User login
New tool better estimates cardiovascular risk in people with lupus
Current risk estimators are inaccurate
A tool that incorporates lupus-related variables with traditional risk factors provides a much more accurate assessment of cardiovascular (CV) risk in patients with systemic lupus erythematosus (SLE), according to data presented at the annual meeting of the Canadian Rheumatology Association.
In the initial clinical assessment of this tool, called the SLECRISK, “it identified high-risk lupus patients who would otherwise be missed by traditional methods of CV risk assessment,” reported May Y. Choi, MD, associate director of translational research at the University of Calgary’s (Alta.) Lupus Centre of Excellence.
It is well known that patients with SLE face an increased risk of CV events starting at an age long before risk begins climbing in the general population, according to Dr. Choi. She cited one study that showed women aged 35-44 years have a 50-fold greater risk of myocardial infarction than healthy individuals.
All major guidelines recognize this increased risk and recommend CV risk assessment in patients with SLE, even though Dr. Choi pointed out that traditional tools, such as the American College of Cardiology atherosclerotic cardiovascular disease (ASCVD) risk calculator or the Framingham Risk Score (FRS) have a limited ability to detect the patients with SLE who are most likely to have an event.
In SLE, current tools are inadequate
“These risk assessment tools perform poorly in SLE patients because they do not capture SLE-related inflammation,” Dr. Choi said. Of several examples, Dr. Choi cited a study showing “seven times more MIs and strokes observed than expected in SLE patients on the basis of the FRS.”
The disparity between expected and observed MIs and strokes is worse with increasing severity of SLE. In a study she presented 3 years ago, rates of CV events were 12 times higher in those with inactive or mild SLE, rising to a 16-fold increase among those with moderate disease and jumping to a 32-fold increase in those with severe SLE.
The SLECRISK tool was developed from the Brigham and Women’s Hospital SLE Registry, which was initiated in 1992. Patients without a history of CV disease were evaluated for traditional CV risk factors and for SLE-specific characteristics such as disease activity, levels of the complement proteins C3 and C4, kidney function, the presence of nephritis, and SLE duration. The value of these characteristics as predictors of CV events were then assessed over a 10-year follow-up period before being assembled into the SLECRISK tool.
In an example of the risk equation, Dr. Choi described a 50-year-old patient with SLE and a 5% 10-year ASCVD risk score, which is low. After adjustment for SLE risks, which included 10 years disease duration, high disease activity, elevated creatinine, and positive anti–double stranded DNA status, the 10-year CV risk score climbed to 16.2%, which is moderate.
The performance of the SLECRISK was evaluated in 1,243 patients providing 8,946.51 person-years of follow-up. During this period, there were 90 major adverse cardiac events (MACE), of which 82% were adjudicated by cardiologists, and 211 secondary events.
Relative to the ASCVD risk score, the SLECRISK identified about twice as many patients with SLE as having moderate risk and 3.5-fold more patients as having high risk. Among patients who experienced CV events, traditional CV risk factors were more common but so were SLE-specific risk factors, including greater disease severity, a greater likelihood of lupus nephritis, increased complement levels, and greater exposure to glucocorticoids, according to Dr. Choi.
Specificities for CV events higher on SLECRISK
In predicting CV events, the differences in specificities were in the same general range, although somewhat higher for the ASCVD risk score in regard to predicting MACE (83% vs. 72%) and MACE plus secondary events (90% vs. 79%). However, the sensitivities were much higher for SLECRISK relative to the ASCVD risk score for MACE alone (64% vs. 41%) and for MACE plus secondary events (58% vs. 35%).
When comparing those who had an MI or stroke, the ASCVD risk score identified 8 (7%) patients missed by SLECRISK, whereas SLECRISK identified 89 (73%) missed by the ASCVD risk score. The remaining 25 patients (20%) were identified by both. The advantage of SLECRISK was similar for MACE plus secondary outcomes.
Dr. Choi noted that all of the SLE-specific variables in SLECRISK are readily obtained and often already available in patient charts. She said that there is a plan to validate the tool in larger groups, but with a goal of creating a tool available online for clinicians and their patients to use. There is also an even more ambitious plan for the future.
“We have funding to look at machine learning to evaluate predictive variables in SLE patients,” Dr. Choi said. Rather than adding SLE-specific variables to traditional risks, the plan is to “start from scratch,” letting artificial intelligence assemble predictors without prejudice to what might or might not be relevant.
A SLE-specific tool for evaluating CV risk is an important “unmet need,” according to Karen H. Costenbader, MD, professor in the division of rheumatology, inflammation, and immunity at Brigham and Women’s Hospital and Harvard Medical School, both in Boston. In an interview, she reiterated that measuring CV risk in SLE is already guideline recommended, but conventional tools have been shown to be inaccurate.
“I can envision it being used in clinical encounters to help guide shared decision-making with patients,” explained Dr. Costenbader, who was not involved in the presentation at the CRA meeting but worked with Dr. Choi in developing SLECRISK. “It would give us more precise estimates, allowing us to risk stratify our patients and informing us as to which modifiable SLE-specific and nonspecific factors are contributing most to CV risk.’
The problem of using conventional risk assessments in SLE has been well recognized. Of those who have written on this subject, Maureen McMahon, MD, site director of the Lupus Clinical Trials Network at the University of California, Los Angeles, said: “There is a critical need for the development of SLE-specific risk assessment tools like SLECRISK.”
Author of several studies looking at alternatives for CV risk assessment in SLE, including a study looking at a panel of biomarkers that was published in ACR Open Rheumatology, Dr. McMahon said in an interview that CV risk in SLE is high but conventional risk assessments are flawed.
“Multiple previous studies have demonstrated that these currently available calculators are not adequate for identifying risk in the lupus patient population,” she said. According to Dr. McMahon, the fact that rheumatologists remain “dependent upon [these conventional] cardiovascular risk calculators” is a well-recognized problem that needs resolution.
Dr. Choi has financial relationships with AstraZeneca, GlaxoSmithKline, Mallinckrodt. MitogenDx, Organon, and Werfen International. Dr. Costenbader reports no potential conflicts of interest. Dr. McMahon has financial relationships with AstraZeneca, Aurinia Pharmaceuticals, Eli Lilly, and GlaxoSmithKline.
Current risk estimators are inaccurate
Current risk estimators are inaccurate
A tool that incorporates lupus-related variables with traditional risk factors provides a much more accurate assessment of cardiovascular (CV) risk in patients with systemic lupus erythematosus (SLE), according to data presented at the annual meeting of the Canadian Rheumatology Association.
In the initial clinical assessment of this tool, called the SLECRISK, “it identified high-risk lupus patients who would otherwise be missed by traditional methods of CV risk assessment,” reported May Y. Choi, MD, associate director of translational research at the University of Calgary’s (Alta.) Lupus Centre of Excellence.
It is well known that patients with SLE face an increased risk of CV events starting at an age long before risk begins climbing in the general population, according to Dr. Choi. She cited one study that showed women aged 35-44 years have a 50-fold greater risk of myocardial infarction than healthy individuals.
All major guidelines recognize this increased risk and recommend CV risk assessment in patients with SLE, even though Dr. Choi pointed out that traditional tools, such as the American College of Cardiology atherosclerotic cardiovascular disease (ASCVD) risk calculator or the Framingham Risk Score (FRS) have a limited ability to detect the patients with SLE who are most likely to have an event.
In SLE, current tools are inadequate
“These risk assessment tools perform poorly in SLE patients because they do not capture SLE-related inflammation,” Dr. Choi said. Of several examples, Dr. Choi cited a study showing “seven times more MIs and strokes observed than expected in SLE patients on the basis of the FRS.”
The disparity between expected and observed MIs and strokes is worse with increasing severity of SLE. In a study she presented 3 years ago, rates of CV events were 12 times higher in those with inactive or mild SLE, rising to a 16-fold increase among those with moderate disease and jumping to a 32-fold increase in those with severe SLE.
The SLECRISK tool was developed from the Brigham and Women’s Hospital SLE Registry, which was initiated in 1992. Patients without a history of CV disease were evaluated for traditional CV risk factors and for SLE-specific characteristics such as disease activity, levels of the complement proteins C3 and C4, kidney function, the presence of nephritis, and SLE duration. The value of these characteristics as predictors of CV events were then assessed over a 10-year follow-up period before being assembled into the SLECRISK tool.
In an example of the risk equation, Dr. Choi described a 50-year-old patient with SLE and a 5% 10-year ASCVD risk score, which is low. After adjustment for SLE risks, which included 10 years disease duration, high disease activity, elevated creatinine, and positive anti–double stranded DNA status, the 10-year CV risk score climbed to 16.2%, which is moderate.
The performance of the SLECRISK was evaluated in 1,243 patients providing 8,946.51 person-years of follow-up. During this period, there were 90 major adverse cardiac events (MACE), of which 82% were adjudicated by cardiologists, and 211 secondary events.
Relative to the ASCVD risk score, the SLECRISK identified about twice as many patients with SLE as having moderate risk and 3.5-fold more patients as having high risk. Among patients who experienced CV events, traditional CV risk factors were more common but so were SLE-specific risk factors, including greater disease severity, a greater likelihood of lupus nephritis, increased complement levels, and greater exposure to glucocorticoids, according to Dr. Choi.
Specificities for CV events higher on SLECRISK
In predicting CV events, the differences in specificities were in the same general range, although somewhat higher for the ASCVD risk score in regard to predicting MACE (83% vs. 72%) and MACE plus secondary events (90% vs. 79%). However, the sensitivities were much higher for SLECRISK relative to the ASCVD risk score for MACE alone (64% vs. 41%) and for MACE plus secondary events (58% vs. 35%).
When comparing those who had an MI or stroke, the ASCVD risk score identified 8 (7%) patients missed by SLECRISK, whereas SLECRISK identified 89 (73%) missed by the ASCVD risk score. The remaining 25 patients (20%) were identified by both. The advantage of SLECRISK was similar for MACE plus secondary outcomes.
Dr. Choi noted that all of the SLE-specific variables in SLECRISK are readily obtained and often already available in patient charts. She said that there is a plan to validate the tool in larger groups, but with a goal of creating a tool available online for clinicians and their patients to use. There is also an even more ambitious plan for the future.
“We have funding to look at machine learning to evaluate predictive variables in SLE patients,” Dr. Choi said. Rather than adding SLE-specific variables to traditional risks, the plan is to “start from scratch,” letting artificial intelligence assemble predictors without prejudice to what might or might not be relevant.
A SLE-specific tool for evaluating CV risk is an important “unmet need,” according to Karen H. Costenbader, MD, professor in the division of rheumatology, inflammation, and immunity at Brigham and Women’s Hospital and Harvard Medical School, both in Boston. In an interview, she reiterated that measuring CV risk in SLE is already guideline recommended, but conventional tools have been shown to be inaccurate.
“I can envision it being used in clinical encounters to help guide shared decision-making with patients,” explained Dr. Costenbader, who was not involved in the presentation at the CRA meeting but worked with Dr. Choi in developing SLECRISK. “It would give us more precise estimates, allowing us to risk stratify our patients and informing us as to which modifiable SLE-specific and nonspecific factors are contributing most to CV risk.’
The problem of using conventional risk assessments in SLE has been well recognized. Of those who have written on this subject, Maureen McMahon, MD, site director of the Lupus Clinical Trials Network at the University of California, Los Angeles, said: “There is a critical need for the development of SLE-specific risk assessment tools like SLECRISK.”
Author of several studies looking at alternatives for CV risk assessment in SLE, including a study looking at a panel of biomarkers that was published in ACR Open Rheumatology, Dr. McMahon said in an interview that CV risk in SLE is high but conventional risk assessments are flawed.
“Multiple previous studies have demonstrated that these currently available calculators are not adequate for identifying risk in the lupus patient population,” she said. According to Dr. McMahon, the fact that rheumatologists remain “dependent upon [these conventional] cardiovascular risk calculators” is a well-recognized problem that needs resolution.
Dr. Choi has financial relationships with AstraZeneca, GlaxoSmithKline, Mallinckrodt. MitogenDx, Organon, and Werfen International. Dr. Costenbader reports no potential conflicts of interest. Dr. McMahon has financial relationships with AstraZeneca, Aurinia Pharmaceuticals, Eli Lilly, and GlaxoSmithKline.
A tool that incorporates lupus-related variables with traditional risk factors provides a much more accurate assessment of cardiovascular (CV) risk in patients with systemic lupus erythematosus (SLE), according to data presented at the annual meeting of the Canadian Rheumatology Association.
In the initial clinical assessment of this tool, called the SLECRISK, “it identified high-risk lupus patients who would otherwise be missed by traditional methods of CV risk assessment,” reported May Y. Choi, MD, associate director of translational research at the University of Calgary’s (Alta.) Lupus Centre of Excellence.
It is well known that patients with SLE face an increased risk of CV events starting at an age long before risk begins climbing in the general population, according to Dr. Choi. She cited one study that showed women aged 35-44 years have a 50-fold greater risk of myocardial infarction than healthy individuals.
All major guidelines recognize this increased risk and recommend CV risk assessment in patients with SLE, even though Dr. Choi pointed out that traditional tools, such as the American College of Cardiology atherosclerotic cardiovascular disease (ASCVD) risk calculator or the Framingham Risk Score (FRS) have a limited ability to detect the patients with SLE who are most likely to have an event.
In SLE, current tools are inadequate
“These risk assessment tools perform poorly in SLE patients because they do not capture SLE-related inflammation,” Dr. Choi said. Of several examples, Dr. Choi cited a study showing “seven times more MIs and strokes observed than expected in SLE patients on the basis of the FRS.”
The disparity between expected and observed MIs and strokes is worse with increasing severity of SLE. In a study she presented 3 years ago, rates of CV events were 12 times higher in those with inactive or mild SLE, rising to a 16-fold increase among those with moderate disease and jumping to a 32-fold increase in those with severe SLE.
The SLECRISK tool was developed from the Brigham and Women’s Hospital SLE Registry, which was initiated in 1992. Patients without a history of CV disease were evaluated for traditional CV risk factors and for SLE-specific characteristics such as disease activity, levels of the complement proteins C3 and C4, kidney function, the presence of nephritis, and SLE duration. The value of these characteristics as predictors of CV events were then assessed over a 10-year follow-up period before being assembled into the SLECRISK tool.
In an example of the risk equation, Dr. Choi described a 50-year-old patient with SLE and a 5% 10-year ASCVD risk score, which is low. After adjustment for SLE risks, which included 10 years disease duration, high disease activity, elevated creatinine, and positive anti–double stranded DNA status, the 10-year CV risk score climbed to 16.2%, which is moderate.
The performance of the SLECRISK was evaluated in 1,243 patients providing 8,946.51 person-years of follow-up. During this period, there were 90 major adverse cardiac events (MACE), of which 82% were adjudicated by cardiologists, and 211 secondary events.
Relative to the ASCVD risk score, the SLECRISK identified about twice as many patients with SLE as having moderate risk and 3.5-fold more patients as having high risk. Among patients who experienced CV events, traditional CV risk factors were more common but so were SLE-specific risk factors, including greater disease severity, a greater likelihood of lupus nephritis, increased complement levels, and greater exposure to glucocorticoids, according to Dr. Choi.
Specificities for CV events higher on SLECRISK
In predicting CV events, the differences in specificities were in the same general range, although somewhat higher for the ASCVD risk score in regard to predicting MACE (83% vs. 72%) and MACE plus secondary events (90% vs. 79%). However, the sensitivities were much higher for SLECRISK relative to the ASCVD risk score for MACE alone (64% vs. 41%) and for MACE plus secondary events (58% vs. 35%).
When comparing those who had an MI or stroke, the ASCVD risk score identified 8 (7%) patients missed by SLECRISK, whereas SLECRISK identified 89 (73%) missed by the ASCVD risk score. The remaining 25 patients (20%) were identified by both. The advantage of SLECRISK was similar for MACE plus secondary outcomes.
Dr. Choi noted that all of the SLE-specific variables in SLECRISK are readily obtained and often already available in patient charts. She said that there is a plan to validate the tool in larger groups, but with a goal of creating a tool available online for clinicians and their patients to use. There is also an even more ambitious plan for the future.
“We have funding to look at machine learning to evaluate predictive variables in SLE patients,” Dr. Choi said. Rather than adding SLE-specific variables to traditional risks, the plan is to “start from scratch,” letting artificial intelligence assemble predictors without prejudice to what might or might not be relevant.
A SLE-specific tool for evaluating CV risk is an important “unmet need,” according to Karen H. Costenbader, MD, professor in the division of rheumatology, inflammation, and immunity at Brigham and Women’s Hospital and Harvard Medical School, both in Boston. In an interview, she reiterated that measuring CV risk in SLE is already guideline recommended, but conventional tools have been shown to be inaccurate.
“I can envision it being used in clinical encounters to help guide shared decision-making with patients,” explained Dr. Costenbader, who was not involved in the presentation at the CRA meeting but worked with Dr. Choi in developing SLECRISK. “It would give us more precise estimates, allowing us to risk stratify our patients and informing us as to which modifiable SLE-specific and nonspecific factors are contributing most to CV risk.’
The problem of using conventional risk assessments in SLE has been well recognized. Of those who have written on this subject, Maureen McMahon, MD, site director of the Lupus Clinical Trials Network at the University of California, Los Angeles, said: “There is a critical need for the development of SLE-specific risk assessment tools like SLECRISK.”
Author of several studies looking at alternatives for CV risk assessment in SLE, including a study looking at a panel of biomarkers that was published in ACR Open Rheumatology, Dr. McMahon said in an interview that CV risk in SLE is high but conventional risk assessments are flawed.
“Multiple previous studies have demonstrated that these currently available calculators are not adequate for identifying risk in the lupus patient population,” she said. According to Dr. McMahon, the fact that rheumatologists remain “dependent upon [these conventional] cardiovascular risk calculators” is a well-recognized problem that needs resolution.
Dr. Choi has financial relationships with AstraZeneca, GlaxoSmithKline, Mallinckrodt. MitogenDx, Organon, and Werfen International. Dr. Costenbader reports no potential conflicts of interest. Dr. McMahon has financial relationships with AstraZeneca, Aurinia Pharmaceuticals, Eli Lilly, and GlaxoSmithKline.
FROM CRA 2023
Drug combo promising in vascular cognitive impairment: LACI-2 trial results
and is seen as a new therapeutic approach for patients with cerebral small-vessel disease. The drugs – isosorbide mononitrate and cilostazol – stabilize endothelial function, which is a new therapeutic target for patients with small-vessel disease stroke.
The phase 2 LACI-2 study, evaluating these drugs individually and in combination in patients with lacunar stroke, showed promising trends toward reductions in recurrent stroke, cognitive impairment, and dependency, some of which became significant when the drugs were given together. There was also some suggestion of positive impacts on mood and quality of life.
“Isosorbide mononitrate was associated with a reduction in recurrent stroke, a tendency toward a reduction in dependency and a reduction in cognitive impairment, and cilostazol also seemed to reduce dependency,” study investigator Joanna M. Wardlaw, MD, professor of applied neuroimaging at Edinburgh University, reported.
“When used together, they seemed to have more benefits than either drug on its own. So this is good preliminary evidence that the drugs are working together in a positive way,” she said. But she cautioned that these potential benefits will need to be confirmed in a larger phase 3 trial.
The LACI-2 study was presented at the International Stroke Conference by Dr. Wardlaw and coinvestigator Philip Bath, DSc, professor of medicine at the University of Nottingham (England).
They both highlighted the effect seen on cognitive impairment at the conference presented by the American Stroke Association, a division of the American Heart Association.
“We saw a significant reduction in the number of patients with cognitive impairment with the two drugs together in this phase 2 study,” Dr. Wardlaw said. “This is very encouraging since no study has previously found any medications that positively affect cognitive impairment in small-vessel disease strokes. We cautiously hope that these medications may have wider implications for other types of small-vessel disease as well.”
Dr. Bath added: “The results on cognitive impairment are particularly important. Many patients rate cognitive impairment as one of the most dreaded outcomes of a stroke even if they also have quite significant physical disability. People simply don’t want to lose their memory and thinking ability.”
“The results of LACI-2 also raise interesting questions about whether these drugs would be beneficial for other types of small-vessel disease which do not present as stroke, but maybe may manifest as headaches or memory impairment,” he noted.
‘Very intriguing results’
Outside experts were enthusiastic about these preliminary results. In an ISC highlights presentation, program chair Tudor Jovin, MD, Cooper Neurological Institute, Cherry Hill, N.J., said: “It is refreshing to finally see some positive signals in studies in small-vessel stroke. This is an area where we haven’t had answers for a long time.”
He described the reduction in cognitive impairment seen in the study as “very intriguing and very important.”
“I think we have underestimated the burden that cognitive impairment has in stroke, and the burden in general in society of vascular cognitive impairment. This is a very promising approach that definitely deserves to be investigated more thoroughly in a larger trial.”
Commenting on the study findings, Mitchell Elkind, MD, professor of neurology and epidemiology at Columbia University Irving Medical Center, New York, said this study “provides evidence that points us in at least two important directions.”
“First, it suggests that endothelial dysfunction, or problems with the lining of the blood vessels, may be an important contributor to small-vessel disease and the cognitive decline that often accompanies it. This is a new mechanism of action and different from blood clotting, blood pressure, and other conventional targets of treatment,” Dr. Elkind said.
“Second, and more generally, it suggests that stroke trials, particularly in the subtype of small-vessel disease, can and should explore not only the incidence of recurrent acute events but also the steady decline that occurs after stroke. Poststroke cognitive decline is a relatively new area of stroke research.”
Dr. Wardlaw noted that lacunar stroke is a common type of ischemic stroke, but it has been rather neglected in terms of research. It is assumed to be caused by atherosclerosis of the small vessel but there is now mounting evidence suggesting that it is a result of problems in the endothelium of the small vessels.
“We looked for potential available drugs that targeted endothelial dysfunction. Both the drugs we tested are already widely used – isosorbide mononitrate for the treatment of coronary artery disease and angina, and cilostazol, mainly in Asia, for stroke prevention,” she said.
LACI-2 was primarily a feasibility study looking at whether it was possible to recruit enough patients who had had a lacunar stroke and would take the drugs, individually or in combination, for up to a year. Outcomes were investigated on an exploratory basis. The study enrolled 363 patients who had experienced lacunar stroke from 26 stroke centers throughout the United Kingdom. They were randomly assigned to one of four treatment groups for 1 year:
- 40-60 mg/day of oral isosorbide mononitrate alone.
- 200 mg/day of oral cilostazol alone.
- Both medications.
- Neither medication.
Patients completed phone surveys at 6 and 12 months to assess health status, including recurrent stroke, myocardial infarction, cognitive tests, symptoms, quality of life surveys, and they also had brain imaging at 12 months.
Results showed 98% of patients were still taking their study medication at 1 year, and the drugs appeared to be safe on top of usual care with few deaths or hemorrhages in the study.
The composite outcome including recurrent stroke, MI, cognitive impairment, dependency (modified Rankin score > 2) and death was reduced by 20% in the isosorbide mononitrate–alone group (adjusted hazard ratio, 0.80; 95% confidence interval, 0.59-1.09).
The composite endpoint was reduced by 23% in the cilostazol group (aHR, 0.77; 95% CI, 0.57-1.05) and by 42% in the combination group (aHR, 0.58, 95% CI, 0.36-0.92) compared with those taking neither drug.
Isosorbide mononitrate alone showed trends toward a reduction in recurrent stroke, cognitive impairment, and dependency, whereas cilostazol alone reduced dependency with a trend toward a reduction in cognitive impairment. When used together, the drugs showed large reductions in cognitive impairment (aHR, 0.44; 95% CI, 0.19-0.99) and dependency (aHR ,0.14; 95% CI, 0.03-0.59).
During the highlights session, Dr. Jovin commented: “It is obvious that the investigators have put a lot of thought into the design of this trial. Presumably because of the composite score they were able to increase the power. We are used to trials which require thousands of patients, but here we are able to see significant results, although exploratory, with just a few hundred patients.”
Dr. Bath stressed that this was only a phase 2 study. “We now need to see if we can confirm these results in a larger phase 3 study.” That study, LACI-3, is planned to start later this year. He also suggested that it would be interesting to investigate whether these drugs would work in other types of ischemic stroke such as those caused by large-artery disease or cardioembolic strokes, as well as other forms of small-vessel disease such as patients with vascular cognitive impairment.
“There are many areas to investigate in future. It might be that in a few years’ time these drugs may be standard of care across many different forms of small-vessel disease,” he said.
Dr. Wardlaw noted that lacunar strokes are generally quite mild strokes, which could be one of the reasons why they have not been the target of much research to date. But Dr. Bath added: “While they may be labeled as a mild stroke on the NIHSS scale, patients can still be quite badly affected. About half of patients with a lacunar stroke develop cognitive impairment and eventually dementia – that is certainly not mild.”
The study was funded primarily by the British Heart Foundation, with support from the UK Alzheimer’s Society, the UK Dementia Research Institute, the Stroke Association, the Fondation Leducq, NHS Research Scotland, and the UK National Institutes of Health Research Clinical Research Networks. Dr. Bath is an adviser to CoMind, DiaMedica, Phagenesis, and Roche. Dr. Wardlaw reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
and is seen as a new therapeutic approach for patients with cerebral small-vessel disease. The drugs – isosorbide mononitrate and cilostazol – stabilize endothelial function, which is a new therapeutic target for patients with small-vessel disease stroke.
The phase 2 LACI-2 study, evaluating these drugs individually and in combination in patients with lacunar stroke, showed promising trends toward reductions in recurrent stroke, cognitive impairment, and dependency, some of which became significant when the drugs were given together. There was also some suggestion of positive impacts on mood and quality of life.
“Isosorbide mononitrate was associated with a reduction in recurrent stroke, a tendency toward a reduction in dependency and a reduction in cognitive impairment, and cilostazol also seemed to reduce dependency,” study investigator Joanna M. Wardlaw, MD, professor of applied neuroimaging at Edinburgh University, reported.
“When used together, they seemed to have more benefits than either drug on its own. So this is good preliminary evidence that the drugs are working together in a positive way,” she said. But she cautioned that these potential benefits will need to be confirmed in a larger phase 3 trial.
The LACI-2 study was presented at the International Stroke Conference by Dr. Wardlaw and coinvestigator Philip Bath, DSc, professor of medicine at the University of Nottingham (England).
They both highlighted the effect seen on cognitive impairment at the conference presented by the American Stroke Association, a division of the American Heart Association.
“We saw a significant reduction in the number of patients with cognitive impairment with the two drugs together in this phase 2 study,” Dr. Wardlaw said. “This is very encouraging since no study has previously found any medications that positively affect cognitive impairment in small-vessel disease strokes. We cautiously hope that these medications may have wider implications for other types of small-vessel disease as well.”
Dr. Bath added: “The results on cognitive impairment are particularly important. Many patients rate cognitive impairment as one of the most dreaded outcomes of a stroke even if they also have quite significant physical disability. People simply don’t want to lose their memory and thinking ability.”
“The results of LACI-2 also raise interesting questions about whether these drugs would be beneficial for other types of small-vessel disease which do not present as stroke, but maybe may manifest as headaches or memory impairment,” he noted.
‘Very intriguing results’
Outside experts were enthusiastic about these preliminary results. In an ISC highlights presentation, program chair Tudor Jovin, MD, Cooper Neurological Institute, Cherry Hill, N.J., said: “It is refreshing to finally see some positive signals in studies in small-vessel stroke. This is an area where we haven’t had answers for a long time.”
He described the reduction in cognitive impairment seen in the study as “very intriguing and very important.”
“I think we have underestimated the burden that cognitive impairment has in stroke, and the burden in general in society of vascular cognitive impairment. This is a very promising approach that definitely deserves to be investigated more thoroughly in a larger trial.”
Commenting on the study findings, Mitchell Elkind, MD, professor of neurology and epidemiology at Columbia University Irving Medical Center, New York, said this study “provides evidence that points us in at least two important directions.”
“First, it suggests that endothelial dysfunction, or problems with the lining of the blood vessels, may be an important contributor to small-vessel disease and the cognitive decline that often accompanies it. This is a new mechanism of action and different from blood clotting, blood pressure, and other conventional targets of treatment,” Dr. Elkind said.
“Second, and more generally, it suggests that stroke trials, particularly in the subtype of small-vessel disease, can and should explore not only the incidence of recurrent acute events but also the steady decline that occurs after stroke. Poststroke cognitive decline is a relatively new area of stroke research.”
Dr. Wardlaw noted that lacunar stroke is a common type of ischemic stroke, but it has been rather neglected in terms of research. It is assumed to be caused by atherosclerosis of the small vessel but there is now mounting evidence suggesting that it is a result of problems in the endothelium of the small vessels.
“We looked for potential available drugs that targeted endothelial dysfunction. Both the drugs we tested are already widely used – isosorbide mononitrate for the treatment of coronary artery disease and angina, and cilostazol, mainly in Asia, for stroke prevention,” she said.
LACI-2 was primarily a feasibility study looking at whether it was possible to recruit enough patients who had had a lacunar stroke and would take the drugs, individually or in combination, for up to a year. Outcomes were investigated on an exploratory basis. The study enrolled 363 patients who had experienced lacunar stroke from 26 stroke centers throughout the United Kingdom. They were randomly assigned to one of four treatment groups for 1 year:
- 40-60 mg/day of oral isosorbide mononitrate alone.
- 200 mg/day of oral cilostazol alone.
- Both medications.
- Neither medication.
Patients completed phone surveys at 6 and 12 months to assess health status, including recurrent stroke, myocardial infarction, cognitive tests, symptoms, quality of life surveys, and they also had brain imaging at 12 months.
Results showed 98% of patients were still taking their study medication at 1 year, and the drugs appeared to be safe on top of usual care with few deaths or hemorrhages in the study.
The composite outcome including recurrent stroke, MI, cognitive impairment, dependency (modified Rankin score > 2) and death was reduced by 20% in the isosorbide mononitrate–alone group (adjusted hazard ratio, 0.80; 95% confidence interval, 0.59-1.09).
The composite endpoint was reduced by 23% in the cilostazol group (aHR, 0.77; 95% CI, 0.57-1.05) and by 42% in the combination group (aHR, 0.58, 95% CI, 0.36-0.92) compared with those taking neither drug.
Isosorbide mononitrate alone showed trends toward a reduction in recurrent stroke, cognitive impairment, and dependency, whereas cilostazol alone reduced dependency with a trend toward a reduction in cognitive impairment. When used together, the drugs showed large reductions in cognitive impairment (aHR, 0.44; 95% CI, 0.19-0.99) and dependency (aHR ,0.14; 95% CI, 0.03-0.59).
During the highlights session, Dr. Jovin commented: “It is obvious that the investigators have put a lot of thought into the design of this trial. Presumably because of the composite score they were able to increase the power. We are used to trials which require thousands of patients, but here we are able to see significant results, although exploratory, with just a few hundred patients.”
Dr. Bath stressed that this was only a phase 2 study. “We now need to see if we can confirm these results in a larger phase 3 study.” That study, LACI-3, is planned to start later this year. He also suggested that it would be interesting to investigate whether these drugs would work in other types of ischemic stroke such as those caused by large-artery disease or cardioembolic strokes, as well as other forms of small-vessel disease such as patients with vascular cognitive impairment.
“There are many areas to investigate in future. It might be that in a few years’ time these drugs may be standard of care across many different forms of small-vessel disease,” he said.
Dr. Wardlaw noted that lacunar strokes are generally quite mild strokes, which could be one of the reasons why they have not been the target of much research to date. But Dr. Bath added: “While they may be labeled as a mild stroke on the NIHSS scale, patients can still be quite badly affected. About half of patients with a lacunar stroke develop cognitive impairment and eventually dementia – that is certainly not mild.”
The study was funded primarily by the British Heart Foundation, with support from the UK Alzheimer’s Society, the UK Dementia Research Institute, the Stroke Association, the Fondation Leducq, NHS Research Scotland, and the UK National Institutes of Health Research Clinical Research Networks. Dr. Bath is an adviser to CoMind, DiaMedica, Phagenesis, and Roche. Dr. Wardlaw reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
and is seen as a new therapeutic approach for patients with cerebral small-vessel disease. The drugs – isosorbide mononitrate and cilostazol – stabilize endothelial function, which is a new therapeutic target for patients with small-vessel disease stroke.
The phase 2 LACI-2 study, evaluating these drugs individually and in combination in patients with lacunar stroke, showed promising trends toward reductions in recurrent stroke, cognitive impairment, and dependency, some of which became significant when the drugs were given together. There was also some suggestion of positive impacts on mood and quality of life.
“Isosorbide mononitrate was associated with a reduction in recurrent stroke, a tendency toward a reduction in dependency and a reduction in cognitive impairment, and cilostazol also seemed to reduce dependency,” study investigator Joanna M. Wardlaw, MD, professor of applied neuroimaging at Edinburgh University, reported.
“When used together, they seemed to have more benefits than either drug on its own. So this is good preliminary evidence that the drugs are working together in a positive way,” she said. But she cautioned that these potential benefits will need to be confirmed in a larger phase 3 trial.
The LACI-2 study was presented at the International Stroke Conference by Dr. Wardlaw and coinvestigator Philip Bath, DSc, professor of medicine at the University of Nottingham (England).
They both highlighted the effect seen on cognitive impairment at the conference presented by the American Stroke Association, a division of the American Heart Association.
“We saw a significant reduction in the number of patients with cognitive impairment with the two drugs together in this phase 2 study,” Dr. Wardlaw said. “This is very encouraging since no study has previously found any medications that positively affect cognitive impairment in small-vessel disease strokes. We cautiously hope that these medications may have wider implications for other types of small-vessel disease as well.”
Dr. Bath added: “The results on cognitive impairment are particularly important. Many patients rate cognitive impairment as one of the most dreaded outcomes of a stroke even if they also have quite significant physical disability. People simply don’t want to lose their memory and thinking ability.”
“The results of LACI-2 also raise interesting questions about whether these drugs would be beneficial for other types of small-vessel disease which do not present as stroke, but maybe may manifest as headaches or memory impairment,” he noted.
‘Very intriguing results’
Outside experts were enthusiastic about these preliminary results. In an ISC highlights presentation, program chair Tudor Jovin, MD, Cooper Neurological Institute, Cherry Hill, N.J., said: “It is refreshing to finally see some positive signals in studies in small-vessel stroke. This is an area where we haven’t had answers for a long time.”
He described the reduction in cognitive impairment seen in the study as “very intriguing and very important.”
“I think we have underestimated the burden that cognitive impairment has in stroke, and the burden in general in society of vascular cognitive impairment. This is a very promising approach that definitely deserves to be investigated more thoroughly in a larger trial.”
Commenting on the study findings, Mitchell Elkind, MD, professor of neurology and epidemiology at Columbia University Irving Medical Center, New York, said this study “provides evidence that points us in at least two important directions.”
“First, it suggests that endothelial dysfunction, or problems with the lining of the blood vessels, may be an important contributor to small-vessel disease and the cognitive decline that often accompanies it. This is a new mechanism of action and different from blood clotting, blood pressure, and other conventional targets of treatment,” Dr. Elkind said.
“Second, and more generally, it suggests that stroke trials, particularly in the subtype of small-vessel disease, can and should explore not only the incidence of recurrent acute events but also the steady decline that occurs after stroke. Poststroke cognitive decline is a relatively new area of stroke research.”
Dr. Wardlaw noted that lacunar stroke is a common type of ischemic stroke, but it has been rather neglected in terms of research. It is assumed to be caused by atherosclerosis of the small vessel but there is now mounting evidence suggesting that it is a result of problems in the endothelium of the small vessels.
“We looked for potential available drugs that targeted endothelial dysfunction. Both the drugs we tested are already widely used – isosorbide mononitrate for the treatment of coronary artery disease and angina, and cilostazol, mainly in Asia, for stroke prevention,” she said.
LACI-2 was primarily a feasibility study looking at whether it was possible to recruit enough patients who had had a lacunar stroke and would take the drugs, individually or in combination, for up to a year. Outcomes were investigated on an exploratory basis. The study enrolled 363 patients who had experienced lacunar stroke from 26 stroke centers throughout the United Kingdom. They were randomly assigned to one of four treatment groups for 1 year:
- 40-60 mg/day of oral isosorbide mononitrate alone.
- 200 mg/day of oral cilostazol alone.
- Both medications.
- Neither medication.
Patients completed phone surveys at 6 and 12 months to assess health status, including recurrent stroke, myocardial infarction, cognitive tests, symptoms, quality of life surveys, and they also had brain imaging at 12 months.
Results showed 98% of patients were still taking their study medication at 1 year, and the drugs appeared to be safe on top of usual care with few deaths or hemorrhages in the study.
The composite outcome including recurrent stroke, MI, cognitive impairment, dependency (modified Rankin score > 2) and death was reduced by 20% in the isosorbide mononitrate–alone group (adjusted hazard ratio, 0.80; 95% confidence interval, 0.59-1.09).
The composite endpoint was reduced by 23% in the cilostazol group (aHR, 0.77; 95% CI, 0.57-1.05) and by 42% in the combination group (aHR, 0.58, 95% CI, 0.36-0.92) compared with those taking neither drug.
Isosorbide mononitrate alone showed trends toward a reduction in recurrent stroke, cognitive impairment, and dependency, whereas cilostazol alone reduced dependency with a trend toward a reduction in cognitive impairment. When used together, the drugs showed large reductions in cognitive impairment (aHR, 0.44; 95% CI, 0.19-0.99) and dependency (aHR ,0.14; 95% CI, 0.03-0.59).
During the highlights session, Dr. Jovin commented: “It is obvious that the investigators have put a lot of thought into the design of this trial. Presumably because of the composite score they were able to increase the power. We are used to trials which require thousands of patients, but here we are able to see significant results, although exploratory, with just a few hundred patients.”
Dr. Bath stressed that this was only a phase 2 study. “We now need to see if we can confirm these results in a larger phase 3 study.” That study, LACI-3, is planned to start later this year. He also suggested that it would be interesting to investigate whether these drugs would work in other types of ischemic stroke such as those caused by large-artery disease or cardioembolic strokes, as well as other forms of small-vessel disease such as patients with vascular cognitive impairment.
“There are many areas to investigate in future. It might be that in a few years’ time these drugs may be standard of care across many different forms of small-vessel disease,” he said.
Dr. Wardlaw noted that lacunar strokes are generally quite mild strokes, which could be one of the reasons why they have not been the target of much research to date. But Dr. Bath added: “While they may be labeled as a mild stroke on the NIHSS scale, patients can still be quite badly affected. About half of patients with a lacunar stroke develop cognitive impairment and eventually dementia – that is certainly not mild.”
The study was funded primarily by the British Heart Foundation, with support from the UK Alzheimer’s Society, the UK Dementia Research Institute, the Stroke Association, the Fondation Leducq, NHS Research Scotland, and the UK National Institutes of Health Research Clinical Research Networks. Dr. Bath is an adviser to CoMind, DiaMedica, Phagenesis, and Roche. Dr. Wardlaw reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ISC 2023
Tenecteplase noninferior to alteplase for ischemic stroke: TRACE-2
, a new study has found. “This was a pivotal trial in establishing the safety and efficacy of tenecteplase as an alternative to alteplase in the thrombolytic treatment of acute ischemic stroke within 4.5 hours in Asian patients,” said study author Shuya Li, MD, associate chief physician, department of neurology, Beijing Tiantan Hospital, Capital Medical University, Beijing.
The findings in this all-Chinese population should have an impact on the use of tenecteplase going forward, said Dr. Li. “The results provide further evidence to support a worldwide switch to tenecteplase as the preferred thrombolytic for acute ischemic stroke.”
The findings were presented at the 2023 International Stroke Conference presented by the American Stroke Association, a division of the American Heart Association.
Single bolus
Use of alteplase (tissue plasminogen activator [tPA]) has for years been the main approach to thrombolytic reperfusion therapy for patients with acute stroke, but tenecteplase has recently emerged as a potential successor.
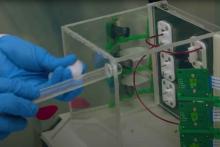
Tenecteplase is a tPA produced by recombinant DNA technology. It has a relatively long half-life and can be delivered in a single bolus instead of requiring an hour-long infusion, as is the case with alteplase.
The phase 3 noninferiority Tenecteplase Reperfusion Therapy in Acute ischemic Cerebrovascular Events (TRACE-2) trial – the first of its kind in an Asian population – included 1,430 adult ischemic stroke patients at 53 Chinese centers. Patients had to have a National Institutes of Health Stroke Scale (NIHSS) score of 5-25 and either not be eligible for or have refused endovascular therapy.
The mean age of study participants was about 66 years, and the percentage of women was about 31%. The mean baseline NIHSS score was 7 in both groups, and the symptom-onset-to-needle time was similar at 180 minutes for the tenecteplase group and 178.5 minutes for the alteplase group.
Researchers randomly assigned patients to receive tenecteplase or alteplase within 4.5 hours of symptom onset.
Those in the tenecteplase group received 0.25 mg/kg of the drug in a single IV bolus (maximum dose, 25 mg). Control group members who were treated with alteplase were given the drug as a 10% bolus, with the remainder given as a 1-hour infusion (0.9 mg/kg with a maximum dose of 90 mg).
Showed noninferiority
The primary efficacy outcome was a modified Rankins scale (mRS) score of 0-1 at 90 days, which is considered excellent function. About 62% of tenecteplase patients and 58% of alteplase patients attained this outcome (risk ratio, 1.09; 95% confidence interval, 1.00-1.18).
The P value was .001 for noninferiority and .06 for superiority, but Dr. Li explained that these values may change when considering the site effect.
There were no statistically significant differences between the two drugs on secondary outcomes of favorable function. For example, 73% of tenecteplase patients and 72% of alteplase patients had an mRS score of 0-2 at 3 months, and 50% in the tenecteplase and 49% in the alteplase group improved by 4 or more points on the NIHSS, or had a score of 1 or less, at 24 hours.
The groups also had comparable scores on the European quality-of-life visual analogue scale and on the Barthel index, which measures functional independence related to personal care and mobility.
Tenecteplase also turned out to be as safe at alteplase. About 2% in both groups had symptomatic intracranial hemorrhage within 36 hours, and both groups had that same percentage for such hemorrhages within 90 days. As well, the groups had a similar rate of any intracranial hemorrhage within 90 days (6% and 7%).
The mortality rate was 7% in the tenecteplase group, compared with 5% in the alteplase group.
Adverse events (AEs) occurred in 86% and 87%, and serious AEs in 16% and 15%, of the tenecteplase and alteplase groups, respectively, again with no statistically significant differences.
The research team aims to test the effectiveness of tenecteplase in other stroke patients, including those with minor strokes, those receiving thrombolysis in a later window, and those receiving endovascular therapy, said Dr. Li.
Strong evidence
Commenting on the study findings, Larry B. Goldstein, MD, professor and chair of neurology, University of Kentucky, Lexington, said it is important to determine the efficacy of tenecteplase among Asians, as they represent “an entirely different population” with unique concerns, such as bleeding complications from anticoagulants.
He noted an advantage of tenecteplase is ease of administration. “You don’t have to go through the loading dose and then the 1-hour infusion,” which poses an “additional hassle” when transferring patients between institutions, he said.
However, he noted that a possible “downside” to having both drugs available in the emergency department is “using the wrong drug at the wrong dose” because of their similar sounding names.
Also commenting on the study, Tudor G. Jovin, MD, professor and chair, department of neurology, Rowan University, Camden, N.J., said he welcomes another trial that confirms that these two drugs are biologically similar.
“I’m very glad this trial was done because it adds another very strong piece of evidence of equivalency.”
But the two drugs are not the same in some important respects, said Dr. Jovin, whose center switched to using tenecteplase almost 3 years ago. That switch has resulted in cutting 17 minutes from the door-to-needle time “which is quite significant,” he said.
“There’s no question that once we used tenecteplase in lieu of tPA, it’s been just so much easier to administer and affects the interhospital transfer protocols, because you’re not transferring the patient with a critical care IV. It’s a win-win situation for everyone.”
The study received funding from the National Science and Technology Major Project, the Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences, the National Natural Science Foundation of China, and the China Shijiazhuang Pharmaceutical Company Recomgen Pharmaceutical (Guangzhou). Dr. Li, Dr. Goldstein, and Dr. Jovin report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, a new study has found. “This was a pivotal trial in establishing the safety and efficacy of tenecteplase as an alternative to alteplase in the thrombolytic treatment of acute ischemic stroke within 4.5 hours in Asian patients,” said study author Shuya Li, MD, associate chief physician, department of neurology, Beijing Tiantan Hospital, Capital Medical University, Beijing.
The findings in this all-Chinese population should have an impact on the use of tenecteplase going forward, said Dr. Li. “The results provide further evidence to support a worldwide switch to tenecteplase as the preferred thrombolytic for acute ischemic stroke.”
The findings were presented at the 2023 International Stroke Conference presented by the American Stroke Association, a division of the American Heart Association.
Single bolus
Use of alteplase (tissue plasminogen activator [tPA]) has for years been the main approach to thrombolytic reperfusion therapy for patients with acute stroke, but tenecteplase has recently emerged as a potential successor.
Tenecteplase is a tPA produced by recombinant DNA technology. It has a relatively long half-life and can be delivered in a single bolus instead of requiring an hour-long infusion, as is the case with alteplase.
The phase 3 noninferiority Tenecteplase Reperfusion Therapy in Acute ischemic Cerebrovascular Events (TRACE-2) trial – the first of its kind in an Asian population – included 1,430 adult ischemic stroke patients at 53 Chinese centers. Patients had to have a National Institutes of Health Stroke Scale (NIHSS) score of 5-25 and either not be eligible for or have refused endovascular therapy.
The mean age of study participants was about 66 years, and the percentage of women was about 31%. The mean baseline NIHSS score was 7 in both groups, and the symptom-onset-to-needle time was similar at 180 minutes for the tenecteplase group and 178.5 minutes for the alteplase group.
Researchers randomly assigned patients to receive tenecteplase or alteplase within 4.5 hours of symptom onset.
Those in the tenecteplase group received 0.25 mg/kg of the drug in a single IV bolus (maximum dose, 25 mg). Control group members who were treated with alteplase were given the drug as a 10% bolus, with the remainder given as a 1-hour infusion (0.9 mg/kg with a maximum dose of 90 mg).
Showed noninferiority
The primary efficacy outcome was a modified Rankins scale (mRS) score of 0-1 at 90 days, which is considered excellent function. About 62% of tenecteplase patients and 58% of alteplase patients attained this outcome (risk ratio, 1.09; 95% confidence interval, 1.00-1.18).
The P value was .001 for noninferiority and .06 for superiority, but Dr. Li explained that these values may change when considering the site effect.
There were no statistically significant differences between the two drugs on secondary outcomes of favorable function. For example, 73% of tenecteplase patients and 72% of alteplase patients had an mRS score of 0-2 at 3 months, and 50% in the tenecteplase and 49% in the alteplase group improved by 4 or more points on the NIHSS, or had a score of 1 or less, at 24 hours.
The groups also had comparable scores on the European quality-of-life visual analogue scale and on the Barthel index, which measures functional independence related to personal care and mobility.
Tenecteplase also turned out to be as safe at alteplase. About 2% in both groups had symptomatic intracranial hemorrhage within 36 hours, and both groups had that same percentage for such hemorrhages within 90 days. As well, the groups had a similar rate of any intracranial hemorrhage within 90 days (6% and 7%).
The mortality rate was 7% in the tenecteplase group, compared with 5% in the alteplase group.
Adverse events (AEs) occurred in 86% and 87%, and serious AEs in 16% and 15%, of the tenecteplase and alteplase groups, respectively, again with no statistically significant differences.
The research team aims to test the effectiveness of tenecteplase in other stroke patients, including those with minor strokes, those receiving thrombolysis in a later window, and those receiving endovascular therapy, said Dr. Li.
Strong evidence
Commenting on the study findings, Larry B. Goldstein, MD, professor and chair of neurology, University of Kentucky, Lexington, said it is important to determine the efficacy of tenecteplase among Asians, as they represent “an entirely different population” with unique concerns, such as bleeding complications from anticoagulants.
He noted an advantage of tenecteplase is ease of administration. “You don’t have to go through the loading dose and then the 1-hour infusion,” which poses an “additional hassle” when transferring patients between institutions, he said.
However, he noted that a possible “downside” to having both drugs available in the emergency department is “using the wrong drug at the wrong dose” because of their similar sounding names.
Also commenting on the study, Tudor G. Jovin, MD, professor and chair, department of neurology, Rowan University, Camden, N.J., said he welcomes another trial that confirms that these two drugs are biologically similar.
“I’m very glad this trial was done because it adds another very strong piece of evidence of equivalency.”
But the two drugs are not the same in some important respects, said Dr. Jovin, whose center switched to using tenecteplase almost 3 years ago. That switch has resulted in cutting 17 minutes from the door-to-needle time “which is quite significant,” he said.
“There’s no question that once we used tenecteplase in lieu of tPA, it’s been just so much easier to administer and affects the interhospital transfer protocols, because you’re not transferring the patient with a critical care IV. It’s a win-win situation for everyone.”
The study received funding from the National Science and Technology Major Project, the Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences, the National Natural Science Foundation of China, and the China Shijiazhuang Pharmaceutical Company Recomgen Pharmaceutical (Guangzhou). Dr. Li, Dr. Goldstein, and Dr. Jovin report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, a new study has found. “This was a pivotal trial in establishing the safety and efficacy of tenecteplase as an alternative to alteplase in the thrombolytic treatment of acute ischemic stroke within 4.5 hours in Asian patients,” said study author Shuya Li, MD, associate chief physician, department of neurology, Beijing Tiantan Hospital, Capital Medical University, Beijing.
The findings in this all-Chinese population should have an impact on the use of tenecteplase going forward, said Dr. Li. “The results provide further evidence to support a worldwide switch to tenecteplase as the preferred thrombolytic for acute ischemic stroke.”
The findings were presented at the 2023 International Stroke Conference presented by the American Stroke Association, a division of the American Heart Association.
Single bolus
Use of alteplase (tissue plasminogen activator [tPA]) has for years been the main approach to thrombolytic reperfusion therapy for patients with acute stroke, but tenecteplase has recently emerged as a potential successor.
Tenecteplase is a tPA produced by recombinant DNA technology. It has a relatively long half-life and can be delivered in a single bolus instead of requiring an hour-long infusion, as is the case with alteplase.
The phase 3 noninferiority Tenecteplase Reperfusion Therapy in Acute ischemic Cerebrovascular Events (TRACE-2) trial – the first of its kind in an Asian population – included 1,430 adult ischemic stroke patients at 53 Chinese centers. Patients had to have a National Institutes of Health Stroke Scale (NIHSS) score of 5-25 and either not be eligible for or have refused endovascular therapy.
The mean age of study participants was about 66 years, and the percentage of women was about 31%. The mean baseline NIHSS score was 7 in both groups, and the symptom-onset-to-needle time was similar at 180 minutes for the tenecteplase group and 178.5 minutes for the alteplase group.
Researchers randomly assigned patients to receive tenecteplase or alteplase within 4.5 hours of symptom onset.
Those in the tenecteplase group received 0.25 mg/kg of the drug in a single IV bolus (maximum dose, 25 mg). Control group members who were treated with alteplase were given the drug as a 10% bolus, with the remainder given as a 1-hour infusion (0.9 mg/kg with a maximum dose of 90 mg).
Showed noninferiority
The primary efficacy outcome was a modified Rankins scale (mRS) score of 0-1 at 90 days, which is considered excellent function. About 62% of tenecteplase patients and 58% of alteplase patients attained this outcome (risk ratio, 1.09; 95% confidence interval, 1.00-1.18).
The P value was .001 for noninferiority and .06 for superiority, but Dr. Li explained that these values may change when considering the site effect.
There were no statistically significant differences between the two drugs on secondary outcomes of favorable function. For example, 73% of tenecteplase patients and 72% of alteplase patients had an mRS score of 0-2 at 3 months, and 50% in the tenecteplase and 49% in the alteplase group improved by 4 or more points on the NIHSS, or had a score of 1 or less, at 24 hours.
The groups also had comparable scores on the European quality-of-life visual analogue scale and on the Barthel index, which measures functional independence related to personal care and mobility.
Tenecteplase also turned out to be as safe at alteplase. About 2% in both groups had symptomatic intracranial hemorrhage within 36 hours, and both groups had that same percentage for such hemorrhages within 90 days. As well, the groups had a similar rate of any intracranial hemorrhage within 90 days (6% and 7%).
The mortality rate was 7% in the tenecteplase group, compared with 5% in the alteplase group.
Adverse events (AEs) occurred in 86% and 87%, and serious AEs in 16% and 15%, of the tenecteplase and alteplase groups, respectively, again with no statistically significant differences.
The research team aims to test the effectiveness of tenecteplase in other stroke patients, including those with minor strokes, those receiving thrombolysis in a later window, and those receiving endovascular therapy, said Dr. Li.
Strong evidence
Commenting on the study findings, Larry B. Goldstein, MD, professor and chair of neurology, University of Kentucky, Lexington, said it is important to determine the efficacy of tenecteplase among Asians, as they represent “an entirely different population” with unique concerns, such as bleeding complications from anticoagulants.
He noted an advantage of tenecteplase is ease of administration. “You don’t have to go through the loading dose and then the 1-hour infusion,” which poses an “additional hassle” when transferring patients between institutions, he said.
However, he noted that a possible “downside” to having both drugs available in the emergency department is “using the wrong drug at the wrong dose” because of their similar sounding names.
Also commenting on the study, Tudor G. Jovin, MD, professor and chair, department of neurology, Rowan University, Camden, N.J., said he welcomes another trial that confirms that these two drugs are biologically similar.
“I’m very glad this trial was done because it adds another very strong piece of evidence of equivalency.”
But the two drugs are not the same in some important respects, said Dr. Jovin, whose center switched to using tenecteplase almost 3 years ago. That switch has resulted in cutting 17 minutes from the door-to-needle time “which is quite significant,” he said.
“There’s no question that once we used tenecteplase in lieu of tPA, it’s been just so much easier to administer and affects the interhospital transfer protocols, because you’re not transferring the patient with a critical care IV. It’s a win-win situation for everyone.”
The study received funding from the National Science and Technology Major Project, the Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences, the National Natural Science Foundation of China, and the China Shijiazhuang Pharmaceutical Company Recomgen Pharmaceutical (Guangzhou). Dr. Li, Dr. Goldstein, and Dr. Jovin report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ISC 2023
No benefit of long-acting antipsychotics in schizophrenia?
In a multicountry, randomized, open-label study of more than 500 adults with schizophrenia, participants received either LAI paliperidone, LAI aripiprazole, or the respective oral formulation of these antipsychotics.
Results showed no significant difference between the combined oral and combined LAI treatment groups in time to all-cause discontinuation.
“We found no substantial advantage for LAI antipsychotic treatment over oral treatment, regarding time to discontinuation in patients with early-phase schizophrenia,” write investigators, led by Inge Winter-van Rossum, PhD, assistant visiting professor at Mount Sinai, New York, and affiliated with King’s College London and UMC Utrecht (the Netherlands).
This indicates that “there is no reason to prescribe LAIs instead of oral antipsychotics if the goal is to prevent discontinuation of antipsychotic medication in daily clinical practice,” they add.
The findings were published online in The Lancet Psychiatry.
Previous conflicting results
Maintenance treatment with antipsychotic medication reduces risk for relapse considerably, with treatment discontinuation being “by far the most important reason for relapse,” the investigators write.
LAIs “seem theoretically to be a way to enhance medication continuation and thereby reduce the risk for relapse,” they add. This is because LAIs enable a rapid response to nonadherence and remove the need for patients to remember to take their medications on a daily basis.
However, previous research has “provided conflicting results,” regarding the effectiveness of LAIs in accomplishing this. Moreover, the subject has not been thoroughly investigated in early-stage schizophrenia, the researchers note.
Therefore, they decided to conduct the EULAST study to compare LAI and oral formulations in terms of all-cause discontinuation.
The trial was conducted at 50 general hospitals and psychiatric specialty clinics located in 15 European countries and Israel and included 511 participants in the intention-to-treat sample (67% men; mean age, 30.5 years).
All were randomly assigned 1:1:1 to receive either LAI paliperidone, LAI aripiprazole, or their respective oral formulations.
The combined OA treatment group consisted of 247 patients; the combined LAI group consisted of 264 patients.
Randomization was stratified by country and illness duration (5 months to 3 years vs. 4-7 years). Participants were followed up to 19 months, with all-cause discontinuation during that time serving as the primary endpoint.
All-cause discontinuation was defined as the allocated treatment was stopped or used at doses outside the allowed range, medication was switched or augmented with another antipsychotic after visit four, the patient missed a monthly visit and did not show up after being reminded, the patient withdrew consent for the study, or the clinician withdrew the patient from the study.
After the baseline visit, patients already taking antipsychotics were also randomly assigned. The next 4 weeks were then used to cross-taper between the prestudy antipsychotic and the agent they would be treated with during the study.
LAIs not superior
Results showed the LAI group did not have lower rates of hospitalization.
In addition, the discontinuation rates between the two combined groups were very similar at 71% for the oral antipsychotics group versus 64% in the LAIs group (hazard ratio, 1.6; 95% confidence interval, 0.94-1.43; P = .18).
Moreover, “no significant difference was found in the time to all-cause discontinuation between the combined oral and combined LAI treatment groups (P = .17),” the researchers report.
Reasons for discontinuation also did not differ significantly between the groups: 12% of patients in the OA group discontinued treatment because of efficacy vs. 17% of patients in the combined LAI group. The difference was not significant and the time to discontinuation also did not differ.
The main reason for discontinuation in both groups was safety concerns, affecting 10% and 13% of the combined OA and LAI groups, respectively, which was not a significant between-group difference.
Illness duration had a significant effect on time to all-cause discontinuation, with patients who had longer illness duration showing a poorer response, compared with those who had shorter duration (HR, 1.26; 95% CI, 1.01-1.56; P = .038).
However, stratifying participants by illness duration showed no significant difference between the subgroups (P = .25 and .34, respectively).
There was a significant between-group difference in discontinuation due to “other reasons,” with 49% vs. 34% of patients in the OA and LAI groups, respectively, discontinuing (HR, 1.51; 95% CI, 1.15-1.98; P = .0034). Moreover, the LAI group showed significantly longer continued use of medication vs the OA group (P = .0029).
“After separating the reasons for discontinuation into no efficacy, safety reasons, and other reasons, we only found a significant difference in favor of LAI for the ‘other reasons’ category; although the number of patients discontinuing medication for this reason over the follow-up period did not differ, patients on LAI continued treatment for a longer time,” the investigators write.
They acknowledge that this finding is “difficult to interpret, given the wide variety of reasons for discontinuation captured in this category,” which prevented an “informative subgroup analysis.”
Nevertheless, since there is “no consistent evidence supporting the use of LAI over oral antipsychotics” in patients with early-phase schizophrenia, their use should be “carefully considered on an individual risk-benefit basis,” they conclude.
No ‘real-world’ implications?
John M. Kane, MD, codirector and professor, Institute of Behavioral Science, Feinstein Institutes for Medical Research, Manhasset, N.Y., said that overall, this was a “large, potentially valuable study.” However, he raised several concerns.
“I think the investigators made a much too emphatic statement about the lack of value of LAIs in early-phase patients when discontinuation is the primary outcome,” he said, noting that other studies have come to the opposite conclusion.
Dr. Kane, who is also a professor of psychiatry at Hofstra/Northwell, New York, was not involved with the current research.
“RCTs [randomized controlled trials] in general are not necessarily the best way to evaluate the impact of LAIs [which] usually represent a small percentage of potentially eligible patients and are likely to include patients who are more adherent than those who would not agree to participate in an RCT,” he said. He added that the investigators “did not report on how many patients were screened and refused to be considered.”
Also, Dr. Kane noted that half of the participants were recruited from inpatient services, and so may have been “more unstable” at baseline. “Patients with residual positive symptoms are more likely to relapse on LAIs than patients who are in remission. This could potentially reduce the advantage of the LAI,” he said.
In addition, he took issue with the definition of all-cause discontinuation, which included the need for augmentation with another antipsychotic or use outside the normal range.
“This happens often in clinical practice. If someone’s symptoms aren’t sufficiently controlled by an LAI alone, for example, they often receive more of that antipsychotic or another drug. This perhaps makes the EULAST study somewhat less ‘real-world’,” Dr. Kane said.
More information needed
In an accompanying editorial, Martina Hahn, PharmD, PhD, department of psychiatry, psychosomatics, and psychotherapy, University Hospital-Goethe University, Frankfurt, Germany, and Sibylle Christine Roll, MD, PHD, department of mental health, Varisano Hospital in Frankfurt, note that comedications were neither documented nor analyzed by the researchers.
“Drug-drug interactions could be responsible for relapse or poor tolerability,” they write.
Moreover, pharmacogenetic information was not available nor were serum concentrations that could have been used for dose optimization after switching antipsychotic formulations, they note.
This information would have provided “a deeper understanding of why some patients do not respond or show side effects,” the editorialists write. “The use of therapeutic drug monitoring, drug interaction checks, and pharmacogenetic testing could improve treatment outcomes in both study settings and clinical practice.”
Financial support and study medication was provided by Lundbeck and Otsuka. Dr. Winter-van Rossum reports no relevant financial relationships. Disclosures for the other investigators are fully listed in the original paper. Dr. Kane is or has been a consultant to or received honoraria for lectures from Alkermes , Biogen, Boehringer Ingelheim, Cerevel, Dainippon Sumitomo, H. Lundbeck, HLS, Intracellular Therapies, Janssen, Karuna, Merck, Newron, Otsuka, Roche, Saladax, Sunovion, and TEVA. He is also a shareholder in The Vanguard Research Group, LB Pharma, Health Rhythms, North Shore Therapeutics, and Medincell. Dr. Hahn reports having received honoraria for lecture from Otsuka and advisory board participation for Rovi. Dr. Roll reports advisory board participation for Recordati, Otsuka, and Janssen.
A version of this article first appeared on Medscape.com.
In a multicountry, randomized, open-label study of more than 500 adults with schizophrenia, participants received either LAI paliperidone, LAI aripiprazole, or the respective oral formulation of these antipsychotics.
Results showed no significant difference between the combined oral and combined LAI treatment groups in time to all-cause discontinuation.
“We found no substantial advantage for LAI antipsychotic treatment over oral treatment, regarding time to discontinuation in patients with early-phase schizophrenia,” write investigators, led by Inge Winter-van Rossum, PhD, assistant visiting professor at Mount Sinai, New York, and affiliated with King’s College London and UMC Utrecht (the Netherlands).
This indicates that “there is no reason to prescribe LAIs instead of oral antipsychotics if the goal is to prevent discontinuation of antipsychotic medication in daily clinical practice,” they add.
The findings were published online in The Lancet Psychiatry.
Previous conflicting results
Maintenance treatment with antipsychotic medication reduces risk for relapse considerably, with treatment discontinuation being “by far the most important reason for relapse,” the investigators write.
LAIs “seem theoretically to be a way to enhance medication continuation and thereby reduce the risk for relapse,” they add. This is because LAIs enable a rapid response to nonadherence and remove the need for patients to remember to take their medications on a daily basis.
However, previous research has “provided conflicting results,” regarding the effectiveness of LAIs in accomplishing this. Moreover, the subject has not been thoroughly investigated in early-stage schizophrenia, the researchers note.
Therefore, they decided to conduct the EULAST study to compare LAI and oral formulations in terms of all-cause discontinuation.
The trial was conducted at 50 general hospitals and psychiatric specialty clinics located in 15 European countries and Israel and included 511 participants in the intention-to-treat sample (67% men; mean age, 30.5 years).
All were randomly assigned 1:1:1 to receive either LAI paliperidone, LAI aripiprazole, or their respective oral formulations.
The combined OA treatment group consisted of 247 patients; the combined LAI group consisted of 264 patients.
Randomization was stratified by country and illness duration (5 months to 3 years vs. 4-7 years). Participants were followed up to 19 months, with all-cause discontinuation during that time serving as the primary endpoint.
All-cause discontinuation was defined as the allocated treatment was stopped or used at doses outside the allowed range, medication was switched or augmented with another antipsychotic after visit four, the patient missed a monthly visit and did not show up after being reminded, the patient withdrew consent for the study, or the clinician withdrew the patient from the study.
After the baseline visit, patients already taking antipsychotics were also randomly assigned. The next 4 weeks were then used to cross-taper between the prestudy antipsychotic and the agent they would be treated with during the study.
LAIs not superior
Results showed the LAI group did not have lower rates of hospitalization.
In addition, the discontinuation rates between the two combined groups were very similar at 71% for the oral antipsychotics group versus 64% in the LAIs group (hazard ratio, 1.6; 95% confidence interval, 0.94-1.43; P = .18).
Moreover, “no significant difference was found in the time to all-cause discontinuation between the combined oral and combined LAI treatment groups (P = .17),” the researchers report.
Reasons for discontinuation also did not differ significantly between the groups: 12% of patients in the OA group discontinued treatment because of efficacy vs. 17% of patients in the combined LAI group. The difference was not significant and the time to discontinuation also did not differ.
The main reason for discontinuation in both groups was safety concerns, affecting 10% and 13% of the combined OA and LAI groups, respectively, which was not a significant between-group difference.
Illness duration had a significant effect on time to all-cause discontinuation, with patients who had longer illness duration showing a poorer response, compared with those who had shorter duration (HR, 1.26; 95% CI, 1.01-1.56; P = .038).
However, stratifying participants by illness duration showed no significant difference between the subgroups (P = .25 and .34, respectively).
There was a significant between-group difference in discontinuation due to “other reasons,” with 49% vs. 34% of patients in the OA and LAI groups, respectively, discontinuing (HR, 1.51; 95% CI, 1.15-1.98; P = .0034). Moreover, the LAI group showed significantly longer continued use of medication vs the OA group (P = .0029).
“After separating the reasons for discontinuation into no efficacy, safety reasons, and other reasons, we only found a significant difference in favor of LAI for the ‘other reasons’ category; although the number of patients discontinuing medication for this reason over the follow-up period did not differ, patients on LAI continued treatment for a longer time,” the investigators write.
They acknowledge that this finding is “difficult to interpret, given the wide variety of reasons for discontinuation captured in this category,” which prevented an “informative subgroup analysis.”
Nevertheless, since there is “no consistent evidence supporting the use of LAI over oral antipsychotics” in patients with early-phase schizophrenia, their use should be “carefully considered on an individual risk-benefit basis,” they conclude.
No ‘real-world’ implications?
John M. Kane, MD, codirector and professor, Institute of Behavioral Science, Feinstein Institutes for Medical Research, Manhasset, N.Y., said that overall, this was a “large, potentially valuable study.” However, he raised several concerns.
“I think the investigators made a much too emphatic statement about the lack of value of LAIs in early-phase patients when discontinuation is the primary outcome,” he said, noting that other studies have come to the opposite conclusion.
Dr. Kane, who is also a professor of psychiatry at Hofstra/Northwell, New York, was not involved with the current research.
“RCTs [randomized controlled trials] in general are not necessarily the best way to evaluate the impact of LAIs [which] usually represent a small percentage of potentially eligible patients and are likely to include patients who are more adherent than those who would not agree to participate in an RCT,” he said. He added that the investigators “did not report on how many patients were screened and refused to be considered.”
Also, Dr. Kane noted that half of the participants were recruited from inpatient services, and so may have been “more unstable” at baseline. “Patients with residual positive symptoms are more likely to relapse on LAIs than patients who are in remission. This could potentially reduce the advantage of the LAI,” he said.
In addition, he took issue with the definition of all-cause discontinuation, which included the need for augmentation with another antipsychotic or use outside the normal range.
“This happens often in clinical practice. If someone’s symptoms aren’t sufficiently controlled by an LAI alone, for example, they often receive more of that antipsychotic or another drug. This perhaps makes the EULAST study somewhat less ‘real-world’,” Dr. Kane said.
More information needed
In an accompanying editorial, Martina Hahn, PharmD, PhD, department of psychiatry, psychosomatics, and psychotherapy, University Hospital-Goethe University, Frankfurt, Germany, and Sibylle Christine Roll, MD, PHD, department of mental health, Varisano Hospital in Frankfurt, note that comedications were neither documented nor analyzed by the researchers.
“Drug-drug interactions could be responsible for relapse or poor tolerability,” they write.
Moreover, pharmacogenetic information was not available nor were serum concentrations that could have been used for dose optimization after switching antipsychotic formulations, they note.
This information would have provided “a deeper understanding of why some patients do not respond or show side effects,” the editorialists write. “The use of therapeutic drug monitoring, drug interaction checks, and pharmacogenetic testing could improve treatment outcomes in both study settings and clinical practice.”
Financial support and study medication was provided by Lundbeck and Otsuka. Dr. Winter-van Rossum reports no relevant financial relationships. Disclosures for the other investigators are fully listed in the original paper. Dr. Kane is or has been a consultant to or received honoraria for lectures from Alkermes , Biogen, Boehringer Ingelheim, Cerevel, Dainippon Sumitomo, H. Lundbeck, HLS, Intracellular Therapies, Janssen, Karuna, Merck, Newron, Otsuka, Roche, Saladax, Sunovion, and TEVA. He is also a shareholder in The Vanguard Research Group, LB Pharma, Health Rhythms, North Shore Therapeutics, and Medincell. Dr. Hahn reports having received honoraria for lecture from Otsuka and advisory board participation for Rovi. Dr. Roll reports advisory board participation for Recordati, Otsuka, and Janssen.
A version of this article first appeared on Medscape.com.
In a multicountry, randomized, open-label study of more than 500 adults with schizophrenia, participants received either LAI paliperidone, LAI aripiprazole, or the respective oral formulation of these antipsychotics.
Results showed no significant difference between the combined oral and combined LAI treatment groups in time to all-cause discontinuation.
“We found no substantial advantage for LAI antipsychotic treatment over oral treatment, regarding time to discontinuation in patients with early-phase schizophrenia,” write investigators, led by Inge Winter-van Rossum, PhD, assistant visiting professor at Mount Sinai, New York, and affiliated with King’s College London and UMC Utrecht (the Netherlands).
This indicates that “there is no reason to prescribe LAIs instead of oral antipsychotics if the goal is to prevent discontinuation of antipsychotic medication in daily clinical practice,” they add.
The findings were published online in The Lancet Psychiatry.
Previous conflicting results
Maintenance treatment with antipsychotic medication reduces risk for relapse considerably, with treatment discontinuation being “by far the most important reason for relapse,” the investigators write.
LAIs “seem theoretically to be a way to enhance medication continuation and thereby reduce the risk for relapse,” they add. This is because LAIs enable a rapid response to nonadherence and remove the need for patients to remember to take their medications on a daily basis.
However, previous research has “provided conflicting results,” regarding the effectiveness of LAIs in accomplishing this. Moreover, the subject has not been thoroughly investigated in early-stage schizophrenia, the researchers note.
Therefore, they decided to conduct the EULAST study to compare LAI and oral formulations in terms of all-cause discontinuation.
The trial was conducted at 50 general hospitals and psychiatric specialty clinics located in 15 European countries and Israel and included 511 participants in the intention-to-treat sample (67% men; mean age, 30.5 years).
All were randomly assigned 1:1:1 to receive either LAI paliperidone, LAI aripiprazole, or their respective oral formulations.
The combined OA treatment group consisted of 247 patients; the combined LAI group consisted of 264 patients.
Randomization was stratified by country and illness duration (5 months to 3 years vs. 4-7 years). Participants were followed up to 19 months, with all-cause discontinuation during that time serving as the primary endpoint.
All-cause discontinuation was defined as the allocated treatment was stopped or used at doses outside the allowed range, medication was switched or augmented with another antipsychotic after visit four, the patient missed a monthly visit and did not show up after being reminded, the patient withdrew consent for the study, or the clinician withdrew the patient from the study.
After the baseline visit, patients already taking antipsychotics were also randomly assigned. The next 4 weeks were then used to cross-taper between the prestudy antipsychotic and the agent they would be treated with during the study.
LAIs not superior
Results showed the LAI group did not have lower rates of hospitalization.
In addition, the discontinuation rates between the two combined groups were very similar at 71% for the oral antipsychotics group versus 64% in the LAIs group (hazard ratio, 1.6; 95% confidence interval, 0.94-1.43; P = .18).
Moreover, “no significant difference was found in the time to all-cause discontinuation between the combined oral and combined LAI treatment groups (P = .17),” the researchers report.
Reasons for discontinuation also did not differ significantly between the groups: 12% of patients in the OA group discontinued treatment because of efficacy vs. 17% of patients in the combined LAI group. The difference was not significant and the time to discontinuation also did not differ.
The main reason for discontinuation in both groups was safety concerns, affecting 10% and 13% of the combined OA and LAI groups, respectively, which was not a significant between-group difference.
Illness duration had a significant effect on time to all-cause discontinuation, with patients who had longer illness duration showing a poorer response, compared with those who had shorter duration (HR, 1.26; 95% CI, 1.01-1.56; P = .038).
However, stratifying participants by illness duration showed no significant difference between the subgroups (P = .25 and .34, respectively).
There was a significant between-group difference in discontinuation due to “other reasons,” with 49% vs. 34% of patients in the OA and LAI groups, respectively, discontinuing (HR, 1.51; 95% CI, 1.15-1.98; P = .0034). Moreover, the LAI group showed significantly longer continued use of medication vs the OA group (P = .0029).
“After separating the reasons for discontinuation into no efficacy, safety reasons, and other reasons, we only found a significant difference in favor of LAI for the ‘other reasons’ category; although the number of patients discontinuing medication for this reason over the follow-up period did not differ, patients on LAI continued treatment for a longer time,” the investigators write.
They acknowledge that this finding is “difficult to interpret, given the wide variety of reasons for discontinuation captured in this category,” which prevented an “informative subgroup analysis.”
Nevertheless, since there is “no consistent evidence supporting the use of LAI over oral antipsychotics” in patients with early-phase schizophrenia, their use should be “carefully considered on an individual risk-benefit basis,” they conclude.
No ‘real-world’ implications?
John M. Kane, MD, codirector and professor, Institute of Behavioral Science, Feinstein Institutes for Medical Research, Manhasset, N.Y., said that overall, this was a “large, potentially valuable study.” However, he raised several concerns.
“I think the investigators made a much too emphatic statement about the lack of value of LAIs in early-phase patients when discontinuation is the primary outcome,” he said, noting that other studies have come to the opposite conclusion.
Dr. Kane, who is also a professor of psychiatry at Hofstra/Northwell, New York, was not involved with the current research.
“RCTs [randomized controlled trials] in general are not necessarily the best way to evaluate the impact of LAIs [which] usually represent a small percentage of potentially eligible patients and are likely to include patients who are more adherent than those who would not agree to participate in an RCT,” he said. He added that the investigators “did not report on how many patients were screened and refused to be considered.”
Also, Dr. Kane noted that half of the participants were recruited from inpatient services, and so may have been “more unstable” at baseline. “Patients with residual positive symptoms are more likely to relapse on LAIs than patients who are in remission. This could potentially reduce the advantage of the LAI,” he said.
In addition, he took issue with the definition of all-cause discontinuation, which included the need for augmentation with another antipsychotic or use outside the normal range.
“This happens often in clinical practice. If someone’s symptoms aren’t sufficiently controlled by an LAI alone, for example, they often receive more of that antipsychotic or another drug. This perhaps makes the EULAST study somewhat less ‘real-world’,” Dr. Kane said.
More information needed
In an accompanying editorial, Martina Hahn, PharmD, PhD, department of psychiatry, psychosomatics, and psychotherapy, University Hospital-Goethe University, Frankfurt, Germany, and Sibylle Christine Roll, MD, PHD, department of mental health, Varisano Hospital in Frankfurt, note that comedications were neither documented nor analyzed by the researchers.
“Drug-drug interactions could be responsible for relapse or poor tolerability,” they write.
Moreover, pharmacogenetic information was not available nor were serum concentrations that could have been used for dose optimization after switching antipsychotic formulations, they note.
This information would have provided “a deeper understanding of why some patients do not respond or show side effects,” the editorialists write. “The use of therapeutic drug monitoring, drug interaction checks, and pharmacogenetic testing could improve treatment outcomes in both study settings and clinical practice.”
Financial support and study medication was provided by Lundbeck and Otsuka. Dr. Winter-van Rossum reports no relevant financial relationships. Disclosures for the other investigators are fully listed in the original paper. Dr. Kane is or has been a consultant to or received honoraria for lectures from Alkermes , Biogen, Boehringer Ingelheim, Cerevel, Dainippon Sumitomo, H. Lundbeck, HLS, Intracellular Therapies, Janssen, Karuna, Merck, Newron, Otsuka, Roche, Saladax, Sunovion, and TEVA. He is also a shareholder in The Vanguard Research Group, LB Pharma, Health Rhythms, North Shore Therapeutics, and Medincell. Dr. Hahn reports having received honoraria for lecture from Otsuka and advisory board participation for Rovi. Dr. Roll reports advisory board participation for Recordati, Otsuka, and Janssen.
A version of this article first appeared on Medscape.com.
FROM THE LANCET PSYCHIATRY
‘Sighing’ tops mindfulness for reduced stress, improved mood
In a randomized controlled study, daily breathwork – especially cyclic breathing, which emphasizes shorter inhalations and prolonged exhalations – was associated with greater improvement in mood and a slower respiratory rate than mindfulness meditation.
“We were pleased that just 5 minutes a day of the breathing exercises positively affected mood and resulted in slower respiratory rate, indicating reduced arousal,” coinvestigator David Spiegel, MD, who directs the Center for Stress and Health at Stanford (Calif.) University, told this news organization.
The findings were published online in Cell Reports Medicine.
Intentional breath control
Controlled breathwork has emerged as a potential tool to manage stress and boost well-being.
In the new study, researchers compared three different daily 5-minute breathwork exercises to an equal amount of mindfulness meditation over 1 month in 108 healthy adults recruited mostly from an undergraduate psychology class at Stanford: 33 participants practiced cyclic hyperventilation, which emphasizes robust inhalation, short retention and rapid exhalation, 30 did exhale-focused cyclic sighing, 21 performed box breathing, which emphasizes equal duration of inhalation, breath retention, and exhalation, and 24 practiced mindfulness meditation (the control group).
The primary endpoints were improvement in mood and anxiety, as well as reduced physiologic arousal (respiratory rate, heart rate, and heart rate variability). Physiological data was collected using a wearable WHOOP strap.
All four groups showed significant daily improvement in mood, as well as reduction in anxiety and negative mood, but there were significant differences between mindfulness meditation and breathwork.
Using a mixed-effects model, the researchers showed that breathwork, especially the exhale-focused cyclic sighing, produced greater improvement in mood (P < .05) and reduction in respiratory rate (P < .05), compared with mindfulness meditation.
Specific patterns vs. passive attention
The finding supports the team’s hypothesis that intentional control over breath with specific breathing patterns produces more benefit to mood than passive attention to one’s breath, as in mindfulness meditation practice.
“It turned out that the cyclic sighing was indeed most soothing,” Dr. Spiegel noted.
“We expected that because of respiratory sinus arrhythmia. Exhaling is accomplished by increasing pressure in the chest, which increases venous return to the heart, triggering parasympathetic slowing of heart rate via the sinoatrial node,” he said.
Dr. Spiegel added that, conversely, inspiration reduces venous return, triggering sympathetic activity and increased heart rate.
“The magnitude of this heart rate variability is associated with better health, including recovery from myocardial infarction and even cancer survival. So self-soothing is a good thing, and we expected an advantage for cyclic sighing,” he said.
“If you’re looking to improve sleep and reduce daytime stress, recover from intense work, life, and/or training, then interventions that facilitate autonomic control (and indeed you can control it), brief (5 minutes) structured breathwork is among the more powerful (and zero cost) tools,” tweeted senior investigator Andrew Huberman, PhD, professor of neurobiology at Stanford.
Immediate application?
Sara Lazar, PhD, Massachusetts General Hospital and Harvard Medical School, Boston, said the findings are “interesting” but cautioned that this is “just one study with a pretty small sample size,” and it only enrolled healthy college students.
Dr. Lazar, who also runs the Lazar Lab for Meditation Research at Mass General, noted that she would want to see a future study “done with working-age adults and with clinical populations.”
“It should also be noted that mindfulness had a bigger effect on negative affect, which could have implications for conditions such as depression or trauma,” said Dr. Lazar, who was not involved with the current research.
Also weighing in, Steven R. Thorp, PhD, professor at California School of Professional Psychology, Alliant International University, San Diego, said in an interview the study is “really interesting and well done.”
“Although breathing exercises and breathing retraining are commonly found in psychosocial interventions, especially for anxiety disorders, there have been few empirical studies comparing different breathing protocols,” Dr. Thorp said.
In this study, the passive observation of breaths (mindfulness) and specific breathwork interventions “all worked to decrease state anxiety; but the breathwork, particularly the cyclic sighing protocol, produced a greater overall reduction in respiratory rate and increase in positive mood,” he noted.
“These techniques can be recommended by all clinicians because all clients have access to their breath at all times – and only 5 minutes of daily practice can yield the benefits. Moreover, as the authors note, the immediate benefits may encourage clients to engage with the breathwork and potentially other aspects of treatment,” Dr. Thorp said.
The study was funded by Victor and Winnie Koo and Tianren Culture and a Stanford School of Medicine Discovery Innovation Award. WHOOP donated the wrist straps used in the study, but was not involved in the study’s design or analysis. Dr. Huberman is an advisor to WHOOP. Dr. Lazar and Dr. Thorp have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a randomized controlled study, daily breathwork – especially cyclic breathing, which emphasizes shorter inhalations and prolonged exhalations – was associated with greater improvement in mood and a slower respiratory rate than mindfulness meditation.
“We were pleased that just 5 minutes a day of the breathing exercises positively affected mood and resulted in slower respiratory rate, indicating reduced arousal,” coinvestigator David Spiegel, MD, who directs the Center for Stress and Health at Stanford (Calif.) University, told this news organization.
The findings were published online in Cell Reports Medicine.
Intentional breath control
Controlled breathwork has emerged as a potential tool to manage stress and boost well-being.
In the new study, researchers compared three different daily 5-minute breathwork exercises to an equal amount of mindfulness meditation over 1 month in 108 healthy adults recruited mostly from an undergraduate psychology class at Stanford: 33 participants practiced cyclic hyperventilation, which emphasizes robust inhalation, short retention and rapid exhalation, 30 did exhale-focused cyclic sighing, 21 performed box breathing, which emphasizes equal duration of inhalation, breath retention, and exhalation, and 24 practiced mindfulness meditation (the control group).
The primary endpoints were improvement in mood and anxiety, as well as reduced physiologic arousal (respiratory rate, heart rate, and heart rate variability). Physiological data was collected using a wearable WHOOP strap.
All four groups showed significant daily improvement in mood, as well as reduction in anxiety and negative mood, but there were significant differences between mindfulness meditation and breathwork.
Using a mixed-effects model, the researchers showed that breathwork, especially the exhale-focused cyclic sighing, produced greater improvement in mood (P < .05) and reduction in respiratory rate (P < .05), compared with mindfulness meditation.
Specific patterns vs. passive attention
The finding supports the team’s hypothesis that intentional control over breath with specific breathing patterns produces more benefit to mood than passive attention to one’s breath, as in mindfulness meditation practice.
“It turned out that the cyclic sighing was indeed most soothing,” Dr. Spiegel noted.
“We expected that because of respiratory sinus arrhythmia. Exhaling is accomplished by increasing pressure in the chest, which increases venous return to the heart, triggering parasympathetic slowing of heart rate via the sinoatrial node,” he said.
Dr. Spiegel added that, conversely, inspiration reduces venous return, triggering sympathetic activity and increased heart rate.
“The magnitude of this heart rate variability is associated with better health, including recovery from myocardial infarction and even cancer survival. So self-soothing is a good thing, and we expected an advantage for cyclic sighing,” he said.
“If you’re looking to improve sleep and reduce daytime stress, recover from intense work, life, and/or training, then interventions that facilitate autonomic control (and indeed you can control it), brief (5 minutes) structured breathwork is among the more powerful (and zero cost) tools,” tweeted senior investigator Andrew Huberman, PhD, professor of neurobiology at Stanford.
Immediate application?
Sara Lazar, PhD, Massachusetts General Hospital and Harvard Medical School, Boston, said the findings are “interesting” but cautioned that this is “just one study with a pretty small sample size,” and it only enrolled healthy college students.
Dr. Lazar, who also runs the Lazar Lab for Meditation Research at Mass General, noted that she would want to see a future study “done with working-age adults and with clinical populations.”
“It should also be noted that mindfulness had a bigger effect on negative affect, which could have implications for conditions such as depression or trauma,” said Dr. Lazar, who was not involved with the current research.
Also weighing in, Steven R. Thorp, PhD, professor at California School of Professional Psychology, Alliant International University, San Diego, said in an interview the study is “really interesting and well done.”
“Although breathing exercises and breathing retraining are commonly found in psychosocial interventions, especially for anxiety disorders, there have been few empirical studies comparing different breathing protocols,” Dr. Thorp said.
In this study, the passive observation of breaths (mindfulness) and specific breathwork interventions “all worked to decrease state anxiety; but the breathwork, particularly the cyclic sighing protocol, produced a greater overall reduction in respiratory rate and increase in positive mood,” he noted.
“These techniques can be recommended by all clinicians because all clients have access to their breath at all times – and only 5 minutes of daily practice can yield the benefits. Moreover, as the authors note, the immediate benefits may encourage clients to engage with the breathwork and potentially other aspects of treatment,” Dr. Thorp said.
The study was funded by Victor and Winnie Koo and Tianren Culture and a Stanford School of Medicine Discovery Innovation Award. WHOOP donated the wrist straps used in the study, but was not involved in the study’s design or analysis. Dr. Huberman is an advisor to WHOOP. Dr. Lazar and Dr. Thorp have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a randomized controlled study, daily breathwork – especially cyclic breathing, which emphasizes shorter inhalations and prolonged exhalations – was associated with greater improvement in mood and a slower respiratory rate than mindfulness meditation.
“We were pleased that just 5 minutes a day of the breathing exercises positively affected mood and resulted in slower respiratory rate, indicating reduced arousal,” coinvestigator David Spiegel, MD, who directs the Center for Stress and Health at Stanford (Calif.) University, told this news organization.
The findings were published online in Cell Reports Medicine.
Intentional breath control
Controlled breathwork has emerged as a potential tool to manage stress and boost well-being.
In the new study, researchers compared three different daily 5-minute breathwork exercises to an equal amount of mindfulness meditation over 1 month in 108 healthy adults recruited mostly from an undergraduate psychology class at Stanford: 33 participants practiced cyclic hyperventilation, which emphasizes robust inhalation, short retention and rapid exhalation, 30 did exhale-focused cyclic sighing, 21 performed box breathing, which emphasizes equal duration of inhalation, breath retention, and exhalation, and 24 practiced mindfulness meditation (the control group).
The primary endpoints were improvement in mood and anxiety, as well as reduced physiologic arousal (respiratory rate, heart rate, and heart rate variability). Physiological data was collected using a wearable WHOOP strap.
All four groups showed significant daily improvement in mood, as well as reduction in anxiety and negative mood, but there were significant differences between mindfulness meditation and breathwork.
Using a mixed-effects model, the researchers showed that breathwork, especially the exhale-focused cyclic sighing, produced greater improvement in mood (P < .05) and reduction in respiratory rate (P < .05), compared with mindfulness meditation.
Specific patterns vs. passive attention
The finding supports the team’s hypothesis that intentional control over breath with specific breathing patterns produces more benefit to mood than passive attention to one’s breath, as in mindfulness meditation practice.
“It turned out that the cyclic sighing was indeed most soothing,” Dr. Spiegel noted.
“We expected that because of respiratory sinus arrhythmia. Exhaling is accomplished by increasing pressure in the chest, which increases venous return to the heart, triggering parasympathetic slowing of heart rate via the sinoatrial node,” he said.
Dr. Spiegel added that, conversely, inspiration reduces venous return, triggering sympathetic activity and increased heart rate.
“The magnitude of this heart rate variability is associated with better health, including recovery from myocardial infarction and even cancer survival. So self-soothing is a good thing, and we expected an advantage for cyclic sighing,” he said.
“If you’re looking to improve sleep and reduce daytime stress, recover from intense work, life, and/or training, then interventions that facilitate autonomic control (and indeed you can control it), brief (5 minutes) structured breathwork is among the more powerful (and zero cost) tools,” tweeted senior investigator Andrew Huberman, PhD, professor of neurobiology at Stanford.
Immediate application?
Sara Lazar, PhD, Massachusetts General Hospital and Harvard Medical School, Boston, said the findings are “interesting” but cautioned that this is “just one study with a pretty small sample size,” and it only enrolled healthy college students.
Dr. Lazar, who also runs the Lazar Lab for Meditation Research at Mass General, noted that she would want to see a future study “done with working-age adults and with clinical populations.”
“It should also be noted that mindfulness had a bigger effect on negative affect, which could have implications for conditions such as depression or trauma,” said Dr. Lazar, who was not involved with the current research.
Also weighing in, Steven R. Thorp, PhD, professor at California School of Professional Psychology, Alliant International University, San Diego, said in an interview the study is “really interesting and well done.”
“Although breathing exercises and breathing retraining are commonly found in psychosocial interventions, especially for anxiety disorders, there have been few empirical studies comparing different breathing protocols,” Dr. Thorp said.
In this study, the passive observation of breaths (mindfulness) and specific breathwork interventions “all worked to decrease state anxiety; but the breathwork, particularly the cyclic sighing protocol, produced a greater overall reduction in respiratory rate and increase in positive mood,” he noted.
“These techniques can be recommended by all clinicians because all clients have access to their breath at all times – and only 5 minutes of daily practice can yield the benefits. Moreover, as the authors note, the immediate benefits may encourage clients to engage with the breathwork and potentially other aspects of treatment,” Dr. Thorp said.
The study was funded by Victor and Winnie Koo and Tianren Culture and a Stanford School of Medicine Discovery Innovation Award. WHOOP donated the wrist straps used in the study, but was not involved in the study’s design or analysis. Dr. Huberman is an advisor to WHOOP. Dr. Lazar and Dr. Thorp have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CELL REPORTS MEDICINE
Medicare ‘offers’ cancer patient a choice: Less life or more debt
We’re gonna need a bigger meth lab
In case you’ve been living under a rock for the past 15 years, the TV show “Breaking Bad” details the spiraling rise and downfall of a high school chemistry teacher who, after developing a case of terminal lung cancer, starts producing methamphetamine to provide for his family in response to the steep cost of treatment for his cancer.
Meanwhile, here in 2023 in the real world, we have Paul Davis, a retired physician in Ohio, who’s being forced to choose between an expensive cancer treatment and bankrupting his family, since Medicare’s decided it doesn’t want to cover the cost. Hey, we’ve seen this one before!
A bit of backstory: In November 2019, Dr. Davis was diagnosed with uveal melanoma, a very rare type of cancer that affects eye tissue. The news got worse in 2022 when the cancer spread to his liver, a move which typically proves fatal within a year. However, in a stroke of great news, the Food and Drug Administration approved the drug Kimmtrak earlier that year, which could be used to treat his cancer. Not cure, of course, but it would give him more time.
His initial treatments with the drug went fine and were covered, but when he transferred his care from a hospital in Columbus to one closer to home, big problem. Medicare decided it didn’t like that hospital and abruptly cut off coverage, denying the local hospital’s claims. That leaves Dr. Davis on the hook for his cancer treatment, and it’s what you might call expensive. Expensive to the tune of $50,000.
A week.
Apparently the coding the local hospital submitted was wrong, indicating that Dr. Davis was receiving Kimmtrak for a type of cancer that the FDA hadn’t approved the drug for. So until the government bureaucracy works itself out, his treatment is on hold, leaving all his faith in Medicare working quickly to rectify its mistake. If it can rectify its mistake. We’re not hopeful.
And in case you were wondering, if Dr. Davis wanted to go full Walter White, the average street price of meth is about $20-$60 per gram, so to pay for his treatment, he’d need to make at least a kilogram of meth every week. That’s, uh, quite a lot of illegal drug, or what we here at the LOTME office would call a fun Saturday night.
When you give a mouse a movie
Researchers have been successfully testing Alzheimer drugs on mice for years, but none of the drugs has proved successful in humans. Recent work, however, might have found the missing link, and it’s a combination no one ever thought of before: mice and movies.
Turns out that Orson Welles’ 1958 film noir classic “Touch of Evil” tapped a part of the mouse brain that has been overlooked: the hippocampus, which is crucial for learning and memory. Previous researchers thought it was just used as a kind of GPS system, but that’s only partially true.
Not only did the mice choose to pay attention to the movie clip, but the hippocampus responded to the visual stimuli only when the rodents saw the scenes from the clip later in the order that they were presented and not in a scrambled order. These findings represent a “major paradigm shift” in studying mouse recall, Mayank Mehta, PhD, of the University of California, Los Angeles, said in a statement from the school.
This breakthrough could run parallel to Alzheimer’s patients struggling with similar defects. “Selective and episodic activation of the mouse hippocampus using a human movie opens up the possibility of directly testing human episodic memory disorders and therapies using mouse neurons, a major step forward,” said coauthor Chinmay Purandare, PhD, who is now at the University of California, San Francisco.
Who would have thought that a classic film would help advance Alzheimer research?
A less human way to study mosquitoes
We here at LOTME have a history with mosquitoes. We know they don’t like us, and they know that we don’t like them. Trust us, they know. So when humans gain a little ground in the war against the buzzy little bloodsuckers, we want to share the joy.
To know the enemy, scientists have to study the enemy, but there is a problem. “Many mosquito experiments still rely on human volunteers and animal subjects,” bioengineering graduate student Kevin Janson, said in a statement from Rice University. Most people don’t like being bitten by mosquitoes, so that kind of testing can be expensive.
Is there a way to automate the collection and processing of mosquito behavior data using inexpensive cameras and machine-learning software? We’re glad you asked, because Mr. Janson and the research team, which includes bioengineers from Rice and tropical medicine experts from Tulane University, have managed to eliminate the need for live volunteers by using patches of synthetic skin made with a 3D printer.
“Each patch of gelatin-like hydrogel comes complete with tiny passageways that can be filled with flowing blood” from a chicken, sheep, or cow, they explained, and proof-of-concept testing showed that mosquitoes would feed on hydrogels without any repellent and stay away from those treated with a repellent.
To conduct the feeding tests, the blood-infused hydrogels are placed in a clear plastic box that is surrounded by cameras.
A bunch of mosquitoes are then tossed in the box and the cameras record all their insect activities: how often they land at each location, how long they stay, whether or not they bite, how long they feed, etc. Humans don’t have to watch and don’t have to be food sources.
Humans don’t have to be food sources, and we just pictured the future of mosquito control. Imagine a dozen Arnold Schwarzenegger–style Terminators, covered in 3D-printed skin, walking through your neighborhood in the summer while wearing sweat-soaked, brightly colored clothing. The mosquitoes wouldn’t be able to stay away, but guess what? They’re feeding off robots with nonhuman skin and nonhuman blood, so we win. It’s good to have a cerebral cortex.
Getting medieval on brain surgery
Let’s get one thing clear: The so-called “Dark Ages” were not nearly as dark as they’re made out to be. For one thing, there’s a world beyond Western Europe. The Roman Empire didn’t collapse everywhere. But even in Western Europe, the centuries between the fall of Rome and the Renaissance were hardly lacking in cultural development.
That said, we wouldn’t want to be in the position of the seventh-century noblewoman whose remains were recently uncovered in a Byzantine fortress in central Italy with multiple cross-shaped incisions in her skull. Yes, this unfortunate woman underwent at least two brain surgeries.
Then again, maybe not. Nothing like it had been discovered at the site, and while the markings – signs of a procedure called trepanation – can be surgical in nature, there are other explanations. For example, the Avar people practiced ritual trepanation during the same time period, but they were hundreds of miles away in the Carpathian mountains, and there was no evidence to support that a different form of ritualistic trepanation ever took place in Byzantine-era Italy.
The investigators then moved on to a form of judicial punishment called decalvatio, which involves mutilation by scalping. Look, the Dark Ages weren’t dark, but no one said they were fun. Anyway, this was discarded, since decalvatio was only meted out to soldiers who deserted the battlefield.
That brings us back to surgery. While one of the trepanations was fully engraved into her skull, indicating that the woman died soon after the surgery, she also bore indications of a healed trepanation. A 50% success rate isn’t terrible for our medieval surgeon. Sure, the Incas managed 80%, but even during the Civil War brain surgery only had a 50% success rate. And that’s the end of the story, nothing more to say about our medieval Italian woman.
Nope. Nothing at all.
Fine. While a surgical procedure was deemed most likely, the study investigators found no direct evidence of a medical condition. No trauma, no tumor, nothing. Just a couple of suggestions of “a systemic pathological condition,” they said. Okay, we swear, it really wasn’t that bad in the Middle [Editor’s note: Approximately 5,000 more words on medieval culture not included. This is a medical column, thank you very much.]
We’re gonna need a bigger meth lab
In case you’ve been living under a rock for the past 15 years, the TV show “Breaking Bad” details the spiraling rise and downfall of a high school chemistry teacher who, after developing a case of terminal lung cancer, starts producing methamphetamine to provide for his family in response to the steep cost of treatment for his cancer.
Meanwhile, here in 2023 in the real world, we have Paul Davis, a retired physician in Ohio, who’s being forced to choose between an expensive cancer treatment and bankrupting his family, since Medicare’s decided it doesn’t want to cover the cost. Hey, we’ve seen this one before!
A bit of backstory: In November 2019, Dr. Davis was diagnosed with uveal melanoma, a very rare type of cancer that affects eye tissue. The news got worse in 2022 when the cancer spread to his liver, a move which typically proves fatal within a year. However, in a stroke of great news, the Food and Drug Administration approved the drug Kimmtrak earlier that year, which could be used to treat his cancer. Not cure, of course, but it would give him more time.
His initial treatments with the drug went fine and were covered, but when he transferred his care from a hospital in Columbus to one closer to home, big problem. Medicare decided it didn’t like that hospital and abruptly cut off coverage, denying the local hospital’s claims. That leaves Dr. Davis on the hook for his cancer treatment, and it’s what you might call expensive. Expensive to the tune of $50,000.
A week.
Apparently the coding the local hospital submitted was wrong, indicating that Dr. Davis was receiving Kimmtrak for a type of cancer that the FDA hadn’t approved the drug for. So until the government bureaucracy works itself out, his treatment is on hold, leaving all his faith in Medicare working quickly to rectify its mistake. If it can rectify its mistake. We’re not hopeful.
And in case you were wondering, if Dr. Davis wanted to go full Walter White, the average street price of meth is about $20-$60 per gram, so to pay for his treatment, he’d need to make at least a kilogram of meth every week. That’s, uh, quite a lot of illegal drug, or what we here at the LOTME office would call a fun Saturday night.
When you give a mouse a movie
Researchers have been successfully testing Alzheimer drugs on mice for years, but none of the drugs has proved successful in humans. Recent work, however, might have found the missing link, and it’s a combination no one ever thought of before: mice and movies.
Turns out that Orson Welles’ 1958 film noir classic “Touch of Evil” tapped a part of the mouse brain that has been overlooked: the hippocampus, which is crucial for learning and memory. Previous researchers thought it was just used as a kind of GPS system, but that’s only partially true.
Not only did the mice choose to pay attention to the movie clip, but the hippocampus responded to the visual stimuli only when the rodents saw the scenes from the clip later in the order that they were presented and not in a scrambled order. These findings represent a “major paradigm shift” in studying mouse recall, Mayank Mehta, PhD, of the University of California, Los Angeles, said in a statement from the school.
This breakthrough could run parallel to Alzheimer’s patients struggling with similar defects. “Selective and episodic activation of the mouse hippocampus using a human movie opens up the possibility of directly testing human episodic memory disorders and therapies using mouse neurons, a major step forward,” said coauthor Chinmay Purandare, PhD, who is now at the University of California, San Francisco.
Who would have thought that a classic film would help advance Alzheimer research?
A less human way to study mosquitoes
We here at LOTME have a history with mosquitoes. We know they don’t like us, and they know that we don’t like them. Trust us, they know. So when humans gain a little ground in the war against the buzzy little bloodsuckers, we want to share the joy.
To know the enemy, scientists have to study the enemy, but there is a problem. “Many mosquito experiments still rely on human volunteers and animal subjects,” bioengineering graduate student Kevin Janson, said in a statement from Rice University. Most people don’t like being bitten by mosquitoes, so that kind of testing can be expensive.
Is there a way to automate the collection and processing of mosquito behavior data using inexpensive cameras and machine-learning software? We’re glad you asked, because Mr. Janson and the research team, which includes bioengineers from Rice and tropical medicine experts from Tulane University, have managed to eliminate the need for live volunteers by using patches of synthetic skin made with a 3D printer.
“Each patch of gelatin-like hydrogel comes complete with tiny passageways that can be filled with flowing blood” from a chicken, sheep, or cow, they explained, and proof-of-concept testing showed that mosquitoes would feed on hydrogels without any repellent and stay away from those treated with a repellent.
To conduct the feeding tests, the blood-infused hydrogels are placed in a clear plastic box that is surrounded by cameras.
A bunch of mosquitoes are then tossed in the box and the cameras record all their insect activities: how often they land at each location, how long they stay, whether or not they bite, how long they feed, etc. Humans don’t have to watch and don’t have to be food sources.
Humans don’t have to be food sources, and we just pictured the future of mosquito control. Imagine a dozen Arnold Schwarzenegger–style Terminators, covered in 3D-printed skin, walking through your neighborhood in the summer while wearing sweat-soaked, brightly colored clothing. The mosquitoes wouldn’t be able to stay away, but guess what? They’re feeding off robots with nonhuman skin and nonhuman blood, so we win. It’s good to have a cerebral cortex.
Getting medieval on brain surgery
Let’s get one thing clear: The so-called “Dark Ages” were not nearly as dark as they’re made out to be. For one thing, there’s a world beyond Western Europe. The Roman Empire didn’t collapse everywhere. But even in Western Europe, the centuries between the fall of Rome and the Renaissance were hardly lacking in cultural development.
That said, we wouldn’t want to be in the position of the seventh-century noblewoman whose remains were recently uncovered in a Byzantine fortress in central Italy with multiple cross-shaped incisions in her skull. Yes, this unfortunate woman underwent at least two brain surgeries.
Then again, maybe not. Nothing like it had been discovered at the site, and while the markings – signs of a procedure called trepanation – can be surgical in nature, there are other explanations. For example, the Avar people practiced ritual trepanation during the same time period, but they were hundreds of miles away in the Carpathian mountains, and there was no evidence to support that a different form of ritualistic trepanation ever took place in Byzantine-era Italy.
The investigators then moved on to a form of judicial punishment called decalvatio, which involves mutilation by scalping. Look, the Dark Ages weren’t dark, but no one said they were fun. Anyway, this was discarded, since decalvatio was only meted out to soldiers who deserted the battlefield.
That brings us back to surgery. While one of the trepanations was fully engraved into her skull, indicating that the woman died soon after the surgery, she also bore indications of a healed trepanation. A 50% success rate isn’t terrible for our medieval surgeon. Sure, the Incas managed 80%, but even during the Civil War brain surgery only had a 50% success rate. And that’s the end of the story, nothing more to say about our medieval Italian woman.
Nope. Nothing at all.
Fine. While a surgical procedure was deemed most likely, the study investigators found no direct evidence of a medical condition. No trauma, no tumor, nothing. Just a couple of suggestions of “a systemic pathological condition,” they said. Okay, we swear, it really wasn’t that bad in the Middle [Editor’s note: Approximately 5,000 more words on medieval culture not included. This is a medical column, thank you very much.]
We’re gonna need a bigger meth lab
In case you’ve been living under a rock for the past 15 years, the TV show “Breaking Bad” details the spiraling rise and downfall of a high school chemistry teacher who, after developing a case of terminal lung cancer, starts producing methamphetamine to provide for his family in response to the steep cost of treatment for his cancer.
Meanwhile, here in 2023 in the real world, we have Paul Davis, a retired physician in Ohio, who’s being forced to choose between an expensive cancer treatment and bankrupting his family, since Medicare’s decided it doesn’t want to cover the cost. Hey, we’ve seen this one before!
A bit of backstory: In November 2019, Dr. Davis was diagnosed with uveal melanoma, a very rare type of cancer that affects eye tissue. The news got worse in 2022 when the cancer spread to his liver, a move which typically proves fatal within a year. However, in a stroke of great news, the Food and Drug Administration approved the drug Kimmtrak earlier that year, which could be used to treat his cancer. Not cure, of course, but it would give him more time.
His initial treatments with the drug went fine and were covered, but when he transferred his care from a hospital in Columbus to one closer to home, big problem. Medicare decided it didn’t like that hospital and abruptly cut off coverage, denying the local hospital’s claims. That leaves Dr. Davis on the hook for his cancer treatment, and it’s what you might call expensive. Expensive to the tune of $50,000.
A week.
Apparently the coding the local hospital submitted was wrong, indicating that Dr. Davis was receiving Kimmtrak for a type of cancer that the FDA hadn’t approved the drug for. So until the government bureaucracy works itself out, his treatment is on hold, leaving all his faith in Medicare working quickly to rectify its mistake. If it can rectify its mistake. We’re not hopeful.
And in case you were wondering, if Dr. Davis wanted to go full Walter White, the average street price of meth is about $20-$60 per gram, so to pay for his treatment, he’d need to make at least a kilogram of meth every week. That’s, uh, quite a lot of illegal drug, or what we here at the LOTME office would call a fun Saturday night.
When you give a mouse a movie
Researchers have been successfully testing Alzheimer drugs on mice for years, but none of the drugs has proved successful in humans. Recent work, however, might have found the missing link, and it’s a combination no one ever thought of before: mice and movies.
Turns out that Orson Welles’ 1958 film noir classic “Touch of Evil” tapped a part of the mouse brain that has been overlooked: the hippocampus, which is crucial for learning and memory. Previous researchers thought it was just used as a kind of GPS system, but that’s only partially true.
Not only did the mice choose to pay attention to the movie clip, but the hippocampus responded to the visual stimuli only when the rodents saw the scenes from the clip later in the order that they were presented and not in a scrambled order. These findings represent a “major paradigm shift” in studying mouse recall, Mayank Mehta, PhD, of the University of California, Los Angeles, said in a statement from the school.
This breakthrough could run parallel to Alzheimer’s patients struggling with similar defects. “Selective and episodic activation of the mouse hippocampus using a human movie opens up the possibility of directly testing human episodic memory disorders and therapies using mouse neurons, a major step forward,” said coauthor Chinmay Purandare, PhD, who is now at the University of California, San Francisco.
Who would have thought that a classic film would help advance Alzheimer research?
A less human way to study mosquitoes
We here at LOTME have a history with mosquitoes. We know they don’t like us, and they know that we don’t like them. Trust us, they know. So when humans gain a little ground in the war against the buzzy little bloodsuckers, we want to share the joy.
To know the enemy, scientists have to study the enemy, but there is a problem. “Many mosquito experiments still rely on human volunteers and animal subjects,” bioengineering graduate student Kevin Janson, said in a statement from Rice University. Most people don’t like being bitten by mosquitoes, so that kind of testing can be expensive.
Is there a way to automate the collection and processing of mosquito behavior data using inexpensive cameras and machine-learning software? We’re glad you asked, because Mr. Janson and the research team, which includes bioengineers from Rice and tropical medicine experts from Tulane University, have managed to eliminate the need for live volunteers by using patches of synthetic skin made with a 3D printer.
“Each patch of gelatin-like hydrogel comes complete with tiny passageways that can be filled with flowing blood” from a chicken, sheep, or cow, they explained, and proof-of-concept testing showed that mosquitoes would feed on hydrogels without any repellent and stay away from those treated with a repellent.
To conduct the feeding tests, the blood-infused hydrogels are placed in a clear plastic box that is surrounded by cameras.
A bunch of mosquitoes are then tossed in the box and the cameras record all their insect activities: how often they land at each location, how long they stay, whether or not they bite, how long they feed, etc. Humans don’t have to watch and don’t have to be food sources.
Humans don’t have to be food sources, and we just pictured the future of mosquito control. Imagine a dozen Arnold Schwarzenegger–style Terminators, covered in 3D-printed skin, walking through your neighborhood in the summer while wearing sweat-soaked, brightly colored clothing. The mosquitoes wouldn’t be able to stay away, but guess what? They’re feeding off robots with nonhuman skin and nonhuman blood, so we win. It’s good to have a cerebral cortex.
Getting medieval on brain surgery
Let’s get one thing clear: The so-called “Dark Ages” were not nearly as dark as they’re made out to be. For one thing, there’s a world beyond Western Europe. The Roman Empire didn’t collapse everywhere. But even in Western Europe, the centuries between the fall of Rome and the Renaissance were hardly lacking in cultural development.
That said, we wouldn’t want to be in the position of the seventh-century noblewoman whose remains were recently uncovered in a Byzantine fortress in central Italy with multiple cross-shaped incisions in her skull. Yes, this unfortunate woman underwent at least two brain surgeries.
Then again, maybe not. Nothing like it had been discovered at the site, and while the markings – signs of a procedure called trepanation – can be surgical in nature, there are other explanations. For example, the Avar people practiced ritual trepanation during the same time period, but they were hundreds of miles away in the Carpathian mountains, and there was no evidence to support that a different form of ritualistic trepanation ever took place in Byzantine-era Italy.
The investigators then moved on to a form of judicial punishment called decalvatio, which involves mutilation by scalping. Look, the Dark Ages weren’t dark, but no one said they were fun. Anyway, this was discarded, since decalvatio was only meted out to soldiers who deserted the battlefield.
That brings us back to surgery. While one of the trepanations was fully engraved into her skull, indicating that the woman died soon after the surgery, she also bore indications of a healed trepanation. A 50% success rate isn’t terrible for our medieval surgeon. Sure, the Incas managed 80%, but even during the Civil War brain surgery only had a 50% success rate. And that’s the end of the story, nothing more to say about our medieval Italian woman.
Nope. Nothing at all.
Fine. While a surgical procedure was deemed most likely, the study investigators found no direct evidence of a medical condition. No trauma, no tumor, nothing. Just a couple of suggestions of “a systemic pathological condition,” they said. Okay, we swear, it really wasn’t that bad in the Middle [Editor’s note: Approximately 5,000 more words on medieval culture not included. This is a medical column, thank you very much.]
PsA prediction tool approaches clinical utility
Easily collected variables establish risk
A new tool for predicting which patients with psoriasis will develop psoriatic arthritis (PsA) is showing promise for such clinical applications as early treatment in those at risk or trials to prevent PsA, according to a summary of progress at the annual meeting of the Canadian Rheumatology Association.
Based on current levels of sensitivity and specificity, psoriasis “can be predicted with reasonable accuracy,” reported Lihi Eder, MD, PhD, director of research in the rheumatology division at the University of Toronto.
The predictive method, called PRESTO (Prediction of Psoriatic Arthritis Tool), is based on variables readily available in clinical practice, according to Dr. Eder. Once values are assigned to the risk factors, the risk of PsA over a 1-year or 5-year time frame can be estimated with a calculator.
She called PRESTO the “first clinical tool for predicting PsA among psoriasis patients.”
The work on this tool began in 2006 when the International Psoriasis and Arthritis Research Team (IPART) initiated a prospectively collected cohort of psoriasis patients. To be enrolled, patients had to be free of signs and symptoms of arthritis upon examination by a rheumatologist. They were then invited to return annually for follow-up that again included screening for joint involvement by a rheumatologist.
At baseline and at follow-up evaluations, 13 predictors were evaluated. These involved psoriasis characteristics, such as nail pitting; symptoms, such as stiffness; comorbidities, such as additional inflammatory diseases; and laboratory values, such as upregulated markers of inflammation.
Symptoms and signs used to predict PsA
Dr. Eder and her colleagues applied regression models to select an optimal combination of variables weighted for predictive value. Variables offering predictive value included higher PASI (Psoriasis Area and Severity Index), greater fatigue score as measured by FACIT (Functional Assessment of Chronic Illness Therapy) score, greater morning stiffness, and greater pain.
When applied to 635 patients in the IPART cohort, in which there were 51 incident PsA cases over 1 year and 75 incident cases over 5 years, the area under the curve (AUC) for PRESTO at the cutoffs studied was 72% for the 1-year time window and 75% for the 5-year time window.
These levels are associated with adequate accuracy, according to Dr. Eder, who explained that “an AUC greater than 70% is considered reasonable” for clinical applicability.
Moreover, the cutoffs can be adjusted for the specific purpose of the predictive tool. For example, to screen patients for risk, lower cutoffs could be employed to increase sensitivity. In order to select patients for a clinical trial to prevent PsA, higher cutoffs could be employed to increase specificity.
But sensitivities and specificities move in opposite directions when cutoffs are adjusted. Showing data from the 5-year prediction model, Dr. Eder reported that specificities climbed from about 58% to 97% as cutoffs were increased. The sensitivities with these adjustments fell from 79% to 14%.
In general, Dr. Eder said there was “excellent calibration” for the cutoffs employed when they compared the predicted and observed rates of PsA according to quintile of predictive probability. The differences were particularly minor over a 1-year time period. Over the 5-year period, observed rates were somewhat higher than predicted in the fourth and fifth quintile, but, again, this discrepancy could be modified for specific applications with cutoff adjustments.
Validation studies are planned
Even though psoriasis patients in IPART represents one of the largest cohorts of prospectively collected psoriasis patients, Dr. Eder acknowledged that the sample size would be considered “moderate” for developing a predictive model. However, the fact that the data were collected prospectively using standardized methodology strengthens the findings and provides the basis for the next step.
“Validation studies are planned with external cohorts,” said Dr. Eder, who indicated that a viable tool for identifying psoriasis patients at risk for PsA is likely. Even if it is not employed routinely in its current form at the level of individual patient care, she predicted that it will have value at a research level for understanding the relationship of psoriasis to PsA.
Christopher T. Ritchlin, MD, a professor and researcher at the University of Rochester (N.Y.), agreed that PRESTO has important potential as a clinical tool. Dr. Ritchlin has been involved in the development of PRESTO but was not involved in the presentation made at the CRA annual meeting.
“The PRESTO tool has the ability to predict the 2- and 5-year risk of developing psoriatic arthritis, which is an important advance if confirmed,” he said in an interview. He pointed out that approximately 25%-30% who develop psoriasis will go on to develop PsA but until now there has been no way to identify them.
“This tool may provide a pathway to early intervention,” he said.
Dr. Eder has financial relationships with AbbVie, Eli Lilly, Fresenius Kabi, Janssen, Novartis, Pfizer, Sandoz, and UCB. Dr. Ritchlin has financial relationships with many of the same companies.
Easily collected variables establish risk
Easily collected variables establish risk
A new tool for predicting which patients with psoriasis will develop psoriatic arthritis (PsA) is showing promise for such clinical applications as early treatment in those at risk or trials to prevent PsA, according to a summary of progress at the annual meeting of the Canadian Rheumatology Association.
Based on current levels of sensitivity and specificity, psoriasis “can be predicted with reasonable accuracy,” reported Lihi Eder, MD, PhD, director of research in the rheumatology division at the University of Toronto.
The predictive method, called PRESTO (Prediction of Psoriatic Arthritis Tool), is based on variables readily available in clinical practice, according to Dr. Eder. Once values are assigned to the risk factors, the risk of PsA over a 1-year or 5-year time frame can be estimated with a calculator.
She called PRESTO the “first clinical tool for predicting PsA among psoriasis patients.”
The work on this tool began in 2006 when the International Psoriasis and Arthritis Research Team (IPART) initiated a prospectively collected cohort of psoriasis patients. To be enrolled, patients had to be free of signs and symptoms of arthritis upon examination by a rheumatologist. They were then invited to return annually for follow-up that again included screening for joint involvement by a rheumatologist.
At baseline and at follow-up evaluations, 13 predictors were evaluated. These involved psoriasis characteristics, such as nail pitting; symptoms, such as stiffness; comorbidities, such as additional inflammatory diseases; and laboratory values, such as upregulated markers of inflammation.
Symptoms and signs used to predict PsA
Dr. Eder and her colleagues applied regression models to select an optimal combination of variables weighted for predictive value. Variables offering predictive value included higher PASI (Psoriasis Area and Severity Index), greater fatigue score as measured by FACIT (Functional Assessment of Chronic Illness Therapy) score, greater morning stiffness, and greater pain.
When applied to 635 patients in the IPART cohort, in which there were 51 incident PsA cases over 1 year and 75 incident cases over 5 years, the area under the curve (AUC) for PRESTO at the cutoffs studied was 72% for the 1-year time window and 75% for the 5-year time window.
These levels are associated with adequate accuracy, according to Dr. Eder, who explained that “an AUC greater than 70% is considered reasonable” for clinical applicability.
Moreover, the cutoffs can be adjusted for the specific purpose of the predictive tool. For example, to screen patients for risk, lower cutoffs could be employed to increase sensitivity. In order to select patients for a clinical trial to prevent PsA, higher cutoffs could be employed to increase specificity.
But sensitivities and specificities move in opposite directions when cutoffs are adjusted. Showing data from the 5-year prediction model, Dr. Eder reported that specificities climbed from about 58% to 97% as cutoffs were increased. The sensitivities with these adjustments fell from 79% to 14%.
In general, Dr. Eder said there was “excellent calibration” for the cutoffs employed when they compared the predicted and observed rates of PsA according to quintile of predictive probability. The differences were particularly minor over a 1-year time period. Over the 5-year period, observed rates were somewhat higher than predicted in the fourth and fifth quintile, but, again, this discrepancy could be modified for specific applications with cutoff adjustments.
Validation studies are planned
Even though psoriasis patients in IPART represents one of the largest cohorts of prospectively collected psoriasis patients, Dr. Eder acknowledged that the sample size would be considered “moderate” for developing a predictive model. However, the fact that the data were collected prospectively using standardized methodology strengthens the findings and provides the basis for the next step.
“Validation studies are planned with external cohorts,” said Dr. Eder, who indicated that a viable tool for identifying psoriasis patients at risk for PsA is likely. Even if it is not employed routinely in its current form at the level of individual patient care, she predicted that it will have value at a research level for understanding the relationship of psoriasis to PsA.
Christopher T. Ritchlin, MD, a professor and researcher at the University of Rochester (N.Y.), agreed that PRESTO has important potential as a clinical tool. Dr. Ritchlin has been involved in the development of PRESTO but was not involved in the presentation made at the CRA annual meeting.
“The PRESTO tool has the ability to predict the 2- and 5-year risk of developing psoriatic arthritis, which is an important advance if confirmed,” he said in an interview. He pointed out that approximately 25%-30% who develop psoriasis will go on to develop PsA but until now there has been no way to identify them.
“This tool may provide a pathway to early intervention,” he said.
Dr. Eder has financial relationships with AbbVie, Eli Lilly, Fresenius Kabi, Janssen, Novartis, Pfizer, Sandoz, and UCB. Dr. Ritchlin has financial relationships with many of the same companies.
A new tool for predicting which patients with psoriasis will develop psoriatic arthritis (PsA) is showing promise for such clinical applications as early treatment in those at risk or trials to prevent PsA, according to a summary of progress at the annual meeting of the Canadian Rheumatology Association.
Based on current levels of sensitivity and specificity, psoriasis “can be predicted with reasonable accuracy,” reported Lihi Eder, MD, PhD, director of research in the rheumatology division at the University of Toronto.
The predictive method, called PRESTO (Prediction of Psoriatic Arthritis Tool), is based on variables readily available in clinical practice, according to Dr. Eder. Once values are assigned to the risk factors, the risk of PsA over a 1-year or 5-year time frame can be estimated with a calculator.
She called PRESTO the “first clinical tool for predicting PsA among psoriasis patients.”
The work on this tool began in 2006 when the International Psoriasis and Arthritis Research Team (IPART) initiated a prospectively collected cohort of psoriasis patients. To be enrolled, patients had to be free of signs and symptoms of arthritis upon examination by a rheumatologist. They were then invited to return annually for follow-up that again included screening for joint involvement by a rheumatologist.
At baseline and at follow-up evaluations, 13 predictors were evaluated. These involved psoriasis characteristics, such as nail pitting; symptoms, such as stiffness; comorbidities, such as additional inflammatory diseases; and laboratory values, such as upregulated markers of inflammation.
Symptoms and signs used to predict PsA
Dr. Eder and her colleagues applied regression models to select an optimal combination of variables weighted for predictive value. Variables offering predictive value included higher PASI (Psoriasis Area and Severity Index), greater fatigue score as measured by FACIT (Functional Assessment of Chronic Illness Therapy) score, greater morning stiffness, and greater pain.
When applied to 635 patients in the IPART cohort, in which there were 51 incident PsA cases over 1 year and 75 incident cases over 5 years, the area under the curve (AUC) for PRESTO at the cutoffs studied was 72% for the 1-year time window and 75% for the 5-year time window.
These levels are associated with adequate accuracy, according to Dr. Eder, who explained that “an AUC greater than 70% is considered reasonable” for clinical applicability.
Moreover, the cutoffs can be adjusted for the specific purpose of the predictive tool. For example, to screen patients for risk, lower cutoffs could be employed to increase sensitivity. In order to select patients for a clinical trial to prevent PsA, higher cutoffs could be employed to increase specificity.
But sensitivities and specificities move in opposite directions when cutoffs are adjusted. Showing data from the 5-year prediction model, Dr. Eder reported that specificities climbed from about 58% to 97% as cutoffs were increased. The sensitivities with these adjustments fell from 79% to 14%.
In general, Dr. Eder said there was “excellent calibration” for the cutoffs employed when they compared the predicted and observed rates of PsA according to quintile of predictive probability. The differences were particularly minor over a 1-year time period. Over the 5-year period, observed rates were somewhat higher than predicted in the fourth and fifth quintile, but, again, this discrepancy could be modified for specific applications with cutoff adjustments.
Validation studies are planned
Even though psoriasis patients in IPART represents one of the largest cohorts of prospectively collected psoriasis patients, Dr. Eder acknowledged that the sample size would be considered “moderate” for developing a predictive model. However, the fact that the data were collected prospectively using standardized methodology strengthens the findings and provides the basis for the next step.
“Validation studies are planned with external cohorts,” said Dr. Eder, who indicated that a viable tool for identifying psoriasis patients at risk for PsA is likely. Even if it is not employed routinely in its current form at the level of individual patient care, she predicted that it will have value at a research level for understanding the relationship of psoriasis to PsA.
Christopher T. Ritchlin, MD, a professor and researcher at the University of Rochester (N.Y.), agreed that PRESTO has important potential as a clinical tool. Dr. Ritchlin has been involved in the development of PRESTO but was not involved in the presentation made at the CRA annual meeting.
“The PRESTO tool has the ability to predict the 2- and 5-year risk of developing psoriatic arthritis, which is an important advance if confirmed,” he said in an interview. He pointed out that approximately 25%-30% who develop psoriasis will go on to develop PsA but until now there has been no way to identify them.
“This tool may provide a pathway to early intervention,” he said.
Dr. Eder has financial relationships with AbbVie, Eli Lilly, Fresenius Kabi, Janssen, Novartis, Pfizer, Sandoz, and UCB. Dr. Ritchlin has financial relationships with many of the same companies.
FROM CRA 2023
Appendicitis more often missed in patients who are Black
This phenomenon, first described in children, occurs in adults as well, according to a study published in JAMA Surgery.
Some hospitals fare better than others: Those with more diverse patient populations were less likely to have missed the diagnosis, the researchers found.
“We don’t think the amount of melanin in your skin predicts how you present with appendicitis,” said Jonathan Carter, MD, professor of surgery at the University of California, San Francisco. “There’s no biological explanation,” Dr. Carter, who wrote an invited commentary on the research, said in an interview. “It’s really what’s going on in the social environment of those emergency rooms.”
For the study, Anne Stey, MD, assistant professor of surgery at Northwestern University in Chicago and her colleagues analyzed data from more than 80,000 men and women in four states – Florida, Maryland, New York, and Wisconsin – who underwent appendectomy in 2016-2017.
They identified those who had been seen for abdominal complaints at a hospital in the week before surgery but did not receive a diagnosis of appendicitis at that time, indicating a missed opportunity to intervene sooner.
Among Black patients, the proportion who had experienced this type of delay was 3.6%, whereas for White patients, it was 2.5%. For Hispanic patients, the share was 2.4%, while for Asian or Pacific Islander patients, the figure was 1.5%.
An analysis that controlled for patient and hospital variables found that among non-Hispanic Black patients, the rate of delayed diagnosis was 1.41 times higher than for non-Hispanic White patients (95% confidence interval, 1.21-1.63).
Other patient factors associated with delayed diagnosis included female sex, comorbidities, and living in a low-income zip code.
A key factor was where patients sought care. A delayed diagnosis of appendicitis was 3.51 times more likely for patients who went to hospitals where most patients are insured by Medicaid. Prior research has shown that “safety-net hospitals have fewer resources and may provide lower-quality care than hospitals with a larger private payer population,” Dr. Stey’s group writes.
On the other hand, going to a hospital with a more diverse patient population reduced the odds of a delayed diagnosis.
“Patients presenting to hospitals with a greater than 50% Black and Hispanic population were 0.73 (95% CI, 0.59-0.91) times less likely to have a delayed diagnosis, compared with patients presenting to hospitals with a less than 25% Black and Hispanic population,” the researchers report.
In the 30 days after discharge following appendectomy, Black patients returned to the hospital at a higher rate than White patients did (17.5% vs. 11.4%), indicating worse outcomes.
“Delayed diagnosis may account for some of the racial and ethnic disparities observed in outcomes after appendicitis,” according to the authors.
“It may be hospitals that are more used to serving racial-ethnic minority patients are better at diagnosing them, because they’re more culturally informed and have a better understanding of these patients,” Dr. Stey said in a news release about their findings.
Great masquerader
Diagnosing appendicitis can be challenging, Dr. Carter said. The early signs can be subtle, and the condition is sometimes called the great masquerader. It is not uncommon for patients to be diagnosed with gastroenteritis or pain associated with their menstrual period, for example, and sent home.
Scoring systems based on patients’ symptoms and liberal use of imaging have improved detection of appendicitis, but “no physician or health care system is perfect in the diagnosis,” he said.
The increased odds of delayed diagnosis for Black patients remained when the researchers focused on healthier patients who had fewer comorbidities, and it also held when they considered patients with private insurance in high-income areas, Dr. Carter noted.
“Once again, with this study we see the association of structural and systematic racism with access to health care, especially for Black patients, in emergency departments and hospitals,” he wrote. “We must redouble our efforts to become anti-racist in ourselves, our institutions, and our profession.”
‘Our health care system itself’
Elizabeth Garner, MD, MPH, a pharmaceutical executive who was not involved in the study, commented on Twitter that the study points to an underlying issue that has existed in medicine “for quite some time.”
“Minority populations are not taken as seriously as their white counterparts,” she wrote. “This needs to change.”
Measures of hospital quality need to be tied to health equity, according to Mofya Diallo, MD, MPH, of the department of anesthesiology at the Children’s Hospital Los Angeles and the University of Southern California, Los Angeles.
“Top hospitals should take pride in outcomes that do not vary based on race, income or literacy,” she tweeted in response to the study.
To better understand possible reasons for delayed diagnosis, future researchers could assess whether patients who are Black are less likely to receive a surgical consultation, imaging studies, or lab work, Dr. Carter told this news organization. He pointed to a recent analysis of patients insured by Medicare that found that Black patients were less likely than White patients to receive a surgical consultation after they were admitted with colorectal, general abdominal, hepatopancreatobiliary, intestinal obstruction, or upper gastrointestinal diagnoses.
While social determinants of health, such as income, education, housing, early childhood development, employment, and social inclusion, may account for a substantial portion of health outcomes, “Our health care system itself can be viewed as another social determinant of health,” Dr. Carter wrote. “Insurance coverage, health care professional availability, health care professional linguistic and cultural competency, and quality of care all have an effect on health outcomes.”
Dr. Stey was supported by grants from the American College of Surgeons and the National Institutes of Health.
A version of this article originally appeared on Medscape.com.
This phenomenon, first described in children, occurs in adults as well, according to a study published in JAMA Surgery.
Some hospitals fare better than others: Those with more diverse patient populations were less likely to have missed the diagnosis, the researchers found.
“We don’t think the amount of melanin in your skin predicts how you present with appendicitis,” said Jonathan Carter, MD, professor of surgery at the University of California, San Francisco. “There’s no biological explanation,” Dr. Carter, who wrote an invited commentary on the research, said in an interview. “It’s really what’s going on in the social environment of those emergency rooms.”
For the study, Anne Stey, MD, assistant professor of surgery at Northwestern University in Chicago and her colleagues analyzed data from more than 80,000 men and women in four states – Florida, Maryland, New York, and Wisconsin – who underwent appendectomy in 2016-2017.
They identified those who had been seen for abdominal complaints at a hospital in the week before surgery but did not receive a diagnosis of appendicitis at that time, indicating a missed opportunity to intervene sooner.
Among Black patients, the proportion who had experienced this type of delay was 3.6%, whereas for White patients, it was 2.5%. For Hispanic patients, the share was 2.4%, while for Asian or Pacific Islander patients, the figure was 1.5%.
An analysis that controlled for patient and hospital variables found that among non-Hispanic Black patients, the rate of delayed diagnosis was 1.41 times higher than for non-Hispanic White patients (95% confidence interval, 1.21-1.63).
Other patient factors associated with delayed diagnosis included female sex, comorbidities, and living in a low-income zip code.
A key factor was where patients sought care. A delayed diagnosis of appendicitis was 3.51 times more likely for patients who went to hospitals where most patients are insured by Medicaid. Prior research has shown that “safety-net hospitals have fewer resources and may provide lower-quality care than hospitals with a larger private payer population,” Dr. Stey’s group writes.
On the other hand, going to a hospital with a more diverse patient population reduced the odds of a delayed diagnosis.
“Patients presenting to hospitals with a greater than 50% Black and Hispanic population were 0.73 (95% CI, 0.59-0.91) times less likely to have a delayed diagnosis, compared with patients presenting to hospitals with a less than 25% Black and Hispanic population,” the researchers report.
In the 30 days after discharge following appendectomy, Black patients returned to the hospital at a higher rate than White patients did (17.5% vs. 11.4%), indicating worse outcomes.
“Delayed diagnosis may account for some of the racial and ethnic disparities observed in outcomes after appendicitis,” according to the authors.
“It may be hospitals that are more used to serving racial-ethnic minority patients are better at diagnosing them, because they’re more culturally informed and have a better understanding of these patients,” Dr. Stey said in a news release about their findings.
Great masquerader
Diagnosing appendicitis can be challenging, Dr. Carter said. The early signs can be subtle, and the condition is sometimes called the great masquerader. It is not uncommon for patients to be diagnosed with gastroenteritis or pain associated with their menstrual period, for example, and sent home.
Scoring systems based on patients’ symptoms and liberal use of imaging have improved detection of appendicitis, but “no physician or health care system is perfect in the diagnosis,” he said.
The increased odds of delayed diagnosis for Black patients remained when the researchers focused on healthier patients who had fewer comorbidities, and it also held when they considered patients with private insurance in high-income areas, Dr. Carter noted.
“Once again, with this study we see the association of structural and systematic racism with access to health care, especially for Black patients, in emergency departments and hospitals,” he wrote. “We must redouble our efforts to become anti-racist in ourselves, our institutions, and our profession.”
‘Our health care system itself’
Elizabeth Garner, MD, MPH, a pharmaceutical executive who was not involved in the study, commented on Twitter that the study points to an underlying issue that has existed in medicine “for quite some time.”
“Minority populations are not taken as seriously as their white counterparts,” she wrote. “This needs to change.”
Measures of hospital quality need to be tied to health equity, according to Mofya Diallo, MD, MPH, of the department of anesthesiology at the Children’s Hospital Los Angeles and the University of Southern California, Los Angeles.
“Top hospitals should take pride in outcomes that do not vary based on race, income or literacy,” she tweeted in response to the study.
To better understand possible reasons for delayed diagnosis, future researchers could assess whether patients who are Black are less likely to receive a surgical consultation, imaging studies, or lab work, Dr. Carter told this news organization. He pointed to a recent analysis of patients insured by Medicare that found that Black patients were less likely than White patients to receive a surgical consultation after they were admitted with colorectal, general abdominal, hepatopancreatobiliary, intestinal obstruction, or upper gastrointestinal diagnoses.
While social determinants of health, such as income, education, housing, early childhood development, employment, and social inclusion, may account for a substantial portion of health outcomes, “Our health care system itself can be viewed as another social determinant of health,” Dr. Carter wrote. “Insurance coverage, health care professional availability, health care professional linguistic and cultural competency, and quality of care all have an effect on health outcomes.”
Dr. Stey was supported by grants from the American College of Surgeons and the National Institutes of Health.
A version of this article originally appeared on Medscape.com.
This phenomenon, first described in children, occurs in adults as well, according to a study published in JAMA Surgery.
Some hospitals fare better than others: Those with more diverse patient populations were less likely to have missed the diagnosis, the researchers found.
“We don’t think the amount of melanin in your skin predicts how you present with appendicitis,” said Jonathan Carter, MD, professor of surgery at the University of California, San Francisco. “There’s no biological explanation,” Dr. Carter, who wrote an invited commentary on the research, said in an interview. “It’s really what’s going on in the social environment of those emergency rooms.”
For the study, Anne Stey, MD, assistant professor of surgery at Northwestern University in Chicago and her colleagues analyzed data from more than 80,000 men and women in four states – Florida, Maryland, New York, and Wisconsin – who underwent appendectomy in 2016-2017.
They identified those who had been seen for abdominal complaints at a hospital in the week before surgery but did not receive a diagnosis of appendicitis at that time, indicating a missed opportunity to intervene sooner.
Among Black patients, the proportion who had experienced this type of delay was 3.6%, whereas for White patients, it was 2.5%. For Hispanic patients, the share was 2.4%, while for Asian or Pacific Islander patients, the figure was 1.5%.
An analysis that controlled for patient and hospital variables found that among non-Hispanic Black patients, the rate of delayed diagnosis was 1.41 times higher than for non-Hispanic White patients (95% confidence interval, 1.21-1.63).
Other patient factors associated with delayed diagnosis included female sex, comorbidities, and living in a low-income zip code.
A key factor was where patients sought care. A delayed diagnosis of appendicitis was 3.51 times more likely for patients who went to hospitals where most patients are insured by Medicaid. Prior research has shown that “safety-net hospitals have fewer resources and may provide lower-quality care than hospitals with a larger private payer population,” Dr. Stey’s group writes.
On the other hand, going to a hospital with a more diverse patient population reduced the odds of a delayed diagnosis.
“Patients presenting to hospitals with a greater than 50% Black and Hispanic population were 0.73 (95% CI, 0.59-0.91) times less likely to have a delayed diagnosis, compared with patients presenting to hospitals with a less than 25% Black and Hispanic population,” the researchers report.
In the 30 days after discharge following appendectomy, Black patients returned to the hospital at a higher rate than White patients did (17.5% vs. 11.4%), indicating worse outcomes.
“Delayed diagnosis may account for some of the racial and ethnic disparities observed in outcomes after appendicitis,” according to the authors.
“It may be hospitals that are more used to serving racial-ethnic minority patients are better at diagnosing them, because they’re more culturally informed and have a better understanding of these patients,” Dr. Stey said in a news release about their findings.
Great masquerader
Diagnosing appendicitis can be challenging, Dr. Carter said. The early signs can be subtle, and the condition is sometimes called the great masquerader. It is not uncommon for patients to be diagnosed with gastroenteritis or pain associated with their menstrual period, for example, and sent home.
Scoring systems based on patients’ symptoms and liberal use of imaging have improved detection of appendicitis, but “no physician or health care system is perfect in the diagnosis,” he said.
The increased odds of delayed diagnosis for Black patients remained when the researchers focused on healthier patients who had fewer comorbidities, and it also held when they considered patients with private insurance in high-income areas, Dr. Carter noted.
“Once again, with this study we see the association of structural and systematic racism with access to health care, especially for Black patients, in emergency departments and hospitals,” he wrote. “We must redouble our efforts to become anti-racist in ourselves, our institutions, and our profession.”
‘Our health care system itself’
Elizabeth Garner, MD, MPH, a pharmaceutical executive who was not involved in the study, commented on Twitter that the study points to an underlying issue that has existed in medicine “for quite some time.”
“Minority populations are not taken as seriously as their white counterparts,” she wrote. “This needs to change.”
Measures of hospital quality need to be tied to health equity, according to Mofya Diallo, MD, MPH, of the department of anesthesiology at the Children’s Hospital Los Angeles and the University of Southern California, Los Angeles.
“Top hospitals should take pride in outcomes that do not vary based on race, income or literacy,” she tweeted in response to the study.
To better understand possible reasons for delayed diagnosis, future researchers could assess whether patients who are Black are less likely to receive a surgical consultation, imaging studies, or lab work, Dr. Carter told this news organization. He pointed to a recent analysis of patients insured by Medicare that found that Black patients were less likely than White patients to receive a surgical consultation after they were admitted with colorectal, general abdominal, hepatopancreatobiliary, intestinal obstruction, or upper gastrointestinal diagnoses.
While social determinants of health, such as income, education, housing, early childhood development, employment, and social inclusion, may account for a substantial portion of health outcomes, “Our health care system itself can be viewed as another social determinant of health,” Dr. Carter wrote. “Insurance coverage, health care professional availability, health care professional linguistic and cultural competency, and quality of care all have an effect on health outcomes.”
Dr. Stey was supported by grants from the American College of Surgeons and the National Institutes of Health.
A version of this article originally appeared on Medscape.com.
FROM JAMA SURGERY
Obstetric violence: How it’s defined and how we face it
In a recent, tragic case, a newborn died from being crushed by its mother, who fell asleep from the fatigue of numerous hours of labor. The case has brought the issue of obstetric violence (OV) to the attention of the Italian media. OV is defined as neglect, physical abuse, or disrespect during childbirth, according to the World Health Organization. The WHO outlined fundamental actions to be taken at various levels for its prevention, especially by health care systems, in a 2014 position paper.
Gender-based abuse
Considered a form of gender-based abuse, OV was first described in Latin America in the early 2000s. It is widespread and is increasing in European countries.
From the scientific literature on the subject, OV seems to be strongly associated with a lack of communication between health care personnel and pregnant women. It appears to have more to do with authoritarian and paternalistic behavior than actual real-life medical issues. Actively involving women in decision-making regarding childbirth and postpartum care seems to reduce the incidence of OV. Pregnant women who are more involved appear to trust health care professionals more and are therefore less likely to report disrespectful and abusive behavior.
Estimates of the prevalence of OV vary, depending on the country, the childbirth facility, and its definition. In Italy, inspired by the web campaign “#Bastatacere: le madri hanno voce [#EnoughSilence: mothers have a voice],” in 2017, the Obstetric Violence Database (OVO) investigated perceptions of having been a victim of OV in a representative sample of Italian women aged 18-54 years who had at least one child.
In 2017, just over 20% of the women interviewed considered themselves victims of OV; 33% felt they had not received adequate care; and around 35% reported serious problems concerning privacy or trust. Following the treatment received, approximately 15% of the women decided not to return to the same health care facility, and 6% did not want to proceed with further pregnancies.
At the time of publication, the results sparked a debate among relevant medical associations (the Association of Obstetricians and Gynecologists of Italian Hospitals, the Italian Society of Gynecology and Obstetrics, and the Association of Italian University Gynecologists), which immediately recognized the importance of the topic and accepted an invitation for further discussion on physician-patient relationships. They expressed reservations concerning the methodologies used by the OVO for data collection, especially regarding the representativeness of the sample.
Lack of communication
“In general, women who claim to have suffered from obstetric violence do not do so because they have been denied an aspect of care but because they have had an overall experience that, for whatever reason, did not conform with their expectations,” said Irene Cetin, MD, PhD, professor of obstetrics and gynecology at the University of Milan and director of the obstetrics and gynecology unit of the Buzzi Hospital in Milan. “Following the OVO’s exposé, the Italian Society of Gynecology and Obstetrics also conducted a large-scale study throughout Italy on all women who had given birth within a 3-month period. That investigation painted a very different picture. It wasn’t the case that no instances of obstetric violence were found, but the results were more contained. This is a very delicate subject, given that every report that we receive in hospital is always valued and looked into in detail, and women come to speak to us about errors and things that were missed.”
She added, “Experience leads me to say that complaints about what happens in the delivery room are extremely rare. What we hear more of, but still not often, are problems experienced during days spent in hospital immediately after childbirth.” There are never enough resources, which is the reason behind most problems. “The real hardships are found in the wards,” continued Dr. Cetin, “where the midwife-to-bed ratio is one or two to 30, and therefore this is where it is more difficult to feel like you’re being listened to. With COVID-19, the situation has gotten even worse, even though in my hospital we have always guaranteed, not without struggle, the presence of the partner in the delivery room.”
Only relatively recently have women’s partners been allowed into the hospital. In addition, a number of services, such as having the right beds and giving the correct explanations and information on how to establish a relationship with the child, are now being offered. These steps are necessary to guarantee what is referred to as a “humanizing birth,” a process in which the woman is at the center of the experience and is the main protagonist of the birth.
Lack of resources
This trend also is observed at the systemic level, where there is a lack of organization and resources. Few staff members are in the ward, even fewer specialists are in the psychological field, and contact is almost nonexistent after discharge from many hospitals and in many regions across Italy. There are, however, some positive aspects and hope for the future. “Just think,” said Dr. Cetin, “of how degree courses in obstetrics have changed over time, with a large part of teaching and training now being centered around the emotional aspects of birth.” From the gynecologist’s side, “most of the problems have been inherited from the past,” said Dr. Cetin. “Let’s not forget that we have only recently been giving birth in hospital. The so-called medicalization of childbirth has been responsible for a decline in the death rate and morbidity rate of pregnant women, but initially, there was little interest or care in how women felt in this situation, including with regard to physical pain. Since the 1970s, with Leboyer from France and Miraglia from Italy [promoters of so-called sweet birth], a path was cleared for a different line of thought. For this reason, I believe that the situation will improve over time.
“To continuously improve physician-patient communication,” concluded Dr. Cetin, “it would perhaps be appropriate to make sure that, even in the preparatory phase, women are well aware of possible complications and of the necessary and rapid emergency procedures that must be implemented by health care personnel. This way, a trusting relationship could be maintained, and the perception of having suffered abuse due to not being involved in strictly medical decisions could be stemmed.”
This article was translated from Univadis Italy. A version of this article appeared on Medscape.com.
In a recent, tragic case, a newborn died from being crushed by its mother, who fell asleep from the fatigue of numerous hours of labor. The case has brought the issue of obstetric violence (OV) to the attention of the Italian media. OV is defined as neglect, physical abuse, or disrespect during childbirth, according to the World Health Organization. The WHO outlined fundamental actions to be taken at various levels for its prevention, especially by health care systems, in a 2014 position paper.
Gender-based abuse
Considered a form of gender-based abuse, OV was first described in Latin America in the early 2000s. It is widespread and is increasing in European countries.
From the scientific literature on the subject, OV seems to be strongly associated with a lack of communication between health care personnel and pregnant women. It appears to have more to do with authoritarian and paternalistic behavior than actual real-life medical issues. Actively involving women in decision-making regarding childbirth and postpartum care seems to reduce the incidence of OV. Pregnant women who are more involved appear to trust health care professionals more and are therefore less likely to report disrespectful and abusive behavior.
Estimates of the prevalence of OV vary, depending on the country, the childbirth facility, and its definition. In Italy, inspired by the web campaign “#Bastatacere: le madri hanno voce [#EnoughSilence: mothers have a voice],” in 2017, the Obstetric Violence Database (OVO) investigated perceptions of having been a victim of OV in a representative sample of Italian women aged 18-54 years who had at least one child.
In 2017, just over 20% of the women interviewed considered themselves victims of OV; 33% felt they had not received adequate care; and around 35% reported serious problems concerning privacy or trust. Following the treatment received, approximately 15% of the women decided not to return to the same health care facility, and 6% did not want to proceed with further pregnancies.
At the time of publication, the results sparked a debate among relevant medical associations (the Association of Obstetricians and Gynecologists of Italian Hospitals, the Italian Society of Gynecology and Obstetrics, and the Association of Italian University Gynecologists), which immediately recognized the importance of the topic and accepted an invitation for further discussion on physician-patient relationships. They expressed reservations concerning the methodologies used by the OVO for data collection, especially regarding the representativeness of the sample.
Lack of communication
“In general, women who claim to have suffered from obstetric violence do not do so because they have been denied an aspect of care but because they have had an overall experience that, for whatever reason, did not conform with their expectations,” said Irene Cetin, MD, PhD, professor of obstetrics and gynecology at the University of Milan and director of the obstetrics and gynecology unit of the Buzzi Hospital in Milan. “Following the OVO’s exposé, the Italian Society of Gynecology and Obstetrics also conducted a large-scale study throughout Italy on all women who had given birth within a 3-month period. That investigation painted a very different picture. It wasn’t the case that no instances of obstetric violence were found, but the results were more contained. This is a very delicate subject, given that every report that we receive in hospital is always valued and looked into in detail, and women come to speak to us about errors and things that were missed.”
She added, “Experience leads me to say that complaints about what happens in the delivery room are extremely rare. What we hear more of, but still not often, are problems experienced during days spent in hospital immediately after childbirth.” There are never enough resources, which is the reason behind most problems. “The real hardships are found in the wards,” continued Dr. Cetin, “where the midwife-to-bed ratio is one or two to 30, and therefore this is where it is more difficult to feel like you’re being listened to. With COVID-19, the situation has gotten even worse, even though in my hospital we have always guaranteed, not without struggle, the presence of the partner in the delivery room.”
Only relatively recently have women’s partners been allowed into the hospital. In addition, a number of services, such as having the right beds and giving the correct explanations and information on how to establish a relationship with the child, are now being offered. These steps are necessary to guarantee what is referred to as a “humanizing birth,” a process in which the woman is at the center of the experience and is the main protagonist of the birth.
Lack of resources
This trend also is observed at the systemic level, where there is a lack of organization and resources. Few staff members are in the ward, even fewer specialists are in the psychological field, and contact is almost nonexistent after discharge from many hospitals and in many regions across Italy. There are, however, some positive aspects and hope for the future. “Just think,” said Dr. Cetin, “of how degree courses in obstetrics have changed over time, with a large part of teaching and training now being centered around the emotional aspects of birth.” From the gynecologist’s side, “most of the problems have been inherited from the past,” said Dr. Cetin. “Let’s not forget that we have only recently been giving birth in hospital. The so-called medicalization of childbirth has been responsible for a decline in the death rate and morbidity rate of pregnant women, but initially, there was little interest or care in how women felt in this situation, including with regard to physical pain. Since the 1970s, with Leboyer from France and Miraglia from Italy [promoters of so-called sweet birth], a path was cleared for a different line of thought. For this reason, I believe that the situation will improve over time.
“To continuously improve physician-patient communication,” concluded Dr. Cetin, “it would perhaps be appropriate to make sure that, even in the preparatory phase, women are well aware of possible complications and of the necessary and rapid emergency procedures that must be implemented by health care personnel. This way, a trusting relationship could be maintained, and the perception of having suffered abuse due to not being involved in strictly medical decisions could be stemmed.”
This article was translated from Univadis Italy. A version of this article appeared on Medscape.com.
In a recent, tragic case, a newborn died from being crushed by its mother, who fell asleep from the fatigue of numerous hours of labor. The case has brought the issue of obstetric violence (OV) to the attention of the Italian media. OV is defined as neglect, physical abuse, or disrespect during childbirth, according to the World Health Organization. The WHO outlined fundamental actions to be taken at various levels for its prevention, especially by health care systems, in a 2014 position paper.
Gender-based abuse
Considered a form of gender-based abuse, OV was first described in Latin America in the early 2000s. It is widespread and is increasing in European countries.
From the scientific literature on the subject, OV seems to be strongly associated with a lack of communication between health care personnel and pregnant women. It appears to have more to do with authoritarian and paternalistic behavior than actual real-life medical issues. Actively involving women in decision-making regarding childbirth and postpartum care seems to reduce the incidence of OV. Pregnant women who are more involved appear to trust health care professionals more and are therefore less likely to report disrespectful and abusive behavior.
Estimates of the prevalence of OV vary, depending on the country, the childbirth facility, and its definition. In Italy, inspired by the web campaign “#Bastatacere: le madri hanno voce [#EnoughSilence: mothers have a voice],” in 2017, the Obstetric Violence Database (OVO) investigated perceptions of having been a victim of OV in a representative sample of Italian women aged 18-54 years who had at least one child.
In 2017, just over 20% of the women interviewed considered themselves victims of OV; 33% felt they had not received adequate care; and around 35% reported serious problems concerning privacy or trust. Following the treatment received, approximately 15% of the women decided not to return to the same health care facility, and 6% did not want to proceed with further pregnancies.
At the time of publication, the results sparked a debate among relevant medical associations (the Association of Obstetricians and Gynecologists of Italian Hospitals, the Italian Society of Gynecology and Obstetrics, and the Association of Italian University Gynecologists), which immediately recognized the importance of the topic and accepted an invitation for further discussion on physician-patient relationships. They expressed reservations concerning the methodologies used by the OVO for data collection, especially regarding the representativeness of the sample.
Lack of communication
“In general, women who claim to have suffered from obstetric violence do not do so because they have been denied an aspect of care but because they have had an overall experience that, for whatever reason, did not conform with their expectations,” said Irene Cetin, MD, PhD, professor of obstetrics and gynecology at the University of Milan and director of the obstetrics and gynecology unit of the Buzzi Hospital in Milan. “Following the OVO’s exposé, the Italian Society of Gynecology and Obstetrics also conducted a large-scale study throughout Italy on all women who had given birth within a 3-month period. That investigation painted a very different picture. It wasn’t the case that no instances of obstetric violence were found, but the results were more contained. This is a very delicate subject, given that every report that we receive in hospital is always valued and looked into in detail, and women come to speak to us about errors and things that were missed.”
She added, “Experience leads me to say that complaints about what happens in the delivery room are extremely rare. What we hear more of, but still not often, are problems experienced during days spent in hospital immediately after childbirth.” There are never enough resources, which is the reason behind most problems. “The real hardships are found in the wards,” continued Dr. Cetin, “where the midwife-to-bed ratio is one or two to 30, and therefore this is where it is more difficult to feel like you’re being listened to. With COVID-19, the situation has gotten even worse, even though in my hospital we have always guaranteed, not without struggle, the presence of the partner in the delivery room.”
Only relatively recently have women’s partners been allowed into the hospital. In addition, a number of services, such as having the right beds and giving the correct explanations and information on how to establish a relationship with the child, are now being offered. These steps are necessary to guarantee what is referred to as a “humanizing birth,” a process in which the woman is at the center of the experience and is the main protagonist of the birth.
Lack of resources
This trend also is observed at the systemic level, where there is a lack of organization and resources. Few staff members are in the ward, even fewer specialists are in the psychological field, and contact is almost nonexistent after discharge from many hospitals and in many regions across Italy. There are, however, some positive aspects and hope for the future. “Just think,” said Dr. Cetin, “of how degree courses in obstetrics have changed over time, with a large part of teaching and training now being centered around the emotional aspects of birth.” From the gynecologist’s side, “most of the problems have been inherited from the past,” said Dr. Cetin. “Let’s not forget that we have only recently been giving birth in hospital. The so-called medicalization of childbirth has been responsible for a decline in the death rate and morbidity rate of pregnant women, but initially, there was little interest or care in how women felt in this situation, including with regard to physical pain. Since the 1970s, with Leboyer from France and Miraglia from Italy [promoters of so-called sweet birth], a path was cleared for a different line of thought. For this reason, I believe that the situation will improve over time.
“To continuously improve physician-patient communication,” concluded Dr. Cetin, “it would perhaps be appropriate to make sure that, even in the preparatory phase, women are well aware of possible complications and of the necessary and rapid emergency procedures that must be implemented by health care personnel. This way, a trusting relationship could be maintained, and the perception of having suffered abuse due to not being involved in strictly medical decisions could be stemmed.”
This article was translated from Univadis Italy. A version of this article appeared on Medscape.com.
Eye drops delay, may even prevent, nearsightedness
Dilating eye drops may delay – and perhaps even prevent – the onset of myopia in children, according to findings from a study published in JAMA. The study was conducted by researchers in Hong Kong.
Myopia is irreversible once it takes root and can contribute to other vision problems, such as macular degeneration, retinal detachment, glaucoma, and cataracts. The incidence of nearsightedness has nearly doubled since the 1970s, rising from 25% of the U.S. population to nearly 42%. Children have been particularly affected by the increase; reasons may include spending more time indoors looking at screens, experts say.
“Myopia is an ongoing and growing worldwide concern. This is of particular importance because of the change in children’s lifestyle, such as decreased outdoor time and increased screen time during and after the COVID-19 pandemic,” Jason C. Yam, MPH, of the department of ophthalmology and visual services at the Chinese University of Hong Kong, said in an interview.
Mr. Yam said that, while encouraging children to engage more in outdoor activity and spend less time using screens would help delay myopia, pharmaceutical interventions are needed, given myopia’s potential lifelong effects.
Putting eye drops to the test
In 2020, Mr. Yam and colleagues reported results of the Low-Concentration Atropine for Myopia Progression (LAMP) study, which showed that eye drops containing a solution of 0.05% atropine worked best at slowing the progression of myopia in 4- to 12-year-olds who already had the condition. Atropine relaxes eye muscles, causing dilation.
In that study, Mr. Yam and colleagues measured the rate of change in the eye’s ability to see at a great distance using a unit of measure known as the diopter. The higher the diopter, the more myopic a person’s vision. The 0.05% atropine solution was better at slowing this decline than placebo or solutions that contained a lower concentration of the substance.
The new study enrolled 474 children who were evenly divided by sex. None of the children had myopia when the trial began. Of that starting group, 353 children (age, 4-9 years) completed the study, which involved receiving eye drops once nightly in both eyes for 2 years.
Some children (n = 116) received 0.05% atropine, others (n = 122) received 0.01% atropine, and the rest (n = 115) received placebo drops. Mr. Yam and colleagues assessed how many children in each group had myopia after 2 years, as measured by a decline of at least a half diopter in one eye.
At the 2-year mark, more than half of children who received the placebo drops (61/115) had developed myopia, as had nearly half of those given 0.01% atropine (56/122). But fewer than one-third of children (33/116, 28.4%) who had received the drops with 0.05% atropine developed myopia during that period, the researchers reported.
The percentage of children with myopia in the placebo group (39/128, 30.5%) was larger by the end of the first year of the study than was the share of children in the 0.05% atropine group by the end of the trial. (Between 12 months and 24 months, 13 children in the placebo group left the study.) The main adverse event, in all treatment groups, was discomfort when exposed to bright light, according to the researchers.
“We are continuing the current study with the total intended follow-up duration of at least 6years,” added Mr. Yam, who hopes to determine whether the 0.05% atropine solution not only delays myopia but also prevents it altogether. While myopia is a concern worldwide, the condition is particularly prevalent in East Asia.
Mark A. Bullimore, MCOptom, PhD, FAAO, an adjunct professor at the University of Houston, and a consultant to ophthalmologic companies, called the trial “a landmark study. Finding children who are eligible and parents who are willing to deal with 2 years of drops is no small feat.
“The 0.05% atropine, on average, delays onset of myopia by a year,” Dr. Bullimore noted. He pointed to the similar percentages of myopia with placebo at 12 months, compared with 0.05% atropine 1 year later. He added that few clinicians in the United States use higher than 0.05% atropine for control of myopia because doing so can lead to excessive dilation and difficulty focusing.
While preventing myopia altogether would be ideal, simply delaying its onset can also be of tangible benefit, Bullimore said. In an article published in January, Dr. Bullimore and Noel A. Brennan of Johnson & Johnson Vision showed that delaying the onset of myopia reduces its severity.
“Optometrists prescribe low-concentration atropine already for myopia control, and there’s no reason now – in the light of this study – that they wouldn’t also do it to delay onset,” Dr. Bullimore said.
But in an editorial accompanying the journal article David A. Berntsen, OD, PhD, and Jeffrey J. Walline, OD, PhD, both of the University of Houston, wrote that a change in practice would be premature.
“The evidence presented does not yet warrant a change in the standard care of children because we do not yet know the long-term effects of delaying the onset of myopia with low-concentration atropine,” they wrote.
Identifying which children to consider for treatment is “a challenge,” they noted, because those who are not nearsighted typically do not undergo routine examination unless they have failed a vision test.
“Ultimately, the implementation of vision screenings that include determining a child’s prescription will likely be needed to identify children most likely to become myopic who may benefit from low-concentration atropine,” Dr. Berntsen and Dr. Walline wrote.
Mr. Yam and coinvestigators have applied for a patent on a 0.05% atropine solution. Dr. Bullimore reported relationships with Alcon Research,CooperVision, CorneaGen, EssilorLuxottica, Eyenovia, Genentech, Johnson & Johnson Vision, Lentechs, Novartis, and Vyluma, and is the sole owner of Ridgevue Publishing and Ridgevue Vision.
A version of this article first appeared on Medscape.com.
Dilating eye drops may delay – and perhaps even prevent – the onset of myopia in children, according to findings from a study published in JAMA. The study was conducted by researchers in Hong Kong.
Myopia is irreversible once it takes root and can contribute to other vision problems, such as macular degeneration, retinal detachment, glaucoma, and cataracts. The incidence of nearsightedness has nearly doubled since the 1970s, rising from 25% of the U.S. population to nearly 42%. Children have been particularly affected by the increase; reasons may include spending more time indoors looking at screens, experts say.
“Myopia is an ongoing and growing worldwide concern. This is of particular importance because of the change in children’s lifestyle, such as decreased outdoor time and increased screen time during and after the COVID-19 pandemic,” Jason C. Yam, MPH, of the department of ophthalmology and visual services at the Chinese University of Hong Kong, said in an interview.
Mr. Yam said that, while encouraging children to engage more in outdoor activity and spend less time using screens would help delay myopia, pharmaceutical interventions are needed, given myopia’s potential lifelong effects.
Putting eye drops to the test
In 2020, Mr. Yam and colleagues reported results of the Low-Concentration Atropine for Myopia Progression (LAMP) study, which showed that eye drops containing a solution of 0.05% atropine worked best at slowing the progression of myopia in 4- to 12-year-olds who already had the condition. Atropine relaxes eye muscles, causing dilation.
In that study, Mr. Yam and colleagues measured the rate of change in the eye’s ability to see at a great distance using a unit of measure known as the diopter. The higher the diopter, the more myopic a person’s vision. The 0.05% atropine solution was better at slowing this decline than placebo or solutions that contained a lower concentration of the substance.
The new study enrolled 474 children who were evenly divided by sex. None of the children had myopia when the trial began. Of that starting group, 353 children (age, 4-9 years) completed the study, which involved receiving eye drops once nightly in both eyes for 2 years.
Some children (n = 116) received 0.05% atropine, others (n = 122) received 0.01% atropine, and the rest (n = 115) received placebo drops. Mr. Yam and colleagues assessed how many children in each group had myopia after 2 years, as measured by a decline of at least a half diopter in one eye.
At the 2-year mark, more than half of children who received the placebo drops (61/115) had developed myopia, as had nearly half of those given 0.01% atropine (56/122). But fewer than one-third of children (33/116, 28.4%) who had received the drops with 0.05% atropine developed myopia during that period, the researchers reported.
The percentage of children with myopia in the placebo group (39/128, 30.5%) was larger by the end of the first year of the study than was the share of children in the 0.05% atropine group by the end of the trial. (Between 12 months and 24 months, 13 children in the placebo group left the study.) The main adverse event, in all treatment groups, was discomfort when exposed to bright light, according to the researchers.
“We are continuing the current study with the total intended follow-up duration of at least 6years,” added Mr. Yam, who hopes to determine whether the 0.05% atropine solution not only delays myopia but also prevents it altogether. While myopia is a concern worldwide, the condition is particularly prevalent in East Asia.
Mark A. Bullimore, MCOptom, PhD, FAAO, an adjunct professor at the University of Houston, and a consultant to ophthalmologic companies, called the trial “a landmark study. Finding children who are eligible and parents who are willing to deal with 2 years of drops is no small feat.
“The 0.05% atropine, on average, delays onset of myopia by a year,” Dr. Bullimore noted. He pointed to the similar percentages of myopia with placebo at 12 months, compared with 0.05% atropine 1 year later. He added that few clinicians in the United States use higher than 0.05% atropine for control of myopia because doing so can lead to excessive dilation and difficulty focusing.
While preventing myopia altogether would be ideal, simply delaying its onset can also be of tangible benefit, Bullimore said. In an article published in January, Dr. Bullimore and Noel A. Brennan of Johnson & Johnson Vision showed that delaying the onset of myopia reduces its severity.
“Optometrists prescribe low-concentration atropine already for myopia control, and there’s no reason now – in the light of this study – that they wouldn’t also do it to delay onset,” Dr. Bullimore said.
But in an editorial accompanying the journal article David A. Berntsen, OD, PhD, and Jeffrey J. Walline, OD, PhD, both of the University of Houston, wrote that a change in practice would be premature.
“The evidence presented does not yet warrant a change in the standard care of children because we do not yet know the long-term effects of delaying the onset of myopia with low-concentration atropine,” they wrote.
Identifying which children to consider for treatment is “a challenge,” they noted, because those who are not nearsighted typically do not undergo routine examination unless they have failed a vision test.
“Ultimately, the implementation of vision screenings that include determining a child’s prescription will likely be needed to identify children most likely to become myopic who may benefit from low-concentration atropine,” Dr. Berntsen and Dr. Walline wrote.
Mr. Yam and coinvestigators have applied for a patent on a 0.05% atropine solution. Dr. Bullimore reported relationships with Alcon Research,CooperVision, CorneaGen, EssilorLuxottica, Eyenovia, Genentech, Johnson & Johnson Vision, Lentechs, Novartis, and Vyluma, and is the sole owner of Ridgevue Publishing and Ridgevue Vision.
A version of this article first appeared on Medscape.com.
Dilating eye drops may delay – and perhaps even prevent – the onset of myopia in children, according to findings from a study published in JAMA. The study was conducted by researchers in Hong Kong.
Myopia is irreversible once it takes root and can contribute to other vision problems, such as macular degeneration, retinal detachment, glaucoma, and cataracts. The incidence of nearsightedness has nearly doubled since the 1970s, rising from 25% of the U.S. population to nearly 42%. Children have been particularly affected by the increase; reasons may include spending more time indoors looking at screens, experts say.
“Myopia is an ongoing and growing worldwide concern. This is of particular importance because of the change in children’s lifestyle, such as decreased outdoor time and increased screen time during and after the COVID-19 pandemic,” Jason C. Yam, MPH, of the department of ophthalmology and visual services at the Chinese University of Hong Kong, said in an interview.
Mr. Yam said that, while encouraging children to engage more in outdoor activity and spend less time using screens would help delay myopia, pharmaceutical interventions are needed, given myopia’s potential lifelong effects.
Putting eye drops to the test
In 2020, Mr. Yam and colleagues reported results of the Low-Concentration Atropine for Myopia Progression (LAMP) study, which showed that eye drops containing a solution of 0.05% atropine worked best at slowing the progression of myopia in 4- to 12-year-olds who already had the condition. Atropine relaxes eye muscles, causing dilation.
In that study, Mr. Yam and colleagues measured the rate of change in the eye’s ability to see at a great distance using a unit of measure known as the diopter. The higher the diopter, the more myopic a person’s vision. The 0.05% atropine solution was better at slowing this decline than placebo or solutions that contained a lower concentration of the substance.
The new study enrolled 474 children who were evenly divided by sex. None of the children had myopia when the trial began. Of that starting group, 353 children (age, 4-9 years) completed the study, which involved receiving eye drops once nightly in both eyes for 2 years.
Some children (n = 116) received 0.05% atropine, others (n = 122) received 0.01% atropine, and the rest (n = 115) received placebo drops. Mr. Yam and colleagues assessed how many children in each group had myopia after 2 years, as measured by a decline of at least a half diopter in one eye.
At the 2-year mark, more than half of children who received the placebo drops (61/115) had developed myopia, as had nearly half of those given 0.01% atropine (56/122). But fewer than one-third of children (33/116, 28.4%) who had received the drops with 0.05% atropine developed myopia during that period, the researchers reported.
The percentage of children with myopia in the placebo group (39/128, 30.5%) was larger by the end of the first year of the study than was the share of children in the 0.05% atropine group by the end of the trial. (Between 12 months and 24 months, 13 children in the placebo group left the study.) The main adverse event, in all treatment groups, was discomfort when exposed to bright light, according to the researchers.
“We are continuing the current study with the total intended follow-up duration of at least 6years,” added Mr. Yam, who hopes to determine whether the 0.05% atropine solution not only delays myopia but also prevents it altogether. While myopia is a concern worldwide, the condition is particularly prevalent in East Asia.
Mark A. Bullimore, MCOptom, PhD, FAAO, an adjunct professor at the University of Houston, and a consultant to ophthalmologic companies, called the trial “a landmark study. Finding children who are eligible and parents who are willing to deal with 2 years of drops is no small feat.
“The 0.05% atropine, on average, delays onset of myopia by a year,” Dr. Bullimore noted. He pointed to the similar percentages of myopia with placebo at 12 months, compared with 0.05% atropine 1 year later. He added that few clinicians in the United States use higher than 0.05% atropine for control of myopia because doing so can lead to excessive dilation and difficulty focusing.
While preventing myopia altogether would be ideal, simply delaying its onset can also be of tangible benefit, Bullimore said. In an article published in January, Dr. Bullimore and Noel A. Brennan of Johnson & Johnson Vision showed that delaying the onset of myopia reduces its severity.
“Optometrists prescribe low-concentration atropine already for myopia control, and there’s no reason now – in the light of this study – that they wouldn’t also do it to delay onset,” Dr. Bullimore said.
But in an editorial accompanying the journal article David A. Berntsen, OD, PhD, and Jeffrey J. Walline, OD, PhD, both of the University of Houston, wrote that a change in practice would be premature.
“The evidence presented does not yet warrant a change in the standard care of children because we do not yet know the long-term effects of delaying the onset of myopia with low-concentration atropine,” they wrote.
Identifying which children to consider for treatment is “a challenge,” they noted, because those who are not nearsighted typically do not undergo routine examination unless they have failed a vision test.
“Ultimately, the implementation of vision screenings that include determining a child’s prescription will likely be needed to identify children most likely to become myopic who may benefit from low-concentration atropine,” Dr. Berntsen and Dr. Walline wrote.
Mr. Yam and coinvestigators have applied for a patent on a 0.05% atropine solution. Dr. Bullimore reported relationships with Alcon Research,CooperVision, CorneaGen, EssilorLuxottica, Eyenovia, Genentech, Johnson & Johnson Vision, Lentechs, Novartis, and Vyluma, and is the sole owner of Ridgevue Publishing and Ridgevue Vision.
A version of this article first appeared on Medscape.com.
FROM JAMA