User login
Insect Repellents and Contact Urticaria: Differential Response to DEET and Picaridin
Psychotic and sexually deviant
CASE: Paranoid and distressed
Mr. P, age 21, is a single, white college student who presents to a psychiatric emergency room with his father at his psychotherapist’s recommendation. The psychotherapist, who has been treating Mr. P for anxiety and depression, recommended he be evaluated because of increased erratic behavior and paranoia. Mr. P reports that he has been feeling increasingly “anxious” and “paranoid” and thinks the security cameras at his college have been following him. He also describes an increased connection with God and hearing God’s voice as a commentary on his behaviors. Mr. P denies euphoria, depression, increased goal-directed activities, distractibility, increased impulsivity, or rapid speech. He is admitted voluntarily to the psychiatric unit for further evaluation.
During the hospitalization, Mr. P discloses that he has been viewing child pornography for 2 years, and during the past 6 months he has been distressed by the intensity of his sexual fantasies involving sexual contact with prepubescent girls. He also continues to experience paranoia and increased religiosity.
Mr. P says he began looking at pornography on the internet at age 14. He says he was watching “regular straight porn” and he would use it to masturbate and achieve orgasm. Mr. P began looking at child pornography at age 19. He stated that “regular porn” was no longer sufficiently arousing for him. Mr. P explains, “First, I started looking for 15- or 16-year-olds. They would work for a while [referring to sexual gratification], but then I would look for younger girls.” He says the images of younger girls are sexually arousing, typically “young girls, 8 to 10 years old” who are nude or involved in sex acts.
Mr. P denies sexual contact with prepubescent individuals and says his thoughts about such contact are “distressing.” He reports that he has viewed child pornography even when he wasn’t experiencing psychotic or mood symptoms. Mr. P’s outpatient psychotherapist reports that Mr. P first disclosed viewing child pornography and his attraction to prepubescent girls 2 years before this admission.
The authors’ observations
DSM-IV-TR diagnostic criteria for pedophilia (Table 1)1 are based on a history of sexual arousal to prepubescent individuals. A subset of sex offenders meet criteria for a paraphilia (Table 2),1 an axis I disorder, and a subset of sex offenders with paraphilia meet diagnostic criteria for pedophilia. Dunsieth et al2 found that among a sample of 113 male sex offenders, 74% had a diagnosable paraphilia, and 50% of individuals with paraphilia met criteria for pedophilia.
Table 1
DSM-IV-TR diagnostic criteria for pedophilia
| A) | Over a period of ≥6 months, recurrent, intense sexually arousing fantasies, sexual urges, or behaviors involving sexual activity with a prepubescent child or children (generally age ≤13) |
| B) | The person has acted on these sexual urges, or the sexual urges or fantasies cause marked distress or interpersonal difficulty |
| C) | The person is age ≥16 and ≥5 years older than the child or children in criterion A |
| Note: Do not include an individual in late adolescence involved in an ongoing sexual relationship with a 12- or 13-year-old | |
| Source: Reference 1 | |
DSM-IV-TR diagnostic criteria for a paraphilia
| The essential features of a paraphilia are recurrent, intense sexually arousing fantasies, sexual urges, or behaviors generally involving: | |
| A) | nonhuman objects, the suffering or humiliation of oneself or one’s partner, or children or other nonconsenting persons that occur over a period of ≥6 months |
| B) | The behavior, sexual urges, or fantasies cause clinically significant distress or impairment in social, occupational, or other important areas of functioning |
| Source: Reference 1 | |
Although most schizophrenia patients without a history of sexual offenses do not exhibit sexual deviancy, sexual content in hallucinations and delusions is common.6 Confusion about sexual identity and the boundaries of one’s body are common and may contribute to sexual deviancy.6 Psychiatric inpatients without a history of sexual offenses—including but not limited to psychotic patients—have higher rates of sexually deviant fantasies and behaviors compared with those without psychiatric illness.6 In one survey, 15% of men with schizophrenia displayed paraphilic behaviors and 20% had atypical sexual thoughts.7
Alish et al4 found that pedophilia was not necessarily linked to psychotic behavior or antisocial personality features when comparing pedophilia rates in individuals with or without schizophrenia. In a sample of 22 adolescent males who sexually molested a child at least once, axis I morbidity was common, and 55% met criteria for bipolar disorder.8
Few experts in paraphilias
A patient who endorses deviant sexual fantasies should be evaluated by a mental health professional with specialized training in paraphilias. Although paraphilias are not recognized as a subspecialty in psychiatry, diagnosing and treating patients with a paraphilia requires additional training. There is a scarcity of psychiatrists trained to evaluate and treat patients with paraphilias.
Sexual evaluation. Evaluating a patient who presents with problematic sexual behaviors includes performing a comprehensive psychiatric history with a focus on sexual history. A psychosexual history is distinct from general psychiatric evaluations because of the level of detail regarding a sexual history (Table 3). In addition to the clinical interview, objective testing to determine sexual interests may be useful in some patients (Table 4).9
Actuarial tools—risk assessment instruments based on statistically significant risk factors—are valid tools for determining the risk of sexual reoffending. There are several validated actuarial tools in the assessment of sex offender recidivism, such as the Static-99R,10 Stable-2007,11 and the Sex Offender Risk Appraisal Guide.12 However, these tools are used for sex offenders, and would not be used for individuals who have not committed a sex offense, such as Mr. P.
Table 3
Psychosexual evaluation
| Aspect of evaluation | Measures |
| Sexual behavior history | History of sexual abuse Childhood exposure to sex Masturbation history Preferred sexual partners Kinsey Scale |
| Sexual addiction or compulsion | Total Sexual Outlet measure Amount of time in sexual fantasy Financial, legal, or social cost of sexual behavior Prior treatment of sexual behavior |
| Sexual interests | Sex, age, and number of partner(s) Review of criteria for all paraphilias (exposing, voyeurism, cross-dressing, sadistic or masochistic interests) |
Objective testing to determine sexual interests
| Test | Results |
|---|---|
| Penile plethysmograph | Measures penis circumference with a mercury-in-rubber strain gauge. Used clinically by measuring circumferential changes in the penis while the patient is listening to audio or video stimuli of various sexual vignettes |
| Abel Assessment for Sexual Interests-3 | An objective method for evaluating deviant sexual interest uses noninvasive means to achieve objective measures of sexual interest. The subject’s visual response time is measured while viewing images of males and females of varying age. Visual reaction time is correlated with sexual interests |
| Source: Reference 9 | |
Medicolegal aspects of a psychosexual evaluation may include mandated reporting, confidentiality, and documentation. Mental health professionals are mandated to report to law enforcement or child welfare agencies when they observe or suspect physical, sexual, or other types of abuse in vulnerable populations such as children. In psychosexual evaluations, the evaluator is legally required to report if a patient discloses current sexual behavior with a child with a plan to continue to engage in the behavior. In Mr. P’s case, there was no duty to report because although he described viewing child pornography and had a sexual interest in prepubescent individuals, he did not report a history of engaging in handson sexual behaviors with children or impulses to do so. When an individual has engaged in sexual contact with a prepubescent individual, reporting is not mandated unless the individual continues to engage in sexual behavior with a minor. Mental health professionals are not responsible for calling the police or alerting authorities after a crime has been committed.
The relationship between viewing child pornography and pedophilia is unclear. Some child pornography viewers are pedophilic, others are sexually compulsive, and others are viewing out of curiosity and have no sexual deviance. Seto et al13 suggested that child pornography offenders show greater sexual arousal to children than to adults. Persistent child pornography use is a stronger diagnostic indicator of pedophilia than sexually offending against child victims.13 A clinician who learns that a patient is viewing child pornography should take a detailed sexual history, including a review of criteria for paraphilias. In addition, when appropriate, the clinician should perform a risk assessment to determine the patient’s risk of engaging in sexual offenses with children.
OUTCOME: Expert consultation
We start Mr. P on risperidone, 1 mg/d, to treat his paranoia and request a consultation with an expert in paraphilias to determine if Mr. P has a paraphilia and to discuss treatment options.
Mr. P’s initial diagnosis is psychotic disorder not otherwise specified. His viewing of child pornography and sexual interest in prepubescent individuals is not limited to his current mental status, and these interests persist in the absence of mood and psychotic states. Mr. P’s viewing of child pornography and sexual attraction to prepubescent girls meet the diagnostic criteria for pedophilia. During hospitalization, we educate Mr. P about his diagnoses and need for continued treatment. We refer him to a sexual disorders outpatient clinic, which continues to address his deviant sexual interests.
The authors’ observations
A meta-analysis indicates that a combination of pharmacologic and behavioral treatments coupled with close legal supervision seems to reduce the risk of repeated sexual offenses.14 Legal supervision is a general term to describe oversight of offenders in the community by supervisory boards, such as probation or parole, and tracking devices such as GPS. Currently, pedophilia treatment focuses on minimizing deviant sexual arousal through behavioral modification, cognitive-behavioral therapies, and testosterone-lowering medications, such as medroxyprogesterone or leuprolide. The decision to prescribe testosterone-lowering medication should be based on informed consent and the patient’s risk of dangerous sexual behaviors.
- Reijnen L, Bulten E, Nijman H. Demographic and personality characteristics of internet child pornography downloaders in comparison to other offenders. J Child Sex Abus. 2009;18(6):611-622.
- Hall RC, Hall RC. A profile of pedophilia: definition, characteristics of offenders, recidivism, treatment outcomes, and forensic issues. Mayo Clin Proc. 2007;82(4):457-471.
- Leuprolide • Eligard, Lupron
- Medroxyprogesterone • Cycrin, Provera
- Risperidone • Risperdal
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
2. Dunsieth NW, Jr, Nelson EB, Brusman-Lovins LA, et al. Psychiatric and legal features of 113 men convicted of sexual offenses. J Clin Psychiatry. 2004;65(3):293-300.
3. Wallace C, Mullen P, Burgess P, et al. Serious criminal offending and mental disorder. Case linkage study. Br J Psychiatry. 1998;172:477-484.
4. Alish Y, Birger M, Manor N, et al. Schizophrenia sex offenders: a clinical and epidemiological comparison study. Int J Law Psychiatry. 2007;30(6):459-466.
5. Smith AD, Taylor PJ. Serious sex offending against women by men with schizophrenia. Relationship of illness and psychiatric symptoms to offending. Br J Psychiatry. 1999;174:233-237.
6. Drake CR, Pathé M. Understanding sexual offending in schizophrenia. Crim Behav Ment Health. 2004;14(2):108-120.
7. Harley EW, Boardman J, Craig T. Sexual problems in schizophrenia prevalence and characteristics: a cross sectional survey. Soc Psychiatry Psychiatr Epidemiol. 2010;45(7):759-766.
8. Galli V, McElroy SL, Soutullo CA, et al. The psychiatric diagnoses of twenty-two adolescents who have sexually molested other children. Compr Psychiatry. 1999;40(2):85-88.
9. Abel GG, Jordan A, Hand CG, et al. Classification models of child molesters utilizing the Abel Assessment for sexual interest. Child Abuse Negl. 2001;25(5):703-718.
10. Hanson RK, Thornton D. Improving risk assessments for sex offenders: a comparison of three actuarial scales. Law Hum Behav. 2000;24(1):119-136.
11. Hanson RK, Harris AJ, Scott TL, et al. Assessing the risk of sexual offenders on community supervision: The Dynamic Supervision Project. Vol 5. Ottawa, Canada: Public Safety Canada; 2007.
12. Quinsey VL, Harris AJ, Rice ME, et al. Violent offenders: appraising and managing risk. 2nd ed. Washington DC: American Psychological Association; 2006.
13. Seto M, Cantor JM, Blanchard R. Child pornography offenses are a valid diagnostic indicator of pedophilia. J Abnorm Psychol. 2006;115(3):610-615.
14. Thibaut F, De La Barra F, Gordon H, et al. WFSBP Task Force on Sexual Disorders. The World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of paraphilias. World J Biol Psychiatry. 2010;11(4):604-655.
CASE: Paranoid and distressed
Mr. P, age 21, is a single, white college student who presents to a psychiatric emergency room with his father at his psychotherapist’s recommendation. The psychotherapist, who has been treating Mr. P for anxiety and depression, recommended he be evaluated because of increased erratic behavior and paranoia. Mr. P reports that he has been feeling increasingly “anxious” and “paranoid” and thinks the security cameras at his college have been following him. He also describes an increased connection with God and hearing God’s voice as a commentary on his behaviors. Mr. P denies euphoria, depression, increased goal-directed activities, distractibility, increased impulsivity, or rapid speech. He is admitted voluntarily to the psychiatric unit for further evaluation.
During the hospitalization, Mr. P discloses that he has been viewing child pornography for 2 years, and during the past 6 months he has been distressed by the intensity of his sexual fantasies involving sexual contact with prepubescent girls. He also continues to experience paranoia and increased religiosity.
Mr. P says he began looking at pornography on the internet at age 14. He says he was watching “regular straight porn” and he would use it to masturbate and achieve orgasm. Mr. P began looking at child pornography at age 19. He stated that “regular porn” was no longer sufficiently arousing for him. Mr. P explains, “First, I started looking for 15- or 16-year-olds. They would work for a while [referring to sexual gratification], but then I would look for younger girls.” He says the images of younger girls are sexually arousing, typically “young girls, 8 to 10 years old” who are nude or involved in sex acts.
Mr. P denies sexual contact with prepubescent individuals and says his thoughts about such contact are “distressing.” He reports that he has viewed child pornography even when he wasn’t experiencing psychotic or mood symptoms. Mr. P’s outpatient psychotherapist reports that Mr. P first disclosed viewing child pornography and his attraction to prepubescent girls 2 years before this admission.
The authors’ observations
DSM-IV-TR diagnostic criteria for pedophilia (Table 1)1 are based on a history of sexual arousal to prepubescent individuals. A subset of sex offenders meet criteria for a paraphilia (Table 2),1 an axis I disorder, and a subset of sex offenders with paraphilia meet diagnostic criteria for pedophilia. Dunsieth et al2 found that among a sample of 113 male sex offenders, 74% had a diagnosable paraphilia, and 50% of individuals with paraphilia met criteria for pedophilia.
Table 1
DSM-IV-TR diagnostic criteria for pedophilia
| A) | Over a period of ≥6 months, recurrent, intense sexually arousing fantasies, sexual urges, or behaviors involving sexual activity with a prepubescent child or children (generally age ≤13) |
| B) | The person has acted on these sexual urges, or the sexual urges or fantasies cause marked distress or interpersonal difficulty |
| C) | The person is age ≥16 and ≥5 years older than the child or children in criterion A |
| Note: Do not include an individual in late adolescence involved in an ongoing sexual relationship with a 12- or 13-year-old | |
| Source: Reference 1 | |
DSM-IV-TR diagnostic criteria for a paraphilia
| The essential features of a paraphilia are recurrent, intense sexually arousing fantasies, sexual urges, or behaviors generally involving: | |
| A) | nonhuman objects, the suffering or humiliation of oneself or one’s partner, or children or other nonconsenting persons that occur over a period of ≥6 months |
| B) | The behavior, sexual urges, or fantasies cause clinically significant distress or impairment in social, occupational, or other important areas of functioning |
| Source: Reference 1 | |
Although most schizophrenia patients without a history of sexual offenses do not exhibit sexual deviancy, sexual content in hallucinations and delusions is common.6 Confusion about sexual identity and the boundaries of one’s body are common and may contribute to sexual deviancy.6 Psychiatric inpatients without a history of sexual offenses—including but not limited to psychotic patients—have higher rates of sexually deviant fantasies and behaviors compared with those without psychiatric illness.6 In one survey, 15% of men with schizophrenia displayed paraphilic behaviors and 20% had atypical sexual thoughts.7
Alish et al4 found that pedophilia was not necessarily linked to psychotic behavior or antisocial personality features when comparing pedophilia rates in individuals with or without schizophrenia. In a sample of 22 adolescent males who sexually molested a child at least once, axis I morbidity was common, and 55% met criteria for bipolar disorder.8
Few experts in paraphilias
A patient who endorses deviant sexual fantasies should be evaluated by a mental health professional with specialized training in paraphilias. Although paraphilias are not recognized as a subspecialty in psychiatry, diagnosing and treating patients with a paraphilia requires additional training. There is a scarcity of psychiatrists trained to evaluate and treat patients with paraphilias.
Sexual evaluation. Evaluating a patient who presents with problematic sexual behaviors includes performing a comprehensive psychiatric history with a focus on sexual history. A psychosexual history is distinct from general psychiatric evaluations because of the level of detail regarding a sexual history (Table 3). In addition to the clinical interview, objective testing to determine sexual interests may be useful in some patients (Table 4).9
Actuarial tools—risk assessment instruments based on statistically significant risk factors—are valid tools for determining the risk of sexual reoffending. There are several validated actuarial tools in the assessment of sex offender recidivism, such as the Static-99R,10 Stable-2007,11 and the Sex Offender Risk Appraisal Guide.12 However, these tools are used for sex offenders, and would not be used for individuals who have not committed a sex offense, such as Mr. P.
Table 3
Psychosexual evaluation
| Aspect of evaluation | Measures |
| Sexual behavior history | History of sexual abuse Childhood exposure to sex Masturbation history Preferred sexual partners Kinsey Scale |
| Sexual addiction or compulsion | Total Sexual Outlet measure Amount of time in sexual fantasy Financial, legal, or social cost of sexual behavior Prior treatment of sexual behavior |
| Sexual interests | Sex, age, and number of partner(s) Review of criteria for all paraphilias (exposing, voyeurism, cross-dressing, sadistic or masochistic interests) |
Objective testing to determine sexual interests
| Test | Results |
|---|---|
| Penile plethysmograph | Measures penis circumference with a mercury-in-rubber strain gauge. Used clinically by measuring circumferential changes in the penis while the patient is listening to audio or video stimuli of various sexual vignettes |
| Abel Assessment for Sexual Interests-3 | An objective method for evaluating deviant sexual interest uses noninvasive means to achieve objective measures of sexual interest. The subject’s visual response time is measured while viewing images of males and females of varying age. Visual reaction time is correlated with sexual interests |
| Source: Reference 9 | |
Medicolegal aspects of a psychosexual evaluation may include mandated reporting, confidentiality, and documentation. Mental health professionals are mandated to report to law enforcement or child welfare agencies when they observe or suspect physical, sexual, or other types of abuse in vulnerable populations such as children. In psychosexual evaluations, the evaluator is legally required to report if a patient discloses current sexual behavior with a child with a plan to continue to engage in the behavior. In Mr. P’s case, there was no duty to report because although he described viewing child pornography and had a sexual interest in prepubescent individuals, he did not report a history of engaging in handson sexual behaviors with children or impulses to do so. When an individual has engaged in sexual contact with a prepubescent individual, reporting is not mandated unless the individual continues to engage in sexual behavior with a minor. Mental health professionals are not responsible for calling the police or alerting authorities after a crime has been committed.
The relationship between viewing child pornography and pedophilia is unclear. Some child pornography viewers are pedophilic, others are sexually compulsive, and others are viewing out of curiosity and have no sexual deviance. Seto et al13 suggested that child pornography offenders show greater sexual arousal to children than to adults. Persistent child pornography use is a stronger diagnostic indicator of pedophilia than sexually offending against child victims.13 A clinician who learns that a patient is viewing child pornography should take a detailed sexual history, including a review of criteria for paraphilias. In addition, when appropriate, the clinician should perform a risk assessment to determine the patient’s risk of engaging in sexual offenses with children.
OUTCOME: Expert consultation
We start Mr. P on risperidone, 1 mg/d, to treat his paranoia and request a consultation with an expert in paraphilias to determine if Mr. P has a paraphilia and to discuss treatment options.
Mr. P’s initial diagnosis is psychotic disorder not otherwise specified. His viewing of child pornography and sexual interest in prepubescent individuals is not limited to his current mental status, and these interests persist in the absence of mood and psychotic states. Mr. P’s viewing of child pornography and sexual attraction to prepubescent girls meet the diagnostic criteria for pedophilia. During hospitalization, we educate Mr. P about his diagnoses and need for continued treatment. We refer him to a sexual disorders outpatient clinic, which continues to address his deviant sexual interests.
The authors’ observations
A meta-analysis indicates that a combination of pharmacologic and behavioral treatments coupled with close legal supervision seems to reduce the risk of repeated sexual offenses.14 Legal supervision is a general term to describe oversight of offenders in the community by supervisory boards, such as probation or parole, and tracking devices such as GPS. Currently, pedophilia treatment focuses on minimizing deviant sexual arousal through behavioral modification, cognitive-behavioral therapies, and testosterone-lowering medications, such as medroxyprogesterone or leuprolide. The decision to prescribe testosterone-lowering medication should be based on informed consent and the patient’s risk of dangerous sexual behaviors.
- Reijnen L, Bulten E, Nijman H. Demographic and personality characteristics of internet child pornography downloaders in comparison to other offenders. J Child Sex Abus. 2009;18(6):611-622.
- Hall RC, Hall RC. A profile of pedophilia: definition, characteristics of offenders, recidivism, treatment outcomes, and forensic issues. Mayo Clin Proc. 2007;82(4):457-471.
- Leuprolide • Eligard, Lupron
- Medroxyprogesterone • Cycrin, Provera
- Risperidone • Risperdal
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE: Paranoid and distressed
Mr. P, age 21, is a single, white college student who presents to a psychiatric emergency room with his father at his psychotherapist’s recommendation. The psychotherapist, who has been treating Mr. P for anxiety and depression, recommended he be evaluated because of increased erratic behavior and paranoia. Mr. P reports that he has been feeling increasingly “anxious” and “paranoid” and thinks the security cameras at his college have been following him. He also describes an increased connection with God and hearing God’s voice as a commentary on his behaviors. Mr. P denies euphoria, depression, increased goal-directed activities, distractibility, increased impulsivity, or rapid speech. He is admitted voluntarily to the psychiatric unit for further evaluation.
During the hospitalization, Mr. P discloses that he has been viewing child pornography for 2 years, and during the past 6 months he has been distressed by the intensity of his sexual fantasies involving sexual contact with prepubescent girls. He also continues to experience paranoia and increased religiosity.
Mr. P says he began looking at pornography on the internet at age 14. He says he was watching “regular straight porn” and he would use it to masturbate and achieve orgasm. Mr. P began looking at child pornography at age 19. He stated that “regular porn” was no longer sufficiently arousing for him. Mr. P explains, “First, I started looking for 15- or 16-year-olds. They would work for a while [referring to sexual gratification], but then I would look for younger girls.” He says the images of younger girls are sexually arousing, typically “young girls, 8 to 10 years old” who are nude or involved in sex acts.
Mr. P denies sexual contact with prepubescent individuals and says his thoughts about such contact are “distressing.” He reports that he has viewed child pornography even when he wasn’t experiencing psychotic or mood symptoms. Mr. P’s outpatient psychotherapist reports that Mr. P first disclosed viewing child pornography and his attraction to prepubescent girls 2 years before this admission.
The authors’ observations
DSM-IV-TR diagnostic criteria for pedophilia (Table 1)1 are based on a history of sexual arousal to prepubescent individuals. A subset of sex offenders meet criteria for a paraphilia (Table 2),1 an axis I disorder, and a subset of sex offenders with paraphilia meet diagnostic criteria for pedophilia. Dunsieth et al2 found that among a sample of 113 male sex offenders, 74% had a diagnosable paraphilia, and 50% of individuals with paraphilia met criteria for pedophilia.
Table 1
DSM-IV-TR diagnostic criteria for pedophilia
| A) | Over a period of ≥6 months, recurrent, intense sexually arousing fantasies, sexual urges, or behaviors involving sexual activity with a prepubescent child or children (generally age ≤13) |
| B) | The person has acted on these sexual urges, or the sexual urges or fantasies cause marked distress or interpersonal difficulty |
| C) | The person is age ≥16 and ≥5 years older than the child or children in criterion A |
| Note: Do not include an individual in late adolescence involved in an ongoing sexual relationship with a 12- or 13-year-old | |
| Source: Reference 1 | |
DSM-IV-TR diagnostic criteria for a paraphilia
| The essential features of a paraphilia are recurrent, intense sexually arousing fantasies, sexual urges, or behaviors generally involving: | |
| A) | nonhuman objects, the suffering or humiliation of oneself or one’s partner, or children or other nonconsenting persons that occur over a period of ≥6 months |
| B) | The behavior, sexual urges, or fantasies cause clinically significant distress or impairment in social, occupational, or other important areas of functioning |
| Source: Reference 1 | |
Although most schizophrenia patients without a history of sexual offenses do not exhibit sexual deviancy, sexual content in hallucinations and delusions is common.6 Confusion about sexual identity and the boundaries of one’s body are common and may contribute to sexual deviancy.6 Psychiatric inpatients without a history of sexual offenses—including but not limited to psychotic patients—have higher rates of sexually deviant fantasies and behaviors compared with those without psychiatric illness.6 In one survey, 15% of men with schizophrenia displayed paraphilic behaviors and 20% had atypical sexual thoughts.7
Alish et al4 found that pedophilia was not necessarily linked to psychotic behavior or antisocial personality features when comparing pedophilia rates in individuals with or without schizophrenia. In a sample of 22 adolescent males who sexually molested a child at least once, axis I morbidity was common, and 55% met criteria for bipolar disorder.8
Few experts in paraphilias
A patient who endorses deviant sexual fantasies should be evaluated by a mental health professional with specialized training in paraphilias. Although paraphilias are not recognized as a subspecialty in psychiatry, diagnosing and treating patients with a paraphilia requires additional training. There is a scarcity of psychiatrists trained to evaluate and treat patients with paraphilias.
Sexual evaluation. Evaluating a patient who presents with problematic sexual behaviors includes performing a comprehensive psychiatric history with a focus on sexual history. A psychosexual history is distinct from general psychiatric evaluations because of the level of detail regarding a sexual history (Table 3). In addition to the clinical interview, objective testing to determine sexual interests may be useful in some patients (Table 4).9
Actuarial tools—risk assessment instruments based on statistically significant risk factors—are valid tools for determining the risk of sexual reoffending. There are several validated actuarial tools in the assessment of sex offender recidivism, such as the Static-99R,10 Stable-2007,11 and the Sex Offender Risk Appraisal Guide.12 However, these tools are used for sex offenders, and would not be used for individuals who have not committed a sex offense, such as Mr. P.
Table 3
Psychosexual evaluation
| Aspect of evaluation | Measures |
| Sexual behavior history | History of sexual abuse Childhood exposure to sex Masturbation history Preferred sexual partners Kinsey Scale |
| Sexual addiction or compulsion | Total Sexual Outlet measure Amount of time in sexual fantasy Financial, legal, or social cost of sexual behavior Prior treatment of sexual behavior |
| Sexual interests | Sex, age, and number of partner(s) Review of criteria for all paraphilias (exposing, voyeurism, cross-dressing, sadistic or masochistic interests) |
Objective testing to determine sexual interests
| Test | Results |
|---|---|
| Penile plethysmograph | Measures penis circumference with a mercury-in-rubber strain gauge. Used clinically by measuring circumferential changes in the penis while the patient is listening to audio or video stimuli of various sexual vignettes |
| Abel Assessment for Sexual Interests-3 | An objective method for evaluating deviant sexual interest uses noninvasive means to achieve objective measures of sexual interest. The subject’s visual response time is measured while viewing images of males and females of varying age. Visual reaction time is correlated with sexual interests |
| Source: Reference 9 | |
Medicolegal aspects of a psychosexual evaluation may include mandated reporting, confidentiality, and documentation. Mental health professionals are mandated to report to law enforcement or child welfare agencies when they observe or suspect physical, sexual, or other types of abuse in vulnerable populations such as children. In psychosexual evaluations, the evaluator is legally required to report if a patient discloses current sexual behavior with a child with a plan to continue to engage in the behavior. In Mr. P’s case, there was no duty to report because although he described viewing child pornography and had a sexual interest in prepubescent individuals, he did not report a history of engaging in handson sexual behaviors with children or impulses to do so. When an individual has engaged in sexual contact with a prepubescent individual, reporting is not mandated unless the individual continues to engage in sexual behavior with a minor. Mental health professionals are not responsible for calling the police or alerting authorities after a crime has been committed.
The relationship between viewing child pornography and pedophilia is unclear. Some child pornography viewers are pedophilic, others are sexually compulsive, and others are viewing out of curiosity and have no sexual deviance. Seto et al13 suggested that child pornography offenders show greater sexual arousal to children than to adults. Persistent child pornography use is a stronger diagnostic indicator of pedophilia than sexually offending against child victims.13 A clinician who learns that a patient is viewing child pornography should take a detailed sexual history, including a review of criteria for paraphilias. In addition, when appropriate, the clinician should perform a risk assessment to determine the patient’s risk of engaging in sexual offenses with children.
OUTCOME: Expert consultation
We start Mr. P on risperidone, 1 mg/d, to treat his paranoia and request a consultation with an expert in paraphilias to determine if Mr. P has a paraphilia and to discuss treatment options.
Mr. P’s initial diagnosis is psychotic disorder not otherwise specified. His viewing of child pornography and sexual interest in prepubescent individuals is not limited to his current mental status, and these interests persist in the absence of mood and psychotic states. Mr. P’s viewing of child pornography and sexual attraction to prepubescent girls meet the diagnostic criteria for pedophilia. During hospitalization, we educate Mr. P about his diagnoses and need for continued treatment. We refer him to a sexual disorders outpatient clinic, which continues to address his deviant sexual interests.
The authors’ observations
A meta-analysis indicates that a combination of pharmacologic and behavioral treatments coupled with close legal supervision seems to reduce the risk of repeated sexual offenses.14 Legal supervision is a general term to describe oversight of offenders in the community by supervisory boards, such as probation or parole, and tracking devices such as GPS. Currently, pedophilia treatment focuses on minimizing deviant sexual arousal through behavioral modification, cognitive-behavioral therapies, and testosterone-lowering medications, such as medroxyprogesterone or leuprolide. The decision to prescribe testosterone-lowering medication should be based on informed consent and the patient’s risk of dangerous sexual behaviors.
- Reijnen L, Bulten E, Nijman H. Demographic and personality characteristics of internet child pornography downloaders in comparison to other offenders. J Child Sex Abus. 2009;18(6):611-622.
- Hall RC, Hall RC. A profile of pedophilia: definition, characteristics of offenders, recidivism, treatment outcomes, and forensic issues. Mayo Clin Proc. 2007;82(4):457-471.
- Leuprolide • Eligard, Lupron
- Medroxyprogesterone • Cycrin, Provera
- Risperidone • Risperdal
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
2. Dunsieth NW, Jr, Nelson EB, Brusman-Lovins LA, et al. Psychiatric and legal features of 113 men convicted of sexual offenses. J Clin Psychiatry. 2004;65(3):293-300.
3. Wallace C, Mullen P, Burgess P, et al. Serious criminal offending and mental disorder. Case linkage study. Br J Psychiatry. 1998;172:477-484.
4. Alish Y, Birger M, Manor N, et al. Schizophrenia sex offenders: a clinical and epidemiological comparison study. Int J Law Psychiatry. 2007;30(6):459-466.
5. Smith AD, Taylor PJ. Serious sex offending against women by men with schizophrenia. Relationship of illness and psychiatric symptoms to offending. Br J Psychiatry. 1999;174:233-237.
6. Drake CR, Pathé M. Understanding sexual offending in schizophrenia. Crim Behav Ment Health. 2004;14(2):108-120.
7. Harley EW, Boardman J, Craig T. Sexual problems in schizophrenia prevalence and characteristics: a cross sectional survey. Soc Psychiatry Psychiatr Epidemiol. 2010;45(7):759-766.
8. Galli V, McElroy SL, Soutullo CA, et al. The psychiatric diagnoses of twenty-two adolescents who have sexually molested other children. Compr Psychiatry. 1999;40(2):85-88.
9. Abel GG, Jordan A, Hand CG, et al. Classification models of child molesters utilizing the Abel Assessment for sexual interest. Child Abuse Negl. 2001;25(5):703-718.
10. Hanson RK, Thornton D. Improving risk assessments for sex offenders: a comparison of three actuarial scales. Law Hum Behav. 2000;24(1):119-136.
11. Hanson RK, Harris AJ, Scott TL, et al. Assessing the risk of sexual offenders on community supervision: The Dynamic Supervision Project. Vol 5. Ottawa, Canada: Public Safety Canada; 2007.
12. Quinsey VL, Harris AJ, Rice ME, et al. Violent offenders: appraising and managing risk. 2nd ed. Washington DC: American Psychological Association; 2006.
13. Seto M, Cantor JM, Blanchard R. Child pornography offenses are a valid diagnostic indicator of pedophilia. J Abnorm Psychol. 2006;115(3):610-615.
14. Thibaut F, De La Barra F, Gordon H, et al. WFSBP Task Force on Sexual Disorders. The World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of paraphilias. World J Biol Psychiatry. 2010;11(4):604-655.
1. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
2. Dunsieth NW, Jr, Nelson EB, Brusman-Lovins LA, et al. Psychiatric and legal features of 113 men convicted of sexual offenses. J Clin Psychiatry. 2004;65(3):293-300.
3. Wallace C, Mullen P, Burgess P, et al. Serious criminal offending and mental disorder. Case linkage study. Br J Psychiatry. 1998;172:477-484.
4. Alish Y, Birger M, Manor N, et al. Schizophrenia sex offenders: a clinical and epidemiological comparison study. Int J Law Psychiatry. 2007;30(6):459-466.
5. Smith AD, Taylor PJ. Serious sex offending against women by men with schizophrenia. Relationship of illness and psychiatric symptoms to offending. Br J Psychiatry. 1999;174:233-237.
6. Drake CR, Pathé M. Understanding sexual offending in schizophrenia. Crim Behav Ment Health. 2004;14(2):108-120.
7. Harley EW, Boardman J, Craig T. Sexual problems in schizophrenia prevalence and characteristics: a cross sectional survey. Soc Psychiatry Psychiatr Epidemiol. 2010;45(7):759-766.
8. Galli V, McElroy SL, Soutullo CA, et al. The psychiatric diagnoses of twenty-two adolescents who have sexually molested other children. Compr Psychiatry. 1999;40(2):85-88.
9. Abel GG, Jordan A, Hand CG, et al. Classification models of child molesters utilizing the Abel Assessment for sexual interest. Child Abuse Negl. 2001;25(5):703-718.
10. Hanson RK, Thornton D. Improving risk assessments for sex offenders: a comparison of three actuarial scales. Law Hum Behav. 2000;24(1):119-136.
11. Hanson RK, Harris AJ, Scott TL, et al. Assessing the risk of sexual offenders on community supervision: The Dynamic Supervision Project. Vol 5. Ottawa, Canada: Public Safety Canada; 2007.
12. Quinsey VL, Harris AJ, Rice ME, et al. Violent offenders: appraising and managing risk. 2nd ed. Washington DC: American Psychological Association; 2006.
13. Seto M, Cantor JM, Blanchard R. Child pornography offenses are a valid diagnostic indicator of pedophilia. J Abnorm Psychol. 2006;115(3):610-615.
14. Thibaut F, De La Barra F, Gordon H, et al. WFSBP Task Force on Sexual Disorders. The World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of paraphilias. World J Biol Psychiatry. 2010;11(4):604-655.
Sildenafil for SSRI-induced sexual dysfunction in women
- Sexual dysfunction can arise from environmental, social, medical, or drug effects and requires a multifaceted approach to treatment.
- When possible, take a baseline sexual dysfunction measurement to assess if selective serotonin reuptake inhibitor use is correlated with onset or worsening of sexual dysfunction.
- Nonpharmacologic options should be considered before and during pharmacotherapy.
- Sildenafil may be useful for treating anorgasmia in women taking serotonergic antidepressants.
- Phosphodiesterase type 5 inhibitors are not FDA-approved for sexual dysfunction in women.
Mrs. L, age 27, has a history of major depressive disorder with symptoms of anxiety. She was managed successfully for 2 years with bupropion XL, 300 mg/d, but was switched to venlafaxine, titrated to 225 mg/d, after she developed seizures secondary to a head injury sustained in a car accident. After the switch, Mrs. L’s mood deteriorated and she was hospitalized. Since then, she’s received several medication trials, including paroxetine, 30 mg/d, a selective serotonin reuptake inhibitor (SSRI), and the tricyclic antidepressant (TCA) nortriptyline, 75 mg/d, but she could not tolerate these medications because of severe xerostomia.
After taking sertraline, 150 mg/d, for 8 weeks, Mrs. L improves and has a Patient Health Questionnaire score of 6, indicating mild depression. Her initial complaints of diarrhea and nausea have resolved, but Mrs. L now reports that she and her husband are having marital difficulties because she cannot achieve orgasm during sexual intercourse. She did not have this problem when she was taking bupropion. Her husband occasionally takes the phosphodiesterase type 5 (PDE5) inhibitor sildenafil before intercourse, and Mrs. L asks you if this medication will help her achieve orgasm.
DSM-IV-TR defines sexual dysfunction as disturbances in sexual desire and/or in the sexual response cycle (excitement, plateau, orgasm, and resolution) that result in marked distress and interpersonal difficulty.1 Sexual dysfunction can occur with the use of any antidepressant with serotonergic activity; it affects an estimated 50% to 70% of patients who take SSRIs.2 Sexual dysfunction can occur with all SSRIs; however, higher rates of sexual dysfunction are found with citalopram, fluoxetine, paroxetine, and sertraline.3 Studies have suggested there may be a dose-side effect relationship with SSRI-induced sexual dysfunction.4
Several factors can increase a patient’s risk of sexual dysfunction and should be considered before prescribing an antidepressant or when a patient presents with new or worsening sexual dysfunction (Table 1).5 In general, nonserotonergic agents such as bupropion, mirtazapine, and nefazodone are associated with lower rates of sexual dysfunction. The pharmacology of these agents explains their decreased propensity to cause sexual dysfunction. These agents increase levels of dopamine in the mesolimbic dopaminergic system either by blocking reuptake (bupropion) or antagonizing the serotonin subtype-2 receptor and facilitating disinhibition of decreased dopamine downstream (nefazodone and mirtazapine).
Table 1
Risk factors for sexual dysfunction
| Sex | Risk factors |
|---|---|
| Women | History of sexual, physical, or emotional abuse, physical inactivity |
| Men | Severe hyperprolactinemia, smoking |
| Both sexes | Poor to fair health, genitourinary disease, diabetes mellitus, cardiovascular disease, hypertension, increasing age, psychiatric disorders, relationship difficulties |
| Source: Reference 5 | |
One option for treating antidepressant-induced sexual dysfunction in women is PDE5 inhibitors, which are used to treat erectile dysfunction (ED). These medications ameliorate ED by inhibiting degradation of cyclic guanosine monophosphate by PDE5, which increases blood flow to the penis during sexual stimulation. Although these medications are not FDA-approved for treating sexual dysfunction in women, adjunctive PDE5 inhibitor treatment may be beneficial for sexual dysfunction in females because similar mediators, such as nitric oxide and cyclic guanosine monophosphate, involved in the nonadrenergic-noncholinergic signaling that controls sexual stimulation in men also are found in female genital tissue.6
When treating a woman with SSRI-induced sexual dysfunction, consider nonpharmacologic treatments both before and during pharmacotherapy (Table 2).7,8 See Table 3 for a comparison of pharmacokinetics, side effects, and drug interactions of the 4 FDA-approved PDE5 inhibitors—avanafil, sildenafil, tadalafil, and vardenafil.
Table 2
Management strategies for SSRI-induced sexual dysfunction
| Intervention | Comments |
|---|---|
| Nonpharmacologic | |
| Lifestyle modifications | Encourage healthy eating, weight loss, smoking cessation, substance abuse treatment, or minimizing alcohol intake to improve patient self-image and overall health |
| Cognitive-behavioral therapy | Patients can identify coping strategies for reducing symptom severity and preventing worsening sexual dysfunction |
| Sex therapy | May benefit patients with relationship difficulties |
| ‘Watch and wait’ | Spontaneous resolving (or ‘adaptation’) of sexual dysfunction with antidepressants can take ≥6 months. Studies have found adaptation rates generally are low (~10%) |
| Pharmacologic | |
| Drug holiday | May be an option for patients taking antidepressants with shorter half-lives and patients taking lower doses. Be cautious of empowering patients to stop their own medications as needed |
| Dosage reduction | Serotonergic antidepressant-induced sexual dysfunction may be related to dose. Little research has been conducted on this method and the patient’s clinical status must be considered |
| Dose timing | Instructing a patient to take the antidepressant after his or her usual time of sexual activity (eg, patients who engage in sexual activity at night should take the antidepressant before falling asleep). This may allow the drug level to be lowest during sexual activity |
| Switching medications | Case reports, retrospective studies, and RCTs suggest switching to a different antidepressant with less serotonergic activity may be appropriate, particularly if the patient has not responded to the current antidepressant |
| Adjunctive therapy | RCTs support adjunctive bupropion (≥300 mg/d) or olanzapine (5 mg/d) as treatment for SSRI-induced sexual dysfunction in women Studies have found no improvement in sexual functioning with adjunctive buspirone, granisetron, amantadine, mirtazapine, yohimbine, ephedrine, or ginkgo biloba in women |
| RCTs: randomized controlled trials; SSRI: selective serotonin reuptake inhibitor Source: Reference 7,8 | |
Table 3
Phosphodiesterase type 5 inhibitors: A comparison
| Medication | Dose rangea | Pharmacokinetics | Side effects | Significant drug interactions |
|---|---|---|---|---|
| Avanafil | 50 to 200 mg, 30 minutes before sexual activity | Bioavailability: N/A (high-fat meal delays Tmax by 60 minutes and reduces Cmax by 24% to 39%; clinically insignificant) Half life: 5 hours Metabolism: CYP3A4 | Headache, flushing, nasal congestion, nasopharyngitis, backache | Strong CYP3A4 inhibitors (increased avanafil levels) Contraindicated within 12 hours of nitrate use (eg, nitroglycerin) |
| Sildenafil | 25 to 100 mg, 1 to 2 hours before sexual activity | Bioavailability: 41% (food/high-fat meal delays Tmax by 60 minutes and reduces Cmax by 29%) Half life: 4 hours Metabolism: CYP3A4 | Headache, flushing, erythema, indigestion, insomnia, visual disturbances (blue vision) | Strong CYP3A4 inhibitors (increased sildenafil levels) Contraindicated within 24 hours of nitrate use |
| Tadalafil | 10 to 20 mg, 30 minutes before sexual activity | Bioavailability: N/A (not affected by food) Half life: 17.5 hours (duration of action up to 36 hours) Metabolism: CYP3A4 | Headache, flushing, indigestion, nasal congestion, dizziness, myalgia, and back pain | Strong CYP3A4 inhibitors (increased tadalafil levels) Contraindicated within 48 hours of nitrate use |
| Vardenafil | 5 to 20 mg, 30 minutes to 2 hours before sexual activity | Bioavailability: 15% for film-coated tablet (high-fat meal reduces Cmax by 18% to 50%) Half life: 4 to 5 hours Metabolism: CYP3A4 | Headache, flushing, indigestion, nasal congestion, dizziness, visual disturbances (blue vision) | Strong CYP3A4 inhibitors (increased vardenafil levels) Contraindicated within 24 hours of nitrate use |
| aTypical dose range for treatment of erectile dysfunction Cmax: maximum concentration; CYP: cytochrome P450; Tmax: time to maximum concentration Source: Micromedex® Healthcare Series [Internet database]. Greenwood Village, CO: Thomson Healthcare. Accessed October 10, 2012 | ||||
Limited evidence for sildenafil
Case reports, a few small open-label trials, and 1 prospective, randomized controlled trial (RCT) have evaluated sildenafil as an adjunctive treatment for serotonergic antidepressant-associated sexual dysfunction in women.6,9 Nurnberg et al6 examined the efficacy of adjunctive sildenafil in women with SSRI-induced sexual dysfunction. This 8-week, placebo-controlled, double-blind, RCT used a flexible dose (50 or 100 mg), intention-to-treat design to assess the effect of sildenafil on 98 premenopausal women whose depression was in remission. Ten patients were taking the serotonin-norepinephrine inhibitor venlafaxine, 1 was taking the TCA clomipramine, and 87 were receiving an SSRI. Patients were instructed to take sildenafil or placebo 1 to 2 hours before sexual activity. The primary outcome was mean change from baseline on the Clinical Global Impression-Sexual Function (CGI-SF) scale.
Women taking sildenafil showed significant improvement compared with those taking placebo, with a treatment difference between groups of 0.8 (95% CI, 0.6 to 1.0; =.001). Additionally, 23% of sildenafil-treated patients reported no improvement with the intervention, compared with 73% of patients receiving placebo. Secondary outcomes using 3 validated scales that evaluated specific phases of sexual function found that patients’ orgasmic function significantly benefited from sildenafil treatment, while desire, arousal, and overall satisfaction were not significantly different.
Although these findings seem to support sildenafil for treating serotonergic antidepressant-associated sexual dysfunction in women, the study had a relatively small treatment effect in a well-defined patient population; therefore, replication in future trials and different patient populations is warranted. Overall, sildenafil was well tolerated, despite patient reports of headaches, flushing, visual disturbances, dyspepsia, nasal congestion, and palpitations. Finally, cost vs benefit should be considered; PDE5 inhibitors may not be covered by insurance or may require prior authorization.
CASE CONTINUED: Symptoms resolve
Bupropion is not an appropriate choice for Mrs. L because of her seizure risk. Mirtazapine is ruled out because in the past she experienced excessive somnolence that impaired her ability to function. You are not comfortable prescribing nefazodone because of its risk of hepatotoxicity or suggesting that Mrs. L take a “drug holiday” (stop taking any antidepressants for a short period) because of the risk of depressive relapse. You suggest that Mrs. L continue to take sertraline because sometimes antidepressant-induced sexual dysfunction resolves after ≥6 months of treatment with the same agent, but she is adamant that her relationship with her husband will deteriorate if she waits that long. She also declines cognitive-behavioral therapy because her job doesn’t allow the time or flexibility to commit to the sessions.
You prescribe sildenafil, 50 mg, and instruct Mrs. L to take 1 tablet 1 to 2 hours before sexual activity. This treatment improves her ability to achieve orgasm. She tolerates the drug well and after 8 weeks of treatment her CGI-SF score improves from 6 at baseline, indicating extreme dysfunction, to 2, indicating normal function. Ten months into her sertraline treatment, Mrs. L discovers she no longer requires sildenafil to achieve orgasm.
Related Resources
- Nurnberg HG. An evidence-based review updating the various treatment and management approaches to serotonin reuptake inhibitor-associated sexual dysfunction. Drugs Today (Barc). 2008;44(2):147-168.
- NIH Medline Plus. Sexual problems in women. www.nlm.nih.gov/medlineplus/sexualproblemsinwomen.html.
- Sturpe DA, Mertens MK, Scoville C. What are the treatment options for SSRI-related sexual dysfunction? J Fam Pract. 2002;51(8):681.
Drug Brand Names
- Amantadine • Symadine, Symmetrel
- Avanafil • Stendra
- Bupropion • Wellbutrin, Zyban
- Buspirone • BuSpar
- Citalopram • Celexa
- Clomipramine • Anafranil
- Fluoxetine • Prozac
- Granisetron • Kytril
- Mirtazapine • Remeron
- Nefazodone • Serzone
- Nitroglycerin • Nitrostat
- Nortriptyline • Pamelor
- Olanzapine • Zyprexa
- Paroxetine • Paxil
- Sertraline • Zoloft
- Sildenafil • Viagra
- Tadalafil • Cialis
- Vardenafil • Levitra
- Venlafaxine • Effexor
Disclosures
Dr. Burghardt receives grant or research support from the University of Michigan Depression Center.
Ms. Gardner reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
2. Montejo AL, Llorca G, Izquierdo JA, et al. Incidence of sexual dysfunction associated with antidepressant agents: a prospective multicenter study of 1022 outpatients. Spanish Working Group for the Study of Psychotropic-Related Sexual Dysfunction. J Clin Psychiatry. 2001;62(suppl 3):10-21.
3. Serretti A, Chiesa A. Treatment-emergent sexual dysfunction related to antidepressants: a meta-analysis. J Clin Psychopharmacol. 2009;29(3):259-266.
4. Clayton AH, Pradko JF, Croft HA, et al. Prevalence of sexual dysfunction among newer antidepressants. J Clin Psychiatry. 2002;63(4):357-366.
5. Lewis RW, Fugl-Meyer KS, Bosch R, et al. Epidemiology/risk factors of sexual dysfunction. J Sex Med. 2004;1(1):35-39.
6. Nurnberg HG, Hensley PL, Heiman JR, et al. Sildenafil treatment of women with antidepressant-associated sexual dysfunction: a randomized controlled trial. JAMA. 2008;300(4):395-404.
7. Taylor MJ, Rudkin L, Hawton K. Strategies for managing antidepressant-induced sexual dysfunction: systematic review of randomised controlled trials. J Affect Disord. 2005;88(3):241-254.
8. Balon R. SSRI-associated sexual dysfunction. Am J Psychiatry. 2006;163(9):1504-1509.
9. Brown DA, Kyle JA, Ferrill MJ. Assessing the clinical efficacy of sildenafil for the treatment of female sexual dysfunction. Ann Pharmacother. 2009;43(7):1275-1285.
- Sexual dysfunction can arise from environmental, social, medical, or drug effects and requires a multifaceted approach to treatment.
- When possible, take a baseline sexual dysfunction measurement to assess if selective serotonin reuptake inhibitor use is correlated with onset or worsening of sexual dysfunction.
- Nonpharmacologic options should be considered before and during pharmacotherapy.
- Sildenafil may be useful for treating anorgasmia in women taking serotonergic antidepressants.
- Phosphodiesterase type 5 inhibitors are not FDA-approved for sexual dysfunction in women.
Mrs. L, age 27, has a history of major depressive disorder with symptoms of anxiety. She was managed successfully for 2 years with bupropion XL, 300 mg/d, but was switched to venlafaxine, titrated to 225 mg/d, after she developed seizures secondary to a head injury sustained in a car accident. After the switch, Mrs. L’s mood deteriorated and she was hospitalized. Since then, she’s received several medication trials, including paroxetine, 30 mg/d, a selective serotonin reuptake inhibitor (SSRI), and the tricyclic antidepressant (TCA) nortriptyline, 75 mg/d, but she could not tolerate these medications because of severe xerostomia.
After taking sertraline, 150 mg/d, for 8 weeks, Mrs. L improves and has a Patient Health Questionnaire score of 6, indicating mild depression. Her initial complaints of diarrhea and nausea have resolved, but Mrs. L now reports that she and her husband are having marital difficulties because she cannot achieve orgasm during sexual intercourse. She did not have this problem when she was taking bupropion. Her husband occasionally takes the phosphodiesterase type 5 (PDE5) inhibitor sildenafil before intercourse, and Mrs. L asks you if this medication will help her achieve orgasm.
DSM-IV-TR defines sexual dysfunction as disturbances in sexual desire and/or in the sexual response cycle (excitement, plateau, orgasm, and resolution) that result in marked distress and interpersonal difficulty.1 Sexual dysfunction can occur with the use of any antidepressant with serotonergic activity; it affects an estimated 50% to 70% of patients who take SSRIs.2 Sexual dysfunction can occur with all SSRIs; however, higher rates of sexual dysfunction are found with citalopram, fluoxetine, paroxetine, and sertraline.3 Studies have suggested there may be a dose-side effect relationship with SSRI-induced sexual dysfunction.4
Several factors can increase a patient’s risk of sexual dysfunction and should be considered before prescribing an antidepressant or when a patient presents with new or worsening sexual dysfunction (Table 1).5 In general, nonserotonergic agents such as bupropion, mirtazapine, and nefazodone are associated with lower rates of sexual dysfunction. The pharmacology of these agents explains their decreased propensity to cause sexual dysfunction. These agents increase levels of dopamine in the mesolimbic dopaminergic system either by blocking reuptake (bupropion) or antagonizing the serotonin subtype-2 receptor and facilitating disinhibition of decreased dopamine downstream (nefazodone and mirtazapine).
Table 1
Risk factors for sexual dysfunction
| Sex | Risk factors |
|---|---|
| Women | History of sexual, physical, or emotional abuse, physical inactivity |
| Men | Severe hyperprolactinemia, smoking |
| Both sexes | Poor to fair health, genitourinary disease, diabetes mellitus, cardiovascular disease, hypertension, increasing age, psychiatric disorders, relationship difficulties |
| Source: Reference 5 | |
One option for treating antidepressant-induced sexual dysfunction in women is PDE5 inhibitors, which are used to treat erectile dysfunction (ED). These medications ameliorate ED by inhibiting degradation of cyclic guanosine monophosphate by PDE5, which increases blood flow to the penis during sexual stimulation. Although these medications are not FDA-approved for treating sexual dysfunction in women, adjunctive PDE5 inhibitor treatment may be beneficial for sexual dysfunction in females because similar mediators, such as nitric oxide and cyclic guanosine monophosphate, involved in the nonadrenergic-noncholinergic signaling that controls sexual stimulation in men also are found in female genital tissue.6
When treating a woman with SSRI-induced sexual dysfunction, consider nonpharmacologic treatments both before and during pharmacotherapy (Table 2).7,8 See Table 3 for a comparison of pharmacokinetics, side effects, and drug interactions of the 4 FDA-approved PDE5 inhibitors—avanafil, sildenafil, tadalafil, and vardenafil.
Table 2
Management strategies for SSRI-induced sexual dysfunction
| Intervention | Comments |
|---|---|
| Nonpharmacologic | |
| Lifestyle modifications | Encourage healthy eating, weight loss, smoking cessation, substance abuse treatment, or minimizing alcohol intake to improve patient self-image and overall health |
| Cognitive-behavioral therapy | Patients can identify coping strategies for reducing symptom severity and preventing worsening sexual dysfunction |
| Sex therapy | May benefit patients with relationship difficulties |
| ‘Watch and wait’ | Spontaneous resolving (or ‘adaptation’) of sexual dysfunction with antidepressants can take ≥6 months. Studies have found adaptation rates generally are low (~10%) |
| Pharmacologic | |
| Drug holiday | May be an option for patients taking antidepressants with shorter half-lives and patients taking lower doses. Be cautious of empowering patients to stop their own medications as needed |
| Dosage reduction | Serotonergic antidepressant-induced sexual dysfunction may be related to dose. Little research has been conducted on this method and the patient’s clinical status must be considered |
| Dose timing | Instructing a patient to take the antidepressant after his or her usual time of sexual activity (eg, patients who engage in sexual activity at night should take the antidepressant before falling asleep). This may allow the drug level to be lowest during sexual activity |
| Switching medications | Case reports, retrospective studies, and RCTs suggest switching to a different antidepressant with less serotonergic activity may be appropriate, particularly if the patient has not responded to the current antidepressant |
| Adjunctive therapy | RCTs support adjunctive bupropion (≥300 mg/d) or olanzapine (5 mg/d) as treatment for SSRI-induced sexual dysfunction in women Studies have found no improvement in sexual functioning with adjunctive buspirone, granisetron, amantadine, mirtazapine, yohimbine, ephedrine, or ginkgo biloba in women |
| RCTs: randomized controlled trials; SSRI: selective serotonin reuptake inhibitor Source: Reference 7,8 | |
Table 3
Phosphodiesterase type 5 inhibitors: A comparison
| Medication | Dose rangea | Pharmacokinetics | Side effects | Significant drug interactions |
|---|---|---|---|---|
| Avanafil | 50 to 200 mg, 30 minutes before sexual activity | Bioavailability: N/A (high-fat meal delays Tmax by 60 minutes and reduces Cmax by 24% to 39%; clinically insignificant) Half life: 5 hours Metabolism: CYP3A4 | Headache, flushing, nasal congestion, nasopharyngitis, backache | Strong CYP3A4 inhibitors (increased avanafil levels) Contraindicated within 12 hours of nitrate use (eg, nitroglycerin) |
| Sildenafil | 25 to 100 mg, 1 to 2 hours before sexual activity | Bioavailability: 41% (food/high-fat meal delays Tmax by 60 minutes and reduces Cmax by 29%) Half life: 4 hours Metabolism: CYP3A4 | Headache, flushing, erythema, indigestion, insomnia, visual disturbances (blue vision) | Strong CYP3A4 inhibitors (increased sildenafil levels) Contraindicated within 24 hours of nitrate use |
| Tadalafil | 10 to 20 mg, 30 minutes before sexual activity | Bioavailability: N/A (not affected by food) Half life: 17.5 hours (duration of action up to 36 hours) Metabolism: CYP3A4 | Headache, flushing, indigestion, nasal congestion, dizziness, myalgia, and back pain | Strong CYP3A4 inhibitors (increased tadalafil levels) Contraindicated within 48 hours of nitrate use |
| Vardenafil | 5 to 20 mg, 30 minutes to 2 hours before sexual activity | Bioavailability: 15% for film-coated tablet (high-fat meal reduces Cmax by 18% to 50%) Half life: 4 to 5 hours Metabolism: CYP3A4 | Headache, flushing, indigestion, nasal congestion, dizziness, visual disturbances (blue vision) | Strong CYP3A4 inhibitors (increased vardenafil levels) Contraindicated within 24 hours of nitrate use |
| aTypical dose range for treatment of erectile dysfunction Cmax: maximum concentration; CYP: cytochrome P450; Tmax: time to maximum concentration Source: Micromedex® Healthcare Series [Internet database]. Greenwood Village, CO: Thomson Healthcare. Accessed October 10, 2012 | ||||
Limited evidence for sildenafil
Case reports, a few small open-label trials, and 1 prospective, randomized controlled trial (RCT) have evaluated sildenafil as an adjunctive treatment for serotonergic antidepressant-associated sexual dysfunction in women.6,9 Nurnberg et al6 examined the efficacy of adjunctive sildenafil in women with SSRI-induced sexual dysfunction. This 8-week, placebo-controlled, double-blind, RCT used a flexible dose (50 or 100 mg), intention-to-treat design to assess the effect of sildenafil on 98 premenopausal women whose depression was in remission. Ten patients were taking the serotonin-norepinephrine inhibitor venlafaxine, 1 was taking the TCA clomipramine, and 87 were receiving an SSRI. Patients were instructed to take sildenafil or placebo 1 to 2 hours before sexual activity. The primary outcome was mean change from baseline on the Clinical Global Impression-Sexual Function (CGI-SF) scale.
Women taking sildenafil showed significant improvement compared with those taking placebo, with a treatment difference between groups of 0.8 (95% CI, 0.6 to 1.0; =.001). Additionally, 23% of sildenafil-treated patients reported no improvement with the intervention, compared with 73% of patients receiving placebo. Secondary outcomes using 3 validated scales that evaluated specific phases of sexual function found that patients’ orgasmic function significantly benefited from sildenafil treatment, while desire, arousal, and overall satisfaction were not significantly different.
Although these findings seem to support sildenafil for treating serotonergic antidepressant-associated sexual dysfunction in women, the study had a relatively small treatment effect in a well-defined patient population; therefore, replication in future trials and different patient populations is warranted. Overall, sildenafil was well tolerated, despite patient reports of headaches, flushing, visual disturbances, dyspepsia, nasal congestion, and palpitations. Finally, cost vs benefit should be considered; PDE5 inhibitors may not be covered by insurance or may require prior authorization.
CASE CONTINUED: Symptoms resolve
Bupropion is not an appropriate choice for Mrs. L because of her seizure risk. Mirtazapine is ruled out because in the past she experienced excessive somnolence that impaired her ability to function. You are not comfortable prescribing nefazodone because of its risk of hepatotoxicity or suggesting that Mrs. L take a “drug holiday” (stop taking any antidepressants for a short period) because of the risk of depressive relapse. You suggest that Mrs. L continue to take sertraline because sometimes antidepressant-induced sexual dysfunction resolves after ≥6 months of treatment with the same agent, but she is adamant that her relationship with her husband will deteriorate if she waits that long. She also declines cognitive-behavioral therapy because her job doesn’t allow the time or flexibility to commit to the sessions.
You prescribe sildenafil, 50 mg, and instruct Mrs. L to take 1 tablet 1 to 2 hours before sexual activity. This treatment improves her ability to achieve orgasm. She tolerates the drug well and after 8 weeks of treatment her CGI-SF score improves from 6 at baseline, indicating extreme dysfunction, to 2, indicating normal function. Ten months into her sertraline treatment, Mrs. L discovers she no longer requires sildenafil to achieve orgasm.
Related Resources
- Nurnberg HG. An evidence-based review updating the various treatment and management approaches to serotonin reuptake inhibitor-associated sexual dysfunction. Drugs Today (Barc). 2008;44(2):147-168.
- NIH Medline Plus. Sexual problems in women. www.nlm.nih.gov/medlineplus/sexualproblemsinwomen.html.
- Sturpe DA, Mertens MK, Scoville C. What are the treatment options for SSRI-related sexual dysfunction? J Fam Pract. 2002;51(8):681.
Drug Brand Names
- Amantadine • Symadine, Symmetrel
- Avanafil • Stendra
- Bupropion • Wellbutrin, Zyban
- Buspirone • BuSpar
- Citalopram • Celexa
- Clomipramine • Anafranil
- Fluoxetine • Prozac
- Granisetron • Kytril
- Mirtazapine • Remeron
- Nefazodone • Serzone
- Nitroglycerin • Nitrostat
- Nortriptyline • Pamelor
- Olanzapine • Zyprexa
- Paroxetine • Paxil
- Sertraline • Zoloft
- Sildenafil • Viagra
- Tadalafil • Cialis
- Vardenafil • Levitra
- Venlafaxine • Effexor
Disclosures
Dr. Burghardt receives grant or research support from the University of Michigan Depression Center.
Ms. Gardner reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
- Sexual dysfunction can arise from environmental, social, medical, or drug effects and requires a multifaceted approach to treatment.
- When possible, take a baseline sexual dysfunction measurement to assess if selective serotonin reuptake inhibitor use is correlated with onset or worsening of sexual dysfunction.
- Nonpharmacologic options should be considered before and during pharmacotherapy.
- Sildenafil may be useful for treating anorgasmia in women taking serotonergic antidepressants.
- Phosphodiesterase type 5 inhibitors are not FDA-approved for sexual dysfunction in women.
Mrs. L, age 27, has a history of major depressive disorder with symptoms of anxiety. She was managed successfully for 2 years with bupropion XL, 300 mg/d, but was switched to venlafaxine, titrated to 225 mg/d, after she developed seizures secondary to a head injury sustained in a car accident. After the switch, Mrs. L’s mood deteriorated and she was hospitalized. Since then, she’s received several medication trials, including paroxetine, 30 mg/d, a selective serotonin reuptake inhibitor (SSRI), and the tricyclic antidepressant (TCA) nortriptyline, 75 mg/d, but she could not tolerate these medications because of severe xerostomia.
After taking sertraline, 150 mg/d, for 8 weeks, Mrs. L improves and has a Patient Health Questionnaire score of 6, indicating mild depression. Her initial complaints of diarrhea and nausea have resolved, but Mrs. L now reports that she and her husband are having marital difficulties because she cannot achieve orgasm during sexual intercourse. She did not have this problem when she was taking bupropion. Her husband occasionally takes the phosphodiesterase type 5 (PDE5) inhibitor sildenafil before intercourse, and Mrs. L asks you if this medication will help her achieve orgasm.
DSM-IV-TR defines sexual dysfunction as disturbances in sexual desire and/or in the sexual response cycle (excitement, plateau, orgasm, and resolution) that result in marked distress and interpersonal difficulty.1 Sexual dysfunction can occur with the use of any antidepressant with serotonergic activity; it affects an estimated 50% to 70% of patients who take SSRIs.2 Sexual dysfunction can occur with all SSRIs; however, higher rates of sexual dysfunction are found with citalopram, fluoxetine, paroxetine, and sertraline.3 Studies have suggested there may be a dose-side effect relationship with SSRI-induced sexual dysfunction.4
Several factors can increase a patient’s risk of sexual dysfunction and should be considered before prescribing an antidepressant or when a patient presents with new or worsening sexual dysfunction (Table 1).5 In general, nonserotonergic agents such as bupropion, mirtazapine, and nefazodone are associated with lower rates of sexual dysfunction. The pharmacology of these agents explains their decreased propensity to cause sexual dysfunction. These agents increase levels of dopamine in the mesolimbic dopaminergic system either by blocking reuptake (bupropion) or antagonizing the serotonin subtype-2 receptor and facilitating disinhibition of decreased dopamine downstream (nefazodone and mirtazapine).
Table 1
Risk factors for sexual dysfunction
| Sex | Risk factors |
|---|---|
| Women | History of sexual, physical, or emotional abuse, physical inactivity |
| Men | Severe hyperprolactinemia, smoking |
| Both sexes | Poor to fair health, genitourinary disease, diabetes mellitus, cardiovascular disease, hypertension, increasing age, psychiatric disorders, relationship difficulties |
| Source: Reference 5 | |
One option for treating antidepressant-induced sexual dysfunction in women is PDE5 inhibitors, which are used to treat erectile dysfunction (ED). These medications ameliorate ED by inhibiting degradation of cyclic guanosine monophosphate by PDE5, which increases blood flow to the penis during sexual stimulation. Although these medications are not FDA-approved for treating sexual dysfunction in women, adjunctive PDE5 inhibitor treatment may be beneficial for sexual dysfunction in females because similar mediators, such as nitric oxide and cyclic guanosine monophosphate, involved in the nonadrenergic-noncholinergic signaling that controls sexual stimulation in men also are found in female genital tissue.6
When treating a woman with SSRI-induced sexual dysfunction, consider nonpharmacologic treatments both before and during pharmacotherapy (Table 2).7,8 See Table 3 for a comparison of pharmacokinetics, side effects, and drug interactions of the 4 FDA-approved PDE5 inhibitors—avanafil, sildenafil, tadalafil, and vardenafil.
Table 2
Management strategies for SSRI-induced sexual dysfunction
| Intervention | Comments |
|---|---|
| Nonpharmacologic | |
| Lifestyle modifications | Encourage healthy eating, weight loss, smoking cessation, substance abuse treatment, or minimizing alcohol intake to improve patient self-image and overall health |
| Cognitive-behavioral therapy | Patients can identify coping strategies for reducing symptom severity and preventing worsening sexual dysfunction |
| Sex therapy | May benefit patients with relationship difficulties |
| ‘Watch and wait’ | Spontaneous resolving (or ‘adaptation’) of sexual dysfunction with antidepressants can take ≥6 months. Studies have found adaptation rates generally are low (~10%) |
| Pharmacologic | |
| Drug holiday | May be an option for patients taking antidepressants with shorter half-lives and patients taking lower doses. Be cautious of empowering patients to stop their own medications as needed |
| Dosage reduction | Serotonergic antidepressant-induced sexual dysfunction may be related to dose. Little research has been conducted on this method and the patient’s clinical status must be considered |
| Dose timing | Instructing a patient to take the antidepressant after his or her usual time of sexual activity (eg, patients who engage in sexual activity at night should take the antidepressant before falling asleep). This may allow the drug level to be lowest during sexual activity |
| Switching medications | Case reports, retrospective studies, and RCTs suggest switching to a different antidepressant with less serotonergic activity may be appropriate, particularly if the patient has not responded to the current antidepressant |
| Adjunctive therapy | RCTs support adjunctive bupropion (≥300 mg/d) or olanzapine (5 mg/d) as treatment for SSRI-induced sexual dysfunction in women Studies have found no improvement in sexual functioning with adjunctive buspirone, granisetron, amantadine, mirtazapine, yohimbine, ephedrine, or ginkgo biloba in women |
| RCTs: randomized controlled trials; SSRI: selective serotonin reuptake inhibitor Source: Reference 7,8 | |
Table 3
Phosphodiesterase type 5 inhibitors: A comparison
| Medication | Dose rangea | Pharmacokinetics | Side effects | Significant drug interactions |
|---|---|---|---|---|
| Avanafil | 50 to 200 mg, 30 minutes before sexual activity | Bioavailability: N/A (high-fat meal delays Tmax by 60 minutes and reduces Cmax by 24% to 39%; clinically insignificant) Half life: 5 hours Metabolism: CYP3A4 | Headache, flushing, nasal congestion, nasopharyngitis, backache | Strong CYP3A4 inhibitors (increased avanafil levels) Contraindicated within 12 hours of nitrate use (eg, nitroglycerin) |
| Sildenafil | 25 to 100 mg, 1 to 2 hours before sexual activity | Bioavailability: 41% (food/high-fat meal delays Tmax by 60 minutes and reduces Cmax by 29%) Half life: 4 hours Metabolism: CYP3A4 | Headache, flushing, erythema, indigestion, insomnia, visual disturbances (blue vision) | Strong CYP3A4 inhibitors (increased sildenafil levels) Contraindicated within 24 hours of nitrate use |
| Tadalafil | 10 to 20 mg, 30 minutes before sexual activity | Bioavailability: N/A (not affected by food) Half life: 17.5 hours (duration of action up to 36 hours) Metabolism: CYP3A4 | Headache, flushing, indigestion, nasal congestion, dizziness, myalgia, and back pain | Strong CYP3A4 inhibitors (increased tadalafil levels) Contraindicated within 48 hours of nitrate use |
| Vardenafil | 5 to 20 mg, 30 minutes to 2 hours before sexual activity | Bioavailability: 15% for film-coated tablet (high-fat meal reduces Cmax by 18% to 50%) Half life: 4 to 5 hours Metabolism: CYP3A4 | Headache, flushing, indigestion, nasal congestion, dizziness, visual disturbances (blue vision) | Strong CYP3A4 inhibitors (increased vardenafil levels) Contraindicated within 24 hours of nitrate use |
| aTypical dose range for treatment of erectile dysfunction Cmax: maximum concentration; CYP: cytochrome P450; Tmax: time to maximum concentration Source: Micromedex® Healthcare Series [Internet database]. Greenwood Village, CO: Thomson Healthcare. Accessed October 10, 2012 | ||||
Limited evidence for sildenafil
Case reports, a few small open-label trials, and 1 prospective, randomized controlled trial (RCT) have evaluated sildenafil as an adjunctive treatment for serotonergic antidepressant-associated sexual dysfunction in women.6,9 Nurnberg et al6 examined the efficacy of adjunctive sildenafil in women with SSRI-induced sexual dysfunction. This 8-week, placebo-controlled, double-blind, RCT used a flexible dose (50 or 100 mg), intention-to-treat design to assess the effect of sildenafil on 98 premenopausal women whose depression was in remission. Ten patients were taking the serotonin-norepinephrine inhibitor venlafaxine, 1 was taking the TCA clomipramine, and 87 were receiving an SSRI. Patients were instructed to take sildenafil or placebo 1 to 2 hours before sexual activity. The primary outcome was mean change from baseline on the Clinical Global Impression-Sexual Function (CGI-SF) scale.
Women taking sildenafil showed significant improvement compared with those taking placebo, with a treatment difference between groups of 0.8 (95% CI, 0.6 to 1.0; =.001). Additionally, 23% of sildenafil-treated patients reported no improvement with the intervention, compared with 73% of patients receiving placebo. Secondary outcomes using 3 validated scales that evaluated specific phases of sexual function found that patients’ orgasmic function significantly benefited from sildenafil treatment, while desire, arousal, and overall satisfaction were not significantly different.
Although these findings seem to support sildenafil for treating serotonergic antidepressant-associated sexual dysfunction in women, the study had a relatively small treatment effect in a well-defined patient population; therefore, replication in future trials and different patient populations is warranted. Overall, sildenafil was well tolerated, despite patient reports of headaches, flushing, visual disturbances, dyspepsia, nasal congestion, and palpitations. Finally, cost vs benefit should be considered; PDE5 inhibitors may not be covered by insurance or may require prior authorization.
CASE CONTINUED: Symptoms resolve
Bupropion is not an appropriate choice for Mrs. L because of her seizure risk. Mirtazapine is ruled out because in the past she experienced excessive somnolence that impaired her ability to function. You are not comfortable prescribing nefazodone because of its risk of hepatotoxicity or suggesting that Mrs. L take a “drug holiday” (stop taking any antidepressants for a short period) because of the risk of depressive relapse. You suggest that Mrs. L continue to take sertraline because sometimes antidepressant-induced sexual dysfunction resolves after ≥6 months of treatment with the same agent, but she is adamant that her relationship with her husband will deteriorate if she waits that long. She also declines cognitive-behavioral therapy because her job doesn’t allow the time or flexibility to commit to the sessions.
You prescribe sildenafil, 50 mg, and instruct Mrs. L to take 1 tablet 1 to 2 hours before sexual activity. This treatment improves her ability to achieve orgasm. She tolerates the drug well and after 8 weeks of treatment her CGI-SF score improves from 6 at baseline, indicating extreme dysfunction, to 2, indicating normal function. Ten months into her sertraline treatment, Mrs. L discovers she no longer requires sildenafil to achieve orgasm.
Related Resources
- Nurnberg HG. An evidence-based review updating the various treatment and management approaches to serotonin reuptake inhibitor-associated sexual dysfunction. Drugs Today (Barc). 2008;44(2):147-168.
- NIH Medline Plus. Sexual problems in women. www.nlm.nih.gov/medlineplus/sexualproblemsinwomen.html.
- Sturpe DA, Mertens MK, Scoville C. What are the treatment options for SSRI-related sexual dysfunction? J Fam Pract. 2002;51(8):681.
Drug Brand Names
- Amantadine • Symadine, Symmetrel
- Avanafil • Stendra
- Bupropion • Wellbutrin, Zyban
- Buspirone • BuSpar
- Citalopram • Celexa
- Clomipramine • Anafranil
- Fluoxetine • Prozac
- Granisetron • Kytril
- Mirtazapine • Remeron
- Nefazodone • Serzone
- Nitroglycerin • Nitrostat
- Nortriptyline • Pamelor
- Olanzapine • Zyprexa
- Paroxetine • Paxil
- Sertraline • Zoloft
- Sildenafil • Viagra
- Tadalafil • Cialis
- Vardenafil • Levitra
- Venlafaxine • Effexor
Disclosures
Dr. Burghardt receives grant or research support from the University of Michigan Depression Center.
Ms. Gardner reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
2. Montejo AL, Llorca G, Izquierdo JA, et al. Incidence of sexual dysfunction associated with antidepressant agents: a prospective multicenter study of 1022 outpatients. Spanish Working Group for the Study of Psychotropic-Related Sexual Dysfunction. J Clin Psychiatry. 2001;62(suppl 3):10-21.
3. Serretti A, Chiesa A. Treatment-emergent sexual dysfunction related to antidepressants: a meta-analysis. J Clin Psychopharmacol. 2009;29(3):259-266.
4. Clayton AH, Pradko JF, Croft HA, et al. Prevalence of sexual dysfunction among newer antidepressants. J Clin Psychiatry. 2002;63(4):357-366.
5. Lewis RW, Fugl-Meyer KS, Bosch R, et al. Epidemiology/risk factors of sexual dysfunction. J Sex Med. 2004;1(1):35-39.
6. Nurnberg HG, Hensley PL, Heiman JR, et al. Sildenafil treatment of women with antidepressant-associated sexual dysfunction: a randomized controlled trial. JAMA. 2008;300(4):395-404.
7. Taylor MJ, Rudkin L, Hawton K. Strategies for managing antidepressant-induced sexual dysfunction: systematic review of randomised controlled trials. J Affect Disord. 2005;88(3):241-254.
8. Balon R. SSRI-associated sexual dysfunction. Am J Psychiatry. 2006;163(9):1504-1509.
9. Brown DA, Kyle JA, Ferrill MJ. Assessing the clinical efficacy of sildenafil for the treatment of female sexual dysfunction. Ann Pharmacother. 2009;43(7):1275-1285.
1. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
2. Montejo AL, Llorca G, Izquierdo JA, et al. Incidence of sexual dysfunction associated with antidepressant agents: a prospective multicenter study of 1022 outpatients. Spanish Working Group for the Study of Psychotropic-Related Sexual Dysfunction. J Clin Psychiatry. 2001;62(suppl 3):10-21.
3. Serretti A, Chiesa A. Treatment-emergent sexual dysfunction related to antidepressants: a meta-analysis. J Clin Psychopharmacol. 2009;29(3):259-266.
4. Clayton AH, Pradko JF, Croft HA, et al. Prevalence of sexual dysfunction among newer antidepressants. J Clin Psychiatry. 2002;63(4):357-366.
5. Lewis RW, Fugl-Meyer KS, Bosch R, et al. Epidemiology/risk factors of sexual dysfunction. J Sex Med. 2004;1(1):35-39.
6. Nurnberg HG, Hensley PL, Heiman JR, et al. Sildenafil treatment of women with antidepressant-associated sexual dysfunction: a randomized controlled trial. JAMA. 2008;300(4):395-404.
7. Taylor MJ, Rudkin L, Hawton K. Strategies for managing antidepressant-induced sexual dysfunction: systematic review of randomised controlled trials. J Affect Disord. 2005;88(3):241-254.
8. Balon R. SSRI-associated sexual dysfunction. Am J Psychiatry. 2006;163(9):1504-1509.
9. Brown DA, Kyle JA, Ferrill MJ. Assessing the clinical efficacy of sildenafil for the treatment of female sexual dysfunction. Ann Pharmacother. 2009;43(7):1275-1285.
Sleepless and paranoid
CASE: Worsening insomnia
Mr. Q, age 44, presents for evaluation of altered mental status characterized by disorientation, impaired attention and concentration, paranoid delusions, and prominent auditory and visual hallucinations. His initial Folstein Mini-Mental State Examination (MMSE) score is 7 of 30, indicating severe impairment. He further describes a recent history of nausea, intermittent vomiting, and anorexia. He takes hydrocodone/acetaminophen, 5/500 mg, 4 times daily for lower back and joint pain. Additionally, he has a pacemaker, which was placed when Mr. Q was in his late 30s to treat sinus bradycardia.
Mr. Q’s fiancée describes his 6-month history of worsening sleep disturbance, noting insomnia, fractured sleep, dream enactment, and daytime fatigue. During this time, Mr. Q averaged 3 to 4 hours of sleep nightly without day-time naps. Ten days ago, he stopped sleeping completely and his cognitive function decompensated rapidly. He became increasingly paranoid, believing government agents had been dispatched to kill him. Several days before admission, Mr. Q developed auditory and visual hallucinations. He reports that he hears voices warning him of Armageddon and sees reincarnated spirits of deceased relatives. He describes his mood as “fine” and “okay” and lacks insight into his psychiatric symptoms other than his sleeplessness.
Mr. Q’s family says he has a history of transient mild depression after his older brother died from an unknown neurologic disease 3 years ago. Mr. Q did not receive pharmacotherapy or psychotherapy but his symptoms resolved. His family says that Mr. Q has been using marijuana daily for several years, but they are unaware of other substance use. They deny a family history of psychiatric illness.
On physical examination, Mr. Q appears thin, agitated, and in mild distress. He has a fever of 99.2°F. His blood pressure drops intermittently from a baseline of 120/70 mm Hg to 100/60 mm Hg, at which point he experiences transient normal sinus tachycardia. Neurologic examination reveals psychomotor agitation and diffuse myoclonic tremor.
The authors’ observations
Table 1
Differential diagnosis of insomnia
| Type of disorder | Examples |
|---|---|
| Sleep disorders | Narcolepsy, REM sleep disorder, periodic limb movement disorder, restless leg syndrome, parasomniac conditions |
| Psychiatric disorders | Mania or hypomania, psychosis, substance intoxication or withdrawal, dementia, delirium |
| Neurologic disorders | Stroke, malignancy, infection or abscess, metabolic or viral encephalopathy, seizure disorder, prion disease |
| Somatic conditions | Cardiorespiratory disease, central or obstructive sleep apnea, congestive heart failure (Cheyne-Stokes respiration), pain, nocturnal movement disorder, gastroesophageal reflux disease, nocturia |
| Other causes | Jet lag, shift work, environment, lifestyle, medication |
| REM: rapid eye movement Source: Reference 1 | |
Medications that can cause or exacerbate insomnia
| Class/category | Medication(s) |
|---|---|
| Stimulants | Bupropion, dextroamphetamine, methylphenidate |
| Decongestants | Pseudoephedrine, phenylephrine |
| Antihypertensives or antiarrythmics | α- and β-antagonists |
| Respiratory medications | Albuterol, theophylline |
| Hormones | Corticosteroids, thyroid medications |
| Anticonvulsants | Lamotrigine |
| Medications that induce rebound insomnia | Benzodiazepines, sedative-hypnotics, opioids |
| Nonprescription medications | Caffeine, alcohol, nicotine, illicit psychostimulants |
EVALUATION: Inconclusive results
Routine laboratory studies reveal mild normocytic anemia and mild hypokalemia. Liver panel, renal function, cardiac profile, brain natriuretic peptide level, folate and vitamin B12 levels, thyroid studies, and human immunodeficiency virus serology are negative or within normal limits. Urinalysis reveals the presence of ketones, indicative of Mr. Q’s recent anorexia. Chest radiography and CT imaging of the head, abdomen, and pelvis also are unremarkable. MRI is contraindicated because of Mr. Q’s implanted pacemaker. Pulse oximetry does not suggest apneic events. Mr. Q and his family refuse a lumbar puncture, which precludes cerebrospinal fluid (CSF) analysis. Electroencephalography (EEG) records normal patterns of wakefulness oscillating with transient periods of stage 1 sleep. A detailed family interview reveals that Mr. Q’s older brother had a history of epilepsy and died at age 49 following a prolonged hospitalization for recurrent seizures and similar insomnia symptoms. History from the patient’s paternal lineage is not available.
The authors’ observations
American Psychiatric Association practice guidelines3 do not support first-line use of benzodiazepines for non-alcohol withdrawal-related delirium. Benzodiazepines are ineffective for treating delirium and may exacerbate symptoms.4 Laboratory evidence confirmed Mr. Q has no history of alcohol or benzodiazepine use. Although treating the underlying cause of delirium is essential, prescribing a sedative-hypnotic medication such as zolpidem for Mr. Q’s insomnia may worsen his condition. These agents are known to impair cognition and may induce or intensify psychosis.5 Melatonin and melatonin receptor agonists, such as ramelteon, promote sleep by regulating the sleep-wake rhythm through their action on melatonin receptors in the hypothalamus.6 Recently, a randomized control trial (RCT)7 found melatonin protected against delirium in hospitalized patients age ≥65. However, no RCT has examined use of exogenous melatonin or melatonin receptor agonists to treat delirium. In Mr. Q’s case, we chose to administer haloperidol. First- and second-generation antipsychotics have shown efficacy in treating acute delirium. Although more clinical experience has accumulated using first-generation agents such as haloperidol, a 2007 Cochrane meta-analysis8 demonstrated equal benefit with second-generation antipsychotics, while noting a decreased incidence of adverse effects.
TREATMENT: Adverse effects
Mr. Q receives an IM injection of haloperidol, 5 mg, for severe agitation, followed 15 hours later by IM aripiprazole, 9.75 mg. Within hours of receiving aripiprazole, Mr. Q develops hyperkinetic perioral and tongue movements. He initially is diagnosed with acute reactionary dystonia, although closer examination reveals myoclonus consistent with his overall presentation. Additionally, his QTc interval increases by 120 ms. Subsequently, all antipsychotics are stopped. We prescribe lorazepam, 1 mg IM every 4 hours as needed, for agitation. Mr. Q receives 2 consecutive doses of lorazepam, although neither effectively reduces his agitation or promotes sleep. Mr. Q is not assessed with positron-emission tomography (PET) or polysomnography.
The authors’ observations
There was no evidence of neurologic disease on Mr. Q’s CT scan and EEG was within normal limits. Other imaging and laboratory studies did not reveal possible infection, malignancy, or cardiovascular disease. Despite its rarity, we considered the possibility of a prion disease, given Mr. Q’s unique presentation and family history. Familial fatal insomnia (FFI) is an autosomal dominant disease caused by a point mutation in the prion protein gene. Prion proteins are theorized to play a role in myelin stability. The aberrant isoform produced in FFI is structurally misfolded so that it resists degradation by proteolytic enzymes. The accumulation of irregular prion proteins in the medial thalamic nucleus results in progressive neurodegeneration. Patients with FFI present with increasingly severe insomnia, mild fever, dysautonomia, spontaneous myoclonus, cognitive dysfunction, and hallucinations.9 Generally, patients die from sudden cardiorespiratory failure or ensuing infections 9 to 24 months after symptom onset. In vivo, FFI diagnosis is suggested by a loss of sleep spindles on polysomnogram and by decreased thalamic metabolism on PET scan. Other imaging modalities and testing, including EEG and CSF analysis, lack sensitivity and/or specificity.10
OUTCOME: Improvement, discharge
On his fourth hospital day, Mr. Q’s symptoms begin to remit spontaneously. His gastrointestinal (GI) upset improves and the following night he sleeps for approximately 4 hours. As his sleep improves, his delusional thinking and hallucinations resolve. Orientation, memory, and concentration gradually improve. Before discharge, his MMSE score is 24 out of 30, indicating improved cognition. His heart rate, blood pressure, and body temperature normalize and his myoclonus improves. Mr. Q is discharged after 6 days in the hospital and returns home. He follows up with his primary care physician, denies any recurrence of sleep disturbance, and reports that his cognition and perception have returned to his baseline.
The authors’ observations
12
Table 3
DSM-IV-TR diagnostic criteria for opioid withdrawal
| A. | Either of the following:
|
| B. | ≥3 of the following, developing within minutes to several days after criterion A:
|
| C. | The symptoms of criterion B cause clinically significant distress or impairment in social, occupational, or other important areas of functioning |
| D. | The symptoms are not due to a general medical condition and are not better accounted for by another mental disorder |
| Source: Reference 11 | |
- Morin CM, Benca R. Chronic insomnia. Lancet. 2012; 379(9821):1129-1141.
- Pressman MR, Orr WC, eds. Understanding sleep: the evolution and treatment of sleep disorders. Washington, DC: American Psychological Association; 1997.
- NIH State-of-the-Science Conference Statement on manifestations and management of chronic insomnia in adults. NIH Consens State Sci Statements. 2005;22(2):1-30.
- Albuterol • Proventil, Ventolin
- Aripiprazole • Abilify
- Bupropion • Wellbutrin, Zyban
- Dextroamphetamine • Dexadrine
- Haloperidol • Haldol
- Hydrocodone/Acetaminophen • Vicodin
- Lamotrigine • Lamictal
- Lorazepam • Ativan
- Methylphenidate • Methylin, Ritalin
- Phenylephrine • Neo-Synephrine
- Pseudoephedrine • Sudafed
- Ramelteon • Rozerem
- Theophylline • Elixophyllin, Slo-Phyllin
- Zolpidem • Ambien
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Mai E, Buysse DJ. Insomnia: prevalence impact, pathogenesis, differential diagnosis, and evaluation. Sleep Med Clin. 2008;3(2):167-174.
2. Kennedy N, Boydell J, Kalidindi S, et al. Gender differences in incidence and age at onset of mania and bipolar disorder over a 35-year period in Camberwell, England. Am J Psychiatry. 2005;162(2):257-262.
3. Cook IA. American Psychiatric Association. Guideline watch: practice guidelines for the treatment of patients with delirium. http://psychiatryonline.org/content.aspx?bookid=28§ionid=1681952. Accessed June 20 2012.
4. Lonergan E, Luxenberg J, Areosa Sastre A, et al. Benzodiazepines for delirium. Cochrane Database Syst Rev. 2009;21(1):CD006379.-
5. Toner LC, Tsambiras BM, Catalano G, et al. Central nervous system side effects associated with zolpidem treatment. Clin Neuropharmacol. 2000;23(1):54-58.
6. Srinivasan V, Pandi-Perumal SR, Trahkt I, et al. Melatonin and melatonergic drugs on sleep: possible mechanisms of action. Int J Neurosci. 2009;119(6):821-846.
7. Al-Aama T, Brymer C, Gutmanis I, et al. Melatonin decreases delirium in elderly patients: a randomized, placebo-controlled trial. Int J Geriatr Psychiatry. 2011;26(7):687-694.
8. Lonergan E, Britton AM, Luxenberg J, et al. Antipsychotics for delirium. Cochrane Database Syst Rev. 2007;18(2):CD005594.-
9. Medori R, Tritschler HJ, LeBlanc A, et al. Fatal familial insomnia, a prion disease with a mutation codon 178 of the prion protein gene. N Engl J Med. 1992;326(7):444-449.
10. Lugaresi E, Provini F, Cortelli P. Agrypnia excitata. Sleep Med. 2011;12(suppl 2):S3-S10.
11. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
12. Jaffe JH, Strain EC. Opioid-related disorders. In: Sadock BJ Sadock VA, eds. Kaplan and Sadock’s comprehensive textbook of psychiatry. 8th ed. Baltimore, MD: Lippincott Williams & Wilkins, 2005:1164, 1272-1274.
CASE: Worsening insomnia
Mr. Q, age 44, presents for evaluation of altered mental status characterized by disorientation, impaired attention and concentration, paranoid delusions, and prominent auditory and visual hallucinations. His initial Folstein Mini-Mental State Examination (MMSE) score is 7 of 30, indicating severe impairment. He further describes a recent history of nausea, intermittent vomiting, and anorexia. He takes hydrocodone/acetaminophen, 5/500 mg, 4 times daily for lower back and joint pain. Additionally, he has a pacemaker, which was placed when Mr. Q was in his late 30s to treat sinus bradycardia.
Mr. Q’s fiancée describes his 6-month history of worsening sleep disturbance, noting insomnia, fractured sleep, dream enactment, and daytime fatigue. During this time, Mr. Q averaged 3 to 4 hours of sleep nightly without day-time naps. Ten days ago, he stopped sleeping completely and his cognitive function decompensated rapidly. He became increasingly paranoid, believing government agents had been dispatched to kill him. Several days before admission, Mr. Q developed auditory and visual hallucinations. He reports that he hears voices warning him of Armageddon and sees reincarnated spirits of deceased relatives. He describes his mood as “fine” and “okay” and lacks insight into his psychiatric symptoms other than his sleeplessness.
Mr. Q’s family says he has a history of transient mild depression after his older brother died from an unknown neurologic disease 3 years ago. Mr. Q did not receive pharmacotherapy or psychotherapy but his symptoms resolved. His family says that Mr. Q has been using marijuana daily for several years, but they are unaware of other substance use. They deny a family history of psychiatric illness.
On physical examination, Mr. Q appears thin, agitated, and in mild distress. He has a fever of 99.2°F. His blood pressure drops intermittently from a baseline of 120/70 mm Hg to 100/60 mm Hg, at which point he experiences transient normal sinus tachycardia. Neurologic examination reveals psychomotor agitation and diffuse myoclonic tremor.
The authors’ observations
Table 1
Differential diagnosis of insomnia
| Type of disorder | Examples |
|---|---|
| Sleep disorders | Narcolepsy, REM sleep disorder, periodic limb movement disorder, restless leg syndrome, parasomniac conditions |
| Psychiatric disorders | Mania or hypomania, psychosis, substance intoxication or withdrawal, dementia, delirium |
| Neurologic disorders | Stroke, malignancy, infection or abscess, metabolic or viral encephalopathy, seizure disorder, prion disease |
| Somatic conditions | Cardiorespiratory disease, central or obstructive sleep apnea, congestive heart failure (Cheyne-Stokes respiration), pain, nocturnal movement disorder, gastroesophageal reflux disease, nocturia |
| Other causes | Jet lag, shift work, environment, lifestyle, medication |
| REM: rapid eye movement Source: Reference 1 | |
Medications that can cause or exacerbate insomnia
| Class/category | Medication(s) |
|---|---|
| Stimulants | Bupropion, dextroamphetamine, methylphenidate |
| Decongestants | Pseudoephedrine, phenylephrine |
| Antihypertensives or antiarrythmics | α- and β-antagonists |
| Respiratory medications | Albuterol, theophylline |
| Hormones | Corticosteroids, thyroid medications |
| Anticonvulsants | Lamotrigine |
| Medications that induce rebound insomnia | Benzodiazepines, sedative-hypnotics, opioids |
| Nonprescription medications | Caffeine, alcohol, nicotine, illicit psychostimulants |
EVALUATION: Inconclusive results
Routine laboratory studies reveal mild normocytic anemia and mild hypokalemia. Liver panel, renal function, cardiac profile, brain natriuretic peptide level, folate and vitamin B12 levels, thyroid studies, and human immunodeficiency virus serology are negative or within normal limits. Urinalysis reveals the presence of ketones, indicative of Mr. Q’s recent anorexia. Chest radiography and CT imaging of the head, abdomen, and pelvis also are unremarkable. MRI is contraindicated because of Mr. Q’s implanted pacemaker. Pulse oximetry does not suggest apneic events. Mr. Q and his family refuse a lumbar puncture, which precludes cerebrospinal fluid (CSF) analysis. Electroencephalography (EEG) records normal patterns of wakefulness oscillating with transient periods of stage 1 sleep. A detailed family interview reveals that Mr. Q’s older brother had a history of epilepsy and died at age 49 following a prolonged hospitalization for recurrent seizures and similar insomnia symptoms. History from the patient’s paternal lineage is not available.
The authors’ observations
American Psychiatric Association practice guidelines3 do not support first-line use of benzodiazepines for non-alcohol withdrawal-related delirium. Benzodiazepines are ineffective for treating delirium and may exacerbate symptoms.4 Laboratory evidence confirmed Mr. Q has no history of alcohol or benzodiazepine use. Although treating the underlying cause of delirium is essential, prescribing a sedative-hypnotic medication such as zolpidem for Mr. Q’s insomnia may worsen his condition. These agents are known to impair cognition and may induce or intensify psychosis.5 Melatonin and melatonin receptor agonists, such as ramelteon, promote sleep by regulating the sleep-wake rhythm through their action on melatonin receptors in the hypothalamus.6 Recently, a randomized control trial (RCT)7 found melatonin protected against delirium in hospitalized patients age ≥65. However, no RCT has examined use of exogenous melatonin or melatonin receptor agonists to treat delirium. In Mr. Q’s case, we chose to administer haloperidol. First- and second-generation antipsychotics have shown efficacy in treating acute delirium. Although more clinical experience has accumulated using first-generation agents such as haloperidol, a 2007 Cochrane meta-analysis8 demonstrated equal benefit with second-generation antipsychotics, while noting a decreased incidence of adverse effects.
TREATMENT: Adverse effects
Mr. Q receives an IM injection of haloperidol, 5 mg, for severe agitation, followed 15 hours later by IM aripiprazole, 9.75 mg. Within hours of receiving aripiprazole, Mr. Q develops hyperkinetic perioral and tongue movements. He initially is diagnosed with acute reactionary dystonia, although closer examination reveals myoclonus consistent with his overall presentation. Additionally, his QTc interval increases by 120 ms. Subsequently, all antipsychotics are stopped. We prescribe lorazepam, 1 mg IM every 4 hours as needed, for agitation. Mr. Q receives 2 consecutive doses of lorazepam, although neither effectively reduces his agitation or promotes sleep. Mr. Q is not assessed with positron-emission tomography (PET) or polysomnography.
The authors’ observations
There was no evidence of neurologic disease on Mr. Q’s CT scan and EEG was within normal limits. Other imaging and laboratory studies did not reveal possible infection, malignancy, or cardiovascular disease. Despite its rarity, we considered the possibility of a prion disease, given Mr. Q’s unique presentation and family history. Familial fatal insomnia (FFI) is an autosomal dominant disease caused by a point mutation in the prion protein gene. Prion proteins are theorized to play a role in myelin stability. The aberrant isoform produced in FFI is structurally misfolded so that it resists degradation by proteolytic enzymes. The accumulation of irregular prion proteins in the medial thalamic nucleus results in progressive neurodegeneration. Patients with FFI present with increasingly severe insomnia, mild fever, dysautonomia, spontaneous myoclonus, cognitive dysfunction, and hallucinations.9 Generally, patients die from sudden cardiorespiratory failure or ensuing infections 9 to 24 months after symptom onset. In vivo, FFI diagnosis is suggested by a loss of sleep spindles on polysomnogram and by decreased thalamic metabolism on PET scan. Other imaging modalities and testing, including EEG and CSF analysis, lack sensitivity and/or specificity.10
OUTCOME: Improvement, discharge
On his fourth hospital day, Mr. Q’s symptoms begin to remit spontaneously. His gastrointestinal (GI) upset improves and the following night he sleeps for approximately 4 hours. As his sleep improves, his delusional thinking and hallucinations resolve. Orientation, memory, and concentration gradually improve. Before discharge, his MMSE score is 24 out of 30, indicating improved cognition. His heart rate, blood pressure, and body temperature normalize and his myoclonus improves. Mr. Q is discharged after 6 days in the hospital and returns home. He follows up with his primary care physician, denies any recurrence of sleep disturbance, and reports that his cognition and perception have returned to his baseline.
The authors’ observations
12
Table 3
DSM-IV-TR diagnostic criteria for opioid withdrawal
| A. | Either of the following:
|
| B. | ≥3 of the following, developing within minutes to several days after criterion A:
|
| C. | The symptoms of criterion B cause clinically significant distress or impairment in social, occupational, or other important areas of functioning |
| D. | The symptoms are not due to a general medical condition and are not better accounted for by another mental disorder |
| Source: Reference 11 | |
- Morin CM, Benca R. Chronic insomnia. Lancet. 2012; 379(9821):1129-1141.
- Pressman MR, Orr WC, eds. Understanding sleep: the evolution and treatment of sleep disorders. Washington, DC: American Psychological Association; 1997.
- NIH State-of-the-Science Conference Statement on manifestations and management of chronic insomnia in adults. NIH Consens State Sci Statements. 2005;22(2):1-30.
- Albuterol • Proventil, Ventolin
- Aripiprazole • Abilify
- Bupropion • Wellbutrin, Zyban
- Dextroamphetamine • Dexadrine
- Haloperidol • Haldol
- Hydrocodone/Acetaminophen • Vicodin
- Lamotrigine • Lamictal
- Lorazepam • Ativan
- Methylphenidate • Methylin, Ritalin
- Phenylephrine • Neo-Synephrine
- Pseudoephedrine • Sudafed
- Ramelteon • Rozerem
- Theophylline • Elixophyllin, Slo-Phyllin
- Zolpidem • Ambien
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE: Worsening insomnia
Mr. Q, age 44, presents for evaluation of altered mental status characterized by disorientation, impaired attention and concentration, paranoid delusions, and prominent auditory and visual hallucinations. His initial Folstein Mini-Mental State Examination (MMSE) score is 7 of 30, indicating severe impairment. He further describes a recent history of nausea, intermittent vomiting, and anorexia. He takes hydrocodone/acetaminophen, 5/500 mg, 4 times daily for lower back and joint pain. Additionally, he has a pacemaker, which was placed when Mr. Q was in his late 30s to treat sinus bradycardia.
Mr. Q’s fiancée describes his 6-month history of worsening sleep disturbance, noting insomnia, fractured sleep, dream enactment, and daytime fatigue. During this time, Mr. Q averaged 3 to 4 hours of sleep nightly without day-time naps. Ten days ago, he stopped sleeping completely and his cognitive function decompensated rapidly. He became increasingly paranoid, believing government agents had been dispatched to kill him. Several days before admission, Mr. Q developed auditory and visual hallucinations. He reports that he hears voices warning him of Armageddon and sees reincarnated spirits of deceased relatives. He describes his mood as “fine” and “okay” and lacks insight into his psychiatric symptoms other than his sleeplessness.
Mr. Q’s family says he has a history of transient mild depression after his older brother died from an unknown neurologic disease 3 years ago. Mr. Q did not receive pharmacotherapy or psychotherapy but his symptoms resolved. His family says that Mr. Q has been using marijuana daily for several years, but they are unaware of other substance use. They deny a family history of psychiatric illness.
On physical examination, Mr. Q appears thin, agitated, and in mild distress. He has a fever of 99.2°F. His blood pressure drops intermittently from a baseline of 120/70 mm Hg to 100/60 mm Hg, at which point he experiences transient normal sinus tachycardia. Neurologic examination reveals psychomotor agitation and diffuse myoclonic tremor.
The authors’ observations
Table 1
Differential diagnosis of insomnia
| Type of disorder | Examples |
|---|---|
| Sleep disorders | Narcolepsy, REM sleep disorder, periodic limb movement disorder, restless leg syndrome, parasomniac conditions |
| Psychiatric disorders | Mania or hypomania, psychosis, substance intoxication or withdrawal, dementia, delirium |
| Neurologic disorders | Stroke, malignancy, infection or abscess, metabolic or viral encephalopathy, seizure disorder, prion disease |
| Somatic conditions | Cardiorespiratory disease, central or obstructive sleep apnea, congestive heart failure (Cheyne-Stokes respiration), pain, nocturnal movement disorder, gastroesophageal reflux disease, nocturia |
| Other causes | Jet lag, shift work, environment, lifestyle, medication |
| REM: rapid eye movement Source: Reference 1 | |
Medications that can cause or exacerbate insomnia
| Class/category | Medication(s) |
|---|---|
| Stimulants | Bupropion, dextroamphetamine, methylphenidate |
| Decongestants | Pseudoephedrine, phenylephrine |
| Antihypertensives or antiarrythmics | α- and β-antagonists |
| Respiratory medications | Albuterol, theophylline |
| Hormones | Corticosteroids, thyroid medications |
| Anticonvulsants | Lamotrigine |
| Medications that induce rebound insomnia | Benzodiazepines, sedative-hypnotics, opioids |
| Nonprescription medications | Caffeine, alcohol, nicotine, illicit psychostimulants |
EVALUATION: Inconclusive results
Routine laboratory studies reveal mild normocytic anemia and mild hypokalemia. Liver panel, renal function, cardiac profile, brain natriuretic peptide level, folate and vitamin B12 levels, thyroid studies, and human immunodeficiency virus serology are negative or within normal limits. Urinalysis reveals the presence of ketones, indicative of Mr. Q’s recent anorexia. Chest radiography and CT imaging of the head, abdomen, and pelvis also are unremarkable. MRI is contraindicated because of Mr. Q’s implanted pacemaker. Pulse oximetry does not suggest apneic events. Mr. Q and his family refuse a lumbar puncture, which precludes cerebrospinal fluid (CSF) analysis. Electroencephalography (EEG) records normal patterns of wakefulness oscillating with transient periods of stage 1 sleep. A detailed family interview reveals that Mr. Q’s older brother had a history of epilepsy and died at age 49 following a prolonged hospitalization for recurrent seizures and similar insomnia symptoms. History from the patient’s paternal lineage is not available.
The authors’ observations
American Psychiatric Association practice guidelines3 do not support first-line use of benzodiazepines for non-alcohol withdrawal-related delirium. Benzodiazepines are ineffective for treating delirium and may exacerbate symptoms.4 Laboratory evidence confirmed Mr. Q has no history of alcohol or benzodiazepine use. Although treating the underlying cause of delirium is essential, prescribing a sedative-hypnotic medication such as zolpidem for Mr. Q’s insomnia may worsen his condition. These agents are known to impair cognition and may induce or intensify psychosis.5 Melatonin and melatonin receptor agonists, such as ramelteon, promote sleep by regulating the sleep-wake rhythm through their action on melatonin receptors in the hypothalamus.6 Recently, a randomized control trial (RCT)7 found melatonin protected against delirium in hospitalized patients age ≥65. However, no RCT has examined use of exogenous melatonin or melatonin receptor agonists to treat delirium. In Mr. Q’s case, we chose to administer haloperidol. First- and second-generation antipsychotics have shown efficacy in treating acute delirium. Although more clinical experience has accumulated using first-generation agents such as haloperidol, a 2007 Cochrane meta-analysis8 demonstrated equal benefit with second-generation antipsychotics, while noting a decreased incidence of adverse effects.
TREATMENT: Adverse effects
Mr. Q receives an IM injection of haloperidol, 5 mg, for severe agitation, followed 15 hours later by IM aripiprazole, 9.75 mg. Within hours of receiving aripiprazole, Mr. Q develops hyperkinetic perioral and tongue movements. He initially is diagnosed with acute reactionary dystonia, although closer examination reveals myoclonus consistent with his overall presentation. Additionally, his QTc interval increases by 120 ms. Subsequently, all antipsychotics are stopped. We prescribe lorazepam, 1 mg IM every 4 hours as needed, for agitation. Mr. Q receives 2 consecutive doses of lorazepam, although neither effectively reduces his agitation or promotes sleep. Mr. Q is not assessed with positron-emission tomography (PET) or polysomnography.
The authors’ observations
There was no evidence of neurologic disease on Mr. Q’s CT scan and EEG was within normal limits. Other imaging and laboratory studies did not reveal possible infection, malignancy, or cardiovascular disease. Despite its rarity, we considered the possibility of a prion disease, given Mr. Q’s unique presentation and family history. Familial fatal insomnia (FFI) is an autosomal dominant disease caused by a point mutation in the prion protein gene. Prion proteins are theorized to play a role in myelin stability. The aberrant isoform produced in FFI is structurally misfolded so that it resists degradation by proteolytic enzymes. The accumulation of irregular prion proteins in the medial thalamic nucleus results in progressive neurodegeneration. Patients with FFI present with increasingly severe insomnia, mild fever, dysautonomia, spontaneous myoclonus, cognitive dysfunction, and hallucinations.9 Generally, patients die from sudden cardiorespiratory failure or ensuing infections 9 to 24 months after symptom onset. In vivo, FFI diagnosis is suggested by a loss of sleep spindles on polysomnogram and by decreased thalamic metabolism on PET scan. Other imaging modalities and testing, including EEG and CSF analysis, lack sensitivity and/or specificity.10
OUTCOME: Improvement, discharge
On his fourth hospital day, Mr. Q’s symptoms begin to remit spontaneously. His gastrointestinal (GI) upset improves and the following night he sleeps for approximately 4 hours. As his sleep improves, his delusional thinking and hallucinations resolve. Orientation, memory, and concentration gradually improve. Before discharge, his MMSE score is 24 out of 30, indicating improved cognition. His heart rate, blood pressure, and body temperature normalize and his myoclonus improves. Mr. Q is discharged after 6 days in the hospital and returns home. He follows up with his primary care physician, denies any recurrence of sleep disturbance, and reports that his cognition and perception have returned to his baseline.
The authors’ observations
12
Table 3
DSM-IV-TR diagnostic criteria for opioid withdrawal
| A. | Either of the following:
|
| B. | ≥3 of the following, developing within minutes to several days after criterion A:
|
| C. | The symptoms of criterion B cause clinically significant distress or impairment in social, occupational, or other important areas of functioning |
| D. | The symptoms are not due to a general medical condition and are not better accounted for by another mental disorder |
| Source: Reference 11 | |
- Morin CM, Benca R. Chronic insomnia. Lancet. 2012; 379(9821):1129-1141.
- Pressman MR, Orr WC, eds. Understanding sleep: the evolution and treatment of sleep disorders. Washington, DC: American Psychological Association; 1997.
- NIH State-of-the-Science Conference Statement on manifestations and management of chronic insomnia in adults. NIH Consens State Sci Statements. 2005;22(2):1-30.
- Albuterol • Proventil, Ventolin
- Aripiprazole • Abilify
- Bupropion • Wellbutrin, Zyban
- Dextroamphetamine • Dexadrine
- Haloperidol • Haldol
- Hydrocodone/Acetaminophen • Vicodin
- Lamotrigine • Lamictal
- Lorazepam • Ativan
- Methylphenidate • Methylin, Ritalin
- Phenylephrine • Neo-Synephrine
- Pseudoephedrine • Sudafed
- Ramelteon • Rozerem
- Theophylline • Elixophyllin, Slo-Phyllin
- Zolpidem • Ambien
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Mai E, Buysse DJ. Insomnia: prevalence impact, pathogenesis, differential diagnosis, and evaluation. Sleep Med Clin. 2008;3(2):167-174.
2. Kennedy N, Boydell J, Kalidindi S, et al. Gender differences in incidence and age at onset of mania and bipolar disorder over a 35-year period in Camberwell, England. Am J Psychiatry. 2005;162(2):257-262.
3. Cook IA. American Psychiatric Association. Guideline watch: practice guidelines for the treatment of patients with delirium. http://psychiatryonline.org/content.aspx?bookid=28§ionid=1681952. Accessed June 20 2012.
4. Lonergan E, Luxenberg J, Areosa Sastre A, et al. Benzodiazepines for delirium. Cochrane Database Syst Rev. 2009;21(1):CD006379.-
5. Toner LC, Tsambiras BM, Catalano G, et al. Central nervous system side effects associated with zolpidem treatment. Clin Neuropharmacol. 2000;23(1):54-58.
6. Srinivasan V, Pandi-Perumal SR, Trahkt I, et al. Melatonin and melatonergic drugs on sleep: possible mechanisms of action. Int J Neurosci. 2009;119(6):821-846.
7. Al-Aama T, Brymer C, Gutmanis I, et al. Melatonin decreases delirium in elderly patients: a randomized, placebo-controlled trial. Int J Geriatr Psychiatry. 2011;26(7):687-694.
8. Lonergan E, Britton AM, Luxenberg J, et al. Antipsychotics for delirium. Cochrane Database Syst Rev. 2007;18(2):CD005594.-
9. Medori R, Tritschler HJ, LeBlanc A, et al. Fatal familial insomnia, a prion disease with a mutation codon 178 of the prion protein gene. N Engl J Med. 1992;326(7):444-449.
10. Lugaresi E, Provini F, Cortelli P. Agrypnia excitata. Sleep Med. 2011;12(suppl 2):S3-S10.
11. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
12. Jaffe JH, Strain EC. Opioid-related disorders. In: Sadock BJ Sadock VA, eds. Kaplan and Sadock’s comprehensive textbook of psychiatry. 8th ed. Baltimore, MD: Lippincott Williams & Wilkins, 2005:1164, 1272-1274.
1. Mai E, Buysse DJ. Insomnia: prevalence impact, pathogenesis, differential diagnosis, and evaluation. Sleep Med Clin. 2008;3(2):167-174.
2. Kennedy N, Boydell J, Kalidindi S, et al. Gender differences in incidence and age at onset of mania and bipolar disorder over a 35-year period in Camberwell, England. Am J Psychiatry. 2005;162(2):257-262.
3. Cook IA. American Psychiatric Association. Guideline watch: practice guidelines for the treatment of patients with delirium. http://psychiatryonline.org/content.aspx?bookid=28§ionid=1681952. Accessed June 20 2012.
4. Lonergan E, Luxenberg J, Areosa Sastre A, et al. Benzodiazepines for delirium. Cochrane Database Syst Rev. 2009;21(1):CD006379.-
5. Toner LC, Tsambiras BM, Catalano G, et al. Central nervous system side effects associated with zolpidem treatment. Clin Neuropharmacol. 2000;23(1):54-58.
6. Srinivasan V, Pandi-Perumal SR, Trahkt I, et al. Melatonin and melatonergic drugs on sleep: possible mechanisms of action. Int J Neurosci. 2009;119(6):821-846.
7. Al-Aama T, Brymer C, Gutmanis I, et al. Melatonin decreases delirium in elderly patients: a randomized, placebo-controlled trial. Int J Geriatr Psychiatry. 2011;26(7):687-694.
8. Lonergan E, Britton AM, Luxenberg J, et al. Antipsychotics for delirium. Cochrane Database Syst Rev. 2007;18(2):CD005594.-
9. Medori R, Tritschler HJ, LeBlanc A, et al. Fatal familial insomnia, a prion disease with a mutation codon 178 of the prion protein gene. N Engl J Med. 1992;326(7):444-449.
10. Lugaresi E, Provini F, Cortelli P. Agrypnia excitata. Sleep Med. 2011;12(suppl 2):S3-S10.
11. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
12. Jaffe JH, Strain EC. Opioid-related disorders. In: Sadock BJ Sadock VA, eds. Kaplan and Sadock’s comprehensive textbook of psychiatry. 8th ed. Baltimore, MD: Lippincott Williams & Wilkins, 2005:1164, 1272-1274.
A taste for the unusual
Discuss this article at www.facebook.com/CurrentPsychiatry
CASE: Nauseous and full
Ms. O, age 48, presents to the emergency department reporting a 3-day history of vomiting approximately 5 minutes after consuming solids or liquids. She’s had 10 vomiting episodes, which were associated with “fullness” and an “aching” sensation she rates as 6 on a 10-point scale pain scale that is diffuse over the upper epigastric area, with no palliative factors. Ms. O has not had a bowel movement for 3 days and her last menstrual period was 8 days ago. She is taking lorazepam, 1 mg/d. Her medical and psychiatric history includes anxiety, depression, personality disorder symptoms of affective dysregulation, obesity (270 lbs; medium height), and pica. She was 352 lbs when she underwent a Roux-en-Y gastric bypass 2 years ago. One year earlier, she had a laparoscopic gastric bezoar removal and an incisional hernia repair. Ms. O had no pica-related surgeries before undergoing gastric bypass surgery.
Ms. O denies shortness of breath, chest pain, allergies, smoking, or alcohol abuse, but reports uncontrollable cravings for paper products, specifically cardboard, which she describes as “just so delicious.” This craving led her to consume large amounts of cardboard and newspaper in the days before she began vomiting.
What may be causing Ms. O’s pica symptoms?
- iron deficiency anemia
- complications from gastric bypass surgery
- personality disorder
- generalized anxiety disorder (GAD)
The authors’ observations
DSM-IV-TR diagnostic criteria for pica include the persistent eating of non-nutritive substances for ≥1 month that is inappropriate for the level of a person’s development and not an acceptable part of one’s culture.1 If pica occurs with other mental disorders, it must be severe enough to indicate further clinical assessment to receive a separate diagnosis. Often associated with pregnancy, iron deficiency anemia, early development, and mental retardation, pica has been observed in post-gastric bypass surgery patients, all of whom presented with pagophagia (compulsive ice eating), and in one case was associated with a bezoar causing obstruction of the GI tract.1,2 With the dramatic increase in gastric bypass surgery and the required presurgical mental health evaluation, the consequences of failing to screen patients for pica behaviors can be devastating.
EVALUATION: Low iron
Ms. O’s vital signs on admission are stable, and physical exam is notable for mild abdominal distention with no guarding, tenderness, rigidity, or masses. No rebound tenderness is elicited. CT scan shows evidence of post-surgical changes involving the small bowel consistent with gastric bypass surgery and a hiatal hernia, but no obstruction, focal inflammation, free fluids, or gas. Lab values for amylase, lipase, urinalysis, coagulation studies, cardiac enzymes, and complete metabolic profile are within normal limits. Although not anemic, Ms. O is iron deficient, with ferritin, 10 ng/mL (normal 10 to 120 ng/mL); B12, 299 pg/mL (normal 100 to 700 pg/mL); and iron, 25 μg/dL (normal 50 to 170 μg/dL).
A foreign body is removed endoscopically and the specimen is sent to pathology. It is determined to be a gastric bezoar, yellowish-green in color, measuring 2.5 cm × 1 cm × 0.8 cm. After bezoar removal, Ms. O tolerates food and is discharged home on vitamin B12, 1,000 mcg/d for 2 weeks; folate, 1 mg/d for 1 month; calcium with vitamin D, 1 g/d; and esomeprazole, 40 mg/d for frequent heartburn. She is referred to psychiatry for behavioral modification therapy and medication management.
How would you treat Ms. O?
- start a selective serotonin reuptake inhibitor (SSRI)
- prescribe an atypical antipsychotic
- continue lorazepam
- begin behavioral therapy
HISTORY: Pica during pregnancy
During psychiatric workup, Ms. O admits to having pica urges most of her life, but experienced an uncontrollable exacerbation after gastric bypass surgery. This led to intense, chaotic periods of pica, resulting in a previous bezoar removal. She is particularly attracted to cardboard and newspaper cartoons, but notes she also has felt the urge to eat charcoal, moist soil, clay, chalk, pencils, and new shoes, which she chews on. In the past, her extreme anxiety and preoccupation with these urges had lead to diagnoses of personality disorder not otherwise specified, GAD, and obsessive-compulsive disorder.
Her first experience with pica was during her first pregnancy at age 15, when she had an impulse to eat soil. The urges briefly stopped until she became pregnant again. During each of her 5 pregnancies her pica symptoms returned. At one point during her last pregnancy she reports having felt out of control, eating 2 to 3 pencils with the eraser per day, after which she would feel intense relaxation. Her mother also exhibited symptoms of pica toward charcoal and soil. Ms. O had been taking unknown dosages of lorazepam for anxiety and fluoxetine for depression, both of which she stopped because she feared side effects during her last pregnancy. However, she never experienced any side effects.
The authors’ observations
Although pica is most commonly observed in young children, it sometimes is seen in pregnant women.1 Pica frequently is associated with other mental disorders, such as pervasive developmental disorder and mental retardation,1 and can be associated with premorbid psychosis and anxiety disorders. Occasional vitamin and mineral deficiencies, such as iron or zinc, have been reported, but usually patients’ lab values are normal. Treatment usually is initiated in the context of medical complications, such as iron deficiency anemia. In Ms. O’s case, the precipitating event was mechanical bowel obstruction due to a bezoar.
Several theories about the origins of pica have been proposed, but none truly are explanatory or satisfactory. The nutritional theory—that patients eat non-nutritive substances to compensate for mineral deficiencies—is popular because of pica’s frequent association with mineral deficiencies, but it is unknown whether pica is the cause or the result of the deficiency. An example of this is anemia due to eating clay instead of foods that contain iron. Another theory is that because pica is normal in early childhood development, it may be a manifestation of delayed development or mental retardation. The cultural theory is attractive because pregnant women in several cultures eat starch or clay as a part of their native rituals, and the incidence of pica is relatively high among pregnant African American women who live in rural areas.3 In the Roux-en-Y procedure, bypass of the duodenum and proximal jejunum can significantly decrease a patient’s iron uptake, leading to iron deficiency anemia, and could trigger pica in a susceptible patient.4
Exacerbation after gastric bypass
Kushner et al4 describes re-emergent pica after bariatric surgery in 2 patients with pagophagia associated with concomitant iron deficiency anemia. A 41-year-old white woman presented with pagophagia and a history of childhood consumption of dirt, chalk, and clay. Another patient, a 34-year-old African American woman, suffered from a lifelong desire to eat dirt, which she was able to resist, but experienced pagophagia during pregnancy and later when she developed iron deficiency anemia.4 In another case series, Kushner et al5 describes a 35-year-old woman with iron deficiency anemia with pagophagia presenting 2 years after Roux-en-Y. Her history was significant for eating clay as a child, but this new-onset pagophagia was so intense she purchased 2 snow cone machines, one for home and one for work, to feed her urges. Another patient, a 45-year-old African American woman, had an irresistible craving for calcium carbonate antacids, eating 40 to 50 a day, as well as several 30-ounce cups of ice.5 A third case report details a 33-year-old woman with iron deficiency anemia who presented with nocturnal pagophagia after Roux-en-Y anastomosis. She repeatedly rose during the night to eat the frost off the ice maker in her refrigerator.6 Another case described a female patient who ate cardboard after having a Roux-en-Y.2
Common themes in these case reports are female sex, Roux-en-Y, and dramatic resurgence of previously noted pica behaviors after gastric bypass surgery. Several studies have shown that pagophagia and pica in patients who are iron deficient or have iron deficiency anemia can be rapidly curbed with iron supplements.5 Ms. O, who has low iron, is taking iron supplementation, yet continues to experience pica cravings, albeit less severely. Her pica could be psychiatric in origin, perhaps related to her history of anxiety.
OUTCOME: Combination therapy
We start Ms. O on ziprasidone, 80 mg twice a day, restart lorazepam, 1 mg/d, and schedule monthly follow-up appointments to monitor her pica symptoms. We prescribe ziprasidone because it could treat paranoia and preoccupations and is considered to be weight-neutral. She continues her supplements, including ferrous sulfate, 325 mg 3 times daily. Ms. O attends weekly behavioral therapy sessions, during which the therapist monitors her mood and cravings with response prevention, which entails purposely avoiding behaviors after initiating a distressing stimulus. Ms. O responds well to medication and psychotherapy 1 month after the gastric bezoar removal, and she reports a decreased urge to eat cardboard. She is able to increase the amount of time she can go without eating non-nutritive substances—once daily, rather than repeatedly throughout the day.
The authors’ observations
Each patient with pica likely needs customized care. Children need to be supervised to prevent ingestion of lead-containing substances such as paint chips. Iron supplements are recommended for iron deficiency anemia and prophylaxis for iron deficiency anemia in Roux-en-Y patients.3,4 Pica in pregnant patients should be addressed to maintain adequate nutrition and prevent accidental poisonings.7 Behavioral intervention strategies are based on positive reinforcement and punishment (Table).8 A report of 3 young children with pica noted successful treatment of one with automatic reinforcement, and the other 2 with a combination of social and automatic reinforcement.9 There are no FDA-approved medications for pica. Positive effects have been seen with SSRIs, bupropion, atypical antipsychotics, buprenorphine, and chlorimipramine.10 Olanzapine has shown positive results as a treatment for pica.11 Most pica patients need concurrent psychotherapy.10
Table
Behavioral interventions for pica
| Intervention | Comments |
|---|---|
| Environmental enrichment | Providing additional stimulus to increase neuronal activity and focus behaviors |
| Noncontingent reinforcement | Presenting reinforcers according to a fixed schedule |
| Differential reinforcement | Desired behaviors are reinforced and inappropriate behaviors are ignored |
| Response blocking | Physically block a patient’s attempts to eat nonedible items |
| Source: Reference 8 | |
Related Resources
- Blinder BJ, Salama C. An update on pica: prevalence, contributing causes, and treatment. Psychiatric Times. www.psychiatrictimes.com/display/article/10168/1159376?pageNumber=1. Published May 1, 2008.
- Nurcombe B. Developmental disorders of attachment, feeding, elimination, & sleeping. In: Ebert MH, Loosen PT, Nurcombe B, et al, eds. CURRENT diagnosis & treatment: psychiatry. 2nd ed. New York, NY: McGraw Hill; 2008.
Drug Brand Names
- Buprenorphine • Subutex
- Bupropion • Wellbutrin, Zyban
- Chlorimipramine • Anafranil
- Esomeprazole • Nexium
- Fluoxetine • Prozac
- Lorazepam • Ativan
- Olanzapine • Zyprexa
- Ziprasidone • Geodon
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
2. Patton W, Gibbs K. Cardboard bezoar complicating laparoscopic gastric bypass. Surg Obes Relat Dis. 2010;6(3):313-315.
3. Nurcombe B. Developmental disorders of attachment feeding, elimination, & sleeping. In: Ebert MH, Loosen PT, Nurcombe B, et al, eds. CURRENT diagnosis & treatment: psychiatry. 2nd ed. New York, NY: McGraw Hill; 2008.
4. Kushner F, Gleason B, Shanta-Retelny V. Reemergence of pica following gastric bypass surgery for obesity: a new presentation of an old problem. J Am Diet Assoc. 2004;104(9):1393-1397.
5. Kushner F, Shanta Retelny V. Emergence of pica (ingestion of non-food substances) accompanying iron deficiency anemia after gastric bypass surgery. Obes Surg. 2005;15(10):1491-1495.
6. Marinella MA. Nocturnal pagophagia complicating gastric bypass. Mayo Clin Proc. 2008;83(8):961.-
7. Bernstein B, Weinstein M. Normal pregnancy & prenatal care. In: DeCherney AH Nathan L, Goodwin TM, et al, eds. CURRENT diagnosis & treatment obstetrics & gynecology. 10th ed. New York, NY: McGraw Hill; 2007.
8. Piazza C, Fisher W, Hanley P, et al. Treatment of pica through multiple analyses of its reinforcing functions. J Appl Behav Anal. 1998;31(2):165-189.
9. Williams DE, McAdam D. Assessment behavioral treatment, and prevention of pica: clinical guidelines and recommendations for practitioners. Res Dev Disabil. 2012;33(6):2050-2057.
10. Blinder BJ, Salama C. An update on pica: prevalence contributing causes, and treatment. Psychiatric Times. http://www.psychiatrictimes.com/display/article/10168/1159376?pageNumber=1. Published May 1, 2008. Accessed January 23, 2013.
11. Lerner AJ. Treatment of pica behavior with olanzapine. CNS Spectr. 2008;13(1):19.-
Discuss this article at www.facebook.com/CurrentPsychiatry
CASE: Nauseous and full
Ms. O, age 48, presents to the emergency department reporting a 3-day history of vomiting approximately 5 minutes after consuming solids or liquids. She’s had 10 vomiting episodes, which were associated with “fullness” and an “aching” sensation she rates as 6 on a 10-point scale pain scale that is diffuse over the upper epigastric area, with no palliative factors. Ms. O has not had a bowel movement for 3 days and her last menstrual period was 8 days ago. She is taking lorazepam, 1 mg/d. Her medical and psychiatric history includes anxiety, depression, personality disorder symptoms of affective dysregulation, obesity (270 lbs; medium height), and pica. She was 352 lbs when she underwent a Roux-en-Y gastric bypass 2 years ago. One year earlier, she had a laparoscopic gastric bezoar removal and an incisional hernia repair. Ms. O had no pica-related surgeries before undergoing gastric bypass surgery.
Ms. O denies shortness of breath, chest pain, allergies, smoking, or alcohol abuse, but reports uncontrollable cravings for paper products, specifically cardboard, which she describes as “just so delicious.” This craving led her to consume large amounts of cardboard and newspaper in the days before she began vomiting.
What may be causing Ms. O’s pica symptoms?
- iron deficiency anemia
- complications from gastric bypass surgery
- personality disorder
- generalized anxiety disorder (GAD)
The authors’ observations
DSM-IV-TR diagnostic criteria for pica include the persistent eating of non-nutritive substances for ≥1 month that is inappropriate for the level of a person’s development and not an acceptable part of one’s culture.1 If pica occurs with other mental disorders, it must be severe enough to indicate further clinical assessment to receive a separate diagnosis. Often associated with pregnancy, iron deficiency anemia, early development, and mental retardation, pica has been observed in post-gastric bypass surgery patients, all of whom presented with pagophagia (compulsive ice eating), and in one case was associated with a bezoar causing obstruction of the GI tract.1,2 With the dramatic increase in gastric bypass surgery and the required presurgical mental health evaluation, the consequences of failing to screen patients for pica behaviors can be devastating.
EVALUATION: Low iron
Ms. O’s vital signs on admission are stable, and physical exam is notable for mild abdominal distention with no guarding, tenderness, rigidity, or masses. No rebound tenderness is elicited. CT scan shows evidence of post-surgical changes involving the small bowel consistent with gastric bypass surgery and a hiatal hernia, but no obstruction, focal inflammation, free fluids, or gas. Lab values for amylase, lipase, urinalysis, coagulation studies, cardiac enzymes, and complete metabolic profile are within normal limits. Although not anemic, Ms. O is iron deficient, with ferritin, 10 ng/mL (normal 10 to 120 ng/mL); B12, 299 pg/mL (normal 100 to 700 pg/mL); and iron, 25 μg/dL (normal 50 to 170 μg/dL).
A foreign body is removed endoscopically and the specimen is sent to pathology. It is determined to be a gastric bezoar, yellowish-green in color, measuring 2.5 cm × 1 cm × 0.8 cm. After bezoar removal, Ms. O tolerates food and is discharged home on vitamin B12, 1,000 mcg/d for 2 weeks; folate, 1 mg/d for 1 month; calcium with vitamin D, 1 g/d; and esomeprazole, 40 mg/d for frequent heartburn. She is referred to psychiatry for behavioral modification therapy and medication management.
How would you treat Ms. O?
- start a selective serotonin reuptake inhibitor (SSRI)
- prescribe an atypical antipsychotic
- continue lorazepam
- begin behavioral therapy
HISTORY: Pica during pregnancy
During psychiatric workup, Ms. O admits to having pica urges most of her life, but experienced an uncontrollable exacerbation after gastric bypass surgery. This led to intense, chaotic periods of pica, resulting in a previous bezoar removal. She is particularly attracted to cardboard and newspaper cartoons, but notes she also has felt the urge to eat charcoal, moist soil, clay, chalk, pencils, and new shoes, which she chews on. In the past, her extreme anxiety and preoccupation with these urges had lead to diagnoses of personality disorder not otherwise specified, GAD, and obsessive-compulsive disorder.
Her first experience with pica was during her first pregnancy at age 15, when she had an impulse to eat soil. The urges briefly stopped until she became pregnant again. During each of her 5 pregnancies her pica symptoms returned. At one point during her last pregnancy she reports having felt out of control, eating 2 to 3 pencils with the eraser per day, after which she would feel intense relaxation. Her mother also exhibited symptoms of pica toward charcoal and soil. Ms. O had been taking unknown dosages of lorazepam for anxiety and fluoxetine for depression, both of which she stopped because she feared side effects during her last pregnancy. However, she never experienced any side effects.
The authors’ observations
Although pica is most commonly observed in young children, it sometimes is seen in pregnant women.1 Pica frequently is associated with other mental disorders, such as pervasive developmental disorder and mental retardation,1 and can be associated with premorbid psychosis and anxiety disorders. Occasional vitamin and mineral deficiencies, such as iron or zinc, have been reported, but usually patients’ lab values are normal. Treatment usually is initiated in the context of medical complications, such as iron deficiency anemia. In Ms. O’s case, the precipitating event was mechanical bowel obstruction due to a bezoar.
Several theories about the origins of pica have been proposed, but none truly are explanatory or satisfactory. The nutritional theory—that patients eat non-nutritive substances to compensate for mineral deficiencies—is popular because of pica’s frequent association with mineral deficiencies, but it is unknown whether pica is the cause or the result of the deficiency. An example of this is anemia due to eating clay instead of foods that contain iron. Another theory is that because pica is normal in early childhood development, it may be a manifestation of delayed development or mental retardation. The cultural theory is attractive because pregnant women in several cultures eat starch or clay as a part of their native rituals, and the incidence of pica is relatively high among pregnant African American women who live in rural areas.3 In the Roux-en-Y procedure, bypass of the duodenum and proximal jejunum can significantly decrease a patient’s iron uptake, leading to iron deficiency anemia, and could trigger pica in a susceptible patient.4
Exacerbation after gastric bypass
Kushner et al4 describes re-emergent pica after bariatric surgery in 2 patients with pagophagia associated with concomitant iron deficiency anemia. A 41-year-old white woman presented with pagophagia and a history of childhood consumption of dirt, chalk, and clay. Another patient, a 34-year-old African American woman, suffered from a lifelong desire to eat dirt, which she was able to resist, but experienced pagophagia during pregnancy and later when she developed iron deficiency anemia.4 In another case series, Kushner et al5 describes a 35-year-old woman with iron deficiency anemia with pagophagia presenting 2 years after Roux-en-Y. Her history was significant for eating clay as a child, but this new-onset pagophagia was so intense she purchased 2 snow cone machines, one for home and one for work, to feed her urges. Another patient, a 45-year-old African American woman, had an irresistible craving for calcium carbonate antacids, eating 40 to 50 a day, as well as several 30-ounce cups of ice.5 A third case report details a 33-year-old woman with iron deficiency anemia who presented with nocturnal pagophagia after Roux-en-Y anastomosis. She repeatedly rose during the night to eat the frost off the ice maker in her refrigerator.6 Another case described a female patient who ate cardboard after having a Roux-en-Y.2
Common themes in these case reports are female sex, Roux-en-Y, and dramatic resurgence of previously noted pica behaviors after gastric bypass surgery. Several studies have shown that pagophagia and pica in patients who are iron deficient or have iron deficiency anemia can be rapidly curbed with iron supplements.5 Ms. O, who has low iron, is taking iron supplementation, yet continues to experience pica cravings, albeit less severely. Her pica could be psychiatric in origin, perhaps related to her history of anxiety.
OUTCOME: Combination therapy
We start Ms. O on ziprasidone, 80 mg twice a day, restart lorazepam, 1 mg/d, and schedule monthly follow-up appointments to monitor her pica symptoms. We prescribe ziprasidone because it could treat paranoia and preoccupations and is considered to be weight-neutral. She continues her supplements, including ferrous sulfate, 325 mg 3 times daily. Ms. O attends weekly behavioral therapy sessions, during which the therapist monitors her mood and cravings with response prevention, which entails purposely avoiding behaviors after initiating a distressing stimulus. Ms. O responds well to medication and psychotherapy 1 month after the gastric bezoar removal, and she reports a decreased urge to eat cardboard. She is able to increase the amount of time she can go without eating non-nutritive substances—once daily, rather than repeatedly throughout the day.
The authors’ observations
Each patient with pica likely needs customized care. Children need to be supervised to prevent ingestion of lead-containing substances such as paint chips. Iron supplements are recommended for iron deficiency anemia and prophylaxis for iron deficiency anemia in Roux-en-Y patients.3,4 Pica in pregnant patients should be addressed to maintain adequate nutrition and prevent accidental poisonings.7 Behavioral intervention strategies are based on positive reinforcement and punishment (Table).8 A report of 3 young children with pica noted successful treatment of one with automatic reinforcement, and the other 2 with a combination of social and automatic reinforcement.9 There are no FDA-approved medications for pica. Positive effects have been seen with SSRIs, bupropion, atypical antipsychotics, buprenorphine, and chlorimipramine.10 Olanzapine has shown positive results as a treatment for pica.11 Most pica patients need concurrent psychotherapy.10
Table
Behavioral interventions for pica
| Intervention | Comments |
|---|---|
| Environmental enrichment | Providing additional stimulus to increase neuronal activity and focus behaviors |
| Noncontingent reinforcement | Presenting reinforcers according to a fixed schedule |
| Differential reinforcement | Desired behaviors are reinforced and inappropriate behaviors are ignored |
| Response blocking | Physically block a patient’s attempts to eat nonedible items |
| Source: Reference 8 | |
Related Resources
- Blinder BJ, Salama C. An update on pica: prevalence, contributing causes, and treatment. Psychiatric Times. www.psychiatrictimes.com/display/article/10168/1159376?pageNumber=1. Published May 1, 2008.
- Nurcombe B. Developmental disorders of attachment, feeding, elimination, & sleeping. In: Ebert MH, Loosen PT, Nurcombe B, et al, eds. CURRENT diagnosis & treatment: psychiatry. 2nd ed. New York, NY: McGraw Hill; 2008.
Drug Brand Names
- Buprenorphine • Subutex
- Bupropion • Wellbutrin, Zyban
- Chlorimipramine • Anafranil
- Esomeprazole • Nexium
- Fluoxetine • Prozac
- Lorazepam • Ativan
- Olanzapine • Zyprexa
- Ziprasidone • Geodon
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Discuss this article at www.facebook.com/CurrentPsychiatry
CASE: Nauseous and full
Ms. O, age 48, presents to the emergency department reporting a 3-day history of vomiting approximately 5 minutes after consuming solids or liquids. She’s had 10 vomiting episodes, which were associated with “fullness” and an “aching” sensation she rates as 6 on a 10-point scale pain scale that is diffuse over the upper epigastric area, with no palliative factors. Ms. O has not had a bowel movement for 3 days and her last menstrual period was 8 days ago. She is taking lorazepam, 1 mg/d. Her medical and psychiatric history includes anxiety, depression, personality disorder symptoms of affective dysregulation, obesity (270 lbs; medium height), and pica. She was 352 lbs when she underwent a Roux-en-Y gastric bypass 2 years ago. One year earlier, she had a laparoscopic gastric bezoar removal and an incisional hernia repair. Ms. O had no pica-related surgeries before undergoing gastric bypass surgery.
Ms. O denies shortness of breath, chest pain, allergies, smoking, or alcohol abuse, but reports uncontrollable cravings for paper products, specifically cardboard, which she describes as “just so delicious.” This craving led her to consume large amounts of cardboard and newspaper in the days before she began vomiting.
What may be causing Ms. O’s pica symptoms?
- iron deficiency anemia
- complications from gastric bypass surgery
- personality disorder
- generalized anxiety disorder (GAD)
The authors’ observations
DSM-IV-TR diagnostic criteria for pica include the persistent eating of non-nutritive substances for ≥1 month that is inappropriate for the level of a person’s development and not an acceptable part of one’s culture.1 If pica occurs with other mental disorders, it must be severe enough to indicate further clinical assessment to receive a separate diagnosis. Often associated with pregnancy, iron deficiency anemia, early development, and mental retardation, pica has been observed in post-gastric bypass surgery patients, all of whom presented with pagophagia (compulsive ice eating), and in one case was associated with a bezoar causing obstruction of the GI tract.1,2 With the dramatic increase in gastric bypass surgery and the required presurgical mental health evaluation, the consequences of failing to screen patients for pica behaviors can be devastating.
EVALUATION: Low iron
Ms. O’s vital signs on admission are stable, and physical exam is notable for mild abdominal distention with no guarding, tenderness, rigidity, or masses. No rebound tenderness is elicited. CT scan shows evidence of post-surgical changes involving the small bowel consistent with gastric bypass surgery and a hiatal hernia, but no obstruction, focal inflammation, free fluids, or gas. Lab values for amylase, lipase, urinalysis, coagulation studies, cardiac enzymes, and complete metabolic profile are within normal limits. Although not anemic, Ms. O is iron deficient, with ferritin, 10 ng/mL (normal 10 to 120 ng/mL); B12, 299 pg/mL (normal 100 to 700 pg/mL); and iron, 25 μg/dL (normal 50 to 170 μg/dL).
A foreign body is removed endoscopically and the specimen is sent to pathology. It is determined to be a gastric bezoar, yellowish-green in color, measuring 2.5 cm × 1 cm × 0.8 cm. After bezoar removal, Ms. O tolerates food and is discharged home on vitamin B12, 1,000 mcg/d for 2 weeks; folate, 1 mg/d for 1 month; calcium with vitamin D, 1 g/d; and esomeprazole, 40 mg/d for frequent heartburn. She is referred to psychiatry for behavioral modification therapy and medication management.
How would you treat Ms. O?
- start a selective serotonin reuptake inhibitor (SSRI)
- prescribe an atypical antipsychotic
- continue lorazepam
- begin behavioral therapy
HISTORY: Pica during pregnancy
During psychiatric workup, Ms. O admits to having pica urges most of her life, but experienced an uncontrollable exacerbation after gastric bypass surgery. This led to intense, chaotic periods of pica, resulting in a previous bezoar removal. She is particularly attracted to cardboard and newspaper cartoons, but notes she also has felt the urge to eat charcoal, moist soil, clay, chalk, pencils, and new shoes, which she chews on. In the past, her extreme anxiety and preoccupation with these urges had lead to diagnoses of personality disorder not otherwise specified, GAD, and obsessive-compulsive disorder.
Her first experience with pica was during her first pregnancy at age 15, when she had an impulse to eat soil. The urges briefly stopped until she became pregnant again. During each of her 5 pregnancies her pica symptoms returned. At one point during her last pregnancy she reports having felt out of control, eating 2 to 3 pencils with the eraser per day, after which she would feel intense relaxation. Her mother also exhibited symptoms of pica toward charcoal and soil. Ms. O had been taking unknown dosages of lorazepam for anxiety and fluoxetine for depression, both of which she stopped because she feared side effects during her last pregnancy. However, she never experienced any side effects.
The authors’ observations
Although pica is most commonly observed in young children, it sometimes is seen in pregnant women.1 Pica frequently is associated with other mental disorders, such as pervasive developmental disorder and mental retardation,1 and can be associated with premorbid psychosis and anxiety disorders. Occasional vitamin and mineral deficiencies, such as iron or zinc, have been reported, but usually patients’ lab values are normal. Treatment usually is initiated in the context of medical complications, such as iron deficiency anemia. In Ms. O’s case, the precipitating event was mechanical bowel obstruction due to a bezoar.
Several theories about the origins of pica have been proposed, but none truly are explanatory or satisfactory. The nutritional theory—that patients eat non-nutritive substances to compensate for mineral deficiencies—is popular because of pica’s frequent association with mineral deficiencies, but it is unknown whether pica is the cause or the result of the deficiency. An example of this is anemia due to eating clay instead of foods that contain iron. Another theory is that because pica is normal in early childhood development, it may be a manifestation of delayed development or mental retardation. The cultural theory is attractive because pregnant women in several cultures eat starch or clay as a part of their native rituals, and the incidence of pica is relatively high among pregnant African American women who live in rural areas.3 In the Roux-en-Y procedure, bypass of the duodenum and proximal jejunum can significantly decrease a patient’s iron uptake, leading to iron deficiency anemia, and could trigger pica in a susceptible patient.4
Exacerbation after gastric bypass
Kushner et al4 describes re-emergent pica after bariatric surgery in 2 patients with pagophagia associated with concomitant iron deficiency anemia. A 41-year-old white woman presented with pagophagia and a history of childhood consumption of dirt, chalk, and clay. Another patient, a 34-year-old African American woman, suffered from a lifelong desire to eat dirt, which she was able to resist, but experienced pagophagia during pregnancy and later when she developed iron deficiency anemia.4 In another case series, Kushner et al5 describes a 35-year-old woman with iron deficiency anemia with pagophagia presenting 2 years after Roux-en-Y. Her history was significant for eating clay as a child, but this new-onset pagophagia was so intense she purchased 2 snow cone machines, one for home and one for work, to feed her urges. Another patient, a 45-year-old African American woman, had an irresistible craving for calcium carbonate antacids, eating 40 to 50 a day, as well as several 30-ounce cups of ice.5 A third case report details a 33-year-old woman with iron deficiency anemia who presented with nocturnal pagophagia after Roux-en-Y anastomosis. She repeatedly rose during the night to eat the frost off the ice maker in her refrigerator.6 Another case described a female patient who ate cardboard after having a Roux-en-Y.2
Common themes in these case reports are female sex, Roux-en-Y, and dramatic resurgence of previously noted pica behaviors after gastric bypass surgery. Several studies have shown that pagophagia and pica in patients who are iron deficient or have iron deficiency anemia can be rapidly curbed with iron supplements.5 Ms. O, who has low iron, is taking iron supplementation, yet continues to experience pica cravings, albeit less severely. Her pica could be psychiatric in origin, perhaps related to her history of anxiety.
OUTCOME: Combination therapy
We start Ms. O on ziprasidone, 80 mg twice a day, restart lorazepam, 1 mg/d, and schedule monthly follow-up appointments to monitor her pica symptoms. We prescribe ziprasidone because it could treat paranoia and preoccupations and is considered to be weight-neutral. She continues her supplements, including ferrous sulfate, 325 mg 3 times daily. Ms. O attends weekly behavioral therapy sessions, during which the therapist monitors her mood and cravings with response prevention, which entails purposely avoiding behaviors after initiating a distressing stimulus. Ms. O responds well to medication and psychotherapy 1 month after the gastric bezoar removal, and she reports a decreased urge to eat cardboard. She is able to increase the amount of time she can go without eating non-nutritive substances—once daily, rather than repeatedly throughout the day.
The authors’ observations
Each patient with pica likely needs customized care. Children need to be supervised to prevent ingestion of lead-containing substances such as paint chips. Iron supplements are recommended for iron deficiency anemia and prophylaxis for iron deficiency anemia in Roux-en-Y patients.3,4 Pica in pregnant patients should be addressed to maintain adequate nutrition and prevent accidental poisonings.7 Behavioral intervention strategies are based on positive reinforcement and punishment (Table).8 A report of 3 young children with pica noted successful treatment of one with automatic reinforcement, and the other 2 with a combination of social and automatic reinforcement.9 There are no FDA-approved medications for pica. Positive effects have been seen with SSRIs, bupropion, atypical antipsychotics, buprenorphine, and chlorimipramine.10 Olanzapine has shown positive results as a treatment for pica.11 Most pica patients need concurrent psychotherapy.10
Table
Behavioral interventions for pica
| Intervention | Comments |
|---|---|
| Environmental enrichment | Providing additional stimulus to increase neuronal activity and focus behaviors |
| Noncontingent reinforcement | Presenting reinforcers according to a fixed schedule |
| Differential reinforcement | Desired behaviors are reinforced and inappropriate behaviors are ignored |
| Response blocking | Physically block a patient’s attempts to eat nonedible items |
| Source: Reference 8 | |
Related Resources
- Blinder BJ, Salama C. An update on pica: prevalence, contributing causes, and treatment. Psychiatric Times. www.psychiatrictimes.com/display/article/10168/1159376?pageNumber=1. Published May 1, 2008.
- Nurcombe B. Developmental disorders of attachment, feeding, elimination, & sleeping. In: Ebert MH, Loosen PT, Nurcombe B, et al, eds. CURRENT diagnosis & treatment: psychiatry. 2nd ed. New York, NY: McGraw Hill; 2008.
Drug Brand Names
- Buprenorphine • Subutex
- Bupropion • Wellbutrin, Zyban
- Chlorimipramine • Anafranil
- Esomeprazole • Nexium
- Fluoxetine • Prozac
- Lorazepam • Ativan
- Olanzapine • Zyprexa
- Ziprasidone • Geodon
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
2. Patton W, Gibbs K. Cardboard bezoar complicating laparoscopic gastric bypass. Surg Obes Relat Dis. 2010;6(3):313-315.
3. Nurcombe B. Developmental disorders of attachment feeding, elimination, & sleeping. In: Ebert MH, Loosen PT, Nurcombe B, et al, eds. CURRENT diagnosis & treatment: psychiatry. 2nd ed. New York, NY: McGraw Hill; 2008.
4. Kushner F, Gleason B, Shanta-Retelny V. Reemergence of pica following gastric bypass surgery for obesity: a new presentation of an old problem. J Am Diet Assoc. 2004;104(9):1393-1397.
5. Kushner F, Shanta Retelny V. Emergence of pica (ingestion of non-food substances) accompanying iron deficiency anemia after gastric bypass surgery. Obes Surg. 2005;15(10):1491-1495.
6. Marinella MA. Nocturnal pagophagia complicating gastric bypass. Mayo Clin Proc. 2008;83(8):961.-
7. Bernstein B, Weinstein M. Normal pregnancy & prenatal care. In: DeCherney AH Nathan L, Goodwin TM, et al, eds. CURRENT diagnosis & treatment obstetrics & gynecology. 10th ed. New York, NY: McGraw Hill; 2007.
8. Piazza C, Fisher W, Hanley P, et al. Treatment of pica through multiple analyses of its reinforcing functions. J Appl Behav Anal. 1998;31(2):165-189.
9. Williams DE, McAdam D. Assessment behavioral treatment, and prevention of pica: clinical guidelines and recommendations for practitioners. Res Dev Disabil. 2012;33(6):2050-2057.
10. Blinder BJ, Salama C. An update on pica: prevalence contributing causes, and treatment. Psychiatric Times. http://www.psychiatrictimes.com/display/article/10168/1159376?pageNumber=1. Published May 1, 2008. Accessed January 23, 2013.
11. Lerner AJ. Treatment of pica behavior with olanzapine. CNS Spectr. 2008;13(1):19.-
1. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
2. Patton W, Gibbs K. Cardboard bezoar complicating laparoscopic gastric bypass. Surg Obes Relat Dis. 2010;6(3):313-315.
3. Nurcombe B. Developmental disorders of attachment feeding, elimination, & sleeping. In: Ebert MH, Loosen PT, Nurcombe B, et al, eds. CURRENT diagnosis & treatment: psychiatry. 2nd ed. New York, NY: McGraw Hill; 2008.
4. Kushner F, Gleason B, Shanta-Retelny V. Reemergence of pica following gastric bypass surgery for obesity: a new presentation of an old problem. J Am Diet Assoc. 2004;104(9):1393-1397.
5. Kushner F, Shanta Retelny V. Emergence of pica (ingestion of non-food substances) accompanying iron deficiency anemia after gastric bypass surgery. Obes Surg. 2005;15(10):1491-1495.
6. Marinella MA. Nocturnal pagophagia complicating gastric bypass. Mayo Clin Proc. 2008;83(8):961.-
7. Bernstein B, Weinstein M. Normal pregnancy & prenatal care. In: DeCherney AH Nathan L, Goodwin TM, et al, eds. CURRENT diagnosis & treatment obstetrics & gynecology. 10th ed. New York, NY: McGraw Hill; 2007.
8. Piazza C, Fisher W, Hanley P, et al. Treatment of pica through multiple analyses of its reinforcing functions. J Appl Behav Anal. 1998;31(2):165-189.
9. Williams DE, McAdam D. Assessment behavioral treatment, and prevention of pica: clinical guidelines and recommendations for practitioners. Res Dev Disabil. 2012;33(6):2050-2057.
10. Blinder BJ, Salama C. An update on pica: prevalence contributing causes, and treatment. Psychiatric Times. http://www.psychiatrictimes.com/display/article/10168/1159376?pageNumber=1. Published May 1, 2008. Accessed January 23, 2013.
11. Lerner AJ. Treatment of pica behavior with olanzapine. CNS Spectr. 2008;13(1):19.-
Bipolar disorder or something else?
CASE: Unclear diagnosis
Police find Ms. S, age 31, extremely intoxicated and drinking alcohol in her car in a city park parking lot. In the emergency room, she becomes increasingly somnolent and clinicians intubate her trachea to protect her airway. Lab testing shows she has elevated acetaminophen and lithium serum levels, and she is transferred to our hospital for further management after being started on N-acetylcysteine to treat acetaminophen toxicity. Her “ex-fiancé,” the father of her 2 children, saw her earlier the day of the episode and says she was distraught, intoxicated, and had several empty pill bottles in her purse.
In our hospital, Ms. S’ lithium level increases from 2.3 mEq/L to a peak of 5.32 mEq/L, and she undergoes hemodialysis. On hospital day 2, her serum lithium level is trending downward. After Ms. S is able to breathe spontaneously, her trachea is extubated and her hemodialysis line is removed. A psychiatric consultation is obtained, but she is unable to provide a coherent history and the treating clinicians believe she has delirium caused by multiple factors.
On hospital day 3, Ms. S’ delirium clears enough for her to engage in an interview, and she is transferred to our inpatient psychiatry ward for further monitoring and stabilization.
She reports that she was diagnosed with bipolar disorder (BD) at age 12, when she faced multiple psychosocial stressors, including physical abuse by her mother’s boyfriend. She took several psychotropics—although she cannot remember which ones—until age 14, when she stopped all medications until the year before her current hospitalization. Although throughout adolescence and adulthood Ms. S experienced chronic irritability, anxiety, impulsive behavior, poor self-esteem, abusive relationships, self-cutting, and depressed mood, she maintains that she felt worse when she was taking psychotropics and doubts the BD diagnosis. She attributes her longstanding mood issues to low self-worth, a “codependent nature,” and a tendency to gravitate toward abusive relationships. Although she admits to experimenting with several illicit drugs during adolescence, she denies more recent substance use and states she drinks alcohol only once every few months.
The authors’ observations
BD is underdiagnosed in several patient populations, such as individuals previously diagnosed with MDD.1-3 Misdiagnosis can have severe implications, including delay in receiving treatment with effective medications (eg, mood stabilizers) or use of agents that can induce mania or rapid-cycling, such as antidepressants. Perhaps in response to this concern, in recent years clinicians increasingly have diagnosed BD in adolescents and adults. An analysis of a national database of physician practices found a 40-fold increase in office visits for BD among youth and a near doubling among adults from 1994 to 2003.4
Although underdiagnosis of BD remains important, some researchers have suggested that overdiagnosis may be more prevalent and equally harmful. In a study of 180 patients being treated for depression in a family care clinic, there was a 21.6% initial underdiagnosis rate among those eventually found to have BD.1 However, among 43 patients with a prior BD diagnosis, the diagnosis was not confirmed in 33%.1 In a study of 700 psychiatric outpatients in Rhode Island, only 43% of 145 patients who reported a prior BD diagnosis had that diagnosis confirmed.5 Three times as many patients were overdiagnosed with BD as underdiagnosed.
Are there characteristics common to individuals incorrectly diagnosed with BD? In a study that compared patients who had been mistakenly diagnosed with BD with those who had not been diagnosed with BD, the overdiagnosis group was significantly more likely to be diagnosed with a personality disorder, in particular borderline or antisocial personality disorder.6 Only lifetime and current BPD, current posttraumatic stress disorder (PTSD), and lifetime impulse control disorders were independently associated with BD overdiagnosis. The odds ratio for overdiagnosis of BD in patients found to have BPD was 3.7.
EVALUATION: Rethink the diagnosis
In the last few months, Ms. S had complained to her primary care provider (PCP) of worsening anxiety and depressed mood. She was the victim of ongoing physical and emotional abuse by her ex-fiancé and was concerned that she may lose custody of her 2 sons. Approximately 8 months before admission, Ms. S’ PCP prescribed lithium, 450 mg, 3 times a day, for “mood stabilization” and depression because she’d already been diagnosed with BD. This was the first mood stabilizer she’d taken since she was 14. She also was taking unknown doses of hydrocodone/acetaminophen, cyclobenzaprine, and tramadol for pain and temazepam for insomnia. Ms. S continued to suffer from labile and depressed mood, and fought with her ex-fiancé and legal authorities to maintain custody of her 2 children until she was found in the park.
Throughout her hospitalization she denies that she attempted suicide that day, and maintains that this incident was caused by unintentional mismanagement of her medications. Although she continues to have a sense of low self-worth, she denies feeling depressed; in contrast, she says she feels like she has a “new lease on life.” During several interviews she cannot provide a history of any prolonged (ie, several days) episodes of elevated mood, increased goal-directed behavior, decreased need for sleep, tangential thought, pressured speech, or other symptoms that suggest hypomania or mania. She does not endorse prolonged periods of neurovegetative symptoms that would indicate a major depressive episode.
We feel that Ms. S’ symptoms of affective dysregulation, impulsivity, and interpersonal dysfunction are consistent with BPD, and we determine that she meets 6 of the 9 DSM-IV-TR diagnostic features of BPD (≥5 are required for a BPD diagnosis) (Table 1).7 Ms. S describes efforts to avoid abandonment, unstable and intense interpersonal relationships, marked and persistent unstable self-image, recurrent suicidal and self-mutilating behavior, affective instability, and chronic feelings of emptiness. She is discharged to follow up with a psychotherapist and family practitioner. She is not continued on any psychotropic medications.
The authors’ observations
Although it can be difficult to accurately diagnose psychiatric illness during a brief inpatient hospitalization, several clinicians who cared for Ms. S felt that her presentation was more consistent with BPD than BD. Her case is an example of the potential harm of incorrectly diagnosing personality-disordered patients with BD. Ms. S is impulsive and used lithium—a medication that is the standard of care for BD—in an overdose, which lead to a costly and dangerous hospitalization marked by a difficult tracheal intubation and hemodialysis.
Table 1
DSM-IV-TR diagnostic criteria for borderline personality disorder
| A pervasive pattern of instability of interpersonal relationships, self-image, and affects, and marked impulsivity, as indicated by ≥5 of the following: |
|
| Source: Reference 7 |
Distinguishing BD and BPD
There is considerable overlap in symptoms of BD and BPD. Although the episodic nature of BD is well differentiated from the more chronic course of BPD, many hypomania and mania symptoms are similar to those of BPD (Table 2).7 For example, patients with BD or BPD may exhibit impulsive behavior and labile moods. Substance use, risky and self-destructive behaviors, and inflammatory interpersonal relationships can occur in both disorders. Some researchers have suggested that pathophysiologically, BPD may fall on a spectrum of bipolar illness, and have proposed a clinical entity they call bipolar type IV or ultra-rapid cycling BD.2,8,9 There may be more co-occurrence of BD with BPD than would be expected by chance10; 1 review of BPD studies found the rate of comorbid BD ranged from 5.6% to 19%.11 However, because of differences in several factors—including phenomenology, family prevalence, longitudinal course, and medication response—some researchers have concluded that evidence does not support categorizing BPD as part of a bipolar spectrum.10-14 Nonetheless, BPD and other personality disorders often co-occur with axis I disorders, including MDD, BD, or PTSD.
Some research has suggested that the increasing availability and marketing campaigns of medications to treat BD may promote diagnosis of the disorder.15 Zimmerman15 hypothesizes that physicians may be more likely to diagnose a condition that responds to medication (ie, BD) than one that is less responsive (ie, BPD). Financial compensation for treating axis I disorders is significantly better than for treating personality disorders.16 The inpatient setting confers barriers to accurately diagnosing personality disorders, including limits on the amount of time that clinicians can spend with patients or ability to communicate with sources of collateral information. A patient’s observed personality and behaviors while hospitalized may not accurately reflect his or her personality and behaviors in that patient’s “natural” environment.
Several diagnostic strategies can help distinguish BPD from BD. For BD to be the primary diagnosis, a patient must have had a hypomanic or manic episode. Sustained episodes of elation or extreme irritability without evident stressors suggest BD rather than BPD.10 According to Gunderson et al,10 “repeated angry outbursts, suicide attempts, or acts of deliberate self harm that are reactive to interpersonal stress and reflect extreme rejection sensitivity are axiomatic of borderline personality disorder.” In a review of clinical practice, Gunderson17 found that hypersensitivity to rejection and fearful preoccupation with expected abandonment are the most distinctive characteristics of BPD patients. He suggested that clinicians can establish the diagnosis by asking patients directly if they believe the criteria for BPD characterize them, which also can help a patient to accept the diagnosis.
Finally, during a short hospitalization, it can be helpful to obtain collateral information from the patient’s friends and family or further characterize the time course of symptoms and diagnostic features in the patient’s natural environment. Clinicians who are reluctant to diagnose BPD in an inpatient setting could suggest the presence of borderline traits or discuss the possibility of the BPD diagnosis in documentation (eg, in the assessment or formulation). Doing so would avoid a premature BPD diagnosis and allow outpatient providers to confirm or rule out personality disorder diagnoses over time. It is important to screen patients with BPD for co-occurring axis I disorders, including BD, MDD, PTSD, and substance abuse.
A false-positive BD diagnosis in patients with BPD has serious treatment implications. Antipsychotics, antidepressants, and anticonvulsants have been used to target BPD symptoms such as affective dysregulation, impulsivity, and cognitive/perceptual abnormalities, but no medications are FDA-approved for treating BPD. American Psychiatric Association guidelines recommend symptom-based pharmacologic strategies for BPD,18 although some researchers believe that these recommendations are out-of-date and not evidence-based.17,19 Some evidence suggests pharmacotherapy can have modest short-term benefits on specific BPD symptoms, but no data suggest that medication can reduce the severity of BPD or lead to remission.19-23 Just 1 randomized controlled trial (N = 17) has examined lithium for BPD and found no effect on mood.11,24
Misdiagnosis of BD in the context of BPD may create unrealistic expectations regarding the potential efficacy of medications for relieving symptoms. Patients may be diverted from potentially helpful psychotherapeutic treatments—such as DBT or mentalization therapy—which evidence suggests can effectively reduce symptoms, the need for additional treatments, and self-harm or suicidal behaviors.10,17,19 Evidence from long-term longitudinal studies suggests that psychosocial or psychotherapeutic treatment may protect against suicide in BPD patients.25
Table 2
DSM-IV-TR diagnostic criteria for a manic episode
|
The DSM-IV-TR diagnostic criteria for a hypomanic episode are similar to criteria for a manic episode, except:
|
| Source: Reference 7 |
Related Resources
- National Education Alliance Borderline Personality Disorder. www.borderlinepersonalitydisorder.com.
- Hoffman PD, Steiner-Grossman P. Borderline personality disorder: meeting the challenges to successful treatment. Philadelphia, PA: Haworth Press; 2008.
Drug Brand Names
- Cyclobenzaprine • Flexeril
- Hydrocodone/acetaminophen • Lorcet, Vicodin, others
- Lithium • Eskalith, Lithobid
- Temazepam • Restoril
- Tramadol • Ultram
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Hirschfeld RM, Cass AR, Holt DC, et al. Screening for bipolar disorder in patients treated for depression in a family medicine clinic. J Am Board Fam Pract. 2005;18(4):233-239.
2. Ghaemi SN, Ko JY, Goodwin FK. “Cade’s disease” and beyond: Misdiagnosis antidepressant use, and a proposed definition for bipolar spectrum disorder. Can J Psychiatry. 2002;47(2):125-134.
3. Bowden CL. Strategies to reduce misdiagnosis of bipolar depression. Psychiatr Serv. 2001;52(1):51-55.
4. Moreno C, Laje G, Blanco C, et al. National trends in the outpatient diagnosis and treatment of bipolar disorder in youth. Arch Gen Psychiatry. 2007;64(9):1032-1039.
5. Zimmerman M, Ruggero CJ, Chelminski I, et al. Is bipolar disorder overdiagnosed? J Clin Psychiatry. 2008;69(6):935-940.
6. Zimmerman M, Ruggero CJ, Chelminski I, et al. Psychiatric diagnoses in patients previously overdiagnosed with bipolar disorder. J Clin Psychiatry. 2010;71(1):26-31.
7. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
8. Akiskal HS. The bipolar spectrum-the shaping of a new paradigm in psychiatry. Curr Psychiatry Rep. 2002;4(1):1-3.
9. Akiskal HS, Pinto O. The evolving bipolar spectrum. Prototypes I II, III, and IV. Psychiatr Clin North Am. 1999;22(3):517-534, vii.
10. Gunderson JG, Weinberg I, Daversa MT, et al. Descriptive and longitudinal observations on the relationship of borderline personality disorder and bipolar disorder. Am J Psychiatry. 2006;163(7):1173-1178.
11. Paris J, Gunderson J, Weinberg I. The interface between borderline personality disorder and bipolar spectrum disorders. Compr Psychiatry. 2007;48(2):145-154.
12. Paris J. Why psychiatrists are reluctant to diagnose: borderline personality disorder. Psychiatry (Edgmont). 2007;4(1):35-39.
13. Paris J. Borderline or bipolar? Distinguishing borderline personality disorder from bipolar spectrum disorders. Harv Rev Psychiatry. 2004;12(3):140-145.
14. Ruggero CJ, Zimmerman M, Chelminski I, et al. Borderline personality disorder and the misdiagnosis of bipolar disorder. J Psychiatr Res. 2010;44(6):405-408.
15. Zimmerman M. Problems diagnosing bipolar disorder in clinical practice. Expert Rev Neurother. 2010;10(7):1019-1021.
16. Stone MH. Relationship of borderline personality disorder and bipolar disorder. Am J Psychiatry. 2006;163(7):1126-1128.
17. Gunderson JG. Clinical practice. Borderline personality disorder. N Engl J Med. 2011;364(21):2037-2042.
18. American Psychiatric Association. Practice guideline for the treatment of patients with borderline personality disorder. Washington D.C.: American Psychiatric Association; 2001.
19. Paris J. The treatment of borderline personality disorder: implications of research on diagnosis etiology, and outcome. Annu Rev Clin Psychol. 2009;5:277-290.
20. Stoffers J, Völlm BA, Rücker G, et al. Pharmacological interventions for borderline personality disorder. Cochrane Database Syst Rev. 2010;(6):CD005653.-
21. Ripoll LH, Triebwasser J, Siever LJ. Evidence-based pharmacotherapy for personality disorders. Int J Neuropsychopharmacol. 2011;14(9):1257-1288.
22. Mercer D, Douglass AB, Links PS. Meta-analyses of mood stabilizers antidepressants and antipsychotics in the treatment of borderline personality disorder: effectiveness for depression and anger symptoms. J Pers Disord. 2009;23(2):156-174.
23. Lieb K, Völlm B, Rücker G, et al. Pharmacotherapy for borderline personality disorder: Cochrane systematic review of randomised trials. Br J Psychiatry. 2010;196(1):4-12.
24. Links PS, Steiner M, Boiago I, et al. Lithium therapy for borderline patients: preliminary findings. J Pers Disord. 1990;4(2):173-181.
25. Goodman M, Roiff T, Oakes AH, et al. Suicidal risk and management in borderline personality disorder. Curr Psychiatry Rep. 2012;14(1):79-85.
CASE: Unclear diagnosis
Police find Ms. S, age 31, extremely intoxicated and drinking alcohol in her car in a city park parking lot. In the emergency room, she becomes increasingly somnolent and clinicians intubate her trachea to protect her airway. Lab testing shows she has elevated acetaminophen and lithium serum levels, and she is transferred to our hospital for further management after being started on N-acetylcysteine to treat acetaminophen toxicity. Her “ex-fiancé,” the father of her 2 children, saw her earlier the day of the episode and says she was distraught, intoxicated, and had several empty pill bottles in her purse.
In our hospital, Ms. S’ lithium level increases from 2.3 mEq/L to a peak of 5.32 mEq/L, and she undergoes hemodialysis. On hospital day 2, her serum lithium level is trending downward. After Ms. S is able to breathe spontaneously, her trachea is extubated and her hemodialysis line is removed. A psychiatric consultation is obtained, but she is unable to provide a coherent history and the treating clinicians believe she has delirium caused by multiple factors.
On hospital day 3, Ms. S’ delirium clears enough for her to engage in an interview, and she is transferred to our inpatient psychiatry ward for further monitoring and stabilization.
She reports that she was diagnosed with bipolar disorder (BD) at age 12, when she faced multiple psychosocial stressors, including physical abuse by her mother’s boyfriend. She took several psychotropics—although she cannot remember which ones—until age 14, when she stopped all medications until the year before her current hospitalization. Although throughout adolescence and adulthood Ms. S experienced chronic irritability, anxiety, impulsive behavior, poor self-esteem, abusive relationships, self-cutting, and depressed mood, she maintains that she felt worse when she was taking psychotropics and doubts the BD diagnosis. She attributes her longstanding mood issues to low self-worth, a “codependent nature,” and a tendency to gravitate toward abusive relationships. Although she admits to experimenting with several illicit drugs during adolescence, she denies more recent substance use and states she drinks alcohol only once every few months.
The authors’ observations
BD is underdiagnosed in several patient populations, such as individuals previously diagnosed with MDD.1-3 Misdiagnosis can have severe implications, including delay in receiving treatment with effective medications (eg, mood stabilizers) or use of agents that can induce mania or rapid-cycling, such as antidepressants. Perhaps in response to this concern, in recent years clinicians increasingly have diagnosed BD in adolescents and adults. An analysis of a national database of physician practices found a 40-fold increase in office visits for BD among youth and a near doubling among adults from 1994 to 2003.4
Although underdiagnosis of BD remains important, some researchers have suggested that overdiagnosis may be more prevalent and equally harmful. In a study of 180 patients being treated for depression in a family care clinic, there was a 21.6% initial underdiagnosis rate among those eventually found to have BD.1 However, among 43 patients with a prior BD diagnosis, the diagnosis was not confirmed in 33%.1 In a study of 700 psychiatric outpatients in Rhode Island, only 43% of 145 patients who reported a prior BD diagnosis had that diagnosis confirmed.5 Three times as many patients were overdiagnosed with BD as underdiagnosed.
Are there characteristics common to individuals incorrectly diagnosed with BD? In a study that compared patients who had been mistakenly diagnosed with BD with those who had not been diagnosed with BD, the overdiagnosis group was significantly more likely to be diagnosed with a personality disorder, in particular borderline or antisocial personality disorder.6 Only lifetime and current BPD, current posttraumatic stress disorder (PTSD), and lifetime impulse control disorders were independently associated with BD overdiagnosis. The odds ratio for overdiagnosis of BD in patients found to have BPD was 3.7.
EVALUATION: Rethink the diagnosis
In the last few months, Ms. S had complained to her primary care provider (PCP) of worsening anxiety and depressed mood. She was the victim of ongoing physical and emotional abuse by her ex-fiancé and was concerned that she may lose custody of her 2 sons. Approximately 8 months before admission, Ms. S’ PCP prescribed lithium, 450 mg, 3 times a day, for “mood stabilization” and depression because she’d already been diagnosed with BD. This was the first mood stabilizer she’d taken since she was 14. She also was taking unknown doses of hydrocodone/acetaminophen, cyclobenzaprine, and tramadol for pain and temazepam for insomnia. Ms. S continued to suffer from labile and depressed mood, and fought with her ex-fiancé and legal authorities to maintain custody of her 2 children until she was found in the park.
Throughout her hospitalization she denies that she attempted suicide that day, and maintains that this incident was caused by unintentional mismanagement of her medications. Although she continues to have a sense of low self-worth, she denies feeling depressed; in contrast, she says she feels like she has a “new lease on life.” During several interviews she cannot provide a history of any prolonged (ie, several days) episodes of elevated mood, increased goal-directed behavior, decreased need for sleep, tangential thought, pressured speech, or other symptoms that suggest hypomania or mania. She does not endorse prolonged periods of neurovegetative symptoms that would indicate a major depressive episode.
We feel that Ms. S’ symptoms of affective dysregulation, impulsivity, and interpersonal dysfunction are consistent with BPD, and we determine that she meets 6 of the 9 DSM-IV-TR diagnostic features of BPD (≥5 are required for a BPD diagnosis) (Table 1).7 Ms. S describes efforts to avoid abandonment, unstable and intense interpersonal relationships, marked and persistent unstable self-image, recurrent suicidal and self-mutilating behavior, affective instability, and chronic feelings of emptiness. She is discharged to follow up with a psychotherapist and family practitioner. She is not continued on any psychotropic medications.
The authors’ observations
Although it can be difficult to accurately diagnose psychiatric illness during a brief inpatient hospitalization, several clinicians who cared for Ms. S felt that her presentation was more consistent with BPD than BD. Her case is an example of the potential harm of incorrectly diagnosing personality-disordered patients with BD. Ms. S is impulsive and used lithium—a medication that is the standard of care for BD—in an overdose, which lead to a costly and dangerous hospitalization marked by a difficult tracheal intubation and hemodialysis.
Table 1
DSM-IV-TR diagnostic criteria for borderline personality disorder
| A pervasive pattern of instability of interpersonal relationships, self-image, and affects, and marked impulsivity, as indicated by ≥5 of the following: |
|
| Source: Reference 7 |
Distinguishing BD and BPD
There is considerable overlap in symptoms of BD and BPD. Although the episodic nature of BD is well differentiated from the more chronic course of BPD, many hypomania and mania symptoms are similar to those of BPD (Table 2).7 For example, patients with BD or BPD may exhibit impulsive behavior and labile moods. Substance use, risky and self-destructive behaviors, and inflammatory interpersonal relationships can occur in both disorders. Some researchers have suggested that pathophysiologically, BPD may fall on a spectrum of bipolar illness, and have proposed a clinical entity they call bipolar type IV or ultra-rapid cycling BD.2,8,9 There may be more co-occurrence of BD with BPD than would be expected by chance10; 1 review of BPD studies found the rate of comorbid BD ranged from 5.6% to 19%.11 However, because of differences in several factors—including phenomenology, family prevalence, longitudinal course, and medication response—some researchers have concluded that evidence does not support categorizing BPD as part of a bipolar spectrum.10-14 Nonetheless, BPD and other personality disorders often co-occur with axis I disorders, including MDD, BD, or PTSD.
Some research has suggested that the increasing availability and marketing campaigns of medications to treat BD may promote diagnosis of the disorder.15 Zimmerman15 hypothesizes that physicians may be more likely to diagnose a condition that responds to medication (ie, BD) than one that is less responsive (ie, BPD). Financial compensation for treating axis I disorders is significantly better than for treating personality disorders.16 The inpatient setting confers barriers to accurately diagnosing personality disorders, including limits on the amount of time that clinicians can spend with patients or ability to communicate with sources of collateral information. A patient’s observed personality and behaviors while hospitalized may not accurately reflect his or her personality and behaviors in that patient’s “natural” environment.
Several diagnostic strategies can help distinguish BPD from BD. For BD to be the primary diagnosis, a patient must have had a hypomanic or manic episode. Sustained episodes of elation or extreme irritability without evident stressors suggest BD rather than BPD.10 According to Gunderson et al,10 “repeated angry outbursts, suicide attempts, or acts of deliberate self harm that are reactive to interpersonal stress and reflect extreme rejection sensitivity are axiomatic of borderline personality disorder.” In a review of clinical practice, Gunderson17 found that hypersensitivity to rejection and fearful preoccupation with expected abandonment are the most distinctive characteristics of BPD patients. He suggested that clinicians can establish the diagnosis by asking patients directly if they believe the criteria for BPD characterize them, which also can help a patient to accept the diagnosis.
Finally, during a short hospitalization, it can be helpful to obtain collateral information from the patient’s friends and family or further characterize the time course of symptoms and diagnostic features in the patient’s natural environment. Clinicians who are reluctant to diagnose BPD in an inpatient setting could suggest the presence of borderline traits or discuss the possibility of the BPD diagnosis in documentation (eg, in the assessment or formulation). Doing so would avoid a premature BPD diagnosis and allow outpatient providers to confirm or rule out personality disorder diagnoses over time. It is important to screen patients with BPD for co-occurring axis I disorders, including BD, MDD, PTSD, and substance abuse.
A false-positive BD diagnosis in patients with BPD has serious treatment implications. Antipsychotics, antidepressants, and anticonvulsants have been used to target BPD symptoms such as affective dysregulation, impulsivity, and cognitive/perceptual abnormalities, but no medications are FDA-approved for treating BPD. American Psychiatric Association guidelines recommend symptom-based pharmacologic strategies for BPD,18 although some researchers believe that these recommendations are out-of-date and not evidence-based.17,19 Some evidence suggests pharmacotherapy can have modest short-term benefits on specific BPD symptoms, but no data suggest that medication can reduce the severity of BPD or lead to remission.19-23 Just 1 randomized controlled trial (N = 17) has examined lithium for BPD and found no effect on mood.11,24
Misdiagnosis of BD in the context of BPD may create unrealistic expectations regarding the potential efficacy of medications for relieving symptoms. Patients may be diverted from potentially helpful psychotherapeutic treatments—such as DBT or mentalization therapy—which evidence suggests can effectively reduce symptoms, the need for additional treatments, and self-harm or suicidal behaviors.10,17,19 Evidence from long-term longitudinal studies suggests that psychosocial or psychotherapeutic treatment may protect against suicide in BPD patients.25
Table 2
DSM-IV-TR diagnostic criteria for a manic episode
|
The DSM-IV-TR diagnostic criteria for a hypomanic episode are similar to criteria for a manic episode, except:
|
| Source: Reference 7 |
Related Resources
- National Education Alliance Borderline Personality Disorder. www.borderlinepersonalitydisorder.com.
- Hoffman PD, Steiner-Grossman P. Borderline personality disorder: meeting the challenges to successful treatment. Philadelphia, PA: Haworth Press; 2008.
Drug Brand Names
- Cyclobenzaprine • Flexeril
- Hydrocodone/acetaminophen • Lorcet, Vicodin, others
- Lithium • Eskalith, Lithobid
- Temazepam • Restoril
- Tramadol • Ultram
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE: Unclear diagnosis
Police find Ms. S, age 31, extremely intoxicated and drinking alcohol in her car in a city park parking lot. In the emergency room, she becomes increasingly somnolent and clinicians intubate her trachea to protect her airway. Lab testing shows she has elevated acetaminophen and lithium serum levels, and she is transferred to our hospital for further management after being started on N-acetylcysteine to treat acetaminophen toxicity. Her “ex-fiancé,” the father of her 2 children, saw her earlier the day of the episode and says she was distraught, intoxicated, and had several empty pill bottles in her purse.
In our hospital, Ms. S’ lithium level increases from 2.3 mEq/L to a peak of 5.32 mEq/L, and she undergoes hemodialysis. On hospital day 2, her serum lithium level is trending downward. After Ms. S is able to breathe spontaneously, her trachea is extubated and her hemodialysis line is removed. A psychiatric consultation is obtained, but she is unable to provide a coherent history and the treating clinicians believe she has delirium caused by multiple factors.
On hospital day 3, Ms. S’ delirium clears enough for her to engage in an interview, and she is transferred to our inpatient psychiatry ward for further monitoring and stabilization.
She reports that she was diagnosed with bipolar disorder (BD) at age 12, when she faced multiple psychosocial stressors, including physical abuse by her mother’s boyfriend. She took several psychotropics—although she cannot remember which ones—until age 14, when she stopped all medications until the year before her current hospitalization. Although throughout adolescence and adulthood Ms. S experienced chronic irritability, anxiety, impulsive behavior, poor self-esteem, abusive relationships, self-cutting, and depressed mood, she maintains that she felt worse when she was taking psychotropics and doubts the BD diagnosis. She attributes her longstanding mood issues to low self-worth, a “codependent nature,” and a tendency to gravitate toward abusive relationships. Although she admits to experimenting with several illicit drugs during adolescence, she denies more recent substance use and states she drinks alcohol only once every few months.
The authors’ observations
BD is underdiagnosed in several patient populations, such as individuals previously diagnosed with MDD.1-3 Misdiagnosis can have severe implications, including delay in receiving treatment with effective medications (eg, mood stabilizers) or use of agents that can induce mania or rapid-cycling, such as antidepressants. Perhaps in response to this concern, in recent years clinicians increasingly have diagnosed BD in adolescents and adults. An analysis of a national database of physician practices found a 40-fold increase in office visits for BD among youth and a near doubling among adults from 1994 to 2003.4
Although underdiagnosis of BD remains important, some researchers have suggested that overdiagnosis may be more prevalent and equally harmful. In a study of 180 patients being treated for depression in a family care clinic, there was a 21.6% initial underdiagnosis rate among those eventually found to have BD.1 However, among 43 patients with a prior BD diagnosis, the diagnosis was not confirmed in 33%.1 In a study of 700 psychiatric outpatients in Rhode Island, only 43% of 145 patients who reported a prior BD diagnosis had that diagnosis confirmed.5 Three times as many patients were overdiagnosed with BD as underdiagnosed.
Are there characteristics common to individuals incorrectly diagnosed with BD? In a study that compared patients who had been mistakenly diagnosed with BD with those who had not been diagnosed with BD, the overdiagnosis group was significantly more likely to be diagnosed with a personality disorder, in particular borderline or antisocial personality disorder.6 Only lifetime and current BPD, current posttraumatic stress disorder (PTSD), and lifetime impulse control disorders were independently associated with BD overdiagnosis. The odds ratio for overdiagnosis of BD in patients found to have BPD was 3.7.
EVALUATION: Rethink the diagnosis
In the last few months, Ms. S had complained to her primary care provider (PCP) of worsening anxiety and depressed mood. She was the victim of ongoing physical and emotional abuse by her ex-fiancé and was concerned that she may lose custody of her 2 sons. Approximately 8 months before admission, Ms. S’ PCP prescribed lithium, 450 mg, 3 times a day, for “mood stabilization” and depression because she’d already been diagnosed with BD. This was the first mood stabilizer she’d taken since she was 14. She also was taking unknown doses of hydrocodone/acetaminophen, cyclobenzaprine, and tramadol for pain and temazepam for insomnia. Ms. S continued to suffer from labile and depressed mood, and fought with her ex-fiancé and legal authorities to maintain custody of her 2 children until she was found in the park.
Throughout her hospitalization she denies that she attempted suicide that day, and maintains that this incident was caused by unintentional mismanagement of her medications. Although she continues to have a sense of low self-worth, she denies feeling depressed; in contrast, she says she feels like she has a “new lease on life.” During several interviews she cannot provide a history of any prolonged (ie, several days) episodes of elevated mood, increased goal-directed behavior, decreased need for sleep, tangential thought, pressured speech, or other symptoms that suggest hypomania or mania. She does not endorse prolonged periods of neurovegetative symptoms that would indicate a major depressive episode.
We feel that Ms. S’ symptoms of affective dysregulation, impulsivity, and interpersonal dysfunction are consistent with BPD, and we determine that she meets 6 of the 9 DSM-IV-TR diagnostic features of BPD (≥5 are required for a BPD diagnosis) (Table 1).7 Ms. S describes efforts to avoid abandonment, unstable and intense interpersonal relationships, marked and persistent unstable self-image, recurrent suicidal and self-mutilating behavior, affective instability, and chronic feelings of emptiness. She is discharged to follow up with a psychotherapist and family practitioner. She is not continued on any psychotropic medications.
The authors’ observations
Although it can be difficult to accurately diagnose psychiatric illness during a brief inpatient hospitalization, several clinicians who cared for Ms. S felt that her presentation was more consistent with BPD than BD. Her case is an example of the potential harm of incorrectly diagnosing personality-disordered patients with BD. Ms. S is impulsive and used lithium—a medication that is the standard of care for BD—in an overdose, which lead to a costly and dangerous hospitalization marked by a difficult tracheal intubation and hemodialysis.
Table 1
DSM-IV-TR diagnostic criteria for borderline personality disorder
| A pervasive pattern of instability of interpersonal relationships, self-image, and affects, and marked impulsivity, as indicated by ≥5 of the following: |
|
| Source: Reference 7 |
Distinguishing BD and BPD
There is considerable overlap in symptoms of BD and BPD. Although the episodic nature of BD is well differentiated from the more chronic course of BPD, many hypomania and mania symptoms are similar to those of BPD (Table 2).7 For example, patients with BD or BPD may exhibit impulsive behavior and labile moods. Substance use, risky and self-destructive behaviors, and inflammatory interpersonal relationships can occur in both disorders. Some researchers have suggested that pathophysiologically, BPD may fall on a spectrum of bipolar illness, and have proposed a clinical entity they call bipolar type IV or ultra-rapid cycling BD.2,8,9 There may be more co-occurrence of BD with BPD than would be expected by chance10; 1 review of BPD studies found the rate of comorbid BD ranged from 5.6% to 19%.11 However, because of differences in several factors—including phenomenology, family prevalence, longitudinal course, and medication response—some researchers have concluded that evidence does not support categorizing BPD as part of a bipolar spectrum.10-14 Nonetheless, BPD and other personality disorders often co-occur with axis I disorders, including MDD, BD, or PTSD.
Some research has suggested that the increasing availability and marketing campaigns of medications to treat BD may promote diagnosis of the disorder.15 Zimmerman15 hypothesizes that physicians may be more likely to diagnose a condition that responds to medication (ie, BD) than one that is less responsive (ie, BPD). Financial compensation for treating axis I disorders is significantly better than for treating personality disorders.16 The inpatient setting confers barriers to accurately diagnosing personality disorders, including limits on the amount of time that clinicians can spend with patients or ability to communicate with sources of collateral information. A patient’s observed personality and behaviors while hospitalized may not accurately reflect his or her personality and behaviors in that patient’s “natural” environment.
Several diagnostic strategies can help distinguish BPD from BD. For BD to be the primary diagnosis, a patient must have had a hypomanic or manic episode. Sustained episodes of elation or extreme irritability without evident stressors suggest BD rather than BPD.10 According to Gunderson et al,10 “repeated angry outbursts, suicide attempts, or acts of deliberate self harm that are reactive to interpersonal stress and reflect extreme rejection sensitivity are axiomatic of borderline personality disorder.” In a review of clinical practice, Gunderson17 found that hypersensitivity to rejection and fearful preoccupation with expected abandonment are the most distinctive characteristics of BPD patients. He suggested that clinicians can establish the diagnosis by asking patients directly if they believe the criteria for BPD characterize them, which also can help a patient to accept the diagnosis.
Finally, during a short hospitalization, it can be helpful to obtain collateral information from the patient’s friends and family or further characterize the time course of symptoms and diagnostic features in the patient’s natural environment. Clinicians who are reluctant to diagnose BPD in an inpatient setting could suggest the presence of borderline traits or discuss the possibility of the BPD diagnosis in documentation (eg, in the assessment or formulation). Doing so would avoid a premature BPD diagnosis and allow outpatient providers to confirm or rule out personality disorder diagnoses over time. It is important to screen patients with BPD for co-occurring axis I disorders, including BD, MDD, PTSD, and substance abuse.
A false-positive BD diagnosis in patients with BPD has serious treatment implications. Antipsychotics, antidepressants, and anticonvulsants have been used to target BPD symptoms such as affective dysregulation, impulsivity, and cognitive/perceptual abnormalities, but no medications are FDA-approved for treating BPD. American Psychiatric Association guidelines recommend symptom-based pharmacologic strategies for BPD,18 although some researchers believe that these recommendations are out-of-date and not evidence-based.17,19 Some evidence suggests pharmacotherapy can have modest short-term benefits on specific BPD symptoms, but no data suggest that medication can reduce the severity of BPD or lead to remission.19-23 Just 1 randomized controlled trial (N = 17) has examined lithium for BPD and found no effect on mood.11,24
Misdiagnosis of BD in the context of BPD may create unrealistic expectations regarding the potential efficacy of medications for relieving symptoms. Patients may be diverted from potentially helpful psychotherapeutic treatments—such as DBT or mentalization therapy—which evidence suggests can effectively reduce symptoms, the need for additional treatments, and self-harm or suicidal behaviors.10,17,19 Evidence from long-term longitudinal studies suggests that psychosocial or psychotherapeutic treatment may protect against suicide in BPD patients.25
Table 2
DSM-IV-TR diagnostic criteria for a manic episode
|
The DSM-IV-TR diagnostic criteria for a hypomanic episode are similar to criteria for a manic episode, except:
|
| Source: Reference 7 |
Related Resources
- National Education Alliance Borderline Personality Disorder. www.borderlinepersonalitydisorder.com.
- Hoffman PD, Steiner-Grossman P. Borderline personality disorder: meeting the challenges to successful treatment. Philadelphia, PA: Haworth Press; 2008.
Drug Brand Names
- Cyclobenzaprine • Flexeril
- Hydrocodone/acetaminophen • Lorcet, Vicodin, others
- Lithium • Eskalith, Lithobid
- Temazepam • Restoril
- Tramadol • Ultram
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Hirschfeld RM, Cass AR, Holt DC, et al. Screening for bipolar disorder in patients treated for depression in a family medicine clinic. J Am Board Fam Pract. 2005;18(4):233-239.
2. Ghaemi SN, Ko JY, Goodwin FK. “Cade’s disease” and beyond: Misdiagnosis antidepressant use, and a proposed definition for bipolar spectrum disorder. Can J Psychiatry. 2002;47(2):125-134.
3. Bowden CL. Strategies to reduce misdiagnosis of bipolar depression. Psychiatr Serv. 2001;52(1):51-55.
4. Moreno C, Laje G, Blanco C, et al. National trends in the outpatient diagnosis and treatment of bipolar disorder in youth. Arch Gen Psychiatry. 2007;64(9):1032-1039.
5. Zimmerman M, Ruggero CJ, Chelminski I, et al. Is bipolar disorder overdiagnosed? J Clin Psychiatry. 2008;69(6):935-940.
6. Zimmerman M, Ruggero CJ, Chelminski I, et al. Psychiatric diagnoses in patients previously overdiagnosed with bipolar disorder. J Clin Psychiatry. 2010;71(1):26-31.
7. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
8. Akiskal HS. The bipolar spectrum-the shaping of a new paradigm in psychiatry. Curr Psychiatry Rep. 2002;4(1):1-3.
9. Akiskal HS, Pinto O. The evolving bipolar spectrum. Prototypes I II, III, and IV. Psychiatr Clin North Am. 1999;22(3):517-534, vii.
10. Gunderson JG, Weinberg I, Daversa MT, et al. Descriptive and longitudinal observations on the relationship of borderline personality disorder and bipolar disorder. Am J Psychiatry. 2006;163(7):1173-1178.
11. Paris J, Gunderson J, Weinberg I. The interface between borderline personality disorder and bipolar spectrum disorders. Compr Psychiatry. 2007;48(2):145-154.
12. Paris J. Why psychiatrists are reluctant to diagnose: borderline personality disorder. Psychiatry (Edgmont). 2007;4(1):35-39.
13. Paris J. Borderline or bipolar? Distinguishing borderline personality disorder from bipolar spectrum disorders. Harv Rev Psychiatry. 2004;12(3):140-145.
14. Ruggero CJ, Zimmerman M, Chelminski I, et al. Borderline personality disorder and the misdiagnosis of bipolar disorder. J Psychiatr Res. 2010;44(6):405-408.
15. Zimmerman M. Problems diagnosing bipolar disorder in clinical practice. Expert Rev Neurother. 2010;10(7):1019-1021.
16. Stone MH. Relationship of borderline personality disorder and bipolar disorder. Am J Psychiatry. 2006;163(7):1126-1128.
17. Gunderson JG. Clinical practice. Borderline personality disorder. N Engl J Med. 2011;364(21):2037-2042.
18. American Psychiatric Association. Practice guideline for the treatment of patients with borderline personality disorder. Washington D.C.: American Psychiatric Association; 2001.
19. Paris J. The treatment of borderline personality disorder: implications of research on diagnosis etiology, and outcome. Annu Rev Clin Psychol. 2009;5:277-290.
20. Stoffers J, Völlm BA, Rücker G, et al. Pharmacological interventions for borderline personality disorder. Cochrane Database Syst Rev. 2010;(6):CD005653.-
21. Ripoll LH, Triebwasser J, Siever LJ. Evidence-based pharmacotherapy for personality disorders. Int J Neuropsychopharmacol. 2011;14(9):1257-1288.
22. Mercer D, Douglass AB, Links PS. Meta-analyses of mood stabilizers antidepressants and antipsychotics in the treatment of borderline personality disorder: effectiveness for depression and anger symptoms. J Pers Disord. 2009;23(2):156-174.
23. Lieb K, Völlm B, Rücker G, et al. Pharmacotherapy for borderline personality disorder: Cochrane systematic review of randomised trials. Br J Psychiatry. 2010;196(1):4-12.
24. Links PS, Steiner M, Boiago I, et al. Lithium therapy for borderline patients: preliminary findings. J Pers Disord. 1990;4(2):173-181.
25. Goodman M, Roiff T, Oakes AH, et al. Suicidal risk and management in borderline personality disorder. Curr Psychiatry Rep. 2012;14(1):79-85.
1. Hirschfeld RM, Cass AR, Holt DC, et al. Screening for bipolar disorder in patients treated for depression in a family medicine clinic. J Am Board Fam Pract. 2005;18(4):233-239.
2. Ghaemi SN, Ko JY, Goodwin FK. “Cade’s disease” and beyond: Misdiagnosis antidepressant use, and a proposed definition for bipolar spectrum disorder. Can J Psychiatry. 2002;47(2):125-134.
3. Bowden CL. Strategies to reduce misdiagnosis of bipolar depression. Psychiatr Serv. 2001;52(1):51-55.
4. Moreno C, Laje G, Blanco C, et al. National trends in the outpatient diagnosis and treatment of bipolar disorder in youth. Arch Gen Psychiatry. 2007;64(9):1032-1039.
5. Zimmerman M, Ruggero CJ, Chelminski I, et al. Is bipolar disorder overdiagnosed? J Clin Psychiatry. 2008;69(6):935-940.
6. Zimmerman M, Ruggero CJ, Chelminski I, et al. Psychiatric diagnoses in patients previously overdiagnosed with bipolar disorder. J Clin Psychiatry. 2010;71(1):26-31.
7. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
8. Akiskal HS. The bipolar spectrum-the shaping of a new paradigm in psychiatry. Curr Psychiatry Rep. 2002;4(1):1-3.
9. Akiskal HS, Pinto O. The evolving bipolar spectrum. Prototypes I II, III, and IV. Psychiatr Clin North Am. 1999;22(3):517-534, vii.
10. Gunderson JG, Weinberg I, Daversa MT, et al. Descriptive and longitudinal observations on the relationship of borderline personality disorder and bipolar disorder. Am J Psychiatry. 2006;163(7):1173-1178.
11. Paris J, Gunderson J, Weinberg I. The interface between borderline personality disorder and bipolar spectrum disorders. Compr Psychiatry. 2007;48(2):145-154.
12. Paris J. Why psychiatrists are reluctant to diagnose: borderline personality disorder. Psychiatry (Edgmont). 2007;4(1):35-39.
13. Paris J. Borderline or bipolar? Distinguishing borderline personality disorder from bipolar spectrum disorders. Harv Rev Psychiatry. 2004;12(3):140-145.
14. Ruggero CJ, Zimmerman M, Chelminski I, et al. Borderline personality disorder and the misdiagnosis of bipolar disorder. J Psychiatr Res. 2010;44(6):405-408.
15. Zimmerman M. Problems diagnosing bipolar disorder in clinical practice. Expert Rev Neurother. 2010;10(7):1019-1021.
16. Stone MH. Relationship of borderline personality disorder and bipolar disorder. Am J Psychiatry. 2006;163(7):1126-1128.
17. Gunderson JG. Clinical practice. Borderline personality disorder. N Engl J Med. 2011;364(21):2037-2042.
18. American Psychiatric Association. Practice guideline for the treatment of patients with borderline personality disorder. Washington D.C.: American Psychiatric Association; 2001.
19. Paris J. The treatment of borderline personality disorder: implications of research on diagnosis etiology, and outcome. Annu Rev Clin Psychol. 2009;5:277-290.
20. Stoffers J, Völlm BA, Rücker G, et al. Pharmacological interventions for borderline personality disorder. Cochrane Database Syst Rev. 2010;(6):CD005653.-
21. Ripoll LH, Triebwasser J, Siever LJ. Evidence-based pharmacotherapy for personality disorders. Int J Neuropsychopharmacol. 2011;14(9):1257-1288.
22. Mercer D, Douglass AB, Links PS. Meta-analyses of mood stabilizers antidepressants and antipsychotics in the treatment of borderline personality disorder: effectiveness for depression and anger symptoms. J Pers Disord. 2009;23(2):156-174.
23. Lieb K, Völlm B, Rücker G, et al. Pharmacotherapy for borderline personality disorder: Cochrane systematic review of randomised trials. Br J Psychiatry. 2010;196(1):4-12.
24. Links PS, Steiner M, Boiago I, et al. Lithium therapy for borderline patients: preliminary findings. J Pers Disord. 1990;4(2):173-181.
25. Goodman M, Roiff T, Oakes AH, et al. Suicidal risk and management in borderline personality disorder. Curr Psychiatry Rep. 2012;14(1):79-85.
Paranoid, agitated, and manipulative
CASE: Agitation
Mrs. M, age 39, presents to the emergency department (ED) with altered mental status. She is escorted by her husband and the police. She has a history of severe alcohol dependence, bipolar disorder (BD), anxiety, borderline personality disorder (BPD), hypothyroidism, and bulimia, and had gastric bypass surgery 4 years ago. Her husband called 911 when he could no longer manage Mrs. M’s agitated state. The police found her to be extremely paranoid, restless, and disoriented. Her husband reports that she shouted “the world is going to end” before she escaped naked into her neighborhood streets.
On several occasions Mrs. M had been admitted to the same hospital for alcohol withdrawal and dependence with subsequent liver failure, leading to jaundice, coagulopathy, and ascites. During these hospitalizations, she exhibited poor behavioral tendencies, unhealthy psychological defenses, and chronic maladaptive coping and defense mechanisms congruent with her BPD diagnosis. Specifically, she engaged in splitting of hospital staff, ranging from extreme flattery to overt devaluation and hostility. Other defense mechanisms included denial, distortion, acting out, and passive-aggressive behavior. During these admissions, Mrs. M often displayed deficits in recall and attention on Mini-Mental State Examination (MMSE), but these deficits were associated with concurrent alcohol use and improved rapidly during her stay.
In her current presentation, Mrs. M’s mental status change is more pronounced and atypical compared with earlier admissions. Her outpatient medication regimen includes lamotrigine, 100 mg/d, levothyroxine, 88 mcg/d, venlafaxine extended release (XR), 75 mg/d, clonazepam, 3 mg/d, docusate as needed for constipation, and a daily multivitamin.
The authors’ observations
Delirium is a disturbance of consciousness manifested by a reduced clarity of awareness (impairment in attention) and change in cognition (impairment in orientation, memory, and language).1,2 The disturbance develops over a short time and tends to fluctuate during the day. Delirium is a direct physiological consequence of a general medical condition, substance use (intoxication or withdrawal), or both (Table).3
Delirium generally is a reversible mental disorder but can progress to irreversible brain damage. Prompt and accurate diagnosis of delirium is essential,4 although the condition often is underdiagnosed or misdiagnosed because of lack of recognition.
Table
DSM-IV-TR diagnostic criteria for delirium
|
| Source: Reference 3 |
Patients who have convoluted histories, such as Mrs. M, are common and difficult to manage and treat. These patients become substantially more complex when they are admitted to inpatient medical or surgical services. The need to clarify between delirium (primarily medical) and depression (primarily psychiatric) becomes paramount when administering treatment and evaluating decision-making capacity.5 In Mrs. M’s case, internal medicine, neurology, and psychiatry teams each had a different approach to altered mental status. Each team’s different terminology, assessment, and objectives further complicated an already challenging case.6
EVALUATION: Confounding results
The ED physicians offer a working diagnosis of acute mental status change, administer IV lorazepam, 4 mg, and order restraints for Mrs. M’s severe agitation. Her initial vital signs reveal slightly elevated blood pressure (140/90 mm Hg) and tachycardia (115 beats per minute). Internal medicine clinicians note that Mrs. M is not in acute distress, although she refuses to speak and has a small amount of dried blood on her lips, presumably from a struggle with the police before coming to the hospital, but this is not certain. Her abdomen is not tender; she has normal bowel sounds, and no asterixis is noted on neurologic exam. Physical exam is otherwise normal. A noncontrast head CT scan shows no acute process. Initial lab values show elevations in ammonia (277 μg/dL) and γ-glutamyl transpeptidase (68 U/L). Thyroid-stimulating hormone is 1.45 mlU/L, prothrombin time is 19.5 s, partial thromboplastin time is 40.3 s, and international normalized ratio is 1.67. The internal medicine team admits Mrs. M to the intensive care unit (ICU) for further management of her mental status change with alcohol withdrawal or hepatic encephalopathy as the most likely etiologies.
Mrs. M’s husband says that his wife has not consumed alcohol in the last 4 months in preparation for a possible liver transplant; however, past interactions with Mrs. M’s family suggest they are unreliable. The Clinical Institute Withdrawal Assessment (CIWA) protocol is implemented in case her symptoms are caused by alcohol withdrawal. Her vital signs are stable and IV lorazepam, 4 mg, is administered once for agitation. Mrs. M’s husband also reports that 1 month ago his wife underwent a transjugular intrahepatic portosystemic shunt (TIPS) procedure for portal hypertension. Outpatient psychotropics (lamotrigine, 100 mg/d, and venlafaxine XR, 75 mg/d) are restarted because withdrawal from these drugs may exacerbate her symptoms. In the ICU Mrs. M experiences a tonic-clonic seizure with fecal incontinence and bitten tongue, which results in a consultation from neurology and the psychiatry consultation-liaison service.
Psychiatry recommends withholding psychotropics, stopping CIWA, and using vital sign parameters along with objective signs of diaphoresis and tremors as indicators of alcohol withdrawal for lorazepam administration. Mrs. M receives IV haloperidol, 1 mg, once during her second day in the hospital for severe agitation, but this medication is discontinued because of concern about lowering her seizure threshold.7 After treatment with lactulose, her ammonia levels trend down to 33 μg/dL, but her altered mental state persists with significant deficits in attention and orientation.
The neurology service performs an EEG that shows no slow-wave, triphasic waves, or epileptiform activity, which likely would be present in delirium or seizures. See Figure 1 for an example of triphasic waves on an EEG and Figure 2 for Mrs. M's EEG results. Subsequent lumbar puncture, MRI, and a second EEG are unremarkable. By the fifth hospital day, Mrs. M is calm and her paranoia has subsided, but she still is confused and disoriented. Psychiatry orders a third EEG while she is in this confused state; it shows no pathologic process. Based on these examinations, neurology posits that Mrs. M is not encephalopathic.
Figure 1: Representative sample of triphasic waves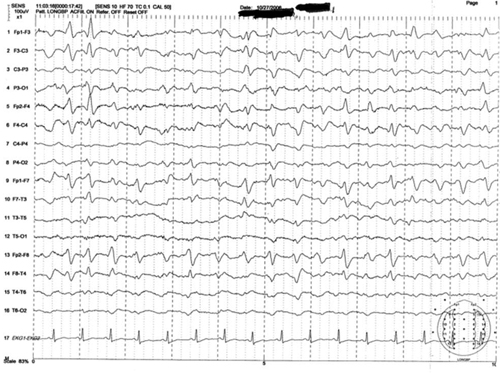
This EEG tracing is from a 54-year-old woman who underwent prolonged abdominal surgery for lysis of adhesions during which she suffered an intraoperative left subinsular stroke followed by nonconvulsive status epilepticus. The tracing demonstrates typical morphology with the positive sharp transient preceded and followed by smaller amplitude negative deflections. Symmetric, frontal predominance of findings seen is this tracing is common
Figure 2: Mrs. M’s EEG results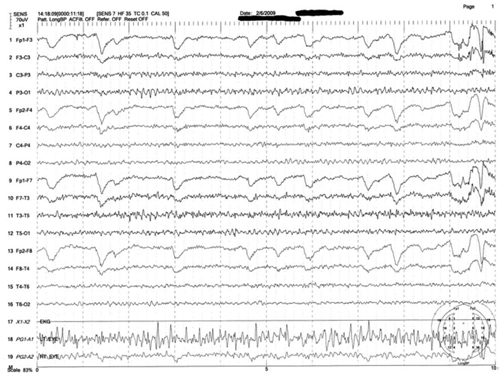
This is a representative tracing of Mrs. M’s 3 EEGs revealing an 8.5 to 9 Hz dominant alpha rhythm. There is superimposed frontally dominant beta fast activity, which is consistent with known administration of benzodiazepines
The authors’ observations
Mrs. M had repeated admissions for alcohol dependence and subsequent liver failure. Her recent hospitalization was complicated by a TIPS procedure done 1 month ago. The incidence of hepatic encephalopathy in patients undergoing TIPS is >30%, especially in the first month post-procedure, which raised suspicion that hepatic encephalopathy played a significant role in Mrs. M’s delirium.8
Because of frequent hospitalization, Mrs. M was well known to the internal medicine, neurology, and psychiatry teams, and each used different terms to describe her mental state. Internal medicine used the phrase “acute mental status change,” which covers a broad differential. Neurology used “encephalopathy,” which also is a general term. Psychiatry used “delirium,” which has narrower and more specific diagnostic criteria. Engel et al9 described the delirious patient as having “cerebral insufficiency” with universally abnormal EEG. Regardless of terminology, based on Mrs. M’s acute confusion, one would expect an abnormal EEG, but repeat EEGs were unremarkable.
Interpreting EEG
EEG is one of the few tools available for measuring acute changes in cerebral function, and an EEG slowing remains a hallmark in encephalopathic processes.10,11 Initially, the 3 specialties agreed that Mrs. M’s presentation likely was caused by underlying medical issues or substances (alcohol or others). EEG can help recognize delirium, and, in some cases, elucidate the underlying cause.10,12 It was surprising that Mrs. M’s EEGs were normal despite a clinical presentation of delirium. Because of the normal EEG findings, neurology leaned toward a primary psychiatric (“functional”) etiology as the cause of her delirium vs a general medical condition or alcohol withdrawal (“organic”).
A literature search in regards to sensitivity of EEG in delirium revealed conflicting statements and data. A standard textbook in neurology and psychiatry states that “a normal EEG virtually excludes a toxic-metabolic encephalopathy.”13 The American Psychiatric Association’s (APA) practice guidelines for delirium states: “The presence of EEG abnormalities has fairly good sensitivities for delirium (in one study, the sensitivity was found to be 75%), but the absence does not rule out the diagnosis; thus the EEG is no substitute for careful clinical observation.”6
At the beginning of Mrs. M’s care, in discussion with the neurology and internal medicine teams, we argued that Mrs. M was experiencing delirium despite her initial normal EEG. We did not expect that 2 subsequent EEGs would be normal, especially because the teams witnessed the final EEG being performed while Mrs. M was clinically evaluated and observed to be in a state of delirium.
OUTCOME: Cause still unknown
By the 6th day of hospitalization, Mrs. M’s vitals are normal and she remains hemodynamically stable. Differential diagnosis remains wide and unclear. The psychiatry team feels she could have atypical catatonia due to an underlying mood disorder. One hour after a trial of IV lorazepam, 1 mg, Mrs. M is more lucid and fully oriented, with MMSE of 28/30 (recall was 1/3), indicating normal cognition. During the exam, a psychiatry resident notes Mrs. M winks and feigns a yawn at the medical students and nurses in the room, displaying her boredom with the interview and simplicity of the mental status exam questions. Later that evening, Mrs. M exhibits bizarre sexual gestures toward male hospital staff, including licking a male nursing staff member’s hand.
Although Mrs. M’s initial confusion resolved, the severity of her comorbid psychiatric history warrants inpatient psychiatric hospitalization. She agrees to transfer to the psychiatric ward after she confesses anxiety regarding death, intense demoralization, and guilt related to her condition and her relationship with her 12-year-old daughter. She tearfully reports that she discontinued her psychotropic medications shortly after stopping alcohol 4 months ago. Shortly before her transfer, psychiatry is called back to the medicine floor because of Mrs. M’s disruptive behavior.
The team finds Mrs. M in her hospital gown, pursuing her husband in the hallway as he is leaving, yelling profanities and blaming him for her horrible experience in the hospital. Based on her demeanor, the team determines that she is back to her baseline mental state despite her mood disorder, and that her upcoming inpatient psychiatric stay likely would be too short to address her comorbid personality disorder. The next day she signs out of the hospital against medical advice.
The authors’ observations
We never clearly identified the specific etiology responsible for Mrs. M’s delirium. We assume at the initial presentation she had toxic-metabolic encephalopathy that rapidly resolved with lactulose treatment and lowering her ammonia. She then had a single tonic-clonic seizure, perhaps related to stopping and then restarting her psychotropics. Her subsequent confusion, bizarre sexual behavior, and demeanor on her final hospital days were more indicative of her psychiatric diagnoses. We now suspect that Mrs. M’s delirium was briefer than presumed and she returned to her baseline borderline personality, resulting in some factitious staging of delirium to confuse her 3 treating teams (a psychoanalyst may say this was a form of projective identification).
We felt that if Mrs. M truly was delirious due to metabolic or hepatic dysfunction or alcohol withdrawal, she would have had abnormal EEG findings. We discovered that the notion of “75% sensitivity” of EEG abnormalities cited in the APA guidelines comes from studies that include patients with “psychogenic” and “organic” delirium. Acute manias and agitated psychoses were termed “psychogenic delirium” and acute confusion due to medical conditions or substance issues was termed “organic delirium.”9,12,14-16
This poses a circular reasoning in the diagnostic criteria and clinical approach to delirium. The fallacy is that, according to DSM-IV-TR, delirium is supposed to be the result of a direct physiological consequence of a general medical condition or substance use (criterion D), and cannot be due to psychosis (eg, schizophrenia) or mania (eg, BD). We question the presumptive 75% sensitivity of EEG abnormalities in patients with delirium because it is possible that when some of these studies were conducted the definition of delirium was not solidified or fully understood. We suspect the sensitivity would be much higher if the correct definition of delirium according to DSM-IV-TR is used in future studies. To improve interdisciplinary communication and future research, it would be constructive if all disciplines could agree on a single term, with the same diagnostic criteria, when evaluating a patient with acute confusion.
Related Resources
- Meagher D. Delirium: the role of psychiatry. Advances in Psychiatric Treatment. 2001;7:433-442.
- Casey DA, DeFazio JV Jr, Vansickle K, et al. Delirium. Quick recognition, careful evaluation, and appropriate treatment. Postgrad Med. 1996;100(1):121-4, 128, 133-134.
Drug Brand Names
- Clonazepam • Klonopin
- Docusate • Surfak
- Haloperidol • Haldol
- Lamotrigine • Lamictal
- Lorazepam • Ativan
- Levothyroxine • Levoxyl, Synthtoid
- Venlafaxine XR • Effexor XR
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgment
The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the U.S. Government. The authors are employees of the U.S. Government. This work was prepared as part of their official duties. Title 17 U.S.C. 105 provides that “Copyright protection under this title is not available for any work of the U.S. Government.” Title 17 U.S.C. 101 defines a U.S. Government work as a work prepared by a military service member or employee of the U.S. Government as part of that person’s official duties.
1. Katz IR, Mossey J, Sussman N, et al. Bedside clinical and electrophysiological assessment: assessment of change in vulnerable patients. Int Psychogeriatr. 1991;3(2):289-300.
2. Inouye SK. Delirium in older persons. N Engl J Med. 2006;354(11):1157-1165.
3. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
4. McPhee SJ, Papadakis M, Rabow MW. CURRENT medical diagnosis and treatment. New York NY: McGraw Hill Medical; 2012.
5. Brody B. Who has capacity? N Engl J Med. 2009;361(3):232-233.
6. Practice guideline for the treatment of patients with delirium. American Psychiatric Association. Am J Psychiatry. 1999;156(5 suppl):1-20.
7. Fricchione GL, Nejad SH, Esses JA, et al. Postoperative delirium. Am J Psychiatry. 2008;165(7):803-812.
8. Sanyal AJ, Freedman AM, Shiffman ML, et al. Portosystemic encephalopathy after transjugular intrahepatic portosystemic shunt: results of a prospective controlled study. Hepatology. 1994;20(1 pt 1):46-55.
9. Engel GL, Romano J. Delirium a syndrome of cerebral insufficiency. 1959. J Neuropsychiatry Clin Neurosci. 2004;16(4):526-538.
10. Pro JD, Wells CE. The use of the electroencephalogram in the diagnosis of delirium. Dis Nerv Syst. 1977;38(10):804-808.
11. Sidhu KS, Balon R, Ajluni V, et al. Standard EEG and the difficult-to-assess mental status. Ann Clin Psychiatry. 2009;21(2):103-108.
12. Brenner RP. Utility of EEG in delirium: past views and current practice. Int Psychogeriatr. 1991;3(2):211-229.
13. Kaufman DM. Clinical neurology for psychiatrists. 5th ed. Philadelphia PA: Saunders; 2001: 230-232.
14. Bond TC. Recognition of acute delirious mania. Arch Gen Psychiatry. 1980;37(5):553-554.
15. Krauthammer C, Klerman GL. Secondary mania: manic syndromes associated with antecedent physical illness or drugs. Arch Gen Psychiatry. 1978;35(11):1333-1339.
16. Larson EW, Richelson E. Organic causes of mania. Mayo Clin Proc. 1988;63(9):906-912.
CASE: Agitation
Mrs. M, age 39, presents to the emergency department (ED) with altered mental status. She is escorted by her husband and the police. She has a history of severe alcohol dependence, bipolar disorder (BD), anxiety, borderline personality disorder (BPD), hypothyroidism, and bulimia, and had gastric bypass surgery 4 years ago. Her husband called 911 when he could no longer manage Mrs. M’s agitated state. The police found her to be extremely paranoid, restless, and disoriented. Her husband reports that she shouted “the world is going to end” before she escaped naked into her neighborhood streets.
On several occasions Mrs. M had been admitted to the same hospital for alcohol withdrawal and dependence with subsequent liver failure, leading to jaundice, coagulopathy, and ascites. During these hospitalizations, she exhibited poor behavioral tendencies, unhealthy psychological defenses, and chronic maladaptive coping and defense mechanisms congruent with her BPD diagnosis. Specifically, she engaged in splitting of hospital staff, ranging from extreme flattery to overt devaluation and hostility. Other defense mechanisms included denial, distortion, acting out, and passive-aggressive behavior. During these admissions, Mrs. M often displayed deficits in recall and attention on Mini-Mental State Examination (MMSE), but these deficits were associated with concurrent alcohol use and improved rapidly during her stay.
In her current presentation, Mrs. M’s mental status change is more pronounced and atypical compared with earlier admissions. Her outpatient medication regimen includes lamotrigine, 100 mg/d, levothyroxine, 88 mcg/d, venlafaxine extended release (XR), 75 mg/d, clonazepam, 3 mg/d, docusate as needed for constipation, and a daily multivitamin.
The authors’ observations
Delirium is a disturbance of consciousness manifested by a reduced clarity of awareness (impairment in attention) and change in cognition (impairment in orientation, memory, and language).1,2 The disturbance develops over a short time and tends to fluctuate during the day. Delirium is a direct physiological consequence of a general medical condition, substance use (intoxication or withdrawal), or both (Table).3
Delirium generally is a reversible mental disorder but can progress to irreversible brain damage. Prompt and accurate diagnosis of delirium is essential,4 although the condition often is underdiagnosed or misdiagnosed because of lack of recognition.
Table
DSM-IV-TR diagnostic criteria for delirium
|
| Source: Reference 3 |
Patients who have convoluted histories, such as Mrs. M, are common and difficult to manage and treat. These patients become substantially more complex when they are admitted to inpatient medical or surgical services. The need to clarify between delirium (primarily medical) and depression (primarily psychiatric) becomes paramount when administering treatment and evaluating decision-making capacity.5 In Mrs. M’s case, internal medicine, neurology, and psychiatry teams each had a different approach to altered mental status. Each team’s different terminology, assessment, and objectives further complicated an already challenging case.6
EVALUATION: Confounding results
The ED physicians offer a working diagnosis of acute mental status change, administer IV lorazepam, 4 mg, and order restraints for Mrs. M’s severe agitation. Her initial vital signs reveal slightly elevated blood pressure (140/90 mm Hg) and tachycardia (115 beats per minute). Internal medicine clinicians note that Mrs. M is not in acute distress, although she refuses to speak and has a small amount of dried blood on her lips, presumably from a struggle with the police before coming to the hospital, but this is not certain. Her abdomen is not tender; she has normal bowel sounds, and no asterixis is noted on neurologic exam. Physical exam is otherwise normal. A noncontrast head CT scan shows no acute process. Initial lab values show elevations in ammonia (277 μg/dL) and γ-glutamyl transpeptidase (68 U/L). Thyroid-stimulating hormone is 1.45 mlU/L, prothrombin time is 19.5 s, partial thromboplastin time is 40.3 s, and international normalized ratio is 1.67. The internal medicine team admits Mrs. M to the intensive care unit (ICU) for further management of her mental status change with alcohol withdrawal or hepatic encephalopathy as the most likely etiologies.
Mrs. M’s husband says that his wife has not consumed alcohol in the last 4 months in preparation for a possible liver transplant; however, past interactions with Mrs. M’s family suggest they are unreliable. The Clinical Institute Withdrawal Assessment (CIWA) protocol is implemented in case her symptoms are caused by alcohol withdrawal. Her vital signs are stable and IV lorazepam, 4 mg, is administered once for agitation. Mrs. M’s husband also reports that 1 month ago his wife underwent a transjugular intrahepatic portosystemic shunt (TIPS) procedure for portal hypertension. Outpatient psychotropics (lamotrigine, 100 mg/d, and venlafaxine XR, 75 mg/d) are restarted because withdrawal from these drugs may exacerbate her symptoms. In the ICU Mrs. M experiences a tonic-clonic seizure with fecal incontinence and bitten tongue, which results in a consultation from neurology and the psychiatry consultation-liaison service.
Psychiatry recommends withholding psychotropics, stopping CIWA, and using vital sign parameters along with objective signs of diaphoresis and tremors as indicators of alcohol withdrawal for lorazepam administration. Mrs. M receives IV haloperidol, 1 mg, once during her second day in the hospital for severe agitation, but this medication is discontinued because of concern about lowering her seizure threshold.7 After treatment with lactulose, her ammonia levels trend down to 33 μg/dL, but her altered mental state persists with significant deficits in attention and orientation.
The neurology service performs an EEG that shows no slow-wave, triphasic waves, or epileptiform activity, which likely would be present in delirium or seizures. See Figure 1 for an example of triphasic waves on an EEG and Figure 2 for Mrs. M's EEG results. Subsequent lumbar puncture, MRI, and a second EEG are unremarkable. By the fifth hospital day, Mrs. M is calm and her paranoia has subsided, but she still is confused and disoriented. Psychiatry orders a third EEG while she is in this confused state; it shows no pathologic process. Based on these examinations, neurology posits that Mrs. M is not encephalopathic.
Figure 1: Representative sample of triphasic waves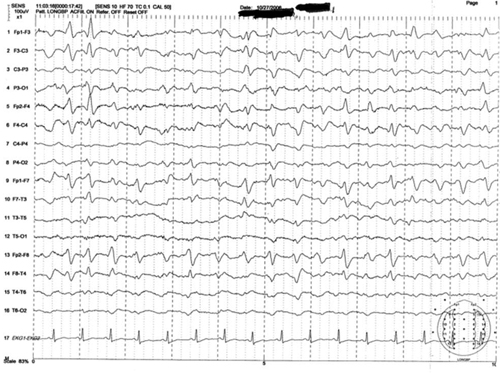
This EEG tracing is from a 54-year-old woman who underwent prolonged abdominal surgery for lysis of adhesions during which she suffered an intraoperative left subinsular stroke followed by nonconvulsive status epilepticus. The tracing demonstrates typical morphology with the positive sharp transient preceded and followed by smaller amplitude negative deflections. Symmetric, frontal predominance of findings seen is this tracing is common
Figure 2: Mrs. M’s EEG results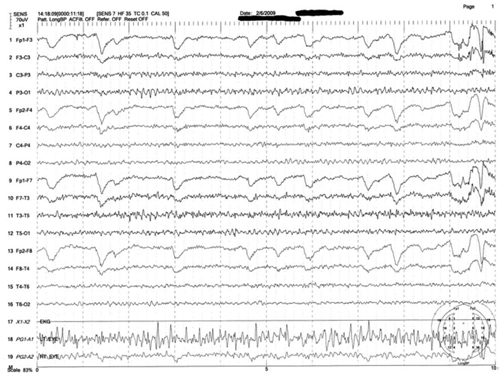
This is a representative tracing of Mrs. M’s 3 EEGs revealing an 8.5 to 9 Hz dominant alpha rhythm. There is superimposed frontally dominant beta fast activity, which is consistent with known administration of benzodiazepines
The authors’ observations
Mrs. M had repeated admissions for alcohol dependence and subsequent liver failure. Her recent hospitalization was complicated by a TIPS procedure done 1 month ago. The incidence of hepatic encephalopathy in patients undergoing TIPS is >30%, especially in the first month post-procedure, which raised suspicion that hepatic encephalopathy played a significant role in Mrs. M’s delirium.8
Because of frequent hospitalization, Mrs. M was well known to the internal medicine, neurology, and psychiatry teams, and each used different terms to describe her mental state. Internal medicine used the phrase “acute mental status change,” which covers a broad differential. Neurology used “encephalopathy,” which also is a general term. Psychiatry used “delirium,” which has narrower and more specific diagnostic criteria. Engel et al9 described the delirious patient as having “cerebral insufficiency” with universally abnormal EEG. Regardless of terminology, based on Mrs. M’s acute confusion, one would expect an abnormal EEG, but repeat EEGs were unremarkable.
Interpreting EEG
EEG is one of the few tools available for measuring acute changes in cerebral function, and an EEG slowing remains a hallmark in encephalopathic processes.10,11 Initially, the 3 specialties agreed that Mrs. M’s presentation likely was caused by underlying medical issues or substances (alcohol or others). EEG can help recognize delirium, and, in some cases, elucidate the underlying cause.10,12 It was surprising that Mrs. M’s EEGs were normal despite a clinical presentation of delirium. Because of the normal EEG findings, neurology leaned toward a primary psychiatric (“functional”) etiology as the cause of her delirium vs a general medical condition or alcohol withdrawal (“organic”).
A literature search in regards to sensitivity of EEG in delirium revealed conflicting statements and data. A standard textbook in neurology and psychiatry states that “a normal EEG virtually excludes a toxic-metabolic encephalopathy.”13 The American Psychiatric Association’s (APA) practice guidelines for delirium states: “The presence of EEG abnormalities has fairly good sensitivities for delirium (in one study, the sensitivity was found to be 75%), but the absence does not rule out the diagnosis; thus the EEG is no substitute for careful clinical observation.”6
At the beginning of Mrs. M’s care, in discussion with the neurology and internal medicine teams, we argued that Mrs. M was experiencing delirium despite her initial normal EEG. We did not expect that 2 subsequent EEGs would be normal, especially because the teams witnessed the final EEG being performed while Mrs. M was clinically evaluated and observed to be in a state of delirium.
OUTCOME: Cause still unknown
By the 6th day of hospitalization, Mrs. M’s vitals are normal and she remains hemodynamically stable. Differential diagnosis remains wide and unclear. The psychiatry team feels she could have atypical catatonia due to an underlying mood disorder. One hour after a trial of IV lorazepam, 1 mg, Mrs. M is more lucid and fully oriented, with MMSE of 28/30 (recall was 1/3), indicating normal cognition. During the exam, a psychiatry resident notes Mrs. M winks and feigns a yawn at the medical students and nurses in the room, displaying her boredom with the interview and simplicity of the mental status exam questions. Later that evening, Mrs. M exhibits bizarre sexual gestures toward male hospital staff, including licking a male nursing staff member’s hand.
Although Mrs. M’s initial confusion resolved, the severity of her comorbid psychiatric history warrants inpatient psychiatric hospitalization. She agrees to transfer to the psychiatric ward after she confesses anxiety regarding death, intense demoralization, and guilt related to her condition and her relationship with her 12-year-old daughter. She tearfully reports that she discontinued her psychotropic medications shortly after stopping alcohol 4 months ago. Shortly before her transfer, psychiatry is called back to the medicine floor because of Mrs. M’s disruptive behavior.
The team finds Mrs. M in her hospital gown, pursuing her husband in the hallway as he is leaving, yelling profanities and blaming him for her horrible experience in the hospital. Based on her demeanor, the team determines that she is back to her baseline mental state despite her mood disorder, and that her upcoming inpatient psychiatric stay likely would be too short to address her comorbid personality disorder. The next day she signs out of the hospital against medical advice.
The authors’ observations
We never clearly identified the specific etiology responsible for Mrs. M’s delirium. We assume at the initial presentation she had toxic-metabolic encephalopathy that rapidly resolved with lactulose treatment and lowering her ammonia. She then had a single tonic-clonic seizure, perhaps related to stopping and then restarting her psychotropics. Her subsequent confusion, bizarre sexual behavior, and demeanor on her final hospital days were more indicative of her psychiatric diagnoses. We now suspect that Mrs. M’s delirium was briefer than presumed and she returned to her baseline borderline personality, resulting in some factitious staging of delirium to confuse her 3 treating teams (a psychoanalyst may say this was a form of projective identification).
We felt that if Mrs. M truly was delirious due to metabolic or hepatic dysfunction or alcohol withdrawal, she would have had abnormal EEG findings. We discovered that the notion of “75% sensitivity” of EEG abnormalities cited in the APA guidelines comes from studies that include patients with “psychogenic” and “organic” delirium. Acute manias and agitated psychoses were termed “psychogenic delirium” and acute confusion due to medical conditions or substance issues was termed “organic delirium.”9,12,14-16
This poses a circular reasoning in the diagnostic criteria and clinical approach to delirium. The fallacy is that, according to DSM-IV-TR, delirium is supposed to be the result of a direct physiological consequence of a general medical condition or substance use (criterion D), and cannot be due to psychosis (eg, schizophrenia) or mania (eg, BD). We question the presumptive 75% sensitivity of EEG abnormalities in patients with delirium because it is possible that when some of these studies were conducted the definition of delirium was not solidified or fully understood. We suspect the sensitivity would be much higher if the correct definition of delirium according to DSM-IV-TR is used in future studies. To improve interdisciplinary communication and future research, it would be constructive if all disciplines could agree on a single term, with the same diagnostic criteria, when evaluating a patient with acute confusion.
Related Resources
- Meagher D. Delirium: the role of psychiatry. Advances in Psychiatric Treatment. 2001;7:433-442.
- Casey DA, DeFazio JV Jr, Vansickle K, et al. Delirium. Quick recognition, careful evaluation, and appropriate treatment. Postgrad Med. 1996;100(1):121-4, 128, 133-134.
Drug Brand Names
- Clonazepam • Klonopin
- Docusate • Surfak
- Haloperidol • Haldol
- Lamotrigine • Lamictal
- Lorazepam • Ativan
- Levothyroxine • Levoxyl, Synthtoid
- Venlafaxine XR • Effexor XR
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgment
The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the U.S. Government. The authors are employees of the U.S. Government. This work was prepared as part of their official duties. Title 17 U.S.C. 105 provides that “Copyright protection under this title is not available for any work of the U.S. Government.” Title 17 U.S.C. 101 defines a U.S. Government work as a work prepared by a military service member or employee of the U.S. Government as part of that person’s official duties.
CASE: Agitation
Mrs. M, age 39, presents to the emergency department (ED) with altered mental status. She is escorted by her husband and the police. She has a history of severe alcohol dependence, bipolar disorder (BD), anxiety, borderline personality disorder (BPD), hypothyroidism, and bulimia, and had gastric bypass surgery 4 years ago. Her husband called 911 when he could no longer manage Mrs. M’s agitated state. The police found her to be extremely paranoid, restless, and disoriented. Her husband reports that she shouted “the world is going to end” before she escaped naked into her neighborhood streets.
On several occasions Mrs. M had been admitted to the same hospital for alcohol withdrawal and dependence with subsequent liver failure, leading to jaundice, coagulopathy, and ascites. During these hospitalizations, she exhibited poor behavioral tendencies, unhealthy psychological defenses, and chronic maladaptive coping and defense mechanisms congruent with her BPD diagnosis. Specifically, she engaged in splitting of hospital staff, ranging from extreme flattery to overt devaluation and hostility. Other defense mechanisms included denial, distortion, acting out, and passive-aggressive behavior. During these admissions, Mrs. M often displayed deficits in recall and attention on Mini-Mental State Examination (MMSE), but these deficits were associated with concurrent alcohol use and improved rapidly during her stay.
In her current presentation, Mrs. M’s mental status change is more pronounced and atypical compared with earlier admissions. Her outpatient medication regimen includes lamotrigine, 100 mg/d, levothyroxine, 88 mcg/d, venlafaxine extended release (XR), 75 mg/d, clonazepam, 3 mg/d, docusate as needed for constipation, and a daily multivitamin.
The authors’ observations
Delirium is a disturbance of consciousness manifested by a reduced clarity of awareness (impairment in attention) and change in cognition (impairment in orientation, memory, and language).1,2 The disturbance develops over a short time and tends to fluctuate during the day. Delirium is a direct physiological consequence of a general medical condition, substance use (intoxication or withdrawal), or both (Table).3
Delirium generally is a reversible mental disorder but can progress to irreversible brain damage. Prompt and accurate diagnosis of delirium is essential,4 although the condition often is underdiagnosed or misdiagnosed because of lack of recognition.
Table
DSM-IV-TR diagnostic criteria for delirium
|
| Source: Reference 3 |
Patients who have convoluted histories, such as Mrs. M, are common and difficult to manage and treat. These patients become substantially more complex when they are admitted to inpatient medical or surgical services. The need to clarify between delirium (primarily medical) and depression (primarily psychiatric) becomes paramount when administering treatment and evaluating decision-making capacity.5 In Mrs. M’s case, internal medicine, neurology, and psychiatry teams each had a different approach to altered mental status. Each team’s different terminology, assessment, and objectives further complicated an already challenging case.6
EVALUATION: Confounding results
The ED physicians offer a working diagnosis of acute mental status change, administer IV lorazepam, 4 mg, and order restraints for Mrs. M’s severe agitation. Her initial vital signs reveal slightly elevated blood pressure (140/90 mm Hg) and tachycardia (115 beats per minute). Internal medicine clinicians note that Mrs. M is not in acute distress, although she refuses to speak and has a small amount of dried blood on her lips, presumably from a struggle with the police before coming to the hospital, but this is not certain. Her abdomen is not tender; she has normal bowel sounds, and no asterixis is noted on neurologic exam. Physical exam is otherwise normal. A noncontrast head CT scan shows no acute process. Initial lab values show elevations in ammonia (277 μg/dL) and γ-glutamyl transpeptidase (68 U/L). Thyroid-stimulating hormone is 1.45 mlU/L, prothrombin time is 19.5 s, partial thromboplastin time is 40.3 s, and international normalized ratio is 1.67. The internal medicine team admits Mrs. M to the intensive care unit (ICU) for further management of her mental status change with alcohol withdrawal or hepatic encephalopathy as the most likely etiologies.
Mrs. M’s husband says that his wife has not consumed alcohol in the last 4 months in preparation for a possible liver transplant; however, past interactions with Mrs. M’s family suggest they are unreliable. The Clinical Institute Withdrawal Assessment (CIWA) protocol is implemented in case her symptoms are caused by alcohol withdrawal. Her vital signs are stable and IV lorazepam, 4 mg, is administered once for agitation. Mrs. M’s husband also reports that 1 month ago his wife underwent a transjugular intrahepatic portosystemic shunt (TIPS) procedure for portal hypertension. Outpatient psychotropics (lamotrigine, 100 mg/d, and venlafaxine XR, 75 mg/d) are restarted because withdrawal from these drugs may exacerbate her symptoms. In the ICU Mrs. M experiences a tonic-clonic seizure with fecal incontinence and bitten tongue, which results in a consultation from neurology and the psychiatry consultation-liaison service.
Psychiatry recommends withholding psychotropics, stopping CIWA, and using vital sign parameters along with objective signs of diaphoresis and tremors as indicators of alcohol withdrawal for lorazepam administration. Mrs. M receives IV haloperidol, 1 mg, once during her second day in the hospital for severe agitation, but this medication is discontinued because of concern about lowering her seizure threshold.7 After treatment with lactulose, her ammonia levels trend down to 33 μg/dL, but her altered mental state persists with significant deficits in attention and orientation.
The neurology service performs an EEG that shows no slow-wave, triphasic waves, or epileptiform activity, which likely would be present in delirium or seizures. See Figure 1 for an example of triphasic waves on an EEG and Figure 2 for Mrs. M's EEG results. Subsequent lumbar puncture, MRI, and a second EEG are unremarkable. By the fifth hospital day, Mrs. M is calm and her paranoia has subsided, but she still is confused and disoriented. Psychiatry orders a third EEG while she is in this confused state; it shows no pathologic process. Based on these examinations, neurology posits that Mrs. M is not encephalopathic.
Figure 1: Representative sample of triphasic waves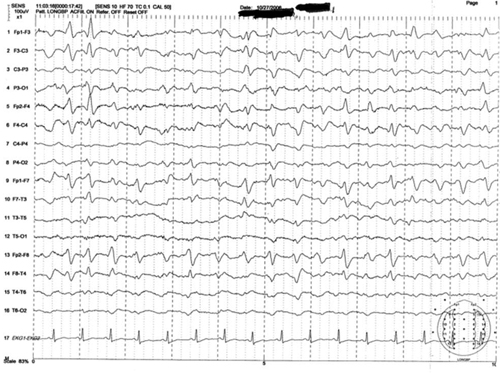
This EEG tracing is from a 54-year-old woman who underwent prolonged abdominal surgery for lysis of adhesions during which she suffered an intraoperative left subinsular stroke followed by nonconvulsive status epilepticus. The tracing demonstrates typical morphology with the positive sharp transient preceded and followed by smaller amplitude negative deflections. Symmetric, frontal predominance of findings seen is this tracing is common
Figure 2: Mrs. M’s EEG results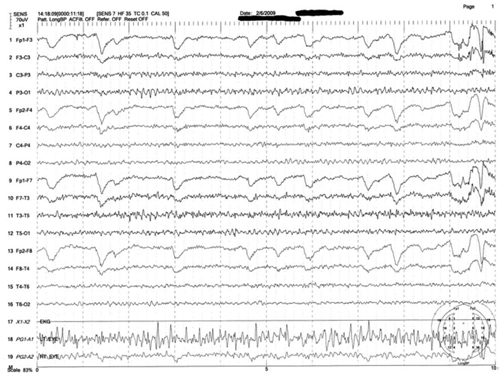
This is a representative tracing of Mrs. M’s 3 EEGs revealing an 8.5 to 9 Hz dominant alpha rhythm. There is superimposed frontally dominant beta fast activity, which is consistent with known administration of benzodiazepines
The authors’ observations
Mrs. M had repeated admissions for alcohol dependence and subsequent liver failure. Her recent hospitalization was complicated by a TIPS procedure done 1 month ago. The incidence of hepatic encephalopathy in patients undergoing TIPS is >30%, especially in the first month post-procedure, which raised suspicion that hepatic encephalopathy played a significant role in Mrs. M’s delirium.8
Because of frequent hospitalization, Mrs. M was well known to the internal medicine, neurology, and psychiatry teams, and each used different terms to describe her mental state. Internal medicine used the phrase “acute mental status change,” which covers a broad differential. Neurology used “encephalopathy,” which also is a general term. Psychiatry used “delirium,” which has narrower and more specific diagnostic criteria. Engel et al9 described the delirious patient as having “cerebral insufficiency” with universally abnormal EEG. Regardless of terminology, based on Mrs. M’s acute confusion, one would expect an abnormal EEG, but repeat EEGs were unremarkable.
Interpreting EEG
EEG is one of the few tools available for measuring acute changes in cerebral function, and an EEG slowing remains a hallmark in encephalopathic processes.10,11 Initially, the 3 specialties agreed that Mrs. M’s presentation likely was caused by underlying medical issues or substances (alcohol or others). EEG can help recognize delirium, and, in some cases, elucidate the underlying cause.10,12 It was surprising that Mrs. M’s EEGs were normal despite a clinical presentation of delirium. Because of the normal EEG findings, neurology leaned toward a primary psychiatric (“functional”) etiology as the cause of her delirium vs a general medical condition or alcohol withdrawal (“organic”).
A literature search in regards to sensitivity of EEG in delirium revealed conflicting statements and data. A standard textbook in neurology and psychiatry states that “a normal EEG virtually excludes a toxic-metabolic encephalopathy.”13 The American Psychiatric Association’s (APA) practice guidelines for delirium states: “The presence of EEG abnormalities has fairly good sensitivities for delirium (in one study, the sensitivity was found to be 75%), but the absence does not rule out the diagnosis; thus the EEG is no substitute for careful clinical observation.”6
At the beginning of Mrs. M’s care, in discussion with the neurology and internal medicine teams, we argued that Mrs. M was experiencing delirium despite her initial normal EEG. We did not expect that 2 subsequent EEGs would be normal, especially because the teams witnessed the final EEG being performed while Mrs. M was clinically evaluated and observed to be in a state of delirium.
OUTCOME: Cause still unknown
By the 6th day of hospitalization, Mrs. M’s vitals are normal and she remains hemodynamically stable. Differential diagnosis remains wide and unclear. The psychiatry team feels she could have atypical catatonia due to an underlying mood disorder. One hour after a trial of IV lorazepam, 1 mg, Mrs. M is more lucid and fully oriented, with MMSE of 28/30 (recall was 1/3), indicating normal cognition. During the exam, a psychiatry resident notes Mrs. M winks and feigns a yawn at the medical students and nurses in the room, displaying her boredom with the interview and simplicity of the mental status exam questions. Later that evening, Mrs. M exhibits bizarre sexual gestures toward male hospital staff, including licking a male nursing staff member’s hand.
Although Mrs. M’s initial confusion resolved, the severity of her comorbid psychiatric history warrants inpatient psychiatric hospitalization. She agrees to transfer to the psychiatric ward after she confesses anxiety regarding death, intense demoralization, and guilt related to her condition and her relationship with her 12-year-old daughter. She tearfully reports that she discontinued her psychotropic medications shortly after stopping alcohol 4 months ago. Shortly before her transfer, psychiatry is called back to the medicine floor because of Mrs. M’s disruptive behavior.
The team finds Mrs. M in her hospital gown, pursuing her husband in the hallway as he is leaving, yelling profanities and blaming him for her horrible experience in the hospital. Based on her demeanor, the team determines that she is back to her baseline mental state despite her mood disorder, and that her upcoming inpatient psychiatric stay likely would be too short to address her comorbid personality disorder. The next day she signs out of the hospital against medical advice.
The authors’ observations
We never clearly identified the specific etiology responsible for Mrs. M’s delirium. We assume at the initial presentation she had toxic-metabolic encephalopathy that rapidly resolved with lactulose treatment and lowering her ammonia. She then had a single tonic-clonic seizure, perhaps related to stopping and then restarting her psychotropics. Her subsequent confusion, bizarre sexual behavior, and demeanor on her final hospital days were more indicative of her psychiatric diagnoses. We now suspect that Mrs. M’s delirium was briefer than presumed and she returned to her baseline borderline personality, resulting in some factitious staging of delirium to confuse her 3 treating teams (a psychoanalyst may say this was a form of projective identification).
We felt that if Mrs. M truly was delirious due to metabolic or hepatic dysfunction or alcohol withdrawal, she would have had abnormal EEG findings. We discovered that the notion of “75% sensitivity” of EEG abnormalities cited in the APA guidelines comes from studies that include patients with “psychogenic” and “organic” delirium. Acute manias and agitated psychoses were termed “psychogenic delirium” and acute confusion due to medical conditions or substance issues was termed “organic delirium.”9,12,14-16
This poses a circular reasoning in the diagnostic criteria and clinical approach to delirium. The fallacy is that, according to DSM-IV-TR, delirium is supposed to be the result of a direct physiological consequence of a general medical condition or substance use (criterion D), and cannot be due to psychosis (eg, schizophrenia) or mania (eg, BD). We question the presumptive 75% sensitivity of EEG abnormalities in patients with delirium because it is possible that when some of these studies were conducted the definition of delirium was not solidified or fully understood. We suspect the sensitivity would be much higher if the correct definition of delirium according to DSM-IV-TR is used in future studies. To improve interdisciplinary communication and future research, it would be constructive if all disciplines could agree on a single term, with the same diagnostic criteria, when evaluating a patient with acute confusion.
Related Resources
- Meagher D. Delirium: the role of psychiatry. Advances in Psychiatric Treatment. 2001;7:433-442.
- Casey DA, DeFazio JV Jr, Vansickle K, et al. Delirium. Quick recognition, careful evaluation, and appropriate treatment. Postgrad Med. 1996;100(1):121-4, 128, 133-134.
Drug Brand Names
- Clonazepam • Klonopin
- Docusate • Surfak
- Haloperidol • Haldol
- Lamotrigine • Lamictal
- Lorazepam • Ativan
- Levothyroxine • Levoxyl, Synthtoid
- Venlafaxine XR • Effexor XR
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgment
The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the U.S. Government. The authors are employees of the U.S. Government. This work was prepared as part of their official duties. Title 17 U.S.C. 105 provides that “Copyright protection under this title is not available for any work of the U.S. Government.” Title 17 U.S.C. 101 defines a U.S. Government work as a work prepared by a military service member or employee of the U.S. Government as part of that person’s official duties.
1. Katz IR, Mossey J, Sussman N, et al. Bedside clinical and electrophysiological assessment: assessment of change in vulnerable patients. Int Psychogeriatr. 1991;3(2):289-300.
2. Inouye SK. Delirium in older persons. N Engl J Med. 2006;354(11):1157-1165.
3. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
4. McPhee SJ, Papadakis M, Rabow MW. CURRENT medical diagnosis and treatment. New York NY: McGraw Hill Medical; 2012.
5. Brody B. Who has capacity? N Engl J Med. 2009;361(3):232-233.
6. Practice guideline for the treatment of patients with delirium. American Psychiatric Association. Am J Psychiatry. 1999;156(5 suppl):1-20.
7. Fricchione GL, Nejad SH, Esses JA, et al. Postoperative delirium. Am J Psychiatry. 2008;165(7):803-812.
8. Sanyal AJ, Freedman AM, Shiffman ML, et al. Portosystemic encephalopathy after transjugular intrahepatic portosystemic shunt: results of a prospective controlled study. Hepatology. 1994;20(1 pt 1):46-55.
9. Engel GL, Romano J. Delirium a syndrome of cerebral insufficiency. 1959. J Neuropsychiatry Clin Neurosci. 2004;16(4):526-538.
10. Pro JD, Wells CE. The use of the electroencephalogram in the diagnosis of delirium. Dis Nerv Syst. 1977;38(10):804-808.
11. Sidhu KS, Balon R, Ajluni V, et al. Standard EEG and the difficult-to-assess mental status. Ann Clin Psychiatry. 2009;21(2):103-108.
12. Brenner RP. Utility of EEG in delirium: past views and current practice. Int Psychogeriatr. 1991;3(2):211-229.
13. Kaufman DM. Clinical neurology for psychiatrists. 5th ed. Philadelphia PA: Saunders; 2001: 230-232.
14. Bond TC. Recognition of acute delirious mania. Arch Gen Psychiatry. 1980;37(5):553-554.
15. Krauthammer C, Klerman GL. Secondary mania: manic syndromes associated with antecedent physical illness or drugs. Arch Gen Psychiatry. 1978;35(11):1333-1339.
16. Larson EW, Richelson E. Organic causes of mania. Mayo Clin Proc. 1988;63(9):906-912.
1. Katz IR, Mossey J, Sussman N, et al. Bedside clinical and electrophysiological assessment: assessment of change in vulnerable patients. Int Psychogeriatr. 1991;3(2):289-300.
2. Inouye SK. Delirium in older persons. N Engl J Med. 2006;354(11):1157-1165.
3. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
4. McPhee SJ, Papadakis M, Rabow MW. CURRENT medical diagnosis and treatment. New York NY: McGraw Hill Medical; 2012.
5. Brody B. Who has capacity? N Engl J Med. 2009;361(3):232-233.
6. Practice guideline for the treatment of patients with delirium. American Psychiatric Association. Am J Psychiatry. 1999;156(5 suppl):1-20.
7. Fricchione GL, Nejad SH, Esses JA, et al. Postoperative delirium. Am J Psychiatry. 2008;165(7):803-812.
8. Sanyal AJ, Freedman AM, Shiffman ML, et al. Portosystemic encephalopathy after transjugular intrahepatic portosystemic shunt: results of a prospective controlled study. Hepatology. 1994;20(1 pt 1):46-55.
9. Engel GL, Romano J. Delirium a syndrome of cerebral insufficiency. 1959. J Neuropsychiatry Clin Neurosci. 2004;16(4):526-538.
10. Pro JD, Wells CE. The use of the electroencephalogram in the diagnosis of delirium. Dis Nerv Syst. 1977;38(10):804-808.
11. Sidhu KS, Balon R, Ajluni V, et al. Standard EEG and the difficult-to-assess mental status. Ann Clin Psychiatry. 2009;21(2):103-108.
12. Brenner RP. Utility of EEG in delirium: past views and current practice. Int Psychogeriatr. 1991;3(2):211-229.
13. Kaufman DM. Clinical neurology for psychiatrists. 5th ed. Philadelphia PA: Saunders; 2001: 230-232.
14. Bond TC. Recognition of acute delirious mania. Arch Gen Psychiatry. 1980;37(5):553-554.
15. Krauthammer C, Klerman GL. Secondary mania: manic syndromes associated with antecedent physical illness or drugs. Arch Gen Psychiatry. 1978;35(11):1333-1339.
16. Larson EW, Richelson E. Organic causes of mania. Mayo Clin Proc. 1988;63(9):906-912.
Drug interactions with tobacco smoke: Implications for patient care
- Tobacco smokers often are treated with medications that are metabolized by hepatic cytochrome (CYP) 1A2 enzymes. Starting or stopping tobacco smoking may cause drug interactions because polycyclic aromatic hydrocarbons in cigarette smoke induce CYP1A2 enzymes.
- Drugs that are significantly metabolized by CYP1A2 (major substrates) are more likely to be impacted by changes in tobacco smoking compared with minor substrates.
- Induction of hepatic CYP1A2 enzymes may be greater in heavy or moderate smokers compared with light smokers (eg, <10 cigarettes per day).
- Evidence-based approaches for treating tobacco use in health care settings should address the risk of CYP1A2 drug interactions in tobacco smokers and how this impacts their clinical care.
Mrs. C, age 51, experiences exacerbated asthma and difficulty breathing and is admitted to a non-smoking hospital. She also has chronic obstructive pulmonary disease, type 2 diabetes mellitus, hypertension, hypercholesterolemia, hypothyroidism, gastroesophageal reflux disease, overactive bladder, muscle spasms, fibromyalgia, bipolar disorder, insomnia, and nicotine and caffeine dependence. She takes 19 prescribed and over-the-counter medications, drinks up to 8 cups of coffee per day, and smokes 20 to 30 cigarettes per day. In the emergency room, she receives albuterol/ipratropium inhalation therapy to help her breathing and a 21-mg nicotine replacement patch to avoid nicotine withdrawal.
In the United States, 19% of adults smoke cigarettes.1 Heavy tobacco smoking and nicotine dependence are common among psychiatric patients and contribute to higher rates of tobacco-related morbidity and mortality.2 When smokers stop smoking or are admitted to smoke-free facilities and are forced to abstain, nicotine withdrawal symptoms and changes in drug metabolism can develop over several days.3-5
Smokers such as Mrs. C are at risk for cytochrome (CYP) P450 drug interactions when they are admitted to or discharged from a smoke-free facility. Nine of Mrs. C’s medications are substrates of CYP1A2 (acetaminophen, caffeine, cyclobenzaprine, diazepam, duloxetine, melatonin, olanzapine, ondansetron, and zolpidem). When Mrs. C stops smoking while in the hospital, she could experience higher serum concentrations and adverse effects of these medications. If Mrs. C resumes smoking after bring discharged, metabolism and clearance of any medications started while she was hospitalized that are substrates of CYP1A2 enzymes could be increased, which could lead to reduced efficacy and poor clinical outcomes.
Pharmacokinetic effects
Polycyclic aromatic hydrocarbons in tobacco smoke induce hepatic CYP1A1, 1A2, and possibly 2E1 isoenzymes.6-12 CYP1A2 is a hepatic enzyme responsible for metabolizing and eliminating several classes of substrates (eg, drugs, hormones, endogenous compounds, and procarcinogens).6,13 Genetic, epigenetic, and environmental factors such as smoking impact the expression and activity of CYP1A2 and result in large interpatient variability in pharmacokinetic drug interactions.6,12,13 CYP1A2 enzymes can be induced or inhibited by drugs and substances, which can result in decreased or increased serum concentrations of substrates, respectively. When individuals stop smoking and switch to other nicotine products or devices, CYP1A2 induction of hepatic enzymes will revert to normal metabolism over several weeks to a month.10 Besides tobacco smoke, other CYP1A2 inducers include charbroiled food, carbamazepine, omeprazole, phenobarbital, primidone, and rifampin.4,5 Nicotine replacement products—such as gum, inhalers, lozenges, patches, and nasal spray—and nicotine delivery devices such as electronic cigarettes do not induce hepatic CYP1A2 enzymes or cause the same drug interactions as cigarette smoking.
Table 13-11 and Table 23-11 list commonly prescribed CYP1A2 substrates that could be affected by tobacco smoke. There are no specific guidelines for how to assess, monitor, or manage pharmacokinetic drug interactions with tobacco smoke.6-13 Induction of hepatic CYP1A2 enzymes by cigarette smoke may require increased dosages of some psychotropics—such as tricyclic antidepressants, duloxetine, mirtazapine, and some first- and second-generation antipsychotics (SGAs)—to achieve serum concentrations adequate for clinical efficacy. Serum concentrations may increase to toxic levels and result in adverse effects when a person quits smoking cigarettes or if a CYP1A2 inhibitor, such as amlodipine, cimetidine, ciprofloxacin, diclofenac, fluoxetine, fluvoxamine, or nifedipine, is added.5
Table 1
Common major cytochrome P450 (CYP) 1A2 substrates
| Drug | Class |
|---|---|
| Alosetron3,5,6 | Irritable bowel syndrome: serotonin 3 antagonist |
| Aminophylline3,5 | Bronchodilator: theophylline derivative |
| Betaxolol3,5 | β-1 selective adrenergic receptor blocking agent |
| Caffeine3-9 | Stimulant |
| Clomipramine3-11 | Tricyclic antidepressant |
| Clozapine3-10 | Second-generation antipsychotic |
| Cyclobenzaprine3-7 | Skeletal muscle relaxant |
| Doxepin3,7,10,11 | Tricyclic antidepressant |
| Duloxetine3-6 | Serotonin-norepinephrine reuptake inhibitor |
| Estradiol3,5-8 | Estrogen (active) |
| Estrogens: conjugated and estropipate3,5; estrone3,7 | Estrogen (derivatives) |
| Fluvoxamine3,8,9 | Selective serotonin reuptake inhibitor |
| Guanabenz3,5-7 | α-2 adrenergic agonist |
| Mirtazapine3-7 | Antidepressant: α-2 antagonist/serotonin 2A, 2C antagonist |
| Olanzapine3-11 | Second-generation antipsychotic |
| Pimozide3,5,7 | First-generation antipsychotic |
| Propranolol3-11 | β-adrenergic blocker |
| Ramelteon3,5,10 | Melatonin receptor agonist |
| Rasagiline3,5 | Antiparkinson: type B monoamine oxidase inhibitor |
| Riluzole3-7,10 | Glutamate inhibitor |
| Ropinirole3,5-7 | Antiparkinson: dopamine agonist |
| Theophylline3-6,8-11 | Bronchodilator: methylxanthine |
| Thiothixene3,5 | First-generation antipsychotic |
| Trifluoperazine3,5,9 | First-generation antipsychotic |
| Several classes of CYP1A2 substrates are not included and may cause toxicity with smoking cessation or require dosage increases in tobacco smokers (eg, antiarrhythmic, antifungal, antimalarial, antineoplastic, antiretroviral, and anthelmintic agents and the antibiotic quinolone). Clinicians should be most concerned about drugs with a narrow therapeutic index and those that may be toxic with smoking cessation (eg, bleeding from warfarin and clopidogrel; high serum concentrations of caffeine, clozapine, olanzapine, propranolol, and theophylline) | |
Table 2
Common minor cytochrome P450 (CYP) 1A2 substrates
| Drug | Class |
|---|---|
| Acetaminophen3-9 | Analgesic |
| Almotriptan6 | Antimigraine: serotonin 1B, 1D receptor agonist |
| Amitriptyline3-7,9-11 | Tricyclic antidepressant |
| Asenapine9 | Second-generation antipsychotic |
| Carvedilol5-7 | β and α adrenergic blocking activity |
| Chlorpromazine3,4,7-9,11 | First-generation antipsychotic |
| Chlorzoxazone4,7 | Skeletal muscle relaxant |
| Clopidogrel5 | Antiplatelet |
| Desipramine4,7,10,11 | Tricyclic antidepressant |
| Diazepam4,7,9,10 | Benzodiazepine |
| Diclofenac5,7 | Nonsteroidal anti-inflammatory drug |
| Diphenhydramine6 | Antihistamine |
| Febuxostat5 | Xanthine oxidase inhibitor |
| Fluphenazine3,9 | First-generation antipsychotic |
| Frovatriptan3 | Antimigraine: serotonin 1 agonist |
| Haloperidol3,4,6,8,9 | First-generation antipsychotic |
| Imipramine3,4,6-11 | Tricyclic antidepressant |
| Maprotiline6 | Tetracyclic antidepressant |
| Melatonin3,4,6,7 | Sleep-regulating hormone |
| Metoclopramide3 | Antiemetic: prokinetic gastrointestinal agent |
| Nabumetone6 | Nonsteroidal anti-inflammatory drug |
| Naproxen3,4,6,7 | Nonsteroidal anti-inflammatory drug |
| Naratriptan10 | Antimigraine: serotonin 1B, 1D receptor agonist |
| Nicardipine3,7 | Calcium channel blocker |
| Nortriptyline4,6,7,9-11 | Tricyclic antidepressant |
| Ondansetron3,4,6,7 | Antiemetic: serotonin 3 antagonist |
| Palonosetron5 | Antiemetic: serotonin 3 antagonist |
| Perphenazine3,7 | First-generation antipsychotic |
| Progesterone5,7 | Progestin |
| Propofol4,6,7 | General anesthetic |
| Ranitidine5,7 | H2 antagonist |
| Rivastigmine10 | Acetylcholinesterase inhibitor |
| Selegiline6,7 | Antiparkinson: type B monoamine oxidase inhibitor |
| Thioridazine3,4,6 | First-generation antipsychotic |
| Tizanidine3-6 | Skeletal muscle relaxant: α-2 adrenergic agonist |
| Trazodone6,9 | Serotonin reuptake inhibitor and antagonist |
| Triamterene6 | Diuretic: potassium sparing |
| Verapamil3,4,6,7,10 | Calcium channel blocker |
| Warfarin3,4,6-10 | Anticoagulant: coumarin derivative |
| Zileuton3,4,6,7 | Asthma agent: 5-lipoxygenase inhibitor |
| Ziprasidone3,4 | Second-generation antipsychotic |
| Zolmitriptan3,6,7 | Antimigraine: serotonin 1B, 1D receptor agonist |
| Zolpidem4,6,7 | Nonbenzodiazepine hypnotic |
| Several classes of CYP1A2 substrates are not included and may cause toxicity with smoking cessation or require dosage increases in tobacco smokers (eg, antiarrhythmic, antifungal, antimalarial, antineoplastic, antiretroviral and anthelmintic agents and the antibiotic quinolone). Clinicians should be most concerned about drugs with a narrow therapeutic index and those that may be toxic with smoking cessation (eg, bleeding from warfarin and clopidogrel; high serum concentrations of caffeine, clozapine, olanzapine, propranolol, and theophylline) | |
SGA such as clozapine and olanzapine are major substrates of CYP1A2 and dosages may need to be adjusted when smoking status changes, depending on clinical efficacy and adverse effects.10,14,15 Maximum induction of clozapine and olanzapine metabolism may occur with 7 to 12 cigarettes per day and smokers may have 40% to 50% lower serum concentrations compared with nonsmokers.14 When a patient stops smoking, clozapine and olanzapine dosages may need to be reduced by 30% to 40% (eg, a stepwise 10% reduction in daily dose until day 4) to avoid elevated serum concentrations and risk of toxicity symptoms.15
Tobacco smokers can tolerate high daily intake of caffeinated beverages because of increased metabolism and clearance of caffeine, a major substrate of CYP1A2.11 When patients stop smoking, increased caffeine serum concentrations may cause anxiety, irritability, restlessness, insomnia, tremors, palpitations, and tachycardia. Caffeine toxicity also can mimic symptoms of nicotine withdrawal; therefore, smokers should be advised to reduce their caffeine intake by half to avoid adverse effects when they stop smoking.10,11
Adjusting dosing
Factors such as the amount and frequency of tobacco smoking, how quickly CYP1A2 enzymes change when starting and stopping smoking, exposure to secondhand smoke, and other concomitant drugs contribute to variability in pharmacokinetic drug interactions. Heavy smokers (≥30 cigarettes per day) should be closely monitored because variations in drug serum concentrations may be affected significantly by changes in smoking status.4,9,11 Dosage reductions of potentially toxic drugs should be done immediately when a heavy tobacco user stops smoking.10 For CYP1A2 substrates with a narrow therapeutic range, a conservative approach is to reduce the daily dose by 10% per day for several days after smoking cessation.11,16 The impact on drug metabolism may continue for weeks to a month after the person stops smoking; therefore, there may be a delay until CYP1A2 enzymes return to normal hepatic metabolism.4,8,9,15 In most situations, smoking cessation reverses induction of hepatic CYP1A2 enzymes back to normal metabolism and causes serum drug concentrations to increase.10 Because secondhand smoke induces hepatic CYP1A2 enzymes, those exposed to smoke may have changes in drug metabolism due to environmental smoke exposure.11
Tobacco smokers who take medications and hormones that are metabolized by CYP1A2 enzymes should be closely monitored because dosage adjustments may be necessary when they start or stop smoking cigarettes. An assessment of CYP drug interactions and routine monitoring of efficacy and/or toxicity should be done to avoid potential adverse effects from medications and to determine if changes in dosages and disease state management are required.
Related Resources
- Rx for Change. Drug interactions with smoking. http://smokingcessationleadership.ucsf.edu/interactions.pdf.
- Fiore MC, Baker TB. Treating smokers in the health care setting. N Engl J Med. 2011;365(13):1222-1231.
Drug Brand Names
- Albuterol/ipratropium • Combivent
- Almotriptan • Axert
- Alosetron • Lotronex
- Aminophylline • Phyllocontin, Truphylline
- Amitriptyline • Elavil
- Amlodipine • Norvasc
- Asenapine • Saphris
- Betaxolol • Kerlone
- Carbamazepine • Carbatrol, Tegretol
- Carvedilol • Coreg
- Chlorpromazine • Thorazine
- Chlorzoxazone • Parafon Forte
- Cimetidine • Tagamet
- Ciprofloxacin • Cipro
- Clomipramine • Anafranil
- Clopidogrel • Plavix
- Clozapine • Clozaril
- Cyclobenzaprine • Flexeril
- Desipramine • Norpramin
- Diazepam • Valium
- Diclofenac • Voltaren
- Diphenhydramine • Benadryl
- Doxepin • Silenor, Sinequan
- Duloxetine • Cymbalta
- Estradiol • Estrace
- Estrogens (conjugated) • Cenestin, Premarin
- Estropipate • Ogen
- Febuxostat • Uloric
- Fluoxetine • Prozac
- Fluphenazine • Prolixin
- Fluvoxamine • Luvox
- Frovatriptan • Frova
- Guanabenz • Wytensin
- Haloperidol • Haldol
- Imipramine • Tofranil
- Maprotiline • Ludiomil
- Metoclopramide • Reglan
- Mirtazapine • Remeron
- Nabumetone • Relafen
- Naratriptan • Amerge
- Nicardipine • Cardene
- Nifedipine • Adalat, Procardia
- Nortriptyline • Aventyl, Pamelor
- Olanzapine • Zyprexa
- Omeprazole • Prilosec
- Ondansetron • Zofran
- Palonosetron • Aloxi
- Perphenazine • Trilafon
- Pimozide • Orap
- Primidone • Mysoline
- Progesterone • Prometrium
- Propofol • Diprivan
- Propranolol • Inderal
- Ramelteon • Rozerem
- Ranitidine • Zantac
- Rasagiline • Azilect
- Rifampin • Rifadin, Rimactane
- Riluzole • Rilutek
- Rivastigmine • Exelon
- Ropinirole • Requip
- Selegiline • Eldepryl, EMSAM, others
- Theophylline • Elixophyllin
- Thioridazine • Mellaril
- Thiothixene • Navane
- Tizanidine • Zanaflex
- Trazodone • Desyrel, Oleptro
- Triamterene • Dyrenium
- Trifluoperazine • Stelazine
- Verapamil • Calan, Verelan
- Warfarin • Coumadin, Jantoven
- Zileuton • Zyflo
- Ziprasidone • Geodon
- Zolmitriptan • Zomig
- Zolpidem • Ambien, Edluar
Disclosure
Ms. Fankhauser reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Centers for Disease Control and Prevention (CDC). Vital signs: current cigarette smoking among adults aged ≥18 years—United States 2005-2010. MMWR Morb Mortal Wkly Rep. 2011;60(35):1207-1212.
2. Ziedonis D, Hitsman B, Beckham JC, et al. Tobacco use and cessation in psychiatric disorders: National Institute of Mental Health report. Nicotine Tob Res. 2008;10(12):1691-1715.
3. Choe JY. Drug actions and interactions. New York NY: McGraw-Hill Medical; 2011.
4. Tatro DS. Drug interaction facts. St. Louis MO: Wolters Kluwer Health; 2011.
5. Lacy CF, Armstrong LL, Goldman MP, et al. eds. Drug information handbook, 20th ed. Hudson, OH: Lexicomp; 2011.
6. Zhou SF, Yang LP, Zhou ZW, et al. Insights into the substrate specificity, inhibitors, regulation, and polymorphisms and the clinical impact of human cytochrome P450 1A2. AAPS J. 2009;11(3):481-494.
7. Rendic S. Summary of information on human CYP enzymes: human P450 metabolism data. Drug Metab Rev. 2002;34(1-2):83-448.
8. Zevin S, Benowitz NL. Drug interactions with tobacco smoking. An update. Clin Pharmacokinet. 1999;36(6):425-438.
9. Desai HD, Seabolt J, Jann MW. Smoking in patients receiving psychotropic medications: a pharmacokinetic perspective. CNS Drugs. 2001;15(6):469-494.
10. Schaffer SD, Yoon S, Zadezensky I. A review of smoking cessation: potentially risky effects on prescribed medications. J Clin Nurs. 2009;18(11):1533-1540.
11. Kroon LA. Drug interactions with smoking. Am J Health Syst Pharm. 2007;64(18):1917-1921.
12. Plowchalk DR, Yeo KR. Prediction of drug clearance in a smoking population: modeling the impact of variable cigarette consumption on the induction of CYP1A2. Eur J Pharmacol. 2012;68(6):951-960.
13. Faber MS, Jetter A, Fuhr U. Assessment of CYP1A2 activity in clinical practice: why how, and when? Basic Clin Pharmacol Toxicol. 2005;97(3):125-134.
14. Haslemo T, Eikeseth PH, Tanum L, et al. The effect of variable cigarette consumption on the interaction with clozapine and olanzapine. Eur J Clin Pharmacol. 2006;62(12):1049-1053.
15. Lowe EJ, Ackman ML. Impact of tobacco smoking cessation on stable clozapine or olanzapine treatment. Ann Pharmacother. 2010;44(4):727-732.
16. Faber MS, Fuhr U. Time response of cytochrome P4501A2 activity on cessation of heavy smoking. Clin Pharmacol Ther. 2004;76(2):178-184.
- Tobacco smokers often are treated with medications that are metabolized by hepatic cytochrome (CYP) 1A2 enzymes. Starting or stopping tobacco smoking may cause drug interactions because polycyclic aromatic hydrocarbons in cigarette smoke induce CYP1A2 enzymes.
- Drugs that are significantly metabolized by CYP1A2 (major substrates) are more likely to be impacted by changes in tobacco smoking compared with minor substrates.
- Induction of hepatic CYP1A2 enzymes may be greater in heavy or moderate smokers compared with light smokers (eg, <10 cigarettes per day).
- Evidence-based approaches for treating tobacco use in health care settings should address the risk of CYP1A2 drug interactions in tobacco smokers and how this impacts their clinical care.
Mrs. C, age 51, experiences exacerbated asthma and difficulty breathing and is admitted to a non-smoking hospital. She also has chronic obstructive pulmonary disease, type 2 diabetes mellitus, hypertension, hypercholesterolemia, hypothyroidism, gastroesophageal reflux disease, overactive bladder, muscle spasms, fibromyalgia, bipolar disorder, insomnia, and nicotine and caffeine dependence. She takes 19 prescribed and over-the-counter medications, drinks up to 8 cups of coffee per day, and smokes 20 to 30 cigarettes per day. In the emergency room, she receives albuterol/ipratropium inhalation therapy to help her breathing and a 21-mg nicotine replacement patch to avoid nicotine withdrawal.
In the United States, 19% of adults smoke cigarettes.1 Heavy tobacco smoking and nicotine dependence are common among psychiatric patients and contribute to higher rates of tobacco-related morbidity and mortality.2 When smokers stop smoking or are admitted to smoke-free facilities and are forced to abstain, nicotine withdrawal symptoms and changes in drug metabolism can develop over several days.3-5
Smokers such as Mrs. C are at risk for cytochrome (CYP) P450 drug interactions when they are admitted to or discharged from a smoke-free facility. Nine of Mrs. C’s medications are substrates of CYP1A2 (acetaminophen, caffeine, cyclobenzaprine, diazepam, duloxetine, melatonin, olanzapine, ondansetron, and zolpidem). When Mrs. C stops smoking while in the hospital, she could experience higher serum concentrations and adverse effects of these medications. If Mrs. C resumes smoking after bring discharged, metabolism and clearance of any medications started while she was hospitalized that are substrates of CYP1A2 enzymes could be increased, which could lead to reduced efficacy and poor clinical outcomes.
Pharmacokinetic effects
Polycyclic aromatic hydrocarbons in tobacco smoke induce hepatic CYP1A1, 1A2, and possibly 2E1 isoenzymes.6-12 CYP1A2 is a hepatic enzyme responsible for metabolizing and eliminating several classes of substrates (eg, drugs, hormones, endogenous compounds, and procarcinogens).6,13 Genetic, epigenetic, and environmental factors such as smoking impact the expression and activity of CYP1A2 and result in large interpatient variability in pharmacokinetic drug interactions.6,12,13 CYP1A2 enzymes can be induced or inhibited by drugs and substances, which can result in decreased or increased serum concentrations of substrates, respectively. When individuals stop smoking and switch to other nicotine products or devices, CYP1A2 induction of hepatic enzymes will revert to normal metabolism over several weeks to a month.10 Besides tobacco smoke, other CYP1A2 inducers include charbroiled food, carbamazepine, omeprazole, phenobarbital, primidone, and rifampin.4,5 Nicotine replacement products—such as gum, inhalers, lozenges, patches, and nasal spray—and nicotine delivery devices such as electronic cigarettes do not induce hepatic CYP1A2 enzymes or cause the same drug interactions as cigarette smoking.
Table 13-11 and Table 23-11 list commonly prescribed CYP1A2 substrates that could be affected by tobacco smoke. There are no specific guidelines for how to assess, monitor, or manage pharmacokinetic drug interactions with tobacco smoke.6-13 Induction of hepatic CYP1A2 enzymes by cigarette smoke may require increased dosages of some psychotropics—such as tricyclic antidepressants, duloxetine, mirtazapine, and some first- and second-generation antipsychotics (SGAs)—to achieve serum concentrations adequate for clinical efficacy. Serum concentrations may increase to toxic levels and result in adverse effects when a person quits smoking cigarettes or if a CYP1A2 inhibitor, such as amlodipine, cimetidine, ciprofloxacin, diclofenac, fluoxetine, fluvoxamine, or nifedipine, is added.5
Table 1
Common major cytochrome P450 (CYP) 1A2 substrates
| Drug | Class |
|---|---|
| Alosetron3,5,6 | Irritable bowel syndrome: serotonin 3 antagonist |
| Aminophylline3,5 | Bronchodilator: theophylline derivative |
| Betaxolol3,5 | β-1 selective adrenergic receptor blocking agent |
| Caffeine3-9 | Stimulant |
| Clomipramine3-11 | Tricyclic antidepressant |
| Clozapine3-10 | Second-generation antipsychotic |
| Cyclobenzaprine3-7 | Skeletal muscle relaxant |
| Doxepin3,7,10,11 | Tricyclic antidepressant |
| Duloxetine3-6 | Serotonin-norepinephrine reuptake inhibitor |
| Estradiol3,5-8 | Estrogen (active) |
| Estrogens: conjugated and estropipate3,5; estrone3,7 | Estrogen (derivatives) |
| Fluvoxamine3,8,9 | Selective serotonin reuptake inhibitor |
| Guanabenz3,5-7 | α-2 adrenergic agonist |
| Mirtazapine3-7 | Antidepressant: α-2 antagonist/serotonin 2A, 2C antagonist |
| Olanzapine3-11 | Second-generation antipsychotic |
| Pimozide3,5,7 | First-generation antipsychotic |
| Propranolol3-11 | β-adrenergic blocker |
| Ramelteon3,5,10 | Melatonin receptor agonist |
| Rasagiline3,5 | Antiparkinson: type B monoamine oxidase inhibitor |
| Riluzole3-7,10 | Glutamate inhibitor |
| Ropinirole3,5-7 | Antiparkinson: dopamine agonist |
| Theophylline3-6,8-11 | Bronchodilator: methylxanthine |
| Thiothixene3,5 | First-generation antipsychotic |
| Trifluoperazine3,5,9 | First-generation antipsychotic |
| Several classes of CYP1A2 substrates are not included and may cause toxicity with smoking cessation or require dosage increases in tobacco smokers (eg, antiarrhythmic, antifungal, antimalarial, antineoplastic, antiretroviral, and anthelmintic agents and the antibiotic quinolone). Clinicians should be most concerned about drugs with a narrow therapeutic index and those that may be toxic with smoking cessation (eg, bleeding from warfarin and clopidogrel; high serum concentrations of caffeine, clozapine, olanzapine, propranolol, and theophylline) | |
Table 2
Common minor cytochrome P450 (CYP) 1A2 substrates
| Drug | Class |
|---|---|
| Acetaminophen3-9 | Analgesic |
| Almotriptan6 | Antimigraine: serotonin 1B, 1D receptor agonist |
| Amitriptyline3-7,9-11 | Tricyclic antidepressant |
| Asenapine9 | Second-generation antipsychotic |
| Carvedilol5-7 | β and α adrenergic blocking activity |
| Chlorpromazine3,4,7-9,11 | First-generation antipsychotic |
| Chlorzoxazone4,7 | Skeletal muscle relaxant |
| Clopidogrel5 | Antiplatelet |
| Desipramine4,7,10,11 | Tricyclic antidepressant |
| Diazepam4,7,9,10 | Benzodiazepine |
| Diclofenac5,7 | Nonsteroidal anti-inflammatory drug |
| Diphenhydramine6 | Antihistamine |
| Febuxostat5 | Xanthine oxidase inhibitor |
| Fluphenazine3,9 | First-generation antipsychotic |
| Frovatriptan3 | Antimigraine: serotonin 1 agonist |
| Haloperidol3,4,6,8,9 | First-generation antipsychotic |
| Imipramine3,4,6-11 | Tricyclic antidepressant |
| Maprotiline6 | Tetracyclic antidepressant |
| Melatonin3,4,6,7 | Sleep-regulating hormone |
| Metoclopramide3 | Antiemetic: prokinetic gastrointestinal agent |
| Nabumetone6 | Nonsteroidal anti-inflammatory drug |
| Naproxen3,4,6,7 | Nonsteroidal anti-inflammatory drug |
| Naratriptan10 | Antimigraine: serotonin 1B, 1D receptor agonist |
| Nicardipine3,7 | Calcium channel blocker |
| Nortriptyline4,6,7,9-11 | Tricyclic antidepressant |
| Ondansetron3,4,6,7 | Antiemetic: serotonin 3 antagonist |
| Palonosetron5 | Antiemetic: serotonin 3 antagonist |
| Perphenazine3,7 | First-generation antipsychotic |
| Progesterone5,7 | Progestin |
| Propofol4,6,7 | General anesthetic |
| Ranitidine5,7 | H2 antagonist |
| Rivastigmine10 | Acetylcholinesterase inhibitor |
| Selegiline6,7 | Antiparkinson: type B monoamine oxidase inhibitor |
| Thioridazine3,4,6 | First-generation antipsychotic |
| Tizanidine3-6 | Skeletal muscle relaxant: α-2 adrenergic agonist |
| Trazodone6,9 | Serotonin reuptake inhibitor and antagonist |
| Triamterene6 | Diuretic: potassium sparing |
| Verapamil3,4,6,7,10 | Calcium channel blocker |
| Warfarin3,4,6-10 | Anticoagulant: coumarin derivative |
| Zileuton3,4,6,7 | Asthma agent: 5-lipoxygenase inhibitor |
| Ziprasidone3,4 | Second-generation antipsychotic |
| Zolmitriptan3,6,7 | Antimigraine: serotonin 1B, 1D receptor agonist |
| Zolpidem4,6,7 | Nonbenzodiazepine hypnotic |
| Several classes of CYP1A2 substrates are not included and may cause toxicity with smoking cessation or require dosage increases in tobacco smokers (eg, antiarrhythmic, antifungal, antimalarial, antineoplastic, antiretroviral and anthelmintic agents and the antibiotic quinolone). Clinicians should be most concerned about drugs with a narrow therapeutic index and those that may be toxic with smoking cessation (eg, bleeding from warfarin and clopidogrel; high serum concentrations of caffeine, clozapine, olanzapine, propranolol, and theophylline) | |
SGA such as clozapine and olanzapine are major substrates of CYP1A2 and dosages may need to be adjusted when smoking status changes, depending on clinical efficacy and adverse effects.10,14,15 Maximum induction of clozapine and olanzapine metabolism may occur with 7 to 12 cigarettes per day and smokers may have 40% to 50% lower serum concentrations compared with nonsmokers.14 When a patient stops smoking, clozapine and olanzapine dosages may need to be reduced by 30% to 40% (eg, a stepwise 10% reduction in daily dose until day 4) to avoid elevated serum concentrations and risk of toxicity symptoms.15
Tobacco smokers can tolerate high daily intake of caffeinated beverages because of increased metabolism and clearance of caffeine, a major substrate of CYP1A2.11 When patients stop smoking, increased caffeine serum concentrations may cause anxiety, irritability, restlessness, insomnia, tremors, palpitations, and tachycardia. Caffeine toxicity also can mimic symptoms of nicotine withdrawal; therefore, smokers should be advised to reduce their caffeine intake by half to avoid adverse effects when they stop smoking.10,11
Adjusting dosing
Factors such as the amount and frequency of tobacco smoking, how quickly CYP1A2 enzymes change when starting and stopping smoking, exposure to secondhand smoke, and other concomitant drugs contribute to variability in pharmacokinetic drug interactions. Heavy smokers (≥30 cigarettes per day) should be closely monitored because variations in drug serum concentrations may be affected significantly by changes in smoking status.4,9,11 Dosage reductions of potentially toxic drugs should be done immediately when a heavy tobacco user stops smoking.10 For CYP1A2 substrates with a narrow therapeutic range, a conservative approach is to reduce the daily dose by 10% per day for several days after smoking cessation.11,16 The impact on drug metabolism may continue for weeks to a month after the person stops smoking; therefore, there may be a delay until CYP1A2 enzymes return to normal hepatic metabolism.4,8,9,15 In most situations, smoking cessation reverses induction of hepatic CYP1A2 enzymes back to normal metabolism and causes serum drug concentrations to increase.10 Because secondhand smoke induces hepatic CYP1A2 enzymes, those exposed to smoke may have changes in drug metabolism due to environmental smoke exposure.11
Tobacco smokers who take medications and hormones that are metabolized by CYP1A2 enzymes should be closely monitored because dosage adjustments may be necessary when they start or stop smoking cigarettes. An assessment of CYP drug interactions and routine monitoring of efficacy and/or toxicity should be done to avoid potential adverse effects from medications and to determine if changes in dosages and disease state management are required.
Related Resources
- Rx for Change. Drug interactions with smoking. http://smokingcessationleadership.ucsf.edu/interactions.pdf.
- Fiore MC, Baker TB. Treating smokers in the health care setting. N Engl J Med. 2011;365(13):1222-1231.
Drug Brand Names
- Albuterol/ipratropium • Combivent
- Almotriptan • Axert
- Alosetron • Lotronex
- Aminophylline • Phyllocontin, Truphylline
- Amitriptyline • Elavil
- Amlodipine • Norvasc
- Asenapine • Saphris
- Betaxolol • Kerlone
- Carbamazepine • Carbatrol, Tegretol
- Carvedilol • Coreg
- Chlorpromazine • Thorazine
- Chlorzoxazone • Parafon Forte
- Cimetidine • Tagamet
- Ciprofloxacin • Cipro
- Clomipramine • Anafranil
- Clopidogrel • Plavix
- Clozapine • Clozaril
- Cyclobenzaprine • Flexeril
- Desipramine • Norpramin
- Diazepam • Valium
- Diclofenac • Voltaren
- Diphenhydramine • Benadryl
- Doxepin • Silenor, Sinequan
- Duloxetine • Cymbalta
- Estradiol • Estrace
- Estrogens (conjugated) • Cenestin, Premarin
- Estropipate • Ogen
- Febuxostat • Uloric
- Fluoxetine • Prozac
- Fluphenazine • Prolixin
- Fluvoxamine • Luvox
- Frovatriptan • Frova
- Guanabenz • Wytensin
- Haloperidol • Haldol
- Imipramine • Tofranil
- Maprotiline • Ludiomil
- Metoclopramide • Reglan
- Mirtazapine • Remeron
- Nabumetone • Relafen
- Naratriptan • Amerge
- Nicardipine • Cardene
- Nifedipine • Adalat, Procardia
- Nortriptyline • Aventyl, Pamelor
- Olanzapine • Zyprexa
- Omeprazole • Prilosec
- Ondansetron • Zofran
- Palonosetron • Aloxi
- Perphenazine • Trilafon
- Pimozide • Orap
- Primidone • Mysoline
- Progesterone • Prometrium
- Propofol • Diprivan
- Propranolol • Inderal
- Ramelteon • Rozerem
- Ranitidine • Zantac
- Rasagiline • Azilect
- Rifampin • Rifadin, Rimactane
- Riluzole • Rilutek
- Rivastigmine • Exelon
- Ropinirole • Requip
- Selegiline • Eldepryl, EMSAM, others
- Theophylline • Elixophyllin
- Thioridazine • Mellaril
- Thiothixene • Navane
- Tizanidine • Zanaflex
- Trazodone • Desyrel, Oleptro
- Triamterene • Dyrenium
- Trifluoperazine • Stelazine
- Verapamil • Calan, Verelan
- Warfarin • Coumadin, Jantoven
- Zileuton • Zyflo
- Ziprasidone • Geodon
- Zolmitriptan • Zomig
- Zolpidem • Ambien, Edluar
Disclosure
Ms. Fankhauser reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
- Tobacco smokers often are treated with medications that are metabolized by hepatic cytochrome (CYP) 1A2 enzymes. Starting or stopping tobacco smoking may cause drug interactions because polycyclic aromatic hydrocarbons in cigarette smoke induce CYP1A2 enzymes.
- Drugs that are significantly metabolized by CYP1A2 (major substrates) are more likely to be impacted by changes in tobacco smoking compared with minor substrates.
- Induction of hepatic CYP1A2 enzymes may be greater in heavy or moderate smokers compared with light smokers (eg, <10 cigarettes per day).
- Evidence-based approaches for treating tobacco use in health care settings should address the risk of CYP1A2 drug interactions in tobacco smokers and how this impacts their clinical care.
Mrs. C, age 51, experiences exacerbated asthma and difficulty breathing and is admitted to a non-smoking hospital. She also has chronic obstructive pulmonary disease, type 2 diabetes mellitus, hypertension, hypercholesterolemia, hypothyroidism, gastroesophageal reflux disease, overactive bladder, muscle spasms, fibromyalgia, bipolar disorder, insomnia, and nicotine and caffeine dependence. She takes 19 prescribed and over-the-counter medications, drinks up to 8 cups of coffee per day, and smokes 20 to 30 cigarettes per day. In the emergency room, she receives albuterol/ipratropium inhalation therapy to help her breathing and a 21-mg nicotine replacement patch to avoid nicotine withdrawal.
In the United States, 19% of adults smoke cigarettes.1 Heavy tobacco smoking and nicotine dependence are common among psychiatric patients and contribute to higher rates of tobacco-related morbidity and mortality.2 When smokers stop smoking or are admitted to smoke-free facilities and are forced to abstain, nicotine withdrawal symptoms and changes in drug metabolism can develop over several days.3-5
Smokers such as Mrs. C are at risk for cytochrome (CYP) P450 drug interactions when they are admitted to or discharged from a smoke-free facility. Nine of Mrs. C’s medications are substrates of CYP1A2 (acetaminophen, caffeine, cyclobenzaprine, diazepam, duloxetine, melatonin, olanzapine, ondansetron, and zolpidem). When Mrs. C stops smoking while in the hospital, she could experience higher serum concentrations and adverse effects of these medications. If Mrs. C resumes smoking after bring discharged, metabolism and clearance of any medications started while she was hospitalized that are substrates of CYP1A2 enzymes could be increased, which could lead to reduced efficacy and poor clinical outcomes.
Pharmacokinetic effects
Polycyclic aromatic hydrocarbons in tobacco smoke induce hepatic CYP1A1, 1A2, and possibly 2E1 isoenzymes.6-12 CYP1A2 is a hepatic enzyme responsible for metabolizing and eliminating several classes of substrates (eg, drugs, hormones, endogenous compounds, and procarcinogens).6,13 Genetic, epigenetic, and environmental factors such as smoking impact the expression and activity of CYP1A2 and result in large interpatient variability in pharmacokinetic drug interactions.6,12,13 CYP1A2 enzymes can be induced or inhibited by drugs and substances, which can result in decreased or increased serum concentrations of substrates, respectively. When individuals stop smoking and switch to other nicotine products or devices, CYP1A2 induction of hepatic enzymes will revert to normal metabolism over several weeks to a month.10 Besides tobacco smoke, other CYP1A2 inducers include charbroiled food, carbamazepine, omeprazole, phenobarbital, primidone, and rifampin.4,5 Nicotine replacement products—such as gum, inhalers, lozenges, patches, and nasal spray—and nicotine delivery devices such as electronic cigarettes do not induce hepatic CYP1A2 enzymes or cause the same drug interactions as cigarette smoking.
Table 13-11 and Table 23-11 list commonly prescribed CYP1A2 substrates that could be affected by tobacco smoke. There are no specific guidelines for how to assess, monitor, or manage pharmacokinetic drug interactions with tobacco smoke.6-13 Induction of hepatic CYP1A2 enzymes by cigarette smoke may require increased dosages of some psychotropics—such as tricyclic antidepressants, duloxetine, mirtazapine, and some first- and second-generation antipsychotics (SGAs)—to achieve serum concentrations adequate for clinical efficacy. Serum concentrations may increase to toxic levels and result in adverse effects when a person quits smoking cigarettes or if a CYP1A2 inhibitor, such as amlodipine, cimetidine, ciprofloxacin, diclofenac, fluoxetine, fluvoxamine, or nifedipine, is added.5
Table 1
Common major cytochrome P450 (CYP) 1A2 substrates
| Drug | Class |
|---|---|
| Alosetron3,5,6 | Irritable bowel syndrome: serotonin 3 antagonist |
| Aminophylline3,5 | Bronchodilator: theophylline derivative |
| Betaxolol3,5 | β-1 selective adrenergic receptor blocking agent |
| Caffeine3-9 | Stimulant |
| Clomipramine3-11 | Tricyclic antidepressant |
| Clozapine3-10 | Second-generation antipsychotic |
| Cyclobenzaprine3-7 | Skeletal muscle relaxant |
| Doxepin3,7,10,11 | Tricyclic antidepressant |
| Duloxetine3-6 | Serotonin-norepinephrine reuptake inhibitor |
| Estradiol3,5-8 | Estrogen (active) |
| Estrogens: conjugated and estropipate3,5; estrone3,7 | Estrogen (derivatives) |
| Fluvoxamine3,8,9 | Selective serotonin reuptake inhibitor |
| Guanabenz3,5-7 | α-2 adrenergic agonist |
| Mirtazapine3-7 | Antidepressant: α-2 antagonist/serotonin 2A, 2C antagonist |
| Olanzapine3-11 | Second-generation antipsychotic |
| Pimozide3,5,7 | First-generation antipsychotic |
| Propranolol3-11 | β-adrenergic blocker |
| Ramelteon3,5,10 | Melatonin receptor agonist |
| Rasagiline3,5 | Antiparkinson: type B monoamine oxidase inhibitor |
| Riluzole3-7,10 | Glutamate inhibitor |
| Ropinirole3,5-7 | Antiparkinson: dopamine agonist |
| Theophylline3-6,8-11 | Bronchodilator: methylxanthine |
| Thiothixene3,5 | First-generation antipsychotic |
| Trifluoperazine3,5,9 | First-generation antipsychotic |
| Several classes of CYP1A2 substrates are not included and may cause toxicity with smoking cessation or require dosage increases in tobacco smokers (eg, antiarrhythmic, antifungal, antimalarial, antineoplastic, antiretroviral, and anthelmintic agents and the antibiotic quinolone). Clinicians should be most concerned about drugs with a narrow therapeutic index and those that may be toxic with smoking cessation (eg, bleeding from warfarin and clopidogrel; high serum concentrations of caffeine, clozapine, olanzapine, propranolol, and theophylline) | |
Table 2
Common minor cytochrome P450 (CYP) 1A2 substrates
| Drug | Class |
|---|---|
| Acetaminophen3-9 | Analgesic |
| Almotriptan6 | Antimigraine: serotonin 1B, 1D receptor agonist |
| Amitriptyline3-7,9-11 | Tricyclic antidepressant |
| Asenapine9 | Second-generation antipsychotic |
| Carvedilol5-7 | β and α adrenergic blocking activity |
| Chlorpromazine3,4,7-9,11 | First-generation antipsychotic |
| Chlorzoxazone4,7 | Skeletal muscle relaxant |
| Clopidogrel5 | Antiplatelet |
| Desipramine4,7,10,11 | Tricyclic antidepressant |
| Diazepam4,7,9,10 | Benzodiazepine |
| Diclofenac5,7 | Nonsteroidal anti-inflammatory drug |
| Diphenhydramine6 | Antihistamine |
| Febuxostat5 | Xanthine oxidase inhibitor |
| Fluphenazine3,9 | First-generation antipsychotic |
| Frovatriptan3 | Antimigraine: serotonin 1 agonist |
| Haloperidol3,4,6,8,9 | First-generation antipsychotic |
| Imipramine3,4,6-11 | Tricyclic antidepressant |
| Maprotiline6 | Tetracyclic antidepressant |
| Melatonin3,4,6,7 | Sleep-regulating hormone |
| Metoclopramide3 | Antiemetic: prokinetic gastrointestinal agent |
| Nabumetone6 | Nonsteroidal anti-inflammatory drug |
| Naproxen3,4,6,7 | Nonsteroidal anti-inflammatory drug |
| Naratriptan10 | Antimigraine: serotonin 1B, 1D receptor agonist |
| Nicardipine3,7 | Calcium channel blocker |
| Nortriptyline4,6,7,9-11 | Tricyclic antidepressant |
| Ondansetron3,4,6,7 | Antiemetic: serotonin 3 antagonist |
| Palonosetron5 | Antiemetic: serotonin 3 antagonist |
| Perphenazine3,7 | First-generation antipsychotic |
| Progesterone5,7 | Progestin |
| Propofol4,6,7 | General anesthetic |
| Ranitidine5,7 | H2 antagonist |
| Rivastigmine10 | Acetylcholinesterase inhibitor |
| Selegiline6,7 | Antiparkinson: type B monoamine oxidase inhibitor |
| Thioridazine3,4,6 | First-generation antipsychotic |
| Tizanidine3-6 | Skeletal muscle relaxant: α-2 adrenergic agonist |
| Trazodone6,9 | Serotonin reuptake inhibitor and antagonist |
| Triamterene6 | Diuretic: potassium sparing |
| Verapamil3,4,6,7,10 | Calcium channel blocker |
| Warfarin3,4,6-10 | Anticoagulant: coumarin derivative |
| Zileuton3,4,6,7 | Asthma agent: 5-lipoxygenase inhibitor |
| Ziprasidone3,4 | Second-generation antipsychotic |
| Zolmitriptan3,6,7 | Antimigraine: serotonin 1B, 1D receptor agonist |
| Zolpidem4,6,7 | Nonbenzodiazepine hypnotic |
| Several classes of CYP1A2 substrates are not included and may cause toxicity with smoking cessation or require dosage increases in tobacco smokers (eg, antiarrhythmic, antifungal, antimalarial, antineoplastic, antiretroviral and anthelmintic agents and the antibiotic quinolone). Clinicians should be most concerned about drugs with a narrow therapeutic index and those that may be toxic with smoking cessation (eg, bleeding from warfarin and clopidogrel; high serum concentrations of caffeine, clozapine, olanzapine, propranolol, and theophylline) | |
SGA such as clozapine and olanzapine are major substrates of CYP1A2 and dosages may need to be adjusted when smoking status changes, depending on clinical efficacy and adverse effects.10,14,15 Maximum induction of clozapine and olanzapine metabolism may occur with 7 to 12 cigarettes per day and smokers may have 40% to 50% lower serum concentrations compared with nonsmokers.14 When a patient stops smoking, clozapine and olanzapine dosages may need to be reduced by 30% to 40% (eg, a stepwise 10% reduction in daily dose until day 4) to avoid elevated serum concentrations and risk of toxicity symptoms.15
Tobacco smokers can tolerate high daily intake of caffeinated beverages because of increased metabolism and clearance of caffeine, a major substrate of CYP1A2.11 When patients stop smoking, increased caffeine serum concentrations may cause anxiety, irritability, restlessness, insomnia, tremors, palpitations, and tachycardia. Caffeine toxicity also can mimic symptoms of nicotine withdrawal; therefore, smokers should be advised to reduce their caffeine intake by half to avoid adverse effects when they stop smoking.10,11
Adjusting dosing
Factors such as the amount and frequency of tobacco smoking, how quickly CYP1A2 enzymes change when starting and stopping smoking, exposure to secondhand smoke, and other concomitant drugs contribute to variability in pharmacokinetic drug interactions. Heavy smokers (≥30 cigarettes per day) should be closely monitored because variations in drug serum concentrations may be affected significantly by changes in smoking status.4,9,11 Dosage reductions of potentially toxic drugs should be done immediately when a heavy tobacco user stops smoking.10 For CYP1A2 substrates with a narrow therapeutic range, a conservative approach is to reduce the daily dose by 10% per day for several days after smoking cessation.11,16 The impact on drug metabolism may continue for weeks to a month after the person stops smoking; therefore, there may be a delay until CYP1A2 enzymes return to normal hepatic metabolism.4,8,9,15 In most situations, smoking cessation reverses induction of hepatic CYP1A2 enzymes back to normal metabolism and causes serum drug concentrations to increase.10 Because secondhand smoke induces hepatic CYP1A2 enzymes, those exposed to smoke may have changes in drug metabolism due to environmental smoke exposure.11
Tobacco smokers who take medications and hormones that are metabolized by CYP1A2 enzymes should be closely monitored because dosage adjustments may be necessary when they start or stop smoking cigarettes. An assessment of CYP drug interactions and routine monitoring of efficacy and/or toxicity should be done to avoid potential adverse effects from medications and to determine if changes in dosages and disease state management are required.
Related Resources
- Rx for Change. Drug interactions with smoking. http://smokingcessationleadership.ucsf.edu/interactions.pdf.
- Fiore MC, Baker TB. Treating smokers in the health care setting. N Engl J Med. 2011;365(13):1222-1231.
Drug Brand Names
- Albuterol/ipratropium • Combivent
- Almotriptan • Axert
- Alosetron • Lotronex
- Aminophylline • Phyllocontin, Truphylline
- Amitriptyline • Elavil
- Amlodipine • Norvasc
- Asenapine • Saphris
- Betaxolol • Kerlone
- Carbamazepine • Carbatrol, Tegretol
- Carvedilol • Coreg
- Chlorpromazine • Thorazine
- Chlorzoxazone • Parafon Forte
- Cimetidine • Tagamet
- Ciprofloxacin • Cipro
- Clomipramine • Anafranil
- Clopidogrel • Plavix
- Clozapine • Clozaril
- Cyclobenzaprine • Flexeril
- Desipramine • Norpramin
- Diazepam • Valium
- Diclofenac • Voltaren
- Diphenhydramine • Benadryl
- Doxepin • Silenor, Sinequan
- Duloxetine • Cymbalta
- Estradiol • Estrace
- Estrogens (conjugated) • Cenestin, Premarin
- Estropipate • Ogen
- Febuxostat • Uloric
- Fluoxetine • Prozac
- Fluphenazine • Prolixin
- Fluvoxamine • Luvox
- Frovatriptan • Frova
- Guanabenz • Wytensin
- Haloperidol • Haldol
- Imipramine • Tofranil
- Maprotiline • Ludiomil
- Metoclopramide • Reglan
- Mirtazapine • Remeron
- Nabumetone • Relafen
- Naratriptan • Amerge
- Nicardipine • Cardene
- Nifedipine • Adalat, Procardia
- Nortriptyline • Aventyl, Pamelor
- Olanzapine • Zyprexa
- Omeprazole • Prilosec
- Ondansetron • Zofran
- Palonosetron • Aloxi
- Perphenazine • Trilafon
- Pimozide • Orap
- Primidone • Mysoline
- Progesterone • Prometrium
- Propofol • Diprivan
- Propranolol • Inderal
- Ramelteon • Rozerem
- Ranitidine • Zantac
- Rasagiline • Azilect
- Rifampin • Rifadin, Rimactane
- Riluzole • Rilutek
- Rivastigmine • Exelon
- Ropinirole • Requip
- Selegiline • Eldepryl, EMSAM, others
- Theophylline • Elixophyllin
- Thioridazine • Mellaril
- Thiothixene • Navane
- Tizanidine • Zanaflex
- Trazodone • Desyrel, Oleptro
- Triamterene • Dyrenium
- Trifluoperazine • Stelazine
- Verapamil • Calan, Verelan
- Warfarin • Coumadin, Jantoven
- Zileuton • Zyflo
- Ziprasidone • Geodon
- Zolmitriptan • Zomig
- Zolpidem • Ambien, Edluar
Disclosure
Ms. Fankhauser reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Centers for Disease Control and Prevention (CDC). Vital signs: current cigarette smoking among adults aged ≥18 years—United States 2005-2010. MMWR Morb Mortal Wkly Rep. 2011;60(35):1207-1212.
2. Ziedonis D, Hitsman B, Beckham JC, et al. Tobacco use and cessation in psychiatric disorders: National Institute of Mental Health report. Nicotine Tob Res. 2008;10(12):1691-1715.
3. Choe JY. Drug actions and interactions. New York NY: McGraw-Hill Medical; 2011.
4. Tatro DS. Drug interaction facts. St. Louis MO: Wolters Kluwer Health; 2011.
5. Lacy CF, Armstrong LL, Goldman MP, et al. eds. Drug information handbook, 20th ed. Hudson, OH: Lexicomp; 2011.
6. Zhou SF, Yang LP, Zhou ZW, et al. Insights into the substrate specificity, inhibitors, regulation, and polymorphisms and the clinical impact of human cytochrome P450 1A2. AAPS J. 2009;11(3):481-494.
7. Rendic S. Summary of information on human CYP enzymes: human P450 metabolism data. Drug Metab Rev. 2002;34(1-2):83-448.
8. Zevin S, Benowitz NL. Drug interactions with tobacco smoking. An update. Clin Pharmacokinet. 1999;36(6):425-438.
9. Desai HD, Seabolt J, Jann MW. Smoking in patients receiving psychotropic medications: a pharmacokinetic perspective. CNS Drugs. 2001;15(6):469-494.
10. Schaffer SD, Yoon S, Zadezensky I. A review of smoking cessation: potentially risky effects on prescribed medications. J Clin Nurs. 2009;18(11):1533-1540.
11. Kroon LA. Drug interactions with smoking. Am J Health Syst Pharm. 2007;64(18):1917-1921.
12. Plowchalk DR, Yeo KR. Prediction of drug clearance in a smoking population: modeling the impact of variable cigarette consumption on the induction of CYP1A2. Eur J Pharmacol. 2012;68(6):951-960.
13. Faber MS, Jetter A, Fuhr U. Assessment of CYP1A2 activity in clinical practice: why how, and when? Basic Clin Pharmacol Toxicol. 2005;97(3):125-134.
14. Haslemo T, Eikeseth PH, Tanum L, et al. The effect of variable cigarette consumption on the interaction with clozapine and olanzapine. Eur J Clin Pharmacol. 2006;62(12):1049-1053.
15. Lowe EJ, Ackman ML. Impact of tobacco smoking cessation on stable clozapine or olanzapine treatment. Ann Pharmacother. 2010;44(4):727-732.
16. Faber MS, Fuhr U. Time response of cytochrome P4501A2 activity on cessation of heavy smoking. Clin Pharmacol Ther. 2004;76(2):178-184.
1. Centers for Disease Control and Prevention (CDC). Vital signs: current cigarette smoking among adults aged ≥18 years—United States 2005-2010. MMWR Morb Mortal Wkly Rep. 2011;60(35):1207-1212.
2. Ziedonis D, Hitsman B, Beckham JC, et al. Tobacco use and cessation in psychiatric disorders: National Institute of Mental Health report. Nicotine Tob Res. 2008;10(12):1691-1715.
3. Choe JY. Drug actions and interactions. New York NY: McGraw-Hill Medical; 2011.
4. Tatro DS. Drug interaction facts. St. Louis MO: Wolters Kluwer Health; 2011.
5. Lacy CF, Armstrong LL, Goldman MP, et al. eds. Drug information handbook, 20th ed. Hudson, OH: Lexicomp; 2011.
6. Zhou SF, Yang LP, Zhou ZW, et al. Insights into the substrate specificity, inhibitors, regulation, and polymorphisms and the clinical impact of human cytochrome P450 1A2. AAPS J. 2009;11(3):481-494.
7. Rendic S. Summary of information on human CYP enzymes: human P450 metabolism data. Drug Metab Rev. 2002;34(1-2):83-448.
8. Zevin S, Benowitz NL. Drug interactions with tobacco smoking. An update. Clin Pharmacokinet. 1999;36(6):425-438.
9. Desai HD, Seabolt J, Jann MW. Smoking in patients receiving psychotropic medications: a pharmacokinetic perspective. CNS Drugs. 2001;15(6):469-494.
10. Schaffer SD, Yoon S, Zadezensky I. A review of smoking cessation: potentially risky effects on prescribed medications. J Clin Nurs. 2009;18(11):1533-1540.
11. Kroon LA. Drug interactions with smoking. Am J Health Syst Pharm. 2007;64(18):1917-1921.
12. Plowchalk DR, Yeo KR. Prediction of drug clearance in a smoking population: modeling the impact of variable cigarette consumption on the induction of CYP1A2. Eur J Pharmacol. 2012;68(6):951-960.
13. Faber MS, Jetter A, Fuhr U. Assessment of CYP1A2 activity in clinical practice: why how, and when? Basic Clin Pharmacol Toxicol. 2005;97(3):125-134.
14. Haslemo T, Eikeseth PH, Tanum L, et al. The effect of variable cigarette consumption on the interaction with clozapine and olanzapine. Eur J Clin Pharmacol. 2006;62(12):1049-1053.
15. Lowe EJ, Ackman ML. Impact of tobacco smoking cessation on stable clozapine or olanzapine treatment. Ann Pharmacother. 2010;44(4):727-732.
16. Faber MS, Fuhr U. Time response of cytochrome P4501A2 activity on cessation of heavy smoking. Clin Pharmacol Ther. 2004;76(2):178-184.
Paranoia and slowed cognition
CASE: Behavioral changes
Mr. K, age 45, is brought to the emergency department (ED) by his wife for severe paranoia, combative behavior, confusion, and slowed cognition. Mr. K tells the ED staff that a chemical abrasion he sustained a few weeks earlier has spread to his penis, and insists that his penis is retracting into his body. He has tied a string around his penis to keep it from disappearing into his body. According to Mr. K’s wife, he went to an urgent care clinic 2 weeks ago after he sustained chemical abrasions from exposure to cleaning solution at home. The provider at the urgent care clinic started Mr. K on an unknown dose of oral prednisone.
Mr. K’s wife reports that her husband had a dysphoric episode approximately 6 months ago when his business was struggling but his mood improved without psychiatric care. Mr. K’s medical history includes episodic sarcoidosis of the eyes, skin, and lungs. In the past these symptoms remitted after he received oral prednisone.
ED clinicians consider neurosarcoidosis and substance-induced delirium in the differential diagnosis (Table).1 A CT scan of the head fails to show lesions suggestive of neurosarcoidosis. Chest radiography does not reveal lesions suggestive of lung sarcoids and Mr. K has no skin lesions.
Table
DSM-IV-TR criteria for substance-induced delirium
|
| Source: Reference 1 |
Mr. K is admitted to the psychiatric inpatient unit for acute stabilization, where he remains aggressive and combative. He throws chairs at his peers and staff on the unit and is placed in physical restraints. He requires several doses of IM haloperidol, 5 mg, lorazepam, 2 mg, and diphenhydramine, 50 mg, for severe agitation. Mr. K is guarded, perseverative, and selectively mute. He avoids eye contact and has poor grooming. He has slow thought processing and displays concrete thought process. Prednisone is discontinued and olanzapine, titrated to 30 mg/d, and mirtazapine, titrated to 30 mg/d, are started for psychosis and depression.
Mr. K’s mood and behavior eventually return to baseline but slowed cognition persists. He is discharged from our facility.
The authors’ observations
Cortisone was first used to treat rheumatoid arthritis in 1948 and corticosteroids have been linked to multiple neuropsychiatric complications that have been broadly defined as steroid psychosis. This syndrome includes reversible behavioral manifestations such as hypomania, irritability, mood reactivity, anxiety, and insomnia in addition to more severe symptoms such as depression, mania, and psychosis.2 Although mild cognitive deficits have been noted in patients taking corticosteroids, most published cases have focused on steroid-induced psychosis.
In 1984, Varney et al3 noted a phenomenon they called “steroid dementia” in 6 patients treated with corticosteroids. On first evaluation, these patients presented with symptoms similar to early Alzheimer’s dementia—impaired memory, attention, and concentration. Three patients initially were diagnosed first with Alzheimer’s dementia until their symptoms spontaneously improved when steroids were reduced or discontinued. Although their presentation resembled Alzheimer’s dementia, patients with steroid dementia had a specific cognitive presentation associated with corticosteroid use. Symptoms included impaired verbal memory and spatial thinking but normal procedural memory. These patients showed intact immediate recall but impaired delayed recall with difficulty tracking conversations and word finding. Overall, patients with steroid dementia showed a predominance of verbal declarative memory deficits out of proportion to other cognitive symptoms. These symptoms and recent corticosteroid exposure differentiated steroid dementia from other forms of dementia.
In a later article, Varney reviewed electroencephalography (EEG) and CT findings associated with steroid dementia, noting bilateral EEG abnormalities and acute cortical atrophy on CT.4 Steroid dementia largely was reversible, resolving 3 to 11 months after corticosteroid discontinuation. Additionally, Varney noted that patients who had psychosis and dementia had more severe and longer-lasting dementia.
TREATMENT: Progressive decline
Mr. K is college educated, has been married for 15 years, has 2 children, age 9 and 11, and owns a successful basketball coaching business. He has no history of substance abuse, legal issues, or violence. He reports a good childhood with normal developmental milestones and no history of trauma.
In the 6 months after his initial psychiatric admission, Mr. K sees various outpatient providers, who change his psychotropics multiple times. He also receives 4 courses of prednisone for ocular sarcoidosis. He is admitted twice to other psychiatric facilities. After he has paranoid interactions with colleagues and families of the youth he coaches, his business fails.
After his third psychiatric inpatient hospitalization, Mr. K becomes severely paranoid, believing his wife is having an affair. He becomes physically abusive to his wife, who obtains a restraining order and leaves with their children. Mr. K barely leaves his house and stops grooming. A friend notes that Mr. K’s home has become uninhabitable, and it goes into foreclosure. After Mr. K’s neighbors report combative behavior and paranoia, police bring him in on an involuntary hold for a fourth psychiatric hospitalization (the second in our facility).
During this hospitalization—6 months after the initial ED presentation—the neurology team conducts a repeat medical workup. EEG shows generalized slowing. Head CT and MRI show diffuse cortical atrophy that was not seen in previous imaging. Mr. K has ocular lesions characteristic of ocular sarcoidosis. His mental status examination is similar to his first presentation except that the psychosis and thought disorganization are considerably worse. His cognitive functioning also shows significant decline. Cognitive screening reveals intact remote memory with impaired recent memory. His thinking is concrete and his verbal memory is markedly impaired. His Mini-Mental State Examination score is 27/30, indicating functional capacity that is better than his clinical presentation. Because of difficulty with concentration and verbal processing, Mr. K is unable to complete the Minnesota Multiphasic Personality Inventory despite substantial assistance. On most days he cannot recall recent conversations with his wife, staff, or physicians. He is taking no medications at this time.
Mr. K is restarted on olanzapine, titrated to 30 mg/d, to control his psychosis; this medication was effective during his last stay in our facility. Oral prednisone is discontinued and methotrexate, 10 mg/week, is initiated for ocular sarcoidosis. Based on recommendations from a case series report,5 we start Mr. K on lithium, titrated to 600 mg twice a day, for steroid-induced mood symptoms, Mr. K’s psychosis and mood improve dramatically once he reaches a therapeutic lithium level; however, his cognition remains slowed and he is unable to care for his basic needs.
The authors’ observations
Steroid dementia may be the result of effects in the medial temporal lobe, specifically dorsolateral prefrontal cortex, which impairs working memory, and the parahippocampal gyrus.6,7 The cognitive presentation of steroid dementia Varney et al3 described has been replicated in healthy volunteers who received corticosteroids.3 Patients with Cushing’s syndrome also have been noted to have diminished hippocampal volume and similar cognitive deficits. Cognitive impairment experienced by patients treated with corticosteroids may be caused by neuronal death in the hippocampus and dorsolateral prefrontal cortex. The etiology of cell death is multifactorial and includes glutamate-mediated excitotoxicity, activation of proinflammatory pathways, inhibited utilization of glucose in the hippocampus, telomere shortening, and diminished cell repair by brain-derived neurotrophic factor. The net result is significant, widespread damage that in some cases is irreversible.8
Because of the severity of Mr. K’s psychosis and personality change from baseline, his cognitive symptoms were largely overlooked during his first psychiatric hospitalization. The affective flattening, delayed verbal response, and markedly concrete thought process were considered within the spectrum of resolving psychosis. After further hospitalizations and abnormal results on cognitive testing, Mr. K’s cognitive impairment was fully noted. His symptoms match those of previously documented cases of steroid dementia, including verbal deficits out of proportion to other impairment, acute cerebral atrophy on CT after corticosteroid treatment, and gradual improvement of symptoms when corticosteroids were discontinued.
Management recommendations
Educate patients taking steroids about possible side effects of mood changes, psychosis, and cognitive deficits. Close monitoring of patients on corticosteroids is paramount. If psychiatric or cognitive symptoms develop, gradually discontinue the corticosteroid and seek other treatments.
Randomized, placebo-controlled trials of lamotrigine and memantine have shown these medications are cognitively protective for patients taking prednisone.9
OUTCOME: Long-term deficits
After a 33-day stay in our adult inpatient psychiatric facility, the county places Mr. K in a permanent conservatorship for severe grave disability. He is discharged to a long-term psychiatric care locked facility for ongoing management. Mr. K spends 20 months in the long-term care facility while his family remains hopeful for his recovery and return home. He is admitted to our facility for acute stabilization of psychotic symptoms after he is released from the locked facility. Although no imaging studies are conducted, he remains significantly forgetful. Additionally, his paranoia persists.
Mr. K is poorly compliant with his psychotropics, which include divalproex, 1,000 mg/d, and olanzapine, 30 mg/d. Although he is discharged home with his family, his functional capacity is less than expected and he requires continuous support. Insisting that Mr. K abstain from steroids after the first psychiatric hospitalization might have prevented this seemingly irreversible dementia.
Related Resources
- Sacks O, Shulman M. Steroid dementia: an overlooked diagnosis? Neurology. 2005;64(4):707-709.
- Cipriani G, Picchi L, Vedovello M, et al. Reversible dementia from corticosteroid therapy. Clinical Geriatrics. 2012;20(7):38-41.
Drug Brand Names
- Diphenhydramine • Benadryl
- Divalproex • Depakote
- Haloperidol • Haldol
- Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid
- Lorazepam • Ativan
- Memantine • Namenda
- Methotrexate • Rheumatrex, Trexall
- Mirtazapine • Remeron
- Olanzapine • Zyprexa
- Prednisone • Deltasone, Meticorten, others
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Diagnostic and statistical manual of mental disorders 4th ed, text rev. Arlington VA: American Psychiatric Association; 2000.
2. Warrington TP, Bostwick JM. Psychiatric adverse effects of corticosteroids. Mayo Clin Proc. 2006;81(10):1361-1367.
3. Varney NR, Alexander B, MacIndoe JH. Reversible steroid dementia in patients without steroid psychosis. Am J Psychiatry. 1984;141(3):369-372.
4. Varney NR. A case of reversible steroid dementia. Arch Clin Neuropsychol. 1997;12(2):167-171.
5. Sirois F. Steroid psychosis: a review. Gen Hosp Psychiatry. 2003;25(1):27-33.
6. Wolkowitz OM, Burke H, Epel ES, et al. Glucocorticoids: mood, memory, and mechanisms. Ann N Y Acad Sci. 2009;1179:19-40.
7. Lupien SJ, McEwen BS. The acute effects of corticosteroids on cognition: integration of animal and human model studies. Brain Res Brain Res Rev. 1997;24(1):1-27.
8. Sapolsky RM. The physiological relevance of glucocorticoid endangerment of the hippocampus. Ann NY Acad Sci. 1994;746:294-304.
9. Brown ES. Effects of glucocorticoids on mood memory and the hippocampus. Treatment and preventative therapy. Ann N Y Acad Sci. 2009;1179:41-55.
CASE: Behavioral changes
Mr. K, age 45, is brought to the emergency department (ED) by his wife for severe paranoia, combative behavior, confusion, and slowed cognition. Mr. K tells the ED staff that a chemical abrasion he sustained a few weeks earlier has spread to his penis, and insists that his penis is retracting into his body. He has tied a string around his penis to keep it from disappearing into his body. According to Mr. K’s wife, he went to an urgent care clinic 2 weeks ago after he sustained chemical abrasions from exposure to cleaning solution at home. The provider at the urgent care clinic started Mr. K on an unknown dose of oral prednisone.
Mr. K’s wife reports that her husband had a dysphoric episode approximately 6 months ago when his business was struggling but his mood improved without psychiatric care. Mr. K’s medical history includes episodic sarcoidosis of the eyes, skin, and lungs. In the past these symptoms remitted after he received oral prednisone.
ED clinicians consider neurosarcoidosis and substance-induced delirium in the differential diagnosis (Table).1 A CT scan of the head fails to show lesions suggestive of neurosarcoidosis. Chest radiography does not reveal lesions suggestive of lung sarcoids and Mr. K has no skin lesions.
Table
DSM-IV-TR criteria for substance-induced delirium
|
| Source: Reference 1 |
Mr. K is admitted to the psychiatric inpatient unit for acute stabilization, where he remains aggressive and combative. He throws chairs at his peers and staff on the unit and is placed in physical restraints. He requires several doses of IM haloperidol, 5 mg, lorazepam, 2 mg, and diphenhydramine, 50 mg, for severe agitation. Mr. K is guarded, perseverative, and selectively mute. He avoids eye contact and has poor grooming. He has slow thought processing and displays concrete thought process. Prednisone is discontinued and olanzapine, titrated to 30 mg/d, and mirtazapine, titrated to 30 mg/d, are started for psychosis and depression.
Mr. K’s mood and behavior eventually return to baseline but slowed cognition persists. He is discharged from our facility.
The authors’ observations
Cortisone was first used to treat rheumatoid arthritis in 1948 and corticosteroids have been linked to multiple neuropsychiatric complications that have been broadly defined as steroid psychosis. This syndrome includes reversible behavioral manifestations such as hypomania, irritability, mood reactivity, anxiety, and insomnia in addition to more severe symptoms such as depression, mania, and psychosis.2 Although mild cognitive deficits have been noted in patients taking corticosteroids, most published cases have focused on steroid-induced psychosis.
In 1984, Varney et al3 noted a phenomenon they called “steroid dementia” in 6 patients treated with corticosteroids. On first evaluation, these patients presented with symptoms similar to early Alzheimer’s dementia—impaired memory, attention, and concentration. Three patients initially were diagnosed first with Alzheimer’s dementia until their symptoms spontaneously improved when steroids were reduced or discontinued. Although their presentation resembled Alzheimer’s dementia, patients with steroid dementia had a specific cognitive presentation associated with corticosteroid use. Symptoms included impaired verbal memory and spatial thinking but normal procedural memory. These patients showed intact immediate recall but impaired delayed recall with difficulty tracking conversations and word finding. Overall, patients with steroid dementia showed a predominance of verbal declarative memory deficits out of proportion to other cognitive symptoms. These symptoms and recent corticosteroid exposure differentiated steroid dementia from other forms of dementia.
In a later article, Varney reviewed electroencephalography (EEG) and CT findings associated with steroid dementia, noting bilateral EEG abnormalities and acute cortical atrophy on CT.4 Steroid dementia largely was reversible, resolving 3 to 11 months after corticosteroid discontinuation. Additionally, Varney noted that patients who had psychosis and dementia had more severe and longer-lasting dementia.
TREATMENT: Progressive decline
Mr. K is college educated, has been married for 15 years, has 2 children, age 9 and 11, and owns a successful basketball coaching business. He has no history of substance abuse, legal issues, or violence. He reports a good childhood with normal developmental milestones and no history of trauma.
In the 6 months after his initial psychiatric admission, Mr. K sees various outpatient providers, who change his psychotropics multiple times. He also receives 4 courses of prednisone for ocular sarcoidosis. He is admitted twice to other psychiatric facilities. After he has paranoid interactions with colleagues and families of the youth he coaches, his business fails.
After his third psychiatric inpatient hospitalization, Mr. K becomes severely paranoid, believing his wife is having an affair. He becomes physically abusive to his wife, who obtains a restraining order and leaves with their children. Mr. K barely leaves his house and stops grooming. A friend notes that Mr. K’s home has become uninhabitable, and it goes into foreclosure. After Mr. K’s neighbors report combative behavior and paranoia, police bring him in on an involuntary hold for a fourth psychiatric hospitalization (the second in our facility).
During this hospitalization—6 months after the initial ED presentation—the neurology team conducts a repeat medical workup. EEG shows generalized slowing. Head CT and MRI show diffuse cortical atrophy that was not seen in previous imaging. Mr. K has ocular lesions characteristic of ocular sarcoidosis. His mental status examination is similar to his first presentation except that the psychosis and thought disorganization are considerably worse. His cognitive functioning also shows significant decline. Cognitive screening reveals intact remote memory with impaired recent memory. His thinking is concrete and his verbal memory is markedly impaired. His Mini-Mental State Examination score is 27/30, indicating functional capacity that is better than his clinical presentation. Because of difficulty with concentration and verbal processing, Mr. K is unable to complete the Minnesota Multiphasic Personality Inventory despite substantial assistance. On most days he cannot recall recent conversations with his wife, staff, or physicians. He is taking no medications at this time.
Mr. K is restarted on olanzapine, titrated to 30 mg/d, to control his psychosis; this medication was effective during his last stay in our facility. Oral prednisone is discontinued and methotrexate, 10 mg/week, is initiated for ocular sarcoidosis. Based on recommendations from a case series report,5 we start Mr. K on lithium, titrated to 600 mg twice a day, for steroid-induced mood symptoms, Mr. K’s psychosis and mood improve dramatically once he reaches a therapeutic lithium level; however, his cognition remains slowed and he is unable to care for his basic needs.
The authors’ observations
Steroid dementia may be the result of effects in the medial temporal lobe, specifically dorsolateral prefrontal cortex, which impairs working memory, and the parahippocampal gyrus.6,7 The cognitive presentation of steroid dementia Varney et al3 described has been replicated in healthy volunteers who received corticosteroids.3 Patients with Cushing’s syndrome also have been noted to have diminished hippocampal volume and similar cognitive deficits. Cognitive impairment experienced by patients treated with corticosteroids may be caused by neuronal death in the hippocampus and dorsolateral prefrontal cortex. The etiology of cell death is multifactorial and includes glutamate-mediated excitotoxicity, activation of proinflammatory pathways, inhibited utilization of glucose in the hippocampus, telomere shortening, and diminished cell repair by brain-derived neurotrophic factor. The net result is significant, widespread damage that in some cases is irreversible.8
Because of the severity of Mr. K’s psychosis and personality change from baseline, his cognitive symptoms were largely overlooked during his first psychiatric hospitalization. The affective flattening, delayed verbal response, and markedly concrete thought process were considered within the spectrum of resolving psychosis. After further hospitalizations and abnormal results on cognitive testing, Mr. K’s cognitive impairment was fully noted. His symptoms match those of previously documented cases of steroid dementia, including verbal deficits out of proportion to other impairment, acute cerebral atrophy on CT after corticosteroid treatment, and gradual improvement of symptoms when corticosteroids were discontinued.
Management recommendations
Educate patients taking steroids about possible side effects of mood changes, psychosis, and cognitive deficits. Close monitoring of patients on corticosteroids is paramount. If psychiatric or cognitive symptoms develop, gradually discontinue the corticosteroid and seek other treatments.
Randomized, placebo-controlled trials of lamotrigine and memantine have shown these medications are cognitively protective for patients taking prednisone.9
OUTCOME: Long-term deficits
After a 33-day stay in our adult inpatient psychiatric facility, the county places Mr. K in a permanent conservatorship for severe grave disability. He is discharged to a long-term psychiatric care locked facility for ongoing management. Mr. K spends 20 months in the long-term care facility while his family remains hopeful for his recovery and return home. He is admitted to our facility for acute stabilization of psychotic symptoms after he is released from the locked facility. Although no imaging studies are conducted, he remains significantly forgetful. Additionally, his paranoia persists.
Mr. K is poorly compliant with his psychotropics, which include divalproex, 1,000 mg/d, and olanzapine, 30 mg/d. Although he is discharged home with his family, his functional capacity is less than expected and he requires continuous support. Insisting that Mr. K abstain from steroids after the first psychiatric hospitalization might have prevented this seemingly irreversible dementia.
Related Resources
- Sacks O, Shulman M. Steroid dementia: an overlooked diagnosis? Neurology. 2005;64(4):707-709.
- Cipriani G, Picchi L, Vedovello M, et al. Reversible dementia from corticosteroid therapy. Clinical Geriatrics. 2012;20(7):38-41.
Drug Brand Names
- Diphenhydramine • Benadryl
- Divalproex • Depakote
- Haloperidol • Haldol
- Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid
- Lorazepam • Ativan
- Memantine • Namenda
- Methotrexate • Rheumatrex, Trexall
- Mirtazapine • Remeron
- Olanzapine • Zyprexa
- Prednisone • Deltasone, Meticorten, others
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE: Behavioral changes
Mr. K, age 45, is brought to the emergency department (ED) by his wife for severe paranoia, combative behavior, confusion, and slowed cognition. Mr. K tells the ED staff that a chemical abrasion he sustained a few weeks earlier has spread to his penis, and insists that his penis is retracting into his body. He has tied a string around his penis to keep it from disappearing into his body. According to Mr. K’s wife, he went to an urgent care clinic 2 weeks ago after he sustained chemical abrasions from exposure to cleaning solution at home. The provider at the urgent care clinic started Mr. K on an unknown dose of oral prednisone.
Mr. K’s wife reports that her husband had a dysphoric episode approximately 6 months ago when his business was struggling but his mood improved without psychiatric care. Mr. K’s medical history includes episodic sarcoidosis of the eyes, skin, and lungs. In the past these symptoms remitted after he received oral prednisone.
ED clinicians consider neurosarcoidosis and substance-induced delirium in the differential diagnosis (Table).1 A CT scan of the head fails to show lesions suggestive of neurosarcoidosis. Chest radiography does not reveal lesions suggestive of lung sarcoids and Mr. K has no skin lesions.
Table
DSM-IV-TR criteria for substance-induced delirium
|
| Source: Reference 1 |
Mr. K is admitted to the psychiatric inpatient unit for acute stabilization, where he remains aggressive and combative. He throws chairs at his peers and staff on the unit and is placed in physical restraints. He requires several doses of IM haloperidol, 5 mg, lorazepam, 2 mg, and diphenhydramine, 50 mg, for severe agitation. Mr. K is guarded, perseverative, and selectively mute. He avoids eye contact and has poor grooming. He has slow thought processing and displays concrete thought process. Prednisone is discontinued and olanzapine, titrated to 30 mg/d, and mirtazapine, titrated to 30 mg/d, are started for psychosis and depression.
Mr. K’s mood and behavior eventually return to baseline but slowed cognition persists. He is discharged from our facility.
The authors’ observations
Cortisone was first used to treat rheumatoid arthritis in 1948 and corticosteroids have been linked to multiple neuropsychiatric complications that have been broadly defined as steroid psychosis. This syndrome includes reversible behavioral manifestations such as hypomania, irritability, mood reactivity, anxiety, and insomnia in addition to more severe symptoms such as depression, mania, and psychosis.2 Although mild cognitive deficits have been noted in patients taking corticosteroids, most published cases have focused on steroid-induced psychosis.
In 1984, Varney et al3 noted a phenomenon they called “steroid dementia” in 6 patients treated with corticosteroids. On first evaluation, these patients presented with symptoms similar to early Alzheimer’s dementia—impaired memory, attention, and concentration. Three patients initially were diagnosed first with Alzheimer’s dementia until their symptoms spontaneously improved when steroids were reduced or discontinued. Although their presentation resembled Alzheimer’s dementia, patients with steroid dementia had a specific cognitive presentation associated with corticosteroid use. Symptoms included impaired verbal memory and spatial thinking but normal procedural memory. These patients showed intact immediate recall but impaired delayed recall with difficulty tracking conversations and word finding. Overall, patients with steroid dementia showed a predominance of verbal declarative memory deficits out of proportion to other cognitive symptoms. These symptoms and recent corticosteroid exposure differentiated steroid dementia from other forms of dementia.
In a later article, Varney reviewed electroencephalography (EEG) and CT findings associated with steroid dementia, noting bilateral EEG abnormalities and acute cortical atrophy on CT.4 Steroid dementia largely was reversible, resolving 3 to 11 months after corticosteroid discontinuation. Additionally, Varney noted that patients who had psychosis and dementia had more severe and longer-lasting dementia.
TREATMENT: Progressive decline
Mr. K is college educated, has been married for 15 years, has 2 children, age 9 and 11, and owns a successful basketball coaching business. He has no history of substance abuse, legal issues, or violence. He reports a good childhood with normal developmental milestones and no history of trauma.
In the 6 months after his initial psychiatric admission, Mr. K sees various outpatient providers, who change his psychotropics multiple times. He also receives 4 courses of prednisone for ocular sarcoidosis. He is admitted twice to other psychiatric facilities. After he has paranoid interactions with colleagues and families of the youth he coaches, his business fails.
After his third psychiatric inpatient hospitalization, Mr. K becomes severely paranoid, believing his wife is having an affair. He becomes physically abusive to his wife, who obtains a restraining order and leaves with their children. Mr. K barely leaves his house and stops grooming. A friend notes that Mr. K’s home has become uninhabitable, and it goes into foreclosure. After Mr. K’s neighbors report combative behavior and paranoia, police bring him in on an involuntary hold for a fourth psychiatric hospitalization (the second in our facility).
During this hospitalization—6 months after the initial ED presentation—the neurology team conducts a repeat medical workup. EEG shows generalized slowing. Head CT and MRI show diffuse cortical atrophy that was not seen in previous imaging. Mr. K has ocular lesions characteristic of ocular sarcoidosis. His mental status examination is similar to his first presentation except that the psychosis and thought disorganization are considerably worse. His cognitive functioning also shows significant decline. Cognitive screening reveals intact remote memory with impaired recent memory. His thinking is concrete and his verbal memory is markedly impaired. His Mini-Mental State Examination score is 27/30, indicating functional capacity that is better than his clinical presentation. Because of difficulty with concentration and verbal processing, Mr. K is unable to complete the Minnesota Multiphasic Personality Inventory despite substantial assistance. On most days he cannot recall recent conversations with his wife, staff, or physicians. He is taking no medications at this time.
Mr. K is restarted on olanzapine, titrated to 30 mg/d, to control his psychosis; this medication was effective during his last stay in our facility. Oral prednisone is discontinued and methotrexate, 10 mg/week, is initiated for ocular sarcoidosis. Based on recommendations from a case series report,5 we start Mr. K on lithium, titrated to 600 mg twice a day, for steroid-induced mood symptoms, Mr. K’s psychosis and mood improve dramatically once he reaches a therapeutic lithium level; however, his cognition remains slowed and he is unable to care for his basic needs.
The authors’ observations
Steroid dementia may be the result of effects in the medial temporal lobe, specifically dorsolateral prefrontal cortex, which impairs working memory, and the parahippocampal gyrus.6,7 The cognitive presentation of steroid dementia Varney et al3 described has been replicated in healthy volunteers who received corticosteroids.3 Patients with Cushing’s syndrome also have been noted to have diminished hippocampal volume and similar cognitive deficits. Cognitive impairment experienced by patients treated with corticosteroids may be caused by neuronal death in the hippocampus and dorsolateral prefrontal cortex. The etiology of cell death is multifactorial and includes glutamate-mediated excitotoxicity, activation of proinflammatory pathways, inhibited utilization of glucose in the hippocampus, telomere shortening, and diminished cell repair by brain-derived neurotrophic factor. The net result is significant, widespread damage that in some cases is irreversible.8
Because of the severity of Mr. K’s psychosis and personality change from baseline, his cognitive symptoms were largely overlooked during his first psychiatric hospitalization. The affective flattening, delayed verbal response, and markedly concrete thought process were considered within the spectrum of resolving psychosis. After further hospitalizations and abnormal results on cognitive testing, Mr. K’s cognitive impairment was fully noted. His symptoms match those of previously documented cases of steroid dementia, including verbal deficits out of proportion to other impairment, acute cerebral atrophy on CT after corticosteroid treatment, and gradual improvement of symptoms when corticosteroids were discontinued.
Management recommendations
Educate patients taking steroids about possible side effects of mood changes, psychosis, and cognitive deficits. Close monitoring of patients on corticosteroids is paramount. If psychiatric or cognitive symptoms develop, gradually discontinue the corticosteroid and seek other treatments.
Randomized, placebo-controlled trials of lamotrigine and memantine have shown these medications are cognitively protective for patients taking prednisone.9
OUTCOME: Long-term deficits
After a 33-day stay in our adult inpatient psychiatric facility, the county places Mr. K in a permanent conservatorship for severe grave disability. He is discharged to a long-term psychiatric care locked facility for ongoing management. Mr. K spends 20 months in the long-term care facility while his family remains hopeful for his recovery and return home. He is admitted to our facility for acute stabilization of psychotic symptoms after he is released from the locked facility. Although no imaging studies are conducted, he remains significantly forgetful. Additionally, his paranoia persists.
Mr. K is poorly compliant with his psychotropics, which include divalproex, 1,000 mg/d, and olanzapine, 30 mg/d. Although he is discharged home with his family, his functional capacity is less than expected and he requires continuous support. Insisting that Mr. K abstain from steroids after the first psychiatric hospitalization might have prevented this seemingly irreversible dementia.
Related Resources
- Sacks O, Shulman M. Steroid dementia: an overlooked diagnosis? Neurology. 2005;64(4):707-709.
- Cipriani G, Picchi L, Vedovello M, et al. Reversible dementia from corticosteroid therapy. Clinical Geriatrics. 2012;20(7):38-41.
Drug Brand Names
- Diphenhydramine • Benadryl
- Divalproex • Depakote
- Haloperidol • Haldol
- Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid
- Lorazepam • Ativan
- Memantine • Namenda
- Methotrexate • Rheumatrex, Trexall
- Mirtazapine • Remeron
- Olanzapine • Zyprexa
- Prednisone • Deltasone, Meticorten, others
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Diagnostic and statistical manual of mental disorders 4th ed, text rev. Arlington VA: American Psychiatric Association; 2000.
2. Warrington TP, Bostwick JM. Psychiatric adverse effects of corticosteroids. Mayo Clin Proc. 2006;81(10):1361-1367.
3. Varney NR, Alexander B, MacIndoe JH. Reversible steroid dementia in patients without steroid psychosis. Am J Psychiatry. 1984;141(3):369-372.
4. Varney NR. A case of reversible steroid dementia. Arch Clin Neuropsychol. 1997;12(2):167-171.
5. Sirois F. Steroid psychosis: a review. Gen Hosp Psychiatry. 2003;25(1):27-33.
6. Wolkowitz OM, Burke H, Epel ES, et al. Glucocorticoids: mood, memory, and mechanisms. Ann N Y Acad Sci. 2009;1179:19-40.
7. Lupien SJ, McEwen BS. The acute effects of corticosteroids on cognition: integration of animal and human model studies. Brain Res Brain Res Rev. 1997;24(1):1-27.
8. Sapolsky RM. The physiological relevance of glucocorticoid endangerment of the hippocampus. Ann NY Acad Sci. 1994;746:294-304.
9. Brown ES. Effects of glucocorticoids on mood memory and the hippocampus. Treatment and preventative therapy. Ann N Y Acad Sci. 2009;1179:41-55.
1. Diagnostic and statistical manual of mental disorders 4th ed, text rev. Arlington VA: American Psychiatric Association; 2000.
2. Warrington TP, Bostwick JM. Psychiatric adverse effects of corticosteroids. Mayo Clin Proc. 2006;81(10):1361-1367.
3. Varney NR, Alexander B, MacIndoe JH. Reversible steroid dementia in patients without steroid psychosis. Am J Psychiatry. 1984;141(3):369-372.
4. Varney NR. A case of reversible steroid dementia. Arch Clin Neuropsychol. 1997;12(2):167-171.
5. Sirois F. Steroid psychosis: a review. Gen Hosp Psychiatry. 2003;25(1):27-33.
6. Wolkowitz OM, Burke H, Epel ES, et al. Glucocorticoids: mood, memory, and mechanisms. Ann N Y Acad Sci. 2009;1179:19-40.
7. Lupien SJ, McEwen BS. The acute effects of corticosteroids on cognition: integration of animal and human model studies. Brain Res Brain Res Rev. 1997;24(1):1-27.
8. Sapolsky RM. The physiological relevance of glucocorticoid endangerment of the hippocampus. Ann NY Acad Sci. 1994;746:294-304.
9. Brown ES. Effects of glucocorticoids on mood memory and the hippocampus. Treatment and preventative therapy. Ann N Y Acad Sci. 2009;1179:41-55.
Something smells different
CASE: Depressed and hopeless
Ms. D, age 69, has a 20-year history of bipolar II disorder, for which she is taking citalopram, 30 mg/d. She presents to her outpatient psychotherapist with a chief complaint of depressed mood. The therapist refers her for psychiatric hospitalization and electroconvulsive therapy consultation. Upon admission, Ms. D reports that her depressed mood has worsened over the past 5 weeks after a trip to the Dominican Republic. Ms. D had a negative encounter with airport security that she attributed to her 2 artificial knees and caused her to miss her flight. She endorses poor appetite, loss of energy, anhedonia, difficulty concentrating, poor memory, and feelings of hopelessness.
Ms. D reports increasingly frequent panic attacks as well as intermittent right-sided discomfort, unusual noxious smells, and increased falls. She says the falls likely are a result of new bilateral lower extremity weakness coupled with long-standing imbalance. Ms. D says she has experienced brief occasions of foul-smelling odors while showering without evidence of an offending substance. She also reports a mild, occipitally located headache.
Four years ago, Ms. D was hospitalized for a depressive episode without psychotic features and diagnosed with generalized anxiety disorder, for which she is taking clonazepam, 1.5 mg/d. Her last hypomanic episode was several years ago, and was characterized by increased energy with decreased need for sleep, flight of ideas, increased productivity, and impulsivity. Her medical history includes non-insulin dependent diabetes mellitus, chronic low back pain, hyperlipidemia, arthritis, and gastroesophageal reflux disease; her medications include pioglitazone, 30 mg/d, oxybutynin, 15 mg/d, rosuvastatin, 20 mg/d, losartan, 50 mg/d, and omeprazole, 20 mg/d. She also had bilateral knee replacements 9 years ago and an L4-S1 spinal fusion 11 years ago. She has no history of head injuries or seizures. Ms. D’s father had major depressive disorder, her mother died of a cerebrovascular accident at an unknown age, and her brother died of a myocardial infarction at age 52.
The authors’ observations
A striking aspect of Ms. D’s presenting complaints was her intermittent experience of foul smells. Although olfactory hallucinations can occur with psychotic and affective states, they also may be harbingers of an organic etiology involving the temporal lobe.1 Olfactory hallucinations associated with a psychiatric disorder often have an accompanying delusional belief regarding the cause of the smell.2
Olfactory hallucinations have been associated with migraines, epilepsy, and Parkinson’s disease.1-3 Neoplasms, cerebrovascular events, or traumatic brain injuries that result in focal mesial temporal lobe lesions can present as a partial complex seizure with olfactory or gustatory hallucinations and progress to automatisms.4 Characteristic odors in these hallucinations are unpleasant; patients with temporal lobe epilepsy describe the smells as “bad,” “rotten,” “sickening,” and “like burning food.”2 Ms. D’s report of unusual smells warranted consideration of an organic etiology for her mood change and a thorough neurologic examination.
EVALUATION: Neurologic signs
At the time of admission, Ms. D has a blood pressure of 127/68 mm Hg, heart rate of 74 beats per minute, respiratory rate of 16 breaths per minute, and temperature of 36.5°C. Neurologic examination reveals a left facial droop of unknown duration. Motor strength is weak throughout with left-sided focal weakness. Ms. D’s daughter notes that her mother’s smile appears “funny” in her admission photograph but is unsure when the asymmetry in her facial appearance began. Ms. D had been ambulatory before admission. Nursing staff observes Ms. D leans toward her left side and exhibits possible left-sided neglect during the first 12 hours of hospitalization.
When asked about her facial droop, Ms. D replies that she had not noticed any change in her appearance lately. She does not appear to be concerned about her worsening ambulation. On hospital day 2, Ms. D seems to have difficulty using utensils to eat breakfast. Ms. D is dismissive of her worsening motor function and asks to be left alone to finish her meal.
The authors’ observations
Ms. D’s focal neurologic deficits and complaint of a headache on admission were concerning because they could be caused by a cerebrovascular event or space-occupying brain lesion with potential for increased intracranial pressure. Neurologic examination with evaluation for papilledema is indicated, followed by medical transport to the closest medical center for emergent brain imaging. Neither Ms. D nor her daughter could pinpoint the onset of Ms. D’s left-sided facial droop, which precluded administering tissue plasminogen activator for a potential acute ischemic stroke.5
Ms. D’s case prompted us to consider what constitutes timely brain imaging in a patient who presents with psychiatric symptoms. Several neurologic conditions may present first with neurobehavioral symptoms before findings on physical exam. Two series of autopsies conducted >70 years ago at psychiatric hospitals found incidences of brain tumors of 3.45%6 and 13.5%.7 In a 5-year retrospective study, 21% of meningioma cases presented with psychiatric symptoms alone.8 These historical cases suggest that affective, behavioral, and psychotic symptoms may be the only clinical indicators of brain lesions that merit surgery.9-11
Imaging and radiation exposure
With the advent of CT scans in the 1970s, psychiatrists gained a new method of investigating potential structural CNS pathology in patients presenting with psychiatric symptoms. The dramatic increase in CT scan use in recent years and resulting radiation exposure is responsible for 1.5% to 2% of all cancers in the United States.12,13 Certainly, physicians must balance the advantage of early detection of brain lesions with cost-effectiveness and exposure to radiation.14
There is no consensus regarding use of brain imaging in a patient who presents with new-onset psychiatric symptoms. Certainly, patients with localizing neurologic deficits or symptoms of increased intracranial pressure should undergo brain imaging. As for psychiatric patients without neurologic findings, Filley and Kleinschmidt-DeMasters15 provide recommendations based on their 1995 case series, and other authors have recommended imaging for patients age ≥4016 vs ≥5017,18 who present with atypical mental status changes.
OUTCOME: Scan, then surgery
Ms. D’s head CT reveals a large right-sided temporoparietal low-density lesion with 8-mm left lower midline shift (Figure). She undergoes a right temporal craniotomy with resection of the mass, which is confirmed by surgical pathology to be a glioblastoma multiforme World Health Organization grade 4 tumor. Postoperative MRI shows evidence of infarction in the right posterior cerebral artery distribution and residual tumor is identified on follow-up imaging. Ms. D is referred to radiation oncology, where she receives a prognostic median life expectancy of 14 months with radiation and temozolomide treatment.19

Figure: Ms. D’s MRI results
MRI with contrast shows a large right temporal heterogeneous mass consistent with glioblastoma multiforme
The authors’ observations
Glioblastoma is a rare cancer that comprises 25% of all malignant nervous system tumors.20 It is associated with a poor prognosis, with a <30% relative survival rate for adults at 1 year and 3% at 5 years.20 Headaches, seizures, motor weakness, and progressive neurologic deficits are common symptoms of glioblastoma at diagnosis.20 Ms. D was offered the standard of care treatment for a high-grade glioma, including surgical resection followed by concomitant external-beam radiotherapy and chemotherapy.21
Consider structural brain lesions in patients who present with neurobehavioral symptoms, although most of these patients will be diagnosed with a primary psychiatric disorder. Ms. D had a known psychiatric disorder that predated the onset of neurologic symptoms and diagnosis of a rare brain cancer. Before she developed neurologic signs, Ms. D experienced symptoms uncharacteristic of her previous depressive episodes, including olfactory hallucinations, that provided an early indicator of a CNS lesion. Consider brain imaging in patients of any age who do not respond to medications targeting the presumed psychiatric diagnosis to ensure that insidious brain tumors are not missed (Table 1).15
Table 1
When to order neuroimaging for psychiatric patients
| Patient’s age | Most common types of brain tumor | MRI vs CT | Indications to image |
|---|---|---|---|
| ≥40 years | Metastases High-grade gliomas Meningiomas | Roughly equivalent for imaging common tumor types. Base on cost, availability, and relative patient contraindications | New-onset cognitive or emotional dysfunction. Patient is not responding to appropriate pharmacotherapy for psychiatric diagnosis |
| <40 years | Low-grade astrocytomas Oligodendrogliomas | MRI preferred | New-onset cognitive or emotional dysfunction with associated somatic symptoms (headache, nausea, vomiting, papilledema, seizures, or focal deficits). Patient is not responding to appropriate pharmacotherapy for the psychiatric diagnosis |
| Source: Reference 15 | |||
Compared with cerebrovascular lesions, neoplasms are more difficult to clinically correlate with their anatomic location. Neurobehavioral symptoms are more frequently associated with tumors originating in the frontal lobe or temporolimbic regions of the brain. The 3 types of frontal lobe syndromes are dorsolateral, orbitofrontal, and medial-frontal (Table 2).15 Temporolimbic tumors may present with hallucinations, mania, panic attacks, or amnesia. A meta-analysis found a statistically significant association between anorexia and hypothalamic tumors.22 Reports of neuropsychiatric symptoms that respond to pharmacologic treatment further confound the clinical picture.16
Table 2
Frontal lobe syndromes
| Syndrome | Characteristics |
|---|---|
| Dorsolateral | Deficits in executive functioning, including organization and behavior planning |
| Orbitofrontal | Prominent disinhibition |
| Medial-frontal | Apathy, abulia |
| Source: Reference 15 | |
It is uncommon for a patient with a long-standing mood disorder to develop a primary brain cancer. However, Ms. D’s case serves as an important reminder to consider medical comorbidities in our aging psychiatric population. In particular, a patient who develops unusual symptoms or does not respond to previously effective treatments should be more closely examined and the differential diagnosis broadened.
Related Resources
- MD Anderson Cancer Center. Brain tumor videos and podcasts. www.mdanderson.org/patient-and-cancer-information/cancer-information/cancer-types/brain-tumor/videos-and-podcasts/index.html.
- Braun CM, Dumont M, Duval J, et al. Brain modules of hallucination: an analysis of multiple patients with brain lesions. J Psychiatry Neurosci. 2003;28(6):432-449.
Drug Brand Names
- Citalopram • Celexa
- Clonazepam • Klonopin
- Losartan • Cozaar
- Omeprazole • Prilosec
- Oxybutynin • Ditropan
- Pioglitazone • Actos
- Rosuvastatin • Crestor
- Temozolomide • Temodar
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Assad G, Shapiro B. Hallucinations: theoretical and clinical overview. Am J Psychiatry. 1986;143(9):1088-1097.
2. Carter JL. Visual somatosensory, olfactory, and gustatory hallucinations. Psychiatr Clin North Am. 1992;15(2):347-358.
3. Fuller GN, Guiloff RJ. Migrainous olfactory hallucinations. J Neurol Neurosurg Psychiatry. 1987;50(12):1688-1690.
4. Chang BS, Lowenstein DH. Mechanisms of disease: epilepsy. N Engl J Med. 2003;349(13):1257-1266.
5. Lansberg MG, Bluhmki E, Thijs VN. Efficacy and safety of tissue plasminogen activator 3 to 4.5 hours after acute ischemic stroke: a metaanalysis. Stroke. 2009;40(7):2438-2441.
6. Hoffman JL. Intracranial neoplasms: their incidence and mental manifestations. Psychiatr Q. 1937;11(4):561-575.
7. Larson CP. Intracranial tumors in mental hospital patients. Am J Psychiatry. 1940;97(1):49-58.
8. Gupta RK, Kumar R. Benign brain tumours and psychiatric morbidity: a 5-years retrospective data analysis. Aust N Z J Psychiatry. 2004;38(5):316-319.
9. Chambers WR. Neurosurgical conditions masquerading as psychiatric diseases. Am J Psychiatry. 1955;112(5):387-389.
10. Trimble MR, Mendez MF, Cummings JL. Neuropsychiatric symptoms from the temporolimbic lobes. J Neuropsychiatry Clin Neurosci. 1997;9(3):429-438.
11. Uribe VM. Psychiatric symptoms and brain tumor. Am Fam Physician. 1986;34(2):95-98.
12. Brenner DJ, Hall EJ. Computed tomography—an increasing source of radiation exposure. N Engl J Med. 2007;357(2):2277-2284.
13. Berrington de González A, Mahesh M, Kim KP, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009;169(22):2071-2077.
14. Weinberger DR. Brain disease and psychiatric illness: when should a psychiatrist order a CAT scan? Am J Psychiatry. 1984;141(12):1521-1526.
15. Filley CM, Kleinschmidt-DeMasters BK. Neurobehavioral presentations of brain neoplasms. West J Med. 1995;163(1):19-25.
16. Moise D, Madhusoodanan S. Psychiatric symptoms associated with brain tumors: a clinical engima. CNS Spectr. 2006;11(1):28-31.
17. Bunevicius A, Deltuva VP, Deltuviene D, et al. Brain lesions manifesting as psychiatric disorders: eight cases. CNS Spectr. 2008;13(11):950-958.
18. Hollister LE, Boutros N. Clinical use of CT and MR scans in psychiatric patients. J Psychiatr Neurosci. 1991;16(4):194-198.
19. Stupp R, Mason WP, van den Bent MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352(10):987-996.
20. Brandes AA, Tosoni A, Franceschi E, et al. Glioblastoma in adults. Crit Rev Oncol Hematol. 2008;67(2):139-152.
21. Chandana SR, Movva S, Arora M, et al. Primary brain tumors in adults. Am Fam Physician. 2008;77(10):1423-1430.
22. Madhusoodanan S, Opler MG, Moise D, et al. Brain tumor location and psychiatric symptoms: is there any association? A meta-analysis of published case studies. Expert Rev Neurother. 2010;10(10):1529-1536.
CASE: Depressed and hopeless
Ms. D, age 69, has a 20-year history of bipolar II disorder, for which she is taking citalopram, 30 mg/d. She presents to her outpatient psychotherapist with a chief complaint of depressed mood. The therapist refers her for psychiatric hospitalization and electroconvulsive therapy consultation. Upon admission, Ms. D reports that her depressed mood has worsened over the past 5 weeks after a trip to the Dominican Republic. Ms. D had a negative encounter with airport security that she attributed to her 2 artificial knees and caused her to miss her flight. She endorses poor appetite, loss of energy, anhedonia, difficulty concentrating, poor memory, and feelings of hopelessness.
Ms. D reports increasingly frequent panic attacks as well as intermittent right-sided discomfort, unusual noxious smells, and increased falls. She says the falls likely are a result of new bilateral lower extremity weakness coupled with long-standing imbalance. Ms. D says she has experienced brief occasions of foul-smelling odors while showering without evidence of an offending substance. She also reports a mild, occipitally located headache.
Four years ago, Ms. D was hospitalized for a depressive episode without psychotic features and diagnosed with generalized anxiety disorder, for which she is taking clonazepam, 1.5 mg/d. Her last hypomanic episode was several years ago, and was characterized by increased energy with decreased need for sleep, flight of ideas, increased productivity, and impulsivity. Her medical history includes non-insulin dependent diabetes mellitus, chronic low back pain, hyperlipidemia, arthritis, and gastroesophageal reflux disease; her medications include pioglitazone, 30 mg/d, oxybutynin, 15 mg/d, rosuvastatin, 20 mg/d, losartan, 50 mg/d, and omeprazole, 20 mg/d. She also had bilateral knee replacements 9 years ago and an L4-S1 spinal fusion 11 years ago. She has no history of head injuries or seizures. Ms. D’s father had major depressive disorder, her mother died of a cerebrovascular accident at an unknown age, and her brother died of a myocardial infarction at age 52.
The authors’ observations
A striking aspect of Ms. D’s presenting complaints was her intermittent experience of foul smells. Although olfactory hallucinations can occur with psychotic and affective states, they also may be harbingers of an organic etiology involving the temporal lobe.1 Olfactory hallucinations associated with a psychiatric disorder often have an accompanying delusional belief regarding the cause of the smell.2
Olfactory hallucinations have been associated with migraines, epilepsy, and Parkinson’s disease.1-3 Neoplasms, cerebrovascular events, or traumatic brain injuries that result in focal mesial temporal lobe lesions can present as a partial complex seizure with olfactory or gustatory hallucinations and progress to automatisms.4 Characteristic odors in these hallucinations are unpleasant; patients with temporal lobe epilepsy describe the smells as “bad,” “rotten,” “sickening,” and “like burning food.”2 Ms. D’s report of unusual smells warranted consideration of an organic etiology for her mood change and a thorough neurologic examination.
EVALUATION: Neurologic signs
At the time of admission, Ms. D has a blood pressure of 127/68 mm Hg, heart rate of 74 beats per minute, respiratory rate of 16 breaths per minute, and temperature of 36.5°C. Neurologic examination reveals a left facial droop of unknown duration. Motor strength is weak throughout with left-sided focal weakness. Ms. D’s daughter notes that her mother’s smile appears “funny” in her admission photograph but is unsure when the asymmetry in her facial appearance began. Ms. D had been ambulatory before admission. Nursing staff observes Ms. D leans toward her left side and exhibits possible left-sided neglect during the first 12 hours of hospitalization.
When asked about her facial droop, Ms. D replies that she had not noticed any change in her appearance lately. She does not appear to be concerned about her worsening ambulation. On hospital day 2, Ms. D seems to have difficulty using utensils to eat breakfast. Ms. D is dismissive of her worsening motor function and asks to be left alone to finish her meal.
The authors’ observations
Ms. D’s focal neurologic deficits and complaint of a headache on admission were concerning because they could be caused by a cerebrovascular event or space-occupying brain lesion with potential for increased intracranial pressure. Neurologic examination with evaluation for papilledema is indicated, followed by medical transport to the closest medical center for emergent brain imaging. Neither Ms. D nor her daughter could pinpoint the onset of Ms. D’s left-sided facial droop, which precluded administering tissue plasminogen activator for a potential acute ischemic stroke.5
Ms. D’s case prompted us to consider what constitutes timely brain imaging in a patient who presents with psychiatric symptoms. Several neurologic conditions may present first with neurobehavioral symptoms before findings on physical exam. Two series of autopsies conducted >70 years ago at psychiatric hospitals found incidences of brain tumors of 3.45%6 and 13.5%.7 In a 5-year retrospective study, 21% of meningioma cases presented with psychiatric symptoms alone.8 These historical cases suggest that affective, behavioral, and psychotic symptoms may be the only clinical indicators of brain lesions that merit surgery.9-11
Imaging and radiation exposure
With the advent of CT scans in the 1970s, psychiatrists gained a new method of investigating potential structural CNS pathology in patients presenting with psychiatric symptoms. The dramatic increase in CT scan use in recent years and resulting radiation exposure is responsible for 1.5% to 2% of all cancers in the United States.12,13 Certainly, physicians must balance the advantage of early detection of brain lesions with cost-effectiveness and exposure to radiation.14
There is no consensus regarding use of brain imaging in a patient who presents with new-onset psychiatric symptoms. Certainly, patients with localizing neurologic deficits or symptoms of increased intracranial pressure should undergo brain imaging. As for psychiatric patients without neurologic findings, Filley and Kleinschmidt-DeMasters15 provide recommendations based on their 1995 case series, and other authors have recommended imaging for patients age ≥4016 vs ≥5017,18 who present with atypical mental status changes.
OUTCOME: Scan, then surgery
Ms. D’s head CT reveals a large right-sided temporoparietal low-density lesion with 8-mm left lower midline shift (Figure). She undergoes a right temporal craniotomy with resection of the mass, which is confirmed by surgical pathology to be a glioblastoma multiforme World Health Organization grade 4 tumor. Postoperative MRI shows evidence of infarction in the right posterior cerebral artery distribution and residual tumor is identified on follow-up imaging. Ms. D is referred to radiation oncology, where she receives a prognostic median life expectancy of 14 months with radiation and temozolomide treatment.19

Figure: Ms. D’s MRI results
MRI with contrast shows a large right temporal heterogeneous mass consistent with glioblastoma multiforme
The authors’ observations
Glioblastoma is a rare cancer that comprises 25% of all malignant nervous system tumors.20 It is associated with a poor prognosis, with a <30% relative survival rate for adults at 1 year and 3% at 5 years.20 Headaches, seizures, motor weakness, and progressive neurologic deficits are common symptoms of glioblastoma at diagnosis.20 Ms. D was offered the standard of care treatment for a high-grade glioma, including surgical resection followed by concomitant external-beam radiotherapy and chemotherapy.21
Consider structural brain lesions in patients who present with neurobehavioral symptoms, although most of these patients will be diagnosed with a primary psychiatric disorder. Ms. D had a known psychiatric disorder that predated the onset of neurologic symptoms and diagnosis of a rare brain cancer. Before she developed neurologic signs, Ms. D experienced symptoms uncharacteristic of her previous depressive episodes, including olfactory hallucinations, that provided an early indicator of a CNS lesion. Consider brain imaging in patients of any age who do not respond to medications targeting the presumed psychiatric diagnosis to ensure that insidious brain tumors are not missed (Table 1).15
Table 1
When to order neuroimaging for psychiatric patients
| Patient’s age | Most common types of brain tumor | MRI vs CT | Indications to image |
|---|---|---|---|
| ≥40 years | Metastases High-grade gliomas Meningiomas | Roughly equivalent for imaging common tumor types. Base on cost, availability, and relative patient contraindications | New-onset cognitive or emotional dysfunction. Patient is not responding to appropriate pharmacotherapy for psychiatric diagnosis |
| <40 years | Low-grade astrocytomas Oligodendrogliomas | MRI preferred | New-onset cognitive or emotional dysfunction with associated somatic symptoms (headache, nausea, vomiting, papilledema, seizures, or focal deficits). Patient is not responding to appropriate pharmacotherapy for the psychiatric diagnosis |
| Source: Reference 15 | |||
Compared with cerebrovascular lesions, neoplasms are more difficult to clinically correlate with their anatomic location. Neurobehavioral symptoms are more frequently associated with tumors originating in the frontal lobe or temporolimbic regions of the brain. The 3 types of frontal lobe syndromes are dorsolateral, orbitofrontal, and medial-frontal (Table 2).15 Temporolimbic tumors may present with hallucinations, mania, panic attacks, or amnesia. A meta-analysis found a statistically significant association between anorexia and hypothalamic tumors.22 Reports of neuropsychiatric symptoms that respond to pharmacologic treatment further confound the clinical picture.16
Table 2
Frontal lobe syndromes
| Syndrome | Characteristics |
|---|---|
| Dorsolateral | Deficits in executive functioning, including organization and behavior planning |
| Orbitofrontal | Prominent disinhibition |
| Medial-frontal | Apathy, abulia |
| Source: Reference 15 | |
It is uncommon for a patient with a long-standing mood disorder to develop a primary brain cancer. However, Ms. D’s case serves as an important reminder to consider medical comorbidities in our aging psychiatric population. In particular, a patient who develops unusual symptoms or does not respond to previously effective treatments should be more closely examined and the differential diagnosis broadened.
Related Resources
- MD Anderson Cancer Center. Brain tumor videos and podcasts. www.mdanderson.org/patient-and-cancer-information/cancer-information/cancer-types/brain-tumor/videos-and-podcasts/index.html.
- Braun CM, Dumont M, Duval J, et al. Brain modules of hallucination: an analysis of multiple patients with brain lesions. J Psychiatry Neurosci. 2003;28(6):432-449.
Drug Brand Names
- Citalopram • Celexa
- Clonazepam • Klonopin
- Losartan • Cozaar
- Omeprazole • Prilosec
- Oxybutynin • Ditropan
- Pioglitazone • Actos
- Rosuvastatin • Crestor
- Temozolomide • Temodar
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE: Depressed and hopeless
Ms. D, age 69, has a 20-year history of bipolar II disorder, for which she is taking citalopram, 30 mg/d. She presents to her outpatient psychotherapist with a chief complaint of depressed mood. The therapist refers her for psychiatric hospitalization and electroconvulsive therapy consultation. Upon admission, Ms. D reports that her depressed mood has worsened over the past 5 weeks after a trip to the Dominican Republic. Ms. D had a negative encounter with airport security that she attributed to her 2 artificial knees and caused her to miss her flight. She endorses poor appetite, loss of energy, anhedonia, difficulty concentrating, poor memory, and feelings of hopelessness.
Ms. D reports increasingly frequent panic attacks as well as intermittent right-sided discomfort, unusual noxious smells, and increased falls. She says the falls likely are a result of new bilateral lower extremity weakness coupled with long-standing imbalance. Ms. D says she has experienced brief occasions of foul-smelling odors while showering without evidence of an offending substance. She also reports a mild, occipitally located headache.
Four years ago, Ms. D was hospitalized for a depressive episode without psychotic features and diagnosed with generalized anxiety disorder, for which she is taking clonazepam, 1.5 mg/d. Her last hypomanic episode was several years ago, and was characterized by increased energy with decreased need for sleep, flight of ideas, increased productivity, and impulsivity. Her medical history includes non-insulin dependent diabetes mellitus, chronic low back pain, hyperlipidemia, arthritis, and gastroesophageal reflux disease; her medications include pioglitazone, 30 mg/d, oxybutynin, 15 mg/d, rosuvastatin, 20 mg/d, losartan, 50 mg/d, and omeprazole, 20 mg/d. She also had bilateral knee replacements 9 years ago and an L4-S1 spinal fusion 11 years ago. She has no history of head injuries or seizures. Ms. D’s father had major depressive disorder, her mother died of a cerebrovascular accident at an unknown age, and her brother died of a myocardial infarction at age 52.
The authors’ observations
A striking aspect of Ms. D’s presenting complaints was her intermittent experience of foul smells. Although olfactory hallucinations can occur with psychotic and affective states, they also may be harbingers of an organic etiology involving the temporal lobe.1 Olfactory hallucinations associated with a psychiatric disorder often have an accompanying delusional belief regarding the cause of the smell.2
Olfactory hallucinations have been associated with migraines, epilepsy, and Parkinson’s disease.1-3 Neoplasms, cerebrovascular events, or traumatic brain injuries that result in focal mesial temporal lobe lesions can present as a partial complex seizure with olfactory or gustatory hallucinations and progress to automatisms.4 Characteristic odors in these hallucinations are unpleasant; patients with temporal lobe epilepsy describe the smells as “bad,” “rotten,” “sickening,” and “like burning food.”2 Ms. D’s report of unusual smells warranted consideration of an organic etiology for her mood change and a thorough neurologic examination.
EVALUATION: Neurologic signs
At the time of admission, Ms. D has a blood pressure of 127/68 mm Hg, heart rate of 74 beats per minute, respiratory rate of 16 breaths per minute, and temperature of 36.5°C. Neurologic examination reveals a left facial droop of unknown duration. Motor strength is weak throughout with left-sided focal weakness. Ms. D’s daughter notes that her mother’s smile appears “funny” in her admission photograph but is unsure when the asymmetry in her facial appearance began. Ms. D had been ambulatory before admission. Nursing staff observes Ms. D leans toward her left side and exhibits possible left-sided neglect during the first 12 hours of hospitalization.
When asked about her facial droop, Ms. D replies that she had not noticed any change in her appearance lately. She does not appear to be concerned about her worsening ambulation. On hospital day 2, Ms. D seems to have difficulty using utensils to eat breakfast. Ms. D is dismissive of her worsening motor function and asks to be left alone to finish her meal.
The authors’ observations
Ms. D’s focal neurologic deficits and complaint of a headache on admission were concerning because they could be caused by a cerebrovascular event or space-occupying brain lesion with potential for increased intracranial pressure. Neurologic examination with evaluation for papilledema is indicated, followed by medical transport to the closest medical center for emergent brain imaging. Neither Ms. D nor her daughter could pinpoint the onset of Ms. D’s left-sided facial droop, which precluded administering tissue plasminogen activator for a potential acute ischemic stroke.5
Ms. D’s case prompted us to consider what constitutes timely brain imaging in a patient who presents with psychiatric symptoms. Several neurologic conditions may present first with neurobehavioral symptoms before findings on physical exam. Two series of autopsies conducted >70 years ago at psychiatric hospitals found incidences of brain tumors of 3.45%6 and 13.5%.7 In a 5-year retrospective study, 21% of meningioma cases presented with psychiatric symptoms alone.8 These historical cases suggest that affective, behavioral, and psychotic symptoms may be the only clinical indicators of brain lesions that merit surgery.9-11
Imaging and radiation exposure
With the advent of CT scans in the 1970s, psychiatrists gained a new method of investigating potential structural CNS pathology in patients presenting with psychiatric symptoms. The dramatic increase in CT scan use in recent years and resulting radiation exposure is responsible for 1.5% to 2% of all cancers in the United States.12,13 Certainly, physicians must balance the advantage of early detection of brain lesions with cost-effectiveness and exposure to radiation.14
There is no consensus regarding use of brain imaging in a patient who presents with new-onset psychiatric symptoms. Certainly, patients with localizing neurologic deficits or symptoms of increased intracranial pressure should undergo brain imaging. As for psychiatric patients without neurologic findings, Filley and Kleinschmidt-DeMasters15 provide recommendations based on their 1995 case series, and other authors have recommended imaging for patients age ≥4016 vs ≥5017,18 who present with atypical mental status changes.
OUTCOME: Scan, then surgery
Ms. D’s head CT reveals a large right-sided temporoparietal low-density lesion with 8-mm left lower midline shift (Figure). She undergoes a right temporal craniotomy with resection of the mass, which is confirmed by surgical pathology to be a glioblastoma multiforme World Health Organization grade 4 tumor. Postoperative MRI shows evidence of infarction in the right posterior cerebral artery distribution and residual tumor is identified on follow-up imaging. Ms. D is referred to radiation oncology, where she receives a prognostic median life expectancy of 14 months with radiation and temozolomide treatment.19

Figure: Ms. D’s MRI results
MRI with contrast shows a large right temporal heterogeneous mass consistent with glioblastoma multiforme
The authors’ observations
Glioblastoma is a rare cancer that comprises 25% of all malignant nervous system tumors.20 It is associated with a poor prognosis, with a <30% relative survival rate for adults at 1 year and 3% at 5 years.20 Headaches, seizures, motor weakness, and progressive neurologic deficits are common symptoms of glioblastoma at diagnosis.20 Ms. D was offered the standard of care treatment for a high-grade glioma, including surgical resection followed by concomitant external-beam radiotherapy and chemotherapy.21
Consider structural brain lesions in patients who present with neurobehavioral symptoms, although most of these patients will be diagnosed with a primary psychiatric disorder. Ms. D had a known psychiatric disorder that predated the onset of neurologic symptoms and diagnosis of a rare brain cancer. Before she developed neurologic signs, Ms. D experienced symptoms uncharacteristic of her previous depressive episodes, including olfactory hallucinations, that provided an early indicator of a CNS lesion. Consider brain imaging in patients of any age who do not respond to medications targeting the presumed psychiatric diagnosis to ensure that insidious brain tumors are not missed (Table 1).15
Table 1
When to order neuroimaging for psychiatric patients
| Patient’s age | Most common types of brain tumor | MRI vs CT | Indications to image |
|---|---|---|---|
| ≥40 years | Metastases High-grade gliomas Meningiomas | Roughly equivalent for imaging common tumor types. Base on cost, availability, and relative patient contraindications | New-onset cognitive or emotional dysfunction. Patient is not responding to appropriate pharmacotherapy for psychiatric diagnosis |
| <40 years | Low-grade astrocytomas Oligodendrogliomas | MRI preferred | New-onset cognitive or emotional dysfunction with associated somatic symptoms (headache, nausea, vomiting, papilledema, seizures, or focal deficits). Patient is not responding to appropriate pharmacotherapy for the psychiatric diagnosis |
| Source: Reference 15 | |||
Compared with cerebrovascular lesions, neoplasms are more difficult to clinically correlate with their anatomic location. Neurobehavioral symptoms are more frequently associated with tumors originating in the frontal lobe or temporolimbic regions of the brain. The 3 types of frontal lobe syndromes are dorsolateral, orbitofrontal, and medial-frontal (Table 2).15 Temporolimbic tumors may present with hallucinations, mania, panic attacks, or amnesia. A meta-analysis found a statistically significant association between anorexia and hypothalamic tumors.22 Reports of neuropsychiatric symptoms that respond to pharmacologic treatment further confound the clinical picture.16
Table 2
Frontal lobe syndromes
| Syndrome | Characteristics |
|---|---|
| Dorsolateral | Deficits in executive functioning, including organization and behavior planning |
| Orbitofrontal | Prominent disinhibition |
| Medial-frontal | Apathy, abulia |
| Source: Reference 15 | |
It is uncommon for a patient with a long-standing mood disorder to develop a primary brain cancer. However, Ms. D’s case serves as an important reminder to consider medical comorbidities in our aging psychiatric population. In particular, a patient who develops unusual symptoms or does not respond to previously effective treatments should be more closely examined and the differential diagnosis broadened.
Related Resources
- MD Anderson Cancer Center. Brain tumor videos and podcasts. www.mdanderson.org/patient-and-cancer-information/cancer-information/cancer-types/brain-tumor/videos-and-podcasts/index.html.
- Braun CM, Dumont M, Duval J, et al. Brain modules of hallucination: an analysis of multiple patients with brain lesions. J Psychiatry Neurosci. 2003;28(6):432-449.
Drug Brand Names
- Citalopram • Celexa
- Clonazepam • Klonopin
- Losartan • Cozaar
- Omeprazole • Prilosec
- Oxybutynin • Ditropan
- Pioglitazone • Actos
- Rosuvastatin • Crestor
- Temozolomide • Temodar
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Assad G, Shapiro B. Hallucinations: theoretical and clinical overview. Am J Psychiatry. 1986;143(9):1088-1097.
2. Carter JL. Visual somatosensory, olfactory, and gustatory hallucinations. Psychiatr Clin North Am. 1992;15(2):347-358.
3. Fuller GN, Guiloff RJ. Migrainous olfactory hallucinations. J Neurol Neurosurg Psychiatry. 1987;50(12):1688-1690.
4. Chang BS, Lowenstein DH. Mechanisms of disease: epilepsy. N Engl J Med. 2003;349(13):1257-1266.
5. Lansberg MG, Bluhmki E, Thijs VN. Efficacy and safety of tissue plasminogen activator 3 to 4.5 hours after acute ischemic stroke: a metaanalysis. Stroke. 2009;40(7):2438-2441.
6. Hoffman JL. Intracranial neoplasms: their incidence and mental manifestations. Psychiatr Q. 1937;11(4):561-575.
7. Larson CP. Intracranial tumors in mental hospital patients. Am J Psychiatry. 1940;97(1):49-58.
8. Gupta RK, Kumar R. Benign brain tumours and psychiatric morbidity: a 5-years retrospective data analysis. Aust N Z J Psychiatry. 2004;38(5):316-319.
9. Chambers WR. Neurosurgical conditions masquerading as psychiatric diseases. Am J Psychiatry. 1955;112(5):387-389.
10. Trimble MR, Mendez MF, Cummings JL. Neuropsychiatric symptoms from the temporolimbic lobes. J Neuropsychiatry Clin Neurosci. 1997;9(3):429-438.
11. Uribe VM. Psychiatric symptoms and brain tumor. Am Fam Physician. 1986;34(2):95-98.
12. Brenner DJ, Hall EJ. Computed tomography—an increasing source of radiation exposure. N Engl J Med. 2007;357(2):2277-2284.
13. Berrington de González A, Mahesh M, Kim KP, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009;169(22):2071-2077.
14. Weinberger DR. Brain disease and psychiatric illness: when should a psychiatrist order a CAT scan? Am J Psychiatry. 1984;141(12):1521-1526.
15. Filley CM, Kleinschmidt-DeMasters BK. Neurobehavioral presentations of brain neoplasms. West J Med. 1995;163(1):19-25.
16. Moise D, Madhusoodanan S. Psychiatric symptoms associated with brain tumors: a clinical engima. CNS Spectr. 2006;11(1):28-31.
17. Bunevicius A, Deltuva VP, Deltuviene D, et al. Brain lesions manifesting as psychiatric disorders: eight cases. CNS Spectr. 2008;13(11):950-958.
18. Hollister LE, Boutros N. Clinical use of CT and MR scans in psychiatric patients. J Psychiatr Neurosci. 1991;16(4):194-198.
19. Stupp R, Mason WP, van den Bent MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352(10):987-996.
20. Brandes AA, Tosoni A, Franceschi E, et al. Glioblastoma in adults. Crit Rev Oncol Hematol. 2008;67(2):139-152.
21. Chandana SR, Movva S, Arora M, et al. Primary brain tumors in adults. Am Fam Physician. 2008;77(10):1423-1430.
22. Madhusoodanan S, Opler MG, Moise D, et al. Brain tumor location and psychiatric symptoms: is there any association? A meta-analysis of published case studies. Expert Rev Neurother. 2010;10(10):1529-1536.
1. Assad G, Shapiro B. Hallucinations: theoretical and clinical overview. Am J Psychiatry. 1986;143(9):1088-1097.
2. Carter JL. Visual somatosensory, olfactory, and gustatory hallucinations. Psychiatr Clin North Am. 1992;15(2):347-358.
3. Fuller GN, Guiloff RJ. Migrainous olfactory hallucinations. J Neurol Neurosurg Psychiatry. 1987;50(12):1688-1690.
4. Chang BS, Lowenstein DH. Mechanisms of disease: epilepsy. N Engl J Med. 2003;349(13):1257-1266.
5. Lansberg MG, Bluhmki E, Thijs VN. Efficacy and safety of tissue plasminogen activator 3 to 4.5 hours after acute ischemic stroke: a metaanalysis. Stroke. 2009;40(7):2438-2441.
6. Hoffman JL. Intracranial neoplasms: their incidence and mental manifestations. Psychiatr Q. 1937;11(4):561-575.
7. Larson CP. Intracranial tumors in mental hospital patients. Am J Psychiatry. 1940;97(1):49-58.
8. Gupta RK, Kumar R. Benign brain tumours and psychiatric morbidity: a 5-years retrospective data analysis. Aust N Z J Psychiatry. 2004;38(5):316-319.
9. Chambers WR. Neurosurgical conditions masquerading as psychiatric diseases. Am J Psychiatry. 1955;112(5):387-389.
10. Trimble MR, Mendez MF, Cummings JL. Neuropsychiatric symptoms from the temporolimbic lobes. J Neuropsychiatry Clin Neurosci. 1997;9(3):429-438.
11. Uribe VM. Psychiatric symptoms and brain tumor. Am Fam Physician. 1986;34(2):95-98.
12. Brenner DJ, Hall EJ. Computed tomography—an increasing source of radiation exposure. N Engl J Med. 2007;357(2):2277-2284.
13. Berrington de González A, Mahesh M, Kim KP, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009;169(22):2071-2077.
14. Weinberger DR. Brain disease and psychiatric illness: when should a psychiatrist order a CAT scan? Am J Psychiatry. 1984;141(12):1521-1526.
15. Filley CM, Kleinschmidt-DeMasters BK. Neurobehavioral presentations of brain neoplasms. West J Med. 1995;163(1):19-25.
16. Moise D, Madhusoodanan S. Psychiatric symptoms associated with brain tumors: a clinical engima. CNS Spectr. 2006;11(1):28-31.
17. Bunevicius A, Deltuva VP, Deltuviene D, et al. Brain lesions manifesting as psychiatric disorders: eight cases. CNS Spectr. 2008;13(11):950-958.
18. Hollister LE, Boutros N. Clinical use of CT and MR scans in psychiatric patients. J Psychiatr Neurosci. 1991;16(4):194-198.
19. Stupp R, Mason WP, van den Bent MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352(10):987-996.
20. Brandes AA, Tosoni A, Franceschi E, et al. Glioblastoma in adults. Crit Rev Oncol Hematol. 2008;67(2):139-152.
21. Chandana SR, Movva S, Arora M, et al. Primary brain tumors in adults. Am Fam Physician. 2008;77(10):1423-1430.
22. Madhusoodanan S, Opler MG, Moise D, et al. Brain tumor location and psychiatric symptoms: is there any association? A meta-analysis of published case studies. Expert Rev Neurother. 2010;10(10):1529-1536.


