User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Higher triglycerides linked to lower dementia risk
TOPLINE:
a large study of community-dwelling older adults suggests.
METHODOLOGY:
- The analysis included 18,294 participants, median age 75 years and median triglyceride level 106 mg/dL, from the Aspirin in Reducing Events in the Elderly (ASPREE) study, a placebo-controlled, randomized trial of daily low-dose aspirin in older people without dementia or history of cardiovascular disease (CVD) at recruitment.
- Researchers repeated their main analyses in a sub-cohort of 13,976 subjects with APOE epsilon-4 genetic data, and an external cohort of 68,200 participants, mean age 66.9 years and a median nonfasting triglyceride of 139 mg/dL, from the UK biobank, followed for a median of 12.5 years.
- The main outcome was incident dementia over 6.4 years and secondary outcomes included changes in composite cognitive function and domain-specific cognition.
- Researchers controlled for a number of potential confounders, including age, sex, race, smoking, alcohol consumption, education, family history of dementia, diabetes, hypertension, and statin use.
TAKEAWAY:
- Every doubling of baseline triglycerides was associated with an 18% lower risk of incident dementia across the entire study cohort (adjusted hazard ratio, 0.82) and in participants with genotypic data (aHR, 0.82) and a 17% lower risk in the external UK Biobank cohort (aHR, 0.83) (P ≤ .01 for all).
- In the entire cohort, the risk for dementia was 15% lower in those with triglyceride levels at 63-106 mg/dL (aHR, 0.85); 24% lower in those at 107-186 mg/dL (aHR, 0.76); and 36% lower for those with levels higher than 187 mg/dL (aHR, 0.64), compared with individuals with levels below 62 mg/dL (P for trend <.001).
- The direction and magnitude of the inverse association between triglycerides and dementia risk were not modified by age, sex, or risk factors related to triglycerides or dementia.
- In the entire study cohort, higher triglyceride levels were significantly associated with slower decline in global cognition (P = .02), composite cognition (P = .03), and a borderline significantly slower decline in episodic memory (P = .05).
IN PRACTICE:
“Triglyceride levels may serve as a useful predictor for dementia risk and cognitive decline in older populations,” the investigators write. Higher triglyceride levels may reflect better overall health and/or lifestyle behaviors that protect against dementia.
SOURCE:
The study was led by Zhen Zhou, of Monash University, Melbourne. It was published online in Neurology.
LIMITATIONS:
The study can’t establish a causal relationship between triglyceride levels and dementia or fully exclude reverse causality. As most ASPREE participants had normal to high-normal triglyceride levels, the results can’t be generalized to those with severe hypertriglyceridemia. The findings are unique to older people without CVD and may not be generalizable to other populations.
DISCLOSURES:
The study received support from the Royal Australian College of General Practitioners (RACGP)/HCF Research Foundation. Dr. Zhou reported receiving salary from the RACGP/HCF Research Foundation.
A version of this article first appeared on Medscape.com.
TOPLINE:
a large study of community-dwelling older adults suggests.
METHODOLOGY:
- The analysis included 18,294 participants, median age 75 years and median triglyceride level 106 mg/dL, from the Aspirin in Reducing Events in the Elderly (ASPREE) study, a placebo-controlled, randomized trial of daily low-dose aspirin in older people without dementia or history of cardiovascular disease (CVD) at recruitment.
- Researchers repeated their main analyses in a sub-cohort of 13,976 subjects with APOE epsilon-4 genetic data, and an external cohort of 68,200 participants, mean age 66.9 years and a median nonfasting triglyceride of 139 mg/dL, from the UK biobank, followed for a median of 12.5 years.
- The main outcome was incident dementia over 6.4 years and secondary outcomes included changes in composite cognitive function and domain-specific cognition.
- Researchers controlled for a number of potential confounders, including age, sex, race, smoking, alcohol consumption, education, family history of dementia, diabetes, hypertension, and statin use.
TAKEAWAY:
- Every doubling of baseline triglycerides was associated with an 18% lower risk of incident dementia across the entire study cohort (adjusted hazard ratio, 0.82) and in participants with genotypic data (aHR, 0.82) and a 17% lower risk in the external UK Biobank cohort (aHR, 0.83) (P ≤ .01 for all).
- In the entire cohort, the risk for dementia was 15% lower in those with triglyceride levels at 63-106 mg/dL (aHR, 0.85); 24% lower in those at 107-186 mg/dL (aHR, 0.76); and 36% lower for those with levels higher than 187 mg/dL (aHR, 0.64), compared with individuals with levels below 62 mg/dL (P for trend <.001).
- The direction and magnitude of the inverse association between triglycerides and dementia risk were not modified by age, sex, or risk factors related to triglycerides or dementia.
- In the entire study cohort, higher triglyceride levels were significantly associated with slower decline in global cognition (P = .02), composite cognition (P = .03), and a borderline significantly slower decline in episodic memory (P = .05).
IN PRACTICE:
“Triglyceride levels may serve as a useful predictor for dementia risk and cognitive decline in older populations,” the investigators write. Higher triglyceride levels may reflect better overall health and/or lifestyle behaviors that protect against dementia.
SOURCE:
The study was led by Zhen Zhou, of Monash University, Melbourne. It was published online in Neurology.
LIMITATIONS:
The study can’t establish a causal relationship between triglyceride levels and dementia or fully exclude reverse causality. As most ASPREE participants had normal to high-normal triglyceride levels, the results can’t be generalized to those with severe hypertriglyceridemia. The findings are unique to older people without CVD and may not be generalizable to other populations.
DISCLOSURES:
The study received support from the Royal Australian College of General Practitioners (RACGP)/HCF Research Foundation. Dr. Zhou reported receiving salary from the RACGP/HCF Research Foundation.
A version of this article first appeared on Medscape.com.
TOPLINE:
a large study of community-dwelling older adults suggests.
METHODOLOGY:
- The analysis included 18,294 participants, median age 75 years and median triglyceride level 106 mg/dL, from the Aspirin in Reducing Events in the Elderly (ASPREE) study, a placebo-controlled, randomized trial of daily low-dose aspirin in older people without dementia or history of cardiovascular disease (CVD) at recruitment.
- Researchers repeated their main analyses in a sub-cohort of 13,976 subjects with APOE epsilon-4 genetic data, and an external cohort of 68,200 participants, mean age 66.9 years and a median nonfasting triglyceride of 139 mg/dL, from the UK biobank, followed for a median of 12.5 years.
- The main outcome was incident dementia over 6.4 years and secondary outcomes included changes in composite cognitive function and domain-specific cognition.
- Researchers controlled for a number of potential confounders, including age, sex, race, smoking, alcohol consumption, education, family history of dementia, diabetes, hypertension, and statin use.
TAKEAWAY:
- Every doubling of baseline triglycerides was associated with an 18% lower risk of incident dementia across the entire study cohort (adjusted hazard ratio, 0.82) and in participants with genotypic data (aHR, 0.82) and a 17% lower risk in the external UK Biobank cohort (aHR, 0.83) (P ≤ .01 for all).
- In the entire cohort, the risk for dementia was 15% lower in those with triglyceride levels at 63-106 mg/dL (aHR, 0.85); 24% lower in those at 107-186 mg/dL (aHR, 0.76); and 36% lower for those with levels higher than 187 mg/dL (aHR, 0.64), compared with individuals with levels below 62 mg/dL (P for trend <.001).
- The direction and magnitude of the inverse association between triglycerides and dementia risk were not modified by age, sex, or risk factors related to triglycerides or dementia.
- In the entire study cohort, higher triglyceride levels were significantly associated with slower decline in global cognition (P = .02), composite cognition (P = .03), and a borderline significantly slower decline in episodic memory (P = .05).
IN PRACTICE:
“Triglyceride levels may serve as a useful predictor for dementia risk and cognitive decline in older populations,” the investigators write. Higher triglyceride levels may reflect better overall health and/or lifestyle behaviors that protect against dementia.
SOURCE:
The study was led by Zhen Zhou, of Monash University, Melbourne. It was published online in Neurology.
LIMITATIONS:
The study can’t establish a causal relationship between triglyceride levels and dementia or fully exclude reverse causality. As most ASPREE participants had normal to high-normal triglyceride levels, the results can’t be generalized to those with severe hypertriglyceridemia. The findings are unique to older people without CVD and may not be generalizable to other populations.
DISCLOSURES:
The study received support from the Royal Australian College of General Practitioners (RACGP)/HCF Research Foundation. Dr. Zhou reported receiving salary from the RACGP/HCF Research Foundation.
A version of this article first appeared on Medscape.com.
Teens streaming on Twitch vulnerable to predators
WASHINGTON – Half of youth broadcasting live streams on the online platform Twitch revealed their real-world location, and nearly half provided their name to viewers, according to research presented at the annual meeting of the American Academy of Pediatrics. It took researchers less than 5 minutes – and sometimes as little as 12 seconds – to find minors in different video game categories, suggesting the environment offers opportunities to predators to gain sensitive information about minors, reported Fiona Dubrosa, BS, BA, a visiting scholar at Cohen Children’s Medical Center, New York, and colleagues.
A ‘clandestine, threatening digital environment’
the authors concluded. “The nature of live streaming makes it particularly dangerous, as there is no way to take back information that has been revealed or regulate content or viewers. Parents and pediatricians should be aware of the dangers presented by Twitch and other live-streaming platforms and counsel children on best practices for Internet safety.”
Twitch is an online streaming platform where people can watch creator’s live content, such as music performances or narrating real-time video game playing. The platform requires live streamers to be 13 years old with a valid email address or phone number to create an account, but no age restrictions or identification requirements exist for viewers, “potentially putting minors in danger of being watched, followed, and groomed by predators,” the researchers noted. They added that people following different streamers receive notifications when those streamers are live. Further, “viewers can donate money to streamers, which can make it easier for predators to manipulate, track, and encourage risky behaviors from minors.”
To better understand the risks the platform might pose to minors, the researchers searched for and analyzed popular video game live streams that appeared to be streamed by minors who had their cameras on and their faces visible. Then the researchers noted the name of the video game, the topics discussed by the streamers, the time it took to find minors under each game, and each streamer’s age, name, follower count, location, streaming schedule, and social media links for money donations.
The researchers analyzed 100 Twitch streamers who were minors, who had a combined 1,755,452 million followers. Nearly half the streamers (47%) provided their presumably real names, and half (50%) gave out their location. Nearly two-thirds (64%) linked other social media accounts they had and encouraged viewers to follow them. Detailed schedules of when they would be live were available for 38% of the streamers, and 37% of the minor streamers were accepting money donations.
Only 11% of the discussion on the streams revealed personal details, most often related to trying on different outfits for viewers and talking about real-world locations they liked to visit. The researchers needed anywhere from 12 seconds to 5 minutes to find a minor in each game category.
”Young users clearly feel a false sense of safety on the platform; a significant proportion were willing to reveal personal information despite having no knowledge of who might be listening,” the researchers said. “The donation system provides a menacing avenue for manipulation and continued exploitation of minors. Our findings reveal the need for stricter age limitations for streamers and more stringent identity verification of audience members on Twitch.”
Open-minded parental guidance is warranted
Jenny Radesky, MD, a developmental behavioral pediatrician and media researcher at University of Michigan Medicine, Ann Arbor, was not surprised that many teens live stream on Twitch since it’s a popular platform for video gaming, but she was surprised at how many revealed their locations and other personal details.
“I suspect that they do this to build closeness with their viewers, by seeming more authentic,” said Dr. Radesky, who was not involved in the study. “It is this type of parasocial relationship with influencers and gamers that keeps an audience engaged, and encourages future viewing and purchases.”
Their willingness to share personal details suggests it’s important to conduct qualitative research to find out how teen live streamers think about privacy risks, what privacy settings they can use and choose to use, and how they handle inappropriate contact from adults, Dr. Radesky said.
Meanwhile, parents should talk with their kids in an open-minded way about what platforms they use and what they like and dislike about them. She recommended parents read the Common Sense Media guide about different social platforms ”to understand what attracts kids to content on specific sites, what their pitfalls are, and what types of privacy and safety settings are available.”
“A child or teen is much more likely to be honest about negative experiences online if they think their parent will hear them out – not judge them or take away their tech. No teen wants to talk with a panicky parent,” Dr. Radesky said.
David Hill, MD, a hospitalist pediatrician for Goldsboro Pediatrics in Wayne County, North Carolina, who also specializes in media communication, said that Twitch is just one example of a social media platform where children can encounter a variety of dangers, including sometimes adult predators.
“This just highlights the importance of parents having an ongoing conversation with their children about how they use their social media platforms and ensuring, just as we do with learning to ride a bicycle or learning to drive a car, that they apply some basic rules of safety,” Dr. Hill said. Then it’s important to keep coming back to that conversation “again and again as they grow and change and as those platforms change to ensure that those kids are continuing to apply those rules consistently.
“The best way for parents to keep up is ask your kids,” he said. “They love to share. They love to teach. They love to be in a position to show you something, especially if it’s something that interests them.”
An example of a rule would be setting personal accounts to private, not public, by default, Dr. Radesky said. “When interviewed, teens often say that they feel intruded upon by older people ‘stalking’ them or trying to connect with them on social platforms,” so making an account private can reduce those opportunities.
For teens who specifically want to create content on social platforms, parent oversight is needed, she said, but she acknowledged it can be a lot of work. “This might take the form of talking about what a teen plans to post before they do, expectations for positive behaviors or language, plans for privacy settings (such as public vs. private accounts), and what to do with trolls or hateful comment,” she said. “Parents may want to follow their child’s account to check in on it.”
Useful advice
Dr. Radesky also provided a handful of talking points that pediatricians can use in talking with patients who use these platforms:
- Keep your account private to just your friends and people you want to interact with. There are a lot of people on the Internet that you don’t want intruding upon your social life.
- Maintain your feed and the accounts you follow to keep it positive, entertaining, and not a source of stress or self-doubt. Content creators are always trying to grab your attention in new ways, some of which are rude or dehumanizing, so don’t waste your time on things that bring you down.
- Talk about why you want to post or live stream. Is it to get reactions or feel validated? If so, can you find other ways to feel validated that don’t require performing for other people? Is it to share a special skill? If so, how do you keep your posts creative and community building rather than attention grabbing? And how can you keep your parents involved so that they can help you navigate challenges?”
Ms. Dubrosa and Dr. Hill had no disclosures. Dr. Radesky is a consultant for Melissa & Doug. No information on external funding was provided.
WASHINGTON – Half of youth broadcasting live streams on the online platform Twitch revealed their real-world location, and nearly half provided their name to viewers, according to research presented at the annual meeting of the American Academy of Pediatrics. It took researchers less than 5 minutes – and sometimes as little as 12 seconds – to find minors in different video game categories, suggesting the environment offers opportunities to predators to gain sensitive information about minors, reported Fiona Dubrosa, BS, BA, a visiting scholar at Cohen Children’s Medical Center, New York, and colleagues.
A ‘clandestine, threatening digital environment’
the authors concluded. “The nature of live streaming makes it particularly dangerous, as there is no way to take back information that has been revealed or regulate content or viewers. Parents and pediatricians should be aware of the dangers presented by Twitch and other live-streaming platforms and counsel children on best practices for Internet safety.”
Twitch is an online streaming platform where people can watch creator’s live content, such as music performances or narrating real-time video game playing. The platform requires live streamers to be 13 years old with a valid email address or phone number to create an account, but no age restrictions or identification requirements exist for viewers, “potentially putting minors in danger of being watched, followed, and groomed by predators,” the researchers noted. They added that people following different streamers receive notifications when those streamers are live. Further, “viewers can donate money to streamers, which can make it easier for predators to manipulate, track, and encourage risky behaviors from minors.”
To better understand the risks the platform might pose to minors, the researchers searched for and analyzed popular video game live streams that appeared to be streamed by minors who had their cameras on and their faces visible. Then the researchers noted the name of the video game, the topics discussed by the streamers, the time it took to find minors under each game, and each streamer’s age, name, follower count, location, streaming schedule, and social media links for money donations.
The researchers analyzed 100 Twitch streamers who were minors, who had a combined 1,755,452 million followers. Nearly half the streamers (47%) provided their presumably real names, and half (50%) gave out their location. Nearly two-thirds (64%) linked other social media accounts they had and encouraged viewers to follow them. Detailed schedules of when they would be live were available for 38% of the streamers, and 37% of the minor streamers were accepting money donations.
Only 11% of the discussion on the streams revealed personal details, most often related to trying on different outfits for viewers and talking about real-world locations they liked to visit. The researchers needed anywhere from 12 seconds to 5 minutes to find a minor in each game category.
”Young users clearly feel a false sense of safety on the platform; a significant proportion were willing to reveal personal information despite having no knowledge of who might be listening,” the researchers said. “The donation system provides a menacing avenue for manipulation and continued exploitation of minors. Our findings reveal the need for stricter age limitations for streamers and more stringent identity verification of audience members on Twitch.”
Open-minded parental guidance is warranted
Jenny Radesky, MD, a developmental behavioral pediatrician and media researcher at University of Michigan Medicine, Ann Arbor, was not surprised that many teens live stream on Twitch since it’s a popular platform for video gaming, but she was surprised at how many revealed their locations and other personal details.
“I suspect that they do this to build closeness with their viewers, by seeming more authentic,” said Dr. Radesky, who was not involved in the study. “It is this type of parasocial relationship with influencers and gamers that keeps an audience engaged, and encourages future viewing and purchases.”
Their willingness to share personal details suggests it’s important to conduct qualitative research to find out how teen live streamers think about privacy risks, what privacy settings they can use and choose to use, and how they handle inappropriate contact from adults, Dr. Radesky said.
Meanwhile, parents should talk with their kids in an open-minded way about what platforms they use and what they like and dislike about them. She recommended parents read the Common Sense Media guide about different social platforms ”to understand what attracts kids to content on specific sites, what their pitfalls are, and what types of privacy and safety settings are available.”
“A child or teen is much more likely to be honest about negative experiences online if they think their parent will hear them out – not judge them or take away their tech. No teen wants to talk with a panicky parent,” Dr. Radesky said.
David Hill, MD, a hospitalist pediatrician for Goldsboro Pediatrics in Wayne County, North Carolina, who also specializes in media communication, said that Twitch is just one example of a social media platform where children can encounter a variety of dangers, including sometimes adult predators.
“This just highlights the importance of parents having an ongoing conversation with their children about how they use their social media platforms and ensuring, just as we do with learning to ride a bicycle or learning to drive a car, that they apply some basic rules of safety,” Dr. Hill said. Then it’s important to keep coming back to that conversation “again and again as they grow and change and as those platforms change to ensure that those kids are continuing to apply those rules consistently.
“The best way for parents to keep up is ask your kids,” he said. “They love to share. They love to teach. They love to be in a position to show you something, especially if it’s something that interests them.”
An example of a rule would be setting personal accounts to private, not public, by default, Dr. Radesky said. “When interviewed, teens often say that they feel intruded upon by older people ‘stalking’ them or trying to connect with them on social platforms,” so making an account private can reduce those opportunities.
For teens who specifically want to create content on social platforms, parent oversight is needed, she said, but she acknowledged it can be a lot of work. “This might take the form of talking about what a teen plans to post before they do, expectations for positive behaviors or language, plans for privacy settings (such as public vs. private accounts), and what to do with trolls or hateful comment,” she said. “Parents may want to follow their child’s account to check in on it.”
Useful advice
Dr. Radesky also provided a handful of talking points that pediatricians can use in talking with patients who use these platforms:
- Keep your account private to just your friends and people you want to interact with. There are a lot of people on the Internet that you don’t want intruding upon your social life.
- Maintain your feed and the accounts you follow to keep it positive, entertaining, and not a source of stress or self-doubt. Content creators are always trying to grab your attention in new ways, some of which are rude or dehumanizing, so don’t waste your time on things that bring you down.
- Talk about why you want to post or live stream. Is it to get reactions or feel validated? If so, can you find other ways to feel validated that don’t require performing for other people? Is it to share a special skill? If so, how do you keep your posts creative and community building rather than attention grabbing? And how can you keep your parents involved so that they can help you navigate challenges?”
Ms. Dubrosa and Dr. Hill had no disclosures. Dr. Radesky is a consultant for Melissa & Doug. No information on external funding was provided.
WASHINGTON – Half of youth broadcasting live streams on the online platform Twitch revealed their real-world location, and nearly half provided their name to viewers, according to research presented at the annual meeting of the American Academy of Pediatrics. It took researchers less than 5 minutes – and sometimes as little as 12 seconds – to find minors in different video game categories, suggesting the environment offers opportunities to predators to gain sensitive information about minors, reported Fiona Dubrosa, BS, BA, a visiting scholar at Cohen Children’s Medical Center, New York, and colleagues.
A ‘clandestine, threatening digital environment’
the authors concluded. “The nature of live streaming makes it particularly dangerous, as there is no way to take back information that has been revealed or regulate content or viewers. Parents and pediatricians should be aware of the dangers presented by Twitch and other live-streaming platforms and counsel children on best practices for Internet safety.”
Twitch is an online streaming platform where people can watch creator’s live content, such as music performances or narrating real-time video game playing. The platform requires live streamers to be 13 years old with a valid email address or phone number to create an account, but no age restrictions or identification requirements exist for viewers, “potentially putting minors in danger of being watched, followed, and groomed by predators,” the researchers noted. They added that people following different streamers receive notifications when those streamers are live. Further, “viewers can donate money to streamers, which can make it easier for predators to manipulate, track, and encourage risky behaviors from minors.”
To better understand the risks the platform might pose to minors, the researchers searched for and analyzed popular video game live streams that appeared to be streamed by minors who had their cameras on and their faces visible. Then the researchers noted the name of the video game, the topics discussed by the streamers, the time it took to find minors under each game, and each streamer’s age, name, follower count, location, streaming schedule, and social media links for money donations.
The researchers analyzed 100 Twitch streamers who were minors, who had a combined 1,755,452 million followers. Nearly half the streamers (47%) provided their presumably real names, and half (50%) gave out their location. Nearly two-thirds (64%) linked other social media accounts they had and encouraged viewers to follow them. Detailed schedules of when they would be live were available for 38% of the streamers, and 37% of the minor streamers were accepting money donations.
Only 11% of the discussion on the streams revealed personal details, most often related to trying on different outfits for viewers and talking about real-world locations they liked to visit. The researchers needed anywhere from 12 seconds to 5 minutes to find a minor in each game category.
”Young users clearly feel a false sense of safety on the platform; a significant proportion were willing to reveal personal information despite having no knowledge of who might be listening,” the researchers said. “The donation system provides a menacing avenue for manipulation and continued exploitation of minors. Our findings reveal the need for stricter age limitations for streamers and more stringent identity verification of audience members on Twitch.”
Open-minded parental guidance is warranted
Jenny Radesky, MD, a developmental behavioral pediatrician and media researcher at University of Michigan Medicine, Ann Arbor, was not surprised that many teens live stream on Twitch since it’s a popular platform for video gaming, but she was surprised at how many revealed their locations and other personal details.
“I suspect that they do this to build closeness with their viewers, by seeming more authentic,” said Dr. Radesky, who was not involved in the study. “It is this type of parasocial relationship with influencers and gamers that keeps an audience engaged, and encourages future viewing and purchases.”
Their willingness to share personal details suggests it’s important to conduct qualitative research to find out how teen live streamers think about privacy risks, what privacy settings they can use and choose to use, and how they handle inappropriate contact from adults, Dr. Radesky said.
Meanwhile, parents should talk with their kids in an open-minded way about what platforms they use and what they like and dislike about them. She recommended parents read the Common Sense Media guide about different social platforms ”to understand what attracts kids to content on specific sites, what their pitfalls are, and what types of privacy and safety settings are available.”
“A child or teen is much more likely to be honest about negative experiences online if they think their parent will hear them out – not judge them or take away their tech. No teen wants to talk with a panicky parent,” Dr. Radesky said.
David Hill, MD, a hospitalist pediatrician for Goldsboro Pediatrics in Wayne County, North Carolina, who also specializes in media communication, said that Twitch is just one example of a social media platform where children can encounter a variety of dangers, including sometimes adult predators.
“This just highlights the importance of parents having an ongoing conversation with their children about how they use their social media platforms and ensuring, just as we do with learning to ride a bicycle or learning to drive a car, that they apply some basic rules of safety,” Dr. Hill said. Then it’s important to keep coming back to that conversation “again and again as they grow and change and as those platforms change to ensure that those kids are continuing to apply those rules consistently.
“The best way for parents to keep up is ask your kids,” he said. “They love to share. They love to teach. They love to be in a position to show you something, especially if it’s something that interests them.”
An example of a rule would be setting personal accounts to private, not public, by default, Dr. Radesky said. “When interviewed, teens often say that they feel intruded upon by older people ‘stalking’ them or trying to connect with them on social platforms,” so making an account private can reduce those opportunities.
For teens who specifically want to create content on social platforms, parent oversight is needed, she said, but she acknowledged it can be a lot of work. “This might take the form of talking about what a teen plans to post before they do, expectations for positive behaviors or language, plans for privacy settings (such as public vs. private accounts), and what to do with trolls or hateful comment,” she said. “Parents may want to follow their child’s account to check in on it.”
Useful advice
Dr. Radesky also provided a handful of talking points that pediatricians can use in talking with patients who use these platforms:
- Keep your account private to just your friends and people you want to interact with. There are a lot of people on the Internet that you don’t want intruding upon your social life.
- Maintain your feed and the accounts you follow to keep it positive, entertaining, and not a source of stress or self-doubt. Content creators are always trying to grab your attention in new ways, some of which are rude or dehumanizing, so don’t waste your time on things that bring you down.
- Talk about why you want to post or live stream. Is it to get reactions or feel validated? If so, can you find other ways to feel validated that don’t require performing for other people? Is it to share a special skill? If so, how do you keep your posts creative and community building rather than attention grabbing? And how can you keep your parents involved so that they can help you navigate challenges?”
Ms. Dubrosa and Dr. Hill had no disclosures. Dr. Radesky is a consultant for Melissa & Doug. No information on external funding was provided.
AT AAP 2023
Psychedelic therapy tied to reduced depression, anxiety
TOPLINE:
Perhaps most surprising to investigators, however, was that treatment was also associated with improved cognitive scores in the veterans, many of whom had traumatic brain injuries.
METHODOLOGY:
- Investigators reviewed clinical charts of 86 SOFVs who received psychedelic-assisted treatment at a therapeutic program in Mexico, 86% of whom sustained head injuries during deployment.
- On the first day of the study, participants received a single oral dose (10 mg/kg) of ibogaine hydrochloride in a group setting with two to five other attendees and spent the next day reflecting on their experience with program staff.
- On the third day, participants inhaled 5-MeO-DMT in three incremental doses for a total of 50 mg and were then invited to reflect on their experience both individually and with the group of peers who shared the experience.
- Follow-up surveys at 1, 3, and 6 months posttreatment between September 2019 to March 2021 measured symptoms of posttraumatic stress disorder, cognitive functioning, generalized anxiety disorder, depression, and quality of life.
TAKEAWAY:
- There were significant improvements in self-reported PTSD symptoms, depression, anxiety, insomnia severity, anger, and a large improvement in self-reported satisfaction with life (P < .001 for all).
- Participants reported significant increases in psychological flexibility (P < .001), cognitive functioning (P < .001), and postconcussive symptoms (P < .001).
- Treatment was also associated with a significant reduction in suicidal ideation from pretreatment to 1-month follow-up (P < .01).
IN PRACTICE:
“If consistently replicated, this could have major implications for the landscape of mental health care if people are able to experience significant and sustained healing with 3 days of intensive treatment, relative to our traditionally available interventions that require 8-12 weeks of weekly therapy (for example, gold standard talk therapies such as [prolonged exposure] or [cognitive processing therapy]), or daily use of a pharmacotherapy such as [a selective serotonin reuptake inhibitor] for months to years,” study authors write.
SOURCE:
Alan Kooi Davis, PhD, of the Center for Psychedelic Drug Research and Education at Ohio State University, led the study, which was published online in the American Journal of Drug and Alcohol Abuse.
LIMITATIONS:
Study assessments are based solely on self-report measures. Future research should implement carefully designed batteries that include both self-report and gold-standard clinician-administered measures to better capture symptom improvement and other information. The sample also lacked diversity with regard to race, religion, and socioeconomic status.
DISCLOSURES:
The study was funded by Veterans Exploring Treatment Solutions. Dr. Davis is a board member at Source Resource Foundation and a lead trainer at Fluence. Full disclosures are included in the original article.
A version of this article first appeared on Medscape.com.
TOPLINE:
Perhaps most surprising to investigators, however, was that treatment was also associated with improved cognitive scores in the veterans, many of whom had traumatic brain injuries.
METHODOLOGY:
- Investigators reviewed clinical charts of 86 SOFVs who received psychedelic-assisted treatment at a therapeutic program in Mexico, 86% of whom sustained head injuries during deployment.
- On the first day of the study, participants received a single oral dose (10 mg/kg) of ibogaine hydrochloride in a group setting with two to five other attendees and spent the next day reflecting on their experience with program staff.
- On the third day, participants inhaled 5-MeO-DMT in three incremental doses for a total of 50 mg and were then invited to reflect on their experience both individually and with the group of peers who shared the experience.
- Follow-up surveys at 1, 3, and 6 months posttreatment between September 2019 to March 2021 measured symptoms of posttraumatic stress disorder, cognitive functioning, generalized anxiety disorder, depression, and quality of life.
TAKEAWAY:
- There were significant improvements in self-reported PTSD symptoms, depression, anxiety, insomnia severity, anger, and a large improvement in self-reported satisfaction with life (P < .001 for all).
- Participants reported significant increases in psychological flexibility (P < .001), cognitive functioning (P < .001), and postconcussive symptoms (P < .001).
- Treatment was also associated with a significant reduction in suicidal ideation from pretreatment to 1-month follow-up (P < .01).
IN PRACTICE:
“If consistently replicated, this could have major implications for the landscape of mental health care if people are able to experience significant and sustained healing with 3 days of intensive treatment, relative to our traditionally available interventions that require 8-12 weeks of weekly therapy (for example, gold standard talk therapies such as [prolonged exposure] or [cognitive processing therapy]), or daily use of a pharmacotherapy such as [a selective serotonin reuptake inhibitor] for months to years,” study authors write.
SOURCE:
Alan Kooi Davis, PhD, of the Center for Psychedelic Drug Research and Education at Ohio State University, led the study, which was published online in the American Journal of Drug and Alcohol Abuse.
LIMITATIONS:
Study assessments are based solely on self-report measures. Future research should implement carefully designed batteries that include both self-report and gold-standard clinician-administered measures to better capture symptom improvement and other information. The sample also lacked diversity with regard to race, religion, and socioeconomic status.
DISCLOSURES:
The study was funded by Veterans Exploring Treatment Solutions. Dr. Davis is a board member at Source Resource Foundation and a lead trainer at Fluence. Full disclosures are included in the original article.
A version of this article first appeared on Medscape.com.
TOPLINE:
Perhaps most surprising to investigators, however, was that treatment was also associated with improved cognitive scores in the veterans, many of whom had traumatic brain injuries.
METHODOLOGY:
- Investigators reviewed clinical charts of 86 SOFVs who received psychedelic-assisted treatment at a therapeutic program in Mexico, 86% of whom sustained head injuries during deployment.
- On the first day of the study, participants received a single oral dose (10 mg/kg) of ibogaine hydrochloride in a group setting with two to five other attendees and spent the next day reflecting on their experience with program staff.
- On the third day, participants inhaled 5-MeO-DMT in three incremental doses for a total of 50 mg and were then invited to reflect on their experience both individually and with the group of peers who shared the experience.
- Follow-up surveys at 1, 3, and 6 months posttreatment between September 2019 to March 2021 measured symptoms of posttraumatic stress disorder, cognitive functioning, generalized anxiety disorder, depression, and quality of life.
TAKEAWAY:
- There were significant improvements in self-reported PTSD symptoms, depression, anxiety, insomnia severity, anger, and a large improvement in self-reported satisfaction with life (P < .001 for all).
- Participants reported significant increases in psychological flexibility (P < .001), cognitive functioning (P < .001), and postconcussive symptoms (P < .001).
- Treatment was also associated with a significant reduction in suicidal ideation from pretreatment to 1-month follow-up (P < .01).
IN PRACTICE:
“If consistently replicated, this could have major implications for the landscape of mental health care if people are able to experience significant and sustained healing with 3 days of intensive treatment, relative to our traditionally available interventions that require 8-12 weeks of weekly therapy (for example, gold standard talk therapies such as [prolonged exposure] or [cognitive processing therapy]), or daily use of a pharmacotherapy such as [a selective serotonin reuptake inhibitor] for months to years,” study authors write.
SOURCE:
Alan Kooi Davis, PhD, of the Center for Psychedelic Drug Research and Education at Ohio State University, led the study, which was published online in the American Journal of Drug and Alcohol Abuse.
LIMITATIONS:
Study assessments are based solely on self-report measures. Future research should implement carefully designed batteries that include both self-report and gold-standard clinician-administered measures to better capture symptom improvement and other information. The sample also lacked diversity with regard to race, religion, and socioeconomic status.
DISCLOSURES:
The study was funded by Veterans Exploring Treatment Solutions. Dr. Davis is a board member at Source Resource Foundation and a lead trainer at Fluence. Full disclosures are included in the original article.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF DRUG AND ALCOHOL ABUSE
Air pollution tied to postpartum depression
TOPLINE:
METHODOLOGY:
- Researchers analyzed data on 340,679 women who had singleton live births at Kaiser Permanente Southern California facilities between 2008 and 2016.
- Ambient air pollution exposures were assessed based on maternal residential addresses using monthly averages of particulate matter ≤ 2.5 mcm (PM2.5), PM ≤ 10 mcm (PM10), nitrogen dioxide, and ozone from Environmental Protection Agency monitoring stations.
- Constituents of PM2.5 (sulfate, nitrate, ammonium, organic matter, and black carbon) were obtained from models based on satellite, ground-based monitor, and chemical transport modeling data.
- Women with an Edinburgh Postnatal Depression Scale score of at least 10 during the first 6 months postpartum were referred for further assessment, including diagnosis and treatment.
TAKEAWAY:
- A total of 25,674 women had PPD (7.5%).
- Positive associations were observed between PPD ozone (adjusted odds ratio, 1.09), PM10 (aOR, 1.02), and PM2.5 (aOR, 1.02), with no statistically significant association with nitrogen dioxide.
- Among PM2.5 constituents, black carbon had the strongest association with PPD (OR 1.04).
- Overall, a higher risk of PPD was associated with ozone exposure during the entire pregnancy and postpartum periods and with PM exposure during the late pregnancy and postpartum periods.
IN PRACTICE:
“These findings suggest that long-term antepartum and postpartum air pollution exposure is a potentially modifiable environmental risk factor for PPD and an important public health issue to address for improved maternal mental health,” the authors wrote.
SOURCE:
The study, with first author Yi Sun, PhD, Chinese Academy of Medical Sciences and Peking Medical College, Beijing, was published online in JAMA Network Open.
LIMITATIONS:
Postpartum exposures were estimated using only maternal address at delivery, which may have led to exposure misclassification. Potential exposure misclassifications may also exist since indoor and personal exposure levels could not be estimated. Although several covariates were adjusted for, some residual or unmeasured covariates were inevitable due to data unavailability, such as psychiatric history, adverse life events, and marital status, which may affect mental health.
DISCLOSURES:
This study was supported by a grant from the National Institute of Environmental Health Sciences. The authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers analyzed data on 340,679 women who had singleton live births at Kaiser Permanente Southern California facilities between 2008 and 2016.
- Ambient air pollution exposures were assessed based on maternal residential addresses using monthly averages of particulate matter ≤ 2.5 mcm (PM2.5), PM ≤ 10 mcm (PM10), nitrogen dioxide, and ozone from Environmental Protection Agency monitoring stations.
- Constituents of PM2.5 (sulfate, nitrate, ammonium, organic matter, and black carbon) were obtained from models based on satellite, ground-based monitor, and chemical transport modeling data.
- Women with an Edinburgh Postnatal Depression Scale score of at least 10 during the first 6 months postpartum were referred for further assessment, including diagnosis and treatment.
TAKEAWAY:
- A total of 25,674 women had PPD (7.5%).
- Positive associations were observed between PPD ozone (adjusted odds ratio, 1.09), PM10 (aOR, 1.02), and PM2.5 (aOR, 1.02), with no statistically significant association with nitrogen dioxide.
- Among PM2.5 constituents, black carbon had the strongest association with PPD (OR 1.04).
- Overall, a higher risk of PPD was associated with ozone exposure during the entire pregnancy and postpartum periods and with PM exposure during the late pregnancy and postpartum periods.
IN PRACTICE:
“These findings suggest that long-term antepartum and postpartum air pollution exposure is a potentially modifiable environmental risk factor for PPD and an important public health issue to address for improved maternal mental health,” the authors wrote.
SOURCE:
The study, with first author Yi Sun, PhD, Chinese Academy of Medical Sciences and Peking Medical College, Beijing, was published online in JAMA Network Open.
LIMITATIONS:
Postpartum exposures were estimated using only maternal address at delivery, which may have led to exposure misclassification. Potential exposure misclassifications may also exist since indoor and personal exposure levels could not be estimated. Although several covariates were adjusted for, some residual or unmeasured covariates were inevitable due to data unavailability, such as psychiatric history, adverse life events, and marital status, which may affect mental health.
DISCLOSURES:
This study was supported by a grant from the National Institute of Environmental Health Sciences. The authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers analyzed data on 340,679 women who had singleton live births at Kaiser Permanente Southern California facilities between 2008 and 2016.
- Ambient air pollution exposures were assessed based on maternal residential addresses using monthly averages of particulate matter ≤ 2.5 mcm (PM2.5), PM ≤ 10 mcm (PM10), nitrogen dioxide, and ozone from Environmental Protection Agency monitoring stations.
- Constituents of PM2.5 (sulfate, nitrate, ammonium, organic matter, and black carbon) were obtained from models based on satellite, ground-based monitor, and chemical transport modeling data.
- Women with an Edinburgh Postnatal Depression Scale score of at least 10 during the first 6 months postpartum were referred for further assessment, including diagnosis and treatment.
TAKEAWAY:
- A total of 25,674 women had PPD (7.5%).
- Positive associations were observed between PPD ozone (adjusted odds ratio, 1.09), PM10 (aOR, 1.02), and PM2.5 (aOR, 1.02), with no statistically significant association with nitrogen dioxide.
- Among PM2.5 constituents, black carbon had the strongest association with PPD (OR 1.04).
- Overall, a higher risk of PPD was associated with ozone exposure during the entire pregnancy and postpartum periods and with PM exposure during the late pregnancy and postpartum periods.
IN PRACTICE:
“These findings suggest that long-term antepartum and postpartum air pollution exposure is a potentially modifiable environmental risk factor for PPD and an important public health issue to address for improved maternal mental health,” the authors wrote.
SOURCE:
The study, with first author Yi Sun, PhD, Chinese Academy of Medical Sciences and Peking Medical College, Beijing, was published online in JAMA Network Open.
LIMITATIONS:
Postpartum exposures were estimated using only maternal address at delivery, which may have led to exposure misclassification. Potential exposure misclassifications may also exist since indoor and personal exposure levels could not be estimated. Although several covariates were adjusted for, some residual or unmeasured covariates were inevitable due to data unavailability, such as psychiatric history, adverse life events, and marital status, which may affect mental health.
DISCLOSURES:
This study was supported by a grant from the National Institute of Environmental Health Sciences. The authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
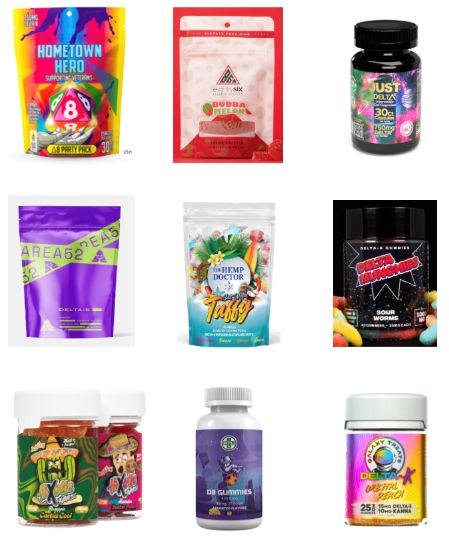
Teens have easy online access to Delta-8 cannabinoid products
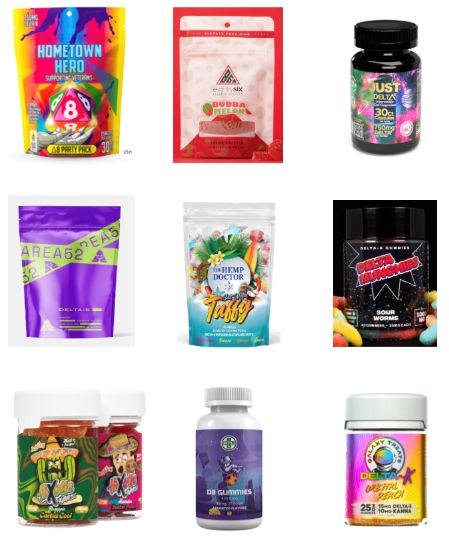
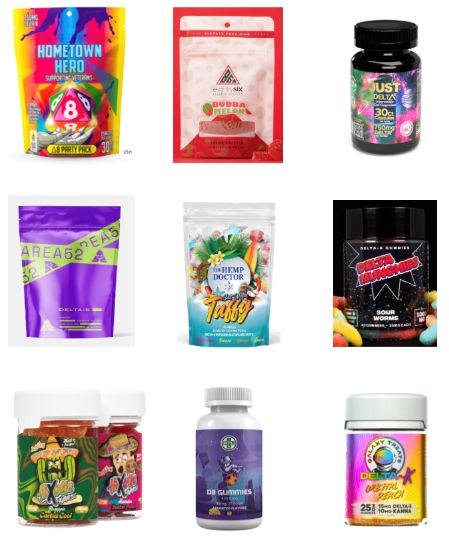
WASHINGTON – , researchers reported at the 2023 annual meeting of the American Academy of Pediatrics. Most of the products identified came in bright, colorful, kid-friendly packaging and cost less than $10, the researchers found, and only 2 out of 45 sites had a third-party age verification requirement for purchases.
Delta-8 THC, also called D8, is a synthetically produced cannabinoid whose chemical structure and effects are nearly identical to traditional THC, the authors explained, and past research has found that D8 products, such as e-cigarettes, can contain toxic byproducts and contaminants.
”Since D8 is not traditional THC, minors may underestimate its strength and potential danger,” wrote lead author Abhijeet Grewal, BS, a research assistant at Cohen Children’s Medical Center, New York, and senior author Ruth Milanaik, DO, director of the Neonatal Neurodevelopmental Program at Cohen Children’s and a developmental/behavioral pediatrician at Northwell Health, also in New York. “Although traditional THC is a federally banned substance, D8 is legal on a federal level and less restricted on a state by state basis, making it easier for individuals to acquire D8.”
Easily accessible
During the first seven moments of 2021, 77% of reports of accidental exposure occurred in people under age 18, including some children who required ICU admission. The U.S. Food and Drug Administration also received 104 reports of adverse events from products containing D8 between December 2020-February 2022, and more than half of those required medical intervention.
To better understand how easy it is to access D8, the authors collected data on 45 websites they identified that sold D8. The researchers looked for age verification questions for accessing the site, third-party age certification, what kinds of products (edibles, smoke products, or tinctures) were sold, the price and dosage of the cheapest product, and examples of packaging, flavors, marketing claims, and warning statements at each site.
More than a third of the sites (36%) did not ask for customers’ age and almost none of the sites asked for proof: 96% of the sites lacked formal third-party age verification procedures. All but one of the sites sold D8 edibles, and most (82%) sold D8 vaping or smoking products. Only 42% sold tinctures, a mix of concentrated D8 with oil that’s orally consumed.
The cheapest product was priced under $5 on one-third of the sites and under $10 on another third of the sites. The cheapest product was between $10-20 on 16% of the sites while the remaining nine sites’ cheapest product was more than $20. In assessing only the cheapest D8 products on each site, nearly half (47%) contained 51 mg or more of D8, and 20% of the products didn’t report the dosage. Another 22% contained 41-50 mg of D8, and the remaining five products contained 20-40 mg.
Kid-friendly D8
More than half of the D8 products were sold in kid-friendly packaging – packages with bright, colorful designs and fonts that resemble candy or snack food, sometimes cartoon characters or fun items like dice on the packaging. Further, 24% of the websites did not include any warnings or other health information about D8.
“The low prices, high dosages available, and eye-popping packaging make these products extremely attractive to teens who are looking for a high,” the researchers concluded. They advised clinicians to talk with teen patients about the dangers of D8 and advocated for policymakers to more strictly regulate online distributors of D8 products, particularly in requiring age verification procedures and prohibiting kid-friendly packaging.
Megan Moreno, MD, MSEd, MPH, an adolescent medicine physician and researcher at the University of Wisconsin, Madison, School of Medicine and Public Health and UWHealthKids, was particularly struck by how eye-catching the packaging was. “The bright colors and font choices are really designed to attract adolescents,” commented Dr. Moreno, who was not involved in the study. But she was not surprised overall by the findings.
“Other studies have found that the cannabis industry leverages online tools and social media, alongside youth-friendly packaging, to attract youth to their products,” she said. “What is disappointing is that these companies do not use industry standard approaches, such as the alcohol industry, to age-gate their websites.”
It’s important for providers who care for adolescents to ask about substance use but to especially include questions about substances that teens might not think of as “drugs,” such as Delta 8, Dr. Moreno said.
“Prior research on other types of substance such as these has found that teens can think these are less dangerous versions of cannabis, so providing accurate information and asking about these products can prevent harm to kids,” Dr. Moreno said. Although this study focused on websites that sell D8 products, she said that “another important area of influence to consider is social media messaging around these products, which may drive traffic to the purchasing site.” It’s clear this industry is not going to self-regulate without policy changes, Dr. Moreno added, so she noted the importance of advocating for policy that regulates these sites.
Mr. Grewal, Dr. Milanaik and Dr. Moreno had no disclosures. No external funding sources were noted.
WASHINGTON – , researchers reported at the 2023 annual meeting of the American Academy of Pediatrics. Most of the products identified came in bright, colorful, kid-friendly packaging and cost less than $10, the researchers found, and only 2 out of 45 sites had a third-party age verification requirement for purchases.
Delta-8 THC, also called D8, is a synthetically produced cannabinoid whose chemical structure and effects are nearly identical to traditional THC, the authors explained, and past research has found that D8 products, such as e-cigarettes, can contain toxic byproducts and contaminants.
”Since D8 is not traditional THC, minors may underestimate its strength and potential danger,” wrote lead author Abhijeet Grewal, BS, a research assistant at Cohen Children’s Medical Center, New York, and senior author Ruth Milanaik, DO, director of the Neonatal Neurodevelopmental Program at Cohen Children’s and a developmental/behavioral pediatrician at Northwell Health, also in New York. “Although traditional THC is a federally banned substance, D8 is legal on a federal level and less restricted on a state by state basis, making it easier for individuals to acquire D8.”
Easily accessible
During the first seven moments of 2021, 77% of reports of accidental exposure occurred in people under age 18, including some children who required ICU admission. The U.S. Food and Drug Administration also received 104 reports of adverse events from products containing D8 between December 2020-February 2022, and more than half of those required medical intervention.
To better understand how easy it is to access D8, the authors collected data on 45 websites they identified that sold D8. The researchers looked for age verification questions for accessing the site, third-party age certification, what kinds of products (edibles, smoke products, or tinctures) were sold, the price and dosage of the cheapest product, and examples of packaging, flavors, marketing claims, and warning statements at each site.
More than a third of the sites (36%) did not ask for customers’ age and almost none of the sites asked for proof: 96% of the sites lacked formal third-party age verification procedures. All but one of the sites sold D8 edibles, and most (82%) sold D8 vaping or smoking products. Only 42% sold tinctures, a mix of concentrated D8 with oil that’s orally consumed.
The cheapest product was priced under $5 on one-third of the sites and under $10 on another third of the sites. The cheapest product was between $10-20 on 16% of the sites while the remaining nine sites’ cheapest product was more than $20. In assessing only the cheapest D8 products on each site, nearly half (47%) contained 51 mg or more of D8, and 20% of the products didn’t report the dosage. Another 22% contained 41-50 mg of D8, and the remaining five products contained 20-40 mg.
Kid-friendly D8
More than half of the D8 products were sold in kid-friendly packaging – packages with bright, colorful designs and fonts that resemble candy or snack food, sometimes cartoon characters or fun items like dice on the packaging. Further, 24% of the websites did not include any warnings or other health information about D8.
“The low prices, high dosages available, and eye-popping packaging make these products extremely attractive to teens who are looking for a high,” the researchers concluded. They advised clinicians to talk with teen patients about the dangers of D8 and advocated for policymakers to more strictly regulate online distributors of D8 products, particularly in requiring age verification procedures and prohibiting kid-friendly packaging.
Megan Moreno, MD, MSEd, MPH, an adolescent medicine physician and researcher at the University of Wisconsin, Madison, School of Medicine and Public Health and UWHealthKids, was particularly struck by how eye-catching the packaging was. “The bright colors and font choices are really designed to attract adolescents,” commented Dr. Moreno, who was not involved in the study. But she was not surprised overall by the findings.
“Other studies have found that the cannabis industry leverages online tools and social media, alongside youth-friendly packaging, to attract youth to their products,” she said. “What is disappointing is that these companies do not use industry standard approaches, such as the alcohol industry, to age-gate their websites.”
It’s important for providers who care for adolescents to ask about substance use but to especially include questions about substances that teens might not think of as “drugs,” such as Delta 8, Dr. Moreno said.
“Prior research on other types of substance such as these has found that teens can think these are less dangerous versions of cannabis, so providing accurate information and asking about these products can prevent harm to kids,” Dr. Moreno said. Although this study focused on websites that sell D8 products, she said that “another important area of influence to consider is social media messaging around these products, which may drive traffic to the purchasing site.” It’s clear this industry is not going to self-regulate without policy changes, Dr. Moreno added, so she noted the importance of advocating for policy that regulates these sites.
Mr. Grewal, Dr. Milanaik and Dr. Moreno had no disclosures. No external funding sources were noted.
WASHINGTON – , researchers reported at the 2023 annual meeting of the American Academy of Pediatrics. Most of the products identified came in bright, colorful, kid-friendly packaging and cost less than $10, the researchers found, and only 2 out of 45 sites had a third-party age verification requirement for purchases.
Delta-8 THC, also called D8, is a synthetically produced cannabinoid whose chemical structure and effects are nearly identical to traditional THC, the authors explained, and past research has found that D8 products, such as e-cigarettes, can contain toxic byproducts and contaminants.
”Since D8 is not traditional THC, minors may underestimate its strength and potential danger,” wrote lead author Abhijeet Grewal, BS, a research assistant at Cohen Children’s Medical Center, New York, and senior author Ruth Milanaik, DO, director of the Neonatal Neurodevelopmental Program at Cohen Children’s and a developmental/behavioral pediatrician at Northwell Health, also in New York. “Although traditional THC is a federally banned substance, D8 is legal on a federal level and less restricted on a state by state basis, making it easier for individuals to acquire D8.”
Easily accessible
During the first seven moments of 2021, 77% of reports of accidental exposure occurred in people under age 18, including some children who required ICU admission. The U.S. Food and Drug Administration also received 104 reports of adverse events from products containing D8 between December 2020-February 2022, and more than half of those required medical intervention.
To better understand how easy it is to access D8, the authors collected data on 45 websites they identified that sold D8. The researchers looked for age verification questions for accessing the site, third-party age certification, what kinds of products (edibles, smoke products, or tinctures) were sold, the price and dosage of the cheapest product, and examples of packaging, flavors, marketing claims, and warning statements at each site.
More than a third of the sites (36%) did not ask for customers’ age and almost none of the sites asked for proof: 96% of the sites lacked formal third-party age verification procedures. All but one of the sites sold D8 edibles, and most (82%) sold D8 vaping or smoking products. Only 42% sold tinctures, a mix of concentrated D8 with oil that’s orally consumed.
The cheapest product was priced under $5 on one-third of the sites and under $10 on another third of the sites. The cheapest product was between $10-20 on 16% of the sites while the remaining nine sites’ cheapest product was more than $20. In assessing only the cheapest D8 products on each site, nearly half (47%) contained 51 mg or more of D8, and 20% of the products didn’t report the dosage. Another 22% contained 41-50 mg of D8, and the remaining five products contained 20-40 mg.
Kid-friendly D8
More than half of the D8 products were sold in kid-friendly packaging – packages with bright, colorful designs and fonts that resemble candy or snack food, sometimes cartoon characters or fun items like dice on the packaging. Further, 24% of the websites did not include any warnings or other health information about D8.
“The low prices, high dosages available, and eye-popping packaging make these products extremely attractive to teens who are looking for a high,” the researchers concluded. They advised clinicians to talk with teen patients about the dangers of D8 and advocated for policymakers to more strictly regulate online distributors of D8 products, particularly in requiring age verification procedures and prohibiting kid-friendly packaging.
Megan Moreno, MD, MSEd, MPH, an adolescent medicine physician and researcher at the University of Wisconsin, Madison, School of Medicine and Public Health and UWHealthKids, was particularly struck by how eye-catching the packaging was. “The bright colors and font choices are really designed to attract adolescents,” commented Dr. Moreno, who was not involved in the study. But she was not surprised overall by the findings.
“Other studies have found that the cannabis industry leverages online tools and social media, alongside youth-friendly packaging, to attract youth to their products,” she said. “What is disappointing is that these companies do not use industry standard approaches, such as the alcohol industry, to age-gate their websites.”
It’s important for providers who care for adolescents to ask about substance use but to especially include questions about substances that teens might not think of as “drugs,” such as Delta 8, Dr. Moreno said.
“Prior research on other types of substance such as these has found that teens can think these are less dangerous versions of cannabis, so providing accurate information and asking about these products can prevent harm to kids,” Dr. Moreno said. Although this study focused on websites that sell D8 products, she said that “another important area of influence to consider is social media messaging around these products, which may drive traffic to the purchasing site.” It’s clear this industry is not going to self-regulate without policy changes, Dr. Moreno added, so she noted the importance of advocating for policy that regulates these sites.
Mr. Grewal, Dr. Milanaik and Dr. Moreno had no disclosures. No external funding sources were noted.
At AAP 2023
Is it time to scrap ultraprocessed foods?
Ultraprocessed foods (UPFs) make up nearly three-quarters of the entire U.S. food supply and about 60% of Americans’ daily caloric intake. A significant body of research has tied consumption of these foods – awash in added sugar, salt, fat, artificial colors, or preservatives – to cancer, diabetes, and heart disease.
Now, a growing number of studies also link them to poor brain health, including an increased risk of dementia, depression, and anxiety, and some experts are calling for public health policies aimed at reducing UPF consumption.
Under srutiny
A mainstay of diets in countries around the world, UPFs have come under increasing scrutiny because of their link to major diseases. The ingredients in UPFs add little or no nutritional value. Their primary function is to increase a product’s shelf life and palatability. Some recent evidence suggests these foods may be as addictive as tobacco. In addition, two pooled analysis studies using the Yale Food Addiction Scale showed that 14% of adults and 12% of children in the United States may have a UPF addiction.
The most widely used measure of what is, and what is not, a UPF was developed in 2009 by researchers in Brazil. The NOVA food classification system assigns food and beverages to one of four groups:
- Unprocessed and minimally processed foods, such as fruits, vegetables, milk, and meat.
- Processed culinary ingredients, including white sugar, butter, and oils derived from seeds, nuts, and fruits.
- Processed foods, such as tomato paste, bacon, canned tuna, and wine.
- Ultraprocessed foods, such as soda, ice cream, breakfast cereal, and prepackaged meals.
Those sounding the alarm about the potential harmful effects of UPFs are particularly concerned about their consumption by young people. The National Health and Nutrition Examination Survey showed that from 1999 to 2018, highly processed foods accounted for the majority of energy intake in those aged 2-19 years.
One of the most commonly used additives in UPFs, the artificial sweetener aspartame, garnered headlines this summer when the World Health Organization classified it as a likely carcinogen in humans. Aspartame is used in thousands of products, from soda to chewing gum to chewable vitamins.
The U.S. Food and Drug Administration strongly disagreed with the WHO’s position and is sticking by its recommended daily limit of 50 mg/kg of body weight – equivalent to 75 packets of the sweetener Equal – as safe for human consumption.
“Aspartame is one of the most studied food additives in the human food supply,” FDA officials said in a statement, adding that the agency found “significant shortcomings” in the studies the WHO used to justify the new classification. “FDA scientists do not have safety concerns when aspartame is used under the approved conditions.”
Increased attention to consumption of UPFs in general and aspartame particularly in recent years has yielded several studies pointing to the foods’ association with compromised brain health.
Link to depression, dementia
A recent report on UPF consumption and mental well-being among nearly 300,000 people across 70 countries showed that 53% of those who consumed UPFs several times a day were distressed or were struggling with their mental well-being, compared with 18% of those who rarely or never consumed UPFs.
Part of the Global Mind Project run by the nonprofit Sapien Labs in Arlington, Va., the report also showed that individuals with the highest rates of UPF consumption reported higher levels of confusion, slowed thinking, unwanted or obsessive thoughts, irritability, and feelings of sadness.
“There seems to be a much broader effect than just depression symptoms,” Tara Thiagarajan, PhD, founder and chief scientist of Sapien Labs and coauthor of the report, said in an interview.
The report, which has not been peer reviewed, comes on the heels of several other studies, including one from the Nurses Health Study II that showed that participants who consumed more than eight servings of UPFs daily had about a 50% higher depression risk, compared with those who consumed half that much.
“We found that UPFs in general, and artificial sweeteners and beverages in particular, were associated with increased risk,” said lead investigator Andrew T. Chan, MD, MPH, professor of medicine at Harvard Medical School and chief of the clinical and translational epidemiology unit, Massachusetts General Hospital, both in Boston.
“This was an interesting finding that correlates with data from animal studies that artificial sweeteners may trigger the transmission of particular signaling molecules in the brain that are important for mood,” he told this news organization.
Cognition may also be affected. An analysis of more than 72,000 people in the UK Biobank showed that those who consumed a high levels of UPFs were 50% more likely to develop dementia than those who consumed fewer processed foods. For every 10% increase in UPF consumption, the odds of developing any kind of dementia increased by 25%.
Another study of nearly 11,000 people showed that higher UPF consumption was associated with a significantly faster decline in executive and global cognitive function.
Epigenetic changes
While these and other studies suggest a link between UPF consumption and brain health, they are designed to demonstrate correlation. To date, no human study has proven that eating highly processed foods directly causes a decline in mental health or cognition.
Animal studies could provide that causal link. Earlier this year, researchers at Florida State University in Tallahassee reported learning and memory deficits in two groups of male mice that completed a maze test after being fed water mixed with aspartame for about 20% of their adult lives, compared with a group of mice that drank water only. Animals that ingested aspartame could finish the test, but it took them longer, and they needed help.
The amount of aspartame used in the study was just 7% and 15% of the FDA’s recommended maximum intake of aspartame (equivalent to two to four 8-ounce diet sodas daily).
Most intriguing was that offspring of the mice in the aspartame groups demonstrated the same levels of cognitive decline and anxiety as their fathers, even though they had never ingested the artificial sweetener. Researchers theorize that in addition to changes in brain gene expression, aspartame also caused epigenetic changes in germ cells.
“Epigenetic changes in germ cells due to environmental exposures are both good and bad,” lead investigator Pradeep G. Bhide, PhD, professor of developmental neuroscience and director of the Center for Brain Repair at FSU, told this news organization. “They are bad because the next generation is affected. But they’re good because as long as the exposure no longer occurs, 2 or 3 generations later, that’s gone.”
The mice, which lacked taste receptors for aspartame, were the same age and weight in all three groups. Because the only difference was exposure to the artificial sweetener, Dr. Bhide says it suggests a causal link.
“Extrapolation of data from well-controlled laboratory experiments in mice to humans is always risky,” Dr. Bhide said. “The extrapolations give us insights into what could happen rather than what will happen.”
Potential mechanisms
Although scientists can’t say for certain how UPFs affect brain health, there are several theories. UPFs may influence an inflammatory immune response, which has been linked to depression and dementia. Consumption of highly processed foods may also disrupt the gut microbiome, Dr. Chan said, which, in turn, may increase depression risk.
“This is an important potential mechanism linking ultraprocessed food to depression since there is emerging evidence that microbes in the gut have been linked with mood through their role in metabolizing and producing proteins that have activity in the brain,” he said.
In addition, with UPFs that contain aspartame, there could be a more direct link to brain function. In the gastrointestinal track, the sweetener is quickly broken down into methanol, aspartic acid, and phenylalanine. All three enter the bloodstream, cross the blood-brain barrier, and are neuroactive.
“Phenylalanine is a precursor for neurotransmitters in the brain, and aspartic acid activates the glutamate excitatory neurotransmitter receptor,” Dr. Bhide said. “The effects we’ve seen could be due to these metabolites that have a direct effect on the brain function.”
Time to act?
Some researchers are building a case for classifying UPFs as addictive substances. Others are calling for additional research on UPF safety that is conducted outside the food industry.
There has also been some discussion of placing warning labels on UPFs. However, there is disagreement about what information should be included and how consumers might interpret it. The question of which food products are UPFs and which are not also isn’t settled. The NOVA system may be widely used, but it still has its detractors who believe it misclassifies some healthy foods as ultraprocessed.
Dr. Chan and other experts say the research conducted thus far requires additional corroboration to inform appropriate public health interventions. That would likely take the form of a large, randomized trial with one group of participants eating a healthy diet and the other consuming large amounts of UPFs.
“This type of study is extremely challenging given the number of people that would have to be willing to participate and be willing to eat a very specific diet over a long period of time,” Dr. Chan said. “I am also not sure it would be ethical to assign people to such a diet, given what we already know about the potential health effects of UPFs.”
Dr. Thiagarajan and others have called on funding agencies to direct more grant monies toward studies of UPFs to better understand their effect on brain health.
“Given the magnitude of the problem and given that there is a fair bit of evidence that points to a potential causal link, then we damn well better put money into this and get to the bottom of it,” she said.
Others are looking to the FDA to increase the agency’s scrutiny of food additives. While some additives such as artificial sweeteners have a place in diets of people with diabetes or obesity, Dr. Bhide suggests it may be wise for healthy individuals to reduce their daily intake of UPFs.
“Our data raise this to a different level because of the transgenerational transmission, which has never been shown before,” he said. “We are saying that the FDA should look in preclinical models at germ cells and maybe transgenerational transmission before approving any food additive.”
A version of this article first appeared on Medscape.com.
Ultraprocessed foods (UPFs) make up nearly three-quarters of the entire U.S. food supply and about 60% of Americans’ daily caloric intake. A significant body of research has tied consumption of these foods – awash in added sugar, salt, fat, artificial colors, or preservatives – to cancer, diabetes, and heart disease.
Now, a growing number of studies also link them to poor brain health, including an increased risk of dementia, depression, and anxiety, and some experts are calling for public health policies aimed at reducing UPF consumption.
Under srutiny
A mainstay of diets in countries around the world, UPFs have come under increasing scrutiny because of their link to major diseases. The ingredients in UPFs add little or no nutritional value. Their primary function is to increase a product’s shelf life and palatability. Some recent evidence suggests these foods may be as addictive as tobacco. In addition, two pooled analysis studies using the Yale Food Addiction Scale showed that 14% of adults and 12% of children in the United States may have a UPF addiction.
The most widely used measure of what is, and what is not, a UPF was developed in 2009 by researchers in Brazil. The NOVA food classification system assigns food and beverages to one of four groups:
- Unprocessed and minimally processed foods, such as fruits, vegetables, milk, and meat.
- Processed culinary ingredients, including white sugar, butter, and oils derived from seeds, nuts, and fruits.
- Processed foods, such as tomato paste, bacon, canned tuna, and wine.
- Ultraprocessed foods, such as soda, ice cream, breakfast cereal, and prepackaged meals.
Those sounding the alarm about the potential harmful effects of UPFs are particularly concerned about their consumption by young people. The National Health and Nutrition Examination Survey showed that from 1999 to 2018, highly processed foods accounted for the majority of energy intake in those aged 2-19 years.
One of the most commonly used additives in UPFs, the artificial sweetener aspartame, garnered headlines this summer when the World Health Organization classified it as a likely carcinogen in humans. Aspartame is used in thousands of products, from soda to chewing gum to chewable vitamins.
The U.S. Food and Drug Administration strongly disagreed with the WHO’s position and is sticking by its recommended daily limit of 50 mg/kg of body weight – equivalent to 75 packets of the sweetener Equal – as safe for human consumption.
“Aspartame is one of the most studied food additives in the human food supply,” FDA officials said in a statement, adding that the agency found “significant shortcomings” in the studies the WHO used to justify the new classification. “FDA scientists do not have safety concerns when aspartame is used under the approved conditions.”
Increased attention to consumption of UPFs in general and aspartame particularly in recent years has yielded several studies pointing to the foods’ association with compromised brain health.
Link to depression, dementia
A recent report on UPF consumption and mental well-being among nearly 300,000 people across 70 countries showed that 53% of those who consumed UPFs several times a day were distressed or were struggling with their mental well-being, compared with 18% of those who rarely or never consumed UPFs.
Part of the Global Mind Project run by the nonprofit Sapien Labs in Arlington, Va., the report also showed that individuals with the highest rates of UPF consumption reported higher levels of confusion, slowed thinking, unwanted or obsessive thoughts, irritability, and feelings of sadness.
“There seems to be a much broader effect than just depression symptoms,” Tara Thiagarajan, PhD, founder and chief scientist of Sapien Labs and coauthor of the report, said in an interview.
The report, which has not been peer reviewed, comes on the heels of several other studies, including one from the Nurses Health Study II that showed that participants who consumed more than eight servings of UPFs daily had about a 50% higher depression risk, compared with those who consumed half that much.
“We found that UPFs in general, and artificial sweeteners and beverages in particular, were associated with increased risk,” said lead investigator Andrew T. Chan, MD, MPH, professor of medicine at Harvard Medical School and chief of the clinical and translational epidemiology unit, Massachusetts General Hospital, both in Boston.
“This was an interesting finding that correlates with data from animal studies that artificial sweeteners may trigger the transmission of particular signaling molecules in the brain that are important for mood,” he told this news organization.
Cognition may also be affected. An analysis of more than 72,000 people in the UK Biobank showed that those who consumed a high levels of UPFs were 50% more likely to develop dementia than those who consumed fewer processed foods. For every 10% increase in UPF consumption, the odds of developing any kind of dementia increased by 25%.
Another study of nearly 11,000 people showed that higher UPF consumption was associated with a significantly faster decline in executive and global cognitive function.
Epigenetic changes
While these and other studies suggest a link between UPF consumption and brain health, they are designed to demonstrate correlation. To date, no human study has proven that eating highly processed foods directly causes a decline in mental health or cognition.
Animal studies could provide that causal link. Earlier this year, researchers at Florida State University in Tallahassee reported learning and memory deficits in two groups of male mice that completed a maze test after being fed water mixed with aspartame for about 20% of their adult lives, compared with a group of mice that drank water only. Animals that ingested aspartame could finish the test, but it took them longer, and they needed help.
The amount of aspartame used in the study was just 7% and 15% of the FDA’s recommended maximum intake of aspartame (equivalent to two to four 8-ounce diet sodas daily).
Most intriguing was that offspring of the mice in the aspartame groups demonstrated the same levels of cognitive decline and anxiety as their fathers, even though they had never ingested the artificial sweetener. Researchers theorize that in addition to changes in brain gene expression, aspartame also caused epigenetic changes in germ cells.
“Epigenetic changes in germ cells due to environmental exposures are both good and bad,” lead investigator Pradeep G. Bhide, PhD, professor of developmental neuroscience and director of the Center for Brain Repair at FSU, told this news organization. “They are bad because the next generation is affected. But they’re good because as long as the exposure no longer occurs, 2 or 3 generations later, that’s gone.”
The mice, which lacked taste receptors for aspartame, were the same age and weight in all three groups. Because the only difference was exposure to the artificial sweetener, Dr. Bhide says it suggests a causal link.
“Extrapolation of data from well-controlled laboratory experiments in mice to humans is always risky,” Dr. Bhide said. “The extrapolations give us insights into what could happen rather than what will happen.”
Potential mechanisms
Although scientists can’t say for certain how UPFs affect brain health, there are several theories. UPFs may influence an inflammatory immune response, which has been linked to depression and dementia. Consumption of highly processed foods may also disrupt the gut microbiome, Dr. Chan said, which, in turn, may increase depression risk.
“This is an important potential mechanism linking ultraprocessed food to depression since there is emerging evidence that microbes in the gut have been linked with mood through their role in metabolizing and producing proteins that have activity in the brain,” he said.
In addition, with UPFs that contain aspartame, there could be a more direct link to brain function. In the gastrointestinal track, the sweetener is quickly broken down into methanol, aspartic acid, and phenylalanine. All three enter the bloodstream, cross the blood-brain barrier, and are neuroactive.
“Phenylalanine is a precursor for neurotransmitters in the brain, and aspartic acid activates the glutamate excitatory neurotransmitter receptor,” Dr. Bhide said. “The effects we’ve seen could be due to these metabolites that have a direct effect on the brain function.”
Time to act?
Some researchers are building a case for classifying UPFs as addictive substances. Others are calling for additional research on UPF safety that is conducted outside the food industry.
There has also been some discussion of placing warning labels on UPFs. However, there is disagreement about what information should be included and how consumers might interpret it. The question of which food products are UPFs and which are not also isn’t settled. The NOVA system may be widely used, but it still has its detractors who believe it misclassifies some healthy foods as ultraprocessed.
Dr. Chan and other experts say the research conducted thus far requires additional corroboration to inform appropriate public health interventions. That would likely take the form of a large, randomized trial with one group of participants eating a healthy diet and the other consuming large amounts of UPFs.
“This type of study is extremely challenging given the number of people that would have to be willing to participate and be willing to eat a very specific diet over a long period of time,” Dr. Chan said. “I am also not sure it would be ethical to assign people to such a diet, given what we already know about the potential health effects of UPFs.”
Dr. Thiagarajan and others have called on funding agencies to direct more grant monies toward studies of UPFs to better understand their effect on brain health.
“Given the magnitude of the problem and given that there is a fair bit of evidence that points to a potential causal link, then we damn well better put money into this and get to the bottom of it,” she said.
Others are looking to the FDA to increase the agency’s scrutiny of food additives. While some additives such as artificial sweeteners have a place in diets of people with diabetes or obesity, Dr. Bhide suggests it may be wise for healthy individuals to reduce their daily intake of UPFs.
“Our data raise this to a different level because of the transgenerational transmission, which has never been shown before,” he said. “We are saying that the FDA should look in preclinical models at germ cells and maybe transgenerational transmission before approving any food additive.”
A version of this article first appeared on Medscape.com.
Ultraprocessed foods (UPFs) make up nearly three-quarters of the entire U.S. food supply and about 60% of Americans’ daily caloric intake. A significant body of research has tied consumption of these foods – awash in added sugar, salt, fat, artificial colors, or preservatives – to cancer, diabetes, and heart disease.
Now, a growing number of studies also link them to poor brain health, including an increased risk of dementia, depression, and anxiety, and some experts are calling for public health policies aimed at reducing UPF consumption.
Under srutiny
A mainstay of diets in countries around the world, UPFs have come under increasing scrutiny because of their link to major diseases. The ingredients in UPFs add little or no nutritional value. Their primary function is to increase a product’s shelf life and palatability. Some recent evidence suggests these foods may be as addictive as tobacco. In addition, two pooled analysis studies using the Yale Food Addiction Scale showed that 14% of adults and 12% of children in the United States may have a UPF addiction.
The most widely used measure of what is, and what is not, a UPF was developed in 2009 by researchers in Brazil. The NOVA food classification system assigns food and beverages to one of four groups:
- Unprocessed and minimally processed foods, such as fruits, vegetables, milk, and meat.
- Processed culinary ingredients, including white sugar, butter, and oils derived from seeds, nuts, and fruits.
- Processed foods, such as tomato paste, bacon, canned tuna, and wine.
- Ultraprocessed foods, such as soda, ice cream, breakfast cereal, and prepackaged meals.
Those sounding the alarm about the potential harmful effects of UPFs are particularly concerned about their consumption by young people. The National Health and Nutrition Examination Survey showed that from 1999 to 2018, highly processed foods accounted for the majority of energy intake in those aged 2-19 years.
One of the most commonly used additives in UPFs, the artificial sweetener aspartame, garnered headlines this summer when the World Health Organization classified it as a likely carcinogen in humans. Aspartame is used in thousands of products, from soda to chewing gum to chewable vitamins.
The U.S. Food and Drug Administration strongly disagreed with the WHO’s position and is sticking by its recommended daily limit of 50 mg/kg of body weight – equivalent to 75 packets of the sweetener Equal – as safe for human consumption.
“Aspartame is one of the most studied food additives in the human food supply,” FDA officials said in a statement, adding that the agency found “significant shortcomings” in the studies the WHO used to justify the new classification. “FDA scientists do not have safety concerns when aspartame is used under the approved conditions.”
Increased attention to consumption of UPFs in general and aspartame particularly in recent years has yielded several studies pointing to the foods’ association with compromised brain health.
Link to depression, dementia
A recent report on UPF consumption and mental well-being among nearly 300,000 people across 70 countries showed that 53% of those who consumed UPFs several times a day were distressed or were struggling with their mental well-being, compared with 18% of those who rarely or never consumed UPFs.
Part of the Global Mind Project run by the nonprofit Sapien Labs in Arlington, Va., the report also showed that individuals with the highest rates of UPF consumption reported higher levels of confusion, slowed thinking, unwanted or obsessive thoughts, irritability, and feelings of sadness.
“There seems to be a much broader effect than just depression symptoms,” Tara Thiagarajan, PhD, founder and chief scientist of Sapien Labs and coauthor of the report, said in an interview.
The report, which has not been peer reviewed, comes on the heels of several other studies, including one from the Nurses Health Study II that showed that participants who consumed more than eight servings of UPFs daily had about a 50% higher depression risk, compared with those who consumed half that much.
“We found that UPFs in general, and artificial sweeteners and beverages in particular, were associated with increased risk,” said lead investigator Andrew T. Chan, MD, MPH, professor of medicine at Harvard Medical School and chief of the clinical and translational epidemiology unit, Massachusetts General Hospital, both in Boston.
“This was an interesting finding that correlates with data from animal studies that artificial sweeteners may trigger the transmission of particular signaling molecules in the brain that are important for mood,” he told this news organization.
Cognition may also be affected. An analysis of more than 72,000 people in the UK Biobank showed that those who consumed a high levels of UPFs were 50% more likely to develop dementia than those who consumed fewer processed foods. For every 10% increase in UPF consumption, the odds of developing any kind of dementia increased by 25%.
Another study of nearly 11,000 people showed that higher UPF consumption was associated with a significantly faster decline in executive and global cognitive function.
Epigenetic changes
While these and other studies suggest a link between UPF consumption and brain health, they are designed to demonstrate correlation. To date, no human study has proven that eating highly processed foods directly causes a decline in mental health or cognition.
Animal studies could provide that causal link. Earlier this year, researchers at Florida State University in Tallahassee reported learning and memory deficits in two groups of male mice that completed a maze test after being fed water mixed with aspartame for about 20% of their adult lives, compared with a group of mice that drank water only. Animals that ingested aspartame could finish the test, but it took them longer, and they needed help.
The amount of aspartame used in the study was just 7% and 15% of the FDA’s recommended maximum intake of aspartame (equivalent to two to four 8-ounce diet sodas daily).
Most intriguing was that offspring of the mice in the aspartame groups demonstrated the same levels of cognitive decline and anxiety as their fathers, even though they had never ingested the artificial sweetener. Researchers theorize that in addition to changes in brain gene expression, aspartame also caused epigenetic changes in germ cells.
“Epigenetic changes in germ cells due to environmental exposures are both good and bad,” lead investigator Pradeep G. Bhide, PhD, professor of developmental neuroscience and director of the Center for Brain Repair at FSU, told this news organization. “They are bad because the next generation is affected. But they’re good because as long as the exposure no longer occurs, 2 or 3 generations later, that’s gone.”
The mice, which lacked taste receptors for aspartame, were the same age and weight in all three groups. Because the only difference was exposure to the artificial sweetener, Dr. Bhide says it suggests a causal link.
“Extrapolation of data from well-controlled laboratory experiments in mice to humans is always risky,” Dr. Bhide said. “The extrapolations give us insights into what could happen rather than what will happen.”
Potential mechanisms
Although scientists can’t say for certain how UPFs affect brain health, there are several theories. UPFs may influence an inflammatory immune response, which has been linked to depression and dementia. Consumption of highly processed foods may also disrupt the gut microbiome, Dr. Chan said, which, in turn, may increase depression risk.
“This is an important potential mechanism linking ultraprocessed food to depression since there is emerging evidence that microbes in the gut have been linked with mood through their role in metabolizing and producing proteins that have activity in the brain,” he said.
In addition, with UPFs that contain aspartame, there could be a more direct link to brain function. In the gastrointestinal track, the sweetener is quickly broken down into methanol, aspartic acid, and phenylalanine. All three enter the bloodstream, cross the blood-brain barrier, and are neuroactive.
“Phenylalanine is a precursor for neurotransmitters in the brain, and aspartic acid activates the glutamate excitatory neurotransmitter receptor,” Dr. Bhide said. “The effects we’ve seen could be due to these metabolites that have a direct effect on the brain function.”
Time to act?
Some researchers are building a case for classifying UPFs as addictive substances. Others are calling for additional research on UPF safety that is conducted outside the food industry.
There has also been some discussion of placing warning labels on UPFs. However, there is disagreement about what information should be included and how consumers might interpret it. The question of which food products are UPFs and which are not also isn’t settled. The NOVA system may be widely used, but it still has its detractors who believe it misclassifies some healthy foods as ultraprocessed.
Dr. Chan and other experts say the research conducted thus far requires additional corroboration to inform appropriate public health interventions. That would likely take the form of a large, randomized trial with one group of participants eating a healthy diet and the other consuming large amounts of UPFs.
“This type of study is extremely challenging given the number of people that would have to be willing to participate and be willing to eat a very specific diet over a long period of time,” Dr. Chan said. “I am also not sure it would be ethical to assign people to such a diet, given what we already know about the potential health effects of UPFs.”
Dr. Thiagarajan and others have called on funding agencies to direct more grant monies toward studies of UPFs to better understand their effect on brain health.
“Given the magnitude of the problem and given that there is a fair bit of evidence that points to a potential causal link, then we damn well better put money into this and get to the bottom of it,” she said.
Others are looking to the FDA to increase the agency’s scrutiny of food additives. While some additives such as artificial sweeteners have a place in diets of people with diabetes or obesity, Dr. Bhide suggests it may be wise for healthy individuals to reduce their daily intake of UPFs.
“Our data raise this to a different level because of the transgenerational transmission, which has never been shown before,” he said. “We are saying that the FDA should look in preclinical models at germ cells and maybe transgenerational transmission before approving any food additive.”
A version of this article first appeared on Medscape.com.
A blood test to diagnose bipolar disorder?
TOPLINE:
(MDD), new research shows. Investigators state that the test could identify up to 30% of patients with BD when used on its own and could be even more effective when combined with a standardized psychometric assessment.
METHODOLOGY:
- In the proof-of-concept study, investigators sought to identify biomarkers to accurately identify BD, which is frequently misdiagnosed as MDD because of overlapping symptoms and the lack of objective diagnostic tools.
- The study included 241 participants (70% female; mean age, 28 years) from the U.K.-based Delta Study who had been diagnosed with MDD within the past 5 years and had depressive symptoms as assessed with the Patient Health Questionnaire-9 (score ≥ 5).
- Participants completed an online questionnaire that included questions from the Mood Disorder Questionnaire and the Warwick-Edinburgh Mental Well-Being Scale and were asked to return a dried blood spot (DBS) fasting blood sample.
- Investigators analyzed the DBS samples for 630 metabolites and contacted participants by phone to establish diagnoses at 6 and 12 months using the World Health Organization World Mental Health Composite International Diagnostic Interview.
TAKEAWAY:
- Investigators used a panel of 17 biomarkers to correctly identify 67 (27.8%) participants with BD who had been previously misdiagnosed with MDD. They confirmed MDD in the remaining 174 patients.
- The biomarkers used in the test were correlated primarily with lifetime manic symptoms and were validated in a separate group of 30 patients.
- The identified biomarker panel provided a mean cross-validated area under the receiver operating characteristic curve of 0.71 (P < .001), with ceramide d18:0/24:1 emerging as the strongest biomarker.
- Combining biomarker readouts with patient-reported data significantly improved the performance of diagnostic models based on extensive demographic data and information from the Patient Health Questionnaire and Mood Disorder Questionnaire (P = .03 for all).
IN PRACTICE:
“The added value of biomarkers was particularly evident in scenarios where data on psychiatric symptoms were unavailable and at intermediate diagnostic thresholds, suggesting that biomarker tests may especially benefit patients who do not report their symptoms and whose diagnoses are uncertain,” the authors write.
SOURCE:
Jakub Tomasik, PhD, of the University of Cambridge (England), led the study, which was published online in JAMA Psychiatry. Stanley Medical Research Institute and Psyomics funded the study.
LIMITATIONS:
Data on confounding factors such as diet and blood pressure were missing. In addition, investigators noted that the sample mostly comprised White Internet users and was not representative of all individuals with BD.
Dr. Tomasik has a patent pending for DBS blood biomarkers. Other disclosures are noted in the original article.
A version of this article first appeared on Medscape.com.
TOPLINE:
(MDD), new research shows. Investigators state that the test could identify up to 30% of patients with BD when used on its own and could be even more effective when combined with a standardized psychometric assessment.
METHODOLOGY:
- In the proof-of-concept study, investigators sought to identify biomarkers to accurately identify BD, which is frequently misdiagnosed as MDD because of overlapping symptoms and the lack of objective diagnostic tools.
- The study included 241 participants (70% female; mean age, 28 years) from the U.K.-based Delta Study who had been diagnosed with MDD within the past 5 years and had depressive symptoms as assessed with the Patient Health Questionnaire-9 (score ≥ 5).
- Participants completed an online questionnaire that included questions from the Mood Disorder Questionnaire and the Warwick-Edinburgh Mental Well-Being Scale and were asked to return a dried blood spot (DBS) fasting blood sample.
- Investigators analyzed the DBS samples for 630 metabolites and contacted participants by phone to establish diagnoses at 6 and 12 months using the World Health Organization World Mental Health Composite International Diagnostic Interview.
TAKEAWAY:
- Investigators used a panel of 17 biomarkers to correctly identify 67 (27.8%) participants with BD who had been previously misdiagnosed with MDD. They confirmed MDD in the remaining 174 patients.
- The biomarkers used in the test were correlated primarily with lifetime manic symptoms and were validated in a separate group of 30 patients.
- The identified biomarker panel provided a mean cross-validated area under the receiver operating characteristic curve of 0.71 (P < .001), with ceramide d18:0/24:1 emerging as the strongest biomarker.
- Combining biomarker readouts with patient-reported data significantly improved the performance of diagnostic models based on extensive demographic data and information from the Patient Health Questionnaire and Mood Disorder Questionnaire (P = .03 for all).
IN PRACTICE:
“The added value of biomarkers was particularly evident in scenarios where data on psychiatric symptoms were unavailable and at intermediate diagnostic thresholds, suggesting that biomarker tests may especially benefit patients who do not report their symptoms and whose diagnoses are uncertain,” the authors write.
SOURCE:
Jakub Tomasik, PhD, of the University of Cambridge (England), led the study, which was published online in JAMA Psychiatry. Stanley Medical Research Institute and Psyomics funded the study.
LIMITATIONS:
Data on confounding factors such as diet and blood pressure were missing. In addition, investigators noted that the sample mostly comprised White Internet users and was not representative of all individuals with BD.
Dr. Tomasik has a patent pending for DBS blood biomarkers. Other disclosures are noted in the original article.
A version of this article first appeared on Medscape.com.
TOPLINE:
(MDD), new research shows. Investigators state that the test could identify up to 30% of patients with BD when used on its own and could be even more effective when combined with a standardized psychometric assessment.
METHODOLOGY:
- In the proof-of-concept study, investigators sought to identify biomarkers to accurately identify BD, which is frequently misdiagnosed as MDD because of overlapping symptoms and the lack of objective diagnostic tools.
- The study included 241 participants (70% female; mean age, 28 years) from the U.K.-based Delta Study who had been diagnosed with MDD within the past 5 years and had depressive symptoms as assessed with the Patient Health Questionnaire-9 (score ≥ 5).
- Participants completed an online questionnaire that included questions from the Mood Disorder Questionnaire and the Warwick-Edinburgh Mental Well-Being Scale and were asked to return a dried blood spot (DBS) fasting blood sample.
- Investigators analyzed the DBS samples for 630 metabolites and contacted participants by phone to establish diagnoses at 6 and 12 months using the World Health Organization World Mental Health Composite International Diagnostic Interview.
TAKEAWAY:
- Investigators used a panel of 17 biomarkers to correctly identify 67 (27.8%) participants with BD who had been previously misdiagnosed with MDD. They confirmed MDD in the remaining 174 patients.
- The biomarkers used in the test were correlated primarily with lifetime manic symptoms and were validated in a separate group of 30 patients.
- The identified biomarker panel provided a mean cross-validated area under the receiver operating characteristic curve of 0.71 (P < .001), with ceramide d18:0/24:1 emerging as the strongest biomarker.
- Combining biomarker readouts with patient-reported data significantly improved the performance of diagnostic models based on extensive demographic data and information from the Patient Health Questionnaire and Mood Disorder Questionnaire (P = .03 for all).
IN PRACTICE:
“The added value of biomarkers was particularly evident in scenarios where data on psychiatric symptoms were unavailable and at intermediate diagnostic thresholds, suggesting that biomarker tests may especially benefit patients who do not report their symptoms and whose diagnoses are uncertain,” the authors write.
SOURCE:
Jakub Tomasik, PhD, of the University of Cambridge (England), led the study, which was published online in JAMA Psychiatry. Stanley Medical Research Institute and Psyomics funded the study.
LIMITATIONS:
Data on confounding factors such as diet and blood pressure were missing. In addition, investigators noted that the sample mostly comprised White Internet users and was not representative of all individuals with BD.
Dr. Tomasik has a patent pending for DBS blood biomarkers. Other disclosures are noted in the original article.
A version of this article first appeared on Medscape.com.
Lag in antidepressant treatment response explained?
BARCELONA – , new imaging data suggest.
In a double-blind study, more than 30 volunteers were randomly assigned to the SSRI escitalopram or placebo for 3-5 weeks. Using PET imaging, the investigators found that over time, synaptic density significantly increased significantly in the neocortex and hippocampus but only in patients taking the active drug.
The results point to two conclusions, said study investigator Gitta Moos Knudsen, MD, PhD, clinical professor and chief physician at the department of clinical medicine, neurology, psychiatry and sensory sciences at Copenhagen (Denmark) University Hospital.
First, they indicate that SSRIs increase synaptic density in brain areas critically involved in depression, a finding that would go some way to indicating that the synaptic density in the brain may be involved in how antidepressants function, “which would give us a target for developing novel drugs against depression,” said Dr. Knudsen.
“Secondly, our data suggest synapses build up over a period of weeks, which would explain why the effects of these drugs take time to kick in,” she added.
The findings were presented at the 36th European College of Neuropsychopharmacology (ECNP) Congress and simultaneously published online in Molecular Psychiatry.
Marked increase in synaptic density
SSRIs are widely used for depression as well as anxiety and obsessive-compulsive disorder. It is thought that they act via neuroplasticity and synaptic remodeling to improve cognition and emotion processing. However, the investigators note clinical evidence is lacking.
For the study, the researchers randomly assigned healthy individuals to either 20-mg escitalopram or placebo for 3-5 weeks.
They performed PET with the 11C-UCB-J tracer, which allows imaging of the synaptic vesicle glycoprotein 2A (SV2A) in the brain, synaptic density, as well as changes in density over time, in the hippocampus and neocortex.
Between May 2020 and October 2021, 17 individuals were assigned to escitalopram and 15 to placebo. There were no significant differences between two groups in terms of age, sex, and PET-related variables. Serum escitalopram measurements confirmed that all participants in the active drug group were compliant.
When synaptic density was assessed at a single time point, an average of 29 days after the intervention, there were no significant differences between the escitalopram and placebo groups in either the neocortex (P = .41) or in the hippocampus (P = .26).
However, when they performed a secondary analysis of the time-dependent effect on SV2A levels, they found a marked difference between the two study groups.
Compared with the placebo group, participants taking escitalopram had a marked increase in synaptic density in both the neocortex (rp value, 0.58; P = .003) and the hippocampus (rp value, 0.41; P = .048).
In contrast, there were no significant changes in synaptic density in either the neocortex (rp value, –0.01; P = .95) or the hippocampus (rp value, –0.06; P = .62) in the hippocampus.
“That is consistent with our clinical observation that it takes time to evolve synaptic density, along with clinical improvement. Does that mean that the increase in synaptic density is a precondition for improvement in symptoms? We don’t know,” said Dr. Knudsen.
Exciting but not conclusive
Session co-chair Oliver Howes, MD, PhD, professor of molecular psychiatry, King’s College London, agreed that the results do not prove the gradual increase in synaptic density the treatment response lag with SSRIs.
“We definitely don’t yet have all the data to know one way or the other,” he said in an interview.
Another potential hypothesis, he said, is that SSRIs are causing shifts in underlying brain circuits that lead to cognitive changes before there is a discernable improvement in mood.
Indeed, Dr. Howes suggested that increases in synaptic density and cognitive changes related to SSRI use are not necessarily dependent on each other and could even be unrelated.
Also commenting on the research, David Nutt, MD, PhD, Edmond J. Safra professor of neuropsychopharmacology at Imperial College London, said that the “delay in therapeutic action of antidepressants has been a puzzle to psychiatrists ever since they were first discerned over 50 years ago. So, these new data in humans, that use cutting edge brain imaging to demonstrate an increase in brain connections developing over the period that the depression lifts, are very exciting.”
Dr. Nutt added that the results provide further evidence that “enhancing serotonin function in the brain can have enduring health benefits.”
Funding support was provided by the Danish Council for Independent Research, the Lundbeck Foundation, Rigshospitalet, and the Swedish Research Council. Open access funding provided by Royal Library, Copenhagen University Library.
Dr. Knudsen declares relationships with Sage Biogen, H. Lundbeck, Onsero, Pangea, Gilgamesh, Abbvie, and PureTechHealth. Another author declares relationships with Cambridge Cognition and PopReach via Cambridge Enterprise.
A version of this article first appeared on Medscape.com.
BARCELONA – , new imaging data suggest.
In a double-blind study, more than 30 volunteers were randomly assigned to the SSRI escitalopram or placebo for 3-5 weeks. Using PET imaging, the investigators found that over time, synaptic density significantly increased significantly in the neocortex and hippocampus but only in patients taking the active drug.
The results point to two conclusions, said study investigator Gitta Moos Knudsen, MD, PhD, clinical professor and chief physician at the department of clinical medicine, neurology, psychiatry and sensory sciences at Copenhagen (Denmark) University Hospital.
First, they indicate that SSRIs increase synaptic density in brain areas critically involved in depression, a finding that would go some way to indicating that the synaptic density in the brain may be involved in how antidepressants function, “which would give us a target for developing novel drugs against depression,” said Dr. Knudsen.
“Secondly, our data suggest synapses build up over a period of weeks, which would explain why the effects of these drugs take time to kick in,” she added.
The findings were presented at the 36th European College of Neuropsychopharmacology (ECNP) Congress and simultaneously published online in Molecular Psychiatry.
Marked increase in synaptic density
SSRIs are widely used for depression as well as anxiety and obsessive-compulsive disorder. It is thought that they act via neuroplasticity and synaptic remodeling to improve cognition and emotion processing. However, the investigators note clinical evidence is lacking.
For the study, the researchers randomly assigned healthy individuals to either 20-mg escitalopram or placebo for 3-5 weeks.
They performed PET with the 11C-UCB-J tracer, which allows imaging of the synaptic vesicle glycoprotein 2A (SV2A) in the brain, synaptic density, as well as changes in density over time, in the hippocampus and neocortex.
Between May 2020 and October 2021, 17 individuals were assigned to escitalopram and 15 to placebo. There were no significant differences between two groups in terms of age, sex, and PET-related variables. Serum escitalopram measurements confirmed that all participants in the active drug group were compliant.
When synaptic density was assessed at a single time point, an average of 29 days after the intervention, there were no significant differences between the escitalopram and placebo groups in either the neocortex (P = .41) or in the hippocampus (P = .26).
However, when they performed a secondary analysis of the time-dependent effect on SV2A levels, they found a marked difference between the two study groups.
Compared with the placebo group, participants taking escitalopram had a marked increase in synaptic density in both the neocortex (rp value, 0.58; P = .003) and the hippocampus (rp value, 0.41; P = .048).
In contrast, there were no significant changes in synaptic density in either the neocortex (rp value, –0.01; P = .95) or the hippocampus (rp value, –0.06; P = .62) in the hippocampus.
“That is consistent with our clinical observation that it takes time to evolve synaptic density, along with clinical improvement. Does that mean that the increase in synaptic density is a precondition for improvement in symptoms? We don’t know,” said Dr. Knudsen.
Exciting but not conclusive
Session co-chair Oliver Howes, MD, PhD, professor of molecular psychiatry, King’s College London, agreed that the results do not prove the gradual increase in synaptic density the treatment response lag with SSRIs.
“We definitely don’t yet have all the data to know one way or the other,” he said in an interview.
Another potential hypothesis, he said, is that SSRIs are causing shifts in underlying brain circuits that lead to cognitive changes before there is a discernable improvement in mood.
Indeed, Dr. Howes suggested that increases in synaptic density and cognitive changes related to SSRI use are not necessarily dependent on each other and could even be unrelated.
Also commenting on the research, David Nutt, MD, PhD, Edmond J. Safra professor of neuropsychopharmacology at Imperial College London, said that the “delay in therapeutic action of antidepressants has been a puzzle to psychiatrists ever since they were first discerned over 50 years ago. So, these new data in humans, that use cutting edge brain imaging to demonstrate an increase in brain connections developing over the period that the depression lifts, are very exciting.”
Dr. Nutt added that the results provide further evidence that “enhancing serotonin function in the brain can have enduring health benefits.”
Funding support was provided by the Danish Council for Independent Research, the Lundbeck Foundation, Rigshospitalet, and the Swedish Research Council. Open access funding provided by Royal Library, Copenhagen University Library.
Dr. Knudsen declares relationships with Sage Biogen, H. Lundbeck, Onsero, Pangea, Gilgamesh, Abbvie, and PureTechHealth. Another author declares relationships with Cambridge Cognition and PopReach via Cambridge Enterprise.
A version of this article first appeared on Medscape.com.
BARCELONA – , new imaging data suggest.
In a double-blind study, more than 30 volunteers were randomly assigned to the SSRI escitalopram or placebo for 3-5 weeks. Using PET imaging, the investigators found that over time, synaptic density significantly increased significantly in the neocortex and hippocampus but only in patients taking the active drug.
The results point to two conclusions, said study investigator Gitta Moos Knudsen, MD, PhD, clinical professor and chief physician at the department of clinical medicine, neurology, psychiatry and sensory sciences at Copenhagen (Denmark) University Hospital.
First, they indicate that SSRIs increase synaptic density in brain areas critically involved in depression, a finding that would go some way to indicating that the synaptic density in the brain may be involved in how antidepressants function, “which would give us a target for developing novel drugs against depression,” said Dr. Knudsen.
“Secondly, our data suggest synapses build up over a period of weeks, which would explain why the effects of these drugs take time to kick in,” she added.
The findings were presented at the 36th European College of Neuropsychopharmacology (ECNP) Congress and simultaneously published online in Molecular Psychiatry.
Marked increase in synaptic density
SSRIs are widely used for depression as well as anxiety and obsessive-compulsive disorder. It is thought that they act via neuroplasticity and synaptic remodeling to improve cognition and emotion processing. However, the investigators note clinical evidence is lacking.
For the study, the researchers randomly assigned healthy individuals to either 20-mg escitalopram or placebo for 3-5 weeks.
They performed PET with the 11C-UCB-J tracer, which allows imaging of the synaptic vesicle glycoprotein 2A (SV2A) in the brain, synaptic density, as well as changes in density over time, in the hippocampus and neocortex.
Between May 2020 and October 2021, 17 individuals were assigned to escitalopram and 15 to placebo. There were no significant differences between two groups in terms of age, sex, and PET-related variables. Serum escitalopram measurements confirmed that all participants in the active drug group were compliant.
When synaptic density was assessed at a single time point, an average of 29 days after the intervention, there were no significant differences between the escitalopram and placebo groups in either the neocortex (P = .41) or in the hippocampus (P = .26).
However, when they performed a secondary analysis of the time-dependent effect on SV2A levels, they found a marked difference between the two study groups.
Compared with the placebo group, participants taking escitalopram had a marked increase in synaptic density in both the neocortex (rp value, 0.58; P = .003) and the hippocampus (rp value, 0.41; P = .048).
In contrast, there were no significant changes in synaptic density in either the neocortex (rp value, –0.01; P = .95) or the hippocampus (rp value, –0.06; P = .62) in the hippocampus.
“That is consistent with our clinical observation that it takes time to evolve synaptic density, along with clinical improvement. Does that mean that the increase in synaptic density is a precondition for improvement in symptoms? We don’t know,” said Dr. Knudsen.
Exciting but not conclusive
Session co-chair Oliver Howes, MD, PhD, professor of molecular psychiatry, King’s College London, agreed that the results do not prove the gradual increase in synaptic density the treatment response lag with SSRIs.
“We definitely don’t yet have all the data to know one way or the other,” he said in an interview.
Another potential hypothesis, he said, is that SSRIs are causing shifts in underlying brain circuits that lead to cognitive changes before there is a discernable improvement in mood.
Indeed, Dr. Howes suggested that increases in synaptic density and cognitive changes related to SSRI use are not necessarily dependent on each other and could even be unrelated.
Also commenting on the research, David Nutt, MD, PhD, Edmond J. Safra professor of neuropsychopharmacology at Imperial College London, said that the “delay in therapeutic action of antidepressants has been a puzzle to psychiatrists ever since they were first discerned over 50 years ago. So, these new data in humans, that use cutting edge brain imaging to demonstrate an increase in brain connections developing over the period that the depression lifts, are very exciting.”
Dr. Nutt added that the results provide further evidence that “enhancing serotonin function in the brain can have enduring health benefits.”
Funding support was provided by the Danish Council for Independent Research, the Lundbeck Foundation, Rigshospitalet, and the Swedish Research Council. Open access funding provided by Royal Library, Copenhagen University Library.
Dr. Knudsen declares relationships with Sage Biogen, H. Lundbeck, Onsero, Pangea, Gilgamesh, Abbvie, and PureTechHealth. Another author declares relationships with Cambridge Cognition and PopReach via Cambridge Enterprise.
A version of this article first appeared on Medscape.com.
AT ECNP 2023
Telehealth linked to better opioid treatment retention
TOPLINE:
METHODOLOGY:
- Researchers analyzed Medicaid claims data from November 2019 through the end of 2020 in Kentucky and Ohio to investigate the impact of a policy change implemented during the COVID-19 pandemic that allowed the use of telehealth to prescribe buprenorphine for OUD.
- The two main outcomes of interest were retention in treatment after initiation (telehealth vs. traditional) and opioid-related nonfatal overdose after initiation.
TAKEAWAY:
- For both states combined, nearly 92,000 adults had a buprenorphine prescription in at least one quarter in 2020, with nearly 43,000 of those individuals starting treatment in 2020.
- Sharp increases in telehealth delivery of buprenorphine were noted at the beginning of 2020 at the pandemic outset, and this was associated with greater retention in treatment (Kentucky adjusted odds ratio, 1.13; 95% confidence interval, 1.01-1.27 and Ohio aOR, 1.19; 95% CI, 1.06-1.32).
- Furthermore, 90-day retention rates were higher among those who started treatment via telehealth versus those who started treatment in nontelehealth settings in Kentucky (48% vs. 44%, respectively) and in Ohio (32% vs. 28%, respectively).
- There was no increased risk of nonfatal overdose with telehealth treatment, providing added evidence to suggest that patients were not harmed by having increased access to buprenorphine treatment via telehealth.
IN PRACTICE:
“These results offer important insights for states with a high burden of OUD looking to policies and methods to reduce barriers to treatment,” the authors write.
SOURCE:
The study, with first author Lindsey Hammerslag, PhD, with University of Kentucky College of Medicine, Lexington, was published online in JAMA Network Open, with an invited commentary by Lindsey Allen, PhD, Northwestern University, Chicago, on navigating the path to effective, equitable, and evidence-based telehealth for OUD treatment.
LIMITATIONS:
The analysis was limited to Medicaid patients in two states over 1 year and there may have been unmeasured confounders, such as perceived patient stability, that influenced the findings. Because Medicaid data were not linked to emergency services or death records, this study considered only medically treated overdose.
DISCLOSURES:
The study was supported by the National Institute on Drug Abuse and carried out in partnership with the Substance Abuse and Mental Health Services Administration. The authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers analyzed Medicaid claims data from November 2019 through the end of 2020 in Kentucky and Ohio to investigate the impact of a policy change implemented during the COVID-19 pandemic that allowed the use of telehealth to prescribe buprenorphine for OUD.
- The two main outcomes of interest were retention in treatment after initiation (telehealth vs. traditional) and opioid-related nonfatal overdose after initiation.
TAKEAWAY:
- For both states combined, nearly 92,000 adults had a buprenorphine prescription in at least one quarter in 2020, with nearly 43,000 of those individuals starting treatment in 2020.
- Sharp increases in telehealth delivery of buprenorphine were noted at the beginning of 2020 at the pandemic outset, and this was associated with greater retention in treatment (Kentucky adjusted odds ratio, 1.13; 95% confidence interval, 1.01-1.27 and Ohio aOR, 1.19; 95% CI, 1.06-1.32).
- Furthermore, 90-day retention rates were higher among those who started treatment via telehealth versus those who started treatment in nontelehealth settings in Kentucky (48% vs. 44%, respectively) and in Ohio (32% vs. 28%, respectively).
- There was no increased risk of nonfatal overdose with telehealth treatment, providing added evidence to suggest that patients were not harmed by having increased access to buprenorphine treatment via telehealth.
IN PRACTICE:
“These results offer important insights for states with a high burden of OUD looking to policies and methods to reduce barriers to treatment,” the authors write.
SOURCE:
The study, with first author Lindsey Hammerslag, PhD, with University of Kentucky College of Medicine, Lexington, was published online in JAMA Network Open, with an invited commentary by Lindsey Allen, PhD, Northwestern University, Chicago, on navigating the path to effective, equitable, and evidence-based telehealth for OUD treatment.
LIMITATIONS:
The analysis was limited to Medicaid patients in two states over 1 year and there may have been unmeasured confounders, such as perceived patient stability, that influenced the findings. Because Medicaid data were not linked to emergency services or death records, this study considered only medically treated overdose.
DISCLOSURES:
The study was supported by the National Institute on Drug Abuse and carried out in partnership with the Substance Abuse and Mental Health Services Administration. The authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers analyzed Medicaid claims data from November 2019 through the end of 2020 in Kentucky and Ohio to investigate the impact of a policy change implemented during the COVID-19 pandemic that allowed the use of telehealth to prescribe buprenorphine for OUD.
- The two main outcomes of interest were retention in treatment after initiation (telehealth vs. traditional) and opioid-related nonfatal overdose after initiation.
TAKEAWAY:
- For both states combined, nearly 92,000 adults had a buprenorphine prescription in at least one quarter in 2020, with nearly 43,000 of those individuals starting treatment in 2020.
- Sharp increases in telehealth delivery of buprenorphine were noted at the beginning of 2020 at the pandemic outset, and this was associated with greater retention in treatment (Kentucky adjusted odds ratio, 1.13; 95% confidence interval, 1.01-1.27 and Ohio aOR, 1.19; 95% CI, 1.06-1.32).
- Furthermore, 90-day retention rates were higher among those who started treatment via telehealth versus those who started treatment in nontelehealth settings in Kentucky (48% vs. 44%, respectively) and in Ohio (32% vs. 28%, respectively).
- There was no increased risk of nonfatal overdose with telehealth treatment, providing added evidence to suggest that patients were not harmed by having increased access to buprenorphine treatment via telehealth.
IN PRACTICE:
“These results offer important insights for states with a high burden of OUD looking to policies and methods to reduce barriers to treatment,” the authors write.
SOURCE:
The study, with first author Lindsey Hammerslag, PhD, with University of Kentucky College of Medicine, Lexington, was published online in JAMA Network Open, with an invited commentary by Lindsey Allen, PhD, Northwestern University, Chicago, on navigating the path to effective, equitable, and evidence-based telehealth for OUD treatment.
LIMITATIONS:
The analysis was limited to Medicaid patients in two states over 1 year and there may have been unmeasured confounders, such as perceived patient stability, that influenced the findings. Because Medicaid data were not linked to emergency services or death records, this study considered only medically treated overdose.
DISCLOSURES:
The study was supported by the National Institute on Drug Abuse and carried out in partnership with the Substance Abuse and Mental Health Services Administration. The authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Pandemic-era telehealth led to fewer therapy disruptions
TOPLINE:
METHODOLOGY:
- Retrospective study using electronic health records and insurance claims data from three large U.S. health systems.
- Sample included 110,089 patients with mental health conditions who attended at least two psychotherapy visits during the 9 months before and 9 months after the onset of COVID-19, defined in this study as March 14, 2020.
- Outcome was disruption in psychotherapy, defined as a gap of more than 45 days between visits.
TAKEAWAY:
- Before the pandemic, 96.9% of psychotherapy visits were in person and 35.4% were followed by a gap of more than 45 days.
- After the onset of the pandemic, more than half of visits (51.8%) were virtual, and only 17.9% were followed by a gap of more than 45 days.
- Prior to the pandemic, the median time between visits was 27 days, and after the pandemic, it dropped to 14 days, suggesting individuals were more likely to return for additional psychotherapy after the widespread shift to virtual care.
- Over the entire study period, individuals with depressive, anxiety, or bipolar disorders were more likely to maintain consistent psychotherapy visits, whereas those with schizophrenia, ADHD, autism, conduct or disruptive disorders, dementia, or personality disorders were more likely to have a disruption in their visits.
IN PRACTICE:
“These findings support continued use of virtual psychotherapy as an option for care when appropriate infrastructure is in place. In addition, these findings support the continuation of policies that provide access to and coverage for virtual psychotherapy,” the authors write.
SOURCE:
The study, led by Brian K. Ahmedani, PhD, with the Center for Health Policy and Health Services Research, Henry Ford Health, Detroit, was published online in Psychiatric Services.
LIMITATIONS:
The study was conducted in three large health systems with virtual care infrastructure already in place. Researchers did not examine use of virtual care for medication management or for types of care other than psychotherapy, which may present different challenges.
DISCLOSURES:
The study was supported by the National Institute of Mental Health. The authors have no relevant disclosures.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Retrospective study using electronic health records and insurance claims data from three large U.S. health systems.
- Sample included 110,089 patients with mental health conditions who attended at least two psychotherapy visits during the 9 months before and 9 months after the onset of COVID-19, defined in this study as March 14, 2020.
- Outcome was disruption in psychotherapy, defined as a gap of more than 45 days between visits.
TAKEAWAY:
- Before the pandemic, 96.9% of psychotherapy visits were in person and 35.4% were followed by a gap of more than 45 days.
- After the onset of the pandemic, more than half of visits (51.8%) were virtual, and only 17.9% were followed by a gap of more than 45 days.
- Prior to the pandemic, the median time between visits was 27 days, and after the pandemic, it dropped to 14 days, suggesting individuals were more likely to return for additional psychotherapy after the widespread shift to virtual care.
- Over the entire study period, individuals with depressive, anxiety, or bipolar disorders were more likely to maintain consistent psychotherapy visits, whereas those with schizophrenia, ADHD, autism, conduct or disruptive disorders, dementia, or personality disorders were more likely to have a disruption in their visits.
IN PRACTICE:
“These findings support continued use of virtual psychotherapy as an option for care when appropriate infrastructure is in place. In addition, these findings support the continuation of policies that provide access to and coverage for virtual psychotherapy,” the authors write.
SOURCE:
The study, led by Brian K. Ahmedani, PhD, with the Center for Health Policy and Health Services Research, Henry Ford Health, Detroit, was published online in Psychiatric Services.
LIMITATIONS:
The study was conducted in three large health systems with virtual care infrastructure already in place. Researchers did not examine use of virtual care for medication management or for types of care other than psychotherapy, which may present different challenges.
DISCLOSURES:
The study was supported by the National Institute of Mental Health. The authors have no relevant disclosures.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Retrospective study using electronic health records and insurance claims data from three large U.S. health systems.
- Sample included 110,089 patients with mental health conditions who attended at least two psychotherapy visits during the 9 months before and 9 months after the onset of COVID-19, defined in this study as March 14, 2020.
- Outcome was disruption in psychotherapy, defined as a gap of more than 45 days between visits.
TAKEAWAY:
- Before the pandemic, 96.9% of psychotherapy visits were in person and 35.4% were followed by a gap of more than 45 days.
- After the onset of the pandemic, more than half of visits (51.8%) were virtual, and only 17.9% were followed by a gap of more than 45 days.
- Prior to the pandemic, the median time between visits was 27 days, and after the pandemic, it dropped to 14 days, suggesting individuals were more likely to return for additional psychotherapy after the widespread shift to virtual care.
- Over the entire study period, individuals with depressive, anxiety, or bipolar disorders were more likely to maintain consistent psychotherapy visits, whereas those with schizophrenia, ADHD, autism, conduct or disruptive disorders, dementia, or personality disorders were more likely to have a disruption in their visits.
IN PRACTICE:
“These findings support continued use of virtual psychotherapy as an option for care when appropriate infrastructure is in place. In addition, these findings support the continuation of policies that provide access to and coverage for virtual psychotherapy,” the authors write.
SOURCE:
The study, led by Brian K. Ahmedani, PhD, with the Center for Health Policy and Health Services Research, Henry Ford Health, Detroit, was published online in Psychiatric Services.
LIMITATIONS:
The study was conducted in three large health systems with virtual care infrastructure already in place. Researchers did not examine use of virtual care for medication management or for types of care other than psychotherapy, which may present different challenges.
DISCLOSURES:
The study was supported by the National Institute of Mental Health. The authors have no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM PSYCHIATRIC SERVICES