User login
Hospitalist movers and shakers – November 2019
Amith Skandhan, MD, SFHM, has been announced as Southeast Health Statera Network’s (Dothan, Ala.) director of physician integration, and chairman of the network’s Physicians Participation Committee. Dr. Skandhan is senior lead hospitalist with Southeast Health, where he has worked for nearly a decade. He also champions the medical group’s clinical documentation improvement faction.
One of just 10 hospitalists in the nation to receive Top Hospitalist recognition by the American College of Physicians in 2018, Dr. Skandhan is also an assistant professor at Alabama College of Osteopathic Medicine and is one of Southeast Health’s Internal Medicine Residency Program’s core faculty members.
Ruby Sahoo, DO, has been promoted by Team Health (Knoxville, Tenn.) as regional performance director of its hospitalist services performance improvement team. Dr. Sahoo joined Team Health in 2016 and has most recently served as medical director and chief of staff at Grand Strand Medical Center (Myrtle Beach, S.C.).
Dr. Sahoo is a highly decorated internist and hospitalist. She was Team Health’s Medical Director of the Year for Hospital Medicine 2018, and a Frist Humanitarian Award winner in 2017. Additionally, Dr. Sahoo is a member of the Society of Hospital Medicine, the American College of Physicians, and the American Association of Physician Leadership.
David Vandenberg, MD, SFHM, recently was elevated to chief medical officer at St. Joseph Mercy Hospital (Ann Arbor and Livingston, Mich.). The hospitalist and senior fellow of hospital medicine previously has been St. Joseph’s vice chair of internal medicine and medical director of care management and documentation integrity. Dr. Vandenberg has spent 20 years as an employee at St. Joseph’s.
Cristian Andrade, MD, has been elevated to vice president of medical affairs with St. Joseph’s Health (Syracuse, N.Y.). A 16-year veteran with St. Joseph’s, Dr. Andrade has been a hospitalist with the system since 2006, and most recently has served as chief of hospitalist services.
Dr. Andrade now will provide guidance focusing on improving length of stay, as well as staff governance, utilization review, and the hospitalist program in general.
Paul DeJac, MD, has received a promotion to chief of hospitalist medicine at Roswell Park Comprehensive Cancer Center (Buffalo, N.Y.). Dr. DeJac was hired at Roswell Park in 2016, becoming lead hospitalist in 2017. He will look to boost professional development on the hospitalist team with a focus on improving patient care.
Independent Emergency Physicians (Farmington, Mich.), which provides hospitalist physicians, ED physicians, scribes, and more at a handful of hospitals in Michigan, has added urgent care facilities in Southfield, Mich., and Novi, Mich., to its portfolio. In addition, IEP has joined with Healthy Urgent Care to create a network of up to 15 urgent care centers in Southeast Michigan.
This is IEP’s first foray into urgent care. The company was founded in 1997 and practices at Ascension Health, Trinity Health, and Henry Ford Health System, covering four different hospitals.
Private hospitalist management provider Sound Physicians (Tacoma, Wash.) has grown once again, acquiring Indigo Health Partners (Traverse City, Mich.), one of Michigan’s largest private hospitalist groups. The new company will be known as Indigo, a division of Sound Inpatient Physicians.
Indigo’s approximately 150 providers are included in the transaction, which includes professionals in hospitals, skilled nursing facilities, and assisted living facilities. Indigo was previously known as Hospitalists of Northwest Michigan, based out of Munson Medical Center.
Amith Skandhan, MD, SFHM, has been announced as Southeast Health Statera Network’s (Dothan, Ala.) director of physician integration, and chairman of the network’s Physicians Participation Committee. Dr. Skandhan is senior lead hospitalist with Southeast Health, where he has worked for nearly a decade. He also champions the medical group’s clinical documentation improvement faction.
One of just 10 hospitalists in the nation to receive Top Hospitalist recognition by the American College of Physicians in 2018, Dr. Skandhan is also an assistant professor at Alabama College of Osteopathic Medicine and is one of Southeast Health’s Internal Medicine Residency Program’s core faculty members.
Ruby Sahoo, DO, has been promoted by Team Health (Knoxville, Tenn.) as regional performance director of its hospitalist services performance improvement team. Dr. Sahoo joined Team Health in 2016 and has most recently served as medical director and chief of staff at Grand Strand Medical Center (Myrtle Beach, S.C.).
Dr. Sahoo is a highly decorated internist and hospitalist. She was Team Health’s Medical Director of the Year for Hospital Medicine 2018, and a Frist Humanitarian Award winner in 2017. Additionally, Dr. Sahoo is a member of the Society of Hospital Medicine, the American College of Physicians, and the American Association of Physician Leadership.
David Vandenberg, MD, SFHM, recently was elevated to chief medical officer at St. Joseph Mercy Hospital (Ann Arbor and Livingston, Mich.). The hospitalist and senior fellow of hospital medicine previously has been St. Joseph’s vice chair of internal medicine and medical director of care management and documentation integrity. Dr. Vandenberg has spent 20 years as an employee at St. Joseph’s.
Cristian Andrade, MD, has been elevated to vice president of medical affairs with St. Joseph’s Health (Syracuse, N.Y.). A 16-year veteran with St. Joseph’s, Dr. Andrade has been a hospitalist with the system since 2006, and most recently has served as chief of hospitalist services.
Dr. Andrade now will provide guidance focusing on improving length of stay, as well as staff governance, utilization review, and the hospitalist program in general.
Paul DeJac, MD, has received a promotion to chief of hospitalist medicine at Roswell Park Comprehensive Cancer Center (Buffalo, N.Y.). Dr. DeJac was hired at Roswell Park in 2016, becoming lead hospitalist in 2017. He will look to boost professional development on the hospitalist team with a focus on improving patient care.
Independent Emergency Physicians (Farmington, Mich.), which provides hospitalist physicians, ED physicians, scribes, and more at a handful of hospitals in Michigan, has added urgent care facilities in Southfield, Mich., and Novi, Mich., to its portfolio. In addition, IEP has joined with Healthy Urgent Care to create a network of up to 15 urgent care centers in Southeast Michigan.
This is IEP’s first foray into urgent care. The company was founded in 1997 and practices at Ascension Health, Trinity Health, and Henry Ford Health System, covering four different hospitals.
Private hospitalist management provider Sound Physicians (Tacoma, Wash.) has grown once again, acquiring Indigo Health Partners (Traverse City, Mich.), one of Michigan’s largest private hospitalist groups. The new company will be known as Indigo, a division of Sound Inpatient Physicians.
Indigo’s approximately 150 providers are included in the transaction, which includes professionals in hospitals, skilled nursing facilities, and assisted living facilities. Indigo was previously known as Hospitalists of Northwest Michigan, based out of Munson Medical Center.
Amith Skandhan, MD, SFHM, has been announced as Southeast Health Statera Network’s (Dothan, Ala.) director of physician integration, and chairman of the network’s Physicians Participation Committee. Dr. Skandhan is senior lead hospitalist with Southeast Health, where he has worked for nearly a decade. He also champions the medical group’s clinical documentation improvement faction.
One of just 10 hospitalists in the nation to receive Top Hospitalist recognition by the American College of Physicians in 2018, Dr. Skandhan is also an assistant professor at Alabama College of Osteopathic Medicine and is one of Southeast Health’s Internal Medicine Residency Program’s core faculty members.
Ruby Sahoo, DO, has been promoted by Team Health (Knoxville, Tenn.) as regional performance director of its hospitalist services performance improvement team. Dr. Sahoo joined Team Health in 2016 and has most recently served as medical director and chief of staff at Grand Strand Medical Center (Myrtle Beach, S.C.).
Dr. Sahoo is a highly decorated internist and hospitalist. She was Team Health’s Medical Director of the Year for Hospital Medicine 2018, and a Frist Humanitarian Award winner in 2017. Additionally, Dr. Sahoo is a member of the Society of Hospital Medicine, the American College of Physicians, and the American Association of Physician Leadership.
David Vandenberg, MD, SFHM, recently was elevated to chief medical officer at St. Joseph Mercy Hospital (Ann Arbor and Livingston, Mich.). The hospitalist and senior fellow of hospital medicine previously has been St. Joseph’s vice chair of internal medicine and medical director of care management and documentation integrity. Dr. Vandenberg has spent 20 years as an employee at St. Joseph’s.
Cristian Andrade, MD, has been elevated to vice president of medical affairs with St. Joseph’s Health (Syracuse, N.Y.). A 16-year veteran with St. Joseph’s, Dr. Andrade has been a hospitalist with the system since 2006, and most recently has served as chief of hospitalist services.
Dr. Andrade now will provide guidance focusing on improving length of stay, as well as staff governance, utilization review, and the hospitalist program in general.
Paul DeJac, MD, has received a promotion to chief of hospitalist medicine at Roswell Park Comprehensive Cancer Center (Buffalo, N.Y.). Dr. DeJac was hired at Roswell Park in 2016, becoming lead hospitalist in 2017. He will look to boost professional development on the hospitalist team with a focus on improving patient care.
Independent Emergency Physicians (Farmington, Mich.), which provides hospitalist physicians, ED physicians, scribes, and more at a handful of hospitals in Michigan, has added urgent care facilities in Southfield, Mich., and Novi, Mich., to its portfolio. In addition, IEP has joined with Healthy Urgent Care to create a network of up to 15 urgent care centers in Southeast Michigan.
This is IEP’s first foray into urgent care. The company was founded in 1997 and practices at Ascension Health, Trinity Health, and Henry Ford Health System, covering four different hospitals.
Private hospitalist management provider Sound Physicians (Tacoma, Wash.) has grown once again, acquiring Indigo Health Partners (Traverse City, Mich.), one of Michigan’s largest private hospitalist groups. The new company will be known as Indigo, a division of Sound Inpatient Physicians.
Indigo’s approximately 150 providers are included in the transaction, which includes professionals in hospitals, skilled nursing facilities, and assisted living facilities. Indigo was previously known as Hospitalists of Northwest Michigan, based out of Munson Medical Center.
PHM19: Mitigating the harm we cause learners in medical education
PHM19 session
Mitigating the harm we cause learners in medical education
Presenters
Benjamin Kinnear, MD, MEd
Andrew Olson, MD
Matthew Kelleher, MD, MEd
Session summary
Dr. Kinnear, Dr. Olson, and Dr. Kelleher expertly led this TED-Talk style session at Pediatric Hospital Medicine 2019, convincing the audience that medical educators persistently harm the learners under their supervision.
Dr. Kinnear, of Cincinnati Children’s Hospital, opened the session noting that the path through medical school presently has a perverse focus on grades as a necessary achievement. As an expert in competency-based assessment, he asserted that the current learner assessment strategy is neither valid nor robust enough to indicate actual competence. Summary assessments presented throughout medical school are lacking continuous constructive feedback, leaving early residents in a state of shock when receiving corrective or negative assessments. He also noted that structurally many rotations create both team and patient discontinuity, leaving the learner with a feeling of detachment and limited ownership of the human patient under his/her/their care.
Dr. Olson of the University of Minnesota next described the need for the USMLE STEP 1 exam to be transitioned to a pass/fail endeavor. He cited the error of measurement of 24 points (i.e., the same test taker could have a 220 one day and a 244 the next) and the potential loss of valuable rotation experiences during the several-month period of intense study. He challenged audience members to complete an esoteric exam question to prove his point and asserted that many learners are lacking in humility, communication skills, and professionalism, and seek only the honors designation on rotations. He likened the experience of medical students on rotation and residents on service weeks to a series of first dates and affirmed the value of longitudinal learner-educator relationships.
Further, he outlined the detachment of learners from patient outcomes, demonstrated by frequent hand-offs and rotation transitions. Dr Olson also cited medical pedagogy as failing to meet the known needs of adult learners to engage in deliberate progressive practice, reflective practice, or to use concepts such as spacing or interleaving to reinforce knowledge.
Dr. Kelleher, also of Cincinnati Children’s Hospital, ended the session by taking those in attendance on an imagined “what-if” journey where each of the wrongs currently done to early learners in medical education were corrected. This included engagement in daily reflection (5 minutes at a time), reporting system issues on rounds that had failed the patient, presenting learners with a CV of attending failures to reinforce the imperfection that is a reality in medicine, praising learners when they admit “they don’t know the answer” to a question posed on rounds, completing assessments in real time in the learner’s presence, rounding until specific feedback can be identified for each learner on the team, having a kiosk on each floor where ANY team member could provide feedback to learners, using cognitive science on rounds for teaching (i.e., Socratic) rather than pimping, modeling interprofessional teamwork daily using a culture of vulnerability rather than infallibility (i.e., airline culture), and by encouraging the attending to care for patients or complete tasks independently, showing the value of education over service and model ideal family-centered communication with the team.
One might wonder, if all of the above were accomplished at the request of our talented presenters, would a pass/fail USMLE world where medical education was learner centered and filled with longitudinal relationships with teams and patients, and outcomes were connected to education produce more engaged, knowledgeable, and holistic physicians? According to this team of presenters, yes.
Key takeaways
• Current processes in medical education are harming today’s adult learner.
• Harms include reliance on numerical rather than competency-based assessment, fragmented learning environments, focus on perfection rather than improvement, ignorance of updates in cognitive science for instructional methodology, and individualist rather than team-based learning.
• Reforms are needed to remedy harms in health professional education, including making USMLE pass/fail, creating a learning-centered rather than service-centered residency environment, encouraging longitudinal relationships between teacher and learner, and connecting education to clinical outcomes.
Dr. King is associate program director, University of Minnesota Pediatric Residency Program, Minneapolis.
PHM19 session
Mitigating the harm we cause learners in medical education
Presenters
Benjamin Kinnear, MD, MEd
Andrew Olson, MD
Matthew Kelleher, MD, MEd
Session summary
Dr. Kinnear, Dr. Olson, and Dr. Kelleher expertly led this TED-Talk style session at Pediatric Hospital Medicine 2019, convincing the audience that medical educators persistently harm the learners under their supervision.
Dr. Kinnear, of Cincinnati Children’s Hospital, opened the session noting that the path through medical school presently has a perverse focus on grades as a necessary achievement. As an expert in competency-based assessment, he asserted that the current learner assessment strategy is neither valid nor robust enough to indicate actual competence. Summary assessments presented throughout medical school are lacking continuous constructive feedback, leaving early residents in a state of shock when receiving corrective or negative assessments. He also noted that structurally many rotations create both team and patient discontinuity, leaving the learner with a feeling of detachment and limited ownership of the human patient under his/her/their care.
Dr. Olson of the University of Minnesota next described the need for the USMLE STEP 1 exam to be transitioned to a pass/fail endeavor. He cited the error of measurement of 24 points (i.e., the same test taker could have a 220 one day and a 244 the next) and the potential loss of valuable rotation experiences during the several-month period of intense study. He challenged audience members to complete an esoteric exam question to prove his point and asserted that many learners are lacking in humility, communication skills, and professionalism, and seek only the honors designation on rotations. He likened the experience of medical students on rotation and residents on service weeks to a series of first dates and affirmed the value of longitudinal learner-educator relationships.
Further, he outlined the detachment of learners from patient outcomes, demonstrated by frequent hand-offs and rotation transitions. Dr Olson also cited medical pedagogy as failing to meet the known needs of adult learners to engage in deliberate progressive practice, reflective practice, or to use concepts such as spacing or interleaving to reinforce knowledge.
Dr. Kelleher, also of Cincinnati Children’s Hospital, ended the session by taking those in attendance on an imagined “what-if” journey where each of the wrongs currently done to early learners in medical education were corrected. This included engagement in daily reflection (5 minutes at a time), reporting system issues on rounds that had failed the patient, presenting learners with a CV of attending failures to reinforce the imperfection that is a reality in medicine, praising learners when they admit “they don’t know the answer” to a question posed on rounds, completing assessments in real time in the learner’s presence, rounding until specific feedback can be identified for each learner on the team, having a kiosk on each floor where ANY team member could provide feedback to learners, using cognitive science on rounds for teaching (i.e., Socratic) rather than pimping, modeling interprofessional teamwork daily using a culture of vulnerability rather than infallibility (i.e., airline culture), and by encouraging the attending to care for patients or complete tasks independently, showing the value of education over service and model ideal family-centered communication with the team.
One might wonder, if all of the above were accomplished at the request of our talented presenters, would a pass/fail USMLE world where medical education was learner centered and filled with longitudinal relationships with teams and patients, and outcomes were connected to education produce more engaged, knowledgeable, and holistic physicians? According to this team of presenters, yes.
Key takeaways
• Current processes in medical education are harming today’s adult learner.
• Harms include reliance on numerical rather than competency-based assessment, fragmented learning environments, focus on perfection rather than improvement, ignorance of updates in cognitive science for instructional methodology, and individualist rather than team-based learning.
• Reforms are needed to remedy harms in health professional education, including making USMLE pass/fail, creating a learning-centered rather than service-centered residency environment, encouraging longitudinal relationships between teacher and learner, and connecting education to clinical outcomes.
Dr. King is associate program director, University of Minnesota Pediatric Residency Program, Minneapolis.
PHM19 session
Mitigating the harm we cause learners in medical education
Presenters
Benjamin Kinnear, MD, MEd
Andrew Olson, MD
Matthew Kelleher, MD, MEd
Session summary
Dr. Kinnear, Dr. Olson, and Dr. Kelleher expertly led this TED-Talk style session at Pediatric Hospital Medicine 2019, convincing the audience that medical educators persistently harm the learners under their supervision.
Dr. Kinnear, of Cincinnati Children’s Hospital, opened the session noting that the path through medical school presently has a perverse focus on grades as a necessary achievement. As an expert in competency-based assessment, he asserted that the current learner assessment strategy is neither valid nor robust enough to indicate actual competence. Summary assessments presented throughout medical school are lacking continuous constructive feedback, leaving early residents in a state of shock when receiving corrective or negative assessments. He also noted that structurally many rotations create both team and patient discontinuity, leaving the learner with a feeling of detachment and limited ownership of the human patient under his/her/their care.
Dr. Olson of the University of Minnesota next described the need for the USMLE STEP 1 exam to be transitioned to a pass/fail endeavor. He cited the error of measurement of 24 points (i.e., the same test taker could have a 220 one day and a 244 the next) and the potential loss of valuable rotation experiences during the several-month period of intense study. He challenged audience members to complete an esoteric exam question to prove his point and asserted that many learners are lacking in humility, communication skills, and professionalism, and seek only the honors designation on rotations. He likened the experience of medical students on rotation and residents on service weeks to a series of first dates and affirmed the value of longitudinal learner-educator relationships.
Further, he outlined the detachment of learners from patient outcomes, demonstrated by frequent hand-offs and rotation transitions. Dr Olson also cited medical pedagogy as failing to meet the known needs of adult learners to engage in deliberate progressive practice, reflective practice, or to use concepts such as spacing or interleaving to reinforce knowledge.
Dr. Kelleher, also of Cincinnati Children’s Hospital, ended the session by taking those in attendance on an imagined “what-if” journey where each of the wrongs currently done to early learners in medical education were corrected. This included engagement in daily reflection (5 minutes at a time), reporting system issues on rounds that had failed the patient, presenting learners with a CV of attending failures to reinforce the imperfection that is a reality in medicine, praising learners when they admit “they don’t know the answer” to a question posed on rounds, completing assessments in real time in the learner’s presence, rounding until specific feedback can be identified for each learner on the team, having a kiosk on each floor where ANY team member could provide feedback to learners, using cognitive science on rounds for teaching (i.e., Socratic) rather than pimping, modeling interprofessional teamwork daily using a culture of vulnerability rather than infallibility (i.e., airline culture), and by encouraging the attending to care for patients or complete tasks independently, showing the value of education over service and model ideal family-centered communication with the team.
One might wonder, if all of the above were accomplished at the request of our talented presenters, would a pass/fail USMLE world where medical education was learner centered and filled with longitudinal relationships with teams and patients, and outcomes were connected to education produce more engaged, knowledgeable, and holistic physicians? According to this team of presenters, yes.
Key takeaways
• Current processes in medical education are harming today’s adult learner.
• Harms include reliance on numerical rather than competency-based assessment, fragmented learning environments, focus on perfection rather than improvement, ignorance of updates in cognitive science for instructional methodology, and individualist rather than team-based learning.
• Reforms are needed to remedy harms in health professional education, including making USMLE pass/fail, creating a learning-centered rather than service-centered residency environment, encouraging longitudinal relationships between teacher and learner, and connecting education to clinical outcomes.
Dr. King is associate program director, University of Minnesota Pediatric Residency Program, Minneapolis.
The SHM Fellow designation: Class of 2020
Society invites applicants in multiple membership categories
In an industry brimming with opportunity and ongoing transformation, it is easy to feel indecisive about your next professional step when ample career paths exist in hospital medicine.
Yingkei Hui, MD, FHM, is an academic hospitalist at St. Vincent Indianapolis, and a Society of Hospital Medicine member since 2015. Seeking to set herself apart as an aspiring patient safety and quality improvement leader while continuing her professional development, she looked to SHM’s Fellow designation as the next piece of her career puzzle.
With more than 14 years of experience in the health care industry, Dr. Hui fell in love with the specialty because of its flexibility and patient-centric focus.
“I have a broad interest in medicine and want to learn everything under the larger umbrella of medicine,” she said. “I also find myself deeply in love with hospital medicine because it provides me with the opportunity to participate in various hospital committees and allows me to enjoy my practice from a macroscopic view of U.S. health care transformation – especially given the popular value-based patient care approach from recent years.”
Dr. Hui’s breadth of experience has allowed her to gain a unique set of perspectives and experiences from international and domestic standpoints. From attending medical school at the Chinese University of Hong Kong to completing her residency on the east coast at Pennsylvania Hospital in Philadelphia – part of the University of Pennsylvania Health System – Dr. Hui has held active medical licenses in New Jersey and currently, Indiana.
“SHM’s Fellow designation allows me to challenge myself in setting my career goal as a patient safety and quality improvement leader in my program,” she said. “It means a lot to me as it is a stand-out recognition of my participation in and contribution to patient care in my institution.”
When asked about the most rewarding aspect of being a part of the hospital medicine community, Dr. Hui identified “satisfaction in the teaching role.” She said she is “motivated by the holistic care for the patients, the integration of medical knowledge and coordination of care, and also the opportunity to conduct quality improvement projects.”
Motivated by her colleagues, Dr. Hui credits SHM with providing her with the inspiration and tools to push herself and advance her career in hospital medicine.
“I enjoy immersing myself in SHM’s patient safety and quality improvement resources; they are perfect for frontline hospitalists and also provide CME [continuing medical education],” she noted. “My previous medical directors were all Senior Fellows; they are my role models and continue to inspire me throughout my career.”
Dr. Hui also said that networking within the SHM community has been encouraging. “I’ve met talented Fellows at a number of hospital medicine annual conferences who have inspired me in the areas of patient care, education, and health promotion,” she explained. “Some of them have extensive publications; they are truly amazing physicians. SHM’s Annual Conference provides great opportunities for networking.”
As Dr. Hui continues to progress her career in hospital medicine, she believes that communication is a key pillar in her success. “Be a true listener and fill your heart with compassion, empathy, and courage,” she said. “Recognize your role as the enabler for the patients to improve their health.”
Completing her Master’s degree in population health management at Johns Hopkins University and expecting to graduate in May 2020, Dr. Hui is the designer of system safety (comprising patient safety, second victim safety, quality improvement, and just culture) in the academic setting of her residency program. She is also chairing a pioneer project for the St. Vincent IM residency program.
Dr. Hui plans to apply for a Senior Fellow designation with SHM in the future.
If you would like to join Dr. Hui and other like-minded hospital medicine leaders in taking your career to the next level, SHM is currently recruiting for the Fellows and Senior Fellows: Class of 2020. Applications are open until Nov. 29 of this year. These designations are available across a variety of membership categories, including physicians, nurse practitioners, physician assistants, and qualified practice administrators. Dedicated to promoting excellence, innovation, and improving the quality of patient care, Fellows designations provide members with a distinguishing credential as established pioneers in the industry.
For more information and to review your eligibility, visit hospitalmedicine.org/fellows.
Ms. Cowan is a marketing communications specialist at the Society of Hospital Medicine.
Society invites applicants in multiple membership categories
Society invites applicants in multiple membership categories
In an industry brimming with opportunity and ongoing transformation, it is easy to feel indecisive about your next professional step when ample career paths exist in hospital medicine.
Yingkei Hui, MD, FHM, is an academic hospitalist at St. Vincent Indianapolis, and a Society of Hospital Medicine member since 2015. Seeking to set herself apart as an aspiring patient safety and quality improvement leader while continuing her professional development, she looked to SHM’s Fellow designation as the next piece of her career puzzle.
With more than 14 years of experience in the health care industry, Dr. Hui fell in love with the specialty because of its flexibility and patient-centric focus.
“I have a broad interest in medicine and want to learn everything under the larger umbrella of medicine,” she said. “I also find myself deeply in love with hospital medicine because it provides me with the opportunity to participate in various hospital committees and allows me to enjoy my practice from a macroscopic view of U.S. health care transformation – especially given the popular value-based patient care approach from recent years.”
Dr. Hui’s breadth of experience has allowed her to gain a unique set of perspectives and experiences from international and domestic standpoints. From attending medical school at the Chinese University of Hong Kong to completing her residency on the east coast at Pennsylvania Hospital in Philadelphia – part of the University of Pennsylvania Health System – Dr. Hui has held active medical licenses in New Jersey and currently, Indiana.
“SHM’s Fellow designation allows me to challenge myself in setting my career goal as a patient safety and quality improvement leader in my program,” she said. “It means a lot to me as it is a stand-out recognition of my participation in and contribution to patient care in my institution.”
When asked about the most rewarding aspect of being a part of the hospital medicine community, Dr. Hui identified “satisfaction in the teaching role.” She said she is “motivated by the holistic care for the patients, the integration of medical knowledge and coordination of care, and also the opportunity to conduct quality improvement projects.”
Motivated by her colleagues, Dr. Hui credits SHM with providing her with the inspiration and tools to push herself and advance her career in hospital medicine.
“I enjoy immersing myself in SHM’s patient safety and quality improvement resources; they are perfect for frontline hospitalists and also provide CME [continuing medical education],” she noted. “My previous medical directors were all Senior Fellows; they are my role models and continue to inspire me throughout my career.”
Dr. Hui also said that networking within the SHM community has been encouraging. “I’ve met talented Fellows at a number of hospital medicine annual conferences who have inspired me in the areas of patient care, education, and health promotion,” she explained. “Some of them have extensive publications; they are truly amazing physicians. SHM’s Annual Conference provides great opportunities for networking.”
As Dr. Hui continues to progress her career in hospital medicine, she believes that communication is a key pillar in her success. “Be a true listener and fill your heart with compassion, empathy, and courage,” she said. “Recognize your role as the enabler for the patients to improve their health.”
Completing her Master’s degree in population health management at Johns Hopkins University and expecting to graduate in May 2020, Dr. Hui is the designer of system safety (comprising patient safety, second victim safety, quality improvement, and just culture) in the academic setting of her residency program. She is also chairing a pioneer project for the St. Vincent IM residency program.
Dr. Hui plans to apply for a Senior Fellow designation with SHM in the future.
If you would like to join Dr. Hui and other like-minded hospital medicine leaders in taking your career to the next level, SHM is currently recruiting for the Fellows and Senior Fellows: Class of 2020. Applications are open until Nov. 29 of this year. These designations are available across a variety of membership categories, including physicians, nurse practitioners, physician assistants, and qualified practice administrators. Dedicated to promoting excellence, innovation, and improving the quality of patient care, Fellows designations provide members with a distinguishing credential as established pioneers in the industry.
For more information and to review your eligibility, visit hospitalmedicine.org/fellows.
Ms. Cowan is a marketing communications specialist at the Society of Hospital Medicine.
In an industry brimming with opportunity and ongoing transformation, it is easy to feel indecisive about your next professional step when ample career paths exist in hospital medicine.
Yingkei Hui, MD, FHM, is an academic hospitalist at St. Vincent Indianapolis, and a Society of Hospital Medicine member since 2015. Seeking to set herself apart as an aspiring patient safety and quality improvement leader while continuing her professional development, she looked to SHM’s Fellow designation as the next piece of her career puzzle.
With more than 14 years of experience in the health care industry, Dr. Hui fell in love with the specialty because of its flexibility and patient-centric focus.
“I have a broad interest in medicine and want to learn everything under the larger umbrella of medicine,” she said. “I also find myself deeply in love with hospital medicine because it provides me with the opportunity to participate in various hospital committees and allows me to enjoy my practice from a macroscopic view of U.S. health care transformation – especially given the popular value-based patient care approach from recent years.”
Dr. Hui’s breadth of experience has allowed her to gain a unique set of perspectives and experiences from international and domestic standpoints. From attending medical school at the Chinese University of Hong Kong to completing her residency on the east coast at Pennsylvania Hospital in Philadelphia – part of the University of Pennsylvania Health System – Dr. Hui has held active medical licenses in New Jersey and currently, Indiana.
“SHM’s Fellow designation allows me to challenge myself in setting my career goal as a patient safety and quality improvement leader in my program,” she said. “It means a lot to me as it is a stand-out recognition of my participation in and contribution to patient care in my institution.”
When asked about the most rewarding aspect of being a part of the hospital medicine community, Dr. Hui identified “satisfaction in the teaching role.” She said she is “motivated by the holistic care for the patients, the integration of medical knowledge and coordination of care, and also the opportunity to conduct quality improvement projects.”
Motivated by her colleagues, Dr. Hui credits SHM with providing her with the inspiration and tools to push herself and advance her career in hospital medicine.
“I enjoy immersing myself in SHM’s patient safety and quality improvement resources; they are perfect for frontline hospitalists and also provide CME [continuing medical education],” she noted. “My previous medical directors were all Senior Fellows; they are my role models and continue to inspire me throughout my career.”
Dr. Hui also said that networking within the SHM community has been encouraging. “I’ve met talented Fellows at a number of hospital medicine annual conferences who have inspired me in the areas of patient care, education, and health promotion,” she explained. “Some of them have extensive publications; they are truly amazing physicians. SHM’s Annual Conference provides great opportunities for networking.”
As Dr. Hui continues to progress her career in hospital medicine, she believes that communication is a key pillar in her success. “Be a true listener and fill your heart with compassion, empathy, and courage,” she said. “Recognize your role as the enabler for the patients to improve their health.”
Completing her Master’s degree in population health management at Johns Hopkins University and expecting to graduate in May 2020, Dr. Hui is the designer of system safety (comprising patient safety, second victim safety, quality improvement, and just culture) in the academic setting of her residency program. She is also chairing a pioneer project for the St. Vincent IM residency program.
Dr. Hui plans to apply for a Senior Fellow designation with SHM in the future.
If you would like to join Dr. Hui and other like-minded hospital medicine leaders in taking your career to the next level, SHM is currently recruiting for the Fellows and Senior Fellows: Class of 2020. Applications are open until Nov. 29 of this year. These designations are available across a variety of membership categories, including physicians, nurse practitioners, physician assistants, and qualified practice administrators. Dedicated to promoting excellence, innovation, and improving the quality of patient care, Fellows designations provide members with a distinguishing credential as established pioneers in the industry.
For more information and to review your eligibility, visit hospitalmedicine.org/fellows.
Ms. Cowan is a marketing communications specialist at the Society of Hospital Medicine.
PHM 19: PREP yourself for the PHM boards
Get ready for the first-ever ABP PHM exam
Presenters
Jared Austin, MD, FAAP
Ryan Bode, MD, FAAP
Jeremy Kern, MD, FAAP
Mary Ottolini, MD, MPH, MEd, FAAP
Stacy Pierson, MD, FAAP
Mary Rocha, MD, MPH, FAAP
Susan Walley, MD, CTTS, FAAP
Session summary
Professional development sessions at the Pediatric Hospital Medicine 2019 conference intended to further educate pediatric hospitalists and advance their careers. In November 2019, many pediatric hospitalists will be taking subspecialty PHM boards for the very first time. This PHM19 session had clear objectives: to describe the American Board of Pediatrics (ABP) PHM board content areas, to analyze common knowledge gaps in PREP PHM, and to examine different approaches to clinical management of PHM patients.
The session opened with a brief history of a vision of PHM and the story of its realization. In 2016, a group of eight stalwart writers, four new writers, and three editors created PREP 2018 and 2019 questions that were released in full prior to November 2019. The ABP will offer the board exam in 2019, 2021, and 2023
The exam content domains include the following:
- Medical conditions.
- Behavioral and mental health conditions.
- Newborn care.
- Children with medical complexity.
- Medical procedures.
- Patient and family centered care.
- Transitions of care.
- Quality improvement, patient safety and system based improvement.
- Evidence-based, high-value care.
- Advocacy and leadership.
- Ethics, legal issues, and human rights.
- Teaching and education.
- Core knowledge in scholarly activities.
Each question consists of a case vignette, question, response choices, critiques, PREP PEARLs, and references. There are also additional PREP Ponder Points that intend to prompt reflection on practice change.
For the remainder of the session presenters reviewed the PHM PREP questions that were most frequently answered incorrectly. Some of the topics included: asthma vs. anaphylaxis, venous thromboembolism prophylaxis in surgical patients, postoperative feeding regimens, transmission-based precautions, febrile neonates, Ebola, medical child abuse, absolute indications for intubation, toxic megacolon, palivizumab prophylaxis guidelines, key driver diagrams, and infantile hemangiomas.
Key takeaway
Pediatric hospitalists all over the United States will for the first time ever take PHM boards in November 2019. The exam content domains were demonstrated in detail, and several often incorrectly answered PREP questions were presented and discussed.
Dr. Giordano is assistant professor in pediatrics at Columbia University Medical Center, New York.
Get ready for the first-ever ABP PHM exam
Get ready for the first-ever ABP PHM exam
Presenters
Jared Austin, MD, FAAP
Ryan Bode, MD, FAAP
Jeremy Kern, MD, FAAP
Mary Ottolini, MD, MPH, MEd, FAAP
Stacy Pierson, MD, FAAP
Mary Rocha, MD, MPH, FAAP
Susan Walley, MD, CTTS, FAAP
Session summary
Professional development sessions at the Pediatric Hospital Medicine 2019 conference intended to further educate pediatric hospitalists and advance their careers. In November 2019, many pediatric hospitalists will be taking subspecialty PHM boards for the very first time. This PHM19 session had clear objectives: to describe the American Board of Pediatrics (ABP) PHM board content areas, to analyze common knowledge gaps in PREP PHM, and to examine different approaches to clinical management of PHM patients.
The session opened with a brief history of a vision of PHM and the story of its realization. In 2016, a group of eight stalwart writers, four new writers, and three editors created PREP 2018 and 2019 questions that were released in full prior to November 2019. The ABP will offer the board exam in 2019, 2021, and 2023
The exam content domains include the following:
- Medical conditions.
- Behavioral and mental health conditions.
- Newborn care.
- Children with medical complexity.
- Medical procedures.
- Patient and family centered care.
- Transitions of care.
- Quality improvement, patient safety and system based improvement.
- Evidence-based, high-value care.
- Advocacy and leadership.
- Ethics, legal issues, and human rights.
- Teaching and education.
- Core knowledge in scholarly activities.
Each question consists of a case vignette, question, response choices, critiques, PREP PEARLs, and references. There are also additional PREP Ponder Points that intend to prompt reflection on practice change.
For the remainder of the session presenters reviewed the PHM PREP questions that were most frequently answered incorrectly. Some of the topics included: asthma vs. anaphylaxis, venous thromboembolism prophylaxis in surgical patients, postoperative feeding regimens, transmission-based precautions, febrile neonates, Ebola, medical child abuse, absolute indications for intubation, toxic megacolon, palivizumab prophylaxis guidelines, key driver diagrams, and infantile hemangiomas.
Key takeaway
Pediatric hospitalists all over the United States will for the first time ever take PHM boards in November 2019. The exam content domains were demonstrated in detail, and several often incorrectly answered PREP questions were presented and discussed.
Dr. Giordano is assistant professor in pediatrics at Columbia University Medical Center, New York.
Presenters
Jared Austin, MD, FAAP
Ryan Bode, MD, FAAP
Jeremy Kern, MD, FAAP
Mary Ottolini, MD, MPH, MEd, FAAP
Stacy Pierson, MD, FAAP
Mary Rocha, MD, MPH, FAAP
Susan Walley, MD, CTTS, FAAP
Session summary
Professional development sessions at the Pediatric Hospital Medicine 2019 conference intended to further educate pediatric hospitalists and advance their careers. In November 2019, many pediatric hospitalists will be taking subspecialty PHM boards for the very first time. This PHM19 session had clear objectives: to describe the American Board of Pediatrics (ABP) PHM board content areas, to analyze common knowledge gaps in PREP PHM, and to examine different approaches to clinical management of PHM patients.
The session opened with a brief history of a vision of PHM and the story of its realization. In 2016, a group of eight stalwart writers, four new writers, and three editors created PREP 2018 and 2019 questions that were released in full prior to November 2019. The ABP will offer the board exam in 2019, 2021, and 2023
The exam content domains include the following:
- Medical conditions.
- Behavioral and mental health conditions.
- Newborn care.
- Children with medical complexity.
- Medical procedures.
- Patient and family centered care.
- Transitions of care.
- Quality improvement, patient safety and system based improvement.
- Evidence-based, high-value care.
- Advocacy and leadership.
- Ethics, legal issues, and human rights.
- Teaching and education.
- Core knowledge in scholarly activities.
Each question consists of a case vignette, question, response choices, critiques, PREP PEARLs, and references. There are also additional PREP Ponder Points that intend to prompt reflection on practice change.
For the remainder of the session presenters reviewed the PHM PREP questions that were most frequently answered incorrectly. Some of the topics included: asthma vs. anaphylaxis, venous thromboembolism prophylaxis in surgical patients, postoperative feeding regimens, transmission-based precautions, febrile neonates, Ebola, medical child abuse, absolute indications for intubation, toxic megacolon, palivizumab prophylaxis guidelines, key driver diagrams, and infantile hemangiomas.
Key takeaway
Pediatric hospitalists all over the United States will for the first time ever take PHM boards in November 2019. The exam content domains were demonstrated in detail, and several often incorrectly answered PREP questions were presented and discussed.
Dr. Giordano is assistant professor in pediatrics at Columbia University Medical Center, New York.
NAM offers recommendations to fight clinician burnout
WASHINGTON – a condition now estimated to affect a third to a half of clinicians in the United States, according to a report from an influential federal panel.
The National Academy of Medicine (NAM) on Oct. 23 released a report, “Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being.” The report calls for a broad and unified approach to tackling the root causes of burnout.
There must be a concerted effort by leaders of many fields of health care to create less stressful workplaces for clinicians, Pascale Carayon, PhD, cochair of the NAM committee that produced the report, said during the NAM press event.
“This is not an easy process,” said Dr. Carayon, a researcher into patient safety issues at the University of Wisconsin–Madison. “There is no single solution.”
The NAM report assigns specific tasks to many different participants in health care through a six-goal approach, as described below.
–Create positive workplaces. Leaders of health care systems should consider how their business and management decisions will affect clinicians’ jobs, taking into account the potential to add to their levels of burnout. Executives need to continuously monitor and evaluate the extent of burnout in their organizations, and report on this at least annually.
–Address burnout in training and in clinicians’ early years. Medical, nursing, and pharmacy schools should consider steps such as monitoring workload, implementing pass-fail grading, improving access to scholarships and affordable loans, and creating new loan repayment systems.
–Reduce administrative burden. Federal and state bodies and organizations such as the National Quality Forum should reconsider how their regulations and recommendations contribute to burnout. Organizations should seek to eliminate tasks that do not improve the care of patients.
–Improve usability and relevance of health information technology (IT). Medical organizations should develop and buy systems that are as user-friendly and easy to operate as possible. They also should look to use IT to reduce documentation demands and automate nonessential tasks.
–Reduce stigma and improve burnout recovery services. State officials and legislative bodies should make it easier for clinicians to use employee assistance programs, peer support programs, and mental health providers without the information being admissible in malpractice litigation. The report notes the recommendations from the Federation of State Medical Boards, American Medical Association, and the American Psychiatric Association on limiting inquiries in licensing applications about a clinician’s mental health. Questions should focus on current impairment rather than reach well into a clinician’s past.
–Create a national research agenda on clinician well-being. By the end of 2020, federal agencies – including the Agency for Healthcare Research and Quality, the National Institute for Occupational Safety and Health, the Health Resources and Services Administration, and the U.S. Department of Veterans Affairs – should develop a coordinated research agenda on clinician burnout, the report said.
In casting a wide net and assigning specific tasks, the NAM report seeks to establish efforts to address clinician burnout as a broad and shared responsibility. It would be too easy for different medical organizations to depict addressing burnout as being outside of their responsibilities, Christine K. Cassel, MD, the cochair of the NAM committee that produced the report, said during the press event.
“Nothing could be farther from the truth. Everyone is necessary to solve this problem,” said Dr. Cassel, who is a former chief executive officer of the National Quality Forum.
Darrell G. Kirch, MD, chief executive of the Association of American Medical Colleges, described the report as a “call to action” at the press event.
Previously published research has found between 35% and 54% of nurses and physicians in the United States have substantial symptoms of burnout, with the prevalence of burnout ranging between 45% and 60% for medical students and residents, the NAM report said.
Leaders of health organizations must consider how the policies they set will add stress for clinicians and make them less effective in caring for patients, said Vindell Washington, MD, chief medical officer of Blue Cross Blue Shield of Louisiana and a member of the NAM committee that wrote the report.
“Those linkages should be incentives and motivations for boards and leaders more broadly to act on the problem,” Dr. Washington said at the NAM event.
Dr. Kirch said he experienced burnout as a first-year medical student. He said a “brilliant aspect” of the NAM report is its emphasis on burnout as a response to the conditions under which medicine is practiced. In the past, burnout has been viewed as being the fault of the physician or nurse experiencing it, with the response then being to try to “fix” this individual, Dr. Kirch said at the event.
The NAM report instead defines burnout as a “work-related phenomenon studied since at least the 1970s,” in which an individual may experience exhaustion and detachment. Depression and other mental health issues such as anxiety disorders and addiction can follow burnout, he said. “That involves a real human toll.”
Joe Rotella, MD, MBA, chief medical officer at American Academy of Hospice and Palliative Medicine, said in an interview that this NAM paper has the potential to spark the kind of transformation that its earlier research did for the quality of care. Then called the Institute of Medicine(IOM), NAM in 1999 issued a report, “To Err Is Human,” which is broadly seen as a key catalyst in efforts in the ensuing decades to improve the quality of care. IOM then followed up with a 2001 report, “Crossing the Quality Chasm.”
“Those papers over a period of time really did change the way we do health care,” said Dr. Rotella, who was not involved with the NAM report.
In Dr. Rotella’s view, the NAM report provides a solid framework for what remains a daunting task, addressing the many factors involved in burnout.
“The most exciting thing about this is that they don’t have 500 recommendations. They had six and that’s something people can organize around,” he said. “They are not small goals. I’m not saying they are simple.”
The NAM report delves into the factors that contribute to burnout. These include a maze of government and commercial insurance plans that create “a confusing and onerous environment for clinicians,” with many of them juggling “multiple payment systems with complex rules, processes, metrics, and incentives that may frequently change.”
Clinicians face a growing field of measurements intended to judge the quality of their performance. While some of these are useful, others are duplicative and some are not relevant to patient care, the NAM report said.
The report also noted that many clinicians describe electronic health records (EHRs) as taking a toll on their work and private lives. Previously published research has found that for every hour spent with a patient, physicians spend an additional 1-2 hours on the EHR at work, with additional time needed to complete this data entry at home after work hours, the report said.
In an interview, Cynda Rushton, RN, PhD, a Johns Hopkins University researcher and a member of the NAM committee that produced the report, said this new publication will support efforts to overhaul many aspects of current medical practice. She said she hopes it will be a “catalyst for bold and fundamental reform.
“It’s taking a deep dive into the evidence to see how we can begin to dismantle the system’s contributions to burnout,” she said. “No longer can we put Band-Aids on a gaping wound.”
WASHINGTON – a condition now estimated to affect a third to a half of clinicians in the United States, according to a report from an influential federal panel.
The National Academy of Medicine (NAM) on Oct. 23 released a report, “Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being.” The report calls for a broad and unified approach to tackling the root causes of burnout.
There must be a concerted effort by leaders of many fields of health care to create less stressful workplaces for clinicians, Pascale Carayon, PhD, cochair of the NAM committee that produced the report, said during the NAM press event.
“This is not an easy process,” said Dr. Carayon, a researcher into patient safety issues at the University of Wisconsin–Madison. “There is no single solution.”
The NAM report assigns specific tasks to many different participants in health care through a six-goal approach, as described below.
–Create positive workplaces. Leaders of health care systems should consider how their business and management decisions will affect clinicians’ jobs, taking into account the potential to add to their levels of burnout. Executives need to continuously monitor and evaluate the extent of burnout in their organizations, and report on this at least annually.
–Address burnout in training and in clinicians’ early years. Medical, nursing, and pharmacy schools should consider steps such as monitoring workload, implementing pass-fail grading, improving access to scholarships and affordable loans, and creating new loan repayment systems.
–Reduce administrative burden. Federal and state bodies and organizations such as the National Quality Forum should reconsider how their regulations and recommendations contribute to burnout. Organizations should seek to eliminate tasks that do not improve the care of patients.
–Improve usability and relevance of health information technology (IT). Medical organizations should develop and buy systems that are as user-friendly and easy to operate as possible. They also should look to use IT to reduce documentation demands and automate nonessential tasks.
–Reduce stigma and improve burnout recovery services. State officials and legislative bodies should make it easier for clinicians to use employee assistance programs, peer support programs, and mental health providers without the information being admissible in malpractice litigation. The report notes the recommendations from the Federation of State Medical Boards, American Medical Association, and the American Psychiatric Association on limiting inquiries in licensing applications about a clinician’s mental health. Questions should focus on current impairment rather than reach well into a clinician’s past.
–Create a national research agenda on clinician well-being. By the end of 2020, federal agencies – including the Agency for Healthcare Research and Quality, the National Institute for Occupational Safety and Health, the Health Resources and Services Administration, and the U.S. Department of Veterans Affairs – should develop a coordinated research agenda on clinician burnout, the report said.
In casting a wide net and assigning specific tasks, the NAM report seeks to establish efforts to address clinician burnout as a broad and shared responsibility. It would be too easy for different medical organizations to depict addressing burnout as being outside of their responsibilities, Christine K. Cassel, MD, the cochair of the NAM committee that produced the report, said during the press event.
“Nothing could be farther from the truth. Everyone is necessary to solve this problem,” said Dr. Cassel, who is a former chief executive officer of the National Quality Forum.
Darrell G. Kirch, MD, chief executive of the Association of American Medical Colleges, described the report as a “call to action” at the press event.
Previously published research has found between 35% and 54% of nurses and physicians in the United States have substantial symptoms of burnout, with the prevalence of burnout ranging between 45% and 60% for medical students and residents, the NAM report said.
Leaders of health organizations must consider how the policies they set will add stress for clinicians and make them less effective in caring for patients, said Vindell Washington, MD, chief medical officer of Blue Cross Blue Shield of Louisiana and a member of the NAM committee that wrote the report.
“Those linkages should be incentives and motivations for boards and leaders more broadly to act on the problem,” Dr. Washington said at the NAM event.
Dr. Kirch said he experienced burnout as a first-year medical student. He said a “brilliant aspect” of the NAM report is its emphasis on burnout as a response to the conditions under which medicine is practiced. In the past, burnout has been viewed as being the fault of the physician or nurse experiencing it, with the response then being to try to “fix” this individual, Dr. Kirch said at the event.
The NAM report instead defines burnout as a “work-related phenomenon studied since at least the 1970s,” in which an individual may experience exhaustion and detachment. Depression and other mental health issues such as anxiety disorders and addiction can follow burnout, he said. “That involves a real human toll.”
Joe Rotella, MD, MBA, chief medical officer at American Academy of Hospice and Palliative Medicine, said in an interview that this NAM paper has the potential to spark the kind of transformation that its earlier research did for the quality of care. Then called the Institute of Medicine(IOM), NAM in 1999 issued a report, “To Err Is Human,” which is broadly seen as a key catalyst in efforts in the ensuing decades to improve the quality of care. IOM then followed up with a 2001 report, “Crossing the Quality Chasm.”
“Those papers over a period of time really did change the way we do health care,” said Dr. Rotella, who was not involved with the NAM report.
In Dr. Rotella’s view, the NAM report provides a solid framework for what remains a daunting task, addressing the many factors involved in burnout.
“The most exciting thing about this is that they don’t have 500 recommendations. They had six and that’s something people can organize around,” he said. “They are not small goals. I’m not saying they are simple.”
The NAM report delves into the factors that contribute to burnout. These include a maze of government and commercial insurance plans that create “a confusing and onerous environment for clinicians,” with many of them juggling “multiple payment systems with complex rules, processes, metrics, and incentives that may frequently change.”
Clinicians face a growing field of measurements intended to judge the quality of their performance. While some of these are useful, others are duplicative and some are not relevant to patient care, the NAM report said.
The report also noted that many clinicians describe electronic health records (EHRs) as taking a toll on their work and private lives. Previously published research has found that for every hour spent with a patient, physicians spend an additional 1-2 hours on the EHR at work, with additional time needed to complete this data entry at home after work hours, the report said.
In an interview, Cynda Rushton, RN, PhD, a Johns Hopkins University researcher and a member of the NAM committee that produced the report, said this new publication will support efforts to overhaul many aspects of current medical practice. She said she hopes it will be a “catalyst for bold and fundamental reform.
“It’s taking a deep dive into the evidence to see how we can begin to dismantle the system’s contributions to burnout,” she said. “No longer can we put Band-Aids on a gaping wound.”
WASHINGTON – a condition now estimated to affect a third to a half of clinicians in the United States, according to a report from an influential federal panel.
The National Academy of Medicine (NAM) on Oct. 23 released a report, “Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being.” The report calls for a broad and unified approach to tackling the root causes of burnout.
There must be a concerted effort by leaders of many fields of health care to create less stressful workplaces for clinicians, Pascale Carayon, PhD, cochair of the NAM committee that produced the report, said during the NAM press event.
“This is not an easy process,” said Dr. Carayon, a researcher into patient safety issues at the University of Wisconsin–Madison. “There is no single solution.”
The NAM report assigns specific tasks to many different participants in health care through a six-goal approach, as described below.
–Create positive workplaces. Leaders of health care systems should consider how their business and management decisions will affect clinicians’ jobs, taking into account the potential to add to their levels of burnout. Executives need to continuously monitor and evaluate the extent of burnout in their organizations, and report on this at least annually.
–Address burnout in training and in clinicians’ early years. Medical, nursing, and pharmacy schools should consider steps such as monitoring workload, implementing pass-fail grading, improving access to scholarships and affordable loans, and creating new loan repayment systems.
–Reduce administrative burden. Federal and state bodies and organizations such as the National Quality Forum should reconsider how their regulations and recommendations contribute to burnout. Organizations should seek to eliminate tasks that do not improve the care of patients.
–Improve usability and relevance of health information technology (IT). Medical organizations should develop and buy systems that are as user-friendly and easy to operate as possible. They also should look to use IT to reduce documentation demands and automate nonessential tasks.
–Reduce stigma and improve burnout recovery services. State officials and legislative bodies should make it easier for clinicians to use employee assistance programs, peer support programs, and mental health providers without the information being admissible in malpractice litigation. The report notes the recommendations from the Federation of State Medical Boards, American Medical Association, and the American Psychiatric Association on limiting inquiries in licensing applications about a clinician’s mental health. Questions should focus on current impairment rather than reach well into a clinician’s past.
–Create a national research agenda on clinician well-being. By the end of 2020, federal agencies – including the Agency for Healthcare Research and Quality, the National Institute for Occupational Safety and Health, the Health Resources and Services Administration, and the U.S. Department of Veterans Affairs – should develop a coordinated research agenda on clinician burnout, the report said.
In casting a wide net and assigning specific tasks, the NAM report seeks to establish efforts to address clinician burnout as a broad and shared responsibility. It would be too easy for different medical organizations to depict addressing burnout as being outside of their responsibilities, Christine K. Cassel, MD, the cochair of the NAM committee that produced the report, said during the press event.
“Nothing could be farther from the truth. Everyone is necessary to solve this problem,” said Dr. Cassel, who is a former chief executive officer of the National Quality Forum.
Darrell G. Kirch, MD, chief executive of the Association of American Medical Colleges, described the report as a “call to action” at the press event.
Previously published research has found between 35% and 54% of nurses and physicians in the United States have substantial symptoms of burnout, with the prevalence of burnout ranging between 45% and 60% for medical students and residents, the NAM report said.
Leaders of health organizations must consider how the policies they set will add stress for clinicians and make them less effective in caring for patients, said Vindell Washington, MD, chief medical officer of Blue Cross Blue Shield of Louisiana and a member of the NAM committee that wrote the report.
“Those linkages should be incentives and motivations for boards and leaders more broadly to act on the problem,” Dr. Washington said at the NAM event.
Dr. Kirch said he experienced burnout as a first-year medical student. He said a “brilliant aspect” of the NAM report is its emphasis on burnout as a response to the conditions under which medicine is practiced. In the past, burnout has been viewed as being the fault of the physician or nurse experiencing it, with the response then being to try to “fix” this individual, Dr. Kirch said at the event.
The NAM report instead defines burnout as a “work-related phenomenon studied since at least the 1970s,” in which an individual may experience exhaustion and detachment. Depression and other mental health issues such as anxiety disorders and addiction can follow burnout, he said. “That involves a real human toll.”
Joe Rotella, MD, MBA, chief medical officer at American Academy of Hospice and Palliative Medicine, said in an interview that this NAM paper has the potential to spark the kind of transformation that its earlier research did for the quality of care. Then called the Institute of Medicine(IOM), NAM in 1999 issued a report, “To Err Is Human,” which is broadly seen as a key catalyst in efforts in the ensuing decades to improve the quality of care. IOM then followed up with a 2001 report, “Crossing the Quality Chasm.”
“Those papers over a period of time really did change the way we do health care,” said Dr. Rotella, who was not involved with the NAM report.
In Dr. Rotella’s view, the NAM report provides a solid framework for what remains a daunting task, addressing the many factors involved in burnout.
“The most exciting thing about this is that they don’t have 500 recommendations. They had six and that’s something people can organize around,” he said. “They are not small goals. I’m not saying they are simple.”
The NAM report delves into the factors that contribute to burnout. These include a maze of government and commercial insurance plans that create “a confusing and onerous environment for clinicians,” with many of them juggling “multiple payment systems with complex rules, processes, metrics, and incentives that may frequently change.”
Clinicians face a growing field of measurements intended to judge the quality of their performance. While some of these are useful, others are duplicative and some are not relevant to patient care, the NAM report said.
The report also noted that many clinicians describe electronic health records (EHRs) as taking a toll on their work and private lives. Previously published research has found that for every hour spent with a patient, physicians spend an additional 1-2 hours on the EHR at work, with additional time needed to complete this data entry at home after work hours, the report said.
In an interview, Cynda Rushton, RN, PhD, a Johns Hopkins University researcher and a member of the NAM committee that produced the report, said this new publication will support efforts to overhaul many aspects of current medical practice. She said she hopes it will be a “catalyst for bold and fundamental reform.
“It’s taking a deep dive into the evidence to see how we can begin to dismantle the system’s contributions to burnout,” she said. “No longer can we put Band-Aids on a gaping wound.”
The growing NP and PA workforce in hospital medicine
High rate of turnover among NPs, PAs
If you were a physician hospitalist in a group serving adults in 2017 you probably worked with nurse practitioners (NPs) and/or physician assistants (PAs). Seventy-seven percent of hospital medicine groups (HMGs) employed NPs and PAs that year.
In addition, the larger the group, the more likely the group was to have NPs and PAs as part of their practice model – 89% of hospital medicine groups with more than 30 physician had NPs and/or PAs as partners. In addition, the mean number of physicians for adult hospital medicine groups was 17.9. The same practices employed an average of 3.5 NPs, and 2.6 PAs.
Based on these numbers, there are just under three physicians per NP and PA in the typical HMG serving adults. This is all according to data from the 2018 State of Hospital Medicine (SoHM) report that was published in 2019 by the Society of Hospital Medicine.
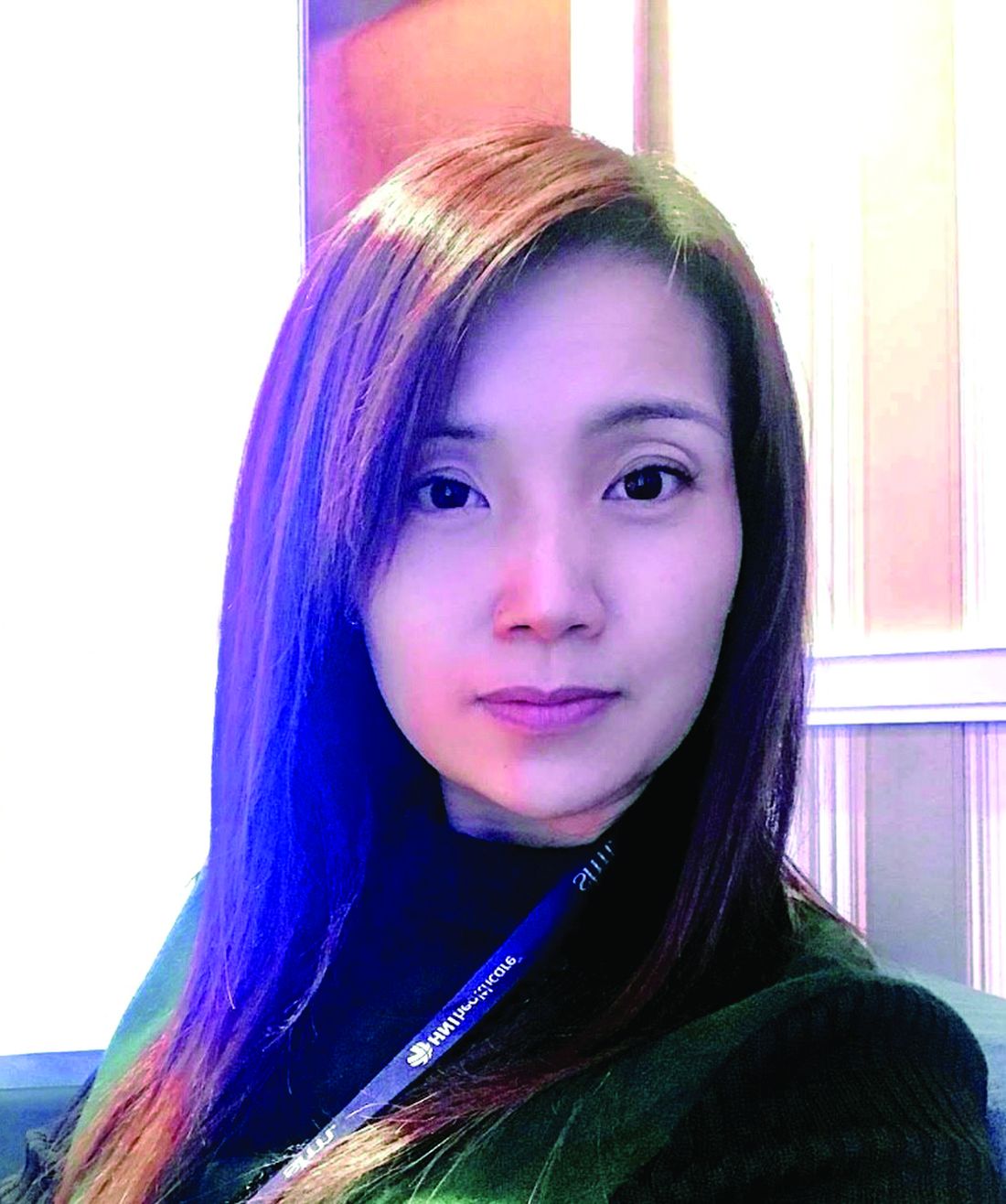
These observations lead to a number of questions. One thing that is not clear from the SoHM is why NPs and PAs are becoming a larger part of the hospital medicine workforce, but there are some insights and conjecture that can be drawn from the data. The first is economics. Over 6 years, the median incomes of NPs and PAs have risen a relatively modest 10%; over the same period physician hospitalists have seen a whopping 23.6% median pay increase.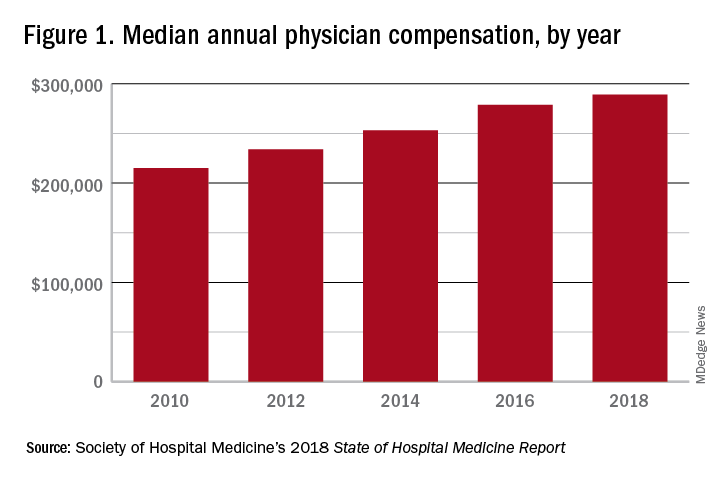
One argument against economics as a driving force behind greater use of NPs and PAs in the hospital medicine workforce is the billing patterns of HMGs that use NPs and PAs. Ten percent of HMGs do not have their NPs and PAs bill at all. The distribution of HMGs that predominantly bill NP and PA services as shared visits, versus having NPs and PAs bill independently, has also not changed much over the years, with 22% of HMGs having NPs and PAs bill independently as a predominant model. This would seem to suggest that some HMGs may not have learned how to deploy NPs and PAs effectively.
While inefficiency can be due to hospital bylaws, the culture of the hospital medicine group, or the skill set of the NPs and PAs working in HMGs – it would seem that if the driving force for the increase in the utilization of NPs and PAs in HMGs was financial, then that would also result in more of these providers billing independently, or alternatively, an increase in hospitalist physician productivity, which the data do not show. However, multistate HMGs may have this figured out better than some of the rest of us – 78% of these HMGs have NPs and PAs billing independently! All other categories of HMGs together are around 13%, with the next highest being hospital or health system integrated delivery systems, where NPs/PAs bill independently about 15% of the time.
In the last 2 years of the survey, there have been marked increases in the number of NPs and PAs at HMGs performing “nontraditional” services. For example, outpatient work has increased from 11% to 17%, and work in the postacute space has increased from 13% to 25%. Work in behavioral health and alcohol and drug rehab facilities has also increased, from 17% to 26%. As HMGs seek to rationalize their workforce while expanding, it is possible that decision makers have felt that it was either more economical to place NPs and PAs in positions where they are seeing these patients, or it was more aligned with the NP/PA skill set, or both. In any event, as the scope of hospital medicine broadens, the use of PAs and NPs has also increased – which is probably not coincidental.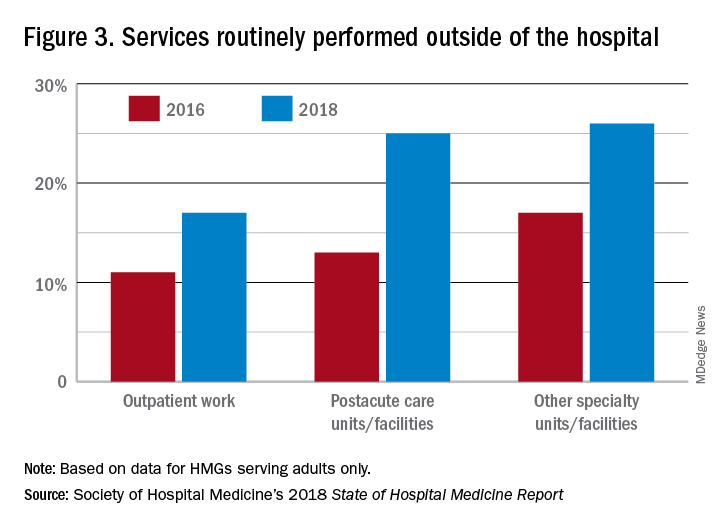
The average hospital medicine group continues to have staff openings. Workforce shortages may be leading to what in the past may have been considered physician openings being filled by NPs and PAs. Only 33% of HMGs reported having all their physician openings filled. Median physician shortage was 12% of total approved staffing. Given concerns in hospital medicine about provider burnout, the number of hospital medicine openings is no doubt a concern to HMG leaders and hospitalists. And necessity being the mother of invention, HMG leadership must be thinking differently than in the past about open positions and the skill mix needed to fill them. I believe this is leading to NPs and PAs being considered more often for a role that would have been open only to a physician in the past.
Just as open positions are a concern, so is turnover. One striking finding in the SoHM is the very high rate of turnover among NPs and PAs – a whopping 19.1% per year. For physicians, the same rate was 7.4% and has been declining every survey for many years. While NPs and PAs may be intended to stabilize the workforce, because of how this is being done in some groups, NPs and PAs may instead be a destabilizing factor. Rapid growth can lead to haphazard onboarding and less than clearly defined roles. NPs and PAs may often be placed into roles for which they are not yet prepared. In addition, the pay disparity between NPs and PAs and physicians has increased. As a new field, and with many HMGs still rapidly growing, increased thoughtfulness and maturity about how NPs and PAs are integrated into hospital medicine practices should lead to less turnover and better HMG stability in the future.
These observations could mark a future that includes higher pay for hospital medicine PAs and NPs (and potentially a slowdown in salary growth for physicians); HMGs taking steps to make the financial model more attractive by having NPs and PAs bill independently more often; and HMGs and their leaders engaging NPs and PAs by more clearly defining roles, shoring up onboarding and mentoring programs, and other measures that decrease turnover. This would help to make hospital medicine a career destination, rather than a stopping off point for NPs and PAs, much as it has become for internists over the past 20 years.
Dr. Frederickson is medical director, hospital medicine and palliative care, at CHI Health, Omaha, Neb., and assistant professor at Creighton University, Omaha.
High rate of turnover among NPs, PAs
High rate of turnover among NPs, PAs
If you were a physician hospitalist in a group serving adults in 2017 you probably worked with nurse practitioners (NPs) and/or physician assistants (PAs). Seventy-seven percent of hospital medicine groups (HMGs) employed NPs and PAs that year.
In addition, the larger the group, the more likely the group was to have NPs and PAs as part of their practice model – 89% of hospital medicine groups with more than 30 physician had NPs and/or PAs as partners. In addition, the mean number of physicians for adult hospital medicine groups was 17.9. The same practices employed an average of 3.5 NPs, and 2.6 PAs.
Based on these numbers, there are just under three physicians per NP and PA in the typical HMG serving adults. This is all according to data from the 2018 State of Hospital Medicine (SoHM) report that was published in 2019 by the Society of Hospital Medicine.
These observations lead to a number of questions. One thing that is not clear from the SoHM is why NPs and PAs are becoming a larger part of the hospital medicine workforce, but there are some insights and conjecture that can be drawn from the data. The first is economics. Over 6 years, the median incomes of NPs and PAs have risen a relatively modest 10%; over the same period physician hospitalists have seen a whopping 23.6% median pay increase.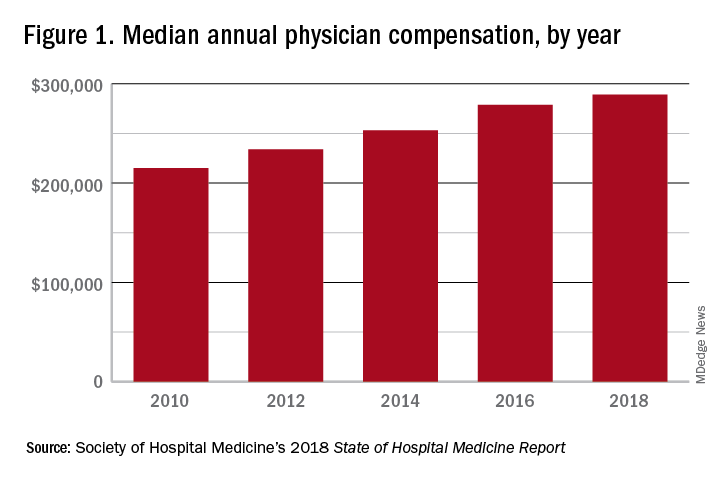
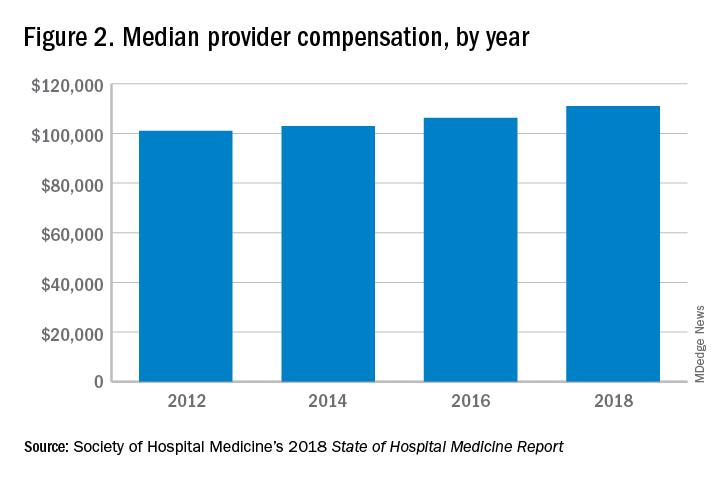
One argument against economics as a driving force behind greater use of NPs and PAs in the hospital medicine workforce is the billing patterns of HMGs that use NPs and PAs. Ten percent of HMGs do not have their NPs and PAs bill at all. The distribution of HMGs that predominantly bill NP and PA services as shared visits, versus having NPs and PAs bill independently, has also not changed much over the years, with 22% of HMGs having NPs and PAs bill independently as a predominant model. This would seem to suggest that some HMGs may not have learned how to deploy NPs and PAs effectively.
While inefficiency can be due to hospital bylaws, the culture of the hospital medicine group, or the skill set of the NPs and PAs working in HMGs – it would seem that if the driving force for the increase in the utilization of NPs and PAs in HMGs was financial, then that would also result in more of these providers billing independently, or alternatively, an increase in hospitalist physician productivity, which the data do not show. However, multistate HMGs may have this figured out better than some of the rest of us – 78% of these HMGs have NPs and PAs billing independently! All other categories of HMGs together are around 13%, with the next highest being hospital or health system integrated delivery systems, where NPs/PAs bill independently about 15% of the time.
In the last 2 years of the survey, there have been marked increases in the number of NPs and PAs at HMGs performing “nontraditional” services. For example, outpatient work has increased from 11% to 17%, and work in the postacute space has increased from 13% to 25%. Work in behavioral health and alcohol and drug rehab facilities has also increased, from 17% to 26%. As HMGs seek to rationalize their workforce while expanding, it is possible that decision makers have felt that it was either more economical to place NPs and PAs in positions where they are seeing these patients, or it was more aligned with the NP/PA skill set, or both. In any event, as the scope of hospital medicine broadens, the use of PAs and NPs has also increased – which is probably not coincidental.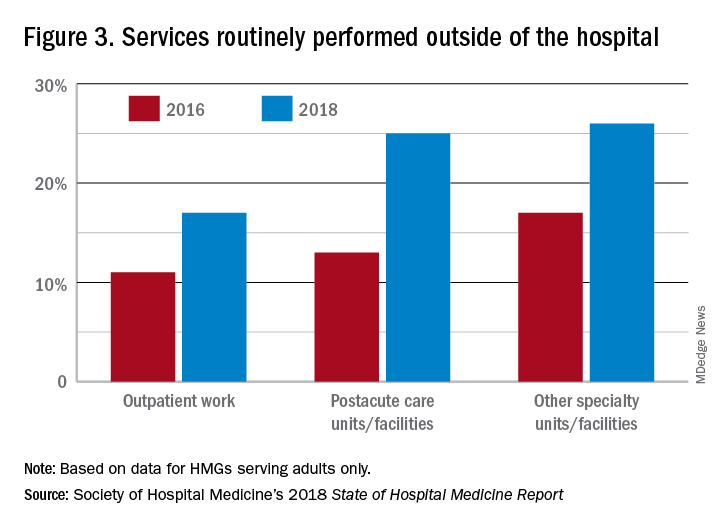
The average hospital medicine group continues to have staff openings. Workforce shortages may be leading to what in the past may have been considered physician openings being filled by NPs and PAs. Only 33% of HMGs reported having all their physician openings filled. Median physician shortage was 12% of total approved staffing. Given concerns in hospital medicine about provider burnout, the number of hospital medicine openings is no doubt a concern to HMG leaders and hospitalists. And necessity being the mother of invention, HMG leadership must be thinking differently than in the past about open positions and the skill mix needed to fill them. I believe this is leading to NPs and PAs being considered more often for a role that would have been open only to a physician in the past.
Just as open positions are a concern, so is turnover. One striking finding in the SoHM is the very high rate of turnover among NPs and PAs – a whopping 19.1% per year. For physicians, the same rate was 7.4% and has been declining every survey for many years. While NPs and PAs may be intended to stabilize the workforce, because of how this is being done in some groups, NPs and PAs may instead be a destabilizing factor. Rapid growth can lead to haphazard onboarding and less than clearly defined roles. NPs and PAs may often be placed into roles for which they are not yet prepared. In addition, the pay disparity between NPs and PAs and physicians has increased. As a new field, and with many HMGs still rapidly growing, increased thoughtfulness and maturity about how NPs and PAs are integrated into hospital medicine practices should lead to less turnover and better HMG stability in the future.
These observations could mark a future that includes higher pay for hospital medicine PAs and NPs (and potentially a slowdown in salary growth for physicians); HMGs taking steps to make the financial model more attractive by having NPs and PAs bill independently more often; and HMGs and their leaders engaging NPs and PAs by more clearly defining roles, shoring up onboarding and mentoring programs, and other measures that decrease turnover. This would help to make hospital medicine a career destination, rather than a stopping off point for NPs and PAs, much as it has become for internists over the past 20 years.
Dr. Frederickson is medical director, hospital medicine and palliative care, at CHI Health, Omaha, Neb., and assistant professor at Creighton University, Omaha.
If you were a physician hospitalist in a group serving adults in 2017 you probably worked with nurse practitioners (NPs) and/or physician assistants (PAs). Seventy-seven percent of hospital medicine groups (HMGs) employed NPs and PAs that year.
In addition, the larger the group, the more likely the group was to have NPs and PAs as part of their practice model – 89% of hospital medicine groups with more than 30 physician had NPs and/or PAs as partners. In addition, the mean number of physicians for adult hospital medicine groups was 17.9. The same practices employed an average of 3.5 NPs, and 2.6 PAs.
Based on these numbers, there are just under three physicians per NP and PA in the typical HMG serving adults. This is all according to data from the 2018 State of Hospital Medicine (SoHM) report that was published in 2019 by the Society of Hospital Medicine.
These observations lead to a number of questions. One thing that is not clear from the SoHM is why NPs and PAs are becoming a larger part of the hospital medicine workforce, but there are some insights and conjecture that can be drawn from the data. The first is economics. Over 6 years, the median incomes of NPs and PAs have risen a relatively modest 10%; over the same period physician hospitalists have seen a whopping 23.6% median pay increase.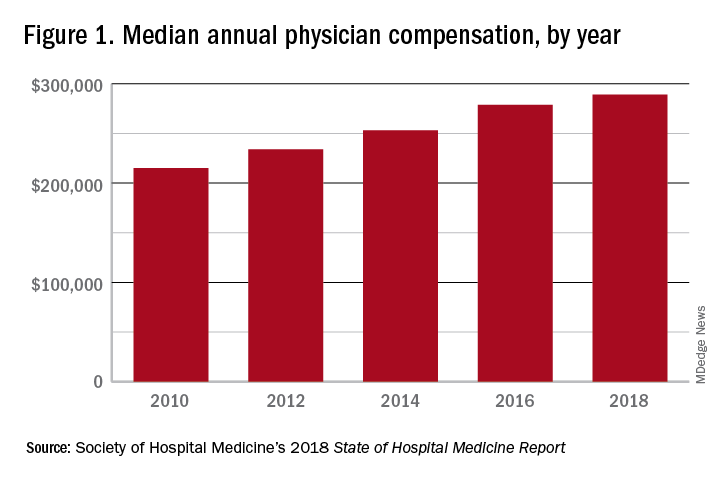
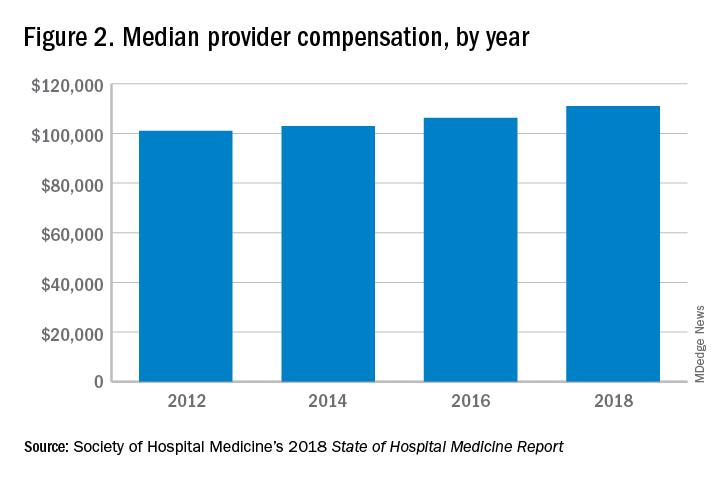
One argument against economics as a driving force behind greater use of NPs and PAs in the hospital medicine workforce is the billing patterns of HMGs that use NPs and PAs. Ten percent of HMGs do not have their NPs and PAs bill at all. The distribution of HMGs that predominantly bill NP and PA services as shared visits, versus having NPs and PAs bill independently, has also not changed much over the years, with 22% of HMGs having NPs and PAs bill independently as a predominant model. This would seem to suggest that some HMGs may not have learned how to deploy NPs and PAs effectively.
While inefficiency can be due to hospital bylaws, the culture of the hospital medicine group, or the skill set of the NPs and PAs working in HMGs – it would seem that if the driving force for the increase in the utilization of NPs and PAs in HMGs was financial, then that would also result in more of these providers billing independently, or alternatively, an increase in hospitalist physician productivity, which the data do not show. However, multistate HMGs may have this figured out better than some of the rest of us – 78% of these HMGs have NPs and PAs billing independently! All other categories of HMGs together are around 13%, with the next highest being hospital or health system integrated delivery systems, where NPs/PAs bill independently about 15% of the time.
In the last 2 years of the survey, there have been marked increases in the number of NPs and PAs at HMGs performing “nontraditional” services. For example, outpatient work has increased from 11% to 17%, and work in the postacute space has increased from 13% to 25%. Work in behavioral health and alcohol and drug rehab facilities has also increased, from 17% to 26%. As HMGs seek to rationalize their workforce while expanding, it is possible that decision makers have felt that it was either more economical to place NPs and PAs in positions where they are seeing these patients, or it was more aligned with the NP/PA skill set, or both. In any event, as the scope of hospital medicine broadens, the use of PAs and NPs has also increased – which is probably not coincidental.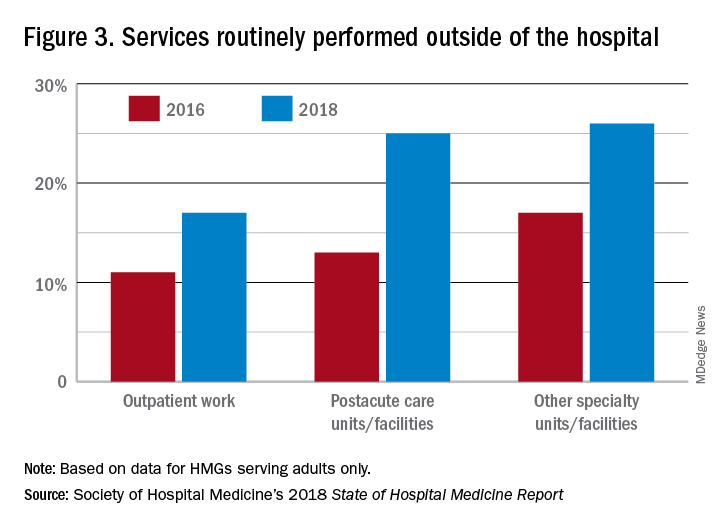
The average hospital medicine group continues to have staff openings. Workforce shortages may be leading to what in the past may have been considered physician openings being filled by NPs and PAs. Only 33% of HMGs reported having all their physician openings filled. Median physician shortage was 12% of total approved staffing. Given concerns in hospital medicine about provider burnout, the number of hospital medicine openings is no doubt a concern to HMG leaders and hospitalists. And necessity being the mother of invention, HMG leadership must be thinking differently than in the past about open positions and the skill mix needed to fill them. I believe this is leading to NPs and PAs being considered more often for a role that would have been open only to a physician in the past.
Just as open positions are a concern, so is turnover. One striking finding in the SoHM is the very high rate of turnover among NPs and PAs – a whopping 19.1% per year. For physicians, the same rate was 7.4% and has been declining every survey for many years. While NPs and PAs may be intended to stabilize the workforce, because of how this is being done in some groups, NPs and PAs may instead be a destabilizing factor. Rapid growth can lead to haphazard onboarding and less than clearly defined roles. NPs and PAs may often be placed into roles for which they are not yet prepared. In addition, the pay disparity between NPs and PAs and physicians has increased. As a new field, and with many HMGs still rapidly growing, increased thoughtfulness and maturity about how NPs and PAs are integrated into hospital medicine practices should lead to less turnover and better HMG stability in the future.
These observations could mark a future that includes higher pay for hospital medicine PAs and NPs (and potentially a slowdown in salary growth for physicians); HMGs taking steps to make the financial model more attractive by having NPs and PAs bill independently more often; and HMGs and their leaders engaging NPs and PAs by more clearly defining roles, shoring up onboarding and mentoring programs, and other measures that decrease turnover. This would help to make hospital medicine a career destination, rather than a stopping off point for NPs and PAs, much as it has become for internists over the past 20 years.
Dr. Frederickson is medical director, hospital medicine and palliative care, at CHI Health, Omaha, Neb., and assistant professor at Creighton University, Omaha.
Gender bias and pediatric hospital medicine
Where do we go from here?
Autumn is a busy time for pediatric hospitalists, with this autumn being particularly eventful as the first American Board of Pediatrics (ABP) certifying exam for Pediatric Hospital Medicine (PHM) will be offered on Nov. 12, 2019.
More than 1,600 med/peds and pediatric hospitalists applied to be eligible for the 2019 exam, 71% of whom were women. At least 3.9% of those applicants were denied eligibility for the 2019 exam.1 These denials resulted in discussions on the American Academy of Pediatrics Section on Hospital Medicine (AAP SOHM) email listserv related to unintentional gender bias.
PHM was first recognized as a subspecialty by the American Board of Medical Specialties in December 2015.2 Since that time, the ABP’s PHM sub-board developed eligibility criteria for practicing pediatric and med/peds hospitalists to apply for the exam. The sub-board identified three paths: a training pathway for applicants who had completed a 2-year PHM fellowship, a practice pathway for those satisfying ABP criteria for clinical activity in PHM, and a combined pathway for applicants who had completed PHM fellowships lasting less than 2 years.
Based on these pathways, 1,627 applicants applied for eligibility for the first PHM board certification exam.1 However, many concerns arose with the practice pathway eligibility criteria.
The PHM practice pathway initially included the following eligibility criteria:
• General pediatrics board certification.
• PHM practice “look back” period ends on or before June 30 of the exam year and starts 4 years earlier.
• More than 0.5 FTE professional PHM-related activities (patient-care, research, administration), defined as more than 900 hours/year every year for the preceding 4 years.
• More than 0.25 FTE direct patient care of hospitalized children, defined as more than 450 hours/year every year for the preceding 4 years.
• Practice covers the full range of hospitalized children with regard to age, diagnoses, and complexity.
• Practice interruptions cannot exceed 3 months in the preceding 4 years, or 6 months in the preceding 5 years.
• Practice experience and hours were acquired in the United States and Canada.1,3
The start date and practice interruptions criteria in the practice pathway posed hurdles for many female applicants. Many women voiced concerns about feeling disadvantaged when applying for the PHM certifying exam and some of these women shared their concerns on the AAP SOHM email listserv. In response to these concerns, the PHM community called for increased transparency from the ABP related to denials, specifically related to unintentional gender bias against women applying for the exam.
David Skey, MD, and Jamee Walters, MD, pediatric hospitalists at Arnold Palmer Medical Center in Orlando, heard these concerns and decided to draft a petition with the help of legal counsel. The petition “demand[ed] immediate action,” and “request[ed] a formal response from the ABP regarding the practice pathway criteria.” The petition also stated that there was insufficient data to determine if the practice pathway “disadvantages women.” The petition asked the ABP to “facilitate a timely analysis to determine if gender bias” was present, or to perform an internal analysis and “release the findings publicly.”4
The petition was shared with the PHM community via the AAP SOHM listserv on July 29, 2019. Dr. Walters stated she was pleased by the response she and Dr. Skey received from the PHM community, on and off the AAP SOHM listserv. The petition was submitted to the ABP on Aug. 6, 2019, with 1,479 signatures.
On Aug. 29, 2019, the ABP’s response was shared on the AAP SOHM email listserv1 and was later published in the Journal of Hospital Medicine as a Special Announcement.5 In its response, the ABP stated that the gender bias allegation was “not supported by the facts” as there was “no significant difference between the percentage of women and men who were denied” eligibility.”5 In addressing the gender bias allegations and clarifying the practice pathway eligibility, the ABP removed the practice interruption criteria and modified the practice pathway criteria as follows:
• General pediatrics board certification.
• PHM practice started on or before July 2015 (for board eligibility in 2019).
• Professional PHM-related activities (patient-care, research, administration), defined as more than 900-1000 hours/year every year for the preceding 4 years.
• Direct patient care of hospitalized children, defined as more than 450-500 hours/year every year for the preceding 4 years.
• Practice covers the full range of hospitalized children with regard to age, diagnoses, and complexity.
• Practice experience and hours were acquired in the United States and Canada.1
Following the release of the ABP’s response, many members of the PHM community remain concerned about the ABP’s revised criteria. Arti Desai, MD, pediatric hospitalist at Seattle Children’s and senior author on a “Perspectives in Hospital Medicine” in the Journal of Hospital Medicine,6 was appreciative that the ABP chose to remove the practice interruptions criterion. However, she and her colleagues remain concerned about lingering gender bias in the ABP’s practice pathway eligibility criteria surrounding the “start date” criterion. The authors state that this criterion differentially affects women, as women may take time off during or after residency for maternity or family leave. Dr. Desai states that this criterion alone can affect a woman’s chance for being eligible for the practice pathway.
Other members of the PHM community also expressed concerns about the ABP’s response to the PHM petition. Beth C. Natt, MD, pediatric hospitalist and director of pediatric hospital medicine regional programs at Connecticut Children’s in Hartford, felt that the population may have been self-selected, as the ABP’s data were limited to individuals who applied for exam eligibility. She was concerned that the data excluded pediatric hospitalists who chose not to apply because of uncertainty about meeting eligibility criteria. Klint Schwenk, MD, pediatric hospitalist at Norton Children’s Hospital in Louisville, Ky., stated that he wished the ABP had addressed the number of pediatric hospitalists who elected not to apply based on fear of ineligibility before concluding that there was no bias. He likened the ABP’s response to that of study authors omitting selection bias when discussing the limitations of their study.
Courtney Edgar-Zarate, MD, med/peds hospitalist and associate program director of the internal medicine/pediatrics residency at the University of Arkansas, expressed concerns that the ABP’s stringent clinical patient care hours criterion may unintentionally result in ineligibility for many mid-career or senior med/peds hospitalists. Dr. Edgar-Zarate also voiced concerns that graduating med/peds residents were electing not to pursue careers in hospital medicine because they would be required to complete a PHM fellowship to become a pediatric hospitalist, when a similar fellowship is not required to practice adult hospital medicine.
The Society of Hospital Medicine shared its position in regard to the ABP’s response in a Special Announcement in the Journal of Hospital Medicine.7 In it, SHM’s pediatric leaders recognized physicians for the excellent care they provide to hospitalized children. They stated that SHM would continue to support all hospitalists, independent of board eligibility status, and would continue to offer these hospitalists the merit-based Fellow designation. SHM’s pediatric leaders also proposed future directions for the ABP, including a Focused Practice Pathway in Hospital Medicine (FPHM), such as what the American Board of Internal Medicine and the American Board of Family Medicine have adopted for board recertification in internal medicine and family medicine. This maintenance of certification program that allows physicians primarily practicing in inpatient settings to focus their continuing education on inpatient practice, and is not a subspecialty.7
Dr. Edgar-Zarate fully supports the future directions for pediatric hospitalists outlined in SHM’s Special Announcement. She hopes that the ABP will support the FPHM. She feels the FPHM will encourage more med/peds physicians to practice med/peds hospital medicine. L. Nell Hodo, MD, a family medicine–trained pediatric hospitalist at Icahn School of Medicine at Mount Sinai in New York, joins Dr. Edgar-Zarate in supporting an FPHM for PHM, and feels that it will open the door for hospitalists who are ineligible for the practice pathway to be able to focus their recertification on the inpatient setting.
Dr. Hodo and Dr. Desai hope that rather than excluding those who are not PHM board eligible/certified, institutions and professional organizations will consider all qualifications when hiring, mentoring, and promoting physicians who care for hospitalized children. Dr. Natt, Dr. Schwenk, Dr. Edgar-Zarate, and Dr. Hodo appreciate that SHM is leading the way, and will continue to allow all hospitalists who care for children to receive Fellow designation.
Dr. Kumar is clinical assistant professor of pediatrics at the Cleveland Clinic Lerner College of Medicine at Case Western Reserve University and a pediatric hospitalist at Cleveland Clinic Children’s. She is the pediatric editor of The Hospitalist.
References
1. The American Board of Pediatrics. The American Board of Pediatrics response to the Pediatric Hospital Medicine petition. https://www.abp.org/sites/abp/files/phm-petition-response.pdf. Published 2019.
2. Barrett DJ, McGuinness GA, Cunha CA, et al. Pediatric hospital medicine: A proposed new subspecialty. Pediatrics. 2017;139(3). doi: 10.1542/peds.2016-1823.
3. The American Board of Pediatrics. Pediatric Hospital Medicine Certification. https://www.abp.org/content/pediatric-hospital-medicine-certification. Published 2019.
4. Skey D. Pediatric Hospitalists, It’s time to take a stand on the PHM Boards Application Process! Five Dog Development, LLC.
5. Nichols DG, Woods SZ. The American Board of Pediatrics response to the Pediatric Hospital Medicine petition. J Hosp Med. 2019 Oct;14(10):586-8. doi: 10.12788/jhm.3322.
6. Gold JM et al. Collective action and effective dialogue to address gender bias in medicine. J Hosp Med. 2019 Oct;14(10):630-2. doi: 10.12788/jhm.3331.
7. Chang WW et al. Society of Hospital Medicine position on the American Board of Pediatrics response to the Pediatric Hospital Medicine petition. J Hosp Med. 2019 Oct;14(10):589-90. doi: 10.12788/jhm.3326.
Where do we go from here?
Where do we go from here?
Autumn is a busy time for pediatric hospitalists, with this autumn being particularly eventful as the first American Board of Pediatrics (ABP) certifying exam for Pediatric Hospital Medicine (PHM) will be offered on Nov. 12, 2019.
More than 1,600 med/peds and pediatric hospitalists applied to be eligible for the 2019 exam, 71% of whom were women. At least 3.9% of those applicants were denied eligibility for the 2019 exam.1 These denials resulted in discussions on the American Academy of Pediatrics Section on Hospital Medicine (AAP SOHM) email listserv related to unintentional gender bias.
PHM was first recognized as a subspecialty by the American Board of Medical Specialties in December 2015.2 Since that time, the ABP’s PHM sub-board developed eligibility criteria for practicing pediatric and med/peds hospitalists to apply for the exam. The sub-board identified three paths: a training pathway for applicants who had completed a 2-year PHM fellowship, a practice pathway for those satisfying ABP criteria for clinical activity in PHM, and a combined pathway for applicants who had completed PHM fellowships lasting less than 2 years.
Based on these pathways, 1,627 applicants applied for eligibility for the first PHM board certification exam.1 However, many concerns arose with the practice pathway eligibility criteria.
The PHM practice pathway initially included the following eligibility criteria:
• General pediatrics board certification.
• PHM practice “look back” period ends on or before June 30 of the exam year and starts 4 years earlier.
• More than 0.5 FTE professional PHM-related activities (patient-care, research, administration), defined as more than 900 hours/year every year for the preceding 4 years.
• More than 0.25 FTE direct patient care of hospitalized children, defined as more than 450 hours/year every year for the preceding 4 years.
• Practice covers the full range of hospitalized children with regard to age, diagnoses, and complexity.
• Practice interruptions cannot exceed 3 months in the preceding 4 years, or 6 months in the preceding 5 years.
• Practice experience and hours were acquired in the United States and Canada.1,3
The start date and practice interruptions criteria in the practice pathway posed hurdles for many female applicants. Many women voiced concerns about feeling disadvantaged when applying for the PHM certifying exam and some of these women shared their concerns on the AAP SOHM email listserv. In response to these concerns, the PHM community called for increased transparency from the ABP related to denials, specifically related to unintentional gender bias against women applying for the exam.
David Skey, MD, and Jamee Walters, MD, pediatric hospitalists at Arnold Palmer Medical Center in Orlando, heard these concerns and decided to draft a petition with the help of legal counsel. The petition “demand[ed] immediate action,” and “request[ed] a formal response from the ABP regarding the practice pathway criteria.” The petition also stated that there was insufficient data to determine if the practice pathway “disadvantages women.” The petition asked the ABP to “facilitate a timely analysis to determine if gender bias” was present, or to perform an internal analysis and “release the findings publicly.”4
The petition was shared with the PHM community via the AAP SOHM listserv on July 29, 2019. Dr. Walters stated she was pleased by the response she and Dr. Skey received from the PHM community, on and off the AAP SOHM listserv. The petition was submitted to the ABP on Aug. 6, 2019, with 1,479 signatures.
On Aug. 29, 2019, the ABP’s response was shared on the AAP SOHM email listserv1 and was later published in the Journal of Hospital Medicine as a Special Announcement.5 In its response, the ABP stated that the gender bias allegation was “not supported by the facts” as there was “no significant difference between the percentage of women and men who were denied” eligibility.”5 In addressing the gender bias allegations and clarifying the practice pathway eligibility, the ABP removed the practice interruption criteria and modified the practice pathway criteria as follows:
• General pediatrics board certification.
• PHM practice started on or before July 2015 (for board eligibility in 2019).
• Professional PHM-related activities (patient-care, research, administration), defined as more than 900-1000 hours/year every year for the preceding 4 years.
• Direct patient care of hospitalized children, defined as more than 450-500 hours/year every year for the preceding 4 years.
• Practice covers the full range of hospitalized children with regard to age, diagnoses, and complexity.
• Practice experience and hours were acquired in the United States and Canada.1
Following the release of the ABP’s response, many members of the PHM community remain concerned about the ABP’s revised criteria. Arti Desai, MD, pediatric hospitalist at Seattle Children’s and senior author on a “Perspectives in Hospital Medicine” in the Journal of Hospital Medicine,6 was appreciative that the ABP chose to remove the practice interruptions criterion. However, she and her colleagues remain concerned about lingering gender bias in the ABP’s practice pathway eligibility criteria surrounding the “start date” criterion. The authors state that this criterion differentially affects women, as women may take time off during or after residency for maternity or family leave. Dr. Desai states that this criterion alone can affect a woman’s chance for being eligible for the practice pathway.
Other members of the PHM community also expressed concerns about the ABP’s response to the PHM petition. Beth C. Natt, MD, pediatric hospitalist and director of pediatric hospital medicine regional programs at Connecticut Children’s in Hartford, felt that the population may have been self-selected, as the ABP’s data were limited to individuals who applied for exam eligibility. She was concerned that the data excluded pediatric hospitalists who chose not to apply because of uncertainty about meeting eligibility criteria. Klint Schwenk, MD, pediatric hospitalist at Norton Children’s Hospital in Louisville, Ky., stated that he wished the ABP had addressed the number of pediatric hospitalists who elected not to apply based on fear of ineligibility before concluding that there was no bias. He likened the ABP’s response to that of study authors omitting selection bias when discussing the limitations of their study.
Courtney Edgar-Zarate, MD, med/peds hospitalist and associate program director of the internal medicine/pediatrics residency at the University of Arkansas, expressed concerns that the ABP’s stringent clinical patient care hours criterion may unintentionally result in ineligibility for many mid-career or senior med/peds hospitalists. Dr. Edgar-Zarate also voiced concerns that graduating med/peds residents were electing not to pursue careers in hospital medicine because they would be required to complete a PHM fellowship to become a pediatric hospitalist, when a similar fellowship is not required to practice adult hospital medicine.
The Society of Hospital Medicine shared its position in regard to the ABP’s response in a Special Announcement in the Journal of Hospital Medicine.7 In it, SHM’s pediatric leaders recognized physicians for the excellent care they provide to hospitalized children. They stated that SHM would continue to support all hospitalists, independent of board eligibility status, and would continue to offer these hospitalists the merit-based Fellow designation. SHM’s pediatric leaders also proposed future directions for the ABP, including a Focused Practice Pathway in Hospital Medicine (FPHM), such as what the American Board of Internal Medicine and the American Board of Family Medicine have adopted for board recertification in internal medicine and family medicine. This maintenance of certification program that allows physicians primarily practicing in inpatient settings to focus their continuing education on inpatient practice, and is not a subspecialty.7
Dr. Edgar-Zarate fully supports the future directions for pediatric hospitalists outlined in SHM’s Special Announcement. She hopes that the ABP will support the FPHM. She feels the FPHM will encourage more med/peds physicians to practice med/peds hospital medicine. L. Nell Hodo, MD, a family medicine–trained pediatric hospitalist at Icahn School of Medicine at Mount Sinai in New York, joins Dr. Edgar-Zarate in supporting an FPHM for PHM, and feels that it will open the door for hospitalists who are ineligible for the practice pathway to be able to focus their recertification on the inpatient setting.
Dr. Hodo and Dr. Desai hope that rather than excluding those who are not PHM board eligible/certified, institutions and professional organizations will consider all qualifications when hiring, mentoring, and promoting physicians who care for hospitalized children. Dr. Natt, Dr. Schwenk, Dr. Edgar-Zarate, and Dr. Hodo appreciate that SHM is leading the way, and will continue to allow all hospitalists who care for children to receive Fellow designation.
Dr. Kumar is clinical assistant professor of pediatrics at the Cleveland Clinic Lerner College of Medicine at Case Western Reserve University and a pediatric hospitalist at Cleveland Clinic Children’s. She is the pediatric editor of The Hospitalist.
References
1. The American Board of Pediatrics. The American Board of Pediatrics response to the Pediatric Hospital Medicine petition. https://www.abp.org/sites/abp/files/phm-petition-response.pdf. Published 2019.
2. Barrett DJ, McGuinness GA, Cunha CA, et al. Pediatric hospital medicine: A proposed new subspecialty. Pediatrics. 2017;139(3). doi: 10.1542/peds.2016-1823.
3. The American Board of Pediatrics. Pediatric Hospital Medicine Certification. https://www.abp.org/content/pediatric-hospital-medicine-certification. Published 2019.
4. Skey D. Pediatric Hospitalists, It’s time to take a stand on the PHM Boards Application Process! Five Dog Development, LLC.
5. Nichols DG, Woods SZ. The American Board of Pediatrics response to the Pediatric Hospital Medicine petition. J Hosp Med. 2019 Oct;14(10):586-8. doi: 10.12788/jhm.3322.
6. Gold JM et al. Collective action and effective dialogue to address gender bias in medicine. J Hosp Med. 2019 Oct;14(10):630-2. doi: 10.12788/jhm.3331.
7. Chang WW et al. Society of Hospital Medicine position on the American Board of Pediatrics response to the Pediatric Hospital Medicine petition. J Hosp Med. 2019 Oct;14(10):589-90. doi: 10.12788/jhm.3326.
Autumn is a busy time for pediatric hospitalists, with this autumn being particularly eventful as the first American Board of Pediatrics (ABP) certifying exam for Pediatric Hospital Medicine (PHM) will be offered on Nov. 12, 2019.
More than 1,600 med/peds and pediatric hospitalists applied to be eligible for the 2019 exam, 71% of whom were women. At least 3.9% of those applicants were denied eligibility for the 2019 exam.1 These denials resulted in discussions on the American Academy of Pediatrics Section on Hospital Medicine (AAP SOHM) email listserv related to unintentional gender bias.
PHM was first recognized as a subspecialty by the American Board of Medical Specialties in December 2015.2 Since that time, the ABP’s PHM sub-board developed eligibility criteria for practicing pediatric and med/peds hospitalists to apply for the exam. The sub-board identified three paths: a training pathway for applicants who had completed a 2-year PHM fellowship, a practice pathway for those satisfying ABP criteria for clinical activity in PHM, and a combined pathway for applicants who had completed PHM fellowships lasting less than 2 years.
Based on these pathways, 1,627 applicants applied for eligibility for the first PHM board certification exam.1 However, many concerns arose with the practice pathway eligibility criteria.
The PHM practice pathway initially included the following eligibility criteria:
• General pediatrics board certification.
• PHM practice “look back” period ends on or before June 30 of the exam year and starts 4 years earlier.
• More than 0.5 FTE professional PHM-related activities (patient-care, research, administration), defined as more than 900 hours/year every year for the preceding 4 years.
• More than 0.25 FTE direct patient care of hospitalized children, defined as more than 450 hours/year every year for the preceding 4 years.
• Practice covers the full range of hospitalized children with regard to age, diagnoses, and complexity.
• Practice interruptions cannot exceed 3 months in the preceding 4 years, or 6 months in the preceding 5 years.
• Practice experience and hours were acquired in the United States and Canada.1,3
The start date and practice interruptions criteria in the practice pathway posed hurdles for many female applicants. Many women voiced concerns about feeling disadvantaged when applying for the PHM certifying exam and some of these women shared their concerns on the AAP SOHM email listserv. In response to these concerns, the PHM community called for increased transparency from the ABP related to denials, specifically related to unintentional gender bias against women applying for the exam.
David Skey, MD, and Jamee Walters, MD, pediatric hospitalists at Arnold Palmer Medical Center in Orlando, heard these concerns and decided to draft a petition with the help of legal counsel. The petition “demand[ed] immediate action,” and “request[ed] a formal response from the ABP regarding the practice pathway criteria.” The petition also stated that there was insufficient data to determine if the practice pathway “disadvantages women.” The petition asked the ABP to “facilitate a timely analysis to determine if gender bias” was present, or to perform an internal analysis and “release the findings publicly.”4
The petition was shared with the PHM community via the AAP SOHM listserv on July 29, 2019. Dr. Walters stated she was pleased by the response she and Dr. Skey received from the PHM community, on and off the AAP SOHM listserv. The petition was submitted to the ABP on Aug. 6, 2019, with 1,479 signatures.
On Aug. 29, 2019, the ABP’s response was shared on the AAP SOHM email listserv1 and was later published in the Journal of Hospital Medicine as a Special Announcement.5 In its response, the ABP stated that the gender bias allegation was “not supported by the facts” as there was “no significant difference between the percentage of women and men who were denied” eligibility.”5 In addressing the gender bias allegations and clarifying the practice pathway eligibility, the ABP removed the practice interruption criteria and modified the practice pathway criteria as follows:
• General pediatrics board certification.
• PHM practice started on or before July 2015 (for board eligibility in 2019).
• Professional PHM-related activities (patient-care, research, administration), defined as more than 900-1000 hours/year every year for the preceding 4 years.
• Direct patient care of hospitalized children, defined as more than 450-500 hours/year every year for the preceding 4 years.
• Practice covers the full range of hospitalized children with regard to age, diagnoses, and complexity.
• Practice experience and hours were acquired in the United States and Canada.1
Following the release of the ABP’s response, many members of the PHM community remain concerned about the ABP’s revised criteria. Arti Desai, MD, pediatric hospitalist at Seattle Children’s and senior author on a “Perspectives in Hospital Medicine” in the Journal of Hospital Medicine,6 was appreciative that the ABP chose to remove the practice interruptions criterion. However, she and her colleagues remain concerned about lingering gender bias in the ABP’s practice pathway eligibility criteria surrounding the “start date” criterion. The authors state that this criterion differentially affects women, as women may take time off during or after residency for maternity or family leave. Dr. Desai states that this criterion alone can affect a woman’s chance for being eligible for the practice pathway.
Other members of the PHM community also expressed concerns about the ABP’s response to the PHM petition. Beth C. Natt, MD, pediatric hospitalist and director of pediatric hospital medicine regional programs at Connecticut Children’s in Hartford, felt that the population may have been self-selected, as the ABP’s data were limited to individuals who applied for exam eligibility. She was concerned that the data excluded pediatric hospitalists who chose not to apply because of uncertainty about meeting eligibility criteria. Klint Schwenk, MD, pediatric hospitalist at Norton Children’s Hospital in Louisville, Ky., stated that he wished the ABP had addressed the number of pediatric hospitalists who elected not to apply based on fear of ineligibility before concluding that there was no bias. He likened the ABP’s response to that of study authors omitting selection bias when discussing the limitations of their study.
Courtney Edgar-Zarate, MD, med/peds hospitalist and associate program director of the internal medicine/pediatrics residency at the University of Arkansas, expressed concerns that the ABP’s stringent clinical patient care hours criterion may unintentionally result in ineligibility for many mid-career or senior med/peds hospitalists. Dr. Edgar-Zarate also voiced concerns that graduating med/peds residents were electing not to pursue careers in hospital medicine because they would be required to complete a PHM fellowship to become a pediatric hospitalist, when a similar fellowship is not required to practice adult hospital medicine.
The Society of Hospital Medicine shared its position in regard to the ABP’s response in a Special Announcement in the Journal of Hospital Medicine.7 In it, SHM’s pediatric leaders recognized physicians for the excellent care they provide to hospitalized children. They stated that SHM would continue to support all hospitalists, independent of board eligibility status, and would continue to offer these hospitalists the merit-based Fellow designation. SHM’s pediatric leaders also proposed future directions for the ABP, including a Focused Practice Pathway in Hospital Medicine (FPHM), such as what the American Board of Internal Medicine and the American Board of Family Medicine have adopted for board recertification in internal medicine and family medicine. This maintenance of certification program that allows physicians primarily practicing in inpatient settings to focus their continuing education on inpatient practice, and is not a subspecialty.7
Dr. Edgar-Zarate fully supports the future directions for pediatric hospitalists outlined in SHM’s Special Announcement. She hopes that the ABP will support the FPHM. She feels the FPHM will encourage more med/peds physicians to practice med/peds hospital medicine. L. Nell Hodo, MD, a family medicine–trained pediatric hospitalist at Icahn School of Medicine at Mount Sinai in New York, joins Dr. Edgar-Zarate in supporting an FPHM for PHM, and feels that it will open the door for hospitalists who are ineligible for the practice pathway to be able to focus their recertification on the inpatient setting.
Dr. Hodo and Dr. Desai hope that rather than excluding those who are not PHM board eligible/certified, institutions and professional organizations will consider all qualifications when hiring, mentoring, and promoting physicians who care for hospitalized children. Dr. Natt, Dr. Schwenk, Dr. Edgar-Zarate, and Dr. Hodo appreciate that SHM is leading the way, and will continue to allow all hospitalists who care for children to receive Fellow designation.
Dr. Kumar is clinical assistant professor of pediatrics at the Cleveland Clinic Lerner College of Medicine at Case Western Reserve University and a pediatric hospitalist at Cleveland Clinic Children’s. She is the pediatric editor of The Hospitalist.
References
1. The American Board of Pediatrics. The American Board of Pediatrics response to the Pediatric Hospital Medicine petition. https://www.abp.org/sites/abp/files/phm-petition-response.pdf. Published 2019.
2. Barrett DJ, McGuinness GA, Cunha CA, et al. Pediatric hospital medicine: A proposed new subspecialty. Pediatrics. 2017;139(3). doi: 10.1542/peds.2016-1823.
3. The American Board of Pediatrics. Pediatric Hospital Medicine Certification. https://www.abp.org/content/pediatric-hospital-medicine-certification. Published 2019.
4. Skey D. Pediatric Hospitalists, It’s time to take a stand on the PHM Boards Application Process! Five Dog Development, LLC.
5. Nichols DG, Woods SZ. The American Board of Pediatrics response to the Pediatric Hospital Medicine petition. J Hosp Med. 2019 Oct;14(10):586-8. doi: 10.12788/jhm.3322.
6. Gold JM et al. Collective action and effective dialogue to address gender bias in medicine. J Hosp Med. 2019 Oct;14(10):630-2. doi: 10.12788/jhm.3331.
7. Chang WW et al. Society of Hospital Medicine position on the American Board of Pediatrics response to the Pediatric Hospital Medicine petition. J Hosp Med. 2019 Oct;14(10):589-90. doi: 10.12788/jhm.3326.
‘Bridging leaders’ link quality, medical education
A new community emerges
In June 2019, a 5-hour preconference seminar at the annual Integrating Quality Conference of the Association of American Medical Colleges (AAMC) in Minneapolis highlighted the emergence of a new concept, and a new community, within the larger field of hospital medicine.
“Bridging leaders” are clinician-educators with a foot in two worlds: leading quality and safety initiatives within their teaching hospitals – with the hospitalist’s customary participation in a broad spectrum of quality improvement (QI) efforts in the hospital – while helping to train future and current physicians. “Bridging” also extends to the third piece of the quality puzzle, the hospital and/or health system’s senior administrators.
“About 8 years ago, another hospitalist and I found ourselves in this role, bridging graduate medical education with hospital quality and safety,” said Jennifer S. Myers, MD, FHM, director of quality and safety education in the department of medicine at the University of Pennsylvania, Philadelphia. “The role has since begun to proliferate, in teaching settings large and small, and about 30-50 of us with somewhat similar job responsibilities have been trying to create a community.”
Following the lead of the American College of Graduate Medical Education1 and its standards for clinical learning environments that include integration of patient safety and quality improvement, these have become graduate medical education (GME) priorities. Students need to learn the theory and practice of safety and quality improvement on the job as part of their professional development. Residency program directors and other trainers thus need to find opportunities for them to practice these techniques in the clinical practice environment.
At the same time, mobilizing those eager medical learners to plan and conduct quality improvement projects can enhance a hospital’s ability to advance its mission in the new health care environment of accountable care and population health.
New concept arises
Is bridging leaders a real thing? The short answer is yes, said Thomas Ciesielski, MD, GME medical director for patient safety, quality education, and clinical learning environment review program development at Washington University in St. Louis. “This is a new trend, but it’s still in the process of defining itself. Every bridging leader has their own identity based on their institution. Some play a bridging role for the entire institution; others play similar roles but only within a specific department or division. There’s a lot of learning going on in our community,” he said.
The first Bridging Leaders track was held last year at AAMC’s 2018 Integrating Quality Conference, an event which has been held annually for the past decade. The concept was also highlighted in a 2017 article in the Journal of Graduate Medical Education2 by bridging leaders, including many of the faculty at the subsequent AAMC sessions, highlighting their roles and programs at six academic medical centers.
One of those coauthors, hospitalist Vineet Arora, MD, MAPP, MHM, was recently appointed to a new position at University of Chicago Medicine: associate chief medical officer for the clinical learning environment – which pulls together many of the threads of the bridging leaders movement into a single job title. Dr. Arora said her job builds on her prior work in GME and improves the clinical learning environment for residents and fellows by integrating them into the health system’s institutional quality, safety, and value missions. It also expands on that work to include faculty and allied health professionals. “I just happen to come from the health system side,” she said.
Natural bridges: From clinical to educational
As with the early days of the hospitalist movement, bridging leaders are trying to build a community of peers with common interests.
“We’re just at the beginning,” Dr. Arora said. “Hospitalists have been the natural torch bearers for quality and safety in their hospitals, and also play roles in the education of residents and medical students, working alongside residency program directors. They are well-versed in quality and in education. So, they are the natural bridges between education and clinical care,” she said. “We also know this is a young group that comes to our meetings. One-third of them have been doing this for only the past 2 years or less – so they are early in their career paths.”
Front-line clinical providers, such as residents, often have good ideas, and bridging leaders can bring these ideas to the health system’s leaders, Dr. Arora said. “Bridging at the leadership level also involves thinking about the larger priorities of the system.” There are trust issues that these leaders can help to bridge, as well as internal communication barriers. “We also realize that health systems have to move quickly in response to a rapidly changing environment,” she noted.
“You don’t want a hundred quality improvement projects being done by students that are unaligned with the organization’s priorities. That leads to waste, and highlights the need for greater alignment,” Dr. Arora added. “Think about using front-line staff as agents of change, of engaging with learners as a win/win – as a way to actually solve the problems we are facing.”
A bridging leader occupies a role in which they can influence and affect these two parts of the mission of health care, somebody whose leadership responsibilities sit at the intersection of these two areas, said Darlene Tad-y, MD, director of GME quality and safety programs at the University of Colorado, Aurora. “Once, these people were mostly in academic medical centers, but that’s not so true anymore. A director of quality for a hospital medicine group is responsible for developing the group’s quality strategy, but at the same time responsible for teaching members of the group – not only doing QI but teaching others how to do it,” she said.
“Hospitalists make terrific bridging leaders. We really are in that sweet spot, and we can and should step into these leadership roles,” Dr. Tad-y said. “Because of our role in the hospital, we know the ins and outs of how processes work or don’t work. We have an insider’s view of the system’s dysfunction, which puts us in a great place to lead these efforts.”
The bridging leaders movement has been a grass-roots development, Dr. Tad-y explained. “It’s not like people started with the job title. But because all of this work was needed, a few people started doing it – and they began seeking each other out. Then they found that there were more than a few of us. We just hadn’t known what it was called.”
What is being bridged?
There has long been a relationship between individuals who lead in the clinical environment and those who lead in education, such as the program directors of residency programs, said Janis Orlowski, MD, chief health care officer for AAMC, which represents 154 MD-granting medical schools and their associated teaching hospitals.
“Our association’s three missions of research, education, and patient care really come together around the bridging leaders concept. So, this movement is well aligned. And as bridging leaders started to develop as a group, they found a home in AAMC and at our Integrating Quality Conference,” she said.
“Where we see this integration is in the teaching of residents and medical students in the clinical environment,” Dr. Orlowski said. “It’s not just their knowledge of disease or treatments or procedural skills that needs to be taught. They also need to understand the safe and effective clinical environment, and the role of learners in patient safety, quality improvement, and efficient and cost-effective hospital care. They need to understand value.” A new field of health systems science is emerging and quality improvement is evolving to incorporate population health. But traditional medical faculty may not be that comfortable teaching it.
Any physician who sees that they have a role in the clinical, administrative, and educational worlds can do the bridging, Dr. Orlowski said. “It could be any environment in which care is provided and learning takes place. I mentioned QI and patient safety, but among the other essential skills for the doctor of tomorrow are teamwork, inter-professional training in how to work with, for example, the pharmacist and dietitian, and understanding the value they bring.”
Whenever quality improvement projects are undertaken as part of post-graduate medical education, they should be aligned with the institution’s quality improvement plan and with the priorities of the health system, said Rob Dressler, MD, MBA, quality and safety officer at Christiana Health Care System in Newark, Del., and president of the Alliance of Independent Academic Medical Centers (AIAMC), which represents 80 hospital and health systems active in the emerging movement for bridging leaders.
“GME needs to keep the C-suite aware of its front-line efforts to improve quality and safety, so the institution’s return on investment can be recognized,” he said. “The AIAMC has consistently advocated for the building of bridges between GME leaders and their C-suites at our member hospitals. If you are doing process improvement, you need to be aligned with the organization and its priorities, or you’ll be less successful.”
AIAMC convenes the National Initiative – a multi-institutional collaborative in which residents lead multi-disciplinary teams in quality improvement projects. A total of 64 hospitals and health systems have participated since the program started in 2007. “We need to train our clinicians to solve the problems of tomorrow,” Dr. Dressler said.
Bridging leaders in action
The leaders contacted for this article offered some examples of bridging in action. Dr. Arora has used “crowd sourcing” – a technique employed extensively in her work with Costs of Care, a global nonprofit trying to drive better health care at lower cost – to implement a local program for front-line clinicians to generate ideas on how to improve value and reduce unnecessary treatment.
“We created our local ‘Choosing Wisely’ challenge for residents and staff at the University of Chicago – with the understanding that the winner would get analytic and time support to pursue their project,” she said. A resident winner was a finalist in the RIV (Research, Innovations and Clinical Vignettes) competition at a recent SHM Annual Conference.
At the University of Colorado, there is an associate program director who is responsible for the quality improvement curriculum for residents, Dr. Tad-y said. Because teaching QI means doing QI, the associate program director had to start implementing QI in the hospital, learning how to choose appropriate QI projects for the residents. That meant looking at quality priorities for the hospital – including VTE prophylaxis, fall prevention, and rates of central line–associated bloodstream infections and catheter-associated urinary tract infections. “A critical priority was to align the learners’ QI projects with what the hospital is already working on,” she explained.
“In our practice, all fellows need education and training in patient safety, how to recognize medical errors and close calls, and how to use our errors reporting system,” Dr. Myers said. “They also need to participate in errors analysis discussions. But we have struggled to get residents to attend those meetings. There’s not enough time in their schedules, and here at Penn, we have 1,500 residents and fellows, and maybe only 20 of these formal medical errors conferences per year,” she said.
Dr. Myers worked with the hospital’s patient safety officer and head of GME to design a simulated approach to fill the gap, a simulation of the root cause analysis process – how it works, the various roles played by different individuals, and what happens after it is done. “In my role, I trained one faculty member in each large residency program in how to identify a case and how to use the simulation,” she said. “They can now teach their own learners and make it more relevant to their specialty.”
Penn also has a blueprint for quality – a road map for how the organization socializes health care quality, safety, and value, Dr. Myers said. “Every 3 or 4 years our CEO looks at the road map and tries to get feedback on its direction from payers and insurers, quality leaders, academic department heads – and residents. I was in a good position to organize a session for a representative group of residents to get together and talk about where they see the quality and safety gaps in their everyday work.”
The role of the bridging leader is a viable career path or target for many hospitalists, Dr. Arora said. “But even if it’s not a career path for you, knowing that hospitalists are at the forefront of the bridging leaders movement could help you energize your health system. If you are seeing gaps in quality and safety, this is an issue you can bring before the system.”
These days doctors are wearing a lot of hats and filling roles that weren’t seen as much before, said Dr. Orlowski. “Bridging leaders are not an exclusive group but open to anyone who finds their passion in teaching quality and safety. Maybe you’re doing quality and safety, but not education, but you recognize its importance, or vice versa. First of all, look to see what this bridging leaders thing really is, and how it might apply to you. You might say: ‘That accurately describes what I’m doing now. I have the interest; I want to learn more.’”
References
1. Accreditation Council for Graduate Medical Education. CLER pathways to excellence.
2. Myers JS et al. Bridging leadership roles in quality and patient safety: Experience of 6 U.S. Academic Medical Centers. J Grad Med Educ. 2017 Feb;9(1): 9-13.
A new community emerges
A new community emerges
In June 2019, a 5-hour preconference seminar at the annual Integrating Quality Conference of the Association of American Medical Colleges (AAMC) in Minneapolis highlighted the emergence of a new concept, and a new community, within the larger field of hospital medicine.
“Bridging leaders” are clinician-educators with a foot in two worlds: leading quality and safety initiatives within their teaching hospitals – with the hospitalist’s customary participation in a broad spectrum of quality improvement (QI) efforts in the hospital – while helping to train future and current physicians. “Bridging” also extends to the third piece of the quality puzzle, the hospital and/or health system’s senior administrators.
“About 8 years ago, another hospitalist and I found ourselves in this role, bridging graduate medical education with hospital quality and safety,” said Jennifer S. Myers, MD, FHM, director of quality and safety education in the department of medicine at the University of Pennsylvania, Philadelphia. “The role has since begun to proliferate, in teaching settings large and small, and about 30-50 of us with somewhat similar job responsibilities have been trying to create a community.”
Following the lead of the American College of Graduate Medical Education1 and its standards for clinical learning environments that include integration of patient safety and quality improvement, these have become graduate medical education (GME) priorities. Students need to learn the theory and practice of safety and quality improvement on the job as part of their professional development. Residency program directors and other trainers thus need to find opportunities for them to practice these techniques in the clinical practice environment.
At the same time, mobilizing those eager medical learners to plan and conduct quality improvement projects can enhance a hospital’s ability to advance its mission in the new health care environment of accountable care and population health.
New concept arises
Is bridging leaders a real thing? The short answer is yes, said Thomas Ciesielski, MD, GME medical director for patient safety, quality education, and clinical learning environment review program development at Washington University in St. Louis. “This is a new trend, but it’s still in the process of defining itself. Every bridging leader has their own identity based on their institution. Some play a bridging role for the entire institution; others play similar roles but only within a specific department or division. There’s a lot of learning going on in our community,” he said.
The first Bridging Leaders track was held last year at AAMC’s 2018 Integrating Quality Conference, an event which has been held annually for the past decade. The concept was also highlighted in a 2017 article in the Journal of Graduate Medical Education2 by bridging leaders, including many of the faculty at the subsequent AAMC sessions, highlighting their roles and programs at six academic medical centers.
One of those coauthors, hospitalist Vineet Arora, MD, MAPP, MHM, was recently appointed to a new position at University of Chicago Medicine: associate chief medical officer for the clinical learning environment – which pulls together many of the threads of the bridging leaders movement into a single job title. Dr. Arora said her job builds on her prior work in GME and improves the clinical learning environment for residents and fellows by integrating them into the health system’s institutional quality, safety, and value missions. It also expands on that work to include faculty and allied health professionals. “I just happen to come from the health system side,” she said.
Natural bridges: From clinical to educational
As with the early days of the hospitalist movement, bridging leaders are trying to build a community of peers with common interests.
“We’re just at the beginning,” Dr. Arora said. “Hospitalists have been the natural torch bearers for quality and safety in their hospitals, and also play roles in the education of residents and medical students, working alongside residency program directors. They are well-versed in quality and in education. So, they are the natural bridges between education and clinical care,” she said. “We also know this is a young group that comes to our meetings. One-third of them have been doing this for only the past 2 years or less – so they are early in their career paths.”
Front-line clinical providers, such as residents, often have good ideas, and bridging leaders can bring these ideas to the health system’s leaders, Dr. Arora said. “Bridging at the leadership level also involves thinking about the larger priorities of the system.” There are trust issues that these leaders can help to bridge, as well as internal communication barriers. “We also realize that health systems have to move quickly in response to a rapidly changing environment,” she noted.
“You don’t want a hundred quality improvement projects being done by students that are unaligned with the organization’s priorities. That leads to waste, and highlights the need for greater alignment,” Dr. Arora added. “Think about using front-line staff as agents of change, of engaging with learners as a win/win – as a way to actually solve the problems we are facing.”
A bridging leader occupies a role in which they can influence and affect these two parts of the mission of health care, somebody whose leadership responsibilities sit at the intersection of these two areas, said Darlene Tad-y, MD, director of GME quality and safety programs at the University of Colorado, Aurora. “Once, these people were mostly in academic medical centers, but that’s not so true anymore. A director of quality for a hospital medicine group is responsible for developing the group’s quality strategy, but at the same time responsible for teaching members of the group – not only doing QI but teaching others how to do it,” she said.
“Hospitalists make terrific bridging leaders. We really are in that sweet spot, and we can and should step into these leadership roles,” Dr. Tad-y said. “Because of our role in the hospital, we know the ins and outs of how processes work or don’t work. We have an insider’s view of the system’s dysfunction, which puts us in a great place to lead these efforts.”
The bridging leaders movement has been a grass-roots development, Dr. Tad-y explained. “It’s not like people started with the job title. But because all of this work was needed, a few people started doing it – and they began seeking each other out. Then they found that there were more than a few of us. We just hadn’t known what it was called.”
What is being bridged?
There has long been a relationship between individuals who lead in the clinical environment and those who lead in education, such as the program directors of residency programs, said Janis Orlowski, MD, chief health care officer for AAMC, which represents 154 MD-granting medical schools and their associated teaching hospitals.
“Our association’s three missions of research, education, and patient care really come together around the bridging leaders concept. So, this movement is well aligned. And as bridging leaders started to develop as a group, they found a home in AAMC and at our Integrating Quality Conference,” she said.
“Where we see this integration is in the teaching of residents and medical students in the clinical environment,” Dr. Orlowski said. “It’s not just their knowledge of disease or treatments or procedural skills that needs to be taught. They also need to understand the safe and effective clinical environment, and the role of learners in patient safety, quality improvement, and efficient and cost-effective hospital care. They need to understand value.” A new field of health systems science is emerging and quality improvement is evolving to incorporate population health. But traditional medical faculty may not be that comfortable teaching it.
Any physician who sees that they have a role in the clinical, administrative, and educational worlds can do the bridging, Dr. Orlowski said. “It could be any environment in which care is provided and learning takes place. I mentioned QI and patient safety, but among the other essential skills for the doctor of tomorrow are teamwork, inter-professional training in how to work with, for example, the pharmacist and dietitian, and understanding the value they bring.”
Whenever quality improvement projects are undertaken as part of post-graduate medical education, they should be aligned with the institution’s quality improvement plan and with the priorities of the health system, said Rob Dressler, MD, MBA, quality and safety officer at Christiana Health Care System in Newark, Del., and president of the Alliance of Independent Academic Medical Centers (AIAMC), which represents 80 hospital and health systems active in the emerging movement for bridging leaders.
“GME needs to keep the C-suite aware of its front-line efforts to improve quality and safety, so the institution’s return on investment can be recognized,” he said. “The AIAMC has consistently advocated for the building of bridges between GME leaders and their C-suites at our member hospitals. If you are doing process improvement, you need to be aligned with the organization and its priorities, or you’ll be less successful.”
AIAMC convenes the National Initiative – a multi-institutional collaborative in which residents lead multi-disciplinary teams in quality improvement projects. A total of 64 hospitals and health systems have participated since the program started in 2007. “We need to train our clinicians to solve the problems of tomorrow,” Dr. Dressler said.
Bridging leaders in action
The leaders contacted for this article offered some examples of bridging in action. Dr. Arora has used “crowd sourcing” – a technique employed extensively in her work with Costs of Care, a global nonprofit trying to drive better health care at lower cost – to implement a local program for front-line clinicians to generate ideas on how to improve value and reduce unnecessary treatment.
“We created our local ‘Choosing Wisely’ challenge for residents and staff at the University of Chicago – with the understanding that the winner would get analytic and time support to pursue their project,” she said. A resident winner was a finalist in the RIV (Research, Innovations and Clinical Vignettes) competition at a recent SHM Annual Conference.
At the University of Colorado, there is an associate program director who is responsible for the quality improvement curriculum for residents, Dr. Tad-y said. Because teaching QI means doing QI, the associate program director had to start implementing QI in the hospital, learning how to choose appropriate QI projects for the residents. That meant looking at quality priorities for the hospital – including VTE prophylaxis, fall prevention, and rates of central line–associated bloodstream infections and catheter-associated urinary tract infections. “A critical priority was to align the learners’ QI projects with what the hospital is already working on,” she explained.
“In our practice, all fellows need education and training in patient safety, how to recognize medical errors and close calls, and how to use our errors reporting system,” Dr. Myers said. “They also need to participate in errors analysis discussions. But we have struggled to get residents to attend those meetings. There’s not enough time in their schedules, and here at Penn, we have 1,500 residents and fellows, and maybe only 20 of these formal medical errors conferences per year,” she said.
Dr. Myers worked with the hospital’s patient safety officer and head of GME to design a simulated approach to fill the gap, a simulation of the root cause analysis process – how it works, the various roles played by different individuals, and what happens after it is done. “In my role, I trained one faculty member in each large residency program in how to identify a case and how to use the simulation,” she said. “They can now teach their own learners and make it more relevant to their specialty.”
Penn also has a blueprint for quality – a road map for how the organization socializes health care quality, safety, and value, Dr. Myers said. “Every 3 or 4 years our CEO looks at the road map and tries to get feedback on its direction from payers and insurers, quality leaders, academic department heads – and residents. I was in a good position to organize a session for a representative group of residents to get together and talk about where they see the quality and safety gaps in their everyday work.”
The role of the bridging leader is a viable career path or target for many hospitalists, Dr. Arora said. “But even if it’s not a career path for you, knowing that hospitalists are at the forefront of the bridging leaders movement could help you energize your health system. If you are seeing gaps in quality and safety, this is an issue you can bring before the system.”
These days doctors are wearing a lot of hats and filling roles that weren’t seen as much before, said Dr. Orlowski. “Bridging leaders are not an exclusive group but open to anyone who finds their passion in teaching quality and safety. Maybe you’re doing quality and safety, but not education, but you recognize its importance, or vice versa. First of all, look to see what this bridging leaders thing really is, and how it might apply to you. You might say: ‘That accurately describes what I’m doing now. I have the interest; I want to learn more.’”
References
1. Accreditation Council for Graduate Medical Education. CLER pathways to excellence.
2. Myers JS et al. Bridging leadership roles in quality and patient safety: Experience of 6 U.S. Academic Medical Centers. J Grad Med Educ. 2017 Feb;9(1): 9-13.
In June 2019, a 5-hour preconference seminar at the annual Integrating Quality Conference of the Association of American Medical Colleges (AAMC) in Minneapolis highlighted the emergence of a new concept, and a new community, within the larger field of hospital medicine.
“Bridging leaders” are clinician-educators with a foot in two worlds: leading quality and safety initiatives within their teaching hospitals – with the hospitalist’s customary participation in a broad spectrum of quality improvement (QI) efforts in the hospital – while helping to train future and current physicians. “Bridging” also extends to the third piece of the quality puzzle, the hospital and/or health system’s senior administrators.
“About 8 years ago, another hospitalist and I found ourselves in this role, bridging graduate medical education with hospital quality and safety,” said Jennifer S. Myers, MD, FHM, director of quality and safety education in the department of medicine at the University of Pennsylvania, Philadelphia. “The role has since begun to proliferate, in teaching settings large and small, and about 30-50 of us with somewhat similar job responsibilities have been trying to create a community.”
Following the lead of the American College of Graduate Medical Education1 and its standards for clinical learning environments that include integration of patient safety and quality improvement, these have become graduate medical education (GME) priorities. Students need to learn the theory and practice of safety and quality improvement on the job as part of their professional development. Residency program directors and other trainers thus need to find opportunities for them to practice these techniques in the clinical practice environment.
At the same time, mobilizing those eager medical learners to plan and conduct quality improvement projects can enhance a hospital’s ability to advance its mission in the new health care environment of accountable care and population health.
New concept arises
Is bridging leaders a real thing? The short answer is yes, said Thomas Ciesielski, MD, GME medical director for patient safety, quality education, and clinical learning environment review program development at Washington University in St. Louis. “This is a new trend, but it’s still in the process of defining itself. Every bridging leader has their own identity based on their institution. Some play a bridging role for the entire institution; others play similar roles but only within a specific department or division. There’s a lot of learning going on in our community,” he said.
The first Bridging Leaders track was held last year at AAMC’s 2018 Integrating Quality Conference, an event which has been held annually for the past decade. The concept was also highlighted in a 2017 article in the Journal of Graduate Medical Education2 by bridging leaders, including many of the faculty at the subsequent AAMC sessions, highlighting their roles and programs at six academic medical centers.
One of those coauthors, hospitalist Vineet Arora, MD, MAPP, MHM, was recently appointed to a new position at University of Chicago Medicine: associate chief medical officer for the clinical learning environment – which pulls together many of the threads of the bridging leaders movement into a single job title. Dr. Arora said her job builds on her prior work in GME and improves the clinical learning environment for residents and fellows by integrating them into the health system’s institutional quality, safety, and value missions. It also expands on that work to include faculty and allied health professionals. “I just happen to come from the health system side,” she said.
Natural bridges: From clinical to educational
As with the early days of the hospitalist movement, bridging leaders are trying to build a community of peers with common interests.
“We’re just at the beginning,” Dr. Arora said. “Hospitalists have been the natural torch bearers for quality and safety in their hospitals, and also play roles in the education of residents and medical students, working alongside residency program directors. They are well-versed in quality and in education. So, they are the natural bridges between education and clinical care,” she said. “We also know this is a young group that comes to our meetings. One-third of them have been doing this for only the past 2 years or less – so they are early in their career paths.”
Front-line clinical providers, such as residents, often have good ideas, and bridging leaders can bring these ideas to the health system’s leaders, Dr. Arora said. “Bridging at the leadership level also involves thinking about the larger priorities of the system.” There are trust issues that these leaders can help to bridge, as well as internal communication barriers. “We also realize that health systems have to move quickly in response to a rapidly changing environment,” she noted.
“You don’t want a hundred quality improvement projects being done by students that are unaligned with the organization’s priorities. That leads to waste, and highlights the need for greater alignment,” Dr. Arora added. “Think about using front-line staff as agents of change, of engaging with learners as a win/win – as a way to actually solve the problems we are facing.”
A bridging leader occupies a role in which they can influence and affect these two parts of the mission of health care, somebody whose leadership responsibilities sit at the intersection of these two areas, said Darlene Tad-y, MD, director of GME quality and safety programs at the University of Colorado, Aurora. “Once, these people were mostly in academic medical centers, but that’s not so true anymore. A director of quality for a hospital medicine group is responsible for developing the group’s quality strategy, but at the same time responsible for teaching members of the group – not only doing QI but teaching others how to do it,” she said.
“Hospitalists make terrific bridging leaders. We really are in that sweet spot, and we can and should step into these leadership roles,” Dr. Tad-y said. “Because of our role in the hospital, we know the ins and outs of how processes work or don’t work. We have an insider’s view of the system’s dysfunction, which puts us in a great place to lead these efforts.”
The bridging leaders movement has been a grass-roots development, Dr. Tad-y explained. “It’s not like people started with the job title. But because all of this work was needed, a few people started doing it – and they began seeking each other out. Then they found that there were more than a few of us. We just hadn’t known what it was called.”
What is being bridged?
There has long been a relationship between individuals who lead in the clinical environment and those who lead in education, such as the program directors of residency programs, said Janis Orlowski, MD, chief health care officer for AAMC, which represents 154 MD-granting medical schools and their associated teaching hospitals.
“Our association’s three missions of research, education, and patient care really come together around the bridging leaders concept. So, this movement is well aligned. And as bridging leaders started to develop as a group, they found a home in AAMC and at our Integrating Quality Conference,” she said.
“Where we see this integration is in the teaching of residents and medical students in the clinical environment,” Dr. Orlowski said. “It’s not just their knowledge of disease or treatments or procedural skills that needs to be taught. They also need to understand the safe and effective clinical environment, and the role of learners in patient safety, quality improvement, and efficient and cost-effective hospital care. They need to understand value.” A new field of health systems science is emerging and quality improvement is evolving to incorporate population health. But traditional medical faculty may not be that comfortable teaching it.
Any physician who sees that they have a role in the clinical, administrative, and educational worlds can do the bridging, Dr. Orlowski said. “It could be any environment in which care is provided and learning takes place. I mentioned QI and patient safety, but among the other essential skills for the doctor of tomorrow are teamwork, inter-professional training in how to work with, for example, the pharmacist and dietitian, and understanding the value they bring.”
Whenever quality improvement projects are undertaken as part of post-graduate medical education, they should be aligned with the institution’s quality improvement plan and with the priorities of the health system, said Rob Dressler, MD, MBA, quality and safety officer at Christiana Health Care System in Newark, Del., and president of the Alliance of Independent Academic Medical Centers (AIAMC), which represents 80 hospital and health systems active in the emerging movement for bridging leaders.
“GME needs to keep the C-suite aware of its front-line efforts to improve quality and safety, so the institution’s return on investment can be recognized,” he said. “The AIAMC has consistently advocated for the building of bridges between GME leaders and their C-suites at our member hospitals. If you are doing process improvement, you need to be aligned with the organization and its priorities, or you’ll be less successful.”
AIAMC convenes the National Initiative – a multi-institutional collaborative in which residents lead multi-disciplinary teams in quality improvement projects. A total of 64 hospitals and health systems have participated since the program started in 2007. “We need to train our clinicians to solve the problems of tomorrow,” Dr. Dressler said.
Bridging leaders in action
The leaders contacted for this article offered some examples of bridging in action. Dr. Arora has used “crowd sourcing” – a technique employed extensively in her work with Costs of Care, a global nonprofit trying to drive better health care at lower cost – to implement a local program for front-line clinicians to generate ideas on how to improve value and reduce unnecessary treatment.
“We created our local ‘Choosing Wisely’ challenge for residents and staff at the University of Chicago – with the understanding that the winner would get analytic and time support to pursue their project,” she said. A resident winner was a finalist in the RIV (Research, Innovations and Clinical Vignettes) competition at a recent SHM Annual Conference.
At the University of Colorado, there is an associate program director who is responsible for the quality improvement curriculum for residents, Dr. Tad-y said. Because teaching QI means doing QI, the associate program director had to start implementing QI in the hospital, learning how to choose appropriate QI projects for the residents. That meant looking at quality priorities for the hospital – including VTE prophylaxis, fall prevention, and rates of central line–associated bloodstream infections and catheter-associated urinary tract infections. “A critical priority was to align the learners’ QI projects with what the hospital is already working on,” she explained.
“In our practice, all fellows need education and training in patient safety, how to recognize medical errors and close calls, and how to use our errors reporting system,” Dr. Myers said. “They also need to participate in errors analysis discussions. But we have struggled to get residents to attend those meetings. There’s not enough time in their schedules, and here at Penn, we have 1,500 residents and fellows, and maybe only 20 of these formal medical errors conferences per year,” she said.
Dr. Myers worked with the hospital’s patient safety officer and head of GME to design a simulated approach to fill the gap, a simulation of the root cause analysis process – how it works, the various roles played by different individuals, and what happens after it is done. “In my role, I trained one faculty member in each large residency program in how to identify a case and how to use the simulation,” she said. “They can now teach their own learners and make it more relevant to their specialty.”
Penn also has a blueprint for quality – a road map for how the organization socializes health care quality, safety, and value, Dr. Myers said. “Every 3 or 4 years our CEO looks at the road map and tries to get feedback on its direction from payers and insurers, quality leaders, academic department heads – and residents. I was in a good position to organize a session for a representative group of residents to get together and talk about where they see the quality and safety gaps in their everyday work.”
The role of the bridging leader is a viable career path or target for many hospitalists, Dr. Arora said. “But even if it’s not a career path for you, knowing that hospitalists are at the forefront of the bridging leaders movement could help you energize your health system. If you are seeing gaps in quality and safety, this is an issue you can bring before the system.”
These days doctors are wearing a lot of hats and filling roles that weren’t seen as much before, said Dr. Orlowski. “Bridging leaders are not an exclusive group but open to anyone who finds their passion in teaching quality and safety. Maybe you’re doing quality and safety, but not education, but you recognize its importance, or vice versa. First of all, look to see what this bridging leaders thing really is, and how it might apply to you. You might say: ‘That accurately describes what I’m doing now. I have the interest; I want to learn more.’”
References
1. Accreditation Council for Graduate Medical Education. CLER pathways to excellence.
2. Myers JS et al. Bridging leadership roles in quality and patient safety: Experience of 6 U.S. Academic Medical Centers. J Grad Med Educ. 2017 Feb;9(1): 9-13.
Judge dismisses doctors’ lawsuit against ABIM
A district court has dismissed a lawsuit levied by a group of physicians against the American Board of Internal Medicine (ABIM) over its maintenance of certification (MOC) program, calling the legal challenge “flawed.”
In a Sept. 26 decision, U.S. District Court Judge for the Eastern District of Pennsylvania Robert F. Kelly Sr. said the plaintiffs failed to demonstrate sufficient evidence for their antitrust and unjust enrichment claims against ABIM. The doctors also did not establish any showing of anticompetitive conduct by ABIM to support a monopolization claim, the judge ruled.
“We disagree with plaintiffs and find that ABIM’s initial certification and MOC products are part of a single product and do not occupy distinct markets,” Judge Kelly wrote in his decision. “Not only are we unconvinced by plaintiffs’ arguments, we find that plaintiffs’ entire framing of the ABIM certification to be flawed. In essence, plaintiffs are arguing that, in order to purchase ABIM’s initial certification, internists are forced to purchase MOC products as well. However, this is not the case. ... Nowhere in the amended complaint do plaintiffs allege that they were forced to buy MOC products in order to purchase the initial certification.”
The judge dismissed the suit, but allowed the plaintiffs 14 days to submit an amended complaint reoutlining their claims of illegal monopolization and racketeering against the board. If the amended complaint passes legal muster, the judge could revive those claims.
ABIM President Richard J. Baron, MD, expressed satisfaction that the court granted the board’s motion to dismiss the case for failure to state a valid claim.
“ABIM is pleased that the United States District Court for the Eastern District of Pennsylvania dismissed in its entirety a lawsuit that alleged physicians were harmed by the requirements for maintaining ABIM board certification,” Dr. Baron said in a statement.
C. Philip Curley, a Chicago-based attorney for the physician plaintiffs, said the case is far from over.
“The four internists who brought the lawsuit were invited to file amended claims, which is certainly being considered,” Mr. Curley said in an interview. “If necessary, all available appeals will also be pursued to the fullest. No one was under the impression that the fight to bring MOC to an end would be quick or easy.”
The original lawsuit, filed Dec. 6, 2018, in a Pennsylvania district court, claims that ABIM is charging inflated monopoly prices for maintaining certification, that the organization is forcing physicians to purchase MOC, and that ABIM is inducing employers and others to require ABIM certification. On Jan. 23 of this year the legal challenge was amended to include racketeering and unjust enrichment claims.
The four plaintiff-physicians want the court to find ABIM in violation of federal antitrust law and to bar the board from continuing its MOC process. The suit is filed as a class action on behalf of all internists and subspecialists required by ABIM to purchase MOC to maintain their ABIM certifications.
Two other lawsuits challenging MOC, one against the American Board of Psychiatry and Neurology and another against the American Board of Radiology, are ongoing. A fourth lawsuit against the American Board of Medical Specialties, the American Board of Emergency Medicine, and the American Board of Anesthesiology was filed in February.
Chicago-based cardiologist Wes Fisher, MD, and fellow physicians with the Practicing Physicians of America are funding the plaintiffs’ legal efforts through a fundraising campaign that has raised more than $300,000.
In an interview, Dr. Fisher called the legal fight against ABIM “a David versus Goliath effort” and said the battle will continue.
“The ABIM may have won this first round, but ... they have only dodged the antitrust tying claim and unjust enrichment claims,” Dr. Fisher said. “The monopoly claim and racketeering claims are still very much open. Plaintiffs have 14 days to amend their compliant.”
A district court has dismissed a lawsuit levied by a group of physicians against the American Board of Internal Medicine (ABIM) over its maintenance of certification (MOC) program, calling the legal challenge “flawed.”
In a Sept. 26 decision, U.S. District Court Judge for the Eastern District of Pennsylvania Robert F. Kelly Sr. said the plaintiffs failed to demonstrate sufficient evidence for their antitrust and unjust enrichment claims against ABIM. The doctors also did not establish any showing of anticompetitive conduct by ABIM to support a monopolization claim, the judge ruled.
“We disagree with plaintiffs and find that ABIM’s initial certification and MOC products are part of a single product and do not occupy distinct markets,” Judge Kelly wrote in his decision. “Not only are we unconvinced by plaintiffs’ arguments, we find that plaintiffs’ entire framing of the ABIM certification to be flawed. In essence, plaintiffs are arguing that, in order to purchase ABIM’s initial certification, internists are forced to purchase MOC products as well. However, this is not the case. ... Nowhere in the amended complaint do plaintiffs allege that they were forced to buy MOC products in order to purchase the initial certification.”
The judge dismissed the suit, but allowed the plaintiffs 14 days to submit an amended complaint reoutlining their claims of illegal monopolization and racketeering against the board. If the amended complaint passes legal muster, the judge could revive those claims.
ABIM President Richard J. Baron, MD, expressed satisfaction that the court granted the board’s motion to dismiss the case for failure to state a valid claim.
“ABIM is pleased that the United States District Court for the Eastern District of Pennsylvania dismissed in its entirety a lawsuit that alleged physicians were harmed by the requirements for maintaining ABIM board certification,” Dr. Baron said in a statement.
C. Philip Curley, a Chicago-based attorney for the physician plaintiffs, said the case is far from over.
“The four internists who brought the lawsuit were invited to file amended claims, which is certainly being considered,” Mr. Curley said in an interview. “If necessary, all available appeals will also be pursued to the fullest. No one was under the impression that the fight to bring MOC to an end would be quick or easy.”
The original lawsuit, filed Dec. 6, 2018, in a Pennsylvania district court, claims that ABIM is charging inflated monopoly prices for maintaining certification, that the organization is forcing physicians to purchase MOC, and that ABIM is inducing employers and others to require ABIM certification. On Jan. 23 of this year the legal challenge was amended to include racketeering and unjust enrichment claims.
The four plaintiff-physicians want the court to find ABIM in violation of federal antitrust law and to bar the board from continuing its MOC process. The suit is filed as a class action on behalf of all internists and subspecialists required by ABIM to purchase MOC to maintain their ABIM certifications.
Two other lawsuits challenging MOC, one against the American Board of Psychiatry and Neurology and another against the American Board of Radiology, are ongoing. A fourth lawsuit against the American Board of Medical Specialties, the American Board of Emergency Medicine, and the American Board of Anesthesiology was filed in February.
Chicago-based cardiologist Wes Fisher, MD, and fellow physicians with the Practicing Physicians of America are funding the plaintiffs’ legal efforts through a fundraising campaign that has raised more than $300,000.
In an interview, Dr. Fisher called the legal fight against ABIM “a David versus Goliath effort” and said the battle will continue.
“The ABIM may have won this first round, but ... they have only dodged the antitrust tying claim and unjust enrichment claims,” Dr. Fisher said. “The monopoly claim and racketeering claims are still very much open. Plaintiffs have 14 days to amend their compliant.”
A district court has dismissed a lawsuit levied by a group of physicians against the American Board of Internal Medicine (ABIM) over its maintenance of certification (MOC) program, calling the legal challenge “flawed.”
In a Sept. 26 decision, U.S. District Court Judge for the Eastern District of Pennsylvania Robert F. Kelly Sr. said the plaintiffs failed to demonstrate sufficient evidence for their antitrust and unjust enrichment claims against ABIM. The doctors also did not establish any showing of anticompetitive conduct by ABIM to support a monopolization claim, the judge ruled.
“We disagree with plaintiffs and find that ABIM’s initial certification and MOC products are part of a single product and do not occupy distinct markets,” Judge Kelly wrote in his decision. “Not only are we unconvinced by plaintiffs’ arguments, we find that plaintiffs’ entire framing of the ABIM certification to be flawed. In essence, plaintiffs are arguing that, in order to purchase ABIM’s initial certification, internists are forced to purchase MOC products as well. However, this is not the case. ... Nowhere in the amended complaint do plaintiffs allege that they were forced to buy MOC products in order to purchase the initial certification.”
The judge dismissed the suit, but allowed the plaintiffs 14 days to submit an amended complaint reoutlining their claims of illegal monopolization and racketeering against the board. If the amended complaint passes legal muster, the judge could revive those claims.
ABIM President Richard J. Baron, MD, expressed satisfaction that the court granted the board’s motion to dismiss the case for failure to state a valid claim.
“ABIM is pleased that the United States District Court for the Eastern District of Pennsylvania dismissed in its entirety a lawsuit that alleged physicians were harmed by the requirements for maintaining ABIM board certification,” Dr. Baron said in a statement.
C. Philip Curley, a Chicago-based attorney for the physician plaintiffs, said the case is far from over.
“The four internists who brought the lawsuit were invited to file amended claims, which is certainly being considered,” Mr. Curley said in an interview. “If necessary, all available appeals will also be pursued to the fullest. No one was under the impression that the fight to bring MOC to an end would be quick or easy.”
The original lawsuit, filed Dec. 6, 2018, in a Pennsylvania district court, claims that ABIM is charging inflated monopoly prices for maintaining certification, that the organization is forcing physicians to purchase MOC, and that ABIM is inducing employers and others to require ABIM certification. On Jan. 23 of this year the legal challenge was amended to include racketeering and unjust enrichment claims.
The four plaintiff-physicians want the court to find ABIM in violation of federal antitrust law and to bar the board from continuing its MOC process. The suit is filed as a class action on behalf of all internists and subspecialists required by ABIM to purchase MOC to maintain their ABIM certifications.
Two other lawsuits challenging MOC, one against the American Board of Psychiatry and Neurology and another against the American Board of Radiology, are ongoing. A fourth lawsuit against the American Board of Medical Specialties, the American Board of Emergency Medicine, and the American Board of Anesthesiology was filed in February.
Chicago-based cardiologist Wes Fisher, MD, and fellow physicians with the Practicing Physicians of America are funding the plaintiffs’ legal efforts through a fundraising campaign that has raised more than $300,000.
In an interview, Dr. Fisher called the legal fight against ABIM “a David versus Goliath effort” and said the battle will continue.
“The ABIM may have won this first round, but ... they have only dodged the antitrust tying claim and unjust enrichment claims,” Dr. Fisher said. “The monopoly claim and racketeering claims are still very much open. Plaintiffs have 14 days to amend their compliant.”
SHM and Jefferson College of Population Health partner to provide vital education for hospitalists
Both the Society of Hospital Medicine and Jefferson College of Population Health, of Thomas Jefferson University in Philadelphia, share a goal to educate physicians to be effective leaders and managers in the pursuit of health care quality, safety, and population health, and they have entered into a partnership with this in mind.
Alexis Skoufalos, EdD, associate dean, strategic development, for Jefferson College of Population Health, recently spoke with The Hospitalist to discuss the importance of population health to hospital medicine professionals, the health care landscape as a whole, and the benefits of this new partnership with SHM.
Can you explain the importance of population health in the current health care landscape?
Many people confuse population health with public health. While they are related, they are different disciplines. Public health focuses on prevention and health promotion (clean water, vaccines, exercise, using seat belts, and so on), but it stops there.
Population health builds on the foundation of public health and goes a step further, working to connect health and health care delivery. It takes a more holistic approach, looking at what we need to do inside and outside the delivery system to help people to get and stay healthy, as well as take better care of them when they do get sick.
We work to identify and understand the health impact of social and environmental factors, while also looking for ways to make health care delivery safer, better, and more affordable and accessible.
This can get complicated. It involves sorting through lots of information to uncover the best way to meet the needs of a specific group, whether that is a community, a neighborhood, or a patient with a particular condition.
It’s about taking the time to really look at things from different vantage points. You won’t see the same view if you are looking at something through a telescope as you would looking through a microscope. That information can help you to adjust your perspective to identify the best course of action.
In order to be successful in improving population health, providers need to understand how to work with the other stakeholders in the health care ecosystem. Collaboration and coordination are the best ways to optimize the resources available.
It is important for delivery systems to establish good working relationships with community nonprofit and service organizations, faith-based organizations, social service providers, school systems, and federal, state, and local government.
At Jefferson, we thought it was important to create a college and programs that would prepare professionals across the workforce for this new challenge.
How did this partnership between SHM and Jefferson College of Population Health come to fruition?
Hospitalists are an important link with a person’s primary care team. The work they do to prepare a person and their family for successful discharge to the community after a hospital stay can make all the difference in a person’s recovery, condition management, and preventing readmission to the hospital.
Because both of our organizations are based in Philadelphia, we have had longstanding connections with SHM leadership. It was only natural for us to talk with SHM about how we can build upon the society’s excellent continuing education offerings and work together to provide members with additional content that can equip them to advance their careers.
How did SHM and Jefferson College of Population Health identify the mutually beneficial educational offerings in each institution that are included in this partnership?
Members of our respective leadership teams got together to complete a detailed review of the offerings from each organization. SHM’s Leadership Academy and JCPH’s Population Health Academy are rigorous continuing education programs that can provide physicians with excellent just-in-time information they can put to use right away.
After a careful examination of the curriculum, JCPH determined that SHM members can apply the credits they earn from completing two qualified sessions from the Leadership Academy to satisfy the elective course requirement for a Master’s degree. (Note: This does not apply to the Population Health Intelligence Program, which does not include an elective course.)
How will this partnership benefit Jefferson College of Population Health?
Our mission is to prepare health care leaders with the skills and tools they need to be effective in improving population health. Clinicians who work in a hospital setting have a key role to play.
We are also dedicated to making a difference right here in Philadelphia. The more students we have in our programs, the more of an impact we (and they) will have in improving outcomes in our own community.
We need to move the needle and get Philadelphia County out of the basement in terms of health rankings. We have a responsibility to do what we can to make a difference, and we appreciate the partnership with SHM to make it happen.
What other components of the partnership are especially noteworthy to highlight?
In addition to what I’ve already discussed, the following are some of the significant benefits that SHM members are entitled to as a result of the partnership with JCPH:
- 15% discount on tuition for any JCPH online graduate degree program.
- Registration discount for JCPH’s Population Health Academy in Philadelphia.
- Special registration rate for Annual Population Health Colloquium.
For more information about this partnership, visit hospitalmedicine.org/jefferson.
Both the Society of Hospital Medicine and Jefferson College of Population Health, of Thomas Jefferson University in Philadelphia, share a goal to educate physicians to be effective leaders and managers in the pursuit of health care quality, safety, and population health, and they have entered into a partnership with this in mind.
Alexis Skoufalos, EdD, associate dean, strategic development, for Jefferson College of Population Health, recently spoke with The Hospitalist to discuss the importance of population health to hospital medicine professionals, the health care landscape as a whole, and the benefits of this new partnership with SHM.
Can you explain the importance of population health in the current health care landscape?
Many people confuse population health with public health. While they are related, they are different disciplines. Public health focuses on prevention and health promotion (clean water, vaccines, exercise, using seat belts, and so on), but it stops there.
Population health builds on the foundation of public health and goes a step further, working to connect health and health care delivery. It takes a more holistic approach, looking at what we need to do inside and outside the delivery system to help people to get and stay healthy, as well as take better care of them when they do get sick.
We work to identify and understand the health impact of social and environmental factors, while also looking for ways to make health care delivery safer, better, and more affordable and accessible.
This can get complicated. It involves sorting through lots of information to uncover the best way to meet the needs of a specific group, whether that is a community, a neighborhood, or a patient with a particular condition.
It’s about taking the time to really look at things from different vantage points. You won’t see the same view if you are looking at something through a telescope as you would looking through a microscope. That information can help you to adjust your perspective to identify the best course of action.
In order to be successful in improving population health, providers need to understand how to work with the other stakeholders in the health care ecosystem. Collaboration and coordination are the best ways to optimize the resources available.
It is important for delivery systems to establish good working relationships with community nonprofit and service organizations, faith-based organizations, social service providers, school systems, and federal, state, and local government.
At Jefferson, we thought it was important to create a college and programs that would prepare professionals across the workforce for this new challenge.
How did this partnership between SHM and Jefferson College of Population Health come to fruition?
Hospitalists are an important link with a person’s primary care team. The work they do to prepare a person and their family for successful discharge to the community after a hospital stay can make all the difference in a person’s recovery, condition management, and preventing readmission to the hospital.
Because both of our organizations are based in Philadelphia, we have had longstanding connections with SHM leadership. It was only natural for us to talk with SHM about how we can build upon the society’s excellent continuing education offerings and work together to provide members with additional content that can equip them to advance their careers.
How did SHM and Jefferson College of Population Health identify the mutually beneficial educational offerings in each institution that are included in this partnership?
Members of our respective leadership teams got together to complete a detailed review of the offerings from each organization. SHM’s Leadership Academy and JCPH’s Population Health Academy are rigorous continuing education programs that can provide physicians with excellent just-in-time information they can put to use right away.
After a careful examination of the curriculum, JCPH determined that SHM members can apply the credits they earn from completing two qualified sessions from the Leadership Academy to satisfy the elective course requirement for a Master’s degree. (Note: This does not apply to the Population Health Intelligence Program, which does not include an elective course.)
How will this partnership benefit Jefferson College of Population Health?
Our mission is to prepare health care leaders with the skills and tools they need to be effective in improving population health. Clinicians who work in a hospital setting have a key role to play.
We are also dedicated to making a difference right here in Philadelphia. The more students we have in our programs, the more of an impact we (and they) will have in improving outcomes in our own community.
We need to move the needle and get Philadelphia County out of the basement in terms of health rankings. We have a responsibility to do what we can to make a difference, and we appreciate the partnership with SHM to make it happen.
What other components of the partnership are especially noteworthy to highlight?
In addition to what I’ve already discussed, the following are some of the significant benefits that SHM members are entitled to as a result of the partnership with JCPH:
- 15% discount on tuition for any JCPH online graduate degree program.
- Registration discount for JCPH’s Population Health Academy in Philadelphia.
- Special registration rate for Annual Population Health Colloquium.
For more information about this partnership, visit hospitalmedicine.org/jefferson.
Both the Society of Hospital Medicine and Jefferson College of Population Health, of Thomas Jefferson University in Philadelphia, share a goal to educate physicians to be effective leaders and managers in the pursuit of health care quality, safety, and population health, and they have entered into a partnership with this in mind.
Alexis Skoufalos, EdD, associate dean, strategic development, for Jefferson College of Population Health, recently spoke with The Hospitalist to discuss the importance of population health to hospital medicine professionals, the health care landscape as a whole, and the benefits of this new partnership with SHM.
Can you explain the importance of population health in the current health care landscape?
Many people confuse population health with public health. While they are related, they are different disciplines. Public health focuses on prevention and health promotion (clean water, vaccines, exercise, using seat belts, and so on), but it stops there.
Population health builds on the foundation of public health and goes a step further, working to connect health and health care delivery. It takes a more holistic approach, looking at what we need to do inside and outside the delivery system to help people to get and stay healthy, as well as take better care of them when they do get sick.
We work to identify and understand the health impact of social and environmental factors, while also looking for ways to make health care delivery safer, better, and more affordable and accessible.
This can get complicated. It involves sorting through lots of information to uncover the best way to meet the needs of a specific group, whether that is a community, a neighborhood, or a patient with a particular condition.
It’s about taking the time to really look at things from different vantage points. You won’t see the same view if you are looking at something through a telescope as you would looking through a microscope. That information can help you to adjust your perspective to identify the best course of action.
In order to be successful in improving population health, providers need to understand how to work with the other stakeholders in the health care ecosystem. Collaboration and coordination are the best ways to optimize the resources available.
It is important for delivery systems to establish good working relationships with community nonprofit and service organizations, faith-based organizations, social service providers, school systems, and federal, state, and local government.
At Jefferson, we thought it was important to create a college and programs that would prepare professionals across the workforce for this new challenge.
How did this partnership between SHM and Jefferson College of Population Health come to fruition?
Hospitalists are an important link with a person’s primary care team. The work they do to prepare a person and their family for successful discharge to the community after a hospital stay can make all the difference in a person’s recovery, condition management, and preventing readmission to the hospital.
Because both of our organizations are based in Philadelphia, we have had longstanding connections with SHM leadership. It was only natural for us to talk with SHM about how we can build upon the society’s excellent continuing education offerings and work together to provide members with additional content that can equip them to advance their careers.
How did SHM and Jefferson College of Population Health identify the mutually beneficial educational offerings in each institution that are included in this partnership?
Members of our respective leadership teams got together to complete a detailed review of the offerings from each organization. SHM’s Leadership Academy and JCPH’s Population Health Academy are rigorous continuing education programs that can provide physicians with excellent just-in-time information they can put to use right away.
After a careful examination of the curriculum, JCPH determined that SHM members can apply the credits they earn from completing two qualified sessions from the Leadership Academy to satisfy the elective course requirement for a Master’s degree. (Note: This does not apply to the Population Health Intelligence Program, which does not include an elective course.)
How will this partnership benefit Jefferson College of Population Health?
Our mission is to prepare health care leaders with the skills and tools they need to be effective in improving population health. Clinicians who work in a hospital setting have a key role to play.
We are also dedicated to making a difference right here in Philadelphia. The more students we have in our programs, the more of an impact we (and they) will have in improving outcomes in our own community.
We need to move the needle and get Philadelphia County out of the basement in terms of health rankings. We have a responsibility to do what we can to make a difference, and we appreciate the partnership with SHM to make it happen.
What other components of the partnership are especially noteworthy to highlight?
In addition to what I’ve already discussed, the following are some of the significant benefits that SHM members are entitled to as a result of the partnership with JCPH:
- 15% discount on tuition for any JCPH online graduate degree program.
- Registration discount for JCPH’s Population Health Academy in Philadelphia.
- Special registration rate for Annual Population Health Colloquium.
For more information about this partnership, visit hospitalmedicine.org/jefferson.