User login
ATX-101: ‘You’re gonna like your new chin’
ISTANBUL – Both clinicians and patients gave favorable marks to a novel injectable pharmacologic treatment for removal of unwanted submental fat – the unsightly double chin – in two phase III randomized trials presented at the annual congress of the European Academy of Dermatology and Venereology.
The investigational chin-fat buster, known as ATX-101, is a proprietary purified synthetic form of deoxycholic acid. Upon injection directly into the submental fat, ATX-101 lyses adipocytes by disrupting their cell membranes.
There is an unmet need for a rigorously studied prescription product for nonsurgical treatment of excess submental fat. Not everyone with a double chin is interested in or a good candidate for the established surgical procedures, observed Dr. Berthold Rzany, a dermatologist at Charité University Hospital, Berlin, who presented a 363-patient, randomized, placebo-controlled phase III trial at the meeting. Participants had to have a body mass index no higher than 30 kg/m2, dissatisfaction with the appearance of their submental area, and a physician rating of moderate to severe submental fat. Three-quarters of the subjects were women, with a mean age of 46 years and a mean BMI of 25.7 kg/m2.
One of the two primary efficacy endpoints required at least a 1-point improvement on the 0- to 4-point Clinician-Reported Submental Fat Rating Scale as assessed 12 weeks after the final treatment. This was achieved in 59% of patients randomized to ATX-101 at a dose of 1mg/cm2 and 65% at 2 mg/cm2, both significantly higher rates than the 23% in placebo-treated controls.
The other primary endpoint required a high level of patient satisfaction with the appearance of their face and chin after treatment as expressed in a Subject Self-Rating Scale score of 4 or more on the 0-6 scale. This endpoint was achieved in 53% of patients treated with ATX-101 at 1 mg/cm2, 66% who received the agent at 2 mg/cm2, and 29% of the placebo group.
ATX-101-treated patients were also significantly more likely to report perceived improvement in the visual and psychological impact of their submental fat. For example, 74% of patients who received ATX-101 at 1 mg/cm2 and 80% at 2 mg/cm2 reported improved definition between their chin and neck, compared with baseline and compared with 28% of placebo-treated controls. In addition, 32% of patients who received the lower dose of ATX-101 and 39% who got the higher dose characterized their submental fat as "a great deal better," compared with baseline, as did a mere 7% of controls.
Also, patients who received ATX-101 reported 12 weeks post treatment that they looked less overweight and were less bothered by and self-conscious about their submental fat, compared with controls.
Treatment-emergent induration, redness, bruising, numbness, and/or swelling variously occurred in one-third to two-thirds of ATX-101 recipients. All of these adverse events were more common than in placebo-treated controls. However, the events were transient and mostly mild or moderate in intensity. The exception was injection site pain, which occurred in roughly 80% of ATX-101-treated patients and was mostly moderate to severe, although it lasted a median of only 1 day, according to Dr. Rzany.
The ATX-101 treatment regimen entails up to 50 2-mL fixed-dose subcutaneous injections 1 cm apart per treatment session. Up to four treatment sessions were permitted, each separated by a minimum of 4 weeks.
In a separate presentation, Dr. Benjamin Ascher reported on 360 randomized patients who participated in the other phase III clinical trial. The two studies had the same design and endpoints.
An improvement of at least 1 point on the Clinician-Reported Submental Fat Rating Scale occurred in 58% of patients randomized to ATX-101 at the 1 mg/cm2 dose, 62% of those who received the higher dose, and 35% on placebo. Moreover, 68% of patients who got ATX-101 at 1 mg/cm2 were satisfied with their resultant appearance as reflected in a Subject Self-Rating Scale score of at least 4. So were 65% of those who received the higher dose and 29% of placebo-treated controls. As in the previously mentioned study, indices of self-image and psychological well being were also improved following the aesthetic therapy. Treatment-related adverse events were mostly transient and mild to moderate in intensity, according to Dr. Ascher, who is in the private practice of aesthetic surgery in Paris.
Both phase III studies were supported by Bayer HealthCare and KYTHERA Biopharmaceuticals. Dr. Rzany and Dr. Ascher serve as advisers to the companies.
ISTANBUL – Both clinicians and patients gave favorable marks to a novel injectable pharmacologic treatment for removal of unwanted submental fat – the unsightly double chin – in two phase III randomized trials presented at the annual congress of the European Academy of Dermatology and Venereology.
The investigational chin-fat buster, known as ATX-101, is a proprietary purified synthetic form of deoxycholic acid. Upon injection directly into the submental fat, ATX-101 lyses adipocytes by disrupting their cell membranes.
There is an unmet need for a rigorously studied prescription product for nonsurgical treatment of excess submental fat. Not everyone with a double chin is interested in or a good candidate for the established surgical procedures, observed Dr. Berthold Rzany, a dermatologist at Charité University Hospital, Berlin, who presented a 363-patient, randomized, placebo-controlled phase III trial at the meeting. Participants had to have a body mass index no higher than 30 kg/m2, dissatisfaction with the appearance of their submental area, and a physician rating of moderate to severe submental fat. Three-quarters of the subjects were women, with a mean age of 46 years and a mean BMI of 25.7 kg/m2.
One of the two primary efficacy endpoints required at least a 1-point improvement on the 0- to 4-point Clinician-Reported Submental Fat Rating Scale as assessed 12 weeks after the final treatment. This was achieved in 59% of patients randomized to ATX-101 at a dose of 1mg/cm2 and 65% at 2 mg/cm2, both significantly higher rates than the 23% in placebo-treated controls.
The other primary endpoint required a high level of patient satisfaction with the appearance of their face and chin after treatment as expressed in a Subject Self-Rating Scale score of 4 or more on the 0-6 scale. This endpoint was achieved in 53% of patients treated with ATX-101 at 1 mg/cm2, 66% who received the agent at 2 mg/cm2, and 29% of the placebo group.
ATX-101-treated patients were also significantly more likely to report perceived improvement in the visual and psychological impact of their submental fat. For example, 74% of patients who received ATX-101 at 1 mg/cm2 and 80% at 2 mg/cm2 reported improved definition between their chin and neck, compared with baseline and compared with 28% of placebo-treated controls. In addition, 32% of patients who received the lower dose of ATX-101 and 39% who got the higher dose characterized their submental fat as "a great deal better," compared with baseline, as did a mere 7% of controls.
Also, patients who received ATX-101 reported 12 weeks post treatment that they looked less overweight and were less bothered by and self-conscious about their submental fat, compared with controls.
Treatment-emergent induration, redness, bruising, numbness, and/or swelling variously occurred in one-third to two-thirds of ATX-101 recipients. All of these adverse events were more common than in placebo-treated controls. However, the events were transient and mostly mild or moderate in intensity. The exception was injection site pain, which occurred in roughly 80% of ATX-101-treated patients and was mostly moderate to severe, although it lasted a median of only 1 day, according to Dr. Rzany.
The ATX-101 treatment regimen entails up to 50 2-mL fixed-dose subcutaneous injections 1 cm apart per treatment session. Up to four treatment sessions were permitted, each separated by a minimum of 4 weeks.
In a separate presentation, Dr. Benjamin Ascher reported on 360 randomized patients who participated in the other phase III clinical trial. The two studies had the same design and endpoints.
An improvement of at least 1 point on the Clinician-Reported Submental Fat Rating Scale occurred in 58% of patients randomized to ATX-101 at the 1 mg/cm2 dose, 62% of those who received the higher dose, and 35% on placebo. Moreover, 68% of patients who got ATX-101 at 1 mg/cm2 were satisfied with their resultant appearance as reflected in a Subject Self-Rating Scale score of at least 4. So were 65% of those who received the higher dose and 29% of placebo-treated controls. As in the previously mentioned study, indices of self-image and psychological well being were also improved following the aesthetic therapy. Treatment-related adverse events were mostly transient and mild to moderate in intensity, according to Dr. Ascher, who is in the private practice of aesthetic surgery in Paris.
Both phase III studies were supported by Bayer HealthCare and KYTHERA Biopharmaceuticals. Dr. Rzany and Dr. Ascher serve as advisers to the companies.
ISTANBUL – Both clinicians and patients gave favorable marks to a novel injectable pharmacologic treatment for removal of unwanted submental fat – the unsightly double chin – in two phase III randomized trials presented at the annual congress of the European Academy of Dermatology and Venereology.
The investigational chin-fat buster, known as ATX-101, is a proprietary purified synthetic form of deoxycholic acid. Upon injection directly into the submental fat, ATX-101 lyses adipocytes by disrupting their cell membranes.
There is an unmet need for a rigorously studied prescription product for nonsurgical treatment of excess submental fat. Not everyone with a double chin is interested in or a good candidate for the established surgical procedures, observed Dr. Berthold Rzany, a dermatologist at Charité University Hospital, Berlin, who presented a 363-patient, randomized, placebo-controlled phase III trial at the meeting. Participants had to have a body mass index no higher than 30 kg/m2, dissatisfaction with the appearance of their submental area, and a physician rating of moderate to severe submental fat. Three-quarters of the subjects were women, with a mean age of 46 years and a mean BMI of 25.7 kg/m2.
One of the two primary efficacy endpoints required at least a 1-point improvement on the 0- to 4-point Clinician-Reported Submental Fat Rating Scale as assessed 12 weeks after the final treatment. This was achieved in 59% of patients randomized to ATX-101 at a dose of 1mg/cm2 and 65% at 2 mg/cm2, both significantly higher rates than the 23% in placebo-treated controls.
The other primary endpoint required a high level of patient satisfaction with the appearance of their face and chin after treatment as expressed in a Subject Self-Rating Scale score of 4 or more on the 0-6 scale. This endpoint was achieved in 53% of patients treated with ATX-101 at 1 mg/cm2, 66% who received the agent at 2 mg/cm2, and 29% of the placebo group.
ATX-101-treated patients were also significantly more likely to report perceived improvement in the visual and psychological impact of their submental fat. For example, 74% of patients who received ATX-101 at 1 mg/cm2 and 80% at 2 mg/cm2 reported improved definition between their chin and neck, compared with baseline and compared with 28% of placebo-treated controls. In addition, 32% of patients who received the lower dose of ATX-101 and 39% who got the higher dose characterized their submental fat as "a great deal better," compared with baseline, as did a mere 7% of controls.
Also, patients who received ATX-101 reported 12 weeks post treatment that they looked less overweight and were less bothered by and self-conscious about their submental fat, compared with controls.
Treatment-emergent induration, redness, bruising, numbness, and/or swelling variously occurred in one-third to two-thirds of ATX-101 recipients. All of these adverse events were more common than in placebo-treated controls. However, the events were transient and mostly mild or moderate in intensity. The exception was injection site pain, which occurred in roughly 80% of ATX-101-treated patients and was mostly moderate to severe, although it lasted a median of only 1 day, according to Dr. Rzany.
The ATX-101 treatment regimen entails up to 50 2-mL fixed-dose subcutaneous injections 1 cm apart per treatment session. Up to four treatment sessions were permitted, each separated by a minimum of 4 weeks.
In a separate presentation, Dr. Benjamin Ascher reported on 360 randomized patients who participated in the other phase III clinical trial. The two studies had the same design and endpoints.
An improvement of at least 1 point on the Clinician-Reported Submental Fat Rating Scale occurred in 58% of patients randomized to ATX-101 at the 1 mg/cm2 dose, 62% of those who received the higher dose, and 35% on placebo. Moreover, 68% of patients who got ATX-101 at 1 mg/cm2 were satisfied with their resultant appearance as reflected in a Subject Self-Rating Scale score of at least 4. So were 65% of those who received the higher dose and 29% of placebo-treated controls. As in the previously mentioned study, indices of self-image and psychological well being were also improved following the aesthetic therapy. Treatment-related adverse events were mostly transient and mild to moderate in intensity, according to Dr. Ascher, who is in the private practice of aesthetic surgery in Paris.
Both phase III studies were supported by Bayer HealthCare and KYTHERA Biopharmaceuticals. Dr. Rzany and Dr. Ascher serve as advisers to the companies.
AT THE EADV CONGRESS
Major finding: Patients with excess submental fat who received treatment using a novel subcutaneously injectable agent for the nonsurgical reduction of double chins were significantly more likely to be satisfied with their chin’s appearance afterward than were placebo-treated controls.
Data source: The two studies included a total of 723 patients with moderate to severe excess submental fat.
Disclosures: The studies were funded by Bayer HealthCare and KYTHERA Biopharmaceuticals. The presenters have received research grants from and serve as advisers to the companies.
A rapid-fire update on lasers in dermatologic surgery
If you have 5 minutes and need an update on the latest advancements in lasers in dermatologic surgery, watch our interview with Dr. Elizabeth Tanzi of Washington Institute of Dermatologic Surgery. Dr. Tanzi talks about the new trends in laser treatments, her two favorite laser machines, and shares her thoughts on the future of lasers.
If you have 5 minutes and need an update on the latest advancements in lasers in dermatologic surgery, watch our interview with Dr. Elizabeth Tanzi of Washington Institute of Dermatologic Surgery. Dr. Tanzi talks about the new trends in laser treatments, her two favorite laser machines, and shares her thoughts on the future of lasers.
If you have 5 minutes and need an update on the latest advancements in lasers in dermatologic surgery, watch our interview with Dr. Elizabeth Tanzi of Washington Institute of Dermatologic Surgery. Dr. Tanzi talks about the new trends in laser treatments, her two favorite laser machines, and shares her thoughts on the future of lasers.
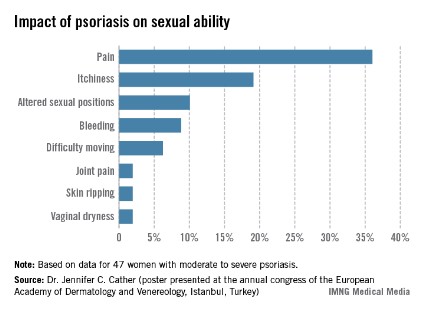
Impact of psoriasis on sexual activity
One third of a group of women with psoriasis reported that the pain associated with their condition interfered with their sexual activity, according to findings from a survey presented by Dr. Jennifer C. Cather.
Based on responses from a survey of 60 women with moderate to severe psoriasis, the specific complaints that were the most common ways in which psoriasis interfered with sexual activity were itchiness (19%), the need to adjust sexual position (10%), and bleeding (9%), Dr. Cather reported at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar. The survey was part of an effort to determine the impact of psoriasis on women’s sexual activity, desires, and relationships.
The data were previously presented in a poster at the annual congress of the European Academy of Dermatology and Venereology (Istanbul.
SDEF and this news organization are owned by Frontline Medical Communications. Dr. Cather disclosed that she is a consultant, speaker, or researcher for AbbVie, Novartis, Leo, Janssen, Amgen, Celgene, Merck, and Pfizer.
One third of a group of women with psoriasis reported that the pain associated with their condition interfered with their sexual activity, according to findings from a survey presented by Dr. Jennifer C. Cather.
Based on responses from a survey of 60 women with moderate to severe psoriasis, the specific complaints that were the most common ways in which psoriasis interfered with sexual activity were itchiness (19%), the need to adjust sexual position (10%), and bleeding (9%), Dr. Cather reported at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar. The survey was part of an effort to determine the impact of psoriasis on women’s sexual activity, desires, and relationships.
The data were previously presented in a poster at the annual congress of the European Academy of Dermatology and Venereology (Istanbul.
SDEF and this news organization are owned by Frontline Medical Communications. Dr. Cather disclosed that she is a consultant, speaker, or researcher for AbbVie, Novartis, Leo, Janssen, Amgen, Celgene, Merck, and Pfizer.
One third of a group of women with psoriasis reported that the pain associated with their condition interfered with their sexual activity, according to findings from a survey presented by Dr. Jennifer C. Cather.
Based on responses from a survey of 60 women with moderate to severe psoriasis, the specific complaints that were the most common ways in which psoriasis interfered with sexual activity were itchiness (19%), the need to adjust sexual position (10%), and bleeding (9%), Dr. Cather reported at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar. The survey was part of an effort to determine the impact of psoriasis on women’s sexual activity, desires, and relationships.
The data were previously presented in a poster at the annual congress of the European Academy of Dermatology and Venereology (Istanbul.
SDEF and this news organization are owned by Frontline Medical Communications. Dr. Cather disclosed that she is a consultant, speaker, or researcher for AbbVie, Novartis, Leo, Janssen, Amgen, Celgene, Merck, and Pfizer.
EXPERT ANALYSIS FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR
Pseudofolliculitis barbae – tips for patients
Pseudofolliculitis barbae (PFB) is a common complaint among darker-skinned patients with coarse curly hair. Patients present with follicular papules in the beard from ingrown hairs that can eventually result in postinflammatory pigmentary alternation and scarring. While these symptoms are most common in men, women may be affected as well, as PFB is not limited to the beard area; it may occur in any other area with thick, coarse curly hair, including the bikini area and axillae.
Some tips for treating PFB:
If the patient doesn’t mind growing a beard, advise him to grow one! The chances of having ingrown hairs that stimulate this condition are less if the hairs are not plucked or shaved, or are kept at least a few millimeters long.
If hair removal/grooming is a must, options include clipping the hairs with a protector; using a self-cleaning electric razor (replacing the blades at least every 2 years); and using thick shaving gel with either a single or twin blade razor, or a chemical depilatory.
Laser hair removal is also an option in the right candidate, particularly with longer pulsed (1,064 nm or 810 nm) lasers in darker-skinned individuals. Eflornithine 12% twice daily for 16 weeks has been shown to work synergistically with laser hair removal. Electrolysis may be helpful for hairs that do not respond to laser hair removal with longer pulsed lasers, such as grey hairs.
If shaving is a must, advise patients to:
• Apply warm compresses to the beard area for a few minutes prior to shaving. In addition, using a mild exfoliant or loofah or toothbrush in a circular motion will help allow any ingrown hairs to be more easily plucked or released at the skin surface.
• Use shaving gel and a sharp razor each time.
• Do not pull the skin taut.
• Do not shave against the direction of hair growth.
• Take short strokes and do not shave back and forth over the same areas.
• After shaving, use a soothing aftershave or hydrocortisone 1% lotion.
Products such as PFB Vanish, which contain salicylic, glycolic, and/or lactic acid, are helpful in some patients after hair removal to prevent ingrown hairs. One version of PFB Vanish contains antipigment ingredients to also address hyperpigmentation.
If inflammatory papules or pustules are present, a combination benzoyl peroxide/clindamycin topical gels (such as Benzaclin, Duac, or Acanya) can be used. Patients with severe inflammation may require oral antibiotics.
Using a topical retinoid at night or a combination retinoid product with hydroquinone can be helpful especially in cases of postinflammatory hyperpigmentation. However, use caution when prescribing retinoids for patients with darker skin, as irritation from these products may lead to postinflammatory pigmentary alteration. Remind patients to avoid drying products, such as toners, if topical retinoids are used.
For severe or refractory postinflammatory hyperpigmentation or inflammatory papules, chemical peels with 20%-30% salicylic acid can be helpful.
What are your PFB solutions? The more we share our clinical insights, the better we will be able to achieve improved treatment results for our patients.
Dr. Wesley practices dermatology in Beverly Hills, Calif. Do you have questions about treating patients with dark skin? If so, send them to [email protected].
Pseudofolliculitis barbae (PFB) is a common complaint among darker-skinned patients with coarse curly hair. Patients present with follicular papules in the beard from ingrown hairs that can eventually result in postinflammatory pigmentary alternation and scarring. While these symptoms are most common in men, women may be affected as well, as PFB is not limited to the beard area; it may occur in any other area with thick, coarse curly hair, including the bikini area and axillae.
Some tips for treating PFB:
If the patient doesn’t mind growing a beard, advise him to grow one! The chances of having ingrown hairs that stimulate this condition are less if the hairs are not plucked or shaved, or are kept at least a few millimeters long.
If hair removal/grooming is a must, options include clipping the hairs with a protector; using a self-cleaning electric razor (replacing the blades at least every 2 years); and using thick shaving gel with either a single or twin blade razor, or a chemical depilatory.
Laser hair removal is also an option in the right candidate, particularly with longer pulsed (1,064 nm or 810 nm) lasers in darker-skinned individuals. Eflornithine 12% twice daily for 16 weeks has been shown to work synergistically with laser hair removal. Electrolysis may be helpful for hairs that do not respond to laser hair removal with longer pulsed lasers, such as grey hairs.
If shaving is a must, advise patients to:
• Apply warm compresses to the beard area for a few minutes prior to shaving. In addition, using a mild exfoliant or loofah or toothbrush in a circular motion will help allow any ingrown hairs to be more easily plucked or released at the skin surface.
• Use shaving gel and a sharp razor each time.
• Do not pull the skin taut.
• Do not shave against the direction of hair growth.
• Take short strokes and do not shave back and forth over the same areas.
• After shaving, use a soothing aftershave or hydrocortisone 1% lotion.
Products such as PFB Vanish, which contain salicylic, glycolic, and/or lactic acid, are helpful in some patients after hair removal to prevent ingrown hairs. One version of PFB Vanish contains antipigment ingredients to also address hyperpigmentation.
If inflammatory papules or pustules are present, a combination benzoyl peroxide/clindamycin topical gels (such as Benzaclin, Duac, or Acanya) can be used. Patients with severe inflammation may require oral antibiotics.
Using a topical retinoid at night or a combination retinoid product with hydroquinone can be helpful especially in cases of postinflammatory hyperpigmentation. However, use caution when prescribing retinoids for patients with darker skin, as irritation from these products may lead to postinflammatory pigmentary alteration. Remind patients to avoid drying products, such as toners, if topical retinoids are used.
For severe or refractory postinflammatory hyperpigmentation or inflammatory papules, chemical peels with 20%-30% salicylic acid can be helpful.
What are your PFB solutions? The more we share our clinical insights, the better we will be able to achieve improved treatment results for our patients.
Dr. Wesley practices dermatology in Beverly Hills, Calif. Do you have questions about treating patients with dark skin? If so, send them to [email protected].
Pseudofolliculitis barbae (PFB) is a common complaint among darker-skinned patients with coarse curly hair. Patients present with follicular papules in the beard from ingrown hairs that can eventually result in postinflammatory pigmentary alternation and scarring. While these symptoms are most common in men, women may be affected as well, as PFB is not limited to the beard area; it may occur in any other area with thick, coarse curly hair, including the bikini area and axillae.
Some tips for treating PFB:
If the patient doesn’t mind growing a beard, advise him to grow one! The chances of having ingrown hairs that stimulate this condition are less if the hairs are not plucked or shaved, or are kept at least a few millimeters long.
If hair removal/grooming is a must, options include clipping the hairs with a protector; using a self-cleaning electric razor (replacing the blades at least every 2 years); and using thick shaving gel with either a single or twin blade razor, or a chemical depilatory.
Laser hair removal is also an option in the right candidate, particularly with longer pulsed (1,064 nm or 810 nm) lasers in darker-skinned individuals. Eflornithine 12% twice daily for 16 weeks has been shown to work synergistically with laser hair removal. Electrolysis may be helpful for hairs that do not respond to laser hair removal with longer pulsed lasers, such as grey hairs.
If shaving is a must, advise patients to:
• Apply warm compresses to the beard area for a few minutes prior to shaving. In addition, using a mild exfoliant or loofah or toothbrush in a circular motion will help allow any ingrown hairs to be more easily plucked or released at the skin surface.
• Use shaving gel and a sharp razor each time.
• Do not pull the skin taut.
• Do not shave against the direction of hair growth.
• Take short strokes and do not shave back and forth over the same areas.
• After shaving, use a soothing aftershave or hydrocortisone 1% lotion.
Products such as PFB Vanish, which contain salicylic, glycolic, and/or lactic acid, are helpful in some patients after hair removal to prevent ingrown hairs. One version of PFB Vanish contains antipigment ingredients to also address hyperpigmentation.
If inflammatory papules or pustules are present, a combination benzoyl peroxide/clindamycin topical gels (such as Benzaclin, Duac, or Acanya) can be used. Patients with severe inflammation may require oral antibiotics.
Using a topical retinoid at night or a combination retinoid product with hydroquinone can be helpful especially in cases of postinflammatory hyperpigmentation. However, use caution when prescribing retinoids for patients with darker skin, as irritation from these products may lead to postinflammatory pigmentary alteration. Remind patients to avoid drying products, such as toners, if topical retinoids are used.
For severe or refractory postinflammatory hyperpigmentation or inflammatory papules, chemical peels with 20%-30% salicylic acid can be helpful.
What are your PFB solutions? The more we share our clinical insights, the better we will be able to achieve improved treatment results for our patients.
Dr. Wesley practices dermatology in Beverly Hills, Calif. Do you have questions about treating patients with dark skin? If so, send them to [email protected].
ASDS 2013 Roundup with Dr. Kavita Mariwalla
Dr. Kavita Mariwalla, the 2013 ASDS annual meeting chair, provides a 3-minute summary of the hot topics discussed at the American Society of Dermatologic Surgery, held in Chicago. For more, visit http://www.skindandallergynews.com.
Dr. Kavita Mariwalla, the 2013 ASDS annual meeting chair, provides a 3-minute summary of the hot topics discussed at the American Society of Dermatologic Surgery, held in Chicago. For more, visit http://www.skindandallergynews.com.
Dr. Kavita Mariwalla, the 2013 ASDS annual meeting chair, provides a 3-minute summary of the hot topics discussed at the American Society of Dermatologic Surgery, held in Chicago. For more, visit http://www.skindandallergynews.com.
When is too young for antiaging procedures?
DANA POINT, CALIF. – When is someone too young for antiaging procedures with cosmetic fillers or laser resurfacing?
Chronologic age "is somewhat irrelevant," in the opinion of Dr. Elizabeth L. Tanzi, codirector of the Washington (D.C.) Institute of Dermatologic Laser Surgery. "I’m looking at dermatologic age, with a critical evaluation of [a patient’s] need," she said at a meeting sponsored by SkinCare Physicians and Northwestern University.
Dr. Tanzi noted that genetics also plays a role in how each person’s skin ages over time. "Some people have inherited facial expressions," she explained. "They may get hyperdynamic movement in certain parts of their face and develop wrinkles much earlier than you would anticipate. Environmental exposure clearly plays a large role. Excessive ultraviolet exposure, growing up with outdoor sporting activities, tanning bed use, or poor habits such as smoking are going to lead to an accelerated aging process," she said.
The importance of establishing realistic patient expectations starts with the first office consultation, when clinicians emphasize that "we can slow down the signs of aging on your skin, but we cannot stop the process completely," said Dr. Tanzi, who is also an assistant professor of dermatology at George Washington University Medical Center, Washington. "I think it’s more important to talk about looking youthful, energetic, and vibrant, not necessarily looking young, because we may be inadvertently delivering the wrong message – that all aging is preventable if treatments are started early enough – and that sets the stage for unrealistic expectations."
Encouraging sun protection behaviors is sensible, and "most dermatologists realize that you can use neuromodulators and fillers strategically early on," Dr. Tanzi said. "But the idea of using fractionated laser resurfacing treatments to promote improved skin function is intriguing to me. We know we can improve the skin cosmetically through a series of fractional laser resurfacing treatments. But can we functionally improve the skin as it’s aging?" she questioned.
Cutting-edge research suggests that may be the case. In 2012, Dan F. Spandau, Ph.D., and his colleagues (J. Invest. Dermatol. 2012;132:1591-6) published data showing that dermal wounding procedures such as fractional resurfacing can "wake up senescent dermal fibroblasts to produce more insulin-like growth factor-1 (IGF-1), which helps the epidermis ward off the damaging effects of UVB on the skin," Dr. Tanzi said. In that case, she continued, "should we be recommending fractional resurfacing as part of a healthy antiaging routine? If so, at what age? These are exciting developments that need additional research to help guide new treatment protocols."
Although she is enthusiastic about preventing some signs of aging and helping patients maintain a youthful appearance, Dr. Tanzi expressed some concerns. "If we are not careful, we could be setting ourselves up for an expectation of being able to stop the aging process, and this can be a slippery slope, especially for women," she said. "Especially when it comes to fillers and neuromodulators, if not done judiciously they can lead to a very artificial look which, ironically, makes women look much older," Dr. Tanzi said. "As thoughtful physicians, it’s important to keep perspective and guide patients to know when enough is enough [in terms of procedures]," she added.
Dr. Tanzi disclosed that she is a consultant for Cynosure/Palomar, Lumenis, and other companies.
DANA POINT, CALIF. – When is someone too young for antiaging procedures with cosmetic fillers or laser resurfacing?
Chronologic age "is somewhat irrelevant," in the opinion of Dr. Elizabeth L. Tanzi, codirector of the Washington (D.C.) Institute of Dermatologic Laser Surgery. "I’m looking at dermatologic age, with a critical evaluation of [a patient’s] need," she said at a meeting sponsored by SkinCare Physicians and Northwestern University.
Dr. Tanzi noted that genetics also plays a role in how each person’s skin ages over time. "Some people have inherited facial expressions," she explained. "They may get hyperdynamic movement in certain parts of their face and develop wrinkles much earlier than you would anticipate. Environmental exposure clearly plays a large role. Excessive ultraviolet exposure, growing up with outdoor sporting activities, tanning bed use, or poor habits such as smoking are going to lead to an accelerated aging process," she said.
The importance of establishing realistic patient expectations starts with the first office consultation, when clinicians emphasize that "we can slow down the signs of aging on your skin, but we cannot stop the process completely," said Dr. Tanzi, who is also an assistant professor of dermatology at George Washington University Medical Center, Washington. "I think it’s more important to talk about looking youthful, energetic, and vibrant, not necessarily looking young, because we may be inadvertently delivering the wrong message – that all aging is preventable if treatments are started early enough – and that sets the stage for unrealistic expectations."
Encouraging sun protection behaviors is sensible, and "most dermatologists realize that you can use neuromodulators and fillers strategically early on," Dr. Tanzi said. "But the idea of using fractionated laser resurfacing treatments to promote improved skin function is intriguing to me. We know we can improve the skin cosmetically through a series of fractional laser resurfacing treatments. But can we functionally improve the skin as it’s aging?" she questioned.
Cutting-edge research suggests that may be the case. In 2012, Dan F. Spandau, Ph.D., and his colleagues (J. Invest. Dermatol. 2012;132:1591-6) published data showing that dermal wounding procedures such as fractional resurfacing can "wake up senescent dermal fibroblasts to produce more insulin-like growth factor-1 (IGF-1), which helps the epidermis ward off the damaging effects of UVB on the skin," Dr. Tanzi said. In that case, she continued, "should we be recommending fractional resurfacing as part of a healthy antiaging routine? If so, at what age? These are exciting developments that need additional research to help guide new treatment protocols."
Although she is enthusiastic about preventing some signs of aging and helping patients maintain a youthful appearance, Dr. Tanzi expressed some concerns. "If we are not careful, we could be setting ourselves up for an expectation of being able to stop the aging process, and this can be a slippery slope, especially for women," she said. "Especially when it comes to fillers and neuromodulators, if not done judiciously they can lead to a very artificial look which, ironically, makes women look much older," Dr. Tanzi said. "As thoughtful physicians, it’s important to keep perspective and guide patients to know when enough is enough [in terms of procedures]," she added.
Dr. Tanzi disclosed that she is a consultant for Cynosure/Palomar, Lumenis, and other companies.
DANA POINT, CALIF. – When is someone too young for antiaging procedures with cosmetic fillers or laser resurfacing?
Chronologic age "is somewhat irrelevant," in the opinion of Dr. Elizabeth L. Tanzi, codirector of the Washington (D.C.) Institute of Dermatologic Laser Surgery. "I’m looking at dermatologic age, with a critical evaluation of [a patient’s] need," she said at a meeting sponsored by SkinCare Physicians and Northwestern University.
Dr. Tanzi noted that genetics also plays a role in how each person’s skin ages over time. "Some people have inherited facial expressions," she explained. "They may get hyperdynamic movement in certain parts of their face and develop wrinkles much earlier than you would anticipate. Environmental exposure clearly plays a large role. Excessive ultraviolet exposure, growing up with outdoor sporting activities, tanning bed use, or poor habits such as smoking are going to lead to an accelerated aging process," she said.
The importance of establishing realistic patient expectations starts with the first office consultation, when clinicians emphasize that "we can slow down the signs of aging on your skin, but we cannot stop the process completely," said Dr. Tanzi, who is also an assistant professor of dermatology at George Washington University Medical Center, Washington. "I think it’s more important to talk about looking youthful, energetic, and vibrant, not necessarily looking young, because we may be inadvertently delivering the wrong message – that all aging is preventable if treatments are started early enough – and that sets the stage for unrealistic expectations."
Encouraging sun protection behaviors is sensible, and "most dermatologists realize that you can use neuromodulators and fillers strategically early on," Dr. Tanzi said. "But the idea of using fractionated laser resurfacing treatments to promote improved skin function is intriguing to me. We know we can improve the skin cosmetically through a series of fractional laser resurfacing treatments. But can we functionally improve the skin as it’s aging?" she questioned.
Cutting-edge research suggests that may be the case. In 2012, Dan F. Spandau, Ph.D., and his colleagues (J. Invest. Dermatol. 2012;132:1591-6) published data showing that dermal wounding procedures such as fractional resurfacing can "wake up senescent dermal fibroblasts to produce more insulin-like growth factor-1 (IGF-1), which helps the epidermis ward off the damaging effects of UVB on the skin," Dr. Tanzi said. In that case, she continued, "should we be recommending fractional resurfacing as part of a healthy antiaging routine? If so, at what age? These are exciting developments that need additional research to help guide new treatment protocols."
Although she is enthusiastic about preventing some signs of aging and helping patients maintain a youthful appearance, Dr. Tanzi expressed some concerns. "If we are not careful, we could be setting ourselves up for an expectation of being able to stop the aging process, and this can be a slippery slope, especially for women," she said. "Especially when it comes to fillers and neuromodulators, if not done judiciously they can lead to a very artificial look which, ironically, makes women look much older," Dr. Tanzi said. "As thoughtful physicians, it’s important to keep perspective and guide patients to know when enough is enough [in terms of procedures]," she added.
Dr. Tanzi disclosed that she is a consultant for Cynosure/Palomar, Lumenis, and other companies.
AT CONTROVERSIES AND CONVERSATIONS IN LASER AND COSMETIC SURGERY
Surgical procedures best for skin tightening, expert says
DANA POINT, CALIF. – For skin tightening, there’s no comparison between surgical and nonsurgical approaches as far as quality, predictability, and longevity, according to Dr. A. Jay Burns.
"Anyone who suggests to patients that nonsurgical contouring and rejuvenation share comparable results is either self-serving, dishonest, grossly naive, or misinformed," said Dr. Burns of the Dallas Plastic Surgery Institute. "In my opinion, surgical treatments are extremely reliable and nonsurgical treatments are extremely variable. But I’m not in an ivory tower. I realize that [surgical approaches result in] more complications and that they’re more expensive."
Surgical skin tightening involves total elevation, full repositioning, centimeter changes, and control, with predictable, clear results, he said at the meeting, sponsored by SkinCare Physicians and Northwestern University.
On the other hand, nonsurgical skin tightening involves no elevation, no repositioning, millimeter changes, and no control. This leads to results that he characterized as "unpredictable and subtle."
Dr. Burns acknowledged certain advantages of nonsurgical skin tightening approaches, such as the fact that they’re typically less expensive (except for brow dynamic line elimination), they eliminate the risk of nerve damage, and they require less downtime. He said he advises clinicians to recommend nonsurgical skin tightening for patients who prioritize downtime, cost, and risk over results. Surgical skin tightening is for those who want optimal results, maximum quality and predictability, and elegance, he said.
Dr. Burns said that there is "a clear place for" nonsurgical skin tightening techniques in his practice, and he emphasized the importance of fostering integrity during patient consultations. This includes informed consent, representing the technology honestly, and being honest with patients about expectations from procedures that you offer. Such practice "shows character and aids your reputation," he said. "It also prioritizes patient care over revenue."
He noted that the ThermiRF, developed by Southlake, Tex.–based ThermiAesthetics, represents a promising advance in noninvasive skin technology because it features a continuous temperature monitor on its internal probe. This radiofrequency device enables the user to administer the precise amount of heat for the collagen layer, Dr. Burns said. "There are some really nice results on the skin and neck," he said.
Dr. Burns disclosed that he has received equipment loans or discounts on equipment from Cynosure, Zeltiq Aesthetics, and other companies. He has held stock or stock options with Skin Medica and Zeltiq and has received honoraria from Solta Medical and Ulthera. He is an advisory board member for Cynosure, Ulthera, and Zeltiq.
DANA POINT, CALIF. – For skin tightening, there’s no comparison between surgical and nonsurgical approaches as far as quality, predictability, and longevity, according to Dr. A. Jay Burns.
"Anyone who suggests to patients that nonsurgical contouring and rejuvenation share comparable results is either self-serving, dishonest, grossly naive, or misinformed," said Dr. Burns of the Dallas Plastic Surgery Institute. "In my opinion, surgical treatments are extremely reliable and nonsurgical treatments are extremely variable. But I’m not in an ivory tower. I realize that [surgical approaches result in] more complications and that they’re more expensive."
Surgical skin tightening involves total elevation, full repositioning, centimeter changes, and control, with predictable, clear results, he said at the meeting, sponsored by SkinCare Physicians and Northwestern University.
On the other hand, nonsurgical skin tightening involves no elevation, no repositioning, millimeter changes, and no control. This leads to results that he characterized as "unpredictable and subtle."
Dr. Burns acknowledged certain advantages of nonsurgical skin tightening approaches, such as the fact that they’re typically less expensive (except for brow dynamic line elimination), they eliminate the risk of nerve damage, and they require less downtime. He said he advises clinicians to recommend nonsurgical skin tightening for patients who prioritize downtime, cost, and risk over results. Surgical skin tightening is for those who want optimal results, maximum quality and predictability, and elegance, he said.
Dr. Burns said that there is "a clear place for" nonsurgical skin tightening techniques in his practice, and he emphasized the importance of fostering integrity during patient consultations. This includes informed consent, representing the technology honestly, and being honest with patients about expectations from procedures that you offer. Such practice "shows character and aids your reputation," he said. "It also prioritizes patient care over revenue."
He noted that the ThermiRF, developed by Southlake, Tex.–based ThermiAesthetics, represents a promising advance in noninvasive skin technology because it features a continuous temperature monitor on its internal probe. This radiofrequency device enables the user to administer the precise amount of heat for the collagen layer, Dr. Burns said. "There are some really nice results on the skin and neck," he said.
Dr. Burns disclosed that he has received equipment loans or discounts on equipment from Cynosure, Zeltiq Aesthetics, and other companies. He has held stock or stock options with Skin Medica and Zeltiq and has received honoraria from Solta Medical and Ulthera. He is an advisory board member for Cynosure, Ulthera, and Zeltiq.
DANA POINT, CALIF. – For skin tightening, there’s no comparison between surgical and nonsurgical approaches as far as quality, predictability, and longevity, according to Dr. A. Jay Burns.
"Anyone who suggests to patients that nonsurgical contouring and rejuvenation share comparable results is either self-serving, dishonest, grossly naive, or misinformed," said Dr. Burns of the Dallas Plastic Surgery Institute. "In my opinion, surgical treatments are extremely reliable and nonsurgical treatments are extremely variable. But I’m not in an ivory tower. I realize that [surgical approaches result in] more complications and that they’re more expensive."
Surgical skin tightening involves total elevation, full repositioning, centimeter changes, and control, with predictable, clear results, he said at the meeting, sponsored by SkinCare Physicians and Northwestern University.
On the other hand, nonsurgical skin tightening involves no elevation, no repositioning, millimeter changes, and no control. This leads to results that he characterized as "unpredictable and subtle."
Dr. Burns acknowledged certain advantages of nonsurgical skin tightening approaches, such as the fact that they’re typically less expensive (except for brow dynamic line elimination), they eliminate the risk of nerve damage, and they require less downtime. He said he advises clinicians to recommend nonsurgical skin tightening for patients who prioritize downtime, cost, and risk over results. Surgical skin tightening is for those who want optimal results, maximum quality and predictability, and elegance, he said.
Dr. Burns said that there is "a clear place for" nonsurgical skin tightening techniques in his practice, and he emphasized the importance of fostering integrity during patient consultations. This includes informed consent, representing the technology honestly, and being honest with patients about expectations from procedures that you offer. Such practice "shows character and aids your reputation," he said. "It also prioritizes patient care over revenue."
He noted that the ThermiRF, developed by Southlake, Tex.–based ThermiAesthetics, represents a promising advance in noninvasive skin technology because it features a continuous temperature monitor on its internal probe. This radiofrequency device enables the user to administer the precise amount of heat for the collagen layer, Dr. Burns said. "There are some really nice results on the skin and neck," he said.
Dr. Burns disclosed that he has received equipment loans or discounts on equipment from Cynosure, Zeltiq Aesthetics, and other companies. He has held stock or stock options with Skin Medica and Zeltiq and has received honoraria from Solta Medical and Ulthera. He is an advisory board member for Cynosure, Ulthera, and Zeltiq.
EXPERT ANALYSIS FROM CONTROVERSIES AND CONVERSATIONS IN LASER AND COSMETIC SURGERY
Use images and analogies to explain hair disorders
NEW YORK – Dr. Paradi Mirmirani has an elegant way of explaining hair loss to her postmenopausal patients.
"Think about [hair production] like an orchestra. When your body is making hair, a whole group of musicians are coming together to make music. But when you’re postmenopausal, the estrogen isn’t there, the head violinist isn’t there, and it’s not going to be the same, but you’re still making music. It’s not going to be same sound, but it’s still there," she said.
Dr. Mirmirani of the University of California, San Francisco, is well recognized for her research in hair disorders, and during her presentation at the American Academy of Dermatology’s summer meeting, she shared her tips on diagnosing and treating different types of hair loss and alopecia in women:
• Telogen effluvium (I’m shedding gobs of hair!)
Find out whether the patient has a history of weight loss or is on new oral contraceptives, Dr. Mirmirani said. Use a hair shaft contrast card and search the scalp for scarring or scaling. Also, perform a "pull test" (for bulb) and "tug test" (for shaft), she advised. For laboratory data, she recommended ferritin and TSH, and possibly tests for antinuclear antibodies and vitamin D levels, and a biopsy of the area. Treat the underlying problem, not the hair, and assure patients that they will not go bald, she said.
• Traction alopecia (I’ve got a bald spot!)
Start by asking these patients what they do for hair care and styling, said Dr. Mirmirani. On exam, look for a telltale "fringe sign," which she and her colleagues described in a paper as "the presence of retained hairs along the frontal and/or temporal rim." (J. Clin. Exp. Dermatol. Res. 2011;2:117).
She recommended ordering ferritin and TSH tests for these patients, and possibly vitamin D. Also, treat any inflammation; consider nonspecific hair growth treatments such as minoxidil, and surgical hair restoration, and remind patients to treat their hair gently, she said.
• Alopecia areata
Ask alopecia areata patients about a personal or family history of atopic disorders, Dr. Mirmirani advised. Treatment options include intralesional corticosteroids (10 mg/cc to 2 cc total); topical corticosteroids; topical minoxidil 5% twice daily; short-contact anthralin (up to 30 minutes); topical immunotherapy; or psoralen + ultraviolet A (PUVA) treatment. Finally, remind patients that alopecia areata is an autoimmune condition that is not contagious, Dr. Mirmirani said. Compare it to an unwelcome house guest, she suggested.
• Female pattern hair loss (midlife hair crisis)
Start care for these patients by ordering (only if virilized) free and total T, dehydroepiandrosterone sulfate, and prolactin tests, Dr. Mirmirani said. Her recommended treatment protocol: minoxidil 2% or 5% solution twice daily, or 5% foam once daily; finasteride (1 mg) or spironolactone. Also, consider hair restoration or cosmetics that bring the scalp’s color closer to hair color and make hair loss less apparent, she suggested. This is when to remind patients that "the orchestra is still playing" (hair may still be produced) although estrogen (the first violinist) is absent, so it may not be quite the same.
• Acquired trichorrhexis nodosa (My hair just won’t grow!)
Acquired trichorrhexis nodosa is the most commonly reported hair shaft defect, Dr. Mirmirani said. It often results from excessive chemical processes and heat applied to hair. She described her typical acquired trichorrhexis nodosa patient as a 24-year-old black woman who washes her every 2 weeks and straightens every 6 weeks, her hair has been breaking off in the back, started after a recent color, with no symptoms.
In these patients, and exam usually shows that the overall hair density is good, no alopecia, a localized area of short hair with blunt ends, and a positive tug test (hair breaks off easily). The scalp often has mild scaling, but no pustules.
Make a hair mount, and show the patient her hair under the microscope; "it’s the easiest and most satisfying thing you can do," said Dr. Mirmirani.
Advise patients to use gentle hair care, trim unhealthy hair, and avoid heat and chemicals, she said. Wigs are fine for these patients, and most will recover the condition of their hair within a year or 2, she added.
• Cicatricial alopecia
Start with a biopsy around the margin of early active area, and then culture the pustules, said Dr. Mirmirani. Dermatopathology can show whether sebaceous glands are absent, and the degree of inflammatory infiltrate.
Explain to these patients that the hair roots or bulbs have been damaged, she added. Tell them regrowth is not possible, but they can relieve the signs and symptoms of the condition and prevent it from spreading. Describe it as "like a wildfire; we want to contain it, and halt the spread," she suggested.
Treat the predominantly lymphocytic patients with anti-inflammatories (intralesionals and topicals; antibiotics and antimalarials; systemic anti-inflammatory therapies), said Dr. Mirmirani. For lichen planopilaris and frontal fibrosing alopecia, try PPAR-gamma agonists; use topical minoxidil or finasteride to promote nonspecific hair growth; or try cosmetic or surgical therapies, she said.
Treat folliculitis decalvans with antibacterial treatments and staph eradication, and treat dissecting cellulitis with intralesionals/anti-inflammatory drugs; perform incision and drainage; use isotretinoin and antitumor-necrosis factor; and consider laser hair removal, she noted.
Dr. Mirmirani said that, in her experience, many dermatologists dread seeing hair-loss patients because of a lack of training in how to care for them. She shared several educational resources, including a reference book she coauthored, "Cicatricial Alopecia: An Approach to Diagnosis and Management," (New York: Springer, 2011) to help clinicians and residents better understand and treat hair disorders, especially the rare kinds. She also recommended the North American Hair Research Society and the Cicatricial Alopecia Research Foundation as useful resources.
Dr. Mirmirani has been an investigator and/or consultant for Johnson & Johnson, as well as Procter & Gamble.
On Twitter @NaseemSMiller
NEW YORK – Dr. Paradi Mirmirani has an elegant way of explaining hair loss to her postmenopausal patients.
"Think about [hair production] like an orchestra. When your body is making hair, a whole group of musicians are coming together to make music. But when you’re postmenopausal, the estrogen isn’t there, the head violinist isn’t there, and it’s not going to be the same, but you’re still making music. It’s not going to be same sound, but it’s still there," she said.
Dr. Mirmirani of the University of California, San Francisco, is well recognized for her research in hair disorders, and during her presentation at the American Academy of Dermatology’s summer meeting, she shared her tips on diagnosing and treating different types of hair loss and alopecia in women:
• Telogen effluvium (I’m shedding gobs of hair!)
Find out whether the patient has a history of weight loss or is on new oral contraceptives, Dr. Mirmirani said. Use a hair shaft contrast card and search the scalp for scarring or scaling. Also, perform a "pull test" (for bulb) and "tug test" (for shaft), she advised. For laboratory data, she recommended ferritin and TSH, and possibly tests for antinuclear antibodies and vitamin D levels, and a biopsy of the area. Treat the underlying problem, not the hair, and assure patients that they will not go bald, she said.
• Traction alopecia (I’ve got a bald spot!)
Start by asking these patients what they do for hair care and styling, said Dr. Mirmirani. On exam, look for a telltale "fringe sign," which she and her colleagues described in a paper as "the presence of retained hairs along the frontal and/or temporal rim." (J. Clin. Exp. Dermatol. Res. 2011;2:117).
She recommended ordering ferritin and TSH tests for these patients, and possibly vitamin D. Also, treat any inflammation; consider nonspecific hair growth treatments such as minoxidil, and surgical hair restoration, and remind patients to treat their hair gently, she said.
• Alopecia areata
Ask alopecia areata patients about a personal or family history of atopic disorders, Dr. Mirmirani advised. Treatment options include intralesional corticosteroids (10 mg/cc to 2 cc total); topical corticosteroids; topical minoxidil 5% twice daily; short-contact anthralin (up to 30 minutes); topical immunotherapy; or psoralen + ultraviolet A (PUVA) treatment. Finally, remind patients that alopecia areata is an autoimmune condition that is not contagious, Dr. Mirmirani said. Compare it to an unwelcome house guest, she suggested.
• Female pattern hair loss (midlife hair crisis)
Start care for these patients by ordering (only if virilized) free and total T, dehydroepiandrosterone sulfate, and prolactin tests, Dr. Mirmirani said. Her recommended treatment protocol: minoxidil 2% or 5% solution twice daily, or 5% foam once daily; finasteride (1 mg) or spironolactone. Also, consider hair restoration or cosmetics that bring the scalp’s color closer to hair color and make hair loss less apparent, she suggested. This is when to remind patients that "the orchestra is still playing" (hair may still be produced) although estrogen (the first violinist) is absent, so it may not be quite the same.
• Acquired trichorrhexis nodosa (My hair just won’t grow!)
Acquired trichorrhexis nodosa is the most commonly reported hair shaft defect, Dr. Mirmirani said. It often results from excessive chemical processes and heat applied to hair. She described her typical acquired trichorrhexis nodosa patient as a 24-year-old black woman who washes her every 2 weeks and straightens every 6 weeks, her hair has been breaking off in the back, started after a recent color, with no symptoms.
In these patients, and exam usually shows that the overall hair density is good, no alopecia, a localized area of short hair with blunt ends, and a positive tug test (hair breaks off easily). The scalp often has mild scaling, but no pustules.
Make a hair mount, and show the patient her hair under the microscope; "it’s the easiest and most satisfying thing you can do," said Dr. Mirmirani.
Advise patients to use gentle hair care, trim unhealthy hair, and avoid heat and chemicals, she said. Wigs are fine for these patients, and most will recover the condition of their hair within a year or 2, she added.
• Cicatricial alopecia
Start with a biopsy around the margin of early active area, and then culture the pustules, said Dr. Mirmirani. Dermatopathology can show whether sebaceous glands are absent, and the degree of inflammatory infiltrate.
Explain to these patients that the hair roots or bulbs have been damaged, she added. Tell them regrowth is not possible, but they can relieve the signs and symptoms of the condition and prevent it from spreading. Describe it as "like a wildfire; we want to contain it, and halt the spread," she suggested.
Treat the predominantly lymphocytic patients with anti-inflammatories (intralesionals and topicals; antibiotics and antimalarials; systemic anti-inflammatory therapies), said Dr. Mirmirani. For lichen planopilaris and frontal fibrosing alopecia, try PPAR-gamma agonists; use topical minoxidil or finasteride to promote nonspecific hair growth; or try cosmetic or surgical therapies, she said.
Treat folliculitis decalvans with antibacterial treatments and staph eradication, and treat dissecting cellulitis with intralesionals/anti-inflammatory drugs; perform incision and drainage; use isotretinoin and antitumor-necrosis factor; and consider laser hair removal, she noted.
Dr. Mirmirani said that, in her experience, many dermatologists dread seeing hair-loss patients because of a lack of training in how to care for them. She shared several educational resources, including a reference book she coauthored, "Cicatricial Alopecia: An Approach to Diagnosis and Management," (New York: Springer, 2011) to help clinicians and residents better understand and treat hair disorders, especially the rare kinds. She also recommended the North American Hair Research Society and the Cicatricial Alopecia Research Foundation as useful resources.
Dr. Mirmirani has been an investigator and/or consultant for Johnson & Johnson, as well as Procter & Gamble.
On Twitter @NaseemSMiller
NEW YORK – Dr. Paradi Mirmirani has an elegant way of explaining hair loss to her postmenopausal patients.
"Think about [hair production] like an orchestra. When your body is making hair, a whole group of musicians are coming together to make music. But when you’re postmenopausal, the estrogen isn’t there, the head violinist isn’t there, and it’s not going to be the same, but you’re still making music. It’s not going to be same sound, but it’s still there," she said.
Dr. Mirmirani of the University of California, San Francisco, is well recognized for her research in hair disorders, and during her presentation at the American Academy of Dermatology’s summer meeting, she shared her tips on diagnosing and treating different types of hair loss and alopecia in women:
• Telogen effluvium (I’m shedding gobs of hair!)
Find out whether the patient has a history of weight loss or is on new oral contraceptives, Dr. Mirmirani said. Use a hair shaft contrast card and search the scalp for scarring or scaling. Also, perform a "pull test" (for bulb) and "tug test" (for shaft), she advised. For laboratory data, she recommended ferritin and TSH, and possibly tests for antinuclear antibodies and vitamin D levels, and a biopsy of the area. Treat the underlying problem, not the hair, and assure patients that they will not go bald, she said.
• Traction alopecia (I’ve got a bald spot!)
Start by asking these patients what they do for hair care and styling, said Dr. Mirmirani. On exam, look for a telltale "fringe sign," which she and her colleagues described in a paper as "the presence of retained hairs along the frontal and/or temporal rim." (J. Clin. Exp. Dermatol. Res. 2011;2:117).
She recommended ordering ferritin and TSH tests for these patients, and possibly vitamin D. Also, treat any inflammation; consider nonspecific hair growth treatments such as minoxidil, and surgical hair restoration, and remind patients to treat their hair gently, she said.
• Alopecia areata
Ask alopecia areata patients about a personal or family history of atopic disorders, Dr. Mirmirani advised. Treatment options include intralesional corticosteroids (10 mg/cc to 2 cc total); topical corticosteroids; topical minoxidil 5% twice daily; short-contact anthralin (up to 30 minutes); topical immunotherapy; or psoralen + ultraviolet A (PUVA) treatment. Finally, remind patients that alopecia areata is an autoimmune condition that is not contagious, Dr. Mirmirani said. Compare it to an unwelcome house guest, she suggested.
• Female pattern hair loss (midlife hair crisis)
Start care for these patients by ordering (only if virilized) free and total T, dehydroepiandrosterone sulfate, and prolactin tests, Dr. Mirmirani said. Her recommended treatment protocol: minoxidil 2% or 5% solution twice daily, or 5% foam once daily; finasteride (1 mg) or spironolactone. Also, consider hair restoration or cosmetics that bring the scalp’s color closer to hair color and make hair loss less apparent, she suggested. This is when to remind patients that "the orchestra is still playing" (hair may still be produced) although estrogen (the first violinist) is absent, so it may not be quite the same.
• Acquired trichorrhexis nodosa (My hair just won’t grow!)
Acquired trichorrhexis nodosa is the most commonly reported hair shaft defect, Dr. Mirmirani said. It often results from excessive chemical processes and heat applied to hair. She described her typical acquired trichorrhexis nodosa patient as a 24-year-old black woman who washes her every 2 weeks and straightens every 6 weeks, her hair has been breaking off in the back, started after a recent color, with no symptoms.
In these patients, and exam usually shows that the overall hair density is good, no alopecia, a localized area of short hair with blunt ends, and a positive tug test (hair breaks off easily). The scalp often has mild scaling, but no pustules.
Make a hair mount, and show the patient her hair under the microscope; "it’s the easiest and most satisfying thing you can do," said Dr. Mirmirani.
Advise patients to use gentle hair care, trim unhealthy hair, and avoid heat and chemicals, she said. Wigs are fine for these patients, and most will recover the condition of their hair within a year or 2, she added.
• Cicatricial alopecia
Start with a biopsy around the margin of early active area, and then culture the pustules, said Dr. Mirmirani. Dermatopathology can show whether sebaceous glands are absent, and the degree of inflammatory infiltrate.
Explain to these patients that the hair roots or bulbs have been damaged, she added. Tell them regrowth is not possible, but they can relieve the signs and symptoms of the condition and prevent it from spreading. Describe it as "like a wildfire; we want to contain it, and halt the spread," she suggested.
Treat the predominantly lymphocytic patients with anti-inflammatories (intralesionals and topicals; antibiotics and antimalarials; systemic anti-inflammatory therapies), said Dr. Mirmirani. For lichen planopilaris and frontal fibrosing alopecia, try PPAR-gamma agonists; use topical minoxidil or finasteride to promote nonspecific hair growth; or try cosmetic or surgical therapies, she said.
Treat folliculitis decalvans with antibacterial treatments and staph eradication, and treat dissecting cellulitis with intralesionals/anti-inflammatory drugs; perform incision and drainage; use isotretinoin and antitumor-necrosis factor; and consider laser hair removal, she noted.
Dr. Mirmirani said that, in her experience, many dermatologists dread seeing hair-loss patients because of a lack of training in how to care for them. She shared several educational resources, including a reference book she coauthored, "Cicatricial Alopecia: An Approach to Diagnosis and Management," (New York: Springer, 2011) to help clinicians and residents better understand and treat hair disorders, especially the rare kinds. She also recommended the North American Hair Research Society and the Cicatricial Alopecia Research Foundation as useful resources.
Dr. Mirmirani has been an investigator and/or consultant for Johnson & Johnson, as well as Procter & Gamble.
On Twitter @NaseemSMiller
Check clinical evidence behind body contouring devices
DANA POINT, CALIF. – If you’re in the market for a body contouring device, Dr. Robert Weiss advises factoring in "solid clinical evidence" before you buy.
"You want to see histologic evidence – apoptosis of fat cells, or at least diminution of fat cells," he said at a meeting sponsored by SkinCare Physicians and Northwestern University. "You want to see ultrasound confirmation of fat reduction, something that’s reproducible and objective. It [the device] also has to have ease of use," he said.
"Most importantly, you want to know if patients themselves see a clinically meaningful response, a significant improvement. If they don’t see improvement, it [the objective value] doesn’t matter," he added.
Other important factors to consider before buying a body contouring device include making sure it has undergone animal studies of internal thermocoupling, and that it has an external temperature monitor for skin. "Infrared camera technology will also help to show how uniform the heating is, and how the skin relates to fat," said Dr. Weiss of the Maryland Laser Skin and Vein Institute, Hunt Valley.
In his practice, Dr. Weiss uses four devices for body contouring: two cryolipolysis devices, one monopolar radiofrequency (RF) device, and one focused-field RF device. The last device, known as the Vanquish, was introduced at the 2013 American Academy of Dermatology meeting. Manufactured by Prague-based BTL Industries, Vanquish is a noncontact device that delivers focused-field RF through panels that are placed over the desired treatment area while the patient is lying horizontally. "The focal point is 10 mm below the skin surface, and it heats to 43-45° C," said Dr. Weiss, who was part of a team of researchers that demonstrated the efficacy of Vanquish in a porcine model (Lasers Surg. Med. 2013;45:235-39). "There are positive and negative fields created within the applicator," Dr. Weiss said. "What happens is that the fat creates more resistance, so the fat heats up but skin and muscle do not. We feel that this [device is] going to be a real game-changer."
In the study, a 70% reduction in abdominal fat was observed in pigs that were treated four times with the Vanquish for 30 minutes each. "Histologic evaluation revealed that epidermis, dermis, and adnexal structures such as hair follicles were unaffected by the treatment, while adipocytes were significantly affected," Dr. Weiss and his colleagues wrote.
Patients who have undergone treatment of excessive abdominal fat with the Vanquish describe a warm sensation during the procedure, with minimal side effects, Dr. Weiss said. "The more hydrated you are, the more selectivity there’s going to be, so we encourage people to drink water before the procedure," he said.
Dr. Weiss disclosed that he is a speaker and investigator for BTL Industries. He also has received honoraria and equipment from the company.
DANA POINT, CALIF. – If you’re in the market for a body contouring device, Dr. Robert Weiss advises factoring in "solid clinical evidence" before you buy.
"You want to see histologic evidence – apoptosis of fat cells, or at least diminution of fat cells," he said at a meeting sponsored by SkinCare Physicians and Northwestern University. "You want to see ultrasound confirmation of fat reduction, something that’s reproducible and objective. It [the device] also has to have ease of use," he said.
"Most importantly, you want to know if patients themselves see a clinically meaningful response, a significant improvement. If they don’t see improvement, it [the objective value] doesn’t matter," he added.
Other important factors to consider before buying a body contouring device include making sure it has undergone animal studies of internal thermocoupling, and that it has an external temperature monitor for skin. "Infrared camera technology will also help to show how uniform the heating is, and how the skin relates to fat," said Dr. Weiss of the Maryland Laser Skin and Vein Institute, Hunt Valley.
In his practice, Dr. Weiss uses four devices for body contouring: two cryolipolysis devices, one monopolar radiofrequency (RF) device, and one focused-field RF device. The last device, known as the Vanquish, was introduced at the 2013 American Academy of Dermatology meeting. Manufactured by Prague-based BTL Industries, Vanquish is a noncontact device that delivers focused-field RF through panels that are placed over the desired treatment area while the patient is lying horizontally. "The focal point is 10 mm below the skin surface, and it heats to 43-45° C," said Dr. Weiss, who was part of a team of researchers that demonstrated the efficacy of Vanquish in a porcine model (Lasers Surg. Med. 2013;45:235-39). "There are positive and negative fields created within the applicator," Dr. Weiss said. "What happens is that the fat creates more resistance, so the fat heats up but skin and muscle do not. We feel that this [device is] going to be a real game-changer."
In the study, a 70% reduction in abdominal fat was observed in pigs that were treated four times with the Vanquish for 30 minutes each. "Histologic evaluation revealed that epidermis, dermis, and adnexal structures such as hair follicles were unaffected by the treatment, while adipocytes were significantly affected," Dr. Weiss and his colleagues wrote.
Patients who have undergone treatment of excessive abdominal fat with the Vanquish describe a warm sensation during the procedure, with minimal side effects, Dr. Weiss said. "The more hydrated you are, the more selectivity there’s going to be, so we encourage people to drink water before the procedure," he said.
Dr. Weiss disclosed that he is a speaker and investigator for BTL Industries. He also has received honoraria and equipment from the company.
DANA POINT, CALIF. – If you’re in the market for a body contouring device, Dr. Robert Weiss advises factoring in "solid clinical evidence" before you buy.
"You want to see histologic evidence – apoptosis of fat cells, or at least diminution of fat cells," he said at a meeting sponsored by SkinCare Physicians and Northwestern University. "You want to see ultrasound confirmation of fat reduction, something that’s reproducible and objective. It [the device] also has to have ease of use," he said.
"Most importantly, you want to know if patients themselves see a clinically meaningful response, a significant improvement. If they don’t see improvement, it [the objective value] doesn’t matter," he added.
Other important factors to consider before buying a body contouring device include making sure it has undergone animal studies of internal thermocoupling, and that it has an external temperature monitor for skin. "Infrared camera technology will also help to show how uniform the heating is, and how the skin relates to fat," said Dr. Weiss of the Maryland Laser Skin and Vein Institute, Hunt Valley.
In his practice, Dr. Weiss uses four devices for body contouring: two cryolipolysis devices, one monopolar radiofrequency (RF) device, and one focused-field RF device. The last device, known as the Vanquish, was introduced at the 2013 American Academy of Dermatology meeting. Manufactured by Prague-based BTL Industries, Vanquish is a noncontact device that delivers focused-field RF through panels that are placed over the desired treatment area while the patient is lying horizontally. "The focal point is 10 mm below the skin surface, and it heats to 43-45° C," said Dr. Weiss, who was part of a team of researchers that demonstrated the efficacy of Vanquish in a porcine model (Lasers Surg. Med. 2013;45:235-39). "There are positive and negative fields created within the applicator," Dr. Weiss said. "What happens is that the fat creates more resistance, so the fat heats up but skin and muscle do not. We feel that this [device is] going to be a real game-changer."
In the study, a 70% reduction in abdominal fat was observed in pigs that were treated four times with the Vanquish for 30 minutes each. "Histologic evaluation revealed that epidermis, dermis, and adnexal structures such as hair follicles were unaffected by the treatment, while adipocytes were significantly affected," Dr. Weiss and his colleagues wrote.
Patients who have undergone treatment of excessive abdominal fat with the Vanquish describe a warm sensation during the procedure, with minimal side effects, Dr. Weiss said. "The more hydrated you are, the more selectivity there’s going to be, so we encourage people to drink water before the procedure," he said.
Dr. Weiss disclosed that he is a speaker and investigator for BTL Industries. He also has received honoraria and equipment from the company.
EXPERT ANALYSIS FROM CONTROVERSIES AND CONVERSATIONS IN LASER AND COSMETIC SURGERY
Forehead wrinkles stay smoother longer with nerve fiber treatment
DANA POINT, CALIF. – Use of a bipolar radiofrequency probe to the frontalis and corrugator branches of the temporal facial nerve resulted in the diminishment of forehead wrinkles that lasts two to three times longer than treatment with botulinum toxin, according to Dr. James Newman.
At a meeting sponsored by SkinCare Physicians and Northwestern University, Dr. Newman described his early clinical experience with the Serene Solution, a Food and Drug Administration–cleared device created by Serene Medical designed to target nerves and create radiofrequency lesions.
"The purpose of this type of treatment is to take a finite probe, which allows the physician to stimulate and target a very specific nerve on the body," said Dr. Newman, a plastic surgeon in private practice in Palo Alto, Calif. "In this case we’re using a bipolar radiofrequency probe within 1-2 mm of the frontalis and corrugator branches of the temporal facial nerve."
The device, which consists of a control unit and 20-gauge dual-purpose probe, enables one or more small radiofrequency lesions to interrupt the motor nerve signal and reduce muscle activity. "The advantage is that the effect is instant," said Dr. Newman, who is chief medical officer for Serene Medical. "It’s long lasting, produces minimal collateral damage, and allows reconnection along the original path of [the] nerve." The effect can last 6-18 months, depending on the lesion, compared with botulinum that lasts for about 3-6 months.
In split-face studies conducted by Dr. Newman and his associates, 20 patients underwent a single treatment with the Serene Solution to create a radiofrequency lesion on the frontalis and corrugator branches of the temporal facial nerve. Six months post treatment, patient wrinkles remained improved compared with baseline, according to evaluation with Merz Aesthetics Scales. "The muscle response to stimulation currently demonstrates that nerve function is fully restored, when compared to the untreated side," Dr. Newman said. "That told us that the nerve sheath is still intact and that we do not have a complete nerve block." The fact that improvement persists long term in the treated side "may be due to a smaller or less-conditioned frontalis muscle," he said.
Dr. Newman and his associates plan to study the hypothesis that creating three radiofrequency lesions along the frontalis nerve will prolong the period of nerve discontinuity by two to three times. "If we create more than one lesion, perhaps we can prolong relaxation of the frontalis muscle and those wrinkle scores might be improved as well," he said.
Dr. Newman disclosed that he is a stockholder in Serene Medical and that he is a speaker for and has received honoraria from Valeant Pharmaceuticals.
DANA POINT, CALIF. – Use of a bipolar radiofrequency probe to the frontalis and corrugator branches of the temporal facial nerve resulted in the diminishment of forehead wrinkles that lasts two to three times longer than treatment with botulinum toxin, according to Dr. James Newman.
At a meeting sponsored by SkinCare Physicians and Northwestern University, Dr. Newman described his early clinical experience with the Serene Solution, a Food and Drug Administration–cleared device created by Serene Medical designed to target nerves and create radiofrequency lesions.
"The purpose of this type of treatment is to take a finite probe, which allows the physician to stimulate and target a very specific nerve on the body," said Dr. Newman, a plastic surgeon in private practice in Palo Alto, Calif. "In this case we’re using a bipolar radiofrequency probe within 1-2 mm of the frontalis and corrugator branches of the temporal facial nerve."
The device, which consists of a control unit and 20-gauge dual-purpose probe, enables one or more small radiofrequency lesions to interrupt the motor nerve signal and reduce muscle activity. "The advantage is that the effect is instant," said Dr. Newman, who is chief medical officer for Serene Medical. "It’s long lasting, produces minimal collateral damage, and allows reconnection along the original path of [the] nerve." The effect can last 6-18 months, depending on the lesion, compared with botulinum that lasts for about 3-6 months.
In split-face studies conducted by Dr. Newman and his associates, 20 patients underwent a single treatment with the Serene Solution to create a radiofrequency lesion on the frontalis and corrugator branches of the temporal facial nerve. Six months post treatment, patient wrinkles remained improved compared with baseline, according to evaluation with Merz Aesthetics Scales. "The muscle response to stimulation currently demonstrates that nerve function is fully restored, when compared to the untreated side," Dr. Newman said. "That told us that the nerve sheath is still intact and that we do not have a complete nerve block." The fact that improvement persists long term in the treated side "may be due to a smaller or less-conditioned frontalis muscle," he said.
Dr. Newman and his associates plan to study the hypothesis that creating three radiofrequency lesions along the frontalis nerve will prolong the period of nerve discontinuity by two to three times. "If we create more than one lesion, perhaps we can prolong relaxation of the frontalis muscle and those wrinkle scores might be improved as well," he said.
Dr. Newman disclosed that he is a stockholder in Serene Medical and that he is a speaker for and has received honoraria from Valeant Pharmaceuticals.
DANA POINT, CALIF. – Use of a bipolar radiofrequency probe to the frontalis and corrugator branches of the temporal facial nerve resulted in the diminishment of forehead wrinkles that lasts two to three times longer than treatment with botulinum toxin, according to Dr. James Newman.
At a meeting sponsored by SkinCare Physicians and Northwestern University, Dr. Newman described his early clinical experience with the Serene Solution, a Food and Drug Administration–cleared device created by Serene Medical designed to target nerves and create radiofrequency lesions.
"The purpose of this type of treatment is to take a finite probe, which allows the physician to stimulate and target a very specific nerve on the body," said Dr. Newman, a plastic surgeon in private practice in Palo Alto, Calif. "In this case we’re using a bipolar radiofrequency probe within 1-2 mm of the frontalis and corrugator branches of the temporal facial nerve."
The device, which consists of a control unit and 20-gauge dual-purpose probe, enables one or more small radiofrequency lesions to interrupt the motor nerve signal and reduce muscle activity. "The advantage is that the effect is instant," said Dr. Newman, who is chief medical officer for Serene Medical. "It’s long lasting, produces minimal collateral damage, and allows reconnection along the original path of [the] nerve." The effect can last 6-18 months, depending on the lesion, compared with botulinum that lasts for about 3-6 months.
In split-face studies conducted by Dr. Newman and his associates, 20 patients underwent a single treatment with the Serene Solution to create a radiofrequency lesion on the frontalis and corrugator branches of the temporal facial nerve. Six months post treatment, patient wrinkles remained improved compared with baseline, according to evaluation with Merz Aesthetics Scales. "The muscle response to stimulation currently demonstrates that nerve function is fully restored, when compared to the untreated side," Dr. Newman said. "That told us that the nerve sheath is still intact and that we do not have a complete nerve block." The fact that improvement persists long term in the treated side "may be due to a smaller or less-conditioned frontalis muscle," he said.
Dr. Newman and his associates plan to study the hypothesis that creating three radiofrequency lesions along the frontalis nerve will prolong the period of nerve discontinuity by two to three times. "If we create more than one lesion, perhaps we can prolong relaxation of the frontalis muscle and those wrinkle scores might be improved as well," he said.
Dr. Newman disclosed that he is a stockholder in Serene Medical and that he is a speaker for and has received honoraria from Valeant Pharmaceuticals.
EXPERT ANALYSIS FROM CONTROVERSIES AND CONVERSATIONS IN LASER AND COSMETIC SURGERY