User login
Hospitalist movers and shakers – March 2020
Swati Mehta, MD, recently was honored as the lone hospitalist on the National Executive Physician Council for Beryl Institute (Nashville, Tenn.). Only 24 total physicians were selected to the council. Dr. Mehta also was named the 2019 Distinguished Physician Award winner at Vituity (Emeryville, Calif.), where she is the executive director of quality and performance.
A nocturnist at Sequoia Hospital (Redwood City, Calif.), Dr. Mehta is a member of the Society of Hospital Medicine’s Patient Experience interest group.
Shannon Phillips, MD, SFHM, has been named to the National Quality Forum’s Board of Directors for 2020. The chief patient experience officer at Intermountain Healthcare (Salt Lake City, Utah), she also is a recent member of the Performance Measurement and Reporting Committee.
Dr. Phillips, whose focus at Intermountain is on catalyzing safety, quality, and experience of care, was named a 2018 Becker’s Hospital Review Hospital and Health System CXO to Know. Previously, she worked at the Cleveland Clinic, where she was its first patient safety officer and an associate chief quality officer.
Vineet Arora, MD, MHM, has been elected as a new member of the National Academy of Medicine, which honors pioneering scientific and professional achievements within the field.
An academic hospitalist at the University of Chicago, Dr. Arora specializes in improving the learning environment for her medical trainees, as well as maintaining a high level of quality, safety, and care for patients. She also is considered an expert in using social media and other new technology to enhance medical education.
The National Academy of Medicine stated that Dr. Arora’s honor was “for pioneering work to optimize resident fatigue and patient safety during long shifts.”
Edmondo Robinson, MD, SFHM, has been named senior vice president and chief digital innovation officer at Moffitt Cancer Center (Tampa, Fla.). The chief digital innovation officer position is a newly created position that the veteran physician has assumed. Dr. Robinson has 16 years’ experience in clinical and technological work.
In this new position, Dr. Robinson, a practicing academic hospitalist, will head Moffitt’s digital innovation while looking to create and test new services, programs, partnerships, and technologies.
Dr. Robinson comes to Moffitt after serving as chief transformation officer and senior vice president at ChristianaCare (Wilmington, Del.). A teacher at Sidney Kimmel Medical College, Philadelphia, Dr. Robinson was the founding medical director of ChristianaCare Hospitalist Partners.
Relias Healthcare (Tupelo, Miss.) has begun providing hospitalist and emergency medicine services for North Mississippi Health Services’ Gilmore-Amory Trauma Center. Relias, a multistate company that has partnered with more than 150 providers, now has a role at four different North Mississippi Health Services facilities.
Mednax (Sunrise, Fla.) has added Arcenio Chacon and Associated Pediatricians of Homestead, a pediatric critical care and hospital practice, as an affiliate.
Chacon and Associated Pediatricians are based out of Miami and have served Baptist Health South Florida for more than 25 years. The four-physician practice provides critical care and pediatric hospitalist services at Baptist Children’s Hospital (Miami) and hospitalist services at Miami Cancer Institute and Homestead (Fla.) Hospital.
Mednax is a health solutions company that provides subspecialty service in all 50 states. Established in 1979, Mednax partners with hospitals, health systems, and health care facilities to offer clinical services, as well as revenue cycle management, patient engagement, and perioperative improvement consulting services.
Swati Mehta, MD, recently was honored as the lone hospitalist on the National Executive Physician Council for Beryl Institute (Nashville, Tenn.). Only 24 total physicians were selected to the council. Dr. Mehta also was named the 2019 Distinguished Physician Award winner at Vituity (Emeryville, Calif.), where she is the executive director of quality and performance.
A nocturnist at Sequoia Hospital (Redwood City, Calif.), Dr. Mehta is a member of the Society of Hospital Medicine’s Patient Experience interest group.
Shannon Phillips, MD, SFHM, has been named to the National Quality Forum’s Board of Directors for 2020. The chief patient experience officer at Intermountain Healthcare (Salt Lake City, Utah), she also is a recent member of the Performance Measurement and Reporting Committee.
Dr. Phillips, whose focus at Intermountain is on catalyzing safety, quality, and experience of care, was named a 2018 Becker’s Hospital Review Hospital and Health System CXO to Know. Previously, she worked at the Cleveland Clinic, where she was its first patient safety officer and an associate chief quality officer.
Vineet Arora, MD, MHM, has been elected as a new member of the National Academy of Medicine, which honors pioneering scientific and professional achievements within the field.
An academic hospitalist at the University of Chicago, Dr. Arora specializes in improving the learning environment for her medical trainees, as well as maintaining a high level of quality, safety, and care for patients. She also is considered an expert in using social media and other new technology to enhance medical education.
The National Academy of Medicine stated that Dr. Arora’s honor was “for pioneering work to optimize resident fatigue and patient safety during long shifts.”
Edmondo Robinson, MD, SFHM, has been named senior vice president and chief digital innovation officer at Moffitt Cancer Center (Tampa, Fla.). The chief digital innovation officer position is a newly created position that the veteran physician has assumed. Dr. Robinson has 16 years’ experience in clinical and technological work.
In this new position, Dr. Robinson, a practicing academic hospitalist, will head Moffitt’s digital innovation while looking to create and test new services, programs, partnerships, and technologies.
Dr. Robinson comes to Moffitt after serving as chief transformation officer and senior vice president at ChristianaCare (Wilmington, Del.). A teacher at Sidney Kimmel Medical College, Philadelphia, Dr. Robinson was the founding medical director of ChristianaCare Hospitalist Partners.
Relias Healthcare (Tupelo, Miss.) has begun providing hospitalist and emergency medicine services for North Mississippi Health Services’ Gilmore-Amory Trauma Center. Relias, a multistate company that has partnered with more than 150 providers, now has a role at four different North Mississippi Health Services facilities.
Mednax (Sunrise, Fla.) has added Arcenio Chacon and Associated Pediatricians of Homestead, a pediatric critical care and hospital practice, as an affiliate.
Chacon and Associated Pediatricians are based out of Miami and have served Baptist Health South Florida for more than 25 years. The four-physician practice provides critical care and pediatric hospitalist services at Baptist Children’s Hospital (Miami) and hospitalist services at Miami Cancer Institute and Homestead (Fla.) Hospital.
Mednax is a health solutions company that provides subspecialty service in all 50 states. Established in 1979, Mednax partners with hospitals, health systems, and health care facilities to offer clinical services, as well as revenue cycle management, patient engagement, and perioperative improvement consulting services.
Swati Mehta, MD, recently was honored as the lone hospitalist on the National Executive Physician Council for Beryl Institute (Nashville, Tenn.). Only 24 total physicians were selected to the council. Dr. Mehta also was named the 2019 Distinguished Physician Award winner at Vituity (Emeryville, Calif.), where she is the executive director of quality and performance.
A nocturnist at Sequoia Hospital (Redwood City, Calif.), Dr. Mehta is a member of the Society of Hospital Medicine’s Patient Experience interest group.
Shannon Phillips, MD, SFHM, has been named to the National Quality Forum’s Board of Directors for 2020. The chief patient experience officer at Intermountain Healthcare (Salt Lake City, Utah), she also is a recent member of the Performance Measurement and Reporting Committee.
Dr. Phillips, whose focus at Intermountain is on catalyzing safety, quality, and experience of care, was named a 2018 Becker’s Hospital Review Hospital and Health System CXO to Know. Previously, she worked at the Cleveland Clinic, where she was its first patient safety officer and an associate chief quality officer.
Vineet Arora, MD, MHM, has been elected as a new member of the National Academy of Medicine, which honors pioneering scientific and professional achievements within the field.
An academic hospitalist at the University of Chicago, Dr. Arora specializes in improving the learning environment for her medical trainees, as well as maintaining a high level of quality, safety, and care for patients. She also is considered an expert in using social media and other new technology to enhance medical education.
The National Academy of Medicine stated that Dr. Arora’s honor was “for pioneering work to optimize resident fatigue and patient safety during long shifts.”
Edmondo Robinson, MD, SFHM, has been named senior vice president and chief digital innovation officer at Moffitt Cancer Center (Tampa, Fla.). The chief digital innovation officer position is a newly created position that the veteran physician has assumed. Dr. Robinson has 16 years’ experience in clinical and technological work.
In this new position, Dr. Robinson, a practicing academic hospitalist, will head Moffitt’s digital innovation while looking to create and test new services, programs, partnerships, and technologies.
Dr. Robinson comes to Moffitt after serving as chief transformation officer and senior vice president at ChristianaCare (Wilmington, Del.). A teacher at Sidney Kimmel Medical College, Philadelphia, Dr. Robinson was the founding medical director of ChristianaCare Hospitalist Partners.
Relias Healthcare (Tupelo, Miss.) has begun providing hospitalist and emergency medicine services for North Mississippi Health Services’ Gilmore-Amory Trauma Center. Relias, a multistate company that has partnered with more than 150 providers, now has a role at four different North Mississippi Health Services facilities.
Mednax (Sunrise, Fla.) has added Arcenio Chacon and Associated Pediatricians of Homestead, a pediatric critical care and hospital practice, as an affiliate.
Chacon and Associated Pediatricians are based out of Miami and have served Baptist Health South Florida for more than 25 years. The four-physician practice provides critical care and pediatric hospitalist services at Baptist Children’s Hospital (Miami) and hospitalist services at Miami Cancer Institute and Homestead (Fla.) Hospital.
Mednax is a health solutions company that provides subspecialty service in all 50 states. Established in 1979, Mednax partners with hospitals, health systems, and health care facilities to offer clinical services, as well as revenue cycle management, patient engagement, and perioperative improvement consulting services.
Hospital medicine physician leaders
The right skills and time to develop them
“When you get someone who knows what quality looks like and pair that with curiosity about new ways to think about leading, you end up with the people who are able to produce dramatic innovations in the field.”1
In medicine, a physician is trained to take charge in emergent situations and make potentially lifesaving efforts. However, when it comes to leading teams of individuals, not only must successful leaders have the right skills, they also need time to dedicate to the work of leadership.
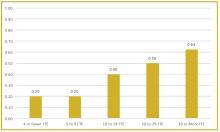
To better understand current approaches to dedicated hospital medicine group (HMG) leadership time, let’s examine the 2018 State of Hospital Medicine (SoHM) Report. The survey, upon which the Report was based, examined two aspects of leadership: 1) how much dedicated time a leader receives to manage the group; and 2) how the leader’s time is compensated. Looking closely at the data displayed in graphs from the SoHM Report (Figures 1, 2, and 3), we can see that dedicated administrative time is directly proportional to the size of the group.
In my current role as a regional medical director in the Dallas-Fort Worth market, I oversee some programs where the size is greater than 30 full-time equivalents (FTEs), and requires a full-time administrative physician leader to manage the group. Their daily administrative duties include, but are not limited to, addressing physician performance and behaviors, managing team performance metrics, dealing with consultants’ expectations, attending and leading various committee meetings at the hospital or the system level, attending and presenting performance reviews, leading and preparing for team meetings, as well as addressing and being innovative in leading new initiatives from the hospital partner system.
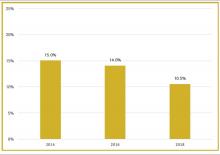
Although physician leaders are paid more for their work, the 2018 SoHM Report reveals a decline in the premium year over year. One of the reasons for the payment decline that I have encountered in various groups is that their incentives for leading the group are based on performance, as opposed to receiving a fixed stipend. Another reason is the presence of dedicated administrative support or the inclusion of a performance improvement staffer, such as an additional nurse or advanced practice provider, in the group.
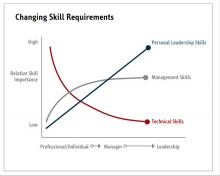
Evidence suggests that organizations and patients benefit when physicians take on leadership roles. Physician leaders play critical roles in providing high-quality patient care. How can the Society of Hospital Medicine help? Management degrees and leadership workshops have become a common pathway for many physicians, including myself. SHM provides one of the most thorough and relevant experiences through the SHM Leadership Academy. The focus of the Leadership Academy is on developing a broad set of additional leadership competencies across a spectrum of experience.5 As hospitalist physicians are often expected to fulfill a broader leadership void, we must pay attention to developing the leadership skills depicted in Figure 3. Hospital medicine is an ideal “proving ground” for future physician executives and leaders, as they often share the same characteristics required for success.
The leadership paths available in my organization, Sound Physicians, were recently highlighted in a New York Times article.3 Sound Physicians employs more than 3,000 physicians across the country, and has a pipeline for doctors to advance through structured rungs of leadership – emphasizing a different mix of clinical, strategic, and business skills at each stage, from individual practitioner to the C-suite. The training includes in-person and online courses, as well as an annual conference, to help doctors develop management and leadership competencies, and learn how to apply these skills within their organizations. Since introducing its leadership development program, the company reports less turnover, higher morale, and better growth. I personally have gone through the leadership training provided by Sound Physicians, and reflecting back, it has been a transformational experience for me. Leadership is a journey, not a destination, and as physicians we should strive to learn more from the health care leaders around us.
The administrative workload for hospital-based physician leaders will increase with the arrival of value-based programs and alternative payment models promoted by the Centers for Medicare and Medicaid Services. Lead hospitalist duties are not limited to daily operations, but can extend to leading the strategic vision of the hospital or health system. The 2020 SoHM Report will reflect these changes, as well as provide further information about how to manage and set expectations for physician leaders, based on group size and employment model.
Dr. Patel is a regional medical director with Sound Physicians. He manages more than 100 FTE hospitalists and advanced-practice providers (APPs) within multiple health systems and hospitals in the Texas market. He also serves as a member of the SHM Practice Analysis Committee and as a vice president of SHM North Texas Chapter.
References
1. Angood P and Birk S. The Value of Physician Leadership. Physician Exec. 2014 May-Jun;40(3):6-20.
2. Rice JA. Expanding the Need for Physician Leaders. Executive Insight, Advance Healthcare Network, Nov 16, 2011. Available at: http://healthcare-executive-insight.advanceweb.com/Features/Articles/Expanding-the-Need-for-Physician-Leaders.aspx.
3. Khullar D. Good leaders make good doctors. New York Times. 2019 Nov 21.
4. Beresford L. The State of Hospital Medicine in 2018. Hospitalist. 2019;23(1):1-11.
5. Harte B. Hospitalists can meet the demand for physician executives. Hospitalist. 2018 Nov 29.
The right skills and time to develop them
The right skills and time to develop them
“When you get someone who knows what quality looks like and pair that with curiosity about new ways to think about leading, you end up with the people who are able to produce dramatic innovations in the field.”1
In medicine, a physician is trained to take charge in emergent situations and make potentially lifesaving efforts. However, when it comes to leading teams of individuals, not only must successful leaders have the right skills, they also need time to dedicate to the work of leadership.
To better understand current approaches to dedicated hospital medicine group (HMG) leadership time, let’s examine the 2018 State of Hospital Medicine (SoHM) Report. The survey, upon which the Report was based, examined two aspects of leadership: 1) how much dedicated time a leader receives to manage the group; and 2) how the leader’s time is compensated. Looking closely at the data displayed in graphs from the SoHM Report (Figures 1, 2, and 3), we can see that dedicated administrative time is directly proportional to the size of the group.
In my current role as a regional medical director in the Dallas-Fort Worth market, I oversee some programs where the size is greater than 30 full-time equivalents (FTEs), and requires a full-time administrative physician leader to manage the group. Their daily administrative duties include, but are not limited to, addressing physician performance and behaviors, managing team performance metrics, dealing with consultants’ expectations, attending and leading various committee meetings at the hospital or the system level, attending and presenting performance reviews, leading and preparing for team meetings, as well as addressing and being innovative in leading new initiatives from the hospital partner system.
Although physician leaders are paid more for their work, the 2018 SoHM Report reveals a decline in the premium year over year. One of the reasons for the payment decline that I have encountered in various groups is that their incentives for leading the group are based on performance, as opposed to receiving a fixed stipend. Another reason is the presence of dedicated administrative support or the inclusion of a performance improvement staffer, such as an additional nurse or advanced practice provider, in the group.
Evidence suggests that organizations and patients benefit when physicians take on leadership roles. Physician leaders play critical roles in providing high-quality patient care. How can the Society of Hospital Medicine help? Management degrees and leadership workshops have become a common pathway for many physicians, including myself. SHM provides one of the most thorough and relevant experiences through the SHM Leadership Academy. The focus of the Leadership Academy is on developing a broad set of additional leadership competencies across a spectrum of experience.5 As hospitalist physicians are often expected to fulfill a broader leadership void, we must pay attention to developing the leadership skills depicted in Figure 3. Hospital medicine is an ideal “proving ground” for future physician executives and leaders, as they often share the same characteristics required for success.
The leadership paths available in my organization, Sound Physicians, were recently highlighted in a New York Times article.3 Sound Physicians employs more than 3,000 physicians across the country, and has a pipeline for doctors to advance through structured rungs of leadership – emphasizing a different mix of clinical, strategic, and business skills at each stage, from individual practitioner to the C-suite. The training includes in-person and online courses, as well as an annual conference, to help doctors develop management and leadership competencies, and learn how to apply these skills within their organizations. Since introducing its leadership development program, the company reports less turnover, higher morale, and better growth. I personally have gone through the leadership training provided by Sound Physicians, and reflecting back, it has been a transformational experience for me. Leadership is a journey, not a destination, and as physicians we should strive to learn more from the health care leaders around us.
The administrative workload for hospital-based physician leaders will increase with the arrival of value-based programs and alternative payment models promoted by the Centers for Medicare and Medicaid Services. Lead hospitalist duties are not limited to daily operations, but can extend to leading the strategic vision of the hospital or health system. The 2020 SoHM Report will reflect these changes, as well as provide further information about how to manage and set expectations for physician leaders, based on group size and employment model.
Dr. Patel is a regional medical director with Sound Physicians. He manages more than 100 FTE hospitalists and advanced-practice providers (APPs) within multiple health systems and hospitals in the Texas market. He also serves as a member of the SHM Practice Analysis Committee and as a vice president of SHM North Texas Chapter.
References
1. Angood P and Birk S. The Value of Physician Leadership. Physician Exec. 2014 May-Jun;40(3):6-20.
2. Rice JA. Expanding the Need for Physician Leaders. Executive Insight, Advance Healthcare Network, Nov 16, 2011. Available at: http://healthcare-executive-insight.advanceweb.com/Features/Articles/Expanding-the-Need-for-Physician-Leaders.aspx.
3. Khullar D. Good leaders make good doctors. New York Times. 2019 Nov 21.
4. Beresford L. The State of Hospital Medicine in 2018. Hospitalist. 2019;23(1):1-11.
5. Harte B. Hospitalists can meet the demand for physician executives. Hospitalist. 2018 Nov 29.
“When you get someone who knows what quality looks like and pair that with curiosity about new ways to think about leading, you end up with the people who are able to produce dramatic innovations in the field.”1
In medicine, a physician is trained to take charge in emergent situations and make potentially lifesaving efforts. However, when it comes to leading teams of individuals, not only must successful leaders have the right skills, they also need time to dedicate to the work of leadership.
To better understand current approaches to dedicated hospital medicine group (HMG) leadership time, let’s examine the 2018 State of Hospital Medicine (SoHM) Report. The survey, upon which the Report was based, examined two aspects of leadership: 1) how much dedicated time a leader receives to manage the group; and 2) how the leader’s time is compensated. Looking closely at the data displayed in graphs from the SoHM Report (Figures 1, 2, and 3), we can see that dedicated administrative time is directly proportional to the size of the group.
In my current role as a regional medical director in the Dallas-Fort Worth market, I oversee some programs where the size is greater than 30 full-time equivalents (FTEs), and requires a full-time administrative physician leader to manage the group. Their daily administrative duties include, but are not limited to, addressing physician performance and behaviors, managing team performance metrics, dealing with consultants’ expectations, attending and leading various committee meetings at the hospital or the system level, attending and presenting performance reviews, leading and preparing for team meetings, as well as addressing and being innovative in leading new initiatives from the hospital partner system.
Although physician leaders are paid more for their work, the 2018 SoHM Report reveals a decline in the premium year over year. One of the reasons for the payment decline that I have encountered in various groups is that their incentives for leading the group are based on performance, as opposed to receiving a fixed stipend. Another reason is the presence of dedicated administrative support or the inclusion of a performance improvement staffer, such as an additional nurse or advanced practice provider, in the group.
Evidence suggests that organizations and patients benefit when physicians take on leadership roles. Physician leaders play critical roles in providing high-quality patient care. How can the Society of Hospital Medicine help? Management degrees and leadership workshops have become a common pathway for many physicians, including myself. SHM provides one of the most thorough and relevant experiences through the SHM Leadership Academy. The focus of the Leadership Academy is on developing a broad set of additional leadership competencies across a spectrum of experience.5 As hospitalist physicians are often expected to fulfill a broader leadership void, we must pay attention to developing the leadership skills depicted in Figure 3. Hospital medicine is an ideal “proving ground” for future physician executives and leaders, as they often share the same characteristics required for success.
The leadership paths available in my organization, Sound Physicians, were recently highlighted in a New York Times article.3 Sound Physicians employs more than 3,000 physicians across the country, and has a pipeline for doctors to advance through structured rungs of leadership – emphasizing a different mix of clinical, strategic, and business skills at each stage, from individual practitioner to the C-suite. The training includes in-person and online courses, as well as an annual conference, to help doctors develop management and leadership competencies, and learn how to apply these skills within their organizations. Since introducing its leadership development program, the company reports less turnover, higher morale, and better growth. I personally have gone through the leadership training provided by Sound Physicians, and reflecting back, it has been a transformational experience for me. Leadership is a journey, not a destination, and as physicians we should strive to learn more from the health care leaders around us.
The administrative workload for hospital-based physician leaders will increase with the arrival of value-based programs and alternative payment models promoted by the Centers for Medicare and Medicaid Services. Lead hospitalist duties are not limited to daily operations, but can extend to leading the strategic vision of the hospital or health system. The 2020 SoHM Report will reflect these changes, as well as provide further information about how to manage and set expectations for physician leaders, based on group size and employment model.
Dr. Patel is a regional medical director with Sound Physicians. He manages more than 100 FTE hospitalists and advanced-practice providers (APPs) within multiple health systems and hospitals in the Texas market. He also serves as a member of the SHM Practice Analysis Committee and as a vice president of SHM North Texas Chapter.
References
1. Angood P and Birk S. The Value of Physician Leadership. Physician Exec. 2014 May-Jun;40(3):6-20.
2. Rice JA. Expanding the Need for Physician Leaders. Executive Insight, Advance Healthcare Network, Nov 16, 2011. Available at: http://healthcare-executive-insight.advanceweb.com/Features/Articles/Expanding-the-Need-for-Physician-Leaders.aspx.
3. Khullar D. Good leaders make good doctors. New York Times. 2019 Nov 21.
4. Beresford L. The State of Hospital Medicine in 2018. Hospitalist. 2019;23(1):1-11.
5. Harte B. Hospitalists can meet the demand for physician executives. Hospitalist. 2018 Nov 29.
A match made in medicine: Match Day 2020
Match Day is the celebration of the National Resident Matching Program® (NRMP®) results, which seals the fate not only of future medical professionals, but of the program placements dedicated to supporting the acceleration of their careers.
Daniel Ricotta, MD, FHM, an academic hospitalist at Beth Israel Deaconess Medical Center (BIDMC) in Boston, and an active SHM member since 2013, offers unique insight into the value of understanding both sides of this interview table.
As the associate program director of BIDMC’s Internal Medicine Residency Program and the director of Simulation Education at the Carl J. Shapiro Center for Education & Research, Dr. Ricotta is able to act on his passions for medical education and clinical care.
“I was attracted to the breadth of medicine and enjoyed learning everything,” Dr. Ricotta said. “I knew I wanted to do academic medicine and education, and I was able to get involved by working with students and residents early on in my career.”
A natural fit for his current roles, Dr. Ricotta has gained a unique perspective on the match process and how it has evolved since he began his residency nine years ago.
Preparing for Match Day includes an extensive checklist of life-altering to-dos that shape your career trajectory. Medical students must have noteworthy CV points, scholarly recommendations, stand-out interviews, and a thoughtful rank list – among many other things to consider throughout the course of the match. Dr. Ricotta said that while this application process has generally remained the same since his participation, he has noticed that the students themselves have changed.
“Students going into residency are more mature and further along professionally,” he explained. “I’ve seen more students go on to do something else for a while and have gained more experience. They’re taking time off for research or getting dual degrees.”
Additionally, according to Dr. Ricotta, students are applying to double the number of programs than in years past, and are even using technology to their benefit. Because interview slots are limited, some students set up “bot automation” to help lock in interviews.
Amidst what can feel like a free-for-all, Dr. Ricotta reminds his students that the match process is a two-sided relationship.
“I certainly didn’t realize how much work goes into recruitment when I was a student,” Dr. Ricotta admitted. “What students don’t think about is the amount of care that goes into trying to match students who share similar values, the mission, or are a good cultural fit.”
He went on to emphasize the importance of environmental compatibility.
“Go somewhere that you feel you will fit in. Where you will thrive,” he said. “Go somewhere that has a mission that resonates with your mission and think about your fellow applicants and potential mentorship. Could you see yourself being their classmate? Does this program have people there who can help you to achieve your goals?”
Keeping in mind questions like these, it is no surprise that because of hospital medicine’s scheduling flexibility and hands-on learning opportunities that more and more students are interested in exploring this specialty.
“What is amazing about hospital medicine is the ample opportunity for you to get involved earlier in your career and build from that,” he said. “There is more face time with patients, more training for medical students available, countless academic opportunities in research and scholarships, and even conferences.”
Because of the multiple career pathways available in hospital medicine, SHM aims to provide students and residents with professional tools and opportunities as early as possible to allow them to get a preview of what they can expect as a hospitalist – no matter which path they choose.
“SHM is about getting involved,” said Dr. Ricotta. “SHM encourages residents to become actively incorporated into the community through chapters, conferences, and other networking opportunities on both local and national levels. That’s really difficult to do as a resident.”
Whether you’re waiting on the NRMP® results this year or you are in the beginning stages of gathering your application materials, one thing is clear according to Dr. Ricotta, you’re not just an applicant number.
Are you a student interested in exploring a career in hospital medicine? SHM supports educational and professional needs at all stages of your career. When you join SHM during your residency training, you receive access to programs, resources, and opportunities that will enhance your skills and raise your professional profile. For more information about our Residents & Fellows membership opportunity, please visit: hospitalmedicine.org/residents.
Ms. Cowan is a marketing communications specialist at the Society of Hospital Medicine.
Match Day is the celebration of the National Resident Matching Program® (NRMP®) results, which seals the fate not only of future medical professionals, but of the program placements dedicated to supporting the acceleration of their careers.
Daniel Ricotta, MD, FHM, an academic hospitalist at Beth Israel Deaconess Medical Center (BIDMC) in Boston, and an active SHM member since 2013, offers unique insight into the value of understanding both sides of this interview table.
As the associate program director of BIDMC’s Internal Medicine Residency Program and the director of Simulation Education at the Carl J. Shapiro Center for Education & Research, Dr. Ricotta is able to act on his passions for medical education and clinical care.
“I was attracted to the breadth of medicine and enjoyed learning everything,” Dr. Ricotta said. “I knew I wanted to do academic medicine and education, and I was able to get involved by working with students and residents early on in my career.”
A natural fit for his current roles, Dr. Ricotta has gained a unique perspective on the match process and how it has evolved since he began his residency nine years ago.
Preparing for Match Day includes an extensive checklist of life-altering to-dos that shape your career trajectory. Medical students must have noteworthy CV points, scholarly recommendations, stand-out interviews, and a thoughtful rank list – among many other things to consider throughout the course of the match. Dr. Ricotta said that while this application process has generally remained the same since his participation, he has noticed that the students themselves have changed.
“Students going into residency are more mature and further along professionally,” he explained. “I’ve seen more students go on to do something else for a while and have gained more experience. They’re taking time off for research or getting dual degrees.”
Additionally, according to Dr. Ricotta, students are applying to double the number of programs than in years past, and are even using technology to their benefit. Because interview slots are limited, some students set up “bot automation” to help lock in interviews.
Amidst what can feel like a free-for-all, Dr. Ricotta reminds his students that the match process is a two-sided relationship.
“I certainly didn’t realize how much work goes into recruitment when I was a student,” Dr. Ricotta admitted. “What students don’t think about is the amount of care that goes into trying to match students who share similar values, the mission, or are a good cultural fit.”
He went on to emphasize the importance of environmental compatibility.
“Go somewhere that you feel you will fit in. Where you will thrive,” he said. “Go somewhere that has a mission that resonates with your mission and think about your fellow applicants and potential mentorship. Could you see yourself being their classmate? Does this program have people there who can help you to achieve your goals?”
Keeping in mind questions like these, it is no surprise that because of hospital medicine’s scheduling flexibility and hands-on learning opportunities that more and more students are interested in exploring this specialty.
“What is amazing about hospital medicine is the ample opportunity for you to get involved earlier in your career and build from that,” he said. “There is more face time with patients, more training for medical students available, countless academic opportunities in research and scholarships, and even conferences.”
Because of the multiple career pathways available in hospital medicine, SHM aims to provide students and residents with professional tools and opportunities as early as possible to allow them to get a preview of what they can expect as a hospitalist – no matter which path they choose.
“SHM is about getting involved,” said Dr. Ricotta. “SHM encourages residents to become actively incorporated into the community through chapters, conferences, and other networking opportunities on both local and national levels. That’s really difficult to do as a resident.”
Whether you’re waiting on the NRMP® results this year or you are in the beginning stages of gathering your application materials, one thing is clear according to Dr. Ricotta, you’re not just an applicant number.
Are you a student interested in exploring a career in hospital medicine? SHM supports educational and professional needs at all stages of your career. When you join SHM during your residency training, you receive access to programs, resources, and opportunities that will enhance your skills and raise your professional profile. For more information about our Residents & Fellows membership opportunity, please visit: hospitalmedicine.org/residents.
Ms. Cowan is a marketing communications specialist at the Society of Hospital Medicine.
Match Day is the celebration of the National Resident Matching Program® (NRMP®) results, which seals the fate not only of future medical professionals, but of the program placements dedicated to supporting the acceleration of their careers.
Daniel Ricotta, MD, FHM, an academic hospitalist at Beth Israel Deaconess Medical Center (BIDMC) in Boston, and an active SHM member since 2013, offers unique insight into the value of understanding both sides of this interview table.
As the associate program director of BIDMC’s Internal Medicine Residency Program and the director of Simulation Education at the Carl J. Shapiro Center for Education & Research, Dr. Ricotta is able to act on his passions for medical education and clinical care.
“I was attracted to the breadth of medicine and enjoyed learning everything,” Dr. Ricotta said. “I knew I wanted to do academic medicine and education, and I was able to get involved by working with students and residents early on in my career.”
A natural fit for his current roles, Dr. Ricotta has gained a unique perspective on the match process and how it has evolved since he began his residency nine years ago.
Preparing for Match Day includes an extensive checklist of life-altering to-dos that shape your career trajectory. Medical students must have noteworthy CV points, scholarly recommendations, stand-out interviews, and a thoughtful rank list – among many other things to consider throughout the course of the match. Dr. Ricotta said that while this application process has generally remained the same since his participation, he has noticed that the students themselves have changed.
“Students going into residency are more mature and further along professionally,” he explained. “I’ve seen more students go on to do something else for a while and have gained more experience. They’re taking time off for research or getting dual degrees.”
Additionally, according to Dr. Ricotta, students are applying to double the number of programs than in years past, and are even using technology to their benefit. Because interview slots are limited, some students set up “bot automation” to help lock in interviews.
Amidst what can feel like a free-for-all, Dr. Ricotta reminds his students that the match process is a two-sided relationship.
“I certainly didn’t realize how much work goes into recruitment when I was a student,” Dr. Ricotta admitted. “What students don’t think about is the amount of care that goes into trying to match students who share similar values, the mission, or are a good cultural fit.”
He went on to emphasize the importance of environmental compatibility.
“Go somewhere that you feel you will fit in. Where you will thrive,” he said. “Go somewhere that has a mission that resonates with your mission and think about your fellow applicants and potential mentorship. Could you see yourself being their classmate? Does this program have people there who can help you to achieve your goals?”
Keeping in mind questions like these, it is no surprise that because of hospital medicine’s scheduling flexibility and hands-on learning opportunities that more and more students are interested in exploring this specialty.
“What is amazing about hospital medicine is the ample opportunity for you to get involved earlier in your career and build from that,” he said. “There is more face time with patients, more training for medical students available, countless academic opportunities in research and scholarships, and even conferences.”
Because of the multiple career pathways available in hospital medicine, SHM aims to provide students and residents with professional tools and opportunities as early as possible to allow them to get a preview of what they can expect as a hospitalist – no matter which path they choose.
“SHM is about getting involved,” said Dr. Ricotta. “SHM encourages residents to become actively incorporated into the community through chapters, conferences, and other networking opportunities on both local and national levels. That’s really difficult to do as a resident.”
Whether you’re waiting on the NRMP® results this year or you are in the beginning stages of gathering your application materials, one thing is clear according to Dr. Ricotta, you’re not just an applicant number.
Are you a student interested in exploring a career in hospital medicine? SHM supports educational and professional needs at all stages of your career. When you join SHM during your residency training, you receive access to programs, resources, and opportunities that will enhance your skills and raise your professional profile. For more information about our Residents & Fellows membership opportunity, please visit: hospitalmedicine.org/residents.
Ms. Cowan is a marketing communications specialist at the Society of Hospital Medicine.
Hospitalist profile: Charu Puri, MD
Charu Puri, MD, FHM, is a hospitalist and medical informaticist at Sutter East Bay Medical Group in Oakland, Calif. She also serves as medical director for onboarding, mentoring, and physician development.
Dr. Puri has been a member of the Society of Hospital Medicine since 2009, and attended the Society’s Leadership Academy, where she was inspired to create a mentorship program at her own institution. She is a member of the San Francisco Bay chapter of SHM and serves on the Performance Measurement and Reporting Committee.
At what point in your education/training did you decide to practice hospital medicine? What about hospital medicine appealed to you?
It was early on in my residency that it became clear to me that I wanted to pursue the hospitalist track. It was a natural fit, and I gravitated toward the hospitalist side of medicine. What appealed to me most was that we had the opportunity and privilege to provide care to patients in their most vulnerable state and experience the effects of that care in real time. I found that very gratifying.
There is also a sense of community and camaraderie that comes with working in a hospital setting. Everyone is working together, trying to help patients. The collegiality and the relationships that develop are very rewarding. I have been fortunate enough to have built strong friendships with the hospitalists in my group as well as colleagues from other disciplines in medicine that work in the hospital.
What is your current role at Sutter Health?
Alta Bates Summit Medical Center is part of the larger Sutter Health system. I have an administrative role with my medical group in addition to the clinical work I do at the medical center, although first and foremost I identify myself as a hospitalist. About 5 years ago I took on a role in clinical informatics, when our hospital implemented an EHR. Since then I have been working as an inpatient physician informaticist. Most recently I took on a new role as medical director for onboarding, mentoring, and physician development in my medical group.
How do you balance the different duties of your various roles?
I am full time in my administration role, between my informatics role and my onboarding role. I technically don’t have to do clinical shifts if I don’t want to, but it’s important to me to continue clinical practice and maintain my skills and connection to the hospital and colleagues. I do about four clinical shifts a month, and plan to continue doing that. In our group you must do 14 shifts a month to be considered full time, so what I do could be considered about one-third of that.
What are your favorite areas of clinical practice and/or research?
I haven’t had a lot of research experience. My residency program was a community-based program, and my current setting is a community hospital. I haven’t been involved much in the academic side of hospital medicine. As far as clinical practices goes, I think it’s the diversity of hospital medicine that appeals to me. You really get to be a jack of all trades, and experience all the different disciplines of medicine. I like the variety.
Both my informatics and onboarding roles came out of a need that I identified, and just began doing the work before there was an official role. When we implemented our EHR, it was essential to get our doctors organized to make sure they were ready to take care of patients that first day of go live. By the time our hospital went live on the EHR, I had a good understanding of how it worked, and so I was able to create a miniature curriculum for our physicians – templates, order sets, workflows, etc. – to help ensure everything went smoothly. A few months after we implemented the EHR, I was officially offered a physician informaticist role.
The onboarding role came about in an interesting way. I was participating in the leadership course offered by SHM and was lucky enough to be in the pilot for the Capstone course. That leadership course is focused around mentoring and sponsorship, and one of the faculty members was Nancy Spector, MD, the associate dean of faculty development at Drexel University, Philadelphia. She talked a lot about mentoring, and I was inspired to set up a mentoring program for our hospitalists. Dr. Spector graciously agreed to mentor me as I worked on my Capstone project, which was to create a mentoring program in a community-based hospitalist group. As I continued to work on the project, coincidentally our medical group decided to redesign our new physician onboarding process. Because I was already involved in the onboarding and training related to our EHR, I became very involved with our medical group's onboarding redesign.
My group's CEO decided to create a new directorship role for onboarding and mentoring, which I recently interviewed for and was offered about two months ago.
I think setting up systems to support our doctors is the common threat between the informatics and the onboarding roles. I want to implement systems that support our doctors, help them succeed, and hopefully make their jobs a little easier.
What are the most challenging aspects of practicing hospital medicine? What are the most rewarding?
We practice in a very urban environment, with many low-income patients who have limited resources and access to health care. That can be very challenging. You always wonder if these patients have all the support they need after leaving the hospital. Sometimes I feel that I am just putting a band-aid on the medical problem, so to speak, but not solving the underlying issue. But it can be very rewarding during those times when the hospital and the broader community can bring our resources together to create interventions to help at-risk patients. It doesn’t happen as frequently as we would like, but when it does happen it feels good.
Another challenging aspect is related to perception. There are a lot of consultants in the hospital who view hospitalists as "house staff." That can be very frustrating, and it’s important to steer the conversations away from that perspective, and really try to establish ourselves as colleagues and peers.
How will hospital medicine change in the next decade or 2?
It’s a relatively young field, and we’re still figuring it out. I really don’t know how hospital medicine is going to change, but I do know that the field will continue to evolve, given the way U.S. health care is rapidly changing.
Do you have any advice for students and residents interested in hospital medicine?
It’s a fun way to practice medicine and I would encourage students to go into hospital medicine. It’s great for work/life balance. The advice I would give is that it is very important to get involved early in your career. Get involved in medical group or hospital committees. Stay away from the “shift mentality” – that I’m going to work my shifts and leave. That can lead to early burnout, which is a real concern in our field now. Early engagement is essential, so you can help lead these conversations at your hospital.
Charu Puri, MD, FHM, is a hospitalist and medical informaticist at Sutter East Bay Medical Group in Oakland, Calif. She also serves as medical director for onboarding, mentoring, and physician development.
Dr. Puri has been a member of the Society of Hospital Medicine since 2009, and attended the Society’s Leadership Academy, where she was inspired to create a mentorship program at her own institution. She is a member of the San Francisco Bay chapter of SHM and serves on the Performance Measurement and Reporting Committee.
At what point in your education/training did you decide to practice hospital medicine? What about hospital medicine appealed to you?
It was early on in my residency that it became clear to me that I wanted to pursue the hospitalist track. It was a natural fit, and I gravitated toward the hospitalist side of medicine. What appealed to me most was that we had the opportunity and privilege to provide care to patients in their most vulnerable state and experience the effects of that care in real time. I found that very gratifying.
There is also a sense of community and camaraderie that comes with working in a hospital setting. Everyone is working together, trying to help patients. The collegiality and the relationships that develop are very rewarding. I have been fortunate enough to have built strong friendships with the hospitalists in my group as well as colleagues from other disciplines in medicine that work in the hospital.
What is your current role at Sutter Health?
Alta Bates Summit Medical Center is part of the larger Sutter Health system. I have an administrative role with my medical group in addition to the clinical work I do at the medical center, although first and foremost I identify myself as a hospitalist. About 5 years ago I took on a role in clinical informatics, when our hospital implemented an EHR. Since then I have been working as an inpatient physician informaticist. Most recently I took on a new role as medical director for onboarding, mentoring, and physician development in my medical group.
How do you balance the different duties of your various roles?
I am full time in my administration role, between my informatics role and my onboarding role. I technically don’t have to do clinical shifts if I don’t want to, but it’s important to me to continue clinical practice and maintain my skills and connection to the hospital and colleagues. I do about four clinical shifts a month, and plan to continue doing that. In our group you must do 14 shifts a month to be considered full time, so what I do could be considered about one-third of that.
What are your favorite areas of clinical practice and/or research?
I haven’t had a lot of research experience. My residency program was a community-based program, and my current setting is a community hospital. I haven’t been involved much in the academic side of hospital medicine. As far as clinical practices goes, I think it’s the diversity of hospital medicine that appeals to me. You really get to be a jack of all trades, and experience all the different disciplines of medicine. I like the variety.
Both my informatics and onboarding roles came out of a need that I identified, and just began doing the work before there was an official role. When we implemented our EHR, it was essential to get our doctors organized to make sure they were ready to take care of patients that first day of go live. By the time our hospital went live on the EHR, I had a good understanding of how it worked, and so I was able to create a miniature curriculum for our physicians – templates, order sets, workflows, etc. – to help ensure everything went smoothly. A few months after we implemented the EHR, I was officially offered a physician informaticist role.
The onboarding role came about in an interesting way. I was participating in the leadership course offered by SHM and was lucky enough to be in the pilot for the Capstone course. That leadership course is focused around mentoring and sponsorship, and one of the faculty members was Nancy Spector, MD, the associate dean of faculty development at Drexel University, Philadelphia. She talked a lot about mentoring, and I was inspired to set up a mentoring program for our hospitalists. Dr. Spector graciously agreed to mentor me as I worked on my Capstone project, which was to create a mentoring program in a community-based hospitalist group. As I continued to work on the project, coincidentally our medical group decided to redesign our new physician onboarding process. Because I was already involved in the onboarding and training related to our EHR, I became very involved with our medical group's onboarding redesign.
My group's CEO decided to create a new directorship role for onboarding and mentoring, which I recently interviewed for and was offered about two months ago.
I think setting up systems to support our doctors is the common threat between the informatics and the onboarding roles. I want to implement systems that support our doctors, help them succeed, and hopefully make their jobs a little easier.
What are the most challenging aspects of practicing hospital medicine? What are the most rewarding?
We practice in a very urban environment, with many low-income patients who have limited resources and access to health care. That can be very challenging. You always wonder if these patients have all the support they need after leaving the hospital. Sometimes I feel that I am just putting a band-aid on the medical problem, so to speak, but not solving the underlying issue. But it can be very rewarding during those times when the hospital and the broader community can bring our resources together to create interventions to help at-risk patients. It doesn’t happen as frequently as we would like, but when it does happen it feels good.
Another challenging aspect is related to perception. There are a lot of consultants in the hospital who view hospitalists as "house staff." That can be very frustrating, and it’s important to steer the conversations away from that perspective, and really try to establish ourselves as colleagues and peers.
How will hospital medicine change in the next decade or 2?
It’s a relatively young field, and we’re still figuring it out. I really don’t know how hospital medicine is going to change, but I do know that the field will continue to evolve, given the way U.S. health care is rapidly changing.
Do you have any advice for students and residents interested in hospital medicine?
It’s a fun way to practice medicine and I would encourage students to go into hospital medicine. It’s great for work/life balance. The advice I would give is that it is very important to get involved early in your career. Get involved in medical group or hospital committees. Stay away from the “shift mentality” – that I’m going to work my shifts and leave. That can lead to early burnout, which is a real concern in our field now. Early engagement is essential, so you can help lead these conversations at your hospital.
Charu Puri, MD, FHM, is a hospitalist and medical informaticist at Sutter East Bay Medical Group in Oakland, Calif. She also serves as medical director for onboarding, mentoring, and physician development.
Dr. Puri has been a member of the Society of Hospital Medicine since 2009, and attended the Society’s Leadership Academy, where she was inspired to create a mentorship program at her own institution. She is a member of the San Francisco Bay chapter of SHM and serves on the Performance Measurement and Reporting Committee.
At what point in your education/training did you decide to practice hospital medicine? What about hospital medicine appealed to you?
It was early on in my residency that it became clear to me that I wanted to pursue the hospitalist track. It was a natural fit, and I gravitated toward the hospitalist side of medicine. What appealed to me most was that we had the opportunity and privilege to provide care to patients in their most vulnerable state and experience the effects of that care in real time. I found that very gratifying.
There is also a sense of community and camaraderie that comes with working in a hospital setting. Everyone is working together, trying to help patients. The collegiality and the relationships that develop are very rewarding. I have been fortunate enough to have built strong friendships with the hospitalists in my group as well as colleagues from other disciplines in medicine that work in the hospital.
What is your current role at Sutter Health?
Alta Bates Summit Medical Center is part of the larger Sutter Health system. I have an administrative role with my medical group in addition to the clinical work I do at the medical center, although first and foremost I identify myself as a hospitalist. About 5 years ago I took on a role in clinical informatics, when our hospital implemented an EHR. Since then I have been working as an inpatient physician informaticist. Most recently I took on a new role as medical director for onboarding, mentoring, and physician development in my medical group.
How do you balance the different duties of your various roles?
I am full time in my administration role, between my informatics role and my onboarding role. I technically don’t have to do clinical shifts if I don’t want to, but it’s important to me to continue clinical practice and maintain my skills and connection to the hospital and colleagues. I do about four clinical shifts a month, and plan to continue doing that. In our group you must do 14 shifts a month to be considered full time, so what I do could be considered about one-third of that.
What are your favorite areas of clinical practice and/or research?
I haven’t had a lot of research experience. My residency program was a community-based program, and my current setting is a community hospital. I haven’t been involved much in the academic side of hospital medicine. As far as clinical practices goes, I think it’s the diversity of hospital medicine that appeals to me. You really get to be a jack of all trades, and experience all the different disciplines of medicine. I like the variety.
Both my informatics and onboarding roles came out of a need that I identified, and just began doing the work before there was an official role. When we implemented our EHR, it was essential to get our doctors organized to make sure they were ready to take care of patients that first day of go live. By the time our hospital went live on the EHR, I had a good understanding of how it worked, and so I was able to create a miniature curriculum for our physicians – templates, order sets, workflows, etc. – to help ensure everything went smoothly. A few months after we implemented the EHR, I was officially offered a physician informaticist role.
The onboarding role came about in an interesting way. I was participating in the leadership course offered by SHM and was lucky enough to be in the pilot for the Capstone course. That leadership course is focused around mentoring and sponsorship, and one of the faculty members was Nancy Spector, MD, the associate dean of faculty development at Drexel University, Philadelphia. She talked a lot about mentoring, and I was inspired to set up a mentoring program for our hospitalists. Dr. Spector graciously agreed to mentor me as I worked on my Capstone project, which was to create a mentoring program in a community-based hospitalist group. As I continued to work on the project, coincidentally our medical group decided to redesign our new physician onboarding process. Because I was already involved in the onboarding and training related to our EHR, I became very involved with our medical group's onboarding redesign.
My group's CEO decided to create a new directorship role for onboarding and mentoring, which I recently interviewed for and was offered about two months ago.
I think setting up systems to support our doctors is the common threat between the informatics and the onboarding roles. I want to implement systems that support our doctors, help them succeed, and hopefully make their jobs a little easier.
What are the most challenging aspects of practicing hospital medicine? What are the most rewarding?
We practice in a very urban environment, with many low-income patients who have limited resources and access to health care. That can be very challenging. You always wonder if these patients have all the support they need after leaving the hospital. Sometimes I feel that I am just putting a band-aid on the medical problem, so to speak, but not solving the underlying issue. But it can be very rewarding during those times when the hospital and the broader community can bring our resources together to create interventions to help at-risk patients. It doesn’t happen as frequently as we would like, but when it does happen it feels good.
Another challenging aspect is related to perception. There are a lot of consultants in the hospital who view hospitalists as "house staff." That can be very frustrating, and it’s important to steer the conversations away from that perspective, and really try to establish ourselves as colleagues and peers.
How will hospital medicine change in the next decade or 2?
It’s a relatively young field, and we’re still figuring it out. I really don’t know how hospital medicine is going to change, but I do know that the field will continue to evolve, given the way U.S. health care is rapidly changing.
Do you have any advice for students and residents interested in hospital medicine?
It’s a fun way to practice medicine and I would encourage students to go into hospital medicine. It’s great for work/life balance. The advice I would give is that it is very important to get involved early in your career. Get involved in medical group or hospital committees. Stay away from the “shift mentality” – that I’m going to work my shifts and leave. That can lead to early burnout, which is a real concern in our field now. Early engagement is essential, so you can help lead these conversations at your hospital.
Hospitalist profile: Ilaria Gadalla, DMSc, PA-C
Ilaria Gadalla, DMSc, PA-C, is a hospitalist at Treasure Coast Hospitalists in Port St. Lucie, Fla., and serves as the physician assistant department chair/program director at South University, West Palm Beach, Fla., where she supervises more than 40 PAs, medical directors, and administrative staff across the South University campuses.
Ms. Gadalla is the chair of SHM’s NP/PA Special Interest Group, which was integral in drafting the society’s recent white paper on NP/PA integration and optimization.
She says that she continuously drives innovative projects for NPs and PAs to demonstrate excellence in collaboration by working closely with C-suite administration to expand quality improvement and education efforts. A prime example is the optimal communication system that she developed within her first week as a hospitalist in the Port St. Lucie area. Nursing, ED, and pharmacy staff had difficulty contacting hospitalists since the electronic medical record would not reflect the assigned hospitalist. She developed a simple contact sheet that included the hospitalist team each day. This method is still in use today.
At what point in your life did you realize you wanted to be a physician assistant?
I worked as a respiratory therapist and had a desire to expand my knowledge to manage critical care patients. I applied to Albany (N.Y.) Medical College, where I received my PA training. I knew before PA school that I was passionate about the medical field and wanted to advance my education and training.
How did you decide to become a PA hospitalist?
From day one at my first job, I knew that I loved inpatient medicine. I had a unique position as a cardiology hospitalist in Baltimore. That was my first experience working in hospital medicine. As a team of PAs, we worked closely with hospitalists in addition to the cardiologists. I really enjoyed the acuity of hospital medicine, and the brilliant hospitalist colleagues I worked with. They fueled my clinical knowledge daily, and that really drew me further into hospital medicine.
What is your current position?
I have a unique position. I work primarily in an academic role, as a program director and department chair of the physician assistant program at South University in West Palm Beach. I provide oversight for four PA program campuses located in Florida. Georgia, and Virginia. I also work clinically as a hospitalist at Treasure Coast Hospitalists in the Port St. Lucie area.
What are some of your favorite parts of your work?
My favorite aspect within the academic environment is what I call the “lightbulb moment” – that instant when you see your students comprehending and applying critical thinking regarding patient care. In clinical practice, I really enjoy educating and navigating a patient through their diagnosis and management. It’s like teaching, in that a patient can also have a lightbulb moment.
What are the most challenging aspects of practicing hospital medicine, from a PA’s perspective?
Medicine is an art, and each patient’s body is different. It’s a challenge to create individualized care in a system where metrics and templates exist. An additional challenge is simply navigating the culture of medicine and its receptiveness to physician assistants.
How does a hospitalist PA work differently than a PA in other health care settings?
PAs in hospital medicine must excel in communication skills. We are frequently the primary liaison between families, patients, specialists, consultants, and various departments daily. PAs in other care settings also communicate with a broad variety of people, but in hospital medicine that communication is required to be much more rapid. Your skills must really rise to the next level.
There is also the opportunity for PAs to integrate within hospital committees and the C-suite. That is very different from other settings.
How can PAs and nurse practitioners fit best into hospital medicine groups?
Initially, a hospital medicine group needs to identify their specific needs when deciding to integrate PAs and NPs. There must be a culture of receptiveness, with proper onboarding. That is a vital necessity, because without a proper onboarding process and a welcoming culture, a group is set up to fail.
What kind of resources do hospitalist PAs require to succeed?
There is a big need for education that targets the hospital C-suite and our physician colleagues about the scope of practice and autonomy that a PA can have. There are significant misconceptions about the capabilities of hospitalist PAs, and the additional value we bring to a team. PAs do not want to replace our MD/DO colleagues.
What do you see on the horizon for PAs and NPs in hospital medicine?
As the chair of SHM’s NP/PA Special Interest Group, we see a significant need for onboarding resources, because there is a hospitalist staffing shortage in the United States, and that gap can be filled with NPs and PAs. There is a lack of understanding about how to onboard and integrate advanced practice providers, so we are working intently on providing a toolkit that will assist groups with this process.
Do you have any advice for students who are interested in becoming hospitalist PAs?
I would encourage students to seek mentoring from a hospitalist PA. This can really help prepare you for the inpatient world, as it’s very different from outpatient medicine with a higher acuity of patient care. I would also encourage students to join SHM, as there are many resources to help improve your skills and increase your confidence as you grow within your career.
Ilaria Gadalla, DMSc, PA-C, is a hospitalist at Treasure Coast Hospitalists in Port St. Lucie, Fla., and serves as the physician assistant department chair/program director at South University, West Palm Beach, Fla., where she supervises more than 40 PAs, medical directors, and administrative staff across the South University campuses.
Ms. Gadalla is the chair of SHM’s NP/PA Special Interest Group, which was integral in drafting the society’s recent white paper on NP/PA integration and optimization.
She says that she continuously drives innovative projects for NPs and PAs to demonstrate excellence in collaboration by working closely with C-suite administration to expand quality improvement and education efforts. A prime example is the optimal communication system that she developed within her first week as a hospitalist in the Port St. Lucie area. Nursing, ED, and pharmacy staff had difficulty contacting hospitalists since the electronic medical record would not reflect the assigned hospitalist. She developed a simple contact sheet that included the hospitalist team each day. This method is still in use today.
At what point in your life did you realize you wanted to be a physician assistant?
I worked as a respiratory therapist and had a desire to expand my knowledge to manage critical care patients. I applied to Albany (N.Y.) Medical College, where I received my PA training. I knew before PA school that I was passionate about the medical field and wanted to advance my education and training.
How did you decide to become a PA hospitalist?
From day one at my first job, I knew that I loved inpatient medicine. I had a unique position as a cardiology hospitalist in Baltimore. That was my first experience working in hospital medicine. As a team of PAs, we worked closely with hospitalists in addition to the cardiologists. I really enjoyed the acuity of hospital medicine, and the brilliant hospitalist colleagues I worked with. They fueled my clinical knowledge daily, and that really drew me further into hospital medicine.
What is your current position?
I have a unique position. I work primarily in an academic role, as a program director and department chair of the physician assistant program at South University in West Palm Beach. I provide oversight for four PA program campuses located in Florida. Georgia, and Virginia. I also work clinically as a hospitalist at Treasure Coast Hospitalists in the Port St. Lucie area.
What are some of your favorite parts of your work?
My favorite aspect within the academic environment is what I call the “lightbulb moment” – that instant when you see your students comprehending and applying critical thinking regarding patient care. In clinical practice, I really enjoy educating and navigating a patient through their diagnosis and management. It’s like teaching, in that a patient can also have a lightbulb moment.
What are the most challenging aspects of practicing hospital medicine, from a PA’s perspective?
Medicine is an art, and each patient’s body is different. It’s a challenge to create individualized care in a system where metrics and templates exist. An additional challenge is simply navigating the culture of medicine and its receptiveness to physician assistants.
How does a hospitalist PA work differently than a PA in other health care settings?
PAs in hospital medicine must excel in communication skills. We are frequently the primary liaison between families, patients, specialists, consultants, and various departments daily. PAs in other care settings also communicate with a broad variety of people, but in hospital medicine that communication is required to be much more rapid. Your skills must really rise to the next level.
There is also the opportunity for PAs to integrate within hospital committees and the C-suite. That is very different from other settings.
How can PAs and nurse practitioners fit best into hospital medicine groups?
Initially, a hospital medicine group needs to identify their specific needs when deciding to integrate PAs and NPs. There must be a culture of receptiveness, with proper onboarding. That is a vital necessity, because without a proper onboarding process and a welcoming culture, a group is set up to fail.
What kind of resources do hospitalist PAs require to succeed?
There is a big need for education that targets the hospital C-suite and our physician colleagues about the scope of practice and autonomy that a PA can have. There are significant misconceptions about the capabilities of hospitalist PAs, and the additional value we bring to a team. PAs do not want to replace our MD/DO colleagues.
What do you see on the horizon for PAs and NPs in hospital medicine?
As the chair of SHM’s NP/PA Special Interest Group, we see a significant need for onboarding resources, because there is a hospitalist staffing shortage in the United States, and that gap can be filled with NPs and PAs. There is a lack of understanding about how to onboard and integrate advanced practice providers, so we are working intently on providing a toolkit that will assist groups with this process.
Do you have any advice for students who are interested in becoming hospitalist PAs?
I would encourage students to seek mentoring from a hospitalist PA. This can really help prepare you for the inpatient world, as it’s very different from outpatient medicine with a higher acuity of patient care. I would also encourage students to join SHM, as there are many resources to help improve your skills and increase your confidence as you grow within your career.
Ilaria Gadalla, DMSc, PA-C, is a hospitalist at Treasure Coast Hospitalists in Port St. Lucie, Fla., and serves as the physician assistant department chair/program director at South University, West Palm Beach, Fla., where she supervises more than 40 PAs, medical directors, and administrative staff across the South University campuses.
Ms. Gadalla is the chair of SHM’s NP/PA Special Interest Group, which was integral in drafting the society’s recent white paper on NP/PA integration and optimization.
She says that she continuously drives innovative projects for NPs and PAs to demonstrate excellence in collaboration by working closely with C-suite administration to expand quality improvement and education efforts. A prime example is the optimal communication system that she developed within her first week as a hospitalist in the Port St. Lucie area. Nursing, ED, and pharmacy staff had difficulty contacting hospitalists since the electronic medical record would not reflect the assigned hospitalist. She developed a simple contact sheet that included the hospitalist team each day. This method is still in use today.
At what point in your life did you realize you wanted to be a physician assistant?
I worked as a respiratory therapist and had a desire to expand my knowledge to manage critical care patients. I applied to Albany (N.Y.) Medical College, where I received my PA training. I knew before PA school that I was passionate about the medical field and wanted to advance my education and training.
How did you decide to become a PA hospitalist?
From day one at my first job, I knew that I loved inpatient medicine. I had a unique position as a cardiology hospitalist in Baltimore. That was my first experience working in hospital medicine. As a team of PAs, we worked closely with hospitalists in addition to the cardiologists. I really enjoyed the acuity of hospital medicine, and the brilliant hospitalist colleagues I worked with. They fueled my clinical knowledge daily, and that really drew me further into hospital medicine.
What is your current position?
I have a unique position. I work primarily in an academic role, as a program director and department chair of the physician assistant program at South University in West Palm Beach. I provide oversight for four PA program campuses located in Florida. Georgia, and Virginia. I also work clinically as a hospitalist at Treasure Coast Hospitalists in the Port St. Lucie area.
What are some of your favorite parts of your work?
My favorite aspect within the academic environment is what I call the “lightbulb moment” – that instant when you see your students comprehending and applying critical thinking regarding patient care. In clinical practice, I really enjoy educating and navigating a patient through their diagnosis and management. It’s like teaching, in that a patient can also have a lightbulb moment.
What are the most challenging aspects of practicing hospital medicine, from a PA’s perspective?
Medicine is an art, and each patient’s body is different. It’s a challenge to create individualized care in a system where metrics and templates exist. An additional challenge is simply navigating the culture of medicine and its receptiveness to physician assistants.
How does a hospitalist PA work differently than a PA in other health care settings?
PAs in hospital medicine must excel in communication skills. We are frequently the primary liaison between families, patients, specialists, consultants, and various departments daily. PAs in other care settings also communicate with a broad variety of people, but in hospital medicine that communication is required to be much more rapid. Your skills must really rise to the next level.
There is also the opportunity for PAs to integrate within hospital committees and the C-suite. That is very different from other settings.
How can PAs and nurse practitioners fit best into hospital medicine groups?
Initially, a hospital medicine group needs to identify their specific needs when deciding to integrate PAs and NPs. There must be a culture of receptiveness, with proper onboarding. That is a vital necessity, because without a proper onboarding process and a welcoming culture, a group is set up to fail.
What kind of resources do hospitalist PAs require to succeed?
There is a big need for education that targets the hospital C-suite and our physician colleagues about the scope of practice and autonomy that a PA can have. There are significant misconceptions about the capabilities of hospitalist PAs, and the additional value we bring to a team. PAs do not want to replace our MD/DO colleagues.
What do you see on the horizon for PAs and NPs in hospital medicine?
As the chair of SHM’s NP/PA Special Interest Group, we see a significant need for onboarding resources, because there is a hospitalist staffing shortage in the United States, and that gap can be filled with NPs and PAs. There is a lack of understanding about how to onboard and integrate advanced practice providers, so we are working intently on providing a toolkit that will assist groups with this process.
Do you have any advice for students who are interested in becoming hospitalist PAs?
I would encourage students to seek mentoring from a hospitalist PA. This can really help prepare you for the inpatient world, as it’s very different from outpatient medicine with a higher acuity of patient care. I would also encourage students to join SHM, as there are many resources to help improve your skills and increase your confidence as you grow within your career.
Hospitalist profile: Amit Vashist, MD, SFHM
Amit Vashist, MD, SFHM, is the senior vice president and chief clinical officer at Ballad Health, an integrated 21-hospital health system serving 29 counties of northeast Tennessee, southwest Virginia, northwest North Carolina, and southeast Kentucky.
Dr. Vashist, who is a member of the Hospitalist’s editorial advisory board, focuses on clinical quality and safety, value-based initiatives to improve quality while reducing cost of care, performance improvement, and oversight of the enterprise-wide clinical delivery of care. He also provides administrative oversight of the Ballad Health Clinical Council – a model of physician partnership for clinical transformation and outcomes improvement.
Dr. Vashist is a dual board-certified internist and psychiatrist and an avid proponent of initiatives aimed at promoting quality, improving safety, reducing cost, and minimizing variation in the delivery of patient care across diverse settings. His work has been instrumental in improving outcomes and reducing mortality in patients with sepsis, earning him several local, regional, and national awards, and his work in promoting a zero-harm culture at Ballad Health has been instrumental in significantly reducing hospital-acquired infections system wide.
Prior to transitioning into the role of the chief clinical officer, Dr. Vashist served as the chair of the Ballad Health Clinical Council and the system chair for Ballad Health’s hospitalist division running a group of over 130 hospitalists.
Why did you choose a career in medicine?
The ability to have a positive impact and help others. In addition, I love learning new information and skills, and medicine affords one the opportunity to be a lifelong learner.
What do you like most about working as a hospitalist?
The relatively fast-paced nature of the work and the ability to tie seemingly fragmented episodes of patient care together. I believe that no other specialty offers that 30,000-foot vantage view of things in clinical medicine.
What do you like the least?
The shift worker mindset emanating from the traditional and rigid 7-on, 7-off model. A sense of team can be lost in this model and, contrary to conventional thinking, this model can accelerate hospitalist burnout.
What’s the best advice you ever received?
“You’ve gotta learn to listen!”
What’s the worst advice you ever received?
“Don’t rock the boat.” I strongly believe that frequent disruption is required to change the established status quo.
What aspect of patient care is most challenging?
A perceived disruption in the continuity of care by virtue of a new hospitalist seeing those patients, and the challenge to build the same level of trust and comfort as the outgoing hospitalist. Superior models of care have developed over the years promoting a better continuity of care but this domain continues to pose a challenge to proponents of hospital medicine.
What’s the biggest change you’ve seen in hospital medicine in your career?
Hospitalists being increasingly perceived as the “quarterbacks” and gatekeepers of quality, costs of care, and clinical outcomes in our hospitals and health care systems.
What’s the biggest change you would like to see in hospital medicine?
Inpatient volumes across the country continue to shrink, and this trend will not change for the foreseeable future. Hospitalists have got to embrace newer models of care faster, like hospitals at home, postacute care, transitional care clinics, hospital at home, etc. Remember what they say: “If you are not at the table, you are on the menu.” Now is our time to be at the table, and be the champions of change and move to true value (quality plus experience/cost), or else, we could end up and vanish like Blockbuster.
Outside of patient care, tell us about your career interests.
Implementing value-driven initiatives, pursuing endeavors aimed at cutting out waste and redundancy in health care, and developing a new generation of physician leaders with these skill sets.
Where do you see yourself in 10 years?
Leveraging my experience, training and expertise in hospital medicine to design better systems of health care that transcend above and beyond the four walls of the hospital, and facilitate true consumerism and “patient centeredness.”
What has been your most meaningful experience with SHM?
Attending the annual SHM meetings for the past several years, which have helped me to not only reap rewards from the numerous educational sessions but has also helped me develop a rich network of friends, colleagues, and mentors whose advice I solicit from time to time.
Amit Vashist, MD, SFHM, is the senior vice president and chief clinical officer at Ballad Health, an integrated 21-hospital health system serving 29 counties of northeast Tennessee, southwest Virginia, northwest North Carolina, and southeast Kentucky.
Dr. Vashist, who is a member of the Hospitalist’s editorial advisory board, focuses on clinical quality and safety, value-based initiatives to improve quality while reducing cost of care, performance improvement, and oversight of the enterprise-wide clinical delivery of care. He also provides administrative oversight of the Ballad Health Clinical Council – a model of physician partnership for clinical transformation and outcomes improvement.
Dr. Vashist is a dual board-certified internist and psychiatrist and an avid proponent of initiatives aimed at promoting quality, improving safety, reducing cost, and minimizing variation in the delivery of patient care across diverse settings. His work has been instrumental in improving outcomes and reducing mortality in patients with sepsis, earning him several local, regional, and national awards, and his work in promoting a zero-harm culture at Ballad Health has been instrumental in significantly reducing hospital-acquired infections system wide.
Prior to transitioning into the role of the chief clinical officer, Dr. Vashist served as the chair of the Ballad Health Clinical Council and the system chair for Ballad Health’s hospitalist division running a group of over 130 hospitalists.
Why did you choose a career in medicine?
The ability to have a positive impact and help others. In addition, I love learning new information and skills, and medicine affords one the opportunity to be a lifelong learner.
What do you like most about working as a hospitalist?
The relatively fast-paced nature of the work and the ability to tie seemingly fragmented episodes of patient care together. I believe that no other specialty offers that 30,000-foot vantage view of things in clinical medicine.
What do you like the least?
The shift worker mindset emanating from the traditional and rigid 7-on, 7-off model. A sense of team can be lost in this model and, contrary to conventional thinking, this model can accelerate hospitalist burnout.
What’s the best advice you ever received?
“You’ve gotta learn to listen!”
What’s the worst advice you ever received?
“Don’t rock the boat.” I strongly believe that frequent disruption is required to change the established status quo.
What aspect of patient care is most challenging?
A perceived disruption in the continuity of care by virtue of a new hospitalist seeing those patients, and the challenge to build the same level of trust and comfort as the outgoing hospitalist. Superior models of care have developed over the years promoting a better continuity of care but this domain continues to pose a challenge to proponents of hospital medicine.
What’s the biggest change you’ve seen in hospital medicine in your career?
Hospitalists being increasingly perceived as the “quarterbacks” and gatekeepers of quality, costs of care, and clinical outcomes in our hospitals and health care systems.
What’s the biggest change you would like to see in hospital medicine?
Inpatient volumes across the country continue to shrink, and this trend will not change for the foreseeable future. Hospitalists have got to embrace newer models of care faster, like hospitals at home, postacute care, transitional care clinics, hospital at home, etc. Remember what they say: “If you are not at the table, you are on the menu.” Now is our time to be at the table, and be the champions of change and move to true value (quality plus experience/cost), or else, we could end up and vanish like Blockbuster.
Outside of patient care, tell us about your career interests.
Implementing value-driven initiatives, pursuing endeavors aimed at cutting out waste and redundancy in health care, and developing a new generation of physician leaders with these skill sets.
Where do you see yourself in 10 years?
Leveraging my experience, training and expertise in hospital medicine to design better systems of health care that transcend above and beyond the four walls of the hospital, and facilitate true consumerism and “patient centeredness.”
What has been your most meaningful experience with SHM?
Attending the annual SHM meetings for the past several years, which have helped me to not only reap rewards from the numerous educational sessions but has also helped me develop a rich network of friends, colleagues, and mentors whose advice I solicit from time to time.
Amit Vashist, MD, SFHM, is the senior vice president and chief clinical officer at Ballad Health, an integrated 21-hospital health system serving 29 counties of northeast Tennessee, southwest Virginia, northwest North Carolina, and southeast Kentucky.
Dr. Vashist, who is a member of the Hospitalist’s editorial advisory board, focuses on clinical quality and safety, value-based initiatives to improve quality while reducing cost of care, performance improvement, and oversight of the enterprise-wide clinical delivery of care. He also provides administrative oversight of the Ballad Health Clinical Council – a model of physician partnership for clinical transformation and outcomes improvement.
Dr. Vashist is a dual board-certified internist and psychiatrist and an avid proponent of initiatives aimed at promoting quality, improving safety, reducing cost, and minimizing variation in the delivery of patient care across diverse settings. His work has been instrumental in improving outcomes and reducing mortality in patients with sepsis, earning him several local, regional, and national awards, and his work in promoting a zero-harm culture at Ballad Health has been instrumental in significantly reducing hospital-acquired infections system wide.
Prior to transitioning into the role of the chief clinical officer, Dr. Vashist served as the chair of the Ballad Health Clinical Council and the system chair for Ballad Health’s hospitalist division running a group of over 130 hospitalists.
Why did you choose a career in medicine?
The ability to have a positive impact and help others. In addition, I love learning new information and skills, and medicine affords one the opportunity to be a lifelong learner.
What do you like most about working as a hospitalist?
The relatively fast-paced nature of the work and the ability to tie seemingly fragmented episodes of patient care together. I believe that no other specialty offers that 30,000-foot vantage view of things in clinical medicine.
What do you like the least?
The shift worker mindset emanating from the traditional and rigid 7-on, 7-off model. A sense of team can be lost in this model and, contrary to conventional thinking, this model can accelerate hospitalist burnout.
What’s the best advice you ever received?
“You’ve gotta learn to listen!”
What’s the worst advice you ever received?
“Don’t rock the boat.” I strongly believe that frequent disruption is required to change the established status quo.
What aspect of patient care is most challenging?
A perceived disruption in the continuity of care by virtue of a new hospitalist seeing those patients, and the challenge to build the same level of trust and comfort as the outgoing hospitalist. Superior models of care have developed over the years promoting a better continuity of care but this domain continues to pose a challenge to proponents of hospital medicine.
What’s the biggest change you’ve seen in hospital medicine in your career?
Hospitalists being increasingly perceived as the “quarterbacks” and gatekeepers of quality, costs of care, and clinical outcomes in our hospitals and health care systems.
What’s the biggest change you would like to see in hospital medicine?
Inpatient volumes across the country continue to shrink, and this trend will not change for the foreseeable future. Hospitalists have got to embrace newer models of care faster, like hospitals at home, postacute care, transitional care clinics, hospital at home, etc. Remember what they say: “If you are not at the table, you are on the menu.” Now is our time to be at the table, and be the champions of change and move to true value (quality plus experience/cost), or else, we could end up and vanish like Blockbuster.
Outside of patient care, tell us about your career interests.
Implementing value-driven initiatives, pursuing endeavors aimed at cutting out waste and redundancy in health care, and developing a new generation of physician leaders with these skill sets.
Where do you see yourself in 10 years?
Leveraging my experience, training and expertise in hospital medicine to design better systems of health care that transcend above and beyond the four walls of the hospital, and facilitate true consumerism and “patient centeredness.”
What has been your most meaningful experience with SHM?
Attending the annual SHM meetings for the past several years, which have helped me to not only reap rewards from the numerous educational sessions but has also helped me develop a rich network of friends, colleagues, and mentors whose advice I solicit from time to time.
Hospitalist profile: Vineet Chopra, MD, MSc, FHM
Vineet Chopra, MD, MSc, FHM, is associate professor of medicine and chief of the Division of Hospital Medicine at Michigan Medicine and the VA Ann Arbor (Michigan) Health System. A career hospitalist, Dr. Chopra’s research is dedicated to improving the safety of hospitalized patients through prevention of hospital-acquired complications. His work focuses on identifying and preventing complications associated with central venous catheters with a particular emphasis on peripherally inserted central catheters (PICCs).
Dr. Chopra is the recipient of numerous teaching and research awards including the 2016 Kaiser Permanente Award for Clinical Teaching, the Jerome W. Conn Award for Outstanding Research in the Department of Medicine, the 2016 Society of Hospital Medicine Award for Excellence in Research, and the 2014 McDevitt Award for Research Excellence. He has published over 100 peer-reviewed articles and has served as associate editor for the American Journal of Medicine and Journal of Hospital Medicine.
At what point in your education/training did you decide to practice hospital medicine? What about hospital medicine appealed to you?
I think I knew very early – toward the middle of my intern year – that I wanted to be a hospitalist. There was much that drew me to the field. First, I loved being in the inpatient setting. The tempo of work, the unexpected nature of what may come next, and the opportunity to truly have an impact on a patients life at their time of greatest need appealed to me. I wasn’t as inclined towards the procedural fields and also loved the cognitive aspects of general medicine – doing the work up on a difficult diagnosis or medically managing a patient with acute coronary syndrome came naturally. I found myself loving the work so much so that it didn’t feel like work. And the rest was history!
What is your current role at Michigan Medicine?
I started at Michigan Medicine in 2008 as a full-time clinician taking care of patients on direct care and resident services. After 3 years of clinical work, I decided it was time to hone in on a specific skill set and went back to a research fellowship.
I become Michigan’s first fellow in hospital medicine – the guinea pig – for what would turn out to be one of the best decisions in my life. After finishing fellowship, I switched my focus from clinical work to research and rose up the ranks to receive tenure as an associate professor of medicine. After attaining tenure, I was among a handful of people in the nation who had success in both the research and the clinical arenas and leadership opportunities began to come my way.
I was fortunate to be recruited as the inaugural division chief of hospital medicine at Michigan Medicine in 2017. The Division of hospital medicine is the 13th in the department of medicine and the first one to be created in over 60 years. As division chief, I oversee all of our clinical, academic, research, and educational endeavors. Currently, we have approximately 130 hospitalists in our group and about 30 advanced practice providers (APPs) with a support and research staff of about 15 individuals. So I like to say we have a big family!
What are your favorite areas of clinical practice and/or research?
I am fortunate to have the ability to enjoy all that hospital medicine has to offer. I still appreciate the challenges that direct care brings, and I continue to do as much as I can in this area. I also enjoy working with residents and medical students at the university and at our VA site – where much of my focus is devoted to making sure all learners on the team are growing while they provide excellent patient care. To meet a new patient and work to develop a therapeutic relationship with them such that we can make positive changes in their disease trajectory remains my favorite part of clinical work.
My research work remains closely linked to my clinical interests around preventing patient harm and improving patient safety – so studying hospital-acquired infections, coming up with new ideas and strategies, and then implementing them when on clinical service represents the perfect blend of the two. My research is largely focused on intravenous devices and catheters, and I focus my work on preventing harms such as bloodstream infection, venous thrombosis, and related adverse events. I have been fortunate to receive national and international attention for my research, including adoption of my work into guidelines and changes to national policies. I am honored to serve on the most important federal advisory committee that advises the government on health care infections (the committee is called HICPAC – Healthcare Infection Control Practice Advisory Committee).
What are the most challenging aspects of practicing hospital medicine? What are the most rewarding?
For me, the most challenging aspects are also the most rewarding. First and foremost, making a connection with a patient and their family to understand their concerns and define a therapeutic alliance is both challenging and rewarding. Second, ensuring that we have the ability to work efficiently and effectively to manage patient care is sometimes challenging but also the most rewarding aspect of the job. I am fortunate to work in a health system where I am surrounded by smart colleagues, important resources, advanced technology, and the support of nurses and advanced practice providers who share this zeal of patient care with me.
Finally, one the greatest challenges and rewards remains time. Our work is hard and grueling, and it is often very challenging to get things done at different times of the day. But the ability to make a diagnosis or see a patient improve makes it all worth it!
How will hospital medicine change in the next decade or two?
I predict our work will shift from a model that is reactive – taking care of patients that are sick and need hospitalization – to a proactive approach where the focus will remain on keeping people out of the hospital. This doesn’t necessarily mean that we will be out of a job – but I see the model of our work shifting to ensure that patients who are discharged remain healthy and well. This means we will need to embrace extensivist models, hospital at home care, and aspects such as bridge clinics.
I also think our work will evolve to harness some of the incredible technology that surrounds us outside health care, but has not yet permeated our work flow. To that end, aspects such as virtual consultations and patient assessments, and remote monitoring that includes biometrics, will all fall into our workflow. And of course, lets not forget about the mighty electronic medical record and how that will affect our experience and work. I see much more of our work shifting toward becoming digital experts, harnessing the power of big data and predictive analytics to provide better care for patients. These are skills that are emerging in our field, but we have not yet mastered the art of managing data.
Do you have any advice for students and residents interested in hospital medicine?
I would highly recommend taking on a rotation with a hospitalist, carrying the pager and working side-by-side with someone who truly loves what they do. Many students and residents just see the on/off nature of the work, but that is truly skin deep in terms of attraction.
The beauty of hospital medicine is that you can be everything for a patient – their doctor, their health care navigator, their friend, and their partner during their hospital stay. Find that joy – you will not regret it!
Vineet Chopra, MD, MSc, FHM, is associate professor of medicine and chief of the Division of Hospital Medicine at Michigan Medicine and the VA Ann Arbor (Michigan) Health System. A career hospitalist, Dr. Chopra’s research is dedicated to improving the safety of hospitalized patients through prevention of hospital-acquired complications. His work focuses on identifying and preventing complications associated with central venous catheters with a particular emphasis on peripherally inserted central catheters (PICCs).
Dr. Chopra is the recipient of numerous teaching and research awards including the 2016 Kaiser Permanente Award for Clinical Teaching, the Jerome W. Conn Award for Outstanding Research in the Department of Medicine, the 2016 Society of Hospital Medicine Award for Excellence in Research, and the 2014 McDevitt Award for Research Excellence. He has published over 100 peer-reviewed articles and has served as associate editor for the American Journal of Medicine and Journal of Hospital Medicine.
At what point in your education/training did you decide to practice hospital medicine? What about hospital medicine appealed to you?
I think I knew very early – toward the middle of my intern year – that I wanted to be a hospitalist. There was much that drew me to the field. First, I loved being in the inpatient setting. The tempo of work, the unexpected nature of what may come next, and the opportunity to truly have an impact on a patients life at their time of greatest need appealed to me. I wasn’t as inclined towards the procedural fields and also loved the cognitive aspects of general medicine – doing the work up on a difficult diagnosis or medically managing a patient with acute coronary syndrome came naturally. I found myself loving the work so much so that it didn’t feel like work. And the rest was history!
What is your current role at Michigan Medicine?
I started at Michigan Medicine in 2008 as a full-time clinician taking care of patients on direct care and resident services. After 3 years of clinical work, I decided it was time to hone in on a specific skill set and went back to a research fellowship.
I become Michigan’s first fellow in hospital medicine – the guinea pig – for what would turn out to be one of the best decisions in my life. After finishing fellowship, I switched my focus from clinical work to research and rose up the ranks to receive tenure as an associate professor of medicine. After attaining tenure, I was among a handful of people in the nation who had success in both the research and the clinical arenas and leadership opportunities began to come my way.
I was fortunate to be recruited as the inaugural division chief of hospital medicine at Michigan Medicine in 2017. The Division of hospital medicine is the 13th in the department of medicine and the first one to be created in over 60 years. As division chief, I oversee all of our clinical, academic, research, and educational endeavors. Currently, we have approximately 130 hospitalists in our group and about 30 advanced practice providers (APPs) with a support and research staff of about 15 individuals. So I like to say we have a big family!
What are your favorite areas of clinical practice and/or research?
I am fortunate to have the ability to enjoy all that hospital medicine has to offer. I still appreciate the challenges that direct care brings, and I continue to do as much as I can in this area. I also enjoy working with residents and medical students at the university and at our VA site – where much of my focus is devoted to making sure all learners on the team are growing while they provide excellent patient care. To meet a new patient and work to develop a therapeutic relationship with them such that we can make positive changes in their disease trajectory remains my favorite part of clinical work.
My research work remains closely linked to my clinical interests around preventing patient harm and improving patient safety – so studying hospital-acquired infections, coming up with new ideas and strategies, and then implementing them when on clinical service represents the perfect blend of the two. My research is largely focused on intravenous devices and catheters, and I focus my work on preventing harms such as bloodstream infection, venous thrombosis, and related adverse events. I have been fortunate to receive national and international attention for my research, including adoption of my work into guidelines and changes to national policies. I am honored to serve on the most important federal advisory committee that advises the government on health care infections (the committee is called HICPAC – Healthcare Infection Control Practice Advisory Committee).
What are the most challenging aspects of practicing hospital medicine? What are the most rewarding?
For me, the most challenging aspects are also the most rewarding. First and foremost, making a connection with a patient and their family to understand their concerns and define a therapeutic alliance is both challenging and rewarding. Second, ensuring that we have the ability to work efficiently and effectively to manage patient care is sometimes challenging but also the most rewarding aspect of the job. I am fortunate to work in a health system where I am surrounded by smart colleagues, important resources, advanced technology, and the support of nurses and advanced practice providers who share this zeal of patient care with me.
Finally, one the greatest challenges and rewards remains time. Our work is hard and grueling, and it is often very challenging to get things done at different times of the day. But the ability to make a diagnosis or see a patient improve makes it all worth it!
How will hospital medicine change in the next decade or two?
I predict our work will shift from a model that is reactive – taking care of patients that are sick and need hospitalization – to a proactive approach where the focus will remain on keeping people out of the hospital. This doesn’t necessarily mean that we will be out of a job – but I see the model of our work shifting to ensure that patients who are discharged remain healthy and well. This means we will need to embrace extensivist models, hospital at home care, and aspects such as bridge clinics.
I also think our work will evolve to harness some of the incredible technology that surrounds us outside health care, but has not yet permeated our work flow. To that end, aspects such as virtual consultations and patient assessments, and remote monitoring that includes biometrics, will all fall into our workflow. And of course, lets not forget about the mighty electronic medical record and how that will affect our experience and work. I see much more of our work shifting toward becoming digital experts, harnessing the power of big data and predictive analytics to provide better care for patients. These are skills that are emerging in our field, but we have not yet mastered the art of managing data.
Do you have any advice for students and residents interested in hospital medicine?
I would highly recommend taking on a rotation with a hospitalist, carrying the pager and working side-by-side with someone who truly loves what they do. Many students and residents just see the on/off nature of the work, but that is truly skin deep in terms of attraction.
The beauty of hospital medicine is that you can be everything for a patient – their doctor, their health care navigator, their friend, and their partner during their hospital stay. Find that joy – you will not regret it!
Vineet Chopra, MD, MSc, FHM, is associate professor of medicine and chief of the Division of Hospital Medicine at Michigan Medicine and the VA Ann Arbor (Michigan) Health System. A career hospitalist, Dr. Chopra’s research is dedicated to improving the safety of hospitalized patients through prevention of hospital-acquired complications. His work focuses on identifying and preventing complications associated with central venous catheters with a particular emphasis on peripherally inserted central catheters (PICCs).
Dr. Chopra is the recipient of numerous teaching and research awards including the 2016 Kaiser Permanente Award for Clinical Teaching, the Jerome W. Conn Award for Outstanding Research in the Department of Medicine, the 2016 Society of Hospital Medicine Award for Excellence in Research, and the 2014 McDevitt Award for Research Excellence. He has published over 100 peer-reviewed articles and has served as associate editor for the American Journal of Medicine and Journal of Hospital Medicine.
At what point in your education/training did you decide to practice hospital medicine? What about hospital medicine appealed to you?
I think I knew very early – toward the middle of my intern year – that I wanted to be a hospitalist. There was much that drew me to the field. First, I loved being in the inpatient setting. The tempo of work, the unexpected nature of what may come next, and the opportunity to truly have an impact on a patients life at their time of greatest need appealed to me. I wasn’t as inclined towards the procedural fields and also loved the cognitive aspects of general medicine – doing the work up on a difficult diagnosis or medically managing a patient with acute coronary syndrome came naturally. I found myself loving the work so much so that it didn’t feel like work. And the rest was history!
What is your current role at Michigan Medicine?
I started at Michigan Medicine in 2008 as a full-time clinician taking care of patients on direct care and resident services. After 3 years of clinical work, I decided it was time to hone in on a specific skill set and went back to a research fellowship.
I become Michigan’s first fellow in hospital medicine – the guinea pig – for what would turn out to be one of the best decisions in my life. After finishing fellowship, I switched my focus from clinical work to research and rose up the ranks to receive tenure as an associate professor of medicine. After attaining tenure, I was among a handful of people in the nation who had success in both the research and the clinical arenas and leadership opportunities began to come my way.
I was fortunate to be recruited as the inaugural division chief of hospital medicine at Michigan Medicine in 2017. The Division of hospital medicine is the 13th in the department of medicine and the first one to be created in over 60 years. As division chief, I oversee all of our clinical, academic, research, and educational endeavors. Currently, we have approximately 130 hospitalists in our group and about 30 advanced practice providers (APPs) with a support and research staff of about 15 individuals. So I like to say we have a big family!
What are your favorite areas of clinical practice and/or research?
I am fortunate to have the ability to enjoy all that hospital medicine has to offer. I still appreciate the challenges that direct care brings, and I continue to do as much as I can in this area. I also enjoy working with residents and medical students at the university and at our VA site – where much of my focus is devoted to making sure all learners on the team are growing while they provide excellent patient care. To meet a new patient and work to develop a therapeutic relationship with them such that we can make positive changes in their disease trajectory remains my favorite part of clinical work.
My research work remains closely linked to my clinical interests around preventing patient harm and improving patient safety – so studying hospital-acquired infections, coming up with new ideas and strategies, and then implementing them when on clinical service represents the perfect blend of the two. My research is largely focused on intravenous devices and catheters, and I focus my work on preventing harms such as bloodstream infection, venous thrombosis, and related adverse events. I have been fortunate to receive national and international attention for my research, including adoption of my work into guidelines and changes to national policies. I am honored to serve on the most important federal advisory committee that advises the government on health care infections (the committee is called HICPAC – Healthcare Infection Control Practice Advisory Committee).
What are the most challenging aspects of practicing hospital medicine? What are the most rewarding?
For me, the most challenging aspects are also the most rewarding. First and foremost, making a connection with a patient and their family to understand their concerns and define a therapeutic alliance is both challenging and rewarding. Second, ensuring that we have the ability to work efficiently and effectively to manage patient care is sometimes challenging but also the most rewarding aspect of the job. I am fortunate to work in a health system where I am surrounded by smart colleagues, important resources, advanced technology, and the support of nurses and advanced practice providers who share this zeal of patient care with me.
Finally, one the greatest challenges and rewards remains time. Our work is hard and grueling, and it is often very challenging to get things done at different times of the day. But the ability to make a diagnosis or see a patient improve makes it all worth it!
How will hospital medicine change in the next decade or two?
I predict our work will shift from a model that is reactive – taking care of patients that are sick and need hospitalization – to a proactive approach where the focus will remain on keeping people out of the hospital. This doesn’t necessarily mean that we will be out of a job – but I see the model of our work shifting to ensure that patients who are discharged remain healthy and well. This means we will need to embrace extensivist models, hospital at home care, and aspects such as bridge clinics.
I also think our work will evolve to harness some of the incredible technology that surrounds us outside health care, but has not yet permeated our work flow. To that end, aspects such as virtual consultations and patient assessments, and remote monitoring that includes biometrics, will all fall into our workflow. And of course, lets not forget about the mighty electronic medical record and how that will affect our experience and work. I see much more of our work shifting toward becoming digital experts, harnessing the power of big data and predictive analytics to provide better care for patients. These are skills that are emerging in our field, but we have not yet mastered the art of managing data.
Do you have any advice for students and residents interested in hospital medicine?
I would highly recommend taking on a rotation with a hospitalist, carrying the pager and working side-by-side with someone who truly loves what they do. Many students and residents just see the on/off nature of the work, but that is truly skin deep in terms of attraction.
The beauty of hospital medicine is that you can be everything for a patient – their doctor, their health care navigator, their friend, and their partner during their hospital stay. Find that joy – you will not regret it!
‘Momentous’ USMLE change: New pass/fail format stuns medicine
News that the United States Medical Licensing Examination (USMLE) program will change its Step 1 scoring from a 3-digit number to pass/fail starting Jan. 1, 2022, has set off a flurry of shocked responses from students and physicians.
J. Bryan Carmody, MD, MPH, an assistant professor at Eastern Virginia Medical School in Norfolk, said in an interview that he was “stunned” when he heard the news on Wednesday and said the switch presents “the single biggest opportunity for medical school education reform since the Flexner Report,” which in 1910 established standards for modern medical education.
Numbers will continue for some tests
The USMLE cosponsors – the Federation of State Medical Boards (FSMB) and the National Board of Medical Examiners (NBME) – said that the Step 2 Clinical Knowledge (CK) exam and Step 3 will continue to be scored numerically. Step 2 Clinical Skills (CS) will continue its pass/fail system.
The change was made after Step 1 had been roundly criticized as playing too big a role in the process of becoming a physician and for causing students to study for the test instead of engaging fully in their medical education.
Ramie Fathy, a third-year medical student at the University of Pennsylvania, Philadelphia, currently studying for Step 1, said in an interview that it would have been nice personally to have the pass/fail choice, but he predicts both good and unintended consequences in the change.
The positive news, Mr. Fathy said, is that less emphasis will be put on the Step 1 test, which includes memorizing basic science details that may or not be relevant depending on later specialty choice.
“It’s not necessarily measuring what the test makers intended, which was whether or not a student can understand and apply basic science concepts to the practice of medicine,” he said.
“The current system encourages students to get as high a score as possible, which – after a certain point – translates to memorizing many little details that become increasingly less practically relevant,” Mr. Fathy said.
Pressure may move elsewhere?
However, Mr. Fathy worries that, without a scoring system to help decide who stands out in Step 1, residency program directors will depend more on the reputation of candidates’ medical school and the clout of the person writing a letter of recommendation – factors that are often influenced by family resources and social standing. That could wedge a further economic divide into the path to becoming a physician.
Mr. Fathy said he and fellow students are watching for information on what the passing bar will be and what happens with Step 2 Clinical Knowledge exam. USMLE has promised more information as soon as it is available.
“The question is whether that test will replace Step 1 as the standardized metric of student competency,” Mr. Fathy said, which would put more pressure on students further down the medical path.
Will Step 2 anxiety increase?
Dr. Carmody agreed that there is the danger that students now will spend their time studying for Step 2 CK at the expense of other parts of their education.
Meaningful reform will depend on the pass/fail move being coupled with other reforms, most importantly application caps, said Dr. Carmody, who teaches preclinical medical students and works with the residency program.
He has been blogging about Step 1 pass/fail for the past year.
Currently students can apply for as many residencies as they can pay for and Carmody said the number of applications per student has been rising over the past decade.
“That puts program directors under an impossible burden,” he said. “With our Step 1-based system, there’s significant inequality in the number of interviews people get. Programs end up overinviting the same group of people who look good on paper.”
People outside that group respond by sending more applications than they need to just to get a few interviews, Dr. Carmody added.
With caps, students would have an incentive to apply to only those programs in which they had a sincere interest, he said. Program directors also would then be better able to evaluate each application.
Switching Step 1 to pass/fail may have some effect on medical school burnout, Dr. Carmody said.
“It’s one thing to work hard when you’re on call and your patients depend on it,” he said. “But I would have a hard time staying up late every night studying something that I know in my heart is not going to help my patients, but I have to do it because I have to do better than the person who’s studying in the apartment next to me.”
Test has strayed from original purpose
Joseph Safdieh, MD, an assistant dean for clinical curriculum and director of the medical student neurology clerkship for the Weill Cornell Medicine, New York, sees the move as positive overall.
“We should not be using any single metric to define or describe our students’ overall profile,” he said in an interview.
“This has been a very significant anxiety point for our medical students for quite a number of years,” Dr. Safdieh said. “They were frustrated that their entire 4 years of medical school seemingly came down to one number.”
The test was created originally as one of three parts of licensure, he pointed out.
“Over the past 10 or 15 years, the exam has morphed to become a litmus test for very specific residency programs,” he said.
However, Dr. Safdieh has concerns that Step 2 will cultivate the same anxiety and may get too big a spotlight without the Step 1 metric, “although one could argue that test does more accurately reflect clinical material,” he said.
He also worries that students who have selected a specialty by the time they take Step 2 may find late in the game that they are less competitive in their field than they thought they were and may have to make a last-minute switch.
Dr. Safdieh said he thinks Step 2 will be next to go the pass/fail route. In reading between the lines of the announcement, he believes the test cosponsors didn’t make both pass/fail at once because it would have been “a nuclear bomb to the system.”
He credited the cosponsors with making what he called a “bold and momentous decision to initiate radical change in the overall transition between undergraduate and graduate medical education.”
Dr. Safdieh added that few in medicine were expecting Wednesday’s announcement.
“I think many of us were expecting them to go to quartile grading, not to go this far,” he said.
Dr. Safdieh suggested that, among those who may see downstream effects from the pass/fail move are offshore schools, such as those in the Caribbean. “Those schools rely on Step 1 to demonstrate that their students are meeting the rigor,” he said. But he hopes that this will lead to more holistic review.
“We’re hoping that this will force change in the system so that residency directors will look at more than just test-taking ability. They’ll look at publications and scholarship, community service and advocacy and performance in medical school,” Dr. Safdieh said.
Alison J. Whelan, MD, chief medical education officer of the Association of American Medical Colleges said in a statement, “The transition from medical school to residency training is a matter of great concern throughout academic medicine.
“The decision by the NBME and FSMB to change USMLE Step 1 score reporting to pass/fail was very carefully considered to balance student learning and student well-being,” she said. “The medical education community must now work together to identify and implement additional changes to improve the overall UME-GME [undergraduate and graduate medical education] transition system for all stakeholders and the AAMC is committed to helping lead this work.”
Dr. Fathy, Dr. Carmody, and Dr. Safdieh have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
News that the United States Medical Licensing Examination (USMLE) program will change its Step 1 scoring from a 3-digit number to pass/fail starting Jan. 1, 2022, has set off a flurry of shocked responses from students and physicians.
J. Bryan Carmody, MD, MPH, an assistant professor at Eastern Virginia Medical School in Norfolk, said in an interview that he was “stunned” when he heard the news on Wednesday and said the switch presents “the single biggest opportunity for medical school education reform since the Flexner Report,” which in 1910 established standards for modern medical education.
Numbers will continue for some tests
The USMLE cosponsors – the Federation of State Medical Boards (FSMB) and the National Board of Medical Examiners (NBME) – said that the Step 2 Clinical Knowledge (CK) exam and Step 3 will continue to be scored numerically. Step 2 Clinical Skills (CS) will continue its pass/fail system.
The change was made after Step 1 had been roundly criticized as playing too big a role in the process of becoming a physician and for causing students to study for the test instead of engaging fully in their medical education.
Ramie Fathy, a third-year medical student at the University of Pennsylvania, Philadelphia, currently studying for Step 1, said in an interview that it would have been nice personally to have the pass/fail choice, but he predicts both good and unintended consequences in the change.
The positive news, Mr. Fathy said, is that less emphasis will be put on the Step 1 test, which includes memorizing basic science details that may or not be relevant depending on later specialty choice.
“It’s not necessarily measuring what the test makers intended, which was whether or not a student can understand and apply basic science concepts to the practice of medicine,” he said.
“The current system encourages students to get as high a score as possible, which – after a certain point – translates to memorizing many little details that become increasingly less practically relevant,” Mr. Fathy said.
Pressure may move elsewhere?
However, Mr. Fathy worries that, without a scoring system to help decide who stands out in Step 1, residency program directors will depend more on the reputation of candidates’ medical school and the clout of the person writing a letter of recommendation – factors that are often influenced by family resources and social standing. That could wedge a further economic divide into the path to becoming a physician.
Mr. Fathy said he and fellow students are watching for information on what the passing bar will be and what happens with Step 2 Clinical Knowledge exam. USMLE has promised more information as soon as it is available.
“The question is whether that test will replace Step 1 as the standardized metric of student competency,” Mr. Fathy said, which would put more pressure on students further down the medical path.
Will Step 2 anxiety increase?
Dr. Carmody agreed that there is the danger that students now will spend their time studying for Step 2 CK at the expense of other parts of their education.
Meaningful reform will depend on the pass/fail move being coupled with other reforms, most importantly application caps, said Dr. Carmody, who teaches preclinical medical students and works with the residency program.
He has been blogging about Step 1 pass/fail for the past year.
Currently students can apply for as many residencies as they can pay for and Carmody said the number of applications per student has been rising over the past decade.
“That puts program directors under an impossible burden,” he said. “With our Step 1-based system, there’s significant inequality in the number of interviews people get. Programs end up overinviting the same group of people who look good on paper.”
People outside that group respond by sending more applications than they need to just to get a few interviews, Dr. Carmody added.
With caps, students would have an incentive to apply to only those programs in which they had a sincere interest, he said. Program directors also would then be better able to evaluate each application.
Switching Step 1 to pass/fail may have some effect on medical school burnout, Dr. Carmody said.
“It’s one thing to work hard when you’re on call and your patients depend on it,” he said. “But I would have a hard time staying up late every night studying something that I know in my heart is not going to help my patients, but I have to do it because I have to do better than the person who’s studying in the apartment next to me.”
Test has strayed from original purpose
Joseph Safdieh, MD, an assistant dean for clinical curriculum and director of the medical student neurology clerkship for the Weill Cornell Medicine, New York, sees the move as positive overall.
“We should not be using any single metric to define or describe our students’ overall profile,” he said in an interview.
“This has been a very significant anxiety point for our medical students for quite a number of years,” Dr. Safdieh said. “They were frustrated that their entire 4 years of medical school seemingly came down to one number.”
The test was created originally as one of three parts of licensure, he pointed out.
“Over the past 10 or 15 years, the exam has morphed to become a litmus test for very specific residency programs,” he said.
However, Dr. Safdieh has concerns that Step 2 will cultivate the same anxiety and may get too big a spotlight without the Step 1 metric, “although one could argue that test does more accurately reflect clinical material,” he said.
He also worries that students who have selected a specialty by the time they take Step 2 may find late in the game that they are less competitive in their field than they thought they were and may have to make a last-minute switch.
Dr. Safdieh said he thinks Step 2 will be next to go the pass/fail route. In reading between the lines of the announcement, he believes the test cosponsors didn’t make both pass/fail at once because it would have been “a nuclear bomb to the system.”
He credited the cosponsors with making what he called a “bold and momentous decision to initiate radical change in the overall transition between undergraduate and graduate medical education.”
Dr. Safdieh added that few in medicine were expecting Wednesday’s announcement.
“I think many of us were expecting them to go to quartile grading, not to go this far,” he said.
Dr. Safdieh suggested that, among those who may see downstream effects from the pass/fail move are offshore schools, such as those in the Caribbean. “Those schools rely on Step 1 to demonstrate that their students are meeting the rigor,” he said. But he hopes that this will lead to more holistic review.
“We’re hoping that this will force change in the system so that residency directors will look at more than just test-taking ability. They’ll look at publications and scholarship, community service and advocacy and performance in medical school,” Dr. Safdieh said.
Alison J. Whelan, MD, chief medical education officer of the Association of American Medical Colleges said in a statement, “The transition from medical school to residency training is a matter of great concern throughout academic medicine.
“The decision by the NBME and FSMB to change USMLE Step 1 score reporting to pass/fail was very carefully considered to balance student learning and student well-being,” she said. “The medical education community must now work together to identify and implement additional changes to improve the overall UME-GME [undergraduate and graduate medical education] transition system for all stakeholders and the AAMC is committed to helping lead this work.”
Dr. Fathy, Dr. Carmody, and Dr. Safdieh have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
News that the United States Medical Licensing Examination (USMLE) program will change its Step 1 scoring from a 3-digit number to pass/fail starting Jan. 1, 2022, has set off a flurry of shocked responses from students and physicians.
J. Bryan Carmody, MD, MPH, an assistant professor at Eastern Virginia Medical School in Norfolk, said in an interview that he was “stunned” when he heard the news on Wednesday and said the switch presents “the single biggest opportunity for medical school education reform since the Flexner Report,” which in 1910 established standards for modern medical education.
Numbers will continue for some tests
The USMLE cosponsors – the Federation of State Medical Boards (FSMB) and the National Board of Medical Examiners (NBME) – said that the Step 2 Clinical Knowledge (CK) exam and Step 3 will continue to be scored numerically. Step 2 Clinical Skills (CS) will continue its pass/fail system.
The change was made after Step 1 had been roundly criticized as playing too big a role in the process of becoming a physician and for causing students to study for the test instead of engaging fully in their medical education.
Ramie Fathy, a third-year medical student at the University of Pennsylvania, Philadelphia, currently studying for Step 1, said in an interview that it would have been nice personally to have the pass/fail choice, but he predicts both good and unintended consequences in the change.
The positive news, Mr. Fathy said, is that less emphasis will be put on the Step 1 test, which includes memorizing basic science details that may or not be relevant depending on later specialty choice.
“It’s not necessarily measuring what the test makers intended, which was whether or not a student can understand and apply basic science concepts to the practice of medicine,” he said.
“The current system encourages students to get as high a score as possible, which – after a certain point – translates to memorizing many little details that become increasingly less practically relevant,” Mr. Fathy said.
Pressure may move elsewhere?
However, Mr. Fathy worries that, without a scoring system to help decide who stands out in Step 1, residency program directors will depend more on the reputation of candidates’ medical school and the clout of the person writing a letter of recommendation – factors that are often influenced by family resources and social standing. That could wedge a further economic divide into the path to becoming a physician.
Mr. Fathy said he and fellow students are watching for information on what the passing bar will be and what happens with Step 2 Clinical Knowledge exam. USMLE has promised more information as soon as it is available.
“The question is whether that test will replace Step 1 as the standardized metric of student competency,” Mr. Fathy said, which would put more pressure on students further down the medical path.
Will Step 2 anxiety increase?
Dr. Carmody agreed that there is the danger that students now will spend their time studying for Step 2 CK at the expense of other parts of their education.
Meaningful reform will depend on the pass/fail move being coupled with other reforms, most importantly application caps, said Dr. Carmody, who teaches preclinical medical students and works with the residency program.
He has been blogging about Step 1 pass/fail for the past year.
Currently students can apply for as many residencies as they can pay for and Carmody said the number of applications per student has been rising over the past decade.
“That puts program directors under an impossible burden,” he said. “With our Step 1-based system, there’s significant inequality in the number of interviews people get. Programs end up overinviting the same group of people who look good on paper.”
People outside that group respond by sending more applications than they need to just to get a few interviews, Dr. Carmody added.
With caps, students would have an incentive to apply to only those programs in which they had a sincere interest, he said. Program directors also would then be better able to evaluate each application.
Switching Step 1 to pass/fail may have some effect on medical school burnout, Dr. Carmody said.
“It’s one thing to work hard when you’re on call and your patients depend on it,” he said. “But I would have a hard time staying up late every night studying something that I know in my heart is not going to help my patients, but I have to do it because I have to do better than the person who’s studying in the apartment next to me.”
Test has strayed from original purpose
Joseph Safdieh, MD, an assistant dean for clinical curriculum and director of the medical student neurology clerkship for the Weill Cornell Medicine, New York, sees the move as positive overall.
“We should not be using any single metric to define or describe our students’ overall profile,” he said in an interview.
“This has been a very significant anxiety point for our medical students for quite a number of years,” Dr. Safdieh said. “They were frustrated that their entire 4 years of medical school seemingly came down to one number.”
The test was created originally as one of three parts of licensure, he pointed out.
“Over the past 10 or 15 years, the exam has morphed to become a litmus test for very specific residency programs,” he said.
However, Dr. Safdieh has concerns that Step 2 will cultivate the same anxiety and may get too big a spotlight without the Step 1 metric, “although one could argue that test does more accurately reflect clinical material,” he said.
He also worries that students who have selected a specialty by the time they take Step 2 may find late in the game that they are less competitive in their field than they thought they were and may have to make a last-minute switch.
Dr. Safdieh said he thinks Step 2 will be next to go the pass/fail route. In reading between the lines of the announcement, he believes the test cosponsors didn’t make both pass/fail at once because it would have been “a nuclear bomb to the system.”
He credited the cosponsors with making what he called a “bold and momentous decision to initiate radical change in the overall transition between undergraduate and graduate medical education.”
Dr. Safdieh added that few in medicine were expecting Wednesday’s announcement.
“I think many of us were expecting them to go to quartile grading, not to go this far,” he said.
Dr. Safdieh suggested that, among those who may see downstream effects from the pass/fail move are offshore schools, such as those in the Caribbean. “Those schools rely on Step 1 to demonstrate that their students are meeting the rigor,” he said. But he hopes that this will lead to more holistic review.
“We’re hoping that this will force change in the system so that residency directors will look at more than just test-taking ability. They’ll look at publications and scholarship, community service and advocacy and performance in medical school,” Dr. Safdieh said.
Alison J. Whelan, MD, chief medical education officer of the Association of American Medical Colleges said in a statement, “The transition from medical school to residency training is a matter of great concern throughout academic medicine.
“The decision by the NBME and FSMB to change USMLE Step 1 score reporting to pass/fail was very carefully considered to balance student learning and student well-being,” she said. “The medical education community must now work together to identify and implement additional changes to improve the overall UME-GME [undergraduate and graduate medical education] transition system for all stakeholders and the AAMC is committed to helping lead this work.”
Dr. Fathy, Dr. Carmody, and Dr. Safdieh have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Resetting your compensation
Using the State of Hospital Medicine Report to bolster your proposal
In the ever-changing world of health care, one thing is for sure: If you’re not paying attention, you’re falling behind. In this column, I will discuss how you may utilize the Society of Hospital Medicine (SHM) State of Hospital Medicine Report (SoHM) to evaluate your current compensation structure and strengthen your business plan for change. For purposes of this exercise, I will focus on data referenced as Internal Medicine only, hospital-owned Hospital Medicine Groups (HMG).
Issues with retention, recruitment, or burnout may be among the first factors that lead you to reevaluate your compensation plan. The SoHM Report can help you to take a dive into feedback for these areas. Look for any indications that compensation may be affecting your turnover, inability to hire, or leaving your current team frustrated with their current pay structure. Feedback surrounding each of these factors may drive you to evaluate your comp plan but remain mindful that money is not always the answer.
You may complete your evaluation and find the data could suggest you are in fact well paid for the work you do. Even though this may be the case, the evaluation and transparency to your provider team may help flush out the real reason you are struggling with recruitment, retention, or burnout. However, if you do find you have an opportunity to improve your compensation structure, remember that you will need a compelling, data-driven case, to present to your C-suite.
Let us start by understanding how the market has changed over time using data from the 2014, 2016, and 2018 SoHM Reports. Of note, each report is based on data from the prior year. Since 2013, hospital owned HMGs have seen a 16% increase in total compensation while experiencing only a 9% increase in collections. Meanwhile RVU productivity has remained relatively stable over time. From this, we see hospitalists are earning more for similar productivity. The hospital reimbursement for professional fees has not grown at the same rate as compensation. Also, the collection per RVU has remained relatively flat over time.
It’s simple: Hospitalists are earning more and professional revenues are not making up the difference. This market change is driving hospitals to invest more money to maintain their HMGs. If your hospital hasn’t been responding to these data, you will need a strong business plan to get buy in from your hospital administration.
Now that you have evaluated the market change, it is time to put some optics on where your compensation falls in the current market. When you combine your total compensation with your total RVU productivity, you can use the SoHM Report to evaluate the current reported benchmarks for Compensation per RVU. Plotting these benchmarks against your own compensation and any proposed changes can help your administration really begin to see whether a change should be considered. Providing that clear picture in relevance to the SoHM benchmark is important, as a chart or graph can simplify your C-suite’s understanding of your proposal.
By simplifying your example using Compensation per RVU, you are making the conversation easier to follow. Your hospital leaders can clearly see the cost for every RVU generated and understand the impact. This is not to say that you should base your compensation around productivity. It is merely a way to roll in all compensation factors, whether quality related, performance based, or productivity driven, and tie them to a metric that is clear and easy for administration to understand.
Remember, when designing your new compensation plan, you can reference the SoHM Report to see how HMGs around the country are providing incentive and what percentage of compensation is based on incentive. There are sections within the report directly outlining these data points.
Now that we have reviewed market change and how to visualize change between your current and proposed future state, I will leave you with some final thoughts regarding other considerations when building your business plan:
- Focus on only physician-generated RVUs.
- Consider Length of Stay impact on productivity.
- Decide if Case Mix Index changes have impacted your staffing needs.
- Understand your E and M coding practices in reference to industry benchmarks. The SoHM Report provides benchmarks for billing practices across the country.
- Lastly, clearly identify the issues you want to address and set goals with measurable outcomes.
There is still time for your group to be part of the 2020 State of Hospital Medicine Report data by participating in the 2020 Survey. Data are being accepted through Feb. 28, 2020. Submit your data at www.hospitalmedicine.org/2020survey.
Mr. Sandroni is director of operations, hospitalists, at Rochester (N.Y.) Regional Health.
Using the State of Hospital Medicine Report to bolster your proposal
Using the State of Hospital Medicine Report to bolster your proposal
In the ever-changing world of health care, one thing is for sure: If you’re not paying attention, you’re falling behind. In this column, I will discuss how you may utilize the Society of Hospital Medicine (SHM) State of Hospital Medicine Report (SoHM) to evaluate your current compensation structure and strengthen your business plan for change. For purposes of this exercise, I will focus on data referenced as Internal Medicine only, hospital-owned Hospital Medicine Groups (HMG).
Issues with retention, recruitment, or burnout may be among the first factors that lead you to reevaluate your compensation plan. The SoHM Report can help you to take a dive into feedback for these areas. Look for any indications that compensation may be affecting your turnover, inability to hire, or leaving your current team frustrated with their current pay structure. Feedback surrounding each of these factors may drive you to evaluate your comp plan but remain mindful that money is not always the answer.
You may complete your evaluation and find the data could suggest you are in fact well paid for the work you do. Even though this may be the case, the evaluation and transparency to your provider team may help flush out the real reason you are struggling with recruitment, retention, or burnout. However, if you do find you have an opportunity to improve your compensation structure, remember that you will need a compelling, data-driven case, to present to your C-suite.
Let us start by understanding how the market has changed over time using data from the 2014, 2016, and 2018 SoHM Reports. Of note, each report is based on data from the prior year. Since 2013, hospital owned HMGs have seen a 16% increase in total compensation while experiencing only a 9% increase in collections. Meanwhile RVU productivity has remained relatively stable over time. From this, we see hospitalists are earning more for similar productivity. The hospital reimbursement for professional fees has not grown at the same rate as compensation. Also, the collection per RVU has remained relatively flat over time.
It’s simple: Hospitalists are earning more and professional revenues are not making up the difference. This market change is driving hospitals to invest more money to maintain their HMGs. If your hospital hasn’t been responding to these data, you will need a strong business plan to get buy in from your hospital administration.
Now that you have evaluated the market change, it is time to put some optics on where your compensation falls in the current market. When you combine your total compensation with your total RVU productivity, you can use the SoHM Report to evaluate the current reported benchmarks for Compensation per RVU. Plotting these benchmarks against your own compensation and any proposed changes can help your administration really begin to see whether a change should be considered. Providing that clear picture in relevance to the SoHM benchmark is important, as a chart or graph can simplify your C-suite’s understanding of your proposal.
By simplifying your example using Compensation per RVU, you are making the conversation easier to follow. Your hospital leaders can clearly see the cost for every RVU generated and understand the impact. This is not to say that you should base your compensation around productivity. It is merely a way to roll in all compensation factors, whether quality related, performance based, or productivity driven, and tie them to a metric that is clear and easy for administration to understand.
Remember, when designing your new compensation plan, you can reference the SoHM Report to see how HMGs around the country are providing incentive and what percentage of compensation is based on incentive. There are sections within the report directly outlining these data points.
Now that we have reviewed market change and how to visualize change between your current and proposed future state, I will leave you with some final thoughts regarding other considerations when building your business plan:
- Focus on only physician-generated RVUs.
- Consider Length of Stay impact on productivity.
- Decide if Case Mix Index changes have impacted your staffing needs.
- Understand your E and M coding practices in reference to industry benchmarks. The SoHM Report provides benchmarks for billing practices across the country.
- Lastly, clearly identify the issues you want to address and set goals with measurable outcomes.
There is still time for your group to be part of the 2020 State of Hospital Medicine Report data by participating in the 2020 Survey. Data are being accepted through Feb. 28, 2020. Submit your data at www.hospitalmedicine.org/2020survey.
Mr. Sandroni is director of operations, hospitalists, at Rochester (N.Y.) Regional Health.
In the ever-changing world of health care, one thing is for sure: If you’re not paying attention, you’re falling behind. In this column, I will discuss how you may utilize the Society of Hospital Medicine (SHM) State of Hospital Medicine Report (SoHM) to evaluate your current compensation structure and strengthen your business plan for change. For purposes of this exercise, I will focus on data referenced as Internal Medicine only, hospital-owned Hospital Medicine Groups (HMG).
Issues with retention, recruitment, or burnout may be among the first factors that lead you to reevaluate your compensation plan. The SoHM Report can help you to take a dive into feedback for these areas. Look for any indications that compensation may be affecting your turnover, inability to hire, or leaving your current team frustrated with their current pay structure. Feedback surrounding each of these factors may drive you to evaluate your comp plan but remain mindful that money is not always the answer.
You may complete your evaluation and find the data could suggest you are in fact well paid for the work you do. Even though this may be the case, the evaluation and transparency to your provider team may help flush out the real reason you are struggling with recruitment, retention, or burnout. However, if you do find you have an opportunity to improve your compensation structure, remember that you will need a compelling, data-driven case, to present to your C-suite.
Let us start by understanding how the market has changed over time using data from the 2014, 2016, and 2018 SoHM Reports. Of note, each report is based on data from the prior year. Since 2013, hospital owned HMGs have seen a 16% increase in total compensation while experiencing only a 9% increase in collections. Meanwhile RVU productivity has remained relatively stable over time. From this, we see hospitalists are earning more for similar productivity. The hospital reimbursement for professional fees has not grown at the same rate as compensation. Also, the collection per RVU has remained relatively flat over time.
It’s simple: Hospitalists are earning more and professional revenues are not making up the difference. This market change is driving hospitals to invest more money to maintain their HMGs. If your hospital hasn’t been responding to these data, you will need a strong business plan to get buy in from your hospital administration.
Now that you have evaluated the market change, it is time to put some optics on where your compensation falls in the current market. When you combine your total compensation with your total RVU productivity, you can use the SoHM Report to evaluate the current reported benchmarks for Compensation per RVU. Plotting these benchmarks against your own compensation and any proposed changes can help your administration really begin to see whether a change should be considered. Providing that clear picture in relevance to the SoHM benchmark is important, as a chart or graph can simplify your C-suite’s understanding of your proposal.
By simplifying your example using Compensation per RVU, you are making the conversation easier to follow. Your hospital leaders can clearly see the cost for every RVU generated and understand the impact. This is not to say that you should base your compensation around productivity. It is merely a way to roll in all compensation factors, whether quality related, performance based, or productivity driven, and tie them to a metric that is clear and easy for administration to understand.
Remember, when designing your new compensation plan, you can reference the SoHM Report to see how HMGs around the country are providing incentive and what percentage of compensation is based on incentive. There are sections within the report directly outlining these data points.
Now that we have reviewed market change and how to visualize change between your current and proposed future state, I will leave you with some final thoughts regarding other considerations when building your business plan:
- Focus on only physician-generated RVUs.
- Consider Length of Stay impact on productivity.
- Decide if Case Mix Index changes have impacted your staffing needs.
- Understand your E and M coding practices in reference to industry benchmarks. The SoHM Report provides benchmarks for billing practices across the country.
- Lastly, clearly identify the issues you want to address and set goals with measurable outcomes.
There is still time for your group to be part of the 2020 State of Hospital Medicine Report data by participating in the 2020 Survey. Data are being accepted through Feb. 28, 2020. Submit your data at www.hospitalmedicine.org/2020survey.
Mr. Sandroni is director of operations, hospitalists, at Rochester (N.Y.) Regional Health.
Work the program for NP/PAs, and the program will work
A ‘knowledge gap’ in best practices exists
Hospital medicine has been the fastest growing medical specialty since the term “hospitalist” was coined by Bob Wachter, MD, in the famous 1996 New England Journal of Medicine article (doi: 10.1056/NEJM199608153350713). The growth and change within this specialty is also reflected in the changing and migrating target of hospitals and hospital systems as they continue to effectively and safely move from fee-for-service to a payer model that rewards value and improvement in the health of a population – both in and outside of hospital walls.
In a short time, nurse practitioners and physician assistants have become a growing population in the hospital medicine workforce. The 2018 State of Hospital Medicine Report notes a 42% increase in 4 years, and about 75% of hospital medicine groups across the country currently incorporate NP/PAs within a hospital medicine practice. This evolution has occurred in the setting of a looming and well-documented physician shortage, a variety of cost pressures on hospitals that reflect the need for an efficient and cost-effective care delivery model, an increasing NP/PA workforce (the Department of Labor notes increases of 35% and 36% respectively by 2036), and data that indicates similar outcomes, for example, HCAHPS (the Hospital Consumer Assessment of Healthcare Providers and Systems), readmission, and morbidity and mortality in NP/PA-driven care.
This evolution, however, reveals a true knowledge gap in best practices related to integration of these providers. This is impacted by wide variability in the preparation of NPs – they may enter hospitalist practice from a variety of clinical exposures and training, for example, adult gerontology acute care, adult, or even, in some states, family NPs. For PAs, this is reflected in the variety of clinical rotations and pregraduate clinical exposure.
This variability is compounded, too, by the lack of standardization of hospital medicine practices, both with site size and patient acuity, a variety of challenges that drive the need for integration of NP/PA providers, and by-laws that define advanced practice clinical models and function.
In that perspective, it is important to define what constitutes a leading and successful advanced practice provider (APP) integration program. I would suggest:
- A structured and formalized transition-to-practice program for all new graduates and those new to hospital medicine. This program should consist of clinical volume progression, formalized didactic congruent with the Society of Hospital Medicine Core Competencies, and a process for evaluating knowledge and decision making throughout the program and upon completion.
- Development of physician competencies related to APP integration. Physicians are not prepared in their medical school training or residency to understand the differences and similarities of NP/PA providers. These competencies should be required and can best be developed through steady leadership, formalized instruction and accountability for professional teamwork.
- Allowance for NP/PA providers to work at the top of their skills and license. This means utilizing NP/PAs as providers who care for patients – not as scribes or clerical workers. The evolution of the acuity of patients provided for may evolve with the skill set and experience of NP/PAs, but it will evolve – especially if steps 1 and 2 are in place.
- Productivity expectations that reach near physician level of volume. In 2016 State of Hospital Medicine Report data, yearly billable encounters for NP/PAs were within 10% of that of physicians. I think 15% is a reasonable goal.
- Implementation and support of APP administrative leadership structure at the system/site level. This can be as simple as having APPs on the same leadership committees as physician team members, being involved in hiring and training newer physicians and NP/PAs or as broad as having all NP/PAs report to an APP leader. Having an intentional leadership structure that demonstrates and reflects inclusivity and belonging is crucial.
Consistent application of these frameworks will provide a strong infrastructure for successful NP/PA practice.
Ms. Cardin is currently the vice president of advanced practice providers at Sound Physicians and serves on SHM’s board of directors as its secretary. This article appeared initially at the Hospital Leader, the official blog of SHM.
A ‘knowledge gap’ in best practices exists
A ‘knowledge gap’ in best practices exists
Hospital medicine has been the fastest growing medical specialty since the term “hospitalist” was coined by Bob Wachter, MD, in the famous 1996 New England Journal of Medicine article (doi: 10.1056/NEJM199608153350713). The growth and change within this specialty is also reflected in the changing and migrating target of hospitals and hospital systems as they continue to effectively and safely move from fee-for-service to a payer model that rewards value and improvement in the health of a population – both in and outside of hospital walls.
In a short time, nurse practitioners and physician assistants have become a growing population in the hospital medicine workforce. The 2018 State of Hospital Medicine Report notes a 42% increase in 4 years, and about 75% of hospital medicine groups across the country currently incorporate NP/PAs within a hospital medicine practice. This evolution has occurred in the setting of a looming and well-documented physician shortage, a variety of cost pressures on hospitals that reflect the need for an efficient and cost-effective care delivery model, an increasing NP/PA workforce (the Department of Labor notes increases of 35% and 36% respectively by 2036), and data that indicates similar outcomes, for example, HCAHPS (the Hospital Consumer Assessment of Healthcare Providers and Systems), readmission, and morbidity and mortality in NP/PA-driven care.
This evolution, however, reveals a true knowledge gap in best practices related to integration of these providers. This is impacted by wide variability in the preparation of NPs – they may enter hospitalist practice from a variety of clinical exposures and training, for example, adult gerontology acute care, adult, or even, in some states, family NPs. For PAs, this is reflected in the variety of clinical rotations and pregraduate clinical exposure.
This variability is compounded, too, by the lack of standardization of hospital medicine practices, both with site size and patient acuity, a variety of challenges that drive the need for integration of NP/PA providers, and by-laws that define advanced practice clinical models and function.
In that perspective, it is important to define what constitutes a leading and successful advanced practice provider (APP) integration program. I would suggest:
- A structured and formalized transition-to-practice program for all new graduates and those new to hospital medicine. This program should consist of clinical volume progression, formalized didactic congruent with the Society of Hospital Medicine Core Competencies, and a process for evaluating knowledge and decision making throughout the program and upon completion.
- Development of physician competencies related to APP integration. Physicians are not prepared in their medical school training or residency to understand the differences and similarities of NP/PA providers. These competencies should be required and can best be developed through steady leadership, formalized instruction and accountability for professional teamwork.
- Allowance for NP/PA providers to work at the top of their skills and license. This means utilizing NP/PAs as providers who care for patients – not as scribes or clerical workers. The evolution of the acuity of patients provided for may evolve with the skill set and experience of NP/PAs, but it will evolve – especially if steps 1 and 2 are in place.
- Productivity expectations that reach near physician level of volume. In 2016 State of Hospital Medicine Report data, yearly billable encounters for NP/PAs were within 10% of that of physicians. I think 15% is a reasonable goal.
- Implementation and support of APP administrative leadership structure at the system/site level. This can be as simple as having APPs on the same leadership committees as physician team members, being involved in hiring and training newer physicians and NP/PAs or as broad as having all NP/PAs report to an APP leader. Having an intentional leadership structure that demonstrates and reflects inclusivity and belonging is crucial.
Consistent application of these frameworks will provide a strong infrastructure for successful NP/PA practice.
Ms. Cardin is currently the vice president of advanced practice providers at Sound Physicians and serves on SHM’s board of directors as its secretary. This article appeared initially at the Hospital Leader, the official blog of SHM.
Hospital medicine has been the fastest growing medical specialty since the term “hospitalist” was coined by Bob Wachter, MD, in the famous 1996 New England Journal of Medicine article (doi: 10.1056/NEJM199608153350713). The growth and change within this specialty is also reflected in the changing and migrating target of hospitals and hospital systems as they continue to effectively and safely move from fee-for-service to a payer model that rewards value and improvement in the health of a population – both in and outside of hospital walls.
In a short time, nurse practitioners and physician assistants have become a growing population in the hospital medicine workforce. The 2018 State of Hospital Medicine Report notes a 42% increase in 4 years, and about 75% of hospital medicine groups across the country currently incorporate NP/PAs within a hospital medicine practice. This evolution has occurred in the setting of a looming and well-documented physician shortage, a variety of cost pressures on hospitals that reflect the need for an efficient and cost-effective care delivery model, an increasing NP/PA workforce (the Department of Labor notes increases of 35% and 36% respectively by 2036), and data that indicates similar outcomes, for example, HCAHPS (the Hospital Consumer Assessment of Healthcare Providers and Systems), readmission, and morbidity and mortality in NP/PA-driven care.
This evolution, however, reveals a true knowledge gap in best practices related to integration of these providers. This is impacted by wide variability in the preparation of NPs – they may enter hospitalist practice from a variety of clinical exposures and training, for example, adult gerontology acute care, adult, or even, in some states, family NPs. For PAs, this is reflected in the variety of clinical rotations and pregraduate clinical exposure.
This variability is compounded, too, by the lack of standardization of hospital medicine practices, both with site size and patient acuity, a variety of challenges that drive the need for integration of NP/PA providers, and by-laws that define advanced practice clinical models and function.
In that perspective, it is important to define what constitutes a leading and successful advanced practice provider (APP) integration program. I would suggest:
- A structured and formalized transition-to-practice program for all new graduates and those new to hospital medicine. This program should consist of clinical volume progression, formalized didactic congruent with the Society of Hospital Medicine Core Competencies, and a process for evaluating knowledge and decision making throughout the program and upon completion.
- Development of physician competencies related to APP integration. Physicians are not prepared in their medical school training or residency to understand the differences and similarities of NP/PA providers. These competencies should be required and can best be developed through steady leadership, formalized instruction and accountability for professional teamwork.
- Allowance for NP/PA providers to work at the top of their skills and license. This means utilizing NP/PAs as providers who care for patients – not as scribes or clerical workers. The evolution of the acuity of patients provided for may evolve with the skill set and experience of NP/PAs, but it will evolve – especially if steps 1 and 2 are in place.
- Productivity expectations that reach near physician level of volume. In 2016 State of Hospital Medicine Report data, yearly billable encounters for NP/PAs were within 10% of that of physicians. I think 15% is a reasonable goal.
- Implementation and support of APP administrative leadership structure at the system/site level. This can be as simple as having APPs on the same leadership committees as physician team members, being involved in hiring and training newer physicians and NP/PAs or as broad as having all NP/PAs report to an APP leader. Having an intentional leadership structure that demonstrates and reflects inclusivity and belonging is crucial.
Consistent application of these frameworks will provide a strong infrastructure for successful NP/PA practice.
Ms. Cardin is currently the vice president of advanced practice providers at Sound Physicians and serves on SHM’s board of directors as its secretary. This article appeared initially at the Hospital Leader, the official blog of SHM.