User login
What Can We Do to Prevent Alzheimer Disease?
Alzheimer disease (AD) and other forms of dementia are pressing public health issues. They diminish quality of life for older adults and their families and impose significant financial costs on individuals and society. Dementia prevention and the development of treatments for dementia are important goals, and as a consequence, the VA Geriatric Research Education and Clinical Centers (GRECCs) have been conducting innovative research for the treatment and prevention of AD and related dementias.
Research conducted at the VISN 20 GRECC at the VA Puget Sound Health Care System (PSHCS) has helped increase clinicians’ understanding of the role of insulin in the development of AD and has evaluated the potential of treatment approaches based on the insulin-related research. More recently, this research has provided the basis for a pilot study aimed at dementia prevention for high-risk patients and for educational outreach about prevention within the VA.
Dementia Studies
The hormone insulin is required for efficient use of glucose throughout the body, including the brain. Insulin may also play a role in regulating cerebral amyloid, which is directly involved in the development of AD neuropathology and in maintaining healthy vascular function and lipid metabolism, both of which are required for brain health.1 Research over the past decade has shown that patients with AD have reduced levels of brain insulin, and individuals with insulin resistance have an increased risk of developing AD. Insulin resistance also has been shown to be related to reduced cerebral glucose metabolism, even in individuals who did not have a memory disorder.2
One recent study, led by Suzanne Craft, PhD, and colleagues at PSHCS, tested the potential of intranasal insulin to treat cognitive impairment.3 Participants with either AD or milder memory deficits used a specially designed device to deliver insulin or a placebo to the nose twice a day. Insulin provided in this way reaches the brain quickly without entering the lungs or affecting glucose metabolism elsewhere in the body. Participants who received the insulin experienced improvements in delayed memory and functional abilities compared with those who received the placebo.
Studies at the same laboratory investigated the role of diet and exercise in insulin metabolism and cognitive function. In a diet-related study, older adults with normal memory and those with mild memory impairment received either a high saturated fat, high glycemic index (GI) diet or a low saturated fat, low GI diet for 4 weeks.4 Plasma insulin levels decreased and delayed visual memory improved for participants who received the low-fat, low-GI diet. AD-related markers in cerebrospinal fluid, however, improved only among participants with mild memory impairment, not among healthy individuals.
In an exercise-related study, older adults with glucose intolerance participated in a 6-month aerobic exercise program.5 Although memory did not improve, cardiorespiratory fitness, executive function, and insulin sensitivity improved for participants in the aerobic exercise program compared with those in a stretching program. The relationship of diet and exercise and cognitive function is complex and likely involves insulin regulation, vascular function, and lipid metabolism, among other factors. More research is needed to fully understand the relationships among diet, exercise, and dementia, but these results suggest that lifestyle modifications may play a role in prevention of dementia.
When patients have problems with memory, attention, or executive function, they may have difficulty managing their medications, making good nutritional choices, and monitoring blood pressure and blood glucose.6 Given the importance of controlling vascular risk factors, helping patients manage their medical conditions may help them prevent or delay the onset of AD.
Pilot Study
A VA-funded pilot study with the goal of dementia prevention among high-risk patients was recently conducted at the PSHCS. This study focused on veterans at significantly elevated risk of dementia: those with both diabetes and hypertension, with poor control of either or both conditions, and who had some degree of memory or attentional impairment. Participants were randomly assigned to continue their usual care or to add a 6-month care management intervention to their usual care.
A registered nurse who helped the veterans overcome the barriers to controlling their medical conditions led the intervention. Barriers ranged from relatively simple problems, such as appropriate use of insulin, to more complex issues, such as learning about healthy nutrition and exercise for people with diabetes. The intervention was adapted to meet each participant’s cognitive level, and family involvement was encouraged, with the veteran’s permission. Preliminary results of this study were presented at the annual meeting of the Gerontological Society of America in 2011 and the Alzheimer’s Association International conference in July 2013.7,8
The VISN 20 GRECC also developed a “Dementia Roadshow” in which GRECC clinicians present educational, research-based lectures on dementia-related topics at VAMCs in VISN 20. One lecture in this series incorporates this recent research about prevention of dementia through control of diabetes and hypertension, as well as depression, posttraumatic stress disorder, and other risk factors; the lecture is presented to frontline clinicians who can then use this information to guide their work with high-risk patients.
The GRECCs are at the forefront of understanding the causes of dementia and how to prevent it. This work will help the VA to develop more effective ways of reducing the public health burden of this disease.
Acknowledgments
The author wishes to thank Debby Tsuang, MD, Stephen Thielke, MD, and Julie Moorer, RN, for helpful feedback on the initial draft of this manuscript. The pilot project described was funded by VA VISN 20.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the Department of Veterans Affairs, the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Craft S, Cholerton B, Baker LD. Insulin and Alzheimer’s disease: Untangling the web. J Alzheimers Dis. 2013;33(suppl 1):S263-S275.
2. Baker LD, Cross DJ, Minoshima S, Belongia D, Watson GS, Craft S. Insulin resistance and Alzheimer-like reductions in regional cerebral glucose metabolism for cognitively normal adults with prediabetes or early type 2 diabetes. Arch Neurol. 2011;68(1):51-57.
3. Craft S, Baker LD, Montine TJ, et al. Intranasal insulin therapy for Alzheimer disease and amnestic mild cognitive impairment: A pilot clinical trial. Arch Neurol. 2012;69(1):29-38.
4. Bayer-Carter JL, Green PS, Montine TJ, et al. Diet intervention and cerebrospinal fluid biomarkers in amnestic mild cognitive impairment. Arch Neurol. 2011;68(6):743-752.
5. Baker LD, Frank LL, Foster-Schubert K, et al. Aerobic exercise improves cognition for older adults with glucose intolerance, a risk factor for Alzheimer’s disease. J Alzheimers Dis. 2010;22(2):569-579.
6. Bonner LM, Craft S. Uncontrolled diabetes plus hypertension: A recipe for dementia? Fed Pract. 2009;26(2):33-35.
7. Bonner LM, Craft S, Robinson G. Screening and care management for dementia prevention and management in VA primary care patients with vascular risk. Poster presented at: Gerontological Society of America Annual Meeting; November 18, 2011; Boston, MA.
8. Bonner LM, Robinson G, Craft S. Care management for VA patients with vascular risk factors and cognitive impairment: A randomized trial. Alzheimer’s Association International Conference. July 2013, Boston, MA.
Alzheimer disease (AD) and other forms of dementia are pressing public health issues. They diminish quality of life for older adults and their families and impose significant financial costs on individuals and society. Dementia prevention and the development of treatments for dementia are important goals, and as a consequence, the VA Geriatric Research Education and Clinical Centers (GRECCs) have been conducting innovative research for the treatment and prevention of AD and related dementias.
Research conducted at the VISN 20 GRECC at the VA Puget Sound Health Care System (PSHCS) has helped increase clinicians’ understanding of the role of insulin in the development of AD and has evaluated the potential of treatment approaches based on the insulin-related research. More recently, this research has provided the basis for a pilot study aimed at dementia prevention for high-risk patients and for educational outreach about prevention within the VA.
Dementia Studies
The hormone insulin is required for efficient use of glucose throughout the body, including the brain. Insulin may also play a role in regulating cerebral amyloid, which is directly involved in the development of AD neuropathology and in maintaining healthy vascular function and lipid metabolism, both of which are required for brain health.1 Research over the past decade has shown that patients with AD have reduced levels of brain insulin, and individuals with insulin resistance have an increased risk of developing AD. Insulin resistance also has been shown to be related to reduced cerebral glucose metabolism, even in individuals who did not have a memory disorder.2
One recent study, led by Suzanne Craft, PhD, and colleagues at PSHCS, tested the potential of intranasal insulin to treat cognitive impairment.3 Participants with either AD or milder memory deficits used a specially designed device to deliver insulin or a placebo to the nose twice a day. Insulin provided in this way reaches the brain quickly without entering the lungs or affecting glucose metabolism elsewhere in the body. Participants who received the insulin experienced improvements in delayed memory and functional abilities compared with those who received the placebo.
Studies at the same laboratory investigated the role of diet and exercise in insulin metabolism and cognitive function. In a diet-related study, older adults with normal memory and those with mild memory impairment received either a high saturated fat, high glycemic index (GI) diet or a low saturated fat, low GI diet for 4 weeks.4 Plasma insulin levels decreased and delayed visual memory improved for participants who received the low-fat, low-GI diet. AD-related markers in cerebrospinal fluid, however, improved only among participants with mild memory impairment, not among healthy individuals.
In an exercise-related study, older adults with glucose intolerance participated in a 6-month aerobic exercise program.5 Although memory did not improve, cardiorespiratory fitness, executive function, and insulin sensitivity improved for participants in the aerobic exercise program compared with those in a stretching program. The relationship of diet and exercise and cognitive function is complex and likely involves insulin regulation, vascular function, and lipid metabolism, among other factors. More research is needed to fully understand the relationships among diet, exercise, and dementia, but these results suggest that lifestyle modifications may play a role in prevention of dementia.
When patients have problems with memory, attention, or executive function, they may have difficulty managing their medications, making good nutritional choices, and monitoring blood pressure and blood glucose.6 Given the importance of controlling vascular risk factors, helping patients manage their medical conditions may help them prevent or delay the onset of AD.
Pilot Study
A VA-funded pilot study with the goal of dementia prevention among high-risk patients was recently conducted at the PSHCS. This study focused on veterans at significantly elevated risk of dementia: those with both diabetes and hypertension, with poor control of either or both conditions, and who had some degree of memory or attentional impairment. Participants were randomly assigned to continue their usual care or to add a 6-month care management intervention to their usual care.
A registered nurse who helped the veterans overcome the barriers to controlling their medical conditions led the intervention. Barriers ranged from relatively simple problems, such as appropriate use of insulin, to more complex issues, such as learning about healthy nutrition and exercise for people with diabetes. The intervention was adapted to meet each participant’s cognitive level, and family involvement was encouraged, with the veteran’s permission. Preliminary results of this study were presented at the annual meeting of the Gerontological Society of America in 2011 and the Alzheimer’s Association International conference in July 2013.7,8
The VISN 20 GRECC also developed a “Dementia Roadshow” in which GRECC clinicians present educational, research-based lectures on dementia-related topics at VAMCs in VISN 20. One lecture in this series incorporates this recent research about prevention of dementia through control of diabetes and hypertension, as well as depression, posttraumatic stress disorder, and other risk factors; the lecture is presented to frontline clinicians who can then use this information to guide their work with high-risk patients.
The GRECCs are at the forefront of understanding the causes of dementia and how to prevent it. This work will help the VA to develop more effective ways of reducing the public health burden of this disease.
Acknowledgments
The author wishes to thank Debby Tsuang, MD, Stephen Thielke, MD, and Julie Moorer, RN, for helpful feedback on the initial draft of this manuscript. The pilot project described was funded by VA VISN 20.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the Department of Veterans Affairs, the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Alzheimer disease (AD) and other forms of dementia are pressing public health issues. They diminish quality of life for older adults and their families and impose significant financial costs on individuals and society. Dementia prevention and the development of treatments for dementia are important goals, and as a consequence, the VA Geriatric Research Education and Clinical Centers (GRECCs) have been conducting innovative research for the treatment and prevention of AD and related dementias.
Research conducted at the VISN 20 GRECC at the VA Puget Sound Health Care System (PSHCS) has helped increase clinicians’ understanding of the role of insulin in the development of AD and has evaluated the potential of treatment approaches based on the insulin-related research. More recently, this research has provided the basis for a pilot study aimed at dementia prevention for high-risk patients and for educational outreach about prevention within the VA.
Dementia Studies
The hormone insulin is required for efficient use of glucose throughout the body, including the brain. Insulin may also play a role in regulating cerebral amyloid, which is directly involved in the development of AD neuropathology and in maintaining healthy vascular function and lipid metabolism, both of which are required for brain health.1 Research over the past decade has shown that patients with AD have reduced levels of brain insulin, and individuals with insulin resistance have an increased risk of developing AD. Insulin resistance also has been shown to be related to reduced cerebral glucose metabolism, even in individuals who did not have a memory disorder.2
One recent study, led by Suzanne Craft, PhD, and colleagues at PSHCS, tested the potential of intranasal insulin to treat cognitive impairment.3 Participants with either AD or milder memory deficits used a specially designed device to deliver insulin or a placebo to the nose twice a day. Insulin provided in this way reaches the brain quickly without entering the lungs or affecting glucose metabolism elsewhere in the body. Participants who received the insulin experienced improvements in delayed memory and functional abilities compared with those who received the placebo.
Studies at the same laboratory investigated the role of diet and exercise in insulin metabolism and cognitive function. In a diet-related study, older adults with normal memory and those with mild memory impairment received either a high saturated fat, high glycemic index (GI) diet or a low saturated fat, low GI diet for 4 weeks.4 Plasma insulin levels decreased and delayed visual memory improved for participants who received the low-fat, low-GI diet. AD-related markers in cerebrospinal fluid, however, improved only among participants with mild memory impairment, not among healthy individuals.
In an exercise-related study, older adults with glucose intolerance participated in a 6-month aerobic exercise program.5 Although memory did not improve, cardiorespiratory fitness, executive function, and insulin sensitivity improved for participants in the aerobic exercise program compared with those in a stretching program. The relationship of diet and exercise and cognitive function is complex and likely involves insulin regulation, vascular function, and lipid metabolism, among other factors. More research is needed to fully understand the relationships among diet, exercise, and dementia, but these results suggest that lifestyle modifications may play a role in prevention of dementia.
When patients have problems with memory, attention, or executive function, they may have difficulty managing their medications, making good nutritional choices, and monitoring blood pressure and blood glucose.6 Given the importance of controlling vascular risk factors, helping patients manage their medical conditions may help them prevent or delay the onset of AD.
Pilot Study
A VA-funded pilot study with the goal of dementia prevention among high-risk patients was recently conducted at the PSHCS. This study focused on veterans at significantly elevated risk of dementia: those with both diabetes and hypertension, with poor control of either or both conditions, and who had some degree of memory or attentional impairment. Participants were randomly assigned to continue their usual care or to add a 6-month care management intervention to their usual care.
A registered nurse who helped the veterans overcome the barriers to controlling their medical conditions led the intervention. Barriers ranged from relatively simple problems, such as appropriate use of insulin, to more complex issues, such as learning about healthy nutrition and exercise for people with diabetes. The intervention was adapted to meet each participant’s cognitive level, and family involvement was encouraged, with the veteran’s permission. Preliminary results of this study were presented at the annual meeting of the Gerontological Society of America in 2011 and the Alzheimer’s Association International conference in July 2013.7,8
The VISN 20 GRECC also developed a “Dementia Roadshow” in which GRECC clinicians present educational, research-based lectures on dementia-related topics at VAMCs in VISN 20. One lecture in this series incorporates this recent research about prevention of dementia through control of diabetes and hypertension, as well as depression, posttraumatic stress disorder, and other risk factors; the lecture is presented to frontline clinicians who can then use this information to guide their work with high-risk patients.
The GRECCs are at the forefront of understanding the causes of dementia and how to prevent it. This work will help the VA to develop more effective ways of reducing the public health burden of this disease.
Acknowledgments
The author wishes to thank Debby Tsuang, MD, Stephen Thielke, MD, and Julie Moorer, RN, for helpful feedback on the initial draft of this manuscript. The pilot project described was funded by VA VISN 20.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the Department of Veterans Affairs, the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Craft S, Cholerton B, Baker LD. Insulin and Alzheimer’s disease: Untangling the web. J Alzheimers Dis. 2013;33(suppl 1):S263-S275.
2. Baker LD, Cross DJ, Minoshima S, Belongia D, Watson GS, Craft S. Insulin resistance and Alzheimer-like reductions in regional cerebral glucose metabolism for cognitively normal adults with prediabetes or early type 2 diabetes. Arch Neurol. 2011;68(1):51-57.
3. Craft S, Baker LD, Montine TJ, et al. Intranasal insulin therapy for Alzheimer disease and amnestic mild cognitive impairment: A pilot clinical trial. Arch Neurol. 2012;69(1):29-38.
4. Bayer-Carter JL, Green PS, Montine TJ, et al. Diet intervention and cerebrospinal fluid biomarkers in amnestic mild cognitive impairment. Arch Neurol. 2011;68(6):743-752.
5. Baker LD, Frank LL, Foster-Schubert K, et al. Aerobic exercise improves cognition for older adults with glucose intolerance, a risk factor for Alzheimer’s disease. J Alzheimers Dis. 2010;22(2):569-579.
6. Bonner LM, Craft S. Uncontrolled diabetes plus hypertension: A recipe for dementia? Fed Pract. 2009;26(2):33-35.
7. Bonner LM, Craft S, Robinson G. Screening and care management for dementia prevention and management in VA primary care patients with vascular risk. Poster presented at: Gerontological Society of America Annual Meeting; November 18, 2011; Boston, MA.
8. Bonner LM, Robinson G, Craft S. Care management for VA patients with vascular risk factors and cognitive impairment: A randomized trial. Alzheimer’s Association International Conference. July 2013, Boston, MA.
1. Craft S, Cholerton B, Baker LD. Insulin and Alzheimer’s disease: Untangling the web. J Alzheimers Dis. 2013;33(suppl 1):S263-S275.
2. Baker LD, Cross DJ, Minoshima S, Belongia D, Watson GS, Craft S. Insulin resistance and Alzheimer-like reductions in regional cerebral glucose metabolism for cognitively normal adults with prediabetes or early type 2 diabetes. Arch Neurol. 2011;68(1):51-57.
3. Craft S, Baker LD, Montine TJ, et al. Intranasal insulin therapy for Alzheimer disease and amnestic mild cognitive impairment: A pilot clinical trial. Arch Neurol. 2012;69(1):29-38.
4. Bayer-Carter JL, Green PS, Montine TJ, et al. Diet intervention and cerebrospinal fluid biomarkers in amnestic mild cognitive impairment. Arch Neurol. 2011;68(6):743-752.
5. Baker LD, Frank LL, Foster-Schubert K, et al. Aerobic exercise improves cognition for older adults with glucose intolerance, a risk factor for Alzheimer’s disease. J Alzheimers Dis. 2010;22(2):569-579.
6. Bonner LM, Craft S. Uncontrolled diabetes plus hypertension: A recipe for dementia? Fed Pract. 2009;26(2):33-35.
7. Bonner LM, Craft S, Robinson G. Screening and care management for dementia prevention and management in VA primary care patients with vascular risk. Poster presented at: Gerontological Society of America Annual Meeting; November 18, 2011; Boston, MA.
8. Bonner LM, Robinson G, Craft S. Care management for VA patients with vascular risk factors and cognitive impairment: A randomized trial. Alzheimer’s Association International Conference. July 2013, Boston, MA.
Pharmacist-Managed Collaborative Practice for Chronic Stable Angina
Coronary artery disease (CAD) continues to have a significant impact on society. The latest update by the American Heart Association estimates that 83.6 million American adults have some form of cardiovascular disease (CVD) with an anticipated 15.4 million attributed to CAD.1 A portion of patients with CAD experience predictable chest pain, which occurs as a result of physical, emotional, or mental stress, more commonly referred to as chronic stable angina (CSA). Based on the most recent estimates, the incidence of patients who experience CSA is about 565,000 and increases in the male population through the eighth decade of life.1
Although it may be common, treatment options for patients with CSA are limited, as these patients may not be ideal candidates for coronary artery bypass graft or percutaneous coronary intervention (PCI) and may often prefer less invasive treatments. It has also been demonstrated that optimal medical management results in similar cardiovascular outcomes when compared with optimal medical management combined with PCI.2,3 Therefore, optimizing medical management is a reasonable alternative for these individuals.
Pharmacists have been successful in implementing collaborative practices for the management of various conditions, including anticoagulation, diabetes, hypertension, and hyperlipidemia.4-7 Pharmacists are heavily involved with cardiovascular risk reduction and management, so it seems opportune that they also treat CSA.8 The latest estimated direct and indirect costs for CVD and stroke were well over $315 billion for 2010, and it is anticipated that the costs will continue to rise.1 Because CSA is typically a medically managed disease and due to its huge medical expense, the development of a pharmacist-managed collaborative practice for treating CSA may prove to be beneficial for both clinical and pharmacoeconomic outcomes.
Clinic Development and Practices
In June 2007, following the approval of ranolazine by the FDA, the VA adopted nonformulary criteria for ranolazine use (Appendix).9,10 In order for patients to receive ranolazine, health care providers (HCPs) within the North Florida/South Georgia Veterans Health System (NFSGVHS) network were required to submit an electronic nonformulary consult using the computerized patient record system (CPRS). Select clinical pharmacists who had knowledge of the health system’s nonformulary criteria and who were granted access to the electronic consults responded to the requests.
The consults primarily consisted of an automated template that required providers to fill out their contact information and the name of the requested nonformulary medication, dose, and clinical rationale for requesting the specified medication, including any previous treatments that the patient could not tolerate or on which the patient failed to achieve an adequate response. It was highly recommended but not required that the HCPs include other supporting information regarding the patient’s cardiovascular status, such as results from diagnostic cardiac catheterization, stress tests, electrocardiograms (ECGs), or echocardiograms if not readily available from the CPRS. If procedures or tests were conducted at outside facilities, then this information was supplied in the request or obtained with the patient’s consent. However, this information was not necessarily required in order to complete the nonformulary consult. Nonformulary requests for ranolazine were typically forwarded to the clinical pharmacists who specialized in cardiology.
A pharmacist-oriented collaborative practice was established to increase cost-effective use, improve monitoring by a HCP because of the drug’s ability to prolong the corrected QT (QTc) interval, and to more firmly establish its safety and efficacy in a veteran population. This practice operated in a clinic, which was staffed by a nurse, postdoctoral pharmacy fellow, clinical pharmacy specialist in cardiology, and a cardiologist. The nurse was responsible for obtaining the patient’s vitals and ECG and documenting them in the CPRS. The pharmacy fellow interviewed the patient and obtained pertinent medical and historical information before discussing any clinical recommendations with the clinical pharmacy specialist.
The recommendations consisted of drug initiation/discontinuation, dose adjustments, and assessing and ordering of pertinent laboratory values and ECGs, which took place under the scope of the clinical pharmacy specialist. The focus of the ECG was to assess for any evidence of excessive QTc prolongation. Due to the variable and subjective nature of CAD, a cardiologist was available at any time and was used to review any relevant information and further discuss any treatment recommendations.
Based in the NFSGVHS Malcom Randall Veterans Affairs Medical Center (VAMC) in Gainesville, Florida, clinic services were primarily offered to patients of that facility due to the limited number of cardiology providers and services offered at other NFSGVHS locations. Despite being driven by requests for ranolazine, especially after cardiac catheterization when further cardiac intervention may not have been feasible, all patients were allowed to enroll in the clinic at the discretion of their primary care provider (PCP) for optimization of their CSA regimen with the intent of adding ranolazine when appropriate.
Patients in outlying regions who met the criteria were supplied with ranolazine and continued to follow up with their HCPs as recommended by the criteria for use. Conversely, if patients from outside areas failed to meet the criteria, their PCPs were supplied with appropriate, alternative guideline-based recommendations for improving CSA with the option to resubmit the nonformulary consult.11 Recommendations regarding cardiovascular risk reduction were also sent to HCPs at that time, which included optimal endpoints for managing other conditions, such as diabetes, hypertension, and hyperlipidemia when necesary.8,11
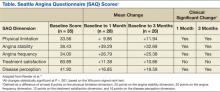
Regardless of whether ranolazine was initiated at baseline, all patients enrolled in the clinic underwent appropriate labs and tests, including a basic metabolic panel, magnesium level, and an ECG, if not otherwise available from the CPRS or documented from outside facilities. A thorough history and description of the patient’s anginal symptoms were also taken at baseline and during follow-up visits. Once it was confirmed that the patients’ electrolytes were within normal limits and there was no evidence of prolongation in the Bazett’s QTc interval or major drug interactions, all patients who met criteria for ranolazine were initiated at 500 mg twice daily.9,12 The Seattle Angina Questionnaire (SAQ) was also completed by patients at the initiation of ranolazine and then again at follow-up visits. The SAQ is an 11-question, self-administered survey that measures functional status of patients with angina.13
All patients initiated on or ensuing dose changes with ranolazine followed up with the clinic at 1 and 3 months with labs and ECGs obtained prior to ensure that there were no electrolyte imbalances or excessive QTc prolongation. Excessive QTc prolongation was defined as an increase of ≥ 60 milliseconds (msec) from baseline or > 500 msec.14 If this boundary was exceeded, ranolazine was discontinued, or for those taking higher doses, it was reduced to the initial 500 mg twice daily as long as there was no previous excessive QTc prolongation. In cases where ranolazine was not added at baseline, doses of antianginal medications were titrated over appropriate intervals to improve angina symptoms with ranolazine subsequently added in conjunction with the nonformulary criteria.
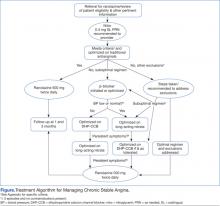
A generalized treatment algorithm was followed by the clinic for the management of CSA (Figure). It was highly recommended that all referred patients have an active prescription in the CPRS for short-acting sublingual nitroglycerin 0.4 mg in case of any acute episodes. Although other forms of short-acting nitroglycerin were available, sublingual nitroglycerin 0.4 mg was the preferred formulary medication at the time of the study.
Depending on whether the patients met nonformulary inclusion or exclusion criteria, they were either initiated or optimized on ranolazine or other traditional antianginals, such as beta-blockers (BBs), dihydropyridine calcium channel blockers (DHP-CCBs), or long-acting nitrates (LANs). Beta-blockers were recommended as first-line treatment for patients with previous myocardial infarction (MI) and left ventricular dysfunction, in accordance with treatment guidelines and because of their benefits in treating patients with CSA.12,15
Once patients were optimized on BBs and/or DHP-CCBs, LANs were added if patients experienced ≥ 3 bothersome episodes of chest pain weekly. Optimization for BBs meant an ideal heart rate of at least about 60 bpm without symptoms suggestive of excessive bradycardia, whereas optimization for all 3 classes (BBs, DHP-CCBs, and LANs) consisted of dose titration until the presence of drug-related adverse effects (AEs) or symptoms suggestive of hypotension. Because LANs have lesser effects on blood pressure (BP) compared with DHP-CCBs, they were preferred in patients with persistent anginal symptoms whose BPs were considered low or normal, according to the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) guidelines.16
If patients with normal or controlled BP continued to have symptoms of angina despite optimal doses of BBs and LANs, an appropriate dose of a DHP-CCB was administered and titrated for as long as the patients tolerated the treatment. If titration of antianginal agents was limited due to the presence of other antihypertensives, then the patient’s medication regimen was modified as necessary to allow for an increased dose of the BB or DHP-CCB due to these medications’ abilities to improve angina symptoms while also lowering BP. If patients achieved an acceptable reduction in their angina symptoms, they were discharged from the clinic, whereas those with contraindications to other classes were referred to their PCP or cardiologist.
Patients successfully treated with ranolazine (defined as a noticeable reduction in angina symptoms in the absence of intolerable AEs and excessive QTc prolongation after 3 months) were discharged from the clinic and instructed to follow up with their PCP at least annually. If the patient was discharged from the clinic at the baseline dose, it was recommended to the HCP that he or she follow up within 3 months after any dose increases. Any patient whose symptoms were consistent with unstable angina (described as occurring in an unpredictable manner, as determined by the clinical pharmacy specialist, lasting longer in duration and/or increasing in frequency, and those who experience symptoms at rest) were immediately evaluated and referred to a cardiologist. Patients who continued to have unacceptable rates or episodes of angina despite an optimal medical regimen were referred to Cardiology for consideration of other treatment modalities.
Results
The initial report of this study population was described by Reeder and colleagues.17 Fifty-seven patients were evaluated for study inclusion, of which 22 were excluded due to ranolazine being managed by an outside HCP or because an SAQ was not obtained at baseline. All study participants were males with an average age of 68 years and were predominantly white (86%). All patients had a past medical history significant for hypertension and hyperlipidemia. More than half (57%) had a prior MI and multivessel disease, although only 1 patient had an ejection fraction of < 35%. The majority of patients enrolled were being treated with BBs (97%) and LANs (94%) with a little more than half prescribed CCBs (60%). A large percentage (97%) of patients were also taking aspirin and a statin.
Improvements in angina symptoms as measured by the SAQ and safety measures, which included details of AEs and discontinuation rates following the initiation of ranolazine within the clinic, have previously been published.17 In summary, it was found that the addition of ranolazine to an optimal medical regimen for CSA improved all dimensions of the SAQ scores at 1 and 3 months compared with baseline (Table). Additionally, it was noted that higher doses may not have been as well tolerated in the veteran population, despite that only a small number of eligible patients were captured. This was because 5 of 7 patients whose dose was increased to 1,000 mg twice daily after 1 month required withdrawal as a result of AEs or lack of efficacy. The AEs reported included dizziness, abdominal pain, blurry vision, nausea and vomiting, dry mouth, and dyspnea.
The pharmacists were able to ensure that relevant electrolytes were replaced during the treatment period and also minimized the number of clinically significant drug interactions. Twenty-one patients received medications at baseline that had known interactions with ranolazine. Two patients required discontinuation of other medications: sotalol and diltiazem. At the time this study was conducted, diltiazem was contraindicated when given concomitantly but has since been allowed per manufacturer recommendations as long as the dose of ranolazine does not exceed 500 mg twice daily. Electrolyte replacement was also required in 3 patients, 2 of whom had hypomagnesemia.
Conclusion
Pharmacists have been influential in managing a variety of chronic diseases. When instituted into collaborative practice agreements, CSA is another unique condition that pharmacists can play a role in treating. Given that pharmacists are heavily involved with cardiovascular risk reduction, combined with the higher cost of ranolazine and the need for monitoring due to its AEs, QTc interval prolongation, and significant drug interactions, the benefits of having pharmacist-oriented clinics can ensure the safe and effective use of medications in the treatment of CSA.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Go AS, Mozaffarian D, Roger VL, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics–2014 update: A report from the American Heart Association. Circulation. 2014;129:e28-e292.
2. Boden WE, O’Rourke RA, Teo KK, et al; COURAGE Trial Research Group. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007;356(15):1503-1516.
3. RITA-2 trial participants. Coronary angioplasty versus medical therapy for angina: The second Randomised Intervention Treatment of Angina (RITA-2) trial. Lancet. 1997;350(9076):461-468.
4. Norton JL, Gibson DL. Establishing an outpatient anticoagulation clinic in a community hospital. Am J Health Syst Pharm. 1996;53(10):1151-1157.
5. Morello CM, Zadvorny EB, Cording MA, Suemoto RT, Skog J, Harari A. Development and clinical outcomes of pharmacist-managed diabetes care clinics. Am J Health Syst Pharm. 2006;63(14):1325-1331.
6. Vivian EM. Improving blood pressure control in a pharmacist-managed hypertension clinic. Pharmacotherapy. 2002;22(12):1533-1540.
7. Cording MA, Engelbrecht-Zadvorny EB, Pettit BJ, Eastham JH, Sandoval R. Development of a pharmacist-managed lipid clinic. Ann Pharmacother. 2002;36(5):892-904.
8. Geber J, Parra D, Beckey NP, Korman L. Optimizing drug therapy in patients with cardiovascular disease: The impact of pharmacist-managed pharmacotherapy clinics in a primary care setting. Pharmacotherapy. 2002; 22(6):738-747.
9. Ranexa [package insert]. Foster City, CA: Gilead Sciences, Inc.; 2013.
10. VHA Pharmacy Benefits Management Strategic Healthcare Group and the Medical Advisory Panel. Ranolazine. National PBM Drug Monograph. U.S. Department of Veterans Affairs Pharmacy Benefits Management Services Website. http://www.pbm.va.gov/clinicalguidance/drugmonographs/Ranolazine.pdf. Published June 2007. Accessed May 7, 2014.
11. Fraker TD Jr, Fihn SD; writing on behalf of the 2002 Chronic Stable Angina Writing Committee. 2007 chronic angina focused update of the ACC/AHA 2002 guidelines for the management of patients with chronic stable angina: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines Writing Group to develop the focused update of the 2002 guidelines for the management of patients with chronic stable angina. Circulation. 2007;116(23):2762-2772.
12. Funck-Brentano C, Jaillon P. Rate-corrected QT interval: Techniques and limitations. Am J Cardiol. 1993;72(6):17B-22B.
13. Spertus JA, Winder JA, Dewhurst TA, et al. Development and evaluation of the Seattle Angina Questionnaire: A new functional status measure for coronary artery disease. J Am Coll Cardiol. 1995;25(2):333-341.
14. Drew BJ, Ackerman MJ, Funk M, et al; American Heart Association Acute Cardiac Care Committee of the Council on Clinical Cardiology, the Council on Cardiovascular Nursing, and the American College of Cardiology Foundation. Prevention of torsade de pointes in hospital settings: A scientific statement from the American Heart Association and the American College of Cardiology Foundation. Circulation. 2010;121(8):1047-1060.
15. Heidenreich PA, McDonald KM, Hastie T, et al. Meta-analysis of trials comparing beta-blockers, calcium antagonists, and nitrates for stable angina. JAMA. 1999;281(20):1927-1936.
16. Chobanian AV, Bakris GL, Black HR, et al; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. The JNC 7 report. JAMA. 2003;289(19):2560-2572.
17. Reeder DN, Gillette MA, Franck AJ, Frohnapple DJ. Clinical experience with ranolazine in a veteran population with chronic stable angina. Ann Pharmacother. 2012;46(1):42-50.
Coronary artery disease (CAD) continues to have a significant impact on society. The latest update by the American Heart Association estimates that 83.6 million American adults have some form of cardiovascular disease (CVD) with an anticipated 15.4 million attributed to CAD.1 A portion of patients with CAD experience predictable chest pain, which occurs as a result of physical, emotional, or mental stress, more commonly referred to as chronic stable angina (CSA). Based on the most recent estimates, the incidence of patients who experience CSA is about 565,000 and increases in the male population through the eighth decade of life.1
Although it may be common, treatment options for patients with CSA are limited, as these patients may not be ideal candidates for coronary artery bypass graft or percutaneous coronary intervention (PCI) and may often prefer less invasive treatments. It has also been demonstrated that optimal medical management results in similar cardiovascular outcomes when compared with optimal medical management combined with PCI.2,3 Therefore, optimizing medical management is a reasonable alternative for these individuals.
Pharmacists have been successful in implementing collaborative practices for the management of various conditions, including anticoagulation, diabetes, hypertension, and hyperlipidemia.4-7 Pharmacists are heavily involved with cardiovascular risk reduction and management, so it seems opportune that they also treat CSA.8 The latest estimated direct and indirect costs for CVD and stroke were well over $315 billion for 2010, and it is anticipated that the costs will continue to rise.1 Because CSA is typically a medically managed disease and due to its huge medical expense, the development of a pharmacist-managed collaborative practice for treating CSA may prove to be beneficial for both clinical and pharmacoeconomic outcomes.
Clinic Development and Practices
In June 2007, following the approval of ranolazine by the FDA, the VA adopted nonformulary criteria for ranolazine use (Appendix).9,10 In order for patients to receive ranolazine, health care providers (HCPs) within the North Florida/South Georgia Veterans Health System (NFSGVHS) network were required to submit an electronic nonformulary consult using the computerized patient record system (CPRS). Select clinical pharmacists who had knowledge of the health system’s nonformulary criteria and who were granted access to the electronic consults responded to the requests.
The consults primarily consisted of an automated template that required providers to fill out their contact information and the name of the requested nonformulary medication, dose, and clinical rationale for requesting the specified medication, including any previous treatments that the patient could not tolerate or on which the patient failed to achieve an adequate response. It was highly recommended but not required that the HCPs include other supporting information regarding the patient’s cardiovascular status, such as results from diagnostic cardiac catheterization, stress tests, electrocardiograms (ECGs), or echocardiograms if not readily available from the CPRS. If procedures or tests were conducted at outside facilities, then this information was supplied in the request or obtained with the patient’s consent. However, this information was not necessarily required in order to complete the nonformulary consult. Nonformulary requests for ranolazine were typically forwarded to the clinical pharmacists who specialized in cardiology.
A pharmacist-oriented collaborative practice was established to increase cost-effective use, improve monitoring by a HCP because of the drug’s ability to prolong the corrected QT (QTc) interval, and to more firmly establish its safety and efficacy in a veteran population. This practice operated in a clinic, which was staffed by a nurse, postdoctoral pharmacy fellow, clinical pharmacy specialist in cardiology, and a cardiologist. The nurse was responsible for obtaining the patient’s vitals and ECG and documenting them in the CPRS. The pharmacy fellow interviewed the patient and obtained pertinent medical and historical information before discussing any clinical recommendations with the clinical pharmacy specialist.
The recommendations consisted of drug initiation/discontinuation, dose adjustments, and assessing and ordering of pertinent laboratory values and ECGs, which took place under the scope of the clinical pharmacy specialist. The focus of the ECG was to assess for any evidence of excessive QTc prolongation. Due to the variable and subjective nature of CAD, a cardiologist was available at any time and was used to review any relevant information and further discuss any treatment recommendations.
Based in the NFSGVHS Malcom Randall Veterans Affairs Medical Center (VAMC) in Gainesville, Florida, clinic services were primarily offered to patients of that facility due to the limited number of cardiology providers and services offered at other NFSGVHS locations. Despite being driven by requests for ranolazine, especially after cardiac catheterization when further cardiac intervention may not have been feasible, all patients were allowed to enroll in the clinic at the discretion of their primary care provider (PCP) for optimization of their CSA regimen with the intent of adding ranolazine when appropriate.
Patients in outlying regions who met the criteria were supplied with ranolazine and continued to follow up with their HCPs as recommended by the criteria for use. Conversely, if patients from outside areas failed to meet the criteria, their PCPs were supplied with appropriate, alternative guideline-based recommendations for improving CSA with the option to resubmit the nonformulary consult.11 Recommendations regarding cardiovascular risk reduction were also sent to HCPs at that time, which included optimal endpoints for managing other conditions, such as diabetes, hypertension, and hyperlipidemia when necesary.8,11
Regardless of whether ranolazine was initiated at baseline, all patients enrolled in the clinic underwent appropriate labs and tests, including a basic metabolic panel, magnesium level, and an ECG, if not otherwise available from the CPRS or documented from outside facilities. A thorough history and description of the patient’s anginal symptoms were also taken at baseline and during follow-up visits. Once it was confirmed that the patients’ electrolytes were within normal limits and there was no evidence of prolongation in the Bazett’s QTc interval or major drug interactions, all patients who met criteria for ranolazine were initiated at 500 mg twice daily.9,12 The Seattle Angina Questionnaire (SAQ) was also completed by patients at the initiation of ranolazine and then again at follow-up visits. The SAQ is an 11-question, self-administered survey that measures functional status of patients with angina.13
All patients initiated on or ensuing dose changes with ranolazine followed up with the clinic at 1 and 3 months with labs and ECGs obtained prior to ensure that there were no electrolyte imbalances or excessive QTc prolongation. Excessive QTc prolongation was defined as an increase of ≥ 60 milliseconds (msec) from baseline or > 500 msec.14 If this boundary was exceeded, ranolazine was discontinued, or for those taking higher doses, it was reduced to the initial 500 mg twice daily as long as there was no previous excessive QTc prolongation. In cases where ranolazine was not added at baseline, doses of antianginal medications were titrated over appropriate intervals to improve angina symptoms with ranolazine subsequently added in conjunction with the nonformulary criteria.
A generalized treatment algorithm was followed by the clinic for the management of CSA (Figure). It was highly recommended that all referred patients have an active prescription in the CPRS for short-acting sublingual nitroglycerin 0.4 mg in case of any acute episodes. Although other forms of short-acting nitroglycerin were available, sublingual nitroglycerin 0.4 mg was the preferred formulary medication at the time of the study.
Depending on whether the patients met nonformulary inclusion or exclusion criteria, they were either initiated or optimized on ranolazine or other traditional antianginals, such as beta-blockers (BBs), dihydropyridine calcium channel blockers (DHP-CCBs), or long-acting nitrates (LANs). Beta-blockers were recommended as first-line treatment for patients with previous myocardial infarction (MI) and left ventricular dysfunction, in accordance with treatment guidelines and because of their benefits in treating patients with CSA.12,15
Once patients were optimized on BBs and/or DHP-CCBs, LANs were added if patients experienced ≥ 3 bothersome episodes of chest pain weekly. Optimization for BBs meant an ideal heart rate of at least about 60 bpm without symptoms suggestive of excessive bradycardia, whereas optimization for all 3 classes (BBs, DHP-CCBs, and LANs) consisted of dose titration until the presence of drug-related adverse effects (AEs) or symptoms suggestive of hypotension. Because LANs have lesser effects on blood pressure (BP) compared with DHP-CCBs, they were preferred in patients with persistent anginal symptoms whose BPs were considered low or normal, according to the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) guidelines.16
If patients with normal or controlled BP continued to have symptoms of angina despite optimal doses of BBs and LANs, an appropriate dose of a DHP-CCB was administered and titrated for as long as the patients tolerated the treatment. If titration of antianginal agents was limited due to the presence of other antihypertensives, then the patient’s medication regimen was modified as necessary to allow for an increased dose of the BB or DHP-CCB due to these medications’ abilities to improve angina symptoms while also lowering BP. If patients achieved an acceptable reduction in their angina symptoms, they were discharged from the clinic, whereas those with contraindications to other classes were referred to their PCP or cardiologist.
Patients successfully treated with ranolazine (defined as a noticeable reduction in angina symptoms in the absence of intolerable AEs and excessive QTc prolongation after 3 months) were discharged from the clinic and instructed to follow up with their PCP at least annually. If the patient was discharged from the clinic at the baseline dose, it was recommended to the HCP that he or she follow up within 3 months after any dose increases. Any patient whose symptoms were consistent with unstable angina (described as occurring in an unpredictable manner, as determined by the clinical pharmacy specialist, lasting longer in duration and/or increasing in frequency, and those who experience symptoms at rest) were immediately evaluated and referred to a cardiologist. Patients who continued to have unacceptable rates or episodes of angina despite an optimal medical regimen were referred to Cardiology for consideration of other treatment modalities.
Results
The initial report of this study population was described by Reeder and colleagues.17 Fifty-seven patients were evaluated for study inclusion, of which 22 were excluded due to ranolazine being managed by an outside HCP or because an SAQ was not obtained at baseline. All study participants were males with an average age of 68 years and were predominantly white (86%). All patients had a past medical history significant for hypertension and hyperlipidemia. More than half (57%) had a prior MI and multivessel disease, although only 1 patient had an ejection fraction of < 35%. The majority of patients enrolled were being treated with BBs (97%) and LANs (94%) with a little more than half prescribed CCBs (60%). A large percentage (97%) of patients were also taking aspirin and a statin.
Improvements in angina symptoms as measured by the SAQ and safety measures, which included details of AEs and discontinuation rates following the initiation of ranolazine within the clinic, have previously been published.17 In summary, it was found that the addition of ranolazine to an optimal medical regimen for CSA improved all dimensions of the SAQ scores at 1 and 3 months compared with baseline (Table). Additionally, it was noted that higher doses may not have been as well tolerated in the veteran population, despite that only a small number of eligible patients were captured. This was because 5 of 7 patients whose dose was increased to 1,000 mg twice daily after 1 month required withdrawal as a result of AEs or lack of efficacy. The AEs reported included dizziness, abdominal pain, blurry vision, nausea and vomiting, dry mouth, and dyspnea.
The pharmacists were able to ensure that relevant electrolytes were replaced during the treatment period and also minimized the number of clinically significant drug interactions. Twenty-one patients received medications at baseline that had known interactions with ranolazine. Two patients required discontinuation of other medications: sotalol and diltiazem. At the time this study was conducted, diltiazem was contraindicated when given concomitantly but has since been allowed per manufacturer recommendations as long as the dose of ranolazine does not exceed 500 mg twice daily. Electrolyte replacement was also required in 3 patients, 2 of whom had hypomagnesemia.
Conclusion
Pharmacists have been influential in managing a variety of chronic diseases. When instituted into collaborative practice agreements, CSA is another unique condition that pharmacists can play a role in treating. Given that pharmacists are heavily involved with cardiovascular risk reduction, combined with the higher cost of ranolazine and the need for monitoring due to its AEs, QTc interval prolongation, and significant drug interactions, the benefits of having pharmacist-oriented clinics can ensure the safe and effective use of medications in the treatment of CSA.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Coronary artery disease (CAD) continues to have a significant impact on society. The latest update by the American Heart Association estimates that 83.6 million American adults have some form of cardiovascular disease (CVD) with an anticipated 15.4 million attributed to CAD.1 A portion of patients with CAD experience predictable chest pain, which occurs as a result of physical, emotional, or mental stress, more commonly referred to as chronic stable angina (CSA). Based on the most recent estimates, the incidence of patients who experience CSA is about 565,000 and increases in the male population through the eighth decade of life.1
Although it may be common, treatment options for patients with CSA are limited, as these patients may not be ideal candidates for coronary artery bypass graft or percutaneous coronary intervention (PCI) and may often prefer less invasive treatments. It has also been demonstrated that optimal medical management results in similar cardiovascular outcomes when compared with optimal medical management combined with PCI.2,3 Therefore, optimizing medical management is a reasonable alternative for these individuals.
Pharmacists have been successful in implementing collaborative practices for the management of various conditions, including anticoagulation, diabetes, hypertension, and hyperlipidemia.4-7 Pharmacists are heavily involved with cardiovascular risk reduction and management, so it seems opportune that they also treat CSA.8 The latest estimated direct and indirect costs for CVD and stroke were well over $315 billion for 2010, and it is anticipated that the costs will continue to rise.1 Because CSA is typically a medically managed disease and due to its huge medical expense, the development of a pharmacist-managed collaborative practice for treating CSA may prove to be beneficial for both clinical and pharmacoeconomic outcomes.
Clinic Development and Practices
In June 2007, following the approval of ranolazine by the FDA, the VA adopted nonformulary criteria for ranolazine use (Appendix).9,10 In order for patients to receive ranolazine, health care providers (HCPs) within the North Florida/South Georgia Veterans Health System (NFSGVHS) network were required to submit an electronic nonformulary consult using the computerized patient record system (CPRS). Select clinical pharmacists who had knowledge of the health system’s nonformulary criteria and who were granted access to the electronic consults responded to the requests.
The consults primarily consisted of an automated template that required providers to fill out their contact information and the name of the requested nonformulary medication, dose, and clinical rationale for requesting the specified medication, including any previous treatments that the patient could not tolerate or on which the patient failed to achieve an adequate response. It was highly recommended but not required that the HCPs include other supporting information regarding the patient’s cardiovascular status, such as results from diagnostic cardiac catheterization, stress tests, electrocardiograms (ECGs), or echocardiograms if not readily available from the CPRS. If procedures or tests were conducted at outside facilities, then this information was supplied in the request or obtained with the patient’s consent. However, this information was not necessarily required in order to complete the nonformulary consult. Nonformulary requests for ranolazine were typically forwarded to the clinical pharmacists who specialized in cardiology.
A pharmacist-oriented collaborative practice was established to increase cost-effective use, improve monitoring by a HCP because of the drug’s ability to prolong the corrected QT (QTc) interval, and to more firmly establish its safety and efficacy in a veteran population. This practice operated in a clinic, which was staffed by a nurse, postdoctoral pharmacy fellow, clinical pharmacy specialist in cardiology, and a cardiologist. The nurse was responsible for obtaining the patient’s vitals and ECG and documenting them in the CPRS. The pharmacy fellow interviewed the patient and obtained pertinent medical and historical information before discussing any clinical recommendations with the clinical pharmacy specialist.
The recommendations consisted of drug initiation/discontinuation, dose adjustments, and assessing and ordering of pertinent laboratory values and ECGs, which took place under the scope of the clinical pharmacy specialist. The focus of the ECG was to assess for any evidence of excessive QTc prolongation. Due to the variable and subjective nature of CAD, a cardiologist was available at any time and was used to review any relevant information and further discuss any treatment recommendations.
Based in the NFSGVHS Malcom Randall Veterans Affairs Medical Center (VAMC) in Gainesville, Florida, clinic services were primarily offered to patients of that facility due to the limited number of cardiology providers and services offered at other NFSGVHS locations. Despite being driven by requests for ranolazine, especially after cardiac catheterization when further cardiac intervention may not have been feasible, all patients were allowed to enroll in the clinic at the discretion of their primary care provider (PCP) for optimization of their CSA regimen with the intent of adding ranolazine when appropriate.
Patients in outlying regions who met the criteria were supplied with ranolazine and continued to follow up with their HCPs as recommended by the criteria for use. Conversely, if patients from outside areas failed to meet the criteria, their PCPs were supplied with appropriate, alternative guideline-based recommendations for improving CSA with the option to resubmit the nonformulary consult.11 Recommendations regarding cardiovascular risk reduction were also sent to HCPs at that time, which included optimal endpoints for managing other conditions, such as diabetes, hypertension, and hyperlipidemia when necesary.8,11
Regardless of whether ranolazine was initiated at baseline, all patients enrolled in the clinic underwent appropriate labs and tests, including a basic metabolic panel, magnesium level, and an ECG, if not otherwise available from the CPRS or documented from outside facilities. A thorough history and description of the patient’s anginal symptoms were also taken at baseline and during follow-up visits. Once it was confirmed that the patients’ electrolytes were within normal limits and there was no evidence of prolongation in the Bazett’s QTc interval or major drug interactions, all patients who met criteria for ranolazine were initiated at 500 mg twice daily.9,12 The Seattle Angina Questionnaire (SAQ) was also completed by patients at the initiation of ranolazine and then again at follow-up visits. The SAQ is an 11-question, self-administered survey that measures functional status of patients with angina.13
All patients initiated on or ensuing dose changes with ranolazine followed up with the clinic at 1 and 3 months with labs and ECGs obtained prior to ensure that there were no electrolyte imbalances or excessive QTc prolongation. Excessive QTc prolongation was defined as an increase of ≥ 60 milliseconds (msec) from baseline or > 500 msec.14 If this boundary was exceeded, ranolazine was discontinued, or for those taking higher doses, it was reduced to the initial 500 mg twice daily as long as there was no previous excessive QTc prolongation. In cases where ranolazine was not added at baseline, doses of antianginal medications were titrated over appropriate intervals to improve angina symptoms with ranolazine subsequently added in conjunction with the nonformulary criteria.
A generalized treatment algorithm was followed by the clinic for the management of CSA (Figure). It was highly recommended that all referred patients have an active prescription in the CPRS for short-acting sublingual nitroglycerin 0.4 mg in case of any acute episodes. Although other forms of short-acting nitroglycerin were available, sublingual nitroglycerin 0.4 mg was the preferred formulary medication at the time of the study.
Depending on whether the patients met nonformulary inclusion or exclusion criteria, they were either initiated or optimized on ranolazine or other traditional antianginals, such as beta-blockers (BBs), dihydropyridine calcium channel blockers (DHP-CCBs), or long-acting nitrates (LANs). Beta-blockers were recommended as first-line treatment for patients with previous myocardial infarction (MI) and left ventricular dysfunction, in accordance with treatment guidelines and because of their benefits in treating patients with CSA.12,15
Once patients were optimized on BBs and/or DHP-CCBs, LANs were added if patients experienced ≥ 3 bothersome episodes of chest pain weekly. Optimization for BBs meant an ideal heart rate of at least about 60 bpm without symptoms suggestive of excessive bradycardia, whereas optimization for all 3 classes (BBs, DHP-CCBs, and LANs) consisted of dose titration until the presence of drug-related adverse effects (AEs) or symptoms suggestive of hypotension. Because LANs have lesser effects on blood pressure (BP) compared with DHP-CCBs, they were preferred in patients with persistent anginal symptoms whose BPs were considered low or normal, according to the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) guidelines.16
If patients with normal or controlled BP continued to have symptoms of angina despite optimal doses of BBs and LANs, an appropriate dose of a DHP-CCB was administered and titrated for as long as the patients tolerated the treatment. If titration of antianginal agents was limited due to the presence of other antihypertensives, then the patient’s medication regimen was modified as necessary to allow for an increased dose of the BB or DHP-CCB due to these medications’ abilities to improve angina symptoms while also lowering BP. If patients achieved an acceptable reduction in their angina symptoms, they were discharged from the clinic, whereas those with contraindications to other classes were referred to their PCP or cardiologist.
Patients successfully treated with ranolazine (defined as a noticeable reduction in angina symptoms in the absence of intolerable AEs and excessive QTc prolongation after 3 months) were discharged from the clinic and instructed to follow up with their PCP at least annually. If the patient was discharged from the clinic at the baseline dose, it was recommended to the HCP that he or she follow up within 3 months after any dose increases. Any patient whose symptoms were consistent with unstable angina (described as occurring in an unpredictable manner, as determined by the clinical pharmacy specialist, lasting longer in duration and/or increasing in frequency, and those who experience symptoms at rest) were immediately evaluated and referred to a cardiologist. Patients who continued to have unacceptable rates or episodes of angina despite an optimal medical regimen were referred to Cardiology for consideration of other treatment modalities.
Results
The initial report of this study population was described by Reeder and colleagues.17 Fifty-seven patients were evaluated for study inclusion, of which 22 were excluded due to ranolazine being managed by an outside HCP or because an SAQ was not obtained at baseline. All study participants were males with an average age of 68 years and were predominantly white (86%). All patients had a past medical history significant for hypertension and hyperlipidemia. More than half (57%) had a prior MI and multivessel disease, although only 1 patient had an ejection fraction of < 35%. The majority of patients enrolled were being treated with BBs (97%) and LANs (94%) with a little more than half prescribed CCBs (60%). A large percentage (97%) of patients were also taking aspirin and a statin.
Improvements in angina symptoms as measured by the SAQ and safety measures, which included details of AEs and discontinuation rates following the initiation of ranolazine within the clinic, have previously been published.17 In summary, it was found that the addition of ranolazine to an optimal medical regimen for CSA improved all dimensions of the SAQ scores at 1 and 3 months compared with baseline (Table). Additionally, it was noted that higher doses may not have been as well tolerated in the veteran population, despite that only a small number of eligible patients were captured. This was because 5 of 7 patients whose dose was increased to 1,000 mg twice daily after 1 month required withdrawal as a result of AEs or lack of efficacy. The AEs reported included dizziness, abdominal pain, blurry vision, nausea and vomiting, dry mouth, and dyspnea.
The pharmacists were able to ensure that relevant electrolytes were replaced during the treatment period and also minimized the number of clinically significant drug interactions. Twenty-one patients received medications at baseline that had known interactions with ranolazine. Two patients required discontinuation of other medications: sotalol and diltiazem. At the time this study was conducted, diltiazem was contraindicated when given concomitantly but has since been allowed per manufacturer recommendations as long as the dose of ranolazine does not exceed 500 mg twice daily. Electrolyte replacement was also required in 3 patients, 2 of whom had hypomagnesemia.
Conclusion
Pharmacists have been influential in managing a variety of chronic diseases. When instituted into collaborative practice agreements, CSA is another unique condition that pharmacists can play a role in treating. Given that pharmacists are heavily involved with cardiovascular risk reduction, combined with the higher cost of ranolazine and the need for monitoring due to its AEs, QTc interval prolongation, and significant drug interactions, the benefits of having pharmacist-oriented clinics can ensure the safe and effective use of medications in the treatment of CSA.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Go AS, Mozaffarian D, Roger VL, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics–2014 update: A report from the American Heart Association. Circulation. 2014;129:e28-e292.
2. Boden WE, O’Rourke RA, Teo KK, et al; COURAGE Trial Research Group. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007;356(15):1503-1516.
3. RITA-2 trial participants. Coronary angioplasty versus medical therapy for angina: The second Randomised Intervention Treatment of Angina (RITA-2) trial. Lancet. 1997;350(9076):461-468.
4. Norton JL, Gibson DL. Establishing an outpatient anticoagulation clinic in a community hospital. Am J Health Syst Pharm. 1996;53(10):1151-1157.
5. Morello CM, Zadvorny EB, Cording MA, Suemoto RT, Skog J, Harari A. Development and clinical outcomes of pharmacist-managed diabetes care clinics. Am J Health Syst Pharm. 2006;63(14):1325-1331.
6. Vivian EM. Improving blood pressure control in a pharmacist-managed hypertension clinic. Pharmacotherapy. 2002;22(12):1533-1540.
7. Cording MA, Engelbrecht-Zadvorny EB, Pettit BJ, Eastham JH, Sandoval R. Development of a pharmacist-managed lipid clinic. Ann Pharmacother. 2002;36(5):892-904.
8. Geber J, Parra D, Beckey NP, Korman L. Optimizing drug therapy in patients with cardiovascular disease: The impact of pharmacist-managed pharmacotherapy clinics in a primary care setting. Pharmacotherapy. 2002; 22(6):738-747.
9. Ranexa [package insert]. Foster City, CA: Gilead Sciences, Inc.; 2013.
10. VHA Pharmacy Benefits Management Strategic Healthcare Group and the Medical Advisory Panel. Ranolazine. National PBM Drug Monograph. U.S. Department of Veterans Affairs Pharmacy Benefits Management Services Website. http://www.pbm.va.gov/clinicalguidance/drugmonographs/Ranolazine.pdf. Published June 2007. Accessed May 7, 2014.
11. Fraker TD Jr, Fihn SD; writing on behalf of the 2002 Chronic Stable Angina Writing Committee. 2007 chronic angina focused update of the ACC/AHA 2002 guidelines for the management of patients with chronic stable angina: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines Writing Group to develop the focused update of the 2002 guidelines for the management of patients with chronic stable angina. Circulation. 2007;116(23):2762-2772.
12. Funck-Brentano C, Jaillon P. Rate-corrected QT interval: Techniques and limitations. Am J Cardiol. 1993;72(6):17B-22B.
13. Spertus JA, Winder JA, Dewhurst TA, et al. Development and evaluation of the Seattle Angina Questionnaire: A new functional status measure for coronary artery disease. J Am Coll Cardiol. 1995;25(2):333-341.
14. Drew BJ, Ackerman MJ, Funk M, et al; American Heart Association Acute Cardiac Care Committee of the Council on Clinical Cardiology, the Council on Cardiovascular Nursing, and the American College of Cardiology Foundation. Prevention of torsade de pointes in hospital settings: A scientific statement from the American Heart Association and the American College of Cardiology Foundation. Circulation. 2010;121(8):1047-1060.
15. Heidenreich PA, McDonald KM, Hastie T, et al. Meta-analysis of trials comparing beta-blockers, calcium antagonists, and nitrates for stable angina. JAMA. 1999;281(20):1927-1936.
16. Chobanian AV, Bakris GL, Black HR, et al; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. The JNC 7 report. JAMA. 2003;289(19):2560-2572.
17. Reeder DN, Gillette MA, Franck AJ, Frohnapple DJ. Clinical experience with ranolazine in a veteran population with chronic stable angina. Ann Pharmacother. 2012;46(1):42-50.
1. Go AS, Mozaffarian D, Roger VL, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics–2014 update: A report from the American Heart Association. Circulation. 2014;129:e28-e292.
2. Boden WE, O’Rourke RA, Teo KK, et al; COURAGE Trial Research Group. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007;356(15):1503-1516.
3. RITA-2 trial participants. Coronary angioplasty versus medical therapy for angina: The second Randomised Intervention Treatment of Angina (RITA-2) trial. Lancet. 1997;350(9076):461-468.
4. Norton JL, Gibson DL. Establishing an outpatient anticoagulation clinic in a community hospital. Am J Health Syst Pharm. 1996;53(10):1151-1157.
5. Morello CM, Zadvorny EB, Cording MA, Suemoto RT, Skog J, Harari A. Development and clinical outcomes of pharmacist-managed diabetes care clinics. Am J Health Syst Pharm. 2006;63(14):1325-1331.
6. Vivian EM. Improving blood pressure control in a pharmacist-managed hypertension clinic. Pharmacotherapy. 2002;22(12):1533-1540.
7. Cording MA, Engelbrecht-Zadvorny EB, Pettit BJ, Eastham JH, Sandoval R. Development of a pharmacist-managed lipid clinic. Ann Pharmacother. 2002;36(5):892-904.
8. Geber J, Parra D, Beckey NP, Korman L. Optimizing drug therapy in patients with cardiovascular disease: The impact of pharmacist-managed pharmacotherapy clinics in a primary care setting. Pharmacotherapy. 2002; 22(6):738-747.
9. Ranexa [package insert]. Foster City, CA: Gilead Sciences, Inc.; 2013.
10. VHA Pharmacy Benefits Management Strategic Healthcare Group and the Medical Advisory Panel. Ranolazine. National PBM Drug Monograph. U.S. Department of Veterans Affairs Pharmacy Benefits Management Services Website. http://www.pbm.va.gov/clinicalguidance/drugmonographs/Ranolazine.pdf. Published June 2007. Accessed May 7, 2014.
11. Fraker TD Jr, Fihn SD; writing on behalf of the 2002 Chronic Stable Angina Writing Committee. 2007 chronic angina focused update of the ACC/AHA 2002 guidelines for the management of patients with chronic stable angina: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines Writing Group to develop the focused update of the 2002 guidelines for the management of patients with chronic stable angina. Circulation. 2007;116(23):2762-2772.
12. Funck-Brentano C, Jaillon P. Rate-corrected QT interval: Techniques and limitations. Am J Cardiol. 1993;72(6):17B-22B.
13. Spertus JA, Winder JA, Dewhurst TA, et al. Development and evaluation of the Seattle Angina Questionnaire: A new functional status measure for coronary artery disease. J Am Coll Cardiol. 1995;25(2):333-341.
14. Drew BJ, Ackerman MJ, Funk M, et al; American Heart Association Acute Cardiac Care Committee of the Council on Clinical Cardiology, the Council on Cardiovascular Nursing, and the American College of Cardiology Foundation. Prevention of torsade de pointes in hospital settings: A scientific statement from the American Heart Association and the American College of Cardiology Foundation. Circulation. 2010;121(8):1047-1060.
15. Heidenreich PA, McDonald KM, Hastie T, et al. Meta-analysis of trials comparing beta-blockers, calcium antagonists, and nitrates for stable angina. JAMA. 1999;281(20):1927-1936.
16. Chobanian AV, Bakris GL, Black HR, et al; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. The JNC 7 report. JAMA. 2003;289(19):2560-2572.
17. Reeder DN, Gillette MA, Franck AJ, Frohnapple DJ. Clinical experience with ranolazine in a veteran population with chronic stable angina. Ann Pharmacother. 2012;46(1):42-50.
Empathic Disclosure of Adverse Events to Patients
In 1987, the chief of staff of the Lexington VAMC and the staff attorney for the VA Regional Counsel Office in Lexington, Kentucky, discovered that a recent patient death was due to a mistake made in the medical care provided at their facility. They decided to disclose what happened to the family who had no knowledge of this mistake in care because “it was the right thing to do.”
The Lexington Model for disclosure, as it became known worldwide, continued to flourish under the leadership of Kraman and Hamm.1,2 The VA National Center for Ethics in Health Care adopted these principles of disclosure in drafting a national VHA policy directive in 2008, which was updated in 2012.3 However, despite the ethical and professional imperatives, disclosing adverse events (AEs) to patients and family members has continued to be one of the most difficult challenges in the practice of medicine.
VHA policy has made a distinction between clinical disclosure, conducted by a clinician with a patient as a routine professional practice, and institutional disclosure, conducted by institutional leadership for an AE rising above a threshold of serious patient harm. According to VHA Director of Risk Management Yuri Walker in a 2013 personal communication, the frequency of institutional disclosure reports from VAMCs since 2011 have reflected significant variation in disclosure practice among facilities of similar size and complexity.
In this report, the authors share their experience developing and delivering a simulation-based disclosure training program in the VHA intended to close the gap between policy expectations and practical challenges for providers and institutions when facing the task of disclosing an AE to patients and families.
Medical Error Disclosure
It is not difficult to understand why health care providers (HCPs) are uncomfortable about disclosing AEs to patients. The study by Delbanco and Bell describes physicians experiencing guilt, shame, and fear of retribution after a patient experiences an AE. The resulting silence and avoidance of the patient only compounds patient harm.4 Many HCPs believe disclosure will lead to tort claims, provide evidence against their defense, encourage reporting to the National Practitioners’ Databank, and damage their reputations with a potentially negative impact on their careers.5-7
In a 2009 survey of 1,891 practicing physicians in the U.S., one-third did not agree with disclosing serious medical errors to patients.8 Another survey of physicians reported wide variations in responses about whether they would offer an apology after making a medical mistake.9 Therefore, a gap between patient expectations and HCP communication when a medical mistake occurs should be expected.10
Few HCPs receive training in empathic communication skills for effective disclosure of AEs to patients and families.11 In a survey of 3,171 physicians in the U.S. and Canada, Waterman and colleagues found that only 10% of physicians believed they had adequate support from their health care organizations (HCOs) after an AE occurred, even though 86% expressed significant interest in receiving training on the disclosure of AEs.12 Despite this gap, some medical educators, such as Katie Watson at Northwestern University, are successfully demonstrating the power of teaching medical students improvisational acting skills to enhance professionalism and communication in future physician–patient interaction.13
Disclosure Training Program
In 2010, the Lexington VAMC was awarded a 3-year VA Systems Improvement Capability Grant, which funded the development of a Disclosure Training Program (DTP). A team of investigators designed a 2-day workshop based on principles of experiential learning. Each workshop incorporated interactive teaching techniques using filmed clinical vignettes to provide a context for facilitated small-group disclosure simulations with professional actors.14 A total of 14 workshops were conducted for 346 participants from December 2011 to September 2012.
The DTP workshop integrates focused didactic sessions with interactive audience-workshop facilitator discussion, debriefing of teaching films, and disclosure simulations, with the majority of time spent the conducting and debriefing of simulations. Core content addressed during workshop activities included the following:
1. Historical origins of disclosure policy at the VHA
2. Ethical obligation, professional duty, and legal mandates for disclosure
3. Empathic communication–cognitive and emotive
4. VHA Handbook 1004.08, Disclosure of Adverse Events to Patient
5. Institutional and Clinical Disclosure of AEs
6. Psychological and physical needs of patients after an AE
7. Disclosure linking risk management to patient safety in a health care system
8. Legal implications for disclosure
9. State apology laws
10. Implementing disclosure programs in health care facilities
11. Facility support for providers after a patient AE
The principles of empathic communication and the core elements of AE disclosure to patients are reinforced during small-group simulations with actors portraying patients or family members. Each small-group simulation typically involves 3 to 4 workshop participants and 1 to 2 actors. Participants are given the task of conducting a clinical or institutional disclosure.
A facilitator manages each simulation, based on a scripted scenario or teaching film viewed by workshop participants. In the simulations attendees assume the roles of hospital staff that might be realistically involved in disclosure conversations, including executive leaders, physicians, nurses, risk managers, pharmacists, chaplains, and social workers.
Simulations average 5 to 7 minutes and are followed by a debriefing, including simulation participants, workshop facilitators, and the professional actor, who remain in character. By the end of each 2-day workshop, all attendees have participated in multiple small-group simulations of both clinical and institutional disclosures. Pre- and postworkshop knowledge questions and program evaluation data are collected with immediate-response polling technology used throughout the workshop.
Between 20 and 40 HCPs attended each workshop, which was designed for clinical and administrative leaders as well as others supporting the disclosure process, such as nurse managers, patient safety managers, social workers, chaplains, and pharmacists. The facility director, chief of staff, risk manager, and lawyers from the Regional Counsel office all play an important role in institutional disclosures and all were strongly encouraged to attend. The DTP facilitators observed the importance of senior executive leadership—participation, which enhanced dialogue in the large group sessions and small-group simulation-based learning.
DTP Workshop Results
Fourteen workshops were conducted for 346 employees from 26 VAMCs in 2012. Audience response technology was used to elicit participant feedback regarding workshop quality and effectiveness. Additional questions were asked as a pre/post-test of subject matter knowledge. Following the workshop, the participants showed a 30% overall improvement over preworkshop tests (Table), and 95% of participants favorably rated the workshop for quality and effectiveness.
There was a positive association between workshops with facility directors and actively engaged chiefs of staff in attendance and higher improvement scores in the test of knowledge. Among the top 7 performers on this test, 6 were individual facilities hosting the workshops and 1 VISN hosting for several facility representatives. Eleven of the 14 workshops with these characteristics (3 of which included VISN directors) evidenced more than 20% improvement on the test knowledge. These findings confirmed the original program design intended for individual facilities with leadership in attendance.
Iterative improvements were made to the program throughout 2012 based on feedback from workshop attendees, the National Office of Risk Management, the National Center for Ethics in Health Care and participating VA facilities and VISNs.
Despite these encouraging results, the DTP has some significant limitations: It is expensive, labor intensive, and dependent on faculty with expertise in clinical medicine, bioethics, and the law. Considering tight federal budgets, justifying the expenses to host a training program is difficult for a VAMC compared with that of other spending priorities. The actual and opportunity costs of travel to host sites for several facilitators and a group of professional actors to conduct a 2-day workshop for busy HCPs is not trivial.
Another limitation is the use of immediate response technology for data collection. Although this method maximizes response rates and seems to keep attendees engaged in presentations and discussions, technical failures could result in dropped responses, and ultimately the choice to respond is dependent on participant willingness to use the device.
Conclusion
Encouraging results suggest a bright future for the DTP, which has relevance for any health care organization, including the VA, academic affiliates, or those in the private sector. Wherever health care is delivered, providers will have the difficult task of disclosing AEs to meet their duty of care when patients experience harm. Learning empathic communication skills and successful strategies for disclosure will enhance this interaction and contribute to the maintenance of trust that is critical to the provider–patient relationship.
The DTP workshop has a flexible design and can be packaged to accommodate host medical centers for workshops of 1 to 2 days’ duration. The didactic presentations are constant, whereas the number of simulations will vary, depending on the length of the workshop (2-3 simulations for 1 day and 5-7 for two days). Participants from every workshop consistently cite that the simulations with professional actors are a powerful learning experience of significant personal value.
The DTP was developed as a unique, simulation-based program for clinicians, administrators, and allied health care personnel to enhance the effective disclosure of AEs to patients. Feedback from participants in 14 workshops in 2012 cited the value of the program with a high favorability rating. In a test of knowledge, participants also demonstrated an increase in learning. This feedback from the health care professionals who have attended the workshops has validated the pedagogic design of the program, which leverages adult learning principles of learning through experience. This approach was described by Aristotle in his best-known work on ethics, Nicomachean Ethics, “For the things we have to learn before we can do them, we learn by doing them.”15
Acknowledgements
For their significant contributions to the development and implementation of the VHA Disclosure Training Program, the authors thank Aaliyah Eaves-Leanos, Mary Duke, Lindsay Hall, and Uzair Munis. We thank the Institute for Healthcare Communication for their assistance in the program development. We express our utmost appreciation to Lee Taft for his many invaluable contributions to this program, including the critical role he continues to assume as a faculty member in the workshops. And, we are grateful for the continued contributions from our talented professional actors of Heyman Talent in Louisville, KY.
We express our sincere gratitude for their continuous feedback and important technical advice informing iterative improvements in the DTP workshops throughout 2012 from Virginia Ashby Sharpe (VA National Center for Ethics in Health Care); Yuri Walker (director of the Risk Management Program); and Barbara Rose (data analyst in the Risk Management Program), all at the VA central office in Washington, DC. And finally, we thank Heather Woodward-Hagg, Director of the VA Center for Applied Systems Engineering in Indianapolis, IN for her continued support in making DTP workshops available to VA Medical Centers throughout the country upon request.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Kraman SS, Hamm G. Risk management: Extreme honesty may be the best policy. Ann Intern Med. 1999;131(12):963-967.
2. Hamm GM, Kraman SS. New standards, new dilemmas: Reflections on managing medical mistakes. Bioethics Forum. 2001;17(2):19-25.
3. Veterans Health Administration. Disclosure of adverse events to patients. Handbook 100408. United States Department of Veterans Affairs Website. http://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=2800. Corrected copy October 12, 2012. Accessed April 3, 2014.
4. Delbanco T, Bell SK. Guilty, afraid, and alone—struggling with medical error. N Engl J Med. 2007;357(17):1682-1683.
5. Taft L. Apology and medical mistake: Opportunity or foil? Ann Health L. 2005;14:55-94.
6. Gallagher TH, Garbutt JM, Waterman AD, et al. Choosing your words carefully: How physicians would disclose harmful medical error to patients. Arch Intern Med. 2006;166(15):1585-1593.
7. Banja J. Medical Errors and Medical Narcissism. Sudbury, MD: Jones and Bartlett; 2005.
8. Iezzoni LI, Rao SR, DesRoches CM, Vogeli C, Campbell EG. Survey shows that at least some physicians are not always open or honest with patients. Health Aff (Millwood). 2012;31(2):383-391.
9. Gallagher TW, Waterman AD, Garbutt JM, et al. US and Canadian physicians’ attitudes and experiences regarding disclosure errors to patients. Arch Intern Med. 2006;166(15):1605-1611.
10. Robbennolt JK. Apologies and medical error. Clin Orthop Relat Res. 2009;467(2):376-382 White AA, Bell SK, Krauss MJ, et al. How trainees would disclose medical errors: Educational implications for training programmes. Med Educ. 201;45(4):372-380.
11. White AA, Bell SK, Krauss MJ, et al. How trainees would disclose medical errors: Educational implications for training programmes. Med Educ. 201;45(4):372-380.
12. Waterman AD, Garbutt J, Hazel E, et al. The emotional impact of medical errors on practicing physicians in the United States and Canada. Jt Comm J Qual Patient Saf. 2007;33(8):467-476.
13. Watson K. Serious play: Teaching medical skills with improvisational theater techniques. Acad Med. 2011;86(10):1260-1265.
14. Eaves-Leanos A, Dunn EJ. Open disclosure of adverse events: Transparency and safety in healthcare. Surg Clin North Am. 2012;92(1):163-177.
15. Aristotle. Nichomachean Ethics (edited by Roger Crisp). Cambridge University Press, New York, NY (2012): Book II, Chapter 1 (1103b), p. 23.
In 1987, the chief of staff of the Lexington VAMC and the staff attorney for the VA Regional Counsel Office in Lexington, Kentucky, discovered that a recent patient death was due to a mistake made in the medical care provided at their facility. They decided to disclose what happened to the family who had no knowledge of this mistake in care because “it was the right thing to do.”
The Lexington Model for disclosure, as it became known worldwide, continued to flourish under the leadership of Kraman and Hamm.1,2 The VA National Center for Ethics in Health Care adopted these principles of disclosure in drafting a national VHA policy directive in 2008, which was updated in 2012.3 However, despite the ethical and professional imperatives, disclosing adverse events (AEs) to patients and family members has continued to be one of the most difficult challenges in the practice of medicine.
VHA policy has made a distinction between clinical disclosure, conducted by a clinician with a patient as a routine professional practice, and institutional disclosure, conducted by institutional leadership for an AE rising above a threshold of serious patient harm. According to VHA Director of Risk Management Yuri Walker in a 2013 personal communication, the frequency of institutional disclosure reports from VAMCs since 2011 have reflected significant variation in disclosure practice among facilities of similar size and complexity.
In this report, the authors share their experience developing and delivering a simulation-based disclosure training program in the VHA intended to close the gap between policy expectations and practical challenges for providers and institutions when facing the task of disclosing an AE to patients and families.
Medical Error Disclosure
It is not difficult to understand why health care providers (HCPs) are uncomfortable about disclosing AEs to patients. The study by Delbanco and Bell describes physicians experiencing guilt, shame, and fear of retribution after a patient experiences an AE. The resulting silence and avoidance of the patient only compounds patient harm.4 Many HCPs believe disclosure will lead to tort claims, provide evidence against their defense, encourage reporting to the National Practitioners’ Databank, and damage their reputations with a potentially negative impact on their careers.5-7
In a 2009 survey of 1,891 practicing physicians in the U.S., one-third did not agree with disclosing serious medical errors to patients.8 Another survey of physicians reported wide variations in responses about whether they would offer an apology after making a medical mistake.9 Therefore, a gap between patient expectations and HCP communication when a medical mistake occurs should be expected.10
Few HCPs receive training in empathic communication skills for effective disclosure of AEs to patients and families.11 In a survey of 3,171 physicians in the U.S. and Canada, Waterman and colleagues found that only 10% of physicians believed they had adequate support from their health care organizations (HCOs) after an AE occurred, even though 86% expressed significant interest in receiving training on the disclosure of AEs.12 Despite this gap, some medical educators, such as Katie Watson at Northwestern University, are successfully demonstrating the power of teaching medical students improvisational acting skills to enhance professionalism and communication in future physician–patient interaction.13
Disclosure Training Program
In 2010, the Lexington VAMC was awarded a 3-year VA Systems Improvement Capability Grant, which funded the development of a Disclosure Training Program (DTP). A team of investigators designed a 2-day workshop based on principles of experiential learning. Each workshop incorporated interactive teaching techniques using filmed clinical vignettes to provide a context for facilitated small-group disclosure simulations with professional actors.14 A total of 14 workshops were conducted for 346 participants from December 2011 to September 2012.
The DTP workshop integrates focused didactic sessions with interactive audience-workshop facilitator discussion, debriefing of teaching films, and disclosure simulations, with the majority of time spent the conducting and debriefing of simulations. Core content addressed during workshop activities included the following:
1. Historical origins of disclosure policy at the VHA
2. Ethical obligation, professional duty, and legal mandates for disclosure
3. Empathic communication–cognitive and emotive
4. VHA Handbook 1004.08, Disclosure of Adverse Events to Patient
5. Institutional and Clinical Disclosure of AEs
6. Psychological and physical needs of patients after an AE
7. Disclosure linking risk management to patient safety in a health care system
8. Legal implications for disclosure
9. State apology laws
10. Implementing disclosure programs in health care facilities
11. Facility support for providers after a patient AE
The principles of empathic communication and the core elements of AE disclosure to patients are reinforced during small-group simulations with actors portraying patients or family members. Each small-group simulation typically involves 3 to 4 workshop participants and 1 to 2 actors. Participants are given the task of conducting a clinical or institutional disclosure.
A facilitator manages each simulation, based on a scripted scenario or teaching film viewed by workshop participants. In the simulations attendees assume the roles of hospital staff that might be realistically involved in disclosure conversations, including executive leaders, physicians, nurses, risk managers, pharmacists, chaplains, and social workers.
Simulations average 5 to 7 minutes and are followed by a debriefing, including simulation participants, workshop facilitators, and the professional actor, who remain in character. By the end of each 2-day workshop, all attendees have participated in multiple small-group simulations of both clinical and institutional disclosures. Pre- and postworkshop knowledge questions and program evaluation data are collected with immediate-response polling technology used throughout the workshop.
Between 20 and 40 HCPs attended each workshop, which was designed for clinical and administrative leaders as well as others supporting the disclosure process, such as nurse managers, patient safety managers, social workers, chaplains, and pharmacists. The facility director, chief of staff, risk manager, and lawyers from the Regional Counsel office all play an important role in institutional disclosures and all were strongly encouraged to attend. The DTP facilitators observed the importance of senior executive leadership—participation, which enhanced dialogue in the large group sessions and small-group simulation-based learning.
DTP Workshop Results
Fourteen workshops were conducted for 346 employees from 26 VAMCs in 2012. Audience response technology was used to elicit participant feedback regarding workshop quality and effectiveness. Additional questions were asked as a pre/post-test of subject matter knowledge. Following the workshop, the participants showed a 30% overall improvement over preworkshop tests (Table), and 95% of participants favorably rated the workshop for quality and effectiveness.
There was a positive association between workshops with facility directors and actively engaged chiefs of staff in attendance and higher improvement scores in the test of knowledge. Among the top 7 performers on this test, 6 were individual facilities hosting the workshops and 1 VISN hosting for several facility representatives. Eleven of the 14 workshops with these characteristics (3 of which included VISN directors) evidenced more than 20% improvement on the test knowledge. These findings confirmed the original program design intended for individual facilities with leadership in attendance.
Iterative improvements were made to the program throughout 2012 based on feedback from workshop attendees, the National Office of Risk Management, the National Center for Ethics in Health Care and participating VA facilities and VISNs.
Despite these encouraging results, the DTP has some significant limitations: It is expensive, labor intensive, and dependent on faculty with expertise in clinical medicine, bioethics, and the law. Considering tight federal budgets, justifying the expenses to host a training program is difficult for a VAMC compared with that of other spending priorities. The actual and opportunity costs of travel to host sites for several facilitators and a group of professional actors to conduct a 2-day workshop for busy HCPs is not trivial.
Another limitation is the use of immediate response technology for data collection. Although this method maximizes response rates and seems to keep attendees engaged in presentations and discussions, technical failures could result in dropped responses, and ultimately the choice to respond is dependent on participant willingness to use the device.
Conclusion
Encouraging results suggest a bright future for the DTP, which has relevance for any health care organization, including the VA, academic affiliates, or those in the private sector. Wherever health care is delivered, providers will have the difficult task of disclosing AEs to meet their duty of care when patients experience harm. Learning empathic communication skills and successful strategies for disclosure will enhance this interaction and contribute to the maintenance of trust that is critical to the provider–patient relationship.
The DTP workshop has a flexible design and can be packaged to accommodate host medical centers for workshops of 1 to 2 days’ duration. The didactic presentations are constant, whereas the number of simulations will vary, depending on the length of the workshop (2-3 simulations for 1 day and 5-7 for two days). Participants from every workshop consistently cite that the simulations with professional actors are a powerful learning experience of significant personal value.
The DTP was developed as a unique, simulation-based program for clinicians, administrators, and allied health care personnel to enhance the effective disclosure of AEs to patients. Feedback from participants in 14 workshops in 2012 cited the value of the program with a high favorability rating. In a test of knowledge, participants also demonstrated an increase in learning. This feedback from the health care professionals who have attended the workshops has validated the pedagogic design of the program, which leverages adult learning principles of learning through experience. This approach was described by Aristotle in his best-known work on ethics, Nicomachean Ethics, “For the things we have to learn before we can do them, we learn by doing them.”15
Acknowledgements
For their significant contributions to the development and implementation of the VHA Disclosure Training Program, the authors thank Aaliyah Eaves-Leanos, Mary Duke, Lindsay Hall, and Uzair Munis. We thank the Institute for Healthcare Communication for their assistance in the program development. We express our utmost appreciation to Lee Taft for his many invaluable contributions to this program, including the critical role he continues to assume as a faculty member in the workshops. And, we are grateful for the continued contributions from our talented professional actors of Heyman Talent in Louisville, KY.
We express our sincere gratitude for their continuous feedback and important technical advice informing iterative improvements in the DTP workshops throughout 2012 from Virginia Ashby Sharpe (VA National Center for Ethics in Health Care); Yuri Walker (director of the Risk Management Program); and Barbara Rose (data analyst in the Risk Management Program), all at the VA central office in Washington, DC. And finally, we thank Heather Woodward-Hagg, Director of the VA Center for Applied Systems Engineering in Indianapolis, IN for her continued support in making DTP workshops available to VA Medical Centers throughout the country upon request.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
In 1987, the chief of staff of the Lexington VAMC and the staff attorney for the VA Regional Counsel Office in Lexington, Kentucky, discovered that a recent patient death was due to a mistake made in the medical care provided at their facility. They decided to disclose what happened to the family who had no knowledge of this mistake in care because “it was the right thing to do.”
The Lexington Model for disclosure, as it became known worldwide, continued to flourish under the leadership of Kraman and Hamm.1,2 The VA National Center for Ethics in Health Care adopted these principles of disclosure in drafting a national VHA policy directive in 2008, which was updated in 2012.3 However, despite the ethical and professional imperatives, disclosing adverse events (AEs) to patients and family members has continued to be one of the most difficult challenges in the practice of medicine.
VHA policy has made a distinction between clinical disclosure, conducted by a clinician with a patient as a routine professional practice, and institutional disclosure, conducted by institutional leadership for an AE rising above a threshold of serious patient harm. According to VHA Director of Risk Management Yuri Walker in a 2013 personal communication, the frequency of institutional disclosure reports from VAMCs since 2011 have reflected significant variation in disclosure practice among facilities of similar size and complexity.
In this report, the authors share their experience developing and delivering a simulation-based disclosure training program in the VHA intended to close the gap between policy expectations and practical challenges for providers and institutions when facing the task of disclosing an AE to patients and families.
Medical Error Disclosure
It is not difficult to understand why health care providers (HCPs) are uncomfortable about disclosing AEs to patients. The study by Delbanco and Bell describes physicians experiencing guilt, shame, and fear of retribution after a patient experiences an AE. The resulting silence and avoidance of the patient only compounds patient harm.4 Many HCPs believe disclosure will lead to tort claims, provide evidence against their defense, encourage reporting to the National Practitioners’ Databank, and damage their reputations with a potentially negative impact on their careers.5-7
In a 2009 survey of 1,891 practicing physicians in the U.S., one-third did not agree with disclosing serious medical errors to patients.8 Another survey of physicians reported wide variations in responses about whether they would offer an apology after making a medical mistake.9 Therefore, a gap between patient expectations and HCP communication when a medical mistake occurs should be expected.10
Few HCPs receive training in empathic communication skills for effective disclosure of AEs to patients and families.11 In a survey of 3,171 physicians in the U.S. and Canada, Waterman and colleagues found that only 10% of physicians believed they had adequate support from their health care organizations (HCOs) after an AE occurred, even though 86% expressed significant interest in receiving training on the disclosure of AEs.12 Despite this gap, some medical educators, such as Katie Watson at Northwestern University, are successfully demonstrating the power of teaching medical students improvisational acting skills to enhance professionalism and communication in future physician–patient interaction.13
Disclosure Training Program
In 2010, the Lexington VAMC was awarded a 3-year VA Systems Improvement Capability Grant, which funded the development of a Disclosure Training Program (DTP). A team of investigators designed a 2-day workshop based on principles of experiential learning. Each workshop incorporated interactive teaching techniques using filmed clinical vignettes to provide a context for facilitated small-group disclosure simulations with professional actors.14 A total of 14 workshops were conducted for 346 participants from December 2011 to September 2012.
The DTP workshop integrates focused didactic sessions with interactive audience-workshop facilitator discussion, debriefing of teaching films, and disclosure simulations, with the majority of time spent the conducting and debriefing of simulations. Core content addressed during workshop activities included the following:
1. Historical origins of disclosure policy at the VHA
2. Ethical obligation, professional duty, and legal mandates for disclosure
3. Empathic communication–cognitive and emotive
4. VHA Handbook 1004.08, Disclosure of Adverse Events to Patient
5. Institutional and Clinical Disclosure of AEs
6. Psychological and physical needs of patients after an AE
7. Disclosure linking risk management to patient safety in a health care system
8. Legal implications for disclosure
9. State apology laws
10. Implementing disclosure programs in health care facilities
11. Facility support for providers after a patient AE
The principles of empathic communication and the core elements of AE disclosure to patients are reinforced during small-group simulations with actors portraying patients or family members. Each small-group simulation typically involves 3 to 4 workshop participants and 1 to 2 actors. Participants are given the task of conducting a clinical or institutional disclosure.
A facilitator manages each simulation, based on a scripted scenario or teaching film viewed by workshop participants. In the simulations attendees assume the roles of hospital staff that might be realistically involved in disclosure conversations, including executive leaders, physicians, nurses, risk managers, pharmacists, chaplains, and social workers.
Simulations average 5 to 7 minutes and are followed by a debriefing, including simulation participants, workshop facilitators, and the professional actor, who remain in character. By the end of each 2-day workshop, all attendees have participated in multiple small-group simulations of both clinical and institutional disclosures. Pre- and postworkshop knowledge questions and program evaluation data are collected with immediate-response polling technology used throughout the workshop.
Between 20 and 40 HCPs attended each workshop, which was designed for clinical and administrative leaders as well as others supporting the disclosure process, such as nurse managers, patient safety managers, social workers, chaplains, and pharmacists. The facility director, chief of staff, risk manager, and lawyers from the Regional Counsel office all play an important role in institutional disclosures and all were strongly encouraged to attend. The DTP facilitators observed the importance of senior executive leadership—participation, which enhanced dialogue in the large group sessions and small-group simulation-based learning.
DTP Workshop Results
Fourteen workshops were conducted for 346 employees from 26 VAMCs in 2012. Audience response technology was used to elicit participant feedback regarding workshop quality and effectiveness. Additional questions were asked as a pre/post-test of subject matter knowledge. Following the workshop, the participants showed a 30% overall improvement over preworkshop tests (Table), and 95% of participants favorably rated the workshop for quality and effectiveness.
There was a positive association between workshops with facility directors and actively engaged chiefs of staff in attendance and higher improvement scores in the test of knowledge. Among the top 7 performers on this test, 6 were individual facilities hosting the workshops and 1 VISN hosting for several facility representatives. Eleven of the 14 workshops with these characteristics (3 of which included VISN directors) evidenced more than 20% improvement on the test knowledge. These findings confirmed the original program design intended for individual facilities with leadership in attendance.
Iterative improvements were made to the program throughout 2012 based on feedback from workshop attendees, the National Office of Risk Management, the National Center for Ethics in Health Care and participating VA facilities and VISNs.
Despite these encouraging results, the DTP has some significant limitations: It is expensive, labor intensive, and dependent on faculty with expertise in clinical medicine, bioethics, and the law. Considering tight federal budgets, justifying the expenses to host a training program is difficult for a VAMC compared with that of other spending priorities. The actual and opportunity costs of travel to host sites for several facilitators and a group of professional actors to conduct a 2-day workshop for busy HCPs is not trivial.
Another limitation is the use of immediate response technology for data collection. Although this method maximizes response rates and seems to keep attendees engaged in presentations and discussions, technical failures could result in dropped responses, and ultimately the choice to respond is dependent on participant willingness to use the device.
Conclusion
Encouraging results suggest a bright future for the DTP, which has relevance for any health care organization, including the VA, academic affiliates, or those in the private sector. Wherever health care is delivered, providers will have the difficult task of disclosing AEs to meet their duty of care when patients experience harm. Learning empathic communication skills and successful strategies for disclosure will enhance this interaction and contribute to the maintenance of trust that is critical to the provider–patient relationship.
The DTP workshop has a flexible design and can be packaged to accommodate host medical centers for workshops of 1 to 2 days’ duration. The didactic presentations are constant, whereas the number of simulations will vary, depending on the length of the workshop (2-3 simulations for 1 day and 5-7 for two days). Participants from every workshop consistently cite that the simulations with professional actors are a powerful learning experience of significant personal value.
The DTP was developed as a unique, simulation-based program for clinicians, administrators, and allied health care personnel to enhance the effective disclosure of AEs to patients. Feedback from participants in 14 workshops in 2012 cited the value of the program with a high favorability rating. In a test of knowledge, participants also demonstrated an increase in learning. This feedback from the health care professionals who have attended the workshops has validated the pedagogic design of the program, which leverages adult learning principles of learning through experience. This approach was described by Aristotle in his best-known work on ethics, Nicomachean Ethics, “For the things we have to learn before we can do them, we learn by doing them.”15
Acknowledgements
For their significant contributions to the development and implementation of the VHA Disclosure Training Program, the authors thank Aaliyah Eaves-Leanos, Mary Duke, Lindsay Hall, and Uzair Munis. We thank the Institute for Healthcare Communication for their assistance in the program development. We express our utmost appreciation to Lee Taft for his many invaluable contributions to this program, including the critical role he continues to assume as a faculty member in the workshops. And, we are grateful for the continued contributions from our talented professional actors of Heyman Talent in Louisville, KY.
We express our sincere gratitude for their continuous feedback and important technical advice informing iterative improvements in the DTP workshops throughout 2012 from Virginia Ashby Sharpe (VA National Center for Ethics in Health Care); Yuri Walker (director of the Risk Management Program); and Barbara Rose (data analyst in the Risk Management Program), all at the VA central office in Washington, DC. And finally, we thank Heather Woodward-Hagg, Director of the VA Center for Applied Systems Engineering in Indianapolis, IN for her continued support in making DTP workshops available to VA Medical Centers throughout the country upon request.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Kraman SS, Hamm G. Risk management: Extreme honesty may be the best policy. Ann Intern Med. 1999;131(12):963-967.
2. Hamm GM, Kraman SS. New standards, new dilemmas: Reflections on managing medical mistakes. Bioethics Forum. 2001;17(2):19-25.
3. Veterans Health Administration. Disclosure of adverse events to patients. Handbook 100408. United States Department of Veterans Affairs Website. http://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=2800. Corrected copy October 12, 2012. Accessed April 3, 2014.
4. Delbanco T, Bell SK. Guilty, afraid, and alone—struggling with medical error. N Engl J Med. 2007;357(17):1682-1683.
5. Taft L. Apology and medical mistake: Opportunity or foil? Ann Health L. 2005;14:55-94.
6. Gallagher TH, Garbutt JM, Waterman AD, et al. Choosing your words carefully: How physicians would disclose harmful medical error to patients. Arch Intern Med. 2006;166(15):1585-1593.
7. Banja J. Medical Errors and Medical Narcissism. Sudbury, MD: Jones and Bartlett; 2005.
8. Iezzoni LI, Rao SR, DesRoches CM, Vogeli C, Campbell EG. Survey shows that at least some physicians are not always open or honest with patients. Health Aff (Millwood). 2012;31(2):383-391.
9. Gallagher TW, Waterman AD, Garbutt JM, et al. US and Canadian physicians’ attitudes and experiences regarding disclosure errors to patients. Arch Intern Med. 2006;166(15):1605-1611.
10. Robbennolt JK. Apologies and medical error. Clin Orthop Relat Res. 2009;467(2):376-382 White AA, Bell SK, Krauss MJ, et al. How trainees would disclose medical errors: Educational implications for training programmes. Med Educ. 201;45(4):372-380.
11. White AA, Bell SK, Krauss MJ, et al. How trainees would disclose medical errors: Educational implications for training programmes. Med Educ. 201;45(4):372-380.
12. Waterman AD, Garbutt J, Hazel E, et al. The emotional impact of medical errors on practicing physicians in the United States and Canada. Jt Comm J Qual Patient Saf. 2007;33(8):467-476.
13. Watson K. Serious play: Teaching medical skills with improvisational theater techniques. Acad Med. 2011;86(10):1260-1265.
14. Eaves-Leanos A, Dunn EJ. Open disclosure of adverse events: Transparency and safety in healthcare. Surg Clin North Am. 2012;92(1):163-177.
15. Aristotle. Nichomachean Ethics (edited by Roger Crisp). Cambridge University Press, New York, NY (2012): Book II, Chapter 1 (1103b), p. 23.
1. Kraman SS, Hamm G. Risk management: Extreme honesty may be the best policy. Ann Intern Med. 1999;131(12):963-967.
2. Hamm GM, Kraman SS. New standards, new dilemmas: Reflections on managing medical mistakes. Bioethics Forum. 2001;17(2):19-25.
3. Veterans Health Administration. Disclosure of adverse events to patients. Handbook 100408. United States Department of Veterans Affairs Website. http://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=2800. Corrected copy October 12, 2012. Accessed April 3, 2014.
4. Delbanco T, Bell SK. Guilty, afraid, and alone—struggling with medical error. N Engl J Med. 2007;357(17):1682-1683.
5. Taft L. Apology and medical mistake: Opportunity or foil? Ann Health L. 2005;14:55-94.
6. Gallagher TH, Garbutt JM, Waterman AD, et al. Choosing your words carefully: How physicians would disclose harmful medical error to patients. Arch Intern Med. 2006;166(15):1585-1593.
7. Banja J. Medical Errors and Medical Narcissism. Sudbury, MD: Jones and Bartlett; 2005.
8. Iezzoni LI, Rao SR, DesRoches CM, Vogeli C, Campbell EG. Survey shows that at least some physicians are not always open or honest with patients. Health Aff (Millwood). 2012;31(2):383-391.
9. Gallagher TW, Waterman AD, Garbutt JM, et al. US and Canadian physicians’ attitudes and experiences regarding disclosure errors to patients. Arch Intern Med. 2006;166(15):1605-1611.
10. Robbennolt JK. Apologies and medical error. Clin Orthop Relat Res. 2009;467(2):376-382 White AA, Bell SK, Krauss MJ, et al. How trainees would disclose medical errors: Educational implications for training programmes. Med Educ. 201;45(4):372-380.
11. White AA, Bell SK, Krauss MJ, et al. How trainees would disclose medical errors: Educational implications for training programmes. Med Educ. 201;45(4):372-380.
12. Waterman AD, Garbutt J, Hazel E, et al. The emotional impact of medical errors on practicing physicians in the United States and Canada. Jt Comm J Qual Patient Saf. 2007;33(8):467-476.
13. Watson K. Serious play: Teaching medical skills with improvisational theater techniques. Acad Med. 2011;86(10):1260-1265.
14. Eaves-Leanos A, Dunn EJ. Open disclosure of adverse events: Transparency and safety in healthcare. Surg Clin North Am. 2012;92(1):163-177.
15. Aristotle. Nichomachean Ethics (edited by Roger Crisp). Cambridge University Press, New York, NY (2012): Book II, Chapter 1 (1103b), p. 23.
Development and Evaluation of a Geriatric Mood Management Program
More older adults suffer from depression in a VHA setting (11%) than those in non-VHA settings (1%-5%).1 Depression and anxiety are evaluated less often in older adults and undertreated compared with younger adults.2-4 Unfortunately, older adults with depression and anxiety are vulnerable to suicide and disability; and they more frequently use medical services, such as the emergency department compared with older adults without these conditions.5-7
However, pharmacologic and behavioral treatments for late-life mood and anxiety disorders are available and are effective.8 These findings raise important questions about improving access to mental health care for older veterans with mood disorders. The VA Palo Alto Health Care System (VAPAHCS) Geriatric Research Education and Clinical Center (GRECC) fulfills one GRECC mission of carrying out transformative clinical demonstration projects by developing programs to address geriatric mood disorders.
The VHA has successfully implemented the nationwide integration of mental health management into primary care settings.9 To design and implement these programs locally, in 2007, all VHAs were invited to submit proposals related to mental health primary care integration. Local sites were given flexibility in their use of different evidence-based models for delivery of this integrated care.
Collaborative Models
Three models of mental health integration into primary care were adopted within VHA. All have resulted in improved patient outcomes.9 The co-located model places a behavioral health specialist within the same setting as primary care providers (PCPs), who shares in the evaluation, treatment planning, and monitoring of mental health outcomes. In the care management model, care managers facilitate evaluation and maintain communication with PCPs, but are not co-located with the PCPs. The third model is a blended model in which both a behavioral health specialist and a care manager may be involved in the management of mental health care. The care management model resulted in better participation in the evaluation and engagement in pharmacotherapy by older veterans in 2 VHA medical centers.10
Persistent Barriers for Older Veterans
The mental health-primary care integration initiative laid important foundations for improving access to mental health care. To provide a truly veteran-centered care option, however, programs require monitoring and analysis of the factors that impact care delivery and access. A recent evaluation of a local integration program, using a co-located model (ie, Primary Care Behavioral Health [PCBH]), demonstrated that there were several factors affecting older veterans’ access to mental health treatment.11 Older veterans with depression were less receptive to a mental health referral; 62% of older veterans refused mental health referrals compared with 32% of younger veterans who refused. Older veterans were less likely to complete at least 1 mental health clinic appointment, which was due in part to clinic location. All veterans were more likely to follow up with a mental health referral if first seen by the PCBH staff vs a referral by PCPs.
Geriatric-Specific Modifications to PCBH
The VAPAHCS GRECC, collaborating with the outpatient psychiatry service and the PCBH, sought to improve current mental health services for older veterans. Several barriers were identified: (1) limitations in types of interventions available to older veterans in the current PCBH and mental health programs; (2) the PCBH staff required geriatrics training, as recommended by the American Psychological Association12; and (3) resistance to receiving care in mental health clinics located several miles from the primary care setting. Therefore, a new pilot program was planned to address these barriers.
The Office of Geriatrics and Extended Care provided the funding for the initial program costs, and in September 2010, the Geriatric Primary Care Behavioral Health program (Geri-PCBH) was launched. The GRECC staff worked closely with the PCBH staff to offer a new service tailored to older veterans’ specific needs, which addressed the previously described program limitations.
Geri-PCBH Program
The Geri-PCBH program is a blended collaborative care model that provides outpatient-based mental health evaluation and treatment of mood disorders for older (aged ≥ 65 years) veterans. It is co-located with PCBH and PCPs within the primary care setting. The program extends PCBH services by providing psychotherapy that is contextually modified for older veterans. Older veterans may present with different therapy concerns than do younger veterans, such as caregiving, death of loved ones, and numerous and chronic medical illnesses. Illnesses may result in polypharmacy, giving rise to the need for understanding potential medication interactions in providing pharmacotherapy.
Within the program, geriatrics-trained psychologists and social workers offer psychotherapy. In addition, a geriatrician with expertise in polypharmacy offers pharmacotherapy. Psychotherapy, pharmacotherapy, or both are offered and initiated following evaluation and discussion with the veteran. Veterans are either referred by the PCBH staff because they screened positive for depression (Patient Health Questionnaire-2 [PHQ-2] ≥ 2) during a regularly scheduled primary care clinic appointment or they are directly referred by primary care physicians for suspected mood problems. Veterans are then contacted immediately by a staff member for a baseline assessment appointment with a geriatrician and one of the therapists. The type of treatment and goals of therapy are determined during the initial meeting. The program is a training site for psychology and social work interns, to increase their geriatric mental health training.
Evaluation and Results
To determine improvements compared to PCBH program outcomes, the patients who attended the initial Geri-PCBH evaluation/intake appointment were tracked. A total of 79 older veterans were referred (average age, 82.7 years; range, aged 66-96 years); 14 veterans were ineligible due to significant cognitive impairment or lack of depressive symptoms. Compared with the 38% rate of attendance at intake for mental health referrals in the PCBH program, the Geri-PCBH program demonstrated a 90% attendance rate at the initial evaluation appointment. Fifty-five older veterans enrolled and received therapy: 39 received only psychotherapy, 14 received psychotherapy and antidepressant therapy, and 2 received only antidepressant therapy. Over the first 2 years of the program, 2 senior therapists and 5 trainees were able to see 53 patients for an average of 7 sessions per patient, which translated to about 14% of each therapist’s time.
To determine the impact on patients, measures of depression (Hamilton Depression Rating Scale [HDRS]; Geriatric Depression Scale Short Form [GDS-SF]; and Patient Health Questionnaire 9 Item [PHQ-9]), anxiety (Mini Psychiatric Evaluation Scale-Generalized Anxiety subscale [MINI-GAD]), overall distress (clinical global inventory), and functional status (12-item World Health Organization Disability Assessment Scale [WHODAS]) were administered at baseline, posttreatment, and 3 months posttreatment. The veterans demonstrated a significant decrease (> 50% decline on mood symptoms) on the HDRS, GDS, PHQ-9, and MINI-GAD subscale, which were all sustained 3 months posttreatment (Figure).
Although the overall disability score did not improve, the percentage of older veterans reporting “bad” or “moderate” health decreased (pre = 42%; post = 31.1%; 3-month follow-up = 20.9%); while those reporting “good” or “very good” health increased (pre = 58%; post = 65.7%; 3-month follow-up = 79.2%) by the 3-month follow-up. Veterans also reported very high satisfaction rates with the program overall (Mean = 30, standard deviation = 2.03; anchors for measure: 0 = not satisfied; 32 = highly satisfied).
Patient Testimonials
“Not in my wildest dreams did I think I’d ever share, on this level, my personal, past and present life…You have been so helpful and allowed me to move forward with pride and self respect.”
“It makes you feel a lot better. I enjoy life more now than I used to. That first time that [my therapist and I] talked, she convinced me just a change in attitude was a big thing. And since I changed my attitude and started listening to people, it’s made a heck of a difference.”
Discussion and Conclusion
The results of the Geri-PCBH evaluation demonstrated improvements in acceptance by older veterans with depression of mental health referrals and in increased access to treatment. The program addressed several identified barriers, such as having a more accessible location, offering treatment by experienced geriatrics-trained providers, and providing a range of mental health services tailored to older veterans’ needs. These factors may have increased older veterans’ willingness to attend mental health referrals to the Geri-PCBH program. Having initial assessments done soon after initial referral (usually < 2 weeks) and calling patients personally to explain the program and make appointments likely improved referral acceptance.
There are some limits to implementing this program in other settings related to variability in staffing, infrastructure, and resources available. The project is currently sustained with the present staff, with the goal of expanding services by telehealth technology to disseminate the program to older veterans in rural settings.
The VHA has made impressive strides toward improving the lives of older veterans with depression and anxiety. The program described here provides an example of how quality improvement efforts, which take into account the specific needs of the older veteran, can lead to a dramatic impact on the services offered and more importantly on veterans’ mental health and functional abilities.
Acknowledgements
This material is the result of work supported with funding by the Office of Geriatrics and Extended Care T21T Fund-10/11 060B2 and resources and use of facilities at the VA Palo Alto Health Care System in Palo Alto, California.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Blow FC, Owen RE. Specialty care for veterans with depression in the VHA 2002 national registry report. Ann Arbor, MI: VHA Health Services Research and Development; 2003.
2. Fischer LR, Wei F, Solberg LI, Rush WA, Heinrich RL. Treatment of elderly and other adult patients for depression in primary care. J Am Geriatr Soc. 2003;51(11):1554-1562.
3. Stanley MA, Roberts RE, Bourland SL, Novy DM. Anxiety disorders among older primary care patients. J Clin Geropsychology. 2001;7(2):105-116.
4. Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: Results from the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62(6):629-640.
5. Conwell Y, Duberstein PR, Caine ED. Risk factors for suicide in later life. Biol Psychiatry. 2002;52(3):193-204.
6. Pérés K, Jagger C, Matthews FE; MRC CFAS. Impact of late-life self-reported emotional problems on disability-free life expectancy: Results from the MRC cognitive function and ageing study. Int J Geriatr Psychiatry. 2008;23(6):643-649.
7. Lee BW, Conwell Y, Shah MN, Barker WH, Delavan RL, Friedman B. Major depression and emergency medical services utilization in community-dwelling elderly persons with disabilities. Int J Geriatr Psychiatry. 2008;23(12):1276-1282.
8. Small GW. Treatment of geriatric depression. Depress Anxiety. 1998;8(suppl 1):32-42.
9. Post EP, Van Stone WW. Veterans health administration primary care-mental health integration initiative. N C Med J. 2008;69(1):49-52.
10. Mavandadi S, Klaus JR, Oslin DW. Age group differences among veterans enrolled in a clinical service for behavioral health issues in primary care. Am J Geriatr Psychiatry. 2012;20(3):205-214.
11. Lindley S, Cacciapaglia H, Noronha D, Carlson E, Schatzberg A. Monitoring mental health treatment acceptance and initial treatment adherence in veterans: Veterans of Operations Enduring Freedom and Iraqi Freedom versus other veterans of other eras. Ann N Y Acad Sci. 2010;1208:104-113.
12. American Psychological Association. Guidelines for psychological practice with older adults. American Psychologist. 2004;59(4):236-260.
More older adults suffer from depression in a VHA setting (11%) than those in non-VHA settings (1%-5%).1 Depression and anxiety are evaluated less often in older adults and undertreated compared with younger adults.2-4 Unfortunately, older adults with depression and anxiety are vulnerable to suicide and disability; and they more frequently use medical services, such as the emergency department compared with older adults without these conditions.5-7
However, pharmacologic and behavioral treatments for late-life mood and anxiety disorders are available and are effective.8 These findings raise important questions about improving access to mental health care for older veterans with mood disorders. The VA Palo Alto Health Care System (VAPAHCS) Geriatric Research Education and Clinical Center (GRECC) fulfills one GRECC mission of carrying out transformative clinical demonstration projects by developing programs to address geriatric mood disorders.
The VHA has successfully implemented the nationwide integration of mental health management into primary care settings.9 To design and implement these programs locally, in 2007, all VHAs were invited to submit proposals related to mental health primary care integration. Local sites were given flexibility in their use of different evidence-based models for delivery of this integrated care.
Collaborative Models
Three models of mental health integration into primary care were adopted within VHA. All have resulted in improved patient outcomes.9 The co-located model places a behavioral health specialist within the same setting as primary care providers (PCPs), who shares in the evaluation, treatment planning, and monitoring of mental health outcomes. In the care management model, care managers facilitate evaluation and maintain communication with PCPs, but are not co-located with the PCPs. The third model is a blended model in which both a behavioral health specialist and a care manager may be involved in the management of mental health care. The care management model resulted in better participation in the evaluation and engagement in pharmacotherapy by older veterans in 2 VHA medical centers.10
Persistent Barriers for Older Veterans
The mental health-primary care integration initiative laid important foundations for improving access to mental health care. To provide a truly veteran-centered care option, however, programs require monitoring and analysis of the factors that impact care delivery and access. A recent evaluation of a local integration program, using a co-located model (ie, Primary Care Behavioral Health [PCBH]), demonstrated that there were several factors affecting older veterans’ access to mental health treatment.11 Older veterans with depression were less receptive to a mental health referral; 62% of older veterans refused mental health referrals compared with 32% of younger veterans who refused. Older veterans were less likely to complete at least 1 mental health clinic appointment, which was due in part to clinic location. All veterans were more likely to follow up with a mental health referral if first seen by the PCBH staff vs a referral by PCPs.
Geriatric-Specific Modifications to PCBH
The VAPAHCS GRECC, collaborating with the outpatient psychiatry service and the PCBH, sought to improve current mental health services for older veterans. Several barriers were identified: (1) limitations in types of interventions available to older veterans in the current PCBH and mental health programs; (2) the PCBH staff required geriatrics training, as recommended by the American Psychological Association12; and (3) resistance to receiving care in mental health clinics located several miles from the primary care setting. Therefore, a new pilot program was planned to address these barriers.
The Office of Geriatrics and Extended Care provided the funding for the initial program costs, and in September 2010, the Geriatric Primary Care Behavioral Health program (Geri-PCBH) was launched. The GRECC staff worked closely with the PCBH staff to offer a new service tailored to older veterans’ specific needs, which addressed the previously described program limitations.
Geri-PCBH Program
The Geri-PCBH program is a blended collaborative care model that provides outpatient-based mental health evaluation and treatment of mood disorders for older (aged ≥ 65 years) veterans. It is co-located with PCBH and PCPs within the primary care setting. The program extends PCBH services by providing psychotherapy that is contextually modified for older veterans. Older veterans may present with different therapy concerns than do younger veterans, such as caregiving, death of loved ones, and numerous and chronic medical illnesses. Illnesses may result in polypharmacy, giving rise to the need for understanding potential medication interactions in providing pharmacotherapy.
Within the program, geriatrics-trained psychologists and social workers offer psychotherapy. In addition, a geriatrician with expertise in polypharmacy offers pharmacotherapy. Psychotherapy, pharmacotherapy, or both are offered and initiated following evaluation and discussion with the veteran. Veterans are either referred by the PCBH staff because they screened positive for depression (Patient Health Questionnaire-2 [PHQ-2] ≥ 2) during a regularly scheduled primary care clinic appointment or they are directly referred by primary care physicians for suspected mood problems. Veterans are then contacted immediately by a staff member for a baseline assessment appointment with a geriatrician and one of the therapists. The type of treatment and goals of therapy are determined during the initial meeting. The program is a training site for psychology and social work interns, to increase their geriatric mental health training.
Evaluation and Results
To determine improvements compared to PCBH program outcomes, the patients who attended the initial Geri-PCBH evaluation/intake appointment were tracked. A total of 79 older veterans were referred (average age, 82.7 years; range, aged 66-96 years); 14 veterans were ineligible due to significant cognitive impairment or lack of depressive symptoms. Compared with the 38% rate of attendance at intake for mental health referrals in the PCBH program, the Geri-PCBH program demonstrated a 90% attendance rate at the initial evaluation appointment. Fifty-five older veterans enrolled and received therapy: 39 received only psychotherapy, 14 received psychotherapy and antidepressant therapy, and 2 received only antidepressant therapy. Over the first 2 years of the program, 2 senior therapists and 5 trainees were able to see 53 patients for an average of 7 sessions per patient, which translated to about 14% of each therapist’s time.
To determine the impact on patients, measures of depression (Hamilton Depression Rating Scale [HDRS]; Geriatric Depression Scale Short Form [GDS-SF]; and Patient Health Questionnaire 9 Item [PHQ-9]), anxiety (Mini Psychiatric Evaluation Scale-Generalized Anxiety subscale [MINI-GAD]), overall distress (clinical global inventory), and functional status (12-item World Health Organization Disability Assessment Scale [WHODAS]) were administered at baseline, posttreatment, and 3 months posttreatment. The veterans demonstrated a significant decrease (> 50% decline on mood symptoms) on the HDRS, GDS, PHQ-9, and MINI-GAD subscale, which were all sustained 3 months posttreatment (Figure).
Although the overall disability score did not improve, the percentage of older veterans reporting “bad” or “moderate” health decreased (pre = 42%; post = 31.1%; 3-month follow-up = 20.9%); while those reporting “good” or “very good” health increased (pre = 58%; post = 65.7%; 3-month follow-up = 79.2%) by the 3-month follow-up. Veterans also reported very high satisfaction rates with the program overall (Mean = 30, standard deviation = 2.03; anchors for measure: 0 = not satisfied; 32 = highly satisfied).
Patient Testimonials
“Not in my wildest dreams did I think I’d ever share, on this level, my personal, past and present life…You have been so helpful and allowed me to move forward with pride and self respect.”
“It makes you feel a lot better. I enjoy life more now than I used to. That first time that [my therapist and I] talked, she convinced me just a change in attitude was a big thing. And since I changed my attitude and started listening to people, it’s made a heck of a difference.”
Discussion and Conclusion
The results of the Geri-PCBH evaluation demonstrated improvements in acceptance by older veterans with depression of mental health referrals and in increased access to treatment. The program addressed several identified barriers, such as having a more accessible location, offering treatment by experienced geriatrics-trained providers, and providing a range of mental health services tailored to older veterans’ needs. These factors may have increased older veterans’ willingness to attend mental health referrals to the Geri-PCBH program. Having initial assessments done soon after initial referral (usually < 2 weeks) and calling patients personally to explain the program and make appointments likely improved referral acceptance.
There are some limits to implementing this program in other settings related to variability in staffing, infrastructure, and resources available. The project is currently sustained with the present staff, with the goal of expanding services by telehealth technology to disseminate the program to older veterans in rural settings.
The VHA has made impressive strides toward improving the lives of older veterans with depression and anxiety. The program described here provides an example of how quality improvement efforts, which take into account the specific needs of the older veteran, can lead to a dramatic impact on the services offered and more importantly on veterans’ mental health and functional abilities.
Acknowledgements
This material is the result of work supported with funding by the Office of Geriatrics and Extended Care T21T Fund-10/11 060B2 and resources and use of facilities at the VA Palo Alto Health Care System in Palo Alto, California.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
More older adults suffer from depression in a VHA setting (11%) than those in non-VHA settings (1%-5%).1 Depression and anxiety are evaluated less often in older adults and undertreated compared with younger adults.2-4 Unfortunately, older adults with depression and anxiety are vulnerable to suicide and disability; and they more frequently use medical services, such as the emergency department compared with older adults without these conditions.5-7
However, pharmacologic and behavioral treatments for late-life mood and anxiety disorders are available and are effective.8 These findings raise important questions about improving access to mental health care for older veterans with mood disorders. The VA Palo Alto Health Care System (VAPAHCS) Geriatric Research Education and Clinical Center (GRECC) fulfills one GRECC mission of carrying out transformative clinical demonstration projects by developing programs to address geriatric mood disorders.
The VHA has successfully implemented the nationwide integration of mental health management into primary care settings.9 To design and implement these programs locally, in 2007, all VHAs were invited to submit proposals related to mental health primary care integration. Local sites were given flexibility in their use of different evidence-based models for delivery of this integrated care.
Collaborative Models
Three models of mental health integration into primary care were adopted within VHA. All have resulted in improved patient outcomes.9 The co-located model places a behavioral health specialist within the same setting as primary care providers (PCPs), who shares in the evaluation, treatment planning, and monitoring of mental health outcomes. In the care management model, care managers facilitate evaluation and maintain communication with PCPs, but are not co-located with the PCPs. The third model is a blended model in which both a behavioral health specialist and a care manager may be involved in the management of mental health care. The care management model resulted in better participation in the evaluation and engagement in pharmacotherapy by older veterans in 2 VHA medical centers.10
Persistent Barriers for Older Veterans
The mental health-primary care integration initiative laid important foundations for improving access to mental health care. To provide a truly veteran-centered care option, however, programs require monitoring and analysis of the factors that impact care delivery and access. A recent evaluation of a local integration program, using a co-located model (ie, Primary Care Behavioral Health [PCBH]), demonstrated that there were several factors affecting older veterans’ access to mental health treatment.11 Older veterans with depression were less receptive to a mental health referral; 62% of older veterans refused mental health referrals compared with 32% of younger veterans who refused. Older veterans were less likely to complete at least 1 mental health clinic appointment, which was due in part to clinic location. All veterans were more likely to follow up with a mental health referral if first seen by the PCBH staff vs a referral by PCPs.
Geriatric-Specific Modifications to PCBH
The VAPAHCS GRECC, collaborating with the outpatient psychiatry service and the PCBH, sought to improve current mental health services for older veterans. Several barriers were identified: (1) limitations in types of interventions available to older veterans in the current PCBH and mental health programs; (2) the PCBH staff required geriatrics training, as recommended by the American Psychological Association12; and (3) resistance to receiving care in mental health clinics located several miles from the primary care setting. Therefore, a new pilot program was planned to address these barriers.
The Office of Geriatrics and Extended Care provided the funding for the initial program costs, and in September 2010, the Geriatric Primary Care Behavioral Health program (Geri-PCBH) was launched. The GRECC staff worked closely with the PCBH staff to offer a new service tailored to older veterans’ specific needs, which addressed the previously described program limitations.
Geri-PCBH Program
The Geri-PCBH program is a blended collaborative care model that provides outpatient-based mental health evaluation and treatment of mood disorders for older (aged ≥ 65 years) veterans. It is co-located with PCBH and PCPs within the primary care setting. The program extends PCBH services by providing psychotherapy that is contextually modified for older veterans. Older veterans may present with different therapy concerns than do younger veterans, such as caregiving, death of loved ones, and numerous and chronic medical illnesses. Illnesses may result in polypharmacy, giving rise to the need for understanding potential medication interactions in providing pharmacotherapy.
Within the program, geriatrics-trained psychologists and social workers offer psychotherapy. In addition, a geriatrician with expertise in polypharmacy offers pharmacotherapy. Psychotherapy, pharmacotherapy, or both are offered and initiated following evaluation and discussion with the veteran. Veterans are either referred by the PCBH staff because they screened positive for depression (Patient Health Questionnaire-2 [PHQ-2] ≥ 2) during a regularly scheduled primary care clinic appointment or they are directly referred by primary care physicians for suspected mood problems. Veterans are then contacted immediately by a staff member for a baseline assessment appointment with a geriatrician and one of the therapists. The type of treatment and goals of therapy are determined during the initial meeting. The program is a training site for psychology and social work interns, to increase their geriatric mental health training.
Evaluation and Results
To determine improvements compared to PCBH program outcomes, the patients who attended the initial Geri-PCBH evaluation/intake appointment were tracked. A total of 79 older veterans were referred (average age, 82.7 years; range, aged 66-96 years); 14 veterans were ineligible due to significant cognitive impairment or lack of depressive symptoms. Compared with the 38% rate of attendance at intake for mental health referrals in the PCBH program, the Geri-PCBH program demonstrated a 90% attendance rate at the initial evaluation appointment. Fifty-five older veterans enrolled and received therapy: 39 received only psychotherapy, 14 received psychotherapy and antidepressant therapy, and 2 received only antidepressant therapy. Over the first 2 years of the program, 2 senior therapists and 5 trainees were able to see 53 patients for an average of 7 sessions per patient, which translated to about 14% of each therapist’s time.
To determine the impact on patients, measures of depression (Hamilton Depression Rating Scale [HDRS]; Geriatric Depression Scale Short Form [GDS-SF]; and Patient Health Questionnaire 9 Item [PHQ-9]), anxiety (Mini Psychiatric Evaluation Scale-Generalized Anxiety subscale [MINI-GAD]), overall distress (clinical global inventory), and functional status (12-item World Health Organization Disability Assessment Scale [WHODAS]) were administered at baseline, posttreatment, and 3 months posttreatment. The veterans demonstrated a significant decrease (> 50% decline on mood symptoms) on the HDRS, GDS, PHQ-9, and MINI-GAD subscale, which were all sustained 3 months posttreatment (Figure).
Although the overall disability score did not improve, the percentage of older veterans reporting “bad” or “moderate” health decreased (pre = 42%; post = 31.1%; 3-month follow-up = 20.9%); while those reporting “good” or “very good” health increased (pre = 58%; post = 65.7%; 3-month follow-up = 79.2%) by the 3-month follow-up. Veterans also reported very high satisfaction rates with the program overall (Mean = 30, standard deviation = 2.03; anchors for measure: 0 = not satisfied; 32 = highly satisfied).
Patient Testimonials
“Not in my wildest dreams did I think I’d ever share, on this level, my personal, past and present life…You have been so helpful and allowed me to move forward with pride and self respect.”
“It makes you feel a lot better. I enjoy life more now than I used to. That first time that [my therapist and I] talked, she convinced me just a change in attitude was a big thing. And since I changed my attitude and started listening to people, it’s made a heck of a difference.”
Discussion and Conclusion
The results of the Geri-PCBH evaluation demonstrated improvements in acceptance by older veterans with depression of mental health referrals and in increased access to treatment. The program addressed several identified barriers, such as having a more accessible location, offering treatment by experienced geriatrics-trained providers, and providing a range of mental health services tailored to older veterans’ needs. These factors may have increased older veterans’ willingness to attend mental health referrals to the Geri-PCBH program. Having initial assessments done soon after initial referral (usually < 2 weeks) and calling patients personally to explain the program and make appointments likely improved referral acceptance.
There are some limits to implementing this program in other settings related to variability in staffing, infrastructure, and resources available. The project is currently sustained with the present staff, with the goal of expanding services by telehealth technology to disseminate the program to older veterans in rural settings.
The VHA has made impressive strides toward improving the lives of older veterans with depression and anxiety. The program described here provides an example of how quality improvement efforts, which take into account the specific needs of the older veteran, can lead to a dramatic impact on the services offered and more importantly on veterans’ mental health and functional abilities.
Acknowledgements
This material is the result of work supported with funding by the Office of Geriatrics and Extended Care T21T Fund-10/11 060B2 and resources and use of facilities at the VA Palo Alto Health Care System in Palo Alto, California.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Blow FC, Owen RE. Specialty care for veterans with depression in the VHA 2002 national registry report. Ann Arbor, MI: VHA Health Services Research and Development; 2003.
2. Fischer LR, Wei F, Solberg LI, Rush WA, Heinrich RL. Treatment of elderly and other adult patients for depression in primary care. J Am Geriatr Soc. 2003;51(11):1554-1562.
3. Stanley MA, Roberts RE, Bourland SL, Novy DM. Anxiety disorders among older primary care patients. J Clin Geropsychology. 2001;7(2):105-116.
4. Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: Results from the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62(6):629-640.
5. Conwell Y, Duberstein PR, Caine ED. Risk factors for suicide in later life. Biol Psychiatry. 2002;52(3):193-204.
6. Pérés K, Jagger C, Matthews FE; MRC CFAS. Impact of late-life self-reported emotional problems on disability-free life expectancy: Results from the MRC cognitive function and ageing study. Int J Geriatr Psychiatry. 2008;23(6):643-649.
7. Lee BW, Conwell Y, Shah MN, Barker WH, Delavan RL, Friedman B. Major depression and emergency medical services utilization in community-dwelling elderly persons with disabilities. Int J Geriatr Psychiatry. 2008;23(12):1276-1282.
8. Small GW. Treatment of geriatric depression. Depress Anxiety. 1998;8(suppl 1):32-42.
9. Post EP, Van Stone WW. Veterans health administration primary care-mental health integration initiative. N C Med J. 2008;69(1):49-52.
10. Mavandadi S, Klaus JR, Oslin DW. Age group differences among veterans enrolled in a clinical service for behavioral health issues in primary care. Am J Geriatr Psychiatry. 2012;20(3):205-214.
11. Lindley S, Cacciapaglia H, Noronha D, Carlson E, Schatzberg A. Monitoring mental health treatment acceptance and initial treatment adherence in veterans: Veterans of Operations Enduring Freedom and Iraqi Freedom versus other veterans of other eras. Ann N Y Acad Sci. 2010;1208:104-113.
12. American Psychological Association. Guidelines for psychological practice with older adults. American Psychologist. 2004;59(4):236-260.
1. Blow FC, Owen RE. Specialty care for veterans with depression in the VHA 2002 national registry report. Ann Arbor, MI: VHA Health Services Research and Development; 2003.
2. Fischer LR, Wei F, Solberg LI, Rush WA, Heinrich RL. Treatment of elderly and other adult patients for depression in primary care. J Am Geriatr Soc. 2003;51(11):1554-1562.
3. Stanley MA, Roberts RE, Bourland SL, Novy DM. Anxiety disorders among older primary care patients. J Clin Geropsychology. 2001;7(2):105-116.
4. Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: Results from the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62(6):629-640.
5. Conwell Y, Duberstein PR, Caine ED. Risk factors for suicide in later life. Biol Psychiatry. 2002;52(3):193-204.
6. Pérés K, Jagger C, Matthews FE; MRC CFAS. Impact of late-life self-reported emotional problems on disability-free life expectancy: Results from the MRC cognitive function and ageing study. Int J Geriatr Psychiatry. 2008;23(6):643-649.
7. Lee BW, Conwell Y, Shah MN, Barker WH, Delavan RL, Friedman B. Major depression and emergency medical services utilization in community-dwelling elderly persons with disabilities. Int J Geriatr Psychiatry. 2008;23(12):1276-1282.
8. Small GW. Treatment of geriatric depression. Depress Anxiety. 1998;8(suppl 1):32-42.
9. Post EP, Van Stone WW. Veterans health administration primary care-mental health integration initiative. N C Med J. 2008;69(1):49-52.
10. Mavandadi S, Klaus JR, Oslin DW. Age group differences among veterans enrolled in a clinical service for behavioral health issues in primary care. Am J Geriatr Psychiatry. 2012;20(3):205-214.
11. Lindley S, Cacciapaglia H, Noronha D, Carlson E, Schatzberg A. Monitoring mental health treatment acceptance and initial treatment adherence in veterans: Veterans of Operations Enduring Freedom and Iraqi Freedom versus other veterans of other eras. Ann N Y Acad Sci. 2010;1208:104-113.
12. American Psychological Association. Guidelines for psychological practice with older adults. American Psychologist. 2004;59(4):236-260.
The Use of Secure Messaging in Medical Specialty Care
Secure messaging (SM) is an encrypted, web-based mode of communication within the My HealtheVet (MHV) website. It was developed for the nonurgent, nonemergency communication of test results and other health information as well as for scheduling appointments and renewing medication prescriptions. Secure messaging is asynchronous, which means that communication between parties is not done at the same time. It was designed to address the need for a secure means of communication between patient and provider.1 Messages can be triaged across teams and saved to the Computerized Patient Record System (CPRS).
The VA patients who use MHV can upgrade their account through an in-person authentication process (IPA), which takes about 10 minutes. Any health care provider (HCP) team or administrator can use SM if set up in the system. Health care providers can only receive messages from patients who have been associated with their triage care group. Patients may only message an HCP with which they are associated. In general, this group would comprise their HCP and 1 or more specialty clinics where they have already been seen. Patients can choose an HCP from a limited drop-down menu.
Patients using SM choose a subject, such as appointments, medications, tests, or general. Patients are then able to type a message, and they are also able to see the threads of previous messages. They may access test results or attachments sent to them by the HCPs. Patients are notified of messages through their previously registered e-mail account, which displays a message asking them to log on to MHV.
Health care providers may access MHV either through the CPRS on the tools menu or as a link in an e-mail. Once HCPs log on, they will see their inbox and messages listed by sender and type of inquiry (ie, prescription refill, test question, and so forth). The HCPs can view escalated messages (those that have not been answered within 3 days), drafts, and sent and completed messages. Health care providers can also create special folders to store their messages.
The health care team can personalize how and to whom messages appear. There are 2 main models used by Specialty Care. The first involves a staff member designated to triage messages for the team. This staff member will see all incoming messages and forward them appropriately. For example, in one clinic model, the program assistant reviews all messages and then forwards them to the appropriate provider. The team pharmacist receives prescription requests, the HCP receives general or test inquiries from patients, and the program assistant retains and answers all communication related to appointments and cancellations. Another model involves employing a staff person or administrator as a co-user with each HCP. The HCP can then forward messages that may need administrative action.
The HCPs receive an e-mail notification with a link when a message has been received. Clicking on the link takes them directly to SM within MHV, where they can sign in to see all their messages. Users can also add a signature block, which will appear on all correspondence. They may also designate a surrogate to answer messages when they are unavailable, such as during administrative or personal leave. The HCPs also have the ability to create a SM even if the patient has not yet messaged them. Users can also send copies of messages to other staff members. Providers and staff have the ability to attach a file, which can be a test result, letter, records, etc. Messages can then be saved in the CPRS if desired.
Patients, however, cannot send attachments to their HCP. Only those HCPs who have seen the patient will be available for communication. This system eliminates the possibility of patients self-referring to a specialist and asking questions of HCPs who have never seen them. The HCPs and staff may also forward messages to the appropriate person.
Secure messaging can provide unique opportunities for communication and improvement in outcome measures in certain specialties. For example, in endocrinology patients may be asked to send home blood sugar or blood pressure (BP) readings in between visits, to allow for more rapid medication titration and achievement of treatment goals. A study by Harris and colleagues showed that the frequent use of electronic SM was associated with improved glycemic control.2
At the Atlanta VAMC, SM was implemented in the Primary Care Service Line prior to the Medicine Specialty Care Service Line. The implementation was a natural fit for the organized Primary Care teams. Implementation within the specialties brought forth a new set of issues. Many specialties were not formally organized with a team leader. There were often multiple HCPs in a division, some full time, some part time, in addition to subspecialty pharmacists, physician assistants, and nurse practitioners. Because the Atlanta VAMC is also a training hospital for the Emory University School of Medicine, new residents and fellows are included in the teams each month. It was, therefore, necessary for each specialty to design a message flow that would best fit its needs. Initially, there was concern that SM would add yet another layer of responsibilities to the already stretched HCPs.
The reality has been the opposite. Secure messaging was found to be an additional type of communication, which could be completed more rapidly than a phone call or generating a results letter. The HCPs were also concerned that patients would attempt to use them as primary care providers (PCPs). However, as patients were able to view both their PCP and their specialty care provider in the drop-down menu, they were generally able to direct their questions appropriately.
At the Atlanta VAMC, 60% of the messages were completed by the provider, 29% by a clinical team member, and 11% by the triage staff from 2013 to 2014 (Figure 1). Some HCPs were concerned that once SM was in place, they would be inundated with messages. The reality seems to be that most patients use SM judiciously, and although they are comfortable in the knowledge that they can communicate directly with their HCP, the need is infrequent. The number of messages has slowly increased over the past year as more patients join MHV and SM (Table). Surprisingly, as the number of inbound messages increased, the percentage of escalated messages (messages not answered within 3 days) declined, indicating a learning curve as HCPs begin using SM.
There are 3 steps to patient enrollment in SM. The first is enrollment in MHV, which can be done either online or at the VAMC. The second step requires the patient to go to the VAMC and present identification to complete the IPA. Finally, the enrolled patients must opt-in to the program. Enrollment in MHV has steadily increased through advertising campaigns on the VAMC website, within the VAMC, and through HCPs and staff (Figure 2).
However, barriers still exist. Some patients do not have an Internet connection and are not computer savvy. Other patients express interest but put it off to another visit. Some patients have been confused about the additional step of IPA that is required for SM and stop at enrollment in MHV only.
Therefore the key challenges for implementing SM are facilitating MHV enrollment, IPA, and completion of the opt-in feature. To encourage participation, VISN 7 mailed postcards to all 33,000 patients who had undergone IPA but had not yet opted-in. The number of patients who opted-in quadrupled, demonstrating that this type of promotion is an effective recruitment tool.
Another ongoing challenge is developing a method to easily generate workload credit for the HCPs’ time spent using SM for patient care. This will be an important parameter to track, as the time spent on SM per provider is expected to increase. It has also been suggested that there be an out-of-office response for nonemergent messages and the assignment of a surrogate to handle incoming messages for HCPs who are on leave. An unforeseen example of a nonemergent message occurs when a patient replies “Thank you” to a message from an HCP. That message is then counted as a new message and must be viewed and completed like any other message. It can also become an escalated message, even though there is no important information being transmitted.
Conclusions
Secure messaging provides a simple means of rapid communication and feedback between HCPs and their patients. An e-mail notification is generated, HCPs access SM through the link, the reply is sent, and a CPRS note is automatically generated. That same communication would require a far more time-consuming and complicated process without SM: The patient must contact the service, usually the program assistant, and leave a message; that message would be passed on via voicemail or e-mail to the appropriate HCP; the provider would need to access the CPRS, phone the patient, discuss the issue if the patient is available, and then document the contact with a note in the CPRS. If the patient was unavailable, this process would require multiple phone calls.
With respect to patients, the benefits of SM are significant and include easy access to prescription refills and a quick response to questions about medications, dosages, or tests. Patients are able to change or cancel appointments, thereby avoiding no-shows. Frustration concerning the inability to reach the correct party or to speak with staff directly is reduced with SM, and overall communication between HCP and patient is streamlined.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Delbanco T, Sands DZ. Electrons in flight—e-mail between doctors and patients. New Engl J Med. 2004;350(17):1705-1707.
2. Harris LT, Haneuse SJ, Martin DP, Ralston JD. Diabetes quality of care and outpatient utilization associated with electronic patient-provider messaging: A cross-sectional analysis. Diabetes Care. 2009;32(7):1182-1187.
Secure messaging (SM) is an encrypted, web-based mode of communication within the My HealtheVet (MHV) website. It was developed for the nonurgent, nonemergency communication of test results and other health information as well as for scheduling appointments and renewing medication prescriptions. Secure messaging is asynchronous, which means that communication between parties is not done at the same time. It was designed to address the need for a secure means of communication between patient and provider.1 Messages can be triaged across teams and saved to the Computerized Patient Record System (CPRS).
The VA patients who use MHV can upgrade their account through an in-person authentication process (IPA), which takes about 10 minutes. Any health care provider (HCP) team or administrator can use SM if set up in the system. Health care providers can only receive messages from patients who have been associated with their triage care group. Patients may only message an HCP with which they are associated. In general, this group would comprise their HCP and 1 or more specialty clinics where they have already been seen. Patients can choose an HCP from a limited drop-down menu.
Patients using SM choose a subject, such as appointments, medications, tests, or general. Patients are then able to type a message, and they are also able to see the threads of previous messages. They may access test results or attachments sent to them by the HCPs. Patients are notified of messages through their previously registered e-mail account, which displays a message asking them to log on to MHV.
Health care providers may access MHV either through the CPRS on the tools menu or as a link in an e-mail. Once HCPs log on, they will see their inbox and messages listed by sender and type of inquiry (ie, prescription refill, test question, and so forth). The HCPs can view escalated messages (those that have not been answered within 3 days), drafts, and sent and completed messages. Health care providers can also create special folders to store their messages.
The health care team can personalize how and to whom messages appear. There are 2 main models used by Specialty Care. The first involves a staff member designated to triage messages for the team. This staff member will see all incoming messages and forward them appropriately. For example, in one clinic model, the program assistant reviews all messages and then forwards them to the appropriate provider. The team pharmacist receives prescription requests, the HCP receives general or test inquiries from patients, and the program assistant retains and answers all communication related to appointments and cancellations. Another model involves employing a staff person or administrator as a co-user with each HCP. The HCP can then forward messages that may need administrative action.
The HCPs receive an e-mail notification with a link when a message has been received. Clicking on the link takes them directly to SM within MHV, where they can sign in to see all their messages. Users can also add a signature block, which will appear on all correspondence. They may also designate a surrogate to answer messages when they are unavailable, such as during administrative or personal leave. The HCPs also have the ability to create a SM even if the patient has not yet messaged them. Users can also send copies of messages to other staff members. Providers and staff have the ability to attach a file, which can be a test result, letter, records, etc. Messages can then be saved in the CPRS if desired.
Patients, however, cannot send attachments to their HCP. Only those HCPs who have seen the patient will be available for communication. This system eliminates the possibility of patients self-referring to a specialist and asking questions of HCPs who have never seen them. The HCPs and staff may also forward messages to the appropriate person.
Secure messaging can provide unique opportunities for communication and improvement in outcome measures in certain specialties. For example, in endocrinology patients may be asked to send home blood sugar or blood pressure (BP) readings in between visits, to allow for more rapid medication titration and achievement of treatment goals. A study by Harris and colleagues showed that the frequent use of electronic SM was associated with improved glycemic control.2
At the Atlanta VAMC, SM was implemented in the Primary Care Service Line prior to the Medicine Specialty Care Service Line. The implementation was a natural fit for the organized Primary Care teams. Implementation within the specialties brought forth a new set of issues. Many specialties were not formally organized with a team leader. There were often multiple HCPs in a division, some full time, some part time, in addition to subspecialty pharmacists, physician assistants, and nurse practitioners. Because the Atlanta VAMC is also a training hospital for the Emory University School of Medicine, new residents and fellows are included in the teams each month. It was, therefore, necessary for each specialty to design a message flow that would best fit its needs. Initially, there was concern that SM would add yet another layer of responsibilities to the already stretched HCPs.
The reality has been the opposite. Secure messaging was found to be an additional type of communication, which could be completed more rapidly than a phone call or generating a results letter. The HCPs were also concerned that patients would attempt to use them as primary care providers (PCPs). However, as patients were able to view both their PCP and their specialty care provider in the drop-down menu, they were generally able to direct their questions appropriately.
At the Atlanta VAMC, 60% of the messages were completed by the provider, 29% by a clinical team member, and 11% by the triage staff from 2013 to 2014 (Figure 1). Some HCPs were concerned that once SM was in place, they would be inundated with messages. The reality seems to be that most patients use SM judiciously, and although they are comfortable in the knowledge that they can communicate directly with their HCP, the need is infrequent. The number of messages has slowly increased over the past year as more patients join MHV and SM (Table). Surprisingly, as the number of inbound messages increased, the percentage of escalated messages (messages not answered within 3 days) declined, indicating a learning curve as HCPs begin using SM.
There are 3 steps to patient enrollment in SM. The first is enrollment in MHV, which can be done either online or at the VAMC. The second step requires the patient to go to the VAMC and present identification to complete the IPA. Finally, the enrolled patients must opt-in to the program. Enrollment in MHV has steadily increased through advertising campaigns on the VAMC website, within the VAMC, and through HCPs and staff (Figure 2).
However, barriers still exist. Some patients do not have an Internet connection and are not computer savvy. Other patients express interest but put it off to another visit. Some patients have been confused about the additional step of IPA that is required for SM and stop at enrollment in MHV only.
Therefore the key challenges for implementing SM are facilitating MHV enrollment, IPA, and completion of the opt-in feature. To encourage participation, VISN 7 mailed postcards to all 33,000 patients who had undergone IPA but had not yet opted-in. The number of patients who opted-in quadrupled, demonstrating that this type of promotion is an effective recruitment tool.
Another ongoing challenge is developing a method to easily generate workload credit for the HCPs’ time spent using SM for patient care. This will be an important parameter to track, as the time spent on SM per provider is expected to increase. It has also been suggested that there be an out-of-office response for nonemergent messages and the assignment of a surrogate to handle incoming messages for HCPs who are on leave. An unforeseen example of a nonemergent message occurs when a patient replies “Thank you” to a message from an HCP. That message is then counted as a new message and must be viewed and completed like any other message. It can also become an escalated message, even though there is no important information being transmitted.
Conclusions
Secure messaging provides a simple means of rapid communication and feedback between HCPs and their patients. An e-mail notification is generated, HCPs access SM through the link, the reply is sent, and a CPRS note is automatically generated. That same communication would require a far more time-consuming and complicated process without SM: The patient must contact the service, usually the program assistant, and leave a message; that message would be passed on via voicemail or e-mail to the appropriate HCP; the provider would need to access the CPRS, phone the patient, discuss the issue if the patient is available, and then document the contact with a note in the CPRS. If the patient was unavailable, this process would require multiple phone calls.
With respect to patients, the benefits of SM are significant and include easy access to prescription refills and a quick response to questions about medications, dosages, or tests. Patients are able to change or cancel appointments, thereby avoiding no-shows. Frustration concerning the inability to reach the correct party or to speak with staff directly is reduced with SM, and overall communication between HCP and patient is streamlined.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Secure messaging (SM) is an encrypted, web-based mode of communication within the My HealtheVet (MHV) website. It was developed for the nonurgent, nonemergency communication of test results and other health information as well as for scheduling appointments and renewing medication prescriptions. Secure messaging is asynchronous, which means that communication between parties is not done at the same time. It was designed to address the need for a secure means of communication between patient and provider.1 Messages can be triaged across teams and saved to the Computerized Patient Record System (CPRS).
The VA patients who use MHV can upgrade their account through an in-person authentication process (IPA), which takes about 10 minutes. Any health care provider (HCP) team or administrator can use SM if set up in the system. Health care providers can only receive messages from patients who have been associated with their triage care group. Patients may only message an HCP with which they are associated. In general, this group would comprise their HCP and 1 or more specialty clinics where they have already been seen. Patients can choose an HCP from a limited drop-down menu.
Patients using SM choose a subject, such as appointments, medications, tests, or general. Patients are then able to type a message, and they are also able to see the threads of previous messages. They may access test results or attachments sent to them by the HCPs. Patients are notified of messages through their previously registered e-mail account, which displays a message asking them to log on to MHV.
Health care providers may access MHV either through the CPRS on the tools menu or as a link in an e-mail. Once HCPs log on, they will see their inbox and messages listed by sender and type of inquiry (ie, prescription refill, test question, and so forth). The HCPs can view escalated messages (those that have not been answered within 3 days), drafts, and sent and completed messages. Health care providers can also create special folders to store their messages.
The health care team can personalize how and to whom messages appear. There are 2 main models used by Specialty Care. The first involves a staff member designated to triage messages for the team. This staff member will see all incoming messages and forward them appropriately. For example, in one clinic model, the program assistant reviews all messages and then forwards them to the appropriate provider. The team pharmacist receives prescription requests, the HCP receives general or test inquiries from patients, and the program assistant retains and answers all communication related to appointments and cancellations. Another model involves employing a staff person or administrator as a co-user with each HCP. The HCP can then forward messages that may need administrative action.
The HCPs receive an e-mail notification with a link when a message has been received. Clicking on the link takes them directly to SM within MHV, where they can sign in to see all their messages. Users can also add a signature block, which will appear on all correspondence. They may also designate a surrogate to answer messages when they are unavailable, such as during administrative or personal leave. The HCPs also have the ability to create a SM even if the patient has not yet messaged them. Users can also send copies of messages to other staff members. Providers and staff have the ability to attach a file, which can be a test result, letter, records, etc. Messages can then be saved in the CPRS if desired.
Patients, however, cannot send attachments to their HCP. Only those HCPs who have seen the patient will be available for communication. This system eliminates the possibility of patients self-referring to a specialist and asking questions of HCPs who have never seen them. The HCPs and staff may also forward messages to the appropriate person.
Secure messaging can provide unique opportunities for communication and improvement in outcome measures in certain specialties. For example, in endocrinology patients may be asked to send home blood sugar or blood pressure (BP) readings in between visits, to allow for more rapid medication titration and achievement of treatment goals. A study by Harris and colleagues showed that the frequent use of electronic SM was associated with improved glycemic control.2
At the Atlanta VAMC, SM was implemented in the Primary Care Service Line prior to the Medicine Specialty Care Service Line. The implementation was a natural fit for the organized Primary Care teams. Implementation within the specialties brought forth a new set of issues. Many specialties were not formally organized with a team leader. There were often multiple HCPs in a division, some full time, some part time, in addition to subspecialty pharmacists, physician assistants, and nurse practitioners. Because the Atlanta VAMC is also a training hospital for the Emory University School of Medicine, new residents and fellows are included in the teams each month. It was, therefore, necessary for each specialty to design a message flow that would best fit its needs. Initially, there was concern that SM would add yet another layer of responsibilities to the already stretched HCPs.
The reality has been the opposite. Secure messaging was found to be an additional type of communication, which could be completed more rapidly than a phone call or generating a results letter. The HCPs were also concerned that patients would attempt to use them as primary care providers (PCPs). However, as patients were able to view both their PCP and their specialty care provider in the drop-down menu, they were generally able to direct their questions appropriately.
At the Atlanta VAMC, 60% of the messages were completed by the provider, 29% by a clinical team member, and 11% by the triage staff from 2013 to 2014 (Figure 1). Some HCPs were concerned that once SM was in place, they would be inundated with messages. The reality seems to be that most patients use SM judiciously, and although they are comfortable in the knowledge that they can communicate directly with their HCP, the need is infrequent. The number of messages has slowly increased over the past year as more patients join MHV and SM (Table). Surprisingly, as the number of inbound messages increased, the percentage of escalated messages (messages not answered within 3 days) declined, indicating a learning curve as HCPs begin using SM.
There are 3 steps to patient enrollment in SM. The first is enrollment in MHV, which can be done either online or at the VAMC. The second step requires the patient to go to the VAMC and present identification to complete the IPA. Finally, the enrolled patients must opt-in to the program. Enrollment in MHV has steadily increased through advertising campaigns on the VAMC website, within the VAMC, and through HCPs and staff (Figure 2).
However, barriers still exist. Some patients do not have an Internet connection and are not computer savvy. Other patients express interest but put it off to another visit. Some patients have been confused about the additional step of IPA that is required for SM and stop at enrollment in MHV only.
Therefore the key challenges for implementing SM are facilitating MHV enrollment, IPA, and completion of the opt-in feature. To encourage participation, VISN 7 mailed postcards to all 33,000 patients who had undergone IPA but had not yet opted-in. The number of patients who opted-in quadrupled, demonstrating that this type of promotion is an effective recruitment tool.
Another ongoing challenge is developing a method to easily generate workload credit for the HCPs’ time spent using SM for patient care. This will be an important parameter to track, as the time spent on SM per provider is expected to increase. It has also been suggested that there be an out-of-office response for nonemergent messages and the assignment of a surrogate to handle incoming messages for HCPs who are on leave. An unforeseen example of a nonemergent message occurs when a patient replies “Thank you” to a message from an HCP. That message is then counted as a new message and must be viewed and completed like any other message. It can also become an escalated message, even though there is no important information being transmitted.
Conclusions
Secure messaging provides a simple means of rapid communication and feedback between HCPs and their patients. An e-mail notification is generated, HCPs access SM through the link, the reply is sent, and a CPRS note is automatically generated. That same communication would require a far more time-consuming and complicated process without SM: The patient must contact the service, usually the program assistant, and leave a message; that message would be passed on via voicemail or e-mail to the appropriate HCP; the provider would need to access the CPRS, phone the patient, discuss the issue if the patient is available, and then document the contact with a note in the CPRS. If the patient was unavailable, this process would require multiple phone calls.
With respect to patients, the benefits of SM are significant and include easy access to prescription refills and a quick response to questions about medications, dosages, or tests. Patients are able to change or cancel appointments, thereby avoiding no-shows. Frustration concerning the inability to reach the correct party or to speak with staff directly is reduced with SM, and overall communication between HCP and patient is streamlined.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Delbanco T, Sands DZ. Electrons in flight—e-mail between doctors and patients. New Engl J Med. 2004;350(17):1705-1707.
2. Harris LT, Haneuse SJ, Martin DP, Ralston JD. Diabetes quality of care and outpatient utilization associated with electronic patient-provider messaging: A cross-sectional analysis. Diabetes Care. 2009;32(7):1182-1187.
1. Delbanco T, Sands DZ. Electrons in flight—e-mail between doctors and patients. New Engl J Med. 2004;350(17):1705-1707.
2. Harris LT, Haneuse SJ, Martin DP, Ralston JD. Diabetes quality of care and outpatient utilization associated with electronic patient-provider messaging: A cross-sectional analysis. Diabetes Care. 2009;32(7):1182-1187.
Enhancing Patient Satisfaction Through the Use of Complementary Therapies
In October 1998, the National Center for Complementary and Alternative Medicine (NCCAM) was funded and established. This center is the federal government’s lead agency for scientific research on complementary and alternative medicine (CAM) and is 1 of the 27 institutes and centers that make up the National Institutes of Health. The mission of the NCCAM is to define, through rigorous scientific investigation, the usefulness and safety of CAM interventions and roles in improving health and health care.
Although a significant number of adults in the U.S. use some form of CAM, physicians rarely recommend these therapies to their patients, and their use is limited in conventional medical settings.1-3 This is often attributed to a lack of knowledge or scientific evidence, despite a belief by many providers of the potential positive effects.3
In an attempt to disseminate knowledge about various CAM therapies investigated by NCCAM, the Complementary and Alternative Resources to Enhance Satisfaction (CARES) program was organized as a resource center at the Louis Stokes Cleveland VA Medical Center (VAMC). It was anticipated that increasing knowledge about CAM and offering these therapies in conjunction with the conventional medical practices at the VAMC would lead to a more comprehensive, patient-centered system of care. In this way, the goal was to transform current thinking from a focus solely on treating the patient’s disease to a holistic approach, which encompassed comfort, family support, and quality of life (QOL).
Background
The number of veterans with chronic illnesses and pain continues to rise. While aggressive efforts have been aimed at safely decreasing pain and discomfort, many veterans report dissatisfaction with traditional treatment methods, which focus on drug therapy and have little emphasis on preventive or holistic care.4 Health care providers often share patients’ frustrations regarding the use of medications that have varying degrees of efficacy and multiple adverse effects. Innovative approaches to improving health and decreasing pain and stress have focused on more holistic and patient-centered philosophies of care. However, there have been few studies to assess feasibility, implementation, and outcomes within an established medical center.
As an ideal goal among patients, families, and HCPs in all care settings, patient-centered care has become a more prominent focus of the VA health care system (VAHCS). The incorporation of patient-centered care, along with an electronic medical record, structural transformation, and greater focus on performance accountability have contributed to dramatic improvements in care within the VAHCS in the past decade.5,6 Mounting evidence continues to validate the positive health outcomes of models of care that engage patients and families with valuable roles in the healing process.7,8 Professional caregiver satisfaction has also been linked to increased patient satisfaction.9
Integral to patient-centered care is the ability of caregivers to see the whole person—body, mind, and soul. The implementation of therapies or environments that complement traditional medicine and provide for physical comfort and pain management can be important in achieving this form of holistic medicine.1,10 By definition, CAM is any method used outside of and in addition to conventional medicine to prevent or treat disease.6 As CAM takes a holistic approach to healing, most therapies involve not only the treatment of the symptoms of the illness, but also the development of a method of healing that focuses on the spiritual and emotional origins from which the illness arises.11
According to the National Health Interview Survey, complementary and alternative therapies were used by one-third of adults in the U.S. in 2002 and by 4 in 10 adults in 2007.11 However, these estimates may be conservative, as other studies have found that at least the majority of adults had used some form of CAM at one time.1 The most common CAM therapies used by adults in 2007 were nonvitamin, nonmineral, natural products, such as fish oil or ginseng; deep breathing exercises; meditation; chiropractic or osteopathic manipulation; massage; and yoga.11 In 2007, adults most commonly used CAM to treat a variety of musculoskeletal problems (ie, back, neck, or joint pain).11
As a patient-centered philosophy, the most general benefit of the use of CAM involves the idea of patient empowerment and participation in the healing process. Many therapies, such as tai chi, meditation, and guided imagery, require active patient involvement, which can encourage feelings of self-control over the disease process. Complementary and alternative medicine has been shown to be effective in decreasing pain, anxiety, stress, and nausea.10,12-14 Increasing evidence supports an association between stress or negative emotions and health outcomes, such as hypertension, diabetes, and heart disease.15,16 When used in conjunction with traditional medical treatment, CAM can help patients cope with devastating symptoms of their disease processes or to avoid some symptoms altogether.
Despite the widespread use of CAM therapies by the public, HCPs rarely recommend CAM therapies to their patients.2,3 This has been attributed to a lack of scientific evidence, a lack of knowledge or comfort, and a lack of an available CAM provider.3 The basic philosophy of self-motivated stress and pain management, which is fundamental to most CAM therapies, is learned and embraced by most HCPs, but the implementation is not often seen in the real world of busy clinical practice. With its numerous benefits, CAM has the potential to significantly improve the health and QOL. Therefore, innovative programs that help HCPs become knowledgeable and competent in incorporating CAM into current systems of care are needed.
In 2010, the Cleveland VAMC was funded through the Innovations in Patient-Centered Care grant to design and implement a complementary therapy resource center. This project was the CARES program and was organized through the Cleveland Geriatric Research Education and Clinical Center (GRECC). The project team included researchers and clinicians within the GRECC as well as other clinical departments. A CAM coordinator was hired to organize lectures, order supplies, and network with various departments within the Cleveland VAMC. Additionally, a major focus of the CARES program was to encourage the involvement of family and friends in the care of the veteran. An integral goal of this project was to bring CAM resources to the bedside of veterans in acute and long-term care on a 24/7 basis.
The rationale for the implementation of a complementary therapy resource center was based on the Planetree model of patient-centered care, which encourages healing in all dimensions and the integration of complementary therapies with conventional medical practices.17 Offering such therapies in an established medical center with knowledgeable HCPs may increase the safety of such use.1 Providing workshops and lectures for HCPs about various complementary therapies would help educate them and provide them with a knowledge base to feel comfortable in recommending therapies to their patients. By opening workshops and lectures about CAM to the public, veterans would be given the opportunity to learn about the therapies available and their efficacy.
Advancing Patient QOL
The Cleveland VAMC has a history of research and policies to advance a culture of patient-centered care with an emphasis on QOL, customer service, and the use of CAM.In 2001, Anthony D’Eramo, a member of the Cleveland VAMC GRECC, developed a program to educate nursing assistants at the Cleveland and Chillicothe VAMCs on complementary therapies, including meditation, spirituality, therapeutic touch, and yoga. The overall response to the program was positive.18 The focus of the training was on the QOL of nursing assistants; most found participation in the training to be a valuable and worthwhile experience. They indicated their intent to use the techniques they learned for themselves, their families, and their patients.18
Also in 2001, researchers at the Cleveland and Pittsburgh VAMCs identified that older veterans with osteoarthritis perceived the use of prayer and meditation as more useful than medications or surgery for the treatment of pain associated with osteoarthritis.19 Since that time, the Cleveland VAMC has worked with the Pittsburgh VAMC to study the use of motivational interviewing—a communication technique that focuses on patient engagement to achieve changes in behavior—for patients with knee osteoarthritis to consider total knee replacement surgery.
In 2004, Antall and Kresevic implemented a program of guided imagery for patients undergoing joint replacement surgery.20 Although the sample size was small, results indicated positive trends for pain relief, decreased anxiety, and decreased length of stay following surgery. Due to the small sample size, statistical comparisons were not performed; however, the mean pain medication use in the 4 days following surgery was morphine 84.76 mg in the control group vs 36.7 mg in the guided imagery group.20 The overall response to the guided imagery tapes was positive, with 75% of the subjects indicating that use of the tapes made them feel more relaxed and decreased their pain.
More recently, the clinical nurse specialist group at the Cleveland VAMC began a study using music and education to decrease pain. In 2009, a Patient-Centered Care Council was established for the medical center to advance a culture of patient-centered care by analyzing the results of performance measures and satisfaction reports. Additionally, the nursing staff at the Cleveland VAMC Community Living Center (CLC) expressed an interest in expanding the use of CAM by creating a wellness center with exercise equipment and aromatherapy. This center was well-received but had only limited access to patients in acute and long-term care and was unable to be sustained due to insufficient staffing.
The CARES Program
The objectives of the CARES program were to (1) change the culture of the medical center to a more holistic approach, encouraging family and patient participation in care and emphasizing comfort and satisfaction; (2) increase knowledge of complementary therapies for relaxation; (3) improve patient and family satisfaction with nursing and medical care; and (4) build on preexisting medical center initiatives for patient-centered care.
The CARES program presented lectures and training workshops on various CAM therapies for all HCPs in order to provide useful information that may not otherwise have been available. Evidence has shown that those who receive training for complementary therapies respond positively and view the experience as valuable.18 It was hoped that these training sessions would empower nurses and other health care staff to provide care while recognizing the importance of treating the entire person. Programs were planned for various times of the day and evening in various patient care locations. (Aims and initiatives of the CARES program are further expanded in the Figure.)
Prior to any educational sessions, a survey was distributed to HCPs about their knowledge and experience with CAM. Though responses to the survey were limited, the results indicate interest in learning more about CAM therapies (Table 1).
Over the course of the yearlong grant, a total of 19 workshops were scheduled and held for HCPs and veterans for a total of 346 participants. This included 3 intensive training sessions for staff, 1 on Reiki and 2 on Healing Touch. All programs, including the intensive training sessions, were available free to participants. Some of the sessions were videotaped and archived for later viewing. (See Table 2 for a list of all training sessions provided by the CARES program.) The project was limited in both time and funds, so only a limited number of topics were able to be covered, and the topics were based mostly on the availability of experts in each field.
Resources
In addition to lectures, organizers of the CARES program purchased 20 comfort carts for inpatient units at the Cleveland VAMC. These were small rolling lockable wooden carts approved by Interior Design, who evaluated and designed previous work spaces at the Cleveland VAMC to make them functional, appealing, and well-suited for the veterans. The carts were stocked with various resources that focused on comfort and entertainment. Specifically related to CAM, these carts contained guided imagery CDs and Playaways. (Playaways are small audio players with included earbud headphones meant for individual use, which are preloaded with a specific guided imagery session.) Additionally, the comfort carts contained books, books on tape, magazines, portable CD players, music CDs, games, exercise bands, healthy snacks, DVDs, and a portable DVD player. Other items purchased to be distributed to various inpatient and outpatient units included Nintendo Wii game consoles and small televisions. Mobile sleepers were purchased for inpatient units to encourage extended-family visitation. These sleepers have been widely adopted throughout the medical center.
Additional resources purchased by the CARES program included educational pamphlets on various health issues affecting veterans, such as the management of stress. In an effort to increase patient education about complementary therapies, the CARES program provided funding for 2 dedicated channels on the patient television system, broadcasting 24-hour, evidence-based relaxation and guided imagery programming. Finally, the CARES program enhanced the Wellness Center begun by the nurses in the CLC. This included the purchase of exercise equipment, computers, aromatherapy, massage tables, and massage cushions. The exercise equipment, including a recumbent stepper, recumbent bike, and treadmill, was provided by funds from the CARES project. The equipment was available 24/7 to veterans and could be accessed once the veteran was cleared by his primary care and admitting physician. Competencies were developed and completed by the staff. The competencies included orienting the patient on use of the equipment, observation and documentation of equipment used, and response. Veterans who had established home exercise routines were able to continue their programs while hospitalized in the CLC. This helped maintain and regain leisure activity and promoted wellness.
Program Outcomes
Evaluations of the training sessions were overwhelmingly positive (Table 3), and many individuals requested further education and training. A total of 204 participants (59%) completed posttraining evaluations. Some common themes identified through comments on program evaluations included requests for training in the evenings and on weekends. Of the 329 HCPs who participated, 36.5% were nurses or nurse practitioners, 13.7% were ancillary staff (eg, nursing assistants), 9.7% were social workers, 8.5% were students, 5.8% were physicians or physician assistants, 5.2% were psychiatry staff members, 4.9% were occupational/physical/recreational therapy staff members, and 15.7% were other/unknown. The remaining 17 individuals who participated were veterans and their family members.
Reiki and guided imagery classes for increasing relaxation and comfort are still offered to veterans. An attendee of the initial level 1 training offered from the first grant progressed in certifications and received Master status. This Master has trained 60% of the nurses in her unit in level 1 Reiki. Weekly sessions are being implemented for veterans. Guided imagery training provided by the initial CARES grant project is sustained via weekly groups. Reports of an increased sense of well-being and relaxation as well as relief from chronic pain have been reported.
Although evaluations were created for the comfort carts, they were not regularly completed by patients. However, direct subjective feedback from nursing staff who spoke to organizers of the project about both the beds and the carts was very positive. Additionally, members of the project were able to talk to some veterans and family members who agreed to discuss their use of these items. They expressed appreciation for the snacks, which helped “tide them over,” and the beds, which allowed them to stay and comfortably visit their sick loved ones. Utilization of the CARES comfort carts and mobile sleepers on the inpatient units continued after completion of this study. The GRECC has continued to function as a resource center by distributing educational materials, restocking the comfort carts, and providing educational programs on CAM.
Objectively measuring satisfaction related to the implementation of the program proved challenging. At program commencement, plans involved an evaluation of the CARES program using overall hospital satisfaction measures. However, different components of the program took effect at different times, and not all components affected all parts of the hospital. Satisfaction measures, such as the National Veteran’s Survey of Healthcare Experiences of Patients (SHEP) and the local Quick-Kards, which report aggregate scores for patient satisfaction, were analyzed prior, during, and after program implementation but could not be clearly correlated to program impact on patient and family satisfaction with health care. Additionally, the categories addressed in the surveys were very broad while the CARES program addressed only some aspects of hospital care. Despite the weak correlation, SHEP results of inpatient services were analyzed and evaluations did increase in the categories of inpatient overall quality and shared decision making from prior-to-program implementation to postprogram implementation. Quick-Kard results remained essentially the same related to patient-provider communication pre- and postprogram implementation. Additional quantitative and qualitative measures of satisfaction linked specifically to program components need to be created or further explored.
Limitations
This project was not able to address all aspects of the wide range of topics under the general term CAM. In a short time, many individuals taught courses in their areas of expertise. However, many areas, such as acupuncture, chiropractic manipulation, and massage therapy, were not included. Additionally, although herbal therapies are likely the most used CAM method, they also present many challenges when combined with medications and other common therapies among veteran patients.11 The study was not intended to provide any general information endorsing the safety of these herbal therapies when combined with medications, so this topic was avoided altogether. However, this is a topic that needs further exploration and medical involvement, as these therapies can have medical consequences despite their casual use and availability.
Conclusions
The most important lesson learned through this program was that CAM is a very “hot topic” at the Cleveland VAMC and many staff members are enthusiastic and open to integrating it into their practice. This was important throughout program implementation as staff buy-in is integral to a successful medical center initiative. Veterans and family members were receptive to learning about CAM and participating in programs. An abundance of local experts outside of the facility were also willing to share their knowledge about their particular therapy.
Securing continuing education (CE) credit hours was challenging, requiring applications and close work with presenters. However, the added benefit of CE credits helped to garner an audience. Marketing the programs in a time sensitive nature to allow staff or family members to arrange schedules was critical.
Multiple opportunities, including initiatives for patient-centered care, CLCs, and management of veterans with pain and delirium can be helpful for maintaining and expanding the CARES program. Most important, it was learned that a small group of clinicians who can think outside the box can make a big difference for veterans. Implementing a holistic and patient-centered program of CAM that brings resources to veterans 24/7 is both feasible and fun.
Future Directions
Plans for future educational programs on CAM will include the use of interactive audio/video technology to expand outreach, yet still allow the active participation of HCPs and possibly veterans. Cleveland VAMC GRECC staff members continue to work on various aspects of the CARES program, such as the use of audio tapes for relaxation and augmentation of pain treatment and to support the Wellness Center. The carts and mobile sleepers are still heavily used to support the “Care Partners” program at the Cleveland VAMC, and they continue to be stocked with items. These items helped meet the project’s goal of providing resources to be available 24/7.
The CARES program and aspects of CAM have continued to be marketed at professional educational activities and to veterans at health fairs at the medical center. Additional funding sources and small grants have helped to sustain the educational programs and restock the carts, particularly the current VA-funded T21 grant to manage patients with delirium. Future funding opportunities continue to be explored. Additionally future directions would include the incorporation of various other methods of CAM, which were unable to be explored in this time-limited project, including acupuncture, chiropractic manipulation, and massage therapy.
Though evaluations of educational programs were very positive and subjective feedback from the use of the carts and mobile sleepers was positive, it was not possible to establish a direct correlation between improved patient and family satisfaction and health care. Future directions of program evaluation should focus on objective measurements, which can be directly linked to program impact on satisfaction. It is hoped that the inclusion of CAM will contribute to continued improvements in quality and patient satisfaction throughout the entire VAHCS.
Acknowledgements
This manuscript and the program described are the results of work funded by the VHA Innovations for Patient Centered Care and supported by the use of resources and facilities at the Louis Stokes Cleveland Department of Veterans Affairs Medical Center, specifically, the Geriatric Research Education and Clinical Center (GRECC).
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
References
1. Vohra S, Feldman K, Johnston B, Waters K, Boon H. Integrating complementary and alternative medicine into academic medical centers: Experience and perceptions of nine leading centers in North America. BMC Health Serv Res. 2005;5:78-84.
2. Kurtz ME, Nolan RB, Rittinger WJ. Primary care physicians’ attitudes and practices regarding complementary and alternative medicine. J Am Osteopath Assoc. 2003;103(12):597-602.
3. Wahner-Roedler DL, Vincent A, Elkin PL, Loehrer LL, Cha SS, Bauer BA. Physician’s attitudes toward complementary and alternative medicine and their knowledge of specific therapies: A survey at an academic medical center. Evid Based Complement Alternat Med. 2006;3(4):495-501.
4. Kroesen K, Baldwin CM, Brooks AJ, Bell IR. U.S. military veterans’ perceptions of the conventional medical care system and their use of complementary and alternative medicine. Fam Pract. 2002;19(1):57-64.
5. Jha AK, Perlin JB, Kizer KW, Dudley RA. Effect of the transformation of the Veterans Affairs Health Care System on the quality of care. N Engl J Med. 2003;348(22):2218-2227.
6. Perlin JB, Kolodner RM, Roswell RH. The Veterans Health Administration: Quality, value, accountability, and information as transforming strategies for patient-centered care. Am J Manag Care. 2004;10(11, pt 2):828-836.
7. Covinsky KE, Goldman L, Cook EF, et al. The impact of serious illness on patients’ families. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. JAMA. 1994;272(23):1839-1844.
8. Cullen L, Titler M, Drahozal R. Family and pet visitation in the critical care unit. Crit Care Nurse. 2003;23(5):62-67.
9. Haas JS, Cook EF, Puopolo AL, Burstin HR, Cleary PD, Brennan TA. Is the professional satisfaction of general internists associated with patient satisfaction? J Gen Intern Med. 2000;15(2):122-128.
10. Kreitzer MJ, Snyder M. Healing the heart: Integrating complementary therapies and healing practices into the care of cardiovascular patients. Prog Cardiovasc Nurs. 2002;17(2):73-80.
11. Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008;12:1-23.
12. Wang C, Collet JP, Lau J. The effect of Tai Chi on health outcomes in patients with chronic conditions: A systematic review. Arch Intern Med. 2004;164(5):493-501.
13. Gregory S, Verdouw J. Therapeutic touch: Its application for residents in aged care. Aust Nurs J. 2005;12(7):23-25.
14. Hilliard RE. Music therapy in hospice and palliative care: A review of empirical data. Evid Based Complement Alternat Med. 2005;2(2):173-178.
15. Jonas BS, Lando JF. Negative affect as a prospective risk factor for hypertension. Psychosom Med. 2000;62(2):188-196.
16. Fredrickson BL, Levenson RW. Positive emotions speed recovery from the cardiovascular sequelae of negative emotions. Cogn Emot. 1998;12(2):191-220.
17. Katz DL, Ali A. Integrating complementary and alternative practices into conventional care. In: Frampton SB, Charmel P, eds. Putting Patients First: Best Practices in Patient-Centered Care. 2nd ed. San Francisco, CA: Jossey-Bass; 2009.
18. D’Eramo AL, Papp KK, Rose JH. A program on complementary therapies for long-term care nursing assistants. Geriatr Nurs. 2001;22(4):201-207.
19. Ibrahim SA, Siminoff LA, Burant CJ, Kwoh CK. Variation in perceptions of treatment and self-care practices in elderly with osteoarthritis: A comparison between African American and white patients. Arthritis Rheum. 2001;45(4):340-345.
20. Antall GF, Kresevic D. The use of guided imagery to manage pain in an elderly orthopaedic population. Orthop Nurs. 2004;23(5):335-340.
In October 1998, the National Center for Complementary and Alternative Medicine (NCCAM) was funded and established. This center is the federal government’s lead agency for scientific research on complementary and alternative medicine (CAM) and is 1 of the 27 institutes and centers that make up the National Institutes of Health. The mission of the NCCAM is to define, through rigorous scientific investigation, the usefulness and safety of CAM interventions and roles in improving health and health care.
Although a significant number of adults in the U.S. use some form of CAM, physicians rarely recommend these therapies to their patients, and their use is limited in conventional medical settings.1-3 This is often attributed to a lack of knowledge or scientific evidence, despite a belief by many providers of the potential positive effects.3
In an attempt to disseminate knowledge about various CAM therapies investigated by NCCAM, the Complementary and Alternative Resources to Enhance Satisfaction (CARES) program was organized as a resource center at the Louis Stokes Cleveland VA Medical Center (VAMC). It was anticipated that increasing knowledge about CAM and offering these therapies in conjunction with the conventional medical practices at the VAMC would lead to a more comprehensive, patient-centered system of care. In this way, the goal was to transform current thinking from a focus solely on treating the patient’s disease to a holistic approach, which encompassed comfort, family support, and quality of life (QOL).
Background
The number of veterans with chronic illnesses and pain continues to rise. While aggressive efforts have been aimed at safely decreasing pain and discomfort, many veterans report dissatisfaction with traditional treatment methods, which focus on drug therapy and have little emphasis on preventive or holistic care.4 Health care providers often share patients’ frustrations regarding the use of medications that have varying degrees of efficacy and multiple adverse effects. Innovative approaches to improving health and decreasing pain and stress have focused on more holistic and patient-centered philosophies of care. However, there have been few studies to assess feasibility, implementation, and outcomes within an established medical center.
As an ideal goal among patients, families, and HCPs in all care settings, patient-centered care has become a more prominent focus of the VA health care system (VAHCS). The incorporation of patient-centered care, along with an electronic medical record, structural transformation, and greater focus on performance accountability have contributed to dramatic improvements in care within the VAHCS in the past decade.5,6 Mounting evidence continues to validate the positive health outcomes of models of care that engage patients and families with valuable roles in the healing process.7,8 Professional caregiver satisfaction has also been linked to increased patient satisfaction.9
Integral to patient-centered care is the ability of caregivers to see the whole person—body, mind, and soul. The implementation of therapies or environments that complement traditional medicine and provide for physical comfort and pain management can be important in achieving this form of holistic medicine.1,10 By definition, CAM is any method used outside of and in addition to conventional medicine to prevent or treat disease.6 As CAM takes a holistic approach to healing, most therapies involve not only the treatment of the symptoms of the illness, but also the development of a method of healing that focuses on the spiritual and emotional origins from which the illness arises.11
According to the National Health Interview Survey, complementary and alternative therapies were used by one-third of adults in the U.S. in 2002 and by 4 in 10 adults in 2007.11 However, these estimates may be conservative, as other studies have found that at least the majority of adults had used some form of CAM at one time.1 The most common CAM therapies used by adults in 2007 were nonvitamin, nonmineral, natural products, such as fish oil or ginseng; deep breathing exercises; meditation; chiropractic or osteopathic manipulation; massage; and yoga.11 In 2007, adults most commonly used CAM to treat a variety of musculoskeletal problems (ie, back, neck, or joint pain).11
As a patient-centered philosophy, the most general benefit of the use of CAM involves the idea of patient empowerment and participation in the healing process. Many therapies, such as tai chi, meditation, and guided imagery, require active patient involvement, which can encourage feelings of self-control over the disease process. Complementary and alternative medicine has been shown to be effective in decreasing pain, anxiety, stress, and nausea.10,12-14 Increasing evidence supports an association between stress or negative emotions and health outcomes, such as hypertension, diabetes, and heart disease.15,16 When used in conjunction with traditional medical treatment, CAM can help patients cope with devastating symptoms of their disease processes or to avoid some symptoms altogether.
Despite the widespread use of CAM therapies by the public, HCPs rarely recommend CAM therapies to their patients.2,3 This has been attributed to a lack of scientific evidence, a lack of knowledge or comfort, and a lack of an available CAM provider.3 The basic philosophy of self-motivated stress and pain management, which is fundamental to most CAM therapies, is learned and embraced by most HCPs, but the implementation is not often seen in the real world of busy clinical practice. With its numerous benefits, CAM has the potential to significantly improve the health and QOL. Therefore, innovative programs that help HCPs become knowledgeable and competent in incorporating CAM into current systems of care are needed.
In 2010, the Cleveland VAMC was funded through the Innovations in Patient-Centered Care grant to design and implement a complementary therapy resource center. This project was the CARES program and was organized through the Cleveland Geriatric Research Education and Clinical Center (GRECC). The project team included researchers and clinicians within the GRECC as well as other clinical departments. A CAM coordinator was hired to organize lectures, order supplies, and network with various departments within the Cleveland VAMC. Additionally, a major focus of the CARES program was to encourage the involvement of family and friends in the care of the veteran. An integral goal of this project was to bring CAM resources to the bedside of veterans in acute and long-term care on a 24/7 basis.
The rationale for the implementation of a complementary therapy resource center was based on the Planetree model of patient-centered care, which encourages healing in all dimensions and the integration of complementary therapies with conventional medical practices.17 Offering such therapies in an established medical center with knowledgeable HCPs may increase the safety of such use.1 Providing workshops and lectures for HCPs about various complementary therapies would help educate them and provide them with a knowledge base to feel comfortable in recommending therapies to their patients. By opening workshops and lectures about CAM to the public, veterans would be given the opportunity to learn about the therapies available and their efficacy.
Advancing Patient QOL
The Cleveland VAMC has a history of research and policies to advance a culture of patient-centered care with an emphasis on QOL, customer service, and the use of CAM.In 2001, Anthony D’Eramo, a member of the Cleveland VAMC GRECC, developed a program to educate nursing assistants at the Cleveland and Chillicothe VAMCs on complementary therapies, including meditation, spirituality, therapeutic touch, and yoga. The overall response to the program was positive.18 The focus of the training was on the QOL of nursing assistants; most found participation in the training to be a valuable and worthwhile experience. They indicated their intent to use the techniques they learned for themselves, their families, and their patients.18
Also in 2001, researchers at the Cleveland and Pittsburgh VAMCs identified that older veterans with osteoarthritis perceived the use of prayer and meditation as more useful than medications or surgery for the treatment of pain associated with osteoarthritis.19 Since that time, the Cleveland VAMC has worked with the Pittsburgh VAMC to study the use of motivational interviewing—a communication technique that focuses on patient engagement to achieve changes in behavior—for patients with knee osteoarthritis to consider total knee replacement surgery.
In 2004, Antall and Kresevic implemented a program of guided imagery for patients undergoing joint replacement surgery.20 Although the sample size was small, results indicated positive trends for pain relief, decreased anxiety, and decreased length of stay following surgery. Due to the small sample size, statistical comparisons were not performed; however, the mean pain medication use in the 4 days following surgery was morphine 84.76 mg in the control group vs 36.7 mg in the guided imagery group.20 The overall response to the guided imagery tapes was positive, with 75% of the subjects indicating that use of the tapes made them feel more relaxed and decreased their pain.
More recently, the clinical nurse specialist group at the Cleveland VAMC began a study using music and education to decrease pain. In 2009, a Patient-Centered Care Council was established for the medical center to advance a culture of patient-centered care by analyzing the results of performance measures and satisfaction reports. Additionally, the nursing staff at the Cleveland VAMC Community Living Center (CLC) expressed an interest in expanding the use of CAM by creating a wellness center with exercise equipment and aromatherapy. This center was well-received but had only limited access to patients in acute and long-term care and was unable to be sustained due to insufficient staffing.
The CARES Program
The objectives of the CARES program were to (1) change the culture of the medical center to a more holistic approach, encouraging family and patient participation in care and emphasizing comfort and satisfaction; (2) increase knowledge of complementary therapies for relaxation; (3) improve patient and family satisfaction with nursing and medical care; and (4) build on preexisting medical center initiatives for patient-centered care.
The CARES program presented lectures and training workshops on various CAM therapies for all HCPs in order to provide useful information that may not otherwise have been available. Evidence has shown that those who receive training for complementary therapies respond positively and view the experience as valuable.18 It was hoped that these training sessions would empower nurses and other health care staff to provide care while recognizing the importance of treating the entire person. Programs were planned for various times of the day and evening in various patient care locations. (Aims and initiatives of the CARES program are further expanded in the Figure.)
Prior to any educational sessions, a survey was distributed to HCPs about their knowledge and experience with CAM. Though responses to the survey were limited, the results indicate interest in learning more about CAM therapies (Table 1).
Over the course of the yearlong grant, a total of 19 workshops were scheduled and held for HCPs and veterans for a total of 346 participants. This included 3 intensive training sessions for staff, 1 on Reiki and 2 on Healing Touch. All programs, including the intensive training sessions, were available free to participants. Some of the sessions were videotaped and archived for later viewing. (See Table 2 for a list of all training sessions provided by the CARES program.) The project was limited in both time and funds, so only a limited number of topics were able to be covered, and the topics were based mostly on the availability of experts in each field.
Resources
In addition to lectures, organizers of the CARES program purchased 20 comfort carts for inpatient units at the Cleveland VAMC. These were small rolling lockable wooden carts approved by Interior Design, who evaluated and designed previous work spaces at the Cleveland VAMC to make them functional, appealing, and well-suited for the veterans. The carts were stocked with various resources that focused on comfort and entertainment. Specifically related to CAM, these carts contained guided imagery CDs and Playaways. (Playaways are small audio players with included earbud headphones meant for individual use, which are preloaded with a specific guided imagery session.) Additionally, the comfort carts contained books, books on tape, magazines, portable CD players, music CDs, games, exercise bands, healthy snacks, DVDs, and a portable DVD player. Other items purchased to be distributed to various inpatient and outpatient units included Nintendo Wii game consoles and small televisions. Mobile sleepers were purchased for inpatient units to encourage extended-family visitation. These sleepers have been widely adopted throughout the medical center.
Additional resources purchased by the CARES program included educational pamphlets on various health issues affecting veterans, such as the management of stress. In an effort to increase patient education about complementary therapies, the CARES program provided funding for 2 dedicated channels on the patient television system, broadcasting 24-hour, evidence-based relaxation and guided imagery programming. Finally, the CARES program enhanced the Wellness Center begun by the nurses in the CLC. This included the purchase of exercise equipment, computers, aromatherapy, massage tables, and massage cushions. The exercise equipment, including a recumbent stepper, recumbent bike, and treadmill, was provided by funds from the CARES project. The equipment was available 24/7 to veterans and could be accessed once the veteran was cleared by his primary care and admitting physician. Competencies were developed and completed by the staff. The competencies included orienting the patient on use of the equipment, observation and documentation of equipment used, and response. Veterans who had established home exercise routines were able to continue their programs while hospitalized in the CLC. This helped maintain and regain leisure activity and promoted wellness.
Program Outcomes
Evaluations of the training sessions were overwhelmingly positive (Table 3), and many individuals requested further education and training. A total of 204 participants (59%) completed posttraining evaluations. Some common themes identified through comments on program evaluations included requests for training in the evenings and on weekends. Of the 329 HCPs who participated, 36.5% were nurses or nurse practitioners, 13.7% were ancillary staff (eg, nursing assistants), 9.7% were social workers, 8.5% were students, 5.8% were physicians or physician assistants, 5.2% were psychiatry staff members, 4.9% were occupational/physical/recreational therapy staff members, and 15.7% were other/unknown. The remaining 17 individuals who participated were veterans and their family members.
Reiki and guided imagery classes for increasing relaxation and comfort are still offered to veterans. An attendee of the initial level 1 training offered from the first grant progressed in certifications and received Master status. This Master has trained 60% of the nurses in her unit in level 1 Reiki. Weekly sessions are being implemented for veterans. Guided imagery training provided by the initial CARES grant project is sustained via weekly groups. Reports of an increased sense of well-being and relaxation as well as relief from chronic pain have been reported.
Although evaluations were created for the comfort carts, they were not regularly completed by patients. However, direct subjective feedback from nursing staff who spoke to organizers of the project about both the beds and the carts was very positive. Additionally, members of the project were able to talk to some veterans and family members who agreed to discuss their use of these items. They expressed appreciation for the snacks, which helped “tide them over,” and the beds, which allowed them to stay and comfortably visit their sick loved ones. Utilization of the CARES comfort carts and mobile sleepers on the inpatient units continued after completion of this study. The GRECC has continued to function as a resource center by distributing educational materials, restocking the comfort carts, and providing educational programs on CAM.
Objectively measuring satisfaction related to the implementation of the program proved challenging. At program commencement, plans involved an evaluation of the CARES program using overall hospital satisfaction measures. However, different components of the program took effect at different times, and not all components affected all parts of the hospital. Satisfaction measures, such as the National Veteran’s Survey of Healthcare Experiences of Patients (SHEP) and the local Quick-Kards, which report aggregate scores for patient satisfaction, were analyzed prior, during, and after program implementation but could not be clearly correlated to program impact on patient and family satisfaction with health care. Additionally, the categories addressed in the surveys were very broad while the CARES program addressed only some aspects of hospital care. Despite the weak correlation, SHEP results of inpatient services were analyzed and evaluations did increase in the categories of inpatient overall quality and shared decision making from prior-to-program implementation to postprogram implementation. Quick-Kard results remained essentially the same related to patient-provider communication pre- and postprogram implementation. Additional quantitative and qualitative measures of satisfaction linked specifically to program components need to be created or further explored.
Limitations
This project was not able to address all aspects of the wide range of topics under the general term CAM. In a short time, many individuals taught courses in their areas of expertise. However, many areas, such as acupuncture, chiropractic manipulation, and massage therapy, were not included. Additionally, although herbal therapies are likely the most used CAM method, they also present many challenges when combined with medications and other common therapies among veteran patients.11 The study was not intended to provide any general information endorsing the safety of these herbal therapies when combined with medications, so this topic was avoided altogether. However, this is a topic that needs further exploration and medical involvement, as these therapies can have medical consequences despite their casual use and availability.
Conclusions
The most important lesson learned through this program was that CAM is a very “hot topic” at the Cleveland VAMC and many staff members are enthusiastic and open to integrating it into their practice. This was important throughout program implementation as staff buy-in is integral to a successful medical center initiative. Veterans and family members were receptive to learning about CAM and participating in programs. An abundance of local experts outside of the facility were also willing to share their knowledge about their particular therapy.
Securing continuing education (CE) credit hours was challenging, requiring applications and close work with presenters. However, the added benefit of CE credits helped to garner an audience. Marketing the programs in a time sensitive nature to allow staff or family members to arrange schedules was critical.
Multiple opportunities, including initiatives for patient-centered care, CLCs, and management of veterans with pain and delirium can be helpful for maintaining and expanding the CARES program. Most important, it was learned that a small group of clinicians who can think outside the box can make a big difference for veterans. Implementing a holistic and patient-centered program of CAM that brings resources to veterans 24/7 is both feasible and fun.
Future Directions
Plans for future educational programs on CAM will include the use of interactive audio/video technology to expand outreach, yet still allow the active participation of HCPs and possibly veterans. Cleveland VAMC GRECC staff members continue to work on various aspects of the CARES program, such as the use of audio tapes for relaxation and augmentation of pain treatment and to support the Wellness Center. The carts and mobile sleepers are still heavily used to support the “Care Partners” program at the Cleveland VAMC, and they continue to be stocked with items. These items helped meet the project’s goal of providing resources to be available 24/7.
The CARES program and aspects of CAM have continued to be marketed at professional educational activities and to veterans at health fairs at the medical center. Additional funding sources and small grants have helped to sustain the educational programs and restock the carts, particularly the current VA-funded T21 grant to manage patients with delirium. Future funding opportunities continue to be explored. Additionally future directions would include the incorporation of various other methods of CAM, which were unable to be explored in this time-limited project, including acupuncture, chiropractic manipulation, and massage therapy.
Though evaluations of educational programs were very positive and subjective feedback from the use of the carts and mobile sleepers was positive, it was not possible to establish a direct correlation between improved patient and family satisfaction and health care. Future directions of program evaluation should focus on objective measurements, which can be directly linked to program impact on satisfaction. It is hoped that the inclusion of CAM will contribute to continued improvements in quality and patient satisfaction throughout the entire VAHCS.
Acknowledgements
This manuscript and the program described are the results of work funded by the VHA Innovations for Patient Centered Care and supported by the use of resources and facilities at the Louis Stokes Cleveland Department of Veterans Affairs Medical Center, specifically, the Geriatric Research Education and Clinical Center (GRECC).
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
References
1. Vohra S, Feldman K, Johnston B, Waters K, Boon H. Integrating complementary and alternative medicine into academic medical centers: Experience and perceptions of nine leading centers in North America. BMC Health Serv Res. 2005;5:78-84.
2. Kurtz ME, Nolan RB, Rittinger WJ. Primary care physicians’ attitudes and practices regarding complementary and alternative medicine. J Am Osteopath Assoc. 2003;103(12):597-602.
3. Wahner-Roedler DL, Vincent A, Elkin PL, Loehrer LL, Cha SS, Bauer BA. Physician’s attitudes toward complementary and alternative medicine and their knowledge of specific therapies: A survey at an academic medical center. Evid Based Complement Alternat Med. 2006;3(4):495-501.
4. Kroesen K, Baldwin CM, Brooks AJ, Bell IR. U.S. military veterans’ perceptions of the conventional medical care system and their use of complementary and alternative medicine. Fam Pract. 2002;19(1):57-64.
5. Jha AK, Perlin JB, Kizer KW, Dudley RA. Effect of the transformation of the Veterans Affairs Health Care System on the quality of care. N Engl J Med. 2003;348(22):2218-2227.
6. Perlin JB, Kolodner RM, Roswell RH. The Veterans Health Administration: Quality, value, accountability, and information as transforming strategies for patient-centered care. Am J Manag Care. 2004;10(11, pt 2):828-836.
7. Covinsky KE, Goldman L, Cook EF, et al. The impact of serious illness on patients’ families. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. JAMA. 1994;272(23):1839-1844.
8. Cullen L, Titler M, Drahozal R. Family and pet visitation in the critical care unit. Crit Care Nurse. 2003;23(5):62-67.
9. Haas JS, Cook EF, Puopolo AL, Burstin HR, Cleary PD, Brennan TA. Is the professional satisfaction of general internists associated with patient satisfaction? J Gen Intern Med. 2000;15(2):122-128.
10. Kreitzer MJ, Snyder M. Healing the heart: Integrating complementary therapies and healing practices into the care of cardiovascular patients. Prog Cardiovasc Nurs. 2002;17(2):73-80.
11. Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008;12:1-23.
12. Wang C, Collet JP, Lau J. The effect of Tai Chi on health outcomes in patients with chronic conditions: A systematic review. Arch Intern Med. 2004;164(5):493-501.
13. Gregory S, Verdouw J. Therapeutic touch: Its application for residents in aged care. Aust Nurs J. 2005;12(7):23-25.
14. Hilliard RE. Music therapy in hospice and palliative care: A review of empirical data. Evid Based Complement Alternat Med. 2005;2(2):173-178.
15. Jonas BS, Lando JF. Negative affect as a prospective risk factor for hypertension. Psychosom Med. 2000;62(2):188-196.
16. Fredrickson BL, Levenson RW. Positive emotions speed recovery from the cardiovascular sequelae of negative emotions. Cogn Emot. 1998;12(2):191-220.
17. Katz DL, Ali A. Integrating complementary and alternative practices into conventional care. In: Frampton SB, Charmel P, eds. Putting Patients First: Best Practices in Patient-Centered Care. 2nd ed. San Francisco, CA: Jossey-Bass; 2009.
18. D’Eramo AL, Papp KK, Rose JH. A program on complementary therapies for long-term care nursing assistants. Geriatr Nurs. 2001;22(4):201-207.
19. Ibrahim SA, Siminoff LA, Burant CJ, Kwoh CK. Variation in perceptions of treatment and self-care practices in elderly with osteoarthritis: A comparison between African American and white patients. Arthritis Rheum. 2001;45(4):340-345.
20. Antall GF, Kresevic D. The use of guided imagery to manage pain in an elderly orthopaedic population. Orthop Nurs. 2004;23(5):335-340.
In October 1998, the National Center for Complementary and Alternative Medicine (NCCAM) was funded and established. This center is the federal government’s lead agency for scientific research on complementary and alternative medicine (CAM) and is 1 of the 27 institutes and centers that make up the National Institutes of Health. The mission of the NCCAM is to define, through rigorous scientific investigation, the usefulness and safety of CAM interventions and roles in improving health and health care.
Although a significant number of adults in the U.S. use some form of CAM, physicians rarely recommend these therapies to their patients, and their use is limited in conventional medical settings.1-3 This is often attributed to a lack of knowledge or scientific evidence, despite a belief by many providers of the potential positive effects.3
In an attempt to disseminate knowledge about various CAM therapies investigated by NCCAM, the Complementary and Alternative Resources to Enhance Satisfaction (CARES) program was organized as a resource center at the Louis Stokes Cleveland VA Medical Center (VAMC). It was anticipated that increasing knowledge about CAM and offering these therapies in conjunction with the conventional medical practices at the VAMC would lead to a more comprehensive, patient-centered system of care. In this way, the goal was to transform current thinking from a focus solely on treating the patient’s disease to a holistic approach, which encompassed comfort, family support, and quality of life (QOL).
Background
The number of veterans with chronic illnesses and pain continues to rise. While aggressive efforts have been aimed at safely decreasing pain and discomfort, many veterans report dissatisfaction with traditional treatment methods, which focus on drug therapy and have little emphasis on preventive or holistic care.4 Health care providers often share patients’ frustrations regarding the use of medications that have varying degrees of efficacy and multiple adverse effects. Innovative approaches to improving health and decreasing pain and stress have focused on more holistic and patient-centered philosophies of care. However, there have been few studies to assess feasibility, implementation, and outcomes within an established medical center.
As an ideal goal among patients, families, and HCPs in all care settings, patient-centered care has become a more prominent focus of the VA health care system (VAHCS). The incorporation of patient-centered care, along with an electronic medical record, structural transformation, and greater focus on performance accountability have contributed to dramatic improvements in care within the VAHCS in the past decade.5,6 Mounting evidence continues to validate the positive health outcomes of models of care that engage patients and families with valuable roles in the healing process.7,8 Professional caregiver satisfaction has also been linked to increased patient satisfaction.9
Integral to patient-centered care is the ability of caregivers to see the whole person—body, mind, and soul. The implementation of therapies or environments that complement traditional medicine and provide for physical comfort and pain management can be important in achieving this form of holistic medicine.1,10 By definition, CAM is any method used outside of and in addition to conventional medicine to prevent or treat disease.6 As CAM takes a holistic approach to healing, most therapies involve not only the treatment of the symptoms of the illness, but also the development of a method of healing that focuses on the spiritual and emotional origins from which the illness arises.11
According to the National Health Interview Survey, complementary and alternative therapies were used by one-third of adults in the U.S. in 2002 and by 4 in 10 adults in 2007.11 However, these estimates may be conservative, as other studies have found that at least the majority of adults had used some form of CAM at one time.1 The most common CAM therapies used by adults in 2007 were nonvitamin, nonmineral, natural products, such as fish oil or ginseng; deep breathing exercises; meditation; chiropractic or osteopathic manipulation; massage; and yoga.11 In 2007, adults most commonly used CAM to treat a variety of musculoskeletal problems (ie, back, neck, or joint pain).11
As a patient-centered philosophy, the most general benefit of the use of CAM involves the idea of patient empowerment and participation in the healing process. Many therapies, such as tai chi, meditation, and guided imagery, require active patient involvement, which can encourage feelings of self-control over the disease process. Complementary and alternative medicine has been shown to be effective in decreasing pain, anxiety, stress, and nausea.10,12-14 Increasing evidence supports an association between stress or negative emotions and health outcomes, such as hypertension, diabetes, and heart disease.15,16 When used in conjunction with traditional medical treatment, CAM can help patients cope with devastating symptoms of their disease processes or to avoid some symptoms altogether.
Despite the widespread use of CAM therapies by the public, HCPs rarely recommend CAM therapies to their patients.2,3 This has been attributed to a lack of scientific evidence, a lack of knowledge or comfort, and a lack of an available CAM provider.3 The basic philosophy of self-motivated stress and pain management, which is fundamental to most CAM therapies, is learned and embraced by most HCPs, but the implementation is not often seen in the real world of busy clinical practice. With its numerous benefits, CAM has the potential to significantly improve the health and QOL. Therefore, innovative programs that help HCPs become knowledgeable and competent in incorporating CAM into current systems of care are needed.
In 2010, the Cleveland VAMC was funded through the Innovations in Patient-Centered Care grant to design and implement a complementary therapy resource center. This project was the CARES program and was organized through the Cleveland Geriatric Research Education and Clinical Center (GRECC). The project team included researchers and clinicians within the GRECC as well as other clinical departments. A CAM coordinator was hired to organize lectures, order supplies, and network with various departments within the Cleveland VAMC. Additionally, a major focus of the CARES program was to encourage the involvement of family and friends in the care of the veteran. An integral goal of this project was to bring CAM resources to the bedside of veterans in acute and long-term care on a 24/7 basis.
The rationale for the implementation of a complementary therapy resource center was based on the Planetree model of patient-centered care, which encourages healing in all dimensions and the integration of complementary therapies with conventional medical practices.17 Offering such therapies in an established medical center with knowledgeable HCPs may increase the safety of such use.1 Providing workshops and lectures for HCPs about various complementary therapies would help educate them and provide them with a knowledge base to feel comfortable in recommending therapies to their patients. By opening workshops and lectures about CAM to the public, veterans would be given the opportunity to learn about the therapies available and their efficacy.
Advancing Patient QOL
The Cleveland VAMC has a history of research and policies to advance a culture of patient-centered care with an emphasis on QOL, customer service, and the use of CAM.In 2001, Anthony D’Eramo, a member of the Cleveland VAMC GRECC, developed a program to educate nursing assistants at the Cleveland and Chillicothe VAMCs on complementary therapies, including meditation, spirituality, therapeutic touch, and yoga. The overall response to the program was positive.18 The focus of the training was on the QOL of nursing assistants; most found participation in the training to be a valuable and worthwhile experience. They indicated their intent to use the techniques they learned for themselves, their families, and their patients.18
Also in 2001, researchers at the Cleveland and Pittsburgh VAMCs identified that older veterans with osteoarthritis perceived the use of prayer and meditation as more useful than medications or surgery for the treatment of pain associated with osteoarthritis.19 Since that time, the Cleveland VAMC has worked with the Pittsburgh VAMC to study the use of motivational interviewing—a communication technique that focuses on patient engagement to achieve changes in behavior—for patients with knee osteoarthritis to consider total knee replacement surgery.
In 2004, Antall and Kresevic implemented a program of guided imagery for patients undergoing joint replacement surgery.20 Although the sample size was small, results indicated positive trends for pain relief, decreased anxiety, and decreased length of stay following surgery. Due to the small sample size, statistical comparisons were not performed; however, the mean pain medication use in the 4 days following surgery was morphine 84.76 mg in the control group vs 36.7 mg in the guided imagery group.20 The overall response to the guided imagery tapes was positive, with 75% of the subjects indicating that use of the tapes made them feel more relaxed and decreased their pain.
More recently, the clinical nurse specialist group at the Cleveland VAMC began a study using music and education to decrease pain. In 2009, a Patient-Centered Care Council was established for the medical center to advance a culture of patient-centered care by analyzing the results of performance measures and satisfaction reports. Additionally, the nursing staff at the Cleveland VAMC Community Living Center (CLC) expressed an interest in expanding the use of CAM by creating a wellness center with exercise equipment and aromatherapy. This center was well-received but had only limited access to patients in acute and long-term care and was unable to be sustained due to insufficient staffing.
The CARES Program
The objectives of the CARES program were to (1) change the culture of the medical center to a more holistic approach, encouraging family and patient participation in care and emphasizing comfort and satisfaction; (2) increase knowledge of complementary therapies for relaxation; (3) improve patient and family satisfaction with nursing and medical care; and (4) build on preexisting medical center initiatives for patient-centered care.
The CARES program presented lectures and training workshops on various CAM therapies for all HCPs in order to provide useful information that may not otherwise have been available. Evidence has shown that those who receive training for complementary therapies respond positively and view the experience as valuable.18 It was hoped that these training sessions would empower nurses and other health care staff to provide care while recognizing the importance of treating the entire person. Programs were planned for various times of the day and evening in various patient care locations. (Aims and initiatives of the CARES program are further expanded in the Figure.)
Prior to any educational sessions, a survey was distributed to HCPs about their knowledge and experience with CAM. Though responses to the survey were limited, the results indicate interest in learning more about CAM therapies (Table 1).
Over the course of the yearlong grant, a total of 19 workshops were scheduled and held for HCPs and veterans for a total of 346 participants. This included 3 intensive training sessions for staff, 1 on Reiki and 2 on Healing Touch. All programs, including the intensive training sessions, were available free to participants. Some of the sessions were videotaped and archived for later viewing. (See Table 2 for a list of all training sessions provided by the CARES program.) The project was limited in both time and funds, so only a limited number of topics were able to be covered, and the topics were based mostly on the availability of experts in each field.
Resources
In addition to lectures, organizers of the CARES program purchased 20 comfort carts for inpatient units at the Cleveland VAMC. These were small rolling lockable wooden carts approved by Interior Design, who evaluated and designed previous work spaces at the Cleveland VAMC to make them functional, appealing, and well-suited for the veterans. The carts were stocked with various resources that focused on comfort and entertainment. Specifically related to CAM, these carts contained guided imagery CDs and Playaways. (Playaways are small audio players with included earbud headphones meant for individual use, which are preloaded with a specific guided imagery session.) Additionally, the comfort carts contained books, books on tape, magazines, portable CD players, music CDs, games, exercise bands, healthy snacks, DVDs, and a portable DVD player. Other items purchased to be distributed to various inpatient and outpatient units included Nintendo Wii game consoles and small televisions. Mobile sleepers were purchased for inpatient units to encourage extended-family visitation. These sleepers have been widely adopted throughout the medical center.
Additional resources purchased by the CARES program included educational pamphlets on various health issues affecting veterans, such as the management of stress. In an effort to increase patient education about complementary therapies, the CARES program provided funding for 2 dedicated channels on the patient television system, broadcasting 24-hour, evidence-based relaxation and guided imagery programming. Finally, the CARES program enhanced the Wellness Center begun by the nurses in the CLC. This included the purchase of exercise equipment, computers, aromatherapy, massage tables, and massage cushions. The exercise equipment, including a recumbent stepper, recumbent bike, and treadmill, was provided by funds from the CARES project. The equipment was available 24/7 to veterans and could be accessed once the veteran was cleared by his primary care and admitting physician. Competencies were developed and completed by the staff. The competencies included orienting the patient on use of the equipment, observation and documentation of equipment used, and response. Veterans who had established home exercise routines were able to continue their programs while hospitalized in the CLC. This helped maintain and regain leisure activity and promoted wellness.
Program Outcomes
Evaluations of the training sessions were overwhelmingly positive (Table 3), and many individuals requested further education and training. A total of 204 participants (59%) completed posttraining evaluations. Some common themes identified through comments on program evaluations included requests for training in the evenings and on weekends. Of the 329 HCPs who participated, 36.5% were nurses or nurse practitioners, 13.7% were ancillary staff (eg, nursing assistants), 9.7% were social workers, 8.5% were students, 5.8% were physicians or physician assistants, 5.2% were psychiatry staff members, 4.9% were occupational/physical/recreational therapy staff members, and 15.7% were other/unknown. The remaining 17 individuals who participated were veterans and their family members.
Reiki and guided imagery classes for increasing relaxation and comfort are still offered to veterans. An attendee of the initial level 1 training offered from the first grant progressed in certifications and received Master status. This Master has trained 60% of the nurses in her unit in level 1 Reiki. Weekly sessions are being implemented for veterans. Guided imagery training provided by the initial CARES grant project is sustained via weekly groups. Reports of an increased sense of well-being and relaxation as well as relief from chronic pain have been reported.
Although evaluations were created for the comfort carts, they were not regularly completed by patients. However, direct subjective feedback from nursing staff who spoke to organizers of the project about both the beds and the carts was very positive. Additionally, members of the project were able to talk to some veterans and family members who agreed to discuss their use of these items. They expressed appreciation for the snacks, which helped “tide them over,” and the beds, which allowed them to stay and comfortably visit their sick loved ones. Utilization of the CARES comfort carts and mobile sleepers on the inpatient units continued after completion of this study. The GRECC has continued to function as a resource center by distributing educational materials, restocking the comfort carts, and providing educational programs on CAM.
Objectively measuring satisfaction related to the implementation of the program proved challenging. At program commencement, plans involved an evaluation of the CARES program using overall hospital satisfaction measures. However, different components of the program took effect at different times, and not all components affected all parts of the hospital. Satisfaction measures, such as the National Veteran’s Survey of Healthcare Experiences of Patients (SHEP) and the local Quick-Kards, which report aggregate scores for patient satisfaction, were analyzed prior, during, and after program implementation but could not be clearly correlated to program impact on patient and family satisfaction with health care. Additionally, the categories addressed in the surveys were very broad while the CARES program addressed only some aspects of hospital care. Despite the weak correlation, SHEP results of inpatient services were analyzed and evaluations did increase in the categories of inpatient overall quality and shared decision making from prior-to-program implementation to postprogram implementation. Quick-Kard results remained essentially the same related to patient-provider communication pre- and postprogram implementation. Additional quantitative and qualitative measures of satisfaction linked specifically to program components need to be created or further explored.
Limitations
This project was not able to address all aspects of the wide range of topics under the general term CAM. In a short time, many individuals taught courses in their areas of expertise. However, many areas, such as acupuncture, chiropractic manipulation, and massage therapy, were not included. Additionally, although herbal therapies are likely the most used CAM method, they also present many challenges when combined with medications and other common therapies among veteran patients.11 The study was not intended to provide any general information endorsing the safety of these herbal therapies when combined with medications, so this topic was avoided altogether. However, this is a topic that needs further exploration and medical involvement, as these therapies can have medical consequences despite their casual use and availability.
Conclusions
The most important lesson learned through this program was that CAM is a very “hot topic” at the Cleveland VAMC and many staff members are enthusiastic and open to integrating it into their practice. This was important throughout program implementation as staff buy-in is integral to a successful medical center initiative. Veterans and family members were receptive to learning about CAM and participating in programs. An abundance of local experts outside of the facility were also willing to share their knowledge about their particular therapy.
Securing continuing education (CE) credit hours was challenging, requiring applications and close work with presenters. However, the added benefit of CE credits helped to garner an audience. Marketing the programs in a time sensitive nature to allow staff or family members to arrange schedules was critical.
Multiple opportunities, including initiatives for patient-centered care, CLCs, and management of veterans with pain and delirium can be helpful for maintaining and expanding the CARES program. Most important, it was learned that a small group of clinicians who can think outside the box can make a big difference for veterans. Implementing a holistic and patient-centered program of CAM that brings resources to veterans 24/7 is both feasible and fun.
Future Directions
Plans for future educational programs on CAM will include the use of interactive audio/video technology to expand outreach, yet still allow the active participation of HCPs and possibly veterans. Cleveland VAMC GRECC staff members continue to work on various aspects of the CARES program, such as the use of audio tapes for relaxation and augmentation of pain treatment and to support the Wellness Center. The carts and mobile sleepers are still heavily used to support the “Care Partners” program at the Cleveland VAMC, and they continue to be stocked with items. These items helped meet the project’s goal of providing resources to be available 24/7.
The CARES program and aspects of CAM have continued to be marketed at professional educational activities and to veterans at health fairs at the medical center. Additional funding sources and small grants have helped to sustain the educational programs and restock the carts, particularly the current VA-funded T21 grant to manage patients with delirium. Future funding opportunities continue to be explored. Additionally future directions would include the incorporation of various other methods of CAM, which were unable to be explored in this time-limited project, including acupuncture, chiropractic manipulation, and massage therapy.
Though evaluations of educational programs were very positive and subjective feedback from the use of the carts and mobile sleepers was positive, it was not possible to establish a direct correlation between improved patient and family satisfaction and health care. Future directions of program evaluation should focus on objective measurements, which can be directly linked to program impact on satisfaction. It is hoped that the inclusion of CAM will contribute to continued improvements in quality and patient satisfaction throughout the entire VAHCS.
Acknowledgements
This manuscript and the program described are the results of work funded by the VHA Innovations for Patient Centered Care and supported by the use of resources and facilities at the Louis Stokes Cleveland Department of Veterans Affairs Medical Center, specifically, the Geriatric Research Education and Clinical Center (GRECC).
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
References
1. Vohra S, Feldman K, Johnston B, Waters K, Boon H. Integrating complementary and alternative medicine into academic medical centers: Experience and perceptions of nine leading centers in North America. BMC Health Serv Res. 2005;5:78-84.
2. Kurtz ME, Nolan RB, Rittinger WJ. Primary care physicians’ attitudes and practices regarding complementary and alternative medicine. J Am Osteopath Assoc. 2003;103(12):597-602.
3. Wahner-Roedler DL, Vincent A, Elkin PL, Loehrer LL, Cha SS, Bauer BA. Physician’s attitudes toward complementary and alternative medicine and their knowledge of specific therapies: A survey at an academic medical center. Evid Based Complement Alternat Med. 2006;3(4):495-501.
4. Kroesen K, Baldwin CM, Brooks AJ, Bell IR. U.S. military veterans’ perceptions of the conventional medical care system and their use of complementary and alternative medicine. Fam Pract. 2002;19(1):57-64.
5. Jha AK, Perlin JB, Kizer KW, Dudley RA. Effect of the transformation of the Veterans Affairs Health Care System on the quality of care. N Engl J Med. 2003;348(22):2218-2227.
6. Perlin JB, Kolodner RM, Roswell RH. The Veterans Health Administration: Quality, value, accountability, and information as transforming strategies for patient-centered care. Am J Manag Care. 2004;10(11, pt 2):828-836.
7. Covinsky KE, Goldman L, Cook EF, et al. The impact of serious illness on patients’ families. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. JAMA. 1994;272(23):1839-1844.
8. Cullen L, Titler M, Drahozal R. Family and pet visitation in the critical care unit. Crit Care Nurse. 2003;23(5):62-67.
9. Haas JS, Cook EF, Puopolo AL, Burstin HR, Cleary PD, Brennan TA. Is the professional satisfaction of general internists associated with patient satisfaction? J Gen Intern Med. 2000;15(2):122-128.
10. Kreitzer MJ, Snyder M. Healing the heart: Integrating complementary therapies and healing practices into the care of cardiovascular patients. Prog Cardiovasc Nurs. 2002;17(2):73-80.
11. Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008;12:1-23.
12. Wang C, Collet JP, Lau J. The effect of Tai Chi on health outcomes in patients with chronic conditions: A systematic review. Arch Intern Med. 2004;164(5):493-501.
13. Gregory S, Verdouw J. Therapeutic touch: Its application for residents in aged care. Aust Nurs J. 2005;12(7):23-25.
14. Hilliard RE. Music therapy in hospice and palliative care: A review of empirical data. Evid Based Complement Alternat Med. 2005;2(2):173-178.
15. Jonas BS, Lando JF. Negative affect as a prospective risk factor for hypertension. Psychosom Med. 2000;62(2):188-196.
16. Fredrickson BL, Levenson RW. Positive emotions speed recovery from the cardiovascular sequelae of negative emotions. Cogn Emot. 1998;12(2):191-220.
17. Katz DL, Ali A. Integrating complementary and alternative practices into conventional care. In: Frampton SB, Charmel P, eds. Putting Patients First: Best Practices in Patient-Centered Care. 2nd ed. San Francisco, CA: Jossey-Bass; 2009.
18. D’Eramo AL, Papp KK, Rose JH. A program on complementary therapies for long-term care nursing assistants. Geriatr Nurs. 2001;22(4):201-207.
19. Ibrahim SA, Siminoff LA, Burant CJ, Kwoh CK. Variation in perceptions of treatment and self-care practices in elderly with osteoarthritis: A comparison between African American and white patients. Arthritis Rheum. 2001;45(4):340-345.
20. Antall GF, Kresevic D. The use of guided imagery to manage pain in an elderly orthopaedic population. Orthop Nurs. 2004;23(5):335-340.
The Clinical Impact of Electronic Consultation in Diabetes Care
In the U.S., the prevalence of diabetes continues to escalate at alarming rates. From 1980-2010 the incidence of diabetes increased by 200% for people aged < 45 years, 124% for people 45 to 64 years, and 126% for people 65 to 74 years. Furthermore, based on the National Institute of Health, diabetes currently affects 25.8 million people in the U.S.1,2 Glycemic control has been demonstrated to reduce the risk of microvascular disease in patients with diabetes.3 Most patients with diabetes are managed by primary care practitioners (PCPs), and as the number of patients with diabetes continues to increase, there is an increasing demand on PCPs to achieve recommended glycemic targets.4
The Veterans Health Administration (VHA) VISN 16 has a notably higher prevalence of diabetes compared with that of the national rate. Failure to achieve glycemic targets continues to impose an escalating economic burden.3 Endocrine assistance is often sought by PCPs, but due to a scarcity of endocrinologists, patients commonly wait weeks or months before being seen. Furthermore, rural patients often must travel for several hours before they can reach a specialty center.
The Office of Specialty Care Transformation has provided a unique opportunity for PCPs to gain greater access to specialty advice via electronic consultations. This initiative allows PCPs and specialists to communicate promptly, to institute definitive solutions for patient care, and to augment the clinical and academic aims of primary and specialty care providers. The Michael E. DeBakey VAMC (MEDVAMC) in Houston, Texas, was chosen to initiate a VISN 16-wide diabetes management e-consult service (DMECS).
Endocrinologists at MEDVAMC developed DMECS to serve as a multifunctional tool to reach as many veterans as possible throughout VISN 16, broaden the scope of the existing diabetes endocrine practice, and engender a collaborative spirit between PCPs and specialty care providers. Initiation of this service has been particularly useful for patients with physical disabilities or financial constraints whose care is managed at the community-based outpatient clinics (CBOCs). The purpose of this article is to discuss the concept and initiation of the DMECS, the structure of the consult note, the implementation process, early provider feedback on the project, and future plans.
The DMECS Process
The DMECS allows endocrinologists to provide advice to PCPs to help improve diabetes care while minimizing travel to specialty centers. The advice generated by the DMECS is electronically conveyed to the referring physician (usually the PCP), not to the patient. The requesting physician is then responsible for implementing the recommendations. The DMECS does not comanage patients with diabetes but rather provides support to the PCP in complex cases that would otherwise require an outside referral.
The diabetes management e-consult team has 1 administrator and 3 health care providers (HCPs). Promotion of the service consisted of electronic distribution of flyers to all primary care teams, posters in the main lobby of the hospital, and electronic distribution of a letter to all VISN 16 HCPs. The DMECS team contacted the chiefs of primary care and CBOC directors to promote the service. Communication was augmented by scheduling videoconferencing with all interested facilities. Presentations were given to the VISN-wide transformational care collaborative and women’s health groups.
Any specialties that assist in diabetes management, including ophthalmology and vascular medicine, were encouraged to refer consults to DMECS if clinically indicated. The recommendation is that PCPs submit an e-consult for any patient with a hemoglobin A1C (A1C) > 9%. The only prerequisite to placing the e-consult order is an A1C > 7.5% within the preceding 3 months. Any patient with reported or objective evidence of hypoglycemia is eligible for an e-consult, regardless of the A1C value. Women who are pregnant and patients on an insulin pump are excluded from the program.
All diabetes e-consults are supervised by a board-certified endocrinologist and are resolved within 2 to 3 business days. On receipt of the consult request, the DMECS provider reviews the chart, including active medication lists, blood glucose levels documented in progress notes, care and coordination of home telehealth data regarding blood glucose levels and changes in diabetes medication management, laboratory results and pharmacy refill patterns.
Recommendations are completed and the DMECS provider alerts the requesting physician by adding them as a cosigner to the note in the Computerized Patient Record System (CPRS). When possible, the patient’s nurse manager is also added to the note. For interfacility consults, the DMECS provider contacts the requesting provider directly via email or telephone. Consistent communication with the requesting physician ensures clarity of understanding between specialist and PCP.
The e-consult recommendations are consolidated into 3 distinct sections. The Impression section provides an explanation to the provider about the specialist’s impression of current diabetes control and the reasoning behind the recommendations. The Recommendation section lists in medical terminology the recommended changes to diabetes medications. A unique component to the e-consult is the Instructions to Patient section, which summarizes both oral and insulin medications that can be provided to the patient. Every note includes a Diabetes Surveillance section and several web links to diabetes education that can be downloaded through the MyHealtheVet website.
Current approaches to e-consult implementation are subject to the discretion of the requesting provider. The most commonly observed approach is that the requesting provider reviews the e-consult note and requests that the patient’s nurse manager instructs the patient on the recommendations. Some providers schedule the patient for a physician or nurse visit to discuss the diabetes management recommendations in a clinic setting. Other providers contact the patient by telephone and mail the instructions to the patient.
To streamline the e-consult implementation process, the DMECS team has the option of placing an e-consult 1 week before a patient’s scheduled clinic visit with the PCP. This helps ensure that the e-consult is completed within 2 to 3 business days before the patient’s scheduled primary care appointment, at which time the recommendations can be implemented. Using the option of a “pre-clinic e-consult” method expedites the implementation process.
Initial Results of DMECS
The first e-consult was completed on January 23, 2012. Since its inception, 3,703 e-consults have been completed. There has been a steady increase in the number of referrals, with an average of 154 e-consults completed monthly from January 2012 to December 2013 (Figure 1). Most e-consults have been completed based on requests submitted by providers in Houston, Texas and affiliated CBOCs. However, a growing number of interfacility consults have been completed for providers at VISN-16 facilities located in Louisiana, Mississippi, Arkansas, and Oklahoma (Figure 2).
The initial response to the e-consult service has been positive. One provider described DMECS as a means to “obtain faster access to an endocrinologist’s input for complex diabetics, which has resulted in faster intervention for patients, particularly those at high risk.”
Additionally, another provider noted, “Along with all the benefits of accelerated access to specialty care recommendations, the patients benefit because they do not have to travel to the VA to receive this care. In many cases, they don’t have to be scheduled to see the endocrinologist, if the treatment recommendations are successful.”
One of the nurse managers explained that “The e-consult service has given me a guide to manage each veteran’s diabetes…One veteran stated that he initially was seeing a private endocrinologist at an outside clinic for his diabetes, but when he lost his insurance and began to receive his care at the VA, he stated that he never realized how high the quality of services for diabetes is at the VA.” With regard to implementation, she noted that “the diabetes instructions as provided by the e-consult specialist enhance the patient’s sense of personalized care.”
Limitations
Another challenge observed by DMECS providers is the variation in the length of time for implementing DMECS recommendations by the requesting providers. Due to the novelty of this service, providers across the VISN are still becoming acquainted with the e-consult process.
In an effort to assist PCPs, DMECS providers perform an objective chart review about 3 months after the e-consult is completed. A note is placed in the CPRS that documents whether e-consult recommendations were implemented and the date of implementation. With time, it is anticipated that a standardized set of recommendations for requesting providers may be instituted to serve as a suggested algorithm for timely and efficient implementation of the e-consult recommendations.
DMECS Goals
In addition to supporting the MEDVAMC initiative to improve glycemic trends among all patients with diabetes within the facility, DMECS providers hope to share in VISN-wide efforts to improve diabetes control by broadening the interfacility referral base. The most successful methods of advertisement and consult recruitment include the recommendation that all patients with diabetes with an A1C > 9% receive an e-consult. Also, when any patient with an A1C > 9% is seen at any of the MEDVAMC eye clinics, an alert is sent to the PCP from the DMECS team, suggesting placement of an e-consult. These strategies have increased the number of referrals within the MEDVAMC, and the goal is to implement similar strategies in all primary care, geriatrics, and women’s health clinics across VISN 16.
There are many sites across the VISN that may not have ready access to certified diabetes educators. In support of the VHA goals to promote virtual health, the DMECS team plans to initiate diabetes patient education sessions through clinical videoconferencing with patients in groups or individually.
In addition to the continued growth of the e-consult service and their efforts at patient education, the DMECS providers are also initiating a CME-accredited course for PCPs and HCPs on outpatient management of diabetes, which will be led by 1 of the 4 endocrinology staff at MEDVAMC. The benefits of provider education have been demonstrated by the University of New Mexico Health Science Center’s Project ECHO, which not only improved the quality of care for hepatitis C in a rural territory, but also increased PCP awareness and capacity to treat and manage complex patients.5 Project ECHO was used as the model for the initiation of the Specialty Care Access Network-Extension for Community Healthcare Outcomes (SCAN-ECHO) program at the VA. Accordingly, the DMECS providers envision that continued efforts at provider education should facilitate an improvement in clinical management strategies used by PCPs to optimize diabetes control.
Now that the diabetes management e-consult program has been set up and seems to play an additive role in the management of outpatient diabetes, the next step is to assess the effect of the diabetes e-consult service on patient clinical outcomes. Currently, DMECS is completing retrospective outcome studies to investigate the baseline characteristics of patients who are referred for the e-consult. These DMECS results will be compared with face-to-face diabetes care and management in a specialty clinic. In addition researchers will attempt to assess whether the time-to-implementation of recommendations has an impact on changes in glycemic parameters.
Conclusion
In support of the VHA goal of veteran-centered care, the diabetes e-consult service for VISN 16 is an innovative and creative addition to the armamentarium of outpatient diabetes management that has accelerated access to endocrine diabetes care. The service has reached > 1,000 veterans with diabetes since its inception and is set to continue expanding its referral base across VISN 16. Through DMECS, specialty care has become more readily accessible to providers and patients across a greater geographic area. The diabetes management e-consult service has been particularly useful for patients with physical disabilities or financial constraints and has been able to bridge the communication gap between primary and specialty care, with the goal of improving diabetes outcomes for veterans across the VISN.
Acknowledgments
The authors would like to express their appreciation for the assistance provided by the program analysts who extracted the number of completed diabetes e-consults from the VISN 16 data warehouse: Pamela Croston, Melody Darbe, and Andrew Spiegelman, PhD.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
References
1. Centers for Disease Control and Prevention. Percentage of civilian non-institutionalized population with diagnosed diabetes, by age, United States, 1980-2010. Centers for Disease Control and Prevention Website. http://www.cdc.gov/Diabetes/statistics/prev/national/figbyage.htm. Accessed February 5, 2014.
2. National Center for Chronic Disease Prevention and Health Promotion. National Diabetes Fact Sheet: National estimates and general information on diabetes and prediabetes in the United States, 2011. Centers for Disease Control and Prevention Website. http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf. Accessed February 4, 2014.
3. Holman RR, Paul SK, Bethel MA, et al. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359(15):1577-1589.
4. American Diabetes Association. Standards of medical care in diabetes—2012. Diabetes Care. 2012;35(suppl 1):S11-S63.
5. Arora S, Thornton K, Murata G, et al. Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med. 2010;364(23):2199-2207.
In the U.S., the prevalence of diabetes continues to escalate at alarming rates. From 1980-2010 the incidence of diabetes increased by 200% for people aged < 45 years, 124% for people 45 to 64 years, and 126% for people 65 to 74 years. Furthermore, based on the National Institute of Health, diabetes currently affects 25.8 million people in the U.S.1,2 Glycemic control has been demonstrated to reduce the risk of microvascular disease in patients with diabetes.3 Most patients with diabetes are managed by primary care practitioners (PCPs), and as the number of patients with diabetes continues to increase, there is an increasing demand on PCPs to achieve recommended glycemic targets.4
The Veterans Health Administration (VHA) VISN 16 has a notably higher prevalence of diabetes compared with that of the national rate. Failure to achieve glycemic targets continues to impose an escalating economic burden.3 Endocrine assistance is often sought by PCPs, but due to a scarcity of endocrinologists, patients commonly wait weeks or months before being seen. Furthermore, rural patients often must travel for several hours before they can reach a specialty center.
The Office of Specialty Care Transformation has provided a unique opportunity for PCPs to gain greater access to specialty advice via electronic consultations. This initiative allows PCPs and specialists to communicate promptly, to institute definitive solutions for patient care, and to augment the clinical and academic aims of primary and specialty care providers. The Michael E. DeBakey VAMC (MEDVAMC) in Houston, Texas, was chosen to initiate a VISN 16-wide diabetes management e-consult service (DMECS).
Endocrinologists at MEDVAMC developed DMECS to serve as a multifunctional tool to reach as many veterans as possible throughout VISN 16, broaden the scope of the existing diabetes endocrine practice, and engender a collaborative spirit between PCPs and specialty care providers. Initiation of this service has been particularly useful for patients with physical disabilities or financial constraints whose care is managed at the community-based outpatient clinics (CBOCs). The purpose of this article is to discuss the concept and initiation of the DMECS, the structure of the consult note, the implementation process, early provider feedback on the project, and future plans.
The DMECS Process
The DMECS allows endocrinologists to provide advice to PCPs to help improve diabetes care while minimizing travel to specialty centers. The advice generated by the DMECS is electronically conveyed to the referring physician (usually the PCP), not to the patient. The requesting physician is then responsible for implementing the recommendations. The DMECS does not comanage patients with diabetes but rather provides support to the PCP in complex cases that would otherwise require an outside referral.
The diabetes management e-consult team has 1 administrator and 3 health care providers (HCPs). Promotion of the service consisted of electronic distribution of flyers to all primary care teams, posters in the main lobby of the hospital, and electronic distribution of a letter to all VISN 16 HCPs. The DMECS team contacted the chiefs of primary care and CBOC directors to promote the service. Communication was augmented by scheduling videoconferencing with all interested facilities. Presentations were given to the VISN-wide transformational care collaborative and women’s health groups.
Any specialties that assist in diabetes management, including ophthalmology and vascular medicine, were encouraged to refer consults to DMECS if clinically indicated. The recommendation is that PCPs submit an e-consult for any patient with a hemoglobin A1C (A1C) > 9%. The only prerequisite to placing the e-consult order is an A1C > 7.5% within the preceding 3 months. Any patient with reported or objective evidence of hypoglycemia is eligible for an e-consult, regardless of the A1C value. Women who are pregnant and patients on an insulin pump are excluded from the program.
All diabetes e-consults are supervised by a board-certified endocrinologist and are resolved within 2 to 3 business days. On receipt of the consult request, the DMECS provider reviews the chart, including active medication lists, blood glucose levels documented in progress notes, care and coordination of home telehealth data regarding blood glucose levels and changes in diabetes medication management, laboratory results and pharmacy refill patterns.
Recommendations are completed and the DMECS provider alerts the requesting physician by adding them as a cosigner to the note in the Computerized Patient Record System (CPRS). When possible, the patient’s nurse manager is also added to the note. For interfacility consults, the DMECS provider contacts the requesting provider directly via email or telephone. Consistent communication with the requesting physician ensures clarity of understanding between specialist and PCP.
The e-consult recommendations are consolidated into 3 distinct sections. The Impression section provides an explanation to the provider about the specialist’s impression of current diabetes control and the reasoning behind the recommendations. The Recommendation section lists in medical terminology the recommended changes to diabetes medications. A unique component to the e-consult is the Instructions to Patient section, which summarizes both oral and insulin medications that can be provided to the patient. Every note includes a Diabetes Surveillance section and several web links to diabetes education that can be downloaded through the MyHealtheVet website.
Current approaches to e-consult implementation are subject to the discretion of the requesting provider. The most commonly observed approach is that the requesting provider reviews the e-consult note and requests that the patient’s nurse manager instructs the patient on the recommendations. Some providers schedule the patient for a physician or nurse visit to discuss the diabetes management recommendations in a clinic setting. Other providers contact the patient by telephone and mail the instructions to the patient.
To streamline the e-consult implementation process, the DMECS team has the option of placing an e-consult 1 week before a patient’s scheduled clinic visit with the PCP. This helps ensure that the e-consult is completed within 2 to 3 business days before the patient’s scheduled primary care appointment, at which time the recommendations can be implemented. Using the option of a “pre-clinic e-consult” method expedites the implementation process.
Initial Results of DMECS
The first e-consult was completed on January 23, 2012. Since its inception, 3,703 e-consults have been completed. There has been a steady increase in the number of referrals, with an average of 154 e-consults completed monthly from January 2012 to December 2013 (Figure 1). Most e-consults have been completed based on requests submitted by providers in Houston, Texas and affiliated CBOCs. However, a growing number of interfacility consults have been completed for providers at VISN-16 facilities located in Louisiana, Mississippi, Arkansas, and Oklahoma (Figure 2).
The initial response to the e-consult service has been positive. One provider described DMECS as a means to “obtain faster access to an endocrinologist’s input for complex diabetics, which has resulted in faster intervention for patients, particularly those at high risk.”
Additionally, another provider noted, “Along with all the benefits of accelerated access to specialty care recommendations, the patients benefit because they do not have to travel to the VA to receive this care. In many cases, they don’t have to be scheduled to see the endocrinologist, if the treatment recommendations are successful.”
One of the nurse managers explained that “The e-consult service has given me a guide to manage each veteran’s diabetes…One veteran stated that he initially was seeing a private endocrinologist at an outside clinic for his diabetes, but when he lost his insurance and began to receive his care at the VA, he stated that he never realized how high the quality of services for diabetes is at the VA.” With regard to implementation, she noted that “the diabetes instructions as provided by the e-consult specialist enhance the patient’s sense of personalized care.”
Limitations
Another challenge observed by DMECS providers is the variation in the length of time for implementing DMECS recommendations by the requesting providers. Due to the novelty of this service, providers across the VISN are still becoming acquainted with the e-consult process.
In an effort to assist PCPs, DMECS providers perform an objective chart review about 3 months after the e-consult is completed. A note is placed in the CPRS that documents whether e-consult recommendations were implemented and the date of implementation. With time, it is anticipated that a standardized set of recommendations for requesting providers may be instituted to serve as a suggested algorithm for timely and efficient implementation of the e-consult recommendations.
DMECS Goals
In addition to supporting the MEDVAMC initiative to improve glycemic trends among all patients with diabetes within the facility, DMECS providers hope to share in VISN-wide efforts to improve diabetes control by broadening the interfacility referral base. The most successful methods of advertisement and consult recruitment include the recommendation that all patients with diabetes with an A1C > 9% receive an e-consult. Also, when any patient with an A1C > 9% is seen at any of the MEDVAMC eye clinics, an alert is sent to the PCP from the DMECS team, suggesting placement of an e-consult. These strategies have increased the number of referrals within the MEDVAMC, and the goal is to implement similar strategies in all primary care, geriatrics, and women’s health clinics across VISN 16.
There are many sites across the VISN that may not have ready access to certified diabetes educators. In support of the VHA goals to promote virtual health, the DMECS team plans to initiate diabetes patient education sessions through clinical videoconferencing with patients in groups or individually.
In addition to the continued growth of the e-consult service and their efforts at patient education, the DMECS providers are also initiating a CME-accredited course for PCPs and HCPs on outpatient management of diabetes, which will be led by 1 of the 4 endocrinology staff at MEDVAMC. The benefits of provider education have been demonstrated by the University of New Mexico Health Science Center’s Project ECHO, which not only improved the quality of care for hepatitis C in a rural territory, but also increased PCP awareness and capacity to treat and manage complex patients.5 Project ECHO was used as the model for the initiation of the Specialty Care Access Network-Extension for Community Healthcare Outcomes (SCAN-ECHO) program at the VA. Accordingly, the DMECS providers envision that continued efforts at provider education should facilitate an improvement in clinical management strategies used by PCPs to optimize diabetes control.
Now that the diabetes management e-consult program has been set up and seems to play an additive role in the management of outpatient diabetes, the next step is to assess the effect of the diabetes e-consult service on patient clinical outcomes. Currently, DMECS is completing retrospective outcome studies to investigate the baseline characteristics of patients who are referred for the e-consult. These DMECS results will be compared with face-to-face diabetes care and management in a specialty clinic. In addition researchers will attempt to assess whether the time-to-implementation of recommendations has an impact on changes in glycemic parameters.
Conclusion
In support of the VHA goal of veteran-centered care, the diabetes e-consult service for VISN 16 is an innovative and creative addition to the armamentarium of outpatient diabetes management that has accelerated access to endocrine diabetes care. The service has reached > 1,000 veterans with diabetes since its inception and is set to continue expanding its referral base across VISN 16. Through DMECS, specialty care has become more readily accessible to providers and patients across a greater geographic area. The diabetes management e-consult service has been particularly useful for patients with physical disabilities or financial constraints and has been able to bridge the communication gap between primary and specialty care, with the goal of improving diabetes outcomes for veterans across the VISN.
Acknowledgments
The authors would like to express their appreciation for the assistance provided by the program analysts who extracted the number of completed diabetes e-consults from the VISN 16 data warehouse: Pamela Croston, Melody Darbe, and Andrew Spiegelman, PhD.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
References
1. Centers for Disease Control and Prevention. Percentage of civilian non-institutionalized population with diagnosed diabetes, by age, United States, 1980-2010. Centers for Disease Control and Prevention Website. http://www.cdc.gov/Diabetes/statistics/prev/national/figbyage.htm. Accessed February 5, 2014.
2. National Center for Chronic Disease Prevention and Health Promotion. National Diabetes Fact Sheet: National estimates and general information on diabetes and prediabetes in the United States, 2011. Centers for Disease Control and Prevention Website. http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf. Accessed February 4, 2014.
3. Holman RR, Paul SK, Bethel MA, et al. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359(15):1577-1589.
4. American Diabetes Association. Standards of medical care in diabetes—2012. Diabetes Care. 2012;35(suppl 1):S11-S63.
5. Arora S, Thornton K, Murata G, et al. Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med. 2010;364(23):2199-2207.
In the U.S., the prevalence of diabetes continues to escalate at alarming rates. From 1980-2010 the incidence of diabetes increased by 200% for people aged < 45 years, 124% for people 45 to 64 years, and 126% for people 65 to 74 years. Furthermore, based on the National Institute of Health, diabetes currently affects 25.8 million people in the U.S.1,2 Glycemic control has been demonstrated to reduce the risk of microvascular disease in patients with diabetes.3 Most patients with diabetes are managed by primary care practitioners (PCPs), and as the number of patients with diabetes continues to increase, there is an increasing demand on PCPs to achieve recommended glycemic targets.4
The Veterans Health Administration (VHA) VISN 16 has a notably higher prevalence of diabetes compared with that of the national rate. Failure to achieve glycemic targets continues to impose an escalating economic burden.3 Endocrine assistance is often sought by PCPs, but due to a scarcity of endocrinologists, patients commonly wait weeks or months before being seen. Furthermore, rural patients often must travel for several hours before they can reach a specialty center.
The Office of Specialty Care Transformation has provided a unique opportunity for PCPs to gain greater access to specialty advice via electronic consultations. This initiative allows PCPs and specialists to communicate promptly, to institute definitive solutions for patient care, and to augment the clinical and academic aims of primary and specialty care providers. The Michael E. DeBakey VAMC (MEDVAMC) in Houston, Texas, was chosen to initiate a VISN 16-wide diabetes management e-consult service (DMECS).
Endocrinologists at MEDVAMC developed DMECS to serve as a multifunctional tool to reach as many veterans as possible throughout VISN 16, broaden the scope of the existing diabetes endocrine practice, and engender a collaborative spirit between PCPs and specialty care providers. Initiation of this service has been particularly useful for patients with physical disabilities or financial constraints whose care is managed at the community-based outpatient clinics (CBOCs). The purpose of this article is to discuss the concept and initiation of the DMECS, the structure of the consult note, the implementation process, early provider feedback on the project, and future plans.
The DMECS Process
The DMECS allows endocrinologists to provide advice to PCPs to help improve diabetes care while minimizing travel to specialty centers. The advice generated by the DMECS is electronically conveyed to the referring physician (usually the PCP), not to the patient. The requesting physician is then responsible for implementing the recommendations. The DMECS does not comanage patients with diabetes but rather provides support to the PCP in complex cases that would otherwise require an outside referral.
The diabetes management e-consult team has 1 administrator and 3 health care providers (HCPs). Promotion of the service consisted of electronic distribution of flyers to all primary care teams, posters in the main lobby of the hospital, and electronic distribution of a letter to all VISN 16 HCPs. The DMECS team contacted the chiefs of primary care and CBOC directors to promote the service. Communication was augmented by scheduling videoconferencing with all interested facilities. Presentations were given to the VISN-wide transformational care collaborative and women’s health groups.
Any specialties that assist in diabetes management, including ophthalmology and vascular medicine, were encouraged to refer consults to DMECS if clinically indicated. The recommendation is that PCPs submit an e-consult for any patient with a hemoglobin A1C (A1C) > 9%. The only prerequisite to placing the e-consult order is an A1C > 7.5% within the preceding 3 months. Any patient with reported or objective evidence of hypoglycemia is eligible for an e-consult, regardless of the A1C value. Women who are pregnant and patients on an insulin pump are excluded from the program.
All diabetes e-consults are supervised by a board-certified endocrinologist and are resolved within 2 to 3 business days. On receipt of the consult request, the DMECS provider reviews the chart, including active medication lists, blood glucose levels documented in progress notes, care and coordination of home telehealth data regarding blood glucose levels and changes in diabetes medication management, laboratory results and pharmacy refill patterns.
Recommendations are completed and the DMECS provider alerts the requesting physician by adding them as a cosigner to the note in the Computerized Patient Record System (CPRS). When possible, the patient’s nurse manager is also added to the note. For interfacility consults, the DMECS provider contacts the requesting provider directly via email or telephone. Consistent communication with the requesting physician ensures clarity of understanding between specialist and PCP.
The e-consult recommendations are consolidated into 3 distinct sections. The Impression section provides an explanation to the provider about the specialist’s impression of current diabetes control and the reasoning behind the recommendations. The Recommendation section lists in medical terminology the recommended changes to diabetes medications. A unique component to the e-consult is the Instructions to Patient section, which summarizes both oral and insulin medications that can be provided to the patient. Every note includes a Diabetes Surveillance section and several web links to diabetes education that can be downloaded through the MyHealtheVet website.
Current approaches to e-consult implementation are subject to the discretion of the requesting provider. The most commonly observed approach is that the requesting provider reviews the e-consult note and requests that the patient’s nurse manager instructs the patient on the recommendations. Some providers schedule the patient for a physician or nurse visit to discuss the diabetes management recommendations in a clinic setting. Other providers contact the patient by telephone and mail the instructions to the patient.
To streamline the e-consult implementation process, the DMECS team has the option of placing an e-consult 1 week before a patient’s scheduled clinic visit with the PCP. This helps ensure that the e-consult is completed within 2 to 3 business days before the patient’s scheduled primary care appointment, at which time the recommendations can be implemented. Using the option of a “pre-clinic e-consult” method expedites the implementation process.
Initial Results of DMECS
The first e-consult was completed on January 23, 2012. Since its inception, 3,703 e-consults have been completed. There has been a steady increase in the number of referrals, with an average of 154 e-consults completed monthly from January 2012 to December 2013 (Figure 1). Most e-consults have been completed based on requests submitted by providers in Houston, Texas and affiliated CBOCs. However, a growing number of interfacility consults have been completed for providers at VISN-16 facilities located in Louisiana, Mississippi, Arkansas, and Oklahoma (Figure 2).
The initial response to the e-consult service has been positive. One provider described DMECS as a means to “obtain faster access to an endocrinologist’s input for complex diabetics, which has resulted in faster intervention for patients, particularly those at high risk.”
Additionally, another provider noted, “Along with all the benefits of accelerated access to specialty care recommendations, the patients benefit because they do not have to travel to the VA to receive this care. In many cases, they don’t have to be scheduled to see the endocrinologist, if the treatment recommendations are successful.”
One of the nurse managers explained that “The e-consult service has given me a guide to manage each veteran’s diabetes…One veteran stated that he initially was seeing a private endocrinologist at an outside clinic for his diabetes, but when he lost his insurance and began to receive his care at the VA, he stated that he never realized how high the quality of services for diabetes is at the VA.” With regard to implementation, she noted that “the diabetes instructions as provided by the e-consult specialist enhance the patient’s sense of personalized care.”
Limitations
Another challenge observed by DMECS providers is the variation in the length of time for implementing DMECS recommendations by the requesting providers. Due to the novelty of this service, providers across the VISN are still becoming acquainted with the e-consult process.
In an effort to assist PCPs, DMECS providers perform an objective chart review about 3 months after the e-consult is completed. A note is placed in the CPRS that documents whether e-consult recommendations were implemented and the date of implementation. With time, it is anticipated that a standardized set of recommendations for requesting providers may be instituted to serve as a suggested algorithm for timely and efficient implementation of the e-consult recommendations.
DMECS Goals
In addition to supporting the MEDVAMC initiative to improve glycemic trends among all patients with diabetes within the facility, DMECS providers hope to share in VISN-wide efforts to improve diabetes control by broadening the interfacility referral base. The most successful methods of advertisement and consult recruitment include the recommendation that all patients with diabetes with an A1C > 9% receive an e-consult. Also, when any patient with an A1C > 9% is seen at any of the MEDVAMC eye clinics, an alert is sent to the PCP from the DMECS team, suggesting placement of an e-consult. These strategies have increased the number of referrals within the MEDVAMC, and the goal is to implement similar strategies in all primary care, geriatrics, and women’s health clinics across VISN 16.
There are many sites across the VISN that may not have ready access to certified diabetes educators. In support of the VHA goals to promote virtual health, the DMECS team plans to initiate diabetes patient education sessions through clinical videoconferencing with patients in groups or individually.
In addition to the continued growth of the e-consult service and their efforts at patient education, the DMECS providers are also initiating a CME-accredited course for PCPs and HCPs on outpatient management of diabetes, which will be led by 1 of the 4 endocrinology staff at MEDVAMC. The benefits of provider education have been demonstrated by the University of New Mexico Health Science Center’s Project ECHO, which not only improved the quality of care for hepatitis C in a rural territory, but also increased PCP awareness and capacity to treat and manage complex patients.5 Project ECHO was used as the model for the initiation of the Specialty Care Access Network-Extension for Community Healthcare Outcomes (SCAN-ECHO) program at the VA. Accordingly, the DMECS providers envision that continued efforts at provider education should facilitate an improvement in clinical management strategies used by PCPs to optimize diabetes control.
Now that the diabetes management e-consult program has been set up and seems to play an additive role in the management of outpatient diabetes, the next step is to assess the effect of the diabetes e-consult service on patient clinical outcomes. Currently, DMECS is completing retrospective outcome studies to investigate the baseline characteristics of patients who are referred for the e-consult. These DMECS results will be compared with face-to-face diabetes care and management in a specialty clinic. In addition researchers will attempt to assess whether the time-to-implementation of recommendations has an impact on changes in glycemic parameters.
Conclusion
In support of the VHA goal of veteran-centered care, the diabetes e-consult service for VISN 16 is an innovative and creative addition to the armamentarium of outpatient diabetes management that has accelerated access to endocrine diabetes care. The service has reached > 1,000 veterans with diabetes since its inception and is set to continue expanding its referral base across VISN 16. Through DMECS, specialty care has become more readily accessible to providers and patients across a greater geographic area. The diabetes management e-consult service has been particularly useful for patients with physical disabilities or financial constraints and has been able to bridge the communication gap between primary and specialty care, with the goal of improving diabetes outcomes for veterans across the VISN.
Acknowledgments
The authors would like to express their appreciation for the assistance provided by the program analysts who extracted the number of completed diabetes e-consults from the VISN 16 data warehouse: Pamela Croston, Melody Darbe, and Andrew Spiegelman, PhD.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
References
1. Centers for Disease Control and Prevention. Percentage of civilian non-institutionalized population with diagnosed diabetes, by age, United States, 1980-2010. Centers for Disease Control and Prevention Website. http://www.cdc.gov/Diabetes/statistics/prev/national/figbyage.htm. Accessed February 5, 2014.
2. National Center for Chronic Disease Prevention and Health Promotion. National Diabetes Fact Sheet: National estimates and general information on diabetes and prediabetes in the United States, 2011. Centers for Disease Control and Prevention Website. http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf. Accessed February 4, 2014.
3. Holman RR, Paul SK, Bethel MA, et al. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359(15):1577-1589.
4. American Diabetes Association. Standards of medical care in diabetes—2012. Diabetes Care. 2012;35(suppl 1):S11-S63.
5. Arora S, Thornton K, Murata G, et al. Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med. 2010;364(23):2199-2207.