User login
Autism tied to higher rates of self-harm, suicide
TOPLINE:
Even after accounting for sociodemographic factors, intellectual disabilities, and psychiatric diagnoses,
METHODOLOGY:
Evidence shows those with autism have over threefold greater odds than their counterparts without the disorder of self-injurious behavior, suicidal ideation, suicide attempt, or suicide death, but reasons for these elevated risks are unclear.
Using various linked databases in the province of Ontario, researchers identified all individuals with an autism diagnosis from April 1, 1988, to March 31, 2018, and matched each on age and sex to four nonautistic individuals for the comparison group.
Investigators created two cohorts to separately evaluate outcomes of self-harm events leading to emergency health care and suicide death with the accrual period for both cohorts beginning at a person’s 10th birthday.
The self-harm cohort included 379,630 individuals while the suicide cohort included 334,690 individuals.
TAKEAWAY:
Over 15 years, autistic females showed the highest cumulative self-harm events, followed by autistic males, nonautistic females, and nonautistic males; over 25 years, autistic males had the highest cumulative incidence of suicide death, followed by autistic females, nonautistic males, and nonautistic females.
Autism had independent associations with self-harm events (females: relative rate, 1.83 [95% confidence interval, 1.61-2.08]; males: RR, 1.47 [95% CI, 1.28-1.69]) even after accounting for sociodemographic factors (varied directions of associations), intellectual disabilities (associated with increased risks), and psychiatric diagnoses including mood and anxiety, psychotic, addiction, and personality disorders (associated with increased risks).
For both females and males, final models showed autism per se was not significantly associated with suicide death, but certain correlates were linked to risk. Among both sexes, intellectual disabilities were associated with reduced risks and psychiatric diagnoses were associated with increased risks.
As a substantial proportion (28.4%) of the suicide cohort did not have data on self-harm, researchers were unable to examine the association of self-harm with suicide death.
IN PRACTICE:
That psychiatric diagnoses increased suicide risks among people with autism suggests supports to reduce such risks “should consider multifactorial mechanisms, with a particular focus on the prevention and timely treatment of psychiatric illnesses,” write the authors.
SOURCE:
The study was conducted by Meng-Chuan Lai, MD, PhD, Centre for Addiction and Mental Health, Toronto, and colleagues. It was published online in JAMA Network Open.
LIMITATIONS:
The autism cohort didn’t capture those diagnosed in private practices or with subtle presentations not yet diagnosed. Misclassification of autistic people in the nonautistic cohort may have resulted in underestimation of suicide-related outcomes. The administrative data don’t reliably identify diagnoses associated with suicide risks such as attention-deficit/hyperactivity disorder or subcategories of mood disorders, and don’t contain information about risk and protective mechanisms of suicide behaviors such as family history.
DISCLOSURES:
The study received support from ICES, an independent nonprofit research institute; the Innovation Fund of the Alternative Funding Plan for the Academic Health Sciences Centres of Ontario; the Academic Scholars Award from the Department of Psychiatry, University of Toronto; and the Canadian Institutes of Health Research Sex and Gender Science Chair. Dr. Lai reported receiving personal fees from SAGE Publications as an editorial honorarium outside the submitted work. One coauthor reported receiving honoraria from the BMJ Group, Archives of Diseases in Childhood.
A version of this article first appeared on Medscape.com.
TOPLINE:
Even after accounting for sociodemographic factors, intellectual disabilities, and psychiatric diagnoses,
METHODOLOGY:
Evidence shows those with autism have over threefold greater odds than their counterparts without the disorder of self-injurious behavior, suicidal ideation, suicide attempt, or suicide death, but reasons for these elevated risks are unclear.
Using various linked databases in the province of Ontario, researchers identified all individuals with an autism diagnosis from April 1, 1988, to March 31, 2018, and matched each on age and sex to four nonautistic individuals for the comparison group.
Investigators created two cohorts to separately evaluate outcomes of self-harm events leading to emergency health care and suicide death with the accrual period for both cohorts beginning at a person’s 10th birthday.
The self-harm cohort included 379,630 individuals while the suicide cohort included 334,690 individuals.
TAKEAWAY:
Over 15 years, autistic females showed the highest cumulative self-harm events, followed by autistic males, nonautistic females, and nonautistic males; over 25 years, autistic males had the highest cumulative incidence of suicide death, followed by autistic females, nonautistic males, and nonautistic females.
Autism had independent associations with self-harm events (females: relative rate, 1.83 [95% confidence interval, 1.61-2.08]; males: RR, 1.47 [95% CI, 1.28-1.69]) even after accounting for sociodemographic factors (varied directions of associations), intellectual disabilities (associated with increased risks), and psychiatric diagnoses including mood and anxiety, psychotic, addiction, and personality disorders (associated with increased risks).
For both females and males, final models showed autism per se was not significantly associated with suicide death, but certain correlates were linked to risk. Among both sexes, intellectual disabilities were associated with reduced risks and psychiatric diagnoses were associated with increased risks.
As a substantial proportion (28.4%) of the suicide cohort did not have data on self-harm, researchers were unable to examine the association of self-harm with suicide death.
IN PRACTICE:
That psychiatric diagnoses increased suicide risks among people with autism suggests supports to reduce such risks “should consider multifactorial mechanisms, with a particular focus on the prevention and timely treatment of psychiatric illnesses,” write the authors.
SOURCE:
The study was conducted by Meng-Chuan Lai, MD, PhD, Centre for Addiction and Mental Health, Toronto, and colleagues. It was published online in JAMA Network Open.
LIMITATIONS:
The autism cohort didn’t capture those diagnosed in private practices or with subtle presentations not yet diagnosed. Misclassification of autistic people in the nonautistic cohort may have resulted in underestimation of suicide-related outcomes. The administrative data don’t reliably identify diagnoses associated with suicide risks such as attention-deficit/hyperactivity disorder or subcategories of mood disorders, and don’t contain information about risk and protective mechanisms of suicide behaviors such as family history.
DISCLOSURES:
The study received support from ICES, an independent nonprofit research institute; the Innovation Fund of the Alternative Funding Plan for the Academic Health Sciences Centres of Ontario; the Academic Scholars Award from the Department of Psychiatry, University of Toronto; and the Canadian Institutes of Health Research Sex and Gender Science Chair. Dr. Lai reported receiving personal fees from SAGE Publications as an editorial honorarium outside the submitted work. One coauthor reported receiving honoraria from the BMJ Group, Archives of Diseases in Childhood.
A version of this article first appeared on Medscape.com.
TOPLINE:
Even after accounting for sociodemographic factors, intellectual disabilities, and psychiatric diagnoses,
METHODOLOGY:
Evidence shows those with autism have over threefold greater odds than their counterparts without the disorder of self-injurious behavior, suicidal ideation, suicide attempt, or suicide death, but reasons for these elevated risks are unclear.
Using various linked databases in the province of Ontario, researchers identified all individuals with an autism diagnosis from April 1, 1988, to March 31, 2018, and matched each on age and sex to four nonautistic individuals for the comparison group.
Investigators created two cohorts to separately evaluate outcomes of self-harm events leading to emergency health care and suicide death with the accrual period for both cohorts beginning at a person’s 10th birthday.
The self-harm cohort included 379,630 individuals while the suicide cohort included 334,690 individuals.
TAKEAWAY:
Over 15 years, autistic females showed the highest cumulative self-harm events, followed by autistic males, nonautistic females, and nonautistic males; over 25 years, autistic males had the highest cumulative incidence of suicide death, followed by autistic females, nonautistic males, and nonautistic females.
Autism had independent associations with self-harm events (females: relative rate, 1.83 [95% confidence interval, 1.61-2.08]; males: RR, 1.47 [95% CI, 1.28-1.69]) even after accounting for sociodemographic factors (varied directions of associations), intellectual disabilities (associated with increased risks), and psychiatric diagnoses including mood and anxiety, psychotic, addiction, and personality disorders (associated with increased risks).
For both females and males, final models showed autism per se was not significantly associated with suicide death, but certain correlates were linked to risk. Among both sexes, intellectual disabilities were associated with reduced risks and psychiatric diagnoses were associated with increased risks.
As a substantial proportion (28.4%) of the suicide cohort did not have data on self-harm, researchers were unable to examine the association of self-harm with suicide death.
IN PRACTICE:
That psychiatric diagnoses increased suicide risks among people with autism suggests supports to reduce such risks “should consider multifactorial mechanisms, with a particular focus on the prevention and timely treatment of psychiatric illnesses,” write the authors.
SOURCE:
The study was conducted by Meng-Chuan Lai, MD, PhD, Centre for Addiction and Mental Health, Toronto, and colleagues. It was published online in JAMA Network Open.
LIMITATIONS:
The autism cohort didn’t capture those diagnosed in private practices or with subtle presentations not yet diagnosed. Misclassification of autistic people in the nonautistic cohort may have resulted in underestimation of suicide-related outcomes. The administrative data don’t reliably identify diagnoses associated with suicide risks such as attention-deficit/hyperactivity disorder or subcategories of mood disorders, and don’t contain information about risk and protective mechanisms of suicide behaviors such as family history.
DISCLOSURES:
The study received support from ICES, an independent nonprofit research institute; the Innovation Fund of the Alternative Funding Plan for the Academic Health Sciences Centres of Ontario; the Academic Scholars Award from the Department of Psychiatry, University of Toronto; and the Canadian Institutes of Health Research Sex and Gender Science Chair. Dr. Lai reported receiving personal fees from SAGE Publications as an editorial honorarium outside the submitted work. One coauthor reported receiving honoraria from the BMJ Group, Archives of Diseases in Childhood.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
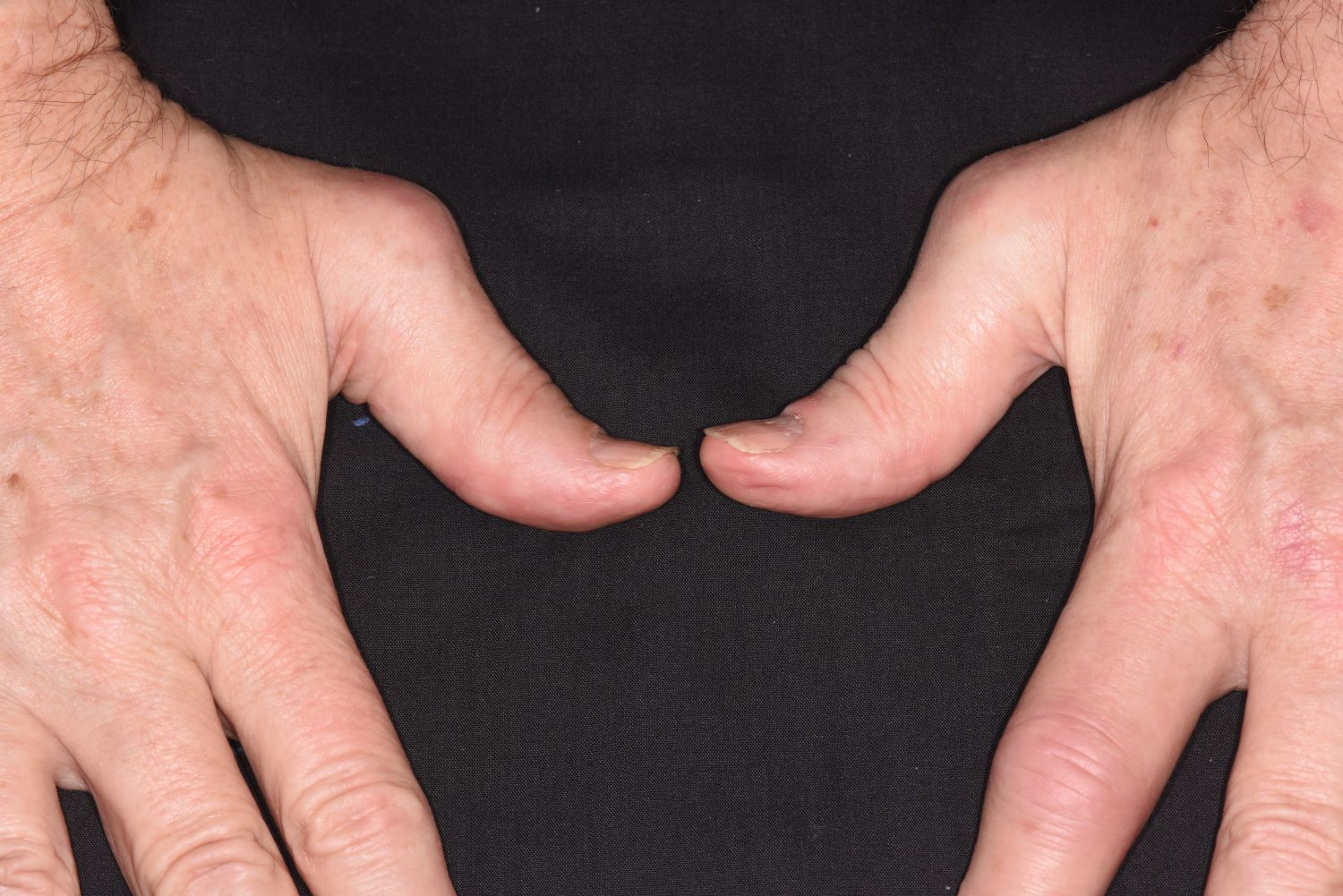
PsA biomarkers move researchers closer to predictive test
In a new study, researchers report that they have found epigenetic methylation markers on 15 genes that appear to foreshadow psoriatic arthritis (PsA), a development that could bring scientists closer to developing a DNA test to predict which patients with psoriasis will develop the condition.
While no predictive test is in sight yet, the findings published in Arthritis & Rheumatology mark an important step, study lead author Omar F. Cruz-Correa, PhD, of the Psoriatic Arthritis Research Program in the University Health Network, Toronto, said in an interview. “In the future, markers like these could be measured by dermatologists and even general practitioners to help identify new psoriasis patients at a high risk of developing PsA,” he said. “Then both the health care team and the patients themselves could be more aware of their increased risk and the pressing need of closer monitoring for musculoskeletal symptoms. Once the first symptoms appear, treatment can be initiated early on, helping to prevent permanent joint damage.”
An estimated 30% of patients with psoriasis will develop PsA, too, putting them at higher risk of disability and death. According to Dr. Cruz-Correa, “one of the more pressing matters in PsA is the lack of means of predicting which psoriasis patients will develop PsA.”
DNA methylation, the topic of the new study, has already been linked to psoriasis and PsA. It’s “relatively easy to measure and helps regulate gene expression in response to environmental effects,” Dr. Cruz-Correa said. “DNA methylation is also appealing because it serves as an intermediary between environment and genetic factors as it’s transmitted between generations of cells and influenced by external factors.”
For the new study, researchers examined the DNA of 117 patients with psoriasis – 58 who went on to develop PsA (“converters”) and another 59 who were matched to converters but did not develop PsA (“nonconverters”). The patients were in a larger group of 700 patients with psoriasis who had the disease for a mean of about 17 years at the time of blood sampling.
Samples from converters were taken an average of 5.16 years (± 12.77 years) before PsA set in.
The researchers report that they found “36 highly relevant methylation markers … across 15 genes and several intergenic regions. A classification model relying on these markers identified converters and nonconverters with an area under the ROC curve of 0.9644.”
Statistically, this number is high and means that “the DNA methylation markers are really good at identifying psoriasis patients who will develop PsA and those that will not,” at least in this specific patient group, Dr. Cruz-Correa said.
At this point, the number of markers is a bit too high to develop a feasible DNA test to predict PsA, he said. “However, the results from our study have also pointed us toward some interesting metabolic pathways that may warrant further study.”
What’s next?
The first step forward “is the validation of these predictive DNA methylation markers in a wider population of patients with varied clinical and demographic characteristics. This would help assess the potential for generalization of such a test,” Dr. Cruz-Correa said. “A second step is to assess the potential impact of these methylation markers on disease activity and treatment response, which are clinical outcomes of great importance to patients.”
Meanwhile, he said, “there are ongoing efforts to shed light into how DNA methylation integrates with other epigenetic mechanisms like micro-RNAs to regulate gene expression in concert with one another. An integrative look into these mechanisms may be able to give insight into the pathogenesis of psoriatic disease in a way that has not been possible before.”
In an interview, Johann E. Gudjonsson, MD, PhD, professor of skin molecular immunology at the University of Michigan, Ann Arbor, said the study “is interesting and important as it indicates that there are changes in the blood that occur before the development of psoriatic arthritis. However, it does not provide much in terms of novel insights into the mechanisms involved and is still a long way away from being useful as a clinical predictor or biomarker.”
The National Psoriasis Foundation, Krembil Foundation, and Canadian Institutes of Health Research provided support for the study. Dr. Cruz-Correa reports support from the National Psoriasis Foundation and the Arthritis Society. Dr. Gudjonsson has no relevant financial relationships.
In a new study, researchers report that they have found epigenetic methylation markers on 15 genes that appear to foreshadow psoriatic arthritis (PsA), a development that could bring scientists closer to developing a DNA test to predict which patients with psoriasis will develop the condition.
While no predictive test is in sight yet, the findings published in Arthritis & Rheumatology mark an important step, study lead author Omar F. Cruz-Correa, PhD, of the Psoriatic Arthritis Research Program in the University Health Network, Toronto, said in an interview. “In the future, markers like these could be measured by dermatologists and even general practitioners to help identify new psoriasis patients at a high risk of developing PsA,” he said. “Then both the health care team and the patients themselves could be more aware of their increased risk and the pressing need of closer monitoring for musculoskeletal symptoms. Once the first symptoms appear, treatment can be initiated early on, helping to prevent permanent joint damage.”
An estimated 30% of patients with psoriasis will develop PsA, too, putting them at higher risk of disability and death. According to Dr. Cruz-Correa, “one of the more pressing matters in PsA is the lack of means of predicting which psoriasis patients will develop PsA.”
DNA methylation, the topic of the new study, has already been linked to psoriasis and PsA. It’s “relatively easy to measure and helps regulate gene expression in response to environmental effects,” Dr. Cruz-Correa said. “DNA methylation is also appealing because it serves as an intermediary between environment and genetic factors as it’s transmitted between generations of cells and influenced by external factors.”
For the new study, researchers examined the DNA of 117 patients with psoriasis – 58 who went on to develop PsA (“converters”) and another 59 who were matched to converters but did not develop PsA (“nonconverters”). The patients were in a larger group of 700 patients with psoriasis who had the disease for a mean of about 17 years at the time of blood sampling.
Samples from converters were taken an average of 5.16 years (± 12.77 years) before PsA set in.
The researchers report that they found “36 highly relevant methylation markers … across 15 genes and several intergenic regions. A classification model relying on these markers identified converters and nonconverters with an area under the ROC curve of 0.9644.”
Statistically, this number is high and means that “the DNA methylation markers are really good at identifying psoriasis patients who will develop PsA and those that will not,” at least in this specific patient group, Dr. Cruz-Correa said.
At this point, the number of markers is a bit too high to develop a feasible DNA test to predict PsA, he said. “However, the results from our study have also pointed us toward some interesting metabolic pathways that may warrant further study.”
What’s next?
The first step forward “is the validation of these predictive DNA methylation markers in a wider population of patients with varied clinical and demographic characteristics. This would help assess the potential for generalization of such a test,” Dr. Cruz-Correa said. “A second step is to assess the potential impact of these methylation markers on disease activity and treatment response, which are clinical outcomes of great importance to patients.”
Meanwhile, he said, “there are ongoing efforts to shed light into how DNA methylation integrates with other epigenetic mechanisms like micro-RNAs to regulate gene expression in concert with one another. An integrative look into these mechanisms may be able to give insight into the pathogenesis of psoriatic disease in a way that has not been possible before.”
In an interview, Johann E. Gudjonsson, MD, PhD, professor of skin molecular immunology at the University of Michigan, Ann Arbor, said the study “is interesting and important as it indicates that there are changes in the blood that occur before the development of psoriatic arthritis. However, it does not provide much in terms of novel insights into the mechanisms involved and is still a long way away from being useful as a clinical predictor or biomarker.”
The National Psoriasis Foundation, Krembil Foundation, and Canadian Institutes of Health Research provided support for the study. Dr. Cruz-Correa reports support from the National Psoriasis Foundation and the Arthritis Society. Dr. Gudjonsson has no relevant financial relationships.
In a new study, researchers report that they have found epigenetic methylation markers on 15 genes that appear to foreshadow psoriatic arthritis (PsA), a development that could bring scientists closer to developing a DNA test to predict which patients with psoriasis will develop the condition.
While no predictive test is in sight yet, the findings published in Arthritis & Rheumatology mark an important step, study lead author Omar F. Cruz-Correa, PhD, of the Psoriatic Arthritis Research Program in the University Health Network, Toronto, said in an interview. “In the future, markers like these could be measured by dermatologists and even general practitioners to help identify new psoriasis patients at a high risk of developing PsA,” he said. “Then both the health care team and the patients themselves could be more aware of their increased risk and the pressing need of closer monitoring for musculoskeletal symptoms. Once the first symptoms appear, treatment can be initiated early on, helping to prevent permanent joint damage.”
An estimated 30% of patients with psoriasis will develop PsA, too, putting them at higher risk of disability and death. According to Dr. Cruz-Correa, “one of the more pressing matters in PsA is the lack of means of predicting which psoriasis patients will develop PsA.”
DNA methylation, the topic of the new study, has already been linked to psoriasis and PsA. It’s “relatively easy to measure and helps regulate gene expression in response to environmental effects,” Dr. Cruz-Correa said. “DNA methylation is also appealing because it serves as an intermediary between environment and genetic factors as it’s transmitted between generations of cells and influenced by external factors.”
For the new study, researchers examined the DNA of 117 patients with psoriasis – 58 who went on to develop PsA (“converters”) and another 59 who were matched to converters but did not develop PsA (“nonconverters”). The patients were in a larger group of 700 patients with psoriasis who had the disease for a mean of about 17 years at the time of blood sampling.
Samples from converters were taken an average of 5.16 years (± 12.77 years) before PsA set in.
The researchers report that they found “36 highly relevant methylation markers … across 15 genes and several intergenic regions. A classification model relying on these markers identified converters and nonconverters with an area under the ROC curve of 0.9644.”
Statistically, this number is high and means that “the DNA methylation markers are really good at identifying psoriasis patients who will develop PsA and those that will not,” at least in this specific patient group, Dr. Cruz-Correa said.
At this point, the number of markers is a bit too high to develop a feasible DNA test to predict PsA, he said. “However, the results from our study have also pointed us toward some interesting metabolic pathways that may warrant further study.”
What’s next?
The first step forward “is the validation of these predictive DNA methylation markers in a wider population of patients with varied clinical and demographic characteristics. This would help assess the potential for generalization of such a test,” Dr. Cruz-Correa said. “A second step is to assess the potential impact of these methylation markers on disease activity and treatment response, which are clinical outcomes of great importance to patients.”
Meanwhile, he said, “there are ongoing efforts to shed light into how DNA methylation integrates with other epigenetic mechanisms like micro-RNAs to regulate gene expression in concert with one another. An integrative look into these mechanisms may be able to give insight into the pathogenesis of psoriatic disease in a way that has not been possible before.”
In an interview, Johann E. Gudjonsson, MD, PhD, professor of skin molecular immunology at the University of Michigan, Ann Arbor, said the study “is interesting and important as it indicates that there are changes in the blood that occur before the development of psoriatic arthritis. However, it does not provide much in terms of novel insights into the mechanisms involved and is still a long way away from being useful as a clinical predictor or biomarker.”
The National Psoriasis Foundation, Krembil Foundation, and Canadian Institutes of Health Research provided support for the study. Dr. Cruz-Correa reports support from the National Psoriasis Foundation and the Arthritis Society. Dr. Gudjonsson has no relevant financial relationships.
FROM ARTHRITIS & RHEUMATOLOGY
Nearly 1 in 100 people diagnosed with IBD in the U.S.
(IBD), and up to 56,000 new cases are diagnosed each year.
“The prevalence of IBD in the United States has been gradually increasing over the last decade, and thus the burden of caring for IBD is likely to increase as life expectancy increases,” said co-principal investigator Andrés Hurtado-Lorenzo, PhD, senior vice president, Translational Research and IBD Ventures, Crohn’s & Colitis Foundation.
These data provide “an initial step toward optimizing health care resources allocation and improving care of individuals with IBD,” said Manasi Agrawal, MD, a gastroenterologist at Mount Sinai Hospital, New York, who wasn’t involved in the study.
The study was published online in Gastroenterology.
For the federally funded study, researchers pooled data from commercial, Medicare, and Medicaid insurance plans to derive a population-based estimate of the incidence and prevalence of IBD throughout the United States.
“In essence, we consider this to be the most extensive study of the incidence and prevalence of IBD in the United States based on physician-diagnosed IBD, which is representative of nearly the entire U.S. population with health insurance,” Dr. Hurtado-Lorenzo said.
Trends identified
Key findings from the study include the following.
- The age- and sex-standardized incidence of IBD was 10.9 per 100,000 person years.
- The incidence of IBD peaks in the third decade of life, decreases to a relatively stable level across the fourth to eighth decades, and declines further beyond age 80.
- Ulcerative colitis is slightly more common than Crohn’s disease in most age groups, except in children, among whom this trend is reversed.
- The adjusted prevalence data show that IBD has been diagnosed in more than 0.7% of Americans, with 721 cases per 100,000, or nearly 1 in 100.
- Historically, IBD was slightly more common in men. Now it’s slightly more common in adult women and male children.
- IBD prevalence is highest in the Northeast and lowest in the western region of the United States.
- The overall prevalence of IBD increased gradually from 2011 to 2020.
“Environmental variables, such as ultra-processed foods, pollution, and urbanization, to name a few, are implicated in IBD risk. Shifts in our modern environment and improving diagnostics may be two reasons why we see rising trends in IBD,” said Dr. Agrawal, assistant professor of medicine at the Icahn School of Medicine at Mount Sinai.
Prevalence highest among Whites
The data also point to significant differences in prevalence among different racial groups in the United States, with Whites having a rate of IBD that is seven times higher than Blacks, six times higher than Hispanics, and 21 times higher than Asians.
The prevalence of IBD per 100,000 population was 812 in Whites, 504 in Blacks, 403 in Asians, and 458 in Hispanics.
“It’s important to note that the reasons for ethnic disparities in IBD prevalence are complex and multifactorial, and further research is needed to better understand the specific mechanisms underlying these disparities,” said Dr. Hurtado-Lorenzo said.
Factors that could contribute to this disparity include genetic and environmental factors, socioeconomic factors, health care disparities, differences in disease awareness and reporting, and underdiagnosis in some populations.
The data suggest a lower prevalence of IBD among children with Medicaid insurance, “which underscores the need for further investigation into the influence of social determinants of health on IBD care,” Dr. Hurtado-Lorenzo said.
Insights important for planning
Because of the fragmented nature of the health care system, it’s been challenging to get an accurate estimate of how many patients in the United States have IBD, said Ashwin Ananthakrishnan, MD, MPH, a gastroenterologist with Massachusetts General Hospital and Harvard Medical School, Boston.
“The authors and involved organizations are to be fully complemented on this really ambitious and important study. Having an idea of how common IBD is and how it is likely to increase in prevalence is important for resource planning for organizations and health care systems,” said Dr. Ananthakrishnan, who was not involved in the study.
Although IBD incidence and prevalence is lower in non-White populations, there is still a “sizeable burden of IBD in those groups, and it’s important to understand the implications of that in terms of disease biology, treatment availability, disparities, and access to care,” he added.
“With the aging of the population and increasing prevalence, it is also important to understand that the ‘face of IBD’ in the coming decades may be different than what we traditionally have estimated it to be. This is also important to incorporate in decision-making,” Dr. Ananthakrishnan said.
Funding for the study was provided by the Centers for Disease Control and Prevention. Dr. Hurtado-Lorenzo, Dr. Agrawal, and Dr. Ananthakrishnan have declared no relevant disclosures.
A version of this article first appeared on Medscape.com.
(IBD), and up to 56,000 new cases are diagnosed each year.
“The prevalence of IBD in the United States has been gradually increasing over the last decade, and thus the burden of caring for IBD is likely to increase as life expectancy increases,” said co-principal investigator Andrés Hurtado-Lorenzo, PhD, senior vice president, Translational Research and IBD Ventures, Crohn’s & Colitis Foundation.
These data provide “an initial step toward optimizing health care resources allocation and improving care of individuals with IBD,” said Manasi Agrawal, MD, a gastroenterologist at Mount Sinai Hospital, New York, who wasn’t involved in the study.
The study was published online in Gastroenterology.
For the federally funded study, researchers pooled data from commercial, Medicare, and Medicaid insurance plans to derive a population-based estimate of the incidence and prevalence of IBD throughout the United States.
“In essence, we consider this to be the most extensive study of the incidence and prevalence of IBD in the United States based on physician-diagnosed IBD, which is representative of nearly the entire U.S. population with health insurance,” Dr. Hurtado-Lorenzo said.
Trends identified
Key findings from the study include the following.
- The age- and sex-standardized incidence of IBD was 10.9 per 100,000 person years.
- The incidence of IBD peaks in the third decade of life, decreases to a relatively stable level across the fourth to eighth decades, and declines further beyond age 80.
- Ulcerative colitis is slightly more common than Crohn’s disease in most age groups, except in children, among whom this trend is reversed.
- The adjusted prevalence data show that IBD has been diagnosed in more than 0.7% of Americans, with 721 cases per 100,000, or nearly 1 in 100.
- Historically, IBD was slightly more common in men. Now it’s slightly more common in adult women and male children.
- IBD prevalence is highest in the Northeast and lowest in the western region of the United States.
- The overall prevalence of IBD increased gradually from 2011 to 2020.
“Environmental variables, such as ultra-processed foods, pollution, and urbanization, to name a few, are implicated in IBD risk. Shifts in our modern environment and improving diagnostics may be two reasons why we see rising trends in IBD,” said Dr. Agrawal, assistant professor of medicine at the Icahn School of Medicine at Mount Sinai.
Prevalence highest among Whites
The data also point to significant differences in prevalence among different racial groups in the United States, with Whites having a rate of IBD that is seven times higher than Blacks, six times higher than Hispanics, and 21 times higher than Asians.
The prevalence of IBD per 100,000 population was 812 in Whites, 504 in Blacks, 403 in Asians, and 458 in Hispanics.
“It’s important to note that the reasons for ethnic disparities in IBD prevalence are complex and multifactorial, and further research is needed to better understand the specific mechanisms underlying these disparities,” said Dr. Hurtado-Lorenzo said.
Factors that could contribute to this disparity include genetic and environmental factors, socioeconomic factors, health care disparities, differences in disease awareness and reporting, and underdiagnosis in some populations.
The data suggest a lower prevalence of IBD among children with Medicaid insurance, “which underscores the need for further investigation into the influence of social determinants of health on IBD care,” Dr. Hurtado-Lorenzo said.
Insights important for planning
Because of the fragmented nature of the health care system, it’s been challenging to get an accurate estimate of how many patients in the United States have IBD, said Ashwin Ananthakrishnan, MD, MPH, a gastroenterologist with Massachusetts General Hospital and Harvard Medical School, Boston.
“The authors and involved organizations are to be fully complemented on this really ambitious and important study. Having an idea of how common IBD is and how it is likely to increase in prevalence is important for resource planning for organizations and health care systems,” said Dr. Ananthakrishnan, who was not involved in the study.
Although IBD incidence and prevalence is lower in non-White populations, there is still a “sizeable burden of IBD in those groups, and it’s important to understand the implications of that in terms of disease biology, treatment availability, disparities, and access to care,” he added.
“With the aging of the population and increasing prevalence, it is also important to understand that the ‘face of IBD’ in the coming decades may be different than what we traditionally have estimated it to be. This is also important to incorporate in decision-making,” Dr. Ananthakrishnan said.
Funding for the study was provided by the Centers for Disease Control and Prevention. Dr. Hurtado-Lorenzo, Dr. Agrawal, and Dr. Ananthakrishnan have declared no relevant disclosures.
A version of this article first appeared on Medscape.com.
(IBD), and up to 56,000 new cases are diagnosed each year.
“The prevalence of IBD in the United States has been gradually increasing over the last decade, and thus the burden of caring for IBD is likely to increase as life expectancy increases,” said co-principal investigator Andrés Hurtado-Lorenzo, PhD, senior vice president, Translational Research and IBD Ventures, Crohn’s & Colitis Foundation.
These data provide “an initial step toward optimizing health care resources allocation and improving care of individuals with IBD,” said Manasi Agrawal, MD, a gastroenterologist at Mount Sinai Hospital, New York, who wasn’t involved in the study.
The study was published online in Gastroenterology.
For the federally funded study, researchers pooled data from commercial, Medicare, and Medicaid insurance plans to derive a population-based estimate of the incidence and prevalence of IBD throughout the United States.
“In essence, we consider this to be the most extensive study of the incidence and prevalence of IBD in the United States based on physician-diagnosed IBD, which is representative of nearly the entire U.S. population with health insurance,” Dr. Hurtado-Lorenzo said.
Trends identified
Key findings from the study include the following.
- The age- and sex-standardized incidence of IBD was 10.9 per 100,000 person years.
- The incidence of IBD peaks in the third decade of life, decreases to a relatively stable level across the fourth to eighth decades, and declines further beyond age 80.
- Ulcerative colitis is slightly more common than Crohn’s disease in most age groups, except in children, among whom this trend is reversed.
- The adjusted prevalence data show that IBD has been diagnosed in more than 0.7% of Americans, with 721 cases per 100,000, or nearly 1 in 100.
- Historically, IBD was slightly more common in men. Now it’s slightly more common in adult women and male children.
- IBD prevalence is highest in the Northeast and lowest in the western region of the United States.
- The overall prevalence of IBD increased gradually from 2011 to 2020.
“Environmental variables, such as ultra-processed foods, pollution, and urbanization, to name a few, are implicated in IBD risk. Shifts in our modern environment and improving diagnostics may be two reasons why we see rising trends in IBD,” said Dr. Agrawal, assistant professor of medicine at the Icahn School of Medicine at Mount Sinai.
Prevalence highest among Whites
The data also point to significant differences in prevalence among different racial groups in the United States, with Whites having a rate of IBD that is seven times higher than Blacks, six times higher than Hispanics, and 21 times higher than Asians.
The prevalence of IBD per 100,000 population was 812 in Whites, 504 in Blacks, 403 in Asians, and 458 in Hispanics.
“It’s important to note that the reasons for ethnic disparities in IBD prevalence are complex and multifactorial, and further research is needed to better understand the specific mechanisms underlying these disparities,” said Dr. Hurtado-Lorenzo said.
Factors that could contribute to this disparity include genetic and environmental factors, socioeconomic factors, health care disparities, differences in disease awareness and reporting, and underdiagnosis in some populations.
The data suggest a lower prevalence of IBD among children with Medicaid insurance, “which underscores the need for further investigation into the influence of social determinants of health on IBD care,” Dr. Hurtado-Lorenzo said.
Insights important for planning
Because of the fragmented nature of the health care system, it’s been challenging to get an accurate estimate of how many patients in the United States have IBD, said Ashwin Ananthakrishnan, MD, MPH, a gastroenterologist with Massachusetts General Hospital and Harvard Medical School, Boston.
“The authors and involved organizations are to be fully complemented on this really ambitious and important study. Having an idea of how common IBD is and how it is likely to increase in prevalence is important for resource planning for organizations and health care systems,” said Dr. Ananthakrishnan, who was not involved in the study.
Although IBD incidence and prevalence is lower in non-White populations, there is still a “sizeable burden of IBD in those groups, and it’s important to understand the implications of that in terms of disease biology, treatment availability, disparities, and access to care,” he added.
“With the aging of the population and increasing prevalence, it is also important to understand that the ‘face of IBD’ in the coming decades may be different than what we traditionally have estimated it to be. This is also important to incorporate in decision-making,” Dr. Ananthakrishnan said.
Funding for the study was provided by the Centers for Disease Control and Prevention. Dr. Hurtado-Lorenzo, Dr. Agrawal, and Dr. Ananthakrishnan have declared no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM GASTROENTEROLOGY
Low-dose colchicine for ASCVD: Your questions answered
This transcript has been edited for clarity.
Dr. O’Donoghue: We’re going to discuss a very important and emerging topic, which is the use of low-dose colchicine. I think there’s much interest in the use of this drug, which now has a Food and Drug Administration indication, which we’ll talk about further, and it’s also been written into both European and American guidelines that have been recently released.
who’s been at the forefront of research into anti-inflammatory therapeutics.
Lifestyle lipid-lowering paramount
Dr. O’Donoghue: As we think about the concept behind the use of colchicine, we’ve obviously done a large amount of research into lipid-lowering drugs, but where does colchicine now fit in?
Dr. Ridker: Let’s make sure we get the basics down. Anti-inflammatory therapy is going to be added on top of quality other care. This is not a replacement for lipids; it’s not a change in diet, exercise, and smoking cessation. The new data are really telling us that a patient who’s aggressively treated to guideline-recommended levels can still do much better in terms of preventing heart attack, stroke, cardiovascular death, and revascularization by adding low-dose colchicine as the first proven anti-inflammatory therapy for atherosclerotic disease.
I have to say, Michelle, for me, it’s been a wonderful end of a journey in many ways. This story starts almost 30 years ago for quite a few of us, thinking about inflammation and atherosclerosis. The whole C-reactive protein (CRP) story is still an ongoing one. We recently showed, for example, that residual inflammatory risk in some 30,000 patients, all taking a statin, was a far better predictor of the likelihood of more cardiovascular events, in particular cardiovascular death, than was residual cholesterol risk.
Think about that. We’re all aggressively giving second lipid-lowering drugs in our very sick patients, but that means inflammation is really the untapped piece of this.
The two clinical trials we have in front of us, the COLCOT trial and the LoDoCo2 trial – both New England Journal of Medicine papers, both with roughly 5,000 patients – provide very clear evidence that following a relatively recent myocardial infarction (that’s COLCOT) in chronic stable atherosclerosis (that’s LoDoCo2), we’re getting 25%-30% relative risk reductions in major adverse cardiovascular events (MACEs) on top of aggressive statin therapy. That’s a big deal. It’s safe, it works, and it’s fully consistent with all the information we have about inflammation being part and parcel of atherosclerosis. It’s a pretty exciting time.
Inflammatory pathway
Dr. O’Donoghue: It beautifully proves the inflammatory hypothesis in many ways. You led CANTOS, and that was a much more specific target. Here, in terms of the effects of colchicine, what do we know about how it may work on the inflammatory cascade?
Dr. Ridker: Our CANTOS trial was proof of principle that you could directly target, with a very specific monoclonal antibody, a specific piece of this innate immune cascade and lower cardiovascular event rates.
Colchicine is a more broad-spectrum drug. It does have a number of antineutrophil effects – that’s important, by the way. Neutrophils are really becoming very important in atherosclerotic disease progression. It’s an indirect inhibitor of the so-called NLRP3 inflammasome, which is where both interleukin-1 (that’s the target for canakinumab) and IL-6 are up-regulated. As you know, it’s been used to treat gout and pericarditis in high doses in short, little bursts.
The change here is this use of low-dose colchicine, that’s 0.5 mg once a day for years to treat chronic, stable atherosclerosis. It is very much like using a statin. The idea here is to prevent the progression of the disease by slowing down and maybe stabilizing the plaque so we have fewer heart attacks and strokes down the road.
It’s entering the armamentarium – at least my armamentarium – as chronic, stable secondary prevention. That’s where the new American College of Cardiology/American Heart Association guidelines also put it. It’s really in as a treatment for chronic, stable atherosclerosis. I think that’s where it belongs.
When to start colchicine, and in whom?
Dr. O’Donoghue: To that point, as we think about the efficacy, I think it’s nice, as you outlined, that we have two complementary trials that are both showing a consistent reduction in MACEs, one in the post–acute coronary syndrome (ACS) state and one for more chronic patients.
At what point do you think would be the appropriate time to start therapy, and who would you be starting it for?
Dr. Ridker: Michelle, that’s a great question. There’s a very interesting analysis that just came out from the LoDoCo2 investigators. It’s kind of a landmark analysis. What they show is that 1 year, 2 years, 3 years, and 4 years since the initiating myocardial infarction, the drug is very effective.
In fact, you could think about starting this drug at your clinic in patients with chronic, stable atherosclerotic disease. That’s just like we would start a statin in people who had a heart attack some time ago, and that’s absolutely fine.
I’m using it for what I call my frequent fliers, those patients who just keep coming back. They’re already on aggressive lipid-lowering therapy. I have them on beta-blockers, aspirin, and all the usual things. I say, look, I can get a large risk reduction by starting them on this drug.
There are a few caveats, Michelle. Like all drugs, colchicine comes with some adverse effects. Most of them are pretty rare, but there are some patients I would not give this drug to, just to be very clear. Colchicine is cleared by the kidney and by the liver. Patients who have severe chronic kidney disease and severe liver disease – this is a no-go for those patients. We should talk about where patients in that realm might want to go.
Then there are some unusual drugs. Colchicine is metabolized by the CYP3A4 and the P-glycoprotein pathway. There are a few drugs, such as ketoconazole, fluconazole, and cyclosporine, that if your primary care doctor or internist is going to start for a short term, you probably want to stop your colchicine for a week or two.
In people with familial Mediterranean fever, for whom colchicine is lifesaving and life-changing and who take it for 20, 30, or 40 years, there’s been no increase in risk for cancer. There have been very few adverse effects. I think it’s interesting that we, who practice in North America, basically never see familial Mediterranean fever. If we were practicing in Lebanon, Israel, or North Africa, this would be a very common therapy that we’d all be extremely familiar with.
Dr. O’Donoghue: To that point, it’s interesting to hear that colchicine was even used by the ancient Greeks and ancient Egyptians. It’s a drug that’s been around for a long time.
In terms of its safety, some people have been talking about the fact that an increase in noncardiovascular death was seen in LoDoCo2. What are your thoughts on that? Is that anything that we should be concerned about?
Colchicine safety and contraindications
Dr. Ridker: First, to set the record straight, a meta-analysis has been done of all-cause mortality in the various colchicine trials, and the hazard ratio is 1.04. I’ll remind you, and all of us know, that the hazard ratios for all-cause mortality in the PCSK9 trials, the bempedoic acid trials, and the ezetimibe trials are also essentially neutral. We’re in a state where we don’t let these trials roll long enough to see benefits necessarily on all-cause mortality. Some of us think we probably should, but that’s just the reality of trials.
One of most interesting things that was part of the FDA review, I suspect, was that there was no specific cause of any of this. It was not like there was a set of particular issues. I suspect that most people think this is probably the play of chance and with time, things will get better.
Again, I do want to emphasize this is not a drug for severe chronic kidney disease and severe liver disease, because those patients will get in trouble with this. The other thing that’s worth knowing is when you start a patient on low-dose colchicine – that’s 0.5 mg/d – there will be some patients who get some short-term gastrointestinal upset. That’s very common when you start colchicine at the much higher doses you might use to treat acute gout or pericarditis. In these trials, the vast majority of patients treated through that, and there were very few episodes long-term. I think it’s generally safe. That’s where we’re at.
Dr. O’Donoghue: Paul, you’ve been a leader, certainly, at looking at CRP as a marker of inflammation. Do you, in your practice, consider CRP levels when making a decision about who is appropriate for this therapy?
Dr. Ridker: That’s another terrific question. I do, because I’m trying to distinguish in my own mind patients who have residual inflammatory risk, in whom the high-sensitivity CRP (hsCRP) level remains high despite being on statins versus those with residual cholesterol risk, in whom I’m really predominantly worried about LDL cholesterol, that I haven’t brought it down far enough.
I do measure it, and if the CRP remains high and the LDL cholesterol is low, to me, that’s residual inflammatory risk and that’s the patient I would target this to. Conversely, if the LDL cholesterol was still, say, above some threshold of 75-100 and I’m worried about that, even if the CRP is low, I’ll probably add a second lipid-lowering drug.
The complexity of this, however, is that CRP was not measured in either LoDoCo2 or COLCOT. That’s mostly because they didn’t have much funding. These trials were done really on a shoestring. They were not sponsored by major pharma at all. We know that the median hsCRP in these trials was probably around 3.5-4 mg/L so I’m pretty comfortable doing that. Others have just advocated giving it to many patients. I must say I like to use biomarkers to think through the biology and who might have the best benefit-to-risk ratio. In my practice, I am doing it that way.
Inpatient vs. outpatient initiation
Dr. O’Donoghue: This is perhaps my last question for you before we wrap up. I know you talked about use of low-dose colchicine for patients with more chronic, stable coronary disease. Now obviously, COLCOT studied patients who were early post ACS, and there we certainly think about the anti-inflammatory effects as potentially having more benefit. What are your thoughts about early initiation of colchicine in that setting, the acute hospitalized setting? Do you think it’s more appropriate for an outpatient start?
Dr. Ridker: Today, I think this is all about chronic, stable atherosclerosis. Yes, COLCOT enrolled their patients within 30 days of a recent myocardial infarction, but as we all know, that’s a pretty stable phase. The vast majority were enrolled after 15 days. There were a small number enrolled within 3 days or something like that, but the benefit is about the same in all these patients.
Conversely, there’s been a small number of trials looking at colchicine in acute coronary ischemia and they’ve not been terribly promising. That makes some sense, though, right? We want to get an artery open. In acute ischemia, that’s about revascularization. It’s about oxygenation. It’s about reperfusion injury. My guess is that 3, 4, 5, or 6 days later, when it becomes a stable situation, is when the drug is probably effective.
Again, there will be some ongoing true intervention trials with large sample sizes for acute coronary ischemia. We don’t have those yet. Right now, I think it’s a therapy for chronic, stable angina. That’s many of our patients.
I would say that if you compare the relative benefit in these trials of adding ezetimibe to a statin, that’s a 5% or 6% benefit. For PCSK9 inhibitors – we all use them – it’s about a 15% benefit. These are 25%-30% risk reductions. If we’re going to think about what’s the next drug to give on top of the statin, serious consideration should be given to low-dose colchicine.
Let me also emphasize that this is not an either/or situation. This is about the fact that we now understand atherosclerosis to be a disorder both of lipid accumulation and a proinflammatory systemic response. We can give these drugs together. I suspect that the best patient care is going to be very aggressive lipid-lowering combined with pretty aggressive inflammation inhibition. I suspect that, down the road, that’s where all of us are going to be.
Dr. O’Donoghue: Thank you so much, Paul, for walking us through that today. I think it was a very nice, succinct review of the evidence, and then also just getting our minds more accustomed to the concept that we can now start to target more orthogonal axes that really get at the pathobiology of what’s going on in the atherosclerotic plaque. I think it’s an important topic.
Dr. O’Donoghue is an associate professor of medicine at Harvard Medical School and an associate physician at Brigham and Women’s Hospital, both in Boston. Dr. Ridker is director of the Center for Cardiovascular Disease Prevention at Brigham and Women’s Hospital. Both Dr. O’Donoghue and Dr. Ridker reported numerous conflicts of interest.
This transcript has been edited for clarity.
Dr. O’Donoghue: We’re going to discuss a very important and emerging topic, which is the use of low-dose colchicine. I think there’s much interest in the use of this drug, which now has a Food and Drug Administration indication, which we’ll talk about further, and it’s also been written into both European and American guidelines that have been recently released.
who’s been at the forefront of research into anti-inflammatory therapeutics.
Lifestyle lipid-lowering paramount
Dr. O’Donoghue: As we think about the concept behind the use of colchicine, we’ve obviously done a large amount of research into lipid-lowering drugs, but where does colchicine now fit in?
Dr. Ridker: Let’s make sure we get the basics down. Anti-inflammatory therapy is going to be added on top of quality other care. This is not a replacement for lipids; it’s not a change in diet, exercise, and smoking cessation. The new data are really telling us that a patient who’s aggressively treated to guideline-recommended levels can still do much better in terms of preventing heart attack, stroke, cardiovascular death, and revascularization by adding low-dose colchicine as the first proven anti-inflammatory therapy for atherosclerotic disease.
I have to say, Michelle, for me, it’s been a wonderful end of a journey in many ways. This story starts almost 30 years ago for quite a few of us, thinking about inflammation and atherosclerosis. The whole C-reactive protein (CRP) story is still an ongoing one. We recently showed, for example, that residual inflammatory risk in some 30,000 patients, all taking a statin, was a far better predictor of the likelihood of more cardiovascular events, in particular cardiovascular death, than was residual cholesterol risk.
Think about that. We’re all aggressively giving second lipid-lowering drugs in our very sick patients, but that means inflammation is really the untapped piece of this.
The two clinical trials we have in front of us, the COLCOT trial and the LoDoCo2 trial – both New England Journal of Medicine papers, both with roughly 5,000 patients – provide very clear evidence that following a relatively recent myocardial infarction (that’s COLCOT) in chronic stable atherosclerosis (that’s LoDoCo2), we’re getting 25%-30% relative risk reductions in major adverse cardiovascular events (MACEs) on top of aggressive statin therapy. That’s a big deal. It’s safe, it works, and it’s fully consistent with all the information we have about inflammation being part and parcel of atherosclerosis. It’s a pretty exciting time.
Inflammatory pathway
Dr. O’Donoghue: It beautifully proves the inflammatory hypothesis in many ways. You led CANTOS, and that was a much more specific target. Here, in terms of the effects of colchicine, what do we know about how it may work on the inflammatory cascade?
Dr. Ridker: Our CANTOS trial was proof of principle that you could directly target, with a very specific monoclonal antibody, a specific piece of this innate immune cascade and lower cardiovascular event rates.
Colchicine is a more broad-spectrum drug. It does have a number of antineutrophil effects – that’s important, by the way. Neutrophils are really becoming very important in atherosclerotic disease progression. It’s an indirect inhibitor of the so-called NLRP3 inflammasome, which is where both interleukin-1 (that’s the target for canakinumab) and IL-6 are up-regulated. As you know, it’s been used to treat gout and pericarditis in high doses in short, little bursts.
The change here is this use of low-dose colchicine, that’s 0.5 mg once a day for years to treat chronic, stable atherosclerosis. It is very much like using a statin. The idea here is to prevent the progression of the disease by slowing down and maybe stabilizing the plaque so we have fewer heart attacks and strokes down the road.
It’s entering the armamentarium – at least my armamentarium – as chronic, stable secondary prevention. That’s where the new American College of Cardiology/American Heart Association guidelines also put it. It’s really in as a treatment for chronic, stable atherosclerosis. I think that’s where it belongs.
When to start colchicine, and in whom?
Dr. O’Donoghue: To that point, as we think about the efficacy, I think it’s nice, as you outlined, that we have two complementary trials that are both showing a consistent reduction in MACEs, one in the post–acute coronary syndrome (ACS) state and one for more chronic patients.
At what point do you think would be the appropriate time to start therapy, and who would you be starting it for?
Dr. Ridker: Michelle, that’s a great question. There’s a very interesting analysis that just came out from the LoDoCo2 investigators. It’s kind of a landmark analysis. What they show is that 1 year, 2 years, 3 years, and 4 years since the initiating myocardial infarction, the drug is very effective.
In fact, you could think about starting this drug at your clinic in patients with chronic, stable atherosclerotic disease. That’s just like we would start a statin in people who had a heart attack some time ago, and that’s absolutely fine.
I’m using it for what I call my frequent fliers, those patients who just keep coming back. They’re already on aggressive lipid-lowering therapy. I have them on beta-blockers, aspirin, and all the usual things. I say, look, I can get a large risk reduction by starting them on this drug.
There are a few caveats, Michelle. Like all drugs, colchicine comes with some adverse effects. Most of them are pretty rare, but there are some patients I would not give this drug to, just to be very clear. Colchicine is cleared by the kidney and by the liver. Patients who have severe chronic kidney disease and severe liver disease – this is a no-go for those patients. We should talk about where patients in that realm might want to go.
Then there are some unusual drugs. Colchicine is metabolized by the CYP3A4 and the P-glycoprotein pathway. There are a few drugs, such as ketoconazole, fluconazole, and cyclosporine, that if your primary care doctor or internist is going to start for a short term, you probably want to stop your colchicine for a week or two.
In people with familial Mediterranean fever, for whom colchicine is lifesaving and life-changing and who take it for 20, 30, or 40 years, there’s been no increase in risk for cancer. There have been very few adverse effects. I think it’s interesting that we, who practice in North America, basically never see familial Mediterranean fever. If we were practicing in Lebanon, Israel, or North Africa, this would be a very common therapy that we’d all be extremely familiar with.
Dr. O’Donoghue: To that point, it’s interesting to hear that colchicine was even used by the ancient Greeks and ancient Egyptians. It’s a drug that’s been around for a long time.
In terms of its safety, some people have been talking about the fact that an increase in noncardiovascular death was seen in LoDoCo2. What are your thoughts on that? Is that anything that we should be concerned about?
Colchicine safety and contraindications
Dr. Ridker: First, to set the record straight, a meta-analysis has been done of all-cause mortality in the various colchicine trials, and the hazard ratio is 1.04. I’ll remind you, and all of us know, that the hazard ratios for all-cause mortality in the PCSK9 trials, the bempedoic acid trials, and the ezetimibe trials are also essentially neutral. We’re in a state where we don’t let these trials roll long enough to see benefits necessarily on all-cause mortality. Some of us think we probably should, but that’s just the reality of trials.
One of most interesting things that was part of the FDA review, I suspect, was that there was no specific cause of any of this. It was not like there was a set of particular issues. I suspect that most people think this is probably the play of chance and with time, things will get better.
Again, I do want to emphasize this is not a drug for severe chronic kidney disease and severe liver disease, because those patients will get in trouble with this. The other thing that’s worth knowing is when you start a patient on low-dose colchicine – that’s 0.5 mg/d – there will be some patients who get some short-term gastrointestinal upset. That’s very common when you start colchicine at the much higher doses you might use to treat acute gout or pericarditis. In these trials, the vast majority of patients treated through that, and there were very few episodes long-term. I think it’s generally safe. That’s where we’re at.
Dr. O’Donoghue: Paul, you’ve been a leader, certainly, at looking at CRP as a marker of inflammation. Do you, in your practice, consider CRP levels when making a decision about who is appropriate for this therapy?
Dr. Ridker: That’s another terrific question. I do, because I’m trying to distinguish in my own mind patients who have residual inflammatory risk, in whom the high-sensitivity CRP (hsCRP) level remains high despite being on statins versus those with residual cholesterol risk, in whom I’m really predominantly worried about LDL cholesterol, that I haven’t brought it down far enough.
I do measure it, and if the CRP remains high and the LDL cholesterol is low, to me, that’s residual inflammatory risk and that’s the patient I would target this to. Conversely, if the LDL cholesterol was still, say, above some threshold of 75-100 and I’m worried about that, even if the CRP is low, I’ll probably add a second lipid-lowering drug.
The complexity of this, however, is that CRP was not measured in either LoDoCo2 or COLCOT. That’s mostly because they didn’t have much funding. These trials were done really on a shoestring. They were not sponsored by major pharma at all. We know that the median hsCRP in these trials was probably around 3.5-4 mg/L so I’m pretty comfortable doing that. Others have just advocated giving it to many patients. I must say I like to use biomarkers to think through the biology and who might have the best benefit-to-risk ratio. In my practice, I am doing it that way.
Inpatient vs. outpatient initiation
Dr. O’Donoghue: This is perhaps my last question for you before we wrap up. I know you talked about use of low-dose colchicine for patients with more chronic, stable coronary disease. Now obviously, COLCOT studied patients who were early post ACS, and there we certainly think about the anti-inflammatory effects as potentially having more benefit. What are your thoughts about early initiation of colchicine in that setting, the acute hospitalized setting? Do you think it’s more appropriate for an outpatient start?
Dr. Ridker: Today, I think this is all about chronic, stable atherosclerosis. Yes, COLCOT enrolled their patients within 30 days of a recent myocardial infarction, but as we all know, that’s a pretty stable phase. The vast majority were enrolled after 15 days. There were a small number enrolled within 3 days or something like that, but the benefit is about the same in all these patients.
Conversely, there’s been a small number of trials looking at colchicine in acute coronary ischemia and they’ve not been terribly promising. That makes some sense, though, right? We want to get an artery open. In acute ischemia, that’s about revascularization. It’s about oxygenation. It’s about reperfusion injury. My guess is that 3, 4, 5, or 6 days later, when it becomes a stable situation, is when the drug is probably effective.
Again, there will be some ongoing true intervention trials with large sample sizes for acute coronary ischemia. We don’t have those yet. Right now, I think it’s a therapy for chronic, stable angina. That’s many of our patients.
I would say that if you compare the relative benefit in these trials of adding ezetimibe to a statin, that’s a 5% or 6% benefit. For PCSK9 inhibitors – we all use them – it’s about a 15% benefit. These are 25%-30% risk reductions. If we’re going to think about what’s the next drug to give on top of the statin, serious consideration should be given to low-dose colchicine.
Let me also emphasize that this is not an either/or situation. This is about the fact that we now understand atherosclerosis to be a disorder both of lipid accumulation and a proinflammatory systemic response. We can give these drugs together. I suspect that the best patient care is going to be very aggressive lipid-lowering combined with pretty aggressive inflammation inhibition. I suspect that, down the road, that’s where all of us are going to be.
Dr. O’Donoghue: Thank you so much, Paul, for walking us through that today. I think it was a very nice, succinct review of the evidence, and then also just getting our minds more accustomed to the concept that we can now start to target more orthogonal axes that really get at the pathobiology of what’s going on in the atherosclerotic plaque. I think it’s an important topic.
Dr. O’Donoghue is an associate professor of medicine at Harvard Medical School and an associate physician at Brigham and Women’s Hospital, both in Boston. Dr. Ridker is director of the Center for Cardiovascular Disease Prevention at Brigham and Women’s Hospital. Both Dr. O’Donoghue and Dr. Ridker reported numerous conflicts of interest.
This transcript has been edited for clarity.
Dr. O’Donoghue: We’re going to discuss a very important and emerging topic, which is the use of low-dose colchicine. I think there’s much interest in the use of this drug, which now has a Food and Drug Administration indication, which we’ll talk about further, and it’s also been written into both European and American guidelines that have been recently released.
who’s been at the forefront of research into anti-inflammatory therapeutics.
Lifestyle lipid-lowering paramount
Dr. O’Donoghue: As we think about the concept behind the use of colchicine, we’ve obviously done a large amount of research into lipid-lowering drugs, but where does colchicine now fit in?
Dr. Ridker: Let’s make sure we get the basics down. Anti-inflammatory therapy is going to be added on top of quality other care. This is not a replacement for lipids; it’s not a change in diet, exercise, and smoking cessation. The new data are really telling us that a patient who’s aggressively treated to guideline-recommended levels can still do much better in terms of preventing heart attack, stroke, cardiovascular death, and revascularization by adding low-dose colchicine as the first proven anti-inflammatory therapy for atherosclerotic disease.
I have to say, Michelle, for me, it’s been a wonderful end of a journey in many ways. This story starts almost 30 years ago for quite a few of us, thinking about inflammation and atherosclerosis. The whole C-reactive protein (CRP) story is still an ongoing one. We recently showed, for example, that residual inflammatory risk in some 30,000 patients, all taking a statin, was a far better predictor of the likelihood of more cardiovascular events, in particular cardiovascular death, than was residual cholesterol risk.
Think about that. We’re all aggressively giving second lipid-lowering drugs in our very sick patients, but that means inflammation is really the untapped piece of this.
The two clinical trials we have in front of us, the COLCOT trial and the LoDoCo2 trial – both New England Journal of Medicine papers, both with roughly 5,000 patients – provide very clear evidence that following a relatively recent myocardial infarction (that’s COLCOT) in chronic stable atherosclerosis (that’s LoDoCo2), we’re getting 25%-30% relative risk reductions in major adverse cardiovascular events (MACEs) on top of aggressive statin therapy. That’s a big deal. It’s safe, it works, and it’s fully consistent with all the information we have about inflammation being part and parcel of atherosclerosis. It’s a pretty exciting time.
Inflammatory pathway
Dr. O’Donoghue: It beautifully proves the inflammatory hypothesis in many ways. You led CANTOS, and that was a much more specific target. Here, in terms of the effects of colchicine, what do we know about how it may work on the inflammatory cascade?
Dr. Ridker: Our CANTOS trial was proof of principle that you could directly target, with a very specific monoclonal antibody, a specific piece of this innate immune cascade and lower cardiovascular event rates.
Colchicine is a more broad-spectrum drug. It does have a number of antineutrophil effects – that’s important, by the way. Neutrophils are really becoming very important in atherosclerotic disease progression. It’s an indirect inhibitor of the so-called NLRP3 inflammasome, which is where both interleukin-1 (that’s the target for canakinumab) and IL-6 are up-regulated. As you know, it’s been used to treat gout and pericarditis in high doses in short, little bursts.
The change here is this use of low-dose colchicine, that’s 0.5 mg once a day for years to treat chronic, stable atherosclerosis. It is very much like using a statin. The idea here is to prevent the progression of the disease by slowing down and maybe stabilizing the plaque so we have fewer heart attacks and strokes down the road.
It’s entering the armamentarium – at least my armamentarium – as chronic, stable secondary prevention. That’s where the new American College of Cardiology/American Heart Association guidelines also put it. It’s really in as a treatment for chronic, stable atherosclerosis. I think that’s where it belongs.
When to start colchicine, and in whom?
Dr. O’Donoghue: To that point, as we think about the efficacy, I think it’s nice, as you outlined, that we have two complementary trials that are both showing a consistent reduction in MACEs, one in the post–acute coronary syndrome (ACS) state and one for more chronic patients.
At what point do you think would be the appropriate time to start therapy, and who would you be starting it for?
Dr. Ridker: Michelle, that’s a great question. There’s a very interesting analysis that just came out from the LoDoCo2 investigators. It’s kind of a landmark analysis. What they show is that 1 year, 2 years, 3 years, and 4 years since the initiating myocardial infarction, the drug is very effective.
In fact, you could think about starting this drug at your clinic in patients with chronic, stable atherosclerotic disease. That’s just like we would start a statin in people who had a heart attack some time ago, and that’s absolutely fine.
I’m using it for what I call my frequent fliers, those patients who just keep coming back. They’re already on aggressive lipid-lowering therapy. I have them on beta-blockers, aspirin, and all the usual things. I say, look, I can get a large risk reduction by starting them on this drug.
There are a few caveats, Michelle. Like all drugs, colchicine comes with some adverse effects. Most of them are pretty rare, but there are some patients I would not give this drug to, just to be very clear. Colchicine is cleared by the kidney and by the liver. Patients who have severe chronic kidney disease and severe liver disease – this is a no-go for those patients. We should talk about where patients in that realm might want to go.
Then there are some unusual drugs. Colchicine is metabolized by the CYP3A4 and the P-glycoprotein pathway. There are a few drugs, such as ketoconazole, fluconazole, and cyclosporine, that if your primary care doctor or internist is going to start for a short term, you probably want to stop your colchicine for a week or two.
In people with familial Mediterranean fever, for whom colchicine is lifesaving and life-changing and who take it for 20, 30, or 40 years, there’s been no increase in risk for cancer. There have been very few adverse effects. I think it’s interesting that we, who practice in North America, basically never see familial Mediterranean fever. If we were practicing in Lebanon, Israel, or North Africa, this would be a very common therapy that we’d all be extremely familiar with.
Dr. O’Donoghue: To that point, it’s interesting to hear that colchicine was even used by the ancient Greeks and ancient Egyptians. It’s a drug that’s been around for a long time.
In terms of its safety, some people have been talking about the fact that an increase in noncardiovascular death was seen in LoDoCo2. What are your thoughts on that? Is that anything that we should be concerned about?
Colchicine safety and contraindications
Dr. Ridker: First, to set the record straight, a meta-analysis has been done of all-cause mortality in the various colchicine trials, and the hazard ratio is 1.04. I’ll remind you, and all of us know, that the hazard ratios for all-cause mortality in the PCSK9 trials, the bempedoic acid trials, and the ezetimibe trials are also essentially neutral. We’re in a state where we don’t let these trials roll long enough to see benefits necessarily on all-cause mortality. Some of us think we probably should, but that’s just the reality of trials.
One of most interesting things that was part of the FDA review, I suspect, was that there was no specific cause of any of this. It was not like there was a set of particular issues. I suspect that most people think this is probably the play of chance and with time, things will get better.
Again, I do want to emphasize this is not a drug for severe chronic kidney disease and severe liver disease, because those patients will get in trouble with this. The other thing that’s worth knowing is when you start a patient on low-dose colchicine – that’s 0.5 mg/d – there will be some patients who get some short-term gastrointestinal upset. That’s very common when you start colchicine at the much higher doses you might use to treat acute gout or pericarditis. In these trials, the vast majority of patients treated through that, and there were very few episodes long-term. I think it’s generally safe. That’s where we’re at.
Dr. O’Donoghue: Paul, you’ve been a leader, certainly, at looking at CRP as a marker of inflammation. Do you, in your practice, consider CRP levels when making a decision about who is appropriate for this therapy?
Dr. Ridker: That’s another terrific question. I do, because I’m trying to distinguish in my own mind patients who have residual inflammatory risk, in whom the high-sensitivity CRP (hsCRP) level remains high despite being on statins versus those with residual cholesterol risk, in whom I’m really predominantly worried about LDL cholesterol, that I haven’t brought it down far enough.
I do measure it, and if the CRP remains high and the LDL cholesterol is low, to me, that’s residual inflammatory risk and that’s the patient I would target this to. Conversely, if the LDL cholesterol was still, say, above some threshold of 75-100 and I’m worried about that, even if the CRP is low, I’ll probably add a second lipid-lowering drug.
The complexity of this, however, is that CRP was not measured in either LoDoCo2 or COLCOT. That’s mostly because they didn’t have much funding. These trials were done really on a shoestring. They were not sponsored by major pharma at all. We know that the median hsCRP in these trials was probably around 3.5-4 mg/L so I’m pretty comfortable doing that. Others have just advocated giving it to many patients. I must say I like to use biomarkers to think through the biology and who might have the best benefit-to-risk ratio. In my practice, I am doing it that way.
Inpatient vs. outpatient initiation
Dr. O’Donoghue: This is perhaps my last question for you before we wrap up. I know you talked about use of low-dose colchicine for patients with more chronic, stable coronary disease. Now obviously, COLCOT studied patients who were early post ACS, and there we certainly think about the anti-inflammatory effects as potentially having more benefit. What are your thoughts about early initiation of colchicine in that setting, the acute hospitalized setting? Do you think it’s more appropriate for an outpatient start?
Dr. Ridker: Today, I think this is all about chronic, stable atherosclerosis. Yes, COLCOT enrolled their patients within 30 days of a recent myocardial infarction, but as we all know, that’s a pretty stable phase. The vast majority were enrolled after 15 days. There were a small number enrolled within 3 days or something like that, but the benefit is about the same in all these patients.
Conversely, there’s been a small number of trials looking at colchicine in acute coronary ischemia and they’ve not been terribly promising. That makes some sense, though, right? We want to get an artery open. In acute ischemia, that’s about revascularization. It’s about oxygenation. It’s about reperfusion injury. My guess is that 3, 4, 5, or 6 days later, when it becomes a stable situation, is when the drug is probably effective.
Again, there will be some ongoing true intervention trials with large sample sizes for acute coronary ischemia. We don’t have those yet. Right now, I think it’s a therapy for chronic, stable angina. That’s many of our patients.
I would say that if you compare the relative benefit in these trials of adding ezetimibe to a statin, that’s a 5% or 6% benefit. For PCSK9 inhibitors – we all use them – it’s about a 15% benefit. These are 25%-30% risk reductions. If we’re going to think about what’s the next drug to give on top of the statin, serious consideration should be given to low-dose colchicine.
Let me also emphasize that this is not an either/or situation. This is about the fact that we now understand atherosclerosis to be a disorder both of lipid accumulation and a proinflammatory systemic response. We can give these drugs together. I suspect that the best patient care is going to be very aggressive lipid-lowering combined with pretty aggressive inflammation inhibition. I suspect that, down the road, that’s where all of us are going to be.
Dr. O’Donoghue: Thank you so much, Paul, for walking us through that today. I think it was a very nice, succinct review of the evidence, and then also just getting our minds more accustomed to the concept that we can now start to target more orthogonal axes that really get at the pathobiology of what’s going on in the atherosclerotic plaque. I think it’s an important topic.
Dr. O’Donoghue is an associate professor of medicine at Harvard Medical School and an associate physician at Brigham and Women’s Hospital, both in Boston. Dr. Ridker is director of the Center for Cardiovascular Disease Prevention at Brigham and Women’s Hospital. Both Dr. O’Donoghue and Dr. Ridker reported numerous conflicts of interest.
Physician-assisted suicide for mental illness – right or wrong?
Until recently, this contentious issue applied only to patients with physical illnesses who want to end their suffering and who seek out a physician willing to assist with that objective. In the United States and other countries, this is the patient population who may be able to avail themselves of this option.
However, newly proposed legislation in Canada – which has the largest number of physician-assisted deaths worldwide – would expand the indication for MAID to include serious mental illness. Originally set to be passed in March 2023, the law has been deferred for final decision until March 2024.
A recent commentary by psychiatrist Dinah Miller, MD, explored the ethics of this proposed legislation for mental health professionals. “To offer the option of death facilitated by the very person who is trying to get [patients with serious mental illness] better seems so counter to everything I have learned and contradicts our role as psychiatrists who work so hard to prevent suicide,” Dr. Miller wrote. “As psychiatrists, do we offer hope to our most vulnerable patients, or do we offer death? Do we rail against suicide, or do we facilitate it?”
Dr. Miller’s piece garnered a huge amount of reader response that included many laudatory comments: a “nuanced and open-ended inquiry here,” “timely and honest,” and “beautifully written.” One reader thanked the author for “this thoughtful, questioning, and open reflection on what it means to be a psychiatrist facing a thorny and deeply personal practice and philosophical question.”
Cognitive distortion or objective reality?
Many readers were opposed to any type of physician involvement in hastening a patient’s death, regardless of whether the condition is medical or psychiatric. “Let others who wish to die make their own arrangement without the aid of the medical profession,” one reader wrote.
But others felt that for those with terminal physical illnesses or intractable pain, it is justified for medical professionals to either facilitate death or, at the very least, withhold life-prolonging treatments.
A critical-care physician described responding to families’ accusations that withdrawal of life-sustaining measures means “playing God.” On the contrary, the physician wrote, “there is a limit to our abilities; and withdrawing those life-prolonging interventions allows nature or God or whatever to play a role and take its course.”
Another U.S. reader pointed out that “multiple polls in this country have shown that the majority of the general public, physicians in general and psychiatrists in particular, support the option of MAID for the terminally ill. They do not find it at variance with their calling as physicians.”
“I and many of my elderly friends don’t fear death but fear prolonged dementia with its dependency and lack of quality of life,” one reader wrote. “We would be much more at peace if we could put in our advanced directive that we request MAID once some point of dependency has been reached.”
Another wrote that in the event of entering a state of “degrading dependency and hardship on the family, please let me go peacefully, without burdening others, into that good night [of death].”
Many felt that not only physical illness but also the prospect of cognitive degeneration – specifically dementia – also justifies assisting patient death.
“Enormous suffering”
One Canadian reader noted that provisions for advance consent are now in place in Canada for those facing the prospect of neurodegenerative disease and who are still mentally competent to make such decisions.
But therein lies the rub – the concept of an advanced directive goes to the question of decisional capacity. Dr. Miller noted that “depression distorts cognition and leads many patients to believe that they would be better off dead and that their loves ones would be better off without them.”
The concept of “cognitive distortion” implies that the illness itself may impede the decisional capacity required for an advanced directive or a decision made in the moment, in the absence of such a directive. Dr. Miller asked, “How do we determine whether patients with serious mental illness are competent to make such a decision or whether it is mental illness that is driving their perception of a future without hope?”
One reader attested to this from personal experience. “As both a physician and a sufferer of severe, often profound depression for 50 years, I can confidently say that ... the pursuit of death is the result of an impaired mental state, which simultaneously prevents a rational decision.”
Another agreed. “As a psychiatrist, I treated suicidal patients almost every day of my 27-year career. I believe in making every effort to prevent the suicide of a healthy depressed person and I do not support MAID for psychiatric conditions. But I do support MAID for the terminally ill.”
Other readers disagreed. In the words of one commentator, “I think that if we are going to help mentally ill people, we have to consider their choices. The stress imposed by a severe/intractable mental illness is as bad as any other devastating medical illness. If no one is going to hold their hand in life (as support services are limited and psychiatric treatments often fail), allow a medical professional to hold their hand through their final moments.”
A psychiatrist described very ill patients with treatment-resistant bipolar disorder who had not only received medications, including ketamine, but had also received electroconvulsive therapy and still did not respond.
“Their suffering is enormous and the truth is that there is no improvement for more than a few days or weeks and later they return to their hell. Appreciating that they would be better off dead for themselves and their families is not always a cognitive distortion but an objective evaluation of their reality.”
However, as another reader pointed out, an issue with the argument presented here is that it presupposes that MAID requires “clinical justification.” But in Canada, “MAID ... is understood as an expression of personal autonomy. Rooted in liberal political philosophy of individualism ... approval for death need not be based on a clinical assessment.” Instead, “death is seen as a ‘right’ that the state must therefore provide.”
Another form of eugenics?
Dr. Miller raised the ethical implications of racial and socioeconomic factors playing a role in the consideration of MAID for those with psychiatric illness.
“Might those who are poor, who have less access to expensive treatment options and social support, be more likely to request facilitated death?” she asks. “Do we risk facilitating a patient’s demise when other options are unavailable because of a lack of access to treatment or when social and financial struggles exacerbate a person’s hopelessness? Should we worry that psychiatric euthanasia will turn into a form of eugenics where those who can’t contribute are made to feel that they should bow out?”
Several readers agreed. “Looking at the disproportionate burden of illness, rates of imprisonment, and application of the death penalty indicates to me that race and socioeconomic status will be an immediate factor in how, where, and with whom MAID for mental illness would be practice in much, if not all, of the U.S.,” wrote one physician.
A Canadian reader expressed similar concerns. “I’ve seen a handful of people, including someone I considered a good friend, opt for MAID because it was easier than living as a disabled person in poverty without adequate mental health care.”
Another Canadian clinician noted that offering people good care can make all the difference. “As a Canadian mental health clinician who served youth with severe mental illness for over 20 years through our socialized medical network, I can attest to the difference good care usually makes in shifting clients from despair and a commitment to death to embracing life once again. Let’s not, as clinicians, embrace easing a government/state-sanctioned pathway to death.”
Some readers believe that these types of issues can’t be solved with a blanket approach, noting that each case is different. “Real life is always more complicated than academic discussions. Having served on a hospital ethics committee, I know that each case is unique,” one reader noted.
Another reader added, “I think all we can do as physicians is to let people decide for themselves and participate only if our conscience allows.”
A version of this article first appeared on Medscape.com.
Until recently, this contentious issue applied only to patients with physical illnesses who want to end their suffering and who seek out a physician willing to assist with that objective. In the United States and other countries, this is the patient population who may be able to avail themselves of this option.
However, newly proposed legislation in Canada – which has the largest number of physician-assisted deaths worldwide – would expand the indication for MAID to include serious mental illness. Originally set to be passed in March 2023, the law has been deferred for final decision until March 2024.
A recent commentary by psychiatrist Dinah Miller, MD, explored the ethics of this proposed legislation for mental health professionals. “To offer the option of death facilitated by the very person who is trying to get [patients with serious mental illness] better seems so counter to everything I have learned and contradicts our role as psychiatrists who work so hard to prevent suicide,” Dr. Miller wrote. “As psychiatrists, do we offer hope to our most vulnerable patients, or do we offer death? Do we rail against suicide, or do we facilitate it?”
Dr. Miller’s piece garnered a huge amount of reader response that included many laudatory comments: a “nuanced and open-ended inquiry here,” “timely and honest,” and “beautifully written.” One reader thanked the author for “this thoughtful, questioning, and open reflection on what it means to be a psychiatrist facing a thorny and deeply personal practice and philosophical question.”
Cognitive distortion or objective reality?
Many readers were opposed to any type of physician involvement in hastening a patient’s death, regardless of whether the condition is medical or psychiatric. “Let others who wish to die make their own arrangement without the aid of the medical profession,” one reader wrote.
But others felt that for those with terminal physical illnesses or intractable pain, it is justified for medical professionals to either facilitate death or, at the very least, withhold life-prolonging treatments.
A critical-care physician described responding to families’ accusations that withdrawal of life-sustaining measures means “playing God.” On the contrary, the physician wrote, “there is a limit to our abilities; and withdrawing those life-prolonging interventions allows nature or God or whatever to play a role and take its course.”
Another U.S. reader pointed out that “multiple polls in this country have shown that the majority of the general public, physicians in general and psychiatrists in particular, support the option of MAID for the terminally ill. They do not find it at variance with their calling as physicians.”
“I and many of my elderly friends don’t fear death but fear prolonged dementia with its dependency and lack of quality of life,” one reader wrote. “We would be much more at peace if we could put in our advanced directive that we request MAID once some point of dependency has been reached.”
Another wrote that in the event of entering a state of “degrading dependency and hardship on the family, please let me go peacefully, without burdening others, into that good night [of death].”
Many felt that not only physical illness but also the prospect of cognitive degeneration – specifically dementia – also justifies assisting patient death.
“Enormous suffering”
One Canadian reader noted that provisions for advance consent are now in place in Canada for those facing the prospect of neurodegenerative disease and who are still mentally competent to make such decisions.
But therein lies the rub – the concept of an advanced directive goes to the question of decisional capacity. Dr. Miller noted that “depression distorts cognition and leads many patients to believe that they would be better off dead and that their loves ones would be better off without them.”
The concept of “cognitive distortion” implies that the illness itself may impede the decisional capacity required for an advanced directive or a decision made in the moment, in the absence of such a directive. Dr. Miller asked, “How do we determine whether patients with serious mental illness are competent to make such a decision or whether it is mental illness that is driving their perception of a future without hope?”
One reader attested to this from personal experience. “As both a physician and a sufferer of severe, often profound depression for 50 years, I can confidently say that ... the pursuit of death is the result of an impaired mental state, which simultaneously prevents a rational decision.”
Another agreed. “As a psychiatrist, I treated suicidal patients almost every day of my 27-year career. I believe in making every effort to prevent the suicide of a healthy depressed person and I do not support MAID for psychiatric conditions. But I do support MAID for the terminally ill.”
Other readers disagreed. In the words of one commentator, “I think that if we are going to help mentally ill people, we have to consider their choices. The stress imposed by a severe/intractable mental illness is as bad as any other devastating medical illness. If no one is going to hold their hand in life (as support services are limited and psychiatric treatments often fail), allow a medical professional to hold their hand through their final moments.”
A psychiatrist described very ill patients with treatment-resistant bipolar disorder who had not only received medications, including ketamine, but had also received electroconvulsive therapy and still did not respond.
“Their suffering is enormous and the truth is that there is no improvement for more than a few days or weeks and later they return to their hell. Appreciating that they would be better off dead for themselves and their families is not always a cognitive distortion but an objective evaluation of their reality.”
However, as another reader pointed out, an issue with the argument presented here is that it presupposes that MAID requires “clinical justification.” But in Canada, “MAID ... is understood as an expression of personal autonomy. Rooted in liberal political philosophy of individualism ... approval for death need not be based on a clinical assessment.” Instead, “death is seen as a ‘right’ that the state must therefore provide.”
Another form of eugenics?
Dr. Miller raised the ethical implications of racial and socioeconomic factors playing a role in the consideration of MAID for those with psychiatric illness.
“Might those who are poor, who have less access to expensive treatment options and social support, be more likely to request facilitated death?” she asks. “Do we risk facilitating a patient’s demise when other options are unavailable because of a lack of access to treatment or when social and financial struggles exacerbate a person’s hopelessness? Should we worry that psychiatric euthanasia will turn into a form of eugenics where those who can’t contribute are made to feel that they should bow out?”
Several readers agreed. “Looking at the disproportionate burden of illness, rates of imprisonment, and application of the death penalty indicates to me that race and socioeconomic status will be an immediate factor in how, where, and with whom MAID for mental illness would be practice in much, if not all, of the U.S.,” wrote one physician.
A Canadian reader expressed similar concerns. “I’ve seen a handful of people, including someone I considered a good friend, opt for MAID because it was easier than living as a disabled person in poverty without adequate mental health care.”
Another Canadian clinician noted that offering people good care can make all the difference. “As a Canadian mental health clinician who served youth with severe mental illness for over 20 years through our socialized medical network, I can attest to the difference good care usually makes in shifting clients from despair and a commitment to death to embracing life once again. Let’s not, as clinicians, embrace easing a government/state-sanctioned pathway to death.”
Some readers believe that these types of issues can’t be solved with a blanket approach, noting that each case is different. “Real life is always more complicated than academic discussions. Having served on a hospital ethics committee, I know that each case is unique,” one reader noted.
Another reader added, “I think all we can do as physicians is to let people decide for themselves and participate only if our conscience allows.”
A version of this article first appeared on Medscape.com.
Until recently, this contentious issue applied only to patients with physical illnesses who want to end their suffering and who seek out a physician willing to assist with that objective. In the United States and other countries, this is the patient population who may be able to avail themselves of this option.
However, newly proposed legislation in Canada – which has the largest number of physician-assisted deaths worldwide – would expand the indication for MAID to include serious mental illness. Originally set to be passed in March 2023, the law has been deferred for final decision until March 2024.
A recent commentary by psychiatrist Dinah Miller, MD, explored the ethics of this proposed legislation for mental health professionals. “To offer the option of death facilitated by the very person who is trying to get [patients with serious mental illness] better seems so counter to everything I have learned and contradicts our role as psychiatrists who work so hard to prevent suicide,” Dr. Miller wrote. “As psychiatrists, do we offer hope to our most vulnerable patients, or do we offer death? Do we rail against suicide, or do we facilitate it?”
Dr. Miller’s piece garnered a huge amount of reader response that included many laudatory comments: a “nuanced and open-ended inquiry here,” “timely and honest,” and “beautifully written.” One reader thanked the author for “this thoughtful, questioning, and open reflection on what it means to be a psychiatrist facing a thorny and deeply personal practice and philosophical question.”
Cognitive distortion or objective reality?
Many readers were opposed to any type of physician involvement in hastening a patient’s death, regardless of whether the condition is medical or psychiatric. “Let others who wish to die make their own arrangement without the aid of the medical profession,” one reader wrote.
But others felt that for those with terminal physical illnesses or intractable pain, it is justified for medical professionals to either facilitate death or, at the very least, withhold life-prolonging treatments.
A critical-care physician described responding to families’ accusations that withdrawal of life-sustaining measures means “playing God.” On the contrary, the physician wrote, “there is a limit to our abilities; and withdrawing those life-prolonging interventions allows nature or God or whatever to play a role and take its course.”
Another U.S. reader pointed out that “multiple polls in this country have shown that the majority of the general public, physicians in general and psychiatrists in particular, support the option of MAID for the terminally ill. They do not find it at variance with their calling as physicians.”
“I and many of my elderly friends don’t fear death but fear prolonged dementia with its dependency and lack of quality of life,” one reader wrote. “We would be much more at peace if we could put in our advanced directive that we request MAID once some point of dependency has been reached.”
Another wrote that in the event of entering a state of “degrading dependency and hardship on the family, please let me go peacefully, without burdening others, into that good night [of death].”
Many felt that not only physical illness but also the prospect of cognitive degeneration – specifically dementia – also justifies assisting patient death.
“Enormous suffering”
One Canadian reader noted that provisions for advance consent are now in place in Canada for those facing the prospect of neurodegenerative disease and who are still mentally competent to make such decisions.
But therein lies the rub – the concept of an advanced directive goes to the question of decisional capacity. Dr. Miller noted that “depression distorts cognition and leads many patients to believe that they would be better off dead and that their loves ones would be better off without them.”
The concept of “cognitive distortion” implies that the illness itself may impede the decisional capacity required for an advanced directive or a decision made in the moment, in the absence of such a directive. Dr. Miller asked, “How do we determine whether patients with serious mental illness are competent to make such a decision or whether it is mental illness that is driving their perception of a future without hope?”
One reader attested to this from personal experience. “As both a physician and a sufferer of severe, often profound depression for 50 years, I can confidently say that ... the pursuit of death is the result of an impaired mental state, which simultaneously prevents a rational decision.”
Another agreed. “As a psychiatrist, I treated suicidal patients almost every day of my 27-year career. I believe in making every effort to prevent the suicide of a healthy depressed person and I do not support MAID for psychiatric conditions. But I do support MAID for the terminally ill.”
Other readers disagreed. In the words of one commentator, “I think that if we are going to help mentally ill people, we have to consider their choices. The stress imposed by a severe/intractable mental illness is as bad as any other devastating medical illness. If no one is going to hold their hand in life (as support services are limited and psychiatric treatments often fail), allow a medical professional to hold their hand through their final moments.”
A psychiatrist described very ill patients with treatment-resistant bipolar disorder who had not only received medications, including ketamine, but had also received electroconvulsive therapy and still did not respond.
“Their suffering is enormous and the truth is that there is no improvement for more than a few days or weeks and later they return to their hell. Appreciating that they would be better off dead for themselves and their families is not always a cognitive distortion but an objective evaluation of their reality.”
However, as another reader pointed out, an issue with the argument presented here is that it presupposes that MAID requires “clinical justification.” But in Canada, “MAID ... is understood as an expression of personal autonomy. Rooted in liberal political philosophy of individualism ... approval for death need not be based on a clinical assessment.” Instead, “death is seen as a ‘right’ that the state must therefore provide.”
Another form of eugenics?
Dr. Miller raised the ethical implications of racial and socioeconomic factors playing a role in the consideration of MAID for those with psychiatric illness.
“Might those who are poor, who have less access to expensive treatment options and social support, be more likely to request facilitated death?” she asks. “Do we risk facilitating a patient’s demise when other options are unavailable because of a lack of access to treatment or when social and financial struggles exacerbate a person’s hopelessness? Should we worry that psychiatric euthanasia will turn into a form of eugenics where those who can’t contribute are made to feel that they should bow out?”
Several readers agreed. “Looking at the disproportionate burden of illness, rates of imprisonment, and application of the death penalty indicates to me that race and socioeconomic status will be an immediate factor in how, where, and with whom MAID for mental illness would be practice in much, if not all, of the U.S.,” wrote one physician.
A Canadian reader expressed similar concerns. “I’ve seen a handful of people, including someone I considered a good friend, opt for MAID because it was easier than living as a disabled person in poverty without adequate mental health care.”
Another Canadian clinician noted that offering people good care can make all the difference. “As a Canadian mental health clinician who served youth with severe mental illness for over 20 years through our socialized medical network, I can attest to the difference good care usually makes in shifting clients from despair and a commitment to death to embracing life once again. Let’s not, as clinicians, embrace easing a government/state-sanctioned pathway to death.”
Some readers believe that these types of issues can’t be solved with a blanket approach, noting that each case is different. “Real life is always more complicated than academic discussions. Having served on a hospital ethics committee, I know that each case is unique,” one reader noted.
Another reader added, “I think all we can do as physicians is to let people decide for themselves and participate only if our conscience allows.”
A version of this article first appeared on Medscape.com.
It may be time to pay attention to COVID again
More than 3 years into the COVID-19 era, most Americans have settled back into their prepandemic lifestyles.
Since April, a new COVID variant has cropped up. According to recent Centers for Disease Control and Prevention data, EG.5 – from the Omicron family – now makes up 17% of all cases in the United States, up from 7.5% in the first week of July.
A summary from the Center for Infectious Disease Research and Policy at the University of Minnesota says that EG.5, nicknamed “Eris” by health trackers, is nearly the same as its parent strain, XBB.1.9.2, but has one extra spike mutation.
Along with the news of EG.5’s growing prevalence, COVID-related hospitalization rates have increased by 12.5% during the week ending on July 29 – the most significant uptick since December. Still, no connection has been made between the new variant and rising hospital admissions. And so far, experts have found no difference in the severity of illness or symptoms between Eris and the strains that came before it.
Cause for concern?
The COVID virus has a great tendency to mutate, said William Schaffner, MD, a professor of infectious diseases at Vanderbilt University, Nashville, Tenn.
“Fortunately, these are relatively minor mutations.” Even so, SARS-CoV-2, the virus that causes COVID-19, continues to be highly contagious. “There isn’t any doubt that it’s spreading – but it’s not more serious.”
So, Dr. Schaffner doesn’t think it’s time to panic. He prefers calling it an “uptick” in cases instead of a “surge,” because a surge “sounds too big.”
While the numbers are still low, compared with 2022’s summer surge, experts still urge people to stay aware of changes in the virus. “I do not think that there is any cause for alarm,” agreed Bernard Camins, MD, an infectious disease specialist at Mount Sinai Hospital, New York.
So why the higher number of cases? “There has been an increase in COVID cases this summer, probably related to travel, socializing, and dwindling masking,” said Anne Liu, MD, an allergy, immunology, and infectious disease specialist at Stanford (Calif.) University. Even so, “because of an existing level of immunity from vaccination and prior infections, it has been limited and case severity has been lower than in prior surges.”
What the official numbers say
The CDC no longer updates its COVID Data Tracker Weekly Review. They stopped in May 2023 when the federal public health emergency ended.
But the agency continues to track COVID-19 cases, hospitalizations, ED visits, and deaths in different ways. The key takeaways include 9,056 new hospitalizations reported for the week ending July 29, 2023. That is relatively low, compared with July 30, 2022, when the weekly new hospitalization numbers topped 44,000.
“Last year, we saw a summer wave with cases peaking around mid-July. In that sense, our summer wave is coming a bit later than last year,” said Pavitra Roychoudhury, PhD, an assistant professor and researcher in the vaccine and infectious disease division at the University of Washington, Seattle.
“It’s unclear how high the peak will be during this current wave. Levels of SARS-CoV-2 in wastewater, as well as the number of hospitalizations, are currently lower than this time last year.”
For part of the pandemic, the CDC recommended people monitor COVID numbers in their own communities. But the agency’s local guidance on COVID is tied to hospital admission levels, which are currently low for more than 99% of the country, even if they are increasing.
So, while it’s good news that hospitalization numbers are smaller, it means the agency’s ability to identify local outbreaks or hot spots of SARS-CoV-2 is now more limited.
It’s not just an uptick in hospitalizations nationwide, as other COVID-19 indicators, including ED visits, positive tests, and wastewater levels, are increasing across the United States.
In terms of other metrics:
- On June 19, 0.47% of ED visits resulted in a positive COVID diagnosis. On Aug. 4, that rate had more than doubled to 1.1%.
- On July 29, 8.9% of people who took a COVID test reported a positive result. The positivity rate has been increasing since June 10, when 4.1% of tests came back positive. This figure only includes test results reported to the CDC. Results of home testing remain largely unknown.
- The weekly percentage of deaths related to COVID-19 was 1% as of July 29. That’s low, compared with previous rates. For example, for the week ending July 30, 2022, it was 5.8%.
What about new COVID vaccines?
As long as the general public continue to make informed decisions and get the new Omicron vaccine or booster once it’s available, experts predict lower hospitalization rates this winter.
“Everyone should get the Omicron booster when it becomes available,” recommended Dean Winslow, MD, a professor of medicine at Stanford University.
In the meantime, “it is important to emphasize that COVID-19 is going to be with us for the foreseeable future,” he said. Since the symptoms linked to these newer Omicron subvariants are generally milder than with earlier variants, “if one has even mild cold symptoms, it is a good idea to test yourself for COVID-19 and start treatment early if one is elderly or otherwise at high risk for severe disease.”
Dr. Schaffner remains optimistic for now. “We anticipate that the vaccines we currently have available, and certainly the vaccine that is being developed for this fall, will continue to prevent severe disease associated with this virus.”
Although it’s difficult to predict an exact time line, Dr. Schaffner said they could be available by the end of September.
His predictions assume “that we don’t have a new nasty variant that crops up somewhere in the world,” he said. “[If] things continue to move the way they have been, we anticipate that this vaccine ... will be really effective and help us keep out of the hospital during this winter, when we expect more of an increase of COVID once again.”
Asked for his outlook on vaccine recommendations, Dr. Camins was less certain. “It is too soon to tell.” Guidance on COVID shots will be based on results of ongoing studies. “It would be prudent, however, for everyone to plan on getting the flu shot in September.”
Stay alert and stay realistic
Cautious optimism and a call to remain vigilant seem like the consensus at the moment. While the numbers remain low so far and the uptick in new cases and hospitalizations are relatively small, compared with past scenarios, “it makes sense to boost our anti-Omicron antibody levels with immunizations before fall and winter,” Dr. Liu said.
“It’s just advisable for everyone – especially those who are at higher risk for hospitalization or death – to be aware,” Dr. Camins said, “so they can form their own decisions to participate in activities that may put them at risk for contracting COVID-19.”
While respiratory virus work best at keeping people with the flu, COVID, or RSV out of the hospital, they’re not as good at preventing milder infections. Dr. Schaffner said: “If we don’t expect perfection, we won’t be so disappointed.”
A version of this article first appeared on WebMD.com.
More than 3 years into the COVID-19 era, most Americans have settled back into their prepandemic lifestyles.
Since April, a new COVID variant has cropped up. According to recent Centers for Disease Control and Prevention data, EG.5 – from the Omicron family – now makes up 17% of all cases in the United States, up from 7.5% in the first week of July.
A summary from the Center for Infectious Disease Research and Policy at the University of Minnesota says that EG.5, nicknamed “Eris” by health trackers, is nearly the same as its parent strain, XBB.1.9.2, but has one extra spike mutation.
Along with the news of EG.5’s growing prevalence, COVID-related hospitalization rates have increased by 12.5% during the week ending on July 29 – the most significant uptick since December. Still, no connection has been made between the new variant and rising hospital admissions. And so far, experts have found no difference in the severity of illness or symptoms between Eris and the strains that came before it.
Cause for concern?
The COVID virus has a great tendency to mutate, said William Schaffner, MD, a professor of infectious diseases at Vanderbilt University, Nashville, Tenn.
“Fortunately, these are relatively minor mutations.” Even so, SARS-CoV-2, the virus that causes COVID-19, continues to be highly contagious. “There isn’t any doubt that it’s spreading – but it’s not more serious.”
So, Dr. Schaffner doesn’t think it’s time to panic. He prefers calling it an “uptick” in cases instead of a “surge,” because a surge “sounds too big.”
While the numbers are still low, compared with 2022’s summer surge, experts still urge people to stay aware of changes in the virus. “I do not think that there is any cause for alarm,” agreed Bernard Camins, MD, an infectious disease specialist at Mount Sinai Hospital, New York.
So why the higher number of cases? “There has been an increase in COVID cases this summer, probably related to travel, socializing, and dwindling masking,” said Anne Liu, MD, an allergy, immunology, and infectious disease specialist at Stanford (Calif.) University. Even so, “because of an existing level of immunity from vaccination and prior infections, it has been limited and case severity has been lower than in prior surges.”
What the official numbers say
The CDC no longer updates its COVID Data Tracker Weekly Review. They stopped in May 2023 when the federal public health emergency ended.
But the agency continues to track COVID-19 cases, hospitalizations, ED visits, and deaths in different ways. The key takeaways include 9,056 new hospitalizations reported for the week ending July 29, 2023. That is relatively low, compared with July 30, 2022, when the weekly new hospitalization numbers topped 44,000.
“Last year, we saw a summer wave with cases peaking around mid-July. In that sense, our summer wave is coming a bit later than last year,” said Pavitra Roychoudhury, PhD, an assistant professor and researcher in the vaccine and infectious disease division at the University of Washington, Seattle.
“It’s unclear how high the peak will be during this current wave. Levels of SARS-CoV-2 in wastewater, as well as the number of hospitalizations, are currently lower than this time last year.”
For part of the pandemic, the CDC recommended people monitor COVID numbers in their own communities. But the agency’s local guidance on COVID is tied to hospital admission levels, which are currently low for more than 99% of the country, even if they are increasing.
So, while it’s good news that hospitalization numbers are smaller, it means the agency’s ability to identify local outbreaks or hot spots of SARS-CoV-2 is now more limited.
It’s not just an uptick in hospitalizations nationwide, as other COVID-19 indicators, including ED visits, positive tests, and wastewater levels, are increasing across the United States.
In terms of other metrics:
- On June 19, 0.47% of ED visits resulted in a positive COVID diagnosis. On Aug. 4, that rate had more than doubled to 1.1%.
- On July 29, 8.9% of people who took a COVID test reported a positive result. The positivity rate has been increasing since June 10, when 4.1% of tests came back positive. This figure only includes test results reported to the CDC. Results of home testing remain largely unknown.
- The weekly percentage of deaths related to COVID-19 was 1% as of July 29. That’s low, compared with previous rates. For example, for the week ending July 30, 2022, it was 5.8%.
What about new COVID vaccines?
As long as the general public continue to make informed decisions and get the new Omicron vaccine or booster once it’s available, experts predict lower hospitalization rates this winter.
“Everyone should get the Omicron booster when it becomes available,” recommended Dean Winslow, MD, a professor of medicine at Stanford University.
In the meantime, “it is important to emphasize that COVID-19 is going to be with us for the foreseeable future,” he said. Since the symptoms linked to these newer Omicron subvariants are generally milder than with earlier variants, “if one has even mild cold symptoms, it is a good idea to test yourself for COVID-19 and start treatment early if one is elderly or otherwise at high risk for severe disease.”
Dr. Schaffner remains optimistic for now. “We anticipate that the vaccines we currently have available, and certainly the vaccine that is being developed for this fall, will continue to prevent severe disease associated with this virus.”
Although it’s difficult to predict an exact time line, Dr. Schaffner said they could be available by the end of September.
His predictions assume “that we don’t have a new nasty variant that crops up somewhere in the world,” he said. “[If] things continue to move the way they have been, we anticipate that this vaccine ... will be really effective and help us keep out of the hospital during this winter, when we expect more of an increase of COVID once again.”
Asked for his outlook on vaccine recommendations, Dr. Camins was less certain. “It is too soon to tell.” Guidance on COVID shots will be based on results of ongoing studies. “It would be prudent, however, for everyone to plan on getting the flu shot in September.”
Stay alert and stay realistic
Cautious optimism and a call to remain vigilant seem like the consensus at the moment. While the numbers remain low so far and the uptick in new cases and hospitalizations are relatively small, compared with past scenarios, “it makes sense to boost our anti-Omicron antibody levels with immunizations before fall and winter,” Dr. Liu said.
“It’s just advisable for everyone – especially those who are at higher risk for hospitalization or death – to be aware,” Dr. Camins said, “so they can form their own decisions to participate in activities that may put them at risk for contracting COVID-19.”
While respiratory virus work best at keeping people with the flu, COVID, or RSV out of the hospital, they’re not as good at preventing milder infections. Dr. Schaffner said: “If we don’t expect perfection, we won’t be so disappointed.”
A version of this article first appeared on WebMD.com.
More than 3 years into the COVID-19 era, most Americans have settled back into their prepandemic lifestyles.
Since April, a new COVID variant has cropped up. According to recent Centers for Disease Control and Prevention data, EG.5 – from the Omicron family – now makes up 17% of all cases in the United States, up from 7.5% in the first week of July.
A summary from the Center for Infectious Disease Research and Policy at the University of Minnesota says that EG.5, nicknamed “Eris” by health trackers, is nearly the same as its parent strain, XBB.1.9.2, but has one extra spike mutation.
Along with the news of EG.5’s growing prevalence, COVID-related hospitalization rates have increased by 12.5% during the week ending on July 29 – the most significant uptick since December. Still, no connection has been made between the new variant and rising hospital admissions. And so far, experts have found no difference in the severity of illness or symptoms between Eris and the strains that came before it.
Cause for concern?
The COVID virus has a great tendency to mutate, said William Schaffner, MD, a professor of infectious diseases at Vanderbilt University, Nashville, Tenn.
“Fortunately, these are relatively minor mutations.” Even so, SARS-CoV-2, the virus that causes COVID-19, continues to be highly contagious. “There isn’t any doubt that it’s spreading – but it’s not more serious.”
So, Dr. Schaffner doesn’t think it’s time to panic. He prefers calling it an “uptick” in cases instead of a “surge,” because a surge “sounds too big.”
While the numbers are still low, compared with 2022’s summer surge, experts still urge people to stay aware of changes in the virus. “I do not think that there is any cause for alarm,” agreed Bernard Camins, MD, an infectious disease specialist at Mount Sinai Hospital, New York.
So why the higher number of cases? “There has been an increase in COVID cases this summer, probably related to travel, socializing, and dwindling masking,” said Anne Liu, MD, an allergy, immunology, and infectious disease specialist at Stanford (Calif.) University. Even so, “because of an existing level of immunity from vaccination and prior infections, it has been limited and case severity has been lower than in prior surges.”
What the official numbers say
The CDC no longer updates its COVID Data Tracker Weekly Review. They stopped in May 2023 when the federal public health emergency ended.
But the agency continues to track COVID-19 cases, hospitalizations, ED visits, and deaths in different ways. The key takeaways include 9,056 new hospitalizations reported for the week ending July 29, 2023. That is relatively low, compared with July 30, 2022, when the weekly new hospitalization numbers topped 44,000.
“Last year, we saw a summer wave with cases peaking around mid-July. In that sense, our summer wave is coming a bit later than last year,” said Pavitra Roychoudhury, PhD, an assistant professor and researcher in the vaccine and infectious disease division at the University of Washington, Seattle.
“It’s unclear how high the peak will be during this current wave. Levels of SARS-CoV-2 in wastewater, as well as the number of hospitalizations, are currently lower than this time last year.”
For part of the pandemic, the CDC recommended people monitor COVID numbers in their own communities. But the agency’s local guidance on COVID is tied to hospital admission levels, which are currently low for more than 99% of the country, even if they are increasing.
So, while it’s good news that hospitalization numbers are smaller, it means the agency’s ability to identify local outbreaks or hot spots of SARS-CoV-2 is now more limited.
It’s not just an uptick in hospitalizations nationwide, as other COVID-19 indicators, including ED visits, positive tests, and wastewater levels, are increasing across the United States.
In terms of other metrics:
- On June 19, 0.47% of ED visits resulted in a positive COVID diagnosis. On Aug. 4, that rate had more than doubled to 1.1%.
- On July 29, 8.9% of people who took a COVID test reported a positive result. The positivity rate has been increasing since June 10, when 4.1% of tests came back positive. This figure only includes test results reported to the CDC. Results of home testing remain largely unknown.
- The weekly percentage of deaths related to COVID-19 was 1% as of July 29. That’s low, compared with previous rates. For example, for the week ending July 30, 2022, it was 5.8%.
What about new COVID vaccines?
As long as the general public continue to make informed decisions and get the new Omicron vaccine or booster once it’s available, experts predict lower hospitalization rates this winter.
“Everyone should get the Omicron booster when it becomes available,” recommended Dean Winslow, MD, a professor of medicine at Stanford University.
In the meantime, “it is important to emphasize that COVID-19 is going to be with us for the foreseeable future,” he said. Since the symptoms linked to these newer Omicron subvariants are generally milder than with earlier variants, “if one has even mild cold symptoms, it is a good idea to test yourself for COVID-19 and start treatment early if one is elderly or otherwise at high risk for severe disease.”
Dr. Schaffner remains optimistic for now. “We anticipate that the vaccines we currently have available, and certainly the vaccine that is being developed for this fall, will continue to prevent severe disease associated with this virus.”
Although it’s difficult to predict an exact time line, Dr. Schaffner said they could be available by the end of September.
His predictions assume “that we don’t have a new nasty variant that crops up somewhere in the world,” he said. “[If] things continue to move the way they have been, we anticipate that this vaccine ... will be really effective and help us keep out of the hospital during this winter, when we expect more of an increase of COVID once again.”
Asked for his outlook on vaccine recommendations, Dr. Camins was less certain. “It is too soon to tell.” Guidance on COVID shots will be based on results of ongoing studies. “It would be prudent, however, for everyone to plan on getting the flu shot in September.”
Stay alert and stay realistic
Cautious optimism and a call to remain vigilant seem like the consensus at the moment. While the numbers remain low so far and the uptick in new cases and hospitalizations are relatively small, compared with past scenarios, “it makes sense to boost our anti-Omicron antibody levels with immunizations before fall and winter,” Dr. Liu said.
“It’s just advisable for everyone – especially those who are at higher risk for hospitalization or death – to be aware,” Dr. Camins said, “so they can form their own decisions to participate in activities that may put them at risk for contracting COVID-19.”
While respiratory virus work best at keeping people with the flu, COVID, or RSV out of the hospital, they’re not as good at preventing milder infections. Dr. Schaffner said: “If we don’t expect perfection, we won’t be so disappointed.”
A version of this article first appeared on WebMD.com.
Study validates use of new psoriatic arthritis prediction tool
Though it requires further validation, researchers led by rheumatologist Lihi Eder, MD, PhD, of the Women’s College Research Institute at Women’s College Hospital, Toronto, characterized the development and validation of PRESTO as “an important first step in the development and testing of interventional strategies that may ultimately halt disease progression,” they wrote in their study of the tool, which published in Arthritis & Rheumatology. Dr. Eder presented a summary of progress on the effort at the 2023 annual meeting of the Canadian Rheumatology Association.
To develop and validate the tool, the researchers evaluated 635 patients from the University of Toronto Psoriasis Cohort, which was launched in 2006 as a prospective longitudinal cohort study to examine risk factors for the development of PsA among patients with psoriasis. Patients enrolled in the cohort have a dermatologist-confirmed diagnosis of psoriasis and are assessed by a rheumatologist prior to enrollment to exclude those with inflammatory arthritis in the past or at the time of assessment.
To develop prediction models for PsA, Dr. Eder and colleagues used information from the patient cohort demographics, psoriasis characteristics, comorbidities, medications, and musculoskeletal symptoms. Next, they used multivariable logistic regression models adjusting for covariates, duration of psoriasis, and the log duration at risk to estimate the probability of developing PsA within 1-year and 5-year time windows from consecutive study visits.
The mean age of the study participants was 47 years, 76% were White, and 57% were male; and they had psoriasis for a mean of 16 years. The researchers found that 51 patients developed PsA during the 1-year follow-up, and 71 developed PsA during the 5-year follow-up. The risk of developing PsA within 1 year was associated with younger age, male sex, family history of psoriasis, back stiffness, nail pitting, joint stiffness, use of biologic medications, patient global health, and pain severity (area under the curve, 72.3).
In addition, the risk of developing PsA within 5 years was associated with morning stiffness, psoriatic nail lesions, psoriasis severity, fatigue, pain, and use of systemic non-biologic medication or phototherapy (AUC, 74.9). Calibration plots showed reasonable agreement between predicted and observed probabilities.
“Interestingly, several previously reported risk factors for PsA, such as HLA-B27, family history of PsA, uveitis, and flexural psoriasis, were not included in the risk prediction model due to their scarcity in our cohort,” the researchers wrote. “This finding may be due to immortal time bias which can complicate the development of risk prediction models for PsA. Genetic factors or their surrogates (e.g., family history of PsA) are associated with the development of PsA concurrently or shortly after the onset of psoriasis.”
They acknowledged certain limitations of the study, including its relatively small sample size and questionable generalizability of the study findings, “as most of the patients were recruited from dermatology clinics leading to overrepresentation of moderate-severe psoriasis. Therefore, PRESTO will require an external validation to assess its performance in other populations of psoriasis patients with different characteristics.”
Saakshi Khattri, MD, a board-certified dermatologist, rheumatologist, and internist at the Icahn School of Medicine at Mount Sinai, New York, who was not involved in the study and was asked to comment on the results, characterized the PRESTO tool as “an interesting step in the right direction, but it’s the first step.”
Since dermatologists are usually the first point of contact for psoriasis patients, she added, “a risk calculator can be helpful, but the question remains: When do we refer them to a rheumatologist? If the risk comes to 5%, is that a low risk that doesn’t need referral to rheumatology? I don’t think those questions have been answered here. From a rheumatology perspective, does the risk calculator help me decide when to intervene? At present, I’m not sure it does. Perhaps a higher score might make us intervene sooner if our clinical exam doesn’t show swollen or tender joints.”
Clinical exam findings and history she considers as a rheumatologist before making treatment recommendations include the following: Are there swollen and tender joints? Does the patient report morning stiffness for upwards of 30 minutes? Do they have enthesitis or dactylitis? Is there axial involvement? “Imaging can help if there isn’t anything on clinical exam and the history is compelling and/or the patient has risk factors for PsA,” she said.
The study’s finding of biologic use being associated with risk of developing PsA at year 1 but not at year 5 is “confusing,” Dr. Khattri added. “My concern is, will that now dissuade our moderate to severe psoriasis patients from using biologics to clear their psoriasis? We know that biologics are indicated for moderate to severe psoriasis. We also know psoriasis is associated with increased cardiovascular risk and there’s data to suggest that treatment with biologics with its resultant decrease in systemic inflammation can decrease cardiovascular risk.”
The study was supported by a New Investigator Grant from the Physician Services Incorporated Foundation. Dr. Eder disclosed that she is supported by the Canada Research Chair in Inflammatory Rheumatic Diseases. Dr. Khattri reported that she is a member of the advisory board for UCB, Janssen, AbbVie, Regeneron, Sanofi, Lilly, Argenx, and Arcutis. She has also received research funds from Incyte, AbbVie, Leo, Galderma, Pfizer, and Acelyrin.
Though it requires further validation, researchers led by rheumatologist Lihi Eder, MD, PhD, of the Women’s College Research Institute at Women’s College Hospital, Toronto, characterized the development and validation of PRESTO as “an important first step in the development and testing of interventional strategies that may ultimately halt disease progression,” they wrote in their study of the tool, which published in Arthritis & Rheumatology. Dr. Eder presented a summary of progress on the effort at the 2023 annual meeting of the Canadian Rheumatology Association.
To develop and validate the tool, the researchers evaluated 635 patients from the University of Toronto Psoriasis Cohort, which was launched in 2006 as a prospective longitudinal cohort study to examine risk factors for the development of PsA among patients with psoriasis. Patients enrolled in the cohort have a dermatologist-confirmed diagnosis of psoriasis and are assessed by a rheumatologist prior to enrollment to exclude those with inflammatory arthritis in the past or at the time of assessment.
To develop prediction models for PsA, Dr. Eder and colleagues used information from the patient cohort demographics, psoriasis characteristics, comorbidities, medications, and musculoskeletal symptoms. Next, they used multivariable logistic regression models adjusting for covariates, duration of psoriasis, and the log duration at risk to estimate the probability of developing PsA within 1-year and 5-year time windows from consecutive study visits.
The mean age of the study participants was 47 years, 76% were White, and 57% were male; and they had psoriasis for a mean of 16 years. The researchers found that 51 patients developed PsA during the 1-year follow-up, and 71 developed PsA during the 5-year follow-up. The risk of developing PsA within 1 year was associated with younger age, male sex, family history of psoriasis, back stiffness, nail pitting, joint stiffness, use of biologic medications, patient global health, and pain severity (area under the curve, 72.3).
In addition, the risk of developing PsA within 5 years was associated with morning stiffness, psoriatic nail lesions, psoriasis severity, fatigue, pain, and use of systemic non-biologic medication or phototherapy (AUC, 74.9). Calibration plots showed reasonable agreement between predicted and observed probabilities.
“Interestingly, several previously reported risk factors for PsA, such as HLA-B27, family history of PsA, uveitis, and flexural psoriasis, were not included in the risk prediction model due to their scarcity in our cohort,” the researchers wrote. “This finding may be due to immortal time bias which can complicate the development of risk prediction models for PsA. Genetic factors or their surrogates (e.g., family history of PsA) are associated with the development of PsA concurrently or shortly after the onset of psoriasis.”
They acknowledged certain limitations of the study, including its relatively small sample size and questionable generalizability of the study findings, “as most of the patients were recruited from dermatology clinics leading to overrepresentation of moderate-severe psoriasis. Therefore, PRESTO will require an external validation to assess its performance in other populations of psoriasis patients with different characteristics.”
Saakshi Khattri, MD, a board-certified dermatologist, rheumatologist, and internist at the Icahn School of Medicine at Mount Sinai, New York, who was not involved in the study and was asked to comment on the results, characterized the PRESTO tool as “an interesting step in the right direction, but it’s the first step.”
Since dermatologists are usually the first point of contact for psoriasis patients, she added, “a risk calculator can be helpful, but the question remains: When do we refer them to a rheumatologist? If the risk comes to 5%, is that a low risk that doesn’t need referral to rheumatology? I don’t think those questions have been answered here. From a rheumatology perspective, does the risk calculator help me decide when to intervene? At present, I’m not sure it does. Perhaps a higher score might make us intervene sooner if our clinical exam doesn’t show swollen or tender joints.”
Clinical exam findings and history she considers as a rheumatologist before making treatment recommendations include the following: Are there swollen and tender joints? Does the patient report morning stiffness for upwards of 30 minutes? Do they have enthesitis or dactylitis? Is there axial involvement? “Imaging can help if there isn’t anything on clinical exam and the history is compelling and/or the patient has risk factors for PsA,” she said.
The study’s finding of biologic use being associated with risk of developing PsA at year 1 but not at year 5 is “confusing,” Dr. Khattri added. “My concern is, will that now dissuade our moderate to severe psoriasis patients from using biologics to clear their psoriasis? We know that biologics are indicated for moderate to severe psoriasis. We also know psoriasis is associated with increased cardiovascular risk and there’s data to suggest that treatment with biologics with its resultant decrease in systemic inflammation can decrease cardiovascular risk.”
The study was supported by a New Investigator Grant from the Physician Services Incorporated Foundation. Dr. Eder disclosed that she is supported by the Canada Research Chair in Inflammatory Rheumatic Diseases. Dr. Khattri reported that she is a member of the advisory board for UCB, Janssen, AbbVie, Regeneron, Sanofi, Lilly, Argenx, and Arcutis. She has also received research funds from Incyte, AbbVie, Leo, Galderma, Pfizer, and Acelyrin.
Though it requires further validation, researchers led by rheumatologist Lihi Eder, MD, PhD, of the Women’s College Research Institute at Women’s College Hospital, Toronto, characterized the development and validation of PRESTO as “an important first step in the development and testing of interventional strategies that may ultimately halt disease progression,” they wrote in their study of the tool, which published in Arthritis & Rheumatology. Dr. Eder presented a summary of progress on the effort at the 2023 annual meeting of the Canadian Rheumatology Association.
To develop and validate the tool, the researchers evaluated 635 patients from the University of Toronto Psoriasis Cohort, which was launched in 2006 as a prospective longitudinal cohort study to examine risk factors for the development of PsA among patients with psoriasis. Patients enrolled in the cohort have a dermatologist-confirmed diagnosis of psoriasis and are assessed by a rheumatologist prior to enrollment to exclude those with inflammatory arthritis in the past or at the time of assessment.
To develop prediction models for PsA, Dr. Eder and colleagues used information from the patient cohort demographics, psoriasis characteristics, comorbidities, medications, and musculoskeletal symptoms. Next, they used multivariable logistic regression models adjusting for covariates, duration of psoriasis, and the log duration at risk to estimate the probability of developing PsA within 1-year and 5-year time windows from consecutive study visits.
The mean age of the study participants was 47 years, 76% were White, and 57% were male; and they had psoriasis for a mean of 16 years. The researchers found that 51 patients developed PsA during the 1-year follow-up, and 71 developed PsA during the 5-year follow-up. The risk of developing PsA within 1 year was associated with younger age, male sex, family history of psoriasis, back stiffness, nail pitting, joint stiffness, use of biologic medications, patient global health, and pain severity (area under the curve, 72.3).
In addition, the risk of developing PsA within 5 years was associated with morning stiffness, psoriatic nail lesions, psoriasis severity, fatigue, pain, and use of systemic non-biologic medication or phototherapy (AUC, 74.9). Calibration plots showed reasonable agreement between predicted and observed probabilities.
“Interestingly, several previously reported risk factors for PsA, such as HLA-B27, family history of PsA, uveitis, and flexural psoriasis, were not included in the risk prediction model due to their scarcity in our cohort,” the researchers wrote. “This finding may be due to immortal time bias which can complicate the development of risk prediction models for PsA. Genetic factors or their surrogates (e.g., family history of PsA) are associated with the development of PsA concurrently or shortly after the onset of psoriasis.”
They acknowledged certain limitations of the study, including its relatively small sample size and questionable generalizability of the study findings, “as most of the patients were recruited from dermatology clinics leading to overrepresentation of moderate-severe psoriasis. Therefore, PRESTO will require an external validation to assess its performance in other populations of psoriasis patients with different characteristics.”
Saakshi Khattri, MD, a board-certified dermatologist, rheumatologist, and internist at the Icahn School of Medicine at Mount Sinai, New York, who was not involved in the study and was asked to comment on the results, characterized the PRESTO tool as “an interesting step in the right direction, but it’s the first step.”
Since dermatologists are usually the first point of contact for psoriasis patients, she added, “a risk calculator can be helpful, but the question remains: When do we refer them to a rheumatologist? If the risk comes to 5%, is that a low risk that doesn’t need referral to rheumatology? I don’t think those questions have been answered here. From a rheumatology perspective, does the risk calculator help me decide when to intervene? At present, I’m not sure it does. Perhaps a higher score might make us intervene sooner if our clinical exam doesn’t show swollen or tender joints.”
Clinical exam findings and history she considers as a rheumatologist before making treatment recommendations include the following: Are there swollen and tender joints? Does the patient report morning stiffness for upwards of 30 minutes? Do they have enthesitis or dactylitis? Is there axial involvement? “Imaging can help if there isn’t anything on clinical exam and the history is compelling and/or the patient has risk factors for PsA,” she said.
The study’s finding of biologic use being associated with risk of developing PsA at year 1 but not at year 5 is “confusing,” Dr. Khattri added. “My concern is, will that now dissuade our moderate to severe psoriasis patients from using biologics to clear their psoriasis? We know that biologics are indicated for moderate to severe psoriasis. We also know psoriasis is associated with increased cardiovascular risk and there’s data to suggest that treatment with biologics with its resultant decrease in systemic inflammation can decrease cardiovascular risk.”
The study was supported by a New Investigator Grant from the Physician Services Incorporated Foundation. Dr. Eder disclosed that she is supported by the Canada Research Chair in Inflammatory Rheumatic Diseases. Dr. Khattri reported that she is a member of the advisory board for UCB, Janssen, AbbVie, Regeneron, Sanofi, Lilly, Argenx, and Arcutis. She has also received research funds from Incyte, AbbVie, Leo, Galderma, Pfizer, and Acelyrin.
FROM ARTHRITIS AND RHEUMATOLOGY
Cause of common gastrointestinal symptoms in diabetes?
The condition – in which the pancreas fails to produce sufficient enzymes to fully digest food – can cause gastrointestinal symptoms, including steatorrhea or other stool changes, bloating, and/or abdominal pain. The preferred test for diagnosis is a 72-hour fecal fat quantification test, but fecal elastase-1 is a less invasive and reliable alternative; values of less than 200 mcg/g indicate EPI. Treatment is pancreatic enzyme replacement therapy (PERT), taken with every meal.
EPI occurs in up to 90% of people with cystic fibrosis and chronic pancreatitis and is commonly associated with acute pancreatitis, autoimmune pancreatitis, and pancreatic cancer. However, those conditions are relatively rare compared to diabetes, yet the EPI association with diabetes is less well-studied, Dana M. Lewis, BA, points out in her review article.
While the data vary across studies, owing to differences in inclusion and exclusion criteria, the overall median prevalence of EPI was 33% among patients with type 1 diabetes (range, 14%-77.5%) and 29% among patients with type 2 diabetes (range, 16.8%-49.2%), Ms. Lewis reports in the article, which was published in Diabetes Technology and Therapeutics.
“Cumulatively, this suggests there may be significant numbers of people with diabetes with EPI who are undiagnosed. People with diabetes who present with gastrointestinal symptoms – such as steatorrhea or changes in stool, bloating, and/or abdominal pain – should be screened for EPI. Diabetes specialists, gastroenterologists, and primary care providers should be aware of the high rates of prevalence of diabetes and EPI and recommend fecal elastase-1 screening for people with diabetes and GI symptoms,” Ms. Lewis writes.
Since the publication of her article, Ms. Lewis told this news organization, “I’ve gotten feedback from multiple diabetes and general providers that they will be changing their practice as a result of this paper, by screening people with diabetes who have GI symptoms for EPI, which is wonderful to hear.”
In addition, she noted that since she began blogging about EPI and diabetes last year following her own delayed diagnosis, “I have had at least half a dozen people with diabetes tell me that they’ve since sought screening for EPI after years of GI symptoms and ended up being diagnosed with EPI as well.”
Asked to comment, Romesh Khardori, MD, PhD, said in an interview, “it would be prudent to investigate EPI and treat it when confirmed. Consultation with a gastroenterologist colleague may be helpful. Treatment is quite rewarding.”
Data limitations; and don’t forget celiac disease and gastroparesis
However, as does Ms. Lewis, Dr. Khardori points to the limitations of the current literature.
“This review suffers from the lack of uniformity amongst the studies in terms of diagnosis and documentation of exocrine pancreatic insufficiency. Many studies lack a control group to draw any meaningful conclusions. Correlations with duration of diabetes, age of onset, symptoms, and glycemic control were mostly lacking,” says Dr. Khardori, now retired but formerly professor of medicine: endocrinology and metabolism at Eastern Virginia Medical School, Norfolk.
In general, the data suggest that PERT is safe and effective for people with diabetes and that it may reduce glycemic variability. However, “there are not many studies looking at glucose outcomes in detail, and only one study that has used CGM [continuous glucose monitoring] data, so this is a big area of need for future study,” Ms. Lewis told this news organization.
Ms. Lewis also reviewed the literature on the prevalence of two other diabetes-related gastrointestinal conditions, celiac disease and gastroparesis, “because anecdotally, it seems as though diabetes care providers and people with diabetes are more aware of those as causes of GI symptoms.”
In type 1 diabetes, the prevalence of both celiac disease and gastroparesis are reported at about 5%, in contrast to the 33% for EPI. Similarly, in type 2 diabetes, the reported prevalence of these two conditions are 1.3% and 1.6%, respectively, vs. 29% for EPI.
“This suggests to me that there is likely disproportionate screening for things like celiac [disease] and gastroparesis in diabetes, and that screening for EPI when people with diabetes present with GI symptoms is warranted,” Ms. Lewis said.
However, Dr. Khardori cautioned that those conditions may also be missed, noting, “Celiac disease often is undiagnosed and gastropathy or gastroparesis may be overlooked in a busy primary care clinic where most patients with diabetes mellitus get their care.”
Ms. Lewis and Dr. Khardori have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The condition – in which the pancreas fails to produce sufficient enzymes to fully digest food – can cause gastrointestinal symptoms, including steatorrhea or other stool changes, bloating, and/or abdominal pain. The preferred test for diagnosis is a 72-hour fecal fat quantification test, but fecal elastase-1 is a less invasive and reliable alternative; values of less than 200 mcg/g indicate EPI. Treatment is pancreatic enzyme replacement therapy (PERT), taken with every meal.
EPI occurs in up to 90% of people with cystic fibrosis and chronic pancreatitis and is commonly associated with acute pancreatitis, autoimmune pancreatitis, and pancreatic cancer. However, those conditions are relatively rare compared to diabetes, yet the EPI association with diabetes is less well-studied, Dana M. Lewis, BA, points out in her review article.
While the data vary across studies, owing to differences in inclusion and exclusion criteria, the overall median prevalence of EPI was 33% among patients with type 1 diabetes (range, 14%-77.5%) and 29% among patients with type 2 diabetes (range, 16.8%-49.2%), Ms. Lewis reports in the article, which was published in Diabetes Technology and Therapeutics.
“Cumulatively, this suggests there may be significant numbers of people with diabetes with EPI who are undiagnosed. People with diabetes who present with gastrointestinal symptoms – such as steatorrhea or changes in stool, bloating, and/or abdominal pain – should be screened for EPI. Diabetes specialists, gastroenterologists, and primary care providers should be aware of the high rates of prevalence of diabetes and EPI and recommend fecal elastase-1 screening for people with diabetes and GI symptoms,” Ms. Lewis writes.
Since the publication of her article, Ms. Lewis told this news organization, “I’ve gotten feedback from multiple diabetes and general providers that they will be changing their practice as a result of this paper, by screening people with diabetes who have GI symptoms for EPI, which is wonderful to hear.”
In addition, she noted that since she began blogging about EPI and diabetes last year following her own delayed diagnosis, “I have had at least half a dozen people with diabetes tell me that they’ve since sought screening for EPI after years of GI symptoms and ended up being diagnosed with EPI as well.”
Asked to comment, Romesh Khardori, MD, PhD, said in an interview, “it would be prudent to investigate EPI and treat it when confirmed. Consultation with a gastroenterologist colleague may be helpful. Treatment is quite rewarding.”
Data limitations; and don’t forget celiac disease and gastroparesis
However, as does Ms. Lewis, Dr. Khardori points to the limitations of the current literature.
“This review suffers from the lack of uniformity amongst the studies in terms of diagnosis and documentation of exocrine pancreatic insufficiency. Many studies lack a control group to draw any meaningful conclusions. Correlations with duration of diabetes, age of onset, symptoms, and glycemic control were mostly lacking,” says Dr. Khardori, now retired but formerly professor of medicine: endocrinology and metabolism at Eastern Virginia Medical School, Norfolk.
In general, the data suggest that PERT is safe and effective for people with diabetes and that it may reduce glycemic variability. However, “there are not many studies looking at glucose outcomes in detail, and only one study that has used CGM [continuous glucose monitoring] data, so this is a big area of need for future study,” Ms. Lewis told this news organization.
Ms. Lewis also reviewed the literature on the prevalence of two other diabetes-related gastrointestinal conditions, celiac disease and gastroparesis, “because anecdotally, it seems as though diabetes care providers and people with diabetes are more aware of those as causes of GI symptoms.”
In type 1 diabetes, the prevalence of both celiac disease and gastroparesis are reported at about 5%, in contrast to the 33% for EPI. Similarly, in type 2 diabetes, the reported prevalence of these two conditions are 1.3% and 1.6%, respectively, vs. 29% for EPI.
“This suggests to me that there is likely disproportionate screening for things like celiac [disease] and gastroparesis in diabetes, and that screening for EPI when people with diabetes present with GI symptoms is warranted,” Ms. Lewis said.
However, Dr. Khardori cautioned that those conditions may also be missed, noting, “Celiac disease often is undiagnosed and gastropathy or gastroparesis may be overlooked in a busy primary care clinic where most patients with diabetes mellitus get their care.”
Ms. Lewis and Dr. Khardori have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The condition – in which the pancreas fails to produce sufficient enzymes to fully digest food – can cause gastrointestinal symptoms, including steatorrhea or other stool changes, bloating, and/or abdominal pain. The preferred test for diagnosis is a 72-hour fecal fat quantification test, but fecal elastase-1 is a less invasive and reliable alternative; values of less than 200 mcg/g indicate EPI. Treatment is pancreatic enzyme replacement therapy (PERT), taken with every meal.
EPI occurs in up to 90% of people with cystic fibrosis and chronic pancreatitis and is commonly associated with acute pancreatitis, autoimmune pancreatitis, and pancreatic cancer. However, those conditions are relatively rare compared to diabetes, yet the EPI association with diabetes is less well-studied, Dana M. Lewis, BA, points out in her review article.
While the data vary across studies, owing to differences in inclusion and exclusion criteria, the overall median prevalence of EPI was 33% among patients with type 1 diabetes (range, 14%-77.5%) and 29% among patients with type 2 diabetes (range, 16.8%-49.2%), Ms. Lewis reports in the article, which was published in Diabetes Technology and Therapeutics.
“Cumulatively, this suggests there may be significant numbers of people with diabetes with EPI who are undiagnosed. People with diabetes who present with gastrointestinal symptoms – such as steatorrhea or changes in stool, bloating, and/or abdominal pain – should be screened for EPI. Diabetes specialists, gastroenterologists, and primary care providers should be aware of the high rates of prevalence of diabetes and EPI and recommend fecal elastase-1 screening for people with diabetes and GI symptoms,” Ms. Lewis writes.
Since the publication of her article, Ms. Lewis told this news organization, “I’ve gotten feedback from multiple diabetes and general providers that they will be changing their practice as a result of this paper, by screening people with diabetes who have GI symptoms for EPI, which is wonderful to hear.”
In addition, she noted that since she began blogging about EPI and diabetes last year following her own delayed diagnosis, “I have had at least half a dozen people with diabetes tell me that they’ve since sought screening for EPI after years of GI symptoms and ended up being diagnosed with EPI as well.”
Asked to comment, Romesh Khardori, MD, PhD, said in an interview, “it would be prudent to investigate EPI and treat it when confirmed. Consultation with a gastroenterologist colleague may be helpful. Treatment is quite rewarding.”
Data limitations; and don’t forget celiac disease and gastroparesis
However, as does Ms. Lewis, Dr. Khardori points to the limitations of the current literature.
“This review suffers from the lack of uniformity amongst the studies in terms of diagnosis and documentation of exocrine pancreatic insufficiency. Many studies lack a control group to draw any meaningful conclusions. Correlations with duration of diabetes, age of onset, symptoms, and glycemic control were mostly lacking,” says Dr. Khardori, now retired but formerly professor of medicine: endocrinology and metabolism at Eastern Virginia Medical School, Norfolk.
In general, the data suggest that PERT is safe and effective for people with diabetes and that it may reduce glycemic variability. However, “there are not many studies looking at glucose outcomes in detail, and only one study that has used CGM [continuous glucose monitoring] data, so this is a big area of need for future study,” Ms. Lewis told this news organization.
Ms. Lewis also reviewed the literature on the prevalence of two other diabetes-related gastrointestinal conditions, celiac disease and gastroparesis, “because anecdotally, it seems as though diabetes care providers and people with diabetes are more aware of those as causes of GI symptoms.”
In type 1 diabetes, the prevalence of both celiac disease and gastroparesis are reported at about 5%, in contrast to the 33% for EPI. Similarly, in type 2 diabetes, the reported prevalence of these two conditions are 1.3% and 1.6%, respectively, vs. 29% for EPI.
“This suggests to me that there is likely disproportionate screening for things like celiac [disease] and gastroparesis in diabetes, and that screening for EPI when people with diabetes present with GI symptoms is warranted,” Ms. Lewis said.
However, Dr. Khardori cautioned that those conditions may also be missed, noting, “Celiac disease often is undiagnosed and gastropathy or gastroparesis may be overlooked in a busy primary care clinic where most patients with diabetes mellitus get their care.”
Ms. Lewis and Dr. Khardori have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM DIABETES TECHNOLOGY AND THERAPEUTICS
My favorite iron pearls
A 45-year-old women presents for evaluation of fatigue. She has been tired for the past 6 months. She has had no problems with sleep and no other new symptoms. Her physical exam is unremarkable. Her Patient Health Questionnaire–9 score is 4. Lab results are as follows: hemoglobin, 13 g/dL; hematocrit, 39%; mean corpuscular volume, 90 fL; blood urea nitrogen, 10 mg/dL; Cr, 1.0 mg/dL; AST, 20 IU/L; ALT, 15 IU/L; ferritin, 35 mcg/mL; thyroid-stimulating hormone, 3.5 mIU/L.
What would you recommend?
A. Sertraline
B. Sleep study
C. Iron supplementation
I would treat this patient with iron. Verdon and colleagues conducted a randomized, double-blind placebo-controlled trial of iron treatment in nonanemic women.1 The women who received iron had a much greater reduction in fatigue score, compared with the women who did not (P < .004). Only women with ferritin levels less than 50 mcg/L benefited. Houston and colleagues performed a systematic review of the literature of iron supplementation for fatigue and concluded that iron should be considered for treatment of fatigue in nonanemic women.2 The key number for benefit was a ferritin level less than 50 mcg/L.
Hair thinning is a common concern for many women. Does iron deficiency have a possible role in this problem? A number of studies have correlated low ferritin levels with hair loss.3 There is less clear evidence of iron treatment being effective. Hard studied 140 women with diffuse hair loss, and found 19% had iron deficiency without anemia.4 All patients with iron deficiency were treated with oral iron and in all patients hair loss ceased, and hair regrowth occurred. The target ferritin goal for treatment is greater than 40 mcg/L.5
Iron deficiency is an important trigger for restless leg syndrome (RLS). All patients who present with RLS should have ferritin checked, and appropriate evaluation for the cause of iron deficiency if ferritin levels are low. Allen and colleagues published clinical practice guidelines for iron treatment of RLS.6 The guidelines conclude that ferric carboxymaltose (1,000 mg) is effective for treating moderate to severe RLS in those with serum ferritin less than 300 mcg/L and could be used as first-line therapy for RLS in adults, with oral iron (65 mg) possibly effective in patients with ferritin levels less than 75 mcg/L.
Pearl: Think of iron as therapy for fatigue in nonanemic women with a ferritin level less than 50 mcg/L, consider a trial of iron for thinning hair in women with ferritin levels less than 50 mcg/L, and a trial of iron in those with RLS with ferritin levels less than 75 mcg/L.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
References
1. Verdon F et al. BMJ. 2003 May 24;326(7399):1124. .
2. Houston BL et al. BMJ Open. 2018 Apr 5;8(4):e019240.
3. Almohanna HM et al. Dermatol Ther (Heidelb). 2019 Mar;9(1):51-70. .
4. Hard S. Acta Derm Venereol. 1963;43:562-9.
5. Kantor J et al. J Invest Dermatol. 2003 Nov;121(5):985-8. .
6. Allen RP et al. Sleep Med. 2018 Jan;41:27-44. .
A 45-year-old women presents for evaluation of fatigue. She has been tired for the past 6 months. She has had no problems with sleep and no other new symptoms. Her physical exam is unremarkable. Her Patient Health Questionnaire–9 score is 4. Lab results are as follows: hemoglobin, 13 g/dL; hematocrit, 39%; mean corpuscular volume, 90 fL; blood urea nitrogen, 10 mg/dL; Cr, 1.0 mg/dL; AST, 20 IU/L; ALT, 15 IU/L; ferritin, 35 mcg/mL; thyroid-stimulating hormone, 3.5 mIU/L.
What would you recommend?
A. Sertraline
B. Sleep study
C. Iron supplementation
I would treat this patient with iron. Verdon and colleagues conducted a randomized, double-blind placebo-controlled trial of iron treatment in nonanemic women.1 The women who received iron had a much greater reduction in fatigue score, compared with the women who did not (P < .004). Only women with ferritin levels less than 50 mcg/L benefited. Houston and colleagues performed a systematic review of the literature of iron supplementation for fatigue and concluded that iron should be considered for treatment of fatigue in nonanemic women.2 The key number for benefit was a ferritin level less than 50 mcg/L.
Hair thinning is a common concern for many women. Does iron deficiency have a possible role in this problem? A number of studies have correlated low ferritin levels with hair loss.3 There is less clear evidence of iron treatment being effective. Hard studied 140 women with diffuse hair loss, and found 19% had iron deficiency without anemia.4 All patients with iron deficiency were treated with oral iron and in all patients hair loss ceased, and hair regrowth occurred. The target ferritin goal for treatment is greater than 40 mcg/L.5
Iron deficiency is an important trigger for restless leg syndrome (RLS). All patients who present with RLS should have ferritin checked, and appropriate evaluation for the cause of iron deficiency if ferritin levels are low. Allen and colleagues published clinical practice guidelines for iron treatment of RLS.6 The guidelines conclude that ferric carboxymaltose (1,000 mg) is effective for treating moderate to severe RLS in those with serum ferritin less than 300 mcg/L and could be used as first-line therapy for RLS in adults, with oral iron (65 mg) possibly effective in patients with ferritin levels less than 75 mcg/L.
Pearl: Think of iron as therapy for fatigue in nonanemic women with a ferritin level less than 50 mcg/L, consider a trial of iron for thinning hair in women with ferritin levels less than 50 mcg/L, and a trial of iron in those with RLS with ferritin levels less than 75 mcg/L.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
References
1. Verdon F et al. BMJ. 2003 May 24;326(7399):1124. .
2. Houston BL et al. BMJ Open. 2018 Apr 5;8(4):e019240.
3. Almohanna HM et al. Dermatol Ther (Heidelb). 2019 Mar;9(1):51-70. .
4. Hard S. Acta Derm Venereol. 1963;43:562-9.
5. Kantor J et al. J Invest Dermatol. 2003 Nov;121(5):985-8. .
6. Allen RP et al. Sleep Med. 2018 Jan;41:27-44. .
A 45-year-old women presents for evaluation of fatigue. She has been tired for the past 6 months. She has had no problems with sleep and no other new symptoms. Her physical exam is unremarkable. Her Patient Health Questionnaire–9 score is 4. Lab results are as follows: hemoglobin, 13 g/dL; hematocrit, 39%; mean corpuscular volume, 90 fL; blood urea nitrogen, 10 mg/dL; Cr, 1.0 mg/dL; AST, 20 IU/L; ALT, 15 IU/L; ferritin, 35 mcg/mL; thyroid-stimulating hormone, 3.5 mIU/L.
What would you recommend?
A. Sertraline
B. Sleep study
C. Iron supplementation
I would treat this patient with iron. Verdon and colleagues conducted a randomized, double-blind placebo-controlled trial of iron treatment in nonanemic women.1 The women who received iron had a much greater reduction in fatigue score, compared with the women who did not (P < .004). Only women with ferritin levels less than 50 mcg/L benefited. Houston and colleagues performed a systematic review of the literature of iron supplementation for fatigue and concluded that iron should be considered for treatment of fatigue in nonanemic women.2 The key number for benefit was a ferritin level less than 50 mcg/L.
Hair thinning is a common concern for many women. Does iron deficiency have a possible role in this problem? A number of studies have correlated low ferritin levels with hair loss.3 There is less clear evidence of iron treatment being effective. Hard studied 140 women with diffuse hair loss, and found 19% had iron deficiency without anemia.4 All patients with iron deficiency were treated with oral iron and in all patients hair loss ceased, and hair regrowth occurred. The target ferritin goal for treatment is greater than 40 mcg/L.5
Iron deficiency is an important trigger for restless leg syndrome (RLS). All patients who present with RLS should have ferritin checked, and appropriate evaluation for the cause of iron deficiency if ferritin levels are low. Allen and colleagues published clinical practice guidelines for iron treatment of RLS.6 The guidelines conclude that ferric carboxymaltose (1,000 mg) is effective for treating moderate to severe RLS in those with serum ferritin less than 300 mcg/L and could be used as first-line therapy for RLS in adults, with oral iron (65 mg) possibly effective in patients with ferritin levels less than 75 mcg/L.
Pearl: Think of iron as therapy for fatigue in nonanemic women with a ferritin level less than 50 mcg/L, consider a trial of iron for thinning hair in women with ferritin levels less than 50 mcg/L, and a trial of iron in those with RLS with ferritin levels less than 75 mcg/L.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
References
1. Verdon F et al. BMJ. 2003 May 24;326(7399):1124. .
2. Houston BL et al. BMJ Open. 2018 Apr 5;8(4):e019240.
3. Almohanna HM et al. Dermatol Ther (Heidelb). 2019 Mar;9(1):51-70. .
4. Hard S. Acta Derm Venereol. 1963;43:562-9.
5. Kantor J et al. J Invest Dermatol. 2003 Nov;121(5):985-8. .
6. Allen RP et al. Sleep Med. 2018 Jan;41:27-44. .
History of plaque psoriasis
The patient's history of psoriasis, along with his current skin and scalp plaque flares, symmetrical joint symptomatology, laboratory studies, and x-rays, suggest a diagnosis of symmetrical psoriatic arthritis (PsA). The rheumatologist considers ordering additional imaging to assess for subclinical enthesitis and dactylitis, and discusses treatment next steps with the patient, given inadequate control with a TNF inhibitor.
Symmetrical polyarthritis is one of the most common types of PsA and involves five or more joints in the hands, wrists, ankles, and/or feet. Among patients with PsA, 60% to 80% experience plaque psoriasis before joint-symptom onset; time to joint-symptom onset in these patients typically occurs within 10 years of a plaque psoriasis diagnosis. Involvement of DIP joints differentiates PsA from rheumatoid arthritis, as does the absence of subcutaneous nodules and a negative result for rheumatoid factor. About 30% of all people with plaque psoriasis will develop PsA, which affects an estimated 1 million people in the United States annually. Symptoms typically appear between the ages of 35 and 55 years; women are more likely than men to develop symmetrical PsA.
There are no specific diagnostic tests for PsA. Rheumatologists generally use the assessment known as the Classification Criteria for Psoriatic Arthritis, (CASPAR), which can help reveal established inflammatory articular disease through a point system based on the presence/absence of various factors. On laboratory studies, the most common characteristic abnormalities of PsA are elevated ESR and CRP levels and negative rheumatoid factor in most patients. Other abnormalities that may be present in patients with PsA include elevated serum uric acid concentration and serum immunoglobulin A, and reduced levels of circulating immune complexes. Physicians also use imaging studies, such as radiography, ultrasonography, and MRI, to help differentiate PsA from other articular diseases.
While the pathogenesis of PsA remains unclear, research has shown that disease development is associated with a complex interplay of immune-mediated inflammatory responses; genetic and environmental factors may also be involved. In addition, patients with PsA are more likely to have a high risk for comorbidities, including obesity, type 2 diabetes, hypertension, hyperlipidemia, and cardiovascular events, compared with the general population.
When patients with PsA experience both skin and joint symptoms, a multidisciplinary approach to care is advised. Multidisciplinary teams play a key role in educating patients about their treatment plans and managing their PsA symptoms. The teams also help patients determine the best approaches to exercise to help maintain current joint function, as well as helpful adjustments in daily activities that will make it easier to accommodate their disease.
Nonsteroidal anti-inflammatory drugs, whether self-prescribed or prescribed by a physician, are a common initial treatment to manage joint symptoms of PsA. Current American College of Rheumatology treatment guidelines, however, encourage early treatment with disease-modifying antirheumatic drugs (DMARDs) because approximately 40% of patients with PsA develop erosive and deforming arthritis. Several DMARDs are available, including older drugs like methotrexate, as well as newer biologic agents, such as TNF inhibitors, interleukin (IL)-17 inhibitors, IL-12/23 inhibitors, and Janus kinase inhibitors. In addition, guidelines recommend early and customized physical therapy and rehabilitation approaches for patients with PsA.
Herbert S. Diamond, MD, Professor of Medicine (retired), Temple University School of Medicine, University of Pittsburgh; Chairman, Department of Medicine Emeritus, Western Pennsylvania Hospital, Pittsburgh, PA.
Herbert S. Diamond, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The patient's history of psoriasis, along with his current skin and scalp plaque flares, symmetrical joint symptomatology, laboratory studies, and x-rays, suggest a diagnosis of symmetrical psoriatic arthritis (PsA). The rheumatologist considers ordering additional imaging to assess for subclinical enthesitis and dactylitis, and discusses treatment next steps with the patient, given inadequate control with a TNF inhibitor.
Symmetrical polyarthritis is one of the most common types of PsA and involves five or more joints in the hands, wrists, ankles, and/or feet. Among patients with PsA, 60% to 80% experience plaque psoriasis before joint-symptom onset; time to joint-symptom onset in these patients typically occurs within 10 years of a plaque psoriasis diagnosis. Involvement of DIP joints differentiates PsA from rheumatoid arthritis, as does the absence of subcutaneous nodules and a negative result for rheumatoid factor. About 30% of all people with plaque psoriasis will develop PsA, which affects an estimated 1 million people in the United States annually. Symptoms typically appear between the ages of 35 and 55 years; women are more likely than men to develop symmetrical PsA.
There are no specific diagnostic tests for PsA. Rheumatologists generally use the assessment known as the Classification Criteria for Psoriatic Arthritis, (CASPAR), which can help reveal established inflammatory articular disease through a point system based on the presence/absence of various factors. On laboratory studies, the most common characteristic abnormalities of PsA are elevated ESR and CRP levels and negative rheumatoid factor in most patients. Other abnormalities that may be present in patients with PsA include elevated serum uric acid concentration and serum immunoglobulin A, and reduced levels of circulating immune complexes. Physicians also use imaging studies, such as radiography, ultrasonography, and MRI, to help differentiate PsA from other articular diseases.
While the pathogenesis of PsA remains unclear, research has shown that disease development is associated with a complex interplay of immune-mediated inflammatory responses; genetic and environmental factors may also be involved. In addition, patients with PsA are more likely to have a high risk for comorbidities, including obesity, type 2 diabetes, hypertension, hyperlipidemia, and cardiovascular events, compared with the general population.
When patients with PsA experience both skin and joint symptoms, a multidisciplinary approach to care is advised. Multidisciplinary teams play a key role in educating patients about their treatment plans and managing their PsA symptoms. The teams also help patients determine the best approaches to exercise to help maintain current joint function, as well as helpful adjustments in daily activities that will make it easier to accommodate their disease.
Nonsteroidal anti-inflammatory drugs, whether self-prescribed or prescribed by a physician, are a common initial treatment to manage joint symptoms of PsA. Current American College of Rheumatology treatment guidelines, however, encourage early treatment with disease-modifying antirheumatic drugs (DMARDs) because approximately 40% of patients with PsA develop erosive and deforming arthritis. Several DMARDs are available, including older drugs like methotrexate, as well as newer biologic agents, such as TNF inhibitors, interleukin (IL)-17 inhibitors, IL-12/23 inhibitors, and Janus kinase inhibitors. In addition, guidelines recommend early and customized physical therapy and rehabilitation approaches for patients with PsA.
Herbert S. Diamond, MD, Professor of Medicine (retired), Temple University School of Medicine, University of Pittsburgh; Chairman, Department of Medicine Emeritus, Western Pennsylvania Hospital, Pittsburgh, PA.
Herbert S. Diamond, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The patient's history of psoriasis, along with his current skin and scalp plaque flares, symmetrical joint symptomatology, laboratory studies, and x-rays, suggest a diagnosis of symmetrical psoriatic arthritis (PsA). The rheumatologist considers ordering additional imaging to assess for subclinical enthesitis and dactylitis, and discusses treatment next steps with the patient, given inadequate control with a TNF inhibitor.
Symmetrical polyarthritis is one of the most common types of PsA and involves five or more joints in the hands, wrists, ankles, and/or feet. Among patients with PsA, 60% to 80% experience plaque psoriasis before joint-symptom onset; time to joint-symptom onset in these patients typically occurs within 10 years of a plaque psoriasis diagnosis. Involvement of DIP joints differentiates PsA from rheumatoid arthritis, as does the absence of subcutaneous nodules and a negative result for rheumatoid factor. About 30% of all people with plaque psoriasis will develop PsA, which affects an estimated 1 million people in the United States annually. Symptoms typically appear between the ages of 35 and 55 years; women are more likely than men to develop symmetrical PsA.
There are no specific diagnostic tests for PsA. Rheumatologists generally use the assessment known as the Classification Criteria for Psoriatic Arthritis, (CASPAR), which can help reveal established inflammatory articular disease through a point system based on the presence/absence of various factors. On laboratory studies, the most common characteristic abnormalities of PsA are elevated ESR and CRP levels and negative rheumatoid factor in most patients. Other abnormalities that may be present in patients with PsA include elevated serum uric acid concentration and serum immunoglobulin A, and reduced levels of circulating immune complexes. Physicians also use imaging studies, such as radiography, ultrasonography, and MRI, to help differentiate PsA from other articular diseases.
While the pathogenesis of PsA remains unclear, research has shown that disease development is associated with a complex interplay of immune-mediated inflammatory responses; genetic and environmental factors may also be involved. In addition, patients with PsA are more likely to have a high risk for comorbidities, including obesity, type 2 diabetes, hypertension, hyperlipidemia, and cardiovascular events, compared with the general population.
When patients with PsA experience both skin and joint symptoms, a multidisciplinary approach to care is advised. Multidisciplinary teams play a key role in educating patients about their treatment plans and managing their PsA symptoms. The teams also help patients determine the best approaches to exercise to help maintain current joint function, as well as helpful adjustments in daily activities that will make it easier to accommodate their disease.
Nonsteroidal anti-inflammatory drugs, whether self-prescribed or prescribed by a physician, are a common initial treatment to manage joint symptoms of PsA. Current American College of Rheumatology treatment guidelines, however, encourage early treatment with disease-modifying antirheumatic drugs (DMARDs) because approximately 40% of patients with PsA develop erosive and deforming arthritis. Several DMARDs are available, including older drugs like methotrexate, as well as newer biologic agents, such as TNF inhibitors, interleukin (IL)-17 inhibitors, IL-12/23 inhibitors, and Janus kinase inhibitors. In addition, guidelines recommend early and customized physical therapy and rehabilitation approaches for patients with PsA.
Herbert S. Diamond, MD, Professor of Medicine (retired), Temple University School of Medicine, University of Pittsburgh; Chairman, Department of Medicine Emeritus, Western Pennsylvania Hospital, Pittsburgh, PA.
Herbert S. Diamond, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 43-year-old White man with a 5-year history of plaque psoriasis presents to a rheumatologist on referral from his dermatologist. He had been taking a tumor necrosis factor (TNF) inhibitor, which had controlled his skin and scalp plaques since diagnosis. Lately, however, some of the plaques have begun to flare up, and the patient reports new tenderness and swelling in three of the same joints on his left and right hands and extensive fatigue. Additional medical history includes type 2 diabetes, which was diagnosed 3 years ago; soon thereafter, he started taking metformin with consistent disease control. The rheumatologist conducts a physical exam and orders laboratory studies and x-rays. Results of the laboratory studies reveal elevated levels of C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR). Radiographs reveal joint-space narrowing in several distal interphalangeal (DIP) joints in both hands, with mild erosive disease.