User login
GET INVOLVED!
- Administrators in Hospital Medicine
- Canadian Hospitalists
- Comanagement/Consultative Hospital Medicine
- Community-Based Hospitalists
- Early-Career Hospitalists
- Education/Curriculum
- Family Practice Hospitalists
- Geriatric Hospitalists
- Information Technology
- International Hospital Medicine
- Medical Directors/Leadership
- Med-Peds Hospitalists
- Nonphysician Providers
- Pediatric Hospitalists
- Quality Improvement
- Researchers/Academic Hospitalists
- Rural Hospitalists
- VA Hospitalists
- Women in Hospital Medicine
- Administrators in Hospital Medicine
- Canadian Hospitalists
- Comanagement/Consultative Hospital Medicine
- Community-Based Hospitalists
- Early-Career Hospitalists
- Education/Curriculum
- Family Practice Hospitalists
- Geriatric Hospitalists
- Information Technology
- International Hospital Medicine
- Medical Directors/Leadership
- Med-Peds Hospitalists
- Nonphysician Providers
- Pediatric Hospitalists
- Quality Improvement
- Researchers/Academic Hospitalists
- Rural Hospitalists
- VA Hospitalists
- Women in Hospital Medicine
- Administrators in Hospital Medicine
- Canadian Hospitalists
- Comanagement/Consultative Hospital Medicine
- Community-Based Hospitalists
- Early-Career Hospitalists
- Education/Curriculum
- Family Practice Hospitalists
- Geriatric Hospitalists
- Information Technology
- International Hospital Medicine
- Medical Directors/Leadership
- Med-Peds Hospitalists
- Nonphysician Providers
- Pediatric Hospitalists
- Quality Improvement
- Researchers/Academic Hospitalists
- Rural Hospitalists
- VA Hospitalists
- Women in Hospital Medicine
MEET AND GREET, TEXAS-STYLE
Ask any veteran of an SHM annual meeting, and they’ll tell you that they come for the people.
The unprecedented growth of HM as a specialty means that more hospitalists have chances to connect throughout the year. But the specialty’s relative youth and the demand for hospitalists make networking with peers a key part of the annual meeting experience.
In response to conference attendees, HM11 will have even more networking opportunities built into the schedule than before. Additional time for lunches and breaks are built into the schedule, and the always-popular Special Interest Forums have been moved to the evening of the first day of the regular meeting, May 11.
The forums are specially designed to bring hospitalists with common interests together to informally share their experiences. “Many hospitalists across the country are tackling similar challenges,” says Geri Barnes, senior director of education and meetings at SHM. “The Special Interest Forums are an opportunity to build community around those challenges and the best practices they’ve developed.”
For hospitalists looking for face time with SHM leadership, the SHM Town Hall (2 p.m., May 13) offers a once-a-year preview into the society’s vision and the chance to ask the nation’s HM leaders about the specialty and its impact on hospitalists.—BS
Ask any veteran of an SHM annual meeting, and they’ll tell you that they come for the people.
The unprecedented growth of HM as a specialty means that more hospitalists have chances to connect throughout the year. But the specialty’s relative youth and the demand for hospitalists make networking with peers a key part of the annual meeting experience.
In response to conference attendees, HM11 will have even more networking opportunities built into the schedule than before. Additional time for lunches and breaks are built into the schedule, and the always-popular Special Interest Forums have been moved to the evening of the first day of the regular meeting, May 11.
The forums are specially designed to bring hospitalists with common interests together to informally share their experiences. “Many hospitalists across the country are tackling similar challenges,” says Geri Barnes, senior director of education and meetings at SHM. “The Special Interest Forums are an opportunity to build community around those challenges and the best practices they’ve developed.”
For hospitalists looking for face time with SHM leadership, the SHM Town Hall (2 p.m., May 13) offers a once-a-year preview into the society’s vision and the chance to ask the nation’s HM leaders about the specialty and its impact on hospitalists.—BS
Ask any veteran of an SHM annual meeting, and they’ll tell you that they come for the people.
The unprecedented growth of HM as a specialty means that more hospitalists have chances to connect throughout the year. But the specialty’s relative youth and the demand for hospitalists make networking with peers a key part of the annual meeting experience.
In response to conference attendees, HM11 will have even more networking opportunities built into the schedule than before. Additional time for lunches and breaks are built into the schedule, and the always-popular Special Interest Forums have been moved to the evening of the first day of the regular meeting, May 11.
The forums are specially designed to bring hospitalists with common interests together to informally share their experiences. “Many hospitalists across the country are tackling similar challenges,” says Geri Barnes, senior director of education and meetings at SHM. “The Special Interest Forums are an opportunity to build community around those challenges and the best practices they’ve developed.”
For hospitalists looking for face time with SHM leadership, the SHM Town Hall (2 p.m., May 13) offers a once-a-year preview into the society’s vision and the chance to ask the nation’s HM leaders about the specialty and its impact on hospitalists.—BS
POLICY CORNER: An inside look at the most pressing policy issues
On Feb. 16, the Agency for Healthcare Research and Quality (AHRQ) listed SHM as a patient safety organization (PSO). A PSO serves as an independent, external, expert organization that can collect, analyze, and aggregate information in order to develop insights into the underlying causes of patient-safety events. PSOs are designed to help clinicians, hospitals, and healthcare organizations improve patient safety and the quality of healthcare delivery.
PSO status allows SHM’s current quality-improvement (QI) activities to be conducted in a secure environment that is protected from legal discovery. AHRQ currently lists 78 PSOs, including the Society for Vascular Surgery PSO, the Emergency Medicine Patient Safety Foundation, and the Biomedical Research and Education Foundation. A full list is available at www.pso.ahrq.gov/listing/psolist.htm.
To achieve PSO status, SHM worked closely with AHRQ to meet specific guidelines and requirements. One of the requirements is that the mission and primary activity of a PSO must be to conduct activities that are designed to improve patient safety and the quality of healthcare delivery.
To comply, SHM formed a separate component within the Quality Initiatives Department strictly to pursue patient safety and quality activities.
The SHM PSO will be unique. While PSOs are required to collect patient-safety data and provide some form of feedback to contracted sites, few have their own QI initiatives, and even fewer are established by a national physician’s professional society.
These differences will help the SHM PSO stand out from the crowd and will present opportunities within the healthcare reform framework. The Affordable Care Act (ACA) requires significant QI among the nation’s hospitals.
Specifically pertaining to PSOs, Section 399KK, a rarely mentioned section of the ACA, requires the Health and Human Services to establish a program for hospitals with high readmission rates to improve their rates through the use of PSOs. The details of this program remain unclear, but based upon the little bit of information currently available, there could be positive overlap between SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions) and the provision.
AHRQ’s recognition of the SHM PSO exemplifies SHM’s commitment to improving the quality of healthcare delivery. It also provides additional value to sites that implement SHM’s QI initiatives and will hopefully open new doors to SHM’s members. TH
On Feb. 16, the Agency for Healthcare Research and Quality (AHRQ) listed SHM as a patient safety organization (PSO). A PSO serves as an independent, external, expert organization that can collect, analyze, and aggregate information in order to develop insights into the underlying causes of patient-safety events. PSOs are designed to help clinicians, hospitals, and healthcare organizations improve patient safety and the quality of healthcare delivery.
PSO status allows SHM’s current quality-improvement (QI) activities to be conducted in a secure environment that is protected from legal discovery. AHRQ currently lists 78 PSOs, including the Society for Vascular Surgery PSO, the Emergency Medicine Patient Safety Foundation, and the Biomedical Research and Education Foundation. A full list is available at www.pso.ahrq.gov/listing/psolist.htm.
To achieve PSO status, SHM worked closely with AHRQ to meet specific guidelines and requirements. One of the requirements is that the mission and primary activity of a PSO must be to conduct activities that are designed to improve patient safety and the quality of healthcare delivery.
To comply, SHM formed a separate component within the Quality Initiatives Department strictly to pursue patient safety and quality activities.
The SHM PSO will be unique. While PSOs are required to collect patient-safety data and provide some form of feedback to contracted sites, few have their own QI initiatives, and even fewer are established by a national physician’s professional society.
These differences will help the SHM PSO stand out from the crowd and will present opportunities within the healthcare reform framework. The Affordable Care Act (ACA) requires significant QI among the nation’s hospitals.
Specifically pertaining to PSOs, Section 399KK, a rarely mentioned section of the ACA, requires the Health and Human Services to establish a program for hospitals with high readmission rates to improve their rates through the use of PSOs. The details of this program remain unclear, but based upon the little bit of information currently available, there could be positive overlap between SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions) and the provision.
AHRQ’s recognition of the SHM PSO exemplifies SHM’s commitment to improving the quality of healthcare delivery. It also provides additional value to sites that implement SHM’s QI initiatives and will hopefully open new doors to SHM’s members. TH
On Feb. 16, the Agency for Healthcare Research and Quality (AHRQ) listed SHM as a patient safety organization (PSO). A PSO serves as an independent, external, expert organization that can collect, analyze, and aggregate information in order to develop insights into the underlying causes of patient-safety events. PSOs are designed to help clinicians, hospitals, and healthcare organizations improve patient safety and the quality of healthcare delivery.
PSO status allows SHM’s current quality-improvement (QI) activities to be conducted in a secure environment that is protected from legal discovery. AHRQ currently lists 78 PSOs, including the Society for Vascular Surgery PSO, the Emergency Medicine Patient Safety Foundation, and the Biomedical Research and Education Foundation. A full list is available at www.pso.ahrq.gov/listing/psolist.htm.
To achieve PSO status, SHM worked closely with AHRQ to meet specific guidelines and requirements. One of the requirements is that the mission and primary activity of a PSO must be to conduct activities that are designed to improve patient safety and the quality of healthcare delivery.
To comply, SHM formed a separate component within the Quality Initiatives Department strictly to pursue patient safety and quality activities.
The SHM PSO will be unique. While PSOs are required to collect patient-safety data and provide some form of feedback to contracted sites, few have their own QI initiatives, and even fewer are established by a national physician’s professional society.
These differences will help the SHM PSO stand out from the crowd and will present opportunities within the healthcare reform framework. The Affordable Care Act (ACA) requires significant QI among the nation’s hospitals.
Specifically pertaining to PSOs, Section 399KK, a rarely mentioned section of the ACA, requires the Health and Human Services to establish a program for hospitals with high readmission rates to improve their rates through the use of PSOs. The details of this program remain unclear, but based upon the little bit of information currently available, there could be positive overlap between SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions) and the provision.
AHRQ’s recognition of the SHM PSO exemplifies SHM’s commitment to improving the quality of healthcare delivery. It also provides additional value to sites that implement SHM’s QI initiatives and will hopefully open new doors to SHM’s members. TH
HM11 BLOGS & BLOGGERS: Hear it through the Grapevine
For hospitalists planning on attending HM11, and those who can’t make it to Dallas in May, SHM’s blogs are a vital connection to the most up-to-date information about the biggest annual event in HM. And many of the specialty’s top bloggers will be speaking or presenting at HM11.
SHM bloggers will keep readers updated before the big event, highlighting can’t-miss issues, sessions, and experts who they’re anxious to see. Plus, they’ll apply the issues of the day to HM11 sessions and pre-courses.
One of HM’s most popular bloggers not only will be blogging about HM11, he’ll be a featured presenter. Robert Wachter, MD, MHM, professor and associate chairman of the Department of Medicine at the University of California at San Francisco, chief of the Division of Hospital Medicine UCSF Medical Center, and author of the blog Wachter’s World, will deliver the May 13 keynote presentation, “Hospital Medicine at 15: The Things I Never Would Have Guessed When the Fun Began.”
Danielle Scheurer, MD, MSc, SFHM, author of the SHM blog Hospital Medicine Quick Hits: Clinical Updates for the Busy Hospitalist and SHM physician advisor, will be teaching the “ABIM Maintenance of Certification (MOC) Learning Session” pre-course May 10. Dr. Scheurer will work with hospitalists to prepare for the ABIM modules and earn up to 20 points toward the Self-Evaluation of Medical Knowledge requirement of the MOC program.
In between teaching and learning, she also will be blogging about HM11. “I do it as a way to include those members that are not able attend,” Dr. Scheurer says, “or those who can’t stay for the whole meeting, as well as people who are at the meeting but who like guidance and synopses.”
With nine tracks and hundreds of educational and networking opportunities, odds are good that her online guidance will be in high demand.—BS
For hospitalists planning on attending HM11, and those who can’t make it to Dallas in May, SHM’s blogs are a vital connection to the most up-to-date information about the biggest annual event in HM. And many of the specialty’s top bloggers will be speaking or presenting at HM11.
SHM bloggers will keep readers updated before the big event, highlighting can’t-miss issues, sessions, and experts who they’re anxious to see. Plus, they’ll apply the issues of the day to HM11 sessions and pre-courses.
One of HM’s most popular bloggers not only will be blogging about HM11, he’ll be a featured presenter. Robert Wachter, MD, MHM, professor and associate chairman of the Department of Medicine at the University of California at San Francisco, chief of the Division of Hospital Medicine UCSF Medical Center, and author of the blog Wachter’s World, will deliver the May 13 keynote presentation, “Hospital Medicine at 15: The Things I Never Would Have Guessed When the Fun Began.”
Danielle Scheurer, MD, MSc, SFHM, author of the SHM blog Hospital Medicine Quick Hits: Clinical Updates for the Busy Hospitalist and SHM physician advisor, will be teaching the “ABIM Maintenance of Certification (MOC) Learning Session” pre-course May 10. Dr. Scheurer will work with hospitalists to prepare for the ABIM modules and earn up to 20 points toward the Self-Evaluation of Medical Knowledge requirement of the MOC program.
In between teaching and learning, she also will be blogging about HM11. “I do it as a way to include those members that are not able attend,” Dr. Scheurer says, “or those who can’t stay for the whole meeting, as well as people who are at the meeting but who like guidance and synopses.”
With nine tracks and hundreds of educational and networking opportunities, odds are good that her online guidance will be in high demand.—BS
For hospitalists planning on attending HM11, and those who can’t make it to Dallas in May, SHM’s blogs are a vital connection to the most up-to-date information about the biggest annual event in HM. And many of the specialty’s top bloggers will be speaking or presenting at HM11.
SHM bloggers will keep readers updated before the big event, highlighting can’t-miss issues, sessions, and experts who they’re anxious to see. Plus, they’ll apply the issues of the day to HM11 sessions and pre-courses.
One of HM’s most popular bloggers not only will be blogging about HM11, he’ll be a featured presenter. Robert Wachter, MD, MHM, professor and associate chairman of the Department of Medicine at the University of California at San Francisco, chief of the Division of Hospital Medicine UCSF Medical Center, and author of the blog Wachter’s World, will deliver the May 13 keynote presentation, “Hospital Medicine at 15: The Things I Never Would Have Guessed When the Fun Began.”
Danielle Scheurer, MD, MSc, SFHM, author of the SHM blog Hospital Medicine Quick Hits: Clinical Updates for the Busy Hospitalist and SHM physician advisor, will be teaching the “ABIM Maintenance of Certification (MOC) Learning Session” pre-course May 10. Dr. Scheurer will work with hospitalists to prepare for the ABIM modules and earn up to 20 points toward the Self-Evaluation of Medical Knowledge requirement of the MOC program.
In between teaching and learning, she also will be blogging about HM11. “I do it as a way to include those members that are not able attend,” Dr. Scheurer says, “or those who can’t stay for the whole meeting, as well as people who are at the meeting but who like guidance and synopses.”
With nine tracks and hundreds of educational and networking opportunities, odds are good that her online guidance will be in high demand.—BS
In the Literature: HM-Related Research You Need to Know
In This Edition
Literature at a Glance
A guide to this month’s studies
- Risk of adverse events with opioid use
- Drug of choice for outpatient treatment of cellulitis
- Preventing hospital falls
- Post-hospital outcomes based on status of PCP follow-up
- LOS, mortality, and readmission based on insurance
- Antiplatelets added to warfarin for atrial fibrillation.
- Cognitive effects of severe sepsis
- Effect of preoperative furosemide use
ED Visits Are Higher among Recipients of Chronic Opioid Therapy
Clinical question: Is there an association between the use of prescription opioids and adverse outcomes?
Background: Chronic opioid therapy is a common strategy for managing chronic, noncancer pain. There has been an increase in overdose deaths and ED visits (EDV) involving the use of prescription opioids.
Study design: Retrospective study from claims records.
Setting: Population in the Health Core Integrated Research Database, containing large, commercial insurance plans in 14 states, and Arkansas Medicaid.
Synopsis: Patients 18 and older without cancer diagnoses who used prescription opioids for at least 90 continuous days within a six-month period from 2000 to 2005 were examined for risk factors for EDVs and alcohol- or drug-related encounters (ADEs) in the 12 months following 90 days or more of prescribed opioids.
Patients with diagnoses of headache, back pain, and pre-existing substance-use disorders had significantly higher EDVs and ADEs. Opioid dose at morphine-equivalent doses over 120 mg per day doubled the risk of ADEs. The use of short-acting Schedule II opioids was associated with EDVs (relative risk, 1.09-1.74). The use of long-acting Schedule II opioids was strongly associated with ADEs (relative risk, 1.64-4.00).
Bottom line: In adults with noncancer pain prescribed opioids for 90 days or more, short-acting Schedule II opioid use was associated with an increased number of EDVs, and long-acting opioid use was associated with an increased number of ADEs. Minimizing Schedule II opioid prescription in these higher-risk patients might be prudent to increase patient safety.
Citation: Braden JB, Russo J, Fan MI, et al. Emergency department visits among recipients of chronic opioid therapy. Arch Intern Med. 2010; 170(16):1425-1432.
Empiric Outpatient Therapy with Trimethoprim-Sulfamethoxazole or Clindamycin Is Preferred for Cellulitis
Clinical question: What is the best empiric outpatient oral antibiotic treatment for cellulitis in areas with a high prevalence of community-associated MRSA infections?
Background: The increasing rates of community-associated MRSA skin and soft-tissue infections have raised concerns that such beta-lactams as cephalexin and other semisynthetic penicillins are not appropriate for empiric outpatient therapy for cellulitis.
Study design: Three-year, retrospective cohort study.
Setting: A teaching clinic of a tertiary-care medical center in Hawaii.
Synopsis: More than 540 patients with cellulitis were identified from January 2005 to December 2007. Of these, 139 patients were excluded for reasons such as hospitalization, surgical intervention, etc. In the final cohort of 405 patients, the three most commonly prescribed oral antibiotics were cephalexin (44%), trimethoprim-sulfamethoxazole (38%), and clindamycin (10%). Other antibiotics accounted for the remaining 8%.
MRSA was recovered in 62% of positive culture specimens. The success rate of trimethoprim-sulfamethoxazole was 91% vs. 74% in the cephalexin group (P<0.001). Clindamycin success rates were higher than those of cephalexin in patients who had subsequently confirmed MRSA infections (P=0.01) and moderately severe cellulitis (P=0.03) and were obese (P=0.04).
Bottom line: Antibiotics with activity against community-acquired MRSA (e.g. trimethroprim-sulfamethoxazole and clinidamycin) are the preferred empiric outpatient therapy for cellulitis in areas with a high prevalence of community-acquired MRSA.
Citation: Khawcharoenporn T, Tice A. Empiric outpatient therapy with trimethoprim-sulfamethoxazole, cephalexin, or clindamycin for cellulitis. Am J Med. 2010;123(10):942-950.
Patient-Specific Screening with Health Information Technology Prevents Falls
Clinical question: Does a fall-prevention toolkit using health information technology decrease patient falls in acute-care hospitals?
Background: Inpatient falls and fall-related injuries result in substantial morbidity and additional healthcare costs. While specific fall-prevention strategies were a longstanding target for intervention, little evidence exists to link them with decreased fall rates.
Study design: Cluster-randomized study.
Setting: Four urban hospitals in Massachusetts.
Synopsis: Comparing patient fall rates in four acute-care hospitals between units providing usual care (5,104 patients) and units using a health information technology (HIT)-linked fall prevention toolkit (5,160 patients), this study demonstrated significant fall reduction in older inpatients. The intervention integrated existing workflow and validated fall risk assessment (Morse Falls Scale) into an HIT software application that tailored fall-prevention interventions to patients’ specific fall risk determinants. The toolkit produced bed posters, patient education handouts, and plans of care communicating patient-specific alerts to key stakeholders.
The primary outcome was patient falls per 1,000 patient-days during the six-month intervention period. The number of patients with falls was significantly different (P=0.02) between control (n=87) and intervention (n=67) units. The toolkit prevented one fall per 862 patient-days.
This nonblinded study was limited by the fact that it was conducted in a single health system. The toolkit was not effective in patients less than 65 years of age. Additionally, the sample size did not have sufficient power to detect effectiveness in preventing repeat falls or falls with injury.
Bottom line: Patient-specific fall prevention strategy coupled with HIT reduces falls in older inpatients.
Citation: Dykes PC, Carroll DL, Hurley A, et al. Fall prevention in acute care hospitals: a randomized trial. JAMA. 2010;304(17):1912-1918.
Lack of Timely Outpatient Follow-Up Results in Higher Readmission Rates
Clinical question: Does timely primary-care-physician (PCP) follow-up improve outcomes and prevent hospital readmissions?
Background: Active PCP involvement is key to interventions aimed at reducing readmissions and ensuring effective ongoing patient care. Some studies suggest increased overall resource utilization when PCP follow-up occurs after hospitalization. Resource utilization and clinical outcomes after hospitalization related to timely PCP follow-up have not been adequately studied.
Study design: Prospective cohort.
Setting: An urban, academic, 425-bed tertiary-care center in Colorado.
Synopsis: From a convenience sample of 121 patients admitted to general medicine services during winter months, 65 patients completed the study. Demographics, diagnosis, payor source, and PCP information were collected upon enrollment. Post-discharge phone calls and patient surveys were used to determine follow-up and readmission status. Timely PCP follow-up was defined as a visit with a PCP or specialist related to the discharge diagnosis within four weeks of hospital discharge.
Thirty-day readmission rates and hospital length of stay were compared for those with timely PCP follow-up and those without. Less than half of general-medicine inpatients received timely PCP follow-up post-discharge. Lack of timely PCP follow-up was associated with younger age, a 10-fold increase in 30-day readmission for the same condition, and a trend toward longer length of stay. However, hospital readmission for any condition did not differ with lack of timely PCP follow-up.
This small, single-center study with convenience sample enrollment might not represent all medical inpatients or diagnoses. Determination of same-condition readmission was potentially subjective.
Bottom line: Patients who lack timely post-discharge follow-up have higher readmission rates for the same medical condition.
Citation: Misky GJ, Wald HL, Coleman EA. Post-hospitalization transitions: examining the effects of timing of primary care provider follow-up. J Hosp Med. 2010;5(7):392-397.
Compared with Uninsured and Medicaid Patients, Privately Insured Patients Admitted for Acute MI, Stroke, and Pneumonia Have Better Mortality Rates
Clinical question: Do outcomes for insured and underinsured patients vary for three of the most common medical conditions for which patients are hospitalized: acute myocardial infarction (AMI), stroke, and pneumonia?
Background: The ideal healthcare system would provide quality care to all individuals regardless of insurance status. Nevertheless, disparities in outcomes for the insured and underinsured or uninsured are well-documented in the outpatient setting but not as well in the inpatient setting. More needs to be done to address these potential disparities.
Study design: Retrospective database analysis.
Setting: Database including 20% of all U.S. community hospitals, including public hospitals, academic medical centers, and specialty hospitals.
Synopsis: This study utilized a database of 8 million discharges from more than 1,000 hospitals and isolated patients 18-64 years old (154,381 patients). Privately insured, uninsured, and Medicaid patients’ data were reviewed for in-hospital mortality, length of stay (LOS), and cost per hospitalization. The analysis took into account disease severity, comorbidities, and the proportion of underinsured patients receiving care in each hospital when insurance-related disparities were examined.
Compared with the privately insured, in-hospital mortality and LOS for AMI and stroke were significantly higher for uninsured and Medicaid patients. Among pneumonia patients, Medicaid patients had significantly higher in-hospital mortality and LOS than the other two groups. Cost per hospitalization was highest for all three conditions in the Medicaid group; the uninsured group had the lowest costs for all three conditions.
Unfortunately, the three conditions analyzed only comprise 8% of annual hospital discharges, so the findings cannot be generalized. Also, deaths occurring soon after hospital discharge were not included, and uninsured and Medicaid patients are likely to have more severe diseases, which, rather than insurance status, could account for the mortality differences.
Bottom line: In-hospital mortality and resource use for three common medical conditions vary significantly between privately insured and uninsured or Medicaid patients, highlighting the need to take measures to close this gap.
Citation: Hasan O, Orav EJ, LeRoi LS. Insurance status and hospital care for myocardial infarction, stroke, and pneumonia. J Hosp Med. 2010;5(8);452-459.
Warfarin Monotherapy Best in Prevention of Thromboembolic Events for Atrial Fibrillation Patients
Clinical question: Is there a benefit to adding an antiplatelet agent to warfarin for the prevention of thromboembolic stroke in atrial fibrillation?
Background: Many physicians prescribe various combinations of aspirin, clopidogrel, and warfarin, as these treatments are endorsed in guidelines and expert statements. The use of these medications, however, has not been studied in a setting large enough to understand the safety of these therapies.
Study design: Retrospective cohort.
Setting: All Danish hospitals.
Synopsis: All hospitalized patients in Denmark from 1997 to 2006 who were identified with new onset atrial fibrillation (n=118,606) were monitored for outcomes and the use of aspirin, clopidogrel, and warfarin. These patients were followed for a mean of 3.3 years with the primary endpoint being admission to a hospital for a diagnosis of bleeding and a secondary endpoint of stroke.
Bleeding occurred in 13,573 patients (11.4%). The incidence of bleeding was highest in the first 180 days and then leveled off. Hazard ratios were computed with warfarin monotherapy as a reference. Only the hazard ratio for aspirin monotherapy (0.93) was lower (confidence interval [CI] 0.88-0.98). The highest risk of bleeding was with the triple therapy warfarin-aspirin-clopidogrel, which had a hazard ratio of 3.70 (CI 2.89-4.76).
For strokes, the hazard ratio was slightly better for warfarin-clopidogrel (0.70), although the CI was wide at 0.35-1.4 compared to warfarin monotherapy as a reference. Hazard ratios for monotherapy with clopidogrel or aspirin, dual therapy, and triple therapy all were worse, ranging from 1.27 to 1.86.
Bottom line: Warfarin as a monotherapy might have a bleeding risk comparable to that of aspirin or clopidogrel alone, and prevents more strokes than various combinations of these medications.
Citation: Hansen ML, Sørensen R, Clausen MT, et al. Risk of bleeding with single, dual, or triple therapy with warfarin, aspirin, and clopidogrel in patients with atrial fibrillation. Arch Intern Med. 2010;170 (16):1433-1441.
Cognitive and Physical Function Declines in Elderly Severe Sepsis Survivors
Clinical question: Is there a change in cognitive and physical functioning after severe sepsis?
Background: Disability is associated with increased mortality, decreased quality of life, and increased burdens by families and healthcare costs. After severe sepsis, the lasting effects of debility have not been investigated in any large studies.
Study design: Prospective cohort.
Setting: Hospitalized Medicare patients participating in the Health and Retirement Study.
Synopsis: Patients (n=1194) were followed for a minimum of one year between 1998 and 2006. The outcomes were measured by multiple personal interviews before and after a severe sepsis episode. Cognitive impairment was measured using three validated questionnaires dependent upon age or if a proxy was the respondent. For functional limitations, a questionnaire concerning instrumental and basic activities of daily living was used.
Cognitive impairment for those with moderate to severe impairment increased to 16.7% from 6.1% after a sepsis episode with an odds ratio of 3.34 (95% confidence interval 1.53-7.25). There was no significant increase in nonsevere sepsis hospitalized comparison patients (n=5574). All survivors with severe sepsis had a functional decline of 1.5 activities. The comparison group had about a 0.4 activity decline. All of these deficits endured throughout the study.
The authors provide comments that there should be a system-based approach in preventing severe sepsis, its burdens, and its costs. Suggestions include preventing delirium, initiating better standards of care, and involving therapists earlier to prevent immobility.
Bottom line: Severe sepsis is independently associated with enduring cognitive and physical functional declines, which strain families and our healthcare system.
Citation: Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304(16):1787-1794.
Furosemide on Day of Elective Noncardiac Surgery Does Not Increase Risk of Intraoperative Hypotension
Clinical question: For patients chronically treated with loop diuretics, does withholding furosemide on the day of elective noncardiac surgery prevent intraoperative hypotension?
Background: Recent studies have questioned the safety of blood-pressure-lowering medications administered on the day of surgery. Beta-blockers have been associated with an increase in strokes and death perioperatively, and angiotensin receptor blockers (ARB) are frequently withheld on the day of surgery to avoid intraoperative hypotension. The effect of loop diuretics is uncertain.
Study design: Double-blind, randomized, placebo-controlled study.
Setting: Three North American university centers.
Synopsis: One hundred ninety-three patients were instructed to take furosemide or placebo on the day they underwent noncardiac surgery. The primary outcome measure was perioperative hypotension defined as a SBP <90 mmHg for more than five minutes, a 35% drop in the mean arterial blood pressure, or the need for a vasopressor agent. The number of cardiovascular complications (acute heart failure, acute coronary syndrome, arrhythmia, acute cerebrovascular event) and deaths also were analyzed.
Concerns have been raised that loop diuretics might predispose patients to a higher risk of intraoperative hypotension during noncardiac surgery. This trial showed no significant difference in the rates of intraoperative hypotension in patients who were administered furosemide versus those who were not. Although cardiovascular complications occurred more frequently in the furosemide group, the difference was not statistically significant.
Important limitations of the study were recognized. A larger population of patients could have revealed a statistically significant difference in cardiovascular outcomes in the furosemide group. Also, an anesthetic protocol was not utilized, which raises questions about the interaction of furosemide and effect on blood pressure with certain anesthetics.
Bottom line: Administering furosemide prior to surgery in chronic users does not appreciably increase the rate of intraoperative hypotension or cardiovascular events.
Citation: Khan NA, Campbell NR, Frost SD, et al. Risk of intraoperative hypotension with loop diuretics: a randomized controlled trial. Am J Med. 2010;123(11):1059e1-1059e8.
In This Edition
Literature at a Glance
A guide to this month’s studies
- Risk of adverse events with opioid use
- Drug of choice for outpatient treatment of cellulitis
- Preventing hospital falls
- Post-hospital outcomes based on status of PCP follow-up
- LOS, mortality, and readmission based on insurance
- Antiplatelets added to warfarin for atrial fibrillation.
- Cognitive effects of severe sepsis
- Effect of preoperative furosemide use
ED Visits Are Higher among Recipients of Chronic Opioid Therapy
Clinical question: Is there an association between the use of prescription opioids and adverse outcomes?
Background: Chronic opioid therapy is a common strategy for managing chronic, noncancer pain. There has been an increase in overdose deaths and ED visits (EDV) involving the use of prescription opioids.
Study design: Retrospective study from claims records.
Setting: Population in the Health Core Integrated Research Database, containing large, commercial insurance plans in 14 states, and Arkansas Medicaid.
Synopsis: Patients 18 and older without cancer diagnoses who used prescription opioids for at least 90 continuous days within a six-month period from 2000 to 2005 were examined for risk factors for EDVs and alcohol- or drug-related encounters (ADEs) in the 12 months following 90 days or more of prescribed opioids.
Patients with diagnoses of headache, back pain, and pre-existing substance-use disorders had significantly higher EDVs and ADEs. Opioid dose at morphine-equivalent doses over 120 mg per day doubled the risk of ADEs. The use of short-acting Schedule II opioids was associated with EDVs (relative risk, 1.09-1.74). The use of long-acting Schedule II opioids was strongly associated with ADEs (relative risk, 1.64-4.00).
Bottom line: In adults with noncancer pain prescribed opioids for 90 days or more, short-acting Schedule II opioid use was associated with an increased number of EDVs, and long-acting opioid use was associated with an increased number of ADEs. Minimizing Schedule II opioid prescription in these higher-risk patients might be prudent to increase patient safety.
Citation: Braden JB, Russo J, Fan MI, et al. Emergency department visits among recipients of chronic opioid therapy. Arch Intern Med. 2010; 170(16):1425-1432.
Empiric Outpatient Therapy with Trimethoprim-Sulfamethoxazole or Clindamycin Is Preferred for Cellulitis
Clinical question: What is the best empiric outpatient oral antibiotic treatment for cellulitis in areas with a high prevalence of community-associated MRSA infections?
Background: The increasing rates of community-associated MRSA skin and soft-tissue infections have raised concerns that such beta-lactams as cephalexin and other semisynthetic penicillins are not appropriate for empiric outpatient therapy for cellulitis.
Study design: Three-year, retrospective cohort study.
Setting: A teaching clinic of a tertiary-care medical center in Hawaii.
Synopsis: More than 540 patients with cellulitis were identified from January 2005 to December 2007. Of these, 139 patients were excluded for reasons such as hospitalization, surgical intervention, etc. In the final cohort of 405 patients, the three most commonly prescribed oral antibiotics were cephalexin (44%), trimethoprim-sulfamethoxazole (38%), and clindamycin (10%). Other antibiotics accounted for the remaining 8%.
MRSA was recovered in 62% of positive culture specimens. The success rate of trimethoprim-sulfamethoxazole was 91% vs. 74% in the cephalexin group (P<0.001). Clindamycin success rates were higher than those of cephalexin in patients who had subsequently confirmed MRSA infections (P=0.01) and moderately severe cellulitis (P=0.03) and were obese (P=0.04).
Bottom line: Antibiotics with activity against community-acquired MRSA (e.g. trimethroprim-sulfamethoxazole and clinidamycin) are the preferred empiric outpatient therapy for cellulitis in areas with a high prevalence of community-acquired MRSA.
Citation: Khawcharoenporn T, Tice A. Empiric outpatient therapy with trimethoprim-sulfamethoxazole, cephalexin, or clindamycin for cellulitis. Am J Med. 2010;123(10):942-950.
Patient-Specific Screening with Health Information Technology Prevents Falls
Clinical question: Does a fall-prevention toolkit using health information technology decrease patient falls in acute-care hospitals?
Background: Inpatient falls and fall-related injuries result in substantial morbidity and additional healthcare costs. While specific fall-prevention strategies were a longstanding target for intervention, little evidence exists to link them with decreased fall rates.
Study design: Cluster-randomized study.
Setting: Four urban hospitals in Massachusetts.
Synopsis: Comparing patient fall rates in four acute-care hospitals between units providing usual care (5,104 patients) and units using a health information technology (HIT)-linked fall prevention toolkit (5,160 patients), this study demonstrated significant fall reduction in older inpatients. The intervention integrated existing workflow and validated fall risk assessment (Morse Falls Scale) into an HIT software application that tailored fall-prevention interventions to patients’ specific fall risk determinants. The toolkit produced bed posters, patient education handouts, and plans of care communicating patient-specific alerts to key stakeholders.
The primary outcome was patient falls per 1,000 patient-days during the six-month intervention period. The number of patients with falls was significantly different (P=0.02) between control (n=87) and intervention (n=67) units. The toolkit prevented one fall per 862 patient-days.
This nonblinded study was limited by the fact that it was conducted in a single health system. The toolkit was not effective in patients less than 65 years of age. Additionally, the sample size did not have sufficient power to detect effectiveness in preventing repeat falls or falls with injury.
Bottom line: Patient-specific fall prevention strategy coupled with HIT reduces falls in older inpatients.
Citation: Dykes PC, Carroll DL, Hurley A, et al. Fall prevention in acute care hospitals: a randomized trial. JAMA. 2010;304(17):1912-1918.
Lack of Timely Outpatient Follow-Up Results in Higher Readmission Rates
Clinical question: Does timely primary-care-physician (PCP) follow-up improve outcomes and prevent hospital readmissions?
Background: Active PCP involvement is key to interventions aimed at reducing readmissions and ensuring effective ongoing patient care. Some studies suggest increased overall resource utilization when PCP follow-up occurs after hospitalization. Resource utilization and clinical outcomes after hospitalization related to timely PCP follow-up have not been adequately studied.
Study design: Prospective cohort.
Setting: An urban, academic, 425-bed tertiary-care center in Colorado.
Synopsis: From a convenience sample of 121 patients admitted to general medicine services during winter months, 65 patients completed the study. Demographics, diagnosis, payor source, and PCP information were collected upon enrollment. Post-discharge phone calls and patient surveys were used to determine follow-up and readmission status. Timely PCP follow-up was defined as a visit with a PCP or specialist related to the discharge diagnosis within four weeks of hospital discharge.
Thirty-day readmission rates and hospital length of stay were compared for those with timely PCP follow-up and those without. Less than half of general-medicine inpatients received timely PCP follow-up post-discharge. Lack of timely PCP follow-up was associated with younger age, a 10-fold increase in 30-day readmission for the same condition, and a trend toward longer length of stay. However, hospital readmission for any condition did not differ with lack of timely PCP follow-up.
This small, single-center study with convenience sample enrollment might not represent all medical inpatients or diagnoses. Determination of same-condition readmission was potentially subjective.
Bottom line: Patients who lack timely post-discharge follow-up have higher readmission rates for the same medical condition.
Citation: Misky GJ, Wald HL, Coleman EA. Post-hospitalization transitions: examining the effects of timing of primary care provider follow-up. J Hosp Med. 2010;5(7):392-397.
Compared with Uninsured and Medicaid Patients, Privately Insured Patients Admitted for Acute MI, Stroke, and Pneumonia Have Better Mortality Rates
Clinical question: Do outcomes for insured and underinsured patients vary for three of the most common medical conditions for which patients are hospitalized: acute myocardial infarction (AMI), stroke, and pneumonia?
Background: The ideal healthcare system would provide quality care to all individuals regardless of insurance status. Nevertheless, disparities in outcomes for the insured and underinsured or uninsured are well-documented in the outpatient setting but not as well in the inpatient setting. More needs to be done to address these potential disparities.
Study design: Retrospective database analysis.
Setting: Database including 20% of all U.S. community hospitals, including public hospitals, academic medical centers, and specialty hospitals.
Synopsis: This study utilized a database of 8 million discharges from more than 1,000 hospitals and isolated patients 18-64 years old (154,381 patients). Privately insured, uninsured, and Medicaid patients’ data were reviewed for in-hospital mortality, length of stay (LOS), and cost per hospitalization. The analysis took into account disease severity, comorbidities, and the proportion of underinsured patients receiving care in each hospital when insurance-related disparities were examined.
Compared with the privately insured, in-hospital mortality and LOS for AMI and stroke were significantly higher for uninsured and Medicaid patients. Among pneumonia patients, Medicaid patients had significantly higher in-hospital mortality and LOS than the other two groups. Cost per hospitalization was highest for all three conditions in the Medicaid group; the uninsured group had the lowest costs for all three conditions.
Unfortunately, the three conditions analyzed only comprise 8% of annual hospital discharges, so the findings cannot be generalized. Also, deaths occurring soon after hospital discharge were not included, and uninsured and Medicaid patients are likely to have more severe diseases, which, rather than insurance status, could account for the mortality differences.
Bottom line: In-hospital mortality and resource use for three common medical conditions vary significantly between privately insured and uninsured or Medicaid patients, highlighting the need to take measures to close this gap.
Citation: Hasan O, Orav EJ, LeRoi LS. Insurance status and hospital care for myocardial infarction, stroke, and pneumonia. J Hosp Med. 2010;5(8);452-459.
Warfarin Monotherapy Best in Prevention of Thromboembolic Events for Atrial Fibrillation Patients
Clinical question: Is there a benefit to adding an antiplatelet agent to warfarin for the prevention of thromboembolic stroke in atrial fibrillation?
Background: Many physicians prescribe various combinations of aspirin, clopidogrel, and warfarin, as these treatments are endorsed in guidelines and expert statements. The use of these medications, however, has not been studied in a setting large enough to understand the safety of these therapies.
Study design: Retrospective cohort.
Setting: All Danish hospitals.
Synopsis: All hospitalized patients in Denmark from 1997 to 2006 who were identified with new onset atrial fibrillation (n=118,606) were monitored for outcomes and the use of aspirin, clopidogrel, and warfarin. These patients were followed for a mean of 3.3 years with the primary endpoint being admission to a hospital for a diagnosis of bleeding and a secondary endpoint of stroke.
Bleeding occurred in 13,573 patients (11.4%). The incidence of bleeding was highest in the first 180 days and then leveled off. Hazard ratios were computed with warfarin monotherapy as a reference. Only the hazard ratio for aspirin monotherapy (0.93) was lower (confidence interval [CI] 0.88-0.98). The highest risk of bleeding was with the triple therapy warfarin-aspirin-clopidogrel, which had a hazard ratio of 3.70 (CI 2.89-4.76).
For strokes, the hazard ratio was slightly better for warfarin-clopidogrel (0.70), although the CI was wide at 0.35-1.4 compared to warfarin monotherapy as a reference. Hazard ratios for monotherapy with clopidogrel or aspirin, dual therapy, and triple therapy all were worse, ranging from 1.27 to 1.86.
Bottom line: Warfarin as a monotherapy might have a bleeding risk comparable to that of aspirin or clopidogrel alone, and prevents more strokes than various combinations of these medications.
Citation: Hansen ML, Sørensen R, Clausen MT, et al. Risk of bleeding with single, dual, or triple therapy with warfarin, aspirin, and clopidogrel in patients with atrial fibrillation. Arch Intern Med. 2010;170 (16):1433-1441.
Cognitive and Physical Function Declines in Elderly Severe Sepsis Survivors
Clinical question: Is there a change in cognitive and physical functioning after severe sepsis?
Background: Disability is associated with increased mortality, decreased quality of life, and increased burdens by families and healthcare costs. After severe sepsis, the lasting effects of debility have not been investigated in any large studies.
Study design: Prospective cohort.
Setting: Hospitalized Medicare patients participating in the Health and Retirement Study.
Synopsis: Patients (n=1194) were followed for a minimum of one year between 1998 and 2006. The outcomes were measured by multiple personal interviews before and after a severe sepsis episode. Cognitive impairment was measured using three validated questionnaires dependent upon age or if a proxy was the respondent. For functional limitations, a questionnaire concerning instrumental and basic activities of daily living was used.
Cognitive impairment for those with moderate to severe impairment increased to 16.7% from 6.1% after a sepsis episode with an odds ratio of 3.34 (95% confidence interval 1.53-7.25). There was no significant increase in nonsevere sepsis hospitalized comparison patients (n=5574). All survivors with severe sepsis had a functional decline of 1.5 activities. The comparison group had about a 0.4 activity decline. All of these deficits endured throughout the study.
The authors provide comments that there should be a system-based approach in preventing severe sepsis, its burdens, and its costs. Suggestions include preventing delirium, initiating better standards of care, and involving therapists earlier to prevent immobility.
Bottom line: Severe sepsis is independently associated with enduring cognitive and physical functional declines, which strain families and our healthcare system.
Citation: Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304(16):1787-1794.
Furosemide on Day of Elective Noncardiac Surgery Does Not Increase Risk of Intraoperative Hypotension
Clinical question: For patients chronically treated with loop diuretics, does withholding furosemide on the day of elective noncardiac surgery prevent intraoperative hypotension?
Background: Recent studies have questioned the safety of blood-pressure-lowering medications administered on the day of surgery. Beta-blockers have been associated with an increase in strokes and death perioperatively, and angiotensin receptor blockers (ARB) are frequently withheld on the day of surgery to avoid intraoperative hypotension. The effect of loop diuretics is uncertain.
Study design: Double-blind, randomized, placebo-controlled study.
Setting: Three North American university centers.
Synopsis: One hundred ninety-three patients were instructed to take furosemide or placebo on the day they underwent noncardiac surgery. The primary outcome measure was perioperative hypotension defined as a SBP <90 mmHg for more than five minutes, a 35% drop in the mean arterial blood pressure, or the need for a vasopressor agent. The number of cardiovascular complications (acute heart failure, acute coronary syndrome, arrhythmia, acute cerebrovascular event) and deaths also were analyzed.
Concerns have been raised that loop diuretics might predispose patients to a higher risk of intraoperative hypotension during noncardiac surgery. This trial showed no significant difference in the rates of intraoperative hypotension in patients who were administered furosemide versus those who were not. Although cardiovascular complications occurred more frequently in the furosemide group, the difference was not statistically significant.
Important limitations of the study were recognized. A larger population of patients could have revealed a statistically significant difference in cardiovascular outcomes in the furosemide group. Also, an anesthetic protocol was not utilized, which raises questions about the interaction of furosemide and effect on blood pressure with certain anesthetics.
Bottom line: Administering furosemide prior to surgery in chronic users does not appreciably increase the rate of intraoperative hypotension or cardiovascular events.
Citation: Khan NA, Campbell NR, Frost SD, et al. Risk of intraoperative hypotension with loop diuretics: a randomized controlled trial. Am J Med. 2010;123(11):1059e1-1059e8.
In This Edition
Literature at a Glance
A guide to this month’s studies
- Risk of adverse events with opioid use
- Drug of choice for outpatient treatment of cellulitis
- Preventing hospital falls
- Post-hospital outcomes based on status of PCP follow-up
- LOS, mortality, and readmission based on insurance
- Antiplatelets added to warfarin for atrial fibrillation.
- Cognitive effects of severe sepsis
- Effect of preoperative furosemide use
ED Visits Are Higher among Recipients of Chronic Opioid Therapy
Clinical question: Is there an association between the use of prescription opioids and adverse outcomes?
Background: Chronic opioid therapy is a common strategy for managing chronic, noncancer pain. There has been an increase in overdose deaths and ED visits (EDV) involving the use of prescription opioids.
Study design: Retrospective study from claims records.
Setting: Population in the Health Core Integrated Research Database, containing large, commercial insurance plans in 14 states, and Arkansas Medicaid.
Synopsis: Patients 18 and older without cancer diagnoses who used prescription opioids for at least 90 continuous days within a six-month period from 2000 to 2005 were examined for risk factors for EDVs and alcohol- or drug-related encounters (ADEs) in the 12 months following 90 days or more of prescribed opioids.
Patients with diagnoses of headache, back pain, and pre-existing substance-use disorders had significantly higher EDVs and ADEs. Opioid dose at morphine-equivalent doses over 120 mg per day doubled the risk of ADEs. The use of short-acting Schedule II opioids was associated with EDVs (relative risk, 1.09-1.74). The use of long-acting Schedule II opioids was strongly associated with ADEs (relative risk, 1.64-4.00).
Bottom line: In adults with noncancer pain prescribed opioids for 90 days or more, short-acting Schedule II opioid use was associated with an increased number of EDVs, and long-acting opioid use was associated with an increased number of ADEs. Minimizing Schedule II opioid prescription in these higher-risk patients might be prudent to increase patient safety.
Citation: Braden JB, Russo J, Fan MI, et al. Emergency department visits among recipients of chronic opioid therapy. Arch Intern Med. 2010; 170(16):1425-1432.
Empiric Outpatient Therapy with Trimethoprim-Sulfamethoxazole or Clindamycin Is Preferred for Cellulitis
Clinical question: What is the best empiric outpatient oral antibiotic treatment for cellulitis in areas with a high prevalence of community-associated MRSA infections?
Background: The increasing rates of community-associated MRSA skin and soft-tissue infections have raised concerns that such beta-lactams as cephalexin and other semisynthetic penicillins are not appropriate for empiric outpatient therapy for cellulitis.
Study design: Three-year, retrospective cohort study.
Setting: A teaching clinic of a tertiary-care medical center in Hawaii.
Synopsis: More than 540 patients with cellulitis were identified from January 2005 to December 2007. Of these, 139 patients were excluded for reasons such as hospitalization, surgical intervention, etc. In the final cohort of 405 patients, the three most commonly prescribed oral antibiotics were cephalexin (44%), trimethoprim-sulfamethoxazole (38%), and clindamycin (10%). Other antibiotics accounted for the remaining 8%.
MRSA was recovered in 62% of positive culture specimens. The success rate of trimethoprim-sulfamethoxazole was 91% vs. 74% in the cephalexin group (P<0.001). Clindamycin success rates were higher than those of cephalexin in patients who had subsequently confirmed MRSA infections (P=0.01) and moderately severe cellulitis (P=0.03) and were obese (P=0.04).
Bottom line: Antibiotics with activity against community-acquired MRSA (e.g. trimethroprim-sulfamethoxazole and clinidamycin) are the preferred empiric outpatient therapy for cellulitis in areas with a high prevalence of community-acquired MRSA.
Citation: Khawcharoenporn T, Tice A. Empiric outpatient therapy with trimethoprim-sulfamethoxazole, cephalexin, or clindamycin for cellulitis. Am J Med. 2010;123(10):942-950.
Patient-Specific Screening with Health Information Technology Prevents Falls
Clinical question: Does a fall-prevention toolkit using health information technology decrease patient falls in acute-care hospitals?
Background: Inpatient falls and fall-related injuries result in substantial morbidity and additional healthcare costs. While specific fall-prevention strategies were a longstanding target for intervention, little evidence exists to link them with decreased fall rates.
Study design: Cluster-randomized study.
Setting: Four urban hospitals in Massachusetts.
Synopsis: Comparing patient fall rates in four acute-care hospitals between units providing usual care (5,104 patients) and units using a health information technology (HIT)-linked fall prevention toolkit (5,160 patients), this study demonstrated significant fall reduction in older inpatients. The intervention integrated existing workflow and validated fall risk assessment (Morse Falls Scale) into an HIT software application that tailored fall-prevention interventions to patients’ specific fall risk determinants. The toolkit produced bed posters, patient education handouts, and plans of care communicating patient-specific alerts to key stakeholders.
The primary outcome was patient falls per 1,000 patient-days during the six-month intervention period. The number of patients with falls was significantly different (P=0.02) between control (n=87) and intervention (n=67) units. The toolkit prevented one fall per 862 patient-days.
This nonblinded study was limited by the fact that it was conducted in a single health system. The toolkit was not effective in patients less than 65 years of age. Additionally, the sample size did not have sufficient power to detect effectiveness in preventing repeat falls or falls with injury.
Bottom line: Patient-specific fall prevention strategy coupled with HIT reduces falls in older inpatients.
Citation: Dykes PC, Carroll DL, Hurley A, et al. Fall prevention in acute care hospitals: a randomized trial. JAMA. 2010;304(17):1912-1918.
Lack of Timely Outpatient Follow-Up Results in Higher Readmission Rates
Clinical question: Does timely primary-care-physician (PCP) follow-up improve outcomes and prevent hospital readmissions?
Background: Active PCP involvement is key to interventions aimed at reducing readmissions and ensuring effective ongoing patient care. Some studies suggest increased overall resource utilization when PCP follow-up occurs after hospitalization. Resource utilization and clinical outcomes after hospitalization related to timely PCP follow-up have not been adequately studied.
Study design: Prospective cohort.
Setting: An urban, academic, 425-bed tertiary-care center in Colorado.
Synopsis: From a convenience sample of 121 patients admitted to general medicine services during winter months, 65 patients completed the study. Demographics, diagnosis, payor source, and PCP information were collected upon enrollment. Post-discharge phone calls and patient surveys were used to determine follow-up and readmission status. Timely PCP follow-up was defined as a visit with a PCP or specialist related to the discharge diagnosis within four weeks of hospital discharge.
Thirty-day readmission rates and hospital length of stay were compared for those with timely PCP follow-up and those without. Less than half of general-medicine inpatients received timely PCP follow-up post-discharge. Lack of timely PCP follow-up was associated with younger age, a 10-fold increase in 30-day readmission for the same condition, and a trend toward longer length of stay. However, hospital readmission for any condition did not differ with lack of timely PCP follow-up.
This small, single-center study with convenience sample enrollment might not represent all medical inpatients or diagnoses. Determination of same-condition readmission was potentially subjective.
Bottom line: Patients who lack timely post-discharge follow-up have higher readmission rates for the same medical condition.
Citation: Misky GJ, Wald HL, Coleman EA. Post-hospitalization transitions: examining the effects of timing of primary care provider follow-up. J Hosp Med. 2010;5(7):392-397.
Compared with Uninsured and Medicaid Patients, Privately Insured Patients Admitted for Acute MI, Stroke, and Pneumonia Have Better Mortality Rates
Clinical question: Do outcomes for insured and underinsured patients vary for three of the most common medical conditions for which patients are hospitalized: acute myocardial infarction (AMI), stroke, and pneumonia?
Background: The ideal healthcare system would provide quality care to all individuals regardless of insurance status. Nevertheless, disparities in outcomes for the insured and underinsured or uninsured are well-documented in the outpatient setting but not as well in the inpatient setting. More needs to be done to address these potential disparities.
Study design: Retrospective database analysis.
Setting: Database including 20% of all U.S. community hospitals, including public hospitals, academic medical centers, and specialty hospitals.
Synopsis: This study utilized a database of 8 million discharges from more than 1,000 hospitals and isolated patients 18-64 years old (154,381 patients). Privately insured, uninsured, and Medicaid patients’ data were reviewed for in-hospital mortality, length of stay (LOS), and cost per hospitalization. The analysis took into account disease severity, comorbidities, and the proportion of underinsured patients receiving care in each hospital when insurance-related disparities were examined.
Compared with the privately insured, in-hospital mortality and LOS for AMI and stroke were significantly higher for uninsured and Medicaid patients. Among pneumonia patients, Medicaid patients had significantly higher in-hospital mortality and LOS than the other two groups. Cost per hospitalization was highest for all three conditions in the Medicaid group; the uninsured group had the lowest costs for all three conditions.
Unfortunately, the three conditions analyzed only comprise 8% of annual hospital discharges, so the findings cannot be generalized. Also, deaths occurring soon after hospital discharge were not included, and uninsured and Medicaid patients are likely to have more severe diseases, which, rather than insurance status, could account for the mortality differences.
Bottom line: In-hospital mortality and resource use for three common medical conditions vary significantly between privately insured and uninsured or Medicaid patients, highlighting the need to take measures to close this gap.
Citation: Hasan O, Orav EJ, LeRoi LS. Insurance status and hospital care for myocardial infarction, stroke, and pneumonia. J Hosp Med. 2010;5(8);452-459.
Warfarin Monotherapy Best in Prevention of Thromboembolic Events for Atrial Fibrillation Patients
Clinical question: Is there a benefit to adding an antiplatelet agent to warfarin for the prevention of thromboembolic stroke in atrial fibrillation?
Background: Many physicians prescribe various combinations of aspirin, clopidogrel, and warfarin, as these treatments are endorsed in guidelines and expert statements. The use of these medications, however, has not been studied in a setting large enough to understand the safety of these therapies.
Study design: Retrospective cohort.
Setting: All Danish hospitals.
Synopsis: All hospitalized patients in Denmark from 1997 to 2006 who were identified with new onset atrial fibrillation (n=118,606) were monitored for outcomes and the use of aspirin, clopidogrel, and warfarin. These patients were followed for a mean of 3.3 years with the primary endpoint being admission to a hospital for a diagnosis of bleeding and a secondary endpoint of stroke.
Bleeding occurred in 13,573 patients (11.4%). The incidence of bleeding was highest in the first 180 days and then leveled off. Hazard ratios were computed with warfarin monotherapy as a reference. Only the hazard ratio for aspirin monotherapy (0.93) was lower (confidence interval [CI] 0.88-0.98). The highest risk of bleeding was with the triple therapy warfarin-aspirin-clopidogrel, which had a hazard ratio of 3.70 (CI 2.89-4.76).
For strokes, the hazard ratio was slightly better for warfarin-clopidogrel (0.70), although the CI was wide at 0.35-1.4 compared to warfarin monotherapy as a reference. Hazard ratios for monotherapy with clopidogrel or aspirin, dual therapy, and triple therapy all were worse, ranging from 1.27 to 1.86.
Bottom line: Warfarin as a monotherapy might have a bleeding risk comparable to that of aspirin or clopidogrel alone, and prevents more strokes than various combinations of these medications.
Citation: Hansen ML, Sørensen R, Clausen MT, et al. Risk of bleeding with single, dual, or triple therapy with warfarin, aspirin, and clopidogrel in patients with atrial fibrillation. Arch Intern Med. 2010;170 (16):1433-1441.
Cognitive and Physical Function Declines in Elderly Severe Sepsis Survivors
Clinical question: Is there a change in cognitive and physical functioning after severe sepsis?
Background: Disability is associated with increased mortality, decreased quality of life, and increased burdens by families and healthcare costs. After severe sepsis, the lasting effects of debility have not been investigated in any large studies.
Study design: Prospective cohort.
Setting: Hospitalized Medicare patients participating in the Health and Retirement Study.
Synopsis: Patients (n=1194) were followed for a minimum of one year between 1998 and 2006. The outcomes were measured by multiple personal interviews before and after a severe sepsis episode. Cognitive impairment was measured using three validated questionnaires dependent upon age or if a proxy was the respondent. For functional limitations, a questionnaire concerning instrumental and basic activities of daily living was used.
Cognitive impairment for those with moderate to severe impairment increased to 16.7% from 6.1% after a sepsis episode with an odds ratio of 3.34 (95% confidence interval 1.53-7.25). There was no significant increase in nonsevere sepsis hospitalized comparison patients (n=5574). All survivors with severe sepsis had a functional decline of 1.5 activities. The comparison group had about a 0.4 activity decline. All of these deficits endured throughout the study.
The authors provide comments that there should be a system-based approach in preventing severe sepsis, its burdens, and its costs. Suggestions include preventing delirium, initiating better standards of care, and involving therapists earlier to prevent immobility.
Bottom line: Severe sepsis is independently associated with enduring cognitive and physical functional declines, which strain families and our healthcare system.
Citation: Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304(16):1787-1794.
Furosemide on Day of Elective Noncardiac Surgery Does Not Increase Risk of Intraoperative Hypotension
Clinical question: For patients chronically treated with loop diuretics, does withholding furosemide on the day of elective noncardiac surgery prevent intraoperative hypotension?
Background: Recent studies have questioned the safety of blood-pressure-lowering medications administered on the day of surgery. Beta-blockers have been associated with an increase in strokes and death perioperatively, and angiotensin receptor blockers (ARB) are frequently withheld on the day of surgery to avoid intraoperative hypotension. The effect of loop diuretics is uncertain.
Study design: Double-blind, randomized, placebo-controlled study.
Setting: Three North American university centers.
Synopsis: One hundred ninety-three patients were instructed to take furosemide or placebo on the day they underwent noncardiac surgery. The primary outcome measure was perioperative hypotension defined as a SBP <90 mmHg for more than five minutes, a 35% drop in the mean arterial blood pressure, or the need for a vasopressor agent. The number of cardiovascular complications (acute heart failure, acute coronary syndrome, arrhythmia, acute cerebrovascular event) and deaths also were analyzed.
Concerns have been raised that loop diuretics might predispose patients to a higher risk of intraoperative hypotension during noncardiac surgery. This trial showed no significant difference in the rates of intraoperative hypotension in patients who were administered furosemide versus those who were not. Although cardiovascular complications occurred more frequently in the furosemide group, the difference was not statistically significant.
Important limitations of the study were recognized. A larger population of patients could have revealed a statistically significant difference in cardiovascular outcomes in the furosemide group. Also, an anesthetic protocol was not utilized, which raises questions about the interaction of furosemide and effect on blood pressure with certain anesthetics.
Bottom line: Administering furosemide prior to surgery in chronic users does not appreciably increase the rate of intraoperative hypotension or cardiovascular events.
Citation: Khan NA, Campbell NR, Frost SD, et al. Risk of intraoperative hypotension with loop diuretics: a randomized controlled trial. Am J Med. 2010;123(11):1059e1-1059e8.
CPT 2011 Update
In the past, observation services typically did not exceed 24 hours or two calendar days. However, changes in healthcare policy coupled with the impetus to reduce wasteful spending have spurred an atmosphere of scrutiny over hospital admissions. Sometimes there are discrepancies between a hospital’s utilization review committee and a payor’s utilization review committee in determining the appropriateness of healthcare services and supplies, in accordance with each party’s definition of medical necessity. This situation has caused an increase in both the number and cost of observation stays.
In response, subsequent observation-care codes (99224-99226) were developed and published in the 2011 edition of Current Procedural Terminology (CPT).1
Codes and Their Uses
CPT outlines three subsequent observation care codes:
- 99224: Subsequent observation care, per day, for the evaluation and management (E/M) of a patient, which requires at least two of these three key components: problem-focused interval history; problem-focused examination; and medical decision-making that is straightforward or of low complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is stable, recovering, or improving. Physicians typically spend 15 minutes at the bedside and on the patient’s hospital floor or unit.
- 99225: Subsequent observation care, per day, for the E/M of a patient, which requires at least two of these three key components: expanded problem focused interval history; expanded problem focused examination; and medical decision-making of moderate complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is responding inadequately to therapy or has developed a minor complication. Physicians typically spend 25 minutes at the bedside and on the patient’s hospital floor or unit.
- 99226: Subsequent observation care, per day, for the E/M of a patient, which requires at least two of these three key components: detailed interval history; detailed examination; and medical decision-making of high complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is unstable or has developed a significant complication or a significant new problem. Physicians typically spend 35 minutes at the bedside and on the patient’s hospital floor or unit.
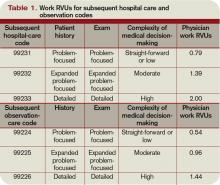
Subsequent observation-care codes replicate the key components and time requirements established for subsequent hospital care services (99231-99233). However, the relative value units (RVUs) of physician work associated with subsequent observation care are not weighted equally (see Table 1, below). Subsequent observation care is a less-intense service, and therefore is valued at a lesser rate.
The attending of record writes the orders to admit the patient to observation (OBS); indicates the reason for the stay; outlines the plan of care; and manages the patient during the stay. Specialists typically are called onto an OBS case for their opinion/advice (i.e. consultants) but do not function as the attending of record.
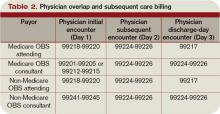
According to CPT 2011, subsequent OBS care codes can be reported by both the attending physician of record and specialists who provide medically necessary, nonoverlapping care to patients on any day other than the admission or discharge day (see Table 2, above). At press time, CMS and private payors had not provided written clarification on the use of subsequent observation-care codes. Therefore, it is imperative to monitor payments, denials, and policy clarifications providing further billing instruction.
On the Horizon
Prior reporting guidelines required the reporting of subsequent observation-care days with established outpatient codes (99212-99215). Some member plans insisted on referrals for all outpatient visits regardless nature of the service. Without the mandated referral for established patient visits performed in the observation setting, physician services were denied for coverage.
The creation of subsequent observation codes might play a role in decreasing these denials. Be sure to review the private payors’ fee schedules for inclusion of 99224-99226 codes. If missing, contact the payor or include it as an agenda item during your contract negotiations.
For more information on observation care services, check out “Observation Care” in the July 2010 issue of The Hospitalist. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is faculty for SHM’s inpatient coding course.
References
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology: Professional Edition. Chicago: American Medical Association Press; 2011.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.8. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 16, 2011.
In the past, observation services typically did not exceed 24 hours or two calendar days. However, changes in healthcare policy coupled with the impetus to reduce wasteful spending have spurred an atmosphere of scrutiny over hospital admissions. Sometimes there are discrepancies between a hospital’s utilization review committee and a payor’s utilization review committee in determining the appropriateness of healthcare services and supplies, in accordance with each party’s definition of medical necessity. This situation has caused an increase in both the number and cost of observation stays.
In response, subsequent observation-care codes (99224-99226) were developed and published in the 2011 edition of Current Procedural Terminology (CPT).1
Codes and Their Uses
CPT outlines three subsequent observation care codes:
- 99224: Subsequent observation care, per day, for the evaluation and management (E/M) of a patient, which requires at least two of these three key components: problem-focused interval history; problem-focused examination; and medical decision-making that is straightforward or of low complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is stable, recovering, or improving. Physicians typically spend 15 minutes at the bedside and on the patient’s hospital floor or unit.
- 99225: Subsequent observation care, per day, for the E/M of a patient, which requires at least two of these three key components: expanded problem focused interval history; expanded problem focused examination; and medical decision-making of moderate complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is responding inadequately to therapy or has developed a minor complication. Physicians typically spend 25 minutes at the bedside and on the patient’s hospital floor or unit.
- 99226: Subsequent observation care, per day, for the E/M of a patient, which requires at least two of these three key components: detailed interval history; detailed examination; and medical decision-making of high complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is unstable or has developed a significant complication or a significant new problem. Physicians typically spend 35 minutes at the bedside and on the patient’s hospital floor or unit.
Subsequent observation-care codes replicate the key components and time requirements established for subsequent hospital care services (99231-99233). However, the relative value units (RVUs) of physician work associated with subsequent observation care are not weighted equally (see Table 1, below). Subsequent observation care is a less-intense service, and therefore is valued at a lesser rate.
The attending of record writes the orders to admit the patient to observation (OBS); indicates the reason for the stay; outlines the plan of care; and manages the patient during the stay. Specialists typically are called onto an OBS case for their opinion/advice (i.e. consultants) but do not function as the attending of record.
According to CPT 2011, subsequent OBS care codes can be reported by both the attending physician of record and specialists who provide medically necessary, nonoverlapping care to patients on any day other than the admission or discharge day (see Table 2, above). At press time, CMS and private payors had not provided written clarification on the use of subsequent observation-care codes. Therefore, it is imperative to monitor payments, denials, and policy clarifications providing further billing instruction.
On the Horizon
Prior reporting guidelines required the reporting of subsequent observation-care days with established outpatient codes (99212-99215). Some member plans insisted on referrals for all outpatient visits regardless nature of the service. Without the mandated referral for established patient visits performed in the observation setting, physician services were denied for coverage.
The creation of subsequent observation codes might play a role in decreasing these denials. Be sure to review the private payors’ fee schedules for inclusion of 99224-99226 codes. If missing, contact the payor or include it as an agenda item during your contract negotiations.
For more information on observation care services, check out “Observation Care” in the July 2010 issue of The Hospitalist. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is faculty for SHM’s inpatient coding course.
References
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology: Professional Edition. Chicago: American Medical Association Press; 2011.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.8. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 16, 2011.
In the past, observation services typically did not exceed 24 hours or two calendar days. However, changes in healthcare policy coupled with the impetus to reduce wasteful spending have spurred an atmosphere of scrutiny over hospital admissions. Sometimes there are discrepancies between a hospital’s utilization review committee and a payor’s utilization review committee in determining the appropriateness of healthcare services and supplies, in accordance with each party’s definition of medical necessity. This situation has caused an increase in both the number and cost of observation stays.
In response, subsequent observation-care codes (99224-99226) were developed and published in the 2011 edition of Current Procedural Terminology (CPT).1
Codes and Their Uses
CPT outlines three subsequent observation care codes:
- 99224: Subsequent observation care, per day, for the evaluation and management (E/M) of a patient, which requires at least two of these three key components: problem-focused interval history; problem-focused examination; and medical decision-making that is straightforward or of low complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is stable, recovering, or improving. Physicians typically spend 15 minutes at the bedside and on the patient’s hospital floor or unit.
- 99225: Subsequent observation care, per day, for the E/M of a patient, which requires at least two of these three key components: expanded problem focused interval history; expanded problem focused examination; and medical decision-making of moderate complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is responding inadequately to therapy or has developed a minor complication. Physicians typically spend 25 minutes at the bedside and on the patient’s hospital floor or unit.
- 99226: Subsequent observation care, per day, for the E/M of a patient, which requires at least two of these three key components: detailed interval history; detailed examination; and medical decision-making of high complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is unstable or has developed a significant complication or a significant new problem. Physicians typically spend 35 minutes at the bedside and on the patient’s hospital floor or unit.
Subsequent observation-care codes replicate the key components and time requirements established for subsequent hospital care services (99231-99233). However, the relative value units (RVUs) of physician work associated with subsequent observation care are not weighted equally (see Table 1, below). Subsequent observation care is a less-intense service, and therefore is valued at a lesser rate.
The attending of record writes the orders to admit the patient to observation (OBS); indicates the reason for the stay; outlines the plan of care; and manages the patient during the stay. Specialists typically are called onto an OBS case for their opinion/advice (i.e. consultants) but do not function as the attending of record.
According to CPT 2011, subsequent OBS care codes can be reported by both the attending physician of record and specialists who provide medically necessary, nonoverlapping care to patients on any day other than the admission or discharge day (see Table 2, above). At press time, CMS and private payors had not provided written clarification on the use of subsequent observation-care codes. Therefore, it is imperative to monitor payments, denials, and policy clarifications providing further billing instruction.
On the Horizon
Prior reporting guidelines required the reporting of subsequent observation-care days with established outpatient codes (99212-99215). Some member plans insisted on referrals for all outpatient visits regardless nature of the service. Without the mandated referral for established patient visits performed in the observation setting, physician services were denied for coverage.
The creation of subsequent observation codes might play a role in decreasing these denials. Be sure to review the private payors’ fee schedules for inclusion of 99224-99226 codes. If missing, contact the payor or include it as an agenda item during your contract negotiations.
For more information on observation care services, check out “Observation Care” in the July 2010 issue of The Hospitalist. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is faculty for SHM’s inpatient coding course.
References
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology: Professional Edition. Chicago: American Medical Association Press; 2011.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.8. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 16, 2011.
Passion for Patient Care
When William D. Atchley Jr., MD, FACP, SFHM, left private practice for hospital medicine in 1995, he didn’t realize he was helping to make history. Dr. Atchley was practicing with an internal-medicine multispecialty group when a medical school withdrew its residency program from the community hospital next door. Soon after, physicians in the group began experiencing frequent disruptions in order to care for a handful of hospitalized patients.
Dr. Atchley and two colleagues, all of whom enjoyed the hospital setting, solved the problem by forming an inpatient rounding team at Sentara Leigh Hospital in Norfolk, Va. They believe it was the first hospitalist program in Virginia.
“When we first started doing this, we were looking at each other saying, ‘Is this something for the long run … or is it going to be something that is a flash in the pan?’ ” says Dr. Atchley, chief of the Division of Hospital Medicine at Sentara Medical Group, which operates hospitalist programs at five sites in southeastern Virginia. “If you had asked me to look into a crystal ball, I would not have projected hospital medicine would have grown so quickly. It truly is phenomenal, and it’s been an exciting ride. It was great to be on the ground floor of this, and it’s been nice to see how things have evolved.”

Question: You studied biomedical engineering prior to medical school. Are there similarities between that field and HM?
Answer: Engineering teaches you how to approach problem-solving. That’s particularly helpful with some of the system issues we talk about, such as dealing with throughput or applications of electronic medical records and computerized physician order entry. It’s given me a good background to understand issues that come up regarding quality and patient safety, and trying to take a systemwide viewpoint about looking at how care is delivered.
Q: What’s the biggest change you’ve seen in HM over the past 16 years?
A: The job I had in 1995 is vastly different from the job I have now. At that time, it was all about taking care of internal-medicine adult patients. We’ve seen the evolution of surgical comanagement, and hospitalists have truly become leaders of change in terms of how care is being delivered in the hospital. Things like patient safety, quality, and learning to deal with the limited resources we have, in terms of the cost of healthcare, were not even on the radar screen 16 years ago.
Q: Why is it important for you to continue seeing patients?
A: To have validity with your fellow hospitalists who are working in the trenches. You can only appreciate what their day-to-day challenges are when you roll up your sleeves and you’re out there with them. I think it gives me “street cred” with them. I still understand the things that are great about the job, but at the same time, I see the things that are frustrating about the job.
Q: What is your biggest professional reward?
A: Being actively engaged in SHM. I served on its board of directors, and I’ve served as secretary and treasurer. I continue to be active in the society. I was honored to be elected as a senior fellow (SFHM) in the organization.
Q: What did it mean to you to be elected a senior fellow?
A: I’m very humbled and gracious to the organization. That’s been my greatest professional achievement.
Q: You also serve as a facilitator with SHM’s Leadership Academy. Why are you so passionate about that program?
A: It gives hospitalists the essential tools they need to be able to roll up their sleeves and start tackling problems at their hospitals. It’s a great opportunity for anybody who is thinking about running a group or taking a leading role in a healthcare system.
Q: What is your biggest professional challenge?
A: It’s learning to be able to lead the next generation of hospitalists, to get them to be as enthusiastic about practicing hospital medicine as I am.
Q: Why is that so challenging?
A: If you have ever practiced in a traditional general internal-medicine practice (office-based), and then you become a hospitalist, you don’t want to go back to office-based. It’s more difficult to generate that enthusiasm for what hospital medicine is all about to people who are just coming on.
Q: Have you found a strategy that works?
A: It’s much easier said than done. It’s really about getting them energized and getting them excited about what they’re doing. Part of that is explaining it’s about more than just the patient in front of them. The hospital really is their site of practice, and there are opportunities for them to advance. If they want to do research or if they want to be involved with quality or patient safety, the opportunities are unlimited.
Q: Do you encourage the next generation of hospitalists to seek out committee assignments, research, or other opportunities outside of clinical work?
A: It’s definitely something for them to embrace. What’s important is crafting a type of staffing or schedule model that allows them to do clinical work but at the same time have a protected time to do their committee work.
In the old model I grew up with, doctors basically did committee work before they started seeing patients or after they were finished. There needs to be time carved out so they can be focused on that and don’t have to do it on the fly. … That’s what makes things successful with hospital medicine. There are programs across the country that (protect physician time), and they serve as a model for what I think our profession should be.
Q: What’s next professionally?
A: Right now, I’m thinking about what I want to be doing for the next 10 years. Is it going back and just doing clinical work? Is it continuing to be the clinical chief, or is it being involved with other things systemwide? I’ll certainly continue to be actively engaged on a national level with SHM, because that’s my passion. But after being a hospitalist for 16 years, I’m pausing and reflecting on what I’ve been doing, what my options are, and what I want to do for the remainder of the time before I retire. TH
Mark Leiser is a freelance writer based in New Jersey.
When William D. Atchley Jr., MD, FACP, SFHM, left private practice for hospital medicine in 1995, he didn’t realize he was helping to make history. Dr. Atchley was practicing with an internal-medicine multispecialty group when a medical school withdrew its residency program from the community hospital next door. Soon after, physicians in the group began experiencing frequent disruptions in order to care for a handful of hospitalized patients.
Dr. Atchley and two colleagues, all of whom enjoyed the hospital setting, solved the problem by forming an inpatient rounding team at Sentara Leigh Hospital in Norfolk, Va. They believe it was the first hospitalist program in Virginia.
“When we first started doing this, we were looking at each other saying, ‘Is this something for the long run … or is it going to be something that is a flash in the pan?’ ” says Dr. Atchley, chief of the Division of Hospital Medicine at Sentara Medical Group, which operates hospitalist programs at five sites in southeastern Virginia. “If you had asked me to look into a crystal ball, I would not have projected hospital medicine would have grown so quickly. It truly is phenomenal, and it’s been an exciting ride. It was great to be on the ground floor of this, and it’s been nice to see how things have evolved.”

Question: You studied biomedical engineering prior to medical school. Are there similarities between that field and HM?
Answer: Engineering teaches you how to approach problem-solving. That’s particularly helpful with some of the system issues we talk about, such as dealing with throughput or applications of electronic medical records and computerized physician order entry. It’s given me a good background to understand issues that come up regarding quality and patient safety, and trying to take a systemwide viewpoint about looking at how care is delivered.
Q: What’s the biggest change you’ve seen in HM over the past 16 years?
A: The job I had in 1995 is vastly different from the job I have now. At that time, it was all about taking care of internal-medicine adult patients. We’ve seen the evolution of surgical comanagement, and hospitalists have truly become leaders of change in terms of how care is being delivered in the hospital. Things like patient safety, quality, and learning to deal with the limited resources we have, in terms of the cost of healthcare, were not even on the radar screen 16 years ago.
Q: Why is it important for you to continue seeing patients?
A: To have validity with your fellow hospitalists who are working in the trenches. You can only appreciate what their day-to-day challenges are when you roll up your sleeves and you’re out there with them. I think it gives me “street cred” with them. I still understand the things that are great about the job, but at the same time, I see the things that are frustrating about the job.
Q: What is your biggest professional reward?
A: Being actively engaged in SHM. I served on its board of directors, and I’ve served as secretary and treasurer. I continue to be active in the society. I was honored to be elected as a senior fellow (SFHM) in the organization.
Q: What did it mean to you to be elected a senior fellow?
A: I’m very humbled and gracious to the organization. That’s been my greatest professional achievement.
Q: You also serve as a facilitator with SHM’s Leadership Academy. Why are you so passionate about that program?
A: It gives hospitalists the essential tools they need to be able to roll up their sleeves and start tackling problems at their hospitals. It’s a great opportunity for anybody who is thinking about running a group or taking a leading role in a healthcare system.
Q: What is your biggest professional challenge?
A: It’s learning to be able to lead the next generation of hospitalists, to get them to be as enthusiastic about practicing hospital medicine as I am.
Q: Why is that so challenging?
A: If you have ever practiced in a traditional general internal-medicine practice (office-based), and then you become a hospitalist, you don’t want to go back to office-based. It’s more difficult to generate that enthusiasm for what hospital medicine is all about to people who are just coming on.
Q: Have you found a strategy that works?
A: It’s much easier said than done. It’s really about getting them energized and getting them excited about what they’re doing. Part of that is explaining it’s about more than just the patient in front of them. The hospital really is their site of practice, and there are opportunities for them to advance. If they want to do research or if they want to be involved with quality or patient safety, the opportunities are unlimited.
Q: Do you encourage the next generation of hospitalists to seek out committee assignments, research, or other opportunities outside of clinical work?
A: It’s definitely something for them to embrace. What’s important is crafting a type of staffing or schedule model that allows them to do clinical work but at the same time have a protected time to do their committee work.
In the old model I grew up with, doctors basically did committee work before they started seeing patients or after they were finished. There needs to be time carved out so they can be focused on that and don’t have to do it on the fly. … That’s what makes things successful with hospital medicine. There are programs across the country that (protect physician time), and they serve as a model for what I think our profession should be.
Q: What’s next professionally?
A: Right now, I’m thinking about what I want to be doing for the next 10 years. Is it going back and just doing clinical work? Is it continuing to be the clinical chief, or is it being involved with other things systemwide? I’ll certainly continue to be actively engaged on a national level with SHM, because that’s my passion. But after being a hospitalist for 16 years, I’m pausing and reflecting on what I’ve been doing, what my options are, and what I want to do for the remainder of the time before I retire. TH
Mark Leiser is a freelance writer based in New Jersey.
When William D. Atchley Jr., MD, FACP, SFHM, left private practice for hospital medicine in 1995, he didn’t realize he was helping to make history. Dr. Atchley was practicing with an internal-medicine multispecialty group when a medical school withdrew its residency program from the community hospital next door. Soon after, physicians in the group began experiencing frequent disruptions in order to care for a handful of hospitalized patients.
Dr. Atchley and two colleagues, all of whom enjoyed the hospital setting, solved the problem by forming an inpatient rounding team at Sentara Leigh Hospital in Norfolk, Va. They believe it was the first hospitalist program in Virginia.
“When we first started doing this, we were looking at each other saying, ‘Is this something for the long run … or is it going to be something that is a flash in the pan?’ ” says Dr. Atchley, chief of the Division of Hospital Medicine at Sentara Medical Group, which operates hospitalist programs at five sites in southeastern Virginia. “If you had asked me to look into a crystal ball, I would not have projected hospital medicine would have grown so quickly. It truly is phenomenal, and it’s been an exciting ride. It was great to be on the ground floor of this, and it’s been nice to see how things have evolved.”

Question: You studied biomedical engineering prior to medical school. Are there similarities between that field and HM?
Answer: Engineering teaches you how to approach problem-solving. That’s particularly helpful with some of the system issues we talk about, such as dealing with throughput or applications of electronic medical records and computerized physician order entry. It’s given me a good background to understand issues that come up regarding quality and patient safety, and trying to take a systemwide viewpoint about looking at how care is delivered.
Q: What’s the biggest change you’ve seen in HM over the past 16 years?
A: The job I had in 1995 is vastly different from the job I have now. At that time, it was all about taking care of internal-medicine adult patients. We’ve seen the evolution of surgical comanagement, and hospitalists have truly become leaders of change in terms of how care is being delivered in the hospital. Things like patient safety, quality, and learning to deal with the limited resources we have, in terms of the cost of healthcare, were not even on the radar screen 16 years ago.
Q: Why is it important for you to continue seeing patients?
A: To have validity with your fellow hospitalists who are working in the trenches. You can only appreciate what their day-to-day challenges are when you roll up your sleeves and you’re out there with them. I think it gives me “street cred” with them. I still understand the things that are great about the job, but at the same time, I see the things that are frustrating about the job.
Q: What is your biggest professional reward?
A: Being actively engaged in SHM. I served on its board of directors, and I’ve served as secretary and treasurer. I continue to be active in the society. I was honored to be elected as a senior fellow (SFHM) in the organization.
Q: What did it mean to you to be elected a senior fellow?
A: I’m very humbled and gracious to the organization. That’s been my greatest professional achievement.
Q: You also serve as a facilitator with SHM’s Leadership Academy. Why are you so passionate about that program?
A: It gives hospitalists the essential tools they need to be able to roll up their sleeves and start tackling problems at their hospitals. It’s a great opportunity for anybody who is thinking about running a group or taking a leading role in a healthcare system.
Q: What is your biggest professional challenge?
A: It’s learning to be able to lead the next generation of hospitalists, to get them to be as enthusiastic about practicing hospital medicine as I am.
Q: Why is that so challenging?
A: If you have ever practiced in a traditional general internal-medicine practice (office-based), and then you become a hospitalist, you don’t want to go back to office-based. It’s more difficult to generate that enthusiasm for what hospital medicine is all about to people who are just coming on.
Q: Have you found a strategy that works?
A: It’s much easier said than done. It’s really about getting them energized and getting them excited about what they’re doing. Part of that is explaining it’s about more than just the patient in front of them. The hospital really is their site of practice, and there are opportunities for them to advance. If they want to do research or if they want to be involved with quality or patient safety, the opportunities are unlimited.
Q: Do you encourage the next generation of hospitalists to seek out committee assignments, research, or other opportunities outside of clinical work?
A: It’s definitely something for them to embrace. What’s important is crafting a type of staffing or schedule model that allows them to do clinical work but at the same time have a protected time to do their committee work.
In the old model I grew up with, doctors basically did committee work before they started seeing patients or after they were finished. There needs to be time carved out so they can be focused on that and don’t have to do it on the fly. … That’s what makes things successful with hospital medicine. There are programs across the country that (protect physician time), and they serve as a model for what I think our profession should be.
Q: What’s next professionally?
A: Right now, I’m thinking about what I want to be doing for the next 10 years. Is it going back and just doing clinical work? Is it continuing to be the clinical chief, or is it being involved with other things systemwide? I’ll certainly continue to be actively engaged on a national level with SHM, because that’s my passion. But after being a hospitalist for 16 years, I’m pausing and reflecting on what I’ve been doing, what my options are, and what I want to do for the remainder of the time before I retire. TH
Mark Leiser is a freelance writer based in New Jersey.
Flexibility Is King
Michael Radzienda, MD, FHM, once worked in a hospitalist program in which physicians were scheduled 30 days straight on clinical duty and 30 days off clinical duty. Although it sounds harsh by today’s standards, that job was so satisfying, he says, the schedule never felt like a burden. Conversely, he’s seen hospitalists work five days on and five days off, and the job was treacherous.
His point: Work schedules are just one influential piece of the job satisfaction pie.
“Satisfaction has more to do with work relationships and opportunities for growth,” says Dr. Radzienda, chief of hospital medicine and director of hospital medicine service at Medical College of Wisconsin/Froedtert Memorial Lutheran General Hospital in Milwaukee.
Shift-based staffing has become the norm, as more than 70% of hospitalist groups use a shift-based staffing model, according to the State of Hospital Medicine: 2010 Report Based on 2009 Data.1 That figure is up 40% from SHM’s 2005-2006 survey. Conversely, the number of HM groups employing call-based and hybrid (some shift, some call) coverage is declining—2.8% of groups employ call-based schedules, and 26.9% use a hybrid schedule. Those figures have dropped significantly from the 2005-2006 report, from 25% and 35%, respectively.
If you are going to make HM a career, you’ll need time to be with your family and pursue other interests, Dr. Radzienda says. As HM groups turn to more shift-based models, in which hospitalists work a set number of predetermined shifts and have no call responsibility, the challenge is setting a schedule that balances productivity and quality time off.
Fixed = Inflexible
The most popular way to schedule is through blocks of five days on/five days off (5/5) or seven days on/seven days off (7/7), in which hospitalists work 12 or 14 hours at a time, says Troy Ahlstrom, MD, FHM, a member of SHM’s Practice Analysis Committee and CFO of Hospitalists of Northern Michigan, a hospitalist-owned and -managed group based in Traverse City, Mich. Many HM groups employ this model because it’s easy to schedule and is attractive to residents who want a fixed schedule. But from a career satisfaction standpoint, the 5/5 and 7/7 schedule models present their own issues.
Fairness is the first potential pitfall. If all of the physicians in a group work the same schedule, they all have to log the same number of shifts and receive the same compensation. This leaves little to no wiggle room for hospitalists who want to make more money by picking up more shifts or those who want to work fewer shifts, Dr. Ahlstrom says. “People have different income goals,” he adds.
Second, physicians have to see the same number of patients throughout the day. This doesn’t take into consideration the reality that some hospitalists naturally work faster than others, thereby forcing the slower-paced doctors to keep up with an imposed patient load. “Invariably, no matter what you do, people are different,” Dr. Ahlstrom says.
Another consideration is that when physicians are working 12 to 14 hours a day, essentially they have no time for activities other than work and sleep, which doesn’t match the realities of life. Inevitably, things in personal lives crop up, which leads to swapping shifts that the group scheduler doesn’t know about or overloading the scheduler with shift-change requests, Dr. Ahlstrom explains.
Additionally, 7/7 schedules and their ilk squeeze a year’s worth of work into a compressed time frame, which can lead to intense stress and burnout, says John Nelson, MD, FACP, MHM, director of the hospitalist practice at Overlake Hospital in Bellevue, Wash., SHM co-founder, and practice management columnist for The Hospitalist. “Maximizing the number of days off is not the holy grail,” he says. “If you choose to shut your life down on days that you work, that is going to be toxic.”
Flexibility Equates to Fairness
Dr. Nelson has long advocated a flexible shift schedule that accommodates individual preferences by giving physicians in the group autonomy in deciding how much or how little they want to work. While the group as a whole has to get all the work done, the flexibility comes from one physician taking more shifts as another takes less.
Dr. Radzienda tries to create teams within his group by pairing hospitalists with similar scheduling preferences. For example, he might have a pair working 5/5 and another working 14/14. “Up front, it takes a lot of work, but once you template it out, it becomes a good strategy,” he says.
He also strives to build robust backup plans and jeopardy models (see “Surge Protection,” September 2010, p. 43) into the schedule for short-notice callouts, as you never know when a hospitalist will need to miss a day or two because of illness or a family emergency. “Psychologically, it helps to know that you don’t have to be a hero if you’re ill or emotionally strained,” Dr. Radzienda says.
Dr. Ahlstrom agrees that a flex-schedule strategy has a positive impact on hospitalists’ career satisfaction and longevity. He suggests hospitalists be allowed to specify how many patients they want to see and be compensated according to their workload through built-in bonuses for physicians who work more. Dr. Nelson suggests paying hospitalists per relative value unit (RVU) of work. “I think hospitalists would like it and find it liberating to be paid on production,” he says.
An added bonus to flexible work hours and patient load, according to Dr. Ahlstrom, is that pay difference “will lead to a far more collegial atmosphere, because physicians know they are getting compensated fairly for the amount of work done.”
Another advantage of a flexible schedule is hospitalists knowing they have the option of ramping up or scaling back the number of shifts they work, Dr. Ahlstrom says—for example, a physician who wants to reduce shifts in order to coach his daughter’s softball team or have Friday nights off to watch her son play high school football.
“You prevent burnout by allowing people to change their work schedule depending on what’s going on in their life,” Dr. Ahlstrom says. TH
Lisa Ryan is a freelance writer based in New Jersey.
Michael Radzienda, MD, FHM, once worked in a hospitalist program in which physicians were scheduled 30 days straight on clinical duty and 30 days off clinical duty. Although it sounds harsh by today’s standards, that job was so satisfying, he says, the schedule never felt like a burden. Conversely, he’s seen hospitalists work five days on and five days off, and the job was treacherous.
His point: Work schedules are just one influential piece of the job satisfaction pie.
“Satisfaction has more to do with work relationships and opportunities for growth,” says Dr. Radzienda, chief of hospital medicine and director of hospital medicine service at Medical College of Wisconsin/Froedtert Memorial Lutheran General Hospital in Milwaukee.
Shift-based staffing has become the norm, as more than 70% of hospitalist groups use a shift-based staffing model, according to the State of Hospital Medicine: 2010 Report Based on 2009 Data.1 That figure is up 40% from SHM’s 2005-2006 survey. Conversely, the number of HM groups employing call-based and hybrid (some shift, some call) coverage is declining—2.8% of groups employ call-based schedules, and 26.9% use a hybrid schedule. Those figures have dropped significantly from the 2005-2006 report, from 25% and 35%, respectively.
If you are going to make HM a career, you’ll need time to be with your family and pursue other interests, Dr. Radzienda says. As HM groups turn to more shift-based models, in which hospitalists work a set number of predetermined shifts and have no call responsibility, the challenge is setting a schedule that balances productivity and quality time off.
Fixed = Inflexible
The most popular way to schedule is through blocks of five days on/five days off (5/5) or seven days on/seven days off (7/7), in which hospitalists work 12 or 14 hours at a time, says Troy Ahlstrom, MD, FHM, a member of SHM’s Practice Analysis Committee and CFO of Hospitalists of Northern Michigan, a hospitalist-owned and -managed group based in Traverse City, Mich. Many HM groups employ this model because it’s easy to schedule and is attractive to residents who want a fixed schedule. But from a career satisfaction standpoint, the 5/5 and 7/7 schedule models present their own issues.
Fairness is the first potential pitfall. If all of the physicians in a group work the same schedule, they all have to log the same number of shifts and receive the same compensation. This leaves little to no wiggle room for hospitalists who want to make more money by picking up more shifts or those who want to work fewer shifts, Dr. Ahlstrom says. “People have different income goals,” he adds.
Second, physicians have to see the same number of patients throughout the day. This doesn’t take into consideration the reality that some hospitalists naturally work faster than others, thereby forcing the slower-paced doctors to keep up with an imposed patient load. “Invariably, no matter what you do, people are different,” Dr. Ahlstrom says.
Another consideration is that when physicians are working 12 to 14 hours a day, essentially they have no time for activities other than work and sleep, which doesn’t match the realities of life. Inevitably, things in personal lives crop up, which leads to swapping shifts that the group scheduler doesn’t know about or overloading the scheduler with shift-change requests, Dr. Ahlstrom explains.
Additionally, 7/7 schedules and their ilk squeeze a year’s worth of work into a compressed time frame, which can lead to intense stress and burnout, says John Nelson, MD, FACP, MHM, director of the hospitalist practice at Overlake Hospital in Bellevue, Wash., SHM co-founder, and practice management columnist for The Hospitalist. “Maximizing the number of days off is not the holy grail,” he says. “If you choose to shut your life down on days that you work, that is going to be toxic.”
Flexibility Equates to Fairness
Dr. Nelson has long advocated a flexible shift schedule that accommodates individual preferences by giving physicians in the group autonomy in deciding how much or how little they want to work. While the group as a whole has to get all the work done, the flexibility comes from one physician taking more shifts as another takes less.
Dr. Radzienda tries to create teams within his group by pairing hospitalists with similar scheduling preferences. For example, he might have a pair working 5/5 and another working 14/14. “Up front, it takes a lot of work, but once you template it out, it becomes a good strategy,” he says.
He also strives to build robust backup plans and jeopardy models (see “Surge Protection,” September 2010, p. 43) into the schedule for short-notice callouts, as you never know when a hospitalist will need to miss a day or two because of illness or a family emergency. “Psychologically, it helps to know that you don’t have to be a hero if you’re ill or emotionally strained,” Dr. Radzienda says.
Dr. Ahlstrom agrees that a flex-schedule strategy has a positive impact on hospitalists’ career satisfaction and longevity. He suggests hospitalists be allowed to specify how many patients they want to see and be compensated according to their workload through built-in bonuses for physicians who work more. Dr. Nelson suggests paying hospitalists per relative value unit (RVU) of work. “I think hospitalists would like it and find it liberating to be paid on production,” he says.
An added bonus to flexible work hours and patient load, according to Dr. Ahlstrom, is that pay difference “will lead to a far more collegial atmosphere, because physicians know they are getting compensated fairly for the amount of work done.”
Another advantage of a flexible schedule is hospitalists knowing they have the option of ramping up or scaling back the number of shifts they work, Dr. Ahlstrom says—for example, a physician who wants to reduce shifts in order to coach his daughter’s softball team or have Friday nights off to watch her son play high school football.
“You prevent burnout by allowing people to change their work schedule depending on what’s going on in their life,” Dr. Ahlstrom says. TH
Lisa Ryan is a freelance writer based in New Jersey.
Michael Radzienda, MD, FHM, once worked in a hospitalist program in which physicians were scheduled 30 days straight on clinical duty and 30 days off clinical duty. Although it sounds harsh by today’s standards, that job was so satisfying, he says, the schedule never felt like a burden. Conversely, he’s seen hospitalists work five days on and five days off, and the job was treacherous.
His point: Work schedules are just one influential piece of the job satisfaction pie.
“Satisfaction has more to do with work relationships and opportunities for growth,” says Dr. Radzienda, chief of hospital medicine and director of hospital medicine service at Medical College of Wisconsin/Froedtert Memorial Lutheran General Hospital in Milwaukee.
Shift-based staffing has become the norm, as more than 70% of hospitalist groups use a shift-based staffing model, according to the State of Hospital Medicine: 2010 Report Based on 2009 Data.1 That figure is up 40% from SHM’s 2005-2006 survey. Conversely, the number of HM groups employing call-based and hybrid (some shift, some call) coverage is declining—2.8% of groups employ call-based schedules, and 26.9% use a hybrid schedule. Those figures have dropped significantly from the 2005-2006 report, from 25% and 35%, respectively.
If you are going to make HM a career, you’ll need time to be with your family and pursue other interests, Dr. Radzienda says. As HM groups turn to more shift-based models, in which hospitalists work a set number of predetermined shifts and have no call responsibility, the challenge is setting a schedule that balances productivity and quality time off.
Fixed = Inflexible
The most popular way to schedule is through blocks of five days on/five days off (5/5) or seven days on/seven days off (7/7), in which hospitalists work 12 or 14 hours at a time, says Troy Ahlstrom, MD, FHM, a member of SHM’s Practice Analysis Committee and CFO of Hospitalists of Northern Michigan, a hospitalist-owned and -managed group based in Traverse City, Mich. Many HM groups employ this model because it’s easy to schedule and is attractive to residents who want a fixed schedule. But from a career satisfaction standpoint, the 5/5 and 7/7 schedule models present their own issues.
Fairness is the first potential pitfall. If all of the physicians in a group work the same schedule, they all have to log the same number of shifts and receive the same compensation. This leaves little to no wiggle room for hospitalists who want to make more money by picking up more shifts or those who want to work fewer shifts, Dr. Ahlstrom says. “People have different income goals,” he adds.
Second, physicians have to see the same number of patients throughout the day. This doesn’t take into consideration the reality that some hospitalists naturally work faster than others, thereby forcing the slower-paced doctors to keep up with an imposed patient load. “Invariably, no matter what you do, people are different,” Dr. Ahlstrom says.
Another consideration is that when physicians are working 12 to 14 hours a day, essentially they have no time for activities other than work and sleep, which doesn’t match the realities of life. Inevitably, things in personal lives crop up, which leads to swapping shifts that the group scheduler doesn’t know about or overloading the scheduler with shift-change requests, Dr. Ahlstrom explains.
Additionally, 7/7 schedules and their ilk squeeze a year’s worth of work into a compressed time frame, which can lead to intense stress and burnout, says John Nelson, MD, FACP, MHM, director of the hospitalist practice at Overlake Hospital in Bellevue, Wash., SHM co-founder, and practice management columnist for The Hospitalist. “Maximizing the number of days off is not the holy grail,” he says. “If you choose to shut your life down on days that you work, that is going to be toxic.”
Flexibility Equates to Fairness
Dr. Nelson has long advocated a flexible shift schedule that accommodates individual preferences by giving physicians in the group autonomy in deciding how much or how little they want to work. While the group as a whole has to get all the work done, the flexibility comes from one physician taking more shifts as another takes less.
Dr. Radzienda tries to create teams within his group by pairing hospitalists with similar scheduling preferences. For example, he might have a pair working 5/5 and another working 14/14. “Up front, it takes a lot of work, but once you template it out, it becomes a good strategy,” he says.
He also strives to build robust backup plans and jeopardy models (see “Surge Protection,” September 2010, p. 43) into the schedule for short-notice callouts, as you never know when a hospitalist will need to miss a day or two because of illness or a family emergency. “Psychologically, it helps to know that you don’t have to be a hero if you’re ill or emotionally strained,” Dr. Radzienda says.
Dr. Ahlstrom agrees that a flex-schedule strategy has a positive impact on hospitalists’ career satisfaction and longevity. He suggests hospitalists be allowed to specify how many patients they want to see and be compensated according to their workload through built-in bonuses for physicians who work more. Dr. Nelson suggests paying hospitalists per relative value unit (RVU) of work. “I think hospitalists would like it and find it liberating to be paid on production,” he says.
An added bonus to flexible work hours and patient load, according to Dr. Ahlstrom, is that pay difference “will lead to a far more collegial atmosphere, because physicians know they are getting compensated fairly for the amount of work done.”
Another advantage of a flexible schedule is hospitalists knowing they have the option of ramping up or scaling back the number of shifts they work, Dr. Ahlstrom says—for example, a physician who wants to reduce shifts in order to coach his daughter’s softball team or have Friday nights off to watch her son play high school football.
“You prevent burnout by allowing people to change their work schedule depending on what’s going on in their life,” Dr. Ahlstrom says. TH
Lisa Ryan is a freelance writer based in New Jersey.
Alternative Access
Effective communication between a physician and their patient is critical to a successful treatment relationship. Even in the best of circumstances, however, we know that physicians and patients often have markedly different impressions of what is said during an interaction or the meaning of information provided. When a language barrier is present, or a patient has a hearing or visual impairment, these communication challenges multiply. How physicians address such challenges has multiple legal implications.
The ADA
Title III of the Americans with Disabilities Act (ADA) prohibits discrimination against visually impaired and deaf and hard-of-hearing people in places of public accommodation. Included within the definition of places of public accommodation is any “professional office of a healthcare provider,” regardless of the size of the office or number of employees. Thus, the ADA applies to doctors, dentists, psychiatrists and psychologists, hospitals, nursing homes and health clinics, and all other providers of mental and physical care. Accordingly, the ADA requires hospitals to provide effective means of communication for patients, family members, and hospital visitors who are visually impaired, deaf, or hard of hearing.
Public accommodations must comply with specific requirements related to effective communication with people with hearing, vision, or speech disabilities. Specifically, unless a hospital or physician can demonstrate that providing communication aids or services would fundamentally alter the nature of the goods or services offered, or would result in an undue burden, a hospital or physician must ensure that no individual with a disability is excluded, denied services, segregated, or otherwise treated differently than other individuals because of the absence of auxiliary aids and services.
Auxiliary aids and services relating to communications, in turn, include:
- Qualified interpreters;
- Note-takers;
- Transcription services;
- Written materials;
- Telephone handset amplifiers;
- Assistive listening devices;
- Assistive listening systems;
- Telephones compatible with hearing aids;
- Closed-caption decoders;
- Open and closed captioning;
- Telecommunications devices for deaf persons (TDDs);
- Videotext displays or other effective methods of making aurally delivered materials available to individuals with hearing impairments;
- Qualified readers;
- Taped texts;
- Audio recordings;
- Braille materials; and
- Large-print materials or other methods of making visually delivered materials available to individuals with visual impairments.
The U.S. Department of Justice (DOJ) has issued memorandums outlining the obligations of physicians and other healthcare providers to provide auxiliary aids or services to people with hearing impairments. The memo recommended that healthcare providers consult with patients about appropriate auxiliary aids and services. The memo noted, however, that private providers are not required to accede to a patient’s specific choice of auxiliary aid or service as long as the provider satisfies his or her obligation to ensure effective communication.
In comparison, healthcare providers working at public entities or hospitals must have a conversation with patients as part of a doctor’s process in providing effective communication, and physicians must give primary consideration to the patient’s choice (see “Americans with Disabilities Act Title II Requirements,” above).
The DOJ has indicated that in determining what constitutes an effective auxiliary aid or service, healthcare providers must consider, among other things, the length and complexity of the communication involved. For example, a note pad and written materials might be sufficient for some routine appointments, to discuss uncomplicated symptoms or minor injuries, or to complete insurance forms or medical history inquiries. When the information is lengthy or complex, however, such as a patient’s discussion of symptoms with medical personnel or a physician’s presentation of diagnosis and treatment options to patients or family members, it might be necessary to provide a qualified sign language interpreter or other interpreter; the use of handwritten notes might be inadequate.
The DOJ also has specified that hospitals should have arrangements in place to ensure that qualified interpreters are readily available on a scheduled basis, and on an unscheduled basis with minimal delay, including on-call arrangements for after-hours emergencies. Larger facilities can choose to have interpreters on staff. Hospitals should develop protocols and provide training to ensure that hospital staff know how to obtain interpreter services and other communication aids and services when needed.
The DOJ has recommended hospitals have signs and other types of notices to advise persons with disabilities that services and assistance are available, along with what they need to do to obtain them. A hospital must be prepared to make and receive relay system calls.
If telephones and televisions are provided in patient rooms, hospitals must provide patients who are deaf or hard of hearing comparable accessible equipment upon request, including TDDs, telephones that are hearing-aid compatible and have volume control, and televisions with closed captioning or decoders. For training or other educational services offered to patients or members of the public, additional aids and services (e.g. note-takers, captioned videos, assistive listening systems) might be necessary for effective communication.
Visual alarms are not required in patient rooms. However, evacuation procedures should include specific measures to ensure the safety of patients and visitors who are deaf or hard of hearing. Certain built-in communication features required for hospitals built or altered after the effective date of the ADA in 1992 include:
- Visual alarms, which must be provided in all public and common-use areas, including restrooms, where audible alarms are provided;
- TDDs, which must be provided at public pay phones serving emergency, recovery, or waiting rooms, and at least one TDD must be provided at other locations where there are four or more pay phones; and
- A certain percentage of public phones that must have other features, such as TDD plug-in capability, volume controls, and hearing-aid compatibility.
Also important: Hospitals and healthcare providers are not allowed to charge patients with a disability to cover the costs of providing auxiliary aids and services. Instead, the costs must be treated as overhead expenses that are passed on to all patients.
New Regulations
Effective March 15, amendments to the ADA regulations will take effect modifying both Title II and Title III. One of the relevant changes to the regulations include video remote interpreting (VRI) services as a kind of auxiliary aid, which could be used to provide effective communication. VRI is an interpreting service that delivers high-quality video images over dedicated lines or wireless technology.
The amended Title II regulations effective March 15 also expand on the explanation of an effective auxiliary aid and provide that “in order to be effective, auxiliary aids and services must be provided in accessible formats, in a timely manner, and in such a way as to protect the privacy and independence of the individual with a disability.” A public entity cannot require an individual with a disability to bring another individual to interpret for him or her, or rely on an adult accompanying an individual with a disability to interpret or facilitate communication, except in the case of an emergency or when the individual with a disability specifically requests that the accompanying adult interpret or facilitate communication, the accompanying adult agrees to provide such assistance, and reliance on that adult for such assistance is appropriate under the circumstances.
Similarly, a public entity cannot rely on a minor child to interpret or facilitate communication, except in an emergency involving an imminent threat to the safety or welfare of an individual or the public and no interpreter is available.
Title IV of Civil Rights Act
Individuals who do not speak English as their primary language and who have a limited ability to read, write, speak, or understand English might be eligible to receive language assistance with respect to particular services, benefits, or encounters.
Title VI and U.S. Department of Health and Human Services (HHS) regulations require recipients of federal financial assistance from HHS to take reasonable steps to provide meaningful access to limited-English-proficiency (LEP) persons. Recipients of HHS assistance might include hospitals, nursing homes, home health agencies, managed-care organizations, universities and other entities with health or social service research programs, and state, county, and local health agencies. It might also include Medicaid agencies, state, county, and local welfare agencies, programs for families, youth, and children, Head Start programs, public and private contractors, subcontractors, and vendors, and physicians and other providers who receive financial assistance from HHS.
HHS has indicated that the obligation to provide meaningful access is fact-dependent and starts with an individualized assessment that balances four factors:
- Number or proportion of LEP persons eligible to be served or likely to be encountered by the program or grantee;
- Frequency with which LEP individuals come into contact with the program;
- Nature and importance of the program, activity or service provided by the recipient to its beneficiaries; and
- Resources available to the grantee/recipient and the costs of interpretation/translation services.
HHS notes that there is no “one size fits all” solution for compliance with respect to LEP persons, and what constitutes “reasonable steps” for large providers might not be reasonable where small providers are concerned.
Use of family members or friends. HHS has indicated that some LEP persons feel more comfortable when a trusted family member or friend acts as an interpreter. When an LEP person attempts to access the services of a recipient of federal financial assistance, who upon application of the four factors is required to provide an interpreter, the recipient should make the LEP person aware that he or she has the option of having the recipient provide an interpreter for them without charge, or of using their own interpreter. Recipients also should consider special circumstances that might affect whether a family member or friend should serve as an interpreter, such as whether the situation is an emergency, and whether there are concerns over competency, confidentiality, privacy, or conflict of interest. Recipients cannot require LEP persons to use family members or friends as interpreters.
Vital documents. Recipients can use the four factors to determine if specific documents or portions of documents should be translated into the language of frequently encountered LEP groups eligible to be served or likely to be affected by the recipient’s program. Recipients should assess whether specific documents or portions of documents are “vital” to the program, information, encounter, or service involved, and the consequences to the LEP person if the information in question is not provided accurately or in a timely manner.
Compliance plans. HHS provides recipients with a “safe harbor” that, if undertaken, will be considered strong evidence that the recipient has satisfied its written translation obligations. If a recipient determines that it should provide language assistance services, a recipient might develop an implementation plan to address the identified needs of the LEP populations it serves. Recipients have considerable flexibility in developing this plan, but should: 1) identify LEP individuals who need language assistance; 2) identify language assistance measures (i.e. how staff can obtain services or respond to LEP callers); 3) train staff; 4) provide notice to LEP persons (e.g. posting signs); and 5) monitor and update the LEP plan.
Voluntary compliance efforts. The Office for Civil Rights and HHS have indicated they are committed to assisting recipients of HHS financial assistance in complying with their obligations under Title VI of the Civil Rights Act of 1964. HHS provides a variety of practical technical assistance to recipients to assist them in serving LEP persons so that they are in compliance with the Title VI regulations. The requirement to provide meaningful access to LEP persons is enforced and implemented by the HHS Office for Civil Rights through the procedures identified in the Title VI regulations. These procedures include complaint investigations, compliance reviews, efforts to secure voluntary compliance, and technical assistance.
Additionally, the American Medical Association has prepared the “Office Guide to Communicating with Limited English Proficient Patients” (download a PDF at www.ama-assn.org/ama1/pub/upload/mm/433/lep_booklet.pdf), which provides useful guidance to physicians.
Conclusion
The requirements for providing assistance to patients presenting with a language barrier, or patients who have hearing or visual impairments, are challenging. Advance planning for interacting with such patients can assist in successful physician-patient communications. Nonetheless, there is no “one size fits all” approach. Accordingly, if you have a question about a specific situation, consult the Office for Civil Rights (www.hhs.gov/ocr), the Department of Justice ADA Information Line (800-514-0301), or an attorney. TH
Carmen Decker is an attorney with Hershey Skinner, LLC, specializing in the representation of healthcare and licensed professionals. Kari Hershey is general counsel to the Colorado Medical Society and an instructor at the University of Colorado Law School.
Effective communication between a physician and their patient is critical to a successful treatment relationship. Even in the best of circumstances, however, we know that physicians and patients often have markedly different impressions of what is said during an interaction or the meaning of information provided. When a language barrier is present, or a patient has a hearing or visual impairment, these communication challenges multiply. How physicians address such challenges has multiple legal implications.
The ADA
Title III of the Americans with Disabilities Act (ADA) prohibits discrimination against visually impaired and deaf and hard-of-hearing people in places of public accommodation. Included within the definition of places of public accommodation is any “professional office of a healthcare provider,” regardless of the size of the office or number of employees. Thus, the ADA applies to doctors, dentists, psychiatrists and psychologists, hospitals, nursing homes and health clinics, and all other providers of mental and physical care. Accordingly, the ADA requires hospitals to provide effective means of communication for patients, family members, and hospital visitors who are visually impaired, deaf, or hard of hearing.
Public accommodations must comply with specific requirements related to effective communication with people with hearing, vision, or speech disabilities. Specifically, unless a hospital or physician can demonstrate that providing communication aids or services would fundamentally alter the nature of the goods or services offered, or would result in an undue burden, a hospital or physician must ensure that no individual with a disability is excluded, denied services, segregated, or otherwise treated differently than other individuals because of the absence of auxiliary aids and services.
Auxiliary aids and services relating to communications, in turn, include:
- Qualified interpreters;
- Note-takers;
- Transcription services;
- Written materials;
- Telephone handset amplifiers;
- Assistive listening devices;
- Assistive listening systems;
- Telephones compatible with hearing aids;
- Closed-caption decoders;
- Open and closed captioning;
- Telecommunications devices for deaf persons (TDDs);
- Videotext displays or other effective methods of making aurally delivered materials available to individuals with hearing impairments;
- Qualified readers;
- Taped texts;
- Audio recordings;
- Braille materials; and
- Large-print materials or other methods of making visually delivered materials available to individuals with visual impairments.
The U.S. Department of Justice (DOJ) has issued memorandums outlining the obligations of physicians and other healthcare providers to provide auxiliary aids or services to people with hearing impairments. The memo recommended that healthcare providers consult with patients about appropriate auxiliary aids and services. The memo noted, however, that private providers are not required to accede to a patient’s specific choice of auxiliary aid or service as long as the provider satisfies his or her obligation to ensure effective communication.
In comparison, healthcare providers working at public entities or hospitals must have a conversation with patients as part of a doctor’s process in providing effective communication, and physicians must give primary consideration to the patient’s choice (see “Americans with Disabilities Act Title II Requirements,” above).
The DOJ has indicated that in determining what constitutes an effective auxiliary aid or service, healthcare providers must consider, among other things, the length and complexity of the communication involved. For example, a note pad and written materials might be sufficient for some routine appointments, to discuss uncomplicated symptoms or minor injuries, or to complete insurance forms or medical history inquiries. When the information is lengthy or complex, however, such as a patient’s discussion of symptoms with medical personnel or a physician’s presentation of diagnosis and treatment options to patients or family members, it might be necessary to provide a qualified sign language interpreter or other interpreter; the use of handwritten notes might be inadequate.
The DOJ also has specified that hospitals should have arrangements in place to ensure that qualified interpreters are readily available on a scheduled basis, and on an unscheduled basis with minimal delay, including on-call arrangements for after-hours emergencies. Larger facilities can choose to have interpreters on staff. Hospitals should develop protocols and provide training to ensure that hospital staff know how to obtain interpreter services and other communication aids and services when needed.
The DOJ has recommended hospitals have signs and other types of notices to advise persons with disabilities that services and assistance are available, along with what they need to do to obtain them. A hospital must be prepared to make and receive relay system calls.
If telephones and televisions are provided in patient rooms, hospitals must provide patients who are deaf or hard of hearing comparable accessible equipment upon request, including TDDs, telephones that are hearing-aid compatible and have volume control, and televisions with closed captioning or decoders. For training or other educational services offered to patients or members of the public, additional aids and services (e.g. note-takers, captioned videos, assistive listening systems) might be necessary for effective communication.
Visual alarms are not required in patient rooms. However, evacuation procedures should include specific measures to ensure the safety of patients and visitors who are deaf or hard of hearing. Certain built-in communication features required for hospitals built or altered after the effective date of the ADA in 1992 include:
- Visual alarms, which must be provided in all public and common-use areas, including restrooms, where audible alarms are provided;
- TDDs, which must be provided at public pay phones serving emergency, recovery, or waiting rooms, and at least one TDD must be provided at other locations where there are four or more pay phones; and
- A certain percentage of public phones that must have other features, such as TDD plug-in capability, volume controls, and hearing-aid compatibility.
Also important: Hospitals and healthcare providers are not allowed to charge patients with a disability to cover the costs of providing auxiliary aids and services. Instead, the costs must be treated as overhead expenses that are passed on to all patients.
New Regulations
Effective March 15, amendments to the ADA regulations will take effect modifying both Title II and Title III. One of the relevant changes to the regulations include video remote interpreting (VRI) services as a kind of auxiliary aid, which could be used to provide effective communication. VRI is an interpreting service that delivers high-quality video images over dedicated lines or wireless technology.
The amended Title II regulations effective March 15 also expand on the explanation of an effective auxiliary aid and provide that “in order to be effective, auxiliary aids and services must be provided in accessible formats, in a timely manner, and in such a way as to protect the privacy and independence of the individual with a disability.” A public entity cannot require an individual with a disability to bring another individual to interpret for him or her, or rely on an adult accompanying an individual with a disability to interpret or facilitate communication, except in the case of an emergency or when the individual with a disability specifically requests that the accompanying adult interpret or facilitate communication, the accompanying adult agrees to provide such assistance, and reliance on that adult for such assistance is appropriate under the circumstances.
Similarly, a public entity cannot rely on a minor child to interpret or facilitate communication, except in an emergency involving an imminent threat to the safety or welfare of an individual or the public and no interpreter is available.
Title IV of Civil Rights Act
Individuals who do not speak English as their primary language and who have a limited ability to read, write, speak, or understand English might be eligible to receive language assistance with respect to particular services, benefits, or encounters.
Title VI and U.S. Department of Health and Human Services (HHS) regulations require recipients of federal financial assistance from HHS to take reasonable steps to provide meaningful access to limited-English-proficiency (LEP) persons. Recipients of HHS assistance might include hospitals, nursing homes, home health agencies, managed-care organizations, universities and other entities with health or social service research programs, and state, county, and local health agencies. It might also include Medicaid agencies, state, county, and local welfare agencies, programs for families, youth, and children, Head Start programs, public and private contractors, subcontractors, and vendors, and physicians and other providers who receive financial assistance from HHS.
HHS has indicated that the obligation to provide meaningful access is fact-dependent and starts with an individualized assessment that balances four factors:
- Number or proportion of LEP persons eligible to be served or likely to be encountered by the program or grantee;
- Frequency with which LEP individuals come into contact with the program;
- Nature and importance of the program, activity or service provided by the recipient to its beneficiaries; and
- Resources available to the grantee/recipient and the costs of interpretation/translation services.
HHS notes that there is no “one size fits all” solution for compliance with respect to LEP persons, and what constitutes “reasonable steps” for large providers might not be reasonable where small providers are concerned.
Use of family members or friends. HHS has indicated that some LEP persons feel more comfortable when a trusted family member or friend acts as an interpreter. When an LEP person attempts to access the services of a recipient of federal financial assistance, who upon application of the four factors is required to provide an interpreter, the recipient should make the LEP person aware that he or she has the option of having the recipient provide an interpreter for them without charge, or of using their own interpreter. Recipients also should consider special circumstances that might affect whether a family member or friend should serve as an interpreter, such as whether the situation is an emergency, and whether there are concerns over competency, confidentiality, privacy, or conflict of interest. Recipients cannot require LEP persons to use family members or friends as interpreters.
Vital documents. Recipients can use the four factors to determine if specific documents or portions of documents should be translated into the language of frequently encountered LEP groups eligible to be served or likely to be affected by the recipient’s program. Recipients should assess whether specific documents or portions of documents are “vital” to the program, information, encounter, or service involved, and the consequences to the LEP person if the information in question is not provided accurately or in a timely manner.
Compliance plans. HHS provides recipients with a “safe harbor” that, if undertaken, will be considered strong evidence that the recipient has satisfied its written translation obligations. If a recipient determines that it should provide language assistance services, a recipient might develop an implementation plan to address the identified needs of the LEP populations it serves. Recipients have considerable flexibility in developing this plan, but should: 1) identify LEP individuals who need language assistance; 2) identify language assistance measures (i.e. how staff can obtain services or respond to LEP callers); 3) train staff; 4) provide notice to LEP persons (e.g. posting signs); and 5) monitor and update the LEP plan.
Voluntary compliance efforts. The Office for Civil Rights and HHS have indicated they are committed to assisting recipients of HHS financial assistance in complying with their obligations under Title VI of the Civil Rights Act of 1964. HHS provides a variety of practical technical assistance to recipients to assist them in serving LEP persons so that they are in compliance with the Title VI regulations. The requirement to provide meaningful access to LEP persons is enforced and implemented by the HHS Office for Civil Rights through the procedures identified in the Title VI regulations. These procedures include complaint investigations, compliance reviews, efforts to secure voluntary compliance, and technical assistance.
Additionally, the American Medical Association has prepared the “Office Guide to Communicating with Limited English Proficient Patients” (download a PDF at www.ama-assn.org/ama1/pub/upload/mm/433/lep_booklet.pdf), which provides useful guidance to physicians.
Conclusion
The requirements for providing assistance to patients presenting with a language barrier, or patients who have hearing or visual impairments, are challenging. Advance planning for interacting with such patients can assist in successful physician-patient communications. Nonetheless, there is no “one size fits all” approach. Accordingly, if you have a question about a specific situation, consult the Office for Civil Rights (www.hhs.gov/ocr), the Department of Justice ADA Information Line (800-514-0301), or an attorney. TH
Carmen Decker is an attorney with Hershey Skinner, LLC, specializing in the representation of healthcare and licensed professionals. Kari Hershey is general counsel to the Colorado Medical Society and an instructor at the University of Colorado Law School.
Effective communication between a physician and their patient is critical to a successful treatment relationship. Even in the best of circumstances, however, we know that physicians and patients often have markedly different impressions of what is said during an interaction or the meaning of information provided. When a language barrier is present, or a patient has a hearing or visual impairment, these communication challenges multiply. How physicians address such challenges has multiple legal implications.
The ADA
Title III of the Americans with Disabilities Act (ADA) prohibits discrimination against visually impaired and deaf and hard-of-hearing people in places of public accommodation. Included within the definition of places of public accommodation is any “professional office of a healthcare provider,” regardless of the size of the office or number of employees. Thus, the ADA applies to doctors, dentists, psychiatrists and psychologists, hospitals, nursing homes and health clinics, and all other providers of mental and physical care. Accordingly, the ADA requires hospitals to provide effective means of communication for patients, family members, and hospital visitors who are visually impaired, deaf, or hard of hearing.
Public accommodations must comply with specific requirements related to effective communication with people with hearing, vision, or speech disabilities. Specifically, unless a hospital or physician can demonstrate that providing communication aids or services would fundamentally alter the nature of the goods or services offered, or would result in an undue burden, a hospital or physician must ensure that no individual with a disability is excluded, denied services, segregated, or otherwise treated differently than other individuals because of the absence of auxiliary aids and services.
Auxiliary aids and services relating to communications, in turn, include:
- Qualified interpreters;
- Note-takers;
- Transcription services;
- Written materials;
- Telephone handset amplifiers;
- Assistive listening devices;
- Assistive listening systems;
- Telephones compatible with hearing aids;
- Closed-caption decoders;
- Open and closed captioning;
- Telecommunications devices for deaf persons (TDDs);
- Videotext displays or other effective methods of making aurally delivered materials available to individuals with hearing impairments;
- Qualified readers;
- Taped texts;
- Audio recordings;
- Braille materials; and
- Large-print materials or other methods of making visually delivered materials available to individuals with visual impairments.
The U.S. Department of Justice (DOJ) has issued memorandums outlining the obligations of physicians and other healthcare providers to provide auxiliary aids or services to people with hearing impairments. The memo recommended that healthcare providers consult with patients about appropriate auxiliary aids and services. The memo noted, however, that private providers are not required to accede to a patient’s specific choice of auxiliary aid or service as long as the provider satisfies his or her obligation to ensure effective communication.
In comparison, healthcare providers working at public entities or hospitals must have a conversation with patients as part of a doctor’s process in providing effective communication, and physicians must give primary consideration to the patient’s choice (see “Americans with Disabilities Act Title II Requirements,” above).
The DOJ has indicated that in determining what constitutes an effective auxiliary aid or service, healthcare providers must consider, among other things, the length and complexity of the communication involved. For example, a note pad and written materials might be sufficient for some routine appointments, to discuss uncomplicated symptoms or minor injuries, or to complete insurance forms or medical history inquiries. When the information is lengthy or complex, however, such as a patient’s discussion of symptoms with medical personnel or a physician’s presentation of diagnosis and treatment options to patients or family members, it might be necessary to provide a qualified sign language interpreter or other interpreter; the use of handwritten notes might be inadequate.
The DOJ also has specified that hospitals should have arrangements in place to ensure that qualified interpreters are readily available on a scheduled basis, and on an unscheduled basis with minimal delay, including on-call arrangements for after-hours emergencies. Larger facilities can choose to have interpreters on staff. Hospitals should develop protocols and provide training to ensure that hospital staff know how to obtain interpreter services and other communication aids and services when needed.
The DOJ has recommended hospitals have signs and other types of notices to advise persons with disabilities that services and assistance are available, along with what they need to do to obtain them. A hospital must be prepared to make and receive relay system calls.
If telephones and televisions are provided in patient rooms, hospitals must provide patients who are deaf or hard of hearing comparable accessible equipment upon request, including TDDs, telephones that are hearing-aid compatible and have volume control, and televisions with closed captioning or decoders. For training or other educational services offered to patients or members of the public, additional aids and services (e.g. note-takers, captioned videos, assistive listening systems) might be necessary for effective communication.
Visual alarms are not required in patient rooms. However, evacuation procedures should include specific measures to ensure the safety of patients and visitors who are deaf or hard of hearing. Certain built-in communication features required for hospitals built or altered after the effective date of the ADA in 1992 include:
- Visual alarms, which must be provided in all public and common-use areas, including restrooms, where audible alarms are provided;
- TDDs, which must be provided at public pay phones serving emergency, recovery, or waiting rooms, and at least one TDD must be provided at other locations where there are four or more pay phones; and
- A certain percentage of public phones that must have other features, such as TDD plug-in capability, volume controls, and hearing-aid compatibility.
Also important: Hospitals and healthcare providers are not allowed to charge patients with a disability to cover the costs of providing auxiliary aids and services. Instead, the costs must be treated as overhead expenses that are passed on to all patients.
New Regulations
Effective March 15, amendments to the ADA regulations will take effect modifying both Title II and Title III. One of the relevant changes to the regulations include video remote interpreting (VRI) services as a kind of auxiliary aid, which could be used to provide effective communication. VRI is an interpreting service that delivers high-quality video images over dedicated lines or wireless technology.
The amended Title II regulations effective March 15 also expand on the explanation of an effective auxiliary aid and provide that “in order to be effective, auxiliary aids and services must be provided in accessible formats, in a timely manner, and in such a way as to protect the privacy and independence of the individual with a disability.” A public entity cannot require an individual with a disability to bring another individual to interpret for him or her, or rely on an adult accompanying an individual with a disability to interpret or facilitate communication, except in the case of an emergency or when the individual with a disability specifically requests that the accompanying adult interpret or facilitate communication, the accompanying adult agrees to provide such assistance, and reliance on that adult for such assistance is appropriate under the circumstances.
Similarly, a public entity cannot rely on a minor child to interpret or facilitate communication, except in an emergency involving an imminent threat to the safety or welfare of an individual or the public and no interpreter is available.
Title IV of Civil Rights Act
Individuals who do not speak English as their primary language and who have a limited ability to read, write, speak, or understand English might be eligible to receive language assistance with respect to particular services, benefits, or encounters.
Title VI and U.S. Department of Health and Human Services (HHS) regulations require recipients of federal financial assistance from HHS to take reasonable steps to provide meaningful access to limited-English-proficiency (LEP) persons. Recipients of HHS assistance might include hospitals, nursing homes, home health agencies, managed-care organizations, universities and other entities with health or social service research programs, and state, county, and local health agencies. It might also include Medicaid agencies, state, county, and local welfare agencies, programs for families, youth, and children, Head Start programs, public and private contractors, subcontractors, and vendors, and physicians and other providers who receive financial assistance from HHS.
HHS has indicated that the obligation to provide meaningful access is fact-dependent and starts with an individualized assessment that balances four factors:
- Number or proportion of LEP persons eligible to be served or likely to be encountered by the program or grantee;
- Frequency with which LEP individuals come into contact with the program;
- Nature and importance of the program, activity or service provided by the recipient to its beneficiaries; and
- Resources available to the grantee/recipient and the costs of interpretation/translation services.
HHS notes that there is no “one size fits all” solution for compliance with respect to LEP persons, and what constitutes “reasonable steps” for large providers might not be reasonable where small providers are concerned.
Use of family members or friends. HHS has indicated that some LEP persons feel more comfortable when a trusted family member or friend acts as an interpreter. When an LEP person attempts to access the services of a recipient of federal financial assistance, who upon application of the four factors is required to provide an interpreter, the recipient should make the LEP person aware that he or she has the option of having the recipient provide an interpreter for them without charge, or of using their own interpreter. Recipients also should consider special circumstances that might affect whether a family member or friend should serve as an interpreter, such as whether the situation is an emergency, and whether there are concerns over competency, confidentiality, privacy, or conflict of interest. Recipients cannot require LEP persons to use family members or friends as interpreters.
Vital documents. Recipients can use the four factors to determine if specific documents or portions of documents should be translated into the language of frequently encountered LEP groups eligible to be served or likely to be affected by the recipient’s program. Recipients should assess whether specific documents or portions of documents are “vital” to the program, information, encounter, or service involved, and the consequences to the LEP person if the information in question is not provided accurately or in a timely manner.
Compliance plans. HHS provides recipients with a “safe harbor” that, if undertaken, will be considered strong evidence that the recipient has satisfied its written translation obligations. If a recipient determines that it should provide language assistance services, a recipient might develop an implementation plan to address the identified needs of the LEP populations it serves. Recipients have considerable flexibility in developing this plan, but should: 1) identify LEP individuals who need language assistance; 2) identify language assistance measures (i.e. how staff can obtain services or respond to LEP callers); 3) train staff; 4) provide notice to LEP persons (e.g. posting signs); and 5) monitor and update the LEP plan.
Voluntary compliance efforts. The Office for Civil Rights and HHS have indicated they are committed to assisting recipients of HHS financial assistance in complying with their obligations under Title VI of the Civil Rights Act of 1964. HHS provides a variety of practical technical assistance to recipients to assist them in serving LEP persons so that they are in compliance with the Title VI regulations. The requirement to provide meaningful access to LEP persons is enforced and implemented by the HHS Office for Civil Rights through the procedures identified in the Title VI regulations. These procedures include complaint investigations, compliance reviews, efforts to secure voluntary compliance, and technical assistance.
Additionally, the American Medical Association has prepared the “Office Guide to Communicating with Limited English Proficient Patients” (download a PDF at www.ama-assn.org/ama1/pub/upload/mm/433/lep_booklet.pdf), which provides useful guidance to physicians.
Conclusion
The requirements for providing assistance to patients presenting with a language barrier, or patients who have hearing or visual impairments, are challenging. Advance planning for interacting with such patients can assist in successful physician-patient communications. Nonetheless, there is no “one size fits all” approach. Accordingly, if you have a question about a specific situation, consult the Office for Civil Rights (www.hhs.gov/ocr), the Department of Justice ADA Information Line (800-514-0301), or an attorney. TH
Carmen Decker is an attorney with Hershey Skinner, LLC, specializing in the representation of healthcare and licensed professionals. Kari Hershey is general counsel to the Colorado Medical Society and an instructor at the University of Colorado Law School.
How You Can Save Your Hospital a Million Bucks
What is value-based purchasing (VBP) and why should I care? Well, for starters, your hospital’s CFO might not know that starting in 2013 (just two years from now), the Centers for Medicare & Medicaid Services (CMS) will be withholding at least 1% of all Medicare payments, but CMS is giving your hospital a chance to get some or all of that money back. For a busy hospital, the withholding will easily be $1 million; for many hospitals, that figure is more like $2 million to $3 million.
SHM thinks hospitalists are uniquely positioned to be champions for the C-suite, helping the hospital’s balance sheet, aiding in staff retention, and providing better care for our patients. And that’s where VBP comes in.
In March 2010, Congress passed the Patient Protection and Affordable Care Act (see “Health Reform Turns 1,” p. 16). This law includes a provision that establishes a VBP program for hospital payments beginning with discharges on Oct. 1, 2012. Payment will be based on hospital performance on quality measures determined by Health and Human Services (HHS). The VBP program will pay hospitals for their actual performance on quality measures, rather than for just reporting those measures, starting in 2013.
This is a null-set game, in which the funding for the best performers is clearly coming out of the hide of low-performing hospitals. Funding will be phased in from 2013 through 2017. Hospitals will have their payments for all Medicare DRGs reduced by 1% in 2013, 1.25% in 2014, 1.5% in 2015, 1.75% in 2016, and 2% in 2017 and beyond. Just ask your CFO what this means at your hospital and see his or her brow furrow.
The good news (i.e. carrot) is that a hospital that meets or exceeds the performance standards will be eligible to earn back all the Medicare money that was withheld and even earn a bonus of as much as 2%.
VBP Metrics
So just what performance will be measured in the new VBP program? While physicians might see quality in clinical terms, the VBP program defines performance more broadly; that means it includes the patient experience. In fact, about 70% of the quality measures will be based on clinical performance, and a full 30% will come from scores on post-discharge patient satisfaction questionnaires (e.g. HCAHPS). To understand the importance of the patient satisfaction part of the VBP equation, just note that Press Ganey, the largest private company helping hospitals understand what their customers are thinking, is jumping into the VBP arena with both feet. Your hospital’s CFO (and lead hospitalist) should contact Press Ganey and run your current performance numbers through their VBP calculator to see if you are on the hilltop or in a deep hole.
The clinical measures will be selected from those used in the current Medicare pay-for-reporting program and likely will include measures for myocardial infarction, heart failure, pneumonia, and surgical care. In addition, HHS is mandated to include measures of efficiency, looking at ways to assess the spending per Medicare beneficiary. This is the real value equation: value = outcomes ÷ cost.
HM to the Rescue
No one in the hospital community sits more at the nexus of clinical care on these measures, efficiency, and the patient experience than hospitalists. This is an opportunity and a risk for hospitalists; that is why SHM is actively planning strategies to help hospitalists assist their hospitals in assessing how their current performance would play out in the payment world post-2013. In addition, SHM will have tools to assist hospitalists in creating change to help their institutions be in the top half of the nation’s hospitals—those who will get their millions of withheld dollars back.
SHM’s board of directors recently passed the following position statement on value-based purchasing:
“SHM supports the Affordable Care Act (ACA) Section 3001 directing the Secretary of HHS to establish a value-based purchasing program under the hospital inpatient prospective payment system. We believe that the Medicare reimbursement system must be changed to promote value, and we strongly support policies that link quality measurement to performance-based payment. We are pleased that under ACA the Secretary will establish performance standards that reward hospitals based on either attaining a certain performance standard or making improvements relative to a previous performance period. Hospitalists, who care for more hospitalized patients than any other physician group and lead system change and quality improvement efforts, will be critical to improving the performance of hospitals under this program.”
As mentioned above, the VBP program poses some risks to hospitalists. We cannot improve our hospital’s performance by ourselves, no matter how well motivated and trained we are. Hospitalists tend to attract a group of patients who traditionally have less satisfaction with their hospital experience (e.g. acutely ill patients admitted through the ED). But for more than a decade, hospitalists have been touting our goal to change the system for the better and to strive to be rewarded for value and performance, not simply for the doing.
In some ways, hospitals’ financial support of hospitalist groups has been predicated on the value we currently provide in efficiency (e.g. decreased length of stay, better use of resources) and effectiveness (e.g. improved measurable quality). The VBP program in ACA is just a first big step for the largest payor of hospital care—CMS—to change the ground rules.
Well-prepared hospitalists can provide leadership and help deliver their institutions to the top half of hospitals (those that will receive bonus payment) and, at the same time, begin to change the culture of their hospital to provide their patients with a better clinical outcome and a better patient experience.
Congress and President Obama are our allies here. A million dollars should get your hospital executives’ attention. Now is the time for hospitalists—with SHM’s help—to step up and show what we can do. TH
Dr. Wellikson is CEO of SHM.
What is value-based purchasing (VBP) and why should I care? Well, for starters, your hospital’s CFO might not know that starting in 2013 (just two years from now), the Centers for Medicare & Medicaid Services (CMS) will be withholding at least 1% of all Medicare payments, but CMS is giving your hospital a chance to get some or all of that money back. For a busy hospital, the withholding will easily be $1 million; for many hospitals, that figure is more like $2 million to $3 million.
SHM thinks hospitalists are uniquely positioned to be champions for the C-suite, helping the hospital’s balance sheet, aiding in staff retention, and providing better care for our patients. And that’s where VBP comes in.
In March 2010, Congress passed the Patient Protection and Affordable Care Act (see “Health Reform Turns 1,” p. 16). This law includes a provision that establishes a VBP program for hospital payments beginning with discharges on Oct. 1, 2012. Payment will be based on hospital performance on quality measures determined by Health and Human Services (HHS). The VBP program will pay hospitals for their actual performance on quality measures, rather than for just reporting those measures, starting in 2013.
This is a null-set game, in which the funding for the best performers is clearly coming out of the hide of low-performing hospitals. Funding will be phased in from 2013 through 2017. Hospitals will have their payments for all Medicare DRGs reduced by 1% in 2013, 1.25% in 2014, 1.5% in 2015, 1.75% in 2016, and 2% in 2017 and beyond. Just ask your CFO what this means at your hospital and see his or her brow furrow.
The good news (i.e. carrot) is that a hospital that meets or exceeds the performance standards will be eligible to earn back all the Medicare money that was withheld and even earn a bonus of as much as 2%.
VBP Metrics
So just what performance will be measured in the new VBP program? While physicians might see quality in clinical terms, the VBP program defines performance more broadly; that means it includes the patient experience. In fact, about 70% of the quality measures will be based on clinical performance, and a full 30% will come from scores on post-discharge patient satisfaction questionnaires (e.g. HCAHPS). To understand the importance of the patient satisfaction part of the VBP equation, just note that Press Ganey, the largest private company helping hospitals understand what their customers are thinking, is jumping into the VBP arena with both feet. Your hospital’s CFO (and lead hospitalist) should contact Press Ganey and run your current performance numbers through their VBP calculator to see if you are on the hilltop or in a deep hole.
The clinical measures will be selected from those used in the current Medicare pay-for-reporting program and likely will include measures for myocardial infarction, heart failure, pneumonia, and surgical care. In addition, HHS is mandated to include measures of efficiency, looking at ways to assess the spending per Medicare beneficiary. This is the real value equation: value = outcomes ÷ cost.
HM to the Rescue
No one in the hospital community sits more at the nexus of clinical care on these measures, efficiency, and the patient experience than hospitalists. This is an opportunity and a risk for hospitalists; that is why SHM is actively planning strategies to help hospitalists assist their hospitals in assessing how their current performance would play out in the payment world post-2013. In addition, SHM will have tools to assist hospitalists in creating change to help their institutions be in the top half of the nation’s hospitals—those who will get their millions of withheld dollars back.
SHM’s board of directors recently passed the following position statement on value-based purchasing:
“SHM supports the Affordable Care Act (ACA) Section 3001 directing the Secretary of HHS to establish a value-based purchasing program under the hospital inpatient prospective payment system. We believe that the Medicare reimbursement system must be changed to promote value, and we strongly support policies that link quality measurement to performance-based payment. We are pleased that under ACA the Secretary will establish performance standards that reward hospitals based on either attaining a certain performance standard or making improvements relative to a previous performance period. Hospitalists, who care for more hospitalized patients than any other physician group and lead system change and quality improvement efforts, will be critical to improving the performance of hospitals under this program.”
As mentioned above, the VBP program poses some risks to hospitalists. We cannot improve our hospital’s performance by ourselves, no matter how well motivated and trained we are. Hospitalists tend to attract a group of patients who traditionally have less satisfaction with their hospital experience (e.g. acutely ill patients admitted through the ED). But for more than a decade, hospitalists have been touting our goal to change the system for the better and to strive to be rewarded for value and performance, not simply for the doing.
In some ways, hospitals’ financial support of hospitalist groups has been predicated on the value we currently provide in efficiency (e.g. decreased length of stay, better use of resources) and effectiveness (e.g. improved measurable quality). The VBP program in ACA is just a first big step for the largest payor of hospital care—CMS—to change the ground rules.
Well-prepared hospitalists can provide leadership and help deliver their institutions to the top half of hospitals (those that will receive bonus payment) and, at the same time, begin to change the culture of their hospital to provide their patients with a better clinical outcome and a better patient experience.
Congress and President Obama are our allies here. A million dollars should get your hospital executives’ attention. Now is the time for hospitalists—with SHM’s help—to step up and show what we can do. TH
Dr. Wellikson is CEO of SHM.
What is value-based purchasing (VBP) and why should I care? Well, for starters, your hospital’s CFO might not know that starting in 2013 (just two years from now), the Centers for Medicare & Medicaid Services (CMS) will be withholding at least 1% of all Medicare payments, but CMS is giving your hospital a chance to get some or all of that money back. For a busy hospital, the withholding will easily be $1 million; for many hospitals, that figure is more like $2 million to $3 million.
SHM thinks hospitalists are uniquely positioned to be champions for the C-suite, helping the hospital’s balance sheet, aiding in staff retention, and providing better care for our patients. And that’s where VBP comes in.
In March 2010, Congress passed the Patient Protection and Affordable Care Act (see “Health Reform Turns 1,” p. 16). This law includes a provision that establishes a VBP program for hospital payments beginning with discharges on Oct. 1, 2012. Payment will be based on hospital performance on quality measures determined by Health and Human Services (HHS). The VBP program will pay hospitals for their actual performance on quality measures, rather than for just reporting those measures, starting in 2013.
This is a null-set game, in which the funding for the best performers is clearly coming out of the hide of low-performing hospitals. Funding will be phased in from 2013 through 2017. Hospitals will have their payments for all Medicare DRGs reduced by 1% in 2013, 1.25% in 2014, 1.5% in 2015, 1.75% in 2016, and 2% in 2017 and beyond. Just ask your CFO what this means at your hospital and see his or her brow furrow.
The good news (i.e. carrot) is that a hospital that meets or exceeds the performance standards will be eligible to earn back all the Medicare money that was withheld and even earn a bonus of as much as 2%.
VBP Metrics
So just what performance will be measured in the new VBP program? While physicians might see quality in clinical terms, the VBP program defines performance more broadly; that means it includes the patient experience. In fact, about 70% of the quality measures will be based on clinical performance, and a full 30% will come from scores on post-discharge patient satisfaction questionnaires (e.g. HCAHPS). To understand the importance of the patient satisfaction part of the VBP equation, just note that Press Ganey, the largest private company helping hospitals understand what their customers are thinking, is jumping into the VBP arena with both feet. Your hospital’s CFO (and lead hospitalist) should contact Press Ganey and run your current performance numbers through their VBP calculator to see if you are on the hilltop or in a deep hole.
The clinical measures will be selected from those used in the current Medicare pay-for-reporting program and likely will include measures for myocardial infarction, heart failure, pneumonia, and surgical care. In addition, HHS is mandated to include measures of efficiency, looking at ways to assess the spending per Medicare beneficiary. This is the real value equation: value = outcomes ÷ cost.
HM to the Rescue
No one in the hospital community sits more at the nexus of clinical care on these measures, efficiency, and the patient experience than hospitalists. This is an opportunity and a risk for hospitalists; that is why SHM is actively planning strategies to help hospitalists assist their hospitals in assessing how their current performance would play out in the payment world post-2013. In addition, SHM will have tools to assist hospitalists in creating change to help their institutions be in the top half of the nation’s hospitals—those who will get their millions of withheld dollars back.
SHM’s board of directors recently passed the following position statement on value-based purchasing:
“SHM supports the Affordable Care Act (ACA) Section 3001 directing the Secretary of HHS to establish a value-based purchasing program under the hospital inpatient prospective payment system. We believe that the Medicare reimbursement system must be changed to promote value, and we strongly support policies that link quality measurement to performance-based payment. We are pleased that under ACA the Secretary will establish performance standards that reward hospitals based on either attaining a certain performance standard or making improvements relative to a previous performance period. Hospitalists, who care for more hospitalized patients than any other physician group and lead system change and quality improvement efforts, will be critical to improving the performance of hospitals under this program.”
As mentioned above, the VBP program poses some risks to hospitalists. We cannot improve our hospital’s performance by ourselves, no matter how well motivated and trained we are. Hospitalists tend to attract a group of patients who traditionally have less satisfaction with their hospital experience (e.g. acutely ill patients admitted through the ED). But for more than a decade, hospitalists have been touting our goal to change the system for the better and to strive to be rewarded for value and performance, not simply for the doing.
In some ways, hospitals’ financial support of hospitalist groups has been predicated on the value we currently provide in efficiency (e.g. decreased length of stay, better use of resources) and effectiveness (e.g. improved measurable quality). The VBP program in ACA is just a first big step for the largest payor of hospital care—CMS—to change the ground rules.
Well-prepared hospitalists can provide leadership and help deliver their institutions to the top half of hospitals (those that will receive bonus payment) and, at the same time, begin to change the culture of their hospital to provide their patients with a better clinical outcome and a better patient experience.
Congress and President Obama are our allies here. A million dollars should get your hospital executives’ attention. Now is the time for hospitalists—with SHM’s help—to step up and show what we can do. TH
Dr. Wellikson is CEO of SHM.