User login
Still No Implementation Date Set for ICD-10
A new implementation date for the 10th revision of the International Statistical Classification of Diseases coding system (ICD-10) isn't expected to be known until after the November election, says a coding specialist. But hospitalists and others should not take that as a sign to just sit around and wait for a date.
"We're probably not going to hear anything until after the election is finished," says Brenda Edwards, CPC, CPMA, a coding and compliance specialist with Kansas Medical Mutual Insurance Co. and a trainer with AAPC. "The thing that's worrisome, though, is people think this delay we have encountered is a time to sit back and do nothing, but really we’re almost burning money by not doing anything."
An outcry from many physicians led the U.S. Department of Health and Human Services to delay the planned October 2013 implementation date. No new date has been announced.
Edwards urges physicians, billing specialists, and group leaders to use the delay as an opportunity to better prepare for the implementation. She suggests checking with vendors and preparing training programs to help adjust to the new coding initiative, which will quadruple the number of billing codes to 68,000.
"Everyone at this point should still be moving forward," she says.
At the same time, the Centers for Medicare & Medicaid Services (CMS) is seeking public comment on a new version of its ICD-10 readiness assessment. Those interested in weighing in can learn more here.
A new implementation date for the 10th revision of the International Statistical Classification of Diseases coding system (ICD-10) isn't expected to be known until after the November election, says a coding specialist. But hospitalists and others should not take that as a sign to just sit around and wait for a date.
"We're probably not going to hear anything until after the election is finished," says Brenda Edwards, CPC, CPMA, a coding and compliance specialist with Kansas Medical Mutual Insurance Co. and a trainer with AAPC. "The thing that's worrisome, though, is people think this delay we have encountered is a time to sit back and do nothing, but really we’re almost burning money by not doing anything."
An outcry from many physicians led the U.S. Department of Health and Human Services to delay the planned October 2013 implementation date. No new date has been announced.
Edwards urges physicians, billing specialists, and group leaders to use the delay as an opportunity to better prepare for the implementation. She suggests checking with vendors and preparing training programs to help adjust to the new coding initiative, which will quadruple the number of billing codes to 68,000.
"Everyone at this point should still be moving forward," she says.
At the same time, the Centers for Medicare & Medicaid Services (CMS) is seeking public comment on a new version of its ICD-10 readiness assessment. Those interested in weighing in can learn more here.
A new implementation date for the 10th revision of the International Statistical Classification of Diseases coding system (ICD-10) isn't expected to be known until after the November election, says a coding specialist. But hospitalists and others should not take that as a sign to just sit around and wait for a date.
"We're probably not going to hear anything until after the election is finished," says Brenda Edwards, CPC, CPMA, a coding and compliance specialist with Kansas Medical Mutual Insurance Co. and a trainer with AAPC. "The thing that's worrisome, though, is people think this delay we have encountered is a time to sit back and do nothing, but really we’re almost burning money by not doing anything."
An outcry from many physicians led the U.S. Department of Health and Human Services to delay the planned October 2013 implementation date. No new date has been announced.
Edwards urges physicians, billing specialists, and group leaders to use the delay as an opportunity to better prepare for the implementation. She suggests checking with vendors and preparing training programs to help adjust to the new coding initiative, which will quadruple the number of billing codes to 68,000.
"Everyone at this point should still be moving forward," she says.
At the same time, the Centers for Medicare & Medicaid Services (CMS) is seeking public comment on a new version of its ICD-10 readiness assessment. Those interested in weighing in can learn more here.
Survey Insights: Better Understand CPT Coding Intensity
Many of the practice-management-related questions we field from members here at SHM are about documentation and coding issues; members are looking for ways to benchmark their group’s coding performance against other similar groups. One helpful metric reported in the SHM/MGMA State of Hospital Medicine report is the ratio of work-RVUs to total encounters, which I refer to as “coding intensity.”
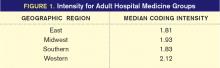
Median coding intensity for adult medicine hospitalists in the 2011 report was 1.90, up slightly from 2010 levels.
The most obvious factor that influences coding intensity is the distribution of CPT codes within specific evaluation and management code sets, such as inpatient admissions (99221-99223) or follow-up visits (99231-99233). Other considerations include the degree to which hospitalists provide high-wRVU services, such as critical care or procedures, the ratio of inpatient vs. observation patients, and the group’s average length of stay.
One interesting finding was that coding intensity varies greatly by geographic region (see Figure 1, right).
What’s going on out there in the Western states? Are those folks receiving different training than the rest of us? Or are they just mavericks, more interested in generating professional fee revenues than hospitalists elsewhere are? It’s hard to say. One big factor is that length of stay (LOS) tends to be shorter in the West than in other parts of the country. That means the typical Western hospitalist will have a larger proportion of high-wRVU value admission and discharge codes relative to their proportion of low-wRVU value subsequent visit codes.
This isn’t the whole story, though. Hospitalists in the West actually did report a significantly more aggressive code distribution for all three CPT code sets for which data were collected (inpatient admissions, subsequent visits, and discharges). And hospitalists in the South, where LOS tends to be longer, also reported the least aggressive code distributions.
Unfortunately, we don’t have a lot of clues as to why these differences exist. We don’t know, for example, whether more hospitalists in the West work in the ICU or perform more procedures compared to other parts of the country. One possibility suggested by report data is that hospitalists in Western states have the highest average proportion of their total compensation allocated to productivity incentives. Hospitalists in the East have the lowest proportion of their compensation based on productivity. So productivity-based compensation might cause hospitalists to care a lot more about doing a good job with documentation and CPT coding.
Other interesting findings include the fact that hospitalists employed by multistate hospitalist-management companies had the lowest median coding intensity, while hospitalists employed by private hospitalist-only groups had the highest coding intensity. And, perhaps not surprisingly, the small proportion of practices that did not receive any financial support had a higher average coding intensity than practices receiving financial support.
While there are no clear answers about variations in CPT coding intensity among hospitalist practices, the State of Hospital Medicine report does offer some intriguing pointers, along with a variety of useful benchmarks about hospitalist CPT coding practices. And stay tuned: The new report, due out in August, will offer even more ways of looking at coding intensity and CPT code distribution.
Leslie Flores, SHM senior advisor
Many of the practice-management-related questions we field from members here at SHM are about documentation and coding issues; members are looking for ways to benchmark their group’s coding performance against other similar groups. One helpful metric reported in the SHM/MGMA State of Hospital Medicine report is the ratio of work-RVUs to total encounters, which I refer to as “coding intensity.”
Median coding intensity for adult medicine hospitalists in the 2011 report was 1.90, up slightly from 2010 levels.
The most obvious factor that influences coding intensity is the distribution of CPT codes within specific evaluation and management code sets, such as inpatient admissions (99221-99223) or follow-up visits (99231-99233). Other considerations include the degree to which hospitalists provide high-wRVU services, such as critical care or procedures, the ratio of inpatient vs. observation patients, and the group’s average length of stay.
One interesting finding was that coding intensity varies greatly by geographic region (see Figure 1, right).
What’s going on out there in the Western states? Are those folks receiving different training than the rest of us? Or are they just mavericks, more interested in generating professional fee revenues than hospitalists elsewhere are? It’s hard to say. One big factor is that length of stay (LOS) tends to be shorter in the West than in other parts of the country. That means the typical Western hospitalist will have a larger proportion of high-wRVU value admission and discharge codes relative to their proportion of low-wRVU value subsequent visit codes.
This isn’t the whole story, though. Hospitalists in the West actually did report a significantly more aggressive code distribution for all three CPT code sets for which data were collected (inpatient admissions, subsequent visits, and discharges). And hospitalists in the South, where LOS tends to be longer, also reported the least aggressive code distributions.
Unfortunately, we don’t have a lot of clues as to why these differences exist. We don’t know, for example, whether more hospitalists in the West work in the ICU or perform more procedures compared to other parts of the country. One possibility suggested by report data is that hospitalists in Western states have the highest average proportion of their total compensation allocated to productivity incentives. Hospitalists in the East have the lowest proportion of their compensation based on productivity. So productivity-based compensation might cause hospitalists to care a lot more about doing a good job with documentation and CPT coding.
Other interesting findings include the fact that hospitalists employed by multistate hospitalist-management companies had the lowest median coding intensity, while hospitalists employed by private hospitalist-only groups had the highest coding intensity. And, perhaps not surprisingly, the small proportion of practices that did not receive any financial support had a higher average coding intensity than practices receiving financial support.
While there are no clear answers about variations in CPT coding intensity among hospitalist practices, the State of Hospital Medicine report does offer some intriguing pointers, along with a variety of useful benchmarks about hospitalist CPT coding practices. And stay tuned: The new report, due out in August, will offer even more ways of looking at coding intensity and CPT code distribution.
Leslie Flores, SHM senior advisor
Many of the practice-management-related questions we field from members here at SHM are about documentation and coding issues; members are looking for ways to benchmark their group’s coding performance against other similar groups. One helpful metric reported in the SHM/MGMA State of Hospital Medicine report is the ratio of work-RVUs to total encounters, which I refer to as “coding intensity.”
Median coding intensity for adult medicine hospitalists in the 2011 report was 1.90, up slightly from 2010 levels.
The most obvious factor that influences coding intensity is the distribution of CPT codes within specific evaluation and management code sets, such as inpatient admissions (99221-99223) or follow-up visits (99231-99233). Other considerations include the degree to which hospitalists provide high-wRVU services, such as critical care or procedures, the ratio of inpatient vs. observation patients, and the group’s average length of stay.
One interesting finding was that coding intensity varies greatly by geographic region (see Figure 1, right).
What’s going on out there in the Western states? Are those folks receiving different training than the rest of us? Or are they just mavericks, more interested in generating professional fee revenues than hospitalists elsewhere are? It’s hard to say. One big factor is that length of stay (LOS) tends to be shorter in the West than in other parts of the country. That means the typical Western hospitalist will have a larger proportion of high-wRVU value admission and discharge codes relative to their proportion of low-wRVU value subsequent visit codes.
This isn’t the whole story, though. Hospitalists in the West actually did report a significantly more aggressive code distribution for all three CPT code sets for which data were collected (inpatient admissions, subsequent visits, and discharges). And hospitalists in the South, where LOS tends to be longer, also reported the least aggressive code distributions.
Unfortunately, we don’t have a lot of clues as to why these differences exist. We don’t know, for example, whether more hospitalists in the West work in the ICU or perform more procedures compared to other parts of the country. One possibility suggested by report data is that hospitalists in Western states have the highest average proportion of their total compensation allocated to productivity incentives. Hospitalists in the East have the lowest proportion of their compensation based on productivity. So productivity-based compensation might cause hospitalists to care a lot more about doing a good job with documentation and CPT coding.
Other interesting findings include the fact that hospitalists employed by multistate hospitalist-management companies had the lowest median coding intensity, while hospitalists employed by private hospitalist-only groups had the highest coding intensity. And, perhaps not surprisingly, the small proportion of practices that did not receive any financial support had a higher average coding intensity than practices receiving financial support.
While there are no clear answers about variations in CPT coding intensity among hospitalist practices, the State of Hospital Medicine report does offer some intriguing pointers, along with a variety of useful benchmarks about hospitalist CPT coding practices. And stay tuned: The new report, due out in August, will offer even more ways of looking at coding intensity and CPT code distribution.
Leslie Flores, SHM senior advisor
Know Surgical Package Requirements before Billing Postoperative Care
Hospitalists often are involved in the postoperative care of the surgical patient. However, HM is emerging in the admitting/attending role for procedural patients. Confusion can arise as to the nature of the hospitalist service, and whether it is deemed billable. Knowing the surgical package requirements can help hospitalists consider the issues.
Global Surgical Package Period1
Surgical procedures, categorized as major or minor surgery, are reimbursed for pre-, intra-, and postoperative care. Postoperative care varies according to the procedure’s assigned global period, which designates zero, 10, or 90 postoperative days. (Physicians can review the global period for any given CPT code in the Medicare Physician Fee Schedule, available at www.cms.gov/apps/physician-fee-schedule/search/search-criteria.aspx.)
Services classified with “XXX” do not have the global period concept. “ZZZ” services denote an “add-on” procedure code that must always be reported with a primary procedure code and assumes the global period assigned to the primary procedure performed.
Major surgery allocates a 90-day global period in which the surgeon is responsible for all related surgical care one day before surgery through 90 postoperative days with no additional charge. Minor surgery, including endoscopy, appoints a zero-day or 10-day postoperative period. The zero-day global period encompasses only services provided on the surgical day, whereas 10-day global periods include services on the surgical day through 10 postoperative days.
Global Surgical Package Components2
The global surgical package comprises a host of responsibilities that include standard facility requirements of filling out all necessary paperwork involved in surgical cases (e.g. preoperative H&P, operative consent forms, preoperative orders). Additionally, the surgeon’s packaged payment includes (at no extra charge):
- Preoperative visits after making the decision for surgery beginning one day prior to surgery;
- All additional postoperative medical or surgical services provided by the surgeon related to complications but not requiring additional trips to the operating room;
- Postoperative visits by the surgeon related to recovery from surgery, including but not limited to dressing changes; local incisional care; removal of cutaneous sutures and staples; line removals; changes and removal of tracheostomy tubes; and discharge services; and
- Postoperative pain management provided by the surgeon.
- Examples of services that are not included in the global surgical package, (i.e. are separately billable and may require an appropriate modifier) are:
- The initial consultation or evaluation of the problem by the surgeon to determine the need for surgery;
- Services of other physicians except where the other physicians are providing coverage for the surgeon or agree on a transfer of care (i.e. a formal agreement in the form of a letter or an annotation in the discharge summary, hospital record, or ASC record);
- Postoperative visits by the surgeon unrelated to the diagnosis for which the surgical procedure is performed, unless the visits occur due to complications of the surgery;
- Diagnostic tests and procedures, including diagnostic radiological procedures;
- Clearly distinct surgical procedures during the postoperative period that do not result in repeat operations or treatment for complications;
- Treatment for postoperative complications that requires a return trip to the operating room (OR), catheterization lab or endoscopy suite;
- Immunosuppressive therapy for organ transplants; and
- Critical-care services (CPT codes 99291 and 99292) unrelated to the surgery where a seriously injured or burned patient is critically ill and requires constant attendance of the surgeon.
Classification of “Surgeon”
For billing purposes, the “surgeon” is a qualified physician who can perform “surgical” services within their scope of practice. All physicians with the same specialty designation in the same group practice as the “surgeon” (i.e. reporting services under the same tax identification number) are considered a single entity and must adhere to the global period billing rules initiated by the “surgeon.”
Alternately, physicians with different specialty designations in the same group practice (e.g. a hospitalist and a cardiologist in a multispecialty group who report services under the same tax identification number) or different group practices can perform and separately report medically necessary services during the surgeon’s global period, as long as a formal (mutually agreed-upon) transfer of care did not occur.
Medical Necessity
With the growth of HM programs and the admission/attending role expansion, involvement in surgical cases comes under scrutiny for medical necessity. Admitting a patient who has active medical conditions (e.g. hypertension, diabetes, emphysema) is reasonable and necessary because the patient has a well-defined need for medical management by the hospitalist. Participation in the care of these patients is separately billable from the surgeon’s global period package.
Alternatively, a hospitalist might be required to admit and follow surgical patients who have no other identifiable chronic or acute conditions aside from the surgical problem. In these cases, hospitalist involvement may satisfy facility policy (quality of care, risk reduction, etc.) and administrative functions (discharge services or coordination of care) rather than active clinical management. This “medical management” will not be considered “medically necessary” by the payor, and may be denied as incidental to the surgeon’s perioperative services. Erroneous payment can occur, which will result in refund requests, as payors do not want to pay twice for duplicate services. Hospitalists can attempt to negotiate other terms with facilities to account for the unpaid time and effort directed toward these types of cases.
Consider the Case
A patient with numerous medical comorbidities is admitted to the hospitalist service for stabilization prior to surgery, which will occur the next day. The hospitalist can report the appropriate admission code (99221-99223) without need for modifiers because the hospitalist is the attending of record and in a different specialty group. If a private insurer denies the claim as inclusive to the surgical service, the hospitalist can appeal with notes and a cover letter, along with the Medicare guidelines for global surgical package. The hospitalist may continue to provide postoperative daily care, as needed, to manage the patient’s chronic conditions, and report each service as subsequent hospital care (99231-99233) without modifier until the day of discharge (99238-99239). Again, if a payor issues a denial (inclusive to surgery), appealing with notes might be necessary.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 40. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf. Accessed May 5, 2012.
- Centers for Medicare & Medicaid Services. ICD-10: HHS proposes one-year delay of ICD-10 compliance date. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Medicare/Coding/ICD10/index.html?redirect=/ICD10. Accessed May 5, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
Hospitalists often are involved in the postoperative care of the surgical patient. However, HM is emerging in the admitting/attending role for procedural patients. Confusion can arise as to the nature of the hospitalist service, and whether it is deemed billable. Knowing the surgical package requirements can help hospitalists consider the issues.
Global Surgical Package Period1
Surgical procedures, categorized as major or minor surgery, are reimbursed for pre-, intra-, and postoperative care. Postoperative care varies according to the procedure’s assigned global period, which designates zero, 10, or 90 postoperative days. (Physicians can review the global period for any given CPT code in the Medicare Physician Fee Schedule, available at www.cms.gov/apps/physician-fee-schedule/search/search-criteria.aspx.)
Services classified with “XXX” do not have the global period concept. “ZZZ” services denote an “add-on” procedure code that must always be reported with a primary procedure code and assumes the global period assigned to the primary procedure performed.
Major surgery allocates a 90-day global period in which the surgeon is responsible for all related surgical care one day before surgery through 90 postoperative days with no additional charge. Minor surgery, including endoscopy, appoints a zero-day or 10-day postoperative period. The zero-day global period encompasses only services provided on the surgical day, whereas 10-day global periods include services on the surgical day through 10 postoperative days.
Global Surgical Package Components2
The global surgical package comprises a host of responsibilities that include standard facility requirements of filling out all necessary paperwork involved in surgical cases (e.g. preoperative H&P, operative consent forms, preoperative orders). Additionally, the surgeon’s packaged payment includes (at no extra charge):
- Preoperative visits after making the decision for surgery beginning one day prior to surgery;
- All additional postoperative medical or surgical services provided by the surgeon related to complications but not requiring additional trips to the operating room;
- Postoperative visits by the surgeon related to recovery from surgery, including but not limited to dressing changes; local incisional care; removal of cutaneous sutures and staples; line removals; changes and removal of tracheostomy tubes; and discharge services; and
- Postoperative pain management provided by the surgeon.
- Examples of services that are not included in the global surgical package, (i.e. are separately billable and may require an appropriate modifier) are:
- The initial consultation or evaluation of the problem by the surgeon to determine the need for surgery;
- Services of other physicians except where the other physicians are providing coverage for the surgeon or agree on a transfer of care (i.e. a formal agreement in the form of a letter or an annotation in the discharge summary, hospital record, or ASC record);
- Postoperative visits by the surgeon unrelated to the diagnosis for which the surgical procedure is performed, unless the visits occur due to complications of the surgery;
- Diagnostic tests and procedures, including diagnostic radiological procedures;
- Clearly distinct surgical procedures during the postoperative period that do not result in repeat operations or treatment for complications;
- Treatment for postoperative complications that requires a return trip to the operating room (OR), catheterization lab or endoscopy suite;
- Immunosuppressive therapy for organ transplants; and
- Critical-care services (CPT codes 99291 and 99292) unrelated to the surgery where a seriously injured or burned patient is critically ill and requires constant attendance of the surgeon.
Classification of “Surgeon”
For billing purposes, the “surgeon” is a qualified physician who can perform “surgical” services within their scope of practice. All physicians with the same specialty designation in the same group practice as the “surgeon” (i.e. reporting services under the same tax identification number) are considered a single entity and must adhere to the global period billing rules initiated by the “surgeon.”
Alternately, physicians with different specialty designations in the same group practice (e.g. a hospitalist and a cardiologist in a multispecialty group who report services under the same tax identification number) or different group practices can perform and separately report medically necessary services during the surgeon’s global period, as long as a formal (mutually agreed-upon) transfer of care did not occur.
Medical Necessity
With the growth of HM programs and the admission/attending role expansion, involvement in surgical cases comes under scrutiny for medical necessity. Admitting a patient who has active medical conditions (e.g. hypertension, diabetes, emphysema) is reasonable and necessary because the patient has a well-defined need for medical management by the hospitalist. Participation in the care of these patients is separately billable from the surgeon’s global period package.
Alternatively, a hospitalist might be required to admit and follow surgical patients who have no other identifiable chronic or acute conditions aside from the surgical problem. In these cases, hospitalist involvement may satisfy facility policy (quality of care, risk reduction, etc.) and administrative functions (discharge services or coordination of care) rather than active clinical management. This “medical management” will not be considered “medically necessary” by the payor, and may be denied as incidental to the surgeon’s perioperative services. Erroneous payment can occur, which will result in refund requests, as payors do not want to pay twice for duplicate services. Hospitalists can attempt to negotiate other terms with facilities to account for the unpaid time and effort directed toward these types of cases.
Consider the Case
A patient with numerous medical comorbidities is admitted to the hospitalist service for stabilization prior to surgery, which will occur the next day. The hospitalist can report the appropriate admission code (99221-99223) without need for modifiers because the hospitalist is the attending of record and in a different specialty group. If a private insurer denies the claim as inclusive to the surgical service, the hospitalist can appeal with notes and a cover letter, along with the Medicare guidelines for global surgical package. The hospitalist may continue to provide postoperative daily care, as needed, to manage the patient’s chronic conditions, and report each service as subsequent hospital care (99231-99233) without modifier until the day of discharge (99238-99239). Again, if a payor issues a denial (inclusive to surgery), appealing with notes might be necessary.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 40. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf. Accessed May 5, 2012.
- Centers for Medicare & Medicaid Services. ICD-10: HHS proposes one-year delay of ICD-10 compliance date. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Medicare/Coding/ICD10/index.html?redirect=/ICD10. Accessed May 5, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
Hospitalists often are involved in the postoperative care of the surgical patient. However, HM is emerging in the admitting/attending role for procedural patients. Confusion can arise as to the nature of the hospitalist service, and whether it is deemed billable. Knowing the surgical package requirements can help hospitalists consider the issues.
Global Surgical Package Period1
Surgical procedures, categorized as major or minor surgery, are reimbursed for pre-, intra-, and postoperative care. Postoperative care varies according to the procedure’s assigned global period, which designates zero, 10, or 90 postoperative days. (Physicians can review the global period for any given CPT code in the Medicare Physician Fee Schedule, available at www.cms.gov/apps/physician-fee-schedule/search/search-criteria.aspx.)
Services classified with “XXX” do not have the global period concept. “ZZZ” services denote an “add-on” procedure code that must always be reported with a primary procedure code and assumes the global period assigned to the primary procedure performed.
Major surgery allocates a 90-day global period in which the surgeon is responsible for all related surgical care one day before surgery through 90 postoperative days with no additional charge. Minor surgery, including endoscopy, appoints a zero-day or 10-day postoperative period. The zero-day global period encompasses only services provided on the surgical day, whereas 10-day global periods include services on the surgical day through 10 postoperative days.
Global Surgical Package Components2
The global surgical package comprises a host of responsibilities that include standard facility requirements of filling out all necessary paperwork involved in surgical cases (e.g. preoperative H&P, operative consent forms, preoperative orders). Additionally, the surgeon’s packaged payment includes (at no extra charge):
- Preoperative visits after making the decision for surgery beginning one day prior to surgery;
- All additional postoperative medical or surgical services provided by the surgeon related to complications but not requiring additional trips to the operating room;
- Postoperative visits by the surgeon related to recovery from surgery, including but not limited to dressing changes; local incisional care; removal of cutaneous sutures and staples; line removals; changes and removal of tracheostomy tubes; and discharge services; and
- Postoperative pain management provided by the surgeon.
- Examples of services that are not included in the global surgical package, (i.e. are separately billable and may require an appropriate modifier) are:
- The initial consultation or evaluation of the problem by the surgeon to determine the need for surgery;
- Services of other physicians except where the other physicians are providing coverage for the surgeon or agree on a transfer of care (i.e. a formal agreement in the form of a letter or an annotation in the discharge summary, hospital record, or ASC record);
- Postoperative visits by the surgeon unrelated to the diagnosis for which the surgical procedure is performed, unless the visits occur due to complications of the surgery;
- Diagnostic tests and procedures, including diagnostic radiological procedures;
- Clearly distinct surgical procedures during the postoperative period that do not result in repeat operations or treatment for complications;
- Treatment for postoperative complications that requires a return trip to the operating room (OR), catheterization lab or endoscopy suite;
- Immunosuppressive therapy for organ transplants; and
- Critical-care services (CPT codes 99291 and 99292) unrelated to the surgery where a seriously injured or burned patient is critically ill and requires constant attendance of the surgeon.
Classification of “Surgeon”
For billing purposes, the “surgeon” is a qualified physician who can perform “surgical” services within their scope of practice. All physicians with the same specialty designation in the same group practice as the “surgeon” (i.e. reporting services under the same tax identification number) are considered a single entity and must adhere to the global period billing rules initiated by the “surgeon.”
Alternately, physicians with different specialty designations in the same group practice (e.g. a hospitalist and a cardiologist in a multispecialty group who report services under the same tax identification number) or different group practices can perform and separately report medically necessary services during the surgeon’s global period, as long as a formal (mutually agreed-upon) transfer of care did not occur.
Medical Necessity
With the growth of HM programs and the admission/attending role expansion, involvement in surgical cases comes under scrutiny for medical necessity. Admitting a patient who has active medical conditions (e.g. hypertension, diabetes, emphysema) is reasonable and necessary because the patient has a well-defined need for medical management by the hospitalist. Participation in the care of these patients is separately billable from the surgeon’s global period package.
Alternatively, a hospitalist might be required to admit and follow surgical patients who have no other identifiable chronic or acute conditions aside from the surgical problem. In these cases, hospitalist involvement may satisfy facility policy (quality of care, risk reduction, etc.) and administrative functions (discharge services or coordination of care) rather than active clinical management. This “medical management” will not be considered “medically necessary” by the payor, and may be denied as incidental to the surgeon’s perioperative services. Erroneous payment can occur, which will result in refund requests, as payors do not want to pay twice for duplicate services. Hospitalists can attempt to negotiate other terms with facilities to account for the unpaid time and effort directed toward these types of cases.
Consider the Case
A patient with numerous medical comorbidities is admitted to the hospitalist service for stabilization prior to surgery, which will occur the next day. The hospitalist can report the appropriate admission code (99221-99223) without need for modifiers because the hospitalist is the attending of record and in a different specialty group. If a private insurer denies the claim as inclusive to the surgical service, the hospitalist can appeal with notes and a cover letter, along with the Medicare guidelines for global surgical package. The hospitalist may continue to provide postoperative daily care, as needed, to manage the patient’s chronic conditions, and report each service as subsequent hospital care (99231-99233) without modifier until the day of discharge (99238-99239). Again, if a payor issues a denial (inclusive to surgery), appealing with notes might be necessary.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 40. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf. Accessed May 5, 2012.
- Centers for Medicare & Medicaid Services. ICD-10: HHS proposes one-year delay of ICD-10 compliance date. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Medicare/Coding/ICD10/index.html?redirect=/ICD10. Accessed May 5, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
Physician Payment Systems Remain Constant
I would like to know where payment for the service of hospitalists fits into the insurance/Medicare payment system. Are hospitalists considered employees of the hospital and, therefore, billed through the hospital system? Are they considered independent doctors and, therefore, do their own direct billing? Do they, in general, accept assignment of benefits from you for your insurance/Medicare? Do they sign contracts with insurance/Medicare to participate in their plans?
Carole L. Hughes
Dr. Hospitalist responds:
For the sake of argument, let’s say that Carole is on the outside looking in—meaning she’s not a healthcare practitioner, but a consumer. It might seem a bit strange to wonder where all these “hospitalists” come from, and who pays for them. Let’s walk through a few scenarios as outlined here.
Are hospitalists considered employees of the hospital? They certainly could be directly employed by the hospital, but it’s just as likely they could be contracted with the hospital for certain services, such as taking ED call for unassigned patients. It’s also entirely possible that the hospitalist has no direct financial relationship with the hospital at all. In this case, a hospitalist is taking cases that are referred from other physicians and for which there is a coverage agreement. The most common situation is a primary-care physician group that is looking for a hospitalist to care for their patients in the hospital. This is usually a handshake agreement, with no money involved.
Do hospitalists do their own direct billing to the insurers? As for this part of the question, it’s time to separate “hospital services” from “hospitalist services.” Hospital services are billed under Medicare Part A, while physician services are billed under Medicare Part B, meaning that even if a physician is employed directly by the hospital, that physician’s professional services are still billed and paid separate from any hospital charges (for things like the bed, supplies, and nursing). Because Medicare sets the ground rules, other insurances typically follow suit. Payment applies similarly to the contracted hospitalists and independent hospitalists.
Do hospitalists have to be credentialed with the insurers? Yes. Whether it is Medicare or Cigna or United, each individual physician must be credentialed with the payors to receive payment. Medicare credentialing for physicians is pretty universal, given that most of our patients have this as their primary insurance. Without it, there is no payment from Medicare to the physician. Many groups or hospitals won’t even let their physicians begin seeing patients until that paperwork is approved. Due to timely filing rules, you can’t just start to see patients and hope to get paid later. And there’s no negotiating with the government—whatever Medicare pays in a region for a specific service is the payment the physician receives.
For the private insurers, it’s generally easier to receive payment if you are credentialed, but I’ve seen a few physician groups negotiate payments without agreeing to a flat contracted rate. I don’t recommend this setup, as the patient can often get caught in the middle with a rather hefty bill. Still, there is some room for negotiation on the private insurer payment rates.
In summary, whether a hospitalist is employed by the hospital, contracted, or truly independent, they all bill Medicare and the insurers for their professional fees. Medicare payments won’t vary, but private insurance payments can. It’s certainly a challenging payment system to understand, from either the provider or the patient point of view.
I would like to know where payment for the service of hospitalists fits into the insurance/Medicare payment system. Are hospitalists considered employees of the hospital and, therefore, billed through the hospital system? Are they considered independent doctors and, therefore, do their own direct billing? Do they, in general, accept assignment of benefits from you for your insurance/Medicare? Do they sign contracts with insurance/Medicare to participate in their plans?
Carole L. Hughes
Dr. Hospitalist responds:
For the sake of argument, let’s say that Carole is on the outside looking in—meaning she’s not a healthcare practitioner, but a consumer. It might seem a bit strange to wonder where all these “hospitalists” come from, and who pays for them. Let’s walk through a few scenarios as outlined here.
Are hospitalists considered employees of the hospital? They certainly could be directly employed by the hospital, but it’s just as likely they could be contracted with the hospital for certain services, such as taking ED call for unassigned patients. It’s also entirely possible that the hospitalist has no direct financial relationship with the hospital at all. In this case, a hospitalist is taking cases that are referred from other physicians and for which there is a coverage agreement. The most common situation is a primary-care physician group that is looking for a hospitalist to care for their patients in the hospital. This is usually a handshake agreement, with no money involved.
Do hospitalists do their own direct billing to the insurers? As for this part of the question, it’s time to separate “hospital services” from “hospitalist services.” Hospital services are billed under Medicare Part A, while physician services are billed under Medicare Part B, meaning that even if a physician is employed directly by the hospital, that physician’s professional services are still billed and paid separate from any hospital charges (for things like the bed, supplies, and nursing). Because Medicare sets the ground rules, other insurances typically follow suit. Payment applies similarly to the contracted hospitalists and independent hospitalists.
Do hospitalists have to be credentialed with the insurers? Yes. Whether it is Medicare or Cigna or United, each individual physician must be credentialed with the payors to receive payment. Medicare credentialing for physicians is pretty universal, given that most of our patients have this as their primary insurance. Without it, there is no payment from Medicare to the physician. Many groups or hospitals won’t even let their physicians begin seeing patients until that paperwork is approved. Due to timely filing rules, you can’t just start to see patients and hope to get paid later. And there’s no negotiating with the government—whatever Medicare pays in a region for a specific service is the payment the physician receives.
For the private insurers, it’s generally easier to receive payment if you are credentialed, but I’ve seen a few physician groups negotiate payments without agreeing to a flat contracted rate. I don’t recommend this setup, as the patient can often get caught in the middle with a rather hefty bill. Still, there is some room for negotiation on the private insurer payment rates.
In summary, whether a hospitalist is employed by the hospital, contracted, or truly independent, they all bill Medicare and the insurers for their professional fees. Medicare payments won’t vary, but private insurance payments can. It’s certainly a challenging payment system to understand, from either the provider or the patient point of view.
I would like to know where payment for the service of hospitalists fits into the insurance/Medicare payment system. Are hospitalists considered employees of the hospital and, therefore, billed through the hospital system? Are they considered independent doctors and, therefore, do their own direct billing? Do they, in general, accept assignment of benefits from you for your insurance/Medicare? Do they sign contracts with insurance/Medicare to participate in their plans?
Carole L. Hughes
Dr. Hospitalist responds:
For the sake of argument, let’s say that Carole is on the outside looking in—meaning she’s not a healthcare practitioner, but a consumer. It might seem a bit strange to wonder where all these “hospitalists” come from, and who pays for them. Let’s walk through a few scenarios as outlined here.
Are hospitalists considered employees of the hospital? They certainly could be directly employed by the hospital, but it’s just as likely they could be contracted with the hospital for certain services, such as taking ED call for unassigned patients. It’s also entirely possible that the hospitalist has no direct financial relationship with the hospital at all. In this case, a hospitalist is taking cases that are referred from other physicians and for which there is a coverage agreement. The most common situation is a primary-care physician group that is looking for a hospitalist to care for their patients in the hospital. This is usually a handshake agreement, with no money involved.
Do hospitalists do their own direct billing to the insurers? As for this part of the question, it’s time to separate “hospital services” from “hospitalist services.” Hospital services are billed under Medicare Part A, while physician services are billed under Medicare Part B, meaning that even if a physician is employed directly by the hospital, that physician’s professional services are still billed and paid separate from any hospital charges (for things like the bed, supplies, and nursing). Because Medicare sets the ground rules, other insurances typically follow suit. Payment applies similarly to the contracted hospitalists and independent hospitalists.
Do hospitalists have to be credentialed with the insurers? Yes. Whether it is Medicare or Cigna or United, each individual physician must be credentialed with the payors to receive payment. Medicare credentialing for physicians is pretty universal, given that most of our patients have this as their primary insurance. Without it, there is no payment from Medicare to the physician. Many groups or hospitals won’t even let their physicians begin seeing patients until that paperwork is approved. Due to timely filing rules, you can’t just start to see patients and hope to get paid later. And there’s no negotiating with the government—whatever Medicare pays in a region for a specific service is the payment the physician receives.
For the private insurers, it’s generally easier to receive payment if you are credentialed, but I’ve seen a few physician groups negotiate payments without agreeing to a flat contracted rate. I don’t recommend this setup, as the patient can often get caught in the middle with a rather hefty bill. Still, there is some room for negotiation on the private insurer payment rates.
In summary, whether a hospitalist is employed by the hospital, contracted, or truly independent, they all bill Medicare and the insurers for their professional fees. Medicare payments won’t vary, but private insurance payments can. It’s certainly a challenging payment system to understand, from either the provider or the patient point of view.
ICD-10 Update
On April 17, the U.S. Department of Health and Human Services (HHS) published a proposed rule to delay the compliance date for the International Classification of Diseases, 10th Edition, diagnosis and procedure codes (ICD-10) from Oct. 1, 2013, to Oct. 1, 2014.2
Per HHS, the ICD-10 compliance date change is part of a proposed rule that would adopt a standard for a unique health plan identifier (HPID), adopt a data element that would serve as an “other entity” identifier (OEID), and add a National Provider Identifier (NPI) requirement. The proposed rule was developed by the Office of E-Health Standards and Services (OESS) as part of its ongoing role, delegated by HHS, to establish standards for electronic healthcare transactions under the Health Insurance Portability and Accountability Act of 1996 (HIPAA).
HHS proposes that covered entities must be in compliance with ICD-10 by Oct. 1, 2014.
On April 17, the U.S. Department of Health and Human Services (HHS) published a proposed rule to delay the compliance date for the International Classification of Diseases, 10th Edition, diagnosis and procedure codes (ICD-10) from Oct. 1, 2013, to Oct. 1, 2014.2
Per HHS, the ICD-10 compliance date change is part of a proposed rule that would adopt a standard for a unique health plan identifier (HPID), adopt a data element that would serve as an “other entity” identifier (OEID), and add a National Provider Identifier (NPI) requirement. The proposed rule was developed by the Office of E-Health Standards and Services (OESS) as part of its ongoing role, delegated by HHS, to establish standards for electronic healthcare transactions under the Health Insurance Portability and Accountability Act of 1996 (HIPAA).
HHS proposes that covered entities must be in compliance with ICD-10 by Oct. 1, 2014.
On April 17, the U.S. Department of Health and Human Services (HHS) published a proposed rule to delay the compliance date for the International Classification of Diseases, 10th Edition, diagnosis and procedure codes (ICD-10) from Oct. 1, 2013, to Oct. 1, 2014.2
Per HHS, the ICD-10 compliance date change is part of a proposed rule that would adopt a standard for a unique health plan identifier (HPID), adopt a data element that would serve as an “other entity” identifier (OEID), and add a National Provider Identifier (NPI) requirement. The proposed rule was developed by the Office of E-Health Standards and Services (OESS) as part of its ongoing role, delegated by HHS, to establish standards for electronic healthcare transactions under the Health Insurance Portability and Accountability Act of 1996 (HIPAA).
HHS proposes that covered entities must be in compliance with ICD-10 by Oct. 1, 2014.
Efficacy, Diagnoses, Frequency Play Parts in Coverage Limitations
Under Section 1862(a)(1)(A) of the Social Security Act, the Medicare program may only pay for items and services that are “reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member,” unless there is another statutory authorization for payment (e.g. colorectal cancer screening).1 Coverage limitations include:2
- Proven clinical efficacy. For example, Medicare deems acupuncture “experimental/investigational” in the diagnosis or treatment of illness or injury;
- Diagnoses. As an example, vitamin B-12 injections are covered, but only for such diagnoses as pernicious anemia and dementias secondary to vitamin B-12 deficiency; and
- Frequency/utilization parameters. For example, a screening colonoscopy (G0105) can be paid once every 24 months for beneficiaries who are at high risk for colorectal cancer; otherwise the service is limited to once every 10 years.
Beyond these factors, individual consideration might be granted. Supportive and unambiguous documentation (medical records, clinical studies, etc.) must be submitted when the clinical circumstances do not appear to support the medical necessity for the service.
Diagnoses Selection
Select the code that best represents the primary reason for the service or procedure on a given date. In the absence of a definitive diagnosis, the code may correspond to a sign or symptom. Physicians never should report a code that represents a probable, suspected, or “rule out” condition. Although facility billing might consider these unconfirmed circumstances (when necessary), physician billing prohibits this practice.
Reporting services for hospitalized patients is challenging when multiple services for the same patient are provided on the same date by the same or different physician, also known as concurrent care. Each physician manages a particular aspect while still considering the patient’s overall condition; each physician should report the corresponding diagnosis for that management. If billed correctly, each physician will have a different primary diagnosis code to justify their involvement, increasing their opportunity for payment.3
The non-primary diagnoses might also be listed on the claim if appropriately addressed in the documentation (i.e. “non-primary” conditions’ indirect role in the focused management of the primary condition). For example, a hospitalist, pulmonologist, and nephrologist manage a patient’s uncontrolled diabetes (250.02), COPD exacerbation (491.21), and CRI (585.9), respectively. Each may report subsequent hospital care (99231-99233) for medically necessary concurrent care:
- Hospitalist: 250.02, 491.21, 585.9;
- Pulmonologist: 491.21, 250.02, 585.9; and
- Nephrologist: 585.9, 492.21, 250.02.
Coverage Determinations
Code comparisons can be made after diagnosis code selection. Coverage determinations identify specific conditions (i.e. ICD-9-CM codes) for which services are considered medically necessary. They also outline the frequency interval at which services can be performed, when applicable.
For example, vascular studies (e.g. CPT 93971) are indicated for the preoperative examination (ICD-9-CM V72.83) of potential harvest vein grafts prior to bypass surgery.4 This is a covered service only when the results of the study are necessary to locate suitable graft vessels. The need for bypass surgery must be determined prior to performance of the test. V72.83 is “covered” only when reported for a unilateral study, not a bilateral study (CPT 93970). Frequency parameters allow for only one preoperative scan.4
Coverage determination can occur on two levels: national and local. The Centers for Medicare & Medicaid Services (CMS) develops national coverage determinations (NCDs) through an evidence-based process, with opportunities for public participation.5 All Medicare administrative contractors must abide by NCDs without imposing further limitations or guidelines. As example, the NCD “Consultations With a Beneficiary’s Family and Associates” permits a physician to provide counseling to family members. Family counseling services are covered only when the primary purpose of such counseling is the treatment of the patient’s condition.6
Non-Medicare payors do not have to follow federal guidelines unless the member participates in a Medicare managed-care plan.
In the absence of a national coverage policy, an item or service may be covered at the discretion of the Medicare contractors based on a local coverage determination (LCD).5 LCDs vary by state, creating an inconsistent approach to medical coverage. The vascular study guidelines listed above do not apply to all contractors. For example, Trailblazer Health Enterprises’ policy does not reference preoperative exams being limited to unilateral studies.7 (A listing of Medicare Contractor LCDs can be found at www.cms.hhs.gov/DeterminationProcess/04_LCDs.asp.)
Other Considerations
Investigate “medical necessity” denials. Do not take them at face value. Billing personnel often assume that the physician reported an incorrect diagnosis code. Consider the service when trying to formulate a response to the denial. Procedures (surgical or diagnostic services) may be denied for an invalid diagnosis. After reviewing the documentation to ensure that it supports the diagnosis, the claim may be resubmitted with a corrected diagnosis code, when applicable. Denials for frequency limitations can only be appealed with documentation that explicitly identifies the need for the service beyond the contractor-stated parameters.
If the “medical necessity” denial involves a covered evaluation and management (E/M) visit, it is less likely to be diagnosis-related. More likely, when dealing with Medicare contractors, the denial is the result of a failed response to a prepayment request for documentation. Medicare typically issues a request to review documentation prior to payment for the following inpatient E/M services: 99223, 99233, 99239, and 99292.
If the documentation is not provided to the Medicare prepayment review department within the designated time frame, the claim is automatically denied with a citation of “not deemed a medical necessity.” Acknowledge this remittance remark and do not assume that the physician assigned an incorrect diagnosis code. Although this is a possibility, it is more likely due to the failed request response. Appealing these claims requires submission of documentation to the Medicare appeals department. Reimbursement is provided once supportive documentation is received.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Social Security Administration. Exclusions from coverage and Medicare as a secondary payer. Social Security Administration website. Available at: http://www.ssa.gov/OP_Home/ssact/title18/1862.htm. Accessed March 1, 2012.
- Highmark Medicare Services. A/B Reference Manual: Chapter 6, Medical Coverage, Medical Necessity, and Medical Policy. Highmark Medicare Services website. Available at: http://www.highmarkmedicareservices.com/refman/chapter-6.html. Accessed March 1, 2012.
- Pohlig C. Daily care conundrums. The Hospitalist. 2008;12(12):18.
- Highmark Medicare Services. LCD L27506: Non-Invasive Peripheral Venous Studies. Highmark Medicare Services website. Available at: http://www.highmarkmedicareservices.com/policy/mac-ab/l27506-r10.html. Accessed March 1, 2012.
- Centers for Medicare & Medicaid Services. Medicare Coverage Determination Process: Overview. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.hhs.gov/DeterminationProcess/01_Overview.asp#TopOfPage. Accessed March 1, 2012.
- Centers for Medicare & Medicaid Services. Medicare National Coverage Determination Manual: Chapter 1, Part 1, Section 70.1. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/ncd103c1_Part1.pdf. Accessed March 1, 2012.
- Trailblazer Health Enterprises. LCD 2866: Non-Invasive Venous Studies. Trailblazer Health Enterprises website. Available at: http://www.trailblazerhealth.com/Tools/LCDs.aspx?ID=2866. Accessed March 1, 2012.
Under Section 1862(a)(1)(A) of the Social Security Act, the Medicare program may only pay for items and services that are “reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member,” unless there is another statutory authorization for payment (e.g. colorectal cancer screening).1 Coverage limitations include:2
- Proven clinical efficacy. For example, Medicare deems acupuncture “experimental/investigational” in the diagnosis or treatment of illness or injury;
- Diagnoses. As an example, vitamin B-12 injections are covered, but only for such diagnoses as pernicious anemia and dementias secondary to vitamin B-12 deficiency; and
- Frequency/utilization parameters. For example, a screening colonoscopy (G0105) can be paid once every 24 months for beneficiaries who are at high risk for colorectal cancer; otherwise the service is limited to once every 10 years.
Beyond these factors, individual consideration might be granted. Supportive and unambiguous documentation (medical records, clinical studies, etc.) must be submitted when the clinical circumstances do not appear to support the medical necessity for the service.
Diagnoses Selection
Select the code that best represents the primary reason for the service or procedure on a given date. In the absence of a definitive diagnosis, the code may correspond to a sign or symptom. Physicians never should report a code that represents a probable, suspected, or “rule out” condition. Although facility billing might consider these unconfirmed circumstances (when necessary), physician billing prohibits this practice.
Reporting services for hospitalized patients is challenging when multiple services for the same patient are provided on the same date by the same or different physician, also known as concurrent care. Each physician manages a particular aspect while still considering the patient’s overall condition; each physician should report the corresponding diagnosis for that management. If billed correctly, each physician will have a different primary diagnosis code to justify their involvement, increasing their opportunity for payment.3
The non-primary diagnoses might also be listed on the claim if appropriately addressed in the documentation (i.e. “non-primary” conditions’ indirect role in the focused management of the primary condition). For example, a hospitalist, pulmonologist, and nephrologist manage a patient’s uncontrolled diabetes (250.02), COPD exacerbation (491.21), and CRI (585.9), respectively. Each may report subsequent hospital care (99231-99233) for medically necessary concurrent care:
- Hospitalist: 250.02, 491.21, 585.9;
- Pulmonologist: 491.21, 250.02, 585.9; and
- Nephrologist: 585.9, 492.21, 250.02.
Coverage Determinations
Code comparisons can be made after diagnosis code selection. Coverage determinations identify specific conditions (i.e. ICD-9-CM codes) for which services are considered medically necessary. They also outline the frequency interval at which services can be performed, when applicable.
For example, vascular studies (e.g. CPT 93971) are indicated for the preoperative examination (ICD-9-CM V72.83) of potential harvest vein grafts prior to bypass surgery.4 This is a covered service only when the results of the study are necessary to locate suitable graft vessels. The need for bypass surgery must be determined prior to performance of the test. V72.83 is “covered” only when reported for a unilateral study, not a bilateral study (CPT 93970). Frequency parameters allow for only one preoperative scan.4
Coverage determination can occur on two levels: national and local. The Centers for Medicare & Medicaid Services (CMS) develops national coverage determinations (NCDs) through an evidence-based process, with opportunities for public participation.5 All Medicare administrative contractors must abide by NCDs without imposing further limitations or guidelines. As example, the NCD “Consultations With a Beneficiary’s Family and Associates” permits a physician to provide counseling to family members. Family counseling services are covered only when the primary purpose of such counseling is the treatment of the patient’s condition.6
Non-Medicare payors do not have to follow federal guidelines unless the member participates in a Medicare managed-care plan.
In the absence of a national coverage policy, an item or service may be covered at the discretion of the Medicare contractors based on a local coverage determination (LCD).5 LCDs vary by state, creating an inconsistent approach to medical coverage. The vascular study guidelines listed above do not apply to all contractors. For example, Trailblazer Health Enterprises’ policy does not reference preoperative exams being limited to unilateral studies.7 (A listing of Medicare Contractor LCDs can be found at www.cms.hhs.gov/DeterminationProcess/04_LCDs.asp.)
Other Considerations
Investigate “medical necessity” denials. Do not take them at face value. Billing personnel often assume that the physician reported an incorrect diagnosis code. Consider the service when trying to formulate a response to the denial. Procedures (surgical or diagnostic services) may be denied for an invalid diagnosis. After reviewing the documentation to ensure that it supports the diagnosis, the claim may be resubmitted with a corrected diagnosis code, when applicable. Denials for frequency limitations can only be appealed with documentation that explicitly identifies the need for the service beyond the contractor-stated parameters.
If the “medical necessity” denial involves a covered evaluation and management (E/M) visit, it is less likely to be diagnosis-related. More likely, when dealing with Medicare contractors, the denial is the result of a failed response to a prepayment request for documentation. Medicare typically issues a request to review documentation prior to payment for the following inpatient E/M services: 99223, 99233, 99239, and 99292.
If the documentation is not provided to the Medicare prepayment review department within the designated time frame, the claim is automatically denied with a citation of “not deemed a medical necessity.” Acknowledge this remittance remark and do not assume that the physician assigned an incorrect diagnosis code. Although this is a possibility, it is more likely due to the failed request response. Appealing these claims requires submission of documentation to the Medicare appeals department. Reimbursement is provided once supportive documentation is received.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Social Security Administration. Exclusions from coverage and Medicare as a secondary payer. Social Security Administration website. Available at: http://www.ssa.gov/OP_Home/ssact/title18/1862.htm. Accessed March 1, 2012.
- Highmark Medicare Services. A/B Reference Manual: Chapter 6, Medical Coverage, Medical Necessity, and Medical Policy. Highmark Medicare Services website. Available at: http://www.highmarkmedicareservices.com/refman/chapter-6.html. Accessed March 1, 2012.
- Pohlig C. Daily care conundrums. The Hospitalist. 2008;12(12):18.
- Highmark Medicare Services. LCD L27506: Non-Invasive Peripheral Venous Studies. Highmark Medicare Services website. Available at: http://www.highmarkmedicareservices.com/policy/mac-ab/l27506-r10.html. Accessed March 1, 2012.
- Centers for Medicare & Medicaid Services. Medicare Coverage Determination Process: Overview. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.hhs.gov/DeterminationProcess/01_Overview.asp#TopOfPage. Accessed March 1, 2012.
- Centers for Medicare & Medicaid Services. Medicare National Coverage Determination Manual: Chapter 1, Part 1, Section 70.1. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/ncd103c1_Part1.pdf. Accessed March 1, 2012.
- Trailblazer Health Enterprises. LCD 2866: Non-Invasive Venous Studies. Trailblazer Health Enterprises website. Available at: http://www.trailblazerhealth.com/Tools/LCDs.aspx?ID=2866. Accessed March 1, 2012.
Under Section 1862(a)(1)(A) of the Social Security Act, the Medicare program may only pay for items and services that are “reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member,” unless there is another statutory authorization for payment (e.g. colorectal cancer screening).1 Coverage limitations include:2
- Proven clinical efficacy. For example, Medicare deems acupuncture “experimental/investigational” in the diagnosis or treatment of illness or injury;
- Diagnoses. As an example, vitamin B-12 injections are covered, but only for such diagnoses as pernicious anemia and dementias secondary to vitamin B-12 deficiency; and
- Frequency/utilization parameters. For example, a screening colonoscopy (G0105) can be paid once every 24 months for beneficiaries who are at high risk for colorectal cancer; otherwise the service is limited to once every 10 years.
Beyond these factors, individual consideration might be granted. Supportive and unambiguous documentation (medical records, clinical studies, etc.) must be submitted when the clinical circumstances do not appear to support the medical necessity for the service.
Diagnoses Selection
Select the code that best represents the primary reason for the service or procedure on a given date. In the absence of a definitive diagnosis, the code may correspond to a sign or symptom. Physicians never should report a code that represents a probable, suspected, or “rule out” condition. Although facility billing might consider these unconfirmed circumstances (when necessary), physician billing prohibits this practice.
Reporting services for hospitalized patients is challenging when multiple services for the same patient are provided on the same date by the same or different physician, also known as concurrent care. Each physician manages a particular aspect while still considering the patient’s overall condition; each physician should report the corresponding diagnosis for that management. If billed correctly, each physician will have a different primary diagnosis code to justify their involvement, increasing their opportunity for payment.3
The non-primary diagnoses might also be listed on the claim if appropriately addressed in the documentation (i.e. “non-primary” conditions’ indirect role in the focused management of the primary condition). For example, a hospitalist, pulmonologist, and nephrologist manage a patient’s uncontrolled diabetes (250.02), COPD exacerbation (491.21), and CRI (585.9), respectively. Each may report subsequent hospital care (99231-99233) for medically necessary concurrent care:
- Hospitalist: 250.02, 491.21, 585.9;
- Pulmonologist: 491.21, 250.02, 585.9; and
- Nephrologist: 585.9, 492.21, 250.02.
Coverage Determinations
Code comparisons can be made after diagnosis code selection. Coverage determinations identify specific conditions (i.e. ICD-9-CM codes) for which services are considered medically necessary. They also outline the frequency interval at which services can be performed, when applicable.
For example, vascular studies (e.g. CPT 93971) are indicated for the preoperative examination (ICD-9-CM V72.83) of potential harvest vein grafts prior to bypass surgery.4 This is a covered service only when the results of the study are necessary to locate suitable graft vessels. The need for bypass surgery must be determined prior to performance of the test. V72.83 is “covered” only when reported for a unilateral study, not a bilateral study (CPT 93970). Frequency parameters allow for only one preoperative scan.4
Coverage determination can occur on two levels: national and local. The Centers for Medicare & Medicaid Services (CMS) develops national coverage determinations (NCDs) through an evidence-based process, with opportunities for public participation.5 All Medicare administrative contractors must abide by NCDs without imposing further limitations or guidelines. As example, the NCD “Consultations With a Beneficiary’s Family and Associates” permits a physician to provide counseling to family members. Family counseling services are covered only when the primary purpose of such counseling is the treatment of the patient’s condition.6
Non-Medicare payors do not have to follow federal guidelines unless the member participates in a Medicare managed-care plan.
In the absence of a national coverage policy, an item or service may be covered at the discretion of the Medicare contractors based on a local coverage determination (LCD).5 LCDs vary by state, creating an inconsistent approach to medical coverage. The vascular study guidelines listed above do not apply to all contractors. For example, Trailblazer Health Enterprises’ policy does not reference preoperative exams being limited to unilateral studies.7 (A listing of Medicare Contractor LCDs can be found at www.cms.hhs.gov/DeterminationProcess/04_LCDs.asp.)
Other Considerations
Investigate “medical necessity” denials. Do not take them at face value. Billing personnel often assume that the physician reported an incorrect diagnosis code. Consider the service when trying to formulate a response to the denial. Procedures (surgical or diagnostic services) may be denied for an invalid diagnosis. After reviewing the documentation to ensure that it supports the diagnosis, the claim may be resubmitted with a corrected diagnosis code, when applicable. Denials for frequency limitations can only be appealed with documentation that explicitly identifies the need for the service beyond the contractor-stated parameters.
If the “medical necessity” denial involves a covered evaluation and management (E/M) visit, it is less likely to be diagnosis-related. More likely, when dealing with Medicare contractors, the denial is the result of a failed response to a prepayment request for documentation. Medicare typically issues a request to review documentation prior to payment for the following inpatient E/M services: 99223, 99233, 99239, and 99292.
If the documentation is not provided to the Medicare prepayment review department within the designated time frame, the claim is automatically denied with a citation of “not deemed a medical necessity.” Acknowledge this remittance remark and do not assume that the physician assigned an incorrect diagnosis code. Although this is a possibility, it is more likely due to the failed request response. Appealing these claims requires submission of documentation to the Medicare appeals department. Reimbursement is provided once supportive documentation is received.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Social Security Administration. Exclusions from coverage and Medicare as a secondary payer. Social Security Administration website. Available at: http://www.ssa.gov/OP_Home/ssact/title18/1862.htm. Accessed March 1, 2012.
- Highmark Medicare Services. A/B Reference Manual: Chapter 6, Medical Coverage, Medical Necessity, and Medical Policy. Highmark Medicare Services website. Available at: http://www.highmarkmedicareservices.com/refman/chapter-6.html. Accessed March 1, 2012.
- Pohlig C. Daily care conundrums. The Hospitalist. 2008;12(12):18.
- Highmark Medicare Services. LCD L27506: Non-Invasive Peripheral Venous Studies. Highmark Medicare Services website. Available at: http://www.highmarkmedicareservices.com/policy/mac-ab/l27506-r10.html. Accessed March 1, 2012.
- Centers for Medicare & Medicaid Services. Medicare Coverage Determination Process: Overview. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.hhs.gov/DeterminationProcess/01_Overview.asp#TopOfPage. Accessed March 1, 2012.
- Centers for Medicare & Medicaid Services. Medicare National Coverage Determination Manual: Chapter 1, Part 1, Section 70.1. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/ncd103c1_Part1.pdf. Accessed March 1, 2012.
- Trailblazer Health Enterprises. LCD 2866: Non-Invasive Venous Studies. Trailblazer Health Enterprises website. Available at: http://www.trailblazerhealth.com/Tools/LCDs.aspx?ID=2866. Accessed March 1, 2012.
HHS Delays ICD-10 Compliance Date
According to a CMS statement regarding part of President Obama’s “commitment to reducing regulatory burden,” Health and Human Services Secretary Kathleen G. Sebelius announced that HHS will initiate a process to “postpone the date” by which certain healthcare entities have to comply with International Classification of Diseases, 10th Edition diagnosis and procedure codes (ICD-10).1
The final rule adopting ICD-10 as a standard was published in January 2009; it set a compliance date of Oct. 1, 2013 (a two-year delay from the 2008 proposed rule). HHS will announce a new compliance date moving forward.
“ICD-10 codes are important to many positive improvements in our healthcare system,” Sebelius said in the statement. “We have heard from many in the provider community who have concerns about the administrative burdens they face in the years ahead. We are committing to work with the provider community to re-examine the pace at which HHS and the nation implement these important improvements to our healthcare system.”
ICD-10 codes provide more robust and specific data that will help improve patient care and enable the exchange of our healthcare data with that of the rest of the world, much of which has long been using ICD-10. Entities covered under the Health Insurance Portability and Accountability Act of 1996 (HIPAA) will be required to use the ICD-10 diagnostic and procedure codes.
All that said, do not postpone any activities toward ICD-10 implementation until further clarification comes from CMS.
—Carol Pohlig
Reference
According to a CMS statement regarding part of President Obama’s “commitment to reducing regulatory burden,” Health and Human Services Secretary Kathleen G. Sebelius announced that HHS will initiate a process to “postpone the date” by which certain healthcare entities have to comply with International Classification of Diseases, 10th Edition diagnosis and procedure codes (ICD-10).1
The final rule adopting ICD-10 as a standard was published in January 2009; it set a compliance date of Oct. 1, 2013 (a two-year delay from the 2008 proposed rule). HHS will announce a new compliance date moving forward.
“ICD-10 codes are important to many positive improvements in our healthcare system,” Sebelius said in the statement. “We have heard from many in the provider community who have concerns about the administrative burdens they face in the years ahead. We are committing to work with the provider community to re-examine the pace at which HHS and the nation implement these important improvements to our healthcare system.”
ICD-10 codes provide more robust and specific data that will help improve patient care and enable the exchange of our healthcare data with that of the rest of the world, much of which has long been using ICD-10. Entities covered under the Health Insurance Portability and Accountability Act of 1996 (HIPAA) will be required to use the ICD-10 diagnostic and procedure codes.
All that said, do not postpone any activities toward ICD-10 implementation until further clarification comes from CMS.
—Carol Pohlig
Reference
According to a CMS statement regarding part of President Obama’s “commitment to reducing regulatory burden,” Health and Human Services Secretary Kathleen G. Sebelius announced that HHS will initiate a process to “postpone the date” by which certain healthcare entities have to comply with International Classification of Diseases, 10th Edition diagnosis and procedure codes (ICD-10).1
The final rule adopting ICD-10 as a standard was published in January 2009; it set a compliance date of Oct. 1, 2013 (a two-year delay from the 2008 proposed rule). HHS will announce a new compliance date moving forward.
“ICD-10 codes are important to many positive improvements in our healthcare system,” Sebelius said in the statement. “We have heard from many in the provider community who have concerns about the administrative burdens they face in the years ahead. We are committing to work with the provider community to re-examine the pace at which HHS and the nation implement these important improvements to our healthcare system.”
ICD-10 codes provide more robust and specific data that will help improve patient care and enable the exchange of our healthcare data with that of the rest of the world, much of which has long been using ICD-10. Entities covered under the Health Insurance Portability and Accountability Act of 1996 (HIPAA) will be required to use the ICD-10 diagnostic and procedure codes.
All that said, do not postpone any activities toward ICD-10 implementation until further clarification comes from CMS.
—Carol Pohlig
Reference
Time-based billing allows hospitalists to avoid
Providers typically rely on the “key components” (history, exam, medical decision-making) when documenting in the medical record. However, there are instances when the majority of the encounter constitutes counseling/coordination of care (C/CC). Physicians might only document a brief history and exam, or nothing at all. Utilizing time-based billing principles allows a physician to disregard the “key component” requirements and select a visit level reflective of this effort.
For example, a 64-year-old female is hospitalized with newly diagnosed diabetes and requires extensive counseling regarding disease management, lifestyle modification, and medication regime, as well as coordination of care for outpatient programs and services. The hospitalist reviews some of the pertinent information with the patient and leaves the room to coordinate the patient’s ongoing care (25 minutes). The hospitalist then asks a resident to assist with the remaining counseling efforts (20 minutes). Code 99232 (inpatient visit, 25 minutes total visit time) would be appropriate to report.
Counseling, Coordination of Care
Time may be used as the determining factor for the visit level, if more than 50% of the total visit time involves C/CC.1 Time is not used for visit-level selection if C/CC is minimal or absent from the patient encounter. Total visit time is acknowledged as the physician’s face-to-face (i.e. bedside) time combined with time spent on the unit/floor reviewing data, obtaining relevant patient information, and discussing the individual case with other involved healthcare providers.
Time associated with activities performed outside of the patient’s unit/floor is not considered when calculating total visit time. Time associated with teaching students/interns also is excluded; only the attending physician’s time counts.
When the requirements have been met, the physician selects the visit level that corresponds with the documented total visit time (see Table 1). In the scenario above, the visit level is chosen based on the attending physician’s documented time (25 minutes). The resident’s time cannot be included.
Documentation Requirements
Physicians must document the interaction during the patient encounter: history and exam, if updated or performed; discussion points; and patient response, if applicable. The medical record entry must contain both the C/CC time and the total visit time.2 “Total visit time=35 minutes; >50% spent counseling/coordinating care” or “20 of 35 minutes spent counseling/coordinating care.”
A payor may prefer one documentation style over another. It is always best to ask about the payor’s policy and review local documentation standards to ensure compliance.
Family Discussions
Physicians are always involved in family discussions. It is appropriate to count this as C/CC time. In the event that the family discussion takes place without the patient present, only count this as C/CC time if:
- The patient is unable or clinically incompetent to participate in discussions;
- The time is spent on the unit/floor with the family members or surrogate decision-makers obtaining a medical history, reviewing the patient’s condition or prognosis, or discussing treatment or limitation(s) of treatment; and
- The conversation bears directly on the management of the patient.4
The medical record should reflect these criteria. Do not consider the time if the discussion takes place in an area outside of the patient’s unit/floor, or if the time is spent counseling family members through their grieving process.
It is not uncommon for the family discussion to take place later in the day, after the physician has made earlier rounds. If the earlier encounter involved C/CC, the physician would report the cumulative time spent for that service date. If the earlier encounter was a typical patient evaluation (i.e. history update and physical) and management service (i.e. care plan review/revision), this second encounter might be regarded as a prolonged care service.
Prolonged Care
Prolonged care codes exist for both outpatient and inpatient services. A hospitalists’ focus involves the inpatient code series:
99356: Prolonged service in the inpatient or observation setting, requiring unit/floor time beyond the usual service, first hour; and
99357: Prolonged service in the inpatient or observation setting, requiring unit/floor time beyond the usual service, each additional 30 minutes.
Code 99356 is reported during the first hour of prolonged services, after the initial 30 minutes is reached; code 99357 is reported for each additional 30 minutes of prolonged care beyond the first hour, after the first 15 minutes of each additional segment. Both are “add on” codes and cannot be reported alone on a claim form; a “primary” code must be reported. Similarly, 99357 cannot be reported without 99356, and 99356 must be reported with one of the following inpatient service (primary) codes: 99218-99220, 99221-99223, 99231-99233, 99251-99255, 99304-99310. Only one unit of 99356 may be reported per patient per physician group per day, whereas multiple units of 99357 may be reported in a single day.
The CPT definition of prolonged care varies from that of the Centers for Medicare & Medicaid Services (CMS). Since 2009, CPT recognizes the total duration spent by a physician on a given date, even if the time spent by the physician on that date is not continuous; the time involves both face-to-face time and unit/floor time.5 CMS only attributes direct face-to-face time between the physician and the patient toward prolonged care billing. Time spent reviewing charts or discussion of a patient with house medical staff, waiting for test results, waiting for changes in the patient’s condition, waiting for end of a therapy session, or waiting for use of facilities cannot be billed as prolonged services.5 This is in direct opposition to its policy for C/CC services, and makes prolonged care services inefficient.
Medicare also identifies “threshold” time (see Table 2). The total physician visit time must exceed the time requirements associated with the “primary” codes by a 30-minute threshold (e.g. 99221+99356=30 minutes+30 minutes=60 minutes threshold time). The physician must document the total face-to-face time spent in separate notes throughout the day or, more realistically, in one cumulative note.
When two providers from the same group and same specialty perform services on the same date (e.g. physician A saw the patient during morning rounds, and physician B spoke with the patient/family in the afternoon), only one physician can report the cumulative service.6 As always, query payors for coverage, because some non-Medicare insurers do not recognize these codes.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.1C. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare National Coverage Determinations Manual: Chapter 1, Section 70.1. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/ncd103c1_Part1.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1C. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011:7-21.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.5. Centers for Medicare & Medicaid Services website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
Providers typically rely on the “key components” (history, exam, medical decision-making) when documenting in the medical record. However, there are instances when the majority of the encounter constitutes counseling/coordination of care (C/CC). Physicians might only document a brief history and exam, or nothing at all. Utilizing time-based billing principles allows a physician to disregard the “key component” requirements and select a visit level reflective of this effort.
For example, a 64-year-old female is hospitalized with newly diagnosed diabetes and requires extensive counseling regarding disease management, lifestyle modification, and medication regime, as well as coordination of care for outpatient programs and services. The hospitalist reviews some of the pertinent information with the patient and leaves the room to coordinate the patient’s ongoing care (25 minutes). The hospitalist then asks a resident to assist with the remaining counseling efforts (20 minutes). Code 99232 (inpatient visit, 25 minutes total visit time) would be appropriate to report.
Counseling, Coordination of Care
Time may be used as the determining factor for the visit level, if more than 50% of the total visit time involves C/CC.1 Time is not used for visit-level selection if C/CC is minimal or absent from the patient encounter. Total visit time is acknowledged as the physician’s face-to-face (i.e. bedside) time combined with time spent on the unit/floor reviewing data, obtaining relevant patient information, and discussing the individual case with other involved healthcare providers.
Time associated with activities performed outside of the patient’s unit/floor is not considered when calculating total visit time. Time associated with teaching students/interns also is excluded; only the attending physician’s time counts.
When the requirements have been met, the physician selects the visit level that corresponds with the documented total visit time (see Table 1). In the scenario above, the visit level is chosen based on the attending physician’s documented time (25 minutes). The resident’s time cannot be included.
Documentation Requirements
Physicians must document the interaction during the patient encounter: history and exam, if updated or performed; discussion points; and patient response, if applicable. The medical record entry must contain both the C/CC time and the total visit time.2 “Total visit time=35 minutes; >50% spent counseling/coordinating care” or “20 of 35 minutes spent counseling/coordinating care.”
A payor may prefer one documentation style over another. It is always best to ask about the payor’s policy and review local documentation standards to ensure compliance.
Family Discussions
Physicians are always involved in family discussions. It is appropriate to count this as C/CC time. In the event that the family discussion takes place without the patient present, only count this as C/CC time if:
- The patient is unable or clinically incompetent to participate in discussions;
- The time is spent on the unit/floor with the family members or surrogate decision-makers obtaining a medical history, reviewing the patient’s condition or prognosis, or discussing treatment or limitation(s) of treatment; and
- The conversation bears directly on the management of the patient.4
The medical record should reflect these criteria. Do not consider the time if the discussion takes place in an area outside of the patient’s unit/floor, or if the time is spent counseling family members through their grieving process.
It is not uncommon for the family discussion to take place later in the day, after the physician has made earlier rounds. If the earlier encounter involved C/CC, the physician would report the cumulative time spent for that service date. If the earlier encounter was a typical patient evaluation (i.e. history update and physical) and management service (i.e. care plan review/revision), this second encounter might be regarded as a prolonged care service.
Prolonged Care
Prolonged care codes exist for both outpatient and inpatient services. A hospitalists’ focus involves the inpatient code series:
99356: Prolonged service in the inpatient or observation setting, requiring unit/floor time beyond the usual service, first hour; and
99357: Prolonged service in the inpatient or observation setting, requiring unit/floor time beyond the usual service, each additional 30 minutes.
Code 99356 is reported during the first hour of prolonged services, after the initial 30 minutes is reached; code 99357 is reported for each additional 30 minutes of prolonged care beyond the first hour, after the first 15 minutes of each additional segment. Both are “add on” codes and cannot be reported alone on a claim form; a “primary” code must be reported. Similarly, 99357 cannot be reported without 99356, and 99356 must be reported with one of the following inpatient service (primary) codes: 99218-99220, 99221-99223, 99231-99233, 99251-99255, 99304-99310. Only one unit of 99356 may be reported per patient per physician group per day, whereas multiple units of 99357 may be reported in a single day.
The CPT definition of prolonged care varies from that of the Centers for Medicare & Medicaid Services (CMS). Since 2009, CPT recognizes the total duration spent by a physician on a given date, even if the time spent by the physician on that date is not continuous; the time involves both face-to-face time and unit/floor time.5 CMS only attributes direct face-to-face time between the physician and the patient toward prolonged care billing. Time spent reviewing charts or discussion of a patient with house medical staff, waiting for test results, waiting for changes in the patient’s condition, waiting for end of a therapy session, or waiting for use of facilities cannot be billed as prolonged services.5 This is in direct opposition to its policy for C/CC services, and makes prolonged care services inefficient.
Medicare also identifies “threshold” time (see Table 2). The total physician visit time must exceed the time requirements associated with the “primary” codes by a 30-minute threshold (e.g. 99221+99356=30 minutes+30 minutes=60 minutes threshold time). The physician must document the total face-to-face time spent in separate notes throughout the day or, more realistically, in one cumulative note.
When two providers from the same group and same specialty perform services on the same date (e.g. physician A saw the patient during morning rounds, and physician B spoke with the patient/family in the afternoon), only one physician can report the cumulative service.6 As always, query payors for coverage, because some non-Medicare insurers do not recognize these codes.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.1C. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare National Coverage Determinations Manual: Chapter 1, Section 70.1. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/ncd103c1_Part1.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1C. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011:7-21.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.5. Centers for Medicare & Medicaid Services website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
Providers typically rely on the “key components” (history, exam, medical decision-making) when documenting in the medical record. However, there are instances when the majority of the encounter constitutes counseling/coordination of care (C/CC). Physicians might only document a brief history and exam, or nothing at all. Utilizing time-based billing principles allows a physician to disregard the “key component” requirements and select a visit level reflective of this effort.
For example, a 64-year-old female is hospitalized with newly diagnosed diabetes and requires extensive counseling regarding disease management, lifestyle modification, and medication regime, as well as coordination of care for outpatient programs and services. The hospitalist reviews some of the pertinent information with the patient and leaves the room to coordinate the patient’s ongoing care (25 minutes). The hospitalist then asks a resident to assist with the remaining counseling efforts (20 minutes). Code 99232 (inpatient visit, 25 minutes total visit time) would be appropriate to report.
Counseling, Coordination of Care
Time may be used as the determining factor for the visit level, if more than 50% of the total visit time involves C/CC.1 Time is not used for visit-level selection if C/CC is minimal or absent from the patient encounter. Total visit time is acknowledged as the physician’s face-to-face (i.e. bedside) time combined with time spent on the unit/floor reviewing data, obtaining relevant patient information, and discussing the individual case with other involved healthcare providers.
Time associated with activities performed outside of the patient’s unit/floor is not considered when calculating total visit time. Time associated with teaching students/interns also is excluded; only the attending physician’s time counts.
When the requirements have been met, the physician selects the visit level that corresponds with the documented total visit time (see Table 1). In the scenario above, the visit level is chosen based on the attending physician’s documented time (25 minutes). The resident’s time cannot be included.
Documentation Requirements
Physicians must document the interaction during the patient encounter: history and exam, if updated or performed; discussion points; and patient response, if applicable. The medical record entry must contain both the C/CC time and the total visit time.2 “Total visit time=35 minutes; >50% spent counseling/coordinating care” or “20 of 35 minutes spent counseling/coordinating care.”
A payor may prefer one documentation style over another. It is always best to ask about the payor’s policy and review local documentation standards to ensure compliance.
Family Discussions
Physicians are always involved in family discussions. It is appropriate to count this as C/CC time. In the event that the family discussion takes place without the patient present, only count this as C/CC time if:
- The patient is unable or clinically incompetent to participate in discussions;
- The time is spent on the unit/floor with the family members or surrogate decision-makers obtaining a medical history, reviewing the patient’s condition or prognosis, or discussing treatment or limitation(s) of treatment; and
- The conversation bears directly on the management of the patient.4
The medical record should reflect these criteria. Do not consider the time if the discussion takes place in an area outside of the patient’s unit/floor, or if the time is spent counseling family members through their grieving process.
It is not uncommon for the family discussion to take place later in the day, after the physician has made earlier rounds. If the earlier encounter involved C/CC, the physician would report the cumulative time spent for that service date. If the earlier encounter was a typical patient evaluation (i.e. history update and physical) and management service (i.e. care plan review/revision), this second encounter might be regarded as a prolonged care service.
Prolonged Care
Prolonged care codes exist for both outpatient and inpatient services. A hospitalists’ focus involves the inpatient code series:
99356: Prolonged service in the inpatient or observation setting, requiring unit/floor time beyond the usual service, first hour; and
99357: Prolonged service in the inpatient or observation setting, requiring unit/floor time beyond the usual service, each additional 30 minutes.
Code 99356 is reported during the first hour of prolonged services, after the initial 30 minutes is reached; code 99357 is reported for each additional 30 minutes of prolonged care beyond the first hour, after the first 15 minutes of each additional segment. Both are “add on” codes and cannot be reported alone on a claim form; a “primary” code must be reported. Similarly, 99357 cannot be reported without 99356, and 99356 must be reported with one of the following inpatient service (primary) codes: 99218-99220, 99221-99223, 99231-99233, 99251-99255, 99304-99310. Only one unit of 99356 may be reported per patient per physician group per day, whereas multiple units of 99357 may be reported in a single day.
The CPT definition of prolonged care varies from that of the Centers for Medicare & Medicaid Services (CMS). Since 2009, CPT recognizes the total duration spent by a physician on a given date, even if the time spent by the physician on that date is not continuous; the time involves both face-to-face time and unit/floor time.5 CMS only attributes direct face-to-face time between the physician and the patient toward prolonged care billing. Time spent reviewing charts or discussion of a patient with house medical staff, waiting for test results, waiting for changes in the patient’s condition, waiting for end of a therapy session, or waiting for use of facilities cannot be billed as prolonged services.5 This is in direct opposition to its policy for C/CC services, and makes prolonged care services inefficient.
Medicare also identifies “threshold” time (see Table 2). The total physician visit time must exceed the time requirements associated with the “primary” codes by a 30-minute threshold (e.g. 99221+99356=30 minutes+30 minutes=60 minutes threshold time). The physician must document the total face-to-face time spent in separate notes throughout the day or, more realistically, in one cumulative note.
When two providers from the same group and same specialty perform services on the same date (e.g. physician A saw the patient during morning rounds, and physician B spoke with the patient/family in the afternoon), only one physician can report the cumulative service.6 As always, query payors for coverage, because some non-Medicare insurers do not recognize these codes.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.1C. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare National Coverage Determinations Manual: Chapter 1, Section 70.1. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/ncd103c1_Part1.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1C. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011:7-21.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.5. Centers for Medicare & Medicaid Services website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
Medical Decision-Making Factors Include Quantity of Information, Complexity
Physicians should formulate a complete and accurate description of a patient’s condition with an equivalent plan of care for each encounter. While acuity and severity can be inferred by healthcare professionals without excessive detail or repetitive documentation of previously entered information, adequate documentation for every service date assists in conveying patient complexity during medical record review.
Regardless of how complex a patient’s condition might be, physicians tend to undervalue their services. This is due, in part, to the routine nature of patient care for seasoned physicians; it is also due in part to a general lack of understanding with respect to the documentation guidelines.
Consider the following scenario: A 68-year-old male with diabetes and a history of chronic obstructive bronchitis was hospitalized after a five-day history of progressive cough with increasing purulent sputum, shortness of breath, and fever. He was treated for an exacerbation of chronic bronchitis within the past six weeks. Upon admission, the patient had an increased temperature (102°F), increased heart rate (96 beats per minute), and increased respiratory rate (28 shallow breaths per minute). His breath sounds included in the right lower lobe rhonchi, and his pulse oximetry was 89% on room air. Chest X-ray confirmed right lower lobe infiltrates along with chronic changes.
Although some physicians would consider this “low complexity” due to the frequency in which they encounter this type of case, others will more appropriately identify this as moderately complex.
MDM Categories
Medical decision-making (MDM) remains consistent in both the 1995 and 1997 guidelines.1,2 Complexity is categorized as straightforward, low, moderate, or high, based on the content of physician documentation. Each visit level is associated with a particular level of complexity. Only the care plan for a given date of service is considered when assigning MDM complexity. For each encounter, the physician receives credit for the number of diagnoses and/or treatment options, the amount and/or complexity of data ordered/reviewed, and the risk of complications/morbidity/mortality (see Table 1).
Number of diagnoses or treatment options. Physicians should document problems addressed and managed daily despite any changes to the treatment plan. Credit is provided for each problem with an associated plan, even if the plan states “continue treatment.” Credit also depends upon the quantity of problems addressed, as well as the problem type. An established problem in which the care plan has been established by the physician or group practice member during the current hospitalization is less complex than a new problem for which a diagnosis, prognosis, or plan has not been determined. Severity of the problem affects the weight of complexity. A worsening problem is more complex than an improving problem. Physician documentation should:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined;
- Indicate the management/treatment option(s) for each problem; and
- When documentation indicates a continuation of current management options (e.g. “continue meds”), be sure that the management options to be continued are noted somewhere in the progress note for that encounter (e.g. medication list).
The plan of care outlines problems that the physician personally manages and those that impact management options, even if another physician directly oversees the problem. For example, the hospitalist might primarily manage diabetes, while the pulmonologist manages pneumonia. Since the pneumonia may impact the hospitalist’s plan for diabetic management, the hospitalist can receive credit for the pneumonia diagnosis if there is a non-overlapping, hospitalist-related care plan or comment about the pneumonia.
Amount and/or complexity of data ordered/reviewed. “Data” is classified as pathology/laboratory testing, radiology, and medicine-based diagnostics. Pertinent orders or results could be noted in the visit record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note. To receive credit:
- Specify tests ordered and rationale in the physician’s progress note or make an entry that refers to another auditor-accessible location for ordered tests and studies;
- Document test review by including a brief entry in the progress note (e.g. “elevated glucose levels” or “CXR shows RLL infiltrates”);
- Summarize key points when reviewing old records or obtaining history from someone other than the patient, as necessary;
- Indicate when images, tracings, or specimens are “personally reviewed”; and
- Summarize any discussions of unexpected or contradictory test results with the physician performing the procedure or diagnostic study.
Risks of complication and/or morbidity or mortality. Risk involves the patient’s presenting problem, diagnostic procedures ordered, and management options selected. It is measured as minimal, low, moderate, or high when compared with corresponding items assigned to each risk level (see Table 2). The highest individual item detected on the table determines the overall patient risk for that encounter.
Chronic conditions and invasive procedures pose more risk than acute, uncomplicated illnesses or non-invasive procedures. Stable or improving problems are not as menacing as progressing problems; minor exacerbations are less hazardous than severe exacerbations; and medication risk varies with the type and potential for adverse effects. A patient maintains the same level of risk for a given medication whether the dosage is increased, decreased, or continued without change. Physicians should:
- Status all problems in the plan of care; identify them as stable, worsening, exacerbating (mild or severe), when applicable;
- Document all diagnostic or therapeutic procedures considered;
- Identify surgical risk factors involving comorbid conditions, when appropriate; and
- Associate the labs ordered to monitor for toxicity with the corresponding medication (e.g. “Continue Coumadin, monitor PT/INR”).
Determining complexity of medical decision-making. The final complexity of MDM depends upon the second-highest MDM category. The physician does not have to meet the requirements for all three MDM categories. For example, if a physician satisfies the requirements for a “multiple” number of diagnoses/treatment options, “limited” data, and “high” risk, the physician achieves moderate complexity decision-making (see Table 3). Remember that decision-making is just one of three components in evaluation and management services, along with history and exam.
Beware of payor variation, as it could have a significant impact on visit-level selection.3 Become acquainted with rules applicable to the geographical area. Review insurer websites for guidelines, policies, and “frequently asked questions” that can help improve documentation skills and support billing practices.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/1995dg.pdf. Accessed Nov. 14, 2011.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/MASTER1.pdf. Accessed Nov. 14, 2011.
- Pohlig, C. Documentation and Coding Evaluation and Management Services. In: Coding for Chest Medicine 2010. Northbrook, IL: American College of Chest Physicians, 2009; 87-118.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2011:1-20.
Physicians should formulate a complete and accurate description of a patient’s condition with an equivalent plan of care for each encounter. While acuity and severity can be inferred by healthcare professionals without excessive detail or repetitive documentation of previously entered information, adequate documentation for every service date assists in conveying patient complexity during medical record review.
Regardless of how complex a patient’s condition might be, physicians tend to undervalue their services. This is due, in part, to the routine nature of patient care for seasoned physicians; it is also due in part to a general lack of understanding with respect to the documentation guidelines.
Consider the following scenario: A 68-year-old male with diabetes and a history of chronic obstructive bronchitis was hospitalized after a five-day history of progressive cough with increasing purulent sputum, shortness of breath, and fever. He was treated for an exacerbation of chronic bronchitis within the past six weeks. Upon admission, the patient had an increased temperature (102°F), increased heart rate (96 beats per minute), and increased respiratory rate (28 shallow breaths per minute). His breath sounds included in the right lower lobe rhonchi, and his pulse oximetry was 89% on room air. Chest X-ray confirmed right lower lobe infiltrates along with chronic changes.
Although some physicians would consider this “low complexity” due to the frequency in which they encounter this type of case, others will more appropriately identify this as moderately complex.
MDM Categories
Medical decision-making (MDM) remains consistent in both the 1995 and 1997 guidelines.1,2 Complexity is categorized as straightforward, low, moderate, or high, based on the content of physician documentation. Each visit level is associated with a particular level of complexity. Only the care plan for a given date of service is considered when assigning MDM complexity. For each encounter, the physician receives credit for the number of diagnoses and/or treatment options, the amount and/or complexity of data ordered/reviewed, and the risk of complications/morbidity/mortality (see Table 1).
Number of diagnoses or treatment options. Physicians should document problems addressed and managed daily despite any changes to the treatment plan. Credit is provided for each problem with an associated plan, even if the plan states “continue treatment.” Credit also depends upon the quantity of problems addressed, as well as the problem type. An established problem in which the care plan has been established by the physician or group practice member during the current hospitalization is less complex than a new problem for which a diagnosis, prognosis, or plan has not been determined. Severity of the problem affects the weight of complexity. A worsening problem is more complex than an improving problem. Physician documentation should:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined;
- Indicate the management/treatment option(s) for each problem; and
- When documentation indicates a continuation of current management options (e.g. “continue meds”), be sure that the management options to be continued are noted somewhere in the progress note for that encounter (e.g. medication list).
The plan of care outlines problems that the physician personally manages and those that impact management options, even if another physician directly oversees the problem. For example, the hospitalist might primarily manage diabetes, while the pulmonologist manages pneumonia. Since the pneumonia may impact the hospitalist’s plan for diabetic management, the hospitalist can receive credit for the pneumonia diagnosis if there is a non-overlapping, hospitalist-related care plan or comment about the pneumonia.
Amount and/or complexity of data ordered/reviewed. “Data” is classified as pathology/laboratory testing, radiology, and medicine-based diagnostics. Pertinent orders or results could be noted in the visit record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note. To receive credit:
- Specify tests ordered and rationale in the physician’s progress note or make an entry that refers to another auditor-accessible location for ordered tests and studies;
- Document test review by including a brief entry in the progress note (e.g. “elevated glucose levels” or “CXR shows RLL infiltrates”);
- Summarize key points when reviewing old records or obtaining history from someone other than the patient, as necessary;
- Indicate when images, tracings, or specimens are “personally reviewed”; and
- Summarize any discussions of unexpected or contradictory test results with the physician performing the procedure or diagnostic study.
Risks of complication and/or morbidity or mortality. Risk involves the patient’s presenting problem, diagnostic procedures ordered, and management options selected. It is measured as minimal, low, moderate, or high when compared with corresponding items assigned to each risk level (see Table 2). The highest individual item detected on the table determines the overall patient risk for that encounter.
Chronic conditions and invasive procedures pose more risk than acute, uncomplicated illnesses or non-invasive procedures. Stable or improving problems are not as menacing as progressing problems; minor exacerbations are less hazardous than severe exacerbations; and medication risk varies with the type and potential for adverse effects. A patient maintains the same level of risk for a given medication whether the dosage is increased, decreased, or continued without change. Physicians should:
- Status all problems in the plan of care; identify them as stable, worsening, exacerbating (mild or severe), when applicable;
- Document all diagnostic or therapeutic procedures considered;
- Identify surgical risk factors involving comorbid conditions, when appropriate; and
- Associate the labs ordered to monitor for toxicity with the corresponding medication (e.g. “Continue Coumadin, monitor PT/INR”).
Determining complexity of medical decision-making. The final complexity of MDM depends upon the second-highest MDM category. The physician does not have to meet the requirements for all three MDM categories. For example, if a physician satisfies the requirements for a “multiple” number of diagnoses/treatment options, “limited” data, and “high” risk, the physician achieves moderate complexity decision-making (see Table 3). Remember that decision-making is just one of three components in evaluation and management services, along with history and exam.
Beware of payor variation, as it could have a significant impact on visit-level selection.3 Become acquainted with rules applicable to the geographical area. Review insurer websites for guidelines, policies, and “frequently asked questions” that can help improve documentation skills and support billing practices.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/1995dg.pdf. Accessed Nov. 14, 2011.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/MASTER1.pdf. Accessed Nov. 14, 2011.
- Pohlig, C. Documentation and Coding Evaluation and Management Services. In: Coding for Chest Medicine 2010. Northbrook, IL: American College of Chest Physicians, 2009; 87-118.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2011:1-20.
Physicians should formulate a complete and accurate description of a patient’s condition with an equivalent plan of care for each encounter. While acuity and severity can be inferred by healthcare professionals without excessive detail or repetitive documentation of previously entered information, adequate documentation for every service date assists in conveying patient complexity during medical record review.
Regardless of how complex a patient’s condition might be, physicians tend to undervalue their services. This is due, in part, to the routine nature of patient care for seasoned physicians; it is also due in part to a general lack of understanding with respect to the documentation guidelines.
Consider the following scenario: A 68-year-old male with diabetes and a history of chronic obstructive bronchitis was hospitalized after a five-day history of progressive cough with increasing purulent sputum, shortness of breath, and fever. He was treated for an exacerbation of chronic bronchitis within the past six weeks. Upon admission, the patient had an increased temperature (102°F), increased heart rate (96 beats per minute), and increased respiratory rate (28 shallow breaths per minute). His breath sounds included in the right lower lobe rhonchi, and his pulse oximetry was 89% on room air. Chest X-ray confirmed right lower lobe infiltrates along with chronic changes.
Although some physicians would consider this “low complexity” due to the frequency in which they encounter this type of case, others will more appropriately identify this as moderately complex.
MDM Categories
Medical decision-making (MDM) remains consistent in both the 1995 and 1997 guidelines.1,2 Complexity is categorized as straightforward, low, moderate, or high, based on the content of physician documentation. Each visit level is associated with a particular level of complexity. Only the care plan for a given date of service is considered when assigning MDM complexity. For each encounter, the physician receives credit for the number of diagnoses and/or treatment options, the amount and/or complexity of data ordered/reviewed, and the risk of complications/morbidity/mortality (see Table 1).
Number of diagnoses or treatment options. Physicians should document problems addressed and managed daily despite any changes to the treatment plan. Credit is provided for each problem with an associated plan, even if the plan states “continue treatment.” Credit also depends upon the quantity of problems addressed, as well as the problem type. An established problem in which the care plan has been established by the physician or group practice member during the current hospitalization is less complex than a new problem for which a diagnosis, prognosis, or plan has not been determined. Severity of the problem affects the weight of complexity. A worsening problem is more complex than an improving problem. Physician documentation should:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined;
- Indicate the management/treatment option(s) for each problem; and
- When documentation indicates a continuation of current management options (e.g. “continue meds”), be sure that the management options to be continued are noted somewhere in the progress note for that encounter (e.g. medication list).
The plan of care outlines problems that the physician personally manages and those that impact management options, even if another physician directly oversees the problem. For example, the hospitalist might primarily manage diabetes, while the pulmonologist manages pneumonia. Since the pneumonia may impact the hospitalist’s plan for diabetic management, the hospitalist can receive credit for the pneumonia diagnosis if there is a non-overlapping, hospitalist-related care plan or comment about the pneumonia.
Amount and/or complexity of data ordered/reviewed. “Data” is classified as pathology/laboratory testing, radiology, and medicine-based diagnostics. Pertinent orders or results could be noted in the visit record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note. To receive credit:
- Specify tests ordered and rationale in the physician’s progress note or make an entry that refers to another auditor-accessible location for ordered tests and studies;
- Document test review by including a brief entry in the progress note (e.g. “elevated glucose levels” or “CXR shows RLL infiltrates”);
- Summarize key points when reviewing old records or obtaining history from someone other than the patient, as necessary;
- Indicate when images, tracings, or specimens are “personally reviewed”; and
- Summarize any discussions of unexpected or contradictory test results with the physician performing the procedure or diagnostic study.
Risks of complication and/or morbidity or mortality. Risk involves the patient’s presenting problem, diagnostic procedures ordered, and management options selected. It is measured as minimal, low, moderate, or high when compared with corresponding items assigned to each risk level (see Table 2). The highest individual item detected on the table determines the overall patient risk for that encounter.
Chronic conditions and invasive procedures pose more risk than acute, uncomplicated illnesses or non-invasive procedures. Stable or improving problems are not as menacing as progressing problems; minor exacerbations are less hazardous than severe exacerbations; and medication risk varies with the type and potential for adverse effects. A patient maintains the same level of risk for a given medication whether the dosage is increased, decreased, or continued without change. Physicians should:
- Status all problems in the plan of care; identify them as stable, worsening, exacerbating (mild or severe), when applicable;
- Document all diagnostic or therapeutic procedures considered;
- Identify surgical risk factors involving comorbid conditions, when appropriate; and
- Associate the labs ordered to monitor for toxicity with the corresponding medication (e.g. “Continue Coumadin, monitor PT/INR”).
Determining complexity of medical decision-making. The final complexity of MDM depends upon the second-highest MDM category. The physician does not have to meet the requirements for all three MDM categories. For example, if a physician satisfies the requirements for a “multiple” number of diagnoses/treatment options, “limited” data, and “high” risk, the physician achieves moderate complexity decision-making (see Table 3). Remember that decision-making is just one of three components in evaluation and management services, along with history and exam.
Beware of payor variation, as it could have a significant impact on visit-level selection.3 Become acquainted with rules applicable to the geographical area. Review insurer websites for guidelines, policies, and “frequently asked questions” that can help improve documentation skills and support billing practices.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/1995dg.pdf. Accessed Nov. 14, 2011.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/MASTER1.pdf. Accessed Nov. 14, 2011.
- Pohlig, C. Documentation and Coding Evaluation and Management Services. In: Coding for Chest Medicine 2010. Northbrook, IL: American College of Chest Physicians, 2009; 87-118.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2011:1-20.
CODE-H: Optimize Revenue with Improved Coding Education
Documentation and coding are facts of life for every HM group. Yet almost every group knows that it could be doing better, according to Barb Pierce, CCS-P, ACS-EM, of Barb Pierce Coding and Consulting Inc.
“Despite being a highly structured system, effective coding still depends on the acumen and experience of the people doing the coding,” she says. “No hospitalist will get it perfect every time, but everyone can improve through training. And that training can improve the practice’s bottom line.”
The challenges of coding optimization are getting more and more difficult as changes in government reimbursements impact both documentation and coding requirements. The financial and compliance imperatives to code accurately—even as these requirements shift—are the major driver behind SHM’s new remote learning series, CODE-H.
Short for “Coding Optimally by Documenting Effectively for Hospitalists,” CODE-H can improve the confidence that practice leaders and administrators have in their documentation and coding efforts through a comprehensive, eight-month program that includes webinars and a variety of other support resources. Six expert-led webinars will cover basic and more nuanced issues of documentation, coding, and compliance, including:
- Basics of E&M Coding for Hospitalists, Part 1 and Part 2
- Coding for Hospitalists’ Expanding Scope of Services
- Staying Out of Trouble
- Integrating Physician Billing & Hospital DRG Assurance
- Optimizing Performance and Compliance
Subscribers also receive exclusive access to an online learning community, pre- and post-webinar tests to evaluate learning, a library of additional resources, and CME or CEU credits, pending approval.
The program kicks off Feb. 1 with the first webinar, led by Pierce, the series course director. She is a veteran faculty member for SHM’s one-day coding pre-course. The remote learning series, which runs through Aug. 29, is offered as a site-based subscription for up to 10 individuals from the same HM group for $1,200. Additional participants from the same practice can be registered for a modest additional fee.
“Practice groups continue to lose tens of thousands of dollars through inappropriate documentation and coding,” says Leslie Flores, MHA, a partner in Nelson Flores Hospital Medicine Consultants and SHM’s senior advisor for practice management. “Investing in CODE-H is a way to recoup some of those losses and is a great value. A practice can provide eight months of coding education and support for 10 people for about the same cost as sending a single doctor to SHM’s all-day coding course.”
Visit www.hospitalmedicine.org/codeh to subscribe.
Documentation and coding are facts of life for every HM group. Yet almost every group knows that it could be doing better, according to Barb Pierce, CCS-P, ACS-EM, of Barb Pierce Coding and Consulting Inc.
“Despite being a highly structured system, effective coding still depends on the acumen and experience of the people doing the coding,” she says. “No hospitalist will get it perfect every time, but everyone can improve through training. And that training can improve the practice’s bottom line.”
The challenges of coding optimization are getting more and more difficult as changes in government reimbursements impact both documentation and coding requirements. The financial and compliance imperatives to code accurately—even as these requirements shift—are the major driver behind SHM’s new remote learning series, CODE-H.
Short for “Coding Optimally by Documenting Effectively for Hospitalists,” CODE-H can improve the confidence that practice leaders and administrators have in their documentation and coding efforts through a comprehensive, eight-month program that includes webinars and a variety of other support resources. Six expert-led webinars will cover basic and more nuanced issues of documentation, coding, and compliance, including:
- Basics of E&M Coding for Hospitalists, Part 1 and Part 2
- Coding for Hospitalists’ Expanding Scope of Services
- Staying Out of Trouble
- Integrating Physician Billing & Hospital DRG Assurance
- Optimizing Performance and Compliance
Subscribers also receive exclusive access to an online learning community, pre- and post-webinar tests to evaluate learning, a library of additional resources, and CME or CEU credits, pending approval.
The program kicks off Feb. 1 with the first webinar, led by Pierce, the series course director. She is a veteran faculty member for SHM’s one-day coding pre-course. The remote learning series, which runs through Aug. 29, is offered as a site-based subscription for up to 10 individuals from the same HM group for $1,200. Additional participants from the same practice can be registered for a modest additional fee.
“Practice groups continue to lose tens of thousands of dollars through inappropriate documentation and coding,” says Leslie Flores, MHA, a partner in Nelson Flores Hospital Medicine Consultants and SHM’s senior advisor for practice management. “Investing in CODE-H is a way to recoup some of those losses and is a great value. A practice can provide eight months of coding education and support for 10 people for about the same cost as sending a single doctor to SHM’s all-day coding course.”
Visit www.hospitalmedicine.org/codeh to subscribe.
Documentation and coding are facts of life for every HM group. Yet almost every group knows that it could be doing better, according to Barb Pierce, CCS-P, ACS-EM, of Barb Pierce Coding and Consulting Inc.
“Despite being a highly structured system, effective coding still depends on the acumen and experience of the people doing the coding,” she says. “No hospitalist will get it perfect every time, but everyone can improve through training. And that training can improve the practice’s bottom line.”
The challenges of coding optimization are getting more and more difficult as changes in government reimbursements impact both documentation and coding requirements. The financial and compliance imperatives to code accurately—even as these requirements shift—are the major driver behind SHM’s new remote learning series, CODE-H.
Short for “Coding Optimally by Documenting Effectively for Hospitalists,” CODE-H can improve the confidence that practice leaders and administrators have in their documentation and coding efforts through a comprehensive, eight-month program that includes webinars and a variety of other support resources. Six expert-led webinars will cover basic and more nuanced issues of documentation, coding, and compliance, including:
- Basics of E&M Coding for Hospitalists, Part 1 and Part 2
- Coding for Hospitalists’ Expanding Scope of Services
- Staying Out of Trouble
- Integrating Physician Billing & Hospital DRG Assurance
- Optimizing Performance and Compliance
Subscribers also receive exclusive access to an online learning community, pre- and post-webinar tests to evaluate learning, a library of additional resources, and CME or CEU credits, pending approval.
The program kicks off Feb. 1 with the first webinar, led by Pierce, the series course director. She is a veteran faculty member for SHM’s one-day coding pre-course. The remote learning series, which runs through Aug. 29, is offered as a site-based subscription for up to 10 individuals from the same HM group for $1,200. Additional participants from the same practice can be registered for a modest additional fee.
“Practice groups continue to lose tens of thousands of dollars through inappropriate documentation and coding,” says Leslie Flores, MHA, a partner in Nelson Flores Hospital Medicine Consultants and SHM’s senior advisor for practice management. “Investing in CODE-H is a way to recoup some of those losses and is a great value. A practice can provide eight months of coding education and support for 10 people for about the same cost as sending a single doctor to SHM’s all-day coding course.”
Visit www.hospitalmedicine.org/codeh to subscribe.