User login
Practicing telepsychiatry: Include backup plans, ground rules
For psychiatrists embarking on a telemedicine consultation, it might be helpful to review a checklist of steps that will reduce the risk of problems when things go wrong, according to an overview of the dangers at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists, sponsored by Medscape Live.
Ideally, telepsychiatry will function much like an inpatient office visit, but the dynamics differ – as do the things that can go wrong, according to Sanjay Gupta, MD, chief medical officer, BryLin Behavioral Health System, Buffalo, N.Y. “Issues can arise suddenly. You need contingency planning.”
At the outset, psychiatrists should establish the location of the patient. This is necessary at every telemedicine encounter. With a remote device, a patient could be essentially anywhere on Earth. Patients might not even remember to mention that they are vacationing in Australia.
The location of the patient is important in the event of an unexpected crisis. This is not only relevant to an unstable patient at risk of dangerous behavior, such as actively attempting suicide, but to patients who have a seizure or some other emergency that inhibits communication. , and this requires confirming that the patient is where he or she was expected to be.
In addition, there should be a plan for technological failure. As everyone knows, these failures, such as dysfunction of a device, a poor connection, or an Internet outage, can happen at any time. Both the clinician and the patient can derive reassurance from at least one if not two or more plans to reconnect in the event of these failures.
The visit should also begin with questions that will establish the patient has a sense of adequate privacy. This is one of the most common obstacles to an effective telemedicine consultation. Dr. Gupta pointed out that phone or computer cameras do not typically permit the clinician to exclude the presence of another individual sitting even a few feet away from the patient. With spouses and children nearby, there might be a tenuous sense of privacy even if they are unlikely to overhear the telemedicine visit.
One strategy that can be used to assess the patient’s level of comfort is to ask for a description of the patient’s surroundings and any other people at the location. Dr. Gupta also said it is appropriate to establish ground rules about recording of the session, which has its own potential to inhibit the interaction.
Warning that some form of consent to a telemedicine visit is mandatory in most states, Dr. Gupta also cautioned that a formal identification check is appropriate for a first-time visit. The risk of an individual offering a false identification is likely to be low, but it can be eliminated entirely by a protocol that verifies consent and identify before the clinical work begins.
Because of the importance of engaging patients quickly, Dr. Gupta called the first few minutes of a telemedicine visit “crucial.” By initiating the visit with a warm and respectful tone, by relaying a competent and professional appearance, and by establishing an atmosphere that encourages communication, the initial minutes of the call can set a tone that facilitates an effective visit.
Simple and established telehealth etiquette strategies should be employed, according to Dr. Gupta. He suggested paying attention to such issues as lighting, background, and camera position. Descriptions of what constitutes adequate lighting and background are easily obtained on free how-to websites, but the goal is to provide patients with a nondistracting and clear view of the clinician.
During a telemedicine visit, the clinician’s focus should remain on the patient, according to Dr. Gupta. He advised against taking notes or documenting the visit on an electronic health record during the course of the visit. Rather, he advised positioning the camera in a way that the patient feels eye contact is being made.
“It can be helpful to periodically summarize what the patient has said to demonstrate that you are fully engaged,” Dr. Gupta suggested.
Telemedicine is very effective for many but not all patients. Some, such as those with active psychosis, are not suited to this approach, but others are simply uncomfortable with this form of communication. Dr. Gupta suggested that clinicians should be mindful of the advantages and the limitations of telepsychiatry.
Ultimately, Dr. Gupta believes that the substantial expansion of telepsychiatry that took place during the COVID-19 pandemic is likely to persist when the pandemic ends, even if many of the changes that permitted its expansion, such as a relaxation of HIPPA requirements, are withdrawn. However, parity reimbursement for visits offered by telemedicine relative to those that are face-to-face, which greatly facilitated the growth of telepsychiatry, is not guaranteed, so this remains an unanswered question.
“The question is what will happen to the billing codes when we see COVID-19 in the rearview mirror, and the answer is that no one knows,” he said.
Uncertainty about future use
Other experts in this field agreed. James (Jay) H. Shore, MD, MPH, director of telemedicine, Helen and Arthur E. Johnson Depression Center, University of Colorado at Denver, Aurora, has long been an advocate for the value of telepsychiatry for reaching patients with limited psychosocial services. The attention drawn to this practice by the COVID-19 pandemic has been welcome, but he does not know how it will affect the future.
“There is too much uncertainty in the system to make a good prediction of where this may end up,” he said.
It is not just reimbursement that is at risk, according to Peter Yellowlees, MBBS, MD, chief wellness officer at the University of California, Davis. Also a longtime advocate of telepsychiatry, particularly to reach the underserved, Dr. Yellowlees pointed out that the ability to prescribe controlled substances through telemedicine and the ability to consult with patients across state lines might also be in jeopardy if and when rules for telemedicine are revisited after the pandemic.
“Many organizations are lobbying to make the pandemic changes permanent because they greatly support telemedicine delivery,” Dr. Yellowlees said, but agreed about the uncertainty regarding what policy makers will do.
Jayasudha Gude, MD, who is completing her residency in psychiatry at Zucker Hillside Hospital, Northwell Health, New York, recently led a literature review evaluating the needs and viability of telepsychiatry during and after the COVID-19 era (Cureus. 2021 Aug;13:e16974). Based on the benefits she identified in her review, she said, “I would definitely want to advocate for the continued use of telepsychiatry after the pandemic is over.” She hopes that psychiatrists who now have experience in this area will join her.
“I am hopeful that a lot of mental health providers will also be advocating since they have experience, and many will want to continue its use,” she said. Medscape Live and this news organization are owned by the same parent company. Dr. Gupta, Dr. Shore, Dr. Yellowlees, and Dr. Gude reported no potential conflicts of interest.
For psychiatrists embarking on a telemedicine consultation, it might be helpful to review a checklist of steps that will reduce the risk of problems when things go wrong, according to an overview of the dangers at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists, sponsored by Medscape Live.
Ideally, telepsychiatry will function much like an inpatient office visit, but the dynamics differ – as do the things that can go wrong, according to Sanjay Gupta, MD, chief medical officer, BryLin Behavioral Health System, Buffalo, N.Y. “Issues can arise suddenly. You need contingency planning.”
At the outset, psychiatrists should establish the location of the patient. This is necessary at every telemedicine encounter. With a remote device, a patient could be essentially anywhere on Earth. Patients might not even remember to mention that they are vacationing in Australia.
The location of the patient is important in the event of an unexpected crisis. This is not only relevant to an unstable patient at risk of dangerous behavior, such as actively attempting suicide, but to patients who have a seizure or some other emergency that inhibits communication. , and this requires confirming that the patient is where he or she was expected to be.
In addition, there should be a plan for technological failure. As everyone knows, these failures, such as dysfunction of a device, a poor connection, or an Internet outage, can happen at any time. Both the clinician and the patient can derive reassurance from at least one if not two or more plans to reconnect in the event of these failures.
The visit should also begin with questions that will establish the patient has a sense of adequate privacy. This is one of the most common obstacles to an effective telemedicine consultation. Dr. Gupta pointed out that phone or computer cameras do not typically permit the clinician to exclude the presence of another individual sitting even a few feet away from the patient. With spouses and children nearby, there might be a tenuous sense of privacy even if they are unlikely to overhear the telemedicine visit.
One strategy that can be used to assess the patient’s level of comfort is to ask for a description of the patient’s surroundings and any other people at the location. Dr. Gupta also said it is appropriate to establish ground rules about recording of the session, which has its own potential to inhibit the interaction.
Warning that some form of consent to a telemedicine visit is mandatory in most states, Dr. Gupta also cautioned that a formal identification check is appropriate for a first-time visit. The risk of an individual offering a false identification is likely to be low, but it can be eliminated entirely by a protocol that verifies consent and identify before the clinical work begins.
Because of the importance of engaging patients quickly, Dr. Gupta called the first few minutes of a telemedicine visit “crucial.” By initiating the visit with a warm and respectful tone, by relaying a competent and professional appearance, and by establishing an atmosphere that encourages communication, the initial minutes of the call can set a tone that facilitates an effective visit.
Simple and established telehealth etiquette strategies should be employed, according to Dr. Gupta. He suggested paying attention to such issues as lighting, background, and camera position. Descriptions of what constitutes adequate lighting and background are easily obtained on free how-to websites, but the goal is to provide patients with a nondistracting and clear view of the clinician.
During a telemedicine visit, the clinician’s focus should remain on the patient, according to Dr. Gupta. He advised against taking notes or documenting the visit on an electronic health record during the course of the visit. Rather, he advised positioning the camera in a way that the patient feels eye contact is being made.
“It can be helpful to periodically summarize what the patient has said to demonstrate that you are fully engaged,” Dr. Gupta suggested.
Telemedicine is very effective for many but not all patients. Some, such as those with active psychosis, are not suited to this approach, but others are simply uncomfortable with this form of communication. Dr. Gupta suggested that clinicians should be mindful of the advantages and the limitations of telepsychiatry.
Ultimately, Dr. Gupta believes that the substantial expansion of telepsychiatry that took place during the COVID-19 pandemic is likely to persist when the pandemic ends, even if many of the changes that permitted its expansion, such as a relaxation of HIPPA requirements, are withdrawn. However, parity reimbursement for visits offered by telemedicine relative to those that are face-to-face, which greatly facilitated the growth of telepsychiatry, is not guaranteed, so this remains an unanswered question.
“The question is what will happen to the billing codes when we see COVID-19 in the rearview mirror, and the answer is that no one knows,” he said.
Uncertainty about future use
Other experts in this field agreed. James (Jay) H. Shore, MD, MPH, director of telemedicine, Helen and Arthur E. Johnson Depression Center, University of Colorado at Denver, Aurora, has long been an advocate for the value of telepsychiatry for reaching patients with limited psychosocial services. The attention drawn to this practice by the COVID-19 pandemic has been welcome, but he does not know how it will affect the future.
“There is too much uncertainty in the system to make a good prediction of where this may end up,” he said.
It is not just reimbursement that is at risk, according to Peter Yellowlees, MBBS, MD, chief wellness officer at the University of California, Davis. Also a longtime advocate of telepsychiatry, particularly to reach the underserved, Dr. Yellowlees pointed out that the ability to prescribe controlled substances through telemedicine and the ability to consult with patients across state lines might also be in jeopardy if and when rules for telemedicine are revisited after the pandemic.
“Many organizations are lobbying to make the pandemic changes permanent because they greatly support telemedicine delivery,” Dr. Yellowlees said, but agreed about the uncertainty regarding what policy makers will do.
Jayasudha Gude, MD, who is completing her residency in psychiatry at Zucker Hillside Hospital, Northwell Health, New York, recently led a literature review evaluating the needs and viability of telepsychiatry during and after the COVID-19 era (Cureus. 2021 Aug;13:e16974). Based on the benefits she identified in her review, she said, “I would definitely want to advocate for the continued use of telepsychiatry after the pandemic is over.” She hopes that psychiatrists who now have experience in this area will join her.
“I am hopeful that a lot of mental health providers will also be advocating since they have experience, and many will want to continue its use,” she said. Medscape Live and this news organization are owned by the same parent company. Dr. Gupta, Dr. Shore, Dr. Yellowlees, and Dr. Gude reported no potential conflicts of interest.
For psychiatrists embarking on a telemedicine consultation, it might be helpful to review a checklist of steps that will reduce the risk of problems when things go wrong, according to an overview of the dangers at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists, sponsored by Medscape Live.
Ideally, telepsychiatry will function much like an inpatient office visit, but the dynamics differ – as do the things that can go wrong, according to Sanjay Gupta, MD, chief medical officer, BryLin Behavioral Health System, Buffalo, N.Y. “Issues can arise suddenly. You need contingency planning.”
At the outset, psychiatrists should establish the location of the patient. This is necessary at every telemedicine encounter. With a remote device, a patient could be essentially anywhere on Earth. Patients might not even remember to mention that they are vacationing in Australia.
The location of the patient is important in the event of an unexpected crisis. This is not only relevant to an unstable patient at risk of dangerous behavior, such as actively attempting suicide, but to patients who have a seizure or some other emergency that inhibits communication. , and this requires confirming that the patient is where he or she was expected to be.
In addition, there should be a plan for technological failure. As everyone knows, these failures, such as dysfunction of a device, a poor connection, or an Internet outage, can happen at any time. Both the clinician and the patient can derive reassurance from at least one if not two or more plans to reconnect in the event of these failures.
The visit should also begin with questions that will establish the patient has a sense of adequate privacy. This is one of the most common obstacles to an effective telemedicine consultation. Dr. Gupta pointed out that phone or computer cameras do not typically permit the clinician to exclude the presence of another individual sitting even a few feet away from the patient. With spouses and children nearby, there might be a tenuous sense of privacy even if they are unlikely to overhear the telemedicine visit.
One strategy that can be used to assess the patient’s level of comfort is to ask for a description of the patient’s surroundings and any other people at the location. Dr. Gupta also said it is appropriate to establish ground rules about recording of the session, which has its own potential to inhibit the interaction.
Warning that some form of consent to a telemedicine visit is mandatory in most states, Dr. Gupta also cautioned that a formal identification check is appropriate for a first-time visit. The risk of an individual offering a false identification is likely to be low, but it can be eliminated entirely by a protocol that verifies consent and identify before the clinical work begins.
Because of the importance of engaging patients quickly, Dr. Gupta called the first few minutes of a telemedicine visit “crucial.” By initiating the visit with a warm and respectful tone, by relaying a competent and professional appearance, and by establishing an atmosphere that encourages communication, the initial minutes of the call can set a tone that facilitates an effective visit.
Simple and established telehealth etiquette strategies should be employed, according to Dr. Gupta. He suggested paying attention to such issues as lighting, background, and camera position. Descriptions of what constitutes adequate lighting and background are easily obtained on free how-to websites, but the goal is to provide patients with a nondistracting and clear view of the clinician.
During a telemedicine visit, the clinician’s focus should remain on the patient, according to Dr. Gupta. He advised against taking notes or documenting the visit on an electronic health record during the course of the visit. Rather, he advised positioning the camera in a way that the patient feels eye contact is being made.
“It can be helpful to periodically summarize what the patient has said to demonstrate that you are fully engaged,” Dr. Gupta suggested.
Telemedicine is very effective for many but not all patients. Some, such as those with active psychosis, are not suited to this approach, but others are simply uncomfortable with this form of communication. Dr. Gupta suggested that clinicians should be mindful of the advantages and the limitations of telepsychiatry.
Ultimately, Dr. Gupta believes that the substantial expansion of telepsychiatry that took place during the COVID-19 pandemic is likely to persist when the pandemic ends, even if many of the changes that permitted its expansion, such as a relaxation of HIPPA requirements, are withdrawn. However, parity reimbursement for visits offered by telemedicine relative to those that are face-to-face, which greatly facilitated the growth of telepsychiatry, is not guaranteed, so this remains an unanswered question.
“The question is what will happen to the billing codes when we see COVID-19 in the rearview mirror, and the answer is that no one knows,” he said.
Uncertainty about future use
Other experts in this field agreed. James (Jay) H. Shore, MD, MPH, director of telemedicine, Helen and Arthur E. Johnson Depression Center, University of Colorado at Denver, Aurora, has long been an advocate for the value of telepsychiatry for reaching patients with limited psychosocial services. The attention drawn to this practice by the COVID-19 pandemic has been welcome, but he does not know how it will affect the future.
“There is too much uncertainty in the system to make a good prediction of where this may end up,” he said.
It is not just reimbursement that is at risk, according to Peter Yellowlees, MBBS, MD, chief wellness officer at the University of California, Davis. Also a longtime advocate of telepsychiatry, particularly to reach the underserved, Dr. Yellowlees pointed out that the ability to prescribe controlled substances through telemedicine and the ability to consult with patients across state lines might also be in jeopardy if and when rules for telemedicine are revisited after the pandemic.
“Many organizations are lobbying to make the pandemic changes permanent because they greatly support telemedicine delivery,” Dr. Yellowlees said, but agreed about the uncertainty regarding what policy makers will do.
Jayasudha Gude, MD, who is completing her residency in psychiatry at Zucker Hillside Hospital, Northwell Health, New York, recently led a literature review evaluating the needs and viability of telepsychiatry during and after the COVID-19 era (Cureus. 2021 Aug;13:e16974). Based on the benefits she identified in her review, she said, “I would definitely want to advocate for the continued use of telepsychiatry after the pandemic is over.” She hopes that psychiatrists who now have experience in this area will join her.
“I am hopeful that a lot of mental health providers will also be advocating since they have experience, and many will want to continue its use,” she said. Medscape Live and this news organization are owned by the same parent company. Dr. Gupta, Dr. Shore, Dr. Yellowlees, and Dr. Gude reported no potential conflicts of interest.
FROM PSYCHOPHARMACOLOGY UPDATE
FDA not recognizing efficacy of psychopharmacologic therapies
Many years ago, drug development in psychiatry turned to control of specific symptoms across disorders rather than within disorders, but regulatory agencies are still not yet on board, according to an expert psychopharmacologist outlining the ongoing evolution at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists, sponsored by Medscape Live.
If this reorientation is going to lead to the broad indications the newer drugs likely deserve, which is control of specific types of symptoms regardless of the diagnosis, “we have to move the [Food and Drug Administration] along,” said Stephen M. Stahl, MD, PhD, chairman of the Neuroscience Institute and an adjunct professor of psychiatry at the University of California, San Diego.
On the side of drug development and clinical practice, the reorientation has already taken place. Dr. Stahl described numerous brain circuits known to produce symptoms when function is altered that are now treatment targets. This includes the ventral medial prefrontal cortex where deficient information processing leads to depression and the orbital frontal cortex where altered function leads to impulsivity.
“It is not like each part of the brain does a little bit of everything. Rather, each part of the brain has an assignment and duty and function,” Dr. Stahl explained. By addressing the disturbed signaling in brain circuits that lead to depression, impulsivity, agitation, or other symptoms, there is an opportunity for control, regardless of the psychiatric diagnosis with which the symptom is associated.
For example, Dr. Stahl predicted that pimavanserin, a highly selective 5-HT2A inverse agonist that is already approved for psychosis in Parkinson’s disease, is now likely to be approved for psychosis associated with other conditions on the basis of recent positive clinical studies in these other disorders.
Brexpiprazole, a serotonin-dopamine activity modulator already known to be useful for control of the agitation characteristic of schizophrenia, is now showing the same type of activity against agitation when it is associated with Alzheimer’s disease. Again, Dr. Stahl thinks this drug is on course for an indication across diseases once studies are conducted in each disease individually.
Another drug being evaluated for agitation, the N-methyl-D-aspartate receptor antagonist dextromethorphan bupropion, is also being tested for treatment of symptoms across multiple disorders, he reported.
However, the FDA has so far taken the position that each drug must be tested separately for a given symptom in each disorder for which it is being considered despite the underlying premise that it is the symptom, not the disease, that is important.
Unlike physiological diseases where symptoms, like a fever or abdominal cramps, are the product of a disease, psychiatric symptoms are the disease and a fundamental target – regardless of the DSM-based diagnosis.
To some degree, the symptoms of psychiatric disorders have always been the focus of treatment, but a pivot toward developing therapies that will control a symptom regardless of the underlying diagnosis is an important conceptual change. It is being made possible by advances in the detail with which the neuropathology of these symptoms is understood .
“By my count, 79 symptoms are described in DSM-5, but they are spread across hundreds of syndromes because they are grouped together in different ways,” Dr. Stahl observed.
He noted that clinicians make a diagnosis on the basis symptom groupings, but their interventions are selected to address the manifestations of the disease, not the disease itself.
“If you are a real psychopharmacologist treating real patients, you are treating the specific symptoms of the specific patient,” according to Dr. Stahl.
So far, the FDA has not made this leap, insisting on trials in these categorical disorders rather than permitting trial designs that allow benefit to be demonstrated against a symptom regardless of the syndrome with which it is associated.
Of egregious examples, Dr. Stahl recounted a recent trial of a 5-HT2 antagonist that looked so promising against psychosis in Alzheimer’s disease that the trialists enrolled patients with psychosis regardless of type of dementia, such as vascular dementia and Lewy body disease. The efficacy was impressive.
“It worked so well that they stopped the trial, but the FDA declined to approve it,” Dr. Stahl recounted. Despite clear evidence of benefit, the regulators insisted that the investigators needed to show a significant benefit in each condition individually.
While the trial investigators acknowledged that there was not enough power in the trial to show a statistically significant benefit in each category, they argued that the overall benefit and the consistent response across categories required them to stop the trial for ethical reasons.
“That’s your problem, the FDA said to the investigators,” according to Dr. Stahl.
The failure of the FDA to recognize the efficacy of psychopharmacologic therapies across symptoms regardless of the associated disease is a failure to stay current with an important evolution in medicine, Dr. Stahl indicated.
“What we have come to understand is the neurobiology of any given symptom is likely to be the same across disorders,” he said.
Agency’s arbitrary decisions cited
“I completely agree with Dr. Stahl,” said Henry A. Nasrallah, MD, professor of psychiatry, neurology, and neuroscience, University of Cincinnati.
In addition to the fact that symptoms are present across multiple categories, many patients manifest multiple symptoms at one time, Dr. Nasrallah pointed out. For neurodegenerative disorders associated with psychosis, depression, anxiety, aggression, and other symptoms, it is already well known that the heterogeneous symptoms “cannot be treated with a single drug,” he said. Rather different drugs targeting each symptom individually is essential for effective management.
Dr. Nasrallah, who chaired the Psychopharmacology Update meeting, has made this point many times in the past, including in his role as the editor of Current Psychiatry. In one editorial 10 years ago, he wrote that “it makes little sense for the FDA to mandate that a drug must work for a DSM diagnosis instead of specific symptoms.”
“The FDA must update its old policy, which has led to the widespread off-label use of psychiatric drugs, an artificial concept, simply because the FDA arbitrarily decided a long time ago that new drugs must be approved for a specific DSM diagnosis,” Dr. Nasrallah said.
Dr. Stahl reported financial relationships with more than 20 pharmaceutical companies, including those that are involved in the development of drugs included in his talk. Medscape Live and this news organization are owned by the same parent company.
Many years ago, drug development in psychiatry turned to control of specific symptoms across disorders rather than within disorders, but regulatory agencies are still not yet on board, according to an expert psychopharmacologist outlining the ongoing evolution at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists, sponsored by Medscape Live.
If this reorientation is going to lead to the broad indications the newer drugs likely deserve, which is control of specific types of symptoms regardless of the diagnosis, “we have to move the [Food and Drug Administration] along,” said Stephen M. Stahl, MD, PhD, chairman of the Neuroscience Institute and an adjunct professor of psychiatry at the University of California, San Diego.
On the side of drug development and clinical practice, the reorientation has already taken place. Dr. Stahl described numerous brain circuits known to produce symptoms when function is altered that are now treatment targets. This includes the ventral medial prefrontal cortex where deficient information processing leads to depression and the orbital frontal cortex where altered function leads to impulsivity.
“It is not like each part of the brain does a little bit of everything. Rather, each part of the brain has an assignment and duty and function,” Dr. Stahl explained. By addressing the disturbed signaling in brain circuits that lead to depression, impulsivity, agitation, or other symptoms, there is an opportunity for control, regardless of the psychiatric diagnosis with which the symptom is associated.
For example, Dr. Stahl predicted that pimavanserin, a highly selective 5-HT2A inverse agonist that is already approved for psychosis in Parkinson’s disease, is now likely to be approved for psychosis associated with other conditions on the basis of recent positive clinical studies in these other disorders.
Brexpiprazole, a serotonin-dopamine activity modulator already known to be useful for control of the agitation characteristic of schizophrenia, is now showing the same type of activity against agitation when it is associated with Alzheimer’s disease. Again, Dr. Stahl thinks this drug is on course for an indication across diseases once studies are conducted in each disease individually.
Another drug being evaluated for agitation, the N-methyl-D-aspartate receptor antagonist dextromethorphan bupropion, is also being tested for treatment of symptoms across multiple disorders, he reported.
However, the FDA has so far taken the position that each drug must be tested separately for a given symptom in each disorder for which it is being considered despite the underlying premise that it is the symptom, not the disease, that is important.
Unlike physiological diseases where symptoms, like a fever or abdominal cramps, are the product of a disease, psychiatric symptoms are the disease and a fundamental target – regardless of the DSM-based diagnosis.
To some degree, the symptoms of psychiatric disorders have always been the focus of treatment, but a pivot toward developing therapies that will control a symptom regardless of the underlying diagnosis is an important conceptual change. It is being made possible by advances in the detail with which the neuropathology of these symptoms is understood .
“By my count, 79 symptoms are described in DSM-5, but they are spread across hundreds of syndromes because they are grouped together in different ways,” Dr. Stahl observed.
He noted that clinicians make a diagnosis on the basis symptom groupings, but their interventions are selected to address the manifestations of the disease, not the disease itself.
“If you are a real psychopharmacologist treating real patients, you are treating the specific symptoms of the specific patient,” according to Dr. Stahl.
So far, the FDA has not made this leap, insisting on trials in these categorical disorders rather than permitting trial designs that allow benefit to be demonstrated against a symptom regardless of the syndrome with which it is associated.
Of egregious examples, Dr. Stahl recounted a recent trial of a 5-HT2 antagonist that looked so promising against psychosis in Alzheimer’s disease that the trialists enrolled patients with psychosis regardless of type of dementia, such as vascular dementia and Lewy body disease. The efficacy was impressive.
“It worked so well that they stopped the trial, but the FDA declined to approve it,” Dr. Stahl recounted. Despite clear evidence of benefit, the regulators insisted that the investigators needed to show a significant benefit in each condition individually.
While the trial investigators acknowledged that there was not enough power in the trial to show a statistically significant benefit in each category, they argued that the overall benefit and the consistent response across categories required them to stop the trial for ethical reasons.
“That’s your problem, the FDA said to the investigators,” according to Dr. Stahl.
The failure of the FDA to recognize the efficacy of psychopharmacologic therapies across symptoms regardless of the associated disease is a failure to stay current with an important evolution in medicine, Dr. Stahl indicated.
“What we have come to understand is the neurobiology of any given symptom is likely to be the same across disorders,” he said.
Agency’s arbitrary decisions cited
“I completely agree with Dr. Stahl,” said Henry A. Nasrallah, MD, professor of psychiatry, neurology, and neuroscience, University of Cincinnati.
In addition to the fact that symptoms are present across multiple categories, many patients manifest multiple symptoms at one time, Dr. Nasrallah pointed out. For neurodegenerative disorders associated with psychosis, depression, anxiety, aggression, and other symptoms, it is already well known that the heterogeneous symptoms “cannot be treated with a single drug,” he said. Rather different drugs targeting each symptom individually is essential for effective management.
Dr. Nasrallah, who chaired the Psychopharmacology Update meeting, has made this point many times in the past, including in his role as the editor of Current Psychiatry. In one editorial 10 years ago, he wrote that “it makes little sense for the FDA to mandate that a drug must work for a DSM diagnosis instead of specific symptoms.”
“The FDA must update its old policy, which has led to the widespread off-label use of psychiatric drugs, an artificial concept, simply because the FDA arbitrarily decided a long time ago that new drugs must be approved for a specific DSM diagnosis,” Dr. Nasrallah said.
Dr. Stahl reported financial relationships with more than 20 pharmaceutical companies, including those that are involved in the development of drugs included in his talk. Medscape Live and this news organization are owned by the same parent company.
Many years ago, drug development in psychiatry turned to control of specific symptoms across disorders rather than within disorders, but regulatory agencies are still not yet on board, according to an expert psychopharmacologist outlining the ongoing evolution at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists, sponsored by Medscape Live.
If this reorientation is going to lead to the broad indications the newer drugs likely deserve, which is control of specific types of symptoms regardless of the diagnosis, “we have to move the [Food and Drug Administration] along,” said Stephen M. Stahl, MD, PhD, chairman of the Neuroscience Institute and an adjunct professor of psychiatry at the University of California, San Diego.
On the side of drug development and clinical practice, the reorientation has already taken place. Dr. Stahl described numerous brain circuits known to produce symptoms when function is altered that are now treatment targets. This includes the ventral medial prefrontal cortex where deficient information processing leads to depression and the orbital frontal cortex where altered function leads to impulsivity.
“It is not like each part of the brain does a little bit of everything. Rather, each part of the brain has an assignment and duty and function,” Dr. Stahl explained. By addressing the disturbed signaling in brain circuits that lead to depression, impulsivity, agitation, or other symptoms, there is an opportunity for control, regardless of the psychiatric diagnosis with which the symptom is associated.
For example, Dr. Stahl predicted that pimavanserin, a highly selective 5-HT2A inverse agonist that is already approved for psychosis in Parkinson’s disease, is now likely to be approved for psychosis associated with other conditions on the basis of recent positive clinical studies in these other disorders.
Brexpiprazole, a serotonin-dopamine activity modulator already known to be useful for control of the agitation characteristic of schizophrenia, is now showing the same type of activity against agitation when it is associated with Alzheimer’s disease. Again, Dr. Stahl thinks this drug is on course for an indication across diseases once studies are conducted in each disease individually.
Another drug being evaluated for agitation, the N-methyl-D-aspartate receptor antagonist dextromethorphan bupropion, is also being tested for treatment of symptoms across multiple disorders, he reported.
However, the FDA has so far taken the position that each drug must be tested separately for a given symptom in each disorder for which it is being considered despite the underlying premise that it is the symptom, not the disease, that is important.
Unlike physiological diseases where symptoms, like a fever or abdominal cramps, are the product of a disease, psychiatric symptoms are the disease and a fundamental target – regardless of the DSM-based diagnosis.
To some degree, the symptoms of psychiatric disorders have always been the focus of treatment, but a pivot toward developing therapies that will control a symptom regardless of the underlying diagnosis is an important conceptual change. It is being made possible by advances in the detail with which the neuropathology of these symptoms is understood .
“By my count, 79 symptoms are described in DSM-5, but they are spread across hundreds of syndromes because they are grouped together in different ways,” Dr. Stahl observed.
He noted that clinicians make a diagnosis on the basis symptom groupings, but their interventions are selected to address the manifestations of the disease, not the disease itself.
“If you are a real psychopharmacologist treating real patients, you are treating the specific symptoms of the specific patient,” according to Dr. Stahl.
So far, the FDA has not made this leap, insisting on trials in these categorical disorders rather than permitting trial designs that allow benefit to be demonstrated against a symptom regardless of the syndrome with which it is associated.
Of egregious examples, Dr. Stahl recounted a recent trial of a 5-HT2 antagonist that looked so promising against psychosis in Alzheimer’s disease that the trialists enrolled patients with psychosis regardless of type of dementia, such as vascular dementia and Lewy body disease. The efficacy was impressive.
“It worked so well that they stopped the trial, but the FDA declined to approve it,” Dr. Stahl recounted. Despite clear evidence of benefit, the regulators insisted that the investigators needed to show a significant benefit in each condition individually.
While the trial investigators acknowledged that there was not enough power in the trial to show a statistically significant benefit in each category, they argued that the overall benefit and the consistent response across categories required them to stop the trial for ethical reasons.
“That’s your problem, the FDA said to the investigators,” according to Dr. Stahl.
The failure of the FDA to recognize the efficacy of psychopharmacologic therapies across symptoms regardless of the associated disease is a failure to stay current with an important evolution in medicine, Dr. Stahl indicated.
“What we have come to understand is the neurobiology of any given symptom is likely to be the same across disorders,” he said.
Agency’s arbitrary decisions cited
“I completely agree with Dr. Stahl,” said Henry A. Nasrallah, MD, professor of psychiatry, neurology, and neuroscience, University of Cincinnati.
In addition to the fact that symptoms are present across multiple categories, many patients manifest multiple symptoms at one time, Dr. Nasrallah pointed out. For neurodegenerative disorders associated with psychosis, depression, anxiety, aggression, and other symptoms, it is already well known that the heterogeneous symptoms “cannot be treated with a single drug,” he said. Rather different drugs targeting each symptom individually is essential for effective management.
Dr. Nasrallah, who chaired the Psychopharmacology Update meeting, has made this point many times in the past, including in his role as the editor of Current Psychiatry. In one editorial 10 years ago, he wrote that “it makes little sense for the FDA to mandate that a drug must work for a DSM diagnosis instead of specific symptoms.”
“The FDA must update its old policy, which has led to the widespread off-label use of psychiatric drugs, an artificial concept, simply because the FDA arbitrarily decided a long time ago that new drugs must be approved for a specific DSM diagnosis,” Dr. Nasrallah said.
Dr. Stahl reported financial relationships with more than 20 pharmaceutical companies, including those that are involved in the development of drugs included in his talk. Medscape Live and this news organization are owned by the same parent company.
FROM PSYCHOPHARMACOLOGY UPDATE
Warn patients about illicit drugs doctored with fentanyl
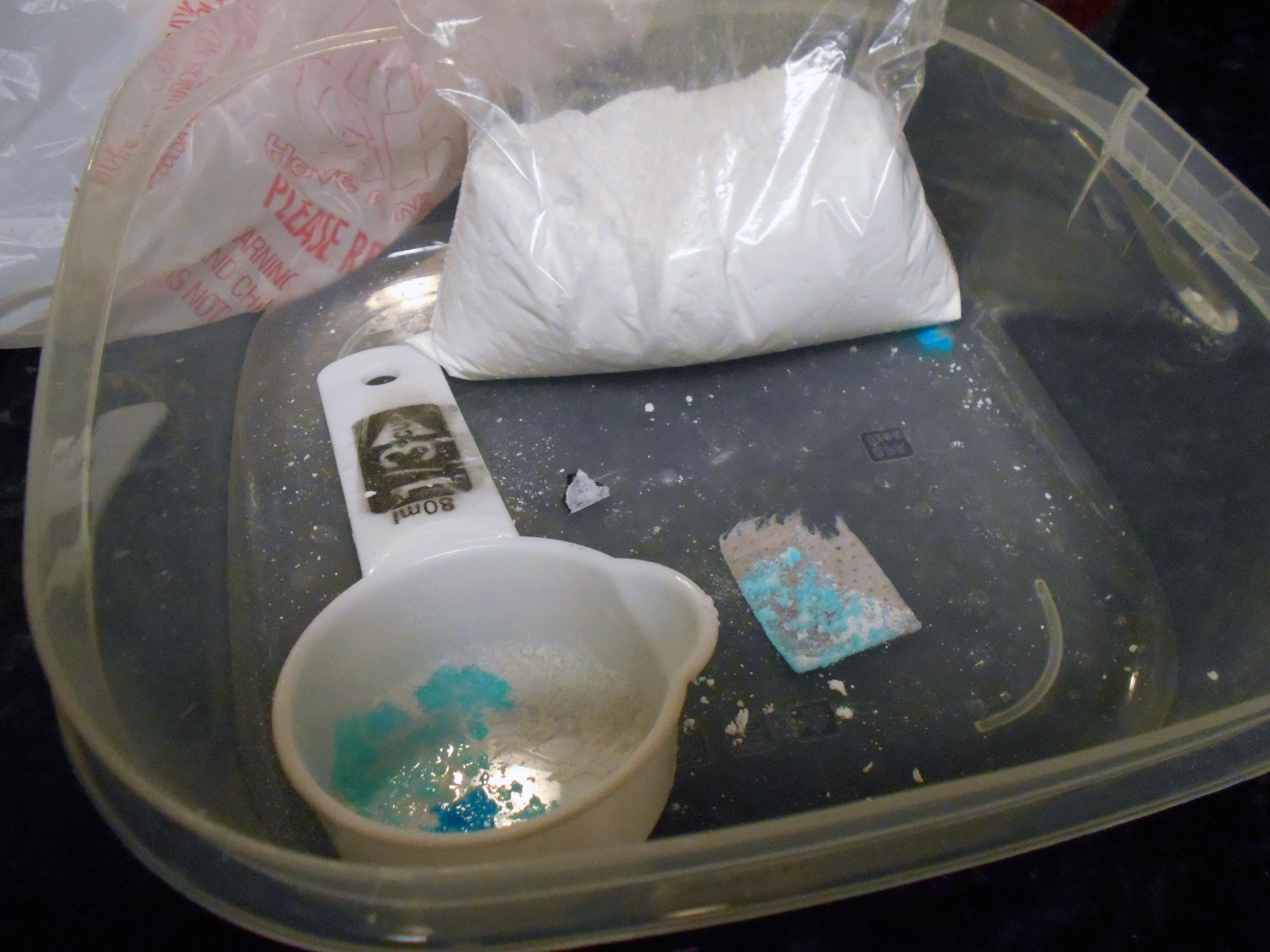
Fentanyl is now threatening overdoses in patients exposed to essentially any of the full array of recreational drugs – not just opioids – that are being sold illicitly, according to an overview of the problem presented at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“Fentanyl can now be found in cocaine and methamphetamine. At this point, there is really no way to predict what is in a [street] drug,” Edwin A. Salsitz, MD, said at the meeting, sponsored by Medscape Live. He is associate clinical professor of medicine who works in the division of chemical dependency at Mount Sinai Beth Israel Medical Center in New York.
As proof of the frequency with which fentanyl is now being used as an additive, most patients with a drug use disorder, regardless of their drug of choice, are testing positive for fentanyl at Dr. Salsitz’s center. Many of those with positive fentanyl tests are unaware that their drugs had been doctored with this agent.
Relative to drugs sold as an opioid, such as heroin or oxycodone, the fentanyl dose in nonopioid drugs is typically more modest, but Dr. Salsitz pointed out that those expecting cocaine or methamphetamine often “have no heroin tolerance, so they are more vulnerable” to the adverse effects of fentanyl, including an overdose.
Although opioid tolerance might improve the chances for surviving a fentanyl overdose, the toxicology of fentanyl is not the same as other opioids. Death from heroin is typically a result of respiratory depression, but the onset is relatively slow, providing a greater opportunity to administer a reversal agent, such as naloxone.
Fentanyl not only produces respiratory depression but skeletal muscle rigidity. The rapid onset of “wooden chest syndrome” can occur within minutes, making the opportunity for intervention much smaller, Dr. Salsitz said.
To illustrate the phenomenon, Dr. Salsitz recounted a case.
After an argument with his mother, a 26-year-old male with a long history of intravenous drug use went to his bedroom. His mother, responding to the sound of a loud thud, rushed to the bedroom to find her son on the floor with a needle still in his arm. Resuscitation efforts by the mother and by the emergency responders, who arrived quickly, failed.
“The speed of his death made it clear that it was fentanyl related, and the postmortem toxicology confirmed that the exposure involved both heroin and fentanyl,” Dr. Salsitz said.
After the first wave of deaths in the opioid epidemic, which was attributed to inappropriate use of prescription opioids, the second wave was driven by heroin. In that wave, patients who became addicted to prescription opioids but were having more difficulty gaining access to them, turned to far cheaper and readily available street heroin. The third wave, driven by fentanyl, began several years ago when sellers of heroin began adding this synthetic opioid, which is relatively cheap, to intensify the high.
It is not expected to end quickly. The fentanyl added to heroin was never a prescription version. Rather, Dr. Salsitz said, it is synthesized in laboratories in China, Mexico, and the United States. It is relatively easy to produce and compact, which makes it easy to transport.
Exacerbating the risks that fentanyl poses when added to street drugs, even more potent versions, such as carfentanil, are also being added to cocaine, methamphetamines, and other nonopioid illicit drugs. When compared on a per-milligram basis, fentanyl is about 100 times more potent than heroin, but carfentanil is about 100 times more potent than fentanyl, according to Dr. Salsitz.
When the third wave of deaths in the opioid epidemic began around 2013, prescriptions of fentanyl, like many other opioid-type therapies were declining. The “perfect storm” that initiated the opioid epidemic was a product of intense focus on pain control and a misperception that prescription opioids posed a low risk of abuse potential, Dr. Salsitz said. By the time fentanyl was driving opioid deaths, the risks of opioids were widely appreciated and their use for prescription analgesia was declining.
Citing several cases, Dr. Salsitz noted that only 20 years after clinicians were being successfully sued for not offering enough analgesia, they were now going to jail for prescribing these drugs too liberally.
According to Dr. Salsitz, While psychiatrists might not have a role in this issue, Dr. Salsitz did see a role for these specialists in protecting patients from the adverse consequences of using illicit drugs doctored with fentanyl.
Noting that individuals with psychiatric disorders are more likely than the general population to self-medicate with drugs purchased illegally, Dr. Salsitz encouraged psychiatrists “to get involved” in asking about drug use and counseling patients on the risks of fentanyl substitution or additives.
“The message is that no one knows what are in these drugs, anymore,” he said.
In addition to making patients aware that many street drugs are now contaminated with fentanyl, Dr. Salsitz provided some safety tips. He suggested instructing patients to take a low dose of any newly acquired drug to gauge its effect, to avoid taking drugs alone, and to avoid mixing drugs. He also recommended using rapid fentanyl test strips in order to detect fentanyl contamination.
Even for the many psychiatrists who do not feel comfortable managing addiction, Dr. Salsitz recommended a proactive approach to address the current threat.
Test strips as an intervention
The seriousness of fentanyl contamination of illicit drugs, including cocaine and methamphetamine, was corroborated by two investigators at the School of Public Health and the Albert Einstein Medical School of Brown University, Providence, R.I. Brandon D.L. Marshall, PhD, associate professor of epidemiology in the School of Public Health, called fentanyl-contaminated cannabis “extremely rare,” but he said that it is being found in counterfeit prescription pills as well as in crystal methamphetamine and in both crack and powder cocaine.
He also advocated the use of fentanyl test strips.
“Test strips are an efficient, inexpensive, and effective way to determine whether fentanyl or related analogs are present in illicit drugs,” he said, noting that he is involved in a trial designed to determine whether fentanyl test strips can reduce the risk of fatal and nonfatal overdoses.
In a pilot study conducted in Baltimore, 69% of the 103 participants engaged in harm reduction behavior after using a fentanyl test strip and receiving a positive result (Addict Behav. 2020;110:106529). It is notable that 86% of the participants had a least one positive result when using the strips. More than half were surprised by the result.
One of the findings from this study was “that the lasting benefit of fentanyl test strip distribution is the opportunity to engage in discussions around safety and relationship building with historically underserved communities,” said the lead author, Ju Nyeong Park, PhD, assistant professor of medicine and epidemiology at Brown University. She moved to Brown after performing this work at Johns Hopkins University, Baltimore.
Dr. Park noted that “many patients in the community already know that they are using drugs containing fentanyl,” but for those who are concerned and wish to avoid contaminated drugs, fentanyl test strips “are a quick screening tool.” However, while the strips are helpful, she cautioned that they cannot be considered a definitive tool for detecting harm in illicit drugs.
“There may also be other chemicals present in tested drugs that confer risk,” she said.
Medscape Live and this news organization are owned by the same parent company. Dr. Salsitz, Dr. Marshall, and Dr. Park reported no potential conflicts of interest.
Fentanyl is now threatening overdoses in patients exposed to essentially any of the full array of recreational drugs – not just opioids – that are being sold illicitly, according to an overview of the problem presented at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“Fentanyl can now be found in cocaine and methamphetamine. At this point, there is really no way to predict what is in a [street] drug,” Edwin A. Salsitz, MD, said at the meeting, sponsored by Medscape Live. He is associate clinical professor of medicine who works in the division of chemical dependency at Mount Sinai Beth Israel Medical Center in New York.
As proof of the frequency with which fentanyl is now being used as an additive, most patients with a drug use disorder, regardless of their drug of choice, are testing positive for fentanyl at Dr. Salsitz’s center. Many of those with positive fentanyl tests are unaware that their drugs had been doctored with this agent.
Relative to drugs sold as an opioid, such as heroin or oxycodone, the fentanyl dose in nonopioid drugs is typically more modest, but Dr. Salsitz pointed out that those expecting cocaine or methamphetamine often “have no heroin tolerance, so they are more vulnerable” to the adverse effects of fentanyl, including an overdose.
Although opioid tolerance might improve the chances for surviving a fentanyl overdose, the toxicology of fentanyl is not the same as other opioids. Death from heroin is typically a result of respiratory depression, but the onset is relatively slow, providing a greater opportunity to administer a reversal agent, such as naloxone.
Fentanyl not only produces respiratory depression but skeletal muscle rigidity. The rapid onset of “wooden chest syndrome” can occur within minutes, making the opportunity for intervention much smaller, Dr. Salsitz said.
To illustrate the phenomenon, Dr. Salsitz recounted a case.
After an argument with his mother, a 26-year-old male with a long history of intravenous drug use went to his bedroom. His mother, responding to the sound of a loud thud, rushed to the bedroom to find her son on the floor with a needle still in his arm. Resuscitation efforts by the mother and by the emergency responders, who arrived quickly, failed.
“The speed of his death made it clear that it was fentanyl related, and the postmortem toxicology confirmed that the exposure involved both heroin and fentanyl,” Dr. Salsitz said.
After the first wave of deaths in the opioid epidemic, which was attributed to inappropriate use of prescription opioids, the second wave was driven by heroin. In that wave, patients who became addicted to prescription opioids but were having more difficulty gaining access to them, turned to far cheaper and readily available street heroin. The third wave, driven by fentanyl, began several years ago when sellers of heroin began adding this synthetic opioid, which is relatively cheap, to intensify the high.
It is not expected to end quickly. The fentanyl added to heroin was never a prescription version. Rather, Dr. Salsitz said, it is synthesized in laboratories in China, Mexico, and the United States. It is relatively easy to produce and compact, which makes it easy to transport.
Exacerbating the risks that fentanyl poses when added to street drugs, even more potent versions, such as carfentanil, are also being added to cocaine, methamphetamines, and other nonopioid illicit drugs. When compared on a per-milligram basis, fentanyl is about 100 times more potent than heroin, but carfentanil is about 100 times more potent than fentanyl, according to Dr. Salsitz.
When the third wave of deaths in the opioid epidemic began around 2013, prescriptions of fentanyl, like many other opioid-type therapies were declining. The “perfect storm” that initiated the opioid epidemic was a product of intense focus on pain control and a misperception that prescription opioids posed a low risk of abuse potential, Dr. Salsitz said. By the time fentanyl was driving opioid deaths, the risks of opioids were widely appreciated and their use for prescription analgesia was declining.
Citing several cases, Dr. Salsitz noted that only 20 years after clinicians were being successfully sued for not offering enough analgesia, they were now going to jail for prescribing these drugs too liberally.
According to Dr. Salsitz, While psychiatrists might not have a role in this issue, Dr. Salsitz did see a role for these specialists in protecting patients from the adverse consequences of using illicit drugs doctored with fentanyl.
Noting that individuals with psychiatric disorders are more likely than the general population to self-medicate with drugs purchased illegally, Dr. Salsitz encouraged psychiatrists “to get involved” in asking about drug use and counseling patients on the risks of fentanyl substitution or additives.
“The message is that no one knows what are in these drugs, anymore,” he said.
In addition to making patients aware that many street drugs are now contaminated with fentanyl, Dr. Salsitz provided some safety tips. He suggested instructing patients to take a low dose of any newly acquired drug to gauge its effect, to avoid taking drugs alone, and to avoid mixing drugs. He also recommended using rapid fentanyl test strips in order to detect fentanyl contamination.
Even for the many psychiatrists who do not feel comfortable managing addiction, Dr. Salsitz recommended a proactive approach to address the current threat.
Test strips as an intervention
The seriousness of fentanyl contamination of illicit drugs, including cocaine and methamphetamine, was corroborated by two investigators at the School of Public Health and the Albert Einstein Medical School of Brown University, Providence, R.I. Brandon D.L. Marshall, PhD, associate professor of epidemiology in the School of Public Health, called fentanyl-contaminated cannabis “extremely rare,” but he said that it is being found in counterfeit prescription pills as well as in crystal methamphetamine and in both crack and powder cocaine.
He also advocated the use of fentanyl test strips.
“Test strips are an efficient, inexpensive, and effective way to determine whether fentanyl or related analogs are present in illicit drugs,” he said, noting that he is involved in a trial designed to determine whether fentanyl test strips can reduce the risk of fatal and nonfatal overdoses.
In a pilot study conducted in Baltimore, 69% of the 103 participants engaged in harm reduction behavior after using a fentanyl test strip and receiving a positive result (Addict Behav. 2020;110:106529). It is notable that 86% of the participants had a least one positive result when using the strips. More than half were surprised by the result.
One of the findings from this study was “that the lasting benefit of fentanyl test strip distribution is the opportunity to engage in discussions around safety and relationship building with historically underserved communities,” said the lead author, Ju Nyeong Park, PhD, assistant professor of medicine and epidemiology at Brown University. She moved to Brown after performing this work at Johns Hopkins University, Baltimore.
Dr. Park noted that “many patients in the community already know that they are using drugs containing fentanyl,” but for those who are concerned and wish to avoid contaminated drugs, fentanyl test strips “are a quick screening tool.” However, while the strips are helpful, she cautioned that they cannot be considered a definitive tool for detecting harm in illicit drugs.
“There may also be other chemicals present in tested drugs that confer risk,” she said.
Medscape Live and this news organization are owned by the same parent company. Dr. Salsitz, Dr. Marshall, and Dr. Park reported no potential conflicts of interest.
Fentanyl is now threatening overdoses in patients exposed to essentially any of the full array of recreational drugs – not just opioids – that are being sold illicitly, according to an overview of the problem presented at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“Fentanyl can now be found in cocaine and methamphetamine. At this point, there is really no way to predict what is in a [street] drug,” Edwin A. Salsitz, MD, said at the meeting, sponsored by Medscape Live. He is associate clinical professor of medicine who works in the division of chemical dependency at Mount Sinai Beth Israel Medical Center in New York.
As proof of the frequency with which fentanyl is now being used as an additive, most patients with a drug use disorder, regardless of their drug of choice, are testing positive for fentanyl at Dr. Salsitz’s center. Many of those with positive fentanyl tests are unaware that their drugs had been doctored with this agent.
Relative to drugs sold as an opioid, such as heroin or oxycodone, the fentanyl dose in nonopioid drugs is typically more modest, but Dr. Salsitz pointed out that those expecting cocaine or methamphetamine often “have no heroin tolerance, so they are more vulnerable” to the adverse effects of fentanyl, including an overdose.
Although opioid tolerance might improve the chances for surviving a fentanyl overdose, the toxicology of fentanyl is not the same as other opioids. Death from heroin is typically a result of respiratory depression, but the onset is relatively slow, providing a greater opportunity to administer a reversal agent, such as naloxone.
Fentanyl not only produces respiratory depression but skeletal muscle rigidity. The rapid onset of “wooden chest syndrome” can occur within minutes, making the opportunity for intervention much smaller, Dr. Salsitz said.
To illustrate the phenomenon, Dr. Salsitz recounted a case.
After an argument with his mother, a 26-year-old male with a long history of intravenous drug use went to his bedroom. His mother, responding to the sound of a loud thud, rushed to the bedroom to find her son on the floor with a needle still in his arm. Resuscitation efforts by the mother and by the emergency responders, who arrived quickly, failed.
“The speed of his death made it clear that it was fentanyl related, and the postmortem toxicology confirmed that the exposure involved both heroin and fentanyl,” Dr. Salsitz said.
After the first wave of deaths in the opioid epidemic, which was attributed to inappropriate use of prescription opioids, the second wave was driven by heroin. In that wave, patients who became addicted to prescription opioids but were having more difficulty gaining access to them, turned to far cheaper and readily available street heroin. The third wave, driven by fentanyl, began several years ago when sellers of heroin began adding this synthetic opioid, which is relatively cheap, to intensify the high.
It is not expected to end quickly. The fentanyl added to heroin was never a prescription version. Rather, Dr. Salsitz said, it is synthesized in laboratories in China, Mexico, and the United States. It is relatively easy to produce and compact, which makes it easy to transport.
Exacerbating the risks that fentanyl poses when added to street drugs, even more potent versions, such as carfentanil, are also being added to cocaine, methamphetamines, and other nonopioid illicit drugs. When compared on a per-milligram basis, fentanyl is about 100 times more potent than heroin, but carfentanil is about 100 times more potent than fentanyl, according to Dr. Salsitz.
When the third wave of deaths in the opioid epidemic began around 2013, prescriptions of fentanyl, like many other opioid-type therapies were declining. The “perfect storm” that initiated the opioid epidemic was a product of intense focus on pain control and a misperception that prescription opioids posed a low risk of abuse potential, Dr. Salsitz said. By the time fentanyl was driving opioid deaths, the risks of opioids were widely appreciated and their use for prescription analgesia was declining.
Citing several cases, Dr. Salsitz noted that only 20 years after clinicians were being successfully sued for not offering enough analgesia, they were now going to jail for prescribing these drugs too liberally.
According to Dr. Salsitz, While psychiatrists might not have a role in this issue, Dr. Salsitz did see a role for these specialists in protecting patients from the adverse consequences of using illicit drugs doctored with fentanyl.
Noting that individuals with psychiatric disorders are more likely than the general population to self-medicate with drugs purchased illegally, Dr. Salsitz encouraged psychiatrists “to get involved” in asking about drug use and counseling patients on the risks of fentanyl substitution or additives.
“The message is that no one knows what are in these drugs, anymore,” he said.
In addition to making patients aware that many street drugs are now contaminated with fentanyl, Dr. Salsitz provided some safety tips. He suggested instructing patients to take a low dose of any newly acquired drug to gauge its effect, to avoid taking drugs alone, and to avoid mixing drugs. He also recommended using rapid fentanyl test strips in order to detect fentanyl contamination.
Even for the many psychiatrists who do not feel comfortable managing addiction, Dr. Salsitz recommended a proactive approach to address the current threat.
Test strips as an intervention
The seriousness of fentanyl contamination of illicit drugs, including cocaine and methamphetamine, was corroborated by two investigators at the School of Public Health and the Albert Einstein Medical School of Brown University, Providence, R.I. Brandon D.L. Marshall, PhD, associate professor of epidemiology in the School of Public Health, called fentanyl-contaminated cannabis “extremely rare,” but he said that it is being found in counterfeit prescription pills as well as in crystal methamphetamine and in both crack and powder cocaine.
He also advocated the use of fentanyl test strips.
“Test strips are an efficient, inexpensive, and effective way to determine whether fentanyl or related analogs are present in illicit drugs,” he said, noting that he is involved in a trial designed to determine whether fentanyl test strips can reduce the risk of fatal and nonfatal overdoses.
In a pilot study conducted in Baltimore, 69% of the 103 participants engaged in harm reduction behavior after using a fentanyl test strip and receiving a positive result (Addict Behav. 2020;110:106529). It is notable that 86% of the participants had a least one positive result when using the strips. More than half were surprised by the result.
One of the findings from this study was “that the lasting benefit of fentanyl test strip distribution is the opportunity to engage in discussions around safety and relationship building with historically underserved communities,” said the lead author, Ju Nyeong Park, PhD, assistant professor of medicine and epidemiology at Brown University. She moved to Brown after performing this work at Johns Hopkins University, Baltimore.
Dr. Park noted that “many patients in the community already know that they are using drugs containing fentanyl,” but for those who are concerned and wish to avoid contaminated drugs, fentanyl test strips “are a quick screening tool.” However, while the strips are helpful, she cautioned that they cannot be considered a definitive tool for detecting harm in illicit drugs.
“There may also be other chemicals present in tested drugs that confer risk,” she said.
Medscape Live and this news organization are owned by the same parent company. Dr. Salsitz, Dr. Marshall, and Dr. Park reported no potential conflicts of interest.
FROM PSYCHOPHARMACOLOGY UPDATE
Cannabis use: Messages remain mixed across diagnoses
Marijuana use is now a legal activity in many parts of the United States, but those managing patients with psychiatric disorders are in the difficult position of determining whether this use is helpful, harmful, or irrelevant to the underlying illness on the basis of limited and largely incomplete data, according to an overview of this issue presented at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
While there is clear evidence that cannabis use relative to the general population “is more prevalent among patients with psychiatric disorders,” it is less certain how often this use is risky, said Diana M. Martinez, MD, professor of psychiatry at Columbia University in New York.
Independent of euphoric effects, cannabis can be perceived by individuals with psychiatric diagnosis as self-medication for feelings of stress, social anxiety, and insomnia, among other symptoms. These are the same reasons why many individuals without psychiatric conditions use cannabis-containing products.
The perception that cannabis use is generally benign presumably explains the successful efforts at legalization, but there are risks for those with or without psychiatric illnesses, Dr. Martinez pointed out at the meeting, sponsored by Medscape Live. Not least, about 20% of regular users of cannabis develop cannabis use disorder (CUD), a condition defined in the DSM-5 as the continued use of cannabis despite adverse consequences, such as dependence.
Impact of severe CUD ‘incapacitating’
“Of those who meet criteria for CUD, 23% have severe CUD, which is an incapacitating form,” reported Dr. Martinez, citing work led by Deborah Hasin, PhD, professor of clinical epidemiology at Columbia University.
However, relative to otherwise healthy individuals, those with a psychiatric diagnosis might face greater benefits or greater risks from cannabis use, according to Dr. Martinez, who cited a 2017 report from the National Academies of Science, Engineering, and Medicine (NASEM).
This report evaluated the potential risks and benefits on the basis of published studies.
There is limited evidence that regular cannabis increases rather than modifies symptoms of mania and hypomania in patients with bipolar disorder, according to the report. The report also cited limited evidence that cannabis use increases severity of posttraumatic stress disorder (PTSD). There was limited evidence of adverse effects on symptoms of anxiety, although this appeared to depend on daily or nearly daily use.
The report found no data of acceptable quality to draw conclusions about the effect of cannabis use on symptoms of depression.
In patients with attention-deficit/hyperactivity disorder (ADHD), “a recent study showed that daily but not occasional use of cannabis increased impulsivity but not inattention, working memory, or verbal intelligence,” said Dr. Martinez, citing a study published this year.
Some evidence also suggests that patients with a psychiatric disorder might benefit from cannabis use, but, again, this evidence is limited. For one example, it includes a potential reduction in symptoms of obsessive-compulsive disorder, Dr. Martinez said.
More support for cannabis in medical disease
Relative to the quality of evidence supporting benefit from cannabis in psychiatric disease, the data appear to be stronger for patients with medical illnesses, such as cancer. For example, Dr. Martinez cited evidence that tetrahydrocannabinol (THC), a major active ingredient in cannabis, improves sleep in the context of a medical illnesses. There is also evidence for anxiolytic effects in patients with a medical illness, although that is weaker.
In patients with or without a psychiatric disorder, marijuana does pose a risk of substance abuse disorder, and it shares the risks of intoxicants, such as inattention leading to increased risk of accidents, including motor vehicle accidents. This pertains to those with or without a psychiatric or medical condition, Dr. Martinez said.
While intermittent light use of cannabis appears to pose no risk or a very low risk of long-term adverse effects on cognition, at least in patients without psychiatric disorders, Dr. Martinez indicated that the risk-benefit ratio for any individual is use dependent. The risk of CUD, for example, increases with the frequency of exposure and the potency of the cannabis.
Empirical evidence for therapeutic role
In published studies, other researchers have expressed interest in a potential therapeutic role of cannabis for psychiatric disorders, but there appears to be a general consensus that the supportive data remain weak. One expert who has written on this topic, Jerome Sarris, PhD, professor of integrative mental health, NICM Health Research Institute, Western Sydney University, Westmead, Australia, said that empirical evidence does support a benefit in selected patients.
“Of course, high THC forms are strongly discouraged in people with schizophrenia or high risk of developing psychotic disorder, or in youths,” Dr. Sarris explained. “However, there is a potential role for use in people with sleep and pain issues, and many find it beneficial to also assist with affective disorder symptoms.”
In a systematic review he led that was published last year, the evidence to support cannabis for psychiatric disorders was characterized as “embryonic.” However, small studies and case reports appear to support benefit for such indications as ADHD if precautions are taken.
“I certainly would not discourage use of prescribed standardized medicinal cannabis therapeutics for all people with psychiatric disorders,” Dr. Sarris said. He suggested that attention should be made to the THC potency and terpene composition of the products that patients with psychiatric disorders are taking.
Marijuana use is now a legal activity in many parts of the United States, but those managing patients with psychiatric disorders are in the difficult position of determining whether this use is helpful, harmful, or irrelevant to the underlying illness on the basis of limited and largely incomplete data, according to an overview of this issue presented at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
While there is clear evidence that cannabis use relative to the general population “is more prevalent among patients with psychiatric disorders,” it is less certain how often this use is risky, said Diana M. Martinez, MD, professor of psychiatry at Columbia University in New York.
Independent of euphoric effects, cannabis can be perceived by individuals with psychiatric diagnosis as self-medication for feelings of stress, social anxiety, and insomnia, among other symptoms. These are the same reasons why many individuals without psychiatric conditions use cannabis-containing products.
The perception that cannabis use is generally benign presumably explains the successful efforts at legalization, but there are risks for those with or without psychiatric illnesses, Dr. Martinez pointed out at the meeting, sponsored by Medscape Live. Not least, about 20% of regular users of cannabis develop cannabis use disorder (CUD), a condition defined in the DSM-5 as the continued use of cannabis despite adverse consequences, such as dependence.
Impact of severe CUD ‘incapacitating’
“Of those who meet criteria for CUD, 23% have severe CUD, which is an incapacitating form,” reported Dr. Martinez, citing work led by Deborah Hasin, PhD, professor of clinical epidemiology at Columbia University.
However, relative to otherwise healthy individuals, those with a psychiatric diagnosis might face greater benefits or greater risks from cannabis use, according to Dr. Martinez, who cited a 2017 report from the National Academies of Science, Engineering, and Medicine (NASEM).
This report evaluated the potential risks and benefits on the basis of published studies.
There is limited evidence that regular cannabis increases rather than modifies symptoms of mania and hypomania in patients with bipolar disorder, according to the report. The report also cited limited evidence that cannabis use increases severity of posttraumatic stress disorder (PTSD). There was limited evidence of adverse effects on symptoms of anxiety, although this appeared to depend on daily or nearly daily use.
The report found no data of acceptable quality to draw conclusions about the effect of cannabis use on symptoms of depression.
In patients with attention-deficit/hyperactivity disorder (ADHD), “a recent study showed that daily but not occasional use of cannabis increased impulsivity but not inattention, working memory, or verbal intelligence,” said Dr. Martinez, citing a study published this year.
Some evidence also suggests that patients with a psychiatric disorder might benefit from cannabis use, but, again, this evidence is limited. For one example, it includes a potential reduction in symptoms of obsessive-compulsive disorder, Dr. Martinez said.
More support for cannabis in medical disease
Relative to the quality of evidence supporting benefit from cannabis in psychiatric disease, the data appear to be stronger for patients with medical illnesses, such as cancer. For example, Dr. Martinez cited evidence that tetrahydrocannabinol (THC), a major active ingredient in cannabis, improves sleep in the context of a medical illnesses. There is also evidence for anxiolytic effects in patients with a medical illness, although that is weaker.
In patients with or without a psychiatric disorder, marijuana does pose a risk of substance abuse disorder, and it shares the risks of intoxicants, such as inattention leading to increased risk of accidents, including motor vehicle accidents. This pertains to those with or without a psychiatric or medical condition, Dr. Martinez said.
While intermittent light use of cannabis appears to pose no risk or a very low risk of long-term adverse effects on cognition, at least in patients without psychiatric disorders, Dr. Martinez indicated that the risk-benefit ratio for any individual is use dependent. The risk of CUD, for example, increases with the frequency of exposure and the potency of the cannabis.
Empirical evidence for therapeutic role
In published studies, other researchers have expressed interest in a potential therapeutic role of cannabis for psychiatric disorders, but there appears to be a general consensus that the supportive data remain weak. One expert who has written on this topic, Jerome Sarris, PhD, professor of integrative mental health, NICM Health Research Institute, Western Sydney University, Westmead, Australia, said that empirical evidence does support a benefit in selected patients.
“Of course, high THC forms are strongly discouraged in people with schizophrenia or high risk of developing psychotic disorder, or in youths,” Dr. Sarris explained. “However, there is a potential role for use in people with sleep and pain issues, and many find it beneficial to also assist with affective disorder symptoms.”
In a systematic review he led that was published last year, the evidence to support cannabis for psychiatric disorders was characterized as “embryonic.” However, small studies and case reports appear to support benefit for such indications as ADHD if precautions are taken.
“I certainly would not discourage use of prescribed standardized medicinal cannabis therapeutics for all people with psychiatric disorders,” Dr. Sarris said. He suggested that attention should be made to the THC potency and terpene composition of the products that patients with psychiatric disorders are taking.
Marijuana use is now a legal activity in many parts of the United States, but those managing patients with psychiatric disorders are in the difficult position of determining whether this use is helpful, harmful, or irrelevant to the underlying illness on the basis of limited and largely incomplete data, according to an overview of this issue presented at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
While there is clear evidence that cannabis use relative to the general population “is more prevalent among patients with psychiatric disorders,” it is less certain how often this use is risky, said Diana M. Martinez, MD, professor of psychiatry at Columbia University in New York.
Independent of euphoric effects, cannabis can be perceived by individuals with psychiatric diagnosis as self-medication for feelings of stress, social anxiety, and insomnia, among other symptoms. These are the same reasons why many individuals without psychiatric conditions use cannabis-containing products.
The perception that cannabis use is generally benign presumably explains the successful efforts at legalization, but there are risks for those with or without psychiatric illnesses, Dr. Martinez pointed out at the meeting, sponsored by Medscape Live. Not least, about 20% of regular users of cannabis develop cannabis use disorder (CUD), a condition defined in the DSM-5 as the continued use of cannabis despite adverse consequences, such as dependence.
Impact of severe CUD ‘incapacitating’
“Of those who meet criteria for CUD, 23% have severe CUD, which is an incapacitating form,” reported Dr. Martinez, citing work led by Deborah Hasin, PhD, professor of clinical epidemiology at Columbia University.
However, relative to otherwise healthy individuals, those with a psychiatric diagnosis might face greater benefits or greater risks from cannabis use, according to Dr. Martinez, who cited a 2017 report from the National Academies of Science, Engineering, and Medicine (NASEM).
This report evaluated the potential risks and benefits on the basis of published studies.
There is limited evidence that regular cannabis increases rather than modifies symptoms of mania and hypomania in patients with bipolar disorder, according to the report. The report also cited limited evidence that cannabis use increases severity of posttraumatic stress disorder (PTSD). There was limited evidence of adverse effects on symptoms of anxiety, although this appeared to depend on daily or nearly daily use.
The report found no data of acceptable quality to draw conclusions about the effect of cannabis use on symptoms of depression.
In patients with attention-deficit/hyperactivity disorder (ADHD), “a recent study showed that daily but not occasional use of cannabis increased impulsivity but not inattention, working memory, or verbal intelligence,” said Dr. Martinez, citing a study published this year.
Some evidence also suggests that patients with a psychiatric disorder might benefit from cannabis use, but, again, this evidence is limited. For one example, it includes a potential reduction in symptoms of obsessive-compulsive disorder, Dr. Martinez said.
More support for cannabis in medical disease
Relative to the quality of evidence supporting benefit from cannabis in psychiatric disease, the data appear to be stronger for patients with medical illnesses, such as cancer. For example, Dr. Martinez cited evidence that tetrahydrocannabinol (THC), a major active ingredient in cannabis, improves sleep in the context of a medical illnesses. There is also evidence for anxiolytic effects in patients with a medical illness, although that is weaker.
In patients with or without a psychiatric disorder, marijuana does pose a risk of substance abuse disorder, and it shares the risks of intoxicants, such as inattention leading to increased risk of accidents, including motor vehicle accidents. This pertains to those with or without a psychiatric or medical condition, Dr. Martinez said.
While intermittent light use of cannabis appears to pose no risk or a very low risk of long-term adverse effects on cognition, at least in patients without psychiatric disorders, Dr. Martinez indicated that the risk-benefit ratio for any individual is use dependent. The risk of CUD, for example, increases with the frequency of exposure and the potency of the cannabis.
Empirical evidence for therapeutic role
In published studies, other researchers have expressed interest in a potential therapeutic role of cannabis for psychiatric disorders, but there appears to be a general consensus that the supportive data remain weak. One expert who has written on this topic, Jerome Sarris, PhD, professor of integrative mental health, NICM Health Research Institute, Western Sydney University, Westmead, Australia, said that empirical evidence does support a benefit in selected patients.
“Of course, high THC forms are strongly discouraged in people with schizophrenia or high risk of developing psychotic disorder, or in youths,” Dr. Sarris explained. “However, there is a potential role for use in people with sleep and pain issues, and many find it beneficial to also assist with affective disorder symptoms.”
In a systematic review he led that was published last year, the evidence to support cannabis for psychiatric disorders was characterized as “embryonic.” However, small studies and case reports appear to support benefit for such indications as ADHD if precautions are taken.
“I certainly would not discourage use of prescribed standardized medicinal cannabis therapeutics for all people with psychiatric disorders,” Dr. Sarris said. He suggested that attention should be made to the THC potency and terpene composition of the products that patients with psychiatric disorders are taking.
FROM PSYCHOPHARMACOLOGY UPDATE