User login
Sepsis mortality greater in Black than White children despite similar interventions
WASHINGTON – , according to research presented at the annual meeting of the American Academy of Pediatrics.
The only other difference between Black and White pediatric patients was the length of hospital stay and the length of time in the ICU among those who died. In both cases, Black children who died spent more time in the hospital and in the ICU, reported Michael H. Stroud, MD, a pediatric critical care physician at the University of Arkansas for Medical Sciences in Little Rock, and his colleagues.
“Further investigations are needed to identify biases, conscious and unconscious, potential socioeconomic factors, and genetic predispositions leading to racial disparities in outcomes of children with pediatric sepsis, severe sepsis, and septic shock,” Dr Stroud and his colleagues said.
Nathan T. Chomilo, MD, adjunct assistant professor of pediatrics at the University of Minnesota, Minneapolis, who was not involved in the study but reviewed it, said the research “builds upon existing evidence that our health care system has work to do to meet its goal of treating patients equitably and provide everyone the opportunity for health.” He found the racial disparity in death particularly striking in 2023. “In the U.S., with all our wealth, knowledge, and resources, very few children should die from this, let alone there be such a stark gap,” Dr. Chomilo wrote.
Racial disparities persist
Dr. Stroud noted that many institutions currently use “automated, real-time, algorithm-based detection of sepsis, severe sepsis, and septic shock incorporated into the electronic medical record,” which leads to earlier recognition and resuscitation and overall better outcomes. Yet racial disparities in sepsis mortality rates persist, and he and his colleagues wanted to explore whether they remained even with these EMR-incorporated systems.
The researchers analyzed data from all patients at Arkansas Children’s Hospital who had sepsis, severe sepsis, or septic shock between January 2018 and April 2022. The hospital uses a best practice advisory (BPA) in the EMR whose activation leads to a bedside huddle and clinical interventions. For this study, the researchers defined a sepsis episode as either a BPA activation or an EMR diagnosis of sepsis, severe sepsis, or septic shock.
Among the 3,514 patients who had a sepsis episode during the study, 60.5% were White (n = 2,126) and 20.9% were Black (n = 736). Overall mortality was 1.65%, but that included 3.13% of Black children versus 1.27% of White children (odds ratio [OR] 2.51, P = .001). No significant differences in mortality were seen in gender or age.
Clinical interventions in the two groups were also similar: Total IV antibiotic days were 23.8 days for Black children and 21.6 days for White children (P = .38); total vasoactive infusion days were 2.2 for Black children and 2.6 for White (P = .18); and extracorporeal membrane oxygenation was necessary for 26.1% of Black children and 18.5% of White children (P = .52).
Length of hospitalization stay, however, was an average 4 days longer for Black children (16.7 days) versus White children (12.7 days) who died (P = .03). ICU stay for Black children who died was also an average 1.9 days longer (7.57 vs. 5.7 days; P = .01). There were no significant differences in the EMR between Black and White patients, however, in the percent who were over the threshold for antibiotic administration and the percent who received an IV fluid bolus.
Contributing factors
Dr. Chomilo said that most BPA systems require staff – including rooming and triage staff, nurses. and physicians – to enter vital signs, order labs, enter the results into the system, and enter other data used by the algorithm. “So even though the time from when those BPA warnings flagged to when clinical interventions were documented didn’t show a significant difference, there are numerous other points along a child’s illness that may be contributing to these numbers,” Dr. Chomilo said.
For example, he pointed out that differences in health insurance coverage could have influenced whether their parent or caregiver was able to bring them in early enough to be diagnosed since studies have revealed disparate access to regular care due to structural racism in the health care system. Studies have also shown disparate rates of patients being triaged or having to wait longer in emergency departments, he added.
“When the child was brought in, how were they triaged? How long did they wait before they had vitals taken? How long until they were seen by a clinician?” Dr. Chomilo said. “Was their care on the inpatient ward the same or different? What was the source of sepsis? Was it all infectious or other issues [since] cancer and autoimmune illnesses can also trigger a sepsis evaluation, for example? Overall, I suspect answers to several of these questions would reveal a disparity due to structural racism that contributed to the ultimate disparity in deaths.”
Other social determinants of health that could have played a role in the outcome disparities here might include the family’s access to transportation options, parental employment or child care options, and nutrition access since baseline nutritional status can be a factor in the outcomes of severe illnesses like sepsis.
”I don’t think this study provided enough information about the potential causative factors to come to any strong conclusions,” Dr. Chomilo said. But it’s important for clinicians to be aware of how biases in the health care system put Black, Indigenous and other communities at higher risk for worse clinical outcomes.
“I would reiterate that clinicians in the hospital can help improve outcomes by being aware of structural racism and structural inequity and how that may contribute to their patient’s risk of severe illness as the decide how to approach their treatment and engaging the patient’s family,” Dr. Chomilo said. “We cannot rely solely on universal tools that don’t take this into account when we are looking to improve clinical outcomes for everyone. Otherwise we will see these gaps persist.”
No external funding sources were noted. Dr. Stroud and Dr. Chomilo had no disclosures.
WASHINGTON – , according to research presented at the annual meeting of the American Academy of Pediatrics.
The only other difference between Black and White pediatric patients was the length of hospital stay and the length of time in the ICU among those who died. In both cases, Black children who died spent more time in the hospital and in the ICU, reported Michael H. Stroud, MD, a pediatric critical care physician at the University of Arkansas for Medical Sciences in Little Rock, and his colleagues.
“Further investigations are needed to identify biases, conscious and unconscious, potential socioeconomic factors, and genetic predispositions leading to racial disparities in outcomes of children with pediatric sepsis, severe sepsis, and septic shock,” Dr Stroud and his colleagues said.
Nathan T. Chomilo, MD, adjunct assistant professor of pediatrics at the University of Minnesota, Minneapolis, who was not involved in the study but reviewed it, said the research “builds upon existing evidence that our health care system has work to do to meet its goal of treating patients equitably and provide everyone the opportunity for health.” He found the racial disparity in death particularly striking in 2023. “In the U.S., with all our wealth, knowledge, and resources, very few children should die from this, let alone there be such a stark gap,” Dr. Chomilo wrote.
Racial disparities persist
Dr. Stroud noted that many institutions currently use “automated, real-time, algorithm-based detection of sepsis, severe sepsis, and septic shock incorporated into the electronic medical record,” which leads to earlier recognition and resuscitation and overall better outcomes. Yet racial disparities in sepsis mortality rates persist, and he and his colleagues wanted to explore whether they remained even with these EMR-incorporated systems.
The researchers analyzed data from all patients at Arkansas Children’s Hospital who had sepsis, severe sepsis, or septic shock between January 2018 and April 2022. The hospital uses a best practice advisory (BPA) in the EMR whose activation leads to a bedside huddle and clinical interventions. For this study, the researchers defined a sepsis episode as either a BPA activation or an EMR diagnosis of sepsis, severe sepsis, or septic shock.
Among the 3,514 patients who had a sepsis episode during the study, 60.5% were White (n = 2,126) and 20.9% were Black (n = 736). Overall mortality was 1.65%, but that included 3.13% of Black children versus 1.27% of White children (odds ratio [OR] 2.51, P = .001). No significant differences in mortality were seen in gender or age.
Clinical interventions in the two groups were also similar: Total IV antibiotic days were 23.8 days for Black children and 21.6 days for White children (P = .38); total vasoactive infusion days were 2.2 for Black children and 2.6 for White (P = .18); and extracorporeal membrane oxygenation was necessary for 26.1% of Black children and 18.5% of White children (P = .52).
Length of hospitalization stay, however, was an average 4 days longer for Black children (16.7 days) versus White children (12.7 days) who died (P = .03). ICU stay for Black children who died was also an average 1.9 days longer (7.57 vs. 5.7 days; P = .01). There were no significant differences in the EMR between Black and White patients, however, in the percent who were over the threshold for antibiotic administration and the percent who received an IV fluid bolus.
Contributing factors
Dr. Chomilo said that most BPA systems require staff – including rooming and triage staff, nurses. and physicians – to enter vital signs, order labs, enter the results into the system, and enter other data used by the algorithm. “So even though the time from when those BPA warnings flagged to when clinical interventions were documented didn’t show a significant difference, there are numerous other points along a child’s illness that may be contributing to these numbers,” Dr. Chomilo said.
For example, he pointed out that differences in health insurance coverage could have influenced whether their parent or caregiver was able to bring them in early enough to be diagnosed since studies have revealed disparate access to regular care due to structural racism in the health care system. Studies have also shown disparate rates of patients being triaged or having to wait longer in emergency departments, he added.
“When the child was brought in, how were they triaged? How long did they wait before they had vitals taken? How long until they were seen by a clinician?” Dr. Chomilo said. “Was their care on the inpatient ward the same or different? What was the source of sepsis? Was it all infectious or other issues [since] cancer and autoimmune illnesses can also trigger a sepsis evaluation, for example? Overall, I suspect answers to several of these questions would reveal a disparity due to structural racism that contributed to the ultimate disparity in deaths.”
Other social determinants of health that could have played a role in the outcome disparities here might include the family’s access to transportation options, parental employment or child care options, and nutrition access since baseline nutritional status can be a factor in the outcomes of severe illnesses like sepsis.
”I don’t think this study provided enough information about the potential causative factors to come to any strong conclusions,” Dr. Chomilo said. But it’s important for clinicians to be aware of how biases in the health care system put Black, Indigenous and other communities at higher risk for worse clinical outcomes.
“I would reiterate that clinicians in the hospital can help improve outcomes by being aware of structural racism and structural inequity and how that may contribute to their patient’s risk of severe illness as the decide how to approach their treatment and engaging the patient’s family,” Dr. Chomilo said. “We cannot rely solely on universal tools that don’t take this into account when we are looking to improve clinical outcomes for everyone. Otherwise we will see these gaps persist.”
No external funding sources were noted. Dr. Stroud and Dr. Chomilo had no disclosures.
WASHINGTON – , according to research presented at the annual meeting of the American Academy of Pediatrics.
The only other difference between Black and White pediatric patients was the length of hospital stay and the length of time in the ICU among those who died. In both cases, Black children who died spent more time in the hospital and in the ICU, reported Michael H. Stroud, MD, a pediatric critical care physician at the University of Arkansas for Medical Sciences in Little Rock, and his colleagues.
“Further investigations are needed to identify biases, conscious and unconscious, potential socioeconomic factors, and genetic predispositions leading to racial disparities in outcomes of children with pediatric sepsis, severe sepsis, and septic shock,” Dr Stroud and his colleagues said.
Nathan T. Chomilo, MD, adjunct assistant professor of pediatrics at the University of Minnesota, Minneapolis, who was not involved in the study but reviewed it, said the research “builds upon existing evidence that our health care system has work to do to meet its goal of treating patients equitably and provide everyone the opportunity for health.” He found the racial disparity in death particularly striking in 2023. “In the U.S., with all our wealth, knowledge, and resources, very few children should die from this, let alone there be such a stark gap,” Dr. Chomilo wrote.
Racial disparities persist
Dr. Stroud noted that many institutions currently use “automated, real-time, algorithm-based detection of sepsis, severe sepsis, and septic shock incorporated into the electronic medical record,” which leads to earlier recognition and resuscitation and overall better outcomes. Yet racial disparities in sepsis mortality rates persist, and he and his colleagues wanted to explore whether they remained even with these EMR-incorporated systems.
The researchers analyzed data from all patients at Arkansas Children’s Hospital who had sepsis, severe sepsis, or septic shock between January 2018 and April 2022. The hospital uses a best practice advisory (BPA) in the EMR whose activation leads to a bedside huddle and clinical interventions. For this study, the researchers defined a sepsis episode as either a BPA activation or an EMR diagnosis of sepsis, severe sepsis, or septic shock.
Among the 3,514 patients who had a sepsis episode during the study, 60.5% were White (n = 2,126) and 20.9% were Black (n = 736). Overall mortality was 1.65%, but that included 3.13% of Black children versus 1.27% of White children (odds ratio [OR] 2.51, P = .001). No significant differences in mortality were seen in gender or age.
Clinical interventions in the two groups were also similar: Total IV antibiotic days were 23.8 days for Black children and 21.6 days for White children (P = .38); total vasoactive infusion days were 2.2 for Black children and 2.6 for White (P = .18); and extracorporeal membrane oxygenation was necessary for 26.1% of Black children and 18.5% of White children (P = .52).
Length of hospitalization stay, however, was an average 4 days longer for Black children (16.7 days) versus White children (12.7 days) who died (P = .03). ICU stay for Black children who died was also an average 1.9 days longer (7.57 vs. 5.7 days; P = .01). There were no significant differences in the EMR between Black and White patients, however, in the percent who were over the threshold for antibiotic administration and the percent who received an IV fluid bolus.
Contributing factors
Dr. Chomilo said that most BPA systems require staff – including rooming and triage staff, nurses. and physicians – to enter vital signs, order labs, enter the results into the system, and enter other data used by the algorithm. “So even though the time from when those BPA warnings flagged to when clinical interventions were documented didn’t show a significant difference, there are numerous other points along a child’s illness that may be contributing to these numbers,” Dr. Chomilo said.
For example, he pointed out that differences in health insurance coverage could have influenced whether their parent or caregiver was able to bring them in early enough to be diagnosed since studies have revealed disparate access to regular care due to structural racism in the health care system. Studies have also shown disparate rates of patients being triaged or having to wait longer in emergency departments, he added.
“When the child was brought in, how were they triaged? How long did they wait before they had vitals taken? How long until they were seen by a clinician?” Dr. Chomilo said. “Was their care on the inpatient ward the same or different? What was the source of sepsis? Was it all infectious or other issues [since] cancer and autoimmune illnesses can also trigger a sepsis evaluation, for example? Overall, I suspect answers to several of these questions would reveal a disparity due to structural racism that contributed to the ultimate disparity in deaths.”
Other social determinants of health that could have played a role in the outcome disparities here might include the family’s access to transportation options, parental employment or child care options, and nutrition access since baseline nutritional status can be a factor in the outcomes of severe illnesses like sepsis.
”I don’t think this study provided enough information about the potential causative factors to come to any strong conclusions,” Dr. Chomilo said. But it’s important for clinicians to be aware of how biases in the health care system put Black, Indigenous and other communities at higher risk for worse clinical outcomes.
“I would reiterate that clinicians in the hospital can help improve outcomes by being aware of structural racism and structural inequity and how that may contribute to their patient’s risk of severe illness as the decide how to approach their treatment and engaging the patient’s family,” Dr. Chomilo said. “We cannot rely solely on universal tools that don’t take this into account when we are looking to improve clinical outcomes for everyone. Otherwise we will see these gaps persist.”
No external funding sources were noted. Dr. Stroud and Dr. Chomilo had no disclosures.
AT AAP 2023
Five times greater suicide risk for trans, gender-diverse teens in ED
WASHINGTON – , according to a study presented at the annual meeting of the American Academy of Pediatrics.
“The take-home message here is this study emphasizes the importance of universal screening to identify gender-diverse youth at risk,” Amanda Burnside, PhD, assistant professor of psychiatry and behavioral sciences at Ann and Robert H. Lurie Children’s Hospital of Chicago and Northwestern University, told attendees. “We really need to develop robust strategies and systems to link better mental health services.”
Suicide rates in transgender and gender-diverse youth are exceptionally high among youth in the U.S., Dr. Burnside said during her presentation. For example, the 2022 LGBTQ health survey from the Trevor Project found that much higher percentages of transgender and gender nonconforming youth had considered suicide in the past year compared with cisgender youth, even within the LGBTQ umbrella. Among nearly 34,000 LGBTQ youth aged 13-24, nearly half of trans females (48%) and more than half of trans males (59%) had considered suicide, compared with 28% of cisgender males and 37% of cisgender females. The rate among nonbinary/genderqueer individuals was 53%, and it was 48% for those questioning their gender.
Current methods of identifying trans and gender-diverse (TGD) youth in the hospital, however, may not actually be capturing the entire population.
“In health care settings, research involving TGD individuals has historically been limited to specialized clinic populations or youth with gender-specific diagnostic codes documented in the electronic medical record,” an approach that “likely significantly underestimates the prevalence of TGD youth in health care settings.” While at least one study has attempted to bridge this gap by searching the EMR for keywords, that study only tried to identify trans youth and not other youth on the gender diversity spectrum, such as nonbinary youth or those questioning their gender identity. Dr. Burnside and her colleagues therefore designed a study that used keywords to identify both trans youth and other gender-diverse youth who visited the ED so they could assess the rate of positive suicide screens in this population.
Underestimating the population at risk?
The researchers conducted a retrospective cross-sectional study of EMR data for all ED visits during which the patient underwent suicide screening. For the period of November 2019 to August 2022, they collected data on the screening results and the patient’s gender identity, age, race/ethnicity, insurance status, chief complaint in the ED and child opportunity index, which assess a youth’s access to resources based on geography. The suicide screener used was the Ask Suicide–Screening Questions (ASQ) tool.
The keywords they looked for in the EMR to identify trans and gender-diverse youth included transgender, pronouns, agender, gender dysphoria, male-to-female, female-to-male, nonbinary, preferred name, and they/them (captured as a complete term, not as “they” and “them” separately).
“If a keyword was present, the surrounding text was extracted and reviewed by two members of our team,” Dr. Burnside explained in her presentation. “We categorized keywords into either indicative of gender-diverse identity or not, and if it wasn’t clear based on the text extracted, we would conduct a manual chart review,” though that only occurred in about 3% of cases, she added.
Among 15,413 ED encounters with a suicide screen, the researchers identified 1,126 of these keywords in the EMR, among which 91.2% were classified as referring to a gender-diverse patient. Nearly all of the words were at least 90% effective in identify a gender-diverse youth, Dr. Burnside said, and all of the 197 instances of “they/them” were classified as gender diverse.
The accuracy was a little lower for the two keywords that appeared most frequently: For “pronouns,” 86.3% of 306 instances were classified as gender diverse, and for “transgender,” 83.1% of 207 instances were classified as gender diverse. Since some providers ask all patients their pronouns, the presence of “pronouns” in the EMR alone did not necessarily indicate the patient was gender diverse, Dr. Burnside said. A common reason the term “transgender” occurred in the EMR of non–gender diverse patients is that the department’s list of crisis resources includes transgender hotlines.
After identifying all the keywords, the researchers determined how many of these occurred in unique ED encounters and removed those with incomplete screening. Overall, they found 565 encounters by 399 gender-diverse individuals who had a suicide screening, representing 4.6% of total visits. This percentage is slightly lower than recent population-based estimates of gender-diverse youth, the researchers noted.
This population ranged from 8 to 23 years old, and 43% were publicly insured. The chief complaint for most of the patients (77.5%) was a mental health one. They were predominantly White (43%) or Hispanic (35%), with 10% Black youth, 4% Asian youth, and 8% youth who were “other” or two or more races. About half (52%) lived in a neighborhood with a “low” or “very low” child opportunity index.
Within this population, 81% of the patients screened positive on the suicide screening, compared with 23% positive screens across all ED visits. One in ten (10%) gender-diverse youth had active suicidal ideation, compared with 3.4% of the rest of the ED patient population. The researchers calculated that gender-diverse youth had 5.35 times greater odds of screening positive than cisgender youth in the ED (95% confidence interval [CI] 8.7-15.92). Further, a quarter (25%) of the trans and gender-diverse youth who screened positive for suicide risk had come to the ED for a primary complaint unrelated to mental health.
“We had a kid who came in because he broke his arm who had active suicidal ideation,” study coauthor Jennifer A. Hoffmann, MD, assistant professor of pediatrics at the Ann & Robert H. Lurie Children’s Hospital of Chicago and Northwestern University, mentioned after the presentation. That particular patient even had a suicide plan, but was identified as actively suicidal only because of the screening. In other cases, she said, a youth may come in with self-inflicted injuries, and while those are the primary complaint, they are linked with suicidal ideation.
Among the study’s limitations are that gender identity is not necessarily being systematically assessed during visits, misspellings might have missed some youth, and their search strategy has not yet been externally validated, though they plan to seek that.
“Overall, however, this study did demonstrate that keyword searching is a promising technique to identify and prioritize gender-diverse youth in health services research,” Dr. Burnside said. In addition to showing the feasibility of using a keyword search strategy for identifying gender-diverse youth, Dr. Burnside noted that 31% of the encounters were identified by just one of the keywords they used, “highlighting the importance of using a comprehensive list of keywords to identify gender-diverse youth.”
Uncovering valuable information
Jason Rafferty, MD, MPH, EdM, clinical assistant professor of pediatrics and of psychiatry and human behavior at Brown University, Providence, R.I., who attended the presentation, noted that the study provides information on a population that’s often difficult to get through traditional EMR research methods.
“A lot of medical record systems don’t have uniform ways of capturing [gender diversity], but what we know as providers is that kids are really struggling and that it’s not a surprise that we’re seeing these disparities with suicidality,” Dr. Rafferty said.
The study also provides more discrete estimates by age than what most other current research measures, which tends to be lifetime suicidality as opposed to suicidal thoughts or attempts within the past year, Dr. Rafferty added.
”What this shows is, for adolescents, the risk of suicide is something we need to be paying attention to. Because it’s not that it’s something that only happens in adults, this really dispels a lot of the misquoting of the data that’s out there.” That kind of information is valuable for determining resource allocation, he said. “A disparity like this really underlies the importance of mental health resources in this field,” he said.
Dr. Burnside, Dr. Hoffmann, and Dr. Rafferty had no disclosures, and no external funding sources were noted.
WASHINGTON – , according to a study presented at the annual meeting of the American Academy of Pediatrics.
“The take-home message here is this study emphasizes the importance of universal screening to identify gender-diverse youth at risk,” Amanda Burnside, PhD, assistant professor of psychiatry and behavioral sciences at Ann and Robert H. Lurie Children’s Hospital of Chicago and Northwestern University, told attendees. “We really need to develop robust strategies and systems to link better mental health services.”
Suicide rates in transgender and gender-diverse youth are exceptionally high among youth in the U.S., Dr. Burnside said during her presentation. For example, the 2022 LGBTQ health survey from the Trevor Project found that much higher percentages of transgender and gender nonconforming youth had considered suicide in the past year compared with cisgender youth, even within the LGBTQ umbrella. Among nearly 34,000 LGBTQ youth aged 13-24, nearly half of trans females (48%) and more than half of trans males (59%) had considered suicide, compared with 28% of cisgender males and 37% of cisgender females. The rate among nonbinary/genderqueer individuals was 53%, and it was 48% for those questioning their gender.
Current methods of identifying trans and gender-diverse (TGD) youth in the hospital, however, may not actually be capturing the entire population.
“In health care settings, research involving TGD individuals has historically been limited to specialized clinic populations or youth with gender-specific diagnostic codes documented in the electronic medical record,” an approach that “likely significantly underestimates the prevalence of TGD youth in health care settings.” While at least one study has attempted to bridge this gap by searching the EMR for keywords, that study only tried to identify trans youth and not other youth on the gender diversity spectrum, such as nonbinary youth or those questioning their gender identity. Dr. Burnside and her colleagues therefore designed a study that used keywords to identify both trans youth and other gender-diverse youth who visited the ED so they could assess the rate of positive suicide screens in this population.
Underestimating the population at risk?
The researchers conducted a retrospective cross-sectional study of EMR data for all ED visits during which the patient underwent suicide screening. For the period of November 2019 to August 2022, they collected data on the screening results and the patient’s gender identity, age, race/ethnicity, insurance status, chief complaint in the ED and child opportunity index, which assess a youth’s access to resources based on geography. The suicide screener used was the Ask Suicide–Screening Questions (ASQ) tool.
The keywords they looked for in the EMR to identify trans and gender-diverse youth included transgender, pronouns, agender, gender dysphoria, male-to-female, female-to-male, nonbinary, preferred name, and they/them (captured as a complete term, not as “they” and “them” separately).
“If a keyword was present, the surrounding text was extracted and reviewed by two members of our team,” Dr. Burnside explained in her presentation. “We categorized keywords into either indicative of gender-diverse identity or not, and if it wasn’t clear based on the text extracted, we would conduct a manual chart review,” though that only occurred in about 3% of cases, she added.
Among 15,413 ED encounters with a suicide screen, the researchers identified 1,126 of these keywords in the EMR, among which 91.2% were classified as referring to a gender-diverse patient. Nearly all of the words were at least 90% effective in identify a gender-diverse youth, Dr. Burnside said, and all of the 197 instances of “they/them” were classified as gender diverse.
The accuracy was a little lower for the two keywords that appeared most frequently: For “pronouns,” 86.3% of 306 instances were classified as gender diverse, and for “transgender,” 83.1% of 207 instances were classified as gender diverse. Since some providers ask all patients their pronouns, the presence of “pronouns” in the EMR alone did not necessarily indicate the patient was gender diverse, Dr. Burnside said. A common reason the term “transgender” occurred in the EMR of non–gender diverse patients is that the department’s list of crisis resources includes transgender hotlines.
After identifying all the keywords, the researchers determined how many of these occurred in unique ED encounters and removed those with incomplete screening. Overall, they found 565 encounters by 399 gender-diverse individuals who had a suicide screening, representing 4.6% of total visits. This percentage is slightly lower than recent population-based estimates of gender-diverse youth, the researchers noted.
This population ranged from 8 to 23 years old, and 43% were publicly insured. The chief complaint for most of the patients (77.5%) was a mental health one. They were predominantly White (43%) or Hispanic (35%), with 10% Black youth, 4% Asian youth, and 8% youth who were “other” or two or more races. About half (52%) lived in a neighborhood with a “low” or “very low” child opportunity index.
Within this population, 81% of the patients screened positive on the suicide screening, compared with 23% positive screens across all ED visits. One in ten (10%) gender-diverse youth had active suicidal ideation, compared with 3.4% of the rest of the ED patient population. The researchers calculated that gender-diverse youth had 5.35 times greater odds of screening positive than cisgender youth in the ED (95% confidence interval [CI] 8.7-15.92). Further, a quarter (25%) of the trans and gender-diverse youth who screened positive for suicide risk had come to the ED for a primary complaint unrelated to mental health.
“We had a kid who came in because he broke his arm who had active suicidal ideation,” study coauthor Jennifer A. Hoffmann, MD, assistant professor of pediatrics at the Ann & Robert H. Lurie Children’s Hospital of Chicago and Northwestern University, mentioned after the presentation. That particular patient even had a suicide plan, but was identified as actively suicidal only because of the screening. In other cases, she said, a youth may come in with self-inflicted injuries, and while those are the primary complaint, they are linked with suicidal ideation.
Among the study’s limitations are that gender identity is not necessarily being systematically assessed during visits, misspellings might have missed some youth, and their search strategy has not yet been externally validated, though they plan to seek that.
“Overall, however, this study did demonstrate that keyword searching is a promising technique to identify and prioritize gender-diverse youth in health services research,” Dr. Burnside said. In addition to showing the feasibility of using a keyword search strategy for identifying gender-diverse youth, Dr. Burnside noted that 31% of the encounters were identified by just one of the keywords they used, “highlighting the importance of using a comprehensive list of keywords to identify gender-diverse youth.”
Uncovering valuable information
Jason Rafferty, MD, MPH, EdM, clinical assistant professor of pediatrics and of psychiatry and human behavior at Brown University, Providence, R.I., who attended the presentation, noted that the study provides information on a population that’s often difficult to get through traditional EMR research methods.
“A lot of medical record systems don’t have uniform ways of capturing [gender diversity], but what we know as providers is that kids are really struggling and that it’s not a surprise that we’re seeing these disparities with suicidality,” Dr. Rafferty said.
The study also provides more discrete estimates by age than what most other current research measures, which tends to be lifetime suicidality as opposed to suicidal thoughts or attempts within the past year, Dr. Rafferty added.
”What this shows is, for adolescents, the risk of suicide is something we need to be paying attention to. Because it’s not that it’s something that only happens in adults, this really dispels a lot of the misquoting of the data that’s out there.” That kind of information is valuable for determining resource allocation, he said. “A disparity like this really underlies the importance of mental health resources in this field,” he said.
Dr. Burnside, Dr. Hoffmann, and Dr. Rafferty had no disclosures, and no external funding sources were noted.
WASHINGTON – , according to a study presented at the annual meeting of the American Academy of Pediatrics.
“The take-home message here is this study emphasizes the importance of universal screening to identify gender-diverse youth at risk,” Amanda Burnside, PhD, assistant professor of psychiatry and behavioral sciences at Ann and Robert H. Lurie Children’s Hospital of Chicago and Northwestern University, told attendees. “We really need to develop robust strategies and systems to link better mental health services.”
Suicide rates in transgender and gender-diverse youth are exceptionally high among youth in the U.S., Dr. Burnside said during her presentation. For example, the 2022 LGBTQ health survey from the Trevor Project found that much higher percentages of transgender and gender nonconforming youth had considered suicide in the past year compared with cisgender youth, even within the LGBTQ umbrella. Among nearly 34,000 LGBTQ youth aged 13-24, nearly half of trans females (48%) and more than half of trans males (59%) had considered suicide, compared with 28% of cisgender males and 37% of cisgender females. The rate among nonbinary/genderqueer individuals was 53%, and it was 48% for those questioning their gender.
Current methods of identifying trans and gender-diverse (TGD) youth in the hospital, however, may not actually be capturing the entire population.
“In health care settings, research involving TGD individuals has historically been limited to specialized clinic populations or youth with gender-specific diagnostic codes documented in the electronic medical record,” an approach that “likely significantly underestimates the prevalence of TGD youth in health care settings.” While at least one study has attempted to bridge this gap by searching the EMR for keywords, that study only tried to identify trans youth and not other youth on the gender diversity spectrum, such as nonbinary youth or those questioning their gender identity. Dr. Burnside and her colleagues therefore designed a study that used keywords to identify both trans youth and other gender-diverse youth who visited the ED so they could assess the rate of positive suicide screens in this population.
Underestimating the population at risk?
The researchers conducted a retrospective cross-sectional study of EMR data for all ED visits during which the patient underwent suicide screening. For the period of November 2019 to August 2022, they collected data on the screening results and the patient’s gender identity, age, race/ethnicity, insurance status, chief complaint in the ED and child opportunity index, which assess a youth’s access to resources based on geography. The suicide screener used was the Ask Suicide–Screening Questions (ASQ) tool.
The keywords they looked for in the EMR to identify trans and gender-diverse youth included transgender, pronouns, agender, gender dysphoria, male-to-female, female-to-male, nonbinary, preferred name, and they/them (captured as a complete term, not as “they” and “them” separately).
“If a keyword was present, the surrounding text was extracted and reviewed by two members of our team,” Dr. Burnside explained in her presentation. “We categorized keywords into either indicative of gender-diverse identity or not, and if it wasn’t clear based on the text extracted, we would conduct a manual chart review,” though that only occurred in about 3% of cases, she added.
Among 15,413 ED encounters with a suicide screen, the researchers identified 1,126 of these keywords in the EMR, among which 91.2% were classified as referring to a gender-diverse patient. Nearly all of the words were at least 90% effective in identify a gender-diverse youth, Dr. Burnside said, and all of the 197 instances of “they/them” were classified as gender diverse.
The accuracy was a little lower for the two keywords that appeared most frequently: For “pronouns,” 86.3% of 306 instances were classified as gender diverse, and for “transgender,” 83.1% of 207 instances were classified as gender diverse. Since some providers ask all patients their pronouns, the presence of “pronouns” in the EMR alone did not necessarily indicate the patient was gender diverse, Dr. Burnside said. A common reason the term “transgender” occurred in the EMR of non–gender diverse patients is that the department’s list of crisis resources includes transgender hotlines.
After identifying all the keywords, the researchers determined how many of these occurred in unique ED encounters and removed those with incomplete screening. Overall, they found 565 encounters by 399 gender-diverse individuals who had a suicide screening, representing 4.6% of total visits. This percentage is slightly lower than recent population-based estimates of gender-diverse youth, the researchers noted.
This population ranged from 8 to 23 years old, and 43% were publicly insured. The chief complaint for most of the patients (77.5%) was a mental health one. They were predominantly White (43%) or Hispanic (35%), with 10% Black youth, 4% Asian youth, and 8% youth who were “other” or two or more races. About half (52%) lived in a neighborhood with a “low” or “very low” child opportunity index.
Within this population, 81% of the patients screened positive on the suicide screening, compared with 23% positive screens across all ED visits. One in ten (10%) gender-diverse youth had active suicidal ideation, compared with 3.4% of the rest of the ED patient population. The researchers calculated that gender-diverse youth had 5.35 times greater odds of screening positive than cisgender youth in the ED (95% confidence interval [CI] 8.7-15.92). Further, a quarter (25%) of the trans and gender-diverse youth who screened positive for suicide risk had come to the ED for a primary complaint unrelated to mental health.
“We had a kid who came in because he broke his arm who had active suicidal ideation,” study coauthor Jennifer A. Hoffmann, MD, assistant professor of pediatrics at the Ann & Robert H. Lurie Children’s Hospital of Chicago and Northwestern University, mentioned after the presentation. That particular patient even had a suicide plan, but was identified as actively suicidal only because of the screening. In other cases, she said, a youth may come in with self-inflicted injuries, and while those are the primary complaint, they are linked with suicidal ideation.
Among the study’s limitations are that gender identity is not necessarily being systematically assessed during visits, misspellings might have missed some youth, and their search strategy has not yet been externally validated, though they plan to seek that.
“Overall, however, this study did demonstrate that keyword searching is a promising technique to identify and prioritize gender-diverse youth in health services research,” Dr. Burnside said. In addition to showing the feasibility of using a keyword search strategy for identifying gender-diverse youth, Dr. Burnside noted that 31% of the encounters were identified by just one of the keywords they used, “highlighting the importance of using a comprehensive list of keywords to identify gender-diverse youth.”
Uncovering valuable information
Jason Rafferty, MD, MPH, EdM, clinical assistant professor of pediatrics and of psychiatry and human behavior at Brown University, Providence, R.I., who attended the presentation, noted that the study provides information on a population that’s often difficult to get through traditional EMR research methods.
“A lot of medical record systems don’t have uniform ways of capturing [gender diversity], but what we know as providers is that kids are really struggling and that it’s not a surprise that we’re seeing these disparities with suicidality,” Dr. Rafferty said.
The study also provides more discrete estimates by age than what most other current research measures, which tends to be lifetime suicidality as opposed to suicidal thoughts or attempts within the past year, Dr. Rafferty added.
”What this shows is, for adolescents, the risk of suicide is something we need to be paying attention to. Because it’s not that it’s something that only happens in adults, this really dispels a lot of the misquoting of the data that’s out there.” That kind of information is valuable for determining resource allocation, he said. “A disparity like this really underlies the importance of mental health resources in this field,” he said.
Dr. Burnside, Dr. Hoffmann, and Dr. Rafferty had no disclosures, and no external funding sources were noted.
AT AAP 2023
Teens streaming on Twitch vulnerable to predators
WASHINGTON – Half of youth broadcasting live streams on the online platform Twitch revealed their real-world location, and nearly half provided their name to viewers, according to research presented at the annual meeting of the American Academy of Pediatrics. It took researchers less than 5 minutes – and sometimes as little as 12 seconds – to find minors in different video game categories, suggesting the environment offers opportunities to predators to gain sensitive information about minors, reported Fiona Dubrosa, BS, BA, a visiting scholar at Cohen Children’s Medical Center, New York, and colleagues.
A ‘clandestine, threatening digital environment’
the authors concluded. “The nature of live streaming makes it particularly dangerous, as there is no way to take back information that has been revealed or regulate content or viewers. Parents and pediatricians should be aware of the dangers presented by Twitch and other live-streaming platforms and counsel children on best practices for Internet safety.”
Twitch is an online streaming platform where people can watch creator’s live content, such as music performances or narrating real-time video game playing. The platform requires live streamers to be 13 years old with a valid email address or phone number to create an account, but no age restrictions or identification requirements exist for viewers, “potentially putting minors in danger of being watched, followed, and groomed by predators,” the researchers noted. They added that people following different streamers receive notifications when those streamers are live. Further, “viewers can donate money to streamers, which can make it easier for predators to manipulate, track, and encourage risky behaviors from minors.”
To better understand the risks the platform might pose to minors, the researchers searched for and analyzed popular video game live streams that appeared to be streamed by minors who had their cameras on and their faces visible. Then the researchers noted the name of the video game, the topics discussed by the streamers, the time it took to find minors under each game, and each streamer’s age, name, follower count, location, streaming schedule, and social media links for money donations.
The researchers analyzed 100 Twitch streamers who were minors, who had a combined 1,755,452 million followers. Nearly half the streamers (47%) provided their presumably real names, and half (50%) gave out their location. Nearly two-thirds (64%) linked other social media accounts they had and encouraged viewers to follow them. Detailed schedules of when they would be live were available for 38% of the streamers, and 37% of the minor streamers were accepting money donations.
Only 11% of the discussion on the streams revealed personal details, most often related to trying on different outfits for viewers and talking about real-world locations they liked to visit. The researchers needed anywhere from 12 seconds to 5 minutes to find a minor in each game category.
”Young users clearly feel a false sense of safety on the platform; a significant proportion were willing to reveal personal information despite having no knowledge of who might be listening,” the researchers said. “The donation system provides a menacing avenue for manipulation and continued exploitation of minors. Our findings reveal the need for stricter age limitations for streamers and more stringent identity verification of audience members on Twitch.”
Open-minded parental guidance is warranted
Jenny Radesky, MD, a developmental behavioral pediatrician and media researcher at University of Michigan Medicine, Ann Arbor, was not surprised that many teens live stream on Twitch since it’s a popular platform for video gaming, but she was surprised at how many revealed their locations and other personal details.
“I suspect that they do this to build closeness with their viewers, by seeming more authentic,” said Dr. Radesky, who was not involved in the study. “It is this type of parasocial relationship with influencers and gamers that keeps an audience engaged, and encourages future viewing and purchases.”
Their willingness to share personal details suggests it’s important to conduct qualitative research to find out how teen live streamers think about privacy risks, what privacy settings they can use and choose to use, and how they handle inappropriate contact from adults, Dr. Radesky said.
Meanwhile, parents should talk with their kids in an open-minded way about what platforms they use and what they like and dislike about them. She recommended parents read the Common Sense Media guide about different social platforms ”to understand what attracts kids to content on specific sites, what their pitfalls are, and what types of privacy and safety settings are available.”
“A child or teen is much more likely to be honest about negative experiences online if they think their parent will hear them out – not judge them or take away their tech. No teen wants to talk with a panicky parent,” Dr. Radesky said.
David Hill, MD, a hospitalist pediatrician for Goldsboro Pediatrics in Wayne County, North Carolina, who also specializes in media communication, said that Twitch is just one example of a social media platform where children can encounter a variety of dangers, including sometimes adult predators.
“This just highlights the importance of parents having an ongoing conversation with their children about how they use their social media platforms and ensuring, just as we do with learning to ride a bicycle or learning to drive a car, that they apply some basic rules of safety,” Dr. Hill said. Then it’s important to keep coming back to that conversation “again and again as they grow and change and as those platforms change to ensure that those kids are continuing to apply those rules consistently.
“The best way for parents to keep up is ask your kids,” he said. “They love to share. They love to teach. They love to be in a position to show you something, especially if it’s something that interests them.”
An example of a rule would be setting personal accounts to private, not public, by default, Dr. Radesky said. “When interviewed, teens often say that they feel intruded upon by older people ‘stalking’ them or trying to connect with them on social platforms,” so making an account private can reduce those opportunities.
For teens who specifically want to create content on social platforms, parent oversight is needed, she said, but she acknowledged it can be a lot of work. “This might take the form of talking about what a teen plans to post before they do, expectations for positive behaviors or language, plans for privacy settings (such as public vs. private accounts), and what to do with trolls or hateful comment,” she said. “Parents may want to follow their child’s account to check in on it.”
Useful advice
Dr. Radesky also provided a handful of talking points that pediatricians can use in talking with patients who use these platforms:
- Keep your account private to just your friends and people you want to interact with. There are a lot of people on the Internet that you don’t want intruding upon your social life.
- Maintain your feed and the accounts you follow to keep it positive, entertaining, and not a source of stress or self-doubt. Content creators are always trying to grab your attention in new ways, some of which are rude or dehumanizing, so don’t waste your time on things that bring you down.
- Talk about why you want to post or live stream. Is it to get reactions or feel validated? If so, can you find other ways to feel validated that don’t require performing for other people? Is it to share a special skill? If so, how do you keep your posts creative and community building rather than attention grabbing? And how can you keep your parents involved so that they can help you navigate challenges?”
Ms. Dubrosa and Dr. Hill had no disclosures. Dr. Radesky is a consultant for Melissa & Doug. No information on external funding was provided.
WASHINGTON – Half of youth broadcasting live streams on the online platform Twitch revealed their real-world location, and nearly half provided their name to viewers, according to research presented at the annual meeting of the American Academy of Pediatrics. It took researchers less than 5 minutes – and sometimes as little as 12 seconds – to find minors in different video game categories, suggesting the environment offers opportunities to predators to gain sensitive information about minors, reported Fiona Dubrosa, BS, BA, a visiting scholar at Cohen Children’s Medical Center, New York, and colleagues.
A ‘clandestine, threatening digital environment’
the authors concluded. “The nature of live streaming makes it particularly dangerous, as there is no way to take back information that has been revealed or regulate content or viewers. Parents and pediatricians should be aware of the dangers presented by Twitch and other live-streaming platforms and counsel children on best practices for Internet safety.”
Twitch is an online streaming platform where people can watch creator’s live content, such as music performances or narrating real-time video game playing. The platform requires live streamers to be 13 years old with a valid email address or phone number to create an account, but no age restrictions or identification requirements exist for viewers, “potentially putting minors in danger of being watched, followed, and groomed by predators,” the researchers noted. They added that people following different streamers receive notifications when those streamers are live. Further, “viewers can donate money to streamers, which can make it easier for predators to manipulate, track, and encourage risky behaviors from minors.”
To better understand the risks the platform might pose to minors, the researchers searched for and analyzed popular video game live streams that appeared to be streamed by minors who had their cameras on and their faces visible. Then the researchers noted the name of the video game, the topics discussed by the streamers, the time it took to find minors under each game, and each streamer’s age, name, follower count, location, streaming schedule, and social media links for money donations.
The researchers analyzed 100 Twitch streamers who were minors, who had a combined 1,755,452 million followers. Nearly half the streamers (47%) provided their presumably real names, and half (50%) gave out their location. Nearly two-thirds (64%) linked other social media accounts they had and encouraged viewers to follow them. Detailed schedules of when they would be live were available for 38% of the streamers, and 37% of the minor streamers were accepting money donations.
Only 11% of the discussion on the streams revealed personal details, most often related to trying on different outfits for viewers and talking about real-world locations they liked to visit. The researchers needed anywhere from 12 seconds to 5 minutes to find a minor in each game category.
”Young users clearly feel a false sense of safety on the platform; a significant proportion were willing to reveal personal information despite having no knowledge of who might be listening,” the researchers said. “The donation system provides a menacing avenue for manipulation and continued exploitation of minors. Our findings reveal the need for stricter age limitations for streamers and more stringent identity verification of audience members on Twitch.”
Open-minded parental guidance is warranted
Jenny Radesky, MD, a developmental behavioral pediatrician and media researcher at University of Michigan Medicine, Ann Arbor, was not surprised that many teens live stream on Twitch since it’s a popular platform for video gaming, but she was surprised at how many revealed their locations and other personal details.
“I suspect that they do this to build closeness with their viewers, by seeming more authentic,” said Dr. Radesky, who was not involved in the study. “It is this type of parasocial relationship with influencers and gamers that keeps an audience engaged, and encourages future viewing and purchases.”
Their willingness to share personal details suggests it’s important to conduct qualitative research to find out how teen live streamers think about privacy risks, what privacy settings they can use and choose to use, and how they handle inappropriate contact from adults, Dr. Radesky said.
Meanwhile, parents should talk with their kids in an open-minded way about what platforms they use and what they like and dislike about them. She recommended parents read the Common Sense Media guide about different social platforms ”to understand what attracts kids to content on specific sites, what their pitfalls are, and what types of privacy and safety settings are available.”
“A child or teen is much more likely to be honest about negative experiences online if they think their parent will hear them out – not judge them or take away their tech. No teen wants to talk with a panicky parent,” Dr. Radesky said.
David Hill, MD, a hospitalist pediatrician for Goldsboro Pediatrics in Wayne County, North Carolina, who also specializes in media communication, said that Twitch is just one example of a social media platform where children can encounter a variety of dangers, including sometimes adult predators.
“This just highlights the importance of parents having an ongoing conversation with their children about how they use their social media platforms and ensuring, just as we do with learning to ride a bicycle or learning to drive a car, that they apply some basic rules of safety,” Dr. Hill said. Then it’s important to keep coming back to that conversation “again and again as they grow and change and as those platforms change to ensure that those kids are continuing to apply those rules consistently.
“The best way for parents to keep up is ask your kids,” he said. “They love to share. They love to teach. They love to be in a position to show you something, especially if it’s something that interests them.”
An example of a rule would be setting personal accounts to private, not public, by default, Dr. Radesky said. “When interviewed, teens often say that they feel intruded upon by older people ‘stalking’ them or trying to connect with them on social platforms,” so making an account private can reduce those opportunities.
For teens who specifically want to create content on social platforms, parent oversight is needed, she said, but she acknowledged it can be a lot of work. “This might take the form of talking about what a teen plans to post before they do, expectations for positive behaviors or language, plans for privacy settings (such as public vs. private accounts), and what to do with trolls or hateful comment,” she said. “Parents may want to follow their child’s account to check in on it.”
Useful advice
Dr. Radesky also provided a handful of talking points that pediatricians can use in talking with patients who use these platforms:
- Keep your account private to just your friends and people you want to interact with. There are a lot of people on the Internet that you don’t want intruding upon your social life.
- Maintain your feed and the accounts you follow to keep it positive, entertaining, and not a source of stress or self-doubt. Content creators are always trying to grab your attention in new ways, some of which are rude or dehumanizing, so don’t waste your time on things that bring you down.
- Talk about why you want to post or live stream. Is it to get reactions or feel validated? If so, can you find other ways to feel validated that don’t require performing for other people? Is it to share a special skill? If so, how do you keep your posts creative and community building rather than attention grabbing? And how can you keep your parents involved so that they can help you navigate challenges?”
Ms. Dubrosa and Dr. Hill had no disclosures. Dr. Radesky is a consultant for Melissa & Doug. No information on external funding was provided.
WASHINGTON – Half of youth broadcasting live streams on the online platform Twitch revealed their real-world location, and nearly half provided their name to viewers, according to research presented at the annual meeting of the American Academy of Pediatrics. It took researchers less than 5 minutes – and sometimes as little as 12 seconds – to find minors in different video game categories, suggesting the environment offers opportunities to predators to gain sensitive information about minors, reported Fiona Dubrosa, BS, BA, a visiting scholar at Cohen Children’s Medical Center, New York, and colleagues.
A ‘clandestine, threatening digital environment’
the authors concluded. “The nature of live streaming makes it particularly dangerous, as there is no way to take back information that has been revealed or regulate content or viewers. Parents and pediatricians should be aware of the dangers presented by Twitch and other live-streaming platforms and counsel children on best practices for Internet safety.”
Twitch is an online streaming platform where people can watch creator’s live content, such as music performances or narrating real-time video game playing. The platform requires live streamers to be 13 years old with a valid email address or phone number to create an account, but no age restrictions or identification requirements exist for viewers, “potentially putting minors in danger of being watched, followed, and groomed by predators,” the researchers noted. They added that people following different streamers receive notifications when those streamers are live. Further, “viewers can donate money to streamers, which can make it easier for predators to manipulate, track, and encourage risky behaviors from minors.”
To better understand the risks the platform might pose to minors, the researchers searched for and analyzed popular video game live streams that appeared to be streamed by minors who had their cameras on and their faces visible. Then the researchers noted the name of the video game, the topics discussed by the streamers, the time it took to find minors under each game, and each streamer’s age, name, follower count, location, streaming schedule, and social media links for money donations.
The researchers analyzed 100 Twitch streamers who were minors, who had a combined 1,755,452 million followers. Nearly half the streamers (47%) provided their presumably real names, and half (50%) gave out their location. Nearly two-thirds (64%) linked other social media accounts they had and encouraged viewers to follow them. Detailed schedules of when they would be live were available for 38% of the streamers, and 37% of the minor streamers were accepting money donations.
Only 11% of the discussion on the streams revealed personal details, most often related to trying on different outfits for viewers and talking about real-world locations they liked to visit. The researchers needed anywhere from 12 seconds to 5 minutes to find a minor in each game category.
”Young users clearly feel a false sense of safety on the platform; a significant proportion were willing to reveal personal information despite having no knowledge of who might be listening,” the researchers said. “The donation system provides a menacing avenue for manipulation and continued exploitation of minors. Our findings reveal the need for stricter age limitations for streamers and more stringent identity verification of audience members on Twitch.”
Open-minded parental guidance is warranted
Jenny Radesky, MD, a developmental behavioral pediatrician and media researcher at University of Michigan Medicine, Ann Arbor, was not surprised that many teens live stream on Twitch since it’s a popular platform for video gaming, but she was surprised at how many revealed their locations and other personal details.
“I suspect that they do this to build closeness with their viewers, by seeming more authentic,” said Dr. Radesky, who was not involved in the study. “It is this type of parasocial relationship with influencers and gamers that keeps an audience engaged, and encourages future viewing and purchases.”
Their willingness to share personal details suggests it’s important to conduct qualitative research to find out how teen live streamers think about privacy risks, what privacy settings they can use and choose to use, and how they handle inappropriate contact from adults, Dr. Radesky said.
Meanwhile, parents should talk with their kids in an open-minded way about what platforms they use and what they like and dislike about them. She recommended parents read the Common Sense Media guide about different social platforms ”to understand what attracts kids to content on specific sites, what their pitfalls are, and what types of privacy and safety settings are available.”
“A child or teen is much more likely to be honest about negative experiences online if they think their parent will hear them out – not judge them or take away their tech. No teen wants to talk with a panicky parent,” Dr. Radesky said.
David Hill, MD, a hospitalist pediatrician for Goldsboro Pediatrics in Wayne County, North Carolina, who also specializes in media communication, said that Twitch is just one example of a social media platform where children can encounter a variety of dangers, including sometimes adult predators.
“This just highlights the importance of parents having an ongoing conversation with their children about how they use their social media platforms and ensuring, just as we do with learning to ride a bicycle or learning to drive a car, that they apply some basic rules of safety,” Dr. Hill said. Then it’s important to keep coming back to that conversation “again and again as they grow and change and as those platforms change to ensure that those kids are continuing to apply those rules consistently.
“The best way for parents to keep up is ask your kids,” he said. “They love to share. They love to teach. They love to be in a position to show you something, especially if it’s something that interests them.”
An example of a rule would be setting personal accounts to private, not public, by default, Dr. Radesky said. “When interviewed, teens often say that they feel intruded upon by older people ‘stalking’ them or trying to connect with them on social platforms,” so making an account private can reduce those opportunities.
For teens who specifically want to create content on social platforms, parent oversight is needed, she said, but she acknowledged it can be a lot of work. “This might take the form of talking about what a teen plans to post before they do, expectations for positive behaviors or language, plans for privacy settings (such as public vs. private accounts), and what to do with trolls or hateful comment,” she said. “Parents may want to follow their child’s account to check in on it.”
Useful advice
Dr. Radesky also provided a handful of talking points that pediatricians can use in talking with patients who use these platforms:
- Keep your account private to just your friends and people you want to interact with. There are a lot of people on the Internet that you don’t want intruding upon your social life.
- Maintain your feed and the accounts you follow to keep it positive, entertaining, and not a source of stress or self-doubt. Content creators are always trying to grab your attention in new ways, some of which are rude or dehumanizing, so don’t waste your time on things that bring you down.
- Talk about why you want to post or live stream. Is it to get reactions or feel validated? If so, can you find other ways to feel validated that don’t require performing for other people? Is it to share a special skill? If so, how do you keep your posts creative and community building rather than attention grabbing? And how can you keep your parents involved so that they can help you navigate challenges?”
Ms. Dubrosa and Dr. Hill had no disclosures. Dr. Radesky is a consultant for Melissa & Doug. No information on external funding was provided.
AT AAP 2023
Teens have easy online access to Delta-8 cannabinoid products
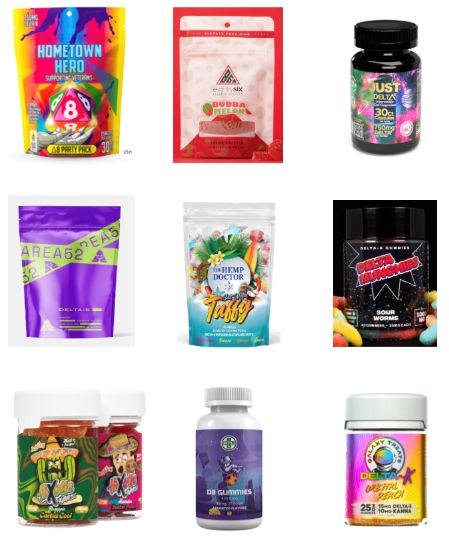
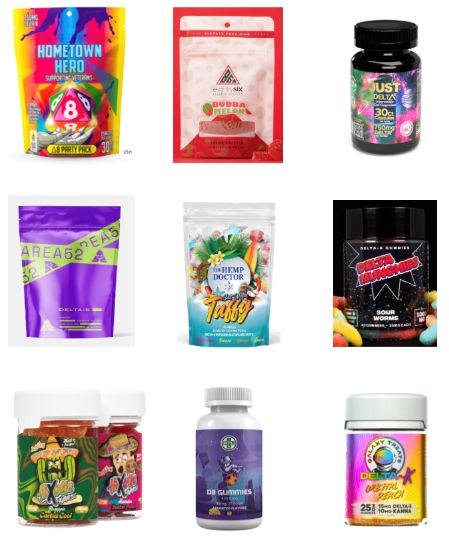
WASHINGTON – , researchers reported at the 2023 annual meeting of the American Academy of Pediatrics. Most of the products identified came in bright, colorful, kid-friendly packaging and cost less than $10, the researchers found, and only 2 out of 45 sites had a third-party age verification requirement for purchases.
Delta-8 THC, also called D8, is a synthetically produced cannabinoid whose chemical structure and effects are nearly identical to traditional THC, the authors explained, and past research has found that D8 products, such as e-cigarettes, can contain toxic byproducts and contaminants.
”Since D8 is not traditional THC, minors may underestimate its strength and potential danger,” wrote lead author Abhijeet Grewal, BS, a research assistant at Cohen Children’s Medical Center, New York, and senior author Ruth Milanaik, DO, director of the Neonatal Neurodevelopmental Program at Cohen Children’s and a developmental/behavioral pediatrician at Northwell Health, also in New York. “Although traditional THC is a federally banned substance, D8 is legal on a federal level and less restricted on a state by state basis, making it easier for individuals to acquire D8.”
Easily accessible
During the first seven moments of 2021, 77% of reports of accidental exposure occurred in people under age 18, including some children who required ICU admission. The U.S. Food and Drug Administration also received 104 reports of adverse events from products containing D8 between December 2020-February 2022, and more than half of those required medical intervention.
To better understand how easy it is to access D8, the authors collected data on 45 websites they identified that sold D8. The researchers looked for age verification questions for accessing the site, third-party age certification, what kinds of products (edibles, smoke products, or tinctures) were sold, the price and dosage of the cheapest product, and examples of packaging, flavors, marketing claims, and warning statements at each site.
More than a third of the sites (36%) did not ask for customers’ age and almost none of the sites asked for proof: 96% of the sites lacked formal third-party age verification procedures. All but one of the sites sold D8 edibles, and most (82%) sold D8 vaping or smoking products. Only 42% sold tinctures, a mix of concentrated D8 with oil that’s orally consumed.
The cheapest product was priced under $5 on one-third of the sites and under $10 on another third of the sites. The cheapest product was between $10-20 on 16% of the sites while the remaining nine sites’ cheapest product was more than $20. In assessing only the cheapest D8 products on each site, nearly half (47%) contained 51 mg or more of D8, and 20% of the products didn’t report the dosage. Another 22% contained 41-50 mg of D8, and the remaining five products contained 20-40 mg.
Kid-friendly D8
More than half of the D8 products were sold in kid-friendly packaging – packages with bright, colorful designs and fonts that resemble candy or snack food, sometimes cartoon characters or fun items like dice on the packaging. Further, 24% of the websites did not include any warnings or other health information about D8.
“The low prices, high dosages available, and eye-popping packaging make these products extremely attractive to teens who are looking for a high,” the researchers concluded. They advised clinicians to talk with teen patients about the dangers of D8 and advocated for policymakers to more strictly regulate online distributors of D8 products, particularly in requiring age verification procedures and prohibiting kid-friendly packaging.
Megan Moreno, MD, MSEd, MPH, an adolescent medicine physician and researcher at the University of Wisconsin, Madison, School of Medicine and Public Health and UWHealthKids, was particularly struck by how eye-catching the packaging was. “The bright colors and font choices are really designed to attract adolescents,” commented Dr. Moreno, who was not involved in the study. But she was not surprised overall by the findings.
“Other studies have found that the cannabis industry leverages online tools and social media, alongside youth-friendly packaging, to attract youth to their products,” she said. “What is disappointing is that these companies do not use industry standard approaches, such as the alcohol industry, to age-gate their websites.”
It’s important for providers who care for adolescents to ask about substance use but to especially include questions about substances that teens might not think of as “drugs,” such as Delta 8, Dr. Moreno said.
“Prior research on other types of substance such as these has found that teens can think these are less dangerous versions of cannabis, so providing accurate information and asking about these products can prevent harm to kids,” Dr. Moreno said. Although this study focused on websites that sell D8 products, she said that “another important area of influence to consider is social media messaging around these products, which may drive traffic to the purchasing site.” It’s clear this industry is not going to self-regulate without policy changes, Dr. Moreno added, so she noted the importance of advocating for policy that regulates these sites.
Mr. Grewal, Dr. Milanaik and Dr. Moreno had no disclosures. No external funding sources were noted.
WASHINGTON – , researchers reported at the 2023 annual meeting of the American Academy of Pediatrics. Most of the products identified came in bright, colorful, kid-friendly packaging and cost less than $10, the researchers found, and only 2 out of 45 sites had a third-party age verification requirement for purchases.
Delta-8 THC, also called D8, is a synthetically produced cannabinoid whose chemical structure and effects are nearly identical to traditional THC, the authors explained, and past research has found that D8 products, such as e-cigarettes, can contain toxic byproducts and contaminants.
”Since D8 is not traditional THC, minors may underestimate its strength and potential danger,” wrote lead author Abhijeet Grewal, BS, a research assistant at Cohen Children’s Medical Center, New York, and senior author Ruth Milanaik, DO, director of the Neonatal Neurodevelopmental Program at Cohen Children’s and a developmental/behavioral pediatrician at Northwell Health, also in New York. “Although traditional THC is a federally banned substance, D8 is legal on a federal level and less restricted on a state by state basis, making it easier for individuals to acquire D8.”
Easily accessible
During the first seven moments of 2021, 77% of reports of accidental exposure occurred in people under age 18, including some children who required ICU admission. The U.S. Food and Drug Administration also received 104 reports of adverse events from products containing D8 between December 2020-February 2022, and more than half of those required medical intervention.
To better understand how easy it is to access D8, the authors collected data on 45 websites they identified that sold D8. The researchers looked for age verification questions for accessing the site, third-party age certification, what kinds of products (edibles, smoke products, or tinctures) were sold, the price and dosage of the cheapest product, and examples of packaging, flavors, marketing claims, and warning statements at each site.
More than a third of the sites (36%) did not ask for customers’ age and almost none of the sites asked for proof: 96% of the sites lacked formal third-party age verification procedures. All but one of the sites sold D8 edibles, and most (82%) sold D8 vaping or smoking products. Only 42% sold tinctures, a mix of concentrated D8 with oil that’s orally consumed.
The cheapest product was priced under $5 on one-third of the sites and under $10 on another third of the sites. The cheapest product was between $10-20 on 16% of the sites while the remaining nine sites’ cheapest product was more than $20. In assessing only the cheapest D8 products on each site, nearly half (47%) contained 51 mg or more of D8, and 20% of the products didn’t report the dosage. Another 22% contained 41-50 mg of D8, and the remaining five products contained 20-40 mg.
Kid-friendly D8
More than half of the D8 products were sold in kid-friendly packaging – packages with bright, colorful designs and fonts that resemble candy or snack food, sometimes cartoon characters or fun items like dice on the packaging. Further, 24% of the websites did not include any warnings or other health information about D8.
“The low prices, high dosages available, and eye-popping packaging make these products extremely attractive to teens who are looking for a high,” the researchers concluded. They advised clinicians to talk with teen patients about the dangers of D8 and advocated for policymakers to more strictly regulate online distributors of D8 products, particularly in requiring age verification procedures and prohibiting kid-friendly packaging.
Megan Moreno, MD, MSEd, MPH, an adolescent medicine physician and researcher at the University of Wisconsin, Madison, School of Medicine and Public Health and UWHealthKids, was particularly struck by how eye-catching the packaging was. “The bright colors and font choices are really designed to attract adolescents,” commented Dr. Moreno, who was not involved in the study. But she was not surprised overall by the findings.
“Other studies have found that the cannabis industry leverages online tools and social media, alongside youth-friendly packaging, to attract youth to their products,” she said. “What is disappointing is that these companies do not use industry standard approaches, such as the alcohol industry, to age-gate their websites.”
It’s important for providers who care for adolescents to ask about substance use but to especially include questions about substances that teens might not think of as “drugs,” such as Delta 8, Dr. Moreno said.
“Prior research on other types of substance such as these has found that teens can think these are less dangerous versions of cannabis, so providing accurate information and asking about these products can prevent harm to kids,” Dr. Moreno said. Although this study focused on websites that sell D8 products, she said that “another important area of influence to consider is social media messaging around these products, which may drive traffic to the purchasing site.” It’s clear this industry is not going to self-regulate without policy changes, Dr. Moreno added, so she noted the importance of advocating for policy that regulates these sites.
Mr. Grewal, Dr. Milanaik and Dr. Moreno had no disclosures. No external funding sources were noted.
WASHINGTON – , researchers reported at the 2023 annual meeting of the American Academy of Pediatrics. Most of the products identified came in bright, colorful, kid-friendly packaging and cost less than $10, the researchers found, and only 2 out of 45 sites had a third-party age verification requirement for purchases.
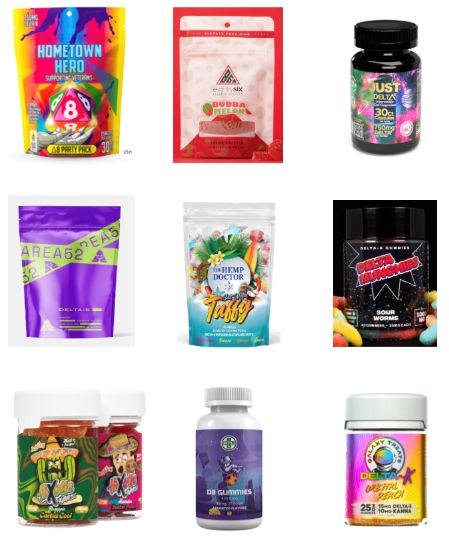
Delta-8 THC, also called D8, is a synthetically produced cannabinoid whose chemical structure and effects are nearly identical to traditional THC, the authors explained, and past research has found that D8 products, such as e-cigarettes, can contain toxic byproducts and contaminants.
”Since D8 is not traditional THC, minors may underestimate its strength and potential danger,” wrote lead author Abhijeet Grewal, BS, a research assistant at Cohen Children’s Medical Center, New York, and senior author Ruth Milanaik, DO, director of the Neonatal Neurodevelopmental Program at Cohen Children’s and a developmental/behavioral pediatrician at Northwell Health, also in New York. “Although traditional THC is a federally banned substance, D8 is legal on a federal level and less restricted on a state by state basis, making it easier for individuals to acquire D8.”
Easily accessible
During the first seven moments of 2021, 77% of reports of accidental exposure occurred in people under age 18, including some children who required ICU admission. The U.S. Food and Drug Administration also received 104 reports of adverse events from products containing D8 between December 2020-February 2022, and more than half of those required medical intervention.
To better understand how easy it is to access D8, the authors collected data on 45 websites they identified that sold D8. The researchers looked for age verification questions for accessing the site, third-party age certification, what kinds of products (edibles, smoke products, or tinctures) were sold, the price and dosage of the cheapest product, and examples of packaging, flavors, marketing claims, and warning statements at each site.
More than a third of the sites (36%) did not ask for customers’ age and almost none of the sites asked for proof: 96% of the sites lacked formal third-party age verification procedures. All but one of the sites sold D8 edibles, and most (82%) sold D8 vaping or smoking products. Only 42% sold tinctures, a mix of concentrated D8 with oil that’s orally consumed.
The cheapest product was priced under $5 on one-third of the sites and under $10 on another third of the sites. The cheapest product was between $10-20 on 16% of the sites while the remaining nine sites’ cheapest product was more than $20. In assessing only the cheapest D8 products on each site, nearly half (47%) contained 51 mg or more of D8, and 20% of the products didn’t report the dosage. Another 22% contained 41-50 mg of D8, and the remaining five products contained 20-40 mg.
Kid-friendly D8
More than half of the D8 products were sold in kid-friendly packaging – packages with bright, colorful designs and fonts that resemble candy or snack food, sometimes cartoon characters or fun items like dice on the packaging. Further, 24% of the websites did not include any warnings or other health information about D8.
“The low prices, high dosages available, and eye-popping packaging make these products extremely attractive to teens who are looking for a high,” the researchers concluded. They advised clinicians to talk with teen patients about the dangers of D8 and advocated for policymakers to more strictly regulate online distributors of D8 products, particularly in requiring age verification procedures and prohibiting kid-friendly packaging.
Megan Moreno, MD, MSEd, MPH, an adolescent medicine physician and researcher at the University of Wisconsin, Madison, School of Medicine and Public Health and UWHealthKids, was particularly struck by how eye-catching the packaging was. “The bright colors and font choices are really designed to attract adolescents,” commented Dr. Moreno, who was not involved in the study. But she was not surprised overall by the findings.
“Other studies have found that the cannabis industry leverages online tools and social media, alongside youth-friendly packaging, to attract youth to their products,” she said. “What is disappointing is that these companies do not use industry standard approaches, such as the alcohol industry, to age-gate their websites.”
It’s important for providers who care for adolescents to ask about substance use but to especially include questions about substances that teens might not think of as “drugs,” such as Delta 8, Dr. Moreno said.
“Prior research on other types of substance such as these has found that teens can think these are less dangerous versions of cannabis, so providing accurate information and asking about these products can prevent harm to kids,” Dr. Moreno said. Although this study focused on websites that sell D8 products, she said that “another important area of influence to consider is social media messaging around these products, which may drive traffic to the purchasing site.” It’s clear this industry is not going to self-regulate without policy changes, Dr. Moreno added, so she noted the importance of advocating for policy that regulates these sites.
Mr. Grewal, Dr. Milanaik and Dr. Moreno had no disclosures. No external funding sources were noted.
At AAP 2023
Online nicotine toothpick vendors ignore age restrictions
WASHINGTON – according to a study of 77 stores and 16 online sites.
Online nicotine toothpick sales are “the Wild West” in terms of regulation, said Abhijeet Grewal, a research assistant at Cohen Children’s Medical Center, in New Hyde Park, N.Y., who presented the findings at the annual meeting of the American Academy of Pediatrics.
Nicotine toothpicks have become popular among teenagers as a relatively inconspicuous way to access the drug, Mr. Grewal said. The nicotine content of the toothpicks varies, but many contain as much as 2-3 mg per pick compared with the 1.1-1.8–mg amount inhaled per the average cigarette, he said. The cheap price and teen-friendly flavors like cherry and mocha add to the appeal of the picks. However, data on the marketplace and accessibility of these products are lacking, Mr. Grewal said.
To find out how easily youth can buy nicotine toothpicks through in-person and online channels, Mr. Grewal and colleagues identified and called 404 brick-and-mortar retailers across the United States by phone and asked whether they required ID for purchase of nicotine toothpicks; of the 77 locations that responded, only 1 said that they would sell nicotine toothpicks without asking for proof of age.
The researchers also collected data on 16 vendor websites that sold nicotine toothpicks with shipment to the United States (identified from pixotine.com).
Overall, 11 sites (69%) prompted users to confirm that they were aged 21 years or older to either view the site or place orders, but 12 sites (75%) required no formal method of verification.
Warnings or disclaimers, such as “nicotine is an addictive chemical,” appeared on 69% of sites. Marketing statements including terms such as “discreet” and “cost-effective” to describe the toothpicks, Mr. Grewal said, and online reviews endorsed the products as “convenient” and “rich in flavor.”
The sites in the study offered a total of 32 different flavors, Mr. Grewal said, and 44% of the sites offered some type of discount on prices, which land in the range of approximately $5 for a tube of 20 toothpicks.
Nicotine toothpicks and flavored toothpicks without nicotine were originally marketed as smoking cessation aids, said Mr. Grewal, but their low price point and ability to be consumed discreetly makes them appealing to teens for nicotine use in many environments.
More research is needed to characterize youth use of nicotine toothpick products, as well as purchasing patterns, he said. However, the results highlight the need for regulation of nicotine toothpick vendors to protect youth from accessing nicotine in this form, he said.
Ask adolescents about toothpicks
“While nicotine replacement therapy [NRT] products may be an effective way for people to quit smoking, these products have the potential to introduce minors to nicotine in a seemingly innocent way resulting in dependence,” senior author Ruth Milanaik, DO, also of Cohen Children’s Medical Center, said in an interview. “Many children are intrigued by these fun flavored products, and our team was interested in examining the availability of these products to minors.”
Overall, “our team was quite pleased with brick-and-mortar stores’ spoken requirements of age verification for purchase, and quite worried about the availability of nic picks through online vendors,” she continued.
Clinicians, educators, and parents should be aware of the existence of nicotine toothpicks and the ease with which minors can attain them through online vendors, Dr. Milanaik said. “While NRT is a part of smoking cessation programs, nicotine toothpicks should not be used by minors without clinical reasons,” she said. “The innocuous and innocent nature of these toothpicks may entice minors to try and regularly use these without regard to future dependence.”
The study received no outside funding. The researchers had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
WASHINGTON – according to a study of 77 stores and 16 online sites.
Online nicotine toothpick sales are “the Wild West” in terms of regulation, said Abhijeet Grewal, a research assistant at Cohen Children’s Medical Center, in New Hyde Park, N.Y., who presented the findings at the annual meeting of the American Academy of Pediatrics.
Nicotine toothpicks have become popular among teenagers as a relatively inconspicuous way to access the drug, Mr. Grewal said. The nicotine content of the toothpicks varies, but many contain as much as 2-3 mg per pick compared with the 1.1-1.8–mg amount inhaled per the average cigarette, he said. The cheap price and teen-friendly flavors like cherry and mocha add to the appeal of the picks. However, data on the marketplace and accessibility of these products are lacking, Mr. Grewal said.
To find out how easily youth can buy nicotine toothpicks through in-person and online channels, Mr. Grewal and colleagues identified and called 404 brick-and-mortar retailers across the United States by phone and asked whether they required ID for purchase of nicotine toothpicks; of the 77 locations that responded, only 1 said that they would sell nicotine toothpicks without asking for proof of age.
The researchers also collected data on 16 vendor websites that sold nicotine toothpicks with shipment to the United States (identified from pixotine.com).
Overall, 11 sites (69%) prompted users to confirm that they were aged 21 years or older to either view the site or place orders, but 12 sites (75%) required no formal method of verification.
Warnings or disclaimers, such as “nicotine is an addictive chemical,” appeared on 69% of sites. Marketing statements including terms such as “discreet” and “cost-effective” to describe the toothpicks, Mr. Grewal said, and online reviews endorsed the products as “convenient” and “rich in flavor.”
The sites in the study offered a total of 32 different flavors, Mr. Grewal said, and 44% of the sites offered some type of discount on prices, which land in the range of approximately $5 for a tube of 20 toothpicks.
Nicotine toothpicks and flavored toothpicks without nicotine were originally marketed as smoking cessation aids, said Mr. Grewal, but their low price point and ability to be consumed discreetly makes them appealing to teens for nicotine use in many environments.
More research is needed to characterize youth use of nicotine toothpick products, as well as purchasing patterns, he said. However, the results highlight the need for regulation of nicotine toothpick vendors to protect youth from accessing nicotine in this form, he said.
Ask adolescents about toothpicks
“While nicotine replacement therapy [NRT] products may be an effective way for people to quit smoking, these products have the potential to introduce minors to nicotine in a seemingly innocent way resulting in dependence,” senior author Ruth Milanaik, DO, also of Cohen Children’s Medical Center, said in an interview. “Many children are intrigued by these fun flavored products, and our team was interested in examining the availability of these products to minors.”
Overall, “our team was quite pleased with brick-and-mortar stores’ spoken requirements of age verification for purchase, and quite worried about the availability of nic picks through online vendors,” she continued.
Clinicians, educators, and parents should be aware of the existence of nicotine toothpicks and the ease with which minors can attain them through online vendors, Dr. Milanaik said. “While NRT is a part of smoking cessation programs, nicotine toothpicks should not be used by minors without clinical reasons,” she said. “The innocuous and innocent nature of these toothpicks may entice minors to try and regularly use these without regard to future dependence.”
The study received no outside funding. The researchers had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
WASHINGTON – according to a study of 77 stores and 16 online sites.
Online nicotine toothpick sales are “the Wild West” in terms of regulation, said Abhijeet Grewal, a research assistant at Cohen Children’s Medical Center, in New Hyde Park, N.Y., who presented the findings at the annual meeting of the American Academy of Pediatrics.
Nicotine toothpicks have become popular among teenagers as a relatively inconspicuous way to access the drug, Mr. Grewal said. The nicotine content of the toothpicks varies, but many contain as much as 2-3 mg per pick compared with the 1.1-1.8–mg amount inhaled per the average cigarette, he said. The cheap price and teen-friendly flavors like cherry and mocha add to the appeal of the picks. However, data on the marketplace and accessibility of these products are lacking, Mr. Grewal said.
To find out how easily youth can buy nicotine toothpicks through in-person and online channels, Mr. Grewal and colleagues identified and called 404 brick-and-mortar retailers across the United States by phone and asked whether they required ID for purchase of nicotine toothpicks; of the 77 locations that responded, only 1 said that they would sell nicotine toothpicks without asking for proof of age.
The researchers also collected data on 16 vendor websites that sold nicotine toothpicks with shipment to the United States (identified from pixotine.com).
Overall, 11 sites (69%) prompted users to confirm that they were aged 21 years or older to either view the site or place orders, but 12 sites (75%) required no formal method of verification.
Warnings or disclaimers, such as “nicotine is an addictive chemical,” appeared on 69% of sites. Marketing statements including terms such as “discreet” and “cost-effective” to describe the toothpicks, Mr. Grewal said, and online reviews endorsed the products as “convenient” and “rich in flavor.”
The sites in the study offered a total of 32 different flavors, Mr. Grewal said, and 44% of the sites offered some type of discount on prices, which land in the range of approximately $5 for a tube of 20 toothpicks.
Nicotine toothpicks and flavored toothpicks without nicotine were originally marketed as smoking cessation aids, said Mr. Grewal, but their low price point and ability to be consumed discreetly makes them appealing to teens for nicotine use in many environments.
More research is needed to characterize youth use of nicotine toothpick products, as well as purchasing patterns, he said. However, the results highlight the need for regulation of nicotine toothpick vendors to protect youth from accessing nicotine in this form, he said.
Ask adolescents about toothpicks
“While nicotine replacement therapy [NRT] products may be an effective way for people to quit smoking, these products have the potential to introduce minors to nicotine in a seemingly innocent way resulting in dependence,” senior author Ruth Milanaik, DO, also of Cohen Children’s Medical Center, said in an interview. “Many children are intrigued by these fun flavored products, and our team was interested in examining the availability of these products to minors.”
Overall, “our team was quite pleased with brick-and-mortar stores’ spoken requirements of age verification for purchase, and quite worried about the availability of nic picks through online vendors,” she continued.
Clinicians, educators, and parents should be aware of the existence of nicotine toothpicks and the ease with which minors can attain them through online vendors, Dr. Milanaik said. “While NRT is a part of smoking cessation programs, nicotine toothpicks should not be used by minors without clinical reasons,” she said. “The innocuous and innocent nature of these toothpicks may entice minors to try and regularly use these without regard to future dependence.”
The study received no outside funding. The researchers had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
AT AAP 2023
Neurologic nuggets of wisdom for pediatric practice
WASHINGTON – Get the back story before rushing to diagnose a seizure disorder in a child, Michael Strunc, MD, said in a presentation at the annual meeting of the American Academy of Pediatrics.
Clinicians should ask parents or caregivers about the child’s behavior before the suspected seizure, whether there were any triggers, and if so, what might they have been, according to Dr. Strunc, a child neurologist and sleep medicine specialist at Children’s Hospital of the King’s Daughters, Norfolk, Va.
“Most seizures don’t have triggers,” he said. Rather, patients often become stiff, experience a motor event that builds in intensity then slows and stops, and finally, the patient is sleepy and tired. Clinicians should also find out whether the event had a beginning, middle, and end.
Approximately 0.6% of children younger than 17 years in the United States have active epilepsy, according to the Centers for Disease Control and Prevention.
Dr. Strunc offered a few more tips for diagnosing a child:
- Ask whether the patient’s eyes were open during the event. If the eyes were closed or squished closed, “it is almost never a seizure,” he said.
- Find out whether the patient was awake or asleep, and how, if at all, caregivers attempted to stop the event.
- Ask if the child’s experiences were repeating and predictable, and inquire about a family history of seizures or other events.
- Inquire about any developmental changes and other changes in the child, such as irritability, regression, or ataxia.
The differential diagnosis for a seizure includes nonepileptic events that occur with and without changes in consciousness or sleep. These events range from breath-holding and hyperventilation to night terrors, narcolepsy, migraine, and attention-deficit/hyperactivity disorder, he said.
Is it epilepsy?
Dr. Strunc shared several cases of neurologic “events” ranging from simple to severe.
In one case, a 10-month-old infant girl with a potential tonic/staring seizure presented with a history of events that involved getting stuck in a stiff position, usually while sitting in a car seat or highchair, with adducting of legs, redness of face, and “zoned-out” expression. The infant was healthy, smart, and precocious, with no illness, fever, or trauma, but the mother was very concerned, Dr. Strunc said.
The diagnosis: Self-gratification, which is benign and usually outgrown, although it can become extreme, he said.
By contrast, “absence,” also known as idiopathic generalized epilepsy, presents as brief events of 4-10 seconds that may occur up to hundreds of times a day. This type of epilepsy is associated with the sudden onset of impaired consciousness and unresponsiveness. These events end abruptly, and the child may be unaware. Absence is more common in girls. It usually occurs after age 4 and usually remits by about age 12, Dr. Strunc said.
However, the onset of absence in patients younger than age 3 is associated with increased odds of neurodevelopmental abnormalities “and probably represents another epilepsy syndrome,” he said.
Absence symptoms may mirror those of children who are simply daydreamers, Dr. Strunc noted. One way to confirm absence is by provoking hyperventilation, which will bring on an episode of absence if present, he said. EEGs provide evidence as well.
Acute ataxia in children has a wide differential that sends kids and families to the pediatrician or emergency department, Dr. Strunc said. Acute cerebellar ataxia is characterized by abrupt and symmetric symptoms, with no mental status changes, no fever, no meningitis, and no headache. A wide, unstable gait is a distinguishing feature, Dr. Strunc said.
However, other causes of acute ataxia should be ruled out, including toxic ingestion, tick paralysis, central nervous system infections, vascular conditions, and genetic conditions.
Don’t miss those ticks
Especially during periods when kids are outdoors, clinicians should consider a tick bite as a source of ataxia and neurologic symptoms in children, Dr. Strunc emphasized. Tick paralysis notably resembles many symptoms of Guillain-Barré syndrome (acute inflammatory demyelinating polyneuropathy).
Dr. Strunc described a case involving a 5-year-old girl who developed sudden problems with gait. The problems worsened quickly and prompted an emergency department visit.
The girl had an unremarkable history, she had not experienced mental status changes, her strength was normal, and she had just returned from a Girl Scouts trip. The patient was presumed to have Guillain-Barré. IVIG was initiated when an emergency nurse found a tick on her scalp. The tick was removed, and the patient left the hospital within 24 hours.
Children with tick paralysis are usually symptomatic after 5-7 days with the tick attached, Dr. Strunc said. They recover within a day after tick removal.
Overall, actual seizures are less common than other neurologic events in children, according to Dr. Strunc. Details on history, lack or presence of neurologic feature, and normal child development can help guide evaluation.
Take advantage of videos, he emphasized, as many parents and caregivers record a child’s neurologic events.
“Ataxia is scary, but exam and associated findings will help you with etiology,” he said.
Dr. Strunc has received research support from Jazz and Harmony and has served on the speakers’ bureau for Jazz Pharmaceuticals, Harmony Biosciences, and Avadel, unrelated to his presentation.
A version of this article first appeared on Medscape.com.
WASHINGTON – Get the back story before rushing to diagnose a seizure disorder in a child, Michael Strunc, MD, said in a presentation at the annual meeting of the American Academy of Pediatrics.
Clinicians should ask parents or caregivers about the child’s behavior before the suspected seizure, whether there were any triggers, and if so, what might they have been, according to Dr. Strunc, a child neurologist and sleep medicine specialist at Children’s Hospital of the King’s Daughters, Norfolk, Va.
“Most seizures don’t have triggers,” he said. Rather, patients often become stiff, experience a motor event that builds in intensity then slows and stops, and finally, the patient is sleepy and tired. Clinicians should also find out whether the event had a beginning, middle, and end.
Approximately 0.6% of children younger than 17 years in the United States have active epilepsy, according to the Centers for Disease Control and Prevention.
Dr. Strunc offered a few more tips for diagnosing a child:
- Ask whether the patient’s eyes were open during the event. If the eyes were closed or squished closed, “it is almost never a seizure,” he said.
- Find out whether the patient was awake or asleep, and how, if at all, caregivers attempted to stop the event.
- Ask if the child’s experiences were repeating and predictable, and inquire about a family history of seizures or other events.
- Inquire about any developmental changes and other changes in the child, such as irritability, regression, or ataxia.
The differential diagnosis for a seizure includes nonepileptic events that occur with and without changes in consciousness or sleep. These events range from breath-holding and hyperventilation to night terrors, narcolepsy, migraine, and attention-deficit/hyperactivity disorder, he said.
Is it epilepsy?
Dr. Strunc shared several cases of neurologic “events” ranging from simple to severe.
In one case, a 10-month-old infant girl with a potential tonic/staring seizure presented with a history of events that involved getting stuck in a stiff position, usually while sitting in a car seat or highchair, with adducting of legs, redness of face, and “zoned-out” expression. The infant was healthy, smart, and precocious, with no illness, fever, or trauma, but the mother was very concerned, Dr. Strunc said.
The diagnosis: Self-gratification, which is benign and usually outgrown, although it can become extreme, he said.
By contrast, “absence,” also known as idiopathic generalized epilepsy, presents as brief events of 4-10 seconds that may occur up to hundreds of times a day. This type of epilepsy is associated with the sudden onset of impaired consciousness and unresponsiveness. These events end abruptly, and the child may be unaware. Absence is more common in girls. It usually occurs after age 4 and usually remits by about age 12, Dr. Strunc said.
However, the onset of absence in patients younger than age 3 is associated with increased odds of neurodevelopmental abnormalities “and probably represents another epilepsy syndrome,” he said.
Absence symptoms may mirror those of children who are simply daydreamers, Dr. Strunc noted. One way to confirm absence is by provoking hyperventilation, which will bring on an episode of absence if present, he said. EEGs provide evidence as well.
Acute ataxia in children has a wide differential that sends kids and families to the pediatrician or emergency department, Dr. Strunc said. Acute cerebellar ataxia is characterized by abrupt and symmetric symptoms, with no mental status changes, no fever, no meningitis, and no headache. A wide, unstable gait is a distinguishing feature, Dr. Strunc said.
However, other causes of acute ataxia should be ruled out, including toxic ingestion, tick paralysis, central nervous system infections, vascular conditions, and genetic conditions.
Don’t miss those ticks
Especially during periods when kids are outdoors, clinicians should consider a tick bite as a source of ataxia and neurologic symptoms in children, Dr. Strunc emphasized. Tick paralysis notably resembles many symptoms of Guillain-Barré syndrome (acute inflammatory demyelinating polyneuropathy).
Dr. Strunc described a case involving a 5-year-old girl who developed sudden problems with gait. The problems worsened quickly and prompted an emergency department visit.
The girl had an unremarkable history, she had not experienced mental status changes, her strength was normal, and she had just returned from a Girl Scouts trip. The patient was presumed to have Guillain-Barré. IVIG was initiated when an emergency nurse found a tick on her scalp. The tick was removed, and the patient left the hospital within 24 hours.
Children with tick paralysis are usually symptomatic after 5-7 days with the tick attached, Dr. Strunc said. They recover within a day after tick removal.
Overall, actual seizures are less common than other neurologic events in children, according to Dr. Strunc. Details on history, lack or presence of neurologic feature, and normal child development can help guide evaluation.
Take advantage of videos, he emphasized, as many parents and caregivers record a child’s neurologic events.
“Ataxia is scary, but exam and associated findings will help you with etiology,” he said.
Dr. Strunc has received research support from Jazz and Harmony and has served on the speakers’ bureau for Jazz Pharmaceuticals, Harmony Biosciences, and Avadel, unrelated to his presentation.
A version of this article first appeared on Medscape.com.
WASHINGTON – Get the back story before rushing to diagnose a seizure disorder in a child, Michael Strunc, MD, said in a presentation at the annual meeting of the American Academy of Pediatrics.
Clinicians should ask parents or caregivers about the child’s behavior before the suspected seizure, whether there were any triggers, and if so, what might they have been, according to Dr. Strunc, a child neurologist and sleep medicine specialist at Children’s Hospital of the King’s Daughters, Norfolk, Va.
“Most seizures don’t have triggers,” he said. Rather, patients often become stiff, experience a motor event that builds in intensity then slows and stops, and finally, the patient is sleepy and tired. Clinicians should also find out whether the event had a beginning, middle, and end.
Approximately 0.6% of children younger than 17 years in the United States have active epilepsy, according to the Centers for Disease Control and Prevention.
Dr. Strunc offered a few more tips for diagnosing a child:
- Ask whether the patient’s eyes were open during the event. If the eyes were closed or squished closed, “it is almost never a seizure,” he said.
- Find out whether the patient was awake or asleep, and how, if at all, caregivers attempted to stop the event.
- Ask if the child’s experiences were repeating and predictable, and inquire about a family history of seizures or other events.
- Inquire about any developmental changes and other changes in the child, such as irritability, regression, or ataxia.
The differential diagnosis for a seizure includes nonepileptic events that occur with and without changes in consciousness or sleep. These events range from breath-holding and hyperventilation to night terrors, narcolepsy, migraine, and attention-deficit/hyperactivity disorder, he said.
Is it epilepsy?
Dr. Strunc shared several cases of neurologic “events” ranging from simple to severe.
In one case, a 10-month-old infant girl with a potential tonic/staring seizure presented with a history of events that involved getting stuck in a stiff position, usually while sitting in a car seat or highchair, with adducting of legs, redness of face, and “zoned-out” expression. The infant was healthy, smart, and precocious, with no illness, fever, or trauma, but the mother was very concerned, Dr. Strunc said.
The diagnosis: Self-gratification, which is benign and usually outgrown, although it can become extreme, he said.
By contrast, “absence,” also known as idiopathic generalized epilepsy, presents as brief events of 4-10 seconds that may occur up to hundreds of times a day. This type of epilepsy is associated with the sudden onset of impaired consciousness and unresponsiveness. These events end abruptly, and the child may be unaware. Absence is more common in girls. It usually occurs after age 4 and usually remits by about age 12, Dr. Strunc said.
However, the onset of absence in patients younger than age 3 is associated with increased odds of neurodevelopmental abnormalities “and probably represents another epilepsy syndrome,” he said.
Absence symptoms may mirror those of children who are simply daydreamers, Dr. Strunc noted. One way to confirm absence is by provoking hyperventilation, which will bring on an episode of absence if present, he said. EEGs provide evidence as well.
Acute ataxia in children has a wide differential that sends kids and families to the pediatrician or emergency department, Dr. Strunc said. Acute cerebellar ataxia is characterized by abrupt and symmetric symptoms, with no mental status changes, no fever, no meningitis, and no headache. A wide, unstable gait is a distinguishing feature, Dr. Strunc said.
However, other causes of acute ataxia should be ruled out, including toxic ingestion, tick paralysis, central nervous system infections, vascular conditions, and genetic conditions.
Don’t miss those ticks
Especially during periods when kids are outdoors, clinicians should consider a tick bite as a source of ataxia and neurologic symptoms in children, Dr. Strunc emphasized. Tick paralysis notably resembles many symptoms of Guillain-Barré syndrome (acute inflammatory demyelinating polyneuropathy).
Dr. Strunc described a case involving a 5-year-old girl who developed sudden problems with gait. The problems worsened quickly and prompted an emergency department visit.
The girl had an unremarkable history, she had not experienced mental status changes, her strength was normal, and she had just returned from a Girl Scouts trip. The patient was presumed to have Guillain-Barré. IVIG was initiated when an emergency nurse found a tick on her scalp. The tick was removed, and the patient left the hospital within 24 hours.
Children with tick paralysis are usually symptomatic after 5-7 days with the tick attached, Dr. Strunc said. They recover within a day after tick removal.
Overall, actual seizures are less common than other neurologic events in children, according to Dr. Strunc. Details on history, lack or presence of neurologic feature, and normal child development can help guide evaluation.
Take advantage of videos, he emphasized, as many parents and caregivers record a child’s neurologic events.
“Ataxia is scary, but exam and associated findings will help you with etiology,” he said.
Dr. Strunc has received research support from Jazz and Harmony and has served on the speakers’ bureau for Jazz Pharmaceuticals, Harmony Biosciences, and Avadel, unrelated to his presentation.
A version of this article first appeared on Medscape.com.
FROM AAP 2023
How clinicians can prepare for and defend against social media attacks
WASHINGTON – The entire video clip is just 15 seconds — 15 seconds that went viral and temporarily upended the entire life and disrupted the medical practice of Nicole Baldwin, MD, a pediatrician in Cincinnati, Ohio, in January 2020. At the annual meeting of the American Academy of Pediatrics, Dr. Baldwin told attendees how her pro-vaccine TikTok video led a horde of anti-vaccine activists to swarm her social media profiles across multiple platforms, leave one-star reviews with false stories about her medical practice on various doctor review sites, and personally threaten her.
The initial response to the video was positive, with 50,000 views in the first 24 hours after the video was posted and more than 1.5 million views the next day. But 2 days after the video was posted, an organized attack that originated on Facebook required Dr. Baldwin to enlist the help of 16 volunteers, working 24/7 for a week, to help ban and block more than 6,000 users on Facebook, Instagram, and TikTok. Just 4 days after she’d posted the video, Dr. Baldwin was reporting personal threats to the police and had begun contacting sites such as Yelp, Google, Healthgrades, Vitals, RateMDs, and WebMD so they could start removing false reviews about her practice.
Today, years after those 2 exhausting, intense weeks of attacks, Dr. Baldwin has found two silver linings in the experience: More people have found her profiles, allowing her to share evidence-based information with an even wider audience, and she can now help other physicians protect themselves and reduce the risk of similar attacks, or at least know how to respond to them if they occur. Dr. Baldwin shared a wealth of tips and resources during her lecture to help pediatricians prepare ahead for the possibility that they will be targeted next, whether the issue is vaccines or another topic.
Online risks and benefits
A Pew survey of U.S. adults in September 2020 found that 41% have personally experienced online harassment, including a quarter of Americans who have experienced severe harassment. More than half of respondents said online harassment and bullying is a major problem – and that was a poll of the entire population, not even just physicians and scientists.
“Now, these numbers would be higher,” Dr. Baldwin said. “A lot has changed in the past 3 years, and the landscape is very different.”
The pandemic contributed to those changes to the landscape, including an increase in harassment of doctors and researchers. A June 2023 study revealed that two-thirds of 359 respondents in an online survey reported harassment on social media, a substantial number even after accounting for selection bias in the individuals who chose to respond to the survey. Although most of the attacks (88%) resulted from the respondent’s advocacy online, nearly half the attacks (45%) were gender based, 27% were based on race/ethnicity, and 13% were based on sexual orientation.
While hateful comments are likely the most common type of online harassment, other types can involve sharing or tagging your profile, creating fake profiles to misrepresent you, fake reviews of your practice, harassing phone calls and hate mail at your office, and doxxing, in which someone online widely shares your personal address, phone number, email, or other contact information.
Despite the risks of all these forms of harassment, Dr. Baldwin emphasized the value of doctors having a social media presence given how much misinformation thrives online. For example, a recent report from the Kaiser Family Foundation revealed how many people weren’t sure whether certain health misinformation claims were true or false. Barely a third of people were sure that COVID-19 vaccines had not caused thousands of deaths in healthy people, and only 22% of people were sure that ivermectin is not an effective treatment for COVID.
“There is so much that we need to be doing and working in these spaces to put evidence-based content out there so that people are not finding all of this crap from everybody else,” Dr. Baldwin said. Having an online presence is particularly important given that the public still has high levels of trust in their doctors, she added.
“They trust their physician, and you may not be their physician online, but I will tell you from experience, when you build a community of followers, you become that trusted source of information for them, and it is so important,” Dr. Baldwin said. “There is room for everybody in this space, and we need all of you.”
Proactive steps for protection
Dr. Baldwin then went through the details of what people should do now to make things easier in the event of an attack later. “The best defense is a good offense,” Dr. Baldwin said, “so make sure all of your accounts are secure.”
She recommended the following steps:
- Use two-factor authentication for all of your logins.
- Use strong, unique passwords for all of your logins.
- Use strong privacy settings on all of your private social media profiles, such as making sure photos are not visible on your personal Facebook account.
- Claim your Google profile and Yelp business profile.
- Claim your doctor and/or business profile on all of the medical review sites where you have one, including Google, Healthgrades, Vitals, RateMDs, and WebMD.
For doctors who are attacked specifically because of pro-vaccine advocacy, Dr. Baldwin recommended contacting Shots Heard Round The World, a site that was created by a physician whose practice was attacked by anti-vaccine activists. The site also has a toolkit that anyone can download for tips on preparing ahead for possible attacks and what to do if you are attacked.
Dr. Baldwin then reviewed how to set up different social media profiles to automatically hide certain comments, including comments with words commonly used by online harassers and trolls:
- Sheep
- Sheeple
- Pharma
- Shill
- Die
- Psychopath
- Clown
- Various curse words
- The clown emoji
In Instagram, go to “Settings and privacy —> Hidden Words” for options on hiding offensive comments and messages and for managing custom words and phrases that should be automatically hidden.
On Facebook, go to “Professional dashboard —> Moderation Assist,” where you can add or edit criteria to automatically hide comments on your Facebook page. In addition to hiding comments with certain keywords, you can hide comments from new accounts, accounts without profile photos, or accounts with no friends or followers.
On TikTok, click the three-line menu icon in the upper right, and choose “Privacy —> Comments —> Filter keywords.”
On the platform formerly known as Twitter, go to “Settings and privacy —> Privacy and safety —> Mute and block —> Muted words.”
On YouTube, under “Manage your community & comments,” select “Learn about comment settings.”
Dr. Baldwin did not discourage doctors from posting about controversial topics, but she said it’s important to know what they are so that you can be prepared for the possibility that a post about one of these topics could lead to online harassment. These hot button topics include vaccines, firearm safety, gender-affirming care, reproductive choice, safe sleep/bedsharing, breastfeeding, and COVID masks.
If you do post on one of these and suspect it could result in harassment, Dr. Baldwin recommends turning on your notifications so you know when attacks begin, alerting your office and call center staff if you think they might receive calls, and, when possible, post your content at a time when you’re more likely to be able to monitor the post. She acknowledged that this last tip isn’t always relevant since attacks can take a few days to start or gain steam.
Defending yourself in an attack
Even after taking all these precautions, it’s not possible to altogether prevent an attack from happening, so Dr. Baldwin provided suggestions on what to do if one occurs, starting with taking a deep breath.
“If you are attacked, first of all, please remain calm, which is a lot easier said than done,” she said. “But know that this too shall pass. These things do come to an end.”
She advises you to get help if you need it, enlisting friends or colleagues to help with moderation and banning/blocking. If necessary, alert your employer to the attack, as attackers may contact your employer. Some people may opt to turn off comments on their post, but doing so “is a really personal decision,” she said. It’s okay to turn off comments if you don’t have the bandwidth or help to deal with them.
However, Dr. Baldwin said she never turns off comments because she wants to be able to ban and block people to reduce the likelihood of a future attack from them, and each comment brings the post higher in the algorithm so that more people are able to see the original content. “So sometimes these things are actually a blessing in disguise,” she said.
If you do have comments turned on, take screenshots of the most egregious or threatening ones and then report them and ban/block them. The screenshots are evidence since blocking will remove the comment.
“Take breaks when you need to,” she said. “Don’t stay up all night” since there are only going to be more in the morning, and if you’re using keywords to help hide many of these comments, that will hide them from your followers while you’re away. She also advised monitoring your online reviews at doctor/practice review sites so you know whether you’re receiving spurious reviews that need to be removed.
Dr. Baldwin also addressed how to handle trolls, the people online who intentionally antagonize others with inflammatory, irrelevant, offensive, or otherwise disruptive comments or content. The No. 1 rule is not to engage – “Don’t feed the trolls” – but Dr. Baldwin acknowledged that she can find that difficult sometimes. So she uses kindness or humor to defuse them or calls them out on their inaccurate information and then thanks them for their engagement. Don’t forget that you are in charge of your own page, so any complaints about “censorship” or infringing “free speech” aren’t relevant.
If the comments are growing out of control and you’re unable to manage them, multiple social media platforms have options for limited interactions or who can comment on your page.
On Instagram under “Settings and privacy,” check out “Limited interactions,” “Comments —> Allow comments from,” and “Tags and mentions” to see ways you can limit who is able to comment, tag or mention your account. If you need a complete break, you can turn off commenting by clicking the three dots in the upper right corner of the post, or make your account temporarily private under “Settings and privacy —> Account privacy.”
On Facebook, click the three dots in the upper right corner of posts to select “Who can comment on your post?” Also, under “Settings —> Privacy —> Your Activity,” you can adjust who sees your future posts. Again, if things are out of control, you can temporarily deactivate your page under “Settings —> Privacy —> Facebook Page information.”
On TikTok, click the three lines in the upper right corner of your profile and select “Privacy —> Comments” to adjust who can comment and to filter comments. Again, you can make your account private under “Settings and privacy —> Privacy —> Private account.”
On the platform formerly known as Twitter, click the three dots in the upper right corner of the tweet to change who can reply to the tweet. If you select “Only people you mentioned,” then no one can reply if you did not mention anyone. You can control tagging under “Settings and privacy —> Privacy and safety —> Audience and tagging.”
If you or your practice receive false reviews on review sites, report the reviews and alert the rating site when you can. In the meantime, lock down your private social media accounts and ensure that no photos of your family are publicly available.
Social media self-care
Dr. Baldwin acknowledged that experiencing a social media attack can be intense and even frightening, but it’s rare and outweighed by the “hundreds and hundreds and hundreds of positive comments all the time.” She also reminded attendees that being on social media doesn’t mean being there all the time.
“Over time, my use of social media has certainly changed. It ebbs and flows,” she said. “There are times when I have a lot of bandwidth and I’m posting a lot, and then I actually have had some struggles with my own mental health, with some anxiety and mild depression, so I took a break from social media for a while. When I came back, I posted about my mental health struggles, and you wouldn’t believe how many people were so appreciative of that.”
Accurate information from a trusted source
Ultimately, Dr. Baldwin sees her work online as an extension of her work educating patients.
“This is where our patients are. They are in your office for maybe 10-15 minutes maybe once a year, but they are on these platforms every single day for hours,” she said. “They need to see this information from medical professionals because there are random people out there that are telling them [misinformation].”
Elizabeth Murray, DO, MBA, an emergency medicine pediatrician at Golisano Children’s Hospital at the University of Rochester, agreed that there’s substantial value in doctors sharing accurate information online.
“Disinformation and misinformation is rampant, and at the end of the day, we know the facts,” Dr. Murray said. “We know what parents want to hear and what they want to learn about, so we need to share that information and get the facts out there.”
Dr. Murray found the session very helpful because there’s so much to learn across different social media platforms and it can feel overwhelming if you aren’t familiar with the tools.
“Social media is always going to be here. We need to learn to live with all of these platforms,” Dr. Murray said. “That’s a skill set. We need to learn the skills and teach our kids the skill set. You never really know what you might put out there that, in your mind is innocent or very science-based, that for whatever reason somebody might take issue with. You might as well be ready because we’re all about prevention in pediatrics.”
There were no funders for the presentation. Dr. Baldwin and Dr. Murray had no disclosures.
WASHINGTON – The entire video clip is just 15 seconds — 15 seconds that went viral and temporarily upended the entire life and disrupted the medical practice of Nicole Baldwin, MD, a pediatrician in Cincinnati, Ohio, in January 2020. At the annual meeting of the American Academy of Pediatrics, Dr. Baldwin told attendees how her pro-vaccine TikTok video led a horde of anti-vaccine activists to swarm her social media profiles across multiple platforms, leave one-star reviews with false stories about her medical practice on various doctor review sites, and personally threaten her.
The initial response to the video was positive, with 50,000 views in the first 24 hours after the video was posted and more than 1.5 million views the next day. But 2 days after the video was posted, an organized attack that originated on Facebook required Dr. Baldwin to enlist the help of 16 volunteers, working 24/7 for a week, to help ban and block more than 6,000 users on Facebook, Instagram, and TikTok. Just 4 days after she’d posted the video, Dr. Baldwin was reporting personal threats to the police and had begun contacting sites such as Yelp, Google, Healthgrades, Vitals, RateMDs, and WebMD so they could start removing false reviews about her practice.
Today, years after those 2 exhausting, intense weeks of attacks, Dr. Baldwin has found two silver linings in the experience: More people have found her profiles, allowing her to share evidence-based information with an even wider audience, and she can now help other physicians protect themselves and reduce the risk of similar attacks, or at least know how to respond to them if they occur. Dr. Baldwin shared a wealth of tips and resources during her lecture to help pediatricians prepare ahead for the possibility that they will be targeted next, whether the issue is vaccines or another topic.
Online risks and benefits
A Pew survey of U.S. adults in September 2020 found that 41% have personally experienced online harassment, including a quarter of Americans who have experienced severe harassment. More than half of respondents said online harassment and bullying is a major problem – and that was a poll of the entire population, not even just physicians and scientists.
“Now, these numbers would be higher,” Dr. Baldwin said. “A lot has changed in the past 3 years, and the landscape is very different.”
The pandemic contributed to those changes to the landscape, including an increase in harassment of doctors and researchers. A June 2023 study revealed that two-thirds of 359 respondents in an online survey reported harassment on social media, a substantial number even after accounting for selection bias in the individuals who chose to respond to the survey. Although most of the attacks (88%) resulted from the respondent’s advocacy online, nearly half the attacks (45%) were gender based, 27% were based on race/ethnicity, and 13% were based on sexual orientation.
While hateful comments are likely the most common type of online harassment, other types can involve sharing or tagging your profile, creating fake profiles to misrepresent you, fake reviews of your practice, harassing phone calls and hate mail at your office, and doxxing, in which someone online widely shares your personal address, phone number, email, or other contact information.
Despite the risks of all these forms of harassment, Dr. Baldwin emphasized the value of doctors having a social media presence given how much misinformation thrives online. For example, a recent report from the Kaiser Family Foundation revealed how many people weren’t sure whether certain health misinformation claims were true or false. Barely a third of people were sure that COVID-19 vaccines had not caused thousands of deaths in healthy people, and only 22% of people were sure that ivermectin is not an effective treatment for COVID.
“There is so much that we need to be doing and working in these spaces to put evidence-based content out there so that people are not finding all of this crap from everybody else,” Dr. Baldwin said. Having an online presence is particularly important given that the public still has high levels of trust in their doctors, she added.
“They trust their physician, and you may not be their physician online, but I will tell you from experience, when you build a community of followers, you become that trusted source of information for them, and it is so important,” Dr. Baldwin said. “There is room for everybody in this space, and we need all of you.”
Proactive steps for protection
Dr. Baldwin then went through the details of what people should do now to make things easier in the event of an attack later. “The best defense is a good offense,” Dr. Baldwin said, “so make sure all of your accounts are secure.”
She recommended the following steps:
- Use two-factor authentication for all of your logins.
- Use strong, unique passwords for all of your logins.
- Use strong privacy settings on all of your private social media profiles, such as making sure photos are not visible on your personal Facebook account.
- Claim your Google profile and Yelp business profile.
- Claim your doctor and/or business profile on all of the medical review sites where you have one, including Google, Healthgrades, Vitals, RateMDs, and WebMD.
For doctors who are attacked specifically because of pro-vaccine advocacy, Dr. Baldwin recommended contacting Shots Heard Round The World, a site that was created by a physician whose practice was attacked by anti-vaccine activists. The site also has a toolkit that anyone can download for tips on preparing ahead for possible attacks and what to do if you are attacked.
Dr. Baldwin then reviewed how to set up different social media profiles to automatically hide certain comments, including comments with words commonly used by online harassers and trolls:
- Sheep
- Sheeple
- Pharma
- Shill
- Die
- Psychopath
- Clown
- Various curse words
- The clown emoji
In Instagram, go to “Settings and privacy —> Hidden Words” for options on hiding offensive comments and messages and for managing custom words and phrases that should be automatically hidden.
On Facebook, go to “Professional dashboard —> Moderation Assist,” where you can add or edit criteria to automatically hide comments on your Facebook page. In addition to hiding comments with certain keywords, you can hide comments from new accounts, accounts without profile photos, or accounts with no friends or followers.
On TikTok, click the three-line menu icon in the upper right, and choose “Privacy —> Comments —> Filter keywords.”
On the platform formerly known as Twitter, go to “Settings and privacy —> Privacy and safety —> Mute and block —> Muted words.”
On YouTube, under “Manage your community & comments,” select “Learn about comment settings.”
Dr. Baldwin did not discourage doctors from posting about controversial topics, but she said it’s important to know what they are so that you can be prepared for the possibility that a post about one of these topics could lead to online harassment. These hot button topics include vaccines, firearm safety, gender-affirming care, reproductive choice, safe sleep/bedsharing, breastfeeding, and COVID masks.
If you do post on one of these and suspect it could result in harassment, Dr. Baldwin recommends turning on your notifications so you know when attacks begin, alerting your office and call center staff if you think they might receive calls, and, when possible, post your content at a time when you’re more likely to be able to monitor the post. She acknowledged that this last tip isn’t always relevant since attacks can take a few days to start or gain steam.
Defending yourself in an attack
Even after taking all these precautions, it’s not possible to altogether prevent an attack from happening, so Dr. Baldwin provided suggestions on what to do if one occurs, starting with taking a deep breath.
“If you are attacked, first of all, please remain calm, which is a lot easier said than done,” she said. “But know that this too shall pass. These things do come to an end.”
She advises you to get help if you need it, enlisting friends or colleagues to help with moderation and banning/blocking. If necessary, alert your employer to the attack, as attackers may contact your employer. Some people may opt to turn off comments on their post, but doing so “is a really personal decision,” she said. It’s okay to turn off comments if you don’t have the bandwidth or help to deal with them.
However, Dr. Baldwin said she never turns off comments because she wants to be able to ban and block people to reduce the likelihood of a future attack from them, and each comment brings the post higher in the algorithm so that more people are able to see the original content. “So sometimes these things are actually a blessing in disguise,” she said.
If you do have comments turned on, take screenshots of the most egregious or threatening ones and then report them and ban/block them. The screenshots are evidence since blocking will remove the comment.
“Take breaks when you need to,” she said. “Don’t stay up all night” since there are only going to be more in the morning, and if you’re using keywords to help hide many of these comments, that will hide them from your followers while you’re away. She also advised monitoring your online reviews at doctor/practice review sites so you know whether you’re receiving spurious reviews that need to be removed.
Dr. Baldwin also addressed how to handle trolls, the people online who intentionally antagonize others with inflammatory, irrelevant, offensive, or otherwise disruptive comments or content. The No. 1 rule is not to engage – “Don’t feed the trolls” – but Dr. Baldwin acknowledged that she can find that difficult sometimes. So she uses kindness or humor to defuse them or calls them out on their inaccurate information and then thanks them for their engagement. Don’t forget that you are in charge of your own page, so any complaints about “censorship” or infringing “free speech” aren’t relevant.
If the comments are growing out of control and you’re unable to manage them, multiple social media platforms have options for limited interactions or who can comment on your page.
On Instagram under “Settings and privacy,” check out “Limited interactions,” “Comments —> Allow comments from,” and “Tags and mentions” to see ways you can limit who is able to comment, tag or mention your account. If you need a complete break, you can turn off commenting by clicking the three dots in the upper right corner of the post, or make your account temporarily private under “Settings and privacy —> Account privacy.”
On Facebook, click the three dots in the upper right corner of posts to select “Who can comment on your post?” Also, under “Settings —> Privacy —> Your Activity,” you can adjust who sees your future posts. Again, if things are out of control, you can temporarily deactivate your page under “Settings —> Privacy —> Facebook Page information.”
On TikTok, click the three lines in the upper right corner of your profile and select “Privacy —> Comments” to adjust who can comment and to filter comments. Again, you can make your account private under “Settings and privacy —> Privacy —> Private account.”
On the platform formerly known as Twitter, click the three dots in the upper right corner of the tweet to change who can reply to the tweet. If you select “Only people you mentioned,” then no one can reply if you did not mention anyone. You can control tagging under “Settings and privacy —> Privacy and safety —> Audience and tagging.”
If you or your practice receive false reviews on review sites, report the reviews and alert the rating site when you can. In the meantime, lock down your private social media accounts and ensure that no photos of your family are publicly available.
Social media self-care
Dr. Baldwin acknowledged that experiencing a social media attack can be intense and even frightening, but it’s rare and outweighed by the “hundreds and hundreds and hundreds of positive comments all the time.” She also reminded attendees that being on social media doesn’t mean being there all the time.
“Over time, my use of social media has certainly changed. It ebbs and flows,” she said. “There are times when I have a lot of bandwidth and I’m posting a lot, and then I actually have had some struggles with my own mental health, with some anxiety and mild depression, so I took a break from social media for a while. When I came back, I posted about my mental health struggles, and you wouldn’t believe how many people were so appreciative of that.”
Accurate information from a trusted source
Ultimately, Dr. Baldwin sees her work online as an extension of her work educating patients.
“This is where our patients are. They are in your office for maybe 10-15 minutes maybe once a year, but they are on these platforms every single day for hours,” she said. “They need to see this information from medical professionals because there are random people out there that are telling them [misinformation].”
Elizabeth Murray, DO, MBA, an emergency medicine pediatrician at Golisano Children’s Hospital at the University of Rochester, agreed that there’s substantial value in doctors sharing accurate information online.
“Disinformation and misinformation is rampant, and at the end of the day, we know the facts,” Dr. Murray said. “We know what parents want to hear and what they want to learn about, so we need to share that information and get the facts out there.”
Dr. Murray found the session very helpful because there’s so much to learn across different social media platforms and it can feel overwhelming if you aren’t familiar with the tools.
“Social media is always going to be here. We need to learn to live with all of these platforms,” Dr. Murray said. “That’s a skill set. We need to learn the skills and teach our kids the skill set. You never really know what you might put out there that, in your mind is innocent or very science-based, that for whatever reason somebody might take issue with. You might as well be ready because we’re all about prevention in pediatrics.”
There were no funders for the presentation. Dr. Baldwin and Dr. Murray had no disclosures.
WASHINGTON – The entire video clip is just 15 seconds — 15 seconds that went viral and temporarily upended the entire life and disrupted the medical practice of Nicole Baldwin, MD, a pediatrician in Cincinnati, Ohio, in January 2020. At the annual meeting of the American Academy of Pediatrics, Dr. Baldwin told attendees how her pro-vaccine TikTok video led a horde of anti-vaccine activists to swarm her social media profiles across multiple platforms, leave one-star reviews with false stories about her medical practice on various doctor review sites, and personally threaten her.
The initial response to the video was positive, with 50,000 views in the first 24 hours after the video was posted and more than 1.5 million views the next day. But 2 days after the video was posted, an organized attack that originated on Facebook required Dr. Baldwin to enlist the help of 16 volunteers, working 24/7 for a week, to help ban and block more than 6,000 users on Facebook, Instagram, and TikTok. Just 4 days after she’d posted the video, Dr. Baldwin was reporting personal threats to the police and had begun contacting sites such as Yelp, Google, Healthgrades, Vitals, RateMDs, and WebMD so they could start removing false reviews about her practice.
Today, years after those 2 exhausting, intense weeks of attacks, Dr. Baldwin has found two silver linings in the experience: More people have found her profiles, allowing her to share evidence-based information with an even wider audience, and she can now help other physicians protect themselves and reduce the risk of similar attacks, or at least know how to respond to them if they occur. Dr. Baldwin shared a wealth of tips and resources during her lecture to help pediatricians prepare ahead for the possibility that they will be targeted next, whether the issue is vaccines or another topic.
Online risks and benefits
A Pew survey of U.S. adults in September 2020 found that 41% have personally experienced online harassment, including a quarter of Americans who have experienced severe harassment. More than half of respondents said online harassment and bullying is a major problem – and that was a poll of the entire population, not even just physicians and scientists.
“Now, these numbers would be higher,” Dr. Baldwin said. “A lot has changed in the past 3 years, and the landscape is very different.”
The pandemic contributed to those changes to the landscape, including an increase in harassment of doctors and researchers. A June 2023 study revealed that two-thirds of 359 respondents in an online survey reported harassment on social media, a substantial number even after accounting for selection bias in the individuals who chose to respond to the survey. Although most of the attacks (88%) resulted from the respondent’s advocacy online, nearly half the attacks (45%) were gender based, 27% were based on race/ethnicity, and 13% were based on sexual orientation.
While hateful comments are likely the most common type of online harassment, other types can involve sharing or tagging your profile, creating fake profiles to misrepresent you, fake reviews of your practice, harassing phone calls and hate mail at your office, and doxxing, in which someone online widely shares your personal address, phone number, email, or other contact information.
Despite the risks of all these forms of harassment, Dr. Baldwin emphasized the value of doctors having a social media presence given how much misinformation thrives online. For example, a recent report from the Kaiser Family Foundation revealed how many people weren’t sure whether certain health misinformation claims were true or false. Barely a third of people were sure that COVID-19 vaccines had not caused thousands of deaths in healthy people, and only 22% of people were sure that ivermectin is not an effective treatment for COVID.
“There is so much that we need to be doing and working in these spaces to put evidence-based content out there so that people are not finding all of this crap from everybody else,” Dr. Baldwin said. Having an online presence is particularly important given that the public still has high levels of trust in their doctors, she added.
“They trust their physician, and you may not be their physician online, but I will tell you from experience, when you build a community of followers, you become that trusted source of information for them, and it is so important,” Dr. Baldwin said. “There is room for everybody in this space, and we need all of you.”
Proactive steps for protection
Dr. Baldwin then went through the details of what people should do now to make things easier in the event of an attack later. “The best defense is a good offense,” Dr. Baldwin said, “so make sure all of your accounts are secure.”
She recommended the following steps:
- Use two-factor authentication for all of your logins.
- Use strong, unique passwords for all of your logins.
- Use strong privacy settings on all of your private social media profiles, such as making sure photos are not visible on your personal Facebook account.
- Claim your Google profile and Yelp business profile.
- Claim your doctor and/or business profile on all of the medical review sites where you have one, including Google, Healthgrades, Vitals, RateMDs, and WebMD.
For doctors who are attacked specifically because of pro-vaccine advocacy, Dr. Baldwin recommended contacting Shots Heard Round The World, a site that was created by a physician whose practice was attacked by anti-vaccine activists. The site also has a toolkit that anyone can download for tips on preparing ahead for possible attacks and what to do if you are attacked.
Dr. Baldwin then reviewed how to set up different social media profiles to automatically hide certain comments, including comments with words commonly used by online harassers and trolls:
- Sheep
- Sheeple
- Pharma
- Shill
- Die
- Psychopath
- Clown
- Various curse words
- The clown emoji
In Instagram, go to “Settings and privacy —> Hidden Words” for options on hiding offensive comments and messages and for managing custom words and phrases that should be automatically hidden.
On Facebook, go to “Professional dashboard —> Moderation Assist,” where you can add or edit criteria to automatically hide comments on your Facebook page. In addition to hiding comments with certain keywords, you can hide comments from new accounts, accounts without profile photos, or accounts with no friends or followers.
On TikTok, click the three-line menu icon in the upper right, and choose “Privacy —> Comments —> Filter keywords.”
On the platform formerly known as Twitter, go to “Settings and privacy —> Privacy and safety —> Mute and block —> Muted words.”
On YouTube, under “Manage your community & comments,” select “Learn about comment settings.”
Dr. Baldwin did not discourage doctors from posting about controversial topics, but she said it’s important to know what they are so that you can be prepared for the possibility that a post about one of these topics could lead to online harassment. These hot button topics include vaccines, firearm safety, gender-affirming care, reproductive choice, safe sleep/bedsharing, breastfeeding, and COVID masks.
If you do post on one of these and suspect it could result in harassment, Dr. Baldwin recommends turning on your notifications so you know when attacks begin, alerting your office and call center staff if you think they might receive calls, and, when possible, post your content at a time when you’re more likely to be able to monitor the post. She acknowledged that this last tip isn’t always relevant since attacks can take a few days to start or gain steam.
Defending yourself in an attack
Even after taking all these precautions, it’s not possible to altogether prevent an attack from happening, so Dr. Baldwin provided suggestions on what to do if one occurs, starting with taking a deep breath.
“If you are attacked, first of all, please remain calm, which is a lot easier said than done,” she said. “But know that this too shall pass. These things do come to an end.”
She advises you to get help if you need it, enlisting friends or colleagues to help with moderation and banning/blocking. If necessary, alert your employer to the attack, as attackers may contact your employer. Some people may opt to turn off comments on their post, but doing so “is a really personal decision,” she said. It’s okay to turn off comments if you don’t have the bandwidth or help to deal with them.
However, Dr. Baldwin said she never turns off comments because she wants to be able to ban and block people to reduce the likelihood of a future attack from them, and each comment brings the post higher in the algorithm so that more people are able to see the original content. “So sometimes these things are actually a blessing in disguise,” she said.
If you do have comments turned on, take screenshots of the most egregious or threatening ones and then report them and ban/block them. The screenshots are evidence since blocking will remove the comment.
“Take breaks when you need to,” she said. “Don’t stay up all night” since there are only going to be more in the morning, and if you’re using keywords to help hide many of these comments, that will hide them from your followers while you’re away. She also advised monitoring your online reviews at doctor/practice review sites so you know whether you’re receiving spurious reviews that need to be removed.
Dr. Baldwin also addressed how to handle trolls, the people online who intentionally antagonize others with inflammatory, irrelevant, offensive, or otherwise disruptive comments or content. The No. 1 rule is not to engage – “Don’t feed the trolls” – but Dr. Baldwin acknowledged that she can find that difficult sometimes. So she uses kindness or humor to defuse them or calls them out on their inaccurate information and then thanks them for their engagement. Don’t forget that you are in charge of your own page, so any complaints about “censorship” or infringing “free speech” aren’t relevant.
If the comments are growing out of control and you’re unable to manage them, multiple social media platforms have options for limited interactions or who can comment on your page.
On Instagram under “Settings and privacy,” check out “Limited interactions,” “Comments —> Allow comments from,” and “Tags and mentions” to see ways you can limit who is able to comment, tag or mention your account. If you need a complete break, you can turn off commenting by clicking the three dots in the upper right corner of the post, or make your account temporarily private under “Settings and privacy —> Account privacy.”
On Facebook, click the three dots in the upper right corner of posts to select “Who can comment on your post?” Also, under “Settings —> Privacy —> Your Activity,” you can adjust who sees your future posts. Again, if things are out of control, you can temporarily deactivate your page under “Settings —> Privacy —> Facebook Page information.”
On TikTok, click the three lines in the upper right corner of your profile and select “Privacy —> Comments” to adjust who can comment and to filter comments. Again, you can make your account private under “Settings and privacy —> Privacy —> Private account.”
On the platform formerly known as Twitter, click the three dots in the upper right corner of the tweet to change who can reply to the tweet. If you select “Only people you mentioned,” then no one can reply if you did not mention anyone. You can control tagging under “Settings and privacy —> Privacy and safety —> Audience and tagging.”
If you or your practice receive false reviews on review sites, report the reviews and alert the rating site when you can. In the meantime, lock down your private social media accounts and ensure that no photos of your family are publicly available.
Social media self-care
Dr. Baldwin acknowledged that experiencing a social media attack can be intense and even frightening, but it’s rare and outweighed by the “hundreds and hundreds and hundreds of positive comments all the time.” She also reminded attendees that being on social media doesn’t mean being there all the time.
“Over time, my use of social media has certainly changed. It ebbs and flows,” she said. “There are times when I have a lot of bandwidth and I’m posting a lot, and then I actually have had some struggles with my own mental health, with some anxiety and mild depression, so I took a break from social media for a while. When I came back, I posted about my mental health struggles, and you wouldn’t believe how many people were so appreciative of that.”
Accurate information from a trusted source
Ultimately, Dr. Baldwin sees her work online as an extension of her work educating patients.
“This is where our patients are. They are in your office for maybe 10-15 minutes maybe once a year, but they are on these platforms every single day for hours,” she said. “They need to see this information from medical professionals because there are random people out there that are telling them [misinformation].”
Elizabeth Murray, DO, MBA, an emergency medicine pediatrician at Golisano Children’s Hospital at the University of Rochester, agreed that there’s substantial value in doctors sharing accurate information online.
“Disinformation and misinformation is rampant, and at the end of the day, we know the facts,” Dr. Murray said. “We know what parents want to hear and what they want to learn about, so we need to share that information and get the facts out there.”
Dr. Murray found the session very helpful because there’s so much to learn across different social media platforms and it can feel overwhelming if you aren’t familiar with the tools.
“Social media is always going to be here. We need to learn to live with all of these platforms,” Dr. Murray said. “That’s a skill set. We need to learn the skills and teach our kids the skill set. You never really know what you might put out there that, in your mind is innocent or very science-based, that for whatever reason somebody might take issue with. You might as well be ready because we’re all about prevention in pediatrics.”
There were no funders for the presentation. Dr. Baldwin and Dr. Murray had no disclosures.
AT AAP 2023
Fathers’ postpartum depression linked to children’s adversity
WASHINGTON – , according to research presented at the annual meeting of the American Academy of Pediatrics.
The findings held even after taking into account postpartum depression in the child’s mother and other factors that might increase risk of adverse childhood experiences, reported Kristine H. Schmitz, MD, an assistant professor of pediatrics at Robert Wood Johnson Medical School, New Brunswick, N.J.
Paternal postpartum depression has not been studied very well, so it’s difficult to pin down its prevalence, but some research has found rates as high as 25%, Dr. Schmitz told attendees.
”We recognize that it’s very under-recognized and often under-reported, but we also know that it has lots of downstream effects on child outcomes, including difficulties with parenting, difficulties with child behavior, as well as school performance and school attainment and employment,” Dr. Schmitz said.
Paternal depression and adverse childhood experiences
The study involved an analysis of six waves of data from the Future of Families & Child Wellbeing Study, which follows a national cohort of children born in large U.S. cities between 1998 and 2000. The cohort includes an intentional over-representation of unmarried mothers, who make up about 75% of the overall population.
The researchers used the World Health Organization’s Composite International Diagnosis Interview Short Form (CIDI-SF) to assess fathers’ depression when their children were 1 year old. Then the researchers looked at the number of adverse childhood experiences (ACEs) children had at 5 years old.
The analysis was adjusted to account for the child’s sex and the father’s age, race/ethnicity, and education as well as whether he was born inside or outside the United States. The findings were also adjusted for the whether the child’s parents were married or cohabiting, whether the child had low birth weight, whether the birth was covered by Medicaid, and whether the mother had postpartum depression.
Among the 1,933 pairs of fathers and children in the analysis, nearly half the fathers were non-Hispanic Black (48%) and more than half (64%) had a high school education or lower level of education. Medicaid paid for half the children’s births.
Nine percent of the fathers experienced depression during their child’s first year, and 70% of the children had at least one ACE at 5 years old. Two in five children (39%) had two ACEs at age 5, and 21% of children had three ACEs.
Children were twice as likely to have three ACEs at 5 years old if their father had depression during the child’s first year (adjusted odds ratio, 2.04; 95% confidence interval, 1.42-2.93). Paternal depression was also significantly associated with children having one ACE (OR, 2.35; 95% CI, 1.45-3.81) and two ACES (OR, 1.89; 95% CI, 1.35-2.63) at age 5.
The ACE with the highest association with paternal depression was the father’s absence from children’s lives (aOR, 2.65; 95% CI, 1.74-4.04). In addition, children of fathers with depression had 60% greater odds of exposure to substance use (aOR, 1.6; 95% CI, 1.08-2.34).
Children also had greater odds of child maltreatment at age 5 if their father had depression in their child’s first year. Odds were greater for psychological maltreatment (aOR, 1.55; 95% CI, 1.02-2.34), neglect (aOR, 1.63; 95% CI, 1.08-2.46), and physical maltreatment (aOR, 1.56; 95% CI, 1.04-2.35). The researchers did not find any association between paternal depression and the ACEs of sexual maltreatment, maternal depression, incarceration of someone in the home, or violence toward the mother.
”We know that dads play a critical role in the family,” Dr. Schmitz said. “We as pediatricians have a really unique position with families, and we should capitalize on that opportunity to engage with fathers just like we do with mothers and postpartum depression. Hopefully by doing that, we’ll reduce hardships for children and families down the road.”
Dr. Schmitz also said it’s important for pediatricians to advocate at a policy level “to really include dads more explicitly in maternal and child health policy and advocate for better father-focused interventions from father-focused research.” She further acknowledged the stigma that exists around men’s mental health in general and the need to find out the best ways to help overcome that stigma.
‘Concerning’ findings may suggest a need for screening
Jason Terk, MD, a pediatrician practicing in north Texas and past president of the Texas Pediatric Society, was not surprised to see a link between depression in fathers and adversity in their children. Dr. Terk was not involved in the research but noted that the 9% rate of paternal depression seen in the study is similar to national rates of depression in U.S. adults.
“I think that the presence of paternal depression being associated with ACEs in their children in their first 5 years of life is certainly concerning and worthy of intervention for both the fathers and their children,” Dr. Terk said. “The key take-home message for clinicians who care for infants and small children is that the presence of paternal depression should increase awareness of adverse effects on those children. We need to consider screening for this at 12 months of age in much the same way we screen for maternal depression for younger infants.”
Dr. Terk noted one limitation of the study was that it didn’t suggest any specific risk factors pediatricians might look for to increase surveillance of potential depression in fathers.
“Also, unlike maternal depression, in which moms may be connected with their obstetricians if they screen positive on an Edinburgh questionnaire, we will be hard-pressed to know where to refer dads who are found to be depressed when their babies are 12 months old,” Dr. Terk said. “Screening must lead to helpful responses if the screening reveals a problem.”
The research was funded by the Robert Wood Johnson Foundation, the National Institutes of Health, and the Health Resources and Services Administration. Dr. Schmitz had no disclosures. Dr. Terk has been a speaker for Sanofi on a topic unrelated to this research.
WASHINGTON – , according to research presented at the annual meeting of the American Academy of Pediatrics.
The findings held even after taking into account postpartum depression in the child’s mother and other factors that might increase risk of adverse childhood experiences, reported Kristine H. Schmitz, MD, an assistant professor of pediatrics at Robert Wood Johnson Medical School, New Brunswick, N.J.
Paternal postpartum depression has not been studied very well, so it’s difficult to pin down its prevalence, but some research has found rates as high as 25%, Dr. Schmitz told attendees.
”We recognize that it’s very under-recognized and often under-reported, but we also know that it has lots of downstream effects on child outcomes, including difficulties with parenting, difficulties with child behavior, as well as school performance and school attainment and employment,” Dr. Schmitz said.
Paternal depression and adverse childhood experiences
The study involved an analysis of six waves of data from the Future of Families & Child Wellbeing Study, which follows a national cohort of children born in large U.S. cities between 1998 and 2000. The cohort includes an intentional over-representation of unmarried mothers, who make up about 75% of the overall population.
The researchers used the World Health Organization’s Composite International Diagnosis Interview Short Form (CIDI-SF) to assess fathers’ depression when their children were 1 year old. Then the researchers looked at the number of adverse childhood experiences (ACEs) children had at 5 years old.
The analysis was adjusted to account for the child’s sex and the father’s age, race/ethnicity, and education as well as whether he was born inside or outside the United States. The findings were also adjusted for the whether the child’s parents were married or cohabiting, whether the child had low birth weight, whether the birth was covered by Medicaid, and whether the mother had postpartum depression.
Among the 1,933 pairs of fathers and children in the analysis, nearly half the fathers were non-Hispanic Black (48%) and more than half (64%) had a high school education or lower level of education. Medicaid paid for half the children’s births.
Nine percent of the fathers experienced depression during their child’s first year, and 70% of the children had at least one ACE at 5 years old. Two in five children (39%) had two ACEs at age 5, and 21% of children had three ACEs.
Children were twice as likely to have three ACEs at 5 years old if their father had depression during the child’s first year (adjusted odds ratio, 2.04; 95% confidence interval, 1.42-2.93). Paternal depression was also significantly associated with children having one ACE (OR, 2.35; 95% CI, 1.45-3.81) and two ACES (OR, 1.89; 95% CI, 1.35-2.63) at age 5.
The ACE with the highest association with paternal depression was the father’s absence from children’s lives (aOR, 2.65; 95% CI, 1.74-4.04). In addition, children of fathers with depression had 60% greater odds of exposure to substance use (aOR, 1.6; 95% CI, 1.08-2.34).
Children also had greater odds of child maltreatment at age 5 if their father had depression in their child’s first year. Odds were greater for psychological maltreatment (aOR, 1.55; 95% CI, 1.02-2.34), neglect (aOR, 1.63; 95% CI, 1.08-2.46), and physical maltreatment (aOR, 1.56; 95% CI, 1.04-2.35). The researchers did not find any association between paternal depression and the ACEs of sexual maltreatment, maternal depression, incarceration of someone in the home, or violence toward the mother.
”We know that dads play a critical role in the family,” Dr. Schmitz said. “We as pediatricians have a really unique position with families, and we should capitalize on that opportunity to engage with fathers just like we do with mothers and postpartum depression. Hopefully by doing that, we’ll reduce hardships for children and families down the road.”
Dr. Schmitz also said it’s important for pediatricians to advocate at a policy level “to really include dads more explicitly in maternal and child health policy and advocate for better father-focused interventions from father-focused research.” She further acknowledged the stigma that exists around men’s mental health in general and the need to find out the best ways to help overcome that stigma.
‘Concerning’ findings may suggest a need for screening
Jason Terk, MD, a pediatrician practicing in north Texas and past president of the Texas Pediatric Society, was not surprised to see a link between depression in fathers and adversity in their children. Dr. Terk was not involved in the research but noted that the 9% rate of paternal depression seen in the study is similar to national rates of depression in U.S. adults.
“I think that the presence of paternal depression being associated with ACEs in their children in their first 5 years of life is certainly concerning and worthy of intervention for both the fathers and their children,” Dr. Terk said. “The key take-home message for clinicians who care for infants and small children is that the presence of paternal depression should increase awareness of adverse effects on those children. We need to consider screening for this at 12 months of age in much the same way we screen for maternal depression for younger infants.”
Dr. Terk noted one limitation of the study was that it didn’t suggest any specific risk factors pediatricians might look for to increase surveillance of potential depression in fathers.
“Also, unlike maternal depression, in which moms may be connected with their obstetricians if they screen positive on an Edinburgh questionnaire, we will be hard-pressed to know where to refer dads who are found to be depressed when their babies are 12 months old,” Dr. Terk said. “Screening must lead to helpful responses if the screening reveals a problem.”
The research was funded by the Robert Wood Johnson Foundation, the National Institutes of Health, and the Health Resources and Services Administration. Dr. Schmitz had no disclosures. Dr. Terk has been a speaker for Sanofi on a topic unrelated to this research.
WASHINGTON – , according to research presented at the annual meeting of the American Academy of Pediatrics.
The findings held even after taking into account postpartum depression in the child’s mother and other factors that might increase risk of adverse childhood experiences, reported Kristine H. Schmitz, MD, an assistant professor of pediatrics at Robert Wood Johnson Medical School, New Brunswick, N.J.
Paternal postpartum depression has not been studied very well, so it’s difficult to pin down its prevalence, but some research has found rates as high as 25%, Dr. Schmitz told attendees.
”We recognize that it’s very under-recognized and often under-reported, but we also know that it has lots of downstream effects on child outcomes, including difficulties with parenting, difficulties with child behavior, as well as school performance and school attainment and employment,” Dr. Schmitz said.
Paternal depression and adverse childhood experiences
The study involved an analysis of six waves of data from the Future of Families & Child Wellbeing Study, which follows a national cohort of children born in large U.S. cities between 1998 and 2000. The cohort includes an intentional over-representation of unmarried mothers, who make up about 75% of the overall population.
The researchers used the World Health Organization’s Composite International Diagnosis Interview Short Form (CIDI-SF) to assess fathers’ depression when their children were 1 year old. Then the researchers looked at the number of adverse childhood experiences (ACEs) children had at 5 years old.
The analysis was adjusted to account for the child’s sex and the father’s age, race/ethnicity, and education as well as whether he was born inside or outside the United States. The findings were also adjusted for the whether the child’s parents were married or cohabiting, whether the child had low birth weight, whether the birth was covered by Medicaid, and whether the mother had postpartum depression.
Among the 1,933 pairs of fathers and children in the analysis, nearly half the fathers were non-Hispanic Black (48%) and more than half (64%) had a high school education or lower level of education. Medicaid paid for half the children’s births.
Nine percent of the fathers experienced depression during their child’s first year, and 70% of the children had at least one ACE at 5 years old. Two in five children (39%) had two ACEs at age 5, and 21% of children had three ACEs.
Children were twice as likely to have three ACEs at 5 years old if their father had depression during the child’s first year (adjusted odds ratio, 2.04; 95% confidence interval, 1.42-2.93). Paternal depression was also significantly associated with children having one ACE (OR, 2.35; 95% CI, 1.45-3.81) and two ACES (OR, 1.89; 95% CI, 1.35-2.63) at age 5.
The ACE with the highest association with paternal depression was the father’s absence from children’s lives (aOR, 2.65; 95% CI, 1.74-4.04). In addition, children of fathers with depression had 60% greater odds of exposure to substance use (aOR, 1.6; 95% CI, 1.08-2.34).
Children also had greater odds of child maltreatment at age 5 if their father had depression in their child’s first year. Odds were greater for psychological maltreatment (aOR, 1.55; 95% CI, 1.02-2.34), neglect (aOR, 1.63; 95% CI, 1.08-2.46), and physical maltreatment (aOR, 1.56; 95% CI, 1.04-2.35). The researchers did not find any association between paternal depression and the ACEs of sexual maltreatment, maternal depression, incarceration of someone in the home, or violence toward the mother.
”We know that dads play a critical role in the family,” Dr. Schmitz said. “We as pediatricians have a really unique position with families, and we should capitalize on that opportunity to engage with fathers just like we do with mothers and postpartum depression. Hopefully by doing that, we’ll reduce hardships for children and families down the road.”
Dr. Schmitz also said it’s important for pediatricians to advocate at a policy level “to really include dads more explicitly in maternal and child health policy and advocate for better father-focused interventions from father-focused research.” She further acknowledged the stigma that exists around men’s mental health in general and the need to find out the best ways to help overcome that stigma.
‘Concerning’ findings may suggest a need for screening
Jason Terk, MD, a pediatrician practicing in north Texas and past president of the Texas Pediatric Society, was not surprised to see a link between depression in fathers and adversity in their children. Dr. Terk was not involved in the research but noted that the 9% rate of paternal depression seen in the study is similar to national rates of depression in U.S. adults.
“I think that the presence of paternal depression being associated with ACEs in their children in their first 5 years of life is certainly concerning and worthy of intervention for both the fathers and their children,” Dr. Terk said. “The key take-home message for clinicians who care for infants and small children is that the presence of paternal depression should increase awareness of adverse effects on those children. We need to consider screening for this at 12 months of age in much the same way we screen for maternal depression for younger infants.”
Dr. Terk noted one limitation of the study was that it didn’t suggest any specific risk factors pediatricians might look for to increase surveillance of potential depression in fathers.
“Also, unlike maternal depression, in which moms may be connected with their obstetricians if they screen positive on an Edinburgh questionnaire, we will be hard-pressed to know where to refer dads who are found to be depressed when their babies are 12 months old,” Dr. Terk said. “Screening must lead to helpful responses if the screening reveals a problem.”
The research was funded by the Robert Wood Johnson Foundation, the National Institutes of Health, and the Health Resources and Services Administration. Dr. Schmitz had no disclosures. Dr. Terk has been a speaker for Sanofi on a topic unrelated to this research.
AT AAP 2023
AAP: ‘Toddler milk’ unnecessary for most kids
WASHINGTON – These products are not nutritionally complete and are not to be confused with formulas for infants younger than 12 months.
“Toddler drinks do not offer anything nutritionally exceptional,” said George J. Fuchs III, MD, a pediatric gastroenterologist at the University of Kentucky, Lexington, who presented a clinical report on toddler formulas from the American Academy of Pediatrics at the group’s annual meeting. The products are not regulated by the U.S. Food and Drug Administration and should not be given to infants younger than 12 months in place of infant formulas, but murky marketing can leave parents and caregivers confused as to whether these products are essential for good health, Dr. Fuchs said.
Despite the rise in marketing of formulas pitched as toddler milks, growth milks, or transition formulas, among other names, the AAP says these formulas are both unregulated and unnecessary for the vast majority of toddlers because they have adequate diets and do not require supplementation.
Clinicians should understand and explain the distinction between products formulated for infants younger than 12 months and those designed for children aged 12 months or older, Dr. Fuchs added.
Formulas for infants younger than 12 months represent a distinct product category for the FDA and are required to be nutritionally complete for this age, Dr. Fuchs said. Infant formulas sold in the United States must meet nutrition requirements as defined by the Infant Formula Act of 1980 (updated in 1986), and the facilities that manufacture them are regularly inspected by the agency.
In contrast, toddler formulas are not regulated or categorized by the FDA and therefore may vary widely in composition and are not nutritionally complete for any age, he said.
One area of concern is that parents or caregivers misunderstand and give these products to infants younger than 12 months instead of infant formulas, he said.
Also, mass-market toddler formulas are inadequate for children with disease-specific requirements, such as malnutrition, gastrointestinal disorders, metabolic disorders, or food allergies.
Questionable composition, misleading marketing
Toddler formulas are not only unnecessary but could be detrimental to children’s health, Dr. Fuchs said. Some formulas have high sodium content relative to cow’s milk or may be high or low in protein. Other products have added sweeteners, which could contribute to an increased preference for sweetened foods as the children get older, he noted.
However, manufacturers of regulated infant products often market them alongside their infant formula, which can be confusing for parents and caregivers. The products often have similar names, images, slogans, and logos, and may suggest benefits such as immune system support, brain development, and digestive health, he added.
A 2020 survey published in Maternal and Child Nutrition found that 60% of approximately 1,000 caregivers of children aged 12-36 months agreed with the marketing claim that toddler formulas or powdered milks provide nutrition that is not available from other food and drinks, Dr. Fuchs said.
Balanced diet is best for healthy children
For infants younger than 12 months, the AAP recommends that the liquid portion of the diet should come from human milk or a standard infant formula that has been reviewed by the FDA based on the Infant Formula Act, Dr. Fuchs said.
Children aged 12 months or older should receive a varied diet with fortified foods. Formula can safely be used as part of a varied diet; however, it offers no nutritional advantage for most children over a well-balanced diet that includes human milk and/or cow milk, “and should not be promoted as such,” Dr. Fuchs noted.
“The category of these toddler drinks has grown and the landscape has changed quite a bit; we thought it was appropriate that we review this category,” Dr. Fuchs said in an interview.
Dr. Fuchs advised pediatricians in practice to follow the AAP’s guidance for breastfeeding infants if possible and progression to formula as needed for infants up to age 1 year, followed by transition to cow milk (or alternatives for those with cow milk allergies) and the addition of a healthy mixed diet.
Formula choices pose practice challenges
In an interview, Cathy Haut, DNP, CPNP-AC, CPNP-PC, a pediatric nurse practitioner in Rehoboth Beach, Del., pointed out that not only are parents often baffled by formula choices, but many are also hesitant to make a switch to regular milk as children get older because they worry that cow’s milk is inadequate for nutrition or is not as “clean” or “sterile” as formula.
In some cases, parents may have had difficulty in acquiring genuine infant formulas, which were relocated to locked cabinets in stores during recent shortages and began using toddler formulas as an alternative for infants younger than 1 year, she added.
“If breastfeeding is not possible, using approved infant formula is preferred, switching to whole cow milk at 1 year of age,” she said. “Nutritional assessment is an important part of well-child visits, with caregiver counseling regarding importance of intake of variety of fortified foods [that] offer vitamins, calcium, iron and zinc,” Ms. Haut added. Although toddler formulas are safe additions to the diets of most young children older than 1 year, supplementation of specific nutrients such as vitamin D if needed is a more effective option, she said.
“National health studies indicate that U.S. toddlers have nutritional gaps in their diet often related to picky eating,” an Abbott spokesperson said in an interview. “When [toddlers] don’t do well transitioning to table foods or won’t drink milk, our toddler drinks contain many of the complementary nutrients, such as vitamins and minerals, that they may be missing in their diet. Toddler drinks may be an option to help fill nutrient gaps for these children 12-36 months of age. Abbott does not recommend or indicate its toddler drinks for infants under 12 months of age,” according to the company.
Dr. Fuchs had no financial conflicts to disclose. Dr. Haut had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
WASHINGTON – These products are not nutritionally complete and are not to be confused with formulas for infants younger than 12 months.
“Toddler drinks do not offer anything nutritionally exceptional,” said George J. Fuchs III, MD, a pediatric gastroenterologist at the University of Kentucky, Lexington, who presented a clinical report on toddler formulas from the American Academy of Pediatrics at the group’s annual meeting. The products are not regulated by the U.S. Food and Drug Administration and should not be given to infants younger than 12 months in place of infant formulas, but murky marketing can leave parents and caregivers confused as to whether these products are essential for good health, Dr. Fuchs said.
Despite the rise in marketing of formulas pitched as toddler milks, growth milks, or transition formulas, among other names, the AAP says these formulas are both unregulated and unnecessary for the vast majority of toddlers because they have adequate diets and do not require supplementation.
Clinicians should understand and explain the distinction between products formulated for infants younger than 12 months and those designed for children aged 12 months or older, Dr. Fuchs added.
Formulas for infants younger than 12 months represent a distinct product category for the FDA and are required to be nutritionally complete for this age, Dr. Fuchs said. Infant formulas sold in the United States must meet nutrition requirements as defined by the Infant Formula Act of 1980 (updated in 1986), and the facilities that manufacture them are regularly inspected by the agency.
In contrast, toddler formulas are not regulated or categorized by the FDA and therefore may vary widely in composition and are not nutritionally complete for any age, he said.
One area of concern is that parents or caregivers misunderstand and give these products to infants younger than 12 months instead of infant formulas, he said.
Also, mass-market toddler formulas are inadequate for children with disease-specific requirements, such as malnutrition, gastrointestinal disorders, metabolic disorders, or food allergies.
Questionable composition, misleading marketing
Toddler formulas are not only unnecessary but could be detrimental to children’s health, Dr. Fuchs said. Some formulas have high sodium content relative to cow’s milk or may be high or low in protein. Other products have added sweeteners, which could contribute to an increased preference for sweetened foods as the children get older, he noted.
However, manufacturers of regulated infant products often market them alongside their infant formula, which can be confusing for parents and caregivers. The products often have similar names, images, slogans, and logos, and may suggest benefits such as immune system support, brain development, and digestive health, he added.
A 2020 survey published in Maternal and Child Nutrition found that 60% of approximately 1,000 caregivers of children aged 12-36 months agreed with the marketing claim that toddler formulas or powdered milks provide nutrition that is not available from other food and drinks, Dr. Fuchs said.
Balanced diet is best for healthy children
For infants younger than 12 months, the AAP recommends that the liquid portion of the diet should come from human milk or a standard infant formula that has been reviewed by the FDA based on the Infant Formula Act, Dr. Fuchs said.
Children aged 12 months or older should receive a varied diet with fortified foods. Formula can safely be used as part of a varied diet; however, it offers no nutritional advantage for most children over a well-balanced diet that includes human milk and/or cow milk, “and should not be promoted as such,” Dr. Fuchs noted.
“The category of these toddler drinks has grown and the landscape has changed quite a bit; we thought it was appropriate that we review this category,” Dr. Fuchs said in an interview.
Dr. Fuchs advised pediatricians in practice to follow the AAP’s guidance for breastfeeding infants if possible and progression to formula as needed for infants up to age 1 year, followed by transition to cow milk (or alternatives for those with cow milk allergies) and the addition of a healthy mixed diet.
Formula choices pose practice challenges
In an interview, Cathy Haut, DNP, CPNP-AC, CPNP-PC, a pediatric nurse practitioner in Rehoboth Beach, Del., pointed out that not only are parents often baffled by formula choices, but many are also hesitant to make a switch to regular milk as children get older because they worry that cow’s milk is inadequate for nutrition or is not as “clean” or “sterile” as formula.
In some cases, parents may have had difficulty in acquiring genuine infant formulas, which were relocated to locked cabinets in stores during recent shortages and began using toddler formulas as an alternative for infants younger than 1 year, she added.
“If breastfeeding is not possible, using approved infant formula is preferred, switching to whole cow milk at 1 year of age,” she said. “Nutritional assessment is an important part of well-child visits, with caregiver counseling regarding importance of intake of variety of fortified foods [that] offer vitamins, calcium, iron and zinc,” Ms. Haut added. Although toddler formulas are safe additions to the diets of most young children older than 1 year, supplementation of specific nutrients such as vitamin D if needed is a more effective option, she said.
“National health studies indicate that U.S. toddlers have nutritional gaps in their diet often related to picky eating,” an Abbott spokesperson said in an interview. “When [toddlers] don’t do well transitioning to table foods or won’t drink milk, our toddler drinks contain many of the complementary nutrients, such as vitamins and minerals, that they may be missing in their diet. Toddler drinks may be an option to help fill nutrient gaps for these children 12-36 months of age. Abbott does not recommend or indicate its toddler drinks for infants under 12 months of age,” according to the company.
Dr. Fuchs had no financial conflicts to disclose. Dr. Haut had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
WASHINGTON – These products are not nutritionally complete and are not to be confused with formulas for infants younger than 12 months.
“Toddler drinks do not offer anything nutritionally exceptional,” said George J. Fuchs III, MD, a pediatric gastroenterologist at the University of Kentucky, Lexington, who presented a clinical report on toddler formulas from the American Academy of Pediatrics at the group’s annual meeting. The products are not regulated by the U.S. Food and Drug Administration and should not be given to infants younger than 12 months in place of infant formulas, but murky marketing can leave parents and caregivers confused as to whether these products are essential for good health, Dr. Fuchs said.
Despite the rise in marketing of formulas pitched as toddler milks, growth milks, or transition formulas, among other names, the AAP says these formulas are both unregulated and unnecessary for the vast majority of toddlers because they have adequate diets and do not require supplementation.
Clinicians should understand and explain the distinction between products formulated for infants younger than 12 months and those designed for children aged 12 months or older, Dr. Fuchs added.
Formulas for infants younger than 12 months represent a distinct product category for the FDA and are required to be nutritionally complete for this age, Dr. Fuchs said. Infant formulas sold in the United States must meet nutrition requirements as defined by the Infant Formula Act of 1980 (updated in 1986), and the facilities that manufacture them are regularly inspected by the agency.
In contrast, toddler formulas are not regulated or categorized by the FDA and therefore may vary widely in composition and are not nutritionally complete for any age, he said.
One area of concern is that parents or caregivers misunderstand and give these products to infants younger than 12 months instead of infant formulas, he said.
Also, mass-market toddler formulas are inadequate for children with disease-specific requirements, such as malnutrition, gastrointestinal disorders, metabolic disorders, or food allergies.
Questionable composition, misleading marketing
Toddler formulas are not only unnecessary but could be detrimental to children’s health, Dr. Fuchs said. Some formulas have high sodium content relative to cow’s milk or may be high or low in protein. Other products have added sweeteners, which could contribute to an increased preference for sweetened foods as the children get older, he noted.
However, manufacturers of regulated infant products often market them alongside their infant formula, which can be confusing for parents and caregivers. The products often have similar names, images, slogans, and logos, and may suggest benefits such as immune system support, brain development, and digestive health, he added.
A 2020 survey published in Maternal and Child Nutrition found that 60% of approximately 1,000 caregivers of children aged 12-36 months agreed with the marketing claim that toddler formulas or powdered milks provide nutrition that is not available from other food and drinks, Dr. Fuchs said.
Balanced diet is best for healthy children
For infants younger than 12 months, the AAP recommends that the liquid portion of the diet should come from human milk or a standard infant formula that has been reviewed by the FDA based on the Infant Formula Act, Dr. Fuchs said.
Children aged 12 months or older should receive a varied diet with fortified foods. Formula can safely be used as part of a varied diet; however, it offers no nutritional advantage for most children over a well-balanced diet that includes human milk and/or cow milk, “and should not be promoted as such,” Dr. Fuchs noted.
“The category of these toddler drinks has grown and the landscape has changed quite a bit; we thought it was appropriate that we review this category,” Dr. Fuchs said in an interview.
Dr. Fuchs advised pediatricians in practice to follow the AAP’s guidance for breastfeeding infants if possible and progression to formula as needed for infants up to age 1 year, followed by transition to cow milk (or alternatives for those with cow milk allergies) and the addition of a healthy mixed diet.
Formula choices pose practice challenges
In an interview, Cathy Haut, DNP, CPNP-AC, CPNP-PC, a pediatric nurse practitioner in Rehoboth Beach, Del., pointed out that not only are parents often baffled by formula choices, but many are also hesitant to make a switch to regular milk as children get older because they worry that cow’s milk is inadequate for nutrition or is not as “clean” or “sterile” as formula.
In some cases, parents may have had difficulty in acquiring genuine infant formulas, which were relocated to locked cabinets in stores during recent shortages and began using toddler formulas as an alternative for infants younger than 1 year, she added.
“If breastfeeding is not possible, using approved infant formula is preferred, switching to whole cow milk at 1 year of age,” she said. “Nutritional assessment is an important part of well-child visits, with caregiver counseling regarding importance of intake of variety of fortified foods [that] offer vitamins, calcium, iron and zinc,” Ms. Haut added. Although toddler formulas are safe additions to the diets of most young children older than 1 year, supplementation of specific nutrients such as vitamin D if needed is a more effective option, she said.
“National health studies indicate that U.S. toddlers have nutritional gaps in their diet often related to picky eating,” an Abbott spokesperson said in an interview. “When [toddlers] don’t do well transitioning to table foods or won’t drink milk, our toddler drinks contain many of the complementary nutrients, such as vitamins and minerals, that they may be missing in their diet. Toddler drinks may be an option to help fill nutrient gaps for these children 12-36 months of age. Abbott does not recommend or indicate its toddler drinks for infants under 12 months of age,” according to the company.
Dr. Fuchs had no financial conflicts to disclose. Dr. Haut had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
AT AAP 2023