User login
Do ICDs still ‘work’ in primary prevention given today’s recommended HF meds?
Contemporary guidelines highly recommend patients with heart failure with reduced ejection fraction (HFrEF) be on all four drug classes that together have shown clinical clout, including improved survival, in major randomized trials.
Although many such patients don’t receive all four drug classes, the more that are prescribed to those with primary-prevention implantable defibrillators (ICD), the better their odds of survival, a new analysis suggests.
The cohort study of almost 5,000 patients with HFrEF and such devices saw their all-cause mortality risk improve stepwise with each additional prescription they were given toward the full quadruple drug combo at the core of modern HFrEF guideline-directed medical therapy (GDMT). The four classes are sodium-glucose cotransporter 2 inhibitors, beta-blockers, mineralocorticoid receptor antagonists (MRA), and renin-angiotensin system (RAS) inhibitors.
That inverse relation between risk and number of GDMT medications held whether patients had solo-ICD or defibrillating cardiac resynchronization therapy (CRT-D) implants, and were independent of device-implantation year and comorbidities, regardless of HFrEF etiology.
“If anybody had doubts about really pushing forward as much of these guideline-directed medical therapies as the patient tolerates, these data confirm that, by doing so, we definitely do better than with two medications or one medication,” Samir Saba, MD, University of Pittsburgh Medical Center, said in an interview.
The analysis begs an old and challenging question: Do primary-prevention ICDs confer clinically important survival gains over those provided by increasingly life-preserving recommended HFrEF medical therapy?
Given the study’s incremental survival bumps with each added GDMT med, “one ought to consider whether ICD therapy can still have an impact on overall survival in this population,” proposes a report published online in JACC Clinical Electrophysiology, with Dr. Saba as senior author.
In the adjusted analysis, the 2-year risk for death from any cause in HFrEF patients with primary-prevention devices fell 36% in those with ICDs and 30% in those with CRT-D devices for each added prescribed GDMT drug, from none up to either three or four such agents (P < .001 in both cases).
Only so much can be made of nonrandomized study results, Saba observed in an interview. But they are enough to justify asking whether primary-prevention ICDs are “still valuable” in HFrEF given current GDMT. One interpretation of the study, the published report noted, is that contemporary GDMT improves HFrEF survival so much that it eclipses any such benefit from a primary-prevention ICD.
Both defibrillators and the four core drug therapies boost survival in such cases, “so the fundamental question is, are they additive. Do we save more lives by having a defibrillator on top of the medications, or is it overlapping?” Dr. Saba asked. “We don’t know the answer.”
For now, at least, the findings could reassure clinicians as they consider whether to recommended a primary-prevention ICD when there might be reasons not to, as long there is full GDMT on board, “especially what we today define as quadruple guideline-directed medical therapy.”
Recently announced North American guidelines defining an HFrEF quadruple regimen prefer – beyond a beta-blocker, MRA, and SGLT2 inhibitor – that the selected RAS inhibitor be sacubitril/valsartan (Entresto, Novartis), with ACE inhibitors or angiotensin-receptor blockers (ARBs) as a substitute, if needed.
Nearly identical European guidelines on HFrEF quad therapy, unveiled in 2021, include but do not necessarily prefer sacubitril/valsartan over ACE inhibitors as the RAS inhibitor of choice.
GDMT a moving target
Primary-prevention defibrillators entered practice at a time when expected background GDMT consisted of beta-blockers and either ACE inhibitors or ARBs, the current report notes. In practice, many patients receive the devices without both drug classes optimally on board. Moreover, many who otherwise meet guidelines for such ICDs won’t tolerate the kind of maximally tolerated GDMT used in the major primary-prevention device trials.
Yet current guidelines give such devices a class I recommendation, based on the highest level of evidence, in HFrEF patients who remain symptomatic despite quad GDMT, observed Gregg C. Fonarow, MD, University of California Los Angeles Medical Center.
The current analysis “further reinforces the importance of providing all four foundational GDMTs” to all eligible HFrEF patients without contraindications who can tolerate them, he said in an interview. Such quad therapy “is associated with incremental 1-year survival advantages” in patients with primary-prevention devices. And in the major trials, “there were reductions in sudden deaths, as well as progressive heart failure deaths.”
But the current study also suggests that in practice “very few patients can actually get to all four drugs on GDMT,” Roderick Tung, MD, University of Arizona, Phoenix, said in an interview. Optimized GDMT in randomized trials probably represents the best-case scenario. “There is a difference between randomized data and real-world data, which is why we need both.”
And it asserts that “the more GDMT you’re on, the better you do,” he said. “But does that obviate the need for an ICD? I think that’s not clear,” in part because of potential confounding in the analysis. For example, patients who can take all four agents tend to be less sick than those who cannot.
“The ones who can get up to four are preselected, because they’re healthier,” Dr. Tung said. “There are real limitations – such as metabolic disturbances, acute kidney injury and cardiorenal syndrome, and hypotension – that actually make it difficult to initiate and titrate these medications.”
Indeed, the major primary-prevention ICD trials usually excluded the sickest patients with the most comorbidities, Dr. Saba observed, which raises issues about their relevance to clinical practice. But his group’s study controlled for many potential confounders by adjusting for, among other things, Elixhauser comorbidity score, ejection fraction, type of cardiomyopathy, and year of device implantation.
“We tried to level the playing field that way, to see if – despite all of this adjustment – the incremental number of heart failure medicines stills make a difference,” Dr. Saba said. “And our results suggest that yes, they still do.”
GDMT coverage in the real world
The analysis of patients with HFrEF involved 3,210 with ICD-only implants and 1,762 with CRT-D devices for primary prevention at a major medical center from 2010 to 2021. Of the total, 5% had not been prescribed any of the four GDMT agents, 20% had been prescribed only one, 52% were prescribed two, and 23% were prescribed three or four. Only 113 patients had been prescribed SGLT2 inhibitors, which have only recently been indicated for HFrEF.
Adjusted hazard ratios for death from any cause at 2 years for each added GDMT drug (P < .001 in each case), were 0.64 (95% confidence interval, 0.56-0.74) for ICD recipients, 0.70 (95% CI, 0.58-0.86) for those with a CRT-D device, 0.70 (95% CI, 0.60-0.81) for those with ischemic cardiomyopathy, and 0.61 (95% CI, 0.51-0.73) for patients with nonischemic disease.
The results “raise questions rather than answers,” Dr. Saba said. “At some point, someone will need to take patients who are optimized on their heart failure medications and then randomize them to defibrillator versus no defibrillator to see whether there is still an additive impact.”
Current best evidence suggests that primary-prevention ICDs in patients with guideline-based indications confer benefits that far outweigh any risks. But if the major primary-prevention ICD trials were to be repeated in patients on contemporary quad-therapy GDMT, Dr. Tung said, “would the benefit of ICD be attenuated? I think most of us believe it likely would.”
Still, he said, a background of modern GDMT could potentially “optimize” such trials by attenuating mortality from heart failure progression and thereby expanding the proportion of deaths that are arrhythmic, “which the defibrillator can prevent.”
Dr. Saba discloses receiving research support from Boston Scientific and Abbott; and serving on advisory boards for Medtronic and Boston Scientific. The other authors reported no relevant relationships. Dr. Tung has disclosed receiving speaker fees from Abbott and Boston Scientific. Dr. Fonarow has reported receiving personal fees from Abbott, Amgen, AstraZeneca, Bayer, Cytokinetics, Edwards, Janssen, Medtronic, Merck, and Novartis.
A version of this article first appeared on Medscape.com.
Contemporary guidelines highly recommend patients with heart failure with reduced ejection fraction (HFrEF) be on all four drug classes that together have shown clinical clout, including improved survival, in major randomized trials.
Although many such patients don’t receive all four drug classes, the more that are prescribed to those with primary-prevention implantable defibrillators (ICD), the better their odds of survival, a new analysis suggests.
The cohort study of almost 5,000 patients with HFrEF and such devices saw their all-cause mortality risk improve stepwise with each additional prescription they were given toward the full quadruple drug combo at the core of modern HFrEF guideline-directed medical therapy (GDMT). The four classes are sodium-glucose cotransporter 2 inhibitors, beta-blockers, mineralocorticoid receptor antagonists (MRA), and renin-angiotensin system (RAS) inhibitors.
That inverse relation between risk and number of GDMT medications held whether patients had solo-ICD or defibrillating cardiac resynchronization therapy (CRT-D) implants, and were independent of device-implantation year and comorbidities, regardless of HFrEF etiology.
“If anybody had doubts about really pushing forward as much of these guideline-directed medical therapies as the patient tolerates, these data confirm that, by doing so, we definitely do better than with two medications or one medication,” Samir Saba, MD, University of Pittsburgh Medical Center, said in an interview.
The analysis begs an old and challenging question: Do primary-prevention ICDs confer clinically important survival gains over those provided by increasingly life-preserving recommended HFrEF medical therapy?
Given the study’s incremental survival bumps with each added GDMT med, “one ought to consider whether ICD therapy can still have an impact on overall survival in this population,” proposes a report published online in JACC Clinical Electrophysiology, with Dr. Saba as senior author.
In the adjusted analysis, the 2-year risk for death from any cause in HFrEF patients with primary-prevention devices fell 36% in those with ICDs and 30% in those with CRT-D devices for each added prescribed GDMT drug, from none up to either three or four such agents (P < .001 in both cases).
Only so much can be made of nonrandomized study results, Saba observed in an interview. But they are enough to justify asking whether primary-prevention ICDs are “still valuable” in HFrEF given current GDMT. One interpretation of the study, the published report noted, is that contemporary GDMT improves HFrEF survival so much that it eclipses any such benefit from a primary-prevention ICD.
Both defibrillators and the four core drug therapies boost survival in such cases, “so the fundamental question is, are they additive. Do we save more lives by having a defibrillator on top of the medications, or is it overlapping?” Dr. Saba asked. “We don’t know the answer.”
For now, at least, the findings could reassure clinicians as they consider whether to recommended a primary-prevention ICD when there might be reasons not to, as long there is full GDMT on board, “especially what we today define as quadruple guideline-directed medical therapy.”
Recently announced North American guidelines defining an HFrEF quadruple regimen prefer – beyond a beta-blocker, MRA, and SGLT2 inhibitor – that the selected RAS inhibitor be sacubitril/valsartan (Entresto, Novartis), with ACE inhibitors or angiotensin-receptor blockers (ARBs) as a substitute, if needed.
Nearly identical European guidelines on HFrEF quad therapy, unveiled in 2021, include but do not necessarily prefer sacubitril/valsartan over ACE inhibitors as the RAS inhibitor of choice.
GDMT a moving target
Primary-prevention defibrillators entered practice at a time when expected background GDMT consisted of beta-blockers and either ACE inhibitors or ARBs, the current report notes. In practice, many patients receive the devices without both drug classes optimally on board. Moreover, many who otherwise meet guidelines for such ICDs won’t tolerate the kind of maximally tolerated GDMT used in the major primary-prevention device trials.
Yet current guidelines give such devices a class I recommendation, based on the highest level of evidence, in HFrEF patients who remain symptomatic despite quad GDMT, observed Gregg C. Fonarow, MD, University of California Los Angeles Medical Center.
The current analysis “further reinforces the importance of providing all four foundational GDMTs” to all eligible HFrEF patients without contraindications who can tolerate them, he said in an interview. Such quad therapy “is associated with incremental 1-year survival advantages” in patients with primary-prevention devices. And in the major trials, “there were reductions in sudden deaths, as well as progressive heart failure deaths.”
But the current study also suggests that in practice “very few patients can actually get to all four drugs on GDMT,” Roderick Tung, MD, University of Arizona, Phoenix, said in an interview. Optimized GDMT in randomized trials probably represents the best-case scenario. “There is a difference between randomized data and real-world data, which is why we need both.”
And it asserts that “the more GDMT you’re on, the better you do,” he said. “But does that obviate the need for an ICD? I think that’s not clear,” in part because of potential confounding in the analysis. For example, patients who can take all four agents tend to be less sick than those who cannot.
“The ones who can get up to four are preselected, because they’re healthier,” Dr. Tung said. “There are real limitations – such as metabolic disturbances, acute kidney injury and cardiorenal syndrome, and hypotension – that actually make it difficult to initiate and titrate these medications.”
Indeed, the major primary-prevention ICD trials usually excluded the sickest patients with the most comorbidities, Dr. Saba observed, which raises issues about their relevance to clinical practice. But his group’s study controlled for many potential confounders by adjusting for, among other things, Elixhauser comorbidity score, ejection fraction, type of cardiomyopathy, and year of device implantation.
“We tried to level the playing field that way, to see if – despite all of this adjustment – the incremental number of heart failure medicines stills make a difference,” Dr. Saba said. “And our results suggest that yes, they still do.”
GDMT coverage in the real world
The analysis of patients with HFrEF involved 3,210 with ICD-only implants and 1,762 with CRT-D devices for primary prevention at a major medical center from 2010 to 2021. Of the total, 5% had not been prescribed any of the four GDMT agents, 20% had been prescribed only one, 52% were prescribed two, and 23% were prescribed three or four. Only 113 patients had been prescribed SGLT2 inhibitors, which have only recently been indicated for HFrEF.
Adjusted hazard ratios for death from any cause at 2 years for each added GDMT drug (P < .001 in each case), were 0.64 (95% confidence interval, 0.56-0.74) for ICD recipients, 0.70 (95% CI, 0.58-0.86) for those with a CRT-D device, 0.70 (95% CI, 0.60-0.81) for those with ischemic cardiomyopathy, and 0.61 (95% CI, 0.51-0.73) for patients with nonischemic disease.
The results “raise questions rather than answers,” Dr. Saba said. “At some point, someone will need to take patients who are optimized on their heart failure medications and then randomize them to defibrillator versus no defibrillator to see whether there is still an additive impact.”
Current best evidence suggests that primary-prevention ICDs in patients with guideline-based indications confer benefits that far outweigh any risks. But if the major primary-prevention ICD trials were to be repeated in patients on contemporary quad-therapy GDMT, Dr. Tung said, “would the benefit of ICD be attenuated? I think most of us believe it likely would.”
Still, he said, a background of modern GDMT could potentially “optimize” such trials by attenuating mortality from heart failure progression and thereby expanding the proportion of deaths that are arrhythmic, “which the defibrillator can prevent.”
Dr. Saba discloses receiving research support from Boston Scientific and Abbott; and serving on advisory boards for Medtronic and Boston Scientific. The other authors reported no relevant relationships. Dr. Tung has disclosed receiving speaker fees from Abbott and Boston Scientific. Dr. Fonarow has reported receiving personal fees from Abbott, Amgen, AstraZeneca, Bayer, Cytokinetics, Edwards, Janssen, Medtronic, Merck, and Novartis.
A version of this article first appeared on Medscape.com.
Contemporary guidelines highly recommend patients with heart failure with reduced ejection fraction (HFrEF) be on all four drug classes that together have shown clinical clout, including improved survival, in major randomized trials.
Although many such patients don’t receive all four drug classes, the more that are prescribed to those with primary-prevention implantable defibrillators (ICD), the better their odds of survival, a new analysis suggests.
The cohort study of almost 5,000 patients with HFrEF and such devices saw their all-cause mortality risk improve stepwise with each additional prescription they were given toward the full quadruple drug combo at the core of modern HFrEF guideline-directed medical therapy (GDMT). The four classes are sodium-glucose cotransporter 2 inhibitors, beta-blockers, mineralocorticoid receptor antagonists (MRA), and renin-angiotensin system (RAS) inhibitors.
That inverse relation between risk and number of GDMT medications held whether patients had solo-ICD or defibrillating cardiac resynchronization therapy (CRT-D) implants, and were independent of device-implantation year and comorbidities, regardless of HFrEF etiology.
“If anybody had doubts about really pushing forward as much of these guideline-directed medical therapies as the patient tolerates, these data confirm that, by doing so, we definitely do better than with two medications or one medication,” Samir Saba, MD, University of Pittsburgh Medical Center, said in an interview.
The analysis begs an old and challenging question: Do primary-prevention ICDs confer clinically important survival gains over those provided by increasingly life-preserving recommended HFrEF medical therapy?
Given the study’s incremental survival bumps with each added GDMT med, “one ought to consider whether ICD therapy can still have an impact on overall survival in this population,” proposes a report published online in JACC Clinical Electrophysiology, with Dr. Saba as senior author.
In the adjusted analysis, the 2-year risk for death from any cause in HFrEF patients with primary-prevention devices fell 36% in those with ICDs and 30% in those with CRT-D devices for each added prescribed GDMT drug, from none up to either three or four such agents (P < .001 in both cases).
Only so much can be made of nonrandomized study results, Saba observed in an interview. But they are enough to justify asking whether primary-prevention ICDs are “still valuable” in HFrEF given current GDMT. One interpretation of the study, the published report noted, is that contemporary GDMT improves HFrEF survival so much that it eclipses any such benefit from a primary-prevention ICD.
Both defibrillators and the four core drug therapies boost survival in such cases, “so the fundamental question is, are they additive. Do we save more lives by having a defibrillator on top of the medications, or is it overlapping?” Dr. Saba asked. “We don’t know the answer.”
For now, at least, the findings could reassure clinicians as they consider whether to recommended a primary-prevention ICD when there might be reasons not to, as long there is full GDMT on board, “especially what we today define as quadruple guideline-directed medical therapy.”
Recently announced North American guidelines defining an HFrEF quadruple regimen prefer – beyond a beta-blocker, MRA, and SGLT2 inhibitor – that the selected RAS inhibitor be sacubitril/valsartan (Entresto, Novartis), with ACE inhibitors or angiotensin-receptor blockers (ARBs) as a substitute, if needed.
Nearly identical European guidelines on HFrEF quad therapy, unveiled in 2021, include but do not necessarily prefer sacubitril/valsartan over ACE inhibitors as the RAS inhibitor of choice.
GDMT a moving target
Primary-prevention defibrillators entered practice at a time when expected background GDMT consisted of beta-blockers and either ACE inhibitors or ARBs, the current report notes. In practice, many patients receive the devices without both drug classes optimally on board. Moreover, many who otherwise meet guidelines for such ICDs won’t tolerate the kind of maximally tolerated GDMT used in the major primary-prevention device trials.
Yet current guidelines give such devices a class I recommendation, based on the highest level of evidence, in HFrEF patients who remain symptomatic despite quad GDMT, observed Gregg C. Fonarow, MD, University of California Los Angeles Medical Center.
The current analysis “further reinforces the importance of providing all four foundational GDMTs” to all eligible HFrEF patients without contraindications who can tolerate them, he said in an interview. Such quad therapy “is associated with incremental 1-year survival advantages” in patients with primary-prevention devices. And in the major trials, “there were reductions in sudden deaths, as well as progressive heart failure deaths.”
But the current study also suggests that in practice “very few patients can actually get to all four drugs on GDMT,” Roderick Tung, MD, University of Arizona, Phoenix, said in an interview. Optimized GDMT in randomized trials probably represents the best-case scenario. “There is a difference between randomized data and real-world data, which is why we need both.”
And it asserts that “the more GDMT you’re on, the better you do,” he said. “But does that obviate the need for an ICD? I think that’s not clear,” in part because of potential confounding in the analysis. For example, patients who can take all four agents tend to be less sick than those who cannot.
“The ones who can get up to four are preselected, because they’re healthier,” Dr. Tung said. “There are real limitations – such as metabolic disturbances, acute kidney injury and cardiorenal syndrome, and hypotension – that actually make it difficult to initiate and titrate these medications.”
Indeed, the major primary-prevention ICD trials usually excluded the sickest patients with the most comorbidities, Dr. Saba observed, which raises issues about their relevance to clinical practice. But his group’s study controlled for many potential confounders by adjusting for, among other things, Elixhauser comorbidity score, ejection fraction, type of cardiomyopathy, and year of device implantation.
“We tried to level the playing field that way, to see if – despite all of this adjustment – the incremental number of heart failure medicines stills make a difference,” Dr. Saba said. “And our results suggest that yes, they still do.”
GDMT coverage in the real world
The analysis of patients with HFrEF involved 3,210 with ICD-only implants and 1,762 with CRT-D devices for primary prevention at a major medical center from 2010 to 2021. Of the total, 5% had not been prescribed any of the four GDMT agents, 20% had been prescribed only one, 52% were prescribed two, and 23% were prescribed three or four. Only 113 patients had been prescribed SGLT2 inhibitors, which have only recently been indicated for HFrEF.
Adjusted hazard ratios for death from any cause at 2 years for each added GDMT drug (P < .001 in each case), were 0.64 (95% confidence interval, 0.56-0.74) for ICD recipients, 0.70 (95% CI, 0.58-0.86) for those with a CRT-D device, 0.70 (95% CI, 0.60-0.81) for those with ischemic cardiomyopathy, and 0.61 (95% CI, 0.51-0.73) for patients with nonischemic disease.
The results “raise questions rather than answers,” Dr. Saba said. “At some point, someone will need to take patients who are optimized on their heart failure medications and then randomize them to defibrillator versus no defibrillator to see whether there is still an additive impact.”
Current best evidence suggests that primary-prevention ICDs in patients with guideline-based indications confer benefits that far outweigh any risks. But if the major primary-prevention ICD trials were to be repeated in patients on contemporary quad-therapy GDMT, Dr. Tung said, “would the benefit of ICD be attenuated? I think most of us believe it likely would.”
Still, he said, a background of modern GDMT could potentially “optimize” such trials by attenuating mortality from heart failure progression and thereby expanding the proportion of deaths that are arrhythmic, “which the defibrillator can prevent.”
Dr. Saba discloses receiving research support from Boston Scientific and Abbott; and serving on advisory boards for Medtronic and Boston Scientific. The other authors reported no relevant relationships. Dr. Tung has disclosed receiving speaker fees from Abbott and Boston Scientific. Dr. Fonarow has reported receiving personal fees from Abbott, Amgen, AstraZeneca, Bayer, Cytokinetics, Edwards, Janssen, Medtronic, Merck, and Novartis.
A version of this article first appeared on Medscape.com.
FROM JACC CLINICAL ELECTROPHYSIOLOGY
For patients with peripheral artery disease, pain can be gain
For people with peripheral artery disease (PAD), even short walks can be exercises in excruciation.
But a new study published in the Journal of the American Heart Association has found that patients who can push through the pain appear to reap significant benefits in ambulation, balance, and leg strength, which have been linked to increased longevity.
“You have to push yourself and get those uncomfortable symptoms, or else you probably won’t get gains,” said Mary McDermott, MD, professor of medicine at Northwestern University, Chicago, and the senior author of the study.
Walking for exercise is critical for people with lower-extremity PAD, Dr. McDermott said, but leg pain dissuades many people with the condition from doing so. She said her group hopes that showing the payoff of the “no pain, no gain” approach gives people with PAD the resolve to walk regularly, even when it’s hard.
The new study, a post hoc analysis of the LITE (Low-Intensity Exercise Intervention in PAD) trial, found that low-intensity exercise did not improve the symptoms of PAD but high-intensity exercise did.
Dr. McDermott and her colleagues compared 109 people with PAD who walked fast enough to cause discomfort versus 101 people who walked at a comfortable pace and 54 people who did not exercise at all. The average age was 69 years, 48% of participants were women, and 61% were Black.
Everyone in the exercise groups walked at home, with visits to a medical center early in the study to get exercise tips and then phone support from exercise coaches throughout the remainder of the study. Researchers encouraged those in the discomfort group to walk fast enough to cause significant pain in their legs, for up to 10 minutes or as long as they could. They then rested before walking again, ideally up to five times per day for 5 days per week.
At 6 months, people in the discomfort group were walking 0.056 m/sec faster than those in the comfort group during a 4-meter walking test (95% confidence interval [CI], 0.19-0.094 m/sec; P < .01), a gap that had grown by 12 months to 0.084 m/sec (95% CI, 0.049-0.120 m/sec; P <.01), according to the researchers. A statistically significant gap also emerged between the discomfort and nonexercising group at 6 months, but it eventually closed.
“It’s a question that people have asked for some time: Is it necessary to get that ischemic pain when you walk?” Dr. McDermott said. “This is the first well-powered clinical trial to provide a definitive answer on that, and the answer is that you do need that discomfort. It wasn’t even close.” Indeed, Dr. McDermott said, it’s possible that walking merely to the point of comfort and never pushing beyond it may harm people with PAD.
At the 6-month mark, the researchers found no statistical difference between the discomfort and comfort groups on a cumulative scale of usual walking speed, ability to rise from a chair, and ability to maintain balance in several positions. By 12 months, the two groups had diverged, with the discomfort group improving by almost 1 point on the scale, whereas the performance of the comfort group declined. No significant differences emerged between the discomfort and nonexercising groups, the researchers reported.
The investigators found, counterintuitively, that some people in the study who did not record exercising did as well as those in the discomfort group,
Dr. McDermott noted that the nonexercise group was smaller than the discomfort group, making firm comparisons between the two challenging to draw. In addition, people whose exercise was not recorded were not asked to take it easy whenever they walked, unlike those in the comfort group. As a result, she said, some people in this group may have walked vigorously.
Dr. McDermott emphasized that these benefits occurred at home rather than at medical centers that can be difficult for some people to visit regularly.
“It’s always good to have this kind of information for patients, to show them that it’s possible for them to continue to improve,” said Jonathan Ehrman, PhD, associate director of preventive cardiology at Henry Ford Medical Center, Detroit. Dr. Ehrman was not involved in this study but said that he is contemplating running a similar home-based study that would use video rather than telephone support for patients.
“There’s emerging data about walking speed being related to longevity and predicting better outcomes in cardiac surgeries,” Dr. Ehrman said. “It seems to be, if you can get people walking faster or they have a better walking pace, related to better health outcomes.”
Dr. McDermott reported relationships with Regeneron, Helixmith, Mars, ArtAssist, ReserveAge, and Hershey. Dr. Ehrman reported no relevant financial conflicts of interest.
A version of this article first appeared on Medscape.com.
For people with peripheral artery disease (PAD), even short walks can be exercises in excruciation.
But a new study published in the Journal of the American Heart Association has found that patients who can push through the pain appear to reap significant benefits in ambulation, balance, and leg strength, which have been linked to increased longevity.
“You have to push yourself and get those uncomfortable symptoms, or else you probably won’t get gains,” said Mary McDermott, MD, professor of medicine at Northwestern University, Chicago, and the senior author of the study.
Walking for exercise is critical for people with lower-extremity PAD, Dr. McDermott said, but leg pain dissuades many people with the condition from doing so. She said her group hopes that showing the payoff of the “no pain, no gain” approach gives people with PAD the resolve to walk regularly, even when it’s hard.
The new study, a post hoc analysis of the LITE (Low-Intensity Exercise Intervention in PAD) trial, found that low-intensity exercise did not improve the symptoms of PAD but high-intensity exercise did.
Dr. McDermott and her colleagues compared 109 people with PAD who walked fast enough to cause discomfort versus 101 people who walked at a comfortable pace and 54 people who did not exercise at all. The average age was 69 years, 48% of participants were women, and 61% were Black.
Everyone in the exercise groups walked at home, with visits to a medical center early in the study to get exercise tips and then phone support from exercise coaches throughout the remainder of the study. Researchers encouraged those in the discomfort group to walk fast enough to cause significant pain in their legs, for up to 10 minutes or as long as they could. They then rested before walking again, ideally up to five times per day for 5 days per week.
At 6 months, people in the discomfort group were walking 0.056 m/sec faster than those in the comfort group during a 4-meter walking test (95% confidence interval [CI], 0.19-0.094 m/sec; P < .01), a gap that had grown by 12 months to 0.084 m/sec (95% CI, 0.049-0.120 m/sec; P <.01), according to the researchers. A statistically significant gap also emerged between the discomfort and nonexercising group at 6 months, but it eventually closed.
“It’s a question that people have asked for some time: Is it necessary to get that ischemic pain when you walk?” Dr. McDermott said. “This is the first well-powered clinical trial to provide a definitive answer on that, and the answer is that you do need that discomfort. It wasn’t even close.” Indeed, Dr. McDermott said, it’s possible that walking merely to the point of comfort and never pushing beyond it may harm people with PAD.
At the 6-month mark, the researchers found no statistical difference between the discomfort and comfort groups on a cumulative scale of usual walking speed, ability to rise from a chair, and ability to maintain balance in several positions. By 12 months, the two groups had diverged, with the discomfort group improving by almost 1 point on the scale, whereas the performance of the comfort group declined. No significant differences emerged between the discomfort and nonexercising groups, the researchers reported.
The investigators found, counterintuitively, that some people in the study who did not record exercising did as well as those in the discomfort group,
Dr. McDermott noted that the nonexercise group was smaller than the discomfort group, making firm comparisons between the two challenging to draw. In addition, people whose exercise was not recorded were not asked to take it easy whenever they walked, unlike those in the comfort group. As a result, she said, some people in this group may have walked vigorously.
Dr. McDermott emphasized that these benefits occurred at home rather than at medical centers that can be difficult for some people to visit regularly.
“It’s always good to have this kind of information for patients, to show them that it’s possible for them to continue to improve,” said Jonathan Ehrman, PhD, associate director of preventive cardiology at Henry Ford Medical Center, Detroit. Dr. Ehrman was not involved in this study but said that he is contemplating running a similar home-based study that would use video rather than telephone support for patients.
“There’s emerging data about walking speed being related to longevity and predicting better outcomes in cardiac surgeries,” Dr. Ehrman said. “It seems to be, if you can get people walking faster or they have a better walking pace, related to better health outcomes.”
Dr. McDermott reported relationships with Regeneron, Helixmith, Mars, ArtAssist, ReserveAge, and Hershey. Dr. Ehrman reported no relevant financial conflicts of interest.
A version of this article first appeared on Medscape.com.
For people with peripheral artery disease (PAD), even short walks can be exercises in excruciation.
But a new study published in the Journal of the American Heart Association has found that patients who can push through the pain appear to reap significant benefits in ambulation, balance, and leg strength, which have been linked to increased longevity.
“You have to push yourself and get those uncomfortable symptoms, or else you probably won’t get gains,” said Mary McDermott, MD, professor of medicine at Northwestern University, Chicago, and the senior author of the study.
Walking for exercise is critical for people with lower-extremity PAD, Dr. McDermott said, but leg pain dissuades many people with the condition from doing so. She said her group hopes that showing the payoff of the “no pain, no gain” approach gives people with PAD the resolve to walk regularly, even when it’s hard.
The new study, a post hoc analysis of the LITE (Low-Intensity Exercise Intervention in PAD) trial, found that low-intensity exercise did not improve the symptoms of PAD but high-intensity exercise did.
Dr. McDermott and her colleagues compared 109 people with PAD who walked fast enough to cause discomfort versus 101 people who walked at a comfortable pace and 54 people who did not exercise at all. The average age was 69 years, 48% of participants were women, and 61% were Black.
Everyone in the exercise groups walked at home, with visits to a medical center early in the study to get exercise tips and then phone support from exercise coaches throughout the remainder of the study. Researchers encouraged those in the discomfort group to walk fast enough to cause significant pain in their legs, for up to 10 minutes or as long as they could. They then rested before walking again, ideally up to five times per day for 5 days per week.
At 6 months, people in the discomfort group were walking 0.056 m/sec faster than those in the comfort group during a 4-meter walking test (95% confidence interval [CI], 0.19-0.094 m/sec; P < .01), a gap that had grown by 12 months to 0.084 m/sec (95% CI, 0.049-0.120 m/sec; P <.01), according to the researchers. A statistically significant gap also emerged between the discomfort and nonexercising group at 6 months, but it eventually closed.
“It’s a question that people have asked for some time: Is it necessary to get that ischemic pain when you walk?” Dr. McDermott said. “This is the first well-powered clinical trial to provide a definitive answer on that, and the answer is that you do need that discomfort. It wasn’t even close.” Indeed, Dr. McDermott said, it’s possible that walking merely to the point of comfort and never pushing beyond it may harm people with PAD.
At the 6-month mark, the researchers found no statistical difference between the discomfort and comfort groups on a cumulative scale of usual walking speed, ability to rise from a chair, and ability to maintain balance in several positions. By 12 months, the two groups had diverged, with the discomfort group improving by almost 1 point on the scale, whereas the performance of the comfort group declined. No significant differences emerged between the discomfort and nonexercising groups, the researchers reported.
The investigators found, counterintuitively, that some people in the study who did not record exercising did as well as those in the discomfort group,
Dr. McDermott noted that the nonexercise group was smaller than the discomfort group, making firm comparisons between the two challenging to draw. In addition, people whose exercise was not recorded were not asked to take it easy whenever they walked, unlike those in the comfort group. As a result, she said, some people in this group may have walked vigorously.
Dr. McDermott emphasized that these benefits occurred at home rather than at medical centers that can be difficult for some people to visit regularly.
“It’s always good to have this kind of information for patients, to show them that it’s possible for them to continue to improve,” said Jonathan Ehrman, PhD, associate director of preventive cardiology at Henry Ford Medical Center, Detroit. Dr. Ehrman was not involved in this study but said that he is contemplating running a similar home-based study that would use video rather than telephone support for patients.
“There’s emerging data about walking speed being related to longevity and predicting better outcomes in cardiac surgeries,” Dr. Ehrman said. “It seems to be, if you can get people walking faster or they have a better walking pace, related to better health outcomes.”
Dr. McDermott reported relationships with Regeneron, Helixmith, Mars, ArtAssist, ReserveAge, and Hershey. Dr. Ehrman reported no relevant financial conflicts of interest.
A version of this article first appeared on Medscape.com.
Avoiding harm in the diagnosis and treatment of food allergies
INDIANAPOLIS – If there’s one truth that David R. Stukus, MD, has come to realize from his 2 years as director of a food allergy treatment center, it’s that
“When they’re given a diagnosis of food allergy, many families do not receive proper education to help them understand the risk as well as self-management and prognosis,” he said at the annual meeting of the Society for Pediatric Dermatology. “They are left to fend for themselves, which leads to increased anxiety. If they don’t understand what it means to manage their child’s food allergy, they’re going to think that they’re a ticking time bomb,” said Dr. Stukus, director of the Food Allergy Treatment Center and professor of pediatrics in the division of allergy and immunology at Nationwide Children’s Hospital in Columbus, Ohio.
During his presentation, he toured clinicians through best practices to diagnose and treat food allergies and shared cautionary tales of unsupported claims, unnecessary testing, and potential harm to misdiagnosed patients.
While food allergies can be serious and life-threatening, they are also manageable, he continued. It doesn’t mean that children with food allergies can’t go to school, attend baseball games, or participate in activities that any other child would. “Telling someone to adopt a restricted diet is not a benign recommendation,” he said. “That can cause real harm.”
Dr. Stukus defined food allergy as an immunologic response to an allergen that results in reproducible symptoms with every exposure. “Most commonly we’re going to see IgE-mediated food allergies, which often occur within minutes of eating certain foods,” he said.
Food intolerance, on the other hand, is a nonimmunologic response to a food that causes gastrointestinal symptoms with exposure. “This can come and go over time,” he said. “The most common example is lactose intolerance.”
Then there’s food sensitivity, which Dr. Stukus said is not a medical term but a marketing term often applied to a variety of symptoms without evidence to support its use.
“On the Internet you will find many companies marketing food sensitivity tests,” he said. “Gluten-free foods are now a billion-dollar industry. There are no validated tests to diagnose food sensitivity. All the blood tests measure IgG, which is memory antibody. If you eat a food, it is a normal response to produce IgG to it, but these companies will test all these things and when it comes back elevated, they say ‘Aha! This is your food sensitivity and this is why you’re not sleeping well at night.’ ” To illustrate the harm that can come from food allergy tests he discussed a 6-year-old girl who presented to his clinic several years ago with typical symptoms of allergic rhinitis. The parent reported a history of sneezing around dogs, itchy, watery eyes in the spring, recurrent cough, and frequent upper respiratory infections.
The referring physician had ordered an allergy panel, which flagged a long list of foods that the girl was supposedly allergic to, including banana, egg white, cod, and peanut. “This family was told to take all of these foods out of her diet,” Dr. Stukus said. “Interestingly, she had been seen by this physician for evaluation of environmental allergies, but the only ones included in the test were cat, cockroach, dog, and dust mite. They didn’t even include the spring pollen allergies. You want to avoid tests like this.”
Food sensitization is not the same as food allergy, he continued, noting that about 30% of all children will have detectable IgE toward peanuts, milk, egg, and shrimp, but that only about 5% are truly allergic to those foods.
“If we go by IgE testing alone, we’re going to overdiagnose the vast majority of people with food allergies that they don’t actually have,” he said. “Food allergy is diagnosed by the history and then confirmed by testing. With IgE-mediated food allergies we know that milk, egg, wheat, soy, finned fish, shellfish, and peanuts account for more than 90% of all food allergy reactions. Can any food potentially cause a food allergy? Yes, potentially, but we know that most fruits and vegetables and grains are very unlikely to cause an allergy.”
IgE-mediated food allergies are objective, immediate onset, and reproducible with every exposure to the offending food, no matter what form. Typical symptoms include hives, swelling, vomiting, runny nose/congestion, wheezing, hypotension, and anaphylaxis.
“We can also accurately identify infants that are more at risk to develop food allergies,” Dr. Stukus said. Infants with refractory atopic dermatitis often progress from eczema to food allergies to allergic rhinitis and asthma, the so-called “allergic march.” “Family history does have a role as well, but it’s not as significant,” he said. As for diagnostic tools, skin prick testing detects the presence of specific IgE bound to cutaneous mast cells and has a high negative predictive value and a low positive predictive value (around 50%).
With serum-specific IgE testing, levels of IgE for food and/or inhalant allergen can be obtained conveniently through routine venipuncture. Results are reported in ranges from 0.1 kU/L to 100 kU/L, and some are reported as arbitrary classes in levels of severity from 1 to 5.
“I highly discourage anybody from paying attention to arbitrary classes [on these reports],” Dr. Stukus said. “Those are meaningless. The absolute value is all that matters.”
He added that both skin and blood testing have high rates of false positive results. “We really need to use the history to help guide what tests we do; they were never designed to be used as screening tests, yet they’re used as screening tests on a regular basis,” he said. “There is also no indication to do shotgun testing. The reason why is because we see lots of cross reactivity on testing. If we have someone with peanut allergy and we start doing specific IgE testing for all legumes, more often than not we’re going to find detectable IgE, but it’s much less likely that they actually have clinical reactivity to foods like soy and beans.”
Dr. Stukus advises clinicians to consider certain questions before they order an allergen panel, the first being: Do I have the knowledge and experience to properly interpret the results?
“If you don’t know how to interpret the test, you probably shouldn’t order it in the first place,” he said. “If you do have the knowledge to interpret the results, will the results help to determine the diagnosis or change management? If not, why are you testing just to test? There is zero clinical indication to order a food allergy panel.” Dr. Stukus recommended a review of unproven tests for adverse reactions to foods published in 2018 in The Journal of Allergy and Clinical Immunology.
According to Dr. Stukus, potential harms from unproven food allergy tests include cost, unnecessary dietary avoidance, and a delay in diagnosis for the underlying condition. During the COVID-19 pandemic, he observed an increase in the number of patients with orthorexia, which he described as an eating disorder characterized by having an unsafe obsession with healthy food that becomes deeply rooted in the individual’s way of thinking to the point that it interferes with daily life.
“If you take someone who has anxiety at baseline, and then you give them a list of foods that they allegedly can’t eat, that’s going to cause worse anxiety,” he added. “We’re seeing that from the results of these tests.”
Dr. Stukus disclosed that he is a consultant for Before Brands, Kaleo, and Novartis. He is also associate editor of the Annals of Allergy, Asthma and Immunology.
INDIANAPOLIS – If there’s one truth that David R. Stukus, MD, has come to realize from his 2 years as director of a food allergy treatment center, it’s that
“When they’re given a diagnosis of food allergy, many families do not receive proper education to help them understand the risk as well as self-management and prognosis,” he said at the annual meeting of the Society for Pediatric Dermatology. “They are left to fend for themselves, which leads to increased anxiety. If they don’t understand what it means to manage their child’s food allergy, they’re going to think that they’re a ticking time bomb,” said Dr. Stukus, director of the Food Allergy Treatment Center and professor of pediatrics in the division of allergy and immunology at Nationwide Children’s Hospital in Columbus, Ohio.
During his presentation, he toured clinicians through best practices to diagnose and treat food allergies and shared cautionary tales of unsupported claims, unnecessary testing, and potential harm to misdiagnosed patients.
While food allergies can be serious and life-threatening, they are also manageable, he continued. It doesn’t mean that children with food allergies can’t go to school, attend baseball games, or participate in activities that any other child would. “Telling someone to adopt a restricted diet is not a benign recommendation,” he said. “That can cause real harm.”
Dr. Stukus defined food allergy as an immunologic response to an allergen that results in reproducible symptoms with every exposure. “Most commonly we’re going to see IgE-mediated food allergies, which often occur within minutes of eating certain foods,” he said.
Food intolerance, on the other hand, is a nonimmunologic response to a food that causes gastrointestinal symptoms with exposure. “This can come and go over time,” he said. “The most common example is lactose intolerance.”
Then there’s food sensitivity, which Dr. Stukus said is not a medical term but a marketing term often applied to a variety of symptoms without evidence to support its use.
“On the Internet you will find many companies marketing food sensitivity tests,” he said. “Gluten-free foods are now a billion-dollar industry. There are no validated tests to diagnose food sensitivity. All the blood tests measure IgG, which is memory antibody. If you eat a food, it is a normal response to produce IgG to it, but these companies will test all these things and when it comes back elevated, they say ‘Aha! This is your food sensitivity and this is why you’re not sleeping well at night.’ ” To illustrate the harm that can come from food allergy tests he discussed a 6-year-old girl who presented to his clinic several years ago with typical symptoms of allergic rhinitis. The parent reported a history of sneezing around dogs, itchy, watery eyes in the spring, recurrent cough, and frequent upper respiratory infections.
The referring physician had ordered an allergy panel, which flagged a long list of foods that the girl was supposedly allergic to, including banana, egg white, cod, and peanut. “This family was told to take all of these foods out of her diet,” Dr. Stukus said. “Interestingly, she had been seen by this physician for evaluation of environmental allergies, but the only ones included in the test were cat, cockroach, dog, and dust mite. They didn’t even include the spring pollen allergies. You want to avoid tests like this.”
Food sensitization is not the same as food allergy, he continued, noting that about 30% of all children will have detectable IgE toward peanuts, milk, egg, and shrimp, but that only about 5% are truly allergic to those foods.
“If we go by IgE testing alone, we’re going to overdiagnose the vast majority of people with food allergies that they don’t actually have,” he said. “Food allergy is diagnosed by the history and then confirmed by testing. With IgE-mediated food allergies we know that milk, egg, wheat, soy, finned fish, shellfish, and peanuts account for more than 90% of all food allergy reactions. Can any food potentially cause a food allergy? Yes, potentially, but we know that most fruits and vegetables and grains are very unlikely to cause an allergy.”
IgE-mediated food allergies are objective, immediate onset, and reproducible with every exposure to the offending food, no matter what form. Typical symptoms include hives, swelling, vomiting, runny nose/congestion, wheezing, hypotension, and anaphylaxis.
“We can also accurately identify infants that are more at risk to develop food allergies,” Dr. Stukus said. Infants with refractory atopic dermatitis often progress from eczema to food allergies to allergic rhinitis and asthma, the so-called “allergic march.” “Family history does have a role as well, but it’s not as significant,” he said. As for diagnostic tools, skin prick testing detects the presence of specific IgE bound to cutaneous mast cells and has a high negative predictive value and a low positive predictive value (around 50%).
With serum-specific IgE testing, levels of IgE for food and/or inhalant allergen can be obtained conveniently through routine venipuncture. Results are reported in ranges from 0.1 kU/L to 100 kU/L, and some are reported as arbitrary classes in levels of severity from 1 to 5.
“I highly discourage anybody from paying attention to arbitrary classes [on these reports],” Dr. Stukus said. “Those are meaningless. The absolute value is all that matters.”
He added that both skin and blood testing have high rates of false positive results. “We really need to use the history to help guide what tests we do; they were never designed to be used as screening tests, yet they’re used as screening tests on a regular basis,” he said. “There is also no indication to do shotgun testing. The reason why is because we see lots of cross reactivity on testing. If we have someone with peanut allergy and we start doing specific IgE testing for all legumes, more often than not we’re going to find detectable IgE, but it’s much less likely that they actually have clinical reactivity to foods like soy and beans.”
Dr. Stukus advises clinicians to consider certain questions before they order an allergen panel, the first being: Do I have the knowledge and experience to properly interpret the results?
“If you don’t know how to interpret the test, you probably shouldn’t order it in the first place,” he said. “If you do have the knowledge to interpret the results, will the results help to determine the diagnosis or change management? If not, why are you testing just to test? There is zero clinical indication to order a food allergy panel.” Dr. Stukus recommended a review of unproven tests for adverse reactions to foods published in 2018 in The Journal of Allergy and Clinical Immunology.
According to Dr. Stukus, potential harms from unproven food allergy tests include cost, unnecessary dietary avoidance, and a delay in diagnosis for the underlying condition. During the COVID-19 pandemic, he observed an increase in the number of patients with orthorexia, which he described as an eating disorder characterized by having an unsafe obsession with healthy food that becomes deeply rooted in the individual’s way of thinking to the point that it interferes with daily life.
“If you take someone who has anxiety at baseline, and then you give them a list of foods that they allegedly can’t eat, that’s going to cause worse anxiety,” he added. “We’re seeing that from the results of these tests.”
Dr. Stukus disclosed that he is a consultant for Before Brands, Kaleo, and Novartis. He is also associate editor of the Annals of Allergy, Asthma and Immunology.
INDIANAPOLIS – If there’s one truth that David R. Stukus, MD, has come to realize from his 2 years as director of a food allergy treatment center, it’s that
“When they’re given a diagnosis of food allergy, many families do not receive proper education to help them understand the risk as well as self-management and prognosis,” he said at the annual meeting of the Society for Pediatric Dermatology. “They are left to fend for themselves, which leads to increased anxiety. If they don’t understand what it means to manage their child’s food allergy, they’re going to think that they’re a ticking time bomb,” said Dr. Stukus, director of the Food Allergy Treatment Center and professor of pediatrics in the division of allergy and immunology at Nationwide Children’s Hospital in Columbus, Ohio.
During his presentation, he toured clinicians through best practices to diagnose and treat food allergies and shared cautionary tales of unsupported claims, unnecessary testing, and potential harm to misdiagnosed patients.
While food allergies can be serious and life-threatening, they are also manageable, he continued. It doesn’t mean that children with food allergies can’t go to school, attend baseball games, or participate in activities that any other child would. “Telling someone to adopt a restricted diet is not a benign recommendation,” he said. “That can cause real harm.”
Dr. Stukus defined food allergy as an immunologic response to an allergen that results in reproducible symptoms with every exposure. “Most commonly we’re going to see IgE-mediated food allergies, which often occur within minutes of eating certain foods,” he said.
Food intolerance, on the other hand, is a nonimmunologic response to a food that causes gastrointestinal symptoms with exposure. “This can come and go over time,” he said. “The most common example is lactose intolerance.”
Then there’s food sensitivity, which Dr. Stukus said is not a medical term but a marketing term often applied to a variety of symptoms without evidence to support its use.
“On the Internet you will find many companies marketing food sensitivity tests,” he said. “Gluten-free foods are now a billion-dollar industry. There are no validated tests to diagnose food sensitivity. All the blood tests measure IgG, which is memory antibody. If you eat a food, it is a normal response to produce IgG to it, but these companies will test all these things and when it comes back elevated, they say ‘Aha! This is your food sensitivity and this is why you’re not sleeping well at night.’ ” To illustrate the harm that can come from food allergy tests he discussed a 6-year-old girl who presented to his clinic several years ago with typical symptoms of allergic rhinitis. The parent reported a history of sneezing around dogs, itchy, watery eyes in the spring, recurrent cough, and frequent upper respiratory infections.
The referring physician had ordered an allergy panel, which flagged a long list of foods that the girl was supposedly allergic to, including banana, egg white, cod, and peanut. “This family was told to take all of these foods out of her diet,” Dr. Stukus said. “Interestingly, she had been seen by this physician for evaluation of environmental allergies, but the only ones included in the test were cat, cockroach, dog, and dust mite. They didn’t even include the spring pollen allergies. You want to avoid tests like this.”
Food sensitization is not the same as food allergy, he continued, noting that about 30% of all children will have detectable IgE toward peanuts, milk, egg, and shrimp, but that only about 5% are truly allergic to those foods.
“If we go by IgE testing alone, we’re going to overdiagnose the vast majority of people with food allergies that they don’t actually have,” he said. “Food allergy is diagnosed by the history and then confirmed by testing. With IgE-mediated food allergies we know that milk, egg, wheat, soy, finned fish, shellfish, and peanuts account for more than 90% of all food allergy reactions. Can any food potentially cause a food allergy? Yes, potentially, but we know that most fruits and vegetables and grains are very unlikely to cause an allergy.”
IgE-mediated food allergies are objective, immediate onset, and reproducible with every exposure to the offending food, no matter what form. Typical symptoms include hives, swelling, vomiting, runny nose/congestion, wheezing, hypotension, and anaphylaxis.
“We can also accurately identify infants that are more at risk to develop food allergies,” Dr. Stukus said. Infants with refractory atopic dermatitis often progress from eczema to food allergies to allergic rhinitis and asthma, the so-called “allergic march.” “Family history does have a role as well, but it’s not as significant,” he said. As for diagnostic tools, skin prick testing detects the presence of specific IgE bound to cutaneous mast cells and has a high negative predictive value and a low positive predictive value (around 50%).
With serum-specific IgE testing, levels of IgE for food and/or inhalant allergen can be obtained conveniently through routine venipuncture. Results are reported in ranges from 0.1 kU/L to 100 kU/L, and some are reported as arbitrary classes in levels of severity from 1 to 5.
“I highly discourage anybody from paying attention to arbitrary classes [on these reports],” Dr. Stukus said. “Those are meaningless. The absolute value is all that matters.”
He added that both skin and blood testing have high rates of false positive results. “We really need to use the history to help guide what tests we do; they were never designed to be used as screening tests, yet they’re used as screening tests on a regular basis,” he said. “There is also no indication to do shotgun testing. The reason why is because we see lots of cross reactivity on testing. If we have someone with peanut allergy and we start doing specific IgE testing for all legumes, more often than not we’re going to find detectable IgE, but it’s much less likely that they actually have clinical reactivity to foods like soy and beans.”
Dr. Stukus advises clinicians to consider certain questions before they order an allergen panel, the first being: Do I have the knowledge and experience to properly interpret the results?
“If you don’t know how to interpret the test, you probably shouldn’t order it in the first place,” he said. “If you do have the knowledge to interpret the results, will the results help to determine the diagnosis or change management? If not, why are you testing just to test? There is zero clinical indication to order a food allergy panel.” Dr. Stukus recommended a review of unproven tests for adverse reactions to foods published in 2018 in The Journal of Allergy and Clinical Immunology.
According to Dr. Stukus, potential harms from unproven food allergy tests include cost, unnecessary dietary avoidance, and a delay in diagnosis for the underlying condition. During the COVID-19 pandemic, he observed an increase in the number of patients with orthorexia, which he described as an eating disorder characterized by having an unsafe obsession with healthy food that becomes deeply rooted in the individual’s way of thinking to the point that it interferes with daily life.
“If you take someone who has anxiety at baseline, and then you give them a list of foods that they allegedly can’t eat, that’s going to cause worse anxiety,” he added. “We’re seeing that from the results of these tests.”
Dr. Stukus disclosed that he is a consultant for Before Brands, Kaleo, and Novartis. He is also associate editor of the Annals of Allergy, Asthma and Immunology.
AT SPD 2022
‘Striking’ disparities in CVD deaths persist across COVID waves
Cardiovascular disease (CVD) mortality rose significantly during the COVID-19 pandemic and persists more than 2 years on and, once again, Blacks and African Americans have been disproportionately affected, an analysis of death certificates shows.
The findings “suggest that the pandemic may reverse years or decades of work aimed at reducing gaps in cardiovascular outcomes,” Sadeer G. Al-Kindi, MD, Case Western Reserve University, Cleveland, said in an interview.
Although the disparities are in line with previous research, he said, “what was surprising is the persistence of excess cardiovascular mortality approximately 2 years after the pandemic started, even during a period of low COVID-19 mortality.”
“This suggests that the pandemic resulted in a disruption of health care access and, along with disparities in COVID-19 infection and its complications, he said, “may have a long-lasting effect on health care disparities, especially among vulnerable populations.”
The study was published online in Mayo Clinic Proceedings with lead author Scott E. Janus, MD, also of Case Western Reserve University.
Impact consistently greater for Blacks
Dr. Al-Kindi and colleagues used 3,598,352 U.S. death files to investigate trends in deaths caused specifically by CVD as well as its subtypes myocardial infarction, stroke, and heart failure (HF) in 2018 and 2019 (prepandemic) and the pandemic years 2020 and 2021. Baseline demographics showed a higher percentage of older, female, and Black individuals among the CVD subtypes of interest.
Overall, there was an excess CVD mortality of 6.7% during the pandemic, compared with prepandemic years, including a 2.5% rise in MI deaths and an 8.5% rise in stroke deaths. HF mortality remained relatively steady, rising only 0.1%.
Subgroup analyses revealed “striking differences” in excess mortality between Blacks and Whites, the authors noted. Blacks had an overall excess mortality of 13.8% versus 5.1% for Whites, compared with the prepandemic years. The differences were consistent across subtypes: MI (9.6% vs. 1.0%); stroke (14.5% vs. 6.9%); and HF (5.1% vs. –1.2%; P value for all < .001).
When the investigators looked at deaths on a yearly basis with 2018 as the baseline, they found CVD deaths increased by 1.5% in 2019, 15.8% in 2020, and 13.5% in 2021 among Black Americans, compared with 0.5%, 5.1%, and 5.7%, respectively, among White Americans.
Excess deaths from MI rose by 9.5% in 2020 and by 6.7% in 2021 among Blacks but fell by 1.2% in 2020 and by 1.0% in 2021 among Whites.
Disparities in excess HF mortality were similar, rising 9.1% and 4.1% in 2020 and 2021 among Blacks, while dipping 0.1% and 0.8% in 2020 and 2021 among Whites.
The “most striking difference” was in excess stroke mortality, which doubled among Blacks compared with whites in 2020 (14.9% vs. 6.7%) and in 2021 (17.5% vs. 8.1%), according to the authors.
Awareness urged
Although the disparities were expected, “there is clear value in documenting and quantifying the magnitude of these disparities,” Amil M. Shah, MD, MPH, of Harvard Medical School and Brigham and Women’s Hospital, both in Boston, said in an interview.
In addition to being observational, the main limitation of the study, he noted, is the quality and resolution of the death certificate data, which may limit the accuracy of the cause of death ascertainment and classification of race or ethnicity. “However, I think these potential inaccuracies are unlikely to materially impact the overall study findings.”
Dr. Shah, who was not involved in the study, said he would like to see additional research into the diversity and heterogeneity in risk among Black communities. “Understanding the environmental, social, and health care factors – both harmful and protective – that influence risk for CVD morbidity and mortality among Black individuals and communities offers the promise to provide actionable insights to mitigate these disparities.”
“Intervention studies testing approaches to mitigate disparities based on race/ethnicity” are also needed, he added. These may be at the policy, community, health system, or individual level, and community involvement in phases will be essential.”
Meanwhile, both Dr. Al-Kindi and Dr. Shah urged clinicians to be aware of the disparities and the need to improve access to care and address social determinants of health in vulnerable populations.
These disparities “are driven by structural factors, and are reinforced by individual behaviors. In this context, implicit bias training is important to help clinicians recognize and mitigate bias in their own practice,” Dr. Shah said. “Supporting diversity, equity, and inclusion efforts, and advocating for anti-racist policies and practices in their health systems” can also help.
Dr. Al-Kindi and Dr. Shah disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Cardiovascular disease (CVD) mortality rose significantly during the COVID-19 pandemic and persists more than 2 years on and, once again, Blacks and African Americans have been disproportionately affected, an analysis of death certificates shows.
The findings “suggest that the pandemic may reverse years or decades of work aimed at reducing gaps in cardiovascular outcomes,” Sadeer G. Al-Kindi, MD, Case Western Reserve University, Cleveland, said in an interview.
Although the disparities are in line with previous research, he said, “what was surprising is the persistence of excess cardiovascular mortality approximately 2 years after the pandemic started, even during a period of low COVID-19 mortality.”
“This suggests that the pandemic resulted in a disruption of health care access and, along with disparities in COVID-19 infection and its complications, he said, “may have a long-lasting effect on health care disparities, especially among vulnerable populations.”
The study was published online in Mayo Clinic Proceedings with lead author Scott E. Janus, MD, also of Case Western Reserve University.
Impact consistently greater for Blacks
Dr. Al-Kindi and colleagues used 3,598,352 U.S. death files to investigate trends in deaths caused specifically by CVD as well as its subtypes myocardial infarction, stroke, and heart failure (HF) in 2018 and 2019 (prepandemic) and the pandemic years 2020 and 2021. Baseline demographics showed a higher percentage of older, female, and Black individuals among the CVD subtypes of interest.
Overall, there was an excess CVD mortality of 6.7% during the pandemic, compared with prepandemic years, including a 2.5% rise in MI deaths and an 8.5% rise in stroke deaths. HF mortality remained relatively steady, rising only 0.1%.
Subgroup analyses revealed “striking differences” in excess mortality between Blacks and Whites, the authors noted. Blacks had an overall excess mortality of 13.8% versus 5.1% for Whites, compared with the prepandemic years. The differences were consistent across subtypes: MI (9.6% vs. 1.0%); stroke (14.5% vs. 6.9%); and HF (5.1% vs. –1.2%; P value for all < .001).
When the investigators looked at deaths on a yearly basis with 2018 as the baseline, they found CVD deaths increased by 1.5% in 2019, 15.8% in 2020, and 13.5% in 2021 among Black Americans, compared with 0.5%, 5.1%, and 5.7%, respectively, among White Americans.
Excess deaths from MI rose by 9.5% in 2020 and by 6.7% in 2021 among Blacks but fell by 1.2% in 2020 and by 1.0% in 2021 among Whites.
Disparities in excess HF mortality were similar, rising 9.1% and 4.1% in 2020 and 2021 among Blacks, while dipping 0.1% and 0.8% in 2020 and 2021 among Whites.
The “most striking difference” was in excess stroke mortality, which doubled among Blacks compared with whites in 2020 (14.9% vs. 6.7%) and in 2021 (17.5% vs. 8.1%), according to the authors.
Awareness urged
Although the disparities were expected, “there is clear value in documenting and quantifying the magnitude of these disparities,” Amil M. Shah, MD, MPH, of Harvard Medical School and Brigham and Women’s Hospital, both in Boston, said in an interview.
In addition to being observational, the main limitation of the study, he noted, is the quality and resolution of the death certificate data, which may limit the accuracy of the cause of death ascertainment and classification of race or ethnicity. “However, I think these potential inaccuracies are unlikely to materially impact the overall study findings.”
Dr. Shah, who was not involved in the study, said he would like to see additional research into the diversity and heterogeneity in risk among Black communities. “Understanding the environmental, social, and health care factors – both harmful and protective – that influence risk for CVD morbidity and mortality among Black individuals and communities offers the promise to provide actionable insights to mitigate these disparities.”
“Intervention studies testing approaches to mitigate disparities based on race/ethnicity” are also needed, he added. These may be at the policy, community, health system, or individual level, and community involvement in phases will be essential.”
Meanwhile, both Dr. Al-Kindi and Dr. Shah urged clinicians to be aware of the disparities and the need to improve access to care and address social determinants of health in vulnerable populations.
These disparities “are driven by structural factors, and are reinforced by individual behaviors. In this context, implicit bias training is important to help clinicians recognize and mitigate bias in their own practice,” Dr. Shah said. “Supporting diversity, equity, and inclusion efforts, and advocating for anti-racist policies and practices in their health systems” can also help.
Dr. Al-Kindi and Dr. Shah disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Cardiovascular disease (CVD) mortality rose significantly during the COVID-19 pandemic and persists more than 2 years on and, once again, Blacks and African Americans have been disproportionately affected, an analysis of death certificates shows.
The findings “suggest that the pandemic may reverse years or decades of work aimed at reducing gaps in cardiovascular outcomes,” Sadeer G. Al-Kindi, MD, Case Western Reserve University, Cleveland, said in an interview.
Although the disparities are in line with previous research, he said, “what was surprising is the persistence of excess cardiovascular mortality approximately 2 years after the pandemic started, even during a period of low COVID-19 mortality.”
“This suggests that the pandemic resulted in a disruption of health care access and, along with disparities in COVID-19 infection and its complications, he said, “may have a long-lasting effect on health care disparities, especially among vulnerable populations.”
The study was published online in Mayo Clinic Proceedings with lead author Scott E. Janus, MD, also of Case Western Reserve University.
Impact consistently greater for Blacks
Dr. Al-Kindi and colleagues used 3,598,352 U.S. death files to investigate trends in deaths caused specifically by CVD as well as its subtypes myocardial infarction, stroke, and heart failure (HF) in 2018 and 2019 (prepandemic) and the pandemic years 2020 and 2021. Baseline demographics showed a higher percentage of older, female, and Black individuals among the CVD subtypes of interest.
Overall, there was an excess CVD mortality of 6.7% during the pandemic, compared with prepandemic years, including a 2.5% rise in MI deaths and an 8.5% rise in stroke deaths. HF mortality remained relatively steady, rising only 0.1%.
Subgroup analyses revealed “striking differences” in excess mortality between Blacks and Whites, the authors noted. Blacks had an overall excess mortality of 13.8% versus 5.1% for Whites, compared with the prepandemic years. The differences were consistent across subtypes: MI (9.6% vs. 1.0%); stroke (14.5% vs. 6.9%); and HF (5.1% vs. –1.2%; P value for all < .001).
When the investigators looked at deaths on a yearly basis with 2018 as the baseline, they found CVD deaths increased by 1.5% in 2019, 15.8% in 2020, and 13.5% in 2021 among Black Americans, compared with 0.5%, 5.1%, and 5.7%, respectively, among White Americans.
Excess deaths from MI rose by 9.5% in 2020 and by 6.7% in 2021 among Blacks but fell by 1.2% in 2020 and by 1.0% in 2021 among Whites.
Disparities in excess HF mortality were similar, rising 9.1% and 4.1% in 2020 and 2021 among Blacks, while dipping 0.1% and 0.8% in 2020 and 2021 among Whites.
The “most striking difference” was in excess stroke mortality, which doubled among Blacks compared with whites in 2020 (14.9% vs. 6.7%) and in 2021 (17.5% vs. 8.1%), according to the authors.
Awareness urged
Although the disparities were expected, “there is clear value in documenting and quantifying the magnitude of these disparities,” Amil M. Shah, MD, MPH, of Harvard Medical School and Brigham and Women’s Hospital, both in Boston, said in an interview.
In addition to being observational, the main limitation of the study, he noted, is the quality and resolution of the death certificate data, which may limit the accuracy of the cause of death ascertainment and classification of race or ethnicity. “However, I think these potential inaccuracies are unlikely to materially impact the overall study findings.”
Dr. Shah, who was not involved in the study, said he would like to see additional research into the diversity and heterogeneity in risk among Black communities. “Understanding the environmental, social, and health care factors – both harmful and protective – that influence risk for CVD morbidity and mortality among Black individuals and communities offers the promise to provide actionable insights to mitigate these disparities.”
“Intervention studies testing approaches to mitigate disparities based on race/ethnicity” are also needed, he added. These may be at the policy, community, health system, or individual level, and community involvement in phases will be essential.”
Meanwhile, both Dr. Al-Kindi and Dr. Shah urged clinicians to be aware of the disparities and the need to improve access to care and address social determinants of health in vulnerable populations.
These disparities “are driven by structural factors, and are reinforced by individual behaviors. In this context, implicit bias training is important to help clinicians recognize and mitigate bias in their own practice,” Dr. Shah said. “Supporting diversity, equity, and inclusion efforts, and advocating for anti-racist policies and practices in their health systems” can also help.
Dr. Al-Kindi and Dr. Shah disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM MAYO CLINIC PROCEEDINGS
What's your diagnosis?
Pancreatic adenocarcinoma arising from main duct intraductal papillary mucinous neoplasm with inadvertent main pancreatic duct stenting.
The FNA was positive for carcinoma with abundant mucin, which, taken together with the imaging findings, was indicative of pancreatic adenocarcinoma arising from main duct intraductal papillary mucinous neoplasm (M-IPMN).
The post-endoscopic retrograde cholangiopancreatography (ERCP) CT revealed inadvertent placement of the fully covered self-expanding metallic stent (fcSEMS) within the main pancreatic duct (MPD) stricture and persistent common bile duct (CBD) obstruction. On post hoc review of the fluoroscopic and cross-sectional imaging, it became evident that the massively dilated MPD was mistaken during ERCP for the CBD and left hepatic duct (Figure F). In addition, the patient also had several cysts within the liver (compatible with incidental polycystic liver disease), which further complicated real-time image interpretation.
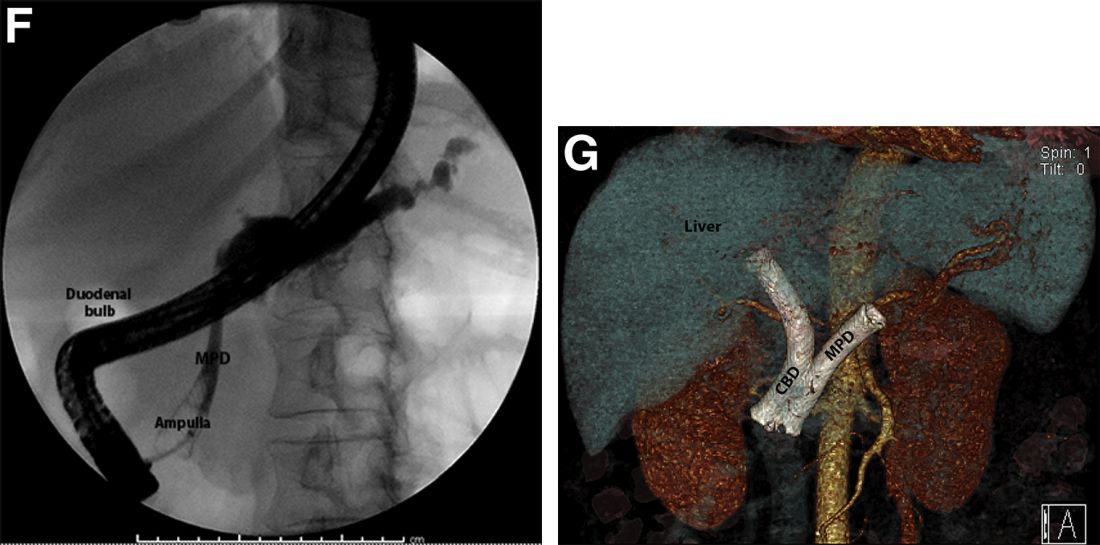
Based on multidisciplinary discussion, the precedent of a prior series of successful palliative MPD stenting in the setting of adenocarcinoma,1 and the notable improvement in the patient's steatorrhea and abdominal pain, the initially placed fcSEMS was left in situ across the MPD stricture, and a second fcSEMS was successfully deployed across the CBD stricture (Figure G), resulting in prompt improvement in serum liver tests. The patient was thereafter initiated on palliative chemotherapy with gemcitabine and abraxane and has maintained clinically stable disease for the last 9 months.
M-IPMN is a premalignant condition in which endoscopy plays an important role. In our patient, because of anatomic and morphologic abnormalities, including the massive dilation of the MPD and severe distal biliary compression in the context of an obstructing pancreatic head mass arising from M-IPMN, initial deployment of the fcSEMS occurred unwittingly into the MPD. Little is known about the impact of fcSEMS in the MPD in patients with pancreatic adenocarcinoma, although in select cases, alleviation of pain caused by MPD obstruction and improvement in quality of life have been reported.2,3 In the case of our patient, fcSEMS placement in the MPD indeed led to symptomatic relief as manifested by a decrease in both diarrhea and pain and an increase in appetite; the addition of a fcSEMS in the CBD led to serum liver test normalization and permitted the initiation of chemotherapy. Further studies are needed to examine the outcomes of palliative MPD stenting in patients with obstructing pancreatic malignancies as well as the epidemiology and biology of M-IPMN and associated pancreatic adenocarcinoma in minority populations.
References
1. Tham TC et al. Am J Gastroenterol. 2000 Apr;95(4):956-60.
2. Grimm IS, Baron TH. Gastroenterology. 2015 Jul;149(1):20-2.
3. Wehrmann T et al. Eur J Gastroenterol Hepatol. 2005 Dec;17(12):1395-400.
Pancreatic adenocarcinoma arising from main duct intraductal papillary mucinous neoplasm with inadvertent main pancreatic duct stenting.
The FNA was positive for carcinoma with abundant mucin, which, taken together with the imaging findings, was indicative of pancreatic adenocarcinoma arising from main duct intraductal papillary mucinous neoplasm (M-IPMN).
The post-endoscopic retrograde cholangiopancreatography (ERCP) CT revealed inadvertent placement of the fully covered self-expanding metallic stent (fcSEMS) within the main pancreatic duct (MPD) stricture and persistent common bile duct (CBD) obstruction. On post hoc review of the fluoroscopic and cross-sectional imaging, it became evident that the massively dilated MPD was mistaken during ERCP for the CBD and left hepatic duct (Figure F). In addition, the patient also had several cysts within the liver (compatible with incidental polycystic liver disease), which further complicated real-time image interpretation.
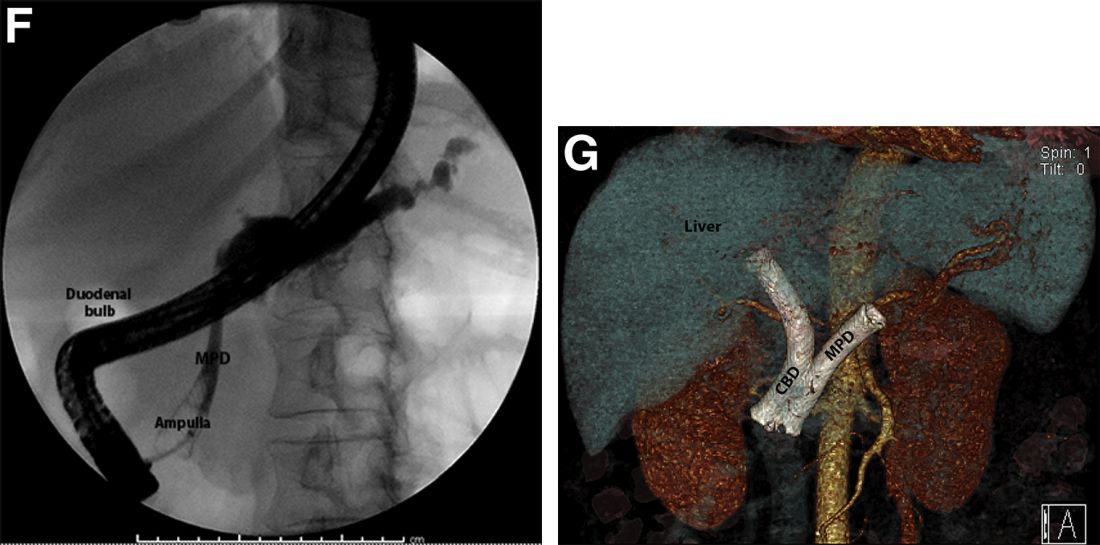
Based on multidisciplinary discussion, the precedent of a prior series of successful palliative MPD stenting in the setting of adenocarcinoma,1 and the notable improvement in the patient's steatorrhea and abdominal pain, the initially placed fcSEMS was left in situ across the MPD stricture, and a second fcSEMS was successfully deployed across the CBD stricture (Figure G), resulting in prompt improvement in serum liver tests. The patient was thereafter initiated on palliative chemotherapy with gemcitabine and abraxane and has maintained clinically stable disease for the last 9 months.
M-IPMN is a premalignant condition in which endoscopy plays an important role. In our patient, because of anatomic and morphologic abnormalities, including the massive dilation of the MPD and severe distal biliary compression in the context of an obstructing pancreatic head mass arising from M-IPMN, initial deployment of the fcSEMS occurred unwittingly into the MPD. Little is known about the impact of fcSEMS in the MPD in patients with pancreatic adenocarcinoma, although in select cases, alleviation of pain caused by MPD obstruction and improvement in quality of life have been reported.2,3 In the case of our patient, fcSEMS placement in the MPD indeed led to symptomatic relief as manifested by a decrease in both diarrhea and pain and an increase in appetite; the addition of a fcSEMS in the CBD led to serum liver test normalization and permitted the initiation of chemotherapy. Further studies are needed to examine the outcomes of palliative MPD stenting in patients with obstructing pancreatic malignancies as well as the epidemiology and biology of M-IPMN and associated pancreatic adenocarcinoma in minority populations.
References
1. Tham TC et al. Am J Gastroenterol. 2000 Apr;95(4):956-60.
2. Grimm IS, Baron TH. Gastroenterology. 2015 Jul;149(1):20-2.
3. Wehrmann T et al. Eur J Gastroenterol Hepatol. 2005 Dec;17(12):1395-400.
Pancreatic adenocarcinoma arising from main duct intraductal papillary mucinous neoplasm with inadvertent main pancreatic duct stenting.
The FNA was positive for carcinoma with abundant mucin, which, taken together with the imaging findings, was indicative of pancreatic adenocarcinoma arising from main duct intraductal papillary mucinous neoplasm (M-IPMN).
The post-endoscopic retrograde cholangiopancreatography (ERCP) CT revealed inadvertent placement of the fully covered self-expanding metallic stent (fcSEMS) within the main pancreatic duct (MPD) stricture and persistent common bile duct (CBD) obstruction. On post hoc review of the fluoroscopic and cross-sectional imaging, it became evident that the massively dilated MPD was mistaken during ERCP for the CBD and left hepatic duct (Figure F). In addition, the patient also had several cysts within the liver (compatible with incidental polycystic liver disease), which further complicated real-time image interpretation.
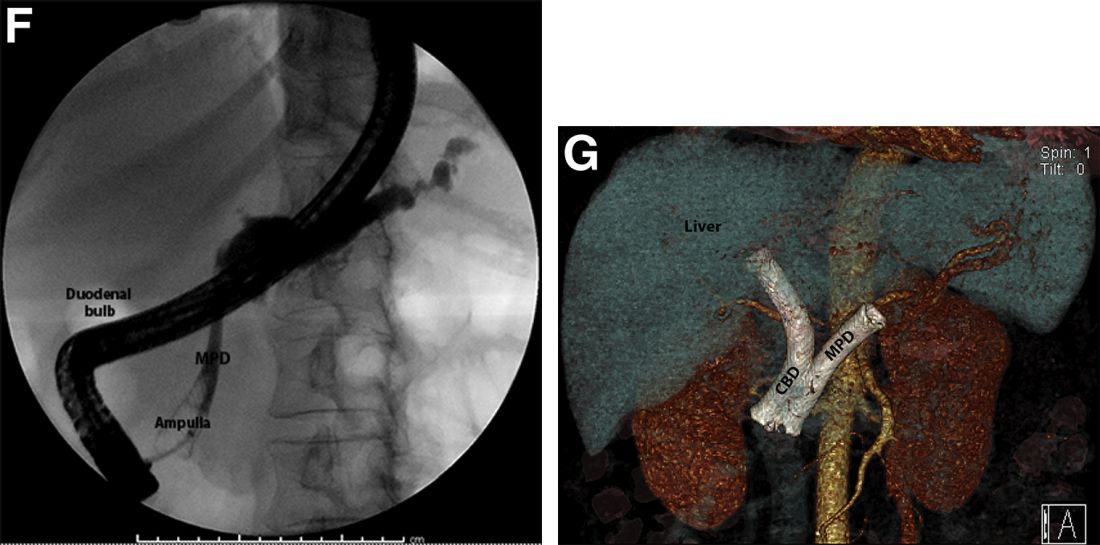
Based on multidisciplinary discussion, the precedent of a prior series of successful palliative MPD stenting in the setting of adenocarcinoma,1 and the notable improvement in the patient's steatorrhea and abdominal pain, the initially placed fcSEMS was left in situ across the MPD stricture, and a second fcSEMS was successfully deployed across the CBD stricture (Figure G), resulting in prompt improvement in serum liver tests. The patient was thereafter initiated on palliative chemotherapy with gemcitabine and abraxane and has maintained clinically stable disease for the last 9 months.
M-IPMN is a premalignant condition in which endoscopy plays an important role. In our patient, because of anatomic and morphologic abnormalities, including the massive dilation of the MPD and severe distal biliary compression in the context of an obstructing pancreatic head mass arising from M-IPMN, initial deployment of the fcSEMS occurred unwittingly into the MPD. Little is known about the impact of fcSEMS in the MPD in patients with pancreatic adenocarcinoma, although in select cases, alleviation of pain caused by MPD obstruction and improvement in quality of life have been reported.2,3 In the case of our patient, fcSEMS placement in the MPD indeed led to symptomatic relief as manifested by a decrease in both diarrhea and pain and an increase in appetite; the addition of a fcSEMS in the CBD led to serum liver test normalization and permitted the initiation of chemotherapy. Further studies are needed to examine the outcomes of palliative MPD stenting in patients with obstructing pancreatic malignancies as well as the epidemiology and biology of M-IPMN and associated pancreatic adenocarcinoma in minority populations.
References
1. Tham TC et al. Am J Gastroenterol. 2000 Apr;95(4):956-60.
2. Grimm IS, Baron TH. Gastroenterology. 2015 Jul;149(1):20-2.
3. Wehrmann T et al. Eur J Gastroenterol Hepatol. 2005 Dec;17(12):1395-400.
A 69-year-old Filipino American woman presented with increasing epigastralgia, worsening appetite, jaundice, and oily diarrhea over the course of 3 months. Her past medical history consisted of diabetes, hypertension, hyperlipidemia, and osteopenia being managed with metformin, losartan, and atorvastatin, respectively.
Physical examination revealed she was thin (body mass index, 22 kg/m2) and jaundiced with moderate tenderness to epigastric palpation and 1+ peripheral pitting edema. Laboratory tests were significant for normal complete blood count and elevated alanine aminotransferase (113 U/L), alkaline phosphatase (235 U/L), bilirubin (7.3 mg/dL), international normalized ratio (1.3), and carbohydrate antigen 19-9 (7886 U/L). A CT scan of the abdomen revealed severe extrahepatic and intrahepatic ductal dilation, with a common bile duct (CBD) and main pancreatic duct (MPD) diameter of 2.5 and 1.7 cm, respectively, as well an infiltrating, malignant-appearing, 4.5-cm spheroid mass in the head of the pancreas (Figure A). The mass involved the superior mesenteric vein at the portal confluence and encased >50% of the superior mesenteric artery.

To further characterize these findings, magnetic resonance cholangiopancreatography was performed, which additionally revealed multifocal cysts throughout the liver ranging from 0.5 to 5.0 cm in greatest diameter, as seen on maximal intensity projection algorithm (Figure B).
The patient was referred for same-session endoscopic ultrasound examination with fine needle aspiration (FNA) and endoscopic retrograde cholangiopancreatography (ERCP) for further diagnosis and treatment. Endoscopic ultrasound demonstrated a large, hypoechoic mass in the pancreatic head with severe CBD and MPD dilation proximally, corresponding with the cross-sectional imaging findings; FNA was performed. ERCP demonstrated a long, distal CBD stricture and what appeared to be nonopacification of the right hepatic ductal system; a 10 × 60-mm fully covered self-expanding metallic stent (fcSEMS) was placed across the stricture (Figure C, D). Over the subsequent 3 days, the patient's diarrhea resolved and epigastralgia improved; however, serum liver tests did not downtrend, thus prompting repeat imaging (Figure E).
Based on the patient's clinical history, cross-sectional imaging findings, and only partial response to therapeutic ERCP, what are the patient's likely diagnoses?
Commentary: Looking at Therapies for Patients With HER2-low Breast Cancer, August 2022
DESTINY-Breast04 is the first randomized clinical trial to show that targeting HER2 provides clinically meaningful benefit for patients with HER2-low metastatic breast cancer. This phase 3 study by Modi and colleagues enrolled 557 patients with hormone receptor (HR)–negative or HR-positive breast cancer and centrally confirmed HER2 low expression in those who had been previously treated with one or two prior lines of chemotherapy for metastatic breast cancer. Patients with HR-positive breast cancer were required to have endocrine therapy–refractory disease. Patients were randomized in a 2:1 ratio to receive either an antibody-drug conjugate, trastuzumab deruxtecan (T-DXd), or the physician's choice of standard chemotherapy (capecitabine, eribulin, gemcitabine, paclitaxel, or nanoparticle albumin–bound paclitaxel [nab-paclitaxel]). Among all 557 patients, T-DXd improved median progression-free survival (PFS) by 4.8 months (9.9 vs 5.1 months; hazard ratio [HR] 0.50; P < .001) and median overall survival (OS) by 6.6 months (23.4 vs 16.8 months; HR 0.64; P = .0010) compared with standard single-agent chemotherapy. Among the 494 (88.7%) HR-positive patients, the median PFS was 10.1 months in the T-DXd group and 5.4 months in the chemotherapy group (HR 0.51; P < .001). Median OS was 23.9 months and 17.5 months, respectively (HR 0.64; P = .003). The rates of grade 3 or higher adverse events were lower with T-DXd than with standard chemotherapy (52.6% vs 67.4%, respectively), although higher rates of drug-related interstitial lung disease or pneumonitis were noted in the T-DXd arm (12.1% vs 0.1%). Lung toxicity continues to be an important safety concern with T-DXd. These practice-changing results open the door to a new treatment option for a substantial group of patients with HER2-low disease and support the need to reclassify HER2-low as a new targetable subset of breast cancer, distinct from HER-negative (HER2-0), and to acquire an understanding of the clinical characteristics of and prognosis for these patients.
Tarantino and colleagues evaluated the biologic and prognostic significance of HER2-low expression in breast cancer and investigated the association between HR status and HER2-low expression. Among 5235 patients with HER2-0 invasive breast cancer, HR expression was significantly more common among HER2-low tumors than among HER2-0 tumors (90.6% vs 81.8%; P < .001). The rate of HER2-low tumors increased progressively as estrogen receptor (ER) expression increased (40.1% of ER-negative, 46.3% of ER-low, 55.2% of ER-moderate, 57.8% of ER-high, and 62.1% of ER-very high [ie, ER > 95%] tumors; P < .001). Among 675 patients receiving neoadjuvant chemotherapy, higher pathologic complete response (pCR) rates were seen among those with HER2-0 tumors (26.8% vs 16.6%; P = .002), although no statistically significant differences in pCR rates were noted between HER2-low and HER2-0 tumors when analyzed by HR and ER status. In contrast to the findings of Modi and colleagues, this analysis saw no prognostic significance in terms of survival outcomes for HER2-low expression among patients who had HR-positive or HER2-0 tumors, suggesting that HER2-low breast cancer may not be a distinct biologic subtype. Further studies are needed to clarify whether HER2-low breast cancer needs to be considered separately in practice.
Immunotherapy, particular checkpoint inhibitors, has revolutionized the treatment of many solid tumors. However, their role in HER2-positive breast cancer remains unclear. IMpassion050 is a double-blind, randomized, phase 3 study evaluating the efficacy and safety of adding atezolizumab, an anti–programmed death-ligand 1 (PD-L1) antibody, to neoadjuvant standard of care (chemotherapy + pertuzumab + trastuzumab [PH]) for high-risk, HER2-positive early breast cancer (EBC). In the study by Huober and colleagues, 454 patients with a primary tumor > 2 cm and histologically confirmed positive lymph node status (N1-3) were randomly assigned in a 1:1 ratio to the atezolizumab or placebo group with dose-dense doxorubicin or cyclophosphamide, followed by paclitaxel and PH. In the adjuvant setting, patients continued atezolizumab or placebo and PH to complete 1 year of HER2-targeted therapy; those with residual disease could switch to trastuzumab emtansine with atezolizumab or placebo. At clinical cutoff (February 5, 2021), rates of pCR in the atezolizumab group vs placebo group were similar among all patients in the study (62.4% vs 62.7%; P = .9551) and in the PD-L1–positive population (64.2% vs 72.5%; P = .1846). Treatment-related grade 3-4 adverse events occurred more frequently in the atezolizumab group compared with the placebo group, both during the neoadjuvant treatment phase (47.3% vs 42.2%) and the adjuvant treatment phase (13.4% vs 9.8%).
In summary, the phase 3 IMpassion050 trial showed no significant improvement in pCR with the addition of atezolizumab to neoadjuvant therapy in patients with high-risk, HER2-positive EBC, including those with PD-L1–positive tumors. At this time, PH and chemotherapy remain the standard of care in this patient population. Longer follow-up is needed in respect to the long-term effect of atezolizumab in this setting.
DESTINY-Breast04 is the first randomized clinical trial to show that targeting HER2 provides clinically meaningful benefit for patients with HER2-low metastatic breast cancer. This phase 3 study by Modi and colleagues enrolled 557 patients with hormone receptor (HR)–negative or HR-positive breast cancer and centrally confirmed HER2 low expression in those who had been previously treated with one or two prior lines of chemotherapy for metastatic breast cancer. Patients with HR-positive breast cancer were required to have endocrine therapy–refractory disease. Patients were randomized in a 2:1 ratio to receive either an antibody-drug conjugate, trastuzumab deruxtecan (T-DXd), or the physician's choice of standard chemotherapy (capecitabine, eribulin, gemcitabine, paclitaxel, or nanoparticle albumin–bound paclitaxel [nab-paclitaxel]). Among all 557 patients, T-DXd improved median progression-free survival (PFS) by 4.8 months (9.9 vs 5.1 months; hazard ratio [HR] 0.50; P < .001) and median overall survival (OS) by 6.6 months (23.4 vs 16.8 months; HR 0.64; P = .0010) compared with standard single-agent chemotherapy. Among the 494 (88.7%) HR-positive patients, the median PFS was 10.1 months in the T-DXd group and 5.4 months in the chemotherapy group (HR 0.51; P < .001). Median OS was 23.9 months and 17.5 months, respectively (HR 0.64; P = .003). The rates of grade 3 or higher adverse events were lower with T-DXd than with standard chemotherapy (52.6% vs 67.4%, respectively), although higher rates of drug-related interstitial lung disease or pneumonitis were noted in the T-DXd arm (12.1% vs 0.1%). Lung toxicity continues to be an important safety concern with T-DXd. These practice-changing results open the door to a new treatment option for a substantial group of patients with HER2-low disease and support the need to reclassify HER2-low as a new targetable subset of breast cancer, distinct from HER-negative (HER2-0), and to acquire an understanding of the clinical characteristics of and prognosis for these patients.
Tarantino and colleagues evaluated the biologic and prognostic significance of HER2-low expression in breast cancer and investigated the association between HR status and HER2-low expression. Among 5235 patients with HER2-0 invasive breast cancer, HR expression was significantly more common among HER2-low tumors than among HER2-0 tumors (90.6% vs 81.8%; P < .001). The rate of HER2-low tumors increased progressively as estrogen receptor (ER) expression increased (40.1% of ER-negative, 46.3% of ER-low, 55.2% of ER-moderate, 57.8% of ER-high, and 62.1% of ER-very high [ie, ER > 95%] tumors; P < .001). Among 675 patients receiving neoadjuvant chemotherapy, higher pathologic complete response (pCR) rates were seen among those with HER2-0 tumors (26.8% vs 16.6%; P = .002), although no statistically significant differences in pCR rates were noted between HER2-low and HER2-0 tumors when analyzed by HR and ER status. In contrast to the findings of Modi and colleagues, this analysis saw no prognostic significance in terms of survival outcomes for HER2-low expression among patients who had HR-positive or HER2-0 tumors, suggesting that HER2-low breast cancer may not be a distinct biologic subtype. Further studies are needed to clarify whether HER2-low breast cancer needs to be considered separately in practice.
Immunotherapy, particular checkpoint inhibitors, has revolutionized the treatment of many solid tumors. However, their role in HER2-positive breast cancer remains unclear. IMpassion050 is a double-blind, randomized, phase 3 study evaluating the efficacy and safety of adding atezolizumab, an anti–programmed death-ligand 1 (PD-L1) antibody, to neoadjuvant standard of care (chemotherapy + pertuzumab + trastuzumab [PH]) for high-risk, HER2-positive early breast cancer (EBC). In the study by Huober and colleagues, 454 patients with a primary tumor > 2 cm and histologically confirmed positive lymph node status (N1-3) were randomly assigned in a 1:1 ratio to the atezolizumab or placebo group with dose-dense doxorubicin or cyclophosphamide, followed by paclitaxel and PH. In the adjuvant setting, patients continued atezolizumab or placebo and PH to complete 1 year of HER2-targeted therapy; those with residual disease could switch to trastuzumab emtansine with atezolizumab or placebo. At clinical cutoff (February 5, 2021), rates of pCR in the atezolizumab group vs placebo group were similar among all patients in the study (62.4% vs 62.7%; P = .9551) and in the PD-L1–positive population (64.2% vs 72.5%; P = .1846). Treatment-related grade 3-4 adverse events occurred more frequently in the atezolizumab group compared with the placebo group, both during the neoadjuvant treatment phase (47.3% vs 42.2%) and the adjuvant treatment phase (13.4% vs 9.8%).
In summary, the phase 3 IMpassion050 trial showed no significant improvement in pCR with the addition of atezolizumab to neoadjuvant therapy in patients with high-risk, HER2-positive EBC, including those with PD-L1–positive tumors. At this time, PH and chemotherapy remain the standard of care in this patient population. Longer follow-up is needed in respect to the long-term effect of atezolizumab in this setting.
DESTINY-Breast04 is the first randomized clinical trial to show that targeting HER2 provides clinically meaningful benefit for patients with HER2-low metastatic breast cancer. This phase 3 study by Modi and colleagues enrolled 557 patients with hormone receptor (HR)–negative or HR-positive breast cancer and centrally confirmed HER2 low expression in those who had been previously treated with one or two prior lines of chemotherapy for metastatic breast cancer. Patients with HR-positive breast cancer were required to have endocrine therapy–refractory disease. Patients were randomized in a 2:1 ratio to receive either an antibody-drug conjugate, trastuzumab deruxtecan (T-DXd), or the physician's choice of standard chemotherapy (capecitabine, eribulin, gemcitabine, paclitaxel, or nanoparticle albumin–bound paclitaxel [nab-paclitaxel]). Among all 557 patients, T-DXd improved median progression-free survival (PFS) by 4.8 months (9.9 vs 5.1 months; hazard ratio [HR] 0.50; P < .001) and median overall survival (OS) by 6.6 months (23.4 vs 16.8 months; HR 0.64; P = .0010) compared with standard single-agent chemotherapy. Among the 494 (88.7%) HR-positive patients, the median PFS was 10.1 months in the T-DXd group and 5.4 months in the chemotherapy group (HR 0.51; P < .001). Median OS was 23.9 months and 17.5 months, respectively (HR 0.64; P = .003). The rates of grade 3 or higher adverse events were lower with T-DXd than with standard chemotherapy (52.6% vs 67.4%, respectively), although higher rates of drug-related interstitial lung disease or pneumonitis were noted in the T-DXd arm (12.1% vs 0.1%). Lung toxicity continues to be an important safety concern with T-DXd. These practice-changing results open the door to a new treatment option for a substantial group of patients with HER2-low disease and support the need to reclassify HER2-low as a new targetable subset of breast cancer, distinct from HER-negative (HER2-0), and to acquire an understanding of the clinical characteristics of and prognosis for these patients.
Tarantino and colleagues evaluated the biologic and prognostic significance of HER2-low expression in breast cancer and investigated the association between HR status and HER2-low expression. Among 5235 patients with HER2-0 invasive breast cancer, HR expression was significantly more common among HER2-low tumors than among HER2-0 tumors (90.6% vs 81.8%; P < .001). The rate of HER2-low tumors increased progressively as estrogen receptor (ER) expression increased (40.1% of ER-negative, 46.3% of ER-low, 55.2% of ER-moderate, 57.8% of ER-high, and 62.1% of ER-very high [ie, ER > 95%] tumors; P < .001). Among 675 patients receiving neoadjuvant chemotherapy, higher pathologic complete response (pCR) rates were seen among those with HER2-0 tumors (26.8% vs 16.6%; P = .002), although no statistically significant differences in pCR rates were noted between HER2-low and HER2-0 tumors when analyzed by HR and ER status. In contrast to the findings of Modi and colleagues, this analysis saw no prognostic significance in terms of survival outcomes for HER2-low expression among patients who had HR-positive or HER2-0 tumors, suggesting that HER2-low breast cancer may not be a distinct biologic subtype. Further studies are needed to clarify whether HER2-low breast cancer needs to be considered separately in practice.
Immunotherapy, particular checkpoint inhibitors, has revolutionized the treatment of many solid tumors. However, their role in HER2-positive breast cancer remains unclear. IMpassion050 is a double-blind, randomized, phase 3 study evaluating the efficacy and safety of adding atezolizumab, an anti–programmed death-ligand 1 (PD-L1) antibody, to neoadjuvant standard of care (chemotherapy + pertuzumab + trastuzumab [PH]) for high-risk, HER2-positive early breast cancer (EBC). In the study by Huober and colleagues, 454 patients with a primary tumor > 2 cm and histologically confirmed positive lymph node status (N1-3) were randomly assigned in a 1:1 ratio to the atezolizumab or placebo group with dose-dense doxorubicin or cyclophosphamide, followed by paclitaxel and PH. In the adjuvant setting, patients continued atezolizumab or placebo and PH to complete 1 year of HER2-targeted therapy; those with residual disease could switch to trastuzumab emtansine with atezolizumab or placebo. At clinical cutoff (February 5, 2021), rates of pCR in the atezolizumab group vs placebo group were similar among all patients in the study (62.4% vs 62.7%; P = .9551) and in the PD-L1–positive population (64.2% vs 72.5%; P = .1846). Treatment-related grade 3-4 adverse events occurred more frequently in the atezolizumab group compared with the placebo group, both during the neoadjuvant treatment phase (47.3% vs 42.2%) and the adjuvant treatment phase (13.4% vs 9.8%).
In summary, the phase 3 IMpassion050 trial showed no significant improvement in pCR with the addition of atezolizumab to neoadjuvant therapy in patients with high-risk, HER2-positive EBC, including those with PD-L1–positive tumors. At this time, PH and chemotherapy remain the standard of care in this patient population. Longer follow-up is needed in respect to the long-term effect of atezolizumab in this setting.
Aesthetics abound for the aging face
At the MedscapeLive’s Women’s and Pediatric Dermatology Seminar, Jacqueline Watchmaker, MD, a dermatologist in Scottsdale, Ariz., provided an overview of current options, along with advice on how to keep patients’ expectations realistic and how to properly choose the best candidates for the best procedures.
“One of the most common concerns patients come to me with are wrinkles on the upper face,” but this is far from their only concern, Dr. Watchmaker said. Wrinkles and sagging of the lower face, areas under the eyes, nasolabial folds, marionette lines, and the neck also draw concern. Uneven coloration is another common concern, she said.
“So, what can we do for all of this?” she asked. The options are plentiful. Wrinkles of the upper face are easy to address with neuromodulators, she said, and soft-tissue fillers help the jawline and cheek areas.
“For the lower face, skin tightening devices really shine,” she added. And lasers can help correct uneven coloration. Surgery, of course, can also produce good results, but many patients want to stick with noninvasive or minimally invasive procedures.
Case: 83-year-old woman
Dr. Watchmaker discussed an 83-year old patient, who had malar mounds and accentuation of the infraorbital hollowness resulting from changes in subcutaneous fat and ligament laxity. She also had uneven coloration from photo damage, wrinkles on the upper face, linear appearance of zygoma related to underlying bony changes and fat compartment descent, and nasolabial folds and jowls related to decreased bony compartments, ligament laxity, and shifting of fat. She was naive to any cosmetic procedure.
Despite her age, this patient had no wrinkling on the upper forehead. Dr. Watchmaker did not inject neuromodulator in the upper forehead, as this patient also had a slightly heavy eyelid. “If you inject too much, it can cause some drooping of the eyelid and eyebrow,” she said.
For filler, she used a combination of high G (firmness, support) hyaluronic acid filler, a medium G acid filler, and a low G filler. The result: The woman’s face became more balanced, the mid-face volumization lifted the lower face, and the glabellar and periocular lines were softer, although still present. “It’s important to counsel patients that neuromodulators won’t make the lines go away the first time, but they will be softened.”
Practice tips
It’s important to titrate neuromodulators to fit the patient, Dr. Watchmaker said. Ask: What are their goals: Reversal of static lines? Softening wrinkles? Maintaining current status? “There’s not one dosing regimen,” and both dosing and frequency of neuromodulators can be titrated to fit each patient’s aesthetic goals, she said. For older patients who want to soften or maintain appearance, she suggested treatment every 4-6 months. And some patients just want to maintain the status quo, she noted.
Ideal candidates
For neuromodulators and fillers, who is an ideal candidate? “I think it’s anyone who has realistic expectations,” she said. Patients need to know how many treatments are needed and how much it will cost. For patients with extensive wrinkling and sagging, she said, she does extensive counseling about what results to expect “because I don’t want them to feel like they wasted their time or their money.”
She also suggests a surgical consult, as some may opt for that route after learning about the options and expected results.
Skin tightening
Both radiofrequency and microfocused ultrasound are noninvasive and additional options. Radiofrequency uses radio waves, with electromagnetic energy to stimulate heat. Ultrasound uses ultrasound waves to stimulate heat. Both approaches cause collagen contraction, neocollagenesis, and skin tightening.
These procedures do well for the lower face, Dr. Watchmaker said, but “I am relatively unimpressed for how well they do for the upper face.” Ideal candidates have mild to moderate skin laxity and want to avoid surgery. She also tells patients that collagen isn’t made overnight. “You won’t see much for 3-6 months after.” The good news? Usually the treatments need to be repeated only every 1.5-2 years, she said.
Lasers
“There are so many lasers out there,” said Dr. Watchmaker, who groups them into three categories: those used for wrinkles, dyschromia, and erythema. Her picks: ablative lasers (CO2 and erbium) and erbium-doped YAG 1550 nm laser for rhytids. Thulium 1927 and QS and picosecond lasers are her picks for dyschromia, and for erythema, pulsed dye and KTP lasers.
Some laser treatments are not a “walk in the park,” as she warns patients. For example, after treatment with ablative lasers, there is pain, post-procedure redness, and crusting.
Take-home points
A combination of noninvasive and minimally invasive procedures can produce appearance-improving results. That’s more likely if dermatologists choose ideal candidates, personalize the treatment, and set realistic expectations. “We have a finite number of tools,” she said, but they can be used in a variety of ways.
At the interactive panel discussion following her presentation, Dr. Watchmaker was asked what she tells patients about sun protection. “I talk a lot about sunscreens,’’ she said, always urging patients to use them. While the options for rejuvenation are numerous, taking care of the skin is still crucial.
Dr. Watchmaker had no disclosures. MedscapeLive and this news organization are owned by the same parent company.
At the MedscapeLive’s Women’s and Pediatric Dermatology Seminar, Jacqueline Watchmaker, MD, a dermatologist in Scottsdale, Ariz., provided an overview of current options, along with advice on how to keep patients’ expectations realistic and how to properly choose the best candidates for the best procedures.
“One of the most common concerns patients come to me with are wrinkles on the upper face,” but this is far from their only concern, Dr. Watchmaker said. Wrinkles and sagging of the lower face, areas under the eyes, nasolabial folds, marionette lines, and the neck also draw concern. Uneven coloration is another common concern, she said.
“So, what can we do for all of this?” she asked. The options are plentiful. Wrinkles of the upper face are easy to address with neuromodulators, she said, and soft-tissue fillers help the jawline and cheek areas.
“For the lower face, skin tightening devices really shine,” she added. And lasers can help correct uneven coloration. Surgery, of course, can also produce good results, but many patients want to stick with noninvasive or minimally invasive procedures.
Case: 83-year-old woman
Dr. Watchmaker discussed an 83-year old patient, who had malar mounds and accentuation of the infraorbital hollowness resulting from changes in subcutaneous fat and ligament laxity. She also had uneven coloration from photo damage, wrinkles on the upper face, linear appearance of zygoma related to underlying bony changes and fat compartment descent, and nasolabial folds and jowls related to decreased bony compartments, ligament laxity, and shifting of fat. She was naive to any cosmetic procedure.
Despite her age, this patient had no wrinkling on the upper forehead. Dr. Watchmaker did not inject neuromodulator in the upper forehead, as this patient also had a slightly heavy eyelid. “If you inject too much, it can cause some drooping of the eyelid and eyebrow,” she said.
For filler, she used a combination of high G (firmness, support) hyaluronic acid filler, a medium G acid filler, and a low G filler. The result: The woman’s face became more balanced, the mid-face volumization lifted the lower face, and the glabellar and periocular lines were softer, although still present. “It’s important to counsel patients that neuromodulators won’t make the lines go away the first time, but they will be softened.”
Practice tips
It’s important to titrate neuromodulators to fit the patient, Dr. Watchmaker said. Ask: What are their goals: Reversal of static lines? Softening wrinkles? Maintaining current status? “There’s not one dosing regimen,” and both dosing and frequency of neuromodulators can be titrated to fit each patient’s aesthetic goals, she said. For older patients who want to soften or maintain appearance, she suggested treatment every 4-6 months. And some patients just want to maintain the status quo, she noted.
Ideal candidates
For neuromodulators and fillers, who is an ideal candidate? “I think it’s anyone who has realistic expectations,” she said. Patients need to know how many treatments are needed and how much it will cost. For patients with extensive wrinkling and sagging, she said, she does extensive counseling about what results to expect “because I don’t want them to feel like they wasted their time or their money.”
She also suggests a surgical consult, as some may opt for that route after learning about the options and expected results.
Skin tightening
Both radiofrequency and microfocused ultrasound are noninvasive and additional options. Radiofrequency uses radio waves, with electromagnetic energy to stimulate heat. Ultrasound uses ultrasound waves to stimulate heat. Both approaches cause collagen contraction, neocollagenesis, and skin tightening.
These procedures do well for the lower face, Dr. Watchmaker said, but “I am relatively unimpressed for how well they do for the upper face.” Ideal candidates have mild to moderate skin laxity and want to avoid surgery. She also tells patients that collagen isn’t made overnight. “You won’t see much for 3-6 months after.” The good news? Usually the treatments need to be repeated only every 1.5-2 years, she said.
Lasers
“There are so many lasers out there,” said Dr. Watchmaker, who groups them into three categories: those used for wrinkles, dyschromia, and erythema. Her picks: ablative lasers (CO2 and erbium) and erbium-doped YAG 1550 nm laser for rhytids. Thulium 1927 and QS and picosecond lasers are her picks for dyschromia, and for erythema, pulsed dye and KTP lasers.
Some laser treatments are not a “walk in the park,” as she warns patients. For example, after treatment with ablative lasers, there is pain, post-procedure redness, and crusting.
Take-home points
A combination of noninvasive and minimally invasive procedures can produce appearance-improving results. That’s more likely if dermatologists choose ideal candidates, personalize the treatment, and set realistic expectations. “We have a finite number of tools,” she said, but they can be used in a variety of ways.
At the interactive panel discussion following her presentation, Dr. Watchmaker was asked what she tells patients about sun protection. “I talk a lot about sunscreens,’’ she said, always urging patients to use them. While the options for rejuvenation are numerous, taking care of the skin is still crucial.
Dr. Watchmaker had no disclosures. MedscapeLive and this news organization are owned by the same parent company.
At the MedscapeLive’s Women’s and Pediatric Dermatology Seminar, Jacqueline Watchmaker, MD, a dermatologist in Scottsdale, Ariz., provided an overview of current options, along with advice on how to keep patients’ expectations realistic and how to properly choose the best candidates for the best procedures.
“One of the most common concerns patients come to me with are wrinkles on the upper face,” but this is far from their only concern, Dr. Watchmaker said. Wrinkles and sagging of the lower face, areas under the eyes, nasolabial folds, marionette lines, and the neck also draw concern. Uneven coloration is another common concern, she said.
“So, what can we do for all of this?” she asked. The options are plentiful. Wrinkles of the upper face are easy to address with neuromodulators, she said, and soft-tissue fillers help the jawline and cheek areas.
“For the lower face, skin tightening devices really shine,” she added. And lasers can help correct uneven coloration. Surgery, of course, can also produce good results, but many patients want to stick with noninvasive or minimally invasive procedures.
Case: 83-year-old woman
Dr. Watchmaker discussed an 83-year old patient, who had malar mounds and accentuation of the infraorbital hollowness resulting from changes in subcutaneous fat and ligament laxity. She also had uneven coloration from photo damage, wrinkles on the upper face, linear appearance of zygoma related to underlying bony changes and fat compartment descent, and nasolabial folds and jowls related to decreased bony compartments, ligament laxity, and shifting of fat. She was naive to any cosmetic procedure.
Despite her age, this patient had no wrinkling on the upper forehead. Dr. Watchmaker did not inject neuromodulator in the upper forehead, as this patient also had a slightly heavy eyelid. “If you inject too much, it can cause some drooping of the eyelid and eyebrow,” she said.
For filler, she used a combination of high G (firmness, support) hyaluronic acid filler, a medium G acid filler, and a low G filler. The result: The woman’s face became more balanced, the mid-face volumization lifted the lower face, and the glabellar and periocular lines were softer, although still present. “It’s important to counsel patients that neuromodulators won’t make the lines go away the first time, but they will be softened.”
Practice tips
It’s important to titrate neuromodulators to fit the patient, Dr. Watchmaker said. Ask: What are their goals: Reversal of static lines? Softening wrinkles? Maintaining current status? “There’s not one dosing regimen,” and both dosing and frequency of neuromodulators can be titrated to fit each patient’s aesthetic goals, she said. For older patients who want to soften or maintain appearance, she suggested treatment every 4-6 months. And some patients just want to maintain the status quo, she noted.
Ideal candidates
For neuromodulators and fillers, who is an ideal candidate? “I think it’s anyone who has realistic expectations,” she said. Patients need to know how many treatments are needed and how much it will cost. For patients with extensive wrinkling and sagging, she said, she does extensive counseling about what results to expect “because I don’t want them to feel like they wasted their time or their money.”
She also suggests a surgical consult, as some may opt for that route after learning about the options and expected results.
Skin tightening
Both radiofrequency and microfocused ultrasound are noninvasive and additional options. Radiofrequency uses radio waves, with electromagnetic energy to stimulate heat. Ultrasound uses ultrasound waves to stimulate heat. Both approaches cause collagen contraction, neocollagenesis, and skin tightening.
These procedures do well for the lower face, Dr. Watchmaker said, but “I am relatively unimpressed for how well they do for the upper face.” Ideal candidates have mild to moderate skin laxity and want to avoid surgery. She also tells patients that collagen isn’t made overnight. “You won’t see much for 3-6 months after.” The good news? Usually the treatments need to be repeated only every 1.5-2 years, she said.
Lasers
“There are so many lasers out there,” said Dr. Watchmaker, who groups them into three categories: those used for wrinkles, dyschromia, and erythema. Her picks: ablative lasers (CO2 and erbium) and erbium-doped YAG 1550 nm laser for rhytids. Thulium 1927 and QS and picosecond lasers are her picks for dyschromia, and for erythema, pulsed dye and KTP lasers.
Some laser treatments are not a “walk in the park,” as she warns patients. For example, after treatment with ablative lasers, there is pain, post-procedure redness, and crusting.
Take-home points
A combination of noninvasive and minimally invasive procedures can produce appearance-improving results. That’s more likely if dermatologists choose ideal candidates, personalize the treatment, and set realistic expectations. “We have a finite number of tools,” she said, but they can be used in a variety of ways.
At the interactive panel discussion following her presentation, Dr. Watchmaker was asked what she tells patients about sun protection. “I talk a lot about sunscreens,’’ she said, always urging patients to use them. While the options for rejuvenation are numerous, taking care of the skin is still crucial.
Dr. Watchmaker had no disclosures. MedscapeLive and this news organization are owned by the same parent company.
FROM MEDSCAPELIVE WOMEN’S & PEDIATRIC DERMATOLOGY SEMINAR
Doxycycline cuts STI risk in men and trans women having sex with men
MONTREAL – (PrEP). The results of the open-label DoxyPEP trial were reported at a press conference at a meeting of the International AIDS Society.
“It is time to take action on the data that we have and really think about incorporating it into guidelines and rolling this out in a safe and thoughtful way,” said co-principal investigator Annie Luetkemeyer, MD, of Zuckerberg San Francisco General Hospital, and professor of medicine at the University of California, San Francisco (UCSF).
The open-label trial, conducted in Seattle and San Francisco, randomized MSM/TGW living with HIV or on PrEP, and with a history of N. gonorrhoeae (GC), C. trachomatis (CT), or early syphilis in the past year, to either doxycycline or none within 72 hours of having condomless sex. It was stopped early in May when a planned interim analysis showed those randomized to take doxycycline had substantially fewer STIs than participants assigned to the control group.
The intent-to-treat analysis included 501 patients with at least one quarter of follow-up: 327 taking PrEP and 174 living with HIV. Among those taking PrEP, new STIs (GC, CT or syphilis) occurred in 31.9% of control participants vs. 10.7% of those taking doxycycline – a reduction of 66% per quarter (P < .001). Among participants living with HIV, new STIs occurred in 30.5% of controls vs. 11.8% taking doxycycline, for a 62% reduction in STIs per quarter (P < .0001).
“Participants reported taking doxycycline 87% of the time after having condomless sex, about half of participants took fewer than 10 doses per month, 30% took 10-20 doses per month, and 16% took more than 20 doses of doxycycline per month,” said Dr. Luetkemeyer, adding that there were no serious – grade 2 or greater – adverse events, and “the majority of participants reported that taking doxy was acceptable or very acceptable.”
Asked how broadly doxycycline prophylaxis could be used in other populations, Dr. Luetkemeyer was cautious. “Our study participants had a very high rate of new STIs – a 30% incidence per quarter and using doxyPEP was well tolerated and very effective to reduce new STIs. However, this is a fairly limited population,” she said. “Whether doxyPEP should be considered for other groups, such as women on PrEP or with an elevated risk for STIs, will need more data which will be forthcoming from ongoing studies.”
Dr. Luetkemeyer said her group is looking at three possible risks of antibiotic resistance with the doxyPEP regimen: the risk to bystander bacteria such as Staphylococcus aureus or commensal neisseria; the impact on the gut; and the risk of resistance to antibiotic treatments for STI.
For the latter, “we don’t really think this is going to be an issue in chlamydia and syphilis, and we’re looking carefully at gonorrhea,” she said, adding that it will be challenging to get definitive data from this particular study because of its short follow-up.
“Available culture data from those who had gonorrhea infections during the study demonstrated a relatively low rate of tetracycline resistance, which is a proxy for doxycycline resistance, at 20%. ... However, larger studies and population-based surveillance of those taking doxycycline as PEP are needed to understand if doxycycline use could drive the element of tetracycline resistance in gonorrhea,” she said, emphasizing that doxycycline is not used to treat active gonorrhea infections.
Calling the doxyPEP regimen a “game-changing strategy,” Sharon Lewin, AO, PhD, president-elect of the International AIDS Society, said many physicians are already prescribing it off label based on the IPERGAY study (N Engl J Med. 2015; 373:2237-46) “but there’s a clear need for more evidence to guide the use of this intervention.”
“This study has huge implications for clinical care,” said Monica Gandhi, MD, MPH, an infectious diseases doctor, professor of medicine, and associate chief in the division of HIV, infectious diseases, and global medicine at UCSF. “Although the data on drug resistance is very important to evaluate, we should certainly consider at this point using doxycycline PEP within 72 hours of condomless sex for our patients for STI prevention,” she said in an interview.
“In our practice, we are very excited about the possibility of a simple one-pill postexposure prophylactic agent (doxycycline 200 mg) to reduce the risk of a number of STIs. We have used PEP for HIV infection for a number of years and are very familiar with the concept of preventing infections after an exposure,” said Dr. Gandhi, director of the UCSF Center for AIDS Research and medical director of the HIV Clinic (“Ward 86”) at San Francisco General Hospital. “We are planning to institute doxycycline as PEP at my clinic after the release of these findings and will follow the remainder of the study findings closely.”
The trial was funded by the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health, through grant R01AI143439. It was conducted at the HIV clinic at Zuckerberg San Francisco General Hospital and the San Francisco City Clinic, both part of the San Francisco Department of Public Health, and the Madison Clinic and the Sexual Health Clinic at Harborview Medical Center, both at the University of Washington. Medications were provided by Mayne Pharmaceuticals, and lab support by Hologic & Cepheid.
Dr. Lewin has the following disclosures: investigator-initiated, industry-funded research for Gilead, Viiv, Merck; scientific advisory board (honoraria paid to her personally) for Gilead, Merck, Viiv, Esfam, Immunocore, Vaxxinity; collaborative research (nonfunded) for AbbVie, Genentech, BMS. Dr. Luetkemeyer and Dr. Gandhi reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
MONTREAL – (PrEP). The results of the open-label DoxyPEP trial were reported at a press conference at a meeting of the International AIDS Society.
“It is time to take action on the data that we have and really think about incorporating it into guidelines and rolling this out in a safe and thoughtful way,” said co-principal investigator Annie Luetkemeyer, MD, of Zuckerberg San Francisco General Hospital, and professor of medicine at the University of California, San Francisco (UCSF).
The open-label trial, conducted in Seattle and San Francisco, randomized MSM/TGW living with HIV or on PrEP, and with a history of N. gonorrhoeae (GC), C. trachomatis (CT), or early syphilis in the past year, to either doxycycline or none within 72 hours of having condomless sex. It was stopped early in May when a planned interim analysis showed those randomized to take doxycycline had substantially fewer STIs than participants assigned to the control group.
The intent-to-treat analysis included 501 patients with at least one quarter of follow-up: 327 taking PrEP and 174 living with HIV. Among those taking PrEP, new STIs (GC, CT or syphilis) occurred in 31.9% of control participants vs. 10.7% of those taking doxycycline – a reduction of 66% per quarter (P < .001). Among participants living with HIV, new STIs occurred in 30.5% of controls vs. 11.8% taking doxycycline, for a 62% reduction in STIs per quarter (P < .0001).
“Participants reported taking doxycycline 87% of the time after having condomless sex, about half of participants took fewer than 10 doses per month, 30% took 10-20 doses per month, and 16% took more than 20 doses of doxycycline per month,” said Dr. Luetkemeyer, adding that there were no serious – grade 2 or greater – adverse events, and “the majority of participants reported that taking doxy was acceptable or very acceptable.”
Asked how broadly doxycycline prophylaxis could be used in other populations, Dr. Luetkemeyer was cautious. “Our study participants had a very high rate of new STIs – a 30% incidence per quarter and using doxyPEP was well tolerated and very effective to reduce new STIs. However, this is a fairly limited population,” she said. “Whether doxyPEP should be considered for other groups, such as women on PrEP or with an elevated risk for STIs, will need more data which will be forthcoming from ongoing studies.”
Dr. Luetkemeyer said her group is looking at three possible risks of antibiotic resistance with the doxyPEP regimen: the risk to bystander bacteria such as Staphylococcus aureus or commensal neisseria; the impact on the gut; and the risk of resistance to antibiotic treatments for STI.
For the latter, “we don’t really think this is going to be an issue in chlamydia and syphilis, and we’re looking carefully at gonorrhea,” she said, adding that it will be challenging to get definitive data from this particular study because of its short follow-up.
“Available culture data from those who had gonorrhea infections during the study demonstrated a relatively low rate of tetracycline resistance, which is a proxy for doxycycline resistance, at 20%. ... However, larger studies and population-based surveillance of those taking doxycycline as PEP are needed to understand if doxycycline use could drive the element of tetracycline resistance in gonorrhea,” she said, emphasizing that doxycycline is not used to treat active gonorrhea infections.
Calling the doxyPEP regimen a “game-changing strategy,” Sharon Lewin, AO, PhD, president-elect of the International AIDS Society, said many physicians are already prescribing it off label based on the IPERGAY study (N Engl J Med. 2015; 373:2237-46) “but there’s a clear need for more evidence to guide the use of this intervention.”
“This study has huge implications for clinical care,” said Monica Gandhi, MD, MPH, an infectious diseases doctor, professor of medicine, and associate chief in the division of HIV, infectious diseases, and global medicine at UCSF. “Although the data on drug resistance is very important to evaluate, we should certainly consider at this point using doxycycline PEP within 72 hours of condomless sex for our patients for STI prevention,” she said in an interview.
“In our practice, we are very excited about the possibility of a simple one-pill postexposure prophylactic agent (doxycycline 200 mg) to reduce the risk of a number of STIs. We have used PEP for HIV infection for a number of years and are very familiar with the concept of preventing infections after an exposure,” said Dr. Gandhi, director of the UCSF Center for AIDS Research and medical director of the HIV Clinic (“Ward 86”) at San Francisco General Hospital. “We are planning to institute doxycycline as PEP at my clinic after the release of these findings and will follow the remainder of the study findings closely.”
The trial was funded by the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health, through grant R01AI143439. It was conducted at the HIV clinic at Zuckerberg San Francisco General Hospital and the San Francisco City Clinic, both part of the San Francisco Department of Public Health, and the Madison Clinic and the Sexual Health Clinic at Harborview Medical Center, both at the University of Washington. Medications were provided by Mayne Pharmaceuticals, and lab support by Hologic & Cepheid.
Dr. Lewin has the following disclosures: investigator-initiated, industry-funded research for Gilead, Viiv, Merck; scientific advisory board (honoraria paid to her personally) for Gilead, Merck, Viiv, Esfam, Immunocore, Vaxxinity; collaborative research (nonfunded) for AbbVie, Genentech, BMS. Dr. Luetkemeyer and Dr. Gandhi reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
MONTREAL – (PrEP). The results of the open-label DoxyPEP trial were reported at a press conference at a meeting of the International AIDS Society.
“It is time to take action on the data that we have and really think about incorporating it into guidelines and rolling this out in a safe and thoughtful way,” said co-principal investigator Annie Luetkemeyer, MD, of Zuckerberg San Francisco General Hospital, and professor of medicine at the University of California, San Francisco (UCSF).
The open-label trial, conducted in Seattle and San Francisco, randomized MSM/TGW living with HIV or on PrEP, and with a history of N. gonorrhoeae (GC), C. trachomatis (CT), or early syphilis in the past year, to either doxycycline or none within 72 hours of having condomless sex. It was stopped early in May when a planned interim analysis showed those randomized to take doxycycline had substantially fewer STIs than participants assigned to the control group.
The intent-to-treat analysis included 501 patients with at least one quarter of follow-up: 327 taking PrEP and 174 living with HIV. Among those taking PrEP, new STIs (GC, CT or syphilis) occurred in 31.9% of control participants vs. 10.7% of those taking doxycycline – a reduction of 66% per quarter (P < .001). Among participants living with HIV, new STIs occurred in 30.5% of controls vs. 11.8% taking doxycycline, for a 62% reduction in STIs per quarter (P < .0001).
“Participants reported taking doxycycline 87% of the time after having condomless sex, about half of participants took fewer than 10 doses per month, 30% took 10-20 doses per month, and 16% took more than 20 doses of doxycycline per month,” said Dr. Luetkemeyer, adding that there were no serious – grade 2 or greater – adverse events, and “the majority of participants reported that taking doxy was acceptable or very acceptable.”
Asked how broadly doxycycline prophylaxis could be used in other populations, Dr. Luetkemeyer was cautious. “Our study participants had a very high rate of new STIs – a 30% incidence per quarter and using doxyPEP was well tolerated and very effective to reduce new STIs. However, this is a fairly limited population,” she said. “Whether doxyPEP should be considered for other groups, such as women on PrEP or with an elevated risk for STIs, will need more data which will be forthcoming from ongoing studies.”
Dr. Luetkemeyer said her group is looking at three possible risks of antibiotic resistance with the doxyPEP regimen: the risk to bystander bacteria such as Staphylococcus aureus or commensal neisseria; the impact on the gut; and the risk of resistance to antibiotic treatments for STI.
For the latter, “we don’t really think this is going to be an issue in chlamydia and syphilis, and we’re looking carefully at gonorrhea,” she said, adding that it will be challenging to get definitive data from this particular study because of its short follow-up.
“Available culture data from those who had gonorrhea infections during the study demonstrated a relatively low rate of tetracycline resistance, which is a proxy for doxycycline resistance, at 20%. ... However, larger studies and population-based surveillance of those taking doxycycline as PEP are needed to understand if doxycycline use could drive the element of tetracycline resistance in gonorrhea,” she said, emphasizing that doxycycline is not used to treat active gonorrhea infections.
Calling the doxyPEP regimen a “game-changing strategy,” Sharon Lewin, AO, PhD, president-elect of the International AIDS Society, said many physicians are already prescribing it off label based on the IPERGAY study (N Engl J Med. 2015; 373:2237-46) “but there’s a clear need for more evidence to guide the use of this intervention.”
“This study has huge implications for clinical care,” said Monica Gandhi, MD, MPH, an infectious diseases doctor, professor of medicine, and associate chief in the division of HIV, infectious diseases, and global medicine at UCSF. “Although the data on drug resistance is very important to evaluate, we should certainly consider at this point using doxycycline PEP within 72 hours of condomless sex for our patients for STI prevention,” she said in an interview.
“In our practice, we are very excited about the possibility of a simple one-pill postexposure prophylactic agent (doxycycline 200 mg) to reduce the risk of a number of STIs. We have used PEP for HIV infection for a number of years and are very familiar with the concept of preventing infections after an exposure,” said Dr. Gandhi, director of the UCSF Center for AIDS Research and medical director of the HIV Clinic (“Ward 86”) at San Francisco General Hospital. “We are planning to institute doxycycline as PEP at my clinic after the release of these findings and will follow the remainder of the study findings closely.”
The trial was funded by the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health, through grant R01AI143439. It was conducted at the HIV clinic at Zuckerberg San Francisco General Hospital and the San Francisco City Clinic, both part of the San Francisco Department of Public Health, and the Madison Clinic and the Sexual Health Clinic at Harborview Medical Center, both at the University of Washington. Medications were provided by Mayne Pharmaceuticals, and lab support by Hologic & Cepheid.
Dr. Lewin has the following disclosures: investigator-initiated, industry-funded research for Gilead, Viiv, Merck; scientific advisory board (honoraria paid to her personally) for Gilead, Merck, Viiv, Esfam, Immunocore, Vaxxinity; collaborative research (nonfunded) for AbbVie, Genentech, BMS. Dr. Luetkemeyer and Dr. Gandhi reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT AIDS 2022
U.S. clears 786,000 monkeypox vaccine doses for distribution
More than 780,000 doses of the JYNNEOS monkeypox vaccine will be available in the United States beginning July 29, the Department of Health & Human Services announced on July 28 in a press call.
HHS Secretary Xavier Becerra urged local and state public health departments to use these doses for preventive vaccination efforts to stay ahead of the virus and end the outbreak, noting that the HHS and Centers for Disease Control and Prevention do not control how vaccines are distributed at state and local levels. “We don’t have the authority to tell them what to do,” he said during the call. “We need them to work with us.”
As of July 28, there were 4,907 reported cases of monkeypox in the United States and officials expect cases will continue to rise in the coming weeks.
The vaccine is manufactured by the small Danish company Bavarian Nordic. These additional 786,000 doses were previously stored at a plant in Denmark, awaiting the completion of an inspection and authorization of the vaccine plant by the Food and Drug Administration. The agency announced on July 27 that both the vaccine doses and the manufacturing plant met standards.
With the announcement of these additional doses, the vaccine allocation plan is also being updated to take into account two important factors: the number of people at high risk in a jurisdiction and the number of new cases reported since the last vaccine allocation.
“This update gives greater weight to prioritizing vaccines to areas with the greatest number of people at risk, which includes men who have sex with men who have HIV or who are eligible for HIV pre-exposure prophylaxis, while still considering where we are seeing cases increase,” said Capt. Jennifer McQuiston, DVM, deputy director of the division of high consequence pathogens and pathology at the CDC.
Capt.McQuiston also provided additional demographic information on the U.S. outbreak. The median age of people with confirmed cases is 35 years old, with a range from 17 to 76. (This does not include the two cases in children reported on July 22.) Of the cases where sex at birth was provided, 99% were individuals assigned male sex at birth. In cases with reported ethnicity and race, 37% were non-Hispanic White people, 31% were Hispanic/Latino, 27% were Black or African American, and 4% were of Asian descent. The most common symptoms were rash – present in 99% of cases – malaise, fever, and swollen lymph nodes.
HHS and CDC did not have data on how many people have received at least one dose of the monkeypox vaccine. When asked how many people need to be fully vaccinated against monkeypox to contain the outbreak, Mr. Becerra did not provide an estimate but implied that preventive vaccination could help limit the number of vaccines needed and expressed optimism about quelling the outbreak in the United States. “We believe that we have done everything we can at the federal level to work with our state and local partners and communities affected to make sure we can stay ahead of this and end this outbreak,” he said, “but everybody’s got to do their part.”
A version of this article first appeared on Medscape.com.
More than 780,000 doses of the JYNNEOS monkeypox vaccine will be available in the United States beginning July 29, the Department of Health & Human Services announced on July 28 in a press call.
HHS Secretary Xavier Becerra urged local and state public health departments to use these doses for preventive vaccination efforts to stay ahead of the virus and end the outbreak, noting that the HHS and Centers for Disease Control and Prevention do not control how vaccines are distributed at state and local levels. “We don’t have the authority to tell them what to do,” he said during the call. “We need them to work with us.”
As of July 28, there were 4,907 reported cases of monkeypox in the United States and officials expect cases will continue to rise in the coming weeks.
The vaccine is manufactured by the small Danish company Bavarian Nordic. These additional 786,000 doses were previously stored at a plant in Denmark, awaiting the completion of an inspection and authorization of the vaccine plant by the Food and Drug Administration. The agency announced on July 27 that both the vaccine doses and the manufacturing plant met standards.
With the announcement of these additional doses, the vaccine allocation plan is also being updated to take into account two important factors: the number of people at high risk in a jurisdiction and the number of new cases reported since the last vaccine allocation.
“This update gives greater weight to prioritizing vaccines to areas with the greatest number of people at risk, which includes men who have sex with men who have HIV or who are eligible for HIV pre-exposure prophylaxis, while still considering where we are seeing cases increase,” said Capt. Jennifer McQuiston, DVM, deputy director of the division of high consequence pathogens and pathology at the CDC.
Capt.McQuiston also provided additional demographic information on the U.S. outbreak. The median age of people with confirmed cases is 35 years old, with a range from 17 to 76. (This does not include the two cases in children reported on July 22.) Of the cases where sex at birth was provided, 99% were individuals assigned male sex at birth. In cases with reported ethnicity and race, 37% were non-Hispanic White people, 31% were Hispanic/Latino, 27% were Black or African American, and 4% were of Asian descent. The most common symptoms were rash – present in 99% of cases – malaise, fever, and swollen lymph nodes.
HHS and CDC did not have data on how many people have received at least one dose of the monkeypox vaccine. When asked how many people need to be fully vaccinated against monkeypox to contain the outbreak, Mr. Becerra did not provide an estimate but implied that preventive vaccination could help limit the number of vaccines needed and expressed optimism about quelling the outbreak in the United States. “We believe that we have done everything we can at the federal level to work with our state and local partners and communities affected to make sure we can stay ahead of this and end this outbreak,” he said, “but everybody’s got to do their part.”
A version of this article first appeared on Medscape.com.
More than 780,000 doses of the JYNNEOS monkeypox vaccine will be available in the United States beginning July 29, the Department of Health & Human Services announced on July 28 in a press call.
HHS Secretary Xavier Becerra urged local and state public health departments to use these doses for preventive vaccination efforts to stay ahead of the virus and end the outbreak, noting that the HHS and Centers for Disease Control and Prevention do not control how vaccines are distributed at state and local levels. “We don’t have the authority to tell them what to do,” he said during the call. “We need them to work with us.”
As of July 28, there were 4,907 reported cases of monkeypox in the United States and officials expect cases will continue to rise in the coming weeks.
The vaccine is manufactured by the small Danish company Bavarian Nordic. These additional 786,000 doses were previously stored at a plant in Denmark, awaiting the completion of an inspection and authorization of the vaccine plant by the Food and Drug Administration. The agency announced on July 27 that both the vaccine doses and the manufacturing plant met standards.
With the announcement of these additional doses, the vaccine allocation plan is also being updated to take into account two important factors: the number of people at high risk in a jurisdiction and the number of new cases reported since the last vaccine allocation.
“This update gives greater weight to prioritizing vaccines to areas with the greatest number of people at risk, which includes men who have sex with men who have HIV or who are eligible for HIV pre-exposure prophylaxis, while still considering where we are seeing cases increase,” said Capt. Jennifer McQuiston, DVM, deputy director of the division of high consequence pathogens and pathology at the CDC.
Capt.McQuiston also provided additional demographic information on the U.S. outbreak. The median age of people with confirmed cases is 35 years old, with a range from 17 to 76. (This does not include the two cases in children reported on July 22.) Of the cases where sex at birth was provided, 99% were individuals assigned male sex at birth. In cases with reported ethnicity and race, 37% were non-Hispanic White people, 31% were Hispanic/Latino, 27% were Black or African American, and 4% were of Asian descent. The most common symptoms were rash – present in 99% of cases – malaise, fever, and swollen lymph nodes.
HHS and CDC did not have data on how many people have received at least one dose of the monkeypox vaccine. When asked how many people need to be fully vaccinated against monkeypox to contain the outbreak, Mr. Becerra did not provide an estimate but implied that preventive vaccination could help limit the number of vaccines needed and expressed optimism about quelling the outbreak in the United States. “We believe that we have done everything we can at the federal level to work with our state and local partners and communities affected to make sure we can stay ahead of this and end this outbreak,” he said, “but everybody’s got to do their part.”
A version of this article first appeared on Medscape.com.
Prolonged remission in patient with HIV may open new avenues to functional cure
MONTREAL – The case of a patient in an HIV study whose viral load dropped to undetectable levels and whose immune cells soared has captured the attention of organizers at a meeting of the International AIDS Society.
Although the 59-year-old woman is one of many who are known as posttreatment controllers (PTCs) – having been in remission for more than 15 years after stopping antiretroviral therapy (ART) –
“This case opens new avenues in the HIV functional-cure field,” lead investigator Núria Climent, PhD, of the HIV unit at Hospital Clinic-IDIBAPS/University of Barcelona, told this news organization.
“As far as we know, this is the first time that the gamma-delta T cells have been identified in a PTC, and concerning the memory-like NK cells, there are very few published data and only sparse information presented in several congresses,” she said, explaining that these cells “have a high capacity to inhibit the replication of the virus in vitro. For that reason, we think that this PTC has cells able to dramatically reduce the virus amount. We think that the potential capacity to increase these cells in this PTC woman could be not only mediated by especial genetic factors ... but also mediated by early ART treatment and might be by the immunomediated treatment.”
The findings suggest the potential for “increasing the amount of those memory-like NK cells and gamma-delta T cells in order to translate this potent antiviral activity in new therapies to achieve an HIV functional cure,” she said, adding: “As far as we know, aiming to increase these specific cells has never been done before in people living with HIV.”
In a press conference during the meeting, Dr. Climent explained that the patient was enrolled in a study in which she received a combination of ART and immunomodulatory therapy. This involved a combination of cyclosporine A, low-dose interleukin 2, granulocyte macrophage colony-stimulating factor, and pegylated interferon alfa-2b.
“None of the other 19 patients included in the trial controlled viral replication,” senior investigator Jose Miro, MD, PhD, also from the HIV unit at Hospital Clinic-IDIBAPS/University of Barcelona, told this news organization.
Sharon Lewin, MD, president-elect of the International AIDS Society, which runs the conference, said in an interview that although the significance of the case is unclear, the IAS selected it as a highlight for the meeting. “It is important for clinicians to understand the complexities in interpreting these case reports. Their patients are probably likely to ask them about the report, and it’s important [that] they can explain it to them.”
Dr. Lewin, who is professor of medicine at the University of Melbourne and director of the Peter Doherty Institute for Infection and Immunity in Melbourne, added that it is impossible to determine the mechanism of action from a single case report. “We don’t know if the intervention played a role or if this person is a ‘posttreatment controller,’ which has been previously described many times,” she said in an interview. “In this patient, the virus is at very low, but controlled, levels, and virus could be grown out. While it’s still exciting and important, this is really what we would consider a remission. The intense study of a single case such as this is certainly worthwhile and important but can only provide new ideas for research. So, I don’t think we can draw any conclusion on the role of NK cells, et cetera. We need much larger case series or controlled trials to reach any conclusion on the reasons for her remission.”
Dr. Climent disclosed no relevant financial conflicts of interest. Dr. Lewin has disclosed investigator-initiated industry-funded research (Gilead, ViiV, Merck), scientific advisory board honoraria paid to her personally (Gilead, Merck, ViiV, Esfam, Immunocore, Vaxxinity), and nonfunded collaborative research (AbbVie, Genentech, Bristol-Myers Squibb).
A version of this article first appeared on Medscape.com.
MONTREAL – The case of a patient in an HIV study whose viral load dropped to undetectable levels and whose immune cells soared has captured the attention of organizers at a meeting of the International AIDS Society.
Although the 59-year-old woman is one of many who are known as posttreatment controllers (PTCs) – having been in remission for more than 15 years after stopping antiretroviral therapy (ART) –
“This case opens new avenues in the HIV functional-cure field,” lead investigator Núria Climent, PhD, of the HIV unit at Hospital Clinic-IDIBAPS/University of Barcelona, told this news organization.
“As far as we know, this is the first time that the gamma-delta T cells have been identified in a PTC, and concerning the memory-like NK cells, there are very few published data and only sparse information presented in several congresses,” she said, explaining that these cells “have a high capacity to inhibit the replication of the virus in vitro. For that reason, we think that this PTC has cells able to dramatically reduce the virus amount. We think that the potential capacity to increase these cells in this PTC woman could be not only mediated by especial genetic factors ... but also mediated by early ART treatment and might be by the immunomediated treatment.”
The findings suggest the potential for “increasing the amount of those memory-like NK cells and gamma-delta T cells in order to translate this potent antiviral activity in new therapies to achieve an HIV functional cure,” she said, adding: “As far as we know, aiming to increase these specific cells has never been done before in people living with HIV.”
In a press conference during the meeting, Dr. Climent explained that the patient was enrolled in a study in which she received a combination of ART and immunomodulatory therapy. This involved a combination of cyclosporine A, low-dose interleukin 2, granulocyte macrophage colony-stimulating factor, and pegylated interferon alfa-2b.
“None of the other 19 patients included in the trial controlled viral replication,” senior investigator Jose Miro, MD, PhD, also from the HIV unit at Hospital Clinic-IDIBAPS/University of Barcelona, told this news organization.
Sharon Lewin, MD, president-elect of the International AIDS Society, which runs the conference, said in an interview that although the significance of the case is unclear, the IAS selected it as a highlight for the meeting. “It is important for clinicians to understand the complexities in interpreting these case reports. Their patients are probably likely to ask them about the report, and it’s important [that] they can explain it to them.”
Dr. Lewin, who is professor of medicine at the University of Melbourne and director of the Peter Doherty Institute for Infection and Immunity in Melbourne, added that it is impossible to determine the mechanism of action from a single case report. “We don’t know if the intervention played a role or if this person is a ‘posttreatment controller,’ which has been previously described many times,” she said in an interview. “In this patient, the virus is at very low, but controlled, levels, and virus could be grown out. While it’s still exciting and important, this is really what we would consider a remission. The intense study of a single case such as this is certainly worthwhile and important but can only provide new ideas for research. So, I don’t think we can draw any conclusion on the role of NK cells, et cetera. We need much larger case series or controlled trials to reach any conclusion on the reasons for her remission.”
Dr. Climent disclosed no relevant financial conflicts of interest. Dr. Lewin has disclosed investigator-initiated industry-funded research (Gilead, ViiV, Merck), scientific advisory board honoraria paid to her personally (Gilead, Merck, ViiV, Esfam, Immunocore, Vaxxinity), and nonfunded collaborative research (AbbVie, Genentech, Bristol-Myers Squibb).
A version of this article first appeared on Medscape.com.
MONTREAL – The case of a patient in an HIV study whose viral load dropped to undetectable levels and whose immune cells soared has captured the attention of organizers at a meeting of the International AIDS Society.
Although the 59-year-old woman is one of many who are known as posttreatment controllers (PTCs) – having been in remission for more than 15 years after stopping antiretroviral therapy (ART) –
“This case opens new avenues in the HIV functional-cure field,” lead investigator Núria Climent, PhD, of the HIV unit at Hospital Clinic-IDIBAPS/University of Barcelona, told this news organization.
“As far as we know, this is the first time that the gamma-delta T cells have been identified in a PTC, and concerning the memory-like NK cells, there are very few published data and only sparse information presented in several congresses,” she said, explaining that these cells “have a high capacity to inhibit the replication of the virus in vitro. For that reason, we think that this PTC has cells able to dramatically reduce the virus amount. We think that the potential capacity to increase these cells in this PTC woman could be not only mediated by especial genetic factors ... but also mediated by early ART treatment and might be by the immunomediated treatment.”
The findings suggest the potential for “increasing the amount of those memory-like NK cells and gamma-delta T cells in order to translate this potent antiviral activity in new therapies to achieve an HIV functional cure,” she said, adding: “As far as we know, aiming to increase these specific cells has never been done before in people living with HIV.”
In a press conference during the meeting, Dr. Climent explained that the patient was enrolled in a study in which she received a combination of ART and immunomodulatory therapy. This involved a combination of cyclosporine A, low-dose interleukin 2, granulocyte macrophage colony-stimulating factor, and pegylated interferon alfa-2b.
“None of the other 19 patients included in the trial controlled viral replication,” senior investigator Jose Miro, MD, PhD, also from the HIV unit at Hospital Clinic-IDIBAPS/University of Barcelona, told this news organization.
Sharon Lewin, MD, president-elect of the International AIDS Society, which runs the conference, said in an interview that although the significance of the case is unclear, the IAS selected it as a highlight for the meeting. “It is important for clinicians to understand the complexities in interpreting these case reports. Their patients are probably likely to ask them about the report, and it’s important [that] they can explain it to them.”
Dr. Lewin, who is professor of medicine at the University of Melbourne and director of the Peter Doherty Institute for Infection and Immunity in Melbourne, added that it is impossible to determine the mechanism of action from a single case report. “We don’t know if the intervention played a role or if this person is a ‘posttreatment controller,’ which has been previously described many times,” she said in an interview. “In this patient, the virus is at very low, but controlled, levels, and virus could be grown out. While it’s still exciting and important, this is really what we would consider a remission. The intense study of a single case such as this is certainly worthwhile and important but can only provide new ideas for research. So, I don’t think we can draw any conclusion on the role of NK cells, et cetera. We need much larger case series or controlled trials to reach any conclusion on the reasons for her remission.”
Dr. Climent disclosed no relevant financial conflicts of interest. Dr. Lewin has disclosed investigator-initiated industry-funded research (Gilead, ViiV, Merck), scientific advisory board honoraria paid to her personally (Gilead, Merck, ViiV, Esfam, Immunocore, Vaxxinity), and nonfunded collaborative research (AbbVie, Genentech, Bristol-Myers Squibb).
A version of this article first appeared on Medscape.com.
AT AIDS 2022


