User login
John Nelson, MD: A New Hospitalist
Ben was just accepted to med school!!! Hopefully, more acceptances will be forthcoming. We are very proud of Ben for all his hard work. Another doctor in the family.
I was delighted to find the above message from an old friend in my inbox. It got me thinking: Will Ben become a hospitalist? Will he join his dad’s hospitalist group? Will his dad encourage him to pursue a hospitalist career or something else?
Early Hospitalist Practice
The author of that email was Ben’s dad, Chuck Wilson. Chuck is the reason I’m a hospitalist. He was a year ahead of me in residency, and while still a resident, he somehow connected with a really busy family physician in town who was looking for someone to manage his hospital patients. Not one to be bound by convention, Chuck agreed to what was at the time a nearly unheard-of arrangement. He finished residency, joined the staff of the community hospital across town from our residency, and began caring for the family physician’s hospital patients. Within days, he was fielding calls from other doctors asking him to do the same for them. Within weeks of arriving, he had begun accepting essentially all unassigned medical admissions from the ED. This was in the 1980s; Chuck was among the nation’s first real hospitalists.
I don’t think Chuck spent any time worrying about how his practice was so different from the traditional internists and family physicians in the community. He was confident he was providing a valuable service to his patients and the medical community. The rapid growth in his patient census was an indicator he was on to something, and soon he and I began talking. He was looking for a partner.
In November of my third year of residency, I decided I would put off my endocrinology fellowship for a year or two and join Chuck in his new practice. From our conversations, I anticipated that I would care for exactly the kinds of patients that filled nearly all of my time as a resident. I wouldn’t need to learn the new skills in ambulatory medicine, and wouldn’t need to make the long-term commitment expected to join a traditional primary-care practice. And I would earn a competitive compensation and have a flexible lifestyle. I soon realized that hospitalist practice provided me with all of these advantages, so more than two decades later, I still haven’t gotten around to completing the application for an endocrine fellowship.
A Loose Arrangement
For the first few years, Chuck and I didn’t bother to have any sort of legal agreement with each other. We shook hands and agreed to a “reap what you till” form of compensation, which meant we didn’t have to work exactly the same amount, and never had disagreements about how practice revenue was divided between us.
Because of Chuck’s influence, we had miniscule overhead expenses, most likely less than 10% of revenue. We each bought our own malpractice insurance, paid our biller a percent of collections, and rented a pager. That was about it for overhead.
We had no rigid scheduling algorithm, the only requirement being that at least one of us needed to be working every day. Both of us worked most weekdays, but we took time off whenever it suited us. Our scheduling meetings were usually held when we bumped into one another while rounding and went something like this:
“You OK if I take five days off starting tomorrow?”
“Sure. That’s fine.”
Meeting adjourned.
For years, we had no official name for our practice. This became a bigger issue when our group had grown to four doctors, so we defaulted to referring to the group by the first letter of the last name of each doctor, in order of tenure: The WNKL Group. A more formal name was to follow a few years later when the group was even larger, but I’ve taken delight in hearing that WNKL has persisted in some places and documents around the hospital years later, even though N, K, and L left the group long ago.
In the first few years, we never thought about developing clinical protocols or measuring our efficiency or clinical effectiveness. Chuck was confident that compared to the traditional primary-care model, we were providing higher-quality care at a lower cost. But I wasn’t so sure. After a few years, we began seeing hospital data showing that our cost per case tended to be lower, and what little data we could get regarding our quality of care suggested that it was about the same, and in some cases might be better.
A principal reason the practice has survived more than 25 years is that other than a small “tax” during their first 18 months (mainly to cover the cost of recruiting them), new doctors were regarded as equals in the business. Chuck and subsequent doctors never tried to gain an advantage over newer doctors by trying to claim a greater share of the practice’s revenue or decision-making authority.
Chuck is still in the same group he founded. In 2000, I was lured away by the chance to start a new group and live in a place that both my wife and I love. He and I have enjoyed watching our field grow up, and we take satisfaction in our roles in its evolution.
Lessons Learned
The hospitalist model of practice didn’t have a single inventor or place of origin, and anyone involved in starting a practice in the 1980s or before should be proud to have invented their practice when no blueprint existed. Creative thinking and openness to a new way of doing things were critical in developing the first hospitalist practices. They also are useful traits in trying to improve modern hospitalist practices or other segments of our healthcare system.
Like many new developments in medicine, the economic effects of our practice—lower hospital cost per case—became apparent, especially to Chuck, before data regarding quality surfaced. I wish we had gotten more serious early on about capturing whatever quality data might have been available—clearly less than what is available today—and those in new healthcare endeavors today should try to measure quality at the outset. Unlike the 1980s, the current marketplace will help ensure that happens.
Coda
There is one other really cool thing about Chuck’s email at the beginning of this column: those three exclamation points! Chuck is typically laconic and understated, and not given to such displays of emotion, but there are few things that generate more enthusiasm than a parent sharing news of a child’s success.
So, Ben, as you start med school next year, I wish you the best. You can be sure I’ll be asking for updates about your progress. The most important thing is that you find a life and career that engages you to do good work for others and provides satisfaction. And whatever you choose to do after med school, I know you’ll continue to make your parents proud.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is course co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Ben was just accepted to med school!!! Hopefully, more acceptances will be forthcoming. We are very proud of Ben for all his hard work. Another doctor in the family.
I was delighted to find the above message from an old friend in my inbox. It got me thinking: Will Ben become a hospitalist? Will he join his dad’s hospitalist group? Will his dad encourage him to pursue a hospitalist career or something else?
Early Hospitalist Practice
The author of that email was Ben’s dad, Chuck Wilson. Chuck is the reason I’m a hospitalist. He was a year ahead of me in residency, and while still a resident, he somehow connected with a really busy family physician in town who was looking for someone to manage his hospital patients. Not one to be bound by convention, Chuck agreed to what was at the time a nearly unheard-of arrangement. He finished residency, joined the staff of the community hospital across town from our residency, and began caring for the family physician’s hospital patients. Within days, he was fielding calls from other doctors asking him to do the same for them. Within weeks of arriving, he had begun accepting essentially all unassigned medical admissions from the ED. This was in the 1980s; Chuck was among the nation’s first real hospitalists.
I don’t think Chuck spent any time worrying about how his practice was so different from the traditional internists and family physicians in the community. He was confident he was providing a valuable service to his patients and the medical community. The rapid growth in his patient census was an indicator he was on to something, and soon he and I began talking. He was looking for a partner.
In November of my third year of residency, I decided I would put off my endocrinology fellowship for a year or two and join Chuck in his new practice. From our conversations, I anticipated that I would care for exactly the kinds of patients that filled nearly all of my time as a resident. I wouldn’t need to learn the new skills in ambulatory medicine, and wouldn’t need to make the long-term commitment expected to join a traditional primary-care practice. And I would earn a competitive compensation and have a flexible lifestyle. I soon realized that hospitalist practice provided me with all of these advantages, so more than two decades later, I still haven’t gotten around to completing the application for an endocrine fellowship.
A Loose Arrangement
For the first few years, Chuck and I didn’t bother to have any sort of legal agreement with each other. We shook hands and agreed to a “reap what you till” form of compensation, which meant we didn’t have to work exactly the same amount, and never had disagreements about how practice revenue was divided between us.
Because of Chuck’s influence, we had miniscule overhead expenses, most likely less than 10% of revenue. We each bought our own malpractice insurance, paid our biller a percent of collections, and rented a pager. That was about it for overhead.
We had no rigid scheduling algorithm, the only requirement being that at least one of us needed to be working every day. Both of us worked most weekdays, but we took time off whenever it suited us. Our scheduling meetings were usually held when we bumped into one another while rounding and went something like this:
“You OK if I take five days off starting tomorrow?”
“Sure. That’s fine.”
Meeting adjourned.
For years, we had no official name for our practice. This became a bigger issue when our group had grown to four doctors, so we defaulted to referring to the group by the first letter of the last name of each doctor, in order of tenure: The WNKL Group. A more formal name was to follow a few years later when the group was even larger, but I’ve taken delight in hearing that WNKL has persisted in some places and documents around the hospital years later, even though N, K, and L left the group long ago.
In the first few years, we never thought about developing clinical protocols or measuring our efficiency or clinical effectiveness. Chuck was confident that compared to the traditional primary-care model, we were providing higher-quality care at a lower cost. But I wasn’t so sure. After a few years, we began seeing hospital data showing that our cost per case tended to be lower, and what little data we could get regarding our quality of care suggested that it was about the same, and in some cases might be better.
A principal reason the practice has survived more than 25 years is that other than a small “tax” during their first 18 months (mainly to cover the cost of recruiting them), new doctors were regarded as equals in the business. Chuck and subsequent doctors never tried to gain an advantage over newer doctors by trying to claim a greater share of the practice’s revenue or decision-making authority.
Chuck is still in the same group he founded. In 2000, I was lured away by the chance to start a new group and live in a place that both my wife and I love. He and I have enjoyed watching our field grow up, and we take satisfaction in our roles in its evolution.
Lessons Learned
The hospitalist model of practice didn’t have a single inventor or place of origin, and anyone involved in starting a practice in the 1980s or before should be proud to have invented their practice when no blueprint existed. Creative thinking and openness to a new way of doing things were critical in developing the first hospitalist practices. They also are useful traits in trying to improve modern hospitalist practices or other segments of our healthcare system.
Like many new developments in medicine, the economic effects of our practice—lower hospital cost per case—became apparent, especially to Chuck, before data regarding quality surfaced. I wish we had gotten more serious early on about capturing whatever quality data might have been available—clearly less than what is available today—and those in new healthcare endeavors today should try to measure quality at the outset. Unlike the 1980s, the current marketplace will help ensure that happens.
Coda
There is one other really cool thing about Chuck’s email at the beginning of this column: those three exclamation points! Chuck is typically laconic and understated, and not given to such displays of emotion, but there are few things that generate more enthusiasm than a parent sharing news of a child’s success.
So, Ben, as you start med school next year, I wish you the best. You can be sure I’ll be asking for updates about your progress. The most important thing is that you find a life and career that engages you to do good work for others and provides satisfaction. And whatever you choose to do after med school, I know you’ll continue to make your parents proud.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is course co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Ben was just accepted to med school!!! Hopefully, more acceptances will be forthcoming. We are very proud of Ben for all his hard work. Another doctor in the family.
I was delighted to find the above message from an old friend in my inbox. It got me thinking: Will Ben become a hospitalist? Will he join his dad’s hospitalist group? Will his dad encourage him to pursue a hospitalist career or something else?
Early Hospitalist Practice
The author of that email was Ben’s dad, Chuck Wilson. Chuck is the reason I’m a hospitalist. He was a year ahead of me in residency, and while still a resident, he somehow connected with a really busy family physician in town who was looking for someone to manage his hospital patients. Not one to be bound by convention, Chuck agreed to what was at the time a nearly unheard-of arrangement. He finished residency, joined the staff of the community hospital across town from our residency, and began caring for the family physician’s hospital patients. Within days, he was fielding calls from other doctors asking him to do the same for them. Within weeks of arriving, he had begun accepting essentially all unassigned medical admissions from the ED. This was in the 1980s; Chuck was among the nation’s first real hospitalists.
I don’t think Chuck spent any time worrying about how his practice was so different from the traditional internists and family physicians in the community. He was confident he was providing a valuable service to his patients and the medical community. The rapid growth in his patient census was an indicator he was on to something, and soon he and I began talking. He was looking for a partner.
In November of my third year of residency, I decided I would put off my endocrinology fellowship for a year or two and join Chuck in his new practice. From our conversations, I anticipated that I would care for exactly the kinds of patients that filled nearly all of my time as a resident. I wouldn’t need to learn the new skills in ambulatory medicine, and wouldn’t need to make the long-term commitment expected to join a traditional primary-care practice. And I would earn a competitive compensation and have a flexible lifestyle. I soon realized that hospitalist practice provided me with all of these advantages, so more than two decades later, I still haven’t gotten around to completing the application for an endocrine fellowship.
A Loose Arrangement
For the first few years, Chuck and I didn’t bother to have any sort of legal agreement with each other. We shook hands and agreed to a “reap what you till” form of compensation, which meant we didn’t have to work exactly the same amount, and never had disagreements about how practice revenue was divided between us.
Because of Chuck’s influence, we had miniscule overhead expenses, most likely less than 10% of revenue. We each bought our own malpractice insurance, paid our biller a percent of collections, and rented a pager. That was about it for overhead.
We had no rigid scheduling algorithm, the only requirement being that at least one of us needed to be working every day. Both of us worked most weekdays, but we took time off whenever it suited us. Our scheduling meetings were usually held when we bumped into one another while rounding and went something like this:
“You OK if I take five days off starting tomorrow?”
“Sure. That’s fine.”
Meeting adjourned.
For years, we had no official name for our practice. This became a bigger issue when our group had grown to four doctors, so we defaulted to referring to the group by the first letter of the last name of each doctor, in order of tenure: The WNKL Group. A more formal name was to follow a few years later when the group was even larger, but I’ve taken delight in hearing that WNKL has persisted in some places and documents around the hospital years later, even though N, K, and L left the group long ago.
In the first few years, we never thought about developing clinical protocols or measuring our efficiency or clinical effectiveness. Chuck was confident that compared to the traditional primary-care model, we were providing higher-quality care at a lower cost. But I wasn’t so sure. After a few years, we began seeing hospital data showing that our cost per case tended to be lower, and what little data we could get regarding our quality of care suggested that it was about the same, and in some cases might be better.
A principal reason the practice has survived more than 25 years is that other than a small “tax” during their first 18 months (mainly to cover the cost of recruiting them), new doctors were regarded as equals in the business. Chuck and subsequent doctors never tried to gain an advantage over newer doctors by trying to claim a greater share of the practice’s revenue or decision-making authority.
Chuck is still in the same group he founded. In 2000, I was lured away by the chance to start a new group and live in a place that both my wife and I love. He and I have enjoyed watching our field grow up, and we take satisfaction in our roles in its evolution.
Lessons Learned
The hospitalist model of practice didn’t have a single inventor or place of origin, and anyone involved in starting a practice in the 1980s or before should be proud to have invented their practice when no blueprint existed. Creative thinking and openness to a new way of doing things were critical in developing the first hospitalist practices. They also are useful traits in trying to improve modern hospitalist practices or other segments of our healthcare system.
Like many new developments in medicine, the economic effects of our practice—lower hospital cost per case—became apparent, especially to Chuck, before data regarding quality surfaced. I wish we had gotten more serious early on about capturing whatever quality data might have been available—clearly less than what is available today—and those in new healthcare endeavors today should try to measure quality at the outset. Unlike the 1980s, the current marketplace will help ensure that happens.
Coda
There is one other really cool thing about Chuck’s email at the beginning of this column: those three exclamation points! Chuck is typically laconic and understated, and not given to such displays of emotion, but there are few things that generate more enthusiasm than a parent sharing news of a child’s success.
So, Ben, as you start med school next year, I wish you the best. You can be sure I’ll be asking for updates about your progress. The most important thing is that you find a life and career that engages you to do good work for others and provides satisfaction. And whatever you choose to do after med school, I know you’ll continue to make your parents proud.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is course co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Host of Factors Play Into Hospitalist Billing for Patient Transfers
Patient Transfers
Hospitalist billing depends on several factors. Know your role and avoid common mistakes Patient transfers can occur for many reasons: advanced technological services required, health insurance coverage, or a change in the level of care, to name a few. Patient care that is provided in the acute-care setting does not always terminate with discharge to home. Frequently, hospitalists are involved in patient transfers to another location to receive additional services: intrafacility (a different unit or related facility within the same physical plant) or interfacility (geographically separate facilities). The hospitalist must identify his or her role in the transfer and the patient’s new environment.
Physician billing in the transferred setting depends upon several factors:1
- Shared or merged medical record;
- The attending of record in each setting;
- The requirements for care rendered by the hospitalist in each setting; and
- Service dates.
Intrafacility Initial Service
Let’s examine a common example: A hospitalist serves as the “attending of record” in an inpatient hospital where acute care is required for an 83-year-old female with hypertension and diabetes who sustained a left hip fracture. The hospitalist plans to discharge the patient to the rehabilitation unit. After transfer, the rehabilitation physician becomes the attending of record, and the hospitalist might be asked to provide ongoing care for the patient’s hypertension and diabetes.
What should the hospitalist report for the initial post-transfer service? The typical options to consider are:2
- Inpatient consultation (99251-99255);
- Initial hospital care (99221-99223); and
- Subsequent hospital care (99231-99233).
Report a consultation only if the rehab attending requests an opinion or advice for an unrelated, new condition instead of previously treated conditions, and the requesting physician’s intent is for opinion or advice on management options rather than the a priori intent for the hospitalist to assume the patient’s medical care. If these requirements are met, the hospitalist may report an inpatient consultation code (99251-99255). Alternatively, if the intent or need represents a continuity of medical care provided during the acute episode of care, report the most appropriate subsequent hospital care code (99231-99233) for the hospitalist’s initial rehab visit and all follow-up services.
Initial hospital care (99221-99223) codes can only be reported for Medicare beneficiaries in place of consultation codes (99251-99255), as Medicare ceased to reimburse consultation codes.3 Most other payors who do not recognize consultation services only allow one initial hospital care code per hospitalization, reserved for the attending of record.
Interfacility Initial Service
Hospitalist groups provide patient care and coverage in many different types of facilities. Confusion often arises when the “attending of record” during acute care and the “subacute” setting (e.g. long-term acute-care hospital) are two different hospitalists from the same group practice. The hospitalist receiving the patient in the transfer facility may decide to report subsequent hospital care (99231-99233), because the group has been providing ongoing care to this patient. In this scenario, the hospitalist group could be losing revenue if an admission service (99221-99223) was not reported.
An initial hospital care service (99221-99223) is permitted when the transfer is between:
- Different hospitals;
- Different facilities under common ownership which do not have merged records; or
- Between the acute-care hospital and a PPS (prospective payment system)-exempt unit within the same hospital when there are no merged records (e.g. Medicare Part A-covered inpatient care in psychiatric, rehabilitation, critical access, and long-term care hospitals).4
In all other transfer circumstances not meeting the elements noted above, the physician should bill only the appropriate level of subsequent hospital care (99231-99233) for the date of transfer.1 Do not equate “merged records” to commonly accessible charts via an electronic medical record system or an electronic storage system. If the medical record for the patient’s acute stay is “closed” and the patient is given a separate medical record and registration for the stay in the transferred facility, consider the transfer stay as a separate admission.
Billing Two Services on Day of Transfer
Whether the transfer is classified as intrafacility or interfacility, an individual hospitalist or two separate hospitalists from the same group practice may provide the acute-care discharge and the transfer admission. A hospital discharge day management service (99238-99239) and an initial hospital care service (99221-99223) can only be reported if they do not occur on the same day.1 Physicians in the same group practice who are in the same specialty must bill and be paid as though they were a single physician; if more than one evaluation and management (face to face) service is provided on the same day to the same patient by the same physician or more than one physician in the same specialty in the same group, only one evaluation and management service may be reported.5
The Exception
CMS will allow a single hospitalist or two hospitalists from the same group practice to report a discharge day management service on the same day as an admission service. When they are billed by the same physician or group with the same date of service, contractors are instructed to pay the hospital discharge day management code (99238-99239) in addition to a nursing facility admission code (99304-99306).6
Conversely, if the patient is admitted to a hospital (99221-99223) following a nursing facility discharge (99315-99316) on the same date by the same physician/group, insurers will only reimburse the initial hospital care code. Payment for the initial hospital care service includes all work performed by the physician/group in all sites of service on that date.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is faculty for SHM’s inpatient coding course.
References available online at the-hospitalist.org
Patient Transfers
Hospitalist billing depends on several factors. Know your role and avoid common mistakes Patient transfers can occur for many reasons: advanced technological services required, health insurance coverage, or a change in the level of care, to name a few. Patient care that is provided in the acute-care setting does not always terminate with discharge to home. Frequently, hospitalists are involved in patient transfers to another location to receive additional services: intrafacility (a different unit or related facility within the same physical plant) or interfacility (geographically separate facilities). The hospitalist must identify his or her role in the transfer and the patient’s new environment.
Physician billing in the transferred setting depends upon several factors:1
- Shared or merged medical record;
- The attending of record in each setting;
- The requirements for care rendered by the hospitalist in each setting; and
- Service dates.
Intrafacility Initial Service
Let’s examine a common example: A hospitalist serves as the “attending of record” in an inpatient hospital where acute care is required for an 83-year-old female with hypertension and diabetes who sustained a left hip fracture. The hospitalist plans to discharge the patient to the rehabilitation unit. After transfer, the rehabilitation physician becomes the attending of record, and the hospitalist might be asked to provide ongoing care for the patient’s hypertension and diabetes.
What should the hospitalist report for the initial post-transfer service? The typical options to consider are:2
- Inpatient consultation (99251-99255);
- Initial hospital care (99221-99223); and
- Subsequent hospital care (99231-99233).
Report a consultation only if the rehab attending requests an opinion or advice for an unrelated, new condition instead of previously treated conditions, and the requesting physician’s intent is for opinion or advice on management options rather than the a priori intent for the hospitalist to assume the patient’s medical care. If these requirements are met, the hospitalist may report an inpatient consultation code (99251-99255). Alternatively, if the intent or need represents a continuity of medical care provided during the acute episode of care, report the most appropriate subsequent hospital care code (99231-99233) for the hospitalist’s initial rehab visit and all follow-up services.
Initial hospital care (99221-99223) codes can only be reported for Medicare beneficiaries in place of consultation codes (99251-99255), as Medicare ceased to reimburse consultation codes.3 Most other payors who do not recognize consultation services only allow one initial hospital care code per hospitalization, reserved for the attending of record.
Interfacility Initial Service
Hospitalist groups provide patient care and coverage in many different types of facilities. Confusion often arises when the “attending of record” during acute care and the “subacute” setting (e.g. long-term acute-care hospital) are two different hospitalists from the same group practice. The hospitalist receiving the patient in the transfer facility may decide to report subsequent hospital care (99231-99233), because the group has been providing ongoing care to this patient. In this scenario, the hospitalist group could be losing revenue if an admission service (99221-99223) was not reported.
An initial hospital care service (99221-99223) is permitted when the transfer is between:
- Different hospitals;
- Different facilities under common ownership which do not have merged records; or
- Between the acute-care hospital and a PPS (prospective payment system)-exempt unit within the same hospital when there are no merged records (e.g. Medicare Part A-covered inpatient care in psychiatric, rehabilitation, critical access, and long-term care hospitals).4
In all other transfer circumstances not meeting the elements noted above, the physician should bill only the appropriate level of subsequent hospital care (99231-99233) for the date of transfer.1 Do not equate “merged records” to commonly accessible charts via an electronic medical record system or an electronic storage system. If the medical record for the patient’s acute stay is “closed” and the patient is given a separate medical record and registration for the stay in the transferred facility, consider the transfer stay as a separate admission.
Billing Two Services on Day of Transfer
Whether the transfer is classified as intrafacility or interfacility, an individual hospitalist or two separate hospitalists from the same group practice may provide the acute-care discharge and the transfer admission. A hospital discharge day management service (99238-99239) and an initial hospital care service (99221-99223) can only be reported if they do not occur on the same day.1 Physicians in the same group practice who are in the same specialty must bill and be paid as though they were a single physician; if more than one evaluation and management (face to face) service is provided on the same day to the same patient by the same physician or more than one physician in the same specialty in the same group, only one evaluation and management service may be reported.5
The Exception
CMS will allow a single hospitalist or two hospitalists from the same group practice to report a discharge day management service on the same day as an admission service. When they are billed by the same physician or group with the same date of service, contractors are instructed to pay the hospital discharge day management code (99238-99239) in addition to a nursing facility admission code (99304-99306).6
Conversely, if the patient is admitted to a hospital (99221-99223) following a nursing facility discharge (99315-99316) on the same date by the same physician/group, insurers will only reimburse the initial hospital care code. Payment for the initial hospital care service includes all work performed by the physician/group in all sites of service on that date.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is faculty for SHM’s inpatient coding course.
References available online at the-hospitalist.org
Patient Transfers
Hospitalist billing depends on several factors. Know your role and avoid common mistakes Patient transfers can occur for many reasons: advanced technological services required, health insurance coverage, or a change in the level of care, to name a few. Patient care that is provided in the acute-care setting does not always terminate with discharge to home. Frequently, hospitalists are involved in patient transfers to another location to receive additional services: intrafacility (a different unit or related facility within the same physical plant) or interfacility (geographically separate facilities). The hospitalist must identify his or her role in the transfer and the patient’s new environment.
Physician billing in the transferred setting depends upon several factors:1
- Shared or merged medical record;
- The attending of record in each setting;
- The requirements for care rendered by the hospitalist in each setting; and
- Service dates.
Intrafacility Initial Service
Let’s examine a common example: A hospitalist serves as the “attending of record” in an inpatient hospital where acute care is required for an 83-year-old female with hypertension and diabetes who sustained a left hip fracture. The hospitalist plans to discharge the patient to the rehabilitation unit. After transfer, the rehabilitation physician becomes the attending of record, and the hospitalist might be asked to provide ongoing care for the patient’s hypertension and diabetes.
What should the hospitalist report for the initial post-transfer service? The typical options to consider are:2
- Inpatient consultation (99251-99255);
- Initial hospital care (99221-99223); and
- Subsequent hospital care (99231-99233).
Report a consultation only if the rehab attending requests an opinion or advice for an unrelated, new condition instead of previously treated conditions, and the requesting physician’s intent is for opinion or advice on management options rather than the a priori intent for the hospitalist to assume the patient’s medical care. If these requirements are met, the hospitalist may report an inpatient consultation code (99251-99255). Alternatively, if the intent or need represents a continuity of medical care provided during the acute episode of care, report the most appropriate subsequent hospital care code (99231-99233) for the hospitalist’s initial rehab visit and all follow-up services.
Initial hospital care (99221-99223) codes can only be reported for Medicare beneficiaries in place of consultation codes (99251-99255), as Medicare ceased to reimburse consultation codes.3 Most other payors who do not recognize consultation services only allow one initial hospital care code per hospitalization, reserved for the attending of record.
Interfacility Initial Service
Hospitalist groups provide patient care and coverage in many different types of facilities. Confusion often arises when the “attending of record” during acute care and the “subacute” setting (e.g. long-term acute-care hospital) are two different hospitalists from the same group practice. The hospitalist receiving the patient in the transfer facility may decide to report subsequent hospital care (99231-99233), because the group has been providing ongoing care to this patient. In this scenario, the hospitalist group could be losing revenue if an admission service (99221-99223) was not reported.
An initial hospital care service (99221-99223) is permitted when the transfer is between:
- Different hospitals;
- Different facilities under common ownership which do not have merged records; or
- Between the acute-care hospital and a PPS (prospective payment system)-exempt unit within the same hospital when there are no merged records (e.g. Medicare Part A-covered inpatient care in psychiatric, rehabilitation, critical access, and long-term care hospitals).4
In all other transfer circumstances not meeting the elements noted above, the physician should bill only the appropriate level of subsequent hospital care (99231-99233) for the date of transfer.1 Do not equate “merged records” to commonly accessible charts via an electronic medical record system or an electronic storage system. If the medical record for the patient’s acute stay is “closed” and the patient is given a separate medical record and registration for the stay in the transferred facility, consider the transfer stay as a separate admission.
Billing Two Services on Day of Transfer
Whether the transfer is classified as intrafacility or interfacility, an individual hospitalist or two separate hospitalists from the same group practice may provide the acute-care discharge and the transfer admission. A hospital discharge day management service (99238-99239) and an initial hospital care service (99221-99223) can only be reported if they do not occur on the same day.1 Physicians in the same group practice who are in the same specialty must bill and be paid as though they were a single physician; if more than one evaluation and management (face to face) service is provided on the same day to the same patient by the same physician or more than one physician in the same specialty in the same group, only one evaluation and management service may be reported.5
The Exception
CMS will allow a single hospitalist or two hospitalists from the same group practice to report a discharge day management service on the same day as an admission service. When they are billed by the same physician or group with the same date of service, contractors are instructed to pay the hospital discharge day management code (99238-99239) in addition to a nursing facility admission code (99304-99306).6
Conversely, if the patient is admitted to a hospital (99221-99223) following a nursing facility discharge (99315-99316) on the same date by the same physician/group, insurers will only reimburse the initial hospital care code. Payment for the initial hospital care service includes all work performed by the physician/group in all sites of service on that date.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is faculty for SHM’s inpatient coding course.
References available online at the-hospitalist.org
Society of Hospital Medicine's CODE-H Returns in January
Staying up to date on the latest techniques for optimal coding can be daunting, but you don't have to do it alone. SHM's exclusive CODE-H program enables hospitalists (and others in their practice) to learn best practices in coding from national experts in the field. It also allows participants to ask questions of other hospitalists who may be experiencing similar coding challenges.
CODE-H works through SHM's new online collaboration space, HMX (www.hmxchange.org), and provides live webinar sessions with expert faculty, downloadable resources, and a discussion forum for participants to ask questions and provide answers.
Previous CODE-H participants can extend their CODE-H subscriptions. The extension is $300, and free for prior participants who refer an individual or group to CODE-H.
For more information, visit www.hospitalmedicine.org/codeh.
Staying up to date on the latest techniques for optimal coding can be daunting, but you don't have to do it alone. SHM's exclusive CODE-H program enables hospitalists (and others in their practice) to learn best practices in coding from national experts in the field. It also allows participants to ask questions of other hospitalists who may be experiencing similar coding challenges.
CODE-H works through SHM's new online collaboration space, HMX (www.hmxchange.org), and provides live webinar sessions with expert faculty, downloadable resources, and a discussion forum for participants to ask questions and provide answers.
Previous CODE-H participants can extend their CODE-H subscriptions. The extension is $300, and free for prior participants who refer an individual or group to CODE-H.
For more information, visit www.hospitalmedicine.org/codeh.
Staying up to date on the latest techniques for optimal coding can be daunting, but you don't have to do it alone. SHM's exclusive CODE-H program enables hospitalists (and others in their practice) to learn best practices in coding from national experts in the field. It also allows participants to ask questions of other hospitalists who may be experiencing similar coding challenges.
CODE-H works through SHM's new online collaboration space, HMX (www.hmxchange.org), and provides live webinar sessions with expert faculty, downloadable resources, and a discussion forum for participants to ask questions and provide answers.
Previous CODE-H participants can extend their CODE-H subscriptions. The extension is $300, and free for prior participants who refer an individual or group to CODE-H.
For more information, visit www.hospitalmedicine.org/codeh.
John Nelson: Peformance Key to Federal Value-Based Payment Modifier Plan
For years, your hospital was paid additional money by Medicare to report its performance on such things as core measures. Medicare then shared that information with the public via www.hospitalcompare.hhs.gov. Even if the hospital never gave Pneumovax when indicated, it was paid more simply for reporting that fact. (Fortunately, there were lots of reasons hospitals wanted to perform well.)
The days of hospitals being paid more simply for reporting ended a long time ago. Now performance, e.g., how often Pneumovax was given when indicated, influences payment. That is, things have transitioned from pay-for-reporting to a pay-for-performance program called hospital value-based purchasing (VBP).
I hope that at least one member of your hospitalist group is keeping up with hospital VBP. It got a lot of attention in the fall because it was the first time Medicare Part A payments to hospitals were adjusted based on performance on some core measures and patient satisfaction domains, as well as readmission rates for congestive heart failure (CHF), acute myocardial infarction (AMI), and pneumonia patients. The dollars at stake and performance metrics change will change every year, so plan to pay attention to hospital VBP on an ongoing basis.
Physicians’ Turn
Medicare payment to physicians is evolving along the same trajectory as hospitals. For several years, doctors have had the option to voluntarily participate in the Physician Quality Reporting System (PQRS). As long as a doctor reported quality performance on a sufficient portion of certain patient types, Medicare would provide a “bonus” at the end of the year. From 2012 through 2014, the “bonus” is 0.5% of that doctor’s total allowable Medicare charges. For example, if that doctor generated $150,000 of Medicare allowable charges over the calendar year, the additional payment for successful reporting PQRS would be $750 (0.5% of $150,000).
Although $750 is only a tiny fraction of collections, the right charge-capture system can make it pretty easy to achieve. And an extra payment of $750 sure is better than the 1.5% penalty for not participating; that program starts in 2015 and increases to a 2% penalty in 2016. If you are still not participating successfully in PQRS in 2015, the reimbursement for that $150,000 in charges will be reduced by $2,250 (1.5% of $150,000). So I strongly recommend that you begin reporting in 2013 so that you have time to work out the kinks well ahead of 2015. Don’t delay, but don’t panic, either, because you can still succeed in 2013 even if you don’t start capturing or reporting PQRS data until late winter or early spring.
At some point in the next year or so, data from as early as January 2013 for doctors reporting through PQRS will be made public on the Centers for Medicare & Medicaid’s (CMS) physician compare website: www.medicare.gov/find-a-doctor/provider-search.aspx. For example, should you choose to report the portion of stroke patients for whom you prescribed DVT prophylaxis, the public will be able to see your data.
The Next Wave of Physician Pay for Performance
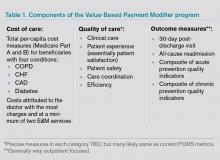
As the name implies, PQRS is a program based on reporting. Now CMS is adding the Value-Based Payment Modifier (VBPM) program, in which performance determines payments (see Table 1). It incorporates quality measures from PQRS, but is for now a separate program. It is very similar in name and structure to the hospital VBP program mentioned above, but incorporates cost of care data as well as quality performance. So it is really about value and not just quality performance (hence the name).
For providers in groups of more than 100 that bill under the same tax ID number (they don’t have to be in the same specialty), VBPM will first influence Part B Medicare reimbursement for physician services in 2015. It will expand to include all providers in 2017.
But don’t think you have until 2015 or 2017 to learn about all of this. There is a two-year lag, so payments in 2015 are based on performance in 2013 and 2017 payments presumably will be based on 2015 performance. In the fall of 2013, CMS plans to provide group-level (not individual) performance reports to all doctors in groups of 100 or more under the same tax ID number. These performance reports are known as quality resource use reports (QRURs). QRURs were trialed on physicians in a few states who received reports in 2012 based on 2011 performance, but in 2013, reports based on 2012 performance will be distributed to all doctors who practice in groups of 100 or more.
The calculation to determine whether a doctor is due additional payment for good performance (more accurately, good value) is awfully complicated. But providers have a choice to make. They can choose to:
- Not report data and accept a 1% penalty (likely to increase in successive years and in addition to the penalty for not reporting PQRS data, for a total penalty of 2.5%);
- Report data but not compete for financial upside or downside; or
- Compete for additional payments (amount to be determined) and risk a penalty of 0.5% or 1% for poor performance.
Look for more details about the VBPM program in future columns and other articles in The Hospitalist. There are a number of good online resources, including a CMS presentation titled “CMS Proposals for the Physician Value-Based Payment Modifier under the Medicare Physician Fee Schedule.” Type “Value-Based Payment Modifier” and “CMS” into any search engine to locate the video.
Parting Recommendations
Just about every hospitalist group should:
- Designate someone in your group to keep up with evolving pay-for-performance programs. It doesn’t have to be an MD, but you do need someone local that can guide your group through it. Consider becoming the most expert physician at your hospital on this topic.
- Start reporting through PQRS in 2013 if you haven’t already.
- Support SHM’s efforts to provide feedback to CMS to ensure that the metrics are meaningful for the type of care we provide.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is course co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Author’s note: For helping to explain all this pay-for-performance stuff, I once again owe thanks to Dr. Pat Torcson, a hospitalist in Covington, La., and member of SHM’s Public Policy Committee. He does an amazing job of keeping up with the evolving pay-for-performance programs, advocating on behalf of hospitalists and the patients we serve, and graciously answers my tedious questions with thoughtful and informative replies. He is a really pleasant guy and a terrific asset to SHM and hospital medicine.
For years, your hospital was paid additional money by Medicare to report its performance on such things as core measures. Medicare then shared that information with the public via www.hospitalcompare.hhs.gov. Even if the hospital never gave Pneumovax when indicated, it was paid more simply for reporting that fact. (Fortunately, there were lots of reasons hospitals wanted to perform well.)
The days of hospitals being paid more simply for reporting ended a long time ago. Now performance, e.g., how often Pneumovax was given when indicated, influences payment. That is, things have transitioned from pay-for-reporting to a pay-for-performance program called hospital value-based purchasing (VBP).
I hope that at least one member of your hospitalist group is keeping up with hospital VBP. It got a lot of attention in the fall because it was the first time Medicare Part A payments to hospitals were adjusted based on performance on some core measures and patient satisfaction domains, as well as readmission rates for congestive heart failure (CHF), acute myocardial infarction (AMI), and pneumonia patients. The dollars at stake and performance metrics change will change every year, so plan to pay attention to hospital VBP on an ongoing basis.
Physicians’ Turn
Medicare payment to physicians is evolving along the same trajectory as hospitals. For several years, doctors have had the option to voluntarily participate in the Physician Quality Reporting System (PQRS). As long as a doctor reported quality performance on a sufficient portion of certain patient types, Medicare would provide a “bonus” at the end of the year. From 2012 through 2014, the “bonus” is 0.5% of that doctor’s total allowable Medicare charges. For example, if that doctor generated $150,000 of Medicare allowable charges over the calendar year, the additional payment for successful reporting PQRS would be $750 (0.5% of $150,000).
Although $750 is only a tiny fraction of collections, the right charge-capture system can make it pretty easy to achieve. And an extra payment of $750 sure is better than the 1.5% penalty for not participating; that program starts in 2015 and increases to a 2% penalty in 2016. If you are still not participating successfully in PQRS in 2015, the reimbursement for that $150,000 in charges will be reduced by $2,250 (1.5% of $150,000). So I strongly recommend that you begin reporting in 2013 so that you have time to work out the kinks well ahead of 2015. Don’t delay, but don’t panic, either, because you can still succeed in 2013 even if you don’t start capturing or reporting PQRS data until late winter or early spring.
At some point in the next year or so, data from as early as January 2013 for doctors reporting through PQRS will be made public on the Centers for Medicare & Medicaid’s (CMS) physician compare website: www.medicare.gov/find-a-doctor/provider-search.aspx. For example, should you choose to report the portion of stroke patients for whom you prescribed DVT prophylaxis, the public will be able to see your data.
The Next Wave of Physician Pay for Performance
As the name implies, PQRS is a program based on reporting. Now CMS is adding the Value-Based Payment Modifier (VBPM) program, in which performance determines payments (see Table 1). It incorporates quality measures from PQRS, but is for now a separate program. It is very similar in name and structure to the hospital VBP program mentioned above, but incorporates cost of care data as well as quality performance. So it is really about value and not just quality performance (hence the name).
For providers in groups of more than 100 that bill under the same tax ID number (they don’t have to be in the same specialty), VBPM will first influence Part B Medicare reimbursement for physician services in 2015. It will expand to include all providers in 2017.
But don’t think you have until 2015 or 2017 to learn about all of this. There is a two-year lag, so payments in 2015 are based on performance in 2013 and 2017 payments presumably will be based on 2015 performance. In the fall of 2013, CMS plans to provide group-level (not individual) performance reports to all doctors in groups of 100 or more under the same tax ID number. These performance reports are known as quality resource use reports (QRURs). QRURs were trialed on physicians in a few states who received reports in 2012 based on 2011 performance, but in 2013, reports based on 2012 performance will be distributed to all doctors who practice in groups of 100 or more.
The calculation to determine whether a doctor is due additional payment for good performance (more accurately, good value) is awfully complicated. But providers have a choice to make. They can choose to:
- Not report data and accept a 1% penalty (likely to increase in successive years and in addition to the penalty for not reporting PQRS data, for a total penalty of 2.5%);
- Report data but not compete for financial upside or downside; or
- Compete for additional payments (amount to be determined) and risk a penalty of 0.5% or 1% for poor performance.
Look for more details about the VBPM program in future columns and other articles in The Hospitalist. There are a number of good online resources, including a CMS presentation titled “CMS Proposals for the Physician Value-Based Payment Modifier under the Medicare Physician Fee Schedule.” Type “Value-Based Payment Modifier” and “CMS” into any search engine to locate the video.
Parting Recommendations
Just about every hospitalist group should:
- Designate someone in your group to keep up with evolving pay-for-performance programs. It doesn’t have to be an MD, but you do need someone local that can guide your group through it. Consider becoming the most expert physician at your hospital on this topic.
- Start reporting through PQRS in 2013 if you haven’t already.
- Support SHM’s efforts to provide feedback to CMS to ensure that the metrics are meaningful for the type of care we provide.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is course co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Author’s note: For helping to explain all this pay-for-performance stuff, I once again owe thanks to Dr. Pat Torcson, a hospitalist in Covington, La., and member of SHM’s Public Policy Committee. He does an amazing job of keeping up with the evolving pay-for-performance programs, advocating on behalf of hospitalists and the patients we serve, and graciously answers my tedious questions with thoughtful and informative replies. He is a really pleasant guy and a terrific asset to SHM and hospital medicine.
For years, your hospital was paid additional money by Medicare to report its performance on such things as core measures. Medicare then shared that information with the public via www.hospitalcompare.hhs.gov. Even if the hospital never gave Pneumovax when indicated, it was paid more simply for reporting that fact. (Fortunately, there were lots of reasons hospitals wanted to perform well.)
The days of hospitals being paid more simply for reporting ended a long time ago. Now performance, e.g., how often Pneumovax was given when indicated, influences payment. That is, things have transitioned from pay-for-reporting to a pay-for-performance program called hospital value-based purchasing (VBP).
I hope that at least one member of your hospitalist group is keeping up with hospital VBP. It got a lot of attention in the fall because it was the first time Medicare Part A payments to hospitals were adjusted based on performance on some core measures and patient satisfaction domains, as well as readmission rates for congestive heart failure (CHF), acute myocardial infarction (AMI), and pneumonia patients. The dollars at stake and performance metrics change will change every year, so plan to pay attention to hospital VBP on an ongoing basis.
Physicians’ Turn
Medicare payment to physicians is evolving along the same trajectory as hospitals. For several years, doctors have had the option to voluntarily participate in the Physician Quality Reporting System (PQRS). As long as a doctor reported quality performance on a sufficient portion of certain patient types, Medicare would provide a “bonus” at the end of the year. From 2012 through 2014, the “bonus” is 0.5% of that doctor’s total allowable Medicare charges. For example, if that doctor generated $150,000 of Medicare allowable charges over the calendar year, the additional payment for successful reporting PQRS would be $750 (0.5% of $150,000).
Although $750 is only a tiny fraction of collections, the right charge-capture system can make it pretty easy to achieve. And an extra payment of $750 sure is better than the 1.5% penalty for not participating; that program starts in 2015 and increases to a 2% penalty in 2016. If you are still not participating successfully in PQRS in 2015, the reimbursement for that $150,000 in charges will be reduced by $2,250 (1.5% of $150,000). So I strongly recommend that you begin reporting in 2013 so that you have time to work out the kinks well ahead of 2015. Don’t delay, but don’t panic, either, because you can still succeed in 2013 even if you don’t start capturing or reporting PQRS data until late winter or early spring.
At some point in the next year or so, data from as early as January 2013 for doctors reporting through PQRS will be made public on the Centers for Medicare & Medicaid’s (CMS) physician compare website: www.medicare.gov/find-a-doctor/provider-search.aspx. For example, should you choose to report the portion of stroke patients for whom you prescribed DVT prophylaxis, the public will be able to see your data.
The Next Wave of Physician Pay for Performance
As the name implies, PQRS is a program based on reporting. Now CMS is adding the Value-Based Payment Modifier (VBPM) program, in which performance determines payments (see Table 1). It incorporates quality measures from PQRS, but is for now a separate program. It is very similar in name and structure to the hospital VBP program mentioned above, but incorporates cost of care data as well as quality performance. So it is really about value and not just quality performance (hence the name).
For providers in groups of more than 100 that bill under the same tax ID number (they don’t have to be in the same specialty), VBPM will first influence Part B Medicare reimbursement for physician services in 2015. It will expand to include all providers in 2017.
But don’t think you have until 2015 or 2017 to learn about all of this. There is a two-year lag, so payments in 2015 are based on performance in 2013 and 2017 payments presumably will be based on 2015 performance. In the fall of 2013, CMS plans to provide group-level (not individual) performance reports to all doctors in groups of 100 or more under the same tax ID number. These performance reports are known as quality resource use reports (QRURs). QRURs were trialed on physicians in a few states who received reports in 2012 based on 2011 performance, but in 2013, reports based on 2012 performance will be distributed to all doctors who practice in groups of 100 or more.
The calculation to determine whether a doctor is due additional payment for good performance (more accurately, good value) is awfully complicated. But providers have a choice to make. They can choose to:
- Not report data and accept a 1% penalty (likely to increase in successive years and in addition to the penalty for not reporting PQRS data, for a total penalty of 2.5%);
- Report data but not compete for financial upside or downside; or
- Compete for additional payments (amount to be determined) and risk a penalty of 0.5% or 1% for poor performance.
Look for more details about the VBPM program in future columns and other articles in The Hospitalist. There are a number of good online resources, including a CMS presentation titled “CMS Proposals for the Physician Value-Based Payment Modifier under the Medicare Physician Fee Schedule.” Type “Value-Based Payment Modifier” and “CMS” into any search engine to locate the video.
Parting Recommendations
Just about every hospitalist group should:
- Designate someone in your group to keep up with evolving pay-for-performance programs. It doesn’t have to be an MD, but you do need someone local that can guide your group through it. Consider becoming the most expert physician at your hospital on this topic.
- Start reporting through PQRS in 2013 if you haven’t already.
- Support SHM’s efforts to provide feedback to CMS to ensure that the metrics are meaningful for the type of care we provide.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is course co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Author’s note: For helping to explain all this pay-for-performance stuff, I once again owe thanks to Dr. Pat Torcson, a hospitalist in Covington, La., and member of SHM’s Public Policy Committee. He does an amazing job of keeping up with the evolving pay-for-performance programs, advocating on behalf of hospitalists and the patients we serve, and graciously answers my tedious questions with thoughtful and informative replies. He is a really pleasant guy and a terrific asset to SHM and hospital medicine.
Pay-for-Performance Challenged as Best Model for Healthcare
Pushing healthcare toward pay-for-performance models that provide financial rewards for patient outcomes might not be the best direction for healthcare, according to an article published by a duo of doctors and a behavioral economist.
“Will Pay for Performance Backfire? Insights from Behavioral Economics” posted at Healthaffairs.org, questions the validity of paying for outcomes, particularly as there is no evidence yet that the model improves patient outcomes.
“You’re not actually paying for quality,” says David Himmelstein, MD, a professor at City University of New York School of Public Health at Hunter College, New York. “What you’re paying for is some very gameable measurement that doctors will find a way to cheat.”
The blog post notes that monetary rewards can actually undermine motivation for tasks that are intrinsically interesting or rewarding, a phenomenon known as “motivational crowd-out.” Dr. Himmelstein says it could focus attention on coding, rather than patients, or encourage providers to avoid noncompliant patients who will make their measured performances look bad.
“Injecting different monetary incentives into healthcare can certainly change it,” according to the article, “but not necessarily in the ways that policy makers would plan, much less hope for.”
Dr. Himmelstein says that without evidence for, or against, pay for performance, it’s difficult to say whether it will improve outcomes over the long term. Given the government push toward pay-for-performance programs—such as value-based purchasing (VBP)—he suggests physicians prepare themselves to comply. Accordingly, SHM supports policies that link "quality measurement to performance-based payment” and has created a toolkit to help hospitalists prepare for VBP, one of the most targeted pay-for-performance programs.
Even as HM moves toward adopting pay for performance as a mantra, Dr. Himmelstein believes hospitalists are in a good position to lead discussions on whether pay for performance is the only way to move forward.
“It can feel like a fait d’accompli, but things can change, and they can change rapidly,” Dr. Himmelstein adds. “The first step is to have real discussions about it. Up to now, much of the medical literature is saying, ‘It’s not working. We must have the wrong incentives.’ What if there are no right incentives?”
Visit our website for more information about pay-for-performance programs.
Pushing healthcare toward pay-for-performance models that provide financial rewards for patient outcomes might not be the best direction for healthcare, according to an article published by a duo of doctors and a behavioral economist.
“Will Pay for Performance Backfire? Insights from Behavioral Economics” posted at Healthaffairs.org, questions the validity of paying for outcomes, particularly as there is no evidence yet that the model improves patient outcomes.
“You’re not actually paying for quality,” says David Himmelstein, MD, a professor at City University of New York School of Public Health at Hunter College, New York. “What you’re paying for is some very gameable measurement that doctors will find a way to cheat.”
The blog post notes that monetary rewards can actually undermine motivation for tasks that are intrinsically interesting or rewarding, a phenomenon known as “motivational crowd-out.” Dr. Himmelstein says it could focus attention on coding, rather than patients, or encourage providers to avoid noncompliant patients who will make their measured performances look bad.
“Injecting different monetary incentives into healthcare can certainly change it,” according to the article, “but not necessarily in the ways that policy makers would plan, much less hope for.”
Dr. Himmelstein says that without evidence for, or against, pay for performance, it’s difficult to say whether it will improve outcomes over the long term. Given the government push toward pay-for-performance programs—such as value-based purchasing (VBP)—he suggests physicians prepare themselves to comply. Accordingly, SHM supports policies that link "quality measurement to performance-based payment” and has created a toolkit to help hospitalists prepare for VBP, one of the most targeted pay-for-performance programs.
Even as HM moves toward adopting pay for performance as a mantra, Dr. Himmelstein believes hospitalists are in a good position to lead discussions on whether pay for performance is the only way to move forward.
“It can feel like a fait d’accompli, but things can change, and they can change rapidly,” Dr. Himmelstein adds. “The first step is to have real discussions about it. Up to now, much of the medical literature is saying, ‘It’s not working. We must have the wrong incentives.’ What if there are no right incentives?”
Visit our website for more information about pay-for-performance programs.
Pushing healthcare toward pay-for-performance models that provide financial rewards for patient outcomes might not be the best direction for healthcare, according to an article published by a duo of doctors and a behavioral economist.
“Will Pay for Performance Backfire? Insights from Behavioral Economics” posted at Healthaffairs.org, questions the validity of paying for outcomes, particularly as there is no evidence yet that the model improves patient outcomes.
“You’re not actually paying for quality,” says David Himmelstein, MD, a professor at City University of New York School of Public Health at Hunter College, New York. “What you’re paying for is some very gameable measurement that doctors will find a way to cheat.”
The blog post notes that monetary rewards can actually undermine motivation for tasks that are intrinsically interesting or rewarding, a phenomenon known as “motivational crowd-out.” Dr. Himmelstein says it could focus attention on coding, rather than patients, or encourage providers to avoid noncompliant patients who will make their measured performances look bad.
“Injecting different monetary incentives into healthcare can certainly change it,” according to the article, “but not necessarily in the ways that policy makers would plan, much less hope for.”
Dr. Himmelstein says that without evidence for, or against, pay for performance, it’s difficult to say whether it will improve outcomes over the long term. Given the government push toward pay-for-performance programs—such as value-based purchasing (VBP)—he suggests physicians prepare themselves to comply. Accordingly, SHM supports policies that link "quality measurement to performance-based payment” and has created a toolkit to help hospitalists prepare for VBP, one of the most targeted pay-for-performance programs.
Even as HM moves toward adopting pay for performance as a mantra, Dr. Himmelstein believes hospitalists are in a good position to lead discussions on whether pay for performance is the only way to move forward.
“It can feel like a fait d’accompli, but things can change, and they can change rapidly,” Dr. Himmelstein adds. “The first step is to have real discussions about it. Up to now, much of the medical literature is saying, ‘It’s not working. We must have the wrong incentives.’ What if there are no right incentives?”
Visit our website for more information about pay-for-performance programs.
John Nelson: Learning CPT Coding and Documentation Tricky for Hospitalists
There is a lot to learn when it comes to proper coding and the documentation requirements that go with it. It can even be tricky for a new residency grad to keep the difference in CPT and ICD-9 coding straight, to say nothing of the difference between documentation requirements for physician reimbursement versus hospital reimbursement. This column addresses only physician CPT coding (I’ll save documentation to support hospital billing for another column).
Although I believe that devoting the large number of brain cells required to keep this stuff straight gets in the way of maintaining necessary clinical knowledge, physicians have no real choice but to do it. (One could argue that having a professional coder read charts to determine proper CPT codes relieves a doctor of the burden of documentation and coding headaches. But this is only partially true. The doctor still needs to ensure that the documentation accurately reflects what was done for the coder to be able to select the appropriate codes, so he still needs to know a lot about this topic.)
All providers have a duty to reasonably ensure that submitted claims (bills) are true and accurate. Failing to document and code correctly risks anything from you or your employer having to return money, potentially with a penalty and interest, to being accused of criminal fraud.
Medicare and other payors generally categorize inaccurate claims as follows:
- Erroneous claims include inadvertent mistakes, innocent errors, or even negligence but still require payments associated with the error to be returned.
- Fraudulent claims are ones judged to be intentionally or recklessly false, and are subject to administrative or civil penalties, such as fines.
- Claims associated with criminal intent to defraud are subject to criminal penalties, which could include jail time.
While I haven’t heard of any hospitalists being accused of fraud, I know of several who have undergone audits and been required to return money. Whether your employer would refund the money or you would have to write a personal check to refund the money depends on your employment situation. For example, in most cases, the hospital would be liable to make the repayment for hospitalists it employs. If you’re an independent contractor, there is a good chance you could be stuck making the repayment yourself.
Trend: Increased Use of Higher-Level Codes
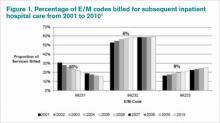
You might have missed it, but there was a recent study of Medicare Part B claims data from 2001 to 2010 showing that “physicians increased their billing of higher-level E/M codes in all types of E/M services.”1 For example, the report showed a steady decrease in use of the 99231 code, the lowest of the three subsequent inpatient hospital care codes, and an increase in the highest level code, 99233 (see Figure 1, below).
I can think of two reasons hospitalists might be increasing the use of higher codes. One, less-sick patients just aren’t seen in the hospital as often as they used to be, so the remaining patients require more intensive services, which could lead to the appropriate use of higher-level codes. Two, doctors have over the past 10 to 15 years invested more energy in learning appropriate documentation and coding, which might have led to correcting historical overuse of lower-level codes.
Did I tell you who conducted the study showing increased use of higher-level codes? It was the federal Office of Inspector General (OIG), which is responsible for preventing and detecting fraud and waste. Although the OIG might agree that the sicker patients and correction of historical undercoding might explain some of the trend, it’s a pretty safe bet they’re also concerned that a significant portion is inappropriate or fraudulent. Some portion of it probably is.
“CMS concurred with [OIG’s] recommendations to (1) continue to educate physicians on proper billing for E/M services and (2) encourage its contractor to review physicians’ billing for E/M services. CMS partially concurred with [OIG’s] third recommendation, to review physicians who bill higher-level E/M codes for appropriate action,” the OIG report noted.1
Plan for Education, Compliance
My sense is that most hospitalists employed by a large entity, such as a hospital or large medical group, have access to a certified coder to perform documentation and coding audits, as well as educational feedback when needed. If your practice doesn’t have access to a certified coder, you should consider photocopying some chart notes (e.g. 10 notes from each of your docs) and send them to an outside coder for an audit. Though they are very valuable, audits usually are not enough to ensure good performance.
In my March 2007 column, I described a reasonably simple chart audit allowing each doctor to compare his or her CPT coding pattern to everyone else in the group. You can compare your own coding to national coding patterns via SHM’s 2012 State of Hospital Medicine Report (www.hospitalmedicine.org/survey) or data from the CMS website, and the Medical Group Management Association (MGMA) will have data in future surveys. Such comparisons might help uncover unusual patterns that are worthy of a closer look.
Other strategies to promote proper documentation and coding include online educational programs, such as:
- SHM’s CODE-H webinars (www.hospitalmedicine.org/codeh), which are available on demand for a fee;
- American Association of Professional Coders Evaluation and Management Online Training (http://www.aapc.com/training/evaluation-management-coding-training.aspx); and
- The American Health Information Management Association’s (AHIMA) Coding Basics Program (www.ahima.org/continuinged/campus/courseinfo/cb.aspx).
If you prefer, an Internet search can turn up in-person courses to learn documentation and coding. Additionally, your in-house or external coding auditors can provide training.
To address tricky issues that come up only occasionally, several in our practice have compiled a “coding manual” by distilling guidance from our certified coders and compliance people on issues as they came up. Some issues would stump all of us, and we’d have to go to the Internet for help. All hospitalists are provided with a copy of the manual during orientation, and an electronic copy is available on the hospital’s Intranet. Topics addressed in the manual include things like how to bill the first inpatient day when a patient has changed from observation status, how to bill initial consult visits for various payors (an issue since Medicare eliminated consult codes a few years ago), how to bill when a patient is seen and discharged from the ED, etc.
Lastly, I suggest someone in your group talk with your hospital’s compliance department about its own coding and billing compliance plan. This could lead to ideas or help develop a compliance plan for your group.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is course co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Reference
There is a lot to learn when it comes to proper coding and the documentation requirements that go with it. It can even be tricky for a new residency grad to keep the difference in CPT and ICD-9 coding straight, to say nothing of the difference between documentation requirements for physician reimbursement versus hospital reimbursement. This column addresses only physician CPT coding (I’ll save documentation to support hospital billing for another column).
Although I believe that devoting the large number of brain cells required to keep this stuff straight gets in the way of maintaining necessary clinical knowledge, physicians have no real choice but to do it. (One could argue that having a professional coder read charts to determine proper CPT codes relieves a doctor of the burden of documentation and coding headaches. But this is only partially true. The doctor still needs to ensure that the documentation accurately reflects what was done for the coder to be able to select the appropriate codes, so he still needs to know a lot about this topic.)
All providers have a duty to reasonably ensure that submitted claims (bills) are true and accurate. Failing to document and code correctly risks anything from you or your employer having to return money, potentially with a penalty and interest, to being accused of criminal fraud.
Medicare and other payors generally categorize inaccurate claims as follows:
- Erroneous claims include inadvertent mistakes, innocent errors, or even negligence but still require payments associated with the error to be returned.
- Fraudulent claims are ones judged to be intentionally or recklessly false, and are subject to administrative or civil penalties, such as fines.
- Claims associated with criminal intent to defraud are subject to criminal penalties, which could include jail time.
While I haven’t heard of any hospitalists being accused of fraud, I know of several who have undergone audits and been required to return money. Whether your employer would refund the money or you would have to write a personal check to refund the money depends on your employment situation. For example, in most cases, the hospital would be liable to make the repayment for hospitalists it employs. If you’re an independent contractor, there is a good chance you could be stuck making the repayment yourself.
Trend: Increased Use of Higher-Level Codes
You might have missed it, but there was a recent study of Medicare Part B claims data from 2001 to 2010 showing that “physicians increased their billing of higher-level E/M codes in all types of E/M services.”1 For example, the report showed a steady decrease in use of the 99231 code, the lowest of the three subsequent inpatient hospital care codes, and an increase in the highest level code, 99233 (see Figure 1, below).
I can think of two reasons hospitalists might be increasing the use of higher codes. One, less-sick patients just aren’t seen in the hospital as often as they used to be, so the remaining patients require more intensive services, which could lead to the appropriate use of higher-level codes. Two, doctors have over the past 10 to 15 years invested more energy in learning appropriate documentation and coding, which might have led to correcting historical overuse of lower-level codes.
Did I tell you who conducted the study showing increased use of higher-level codes? It was the federal Office of Inspector General (OIG), which is responsible for preventing and detecting fraud and waste. Although the OIG might agree that the sicker patients and correction of historical undercoding might explain some of the trend, it’s a pretty safe bet they’re also concerned that a significant portion is inappropriate or fraudulent. Some portion of it probably is.
“CMS concurred with [OIG’s] recommendations to (1) continue to educate physicians on proper billing for E/M services and (2) encourage its contractor to review physicians’ billing for E/M services. CMS partially concurred with [OIG’s] third recommendation, to review physicians who bill higher-level E/M codes for appropriate action,” the OIG report noted.1
Plan for Education, Compliance
My sense is that most hospitalists employed by a large entity, such as a hospital or large medical group, have access to a certified coder to perform documentation and coding audits, as well as educational feedback when needed. If your practice doesn’t have access to a certified coder, you should consider photocopying some chart notes (e.g. 10 notes from each of your docs) and send them to an outside coder for an audit. Though they are very valuable, audits usually are not enough to ensure good performance.
In my March 2007 column, I described a reasonably simple chart audit allowing each doctor to compare his or her CPT coding pattern to everyone else in the group. You can compare your own coding to national coding patterns via SHM’s 2012 State of Hospital Medicine Report (www.hospitalmedicine.org/survey) or data from the CMS website, and the Medical Group Management Association (MGMA) will have data in future surveys. Such comparisons might help uncover unusual patterns that are worthy of a closer look.
Other strategies to promote proper documentation and coding include online educational programs, such as:
- SHM’s CODE-H webinars (www.hospitalmedicine.org/codeh), which are available on demand for a fee;
- American Association of Professional Coders Evaluation and Management Online Training (http://www.aapc.com/training/evaluation-management-coding-training.aspx); and
- The American Health Information Management Association’s (AHIMA) Coding Basics Program (www.ahima.org/continuinged/campus/courseinfo/cb.aspx).
If you prefer, an Internet search can turn up in-person courses to learn documentation and coding. Additionally, your in-house or external coding auditors can provide training.
To address tricky issues that come up only occasionally, several in our practice have compiled a “coding manual” by distilling guidance from our certified coders and compliance people on issues as they came up. Some issues would stump all of us, and we’d have to go to the Internet for help. All hospitalists are provided with a copy of the manual during orientation, and an electronic copy is available on the hospital’s Intranet. Topics addressed in the manual include things like how to bill the first inpatient day when a patient has changed from observation status, how to bill initial consult visits for various payors (an issue since Medicare eliminated consult codes a few years ago), how to bill when a patient is seen and discharged from the ED, etc.
Lastly, I suggest someone in your group talk with your hospital’s compliance department about its own coding and billing compliance plan. This could lead to ideas or help develop a compliance plan for your group.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is course co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Reference
There is a lot to learn when it comes to proper coding and the documentation requirements that go with it. It can even be tricky for a new residency grad to keep the difference in CPT and ICD-9 coding straight, to say nothing of the difference between documentation requirements for physician reimbursement versus hospital reimbursement. This column addresses only physician CPT coding (I’ll save documentation to support hospital billing for another column).
Although I believe that devoting the large number of brain cells required to keep this stuff straight gets in the way of maintaining necessary clinical knowledge, physicians have no real choice but to do it. (One could argue that having a professional coder read charts to determine proper CPT codes relieves a doctor of the burden of documentation and coding headaches. But this is only partially true. The doctor still needs to ensure that the documentation accurately reflects what was done for the coder to be able to select the appropriate codes, so he still needs to know a lot about this topic.)
All providers have a duty to reasonably ensure that submitted claims (bills) are true and accurate. Failing to document and code correctly risks anything from you or your employer having to return money, potentially with a penalty and interest, to being accused of criminal fraud.
Medicare and other payors generally categorize inaccurate claims as follows:
- Erroneous claims include inadvertent mistakes, innocent errors, or even negligence but still require payments associated with the error to be returned.
- Fraudulent claims are ones judged to be intentionally or recklessly false, and are subject to administrative or civil penalties, such as fines.
- Claims associated with criminal intent to defraud are subject to criminal penalties, which could include jail time.
While I haven’t heard of any hospitalists being accused of fraud, I know of several who have undergone audits and been required to return money. Whether your employer would refund the money or you would have to write a personal check to refund the money depends on your employment situation. For example, in most cases, the hospital would be liable to make the repayment for hospitalists it employs. If you’re an independent contractor, there is a good chance you could be stuck making the repayment yourself.
Trend: Increased Use of Higher-Level Codes
You might have missed it, but there was a recent study of Medicare Part B claims data from 2001 to 2010 showing that “physicians increased their billing of higher-level E/M codes in all types of E/M services.”1 For example, the report showed a steady decrease in use of the 99231 code, the lowest of the three subsequent inpatient hospital care codes, and an increase in the highest level code, 99233 (see Figure 1, below).
I can think of two reasons hospitalists might be increasing the use of higher codes. One, less-sick patients just aren’t seen in the hospital as often as they used to be, so the remaining patients require more intensive services, which could lead to the appropriate use of higher-level codes. Two, doctors have over the past 10 to 15 years invested more energy in learning appropriate documentation and coding, which might have led to correcting historical overuse of lower-level codes.
Did I tell you who conducted the study showing increased use of higher-level codes? It was the federal Office of Inspector General (OIG), which is responsible for preventing and detecting fraud and waste. Although the OIG might agree that the sicker patients and correction of historical undercoding might explain some of the trend, it’s a pretty safe bet they’re also concerned that a significant portion is inappropriate or fraudulent. Some portion of it probably is.
“CMS concurred with [OIG’s] recommendations to (1) continue to educate physicians on proper billing for E/M services and (2) encourage its contractor to review physicians’ billing for E/M services. CMS partially concurred with [OIG’s] third recommendation, to review physicians who bill higher-level E/M codes for appropriate action,” the OIG report noted.1
Plan for Education, Compliance
My sense is that most hospitalists employed by a large entity, such as a hospital or large medical group, have access to a certified coder to perform documentation and coding audits, as well as educational feedback when needed. If your practice doesn’t have access to a certified coder, you should consider photocopying some chart notes (e.g. 10 notes from each of your docs) and send them to an outside coder for an audit. Though they are very valuable, audits usually are not enough to ensure good performance.
In my March 2007 column, I described a reasonably simple chart audit allowing each doctor to compare his or her CPT coding pattern to everyone else in the group. You can compare your own coding to national coding patterns via SHM’s 2012 State of Hospital Medicine Report (www.hospitalmedicine.org/survey) or data from the CMS website, and the Medical Group Management Association (MGMA) will have data in future surveys. Such comparisons might help uncover unusual patterns that are worthy of a closer look.
Other strategies to promote proper documentation and coding include online educational programs, such as:
- SHM’s CODE-H webinars (www.hospitalmedicine.org/codeh), which are available on demand for a fee;
- American Association of Professional Coders Evaluation and Management Online Training (http://www.aapc.com/training/evaluation-management-coding-training.aspx); and
- The American Health Information Management Association’s (AHIMA) Coding Basics Program (www.ahima.org/continuinged/campus/courseinfo/cb.aspx).
If you prefer, an Internet search can turn up in-person courses to learn documentation and coding. Additionally, your in-house or external coding auditors can provide training.
To address tricky issues that come up only occasionally, several in our practice have compiled a “coding manual” by distilling guidance from our certified coders and compliance people on issues as they came up. Some issues would stump all of us, and we’d have to go to the Internet for help. All hospitalists are provided with a copy of the manual during orientation, and an electronic copy is available on the hospital’s Intranet. Topics addressed in the manual include things like how to bill the first inpatient day when a patient has changed from observation status, how to bill initial consult visits for various payors (an issue since Medicare eliminated consult codes a few years ago), how to bill when a patient is seen and discharged from the ED, etc.
Lastly, I suggest someone in your group talk with your hospital’s compliance department about its own coding and billing compliance plan. This could lead to ideas or help develop a compliance plan for your group.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is course co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Reference
Medical Coding: Hospice Care vs. Palliative Care
Hospice care” and “palliative care” are not synonymous terms. Hospice care is defined as a comprehensive set of services (see “Hospice Coverage,” below) identified and coordinated by an interdisciplinary group to provide for the physical, psychosocial, spiritual, and emotional needs of a terminally ill patient and/or family members, as delineated in a specific patient plan of care.1 Palliative care is defined as patient- and family-centered care that optimizes quality of life by anticipating, preventing, and treating suffering. Palliative care throughout the continuum of illness involves addressing physical, intellectual, emotional, social, and spiritual needs, and facilitates patient autonomy, access to information, and choice.1
As an approach, hospice care of terminally ill individuals involves palliative care (relief of pain and uncomfortable symptoms), and emphasizes maintaining the patient at home with family and friends as long as possible. Hospice services can be provided in a home, center, skilled-nursing facility, or hospital setting. In contrast, palliative-care services can be provided during hospice care, or coincide with care that is focused on a cure.
Many hospitalists provide both hospice care and palliative-care services to their patients. Different factors affect how to report these services. These programs can be quite costly, as they involve several team members and a substantial amount of time delivering these services. Capturing services appropriately and obtaining reimbursement to help continue program initiatives are significant issues.
Hospice Care
When a patient enrolls in hospice, all rights to Medicare Part B payments are waived during the benefit period involving professional services related to the treatment and management of the terminal illness. Payment is made through the Part A benefit for the associated costs of daily care and the services provided by the hospice-employed physician. An exception occurs for professional services of an independent attending physician who is not an employee of the designated hospice and does not receive compensation from the hospice for those services. The “attending physician” for hospice services must be an individual who is a doctor of medicine or osteopathy, or a nurse practitioner identified by the individual, at the time they elect hospice coverage, as having the most significant role in the determination and delivery of their medical care.2
Patients often receive hospice in the hospital setting, where the hospitalist manages the patient’s daily care. If the hospitalist is designated as the “attending physician” for hospice services, the visits should be reported to Medicare Part B with modifier GV (e.g. 99232-GV).3 This will allow for separate payment to the hospitalist (the independent attending physician), while the hospice agency maintains its daily-care rate. Reporting services absent this modifier will result in denial.
In some cases, the hospitalist is not identified as the “attending physician” for hospice services but occasionally provides care related to the terminal illness. This situation proves most difficult. Although the hospitalist might be the most accessible physician to the staff and is putting the patient’s needs first, reimbursement is unlikely. Regulations stipulate that patients must not see independent physicians other than their “attending physician” for care related to their terminal illness unless the hospice arranges it. When the service is related to the hospice patient’s terminal illness but was furnished by someone other than the designated “attending physician,” this “other physician” must look to the hospice for payment.3
Nonhospice Palliative Care
Members of the palliative-care team often are called to provide management options to assist in reducing pain and suffering. When the palliative-care specialist is asked to provide opinions or advice, the initial service may qualify as a consultation for those payors that still recognize these codes. However, all of the requirements4 must be met in order to report the service as an inpatient consultation (99251-99255):3
- There must be a written request from a qualified healthcare provider who is involved in the patient’s care (e.g. physician, resident, nurse practitioner); this may be documented as a physician order or in the assessment/plan of the requesting provider’s progress note. Standing orders for consultation are not permitted.
- The requesting provider should clearly and accurately identify the reason for consult request to support the medical necessity of the service.
- The palliative-care physician renders and documents the service.
- The palliative-care physician reports his or her findings to the requesting physician via written communication; because the requesting physician and the consultant share a common inpatient medical record, the consultant’s inpatient progress note satisfies the “written report” requirement.
Consider the nature of the request when reporting a consultation. If the request demonstrates the need for opinions or advice from the palliative-care specialist, the service can be reported as a consultation. If the indication cites “medical management” or “palliative management,” payors are less likely to consider the service as a consultation because the physician is not seeking opinions or advice from the consultant to incorporate into his or her own plan of care for the patient and would rather the consultant just take over that portion of patient care. When consultations do not meet the requirements, subsequent hospital care services should be reported (99231-99233).3
The requesting physician can be in the same or a different provider group as the consultant. The consultant must possess expertise in an area that is beyond that of the requesting provider. Because most hospitalists carry a specialty designation of internal medicine (physician specialty code 11), hospitalists providing palliative-care services can distinguish themselves by their own code (physician specialty code 17, hospice and palliative care).5 Payor concerns arise when physicians of the same designated specialty submit a claim for the same patient on the same date. The payor is likely to pay the first claim received and deny the second claim received pending review of documentation. If this occurs, submit a copy of both progress notes for the date in question to distinguish the services provided. The payor may still require that both encounters be reported as one cumulative service under one physician.
Consultations are not an option for Medicare beneficiaries. Hospitalists providing palliative care can report initial hospital care codes (99221-99223) for their first encounter with the patient.3 This is only acceptable when no other hospitalist from the group has reported initial hospital care during the patient stay, unless the palliative-care hospitalist carries the corresponding designation (i.e. enrolled with Medicare as physician specialty code 17). Without this separate designation, the palliative-care hospitalist can only report subsequent hospital care codes (99231-99233) as the patient was seen previously by a hospitalist in the same group.3
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- U.S. Government Printing Office. Electronic Code of Federal Regulations: Title 42: Public Health, Part 418: Hospice Care, §418.3. June 2012. U.S. Government Printing Office website. Available at: http://ecfr.gpoaccess.gov/cgi/t/text/text-idx?c=ecfr&sid=818258235647b14d2961ad30fa3e68e6&rgn=div5&view=text&node=42:3.0.1.1.5&idno=42#42:3.0.1.1.5.1.3.3. Accessed June 23, 2012.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 11: processing hospice claims. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c11.pdf. Accessed June 23, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
- American Medical Association. Consultation services and transfer of care. American Medical Association website. Available at: http://www.ama-assn.org/resources/doc/cpt/cpt-consultation-services.pdf. Accessed June 23, 2012.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 26: completing and processing form CMS-1500 data set. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c26.pdf. Accessed June 23, 2012. Department of Health and Human Services.
- Hospice Payment System: payment system fact sheet series. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/hospice_pay_sys_fs.pdf. Accessed June 23, 2012.
Hospice care” and “palliative care” are not synonymous terms. Hospice care is defined as a comprehensive set of services (see “Hospice Coverage,” below) identified and coordinated by an interdisciplinary group to provide for the physical, psychosocial, spiritual, and emotional needs of a terminally ill patient and/or family members, as delineated in a specific patient plan of care.1 Palliative care is defined as patient- and family-centered care that optimizes quality of life by anticipating, preventing, and treating suffering. Palliative care throughout the continuum of illness involves addressing physical, intellectual, emotional, social, and spiritual needs, and facilitates patient autonomy, access to information, and choice.1
As an approach, hospice care of terminally ill individuals involves palliative care (relief of pain and uncomfortable symptoms), and emphasizes maintaining the patient at home with family and friends as long as possible. Hospice services can be provided in a home, center, skilled-nursing facility, or hospital setting. In contrast, palliative-care services can be provided during hospice care, or coincide with care that is focused on a cure.
Many hospitalists provide both hospice care and palliative-care services to their patients. Different factors affect how to report these services. These programs can be quite costly, as they involve several team members and a substantial amount of time delivering these services. Capturing services appropriately and obtaining reimbursement to help continue program initiatives are significant issues.
Hospice Care
When a patient enrolls in hospice, all rights to Medicare Part B payments are waived during the benefit period involving professional services related to the treatment and management of the terminal illness. Payment is made through the Part A benefit for the associated costs of daily care and the services provided by the hospice-employed physician. An exception occurs for professional services of an independent attending physician who is not an employee of the designated hospice and does not receive compensation from the hospice for those services. The “attending physician” for hospice services must be an individual who is a doctor of medicine or osteopathy, or a nurse practitioner identified by the individual, at the time they elect hospice coverage, as having the most significant role in the determination and delivery of their medical care.2
Patients often receive hospice in the hospital setting, where the hospitalist manages the patient’s daily care. If the hospitalist is designated as the “attending physician” for hospice services, the visits should be reported to Medicare Part B with modifier GV (e.g. 99232-GV).3 This will allow for separate payment to the hospitalist (the independent attending physician), while the hospice agency maintains its daily-care rate. Reporting services absent this modifier will result in denial.
In some cases, the hospitalist is not identified as the “attending physician” for hospice services but occasionally provides care related to the terminal illness. This situation proves most difficult. Although the hospitalist might be the most accessible physician to the staff and is putting the patient’s needs first, reimbursement is unlikely. Regulations stipulate that patients must not see independent physicians other than their “attending physician” for care related to their terminal illness unless the hospice arranges it. When the service is related to the hospice patient’s terminal illness but was furnished by someone other than the designated “attending physician,” this “other physician” must look to the hospice for payment.3
Nonhospice Palliative Care
Members of the palliative-care team often are called to provide management options to assist in reducing pain and suffering. When the palliative-care specialist is asked to provide opinions or advice, the initial service may qualify as a consultation for those payors that still recognize these codes. However, all of the requirements4 must be met in order to report the service as an inpatient consultation (99251-99255):3
- There must be a written request from a qualified healthcare provider who is involved in the patient’s care (e.g. physician, resident, nurse practitioner); this may be documented as a physician order or in the assessment/plan of the requesting provider’s progress note. Standing orders for consultation are not permitted.
- The requesting provider should clearly and accurately identify the reason for consult request to support the medical necessity of the service.
- The palliative-care physician renders and documents the service.
- The palliative-care physician reports his or her findings to the requesting physician via written communication; because the requesting physician and the consultant share a common inpatient medical record, the consultant’s inpatient progress note satisfies the “written report” requirement.
Consider the nature of the request when reporting a consultation. If the request demonstrates the need for opinions or advice from the palliative-care specialist, the service can be reported as a consultation. If the indication cites “medical management” or “palliative management,” payors are less likely to consider the service as a consultation because the physician is not seeking opinions or advice from the consultant to incorporate into his or her own plan of care for the patient and would rather the consultant just take over that portion of patient care. When consultations do not meet the requirements, subsequent hospital care services should be reported (99231-99233).3
The requesting physician can be in the same or a different provider group as the consultant. The consultant must possess expertise in an area that is beyond that of the requesting provider. Because most hospitalists carry a specialty designation of internal medicine (physician specialty code 11), hospitalists providing palliative-care services can distinguish themselves by their own code (physician specialty code 17, hospice and palliative care).5 Payor concerns arise when physicians of the same designated specialty submit a claim for the same patient on the same date. The payor is likely to pay the first claim received and deny the second claim received pending review of documentation. If this occurs, submit a copy of both progress notes for the date in question to distinguish the services provided. The payor may still require that both encounters be reported as one cumulative service under one physician.
Consultations are not an option for Medicare beneficiaries. Hospitalists providing palliative care can report initial hospital care codes (99221-99223) for their first encounter with the patient.3 This is only acceptable when no other hospitalist from the group has reported initial hospital care during the patient stay, unless the palliative-care hospitalist carries the corresponding designation (i.e. enrolled with Medicare as physician specialty code 17). Without this separate designation, the palliative-care hospitalist can only report subsequent hospital care codes (99231-99233) as the patient was seen previously by a hospitalist in the same group.3
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- U.S. Government Printing Office. Electronic Code of Federal Regulations: Title 42: Public Health, Part 418: Hospice Care, §418.3. June 2012. U.S. Government Printing Office website. Available at: http://ecfr.gpoaccess.gov/cgi/t/text/text-idx?c=ecfr&sid=818258235647b14d2961ad30fa3e68e6&rgn=div5&view=text&node=42:3.0.1.1.5&idno=42#42:3.0.1.1.5.1.3.3. Accessed June 23, 2012.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 11: processing hospice claims. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c11.pdf. Accessed June 23, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
- American Medical Association. Consultation services and transfer of care. American Medical Association website. Available at: http://www.ama-assn.org/resources/doc/cpt/cpt-consultation-services.pdf. Accessed June 23, 2012.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 26: completing and processing form CMS-1500 data set. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c26.pdf. Accessed June 23, 2012. Department of Health and Human Services.
- Hospice Payment System: payment system fact sheet series. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/hospice_pay_sys_fs.pdf. Accessed June 23, 2012.
Hospice care” and “palliative care” are not synonymous terms. Hospice care is defined as a comprehensive set of services (see “Hospice Coverage,” below) identified and coordinated by an interdisciplinary group to provide for the physical, psychosocial, spiritual, and emotional needs of a terminally ill patient and/or family members, as delineated in a specific patient plan of care.1 Palliative care is defined as patient- and family-centered care that optimizes quality of life by anticipating, preventing, and treating suffering. Palliative care throughout the continuum of illness involves addressing physical, intellectual, emotional, social, and spiritual needs, and facilitates patient autonomy, access to information, and choice.1
As an approach, hospice care of terminally ill individuals involves palliative care (relief of pain and uncomfortable symptoms), and emphasizes maintaining the patient at home with family and friends as long as possible. Hospice services can be provided in a home, center, skilled-nursing facility, or hospital setting. In contrast, palliative-care services can be provided during hospice care, or coincide with care that is focused on a cure.
Many hospitalists provide both hospice care and palliative-care services to their patients. Different factors affect how to report these services. These programs can be quite costly, as they involve several team members and a substantial amount of time delivering these services. Capturing services appropriately and obtaining reimbursement to help continue program initiatives are significant issues.
Hospice Care
When a patient enrolls in hospice, all rights to Medicare Part B payments are waived during the benefit period involving professional services related to the treatment and management of the terminal illness. Payment is made through the Part A benefit for the associated costs of daily care and the services provided by the hospice-employed physician. An exception occurs for professional services of an independent attending physician who is not an employee of the designated hospice and does not receive compensation from the hospice for those services. The “attending physician” for hospice services must be an individual who is a doctor of medicine or osteopathy, or a nurse practitioner identified by the individual, at the time they elect hospice coverage, as having the most significant role in the determination and delivery of their medical care.2
Patients often receive hospice in the hospital setting, where the hospitalist manages the patient’s daily care. If the hospitalist is designated as the “attending physician” for hospice services, the visits should be reported to Medicare Part B with modifier GV (e.g. 99232-GV).3 This will allow for separate payment to the hospitalist (the independent attending physician), while the hospice agency maintains its daily-care rate. Reporting services absent this modifier will result in denial.
In some cases, the hospitalist is not identified as the “attending physician” for hospice services but occasionally provides care related to the terminal illness. This situation proves most difficult. Although the hospitalist might be the most accessible physician to the staff and is putting the patient’s needs first, reimbursement is unlikely. Regulations stipulate that patients must not see independent physicians other than their “attending physician” for care related to their terminal illness unless the hospice arranges it. When the service is related to the hospice patient’s terminal illness but was furnished by someone other than the designated “attending physician,” this “other physician” must look to the hospice for payment.3
Nonhospice Palliative Care
Members of the palliative-care team often are called to provide management options to assist in reducing pain and suffering. When the palliative-care specialist is asked to provide opinions or advice, the initial service may qualify as a consultation for those payors that still recognize these codes. However, all of the requirements4 must be met in order to report the service as an inpatient consultation (99251-99255):3
- There must be a written request from a qualified healthcare provider who is involved in the patient’s care (e.g. physician, resident, nurse practitioner); this may be documented as a physician order or in the assessment/plan of the requesting provider’s progress note. Standing orders for consultation are not permitted.
- The requesting provider should clearly and accurately identify the reason for consult request to support the medical necessity of the service.
- The palliative-care physician renders and documents the service.
- The palliative-care physician reports his or her findings to the requesting physician via written communication; because the requesting physician and the consultant share a common inpatient medical record, the consultant’s inpatient progress note satisfies the “written report” requirement.
Consider the nature of the request when reporting a consultation. If the request demonstrates the need for opinions or advice from the palliative-care specialist, the service can be reported as a consultation. If the indication cites “medical management” or “palliative management,” payors are less likely to consider the service as a consultation because the physician is not seeking opinions or advice from the consultant to incorporate into his or her own plan of care for the patient and would rather the consultant just take over that portion of patient care. When consultations do not meet the requirements, subsequent hospital care services should be reported (99231-99233).3
The requesting physician can be in the same or a different provider group as the consultant. The consultant must possess expertise in an area that is beyond that of the requesting provider. Because most hospitalists carry a specialty designation of internal medicine (physician specialty code 11), hospitalists providing palliative-care services can distinguish themselves by their own code (physician specialty code 17, hospice and palliative care).5 Payor concerns arise when physicians of the same designated specialty submit a claim for the same patient on the same date. The payor is likely to pay the first claim received and deny the second claim received pending review of documentation. If this occurs, submit a copy of both progress notes for the date in question to distinguish the services provided. The payor may still require that both encounters be reported as one cumulative service under one physician.
Consultations are not an option for Medicare beneficiaries. Hospitalists providing palliative care can report initial hospital care codes (99221-99223) for their first encounter with the patient.3 This is only acceptable when no other hospitalist from the group has reported initial hospital care during the patient stay, unless the palliative-care hospitalist carries the corresponding designation (i.e. enrolled with Medicare as physician specialty code 17). Without this separate designation, the palliative-care hospitalist can only report subsequent hospital care codes (99231-99233) as the patient was seen previously by a hospitalist in the same group.3
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- U.S. Government Printing Office. Electronic Code of Federal Regulations: Title 42: Public Health, Part 418: Hospice Care, §418.3. June 2012. U.S. Government Printing Office website. Available at: http://ecfr.gpoaccess.gov/cgi/t/text/text-idx?c=ecfr&sid=818258235647b14d2961ad30fa3e68e6&rgn=div5&view=text&node=42:3.0.1.1.5&idno=42#42:3.0.1.1.5.1.3.3. Accessed June 23, 2012.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 11: processing hospice claims. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c11.pdf. Accessed June 23, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
- American Medical Association. Consultation services and transfer of care. American Medical Association website. Available at: http://www.ama-assn.org/resources/doc/cpt/cpt-consultation-services.pdf. Accessed June 23, 2012.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 26: completing and processing form CMS-1500 data set. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c26.pdf. Accessed June 23, 2012. Department of Health and Human Services.
- Hospice Payment System: payment system fact sheet series. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/hospice_pay_sys_fs.pdf. Accessed June 23, 2012.
Physician Value-Based Payment Initiative Would Change Medicare Reimbursement
The healthcare market is saturated with fee-for-service reimbursement schemes. The Bureau of Labor Statistics estimates that 78% of employer-sponsored health insurance plans are some type of fee-for-service plan.1 In Medicare, about 75% of beneficiaries use the traditional fee-for-service program.2 Fee-for-service denotes that payments are made on individual services, billed separately, irrespective of outcome and, in some cases, necessity.
The physician value-based payment modifier (VBPM) is an initiative that will begin shifting Medicare reimbursement for physicians away from fee-for-service schemes and toward some type of pay-for-performance model.
For hospitalists, this will have a marked impact on HM practice and might have reverberating effects in the field itself.
Established under the 2008 Medicare Improvements for Patients and Providers Act (MIPPA) and expanded under the 2010 Affordable Care Act (ACA), the VBPM will be applied to all physicians by 2017.
The VBPM program is the physician version of hospital value-based purchasing; both are designed to move the basis of payment toward the quality of care delivered, not simply for the quantity of services rendered. By linking quality measurement with payment, the Centers for Medicare & Medicaid Services (CMS) hopes to start paying for value.
While legislation required the creation of pay-for-performance programs for physicians and hospitals, the design and implementation details have been delegated to CMS, part of the U.S. Department of Health and Human Services. Thus, CMS has oversight on the specifics of the program. These specifics are promulgated through the federal rulemaking process, which requires such agencies as CMS to seek input from the general public—as well as medical societies, including SHM—as rules are proposed and finalized. Generally, there is a 30- to 90-day period after a rule is proposed for public comment, after which a rule will be finalized.
For the VBPM and its performance period starting next year, the guidelines were published for public comment in a proposed rule for the fiscal-year 2013 Physician Fee Schedule. The final rule, which will provide more definitive guidance for hospitalists, is slated to come out in November.
Hospitalists should be cognizant of how quality measurements apply to their practice and find ways to participate in such quality measurement programs as the Physician Quality Reporting System (PQRS). PQRS will become the evaluative backbone of the VBPM. It is imperative that hospitalists stay abreast of these transformative changes in the healthcare system and work to ensure that their practice patterns, which fill critical gaps in patient care, are adequately represented in these changes.
Although legislation and legislative advocacy are undoubtedly important features of policymaking, participating in the federal rulemaking process is a vital tool for helping to shape healthcare. SHM actively pursues regulatory issues in order to advocate for hospitalists and their patients. The experiences and expertise of members are critical for SHM to be able to accurately represent the specialty.
By staying informed on health policy and being engaged with SHM, members can provide invaluable perspectives to help transform the field and revolutionize the healthcare system.
Josh Lapps is SHM's government relations specialist.
References
- U.S. Bureau of Labor Statistics. Program Perspectives: fee-for-service plans. U.S. Bureau of Labor Statistics website. Available at: http://www.bls.gov/opub/perspectives/program_perspectives_vol2_issue5.pdf. Accessed Aug. 15, 2012.
- The Henry J. Kaiser Family Foundation. Medicare at a glance. The Henry J. Kaiser Family Foundation website. Available at: http://www.kff.org/medicare/upload/1066_11.pdf. Accessed Aug. 29, 2012.
The healthcare market is saturated with fee-for-service reimbursement schemes. The Bureau of Labor Statistics estimates that 78% of employer-sponsored health insurance plans are some type of fee-for-service plan.1 In Medicare, about 75% of beneficiaries use the traditional fee-for-service program.2 Fee-for-service denotes that payments are made on individual services, billed separately, irrespective of outcome and, in some cases, necessity.
The physician value-based payment modifier (VBPM) is an initiative that will begin shifting Medicare reimbursement for physicians away from fee-for-service schemes and toward some type of pay-for-performance model.
For hospitalists, this will have a marked impact on HM practice and might have reverberating effects in the field itself.
Established under the 2008 Medicare Improvements for Patients and Providers Act (MIPPA) and expanded under the 2010 Affordable Care Act (ACA), the VBPM will be applied to all physicians by 2017.
The VBPM program is the physician version of hospital value-based purchasing; both are designed to move the basis of payment toward the quality of care delivered, not simply for the quantity of services rendered. By linking quality measurement with payment, the Centers for Medicare & Medicaid Services (CMS) hopes to start paying for value.
While legislation required the creation of pay-for-performance programs for physicians and hospitals, the design and implementation details have been delegated to CMS, part of the U.S. Department of Health and Human Services. Thus, CMS has oversight on the specifics of the program. These specifics are promulgated through the federal rulemaking process, which requires such agencies as CMS to seek input from the general public—as well as medical societies, including SHM—as rules are proposed and finalized. Generally, there is a 30- to 90-day period after a rule is proposed for public comment, after which a rule will be finalized.
For the VBPM and its performance period starting next year, the guidelines were published for public comment in a proposed rule for the fiscal-year 2013 Physician Fee Schedule. The final rule, which will provide more definitive guidance for hospitalists, is slated to come out in November.
Hospitalists should be cognizant of how quality measurements apply to their practice and find ways to participate in such quality measurement programs as the Physician Quality Reporting System (PQRS). PQRS will become the evaluative backbone of the VBPM. It is imperative that hospitalists stay abreast of these transformative changes in the healthcare system and work to ensure that their practice patterns, which fill critical gaps in patient care, are adequately represented in these changes.
Although legislation and legislative advocacy are undoubtedly important features of policymaking, participating in the federal rulemaking process is a vital tool for helping to shape healthcare. SHM actively pursues regulatory issues in order to advocate for hospitalists and their patients. The experiences and expertise of members are critical for SHM to be able to accurately represent the specialty.
By staying informed on health policy and being engaged with SHM, members can provide invaluable perspectives to help transform the field and revolutionize the healthcare system.
Josh Lapps is SHM's government relations specialist.
References
- U.S. Bureau of Labor Statistics. Program Perspectives: fee-for-service plans. U.S. Bureau of Labor Statistics website. Available at: http://www.bls.gov/opub/perspectives/program_perspectives_vol2_issue5.pdf. Accessed Aug. 15, 2012.
- The Henry J. Kaiser Family Foundation. Medicare at a glance. The Henry J. Kaiser Family Foundation website. Available at: http://www.kff.org/medicare/upload/1066_11.pdf. Accessed Aug. 29, 2012.
The healthcare market is saturated with fee-for-service reimbursement schemes. The Bureau of Labor Statistics estimates that 78% of employer-sponsored health insurance plans are some type of fee-for-service plan.1 In Medicare, about 75% of beneficiaries use the traditional fee-for-service program.2 Fee-for-service denotes that payments are made on individual services, billed separately, irrespective of outcome and, in some cases, necessity.
The physician value-based payment modifier (VBPM) is an initiative that will begin shifting Medicare reimbursement for physicians away from fee-for-service schemes and toward some type of pay-for-performance model.
For hospitalists, this will have a marked impact on HM practice and might have reverberating effects in the field itself.
Established under the 2008 Medicare Improvements for Patients and Providers Act (MIPPA) and expanded under the 2010 Affordable Care Act (ACA), the VBPM will be applied to all physicians by 2017.
The VBPM program is the physician version of hospital value-based purchasing; both are designed to move the basis of payment toward the quality of care delivered, not simply for the quantity of services rendered. By linking quality measurement with payment, the Centers for Medicare & Medicaid Services (CMS) hopes to start paying for value.
While legislation required the creation of pay-for-performance programs for physicians and hospitals, the design and implementation details have been delegated to CMS, part of the U.S. Department of Health and Human Services. Thus, CMS has oversight on the specifics of the program. These specifics are promulgated through the federal rulemaking process, which requires such agencies as CMS to seek input from the general public—as well as medical societies, including SHM—as rules are proposed and finalized. Generally, there is a 30- to 90-day period after a rule is proposed for public comment, after which a rule will be finalized.
For the VBPM and its performance period starting next year, the guidelines were published for public comment in a proposed rule for the fiscal-year 2013 Physician Fee Schedule. The final rule, which will provide more definitive guidance for hospitalists, is slated to come out in November.
Hospitalists should be cognizant of how quality measurements apply to their practice and find ways to participate in such quality measurement programs as the Physician Quality Reporting System (PQRS). PQRS will become the evaluative backbone of the VBPM. It is imperative that hospitalists stay abreast of these transformative changes in the healthcare system and work to ensure that their practice patterns, which fill critical gaps in patient care, are adequately represented in these changes.
Although legislation and legislative advocacy are undoubtedly important features of policymaking, participating in the federal rulemaking process is a vital tool for helping to shape healthcare. SHM actively pursues regulatory issues in order to advocate for hospitalists and their patients. The experiences and expertise of members are critical for SHM to be able to accurately represent the specialty.
By staying informed on health policy and being engaged with SHM, members can provide invaluable perspectives to help transform the field and revolutionize the healthcare system.
Josh Lapps is SHM's government relations specialist.
References
- U.S. Bureau of Labor Statistics. Program Perspectives: fee-for-service plans. U.S. Bureau of Labor Statistics website. Available at: http://www.bls.gov/opub/perspectives/program_perspectives_vol2_issue5.pdf. Accessed Aug. 15, 2012.
- The Henry J. Kaiser Family Foundation. Medicare at a glance. The Henry J. Kaiser Family Foundation website. Available at: http://www.kff.org/medicare/upload/1066_11.pdf. Accessed Aug. 29, 2012.
Code-H: Learn Hospital-Based Coding from National Experts
What’s better than learning from national experts in hospital-based coding? Learning from them, being able to ask them questions, and sharing your own experiences with others, all at the same time.
CODE-H, which will be offered again this fall, is presented via live webinar at SHM’s new online community, Hospital Medicine Exchange, which enables CODE-H users to post messages to other users and the faculty. Using Hospital Medicine Exchange, CODE-H users can also share their own resources and documents.
Each webinar is archived on the CODE-H site, so participants can log in and learn at any time.
Best of all, one subscription is good for up to 10 participants at each hospital or site, so inviting others at your hospital to participate increases the value.
Used first for CODE-H and SHM’s Hospital Value-Based Purchasing toolkit, Hospital Medicine Exchange will soon be available to all hospitalists as a forum for learning and sharing best practices.
To register for CODE-H, visit www.hospitalmedicine.org/codeh.
What’s better than learning from national experts in hospital-based coding? Learning from them, being able to ask them questions, and sharing your own experiences with others, all at the same time.
CODE-H, which will be offered again this fall, is presented via live webinar at SHM’s new online community, Hospital Medicine Exchange, which enables CODE-H users to post messages to other users and the faculty. Using Hospital Medicine Exchange, CODE-H users can also share their own resources and documents.
Each webinar is archived on the CODE-H site, so participants can log in and learn at any time.
Best of all, one subscription is good for up to 10 participants at each hospital or site, so inviting others at your hospital to participate increases the value.
Used first for CODE-H and SHM’s Hospital Value-Based Purchasing toolkit, Hospital Medicine Exchange will soon be available to all hospitalists as a forum for learning and sharing best practices.
To register for CODE-H, visit www.hospitalmedicine.org/codeh.
What’s better than learning from national experts in hospital-based coding? Learning from them, being able to ask them questions, and sharing your own experiences with others, all at the same time.
CODE-H, which will be offered again this fall, is presented via live webinar at SHM’s new online community, Hospital Medicine Exchange, which enables CODE-H users to post messages to other users and the faculty. Using Hospital Medicine Exchange, CODE-H users can also share their own resources and documents.
Each webinar is archived on the CODE-H site, so participants can log in and learn at any time.
Best of all, one subscription is good for up to 10 participants at each hospital or site, so inviting others at your hospital to participate increases the value.
Used first for CODE-H and SHM’s Hospital Value-Based Purchasing toolkit, Hospital Medicine Exchange will soon be available to all hospitalists as a forum for learning and sharing best practices.
To register for CODE-H, visit www.hospitalmedicine.org/codeh.
Response: Properly Coding an Uncertain Diagnosis
Dr. Pinson:
Thank you for your inquiry to my June column, which outlined physician reporting of ICD-9-CM diagnoses. Confusion arises because there are two mechanisms for reporting facility-based claims: the professional (physician) bill and the facility bill. ICD-9-CM has been adopted under HIPAA for all healthcare settings. Several components of the ICD-9-CM manual offer instructions on its use. “How to Use the ICD-9-CM for Physicians (Volumes 1&2)” identifies “10 Steps to Correct Coding.”2,3 Step 1 explicitly denotes the inability to use “rule out,” “suspected,” “probable,” or “questionable” diagnoses, and applies to all professional claims submitted on CMS1500 or electronic equivalent.3
The “ICD-9-CM Official Guidelines for Coding and Reporting” are a set of rules developed to accompany and complement the official conventions and instructions provided within ICD-9-CM and approved by the four organizations that make up the Cooperating Parties for the ICD-9-CM: the American Hospital Association (AHA), the American Health Information Management Association (AHIMA), the Centers for Medicare & Medicaid Services (CMS), and NCHS. These guidelines are included on the official government version of the ICD-9-CM, and also appear in “Coding Clinic for ICD-9-CM” published by the AHA.3
While Section I of these guidelines applies to all locations, Sections II and III refer to the selection of the principal diagnosis (the condition established after study to be chiefly responsible for the admission) reported by facilities for DRG payment on CMS1450 or its electronic equivalent.2 Since DRG payment is based on the average resources used to treat inpatients, it is allowable to code a properly documented, “uncertain” condition as if it existed or was established. It does not apply to the outpatient setting. Outpatient, facility-based (Section IV) claims follow the same standards as professional claims, which should not list any diagnosis documented as “probable,” “suspected,” “questionable,” “rule out” or “working diagnosis,” or other similar terms indicating uncertainty.
Carol Pohlig, BSN, RN, CPC, ACS, is a contributing writer to The Hospitalist.
References
- Hart AC, Stegman MS, Ford B, eds. ICD-9-CM for Physicians Volumes 1 & 2 2012 Expert Edition. OptimumInsight; 2011. Page vi.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual. Chapter 23, Section 10A. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c23.pdf. Accessed July 24, 2012.
- Hart AC, Stegman MS, Ford B. ICD-9-CM for Physicians Volumes 1 & 2 2012 Expert Edition. OptimumInsight; 2011. Page 1.
Dr. Pinson:
Thank you for your inquiry to my June column, which outlined physician reporting of ICD-9-CM diagnoses. Confusion arises because there are two mechanisms for reporting facility-based claims: the professional (physician) bill and the facility bill. ICD-9-CM has been adopted under HIPAA for all healthcare settings. Several components of the ICD-9-CM manual offer instructions on its use. “How to Use the ICD-9-CM for Physicians (Volumes 1&2)” identifies “10 Steps to Correct Coding.”2,3 Step 1 explicitly denotes the inability to use “rule out,” “suspected,” “probable,” or “questionable” diagnoses, and applies to all professional claims submitted on CMS1500 or electronic equivalent.3
The “ICD-9-CM Official Guidelines for Coding and Reporting” are a set of rules developed to accompany and complement the official conventions and instructions provided within ICD-9-CM and approved by the four organizations that make up the Cooperating Parties for the ICD-9-CM: the American Hospital Association (AHA), the American Health Information Management Association (AHIMA), the Centers for Medicare & Medicaid Services (CMS), and NCHS. These guidelines are included on the official government version of the ICD-9-CM, and also appear in “Coding Clinic for ICD-9-CM” published by the AHA.3
While Section I of these guidelines applies to all locations, Sections II and III refer to the selection of the principal diagnosis (the condition established after study to be chiefly responsible for the admission) reported by facilities for DRG payment on CMS1450 or its electronic equivalent.2 Since DRG payment is based on the average resources used to treat inpatients, it is allowable to code a properly documented, “uncertain” condition as if it existed or was established. It does not apply to the outpatient setting. Outpatient, facility-based (Section IV) claims follow the same standards as professional claims, which should not list any diagnosis documented as “probable,” “suspected,” “questionable,” “rule out” or “working diagnosis,” or other similar terms indicating uncertainty.
Carol Pohlig, BSN, RN, CPC, ACS, is a contributing writer to The Hospitalist.
References
- Hart AC, Stegman MS, Ford B, eds. ICD-9-CM for Physicians Volumes 1 & 2 2012 Expert Edition. OptimumInsight; 2011. Page vi.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual. Chapter 23, Section 10A. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c23.pdf. Accessed July 24, 2012.
- Hart AC, Stegman MS, Ford B. ICD-9-CM for Physicians Volumes 1 & 2 2012 Expert Edition. OptimumInsight; 2011. Page 1.
Dr. Pinson:
Thank you for your inquiry to my June column, which outlined physician reporting of ICD-9-CM diagnoses. Confusion arises because there are two mechanisms for reporting facility-based claims: the professional (physician) bill and the facility bill. ICD-9-CM has been adopted under HIPAA for all healthcare settings. Several components of the ICD-9-CM manual offer instructions on its use. “How to Use the ICD-9-CM for Physicians (Volumes 1&2)” identifies “10 Steps to Correct Coding.”2,3 Step 1 explicitly denotes the inability to use “rule out,” “suspected,” “probable,” or “questionable” diagnoses, and applies to all professional claims submitted on CMS1500 or electronic equivalent.3
The “ICD-9-CM Official Guidelines for Coding and Reporting” are a set of rules developed to accompany and complement the official conventions and instructions provided within ICD-9-CM and approved by the four organizations that make up the Cooperating Parties for the ICD-9-CM: the American Hospital Association (AHA), the American Health Information Management Association (AHIMA), the Centers for Medicare & Medicaid Services (CMS), and NCHS. These guidelines are included on the official government version of the ICD-9-CM, and also appear in “Coding Clinic for ICD-9-CM” published by the AHA.3
While Section I of these guidelines applies to all locations, Sections II and III refer to the selection of the principal diagnosis (the condition established after study to be chiefly responsible for the admission) reported by facilities for DRG payment on CMS1450 or its electronic equivalent.2 Since DRG payment is based on the average resources used to treat inpatients, it is allowable to code a properly documented, “uncertain” condition as if it existed or was established. It does not apply to the outpatient setting. Outpatient, facility-based (Section IV) claims follow the same standards as professional claims, which should not list any diagnosis documented as “probable,” “suspected,” “questionable,” “rule out” or “working diagnosis,” or other similar terms indicating uncertainty.
Carol Pohlig, BSN, RN, CPC, ACS, is a contributing writer to The Hospitalist.
References
- Hart AC, Stegman MS, Ford B, eds. ICD-9-CM for Physicians Volumes 1 & 2 2012 Expert Edition. OptimumInsight; 2011. Page vi.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual. Chapter 23, Section 10A. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c23.pdf. Accessed July 24, 2012.
- Hart AC, Stegman MS, Ford B. ICD-9-CM for Physicians Volumes 1 & 2 2012 Expert Edition. OptimumInsight; 2011. Page 1.