User login
Performance Partnership
With 37,000 individual members and nearly 5,000 hospitals and other provider groups on its roster, the American Hospital Association (AHA) is a major player in national healthcare debates and in shaping policies aimed at improving quality.
John Combes, MD, AHA senior vice president and president and chief operating officer of the association-affiliated Center for Healthcare Governance, serves on several national advisory groups on medical ethics, palliative care, and reducing medication errors.
Among his many duties, he is a principal investigator for a national project aimed at reducing hospital-acquired infections called “On the CUSP: Stop Bloodstream Infections,” sponsored by the Agency for Healthcare Research and Quality (AHRQ). (CUSP is the Comprehensive Unit-based Safety Program, developed by Johns Hopkins University and the Michigan Hospital Association.)
Dr. Combes recently talked with The Hospitalist about the AHA’s vision for healthcare reform, integrated care, and the role of hospitalists in redesigning hospital-based care.
Question: What are the AHA’s biggest priorities over the next year?
Answer: Healthcare reform and making sure that we can increase coverage for patients without insurance. There are 48 million uninsured in this country, and we are very supportive of increasing that coverage to make sure that people have good access to healthcare.
Q: The AHA has stated that “clinical integration holds the promise of greater quality and improved efficiency in delivering patient-centered care.” What’s your vision for clinical integration?
A: What we recognize is that in a reformed delivery system, we have to have a lot of partnerships between hospitals and clinicians—physicians in particular—and between hospitals and other facilities, such as long-term care facilities and post-acute facilities. We need to be able to bring better-coordinated care that meets the patient’s needs, and we need to work with each other to constantly improve that care. So that’s why we’re looking at an integrated delivery system. In our minds, it really means one registration, one bill, one experience for the patient.
Practically speaking, if you look at the healthcare reform legislation … there are pilots in there for accountable-care organizations (ACOs) and other payment reforms. And we’re very interested in making sure that hospitals can participate and take a leadership role in the development of those kinds of new structures.
Q: What role do you expect hospitalists to play in the continued drive for higher quality and more efficient care?
A: I think hospitalists can become a critical partner with the hospital in helping us redesign inpatient care to make it more efficient and effective. Additionally, hospitalists have a key role in engaging and keeping involved the community-based PCP, and making sure that they are considered part of the care team, even though they may not be present in the hospital, since they have the continuing responsibility for the patient.
I think as we look at other models of care delivery, such as the patient-centered medical home, it’s critical that hospitalists really develop some strong relationships and communication networks with those groups as well, so that the care for the patient can become seamless and transitions are not as dangerous as they’ve been in the past, in terms of missed opportunities and missed handoffs.

Q: What are the necessary ingredients for any successful quality incentive payment program?
A: One of our big concerns is that there are lots of regulatory obstacles to true integration, where you can design some of those payment structures in terms of gainsharing and also in terms of payment for high-level-quality performance. One of the concerns of the AHM is to make sure that as we pursue these new models of care that require high levels of integration, we also look at some regulatory relief.
The promise is that if we can integrate the delivery system, we can then get focused on improving care and then rewarding high-quality delivery of care. And that can come through incentive programs or pay-for-performance programs and things of that nature that can be worked out between the hospitals and the physicians.
Q: What can be done to reduce the rates of hospital-acquired infections?
A: The idea of CUSP is that you create teams and a culture on units that will then implement the evidence-based intervention—in this case, eliminating central-line infections.
Hospitalists can play a critical role in helping create that culture of mutual accountability at the team level [and] holding each other accountable to use the evidence-based techniques for, in this case, line insertion, or for any kind of safety intervention. I think eliminating infections is a goal that’s achievable. I think we have come to the understanding over the last five or so years that these complications are avoidable in many, many cases, and that it takes teamwork, communication, and use of evidence-based procedures to get the work done.
Q: What can be done to help reduce preventable hospital readmissions?
A: There are so many things that go into readmissions. And the issue is: What is truly preventable in terms of treatments within the hospital, the coordination of discharge, and aftercare followup? A lot of readmissions are related to social determinants of health. And those have to do with people’s ability to afford their medications, people’s ability to access care, people’s home environment, and things of that nature. It’s going to take an approach by hospitals on those things that are controllable in partnerships with the physicians. But for many, many readmissions, it’s related to other issues that we as a society really have to hold ourselves accountable to.
Q: Some critics have charged that the overuse of medical technology is helping to drive up healthcare costs. Would there be more of a role for hospitals in decision-making about the appropriateness of tests within a model like an ACO?
A: In an ACO, that’s a partnership between hospitals and physicians operating as one entity. So that’s the difference, because there, everybody is aligned to make sure that we deliver the most effective care. There’s going to be much more time spent on physicians ordering the most appropriate technology or treatments for that condition that will deliver value to the patient and to the payor of that care.
But that’s in a totally integrated system. Right now we don’t have that. So where the interests of the physicians may be different from the interests of the hospital and the intentions are not aligned, it’s very hard to get at talking about what’s the most effective care.
Q: Is there a measure that hasn’t received as much attention that you would like to see more focus on to help improve the quality or cost-effectiveness of healthcare?
A: I think the one area that we’re always challenged with—and I think we’ve seen it in the healthcare debate, and I think it’s an appropriate role for us as healthcare providers to pay attention to—is palliative and end-of-life care. I don’t think we’ve done enough work, as a profession, to make sure that we deliver very-high-quality care of patients with chronic and acute catastrophic illnesses.
We need to better understand what the needs of those patients are, to ask them to work with us to set the goals with them, what they want from us.
So I think it’s an opportunity for us to have a real partnership with patients at a critical time in their lives. TH
Bryn Nelson is a freelance medical writer based in Seattle.
With 37,000 individual members and nearly 5,000 hospitals and other provider groups on its roster, the American Hospital Association (AHA) is a major player in national healthcare debates and in shaping policies aimed at improving quality.
John Combes, MD, AHA senior vice president and president and chief operating officer of the association-affiliated Center for Healthcare Governance, serves on several national advisory groups on medical ethics, palliative care, and reducing medication errors.
Among his many duties, he is a principal investigator for a national project aimed at reducing hospital-acquired infections called “On the CUSP: Stop Bloodstream Infections,” sponsored by the Agency for Healthcare Research and Quality (AHRQ). (CUSP is the Comprehensive Unit-based Safety Program, developed by Johns Hopkins University and the Michigan Hospital Association.)
Dr. Combes recently talked with The Hospitalist about the AHA’s vision for healthcare reform, integrated care, and the role of hospitalists in redesigning hospital-based care.
Question: What are the AHA’s biggest priorities over the next year?
Answer: Healthcare reform and making sure that we can increase coverage for patients without insurance. There are 48 million uninsured in this country, and we are very supportive of increasing that coverage to make sure that people have good access to healthcare.
Q: The AHA has stated that “clinical integration holds the promise of greater quality and improved efficiency in delivering patient-centered care.” What’s your vision for clinical integration?
A: What we recognize is that in a reformed delivery system, we have to have a lot of partnerships between hospitals and clinicians—physicians in particular—and between hospitals and other facilities, such as long-term care facilities and post-acute facilities. We need to be able to bring better-coordinated care that meets the patient’s needs, and we need to work with each other to constantly improve that care. So that’s why we’re looking at an integrated delivery system. In our minds, it really means one registration, one bill, one experience for the patient.
Practically speaking, if you look at the healthcare reform legislation … there are pilots in there for accountable-care organizations (ACOs) and other payment reforms. And we’re very interested in making sure that hospitals can participate and take a leadership role in the development of those kinds of new structures.
Q: What role do you expect hospitalists to play in the continued drive for higher quality and more efficient care?
A: I think hospitalists can become a critical partner with the hospital in helping us redesign inpatient care to make it more efficient and effective. Additionally, hospitalists have a key role in engaging and keeping involved the community-based PCP, and making sure that they are considered part of the care team, even though they may not be present in the hospital, since they have the continuing responsibility for the patient.
I think as we look at other models of care delivery, such as the patient-centered medical home, it’s critical that hospitalists really develop some strong relationships and communication networks with those groups as well, so that the care for the patient can become seamless and transitions are not as dangerous as they’ve been in the past, in terms of missed opportunities and missed handoffs.

Q: What are the necessary ingredients for any successful quality incentive payment program?
A: One of our big concerns is that there are lots of regulatory obstacles to true integration, where you can design some of those payment structures in terms of gainsharing and also in terms of payment for high-level-quality performance. One of the concerns of the AHM is to make sure that as we pursue these new models of care that require high levels of integration, we also look at some regulatory relief.
The promise is that if we can integrate the delivery system, we can then get focused on improving care and then rewarding high-quality delivery of care. And that can come through incentive programs or pay-for-performance programs and things of that nature that can be worked out between the hospitals and the physicians.
Q: What can be done to reduce the rates of hospital-acquired infections?
A: The idea of CUSP is that you create teams and a culture on units that will then implement the evidence-based intervention—in this case, eliminating central-line infections.
Hospitalists can play a critical role in helping create that culture of mutual accountability at the team level [and] holding each other accountable to use the evidence-based techniques for, in this case, line insertion, or for any kind of safety intervention. I think eliminating infections is a goal that’s achievable. I think we have come to the understanding over the last five or so years that these complications are avoidable in many, many cases, and that it takes teamwork, communication, and use of evidence-based procedures to get the work done.
Q: What can be done to help reduce preventable hospital readmissions?
A: There are so many things that go into readmissions. And the issue is: What is truly preventable in terms of treatments within the hospital, the coordination of discharge, and aftercare followup? A lot of readmissions are related to social determinants of health. And those have to do with people’s ability to afford their medications, people’s ability to access care, people’s home environment, and things of that nature. It’s going to take an approach by hospitals on those things that are controllable in partnerships with the physicians. But for many, many readmissions, it’s related to other issues that we as a society really have to hold ourselves accountable to.
Q: Some critics have charged that the overuse of medical technology is helping to drive up healthcare costs. Would there be more of a role for hospitals in decision-making about the appropriateness of tests within a model like an ACO?
A: In an ACO, that’s a partnership between hospitals and physicians operating as one entity. So that’s the difference, because there, everybody is aligned to make sure that we deliver the most effective care. There’s going to be much more time spent on physicians ordering the most appropriate technology or treatments for that condition that will deliver value to the patient and to the payor of that care.
But that’s in a totally integrated system. Right now we don’t have that. So where the interests of the physicians may be different from the interests of the hospital and the intentions are not aligned, it’s very hard to get at talking about what’s the most effective care.
Q: Is there a measure that hasn’t received as much attention that you would like to see more focus on to help improve the quality or cost-effectiveness of healthcare?
A: I think the one area that we’re always challenged with—and I think we’ve seen it in the healthcare debate, and I think it’s an appropriate role for us as healthcare providers to pay attention to—is palliative and end-of-life care. I don’t think we’ve done enough work, as a profession, to make sure that we deliver very-high-quality care of patients with chronic and acute catastrophic illnesses.
We need to better understand what the needs of those patients are, to ask them to work with us to set the goals with them, what they want from us.
So I think it’s an opportunity for us to have a real partnership with patients at a critical time in their lives. TH
Bryn Nelson is a freelance medical writer based in Seattle.
With 37,000 individual members and nearly 5,000 hospitals and other provider groups on its roster, the American Hospital Association (AHA) is a major player in national healthcare debates and in shaping policies aimed at improving quality.
John Combes, MD, AHA senior vice president and president and chief operating officer of the association-affiliated Center for Healthcare Governance, serves on several national advisory groups on medical ethics, palliative care, and reducing medication errors.
Among his many duties, he is a principal investigator for a national project aimed at reducing hospital-acquired infections called “On the CUSP: Stop Bloodstream Infections,” sponsored by the Agency for Healthcare Research and Quality (AHRQ). (CUSP is the Comprehensive Unit-based Safety Program, developed by Johns Hopkins University and the Michigan Hospital Association.)
Dr. Combes recently talked with The Hospitalist about the AHA’s vision for healthcare reform, integrated care, and the role of hospitalists in redesigning hospital-based care.
Question: What are the AHA’s biggest priorities over the next year?
Answer: Healthcare reform and making sure that we can increase coverage for patients without insurance. There are 48 million uninsured in this country, and we are very supportive of increasing that coverage to make sure that people have good access to healthcare.
Q: The AHA has stated that “clinical integration holds the promise of greater quality and improved efficiency in delivering patient-centered care.” What’s your vision for clinical integration?
A: What we recognize is that in a reformed delivery system, we have to have a lot of partnerships between hospitals and clinicians—physicians in particular—and between hospitals and other facilities, such as long-term care facilities and post-acute facilities. We need to be able to bring better-coordinated care that meets the patient’s needs, and we need to work with each other to constantly improve that care. So that’s why we’re looking at an integrated delivery system. In our minds, it really means one registration, one bill, one experience for the patient.
Practically speaking, if you look at the healthcare reform legislation … there are pilots in there for accountable-care organizations (ACOs) and other payment reforms. And we’re very interested in making sure that hospitals can participate and take a leadership role in the development of those kinds of new structures.
Q: What role do you expect hospitalists to play in the continued drive for higher quality and more efficient care?
A: I think hospitalists can become a critical partner with the hospital in helping us redesign inpatient care to make it more efficient and effective. Additionally, hospitalists have a key role in engaging and keeping involved the community-based PCP, and making sure that they are considered part of the care team, even though they may not be present in the hospital, since they have the continuing responsibility for the patient.
I think as we look at other models of care delivery, such as the patient-centered medical home, it’s critical that hospitalists really develop some strong relationships and communication networks with those groups as well, so that the care for the patient can become seamless and transitions are not as dangerous as they’ve been in the past, in terms of missed opportunities and missed handoffs.

Q: What are the necessary ingredients for any successful quality incentive payment program?
A: One of our big concerns is that there are lots of regulatory obstacles to true integration, where you can design some of those payment structures in terms of gainsharing and also in terms of payment for high-level-quality performance. One of the concerns of the AHM is to make sure that as we pursue these new models of care that require high levels of integration, we also look at some regulatory relief.
The promise is that if we can integrate the delivery system, we can then get focused on improving care and then rewarding high-quality delivery of care. And that can come through incentive programs or pay-for-performance programs and things of that nature that can be worked out between the hospitals and the physicians.
Q: What can be done to reduce the rates of hospital-acquired infections?
A: The idea of CUSP is that you create teams and a culture on units that will then implement the evidence-based intervention—in this case, eliminating central-line infections.
Hospitalists can play a critical role in helping create that culture of mutual accountability at the team level [and] holding each other accountable to use the evidence-based techniques for, in this case, line insertion, or for any kind of safety intervention. I think eliminating infections is a goal that’s achievable. I think we have come to the understanding over the last five or so years that these complications are avoidable in many, many cases, and that it takes teamwork, communication, and use of evidence-based procedures to get the work done.
Q: What can be done to help reduce preventable hospital readmissions?
A: There are so many things that go into readmissions. And the issue is: What is truly preventable in terms of treatments within the hospital, the coordination of discharge, and aftercare followup? A lot of readmissions are related to social determinants of health. And those have to do with people’s ability to afford their medications, people’s ability to access care, people’s home environment, and things of that nature. It’s going to take an approach by hospitals on those things that are controllable in partnerships with the physicians. But for many, many readmissions, it’s related to other issues that we as a society really have to hold ourselves accountable to.
Q: Some critics have charged that the overuse of medical technology is helping to drive up healthcare costs. Would there be more of a role for hospitals in decision-making about the appropriateness of tests within a model like an ACO?
A: In an ACO, that’s a partnership between hospitals and physicians operating as one entity. So that’s the difference, because there, everybody is aligned to make sure that we deliver the most effective care. There’s going to be much more time spent on physicians ordering the most appropriate technology or treatments for that condition that will deliver value to the patient and to the payor of that care.
But that’s in a totally integrated system. Right now we don’t have that. So where the interests of the physicians may be different from the interests of the hospital and the intentions are not aligned, it’s very hard to get at talking about what’s the most effective care.
Q: Is there a measure that hasn’t received as much attention that you would like to see more focus on to help improve the quality or cost-effectiveness of healthcare?
A: I think the one area that we’re always challenged with—and I think we’ve seen it in the healthcare debate, and I think it’s an appropriate role for us as healthcare providers to pay attention to—is palliative and end-of-life care. I don’t think we’ve done enough work, as a profession, to make sure that we deliver very-high-quality care of patients with chronic and acute catastrophic illnesses.
We need to better understand what the needs of those patients are, to ask them to work with us to set the goals with them, what they want from us.
So I think it’s an opportunity for us to have a real partnership with patients at a critical time in their lives. TH
Bryn Nelson is a freelance medical writer based in Seattle.
Focused Practice in Hospital Medicine
Some in her HM group think Cathleen Ammann, MD, is the guinea pig. Dr. Ammann, the medical director of the hospital medicine division at Wentworth-Douglass Hospital in Dover, N.H., will be one of the first to complete her American Board of Internal Medicine’s (ABIM) Maintenance of Certification (MOC) through the new Focused Practice in Hospital Medicine (FPHM) pathway. Dr. Ammann—and the hospital administration—sees things a little differently.
“Am I the guinea pig or a pioneer?” a hospitalist in Dr. Ammann’s group asked her recently. “I definitely see it as being a pioneer. When you look back in another 10 years, hospital medicine might be a specialty with its own certification. I know it’s a little corny, but I look forward to getting in on that at the ground floor.”
Dr. Ammann is one of about 175 hospitalists who have signed up to recertify through FPHM. Her internal-medicine (IM) certification expires at the end of the year, so she will be taking the recertification exam Oct. 25.
“I hope the test focuses more on what I’m doing … stroke, quality measures,” she says. “Hospitalists know that stuff like the back of our hand. … I think it will work out well for me, but I also think it will be great for our program to have a director who has a Focused Practice in Hospital Medicine. It shows my commitment, and we can hold that up to the rest of the organization and say we really have someone who is concentrated in this field.”
Dr. Ammann sums up the thinking of many HM leaders who’ve been working with ABIM and the American Board of Medical Specialties to launch the MOC pathway for hospitalists: Not only does a focused practice certification allow the more than 30,000 hospitalists in the U.S. to define themselves as different, it also provides hospitalists an MOC process and secured examination more acutely tailored to their skill sets and daily practice. The new pathway also requires ACLS certification and stresses continued “maintenance of competency,” according to SHM leaders, through a triennial self-evaluation requirement (60 self-evaluation points, with at least 20 points from medical knowledge modules and 40 points from completion of practice performance modules). The traditional IM MOC requires a practice-improvement module (PIM) every 10 years.
“The process will ask diplomates to participate in practice improvement every three years, which will focus on the ongoing need for performance improvement,” says Jeff Wiese, MD, FACP, SFHM, SHM president and chair of the ABIM Hospital Medicine MOC Question Writing Committee. “It will separate out the authentic hospitalist who is representing the goals and virtues that we are espousing as a society, particularly with regards to quality healthcare and safe healthcare. But I also think there are unique benefits for the patient that will be receiving the healthcare, because through this process, I believe, every diplomate will be a better hospitalist as a product of having done it.”
Here’s a brief look at what hospitalists interested in the FPHM MOC can expect:
The Process and Timeline
ABIM and SHM began working toward an HM-focused pathway about five years ago, and the two groups announced the FPHM program in September 2009. ABIM is in the process of retooling its website for the new MOC pathway. The entry system—to sign up and begin the MOC’s attestation process—was made public in March. The registration interface for the secure exam opened to the hospitalist community May 1, says Eric Holmboe, MD, ABIM’s chief medical officer.
“Diplomates can signify their interest and start the attestation process, which will allow them to get formal entry into the pathway,” Dr. Holmboe says. “Once they receive the attestation confirmation back, they can start doing the requirements around the medical knowledge and performance and practice requirements. Those are all available on the website. … We’re excited. The first phase of the project is live. This is a brand-new pathway for MOC, and we’re really hopeful people will find it valuable and useful.”
Board recertification is no easy task, and prospective diplomates should organize a plan of attack based upon individual workloads and regular involvement in performance-improvement programs. Some hospitalists will only need six to nine months to complete all the requirements and take the exam; others might take a conservative approach and need one to two years.
“Eighteen months is very reasonable,” Dr. Holmboe says. “Because of the 40-point requirement for the evaluation of performance and practice, that means you have to do the hospital-based PIM or self-directed PIM, or some combination thereof, twice. So if you haven’t been active in QI projects in your hospital, you really need to get going.”
Some hospitalists and HM groups work on quality-improvement (QI) projects regularly. Dr. Ammann plans to use a recent QI project looking at her group’s compliance with antibiotic selection for pneumonia to satisfy one of her required PIMs.
“[The three-year] requirement should be easy for directors because we’re always doing that kind of work anyway,” she says. “We just finished a project where we had to improve our compliance with antibiotic selection. We looked at our processes and found that our pathway wasn’t clear, and it could be interpreted a couple different ways. So our chief of medicine and I just changed the pathway, put it out there, and since then, our compliance has consistently been 100%.
We have two quarters of data, and I’m going to use that for my PIM, which is nice, because it’s done.”
For hospitalists whose certification runs out in 2011 or beyond, Dr. Holmboe suggests the following timeline:
Now through end of 2010
- Register for the Focused Practice in Hospital Medicine MOC pathway on ABIM’ website (www.abim.org/moc/policies. aspx);
- Complete the attestation process;
- Get involved in an appropriate (hospital-based) performance-improvement activity; and
- Complete Update in Hospital Medicine using ABIM or ACP medical education modules.

—Cathleen Ammann, MD, medical director, hospital medicine division, Wentworth-Douglass Hospital, Dover, N.H.
First six months of 2011
- Complete the next yearly Update in HM module;
- Develop a strategy to prepare for the exam, which is given in the fall; and
- Plan and complete your second performance improvement activity.
Second half of 2011
- Prepare for the exam; and
- Pass the exam.
Start Process Now, Start Earning Points
ABIM is encouraging prospective FPHM diplomates to begin working on medical-knowledge modules. Most are designed to “stretch folks and to get them to look things up.”
“ACP, to their credit, also has hospital-based modules,” Dr. Holmboe says. “So if somebody is a dual member, they can certainly use the ACP’s MKSAP (Medical Knowledge Self-Assessment Program) hospital-based modules as well. We’re also working with SHM, looking for areas they might fill in around knowledge and updates—things that could be brought into the program over time.”
In regard to the evaluation and performance modules, ABIM offers three main pathways, including the Hospital-Based PIM, which targets core measure sets like community-acquired pneumonia and congestive heart failure and DVT prophylaxis. “Hospitalists can use those PIMs to start a quality-improvement program, or they can use it to report on one they are working on,” Dr. Holmboe says, adding the Hospital Based PIM’s online module will be redesigned this summer to improve the user experience.
Two other approaches are the Self-Directed PIM and the Accepted Quality Improvement programs. “That would be for hospitalists who may not be working on the core measure sets in the hospital-based PIM, but are still important,” he says. “They can use that module to report on those activities and get the points they need.”
Dr. Holmboe also points out that diplomates do not have to complete all the other requirements before they take the exam. “Some people get confused; you don’t have to cram in the 100 points before the exam,” Dr. Holmboe explains. He notes that the exam can, for example, be taken this year and the remainder of the requirements completed at a later date.
“If it was up to me, you should do a [PIM] every year,” says Larry Wellikson, MD, SFHM, CEO of SHM and one of the architects of the new FPHM pathway. “If you are a real hospitalist, completing a PIM every three years shouldn’t be a big deal. You should be able to say, ‘I’ve looked at 10 things: how I’m doing in pneumonia, how I’m doing in DVT, how I’m doing in glycemic control. This isn’t work for me; it’s part of my workflow.’ It’s like asking a salesman how many sales calls have you made, how many miles have you driven, and how many sales have you closed.”
The Examination
Dr. Wiese, associate dean of Graduate Medical Education and professor of medicine at Tulane University in New Orleans, completed his 10-year MOC in 2008, and he says the process made him “a better physician.” As president of SHM and chair of the FPHM test-writing committee, he envisions that the new MOC pathway will help “ramp up the quality of care for the hospitalized patient.”
“The FPHM MOC process is much more than just a different exam,” he says. “It is true the secure examination will have a lot more hospital-medicine-patient content focus, but not to the exclusion of ambulatory content.”

—Jeff Wiese, SHM president, ABIM Focused Practice in Hospital Medicine Test Writing Committee chair
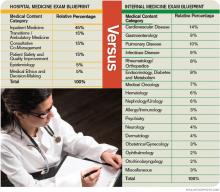
The content-area blueprint (see “Traditional IM Test vs. Focused Practice in HM Test” below) for the FPHM exam includes 15% of questions in the areas of quality and patient safety, along with another 15% in consultative and comanagement topics. Transitions of care and ambulatory questions make up another 15% of the exam.
“If there is one component of the exam that will [be HM-focused], it’s the questions of the exam that are focusing on the core principles of quality and patient safety,” Dr. Wiese says.
That’s music to the ears of many hospitalists—including Dr. Ammann—who know questions about managing cholesterol aren’t relevant to hospitalists. Dr. Ammann was an office-based physician before becoming a hospitalist in 2005. One year later, she was promoted to director of her group, which includes 14 physicians and two nonphysician providers.
“I was really hoping I would be able to [MOC] through the focused practice in HM,” she says. “I did practice office medicine, so I probably have a little advantage. But I was not looking forward to spending time learning and brushing up on things that I am not doing anymore—not only because I’m not doing it anymore, but it would be a waste of time because I’m not going to be doing it, either.”
One of her hospitalist colleagues is taking the traditional IM pathway to MOC, Dr. Ammann says, because “she doesn’t want to limit her scope.” But that’s not how Dr. Ammann sees the FPHM. She is committed to HM and doesn’t have “any problems kissing office medicine goodbye.”
“I think it will work out well for me, but I also think it will be great for our program to have a director who has a Focused Practice in Hospital Medicine,” she says. “It shows my commitment, and we can hold that up to the rest of the organization and say we really have someone who is concentrated in this field.”
Educational Efforts
Vikas Parekh, MD, FHM, is in his second year as the chair of SHM’s Education Committee, and says the first task at hand is to educate hospitalists about the new FPHM pathway to MOC. The University of Michigan hospitalist says his committee, working with ABIM and SHM staff, is focused on two major educational efforts: developing the SHM strategy to assist hospitalists with the new FPHM MOC pathway, and “fulfilling the needs of hospitalists, in terms of the resources they have for the MOC process.”
“We’ve already started down this route, in terms of developing resources,” Dr. Parekh says. “We’ve done a few things that have been easy. One is the ABIM learning session pre-course at the annual meeting. … It earns you points toward the medical-knowledge component.”
ABIM and ACP are the traditional avenues for medical-knowledge and practice-improvement requirements for the MOC process. SHM and ABIM currently are working to develop medical-knowledge modules in the domains of patient safety and quality improvement, areas most relevant to HM. Dr. Parekh expects those components to be available in early 2011.
“Practice improvement is likely to be our second main effort,” Dr. Parekh says. “SHM has a lot of resources within our resource rooms that have the shell of what you would really need to meet ABIM requirements for a PIM but aren’t quite complete or thorough enough, or have all the bells and whistles that ABIM wants them to have. … We think we can do a much better job focusing the PIMs to hospitalists.”
At a more granular level, Dr. Wellikson envisions a “suite of products” to assist members in the MOC process. “What we are trying to do is develop resources that help people practice better medicine,” he says, “and while we are helping you practice better medicine, you can also use that to prove to [ABIM] that you have done it.
“So if you log onto the website today and downloaded and completed any of those SHM resource rooms, somewhere in the next several months you will be able to click on a form, enter the results, send it to ABIM, and you’ll have satisfied a PIM,” Dr. Wellikson says. “You can do the work today.”
SHM’s Project BOOST (Better Outcomes for Older Adults through Safer Transitions) and Glycemic Control Mentored Implementation programs are prime candidates for Web-based PIMs, according to Dr. Holmboe.
“I think it is still very early, but we are very excited about this,” Dr. Parekh says. “I think a lot of people still have questions about what exactly this mean to me, and why should I recertify through this focused practice as opposed to the traditional general pathway? We hope to change that by making the resources focused to their practice.” TH
Jason Carris is editor of The Hospitalist.
Some in her HM group think Cathleen Ammann, MD, is the guinea pig. Dr. Ammann, the medical director of the hospital medicine division at Wentworth-Douglass Hospital in Dover, N.H., will be one of the first to complete her American Board of Internal Medicine’s (ABIM) Maintenance of Certification (MOC) through the new Focused Practice in Hospital Medicine (FPHM) pathway. Dr. Ammann—and the hospital administration—sees things a little differently.
“Am I the guinea pig or a pioneer?” a hospitalist in Dr. Ammann’s group asked her recently. “I definitely see it as being a pioneer. When you look back in another 10 years, hospital medicine might be a specialty with its own certification. I know it’s a little corny, but I look forward to getting in on that at the ground floor.”
Dr. Ammann is one of about 175 hospitalists who have signed up to recertify through FPHM. Her internal-medicine (IM) certification expires at the end of the year, so she will be taking the recertification exam Oct. 25.
“I hope the test focuses more on what I’m doing … stroke, quality measures,” she says. “Hospitalists know that stuff like the back of our hand. … I think it will work out well for me, but I also think it will be great for our program to have a director who has a Focused Practice in Hospital Medicine. It shows my commitment, and we can hold that up to the rest of the organization and say we really have someone who is concentrated in this field.”
Dr. Ammann sums up the thinking of many HM leaders who’ve been working with ABIM and the American Board of Medical Specialties to launch the MOC pathway for hospitalists: Not only does a focused practice certification allow the more than 30,000 hospitalists in the U.S. to define themselves as different, it also provides hospitalists an MOC process and secured examination more acutely tailored to their skill sets and daily practice. The new pathway also requires ACLS certification and stresses continued “maintenance of competency,” according to SHM leaders, through a triennial self-evaluation requirement (60 self-evaluation points, with at least 20 points from medical knowledge modules and 40 points from completion of practice performance modules). The traditional IM MOC requires a practice-improvement module (PIM) every 10 years.
“The process will ask diplomates to participate in practice improvement every three years, which will focus on the ongoing need for performance improvement,” says Jeff Wiese, MD, FACP, SFHM, SHM president and chair of the ABIM Hospital Medicine MOC Question Writing Committee. “It will separate out the authentic hospitalist who is representing the goals and virtues that we are espousing as a society, particularly with regards to quality healthcare and safe healthcare. But I also think there are unique benefits for the patient that will be receiving the healthcare, because through this process, I believe, every diplomate will be a better hospitalist as a product of having done it.”
Here’s a brief look at what hospitalists interested in the FPHM MOC can expect:
The Process and Timeline
ABIM and SHM began working toward an HM-focused pathway about five years ago, and the two groups announced the FPHM program in September 2009. ABIM is in the process of retooling its website for the new MOC pathway. The entry system—to sign up and begin the MOC’s attestation process—was made public in March. The registration interface for the secure exam opened to the hospitalist community May 1, says Eric Holmboe, MD, ABIM’s chief medical officer.
“Diplomates can signify their interest and start the attestation process, which will allow them to get formal entry into the pathway,” Dr. Holmboe says. “Once they receive the attestation confirmation back, they can start doing the requirements around the medical knowledge and performance and practice requirements. Those are all available on the website. … We’re excited. The first phase of the project is live. This is a brand-new pathway for MOC, and we’re really hopeful people will find it valuable and useful.”
Board recertification is no easy task, and prospective diplomates should organize a plan of attack based upon individual workloads and regular involvement in performance-improvement programs. Some hospitalists will only need six to nine months to complete all the requirements and take the exam; others might take a conservative approach and need one to two years.
“Eighteen months is very reasonable,” Dr. Holmboe says. “Because of the 40-point requirement for the evaluation of performance and practice, that means you have to do the hospital-based PIM or self-directed PIM, or some combination thereof, twice. So if you haven’t been active in QI projects in your hospital, you really need to get going.”
Some hospitalists and HM groups work on quality-improvement (QI) projects regularly. Dr. Ammann plans to use a recent QI project looking at her group’s compliance with antibiotic selection for pneumonia to satisfy one of her required PIMs.
“[The three-year] requirement should be easy for directors because we’re always doing that kind of work anyway,” she says. “We just finished a project where we had to improve our compliance with antibiotic selection. We looked at our processes and found that our pathway wasn’t clear, and it could be interpreted a couple different ways. So our chief of medicine and I just changed the pathway, put it out there, and since then, our compliance has consistently been 100%.
We have two quarters of data, and I’m going to use that for my PIM, which is nice, because it’s done.”
For hospitalists whose certification runs out in 2011 or beyond, Dr. Holmboe suggests the following timeline:
Now through end of 2010
- Register for the Focused Practice in Hospital Medicine MOC pathway on ABIM’ website (www.abim.org/moc/policies. aspx);
- Complete the attestation process;
- Get involved in an appropriate (hospital-based) performance-improvement activity; and
- Complete Update in Hospital Medicine using ABIM or ACP medical education modules.

—Cathleen Ammann, MD, medical director, hospital medicine division, Wentworth-Douglass Hospital, Dover, N.H.
First six months of 2011
- Complete the next yearly Update in HM module;
- Develop a strategy to prepare for the exam, which is given in the fall; and
- Plan and complete your second performance improvement activity.
Second half of 2011
- Prepare for the exam; and
- Pass the exam.
Start Process Now, Start Earning Points
ABIM is encouraging prospective FPHM diplomates to begin working on medical-knowledge modules. Most are designed to “stretch folks and to get them to look things up.”
“ACP, to their credit, also has hospital-based modules,” Dr. Holmboe says. “So if somebody is a dual member, they can certainly use the ACP’s MKSAP (Medical Knowledge Self-Assessment Program) hospital-based modules as well. We’re also working with SHM, looking for areas they might fill in around knowledge and updates—things that could be brought into the program over time.”
In regard to the evaluation and performance modules, ABIM offers three main pathways, including the Hospital-Based PIM, which targets core measure sets like community-acquired pneumonia and congestive heart failure and DVT prophylaxis. “Hospitalists can use those PIMs to start a quality-improvement program, or they can use it to report on one they are working on,” Dr. Holmboe says, adding the Hospital Based PIM’s online module will be redesigned this summer to improve the user experience.
Two other approaches are the Self-Directed PIM and the Accepted Quality Improvement programs. “That would be for hospitalists who may not be working on the core measure sets in the hospital-based PIM, but are still important,” he says. “They can use that module to report on those activities and get the points they need.”
Dr. Holmboe also points out that diplomates do not have to complete all the other requirements before they take the exam. “Some people get confused; you don’t have to cram in the 100 points before the exam,” Dr. Holmboe explains. He notes that the exam can, for example, be taken this year and the remainder of the requirements completed at a later date.
“If it was up to me, you should do a [PIM] every year,” says Larry Wellikson, MD, SFHM, CEO of SHM and one of the architects of the new FPHM pathway. “If you are a real hospitalist, completing a PIM every three years shouldn’t be a big deal. You should be able to say, ‘I’ve looked at 10 things: how I’m doing in pneumonia, how I’m doing in DVT, how I’m doing in glycemic control. This isn’t work for me; it’s part of my workflow.’ It’s like asking a salesman how many sales calls have you made, how many miles have you driven, and how many sales have you closed.”
The Examination
Dr. Wiese, associate dean of Graduate Medical Education and professor of medicine at Tulane University in New Orleans, completed his 10-year MOC in 2008, and he says the process made him “a better physician.” As president of SHM and chair of the FPHM test-writing committee, he envisions that the new MOC pathway will help “ramp up the quality of care for the hospitalized patient.”
“The FPHM MOC process is much more than just a different exam,” he says. “It is true the secure examination will have a lot more hospital-medicine-patient content focus, but not to the exclusion of ambulatory content.”

—Jeff Wiese, SHM president, ABIM Focused Practice in Hospital Medicine Test Writing Committee chair
The content-area blueprint (see “Traditional IM Test vs. Focused Practice in HM Test” below) for the FPHM exam includes 15% of questions in the areas of quality and patient safety, along with another 15% in consultative and comanagement topics. Transitions of care and ambulatory questions make up another 15% of the exam.
“If there is one component of the exam that will [be HM-focused], it’s the questions of the exam that are focusing on the core principles of quality and patient safety,” Dr. Wiese says.
That’s music to the ears of many hospitalists—including Dr. Ammann—who know questions about managing cholesterol aren’t relevant to hospitalists. Dr. Ammann was an office-based physician before becoming a hospitalist in 2005. One year later, she was promoted to director of her group, which includes 14 physicians and two nonphysician providers.
“I was really hoping I would be able to [MOC] through the focused practice in HM,” she says. “I did practice office medicine, so I probably have a little advantage. But I was not looking forward to spending time learning and brushing up on things that I am not doing anymore—not only because I’m not doing it anymore, but it would be a waste of time because I’m not going to be doing it, either.”
One of her hospitalist colleagues is taking the traditional IM pathway to MOC, Dr. Ammann says, because “she doesn’t want to limit her scope.” But that’s not how Dr. Ammann sees the FPHM. She is committed to HM and doesn’t have “any problems kissing office medicine goodbye.”
“I think it will work out well for me, but I also think it will be great for our program to have a director who has a Focused Practice in Hospital Medicine,” she says. “It shows my commitment, and we can hold that up to the rest of the organization and say we really have someone who is concentrated in this field.”
Educational Efforts
Vikas Parekh, MD, FHM, is in his second year as the chair of SHM’s Education Committee, and says the first task at hand is to educate hospitalists about the new FPHM pathway to MOC. The University of Michigan hospitalist says his committee, working with ABIM and SHM staff, is focused on two major educational efforts: developing the SHM strategy to assist hospitalists with the new FPHM MOC pathway, and “fulfilling the needs of hospitalists, in terms of the resources they have for the MOC process.”
“We’ve already started down this route, in terms of developing resources,” Dr. Parekh says. “We’ve done a few things that have been easy. One is the ABIM learning session pre-course at the annual meeting. … It earns you points toward the medical-knowledge component.”
ABIM and ACP are the traditional avenues for medical-knowledge and practice-improvement requirements for the MOC process. SHM and ABIM currently are working to develop medical-knowledge modules in the domains of patient safety and quality improvement, areas most relevant to HM. Dr. Parekh expects those components to be available in early 2011.
“Practice improvement is likely to be our second main effort,” Dr. Parekh says. “SHM has a lot of resources within our resource rooms that have the shell of what you would really need to meet ABIM requirements for a PIM but aren’t quite complete or thorough enough, or have all the bells and whistles that ABIM wants them to have. … We think we can do a much better job focusing the PIMs to hospitalists.”
At a more granular level, Dr. Wellikson envisions a “suite of products” to assist members in the MOC process. “What we are trying to do is develop resources that help people practice better medicine,” he says, “and while we are helping you practice better medicine, you can also use that to prove to [ABIM] that you have done it.
“So if you log onto the website today and downloaded and completed any of those SHM resource rooms, somewhere in the next several months you will be able to click on a form, enter the results, send it to ABIM, and you’ll have satisfied a PIM,” Dr. Wellikson says. “You can do the work today.”
SHM’s Project BOOST (Better Outcomes for Older Adults through Safer Transitions) and Glycemic Control Mentored Implementation programs are prime candidates for Web-based PIMs, according to Dr. Holmboe.
“I think it is still very early, but we are very excited about this,” Dr. Parekh says. “I think a lot of people still have questions about what exactly this mean to me, and why should I recertify through this focused practice as opposed to the traditional general pathway? We hope to change that by making the resources focused to their practice.” TH
Jason Carris is editor of The Hospitalist.
Some in her HM group think Cathleen Ammann, MD, is the guinea pig. Dr. Ammann, the medical director of the hospital medicine division at Wentworth-Douglass Hospital in Dover, N.H., will be one of the first to complete her American Board of Internal Medicine’s (ABIM) Maintenance of Certification (MOC) through the new Focused Practice in Hospital Medicine (FPHM) pathway. Dr. Ammann—and the hospital administration—sees things a little differently.
“Am I the guinea pig or a pioneer?” a hospitalist in Dr. Ammann’s group asked her recently. “I definitely see it as being a pioneer. When you look back in another 10 years, hospital medicine might be a specialty with its own certification. I know it’s a little corny, but I look forward to getting in on that at the ground floor.”
Dr. Ammann is one of about 175 hospitalists who have signed up to recertify through FPHM. Her internal-medicine (IM) certification expires at the end of the year, so she will be taking the recertification exam Oct. 25.
“I hope the test focuses more on what I’m doing … stroke, quality measures,” she says. “Hospitalists know that stuff like the back of our hand. … I think it will work out well for me, but I also think it will be great for our program to have a director who has a Focused Practice in Hospital Medicine. It shows my commitment, and we can hold that up to the rest of the organization and say we really have someone who is concentrated in this field.”
Dr. Ammann sums up the thinking of many HM leaders who’ve been working with ABIM and the American Board of Medical Specialties to launch the MOC pathway for hospitalists: Not only does a focused practice certification allow the more than 30,000 hospitalists in the U.S. to define themselves as different, it also provides hospitalists an MOC process and secured examination more acutely tailored to their skill sets and daily practice. The new pathway also requires ACLS certification and stresses continued “maintenance of competency,” according to SHM leaders, through a triennial self-evaluation requirement (60 self-evaluation points, with at least 20 points from medical knowledge modules and 40 points from completion of practice performance modules). The traditional IM MOC requires a practice-improvement module (PIM) every 10 years.
“The process will ask diplomates to participate in practice improvement every three years, which will focus on the ongoing need for performance improvement,” says Jeff Wiese, MD, FACP, SFHM, SHM president and chair of the ABIM Hospital Medicine MOC Question Writing Committee. “It will separate out the authentic hospitalist who is representing the goals and virtues that we are espousing as a society, particularly with regards to quality healthcare and safe healthcare. But I also think there are unique benefits for the patient that will be receiving the healthcare, because through this process, I believe, every diplomate will be a better hospitalist as a product of having done it.”
Here’s a brief look at what hospitalists interested in the FPHM MOC can expect:
The Process and Timeline
ABIM and SHM began working toward an HM-focused pathway about five years ago, and the two groups announced the FPHM program in September 2009. ABIM is in the process of retooling its website for the new MOC pathway. The entry system—to sign up and begin the MOC’s attestation process—was made public in March. The registration interface for the secure exam opened to the hospitalist community May 1, says Eric Holmboe, MD, ABIM’s chief medical officer.
“Diplomates can signify their interest and start the attestation process, which will allow them to get formal entry into the pathway,” Dr. Holmboe says. “Once they receive the attestation confirmation back, they can start doing the requirements around the medical knowledge and performance and practice requirements. Those are all available on the website. … We’re excited. The first phase of the project is live. This is a brand-new pathway for MOC, and we’re really hopeful people will find it valuable and useful.”
Board recertification is no easy task, and prospective diplomates should organize a plan of attack based upon individual workloads and regular involvement in performance-improvement programs. Some hospitalists will only need six to nine months to complete all the requirements and take the exam; others might take a conservative approach and need one to two years.
“Eighteen months is very reasonable,” Dr. Holmboe says. “Because of the 40-point requirement for the evaluation of performance and practice, that means you have to do the hospital-based PIM or self-directed PIM, or some combination thereof, twice. So if you haven’t been active in QI projects in your hospital, you really need to get going.”
Some hospitalists and HM groups work on quality-improvement (QI) projects regularly. Dr. Ammann plans to use a recent QI project looking at her group’s compliance with antibiotic selection for pneumonia to satisfy one of her required PIMs.
“[The three-year] requirement should be easy for directors because we’re always doing that kind of work anyway,” she says. “We just finished a project where we had to improve our compliance with antibiotic selection. We looked at our processes and found that our pathway wasn’t clear, and it could be interpreted a couple different ways. So our chief of medicine and I just changed the pathway, put it out there, and since then, our compliance has consistently been 100%.
We have two quarters of data, and I’m going to use that for my PIM, which is nice, because it’s done.”
For hospitalists whose certification runs out in 2011 or beyond, Dr. Holmboe suggests the following timeline:
Now through end of 2010
- Register for the Focused Practice in Hospital Medicine MOC pathway on ABIM’ website (www.abim.org/moc/policies. aspx);
- Complete the attestation process;
- Get involved in an appropriate (hospital-based) performance-improvement activity; and
- Complete Update in Hospital Medicine using ABIM or ACP medical education modules.

—Cathleen Ammann, MD, medical director, hospital medicine division, Wentworth-Douglass Hospital, Dover, N.H.
First six months of 2011
- Complete the next yearly Update in HM module;
- Develop a strategy to prepare for the exam, which is given in the fall; and
- Plan and complete your second performance improvement activity.
Second half of 2011
- Prepare for the exam; and
- Pass the exam.
Start Process Now, Start Earning Points
ABIM is encouraging prospective FPHM diplomates to begin working on medical-knowledge modules. Most are designed to “stretch folks and to get them to look things up.”
“ACP, to their credit, also has hospital-based modules,” Dr. Holmboe says. “So if somebody is a dual member, they can certainly use the ACP’s MKSAP (Medical Knowledge Self-Assessment Program) hospital-based modules as well. We’re also working with SHM, looking for areas they might fill in around knowledge and updates—things that could be brought into the program over time.”
In regard to the evaluation and performance modules, ABIM offers three main pathways, including the Hospital-Based PIM, which targets core measure sets like community-acquired pneumonia and congestive heart failure and DVT prophylaxis. “Hospitalists can use those PIMs to start a quality-improvement program, or they can use it to report on one they are working on,” Dr. Holmboe says, adding the Hospital Based PIM’s online module will be redesigned this summer to improve the user experience.
Two other approaches are the Self-Directed PIM and the Accepted Quality Improvement programs. “That would be for hospitalists who may not be working on the core measure sets in the hospital-based PIM, but are still important,” he says. “They can use that module to report on those activities and get the points they need.”
Dr. Holmboe also points out that diplomates do not have to complete all the other requirements before they take the exam. “Some people get confused; you don’t have to cram in the 100 points before the exam,” Dr. Holmboe explains. He notes that the exam can, for example, be taken this year and the remainder of the requirements completed at a later date.
“If it was up to me, you should do a [PIM] every year,” says Larry Wellikson, MD, SFHM, CEO of SHM and one of the architects of the new FPHM pathway. “If you are a real hospitalist, completing a PIM every three years shouldn’t be a big deal. You should be able to say, ‘I’ve looked at 10 things: how I’m doing in pneumonia, how I’m doing in DVT, how I’m doing in glycemic control. This isn’t work for me; it’s part of my workflow.’ It’s like asking a salesman how many sales calls have you made, how many miles have you driven, and how many sales have you closed.”
The Examination
Dr. Wiese, associate dean of Graduate Medical Education and professor of medicine at Tulane University in New Orleans, completed his 10-year MOC in 2008, and he says the process made him “a better physician.” As president of SHM and chair of the FPHM test-writing committee, he envisions that the new MOC pathway will help “ramp up the quality of care for the hospitalized patient.”
“The FPHM MOC process is much more than just a different exam,” he says. “It is true the secure examination will have a lot more hospital-medicine-patient content focus, but not to the exclusion of ambulatory content.”

—Jeff Wiese, SHM president, ABIM Focused Practice in Hospital Medicine Test Writing Committee chair
The content-area blueprint (see “Traditional IM Test vs. Focused Practice in HM Test” below) for the FPHM exam includes 15% of questions in the areas of quality and patient safety, along with another 15% in consultative and comanagement topics. Transitions of care and ambulatory questions make up another 15% of the exam.
“If there is one component of the exam that will [be HM-focused], it’s the questions of the exam that are focusing on the core principles of quality and patient safety,” Dr. Wiese says.
That’s music to the ears of many hospitalists—including Dr. Ammann—who know questions about managing cholesterol aren’t relevant to hospitalists. Dr. Ammann was an office-based physician before becoming a hospitalist in 2005. One year later, she was promoted to director of her group, which includes 14 physicians and two nonphysician providers.
“I was really hoping I would be able to [MOC] through the focused practice in HM,” she says. “I did practice office medicine, so I probably have a little advantage. But I was not looking forward to spending time learning and brushing up on things that I am not doing anymore—not only because I’m not doing it anymore, but it would be a waste of time because I’m not going to be doing it, either.”
One of her hospitalist colleagues is taking the traditional IM pathway to MOC, Dr. Ammann says, because “she doesn’t want to limit her scope.” But that’s not how Dr. Ammann sees the FPHM. She is committed to HM and doesn’t have “any problems kissing office medicine goodbye.”
“I think it will work out well for me, but I also think it will be great for our program to have a director who has a Focused Practice in Hospital Medicine,” she says. “It shows my commitment, and we can hold that up to the rest of the organization and say we really have someone who is concentrated in this field.”
Educational Efforts
Vikas Parekh, MD, FHM, is in his second year as the chair of SHM’s Education Committee, and says the first task at hand is to educate hospitalists about the new FPHM pathway to MOC. The University of Michigan hospitalist says his committee, working with ABIM and SHM staff, is focused on two major educational efforts: developing the SHM strategy to assist hospitalists with the new FPHM MOC pathway, and “fulfilling the needs of hospitalists, in terms of the resources they have for the MOC process.”
“We’ve already started down this route, in terms of developing resources,” Dr. Parekh says. “We’ve done a few things that have been easy. One is the ABIM learning session pre-course at the annual meeting. … It earns you points toward the medical-knowledge component.”
ABIM and ACP are the traditional avenues for medical-knowledge and practice-improvement requirements for the MOC process. SHM and ABIM currently are working to develop medical-knowledge modules in the domains of patient safety and quality improvement, areas most relevant to HM. Dr. Parekh expects those components to be available in early 2011.
“Practice improvement is likely to be our second main effort,” Dr. Parekh says. “SHM has a lot of resources within our resource rooms that have the shell of what you would really need to meet ABIM requirements for a PIM but aren’t quite complete or thorough enough, or have all the bells and whistles that ABIM wants them to have. … We think we can do a much better job focusing the PIMs to hospitalists.”
At a more granular level, Dr. Wellikson envisions a “suite of products” to assist members in the MOC process. “What we are trying to do is develop resources that help people practice better medicine,” he says, “and while we are helping you practice better medicine, you can also use that to prove to [ABIM] that you have done it.
“So if you log onto the website today and downloaded and completed any of those SHM resource rooms, somewhere in the next several months you will be able to click on a form, enter the results, send it to ABIM, and you’ll have satisfied a PIM,” Dr. Wellikson says. “You can do the work today.”
SHM’s Project BOOST (Better Outcomes for Older Adults through Safer Transitions) and Glycemic Control Mentored Implementation programs are prime candidates for Web-based PIMs, according to Dr. Holmboe.
“I think it is still very early, but we are very excited about this,” Dr. Parekh says. “I think a lot of people still have questions about what exactly this mean to me, and why should I recertify through this focused practice as opposed to the traditional general pathway? We hope to change that by making the resources focused to their practice.” TH
Jason Carris is editor of The Hospitalist.
Wachter’s World
NATIONAL HARBOR, Md.—Democrats and Republicans have trumpeted that unprecedented changes in the healthcare system are on the way, but the dean of HM cautions that significant change is still years away.
“The reform bill, to my mind, mostly kicked the hard decision for cost, quality, and safety down the road,” said Bob Wachter, MD, MHM, chief of the hospitalist division, professor, and associate chair of the Department of Medicine at the University of California at San Francisco. “All of these issues have been raised, though.”
Dr. Wachter, former SHM president, author of the blog Wachter’s World (www.wachters world.com), and recently named the 10th-most-powerful physician executive in the nation by Modern Healthcare, used his annual HM10 address to paint a cautiously optimistic picture of HM playing a leading role in quality, safety, and innovation in the delivery of healthcare.
“It is a completely open question, whether we will be capable of snapping our fingers and creating a set of incentives or policy drivers that will allow the creation of the next Geisinger [Health System] without waiting 50 years,” Dr. Wachter said. “These cultures take a long time to develop. It’s not just about the [organizational] chart and the way money flows. You have to develop the culture of shared governance.”
In what has become a rite, Dr. Wachter gives the closing address at SHM’s annual meeting. This year’s title: “Use Your Words: Understanding the New Language of Healthcare Reform.” He focused most of his speech on finding the balance between high-quality and low-cost patient care, particularly when viewed through the prism of the “cost curve,” the economic principle that measures benefits against their cost.
Medical care on the “flat part of the curve” equates to tests, procedures, or other engagements that might have prophylactic value but little clinical benefit. From a purely clinical point of view, that is acceptable, but layering in a cost-benefit analysis adds a more objective way of deciding whether the care delivered is “worth the cost,” Dr. Wachter said.
—Bob Wachter, MD, MHM, chief of the hospitalist division, professor, and associate chair of the Department of Medicine at the University of California at San Francisco
“The question is: Where do we want to live on this curve?” he added. “As you spend more money, you may be getting more benefit, but the incremental amount . . . pushes out past the flat part of curve.”
Dr. Wachter boiled his lesson down to two philosophies. In one, the practice of HM means a test, a procedure, or a consult is ordered because the benefits outweigh the risks. In the other, that same episodic treatment is ordered only if every less-expensive option has already been attempted. “These are absolutely fundamental tensions,” he admitted.
But not all that is reform must be contentious, he said. Take the renewed push toward “accountable-care organizations,” in which providers partner and share responsibility for both the quality and cost of healthcare for a specific population of beneficiaries. The healthcare reform bill contains incentives for such a structure, which Dr. Wachter views as the government’s latest attempt to improve care by controlling how much reimbursement physicians and their employers receive.
While other specialists might not be experienced with data-point discussions on cost savings with hospital administrators, HM leaders are all too familiar with the concept, as most have those discussions during annual hospital subsidy negotiations. Correspondingly, those who listened to Dr. Wachter’s advice agreed that there is ample opportunity to lead the charge for quality and safety improvement—and the likely savings to be associated with those changes.
“Let’s be patient for what’s coming around the corner,” said Daniel Dressler, MD, SFHM, director of hospital medicine at Emory University Hospital in Atlanta and an SHM board member. “But let’s not miss the boat.” HM2010
Richard Quinn is a freelance writer based in New Jersey.
NATIONAL HARBOR, Md.—Democrats and Republicans have trumpeted that unprecedented changes in the healthcare system are on the way, but the dean of HM cautions that significant change is still years away.
“The reform bill, to my mind, mostly kicked the hard decision for cost, quality, and safety down the road,” said Bob Wachter, MD, MHM, chief of the hospitalist division, professor, and associate chair of the Department of Medicine at the University of California at San Francisco. “All of these issues have been raised, though.”
Dr. Wachter, former SHM president, author of the blog Wachter’s World (www.wachters world.com), and recently named the 10th-most-powerful physician executive in the nation by Modern Healthcare, used his annual HM10 address to paint a cautiously optimistic picture of HM playing a leading role in quality, safety, and innovation in the delivery of healthcare.
“It is a completely open question, whether we will be capable of snapping our fingers and creating a set of incentives or policy drivers that will allow the creation of the next Geisinger [Health System] without waiting 50 years,” Dr. Wachter said. “These cultures take a long time to develop. It’s not just about the [organizational] chart and the way money flows. You have to develop the culture of shared governance.”
In what has become a rite, Dr. Wachter gives the closing address at SHM’s annual meeting. This year’s title: “Use Your Words: Understanding the New Language of Healthcare Reform.” He focused most of his speech on finding the balance between high-quality and low-cost patient care, particularly when viewed through the prism of the “cost curve,” the economic principle that measures benefits against their cost.
Medical care on the “flat part of the curve” equates to tests, procedures, or other engagements that might have prophylactic value but little clinical benefit. From a purely clinical point of view, that is acceptable, but layering in a cost-benefit analysis adds a more objective way of deciding whether the care delivered is “worth the cost,” Dr. Wachter said.
—Bob Wachter, MD, MHM, chief of the hospitalist division, professor, and associate chair of the Department of Medicine at the University of California at San Francisco
“The question is: Where do we want to live on this curve?” he added. “As you spend more money, you may be getting more benefit, but the incremental amount . . . pushes out past the flat part of curve.”
Dr. Wachter boiled his lesson down to two philosophies. In one, the practice of HM means a test, a procedure, or a consult is ordered because the benefits outweigh the risks. In the other, that same episodic treatment is ordered only if every less-expensive option has already been attempted. “These are absolutely fundamental tensions,” he admitted.
But not all that is reform must be contentious, he said. Take the renewed push toward “accountable-care organizations,” in which providers partner and share responsibility for both the quality and cost of healthcare for a specific population of beneficiaries. The healthcare reform bill contains incentives for such a structure, which Dr. Wachter views as the government’s latest attempt to improve care by controlling how much reimbursement physicians and their employers receive.
While other specialists might not be experienced with data-point discussions on cost savings with hospital administrators, HM leaders are all too familiar with the concept, as most have those discussions during annual hospital subsidy negotiations. Correspondingly, those who listened to Dr. Wachter’s advice agreed that there is ample opportunity to lead the charge for quality and safety improvement—and the likely savings to be associated with those changes.
“Let’s be patient for what’s coming around the corner,” said Daniel Dressler, MD, SFHM, director of hospital medicine at Emory University Hospital in Atlanta and an SHM board member. “But let’s not miss the boat.” HM2010
Richard Quinn is a freelance writer based in New Jersey.
NATIONAL HARBOR, Md.—Democrats and Republicans have trumpeted that unprecedented changes in the healthcare system are on the way, but the dean of HM cautions that significant change is still years away.
“The reform bill, to my mind, mostly kicked the hard decision for cost, quality, and safety down the road,” said Bob Wachter, MD, MHM, chief of the hospitalist division, professor, and associate chair of the Department of Medicine at the University of California at San Francisco. “All of these issues have been raised, though.”
Dr. Wachter, former SHM president, author of the blog Wachter’s World (www.wachters world.com), and recently named the 10th-most-powerful physician executive in the nation by Modern Healthcare, used his annual HM10 address to paint a cautiously optimistic picture of HM playing a leading role in quality, safety, and innovation in the delivery of healthcare.
“It is a completely open question, whether we will be capable of snapping our fingers and creating a set of incentives or policy drivers that will allow the creation of the next Geisinger [Health System] without waiting 50 years,” Dr. Wachter said. “These cultures take a long time to develop. It’s not just about the [organizational] chart and the way money flows. You have to develop the culture of shared governance.”
In what has become a rite, Dr. Wachter gives the closing address at SHM’s annual meeting. This year’s title: “Use Your Words: Understanding the New Language of Healthcare Reform.” He focused most of his speech on finding the balance between high-quality and low-cost patient care, particularly when viewed through the prism of the “cost curve,” the economic principle that measures benefits against their cost.
Medical care on the “flat part of the curve” equates to tests, procedures, or other engagements that might have prophylactic value but little clinical benefit. From a purely clinical point of view, that is acceptable, but layering in a cost-benefit analysis adds a more objective way of deciding whether the care delivered is “worth the cost,” Dr. Wachter said.
—Bob Wachter, MD, MHM, chief of the hospitalist division, professor, and associate chair of the Department of Medicine at the University of California at San Francisco
“The question is: Where do we want to live on this curve?” he added. “As you spend more money, you may be getting more benefit, but the incremental amount . . . pushes out past the flat part of curve.”
Dr. Wachter boiled his lesson down to two philosophies. In one, the practice of HM means a test, a procedure, or a consult is ordered because the benefits outweigh the risks. In the other, that same episodic treatment is ordered only if every less-expensive option has already been attempted. “These are absolutely fundamental tensions,” he admitted.
But not all that is reform must be contentious, he said. Take the renewed push toward “accountable-care organizations,” in which providers partner and share responsibility for both the quality and cost of healthcare for a specific population of beneficiaries. The healthcare reform bill contains incentives for such a structure, which Dr. Wachter views as the government’s latest attempt to improve care by controlling how much reimbursement physicians and their employers receive.
While other specialists might not be experienced with data-point discussions on cost savings with hospital administrators, HM leaders are all too familiar with the concept, as most have those discussions during annual hospital subsidy negotiations. Correspondingly, those who listened to Dr. Wachter’s advice agreed that there is ample opportunity to lead the charge for quality and safety improvement—and the likely savings to be associated with those changes.
“Let’s be patient for what’s coming around the corner,” said Daniel Dressler, MD, SFHM, director of hospital medicine at Emory University Hospital in Atlanta and an SHM board member. “But let’s not miss the boat.” HM2010
Richard Quinn is a freelance writer based in New Jersey.
Special Interests
HOSPITALISTS FROM ALL PARTS OF THE COUNTRY—and a few other countries—discussed a wide swath of topics during a community-based HM special-interest forum at HM10. Issues that were discussed included unit-based rounding, changes to Medicare consult codes, strategies for avoiding “dumps,” and working with specialists.
Two established community hospitalists—SHM co-founders John Nelson, MD, MHM, and Winthrop Whitcomb, MD, MHM—moderated the one-hour session.
Much of the debate centered on defining a hospitalist’s role and relationships with others in the hospital. One hospitalist said he’d noticed significant changes in the 15 years since he began HM practice; however, some issues remain unresolved: Primary-care physicians (PCPs) still know the patients better, and medical specialists still want hospitalists to be their “interns.”
“We have two things to sell: your expertise and your availability. It’s up to your group to determine which one you want to sell,” said Tony Lin, MD, FHM, a hospitalist and chief of the Department of Internal Medicine at Kelsey-Seybold Clinic in Houston. “I don’t think you have to pick one. So I think you have to ask yourself: What does our group want to sell to the specialist? Sometimes you might have to turn them down to make that point.”
Dr. Lin also described a phenomena emerging in the Houston area: independent, one-physician HM groups taking root in community hospitals. “A lot of the surgeons are using them because they are willing to work as the interns and residents, the first people the nurses call at 2 a.m.,” he said. “There is a market for them.”
Dr. Nelson advised community hospitalists to avoid doing “the things that make you appear different from everyone else. Build social connections with specialists; call them by their first name; eat lunch in the cafeteria; and dress professionally.”
•
One community hospitalist spoke of an ethical situation she regularly encounters at her hospital, which contracts with multiple HM groups. Anna Rodriguez, MD, of Chesapeake Hospitalists in Chesapeake, Va., explained that her group’s issue is acutely ill patients who are assigned to one of the other HM group services—which, unlike Dr. Rodriguez’s group, are not responsible for codes or 24/7 patient coverage. So what happens when the “other” group’s patient has a sudden deterioration and the hospital staff calls us to run the rapid response? Dr. Rodriguez asked the group.
Dr. Whitcomb suggested Dr. Rodriguez’s group, which is not contracted to run the code, work to iron that situation out. “Then, that is your job and contractually recognized,” he said.
“We get into the exact same situation in our hospital. We created a hospital medicine section and … established expectations for who responds to codes,” said Dennis Kold, MD, medical director of the hospitalist service Tri-Health in Cincinnati. “If the patient is declining, we will respond to code, but we have it set up where the expectation is that the [attending] will be in to take care of the patient in one hour, or if the patient is admitted overnight to the ICU at 10 p.m., that the [admitting] will be in the ICU to take care of the patient within four hours.” Dr. Kold added that when the attending doesn’t show up in time that penalties are enforced (e.g., taken off the ER call schedule, restriction of hospital privileges).
“If you are not dealing with rapid response, then you are just hurting yourself,” added Edward Rosenfeld, MD, a hospitalist with Lehigh Valley Medical Associates in Allentown, Pa. “You need to do it; that’s your code prevention.”
•
Community hospitalists also discussed bundled payments and the recent changes in Medicare consult codes. “As a hospitalist service, I want to be involved in divvying up the money,” said Dan Allen, MD, a group director in Des Moines, Iowa. “I don’t know where it’s going, but I want to have a seat at the table.”
When asked by Dr. Nelson if they had noticed a significant change in reimbursement due to Medicare’s elimination of consultation codes, few in the room raised their hands. In fact, Dr. Nelson explained, “you can bill initial hospital care instead of initial hospital consult.”
“If done right, you might get paid better,” Dr. Rosenfeld added.
—Jason Carris
Health Information Technology on the Hospitalist Radar
Health information technology (HIT) isn’t for geeks anymore. A year after a mostly tech-savvy room discussed the basics of introducing more IT aspects to HM, nearly three dozen hospitalists clamored for SHM to take advocacy positions on everything from best practices to best vendors.
“SHM could help us all speak the language we need to speak,” said Tosha Wetterneck, MD, MS, a hospitalist with the University of Wisconsin Clinic in Madison. “Visibility, transparency—give us the words.”
Participants in last year’s group focused on the technical side of IT. This year’s attendees talked about the need for SHM to create portals for shared information, message boards to spur interinstitution conversations, and, perhaps, a weekend boot-camp-style course to introduce novices to basic IT information.
“SHM needs to take a stand now,” said Damascene Kurukulasuriya, MD, FACP, CMD, CCD, a hospitalist in perioperative medicine at the University of Missouri Health System in Columbia. “We need to be part of the solution.”
To that end, Kendall Rogers, MD, assistant professor at the University of New Mexico School of Medicine and chair of SHM’s IT Task Force, says the society is making progress. More hospitalists have been encouraged to sign up for the BioMedical Informatics course at the Marine Biology Laboratory in Woods Hole, Mass. The weeklong course is an introduction to the use of computer technologies and information science related to biomedicine and health science, according to the program’s Web site (www.courses.mbl.edu/mi/). The cost of travel, housing, and meals are fully paid for by the National Library of Medicine, making the fellowship even more appealing for cash-strapped hospitals and HM groups. “It’s a hidden program,” Dr. Rogers said.
Dr. Rogers and SHM CEO Larry Wellikson have toured the country meeting with top officials from the largest IT vendors, including Cerner and GE Healthcare. An IT committee has formed, with subcommittees dedicated to policy, quality, and leadership/education. But Bob Lineberger, MD, medical information officer at Durham Regional Hospital in North Carolina, says a nuanced message will take time.
“Our focus is just coming into focus,” Dr. Lineberger conceded. “We do need to come up with a position statement.”
—Richard Quinn
Education in HM: How to Grow Rock Stars and Champions
What skills does a hospitalist need to know to practice well that they didn’t learn in residency? That was the question new SHM President Jeff Weise, MD, SFHM, posed to about 20 hospitalists attending the special-interest forum on educational initiatives at HM10. Led by Dr. Wiese and SHM Education Committee co-chair Vikas Parekh, MD, FHM, the discussion focused on what SHM can do—or perhaps do better—in this capacity.
Dr. Parekh said hospitalists should be experts in quality-improvement (QI) and patient safety, and HM must incorporate that expertise into daily practice. However, he said, SHM’s largest educational focus is the new Focused Practice in Hospital Medicine pathway to American Board of Internal Medicine’s (ABIM) recertification.
In describing the future of this dynamic field, Dr. Weise raised concerns about managing the pipeline of approximately 2,500 new residents turning out each year and the potential for “losing intimacy” among SHM members—which he described as “the curse of being a champion.”
“IT is the only solution,” he added, “and identifying new and better ways of communicating.”
Competency-Based Train-ing (CBT) is critical to the development of new hospitalists, Dr. Wiese explained, as a supplement for what isn’t taught in residency. He posed a question: Should residencies last four or five years to incorporate additional training and career planning? “It’s an MBA paradigm of learning what we do,” he said. “What compels residents to join fellowship programs and earn $50K per year when they can start practicing and earning $150K?”
Educating the membership requires innovation and more than just bench-to-bedside research, Dr. Wiese added. Translational research and best-evidence practices will improve the field. “Five or 10 programs are rock stars,” he said, “but there are 377 that are terrible.”
Future SHM goals include a vision of having hospitalists hold 20% of all Internal Medicine Residency Program Director positions; developing best practices, not unfunded mandates; establishing protected academic time; and encouraging mentorship that positions hospitalists as heroes for the next generation.
An education committee sub-group has been tasked to focus on the recruitment of hospitalists and expose them to the best the society and field have to offer. HM10
—Phaedra Cress
HOSPITALISTS FROM ALL PARTS OF THE COUNTRY—and a few other countries—discussed a wide swath of topics during a community-based HM special-interest forum at HM10. Issues that were discussed included unit-based rounding, changes to Medicare consult codes, strategies for avoiding “dumps,” and working with specialists.
Two established community hospitalists—SHM co-founders John Nelson, MD, MHM, and Winthrop Whitcomb, MD, MHM—moderated the one-hour session.
Much of the debate centered on defining a hospitalist’s role and relationships with others in the hospital. One hospitalist said he’d noticed significant changes in the 15 years since he began HM practice; however, some issues remain unresolved: Primary-care physicians (PCPs) still know the patients better, and medical specialists still want hospitalists to be their “interns.”
“We have two things to sell: your expertise and your availability. It’s up to your group to determine which one you want to sell,” said Tony Lin, MD, FHM, a hospitalist and chief of the Department of Internal Medicine at Kelsey-Seybold Clinic in Houston. “I don’t think you have to pick one. So I think you have to ask yourself: What does our group want to sell to the specialist? Sometimes you might have to turn them down to make that point.”
Dr. Lin also described a phenomena emerging in the Houston area: independent, one-physician HM groups taking root in community hospitals. “A lot of the surgeons are using them because they are willing to work as the interns and residents, the first people the nurses call at 2 a.m.,” he said. “There is a market for them.”
Dr. Nelson advised community hospitalists to avoid doing “the things that make you appear different from everyone else. Build social connections with specialists; call them by their first name; eat lunch in the cafeteria; and dress professionally.”
•
One community hospitalist spoke of an ethical situation she regularly encounters at her hospital, which contracts with multiple HM groups. Anna Rodriguez, MD, of Chesapeake Hospitalists in Chesapeake, Va., explained that her group’s issue is acutely ill patients who are assigned to one of the other HM group services—which, unlike Dr. Rodriguez’s group, are not responsible for codes or 24/7 patient coverage. So what happens when the “other” group’s patient has a sudden deterioration and the hospital staff calls us to run the rapid response? Dr. Rodriguez asked the group.
Dr. Whitcomb suggested Dr. Rodriguez’s group, which is not contracted to run the code, work to iron that situation out. “Then, that is your job and contractually recognized,” he said.
“We get into the exact same situation in our hospital. We created a hospital medicine section and … established expectations for who responds to codes,” said Dennis Kold, MD, medical director of the hospitalist service Tri-Health in Cincinnati. “If the patient is declining, we will respond to code, but we have it set up where the expectation is that the [attending] will be in to take care of the patient in one hour, or if the patient is admitted overnight to the ICU at 10 p.m., that the [admitting] will be in the ICU to take care of the patient within four hours.” Dr. Kold added that when the attending doesn’t show up in time that penalties are enforced (e.g., taken off the ER call schedule, restriction of hospital privileges).
“If you are not dealing with rapid response, then you are just hurting yourself,” added Edward Rosenfeld, MD, a hospitalist with Lehigh Valley Medical Associates in Allentown, Pa. “You need to do it; that’s your code prevention.”
•
Community hospitalists also discussed bundled payments and the recent changes in Medicare consult codes. “As a hospitalist service, I want to be involved in divvying up the money,” said Dan Allen, MD, a group director in Des Moines, Iowa. “I don’t know where it’s going, but I want to have a seat at the table.”
When asked by Dr. Nelson if they had noticed a significant change in reimbursement due to Medicare’s elimination of consultation codes, few in the room raised their hands. In fact, Dr. Nelson explained, “you can bill initial hospital care instead of initial hospital consult.”
“If done right, you might get paid better,” Dr. Rosenfeld added.
—Jason Carris
Health Information Technology on the Hospitalist Radar
Health information technology (HIT) isn’t for geeks anymore. A year after a mostly tech-savvy room discussed the basics of introducing more IT aspects to HM, nearly three dozen hospitalists clamored for SHM to take advocacy positions on everything from best practices to best vendors.
“SHM could help us all speak the language we need to speak,” said Tosha Wetterneck, MD, MS, a hospitalist with the University of Wisconsin Clinic in Madison. “Visibility, transparency—give us the words.”
Participants in last year’s group focused on the technical side of IT. This year’s attendees talked about the need for SHM to create portals for shared information, message boards to spur interinstitution conversations, and, perhaps, a weekend boot-camp-style course to introduce novices to basic IT information.
“SHM needs to take a stand now,” said Damascene Kurukulasuriya, MD, FACP, CMD, CCD, a hospitalist in perioperative medicine at the University of Missouri Health System in Columbia. “We need to be part of the solution.”
To that end, Kendall Rogers, MD, assistant professor at the University of New Mexico School of Medicine and chair of SHM’s IT Task Force, says the society is making progress. More hospitalists have been encouraged to sign up for the BioMedical Informatics course at the Marine Biology Laboratory in Woods Hole, Mass. The weeklong course is an introduction to the use of computer technologies and information science related to biomedicine and health science, according to the program’s Web site (www.courses.mbl.edu/mi/). The cost of travel, housing, and meals are fully paid for by the National Library of Medicine, making the fellowship even more appealing for cash-strapped hospitals and HM groups. “It’s a hidden program,” Dr. Rogers said.
Dr. Rogers and SHM CEO Larry Wellikson have toured the country meeting with top officials from the largest IT vendors, including Cerner and GE Healthcare. An IT committee has formed, with subcommittees dedicated to policy, quality, and leadership/education. But Bob Lineberger, MD, medical information officer at Durham Regional Hospital in North Carolina, says a nuanced message will take time.
“Our focus is just coming into focus,” Dr. Lineberger conceded. “We do need to come up with a position statement.”
—Richard Quinn
Education in HM: How to Grow Rock Stars and Champions
What skills does a hospitalist need to know to practice well that they didn’t learn in residency? That was the question new SHM President Jeff Weise, MD, SFHM, posed to about 20 hospitalists attending the special-interest forum on educational initiatives at HM10. Led by Dr. Wiese and SHM Education Committee co-chair Vikas Parekh, MD, FHM, the discussion focused on what SHM can do—or perhaps do better—in this capacity.
Dr. Parekh said hospitalists should be experts in quality-improvement (QI) and patient safety, and HM must incorporate that expertise into daily practice. However, he said, SHM’s largest educational focus is the new Focused Practice in Hospital Medicine pathway to American Board of Internal Medicine’s (ABIM) recertification.
In describing the future of this dynamic field, Dr. Weise raised concerns about managing the pipeline of approximately 2,500 new residents turning out each year and the potential for “losing intimacy” among SHM members—which he described as “the curse of being a champion.”
“IT is the only solution,” he added, “and identifying new and better ways of communicating.”
Competency-Based Train-ing (CBT) is critical to the development of new hospitalists, Dr. Wiese explained, as a supplement for what isn’t taught in residency. He posed a question: Should residencies last four or five years to incorporate additional training and career planning? “It’s an MBA paradigm of learning what we do,” he said. “What compels residents to join fellowship programs and earn $50K per year when they can start practicing and earning $150K?”
Educating the membership requires innovation and more than just bench-to-bedside research, Dr. Wiese added. Translational research and best-evidence practices will improve the field. “Five or 10 programs are rock stars,” he said, “but there are 377 that are terrible.”
Future SHM goals include a vision of having hospitalists hold 20% of all Internal Medicine Residency Program Director positions; developing best practices, not unfunded mandates; establishing protected academic time; and encouraging mentorship that positions hospitalists as heroes for the next generation.
An education committee sub-group has been tasked to focus on the recruitment of hospitalists and expose them to the best the society and field have to offer. HM10
—Phaedra Cress
HOSPITALISTS FROM ALL PARTS OF THE COUNTRY—and a few other countries—discussed a wide swath of topics during a community-based HM special-interest forum at HM10. Issues that were discussed included unit-based rounding, changes to Medicare consult codes, strategies for avoiding “dumps,” and working with specialists.
Two established community hospitalists—SHM co-founders John Nelson, MD, MHM, and Winthrop Whitcomb, MD, MHM—moderated the one-hour session.
Much of the debate centered on defining a hospitalist’s role and relationships with others in the hospital. One hospitalist said he’d noticed significant changes in the 15 years since he began HM practice; however, some issues remain unresolved: Primary-care physicians (PCPs) still know the patients better, and medical specialists still want hospitalists to be their “interns.”
“We have two things to sell: your expertise and your availability. It’s up to your group to determine which one you want to sell,” said Tony Lin, MD, FHM, a hospitalist and chief of the Department of Internal Medicine at Kelsey-Seybold Clinic in Houston. “I don’t think you have to pick one. So I think you have to ask yourself: What does our group want to sell to the specialist? Sometimes you might have to turn them down to make that point.”
Dr. Lin also described a phenomena emerging in the Houston area: independent, one-physician HM groups taking root in community hospitals. “A lot of the surgeons are using them because they are willing to work as the interns and residents, the first people the nurses call at 2 a.m.,” he said. “There is a market for them.”
Dr. Nelson advised community hospitalists to avoid doing “the things that make you appear different from everyone else. Build social connections with specialists; call them by their first name; eat lunch in the cafeteria; and dress professionally.”
•
One community hospitalist spoke of an ethical situation she regularly encounters at her hospital, which contracts with multiple HM groups. Anna Rodriguez, MD, of Chesapeake Hospitalists in Chesapeake, Va., explained that her group’s issue is acutely ill patients who are assigned to one of the other HM group services—which, unlike Dr. Rodriguez’s group, are not responsible for codes or 24/7 patient coverage. So what happens when the “other” group’s patient has a sudden deterioration and the hospital staff calls us to run the rapid response? Dr. Rodriguez asked the group.
Dr. Whitcomb suggested Dr. Rodriguez’s group, which is not contracted to run the code, work to iron that situation out. “Then, that is your job and contractually recognized,” he said.
“We get into the exact same situation in our hospital. We created a hospital medicine section and … established expectations for who responds to codes,” said Dennis Kold, MD, medical director of the hospitalist service Tri-Health in Cincinnati. “If the patient is declining, we will respond to code, but we have it set up where the expectation is that the [attending] will be in to take care of the patient in one hour, or if the patient is admitted overnight to the ICU at 10 p.m., that the [admitting] will be in the ICU to take care of the patient within four hours.” Dr. Kold added that when the attending doesn’t show up in time that penalties are enforced (e.g., taken off the ER call schedule, restriction of hospital privileges).
“If you are not dealing with rapid response, then you are just hurting yourself,” added Edward Rosenfeld, MD, a hospitalist with Lehigh Valley Medical Associates in Allentown, Pa. “You need to do it; that’s your code prevention.”
•
Community hospitalists also discussed bundled payments and the recent changes in Medicare consult codes. “As a hospitalist service, I want to be involved in divvying up the money,” said Dan Allen, MD, a group director in Des Moines, Iowa. “I don’t know where it’s going, but I want to have a seat at the table.”
When asked by Dr. Nelson if they had noticed a significant change in reimbursement due to Medicare’s elimination of consultation codes, few in the room raised their hands. In fact, Dr. Nelson explained, “you can bill initial hospital care instead of initial hospital consult.”
“If done right, you might get paid better,” Dr. Rosenfeld added.
—Jason Carris
Health Information Technology on the Hospitalist Radar
Health information technology (HIT) isn’t for geeks anymore. A year after a mostly tech-savvy room discussed the basics of introducing more IT aspects to HM, nearly three dozen hospitalists clamored for SHM to take advocacy positions on everything from best practices to best vendors.
“SHM could help us all speak the language we need to speak,” said Tosha Wetterneck, MD, MS, a hospitalist with the University of Wisconsin Clinic in Madison. “Visibility, transparency—give us the words.”
Participants in last year’s group focused on the technical side of IT. This year’s attendees talked about the need for SHM to create portals for shared information, message boards to spur interinstitution conversations, and, perhaps, a weekend boot-camp-style course to introduce novices to basic IT information.
“SHM needs to take a stand now,” said Damascene Kurukulasuriya, MD, FACP, CMD, CCD, a hospitalist in perioperative medicine at the University of Missouri Health System in Columbia. “We need to be part of the solution.”
To that end, Kendall Rogers, MD, assistant professor at the University of New Mexico School of Medicine and chair of SHM’s IT Task Force, says the society is making progress. More hospitalists have been encouraged to sign up for the BioMedical Informatics course at the Marine Biology Laboratory in Woods Hole, Mass. The weeklong course is an introduction to the use of computer technologies and information science related to biomedicine and health science, according to the program’s Web site (www.courses.mbl.edu/mi/). The cost of travel, housing, and meals are fully paid for by the National Library of Medicine, making the fellowship even more appealing for cash-strapped hospitals and HM groups. “It’s a hidden program,” Dr. Rogers said.
Dr. Rogers and SHM CEO Larry Wellikson have toured the country meeting with top officials from the largest IT vendors, including Cerner and GE Healthcare. An IT committee has formed, with subcommittees dedicated to policy, quality, and leadership/education. But Bob Lineberger, MD, medical information officer at Durham Regional Hospital in North Carolina, says a nuanced message will take time.
“Our focus is just coming into focus,” Dr. Lineberger conceded. “We do need to come up with a position statement.”
—Richard Quinn
Education in HM: How to Grow Rock Stars and Champions
What skills does a hospitalist need to know to practice well that they didn’t learn in residency? That was the question new SHM President Jeff Weise, MD, SFHM, posed to about 20 hospitalists attending the special-interest forum on educational initiatives at HM10. Led by Dr. Wiese and SHM Education Committee co-chair Vikas Parekh, MD, FHM, the discussion focused on what SHM can do—or perhaps do better—in this capacity.
Dr. Parekh said hospitalists should be experts in quality-improvement (QI) and patient safety, and HM must incorporate that expertise into daily practice. However, he said, SHM’s largest educational focus is the new Focused Practice in Hospital Medicine pathway to American Board of Internal Medicine’s (ABIM) recertification.
In describing the future of this dynamic field, Dr. Weise raised concerns about managing the pipeline of approximately 2,500 new residents turning out each year and the potential for “losing intimacy” among SHM members—which he described as “the curse of being a champion.”
“IT is the only solution,” he added, “and identifying new and better ways of communicating.”
Competency-Based Train-ing (CBT) is critical to the development of new hospitalists, Dr. Wiese explained, as a supplement for what isn’t taught in residency. He posed a question: Should residencies last four or five years to incorporate additional training and career planning? “It’s an MBA paradigm of learning what we do,” he said. “What compels residents to join fellowship programs and earn $50K per year when they can start practicing and earning $150K?”
Educating the membership requires innovation and more than just bench-to-bedside research, Dr. Wiese added. Translational research and best-evidence practices will improve the field. “Five or 10 programs are rock stars,” he said, “but there are 377 that are terrible.”
Future SHM goals include a vision of having hospitalists hold 20% of all Internal Medicine Residency Program Director positions; developing best practices, not unfunded mandates; establishing protected academic time; and encouraging mentorship that positions hospitalists as heroes for the next generation.
An education committee sub-group has been tasked to focus on the recruitment of hospitalists and expose them to the best the society and field have to offer. HM10
—Phaedra Cress
Jam-Packed & Well Worth It
IT’S 11 MINUTES to 8 o’clock, and the sun is still climbing over the Potomac River just outside the Gaylord National Resort & Convention Center in National Harbor, Md. Day two of SHM’s annual meeting is about to begin.
Hospitalists file into a cavernous ballroom as the day kicks off with a panel discussion on healthcare reform and a speech by that rarest of breed: a popular hospital CEO. The back of the room fills quickly, but front and center, second row—that’s the seat for Nasim Afsarmanesh, MD, director of quality for HM and neurosurgery at Ronald Reagan UCLA Medical Center in Los Angeles.
“If I’m not in the front, I zone out,” she admits.
Dr. Afsarmanesh (who often adds a hyphen to her surname— Afsar-manesh—to help others pronounce it) knows herself and she knows how to plan ahead, from taking notes on her mini-laptop to knowing when to sit up front. And this day in her life is no different. Her schedule is a 12-hour dervish, yet it’s a simple roadmap of how to navigate HM10 and its scores of sessions, speeches, and seminars.
Innovator at Heart
Dr. Afsarmanesh did her residency in 2007 at UCLA. She stayed on to take a faculty position and is now assistant clinical professor of internal medicine (IM) and neurosurgery. Her days are split about 35% clinical practice, 40% on neurology quality issues, and 25% on hospital QI projects. In her free time, she’s an SHM activist and the incoming chair of its Hospital Quality and Patient Safety (HQPS) Committee.
“I get to be an innovator,” she boasts as she picks up a Danish, a chocolate pastry, and a cup of tea following two hours of listening to others talk. “I love that. You can’t really be an innovator when you’re [purely] practicing clinical medicine.”
Innovation requires preparation, though. Dr. Afsarmanesh spends countless hours creating PowerPoint presentations, so she hit a new feature at this year’s meeting: a limited-seating workshop on drawing up effective slides. The presentation is helpful, but she’s partially distracted. “Look up healthcare from talk,” she types as a note to herself for later. She follows that with “Look up Levy’s talk” (a nod to Paul Levy, the well-liked CEO of Beth Israel Deaconess in Boston).
Facial Recognition
The distraction ratchets up as she’s already looking forward to introducing herself to the editorial board of the Journal of Hospital Medicine, where she serves as an assistant editor. There are a few people she’d like to meet in person, so she gracefully sneaks out the side door a few minutes before noon. Handshakes, a box lunch, and a chat with 40 other journal editors ensue for the next hour.
“You can meet people you talk on the phone with for several years,” she says. “You can put a face to the name. That’s important.”
Hobnobbing at a board meeting is only a brief respite, however, before it’s back to professional development. At 1:15, there’s a 60-minute lesson on how to improve care from the patient perspective. Dr. Afsarmanesh, again, is distracted. She’s a first-time presenter in a few minutes, part of a four-woman panel on building a QI educational curriculum for medical students, residents, fellows, faculty, and other healthcare providers.
She scrolls through slides, rehearsing her thoughts. She wonders whether her PowerPoint presentation would have made the grade at this morning’s session.
She is smart enough not to judge her performance too soon—someone in an audience once reached out to her a year later—as she knows the impact of a training session is more than the round of applause at its end.
“You hope that you generate a discussion more than the traditional didactics,” she says. “These meetings are meant to start a discussion and, hopefully, create a network and a community where people can continue to [share ideas and learn from each other]. … I hope that along with some of the content that people take away, the bigger thing is those connections that they make.”
—Nasim Afsarmanesh, MD, director, HM quality initiatives, Ronald Reagan UCLA Medical Center, Los Angeles
Work Never Ends
It’s 4:30 p.m. and Dr. Afsarmanesh still has a sales pitch to rehearse. This time, it’s self-promotion for her soon-to-begin poster presentation: “The ABCs of Hospitalized Patients: A Multi-Disciplinary Checklist for Improving Quality of Patient Care."
After umpteen repetitions of her spiel, the presentation doesn’t win a prize, but, once again, she showcases her attention to detail: A stack of 8.5”x 11” versions of her poster are available for handouts, a feature few others in the competition have.
Some 12 hours into her tour of this massive convention center, the day is coming to a close. But not before SHM CEO Larry Wellikson, MD, SFHM, drops by to say hello.
He points out how strong her research is. Unfortunately, he uses a pen in the process.
“Don’t poke a hole in my poster,” she jokes.
Moments later, it’s back to working the line queued up at her poster. “Hi, would you like to hear about my poster?” HM2010
Richard Quinn is a freelance writer based in New Jersey.
IT’S 11 MINUTES to 8 o’clock, and the sun is still climbing over the Potomac River just outside the Gaylord National Resort & Convention Center in National Harbor, Md. Day two of SHM’s annual meeting is about to begin.
Hospitalists file into a cavernous ballroom as the day kicks off with a panel discussion on healthcare reform and a speech by that rarest of breed: a popular hospital CEO. The back of the room fills quickly, but front and center, second row—that’s the seat for Nasim Afsarmanesh, MD, director of quality for HM and neurosurgery at Ronald Reagan UCLA Medical Center in Los Angeles.
“If I’m not in the front, I zone out,” she admits.
Dr. Afsarmanesh (who often adds a hyphen to her surname— Afsar-manesh—to help others pronounce it) knows herself and she knows how to plan ahead, from taking notes on her mini-laptop to knowing when to sit up front. And this day in her life is no different. Her schedule is a 12-hour dervish, yet it’s a simple roadmap of how to navigate HM10 and its scores of sessions, speeches, and seminars.
Innovator at Heart
Dr. Afsarmanesh did her residency in 2007 at UCLA. She stayed on to take a faculty position and is now assistant clinical professor of internal medicine (IM) and neurosurgery. Her days are split about 35% clinical practice, 40% on neurology quality issues, and 25% on hospital QI projects. In her free time, she’s an SHM activist and the incoming chair of its Hospital Quality and Patient Safety (HQPS) Committee.
“I get to be an innovator,” she boasts as she picks up a Danish, a chocolate pastry, and a cup of tea following two hours of listening to others talk. “I love that. You can’t really be an innovator when you’re [purely] practicing clinical medicine.”
Innovation requires preparation, though. Dr. Afsarmanesh spends countless hours creating PowerPoint presentations, so she hit a new feature at this year’s meeting: a limited-seating workshop on drawing up effective slides. The presentation is helpful, but she’s partially distracted. “Look up healthcare from talk,” she types as a note to herself for later. She follows that with “Look up Levy’s talk” (a nod to Paul Levy, the well-liked CEO of Beth Israel Deaconess in Boston).
Facial Recognition
The distraction ratchets up as she’s already looking forward to introducing herself to the editorial board of the Journal of Hospital Medicine, where she serves as an assistant editor. There are a few people she’d like to meet in person, so she gracefully sneaks out the side door a few minutes before noon. Handshakes, a box lunch, and a chat with 40 other journal editors ensue for the next hour.
“You can meet people you talk on the phone with for several years,” she says. “You can put a face to the name. That’s important.”
Hobnobbing at a board meeting is only a brief respite, however, before it’s back to professional development. At 1:15, there’s a 60-minute lesson on how to improve care from the patient perspective. Dr. Afsarmanesh, again, is distracted. She’s a first-time presenter in a few minutes, part of a four-woman panel on building a QI educational curriculum for medical students, residents, fellows, faculty, and other healthcare providers.
She scrolls through slides, rehearsing her thoughts. She wonders whether her PowerPoint presentation would have made the grade at this morning’s session.
She is smart enough not to judge her performance too soon—someone in an audience once reached out to her a year later—as she knows the impact of a training session is more than the round of applause at its end.
“You hope that you generate a discussion more than the traditional didactics,” she says. “These meetings are meant to start a discussion and, hopefully, create a network and a community where people can continue to [share ideas and learn from each other]. … I hope that along with some of the content that people take away, the bigger thing is those connections that they make.”
—Nasim Afsarmanesh, MD, director, HM quality initiatives, Ronald Reagan UCLA Medical Center, Los Angeles
Work Never Ends
It’s 4:30 p.m. and Dr. Afsarmanesh still has a sales pitch to rehearse. This time, it’s self-promotion for her soon-to-begin poster presentation: “The ABCs of Hospitalized Patients: A Multi-Disciplinary Checklist for Improving Quality of Patient Care."
After umpteen repetitions of her spiel, the presentation doesn’t win a prize, but, once again, she showcases her attention to detail: A stack of 8.5”x 11” versions of her poster are available for handouts, a feature few others in the competition have.
Some 12 hours into her tour of this massive convention center, the day is coming to a close. But not before SHM CEO Larry Wellikson, MD, SFHM, drops by to say hello.
He points out how strong her research is. Unfortunately, he uses a pen in the process.
“Don’t poke a hole in my poster,” she jokes.
Moments later, it’s back to working the line queued up at her poster. “Hi, would you like to hear about my poster?” HM2010
Richard Quinn is a freelance writer based in New Jersey.
IT’S 11 MINUTES to 8 o’clock, and the sun is still climbing over the Potomac River just outside the Gaylord National Resort & Convention Center in National Harbor, Md. Day two of SHM’s annual meeting is about to begin.
Hospitalists file into a cavernous ballroom as the day kicks off with a panel discussion on healthcare reform and a speech by that rarest of breed: a popular hospital CEO. The back of the room fills quickly, but front and center, second row—that’s the seat for Nasim Afsarmanesh, MD, director of quality for HM and neurosurgery at Ronald Reagan UCLA Medical Center in Los Angeles.
“If I’m not in the front, I zone out,” she admits.
Dr. Afsarmanesh (who often adds a hyphen to her surname— Afsar-manesh—to help others pronounce it) knows herself and she knows how to plan ahead, from taking notes on her mini-laptop to knowing when to sit up front. And this day in her life is no different. Her schedule is a 12-hour dervish, yet it’s a simple roadmap of how to navigate HM10 and its scores of sessions, speeches, and seminars.
Innovator at Heart
Dr. Afsarmanesh did her residency in 2007 at UCLA. She stayed on to take a faculty position and is now assistant clinical professor of internal medicine (IM) and neurosurgery. Her days are split about 35% clinical practice, 40% on neurology quality issues, and 25% on hospital QI projects. In her free time, she’s an SHM activist and the incoming chair of its Hospital Quality and Patient Safety (HQPS) Committee.
“I get to be an innovator,” she boasts as she picks up a Danish, a chocolate pastry, and a cup of tea following two hours of listening to others talk. “I love that. You can’t really be an innovator when you’re [purely] practicing clinical medicine.”
Innovation requires preparation, though. Dr. Afsarmanesh spends countless hours creating PowerPoint presentations, so she hit a new feature at this year’s meeting: a limited-seating workshop on drawing up effective slides. The presentation is helpful, but she’s partially distracted. “Look up healthcare from talk,” she types as a note to herself for later. She follows that with “Look up Levy’s talk” (a nod to Paul Levy, the well-liked CEO of Beth Israel Deaconess in Boston).
Facial Recognition
The distraction ratchets up as she’s already looking forward to introducing herself to the editorial board of the Journal of Hospital Medicine, where she serves as an assistant editor. There are a few people she’d like to meet in person, so she gracefully sneaks out the side door a few minutes before noon. Handshakes, a box lunch, and a chat with 40 other journal editors ensue for the next hour.
“You can meet people you talk on the phone with for several years,” she says. “You can put a face to the name. That’s important.”
Hobnobbing at a board meeting is only a brief respite, however, before it’s back to professional development. At 1:15, there’s a 60-minute lesson on how to improve care from the patient perspective. Dr. Afsarmanesh, again, is distracted. She’s a first-time presenter in a few minutes, part of a four-woman panel on building a QI educational curriculum for medical students, residents, fellows, faculty, and other healthcare providers.
She scrolls through slides, rehearsing her thoughts. She wonders whether her PowerPoint presentation would have made the grade at this morning’s session.
She is smart enough not to judge her performance too soon—someone in an audience once reached out to her a year later—as she knows the impact of a training session is more than the round of applause at its end.
“You hope that you generate a discussion more than the traditional didactics,” she says. “These meetings are meant to start a discussion and, hopefully, create a network and a community where people can continue to [share ideas and learn from each other]. … I hope that along with some of the content that people take away, the bigger thing is those connections that they make.”
—Nasim Afsarmanesh, MD, director, HM quality initiatives, Ronald Reagan UCLA Medical Center, Los Angeles
Work Never Ends
It’s 4:30 p.m. and Dr. Afsarmanesh still has a sales pitch to rehearse. This time, it’s self-promotion for her soon-to-begin poster presentation: “The ABCs of Hospitalized Patients: A Multi-Disciplinary Checklist for Improving Quality of Patient Care."
After umpteen repetitions of her spiel, the presentation doesn’t win a prize, but, once again, she showcases her attention to detail: A stack of 8.5”x 11” versions of her poster are available for handouts, a feature few others in the competition have.
Some 12 hours into her tour of this massive convention center, the day is coming to a close. But not before SHM CEO Larry Wellikson, MD, SFHM, drops by to say hello.
He points out how strong her research is. Unfortunately, he uses a pen in the process.
“Don’t poke a hole in my poster,” she jokes.
Moments later, it’s back to working the line queued up at her poster. “Hi, would you like to hear about my poster?” HM2010
Richard Quinn is a freelance writer based in New Jersey.
Core Competencies Lay Pediatric HM Foundation
NATIONAL HARBOR, Md. HM10 kicked off with a pediatric hospitalist leading the way. Patrick Conway, MD, MSc, a chief medical officer with the U.S. Department of Health and Human Services, and one of pediatric HM’s own, was a part of the opening panel discussion that reviewed the implications of healthcare reform. And as the pediatric track coursed over the next two days, amidst the hustle and bustle of value-laden content, the final pediatric presentation just might have escaped routine notice.
Two days after its electronic release, a live preview of the “Pediatric Hospital Medicine Core Competencies” debuted at HM 2010.1 (The core competencies were printed as a supplement in the April issue of the Journal of Hospital Medicine.)
Mary Ottolini, MD, of Children’s National Medical Center in Washington, D.C., graciously thanked Erin Stucky, MD, Rady Children’s Hospital in San Diego, and Jennifer Maniscalco, MD, Children’s Hospital in Los Angeles, for their collaboration in the core competencies effort, which represented the culmination of years of perseverance and dedication. The core competencies underwent a rigorous development and review process; notably, draft copies were sent to more than 30 academic and certifying societies and stakeholder agencies for input. Vibrant discussion ensued as pediatric, family practice, and med-ped hospitalists engaged in both thoughtful reflection and optimistic forecasts of the relevance and utility of a practical framework to define the field.
These guidelines, however, are just the beginning. Much dialogue centered on the future role of the core competencies in such arenas as education and professional development. It became clear that work remains if pediatric hospitalists are to make the best use of this sentinel publication.
Nonetheless, this journey that is the advancement of a vibrant—and now well-defined—field of medicine has a stellar launching pad from which to take flight. HM10
Dr. Shen is a pediatric hospitalist and director of the hospital medicine program at Dell Children’s Hospital in Austin, Texas.
Reference
- Stucky ER, Maniscalco J, Ottolini MC, et al. The pediatric hospital medicine core competencies. J Hosp Med. 2010;5(S2):1-82.
NATIONAL HARBOR, Md. HM10 kicked off with a pediatric hospitalist leading the way. Patrick Conway, MD, MSc, a chief medical officer with the U.S. Department of Health and Human Services, and one of pediatric HM’s own, was a part of the opening panel discussion that reviewed the implications of healthcare reform. And as the pediatric track coursed over the next two days, amidst the hustle and bustle of value-laden content, the final pediatric presentation just might have escaped routine notice.
Two days after its electronic release, a live preview of the “Pediatric Hospital Medicine Core Competencies” debuted at HM 2010.1 (The core competencies were printed as a supplement in the April issue of the Journal of Hospital Medicine.)
Mary Ottolini, MD, of Children’s National Medical Center in Washington, D.C., graciously thanked Erin Stucky, MD, Rady Children’s Hospital in San Diego, and Jennifer Maniscalco, MD, Children’s Hospital in Los Angeles, for their collaboration in the core competencies effort, which represented the culmination of years of perseverance and dedication. The core competencies underwent a rigorous development and review process; notably, draft copies were sent to more than 30 academic and certifying societies and stakeholder agencies for input. Vibrant discussion ensued as pediatric, family practice, and med-ped hospitalists engaged in both thoughtful reflection and optimistic forecasts of the relevance and utility of a practical framework to define the field.
These guidelines, however, are just the beginning. Much dialogue centered on the future role of the core competencies in such arenas as education and professional development. It became clear that work remains if pediatric hospitalists are to make the best use of this sentinel publication.
Nonetheless, this journey that is the advancement of a vibrant—and now well-defined—field of medicine has a stellar launching pad from which to take flight. HM10
Dr. Shen is a pediatric hospitalist and director of the hospital medicine program at Dell Children’s Hospital in Austin, Texas.
Reference
- Stucky ER, Maniscalco J, Ottolini MC, et al. The pediatric hospital medicine core competencies. J Hosp Med. 2010;5(S2):1-82.
NATIONAL HARBOR, Md. HM10 kicked off with a pediatric hospitalist leading the way. Patrick Conway, MD, MSc, a chief medical officer with the U.S. Department of Health and Human Services, and one of pediatric HM’s own, was a part of the opening panel discussion that reviewed the implications of healthcare reform. And as the pediatric track coursed over the next two days, amidst the hustle and bustle of value-laden content, the final pediatric presentation just might have escaped routine notice.
Two days after its electronic release, a live preview of the “Pediatric Hospital Medicine Core Competencies” debuted at HM 2010.1 (The core competencies were printed as a supplement in the April issue of the Journal of Hospital Medicine.)
Mary Ottolini, MD, of Children’s National Medical Center in Washington, D.C., graciously thanked Erin Stucky, MD, Rady Children’s Hospital in San Diego, and Jennifer Maniscalco, MD, Children’s Hospital in Los Angeles, for their collaboration in the core competencies effort, which represented the culmination of years of perseverance and dedication. The core competencies underwent a rigorous development and review process; notably, draft copies were sent to more than 30 academic and certifying societies and stakeholder agencies for input. Vibrant discussion ensued as pediatric, family practice, and med-ped hospitalists engaged in both thoughtful reflection and optimistic forecasts of the relevance and utility of a practical framework to define the field.
These guidelines, however, are just the beginning. Much dialogue centered on the future role of the core competencies in such arenas as education and professional development. It became clear that work remains if pediatric hospitalists are to make the best use of this sentinel publication.
Nonetheless, this journey that is the advancement of a vibrant—and now well-defined—field of medicine has a stellar launching pad from which to take flight. HM10
Dr. Shen is a pediatric hospitalist and director of the hospital medicine program at Dell Children’s Hospital in Austin, Texas.
Reference
- Stucky ER, Maniscalco J, Ottolini MC, et al. The pediatric hospital medicine core competencies. J Hosp Med. 2010;5(S2):1-82.
Clinical Session: “The New C. Diff”
JOHN G. BARTLETT, MD, professor of medicine in the Department of Infectious Diseases at Johns Hopkins University School of Medicine in Baltimore, mesmerized a standing-room-only crowd of more than 500 at his lecture about the increase of Clostridium difficile in U.S. hospitals.
C. diff incidence has more than doubled since the mid-1990s, to more than 160 cases per 100,000 patients, and currently outnumbers the annual total of MRSA cases in the U.S., according to Dr. Bartlett, one of the foremost scholars on the subject. For hospitalists encountering patients with questions about the disease and where it comes from, Dr. Bartlett encouraged providers to punt that question: “The fact is, we don’t know most of the time.”
Most patients acquire C. diff during a hospital stay (74%) or a previous hospital stay (21%), and research shows the longer patients stay in the hospital, the more likely they are to acquire the disease.
—John G. Bartlett, professor, Department of Infectious Diseases, Johns Hopkins University School of Medicine, Baltimore
“It’s embedded in the fabric of hospitals,” Dr. Bartlett said. “The longer you are in the hospital, the more likely you are to get colonized.”
Prevention guidelines include:
- Hand hygiene;
- Advocate gloves and gowns;
- Patients with C. diff should be in single rooms;
- Maintain precautions until diarrhea resolves; and
- Clean with chlorine antiseptic.
Dr. Bartlett was excited to share his experience with RT-PCR testing, which he termed the “new, slick, fast” testing option for C. diff. In trials, it has been shown to be 99% sensitive and 98% specific. “If your lab does PCR, it is the best test currently available,” Dr. Bartlett said, although he cautioned that “this test detects the bug, not the toxin.”
Treatment of C. diff disease happens in the colon, and medications must make it there to be effective. The most common treatments, vancomycin and metronidazole, have pluses and minuses, Dr. Bartlett explained. Vancomycin is FDA-approved and unbeaten in clinical trials; however, it is the more expensive choice. Metronidazole is cheaper ($5 per day) and proven to be effective in mild to moderate cases, but is not FDA-approved and is unproven in severe cases.
Dr. Bartlett’s guidelines for C. diff treatment:
- Mild cases: no treatment;
- Moderate: metronidazole 250 mg four times a day for 10 to 14 days; and
- Serious: vancomycin 125 mg four times a day for 10 to 14 days.
“If metro doesn’t work, switch to oral vanco,” Dr. Bartlett said. HM10
JOHN G. BARTLETT, MD, professor of medicine in the Department of Infectious Diseases at Johns Hopkins University School of Medicine in Baltimore, mesmerized a standing-room-only crowd of more than 500 at his lecture about the increase of Clostridium difficile in U.S. hospitals.
C. diff incidence has more than doubled since the mid-1990s, to more than 160 cases per 100,000 patients, and currently outnumbers the annual total of MRSA cases in the U.S., according to Dr. Bartlett, one of the foremost scholars on the subject. For hospitalists encountering patients with questions about the disease and where it comes from, Dr. Bartlett encouraged providers to punt that question: “The fact is, we don’t know most of the time.”
Most patients acquire C. diff during a hospital stay (74%) or a previous hospital stay (21%), and research shows the longer patients stay in the hospital, the more likely they are to acquire the disease.
—John G. Bartlett, professor, Department of Infectious Diseases, Johns Hopkins University School of Medicine, Baltimore
“It’s embedded in the fabric of hospitals,” Dr. Bartlett said. “The longer you are in the hospital, the more likely you are to get colonized.”
Prevention guidelines include:
- Hand hygiene;
- Advocate gloves and gowns;
- Patients with C. diff should be in single rooms;
- Maintain precautions until diarrhea resolves; and
- Clean with chlorine antiseptic.
Dr. Bartlett was excited to share his experience with RT-PCR testing, which he termed the “new, slick, fast” testing option for C. diff. In trials, it has been shown to be 99% sensitive and 98% specific. “If your lab does PCR, it is the best test currently available,” Dr. Bartlett said, although he cautioned that “this test detects the bug, not the toxin.”
Treatment of C. diff disease happens in the colon, and medications must make it there to be effective. The most common treatments, vancomycin and metronidazole, have pluses and minuses, Dr. Bartlett explained. Vancomycin is FDA-approved and unbeaten in clinical trials; however, it is the more expensive choice. Metronidazole is cheaper ($5 per day) and proven to be effective in mild to moderate cases, but is not FDA-approved and is unproven in severe cases.
Dr. Bartlett’s guidelines for C. diff treatment:
- Mild cases: no treatment;
- Moderate: metronidazole 250 mg four times a day for 10 to 14 days; and
- Serious: vancomycin 125 mg four times a day for 10 to 14 days.
“If metro doesn’t work, switch to oral vanco,” Dr. Bartlett said. HM10
JOHN G. BARTLETT, MD, professor of medicine in the Department of Infectious Diseases at Johns Hopkins University School of Medicine in Baltimore, mesmerized a standing-room-only crowd of more than 500 at his lecture about the increase of Clostridium difficile in U.S. hospitals.
C. diff incidence has more than doubled since the mid-1990s, to more than 160 cases per 100,000 patients, and currently outnumbers the annual total of MRSA cases in the U.S., according to Dr. Bartlett, one of the foremost scholars on the subject. For hospitalists encountering patients with questions about the disease and where it comes from, Dr. Bartlett encouraged providers to punt that question: “The fact is, we don’t know most of the time.”
Most patients acquire C. diff during a hospital stay (74%) or a previous hospital stay (21%), and research shows the longer patients stay in the hospital, the more likely they are to acquire the disease.
—John G. Bartlett, professor, Department of Infectious Diseases, Johns Hopkins University School of Medicine, Baltimore
“It’s embedded in the fabric of hospitals,” Dr. Bartlett said. “The longer you are in the hospital, the more likely you are to get colonized.”
Prevention guidelines include:
- Hand hygiene;
- Advocate gloves and gowns;
- Patients with C. diff should be in single rooms;
- Maintain precautions until diarrhea resolves; and
- Clean with chlorine antiseptic.
Dr. Bartlett was excited to share his experience with RT-PCR testing, which he termed the “new, slick, fast” testing option for C. diff. In trials, it has been shown to be 99% sensitive and 98% specific. “If your lab does PCR, it is the best test currently available,” Dr. Bartlett said, although he cautioned that “this test detects the bug, not the toxin.”
Treatment of C. diff disease happens in the colon, and medications must make it there to be effective. The most common treatments, vancomycin and metronidazole, have pluses and minuses, Dr. Bartlett explained. Vancomycin is FDA-approved and unbeaten in clinical trials; however, it is the more expensive choice. Metronidazole is cheaper ($5 per day) and proven to be effective in mild to moderate cases, but is not FDA-approved and is unproven in severe cases.
Dr. Bartlett’s guidelines for C. diff treatment:
- Mild cases: no treatment;
- Moderate: metronidazole 250 mg four times a day for 10 to 14 days; and
- Serious: vancomycin 125 mg four times a day for 10 to 14 days.
“If metro doesn’t work, switch to oral vanco,” Dr. Bartlett said. HM10
Practice Management Session
PHYSICIAN ASSISTANTS (PAs) and nurse practitioners can do almost anything a physician can do, and many have skill sets physicians lack, according to David Friar, MD, FHM, president of Hospitalists of Northwest Michigan based in Traverse City.
“As we go forward, with continued physician shortages and with the growing responsibilities of the hospitalist movement, we are going to need more and more people with different skill sets,” Dr. Friar said during his presentation at HM10. “I think one of those important areas is nonphysician providers.”
A quick survey of the 300 or so hospitalists at the session showed most HM groups employ NPPs, but less than a third of those thought they were “using NPPs well.” Dr. Friar, who has worked with NPs and PAs for 14 years, said he has found NPPs “to be an integral part of our practice. They have become indispensable to us in the way we provide services to our hospitals and patients.”
Still, many hospitalist groups waste NPP potential, Dr. Friar explained. He suggested HM groups evaluate their NPP roster and duties, and make necessary changes. “Make sure you treat them as if they are part of the team. That is very important,” he said. “NPPs can and should take care of patients throughout all stages of the hospital stay, from admission to discharge.”
When hiring NPPs, look for team players who are flexible and willing to learn. Make sure the NPP knows their limits and is comfortable asking for help. Target local training programs or other departments in the hospital as fertile ground for new hires. But, most importantly, know what you are getting when you hire an NPP.
“Don’t underestimate the cost of the inexperienced NPP in terms of training. If you think it’s two weeks or two months, you are fooling yourself,” Dr. Friar emphasized, adding an inexperienced NPP could take from six months to two years to reach full competency in hospitalist service. “Know the tradeoffs,” he said. “It might be more important for you to hire the more experienced—and more costly—NPP so you don’t have to spend two years to get them up to speed.” HM10
PHYSICIAN ASSISTANTS (PAs) and nurse practitioners can do almost anything a physician can do, and many have skill sets physicians lack, according to David Friar, MD, FHM, president of Hospitalists of Northwest Michigan based in Traverse City.
“As we go forward, with continued physician shortages and with the growing responsibilities of the hospitalist movement, we are going to need more and more people with different skill sets,” Dr. Friar said during his presentation at HM10. “I think one of those important areas is nonphysician providers.”
A quick survey of the 300 or so hospitalists at the session showed most HM groups employ NPPs, but less than a third of those thought they were “using NPPs well.” Dr. Friar, who has worked with NPs and PAs for 14 years, said he has found NPPs “to be an integral part of our practice. They have become indispensable to us in the way we provide services to our hospitals and patients.”
Still, many hospitalist groups waste NPP potential, Dr. Friar explained. He suggested HM groups evaluate their NPP roster and duties, and make necessary changes. “Make sure you treat them as if they are part of the team. That is very important,” he said. “NPPs can and should take care of patients throughout all stages of the hospital stay, from admission to discharge.”
When hiring NPPs, look for team players who are flexible and willing to learn. Make sure the NPP knows their limits and is comfortable asking for help. Target local training programs or other departments in the hospital as fertile ground for new hires. But, most importantly, know what you are getting when you hire an NPP.
“Don’t underestimate the cost of the inexperienced NPP in terms of training. If you think it’s two weeks or two months, you are fooling yourself,” Dr. Friar emphasized, adding an inexperienced NPP could take from six months to two years to reach full competency in hospitalist service. “Know the tradeoffs,” he said. “It might be more important for you to hire the more experienced—and more costly—NPP so you don’t have to spend two years to get them up to speed.” HM10
PHYSICIAN ASSISTANTS (PAs) and nurse practitioners can do almost anything a physician can do, and many have skill sets physicians lack, according to David Friar, MD, FHM, president of Hospitalists of Northwest Michigan based in Traverse City.
“As we go forward, with continued physician shortages and with the growing responsibilities of the hospitalist movement, we are going to need more and more people with different skill sets,” Dr. Friar said during his presentation at HM10. “I think one of those important areas is nonphysician providers.”
A quick survey of the 300 or so hospitalists at the session showed most HM groups employ NPPs, but less than a third of those thought they were “using NPPs well.” Dr. Friar, who has worked with NPs and PAs for 14 years, said he has found NPPs “to be an integral part of our practice. They have become indispensable to us in the way we provide services to our hospitals and patients.”
Still, many hospitalist groups waste NPP potential, Dr. Friar explained. He suggested HM groups evaluate their NPP roster and duties, and make necessary changes. “Make sure you treat them as if they are part of the team. That is very important,” he said. “NPPs can and should take care of patients throughout all stages of the hospital stay, from admission to discharge.”
When hiring NPPs, look for team players who are flexible and willing to learn. Make sure the NPP knows their limits and is comfortable asking for help. Target local training programs or other departments in the hospital as fertile ground for new hires. But, most importantly, know what you are getting when you hire an NPP.
“Don’t underestimate the cost of the inexperienced NPP in terms of training. If you think it’s two weeks or two months, you are fooling yourself,” Dr. Friar emphasized, adding an inexperienced NPP could take from six months to two years to reach full competency in hospitalist service. “Know the tradeoffs,” he said. “It might be more important for you to hire the more experienced—and more costly—NPP so you don’t have to spend two years to get them up to speed.” HM10
Clinical Session
ELIZABETH BARLOW, MD, MPP, wants all hospitalists to know that upper-extremity DVT (UEDVT) is on the rise. Although most think of it “as a lesser entity,” Dr. Barlow told a jam-packed clinical-track session at HM10 the data show a higher rate of pulmonary em-bolism [PE] occurrence in UEDVT than was first thought. “So I think treating it seriously is important,” she said.
Dr. Barlow, a hospitalist at the University of Chicago Medical Center, outlined the case for greater attention to UEDVT during “Controversies in Anticoagu-lation and Thrombosis. “UEDVTs make up 1% to 4% of all DVTs in the U.S., and nearly 80% of UEDVT cases are provoked.
Much of the rise in—and controversy—UEDVT is due to the increased use of in-dwelling catheters, primarily how long to leave the catheter in place and when to remove it. “Judicious use of catheters is necessary. You should leave it in, if you need it,” Dr. Barlow said, adding that hospitalists should weigh the benefits and risks of PICC lines.
Some of Dr. Barlow’s key take-home points:
- Treat UEDVT seriously;
- Understand there is a higher rate of PE than previously thought;
- Insert central-vein catheters judiciously, and keep them in if you still need them;
- Manage the duration of therapy parallel to that of lower extremity DVT; and
- Routine thrombolytics use isn’t indicated at this time. HM10
ELIZABETH BARLOW, MD, MPP, wants all hospitalists to know that upper-extremity DVT (UEDVT) is on the rise. Although most think of it “as a lesser entity,” Dr. Barlow told a jam-packed clinical-track session at HM10 the data show a higher rate of pulmonary em-bolism [PE] occurrence in UEDVT than was first thought. “So I think treating it seriously is important,” she said.
Dr. Barlow, a hospitalist at the University of Chicago Medical Center, outlined the case for greater attention to UEDVT during “Controversies in Anticoagu-lation and Thrombosis. “UEDVTs make up 1% to 4% of all DVTs in the U.S., and nearly 80% of UEDVT cases are provoked.
Much of the rise in—and controversy—UEDVT is due to the increased use of in-dwelling catheters, primarily how long to leave the catheter in place and when to remove it. “Judicious use of catheters is necessary. You should leave it in, if you need it,” Dr. Barlow said, adding that hospitalists should weigh the benefits and risks of PICC lines.
Some of Dr. Barlow’s key take-home points:
- Treat UEDVT seriously;
- Understand there is a higher rate of PE than previously thought;
- Insert central-vein catheters judiciously, and keep them in if you still need them;
- Manage the duration of therapy parallel to that of lower extremity DVT; and
- Routine thrombolytics use isn’t indicated at this time. HM10
ELIZABETH BARLOW, MD, MPP, wants all hospitalists to know that upper-extremity DVT (UEDVT) is on the rise. Although most think of it “as a lesser entity,” Dr. Barlow told a jam-packed clinical-track session at HM10 the data show a higher rate of pulmonary em-bolism [PE] occurrence in UEDVT than was first thought. “So I think treating it seriously is important,” she said.
Dr. Barlow, a hospitalist at the University of Chicago Medical Center, outlined the case for greater attention to UEDVT during “Controversies in Anticoagu-lation and Thrombosis. “UEDVTs make up 1% to 4% of all DVTs in the U.S., and nearly 80% of UEDVT cases are provoked.
Much of the rise in—and controversy—UEDVT is due to the increased use of in-dwelling catheters, primarily how long to leave the catheter in place and when to remove it. “Judicious use of catheters is necessary. You should leave it in, if you need it,” Dr. Barlow said, adding that hospitalists should weigh the benefits and risks of PICC lines.
Some of Dr. Barlow’s key take-home points:
- Treat UEDVT seriously;
- Understand there is a higher rate of PE than previously thought;
- Insert central-vein catheters judiciously, and keep them in if you still need them;
- Manage the duration of therapy parallel to that of lower extremity DVT; and
- Routine thrombolytics use isn’t indicated at this time. HM10
Quality Session
BUILDING QUALITY improvement (QI) into the healthcare process starts with education, but to date, standardized QI curriculums have not taken root across academic medical centers.
A quartet of academic hospitalists pushed the concept during an HM10 session titled “Quality Improvement Curriculum: How to Get Started and to Keep Going.” All four speakers agreed that QI “empowers providers to create change.”
The presentation was based on a 1998 book from first author David Kern, MD, MPH, FACP, professor at the Johns Hopkins University School of Medicine in Baltimore: “Curriculum Development for Medical Education: A Six-Step Process.” Some of the take-home points included:
- Problem identification and a general-needs assessment, followed by a targeted needs assessment. Combined, the two steps create a construct for an issue, such as “residents lack knowledge skills in QI,” and then hone in with such queries as “What is the baseline knowledge?”
- Goals and objectives. There is a difference between the two. Goals are broad-based with little specificity; objectives are measurable items that gauge progress.
- Educational strategies. Cognitive objectives can be taught via lectures or team-based projects; however, skill-based objectives traditionally are better taught via hands-on experience.
- Implementation, evaluation, and feedback. Many programs try to move too quickly and put something in place before fully planning out the curriculum.
“Take a step back,” said Arpana Vidyarthi, MD, assistant professor and director of quality University of California at San Francisco. “What you do in implementing your curriculum ought to be connected to what your goals and objectives are.” HM10
BUILDING QUALITY improvement (QI) into the healthcare process starts with education, but to date, standardized QI curriculums have not taken root across academic medical centers.
A quartet of academic hospitalists pushed the concept during an HM10 session titled “Quality Improvement Curriculum: How to Get Started and to Keep Going.” All four speakers agreed that QI “empowers providers to create change.”
The presentation was based on a 1998 book from first author David Kern, MD, MPH, FACP, professor at the Johns Hopkins University School of Medicine in Baltimore: “Curriculum Development for Medical Education: A Six-Step Process.” Some of the take-home points included:
- Problem identification and a general-needs assessment, followed by a targeted needs assessment. Combined, the two steps create a construct for an issue, such as “residents lack knowledge skills in QI,” and then hone in with such queries as “What is the baseline knowledge?”
- Goals and objectives. There is a difference between the two. Goals are broad-based with little specificity; objectives are measurable items that gauge progress.
- Educational strategies. Cognitive objectives can be taught via lectures or team-based projects; however, skill-based objectives traditionally are better taught via hands-on experience.
- Implementation, evaluation, and feedback. Many programs try to move too quickly and put something in place before fully planning out the curriculum.
“Take a step back,” said Arpana Vidyarthi, MD, assistant professor and director of quality University of California at San Francisco. “What you do in implementing your curriculum ought to be connected to what your goals and objectives are.” HM10
BUILDING QUALITY improvement (QI) into the healthcare process starts with education, but to date, standardized QI curriculums have not taken root across academic medical centers.
A quartet of academic hospitalists pushed the concept during an HM10 session titled “Quality Improvement Curriculum: How to Get Started and to Keep Going.” All four speakers agreed that QI “empowers providers to create change.”
The presentation was based on a 1998 book from first author David Kern, MD, MPH, FACP, professor at the Johns Hopkins University School of Medicine in Baltimore: “Curriculum Development for Medical Education: A Six-Step Process.” Some of the take-home points included:
- Problem identification and a general-needs assessment, followed by a targeted needs assessment. Combined, the two steps create a construct for an issue, such as “residents lack knowledge skills in QI,” and then hone in with such queries as “What is the baseline knowledge?”
- Goals and objectives. There is a difference between the two. Goals are broad-based with little specificity; objectives are measurable items that gauge progress.
- Educational strategies. Cognitive objectives can be taught via lectures or team-based projects; however, skill-based objectives traditionally are better taught via hands-on experience.
- Implementation, evaluation, and feedback. Many programs try to move too quickly and put something in place before fully planning out the curriculum.
“Take a step back,” said Arpana Vidyarthi, MD, assistant professor and director of quality University of California at San Francisco. “What you do in implementing your curriculum ought to be connected to what your goals and objectives are.” HM10