User login
Educational, Networking Opportunities for Hospitalists Abound at HM13
Ask Dan Brotman, MD, FACP, SFHM, how to get the most out of the annual meeting of hospitalists and you’ll get a simple, one-word answer: Go.
“It sounds so trivial,” says Dr. Brotman, HM13 course director. “But there are a lot more hospitalists out there than we see at the meeting, and I think that [we should be] getting out the word that this is the best single opportunity that hospitalists have to network and learn about their field, not only content knowledge but also understanding where the field is going from thought leaders.”
The annual pilgrimage of hospitalists is expected to be larger than ever this year, with SHM expecting nearly 3,000 hospitalists to attend. Last year, roughly 2,700 hospitalists attended in San Diego.
But navigating a four-day maze of pre-courses, plenaries, and presentations can overwhelm even the most experienced attendee, much less a first-timer. And that’s before the annual rite that is the Research, Innovation, and Clinical Vignettes (RIV) poster competition and the Hospitalists on the Hill event that is particularly fitting this year as Capitol Hill happens to be just a few miles away.
So what’s the best advice to have the best meeting experience? Planning, planning, and a little more planning.
Ken Simone, DO, SFHM, principal of Hospitalist and Practice Solutions in Veazie, Maine, says the plethora of workshops, keynote speakers, and formalized educational offerings means attendees should “game plan” their schedule as much as possible.
“It behooves everyone to really study the offerings each day and each hour and plan their schedule accordingly,” says Dr. Simone, a Team Hospitalist member. “I typically create my schedule before I leave home for the conference.”
But don’t plan too much, he adds. Having a list of sessions to attend is important, but part of the meeting’s allure is the ability to mingle with clinical, administrative, and society leaders from around the country.
“Flexibility is the key,” he says. “Having something well planned doesn’t mean you can’t be flexible.”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Dr. Brotman says meeting organizers take the same approach. While some topics are old favorites, SHM adds new offerings each year to adapt in real time to important trends. For example, he says, a new track this year focused on comanagement will appeal to hospitalists and subspecialists who take care of stroke patients, surgical patients, and pregnant women, among others.
The new track is in addition to the existing offerings: clinical, academic/research, rapid fire, pediatric, practice management, quality, and potpourri. The last item is in its second year and offers a break from the didactic and lecture approaches taken in nearly all of the annual meeting’s other breakout sessions. A particularly popular event is expected to be “History of Hospitals,” presented by hospitalist historian Jordan Messler, MD, SFHM.
There are two new pre-courses this year: “Bugs, Drugs and You: Infectious Disease Essentials for the Hospitalist” and “What Keeps You Awake at Night? Hot Topics in Hospitalist Practice Management.” Pre-course mainstays scheduled again this year include “ABIM Maintenance Certification,” “Medical Procedures for the Hospitalist,” and “Portable Ultrasounds for the Hospitalist.”
“As the society has gotten bigger, the meeting has gotten bigger in terms of its scope,” says Dr. Brotman, whose day job is director of the hospitalist program at Johns Hopkins Hospital in Baltimore. “So we have Friday, Saturday, and Sunday, plus the evening activities, plus the pre-courses. One of the adjustments that we’ve made over time is that we do recognize that with a larger constituency and a larger amount of topical information that we’d like to cover, the meeting does get longer. The hope is that people can commit close to a week toward advancing their knowledge; it’s well worth the time.”
Richard Quinn is a freelance writer in New Jersey.
Ask Dan Brotman, MD, FACP, SFHM, how to get the most out of the annual meeting of hospitalists and you’ll get a simple, one-word answer: Go.
“It sounds so trivial,” says Dr. Brotman, HM13 course director. “But there are a lot more hospitalists out there than we see at the meeting, and I think that [we should be] getting out the word that this is the best single opportunity that hospitalists have to network and learn about their field, not only content knowledge but also understanding where the field is going from thought leaders.”
The annual pilgrimage of hospitalists is expected to be larger than ever this year, with SHM expecting nearly 3,000 hospitalists to attend. Last year, roughly 2,700 hospitalists attended in San Diego.
But navigating a four-day maze of pre-courses, plenaries, and presentations can overwhelm even the most experienced attendee, much less a first-timer. And that’s before the annual rite that is the Research, Innovation, and Clinical Vignettes (RIV) poster competition and the Hospitalists on the Hill event that is particularly fitting this year as Capitol Hill happens to be just a few miles away.
So what’s the best advice to have the best meeting experience? Planning, planning, and a little more planning.
Ken Simone, DO, SFHM, principal of Hospitalist and Practice Solutions in Veazie, Maine, says the plethora of workshops, keynote speakers, and formalized educational offerings means attendees should “game plan” their schedule as much as possible.
“It behooves everyone to really study the offerings each day and each hour and plan their schedule accordingly,” says Dr. Simone, a Team Hospitalist member. “I typically create my schedule before I leave home for the conference.”
But don’t plan too much, he adds. Having a list of sessions to attend is important, but part of the meeting’s allure is the ability to mingle with clinical, administrative, and society leaders from around the country.
“Flexibility is the key,” he says. “Having something well planned doesn’t mean you can’t be flexible.”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Dr. Brotman says meeting organizers take the same approach. While some topics are old favorites, SHM adds new offerings each year to adapt in real time to important trends. For example, he says, a new track this year focused on comanagement will appeal to hospitalists and subspecialists who take care of stroke patients, surgical patients, and pregnant women, among others.
The new track is in addition to the existing offerings: clinical, academic/research, rapid fire, pediatric, practice management, quality, and potpourri. The last item is in its second year and offers a break from the didactic and lecture approaches taken in nearly all of the annual meeting’s other breakout sessions. A particularly popular event is expected to be “History of Hospitals,” presented by hospitalist historian Jordan Messler, MD, SFHM.
There are two new pre-courses this year: “Bugs, Drugs and You: Infectious Disease Essentials for the Hospitalist” and “What Keeps You Awake at Night? Hot Topics in Hospitalist Practice Management.” Pre-course mainstays scheduled again this year include “ABIM Maintenance Certification,” “Medical Procedures for the Hospitalist,” and “Portable Ultrasounds for the Hospitalist.”
“As the society has gotten bigger, the meeting has gotten bigger in terms of its scope,” says Dr. Brotman, whose day job is director of the hospitalist program at Johns Hopkins Hospital in Baltimore. “So we have Friday, Saturday, and Sunday, plus the evening activities, plus the pre-courses. One of the adjustments that we’ve made over time is that we do recognize that with a larger constituency and a larger amount of topical information that we’d like to cover, the meeting does get longer. The hope is that people can commit close to a week toward advancing their knowledge; it’s well worth the time.”
Richard Quinn is a freelance writer in New Jersey.
Ask Dan Brotman, MD, FACP, SFHM, how to get the most out of the annual meeting of hospitalists and you’ll get a simple, one-word answer: Go.
“It sounds so trivial,” says Dr. Brotman, HM13 course director. “But there are a lot more hospitalists out there than we see at the meeting, and I think that [we should be] getting out the word that this is the best single opportunity that hospitalists have to network and learn about their field, not only content knowledge but also understanding where the field is going from thought leaders.”
The annual pilgrimage of hospitalists is expected to be larger than ever this year, with SHM expecting nearly 3,000 hospitalists to attend. Last year, roughly 2,700 hospitalists attended in San Diego.
But navigating a four-day maze of pre-courses, plenaries, and presentations can overwhelm even the most experienced attendee, much less a first-timer. And that’s before the annual rite that is the Research, Innovation, and Clinical Vignettes (RIV) poster competition and the Hospitalists on the Hill event that is particularly fitting this year as Capitol Hill happens to be just a few miles away.
So what’s the best advice to have the best meeting experience? Planning, planning, and a little more planning.
Ken Simone, DO, SFHM, principal of Hospitalist and Practice Solutions in Veazie, Maine, says the plethora of workshops, keynote speakers, and formalized educational offerings means attendees should “game plan” their schedule as much as possible.
“It behooves everyone to really study the offerings each day and each hour and plan their schedule accordingly,” says Dr. Simone, a Team Hospitalist member. “I typically create my schedule before I leave home for the conference.”
But don’t plan too much, he adds. Having a list of sessions to attend is important, but part of the meeting’s allure is the ability to mingle with clinical, administrative, and society leaders from around the country.
“Flexibility is the key,” he says. “Having something well planned doesn’t mean you can’t be flexible.”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Dr. Brotman says meeting organizers take the same approach. While some topics are old favorites, SHM adds new offerings each year to adapt in real time to important trends. For example, he says, a new track this year focused on comanagement will appeal to hospitalists and subspecialists who take care of stroke patients, surgical patients, and pregnant women, among others.
The new track is in addition to the existing offerings: clinical, academic/research, rapid fire, pediatric, practice management, quality, and potpourri. The last item is in its second year and offers a break from the didactic and lecture approaches taken in nearly all of the annual meeting’s other breakout sessions. A particularly popular event is expected to be “History of Hospitals,” presented by hospitalist historian Jordan Messler, MD, SFHM.
There are two new pre-courses this year: “Bugs, Drugs and You: Infectious Disease Essentials for the Hospitalist” and “What Keeps You Awake at Night? Hot Topics in Hospitalist Practice Management.” Pre-course mainstays scheduled again this year include “ABIM Maintenance Certification,” “Medical Procedures for the Hospitalist,” and “Portable Ultrasounds for the Hospitalist.”
“As the society has gotten bigger, the meeting has gotten bigger in terms of its scope,” says Dr. Brotman, whose day job is director of the hospitalist program at Johns Hopkins Hospital in Baltimore. “So we have Friday, Saturday, and Sunday, plus the evening activities, plus the pre-courses. One of the adjustments that we’ve made over time is that we do recognize that with a larger constituency and a larger amount of topical information that we’d like to cover, the meeting does get longer. The hope is that people can commit close to a week toward advancing their knowledge; it’s well worth the time.”
Richard Quinn is a freelance writer in New Jersey.
Hospitalists Gear Up to Lobby Congress on Health Care Policy
Mangla Gulati, MD, FACP, FHM, an academic hospitalist and medical director of clinical effectiveness at University of Maryland Medical Center in Baltimore, had never been involved in a lobbying trip before the waning days of last year. But then, just as members of Congress were wrestling with potential Draconian cuts to Medicare reimbursements and a $10 million slash in Medicare funding for the National Quality Forum (NQF), Dr. Gulati found herself on a daylong trip with SHM government guru Laura Allendorf and an NQF representative to make a series of in-person appeals to politicians in Washington, D.C. “When you’re a practicing physician, even though you know there’s regulation and compliance and mandates, you really don’t understand how they come to fruition and what the thought process is,” says Dr. Gulati, secretary of SHM’s Maryland chapter. “It was really interesting to see the other side of that and how people up on the Hill make a lot of decisions based on the information that’s given to them.”
The Hill she’s referring to is none other than Capitol Hill, and Dr. Gulati is making a return just a few months after her visit. And this time, she’s bringing a few hundred hospitalists with her. Hospitalists on the Hill 2013 (www.hospitalmedicine 2013.org/advocacy) is the annual trek made by SHM leadership and rank-and-file members to lobby legislators and federal staffers “on the way policies affect your practice and your patients,” SHM says on its website. This year, the showing in Washington is expected to be among the best ever, as the lobbying trip is May 16, just before HM13’s full program kicks off at the Gaylord National Resort & Convention Center in National Harbor, Md.
The all-day affair kicks off in the morning, as participants will receive briefings from SHM Public Policy Committee Chair Ron Greeno, MD, FCCP, MHM, and Allendorf, SHM’s senior advisor for advocacy and government affairs. Then comes a two-hour training course from Advocacy Associates (http://advocacyassociates.com), a boutique communications firm that helps organizations, such as SHM, tailor their message to policymakers. After that, it’s a six-hour whirlwind of meetings with home-state legislators, career administrators, and aide-de-camps that one former participant described as “almost like speed-dial dating with congressmen and -women.” Lastly, participants regroup at day’s end for a debriefing.
“I think what’s different at SHM is we go to Washington with an agenda of how we can improve patient safety and quality outcomes,” says Patrick Torcson, MD, MMM, FACP, SFHM, chair of SHM’s Performance Measurement and Reporting Committee. “We’re not there about just protecting our turf and making sure that our reimbursement stays at a reasonable level. We’ve been very clear to offer innovations about care transitions and Project BOOST, and different things that can be done to improve things like quality and service for Medicare beneficiaries.”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Dr. Torcson says congressional contacts he’s made in past years “always look forward to our visits, because we really do come with an attitude of how can we help fix a broken system.”
He counts several victories as fruit of the annual trip. First, he believes the trip has “clearly educated our politicians, congressional staffers, and CMS [the Centers for Medicare & Medicaid Services] that the predominant model of the way patients are taken care of in the hospital is by a hospitalist.”
Second, and more granularly, SHM really gets into the weeds. Take CMS’ Quality and Resource Use Report (QRUR), which is part of the rollout of its value-based purchasing modifier (VBPM). Dr. Torcson says SHM carefully reviewed the report to register its concerns about proper attribution, fair comparisons, relevant metrics, and other issues. In turn, CMS signaled its appreciation of SHM’s due diligence and has indicated a willingness to work with SHM to address its concerns.
CMS chief medical officer Patrick Conway, MD, MSc, FAAP, SFHM, sees it from both sides of the equation. A pediatric hospitalist by training, he has been on trips to push federal officials to promulgate rules that make the most sense for HM. But in his current job, he’s often the one being pushed—and he welcomes the visits.
“We’re trying to partner up with physicians,” he says.
Dr. Conway believes lobbying trips like SHM’s are critical to informing both politicians and professionals on what physicians need or want most.
“People often think, ‘How could it matter?’ Sure, some of it will be hits and misses. But you’ll hit some key points that resonate,” he says.
Hospitalist Rick Hilger, MD, SFHM, director of resident education and adjunct associate professor of medicine at the University of Minnesota Medical School in Minneapolis, learned that lesson last year during his first Hospitalists on the Hill. A first-time member of SHM’s Public Policy Committee, he met with the legislative assistants for U.S. Sens.
Al Franken (D-Minn.) and Amy Klobuchar (D-Minn.), as well as had a face-to-face meeting with U.S. Rep. Allyson Schwartz (D-Pa.). The latter has been a staunch advocate of Medicare payment reform, sponsoring several bills—with SHM’s support—to repeal the sustainable growth rate (SGR) formula.
“It’s an investment in time, and especially for the senators and congressmen and -women from your own state, it’s more about trying to develop a relationship,” Dr. Hilger says. “I’ve already exchanged emails with the aides that I met that day concerning other healthcare issues. … I’m not sure I can completely answer for the long-term impact, but it definitely feels better than doing nothing.”
Richard Quinn is a freelance writer in New Jersey.
Mangla Gulati, MD, FACP, FHM, an academic hospitalist and medical director of clinical effectiveness at University of Maryland Medical Center in Baltimore, had never been involved in a lobbying trip before the waning days of last year. But then, just as members of Congress were wrestling with potential Draconian cuts to Medicare reimbursements and a $10 million slash in Medicare funding for the National Quality Forum (NQF), Dr. Gulati found herself on a daylong trip with SHM government guru Laura Allendorf and an NQF representative to make a series of in-person appeals to politicians in Washington, D.C. “When you’re a practicing physician, even though you know there’s regulation and compliance and mandates, you really don’t understand how they come to fruition and what the thought process is,” says Dr. Gulati, secretary of SHM’s Maryland chapter. “It was really interesting to see the other side of that and how people up on the Hill make a lot of decisions based on the information that’s given to them.”
The Hill she’s referring to is none other than Capitol Hill, and Dr. Gulati is making a return just a few months after her visit. And this time, she’s bringing a few hundred hospitalists with her. Hospitalists on the Hill 2013 (www.hospitalmedicine 2013.org/advocacy) is the annual trek made by SHM leadership and rank-and-file members to lobby legislators and federal staffers “on the way policies affect your practice and your patients,” SHM says on its website. This year, the showing in Washington is expected to be among the best ever, as the lobbying trip is May 16, just before HM13’s full program kicks off at the Gaylord National Resort & Convention Center in National Harbor, Md.
The all-day affair kicks off in the morning, as participants will receive briefings from SHM Public Policy Committee Chair Ron Greeno, MD, FCCP, MHM, and Allendorf, SHM’s senior advisor for advocacy and government affairs. Then comes a two-hour training course from Advocacy Associates (http://advocacyassociates.com), a boutique communications firm that helps organizations, such as SHM, tailor their message to policymakers. After that, it’s a six-hour whirlwind of meetings with home-state legislators, career administrators, and aide-de-camps that one former participant described as “almost like speed-dial dating with congressmen and -women.” Lastly, participants regroup at day’s end for a debriefing.
“I think what’s different at SHM is we go to Washington with an agenda of how we can improve patient safety and quality outcomes,” says Patrick Torcson, MD, MMM, FACP, SFHM, chair of SHM’s Performance Measurement and Reporting Committee. “We’re not there about just protecting our turf and making sure that our reimbursement stays at a reasonable level. We’ve been very clear to offer innovations about care transitions and Project BOOST, and different things that can be done to improve things like quality and service for Medicare beneficiaries.”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Dr. Torcson says congressional contacts he’s made in past years “always look forward to our visits, because we really do come with an attitude of how can we help fix a broken system.”
He counts several victories as fruit of the annual trip. First, he believes the trip has “clearly educated our politicians, congressional staffers, and CMS [the Centers for Medicare & Medicaid Services] that the predominant model of the way patients are taken care of in the hospital is by a hospitalist.”
Second, and more granularly, SHM really gets into the weeds. Take CMS’ Quality and Resource Use Report (QRUR), which is part of the rollout of its value-based purchasing modifier (VBPM). Dr. Torcson says SHM carefully reviewed the report to register its concerns about proper attribution, fair comparisons, relevant metrics, and other issues. In turn, CMS signaled its appreciation of SHM’s due diligence and has indicated a willingness to work with SHM to address its concerns.
CMS chief medical officer Patrick Conway, MD, MSc, FAAP, SFHM, sees it from both sides of the equation. A pediatric hospitalist by training, he has been on trips to push federal officials to promulgate rules that make the most sense for HM. But in his current job, he’s often the one being pushed—and he welcomes the visits.
“We’re trying to partner up with physicians,” he says.
Dr. Conway believes lobbying trips like SHM’s are critical to informing both politicians and professionals on what physicians need or want most.
“People often think, ‘How could it matter?’ Sure, some of it will be hits and misses. But you’ll hit some key points that resonate,” he says.
Hospitalist Rick Hilger, MD, SFHM, director of resident education and adjunct associate professor of medicine at the University of Minnesota Medical School in Minneapolis, learned that lesson last year during his first Hospitalists on the Hill. A first-time member of SHM’s Public Policy Committee, he met with the legislative assistants for U.S. Sens.
Al Franken (D-Minn.) and Amy Klobuchar (D-Minn.), as well as had a face-to-face meeting with U.S. Rep. Allyson Schwartz (D-Pa.). The latter has been a staunch advocate of Medicare payment reform, sponsoring several bills—with SHM’s support—to repeal the sustainable growth rate (SGR) formula.
“It’s an investment in time, and especially for the senators and congressmen and -women from your own state, it’s more about trying to develop a relationship,” Dr. Hilger says. “I’ve already exchanged emails with the aides that I met that day concerning other healthcare issues. … I’m not sure I can completely answer for the long-term impact, but it definitely feels better than doing nothing.”
Richard Quinn is a freelance writer in New Jersey.
Mangla Gulati, MD, FACP, FHM, an academic hospitalist and medical director of clinical effectiveness at University of Maryland Medical Center in Baltimore, had never been involved in a lobbying trip before the waning days of last year. But then, just as members of Congress were wrestling with potential Draconian cuts to Medicare reimbursements and a $10 million slash in Medicare funding for the National Quality Forum (NQF), Dr. Gulati found herself on a daylong trip with SHM government guru Laura Allendorf and an NQF representative to make a series of in-person appeals to politicians in Washington, D.C. “When you’re a practicing physician, even though you know there’s regulation and compliance and mandates, you really don’t understand how they come to fruition and what the thought process is,” says Dr. Gulati, secretary of SHM’s Maryland chapter. “It was really interesting to see the other side of that and how people up on the Hill make a lot of decisions based on the information that’s given to them.”
The Hill she’s referring to is none other than Capitol Hill, and Dr. Gulati is making a return just a few months after her visit. And this time, she’s bringing a few hundred hospitalists with her. Hospitalists on the Hill 2013 (www.hospitalmedicine 2013.org/advocacy) is the annual trek made by SHM leadership and rank-and-file members to lobby legislators and federal staffers “on the way policies affect your practice and your patients,” SHM says on its website. This year, the showing in Washington is expected to be among the best ever, as the lobbying trip is May 16, just before HM13’s full program kicks off at the Gaylord National Resort & Convention Center in National Harbor, Md.
The all-day affair kicks off in the morning, as participants will receive briefings from SHM Public Policy Committee Chair Ron Greeno, MD, FCCP, MHM, and Allendorf, SHM’s senior advisor for advocacy and government affairs. Then comes a two-hour training course from Advocacy Associates (http://advocacyassociates.com), a boutique communications firm that helps organizations, such as SHM, tailor their message to policymakers. After that, it’s a six-hour whirlwind of meetings with home-state legislators, career administrators, and aide-de-camps that one former participant described as “almost like speed-dial dating with congressmen and -women.” Lastly, participants regroup at day’s end for a debriefing.
“I think what’s different at SHM is we go to Washington with an agenda of how we can improve patient safety and quality outcomes,” says Patrick Torcson, MD, MMM, FACP, SFHM, chair of SHM’s Performance Measurement and Reporting Committee. “We’re not there about just protecting our turf and making sure that our reimbursement stays at a reasonable level. We’ve been very clear to offer innovations about care transitions and Project BOOST, and different things that can be done to improve things like quality and service for Medicare beneficiaries.”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Dr. Torcson says congressional contacts he’s made in past years “always look forward to our visits, because we really do come with an attitude of how can we help fix a broken system.”
He counts several victories as fruit of the annual trip. First, he believes the trip has “clearly educated our politicians, congressional staffers, and CMS [the Centers for Medicare & Medicaid Services] that the predominant model of the way patients are taken care of in the hospital is by a hospitalist.”
Second, and more granularly, SHM really gets into the weeds. Take CMS’ Quality and Resource Use Report (QRUR), which is part of the rollout of its value-based purchasing modifier (VBPM). Dr. Torcson says SHM carefully reviewed the report to register its concerns about proper attribution, fair comparisons, relevant metrics, and other issues. In turn, CMS signaled its appreciation of SHM’s due diligence and has indicated a willingness to work with SHM to address its concerns.
CMS chief medical officer Patrick Conway, MD, MSc, FAAP, SFHM, sees it from both sides of the equation. A pediatric hospitalist by training, he has been on trips to push federal officials to promulgate rules that make the most sense for HM. But in his current job, he’s often the one being pushed—and he welcomes the visits.
“We’re trying to partner up with physicians,” he says.
Dr. Conway believes lobbying trips like SHM’s are critical to informing both politicians and professionals on what physicians need or want most.
“People often think, ‘How could it matter?’ Sure, some of it will be hits and misses. But you’ll hit some key points that resonate,” he says.
Hospitalist Rick Hilger, MD, SFHM, director of resident education and adjunct associate professor of medicine at the University of Minnesota Medical School in Minneapolis, learned that lesson last year during his first Hospitalists on the Hill. A first-time member of SHM’s Public Policy Committee, he met with the legislative assistants for U.S. Sens.
Al Franken (D-Minn.) and Amy Klobuchar (D-Minn.), as well as had a face-to-face meeting with U.S. Rep. Allyson Schwartz (D-Pa.). The latter has been a staunch advocate of Medicare payment reform, sponsoring several bills—with SHM’s support—to repeal the sustainable growth rate (SGR) formula.
“It’s an investment in time, and especially for the senators and congressmen and -women from your own state, it’s more about trying to develop a relationship,” Dr. Hilger says. “I’ve already exchanged emails with the aides that I met that day concerning other healthcare issues. … I’m not sure I can completely answer for the long-term impact, but it definitely feels better than doing nothing.”
Richard Quinn is a freelance writer in New Jersey.
Continuing Medical Education (CME) Courses for Hospitalists Thrive Online
Hospitalist Lenny Feldman, MD, FACP, FAAP, SFHM, of John Hopkins School of Medicine in Baltimore, is the proverbial study in contrasts. He is the longtime editor of SHM’s Consultative & Perioperative Medicine Essentials for Hospitalists, a free continuing medical education (CME) repository more commonly known as SHMConsults (www.shmconsults.com). But in February, he helped lead “Updates in Hospital Medicine 2013: Evidence-Based Reviews on the Management of Hospitalized Patients.” That program, arranged by Canadian education provider CMEatSea (www.cmeatsea.org) and held aboard a cruise ship in the eastern Caribbean, attracted some 60 hospitalists, nurse practitioners, and physician assistants interested in earning up to 14 credits.
On the one hand, Dr. Feldman is a pioneer of free virtual CME. On the other, he is an example of the big-ticket CME events that were much more commonplace five or 10 years ago.
“It’s tough,” Dr. Feldman says. “There’s no doubt that once you’ve built that virtual infrastructure, it allows many more people access to CME than if they have to come together. But with that said, particularly at a meeting like HM13, there’s so much more to it than just the CME. The networking is a huge part of that.”
This is the current state of CME, in which ever-tightening physician budgets plus a massive pullback of pharmaceutical industry support equals a landscape of fewer and fewer big-ticket events and more and more online offerings. The expense of large-scale offerings means that many physicians look for more than just the credits available when deciding which events to attend.
For many hospitalists, of course, SHM’s annual meeting remains the best opportunity of the year for CME. Accordingly, those credits are often cited as one of the biggest lures for many of the nearly 3,000 hospitalists who are expected to convene May 16-19 at the Gaylord National Resort & Convention Center in National Harbor, Md.
“You can always get CME credits locally by attending lectures at your own institution, but so often the content of these lectures is really not something that has been vetted and put forward by hospitalists,” says HM13 course director Daniel Brotman, MD, FACP, SFHM. “I think the people who attend this meeting know where the field is going, not only because of the content that’s offered, but because of who else is there. That’s different than going to an hourlong lecture by a cardiologist at your institution on atrial fibrillation.”

—Lenny Feldman, MD, FACP, FAAP, SFHM, John Hopkins School of Medicine, Baltimore
Pharma Pullback
CME budgets typically run $3,000 to $3,500 per physician, but can range from as low as $2,000 to as high as $5,000 annually, according to rough estimates from industry leaders. Opinions are mixed on whether those budgets have been significantly reduced over the past few years, but “they’re certainly not going up,” Dr. Feldman says.
What is falling year after year is the amount of money that the pharmaceutical industry is providing to support CME, says Daniel Guinee, executive vice president of educational firm ASiM of Somerville, N.J. The drug industry funded $1.2 billion of CME in 2007, according to the Accreditation Council for Continuing Medical Education (ACCME). That number dropped to $736 million in 2011, the latest year for which ACCME has statistics. Guinee says many expect the total for 2012 to be approximately $600 million, then level off.
Some applaud the drop-off in industry funding as a needed correction to ensure any potential bias is eliminated. To that end, the American Medical Association’s (AMA) Council on Ethical and Judicial Affairs in 2011 adopted a policy urging the avoidance of industry funding of CME when possible. But just 42% of physicians in one study said they were willing to pay higher fees to eliminate that funding source (Arch Intern Med. 2011;171(9):840-846).
Guinee attributes much of the drug industry’s pullback in funding to companies’ uncertainty over transparency and reporting required by ACCME, the FDA, and the U.S. Department of Health & Human Services (HHS).
“The companies want to use their money as they want to,” Guinee says. “Instead of putting the money out there … as way to support medical education, they’re saying, ‘You know what? We’ll just hang on to it and spend it in other ways.’”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Dr. Feldman, whose SHMConsults project has been supported by the pharmaceutical industry for seven years, says it’s unclear where future funding will come from in order to support CME. But ACCME president and chief executive officer Murray Kopelow, MD, says that while commercial support—the industry term for pharmaceutical funding—has steadily fallen, “other income” rose 221% from 2006 to 2011 for ACCME-accredited providers and ACCME–recognized, state-accredited providers. ACCME says that income can include activity registration fees, government or nonprofit foundation grants, and allocations from accredited providers’ parent organizations.
“The balance of revenue has shifted,” Dr. Kopelow says.
Education When You Need It
Also shifting is the nature of CME delivery. Since 2007, the number of live Internet CME activities has risen 33%, while the number of journal CME activities has risen 13%, according to ACCME figures. The number of courses in which participants physically attend is virtually static.
SHM has embraced the virtual concept and is looking to add as many online learning opportunities as feasible, says Catharine Smith, SHM’s senior director for education. That includes updates to SHMConsults and the Hospital Quality and Patient Safety Online Academy (www.hospitalmedicine.org/hqps), as well as future offerings based on core competencies. Virtual CME allows hospitalists to meet CME requirements when it is convenient for them and allows providers to set up both live events and enduring materials, Smith says.
“More online CME opportunities from SHM’s Learning Portal is about bringing quality content to hospitalists,” Smith said in a statement. “This reflects SHM’s understanding of the professional needs of hospitalists.”
She added that measuring outcomes can be easier online, as data recording in that manner is easier than during a big meeting. Then again, it’s also difficult to gauge just how well a learned lesson is then incorporated into practice.
For all its advantages, online CME shouldn’t replace all face-to-face learning, Dr. Kopelow says.
“Physicians consult colleagues and reflect on what they have learned before integrating the new information into their practice for the benefit of patients,” he adds. “It is this process that accredited CME promotes and supports. Online CME supports this process, but it does not replace the total process of continuing professional development.”
Dr. Feldman says physicians will have to decide for themselves what works for them, particularly if reduced CME spending by the drug industry continues to crimp offerings.
“There’s going to be a huge sea change there in terms of folks needing to decide where they’re going to want to spend their CME money,” he adds. “Are they going to choose some of these easier-to-use, online CME offerings if they think that going to meetings is becoming prohibitively expensive? Only time is going to tell.”
Hospitalist Lenny Feldman, MD, FACP, FAAP, SFHM, of John Hopkins School of Medicine in Baltimore, is the proverbial study in contrasts. He is the longtime editor of SHM’s Consultative & Perioperative Medicine Essentials for Hospitalists, a free continuing medical education (CME) repository more commonly known as SHMConsults (www.shmconsults.com). But in February, he helped lead “Updates in Hospital Medicine 2013: Evidence-Based Reviews on the Management of Hospitalized Patients.” That program, arranged by Canadian education provider CMEatSea (www.cmeatsea.org) and held aboard a cruise ship in the eastern Caribbean, attracted some 60 hospitalists, nurse practitioners, and physician assistants interested in earning up to 14 credits.
On the one hand, Dr. Feldman is a pioneer of free virtual CME. On the other, he is an example of the big-ticket CME events that were much more commonplace five or 10 years ago.
“It’s tough,” Dr. Feldman says. “There’s no doubt that once you’ve built that virtual infrastructure, it allows many more people access to CME than if they have to come together. But with that said, particularly at a meeting like HM13, there’s so much more to it than just the CME. The networking is a huge part of that.”
This is the current state of CME, in which ever-tightening physician budgets plus a massive pullback of pharmaceutical industry support equals a landscape of fewer and fewer big-ticket events and more and more online offerings. The expense of large-scale offerings means that many physicians look for more than just the credits available when deciding which events to attend.
For many hospitalists, of course, SHM’s annual meeting remains the best opportunity of the year for CME. Accordingly, those credits are often cited as one of the biggest lures for many of the nearly 3,000 hospitalists who are expected to convene May 16-19 at the Gaylord National Resort & Convention Center in National Harbor, Md.
“You can always get CME credits locally by attending lectures at your own institution, but so often the content of these lectures is really not something that has been vetted and put forward by hospitalists,” says HM13 course director Daniel Brotman, MD, FACP, SFHM. “I think the people who attend this meeting know where the field is going, not only because of the content that’s offered, but because of who else is there. That’s different than going to an hourlong lecture by a cardiologist at your institution on atrial fibrillation.”

—Lenny Feldman, MD, FACP, FAAP, SFHM, John Hopkins School of Medicine, Baltimore
Pharma Pullback
CME budgets typically run $3,000 to $3,500 per physician, but can range from as low as $2,000 to as high as $5,000 annually, according to rough estimates from industry leaders. Opinions are mixed on whether those budgets have been significantly reduced over the past few years, but “they’re certainly not going up,” Dr. Feldman says.
What is falling year after year is the amount of money that the pharmaceutical industry is providing to support CME, says Daniel Guinee, executive vice president of educational firm ASiM of Somerville, N.J. The drug industry funded $1.2 billion of CME in 2007, according to the Accreditation Council for Continuing Medical Education (ACCME). That number dropped to $736 million in 2011, the latest year for which ACCME has statistics. Guinee says many expect the total for 2012 to be approximately $600 million, then level off.
Some applaud the drop-off in industry funding as a needed correction to ensure any potential bias is eliminated. To that end, the American Medical Association’s (AMA) Council on Ethical and Judicial Affairs in 2011 adopted a policy urging the avoidance of industry funding of CME when possible. But just 42% of physicians in one study said they were willing to pay higher fees to eliminate that funding source (Arch Intern Med. 2011;171(9):840-846).
Guinee attributes much of the drug industry’s pullback in funding to companies’ uncertainty over transparency and reporting required by ACCME, the FDA, and the U.S. Department of Health & Human Services (HHS).
“The companies want to use their money as they want to,” Guinee says. “Instead of putting the money out there … as way to support medical education, they’re saying, ‘You know what? We’ll just hang on to it and spend it in other ways.’”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Dr. Feldman, whose SHMConsults project has been supported by the pharmaceutical industry for seven years, says it’s unclear where future funding will come from in order to support CME. But ACCME president and chief executive officer Murray Kopelow, MD, says that while commercial support—the industry term for pharmaceutical funding—has steadily fallen, “other income” rose 221% from 2006 to 2011 for ACCME-accredited providers and ACCME–recognized, state-accredited providers. ACCME says that income can include activity registration fees, government or nonprofit foundation grants, and allocations from accredited providers’ parent organizations.
“The balance of revenue has shifted,” Dr. Kopelow says.
Education When You Need It
Also shifting is the nature of CME delivery. Since 2007, the number of live Internet CME activities has risen 33%, while the number of journal CME activities has risen 13%, according to ACCME figures. The number of courses in which participants physically attend is virtually static.
SHM has embraced the virtual concept and is looking to add as many online learning opportunities as feasible, says Catharine Smith, SHM’s senior director for education. That includes updates to SHMConsults and the Hospital Quality and Patient Safety Online Academy (www.hospitalmedicine.org/hqps), as well as future offerings based on core competencies. Virtual CME allows hospitalists to meet CME requirements when it is convenient for them and allows providers to set up both live events and enduring materials, Smith says.
“More online CME opportunities from SHM’s Learning Portal is about bringing quality content to hospitalists,” Smith said in a statement. “This reflects SHM’s understanding of the professional needs of hospitalists.”
She added that measuring outcomes can be easier online, as data recording in that manner is easier than during a big meeting. Then again, it’s also difficult to gauge just how well a learned lesson is then incorporated into practice.
For all its advantages, online CME shouldn’t replace all face-to-face learning, Dr. Kopelow says.
“Physicians consult colleagues and reflect on what they have learned before integrating the new information into their practice for the benefit of patients,” he adds. “It is this process that accredited CME promotes and supports. Online CME supports this process, but it does not replace the total process of continuing professional development.”
Dr. Feldman says physicians will have to decide for themselves what works for them, particularly if reduced CME spending by the drug industry continues to crimp offerings.
“There’s going to be a huge sea change there in terms of folks needing to decide where they’re going to want to spend their CME money,” he adds. “Are they going to choose some of these easier-to-use, online CME offerings if they think that going to meetings is becoming prohibitively expensive? Only time is going to tell.”
Hospitalist Lenny Feldman, MD, FACP, FAAP, SFHM, of John Hopkins School of Medicine in Baltimore, is the proverbial study in contrasts. He is the longtime editor of SHM’s Consultative & Perioperative Medicine Essentials for Hospitalists, a free continuing medical education (CME) repository more commonly known as SHMConsults (www.shmconsults.com). But in February, he helped lead “Updates in Hospital Medicine 2013: Evidence-Based Reviews on the Management of Hospitalized Patients.” That program, arranged by Canadian education provider CMEatSea (www.cmeatsea.org) and held aboard a cruise ship in the eastern Caribbean, attracted some 60 hospitalists, nurse practitioners, and physician assistants interested in earning up to 14 credits.
On the one hand, Dr. Feldman is a pioneer of free virtual CME. On the other, he is an example of the big-ticket CME events that were much more commonplace five or 10 years ago.
“It’s tough,” Dr. Feldman says. “There’s no doubt that once you’ve built that virtual infrastructure, it allows many more people access to CME than if they have to come together. But with that said, particularly at a meeting like HM13, there’s so much more to it than just the CME. The networking is a huge part of that.”
This is the current state of CME, in which ever-tightening physician budgets plus a massive pullback of pharmaceutical industry support equals a landscape of fewer and fewer big-ticket events and more and more online offerings. The expense of large-scale offerings means that many physicians look for more than just the credits available when deciding which events to attend.
For many hospitalists, of course, SHM’s annual meeting remains the best opportunity of the year for CME. Accordingly, those credits are often cited as one of the biggest lures for many of the nearly 3,000 hospitalists who are expected to convene May 16-19 at the Gaylord National Resort & Convention Center in National Harbor, Md.
“You can always get CME credits locally by attending lectures at your own institution, but so often the content of these lectures is really not something that has been vetted and put forward by hospitalists,” says HM13 course director Daniel Brotman, MD, FACP, SFHM. “I think the people who attend this meeting know where the field is going, not only because of the content that’s offered, but because of who else is there. That’s different than going to an hourlong lecture by a cardiologist at your institution on atrial fibrillation.”

—Lenny Feldman, MD, FACP, FAAP, SFHM, John Hopkins School of Medicine, Baltimore
Pharma Pullback
CME budgets typically run $3,000 to $3,500 per physician, but can range from as low as $2,000 to as high as $5,000 annually, according to rough estimates from industry leaders. Opinions are mixed on whether those budgets have been significantly reduced over the past few years, but “they’re certainly not going up,” Dr. Feldman says.
What is falling year after year is the amount of money that the pharmaceutical industry is providing to support CME, says Daniel Guinee, executive vice president of educational firm ASiM of Somerville, N.J. The drug industry funded $1.2 billion of CME in 2007, according to the Accreditation Council for Continuing Medical Education (ACCME). That number dropped to $736 million in 2011, the latest year for which ACCME has statistics. Guinee says many expect the total for 2012 to be approximately $600 million, then level off.
Some applaud the drop-off in industry funding as a needed correction to ensure any potential bias is eliminated. To that end, the American Medical Association’s (AMA) Council on Ethical and Judicial Affairs in 2011 adopted a policy urging the avoidance of industry funding of CME when possible. But just 42% of physicians in one study said they were willing to pay higher fees to eliminate that funding source (Arch Intern Med. 2011;171(9):840-846).
Guinee attributes much of the drug industry’s pullback in funding to companies’ uncertainty over transparency and reporting required by ACCME, the FDA, and the U.S. Department of Health & Human Services (HHS).
“The companies want to use their money as they want to,” Guinee says. “Instead of putting the money out there … as way to support medical education, they’re saying, ‘You know what? We’ll just hang on to it and spend it in other ways.’”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Dr. Feldman, whose SHMConsults project has been supported by the pharmaceutical industry for seven years, says it’s unclear where future funding will come from in order to support CME. But ACCME president and chief executive officer Murray Kopelow, MD, says that while commercial support—the industry term for pharmaceutical funding—has steadily fallen, “other income” rose 221% from 2006 to 2011 for ACCME-accredited providers and ACCME–recognized, state-accredited providers. ACCME says that income can include activity registration fees, government or nonprofit foundation grants, and allocations from accredited providers’ parent organizations.
“The balance of revenue has shifted,” Dr. Kopelow says.
Education When You Need It
Also shifting is the nature of CME delivery. Since 2007, the number of live Internet CME activities has risen 33%, while the number of journal CME activities has risen 13%, according to ACCME figures. The number of courses in which participants physically attend is virtually static.
SHM has embraced the virtual concept and is looking to add as many online learning opportunities as feasible, says Catharine Smith, SHM’s senior director for education. That includes updates to SHMConsults and the Hospital Quality and Patient Safety Online Academy (www.hospitalmedicine.org/hqps), as well as future offerings based on core competencies. Virtual CME allows hospitalists to meet CME requirements when it is convenient for them and allows providers to set up both live events and enduring materials, Smith says.
“More online CME opportunities from SHM’s Learning Portal is about bringing quality content to hospitalists,” Smith said in a statement. “This reflects SHM’s understanding of the professional needs of hospitalists.”
She added that measuring outcomes can be easier online, as data recording in that manner is easier than during a big meeting. Then again, it’s also difficult to gauge just how well a learned lesson is then incorporated into practice.
For all its advantages, online CME shouldn’t replace all face-to-face learning, Dr. Kopelow says.
“Physicians consult colleagues and reflect on what they have learned before integrating the new information into their practice for the benefit of patients,” he adds. “It is this process that accredited CME promotes and supports. Online CME supports this process, but it does not replace the total process of continuing professional development.”
Dr. Feldman says physicians will have to decide for themselves what works for them, particularly if reduced CME spending by the drug industry continues to crimp offerings.
“There’s going to be a huge sea change there in terms of folks needing to decide where they’re going to want to spend their CME money,” he adds. “Are they going to choose some of these easier-to-use, online CME offerings if they think that going to meetings is becoming prohibitively expensive? Only time is going to tell.”
Team Hospitalist Recommends Nine Don’t-Miss Sessions at HM13
Eight educational tracks, an equal number of credit bearing pre-courses, a score of small-group forums, three plenaries, and an SHM Town Hall meeting offers a lot of professional development in a four-day span. But that’s just a sampling of what HM13 has slated May 16-19 at the Gaylord National Resort & Convention Center in National Harbor, Md., just outside Washington, D.C.
So how does one get the most value out of the conference?
“The highest-yield content is going to depend on what your background is and how to spend that time in a way that augments your knowledge, your perspective, or your exposure to like-minded colleagues in a very individual way,” says HM13 course director Daniel Brotman, MD, FACP, SFHM, director of the hospitalist program at Johns Hopkins Hospital in Baltimore. “One of the things that’s so cool about hospital medicine is its diversity.”
But don’t take Dr. Brotman’s well-educated word for it. Here’s a list of recommendations from Team Hospitalist, the only reader-involvement group of its kind in HM, on events they would not miss this year.
The New Anticoagulants: When Should We Be Using Them?
2:45 p.m., May 17
Dr. Ma: “I’m very interested about the new anticoagulants talk. What I’m curious to see is what the speaker thinks about the survivability of these medications in our society, with so many lawyers. Pradaxa already has fallen out of favor. Let’s see what happens to Xarelto.”
How do CFOs Value Their Hospitalist Programs?
2:50 p.m., May 18
Dr. Ma: “The problem today is CFOs have to valuate their hospitalists in the setting of other specialists who also receive subsidies. There is less money to be spent on hospitalists, as other specialists vie for this allotment of savings from hospital-based value purchasing.”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Mentoring/Coaching an Improvement Team: Lessons from SHM’s Mentored Implementation Programs
2:45 p.m., May 17
Dr. Perumalswami: “As a Project BOOST physician mentor in Illinois, I would highly recommend the session because the discussion will involve an inside look into valuable experience-based observations and analysis for the success of any process improvement team. The nature of teams and the culture of improvement at various sites will also be discussed. There will be a mentee side of the presentation, too, which will help other mentors of implementation programs better understand what the issues are ‘from the other side.’”
Strategies to Improve Communication with Patients and Families to Improve Care
2:45 p.m., May 17
Dr. Hale: “It is well known in pediatrics that you are treating two patients: both the child and the parents. If the family has a shared understanding of the child’s illness and there is collaboration for the care plan, there will be improved care.”
Neonatal HSV: When to Consider It, How to Evaluate for It, and How to Treat It
11 a.m., May 18
Dr. Hale: “Neonatal HSV is a devastating disease. It is essential to recognize high-risk patients to decrease morbidity and mortality for this illness. There have been recent updates in the understanding of epidemiology of this disease that can assist the provider in recognizing high-risk patients.”
Supporting Transition for Youth with Special Healthcare Needs: Coordinating Care and Preparing to Pass the Baton
4:15 p.m., May 18
Dr. Hale: “The transition of adolescents and young adults from pediatric-care teams to adult-medicine-care teams should be seamless for the sake of the patient, but often it is a blurry transition over the course of years. This session is high-yield for both pediatric and adult hospitalists.”
Getting Ready for Physician Value-Based Purchasing
9:50 a.m., May 19
Dr. Simone: “Dr. [Pat] Torcson’s presentation last year was one of the best at HM12, and I expect this year to be the same. He chairs SHM’s Performance Measurement and Reporting Committee and is well versed in these matters. He speaks in terms that will capture all audiences, whether they are experienced or new to the business aspects of medicine. Highly recommended.”
BOOSTing the Hospital Discharge Process: What Works and What Doesn’t
10:35 a.m., May 17
Dr. Simone: “Both panelists are excellent presenters as well as leading authorities when it comes to discharge processes. This presentation is very timely with the new CMS payment system, which penalizes unnecessary and unexpected readmissions.”
Success Stories: How to Integrate NPs and PAs into a Hospitalist Practice
4:15 p.m., May 18
Cardin: “This is an important session because, as every hard-working hospitalist knows, there simply aren’t enough physicians to fill the needs of our medically complex hospitalized patients. It is simply a reality that there will be an increased need in the future for mid-level providers, and it is valuable to maximize the success of a program by learning how to assimilate them into hospitalized practice.”
Diagnostic Errors and the Hospitalist: Why They Happen and How to Avoid Them
12:45 p.m., May 17
Cardin: “Half of practicing medicine is pattern recognition, and if there are patterns to making diagnostic errors, it would be so valuable to be aware of them. We have tremendous responsibility when caring for patients, and I think it is always beneficial to learn from mistakes.”
Richard Quinn is a freelance writer in New Jersey.
Eight educational tracks, an equal number of credit bearing pre-courses, a score of small-group forums, three plenaries, and an SHM Town Hall meeting offers a lot of professional development in a four-day span. But that’s just a sampling of what HM13 has slated May 16-19 at the Gaylord National Resort & Convention Center in National Harbor, Md., just outside Washington, D.C.
So how does one get the most value out of the conference?
“The highest-yield content is going to depend on what your background is and how to spend that time in a way that augments your knowledge, your perspective, or your exposure to like-minded colleagues in a very individual way,” says HM13 course director Daniel Brotman, MD, FACP, SFHM, director of the hospitalist program at Johns Hopkins Hospital in Baltimore. “One of the things that’s so cool about hospital medicine is its diversity.”
But don’t take Dr. Brotman’s well-educated word for it. Here’s a list of recommendations from Team Hospitalist, the only reader-involvement group of its kind in HM, on events they would not miss this year.
The New Anticoagulants: When Should We Be Using Them?
2:45 p.m., May 17
Dr. Ma: “I’m very interested about the new anticoagulants talk. What I’m curious to see is what the speaker thinks about the survivability of these medications in our society, with so many lawyers. Pradaxa already has fallen out of favor. Let’s see what happens to Xarelto.”
How do CFOs Value Their Hospitalist Programs?
2:50 p.m., May 18
Dr. Ma: “The problem today is CFOs have to valuate their hospitalists in the setting of other specialists who also receive subsidies. There is less money to be spent on hospitalists, as other specialists vie for this allotment of savings from hospital-based value purchasing.”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Mentoring/Coaching an Improvement Team: Lessons from SHM’s Mentored Implementation Programs
2:45 p.m., May 17
Dr. Perumalswami: “As a Project BOOST physician mentor in Illinois, I would highly recommend the session because the discussion will involve an inside look into valuable experience-based observations and analysis for the success of any process improvement team. The nature of teams and the culture of improvement at various sites will also be discussed. There will be a mentee side of the presentation, too, which will help other mentors of implementation programs better understand what the issues are ‘from the other side.’”
Strategies to Improve Communication with Patients and Families to Improve Care
2:45 p.m., May 17
Dr. Hale: “It is well known in pediatrics that you are treating two patients: both the child and the parents. If the family has a shared understanding of the child’s illness and there is collaboration for the care plan, there will be improved care.”
Neonatal HSV: When to Consider It, How to Evaluate for It, and How to Treat It
11 a.m., May 18
Dr. Hale: “Neonatal HSV is a devastating disease. It is essential to recognize high-risk patients to decrease morbidity and mortality for this illness. There have been recent updates in the understanding of epidemiology of this disease that can assist the provider in recognizing high-risk patients.”
Supporting Transition for Youth with Special Healthcare Needs: Coordinating Care and Preparing to Pass the Baton
4:15 p.m., May 18
Dr. Hale: “The transition of adolescents and young adults from pediatric-care teams to adult-medicine-care teams should be seamless for the sake of the patient, but often it is a blurry transition over the course of years. This session is high-yield for both pediatric and adult hospitalists.”
Getting Ready for Physician Value-Based Purchasing
9:50 a.m., May 19
Dr. Simone: “Dr. [Pat] Torcson’s presentation last year was one of the best at HM12, and I expect this year to be the same. He chairs SHM’s Performance Measurement and Reporting Committee and is well versed in these matters. He speaks in terms that will capture all audiences, whether they are experienced or new to the business aspects of medicine. Highly recommended.”
BOOSTing the Hospital Discharge Process: What Works and What Doesn’t
10:35 a.m., May 17
Dr. Simone: “Both panelists are excellent presenters as well as leading authorities when it comes to discharge processes. This presentation is very timely with the new CMS payment system, which penalizes unnecessary and unexpected readmissions.”
Success Stories: How to Integrate NPs and PAs into a Hospitalist Practice
4:15 p.m., May 18
Cardin: “This is an important session because, as every hard-working hospitalist knows, there simply aren’t enough physicians to fill the needs of our medically complex hospitalized patients. It is simply a reality that there will be an increased need in the future for mid-level providers, and it is valuable to maximize the success of a program by learning how to assimilate them into hospitalized practice.”
Diagnostic Errors and the Hospitalist: Why They Happen and How to Avoid Them
12:45 p.m., May 17
Cardin: “Half of practicing medicine is pattern recognition, and if there are patterns to making diagnostic errors, it would be so valuable to be aware of them. We have tremendous responsibility when caring for patients, and I think it is always beneficial to learn from mistakes.”
Richard Quinn is a freelance writer in New Jersey.
Eight educational tracks, an equal number of credit bearing pre-courses, a score of small-group forums, three plenaries, and an SHM Town Hall meeting offers a lot of professional development in a four-day span. But that’s just a sampling of what HM13 has slated May 16-19 at the Gaylord National Resort & Convention Center in National Harbor, Md., just outside Washington, D.C.
So how does one get the most value out of the conference?
“The highest-yield content is going to depend on what your background is and how to spend that time in a way that augments your knowledge, your perspective, or your exposure to like-minded colleagues in a very individual way,” says HM13 course director Daniel Brotman, MD, FACP, SFHM, director of the hospitalist program at Johns Hopkins Hospital in Baltimore. “One of the things that’s so cool about hospital medicine is its diversity.”
But don’t take Dr. Brotman’s well-educated word for it. Here’s a list of recommendations from Team Hospitalist, the only reader-involvement group of its kind in HM, on events they would not miss this year.
The New Anticoagulants: When Should We Be Using Them?
2:45 p.m., May 17
Dr. Ma: “I’m very interested about the new anticoagulants talk. What I’m curious to see is what the speaker thinks about the survivability of these medications in our society, with so many lawyers. Pradaxa already has fallen out of favor. Let’s see what happens to Xarelto.”
How do CFOs Value Their Hospitalist Programs?
2:50 p.m., May 18
Dr. Ma: “The problem today is CFOs have to valuate their hospitalists in the setting of other specialists who also receive subsidies. There is less money to be spent on hospitalists, as other specialists vie for this allotment of savings from hospital-based value purchasing.”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Mentoring/Coaching an Improvement Team: Lessons from SHM’s Mentored Implementation Programs
2:45 p.m., May 17
Dr. Perumalswami: “As a Project BOOST physician mentor in Illinois, I would highly recommend the session because the discussion will involve an inside look into valuable experience-based observations and analysis for the success of any process improvement team. The nature of teams and the culture of improvement at various sites will also be discussed. There will be a mentee side of the presentation, too, which will help other mentors of implementation programs better understand what the issues are ‘from the other side.’”
Strategies to Improve Communication with Patients and Families to Improve Care
2:45 p.m., May 17
Dr. Hale: “It is well known in pediatrics that you are treating two patients: both the child and the parents. If the family has a shared understanding of the child’s illness and there is collaboration for the care plan, there will be improved care.”
Neonatal HSV: When to Consider It, How to Evaluate for It, and How to Treat It
11 a.m., May 18
Dr. Hale: “Neonatal HSV is a devastating disease. It is essential to recognize high-risk patients to decrease morbidity and mortality for this illness. There have been recent updates in the understanding of epidemiology of this disease that can assist the provider in recognizing high-risk patients.”
Supporting Transition for Youth with Special Healthcare Needs: Coordinating Care and Preparing to Pass the Baton
4:15 p.m., May 18
Dr. Hale: “The transition of adolescents and young adults from pediatric-care teams to adult-medicine-care teams should be seamless for the sake of the patient, but often it is a blurry transition over the course of years. This session is high-yield for both pediatric and adult hospitalists.”
Getting Ready for Physician Value-Based Purchasing
9:50 a.m., May 19
Dr. Simone: “Dr. [Pat] Torcson’s presentation last year was one of the best at HM12, and I expect this year to be the same. He chairs SHM’s Performance Measurement and Reporting Committee and is well versed in these matters. He speaks in terms that will capture all audiences, whether they are experienced or new to the business aspects of medicine. Highly recommended.”
BOOSTing the Hospital Discharge Process: What Works and What Doesn’t
10:35 a.m., May 17
Dr. Simone: “Both panelists are excellent presenters as well as leading authorities when it comes to discharge processes. This presentation is very timely with the new CMS payment system, which penalizes unnecessary and unexpected readmissions.”
Success Stories: How to Integrate NPs and PAs into a Hospitalist Practice
4:15 p.m., May 18
Cardin: “This is an important session because, as every hard-working hospitalist knows, there simply aren’t enough physicians to fill the needs of our medically complex hospitalized patients. It is simply a reality that there will be an increased need in the future for mid-level providers, and it is valuable to maximize the success of a program by learning how to assimilate them into hospitalized practice.”
Diagnostic Errors and the Hospitalist: Why They Happen and How to Avoid Them
12:45 p.m., May 17
Cardin: “Half of practicing medicine is pattern recognition, and if there are patterns to making diagnostic errors, it would be so valuable to be aware of them. We have tremendous responsibility when caring for patients, and I think it is always beneficial to learn from mistakes.”
Richard Quinn is a freelance writer in New Jersey.
Danielle Scheurer: Thousands of Hospitalists Set Their Sights on HM13
SHM’s annual meeting—or annui conventus, for you Latin lovers—is right around the corner, so be sure to cement your intentions and prepare to go if you have not already.
Now a “longstanding” tradition, the annual meeting serves many purposes, one of which is to act as a reservoir of time for individual hospitalists and for hospitalist groups to reflect on where they have been, where they are now, and where they are (or would like to be) going. A brief history of the SHM annual meeting makes us quickly realize how far we have come, and how far we have to go.
Where We’ve Been
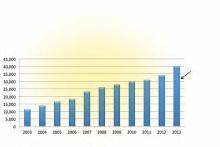
The annual meeting’s history dates back to 1998, when a rogue gathering of about 100 self-proclaimed hospitalists gathered at the National Association of Inpatient Physicians (NAIP) meeting in San Diego. From the year before the first annual meeting to the year after the first annual meeting, membership in NAIP had grown from about 20 hospitalists to about 800 hospitalists. That rapidity of growth had never been seen by another specialty in the history of modern medicine. By the 2003 annual meeting in San Diego, the name had officially changed to the Society of Hospital Medicine, and membership had grown to more than 3,000; less than 10 years later, when the meeting returned to San Diego, membership had grown to more than 10,000. These continued steady increases in both membership size and attendance at the meeting serves as a testimony to the strength of the field and the leadership of the society.
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Where We Are Now
Growth: SHM’s annual meeting now has a track record to be reckoned with. The number of attendees expected for 2013 is a staggering 3,000, which is only a portion of the more than 11,000 SHM members who can actually take time away from their busy practices to attend. The event has now expanded to more than three and a half days, including eight pre-courses and more than 100 workshops/breakout sessions to meet the needs of most any hospitalist. The number of submissions for the Research, Innovations, and Clinical Vignettes competition has steadily risen over the years, topping an all-time record of 800 submissions in 2013. This is a testimony to the curiosity and productivity of so many hospitalists and HM groups.
Advocacy: SHM has been a longstanding and considerable advocate for healthcare reform for more than a decade. With the annual meeting in Washington, D.C., this year, and in lieu of the pre-courses, more than 100 hospitalists and SHM staff will be making a field trip to Capitol Hill to advocate for changes in the structure and payment within the medical industry, to promote good patient care for those we serve, and to promote continued research for better ways of delivering care in the future. Over the course of 2012, SHM submitted more than 20 influential advocacy letters to a variety of stakeholders on topics ranging from sustainable growth rate (SGR) repeal to Agency for Healthcare Research and Quality (AHRQ) funding.
Impact: The annual meeting is not just bigger and longer; it is better. The quality and reputation of the plenary, breakout, and workshop speakers is tremendous, with this year’s plenary speakers including Patrick Conway, chief medical officer of CMS, and David Feinberg, president of UCLA Health System and CEO of UCLA Hospital System. The annual award ceremony will recognize a highly qualified repertoire of dedicated hospitalists and teams and reflect the number and quality of those involved in HM in the areas of clinical excellence, teaching, research, service, and teamwork. The annual Fellows in Hospital Medicine induction will include more than 300 additional fellows and senior fellows, which is a testimony to the level of involvement so many hospitalists have within our specialty.
Where We Are Going
Growth: I suspect the annual meeting will continue to grow in size, and it will expand to better serve the needs of other types of hospital-based physicians (neurologists, obstetricians, etc.), other types of practitioners (NPs, PAs, other specialty nurses), and other types of professionals (administrators and executives). It likely will attract an international community of hospitalists as other nations identify and execute better models of care for hospitalized patients.
Advocacy: SHM and the annual meeting will continue to serve as a nidus for directing the best pathways toward a better healthcare system. It will continue to serve as an avenue by which we partner with and/or influence impactful organizations, such as federal, state, and local governments, the Centers for Medicare & Medicaid Services (CMS), the Joint Commission, and the American Hospital Association, to name a few.
Impact: SHM and the annual meeting will expand its role as the focus for learning and sharing new research and innovations within the field. It will serve as a platform for initiating and spreading standardized evidence-based implementation of best practices through a repertoire of mentored implementation programs. And it will continue to serve as proof of the strength of our hospital medicine community as we spread into every U.S. hospital system and beyond.
Reputation: The future of our annual meeting and reputation will be dependent on how fast and how carefully we craft the pathway for HM. Currently, about half of all the nation’s hospitalists have been in practice for five years or less. We will need to carefully focus on how to be compassionate providers and system advocates—not just shift workers and billing specialists. We will have to be the mentors by which other countries define best practice for inpatient care, including what ideal training for a hospitalist should look like, and what their scope of practice should entail.
If you ask one of the attendees of the first annui conventus what it was like, they will say it was a small mom-and-pop gathering of disparate physicians, with a pie-in-the-sky idea of the future of hospitalist practice. And someday, when our current generation of hospitalists attends an international conference of hospitalists, in Prague, in 2033, we can say, “Remember when we met in that tiny hotel in D.C. in 2013?”
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
SHM’s annual meeting—or annui conventus, for you Latin lovers—is right around the corner, so be sure to cement your intentions and prepare to go if you have not already.
Now a “longstanding” tradition, the annual meeting serves many purposes, one of which is to act as a reservoir of time for individual hospitalists and for hospitalist groups to reflect on where they have been, where they are now, and where they are (or would like to be) going. A brief history of the SHM annual meeting makes us quickly realize how far we have come, and how far we have to go.
Where We’ve Been
The annual meeting’s history dates back to 1998, when a rogue gathering of about 100 self-proclaimed hospitalists gathered at the National Association of Inpatient Physicians (NAIP) meeting in San Diego. From the year before the first annual meeting to the year after the first annual meeting, membership in NAIP had grown from about 20 hospitalists to about 800 hospitalists. That rapidity of growth had never been seen by another specialty in the history of modern medicine. By the 2003 annual meeting in San Diego, the name had officially changed to the Society of Hospital Medicine, and membership had grown to more than 3,000; less than 10 years later, when the meeting returned to San Diego, membership had grown to more than 10,000. These continued steady increases in both membership size and attendance at the meeting serves as a testimony to the strength of the field and the leadership of the society.
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Where We Are Now
Growth: SHM’s annual meeting now has a track record to be reckoned with. The number of attendees expected for 2013 is a staggering 3,000, which is only a portion of the more than 11,000 SHM members who can actually take time away from their busy practices to attend. The event has now expanded to more than three and a half days, including eight pre-courses and more than 100 workshops/breakout sessions to meet the needs of most any hospitalist. The number of submissions for the Research, Innovations, and Clinical Vignettes competition has steadily risen over the years, topping an all-time record of 800 submissions in 2013. This is a testimony to the curiosity and productivity of so many hospitalists and HM groups.
Advocacy: SHM has been a longstanding and considerable advocate for healthcare reform for more than a decade. With the annual meeting in Washington, D.C., this year, and in lieu of the pre-courses, more than 100 hospitalists and SHM staff will be making a field trip to Capitol Hill to advocate for changes in the structure and payment within the medical industry, to promote good patient care for those we serve, and to promote continued research for better ways of delivering care in the future. Over the course of 2012, SHM submitted more than 20 influential advocacy letters to a variety of stakeholders on topics ranging from sustainable growth rate (SGR) repeal to Agency for Healthcare Research and Quality (AHRQ) funding.
Impact: The annual meeting is not just bigger and longer; it is better. The quality and reputation of the plenary, breakout, and workshop speakers is tremendous, with this year’s plenary speakers including Patrick Conway, chief medical officer of CMS, and David Feinberg, president of UCLA Health System and CEO of UCLA Hospital System. The annual award ceremony will recognize a highly qualified repertoire of dedicated hospitalists and teams and reflect the number and quality of those involved in HM in the areas of clinical excellence, teaching, research, service, and teamwork. The annual Fellows in Hospital Medicine induction will include more than 300 additional fellows and senior fellows, which is a testimony to the level of involvement so many hospitalists have within our specialty.
Where We Are Going
Growth: I suspect the annual meeting will continue to grow in size, and it will expand to better serve the needs of other types of hospital-based physicians (neurologists, obstetricians, etc.), other types of practitioners (NPs, PAs, other specialty nurses), and other types of professionals (administrators and executives). It likely will attract an international community of hospitalists as other nations identify and execute better models of care for hospitalized patients.
Advocacy: SHM and the annual meeting will continue to serve as a nidus for directing the best pathways toward a better healthcare system. It will continue to serve as an avenue by which we partner with and/or influence impactful organizations, such as federal, state, and local governments, the Centers for Medicare & Medicaid Services (CMS), the Joint Commission, and the American Hospital Association, to name a few.
Impact: SHM and the annual meeting will expand its role as the focus for learning and sharing new research and innovations within the field. It will serve as a platform for initiating and spreading standardized evidence-based implementation of best practices through a repertoire of mentored implementation programs. And it will continue to serve as proof of the strength of our hospital medicine community as we spread into every U.S. hospital system and beyond.
Reputation: The future of our annual meeting and reputation will be dependent on how fast and how carefully we craft the pathway for HM. Currently, about half of all the nation’s hospitalists have been in practice for five years or less. We will need to carefully focus on how to be compassionate providers and system advocates—not just shift workers and billing specialists. We will have to be the mentors by which other countries define best practice for inpatient care, including what ideal training for a hospitalist should look like, and what their scope of practice should entail.
If you ask one of the attendees of the first annui conventus what it was like, they will say it was a small mom-and-pop gathering of disparate physicians, with a pie-in-the-sky idea of the future of hospitalist practice. And someday, when our current generation of hospitalists attends an international conference of hospitalists, in Prague, in 2033, we can say, “Remember when we met in that tiny hotel in D.C. in 2013?”
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
SHM’s annual meeting—or annui conventus, for you Latin lovers—is right around the corner, so be sure to cement your intentions and prepare to go if you have not already.
Now a “longstanding” tradition, the annual meeting serves many purposes, one of which is to act as a reservoir of time for individual hospitalists and for hospitalist groups to reflect on where they have been, where they are now, and where they are (or would like to be) going. A brief history of the SHM annual meeting makes us quickly realize how far we have come, and how far we have to go.
Where We’ve Been
The annual meeting’s history dates back to 1998, when a rogue gathering of about 100 self-proclaimed hospitalists gathered at the National Association of Inpatient Physicians (NAIP) meeting in San Diego. From the year before the first annual meeting to the year after the first annual meeting, membership in NAIP had grown from about 20 hospitalists to about 800 hospitalists. That rapidity of growth had never been seen by another specialty in the history of modern medicine. By the 2003 annual meeting in San Diego, the name had officially changed to the Society of Hospital Medicine, and membership had grown to more than 3,000; less than 10 years later, when the meeting returned to San Diego, membership had grown to more than 10,000. These continued steady increases in both membership size and attendance at the meeting serves as a testimony to the strength of the field and the leadership of the society.
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Where We Are Now
Growth: SHM’s annual meeting now has a track record to be reckoned with. The number of attendees expected for 2013 is a staggering 3,000, which is only a portion of the more than 11,000 SHM members who can actually take time away from their busy practices to attend. The event has now expanded to more than three and a half days, including eight pre-courses and more than 100 workshops/breakout sessions to meet the needs of most any hospitalist. The number of submissions for the Research, Innovations, and Clinical Vignettes competition has steadily risen over the years, topping an all-time record of 800 submissions in 2013. This is a testimony to the curiosity and productivity of so many hospitalists and HM groups.
Advocacy: SHM has been a longstanding and considerable advocate for healthcare reform for more than a decade. With the annual meeting in Washington, D.C., this year, and in lieu of the pre-courses, more than 100 hospitalists and SHM staff will be making a field trip to Capitol Hill to advocate for changes in the structure and payment within the medical industry, to promote good patient care for those we serve, and to promote continued research for better ways of delivering care in the future. Over the course of 2012, SHM submitted more than 20 influential advocacy letters to a variety of stakeholders on topics ranging from sustainable growth rate (SGR) repeal to Agency for Healthcare Research and Quality (AHRQ) funding.
Impact: The annual meeting is not just bigger and longer; it is better. The quality and reputation of the plenary, breakout, and workshop speakers is tremendous, with this year’s plenary speakers including Patrick Conway, chief medical officer of CMS, and David Feinberg, president of UCLA Health System and CEO of UCLA Hospital System. The annual award ceremony will recognize a highly qualified repertoire of dedicated hospitalists and teams and reflect the number and quality of those involved in HM in the areas of clinical excellence, teaching, research, service, and teamwork. The annual Fellows in Hospital Medicine induction will include more than 300 additional fellows and senior fellows, which is a testimony to the level of involvement so many hospitalists have within our specialty.
Where We Are Going
Growth: I suspect the annual meeting will continue to grow in size, and it will expand to better serve the needs of other types of hospital-based physicians (neurologists, obstetricians, etc.), other types of practitioners (NPs, PAs, other specialty nurses), and other types of professionals (administrators and executives). It likely will attract an international community of hospitalists as other nations identify and execute better models of care for hospitalized patients.
Advocacy: SHM and the annual meeting will continue to serve as a nidus for directing the best pathways toward a better healthcare system. It will continue to serve as an avenue by which we partner with and/or influence impactful organizations, such as federal, state, and local governments, the Centers for Medicare & Medicaid Services (CMS), the Joint Commission, and the American Hospital Association, to name a few.
Impact: SHM and the annual meeting will expand its role as the focus for learning and sharing new research and innovations within the field. It will serve as a platform for initiating and spreading standardized evidence-based implementation of best practices through a repertoire of mentored implementation programs. And it will continue to serve as proof of the strength of our hospital medicine community as we spread into every U.S. hospital system and beyond.
Reputation: The future of our annual meeting and reputation will be dependent on how fast and how carefully we craft the pathway for HM. Currently, about half of all the nation’s hospitalists have been in practice for five years or less. We will need to carefully focus on how to be compassionate providers and system advocates—not just shift workers and billing specialists. We will have to be the mentors by which other countries define best practice for inpatient care, including what ideal training for a hospitalist should look like, and what their scope of practice should entail.
If you ask one of the attendees of the first annui conventus what it was like, they will say it was a small mom-and-pop gathering of disparate physicians, with a pie-in-the-sky idea of the future of hospitalist practice. And someday, when our current generation of hospitalists attends an international conference of hospitalists, in Prague, in 2033, we can say, “Remember when we met in that tiny hotel in D.C. in 2013?”
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
Two Accountable Care Organizations (ACOs) Share Their Strategies for Success
Success as an ACO likely won’t come from any one strategy, but from many. Christopher Kim, MD, MBA, SFHM, a hospitalist and associate professor of internal medicine at the University of Michigan, says the Michigan Pioneer ACO serving roughly 20,000 beneficiaries in the state’s southeastern region has benefited greatly from a variety of pre-existing relationships and initiatives. The university’s medical center, one of 10 participants in a Medicare ACO precursor called the Physician Group Practice demonstration project, was among the few sites to successfully meet the requirements and gain the full cost savings benefits in all five years.
The newer ACO, which officially launched in January 2012, pairs the university’s Faculty Group Practice with Integrated Health Associates Inc. (IHA), a large multispecialty private-practice group. Many IHA providers already had access to the university’s electronic health records so they could track admitted patients. One preliminary collaborative effort between the two entities hinted at a trend toward lower readmission rates among a small group of patients who were seen by a primary-care provider within seven days of a hospital discharge, underscoring the importance of a smooth transition.
Providers also have been able to tap into statewide initiatives aimed at improving quality and care coordination in key areas, such as cardiovascular disease, cancer, and hospital care transitions (sponsored by Blue Cross Blue Shield of Michigan).

—Christopher Kim, MD, MBA, SFHM, associate professor of internal medicine, University of Michigan Health System, Ann Arbor
“These programs helped physician organizations and hospitals throughout the state become familiar with best practices related to these kinds of conditions,” Dr. Kim says, “and I think partly because of that, we were very prepared to work on a quality-improvement initiative such as this while also improving efficiency.”
Listen to Dr. Kim discuss the added responsibility hospitalists in ACOs like the one formed between the university faculty and a large multi-specialty practice called Integrated Health Associates, Inc.
For stratifying beneficiaries by risk, the ACO has benefited from a separate initiative called the Michigan Primary Care Transformation Project, which uses the concept of a pyramid to classify increasingly complicated patients. A complex-case manager, typically an advanced practice nurse, acts as the point person for guiding patients in the upper half of the pyramid toward the best resources while preventing unnecessary duplication of tasks or consultation referrals. Optimal coordination means that hospitalists need to communicate effectively with these managers as well as with other providers.
From Medicare claims supplied by CMS, Beth Israel Deaconess Physician Organization (BIDPO) in the Boston metropolitan region has used software to identify its highest-risk patients, or those most likely to be admitted to the hospital within the next 12 months. As part of the process, BIDPO officials asked doctors to validate the results based on their own patient records and observations.
The ACO has hired nurse practitioners through a company called INSPIRIS Massachusetts to visit its sickest and frailest Medicare beneficiaries at home to prevent hospital admissions and to avoid post-discharge readmissions among the highest-risk patients. BIDPO also uses nurse care managers to do telephone-based care management for less acute patients, and is asking emergency department staff to recognize patients who could be sent home safely with appropriate care rather than be admitted. Patients with cellulitis, for example, could be treated via IV antibiotic therapy at home, a service made possible through a collaboration with a home infusion company.
Dr. Parker, BIDPO’s medical director, says hospitalists will be key to understanding the need for excellent inpatient care and thoughtful, comprehensive discharge planning that helps avoid adverse events post-discharge.
Success as an ACO likely won’t come from any one strategy, but from many. Christopher Kim, MD, MBA, SFHM, a hospitalist and associate professor of internal medicine at the University of Michigan, says the Michigan Pioneer ACO serving roughly 20,000 beneficiaries in the state’s southeastern region has benefited greatly from a variety of pre-existing relationships and initiatives. The university’s medical center, one of 10 participants in a Medicare ACO precursor called the Physician Group Practice demonstration project, was among the few sites to successfully meet the requirements and gain the full cost savings benefits in all five years.
The newer ACO, which officially launched in January 2012, pairs the university’s Faculty Group Practice with Integrated Health Associates Inc. (IHA), a large multispecialty private-practice group. Many IHA providers already had access to the university’s electronic health records so they could track admitted patients. One preliminary collaborative effort between the two entities hinted at a trend toward lower readmission rates among a small group of patients who were seen by a primary-care provider within seven days of a hospital discharge, underscoring the importance of a smooth transition.
Providers also have been able to tap into statewide initiatives aimed at improving quality and care coordination in key areas, such as cardiovascular disease, cancer, and hospital care transitions (sponsored by Blue Cross Blue Shield of Michigan).

—Christopher Kim, MD, MBA, SFHM, associate professor of internal medicine, University of Michigan Health System, Ann Arbor
“These programs helped physician organizations and hospitals throughout the state become familiar with best practices related to these kinds of conditions,” Dr. Kim says, “and I think partly because of that, we were very prepared to work on a quality-improvement initiative such as this while also improving efficiency.”
Listen to Dr. Kim discuss the added responsibility hospitalists in ACOs like the one formed between the university faculty and a large multi-specialty practice called Integrated Health Associates, Inc.
For stratifying beneficiaries by risk, the ACO has benefited from a separate initiative called the Michigan Primary Care Transformation Project, which uses the concept of a pyramid to classify increasingly complicated patients. A complex-case manager, typically an advanced practice nurse, acts as the point person for guiding patients in the upper half of the pyramid toward the best resources while preventing unnecessary duplication of tasks or consultation referrals. Optimal coordination means that hospitalists need to communicate effectively with these managers as well as with other providers.
From Medicare claims supplied by CMS, Beth Israel Deaconess Physician Organization (BIDPO) in the Boston metropolitan region has used software to identify its highest-risk patients, or those most likely to be admitted to the hospital within the next 12 months. As part of the process, BIDPO officials asked doctors to validate the results based on their own patient records and observations.
The ACO has hired nurse practitioners through a company called INSPIRIS Massachusetts to visit its sickest and frailest Medicare beneficiaries at home to prevent hospital admissions and to avoid post-discharge readmissions among the highest-risk patients. BIDPO also uses nurse care managers to do telephone-based care management for less acute patients, and is asking emergency department staff to recognize patients who could be sent home safely with appropriate care rather than be admitted. Patients with cellulitis, for example, could be treated via IV antibiotic therapy at home, a service made possible through a collaboration with a home infusion company.
Dr. Parker, BIDPO’s medical director, says hospitalists will be key to understanding the need for excellent inpatient care and thoughtful, comprehensive discharge planning that helps avoid adverse events post-discharge.
Success as an ACO likely won’t come from any one strategy, but from many. Christopher Kim, MD, MBA, SFHM, a hospitalist and associate professor of internal medicine at the University of Michigan, says the Michigan Pioneer ACO serving roughly 20,000 beneficiaries in the state’s southeastern region has benefited greatly from a variety of pre-existing relationships and initiatives. The university’s medical center, one of 10 participants in a Medicare ACO precursor called the Physician Group Practice demonstration project, was among the few sites to successfully meet the requirements and gain the full cost savings benefits in all five years.
The newer ACO, which officially launched in January 2012, pairs the university’s Faculty Group Practice with Integrated Health Associates Inc. (IHA), a large multispecialty private-practice group. Many IHA providers already had access to the university’s electronic health records so they could track admitted patients. One preliminary collaborative effort between the two entities hinted at a trend toward lower readmission rates among a small group of patients who were seen by a primary-care provider within seven days of a hospital discharge, underscoring the importance of a smooth transition.
Providers also have been able to tap into statewide initiatives aimed at improving quality and care coordination in key areas, such as cardiovascular disease, cancer, and hospital care transitions (sponsored by Blue Cross Blue Shield of Michigan).

—Christopher Kim, MD, MBA, SFHM, associate professor of internal medicine, University of Michigan Health System, Ann Arbor
“These programs helped physician organizations and hospitals throughout the state become familiar with best practices related to these kinds of conditions,” Dr. Kim says, “and I think partly because of that, we were very prepared to work on a quality-improvement initiative such as this while also improving efficiency.”
Listen to Dr. Kim discuss the added responsibility hospitalists in ACOs like the one formed between the university faculty and a large multi-specialty practice called Integrated Health Associates, Inc.
For stratifying beneficiaries by risk, the ACO has benefited from a separate initiative called the Michigan Primary Care Transformation Project, which uses the concept of a pyramid to classify increasingly complicated patients. A complex-case manager, typically an advanced practice nurse, acts as the point person for guiding patients in the upper half of the pyramid toward the best resources while preventing unnecessary duplication of tasks or consultation referrals. Optimal coordination means that hospitalists need to communicate effectively with these managers as well as with other providers.
From Medicare claims supplied by CMS, Beth Israel Deaconess Physician Organization (BIDPO) in the Boston metropolitan region has used software to identify its highest-risk patients, or those most likely to be admitted to the hospital within the next 12 months. As part of the process, BIDPO officials asked doctors to validate the results based on their own patient records and observations.
The ACO has hired nurse practitioners through a company called INSPIRIS Massachusetts to visit its sickest and frailest Medicare beneficiaries at home to prevent hospital admissions and to avoid post-discharge readmissions among the highest-risk patients. BIDPO also uses nurse care managers to do telephone-based care management for less acute patients, and is asking emergency department staff to recognize patients who could be sent home safely with appropriate care rather than be admitted. Patients with cellulitis, for example, could be treated via IV antibiotic therapy at home, a service made possible through a collaboration with a home infusion company.
Dr. Parker, BIDPO’s medical director, says hospitalists will be key to understanding the need for excellent inpatient care and thoughtful, comprehensive discharge planning that helps avoid adverse events post-discharge.
Accountable Care Organizations (ACO) Gain Popularity with Physicians in Wake of Added Incentives, Revised Federal Rules
Throughout much of 2011, ambivalence plagued efforts by the Centers for Medicare & Medicaid Services (CMS) to expand the federal government’s reach into integrated care delivery to help improve patient outcomes while lowering costs. Critics panned the initial draft of regulations for a large accountable-care demonstration project called the Shared Savings Program, and prominent medical groups announced their intention to sit on the sidelines.
At the start of 2013, the atmosphere couldn’t be more different. CMS won over most of its critics with a well-received final version of the rules that provided more incentives for groups to form accountable-care organizations (ACOs), and the presidential election provided more clarity about the future of healthcare reform. Medical groups around the country are readily jumping on the ACO bandwagon, with its emphasis on shared responsibility among provider groups for a defined pool of patients.
Few medical groups have enough data to suggest whether their varied approaches to managing patient populations will lead to better-quality care that’s also more affordable; the first batch of Medicare ACO data isn’t expected until later this spring. And healthcare experts differ on which models and components are likely to make the biggest long-term impact; even the precise definition of an ACO remains a moving target. But industry observers say they’re surprised and encouraged not only by the speed with which the movement has taken off, but also by the breadth of models being investigated, the strong engagement of the private sector, and a spreading sense of cautious optimism.
“This is actually moving faster than I thought—faster than I think anybody thought,” says SHM Public Policy Committee chair Ron Greeno, MD, FCCP, MHM.
Although CMS still is in the beginning stages of its work and has focused most of its efforts on reviewing applications and providing feedback on organizations’ historical expenditure and utilization patterns, agency officials say the ACO initiative has not encountered any unexpected setbacks. “As with any new program, there are bumps along the way, but I don’t think we’ve experienced anything that is out of the ordinary,” says John Pilotte, director of Performance-Based Payment Policy in the Center for Medicare. “We’re pretty happy with where we are with the program.”
The Shared Savings Program, which Pilotte describes as “an easier on-ramp” to population management for providers and offers low financial risk in exchange for a modest level of shared cost savings, is proving especially popular. Combined, several hundred organizations submitted applications for the program’s second and third rounds, which began July 1, 2012, and Jan. 1, 2013, respectively.
“Two hundred twenty ACOs are currently up and running, and we expect to continue to add ACOs to the program annually,” Pilotte says.

—David Muhlestein, analyst, Leavitt Partners
Last January, another 32 groups joined Medicare’s Pioneer ACO program, designed for more experienced organizations with more resources. The groups assume more risk, and in return are more handsomely rewarded if they meet benchmarks.
All told, the tally of confirmed ACOs in the U.S. reached 428 by the end of January, according to Leavitt Partners, a Salt Lake City-based healthcare consulting firm that is tracking the growth of accountable care (see “A Sampling of Significant ACO Programs,” below). David Muhlestein, an analyst with Leavitt Partners, says private ACOs now account for roughly half of that total, a trend driven by their ability to experiment with different approaches and more easily track costs through clearly defined patient populations.
The central role for hospitalists within most ACOs is rooted in the reality that hospital care is the most expensive part of healthcare. Successfully implementing a plan to coordinate care and prevent hospital readmissions might not correlate directly with improved quality metrics, but it can lead to significant savings.
The diverse ACO models now being tested, however, could result in varying responsibilities for hospitalists, depending on the focal points of the sponsoring entities. After patients have been admitted to a hospital, for example, many hospitalists assume responsibility for managing inpatient care and the inpatient-outpatient handoff. A main goal of a physician-owned medical group, such as an independent practice association (IPA), by contrast, is to keep patients out of the hospital altogether, placing more of the focus on primary and specialty care. An IPA that forms an ACO, Muhlestein says, might hire its own hospitalists to monitor the care of patients in affiliated hospitals while using the association’s approach to limiting costs.
ACO participants also have varied widely in the effort expended to get up to speed. “Some people have said they haven’t had to make any major changes to their organization, while some people have had to drastically think how they provide care,” Muhlestein says. In general, many of the former have had the luxury of working within relatively integrated facilities and building upon existing frameworks, whereas many of the latter previously toiled away in silos and are now scrambling to establish more cohesive working relationships from scratch.
Optimism Abounds
Though many ACOs have only limited data so far, Muhlestein says most are generally optimistic that their early results will be positive. Even so, Dr. Greeno says, he fully expects the Pioneer ACOs to produce the best results among the Medicare demonstration projects. Those organizations already have successful track records in managing patient populations, and the Pioneer model’s incentives are stronger because the groups are assuming more risk. If the Pioneer ACO results are eclipsed by those of the Shared Savings Program, he says, “I’d fall out of my chair.”
The Beth Israel Deaconess Physician Organization (BIDPO) now has four global payment contracts, including its Pioneer ACO arrangement with CMS that serves 33,000 beneficiaries in the Boston metropolitan region. “The decision-making around joining was a recognition that the fee-for-service model is highly dysfunctional,” says Richard Parker, MD, BIDPO’s medical director. “Our organization and our leadership believed that most of the country, both private payor and governmental payor, would be moving toward global payment and that it would be to our advantage to get in early.”
Despite the complicated rollout and delays in receiving Medicare data on patients from CMS, Dr. Parker says, the feedback from both providers and patients has been mostly positive. “I would say, anecdotally, that the doctors seem appreciative that we’re trying to fix some of these gaps in care that we all know have existed for some time,” he says. “And, anecdotally from the patients, we get appreciation that we’re trying to take better care of them.”
Chris Coleman, chief financial officer for Phoenix-based Banner Health Network, another Pioneer ACO participant, says the project fits in well with his company’s decision “to transform itself into more of a value-based, performance-based provider.” Banner’s ACO, which serves about 50,000 beneficiaries, is still setting up needed systems, including a consistent platform for electronic medical records throughout the entire provider network. Even during the building phase, however, Coleman says company officials have been pleasantly surprised by the ACO’s positive effect on utilization, patient care, and apparent savings.
Although the company has only a partial year of Medicare claims to go by, Coleman says the data look “pretty good” so far and suggest the ACO is on track for modest savings of perhaps 3% or 4%. Like BIDPO, Banner has other shared-risk agreements in place, including one for a Medicare Advantage population and another with a private payor. So far, Coleman says, those arrangements also seem to be “performing positively.”
Dr. Greeno and other experts see the best ACO results coming from such rapidly growing private arrangements, and early published data have been generally encouraging.1 The ability to more narrowly define patient groups and assume more control over payments, he says, has allowed private ACOs to keep better track of costs and implement innovative population health interventions.

—Ron Greeno, MD, FCCP, MHM, SHM Public Policy Committee chair
Built to Last?
Whether public, private, or a hybrid between the two, some ACOs are trying to manage the care of their entire patient pool and look at everything that might help them accrue cost savings. Others are focusing only on the sickest patients to reach their quality improvement (QI) and savings goals, and targeting specific parameters, such as blood pressure or medication adherence, for patients with myocardial infarction.
Joane Goodroe, an Atlanta-based healthcare consultant, favors the latter approach, at least for new ACOs. Goodroe recommends adopting a streamlined strategy that will get an ACO up and running, then allow the group to gradually add to it, rather than waiting until all of the right pieces fall into place. Her own data analysis of Medicare patients, for example, suggests that a diabetic who’s been an inpatient can average $50,000 in yearly costs, compared with $2,400 for a diabetic who has never been admitted to a hospital.
Setting up a system to manage every diabetic patient from the start, she says, would require too much time and money. “If you try to build the perfect ACO structure, it’s going to be too expensive for the results you initially get back,” she says, making it seem like the ACO is an unsustainable failure. “You’ve got to figure out how to build a cost-effective infrastructure while you’re also improving the care of the patients, and the best place to go is to target your sickest patients first.”
CMS’ Advance Payment ACO Model is designed to help by providing upfront payments to smaller ACO organizations that might lack capital, giving them an advance on potential shared savings so they can install the infrastructure and support structures necessary to redesign care.
To maximize the overall chances of success, Dr. Parker says, ACO leadership should be fully engaged, and each organization should have enough resources to address its own care management and information technology needs. “My goal as medical director is to improve the quality of care of the patients and, hopefully, also improve the working life of the doctors and staff,” he says. “And my belief and expectation is that if we do that, the cost of care will ultimately go down.”
Bryn Nelson is a freelance medical writer in Seattle.
Reference
Throughout much of 2011, ambivalence plagued efforts by the Centers for Medicare & Medicaid Services (CMS) to expand the federal government’s reach into integrated care delivery to help improve patient outcomes while lowering costs. Critics panned the initial draft of regulations for a large accountable-care demonstration project called the Shared Savings Program, and prominent medical groups announced their intention to sit on the sidelines.
At the start of 2013, the atmosphere couldn’t be more different. CMS won over most of its critics with a well-received final version of the rules that provided more incentives for groups to form accountable-care organizations (ACOs), and the presidential election provided more clarity about the future of healthcare reform. Medical groups around the country are readily jumping on the ACO bandwagon, with its emphasis on shared responsibility among provider groups for a defined pool of patients.
Few medical groups have enough data to suggest whether their varied approaches to managing patient populations will lead to better-quality care that’s also more affordable; the first batch of Medicare ACO data isn’t expected until later this spring. And healthcare experts differ on which models and components are likely to make the biggest long-term impact; even the precise definition of an ACO remains a moving target. But industry observers say they’re surprised and encouraged not only by the speed with which the movement has taken off, but also by the breadth of models being investigated, the strong engagement of the private sector, and a spreading sense of cautious optimism.
“This is actually moving faster than I thought—faster than I think anybody thought,” says SHM Public Policy Committee chair Ron Greeno, MD, FCCP, MHM.
Although CMS still is in the beginning stages of its work and has focused most of its efforts on reviewing applications and providing feedback on organizations’ historical expenditure and utilization patterns, agency officials say the ACO initiative has not encountered any unexpected setbacks. “As with any new program, there are bumps along the way, but I don’t think we’ve experienced anything that is out of the ordinary,” says John Pilotte, director of Performance-Based Payment Policy in the Center for Medicare. “We’re pretty happy with where we are with the program.”
The Shared Savings Program, which Pilotte describes as “an easier on-ramp” to population management for providers and offers low financial risk in exchange for a modest level of shared cost savings, is proving especially popular. Combined, several hundred organizations submitted applications for the program’s second and third rounds, which began July 1, 2012, and Jan. 1, 2013, respectively.
“Two hundred twenty ACOs are currently up and running, and we expect to continue to add ACOs to the program annually,” Pilotte says.

—David Muhlestein, analyst, Leavitt Partners
Last January, another 32 groups joined Medicare’s Pioneer ACO program, designed for more experienced organizations with more resources. The groups assume more risk, and in return are more handsomely rewarded if they meet benchmarks.
All told, the tally of confirmed ACOs in the U.S. reached 428 by the end of January, according to Leavitt Partners, a Salt Lake City-based healthcare consulting firm that is tracking the growth of accountable care (see “A Sampling of Significant ACO Programs,” below). David Muhlestein, an analyst with Leavitt Partners, says private ACOs now account for roughly half of that total, a trend driven by their ability to experiment with different approaches and more easily track costs through clearly defined patient populations.
The central role for hospitalists within most ACOs is rooted in the reality that hospital care is the most expensive part of healthcare. Successfully implementing a plan to coordinate care and prevent hospital readmissions might not correlate directly with improved quality metrics, but it can lead to significant savings.
The diverse ACO models now being tested, however, could result in varying responsibilities for hospitalists, depending on the focal points of the sponsoring entities. After patients have been admitted to a hospital, for example, many hospitalists assume responsibility for managing inpatient care and the inpatient-outpatient handoff. A main goal of a physician-owned medical group, such as an independent practice association (IPA), by contrast, is to keep patients out of the hospital altogether, placing more of the focus on primary and specialty care. An IPA that forms an ACO, Muhlestein says, might hire its own hospitalists to monitor the care of patients in affiliated hospitals while using the association’s approach to limiting costs.
ACO participants also have varied widely in the effort expended to get up to speed. “Some people have said they haven’t had to make any major changes to their organization, while some people have had to drastically think how they provide care,” Muhlestein says. In general, many of the former have had the luxury of working within relatively integrated facilities and building upon existing frameworks, whereas many of the latter previously toiled away in silos and are now scrambling to establish more cohesive working relationships from scratch.
Optimism Abounds
Though many ACOs have only limited data so far, Muhlestein says most are generally optimistic that their early results will be positive. Even so, Dr. Greeno says, he fully expects the Pioneer ACOs to produce the best results among the Medicare demonstration projects. Those organizations already have successful track records in managing patient populations, and the Pioneer model’s incentives are stronger because the groups are assuming more risk. If the Pioneer ACO results are eclipsed by those of the Shared Savings Program, he says, “I’d fall out of my chair.”
The Beth Israel Deaconess Physician Organization (BIDPO) now has four global payment contracts, including its Pioneer ACO arrangement with CMS that serves 33,000 beneficiaries in the Boston metropolitan region. “The decision-making around joining was a recognition that the fee-for-service model is highly dysfunctional,” says Richard Parker, MD, BIDPO’s medical director. “Our organization and our leadership believed that most of the country, both private payor and governmental payor, would be moving toward global payment and that it would be to our advantage to get in early.”
Despite the complicated rollout and delays in receiving Medicare data on patients from CMS, Dr. Parker says, the feedback from both providers and patients has been mostly positive. “I would say, anecdotally, that the doctors seem appreciative that we’re trying to fix some of these gaps in care that we all know have existed for some time,” he says. “And, anecdotally from the patients, we get appreciation that we’re trying to take better care of them.”
Chris Coleman, chief financial officer for Phoenix-based Banner Health Network, another Pioneer ACO participant, says the project fits in well with his company’s decision “to transform itself into more of a value-based, performance-based provider.” Banner’s ACO, which serves about 50,000 beneficiaries, is still setting up needed systems, including a consistent platform for electronic medical records throughout the entire provider network. Even during the building phase, however, Coleman says company officials have been pleasantly surprised by the ACO’s positive effect on utilization, patient care, and apparent savings.
Although the company has only a partial year of Medicare claims to go by, Coleman says the data look “pretty good” so far and suggest the ACO is on track for modest savings of perhaps 3% or 4%. Like BIDPO, Banner has other shared-risk agreements in place, including one for a Medicare Advantage population and another with a private payor. So far, Coleman says, those arrangements also seem to be “performing positively.”
Dr. Greeno and other experts see the best ACO results coming from such rapidly growing private arrangements, and early published data have been generally encouraging.1 The ability to more narrowly define patient groups and assume more control over payments, he says, has allowed private ACOs to keep better track of costs and implement innovative population health interventions.

—Ron Greeno, MD, FCCP, MHM, SHM Public Policy Committee chair
Built to Last?
Whether public, private, or a hybrid between the two, some ACOs are trying to manage the care of their entire patient pool and look at everything that might help them accrue cost savings. Others are focusing only on the sickest patients to reach their quality improvement (QI) and savings goals, and targeting specific parameters, such as blood pressure or medication adherence, for patients with myocardial infarction.
Joane Goodroe, an Atlanta-based healthcare consultant, favors the latter approach, at least for new ACOs. Goodroe recommends adopting a streamlined strategy that will get an ACO up and running, then allow the group to gradually add to it, rather than waiting until all of the right pieces fall into place. Her own data analysis of Medicare patients, for example, suggests that a diabetic who’s been an inpatient can average $50,000 in yearly costs, compared with $2,400 for a diabetic who has never been admitted to a hospital.
Setting up a system to manage every diabetic patient from the start, she says, would require too much time and money. “If you try to build the perfect ACO structure, it’s going to be too expensive for the results you initially get back,” she says, making it seem like the ACO is an unsustainable failure. “You’ve got to figure out how to build a cost-effective infrastructure while you’re also improving the care of the patients, and the best place to go is to target your sickest patients first.”
CMS’ Advance Payment ACO Model is designed to help by providing upfront payments to smaller ACO organizations that might lack capital, giving them an advance on potential shared savings so they can install the infrastructure and support structures necessary to redesign care.
To maximize the overall chances of success, Dr. Parker says, ACO leadership should be fully engaged, and each organization should have enough resources to address its own care management and information technology needs. “My goal as medical director is to improve the quality of care of the patients and, hopefully, also improve the working life of the doctors and staff,” he says. “And my belief and expectation is that if we do that, the cost of care will ultimately go down.”
Bryn Nelson is a freelance medical writer in Seattle.
Reference
Throughout much of 2011, ambivalence plagued efforts by the Centers for Medicare & Medicaid Services (CMS) to expand the federal government’s reach into integrated care delivery to help improve patient outcomes while lowering costs. Critics panned the initial draft of regulations for a large accountable-care demonstration project called the Shared Savings Program, and prominent medical groups announced their intention to sit on the sidelines.
At the start of 2013, the atmosphere couldn’t be more different. CMS won over most of its critics with a well-received final version of the rules that provided more incentives for groups to form accountable-care organizations (ACOs), and the presidential election provided more clarity about the future of healthcare reform. Medical groups around the country are readily jumping on the ACO bandwagon, with its emphasis on shared responsibility among provider groups for a defined pool of patients.
Few medical groups have enough data to suggest whether their varied approaches to managing patient populations will lead to better-quality care that’s also more affordable; the first batch of Medicare ACO data isn’t expected until later this spring. And healthcare experts differ on which models and components are likely to make the biggest long-term impact; even the precise definition of an ACO remains a moving target. But industry observers say they’re surprised and encouraged not only by the speed with which the movement has taken off, but also by the breadth of models being investigated, the strong engagement of the private sector, and a spreading sense of cautious optimism.
“This is actually moving faster than I thought—faster than I think anybody thought,” says SHM Public Policy Committee chair Ron Greeno, MD, FCCP, MHM.
Although CMS still is in the beginning stages of its work and has focused most of its efforts on reviewing applications and providing feedback on organizations’ historical expenditure and utilization patterns, agency officials say the ACO initiative has not encountered any unexpected setbacks. “As with any new program, there are bumps along the way, but I don’t think we’ve experienced anything that is out of the ordinary,” says John Pilotte, director of Performance-Based Payment Policy in the Center for Medicare. “We’re pretty happy with where we are with the program.”
The Shared Savings Program, which Pilotte describes as “an easier on-ramp” to population management for providers and offers low financial risk in exchange for a modest level of shared cost savings, is proving especially popular. Combined, several hundred organizations submitted applications for the program’s second and third rounds, which began July 1, 2012, and Jan. 1, 2013, respectively.
“Two hundred twenty ACOs are currently up and running, and we expect to continue to add ACOs to the program annually,” Pilotte says.

—David Muhlestein, analyst, Leavitt Partners
Last January, another 32 groups joined Medicare’s Pioneer ACO program, designed for more experienced organizations with more resources. The groups assume more risk, and in return are more handsomely rewarded if they meet benchmarks.
All told, the tally of confirmed ACOs in the U.S. reached 428 by the end of January, according to Leavitt Partners, a Salt Lake City-based healthcare consulting firm that is tracking the growth of accountable care (see “A Sampling of Significant ACO Programs,” below). David Muhlestein, an analyst with Leavitt Partners, says private ACOs now account for roughly half of that total, a trend driven by their ability to experiment with different approaches and more easily track costs through clearly defined patient populations.
The central role for hospitalists within most ACOs is rooted in the reality that hospital care is the most expensive part of healthcare. Successfully implementing a plan to coordinate care and prevent hospital readmissions might not correlate directly with improved quality metrics, but it can lead to significant savings.
The diverse ACO models now being tested, however, could result in varying responsibilities for hospitalists, depending on the focal points of the sponsoring entities. After patients have been admitted to a hospital, for example, many hospitalists assume responsibility for managing inpatient care and the inpatient-outpatient handoff. A main goal of a physician-owned medical group, such as an independent practice association (IPA), by contrast, is to keep patients out of the hospital altogether, placing more of the focus on primary and specialty care. An IPA that forms an ACO, Muhlestein says, might hire its own hospitalists to monitor the care of patients in affiliated hospitals while using the association’s approach to limiting costs.
ACO participants also have varied widely in the effort expended to get up to speed. “Some people have said they haven’t had to make any major changes to their organization, while some people have had to drastically think how they provide care,” Muhlestein says. In general, many of the former have had the luxury of working within relatively integrated facilities and building upon existing frameworks, whereas many of the latter previously toiled away in silos and are now scrambling to establish more cohesive working relationships from scratch.
Optimism Abounds
Though many ACOs have only limited data so far, Muhlestein says most are generally optimistic that their early results will be positive. Even so, Dr. Greeno says, he fully expects the Pioneer ACOs to produce the best results among the Medicare demonstration projects. Those organizations already have successful track records in managing patient populations, and the Pioneer model’s incentives are stronger because the groups are assuming more risk. If the Pioneer ACO results are eclipsed by those of the Shared Savings Program, he says, “I’d fall out of my chair.”
The Beth Israel Deaconess Physician Organization (BIDPO) now has four global payment contracts, including its Pioneer ACO arrangement with CMS that serves 33,000 beneficiaries in the Boston metropolitan region. “The decision-making around joining was a recognition that the fee-for-service model is highly dysfunctional,” says Richard Parker, MD, BIDPO’s medical director. “Our organization and our leadership believed that most of the country, both private payor and governmental payor, would be moving toward global payment and that it would be to our advantage to get in early.”
Despite the complicated rollout and delays in receiving Medicare data on patients from CMS, Dr. Parker says, the feedback from both providers and patients has been mostly positive. “I would say, anecdotally, that the doctors seem appreciative that we’re trying to fix some of these gaps in care that we all know have existed for some time,” he says. “And, anecdotally from the patients, we get appreciation that we’re trying to take better care of them.”
Chris Coleman, chief financial officer for Phoenix-based Banner Health Network, another Pioneer ACO participant, says the project fits in well with his company’s decision “to transform itself into more of a value-based, performance-based provider.” Banner’s ACO, which serves about 50,000 beneficiaries, is still setting up needed systems, including a consistent platform for electronic medical records throughout the entire provider network. Even during the building phase, however, Coleman says company officials have been pleasantly surprised by the ACO’s positive effect on utilization, patient care, and apparent savings.
Although the company has only a partial year of Medicare claims to go by, Coleman says the data look “pretty good” so far and suggest the ACO is on track for modest savings of perhaps 3% or 4%. Like BIDPO, Banner has other shared-risk agreements in place, including one for a Medicare Advantage population and another with a private payor. So far, Coleman says, those arrangements also seem to be “performing positively.”
Dr. Greeno and other experts see the best ACO results coming from such rapidly growing private arrangements, and early published data have been generally encouraging.1 The ability to more narrowly define patient groups and assume more control over payments, he says, has allowed private ACOs to keep better track of costs and implement innovative population health interventions.

—Ron Greeno, MD, FCCP, MHM, SHM Public Policy Committee chair
Built to Last?
Whether public, private, or a hybrid between the two, some ACOs are trying to manage the care of their entire patient pool and look at everything that might help them accrue cost savings. Others are focusing only on the sickest patients to reach their quality improvement (QI) and savings goals, and targeting specific parameters, such as blood pressure or medication adherence, for patients with myocardial infarction.
Joane Goodroe, an Atlanta-based healthcare consultant, favors the latter approach, at least for new ACOs. Goodroe recommends adopting a streamlined strategy that will get an ACO up and running, then allow the group to gradually add to it, rather than waiting until all of the right pieces fall into place. Her own data analysis of Medicare patients, for example, suggests that a diabetic who’s been an inpatient can average $50,000 in yearly costs, compared with $2,400 for a diabetic who has never been admitted to a hospital.
Setting up a system to manage every diabetic patient from the start, she says, would require too much time and money. “If you try to build the perfect ACO structure, it’s going to be too expensive for the results you initially get back,” she says, making it seem like the ACO is an unsustainable failure. “You’ve got to figure out how to build a cost-effective infrastructure while you’re also improving the care of the patients, and the best place to go is to target your sickest patients first.”
CMS’ Advance Payment ACO Model is designed to help by providing upfront payments to smaller ACO organizations that might lack capital, giving them an advance on potential shared savings so they can install the infrastructure and support structures necessary to redesign care.
To maximize the overall chances of success, Dr. Parker says, ACO leadership should be fully engaged, and each organization should have enough resources to address its own care management and information technology needs. “My goal as medical director is to improve the quality of care of the patients and, hopefully, also improve the working life of the doctors and staff,” he says. “And my belief and expectation is that if we do that, the cost of care will ultimately go down.”
Bryn Nelson is a freelance medical writer in Seattle.
Reference
20 Things Psychiatrists Think Hospitalists Need to Know
20 Things At A Glance
- Acknowledge that collaboration between health professionals is important, even when schedules are hectic and reimbursement doesn’t cover these discussions.
- Secure patient consent before consulting a psychiatrist.
- Present the psychiatrist’s anticipated insight as a benefit to the patient.
- Ask the patient if it’s all right to discuss their health status and needs with family members.
- Recognize that psychiatric illness is real, not imaginary.
- Realize that not all sadness constitutes depression.
- Don’t gloss over the possibility of delirium.
- Take the time to really listen.
- Always remain conscious of alcohol and substance abuse.
- Monitor patients’ vital signs for autonomic instability.
- Avoid arguments and power struggles with difficult or demanding patients.
- Adapt your vocabulary to the patient’s and family’s level of understanding.
- Be mindful of your nonverbal cues.
- Always take suicide risk seriously.
- Beware of patients who exhibit attention-seeking behavior, which can have a negative impact on the healthcare team and the care provided to the patient.
- Consider the possibility of a factitious disorder when there is a lack of objective evidence for pathology to explain a patient’s symptoms despite extensive evaluation.
- Choose an intravenous psychiatric medication when a patient with severe and persistent mental illness should avoid oral medication for a procedure.
- Listen to your instincts.
- Arrange for post-discharge follow-up with a primary-care physician or psychiatrist.
- Extend genuine compassion to your patients.
Patients can be hospitalized with chest pain, a kidney infection, pneumonia, or myriad other medical conditions. Hospital stays on occasion upend a patient’s mental state, with upcoming tests, surgery, or other procedures triggering anxiety or other conditions.
That doesn’t mean these patients have psychiatric or psychological problems, but some of them might. Hospitalists walk a fine line in deciding when to consult a psychiatrist in certain cases.
“A common mistake, when it comes to psychiatry, for hospitalists is to either think they know too much or they know too little,” says Philip R. Muskin, MD, professor of clinical psychiatry at Columbia University College of Physicians & Surgeons in New York City. “Sometimes they’re too quick to call a psychiatrist, and sometimes they’re too slow to call a specialist because they don’t think it’s a psychiatric problem.”
The Hospitalist asked more than half a dozen specialists in psychiatry and hospital medicine to shed light on when to seek additional expertise—and how to inform patients about your request to do so. “If I say, ‘You need to see a psychiatrist,’ it carries some stigma,” says Dr. Muskin, who is the chief of consultation for liaison psychiatry at New York-Presbyterian Medical Center’s Columbia campus. “We have to be sensitive to that.”
So how can you more comfortably approach psychiatric or psychological issues in the hospital setting?
1. Acknowledge that collaboration between health professionals is important, even when schedules are hectic and reimbursement doesn’t cover these discussions.
“Because of the overwhelming comorbidity between psychiatric illness and medical illness, it’s important to have some communication between the emergency room, caregiver, the hospitalist, and the psychiatrist,” says Ken Duckworth, MD, medical director of the National Alliance on Mental Illness (NAMI) and an assistant clinical professor of psychiatry at Harvard Medical School in Boston. “We know that people with mental health vulnerabilities consume a much higher amount of medical services. That’s a well-known phenomenon.”
2. Secure patient consent before consulting a psychiatrist.
“You need the patient’s permission,” Dr. Duckworth says. “That’s an important piece of the equation.” There are exceptions in emergencies, and the laws pertaining to this vary by state. Verbal consent may suffice if written authorization is already on file. If a patient declines, a hospitalist has to respect those wishes.
3. Present the psychiatrist’s anticipated insight as a benefit to the patient.
Physicians sometimes are uncomfortable informing their patients that they’re asking for a psychiatric consultation. They fear a bad reaction, such as “You think I’m crazy?” The consultation will be more useful if the patient is open and accepting of the process. For example, tell your patient at the outset: “I’d really like you to talk to one of my colleagues, whom I trust a great deal. He/she is an expert in the overlapping area between the body and the brain. I need their help so that I can take better care of you,’” says Linda L.M. Worley, MD, FAPM, professor of psychiatry and obstetrics and gynecology at the University of Arkansas for Medical Sciences in Little Rock.
4. Ask the patient if it’s all right to discuss their health status and needs with family members.
Get to know their names. Identify the medical expert in the family and be certain to involve them in overall discussions and the decision-making process, Dr. Worley says.
5. Recognize that psychiatric illness is real, not imaginary.
The illness “should be placed in exactly the same arena as other medical problems,” Dr. Muskin says. Patients with psychiatric conditions are “not weak. They’re not dumb. It’s not all in their head.” Their mental health “deserves the same attention as their heart, stomach, or kidneys.”
6. Realize that not all sadness constitutes depression.
“There are many reasons why people cry or feel down, and most are not psychiatric illnesses. Depression is often overdiagnosed, leading to wasted time and inappropriate medications,” says Robert Boland, MD, professor of psychiatry and human behavior at Brown University’s Warren Alpert School of Medicine in Providence, R.I. “Unfortunately, the opposite is also true. Depression is often missed in the hospital.”
So how does a hospitalist reconcile those extremes? First, consider depression in any patient who is predisposed, then rely on a consistent way of working it up. The Diagnostic and Statistical Manual of Mental Disorders (DSM, http://www.dsm5.org) offers a conservative approach, so you usually can’t go wrong by following it.
7. Don’t gloss over the possibility of delirium.
It is probably the most frequently missed diagnosis in the general hospital. “We usually recognize it when patients are agitated, but most patients aren’t,” Dr. Boland says. “If anything, they are hypoactive or change throughout the day. When a patient seems confused, we want to find a cause, but that cause isn’t always obvious.”
These situations are particularly true in fragile patients (e.g. the very old or those with dementia). Sometimes medical problems that seem very minor can “push them over the edge,” he adds. When you do expect dementia, the main treatments revolve around medically stabilizing the patient, and psychiatric medications are a minor part of the management, if at all.
8. Take the time to really listen.
Patients’ biggest complaint is that physicians don’t listen. “The best doctors in any specialty know how to communicate with patients,” Dr. Boland says. “It doesn’t take longer—in fact, good communication usually saves time. But it does take attention and focus to let the patient try and explain what is going on with them. It always pays off in the end.”
9. Always remain conscious of alcohol and substance abuse.
Although it might not be the reason patients are hospitalized, it is one of the more common underlying causes. When this is the case, don’t be nihilistic. Many patients improve with treatment, and some get better simply because a physician explained how damaging substance abuse can be to their health, Dr. Boland says.
For those in complete remission from a past addiction to alcohol, benzodiazepines, opiates, or a combination thereof, beware that prescribing certain medications puts them at substantially increased risk for relapse. Use alternative treatments whenever possible; if clinically indicated, be certain that these patients have a safety net to prevent relapse. Patients with severe pain need effective relief.
“If a patient has been exposed to significant dosages of pain medications in the past, their neurotransmitters will have physically adapted,” says Dr. Worley, president-elect of the Academy of Psychosomatic Medicine. “They will require higher doses than normal for effective pain relief.”

—Gregory Ruhnke, MD, assistant professor in the section of hospital medicine, University of Chicago Pritzker School of Medicine
10. Monitor patients’ vital signs for autonomic instability.
“Patients in withdrawal from physiologically addictive medications may have forgotten to tell you that they were taking these medications,” Dr. Worley says. “Abrupt discontinuation can cause incapacitating anxiety and life-threatening delirium.”
11. Avoid arguments and power struggles with difficult or demanding patients.
Put on your thick skin. Don’t take insults or slights personally. And resist the urge to flee or counterattack. Instead, Dr. Worley suggests hospitalists stay calm and focused on providing the best medical care that they can. “Chronically noncompliant patients can be excruciatingly frustrating to care for when they don’t follow through on what they are repeatedly advised to do, but lecturing more vigorously at them won’t help,” she says. “It only makes them shut down more and feel more helpless and you more exhausted. Shift to more of a listening mode and inquire about what they hope to accomplish by coming to you for help.”
12. Adapt your vocabulary to the patient’s and family’s level of understanding.
After your explanation, ask them, “Do me a favor and explain back to me in your words what I said. I want to be sure I got across what I wanted to say.” Then ask whether they have any questions. Also know that all too often patients are so anxious and upset that they are “emotionally flooded” and unable to hear much of what you communicated. You can save a lot of time if they understand you in the first place.
13. Be mindful of your nonverbal cues.
A majority of communication is nonverbal, and your facial expressions, gestures, and body posture speak volumes to patients and family members. “The innocent tilt of a chin upwards while peering through bifocals can be misperceived as arrogance,” Dr. Worley says. “The thoughtful furled brow of contemplation may be misconstrued as irritability or disapproval.”
14. Always take suicide risk seriously.
It’s better to call a psychiatrist unnecessarily than to overlook a patient at risk for suicide. Benzodiazepines, alcohol, or a combination of the two might reduce inhibition and increase the likelihood of a suicide attempt. Be sure to assess suicidal ideation, intent, and lethality of suicide attempt.
“Hopelessness about the future correlates with completed suicide,” says Gregory Ruhnke, MD, assistant professor in the section of hospital medicine at the University of Chicago Pritzker School of Medicine. “Additionally, it is helpful to ask about the four H’s: Hate, humiliation, hostility, handguns.”
15. Beware of patients who exhibit attention-seeking behavior, which can have a negative impact on the healthcare team and the care provided to the patient.
“The patient may become angry and engage in splitting, whereby he or she emphatically expresses the view that certain caregivers are all good or all bad. This may reflect such [a] patient’s desire to divide the caregivers into opposing factions. It’s a maladaptive way of coping,” says Marie Tobin, MD, associate professor of psychiatry and consult-liaison psychiatrist at the Pritzker School of Medicine. This can be very time-consuming, and it can breed hostility among colleagues. “Communication between caregivers is really important in creating a unified treatment plan that is coherently presented to the patient in a single voice.”
Fortunately, she says, “even though these situations can arise, they are the exception rather than the rule.”

—Marie Tobin, MD, associate professor of psychiatry and consult-liaison psychiatrist, University of Chicago Pritzker School of Medicine
16. Consider the possibility of a factitious disorder when there is a lack of objective evidence for pathology to explain a patient’s symptoms despite extensive evaluation.
For example, Dr. Ruhnke says, if a patient complains of hemoptysis and hematochezia with negative endoscopies, talk to the nurse about the patient’s diet, and be suspicious if it includes only red foods and liquids. The most common symptoms among patients who come to medical attention because of factitious disorders are diarrhea, fever of unknown origin, gastrointestinal bleeding, hematuria, seizures, and hypoglycemia.
17. Choose an intravenous psychiatric medication when a patient with severe and persistent mental illness should avoid oral medication for a procedure.
A patient with schizophrenia or bipolar disorder could experience a severe psychiatric episode without psychiatric medication. An appropriate alternative, perhaps administered intravenously if necessary, “can make all the difference in the world,” says Christopher Dobbelstein, MD, assistant professor of psychiatry at the University of Pittsburgh School of Medicine.
18. Listen to your instincts.
Medical teams can handle many psychiatric issues. Straightforward delirium is a good example. The bigger question, which takes experience and confidence, is to recognize when a line has been crossed. “The decision to consult psychiatry is not formulaic,” Dr. Dobbelstein says.
Sometimes a patient is acting strangely, and the team can’t explain why a psychiatrist could offer sound advice. “That’s when they should trust their instincts and consult us,” he says, “because the patient likely does have something more complex going on.”
19. Arrange for post-discharge follow-up with a primary-care physician or psychiatrist.
Sometimes psychiatric medications are started without good oversight. Suicide risk is highest during the weeks following an inpatient psychiatric admission, so a patient should see an outpatient mental health provider within seven days after hospital discharge, says NAMI’s Dr. Duckworth.
20. Extend genuine compassion to your patients.
“This is the secret to achieving a lifelong rewarding career in medicine,” Dr. Worley says, “and is the most important ingredient in positive outcomes.”
Susan Kreimer is a freelance writer in New York.
20 Things At A Glance
- Acknowledge that collaboration between health professionals is important, even when schedules are hectic and reimbursement doesn’t cover these discussions.
- Secure patient consent before consulting a psychiatrist.
- Present the psychiatrist’s anticipated insight as a benefit to the patient.
- Ask the patient if it’s all right to discuss their health status and needs with family members.
- Recognize that psychiatric illness is real, not imaginary.
- Realize that not all sadness constitutes depression.
- Don’t gloss over the possibility of delirium.
- Take the time to really listen.
- Always remain conscious of alcohol and substance abuse.
- Monitor patients’ vital signs for autonomic instability.
- Avoid arguments and power struggles with difficult or demanding patients.
- Adapt your vocabulary to the patient’s and family’s level of understanding.
- Be mindful of your nonverbal cues.
- Always take suicide risk seriously.
- Beware of patients who exhibit attention-seeking behavior, which can have a negative impact on the healthcare team and the care provided to the patient.
- Consider the possibility of a factitious disorder when there is a lack of objective evidence for pathology to explain a patient’s symptoms despite extensive evaluation.
- Choose an intravenous psychiatric medication when a patient with severe and persistent mental illness should avoid oral medication for a procedure.
- Listen to your instincts.
- Arrange for post-discharge follow-up with a primary-care physician or psychiatrist.
- Extend genuine compassion to your patients.
Patients can be hospitalized with chest pain, a kidney infection, pneumonia, or myriad other medical conditions. Hospital stays on occasion upend a patient’s mental state, with upcoming tests, surgery, or other procedures triggering anxiety or other conditions.
That doesn’t mean these patients have psychiatric or psychological problems, but some of them might. Hospitalists walk a fine line in deciding when to consult a psychiatrist in certain cases.
“A common mistake, when it comes to psychiatry, for hospitalists is to either think they know too much or they know too little,” says Philip R. Muskin, MD, professor of clinical psychiatry at Columbia University College of Physicians & Surgeons in New York City. “Sometimes they’re too quick to call a psychiatrist, and sometimes they’re too slow to call a specialist because they don’t think it’s a psychiatric problem.”
The Hospitalist asked more than half a dozen specialists in psychiatry and hospital medicine to shed light on when to seek additional expertise—and how to inform patients about your request to do so. “If I say, ‘You need to see a psychiatrist,’ it carries some stigma,” says Dr. Muskin, who is the chief of consultation for liaison psychiatry at New York-Presbyterian Medical Center’s Columbia campus. “We have to be sensitive to that.”
So how can you more comfortably approach psychiatric or psychological issues in the hospital setting?
1. Acknowledge that collaboration between health professionals is important, even when schedules are hectic and reimbursement doesn’t cover these discussions.
“Because of the overwhelming comorbidity between psychiatric illness and medical illness, it’s important to have some communication between the emergency room, caregiver, the hospitalist, and the psychiatrist,” says Ken Duckworth, MD, medical director of the National Alliance on Mental Illness (NAMI) and an assistant clinical professor of psychiatry at Harvard Medical School in Boston. “We know that people with mental health vulnerabilities consume a much higher amount of medical services. That’s a well-known phenomenon.”
2. Secure patient consent before consulting a psychiatrist.
“You need the patient’s permission,” Dr. Duckworth says. “That’s an important piece of the equation.” There are exceptions in emergencies, and the laws pertaining to this vary by state. Verbal consent may suffice if written authorization is already on file. If a patient declines, a hospitalist has to respect those wishes.
3. Present the psychiatrist’s anticipated insight as a benefit to the patient.
Physicians sometimes are uncomfortable informing their patients that they’re asking for a psychiatric consultation. They fear a bad reaction, such as “You think I’m crazy?” The consultation will be more useful if the patient is open and accepting of the process. For example, tell your patient at the outset: “I’d really like you to talk to one of my colleagues, whom I trust a great deal. He/she is an expert in the overlapping area between the body and the brain. I need their help so that I can take better care of you,’” says Linda L.M. Worley, MD, FAPM, professor of psychiatry and obstetrics and gynecology at the University of Arkansas for Medical Sciences in Little Rock.
4. Ask the patient if it’s all right to discuss their health status and needs with family members.
Get to know their names. Identify the medical expert in the family and be certain to involve them in overall discussions and the decision-making process, Dr. Worley says.
5. Recognize that psychiatric illness is real, not imaginary.
The illness “should be placed in exactly the same arena as other medical problems,” Dr. Muskin says. Patients with psychiatric conditions are “not weak. They’re not dumb. It’s not all in their head.” Their mental health “deserves the same attention as their heart, stomach, or kidneys.”
6. Realize that not all sadness constitutes depression.
“There are many reasons why people cry or feel down, and most are not psychiatric illnesses. Depression is often overdiagnosed, leading to wasted time and inappropriate medications,” says Robert Boland, MD, professor of psychiatry and human behavior at Brown University’s Warren Alpert School of Medicine in Providence, R.I. “Unfortunately, the opposite is also true. Depression is often missed in the hospital.”
So how does a hospitalist reconcile those extremes? First, consider depression in any patient who is predisposed, then rely on a consistent way of working it up. The Diagnostic and Statistical Manual of Mental Disorders (DSM, http://www.dsm5.org) offers a conservative approach, so you usually can’t go wrong by following it.
7. Don’t gloss over the possibility of delirium.
It is probably the most frequently missed diagnosis in the general hospital. “We usually recognize it when patients are agitated, but most patients aren’t,” Dr. Boland says. “If anything, they are hypoactive or change throughout the day. When a patient seems confused, we want to find a cause, but that cause isn’t always obvious.”
These situations are particularly true in fragile patients (e.g. the very old or those with dementia). Sometimes medical problems that seem very minor can “push them over the edge,” he adds. When you do expect dementia, the main treatments revolve around medically stabilizing the patient, and psychiatric medications are a minor part of the management, if at all.
8. Take the time to really listen.
Patients’ biggest complaint is that physicians don’t listen. “The best doctors in any specialty know how to communicate with patients,” Dr. Boland says. “It doesn’t take longer—in fact, good communication usually saves time. But it does take attention and focus to let the patient try and explain what is going on with them. It always pays off in the end.”
9. Always remain conscious of alcohol and substance abuse.
Although it might not be the reason patients are hospitalized, it is one of the more common underlying causes. When this is the case, don’t be nihilistic. Many patients improve with treatment, and some get better simply because a physician explained how damaging substance abuse can be to their health, Dr. Boland says.
For those in complete remission from a past addiction to alcohol, benzodiazepines, opiates, or a combination thereof, beware that prescribing certain medications puts them at substantially increased risk for relapse. Use alternative treatments whenever possible; if clinically indicated, be certain that these patients have a safety net to prevent relapse. Patients with severe pain need effective relief.
“If a patient has been exposed to significant dosages of pain medications in the past, their neurotransmitters will have physically adapted,” says Dr. Worley, president-elect of the Academy of Psychosomatic Medicine. “They will require higher doses than normal for effective pain relief.”

—Gregory Ruhnke, MD, assistant professor in the section of hospital medicine, University of Chicago Pritzker School of Medicine
10. Monitor patients’ vital signs for autonomic instability.
“Patients in withdrawal from physiologically addictive medications may have forgotten to tell you that they were taking these medications,” Dr. Worley says. “Abrupt discontinuation can cause incapacitating anxiety and life-threatening delirium.”
11. Avoid arguments and power struggles with difficult or demanding patients.
Put on your thick skin. Don’t take insults or slights personally. And resist the urge to flee or counterattack. Instead, Dr. Worley suggests hospitalists stay calm and focused on providing the best medical care that they can. “Chronically noncompliant patients can be excruciatingly frustrating to care for when they don’t follow through on what they are repeatedly advised to do, but lecturing more vigorously at them won’t help,” she says. “It only makes them shut down more and feel more helpless and you more exhausted. Shift to more of a listening mode and inquire about what they hope to accomplish by coming to you for help.”
12. Adapt your vocabulary to the patient’s and family’s level of understanding.
After your explanation, ask them, “Do me a favor and explain back to me in your words what I said. I want to be sure I got across what I wanted to say.” Then ask whether they have any questions. Also know that all too often patients are so anxious and upset that they are “emotionally flooded” and unable to hear much of what you communicated. You can save a lot of time if they understand you in the first place.
13. Be mindful of your nonverbal cues.
A majority of communication is nonverbal, and your facial expressions, gestures, and body posture speak volumes to patients and family members. “The innocent tilt of a chin upwards while peering through bifocals can be misperceived as arrogance,” Dr. Worley says. “The thoughtful furled brow of contemplation may be misconstrued as irritability or disapproval.”
14. Always take suicide risk seriously.
It’s better to call a psychiatrist unnecessarily than to overlook a patient at risk for suicide. Benzodiazepines, alcohol, or a combination of the two might reduce inhibition and increase the likelihood of a suicide attempt. Be sure to assess suicidal ideation, intent, and lethality of suicide attempt.
“Hopelessness about the future correlates with completed suicide,” says Gregory Ruhnke, MD, assistant professor in the section of hospital medicine at the University of Chicago Pritzker School of Medicine. “Additionally, it is helpful to ask about the four H’s: Hate, humiliation, hostility, handguns.”
15. Beware of patients who exhibit attention-seeking behavior, which can have a negative impact on the healthcare team and the care provided to the patient.
“The patient may become angry and engage in splitting, whereby he or she emphatically expresses the view that certain caregivers are all good or all bad. This may reflect such [a] patient’s desire to divide the caregivers into opposing factions. It’s a maladaptive way of coping,” says Marie Tobin, MD, associate professor of psychiatry and consult-liaison psychiatrist at the Pritzker School of Medicine. This can be very time-consuming, and it can breed hostility among colleagues. “Communication between caregivers is really important in creating a unified treatment plan that is coherently presented to the patient in a single voice.”
Fortunately, she says, “even though these situations can arise, they are the exception rather than the rule.”

—Marie Tobin, MD, associate professor of psychiatry and consult-liaison psychiatrist, University of Chicago Pritzker School of Medicine
16. Consider the possibility of a factitious disorder when there is a lack of objective evidence for pathology to explain a patient’s symptoms despite extensive evaluation.
For example, Dr. Ruhnke says, if a patient complains of hemoptysis and hematochezia with negative endoscopies, talk to the nurse about the patient’s diet, and be suspicious if it includes only red foods and liquids. The most common symptoms among patients who come to medical attention because of factitious disorders are diarrhea, fever of unknown origin, gastrointestinal bleeding, hematuria, seizures, and hypoglycemia.
17. Choose an intravenous psychiatric medication when a patient with severe and persistent mental illness should avoid oral medication for a procedure.
A patient with schizophrenia or bipolar disorder could experience a severe psychiatric episode without psychiatric medication. An appropriate alternative, perhaps administered intravenously if necessary, “can make all the difference in the world,” says Christopher Dobbelstein, MD, assistant professor of psychiatry at the University of Pittsburgh School of Medicine.
18. Listen to your instincts.
Medical teams can handle many psychiatric issues. Straightforward delirium is a good example. The bigger question, which takes experience and confidence, is to recognize when a line has been crossed. “The decision to consult psychiatry is not formulaic,” Dr. Dobbelstein says.
Sometimes a patient is acting strangely, and the team can’t explain why a psychiatrist could offer sound advice. “That’s when they should trust their instincts and consult us,” he says, “because the patient likely does have something more complex going on.”
19. Arrange for post-discharge follow-up with a primary-care physician or psychiatrist.
Sometimes psychiatric medications are started without good oversight. Suicide risk is highest during the weeks following an inpatient psychiatric admission, so a patient should see an outpatient mental health provider within seven days after hospital discharge, says NAMI’s Dr. Duckworth.
20. Extend genuine compassion to your patients.
“This is the secret to achieving a lifelong rewarding career in medicine,” Dr. Worley says, “and is the most important ingredient in positive outcomes.”
Susan Kreimer is a freelance writer in New York.
20 Things At A Glance
- Acknowledge that collaboration between health professionals is important, even when schedules are hectic and reimbursement doesn’t cover these discussions.
- Secure patient consent before consulting a psychiatrist.
- Present the psychiatrist’s anticipated insight as a benefit to the patient.
- Ask the patient if it’s all right to discuss their health status and needs with family members.
- Recognize that psychiatric illness is real, not imaginary.
- Realize that not all sadness constitutes depression.
- Don’t gloss over the possibility of delirium.
- Take the time to really listen.
- Always remain conscious of alcohol and substance abuse.
- Monitor patients’ vital signs for autonomic instability.
- Avoid arguments and power struggles with difficult or demanding patients.
- Adapt your vocabulary to the patient’s and family’s level of understanding.
- Be mindful of your nonverbal cues.
- Always take suicide risk seriously.
- Beware of patients who exhibit attention-seeking behavior, which can have a negative impact on the healthcare team and the care provided to the patient.
- Consider the possibility of a factitious disorder when there is a lack of objective evidence for pathology to explain a patient’s symptoms despite extensive evaluation.
- Choose an intravenous psychiatric medication when a patient with severe and persistent mental illness should avoid oral medication for a procedure.
- Listen to your instincts.
- Arrange for post-discharge follow-up with a primary-care physician or psychiatrist.
- Extend genuine compassion to your patients.
Patients can be hospitalized with chest pain, a kidney infection, pneumonia, or myriad other medical conditions. Hospital stays on occasion upend a patient’s mental state, with upcoming tests, surgery, or other procedures triggering anxiety or other conditions.
That doesn’t mean these patients have psychiatric or psychological problems, but some of them might. Hospitalists walk a fine line in deciding when to consult a psychiatrist in certain cases.
“A common mistake, when it comes to psychiatry, for hospitalists is to either think they know too much or they know too little,” says Philip R. Muskin, MD, professor of clinical psychiatry at Columbia University College of Physicians & Surgeons in New York City. “Sometimes they’re too quick to call a psychiatrist, and sometimes they’re too slow to call a specialist because they don’t think it’s a psychiatric problem.”
The Hospitalist asked more than half a dozen specialists in psychiatry and hospital medicine to shed light on when to seek additional expertise—and how to inform patients about your request to do so. “If I say, ‘You need to see a psychiatrist,’ it carries some stigma,” says Dr. Muskin, who is the chief of consultation for liaison psychiatry at New York-Presbyterian Medical Center’s Columbia campus. “We have to be sensitive to that.”
So how can you more comfortably approach psychiatric or psychological issues in the hospital setting?
1. Acknowledge that collaboration between health professionals is important, even when schedules are hectic and reimbursement doesn’t cover these discussions.
“Because of the overwhelming comorbidity between psychiatric illness and medical illness, it’s important to have some communication between the emergency room, caregiver, the hospitalist, and the psychiatrist,” says Ken Duckworth, MD, medical director of the National Alliance on Mental Illness (NAMI) and an assistant clinical professor of psychiatry at Harvard Medical School in Boston. “We know that people with mental health vulnerabilities consume a much higher amount of medical services. That’s a well-known phenomenon.”
2. Secure patient consent before consulting a psychiatrist.
“You need the patient’s permission,” Dr. Duckworth says. “That’s an important piece of the equation.” There are exceptions in emergencies, and the laws pertaining to this vary by state. Verbal consent may suffice if written authorization is already on file. If a patient declines, a hospitalist has to respect those wishes.
3. Present the psychiatrist’s anticipated insight as a benefit to the patient.
Physicians sometimes are uncomfortable informing their patients that they’re asking for a psychiatric consultation. They fear a bad reaction, such as “You think I’m crazy?” The consultation will be more useful if the patient is open and accepting of the process. For example, tell your patient at the outset: “I’d really like you to talk to one of my colleagues, whom I trust a great deal. He/she is an expert in the overlapping area between the body and the brain. I need their help so that I can take better care of you,’” says Linda L.M. Worley, MD, FAPM, professor of psychiatry and obstetrics and gynecology at the University of Arkansas for Medical Sciences in Little Rock.
4. Ask the patient if it’s all right to discuss their health status and needs with family members.
Get to know their names. Identify the medical expert in the family and be certain to involve them in overall discussions and the decision-making process, Dr. Worley says.
5. Recognize that psychiatric illness is real, not imaginary.
The illness “should be placed in exactly the same arena as other medical problems,” Dr. Muskin says. Patients with psychiatric conditions are “not weak. They’re not dumb. It’s not all in their head.” Their mental health “deserves the same attention as their heart, stomach, or kidneys.”
6. Realize that not all sadness constitutes depression.
“There are many reasons why people cry or feel down, and most are not psychiatric illnesses. Depression is often overdiagnosed, leading to wasted time and inappropriate medications,” says Robert Boland, MD, professor of psychiatry and human behavior at Brown University’s Warren Alpert School of Medicine in Providence, R.I. “Unfortunately, the opposite is also true. Depression is often missed in the hospital.”
So how does a hospitalist reconcile those extremes? First, consider depression in any patient who is predisposed, then rely on a consistent way of working it up. The Diagnostic and Statistical Manual of Mental Disorders (DSM, http://www.dsm5.org) offers a conservative approach, so you usually can’t go wrong by following it.
7. Don’t gloss over the possibility of delirium.
It is probably the most frequently missed diagnosis in the general hospital. “We usually recognize it when patients are agitated, but most patients aren’t,” Dr. Boland says. “If anything, they are hypoactive or change throughout the day. When a patient seems confused, we want to find a cause, but that cause isn’t always obvious.”
These situations are particularly true in fragile patients (e.g. the very old or those with dementia). Sometimes medical problems that seem very minor can “push them over the edge,” he adds. When you do expect dementia, the main treatments revolve around medically stabilizing the patient, and psychiatric medications are a minor part of the management, if at all.
8. Take the time to really listen.
Patients’ biggest complaint is that physicians don’t listen. “The best doctors in any specialty know how to communicate with patients,” Dr. Boland says. “It doesn’t take longer—in fact, good communication usually saves time. But it does take attention and focus to let the patient try and explain what is going on with them. It always pays off in the end.”
9. Always remain conscious of alcohol and substance abuse.
Although it might not be the reason patients are hospitalized, it is one of the more common underlying causes. When this is the case, don’t be nihilistic. Many patients improve with treatment, and some get better simply because a physician explained how damaging substance abuse can be to their health, Dr. Boland says.
For those in complete remission from a past addiction to alcohol, benzodiazepines, opiates, or a combination thereof, beware that prescribing certain medications puts them at substantially increased risk for relapse. Use alternative treatments whenever possible; if clinically indicated, be certain that these patients have a safety net to prevent relapse. Patients with severe pain need effective relief.
“If a patient has been exposed to significant dosages of pain medications in the past, their neurotransmitters will have physically adapted,” says Dr. Worley, president-elect of the Academy of Psychosomatic Medicine. “They will require higher doses than normal for effective pain relief.”

—Gregory Ruhnke, MD, assistant professor in the section of hospital medicine, University of Chicago Pritzker School of Medicine
10. Monitor patients’ vital signs for autonomic instability.
“Patients in withdrawal from physiologically addictive medications may have forgotten to tell you that they were taking these medications,” Dr. Worley says. “Abrupt discontinuation can cause incapacitating anxiety and life-threatening delirium.”
11. Avoid arguments and power struggles with difficult or demanding patients.
Put on your thick skin. Don’t take insults or slights personally. And resist the urge to flee or counterattack. Instead, Dr. Worley suggests hospitalists stay calm and focused on providing the best medical care that they can. “Chronically noncompliant patients can be excruciatingly frustrating to care for when they don’t follow through on what they are repeatedly advised to do, but lecturing more vigorously at them won’t help,” she says. “It only makes them shut down more and feel more helpless and you more exhausted. Shift to more of a listening mode and inquire about what they hope to accomplish by coming to you for help.”
12. Adapt your vocabulary to the patient’s and family’s level of understanding.
After your explanation, ask them, “Do me a favor and explain back to me in your words what I said. I want to be sure I got across what I wanted to say.” Then ask whether they have any questions. Also know that all too often patients are so anxious and upset that they are “emotionally flooded” and unable to hear much of what you communicated. You can save a lot of time if they understand you in the first place.
13. Be mindful of your nonverbal cues.
A majority of communication is nonverbal, and your facial expressions, gestures, and body posture speak volumes to patients and family members. “The innocent tilt of a chin upwards while peering through bifocals can be misperceived as arrogance,” Dr. Worley says. “The thoughtful furled brow of contemplation may be misconstrued as irritability or disapproval.”
14. Always take suicide risk seriously.
It’s better to call a psychiatrist unnecessarily than to overlook a patient at risk for suicide. Benzodiazepines, alcohol, or a combination of the two might reduce inhibition and increase the likelihood of a suicide attempt. Be sure to assess suicidal ideation, intent, and lethality of suicide attempt.
“Hopelessness about the future correlates with completed suicide,” says Gregory Ruhnke, MD, assistant professor in the section of hospital medicine at the University of Chicago Pritzker School of Medicine. “Additionally, it is helpful to ask about the four H’s: Hate, humiliation, hostility, handguns.”
15. Beware of patients who exhibit attention-seeking behavior, which can have a negative impact on the healthcare team and the care provided to the patient.
“The patient may become angry and engage in splitting, whereby he or she emphatically expresses the view that certain caregivers are all good or all bad. This may reflect such [a] patient’s desire to divide the caregivers into opposing factions. It’s a maladaptive way of coping,” says Marie Tobin, MD, associate professor of psychiatry and consult-liaison psychiatrist at the Pritzker School of Medicine. This can be very time-consuming, and it can breed hostility among colleagues. “Communication between caregivers is really important in creating a unified treatment plan that is coherently presented to the patient in a single voice.”
Fortunately, she says, “even though these situations can arise, they are the exception rather than the rule.”

—Marie Tobin, MD, associate professor of psychiatry and consult-liaison psychiatrist, University of Chicago Pritzker School of Medicine
16. Consider the possibility of a factitious disorder when there is a lack of objective evidence for pathology to explain a patient’s symptoms despite extensive evaluation.
For example, Dr. Ruhnke says, if a patient complains of hemoptysis and hematochezia with negative endoscopies, talk to the nurse about the patient’s diet, and be suspicious if it includes only red foods and liquids. The most common symptoms among patients who come to medical attention because of factitious disorders are diarrhea, fever of unknown origin, gastrointestinal bleeding, hematuria, seizures, and hypoglycemia.
17. Choose an intravenous psychiatric medication when a patient with severe and persistent mental illness should avoid oral medication for a procedure.
A patient with schizophrenia or bipolar disorder could experience a severe psychiatric episode without psychiatric medication. An appropriate alternative, perhaps administered intravenously if necessary, “can make all the difference in the world,” says Christopher Dobbelstein, MD, assistant professor of psychiatry at the University of Pittsburgh School of Medicine.
18. Listen to your instincts.
Medical teams can handle many psychiatric issues. Straightforward delirium is a good example. The bigger question, which takes experience and confidence, is to recognize when a line has been crossed. “The decision to consult psychiatry is not formulaic,” Dr. Dobbelstein says.
Sometimes a patient is acting strangely, and the team can’t explain why a psychiatrist could offer sound advice. “That’s when they should trust their instincts and consult us,” he says, “because the patient likely does have something more complex going on.”
19. Arrange for post-discharge follow-up with a primary-care physician or psychiatrist.
Sometimes psychiatric medications are started without good oversight. Suicide risk is highest during the weeks following an inpatient psychiatric admission, so a patient should see an outpatient mental health provider within seven days after hospital discharge, says NAMI’s Dr. Duckworth.
20. Extend genuine compassion to your patients.
“This is the secret to achieving a lifelong rewarding career in medicine,” Dr. Worley says, “and is the most important ingredient in positive outcomes.”
Susan Kreimer is a freelance writer in New York.
The Future of ACOs Remains Cloudy
Experts disagree on what a sustainable accountable-care organization (ACO) will look like in the future. The shared savings model currently dominates the ACO landscape, but David Muhlestein, an analyst with Washington, D.C.-based healthcare consulting firm Leavitt Partners, says his firm’s interviews with participants suggest that very few see the approach as the best long-term answer. Some believe those capitated models of the 1990s—the much-despised HMOs with their narrowly defined networks and global payments to provider groups—could make a comeback in a slightly altered form. Others feel strongly that a bundled payment model, which provides more flexibility in where patients can go for care, will instead dominate. A few providers have even suggested that the shared savings experiment will eventually revert back to a fee-for-service approach.

—David Muhlestein, analyst, Leavitt Partners, Washington, D.C.
SHM Public Policy Committee chair Ron Greeno, MD, FCCP, MHM, says bundled payments and shared savings alone are unlikely to deliver optimal value within the integrated care structure.
“There’s just not enough incentive, and the organization that’s taking risk doesn’t have enough flexibility in terms of how they use resources,” says Dr. Greeno, chief medical officer of Cogent HMG. The real improvements, Dr. Greeno says, might not come until ACOs assume a more capitated structure in which they accept global risk and are given unfettered freedom in how they allocate payments. In the meantime, he says, Medicare could be simply trying to encourage organizations “to start dipping their toe in the water of integrated care.”
John Pilotte, director of performance-based payment policy in the Center for Medicare at CMS, agreed that one major aim of its Shared Savings Program is to provide a “new avenue for providers to work together to better coordinate care for Medicare fee-for-service beneficiaries, and to move away from volume-based incentives and to recognize and reward them for improving the quality and efficiency and effectiveness of the care they deliver.”
Muhlestein says his firm has spoken with many organizations that are carefully monitoring how the current ACOs are faring. “Right now, the ACOs that have formed are people who want to forge their own trail,” he says. “There are many more providers that want to follow some path, and they want to follow a path that has some evidence that it has been successful.”
The more paths that are taken, he says, the greater the likelihood that one or more will achieve success. And although healthcare analysts often talk about success in terms of controlling costs, Muhlestein says, quality improvement (QI) and better outcomes alone could prove alluring to would-be ACOs.
“Even if we don’t see a moderation in cost growth, but we do see an improvement in quality, there is the chance that the model could still stick around, because that’s enough,” he says. “Even if we’re paying the same amount, we’re getting better results, so our value has improved.”
Regardless of how the ACO experiment plays out, Dr. Greeno says, it represents a fundamental shift toward a more integrated, pay-for-performance healthcare system that will not be optional for providers in the near future.
“Everyone is going to be asked to perform at a higher level, and there’s going to be tremendous pressure on hospitalists to lead that performance,” he says. “My advice would be to embrace it—it’s a great opportunity to bring value to the healthcare system.” TH
Bryn Nelson is a freelance medical writer in Seattle.
Experts disagree on what a sustainable accountable-care organization (ACO) will look like in the future. The shared savings model currently dominates the ACO landscape, but David Muhlestein, an analyst with Washington, D.C.-based healthcare consulting firm Leavitt Partners, says his firm’s interviews with participants suggest that very few see the approach as the best long-term answer. Some believe those capitated models of the 1990s—the much-despised HMOs with their narrowly defined networks and global payments to provider groups—could make a comeback in a slightly altered form. Others feel strongly that a bundled payment model, which provides more flexibility in where patients can go for care, will instead dominate. A few providers have even suggested that the shared savings experiment will eventually revert back to a fee-for-service approach.

—David Muhlestein, analyst, Leavitt Partners, Washington, D.C.
SHM Public Policy Committee chair Ron Greeno, MD, FCCP, MHM, says bundled payments and shared savings alone are unlikely to deliver optimal value within the integrated care structure.
“There’s just not enough incentive, and the organization that’s taking risk doesn’t have enough flexibility in terms of how they use resources,” says Dr. Greeno, chief medical officer of Cogent HMG. The real improvements, Dr. Greeno says, might not come until ACOs assume a more capitated structure in which they accept global risk and are given unfettered freedom in how they allocate payments. In the meantime, he says, Medicare could be simply trying to encourage organizations “to start dipping their toe in the water of integrated care.”
John Pilotte, director of performance-based payment policy in the Center for Medicare at CMS, agreed that one major aim of its Shared Savings Program is to provide a “new avenue for providers to work together to better coordinate care for Medicare fee-for-service beneficiaries, and to move away from volume-based incentives and to recognize and reward them for improving the quality and efficiency and effectiveness of the care they deliver.”
Muhlestein says his firm has spoken with many organizations that are carefully monitoring how the current ACOs are faring. “Right now, the ACOs that have formed are people who want to forge their own trail,” he says. “There are many more providers that want to follow some path, and they want to follow a path that has some evidence that it has been successful.”
The more paths that are taken, he says, the greater the likelihood that one or more will achieve success. And although healthcare analysts often talk about success in terms of controlling costs, Muhlestein says, quality improvement (QI) and better outcomes alone could prove alluring to would-be ACOs.
“Even if we don’t see a moderation in cost growth, but we do see an improvement in quality, there is the chance that the model could still stick around, because that’s enough,” he says. “Even if we’re paying the same amount, we’re getting better results, so our value has improved.”
Regardless of how the ACO experiment plays out, Dr. Greeno says, it represents a fundamental shift toward a more integrated, pay-for-performance healthcare system that will not be optional for providers in the near future.
“Everyone is going to be asked to perform at a higher level, and there’s going to be tremendous pressure on hospitalists to lead that performance,” he says. “My advice would be to embrace it—it’s a great opportunity to bring value to the healthcare system.” TH
Bryn Nelson is a freelance medical writer in Seattle.
Experts disagree on what a sustainable accountable-care organization (ACO) will look like in the future. The shared savings model currently dominates the ACO landscape, but David Muhlestein, an analyst with Washington, D.C.-based healthcare consulting firm Leavitt Partners, says his firm’s interviews with participants suggest that very few see the approach as the best long-term answer. Some believe those capitated models of the 1990s—the much-despised HMOs with their narrowly defined networks and global payments to provider groups—could make a comeback in a slightly altered form. Others feel strongly that a bundled payment model, which provides more flexibility in where patients can go for care, will instead dominate. A few providers have even suggested that the shared savings experiment will eventually revert back to a fee-for-service approach.

—David Muhlestein, analyst, Leavitt Partners, Washington, D.C.
SHM Public Policy Committee chair Ron Greeno, MD, FCCP, MHM, says bundled payments and shared savings alone are unlikely to deliver optimal value within the integrated care structure.
“There’s just not enough incentive, and the organization that’s taking risk doesn’t have enough flexibility in terms of how they use resources,” says Dr. Greeno, chief medical officer of Cogent HMG. The real improvements, Dr. Greeno says, might not come until ACOs assume a more capitated structure in which they accept global risk and are given unfettered freedom in how they allocate payments. In the meantime, he says, Medicare could be simply trying to encourage organizations “to start dipping their toe in the water of integrated care.”
John Pilotte, director of performance-based payment policy in the Center for Medicare at CMS, agreed that one major aim of its Shared Savings Program is to provide a “new avenue for providers to work together to better coordinate care for Medicare fee-for-service beneficiaries, and to move away from volume-based incentives and to recognize and reward them for improving the quality and efficiency and effectiveness of the care they deliver.”
Muhlestein says his firm has spoken with many organizations that are carefully monitoring how the current ACOs are faring. “Right now, the ACOs that have formed are people who want to forge their own trail,” he says. “There are many more providers that want to follow some path, and they want to follow a path that has some evidence that it has been successful.”
The more paths that are taken, he says, the greater the likelihood that one or more will achieve success. And although healthcare analysts often talk about success in terms of controlling costs, Muhlestein says, quality improvement (QI) and better outcomes alone could prove alluring to would-be ACOs.
“Even if we don’t see a moderation in cost growth, but we do see an improvement in quality, there is the chance that the model could still stick around, because that’s enough,” he says. “Even if we’re paying the same amount, we’re getting better results, so our value has improved.”
Regardless of how the ACO experiment plays out, Dr. Greeno says, it represents a fundamental shift toward a more integrated, pay-for-performance healthcare system that will not be optional for providers in the near future.
“Everyone is going to be asked to perform at a higher level, and there’s going to be tremendous pressure on hospitalists to lead that performance,” he says. “My advice would be to embrace it—it’s a great opportunity to bring value to the healthcare system.” TH
Bryn Nelson is a freelance medical writer in Seattle.
Keep an Eye Out for Factitious Disorders
Among the challenging psychiatric conditions hospitalists encounter are factitious disorders in which patients fabricate symptoms to draw attention, elicit empathy, and intentionally take on a sick role.
For example, at the University of Chicago, a patient in her 30s complained of blood in her urine, stool, and vomit. The staff performed an extensive evaluation, including laboratory analyses and upper and lower gastrointestinal endoscopies, but they found no source of the alleged bleeding, says Gregory Ruhnke, MD, MS, MPH, assistant professor in the section of hospital medicine at the university’s Pritzker School of Medicine.
In this instance, the patient’s objective was “to stay in the hospital,” says Marie Tobin, MD, associate professor of psychiatry and consult-liaison psychiatrist at the University of Chicago. “That’s the goal—to be taken care of as a patient.”
The staff later learned that the patient had engaged in similar tactics at other hospitals. When physicians wanted to obtain medical records from those facilities, the patient declined to grant permission.
“We do have to respect the patient’s confidentiality,” Dr. Tobin says. “If they refuse, we really can’t [obtain their records].”
Aside from previous records, “room searches can help confirm suspicions,” Dr. Ruhnke says. Security personnel should conduct a room search when necessary. This preserves the patient’s therapeutic rapport with healthcare providers. A search could uncover knives or needles, which a patient could use to inflict harm. More important, room searches can resolve inconsistencies and help hospitalists avoid ordering unjustified tests and procedures.
“It’s not a pleasant situation, but it is for safety,” Dr. Tobin says of investigations.
“These are people who can be at high risk to themselves.” TH
Susan Kreimer is a freelance writer in New York.
Among the challenging psychiatric conditions hospitalists encounter are factitious disorders in which patients fabricate symptoms to draw attention, elicit empathy, and intentionally take on a sick role.
For example, at the University of Chicago, a patient in her 30s complained of blood in her urine, stool, and vomit. The staff performed an extensive evaluation, including laboratory analyses and upper and lower gastrointestinal endoscopies, but they found no source of the alleged bleeding, says Gregory Ruhnke, MD, MS, MPH, assistant professor in the section of hospital medicine at the university’s Pritzker School of Medicine.
In this instance, the patient’s objective was “to stay in the hospital,” says Marie Tobin, MD, associate professor of psychiatry and consult-liaison psychiatrist at the University of Chicago. “That’s the goal—to be taken care of as a patient.”
The staff later learned that the patient had engaged in similar tactics at other hospitals. When physicians wanted to obtain medical records from those facilities, the patient declined to grant permission.
“We do have to respect the patient’s confidentiality,” Dr. Tobin says. “If they refuse, we really can’t [obtain their records].”
Aside from previous records, “room searches can help confirm suspicions,” Dr. Ruhnke says. Security personnel should conduct a room search when necessary. This preserves the patient’s therapeutic rapport with healthcare providers. A search could uncover knives or needles, which a patient could use to inflict harm. More important, room searches can resolve inconsistencies and help hospitalists avoid ordering unjustified tests and procedures.
“It’s not a pleasant situation, but it is for safety,” Dr. Tobin says of investigations.
“These are people who can be at high risk to themselves.” TH
Susan Kreimer is a freelance writer in New York.
Among the challenging psychiatric conditions hospitalists encounter are factitious disorders in which patients fabricate symptoms to draw attention, elicit empathy, and intentionally take on a sick role.
For example, at the University of Chicago, a patient in her 30s complained of blood in her urine, stool, and vomit. The staff performed an extensive evaluation, including laboratory analyses and upper and lower gastrointestinal endoscopies, but they found no source of the alleged bleeding, says Gregory Ruhnke, MD, MS, MPH, assistant professor in the section of hospital medicine at the university’s Pritzker School of Medicine.
In this instance, the patient’s objective was “to stay in the hospital,” says Marie Tobin, MD, associate professor of psychiatry and consult-liaison psychiatrist at the University of Chicago. “That’s the goal—to be taken care of as a patient.”
The staff later learned that the patient had engaged in similar tactics at other hospitals. When physicians wanted to obtain medical records from those facilities, the patient declined to grant permission.
“We do have to respect the patient’s confidentiality,” Dr. Tobin says. “If they refuse, we really can’t [obtain their records].”
Aside from previous records, “room searches can help confirm suspicions,” Dr. Ruhnke says. Security personnel should conduct a room search when necessary. This preserves the patient’s therapeutic rapport with healthcare providers. A search could uncover knives or needles, which a patient could use to inflict harm. More important, room searches can resolve inconsistencies and help hospitalists avoid ordering unjustified tests and procedures.
“It’s not a pleasant situation, but it is for safety,” Dr. Tobin says of investigations.
“These are people who can be at high risk to themselves.” TH
Susan Kreimer is a freelance writer in New York.