User login
Skin Disease Education Foundation (SDEF): Las Vegas Dermatology Seminar
Palm lines predict worse outcomes in atopic dermatitis
LAS VEGAS – Hyperlinearity in the palms of atopic dermatitis patients may indicate filaggrin deficiency, which increases the likelihood of more severe and persistent disease and associated problems, according to Dr. Jacob Thyssen of the National Allergy Research Centre at Copenhagen University.
"If you can’t genotype" the filaggrin gene to check for mutations that decrease or eliminate the protective skin barrier protein, "check the palms of your patients and their parents" for deeper, more numerous, and slightly erythematous lines, said Dr. Thyssen. "I do that routinely. It’s harder in children, but it gets easier as they age," he said at the Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
When such lines are present, it’s probably a good idea to tell patients they may have a more severe case of atopic dermatitis and need to follow treatments and advice carefully, he said.
Filaggrin mutations were first identified in 2006 as the cause of ichthyosis vulgaris – a related condition associated with palm and plantar hyperlinearity – plus keratosis pilaris and fissured, dry, and scaly skin. The mutations have since been identified in about half of all severe atopic dermatitis patients, and risk of the disease increases 150-fold in homozygous mutation carriers who produce no filaggrin at all. Perhaps 10% of people of European ancestry carry filaggrin mutations, and it is less common in people of Asian or African descent, Dr. Thyssen noted.
"The filaggrin deficient group needs emollients," perhaps more so than other atopic dermatitis patients, and may benefit less from anti-inflammatory treatments, he said. "Barrier restoration [with hypoallergenic emollients] should be the main issue," he emphasized.
Moisturizers with ceramides and filaggrin breakdown products haven’t been heavily promoted in Europe. Although they may be effective, at this point "we just try to use very lipid-rich emollients," Dr. Thyssen said.
Filaggrin mutations in atopic dermatitis patients have been associated with allergic rhinitis and asthma, Dr. Thyssen said. Deficient patients also may be more susceptible to sun sensitivity, skin dehydration, skin infections, food allergies, and. contact dermatitis. The reason for these associations remains unclear; perhaps allergens have an easier time penetrating the skin and engaging the immune system when filaggrin is lacking, he said. Patients also seem to self-select for careers that avoid skin irritants such as nickel, he added.
Research is ongoing to devise treatments that directly correct the deficiency. However, it is likely that atopic dermatitis represents "many diseases with one face," said Dr. Thyssen. "Today, we treat all cases the same, but we are beginning to dissect" the various factors at play in individuals, and may one day be able to individualize treatment approaches, he said.
Dr. Thyssen had no relevant disclosures.
SDEF and this news organization are owned by Frontline Medical Communications.
LAS VEGAS – Hyperlinearity in the palms of atopic dermatitis patients may indicate filaggrin deficiency, which increases the likelihood of more severe and persistent disease and associated problems, according to Dr. Jacob Thyssen of the National Allergy Research Centre at Copenhagen University.
"If you can’t genotype" the filaggrin gene to check for mutations that decrease or eliminate the protective skin barrier protein, "check the palms of your patients and their parents" for deeper, more numerous, and slightly erythematous lines, said Dr. Thyssen. "I do that routinely. It’s harder in children, but it gets easier as they age," he said at the Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
When such lines are present, it’s probably a good idea to tell patients they may have a more severe case of atopic dermatitis and need to follow treatments and advice carefully, he said.
Filaggrin mutations were first identified in 2006 as the cause of ichthyosis vulgaris – a related condition associated with palm and plantar hyperlinearity – plus keratosis pilaris and fissured, dry, and scaly skin. The mutations have since been identified in about half of all severe atopic dermatitis patients, and risk of the disease increases 150-fold in homozygous mutation carriers who produce no filaggrin at all. Perhaps 10% of people of European ancestry carry filaggrin mutations, and it is less common in people of Asian or African descent, Dr. Thyssen noted.
"The filaggrin deficient group needs emollients," perhaps more so than other atopic dermatitis patients, and may benefit less from anti-inflammatory treatments, he said. "Barrier restoration [with hypoallergenic emollients] should be the main issue," he emphasized.
Moisturizers with ceramides and filaggrin breakdown products haven’t been heavily promoted in Europe. Although they may be effective, at this point "we just try to use very lipid-rich emollients," Dr. Thyssen said.
Filaggrin mutations in atopic dermatitis patients have been associated with allergic rhinitis and asthma, Dr. Thyssen said. Deficient patients also may be more susceptible to sun sensitivity, skin dehydration, skin infections, food allergies, and. contact dermatitis. The reason for these associations remains unclear; perhaps allergens have an easier time penetrating the skin and engaging the immune system when filaggrin is lacking, he said. Patients also seem to self-select for careers that avoid skin irritants such as nickel, he added.
Research is ongoing to devise treatments that directly correct the deficiency. However, it is likely that atopic dermatitis represents "many diseases with one face," said Dr. Thyssen. "Today, we treat all cases the same, but we are beginning to dissect" the various factors at play in individuals, and may one day be able to individualize treatment approaches, he said.
Dr. Thyssen had no relevant disclosures.
SDEF and this news organization are owned by Frontline Medical Communications.
LAS VEGAS – Hyperlinearity in the palms of atopic dermatitis patients may indicate filaggrin deficiency, which increases the likelihood of more severe and persistent disease and associated problems, according to Dr. Jacob Thyssen of the National Allergy Research Centre at Copenhagen University.
"If you can’t genotype" the filaggrin gene to check for mutations that decrease or eliminate the protective skin barrier protein, "check the palms of your patients and their parents" for deeper, more numerous, and slightly erythematous lines, said Dr. Thyssen. "I do that routinely. It’s harder in children, but it gets easier as they age," he said at the Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
When such lines are present, it’s probably a good idea to tell patients they may have a more severe case of atopic dermatitis and need to follow treatments and advice carefully, he said.
Filaggrin mutations were first identified in 2006 as the cause of ichthyosis vulgaris – a related condition associated with palm and plantar hyperlinearity – plus keratosis pilaris and fissured, dry, and scaly skin. The mutations have since been identified in about half of all severe atopic dermatitis patients, and risk of the disease increases 150-fold in homozygous mutation carriers who produce no filaggrin at all. Perhaps 10% of people of European ancestry carry filaggrin mutations, and it is less common in people of Asian or African descent, Dr. Thyssen noted.
"The filaggrin deficient group needs emollients," perhaps more so than other atopic dermatitis patients, and may benefit less from anti-inflammatory treatments, he said. "Barrier restoration [with hypoallergenic emollients] should be the main issue," he emphasized.
Moisturizers with ceramides and filaggrin breakdown products haven’t been heavily promoted in Europe. Although they may be effective, at this point "we just try to use very lipid-rich emollients," Dr. Thyssen said.
Filaggrin mutations in atopic dermatitis patients have been associated with allergic rhinitis and asthma, Dr. Thyssen said. Deficient patients also may be more susceptible to sun sensitivity, skin dehydration, skin infections, food allergies, and. contact dermatitis. The reason for these associations remains unclear; perhaps allergens have an easier time penetrating the skin and engaging the immune system when filaggrin is lacking, he said. Patients also seem to self-select for careers that avoid skin irritants such as nickel, he added.
Research is ongoing to devise treatments that directly correct the deficiency. However, it is likely that atopic dermatitis represents "many diseases with one face," said Dr. Thyssen. "Today, we treat all cases the same, but we are beginning to dissect" the various factors at play in individuals, and may one day be able to individualize treatment approaches, he said.
Dr. Thyssen had no relevant disclosures.
SDEF and this news organization are owned by Frontline Medical Communications.
AT SDEF LAS VEGAS DERMATOLOGY SEMINAR
Replace Narcotics for Skin Pain
LAS VEGAS – A topical mixture of amitriptyline and ketamine controls pain in a variety of skin conditions, even when more traditional options fail, according to Dr. Mark Davis, chair of the division of clinical dermatology at the Mayo Clinic in Rochester, Minn.
"We are getting patients off systemic narcotics with these mixtures," he said at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
Lidocaine patches are allowing leg ulcer patients to drop narcotics, too, and are greatly helping those with erythromelalgia, an often-misdiagnosed condition involving intermittent and excruciating, burning pain in the feet, hands, and sometimes ears. "To have something topical [for such pain] is terrific," Dr. Davis said.
The Mayo Clinic uses topical amitriptyline and ketamine for brachioradial pruritus, erythromelalgia, rectogenital and perineal pain, and other localized skin pain recalcitrant to oral medications and other standard approaches. Dr. Davis and his colleagues recently published several reviews and retrospective studies on the use of topical pain relievers, including a recent article showing that more than half the patients who used topical amitriptyline-ketamine for pain reported substantial or complete relief (Pain Physician 2012;15:485-8).
Pharmaceutical companies are working to bring the combination to market, but it’s not yet available commercially, so Mayo Clinic dermatologists have their pharmacists compound it in two strengths – 2% amitriptyline and either 0.5% or 5% ketamine – using Lipoderm cream as the base, according to Dr. Davis. Patients apply the mixture three times daily. Why it works isn’t clear; the drugs have different and perhaps synergistic effects on skin pain.
"I try to get people to use it [the product] on small parts of the body, such as the hands and feet, and, in patients with brachioradial pruritus, both arms," said Dr. Davis. "I’ve never used it any more extensively than that; I am afraid patients would absorb too much ketamine," he said.
Of more than 1,000 Mayo Clinic patients who have tried the combination, "I’d say less than 1% has told me that they’ve ever had a side effect," he said. "I’ve had just two or three patients tell me they’ve gotten nightmares," a known effect of ketamine. "This is a product that has great promise," he noted.
Meanwhile, some erythromelalgia patients at the Mayo Clinic have been able to walk again after applying lidocaine patches to their feet, and the clinicians there consider the patches first-line treatment for the condition. "Many patients are well controlled just by using [the patches], and I don’t think I’ve come across any side effects in the hundreds of patients I’ve treated," Dr. Davis said. In the inherited form of the disease, which accounts for perhaps 5% of cases, erythromelalgia is caused by a genetic sodium channel glitch that keeps nerves in the skin firing once they are stimulated.
Lidocaine patches also are "really useful for patients with bad, painful ulcers; I use [them] over whatever wound care I am using," Dr. Davis noted. Sometimes these patients can discontinue, or at least reduce, their use of narcotics, he said.
Lidocaine helps with debridement, too. "For leg ulcers, our nurses take 4 x 4-inch gauze and soak it in lidocaine 4% solution, and leave it on the ulcer for about 20 minutes. We are usually able to debride those ulcers [after that] even if they were very painful to start," he said.
Dr. Davis has no relevant disclosures. SDEF and this news organization are owned by Frontline Medical Communications.
LAS VEGAS – A topical mixture of amitriptyline and ketamine controls pain in a variety of skin conditions, even when more traditional options fail, according to Dr. Mark Davis, chair of the division of clinical dermatology at the Mayo Clinic in Rochester, Minn.
"We are getting patients off systemic narcotics with these mixtures," he said at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
Lidocaine patches are allowing leg ulcer patients to drop narcotics, too, and are greatly helping those with erythromelalgia, an often-misdiagnosed condition involving intermittent and excruciating, burning pain in the feet, hands, and sometimes ears. "To have something topical [for such pain] is terrific," Dr. Davis said.
The Mayo Clinic uses topical amitriptyline and ketamine for brachioradial pruritus, erythromelalgia, rectogenital and perineal pain, and other localized skin pain recalcitrant to oral medications and other standard approaches. Dr. Davis and his colleagues recently published several reviews and retrospective studies on the use of topical pain relievers, including a recent article showing that more than half the patients who used topical amitriptyline-ketamine for pain reported substantial or complete relief (Pain Physician 2012;15:485-8).
Pharmaceutical companies are working to bring the combination to market, but it’s not yet available commercially, so Mayo Clinic dermatologists have their pharmacists compound it in two strengths – 2% amitriptyline and either 0.5% or 5% ketamine – using Lipoderm cream as the base, according to Dr. Davis. Patients apply the mixture three times daily. Why it works isn’t clear; the drugs have different and perhaps synergistic effects on skin pain.
"I try to get people to use it [the product] on small parts of the body, such as the hands and feet, and, in patients with brachioradial pruritus, both arms," said Dr. Davis. "I’ve never used it any more extensively than that; I am afraid patients would absorb too much ketamine," he said.
Of more than 1,000 Mayo Clinic patients who have tried the combination, "I’d say less than 1% has told me that they’ve ever had a side effect," he said. "I’ve had just two or three patients tell me they’ve gotten nightmares," a known effect of ketamine. "This is a product that has great promise," he noted.
Meanwhile, some erythromelalgia patients at the Mayo Clinic have been able to walk again after applying lidocaine patches to their feet, and the clinicians there consider the patches first-line treatment for the condition. "Many patients are well controlled just by using [the patches], and I don’t think I’ve come across any side effects in the hundreds of patients I’ve treated," Dr. Davis said. In the inherited form of the disease, which accounts for perhaps 5% of cases, erythromelalgia is caused by a genetic sodium channel glitch that keeps nerves in the skin firing once they are stimulated.
Lidocaine patches also are "really useful for patients with bad, painful ulcers; I use [them] over whatever wound care I am using," Dr. Davis noted. Sometimes these patients can discontinue, or at least reduce, their use of narcotics, he said.
Lidocaine helps with debridement, too. "For leg ulcers, our nurses take 4 x 4-inch gauze and soak it in lidocaine 4% solution, and leave it on the ulcer for about 20 minutes. We are usually able to debride those ulcers [after that] even if they were very painful to start," he said.
Dr. Davis has no relevant disclosures. SDEF and this news organization are owned by Frontline Medical Communications.
LAS VEGAS – A topical mixture of amitriptyline and ketamine controls pain in a variety of skin conditions, even when more traditional options fail, according to Dr. Mark Davis, chair of the division of clinical dermatology at the Mayo Clinic in Rochester, Minn.
"We are getting patients off systemic narcotics with these mixtures," he said at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
Lidocaine patches are allowing leg ulcer patients to drop narcotics, too, and are greatly helping those with erythromelalgia, an often-misdiagnosed condition involving intermittent and excruciating, burning pain in the feet, hands, and sometimes ears. "To have something topical [for such pain] is terrific," Dr. Davis said.
The Mayo Clinic uses topical amitriptyline and ketamine for brachioradial pruritus, erythromelalgia, rectogenital and perineal pain, and other localized skin pain recalcitrant to oral medications and other standard approaches. Dr. Davis and his colleagues recently published several reviews and retrospective studies on the use of topical pain relievers, including a recent article showing that more than half the patients who used topical amitriptyline-ketamine for pain reported substantial or complete relief (Pain Physician 2012;15:485-8).
Pharmaceutical companies are working to bring the combination to market, but it’s not yet available commercially, so Mayo Clinic dermatologists have their pharmacists compound it in two strengths – 2% amitriptyline and either 0.5% or 5% ketamine – using Lipoderm cream as the base, according to Dr. Davis. Patients apply the mixture three times daily. Why it works isn’t clear; the drugs have different and perhaps synergistic effects on skin pain.
"I try to get people to use it [the product] on small parts of the body, such as the hands and feet, and, in patients with brachioradial pruritus, both arms," said Dr. Davis. "I’ve never used it any more extensively than that; I am afraid patients would absorb too much ketamine," he said.
Of more than 1,000 Mayo Clinic patients who have tried the combination, "I’d say less than 1% has told me that they’ve ever had a side effect," he said. "I’ve had just two or three patients tell me they’ve gotten nightmares," a known effect of ketamine. "This is a product that has great promise," he noted.
Meanwhile, some erythromelalgia patients at the Mayo Clinic have been able to walk again after applying lidocaine patches to their feet, and the clinicians there consider the patches first-line treatment for the condition. "Many patients are well controlled just by using [the patches], and I don’t think I’ve come across any side effects in the hundreds of patients I’ve treated," Dr. Davis said. In the inherited form of the disease, which accounts for perhaps 5% of cases, erythromelalgia is caused by a genetic sodium channel glitch that keeps nerves in the skin firing once they are stimulated.
Lidocaine patches also are "really useful for patients with bad, painful ulcers; I use [them] over whatever wound care I am using," Dr. Davis noted. Sometimes these patients can discontinue, or at least reduce, their use of narcotics, he said.
Lidocaine helps with debridement, too. "For leg ulcers, our nurses take 4 x 4-inch gauze and soak it in lidocaine 4% solution, and leave it on the ulcer for about 20 minutes. We are usually able to debride those ulcers [after that] even if they were very painful to start," he said.
Dr. Davis has no relevant disclosures. SDEF and this news organization are owned by Frontline Medical Communications.
EXPERT ANALYSIS FROM THE SDEF LAS VEGAS DERMATOLOGY SEMINAR
Creams and patches can replace narcotics for skin pain
LAS VEGAS – A topical mixture of amitriptyline and ketamine controls pain in a variety of skin conditions, even when more traditional options fail, according to Dr. Mark Davis, chair of the division of clinical dermatology at the Mayo Clinic in Rochester, Minn.
"We are getting patients off systemic narcotics with these mixtures," he said at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
Lidocaine patches are allowing leg ulcer patients to drop narcotics, too, and are greatly helping those with erythromelalgia, an often-misdiagnosed condition involving intermittent and excruciating, burning pain in the feet, hands, and sometimes ears. "To have something topical [for such pain] is terrific," Dr. Davis said.
The Mayo Clinic uses topical amitriptyline and ketamine for brachioradial pruritus, erythromelalgia, rectogenital and perineal pain, and other localized skin pain recalcitrant to oral medications and other standard approaches. Dr. Davis and his colleagues recently published several reviews and retrospective studies on the use of topical pain relievers, including a recent article showing that more than half the patients who used topical amitriptyline-ketamine for pain reported substantial or complete relief (Pain Physician 2012;15:485-8).
Pharmaceutical companies are working to bring the combination to market, but it’s not yet available commercially, so Mayo Clinic dermatologists have their pharmacists compound it in two strengths – 2% amitriptyline and either 0.5% or 5% ketamine – using Lipoderm cream as the base, according to Dr. Davis. Patients apply the mixture three times daily. Why it works isn’t clear; the drugs have different and perhaps synergistic effects on skin pain.
"I try to get people to use it [the product] on small parts of the body, such as the hands and feet, and, in patients with brachioradial pruritus, both arms," said Dr. Davis. "I’ve never used it any more extensively than that; I am afraid patients would absorb too much ketamine," he said.
Of more than 1,000 Mayo Clinic patients who have tried the combination, "I’d say less than 1% has told me that they’ve ever had a side effect," he said. "I’ve had just two or three patients tell me they’ve gotten nightmares," a known effect of ketamine. "This is a product that has great promise," he noted.
Meanwhile, some erythromelalgia patients at the Mayo Clinic have been able to walk again after applying lidocaine patches to their feet, and the clinicians there consider the patches first-line treatment for the condition. "Many patients are well controlled just by using [the patches], and I don’t think I’ve come across any side effects in the hundreds of patients I’ve treated," Dr. Davis said. In the inherited form of the disease, which accounts for perhaps 5% of cases, erythromelalgia is caused by a genetic sodium channel glitch that keeps nerves in the skin firing once they are stimulated.
Lidocaine patches also are "really useful for patients with bad, painful ulcers; I use [them] over whatever wound care I am using," Dr. Davis noted. Sometimes these patients can discontinue, or at least reduce, their use of narcotics, he said.
Lidocaine helps with debridement, too. "For leg ulcers, our nurses take 4 x 4-inch gauze and soak it in lidocaine 4% solution, and leave it on the ulcer for about 20 minutes. We are usually able to debride those ulcers [after that] even if they were very painful to start," he said.
Dr. Davis has no relevant disclosures. SDEF and this news organization are owned by Frontline Medical Communications.
LAS VEGAS – A topical mixture of amitriptyline and ketamine controls pain in a variety of skin conditions, even when more traditional options fail, according to Dr. Mark Davis, chair of the division of clinical dermatology at the Mayo Clinic in Rochester, Minn.
"We are getting patients off systemic narcotics with these mixtures," he said at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
Lidocaine patches are allowing leg ulcer patients to drop narcotics, too, and are greatly helping those with erythromelalgia, an often-misdiagnosed condition involving intermittent and excruciating, burning pain in the feet, hands, and sometimes ears. "To have something topical [for such pain] is terrific," Dr. Davis said.
The Mayo Clinic uses topical amitriptyline and ketamine for brachioradial pruritus, erythromelalgia, rectogenital and perineal pain, and other localized skin pain recalcitrant to oral medications and other standard approaches. Dr. Davis and his colleagues recently published several reviews and retrospective studies on the use of topical pain relievers, including a recent article showing that more than half the patients who used topical amitriptyline-ketamine for pain reported substantial or complete relief (Pain Physician 2012;15:485-8).
Pharmaceutical companies are working to bring the combination to market, but it’s not yet available commercially, so Mayo Clinic dermatologists have their pharmacists compound it in two strengths – 2% amitriptyline and either 0.5% or 5% ketamine – using Lipoderm cream as the base, according to Dr. Davis. Patients apply the mixture three times daily. Why it works isn’t clear; the drugs have different and perhaps synergistic effects on skin pain.
"I try to get people to use it [the product] on small parts of the body, such as the hands and feet, and, in patients with brachioradial pruritus, both arms," said Dr. Davis. "I’ve never used it any more extensively than that; I am afraid patients would absorb too much ketamine," he said.
Of more than 1,000 Mayo Clinic patients who have tried the combination, "I’d say less than 1% has told me that they’ve ever had a side effect," he said. "I’ve had just two or three patients tell me they’ve gotten nightmares," a known effect of ketamine. "This is a product that has great promise," he noted.
Meanwhile, some erythromelalgia patients at the Mayo Clinic have been able to walk again after applying lidocaine patches to their feet, and the clinicians there consider the patches first-line treatment for the condition. "Many patients are well controlled just by using [the patches], and I don’t think I’ve come across any side effects in the hundreds of patients I’ve treated," Dr. Davis said. In the inherited form of the disease, which accounts for perhaps 5% of cases, erythromelalgia is caused by a genetic sodium channel glitch that keeps nerves in the skin firing once they are stimulated.
Lidocaine patches also are "really useful for patients with bad, painful ulcers; I use [them] over whatever wound care I am using," Dr. Davis noted. Sometimes these patients can discontinue, or at least reduce, their use of narcotics, he said.
Lidocaine helps with debridement, too. "For leg ulcers, our nurses take 4 x 4-inch gauze and soak it in lidocaine 4% solution, and leave it on the ulcer for about 20 minutes. We are usually able to debride those ulcers [after that] even if they were very painful to start," he said.
Dr. Davis has no relevant disclosures. SDEF and this news organization are owned by Frontline Medical Communications.
LAS VEGAS – A topical mixture of amitriptyline and ketamine controls pain in a variety of skin conditions, even when more traditional options fail, according to Dr. Mark Davis, chair of the division of clinical dermatology at the Mayo Clinic in Rochester, Minn.
"We are getting patients off systemic narcotics with these mixtures," he said at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
Lidocaine patches are allowing leg ulcer patients to drop narcotics, too, and are greatly helping those with erythromelalgia, an often-misdiagnosed condition involving intermittent and excruciating, burning pain in the feet, hands, and sometimes ears. "To have something topical [for such pain] is terrific," Dr. Davis said.
The Mayo Clinic uses topical amitriptyline and ketamine for brachioradial pruritus, erythromelalgia, rectogenital and perineal pain, and other localized skin pain recalcitrant to oral medications and other standard approaches. Dr. Davis and his colleagues recently published several reviews and retrospective studies on the use of topical pain relievers, including a recent article showing that more than half the patients who used topical amitriptyline-ketamine for pain reported substantial or complete relief (Pain Physician 2012;15:485-8).
Pharmaceutical companies are working to bring the combination to market, but it’s not yet available commercially, so Mayo Clinic dermatologists have their pharmacists compound it in two strengths – 2% amitriptyline and either 0.5% or 5% ketamine – using Lipoderm cream as the base, according to Dr. Davis. Patients apply the mixture three times daily. Why it works isn’t clear; the drugs have different and perhaps synergistic effects on skin pain.
"I try to get people to use it [the product] on small parts of the body, such as the hands and feet, and, in patients with brachioradial pruritus, both arms," said Dr. Davis. "I’ve never used it any more extensively than that; I am afraid patients would absorb too much ketamine," he said.
Of more than 1,000 Mayo Clinic patients who have tried the combination, "I’d say less than 1% has told me that they’ve ever had a side effect," he said. "I’ve had just two or three patients tell me they’ve gotten nightmares," a known effect of ketamine. "This is a product that has great promise," he noted.
Meanwhile, some erythromelalgia patients at the Mayo Clinic have been able to walk again after applying lidocaine patches to their feet, and the clinicians there consider the patches first-line treatment for the condition. "Many patients are well controlled just by using [the patches], and I don’t think I’ve come across any side effects in the hundreds of patients I’ve treated," Dr. Davis said. In the inherited form of the disease, which accounts for perhaps 5% of cases, erythromelalgia is caused by a genetic sodium channel glitch that keeps nerves in the skin firing once they are stimulated.
Lidocaine patches also are "really useful for patients with bad, painful ulcers; I use [them] over whatever wound care I am using," Dr. Davis noted. Sometimes these patients can discontinue, or at least reduce, their use of narcotics, he said.
Lidocaine helps with debridement, too. "For leg ulcers, our nurses take 4 x 4-inch gauze and soak it in lidocaine 4% solution, and leave it on the ulcer for about 20 minutes. We are usually able to debride those ulcers [after that] even if they were very painful to start," he said.
Dr. Davis has no relevant disclosures. SDEF and this news organization are owned by Frontline Medical Communications.
EXPERT ANALYSIS FROM THE SDEF LAS VEGAS DERMATOLOGY SEMINAR
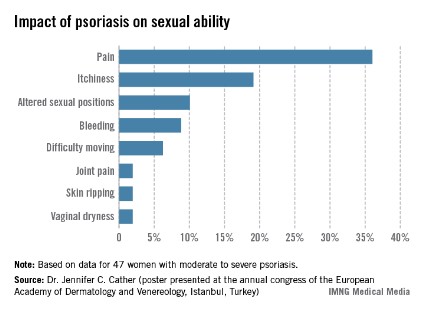
Impact of psoriasis on sexual activity
One third of a group of women with psoriasis reported that the pain associated with their condition interfered with their sexual activity, according to findings from a survey presented by Dr. Jennifer C. Cather.
Based on responses from a survey of 60 women with moderate to severe psoriasis, the specific complaints that were the most common ways in which psoriasis interfered with sexual activity were itchiness (19%), the need to adjust sexual position (10%), and bleeding (9%), Dr. Cather reported at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar. The survey was part of an effort to determine the impact of psoriasis on women’s sexual activity, desires, and relationships.
The data were previously presented in a poster at the annual congress of the European Academy of Dermatology and Venereology (Istanbul.
SDEF and this news organization are owned by Frontline Medical Communications. Dr. Cather disclosed that she is a consultant, speaker, or researcher for AbbVie, Novartis, Leo, Janssen, Amgen, Celgene, Merck, and Pfizer.
One third of a group of women with psoriasis reported that the pain associated with their condition interfered with their sexual activity, according to findings from a survey presented by Dr. Jennifer C. Cather.
Based on responses from a survey of 60 women with moderate to severe psoriasis, the specific complaints that were the most common ways in which psoriasis interfered with sexual activity were itchiness (19%), the need to adjust sexual position (10%), and bleeding (9%), Dr. Cather reported at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar. The survey was part of an effort to determine the impact of psoriasis on women’s sexual activity, desires, and relationships.
The data were previously presented in a poster at the annual congress of the European Academy of Dermatology and Venereology (Istanbul.
SDEF and this news organization are owned by Frontline Medical Communications. Dr. Cather disclosed that she is a consultant, speaker, or researcher for AbbVie, Novartis, Leo, Janssen, Amgen, Celgene, Merck, and Pfizer.
One third of a group of women with psoriasis reported that the pain associated with their condition interfered with their sexual activity, according to findings from a survey presented by Dr. Jennifer C. Cather.
Based on responses from a survey of 60 women with moderate to severe psoriasis, the specific complaints that were the most common ways in which psoriasis interfered with sexual activity were itchiness (19%), the need to adjust sexual position (10%), and bleeding (9%), Dr. Cather reported at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar. The survey was part of an effort to determine the impact of psoriasis on women’s sexual activity, desires, and relationships.
The data were previously presented in a poster at the annual congress of the European Academy of Dermatology and Venereology (Istanbul.
SDEF and this news organization are owned by Frontline Medical Communications. Dr. Cather disclosed that she is a consultant, speaker, or researcher for AbbVie, Novartis, Leo, Janssen, Amgen, Celgene, Merck, and Pfizer.
EXPERT ANALYSIS FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR
Women’s Sexuality Diminished by Psoriasis
LAS VEGAS – Psoriasis has a negative impact on women’s sexual desire, sexual ability, and sexual relationships, according to Dr. Jennifer Cather of the Modern Dermatology-Aesthetics Center in Dallas.
Dr. Cather and her colleagues are developing a clinical tool to assess the disease’s sexual impact; as part of those efforts, they conducted 60 interviews with moderately to severely psoriatic women with a mean age of 41 years.
The survey results showed that sexuality was clearly another reason why it’s important to keep psoriasis in check. Pain and itchiness during sex, self-consciousness and embarrassment, and avoidance of dating and intimate relationships were among the most common problems the women reported.
"We really didn’t appreciate the impact psoriasis had on relationships" before the survey, Dr. Cather said at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar. "The sexual impact has been underappreciated," she said.
Those problems might help explain why women with psoriasis, especially those aged younger than 35 years, tend to have fewer babies, she added. Psoriatic women also have higher rates of induced and spontaneous abortions and are more likely to have preterm and underweight births.
Some of the women surveyed said that they worried about passing psoriasis to their children. "Maybe there’s voluntary childlessness," Dr. Cather said. But when women in her practice mention they don’t want kids for fear of passing on the disease, "I answer right back, ‘You don’t have to have what you have. I can help you with it,’ " she said.
Methotrexate, acitretin, and psoralen photochemotherapy (PUVA) are contraindicated during pregnancy, but ultraviolet B (UVB) treatments are safe, said Dr. Cather. She also uses tumor necrosis factor inhibitors, which are FDA pregnancy category B agents; she prefers etanercept for its short half-life (just over 4 days) and because ob.gyns. are usually familiar with it. The Organization of Teratology Information Specialists (OTIS) keeps the etanercept and adalimumab pregnancy registries, and "there’s [been] no signal to date" for those drugs, she said.
Psoriatic women should know that the odds are with them for having a normal pregnancy, and that pregnancy is likely to help clear their skin, Dr. Cather said.
But because half of the pregnancies in the United States are unplanned, it’s important to discuss pregnancy – and psoriasis treatment during pregnancy – as part of routine care. "It’s difficult if a psoriasis patient calls you in a panic because they’re not sure their drug is safe, and not sure their doctor will let them continue it,’ she said. Some ob.gyns. are comfortable with letting women stay on their psoriasis therapy, while others want them to quit everything, even topical steroids.
"In my clinic, when a psoriasis patient gets pregnant, usually we’ve planned for it and are excited about it, and we’ve had some dialogue with the ob.gyn.," she explained.
SDEF and this news organization are owned by Frontline Medical Communications. Dr. Cather is a consultant, speaker, or researcher for AbbVie, Novartis, Leo, Janssen, Amgen, Celgene, Merck, and Pfizer.
LAS VEGAS – Psoriasis has a negative impact on women’s sexual desire, sexual ability, and sexual relationships, according to Dr. Jennifer Cather of the Modern Dermatology-Aesthetics Center in Dallas.
Dr. Cather and her colleagues are developing a clinical tool to assess the disease’s sexual impact; as part of those efforts, they conducted 60 interviews with moderately to severely psoriatic women with a mean age of 41 years.
The survey results showed that sexuality was clearly another reason why it’s important to keep psoriasis in check. Pain and itchiness during sex, self-consciousness and embarrassment, and avoidance of dating and intimate relationships were among the most common problems the women reported.
"We really didn’t appreciate the impact psoriasis had on relationships" before the survey, Dr. Cather said at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar. "The sexual impact has been underappreciated," she said.
Those problems might help explain why women with psoriasis, especially those aged younger than 35 years, tend to have fewer babies, she added. Psoriatic women also have higher rates of induced and spontaneous abortions and are more likely to have preterm and underweight births.
Some of the women surveyed said that they worried about passing psoriasis to their children. "Maybe there’s voluntary childlessness," Dr. Cather said. But when women in her practice mention they don’t want kids for fear of passing on the disease, "I answer right back, ‘You don’t have to have what you have. I can help you with it,’ " she said.
Methotrexate, acitretin, and psoralen photochemotherapy (PUVA) are contraindicated during pregnancy, but ultraviolet B (UVB) treatments are safe, said Dr. Cather. She also uses tumor necrosis factor inhibitors, which are FDA pregnancy category B agents; she prefers etanercept for its short half-life (just over 4 days) and because ob.gyns. are usually familiar with it. The Organization of Teratology Information Specialists (OTIS) keeps the etanercept and adalimumab pregnancy registries, and "there’s [been] no signal to date" for those drugs, she said.
Psoriatic women should know that the odds are with them for having a normal pregnancy, and that pregnancy is likely to help clear their skin, Dr. Cather said.
But because half of the pregnancies in the United States are unplanned, it’s important to discuss pregnancy – and psoriasis treatment during pregnancy – as part of routine care. "It’s difficult if a psoriasis patient calls you in a panic because they’re not sure their drug is safe, and not sure their doctor will let them continue it,’ she said. Some ob.gyns. are comfortable with letting women stay on their psoriasis therapy, while others want them to quit everything, even topical steroids.
"In my clinic, when a psoriasis patient gets pregnant, usually we’ve planned for it and are excited about it, and we’ve had some dialogue with the ob.gyn.," she explained.
SDEF and this news organization are owned by Frontline Medical Communications. Dr. Cather is a consultant, speaker, or researcher for AbbVie, Novartis, Leo, Janssen, Amgen, Celgene, Merck, and Pfizer.
LAS VEGAS – Psoriasis has a negative impact on women’s sexual desire, sexual ability, and sexual relationships, according to Dr. Jennifer Cather of the Modern Dermatology-Aesthetics Center in Dallas.
Dr. Cather and her colleagues are developing a clinical tool to assess the disease’s sexual impact; as part of those efforts, they conducted 60 interviews with moderately to severely psoriatic women with a mean age of 41 years.
The survey results showed that sexuality was clearly another reason why it’s important to keep psoriasis in check. Pain and itchiness during sex, self-consciousness and embarrassment, and avoidance of dating and intimate relationships were among the most common problems the women reported.
"We really didn’t appreciate the impact psoriasis had on relationships" before the survey, Dr. Cather said at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar. "The sexual impact has been underappreciated," she said.
Those problems might help explain why women with psoriasis, especially those aged younger than 35 years, tend to have fewer babies, she added. Psoriatic women also have higher rates of induced and spontaneous abortions and are more likely to have preterm and underweight births.
Some of the women surveyed said that they worried about passing psoriasis to their children. "Maybe there’s voluntary childlessness," Dr. Cather said. But when women in her practice mention they don’t want kids for fear of passing on the disease, "I answer right back, ‘You don’t have to have what you have. I can help you with it,’ " she said.
Methotrexate, acitretin, and psoralen photochemotherapy (PUVA) are contraindicated during pregnancy, but ultraviolet B (UVB) treatments are safe, said Dr. Cather. She also uses tumor necrosis factor inhibitors, which are FDA pregnancy category B agents; she prefers etanercept for its short half-life (just over 4 days) and because ob.gyns. are usually familiar with it. The Organization of Teratology Information Specialists (OTIS) keeps the etanercept and adalimumab pregnancy registries, and "there’s [been] no signal to date" for those drugs, she said.
Psoriatic women should know that the odds are with them for having a normal pregnancy, and that pregnancy is likely to help clear their skin, Dr. Cather said.
But because half of the pregnancies in the United States are unplanned, it’s important to discuss pregnancy – and psoriasis treatment during pregnancy – as part of routine care. "It’s difficult if a psoriasis patient calls you in a panic because they’re not sure their drug is safe, and not sure their doctor will let them continue it,’ she said. Some ob.gyns. are comfortable with letting women stay on their psoriasis therapy, while others want them to quit everything, even topical steroids.
"In my clinic, when a psoriasis patient gets pregnant, usually we’ve planned for it and are excited about it, and we’ve had some dialogue with the ob.gyn.," she explained.
SDEF and this news organization are owned by Frontline Medical Communications. Dr. Cather is a consultant, speaker, or researcher for AbbVie, Novartis, Leo, Janssen, Amgen, Celgene, Merck, and Pfizer.
EXPERT ANALYSIS FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR
Women’s sexuality diminished by psoriasis
LAS VEGAS – Psoriasis has a negative impact on women’s sexual desire, sexual ability, and sexual relationships, according to Dr. Jennifer Cather of the Modern Dermatology-Aesthetics Center in Dallas.
Dr. Cather and her colleagues are developing a clinical tool to assess the disease’s sexual impact; as part of those efforts, they conducted 60 interviews with moderately to severely psoriatic women with a mean age of 41 years.
The survey results showed that sexuality was clearly another reason why it’s important to keep psoriasis in check. Pain and itchiness during sex, self-consciousness and embarrassment, and avoidance of dating and intimate relationships were among the most common problems the women reported.
"We really didn’t appreciate the impact psoriasis had on relationships" before the survey, Dr. Cather said at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar. "The sexual impact has been underappreciated," she said.
Those problems might help explain why women with psoriasis, especially those aged younger than 35 years, tend to have fewer babies, she added. Psoriatic women also have higher rates of induced and spontaneous abortions and are more likely to have preterm and underweight births.
Some of the women surveyed said that they worried about passing psoriasis to their children. "Maybe there’s voluntary childlessness," Dr. Cather said. But when women in her practice mention they don’t want kids for fear of passing on the disease, "I answer right back, ‘You don’t have to have what you have. I can help you with it,’ " she said.
Methotrexate, acitretin, and psoralen photochemotherapy (PUVA) are contraindicated during pregnancy, but ultraviolet B (UVB) treatments are safe, said Dr. Cather. She also uses tumor necrosis factor inhibitors, which are FDA pregnancy category B agents; she prefers etanercept for its short half-life (just over 4 days) and because ob.gyns. are usually familiar with it. The Organization of Teratology Information Specialists (OTIS) keeps the etanercept and adalimumab pregnancy registries, and "there’s [been] no signal to date" for those drugs, she said.
Psoriatic women should know that the odds are with them for having a normal pregnancy, and that pregnancy is likely to help clear their skin, Dr. Cather said.
But because half of the pregnancies in the United States are unplanned, it’s important to discuss pregnancy – and psoriasis treatment during pregnancy – as part of routine care. "It’s difficult if a psoriasis patient calls you in a panic because they’re not sure their drug is safe, and not sure their doctor will let them continue it,’ she said. Some ob.gyns. are comfortable with letting women stay on their psoriasis therapy, while others want them to quit everything, even topical steroids.
"In my clinic, when a psoriasis patient gets pregnant, usually we’ve planned for it and are excited about it, and we’ve had some dialogue with the ob.gyn.," she explained.
SDEF and this news organization are owned by Frontline Medical Communications. Dr. Cather is a consultant, speaker, or researcher for AbbVie, Novartis, Leo, Janssen, Amgen, Celgene, Merck, and Pfizer.
LAS VEGAS – Psoriasis has a negative impact on women’s sexual desire, sexual ability, and sexual relationships, according to Dr. Jennifer Cather of the Modern Dermatology-Aesthetics Center in Dallas.
Dr. Cather and her colleagues are developing a clinical tool to assess the disease’s sexual impact; as part of those efforts, they conducted 60 interviews with moderately to severely psoriatic women with a mean age of 41 years.
The survey results showed that sexuality was clearly another reason why it’s important to keep psoriasis in check. Pain and itchiness during sex, self-consciousness and embarrassment, and avoidance of dating and intimate relationships were among the most common problems the women reported.
"We really didn’t appreciate the impact psoriasis had on relationships" before the survey, Dr. Cather said at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar. "The sexual impact has been underappreciated," she said.
Those problems might help explain why women with psoriasis, especially those aged younger than 35 years, tend to have fewer babies, she added. Psoriatic women also have higher rates of induced and spontaneous abortions and are more likely to have preterm and underweight births.
Some of the women surveyed said that they worried about passing psoriasis to their children. "Maybe there’s voluntary childlessness," Dr. Cather said. But when women in her practice mention they don’t want kids for fear of passing on the disease, "I answer right back, ‘You don’t have to have what you have. I can help you with it,’ " she said.
Methotrexate, acitretin, and psoralen photochemotherapy (PUVA) are contraindicated during pregnancy, but ultraviolet B (UVB) treatments are safe, said Dr. Cather. She also uses tumor necrosis factor inhibitors, which are FDA pregnancy category B agents; she prefers etanercept for its short half-life (just over 4 days) and because ob.gyns. are usually familiar with it. The Organization of Teratology Information Specialists (OTIS) keeps the etanercept and adalimumab pregnancy registries, and "there’s [been] no signal to date" for those drugs, she said.
Psoriatic women should know that the odds are with them for having a normal pregnancy, and that pregnancy is likely to help clear their skin, Dr. Cather said.
But because half of the pregnancies in the United States are unplanned, it’s important to discuss pregnancy – and psoriasis treatment during pregnancy – as part of routine care. "It’s difficult if a psoriasis patient calls you in a panic because they’re not sure their drug is safe, and not sure their doctor will let them continue it,’ she said. Some ob.gyns. are comfortable with letting women stay on their psoriasis therapy, while others want them to quit everything, even topical steroids.
"In my clinic, when a psoriasis patient gets pregnant, usually we’ve planned for it and are excited about it, and we’ve had some dialogue with the ob.gyn.," she explained.
SDEF and this news organization are owned by Frontline Medical Communications. Dr. Cather is a consultant, speaker, or researcher for AbbVie, Novartis, Leo, Janssen, Amgen, Celgene, Merck, and Pfizer.
LAS VEGAS – Psoriasis has a negative impact on women’s sexual desire, sexual ability, and sexual relationships, according to Dr. Jennifer Cather of the Modern Dermatology-Aesthetics Center in Dallas.
Dr. Cather and her colleagues are developing a clinical tool to assess the disease’s sexual impact; as part of those efforts, they conducted 60 interviews with moderately to severely psoriatic women with a mean age of 41 years.
The survey results showed that sexuality was clearly another reason why it’s important to keep psoriasis in check. Pain and itchiness during sex, self-consciousness and embarrassment, and avoidance of dating and intimate relationships were among the most common problems the women reported.
"We really didn’t appreciate the impact psoriasis had on relationships" before the survey, Dr. Cather said at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar. "The sexual impact has been underappreciated," she said.
Those problems might help explain why women with psoriasis, especially those aged younger than 35 years, tend to have fewer babies, she added. Psoriatic women also have higher rates of induced and spontaneous abortions and are more likely to have preterm and underweight births.
Some of the women surveyed said that they worried about passing psoriasis to their children. "Maybe there’s voluntary childlessness," Dr. Cather said. But when women in her practice mention they don’t want kids for fear of passing on the disease, "I answer right back, ‘You don’t have to have what you have. I can help you with it,’ " she said.
Methotrexate, acitretin, and psoralen photochemotherapy (PUVA) are contraindicated during pregnancy, but ultraviolet B (UVB) treatments are safe, said Dr. Cather. She also uses tumor necrosis factor inhibitors, which are FDA pregnancy category B agents; she prefers etanercept for its short half-life (just over 4 days) and because ob.gyns. are usually familiar with it. The Organization of Teratology Information Specialists (OTIS) keeps the etanercept and adalimumab pregnancy registries, and "there’s [been] no signal to date" for those drugs, she said.
Psoriatic women should know that the odds are with them for having a normal pregnancy, and that pregnancy is likely to help clear their skin, Dr. Cather said.
But because half of the pregnancies in the United States are unplanned, it’s important to discuss pregnancy – and psoriasis treatment during pregnancy – as part of routine care. "It’s difficult if a psoriasis patient calls you in a panic because they’re not sure their drug is safe, and not sure their doctor will let them continue it,’ she said. Some ob.gyns. are comfortable with letting women stay on their psoriasis therapy, while others want them to quit everything, even topical steroids.
"In my clinic, when a psoriasis patient gets pregnant, usually we’ve planned for it and are excited about it, and we’ve had some dialogue with the ob.gyn.," she explained.
SDEF and this news organization are owned by Frontline Medical Communications. Dr. Cather is a consultant, speaker, or researcher for AbbVie, Novartis, Leo, Janssen, Amgen, Celgene, Merck, and Pfizer.
EXPERT ANALYSIS FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR
Wet Dressings Work for Pruritus When Other Options Fail
LAS VEGAS – Wet dressing, a technique forgotten in most places but in continual use at the Mayo Clinic for more than 80 years, knocks out intractable pruritus – whatever its cause – in children and adults, according to Dr. Mark Davis, chair of the division of clinical dermatology at the clinic in Rochester, Minn.
"It’s a simple technique that works extraordinarily well for any itchy condition from head to toe, and has virtually no side effects. It stops itching reliably, when nothing else has worked," including prednisone, methotrexate, phototherapy, and elimination diets, among other strategies, he said at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
Even so, "there’s remarkably little on this in the literature, and what’s published is mostly just in kids, but in adults it works brilliantly, too, particularly for atopic dermatitis. We use it when people come in itching from anything, like psoriasis," he said (J. Am. Acad. Dermatol. 2009;60:792-800).
"The commonest question [we hear from people] is ‘I’ve been going to doctors for years. Why didn’t anybody tell me about this?’ " said Dr. Davis.
If their pruritus is severe enough, patients will be admitted to the Mayo Clinic and have wet cloths applied to wherever the itch happens to be – above the waist, below the waist, the feet, or even the entire body, including the face – with a dry blanket on top if needed to ward of the chill. Patients can get up from bed for a bathroom break when the dressings are changed every 3 hours.
Topical steroids are used with the dressings up to three times a day; 1% percent hydrocortisone for the face or genitals, 0.1% or 0.05% triamcinolone elsewhere. The Mayo Clinic has never had a case of hypothalamic-pituitary-adrenal axis suppression with the technique, and insurance usually covers the cost for 3 days, Dr. Davis said.
When outpatient treatment is sufficient, pruritic patients are instructed to put on wet pajamas or long johns, or hop into the shower in dry ones, and then leave them on for 30 minutes to an hour, 3-4 times a day. Nurses, with the help of handouts and videos, teach patients how to do this, and call them every 24 hours to see how they are getting along.
Hospital patients get the same instructions at discharge. "Initially, they have to do [it] at least once a day for a number of weeks, and then they can use [the technique] on an as-needed basis, maybe once or twice a week," Dr. Davis said.
"Wet dressings went out of favor" in most places because "they are just so much trouble," he said. At present, the technique is "largely unknown," as is the reason why it works, he added.
Dr. Davis has no relevant disclosures. SDEF and this news organization are owned by Frontline Medical Communications.
LAS VEGAS – Wet dressing, a technique forgotten in most places but in continual use at the Mayo Clinic for more than 80 years, knocks out intractable pruritus – whatever its cause – in children and adults, according to Dr. Mark Davis, chair of the division of clinical dermatology at the clinic in Rochester, Minn.
"It’s a simple technique that works extraordinarily well for any itchy condition from head to toe, and has virtually no side effects. It stops itching reliably, when nothing else has worked," including prednisone, methotrexate, phototherapy, and elimination diets, among other strategies, he said at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
Even so, "there’s remarkably little on this in the literature, and what’s published is mostly just in kids, but in adults it works brilliantly, too, particularly for atopic dermatitis. We use it when people come in itching from anything, like psoriasis," he said (J. Am. Acad. Dermatol. 2009;60:792-800).
"The commonest question [we hear from people] is ‘I’ve been going to doctors for years. Why didn’t anybody tell me about this?’ " said Dr. Davis.
If their pruritus is severe enough, patients will be admitted to the Mayo Clinic and have wet cloths applied to wherever the itch happens to be – above the waist, below the waist, the feet, or even the entire body, including the face – with a dry blanket on top if needed to ward of the chill. Patients can get up from bed for a bathroom break when the dressings are changed every 3 hours.
Topical steroids are used with the dressings up to three times a day; 1% percent hydrocortisone for the face or genitals, 0.1% or 0.05% triamcinolone elsewhere. The Mayo Clinic has never had a case of hypothalamic-pituitary-adrenal axis suppression with the technique, and insurance usually covers the cost for 3 days, Dr. Davis said.
When outpatient treatment is sufficient, pruritic patients are instructed to put on wet pajamas or long johns, or hop into the shower in dry ones, and then leave them on for 30 minutes to an hour, 3-4 times a day. Nurses, with the help of handouts and videos, teach patients how to do this, and call them every 24 hours to see how they are getting along.
Hospital patients get the same instructions at discharge. "Initially, they have to do [it] at least once a day for a number of weeks, and then they can use [the technique] on an as-needed basis, maybe once or twice a week," Dr. Davis said.
"Wet dressings went out of favor" in most places because "they are just so much trouble," he said. At present, the technique is "largely unknown," as is the reason why it works, he added.
Dr. Davis has no relevant disclosures. SDEF and this news organization are owned by Frontline Medical Communications.
LAS VEGAS – Wet dressing, a technique forgotten in most places but in continual use at the Mayo Clinic for more than 80 years, knocks out intractable pruritus – whatever its cause – in children and adults, according to Dr. Mark Davis, chair of the division of clinical dermatology at the clinic in Rochester, Minn.
"It’s a simple technique that works extraordinarily well for any itchy condition from head to toe, and has virtually no side effects. It stops itching reliably, when nothing else has worked," including prednisone, methotrexate, phototherapy, and elimination diets, among other strategies, he said at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
Even so, "there’s remarkably little on this in the literature, and what’s published is mostly just in kids, but in adults it works brilliantly, too, particularly for atopic dermatitis. We use it when people come in itching from anything, like psoriasis," he said (J. Am. Acad. Dermatol. 2009;60:792-800).
"The commonest question [we hear from people] is ‘I’ve been going to doctors for years. Why didn’t anybody tell me about this?’ " said Dr. Davis.
If their pruritus is severe enough, patients will be admitted to the Mayo Clinic and have wet cloths applied to wherever the itch happens to be – above the waist, below the waist, the feet, or even the entire body, including the face – with a dry blanket on top if needed to ward of the chill. Patients can get up from bed for a bathroom break when the dressings are changed every 3 hours.
Topical steroids are used with the dressings up to three times a day; 1% percent hydrocortisone for the face or genitals, 0.1% or 0.05% triamcinolone elsewhere. The Mayo Clinic has never had a case of hypothalamic-pituitary-adrenal axis suppression with the technique, and insurance usually covers the cost for 3 days, Dr. Davis said.
When outpatient treatment is sufficient, pruritic patients are instructed to put on wet pajamas or long johns, or hop into the shower in dry ones, and then leave them on for 30 minutes to an hour, 3-4 times a day. Nurses, with the help of handouts and videos, teach patients how to do this, and call them every 24 hours to see how they are getting along.
Hospital patients get the same instructions at discharge. "Initially, they have to do [it] at least once a day for a number of weeks, and then they can use [the technique] on an as-needed basis, maybe once or twice a week," Dr. Davis said.
"Wet dressings went out of favor" in most places because "they are just so much trouble," he said. At present, the technique is "largely unknown," as is the reason why it works, he added.
Dr. Davis has no relevant disclosures. SDEF and this news organization are owned by Frontline Medical Communications.
AT SDEF LAS VEGAS DERMATOLOGY SEMINAR
Wet dressings work for pruritus when other options fail
LAS VEGAS – Wet dressing, a technique forgotten in most places but in continual use at the Mayo Clinic for more than 80 years, knocks out intractable pruritus – whatever its cause – in children and adults, according to Dr. Mark Davis, chair of the division of clinical dermatology at the clinic in Rochester, Minn.
"It’s a simple technique that works extraordinarily well for any itchy condition from head to toe, and has virtually no side effects. It stops itching reliably, when nothing else has worked," including prednisone, methotrexate, phototherapy, and elimination diets, among other strategies, he said at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
Even so, "there’s remarkably little on this in the literature, and what’s published is mostly just in kids, but in adults it works brilliantly, too, particularly for atopic dermatitis. We use it when people come in itching from anything, like psoriasis," he said (J. Am. Acad. Dermatol. 2009;60:792-800).
"The commonest question [we hear from people] is ‘I’ve been going to doctors for years. Why didn’t anybody tell me about this?’ " said Dr. Davis.
If their pruritus is severe enough, patients will be admitted to the Mayo Clinic and have wet cloths applied to wherever the itch happens to be – above the waist, below the waist, the feet, or even the entire body, including the face – with a dry blanket on top if needed to ward of the chill. Patients can get up from bed for a bathroom break when the dressings are changed every 3 hours.
Topical steroids are used with the dressings up to three times a day; 1% percent hydrocortisone for the face or genitals, 0.1% or 0.05% triamcinolone elsewhere. The Mayo Clinic has never had a case of hypothalamic-pituitary-adrenal axis suppression with the technique, and insurance usually covers the cost for 3 days, Dr. Davis said.
When outpatient treatment is sufficient, pruritic patients are instructed to put on wet pajamas or long johns, or hop into the shower in dry ones, and then leave them on for 30 minutes to an hour, 3-4 times a day. Nurses, with the help of handouts and videos, teach patients how to do this, and call them every 24 hours to see how they are getting along.
Hospital patients get the same instructions at discharge. "Initially, they have to do [it] at least once a day for a number of weeks, and then they can use [the technique] on an as-needed basis, maybe once or twice a week," Dr. Davis said.
"Wet dressings went out of favor" in most places because "they are just so much trouble," he said. At present, the technique is "largely unknown," as is the reason why it works, he added.
Dr. Davis has no relevant disclosures. SDEF and this news organization are owned by Frontline Medical Communications.
LAS VEGAS – Wet dressing, a technique forgotten in most places but in continual use at the Mayo Clinic for more than 80 years, knocks out intractable pruritus – whatever its cause – in children and adults, according to Dr. Mark Davis, chair of the division of clinical dermatology at the clinic in Rochester, Minn.
"It’s a simple technique that works extraordinarily well for any itchy condition from head to toe, and has virtually no side effects. It stops itching reliably, when nothing else has worked," including prednisone, methotrexate, phototherapy, and elimination diets, among other strategies, he said at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
Even so, "there’s remarkably little on this in the literature, and what’s published is mostly just in kids, but in adults it works brilliantly, too, particularly for atopic dermatitis. We use it when people come in itching from anything, like psoriasis," he said (J. Am. Acad. Dermatol. 2009;60:792-800).
"The commonest question [we hear from people] is ‘I’ve been going to doctors for years. Why didn’t anybody tell me about this?’ " said Dr. Davis.
If their pruritus is severe enough, patients will be admitted to the Mayo Clinic and have wet cloths applied to wherever the itch happens to be – above the waist, below the waist, the feet, or even the entire body, including the face – with a dry blanket on top if needed to ward of the chill. Patients can get up from bed for a bathroom break when the dressings are changed every 3 hours.
Topical steroids are used with the dressings up to three times a day; 1% percent hydrocortisone for the face or genitals, 0.1% or 0.05% triamcinolone elsewhere. The Mayo Clinic has never had a case of hypothalamic-pituitary-adrenal axis suppression with the technique, and insurance usually covers the cost for 3 days, Dr. Davis said.
When outpatient treatment is sufficient, pruritic patients are instructed to put on wet pajamas or long johns, or hop into the shower in dry ones, and then leave them on for 30 minutes to an hour, 3-4 times a day. Nurses, with the help of handouts and videos, teach patients how to do this, and call them every 24 hours to see how they are getting along.
Hospital patients get the same instructions at discharge. "Initially, they have to do [it] at least once a day for a number of weeks, and then they can use [the technique] on an as-needed basis, maybe once or twice a week," Dr. Davis said.
"Wet dressings went out of favor" in most places because "they are just so much trouble," he said. At present, the technique is "largely unknown," as is the reason why it works, he added.
Dr. Davis has no relevant disclosures. SDEF and this news organization are owned by Frontline Medical Communications.
LAS VEGAS – Wet dressing, a technique forgotten in most places but in continual use at the Mayo Clinic for more than 80 years, knocks out intractable pruritus – whatever its cause – in children and adults, according to Dr. Mark Davis, chair of the division of clinical dermatology at the clinic in Rochester, Minn.
"It’s a simple technique that works extraordinarily well for any itchy condition from head to toe, and has virtually no side effects. It stops itching reliably, when nothing else has worked," including prednisone, methotrexate, phototherapy, and elimination diets, among other strategies, he said at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
Even so, "there’s remarkably little on this in the literature, and what’s published is mostly just in kids, but in adults it works brilliantly, too, particularly for atopic dermatitis. We use it when people come in itching from anything, like psoriasis," he said (J. Am. Acad. Dermatol. 2009;60:792-800).
"The commonest question [we hear from people] is ‘I’ve been going to doctors for years. Why didn’t anybody tell me about this?’ " said Dr. Davis.
If their pruritus is severe enough, patients will be admitted to the Mayo Clinic and have wet cloths applied to wherever the itch happens to be – above the waist, below the waist, the feet, or even the entire body, including the face – with a dry blanket on top if needed to ward of the chill. Patients can get up from bed for a bathroom break when the dressings are changed every 3 hours.
Topical steroids are used with the dressings up to three times a day; 1% percent hydrocortisone for the face or genitals, 0.1% or 0.05% triamcinolone elsewhere. The Mayo Clinic has never had a case of hypothalamic-pituitary-adrenal axis suppression with the technique, and insurance usually covers the cost for 3 days, Dr. Davis said.
When outpatient treatment is sufficient, pruritic patients are instructed to put on wet pajamas or long johns, or hop into the shower in dry ones, and then leave them on for 30 minutes to an hour, 3-4 times a day. Nurses, with the help of handouts and videos, teach patients how to do this, and call them every 24 hours to see how they are getting along.
Hospital patients get the same instructions at discharge. "Initially, they have to do [it] at least once a day for a number of weeks, and then they can use [the technique] on an as-needed basis, maybe once or twice a week," Dr. Davis said.
"Wet dressings went out of favor" in most places because "they are just so much trouble," he said. At present, the technique is "largely unknown," as is the reason why it works, he added.
Dr. Davis has no relevant disclosures. SDEF and this news organization are owned by Frontline Medical Communications.
AT SDEF LAS VEGAS DERMATOLOGY SEMINAR
Patient Education on Heart Failure Risk is Crucial in Psoriasis
As evidence supporting an association between psoriasis and cardiovascular disease continues to mount, dermatologists may be the first line of defense in lowering heart failure risk.
"The increased risk of cardiovascular disease for patients with psoriasis may be of a similar magnitude as other well-described CV risk factors, such as uncontrolled hypertension," said Dr. Bruce E. Strober of the University of Connecticut, Farmington. "Further, epidemiological studies show that psoriasis patients have a shortened life expectancy, likely as a result of their experience with CV comorbitidies."
Patient education is essential, he noted at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar. "At the very least, dermatologists should alert patients of the link between psoriasis and CV disease, and remind these patients of the necessity of having a primary care physician who monitors conventional risk factors of CV disease. Patients should be reminded that psoriasis is ‘systemic disease of inflammation’ that creates risks beyond the skin and may shorten life expectancy."
"Dermatologists who care for moderate to severe psoriasis patients should measure blood pressure and draw baseline blood tests assessing for abnormalities of cholesterol, triglycerides, kidney function, liver function, and blood glucose. Abnormalities should prompt an appropriate referral to a primary care physician," he noted.
In a population-based Dutch study presented at the annual congress of the European Society of Cardiology in September, adults with mild psoriasis developed 4.02 cases of new-onset heart failure per 1,000 person-years of follow-up, compared with 4.50/1,000 person-years in patients with severe psoriasis; both of which were significantly higher than the rate of 2.27/1,000 person-years in the general population.
Data from a 2006 study found that diabetes, hypertension, hyperlipidemia, and obesity were more prevalent in psoriasis patients, when compared with controls (J. Am. Acad. Dermatol. 2006;55:829-35). Diabetes and obesity were significantly more prevalent in patients with severe psoriasis, compared with patients with mild psoriasis.
Although the reasons for the increased cardiovascular risk in psoriasis patients remain unknown, possible causes include the use of dyslipidemic therapies, including corticosteroids, acitretin, and cyclosporine, as well as uncontrolled inflammation that could lead to endothelial dysfunction and dyslipidemia, said Dr. Strober. The prevalence of other associated and/or independent risk factors including obesity, hypertension, smoking, and alcohol misuse in psoriasis patients, also could play a role.
Dr. Strober disclosed relationships with multiple pharmaceutical companies including Abbott, Amgen, Janssen, Pfizer, Novartis, and Celgene. SDEF and this news organization are owned by Frontline Medical Communications.
As evidence supporting an association between psoriasis and cardiovascular disease continues to mount, dermatologists may be the first line of defense in lowering heart failure risk.
"The increased risk of cardiovascular disease for patients with psoriasis may be of a similar magnitude as other well-described CV risk factors, such as uncontrolled hypertension," said Dr. Bruce E. Strober of the University of Connecticut, Farmington. "Further, epidemiological studies show that psoriasis patients have a shortened life expectancy, likely as a result of their experience with CV comorbitidies."
Patient education is essential, he noted at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar. "At the very least, dermatologists should alert patients of the link between psoriasis and CV disease, and remind these patients of the necessity of having a primary care physician who monitors conventional risk factors of CV disease. Patients should be reminded that psoriasis is ‘systemic disease of inflammation’ that creates risks beyond the skin and may shorten life expectancy."
"Dermatologists who care for moderate to severe psoriasis patients should measure blood pressure and draw baseline blood tests assessing for abnormalities of cholesterol, triglycerides, kidney function, liver function, and blood glucose. Abnormalities should prompt an appropriate referral to a primary care physician," he noted.
In a population-based Dutch study presented at the annual congress of the European Society of Cardiology in September, adults with mild psoriasis developed 4.02 cases of new-onset heart failure per 1,000 person-years of follow-up, compared with 4.50/1,000 person-years in patients with severe psoriasis; both of which were significantly higher than the rate of 2.27/1,000 person-years in the general population.
Data from a 2006 study found that diabetes, hypertension, hyperlipidemia, and obesity were more prevalent in psoriasis patients, when compared with controls (J. Am. Acad. Dermatol. 2006;55:829-35). Diabetes and obesity were significantly more prevalent in patients with severe psoriasis, compared with patients with mild psoriasis.
Although the reasons for the increased cardiovascular risk in psoriasis patients remain unknown, possible causes include the use of dyslipidemic therapies, including corticosteroids, acitretin, and cyclosporine, as well as uncontrolled inflammation that could lead to endothelial dysfunction and dyslipidemia, said Dr. Strober. The prevalence of other associated and/or independent risk factors including obesity, hypertension, smoking, and alcohol misuse in psoriasis patients, also could play a role.
Dr. Strober disclosed relationships with multiple pharmaceutical companies including Abbott, Amgen, Janssen, Pfizer, Novartis, and Celgene. SDEF and this news organization are owned by Frontline Medical Communications.
As evidence supporting an association between psoriasis and cardiovascular disease continues to mount, dermatologists may be the first line of defense in lowering heart failure risk.
"The increased risk of cardiovascular disease for patients with psoriasis may be of a similar magnitude as other well-described CV risk factors, such as uncontrolled hypertension," said Dr. Bruce E. Strober of the University of Connecticut, Farmington. "Further, epidemiological studies show that psoriasis patients have a shortened life expectancy, likely as a result of their experience with CV comorbitidies."
Patient education is essential, he noted at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar. "At the very least, dermatologists should alert patients of the link between psoriasis and CV disease, and remind these patients of the necessity of having a primary care physician who monitors conventional risk factors of CV disease. Patients should be reminded that psoriasis is ‘systemic disease of inflammation’ that creates risks beyond the skin and may shorten life expectancy."
"Dermatologists who care for moderate to severe psoriasis patients should measure blood pressure and draw baseline blood tests assessing for abnormalities of cholesterol, triglycerides, kidney function, liver function, and blood glucose. Abnormalities should prompt an appropriate referral to a primary care physician," he noted.
In a population-based Dutch study presented at the annual congress of the European Society of Cardiology in September, adults with mild psoriasis developed 4.02 cases of new-onset heart failure per 1,000 person-years of follow-up, compared with 4.50/1,000 person-years in patients with severe psoriasis; both of which were significantly higher than the rate of 2.27/1,000 person-years in the general population.
Data from a 2006 study found that diabetes, hypertension, hyperlipidemia, and obesity were more prevalent in psoriasis patients, when compared with controls (J. Am. Acad. Dermatol. 2006;55:829-35). Diabetes and obesity were significantly more prevalent in patients with severe psoriasis, compared with patients with mild psoriasis.
Although the reasons for the increased cardiovascular risk in psoriasis patients remain unknown, possible causes include the use of dyslipidemic therapies, including corticosteroids, acitretin, and cyclosporine, as well as uncontrolled inflammation that could lead to endothelial dysfunction and dyslipidemia, said Dr. Strober. The prevalence of other associated and/or independent risk factors including obesity, hypertension, smoking, and alcohol misuse in psoriasis patients, also could play a role.
Dr. Strober disclosed relationships with multiple pharmaceutical companies including Abbott, Amgen, Janssen, Pfizer, Novartis, and Celgene. SDEF and this news organization are owned by Frontline Medical Communications.
EXPERT ANALYSIS FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR
Patient education on heart failure risk is crucial in psoriasis
As evidence supporting an association between psoriasis and cardiovascular disease continues to mount, dermatologists may be the first line of defense in lowering heart failure risk.
"The increased risk of cardiovascular disease for patients with psoriasis may be of a similar magnitude as other well-described CV risk factors, such as uncontrolled hypertension," said Dr. Bruce E. Strober of the University of Connecticut, Farmington. "Further, epidemiological studies show that psoriasis patients have a shortened life expectancy, likely as a result of their experience with CV comorbitidies."
Patient education is essential, he noted at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar. "At the very least, dermatologists should alert patients of the link between psoriasis and CV disease, and remind these patients of the necessity of having a primary care physician who monitors conventional risk factors of CV disease. Patients should be reminded that psoriasis is ‘systemic disease of inflammation’ that creates risks beyond the skin and may shorten life expectancy."
"Dermatologists who care for moderate to severe psoriasis patients should measure blood pressure and draw baseline blood tests assessing for abnormalities of cholesterol, triglycerides, kidney function, liver function, and blood glucose. Abnormalities should prompt an appropriate referral to a primary care physician," he noted.
In a population-based Dutch study presented at the annual congress of the European Society of Cardiology in September, adults with mild psoriasis developed 4.02 cases of new-onset heart failure per 1,000 person-years of follow-up, compared with 4.50/1,000 person-years in patients with severe psoriasis; both of which were significantly higher than the rate of 2.27/1,000 person-years in the general population.
Data from a 2006 study found that diabetes, hypertension, hyperlipidemia, and obesity were more prevalent in psoriasis patients, when compared with controls (J. Am. Acad. Dermatol. 2006;55:829-35). Diabetes and obesity were significantly more prevalent in patients with severe psoriasis, compared with patients with mild psoriasis.
Although the reasons for the increased cardiovascular risk in psoriasis patients remain unknown, possible causes include the use of dyslipidemic therapies, including corticosteroids, acitretin, and cyclosporine, as well as uncontrolled inflammation that could lead to endothelial dysfunction and dyslipidemia, said Dr. Strober. The prevalence of other associated and/or independent risk factors including obesity, hypertension, smoking, and alcohol misuse in psoriasis patients, also could play a role.
Dr. Strober disclosed relationships with multiple pharmaceutical companies including Abbott, Amgen, Janssen, Pfizer, Novartis, and Celgene. SDEF and this news organization are owned by Frontline Medical Communications.
As evidence supporting an association between psoriasis and cardiovascular disease continues to mount, dermatologists may be the first line of defense in lowering heart failure risk.
"The increased risk of cardiovascular disease for patients with psoriasis may be of a similar magnitude as other well-described CV risk factors, such as uncontrolled hypertension," said Dr. Bruce E. Strober of the University of Connecticut, Farmington. "Further, epidemiological studies show that psoriasis patients have a shortened life expectancy, likely as a result of their experience with CV comorbitidies."
Patient education is essential, he noted at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar. "At the very least, dermatologists should alert patients of the link between psoriasis and CV disease, and remind these patients of the necessity of having a primary care physician who monitors conventional risk factors of CV disease. Patients should be reminded that psoriasis is ‘systemic disease of inflammation’ that creates risks beyond the skin and may shorten life expectancy."
"Dermatologists who care for moderate to severe psoriasis patients should measure blood pressure and draw baseline blood tests assessing for abnormalities of cholesterol, triglycerides, kidney function, liver function, and blood glucose. Abnormalities should prompt an appropriate referral to a primary care physician," he noted.
In a population-based Dutch study presented at the annual congress of the European Society of Cardiology in September, adults with mild psoriasis developed 4.02 cases of new-onset heart failure per 1,000 person-years of follow-up, compared with 4.50/1,000 person-years in patients with severe psoriasis; both of which were significantly higher than the rate of 2.27/1,000 person-years in the general population.
Data from a 2006 study found that diabetes, hypertension, hyperlipidemia, and obesity were more prevalent in psoriasis patients, when compared with controls (J. Am. Acad. Dermatol. 2006;55:829-35). Diabetes and obesity were significantly more prevalent in patients with severe psoriasis, compared with patients with mild psoriasis.
Although the reasons for the increased cardiovascular risk in psoriasis patients remain unknown, possible causes include the use of dyslipidemic therapies, including corticosteroids, acitretin, and cyclosporine, as well as uncontrolled inflammation that could lead to endothelial dysfunction and dyslipidemia, said Dr. Strober. The prevalence of other associated and/or independent risk factors including obesity, hypertension, smoking, and alcohol misuse in psoriasis patients, also could play a role.
Dr. Strober disclosed relationships with multiple pharmaceutical companies including Abbott, Amgen, Janssen, Pfizer, Novartis, and Celgene. SDEF and this news organization are owned by Frontline Medical Communications.
As evidence supporting an association between psoriasis and cardiovascular disease continues to mount, dermatologists may be the first line of defense in lowering heart failure risk.
"The increased risk of cardiovascular disease for patients with psoriasis may be of a similar magnitude as other well-described CV risk factors, such as uncontrolled hypertension," said Dr. Bruce E. Strober of the University of Connecticut, Farmington. "Further, epidemiological studies show that psoriasis patients have a shortened life expectancy, likely as a result of their experience with CV comorbitidies."
Patient education is essential, he noted at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar. "At the very least, dermatologists should alert patients of the link between psoriasis and CV disease, and remind these patients of the necessity of having a primary care physician who monitors conventional risk factors of CV disease. Patients should be reminded that psoriasis is ‘systemic disease of inflammation’ that creates risks beyond the skin and may shorten life expectancy."
"Dermatologists who care for moderate to severe psoriasis patients should measure blood pressure and draw baseline blood tests assessing for abnormalities of cholesterol, triglycerides, kidney function, liver function, and blood glucose. Abnormalities should prompt an appropriate referral to a primary care physician," he noted.
In a population-based Dutch study presented at the annual congress of the European Society of Cardiology in September, adults with mild psoriasis developed 4.02 cases of new-onset heart failure per 1,000 person-years of follow-up, compared with 4.50/1,000 person-years in patients with severe psoriasis; both of which were significantly higher than the rate of 2.27/1,000 person-years in the general population.
Data from a 2006 study found that diabetes, hypertension, hyperlipidemia, and obesity were more prevalent in psoriasis patients, when compared with controls (J. Am. Acad. Dermatol. 2006;55:829-35). Diabetes and obesity were significantly more prevalent in patients with severe psoriasis, compared with patients with mild psoriasis.
Although the reasons for the increased cardiovascular risk in psoriasis patients remain unknown, possible causes include the use of dyslipidemic therapies, including corticosteroids, acitretin, and cyclosporine, as well as uncontrolled inflammation that could lead to endothelial dysfunction and dyslipidemia, said Dr. Strober. The prevalence of other associated and/or independent risk factors including obesity, hypertension, smoking, and alcohol misuse in psoriasis patients, also could play a role.
Dr. Strober disclosed relationships with multiple pharmaceutical companies including Abbott, Amgen, Janssen, Pfizer, Novartis, and Celgene. SDEF and this news organization are owned by Frontline Medical Communications.
EXPERT ANALYSIS FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR