User login
What you absolutely need to know about tail coverage
A 28-year-old pediatrician working in a large group practice in California found a new job in Pennsylvania. The job would allow her to live with her husband, who was a nonphysician.
On her last day of work at the California job, the practice’s office manager asked her, “Do you know about the tail coverage?”
He explained that it is malpractice insurance for any cases filed against her after leaving the job. Without it, he said, she would not be covered for those claims.
The physician (who asked not to be identified) had very little savings and suddenly had to pay a five-figure bill for tail coverage. To provide the extra malpractice coverage, she and her husband had to use savings they’d set aside to buy a house.
Getting tail coverage, known formally as an extended reporting endorsement, often comes as a complete and costly surprise for new doctors, says Dennis Hursh, Esq, a health care attorney based in Middletown, Penn., who deals with physicians’ employment contracts.
“Having to pay for a tail can disrupt lives,” Hursh said. “A tail can cost about one third of a young doctor’s salary. If you don’t feel you can afford to pay that, you may be forced to stay with a job you don’t like.”
Most medical residents don’t think about tail coverage until they apply for their first job, but last year, residents at Hahnemann University Hospital in Philadelphia got a painful early lesson.
In the summer, the hospital went out of business because of financial problems. Hundreds of medical residents and fellows not only were forced to find new programs but also had to prepare to buy tail coverage for their training years at Hahnemann.
“All the guarantees have been yanked out from under us,” said Tom Sibert, MD, a former internal medicine resident at the hospital, who is now finishing his training in California. “Residents don’t have that kind of money.”
Hahnemann trainees have asked the judge in the bankruptcy proceedings to put them ahead of other creditors and to ensure their tail coverage is paid. As of early February, the issue had not been resolved.
Meanwhile, Sibert and many other former trainees were trying to get quotes for purchasing tail coverage. They have been shocked by the amounts they would have to pay.
How tail coverage works
Medical malpractice tail coverage protects from incidents that took place when doctors were at their previous jobs but that later resulted in malpractice claims after they had left that employer.
One type of malpractice insurance, an occurrence policy, does not need tail coverage. Occurrence policies cover any incident that occurred when the policy was in force, no matter when a claim was filed – even if it is filed many years after the claims-filing period of the policy ends.
However, most malpractice policies – as many as 85%, according to one estimate – are claims-made policies. Claims-made policies are more much common because they’re significantly less expensive than occurrence policies.
Under a claims-made policy, coverage for malpractice claims completely stops when the policy ends. It does not cover incidents that occurred when the policy was in force but for which the patients later filed claims, as the occurrence policy does. So a tail is needed to cover these claims.
Physicians in all stages of their career may need tail coverage when they leave a job, change malpractice carriers, or retire.
But young physicians often have greater problems with tail coverage, for several reasons. They tend to be employed, and as such, they cannot choose the coverage they want. As a result, they most likely get claims-made coverage. In addition, the job turnover tends to be higher for these doctors. When leaving a job, the tail comes into play. More than half of new physicians leave their first job within 5 years, and of those, more than half leave after only 1 or 2 years.
Young physicians have no experience with tails and may not even know what they are. “In training, malpractice coverage is not a problem because the program handles it,” Mr. Hursh said. Accreditation standards require that teaching hospitals buy coverage, including a tail when residents leave.
So when young physicians are offered their first job and are handed an employment contract to sign, they may not even look for tail coverage, says Mr. Hursh, who wrote The Final Hurdle, a Physician’s Guide to Negotiating a Fair Employment Agreement. Instead, “young physicians tend to focus on issues like salary, benefits, and signing bonuses,” he said.
Mr. Hursh says the tail is usually the most expensive potential cost in the contract.
There’s no easy way to get out of paying the tail coverage once it is enshrined in the contract. The full tail can cost five or even six figures, depending on the physicians’ specialty, the local malpractice premium, and the physician’s own claims history.
Can you negotiate your tail coverage?
Negotiating tail coverage in the employment contract involves some familiarity with medical malpractice insurance and a close reading of the contract. First, you have to determine that the employer is providing claims-made coverage, which would require a tail if you leave. Then you have to determine whether the employer will pay for the tail coverage.
Often, the contract does not even mention tail coverage. “It could merely state that the practice will be responsible for malpractice coverage while you are working there,” Mr. Hursh said. Although it never specifies the tail, this language indicates that you will be paying for it, he says.
Therefore, it’s wise to have a conversation with your prospective employer about the tail. “Some new doctors never ask the question ‘What happens if I leave? Do I get tail coverage?’ ” said Israel Teitelbaum, an attorney who is chairman of Contemporary Insurance Services, an insurance broker in Silver Spring, Md.
Talking about the tail, however, can be a touchy subject for many young doctors applying for their first job. The tail matters only if you leave the job, and you may not want to imply that you would ever want to leave. Too much money, however, is on the line for you not to ask, Mr. Teitelbaum said.
Even if the employer verbally agrees to pay for the tail coverage, experts advise that you try to get the employer’s commitment in writing and have it put it into the contract.
Getting the employer to cover the tail in the initial contract is crucial because once you have agreed to work there, “it’s much more difficult to get it changed,” Mr. Teitelbaum said. However, even if tail coverage is not in the first contract, you shouldn’t give up, he says. You should try again in the next contract a few years later.
“It’s never too late to bring it up,” Mr. Teitelbaum said. After a few years of employment, you have a track record at the job. “A doctor who is very desirable to the employer may be able to get tail coverage on contract renewal.”
Coverage: Large employers vs. small employers
Willingness to pay for an employee’s tail coverage varies depending on the size of the employer. Large employers – systems, hospitals, and large practices – are much more likely to cover the tail than small and medium-sized practices.
Large employers tend to pay for at least part of the tail because they realize that it is in their interest to do so. Since they have the deepest pockets, they’re often the first to be named in a lawsuit. They might have to pay the whole claim if the physician did not have tail coverage.
However, many large employers want to use tail coverage as a bargaining chip to make sure doctors stay for a while at least. One typical arrangement, Mr. Hursh says, is to pay only one-fifth of the tail if the physician leaves in the first year of employment and then to pay one fifth more in each succeeding year until year five, when the employer assumes the entire cost of the tail.
Smaller practices, on the other hand, are usually close-fisted about tail coverage. “They tend to view the tail as an unnecessary expense,” Mr. Hursh said. “They don’t want to pay for a doctor who is not generating revenue for them any more.”
Traditionally, when physicians become partners, practices are more generous and agree to pay their tails if they leave, Mr. Hursh says. But he thinks this is changing, too – recent partnership contracts he has reviewed did not provide for tail coverage.
Times you don’t need to pay for tail coverage
Even if you’re responsible for the tail coverage, your insurance arrangement may be such that you don’t have to pay for it, says Michelle Perron, a malpractice insurance broker in North Hampton, N.H.
For example, if the carrier at your new job is the same as the one at your old job, your coverage would continue with no break, and you would not need a tail, she says. Even if you move to another state, your old carrier might also sell policies there, and you would then likely have seamless coverage, Ms. Perron says. This would be handy if you could choose your new carrier.
Even when you change carriers, Ms. Perron says, the new one might agree to pick up the old carrier’s coverage in return for getting your business, assuming you are an independent physician buying your own coverage. The new carrier would issue prior acts coverage, also known as nose coverage.
Older doctors going into retirement also have a potential tail coverage problem, but their tail coverage premium is often waived, Ms. Perron says. The need for a tail has to do with claims arising post retirement, after your coverage has ended. Typically, if you have been with the carrier for at least 5 years and you are age 55 years or older, your carrier will waive the tail coverage premium, she says.
However, if the retired doctor starts practicing again, even part time, the carrier may want to take back the free tail, she says. Some retired doctors get around this by buying a lower-priced tail from another company, but the former carrier may still want its money back, Ms. Perron says.
Can you just go without tail coverage?
What happens if physicians with a tail commitment choose to wing it and not pay for the tail? If a claim was never made against them, they may believe that the expense is unnecessary. The situation, however, is not so simple.
Some states require having tail coverage. Malpractice coverage is required in seven states, and at least some of those states explicitly extend this requirement to tails. They are Colorado, Connecticut, Kansas, Massachusetts, New Jersey, Rhode Island, and Wisconsin. Eleven more states tie malpractice coverage, perhaps including tails, to some benefit for the doctor, such as tort reform. These states include Indiana, Nebraska, New Mexico, New York, and Pennsylvania.
Many hospitals require tail coverage for privileges, and some insurers do as well. In addition, Ms. Perron says a missing tail reduces your prospects when looking for a job. “For the employer, having to pay coverage for a new hire will cost more than starting fresh with someone else,” she said.
Still, it’s important to remember the risk of being sued. “If you don’t buy the tail coverage, you are at risk for a lawsuit for many years to come,” Mr. Teitelbaum said.
Doctors should consider their potential lifetime risk, not just their current risk. Although only 8% of doctors younger than age 40 have been sued for malpractice, that figure climbs to almost half by the time doctors reach age 55.
The risks are higher in some specialties. About 63% of general surgeons and ob.gyns. have been sued.
Many of these claims are without merit, and doctors pay only the legal expenses of defending the case. Some doctors may think they could risk frivolous suits and cover legal expenses out of pocket. An American Medical Association survey showed that 68% of closed claims against doctors were dropped, dismissed, or withdrawn. It said these claims cost an average of more than $30,000 to defend.
However, Mr. Teitelbaum puts the defense costs for so-called frivolous suits much higher than the AMA, at $250,000 or more. “Even if you’re sure you won’t have to pay a claim, you still have to defend yourself against frivolous suits,” he said. “You won’t recover those expenses.”
How to lower your tail coverage cost
Physicians typically have 60 days to buy tail coverage after their regular coverage has ended. Specialized brokers such as Mr. Teitelbaum and Ms. Perron help physicians look for the best tails to buy.
The cost of the tail depends on how long you’ve been at your job when you leave it, Ms. Perron says. If you leave in the first 1 or 2 years of the policy, she says, the tail price will be lower because the coverage period is shorter.
Usually the most expensive tail available is from the carrier that issued the original policy. Why is this? “Carriers rarely sell a tail that undercuts their retail price,” Mr. Teitelbaum said. “They don’t want to compete with themselves, and in fact doing so could pose regulatory problems for them.”
Instead of buying from their own carrier, doctors can purchase stand-alone tails from competitors, which Mr. Teitelbaum says are 10%-30% less expensive than the policy the original carrier issues. However, stand-alone tails are not always easy to find, especially for high-cost specialties such as neurosurgery and ob.gyn., he says.
Some physicians try to bring down the cost of the tail by limiting the duration of the tail. You can buy tails that only cover claims filed 1-5 years after the incident took place, rather than indefinitely. These limits mirror the typical statute of limitations – the time limit to file a claim in each state. This limit is as little as 2 years in some states, though it can be as long as 6 years in others.
However, some states make exceptions to the statute of limitations. The 2- to 6-year clock doesn’t start ticking until the mistake is discovered or, in the case of children, when they reach adulthood. “This means that with a limited tail, you always have risk,” Perron said.
And yet some doctors insist on these time-limited tails. “If a doctor opts for 3 years’ coverage, that’s better than no years,” Mr. Teitelbaum said. “But I would advise them to take at least 5 years because that gives you coverage for the basic statute of limitations in most states. Three-year tails do yield savings, but often they’re not enough to warrant the risk.”
Another way to reduce costs is to lower the coverage limits of the tail. The standard coverage limit is $1 million per case and $3 million per year, so doctors might be able to save money on the premium by buying limits of $200,000/$600,000. But Mr. Teitelbaum says most companies would refuse to sell a policy with a limit lower than that of the expiring policy.
Further ways to reduce the cost of the tail include buying tail coverage that doesn’t give the physician the right to approve a settlement or that doesn’t include legal fees in the coverage limits. But these options, too, raise the physician’s risks. Whichever option you choose, the important thing is to protect yourself against costly lawsuits.
This article first appeared on Medscape.com.
A 28-year-old pediatrician working in a large group practice in California found a new job in Pennsylvania. The job would allow her to live with her husband, who was a nonphysician.
On her last day of work at the California job, the practice’s office manager asked her, “Do you know about the tail coverage?”
He explained that it is malpractice insurance for any cases filed against her after leaving the job. Without it, he said, she would not be covered for those claims.
The physician (who asked not to be identified) had very little savings and suddenly had to pay a five-figure bill for tail coverage. To provide the extra malpractice coverage, she and her husband had to use savings they’d set aside to buy a house.
Getting tail coverage, known formally as an extended reporting endorsement, often comes as a complete and costly surprise for new doctors, says Dennis Hursh, Esq, a health care attorney based in Middletown, Penn., who deals with physicians’ employment contracts.
“Having to pay for a tail can disrupt lives,” Hursh said. “A tail can cost about one third of a young doctor’s salary. If you don’t feel you can afford to pay that, you may be forced to stay with a job you don’t like.”
Most medical residents don’t think about tail coverage until they apply for their first job, but last year, residents at Hahnemann University Hospital in Philadelphia got a painful early lesson.
In the summer, the hospital went out of business because of financial problems. Hundreds of medical residents and fellows not only were forced to find new programs but also had to prepare to buy tail coverage for their training years at Hahnemann.
“All the guarantees have been yanked out from under us,” said Tom Sibert, MD, a former internal medicine resident at the hospital, who is now finishing his training in California. “Residents don’t have that kind of money.”
Hahnemann trainees have asked the judge in the bankruptcy proceedings to put them ahead of other creditors and to ensure their tail coverage is paid. As of early February, the issue had not been resolved.
Meanwhile, Sibert and many other former trainees were trying to get quotes for purchasing tail coverage. They have been shocked by the amounts they would have to pay.
How tail coverage works
Medical malpractice tail coverage protects from incidents that took place when doctors were at their previous jobs but that later resulted in malpractice claims after they had left that employer.
One type of malpractice insurance, an occurrence policy, does not need tail coverage. Occurrence policies cover any incident that occurred when the policy was in force, no matter when a claim was filed – even if it is filed many years after the claims-filing period of the policy ends.
However, most malpractice policies – as many as 85%, according to one estimate – are claims-made policies. Claims-made policies are more much common because they’re significantly less expensive than occurrence policies.
Under a claims-made policy, coverage for malpractice claims completely stops when the policy ends. It does not cover incidents that occurred when the policy was in force but for which the patients later filed claims, as the occurrence policy does. So a tail is needed to cover these claims.
Physicians in all stages of their career may need tail coverage when they leave a job, change malpractice carriers, or retire.
But young physicians often have greater problems with tail coverage, for several reasons. They tend to be employed, and as such, they cannot choose the coverage they want. As a result, they most likely get claims-made coverage. In addition, the job turnover tends to be higher for these doctors. When leaving a job, the tail comes into play. More than half of new physicians leave their first job within 5 years, and of those, more than half leave after only 1 or 2 years.
Young physicians have no experience with tails and may not even know what they are. “In training, malpractice coverage is not a problem because the program handles it,” Mr. Hursh said. Accreditation standards require that teaching hospitals buy coverage, including a tail when residents leave.
So when young physicians are offered their first job and are handed an employment contract to sign, they may not even look for tail coverage, says Mr. Hursh, who wrote The Final Hurdle, a Physician’s Guide to Negotiating a Fair Employment Agreement. Instead, “young physicians tend to focus on issues like salary, benefits, and signing bonuses,” he said.
Mr. Hursh says the tail is usually the most expensive potential cost in the contract.
There’s no easy way to get out of paying the tail coverage once it is enshrined in the contract. The full tail can cost five or even six figures, depending on the physicians’ specialty, the local malpractice premium, and the physician’s own claims history.
Can you negotiate your tail coverage?
Negotiating tail coverage in the employment contract involves some familiarity with medical malpractice insurance and a close reading of the contract. First, you have to determine that the employer is providing claims-made coverage, which would require a tail if you leave. Then you have to determine whether the employer will pay for the tail coverage.
Often, the contract does not even mention tail coverage. “It could merely state that the practice will be responsible for malpractice coverage while you are working there,” Mr. Hursh said. Although it never specifies the tail, this language indicates that you will be paying for it, he says.
Therefore, it’s wise to have a conversation with your prospective employer about the tail. “Some new doctors never ask the question ‘What happens if I leave? Do I get tail coverage?’ ” said Israel Teitelbaum, an attorney who is chairman of Contemporary Insurance Services, an insurance broker in Silver Spring, Md.
Talking about the tail, however, can be a touchy subject for many young doctors applying for their first job. The tail matters only if you leave the job, and you may not want to imply that you would ever want to leave. Too much money, however, is on the line for you not to ask, Mr. Teitelbaum said.
Even if the employer verbally agrees to pay for the tail coverage, experts advise that you try to get the employer’s commitment in writing and have it put it into the contract.
Getting the employer to cover the tail in the initial contract is crucial because once you have agreed to work there, “it’s much more difficult to get it changed,” Mr. Teitelbaum said. However, even if tail coverage is not in the first contract, you shouldn’t give up, he says. You should try again in the next contract a few years later.
“It’s never too late to bring it up,” Mr. Teitelbaum said. After a few years of employment, you have a track record at the job. “A doctor who is very desirable to the employer may be able to get tail coverage on contract renewal.”
Coverage: Large employers vs. small employers
Willingness to pay for an employee’s tail coverage varies depending on the size of the employer. Large employers – systems, hospitals, and large practices – are much more likely to cover the tail than small and medium-sized practices.
Large employers tend to pay for at least part of the tail because they realize that it is in their interest to do so. Since they have the deepest pockets, they’re often the first to be named in a lawsuit. They might have to pay the whole claim if the physician did not have tail coverage.
However, many large employers want to use tail coverage as a bargaining chip to make sure doctors stay for a while at least. One typical arrangement, Mr. Hursh says, is to pay only one-fifth of the tail if the physician leaves in the first year of employment and then to pay one fifth more in each succeeding year until year five, when the employer assumes the entire cost of the tail.
Smaller practices, on the other hand, are usually close-fisted about tail coverage. “They tend to view the tail as an unnecessary expense,” Mr. Hursh said. “They don’t want to pay for a doctor who is not generating revenue for them any more.”
Traditionally, when physicians become partners, practices are more generous and agree to pay their tails if they leave, Mr. Hursh says. But he thinks this is changing, too – recent partnership contracts he has reviewed did not provide for tail coverage.
Times you don’t need to pay for tail coverage
Even if you’re responsible for the tail coverage, your insurance arrangement may be such that you don’t have to pay for it, says Michelle Perron, a malpractice insurance broker in North Hampton, N.H.
For example, if the carrier at your new job is the same as the one at your old job, your coverage would continue with no break, and you would not need a tail, she says. Even if you move to another state, your old carrier might also sell policies there, and you would then likely have seamless coverage, Ms. Perron says. This would be handy if you could choose your new carrier.
Even when you change carriers, Ms. Perron says, the new one might agree to pick up the old carrier’s coverage in return for getting your business, assuming you are an independent physician buying your own coverage. The new carrier would issue prior acts coverage, also known as nose coverage.
Older doctors going into retirement also have a potential tail coverage problem, but their tail coverage premium is often waived, Ms. Perron says. The need for a tail has to do with claims arising post retirement, after your coverage has ended. Typically, if you have been with the carrier for at least 5 years and you are age 55 years or older, your carrier will waive the tail coverage premium, she says.
However, if the retired doctor starts practicing again, even part time, the carrier may want to take back the free tail, she says. Some retired doctors get around this by buying a lower-priced tail from another company, but the former carrier may still want its money back, Ms. Perron says.
Can you just go without tail coverage?
What happens if physicians with a tail commitment choose to wing it and not pay for the tail? If a claim was never made against them, they may believe that the expense is unnecessary. The situation, however, is not so simple.
Some states require having tail coverage. Malpractice coverage is required in seven states, and at least some of those states explicitly extend this requirement to tails. They are Colorado, Connecticut, Kansas, Massachusetts, New Jersey, Rhode Island, and Wisconsin. Eleven more states tie malpractice coverage, perhaps including tails, to some benefit for the doctor, such as tort reform. These states include Indiana, Nebraska, New Mexico, New York, and Pennsylvania.
Many hospitals require tail coverage for privileges, and some insurers do as well. In addition, Ms. Perron says a missing tail reduces your prospects when looking for a job. “For the employer, having to pay coverage for a new hire will cost more than starting fresh with someone else,” she said.
Still, it’s important to remember the risk of being sued. “If you don’t buy the tail coverage, you are at risk for a lawsuit for many years to come,” Mr. Teitelbaum said.
Doctors should consider their potential lifetime risk, not just their current risk. Although only 8% of doctors younger than age 40 have been sued for malpractice, that figure climbs to almost half by the time doctors reach age 55.
The risks are higher in some specialties. About 63% of general surgeons and ob.gyns. have been sued.
Many of these claims are without merit, and doctors pay only the legal expenses of defending the case. Some doctors may think they could risk frivolous suits and cover legal expenses out of pocket. An American Medical Association survey showed that 68% of closed claims against doctors were dropped, dismissed, or withdrawn. It said these claims cost an average of more than $30,000 to defend.
However, Mr. Teitelbaum puts the defense costs for so-called frivolous suits much higher than the AMA, at $250,000 or more. “Even if you’re sure you won’t have to pay a claim, you still have to defend yourself against frivolous suits,” he said. “You won’t recover those expenses.”
How to lower your tail coverage cost
Physicians typically have 60 days to buy tail coverage after their regular coverage has ended. Specialized brokers such as Mr. Teitelbaum and Ms. Perron help physicians look for the best tails to buy.
The cost of the tail depends on how long you’ve been at your job when you leave it, Ms. Perron says. If you leave in the first 1 or 2 years of the policy, she says, the tail price will be lower because the coverage period is shorter.
Usually the most expensive tail available is from the carrier that issued the original policy. Why is this? “Carriers rarely sell a tail that undercuts their retail price,” Mr. Teitelbaum said. “They don’t want to compete with themselves, and in fact doing so could pose regulatory problems for them.”
Instead of buying from their own carrier, doctors can purchase stand-alone tails from competitors, which Mr. Teitelbaum says are 10%-30% less expensive than the policy the original carrier issues. However, stand-alone tails are not always easy to find, especially for high-cost specialties such as neurosurgery and ob.gyn., he says.
Some physicians try to bring down the cost of the tail by limiting the duration of the tail. You can buy tails that only cover claims filed 1-5 years after the incident took place, rather than indefinitely. These limits mirror the typical statute of limitations – the time limit to file a claim in each state. This limit is as little as 2 years in some states, though it can be as long as 6 years in others.
However, some states make exceptions to the statute of limitations. The 2- to 6-year clock doesn’t start ticking until the mistake is discovered or, in the case of children, when they reach adulthood. “This means that with a limited tail, you always have risk,” Perron said.
And yet some doctors insist on these time-limited tails. “If a doctor opts for 3 years’ coverage, that’s better than no years,” Mr. Teitelbaum said. “But I would advise them to take at least 5 years because that gives you coverage for the basic statute of limitations in most states. Three-year tails do yield savings, but often they’re not enough to warrant the risk.”
Another way to reduce costs is to lower the coverage limits of the tail. The standard coverage limit is $1 million per case and $3 million per year, so doctors might be able to save money on the premium by buying limits of $200,000/$600,000. But Mr. Teitelbaum says most companies would refuse to sell a policy with a limit lower than that of the expiring policy.
Further ways to reduce the cost of the tail include buying tail coverage that doesn’t give the physician the right to approve a settlement or that doesn’t include legal fees in the coverage limits. But these options, too, raise the physician’s risks. Whichever option you choose, the important thing is to protect yourself against costly lawsuits.
This article first appeared on Medscape.com.
A 28-year-old pediatrician working in a large group practice in California found a new job in Pennsylvania. The job would allow her to live with her husband, who was a nonphysician.
On her last day of work at the California job, the practice’s office manager asked her, “Do you know about the tail coverage?”
He explained that it is malpractice insurance for any cases filed against her after leaving the job. Without it, he said, she would not be covered for those claims.
The physician (who asked not to be identified) had very little savings and suddenly had to pay a five-figure bill for tail coverage. To provide the extra malpractice coverage, she and her husband had to use savings they’d set aside to buy a house.
Getting tail coverage, known formally as an extended reporting endorsement, often comes as a complete and costly surprise for new doctors, says Dennis Hursh, Esq, a health care attorney based in Middletown, Penn., who deals with physicians’ employment contracts.
“Having to pay for a tail can disrupt lives,” Hursh said. “A tail can cost about one third of a young doctor’s salary. If you don’t feel you can afford to pay that, you may be forced to stay with a job you don’t like.”
Most medical residents don’t think about tail coverage until they apply for their first job, but last year, residents at Hahnemann University Hospital in Philadelphia got a painful early lesson.
In the summer, the hospital went out of business because of financial problems. Hundreds of medical residents and fellows not only were forced to find new programs but also had to prepare to buy tail coverage for their training years at Hahnemann.
“All the guarantees have been yanked out from under us,” said Tom Sibert, MD, a former internal medicine resident at the hospital, who is now finishing his training in California. “Residents don’t have that kind of money.”
Hahnemann trainees have asked the judge in the bankruptcy proceedings to put them ahead of other creditors and to ensure their tail coverage is paid. As of early February, the issue had not been resolved.
Meanwhile, Sibert and many other former trainees were trying to get quotes for purchasing tail coverage. They have been shocked by the amounts they would have to pay.
How tail coverage works
Medical malpractice tail coverage protects from incidents that took place when doctors were at their previous jobs but that later resulted in malpractice claims after they had left that employer.
One type of malpractice insurance, an occurrence policy, does not need tail coverage. Occurrence policies cover any incident that occurred when the policy was in force, no matter when a claim was filed – even if it is filed many years after the claims-filing period of the policy ends.
However, most malpractice policies – as many as 85%, according to one estimate – are claims-made policies. Claims-made policies are more much common because they’re significantly less expensive than occurrence policies.
Under a claims-made policy, coverage for malpractice claims completely stops when the policy ends. It does not cover incidents that occurred when the policy was in force but for which the patients later filed claims, as the occurrence policy does. So a tail is needed to cover these claims.
Physicians in all stages of their career may need tail coverage when they leave a job, change malpractice carriers, or retire.
But young physicians often have greater problems with tail coverage, for several reasons. They tend to be employed, and as such, they cannot choose the coverage they want. As a result, they most likely get claims-made coverage. In addition, the job turnover tends to be higher for these doctors. When leaving a job, the tail comes into play. More than half of new physicians leave their first job within 5 years, and of those, more than half leave after only 1 or 2 years.
Young physicians have no experience with tails and may not even know what they are. “In training, malpractice coverage is not a problem because the program handles it,” Mr. Hursh said. Accreditation standards require that teaching hospitals buy coverage, including a tail when residents leave.
So when young physicians are offered their first job and are handed an employment contract to sign, they may not even look for tail coverage, says Mr. Hursh, who wrote The Final Hurdle, a Physician’s Guide to Negotiating a Fair Employment Agreement. Instead, “young physicians tend to focus on issues like salary, benefits, and signing bonuses,” he said.
Mr. Hursh says the tail is usually the most expensive potential cost in the contract.
There’s no easy way to get out of paying the tail coverage once it is enshrined in the contract. The full tail can cost five or even six figures, depending on the physicians’ specialty, the local malpractice premium, and the physician’s own claims history.
Can you negotiate your tail coverage?
Negotiating tail coverage in the employment contract involves some familiarity with medical malpractice insurance and a close reading of the contract. First, you have to determine that the employer is providing claims-made coverage, which would require a tail if you leave. Then you have to determine whether the employer will pay for the tail coverage.
Often, the contract does not even mention tail coverage. “It could merely state that the practice will be responsible for malpractice coverage while you are working there,” Mr. Hursh said. Although it never specifies the tail, this language indicates that you will be paying for it, he says.
Therefore, it’s wise to have a conversation with your prospective employer about the tail. “Some new doctors never ask the question ‘What happens if I leave? Do I get tail coverage?’ ” said Israel Teitelbaum, an attorney who is chairman of Contemporary Insurance Services, an insurance broker in Silver Spring, Md.
Talking about the tail, however, can be a touchy subject for many young doctors applying for their first job. The tail matters only if you leave the job, and you may not want to imply that you would ever want to leave. Too much money, however, is on the line for you not to ask, Mr. Teitelbaum said.
Even if the employer verbally agrees to pay for the tail coverage, experts advise that you try to get the employer’s commitment in writing and have it put it into the contract.
Getting the employer to cover the tail in the initial contract is crucial because once you have agreed to work there, “it’s much more difficult to get it changed,” Mr. Teitelbaum said. However, even if tail coverage is not in the first contract, you shouldn’t give up, he says. You should try again in the next contract a few years later.
“It’s never too late to bring it up,” Mr. Teitelbaum said. After a few years of employment, you have a track record at the job. “A doctor who is very desirable to the employer may be able to get tail coverage on contract renewal.”
Coverage: Large employers vs. small employers
Willingness to pay for an employee’s tail coverage varies depending on the size of the employer. Large employers – systems, hospitals, and large practices – are much more likely to cover the tail than small and medium-sized practices.
Large employers tend to pay for at least part of the tail because they realize that it is in their interest to do so. Since they have the deepest pockets, they’re often the first to be named in a lawsuit. They might have to pay the whole claim if the physician did not have tail coverage.
However, many large employers want to use tail coverage as a bargaining chip to make sure doctors stay for a while at least. One typical arrangement, Mr. Hursh says, is to pay only one-fifth of the tail if the physician leaves in the first year of employment and then to pay one fifth more in each succeeding year until year five, when the employer assumes the entire cost of the tail.
Smaller practices, on the other hand, are usually close-fisted about tail coverage. “They tend to view the tail as an unnecessary expense,” Mr. Hursh said. “They don’t want to pay for a doctor who is not generating revenue for them any more.”
Traditionally, when physicians become partners, practices are more generous and agree to pay their tails if they leave, Mr. Hursh says. But he thinks this is changing, too – recent partnership contracts he has reviewed did not provide for tail coverage.
Times you don’t need to pay for tail coverage
Even if you’re responsible for the tail coverage, your insurance arrangement may be such that you don’t have to pay for it, says Michelle Perron, a malpractice insurance broker in North Hampton, N.H.
For example, if the carrier at your new job is the same as the one at your old job, your coverage would continue with no break, and you would not need a tail, she says. Even if you move to another state, your old carrier might also sell policies there, and you would then likely have seamless coverage, Ms. Perron says. This would be handy if you could choose your new carrier.
Even when you change carriers, Ms. Perron says, the new one might agree to pick up the old carrier’s coverage in return for getting your business, assuming you are an independent physician buying your own coverage. The new carrier would issue prior acts coverage, also known as nose coverage.
Older doctors going into retirement also have a potential tail coverage problem, but their tail coverage premium is often waived, Ms. Perron says. The need for a tail has to do with claims arising post retirement, after your coverage has ended. Typically, if you have been with the carrier for at least 5 years and you are age 55 years or older, your carrier will waive the tail coverage premium, she says.
However, if the retired doctor starts practicing again, even part time, the carrier may want to take back the free tail, she says. Some retired doctors get around this by buying a lower-priced tail from another company, but the former carrier may still want its money back, Ms. Perron says.
Can you just go without tail coverage?
What happens if physicians with a tail commitment choose to wing it and not pay for the tail? If a claim was never made against them, they may believe that the expense is unnecessary. The situation, however, is not so simple.
Some states require having tail coverage. Malpractice coverage is required in seven states, and at least some of those states explicitly extend this requirement to tails. They are Colorado, Connecticut, Kansas, Massachusetts, New Jersey, Rhode Island, and Wisconsin. Eleven more states tie malpractice coverage, perhaps including tails, to some benefit for the doctor, such as tort reform. These states include Indiana, Nebraska, New Mexico, New York, and Pennsylvania.
Many hospitals require tail coverage for privileges, and some insurers do as well. In addition, Ms. Perron says a missing tail reduces your prospects when looking for a job. “For the employer, having to pay coverage for a new hire will cost more than starting fresh with someone else,” she said.
Still, it’s important to remember the risk of being sued. “If you don’t buy the tail coverage, you are at risk for a lawsuit for many years to come,” Mr. Teitelbaum said.
Doctors should consider their potential lifetime risk, not just their current risk. Although only 8% of doctors younger than age 40 have been sued for malpractice, that figure climbs to almost half by the time doctors reach age 55.
The risks are higher in some specialties. About 63% of general surgeons and ob.gyns. have been sued.
Many of these claims are without merit, and doctors pay only the legal expenses of defending the case. Some doctors may think they could risk frivolous suits and cover legal expenses out of pocket. An American Medical Association survey showed that 68% of closed claims against doctors were dropped, dismissed, or withdrawn. It said these claims cost an average of more than $30,000 to defend.
However, Mr. Teitelbaum puts the defense costs for so-called frivolous suits much higher than the AMA, at $250,000 or more. “Even if you’re sure you won’t have to pay a claim, you still have to defend yourself against frivolous suits,” he said. “You won’t recover those expenses.”
How to lower your tail coverage cost
Physicians typically have 60 days to buy tail coverage after their regular coverage has ended. Specialized brokers such as Mr. Teitelbaum and Ms. Perron help physicians look for the best tails to buy.
The cost of the tail depends on how long you’ve been at your job when you leave it, Ms. Perron says. If you leave in the first 1 or 2 years of the policy, she says, the tail price will be lower because the coverage period is shorter.
Usually the most expensive tail available is from the carrier that issued the original policy. Why is this? “Carriers rarely sell a tail that undercuts their retail price,” Mr. Teitelbaum said. “They don’t want to compete with themselves, and in fact doing so could pose regulatory problems for them.”
Instead of buying from their own carrier, doctors can purchase stand-alone tails from competitors, which Mr. Teitelbaum says are 10%-30% less expensive than the policy the original carrier issues. However, stand-alone tails are not always easy to find, especially for high-cost specialties such as neurosurgery and ob.gyn., he says.
Some physicians try to bring down the cost of the tail by limiting the duration of the tail. You can buy tails that only cover claims filed 1-5 years after the incident took place, rather than indefinitely. These limits mirror the typical statute of limitations – the time limit to file a claim in each state. This limit is as little as 2 years in some states, though it can be as long as 6 years in others.
However, some states make exceptions to the statute of limitations. The 2- to 6-year clock doesn’t start ticking until the mistake is discovered or, in the case of children, when they reach adulthood. “This means that with a limited tail, you always have risk,” Perron said.
And yet some doctors insist on these time-limited tails. “If a doctor opts for 3 years’ coverage, that’s better than no years,” Mr. Teitelbaum said. “But I would advise them to take at least 5 years because that gives you coverage for the basic statute of limitations in most states. Three-year tails do yield savings, but often they’re not enough to warrant the risk.”
Another way to reduce costs is to lower the coverage limits of the tail. The standard coverage limit is $1 million per case and $3 million per year, so doctors might be able to save money on the premium by buying limits of $200,000/$600,000. But Mr. Teitelbaum says most companies would refuse to sell a policy with a limit lower than that of the expiring policy.
Further ways to reduce the cost of the tail include buying tail coverage that doesn’t give the physician the right to approve a settlement or that doesn’t include legal fees in the coverage limits. But these options, too, raise the physician’s risks. Whichever option you choose, the important thing is to protect yourself against costly lawsuits.
This article first appeared on Medscape.com.
Hospitalist movers and shakers – January 2020
Hyung (Harry) Cho, MD, SFHM, and Christopher Moriates, MD, SFHM, have been honored by Modern Healthcare as two of 25 emerging young executives in health care management.
Dr. Cho is chief value officer for NYC Health and Hospitals, where his focus is on eliminating unnecessary testing and treatments within the New York City public health system, which includes 11 hospitals and five post-acute care facilities. Before landing with NYC Health and Hospitals, Dr. Cho was director of quality, safety and value at the Icahn School of Medicine at Mount Sinai, New York.
Dr. Moriates is assistant dean for health care and value at the University of Texas at Austin’s Dell Medical School, where he has created the Discovering Value-Based Health Care online learning platform. In addition, Dr. Moriates has helped design a care model to enhance the treatment of patients who suffer from opioid use disorder. Prior to arriving at Dell, he helped create curriculum to educate students about costs and value at the University of California, San Francisco.
Trina Abla, DO, was appointed chief medical officer at Mercy Catholic Medical Center in Darby, Pa. A practicing hospitalist, Dr. Abla will be in charge of the hospital budget, the recruiting and training of physicians, and maintaining safety standards and quality care at the facility.
Prior to taking the position at Mercy Catholic, Dr. Abla was chief quality officer and associate CMO at Penn State Health St. Joseph in Reading, Pa.
Ghania El Akiki, MD, has been named to the board of advisors at Beth Israel Deaconess Hospital in Needham, Mass. Dr. Akiki is chief of hospitalist services at Beth Israel Deaconess, landing there after a fellowship in geriatrics at Beth Israel Deaconess Medical Center.
Dr. Akiki completed a physician leadership program at BID Medical Center in 2018, and serves as instructor of medicine at Harvard Medical School, Boston.
Michael Schandorf-Lartey, MD, has been named the chief medical officer at Doctors Hospital in Sarasota, Fla. Dr. Schandorf-Lartey has been a hospitalist at Doctors Hospital for the past 12 years.
In his time at Doctors, Dr. Schandorf-Lartey also has been chief of medicine, president-elect, and president of the medical staff. A native of Ghana, he has had experience working in rural and urban hospitals in Africa before coming to the United States.
Michael Roberts, MD, was named chief of staff at East Alabama Medical Center in Opeleika, Ala. He has been part of EAMC since 2008, when he became a hospitalist there through Internal Medicine Associates.
As chief of staff, Dr. Roberts will work with different components of the medical staff and serve as a liaison between the hospital board and its staff; assist in developing policies alongside the chief medical officer; and serve on many of the medical staff’s committees.
Brian Dawson, MD, has been named chief medical officer for Ballad Health, Southwest Region, based in Johnson City, Tenn. Dr. Dawson will lead Ballad Health locations in Washington County, which include Franklin Woods Community Hospital, Johnson City Medical Center, Niswonger Children Hospital, and Woodridge Hospital.
Dr. Dawson comes to Ballad Health after serving as vice president at VEP Healthcare, where he focused on contract management for the emergency medicine and hospitalist firm. Previously, he was chief of staff and Northeast regional director for emergency medicine at Johnston Memorial Hospital, Abington, Va.
Eagle Telemedicine (Atlanta, Ga.) recently agreed to begin a telehospitalist program at Jersey Community Hospital in Jerseyville, Ill. Eagle Telemedicine offers telehospitalist services to more than 150 hospitals nationwide.
A rural facility with fewer than 50 beds, JCH will use Eagle to make up for the lack of a full-time, onsite hospitalist program, taking strain off of physicians handling emergency calls. At JCH, telehospitalists work closely with onsite nurse practitioners to guide patients through their hospital stay.
Hyung (Harry) Cho, MD, SFHM, and Christopher Moriates, MD, SFHM, have been honored by Modern Healthcare as two of 25 emerging young executives in health care management.
Dr. Cho is chief value officer for NYC Health and Hospitals, where his focus is on eliminating unnecessary testing and treatments within the New York City public health system, which includes 11 hospitals and five post-acute care facilities. Before landing with NYC Health and Hospitals, Dr. Cho was director of quality, safety and value at the Icahn School of Medicine at Mount Sinai, New York.
Dr. Moriates is assistant dean for health care and value at the University of Texas at Austin’s Dell Medical School, where he has created the Discovering Value-Based Health Care online learning platform. In addition, Dr. Moriates has helped design a care model to enhance the treatment of patients who suffer from opioid use disorder. Prior to arriving at Dell, he helped create curriculum to educate students about costs and value at the University of California, San Francisco.
Trina Abla, DO, was appointed chief medical officer at Mercy Catholic Medical Center in Darby, Pa. A practicing hospitalist, Dr. Abla will be in charge of the hospital budget, the recruiting and training of physicians, and maintaining safety standards and quality care at the facility.
Prior to taking the position at Mercy Catholic, Dr. Abla was chief quality officer and associate CMO at Penn State Health St. Joseph in Reading, Pa.
Ghania El Akiki, MD, has been named to the board of advisors at Beth Israel Deaconess Hospital in Needham, Mass. Dr. Akiki is chief of hospitalist services at Beth Israel Deaconess, landing there after a fellowship in geriatrics at Beth Israel Deaconess Medical Center.
Dr. Akiki completed a physician leadership program at BID Medical Center in 2018, and serves as instructor of medicine at Harvard Medical School, Boston.
Michael Schandorf-Lartey, MD, has been named the chief medical officer at Doctors Hospital in Sarasota, Fla. Dr. Schandorf-Lartey has been a hospitalist at Doctors Hospital for the past 12 years.
In his time at Doctors, Dr. Schandorf-Lartey also has been chief of medicine, president-elect, and president of the medical staff. A native of Ghana, he has had experience working in rural and urban hospitals in Africa before coming to the United States.
Michael Roberts, MD, was named chief of staff at East Alabama Medical Center in Opeleika, Ala. He has been part of EAMC since 2008, when he became a hospitalist there through Internal Medicine Associates.
As chief of staff, Dr. Roberts will work with different components of the medical staff and serve as a liaison between the hospital board and its staff; assist in developing policies alongside the chief medical officer; and serve on many of the medical staff’s committees.
Brian Dawson, MD, has been named chief medical officer for Ballad Health, Southwest Region, based in Johnson City, Tenn. Dr. Dawson will lead Ballad Health locations in Washington County, which include Franklin Woods Community Hospital, Johnson City Medical Center, Niswonger Children Hospital, and Woodridge Hospital.
Dr. Dawson comes to Ballad Health after serving as vice president at VEP Healthcare, where he focused on contract management for the emergency medicine and hospitalist firm. Previously, he was chief of staff and Northeast regional director for emergency medicine at Johnston Memorial Hospital, Abington, Va.
Eagle Telemedicine (Atlanta, Ga.) recently agreed to begin a telehospitalist program at Jersey Community Hospital in Jerseyville, Ill. Eagle Telemedicine offers telehospitalist services to more than 150 hospitals nationwide.
A rural facility with fewer than 50 beds, JCH will use Eagle to make up for the lack of a full-time, onsite hospitalist program, taking strain off of physicians handling emergency calls. At JCH, telehospitalists work closely with onsite nurse practitioners to guide patients through their hospital stay.
Hyung (Harry) Cho, MD, SFHM, and Christopher Moriates, MD, SFHM, have been honored by Modern Healthcare as two of 25 emerging young executives in health care management.
Dr. Cho is chief value officer for NYC Health and Hospitals, where his focus is on eliminating unnecessary testing and treatments within the New York City public health system, which includes 11 hospitals and five post-acute care facilities. Before landing with NYC Health and Hospitals, Dr. Cho was director of quality, safety and value at the Icahn School of Medicine at Mount Sinai, New York.
Dr. Moriates is assistant dean for health care and value at the University of Texas at Austin’s Dell Medical School, where he has created the Discovering Value-Based Health Care online learning platform. In addition, Dr. Moriates has helped design a care model to enhance the treatment of patients who suffer from opioid use disorder. Prior to arriving at Dell, he helped create curriculum to educate students about costs and value at the University of California, San Francisco.
Trina Abla, DO, was appointed chief medical officer at Mercy Catholic Medical Center in Darby, Pa. A practicing hospitalist, Dr. Abla will be in charge of the hospital budget, the recruiting and training of physicians, and maintaining safety standards and quality care at the facility.
Prior to taking the position at Mercy Catholic, Dr. Abla was chief quality officer and associate CMO at Penn State Health St. Joseph in Reading, Pa.
Ghania El Akiki, MD, has been named to the board of advisors at Beth Israel Deaconess Hospital in Needham, Mass. Dr. Akiki is chief of hospitalist services at Beth Israel Deaconess, landing there after a fellowship in geriatrics at Beth Israel Deaconess Medical Center.
Dr. Akiki completed a physician leadership program at BID Medical Center in 2018, and serves as instructor of medicine at Harvard Medical School, Boston.
Michael Schandorf-Lartey, MD, has been named the chief medical officer at Doctors Hospital in Sarasota, Fla. Dr. Schandorf-Lartey has been a hospitalist at Doctors Hospital for the past 12 years.
In his time at Doctors, Dr. Schandorf-Lartey also has been chief of medicine, president-elect, and president of the medical staff. A native of Ghana, he has had experience working in rural and urban hospitals in Africa before coming to the United States.
Michael Roberts, MD, was named chief of staff at East Alabama Medical Center in Opeleika, Ala. He has been part of EAMC since 2008, when he became a hospitalist there through Internal Medicine Associates.
As chief of staff, Dr. Roberts will work with different components of the medical staff and serve as a liaison between the hospital board and its staff; assist in developing policies alongside the chief medical officer; and serve on many of the medical staff’s committees.
Brian Dawson, MD, has been named chief medical officer for Ballad Health, Southwest Region, based in Johnson City, Tenn. Dr. Dawson will lead Ballad Health locations in Washington County, which include Franklin Woods Community Hospital, Johnson City Medical Center, Niswonger Children Hospital, and Woodridge Hospital.
Dr. Dawson comes to Ballad Health after serving as vice president at VEP Healthcare, where he focused on contract management for the emergency medicine and hospitalist firm. Previously, he was chief of staff and Northeast regional director for emergency medicine at Johnston Memorial Hospital, Abington, Va.
Eagle Telemedicine (Atlanta, Ga.) recently agreed to begin a telehospitalist program at Jersey Community Hospital in Jerseyville, Ill. Eagle Telemedicine offers telehospitalist services to more than 150 hospitals nationwide.
A rural facility with fewer than 50 beds, JCH will use Eagle to make up for the lack of a full-time, onsite hospitalist program, taking strain off of physicians handling emergency calls. At JCH, telehospitalists work closely with onsite nurse practitioners to guide patients through their hospital stay.
Medscape survey points to generational differences in physician burnout
Burnout among physicians appears to have decreased slightly in the past few years, but remains a significant problem for the medical profession, according to the Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide.
A survey of more than 15,000 physicians revealed that 42% reported being burned out, down from 46% who responded to the survey 5 years ago. However, there are variations in the rates based on certain demographic factors such as specialty, age, and gender.
Urology sits at the top of the list as the specialty that is experiencing the highest rate of burnout, with 54% of urologists responding to the survey reporting burnout. Neurology and nephrology followed with rates of burnout at 50% and 49%, respectively. The next five specialties on the list all reported burnout rates of 46%: diabetes and endocrinology, family medicine, radiology, ob.gyn., and rheumatology. Pulmonology specialists reported a burnout rate of 41%. Gastroenterologists reported burnout rates of 37%.
The survey divided participants into three age categories – Millennial (ages 25-39 years), Generation X (ages 40-54 years), and Baby Boomer (ages 55-73 years). Both Millennials and Baby Boomers reported similar rates of burnout (38% and 39%, respectively) and those in Generation X reported a higher rate of burnout (48%).
This higher rate is not unexpected. The survey results cite Carol Bernstein, MD, of the Albert Einstein College of Medicine, New York, as noting that midcareer “is typically the time of highest burnout, which is where Gen Xers are in their career trajectory, suggesting a number of factors outside of work such as caring for children and elderly parents, planning for retirement, can play a role in contributing to burnout.”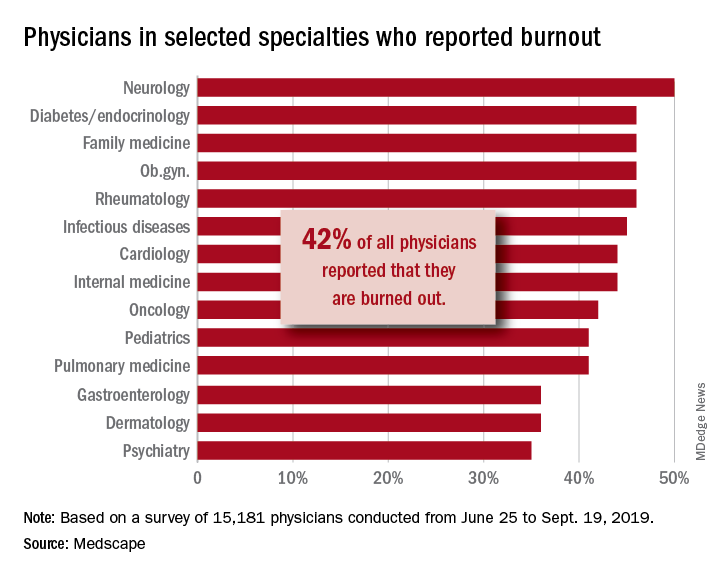
Women also reported a higher rate of burnout, although the rate has dropped from the survey conducted 5 years ago. The rate of burnout among women reported for the 2020 survey was 48%, down from 51% reported 5 years ago. By comparison, the rate of burnout for men was 37% in 2020, down from 43% in 2015.
In terms of what is causing burnout, the biggest contributor is the bureaucratic tasks (charting and paperwork, for example) that physicians must complete, which 55% of respondents to the survey said was the leading cause of burnout. Next was spending too many hours at work (33%); lack of respect from administrators, employers, colleagues, and staff (32%); and the increased computerization of the practice, including the use of electronic health records (30%).
When broken down by age category, the bureaucratic tasks was tops in all three groups (57% for Millennials, 56% for Generation X, and 54% for Baby Boomers), but what ranks next differs slightly by age group. For Millennials, the next two factors were too many hours at work (38%) and lack of respect (35%). Generation X respondents cited the same two factors, both at 33%. Baby Boomers cited computerization as their second-highest factor (41%) and spending too many hours at work as the third-highest factor (31%).
The generations had different approaches to coping with burnout. Millennials (56%) reported sleep as their top-ranked coping strategy, while Gen Xers and Baby Boomers ranked exercise and personal isolation as their top choice. For these two older groups, sleep was ranked last, after other activities such as talking with family and friends.
The survey also asked about depression, and respondents reported a similar rate across all age groups (15%, 18%, and 16%, respectively). Among those who said they were depressed, the three age groups had similar rates of suicidal thoughts (21%, 24%, and 22%).
Perhaps the most striking finding of the survey is the number of physicians who would take a pay cut to achieve a better work-life balance. Among Millennials, 52% would accept a pay cut, compared with 48% of Generation X and 49% of Baby Boomers. A surprising number (36%, 34%, and 31%, respectively, reported that they would accept a $10,000-$20,000 pay cut to have a 20% reduction in work hours. [email protected]
*This story was updated on 1/22/2020.
SOURCE: Kane L et al. Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide. Medscape. 2020 Jan 15.
Burnout among physicians appears to have decreased slightly in the past few years, but remains a significant problem for the medical profession, according to the Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide.
A survey of more than 15,000 physicians revealed that 42% reported being burned out, down from 46% who responded to the survey 5 years ago. However, there are variations in the rates based on certain demographic factors such as specialty, age, and gender.
Urology sits at the top of the list as the specialty that is experiencing the highest rate of burnout, with 54% of urologists responding to the survey reporting burnout. Neurology and nephrology followed with rates of burnout at 50% and 49%, respectively. The next five specialties on the list all reported burnout rates of 46%: diabetes and endocrinology, family medicine, radiology, ob.gyn., and rheumatology. Pulmonology specialists reported a burnout rate of 41%. Gastroenterologists reported burnout rates of 37%.
The survey divided participants into three age categories – Millennial (ages 25-39 years), Generation X (ages 40-54 years), and Baby Boomer (ages 55-73 years). Both Millennials and Baby Boomers reported similar rates of burnout (38% and 39%, respectively) and those in Generation X reported a higher rate of burnout (48%).
This higher rate is not unexpected. The survey results cite Carol Bernstein, MD, of the Albert Einstein College of Medicine, New York, as noting that midcareer “is typically the time of highest burnout, which is where Gen Xers are in their career trajectory, suggesting a number of factors outside of work such as caring for children and elderly parents, planning for retirement, can play a role in contributing to burnout.”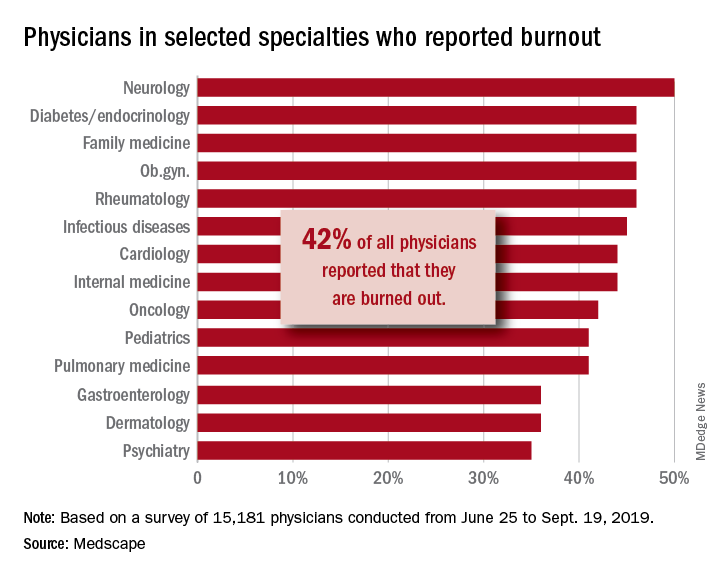
Women also reported a higher rate of burnout, although the rate has dropped from the survey conducted 5 years ago. The rate of burnout among women reported for the 2020 survey was 48%, down from 51% reported 5 years ago. By comparison, the rate of burnout for men was 37% in 2020, down from 43% in 2015.
In terms of what is causing burnout, the biggest contributor is the bureaucratic tasks (charting and paperwork, for example) that physicians must complete, which 55% of respondents to the survey said was the leading cause of burnout. Next was spending too many hours at work (33%); lack of respect from administrators, employers, colleagues, and staff (32%); and the increased computerization of the practice, including the use of electronic health records (30%).
When broken down by age category, the bureaucratic tasks was tops in all three groups (57% for Millennials, 56% for Generation X, and 54% for Baby Boomers), but what ranks next differs slightly by age group. For Millennials, the next two factors were too many hours at work (38%) and lack of respect (35%). Generation X respondents cited the same two factors, both at 33%. Baby Boomers cited computerization as their second-highest factor (41%) and spending too many hours at work as the third-highest factor (31%).
The generations had different approaches to coping with burnout. Millennials (56%) reported sleep as their top-ranked coping strategy, while Gen Xers and Baby Boomers ranked exercise and personal isolation as their top choice. For these two older groups, sleep was ranked last, after other activities such as talking with family and friends.
The survey also asked about depression, and respondents reported a similar rate across all age groups (15%, 18%, and 16%, respectively). Among those who said they were depressed, the three age groups had similar rates of suicidal thoughts (21%, 24%, and 22%).
Perhaps the most striking finding of the survey is the number of physicians who would take a pay cut to achieve a better work-life balance. Among Millennials, 52% would accept a pay cut, compared with 48% of Generation X and 49% of Baby Boomers. A surprising number (36%, 34%, and 31%, respectively, reported that they would accept a $10,000-$20,000 pay cut to have a 20% reduction in work hours. [email protected]
*This story was updated on 1/22/2020.
SOURCE: Kane L et al. Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide. Medscape. 2020 Jan 15.
Burnout among physicians appears to have decreased slightly in the past few years, but remains a significant problem for the medical profession, according to the Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide.
A survey of more than 15,000 physicians revealed that 42% reported being burned out, down from 46% who responded to the survey 5 years ago. However, there are variations in the rates based on certain demographic factors such as specialty, age, and gender.
Urology sits at the top of the list as the specialty that is experiencing the highest rate of burnout, with 54% of urologists responding to the survey reporting burnout. Neurology and nephrology followed with rates of burnout at 50% and 49%, respectively. The next five specialties on the list all reported burnout rates of 46%: diabetes and endocrinology, family medicine, radiology, ob.gyn., and rheumatology. Pulmonology specialists reported a burnout rate of 41%. Gastroenterologists reported burnout rates of 37%.
The survey divided participants into three age categories – Millennial (ages 25-39 years), Generation X (ages 40-54 years), and Baby Boomer (ages 55-73 years). Both Millennials and Baby Boomers reported similar rates of burnout (38% and 39%, respectively) and those in Generation X reported a higher rate of burnout (48%).
This higher rate is not unexpected. The survey results cite Carol Bernstein, MD, of the Albert Einstein College of Medicine, New York, as noting that midcareer “is typically the time of highest burnout, which is where Gen Xers are in their career trajectory, suggesting a number of factors outside of work such as caring for children and elderly parents, planning for retirement, can play a role in contributing to burnout.”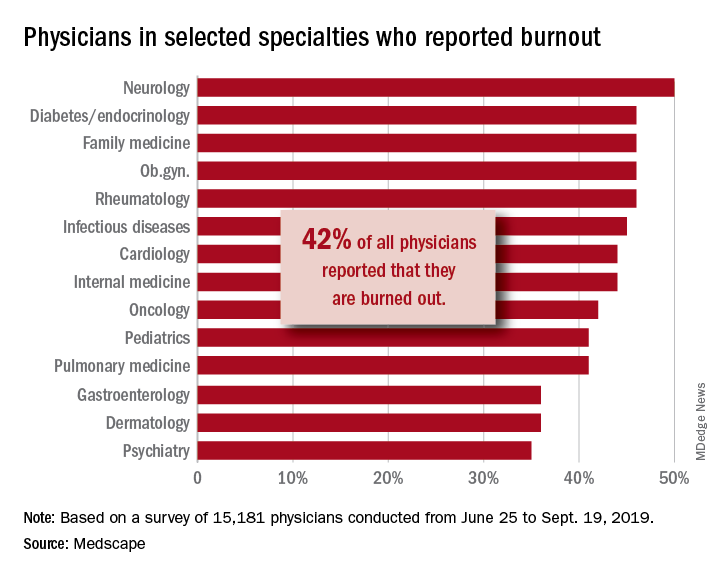
Women also reported a higher rate of burnout, although the rate has dropped from the survey conducted 5 years ago. The rate of burnout among women reported for the 2020 survey was 48%, down from 51% reported 5 years ago. By comparison, the rate of burnout for men was 37% in 2020, down from 43% in 2015.
In terms of what is causing burnout, the biggest contributor is the bureaucratic tasks (charting and paperwork, for example) that physicians must complete, which 55% of respondents to the survey said was the leading cause of burnout. Next was spending too many hours at work (33%); lack of respect from administrators, employers, colleagues, and staff (32%); and the increased computerization of the practice, including the use of electronic health records (30%).
When broken down by age category, the bureaucratic tasks was tops in all three groups (57% for Millennials, 56% for Generation X, and 54% for Baby Boomers), but what ranks next differs slightly by age group. For Millennials, the next two factors were too many hours at work (38%) and lack of respect (35%). Generation X respondents cited the same two factors, both at 33%. Baby Boomers cited computerization as their second-highest factor (41%) and spending too many hours at work as the third-highest factor (31%).
The generations had different approaches to coping with burnout. Millennials (56%) reported sleep as their top-ranked coping strategy, while Gen Xers and Baby Boomers ranked exercise and personal isolation as their top choice. For these two older groups, sleep was ranked last, after other activities such as talking with family and friends.
The survey also asked about depression, and respondents reported a similar rate across all age groups (15%, 18%, and 16%, respectively). Among those who said they were depressed, the three age groups had similar rates of suicidal thoughts (21%, 24%, and 22%).
Perhaps the most striking finding of the survey is the number of physicians who would take a pay cut to achieve a better work-life balance. Among Millennials, 52% would accept a pay cut, compared with 48% of Generation X and 49% of Baby Boomers. A surprising number (36%, 34%, and 31%, respectively, reported that they would accept a $10,000-$20,000 pay cut to have a 20% reduction in work hours. [email protected]
*This story was updated on 1/22/2020.
SOURCE: Kane L et al. Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide. Medscape. 2020 Jan 15.
For everything there is a season
2020 SoHM Survey ready to launch
Wow, the last 2 years have just flown by! I can’t believe it’s already time to launch the Society of Hospital Medicine State of Hospital Medicine survey again! Right now is the season for you to roll up your sleeves and get to work helping SHM develop the nation’s definitive resource on the current state of hospital medicine practice.
I’m really excited about this year’s survey. SHM’s Practice Analysis Committee has redesigned it to eliminate some out-of-date or little-used questions and to add a few new, more relevant questions. Even more exciting, we have a new survey platform that should massively improve your experience of submitting data for the survey and also make the back-end data tabulation and analysis much quicker and more accurate. Multisite groups will now have two options for submitting data – a redesigned, more user-friendly Excel tool, or a new pathway to submit data in the reporting platform by replicating responses.
In addition, our new survey platform should help us produce the final report a little more quickly and improve its usability.
New-for-2020 survey topics will include:
- Expanded information on nurse practitioner/physician assistant roles
- Diversity in hospital medicine physician leadership
- Specific questions for hospital medicine groups (HMGs) serving children that will better capture unique attributes of these hospital medicine practices
Why participate?
I can’t emphasize enough that each and every survey submission matters a lot. The State of Hospital Medicine report claims to be the authoritative resource for information about the specialty of hospital medicine. But the report can’t fulfill this claim if the underlying data is skimpy because people were too busy, couldn’t be bothered to participate, or if participation is not broadly representative of the amazing diversity of hospital medicine practices out there.
Your participation will help ensure that you are contributing to a robust hospital medicine database, and that your own group’s information is represented in the survey results. By doing so you will be helping to ensure hospital medicine’s place as perhaps the crucial specialty for U.S. health care in the coming decade.
In addition, participants will receive free access to the survey results, so there’s a direct benefit to you and your HMG as well.
How can you participate?
Here’s what you need to know:
1. The survey opens on Jan.6, 2020, and closes on Feb. 14, 2020.
2. You can find general information about the survey at this link: https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/, and register to participate by using this link: https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/sohm-survey/.
3. To participate, you’ll want to collect the following general types of information for your hospital medicine group:
- Basic group descriptive information (for example, types of patients seen, number of hospitals covered, teaching status, etc.)
- Scope of clinical services
- Nurse practitioners and physician assistants in the HMG
- Full-time equivalent (FTE) information
- Information about the physician leader(s)
- Staffing/scheduling arrangements, including backup plans, paid time off, unfilled positions, predominant scheduling pattern, night coverage arrangements, dedicated admitters, unit-based assignments, etc.
- Compensation model (but not specific amounts)
- Value of employee benefits and CME
- Total work relative value units generated by the HMG, and number of times the following CPT codes were billed: 99221, 99222, 99223, 99231, 99232, 99233, 99238, 99239
- Information about financial support provided to the HMG
- Specific questions for academic HMGs, including financial support for nonclinical work, and allocation of FTEs
- Specific questions for HMGs serving children, including the hospital settings served, proportion of part-time staff, FTE definition, and information about board certification in pediatric hospital medicine
I’m hoping that all of you will join me in working to make the 2020 State of Hospital Medicine survey and report the best one yet!
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Meeting Committees, and helps to coordinate SHM’s biannual State of Hospital Medicine survey.
2020 SoHM Survey ready to launch
2020 SoHM Survey ready to launch
Wow, the last 2 years have just flown by! I can’t believe it’s already time to launch the Society of Hospital Medicine State of Hospital Medicine survey again! Right now is the season for you to roll up your sleeves and get to work helping SHM develop the nation’s definitive resource on the current state of hospital medicine practice.
I’m really excited about this year’s survey. SHM’s Practice Analysis Committee has redesigned it to eliminate some out-of-date or little-used questions and to add a few new, more relevant questions. Even more exciting, we have a new survey platform that should massively improve your experience of submitting data for the survey and also make the back-end data tabulation and analysis much quicker and more accurate. Multisite groups will now have two options for submitting data – a redesigned, more user-friendly Excel tool, or a new pathway to submit data in the reporting platform by replicating responses.
In addition, our new survey platform should help us produce the final report a little more quickly and improve its usability.
New-for-2020 survey topics will include:
- Expanded information on nurse practitioner/physician assistant roles
- Diversity in hospital medicine physician leadership
- Specific questions for hospital medicine groups (HMGs) serving children that will better capture unique attributes of these hospital medicine practices
Why participate?
I can’t emphasize enough that each and every survey submission matters a lot. The State of Hospital Medicine report claims to be the authoritative resource for information about the specialty of hospital medicine. But the report can’t fulfill this claim if the underlying data is skimpy because people were too busy, couldn’t be bothered to participate, or if participation is not broadly representative of the amazing diversity of hospital medicine practices out there.
Your participation will help ensure that you are contributing to a robust hospital medicine database, and that your own group’s information is represented in the survey results. By doing so you will be helping to ensure hospital medicine’s place as perhaps the crucial specialty for U.S. health care in the coming decade.
In addition, participants will receive free access to the survey results, so there’s a direct benefit to you and your HMG as well.
How can you participate?
Here’s what you need to know:
1. The survey opens on Jan.6, 2020, and closes on Feb. 14, 2020.
2. You can find general information about the survey at this link: https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/, and register to participate by using this link: https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/sohm-survey/.
3. To participate, you’ll want to collect the following general types of information for your hospital medicine group:
- Basic group descriptive information (for example, types of patients seen, number of hospitals covered, teaching status, etc.)
- Scope of clinical services
- Nurse practitioners and physician assistants in the HMG
- Full-time equivalent (FTE) information
- Information about the physician leader(s)
- Staffing/scheduling arrangements, including backup plans, paid time off, unfilled positions, predominant scheduling pattern, night coverage arrangements, dedicated admitters, unit-based assignments, etc.
- Compensation model (but not specific amounts)
- Value of employee benefits and CME
- Total work relative value units generated by the HMG, and number of times the following CPT codes were billed: 99221, 99222, 99223, 99231, 99232, 99233, 99238, 99239
- Information about financial support provided to the HMG
- Specific questions for academic HMGs, including financial support for nonclinical work, and allocation of FTEs
- Specific questions for HMGs serving children, including the hospital settings served, proportion of part-time staff, FTE definition, and information about board certification in pediatric hospital medicine
I’m hoping that all of you will join me in working to make the 2020 State of Hospital Medicine survey and report the best one yet!
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Meeting Committees, and helps to coordinate SHM’s biannual State of Hospital Medicine survey.
Wow, the last 2 years have just flown by! I can’t believe it’s already time to launch the Society of Hospital Medicine State of Hospital Medicine survey again! Right now is the season for you to roll up your sleeves and get to work helping SHM develop the nation’s definitive resource on the current state of hospital medicine practice.
I’m really excited about this year’s survey. SHM’s Practice Analysis Committee has redesigned it to eliminate some out-of-date or little-used questions and to add a few new, more relevant questions. Even more exciting, we have a new survey platform that should massively improve your experience of submitting data for the survey and also make the back-end data tabulation and analysis much quicker and more accurate. Multisite groups will now have two options for submitting data – a redesigned, more user-friendly Excel tool, or a new pathway to submit data in the reporting platform by replicating responses.
In addition, our new survey platform should help us produce the final report a little more quickly and improve its usability.
New-for-2020 survey topics will include:
- Expanded information on nurse practitioner/physician assistant roles
- Diversity in hospital medicine physician leadership
- Specific questions for hospital medicine groups (HMGs) serving children that will better capture unique attributes of these hospital medicine practices
Why participate?
I can’t emphasize enough that each and every survey submission matters a lot. The State of Hospital Medicine report claims to be the authoritative resource for information about the specialty of hospital medicine. But the report can’t fulfill this claim if the underlying data is skimpy because people were too busy, couldn’t be bothered to participate, or if participation is not broadly representative of the amazing diversity of hospital medicine practices out there.
Your participation will help ensure that you are contributing to a robust hospital medicine database, and that your own group’s information is represented in the survey results. By doing so you will be helping to ensure hospital medicine’s place as perhaps the crucial specialty for U.S. health care in the coming decade.
In addition, participants will receive free access to the survey results, so there’s a direct benefit to you and your HMG as well.
How can you participate?
Here’s what you need to know:
1. The survey opens on Jan.6, 2020, and closes on Feb. 14, 2020.
2. You can find general information about the survey at this link: https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/, and register to participate by using this link: https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/sohm-survey/.
3. To participate, you’ll want to collect the following general types of information for your hospital medicine group:
- Basic group descriptive information (for example, types of patients seen, number of hospitals covered, teaching status, etc.)
- Scope of clinical services
- Nurse practitioners and physician assistants in the HMG
- Full-time equivalent (FTE) information
- Information about the physician leader(s)
- Staffing/scheduling arrangements, including backup plans, paid time off, unfilled positions, predominant scheduling pattern, night coverage arrangements, dedicated admitters, unit-based assignments, etc.
- Compensation model (but not specific amounts)
- Value of employee benefits and CME
- Total work relative value units generated by the HMG, and number of times the following CPT codes were billed: 99221, 99222, 99223, 99231, 99232, 99233, 99238, 99239
- Information about financial support provided to the HMG
- Specific questions for academic HMGs, including financial support for nonclinical work, and allocation of FTEs
- Specific questions for HMGs serving children, including the hospital settings served, proportion of part-time staff, FTE definition, and information about board certification in pediatric hospital medicine
I’m hoping that all of you will join me in working to make the 2020 State of Hospital Medicine survey and report the best one yet!
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Meeting Committees, and helps to coordinate SHM’s biannual State of Hospital Medicine survey.
Accelerating the careers of future hospitalists
Grant program provides funding, research support
When it comes to what future hospitalists should be doing to accelerate their careers, is there such a thing as a “no-brainer” opportunity? Aram Namavar, MD, MS, thinks so.
Dr. Namavar is a first-year internal medicine resident at UC San Diego pursuing a career as an academic hospitalist. He is passionate about building interdisciplinary platforms for patient care enhancement and serving disadvantaged and underserved communities.
Membership in the Society of Hospital Medicine is free for medical students and offers a diverse array of resources specifically curated for the ever-expanding needs of the specialty and its aspiring leaders. An active member of SHM since 2015, Dr. Namavar has looked to the organization for leading career-enhancing opportunities and resources in hospital medicine to help him achieve his altruistic career goals.
For Dr. Namavar, a few of these professional development–focused opportunities include becoming an active member of the Physicians-in-Training Committee, a founding member of the Resident and Student Special Interest Group, and a recipient of the Student Hospitalist Scholar Grant.
“I applied for the Student Hospitalist Scholar Grant to have a dedicated summer of learning quality improvement through being in meetings with hospital medicine leaders and leading my research initiatives alongside my team,” Dr. Namavar said. He described the experience as pivotal to his growth within hospital medicine and as a medical student.
The key component to SHM’s Student Hospitalist Scholar Grant opportunity is the ability for first- and second-year medical students to work alongside leading hospital medicine professionals in scholarly projects to help interested students gain perspective on working within the specialty.
“As a young, interested trainee in hospital medicine, working with a mentor who is established in the field allows one to learn what steps to take in the future to become a leader,” he said. “[It allowed me to] gain insight into leadership style and develop a strong network for the future.”
In addition to the program’s mentorship benefits, grant recipients also receive complimentary registration to SHM’s Annual Conference with the added perks of funding and research support, accommodation expenses, and acceptance into SHM’s RIV Poster Competition.
“I attended the SHM Annual Conference previously,” Dr. Namavar said. “However, as a grant recipient, you have the chance to connect with faculty who will come to your poster presentation and want to learn about your project. This platform allows you to meet individuals from across the nation and connect with those interested in helping trainees thrive within hospital medicine.”
With the grant funding, Dr. Namavar completed his project, “Evaluation of Decisional Conflict as a Simple Tool to Assess Risk of Readmission.” He described this endeavor as a multidimensional project that took on a holistic view of patient-centered readmissions. “We evaluated patient conflict in posthospitalization resources as a marker of readmission, social determinants of health, and health literacy as risk factors for hospital readmission.”
Described by Dr. Namavar as a “no-brainer” opportunity, SHM’s Student Hospitalist Scholar Grant “offers some of the best benefits overall – funding for your project, automatic acceptance at the Annual Conference, the chance to have your work highlighted in blog posts, networking opportunities with faculty across the nation, and travel reimbursement for the conference.”
Building your networks or establishing your professional career path does not stop at individual networking events or scholarship programs, Dr. Namavar said. It’s about piecing together the building blocks to set yourself up for success.
“My long-term involvement in SHM through working on a committee, leading a special interest group, attending annual meetings, and receiving the grant from SHM has helped me to build new, long-lasting connections in the field,” he said. “Because of this, I plan to continue to serve within SHM in multiple capacities throughout my career in hospital medicine.”
Are you a first- or second-year medical student interested in taking the next step in your hospital medicine career? Apply to SHM’s Student Hospitalist Scholar Grant program through late January 2020 at hospitalmedicine.org/scholargrant.
Ms. Cowan is a marketing communications specialist at the Society of Hospital Medicine.
Grant program provides funding, research support
Grant program provides funding, research support
When it comes to what future hospitalists should be doing to accelerate their careers, is there such a thing as a “no-brainer” opportunity? Aram Namavar, MD, MS, thinks so.
Dr. Namavar is a first-year internal medicine resident at UC San Diego pursuing a career as an academic hospitalist. He is passionate about building interdisciplinary platforms for patient care enhancement and serving disadvantaged and underserved communities.
Membership in the Society of Hospital Medicine is free for medical students and offers a diverse array of resources specifically curated for the ever-expanding needs of the specialty and its aspiring leaders. An active member of SHM since 2015, Dr. Namavar has looked to the organization for leading career-enhancing opportunities and resources in hospital medicine to help him achieve his altruistic career goals.
For Dr. Namavar, a few of these professional development–focused opportunities include becoming an active member of the Physicians-in-Training Committee, a founding member of the Resident and Student Special Interest Group, and a recipient of the Student Hospitalist Scholar Grant.
“I applied for the Student Hospitalist Scholar Grant to have a dedicated summer of learning quality improvement through being in meetings with hospital medicine leaders and leading my research initiatives alongside my team,” Dr. Namavar said. He described the experience as pivotal to his growth within hospital medicine and as a medical student.
The key component to SHM’s Student Hospitalist Scholar Grant opportunity is the ability for first- and second-year medical students to work alongside leading hospital medicine professionals in scholarly projects to help interested students gain perspective on working within the specialty.
“As a young, interested trainee in hospital medicine, working with a mentor who is established in the field allows one to learn what steps to take in the future to become a leader,” he said. “[It allowed me to] gain insight into leadership style and develop a strong network for the future.”
In addition to the program’s mentorship benefits, grant recipients also receive complimentary registration to SHM’s Annual Conference with the added perks of funding and research support, accommodation expenses, and acceptance into SHM’s RIV Poster Competition.
“I attended the SHM Annual Conference previously,” Dr. Namavar said. “However, as a grant recipient, you have the chance to connect with faculty who will come to your poster presentation and want to learn about your project. This platform allows you to meet individuals from across the nation and connect with those interested in helping trainees thrive within hospital medicine.”
With the grant funding, Dr. Namavar completed his project, “Evaluation of Decisional Conflict as a Simple Tool to Assess Risk of Readmission.” He described this endeavor as a multidimensional project that took on a holistic view of patient-centered readmissions. “We evaluated patient conflict in posthospitalization resources as a marker of readmission, social determinants of health, and health literacy as risk factors for hospital readmission.”
Described by Dr. Namavar as a “no-brainer” opportunity, SHM’s Student Hospitalist Scholar Grant “offers some of the best benefits overall – funding for your project, automatic acceptance at the Annual Conference, the chance to have your work highlighted in blog posts, networking opportunities with faculty across the nation, and travel reimbursement for the conference.”
Building your networks or establishing your professional career path does not stop at individual networking events or scholarship programs, Dr. Namavar said. It’s about piecing together the building blocks to set yourself up for success.
“My long-term involvement in SHM through working on a committee, leading a special interest group, attending annual meetings, and receiving the grant from SHM has helped me to build new, long-lasting connections in the field,” he said. “Because of this, I plan to continue to serve within SHM in multiple capacities throughout my career in hospital medicine.”
Are you a first- or second-year medical student interested in taking the next step in your hospital medicine career? Apply to SHM’s Student Hospitalist Scholar Grant program through late January 2020 at hospitalmedicine.org/scholargrant.
Ms. Cowan is a marketing communications specialist at the Society of Hospital Medicine.
When it comes to what future hospitalists should be doing to accelerate their careers, is there such a thing as a “no-brainer” opportunity? Aram Namavar, MD, MS, thinks so.
Dr. Namavar is a first-year internal medicine resident at UC San Diego pursuing a career as an academic hospitalist. He is passionate about building interdisciplinary platforms for patient care enhancement and serving disadvantaged and underserved communities.
Membership in the Society of Hospital Medicine is free for medical students and offers a diverse array of resources specifically curated for the ever-expanding needs of the specialty and its aspiring leaders. An active member of SHM since 2015, Dr. Namavar has looked to the organization for leading career-enhancing opportunities and resources in hospital medicine to help him achieve his altruistic career goals.
For Dr. Namavar, a few of these professional development–focused opportunities include becoming an active member of the Physicians-in-Training Committee, a founding member of the Resident and Student Special Interest Group, and a recipient of the Student Hospitalist Scholar Grant.
“I applied for the Student Hospitalist Scholar Grant to have a dedicated summer of learning quality improvement through being in meetings with hospital medicine leaders and leading my research initiatives alongside my team,” Dr. Namavar said. He described the experience as pivotal to his growth within hospital medicine and as a medical student.
The key component to SHM’s Student Hospitalist Scholar Grant opportunity is the ability for first- and second-year medical students to work alongside leading hospital medicine professionals in scholarly projects to help interested students gain perspective on working within the specialty.
“As a young, interested trainee in hospital medicine, working with a mentor who is established in the field allows one to learn what steps to take in the future to become a leader,” he said. “[It allowed me to] gain insight into leadership style and develop a strong network for the future.”
In addition to the program’s mentorship benefits, grant recipients also receive complimentary registration to SHM’s Annual Conference with the added perks of funding and research support, accommodation expenses, and acceptance into SHM’s RIV Poster Competition.
“I attended the SHM Annual Conference previously,” Dr. Namavar said. “However, as a grant recipient, you have the chance to connect with faculty who will come to your poster presentation and want to learn about your project. This platform allows you to meet individuals from across the nation and connect with those interested in helping trainees thrive within hospital medicine.”
With the grant funding, Dr. Namavar completed his project, “Evaluation of Decisional Conflict as a Simple Tool to Assess Risk of Readmission.” He described this endeavor as a multidimensional project that took on a holistic view of patient-centered readmissions. “We evaluated patient conflict in posthospitalization resources as a marker of readmission, social determinants of health, and health literacy as risk factors for hospital readmission.”
Described by Dr. Namavar as a “no-brainer” opportunity, SHM’s Student Hospitalist Scholar Grant “offers some of the best benefits overall – funding for your project, automatic acceptance at the Annual Conference, the chance to have your work highlighted in blog posts, networking opportunities with faculty across the nation, and travel reimbursement for the conference.”
Building your networks or establishing your professional career path does not stop at individual networking events or scholarship programs, Dr. Namavar said. It’s about piecing together the building blocks to set yourself up for success.
“My long-term involvement in SHM through working on a committee, leading a special interest group, attending annual meetings, and receiving the grant from SHM has helped me to build new, long-lasting connections in the field,” he said. “Because of this, I plan to continue to serve within SHM in multiple capacities throughout my career in hospital medicine.”
Are you a first- or second-year medical student interested in taking the next step in your hospital medicine career? Apply to SHM’s Student Hospitalist Scholar Grant program through late January 2020 at hospitalmedicine.org/scholargrant.
Ms. Cowan is a marketing communications specialist at the Society of Hospital Medicine.
Hospitalists deal with patient discrimination
Encounters with bias are underreported
In the fall of 2016, Hyma Polimera, MD, a hospitalist at Penn State Health in Hershey, Pa., approached the bedside of a patient with dementia and several other chronic conditions, and introduced herself to him and his family.
The patient’s daughter, who had power of attorney, took one look at Dr. Polimera and told her, “I’d like to see an American doctor.” Dr. Polimera is originally from India, but moved to Europe in 2005 and did her residency in Pennsylvania. She stayed calm and confident – she understood that she had done nothing wrong – but didn’t really know what to do next. All of the other hospitalists on the ward at the time were nonwhite and were also rejected by the patient’s daughter.
“I was wondering what was going to happen and who would provide care to this patient?” she said.
Dr. Polimera is far from alone. Nonwhite physicians, nurses, and other health care providers say they increasingly encounter patients who demand that only “white” health professionals take care of them. The number of these reassignment requests has ticked upward in the last few years, they say, coinciding with the 2016 U.S. presidential campaign and the subsequent election of Donald Trump.
The requests often come at medical centers with no policy in place for how to deal with them. And the unpleasant encounters find providers unprepared for how to respond, not knowing whether or how to resolve the situation with patients and their families. Clinicians sometimes wonder whether they are allowed to care for a patient even if they are willing to do so, and how to go about reassigning a patient to another clinician if that is the choice that the family makes.
To many hospitalists working in the field, it seems obvious that such situations are encouraged by a political environment in which discriminatory beliefs – once considered shameful to express publicly – are now deemed acceptable, even in health care encounters. Indeed, the health care encounter is perhaps the only time some patients will find themselves in intimate interactions with people of other ethnicities.
Responding to discrimination
A workshop at the 2019 Society of Hospital Medicine Annual Conference offered hospitalists an opportunity to discuss encounters with patients who expressed discriminatory attitudes. One physician, of South Asian descent, said that she had encountered no reassignment requests rooted in racial intolerance over more than a decade of work, but has encountered several in the last year or two.
Sabrina Chaklos, MD, a hospitalist at Burlington, Mass.–based Lahey Hospital & Medical Center and clinical assistant professor at Tufts University, said she has had a similar experience.
“It was blatantly bad behavior for 2018,” she said. Dr. Chaklos said she and other clinicians of color have been told, “I want an American doctor,” and that some patients see her darker complexion and conclude, “You must not be an American.”
Given the charged political environment since 2016, some medical facilities have been adapting how they respond to these comments and requests.
“The policy of the organization prior to 2016 was to give patients a new doctor,” Dr. Chaklos said. “Within the past year or so, they’re finally allowing people to say, ‘Look, you cannot just pick and choose your doctor,’ based on arbitrary reasons that are discriminatory in nature.”
Emily Whitgob, MD, MEd, a developmental-behavioral pediatrician at Santa Clara Valley Medical Center in San Jose, Calif., said that, several years ago, a scenario unfolded that led her to study the issue. An intern she was overseeing told her that the father of a pediatric patient had scrutinized the intern’s name tag and said, “Is that a Jewish last name? I don’t want a Jewish doctor.”
“I didn’t know what to do,” Dr. Whitgob said. Later, she brought up the situation at a meeting of 30 staff members. It led to an outpouring of sharing about similar incidents that other clinicians had experienced but had never talked about with colleagues.
“Half the room, by the end, was in tears talking about their experiences,” Dr. Whitgob said.
Since then, she has led research into how physicians typically handle such situations, performing semistructured interviews to survey pediatricians about their experiences with patients who discriminate on racial and ethnic grounds.
One important step, she said, is assessing the acuity of the illness involved to help determine whether the transfer of a patient from one provider to another should even be considered. In a dire situation, or when the physician involved is the foremost expert on a given condition, it might not be realistic.
Dr. Whitgob said some clinicians advocated cultivating a kind of alliance with the parents of pediatric patients, informing them that they’re part of a team that interacts with many types of providers, and redirecting them to focus on their child’s care.
“This takes time, and in a busy setting, that might not happen,” she acknowledged.
Physicians surveyed also said they try to depersonalize the uncomfortable encounter, remembering that discrimination is often motivated by a patient’s fears and a lack of control.
An important consideration, researchers found, was ensuring a safe learning environment for trainees, telling patients they would trust the physician with the care of their own children, escalating a complaint to hospital administration when appropriate, and empowering trainees to choose the next step in a situation.
Dr. Whitgob said that handling a reassignment request based on discriminatory sentiments is not as easy as “calling out ‘Code Bigotry.’ ”
“It’s not that simple,” Dr. Whitgob said. “There’s not going to be a one-size-fits-all or even a one-size-fits-most solution. Each case is an individual case.”
Taking action
Penn State Health is based in Hershey, Pa., a city that tends to vote Democratic in local and national elections but is encircled by Republican-leaning counties. Dr. Polimera’s encounter with her patient’s daughter led to changes in the way the health system handles encounters like hers.
When Dr. Polimera explained the situation to physician leadership, she was asked whether she was still comfortable taking care of the patient, and she said yes. The physician leaders informed the family that they could not change providers simply because of ethnicity. But that was just the first step.
Ultimately, the health system undertook a survey of all its health care providers, to determine whether others had similar experiences with patients or families, and had to deal with rude comments or were rejected as caregivers based on their race, gender, or religion.
“The feedback we received was massive and detailed,” Dr. Polimera said.
Brian McGillen, MD, section chief of hospital medicine and associate professor in the department of medicine at Penn State Health, said physician leaders took the survey results to the dean’s executive council, a who’s-who of medical leadership at the health system.
“I read aloud to the executive council what our folks were facing out on the floors,” Dr. McGillen said. “And I was halfway through my third story when the dean threw his hands up in the air and said, ‘We have to do something.’ ”
As a result, the health system’s policy on patient responsibility was changed to protect all health care providers from threats, violence, disrespectful communication, or harassment by patients, families, and other visitors. Before the change, the policy covered only discriminatory acts by patients themselves.
Penn State Health is now embarking on a training program for faculty, residents, and students that uses simulations of common hospital encounters. The health system also is engaging its patient relations staff to help mediate patient reassignment requests, and is trying to increase real-time debriefing of these events to further improve awareness and training.
Dr. McGillen noted that researchers at the University of North Texas, using data from the Anti-Defamation League, found that counties in which President Trump held campaign rallies – such as Dauphin County, Pa., where Hershey is located – had a 226% increase in hate crimes in the months after the rallies.
“This isn’t to say that every county and every person in these counties that voted for Mr. Trump is racist, but we surely know that his campaign unlocked an undercurrent of political incorrectness that has existed for ages,” he said. “We had to do something as an organization.”
Adapting to change
While some health systems are acting to limit the harm caused by discrimination, there is still much awareness to be raised and work to be done on this issue nationally. Some hospitalists at the 2019 SHM Annual Conference said they suspect that discriminatory incidents involving patients are still so underreported that the C-suite leaders at their hospitals do not recognize how serious a problem it is. Attendees at the HM19 workshop said discriminatory behavior by patients could affect hospitalist turnover and lead to burnout.
Multiple hospitalists at the workshop said that if a transfer of a patient is going to take place – if the patient requests a “white” doctor and there is not one available where the patient is admitted – they are unsure whether it is their responsibility to make the necessary phone calls. Some hospitalists say that if that job does fall to them, it interrupts work flow.
Susan Hakes, MHA, director of hospital administration at the Guthrie Clinic in Ithaca, N.Y., said that when a patient recently asked for a “white” doctor and there was not one available at the time of the request, the patient changed her mind when costs were considered.
“I was willing to have this patient transferred to another one of our hospitals that did have a white doctor, but it would have been at her expense since insurance wouldn’t cover the ambulance ride,” Ms. Hakes said. “She had second thoughts after learning that.”
Ms. Hakes said that the broader community in her region – which is predominantly white – needs to adapt to a changing health care scene.
“We’re recruiting international nurses now, due to the nursing shortage,” she said. “It will serve our community well to be receptive and welcome this additional resource.”
Kunal P. Bhagat, MD, chief of hospital medicine at Christiana Care Health System in Newark, Del., said that medical centers should set parameters for action when a patient discriminates, but that clinicians should not expect to fundamentally change a patient’s mindset.
“I think it is important to set limits,” Dr. Bhagat said. “It’s like with your kids. Your children may behave in certain ways, at certain times, that you don’t like. You can tell them, ‘You know, you may not like behaving the way I want you to behave, but the way you’re behaving now is not acceptable.’ If our goal is to try to completely change their world-view at that moment, I think we’re going to be set up for failure. That’s more of a long-term issue for society to address.”
Encounters with bias are underreported
Encounters with bias are underreported
In the fall of 2016, Hyma Polimera, MD, a hospitalist at Penn State Health in Hershey, Pa., approached the bedside of a patient with dementia and several other chronic conditions, and introduced herself to him and his family.
The patient’s daughter, who had power of attorney, took one look at Dr. Polimera and told her, “I’d like to see an American doctor.” Dr. Polimera is originally from India, but moved to Europe in 2005 and did her residency in Pennsylvania. She stayed calm and confident – she understood that she had done nothing wrong – but didn’t really know what to do next. All of the other hospitalists on the ward at the time were nonwhite and were also rejected by the patient’s daughter.
“I was wondering what was going to happen and who would provide care to this patient?” she said.
Dr. Polimera is far from alone. Nonwhite physicians, nurses, and other health care providers say they increasingly encounter patients who demand that only “white” health professionals take care of them. The number of these reassignment requests has ticked upward in the last few years, they say, coinciding with the 2016 U.S. presidential campaign and the subsequent election of Donald Trump.
The requests often come at medical centers with no policy in place for how to deal with them. And the unpleasant encounters find providers unprepared for how to respond, not knowing whether or how to resolve the situation with patients and their families. Clinicians sometimes wonder whether they are allowed to care for a patient even if they are willing to do so, and how to go about reassigning a patient to another clinician if that is the choice that the family makes.
To many hospitalists working in the field, it seems obvious that such situations are encouraged by a political environment in which discriminatory beliefs – once considered shameful to express publicly – are now deemed acceptable, even in health care encounters. Indeed, the health care encounter is perhaps the only time some patients will find themselves in intimate interactions with people of other ethnicities.
Responding to discrimination
A workshop at the 2019 Society of Hospital Medicine Annual Conference offered hospitalists an opportunity to discuss encounters with patients who expressed discriminatory attitudes. One physician, of South Asian descent, said that she had encountered no reassignment requests rooted in racial intolerance over more than a decade of work, but has encountered several in the last year or two.
Sabrina Chaklos, MD, a hospitalist at Burlington, Mass.–based Lahey Hospital & Medical Center and clinical assistant professor at Tufts University, said she has had a similar experience.
“It was blatantly bad behavior for 2018,” she said. Dr. Chaklos said she and other clinicians of color have been told, “I want an American doctor,” and that some patients see her darker complexion and conclude, “You must not be an American.”
Given the charged political environment since 2016, some medical facilities have been adapting how they respond to these comments and requests.
“The policy of the organization prior to 2016 was to give patients a new doctor,” Dr. Chaklos said. “Within the past year or so, they’re finally allowing people to say, ‘Look, you cannot just pick and choose your doctor,’ based on arbitrary reasons that are discriminatory in nature.”
Emily Whitgob, MD, MEd, a developmental-behavioral pediatrician at Santa Clara Valley Medical Center in San Jose, Calif., said that, several years ago, a scenario unfolded that led her to study the issue. An intern she was overseeing told her that the father of a pediatric patient had scrutinized the intern’s name tag and said, “Is that a Jewish last name? I don’t want a Jewish doctor.”
“I didn’t know what to do,” Dr. Whitgob said. Later, she brought up the situation at a meeting of 30 staff members. It led to an outpouring of sharing about similar incidents that other clinicians had experienced but had never talked about with colleagues.
“Half the room, by the end, was in tears talking about their experiences,” Dr. Whitgob said.
Since then, she has led research into how physicians typically handle such situations, performing semistructured interviews to survey pediatricians about their experiences with patients who discriminate on racial and ethnic grounds.
One important step, she said, is assessing the acuity of the illness involved to help determine whether the transfer of a patient from one provider to another should even be considered. In a dire situation, or when the physician involved is the foremost expert on a given condition, it might not be realistic.
Dr. Whitgob said some clinicians advocated cultivating a kind of alliance with the parents of pediatric patients, informing them that they’re part of a team that interacts with many types of providers, and redirecting them to focus on their child’s care.
“This takes time, and in a busy setting, that might not happen,” she acknowledged.
Physicians surveyed also said they try to depersonalize the uncomfortable encounter, remembering that discrimination is often motivated by a patient’s fears and a lack of control.
An important consideration, researchers found, was ensuring a safe learning environment for trainees, telling patients they would trust the physician with the care of their own children, escalating a complaint to hospital administration when appropriate, and empowering trainees to choose the next step in a situation.
Dr. Whitgob said that handling a reassignment request based on discriminatory sentiments is not as easy as “calling out ‘Code Bigotry.’ ”
“It’s not that simple,” Dr. Whitgob said. “There’s not going to be a one-size-fits-all or even a one-size-fits-most solution. Each case is an individual case.”
Taking action
Penn State Health is based in Hershey, Pa., a city that tends to vote Democratic in local and national elections but is encircled by Republican-leaning counties. Dr. Polimera’s encounter with her patient’s daughter led to changes in the way the health system handles encounters like hers.
When Dr. Polimera explained the situation to physician leadership, she was asked whether she was still comfortable taking care of the patient, and she said yes. The physician leaders informed the family that they could not change providers simply because of ethnicity. But that was just the first step.
Ultimately, the health system undertook a survey of all its health care providers, to determine whether others had similar experiences with patients or families, and had to deal with rude comments or were rejected as caregivers based on their race, gender, or religion.
“The feedback we received was massive and detailed,” Dr. Polimera said.
Brian McGillen, MD, section chief of hospital medicine and associate professor in the department of medicine at Penn State Health, said physician leaders took the survey results to the dean’s executive council, a who’s-who of medical leadership at the health system.
“I read aloud to the executive council what our folks were facing out on the floors,” Dr. McGillen said. “And I was halfway through my third story when the dean threw his hands up in the air and said, ‘We have to do something.’ ”
As a result, the health system’s policy on patient responsibility was changed to protect all health care providers from threats, violence, disrespectful communication, or harassment by patients, families, and other visitors. Before the change, the policy covered only discriminatory acts by patients themselves.
Penn State Health is now embarking on a training program for faculty, residents, and students that uses simulations of common hospital encounters. The health system also is engaging its patient relations staff to help mediate patient reassignment requests, and is trying to increase real-time debriefing of these events to further improve awareness and training.
Dr. McGillen noted that researchers at the University of North Texas, using data from the Anti-Defamation League, found that counties in which President Trump held campaign rallies – such as Dauphin County, Pa., where Hershey is located – had a 226% increase in hate crimes in the months after the rallies.
“This isn’t to say that every county and every person in these counties that voted for Mr. Trump is racist, but we surely know that his campaign unlocked an undercurrent of political incorrectness that has existed for ages,” he said. “We had to do something as an organization.”
Adapting to change
While some health systems are acting to limit the harm caused by discrimination, there is still much awareness to be raised and work to be done on this issue nationally. Some hospitalists at the 2019 SHM Annual Conference said they suspect that discriminatory incidents involving patients are still so underreported that the C-suite leaders at their hospitals do not recognize how serious a problem it is. Attendees at the HM19 workshop said discriminatory behavior by patients could affect hospitalist turnover and lead to burnout.
Multiple hospitalists at the workshop said that if a transfer of a patient is going to take place – if the patient requests a “white” doctor and there is not one available where the patient is admitted – they are unsure whether it is their responsibility to make the necessary phone calls. Some hospitalists say that if that job does fall to them, it interrupts work flow.
Susan Hakes, MHA, director of hospital administration at the Guthrie Clinic in Ithaca, N.Y., said that when a patient recently asked for a “white” doctor and there was not one available at the time of the request, the patient changed her mind when costs were considered.
“I was willing to have this patient transferred to another one of our hospitals that did have a white doctor, but it would have been at her expense since insurance wouldn’t cover the ambulance ride,” Ms. Hakes said. “She had second thoughts after learning that.”
Ms. Hakes said that the broader community in her region – which is predominantly white – needs to adapt to a changing health care scene.
“We’re recruiting international nurses now, due to the nursing shortage,” she said. “It will serve our community well to be receptive and welcome this additional resource.”
Kunal P. Bhagat, MD, chief of hospital medicine at Christiana Care Health System in Newark, Del., said that medical centers should set parameters for action when a patient discriminates, but that clinicians should not expect to fundamentally change a patient’s mindset.
“I think it is important to set limits,” Dr. Bhagat said. “It’s like with your kids. Your children may behave in certain ways, at certain times, that you don’t like. You can tell them, ‘You know, you may not like behaving the way I want you to behave, but the way you’re behaving now is not acceptable.’ If our goal is to try to completely change their world-view at that moment, I think we’re going to be set up for failure. That’s more of a long-term issue for society to address.”
In the fall of 2016, Hyma Polimera, MD, a hospitalist at Penn State Health in Hershey, Pa., approached the bedside of a patient with dementia and several other chronic conditions, and introduced herself to him and his family.
The patient’s daughter, who had power of attorney, took one look at Dr. Polimera and told her, “I’d like to see an American doctor.” Dr. Polimera is originally from India, but moved to Europe in 2005 and did her residency in Pennsylvania. She stayed calm and confident – she understood that she had done nothing wrong – but didn’t really know what to do next. All of the other hospitalists on the ward at the time were nonwhite and were also rejected by the patient’s daughter.
“I was wondering what was going to happen and who would provide care to this patient?” she said.
Dr. Polimera is far from alone. Nonwhite physicians, nurses, and other health care providers say they increasingly encounter patients who demand that only “white” health professionals take care of them. The number of these reassignment requests has ticked upward in the last few years, they say, coinciding with the 2016 U.S. presidential campaign and the subsequent election of Donald Trump.
The requests often come at medical centers with no policy in place for how to deal with them. And the unpleasant encounters find providers unprepared for how to respond, not knowing whether or how to resolve the situation with patients and their families. Clinicians sometimes wonder whether they are allowed to care for a patient even if they are willing to do so, and how to go about reassigning a patient to another clinician if that is the choice that the family makes.
To many hospitalists working in the field, it seems obvious that such situations are encouraged by a political environment in which discriminatory beliefs – once considered shameful to express publicly – are now deemed acceptable, even in health care encounters. Indeed, the health care encounter is perhaps the only time some patients will find themselves in intimate interactions with people of other ethnicities.
Responding to discrimination
A workshop at the 2019 Society of Hospital Medicine Annual Conference offered hospitalists an opportunity to discuss encounters with patients who expressed discriminatory attitudes. One physician, of South Asian descent, said that she had encountered no reassignment requests rooted in racial intolerance over more than a decade of work, but has encountered several in the last year or two.
Sabrina Chaklos, MD, a hospitalist at Burlington, Mass.–based Lahey Hospital & Medical Center and clinical assistant professor at Tufts University, said she has had a similar experience.
“It was blatantly bad behavior for 2018,” she said. Dr. Chaklos said she and other clinicians of color have been told, “I want an American doctor,” and that some patients see her darker complexion and conclude, “You must not be an American.”
Given the charged political environment since 2016, some medical facilities have been adapting how they respond to these comments and requests.
“The policy of the organization prior to 2016 was to give patients a new doctor,” Dr. Chaklos said. “Within the past year or so, they’re finally allowing people to say, ‘Look, you cannot just pick and choose your doctor,’ based on arbitrary reasons that are discriminatory in nature.”
Emily Whitgob, MD, MEd, a developmental-behavioral pediatrician at Santa Clara Valley Medical Center in San Jose, Calif., said that, several years ago, a scenario unfolded that led her to study the issue. An intern she was overseeing told her that the father of a pediatric patient had scrutinized the intern’s name tag and said, “Is that a Jewish last name? I don’t want a Jewish doctor.”
“I didn’t know what to do,” Dr. Whitgob said. Later, she brought up the situation at a meeting of 30 staff members. It led to an outpouring of sharing about similar incidents that other clinicians had experienced but had never talked about with colleagues.
“Half the room, by the end, was in tears talking about their experiences,” Dr. Whitgob said.
Since then, she has led research into how physicians typically handle such situations, performing semistructured interviews to survey pediatricians about their experiences with patients who discriminate on racial and ethnic grounds.
One important step, she said, is assessing the acuity of the illness involved to help determine whether the transfer of a patient from one provider to another should even be considered. In a dire situation, or when the physician involved is the foremost expert on a given condition, it might not be realistic.
Dr. Whitgob said some clinicians advocated cultivating a kind of alliance with the parents of pediatric patients, informing them that they’re part of a team that interacts with many types of providers, and redirecting them to focus on their child’s care.
“This takes time, and in a busy setting, that might not happen,” she acknowledged.
Physicians surveyed also said they try to depersonalize the uncomfortable encounter, remembering that discrimination is often motivated by a patient’s fears and a lack of control.
An important consideration, researchers found, was ensuring a safe learning environment for trainees, telling patients they would trust the physician with the care of their own children, escalating a complaint to hospital administration when appropriate, and empowering trainees to choose the next step in a situation.
Dr. Whitgob said that handling a reassignment request based on discriminatory sentiments is not as easy as “calling out ‘Code Bigotry.’ ”
“It’s not that simple,” Dr. Whitgob said. “There’s not going to be a one-size-fits-all or even a one-size-fits-most solution. Each case is an individual case.”
Taking action
Penn State Health is based in Hershey, Pa., a city that tends to vote Democratic in local and national elections but is encircled by Republican-leaning counties. Dr. Polimera’s encounter with her patient’s daughter led to changes in the way the health system handles encounters like hers.
When Dr. Polimera explained the situation to physician leadership, she was asked whether she was still comfortable taking care of the patient, and she said yes. The physician leaders informed the family that they could not change providers simply because of ethnicity. But that was just the first step.
Ultimately, the health system undertook a survey of all its health care providers, to determine whether others had similar experiences with patients or families, and had to deal with rude comments or were rejected as caregivers based on their race, gender, or religion.
“The feedback we received was massive and detailed,” Dr. Polimera said.
Brian McGillen, MD, section chief of hospital medicine and associate professor in the department of medicine at Penn State Health, said physician leaders took the survey results to the dean’s executive council, a who’s-who of medical leadership at the health system.
“I read aloud to the executive council what our folks were facing out on the floors,” Dr. McGillen said. “And I was halfway through my third story when the dean threw his hands up in the air and said, ‘We have to do something.’ ”
As a result, the health system’s policy on patient responsibility was changed to protect all health care providers from threats, violence, disrespectful communication, or harassment by patients, families, and other visitors. Before the change, the policy covered only discriminatory acts by patients themselves.
Penn State Health is now embarking on a training program for faculty, residents, and students that uses simulations of common hospital encounters. The health system also is engaging its patient relations staff to help mediate patient reassignment requests, and is trying to increase real-time debriefing of these events to further improve awareness and training.
Dr. McGillen noted that researchers at the University of North Texas, using data from the Anti-Defamation League, found that counties in which President Trump held campaign rallies – such as Dauphin County, Pa., where Hershey is located – had a 226% increase in hate crimes in the months after the rallies.
“This isn’t to say that every county and every person in these counties that voted for Mr. Trump is racist, but we surely know that his campaign unlocked an undercurrent of political incorrectness that has existed for ages,” he said. “We had to do something as an organization.”
Adapting to change
While some health systems are acting to limit the harm caused by discrimination, there is still much awareness to be raised and work to be done on this issue nationally. Some hospitalists at the 2019 SHM Annual Conference said they suspect that discriminatory incidents involving patients are still so underreported that the C-suite leaders at their hospitals do not recognize how serious a problem it is. Attendees at the HM19 workshop said discriminatory behavior by patients could affect hospitalist turnover and lead to burnout.
Multiple hospitalists at the workshop said that if a transfer of a patient is going to take place – if the patient requests a “white” doctor and there is not one available where the patient is admitted – they are unsure whether it is their responsibility to make the necessary phone calls. Some hospitalists say that if that job does fall to them, it interrupts work flow.
Susan Hakes, MHA, director of hospital administration at the Guthrie Clinic in Ithaca, N.Y., said that when a patient recently asked for a “white” doctor and there was not one available at the time of the request, the patient changed her mind when costs were considered.
“I was willing to have this patient transferred to another one of our hospitals that did have a white doctor, but it would have been at her expense since insurance wouldn’t cover the ambulance ride,” Ms. Hakes said. “She had second thoughts after learning that.”
Ms. Hakes said that the broader community in her region – which is predominantly white – needs to adapt to a changing health care scene.
“We’re recruiting international nurses now, due to the nursing shortage,” she said. “It will serve our community well to be receptive and welcome this additional resource.”
Kunal P. Bhagat, MD, chief of hospital medicine at Christiana Care Health System in Newark, Del., said that medical centers should set parameters for action when a patient discriminates, but that clinicians should not expect to fundamentally change a patient’s mindset.
“I think it is important to set limits,” Dr. Bhagat said. “It’s like with your kids. Your children may behave in certain ways, at certain times, that you don’t like. You can tell them, ‘You know, you may not like behaving the way I want you to behave, but the way you’re behaving now is not acceptable.’ If our goal is to try to completely change their world-view at that moment, I think we’re going to be set up for failure. That’s more of a long-term issue for society to address.”
Aligning scheduling and satisfaction
Research reveals counterintuitive results
Hospitalist work schedules have been the subject of much reporting – and recent research. Studies have shown that control over work hours and schedule flexibility are predictors of clinicians’ career satisfaction and burnout, factors linked to quality of patient care and retention.
Starting in January 2017, an academic hospital medicine group at the University of Colorado at Denver, Aurora, undertook a scheduling redesign using improvement methodology, combined with purchased scheduling software. Tyler Anstett, DO, a hospitalist and assistant professor at the university, and colleagues presented the results in an abstract published during the SHM 2019 annual conference last March.
“We wrote this abstract as a report of the work that we did over several years in our hospital medicine group to improve hospitalist satisfaction with their schedules,” said Dr. Anstett. “We identified that, despite not following the traditional seven-on, seven-off model and 100% fulfillment of individual schedule requests, the majority of clinicians were dissatisfied with the scheduling process and their overall clinical schedules. Further, building these complex, individualized schedules resulted in a heavy administrative burden. We strove to provide better alignment of schedule satisfaction and the administrative burden of incorporating individualized schedule requests.”
Prior to January 2017, service stretches had ranged from 5 to 9 days, and there were few limits on time-off requests.
“Through sequential interventions, we standardized service stretches to 7 days (Tuesday-Monday), introduced a limited number of guaranteed 7-day time-off requests (Tuesday-Monday), and added a limited number of nonguaranteed 3-day flexible time-off requests,” according to the authors. “This simplification improved the automation of the scheduling software, which increased the schedule release lead time to an average of 16 weeks. Further, despite standardizing service stretches to 7 days and limiting time-off requests, physicians surveyed reported improved satisfaction with both their scheduling process (34% of participants ‘satisfied’ in 2017 to 67% in 2018) and their overall clinical schedules (50% of participants ‘satisfied’ in 2017 to 75% in 2018).”So counterintuitively, creating individualized schedules may not result in improved satisfaction and likely results in heavy administrative burden, Dr. Anstett said. “Standardization of schedule creation with allowance of a ‘free-market’ system, allowing clinicians to self-individualize their schedules may also result in less administrative burden and improved satisfaction.”
Reference
1. Anstett T et al. K.I.S.S. (Keep It Simple … Schedules): How Standardization and Simplification Can Improve Scheduling and Physician Satisfaction. SHM 2019, Abstract 112. Accessed June 4, 2019.
Research reveals counterintuitive results
Research reveals counterintuitive results
Hospitalist work schedules have been the subject of much reporting – and recent research. Studies have shown that control over work hours and schedule flexibility are predictors of clinicians’ career satisfaction and burnout, factors linked to quality of patient care and retention.
Starting in January 2017, an academic hospital medicine group at the University of Colorado at Denver, Aurora, undertook a scheduling redesign using improvement methodology, combined with purchased scheduling software. Tyler Anstett, DO, a hospitalist and assistant professor at the university, and colleagues presented the results in an abstract published during the SHM 2019 annual conference last March.
“We wrote this abstract as a report of the work that we did over several years in our hospital medicine group to improve hospitalist satisfaction with their schedules,” said Dr. Anstett. “We identified that, despite not following the traditional seven-on, seven-off model and 100% fulfillment of individual schedule requests, the majority of clinicians were dissatisfied with the scheduling process and their overall clinical schedules. Further, building these complex, individualized schedules resulted in a heavy administrative burden. We strove to provide better alignment of schedule satisfaction and the administrative burden of incorporating individualized schedule requests.”
Prior to January 2017, service stretches had ranged from 5 to 9 days, and there were few limits on time-off requests.
“Through sequential interventions, we standardized service stretches to 7 days (Tuesday-Monday), introduced a limited number of guaranteed 7-day time-off requests (Tuesday-Monday), and added a limited number of nonguaranteed 3-day flexible time-off requests,” according to the authors. “This simplification improved the automation of the scheduling software, which increased the schedule release lead time to an average of 16 weeks. Further, despite standardizing service stretches to 7 days and limiting time-off requests, physicians surveyed reported improved satisfaction with both their scheduling process (34% of participants ‘satisfied’ in 2017 to 67% in 2018) and their overall clinical schedules (50% of participants ‘satisfied’ in 2017 to 75% in 2018).”So counterintuitively, creating individualized schedules may not result in improved satisfaction and likely results in heavy administrative burden, Dr. Anstett said. “Standardization of schedule creation with allowance of a ‘free-market’ system, allowing clinicians to self-individualize their schedules may also result in less administrative burden and improved satisfaction.”
Reference
1. Anstett T et al. K.I.S.S. (Keep It Simple … Schedules): How Standardization and Simplification Can Improve Scheduling and Physician Satisfaction. SHM 2019, Abstract 112. Accessed June 4, 2019.
Hospitalist work schedules have been the subject of much reporting – and recent research. Studies have shown that control over work hours and schedule flexibility are predictors of clinicians’ career satisfaction and burnout, factors linked to quality of patient care and retention.
Starting in January 2017, an academic hospital medicine group at the University of Colorado at Denver, Aurora, undertook a scheduling redesign using improvement methodology, combined with purchased scheduling software. Tyler Anstett, DO, a hospitalist and assistant professor at the university, and colleagues presented the results in an abstract published during the SHM 2019 annual conference last March.
“We wrote this abstract as a report of the work that we did over several years in our hospital medicine group to improve hospitalist satisfaction with their schedules,” said Dr. Anstett. “We identified that, despite not following the traditional seven-on, seven-off model and 100% fulfillment of individual schedule requests, the majority of clinicians were dissatisfied with the scheduling process and their overall clinical schedules. Further, building these complex, individualized schedules resulted in a heavy administrative burden. We strove to provide better alignment of schedule satisfaction and the administrative burden of incorporating individualized schedule requests.”
Prior to January 2017, service stretches had ranged from 5 to 9 days, and there were few limits on time-off requests.
“Through sequential interventions, we standardized service stretches to 7 days (Tuesday-Monday), introduced a limited number of guaranteed 7-day time-off requests (Tuesday-Monday), and added a limited number of nonguaranteed 3-day flexible time-off requests,” according to the authors. “This simplification improved the automation of the scheduling software, which increased the schedule release lead time to an average of 16 weeks. Further, despite standardizing service stretches to 7 days and limiting time-off requests, physicians surveyed reported improved satisfaction with both their scheduling process (34% of participants ‘satisfied’ in 2017 to 67% in 2018) and their overall clinical schedules (50% of participants ‘satisfied’ in 2017 to 75% in 2018).”So counterintuitively, creating individualized schedules may not result in improved satisfaction and likely results in heavy administrative burden, Dr. Anstett said. “Standardization of schedule creation with allowance of a ‘free-market’ system, allowing clinicians to self-individualize their schedules may also result in less administrative burden and improved satisfaction.”
Reference
1. Anstett T et al. K.I.S.S. (Keep It Simple … Schedules): How Standardization and Simplification Can Improve Scheduling and Physician Satisfaction. SHM 2019, Abstract 112. Accessed June 4, 2019.
The branching tree of hospital medicine
Diversity of training backgrounds
You’ve probably heard of a “nocturnist,” but have you ever heard of a “weekendist?”
The field of hospital medicine (HM) has evolved dramatically since the term “hospitalist” was introduced in the literature in 1996.1 There is a saying in HM that “if you know one HM program, you know one HM program,” alluding to the fact that every HM program is unique. The diversity of individual HM programs combined with the overall evolution of the field has expanded the range of jobs available in HM.
The nomenclature of adding an -ist to the end of the specific roles (e.g., nocturnist, weekendist) has become commonplace. These roles have developed with the increasing need for day and night staffing at many hospitals secondary to increased and more complex patients, less availability of residents because of work hour restrictions, and the Accreditation Council for Graduate Medical Education (ACGME) rules that require overnight supervision of residents
Additionally, the field of HM increasingly includes physicians trained in internal medicine, family medicine, pediatrics, and medicine-pediatrics (med-peds). In this article, we describe the variety of roles available to trainees joining HM and the multitude of different training backgrounds hospitalists come from.
Nocturnists
The 2018 State of Hospital Medicine Report notes that 76.1% of adult-only HM groups have nocturnists, hospitalists who work primarily at night to admit and to provide coverage for admitted patients.2 Nocturnists often provide benefit to the rest of their hospitalist group by allowing fewer required night shifts for those that prefer to work during the day.
Nocturnists may choose a nighttime schedule for several reasons, including the ability to be home more during the day. They also have the potential to work fewer total hours or shifts while still earning a similar or increased income, compared with predominantly daytime hospitalists, increasing their flexibility to pursue other interests. These nocturnists become experts in navigating the admission process and responding to inpatient emergencies often with less support when compared with daytime hospitalists.
In addition to career nocturnist work, nocturnist jobs can be a great fit for those residency graduates who are undecided about fellowship and enjoy the acuity of inpatient medicine. It provides an opportunity to hone their clinical skill set prior to specialized training while earning an attending salary, and offers flexible hours which may allow for research or other endeavors. In academic centers, nocturnist educational roles take on a different character as well and may involve more 1:1 educational experiences. The role of nocturnists as educators is expanding as ACGME rules call for more oversight and educational opportunities for residents who are working at night.
However, challenges exist for nocturnists, including keeping abreast of new changes in their HM groups and hospital systems and engaging in quality initiatives, given that most meetings occur during the day. Additionally, nocturnists must adapt to sleeping during the day, potentially getting less sleep then they would otherwise and being “off cycle” with family and friends. For nocturnists raising children, being off cycle may be advantageous as it can allow them to be home with their children after school.
Weekendists
Another common hospitalist role is the weekendist, hospitalists who spend much of their clinical time preferentially working weekends. Similar to nocturnists, weekendists provide benefit to their hospitalist group by allowing others to have more weekends off.
Weekendists may prefer working weekends because of fewer total shifts or hours and/or higher compensation per shift. Additionally, weekendists have the flexibility to do other work on weekdays, such as research or another hospitalist job. For those that do nonclinical work during the week, a weekendist position may allow them to keep their clinical skills up to date. However, weekendists may face intense clinical days with a higher census because of fewer hospitalists rounding on the weekends.
Weekendists must balance having more potential time available during the weekdays but less time on the weekends to devote to family and friends. Furthermore, weekendists may feel less engaged with nonclinical opportunities, including quality improvement, educational offerings, and teaching opportunities.
SNFists
With increasing emphasis on transitions of care and the desire to avoid readmission penalties, some hospitalists have transitioned to work partly or primarily in skilled nursing facilities (SNF) and have been referred to as “SNFists.” Some of these hospitalists may split their clinical time between SNFs and acute care hospitals, while others may work exclusively at SNFs.
SNFists have the potential to be invaluable in improving transitions of care after discharge to post–acute care facilities because of increased provider presence in these facilities, comfort with medically complex patients, and appreciation of government regulations.4 SNFists may face potential challenges of needing to staff more than one post–acute care hospital and of having less resources available, compared with an acute care hospital.
Specific specialty hospitalists
For a variety of reasons including clinical interest, many hospitalists have become specialized with regards to their primary inpatient population. Some hospitalists spend the majority of their clinical time on a specific service in the hospital, often working closely with the subspecialist caring for that patient. These hospitalists may focus on hematology, oncology, bone-marrow transplant, neurology, cardiology, surgery services, or critical care, among others. Hospitalists focused on a specific service often become knowledge experts in that specialty. Conversely, by focusing on a specific service, certain pathologies may be less commonly seen, which may narrow the breadth of the hospital medicine job.
Hospitalist training
Internal medicine hospitalists may be the most common hospitalists encountered in many hospitals and at each Society of Hospital Medicine annual conference, but there has also been rapid growth in hospitalists from other specialties and backgrounds.
Family medicine hospitalists are a part of 64.9% of HM groups and about 9% of family medicine graduates are choosing HM as a career path.2,3 Most family medicine hospitalists work in adult HM groups, but some, particularly in rural or academic settings, care for pediatric, newborn, and/or maternity patients. Similarly, pediatric hospitalists have become entrenched at many hospitals where children are admitted. These pediatric hospitalists, like adult hospitalists, may work in a variety of different clinical roles including in EDs, newborn nurseries, and inpatient wards or ICUs; they may also provide consult, sedation, or procedural services.
Med-peds hospitalists that split time between internal medicine and pediatrics are becoming more commonplace in the field. Many work at academic centers where they often work on each side separately, doing the same work as their internal medicine or pediatrics colleagues, and then switching to the other side after a period of time. Some centers offer unique roles for med-peds hospitalists including working on adult consult teams in children’s hospitals, where they provide consult care to older patients that may still receive their care at a children’s hospital. There are also nonacademic hospitals that primarily staff med-peds hospitalists, where they can provide the full spectrum of care from the newborn nursery to the inpatient pediatric and adult wards.
Hospital medicine is a young field that is constantly changing with new and developing roles for hospitalists from a wide variety of backgrounds. Stick around to see which “-ist” will come next in HM.
Dr. Hall is a med-peds hospitalist and assistant professor at the University of Kentucky, Lexington. Dr. Sanyal-Dey is an academic hospitalist at Zuckerberg San Francisco General Hospital and Trauma Center and the University of California, San Francisco, where she is the director of clinical operations, and director of the faculty inpatient service. Dr. Chang is associate professor and interprofessional education thread director (MD curriculum) at Washington University, St. Louis. Dr. Kwan is a hospitalist at the Veterans Affairs San Diego Healthcare System and associate professor at the University of California, San Diego. He is the chair of SHM’s Physicians in Training committee. Dr. Seymour is family medicine hospitalist education director at the University of Massachusetts Memorial Medical Center, Worcester, and associate professor at the University of Massachusetts.
References
1. Wachter RM, Goldman L. The Emerging Role of “Hospitalists” in the American Health Care System. N Engl J Med. 1996;335(7):514-7.
2. 2018 State of Hospital Medicine Report. Philadelphia: Society of Hospital Medicine, 2018.
3. Weaver SP, Hill J. Academician Attitudes and Beliefs Regarding the Use of Hospitalists: A CERA Study. Fam Med. 2015;47(5):357-61.
4. Teno JM et al. Temporal Trends in the Numbers of Skilled Nursing Facility Specialists From 2007 Through 2014. JAMA Intern Med. 2017;177(9):1376-8.
Diversity of training backgrounds
Diversity of training backgrounds
You’ve probably heard of a “nocturnist,” but have you ever heard of a “weekendist?”
The field of hospital medicine (HM) has evolved dramatically since the term “hospitalist” was introduced in the literature in 1996.1 There is a saying in HM that “if you know one HM program, you know one HM program,” alluding to the fact that every HM program is unique. The diversity of individual HM programs combined with the overall evolution of the field has expanded the range of jobs available in HM.
The nomenclature of adding an -ist to the end of the specific roles (e.g., nocturnist, weekendist) has become commonplace. These roles have developed with the increasing need for day and night staffing at many hospitals secondary to increased and more complex patients, less availability of residents because of work hour restrictions, and the Accreditation Council for Graduate Medical Education (ACGME) rules that require overnight supervision of residents
Additionally, the field of HM increasingly includes physicians trained in internal medicine, family medicine, pediatrics, and medicine-pediatrics (med-peds). In this article, we describe the variety of roles available to trainees joining HM and the multitude of different training backgrounds hospitalists come from.
Nocturnists
The 2018 State of Hospital Medicine Report notes that 76.1% of adult-only HM groups have nocturnists, hospitalists who work primarily at night to admit and to provide coverage for admitted patients.2 Nocturnists often provide benefit to the rest of their hospitalist group by allowing fewer required night shifts for those that prefer to work during the day.
Nocturnists may choose a nighttime schedule for several reasons, including the ability to be home more during the day. They also have the potential to work fewer total hours or shifts while still earning a similar or increased income, compared with predominantly daytime hospitalists, increasing their flexibility to pursue other interests. These nocturnists become experts in navigating the admission process and responding to inpatient emergencies often with less support when compared with daytime hospitalists.
In addition to career nocturnist work, nocturnist jobs can be a great fit for those residency graduates who are undecided about fellowship and enjoy the acuity of inpatient medicine. It provides an opportunity to hone their clinical skill set prior to specialized training while earning an attending salary, and offers flexible hours which may allow for research or other endeavors. In academic centers, nocturnist educational roles take on a different character as well and may involve more 1:1 educational experiences. The role of nocturnists as educators is expanding as ACGME rules call for more oversight and educational opportunities for residents who are working at night.
However, challenges exist for nocturnists, including keeping abreast of new changes in their HM groups and hospital systems and engaging in quality initiatives, given that most meetings occur during the day. Additionally, nocturnists must adapt to sleeping during the day, potentially getting less sleep then they would otherwise and being “off cycle” with family and friends. For nocturnists raising children, being off cycle may be advantageous as it can allow them to be home with their children after school.
Weekendists
Another common hospitalist role is the weekendist, hospitalists who spend much of their clinical time preferentially working weekends. Similar to nocturnists, weekendists provide benefit to their hospitalist group by allowing others to have more weekends off.
Weekendists may prefer working weekends because of fewer total shifts or hours and/or higher compensation per shift. Additionally, weekendists have the flexibility to do other work on weekdays, such as research or another hospitalist job. For those that do nonclinical work during the week, a weekendist position may allow them to keep their clinical skills up to date. However, weekendists may face intense clinical days with a higher census because of fewer hospitalists rounding on the weekends.
Weekendists must balance having more potential time available during the weekdays but less time on the weekends to devote to family and friends. Furthermore, weekendists may feel less engaged with nonclinical opportunities, including quality improvement, educational offerings, and teaching opportunities.
SNFists
With increasing emphasis on transitions of care and the desire to avoid readmission penalties, some hospitalists have transitioned to work partly or primarily in skilled nursing facilities (SNF) and have been referred to as “SNFists.” Some of these hospitalists may split their clinical time between SNFs and acute care hospitals, while others may work exclusively at SNFs.
SNFists have the potential to be invaluable in improving transitions of care after discharge to post–acute care facilities because of increased provider presence in these facilities, comfort with medically complex patients, and appreciation of government regulations.4 SNFists may face potential challenges of needing to staff more than one post–acute care hospital and of having less resources available, compared with an acute care hospital.
Specific specialty hospitalists
For a variety of reasons including clinical interest, many hospitalists have become specialized with regards to their primary inpatient population. Some hospitalists spend the majority of their clinical time on a specific service in the hospital, often working closely with the subspecialist caring for that patient. These hospitalists may focus on hematology, oncology, bone-marrow transplant, neurology, cardiology, surgery services, or critical care, among others. Hospitalists focused on a specific service often become knowledge experts in that specialty. Conversely, by focusing on a specific service, certain pathologies may be less commonly seen, which may narrow the breadth of the hospital medicine job.
Hospitalist training
Internal medicine hospitalists may be the most common hospitalists encountered in many hospitals and at each Society of Hospital Medicine annual conference, but there has also been rapid growth in hospitalists from other specialties and backgrounds.
Family medicine hospitalists are a part of 64.9% of HM groups and about 9% of family medicine graduates are choosing HM as a career path.2,3 Most family medicine hospitalists work in adult HM groups, but some, particularly in rural or academic settings, care for pediatric, newborn, and/or maternity patients. Similarly, pediatric hospitalists have become entrenched at many hospitals where children are admitted. These pediatric hospitalists, like adult hospitalists, may work in a variety of different clinical roles including in EDs, newborn nurseries, and inpatient wards or ICUs; they may also provide consult, sedation, or procedural services.
Med-peds hospitalists that split time between internal medicine and pediatrics are becoming more commonplace in the field. Many work at academic centers where they often work on each side separately, doing the same work as their internal medicine or pediatrics colleagues, and then switching to the other side after a period of time. Some centers offer unique roles for med-peds hospitalists including working on adult consult teams in children’s hospitals, where they provide consult care to older patients that may still receive their care at a children’s hospital. There are also nonacademic hospitals that primarily staff med-peds hospitalists, where they can provide the full spectrum of care from the newborn nursery to the inpatient pediatric and adult wards.
Hospital medicine is a young field that is constantly changing with new and developing roles for hospitalists from a wide variety of backgrounds. Stick around to see which “-ist” will come next in HM.
Dr. Hall is a med-peds hospitalist and assistant professor at the University of Kentucky, Lexington. Dr. Sanyal-Dey is an academic hospitalist at Zuckerberg San Francisco General Hospital and Trauma Center and the University of California, San Francisco, where she is the director of clinical operations, and director of the faculty inpatient service. Dr. Chang is associate professor and interprofessional education thread director (MD curriculum) at Washington University, St. Louis. Dr. Kwan is a hospitalist at the Veterans Affairs San Diego Healthcare System and associate professor at the University of California, San Diego. He is the chair of SHM’s Physicians in Training committee. Dr. Seymour is family medicine hospitalist education director at the University of Massachusetts Memorial Medical Center, Worcester, and associate professor at the University of Massachusetts.
References
1. Wachter RM, Goldman L. The Emerging Role of “Hospitalists” in the American Health Care System. N Engl J Med. 1996;335(7):514-7.
2. 2018 State of Hospital Medicine Report. Philadelphia: Society of Hospital Medicine, 2018.
3. Weaver SP, Hill J. Academician Attitudes and Beliefs Regarding the Use of Hospitalists: A CERA Study. Fam Med. 2015;47(5):357-61.
4. Teno JM et al. Temporal Trends in the Numbers of Skilled Nursing Facility Specialists From 2007 Through 2014. JAMA Intern Med. 2017;177(9):1376-8.
You’ve probably heard of a “nocturnist,” but have you ever heard of a “weekendist?”
The field of hospital medicine (HM) has evolved dramatically since the term “hospitalist” was introduced in the literature in 1996.1 There is a saying in HM that “if you know one HM program, you know one HM program,” alluding to the fact that every HM program is unique. The diversity of individual HM programs combined with the overall evolution of the field has expanded the range of jobs available in HM.
The nomenclature of adding an -ist to the end of the specific roles (e.g., nocturnist, weekendist) has become commonplace. These roles have developed with the increasing need for day and night staffing at many hospitals secondary to increased and more complex patients, less availability of residents because of work hour restrictions, and the Accreditation Council for Graduate Medical Education (ACGME) rules that require overnight supervision of residents
Additionally, the field of HM increasingly includes physicians trained in internal medicine, family medicine, pediatrics, and medicine-pediatrics (med-peds). In this article, we describe the variety of roles available to trainees joining HM and the multitude of different training backgrounds hospitalists come from.
Nocturnists
The 2018 State of Hospital Medicine Report notes that 76.1% of adult-only HM groups have nocturnists, hospitalists who work primarily at night to admit and to provide coverage for admitted patients.2 Nocturnists often provide benefit to the rest of their hospitalist group by allowing fewer required night shifts for those that prefer to work during the day.
Nocturnists may choose a nighttime schedule for several reasons, including the ability to be home more during the day. They also have the potential to work fewer total hours or shifts while still earning a similar or increased income, compared with predominantly daytime hospitalists, increasing their flexibility to pursue other interests. These nocturnists become experts in navigating the admission process and responding to inpatient emergencies often with less support when compared with daytime hospitalists.
In addition to career nocturnist work, nocturnist jobs can be a great fit for those residency graduates who are undecided about fellowship and enjoy the acuity of inpatient medicine. It provides an opportunity to hone their clinical skill set prior to specialized training while earning an attending salary, and offers flexible hours which may allow for research or other endeavors. In academic centers, nocturnist educational roles take on a different character as well and may involve more 1:1 educational experiences. The role of nocturnists as educators is expanding as ACGME rules call for more oversight and educational opportunities for residents who are working at night.
However, challenges exist for nocturnists, including keeping abreast of new changes in their HM groups and hospital systems and engaging in quality initiatives, given that most meetings occur during the day. Additionally, nocturnists must adapt to sleeping during the day, potentially getting less sleep then they would otherwise and being “off cycle” with family and friends. For nocturnists raising children, being off cycle may be advantageous as it can allow them to be home with their children after school.
Weekendists
Another common hospitalist role is the weekendist, hospitalists who spend much of their clinical time preferentially working weekends. Similar to nocturnists, weekendists provide benefit to their hospitalist group by allowing others to have more weekends off.
Weekendists may prefer working weekends because of fewer total shifts or hours and/or higher compensation per shift. Additionally, weekendists have the flexibility to do other work on weekdays, such as research or another hospitalist job. For those that do nonclinical work during the week, a weekendist position may allow them to keep their clinical skills up to date. However, weekendists may face intense clinical days with a higher census because of fewer hospitalists rounding on the weekends.
Weekendists must balance having more potential time available during the weekdays but less time on the weekends to devote to family and friends. Furthermore, weekendists may feel less engaged with nonclinical opportunities, including quality improvement, educational offerings, and teaching opportunities.
SNFists
With increasing emphasis on transitions of care and the desire to avoid readmission penalties, some hospitalists have transitioned to work partly or primarily in skilled nursing facilities (SNF) and have been referred to as “SNFists.” Some of these hospitalists may split their clinical time between SNFs and acute care hospitals, while others may work exclusively at SNFs.
SNFists have the potential to be invaluable in improving transitions of care after discharge to post–acute care facilities because of increased provider presence in these facilities, comfort with medically complex patients, and appreciation of government regulations.4 SNFists may face potential challenges of needing to staff more than one post–acute care hospital and of having less resources available, compared with an acute care hospital.
Specific specialty hospitalists
For a variety of reasons including clinical interest, many hospitalists have become specialized with regards to their primary inpatient population. Some hospitalists spend the majority of their clinical time on a specific service in the hospital, often working closely with the subspecialist caring for that patient. These hospitalists may focus on hematology, oncology, bone-marrow transplant, neurology, cardiology, surgery services, or critical care, among others. Hospitalists focused on a specific service often become knowledge experts in that specialty. Conversely, by focusing on a specific service, certain pathologies may be less commonly seen, which may narrow the breadth of the hospital medicine job.
Hospitalist training
Internal medicine hospitalists may be the most common hospitalists encountered in many hospitals and at each Society of Hospital Medicine annual conference, but there has also been rapid growth in hospitalists from other specialties and backgrounds.
Family medicine hospitalists are a part of 64.9% of HM groups and about 9% of family medicine graduates are choosing HM as a career path.2,3 Most family medicine hospitalists work in adult HM groups, but some, particularly in rural or academic settings, care for pediatric, newborn, and/or maternity patients. Similarly, pediatric hospitalists have become entrenched at many hospitals where children are admitted. These pediatric hospitalists, like adult hospitalists, may work in a variety of different clinical roles including in EDs, newborn nurseries, and inpatient wards or ICUs; they may also provide consult, sedation, or procedural services.
Med-peds hospitalists that split time between internal medicine and pediatrics are becoming more commonplace in the field. Many work at academic centers where they often work on each side separately, doing the same work as their internal medicine or pediatrics colleagues, and then switching to the other side after a period of time. Some centers offer unique roles for med-peds hospitalists including working on adult consult teams in children’s hospitals, where they provide consult care to older patients that may still receive their care at a children’s hospital. There are also nonacademic hospitals that primarily staff med-peds hospitalists, where they can provide the full spectrum of care from the newborn nursery to the inpatient pediatric and adult wards.
Hospital medicine is a young field that is constantly changing with new and developing roles for hospitalists from a wide variety of backgrounds. Stick around to see which “-ist” will come next in HM.
Dr. Hall is a med-peds hospitalist and assistant professor at the University of Kentucky, Lexington. Dr. Sanyal-Dey is an academic hospitalist at Zuckerberg San Francisco General Hospital and Trauma Center and the University of California, San Francisco, where she is the director of clinical operations, and director of the faculty inpatient service. Dr. Chang is associate professor and interprofessional education thread director (MD curriculum) at Washington University, St. Louis. Dr. Kwan is a hospitalist at the Veterans Affairs San Diego Healthcare System and associate professor at the University of California, San Diego. He is the chair of SHM’s Physicians in Training committee. Dr. Seymour is family medicine hospitalist education director at the University of Massachusetts Memorial Medical Center, Worcester, and associate professor at the University of Massachusetts.
References
1. Wachter RM, Goldman L. The Emerging Role of “Hospitalists” in the American Health Care System. N Engl J Med. 1996;335(7):514-7.
2. 2018 State of Hospital Medicine Report. Philadelphia: Society of Hospital Medicine, 2018.
3. Weaver SP, Hill J. Academician Attitudes and Beliefs Regarding the Use of Hospitalists: A CERA Study. Fam Med. 2015;47(5):357-61.
4. Teno JM et al. Temporal Trends in the Numbers of Skilled Nursing Facility Specialists From 2007 Through 2014. JAMA Intern Med. 2017;177(9):1376-8.
PHM19: MOC Part 4 projects for community pediatric hospitalists
PHM19 session
MOC Part 4 projects for community pediatric hospitalists
Presenters
Jack M. Percelay, MD, MPH, FAAP, MHM
Nancy Chen, MD, FAAP
Elizabeth Dobler, MD, FAAP
Lindsay Fox, MD
Beth C. Natt, MD, MPH, SFHM
Clota Snow, MD, FAAP
Session summary
Dr. Jack Percelay, of Sutter Health in San Francisco, started this session at Pediatric Hospital Medicine 2019 by outlining the process of submitting a small group (n = 1-10) project for Maintenance of Certification (MOC) Part 4 credit including the basics of what is needed for the application:
- Aim statement.
- Metrics used.
- Data required (3 data points: pre, post, and sustain).
He also shared the requirement of “meaningful participation” for participants to be eligible for MOC Part 4 credit.
Examples of successful projects were shared by members of the presenting group:
- Dr. Natt: Improving the timing of the birth dose of the hepatitis B vaccination.
- Dr. Dobler: Improving the hepatitis B vaccination rate within 24 hours of birth.
- Dr. Snow: Supplementing vitamin D in the newborn nursery.
- Dr. Fox: Improving newborn discharge efficiency, improving screening for smoking exposure, and offering smoking cessation.
- Dr. Percelay: Improving hospitalist billing and coding using time as a factor.
- Dr. Chen: Improving patient satisfaction through improvement of family-centered rounds.
The workshop audience divided into groups to brainstorm/troubleshoot projects and to elicit general advice regarding the process. Sample submissions were provided.
Key takeaways
- Even small projects (i.e. single metric) can be submitted/accepted with pre- and postintervention data.
- Be creative! Think about changes you are making at your institution and gather the data to support the intervention.
- Always double-dip on QI projects to gain valuable MOC Part 4 credit!
Dr. Fox is site director, Pediatric Hospital Medicine Division at MetroWest Medical Center, Framingham, Mass.
PHM19 session
MOC Part 4 projects for community pediatric hospitalists
Presenters
Jack M. Percelay, MD, MPH, FAAP, MHM
Nancy Chen, MD, FAAP
Elizabeth Dobler, MD, FAAP
Lindsay Fox, MD
Beth C. Natt, MD, MPH, SFHM
Clota Snow, MD, FAAP
Session summary
Dr. Jack Percelay, of Sutter Health in San Francisco, started this session at Pediatric Hospital Medicine 2019 by outlining the process of submitting a small group (n = 1-10) project for Maintenance of Certification (MOC) Part 4 credit including the basics of what is needed for the application:
- Aim statement.
- Metrics used.
- Data required (3 data points: pre, post, and sustain).
He also shared the requirement of “meaningful participation” for participants to be eligible for MOC Part 4 credit.
Examples of successful projects were shared by members of the presenting group:
- Dr. Natt: Improving the timing of the birth dose of the hepatitis B vaccination.
- Dr. Dobler: Improving the hepatitis B vaccination rate within 24 hours of birth.
- Dr. Snow: Supplementing vitamin D in the newborn nursery.
- Dr. Fox: Improving newborn discharge efficiency, improving screening for smoking exposure, and offering smoking cessation.
- Dr. Percelay: Improving hospitalist billing and coding using time as a factor.
- Dr. Chen: Improving patient satisfaction through improvement of family-centered rounds.
The workshop audience divided into groups to brainstorm/troubleshoot projects and to elicit general advice regarding the process. Sample submissions were provided.
Key takeaways
- Even small projects (i.e. single metric) can be submitted/accepted with pre- and postintervention data.
- Be creative! Think about changes you are making at your institution and gather the data to support the intervention.
- Always double-dip on QI projects to gain valuable MOC Part 4 credit!
Dr. Fox is site director, Pediatric Hospital Medicine Division at MetroWest Medical Center, Framingham, Mass.
PHM19 session
MOC Part 4 projects for community pediatric hospitalists
Presenters
Jack M. Percelay, MD, MPH, FAAP, MHM
Nancy Chen, MD, FAAP
Elizabeth Dobler, MD, FAAP
Lindsay Fox, MD
Beth C. Natt, MD, MPH, SFHM
Clota Snow, MD, FAAP
Session summary
Dr. Jack Percelay, of Sutter Health in San Francisco, started this session at Pediatric Hospital Medicine 2019 by outlining the process of submitting a small group (n = 1-10) project for Maintenance of Certification (MOC) Part 4 credit including the basics of what is needed for the application:
- Aim statement.
- Metrics used.
- Data required (3 data points: pre, post, and sustain).
He also shared the requirement of “meaningful participation” for participants to be eligible for MOC Part 4 credit.
Examples of successful projects were shared by members of the presenting group:
- Dr. Natt: Improving the timing of the birth dose of the hepatitis B vaccination.
- Dr. Dobler: Improving the hepatitis B vaccination rate within 24 hours of birth.
- Dr. Snow: Supplementing vitamin D in the newborn nursery.
- Dr. Fox: Improving newborn discharge efficiency, improving screening for smoking exposure, and offering smoking cessation.
- Dr. Percelay: Improving hospitalist billing and coding using time as a factor.
- Dr. Chen: Improving patient satisfaction through improvement of family-centered rounds.
The workshop audience divided into groups to brainstorm/troubleshoot projects and to elicit general advice regarding the process. Sample submissions were provided.
Key takeaways
- Even small projects (i.e. single metric) can be submitted/accepted with pre- and postintervention data.
- Be creative! Think about changes you are making at your institution and gather the data to support the intervention.
- Always double-dip on QI projects to gain valuable MOC Part 4 credit!
Dr. Fox is site director, Pediatric Hospital Medicine Division at MetroWest Medical Center, Framingham, Mass.
ACGME deepening its commitment to physician well-being, leader says
NEW ORLEANS – When Timothy P. Brigham, MDiv, PhD, thinks about the impact of burnout and stress on the ability of physicians to practice medicine, Lewin’s equation comes to mind.
Developed by psychologist Kurt Lewin in 1936, the equation holds that behavior stems from a person’s personality and the environment that person inhabits.
Dr. Brigham, chief of staff and chief education and organizational development officer at the Chicago-based Accreditation Council for Graduate Medical Education (ACGME), said at the annual meeting of the American Academy of Pediatrics.
“It’s a toxic mine, in some ways. What we tend to do is when we detect that physicians in general are, or a particular residency program is, too stressed out or burned out, we give them resilience training. Not that that’s unimportant, but it’s like putting a canary in a toxic mine full of poison and saying, ‘We’re going to teach you to hold your breath a little bit longer.’ Our job is to detoxify the mine.”
Troubled by the rise of suicides among physicians in recent years as well as mounting evidence about the adverse impact of burnout and stress on the practice of medicine, Dr. Brigham said that the ACGME is deepening its commitment to the well-being of faculty, residents, patients, and all members of the health care team. Since launching a “call to arms” on the topic at its annual educational conference in 2015, the ACGME has added courses on well-being to its annual meeting and remolded its Clinical Learning Environmental Review program to include all clinicians, “because everybody is affected by this: nurses, coordinators, et cetera,” he said. The ACGME also has revised Common Program Requirements, disseminated tools and resources to promote well-being and new knowledge on the topic, and partnered with the National Academy of Medicine Action Collaborative on Clinician Well-Being and Resilience – all in an effort to bring about culture change.
“But we’re well aware that the ACGME can’t do this alone,” Dr. Brigham said. “We can’t ‘requirement’ our way out of this problem. It’s going to take a culture shift. Only you physicians, in collaboration with everyone in your community of learning, can create the systemic change required to improve our culture. We have a good handle on the problem at this point, but the solutions are a little bit more difficult to get a hold of. As Martin Luther King Jr. once said, ‘You don’t have to see the whole staircase, just take the first step.’ ”
The ACGME wants to work with physicians “to collect data and do joint research, to share insights, and to share tools and resources to create a better world for practicing physicians, for other members of the health care team, and for patients. After all, clinicians who care for themselves provide better care for others. They’re less likely to make errors or leave the profession,” Dr. Brigham told attendees.
He added that clinicians can gauge their risk for burnout by asking themselves three simple questions about their work environment: Does it support self-care? Does it increase and support connection with colleagues? Does it connect people to purpose and meaningful work?
“One of the problems with our resident clinical work hours is not terrible program directors saying, ‘work longer.’ It’s residents who want to take care of families for 1 more hour,” Dr. Brigham continued. “It’s residents who want to take care of patients who are going through a difficult time. You represent the top 2% in the world in terms of your intelligence and achievement, yet that’s not what makes you special. What makes you special is that the level of self-doubt in this room exceeds that of the general population by about 10 times. You also tend to run toward what everyone else runs away from: disease, despair, people who are injured and suffering. That takes a toll.”
He emphasized that positive social relationships with others are crucial to joy and well-being in the practice of medicine. “Burnout isn’t just about exhaustion; it’s about loneliness,” Dr. Brigham said. “There’s a surprising power in just asking people how they’re doing, and really wanting to know the answer.”
Negative social connections are highly correlated with burnout and depression, such as harassment, bullying, mistreatment, discrimination, “and using the power gradient to squash somebody who’s trying their best to be a physician,” he said.
Dr. Brigham acknowledged the tall task of bringing a spotlight to well-being as physicians continue to engage in tasks such as the burden and lack of standardization of prior authorization requirements, the burden of clinical documentation requirements, electronic health records and related work flow, and quality payment programs. “This is what we need to shift; this is what we need to take away so you can get back in touch with why you became a physician in the first place.”
Dr. Brigham reported having no financial disclosures.
NEW ORLEANS – When Timothy P. Brigham, MDiv, PhD, thinks about the impact of burnout and stress on the ability of physicians to practice medicine, Lewin’s equation comes to mind.
Developed by psychologist Kurt Lewin in 1936, the equation holds that behavior stems from a person’s personality and the environment that person inhabits.
Dr. Brigham, chief of staff and chief education and organizational development officer at the Chicago-based Accreditation Council for Graduate Medical Education (ACGME), said at the annual meeting of the American Academy of Pediatrics.
“It’s a toxic mine, in some ways. What we tend to do is when we detect that physicians in general are, or a particular residency program is, too stressed out or burned out, we give them resilience training. Not that that’s unimportant, but it’s like putting a canary in a toxic mine full of poison and saying, ‘We’re going to teach you to hold your breath a little bit longer.’ Our job is to detoxify the mine.”
Troubled by the rise of suicides among physicians in recent years as well as mounting evidence about the adverse impact of burnout and stress on the practice of medicine, Dr. Brigham said that the ACGME is deepening its commitment to the well-being of faculty, residents, patients, and all members of the health care team. Since launching a “call to arms” on the topic at its annual educational conference in 2015, the ACGME has added courses on well-being to its annual meeting and remolded its Clinical Learning Environmental Review program to include all clinicians, “because everybody is affected by this: nurses, coordinators, et cetera,” he said. The ACGME also has revised Common Program Requirements, disseminated tools and resources to promote well-being and new knowledge on the topic, and partnered with the National Academy of Medicine Action Collaborative on Clinician Well-Being and Resilience – all in an effort to bring about culture change.
“But we’re well aware that the ACGME can’t do this alone,” Dr. Brigham said. “We can’t ‘requirement’ our way out of this problem. It’s going to take a culture shift. Only you physicians, in collaboration with everyone in your community of learning, can create the systemic change required to improve our culture. We have a good handle on the problem at this point, but the solutions are a little bit more difficult to get a hold of. As Martin Luther King Jr. once said, ‘You don’t have to see the whole staircase, just take the first step.’ ”
The ACGME wants to work with physicians “to collect data and do joint research, to share insights, and to share tools and resources to create a better world for practicing physicians, for other members of the health care team, and for patients. After all, clinicians who care for themselves provide better care for others. They’re less likely to make errors or leave the profession,” Dr. Brigham told attendees.
He added that clinicians can gauge their risk for burnout by asking themselves three simple questions about their work environment: Does it support self-care? Does it increase and support connection with colleagues? Does it connect people to purpose and meaningful work?
“One of the problems with our resident clinical work hours is not terrible program directors saying, ‘work longer.’ It’s residents who want to take care of families for 1 more hour,” Dr. Brigham continued. “It’s residents who want to take care of patients who are going through a difficult time. You represent the top 2% in the world in terms of your intelligence and achievement, yet that’s not what makes you special. What makes you special is that the level of self-doubt in this room exceeds that of the general population by about 10 times. You also tend to run toward what everyone else runs away from: disease, despair, people who are injured and suffering. That takes a toll.”
He emphasized that positive social relationships with others are crucial to joy and well-being in the practice of medicine. “Burnout isn’t just about exhaustion; it’s about loneliness,” Dr. Brigham said. “There’s a surprising power in just asking people how they’re doing, and really wanting to know the answer.”
Negative social connections are highly correlated with burnout and depression, such as harassment, bullying, mistreatment, discrimination, “and using the power gradient to squash somebody who’s trying their best to be a physician,” he said.
Dr. Brigham acknowledged the tall task of bringing a spotlight to well-being as physicians continue to engage in tasks such as the burden and lack of standardization of prior authorization requirements, the burden of clinical documentation requirements, electronic health records and related work flow, and quality payment programs. “This is what we need to shift; this is what we need to take away so you can get back in touch with why you became a physician in the first place.”
Dr. Brigham reported having no financial disclosures.
NEW ORLEANS – When Timothy P. Brigham, MDiv, PhD, thinks about the impact of burnout and stress on the ability of physicians to practice medicine, Lewin’s equation comes to mind.
Developed by psychologist Kurt Lewin in 1936, the equation holds that behavior stems from a person’s personality and the environment that person inhabits.
Dr. Brigham, chief of staff and chief education and organizational development officer at the Chicago-based Accreditation Council for Graduate Medical Education (ACGME), said at the annual meeting of the American Academy of Pediatrics.
“It’s a toxic mine, in some ways. What we tend to do is when we detect that physicians in general are, or a particular residency program is, too stressed out or burned out, we give them resilience training. Not that that’s unimportant, but it’s like putting a canary in a toxic mine full of poison and saying, ‘We’re going to teach you to hold your breath a little bit longer.’ Our job is to detoxify the mine.”
Troubled by the rise of suicides among physicians in recent years as well as mounting evidence about the adverse impact of burnout and stress on the practice of medicine, Dr. Brigham said that the ACGME is deepening its commitment to the well-being of faculty, residents, patients, and all members of the health care team. Since launching a “call to arms” on the topic at its annual educational conference in 2015, the ACGME has added courses on well-being to its annual meeting and remolded its Clinical Learning Environmental Review program to include all clinicians, “because everybody is affected by this: nurses, coordinators, et cetera,” he said. The ACGME also has revised Common Program Requirements, disseminated tools and resources to promote well-being and new knowledge on the topic, and partnered with the National Academy of Medicine Action Collaborative on Clinician Well-Being and Resilience – all in an effort to bring about culture change.
“But we’re well aware that the ACGME can’t do this alone,” Dr. Brigham said. “We can’t ‘requirement’ our way out of this problem. It’s going to take a culture shift. Only you physicians, in collaboration with everyone in your community of learning, can create the systemic change required to improve our culture. We have a good handle on the problem at this point, but the solutions are a little bit more difficult to get a hold of. As Martin Luther King Jr. once said, ‘You don’t have to see the whole staircase, just take the first step.’ ”
The ACGME wants to work with physicians “to collect data and do joint research, to share insights, and to share tools and resources to create a better world for practicing physicians, for other members of the health care team, and for patients. After all, clinicians who care for themselves provide better care for others. They’re less likely to make errors or leave the profession,” Dr. Brigham told attendees.
He added that clinicians can gauge their risk for burnout by asking themselves three simple questions about their work environment: Does it support self-care? Does it increase and support connection with colleagues? Does it connect people to purpose and meaningful work?
“One of the problems with our resident clinical work hours is not terrible program directors saying, ‘work longer.’ It’s residents who want to take care of families for 1 more hour,” Dr. Brigham continued. “It’s residents who want to take care of patients who are going through a difficult time. You represent the top 2% in the world in terms of your intelligence and achievement, yet that’s not what makes you special. What makes you special is that the level of self-doubt in this room exceeds that of the general population by about 10 times. You also tend to run toward what everyone else runs away from: disease, despair, people who are injured and suffering. That takes a toll.”
He emphasized that positive social relationships with others are crucial to joy and well-being in the practice of medicine. “Burnout isn’t just about exhaustion; it’s about loneliness,” Dr. Brigham said. “There’s a surprising power in just asking people how they’re doing, and really wanting to know the answer.”
Negative social connections are highly correlated with burnout and depression, such as harassment, bullying, mistreatment, discrimination, “and using the power gradient to squash somebody who’s trying their best to be a physician,” he said.
Dr. Brigham acknowledged the tall task of bringing a spotlight to well-being as physicians continue to engage in tasks such as the burden and lack of standardization of prior authorization requirements, the burden of clinical documentation requirements, electronic health records and related work flow, and quality payment programs. “This is what we need to shift; this is what we need to take away so you can get back in touch with why you became a physician in the first place.”
Dr. Brigham reported having no financial disclosures.
EXPERT ANALYSIS AT AAP 2019