted univariate and multivariate regression analyses. Compared with controls, the results suggest psoriatic arthritis patients have a higher risk for diabetes mellitus (odds ratio, 1.48), hypothyroidism (OR, 1.56), and osteoporosis (OR, 1.52). The risk for Cushing’s disease was notably higher (OR, 5.31) in the univariate analysis.
Risks for these endocrine conditions remained higher for the psoriatic arthritis patients in a multivariate regression analysis as well. For example, risk for diabetes mellitus (OR, 1.30) remained after adjusting for age, gender, smoking, obesity, and steroid use. Risk of hypothyroidism (OR, 1.61) remained after adjusting for age and gender; risk of osteoporosis (OR, 1.50) after adjusting for age, gender, steroid use, and smoking; and risk of Cushing’s disease (OR, 3.79) after adjustment for age, gender, and steroid use.
The large, population-based cohort is a strength of the study. “We are now going back to see how many of these patients were seen by rheumatologists,” Dr. Haddad said. A lack of association with disease burden is a potential limitation, he added.
Thirty percent of patients were treated with biologics and about 67% with steroids. “That number treated with steroids seems high,” a meeting attendee commented. Dr. Haddad explained that it is the percentage ever treated with steroids, not necessarily currently on steroids.
In a separate session at the GRAPPA meeting addressing psoriatic disease treatment recommendations, an attendee asked about specific recommendations for comorbidities. For now, GRAPPA plans to include comorbidities within its overall recommendations, as it did in its most recent update, released in January 2016. A limited amount of data is a primary reason.
“As the evidence on comorbidities gets better, we may someday have separate recommendations for comorbidities,” said Laura Coates, MD, a clinical lecturer in rheumatology at the University of Leeds (England).
“The comorbidities are very important,” said Arthur F. Kavanaugh, MD, professor of medicine at the University of California, San Diego. “That’s trickier and deals with the international nature of GRAPPA. It’s hard to say, ‘Go see this specialist,’ because that might not be standard of care in that country.”
Dr. Haddad, Dr. Coates, and Dr. Kavanaugh reported having no relevant financial disclosures.
MIAMI – Diabetes mellitus, hypothyroidism, Cushing’s disease, and osteoporosis occur more frequently in people with psoriatic arthritis than in controls, a large cohort study reveals. Prevalence of these endocrine conditions was greater in a group of 3,161 patients with psoriatic arthritis, compared with 31,610 matched controls.
“We recommend that physicians should be aware of comorbid associations to provide comprehensive medical care to patients with psoriatic arthritis,” said Amir Haddad, MD, of the department of rheumatology at Carmel Medical Center in Haifa, Israel.
Dr. Haddad and his colleagues, however, found no significant differences in the prevalence of hyperthyroidism, hypo- and hyperparathyroidism, hyperprolactinemia, Addison’s disease, diabetes insipidus, pituitary adenoma, or acromegaly between groups in this retrospective, cross-sectional study.
They identified 1,474 men and 1,687 women diagnosed with psoriatic disease from 2000 to 2013 using the Clalit health services database in Israel. This group was a mean of 58 years old and 53% were women. Each patient was matched with 10 age- and gender-matched controls without psoriatic disease for the study.
“This is, to our knowledge, one of the largest real-life cohorts of psoriatic patient registries,” Dr. Haddad said at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA).
In the psoriatic arthritis group versus controls, diabetes mellitus prevalence was 27.9% vs. 20.7%; for hypothyroidism it was 12.7% vs. 8.6%; and for Cushing’s disease it was 0.3% vs. 0.1%. All these differences were statically significant (P less than 0.0001). Osteoporosis prevalence also differed significantly between the psoriatic arthritis and control groups: 13.2% vs. 9.1% (P less than 0.001).
Greater awareness of nonskin and nonjoint comorbidities is important, Dr. Haddad said, because it can influence choice of therapy and management of patients with psoriatic arthritis.
The investigators also conducted univariate and multivariate regression analyses. Compared with controls, the results suggest psoriatic arthritis patients have a higher risk for diabetes mellitus (odds ratio, 1.48), hypothyroidism (OR, 1.56), and osteoporosis (OR, 1.52). The risk for Cushing’s disease was notably higher (OR, 5.31) in the univariate analysis.
Risks for these endocrine conditions remained higher for the psoriatic arthritis patients in a multivariate regression analysis as well. For example, risk for diabetes mellitus (OR, 1.30) remained after adjusting for age, gender, smoking, obesity, and steroid use. Risk of hypothyroidism (OR, 1.61) remained after adjusting for age and gender; risk of osteoporosis (OR, 1.50) after adjusting for age, gender, steroid use, and smoking; and risk of Cushing’s disease (OR, 3.79) after adjustment for age, gender, and steroid use.
The large, population-based cohort is a strength of the study. “We are now going back to see how many of these patients were seen by rheumatologists,” Dr. Haddad said. A lack of association with disease burden is a potential limitation, he added.
Thirty percent of patients were treated with biologics and about 67% with steroids. “That number treated with steroids seems high,” a meeting attendee commented. Dr. Haddad explained that it is the percentage ever treated with steroids, not necessarily currently on steroids.
In a separate session at the GRAPPA meeting addressing psoriatic disease treatment recommendations, an attendee asked about specific recommendations for comorbidities. For now, GRAPPA plans to include comorbidities within its overall recommendations, as it did in its most recent update, released in January 2016. A limited amount of data is a primary reason.
“As the evidence on comorbidities gets better, we may someday have separate recommendations for comorbidities,” said Laura Coates, MD, a clinical lecturer in rheumatology at the University of Leeds (England).
“The comorbidities are very important,” said Arthur F. Kavanaugh, MD, professor of medicine at the University of California, San Diego. “That’s trickier and deals with the international nature of GRAPPA. It’s hard to say, ‘Go see this specialist,’ because that might not be standard of care in that country.”
Dr. Haddad, Dr. Coates, and Dr. Kavanaugh reported having no relevant financial disclosures.
AT 2016 GRAPPA ANNUAL MEETING
Key clinical point:Patients with psoriatic disease had a significantly higher prevalence of diabetes mellitus and some other endocrine comorbidities.
Major finding: In a univariate analysis, the risk for Cushing’s disease was notably higher among psoriatic arthritis patients, compared with controls (odds ratio, 5.31).
Data source: Retrospective, cross-sectional comparison of 3,161 patients with psoriatic arthritis and 31,610 matched controls.
Disclosures: Dr. Haddad, Dr. Coates, and Dr. Kavanaugh reported having no relevant financial disclosures.
Benefits, challenges emerge in evolution of rheumatology-dermatology clinics
MIAMI – Combined rheumatology-dermatology clinics to help people with psoriasis, psoriatic arthritis, and other relevant overlapping conditions continue to evolve, with evidence suggesting advantages and challenges for both patients and physicians.
Physicians like the improved communication and greater collaboration but still have reservations about billing and scheduling, according to preliminary results of a survey conducted by the Psoriasis and Psoriatic Arthritis Clinic Multicenter Advancement Network (PPACMAN). For patients, the advantages go beyond convenience, according to a 1-year study of outcomes at a Rhode Island Hospital–Brown University combined clinic in Providence.
“The goal of the combined clinics survey is to gauge strengths, barriers, and challenges to creating these models, to learn from one another to improve current clinical care, and to support propagation of these models,” said Joseph F. Merola, MD, at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
Multiple clinic models
The clinic setups differ. In those settings where rheumatologists and dermatologists see patients on the same day, approximately three-quarters provide care together in the same room. The remaining clinics see patients through serial visits. Another 30% of respondents said dermatologists and rheumatologists generally see patients in a combined clinic on different days.
“Rheumatologists said it is a satisfying and rewarding endeavor, they form closer ties with colleagues, and it allows early, improved communication,” said Dr. Merola, a rheumatologist and dermatologist who is co-director of the Center for Skin and Related Musculoskeletal Diseases, a combined clinic at Brigham and Women’s Hospital in Boston.
Some common benefits, each cited by more than 80% of respondents, include a prompt and accurate diagnosis of psoriatic arthritis, the ability of physicians to learn from each other, and multiple training opportunities for residents and fellows. In fact, 72% said their combined clinic has rheumatology fellows, 82% have dermatology residents, and 27% incorporate internal medicine trainees.
Other than rheumatologists and dermatologists, 31% said their clinic has dedicated nursing, 15% have a cardiologist, and 15% have a psychiatrist.
A majority of physicians (92%) said they bill through their own department. At a subsequent roundtable discussion, Dr. Merola noted that patients pay separate copays at the combined clinic. “We’ve had some complaints from patients. They don’t like having two copayments.”
“You have to tell patients in advance,” suggested Soumya M. Reddy, MD, a rheumatologist at NYU Langone Medical Center in New York and co-director of its Psoriasis and Psoriatic Arthritis Center.
Common conditions and challenges
Not surprisingly, psoriasis and psoriatic arthritis are the most common conditions treated in these clinics, followed by lupus and dermatomyositis. Most clinics see patients either once weekly or once monthly.
A major concern expressed by 75% surrounds scheduling. More than half, 58%, worry about demonstrating value to their institution. Only a minority, 17%, responded that achieving consensus on patient management is a challenge.
In general, rheumatology evaluations take more time than dermatology assessments, presenting a challenge for scheduling and maximizing physician time. “You don’t really want the dermatologist sitting there for 20 minutes not really doing a lot,” said Alison Ehrlich, MD, professor and chair of dermatology at George Washington University in Washington.
The solution at Brigham and Women’s Hospital is to staff the clinic with two dermatologists and one rheumatologist. The two dermatologists see about 20 patients each in a half-day; the rheumatologist probably treats about 6 to 8 of those 40 patients, Dr. Merola said. At George Washington, Dr. Ehrlich sees patients along with the rheumatologist, leaves the room to treat other patients, later consults with her colleague, and they go back in together as necessary.
“The patients are incredibly appreciative” of the combined clinic, Dr. Ehrlich said. “They really love it.”
The survey is ongoing. The preliminary responses above are based on 17 responses, a 52% response rate. Of the respondents, 10 are dermatologists, 6 are rheumatologists, and 1 is dual trained. Since the meeting, Dr. Merola indicated that another two dermatologists and three rheumatologists have responded to the survey.
The Brown University experience
Charis Gn, MD, and colleagues studied outcomes for 167 patients treated at a combined clinic at Rhode Island Hospital. The ultimate goal of the clinic is “to identify patients with psoriatic arthritis early on,” Dr. Gn said at a poster presentation at the GRAPPA annual meeting. “We wanted to see what kind of outcomes [we get] for patients who see rheumatology and dermatology.”
About one-third of patients left the clinic with changes in diagnosis. About 1 in 5 patients with psoriasis were diagnosed with psoriatic arthritis as well. For the psoriasis patients newly diagnosed with psoriatic arthritis, 80% had an escalation in treatment, said Dr. Gn, an internal medicine resident.
Of the 41 patients with psoriasis, 17 (41%) had a treatment escalation. The same was true for 15 (79%) of the 19 patients with psoriatic arthritis post-evaluation.
Regarding the combined clinic, “it’s shown to be very beneficial for patients with psoriatic arthritis,” Dr. Gn said.
The record review from July 2014 to February 2016 shows the clinic also serves patients with cutaneous lupus, dermatomyositis, pyoderma gangrenosum, vasculitis, and rheumatoid arthritis, among others.
The presenters had no relevant disclosures.
MIAMI – Combined rheumatology-dermatology clinics to help people with psoriasis, psoriatic arthritis, and other relevant overlapping conditions continue to evolve, with evidence suggesting advantages and challenges for both patients and physicians.
Physicians like the improved communication and greater collaboration but still have reservations about billing and scheduling, according to preliminary results of a survey conducted by the Psoriasis and Psoriatic Arthritis Clinic Multicenter Advancement Network (PPACMAN). For patients, the advantages go beyond convenience, according to a 1-year study of outcomes at a Rhode Island Hospital–Brown University combined clinic in Providence.
“The goal of the combined clinics survey is to gauge strengths, barriers, and challenges to creating these models, to learn from one another to improve current clinical care, and to support propagation of these models,” said Joseph F. Merola, MD, at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
Multiple clinic models
The clinic setups differ. In those settings where rheumatologists and dermatologists see patients on the same day, approximately three-quarters provide care together in the same room. The remaining clinics see patients through serial visits. Another 30% of respondents said dermatologists and rheumatologists generally see patients in a combined clinic on different days.
“Rheumatologists said it is a satisfying and rewarding endeavor, they form closer ties with colleagues, and it allows early, improved communication,” said Dr. Merola, a rheumatologist and dermatologist who is co-director of the Center for Skin and Related Musculoskeletal Diseases, a combined clinic at Brigham and Women’s Hospital in Boston.
Some common benefits, each cited by more than 80% of respondents, include a prompt and accurate diagnosis of psoriatic arthritis, the ability of physicians to learn from each other, and multiple training opportunities for residents and fellows. In fact, 72% said their combined clinic has rheumatology fellows, 82% have dermatology residents, and 27% incorporate internal medicine trainees.
Other than rheumatologists and dermatologists, 31% said their clinic has dedicated nursing, 15% have a cardiologist, and 15% have a psychiatrist.
A majority of physicians (92%) said they bill through their own department. At a subsequent roundtable discussion, Dr. Merola noted that patients pay separate copays at the combined clinic. “We’ve had some complaints from patients. They don’t like having two copayments.”
“You have to tell patients in advance,” suggested Soumya M. Reddy, MD, a rheumatologist at NYU Langone Medical Center in New York and co-director of its Psoriasis and Psoriatic Arthritis Center.
Common conditions and challenges
Not surprisingly, psoriasis and psoriatic arthritis are the most common conditions treated in these clinics, followed by lupus and dermatomyositis. Most clinics see patients either once weekly or once monthly.
A major concern expressed by 75% surrounds scheduling. More than half, 58%, worry about demonstrating value to their institution. Only a minority, 17%, responded that achieving consensus on patient management is a challenge.
In general, rheumatology evaluations take more time than dermatology assessments, presenting a challenge for scheduling and maximizing physician time. “You don’t really want the dermatologist sitting there for 20 minutes not really doing a lot,” said Alison Ehrlich, MD, professor and chair of dermatology at George Washington University in Washington.
The solution at Brigham and Women’s Hospital is to staff the clinic with two dermatologists and one rheumatologist. The two dermatologists see about 20 patients each in a half-day; the rheumatologist probably treats about 6 to 8 of those 40 patients, Dr. Merola said. At George Washington, Dr. Ehrlich sees patients along with the rheumatologist, leaves the room to treat other patients, later consults with her colleague, and they go back in together as necessary.
“The patients are incredibly appreciative” of the combined clinic, Dr. Ehrlich said. “They really love it.”
The survey is ongoing. The preliminary responses above are based on 17 responses, a 52% response rate. Of the respondents, 10 are dermatologists, 6 are rheumatologists, and 1 is dual trained. Since the meeting, Dr. Merola indicated that another two dermatologists and three rheumatologists have responded to the survey.
The Brown University experience
Charis Gn, MD, and colleagues studied outcomes for 167 patients treated at a combined clinic at Rhode Island Hospital. The ultimate goal of the clinic is “to identify patients with psoriatic arthritis early on,” Dr. Gn said at a poster presentation at the GRAPPA annual meeting. “We wanted to see what kind of outcomes [we get] for patients who see rheumatology and dermatology.”
About one-third of patients left the clinic with changes in diagnosis. About 1 in 5 patients with psoriasis were diagnosed with psoriatic arthritis as well. For the psoriasis patients newly diagnosed with psoriatic arthritis, 80% had an escalation in treatment, said Dr. Gn, an internal medicine resident.
Of the 41 patients with psoriasis, 17 (41%) had a treatment escalation. The same was true for 15 (79%) of the 19 patients with psoriatic arthritis post-evaluation.
Regarding the combined clinic, “it’s shown to be very beneficial for patients with psoriatic arthritis,” Dr. Gn said.
The record review from July 2014 to February 2016 shows the clinic also serves patients with cutaneous lupus, dermatomyositis, pyoderma gangrenosum, vasculitis, and rheumatoid arthritis, among others.
The presenters had no relevant disclosures.
MIAMI – Combined rheumatology-dermatology clinics to help people with psoriasis, psoriatic arthritis, and other relevant overlapping conditions continue to evolve, with evidence suggesting advantages and challenges for both patients and physicians.
Physicians like the improved communication and greater collaboration but still have reservations about billing and scheduling, according to preliminary results of a survey conducted by the Psoriasis and Psoriatic Arthritis Clinic Multicenter Advancement Network (PPACMAN). For patients, the advantages go beyond convenience, according to a 1-year study of outcomes at a Rhode Island Hospital–Brown University combined clinic in Providence.
“The goal of the combined clinics survey is to gauge strengths, barriers, and challenges to creating these models, to learn from one another to improve current clinical care, and to support propagation of these models,” said Joseph F. Merola, MD, at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
Multiple clinic models
The clinic setups differ. In those settings where rheumatologists and dermatologists see patients on the same day, approximately three-quarters provide care together in the same room. The remaining clinics see patients through serial visits. Another 30% of respondents said dermatologists and rheumatologists generally see patients in a combined clinic on different days.
“Rheumatologists said it is a satisfying and rewarding endeavor, they form closer ties with colleagues, and it allows early, improved communication,” said Dr. Merola, a rheumatologist and dermatologist who is co-director of the Center for Skin and Related Musculoskeletal Diseases, a combined clinic at Brigham and Women’s Hospital in Boston.
Some common benefits, each cited by more than 80% of respondents, include a prompt and accurate diagnosis of psoriatic arthritis, the ability of physicians to learn from each other, and multiple training opportunities for residents and fellows. In fact, 72% said their combined clinic has rheumatology fellows, 82% have dermatology residents, and 27% incorporate internal medicine trainees.
Other than rheumatologists and dermatologists, 31% said their clinic has dedicated nursing, 15% have a cardiologist, and 15% have a psychiatrist.
A majority of physicians (92%) said they bill through their own department. At a subsequent roundtable discussion, Dr. Merola noted that patients pay separate copays at the combined clinic. “We’ve had some complaints from patients. They don’t like having two copayments.”
“You have to tell patients in advance,” suggested Soumya M. Reddy, MD, a rheumatologist at NYU Langone Medical Center in New York and co-director of its Psoriasis and Psoriatic Arthritis Center.
Common conditions and challenges
Not surprisingly, psoriasis and psoriatic arthritis are the most common conditions treated in these clinics, followed by lupus and dermatomyositis. Most clinics see patients either once weekly or once monthly.
A major concern expressed by 75% surrounds scheduling. More than half, 58%, worry about demonstrating value to their institution. Only a minority, 17%, responded that achieving consensus on patient management is a challenge.
In general, rheumatology evaluations take more time than dermatology assessments, presenting a challenge for scheduling and maximizing physician time. “You don’t really want the dermatologist sitting there for 20 minutes not really doing a lot,” said Alison Ehrlich, MD, professor and chair of dermatology at George Washington University in Washington.
The solution at Brigham and Women’s Hospital is to staff the clinic with two dermatologists and one rheumatologist. The two dermatologists see about 20 patients each in a half-day; the rheumatologist probably treats about 6 to 8 of those 40 patients, Dr. Merola said. At George Washington, Dr. Ehrlich sees patients along with the rheumatologist, leaves the room to treat other patients, later consults with her colleague, and they go back in together as necessary.
“The patients are incredibly appreciative” of the combined clinic, Dr. Ehrlich said. “They really love it.”
The survey is ongoing. The preliminary responses above are based on 17 responses, a 52% response rate. Of the respondents, 10 are dermatologists, 6 are rheumatologists, and 1 is dual trained. Since the meeting, Dr. Merola indicated that another two dermatologists and three rheumatologists have responded to the survey.
The Brown University experience
Charis Gn, MD, and colleagues studied outcomes for 167 patients treated at a combined clinic at Rhode Island Hospital. The ultimate goal of the clinic is “to identify patients with psoriatic arthritis early on,” Dr. Gn said at a poster presentation at the GRAPPA annual meeting. “We wanted to see what kind of outcomes [we get] for patients who see rheumatology and dermatology.”
About one-third of patients left the clinic with changes in diagnosis. About 1 in 5 patients with psoriasis were diagnosed with psoriatic arthritis as well. For the psoriasis patients newly diagnosed with psoriatic arthritis, 80% had an escalation in treatment, said Dr. Gn, an internal medicine resident.
Of the 41 patients with psoriasis, 17 (41%) had a treatment escalation. The same was true for 15 (79%) of the 19 patients with psoriatic arthritis post-evaluation.
Regarding the combined clinic, “it’s shown to be very beneficial for patients with psoriatic arthritis,” Dr. Gn said.
The record review from July 2014 to February 2016 shows the clinic also serves patients with cutaneous lupus, dermatomyositis, pyoderma gangrenosum, vasculitis, and rheumatoid arthritis, among others.
The presenters had no relevant disclosures.
AT 2016 GRAPPA ANNUAL MEETING
Psoriatic arthritis patients have elevated risk for coronary artery plaque
MIAMI – Patients with psoriatic arthritis had a higher prevalence and greater extent of coronary artery plaque in a pilot study comparison with healthy control patients that may point to increased risk independent of traditional cardiovascular risk factors.
In the study, coronary artery plaque as assessed by cardiac computed tomography angiography (CCTA) occurred in 39 (78%) of 50 patients with psoriatic arthritis, a significantly higher rate than that observed for healthy controls (11 of 25, 44%).
Investigators not only measured plaque volume, but also assessed the type of plaque: calcified, noncalcified, or mixed. Mixed plaque predominated. This could be important because “noncalcified and mixed carry higher risk for rupture and later cardiovascular events,” Agnes Szentpetery, MD, a research fellow at St. Vincent’s University Hospital in Dublin, said at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
She and her colleagues also found more clinically significant stenosis among the 50 participants with psoriatic arthritis, compared with 25 healthy controls matched for age, sex, smoking status, and presence of metabolic syndrome. “This pilot study is the first to assess coronary plaques in asymptomatic patients with psoriatic arthritis with CCTA,” Dr. Szentpetery said.
Total plaque volume was higher in the psoriatic arthritis group versus controls, and higher in the left main artery for psoriatic arthritis patients, both with and without metabolic syndrome.
The study points to increased risk independent of traditional cardiovascular risk factors. For example, CCTA revealed no difference in plaque volume between patients with and without metabolic disease. In addition, a previous study suggests “the burden of carotid artery plaques is higher in patients with psoriatic arthritis compared to those with psoriasis alone,” Dr. Szentpetery said, citing a cross-sectional study comparing 125 people with psoriasis to 114 others with psoriatic arthritis (Ann Rheum Dis. 2013 May;72[5]:715-20).
Perhaps not surprisingly, inflammation could be driving the association between psoriatic and cardiovascular disease risk. Other investigators suggest chronic, low-grade inflammation leads to atherosclerosis through a maladaptive immune response and altered lipid metabolism, for example (Nat Med. 2011 Nov;17[11]:1410-22).
In the current study, the patients with psoriatic arthritis had well-established disease, occurring for a mean duration of 19 years. Mean age was 58 years, and 54% were men. Approximately 60% were taking disease-modifying antirheumatic drugs, two-thirds were taking biologics, and about one-third were on combination treatment. Controls were similar demographically with a mean age of 57 years, and 52% were men.
Interestingly, Psoriasis Area and Severity Index (PASI) scores did not correlate with increased risk. During discussion after the presentation of the study, a researcher unaffiliated with the study offered an answer. “It could be their skin disease was controlled by the biologics. You had 67% on biologics,” said Nehal Mehta, MD, Clinical Research Scholar in the section of inflammation and cardiometabolic disease at the National Heart, Lung, and Blood Institute. “We at the NIH see a strong correlation between PASI and coronary artery disease risk.”
“We know methotrexate and anti-TNF agents can have a protective effect on atherosclerosis, but we did not look at this specifically,” Dr. Szentpetery said. Overall, PASI scores were relatively low in the study population, she added, which “may explain why we did not see the correlation with PASI scores.”
Dr. Szentpetery and Dr. Mehta had no relevant financial disclosures.
MIAMI – Patients with psoriatic arthritis had a higher prevalence and greater extent of coronary artery plaque in a pilot study comparison with healthy control patients that may point to increased risk independent of traditional cardiovascular risk factors.
In the study, coronary artery plaque as assessed by cardiac computed tomography angiography (CCTA) occurred in 39 (78%) of 50 patients with psoriatic arthritis, a significantly higher rate than that observed for healthy controls (11 of 25, 44%).
Investigators not only measured plaque volume, but also assessed the type of plaque: calcified, noncalcified, or mixed. Mixed plaque predominated. This could be important because “noncalcified and mixed carry higher risk for rupture and later cardiovascular events,” Agnes Szentpetery, MD, a research fellow at St. Vincent’s University Hospital in Dublin, said at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
She and her colleagues also found more clinically significant stenosis among the 50 participants with psoriatic arthritis, compared with 25 healthy controls matched for age, sex, smoking status, and presence of metabolic syndrome. “This pilot study is the first to assess coronary plaques in asymptomatic patients with psoriatic arthritis with CCTA,” Dr. Szentpetery said.
Total plaque volume was higher in the psoriatic arthritis group versus controls, and higher in the left main artery for psoriatic arthritis patients, both with and without metabolic syndrome.
The study points to increased risk independent of traditional cardiovascular risk factors. For example, CCTA revealed no difference in plaque volume between patients with and without metabolic disease. In addition, a previous study suggests “the burden of carotid artery plaques is higher in patients with psoriatic arthritis compared to those with psoriasis alone,” Dr. Szentpetery said, citing a cross-sectional study comparing 125 people with psoriasis to 114 others with psoriatic arthritis (Ann Rheum Dis. 2013 May;72[5]:715-20).
Perhaps not surprisingly, inflammation could be driving the association between psoriatic and cardiovascular disease risk. Other investigators suggest chronic, low-grade inflammation leads to atherosclerosis through a maladaptive immune response and altered lipid metabolism, for example (Nat Med. 2011 Nov;17[11]:1410-22).
In the current study, the patients with psoriatic arthritis had well-established disease, occurring for a mean duration of 19 years. Mean age was 58 years, and 54% were men. Approximately 60% were taking disease-modifying antirheumatic drugs, two-thirds were taking biologics, and about one-third were on combination treatment. Controls were similar demographically with a mean age of 57 years, and 52% were men.
Interestingly, Psoriasis Area and Severity Index (PASI) scores did not correlate with increased risk. During discussion after the presentation of the study, a researcher unaffiliated with the study offered an answer. “It could be their skin disease was controlled by the biologics. You had 67% on biologics,” said Nehal Mehta, MD, Clinical Research Scholar in the section of inflammation and cardiometabolic disease at the National Heart, Lung, and Blood Institute. “We at the NIH see a strong correlation between PASI and coronary artery disease risk.”
“We know methotrexate and anti-TNF agents can have a protective effect on atherosclerosis, but we did not look at this specifically,” Dr. Szentpetery said. Overall, PASI scores were relatively low in the study population, she added, which “may explain why we did not see the correlation with PASI scores.”
Dr. Szentpetery and Dr. Mehta had no relevant financial disclosures.
MIAMI – Patients with psoriatic arthritis had a higher prevalence and greater extent of coronary artery plaque in a pilot study comparison with healthy control patients that may point to increased risk independent of traditional cardiovascular risk factors.
In the study, coronary artery plaque as assessed by cardiac computed tomography angiography (CCTA) occurred in 39 (78%) of 50 patients with psoriatic arthritis, a significantly higher rate than that observed for healthy controls (11 of 25, 44%).
Investigators not only measured plaque volume, but also assessed the type of plaque: calcified, noncalcified, or mixed. Mixed plaque predominated. This could be important because “noncalcified and mixed carry higher risk for rupture and later cardiovascular events,” Agnes Szentpetery, MD, a research fellow at St. Vincent’s University Hospital in Dublin, said at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
She and her colleagues also found more clinically significant stenosis among the 50 participants with psoriatic arthritis, compared with 25 healthy controls matched for age, sex, smoking status, and presence of metabolic syndrome. “This pilot study is the first to assess coronary plaques in asymptomatic patients with psoriatic arthritis with CCTA,” Dr. Szentpetery said.
Total plaque volume was higher in the psoriatic arthritis group versus controls, and higher in the left main artery for psoriatic arthritis patients, both with and without metabolic syndrome.
The study points to increased risk independent of traditional cardiovascular risk factors. For example, CCTA revealed no difference in plaque volume between patients with and without metabolic disease. In addition, a previous study suggests “the burden of carotid artery plaques is higher in patients with psoriatic arthritis compared to those with psoriasis alone,” Dr. Szentpetery said, citing a cross-sectional study comparing 125 people with psoriasis to 114 others with psoriatic arthritis (Ann Rheum Dis. 2013 May;72[5]:715-20).
Perhaps not surprisingly, inflammation could be driving the association between psoriatic and cardiovascular disease risk. Other investigators suggest chronic, low-grade inflammation leads to atherosclerosis through a maladaptive immune response and altered lipid metabolism, for example (Nat Med. 2011 Nov;17[11]:1410-22).
In the current study, the patients with psoriatic arthritis had well-established disease, occurring for a mean duration of 19 years. Mean age was 58 years, and 54% were men. Approximately 60% were taking disease-modifying antirheumatic drugs, two-thirds were taking biologics, and about one-third were on combination treatment. Controls were similar demographically with a mean age of 57 years, and 52% were men.
Interestingly, Psoriasis Area and Severity Index (PASI) scores did not correlate with increased risk. During discussion after the presentation of the study, a researcher unaffiliated with the study offered an answer. “It could be their skin disease was controlled by the biologics. You had 67% on biologics,” said Nehal Mehta, MD, Clinical Research Scholar in the section of inflammation and cardiometabolic disease at the National Heart, Lung, and Blood Institute. “We at the NIH see a strong correlation between PASI and coronary artery disease risk.”
“We know methotrexate and anti-TNF agents can have a protective effect on atherosclerosis, but we did not look at this specifically,” Dr. Szentpetery said. Overall, PASI scores were relatively low in the study population, she added, which “may explain why we did not see the correlation with PASI scores.”
Dr. Szentpetery and Dr. Mehta had no relevant financial disclosures.
AT 2016 GRAPPA ANNUAL MEETING
Key clinical point:Imaging reveals a higher rate and greater extent of coronary plaque in people with psoriatic arthritis versus healthy controls.
Major finding: 78% of people with PsA had coronary artery plaque versus 44% of controls, a significant difference.
Data source: Comparison of 50 people with PsA versus 25 healthy controls undergoing CCTA.
Disclosures: Dr. Szentpetery and Dr. Mehta had no relevant disclosures.