User login
Antimicrobial resistance threat continues during COVID-19
The stark realities of antimicrobial resistance – including rising rates of difficult-to-treat infections, lack of a robust pipeline of future antimicrobials, and COVID-19 treatments that leave people more vulnerable to infections – remain urgent priorities, experts say.
For some patients, the pandemic and antimicrobial resistance (AMR) are intertwined.
“One patient I’m seeing now in service really underscores how the two interact,” Vance Fowler, MD, said during a June 30 media briefing sponsored by the Infectious Diseases Society of America (IDSA). A man in his mid-40s, married with a small child, developed COVID-19 in early January 2021. He was intubated, spent about 1 month in the ICU, and managed to survive.
“But since then he has been struck with a series of progressively more drug resistant bacteria,” said Dr. Fowler, professor of medicine at Duke University, Durham, N.C., and chair of the IDSA Antimicrobial Resistance Committee.
The patient acquired Pseudomonas ventilator-associated pneumonia. Although the infection initially responded to standard antibiotics, he has experienced relapses over the past few months. Through these multiple infections the Pseudomonas grew increasingly pan-resistant to treatment.
The only remaining antimicrobial agent for this patient, Dr. Fowler said, is “a case study in what we are describing ... a drug that is used relatively infrequently, that is fairly expensive, but for that particular patient is absolutely vital.”
A ‘terrifying’ personal experience
Tori Kinamon, a Duke University medical student and Food and Drug Administration antibacterial drug resistance fellow, joined Dr. Fowler at the IDSA briefing. She shared her personal journey of surviving a methicillin-resistant Staphylococcus aureus (MRSA) infection, one that sparked her interest in becoming a physician.
“I had a very frightening and unexpected confrontation with antimicrobial resistance when I was a freshman in college,” Ms. Kinamon said.
A few days after competing in a Division One gymnastics championship, she felt a gradual onset of pain in her left hamstring. The pain grew acutely worse and, within days, her leg become red, swollen, and painful to the touch.
Ms. Kinamon was admitted to the hospital for suspected cellulitis and put on intravenous antibiotics.
“However, my clinical condition continued to decline,” she recalled. “Imaging studies revealed a 15-cm abscess deep in my hamstring.”
The limb- and life-threatening infection left her wondering if she would come out of surgery with both legs.
“Ultimately, I had eight surgeries in 2 weeks,” she said.
“As a 19-year-old collegiate athlete, that’s terrifying. And I never imagined that something like that would happen to me – until it did,” said Ms. Kinamon, who is an NCAA infection prevention advocate.
When Ms. Kinamon’s kidneys could no longer tolerate vancomycin, she was switched to daptomycin.
“I reflect quite frequently on how having that one extra drug in the stockpile had a significant impact on my outcome,” she said.
Incentivizing new antimicrobial agents
A lack of new antimicrobials in development is not a new story.
“There’s been a chill that’s been sustained on the antibiotic development field. Most large pharmaceutical companies have left the area of anti-infectants and the bulk of research and development is now in small pharmaceutical companies,” Dr. Fowler said. “And they’re struggling.”
One potential solution is the Pasteur Act, a bipartisan bill reintroduced in Congress and supported by IDSA. The bill encourages pharmaceutical companies to develop new antimicrobial agents with funding not linked to sales or use of the drugs.
Furthermore, the bill emphasizes appropriate use of these agents through effective stewardship programs.
Although some institutions shifted resources away from AMR out of necessity when COVID-19 struck, “I can say certainly from our experience at Duke that at least stewardship was alive and well. It was not relegated to the side,” Dr. Fowler said.
“In fact,” he added, “if anything, COVID really emphasized the importance of stewardship” by helping clinicians with guidance on the use of remdesivir and other antivirals during the pandemic.
Also, in some instances, treatments used to keep people with COVID-19 alive can paradoxically place them at higher risk for other infections, Dr. Fowler said, citing corticosteroids as an example.
Everyone’s concern
AMR isn’t just an issue in hospital settings, either. Ms. Kinamon reiterated that she picked up the infection in an athletic environment.
“Antimicrobial resistance is not just a problem for ICU patients in the hospital. I was the healthiest I had ever been and just very nearly escaped death due to one of these infections,” she said. ”As rates of resistance rise as these pathogens become more virulent, AMR is becoming more and more of a community threat,” she added.
Furthermore, consumers are partially to blame as well, Dr. Fowler noted.
“It’s interesting when you look at the surveys of the numbers of patients that have used someone else’s antibiotics” or leftover antimicrobial agents from a prior infection.
“It’s really startling ... that’s the sort of antibiotic overuse that directly contributes to antibacterial resistance,” he said.
Reasons for optimism
Promising advances in diagnostics, treatment, and prevention of AMRs are underway, Dr. Fowler said.
“It always gets me really excited to talk about it. It’s amazing what technology and scientific discovery can bring to this discussion and to this threat,” he said.
For example, there is a “silent revolution” in diagnostics with the aim to rapidly provide life-saving actionable data on a real patient in nearly real time.
Traditionally, “you start off by treating what should be there” while awaiting results of tests to narrow down therapy, Dr. Fowler said. However, a whole host of new platforms are in development to reduce the time to susceptibility results. This kind of technology has “the potential to transform our ability to take care of patients, giving them the right drug at the right time and no more,” he said.
Another promising avenue of research involves bacteriophages. Dr. Fowler is principal investigator on a clinical trial underway to evaluate bacteriophages as adjunct therapy for MRSA bacteremia.
When it comes to prevention on AMR infections in the future, “I continue to be optimistic about the possibility of vaccines to prevent many of these infections,” Dr. Fowler said, adding that companies are working on vaccines against these kinds of infections caused by MRSA or Escherichia coli, for example.
Patient outcomes
The man in his 40s with the multidrug resistant Pseudomonas infections “is now to the point where he’s walking in the halls and I think he’ll get out of the hospital eventually,” Dr. Fowler said.
“But his life is forever changed,” he added.
Ms. Kinamon’s recovery from MRSA included time in the ICU, 1 month in a regular hospital setting, and 5 months at home.
“It sparked my interest in antibiotic research and development because I see myself as a direct beneficiary of the stockpile of antibiotics that were available to treat my infection,” Ms. Kinamon said. “Now as a medical student working with patients who have similar infections, I feel a deep empathy and connectedness to them because they ask the same questions that I did.”
A version of this article first appeared on WebMD.com.
The stark realities of antimicrobial resistance – including rising rates of difficult-to-treat infections, lack of a robust pipeline of future antimicrobials, and COVID-19 treatments that leave people more vulnerable to infections – remain urgent priorities, experts say.
For some patients, the pandemic and antimicrobial resistance (AMR) are intertwined.
“One patient I’m seeing now in service really underscores how the two interact,” Vance Fowler, MD, said during a June 30 media briefing sponsored by the Infectious Diseases Society of America (IDSA). A man in his mid-40s, married with a small child, developed COVID-19 in early January 2021. He was intubated, spent about 1 month in the ICU, and managed to survive.
“But since then he has been struck with a series of progressively more drug resistant bacteria,” said Dr. Fowler, professor of medicine at Duke University, Durham, N.C., and chair of the IDSA Antimicrobial Resistance Committee.
The patient acquired Pseudomonas ventilator-associated pneumonia. Although the infection initially responded to standard antibiotics, he has experienced relapses over the past few months. Through these multiple infections the Pseudomonas grew increasingly pan-resistant to treatment.
The only remaining antimicrobial agent for this patient, Dr. Fowler said, is “a case study in what we are describing ... a drug that is used relatively infrequently, that is fairly expensive, but for that particular patient is absolutely vital.”
A ‘terrifying’ personal experience
Tori Kinamon, a Duke University medical student and Food and Drug Administration antibacterial drug resistance fellow, joined Dr. Fowler at the IDSA briefing. She shared her personal journey of surviving a methicillin-resistant Staphylococcus aureus (MRSA) infection, one that sparked her interest in becoming a physician.
“I had a very frightening and unexpected confrontation with antimicrobial resistance when I was a freshman in college,” Ms. Kinamon said.
A few days after competing in a Division One gymnastics championship, she felt a gradual onset of pain in her left hamstring. The pain grew acutely worse and, within days, her leg become red, swollen, and painful to the touch.
Ms. Kinamon was admitted to the hospital for suspected cellulitis and put on intravenous antibiotics.
“However, my clinical condition continued to decline,” she recalled. “Imaging studies revealed a 15-cm abscess deep in my hamstring.”
The limb- and life-threatening infection left her wondering if she would come out of surgery with both legs.
“Ultimately, I had eight surgeries in 2 weeks,” she said.
“As a 19-year-old collegiate athlete, that’s terrifying. And I never imagined that something like that would happen to me – until it did,” said Ms. Kinamon, who is an NCAA infection prevention advocate.
When Ms. Kinamon’s kidneys could no longer tolerate vancomycin, she was switched to daptomycin.
“I reflect quite frequently on how having that one extra drug in the stockpile had a significant impact on my outcome,” she said.
Incentivizing new antimicrobial agents
A lack of new antimicrobials in development is not a new story.
“There’s been a chill that’s been sustained on the antibiotic development field. Most large pharmaceutical companies have left the area of anti-infectants and the bulk of research and development is now in small pharmaceutical companies,” Dr. Fowler said. “And they’re struggling.”
One potential solution is the Pasteur Act, a bipartisan bill reintroduced in Congress and supported by IDSA. The bill encourages pharmaceutical companies to develop new antimicrobial agents with funding not linked to sales or use of the drugs.
Furthermore, the bill emphasizes appropriate use of these agents through effective stewardship programs.
Although some institutions shifted resources away from AMR out of necessity when COVID-19 struck, “I can say certainly from our experience at Duke that at least stewardship was alive and well. It was not relegated to the side,” Dr. Fowler said.
“In fact,” he added, “if anything, COVID really emphasized the importance of stewardship” by helping clinicians with guidance on the use of remdesivir and other antivirals during the pandemic.
Also, in some instances, treatments used to keep people with COVID-19 alive can paradoxically place them at higher risk for other infections, Dr. Fowler said, citing corticosteroids as an example.
Everyone’s concern
AMR isn’t just an issue in hospital settings, either. Ms. Kinamon reiterated that she picked up the infection in an athletic environment.
“Antimicrobial resistance is not just a problem for ICU patients in the hospital. I was the healthiest I had ever been and just very nearly escaped death due to one of these infections,” she said. ”As rates of resistance rise as these pathogens become more virulent, AMR is becoming more and more of a community threat,” she added.
Furthermore, consumers are partially to blame as well, Dr. Fowler noted.
“It’s interesting when you look at the surveys of the numbers of patients that have used someone else’s antibiotics” or leftover antimicrobial agents from a prior infection.
“It’s really startling ... that’s the sort of antibiotic overuse that directly contributes to antibacterial resistance,” he said.
Reasons for optimism
Promising advances in diagnostics, treatment, and prevention of AMRs are underway, Dr. Fowler said.
“It always gets me really excited to talk about it. It’s amazing what technology and scientific discovery can bring to this discussion and to this threat,” he said.
For example, there is a “silent revolution” in diagnostics with the aim to rapidly provide life-saving actionable data on a real patient in nearly real time.
Traditionally, “you start off by treating what should be there” while awaiting results of tests to narrow down therapy, Dr. Fowler said. However, a whole host of new platforms are in development to reduce the time to susceptibility results. This kind of technology has “the potential to transform our ability to take care of patients, giving them the right drug at the right time and no more,” he said.
Another promising avenue of research involves bacteriophages. Dr. Fowler is principal investigator on a clinical trial underway to evaluate bacteriophages as adjunct therapy for MRSA bacteremia.
When it comes to prevention on AMR infections in the future, “I continue to be optimistic about the possibility of vaccines to prevent many of these infections,” Dr. Fowler said, adding that companies are working on vaccines against these kinds of infections caused by MRSA or Escherichia coli, for example.
Patient outcomes
The man in his 40s with the multidrug resistant Pseudomonas infections “is now to the point where he’s walking in the halls and I think he’ll get out of the hospital eventually,” Dr. Fowler said.
“But his life is forever changed,” he added.
Ms. Kinamon’s recovery from MRSA included time in the ICU, 1 month in a regular hospital setting, and 5 months at home.
“It sparked my interest in antibiotic research and development because I see myself as a direct beneficiary of the stockpile of antibiotics that were available to treat my infection,” Ms. Kinamon said. “Now as a medical student working with patients who have similar infections, I feel a deep empathy and connectedness to them because they ask the same questions that I did.”
A version of this article first appeared on WebMD.com.
The stark realities of antimicrobial resistance – including rising rates of difficult-to-treat infections, lack of a robust pipeline of future antimicrobials, and COVID-19 treatments that leave people more vulnerable to infections – remain urgent priorities, experts say.
For some patients, the pandemic and antimicrobial resistance (AMR) are intertwined.
“One patient I’m seeing now in service really underscores how the two interact,” Vance Fowler, MD, said during a June 30 media briefing sponsored by the Infectious Diseases Society of America (IDSA). A man in his mid-40s, married with a small child, developed COVID-19 in early January 2021. He was intubated, spent about 1 month in the ICU, and managed to survive.
“But since then he has been struck with a series of progressively more drug resistant bacteria,” said Dr. Fowler, professor of medicine at Duke University, Durham, N.C., and chair of the IDSA Antimicrobial Resistance Committee.
The patient acquired Pseudomonas ventilator-associated pneumonia. Although the infection initially responded to standard antibiotics, he has experienced relapses over the past few months. Through these multiple infections the Pseudomonas grew increasingly pan-resistant to treatment.
The only remaining antimicrobial agent for this patient, Dr. Fowler said, is “a case study in what we are describing ... a drug that is used relatively infrequently, that is fairly expensive, but for that particular patient is absolutely vital.”
A ‘terrifying’ personal experience
Tori Kinamon, a Duke University medical student and Food and Drug Administration antibacterial drug resistance fellow, joined Dr. Fowler at the IDSA briefing. She shared her personal journey of surviving a methicillin-resistant Staphylococcus aureus (MRSA) infection, one that sparked her interest in becoming a physician.
“I had a very frightening and unexpected confrontation with antimicrobial resistance when I was a freshman in college,” Ms. Kinamon said.
A few days after competing in a Division One gymnastics championship, she felt a gradual onset of pain in her left hamstring. The pain grew acutely worse and, within days, her leg become red, swollen, and painful to the touch.
Ms. Kinamon was admitted to the hospital for suspected cellulitis and put on intravenous antibiotics.
“However, my clinical condition continued to decline,” she recalled. “Imaging studies revealed a 15-cm abscess deep in my hamstring.”
The limb- and life-threatening infection left her wondering if she would come out of surgery with both legs.
“Ultimately, I had eight surgeries in 2 weeks,” she said.
“As a 19-year-old collegiate athlete, that’s terrifying. And I never imagined that something like that would happen to me – until it did,” said Ms. Kinamon, who is an NCAA infection prevention advocate.
When Ms. Kinamon’s kidneys could no longer tolerate vancomycin, she was switched to daptomycin.
“I reflect quite frequently on how having that one extra drug in the stockpile had a significant impact on my outcome,” she said.
Incentivizing new antimicrobial agents
A lack of new antimicrobials in development is not a new story.
“There’s been a chill that’s been sustained on the antibiotic development field. Most large pharmaceutical companies have left the area of anti-infectants and the bulk of research and development is now in small pharmaceutical companies,” Dr. Fowler said. “And they’re struggling.”
One potential solution is the Pasteur Act, a bipartisan bill reintroduced in Congress and supported by IDSA. The bill encourages pharmaceutical companies to develop new antimicrobial agents with funding not linked to sales or use of the drugs.
Furthermore, the bill emphasizes appropriate use of these agents through effective stewardship programs.
Although some institutions shifted resources away from AMR out of necessity when COVID-19 struck, “I can say certainly from our experience at Duke that at least stewardship was alive and well. It was not relegated to the side,” Dr. Fowler said.
“In fact,” he added, “if anything, COVID really emphasized the importance of stewardship” by helping clinicians with guidance on the use of remdesivir and other antivirals during the pandemic.
Also, in some instances, treatments used to keep people with COVID-19 alive can paradoxically place them at higher risk for other infections, Dr. Fowler said, citing corticosteroids as an example.
Everyone’s concern
AMR isn’t just an issue in hospital settings, either. Ms. Kinamon reiterated that she picked up the infection in an athletic environment.
“Antimicrobial resistance is not just a problem for ICU patients in the hospital. I was the healthiest I had ever been and just very nearly escaped death due to one of these infections,” she said. ”As rates of resistance rise as these pathogens become more virulent, AMR is becoming more and more of a community threat,” she added.
Furthermore, consumers are partially to blame as well, Dr. Fowler noted.
“It’s interesting when you look at the surveys of the numbers of patients that have used someone else’s antibiotics” or leftover antimicrobial agents from a prior infection.
“It’s really startling ... that’s the sort of antibiotic overuse that directly contributes to antibacterial resistance,” he said.
Reasons for optimism
Promising advances in diagnostics, treatment, and prevention of AMRs are underway, Dr. Fowler said.
“It always gets me really excited to talk about it. It’s amazing what technology and scientific discovery can bring to this discussion and to this threat,” he said.
For example, there is a “silent revolution” in diagnostics with the aim to rapidly provide life-saving actionable data on a real patient in nearly real time.
Traditionally, “you start off by treating what should be there” while awaiting results of tests to narrow down therapy, Dr. Fowler said. However, a whole host of new platforms are in development to reduce the time to susceptibility results. This kind of technology has “the potential to transform our ability to take care of patients, giving them the right drug at the right time and no more,” he said.
Another promising avenue of research involves bacteriophages. Dr. Fowler is principal investigator on a clinical trial underway to evaluate bacteriophages as adjunct therapy for MRSA bacteremia.
When it comes to prevention on AMR infections in the future, “I continue to be optimistic about the possibility of vaccines to prevent many of these infections,” Dr. Fowler said, adding that companies are working on vaccines against these kinds of infections caused by MRSA or Escherichia coli, for example.
Patient outcomes
The man in his 40s with the multidrug resistant Pseudomonas infections “is now to the point where he’s walking in the halls and I think he’ll get out of the hospital eventually,” Dr. Fowler said.
“But his life is forever changed,” he added.
Ms. Kinamon’s recovery from MRSA included time in the ICU, 1 month in a regular hospital setting, and 5 months at home.
“It sparked my interest in antibiotic research and development because I see myself as a direct beneficiary of the stockpile of antibiotics that were available to treat my infection,” Ms. Kinamon said. “Now as a medical student working with patients who have similar infections, I feel a deep empathy and connectedness to them because they ask the same questions that I did.”
A version of this article first appeared on WebMD.com.
Asymptomatic C. diff carriers have increased risk of symptomatic infection
Background: C. difficile infections (CDI) are significant with more than 400,000 cases and almost 30,000 deaths annually. However, there is uncertainty regarding asymptomatic C. difficile carriers and whether they have higher rates of progression to symptomatic infections.
Study design: Prospective cohort study.
Setting: Large university hospital in the New York from July 2017 through March 2018.
Synopsis: Patients admitted were screened, enrolled, and tested to include an adequate sample of nursing facility residents because of prior studies that showed nursing facility residents with a higher prevalence of carriage. Patients underwent perirectal swabbing and stool swabbing if available. Test swab soilage, noted as any visible material on the swab, was noted and recorded. Two stool-testing methods were used to test for carriage. A C. difficile carrier was defined as any patient with a positive test without diarrhea. Patients were followed for 6 months or until death; 220 patients were enrolled, with 21 patients (9.6%) asymptomatic C. difficile carriers. Having a soiled swab was the only statistically significant characteristic, including previous antibiotic exposure within the past 90 days, to be associated with carriage; 8 of 21 (38.1%) carriage patients progressed to CDI within 6 months versus 4 of 199 (2.0%) noncarriage patients. Most carriers that progressed to CDI did so within 2 weeks of enrollment. Limitations included lower numbers of expected carriage patients, diarrhea diagnosing variability, and perirectal swabbing was used rather than rectal swabbing/stool testing.
Bottom line: Asymptomatic carriage of C. difficile has increased risk of progression to symptomatic CDI and could present an opportunity for screening to reduce CDI in the inpatient setting.
Citation: Baron SW et al. Screening of Clostridioides difficile carriers in an urban academic medical center: Understanding implications of disease. Infect Control Hosp Epidemiol. 2020;41(2):149-53.
Dr. Wang is a hospitalist and associate professor of medicine at University of Texas Health, San Antonio.
Background: C. difficile infections (CDI) are significant with more than 400,000 cases and almost 30,000 deaths annually. However, there is uncertainty regarding asymptomatic C. difficile carriers and whether they have higher rates of progression to symptomatic infections.
Study design: Prospective cohort study.
Setting: Large university hospital in the New York from July 2017 through March 2018.
Synopsis: Patients admitted were screened, enrolled, and tested to include an adequate sample of nursing facility residents because of prior studies that showed nursing facility residents with a higher prevalence of carriage. Patients underwent perirectal swabbing and stool swabbing if available. Test swab soilage, noted as any visible material on the swab, was noted and recorded. Two stool-testing methods were used to test for carriage. A C. difficile carrier was defined as any patient with a positive test without diarrhea. Patients were followed for 6 months or until death; 220 patients were enrolled, with 21 patients (9.6%) asymptomatic C. difficile carriers. Having a soiled swab was the only statistically significant characteristic, including previous antibiotic exposure within the past 90 days, to be associated with carriage; 8 of 21 (38.1%) carriage patients progressed to CDI within 6 months versus 4 of 199 (2.0%) noncarriage patients. Most carriers that progressed to CDI did so within 2 weeks of enrollment. Limitations included lower numbers of expected carriage patients, diarrhea diagnosing variability, and perirectal swabbing was used rather than rectal swabbing/stool testing.
Bottom line: Asymptomatic carriage of C. difficile has increased risk of progression to symptomatic CDI and could present an opportunity for screening to reduce CDI in the inpatient setting.
Citation: Baron SW et al. Screening of Clostridioides difficile carriers in an urban academic medical center: Understanding implications of disease. Infect Control Hosp Epidemiol. 2020;41(2):149-53.
Dr. Wang is a hospitalist and associate professor of medicine at University of Texas Health, San Antonio.
Background: C. difficile infections (CDI) are significant with more than 400,000 cases and almost 30,000 deaths annually. However, there is uncertainty regarding asymptomatic C. difficile carriers and whether they have higher rates of progression to symptomatic infections.
Study design: Prospective cohort study.
Setting: Large university hospital in the New York from July 2017 through March 2018.
Synopsis: Patients admitted were screened, enrolled, and tested to include an adequate sample of nursing facility residents because of prior studies that showed nursing facility residents with a higher prevalence of carriage. Patients underwent perirectal swabbing and stool swabbing if available. Test swab soilage, noted as any visible material on the swab, was noted and recorded. Two stool-testing methods were used to test for carriage. A C. difficile carrier was defined as any patient with a positive test without diarrhea. Patients were followed for 6 months or until death; 220 patients were enrolled, with 21 patients (9.6%) asymptomatic C. difficile carriers. Having a soiled swab was the only statistically significant characteristic, including previous antibiotic exposure within the past 90 days, to be associated with carriage; 8 of 21 (38.1%) carriage patients progressed to CDI within 6 months versus 4 of 199 (2.0%) noncarriage patients. Most carriers that progressed to CDI did so within 2 weeks of enrollment. Limitations included lower numbers of expected carriage patients, diarrhea diagnosing variability, and perirectal swabbing was used rather than rectal swabbing/stool testing.
Bottom line: Asymptomatic carriage of C. difficile has increased risk of progression to symptomatic CDI and could present an opportunity for screening to reduce CDI in the inpatient setting.
Citation: Baron SW et al. Screening of Clostridioides difficile carriers in an urban academic medical center: Understanding implications of disease. Infect Control Hosp Epidemiol. 2020;41(2):149-53.
Dr. Wang is a hospitalist and associate professor of medicine at University of Texas Health, San Antonio.
Default EMR settings can influence opioid prescribing
Background: The opioid crisis is in the forefront as a public health emergency and there are concerns regarding addiction stemming from opioid prescriptions written in the acute setting, such as the ED and hospitals.
Study design: Quality improvement project, randomized.
Setting: Two large EDs in San Francisco and Oakland, Calif.
Synopsis: In five 4-week blocks, the prepopulated opioid dispense quantities were altered on a block randomized treatment schedule without prior knowledge by the prescribing practitioners with the default dispense quantities of 5, 10, 15, and null (prescriber determined dispense quantity). Opiates included oxycodone, oxycodone/acetaminophen, and hydrocodone/acetaminophen. The primary outcome was number of opioid tablets prescribed at discharge from the ED. In this study, a total of 104 health care professionals issued 4,320 opioid study prescriptions. With use of linear regression, an increase of 0.19 tablets prescribed was found for each tablet increase in default quantity. When comparing default pairs – that is, 5 versus 15 tablets – a lower default was associated with a lower number of pills prescribed in more than half of the comparisons. Limitations of this study include a small sample of EDs, and local prescribing patterns can vary greatly for opioid prescriptions written. In addition, the reasons for the prescriptions were not noted.
Bottom line: Default EMR opioid quantity settings can be used to decrease the quantity of opioids prescribed.
Citation: Montoy JCC et al. Association of default electronic medical record settings with health care professional patterns of opioid prescribing in emergency departments: A randomized quality improvement study. JAMA Intern Med. 2020;180(4):487-93.
Dr. Wang is a hospitalist and associate professor of medicine at University of Texas Health, San Antonio.
Background: The opioid crisis is in the forefront as a public health emergency and there are concerns regarding addiction stemming from opioid prescriptions written in the acute setting, such as the ED and hospitals.
Study design: Quality improvement project, randomized.
Setting: Two large EDs in San Francisco and Oakland, Calif.
Synopsis: In five 4-week blocks, the prepopulated opioid dispense quantities were altered on a block randomized treatment schedule without prior knowledge by the prescribing practitioners with the default dispense quantities of 5, 10, 15, and null (prescriber determined dispense quantity). Opiates included oxycodone, oxycodone/acetaminophen, and hydrocodone/acetaminophen. The primary outcome was number of opioid tablets prescribed at discharge from the ED. In this study, a total of 104 health care professionals issued 4,320 opioid study prescriptions. With use of linear regression, an increase of 0.19 tablets prescribed was found for each tablet increase in default quantity. When comparing default pairs – that is, 5 versus 15 tablets – a lower default was associated with a lower number of pills prescribed in more than half of the comparisons. Limitations of this study include a small sample of EDs, and local prescribing patterns can vary greatly for opioid prescriptions written. In addition, the reasons for the prescriptions were not noted.
Bottom line: Default EMR opioid quantity settings can be used to decrease the quantity of opioids prescribed.
Citation: Montoy JCC et al. Association of default electronic medical record settings with health care professional patterns of opioid prescribing in emergency departments: A randomized quality improvement study. JAMA Intern Med. 2020;180(4):487-93.
Dr. Wang is a hospitalist and associate professor of medicine at University of Texas Health, San Antonio.
Background: The opioid crisis is in the forefront as a public health emergency and there are concerns regarding addiction stemming from opioid prescriptions written in the acute setting, such as the ED and hospitals.
Study design: Quality improvement project, randomized.
Setting: Two large EDs in San Francisco and Oakland, Calif.
Synopsis: In five 4-week blocks, the prepopulated opioid dispense quantities were altered on a block randomized treatment schedule without prior knowledge by the prescribing practitioners with the default dispense quantities of 5, 10, 15, and null (prescriber determined dispense quantity). Opiates included oxycodone, oxycodone/acetaminophen, and hydrocodone/acetaminophen. The primary outcome was number of opioid tablets prescribed at discharge from the ED. In this study, a total of 104 health care professionals issued 4,320 opioid study prescriptions. With use of linear regression, an increase of 0.19 tablets prescribed was found for each tablet increase in default quantity. When comparing default pairs – that is, 5 versus 15 tablets – a lower default was associated with a lower number of pills prescribed in more than half of the comparisons. Limitations of this study include a small sample of EDs, and local prescribing patterns can vary greatly for opioid prescriptions written. In addition, the reasons for the prescriptions were not noted.
Bottom line: Default EMR opioid quantity settings can be used to decrease the quantity of opioids prescribed.
Citation: Montoy JCC et al. Association of default electronic medical record settings with health care professional patterns of opioid prescribing in emergency departments: A randomized quality improvement study. JAMA Intern Med. 2020;180(4):487-93.
Dr. Wang is a hospitalist and associate professor of medicine at University of Texas Health, San Antonio.
Clinician practices to connect with patients
Background: As technology and medical advances improve patient care, physicians and patients have become more dissatisfied with their interactions and relationships. Practices are needed to improve the connection between physician and patient.
Study design: Mixed-methods.
Setting: Three diverse primary care settings (academic medical center, Veterans Affairs facility, federally qualified health center).
Synopsis: Initial evidence- and narrative-based practices were identified from a systematic literature review, clinical observations of primary care encounters, and qualitative discussions with physicians, patients, and nonmedical professionals. A three-round modified Delphi process was performed with experts representing different aspects of the patient-physician relationship.
Five recommended clinical practices were recognized to foster presence and meaningful connections with patients: 1. Prepare with intention (becoming familiar with the patient before you meet them); 2. Listen intently and completely (sit down, lean forward, and don’t interrupt, but listen); 3. Agree on what matters most (discover your patient’s goals and fit them into the visit); 4. Connect with the patient’s story (take notice of efforts by the patient and successes); 5. Explore emotional cues (be aware of your patient’s emotions). Limitations of this study include the use of convenience sampling for the qualitative research, lack of international diversity of the expert panelists, and the lack of validation of the five practices as a whole.
Bottom line: The five practices of prepare with intention, listen intently and completely, agree on what matters most, connect with the patient’s story, and explore emotional cues may improve the patient-physician connection.
Citation: Zulman DM et al. Practices to foster physician presence and connection with patients in the clinical encounter. JAMA. 2020;323(1):70-81.
Dr. Trammell-Velasquez is a hospitalist and associate professor of medicine at University of Texas Health, San Antonio.
Background: As technology and medical advances improve patient care, physicians and patients have become more dissatisfied with their interactions and relationships. Practices are needed to improve the connection between physician and patient.
Study design: Mixed-methods.
Setting: Three diverse primary care settings (academic medical center, Veterans Affairs facility, federally qualified health center).
Synopsis: Initial evidence- and narrative-based practices were identified from a systematic literature review, clinical observations of primary care encounters, and qualitative discussions with physicians, patients, and nonmedical professionals. A three-round modified Delphi process was performed with experts representing different aspects of the patient-physician relationship.
Five recommended clinical practices were recognized to foster presence and meaningful connections with patients: 1. Prepare with intention (becoming familiar with the patient before you meet them); 2. Listen intently and completely (sit down, lean forward, and don’t interrupt, but listen); 3. Agree on what matters most (discover your patient’s goals and fit them into the visit); 4. Connect with the patient’s story (take notice of efforts by the patient and successes); 5. Explore emotional cues (be aware of your patient’s emotions). Limitations of this study include the use of convenience sampling for the qualitative research, lack of international diversity of the expert panelists, and the lack of validation of the five practices as a whole.
Bottom line: The five practices of prepare with intention, listen intently and completely, agree on what matters most, connect with the patient’s story, and explore emotional cues may improve the patient-physician connection.
Citation: Zulman DM et al. Practices to foster physician presence and connection with patients in the clinical encounter. JAMA. 2020;323(1):70-81.
Dr. Trammell-Velasquez is a hospitalist and associate professor of medicine at University of Texas Health, San Antonio.
Background: As technology and medical advances improve patient care, physicians and patients have become more dissatisfied with their interactions and relationships. Practices are needed to improve the connection between physician and patient.
Study design: Mixed-methods.
Setting: Three diverse primary care settings (academic medical center, Veterans Affairs facility, federally qualified health center).
Synopsis: Initial evidence- and narrative-based practices were identified from a systematic literature review, clinical observations of primary care encounters, and qualitative discussions with physicians, patients, and nonmedical professionals. A three-round modified Delphi process was performed with experts representing different aspects of the patient-physician relationship.
Five recommended clinical practices were recognized to foster presence and meaningful connections with patients: 1. Prepare with intention (becoming familiar with the patient before you meet them); 2. Listen intently and completely (sit down, lean forward, and don’t interrupt, but listen); 3. Agree on what matters most (discover your patient’s goals and fit them into the visit); 4. Connect with the patient’s story (take notice of efforts by the patient and successes); 5. Explore emotional cues (be aware of your patient’s emotions). Limitations of this study include the use of convenience sampling for the qualitative research, lack of international diversity of the expert panelists, and the lack of validation of the five practices as a whole.
Bottom line: The five practices of prepare with intention, listen intently and completely, agree on what matters most, connect with the patient’s story, and explore emotional cues may improve the patient-physician connection.
Citation: Zulman DM et al. Practices to foster physician presence and connection with patients in the clinical encounter. JAMA. 2020;323(1):70-81.
Dr. Trammell-Velasquez is a hospitalist and associate professor of medicine at University of Texas Health, San Antonio.
New details of myocarditis linked to COVID vaccines
Further details from multiple cases of myocarditis linked to the Pfizer and Moderna mRNA COVID vaccines have been described in recent papers in the medical literature.
The cases appear to occur almost exclusively in males and most often in younger age groups. While symptoms and signs of myocarditis mostly resolved with a few days of supportive care, long-term effects are unknown at present.
The authors of all the reports and of two accompanying editorials in JAMA Cardiology are unanimous in their opinion that the benefits of vaccination still outweigh the risks.
The Centers for Disease Control and Prevention’s but committee members delivered a strong endorsement for continuing to vaccinate young people with the mRNA vaccines.
The current case reports are published in two papers in JAMA Cardiology and in three in Circulation.
U.S. military reports 23 cases
In one report in JAMA Cardiology, authors led by Jay Montgomery, MD, from Walter Reed National Military Medical Center in Bethesda, Md., described 23 cases from the U.S. Military Health System of individuals with acute myocarditis who presented within 4 days after mRNA-based COVID-19 vaccination (7 Pfizer and 16 Moderna).
All patients were male, 22 of 23 were on active duty, and the median age was 25 years (range, 20-51); 20 of the 23 cases occurred after receipt of a second dose of an mRNA COVID-19 vaccine.
The patients all presented with acute onset of marked chest pain. All patients had significantly elevated cardiac troponin levels. Among eight patients who underwent cardiac MRI (cMRI), all had findings consistent with the clinical diagnosis of myocarditis.
Additional testing did not identify other possible causes of myocarditis. All patients received brief supportive care and were recovered or recovering.
The authors reported that the military administered more than 2.8 million doses of mRNA COVID-19 vaccine in this period, and while the observed number of myocarditis cases was small, the number was “substantially higher” than expected among male military members after a second vaccine dose.
They noted that, based on historical data, among the 544,000 second doses to military members there may have been 0-10 expected myocarditis cases, but they observed 19 cases.
“All patients in this series reflect substantial similarities in demographic characteristics, proximate vaccine dose, onset interval, and character of vaccine-associated myocarditis. The consistent pattern of clinical presentation, rapid recovery, and absence of evidence of other causes support the diagnosis of hypersensitivity myocarditis,” they stated.
They added that presentation after a second vaccine dose or, in three patients, when vaccination followed SARS-CoV-2 infection, suggests that prior exposure was relevant in the hypersensitivity response.
“The spectrum of clinical presentation and reliance on patients seeking health care and on health care professionals recognizing a rare vaccine-associated adverse event limits determination of the true incidence of this condition,” the authors wrote.
They stressed that recognition of vaccine-associated myocarditis is clinically important because diagnosis impacts management, recommendations for exercise, and monitoring for cardiomyopathy.
But the authors also acknowledged that it is important to frame concerns about potential vaccine-associated myocarditis within the context of the current pandemic.
“Infection with SARS-CoV-2 is a clear cause of serious cardiac injury in many patients. ... Prevalence of cardiac injury may be as high as 60% in seriously ill patients. Notably, nearly 1% of highly fit athletes with mild COVID-19 infection have evidence of myocarditis on cMRI,” they wrote.
“Given that COVID-19 vaccines are remarkably effective at preventing infection, any risk of rare adverse events following immunization must be carefully weighed against the very substantial benefit of vaccination,” they concluded.
Four cases at Duke
In the second paper in JAMA Cardiology, a group led by Han W. Kim, MD, reported four patients with acute myocarditis occurring within days of mRNA COVID-19 vaccination (two Pfizer and two Moderna) in patients treated at Duke University Medical Center, Durham, N.C. The hospital courses of the four patients with myocarditis following COVID-19 vaccination were uneventful, and they were discharged within 2-4 days.
The authors said that, although a causal relationship cannot be established, none of the patients had a viral prodrome or had coincident testing that revealed an alternative explanation.
They stated that these four patients represent the majority of patients with acute myocarditis identified in the past 3 months at their institution, and this led to the highest total number of patients with acute myocarditis, compared with the same 3-month period for the past 5 years.
“Additionally, we identified only those patients with severe unremitting chest pain who sought medical attention. Those with mild or moderate chest pain might not seek medical attention, and it is possible that subclinical myocarditis may occur and could be detected by active surveillance, as has been described with smallpox vaccination,” they wrote.
Further case reports
In one of the papers in Circulation, a group led by Kathryn F. Larson, MD, from the Mayo Clinic in Rochester, Minn., described eight patients hospitalized with chest pain who were diagnosed with myocarditis within 2-4 days of receiving either the Pfizer or Moderna vaccine.
Two of the patients had previously been infected by SARS-CoV-2 without need for hospitalization. All individuals were otherwise healthy males between the ages of 21 and 56 years. All but one patient developed symptoms after their second dose, and the one patient who developed myocarditis after the first vaccine dose had previously been infected with SARS-CoV-2.
Systemic symptoms began within 24 hours after vaccine administration in five of eight patients, with chest pain presenting between 48 and 96 hours later. Troponin values were elevated in all individuals and appeared to peak the day after admission, whereas none had eosinophilia.
Cardiac MRI revealed findings consistent with myocarditis in all patients. All patients had resolution of their chest pain and were discharged from the hospital in stable condition.
“The patients presented here demonstrated typical signs, symptoms, and diagnostic features of acute myocarditis. The temporal association between receiving an mRNA-based COVID-19 vaccine and the development of myocarditis is notable,” the authors said.
They added that they would consider the use of corticosteroids in these patients but cautioned that this could reduce the specific immune response against SARS-COV-2 triggered by the vaccine. “Thus, the duration of corticosteroid administration should be limited to the resolution of the symptoms or ventricular arrhythmias or the recovery of the left ventricular ejection fraction.”
Pending publication of long-term outcome data after SARS-CoV-2 vaccine–related myocarditis, they suggest adherence to the current consensus recommendation to abstain from competitive sports for a period of 3-6 months with reevaluation prior to sports participation.
In another of the Circulation papers, a group led by Carolyn M. Rosner, MSN, presented a case series of seven patients hospitalized for acute myocarditis-like illness following COVID-19 vaccination, from two U.S. medical centers, in Falls Church, Va., and Dallas. All patients were males below the age of 40 years and of White or Hispanic race/ethnicity. Only one patient reported prior history of COVID-19 infection. Six patients received mRNA (Moderna or Pfizer) and one received the adenovirus (Johnson & Johnson) vaccine. All patients presented 3-7 days post vaccination with acute onset chest pain and biochemical evidence of myocardial injury.
Hospital length of stay was 3 days, and all patients’ symptoms resolved by hospital discharge.
And finally, the third paper in Circulation reported a detailed description of one patient – a 52-year-old, previously healthy male who presented with acute myocarditis 3 days after the administration of the second dose of Moderna’s COVID-19 vaccine. The symptoms resolved, and there was a gradual improvement in cMRI findings. Ischemic injury and other potential causes of acute myocardial injury were excluded, as were other potential infectious causes of myocarditis, and there was no evidence of systemic autoimmune disease.
“Clinicians should be aware that myocarditis may be present in patients exhibiting cardiac signs and symptoms 2-4 days after COVID-19 vaccination,” the authors said.
They added that additional surveillance of such adverse events post–COVID-19 vaccination will help identify subgroups at higher risk for this vaccine-related effect, and whether additional precautions are necessary.
‘Benefits outweigh risk’
In an accompanying editorial in JAMA Cardiology, three doctors from the CDC cite several other reports of myocarditis after mRNA COVID vaccination. These include a case report published in Pediatrics of seven male adolescents aged 14-19 years who presented with myocarditis or myopericarditis within 4 days after receipt of a second dose of the Pfizer vaccine.
But the editorialists noted that the most comprehensive data about the risk for myocarditis following immunization with mRNA vaccines comes from Israel.
The Israeli Ministry of Health recently posted data describing 121 myocarditis cases occurring within 30 days of a second dose of mRNA vaccine among 5,049,424 persons, suggesting a crude incidence rate of approximately 24 cases per million.
On the current case reports, the CDC doctors wrote: “The striking clinical similarities in the presentations of these patients, their recent vaccination with an mRNA-based COVID-19 vaccine, and the lack of any alternative etiologies for acute myocarditis suggest an association with immunization.”
They said that acute onset of chest pain 3-5 days after vaccine administration, usually after a second dose, is a typical feature of reported cases and suggests an immune-mediated mechanism.
But SARS-CoV-2 infection also causes cardiac injury which may result in severe outcomes, and based on currently available data, myocarditis following immunization with current mRNA-based vaccines is rare.
“At present, the benefits of immunization in preventing severe morbidity favors continued COVID-19 vaccination, particularly considering the increasing COVID-19 hospitalization rates among adolescents reported during spring 2021,” the editorialists stated.
But they added that many questions remain. These include whether modifications are needed to the vaccine schedule among persons with a history of possible or confirmed myocarditis after COVID vaccine, how should postvaccine myocarditis be managed, how often should follow-up assessments be performed, how might follow-up assessments affect recommendations to avoid vigorous physical activity following the diagnosis of myocarditis, and do all likely cases of acute myocarditis that appear to be uncomplicated require cardiac MRI for more definitive diagnosis?
“While the data needed to answer such questions are being collected, there is an opportunity for researchers with expertise in myocarditis to develop a comprehensive, national assessment of the natural history, pathogenesis, and treatment of acute myocarditis associated with receipt of mRNA-based COVID-19 vaccines,” they concluded.
In a second editorial in JAMA Cardiology, a group of editors from the journal acknowledged that publication of the current case reports may contribute to additional public concern regarding immunization. But they added that clinicians discussing immunization with patients should recognize that these case series suggest that the symptomatic events consistent with myocarditis are still very rare and appear to be self-limiting.
“Given the risks of COVID-19, including the risk of myocarditis from COVID-19 infection, the editors do not believe these case reports are sufficient to interrupt the march toward maximal vaccination against SARS-CoV-2 as expeditiously as possible,” they said.
A version of this article first appeared on Medscape.com.
Further details from multiple cases of myocarditis linked to the Pfizer and Moderna mRNA COVID vaccines have been described in recent papers in the medical literature.
The cases appear to occur almost exclusively in males and most often in younger age groups. While symptoms and signs of myocarditis mostly resolved with a few days of supportive care, long-term effects are unknown at present.
The authors of all the reports and of two accompanying editorials in JAMA Cardiology are unanimous in their opinion that the benefits of vaccination still outweigh the risks.
The Centers for Disease Control and Prevention’s but committee members delivered a strong endorsement for continuing to vaccinate young people with the mRNA vaccines.
The current case reports are published in two papers in JAMA Cardiology and in three in Circulation.
U.S. military reports 23 cases
In one report in JAMA Cardiology, authors led by Jay Montgomery, MD, from Walter Reed National Military Medical Center in Bethesda, Md., described 23 cases from the U.S. Military Health System of individuals with acute myocarditis who presented within 4 days after mRNA-based COVID-19 vaccination (7 Pfizer and 16 Moderna).
All patients were male, 22 of 23 were on active duty, and the median age was 25 years (range, 20-51); 20 of the 23 cases occurred after receipt of a second dose of an mRNA COVID-19 vaccine.
The patients all presented with acute onset of marked chest pain. All patients had significantly elevated cardiac troponin levels. Among eight patients who underwent cardiac MRI (cMRI), all had findings consistent with the clinical diagnosis of myocarditis.
Additional testing did not identify other possible causes of myocarditis. All patients received brief supportive care and were recovered or recovering.
The authors reported that the military administered more than 2.8 million doses of mRNA COVID-19 vaccine in this period, and while the observed number of myocarditis cases was small, the number was “substantially higher” than expected among male military members after a second vaccine dose.
They noted that, based on historical data, among the 544,000 second doses to military members there may have been 0-10 expected myocarditis cases, but they observed 19 cases.
“All patients in this series reflect substantial similarities in demographic characteristics, proximate vaccine dose, onset interval, and character of vaccine-associated myocarditis. The consistent pattern of clinical presentation, rapid recovery, and absence of evidence of other causes support the diagnosis of hypersensitivity myocarditis,” they stated.
They added that presentation after a second vaccine dose or, in three patients, when vaccination followed SARS-CoV-2 infection, suggests that prior exposure was relevant in the hypersensitivity response.
“The spectrum of clinical presentation and reliance on patients seeking health care and on health care professionals recognizing a rare vaccine-associated adverse event limits determination of the true incidence of this condition,” the authors wrote.
They stressed that recognition of vaccine-associated myocarditis is clinically important because diagnosis impacts management, recommendations for exercise, and monitoring for cardiomyopathy.
But the authors also acknowledged that it is important to frame concerns about potential vaccine-associated myocarditis within the context of the current pandemic.
“Infection with SARS-CoV-2 is a clear cause of serious cardiac injury in many patients. ... Prevalence of cardiac injury may be as high as 60% in seriously ill patients. Notably, nearly 1% of highly fit athletes with mild COVID-19 infection have evidence of myocarditis on cMRI,” they wrote.
“Given that COVID-19 vaccines are remarkably effective at preventing infection, any risk of rare adverse events following immunization must be carefully weighed against the very substantial benefit of vaccination,” they concluded.
Four cases at Duke
In the second paper in JAMA Cardiology, a group led by Han W. Kim, MD, reported four patients with acute myocarditis occurring within days of mRNA COVID-19 vaccination (two Pfizer and two Moderna) in patients treated at Duke University Medical Center, Durham, N.C. The hospital courses of the four patients with myocarditis following COVID-19 vaccination were uneventful, and they were discharged within 2-4 days.
The authors said that, although a causal relationship cannot be established, none of the patients had a viral prodrome or had coincident testing that revealed an alternative explanation.
They stated that these four patients represent the majority of patients with acute myocarditis identified in the past 3 months at their institution, and this led to the highest total number of patients with acute myocarditis, compared with the same 3-month period for the past 5 years.
“Additionally, we identified only those patients with severe unremitting chest pain who sought medical attention. Those with mild or moderate chest pain might not seek medical attention, and it is possible that subclinical myocarditis may occur and could be detected by active surveillance, as has been described with smallpox vaccination,” they wrote.
Further case reports
In one of the papers in Circulation, a group led by Kathryn F. Larson, MD, from the Mayo Clinic in Rochester, Minn., described eight patients hospitalized with chest pain who were diagnosed with myocarditis within 2-4 days of receiving either the Pfizer or Moderna vaccine.
Two of the patients had previously been infected by SARS-CoV-2 without need for hospitalization. All individuals were otherwise healthy males between the ages of 21 and 56 years. All but one patient developed symptoms after their second dose, and the one patient who developed myocarditis after the first vaccine dose had previously been infected with SARS-CoV-2.
Systemic symptoms began within 24 hours after vaccine administration in five of eight patients, with chest pain presenting between 48 and 96 hours later. Troponin values were elevated in all individuals and appeared to peak the day after admission, whereas none had eosinophilia.
Cardiac MRI revealed findings consistent with myocarditis in all patients. All patients had resolution of their chest pain and were discharged from the hospital in stable condition.
“The patients presented here demonstrated typical signs, symptoms, and diagnostic features of acute myocarditis. The temporal association between receiving an mRNA-based COVID-19 vaccine and the development of myocarditis is notable,” the authors said.
They added that they would consider the use of corticosteroids in these patients but cautioned that this could reduce the specific immune response against SARS-COV-2 triggered by the vaccine. “Thus, the duration of corticosteroid administration should be limited to the resolution of the symptoms or ventricular arrhythmias or the recovery of the left ventricular ejection fraction.”
Pending publication of long-term outcome data after SARS-CoV-2 vaccine–related myocarditis, they suggest adherence to the current consensus recommendation to abstain from competitive sports for a period of 3-6 months with reevaluation prior to sports participation.
In another of the Circulation papers, a group led by Carolyn M. Rosner, MSN, presented a case series of seven patients hospitalized for acute myocarditis-like illness following COVID-19 vaccination, from two U.S. medical centers, in Falls Church, Va., and Dallas. All patients were males below the age of 40 years and of White or Hispanic race/ethnicity. Only one patient reported prior history of COVID-19 infection. Six patients received mRNA (Moderna or Pfizer) and one received the adenovirus (Johnson & Johnson) vaccine. All patients presented 3-7 days post vaccination with acute onset chest pain and biochemical evidence of myocardial injury.
Hospital length of stay was 3 days, and all patients’ symptoms resolved by hospital discharge.
And finally, the third paper in Circulation reported a detailed description of one patient – a 52-year-old, previously healthy male who presented with acute myocarditis 3 days after the administration of the second dose of Moderna’s COVID-19 vaccine. The symptoms resolved, and there was a gradual improvement in cMRI findings. Ischemic injury and other potential causes of acute myocardial injury were excluded, as were other potential infectious causes of myocarditis, and there was no evidence of systemic autoimmune disease.
“Clinicians should be aware that myocarditis may be present in patients exhibiting cardiac signs and symptoms 2-4 days after COVID-19 vaccination,” the authors said.
They added that additional surveillance of such adverse events post–COVID-19 vaccination will help identify subgroups at higher risk for this vaccine-related effect, and whether additional precautions are necessary.
‘Benefits outweigh risk’
In an accompanying editorial in JAMA Cardiology, three doctors from the CDC cite several other reports of myocarditis after mRNA COVID vaccination. These include a case report published in Pediatrics of seven male adolescents aged 14-19 years who presented with myocarditis or myopericarditis within 4 days after receipt of a second dose of the Pfizer vaccine.
But the editorialists noted that the most comprehensive data about the risk for myocarditis following immunization with mRNA vaccines comes from Israel.
The Israeli Ministry of Health recently posted data describing 121 myocarditis cases occurring within 30 days of a second dose of mRNA vaccine among 5,049,424 persons, suggesting a crude incidence rate of approximately 24 cases per million.
On the current case reports, the CDC doctors wrote: “The striking clinical similarities in the presentations of these patients, their recent vaccination with an mRNA-based COVID-19 vaccine, and the lack of any alternative etiologies for acute myocarditis suggest an association with immunization.”
They said that acute onset of chest pain 3-5 days after vaccine administration, usually after a second dose, is a typical feature of reported cases and suggests an immune-mediated mechanism.
But SARS-CoV-2 infection also causes cardiac injury which may result in severe outcomes, and based on currently available data, myocarditis following immunization with current mRNA-based vaccines is rare.
“At present, the benefits of immunization in preventing severe morbidity favors continued COVID-19 vaccination, particularly considering the increasing COVID-19 hospitalization rates among adolescents reported during spring 2021,” the editorialists stated.
But they added that many questions remain. These include whether modifications are needed to the vaccine schedule among persons with a history of possible or confirmed myocarditis after COVID vaccine, how should postvaccine myocarditis be managed, how often should follow-up assessments be performed, how might follow-up assessments affect recommendations to avoid vigorous physical activity following the diagnosis of myocarditis, and do all likely cases of acute myocarditis that appear to be uncomplicated require cardiac MRI for more definitive diagnosis?
“While the data needed to answer such questions are being collected, there is an opportunity for researchers with expertise in myocarditis to develop a comprehensive, national assessment of the natural history, pathogenesis, and treatment of acute myocarditis associated with receipt of mRNA-based COVID-19 vaccines,” they concluded.
In a second editorial in JAMA Cardiology, a group of editors from the journal acknowledged that publication of the current case reports may contribute to additional public concern regarding immunization. But they added that clinicians discussing immunization with patients should recognize that these case series suggest that the symptomatic events consistent with myocarditis are still very rare and appear to be self-limiting.
“Given the risks of COVID-19, including the risk of myocarditis from COVID-19 infection, the editors do not believe these case reports are sufficient to interrupt the march toward maximal vaccination against SARS-CoV-2 as expeditiously as possible,” they said.
A version of this article first appeared on Medscape.com.
Further details from multiple cases of myocarditis linked to the Pfizer and Moderna mRNA COVID vaccines have been described in recent papers in the medical literature.
The cases appear to occur almost exclusively in males and most often in younger age groups. While symptoms and signs of myocarditis mostly resolved with a few days of supportive care, long-term effects are unknown at present.
The authors of all the reports and of two accompanying editorials in JAMA Cardiology are unanimous in their opinion that the benefits of vaccination still outweigh the risks.
The Centers for Disease Control and Prevention’s but committee members delivered a strong endorsement for continuing to vaccinate young people with the mRNA vaccines.
The current case reports are published in two papers in JAMA Cardiology and in three in Circulation.
U.S. military reports 23 cases
In one report in JAMA Cardiology, authors led by Jay Montgomery, MD, from Walter Reed National Military Medical Center in Bethesda, Md., described 23 cases from the U.S. Military Health System of individuals with acute myocarditis who presented within 4 days after mRNA-based COVID-19 vaccination (7 Pfizer and 16 Moderna).
All patients were male, 22 of 23 were on active duty, and the median age was 25 years (range, 20-51); 20 of the 23 cases occurred after receipt of a second dose of an mRNA COVID-19 vaccine.
The patients all presented with acute onset of marked chest pain. All patients had significantly elevated cardiac troponin levels. Among eight patients who underwent cardiac MRI (cMRI), all had findings consistent with the clinical diagnosis of myocarditis.
Additional testing did not identify other possible causes of myocarditis. All patients received brief supportive care and were recovered or recovering.
The authors reported that the military administered more than 2.8 million doses of mRNA COVID-19 vaccine in this period, and while the observed number of myocarditis cases was small, the number was “substantially higher” than expected among male military members after a second vaccine dose.
They noted that, based on historical data, among the 544,000 second doses to military members there may have been 0-10 expected myocarditis cases, but they observed 19 cases.
“All patients in this series reflect substantial similarities in demographic characteristics, proximate vaccine dose, onset interval, and character of vaccine-associated myocarditis. The consistent pattern of clinical presentation, rapid recovery, and absence of evidence of other causes support the diagnosis of hypersensitivity myocarditis,” they stated.
They added that presentation after a second vaccine dose or, in three patients, when vaccination followed SARS-CoV-2 infection, suggests that prior exposure was relevant in the hypersensitivity response.
“The spectrum of clinical presentation and reliance on patients seeking health care and on health care professionals recognizing a rare vaccine-associated adverse event limits determination of the true incidence of this condition,” the authors wrote.
They stressed that recognition of vaccine-associated myocarditis is clinically important because diagnosis impacts management, recommendations for exercise, and monitoring for cardiomyopathy.
But the authors also acknowledged that it is important to frame concerns about potential vaccine-associated myocarditis within the context of the current pandemic.
“Infection with SARS-CoV-2 is a clear cause of serious cardiac injury in many patients. ... Prevalence of cardiac injury may be as high as 60% in seriously ill patients. Notably, nearly 1% of highly fit athletes with mild COVID-19 infection have evidence of myocarditis on cMRI,” they wrote.
“Given that COVID-19 vaccines are remarkably effective at preventing infection, any risk of rare adverse events following immunization must be carefully weighed against the very substantial benefit of vaccination,” they concluded.
Four cases at Duke
In the second paper in JAMA Cardiology, a group led by Han W. Kim, MD, reported four patients with acute myocarditis occurring within days of mRNA COVID-19 vaccination (two Pfizer and two Moderna) in patients treated at Duke University Medical Center, Durham, N.C. The hospital courses of the four patients with myocarditis following COVID-19 vaccination were uneventful, and they were discharged within 2-4 days.
The authors said that, although a causal relationship cannot be established, none of the patients had a viral prodrome or had coincident testing that revealed an alternative explanation.
They stated that these four patients represent the majority of patients with acute myocarditis identified in the past 3 months at their institution, and this led to the highest total number of patients with acute myocarditis, compared with the same 3-month period for the past 5 years.
“Additionally, we identified only those patients with severe unremitting chest pain who sought medical attention. Those with mild or moderate chest pain might not seek medical attention, and it is possible that subclinical myocarditis may occur and could be detected by active surveillance, as has been described with smallpox vaccination,” they wrote.
Further case reports
In one of the papers in Circulation, a group led by Kathryn F. Larson, MD, from the Mayo Clinic in Rochester, Minn., described eight patients hospitalized with chest pain who were diagnosed with myocarditis within 2-4 days of receiving either the Pfizer or Moderna vaccine.
Two of the patients had previously been infected by SARS-CoV-2 without need for hospitalization. All individuals were otherwise healthy males between the ages of 21 and 56 years. All but one patient developed symptoms after their second dose, and the one patient who developed myocarditis after the first vaccine dose had previously been infected with SARS-CoV-2.
Systemic symptoms began within 24 hours after vaccine administration in five of eight patients, with chest pain presenting between 48 and 96 hours later. Troponin values were elevated in all individuals and appeared to peak the day after admission, whereas none had eosinophilia.
Cardiac MRI revealed findings consistent with myocarditis in all patients. All patients had resolution of their chest pain and were discharged from the hospital in stable condition.
“The patients presented here demonstrated typical signs, symptoms, and diagnostic features of acute myocarditis. The temporal association between receiving an mRNA-based COVID-19 vaccine and the development of myocarditis is notable,” the authors said.
They added that they would consider the use of corticosteroids in these patients but cautioned that this could reduce the specific immune response against SARS-COV-2 triggered by the vaccine. “Thus, the duration of corticosteroid administration should be limited to the resolution of the symptoms or ventricular arrhythmias or the recovery of the left ventricular ejection fraction.”
Pending publication of long-term outcome data after SARS-CoV-2 vaccine–related myocarditis, they suggest adherence to the current consensus recommendation to abstain from competitive sports for a period of 3-6 months with reevaluation prior to sports participation.
In another of the Circulation papers, a group led by Carolyn M. Rosner, MSN, presented a case series of seven patients hospitalized for acute myocarditis-like illness following COVID-19 vaccination, from two U.S. medical centers, in Falls Church, Va., and Dallas. All patients were males below the age of 40 years and of White or Hispanic race/ethnicity. Only one patient reported prior history of COVID-19 infection. Six patients received mRNA (Moderna or Pfizer) and one received the adenovirus (Johnson & Johnson) vaccine. All patients presented 3-7 days post vaccination with acute onset chest pain and biochemical evidence of myocardial injury.
Hospital length of stay was 3 days, and all patients’ symptoms resolved by hospital discharge.
And finally, the third paper in Circulation reported a detailed description of one patient – a 52-year-old, previously healthy male who presented with acute myocarditis 3 days after the administration of the second dose of Moderna’s COVID-19 vaccine. The symptoms resolved, and there was a gradual improvement in cMRI findings. Ischemic injury and other potential causes of acute myocardial injury were excluded, as were other potential infectious causes of myocarditis, and there was no evidence of systemic autoimmune disease.
“Clinicians should be aware that myocarditis may be present in patients exhibiting cardiac signs and symptoms 2-4 days after COVID-19 vaccination,” the authors said.
They added that additional surveillance of such adverse events post–COVID-19 vaccination will help identify subgroups at higher risk for this vaccine-related effect, and whether additional precautions are necessary.
‘Benefits outweigh risk’
In an accompanying editorial in JAMA Cardiology, three doctors from the CDC cite several other reports of myocarditis after mRNA COVID vaccination. These include a case report published in Pediatrics of seven male adolescents aged 14-19 years who presented with myocarditis or myopericarditis within 4 days after receipt of a second dose of the Pfizer vaccine.
But the editorialists noted that the most comprehensive data about the risk for myocarditis following immunization with mRNA vaccines comes from Israel.
The Israeli Ministry of Health recently posted data describing 121 myocarditis cases occurring within 30 days of a second dose of mRNA vaccine among 5,049,424 persons, suggesting a crude incidence rate of approximately 24 cases per million.
On the current case reports, the CDC doctors wrote: “The striking clinical similarities in the presentations of these patients, their recent vaccination with an mRNA-based COVID-19 vaccine, and the lack of any alternative etiologies for acute myocarditis suggest an association with immunization.”
They said that acute onset of chest pain 3-5 days after vaccine administration, usually after a second dose, is a typical feature of reported cases and suggests an immune-mediated mechanism.
But SARS-CoV-2 infection also causes cardiac injury which may result in severe outcomes, and based on currently available data, myocarditis following immunization with current mRNA-based vaccines is rare.
“At present, the benefits of immunization in preventing severe morbidity favors continued COVID-19 vaccination, particularly considering the increasing COVID-19 hospitalization rates among adolescents reported during spring 2021,” the editorialists stated.
But they added that many questions remain. These include whether modifications are needed to the vaccine schedule among persons with a history of possible or confirmed myocarditis after COVID vaccine, how should postvaccine myocarditis be managed, how often should follow-up assessments be performed, how might follow-up assessments affect recommendations to avoid vigorous physical activity following the diagnosis of myocarditis, and do all likely cases of acute myocarditis that appear to be uncomplicated require cardiac MRI for more definitive diagnosis?
“While the data needed to answer such questions are being collected, there is an opportunity for researchers with expertise in myocarditis to develop a comprehensive, national assessment of the natural history, pathogenesis, and treatment of acute myocarditis associated with receipt of mRNA-based COVID-19 vaccines,” they concluded.
In a second editorial in JAMA Cardiology, a group of editors from the journal acknowledged that publication of the current case reports may contribute to additional public concern regarding immunization. But they added that clinicians discussing immunization with patients should recognize that these case series suggest that the symptomatic events consistent with myocarditis are still very rare and appear to be self-limiting.
“Given the risks of COVID-19, including the risk of myocarditis from COVID-19 infection, the editors do not believe these case reports are sufficient to interrupt the march toward maximal vaccination against SARS-CoV-2 as expeditiously as possible,” they said.
A version of this article first appeared on Medscape.com.
Post–COVID-19 lung injury: What we know so far
With vaccination rates increasing and new infections declining, we all hope the worst of the COVID-19 pandemic is over (fingers crossed really tight). Regardless, the post–COVID-19 syndrome pandemic has already begun. What is post–COVID-19 syndrome (or long-haulers or long-COVID)? Is it standard postviral fatigue? Prolonged deconditioning following debilitating illness? Permanent lung or vascular injury? Common sense and past experience say it’s all of these.
In theory, the burden of actual lung injury post COVID-19 should be the easiest to quantify, so let’s discuss what we think we know. I’ve heard experts break post–COVID-19 lung injury into three broad categories:
- Preexisting lung disease that is exacerbated by acute COVID-19 infection.
- Acute COVID-19 infection that causes acute respiratory distress syndrome (ARDS) or other acute lung injury (ALI).
- Non–critically ill acute COVID-19 with residual lung damage and abnormal repair.
These categories are necessarily imprecise, making it challenging to fit some patients neatly into a single definition.
For patients in the first category, management will be dictated largely by the nature of the preexisting lung disease. For those in category two, we already know a lot about what their recovery from ARDS will look like. There’s no longer reason to believe that COVID-19–related ARDS is particularly unique, and all things being equal, lung recovery should mimic that seen with non–COVID-19 ARDS.
It’s going to take patience and time, and beyond targeted rehabilitation it’s not clear that we have anything available to expedite the process.
The third category of patients is the most intriguing. Is there a group of patients who have residual lung injury but didn’t have evident ARDS/ALI during their acute COVID-19 infection? Anecdotally we think so, but we know little about prevalence and less about management. A recent study published in Annals of the American Thoracic Society addresses both issues. In an observational report on patients recovering after being hospitalized with COVID-19 infection, the authors found that 3.6% of patients had residual lung injury that improved with 3 weeks of corticosteroid treatment.
The report is timely and helpful but hardly definitive. It’s observational, and patients required extensive screening and identification by a multidisciplinary committee of experts in interstitial lung disease. Patients were diagnosed as having organizing pneumonia (OP) as their “lung injury” if certain radiographic criteria were met. There were no biopsies. Last, there was no control group. Still, this report is critically important. It tells us that at 6 weeks post discharge, about 3.6% of patients who were hospitalized for COVID-19 will have persistent symptoms, radiographic abnormalities, and a plateau in their recovery.
Beyond that, it tells us little. Did these patients really have OP? It’s impossible to know. The CT findings used to establish the diagnosis are nonspecific. Response to steroids is consistent with OP, but the treatment course was quite short. If truly OP, one would expect a high relapse rate after steroid withdrawal. Patients weren’t followed long enough to monitor recurrence rates. Also, as appropriately discussed in the accompanying editorial, there’s no control group so we can’t know whether the patients treated with steroids would have recovered without treatment. There was objective improvement in lung function for the two to three patients they followed who did not receive steroids. However, it was of lesser magnitude than in the steroid group.
Post–COVID-19 symptoms will remain a challenge for the foreseeable future. More than 30 million patients have been diagnosed with COVID-19 in the United States and close to half will experience persistent dyspnea. Putting the numbers together, I conclude that the vast majority will not have identifiable lung injury that will benefit from steroids. I wish I could prescribe patience to both physicians and patients.
Dr. Holley is associate professor of medicine at Uniformed Services University and program director of pulmonary and critical care medicine at Walter Reed National Military Medical Center. He covers a wide range of topics in pulmonary, critical care, and sleep medicine.
A version of this article first appeared on Medscape.com.
With vaccination rates increasing and new infections declining, we all hope the worst of the COVID-19 pandemic is over (fingers crossed really tight). Regardless, the post–COVID-19 syndrome pandemic has already begun. What is post–COVID-19 syndrome (or long-haulers or long-COVID)? Is it standard postviral fatigue? Prolonged deconditioning following debilitating illness? Permanent lung or vascular injury? Common sense and past experience say it’s all of these.
In theory, the burden of actual lung injury post COVID-19 should be the easiest to quantify, so let’s discuss what we think we know. I’ve heard experts break post–COVID-19 lung injury into three broad categories:
- Preexisting lung disease that is exacerbated by acute COVID-19 infection.
- Acute COVID-19 infection that causes acute respiratory distress syndrome (ARDS) or other acute lung injury (ALI).
- Non–critically ill acute COVID-19 with residual lung damage and abnormal repair.
These categories are necessarily imprecise, making it challenging to fit some patients neatly into a single definition.
For patients in the first category, management will be dictated largely by the nature of the preexisting lung disease. For those in category two, we already know a lot about what their recovery from ARDS will look like. There’s no longer reason to believe that COVID-19–related ARDS is particularly unique, and all things being equal, lung recovery should mimic that seen with non–COVID-19 ARDS.
It’s going to take patience and time, and beyond targeted rehabilitation it’s not clear that we have anything available to expedite the process.
The third category of patients is the most intriguing. Is there a group of patients who have residual lung injury but didn’t have evident ARDS/ALI during their acute COVID-19 infection? Anecdotally we think so, but we know little about prevalence and less about management. A recent study published in Annals of the American Thoracic Society addresses both issues. In an observational report on patients recovering after being hospitalized with COVID-19 infection, the authors found that 3.6% of patients had residual lung injury that improved with 3 weeks of corticosteroid treatment.
The report is timely and helpful but hardly definitive. It’s observational, and patients required extensive screening and identification by a multidisciplinary committee of experts in interstitial lung disease. Patients were diagnosed as having organizing pneumonia (OP) as their “lung injury” if certain radiographic criteria were met. There were no biopsies. Last, there was no control group. Still, this report is critically important. It tells us that at 6 weeks post discharge, about 3.6% of patients who were hospitalized for COVID-19 will have persistent symptoms, radiographic abnormalities, and a plateau in their recovery.
Beyond that, it tells us little. Did these patients really have OP? It’s impossible to know. The CT findings used to establish the diagnosis are nonspecific. Response to steroids is consistent with OP, but the treatment course was quite short. If truly OP, one would expect a high relapse rate after steroid withdrawal. Patients weren’t followed long enough to monitor recurrence rates. Also, as appropriately discussed in the accompanying editorial, there’s no control group so we can’t know whether the patients treated with steroids would have recovered without treatment. There was objective improvement in lung function for the two to three patients they followed who did not receive steroids. However, it was of lesser magnitude than in the steroid group.
Post–COVID-19 symptoms will remain a challenge for the foreseeable future. More than 30 million patients have been diagnosed with COVID-19 in the United States and close to half will experience persistent dyspnea. Putting the numbers together, I conclude that the vast majority will not have identifiable lung injury that will benefit from steroids. I wish I could prescribe patience to both physicians and patients.
Dr. Holley is associate professor of medicine at Uniformed Services University and program director of pulmonary and critical care medicine at Walter Reed National Military Medical Center. He covers a wide range of topics in pulmonary, critical care, and sleep medicine.
A version of this article first appeared on Medscape.com.
With vaccination rates increasing and new infections declining, we all hope the worst of the COVID-19 pandemic is over (fingers crossed really tight). Regardless, the post–COVID-19 syndrome pandemic has already begun. What is post–COVID-19 syndrome (or long-haulers or long-COVID)? Is it standard postviral fatigue? Prolonged deconditioning following debilitating illness? Permanent lung or vascular injury? Common sense and past experience say it’s all of these.
In theory, the burden of actual lung injury post COVID-19 should be the easiest to quantify, so let’s discuss what we think we know. I’ve heard experts break post–COVID-19 lung injury into three broad categories:
- Preexisting lung disease that is exacerbated by acute COVID-19 infection.
- Acute COVID-19 infection that causes acute respiratory distress syndrome (ARDS) or other acute lung injury (ALI).
- Non–critically ill acute COVID-19 with residual lung damage and abnormal repair.
These categories are necessarily imprecise, making it challenging to fit some patients neatly into a single definition.
For patients in the first category, management will be dictated largely by the nature of the preexisting lung disease. For those in category two, we already know a lot about what their recovery from ARDS will look like. There’s no longer reason to believe that COVID-19–related ARDS is particularly unique, and all things being equal, lung recovery should mimic that seen with non–COVID-19 ARDS.
It’s going to take patience and time, and beyond targeted rehabilitation it’s not clear that we have anything available to expedite the process.
The third category of patients is the most intriguing. Is there a group of patients who have residual lung injury but didn’t have evident ARDS/ALI during their acute COVID-19 infection? Anecdotally we think so, but we know little about prevalence and less about management. A recent study published in Annals of the American Thoracic Society addresses both issues. In an observational report on patients recovering after being hospitalized with COVID-19 infection, the authors found that 3.6% of patients had residual lung injury that improved with 3 weeks of corticosteroid treatment.
The report is timely and helpful but hardly definitive. It’s observational, and patients required extensive screening and identification by a multidisciplinary committee of experts in interstitial lung disease. Patients were diagnosed as having organizing pneumonia (OP) as their “lung injury” if certain radiographic criteria were met. There were no biopsies. Last, there was no control group. Still, this report is critically important. It tells us that at 6 weeks post discharge, about 3.6% of patients who were hospitalized for COVID-19 will have persistent symptoms, radiographic abnormalities, and a plateau in their recovery.
Beyond that, it tells us little. Did these patients really have OP? It’s impossible to know. The CT findings used to establish the diagnosis are nonspecific. Response to steroids is consistent with OP, but the treatment course was quite short. If truly OP, one would expect a high relapse rate after steroid withdrawal. Patients weren’t followed long enough to monitor recurrence rates. Also, as appropriately discussed in the accompanying editorial, there’s no control group so we can’t know whether the patients treated with steroids would have recovered without treatment. There was objective improvement in lung function for the two to three patients they followed who did not receive steroids. However, it was of lesser magnitude than in the steroid group.
Post–COVID-19 symptoms will remain a challenge for the foreseeable future. More than 30 million patients have been diagnosed with COVID-19 in the United States and close to half will experience persistent dyspnea. Putting the numbers together, I conclude that the vast majority will not have identifiable lung injury that will benefit from steroids. I wish I could prescribe patience to both physicians and patients.
Dr. Holley is associate professor of medicine at Uniformed Services University and program director of pulmonary and critical care medicine at Walter Reed National Military Medical Center. He covers a wide range of topics in pulmonary, critical care, and sleep medicine.
A version of this article first appeared on Medscape.com.
Almost all U.S. COVID-19 deaths now in the unvaccinated
If you, a friend, or a loved one remain unvaccinated against COVID-19 at this point – for whatever reason – you are at higher risk of dying if you become infected.
That’s the conclusion of a new report released by the Associated Press looking at COVID-19 deaths during May 2021.
Of more than 18,000 people who died from COVID-19, for example, only about 150 were fully vaccinated. That’s less than 1%.
“Recently, I was working in the emergency room [and] I saw a 21-year-old African American who came in with shortness of breath,” said Vino K. Palli, MD, MPH, a physician specializing in emergency medicine, internal medicine, and urgent care.
The patient rapidly deteriorated and required intubation and ventilation. She was transferred to a specialized hospital for possible extracorporeal membrane oxygenation (ECMO) treatment.
“This patient was unvaccinated, along with her entire family. This would have been easily preventable,” added Dr. Palli, who is also founder and CEO of MiDoctor Urgent Care in New York City.
“Vaccine misinformation, compounded with vaccine inertia and vaccine access, have contributed to this,” he added. “Even though we have a surplus amount of vaccines at this time, we are only seeing 50% to 55% of completely vaccinated patients.”
Authors of the Associated Press report also acknowledge that some people who are fully vaccinated can get a breakthrough infection. These occurred in fewer than 1,200 of more than 853,000 people hospitalized for COVID-19 in May, or about 0.1%.
The Associated Press came up with these numbers using data from the Centers for Disease Control and Prevention. The CDC tracks the numbers of cases, hospitalizations, and deaths but does not breakdown rates by vaccination status.
Stronger argument for vaccination?
“The fact that only 0.8% of COVID-19 deaths are in the fully vaccinated should persuade those people still hesitant about vaccination,” said Hugh Cassiere, MD, medical director of Respiratory Therapy Services at North Shore University Hospital in Manhasset, New York.
Stuart C. Ray, MD, professor of medicine and oncology in the Division of Infectious Diseases at Johns Hopkins University, Baltimore, agreed. “It seems compelling, even for skeptics, that unvaccinated people represent 99% of those now dying from COVID-19 when they represent less than 50% of the adult population in the United States.”
The findings from the study could be more persuasive than previous arguments made in favor of immunization, Dr. Ray said. “These recent findings of striking reductions in risk of death in the vaccinated are more directly attributable and harder to ignore or dismiss.”
Brian Labus, PhD, MPH, of the University of Nevada Las Vegas (UNLV) is less convinced. “While this might change some peoples’ minds, it probably won’t make a major difference. People have many different reasons for not getting vaccinated, and this is only one of the things they consider.”
The study adds information that was not available before, said Dr. Labus, assistant professor in the Department of Epidemiology and Biostatistics at the UNLV School of Public Health. “We study the vaccine under tightly controlled, ideal conditions. This is the evidence that it works as well in the real world as it did in the trials, and that is what is most important in implementing a vaccination program,” added Dr. Labus.
“The scientific data has honed in on one thing: Vaccines are effective in preventing hospitalizations, ICU admissions, ventilations, and deaths,” agreed Dr. Palli.
“We now know that almost all deaths occurred in patients who were not vaccinated. We also know that all vaccines are effective against various strains that are in circulation right now, including the Delta variant, which is rapidly spreading,” Dr. Palli said.
Dr. Cassiere pointed out that the unvaccinated are not only at higher risk of developing COVID-19 but also of spreading, being hospitalized for, and dying from the infection. Avoiding “long hauler” symptoms is another argument in favor of immunization, he added.
As of June 28, the CDC reports that 63% of Americans 12 years and older have received at least one dose of a COVID-19 vaccine, and 54% are fully vaccinated.
Worldwide worry?
Although overall rates of U.S. COVID-19 hospitalizations and deaths are down, the outlook may not remain as encouraging. “I hope I’m wrong about this, but I anticipate that the coming fall and winter will bring increasingly localized versions of similar findings – severe disease and death due to SARS-CoV-2 infection in regions or groups with lower vaccination rates,” Dr. Ray said.
There could be a silver lining, he added: “If this unfortunate surge occurs, the health and economic consequences seem likely to erode much of the remaining hesitancy regarding vaccination.”
The rise of more infectious SARS-CoV-2 variants, such as the Delta variant, could also throw a wrench in controlling COVID-19. “This isn’t just a domestic issue,” Dr. Ray said. “We have learned that the world is a small place in pandemic times.”
The Associated Press investigators state that their findings support the high efficacy of the vaccine. Also, given the current widespread availability of COVID-19 vaccines in the United States, they believe many of the COVID-19 deaths now occurring are preventable.
Public health measures should have continued longer to protect unvaccinated individuals, especially Black Americans, Hispanic Americans, and other minorities, Dr. Palli said. “Only time will tell if re-opening and abandoning all public health measures by the CDC was premature.”
A version of this article first appeared on Medscape.com.
If you, a friend, or a loved one remain unvaccinated against COVID-19 at this point – for whatever reason – you are at higher risk of dying if you become infected.
That’s the conclusion of a new report released by the Associated Press looking at COVID-19 deaths during May 2021.
Of more than 18,000 people who died from COVID-19, for example, only about 150 were fully vaccinated. That’s less than 1%.
“Recently, I was working in the emergency room [and] I saw a 21-year-old African American who came in with shortness of breath,” said Vino K. Palli, MD, MPH, a physician specializing in emergency medicine, internal medicine, and urgent care.
The patient rapidly deteriorated and required intubation and ventilation. She was transferred to a specialized hospital for possible extracorporeal membrane oxygenation (ECMO) treatment.
“This patient was unvaccinated, along with her entire family. This would have been easily preventable,” added Dr. Palli, who is also founder and CEO of MiDoctor Urgent Care in New York City.
“Vaccine misinformation, compounded with vaccine inertia and vaccine access, have contributed to this,” he added. “Even though we have a surplus amount of vaccines at this time, we are only seeing 50% to 55% of completely vaccinated patients.”
Authors of the Associated Press report also acknowledge that some people who are fully vaccinated can get a breakthrough infection. These occurred in fewer than 1,200 of more than 853,000 people hospitalized for COVID-19 in May, or about 0.1%.
The Associated Press came up with these numbers using data from the Centers for Disease Control and Prevention. The CDC tracks the numbers of cases, hospitalizations, and deaths but does not breakdown rates by vaccination status.
Stronger argument for vaccination?
“The fact that only 0.8% of COVID-19 deaths are in the fully vaccinated should persuade those people still hesitant about vaccination,” said Hugh Cassiere, MD, medical director of Respiratory Therapy Services at North Shore University Hospital in Manhasset, New York.
Stuart C. Ray, MD, professor of medicine and oncology in the Division of Infectious Diseases at Johns Hopkins University, Baltimore, agreed. “It seems compelling, even for skeptics, that unvaccinated people represent 99% of those now dying from COVID-19 when they represent less than 50% of the adult population in the United States.”
The findings from the study could be more persuasive than previous arguments made in favor of immunization, Dr. Ray said. “These recent findings of striking reductions in risk of death in the vaccinated are more directly attributable and harder to ignore or dismiss.”
Brian Labus, PhD, MPH, of the University of Nevada Las Vegas (UNLV) is less convinced. “While this might change some peoples’ minds, it probably won’t make a major difference. People have many different reasons for not getting vaccinated, and this is only one of the things they consider.”
The study adds information that was not available before, said Dr. Labus, assistant professor in the Department of Epidemiology and Biostatistics at the UNLV School of Public Health. “We study the vaccine under tightly controlled, ideal conditions. This is the evidence that it works as well in the real world as it did in the trials, and that is what is most important in implementing a vaccination program,” added Dr. Labus.
“The scientific data has honed in on one thing: Vaccines are effective in preventing hospitalizations, ICU admissions, ventilations, and deaths,” agreed Dr. Palli.
“We now know that almost all deaths occurred in patients who were not vaccinated. We also know that all vaccines are effective against various strains that are in circulation right now, including the Delta variant, which is rapidly spreading,” Dr. Palli said.
Dr. Cassiere pointed out that the unvaccinated are not only at higher risk of developing COVID-19 but also of spreading, being hospitalized for, and dying from the infection. Avoiding “long hauler” symptoms is another argument in favor of immunization, he added.
As of June 28, the CDC reports that 63% of Americans 12 years and older have received at least one dose of a COVID-19 vaccine, and 54% are fully vaccinated.
Worldwide worry?
Although overall rates of U.S. COVID-19 hospitalizations and deaths are down, the outlook may not remain as encouraging. “I hope I’m wrong about this, but I anticipate that the coming fall and winter will bring increasingly localized versions of similar findings – severe disease and death due to SARS-CoV-2 infection in regions or groups with lower vaccination rates,” Dr. Ray said.
There could be a silver lining, he added: “If this unfortunate surge occurs, the health and economic consequences seem likely to erode much of the remaining hesitancy regarding vaccination.”
The rise of more infectious SARS-CoV-2 variants, such as the Delta variant, could also throw a wrench in controlling COVID-19. “This isn’t just a domestic issue,” Dr. Ray said. “We have learned that the world is a small place in pandemic times.”
The Associated Press investigators state that their findings support the high efficacy of the vaccine. Also, given the current widespread availability of COVID-19 vaccines in the United States, they believe many of the COVID-19 deaths now occurring are preventable.
Public health measures should have continued longer to protect unvaccinated individuals, especially Black Americans, Hispanic Americans, and other minorities, Dr. Palli said. “Only time will tell if re-opening and abandoning all public health measures by the CDC was premature.”
A version of this article first appeared on Medscape.com.
If you, a friend, or a loved one remain unvaccinated against COVID-19 at this point – for whatever reason – you are at higher risk of dying if you become infected.
That’s the conclusion of a new report released by the Associated Press looking at COVID-19 deaths during May 2021.
Of more than 18,000 people who died from COVID-19, for example, only about 150 were fully vaccinated. That’s less than 1%.
“Recently, I was working in the emergency room [and] I saw a 21-year-old African American who came in with shortness of breath,” said Vino K. Palli, MD, MPH, a physician specializing in emergency medicine, internal medicine, and urgent care.
The patient rapidly deteriorated and required intubation and ventilation. She was transferred to a specialized hospital for possible extracorporeal membrane oxygenation (ECMO) treatment.
“This patient was unvaccinated, along with her entire family. This would have been easily preventable,” added Dr. Palli, who is also founder and CEO of MiDoctor Urgent Care in New York City.
“Vaccine misinformation, compounded with vaccine inertia and vaccine access, have contributed to this,” he added. “Even though we have a surplus amount of vaccines at this time, we are only seeing 50% to 55% of completely vaccinated patients.”
Authors of the Associated Press report also acknowledge that some people who are fully vaccinated can get a breakthrough infection. These occurred in fewer than 1,200 of more than 853,000 people hospitalized for COVID-19 in May, or about 0.1%.
The Associated Press came up with these numbers using data from the Centers for Disease Control and Prevention. The CDC tracks the numbers of cases, hospitalizations, and deaths but does not breakdown rates by vaccination status.
Stronger argument for vaccination?
“The fact that only 0.8% of COVID-19 deaths are in the fully vaccinated should persuade those people still hesitant about vaccination,” said Hugh Cassiere, MD, medical director of Respiratory Therapy Services at North Shore University Hospital in Manhasset, New York.
Stuart C. Ray, MD, professor of medicine and oncology in the Division of Infectious Diseases at Johns Hopkins University, Baltimore, agreed. “It seems compelling, even for skeptics, that unvaccinated people represent 99% of those now dying from COVID-19 when they represent less than 50% of the adult population in the United States.”
The findings from the study could be more persuasive than previous arguments made in favor of immunization, Dr. Ray said. “These recent findings of striking reductions in risk of death in the vaccinated are more directly attributable and harder to ignore or dismiss.”
Brian Labus, PhD, MPH, of the University of Nevada Las Vegas (UNLV) is less convinced. “While this might change some peoples’ minds, it probably won’t make a major difference. People have many different reasons for not getting vaccinated, and this is only one of the things they consider.”
The study adds information that was not available before, said Dr. Labus, assistant professor in the Department of Epidemiology and Biostatistics at the UNLV School of Public Health. “We study the vaccine under tightly controlled, ideal conditions. This is the evidence that it works as well in the real world as it did in the trials, and that is what is most important in implementing a vaccination program,” added Dr. Labus.
“The scientific data has honed in on one thing: Vaccines are effective in preventing hospitalizations, ICU admissions, ventilations, and deaths,” agreed Dr. Palli.
“We now know that almost all deaths occurred in patients who were not vaccinated. We also know that all vaccines are effective against various strains that are in circulation right now, including the Delta variant, which is rapidly spreading,” Dr. Palli said.
Dr. Cassiere pointed out that the unvaccinated are not only at higher risk of developing COVID-19 but also of spreading, being hospitalized for, and dying from the infection. Avoiding “long hauler” symptoms is another argument in favor of immunization, he added.
As of June 28, the CDC reports that 63% of Americans 12 years and older have received at least one dose of a COVID-19 vaccine, and 54% are fully vaccinated.
Worldwide worry?
Although overall rates of U.S. COVID-19 hospitalizations and deaths are down, the outlook may not remain as encouraging. “I hope I’m wrong about this, but I anticipate that the coming fall and winter will bring increasingly localized versions of similar findings – severe disease and death due to SARS-CoV-2 infection in regions or groups with lower vaccination rates,” Dr. Ray said.
There could be a silver lining, he added: “If this unfortunate surge occurs, the health and economic consequences seem likely to erode much of the remaining hesitancy regarding vaccination.”
The rise of more infectious SARS-CoV-2 variants, such as the Delta variant, could also throw a wrench in controlling COVID-19. “This isn’t just a domestic issue,” Dr. Ray said. “We have learned that the world is a small place in pandemic times.”
The Associated Press investigators state that their findings support the high efficacy of the vaccine. Also, given the current widespread availability of COVID-19 vaccines in the United States, they believe many of the COVID-19 deaths now occurring are preventable.
Public health measures should have continued longer to protect unvaccinated individuals, especially Black Americans, Hispanic Americans, and other minorities, Dr. Palli said. “Only time will tell if re-opening and abandoning all public health measures by the CDC was premature.”
A version of this article first appeared on Medscape.com.
Lack of fever in ESRD with S. aureus bacteremia is common
Background: Fever is a common symptom in patients presenting to the ED. In patients with hemodialysis-dependent ESRD, the literature on febrile response during infection is scarce. In this study, authors compared ED triage temperatures of S. aureus bacteremic patients with and without hemodialysis-dependent ESRD.
Study design: Paired, retrospective cohort study.
Setting: Tertiary care referral center.
Synopsis: A total of 74 patients with methicillin-resistant or methicillin-susceptible S. aureus bacteremia were included in this study (37 patients with and 37 patients without hemodialysis-dependent ESRD). Upon triage, 54% (95% confidence interval, 38%-70%) and 82% (95% CI, 65%-91%) of hemodialysis and nonhemodialysis patients did not have a detectable fever (less than 100.4° F), respectively. The estimated mean ED triage temperatures were 100.5° F in the hemodialysis-dependent patients and 99.0° F in the non–hemodialysis-dependent patients (P < .001). The authors note the significant lack of fevers may be the result of insensitive methods for measuring body temperature, such as peripheral thermometers.
Bottom line: In this small retrospective cohort study, these data suggest a high incidence of afebrile bacteremia in patients with ESRD, especially those patients not dialysis dependent. This may lead to delays in obtaining blood cultures and initiating antibiotics. However, given the study design, the authors were unable to conclude a causal relationship between ESRD and febrile response.
Citation: Weatherall SL et al. Do bacteremic patients with end-stage renal disease have a fever when presenting to the emergency department? A paired, retrospective cohort study. BMC Emerg Med. 2020;20:2.
Dr. Schmit is a hospitalist and associate professor of medicine at University of Texas Health, San Antonio.
Background: Fever is a common symptom in patients presenting to the ED. In patients with hemodialysis-dependent ESRD, the literature on febrile response during infection is scarce. In this study, authors compared ED triage temperatures of S. aureus bacteremic patients with and without hemodialysis-dependent ESRD.
Study design: Paired, retrospective cohort study.
Setting: Tertiary care referral center.
Synopsis: A total of 74 patients with methicillin-resistant or methicillin-susceptible S. aureus bacteremia were included in this study (37 patients with and 37 patients without hemodialysis-dependent ESRD). Upon triage, 54% (95% confidence interval, 38%-70%) and 82% (95% CI, 65%-91%) of hemodialysis and nonhemodialysis patients did not have a detectable fever (less than 100.4° F), respectively. The estimated mean ED triage temperatures were 100.5° F in the hemodialysis-dependent patients and 99.0° F in the non–hemodialysis-dependent patients (P < .001). The authors note the significant lack of fevers may be the result of insensitive methods for measuring body temperature, such as peripheral thermometers.
Bottom line: In this small retrospective cohort study, these data suggest a high incidence of afebrile bacteremia in patients with ESRD, especially those patients not dialysis dependent. This may lead to delays in obtaining blood cultures and initiating antibiotics. However, given the study design, the authors were unable to conclude a causal relationship between ESRD and febrile response.
Citation: Weatherall SL et al. Do bacteremic patients with end-stage renal disease have a fever when presenting to the emergency department? A paired, retrospective cohort study. BMC Emerg Med. 2020;20:2.
Dr. Schmit is a hospitalist and associate professor of medicine at University of Texas Health, San Antonio.
Background: Fever is a common symptom in patients presenting to the ED. In patients with hemodialysis-dependent ESRD, the literature on febrile response during infection is scarce. In this study, authors compared ED triage temperatures of S. aureus bacteremic patients with and without hemodialysis-dependent ESRD.
Study design: Paired, retrospective cohort study.
Setting: Tertiary care referral center.
Synopsis: A total of 74 patients with methicillin-resistant or methicillin-susceptible S. aureus bacteremia were included in this study (37 patients with and 37 patients without hemodialysis-dependent ESRD). Upon triage, 54% (95% confidence interval, 38%-70%) and 82% (95% CI, 65%-91%) of hemodialysis and nonhemodialysis patients did not have a detectable fever (less than 100.4° F), respectively. The estimated mean ED triage temperatures were 100.5° F in the hemodialysis-dependent patients and 99.0° F in the non–hemodialysis-dependent patients (P < .001). The authors note the significant lack of fevers may be the result of insensitive methods for measuring body temperature, such as peripheral thermometers.
Bottom line: In this small retrospective cohort study, these data suggest a high incidence of afebrile bacteremia in patients with ESRD, especially those patients not dialysis dependent. This may lead to delays in obtaining blood cultures and initiating antibiotics. However, given the study design, the authors were unable to conclude a causal relationship between ESRD and febrile response.
Citation: Weatherall SL et al. Do bacteremic patients with end-stage renal disease have a fever when presenting to the emergency department? A paired, retrospective cohort study. BMC Emerg Med. 2020;20:2.
Dr. Schmit is a hospitalist and associate professor of medicine at University of Texas Health, San Antonio.
Conservative treatment for spontaneous pneumothorax?
Background: Management of primary spontaneous pneumothorax is usually with the insertion of a chest tube and typically requires hospitalization. This procedure can result in pain, organ injury, bleeding, and infection, and, if unresolved, may require surgery, introducing additional risks and complications. Few data exist from randomized trials comparing conservative versus interventional management.
Study design: Open-label, multicenter, prospective, randomized, noninferiority trial.
Setting: A total of 39 metropolitan and rural hospitals in Australia and New Zealand.
Synopsis: Overall, 316 patients with moderate to large primary spontaneous pneumothorax were randomized (154 to the intervention group and 162 in the conservative group). In the conservative group, 25 patients (15.4%) required eventual intervention for prespecified reasons (uncontrolled pain, chest pain or shortness of breath preventing mobilization, clinical instability, enlarging pneumothorax).
In complete-case analysis, 129 out of 131 (98.5%) patients in the intervention group had resolution within 8 weeks, compared with 118 of 125 (94.4%) in the conservative group (risk difference, –4.1 percentage points; 95% confidence interval, –8.6 to 0.5, P = .02 for noninferiority).
In sensitivity analysis, in which missing data after the 8-week period were imputed as treatment failures, re-expansion occurred in 129 out of 138 (93.5%) patients in the intervention group and 118 out of 143 (82.5%) in the conservative group (risk difference, –11.0 percentage points; 95% CI, –18.4 to –3.5), which is outside the noninferiority margin of –9.0.
Overall, 41 patients in the intervention group and 13 in the conservative group had at least one adverse event.
Bottom line: Missing data limit the ability to make strong conclusions, but this trial suggests that conservative management of primary spontaneous pneumothorax was noninferior to interventional management with lower risk of serious adverse events.
Citation: Brown SG et al. Conservative versus interventional treatment for spontaneous pneumothorax. N Engl J Med. 2020; 382:405-15.
Dr. Schmit is a hospitalist and associate professor of medicine at University of Texas Health, San Antonio.
Background: Management of primary spontaneous pneumothorax is usually with the insertion of a chest tube and typically requires hospitalization. This procedure can result in pain, organ injury, bleeding, and infection, and, if unresolved, may require surgery, introducing additional risks and complications. Few data exist from randomized trials comparing conservative versus interventional management.
Study design: Open-label, multicenter, prospective, randomized, noninferiority trial.
Setting: A total of 39 metropolitan and rural hospitals in Australia and New Zealand.
Synopsis: Overall, 316 patients with moderate to large primary spontaneous pneumothorax were randomized (154 to the intervention group and 162 in the conservative group). In the conservative group, 25 patients (15.4%) required eventual intervention for prespecified reasons (uncontrolled pain, chest pain or shortness of breath preventing mobilization, clinical instability, enlarging pneumothorax).
In complete-case analysis, 129 out of 131 (98.5%) patients in the intervention group had resolution within 8 weeks, compared with 118 of 125 (94.4%) in the conservative group (risk difference, –4.1 percentage points; 95% confidence interval, –8.6 to 0.5, P = .02 for noninferiority).
In sensitivity analysis, in which missing data after the 8-week period were imputed as treatment failures, re-expansion occurred in 129 out of 138 (93.5%) patients in the intervention group and 118 out of 143 (82.5%) in the conservative group (risk difference, –11.0 percentage points; 95% CI, –18.4 to –3.5), which is outside the noninferiority margin of –9.0.
Overall, 41 patients in the intervention group and 13 in the conservative group had at least one adverse event.
Bottom line: Missing data limit the ability to make strong conclusions, but this trial suggests that conservative management of primary spontaneous pneumothorax was noninferior to interventional management with lower risk of serious adverse events.
Citation: Brown SG et al. Conservative versus interventional treatment for spontaneous pneumothorax. N Engl J Med. 2020; 382:405-15.
Dr. Schmit is a hospitalist and associate professor of medicine at University of Texas Health, San Antonio.
Background: Management of primary spontaneous pneumothorax is usually with the insertion of a chest tube and typically requires hospitalization. This procedure can result in pain, organ injury, bleeding, and infection, and, if unresolved, may require surgery, introducing additional risks and complications. Few data exist from randomized trials comparing conservative versus interventional management.
Study design: Open-label, multicenter, prospective, randomized, noninferiority trial.
Setting: A total of 39 metropolitan and rural hospitals in Australia and New Zealand.
Synopsis: Overall, 316 patients with moderate to large primary spontaneous pneumothorax were randomized (154 to the intervention group and 162 in the conservative group). In the conservative group, 25 patients (15.4%) required eventual intervention for prespecified reasons (uncontrolled pain, chest pain or shortness of breath preventing mobilization, clinical instability, enlarging pneumothorax).
In complete-case analysis, 129 out of 131 (98.5%) patients in the intervention group had resolution within 8 weeks, compared with 118 of 125 (94.4%) in the conservative group (risk difference, –4.1 percentage points; 95% confidence interval, –8.6 to 0.5, P = .02 for noninferiority).
In sensitivity analysis, in which missing data after the 8-week period were imputed as treatment failures, re-expansion occurred in 129 out of 138 (93.5%) patients in the intervention group and 118 out of 143 (82.5%) in the conservative group (risk difference, –11.0 percentage points; 95% CI, –18.4 to –3.5), which is outside the noninferiority margin of –9.0.
Overall, 41 patients in the intervention group and 13 in the conservative group had at least one adverse event.
Bottom line: Missing data limit the ability to make strong conclusions, but this trial suggests that conservative management of primary spontaneous pneumothorax was noninferior to interventional management with lower risk of serious adverse events.
Citation: Brown SG et al. Conservative versus interventional treatment for spontaneous pneumothorax. N Engl J Med. 2020; 382:405-15.
Dr. Schmit is a hospitalist and associate professor of medicine at University of Texas Health, San Antonio.
Disturbing number of hospital workers still unvaccinated
Tim Oswalt had been in a Fort Worth, Texas, hospital for over a month, receiving treatment for a grapefruit-sized tumor in his chest that was pressing on his heart and lungs. It turned out to be stage 3 non-Hodgkin lymphoma.
Then one day in January, he was moved from his semi-private room to an isolated one with special ventilation. The staff explained he had been infected by the virus that was once again surging in many areas of the country, including Texas.
“How the hell did I catch COVID?” he asked the staff, who now approached him in full moon-suit personal protective equipment (PPE).
The hospital was locked down, and Mr. Oswalt hadn’t had any visitors in weeks. Neither of his two roommates tested positive. He’d been tested for COVID several times over the course of his nearly 5-week stay and was always negative.
“‘Well, you know, it’s easy to [catch it] in a hospital,’” Mr. Oswalt said he was told by hospital staff. “‘We’re having a bad outbreak. So you were just exposed somehow.’”

Officials at John Peter Smith Hospital, where Mr. Oswalt was treated, said they are puzzled by his case. According to their infection prevention team, none of his caregivers tested positive for COVID-19, nor did Mr. Oswalt share space with any other COVID-positive patients. And yet, local media reported a surge in cases among JPS hospital staff in December.
“Infection of any kind is a constant battle within hospitals and one that we all take seriously,” said Rob Stephenson, MD, chief quality officer at JPS Health Network. “Anyone in a vulnerable health condition at the height of the pandemic would have been at greater risk for contracting COVID-19 inside – or even more so, outside – the hospital.”
Mr. Oswalt was diagnosed with COVID in early January. JPS Hospital began vaccinating its health care workers about 2 weeks earlier, so there had not yet been enough time for any of them to develop full protection against catching or spreading the virus.
Today, the hospital said 74% of its staff – 5,300 of 7,200 workers – are now vaccinated.
against the SARS-CoV2 virus.
Refusing vaccinations
In fact, nationwide, 1 in 4 hospital workers who have direct contact with patients had not yet received a single dose of a COVID vaccine by the end of May, according to a WebMD and Medscape Medical News analysis of data collected by the U.S. Department of Health and Human Services (HHS) from 2,500 hospitals across the United States.
Among the nation’s 50 largest hospitals, the percentage of unvaccinated health care workers appears to be even larger, about 1 in 3. Vaccination rates range from a high of 99% at Houston Methodist Hospital, which was the first in the nation to mandate the shots for its workers, to a low between 30% and 40% at some hospitals in Florida.
Memorial Hermann Texas Medical Center in Houston has 1,180 beds and sits less than half a mile from Houston Methodist Hospital. But in terms of worker vaccinations, it is farther away.
Memorial Hermann reported to HHS that about 32% of its 28,000 workers haven’t been inoculated. The hospital’s PR office contests that figure, putting it closer to 25% unvaccinated across their health system. The hospital said it is boosting participation by offering a $300 “shot of hope” bonus to workers who start their vaccination series by the end of June.
Lakeland Regional Medical Center in Lakeland, Fla., reported to HHS that 63% of its health care personnel are still unvaccinated. The hospital did not return a call to verify that number.
To boost vaccination rates, more hospitals are starting to require the shots, after the Equal Employment Opportunity Commission gave its green light to mandates in May.
“It’s a real problem that you have such high levels of unvaccinated individuals in hospitals,” said Lawrence Gostin, JD, director of the O’Neill Institute for National and Global Health Law at Georgetown University, Washington.
“We have to protect our health workforce, and we have to protect our patients. Hospitals should be the safest places in the country, and the only way to make them safe is to have a fully vaccinated workforce,” Mr. Gostin said.
Is the data misleading?
The HHS system designed to amass hospital data was set up quickly, to respond to an emergency. For that reason, experts say the information hasn’t been as carefully collected or vetted as it normally would have been. Some hospitals may have misunderstood how to report their vaccination numbers.
In addition, reporting data on worker vaccinations is voluntary. Only about half of hospitals have chosen to share their numbers. In other cases, like Texas, states have blocked the public release of these statistics.
AdventHealth Orlando, a 1,300-bed hospital in Florida, reported to HHS that 56% of its staff have not started their shots. But spokesman Jeff Grainger said the figures probably overstate the number of unvaccinated workers because the hospital doesn’t always know when people get vaccinated outside of its campus, at a local pharmacy, for example.
For those reasons, the picture of health care worker vaccinations across the country is incomplete.
Where hospitals fall behind
Even if the data are flawed, the vaccination rates from hospitals mirror the general population. A May Gallup poll, for example, found 24% of Americans said they definitely won’t get the vaccine. Another 12% say they plan to get it but are waiting.
The data also align with recent studies. A review of 35 studies by researchers at New Mexico State University that assessed hesitancy in more than 76,000 health care workers around the world found about 23% of them were reluctant to get the shots.
An ongoing monthly survey of more than 1.9 million U.S. Facebook users led by researchers at Carnegie Mellon University, Pittsburgh recently looked at vaccine hesitancy by occupation. It revealed a spectrum of hesitancy among health care workers corresponding to income and education, ranging from a low of 9% among pharmacists to highs of 20%-23% among nursing aides and emergency medical technicians. About 12% of registered nurses and doctors admitted to being hesitant to get a shot.
“Health care workers are not monolithic,” said study author Jagdish Khubchandani, professor of public health sciences at New Mexico State.
“There’s a big divide between males, doctoral degree holders, older people and the younger low-income, low-education frontline, female, health care workers. They are the most hesitant,” he said. Support staff typically outnumbers doctors at hospitals about 3 to 1.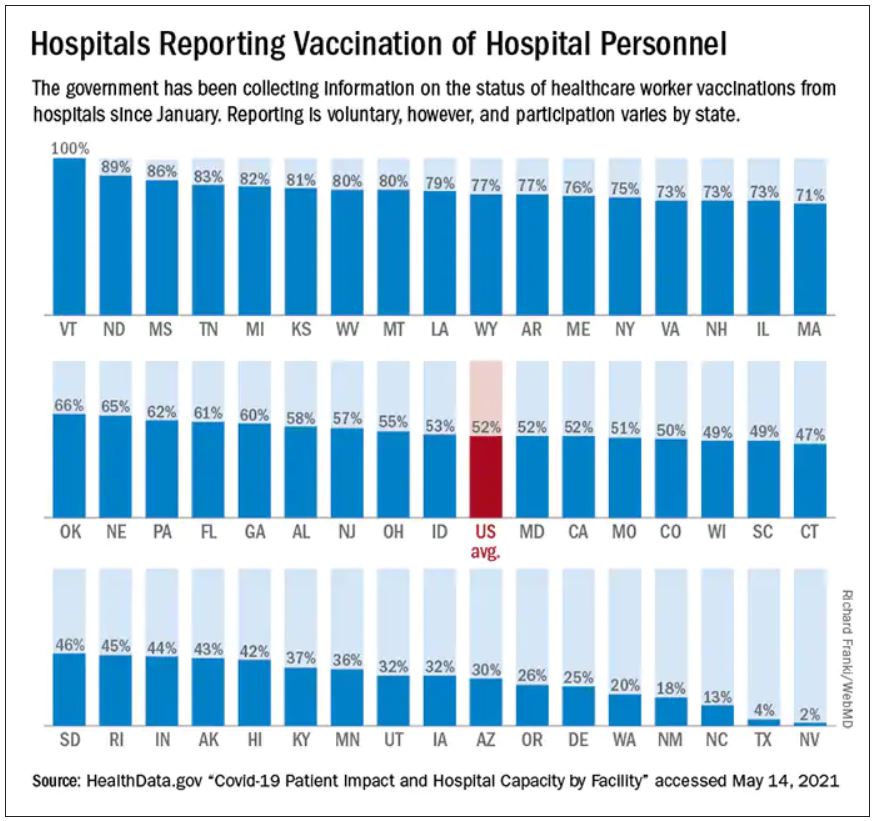
“There is outreach work to be done there,” said Robin Mejia, PhD, director of the Statistics and Human Rights Program at Carnegie Mellon, who is leading the study on Facebook’s survey data. “These are also high-contact professions. These are people who are seeing patients on a regular basis.”
That’s why, when the Centers for Disease Control and Prevention was planning the national vaccine rollout, they prioritized health care workers for the initially scarce first doses. The intent was to protect vulnerable workers and their patients who are at high risk of infection. But the CDC had another reason for putting health care workers first: After they were safely vaccinated, the hope was that they would encourage wary patients to do the same.
Hospitals were supposed to be hubs of education to help build trust within less confident communities. But not all hospitals have risen to that challenge.
Political affiliation seems to be one contributing factor in vaccine hesitancy. Take for example Calhoun, Ga., the seat of Gordon County, where residents voted for Donald Trump over Joe Biden by a 67-point margin in the 2020 general election. Studies have found that Republicans are more likely to decline vaccines than Democrats.
People who live in rural areas are less likely to be vaccinated than those who live in cities, and that’s true in Gordon County too. Vaccinations are lagging in this northwest corner of Georgia where factory jobs in chicken processing plants and carpet manufacturing energize the local economy. Just 24% of Gordon County residents are fully vaccinated, according to the Georgia Department of Public Health.
At AdventHealth Gordon, a 112-bed hospital in Calhoun, just 35% of the 1,723 workers that serve the hospital are at least partially vaccinated, according to data reported to HHS.
‘I am not vaccinated’
One reason some hospital staff say they are resisting COVID vaccination is because it’s so new and not yet fully approved by the FDA.
“I am not vaccinated,” said a social services worker for AdventHealth Gordon who asked that her name not be used because she was unauthorized to speak to this news organization and Georgia Health News (who collaborated on this project). “I just have not felt the need to do that at this time.”
The woman said she doesn’t have a problem with vaccines. She gets the flu shot every year. “I’ve been vaccinated all my life,” she said. But she doesn’t view COVID-19 vaccination in the same way.
“I want to see more testing done,” she said. “It took a long time to get a flu vaccine, and we made a COVID vaccine in 6 months. I want to know, before I start putting something into my body, that the testing is done.”
Staff at her hospital were given the option to be vaccinated or wear a mask. She chose the mask.
Many of her coworkers share her feelings, she said.
Mask expert Linsey Marr, PhD, a professor of civil and environmental engineering at Virginia Tech University, Blacksburg, Va., said N95 masks and vaccines are both highly effective, but the protection from the vaccine is superior because it is continuous.
“It’s hard to wear an N95 at all times. You have to take it off to eat, for example, in a break room in a hospital. I should point out that you can be exposed to the virus in other buildings besides a hospital – restaurants, stores, people’s homes – and because someone can be infected without symptoms, you could easily be around an infected person without knowing it,” she said.
Eventually, staff at AdventHealth Gordon may get a stronger nudge to get the shots. Chief Medical Officer Joseph Joyave, MD, said AdventHealth asks workers to get flu vaccines or provide the hospital with a reason why they won’t. He expects a similar policy will be adopted for COVID vaccines once they are fully licensed by the FDA.
In the meantime, he does not believe that the hospital is putting patients at risk with its low vaccination rate. “We continue to use PPE, masking in all clinical areas, and continue to screen daily all employees and visitors,” he said.
AdventHealth, the 12th largest hospital system in the nation with 49 hospitals, has at least 20 hospitals with vaccination rates lower than 50%, according to HHS data.
Other hospital systems have approached hesitation around the COVID vaccines differently.
When infectious disease experts at Vanderbilt Hospital in Nashville realized early on that many of their workers felt unsure about the vaccines, they set out to provide a wealth of information.
“There was a lot of hesitancy and skepticism,” said William Schaffner, MD, a professor of preventive medicine and infectious disease at Vanderbilt. So the infectious disease division put together a multifaceted program including Q&As, educational sessions, and one-on-one visits with employees “from the custodians all the way up to the C-Suite,” he said.
Today, HHS data shows the hospital is 83% vaccinated. Dr. Schaffner thinks the true number is probably higher, about 90%. “We’re very pleased with that,” he said.
In his experience with flu vaccinations, it was extremely difficult in the first year to get workers to take flu shots. The second year it was easier. By the third year it was humdrum, he said, because it had become a cultural norm.
Dr. Schaffner expects winning people over to the COVID vaccines will follow a similar course, but “we’re not there yet,” he said.
Protecting patients and caregivers
There is no question that health care workers carried a heavy load through the worst months of the pandemic. Many of them worked to the point of exhaustion and burnout. Some were the only conduits between isolated patients and their families, holding hands and mobile phones so distanced loved ones could video chat. Many were left inadequately protected because of shortages of masks, gowns, gloves, and other gear.
An investigation by Kaiser Health News and The Guardian recently revealed that more than 3,600 health care workers died in COVID’s first year in the United States.
Vaccination of health care workers is important to protect these frontline workers and their families who will continue to be at risk of coming into contact with the infection, even as the number of cases falls.
Hesitancy in health care is also dangerous because these clinicians and allied health workers – who may not show any symptoms – can also carry the virus to someone who wouldn’t survive an infection, including patients with organ transplants, those with autoimmune diseases, premature infants, and the elderly.
It is not known how often patients in the United States are infected with COVID in health care settings, but case reports reveal that hospitals are still experiencing outbreaks.
On June 1, Northern Lights A.R. Gould Hospital in Presque Isle, Maine, announced a COVID outbreak on its medical-surgical unit. As of June 22, 13 residents and staff have caught the virus, according to the Maine Centers for Disease Control, which is investigating. Four of the first five staff members to test positive had not been fully vaccinated.
According to HHS data, about 20% of the health care workers at that hospital are still unvaccinated.
Oregon Health & Science University experienced a COVID outbreak connected to the hospital’s cardiovascular care unit from April to mid-May of this year. According to hospital spokesperson Tracy Brawley, a patient visitor brought the infection to campus, where it ultimately spread to 14 others, including “patients, visitors, employees, and learners.”
In a written statement, the hospital said “nearly all” health care workers who tested positive were previously vaccinated and experienced no symptoms or only minor ones. The hospital said it hasn’t identified any onward transmission from health care workers to patients, and also stated: “It is not yet understood how transmission may have occurred between patients, visitors, and health care workers.”
In March, an unvaccinated health care worker in Kentucky carried a SARS-CoV-2 variant back to the nursing home where the person worked. Some 90% of the residents were fully vaccinated. Ultimately, 26 patients were infected; 18 of them were fully vaccinated. And 20 health care workers, four of whom were vaccinated, were infected.
Vaccines slowed the virus down and made infections less severe, but in this fragile population, they couldn’t stop it completely. One resident, who had survived a bout of COVID almost a year earlier, died. According to the CDC’s Morbidity and Mortality Weekly Report, 47% of the workers in that facility were unvaccinated.
In the United Kingdom, statistics collected through that country’s National Health Service also suggest a heavy toll. More than 32,300 patients caught COVID in English hospitals since March 2020. Up to 8,700 of them died, according to a recent analysis by The Guardian. The U.K. government recently made COVID vaccinations mandatory for health care workers.
COVID delays cancer care
When Mr. Oswalt, the Fort Worth, Texas man with non-Hodgkin lymphoma, contracted COVID-19, the virus took down his kidneys first. Toxins were building up in his blood, so doctors prescribed dialysis to support his body and buy his kidneys time to heal.
He was in one of these dialysis treatments when his lungs succumbed.
“Look, I can’t breathe,” he told the nurse who was supervising his treatment. The nurse gestured to an oxygen tank already hanging by his side, and said, “You should be OK.”
But he wasn’t.
“I can’t breathe,” Mr. Oswalt said again. Then the air hunger hit. Mr. Oswalt began gasping and couldn’t stop. Today, his voice breaks when he describes this moment. “A lot of it becomes a blur.”
When Mr. Oswalt, 61, regained consciousness, he was hooked up to a ventilator to ease his breathing.
For days, Mr. Oswalt clung to the edge of life. His wife, Molly, who wasn’t allowed to see him in the hospital, got a call that he might not make it through the night. She made frantic phone calls to her brother and sister and prayed.
Mr. Oswalt was on a ventilator for about a week. His kidneys and lungs healed enough so that he could restart his chemotherapy. He was eventually discharged home on January 22.
The last time he was scanned, the large tumor in his chest had shrunk from the size of a grapefruit to the size of a dime.
But having COVID on top of cancer has had a devastating effect on his life. Before he got sick, Molly said, he couldn’t stay still. He was busy all the time. After spending months in the hospital, his energy was depleted. He couldn’t keep his swimming pool installation business going.
He and Molly had to give up their house in Fort Worth and move in with family in Amarillo. He has had to pause his cancer treatments while doctors wait for his kidneys to heal. Relatives have been raising money on GoFundMe to pay their bills.
Months after moving across the state to Amarillo and hoping for better days, Tim said he got good news this week: He no longer needs dialysis. A new round of tests found no signs of cancer. His white blood cell count is back to normal. His lymph nodes are no longer swollen.
He goes back for another scan in a few weeks, but the doctor told him she isn’t going to recommend any further chemo at this point.
“It was shocking, to tell you the truth. It still is. When I talk about it, I get kind of emotional” about his recovery, he said.
Tim said he was really dreading more chemotherapy. His hair has just started growing back. He can finally taste food again. He wasn’t ready to face more side effects from the treatments, or the COVID – he no longer knows exactly which diagnosis led to his most debilitating symptoms.
He said his ordeal has left him with no patience for health care workers who don’t think they need to be vaccinated.
The way he sees it, it’s no different than the electrical training he had to get before he could wire the lights and pumps in a swimming pool.
“You know, if I don’t certify and keep my license, I can’t work on anything electrical. So, if I’ve made the choice not to go down and take the test and get a license, then I made the choice not to work on electrical stuff,” he said.
He supports the growing number of hospitals that have made vaccination mandatory for their workers.
“They don’t let electricians put people at risk. And they shouldn’t let health care workers for sure,” he said.
A version of this article first appeared on Medscape.com.
Tim Oswalt had been in a Fort Worth, Texas, hospital for over a month, receiving treatment for a grapefruit-sized tumor in his chest that was pressing on his heart and lungs. It turned out to be stage 3 non-Hodgkin lymphoma.
Then one day in January, he was moved from his semi-private room to an isolated one with special ventilation. The staff explained he had been infected by the virus that was once again surging in many areas of the country, including Texas.
“How the hell did I catch COVID?” he asked the staff, who now approached him in full moon-suit personal protective equipment (PPE).
The hospital was locked down, and Mr. Oswalt hadn’t had any visitors in weeks. Neither of his two roommates tested positive. He’d been tested for COVID several times over the course of his nearly 5-week stay and was always negative.
“‘Well, you know, it’s easy to [catch it] in a hospital,’” Mr. Oswalt said he was told by hospital staff. “‘We’re having a bad outbreak. So you were just exposed somehow.’”

Officials at John Peter Smith Hospital, where Mr. Oswalt was treated, said they are puzzled by his case. According to their infection prevention team, none of his caregivers tested positive for COVID-19, nor did Mr. Oswalt share space with any other COVID-positive patients. And yet, local media reported a surge in cases among JPS hospital staff in December.
“Infection of any kind is a constant battle within hospitals and one that we all take seriously,” said Rob Stephenson, MD, chief quality officer at JPS Health Network. “Anyone in a vulnerable health condition at the height of the pandemic would have been at greater risk for contracting COVID-19 inside – or even more so, outside – the hospital.”
Mr. Oswalt was diagnosed with COVID in early January. JPS Hospital began vaccinating its health care workers about 2 weeks earlier, so there had not yet been enough time for any of them to develop full protection against catching or spreading the virus.
Today, the hospital said 74% of its staff – 5,300 of 7,200 workers – are now vaccinated.
against the SARS-CoV2 virus.
Refusing vaccinations
In fact, nationwide, 1 in 4 hospital workers who have direct contact with patients had not yet received a single dose of a COVID vaccine by the end of May, according to a WebMD and Medscape Medical News analysis of data collected by the U.S. Department of Health and Human Services (HHS) from 2,500 hospitals across the United States.
Among the nation’s 50 largest hospitals, the percentage of unvaccinated health care workers appears to be even larger, about 1 in 3. Vaccination rates range from a high of 99% at Houston Methodist Hospital, which was the first in the nation to mandate the shots for its workers, to a low between 30% and 40% at some hospitals in Florida.
Memorial Hermann Texas Medical Center in Houston has 1,180 beds and sits less than half a mile from Houston Methodist Hospital. But in terms of worker vaccinations, it is farther away.
Memorial Hermann reported to HHS that about 32% of its 28,000 workers haven’t been inoculated. The hospital’s PR office contests that figure, putting it closer to 25% unvaccinated across their health system. The hospital said it is boosting participation by offering a $300 “shot of hope” bonus to workers who start their vaccination series by the end of June.
Lakeland Regional Medical Center in Lakeland, Fla., reported to HHS that 63% of its health care personnel are still unvaccinated. The hospital did not return a call to verify that number.
To boost vaccination rates, more hospitals are starting to require the shots, after the Equal Employment Opportunity Commission gave its green light to mandates in May.
“It’s a real problem that you have such high levels of unvaccinated individuals in hospitals,” said Lawrence Gostin, JD, director of the O’Neill Institute for National and Global Health Law at Georgetown University, Washington.
“We have to protect our health workforce, and we have to protect our patients. Hospitals should be the safest places in the country, and the only way to make them safe is to have a fully vaccinated workforce,” Mr. Gostin said.
Is the data misleading?
The HHS system designed to amass hospital data was set up quickly, to respond to an emergency. For that reason, experts say the information hasn’t been as carefully collected or vetted as it normally would have been. Some hospitals may have misunderstood how to report their vaccination numbers.
In addition, reporting data on worker vaccinations is voluntary. Only about half of hospitals have chosen to share their numbers. In other cases, like Texas, states have blocked the public release of these statistics.
AdventHealth Orlando, a 1,300-bed hospital in Florida, reported to HHS that 56% of its staff have not started their shots. But spokesman Jeff Grainger said the figures probably overstate the number of unvaccinated workers because the hospital doesn’t always know when people get vaccinated outside of its campus, at a local pharmacy, for example.
For those reasons, the picture of health care worker vaccinations across the country is incomplete.
Where hospitals fall behind
Even if the data are flawed, the vaccination rates from hospitals mirror the general population. A May Gallup poll, for example, found 24% of Americans said they definitely won’t get the vaccine. Another 12% say they plan to get it but are waiting.
The data also align with recent studies. A review of 35 studies by researchers at New Mexico State University that assessed hesitancy in more than 76,000 health care workers around the world found about 23% of them were reluctant to get the shots.
An ongoing monthly survey of more than 1.9 million U.S. Facebook users led by researchers at Carnegie Mellon University, Pittsburgh recently looked at vaccine hesitancy by occupation. It revealed a spectrum of hesitancy among health care workers corresponding to income and education, ranging from a low of 9% among pharmacists to highs of 20%-23% among nursing aides and emergency medical technicians. About 12% of registered nurses and doctors admitted to being hesitant to get a shot.
“Health care workers are not monolithic,” said study author Jagdish Khubchandani, professor of public health sciences at New Mexico State.
“There’s a big divide between males, doctoral degree holders, older people and the younger low-income, low-education frontline, female, health care workers. They are the most hesitant,” he said. Support staff typically outnumbers doctors at hospitals about 3 to 1.
“There is outreach work to be done there,” said Robin Mejia, PhD, director of the Statistics and Human Rights Program at Carnegie Mellon, who is leading the study on Facebook’s survey data. “These are also high-contact professions. These are people who are seeing patients on a regular basis.”
That’s why, when the Centers for Disease Control and Prevention was planning the national vaccine rollout, they prioritized health care workers for the initially scarce first doses. The intent was to protect vulnerable workers and their patients who are at high risk of infection. But the CDC had another reason for putting health care workers first: After they were safely vaccinated, the hope was that they would encourage wary patients to do the same.
Hospitals were supposed to be hubs of education to help build trust within less confident communities. But not all hospitals have risen to that challenge.
Political affiliation seems to be one contributing factor in vaccine hesitancy. Take for example Calhoun, Ga., the seat of Gordon County, where residents voted for Donald Trump over Joe Biden by a 67-point margin in the 2020 general election. Studies have found that Republicans are more likely to decline vaccines than Democrats.
People who live in rural areas are less likely to be vaccinated than those who live in cities, and that’s true in Gordon County too. Vaccinations are lagging in this northwest corner of Georgia where factory jobs in chicken processing plants and carpet manufacturing energize the local economy. Just 24% of Gordon County residents are fully vaccinated, according to the Georgia Department of Public Health.
At AdventHealth Gordon, a 112-bed hospital in Calhoun, just 35% of the 1,723 workers that serve the hospital are at least partially vaccinated, according to data reported to HHS.
‘I am not vaccinated’
One reason some hospital staff say they are resisting COVID vaccination is because it’s so new and not yet fully approved by the FDA.
“I am not vaccinated,” said a social services worker for AdventHealth Gordon who asked that her name not be used because she was unauthorized to speak to this news organization and Georgia Health News (who collaborated on this project). “I just have not felt the need to do that at this time.”
The woman said she doesn’t have a problem with vaccines. She gets the flu shot every year. “I’ve been vaccinated all my life,” she said. But she doesn’t view COVID-19 vaccination in the same way.
“I want to see more testing done,” she said. “It took a long time to get a flu vaccine, and we made a COVID vaccine in 6 months. I want to know, before I start putting something into my body, that the testing is done.”
Staff at her hospital were given the option to be vaccinated or wear a mask. She chose the mask.
Many of her coworkers share her feelings, she said.
Mask expert Linsey Marr, PhD, a professor of civil and environmental engineering at Virginia Tech University, Blacksburg, Va., said N95 masks and vaccines are both highly effective, but the protection from the vaccine is superior because it is continuous.
“It’s hard to wear an N95 at all times. You have to take it off to eat, for example, in a break room in a hospital. I should point out that you can be exposed to the virus in other buildings besides a hospital – restaurants, stores, people’s homes – and because someone can be infected without symptoms, you could easily be around an infected person without knowing it,” she said.
Eventually, staff at AdventHealth Gordon may get a stronger nudge to get the shots. Chief Medical Officer Joseph Joyave, MD, said AdventHealth asks workers to get flu vaccines or provide the hospital with a reason why they won’t. He expects a similar policy will be adopted for COVID vaccines once they are fully licensed by the FDA.
In the meantime, he does not believe that the hospital is putting patients at risk with its low vaccination rate. “We continue to use PPE, masking in all clinical areas, and continue to screen daily all employees and visitors,” he said.
AdventHealth, the 12th largest hospital system in the nation with 49 hospitals, has at least 20 hospitals with vaccination rates lower than 50%, according to HHS data.
Other hospital systems have approached hesitation around the COVID vaccines differently.
When infectious disease experts at Vanderbilt Hospital in Nashville realized early on that many of their workers felt unsure about the vaccines, they set out to provide a wealth of information.
“There was a lot of hesitancy and skepticism,” said William Schaffner, MD, a professor of preventive medicine and infectious disease at Vanderbilt. So the infectious disease division put together a multifaceted program including Q&As, educational sessions, and one-on-one visits with employees “from the custodians all the way up to the C-Suite,” he said.
Today, HHS data shows the hospital is 83% vaccinated. Dr. Schaffner thinks the true number is probably higher, about 90%. “We’re very pleased with that,” he said.
In his experience with flu vaccinations, it was extremely difficult in the first year to get workers to take flu shots. The second year it was easier. By the third year it was humdrum, he said, because it had become a cultural norm.
Dr. Schaffner expects winning people over to the COVID vaccines will follow a similar course, but “we’re not there yet,” he said.
Protecting patients and caregivers
There is no question that health care workers carried a heavy load through the worst months of the pandemic. Many of them worked to the point of exhaustion and burnout. Some were the only conduits between isolated patients and their families, holding hands and mobile phones so distanced loved ones could video chat. Many were left inadequately protected because of shortages of masks, gowns, gloves, and other gear.
An investigation by Kaiser Health News and The Guardian recently revealed that more than 3,600 health care workers died in COVID’s first year in the United States.
Vaccination of health care workers is important to protect these frontline workers and their families who will continue to be at risk of coming into contact with the infection, even as the number of cases falls.
Hesitancy in health care is also dangerous because these clinicians and allied health workers – who may not show any symptoms – can also carry the virus to someone who wouldn’t survive an infection, including patients with organ transplants, those with autoimmune diseases, premature infants, and the elderly.
It is not known how often patients in the United States are infected with COVID in health care settings, but case reports reveal that hospitals are still experiencing outbreaks.
On June 1, Northern Lights A.R. Gould Hospital in Presque Isle, Maine, announced a COVID outbreak on its medical-surgical unit. As of June 22, 13 residents and staff have caught the virus, according to the Maine Centers for Disease Control, which is investigating. Four of the first five staff members to test positive had not been fully vaccinated.
According to HHS data, about 20% of the health care workers at that hospital are still unvaccinated.
Oregon Health & Science University experienced a COVID outbreak connected to the hospital’s cardiovascular care unit from April to mid-May of this year. According to hospital spokesperson Tracy Brawley, a patient visitor brought the infection to campus, where it ultimately spread to 14 others, including “patients, visitors, employees, and learners.”
In a written statement, the hospital said “nearly all” health care workers who tested positive were previously vaccinated and experienced no symptoms or only minor ones. The hospital said it hasn’t identified any onward transmission from health care workers to patients, and also stated: “It is not yet understood how transmission may have occurred between patients, visitors, and health care workers.”
In March, an unvaccinated health care worker in Kentucky carried a SARS-CoV-2 variant back to the nursing home where the person worked. Some 90% of the residents were fully vaccinated. Ultimately, 26 patients were infected; 18 of them were fully vaccinated. And 20 health care workers, four of whom were vaccinated, were infected.
Vaccines slowed the virus down and made infections less severe, but in this fragile population, they couldn’t stop it completely. One resident, who had survived a bout of COVID almost a year earlier, died. According to the CDC’s Morbidity and Mortality Weekly Report, 47% of the workers in that facility were unvaccinated.
In the United Kingdom, statistics collected through that country’s National Health Service also suggest a heavy toll. More than 32,300 patients caught COVID in English hospitals since March 2020. Up to 8,700 of them died, according to a recent analysis by The Guardian. The U.K. government recently made COVID vaccinations mandatory for health care workers.
COVID delays cancer care
When Mr. Oswalt, the Fort Worth, Texas man with non-Hodgkin lymphoma, contracted COVID-19, the virus took down his kidneys first. Toxins were building up in his blood, so doctors prescribed dialysis to support his body and buy his kidneys time to heal.
He was in one of these dialysis treatments when his lungs succumbed.
“Look, I can’t breathe,” he told the nurse who was supervising his treatment. The nurse gestured to an oxygen tank already hanging by his side, and said, “You should be OK.”
But he wasn’t.
“I can’t breathe,” Mr. Oswalt said again. Then the air hunger hit. Mr. Oswalt began gasping and couldn’t stop. Today, his voice breaks when he describes this moment. “A lot of it becomes a blur.”
When Mr. Oswalt, 61, regained consciousness, he was hooked up to a ventilator to ease his breathing.
For days, Mr. Oswalt clung to the edge of life. His wife, Molly, who wasn’t allowed to see him in the hospital, got a call that he might not make it through the night. She made frantic phone calls to her brother and sister and prayed.
Mr. Oswalt was on a ventilator for about a week. His kidneys and lungs healed enough so that he could restart his chemotherapy. He was eventually discharged home on January 22.
The last time he was scanned, the large tumor in his chest had shrunk from the size of a grapefruit to the size of a dime.
But having COVID on top of cancer has had a devastating effect on his life. Before he got sick, Molly said, he couldn’t stay still. He was busy all the time. After spending months in the hospital, his energy was depleted. He couldn’t keep his swimming pool installation business going.
He and Molly had to give up their house in Fort Worth and move in with family in Amarillo. He has had to pause his cancer treatments while doctors wait for his kidneys to heal. Relatives have been raising money on GoFundMe to pay their bills.
Months after moving across the state to Amarillo and hoping for better days, Tim said he got good news this week: He no longer needs dialysis. A new round of tests found no signs of cancer. His white blood cell count is back to normal. His lymph nodes are no longer swollen.
He goes back for another scan in a few weeks, but the doctor told him she isn’t going to recommend any further chemo at this point.
“It was shocking, to tell you the truth. It still is. When I talk about it, I get kind of emotional” about his recovery, he said.
Tim said he was really dreading more chemotherapy. His hair has just started growing back. He can finally taste food again. He wasn’t ready to face more side effects from the treatments, or the COVID – he no longer knows exactly which diagnosis led to his most debilitating symptoms.
He said his ordeal has left him with no patience for health care workers who don’t think they need to be vaccinated.
The way he sees it, it’s no different than the electrical training he had to get before he could wire the lights and pumps in a swimming pool.
“You know, if I don’t certify and keep my license, I can’t work on anything electrical. So, if I’ve made the choice not to go down and take the test and get a license, then I made the choice not to work on electrical stuff,” he said.
He supports the growing number of hospitals that have made vaccination mandatory for their workers.
“They don’t let electricians put people at risk. And they shouldn’t let health care workers for sure,” he said.
A version of this article first appeared on Medscape.com.
Tim Oswalt had been in a Fort Worth, Texas, hospital for over a month, receiving treatment for a grapefruit-sized tumor in his chest that was pressing on his heart and lungs. It turned out to be stage 3 non-Hodgkin lymphoma.
Then one day in January, he was moved from his semi-private room to an isolated one with special ventilation. The staff explained he had been infected by the virus that was once again surging in many areas of the country, including Texas.
“How the hell did I catch COVID?” he asked the staff, who now approached him in full moon-suit personal protective equipment (PPE).
The hospital was locked down, and Mr. Oswalt hadn’t had any visitors in weeks. Neither of his two roommates tested positive. He’d been tested for COVID several times over the course of his nearly 5-week stay and was always negative.
“‘Well, you know, it’s easy to [catch it] in a hospital,’” Mr. Oswalt said he was told by hospital staff. “‘We’re having a bad outbreak. So you were just exposed somehow.’”

Officials at John Peter Smith Hospital, where Mr. Oswalt was treated, said they are puzzled by his case. According to their infection prevention team, none of his caregivers tested positive for COVID-19, nor did Mr. Oswalt share space with any other COVID-positive patients. And yet, local media reported a surge in cases among JPS hospital staff in December.
“Infection of any kind is a constant battle within hospitals and one that we all take seriously,” said Rob Stephenson, MD, chief quality officer at JPS Health Network. “Anyone in a vulnerable health condition at the height of the pandemic would have been at greater risk for contracting COVID-19 inside – or even more so, outside – the hospital.”
Mr. Oswalt was diagnosed with COVID in early January. JPS Hospital began vaccinating its health care workers about 2 weeks earlier, so there had not yet been enough time for any of them to develop full protection against catching or spreading the virus.
Today, the hospital said 74% of its staff – 5,300 of 7,200 workers – are now vaccinated.
against the SARS-CoV2 virus.
Refusing vaccinations
In fact, nationwide, 1 in 4 hospital workers who have direct contact with patients had not yet received a single dose of a COVID vaccine by the end of May, according to a WebMD and Medscape Medical News analysis of data collected by the U.S. Department of Health and Human Services (HHS) from 2,500 hospitals across the United States.
Among the nation’s 50 largest hospitals, the percentage of unvaccinated health care workers appears to be even larger, about 1 in 3. Vaccination rates range from a high of 99% at Houston Methodist Hospital, which was the first in the nation to mandate the shots for its workers, to a low between 30% and 40% at some hospitals in Florida.
Memorial Hermann Texas Medical Center in Houston has 1,180 beds and sits less than half a mile from Houston Methodist Hospital. But in terms of worker vaccinations, it is farther away.
Memorial Hermann reported to HHS that about 32% of its 28,000 workers haven’t been inoculated. The hospital’s PR office contests that figure, putting it closer to 25% unvaccinated across their health system. The hospital said it is boosting participation by offering a $300 “shot of hope” bonus to workers who start their vaccination series by the end of June.
Lakeland Regional Medical Center in Lakeland, Fla., reported to HHS that 63% of its health care personnel are still unvaccinated. The hospital did not return a call to verify that number.
To boost vaccination rates, more hospitals are starting to require the shots, after the Equal Employment Opportunity Commission gave its green light to mandates in May.
“It’s a real problem that you have such high levels of unvaccinated individuals in hospitals,” said Lawrence Gostin, JD, director of the O’Neill Institute for National and Global Health Law at Georgetown University, Washington.
“We have to protect our health workforce, and we have to protect our patients. Hospitals should be the safest places in the country, and the only way to make them safe is to have a fully vaccinated workforce,” Mr. Gostin said.
Is the data misleading?
The HHS system designed to amass hospital data was set up quickly, to respond to an emergency. For that reason, experts say the information hasn’t been as carefully collected or vetted as it normally would have been. Some hospitals may have misunderstood how to report their vaccination numbers.
In addition, reporting data on worker vaccinations is voluntary. Only about half of hospitals have chosen to share their numbers. In other cases, like Texas, states have blocked the public release of these statistics.
AdventHealth Orlando, a 1,300-bed hospital in Florida, reported to HHS that 56% of its staff have not started their shots. But spokesman Jeff Grainger said the figures probably overstate the number of unvaccinated workers because the hospital doesn’t always know when people get vaccinated outside of its campus, at a local pharmacy, for example.
For those reasons, the picture of health care worker vaccinations across the country is incomplete.
Where hospitals fall behind
Even if the data are flawed, the vaccination rates from hospitals mirror the general population. A May Gallup poll, for example, found 24% of Americans said they definitely won’t get the vaccine. Another 12% say they plan to get it but are waiting.
The data also align with recent studies. A review of 35 studies by researchers at New Mexico State University that assessed hesitancy in more than 76,000 health care workers around the world found about 23% of them were reluctant to get the shots.
An ongoing monthly survey of more than 1.9 million U.S. Facebook users led by researchers at Carnegie Mellon University, Pittsburgh recently looked at vaccine hesitancy by occupation. It revealed a spectrum of hesitancy among health care workers corresponding to income and education, ranging from a low of 9% among pharmacists to highs of 20%-23% among nursing aides and emergency medical technicians. About 12% of registered nurses and doctors admitted to being hesitant to get a shot.
“Health care workers are not monolithic,” said study author Jagdish Khubchandani, professor of public health sciences at New Mexico State.
“There’s a big divide between males, doctoral degree holders, older people and the younger low-income, low-education frontline, female, health care workers. They are the most hesitant,” he said. Support staff typically outnumbers doctors at hospitals about 3 to 1.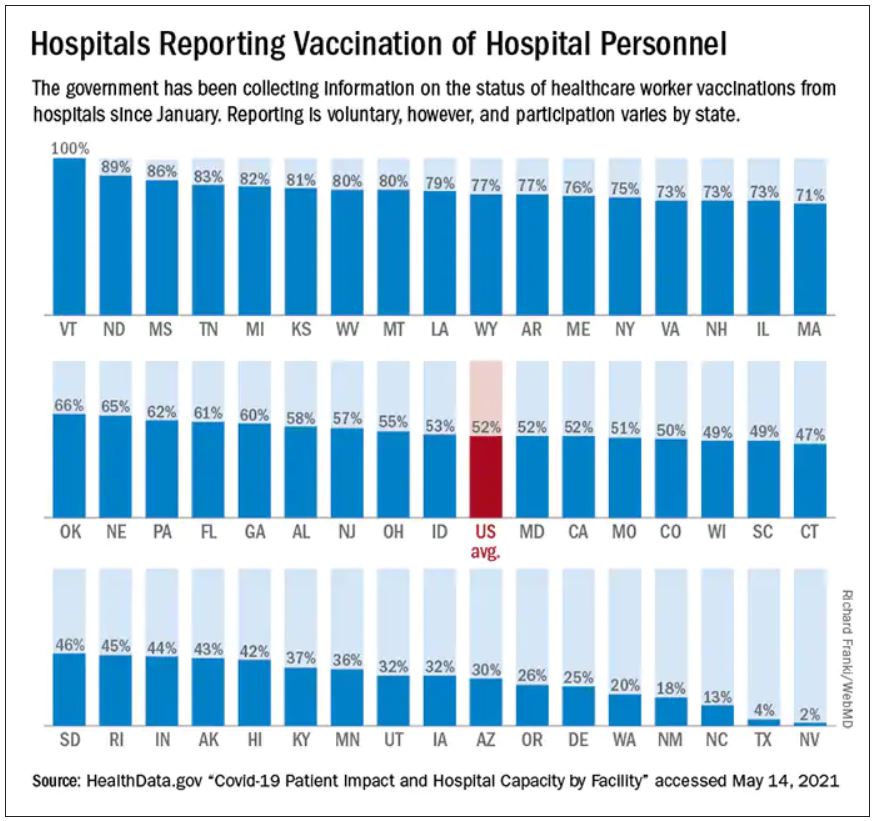
“There is outreach work to be done there,” said Robin Mejia, PhD, director of the Statistics and Human Rights Program at Carnegie Mellon, who is leading the study on Facebook’s survey data. “These are also high-contact professions. These are people who are seeing patients on a regular basis.”
That’s why, when the Centers for Disease Control and Prevention was planning the national vaccine rollout, they prioritized health care workers for the initially scarce first doses. The intent was to protect vulnerable workers and their patients who are at high risk of infection. But the CDC had another reason for putting health care workers first: After they were safely vaccinated, the hope was that they would encourage wary patients to do the same.
Hospitals were supposed to be hubs of education to help build trust within less confident communities. But not all hospitals have risen to that challenge.
Political affiliation seems to be one contributing factor in vaccine hesitancy. Take for example Calhoun, Ga., the seat of Gordon County, where residents voted for Donald Trump over Joe Biden by a 67-point margin in the 2020 general election. Studies have found that Republicans are more likely to decline vaccines than Democrats.
People who live in rural areas are less likely to be vaccinated than those who live in cities, and that’s true in Gordon County too. Vaccinations are lagging in this northwest corner of Georgia where factory jobs in chicken processing plants and carpet manufacturing energize the local economy. Just 24% of Gordon County residents are fully vaccinated, according to the Georgia Department of Public Health.
At AdventHealth Gordon, a 112-bed hospital in Calhoun, just 35% of the 1,723 workers that serve the hospital are at least partially vaccinated, according to data reported to HHS.
‘I am not vaccinated’
One reason some hospital staff say they are resisting COVID vaccination is because it’s so new and not yet fully approved by the FDA.
“I am not vaccinated,” said a social services worker for AdventHealth Gordon who asked that her name not be used because she was unauthorized to speak to this news organization and Georgia Health News (who collaborated on this project). “I just have not felt the need to do that at this time.”
The woman said she doesn’t have a problem with vaccines. She gets the flu shot every year. “I’ve been vaccinated all my life,” she said. But she doesn’t view COVID-19 vaccination in the same way.
“I want to see more testing done,” she said. “It took a long time to get a flu vaccine, and we made a COVID vaccine in 6 months. I want to know, before I start putting something into my body, that the testing is done.”
Staff at her hospital were given the option to be vaccinated or wear a mask. She chose the mask.
Many of her coworkers share her feelings, she said.
Mask expert Linsey Marr, PhD, a professor of civil and environmental engineering at Virginia Tech University, Blacksburg, Va., said N95 masks and vaccines are both highly effective, but the protection from the vaccine is superior because it is continuous.
“It’s hard to wear an N95 at all times. You have to take it off to eat, for example, in a break room in a hospital. I should point out that you can be exposed to the virus in other buildings besides a hospital – restaurants, stores, people’s homes – and because someone can be infected without symptoms, you could easily be around an infected person without knowing it,” she said.
Eventually, staff at AdventHealth Gordon may get a stronger nudge to get the shots. Chief Medical Officer Joseph Joyave, MD, said AdventHealth asks workers to get flu vaccines or provide the hospital with a reason why they won’t. He expects a similar policy will be adopted for COVID vaccines once they are fully licensed by the FDA.
In the meantime, he does not believe that the hospital is putting patients at risk with its low vaccination rate. “We continue to use PPE, masking in all clinical areas, and continue to screen daily all employees and visitors,” he said.
AdventHealth, the 12th largest hospital system in the nation with 49 hospitals, has at least 20 hospitals with vaccination rates lower than 50%, according to HHS data.
Other hospital systems have approached hesitation around the COVID vaccines differently.
When infectious disease experts at Vanderbilt Hospital in Nashville realized early on that many of their workers felt unsure about the vaccines, they set out to provide a wealth of information.
“There was a lot of hesitancy and skepticism,” said William Schaffner, MD, a professor of preventive medicine and infectious disease at Vanderbilt. So the infectious disease division put together a multifaceted program including Q&As, educational sessions, and one-on-one visits with employees “from the custodians all the way up to the C-Suite,” he said.
Today, HHS data shows the hospital is 83% vaccinated. Dr. Schaffner thinks the true number is probably higher, about 90%. “We’re very pleased with that,” he said.
In his experience with flu vaccinations, it was extremely difficult in the first year to get workers to take flu shots. The second year it was easier. By the third year it was humdrum, he said, because it had become a cultural norm.
Dr. Schaffner expects winning people over to the COVID vaccines will follow a similar course, but “we’re not there yet,” he said.
Protecting patients and caregivers
There is no question that health care workers carried a heavy load through the worst months of the pandemic. Many of them worked to the point of exhaustion and burnout. Some were the only conduits between isolated patients and their families, holding hands and mobile phones so distanced loved ones could video chat. Many were left inadequately protected because of shortages of masks, gowns, gloves, and other gear.
An investigation by Kaiser Health News and The Guardian recently revealed that more than 3,600 health care workers died in COVID’s first year in the United States.
Vaccination of health care workers is important to protect these frontline workers and their families who will continue to be at risk of coming into contact with the infection, even as the number of cases falls.
Hesitancy in health care is also dangerous because these clinicians and allied health workers – who may not show any symptoms – can also carry the virus to someone who wouldn’t survive an infection, including patients with organ transplants, those with autoimmune diseases, premature infants, and the elderly.
It is not known how often patients in the United States are infected with COVID in health care settings, but case reports reveal that hospitals are still experiencing outbreaks.
On June 1, Northern Lights A.R. Gould Hospital in Presque Isle, Maine, announced a COVID outbreak on its medical-surgical unit. As of June 22, 13 residents and staff have caught the virus, according to the Maine Centers for Disease Control, which is investigating. Four of the first five staff members to test positive had not been fully vaccinated.
According to HHS data, about 20% of the health care workers at that hospital are still unvaccinated.
Oregon Health & Science University experienced a COVID outbreak connected to the hospital’s cardiovascular care unit from April to mid-May of this year. According to hospital spokesperson Tracy Brawley, a patient visitor brought the infection to campus, where it ultimately spread to 14 others, including “patients, visitors, employees, and learners.”
In a written statement, the hospital said “nearly all” health care workers who tested positive were previously vaccinated and experienced no symptoms or only minor ones. The hospital said it hasn’t identified any onward transmission from health care workers to patients, and also stated: “It is not yet understood how transmission may have occurred between patients, visitors, and health care workers.”
In March, an unvaccinated health care worker in Kentucky carried a SARS-CoV-2 variant back to the nursing home where the person worked. Some 90% of the residents were fully vaccinated. Ultimately, 26 patients were infected; 18 of them were fully vaccinated. And 20 health care workers, four of whom were vaccinated, were infected.
Vaccines slowed the virus down and made infections less severe, but in this fragile population, they couldn’t stop it completely. One resident, who had survived a bout of COVID almost a year earlier, died. According to the CDC’s Morbidity and Mortality Weekly Report, 47% of the workers in that facility were unvaccinated.
In the United Kingdom, statistics collected through that country’s National Health Service also suggest a heavy toll. More than 32,300 patients caught COVID in English hospitals since March 2020. Up to 8,700 of them died, according to a recent analysis by The Guardian. The U.K. government recently made COVID vaccinations mandatory for health care workers.
COVID delays cancer care
When Mr. Oswalt, the Fort Worth, Texas man with non-Hodgkin lymphoma, contracted COVID-19, the virus took down his kidneys first. Toxins were building up in his blood, so doctors prescribed dialysis to support his body and buy his kidneys time to heal.
He was in one of these dialysis treatments when his lungs succumbed.
“Look, I can’t breathe,” he told the nurse who was supervising his treatment. The nurse gestured to an oxygen tank already hanging by his side, and said, “You should be OK.”
But he wasn’t.
“I can’t breathe,” Mr. Oswalt said again. Then the air hunger hit. Mr. Oswalt began gasping and couldn’t stop. Today, his voice breaks when he describes this moment. “A lot of it becomes a blur.”
When Mr. Oswalt, 61, regained consciousness, he was hooked up to a ventilator to ease his breathing.
For days, Mr. Oswalt clung to the edge of life. His wife, Molly, who wasn’t allowed to see him in the hospital, got a call that he might not make it through the night. She made frantic phone calls to her brother and sister and prayed.
Mr. Oswalt was on a ventilator for about a week. His kidneys and lungs healed enough so that he could restart his chemotherapy. He was eventually discharged home on January 22.
The last time he was scanned, the large tumor in his chest had shrunk from the size of a grapefruit to the size of a dime.
But having COVID on top of cancer has had a devastating effect on his life. Before he got sick, Molly said, he couldn’t stay still. He was busy all the time. After spending months in the hospital, his energy was depleted. He couldn’t keep his swimming pool installation business going.
He and Molly had to give up their house in Fort Worth and move in with family in Amarillo. He has had to pause his cancer treatments while doctors wait for his kidneys to heal. Relatives have been raising money on GoFundMe to pay their bills.
Months after moving across the state to Amarillo and hoping for better days, Tim said he got good news this week: He no longer needs dialysis. A new round of tests found no signs of cancer. His white blood cell count is back to normal. His lymph nodes are no longer swollen.
He goes back for another scan in a few weeks, but the doctor told him she isn’t going to recommend any further chemo at this point.
“It was shocking, to tell you the truth. It still is. When I talk about it, I get kind of emotional” about his recovery, he said.
Tim said he was really dreading more chemotherapy. His hair has just started growing back. He can finally taste food again. He wasn’t ready to face more side effects from the treatments, or the COVID – he no longer knows exactly which diagnosis led to his most debilitating symptoms.
He said his ordeal has left him with no patience for health care workers who don’t think they need to be vaccinated.
The way he sees it, it’s no different than the electrical training he had to get before he could wire the lights and pumps in a swimming pool.
“You know, if I don’t certify and keep my license, I can’t work on anything electrical. So, if I’ve made the choice not to go down and take the test and get a license, then I made the choice not to work on electrical stuff,” he said.
He supports the growing number of hospitals that have made vaccination mandatory for their workers.
“They don’t let electricians put people at risk. And they shouldn’t let health care workers for sure,” he said.
A version of this article first appeared on Medscape.com.