User login
Hospitalist Career Goals Should Flow from Passion and Purpose
By Surinder Yadav, MD
For many new or job-changing hospitalists, finding your next position may be your main focus. It’s easy to imagine that once you land a job, the rest of your career will fall easily into place.
But hospital medicine is demanding stuff, and you can get so busy meeting the needs of others that you lose sight of your own. Eventually survival mode kicks in, and your drive and passion begin to fade.
In order to maintain a sense of forward momentum and job satisfaction, it helps to set annual goals. What could you accomplish this year that would really get you excited about your career? What skills could take your practice to the next level? Are your current actions in sync with your values and life purpose?
Here are some tips I've learned through the years:
Base goals on your passion
To get the most satisfaction from your career, start by identifying your passion. Why did you select medicine as a career, and how does it relate to your life purpose? Once you are clear on what motivates you to get up in the morning, you can set your goals to help drive and sustain that passion.
Set goals that are measurable
If you don’t have goals you can measure, it’s too easy to let them slide when you get busy with other obligations. Examples of some measurable goals I’ve set for my own career include taking leadership courses in project management and people management.
Once you’ve established your goals and determined how you will measure your progress and success, create a timeline for achieving each milestone. Also, consider finding an accountability partner who will check in with you now and then to make sure you're on track.
Be realistic
Goals that are admirable but not attainable are a waste of the paper they are written on. Make sure you have the resources you need to achieve your specific goals so that you have no roadblocks to success.
A final thought: One of the benefits of working for a physician partnership like Vituity is flexibility. You'll have more leeway to create a work schedule that allows you time for yourself. Work-life balance is great for your career longevity, and we believe it’s also good for your patients. When you feel rested and fulfilled, you have more energy and compassion to give to others.
Surinder Yadav, MD, is Vituity’s Vice President of Hospital Medicine Operations.
To learn more about satisfying medical careers at Vituity, please visit http://www.vituity.com/careers.
By Surinder Yadav, MD
For many new or job-changing hospitalists, finding your next position may be your main focus. It’s easy to imagine that once you land a job, the rest of your career will fall easily into place.
But hospital medicine is demanding stuff, and you can get so busy meeting the needs of others that you lose sight of your own. Eventually survival mode kicks in, and your drive and passion begin to fade.
In order to maintain a sense of forward momentum and job satisfaction, it helps to set annual goals. What could you accomplish this year that would really get you excited about your career? What skills could take your practice to the next level? Are your current actions in sync with your values and life purpose?
Here are some tips I've learned through the years:
Base goals on your passion
To get the most satisfaction from your career, start by identifying your passion. Why did you select medicine as a career, and how does it relate to your life purpose? Once you are clear on what motivates you to get up in the morning, you can set your goals to help drive and sustain that passion.
Set goals that are measurable
If you don’t have goals you can measure, it’s too easy to let them slide when you get busy with other obligations. Examples of some measurable goals I’ve set for my own career include taking leadership courses in project management and people management.
Once you’ve established your goals and determined how you will measure your progress and success, create a timeline for achieving each milestone. Also, consider finding an accountability partner who will check in with you now and then to make sure you're on track.
Be realistic
Goals that are admirable but not attainable are a waste of the paper they are written on. Make sure you have the resources you need to achieve your specific goals so that you have no roadblocks to success.
A final thought: One of the benefits of working for a physician partnership like Vituity is flexibility. You'll have more leeway to create a work schedule that allows you time for yourself. Work-life balance is great for your career longevity, and we believe it’s also good for your patients. When you feel rested and fulfilled, you have more energy and compassion to give to others.
Surinder Yadav, MD, is Vituity’s Vice President of Hospital Medicine Operations.
To learn more about satisfying medical careers at Vituity, please visit http://www.vituity.com/careers.
By Surinder Yadav, MD
For many new or job-changing hospitalists, finding your next position may be your main focus. It’s easy to imagine that once you land a job, the rest of your career will fall easily into place.
But hospital medicine is demanding stuff, and you can get so busy meeting the needs of others that you lose sight of your own. Eventually survival mode kicks in, and your drive and passion begin to fade.
In order to maintain a sense of forward momentum and job satisfaction, it helps to set annual goals. What could you accomplish this year that would really get you excited about your career? What skills could take your practice to the next level? Are your current actions in sync with your values and life purpose?
Here are some tips I've learned through the years:
Base goals on your passion
To get the most satisfaction from your career, start by identifying your passion. Why did you select medicine as a career, and how does it relate to your life purpose? Once you are clear on what motivates you to get up in the morning, you can set your goals to help drive and sustain that passion.
Set goals that are measurable
If you don’t have goals you can measure, it’s too easy to let them slide when you get busy with other obligations. Examples of some measurable goals I’ve set for my own career include taking leadership courses in project management and people management.
Once you’ve established your goals and determined how you will measure your progress and success, create a timeline for achieving each milestone. Also, consider finding an accountability partner who will check in with you now and then to make sure you're on track.
Be realistic
Goals that are admirable but not attainable are a waste of the paper they are written on. Make sure you have the resources you need to achieve your specific goals so that you have no roadblocks to success.
A final thought: One of the benefits of working for a physician partnership like Vituity is flexibility. You'll have more leeway to create a work schedule that allows you time for yourself. Work-life balance is great for your career longevity, and we believe it’s also good for your patients. When you feel rested and fulfilled, you have more energy and compassion to give to others.
Surinder Yadav, MD, is Vituity’s Vice President of Hospital Medicine Operations.
To learn more about satisfying medical careers at Vituity, please visit http://www.vituity.com/careers.
AI will change the practice of medicine
Remembering the importance of caring
As artificial intelligence (AI) takes on more and more tasks in medical care that mimic human cognition, hospitalists and other physicians will need to adapt to a changing role.
Today AI can identify tuberculosis infections in chest radiographs with almost complete accuracy, diagnose melanoma from images of skin lesions more accurately than dermatologists can, and identify metastatic cells in images of lymph node tissue more accurately than pathologists can. The next 20 years are likely to see further acceleration in the capabilities, according to a recent article by S. Claiborne Johnston, MD, PhD.
“AI will change the practice of medicine. The art of medicine, including all the humanistic components, will only become more important over time. As dean of a medical school, I’m training students who will be practicing in 2065,” Dr. Johnston said. “If I’m not thinking about the future, I’m failing my students and the society they will serve.”
The contributions of AI will shift the emphasis for human caregivers to the caring. Studies have shown that the skills of caring are associated with improved patient outcomes, but most medical schools allocate substantial time in the curriculum to memorization and analysis – tasks that will become less demanding as artificial intelligence improves. The art of caring – communication, empathy, shared decision making, leadership, and team building – is usually a minor part of the medical school curriculum.
Effective leadership and creativity are distant aspirations for artificial intelligence but are growing needs in a system of care that is ever more complex.
At Dr. Johnston’s school, the Dell Medical School at the University of Texas at Austin, they have reduced the duration of basic science instruction to 12 months and emphasized group problem solving, while deemphasizing memorization. This has freed up additional time for instruction in the art of caring, leadership, and creativity.
“Hospitalists should acknowledge the value of caring,” Dr. Johnston said. “They do it every day with every patient. It is important today, and will be more important tomorrow.”
Reference
Johnston SC. Anticipating and training the physician of the future: The importance of caring in an age of artificial intelligence. Acad Med. 2018;93(8):1105-6. doi: 10.1097/ACM.0000000000002175.
Remembering the importance of caring
Remembering the importance of caring
As artificial intelligence (AI) takes on more and more tasks in medical care that mimic human cognition, hospitalists and other physicians will need to adapt to a changing role.
Today AI can identify tuberculosis infections in chest radiographs with almost complete accuracy, diagnose melanoma from images of skin lesions more accurately than dermatologists can, and identify metastatic cells in images of lymph node tissue more accurately than pathologists can. The next 20 years are likely to see further acceleration in the capabilities, according to a recent article by S. Claiborne Johnston, MD, PhD.
“AI will change the practice of medicine. The art of medicine, including all the humanistic components, will only become more important over time. As dean of a medical school, I’m training students who will be practicing in 2065,” Dr. Johnston said. “If I’m not thinking about the future, I’m failing my students and the society they will serve.”
The contributions of AI will shift the emphasis for human caregivers to the caring. Studies have shown that the skills of caring are associated with improved patient outcomes, but most medical schools allocate substantial time in the curriculum to memorization and analysis – tasks that will become less demanding as artificial intelligence improves. The art of caring – communication, empathy, shared decision making, leadership, and team building – is usually a minor part of the medical school curriculum.
Effective leadership and creativity are distant aspirations for artificial intelligence but are growing needs in a system of care that is ever more complex.
At Dr. Johnston’s school, the Dell Medical School at the University of Texas at Austin, they have reduced the duration of basic science instruction to 12 months and emphasized group problem solving, while deemphasizing memorization. This has freed up additional time for instruction in the art of caring, leadership, and creativity.
“Hospitalists should acknowledge the value of caring,” Dr. Johnston said. “They do it every day with every patient. It is important today, and will be more important tomorrow.”
Reference
Johnston SC. Anticipating and training the physician of the future: The importance of caring in an age of artificial intelligence. Acad Med. 2018;93(8):1105-6. doi: 10.1097/ACM.0000000000002175.
As artificial intelligence (AI) takes on more and more tasks in medical care that mimic human cognition, hospitalists and other physicians will need to adapt to a changing role.
Today AI can identify tuberculosis infections in chest radiographs with almost complete accuracy, diagnose melanoma from images of skin lesions more accurately than dermatologists can, and identify metastatic cells in images of lymph node tissue more accurately than pathologists can. The next 20 years are likely to see further acceleration in the capabilities, according to a recent article by S. Claiborne Johnston, MD, PhD.
“AI will change the practice of medicine. The art of medicine, including all the humanistic components, will only become more important over time. As dean of a medical school, I’m training students who will be practicing in 2065,” Dr. Johnston said. “If I’m not thinking about the future, I’m failing my students and the society they will serve.”
The contributions of AI will shift the emphasis for human caregivers to the caring. Studies have shown that the skills of caring are associated with improved patient outcomes, but most medical schools allocate substantial time in the curriculum to memorization and analysis – tasks that will become less demanding as artificial intelligence improves. The art of caring – communication, empathy, shared decision making, leadership, and team building – is usually a minor part of the medical school curriculum.
Effective leadership and creativity are distant aspirations for artificial intelligence but are growing needs in a system of care that is ever more complex.
At Dr. Johnston’s school, the Dell Medical School at the University of Texas at Austin, they have reduced the duration of basic science instruction to 12 months and emphasized group problem solving, while deemphasizing memorization. This has freed up additional time for instruction in the art of caring, leadership, and creativity.
“Hospitalists should acknowledge the value of caring,” Dr. Johnston said. “They do it every day with every patient. It is important today, and will be more important tomorrow.”
Reference
Johnston SC. Anticipating and training the physician of the future: The importance of caring in an age of artificial intelligence. Acad Med. 2018;93(8):1105-6. doi: 10.1097/ACM.0000000000002175.
Gender wage gap varies by specialty
There is no specialty in which women physicians make as much as men, but hematology came the closest in 2018, according to a new survey by the medical social network Doximity.
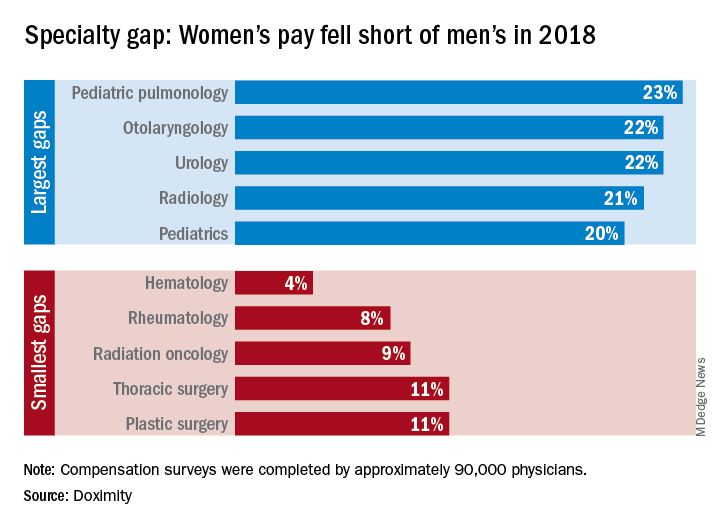
Female hematologists averaged $309,000 in earnings in 2018, just 4% less than their male counterparts, who brought in an average of $323,000. Rheumatology had the next-smallest gap, 8%, between women and men, followed by radiation oncology at 9% and thoracic surgery and plastic surgery at 11% each, Doximity reported March 26. All of the 90,000 physicians involved in the survey worked at least 40 hours per week.
At the other end of the scale is pediatric pulmonology, home of the largest gender wage gap. Average compensation for women in the specialty was $195,000, or 23% less than the $253,000 that men received. Women in otolaryngology and urology were next, earning 22% less than men in those specialties, while women in radiology and pediatrics averaged 21% and 20% less, respectively, than men, Doximity said in its report.
The gender wage gap has been persistent, but the latest data show that it is starting to close as the earnings curve for male physicians flattened in 2018 while pay increased for female physicians.
“Compensation transparency is a powerful force. As more data becomes available to us, exposing the pay gap between men and women, we see more movements to rectify this issue,” said Christopher Whaley, PhD, of the University of California, Berkeley, School of Public Health, who was lead author of the study.
To account for differences in specialty, geography, and physician-specific factors, the Doximity researchers used “a multivariate regression with fixed effects for provider specialty and [metropolitan statistical area].” They also controlled for how long each physician has been in practice and their self-reported average hours worked.
There is no specialty in which women physicians make as much as men, but hematology came the closest in 2018, according to a new survey by the medical social network Doximity.
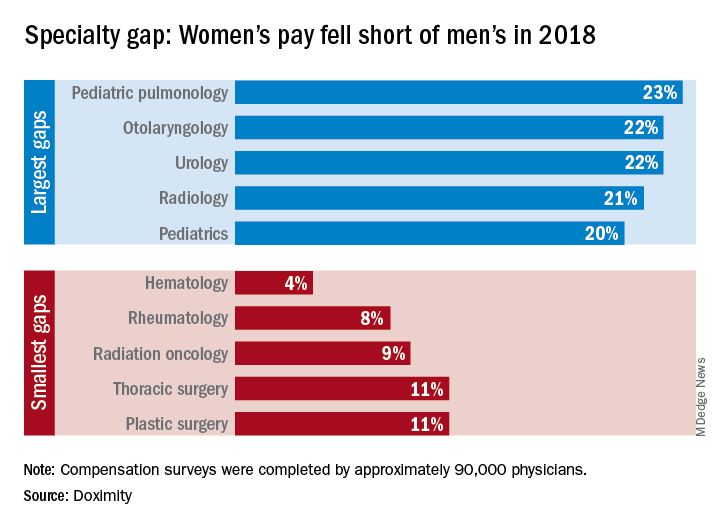
Female hematologists averaged $309,000 in earnings in 2018, just 4% less than their male counterparts, who brought in an average of $323,000. Rheumatology had the next-smallest gap, 8%, between women and men, followed by radiation oncology at 9% and thoracic surgery and plastic surgery at 11% each, Doximity reported March 26. All of the 90,000 physicians involved in the survey worked at least 40 hours per week.
At the other end of the scale is pediatric pulmonology, home of the largest gender wage gap. Average compensation for women in the specialty was $195,000, or 23% less than the $253,000 that men received. Women in otolaryngology and urology were next, earning 22% less than men in those specialties, while women in radiology and pediatrics averaged 21% and 20% less, respectively, than men, Doximity said in its report.
The gender wage gap has been persistent, but the latest data show that it is starting to close as the earnings curve for male physicians flattened in 2018 while pay increased for female physicians.
“Compensation transparency is a powerful force. As more data becomes available to us, exposing the pay gap between men and women, we see more movements to rectify this issue,” said Christopher Whaley, PhD, of the University of California, Berkeley, School of Public Health, who was lead author of the study.
To account for differences in specialty, geography, and physician-specific factors, the Doximity researchers used “a multivariate regression with fixed effects for provider specialty and [metropolitan statistical area].” They also controlled for how long each physician has been in practice and their self-reported average hours worked.
There is no specialty in which women physicians make as much as men, but hematology came the closest in 2018, according to a new survey by the medical social network Doximity.
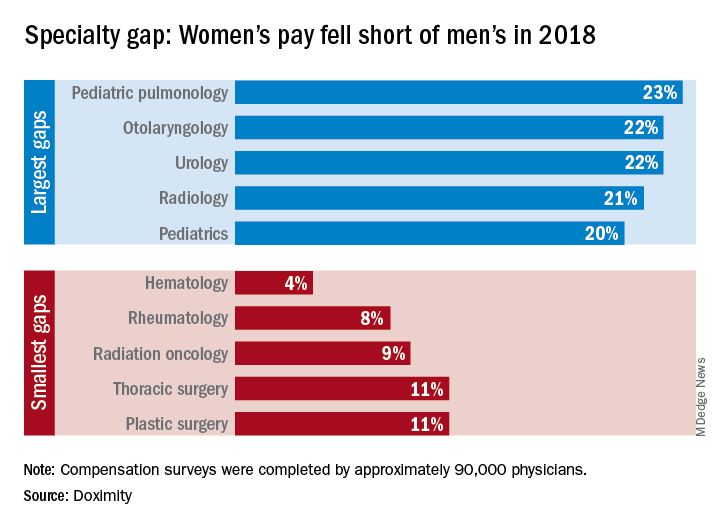
Female hematologists averaged $309,000 in earnings in 2018, just 4% less than their male counterparts, who brought in an average of $323,000. Rheumatology had the next-smallest gap, 8%, between women and men, followed by radiation oncology at 9% and thoracic surgery and plastic surgery at 11% each, Doximity reported March 26. All of the 90,000 physicians involved in the survey worked at least 40 hours per week.
At the other end of the scale is pediatric pulmonology, home of the largest gender wage gap. Average compensation for women in the specialty was $195,000, or 23% less than the $253,000 that men received. Women in otolaryngology and urology were next, earning 22% less than men in those specialties, while women in radiology and pediatrics averaged 21% and 20% less, respectively, than men, Doximity said in its report.
The gender wage gap has been persistent, but the latest data show that it is starting to close as the earnings curve for male physicians flattened in 2018 while pay increased for female physicians.
“Compensation transparency is a powerful force. As more data becomes available to us, exposing the pay gap between men and women, we see more movements to rectify this issue,” said Christopher Whaley, PhD, of the University of California, Berkeley, School of Public Health, who was lead author of the study.
To account for differences in specialty, geography, and physician-specific factors, the Doximity researchers used “a multivariate regression with fixed effects for provider specialty and [metropolitan statistical area].” They also controlled for how long each physician has been in practice and their self-reported average hours worked.
ABIM contests class-action lawsuit, asks judge to dismiss
Attorneys for the American Board of Internal Medicine have asked Judge Robert Kelly of the United States District Court for the Eastern District of Pennsylvania to dismiss a class-action lawsuit against the board’s maintenance of certification (MOC) program.
The legal challenge, filed Dec. 6, 2018, claims that ABIM charges inflated monopoly prices for maintaining certification, that the organization is forcing physicians to purchase MOC, and that ABIM is inducing employers and others to require ABIM certification as a condition of employment.
The four plaintiff-physicians are asking a judge to find ABIM in violation of federal antitrust law and to bar the board from continuing its MOC process. The suit is filed as a class action on behalf of all internists and subspecialists required by ABIM to purchase MOC to maintain their certification. On Jan. 23 of this year, the suit was amended to include racketeering and unjust enrichment claims.
In a motion filed March 18, attorneys for ABIM asserted that the plaintiffs fail to prove that board certification – initial certification and continuing certification – are two separate products that ABIM is unlawfully tying, and for that reason, their antitrust claims are invalid, according to the motion.
“Plaintiffs may disagree with ABIM and members of the medical community on whether ABIM certification provides them value, but their claims have no basis in the law,” Richard J. Baron, MD, ABIM president and CEO said in a statement. “With advances in medical science and technology occurring constantly, periodic assessments are critical to ensure internists are staying current and continuing to meet high performance standards in their field.”
Two other lawsuits challenging MOC, one against the American Board of Psychiatry and Neurology and another against the American Board of Radiology, are ongoing.
More than $200,000 has been raised by doctors and their supporters nationwide through a GoFundMe campaign launched by Practicing Physicians of America to pay for the plaintiffs’ legal costs.
Attorneys for the American Board of Internal Medicine have asked Judge Robert Kelly of the United States District Court for the Eastern District of Pennsylvania to dismiss a class-action lawsuit against the board’s maintenance of certification (MOC) program.
The legal challenge, filed Dec. 6, 2018, claims that ABIM charges inflated monopoly prices for maintaining certification, that the organization is forcing physicians to purchase MOC, and that ABIM is inducing employers and others to require ABIM certification as a condition of employment.
The four plaintiff-physicians are asking a judge to find ABIM in violation of federal antitrust law and to bar the board from continuing its MOC process. The suit is filed as a class action on behalf of all internists and subspecialists required by ABIM to purchase MOC to maintain their certification. On Jan. 23 of this year, the suit was amended to include racketeering and unjust enrichment claims.
In a motion filed March 18, attorneys for ABIM asserted that the plaintiffs fail to prove that board certification – initial certification and continuing certification – are two separate products that ABIM is unlawfully tying, and for that reason, their antitrust claims are invalid, according to the motion.
“Plaintiffs may disagree with ABIM and members of the medical community on whether ABIM certification provides them value, but their claims have no basis in the law,” Richard J. Baron, MD, ABIM president and CEO said in a statement. “With advances in medical science and technology occurring constantly, periodic assessments are critical to ensure internists are staying current and continuing to meet high performance standards in their field.”
Two other lawsuits challenging MOC, one against the American Board of Psychiatry and Neurology and another against the American Board of Radiology, are ongoing.
More than $200,000 has been raised by doctors and their supporters nationwide through a GoFundMe campaign launched by Practicing Physicians of America to pay for the plaintiffs’ legal costs.
Attorneys for the American Board of Internal Medicine have asked Judge Robert Kelly of the United States District Court for the Eastern District of Pennsylvania to dismiss a class-action lawsuit against the board’s maintenance of certification (MOC) program.
The legal challenge, filed Dec. 6, 2018, claims that ABIM charges inflated monopoly prices for maintaining certification, that the organization is forcing physicians to purchase MOC, and that ABIM is inducing employers and others to require ABIM certification as a condition of employment.
The four plaintiff-physicians are asking a judge to find ABIM in violation of federal antitrust law and to bar the board from continuing its MOC process. The suit is filed as a class action on behalf of all internists and subspecialists required by ABIM to purchase MOC to maintain their certification. On Jan. 23 of this year, the suit was amended to include racketeering and unjust enrichment claims.
In a motion filed March 18, attorneys for ABIM asserted that the plaintiffs fail to prove that board certification – initial certification and continuing certification – are two separate products that ABIM is unlawfully tying, and for that reason, their antitrust claims are invalid, according to the motion.
“Plaintiffs may disagree with ABIM and members of the medical community on whether ABIM certification provides them value, but their claims have no basis in the law,” Richard J. Baron, MD, ABIM president and CEO said in a statement. “With advances in medical science and technology occurring constantly, periodic assessments are critical to ensure internists are staying current and continuing to meet high performance standards in their field.”
Two other lawsuits challenging MOC, one against the American Board of Psychiatry and Neurology and another against the American Board of Radiology, are ongoing.
More than $200,000 has been raised by doctors and their supporters nationwide through a GoFundMe campaign launched by Practicing Physicians of America to pay for the plaintiffs’ legal costs.
What’s driving burnout?
Working fewer hours but still struggling
According to a new survey report released by The Physicians Foundation, 80% of physicians across all specialties report being at full capacity or overextended, and 78% reported sometimes, often, or always experiencing feelings of burnout.
Sixty-two percent of U.S. doctors are pessimistic about the future of medicine, and 49% wouldn’t recommend medicine as a career to their children. This paints a pretty grim picture of medical practice in the United States in 2018.
The survey is conducted every other year by The Physicians Foundation with the assistance of Merritt Hawkins, and I wrote a blog post about the 2016 survey results, which showed alarming levels of disengagement and burnout. So, I thought it would be worthwhile looking over the 2018 report to see if anything has improved.
It appears that things haven’t changed much for doctors since 2016 regarding their attitudes toward their work. The biggest take-away from this year’s survey is that doctors overall are working fewer hours and seeing fewer patients but still struggling with morale and burnout. One important trend that was highlighted is the move toward employment by hospitals or integrated delivery systems; only 31% of physicians are independent practice owners or partners, vs. 49% in the first such survey conducted in 2012. Interestingly, employed doctors tend to work longer hours but see fewer patients compared with their practice-owner colleagues.
The 39-question survey is sent out via e-mail to more than 700,000 physicians (everyone the AMA or Merritt Hawkins has in their databases), and this year 8,774 physicians responded; the statistics geniuses at the University of Tennessee say the survey results have a margin of error of +/– 1.057%. Interestingly, that’s less than half of the 17,236 physicians who responded to the survey in 2016, and I wonder if the reduction in response rate itself indicates an increased level of disengagement among doctors.
Doctors expressed similar frustrations with specific aspects of their work this year, compared with 2016. The single biggest frustration cited by doctors was EHRs (39% this year vs. 27% in 2016), followed by regulatory/insurance requirements (down to 38% from 58% in 2016) and loss of clinical autonomy (37% vs. 32% in 2016). Survey respondents reported working an average of 51.4 hours per week, of which 11.4 hours (22%) are spent on nonclinical (paperwork) duties.
Read the full post at hospitalleader.org.
Also on The Hospital Leader
- I don’t want someone like you caring for me by Gopi Astik, MD
- CMS added care transition codes a few years back. How’s that goin’? by Brad Flansbaum, DO, MPH, MHM
- Sleepless in the hospital no more: Lessons learned during the SIESTA Study by Vineet Arora, MD, MAPP, MHM
- Are you committing malpractice by not treating opioid use disorder in the hospital? by Chris Moriates, MD
Working fewer hours but still struggling
Working fewer hours but still struggling
According to a new survey report released by The Physicians Foundation, 80% of physicians across all specialties report being at full capacity or overextended, and 78% reported sometimes, often, or always experiencing feelings of burnout.
Sixty-two percent of U.S. doctors are pessimistic about the future of medicine, and 49% wouldn’t recommend medicine as a career to their children. This paints a pretty grim picture of medical practice in the United States in 2018.
The survey is conducted every other year by The Physicians Foundation with the assistance of Merritt Hawkins, and I wrote a blog post about the 2016 survey results, which showed alarming levels of disengagement and burnout. So, I thought it would be worthwhile looking over the 2018 report to see if anything has improved.
It appears that things haven’t changed much for doctors since 2016 regarding their attitudes toward their work. The biggest take-away from this year’s survey is that doctors overall are working fewer hours and seeing fewer patients but still struggling with morale and burnout. One important trend that was highlighted is the move toward employment by hospitals or integrated delivery systems; only 31% of physicians are independent practice owners or partners, vs. 49% in the first such survey conducted in 2012. Interestingly, employed doctors tend to work longer hours but see fewer patients compared with their practice-owner colleagues.
The 39-question survey is sent out via e-mail to more than 700,000 physicians (everyone the AMA or Merritt Hawkins has in their databases), and this year 8,774 physicians responded; the statistics geniuses at the University of Tennessee say the survey results have a margin of error of +/– 1.057%. Interestingly, that’s less than half of the 17,236 physicians who responded to the survey in 2016, and I wonder if the reduction in response rate itself indicates an increased level of disengagement among doctors.
Doctors expressed similar frustrations with specific aspects of their work this year, compared with 2016. The single biggest frustration cited by doctors was EHRs (39% this year vs. 27% in 2016), followed by regulatory/insurance requirements (down to 38% from 58% in 2016) and loss of clinical autonomy (37% vs. 32% in 2016). Survey respondents reported working an average of 51.4 hours per week, of which 11.4 hours (22%) are spent on nonclinical (paperwork) duties.
Read the full post at hospitalleader.org.
Also on The Hospital Leader
- I don’t want someone like you caring for me by Gopi Astik, MD
- CMS added care transition codes a few years back. How’s that goin’? by Brad Flansbaum, DO, MPH, MHM
- Sleepless in the hospital no more: Lessons learned during the SIESTA Study by Vineet Arora, MD, MAPP, MHM
- Are you committing malpractice by not treating opioid use disorder in the hospital? by Chris Moriates, MD
According to a new survey report released by The Physicians Foundation, 80% of physicians across all specialties report being at full capacity or overextended, and 78% reported sometimes, often, or always experiencing feelings of burnout.
Sixty-two percent of U.S. doctors are pessimistic about the future of medicine, and 49% wouldn’t recommend medicine as a career to their children. This paints a pretty grim picture of medical practice in the United States in 2018.
The survey is conducted every other year by The Physicians Foundation with the assistance of Merritt Hawkins, and I wrote a blog post about the 2016 survey results, which showed alarming levels of disengagement and burnout. So, I thought it would be worthwhile looking over the 2018 report to see if anything has improved.
It appears that things haven’t changed much for doctors since 2016 regarding their attitudes toward their work. The biggest take-away from this year’s survey is that doctors overall are working fewer hours and seeing fewer patients but still struggling with morale and burnout. One important trend that was highlighted is the move toward employment by hospitals or integrated delivery systems; only 31% of physicians are independent practice owners or partners, vs. 49% in the first such survey conducted in 2012. Interestingly, employed doctors tend to work longer hours but see fewer patients compared with their practice-owner colleagues.
The 39-question survey is sent out via e-mail to more than 700,000 physicians (everyone the AMA or Merritt Hawkins has in their databases), and this year 8,774 physicians responded; the statistics geniuses at the University of Tennessee say the survey results have a margin of error of +/– 1.057%. Interestingly, that’s less than half of the 17,236 physicians who responded to the survey in 2016, and I wonder if the reduction in response rate itself indicates an increased level of disengagement among doctors.
Doctors expressed similar frustrations with specific aspects of their work this year, compared with 2016. The single biggest frustration cited by doctors was EHRs (39% this year vs. 27% in 2016), followed by regulatory/insurance requirements (down to 38% from 58% in 2016) and loss of clinical autonomy (37% vs. 32% in 2016). Survey respondents reported working an average of 51.4 hours per week, of which 11.4 hours (22%) are spent on nonclinical (paperwork) duties.
Read the full post at hospitalleader.org.
Also on The Hospital Leader
- I don’t want someone like you caring for me by Gopi Astik, MD
- CMS added care transition codes a few years back. How’s that goin’? by Brad Flansbaum, DO, MPH, MHM
- Sleepless in the hospital no more: Lessons learned during the SIESTA Study by Vineet Arora, MD, MAPP, MHM
- Are you committing malpractice by not treating opioid use disorder in the hospital? by Chris Moriates, MD
Hospitalist movers and shakers – March 2019
Flora Kisuule, MD, SFHM, has been awarded the 2018 Excellence in Service and Professionalism Award by Johns Hopkins Bayview Medical Center, Baltimore. Dr. Kisuule is associate director of the division of hospital medicine at Johns Hopkins Bayview, assistant professor at Johns Hopkins University School of Medicine, and assistant professor in the Johns Hopkins Bloomberg School of Public Health.
Dr. Kisuule codeveloped a hospitalist fellowship program for Johns Hopkins University, which she now directs. She has served on several Society of Hospital Medicine committees and consulted on hospitalist programs around the world. Dr. Kisuule is joining the SHM Board of Directors in March 2019.
Paul Hain, DO, was promoted recently to chief medical officer and senior vice president of market delivery for Blue Cross/Blue Shield of Texas. Dr. Hain has a wealth of experience in leadership, including helping create the pediatric hospitalist program at Vanderbilt Children’s Hospital in Nashville, Tenn.
With BC/BS, Dr. Hain will oversee the region’s public relations, community investments, government relations, and lobbying. He will help sponsor Medicare and Medicaid in the state, while also supporting enterprise and marketing efforts. Dr. Hain joins BC/BS after serving as vice president and medical director of population health and network development at the Children’s Medical Center of Dallas.
Laura M. Rosch, DO, recently was selected by Kansas City University as the new campus dean in the Joplin (Mo.) College of Osteopathic Medicine. Dr. Rosch is a practicing hospitalist in Illinois, where she was chair of internal medicine at the Chicago College of Osteopathic Medicine prior to taking her current position.
Dr. Rosch will manage daily operations for the Joplin medical school, streamlining the school with the main campus. She is a former president of the Illinois Osteopathic Medicine Society and holds a master’s degree in nutrition science.
Suzan Lowry, MD, has been named health officer for Charles County, Md., by the county Department of Health and Charles County Commissioners. A longtime pediatrician with 20 years’ experience, Dr. Lowry has served as a pediatric hospitalist educator at Children’s National Medical Center in Washington, D.C.
Dr. Lowry has spent a majority of her career working on behalf of public health. Most recently, she has worked at the United States Marine Corps Quantico Health Clinic in Virginia.
Robyn Chase, DO, a staff hospitalist at Yavapai Regional Medical Center (Prescott, Ariz.), recently was selected as the hospital’s Physician of the Year for 2018.
Dr. Chase has practiced at YRMC since 2010 and is a board-certified internist. She also serves as an associate professor at the University of Arizona, Phoenix.
Kevin Dishman, MD, has been elevated to senior vice president and chief medical officer at Stormont Vail Health (Topeka, Kan.). Dr. Dishman also will be president of Stormont medical services division’s medical staff.
Dr. Dishman came to Stormont in 2000 to work as a hospitalist. Most recently, he has served as the center’s vice president of acute care services. In his new role, Dr. Dishman will be charged with, among other duties, seeking out physicians to bring to Stormont’s Topeka location.
BUSINESS MOVES
The Hazel Hawkins Memorial Hospital Women’s Center (Hollister, Calif.) recently established a relationship with Pediatrix Medical Group (Sunrise, Fla.) to provide pediatric hospitalists to help with high-risk delivery of newborns. The hospitalists also will advise Hazel Hawkins staff with regards to critical care transport and assist with the care of newborns and the treatment of child and teen patients.
Hazel Hawkins has been in operation for the past 5 years. Pediatrix hospitalists will be used as consultants for attending staff and emergency physicians and will help treat patients in emergency situations.
American Physician Partners (Brentwood, Tenn.), a national hospital medicine management services company, has acquired private physician group Progressive Medical Associates (Mesa, Ariz.). Progressive’s 37 physicians and 21 private clinicians – working at Banner Health’s 28 nonprofit hospitals covering six states – join the APP team.
Flora Kisuule, MD, SFHM, has been awarded the 2018 Excellence in Service and Professionalism Award by Johns Hopkins Bayview Medical Center, Baltimore. Dr. Kisuule is associate director of the division of hospital medicine at Johns Hopkins Bayview, assistant professor at Johns Hopkins University School of Medicine, and assistant professor in the Johns Hopkins Bloomberg School of Public Health.
Dr. Kisuule codeveloped a hospitalist fellowship program for Johns Hopkins University, which she now directs. She has served on several Society of Hospital Medicine committees and consulted on hospitalist programs around the world. Dr. Kisuule is joining the SHM Board of Directors in March 2019.
Paul Hain, DO, was promoted recently to chief medical officer and senior vice president of market delivery for Blue Cross/Blue Shield of Texas. Dr. Hain has a wealth of experience in leadership, including helping create the pediatric hospitalist program at Vanderbilt Children’s Hospital in Nashville, Tenn.
With BC/BS, Dr. Hain will oversee the region’s public relations, community investments, government relations, and lobbying. He will help sponsor Medicare and Medicaid in the state, while also supporting enterprise and marketing efforts. Dr. Hain joins BC/BS after serving as vice president and medical director of population health and network development at the Children’s Medical Center of Dallas.
Laura M. Rosch, DO, recently was selected by Kansas City University as the new campus dean in the Joplin (Mo.) College of Osteopathic Medicine. Dr. Rosch is a practicing hospitalist in Illinois, where she was chair of internal medicine at the Chicago College of Osteopathic Medicine prior to taking her current position.
Dr. Rosch will manage daily operations for the Joplin medical school, streamlining the school with the main campus. She is a former president of the Illinois Osteopathic Medicine Society and holds a master’s degree in nutrition science.
Suzan Lowry, MD, has been named health officer for Charles County, Md., by the county Department of Health and Charles County Commissioners. A longtime pediatrician with 20 years’ experience, Dr. Lowry has served as a pediatric hospitalist educator at Children’s National Medical Center in Washington, D.C.
Dr. Lowry has spent a majority of her career working on behalf of public health. Most recently, she has worked at the United States Marine Corps Quantico Health Clinic in Virginia.
Robyn Chase, DO, a staff hospitalist at Yavapai Regional Medical Center (Prescott, Ariz.), recently was selected as the hospital’s Physician of the Year for 2018.
Dr. Chase has practiced at YRMC since 2010 and is a board-certified internist. She also serves as an associate professor at the University of Arizona, Phoenix.
Kevin Dishman, MD, has been elevated to senior vice president and chief medical officer at Stormont Vail Health (Topeka, Kan.). Dr. Dishman also will be president of Stormont medical services division’s medical staff.
Dr. Dishman came to Stormont in 2000 to work as a hospitalist. Most recently, he has served as the center’s vice president of acute care services. In his new role, Dr. Dishman will be charged with, among other duties, seeking out physicians to bring to Stormont’s Topeka location.
BUSINESS MOVES
The Hazel Hawkins Memorial Hospital Women’s Center (Hollister, Calif.) recently established a relationship with Pediatrix Medical Group (Sunrise, Fla.) to provide pediatric hospitalists to help with high-risk delivery of newborns. The hospitalists also will advise Hazel Hawkins staff with regards to critical care transport and assist with the care of newborns and the treatment of child and teen patients.
Hazel Hawkins has been in operation for the past 5 years. Pediatrix hospitalists will be used as consultants for attending staff and emergency physicians and will help treat patients in emergency situations.
American Physician Partners (Brentwood, Tenn.), a national hospital medicine management services company, has acquired private physician group Progressive Medical Associates (Mesa, Ariz.). Progressive’s 37 physicians and 21 private clinicians – working at Banner Health’s 28 nonprofit hospitals covering six states – join the APP team.
Flora Kisuule, MD, SFHM, has been awarded the 2018 Excellence in Service and Professionalism Award by Johns Hopkins Bayview Medical Center, Baltimore. Dr. Kisuule is associate director of the division of hospital medicine at Johns Hopkins Bayview, assistant professor at Johns Hopkins University School of Medicine, and assistant professor in the Johns Hopkins Bloomberg School of Public Health.
Dr. Kisuule codeveloped a hospitalist fellowship program for Johns Hopkins University, which she now directs. She has served on several Society of Hospital Medicine committees and consulted on hospitalist programs around the world. Dr. Kisuule is joining the SHM Board of Directors in March 2019.
Paul Hain, DO, was promoted recently to chief medical officer and senior vice president of market delivery for Blue Cross/Blue Shield of Texas. Dr. Hain has a wealth of experience in leadership, including helping create the pediatric hospitalist program at Vanderbilt Children’s Hospital in Nashville, Tenn.
With BC/BS, Dr. Hain will oversee the region’s public relations, community investments, government relations, and lobbying. He will help sponsor Medicare and Medicaid in the state, while also supporting enterprise and marketing efforts. Dr. Hain joins BC/BS after serving as vice president and medical director of population health and network development at the Children’s Medical Center of Dallas.
Laura M. Rosch, DO, recently was selected by Kansas City University as the new campus dean in the Joplin (Mo.) College of Osteopathic Medicine. Dr. Rosch is a practicing hospitalist in Illinois, where she was chair of internal medicine at the Chicago College of Osteopathic Medicine prior to taking her current position.
Dr. Rosch will manage daily operations for the Joplin medical school, streamlining the school with the main campus. She is a former president of the Illinois Osteopathic Medicine Society and holds a master’s degree in nutrition science.
Suzan Lowry, MD, has been named health officer for Charles County, Md., by the county Department of Health and Charles County Commissioners. A longtime pediatrician with 20 years’ experience, Dr. Lowry has served as a pediatric hospitalist educator at Children’s National Medical Center in Washington, D.C.
Dr. Lowry has spent a majority of her career working on behalf of public health. Most recently, she has worked at the United States Marine Corps Quantico Health Clinic in Virginia.
Robyn Chase, DO, a staff hospitalist at Yavapai Regional Medical Center (Prescott, Ariz.), recently was selected as the hospital’s Physician of the Year for 2018.
Dr. Chase has practiced at YRMC since 2010 and is a board-certified internist. She also serves as an associate professor at the University of Arizona, Phoenix.
Kevin Dishman, MD, has been elevated to senior vice president and chief medical officer at Stormont Vail Health (Topeka, Kan.). Dr. Dishman also will be president of Stormont medical services division’s medical staff.
Dr. Dishman came to Stormont in 2000 to work as a hospitalist. Most recently, he has served as the center’s vice president of acute care services. In his new role, Dr. Dishman will be charged with, among other duties, seeking out physicians to bring to Stormont’s Topeka location.
BUSINESS MOVES
The Hazel Hawkins Memorial Hospital Women’s Center (Hollister, Calif.) recently established a relationship with Pediatrix Medical Group (Sunrise, Fla.) to provide pediatric hospitalists to help with high-risk delivery of newborns. The hospitalists also will advise Hazel Hawkins staff with regards to critical care transport and assist with the care of newborns and the treatment of child and teen patients.
Hazel Hawkins has been in operation for the past 5 years. Pediatrix hospitalists will be used as consultants for attending staff and emergency physicians and will help treat patients in emergency situations.
American Physician Partners (Brentwood, Tenn.), a national hospital medicine management services company, has acquired private physician group Progressive Medical Associates (Mesa, Ariz.). Progressive’s 37 physicians and 21 private clinicians – working at Banner Health’s 28 nonprofit hospitals covering six states – join the APP team.
Advancing coherence: Your “meta-leadership” objective
Learn to balance organizational priorities
For the many people who expect you to lead, your role – among others – is to create coherence. That coherence characterizes the logic and consistency of what you do in your organization. It assembles the individual work of many different people into a whole that functions well. Coherence in your workplace helps people make sense of what they are doing and why it matters.
Our very rational brain craves coherence. We assemble facts, emotions, ambitions and our life stories into narratives that define who we are, what we are doing, and why it is important. An effective organizational “metaleader” encourages that process for followers. It helps people make sense of the work side of their life.
When coherence is absent, the workplace is riddled with contradictions, unpredictability, and dissonance. People are expected to accomplish tasks for which the time, tools, and talent are missing. There is a perplexed swirl of high activity and low productivity. Expectations for high quality of care and patient satisfaction are contradicted by an overbearing workload, reams of paper work, and the low morale that leaves the work force lethargic. “What we are doing here and how we are doing it doesn’t make sense,” exemplifies the exasperation of working amid incoherence. The department does not drive together toward success-oriented performance. Instead, different people, priorities, and opportunities will be positioned in conflict with one another. For people in your group and those surrounding it, morale and motivation suffer. There is the risk that people will descend into malaise.
Creating coherence is a complex metaleadership process. A large health care center is a cacophony of priorities, of which advancing quality of care is but one. There are other objectives, some contradictory, that also absorb time and attention: achievement of financial benchmarks, promotion of professional careers, and the individual hopes and desires of patients. Systematically aligning those many priorities and objectives is a process of both design and leadership.
The metaleadership model is a strategy for building coherence amid the complexity of health care operations. For those unfamiliar with metaleadership: The prefix “meta-” refers to a wider perspective on what is happening, the people involved, and the overall combination of objectives. The three dimensions of practice are: 1) the Person of the metaleader – your own priorities, values and emotional intelligence; 2) the Situation – what is happening and what ought to be done about it; and 3) Connectivity of Effort, which leads down to subordinates, up to bosses, across to other internal departments, and beyond to external organizations and professionals.
In building connectivity of effort, the metaleader links the many sides of the work being accomplished. The intent is to balance – purposefully – different organizational objectives into a combined whole that gets the jobs done. Furthermore, that coherence links and adapts what people are doing to the situation at hand. And in essence, the person of the leader cannot lead broader coherence if not coherent in her or his own thinking, attitudes, and behaviors, so achievement of personal and professional clarity of purpose is important.
The question for you: How do you as a hospitalist leader create coherence in what you are leading given the changing priorities, actions, and turbulence of current health policy and the market?
The answers lie in the communication you foster and clarify. That communication demands clarity and diplomacy. It is multidirectional such that messages and information in your leading down, up, across, and beyond complement and inform one another.
An illustration of one pathway: You learn from senior management about cuts in the budget. You reflect with them on the choices implicit in those cuts. Perhaps there are better ways to reduce expenditures and increase revenues that offer an alternative pathway to a balanced budget? When communicating with your subordinates, you open conversation on ways to enhance efficiencies and assure quality. You explore avenues to partner with other departments within your institution on how you can link and leverage services and capabilities. And you consider your marketplace and the actions you can take to reinforce your department and assure the volume necessary to achieve budget and quality objectives. And through it all, you monitor the situation. What are the effects of the budget adjustments, and what can be done to sustain the coherence of the work and output of the department? It is a leadership process of constant situational awareness, personal commitment, and connectivity of effort.
An illustration of another pathway: Resist the change and argue forcefully for holding onto the current budget and workforce. Though you do not possess the authority to control larger budgetary decisions, you employ influence well beyond your authority. You recruit allies to your cause, advocates who believe in the purpose you are promoting. You build an alternative coherence, mindful of fostering friendship and minimizing alienation. You are recognized for the passion of your professional commitment and your capacity to uphold quality care and organizational balance.
Two very different pathways to crafting coherence. Leaders of each perceive their actions to advance priority coherence objectives. Apply this question to your own complex problem solving.
Metaleaders forge coherence through the narratives they build and the consistency with those themes and priorities. When everyone on your staff, from physicians to housekeeping personnel, can say “I am here to help save lives,” you know that your followers are on board with a shared mission. They recognize that their efforts contribute to that overall mission. Each person has a role to play, and her or his work fits with the efforts of others, and the bottom line accomplishments of the department.
The coherence you forge assists your followers to make sense of what they are doing and how it fits what others are doing. Work is fulfilling. Beyond that, in a turbulent health care system, you anticipate both problems and opportunities with strategies to meet them. You stay ahead of the game to ensure that people within and outside the department are aligned to maximize opportunities for success.
This is particularly important for the hospitalist. Your job is to fashion coherence on many levels. First, coherent patient care for the patient. Second, coherent interactions among professionals. Finally, organizational coherence, so one piece of the puzzle fits with others. And, when there is a need to recalculate, you adapt and develop solutions that fit the people and situation at hand.
Dr. Marcus is coauthor of Renegotiating Health Care: Resolving Conflict to Build Collaboration, Second Edition (San Francisco: Jossey-Bass Publishers, 2011) and is Director of the Program for Health Care Negotiation and Conflict Resolution, Harvard T.H. Chan School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected].
Learn to balance organizational priorities
Learn to balance organizational priorities
For the many people who expect you to lead, your role – among others – is to create coherence. That coherence characterizes the logic and consistency of what you do in your organization. It assembles the individual work of many different people into a whole that functions well. Coherence in your workplace helps people make sense of what they are doing and why it matters.
Our very rational brain craves coherence. We assemble facts, emotions, ambitions and our life stories into narratives that define who we are, what we are doing, and why it is important. An effective organizational “metaleader” encourages that process for followers. It helps people make sense of the work side of their life.
When coherence is absent, the workplace is riddled with contradictions, unpredictability, and dissonance. People are expected to accomplish tasks for which the time, tools, and talent are missing. There is a perplexed swirl of high activity and low productivity. Expectations for high quality of care and patient satisfaction are contradicted by an overbearing workload, reams of paper work, and the low morale that leaves the work force lethargic. “What we are doing here and how we are doing it doesn’t make sense,” exemplifies the exasperation of working amid incoherence. The department does not drive together toward success-oriented performance. Instead, different people, priorities, and opportunities will be positioned in conflict with one another. For people in your group and those surrounding it, morale and motivation suffer. There is the risk that people will descend into malaise.
Creating coherence is a complex metaleadership process. A large health care center is a cacophony of priorities, of which advancing quality of care is but one. There are other objectives, some contradictory, that also absorb time and attention: achievement of financial benchmarks, promotion of professional careers, and the individual hopes and desires of patients. Systematically aligning those many priorities and objectives is a process of both design and leadership.
The metaleadership model is a strategy for building coherence amid the complexity of health care operations. For those unfamiliar with metaleadership: The prefix “meta-” refers to a wider perspective on what is happening, the people involved, and the overall combination of objectives. The three dimensions of practice are: 1) the Person of the metaleader – your own priorities, values and emotional intelligence; 2) the Situation – what is happening and what ought to be done about it; and 3) Connectivity of Effort, which leads down to subordinates, up to bosses, across to other internal departments, and beyond to external organizations and professionals.
In building connectivity of effort, the metaleader links the many sides of the work being accomplished. The intent is to balance – purposefully – different organizational objectives into a combined whole that gets the jobs done. Furthermore, that coherence links and adapts what people are doing to the situation at hand. And in essence, the person of the leader cannot lead broader coherence if not coherent in her or his own thinking, attitudes, and behaviors, so achievement of personal and professional clarity of purpose is important.
The question for you: How do you as a hospitalist leader create coherence in what you are leading given the changing priorities, actions, and turbulence of current health policy and the market?
The answers lie in the communication you foster and clarify. That communication demands clarity and diplomacy. It is multidirectional such that messages and information in your leading down, up, across, and beyond complement and inform one another.
An illustration of one pathway: You learn from senior management about cuts in the budget. You reflect with them on the choices implicit in those cuts. Perhaps there are better ways to reduce expenditures and increase revenues that offer an alternative pathway to a balanced budget? When communicating with your subordinates, you open conversation on ways to enhance efficiencies and assure quality. You explore avenues to partner with other departments within your institution on how you can link and leverage services and capabilities. And you consider your marketplace and the actions you can take to reinforce your department and assure the volume necessary to achieve budget and quality objectives. And through it all, you monitor the situation. What are the effects of the budget adjustments, and what can be done to sustain the coherence of the work and output of the department? It is a leadership process of constant situational awareness, personal commitment, and connectivity of effort.
An illustration of another pathway: Resist the change and argue forcefully for holding onto the current budget and workforce. Though you do not possess the authority to control larger budgetary decisions, you employ influence well beyond your authority. You recruit allies to your cause, advocates who believe in the purpose you are promoting. You build an alternative coherence, mindful of fostering friendship and minimizing alienation. You are recognized for the passion of your professional commitment and your capacity to uphold quality care and organizational balance.
Two very different pathways to crafting coherence. Leaders of each perceive their actions to advance priority coherence objectives. Apply this question to your own complex problem solving.
Metaleaders forge coherence through the narratives they build and the consistency with those themes and priorities. When everyone on your staff, from physicians to housekeeping personnel, can say “I am here to help save lives,” you know that your followers are on board with a shared mission. They recognize that their efforts contribute to that overall mission. Each person has a role to play, and her or his work fits with the efforts of others, and the bottom line accomplishments of the department.
The coherence you forge assists your followers to make sense of what they are doing and how it fits what others are doing. Work is fulfilling. Beyond that, in a turbulent health care system, you anticipate both problems and opportunities with strategies to meet them. You stay ahead of the game to ensure that people within and outside the department are aligned to maximize opportunities for success.
This is particularly important for the hospitalist. Your job is to fashion coherence on many levels. First, coherent patient care for the patient. Second, coherent interactions among professionals. Finally, organizational coherence, so one piece of the puzzle fits with others. And, when there is a need to recalculate, you adapt and develop solutions that fit the people and situation at hand.
Dr. Marcus is coauthor of Renegotiating Health Care: Resolving Conflict to Build Collaboration, Second Edition (San Francisco: Jossey-Bass Publishers, 2011) and is Director of the Program for Health Care Negotiation and Conflict Resolution, Harvard T.H. Chan School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected].
For the many people who expect you to lead, your role – among others – is to create coherence. That coherence characterizes the logic and consistency of what you do in your organization. It assembles the individual work of many different people into a whole that functions well. Coherence in your workplace helps people make sense of what they are doing and why it matters.
Our very rational brain craves coherence. We assemble facts, emotions, ambitions and our life stories into narratives that define who we are, what we are doing, and why it is important. An effective organizational “metaleader” encourages that process for followers. It helps people make sense of the work side of their life.
When coherence is absent, the workplace is riddled with contradictions, unpredictability, and dissonance. People are expected to accomplish tasks for which the time, tools, and talent are missing. There is a perplexed swirl of high activity and low productivity. Expectations for high quality of care and patient satisfaction are contradicted by an overbearing workload, reams of paper work, and the low morale that leaves the work force lethargic. “What we are doing here and how we are doing it doesn’t make sense,” exemplifies the exasperation of working amid incoherence. The department does not drive together toward success-oriented performance. Instead, different people, priorities, and opportunities will be positioned in conflict with one another. For people in your group and those surrounding it, morale and motivation suffer. There is the risk that people will descend into malaise.
Creating coherence is a complex metaleadership process. A large health care center is a cacophony of priorities, of which advancing quality of care is but one. There are other objectives, some contradictory, that also absorb time and attention: achievement of financial benchmarks, promotion of professional careers, and the individual hopes and desires of patients. Systematically aligning those many priorities and objectives is a process of both design and leadership.
The metaleadership model is a strategy for building coherence amid the complexity of health care operations. For those unfamiliar with metaleadership: The prefix “meta-” refers to a wider perspective on what is happening, the people involved, and the overall combination of objectives. The three dimensions of practice are: 1) the Person of the metaleader – your own priorities, values and emotional intelligence; 2) the Situation – what is happening and what ought to be done about it; and 3) Connectivity of Effort, which leads down to subordinates, up to bosses, across to other internal departments, and beyond to external organizations and professionals.
In building connectivity of effort, the metaleader links the many sides of the work being accomplished. The intent is to balance – purposefully – different organizational objectives into a combined whole that gets the jobs done. Furthermore, that coherence links and adapts what people are doing to the situation at hand. And in essence, the person of the leader cannot lead broader coherence if not coherent in her or his own thinking, attitudes, and behaviors, so achievement of personal and professional clarity of purpose is important.
The question for you: How do you as a hospitalist leader create coherence in what you are leading given the changing priorities, actions, and turbulence of current health policy and the market?
The answers lie in the communication you foster and clarify. That communication demands clarity and diplomacy. It is multidirectional such that messages and information in your leading down, up, across, and beyond complement and inform one another.
An illustration of one pathway: You learn from senior management about cuts in the budget. You reflect with them on the choices implicit in those cuts. Perhaps there are better ways to reduce expenditures and increase revenues that offer an alternative pathway to a balanced budget? When communicating with your subordinates, you open conversation on ways to enhance efficiencies and assure quality. You explore avenues to partner with other departments within your institution on how you can link and leverage services and capabilities. And you consider your marketplace and the actions you can take to reinforce your department and assure the volume necessary to achieve budget and quality objectives. And through it all, you monitor the situation. What are the effects of the budget adjustments, and what can be done to sustain the coherence of the work and output of the department? It is a leadership process of constant situational awareness, personal commitment, and connectivity of effort.
An illustration of another pathway: Resist the change and argue forcefully for holding onto the current budget and workforce. Though you do not possess the authority to control larger budgetary decisions, you employ influence well beyond your authority. You recruit allies to your cause, advocates who believe in the purpose you are promoting. You build an alternative coherence, mindful of fostering friendship and minimizing alienation. You are recognized for the passion of your professional commitment and your capacity to uphold quality care and organizational balance.
Two very different pathways to crafting coherence. Leaders of each perceive their actions to advance priority coherence objectives. Apply this question to your own complex problem solving.
Metaleaders forge coherence through the narratives they build and the consistency with those themes and priorities. When everyone on your staff, from physicians to housekeeping personnel, can say “I am here to help save lives,” you know that your followers are on board with a shared mission. They recognize that their efforts contribute to that overall mission. Each person has a role to play, and her or his work fits with the efforts of others, and the bottom line accomplishments of the department.
The coherence you forge assists your followers to make sense of what they are doing and how it fits what others are doing. Work is fulfilling. Beyond that, in a turbulent health care system, you anticipate both problems and opportunities with strategies to meet them. You stay ahead of the game to ensure that people within and outside the department are aligned to maximize opportunities for success.
This is particularly important for the hospitalist. Your job is to fashion coherence on many levels. First, coherent patient care for the patient. Second, coherent interactions among professionals. Finally, organizational coherence, so one piece of the puzzle fits with others. And, when there is a need to recalculate, you adapt and develop solutions that fit the people and situation at hand.
Dr. Marcus is coauthor of Renegotiating Health Care: Resolving Conflict to Build Collaboration, Second Edition (San Francisco: Jossey-Bass Publishers, 2011) and is Director of the Program for Health Care Negotiation and Conflict Resolution, Harvard T.H. Chan School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected].
Final ‘Vision’ report addresses MOC woes
Whatever you do, change the name.
That was key among the final recommendations the Vision Initiative Commission submitted to the American Board of Medical Specialties on how to improve the maintenance of certification process.
“A new term that communicates the concept, intent, and expectations of continuing certification programs should be adopted by the ABMS in order to reengage disaffected diplomates and assure the public and other stakeholders that the certificate has enduring meaning and value,” according to the final report. A new term was not suggested.
The commission recommended a continuing certification system with four aims:
- Become a meaningful, contemporary, and relevant professional development activity for diplomates that ensures they remain up-to-date in their specialty.
- Demonstrate a commitment to professional self-regulation to both diplomates and the public.
- Align with international and national standards for certification programs.
- Provide a specialty-based credential that would be of value to diplomates and to multiple stakeholders, including patients, families, the public, and health care institutions.
Testing methods and situations must be simplified and updated, according to the report, which was submitted to ABMS on Feb. 12. Continuing certification “must change to incorporate longitudinal and other innovative formative assessment strategies that support learning, identify knowledge and skills gaps, and help diplomates stay current. The ABMS Boards must offer an alternative to burdensome highly secure, point-in-time examinations of knowledge.” In addition, the boards “must no longer use a single point-in-time examination or a series of single point-in-time assessments as the sole method to determine certification status.”
Instead, the commission recommends that ABMS “move quickly to formative assessment formats that are not characterized by high-stakes summative outcomes (pass/fail), specified time frames for high-stakes assessment, or require burdensome testing formats (such as testing centers or remote proctoring) that are inconsistent with the desired goals for continuing certification – support learning; identify knowledge and skills gaps; and help diplomates stay current.”
The commission also defined how the certification process should be used by other stakeholders.
“ABMS must demonstrate and communicate that continuing certification has value, meaning, and purpose in the health care environment,” the report states. “Hospitals, health systems, payers, and other health care organizations can independently decide what factors are used in credentialing and privileging decisions. ABMS must inform these organizations that continuing certification should not be the only criterion used in these decisions, and these organizations should use a wide portfolio of criteria in these decisions. ABMS must encourage hospitals, health systems, payers, and other health care organizations to not deny credentialing or privileging to a physician solely on the basis of certification status.”
Additionally, the commission report states that “ABMS and the ABMS Boards should collaborate with specialty societies, the [continuing medical education/continuing professional development] community, and other expert stakeholders to develop the infrastructure to support learning activities that produce data-driven advances in clinical practice. The ABMS Boards must ensure that their continuing certification programs recognize and document participation in a wide range of quality assessment activities in which diplomates already engage.”
The report adds that the boards “should readily accept existing activities that diplomates are doing to advance their clinical practice and to provide credit for performing low-resource, high-impact activities as part of their daily practice routine.”
The commission’s final report incorporates a number of changes that physicians offered based on a draft version of the report.
The American College of Physicians commented that it “objects to the use of data regarding quality measures for individual diplomate certification status, because physician-level measures of quality are flawed, and because physician-level data inevitably leads to physician-level documentation burden. Flawed performance measures also often inadequately adjust for patient comorbidities and socioeconomic status, which leads to assessments that do not reflect the actual quality of care.”
Similarly, the American Society of Hematology noted in a statement that it “disagrees with the commission’s recommendation to retain the reporting of practice improvement activities as part of continuous certification due to direct and indirect costs needed to fulfill this requirement on top of requirements for engagement in quality improvement mandated by insurers, institutions, and health systems.”
While the draft report recommended that specialty boards provide aggregated feedback to medical societies, a more individualized dissemination on the gaps in knowledge would be more helpful, according to Doug Henley, MD, CEO of the American Academy of Family Physicians, who said that a more individualized approach would help his organization better provide CME to its members to help fill in the knowledge gaps.
“If we can identify these and use other processes and then target at the individual level to seek improvement, I think that will be a better outcome rather than just x learners don’t do well in diabetic care,” he said in an interview. “That doesn’t really help me in terms of who needs the real education in diabetic care versus who needs it for heart failure.”
The final recommendation notes that ABMS member boards “must collaborate with professional and/or CME/CPD organizations to share data and information to guide and support diplomate engagement in continuing certification.”
The document further clarifies that the boards should examine “the aggregated results from assessments to identify knowledge, skills, and other competency gaps,” and the aggregated data should be shared with specialty societies, CME/CPD providers, quality improvement professionals, and other health care organizations.
One weakness in the draft noted by Dr. Henley was the lack of a more forceful tone within the recommendations. Even though AMBS is not bound by its recommendations, he said that he would like to see stronger language throughout the document.
“We would certainly hope that the ABMS and the member boards will follow the direction of the Vision Commission very directly and succinctly,” he said. “That is why we suggested that some of the recommendations from the Vision Commission should use words like ‘should’ and ‘must’ and not just ‘encourage’ and words like that.”
That recommendation was taken and implemented in the final document.
Societies differed in how often participation in the certification process should occur.
The American College of Rheumatology in its comments challenged a recommendation that certification should be structured to expect participation on an annual basis.
“The ACR supports the importance of ongoing learning,” it stated. “However, no discussion is provided as to how and why the recommendation for annual participation by diplomates was conceived. For some ABMS Boards, an annual requirement will increase physician burden unless continuing certification is modified to a formative pathway. If this recommendation is to be retained, the commission would be encouraged to emphasize that inclusion of annual participation should be part of an overall program structure plan that supports a formative approach to assessment. In addition, the ACR requests that ABMS Boards allow exceptions without penalty to be made to this annual requirement to all for live events.”
The American College of Cardiology took a different point of view with regard to this recommendation.
In its comments, ACC stated that it “concurs with this recommendation. Annual participation is a feature of the ACC’s proposed maintenance of certification solution. The ACC believes that ABMS boards should recognize, and make allowances for, physicians who may, for valid reasons (illness, sabbatical, medical or family issue) may not participate in MOC for a period of a year.” ACC generally concurred with the recommendations in the draft.
The final document presented the commission’s view that the ABMS member boards “need to engage with diplomates on an ongoing basis instead of every 2, 5, or 10 years. The ABMS Boards should develop a diplomate engagement strategy and support the idea that diplomates are committed to learning and continually improving their practice, skills, and competencies. The ABMS Boards should expect that diplomates would engage in some learning, assessment, or advancing practice work annually.”
The American Gastroenterological Association, in its comment letter on the draft, said it was “greatly concerned” about the inclusion of practice improvement data, noting it is “debatable whether it is even within the appropriate domain of the boards to assume responsibility for clinical practice performance and quality assurance.”
The final report states that ABMS “must ensure that their continuing certification programs recognize and document participation in a wide range of quality assessment activities in which diplomates already engage,” and added that “when appropriate, taking advantage of other organizations’ quality improvement and reporting activities should be maximized to avoid additional burdens on diplomates.”
ABMS and its board are not bound to follow any of the recommendations contained within the report, but the commission states that it “expects that the ABMS and the ABMS Boards, in collaboration with professional organizations and other stakeholders, will prioritize these recommendations and develop the necessary strategies and infrastructure to implement them.”
Whatever you do, change the name.
That was key among the final recommendations the Vision Initiative Commission submitted to the American Board of Medical Specialties on how to improve the maintenance of certification process.
“A new term that communicates the concept, intent, and expectations of continuing certification programs should be adopted by the ABMS in order to reengage disaffected diplomates and assure the public and other stakeholders that the certificate has enduring meaning and value,” according to the final report. A new term was not suggested.
The commission recommended a continuing certification system with four aims:
- Become a meaningful, contemporary, and relevant professional development activity for diplomates that ensures they remain up-to-date in their specialty.
- Demonstrate a commitment to professional self-regulation to both diplomates and the public.
- Align with international and national standards for certification programs.
- Provide a specialty-based credential that would be of value to diplomates and to multiple stakeholders, including patients, families, the public, and health care institutions.
Testing methods and situations must be simplified and updated, according to the report, which was submitted to ABMS on Feb. 12. Continuing certification “must change to incorporate longitudinal and other innovative formative assessment strategies that support learning, identify knowledge and skills gaps, and help diplomates stay current. The ABMS Boards must offer an alternative to burdensome highly secure, point-in-time examinations of knowledge.” In addition, the boards “must no longer use a single point-in-time examination or a series of single point-in-time assessments as the sole method to determine certification status.”
Instead, the commission recommends that ABMS “move quickly to formative assessment formats that are not characterized by high-stakes summative outcomes (pass/fail), specified time frames for high-stakes assessment, or require burdensome testing formats (such as testing centers or remote proctoring) that are inconsistent with the desired goals for continuing certification – support learning; identify knowledge and skills gaps; and help diplomates stay current.”
The commission also defined how the certification process should be used by other stakeholders.
“ABMS must demonstrate and communicate that continuing certification has value, meaning, and purpose in the health care environment,” the report states. “Hospitals, health systems, payers, and other health care organizations can independently decide what factors are used in credentialing and privileging decisions. ABMS must inform these organizations that continuing certification should not be the only criterion used in these decisions, and these organizations should use a wide portfolio of criteria in these decisions. ABMS must encourage hospitals, health systems, payers, and other health care organizations to not deny credentialing or privileging to a physician solely on the basis of certification status.”
Additionally, the commission report states that “ABMS and the ABMS Boards should collaborate with specialty societies, the [continuing medical education/continuing professional development] community, and other expert stakeholders to develop the infrastructure to support learning activities that produce data-driven advances in clinical practice. The ABMS Boards must ensure that their continuing certification programs recognize and document participation in a wide range of quality assessment activities in which diplomates already engage.”
The report adds that the boards “should readily accept existing activities that diplomates are doing to advance their clinical practice and to provide credit for performing low-resource, high-impact activities as part of their daily practice routine.”
The commission’s final report incorporates a number of changes that physicians offered based on a draft version of the report.
The American College of Physicians commented that it “objects to the use of data regarding quality measures for individual diplomate certification status, because physician-level measures of quality are flawed, and because physician-level data inevitably leads to physician-level documentation burden. Flawed performance measures also often inadequately adjust for patient comorbidities and socioeconomic status, which leads to assessments that do not reflect the actual quality of care.”
Similarly, the American Society of Hematology noted in a statement that it “disagrees with the commission’s recommendation to retain the reporting of practice improvement activities as part of continuous certification due to direct and indirect costs needed to fulfill this requirement on top of requirements for engagement in quality improvement mandated by insurers, institutions, and health systems.”
While the draft report recommended that specialty boards provide aggregated feedback to medical societies, a more individualized dissemination on the gaps in knowledge would be more helpful, according to Doug Henley, MD, CEO of the American Academy of Family Physicians, who said that a more individualized approach would help his organization better provide CME to its members to help fill in the knowledge gaps.
“If we can identify these and use other processes and then target at the individual level to seek improvement, I think that will be a better outcome rather than just x learners don’t do well in diabetic care,” he said in an interview. “That doesn’t really help me in terms of who needs the real education in diabetic care versus who needs it for heart failure.”
The final recommendation notes that ABMS member boards “must collaborate with professional and/or CME/CPD organizations to share data and information to guide and support diplomate engagement in continuing certification.”
The document further clarifies that the boards should examine “the aggregated results from assessments to identify knowledge, skills, and other competency gaps,” and the aggregated data should be shared with specialty societies, CME/CPD providers, quality improvement professionals, and other health care organizations.
One weakness in the draft noted by Dr. Henley was the lack of a more forceful tone within the recommendations. Even though AMBS is not bound by its recommendations, he said that he would like to see stronger language throughout the document.
“We would certainly hope that the ABMS and the member boards will follow the direction of the Vision Commission very directly and succinctly,” he said. “That is why we suggested that some of the recommendations from the Vision Commission should use words like ‘should’ and ‘must’ and not just ‘encourage’ and words like that.”
That recommendation was taken and implemented in the final document.
Societies differed in how often participation in the certification process should occur.
The American College of Rheumatology in its comments challenged a recommendation that certification should be structured to expect participation on an annual basis.
“The ACR supports the importance of ongoing learning,” it stated. “However, no discussion is provided as to how and why the recommendation for annual participation by diplomates was conceived. For some ABMS Boards, an annual requirement will increase physician burden unless continuing certification is modified to a formative pathway. If this recommendation is to be retained, the commission would be encouraged to emphasize that inclusion of annual participation should be part of an overall program structure plan that supports a formative approach to assessment. In addition, the ACR requests that ABMS Boards allow exceptions without penalty to be made to this annual requirement to all for live events.”
The American College of Cardiology took a different point of view with regard to this recommendation.
In its comments, ACC stated that it “concurs with this recommendation. Annual participation is a feature of the ACC’s proposed maintenance of certification solution. The ACC believes that ABMS boards should recognize, and make allowances for, physicians who may, for valid reasons (illness, sabbatical, medical or family issue) may not participate in MOC for a period of a year.” ACC generally concurred with the recommendations in the draft.
The final document presented the commission’s view that the ABMS member boards “need to engage with diplomates on an ongoing basis instead of every 2, 5, or 10 years. The ABMS Boards should develop a diplomate engagement strategy and support the idea that diplomates are committed to learning and continually improving their practice, skills, and competencies. The ABMS Boards should expect that diplomates would engage in some learning, assessment, or advancing practice work annually.”
The American Gastroenterological Association, in its comment letter on the draft, said it was “greatly concerned” about the inclusion of practice improvement data, noting it is “debatable whether it is even within the appropriate domain of the boards to assume responsibility for clinical practice performance and quality assurance.”
The final report states that ABMS “must ensure that their continuing certification programs recognize and document participation in a wide range of quality assessment activities in which diplomates already engage,” and added that “when appropriate, taking advantage of other organizations’ quality improvement and reporting activities should be maximized to avoid additional burdens on diplomates.”
ABMS and its board are not bound to follow any of the recommendations contained within the report, but the commission states that it “expects that the ABMS and the ABMS Boards, in collaboration with professional organizations and other stakeholders, will prioritize these recommendations and develop the necessary strategies and infrastructure to implement them.”
Whatever you do, change the name.
That was key among the final recommendations the Vision Initiative Commission submitted to the American Board of Medical Specialties on how to improve the maintenance of certification process.
“A new term that communicates the concept, intent, and expectations of continuing certification programs should be adopted by the ABMS in order to reengage disaffected diplomates and assure the public and other stakeholders that the certificate has enduring meaning and value,” according to the final report. A new term was not suggested.
The commission recommended a continuing certification system with four aims:
- Become a meaningful, contemporary, and relevant professional development activity for diplomates that ensures they remain up-to-date in their specialty.
- Demonstrate a commitment to professional self-regulation to both diplomates and the public.
- Align with international and national standards for certification programs.
- Provide a specialty-based credential that would be of value to diplomates and to multiple stakeholders, including patients, families, the public, and health care institutions.
Testing methods and situations must be simplified and updated, according to the report, which was submitted to ABMS on Feb. 12. Continuing certification “must change to incorporate longitudinal and other innovative formative assessment strategies that support learning, identify knowledge and skills gaps, and help diplomates stay current. The ABMS Boards must offer an alternative to burdensome highly secure, point-in-time examinations of knowledge.” In addition, the boards “must no longer use a single point-in-time examination or a series of single point-in-time assessments as the sole method to determine certification status.”
Instead, the commission recommends that ABMS “move quickly to formative assessment formats that are not characterized by high-stakes summative outcomes (pass/fail), specified time frames for high-stakes assessment, or require burdensome testing formats (such as testing centers or remote proctoring) that are inconsistent with the desired goals for continuing certification – support learning; identify knowledge and skills gaps; and help diplomates stay current.”
The commission also defined how the certification process should be used by other stakeholders.
“ABMS must demonstrate and communicate that continuing certification has value, meaning, and purpose in the health care environment,” the report states. “Hospitals, health systems, payers, and other health care organizations can independently decide what factors are used in credentialing and privileging decisions. ABMS must inform these organizations that continuing certification should not be the only criterion used in these decisions, and these organizations should use a wide portfolio of criteria in these decisions. ABMS must encourage hospitals, health systems, payers, and other health care organizations to not deny credentialing or privileging to a physician solely on the basis of certification status.”
Additionally, the commission report states that “ABMS and the ABMS Boards should collaborate with specialty societies, the [continuing medical education/continuing professional development] community, and other expert stakeholders to develop the infrastructure to support learning activities that produce data-driven advances in clinical practice. The ABMS Boards must ensure that their continuing certification programs recognize and document participation in a wide range of quality assessment activities in which diplomates already engage.”
The report adds that the boards “should readily accept existing activities that diplomates are doing to advance their clinical practice and to provide credit for performing low-resource, high-impact activities as part of their daily practice routine.”
The commission’s final report incorporates a number of changes that physicians offered based on a draft version of the report.
The American College of Physicians commented that it “objects to the use of data regarding quality measures for individual diplomate certification status, because physician-level measures of quality are flawed, and because physician-level data inevitably leads to physician-level documentation burden. Flawed performance measures also often inadequately adjust for patient comorbidities and socioeconomic status, which leads to assessments that do not reflect the actual quality of care.”
Similarly, the American Society of Hematology noted in a statement that it “disagrees with the commission’s recommendation to retain the reporting of practice improvement activities as part of continuous certification due to direct and indirect costs needed to fulfill this requirement on top of requirements for engagement in quality improvement mandated by insurers, institutions, and health systems.”
While the draft report recommended that specialty boards provide aggregated feedback to medical societies, a more individualized dissemination on the gaps in knowledge would be more helpful, according to Doug Henley, MD, CEO of the American Academy of Family Physicians, who said that a more individualized approach would help his organization better provide CME to its members to help fill in the knowledge gaps.
“If we can identify these and use other processes and then target at the individual level to seek improvement, I think that will be a better outcome rather than just x learners don’t do well in diabetic care,” he said in an interview. “That doesn’t really help me in terms of who needs the real education in diabetic care versus who needs it for heart failure.”
The final recommendation notes that ABMS member boards “must collaborate with professional and/or CME/CPD organizations to share data and information to guide and support diplomate engagement in continuing certification.”
The document further clarifies that the boards should examine “the aggregated results from assessments to identify knowledge, skills, and other competency gaps,” and the aggregated data should be shared with specialty societies, CME/CPD providers, quality improvement professionals, and other health care organizations.
One weakness in the draft noted by Dr. Henley was the lack of a more forceful tone within the recommendations. Even though AMBS is not bound by its recommendations, he said that he would like to see stronger language throughout the document.
“We would certainly hope that the ABMS and the member boards will follow the direction of the Vision Commission very directly and succinctly,” he said. “That is why we suggested that some of the recommendations from the Vision Commission should use words like ‘should’ and ‘must’ and not just ‘encourage’ and words like that.”
That recommendation was taken and implemented in the final document.
Societies differed in how often participation in the certification process should occur.
The American College of Rheumatology in its comments challenged a recommendation that certification should be structured to expect participation on an annual basis.
“The ACR supports the importance of ongoing learning,” it stated. “However, no discussion is provided as to how and why the recommendation for annual participation by diplomates was conceived. For some ABMS Boards, an annual requirement will increase physician burden unless continuing certification is modified to a formative pathway. If this recommendation is to be retained, the commission would be encouraged to emphasize that inclusion of annual participation should be part of an overall program structure plan that supports a formative approach to assessment. In addition, the ACR requests that ABMS Boards allow exceptions without penalty to be made to this annual requirement to all for live events.”
The American College of Cardiology took a different point of view with regard to this recommendation.
In its comments, ACC stated that it “concurs with this recommendation. Annual participation is a feature of the ACC’s proposed maintenance of certification solution. The ACC believes that ABMS boards should recognize, and make allowances for, physicians who may, for valid reasons (illness, sabbatical, medical or family issue) may not participate in MOC for a period of a year.” ACC generally concurred with the recommendations in the draft.
The final document presented the commission’s view that the ABMS member boards “need to engage with diplomates on an ongoing basis instead of every 2, 5, or 10 years. The ABMS Boards should develop a diplomate engagement strategy and support the idea that diplomates are committed to learning and continually improving their practice, skills, and competencies. The ABMS Boards should expect that diplomates would engage in some learning, assessment, or advancing practice work annually.”
The American Gastroenterological Association, in its comment letter on the draft, said it was “greatly concerned” about the inclusion of practice improvement data, noting it is “debatable whether it is even within the appropriate domain of the boards to assume responsibility for clinical practice performance and quality assurance.”
The final report states that ABMS “must ensure that their continuing certification programs recognize and document participation in a wide range of quality assessment activities in which diplomates already engage,” and added that “when appropriate, taking advantage of other organizations’ quality improvement and reporting activities should be maximized to avoid additional burdens on diplomates.”
ABMS and its board are not bound to follow any of the recommendations contained within the report, but the commission states that it “expects that the ABMS and the ABMS Boards, in collaboration with professional organizations and other stakeholders, will prioritize these recommendations and develop the necessary strategies and infrastructure to implement them.”
Shaping the future of hospital medicine
Dr. Therese Franco leads SHM’s Pacific Northwest chapter
Therese Franco, MD, SFHM, a hospitalist at the Virginia Mason Medical Center in Seattle, is the current president of SHM’s Pacific Northwest chapter.
The Hospitalist recently sat down with her to learn about her background and discuss some of the initiatives that the Pacific Northwest chapter has been working on.
Can you tell us about your education and training on the way to becoming a hospitalist?
My undergraduate degree is in engineering from Michigan State University. I then went to the University of Michigan in Ann Arbor and did one degree at the School of Public Health in environmental and industrial health, and another degree in the College of Engineering in industrial and operations engineering. In my work with the safety department at an automotive company, I found I was spending a lot of time looking at data, and not talking to people. I got into a conversation with one of the occupational medicine physicians there, and he said, “You ought to try this.” I spoke with a good friend, who was a medical student, and she agreed.
So then I went to medical school thinking that I would practice occupational medicine. I went to medical school at Wayne State University in Detroit and did a couple of rotations in occupational medicine. I wasn’t sure that was the right fit, so I then went off to residency in internal medicine at the University of Connecticut and really enjoyed my wards experience. I liked the pace, I liked the variety, and just really liked all of hospital medicine. So that’s what I decided to do.
What are your areas of research interest?
This year I’m doing a research fellowship through the Center for Healthcare Improvement Science, at Virginia Mason. Through SHM’s mentored implementation program, I have done a lot of work on diabetes and glycemic control but never really published much of it. I think it is so important to share what you learn, so I’m working on publishing some of our results from the diabetes work.
Another area of interest is advanced-practice providers in hospital medicine, which I think is very important, given all the issues that health care is facing. I think that medicine has gotten more complex and that we’re going to have to look at working in a collaborative, inter-professional, multidisciplinary way. I think that advanced practice can really improve the care of hospitalized patients, if we practice appropriate skill-task alignment, develop a culture of mutual respect, and find the best ways to deploy our advanced-practice providers and our physicians.
That can be challenging. Some people, I think, are worried about losing their jobs, and some people feel like they want to “own” all of the patient, because it’s such a part of the culture of medicine. So it’s a really complicated issue, and I think that doctors are going to have to get used to delegating tasks that they used to perform.
So a collaborative practice requires both a professional and a cultural shift?
I think so. I was our inaugural program director for an advanced-practice fellowship in hospital medicine, and in that role, I attended conferences and learning events for program development. I think that many institutions are facing some of the same challenges. For the most part, I’m optimistic about things. I think we’re on the right track, and help is on the way – we just have to figure out how to use it.
Has your institution made any changes along these lines?
We’re primarily using the fellowship as a tool to recruit and retain some of the brightest and best. We’ve got three fellows that matriculated from our program and are currently working in the section of hospital medicine. Everyone’s been really flexible and open to the idea that the job description is emerging. I think my colleagues are very appreciative of our advanced-practice providers. We’ve got two nurse practitioners and one physician assistant who is also a PhD-trained pharmacist. They’ve been great additions to our team.
What are some of the other issues that the Pacific Northwest chapter members are concerned about?
One of our most successful meetings was around telemedicine. There’s a lot of interest in that, and it’s very financially and technically complex. Some hospitals in the area are really doing novel things. One of the most interesting things is an addiction medicine teleconsult.
That’s out of Swedish Medical Center, Seattle. Of course there’s telestroke, which I think is picking up in popularity. We had speakers from Virginia Mason who presented on telestroke. Some institutions are even doing admissions this way. The University of Washington is doing some good antimicrobial stewardship work. They present cases and they teleconference and have an infectious disease consultant. It’s not a program directed at revenue generation, but is focused instead on sharing and spreading expertise.
Our chapter also hosted a presentation on burnout that was pretty well attended. And then, unfortunately, we did lose a hospitalist to suicide over the summer. That was the inspiration for offering the screening of the movie, “Do No Harm: Exposing the Hippocratic Hoax.”
What was the program that you put together around the screening?
We had the filmmaker come for the screening, and we organized a panel discussion with a wellness officer from a local clinic and a psychiatrist who used to be on the board of the Physician Health Program. John Nelson, MD, MHM, one of SHM’s cofounders and a local hospitalist here, also participated as a panelist.
Overall, the event was well received. There were some things that I didn’t really expect. I’m not sure that the film resonated with too many people in the room. It is very much directed at the educational process – med students and residents – and at times the dialogue is a little inflammatory.
I learned a few important things from the film. I did not realize that the tragedy of physician suicide is not unique to the United States – it’s an international issue. And we sometimes use the term “pimping” to talk about questioning interns or residents on rounds. Apparently, that stands for “put in my place,” which is very condescending and unacceptable. I will not use the term again.
I think future conversations need to come from thoughtful, rational, respectful leaders who are willing to work with regulatory agencies, hospitals, and administrators. If we want to move forward, physicians, administrators, and the public need to come together in the best interest of the patient and of public health. And I don’t know who leads that conversation.
Will your chapter have another event around that subject?
We will do what our membership wants and needs. We meet quarterly, and once a year we hold a people’s choice meeting and I solicit topics. If members want to keep the conversation moving, I’m going to do what I can to support them.
What are some other issues that stand out as important to your chapter?
One key topic is the financial side of hospitalist practice, and dealing with issues that seem to create inefficiencies – regulatory issues, documentation issues, things that are important because we want to tell the story of what we’re doing. We certainly want to be reimbursed for the value-added work that we’re doing, but a lot of value-added work creates inefficiencies of practice, and I hear a lot of dissatisfaction around documentation, coding, billing, and other issues related to reimbursement. While people are concerned about these problems, nobody wants to talk about them. They just want somebody to fix it. So I’m not sure what to do with that, because I think if I had a meeting about coding and billing, I would have three attendees.
But our annual poster meeting is always well attended. We always do it at the end of the year, to kick off the holiday season. It’s a nice opportunity to connect socially with colleagues because you mix and you mingle and look at the posters. We had some really great posters, and our top three prize winners were medical students, which is inspirational. They make you feel good about the future.
Our chapter is trying to diversify geographically and clinically. We were fortunate to receive a development funds grant to use technology to do streaming meetings. Our hope is that we can host streaming meetings and eventually transition hosting to rotate around the state. Once there’s large enough attendance, the different delegates can develop their own leadership teams and, eventually, their own chapter. We’re hoping to grow the organization that way.
What else is on the horizon for hospitalists in the Pacific Northwest?
I’d like to see more frequent meetings and a greater variety of meetings. I think there’s interest in adding some kind of service element to the chapter. Maybe we can do a blood pressure screening at a sporting event.
I think we’ll also be focusing on students and residents and trying to create support for them. We held a student event around financial planning, and that was very well attended. I think we would like to do something around mentorship. Of course it’s hard to find mentors, because everybody is so busy.
Our chapter really needs to leverage our technology if we want to have the reach that I’m talking about. I’m looking forward to piloting the streaming meeting concept, and I hope to do some live polling of our meeting attendees to get them engaged. I hope we continue to grow and keep the dialogue going about what matters in hospital medicine, and do our part to shape the future in the way we want it.
Dr. Therese Franco leads SHM’s Pacific Northwest chapter
Dr. Therese Franco leads SHM’s Pacific Northwest chapter
Therese Franco, MD, SFHM, a hospitalist at the Virginia Mason Medical Center in Seattle, is the current president of SHM’s Pacific Northwest chapter.
The Hospitalist recently sat down with her to learn about her background and discuss some of the initiatives that the Pacific Northwest chapter has been working on.
Can you tell us about your education and training on the way to becoming a hospitalist?
My undergraduate degree is in engineering from Michigan State University. I then went to the University of Michigan in Ann Arbor and did one degree at the School of Public Health in environmental and industrial health, and another degree in the College of Engineering in industrial and operations engineering. In my work with the safety department at an automotive company, I found I was spending a lot of time looking at data, and not talking to people. I got into a conversation with one of the occupational medicine physicians there, and he said, “You ought to try this.” I spoke with a good friend, who was a medical student, and she agreed.
So then I went to medical school thinking that I would practice occupational medicine. I went to medical school at Wayne State University in Detroit and did a couple of rotations in occupational medicine. I wasn’t sure that was the right fit, so I then went off to residency in internal medicine at the University of Connecticut and really enjoyed my wards experience. I liked the pace, I liked the variety, and just really liked all of hospital medicine. So that’s what I decided to do.
What are your areas of research interest?
This year I’m doing a research fellowship through the Center for Healthcare Improvement Science, at Virginia Mason. Through SHM’s mentored implementation program, I have done a lot of work on diabetes and glycemic control but never really published much of it. I think it is so important to share what you learn, so I’m working on publishing some of our results from the diabetes work.
Another area of interest is advanced-practice providers in hospital medicine, which I think is very important, given all the issues that health care is facing. I think that medicine has gotten more complex and that we’re going to have to look at working in a collaborative, inter-professional, multidisciplinary way. I think that advanced practice can really improve the care of hospitalized patients, if we practice appropriate skill-task alignment, develop a culture of mutual respect, and find the best ways to deploy our advanced-practice providers and our physicians.
That can be challenging. Some people, I think, are worried about losing their jobs, and some people feel like they want to “own” all of the patient, because it’s such a part of the culture of medicine. So it’s a really complicated issue, and I think that doctors are going to have to get used to delegating tasks that they used to perform.
So a collaborative practice requires both a professional and a cultural shift?
I think so. I was our inaugural program director for an advanced-practice fellowship in hospital medicine, and in that role, I attended conferences and learning events for program development. I think that many institutions are facing some of the same challenges. For the most part, I’m optimistic about things. I think we’re on the right track, and help is on the way – we just have to figure out how to use it.
Has your institution made any changes along these lines?
We’re primarily using the fellowship as a tool to recruit and retain some of the brightest and best. We’ve got three fellows that matriculated from our program and are currently working in the section of hospital medicine. Everyone’s been really flexible and open to the idea that the job description is emerging. I think my colleagues are very appreciative of our advanced-practice providers. We’ve got two nurse practitioners and one physician assistant who is also a PhD-trained pharmacist. They’ve been great additions to our team.
What are some of the other issues that the Pacific Northwest chapter members are concerned about?
One of our most successful meetings was around telemedicine. There’s a lot of interest in that, and it’s very financially and technically complex. Some hospitals in the area are really doing novel things. One of the most interesting things is an addiction medicine teleconsult.
That’s out of Swedish Medical Center, Seattle. Of course there’s telestroke, which I think is picking up in popularity. We had speakers from Virginia Mason who presented on telestroke. Some institutions are even doing admissions this way. The University of Washington is doing some good antimicrobial stewardship work. They present cases and they teleconference and have an infectious disease consultant. It’s not a program directed at revenue generation, but is focused instead on sharing and spreading expertise.
Our chapter also hosted a presentation on burnout that was pretty well attended. And then, unfortunately, we did lose a hospitalist to suicide over the summer. That was the inspiration for offering the screening of the movie, “Do No Harm: Exposing the Hippocratic Hoax.”
What was the program that you put together around the screening?
We had the filmmaker come for the screening, and we organized a panel discussion with a wellness officer from a local clinic and a psychiatrist who used to be on the board of the Physician Health Program. John Nelson, MD, MHM, one of SHM’s cofounders and a local hospitalist here, also participated as a panelist.
Overall, the event was well received. There were some things that I didn’t really expect. I’m not sure that the film resonated with too many people in the room. It is very much directed at the educational process – med students and residents – and at times the dialogue is a little inflammatory.
I learned a few important things from the film. I did not realize that the tragedy of physician suicide is not unique to the United States – it’s an international issue. And we sometimes use the term “pimping” to talk about questioning interns or residents on rounds. Apparently, that stands for “put in my place,” which is very condescending and unacceptable. I will not use the term again.
I think future conversations need to come from thoughtful, rational, respectful leaders who are willing to work with regulatory agencies, hospitals, and administrators. If we want to move forward, physicians, administrators, and the public need to come together in the best interest of the patient and of public health. And I don’t know who leads that conversation.
Will your chapter have another event around that subject?
We will do what our membership wants and needs. We meet quarterly, and once a year we hold a people’s choice meeting and I solicit topics. If members want to keep the conversation moving, I’m going to do what I can to support them.
What are some other issues that stand out as important to your chapter?
One key topic is the financial side of hospitalist practice, and dealing with issues that seem to create inefficiencies – regulatory issues, documentation issues, things that are important because we want to tell the story of what we’re doing. We certainly want to be reimbursed for the value-added work that we’re doing, but a lot of value-added work creates inefficiencies of practice, and I hear a lot of dissatisfaction around documentation, coding, billing, and other issues related to reimbursement. While people are concerned about these problems, nobody wants to talk about them. They just want somebody to fix it. So I’m not sure what to do with that, because I think if I had a meeting about coding and billing, I would have three attendees.
But our annual poster meeting is always well attended. We always do it at the end of the year, to kick off the holiday season. It’s a nice opportunity to connect socially with colleagues because you mix and you mingle and look at the posters. We had some really great posters, and our top three prize winners were medical students, which is inspirational. They make you feel good about the future.
Our chapter is trying to diversify geographically and clinically. We were fortunate to receive a development funds grant to use technology to do streaming meetings. Our hope is that we can host streaming meetings and eventually transition hosting to rotate around the state. Once there’s large enough attendance, the different delegates can develop their own leadership teams and, eventually, their own chapter. We’re hoping to grow the organization that way.
What else is on the horizon for hospitalists in the Pacific Northwest?
I’d like to see more frequent meetings and a greater variety of meetings. I think there’s interest in adding some kind of service element to the chapter. Maybe we can do a blood pressure screening at a sporting event.
I think we’ll also be focusing on students and residents and trying to create support for them. We held a student event around financial planning, and that was very well attended. I think we would like to do something around mentorship. Of course it’s hard to find mentors, because everybody is so busy.
Our chapter really needs to leverage our technology if we want to have the reach that I’m talking about. I’m looking forward to piloting the streaming meeting concept, and I hope to do some live polling of our meeting attendees to get them engaged. I hope we continue to grow and keep the dialogue going about what matters in hospital medicine, and do our part to shape the future in the way we want it.
Therese Franco, MD, SFHM, a hospitalist at the Virginia Mason Medical Center in Seattle, is the current president of SHM’s Pacific Northwest chapter.
The Hospitalist recently sat down with her to learn about her background and discuss some of the initiatives that the Pacific Northwest chapter has been working on.
Can you tell us about your education and training on the way to becoming a hospitalist?
My undergraduate degree is in engineering from Michigan State University. I then went to the University of Michigan in Ann Arbor and did one degree at the School of Public Health in environmental and industrial health, and another degree in the College of Engineering in industrial and operations engineering. In my work with the safety department at an automotive company, I found I was spending a lot of time looking at data, and not talking to people. I got into a conversation with one of the occupational medicine physicians there, and he said, “You ought to try this.” I spoke with a good friend, who was a medical student, and she agreed.
So then I went to medical school thinking that I would practice occupational medicine. I went to medical school at Wayne State University in Detroit and did a couple of rotations in occupational medicine. I wasn’t sure that was the right fit, so I then went off to residency in internal medicine at the University of Connecticut and really enjoyed my wards experience. I liked the pace, I liked the variety, and just really liked all of hospital medicine. So that’s what I decided to do.
What are your areas of research interest?
This year I’m doing a research fellowship through the Center for Healthcare Improvement Science, at Virginia Mason. Through SHM’s mentored implementation program, I have done a lot of work on diabetes and glycemic control but never really published much of it. I think it is so important to share what you learn, so I’m working on publishing some of our results from the diabetes work.
Another area of interest is advanced-practice providers in hospital medicine, which I think is very important, given all the issues that health care is facing. I think that medicine has gotten more complex and that we’re going to have to look at working in a collaborative, inter-professional, multidisciplinary way. I think that advanced practice can really improve the care of hospitalized patients, if we practice appropriate skill-task alignment, develop a culture of mutual respect, and find the best ways to deploy our advanced-practice providers and our physicians.
That can be challenging. Some people, I think, are worried about losing their jobs, and some people feel like they want to “own” all of the patient, because it’s such a part of the culture of medicine. So it’s a really complicated issue, and I think that doctors are going to have to get used to delegating tasks that they used to perform.
So a collaborative practice requires both a professional and a cultural shift?
I think so. I was our inaugural program director for an advanced-practice fellowship in hospital medicine, and in that role, I attended conferences and learning events for program development. I think that many institutions are facing some of the same challenges. For the most part, I’m optimistic about things. I think we’re on the right track, and help is on the way – we just have to figure out how to use it.
Has your institution made any changes along these lines?
We’re primarily using the fellowship as a tool to recruit and retain some of the brightest and best. We’ve got three fellows that matriculated from our program and are currently working in the section of hospital medicine. Everyone’s been really flexible and open to the idea that the job description is emerging. I think my colleagues are very appreciative of our advanced-practice providers. We’ve got two nurse practitioners and one physician assistant who is also a PhD-trained pharmacist. They’ve been great additions to our team.
What are some of the other issues that the Pacific Northwest chapter members are concerned about?
One of our most successful meetings was around telemedicine. There’s a lot of interest in that, and it’s very financially and technically complex. Some hospitals in the area are really doing novel things. One of the most interesting things is an addiction medicine teleconsult.
That’s out of Swedish Medical Center, Seattle. Of course there’s telestroke, which I think is picking up in popularity. We had speakers from Virginia Mason who presented on telestroke. Some institutions are even doing admissions this way. The University of Washington is doing some good antimicrobial stewardship work. They present cases and they teleconference and have an infectious disease consultant. It’s not a program directed at revenue generation, but is focused instead on sharing and spreading expertise.
Our chapter also hosted a presentation on burnout that was pretty well attended. And then, unfortunately, we did lose a hospitalist to suicide over the summer. That was the inspiration for offering the screening of the movie, “Do No Harm: Exposing the Hippocratic Hoax.”
What was the program that you put together around the screening?
We had the filmmaker come for the screening, and we organized a panel discussion with a wellness officer from a local clinic and a psychiatrist who used to be on the board of the Physician Health Program. John Nelson, MD, MHM, one of SHM’s cofounders and a local hospitalist here, also participated as a panelist.
Overall, the event was well received. There were some things that I didn’t really expect. I’m not sure that the film resonated with too many people in the room. It is very much directed at the educational process – med students and residents – and at times the dialogue is a little inflammatory.
I learned a few important things from the film. I did not realize that the tragedy of physician suicide is not unique to the United States – it’s an international issue. And we sometimes use the term “pimping” to talk about questioning interns or residents on rounds. Apparently, that stands for “put in my place,” which is very condescending and unacceptable. I will not use the term again.
I think future conversations need to come from thoughtful, rational, respectful leaders who are willing to work with regulatory agencies, hospitals, and administrators. If we want to move forward, physicians, administrators, and the public need to come together in the best interest of the patient and of public health. And I don’t know who leads that conversation.
Will your chapter have another event around that subject?
We will do what our membership wants and needs. We meet quarterly, and once a year we hold a people’s choice meeting and I solicit topics. If members want to keep the conversation moving, I’m going to do what I can to support them.
What are some other issues that stand out as important to your chapter?
One key topic is the financial side of hospitalist practice, and dealing with issues that seem to create inefficiencies – regulatory issues, documentation issues, things that are important because we want to tell the story of what we’re doing. We certainly want to be reimbursed for the value-added work that we’re doing, but a lot of value-added work creates inefficiencies of practice, and I hear a lot of dissatisfaction around documentation, coding, billing, and other issues related to reimbursement. While people are concerned about these problems, nobody wants to talk about them. They just want somebody to fix it. So I’m not sure what to do with that, because I think if I had a meeting about coding and billing, I would have three attendees.
But our annual poster meeting is always well attended. We always do it at the end of the year, to kick off the holiday season. It’s a nice opportunity to connect socially with colleagues because you mix and you mingle and look at the posters. We had some really great posters, and our top three prize winners were medical students, which is inspirational. They make you feel good about the future.
Our chapter is trying to diversify geographically and clinically. We were fortunate to receive a development funds grant to use technology to do streaming meetings. Our hope is that we can host streaming meetings and eventually transition hosting to rotate around the state. Once there’s large enough attendance, the different delegates can develop their own leadership teams and, eventually, their own chapter. We’re hoping to grow the organization that way.
What else is on the horizon for hospitalists in the Pacific Northwest?
I’d like to see more frequent meetings and a greater variety of meetings. I think there’s interest in adding some kind of service element to the chapter. Maybe we can do a blood pressure screening at a sporting event.
I think we’ll also be focusing on students and residents and trying to create support for them. We held a student event around financial planning, and that was very well attended. I think we would like to do something around mentorship. Of course it’s hard to find mentors, because everybody is so busy.
Our chapter really needs to leverage our technology if we want to have the reach that I’m talking about. I’m looking forward to piloting the streaming meeting concept, and I hope to do some live polling of our meeting attendees to get them engaged. I hope we continue to grow and keep the dialogue going about what matters in hospital medicine, and do our part to shape the future in the way we want it.
The amazing work we get to do
Serving people, connecting, and improving care
Stories are told of the first meeting, 20 years ago, where a hat was passed to collect donations to develop a fledgling organization of inpatient physicians. Today, 90% of hospitals with 200+ beds operate with a hospitalist model. Today, we are the Society of Hospital Medicine.
In the early 1900s, health care in many ways was simple. It was a doctor with a shingle hung. It was house calls. Remedies were limited. In the 1940s, companies developed insurance benefits to lure workers during World War II; this third party, the payer, added complexity. Meanwhile, treatment options began to diversify. Then, in the 1960s, Medicare was passed, and the government came into the mix, further increasing this complexity. Diagnostic and treatment options continued to diversify, seemingly exponentially. Some would say it took 30 years for our country to recognize that it had created the most advanced and expensive, as well as one of the least quality-controlled, health systems in the world. Thus, as hospital medicine was conceived in the 1990s, our national health system was awakening to the need – the creative niche – that hospitalists would fill.
When I began my career, I was unaware that I was a hospitalist. The title didn’t exist. Yes, I was working solely in the hospital. I was developing programs to improve care delivery. I was rounding, teaching, collaborating, connecting – everything that we now call hospital medicine. That first job has evolved into my career, one that I find both honorable and enjoyable.
As health care changes with the passing years, being a hospitalist continues to be about serving people, connecting, and improving care. Being a hospitalist is being innovative, willing, and even daring. Dare to try, dare to fail, dare to redesign and try again. Hospital medicine is thinking outside of the box while knowing how to color between the lines. In the coming decades, health care will continue to evolve, and hospital medicine will too. We now encompass surgical comanagement and perioperative care, palliative care, postacute care, and transitions of care services. In corners, hospital medicine is already experimenting with telecare, virtual health, and hospital at home. Our hospital medicine workforce is innovative, diverse, tech savvy and poised for leading.
We are ready and willing to face the pressures affecting health care in the United States today: the recognition of an overwhelming expense to society, the relative underperformance with regard to quality, the increasing complexity of illness and treatment options, the worsening health of the average American citizen, the aging population, the role of medical error in patient harm, the increasing engagement of people in their own care, and the desire to make care better. What our country is facing is actually a phenomenal opportunity, no matter what side of the political aisle you live on. Being in hospital medicine today is being at the center front of this evolutionary stage.
Since joining the SHM board of directors, I continue to find examples of the stellar work of our staff and our members across the country. Having the privilege as a board member to join several Chapter meetings, I have witnessed firsthand the camaraderie, the compassion, the team that makes our Society work. From Houston to San Francisco and from St. Louis to Seattle, I have been honored to work with SHM members that create and nurture local and regional networks with the support of SHM’s Chapters program – a program that now houses more than 50 chapters and has launched regional districts to further support networking and growth. SHM’s chapter venues allow our larger hospital medicine team – yes, the national one – to connect and collaborate.
Take the Pacific Northwest Chapter. In its early years hospitalists from various and competing health systems would convene at a restaurant and just talk. They spoke of how to staff, how to pay, and how to negotiate with hospital leadership. As I have joined chapter meetings in recent years, meetings continue to be the place to share ideas – how to develop new programs; what is the most recent approach to glycemic control, sepsis care, or antibiotic stewardship; how best to approach diagnosis without “anchoring”; and even how to care for each other in the time of loss of a colleague to suicide. It is here in our community that we share experiences, knowledge, new ideas – and this sharing makes us all stronger.
Our hospital medicine community also comes together through areas of shared interest. There are 18 Special Interest Groups (SIGs), focused on specific topic areas. I have been privileged as a board member to work with our Perioperative/Comanagement SIG as it launched in 2017 and has grown rapidly. Currently, the community hosts a “case of the month” hospital medicine discussion as well as a regular journal club webinar that allows participants to review recent literature and interact directly with the authors. As this SIG has grown, shared resources and ideas have allowed for diffusion of knowledge, providing our nation with infrastructure for improving perioperative care. It is networks like this that support our national hospital medicine team to build strength through sharing.
It is our society, our people, that have taken us from the passing of a hat to developing our national community and network. This March, we get to celebrate our field in a new way – Thursday, March 7, 2019, marks the inaugural National Hospitalist Day. Then, March 24-27, our annual conference, Hospital Medicine 2019, will bring thousands of our national team to National Harbor, Maryland. Join your colleagues. Find your niche and your community. Be a part of the change you want to see. While you are there, come introduce yourself to me and let me thank you for the amazing work you are doing.
We are all a part of this movement transforming patient care both on a local and national level. As we move to the future, our innovative, diverse, and connected network of hospital medicine will continue to create and guide health care advances in our country.
Dr. Thompson is professor and chief of the section of hospital medicine at University of Nebraska Medical Center, and medical director of clinical care transitions at Nebraska Medicine, Omaha.
Serving people, connecting, and improving care
Serving people, connecting, and improving care
Stories are told of the first meeting, 20 years ago, where a hat was passed to collect donations to develop a fledgling organization of inpatient physicians. Today, 90% of hospitals with 200+ beds operate with a hospitalist model. Today, we are the Society of Hospital Medicine.
In the early 1900s, health care in many ways was simple. It was a doctor with a shingle hung. It was house calls. Remedies were limited. In the 1940s, companies developed insurance benefits to lure workers during World War II; this third party, the payer, added complexity. Meanwhile, treatment options began to diversify. Then, in the 1960s, Medicare was passed, and the government came into the mix, further increasing this complexity. Diagnostic and treatment options continued to diversify, seemingly exponentially. Some would say it took 30 years for our country to recognize that it had created the most advanced and expensive, as well as one of the least quality-controlled, health systems in the world. Thus, as hospital medicine was conceived in the 1990s, our national health system was awakening to the need – the creative niche – that hospitalists would fill.
When I began my career, I was unaware that I was a hospitalist. The title didn’t exist. Yes, I was working solely in the hospital. I was developing programs to improve care delivery. I was rounding, teaching, collaborating, connecting – everything that we now call hospital medicine. That first job has evolved into my career, one that I find both honorable and enjoyable.
As health care changes with the passing years, being a hospitalist continues to be about serving people, connecting, and improving care. Being a hospitalist is being innovative, willing, and even daring. Dare to try, dare to fail, dare to redesign and try again. Hospital medicine is thinking outside of the box while knowing how to color between the lines. In the coming decades, health care will continue to evolve, and hospital medicine will too. We now encompass surgical comanagement and perioperative care, palliative care, postacute care, and transitions of care services. In corners, hospital medicine is already experimenting with telecare, virtual health, and hospital at home. Our hospital medicine workforce is innovative, diverse, tech savvy and poised for leading.
We are ready and willing to face the pressures affecting health care in the United States today: the recognition of an overwhelming expense to society, the relative underperformance with regard to quality, the increasing complexity of illness and treatment options, the worsening health of the average American citizen, the aging population, the role of medical error in patient harm, the increasing engagement of people in their own care, and the desire to make care better. What our country is facing is actually a phenomenal opportunity, no matter what side of the political aisle you live on. Being in hospital medicine today is being at the center front of this evolutionary stage.
Since joining the SHM board of directors, I continue to find examples of the stellar work of our staff and our members across the country. Having the privilege as a board member to join several Chapter meetings, I have witnessed firsthand the camaraderie, the compassion, the team that makes our Society work. From Houston to San Francisco and from St. Louis to Seattle, I have been honored to work with SHM members that create and nurture local and regional networks with the support of SHM’s Chapters program – a program that now houses more than 50 chapters and has launched regional districts to further support networking and growth. SHM’s chapter venues allow our larger hospital medicine team – yes, the national one – to connect and collaborate.
Take the Pacific Northwest Chapter. In its early years hospitalists from various and competing health systems would convene at a restaurant and just talk. They spoke of how to staff, how to pay, and how to negotiate with hospital leadership. As I have joined chapter meetings in recent years, meetings continue to be the place to share ideas – how to develop new programs; what is the most recent approach to glycemic control, sepsis care, or antibiotic stewardship; how best to approach diagnosis without “anchoring”; and even how to care for each other in the time of loss of a colleague to suicide. It is here in our community that we share experiences, knowledge, new ideas – and this sharing makes us all stronger.
Our hospital medicine community also comes together through areas of shared interest. There are 18 Special Interest Groups (SIGs), focused on specific topic areas. I have been privileged as a board member to work with our Perioperative/Comanagement SIG as it launched in 2017 and has grown rapidly. Currently, the community hosts a “case of the month” hospital medicine discussion as well as a regular journal club webinar that allows participants to review recent literature and interact directly with the authors. As this SIG has grown, shared resources and ideas have allowed for diffusion of knowledge, providing our nation with infrastructure for improving perioperative care. It is networks like this that support our national hospital medicine team to build strength through sharing.
It is our society, our people, that have taken us from the passing of a hat to developing our national community and network. This March, we get to celebrate our field in a new way – Thursday, March 7, 2019, marks the inaugural National Hospitalist Day. Then, March 24-27, our annual conference, Hospital Medicine 2019, will bring thousands of our national team to National Harbor, Maryland. Join your colleagues. Find your niche and your community. Be a part of the change you want to see. While you are there, come introduce yourself to me and let me thank you for the amazing work you are doing.
We are all a part of this movement transforming patient care both on a local and national level. As we move to the future, our innovative, diverse, and connected network of hospital medicine will continue to create and guide health care advances in our country.
Dr. Thompson is professor and chief of the section of hospital medicine at University of Nebraska Medical Center, and medical director of clinical care transitions at Nebraska Medicine, Omaha.
Stories are told of the first meeting, 20 years ago, where a hat was passed to collect donations to develop a fledgling organization of inpatient physicians. Today, 90% of hospitals with 200+ beds operate with a hospitalist model. Today, we are the Society of Hospital Medicine.
In the early 1900s, health care in many ways was simple. It was a doctor with a shingle hung. It was house calls. Remedies were limited. In the 1940s, companies developed insurance benefits to lure workers during World War II; this third party, the payer, added complexity. Meanwhile, treatment options began to diversify. Then, in the 1960s, Medicare was passed, and the government came into the mix, further increasing this complexity. Diagnostic and treatment options continued to diversify, seemingly exponentially. Some would say it took 30 years for our country to recognize that it had created the most advanced and expensive, as well as one of the least quality-controlled, health systems in the world. Thus, as hospital medicine was conceived in the 1990s, our national health system was awakening to the need – the creative niche – that hospitalists would fill.
When I began my career, I was unaware that I was a hospitalist. The title didn’t exist. Yes, I was working solely in the hospital. I was developing programs to improve care delivery. I was rounding, teaching, collaborating, connecting – everything that we now call hospital medicine. That first job has evolved into my career, one that I find both honorable and enjoyable.
As health care changes with the passing years, being a hospitalist continues to be about serving people, connecting, and improving care. Being a hospitalist is being innovative, willing, and even daring. Dare to try, dare to fail, dare to redesign and try again. Hospital medicine is thinking outside of the box while knowing how to color between the lines. In the coming decades, health care will continue to evolve, and hospital medicine will too. We now encompass surgical comanagement and perioperative care, palliative care, postacute care, and transitions of care services. In corners, hospital medicine is already experimenting with telecare, virtual health, and hospital at home. Our hospital medicine workforce is innovative, diverse, tech savvy and poised for leading.
We are ready and willing to face the pressures affecting health care in the United States today: the recognition of an overwhelming expense to society, the relative underperformance with regard to quality, the increasing complexity of illness and treatment options, the worsening health of the average American citizen, the aging population, the role of medical error in patient harm, the increasing engagement of people in their own care, and the desire to make care better. What our country is facing is actually a phenomenal opportunity, no matter what side of the political aisle you live on. Being in hospital medicine today is being at the center front of this evolutionary stage.
Since joining the SHM board of directors, I continue to find examples of the stellar work of our staff and our members across the country. Having the privilege as a board member to join several Chapter meetings, I have witnessed firsthand the camaraderie, the compassion, the team that makes our Society work. From Houston to San Francisco and from St. Louis to Seattle, I have been honored to work with SHM members that create and nurture local and regional networks with the support of SHM’s Chapters program – a program that now houses more than 50 chapters and has launched regional districts to further support networking and growth. SHM’s chapter venues allow our larger hospital medicine team – yes, the national one – to connect and collaborate.
Take the Pacific Northwest Chapter. In its early years hospitalists from various and competing health systems would convene at a restaurant and just talk. They spoke of how to staff, how to pay, and how to negotiate with hospital leadership. As I have joined chapter meetings in recent years, meetings continue to be the place to share ideas – how to develop new programs; what is the most recent approach to glycemic control, sepsis care, or antibiotic stewardship; how best to approach diagnosis without “anchoring”; and even how to care for each other in the time of loss of a colleague to suicide. It is here in our community that we share experiences, knowledge, new ideas – and this sharing makes us all stronger.
Our hospital medicine community also comes together through areas of shared interest. There are 18 Special Interest Groups (SIGs), focused on specific topic areas. I have been privileged as a board member to work with our Perioperative/Comanagement SIG as it launched in 2017 and has grown rapidly. Currently, the community hosts a “case of the month” hospital medicine discussion as well as a regular journal club webinar that allows participants to review recent literature and interact directly with the authors. As this SIG has grown, shared resources and ideas have allowed for diffusion of knowledge, providing our nation with infrastructure for improving perioperative care. It is networks like this that support our national hospital medicine team to build strength through sharing.
It is our society, our people, that have taken us from the passing of a hat to developing our national community and network. This March, we get to celebrate our field in a new way – Thursday, March 7, 2019, marks the inaugural National Hospitalist Day. Then, March 24-27, our annual conference, Hospital Medicine 2019, will bring thousands of our national team to National Harbor, Maryland. Join your colleagues. Find your niche and your community. Be a part of the change you want to see. While you are there, come introduce yourself to me and let me thank you for the amazing work you are doing.
We are all a part of this movement transforming patient care both on a local and national level. As we move to the future, our innovative, diverse, and connected network of hospital medicine will continue to create and guide health care advances in our country.
Dr. Thompson is professor and chief of the section of hospital medicine at University of Nebraska Medical Center, and medical director of clinical care transitions at Nebraska Medicine, Omaha.