User login
Retinyl palmitate
Retinyl palmitate, a storage and ester form of retinol (vitamin A) and the prevailing type of vitamin A found naturally in the skin (Toxicol. Ind. Health 2005;21:167-75), has become increasingly popular during the past 2 decades. It is widely used in more than 600 skin care products, including cosmetics and sunscreens, and, with FDA approval, over-the-counter and prescription drugs (Photodermatol. Photoimmunol. Photomed. 2011;27:58-67). It was also the subject of a controversial summer 2010 report by the Environmental Working Group (EWG) in which the organization warned of possible photocarcinogenicity associated with retinyl palmitate (RP)-containing sunscreens.
Although vitamin A storage in the epidermis takes the form of retinyl esters and retinols, they act differently when exposed to UV light. The retinols display UVB-resistant and UVB-sensitive characteristics not exhibited by retinyl esters such as RP (Dermatology 1999;199:302-7). The EWG used "vitamin A" and "retinyl palmitate" interchangeably in their criticisms and follow-ups, which is misleading. The vitamin A family of drugs includes retinyl esters, retinol, tretinoin, adapalene, tazarotene, and oral isotretinoin (Accutane), in addition to four carotenoids, including beta-carotene, many of which have been shown to prevent or protect against cancer (Br. J. Cancer 1988;57:428-33; Cancer Epidemiol. Biomarkers Prev. 1997;6:949-56; J. Invest. Dermatol. 1981;76:178-80; Arch. Dermatol. Res. 1981;270:453-62). That does not mean that RP prevents cancer just because oral retinol, beta-carotene, or tretinoin have been shown to do so, for example. In fact, the study that the EWG refers to shows evidence that RP may lead to skin tumors in mice.
In response to the EWG report, Wang et al. acknowledged that of the eight in vitro studies published by the Food and Drug Administration from 2002 to 2009, four revealed that reactive oxygen species were produced by RP after UVA exposure (J. Am. Acad. Dermatol. 2010;63:903-6; Photodermatol. Photoimmunol. Photomed. 2011;27:58-67; Toxicol. Ind. Health 2007;23:625-31; Toxicol. Lett. 2006;163:30-43; Int. J. Environ. Res. Public Health 2006;3:185-90; Chem. Res. Toxicol. 2005;18:129-38). However, they questioned the relevance of these results in the context of the convoluted mechanisms of the antioxidant setting in human skin. They also contended that the National Toxicology Program (NTP) study on which the EWG based its report failed to prove that the combination of RP and UV results in photocarcinogenesis and, in fact, was rife with reasons for skepticism (J. Am. Acad. Dermatol. 2010;63:903-6; Photodermatol. Photoimmunol. Photomed. 2011;27:58-67). The EWG offered its own counterarguments and stood by its report. Rather than wade further into the debate that occurred in 2010 and found its way into the pages of the Journal of the American Academy of Dermatology (2010;63:903-6), let’s review what is known about RP.
What else do we know about RP?
In 1997, Duell et al. showed that unoccluded retinol is more effective at penetrating human skin in vivo than RP or retinoic acid (J. Invest. Dermatol. 1997;109:301-5).
In 2003, Antille et al. used an in vitro model to evaluate the photoprotective activity of RP, and then applied topical RP on the back of hairless mice before exposing them to UVB. They also applied topical RP or a sunscreen on the buttocks of human volunteers before exposing them to four minimal erythema doses of UVB. The investigators found that RP was as efficient in vitro as the commercial filter octylmethoxycinnamate in preventing UVB-induced fluorescence or photobleaching of fluorescent markers. Topical RP also significantly suppressed the formation of thymine dimers in mouse epidermis and human skin. In the volunteers, topical RP was as efficient as an SPF (sun protection factor) 20 sunscreen in preventing sunburn erythema (J. Invest. Dermatol. 2003;121:1163-7).
In 2005, Yan et al. studied the phototoxicity of RP, anhydroretinol (AR), and 5,6-epoxyretinyl palmitate (5,6-epoxy-RP) in human skin Jurkat T cells with and without light irradiation. Irradiation of cells in the absence of a retinoid rendered little damage, but the presence of RP, 5,6-epoxy-RP, or AR (50, 100, 150, and 200 micromol/L) yielded DNA fragmentation, with cell death occurring at retinoid concentrations of 100 micromol/L or greater. The investigators concluded that DNA damage and cytotoxicity are engendered by RP and its photodecomposition products in association with UVA and visible light exposure. They also determined that UVA irradiation of these retinoids produces free radicals that spur DNA strand cleavage (Toxicol. Ind. Health 2005;21:167-75).
RP accounts for most of the retinyl esters endogenously formed in skin. In 2006, Yan et al., noting that exogenous RP accumulates via topically applied cosmetic and skin care formulations, investigated the time course for buildup and disappearance of RP and retinol in the stratified layers of skin from female SKH-1 mice singly or repeatedly dosed with topical creams containing 0.5% or 2% RP. The researchers observed that within 24 hours of application, RP quickly diffused into the stratum corneum and epidermal skin layers. RP and retinol levels were lowest in the dermis, intermediate in the stratum corneum, and highest in the epidermis. In separated skin layers and intact skin, RP and retinol levels declined over time, but for 18 days, RP levels remained higher than control values. The investigators concluded that topically applied RP changed the normal physiological levels of RP and retinol in the skin of mice (Toxicol. Ind. Health 2006;22:181-91).
Having previously shown that irradiation of RP with UVA leads to the formation of photodecomposition products, synthesis of reactive oxygen species, and lipid peroxidation induction, Xia et al. demonstrated comparable results, identifying RP as a photosensitizer following irradiation with UVB light (Int. J. Environ. Res. Public Health 2006;3:185-90).
Recommendations
In light of the controversy swirling around RP and the appropriate concern it has engendered, in addition to the weight of evidence as well as experience from personal observation, I advise patients to avoid daytime use of products with RP high on the ingredient list. I add that it poses real risks while offering minimal benefits. Such patients should be using retinol or tretinoin. I recommend the use of retinoids at night, to avoid the photosensitizing action induced by UVA or UVB on retinoids left on the skin.
Conclusion
Retinyl palmitate does not penetrate very well into the skin. Consequently, for over-the-counter topical formulations, I recommend retinol instead. Because of the slow penetration of RP into the skin, the RP that remains on the skin will undergo photoreaction more than a substance that is rapidly absorbed. When exposed to light, RP on the skin may undergo metabolism and/or photoreaction to generate reactive oxygen species. These reactive oxygen species or free radicals can theoretically lead to increased skin cancer. That said, sufficient evidence to establish a causal link between RP and skin cancer has not been produced. Nor, I’m afraid, are there any good reasons to recommend the use of RP. More research on this subject is needed and will likely emerge in a timely fashion.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected]. This column, "Cosmeceutical Critique," appears regularly in Skin & Allergy News.
Retinyl palmitate, a storage and ester form of retinol (vitamin A) and the prevailing type of vitamin A found naturally in the skin (Toxicol. Ind. Health 2005;21:167-75), has become increasingly popular during the past 2 decades. It is widely used in more than 600 skin care products, including cosmetics and sunscreens, and, with FDA approval, over-the-counter and prescription drugs (Photodermatol. Photoimmunol. Photomed. 2011;27:58-67). It was also the subject of a controversial summer 2010 report by the Environmental Working Group (EWG) in which the organization warned of possible photocarcinogenicity associated with retinyl palmitate (RP)-containing sunscreens.
Although vitamin A storage in the epidermis takes the form of retinyl esters and retinols, they act differently when exposed to UV light. The retinols display UVB-resistant and UVB-sensitive characteristics not exhibited by retinyl esters such as RP (Dermatology 1999;199:302-7). The EWG used "vitamin A" and "retinyl palmitate" interchangeably in their criticisms and follow-ups, which is misleading. The vitamin A family of drugs includes retinyl esters, retinol, tretinoin, adapalene, tazarotene, and oral isotretinoin (Accutane), in addition to four carotenoids, including beta-carotene, many of which have been shown to prevent or protect against cancer (Br. J. Cancer 1988;57:428-33; Cancer Epidemiol. Biomarkers Prev. 1997;6:949-56; J. Invest. Dermatol. 1981;76:178-80; Arch. Dermatol. Res. 1981;270:453-62). That does not mean that RP prevents cancer just because oral retinol, beta-carotene, or tretinoin have been shown to do so, for example. In fact, the study that the EWG refers to shows evidence that RP may lead to skin tumors in mice.
In response to the EWG report, Wang et al. acknowledged that of the eight in vitro studies published by the Food and Drug Administration from 2002 to 2009, four revealed that reactive oxygen species were produced by RP after UVA exposure (J. Am. Acad. Dermatol. 2010;63:903-6; Photodermatol. Photoimmunol. Photomed. 2011;27:58-67; Toxicol. Ind. Health 2007;23:625-31; Toxicol. Lett. 2006;163:30-43; Int. J. Environ. Res. Public Health 2006;3:185-90; Chem. Res. Toxicol. 2005;18:129-38). However, they questioned the relevance of these results in the context of the convoluted mechanisms of the antioxidant setting in human skin. They also contended that the National Toxicology Program (NTP) study on which the EWG based its report failed to prove that the combination of RP and UV results in photocarcinogenesis and, in fact, was rife with reasons for skepticism (J. Am. Acad. Dermatol. 2010;63:903-6; Photodermatol. Photoimmunol. Photomed. 2011;27:58-67). The EWG offered its own counterarguments and stood by its report. Rather than wade further into the debate that occurred in 2010 and found its way into the pages of the Journal of the American Academy of Dermatology (2010;63:903-6), let’s review what is known about RP.
What else do we know about RP?
In 1997, Duell et al. showed that unoccluded retinol is more effective at penetrating human skin in vivo than RP or retinoic acid (J. Invest. Dermatol. 1997;109:301-5).
In 2003, Antille et al. used an in vitro model to evaluate the photoprotective activity of RP, and then applied topical RP on the back of hairless mice before exposing them to UVB. They also applied topical RP or a sunscreen on the buttocks of human volunteers before exposing them to four minimal erythema doses of UVB. The investigators found that RP was as efficient in vitro as the commercial filter octylmethoxycinnamate in preventing UVB-induced fluorescence or photobleaching of fluorescent markers. Topical RP also significantly suppressed the formation of thymine dimers in mouse epidermis and human skin. In the volunteers, topical RP was as efficient as an SPF (sun protection factor) 20 sunscreen in preventing sunburn erythema (J. Invest. Dermatol. 2003;121:1163-7).
In 2005, Yan et al. studied the phototoxicity of RP, anhydroretinol (AR), and 5,6-epoxyretinyl palmitate (5,6-epoxy-RP) in human skin Jurkat T cells with and without light irradiation. Irradiation of cells in the absence of a retinoid rendered little damage, but the presence of RP, 5,6-epoxy-RP, or AR (50, 100, 150, and 200 micromol/L) yielded DNA fragmentation, with cell death occurring at retinoid concentrations of 100 micromol/L or greater. The investigators concluded that DNA damage and cytotoxicity are engendered by RP and its photodecomposition products in association with UVA and visible light exposure. They also determined that UVA irradiation of these retinoids produces free radicals that spur DNA strand cleavage (Toxicol. Ind. Health 2005;21:167-75).
RP accounts for most of the retinyl esters endogenously formed in skin. In 2006, Yan et al., noting that exogenous RP accumulates via topically applied cosmetic and skin care formulations, investigated the time course for buildup and disappearance of RP and retinol in the stratified layers of skin from female SKH-1 mice singly or repeatedly dosed with topical creams containing 0.5% or 2% RP. The researchers observed that within 24 hours of application, RP quickly diffused into the stratum corneum and epidermal skin layers. RP and retinol levels were lowest in the dermis, intermediate in the stratum corneum, and highest in the epidermis. In separated skin layers and intact skin, RP and retinol levels declined over time, but for 18 days, RP levels remained higher than control values. The investigators concluded that topically applied RP changed the normal physiological levels of RP and retinol in the skin of mice (Toxicol. Ind. Health 2006;22:181-91).
Having previously shown that irradiation of RP with UVA leads to the formation of photodecomposition products, synthesis of reactive oxygen species, and lipid peroxidation induction, Xia et al. demonstrated comparable results, identifying RP as a photosensitizer following irradiation with UVB light (Int. J. Environ. Res. Public Health 2006;3:185-90).
Recommendations
In light of the controversy swirling around RP and the appropriate concern it has engendered, in addition to the weight of evidence as well as experience from personal observation, I advise patients to avoid daytime use of products with RP high on the ingredient list. I add that it poses real risks while offering minimal benefits. Such patients should be using retinol or tretinoin. I recommend the use of retinoids at night, to avoid the photosensitizing action induced by UVA or UVB on retinoids left on the skin.
Conclusion
Retinyl palmitate does not penetrate very well into the skin. Consequently, for over-the-counter topical formulations, I recommend retinol instead. Because of the slow penetration of RP into the skin, the RP that remains on the skin will undergo photoreaction more than a substance that is rapidly absorbed. When exposed to light, RP on the skin may undergo metabolism and/or photoreaction to generate reactive oxygen species. These reactive oxygen species or free radicals can theoretically lead to increased skin cancer. That said, sufficient evidence to establish a causal link between RP and skin cancer has not been produced. Nor, I’m afraid, are there any good reasons to recommend the use of RP. More research on this subject is needed and will likely emerge in a timely fashion.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected]. This column, "Cosmeceutical Critique," appears regularly in Skin & Allergy News.
Retinyl palmitate, a storage and ester form of retinol (vitamin A) and the prevailing type of vitamin A found naturally in the skin (Toxicol. Ind. Health 2005;21:167-75), has become increasingly popular during the past 2 decades. It is widely used in more than 600 skin care products, including cosmetics and sunscreens, and, with FDA approval, over-the-counter and prescription drugs (Photodermatol. Photoimmunol. Photomed. 2011;27:58-67). It was also the subject of a controversial summer 2010 report by the Environmental Working Group (EWG) in which the organization warned of possible photocarcinogenicity associated with retinyl palmitate (RP)-containing sunscreens.
Although vitamin A storage in the epidermis takes the form of retinyl esters and retinols, they act differently when exposed to UV light. The retinols display UVB-resistant and UVB-sensitive characteristics not exhibited by retinyl esters such as RP (Dermatology 1999;199:302-7). The EWG used "vitamin A" and "retinyl palmitate" interchangeably in their criticisms and follow-ups, which is misleading. The vitamin A family of drugs includes retinyl esters, retinol, tretinoin, adapalene, tazarotene, and oral isotretinoin (Accutane), in addition to four carotenoids, including beta-carotene, many of which have been shown to prevent or protect against cancer (Br. J. Cancer 1988;57:428-33; Cancer Epidemiol. Biomarkers Prev. 1997;6:949-56; J. Invest. Dermatol. 1981;76:178-80; Arch. Dermatol. Res. 1981;270:453-62). That does not mean that RP prevents cancer just because oral retinol, beta-carotene, or tretinoin have been shown to do so, for example. In fact, the study that the EWG refers to shows evidence that RP may lead to skin tumors in mice.
In response to the EWG report, Wang et al. acknowledged that of the eight in vitro studies published by the Food and Drug Administration from 2002 to 2009, four revealed that reactive oxygen species were produced by RP after UVA exposure (J. Am. Acad. Dermatol. 2010;63:903-6; Photodermatol. Photoimmunol. Photomed. 2011;27:58-67; Toxicol. Ind. Health 2007;23:625-31; Toxicol. Lett. 2006;163:30-43; Int. J. Environ. Res. Public Health 2006;3:185-90; Chem. Res. Toxicol. 2005;18:129-38). However, they questioned the relevance of these results in the context of the convoluted mechanisms of the antioxidant setting in human skin. They also contended that the National Toxicology Program (NTP) study on which the EWG based its report failed to prove that the combination of RP and UV results in photocarcinogenesis and, in fact, was rife with reasons for skepticism (J. Am. Acad. Dermatol. 2010;63:903-6; Photodermatol. Photoimmunol. Photomed. 2011;27:58-67). The EWG offered its own counterarguments and stood by its report. Rather than wade further into the debate that occurred in 2010 and found its way into the pages of the Journal of the American Academy of Dermatology (2010;63:903-6), let’s review what is known about RP.
What else do we know about RP?
In 1997, Duell et al. showed that unoccluded retinol is more effective at penetrating human skin in vivo than RP or retinoic acid (J. Invest. Dermatol. 1997;109:301-5).
In 2003, Antille et al. used an in vitro model to evaluate the photoprotective activity of RP, and then applied topical RP on the back of hairless mice before exposing them to UVB. They also applied topical RP or a sunscreen on the buttocks of human volunteers before exposing them to four minimal erythema doses of UVB. The investigators found that RP was as efficient in vitro as the commercial filter octylmethoxycinnamate in preventing UVB-induced fluorescence or photobleaching of fluorescent markers. Topical RP also significantly suppressed the formation of thymine dimers in mouse epidermis and human skin. In the volunteers, topical RP was as efficient as an SPF (sun protection factor) 20 sunscreen in preventing sunburn erythema (J. Invest. Dermatol. 2003;121:1163-7).
In 2005, Yan et al. studied the phototoxicity of RP, anhydroretinol (AR), and 5,6-epoxyretinyl palmitate (5,6-epoxy-RP) in human skin Jurkat T cells with and without light irradiation. Irradiation of cells in the absence of a retinoid rendered little damage, but the presence of RP, 5,6-epoxy-RP, or AR (50, 100, 150, and 200 micromol/L) yielded DNA fragmentation, with cell death occurring at retinoid concentrations of 100 micromol/L or greater. The investigators concluded that DNA damage and cytotoxicity are engendered by RP and its photodecomposition products in association with UVA and visible light exposure. They also determined that UVA irradiation of these retinoids produces free radicals that spur DNA strand cleavage (Toxicol. Ind. Health 2005;21:167-75).
RP accounts for most of the retinyl esters endogenously formed in skin. In 2006, Yan et al., noting that exogenous RP accumulates via topically applied cosmetic and skin care formulations, investigated the time course for buildup and disappearance of RP and retinol in the stratified layers of skin from female SKH-1 mice singly or repeatedly dosed with topical creams containing 0.5% or 2% RP. The researchers observed that within 24 hours of application, RP quickly diffused into the stratum corneum and epidermal skin layers. RP and retinol levels were lowest in the dermis, intermediate in the stratum corneum, and highest in the epidermis. In separated skin layers and intact skin, RP and retinol levels declined over time, but for 18 days, RP levels remained higher than control values. The investigators concluded that topically applied RP changed the normal physiological levels of RP and retinol in the skin of mice (Toxicol. Ind. Health 2006;22:181-91).
Having previously shown that irradiation of RP with UVA leads to the formation of photodecomposition products, synthesis of reactive oxygen species, and lipid peroxidation induction, Xia et al. demonstrated comparable results, identifying RP as a photosensitizer following irradiation with UVB light (Int. J. Environ. Res. Public Health 2006;3:185-90).
Recommendations
In light of the controversy swirling around RP and the appropriate concern it has engendered, in addition to the weight of evidence as well as experience from personal observation, I advise patients to avoid daytime use of products with RP high on the ingredient list. I add that it poses real risks while offering minimal benefits. Such patients should be using retinol or tretinoin. I recommend the use of retinoids at night, to avoid the photosensitizing action induced by UVA or UVB on retinoids left on the skin.
Conclusion
Retinyl palmitate does not penetrate very well into the skin. Consequently, for over-the-counter topical formulations, I recommend retinol instead. Because of the slow penetration of RP into the skin, the RP that remains on the skin will undergo photoreaction more than a substance that is rapidly absorbed. When exposed to light, RP on the skin may undergo metabolism and/or photoreaction to generate reactive oxygen species. These reactive oxygen species or free radicals can theoretically lead to increased skin cancer. That said, sufficient evidence to establish a causal link between RP and skin cancer has not been produced. Nor, I’m afraid, are there any good reasons to recommend the use of RP. More research on this subject is needed and will likely emerge in a timely fashion.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected]. This column, "Cosmeceutical Critique," appears regularly in Skin & Allergy News.
Flaxseed
Linum usitatissimum, an annual plant native to the eastern Mediterranean and India and better known as flax (or linseed, several decades ago), was cultivated in ancient Egypt and Ethiopia and used for many purposes, including as an ingredient in medicine, soap, and hair products. The oil from the seeds of the plant is thought to possess significant health benefits. Flaxseed oil is one of the richest sources of omega-3 fatty acids, in particular, alpha-linolenic acid (ALA), which represents more than 50% of its total fatty acid content (Br. J. Nutr. 2009;101:440-5; Medical Herbalism: The science and practice of herbal medicine. Healing Arts Press: Rochester, Vt., 2003, p. 57). In addition, flaxseeds are rich in dietary fiber and lignans, which are phytoestrogens with antioxidant properties.
Antioxidant, anti-inflammatory, and antiapoptotic properties have been associated with flaxseed oil and warrant medical consideration. The substantial anti-inflammatory activity of L. usitatissimum has been ascribed to its primary active constituent, ALA (57%), which suppresses arachidonic acid metabolism, thus inhibiting the synthesis of proinflammatory n-6 eicosanoids and reducing vascular permeability (Inflammopharmacology 2010;18:127-36).
In a randomized, double-blind, placebo-controlled application test in 2009, De Spirt et al. studied the cutaneous effects of supplementation with flaxseed or borage oil for 12 weeks in two groups of women (n = 45) aged 18-65 years with sensitive and dry skin. Fifteen women were included in each group, and 15 were randomized to a placebo control group. The placebo group received medium-chain fatty acids. The flaxseed oil included ALA and linoleic acid, and the borage oil contained linoleic and gamma-linolenic acids. ALA contributed to the significant rise in total fatty acids in plasma seen in the flaxseed oil group at weeks 6 and 12. An increase in gamma-linolenic acid was noted in the borage oil group. Erythema, roughness, and scaling were decreased in both treatment groups compared with baseline, while skin hydration was markedly elevated after 12 weeks. In addition, transepidermal water loss was diminished by 10% after 6 weeks in both oil treatment groups, with further reductions after 12 weeks in the flaxseed oil group. The investigators concluded that intervention with dietary lipids can manifest as skin improvements (Br. J. Nutr. 2009;101:440-5).
In 2010, Kaithwas and Majumdar evaluated the anti-inflammatory potential of flaxseed fixed oil against castor oil–induced diarrhea, turpentine oil–induced joint edema, and formaldehyde-induced and complete Freund’s adjuvant (CFA)-induced arthritis in Wistar albino rats. They found that flaxseed oil dose-dependently inhibited the adverse effects of castor oil and turpentine oil as well as CFA, and a significant inhibitory effect was also exerted by flaxseed oil against formaldehyde-induced proliferation of global edematous arthritis. Flaxseed oil also significantly diminished the secondary lesions engendered by CFA by dint of a delayed hypersensitivity reaction. The authors concluded that the significant anti-inflammatory activity imparted by L. usitatissimum fixed oil suggests its therapeutic viability for inflammatory conditions, such as rheumatoid arthritis (Inflammopharmacology 2010;18:127-36).
Recently, de Souza et al. studied the effects on skin wounds in rats of a semisolid formulation of flaxseed oil (1%, 5%, or 10%). The investigators assessed the contraction/re-epithelialization of the wound and resistance to mechanical traction in incisional and excisional models, respectively. They found that the groups treated with flaxseed oil concentrations of 1% or 5% largely started re-epithelialization earlier than the petroleum jelly control group, and achieved 100% re-epithelialization on the 14th day after injury, as compared to 33% of animals in the petroleum jelly group. The investigators concluded that flaxseed oil, at low concentrations, exhibits potential in a solid pharmaceutical preparation, for use in dermal repair (Evid. Based. Complement. Alternat. Med. 2012;2012:270752).
Early in 2012, Tülüce et al. set out to ascertain the antioxidant and antiapoptotic effects of flaxseed oil exerted against ultraviolet C–induced damage in rats. They divided animals into three groups: control, UVC alone, and UVC and flaxseed oil. UVC light exposure lasted for 1 hour twice daily for four weeks in the two exposure groups. In the flaxseed oil group, the oil was administered by gavage prior to each irradiation (4 mL/kg ). The investigators noted that malondialdehyde and protein carbonyl levels were higher in the UVC group than in the controls, but such levels were reduced in the flaxseed oil group compared with the UVC-only group, in skin, lens, and sera. Also, the activities of glutathione peroxidase and superoxide dismutase were found to be higher in the skin, lens, and sera of the flaxseed oil group as compared to the UVC-only group. In addition, retinal apoptosis was lower in the flaxseed group than in the UVC group. The researchers concluded that flaxseed oil may be useful in conferring a photoprotective effect against UVC-induced damage, as manifested in protein carbonylation and reactive oxygen species generation, in rats (Toxicol. Ind. Health. 2012;28:99-107).
Conclusion
Flaxseed oil has gained recent attention for its salutary effects as part of the diet. Rich in omega-3 essential fatty acids and lignans, flaxseed oil has been found to improve fatty acid profiles. Significantly, emerging evidence points to beneficial cutaneous effects derived from dietary use of flaxseed oil. However, more research is necessary to determine whether the beneficial constituents of flaxseed oil can be harnessed in topical products.
Dr. Baumann is in private practice in Miami Beach.
Linum usitatissimum, an annual plant native to the eastern Mediterranean and India and better known as flax (or linseed, several decades ago), was cultivated in ancient Egypt and Ethiopia and used for many purposes, including as an ingredient in medicine, soap, and hair products. The oil from the seeds of the plant is thought to possess significant health benefits. Flaxseed oil is one of the richest sources of omega-3 fatty acids, in particular, alpha-linolenic acid (ALA), which represents more than 50% of its total fatty acid content (Br. J. Nutr. 2009;101:440-5; Medical Herbalism: The science and practice of herbal medicine. Healing Arts Press: Rochester, Vt., 2003, p. 57). In addition, flaxseeds are rich in dietary fiber and lignans, which are phytoestrogens with antioxidant properties.
Antioxidant, anti-inflammatory, and antiapoptotic properties have been associated with flaxseed oil and warrant medical consideration. The substantial anti-inflammatory activity of L. usitatissimum has been ascribed to its primary active constituent, ALA (57%), which suppresses arachidonic acid metabolism, thus inhibiting the synthesis of proinflammatory n-6 eicosanoids and reducing vascular permeability (Inflammopharmacology 2010;18:127-36).
In a randomized, double-blind, placebo-controlled application test in 2009, De Spirt et al. studied the cutaneous effects of supplementation with flaxseed or borage oil for 12 weeks in two groups of women (n = 45) aged 18-65 years with sensitive and dry skin. Fifteen women were included in each group, and 15 were randomized to a placebo control group. The placebo group received medium-chain fatty acids. The flaxseed oil included ALA and linoleic acid, and the borage oil contained linoleic and gamma-linolenic acids. ALA contributed to the significant rise in total fatty acids in plasma seen in the flaxseed oil group at weeks 6 and 12. An increase in gamma-linolenic acid was noted in the borage oil group. Erythema, roughness, and scaling were decreased in both treatment groups compared with baseline, while skin hydration was markedly elevated after 12 weeks. In addition, transepidermal water loss was diminished by 10% after 6 weeks in both oil treatment groups, with further reductions after 12 weeks in the flaxseed oil group. The investigators concluded that intervention with dietary lipids can manifest as skin improvements (Br. J. Nutr. 2009;101:440-5).
In 2010, Kaithwas and Majumdar evaluated the anti-inflammatory potential of flaxseed fixed oil against castor oil–induced diarrhea, turpentine oil–induced joint edema, and formaldehyde-induced and complete Freund’s adjuvant (CFA)-induced arthritis in Wistar albino rats. They found that flaxseed oil dose-dependently inhibited the adverse effects of castor oil and turpentine oil as well as CFA, and a significant inhibitory effect was also exerted by flaxseed oil against formaldehyde-induced proliferation of global edematous arthritis. Flaxseed oil also significantly diminished the secondary lesions engendered by CFA by dint of a delayed hypersensitivity reaction. The authors concluded that the significant anti-inflammatory activity imparted by L. usitatissimum fixed oil suggests its therapeutic viability for inflammatory conditions, such as rheumatoid arthritis (Inflammopharmacology 2010;18:127-36).
Recently, de Souza et al. studied the effects on skin wounds in rats of a semisolid formulation of flaxseed oil (1%, 5%, or 10%). The investigators assessed the contraction/re-epithelialization of the wound and resistance to mechanical traction in incisional and excisional models, respectively. They found that the groups treated with flaxseed oil concentrations of 1% or 5% largely started re-epithelialization earlier than the petroleum jelly control group, and achieved 100% re-epithelialization on the 14th day after injury, as compared to 33% of animals in the petroleum jelly group. The investigators concluded that flaxseed oil, at low concentrations, exhibits potential in a solid pharmaceutical preparation, for use in dermal repair (Evid. Based. Complement. Alternat. Med. 2012;2012:270752).
Early in 2012, Tülüce et al. set out to ascertain the antioxidant and antiapoptotic effects of flaxseed oil exerted against ultraviolet C–induced damage in rats. They divided animals into three groups: control, UVC alone, and UVC and flaxseed oil. UVC light exposure lasted for 1 hour twice daily for four weeks in the two exposure groups. In the flaxseed oil group, the oil was administered by gavage prior to each irradiation (4 mL/kg ). The investigators noted that malondialdehyde and protein carbonyl levels were higher in the UVC group than in the controls, but such levels were reduced in the flaxseed oil group compared with the UVC-only group, in skin, lens, and sera. Also, the activities of glutathione peroxidase and superoxide dismutase were found to be higher in the skin, lens, and sera of the flaxseed oil group as compared to the UVC-only group. In addition, retinal apoptosis was lower in the flaxseed group than in the UVC group. The researchers concluded that flaxseed oil may be useful in conferring a photoprotective effect against UVC-induced damage, as manifested in protein carbonylation and reactive oxygen species generation, in rats (Toxicol. Ind. Health. 2012;28:99-107).
Conclusion
Flaxseed oil has gained recent attention for its salutary effects as part of the diet. Rich in omega-3 essential fatty acids and lignans, flaxseed oil has been found to improve fatty acid profiles. Significantly, emerging evidence points to beneficial cutaneous effects derived from dietary use of flaxseed oil. However, more research is necessary to determine whether the beneficial constituents of flaxseed oil can be harnessed in topical products.
Dr. Baumann is in private practice in Miami Beach.
Linum usitatissimum, an annual plant native to the eastern Mediterranean and India and better known as flax (or linseed, several decades ago), was cultivated in ancient Egypt and Ethiopia and used for many purposes, including as an ingredient in medicine, soap, and hair products. The oil from the seeds of the plant is thought to possess significant health benefits. Flaxseed oil is one of the richest sources of omega-3 fatty acids, in particular, alpha-linolenic acid (ALA), which represents more than 50% of its total fatty acid content (Br. J. Nutr. 2009;101:440-5; Medical Herbalism: The science and practice of herbal medicine. Healing Arts Press: Rochester, Vt., 2003, p. 57). In addition, flaxseeds are rich in dietary fiber and lignans, which are phytoestrogens with antioxidant properties.
Antioxidant, anti-inflammatory, and antiapoptotic properties have been associated with flaxseed oil and warrant medical consideration. The substantial anti-inflammatory activity of L. usitatissimum has been ascribed to its primary active constituent, ALA (57%), which suppresses arachidonic acid metabolism, thus inhibiting the synthesis of proinflammatory n-6 eicosanoids and reducing vascular permeability (Inflammopharmacology 2010;18:127-36).
In a randomized, double-blind, placebo-controlled application test in 2009, De Spirt et al. studied the cutaneous effects of supplementation with flaxseed or borage oil for 12 weeks in two groups of women (n = 45) aged 18-65 years with sensitive and dry skin. Fifteen women were included in each group, and 15 were randomized to a placebo control group. The placebo group received medium-chain fatty acids. The flaxseed oil included ALA and linoleic acid, and the borage oil contained linoleic and gamma-linolenic acids. ALA contributed to the significant rise in total fatty acids in plasma seen in the flaxseed oil group at weeks 6 and 12. An increase in gamma-linolenic acid was noted in the borage oil group. Erythema, roughness, and scaling were decreased in both treatment groups compared with baseline, while skin hydration was markedly elevated after 12 weeks. In addition, transepidermal water loss was diminished by 10% after 6 weeks in both oil treatment groups, with further reductions after 12 weeks in the flaxseed oil group. The investigators concluded that intervention with dietary lipids can manifest as skin improvements (Br. J. Nutr. 2009;101:440-5).
In 2010, Kaithwas and Majumdar evaluated the anti-inflammatory potential of flaxseed fixed oil against castor oil–induced diarrhea, turpentine oil–induced joint edema, and formaldehyde-induced and complete Freund’s adjuvant (CFA)-induced arthritis in Wistar albino rats. They found that flaxseed oil dose-dependently inhibited the adverse effects of castor oil and turpentine oil as well as CFA, and a significant inhibitory effect was also exerted by flaxseed oil against formaldehyde-induced proliferation of global edematous arthritis. Flaxseed oil also significantly diminished the secondary lesions engendered by CFA by dint of a delayed hypersensitivity reaction. The authors concluded that the significant anti-inflammatory activity imparted by L. usitatissimum fixed oil suggests its therapeutic viability for inflammatory conditions, such as rheumatoid arthritis (Inflammopharmacology 2010;18:127-36).
Recently, de Souza et al. studied the effects on skin wounds in rats of a semisolid formulation of flaxseed oil (1%, 5%, or 10%). The investigators assessed the contraction/re-epithelialization of the wound and resistance to mechanical traction in incisional and excisional models, respectively. They found that the groups treated with flaxseed oil concentrations of 1% or 5% largely started re-epithelialization earlier than the petroleum jelly control group, and achieved 100% re-epithelialization on the 14th day after injury, as compared to 33% of animals in the petroleum jelly group. The investigators concluded that flaxseed oil, at low concentrations, exhibits potential in a solid pharmaceutical preparation, for use in dermal repair (Evid. Based. Complement. Alternat. Med. 2012;2012:270752).
Early in 2012, Tülüce et al. set out to ascertain the antioxidant and antiapoptotic effects of flaxseed oil exerted against ultraviolet C–induced damage in rats. They divided animals into three groups: control, UVC alone, and UVC and flaxseed oil. UVC light exposure lasted for 1 hour twice daily for four weeks in the two exposure groups. In the flaxseed oil group, the oil was administered by gavage prior to each irradiation (4 mL/kg ). The investigators noted that malondialdehyde and protein carbonyl levels were higher in the UVC group than in the controls, but such levels were reduced in the flaxseed oil group compared with the UVC-only group, in skin, lens, and sera. Also, the activities of glutathione peroxidase and superoxide dismutase were found to be higher in the skin, lens, and sera of the flaxseed oil group as compared to the UVC-only group. In addition, retinal apoptosis was lower in the flaxseed group than in the UVC group. The researchers concluded that flaxseed oil may be useful in conferring a photoprotective effect against UVC-induced damage, as manifested in protein carbonylation and reactive oxygen species generation, in rats (Toxicol. Ind. Health. 2012;28:99-107).
Conclusion
Flaxseed oil has gained recent attention for its salutary effects as part of the diet. Rich in omega-3 essential fatty acids and lignans, flaxseed oil has been found to improve fatty acid profiles. Significantly, emerging evidence points to beneficial cutaneous effects derived from dietary use of flaxseed oil. However, more research is necessary to determine whether the beneficial constituents of flaxseed oil can be harnessed in topical products.
Dr. Baumann is in private practice in Miami Beach.
Melissa Officinalis
Used in foods, some traditional medicines, herbal tea, herbal toothpastes, and aromatherapy, Melissa officinalis (lemon balm) is a perennial herb in the Lamiaceae (mint) family found in southern Europe and the Mediterranean area. The medicinal use of lemon balm dates back at least 2,000 years (Ann. N. Y. Acad. Sci. 1965;130:474-82). Lower abdominal distress and nervous conditions are some of the ailments treated with lemon balm in folk medicine; herpes lesions are a modern indication (Nat. Prod. Res. 2008;22:1433-40). The essential oil and phenylpropanoid derivatives are thought to be the two primary groups of active constituents in lemon balm (Phytochemistry. 2011;72:572-8).
The main individual components of M. officinalis essential oil have been identified as the monoterpenaldehydes citral a, citral b, and citronellal (Phytomedicine. 2008;15:734-40). The chief phenolic compounds are rosmarinic acid, which is an ester of caffeic acid and 3,4-dihydroxyphenyllactic acid, as well as caffeic acid, which is isolated from the fresh leaves and stems (J. Nat. Prod. 2009;72:1512-5Phytochemistry. 2011;72:572-8). Six flavonoids, including luteolin and apigenin, have also been isolated from the leaves of lemon balm (Acta. Pol. Pharm. 2002;59:139-43; J. Nat. Prod. 2007;70:1889-94). Given the presence of such ingredients known to exhibit antioxidant properties, it is not surprising that such a capacity is considered one of the main medicinal benefits of M. officinalis. Indeed, lemon balm is reputed to display significant antioxidant, anxiolytic (Med. J. Nutrition. Metab. 2011;4:211-8; Phytomedicine. 2010;17:397-403; Psychosom. Med. 2004;66:607-13), and antiviral (particularly antiherpetic) activity (Proc. Soc. Exp. Biol. Med. 1964;117:431-4; Virol. J. 2011;8:188). M. officinalis is also a component, with two other herbs, in a mixture (Ob-X) recently shown to lower body weight gain and adipose tissue mass in genetically obese mice (Pharm. Biol. 2011;49:614-9).
Antioxidant Activity
In a 2009 study, investigators examined the antioxidant potential of three plants (M. officinalis, Matricaria recutita (German chamomile), and Cymbopogon citrus [lemon grass]) used in Brazil to treat neurologic conditions. M. officinalis was found to deliver the greatest reduction in thiobarbituric acid reactive species (TBARS) and the most salient antioxidant effect as evaluated by the 2,2-diphenyl-1-picrylhydrazyl (DPPH) assay. The investigators concluded that M. officinalis warrants consideration as a treatment for oxidative stress–associated neurologic diseases (Neurochem. Res. 2009;34:973-83).
Additional evidence of its antioxidant activity is emerging. In early 2012, Martins et al. reported on their study in which an aqueous extract of M. officinalis significantly mitigated manganese-induced brain oxidative stress in mice. They found that the extract attenuated oxidative damage (TBARS) and reduced total thiol levels, and concluded that their findings show the potent antioxidant activity of M. officinalis (Brain. Res. Bull. 2012;87;74-9). In addition, a recent study found that lemon balm infusion in a tea, after 30 days of daily consumption, significantly lowered oxidative stress and DNA damage in radiology staff exposed to low doses of radiation at work (Toxicol. Ind. Health. 2011;27:205-12).
Antiviral Activity
In 2006, Gaby reported on various natural substances, used in the diet or topically, that exert activity against herpes simplex lesions and prevent recurrences, serving as effective alternatives to acyclovir and its attendant side effects. He cited lemon balm as having exhibited antiviral properties in two studies in the 1990s (Altern. Med. Rev. 2006;11:93-101).
In 1994, 116 patients with acute herpes simplex applied a standardized lemon balm cream (containing 1% Lo-701) or a placebo cream two to four times daily in a randomized, double-blind trial over a 5- to 10-day period within 72 hours of symptom onset. While only 19% of the placebo group reported satisfactory healing, 41% of the active treatment group was satisfied (Phytomedicine. 1994;1:25-31). In 1999, a double-blind, placebo-controlled trial randomized 66 patients with a minimum of four herpes simplex episodes per year to treatment (four times daily for 5 days) with the same standardized lemon balm cream or placebo. Symptom scores were significantly lower in the treatment group than the control group by the second day of the protocol, though the trend supporting active treatment over 5 days was not significant (Phytomedicine 1999;6:225-30).
In 2008, Mazzanti et al. evaluated the antiviral activity against herpes simplex virus type 2 (HSV-2) of a hydroalcoholic extract of lemon balm leaves using a cytopathic effect inhibition assay on Vero cells. They found that lemon balm diminished the cytopathic effect of HSV-2 on Vero cells, with a maximum suppression effect with 0.5 mg/mL. The extract, shown through NMR (nuclear magnetic resonance) and HPLC (high-performance liquid chromatography) analysis to contain rosmarinic acid (4.1% w/w), did not prevent the entry of HSV-2 into cells, indicating postpenetration activity by the botanical agent. The investigators concluded that their work supports the use of lemon balm for treating herpes lesions, and justifies its further study in clinical trials (Nat. Prod. Res. 2008;22:1433-40).
Also that year, Schnitzler et al. evaluated the antiviral effect of lemon balm oil on HSV-1 and HSV-2 in vitro on monkey kidney cells. They found that plaque formation was significantly lowered (by 98.8% for HSV-1 and 97.2% for HSV-2) by noncytotoxic lemon balm oil concentrations, with higher concentrations nearly eradicating infections. Using time-on-addition assays, the investigators determined that pretreatment with lemon balm oil significantly suppressed both viruses before infection of cells, suggesting that the oil impacted the virus prior to adsorption, but not after reaching the host cell. They concluded that this implies the capacity for direct antiviral activity. The authors added that the lipophilic nature of lemon balm oil allows for its penetration into the skin, further supporting its suitability as a topical treatment of herpes (Phytomedicine. 2008;15:734-40).
In a more recent in vitro experiment evaluating antiviral activity against HSV-1, Astani et al. compared an aqueous extract of M. officinalis and phenolic extract compounds (caffeic acid, p-coumaric acid, and rosmarinic acid). The lemon balm extract exhibited high virucidal activity against HSV-1, even at concentrations of 1.5 mcg/mL; phenolic compounds showed similar results only at concentrations 100 times greater. Further, lemon balm extract and rosmarinic acid dose-dependently suppressed HSV-1 attachment to host cells. The researchers concluded that rosmarinic acid was the primary constituent responsible for the antiviral activity displayed by lemon balm, but noted that M. officinalis extract, which imparted virucidal activity against HSV-1 in vitro with low toxicity, has a greater selectivity index against HSV than that of its constituents alone (Chemotherapy. 2012;58:70-7).
In 2008, Geuenich et al. investigated several species of the Lamiaceae family (including lemon balm) for their potency in suppressing HIV-1 infection. The aqueous extracts from the leaves of lemon balm (as well as peppermint and sage) dose-dependently displayed substantial activity against HIV-1 infection in T-cell lines, primary macrophages, and in ex vivo tonsil histocultures. The investigators also found that exposure of extracts to free virions strongly and quickly suppressed infections, though no antiviral effect was seen in exposure to surface-bound virions or target cells alone. Noting the antiherpetic activity of these Lamiaceae family extracts, the investigators suggested that the development of virucidal topical microbicides using such ingredients is warranted (Retrovirology. 2008;5:27).
Hypopigmentary Potential
A potential hypopigmentary application of lemon balm also may be emerging. In 2011, Fujita et al. isolated 16-hydroxy-9-oxo-10E,12E,14E-octadecatrienoic acid (also called Corchorifatty acid B [CFAB]) from the ethanol extracts of the aerial parts of M. officinalis, and found that it suppresses pigmentation in human melanocytes and murine melanoma B16 cells, probably by promoting accelerated degradation of tyrosinase in B16 cells. Further, they noted that the mechanism of action of CFAB is markedly different from those of many other hypopigmentary agents, which facilitate tyrosinase degradation in proteasomes or lysosomes. That is, the reductions in tyrosinase caused by CFAB are thought to take place in post–Golgi complex areas, not in proteasomal or lysosomal ones (Exp. Dermatol. 2011;20(5):420-4).
Conclusions
Like many botanical ingredients studied and harnessed in our modern pharmacopeia, lemon balm has a history of use in traditional medicine. Recent studies suggest antioxidant, anxiolytic, and, especially, antiviral properties, notably in the treatment of herpes viruses. More research is necessary, however, to establish a broader role for M. officinalis in the dermatologic armamentarium.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to Dr. Baumann at [email protected].
Used in foods, some traditional medicines, herbal tea, herbal toothpastes, and aromatherapy, Melissa officinalis (lemon balm) is a perennial herb in the Lamiaceae (mint) family found in southern Europe and the Mediterranean area. The medicinal use of lemon balm dates back at least 2,000 years (Ann. N. Y. Acad. Sci. 1965;130:474-82). Lower abdominal distress and nervous conditions are some of the ailments treated with lemon balm in folk medicine; herpes lesions are a modern indication (Nat. Prod. Res. 2008;22:1433-40). The essential oil and phenylpropanoid derivatives are thought to be the two primary groups of active constituents in lemon balm (Phytochemistry. 2011;72:572-8).
The main individual components of M. officinalis essential oil have been identified as the monoterpenaldehydes citral a, citral b, and citronellal (Phytomedicine. 2008;15:734-40). The chief phenolic compounds are rosmarinic acid, which is an ester of caffeic acid and 3,4-dihydroxyphenyllactic acid, as well as caffeic acid, which is isolated from the fresh leaves and stems (J. Nat. Prod. 2009;72:1512-5Phytochemistry. 2011;72:572-8). Six flavonoids, including luteolin and apigenin, have also been isolated from the leaves of lemon balm (Acta. Pol. Pharm. 2002;59:139-43; J. Nat. Prod. 2007;70:1889-94). Given the presence of such ingredients known to exhibit antioxidant properties, it is not surprising that such a capacity is considered one of the main medicinal benefits of M. officinalis. Indeed, lemon balm is reputed to display significant antioxidant, anxiolytic (Med. J. Nutrition. Metab. 2011;4:211-8; Phytomedicine. 2010;17:397-403; Psychosom. Med. 2004;66:607-13), and antiviral (particularly antiherpetic) activity (Proc. Soc. Exp. Biol. Med. 1964;117:431-4; Virol. J. 2011;8:188). M. officinalis is also a component, with two other herbs, in a mixture (Ob-X) recently shown to lower body weight gain and adipose tissue mass in genetically obese mice (Pharm. Biol. 2011;49:614-9).
Antioxidant Activity
In a 2009 study, investigators examined the antioxidant potential of three plants (M. officinalis, Matricaria recutita (German chamomile), and Cymbopogon citrus [lemon grass]) used in Brazil to treat neurologic conditions. M. officinalis was found to deliver the greatest reduction in thiobarbituric acid reactive species (TBARS) and the most salient antioxidant effect as evaluated by the 2,2-diphenyl-1-picrylhydrazyl (DPPH) assay. The investigators concluded that M. officinalis warrants consideration as a treatment for oxidative stress–associated neurologic diseases (Neurochem. Res. 2009;34:973-83).
Additional evidence of its antioxidant activity is emerging. In early 2012, Martins et al. reported on their study in which an aqueous extract of M. officinalis significantly mitigated manganese-induced brain oxidative stress in mice. They found that the extract attenuated oxidative damage (TBARS) and reduced total thiol levels, and concluded that their findings show the potent antioxidant activity of M. officinalis (Brain. Res. Bull. 2012;87;74-9). In addition, a recent study found that lemon balm infusion in a tea, after 30 days of daily consumption, significantly lowered oxidative stress and DNA damage in radiology staff exposed to low doses of radiation at work (Toxicol. Ind. Health. 2011;27:205-12).
Antiviral Activity
In 2006, Gaby reported on various natural substances, used in the diet or topically, that exert activity against herpes simplex lesions and prevent recurrences, serving as effective alternatives to acyclovir and its attendant side effects. He cited lemon balm as having exhibited antiviral properties in two studies in the 1990s (Altern. Med. Rev. 2006;11:93-101).
In 1994, 116 patients with acute herpes simplex applied a standardized lemon balm cream (containing 1% Lo-701) or a placebo cream two to four times daily in a randomized, double-blind trial over a 5- to 10-day period within 72 hours of symptom onset. While only 19% of the placebo group reported satisfactory healing, 41% of the active treatment group was satisfied (Phytomedicine. 1994;1:25-31). In 1999, a double-blind, placebo-controlled trial randomized 66 patients with a minimum of four herpes simplex episodes per year to treatment (four times daily for 5 days) with the same standardized lemon balm cream or placebo. Symptom scores were significantly lower in the treatment group than the control group by the second day of the protocol, though the trend supporting active treatment over 5 days was not significant (Phytomedicine 1999;6:225-30).
In 2008, Mazzanti et al. evaluated the antiviral activity against herpes simplex virus type 2 (HSV-2) of a hydroalcoholic extract of lemon balm leaves using a cytopathic effect inhibition assay on Vero cells. They found that lemon balm diminished the cytopathic effect of HSV-2 on Vero cells, with a maximum suppression effect with 0.5 mg/mL. The extract, shown through NMR (nuclear magnetic resonance) and HPLC (high-performance liquid chromatography) analysis to contain rosmarinic acid (4.1% w/w), did not prevent the entry of HSV-2 into cells, indicating postpenetration activity by the botanical agent. The investigators concluded that their work supports the use of lemon balm for treating herpes lesions, and justifies its further study in clinical trials (Nat. Prod. Res. 2008;22:1433-40).
Also that year, Schnitzler et al. evaluated the antiviral effect of lemon balm oil on HSV-1 and HSV-2 in vitro on monkey kidney cells. They found that plaque formation was significantly lowered (by 98.8% for HSV-1 and 97.2% for HSV-2) by noncytotoxic lemon balm oil concentrations, with higher concentrations nearly eradicating infections. Using time-on-addition assays, the investigators determined that pretreatment with lemon balm oil significantly suppressed both viruses before infection of cells, suggesting that the oil impacted the virus prior to adsorption, but not after reaching the host cell. They concluded that this implies the capacity for direct antiviral activity. The authors added that the lipophilic nature of lemon balm oil allows for its penetration into the skin, further supporting its suitability as a topical treatment of herpes (Phytomedicine. 2008;15:734-40).
In a more recent in vitro experiment evaluating antiviral activity against HSV-1, Astani et al. compared an aqueous extract of M. officinalis and phenolic extract compounds (caffeic acid, p-coumaric acid, and rosmarinic acid). The lemon balm extract exhibited high virucidal activity against HSV-1, even at concentrations of 1.5 mcg/mL; phenolic compounds showed similar results only at concentrations 100 times greater. Further, lemon balm extract and rosmarinic acid dose-dependently suppressed HSV-1 attachment to host cells. The researchers concluded that rosmarinic acid was the primary constituent responsible for the antiviral activity displayed by lemon balm, but noted that M. officinalis extract, which imparted virucidal activity against HSV-1 in vitro with low toxicity, has a greater selectivity index against HSV than that of its constituents alone (Chemotherapy. 2012;58:70-7).
In 2008, Geuenich et al. investigated several species of the Lamiaceae family (including lemon balm) for their potency in suppressing HIV-1 infection. The aqueous extracts from the leaves of lemon balm (as well as peppermint and sage) dose-dependently displayed substantial activity against HIV-1 infection in T-cell lines, primary macrophages, and in ex vivo tonsil histocultures. The investigators also found that exposure of extracts to free virions strongly and quickly suppressed infections, though no antiviral effect was seen in exposure to surface-bound virions or target cells alone. Noting the antiherpetic activity of these Lamiaceae family extracts, the investigators suggested that the development of virucidal topical microbicides using such ingredients is warranted (Retrovirology. 2008;5:27).
Hypopigmentary Potential
A potential hypopigmentary application of lemon balm also may be emerging. In 2011, Fujita et al. isolated 16-hydroxy-9-oxo-10E,12E,14E-octadecatrienoic acid (also called Corchorifatty acid B [CFAB]) from the ethanol extracts of the aerial parts of M. officinalis, and found that it suppresses pigmentation in human melanocytes and murine melanoma B16 cells, probably by promoting accelerated degradation of tyrosinase in B16 cells. Further, they noted that the mechanism of action of CFAB is markedly different from those of many other hypopigmentary agents, which facilitate tyrosinase degradation in proteasomes or lysosomes. That is, the reductions in tyrosinase caused by CFAB are thought to take place in post–Golgi complex areas, not in proteasomal or lysosomal ones (Exp. Dermatol. 2011;20(5):420-4).
Conclusions
Like many botanical ingredients studied and harnessed in our modern pharmacopeia, lemon balm has a history of use in traditional medicine. Recent studies suggest antioxidant, anxiolytic, and, especially, antiviral properties, notably in the treatment of herpes viruses. More research is necessary, however, to establish a broader role for M. officinalis in the dermatologic armamentarium.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to Dr. Baumann at [email protected].
Used in foods, some traditional medicines, herbal tea, herbal toothpastes, and aromatherapy, Melissa officinalis (lemon balm) is a perennial herb in the Lamiaceae (mint) family found in southern Europe and the Mediterranean area. The medicinal use of lemon balm dates back at least 2,000 years (Ann. N. Y. Acad. Sci. 1965;130:474-82). Lower abdominal distress and nervous conditions are some of the ailments treated with lemon balm in folk medicine; herpes lesions are a modern indication (Nat. Prod. Res. 2008;22:1433-40). The essential oil and phenylpropanoid derivatives are thought to be the two primary groups of active constituents in lemon balm (Phytochemistry. 2011;72:572-8).
The main individual components of M. officinalis essential oil have been identified as the monoterpenaldehydes citral a, citral b, and citronellal (Phytomedicine. 2008;15:734-40). The chief phenolic compounds are rosmarinic acid, which is an ester of caffeic acid and 3,4-dihydroxyphenyllactic acid, as well as caffeic acid, which is isolated from the fresh leaves and stems (J. Nat. Prod. 2009;72:1512-5Phytochemistry. 2011;72:572-8). Six flavonoids, including luteolin and apigenin, have also been isolated from the leaves of lemon balm (Acta. Pol. Pharm. 2002;59:139-43; J. Nat. Prod. 2007;70:1889-94). Given the presence of such ingredients known to exhibit antioxidant properties, it is not surprising that such a capacity is considered one of the main medicinal benefits of M. officinalis. Indeed, lemon balm is reputed to display significant antioxidant, anxiolytic (Med. J. Nutrition. Metab. 2011;4:211-8; Phytomedicine. 2010;17:397-403; Psychosom. Med. 2004;66:607-13), and antiviral (particularly antiherpetic) activity (Proc. Soc. Exp. Biol. Med. 1964;117:431-4; Virol. J. 2011;8:188). M. officinalis is also a component, with two other herbs, in a mixture (Ob-X) recently shown to lower body weight gain and adipose tissue mass in genetically obese mice (Pharm. Biol. 2011;49:614-9).
Antioxidant Activity
In a 2009 study, investigators examined the antioxidant potential of three plants (M. officinalis, Matricaria recutita (German chamomile), and Cymbopogon citrus [lemon grass]) used in Brazil to treat neurologic conditions. M. officinalis was found to deliver the greatest reduction in thiobarbituric acid reactive species (TBARS) and the most salient antioxidant effect as evaluated by the 2,2-diphenyl-1-picrylhydrazyl (DPPH) assay. The investigators concluded that M. officinalis warrants consideration as a treatment for oxidative stress–associated neurologic diseases (Neurochem. Res. 2009;34:973-83).
Additional evidence of its antioxidant activity is emerging. In early 2012, Martins et al. reported on their study in which an aqueous extract of M. officinalis significantly mitigated manganese-induced brain oxidative stress in mice. They found that the extract attenuated oxidative damage (TBARS) and reduced total thiol levels, and concluded that their findings show the potent antioxidant activity of M. officinalis (Brain. Res. Bull. 2012;87;74-9). In addition, a recent study found that lemon balm infusion in a tea, after 30 days of daily consumption, significantly lowered oxidative stress and DNA damage in radiology staff exposed to low doses of radiation at work (Toxicol. Ind. Health. 2011;27:205-12).
Antiviral Activity
In 2006, Gaby reported on various natural substances, used in the diet or topically, that exert activity against herpes simplex lesions and prevent recurrences, serving as effective alternatives to acyclovir and its attendant side effects. He cited lemon balm as having exhibited antiviral properties in two studies in the 1990s (Altern. Med. Rev. 2006;11:93-101).
In 1994, 116 patients with acute herpes simplex applied a standardized lemon balm cream (containing 1% Lo-701) or a placebo cream two to four times daily in a randomized, double-blind trial over a 5- to 10-day period within 72 hours of symptom onset. While only 19% of the placebo group reported satisfactory healing, 41% of the active treatment group was satisfied (Phytomedicine. 1994;1:25-31). In 1999, a double-blind, placebo-controlled trial randomized 66 patients with a minimum of four herpes simplex episodes per year to treatment (four times daily for 5 days) with the same standardized lemon balm cream or placebo. Symptom scores were significantly lower in the treatment group than the control group by the second day of the protocol, though the trend supporting active treatment over 5 days was not significant (Phytomedicine 1999;6:225-30).
In 2008, Mazzanti et al. evaluated the antiviral activity against herpes simplex virus type 2 (HSV-2) of a hydroalcoholic extract of lemon balm leaves using a cytopathic effect inhibition assay on Vero cells. They found that lemon balm diminished the cytopathic effect of HSV-2 on Vero cells, with a maximum suppression effect with 0.5 mg/mL. The extract, shown through NMR (nuclear magnetic resonance) and HPLC (high-performance liquid chromatography) analysis to contain rosmarinic acid (4.1% w/w), did not prevent the entry of HSV-2 into cells, indicating postpenetration activity by the botanical agent. The investigators concluded that their work supports the use of lemon balm for treating herpes lesions, and justifies its further study in clinical trials (Nat. Prod. Res. 2008;22:1433-40).
Also that year, Schnitzler et al. evaluated the antiviral effect of lemon balm oil on HSV-1 and HSV-2 in vitro on monkey kidney cells. They found that plaque formation was significantly lowered (by 98.8% for HSV-1 and 97.2% for HSV-2) by noncytotoxic lemon balm oil concentrations, with higher concentrations nearly eradicating infections. Using time-on-addition assays, the investigators determined that pretreatment with lemon balm oil significantly suppressed both viruses before infection of cells, suggesting that the oil impacted the virus prior to adsorption, but not after reaching the host cell. They concluded that this implies the capacity for direct antiviral activity. The authors added that the lipophilic nature of lemon balm oil allows for its penetration into the skin, further supporting its suitability as a topical treatment of herpes (Phytomedicine. 2008;15:734-40).
In a more recent in vitro experiment evaluating antiviral activity against HSV-1, Astani et al. compared an aqueous extract of M. officinalis and phenolic extract compounds (caffeic acid, p-coumaric acid, and rosmarinic acid). The lemon balm extract exhibited high virucidal activity against HSV-1, even at concentrations of 1.5 mcg/mL; phenolic compounds showed similar results only at concentrations 100 times greater. Further, lemon balm extract and rosmarinic acid dose-dependently suppressed HSV-1 attachment to host cells. The researchers concluded that rosmarinic acid was the primary constituent responsible for the antiviral activity displayed by lemon balm, but noted that M. officinalis extract, which imparted virucidal activity against HSV-1 in vitro with low toxicity, has a greater selectivity index against HSV than that of its constituents alone (Chemotherapy. 2012;58:70-7).
In 2008, Geuenich et al. investigated several species of the Lamiaceae family (including lemon balm) for their potency in suppressing HIV-1 infection. The aqueous extracts from the leaves of lemon balm (as well as peppermint and sage) dose-dependently displayed substantial activity against HIV-1 infection in T-cell lines, primary macrophages, and in ex vivo tonsil histocultures. The investigators also found that exposure of extracts to free virions strongly and quickly suppressed infections, though no antiviral effect was seen in exposure to surface-bound virions or target cells alone. Noting the antiherpetic activity of these Lamiaceae family extracts, the investigators suggested that the development of virucidal topical microbicides using such ingredients is warranted (Retrovirology. 2008;5:27).
Hypopigmentary Potential
A potential hypopigmentary application of lemon balm also may be emerging. In 2011, Fujita et al. isolated 16-hydroxy-9-oxo-10E,12E,14E-octadecatrienoic acid (also called Corchorifatty acid B [CFAB]) from the ethanol extracts of the aerial parts of M. officinalis, and found that it suppresses pigmentation in human melanocytes and murine melanoma B16 cells, probably by promoting accelerated degradation of tyrosinase in B16 cells. Further, they noted that the mechanism of action of CFAB is markedly different from those of many other hypopigmentary agents, which facilitate tyrosinase degradation in proteasomes or lysosomes. That is, the reductions in tyrosinase caused by CFAB are thought to take place in post–Golgi complex areas, not in proteasomal or lysosomal ones (Exp. Dermatol. 2011;20(5):420-4).
Conclusions
Like many botanical ingredients studied and harnessed in our modern pharmacopeia, lemon balm has a history of use in traditional medicine. Recent studies suggest antioxidant, anxiolytic, and, especially, antiviral properties, notably in the treatment of herpes viruses. More research is necessary, however, to establish a broader role for M. officinalis in the dermatologic armamentarium.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to Dr. Baumann at [email protected].
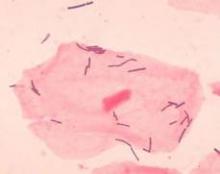
Dill
Dill (Anethum graveolens), an aromatic perennial herb often used as a culinary spice, has been utilized for medical purposes for hundreds of years, at least since medieval times (Wurzbg. Medizinhist. Forsch. 1982;24:411-24). A member of the Umbelliferae (carrot or parsley) family, dill is used in traditional Chinese medicine, and its use in cooking and Uygur medicine is believed to date back to ancient times in China (Evid. Based Complement. Alternat. Med. 2011;2011:659-704).
Based on such past uses, as well as modern research, dill is known for having demonstrated anti-inflammatory, antispasmodic, carminative, aromatic, and galactagogue activity (Medical Herbalism: The Science and Practice of Herbal Medicine. Rochester, Vt.: Healing Arts Press, 2003).
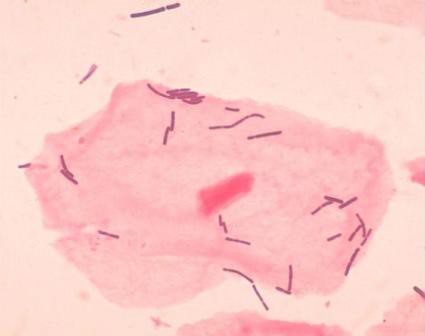
Antimicrobial Activity
In a 2003 study of the essential oil of seeds of dill stored for more than 35 years, Bulgarian researchers tested its antimicrobial activity using various microorganisms. They noted high activity of the essential A. graveolens oil against the mold Aspergillus niger and the yeasts Saccharomyces cerevisiae and Candida albicans (J. Agric. Food. Chem. 2003;51:3854-7). Worth noting from this study is not only the anticandidal properties of dill but its potency even after a long time in storage.
In 2009, Kaur and Arora examined the spices dill, fennel (Foeniculum vulgare), and ajwain (Trachyspermum ammi) for their antibacterial activity. The investigators ascertained antibacterial activity by using agar diffusion assay, minimum inhibitory concentration, and viable cell count studies, and compared effects with those of some standard antibiotics. All three spices in the study exhibited significant activity against a wide range of bacteria, with the exception of Klebsiella pneumoniae and a strain of Pseudomonas aeruginosa. The researchers concluded that the results reveal a scientific basis for the reputed antibacterial effects of these plants and lend credence to their traditional medicinal applications. Further, they suggested that future work may lead to viable antibacterial agents based on these ingredients (BMC Complement. Altern. Med. 2009;9:30).
In 2011, Zeng et al. found that the essential oil produced from dill displays properties effective against vulvovaginal candidiasis in immunosuppressed mice (Evid. Based Complement. Alternat. Med. 2011;659704).
In addition, dill has been found to play an adjuvant role in augmenting the antibacterial activity of nitrofurantoin, which is used to treat urinary tract infections. Researchers used disk-diffusion and agar-dilution methods to determine the effects of essential oils of spearmint (Mentha spicata), dill (A. graveolens), and peppermint (Mentha piperita) and their components on the antibacterial activity of nitrofurantoin against Enterobacter cloacae. They used gas chromatography-mass spectrometry to examine essential oil composition. Dill and spearmint were found to exhibit the most significant effects, with pure carvone and piperitone identified as the most active constituents (Chemotherapy 2007;53:21-5).
Elastogenesis Promotion
In 2006, Cenizo et al. set out to induce elastogenesis in adult dermal fibroblasts by targeting lysyl oxidase (LOX) and lysyl oxidase–like (LOXL) enzymes, which are responsible for elastin cross-linking. LOX and LOXL have been identified as the rate-limiting step in synthesizing mature elastin in adult skin. The expression of LOXL in particular decreases with age. Copious amounts of LOX and LOXL allow the catalysis of immature elastin into desmosine and isodesmosine.
In studying these enzymes, Cenizo and colleagues screened more than 1,000 active ingredients to identify agents that could spur LOXL gene expression in adult dermal fibroblasts. They found that a dill extract was capable of penetrating into the epidermis and dermis in skin engineering and in vitro models, significantly stimulating LOXL gene expression in dermal equivalents (an increase of 64% in mRNA level compared with controls). The researchers also noted increases in elastin detection in dermal equivalents under the dermal-epidermal junction without a corresponding elevation in elastin mRNA. They concluded that LOXL is a suitable target for stimulating elastogenesis, and that dill extract appears to foster such activity (Exp. Dermatol. 2006;15:574-81).
Having shown that dill increases LOX and LOXL expression, along with their respective mRNAs, in 2011, some of the same investigators, this time led by Sohm, assessed the capacity of dill extract to enhance skin elasticity in vitro and in vivo. They reported that skin firmness and elasticity did indeed improve significantly in subjects treated for 56 days with a 1% topical application of dill extract, compared with subjects treated with placebo, based on cutometer measurements, biotribometer measurements, investigator evaluations, subject assessments, and photography. Most volunteers treated with dill extract identified marked enhancements in elasticity, firmness, and jaw line slackness. After 84 days, subjects treated with dill also exhibited significantly reduced mean wrinkle area and length compared with those taking the placebo formulation (Int. J. Cosmet. Sci. 2011;33:157-63). This greater elasticity might be attributed to increased LOX expression stimulated by dill extract application, though this study did not measure LOX or LOXL.
Antioxidant Activity
Recently, investigators compared the radical scavenging and antioxidant activities of the phenolic compounds in six spice plants using spectrophotometric and chromatographic methods. They analyzed onion (Allium cepa), parsley (Petroselinum crispum) roots and leaves, and celery (Apium graveolens) roots and leaves, as well as dill (A. graveolens) leaves, and found that the total amounts of phenolic compounds and radical scavenging activity were greatest in celery leaves and dill extracts (J. Sep. Sci. 2011;34:1261-7).
Combination Therapy
It is worth noting that significant improvement in most measures of photoaged skin was observed after the use of a day and night regimen containing dill extract, blackberry leaf extract, and Zn-Cu(II) bi-mineral complex in patients with mild to moderate photodamage in a small (n = 33), single-center, open-label study led by the author (Baumann LS, Figueras KA, Bell M, Flitter CJ. Unpublished results). This small study supports the notion of dill contributing to cutaneous improvement in combination therapy.
Conclusion
Dill is a culinary spice used worldwide and has a history of traditional use in medicine. Current results suggest reasons for optimism in harnessing the medicinal properties of this plant for various uses in the modern armamentarium, particularly as an antibacterial agent. Much more research is necessary, of course, but recent findings regarding the elastogenesis effects of dill are encouraging and suggest the potential for dermatologic, particularly antiaging, applications.
Dill (Anethum graveolens), an aromatic perennial herb often used as a culinary spice, has been utilized for medical purposes for hundreds of years, at least since medieval times (Wurzbg. Medizinhist. Forsch. 1982;24:411-24). A member of the Umbelliferae (carrot or parsley) family, dill is used in traditional Chinese medicine, and its use in cooking and Uygur medicine is believed to date back to ancient times in China (Evid. Based Complement. Alternat. Med. 2011;2011:659-704).
Based on such past uses, as well as modern research, dill is known for having demonstrated anti-inflammatory, antispasmodic, carminative, aromatic, and galactagogue activity (Medical Herbalism: The Science and Practice of Herbal Medicine. Rochester, Vt.: Healing Arts Press, 2003).
Antimicrobial Activity
In a 2003 study of the essential oil of seeds of dill stored for more than 35 years, Bulgarian researchers tested its antimicrobial activity using various microorganisms. They noted high activity of the essential A. graveolens oil against the mold Aspergillus niger and the yeasts Saccharomyces cerevisiae and Candida albicans (J. Agric. Food. Chem. 2003;51:3854-7). Worth noting from this study is not only the anticandidal properties of dill but its potency even after a long time in storage.
In 2009, Kaur and Arora examined the spices dill, fennel (Foeniculum vulgare), and ajwain (Trachyspermum ammi) for their antibacterial activity. The investigators ascertained antibacterial activity by using agar diffusion assay, minimum inhibitory concentration, and viable cell count studies, and compared effects with those of some standard antibiotics. All three spices in the study exhibited significant activity against a wide range of bacteria, with the exception of Klebsiella pneumoniae and a strain of Pseudomonas aeruginosa. The researchers concluded that the results reveal a scientific basis for the reputed antibacterial effects of these plants and lend credence to their traditional medicinal applications. Further, they suggested that future work may lead to viable antibacterial agents based on these ingredients (BMC Complement. Altern. Med. 2009;9:30).
In 2011, Zeng et al. found that the essential oil produced from dill displays properties effective against vulvovaginal candidiasis in immunosuppressed mice (Evid. Based Complement. Alternat. Med. 2011;659704).
In addition, dill has been found to play an adjuvant role in augmenting the antibacterial activity of nitrofurantoin, which is used to treat urinary tract infections. Researchers used disk-diffusion and agar-dilution methods to determine the effects of essential oils of spearmint (Mentha spicata), dill (A. graveolens), and peppermint (Mentha piperita) and their components on the antibacterial activity of nitrofurantoin against Enterobacter cloacae. They used gas chromatography-mass spectrometry to examine essential oil composition. Dill and spearmint were found to exhibit the most significant effects, with pure carvone and piperitone identified as the most active constituents (Chemotherapy 2007;53:21-5).
Elastogenesis Promotion
In 2006, Cenizo et al. set out to induce elastogenesis in adult dermal fibroblasts by targeting lysyl oxidase (LOX) and lysyl oxidase–like (LOXL) enzymes, which are responsible for elastin cross-linking. LOX and LOXL have been identified as the rate-limiting step in synthesizing mature elastin in adult skin. The expression of LOXL in particular decreases with age. Copious amounts of LOX and LOXL allow the catalysis of immature elastin into desmosine and isodesmosine.
In studying these enzymes, Cenizo and colleagues screened more than 1,000 active ingredients to identify agents that could spur LOXL gene expression in adult dermal fibroblasts. They found that a dill extract was capable of penetrating into the epidermis and dermis in skin engineering and in vitro models, significantly stimulating LOXL gene expression in dermal equivalents (an increase of 64% in mRNA level compared with controls). The researchers also noted increases in elastin detection in dermal equivalents under the dermal-epidermal junction without a corresponding elevation in elastin mRNA. They concluded that LOXL is a suitable target for stimulating elastogenesis, and that dill extract appears to foster such activity (Exp. Dermatol. 2006;15:574-81).
Having shown that dill increases LOX and LOXL expression, along with their respective mRNAs, in 2011, some of the same investigators, this time led by Sohm, assessed the capacity of dill extract to enhance skin elasticity in vitro and in vivo. They reported that skin firmness and elasticity did indeed improve significantly in subjects treated for 56 days with a 1% topical application of dill extract, compared with subjects treated with placebo, based on cutometer measurements, biotribometer measurements, investigator evaluations, subject assessments, and photography. Most volunteers treated with dill extract identified marked enhancements in elasticity, firmness, and jaw line slackness. After 84 days, subjects treated with dill also exhibited significantly reduced mean wrinkle area and length compared with those taking the placebo formulation (Int. J. Cosmet. Sci. 2011;33:157-63). This greater elasticity might be attributed to increased LOX expression stimulated by dill extract application, though this study did not measure LOX or LOXL.
Antioxidant Activity
Recently, investigators compared the radical scavenging and antioxidant activities of the phenolic compounds in six spice plants using spectrophotometric and chromatographic methods. They analyzed onion (Allium cepa), parsley (Petroselinum crispum) roots and leaves, and celery (Apium graveolens) roots and leaves, as well as dill (A. graveolens) leaves, and found that the total amounts of phenolic compounds and radical scavenging activity were greatest in celery leaves and dill extracts (J. Sep. Sci. 2011;34:1261-7).
Combination Therapy
It is worth noting that significant improvement in most measures of photoaged skin was observed after the use of a day and night regimen containing dill extract, blackberry leaf extract, and Zn-Cu(II) bi-mineral complex in patients with mild to moderate photodamage in a small (n = 33), single-center, open-label study led by the author (Baumann LS, Figueras KA, Bell M, Flitter CJ. Unpublished results). This small study supports the notion of dill contributing to cutaneous improvement in combination therapy.
Conclusion
Dill is a culinary spice used worldwide and has a history of traditional use in medicine. Current results suggest reasons for optimism in harnessing the medicinal properties of this plant for various uses in the modern armamentarium, particularly as an antibacterial agent. Much more research is necessary, of course, but recent findings regarding the elastogenesis effects of dill are encouraging and suggest the potential for dermatologic, particularly antiaging, applications.
Dill (Anethum graveolens), an aromatic perennial herb often used as a culinary spice, has been utilized for medical purposes for hundreds of years, at least since medieval times (Wurzbg. Medizinhist. Forsch. 1982;24:411-24). A member of the Umbelliferae (carrot or parsley) family, dill is used in traditional Chinese medicine, and its use in cooking and Uygur medicine is believed to date back to ancient times in China (Evid. Based Complement. Alternat. Med. 2011;2011:659-704).
Based on such past uses, as well as modern research, dill is known for having demonstrated anti-inflammatory, antispasmodic, carminative, aromatic, and galactagogue activity (Medical Herbalism: The Science and Practice of Herbal Medicine. Rochester, Vt.: Healing Arts Press, 2003).
Antimicrobial Activity
In a 2003 study of the essential oil of seeds of dill stored for more than 35 years, Bulgarian researchers tested its antimicrobial activity using various microorganisms. They noted high activity of the essential A. graveolens oil against the mold Aspergillus niger and the yeasts Saccharomyces cerevisiae and Candida albicans (J. Agric. Food. Chem. 2003;51:3854-7). Worth noting from this study is not only the anticandidal properties of dill but its potency even after a long time in storage.
In 2009, Kaur and Arora examined the spices dill, fennel (Foeniculum vulgare), and ajwain (Trachyspermum ammi) for their antibacterial activity. The investigators ascertained antibacterial activity by using agar diffusion assay, minimum inhibitory concentration, and viable cell count studies, and compared effects with those of some standard antibiotics. All three spices in the study exhibited significant activity against a wide range of bacteria, with the exception of Klebsiella pneumoniae and a strain of Pseudomonas aeruginosa. The researchers concluded that the results reveal a scientific basis for the reputed antibacterial effects of these plants and lend credence to their traditional medicinal applications. Further, they suggested that future work may lead to viable antibacterial agents based on these ingredients (BMC Complement. Altern. Med. 2009;9:30).
In 2011, Zeng et al. found that the essential oil produced from dill displays properties effective against vulvovaginal candidiasis in immunosuppressed mice (Evid. Based Complement. Alternat. Med. 2011;659704).
In addition, dill has been found to play an adjuvant role in augmenting the antibacterial activity of nitrofurantoin, which is used to treat urinary tract infections. Researchers used disk-diffusion and agar-dilution methods to determine the effects of essential oils of spearmint (Mentha spicata), dill (A. graveolens), and peppermint (Mentha piperita) and their components on the antibacterial activity of nitrofurantoin against Enterobacter cloacae. They used gas chromatography-mass spectrometry to examine essential oil composition. Dill and spearmint were found to exhibit the most significant effects, with pure carvone and piperitone identified as the most active constituents (Chemotherapy 2007;53:21-5).
Elastogenesis Promotion
In 2006, Cenizo et al. set out to induce elastogenesis in adult dermal fibroblasts by targeting lysyl oxidase (LOX) and lysyl oxidase–like (LOXL) enzymes, which are responsible for elastin cross-linking. LOX and LOXL have been identified as the rate-limiting step in synthesizing mature elastin in adult skin. The expression of LOXL in particular decreases with age. Copious amounts of LOX and LOXL allow the catalysis of immature elastin into desmosine and isodesmosine.
In studying these enzymes, Cenizo and colleagues screened more than 1,000 active ingredients to identify agents that could spur LOXL gene expression in adult dermal fibroblasts. They found that a dill extract was capable of penetrating into the epidermis and dermis in skin engineering and in vitro models, significantly stimulating LOXL gene expression in dermal equivalents (an increase of 64% in mRNA level compared with controls). The researchers also noted increases in elastin detection in dermal equivalents under the dermal-epidermal junction without a corresponding elevation in elastin mRNA. They concluded that LOXL is a suitable target for stimulating elastogenesis, and that dill extract appears to foster such activity (Exp. Dermatol. 2006;15:574-81).
Having shown that dill increases LOX and LOXL expression, along with their respective mRNAs, in 2011, some of the same investigators, this time led by Sohm, assessed the capacity of dill extract to enhance skin elasticity in vitro and in vivo. They reported that skin firmness and elasticity did indeed improve significantly in subjects treated for 56 days with a 1% topical application of dill extract, compared with subjects treated with placebo, based on cutometer measurements, biotribometer measurements, investigator evaluations, subject assessments, and photography. Most volunteers treated with dill extract identified marked enhancements in elasticity, firmness, and jaw line slackness. After 84 days, subjects treated with dill also exhibited significantly reduced mean wrinkle area and length compared with those taking the placebo formulation (Int. J. Cosmet. Sci. 2011;33:157-63). This greater elasticity might be attributed to increased LOX expression stimulated by dill extract application, though this study did not measure LOX or LOXL.
Antioxidant Activity
Recently, investigators compared the radical scavenging and antioxidant activities of the phenolic compounds in six spice plants using spectrophotometric and chromatographic methods. They analyzed onion (Allium cepa), parsley (Petroselinum crispum) roots and leaves, and celery (Apium graveolens) roots and leaves, as well as dill (A. graveolens) leaves, and found that the total amounts of phenolic compounds and radical scavenging activity were greatest in celery leaves and dill extracts (J. Sep. Sci. 2011;34:1261-7).
Combination Therapy
It is worth noting that significant improvement in most measures of photoaged skin was observed after the use of a day and night regimen containing dill extract, blackberry leaf extract, and Zn-Cu(II) bi-mineral complex in patients with mild to moderate photodamage in a small (n = 33), single-center, open-label study led by the author (Baumann LS, Figueras KA, Bell M, Flitter CJ. Unpublished results). This small study supports the notion of dill contributing to cutaneous improvement in combination therapy.
Conclusion
Dill is a culinary spice used worldwide and has a history of traditional use in medicine. Current results suggest reasons for optimism in harnessing the medicinal properties of this plant for various uses in the modern armamentarium, particularly as an antibacterial agent. Much more research is necessary, of course, but recent findings regarding the elastogenesis effects of dill are encouraging and suggest the potential for dermatologic, particularly antiaging, applications.
Cucumber
Cucumis sativus is a member of the Cucurbitaceae family, which also includes pumpkin, zucchini, watermelon, and squash. Found growing wild in the Himalayan region and commonly referred to as cucumber in English, khira in Hindi, and sakusa in Sanskrit, the plant is cultivated throughout India and China, in particular, as well as in Europe and the United States (J. Young. Pharm. 2010;2:365-8).
It is grown as a food crop, with its fruit (the cucumber) found in many cuisines as well as a component in traditional medicine and folk cosmetics (Planta. Med. 2008;74:1785-8). Headache was one traditional indication; the fruit juice was used as a demulcent in antiacne lotions and the seeds were noted for their cooling and diuretic effects (J. Young. Pharm. 2010;2:365-8). In traditional Chinese medicine, the leaves, roots, and stems of the plant have been used to detoxify as well as to treat diarrhea and gonorrhea (Planta. Med. 2008;74:1785-8). Popularly, the application of cucumber slices to ameliorate swelling or dark circles under the eyes has long been accepted throughout the world as an effective treatment.
Antioxidant Activity
In 2002, Villaseñor and coinvestigators assessed the comparative effectiveness of sugar beet roots, cucumber fruits, New Zealand spinach leaves, and turmeric rhizomes against dimethylbenz[a]anthracene-initiated and croton oil–promoted skin tumors in a Swiss Webster albino mouse model using three different protocols. The four species were selected based on prior findings of antioxidant activity and effectiveness in preventing skin tumors induced in laboratory settings. All four displayed antioxidant activity, and all were found to be effective in lowering skin tumor incidence and the number of skin tumors as well as delaying the onset of skin tumor formation, compared with the control, with turmeric exhibiting the greatest potency (Nutr. Cancer. 2002;44:66-70).
Melanin Suppressing Properties
In 2008, Kai and coinvestigators assessed six plant parts of C. sativus to compare their inhibitory effects on melanogenesis. They found that methanol extracts of the leaves and stems suppressed melanin production in cultured B16 mouse melanoma cells. Although they did not alter mushroom tyrosinase activity or crude enzyme lysate activity in these cells, the methanol extracts did reduce tyrosinase expression at the protein level. The researchers suggested that these findings indicate that the depigmenting activity of C. sativus extracts is associated with tyrosinase expression. They also found that lutein, of eight compounds isolated from the leaves, inhibited melanogenesis, significantly lowering tyrosinase expression. The investigators concluded that the leaves, and lutein in particular, of C. sativus effectively suppress tyrosinase expression and warrant consideration as a skin-whitening agent (Planta. Med. 2008;74:1785-8). Tyrosinase-inhibitory activity exhibited by cucumber extracts had also been previously attributed to enzymes found in cucumber skin (J. Agric. Food. Chem. 2003;51:7764-9).
In 2010, Kumar and coinvestigators evaluated the aqueous fruit extract of C. sativus for free radical scavenging and analgesic activities using in vitro and in vivo models. Preliminary phytochemical screening indicated that cucumber contains various classes of compounds known to exert antioxidant as well as analgesic activity, including flavonoids and tannins. The investigators found that the fruit extract showed maximum antioxidant and analgesic effect at 500 mcg/mL and 500 mg/kg, respectively, although the exact constituents of C. sativus fruits responsible for the promising effects were not elucidated by the study (J. Young. Pharm. 2010;2:365-8).
Research on Skin Care Properties
Early in 2011, Akhtar and coinvestigators reported on their efforts to formulate a topical water in oil (without) emulsion of 3% cucumber extracts, and to assess it according to multiple parameters, compared with its base (lacking cucumber ingredients) as a control, in 21 healthy volunteers over 4 weeks. The cucumber formulation demonstrated statistically significant reductions in sebum, as well as a decline in melanin content that was not statistically significant. Transepidermal water loss and erythema were elevated by the test formulation, but these changes were also not statistically significant. While identifying the need for more research, the authors concluded that their findings point to the potential for cucumber extracts to be effective ingredients in skin care agents for medical and cosmetic purposes (African J. Biotechnol. 2011;10:1206-16).
Later in 2011, Nema and coinvestigators subjected the lyophilized juice of C. sativus fruit to 1,1-diphenyl-2-picrylhydrazyl and superoxide radical scavenging assays in reference to butylated hydroxytoluene, and hyaluronoidase and elastase inhibitory assays in reference to oleanolic acid. The cucumber juice, rich in ascorbic acid, was found to exhibit significant free radical scavenging activity as well as potent antihyaluronidase and antielastase activity. The researchers concluded that C. sativus warrants consideration for its potential used as an antiwrinkle ingredient in cosmetic formulations (Arch. Dermatol. Res. 2011;303;247-52).
Cucumber extracts can currently be found in a wide range of over-the-counter skin care creams and eye gels.
Conclusion
Cucumber has captured the popular imagination as an effective, temporary agent for the relief of swollen eyes, or dark circles under the eyes. It has developed an anecdotal reputation as a diuretic that systemically and topically acts against water retention, thus ameliorating burns, dermatitis, and swollen eyes. This folk medicine success or popularity has, perhaps, spurred the inclusion of C. sativa in various skin care products. There is a dearth of research on the dermatologic benefits of the plant, however, as well as its usefulness in skin care products. That said, some emerging evidence regarding its inhibitory effect on melanin production bears watching. Much more research is necessary to determine the appropriate role of cucumber in dermatology.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest.
Cucumis sativus is a member of the Cucurbitaceae family, which also includes pumpkin, zucchini, watermelon, and squash. Found growing wild in the Himalayan region and commonly referred to as cucumber in English, khira in Hindi, and sakusa in Sanskrit, the plant is cultivated throughout India and China, in particular, as well as in Europe and the United States (J. Young. Pharm. 2010;2:365-8).
It is grown as a food crop, with its fruit (the cucumber) found in many cuisines as well as a component in traditional medicine and folk cosmetics (Planta. Med. 2008;74:1785-8). Headache was one traditional indication; the fruit juice was used as a demulcent in antiacne lotions and the seeds were noted for their cooling and diuretic effects (J. Young. Pharm. 2010;2:365-8). In traditional Chinese medicine, the leaves, roots, and stems of the plant have been used to detoxify as well as to treat diarrhea and gonorrhea (Planta. Med. 2008;74:1785-8). Popularly, the application of cucumber slices to ameliorate swelling or dark circles under the eyes has long been accepted throughout the world as an effective treatment.
Antioxidant Activity
In 2002, Villaseñor and coinvestigators assessed the comparative effectiveness of sugar beet roots, cucumber fruits, New Zealand spinach leaves, and turmeric rhizomes against dimethylbenz[a]anthracene-initiated and croton oil–promoted skin tumors in a Swiss Webster albino mouse model using three different protocols. The four species were selected based on prior findings of antioxidant activity and effectiveness in preventing skin tumors induced in laboratory settings. All four displayed antioxidant activity, and all were found to be effective in lowering skin tumor incidence and the number of skin tumors as well as delaying the onset of skin tumor formation, compared with the control, with turmeric exhibiting the greatest potency (Nutr. Cancer. 2002;44:66-70).
Melanin Suppressing Properties
In 2008, Kai and coinvestigators assessed six plant parts of C. sativus to compare their inhibitory effects on melanogenesis. They found that methanol extracts of the leaves and stems suppressed melanin production in cultured B16 mouse melanoma cells. Although they did not alter mushroom tyrosinase activity or crude enzyme lysate activity in these cells, the methanol extracts did reduce tyrosinase expression at the protein level. The researchers suggested that these findings indicate that the depigmenting activity of C. sativus extracts is associated with tyrosinase expression. They also found that lutein, of eight compounds isolated from the leaves, inhibited melanogenesis, significantly lowering tyrosinase expression. The investigators concluded that the leaves, and lutein in particular, of C. sativus effectively suppress tyrosinase expression and warrant consideration as a skin-whitening agent (Planta. Med. 2008;74:1785-8). Tyrosinase-inhibitory activity exhibited by cucumber extracts had also been previously attributed to enzymes found in cucumber skin (J. Agric. Food. Chem. 2003;51:7764-9).
In 2010, Kumar and coinvestigators evaluated the aqueous fruit extract of C. sativus for free radical scavenging and analgesic activities using in vitro and in vivo models. Preliminary phytochemical screening indicated that cucumber contains various classes of compounds known to exert antioxidant as well as analgesic activity, including flavonoids and tannins. The investigators found that the fruit extract showed maximum antioxidant and analgesic effect at 500 mcg/mL and 500 mg/kg, respectively, although the exact constituents of C. sativus fruits responsible for the promising effects were not elucidated by the study (J. Young. Pharm. 2010;2:365-8).
Research on Skin Care Properties
Early in 2011, Akhtar and coinvestigators reported on their efforts to formulate a topical water in oil (without) emulsion of 3% cucumber extracts, and to assess it according to multiple parameters, compared with its base (lacking cucumber ingredients) as a control, in 21 healthy volunteers over 4 weeks. The cucumber formulation demonstrated statistically significant reductions in sebum, as well as a decline in melanin content that was not statistically significant. Transepidermal water loss and erythema were elevated by the test formulation, but these changes were also not statistically significant. While identifying the need for more research, the authors concluded that their findings point to the potential for cucumber extracts to be effective ingredients in skin care agents for medical and cosmetic purposes (African J. Biotechnol. 2011;10:1206-16).
Later in 2011, Nema and coinvestigators subjected the lyophilized juice of C. sativus fruit to 1,1-diphenyl-2-picrylhydrazyl and superoxide radical scavenging assays in reference to butylated hydroxytoluene, and hyaluronoidase and elastase inhibitory assays in reference to oleanolic acid. The cucumber juice, rich in ascorbic acid, was found to exhibit significant free radical scavenging activity as well as potent antihyaluronidase and antielastase activity. The researchers concluded that C. sativus warrants consideration for its potential used as an antiwrinkle ingredient in cosmetic formulations (Arch. Dermatol. Res. 2011;303;247-52).
Cucumber extracts can currently be found in a wide range of over-the-counter skin care creams and eye gels.
Conclusion
Cucumber has captured the popular imagination as an effective, temporary agent for the relief of swollen eyes, or dark circles under the eyes. It has developed an anecdotal reputation as a diuretic that systemically and topically acts against water retention, thus ameliorating burns, dermatitis, and swollen eyes. This folk medicine success or popularity has, perhaps, spurred the inclusion of C. sativa in various skin care products. There is a dearth of research on the dermatologic benefits of the plant, however, as well as its usefulness in skin care products. That said, some emerging evidence regarding its inhibitory effect on melanin production bears watching. Much more research is necessary to determine the appropriate role of cucumber in dermatology.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest.
Cucumis sativus is a member of the Cucurbitaceae family, which also includes pumpkin, zucchini, watermelon, and squash. Found growing wild in the Himalayan region and commonly referred to as cucumber in English, khira in Hindi, and sakusa in Sanskrit, the plant is cultivated throughout India and China, in particular, as well as in Europe and the United States (J. Young. Pharm. 2010;2:365-8).
It is grown as a food crop, with its fruit (the cucumber) found in many cuisines as well as a component in traditional medicine and folk cosmetics (Planta. Med. 2008;74:1785-8). Headache was one traditional indication; the fruit juice was used as a demulcent in antiacne lotions and the seeds were noted for their cooling and diuretic effects (J. Young. Pharm. 2010;2:365-8). In traditional Chinese medicine, the leaves, roots, and stems of the plant have been used to detoxify as well as to treat diarrhea and gonorrhea (Planta. Med. 2008;74:1785-8). Popularly, the application of cucumber slices to ameliorate swelling or dark circles under the eyes has long been accepted throughout the world as an effective treatment.
Antioxidant Activity
In 2002, Villaseñor and coinvestigators assessed the comparative effectiveness of sugar beet roots, cucumber fruits, New Zealand spinach leaves, and turmeric rhizomes against dimethylbenz[a]anthracene-initiated and croton oil–promoted skin tumors in a Swiss Webster albino mouse model using three different protocols. The four species were selected based on prior findings of antioxidant activity and effectiveness in preventing skin tumors induced in laboratory settings. All four displayed antioxidant activity, and all were found to be effective in lowering skin tumor incidence and the number of skin tumors as well as delaying the onset of skin tumor formation, compared with the control, with turmeric exhibiting the greatest potency (Nutr. Cancer. 2002;44:66-70).
Melanin Suppressing Properties
In 2008, Kai and coinvestigators assessed six plant parts of C. sativus to compare their inhibitory effects on melanogenesis. They found that methanol extracts of the leaves and stems suppressed melanin production in cultured B16 mouse melanoma cells. Although they did not alter mushroom tyrosinase activity or crude enzyme lysate activity in these cells, the methanol extracts did reduce tyrosinase expression at the protein level. The researchers suggested that these findings indicate that the depigmenting activity of C. sativus extracts is associated with tyrosinase expression. They also found that lutein, of eight compounds isolated from the leaves, inhibited melanogenesis, significantly lowering tyrosinase expression. The investigators concluded that the leaves, and lutein in particular, of C. sativus effectively suppress tyrosinase expression and warrant consideration as a skin-whitening agent (Planta. Med. 2008;74:1785-8). Tyrosinase-inhibitory activity exhibited by cucumber extracts had also been previously attributed to enzymes found in cucumber skin (J. Agric. Food. Chem. 2003;51:7764-9).
In 2010, Kumar and coinvestigators evaluated the aqueous fruit extract of C. sativus for free radical scavenging and analgesic activities using in vitro and in vivo models. Preliminary phytochemical screening indicated that cucumber contains various classes of compounds known to exert antioxidant as well as analgesic activity, including flavonoids and tannins. The investigators found that the fruit extract showed maximum antioxidant and analgesic effect at 500 mcg/mL and 500 mg/kg, respectively, although the exact constituents of C. sativus fruits responsible for the promising effects were not elucidated by the study (J. Young. Pharm. 2010;2:365-8).
Research on Skin Care Properties
Early in 2011, Akhtar and coinvestigators reported on their efforts to formulate a topical water in oil (without) emulsion of 3% cucumber extracts, and to assess it according to multiple parameters, compared with its base (lacking cucumber ingredients) as a control, in 21 healthy volunteers over 4 weeks. The cucumber formulation demonstrated statistically significant reductions in sebum, as well as a decline in melanin content that was not statistically significant. Transepidermal water loss and erythema were elevated by the test formulation, but these changes were also not statistically significant. While identifying the need for more research, the authors concluded that their findings point to the potential for cucumber extracts to be effective ingredients in skin care agents for medical and cosmetic purposes (African J. Biotechnol. 2011;10:1206-16).
Later in 2011, Nema and coinvestigators subjected the lyophilized juice of C. sativus fruit to 1,1-diphenyl-2-picrylhydrazyl and superoxide radical scavenging assays in reference to butylated hydroxytoluene, and hyaluronoidase and elastase inhibitory assays in reference to oleanolic acid. The cucumber juice, rich in ascorbic acid, was found to exhibit significant free radical scavenging activity as well as potent antihyaluronidase and antielastase activity. The researchers concluded that C. sativus warrants consideration for its potential used as an antiwrinkle ingredient in cosmetic formulations (Arch. Dermatol. Res. 2011;303;247-52).
Cucumber extracts can currently be found in a wide range of over-the-counter skin care creams and eye gels.
Conclusion
Cucumber has captured the popular imagination as an effective, temporary agent for the relief of swollen eyes, or dark circles under the eyes. It has developed an anecdotal reputation as a diuretic that systemically and topically acts against water retention, thus ameliorating burns, dermatitis, and swollen eyes. This folk medicine success or popularity has, perhaps, spurred the inclusion of C. sativa in various skin care products. There is a dearth of research on the dermatologic benefits of the plant, however, as well as its usefulness in skin care products. That said, some emerging evidence regarding its inhibitory effect on melanin production bears watching. Much more research is necessary to determine the appropriate role of cucumber in dermatology.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest.
Probiotics
Probiotics are live microorganisms that impart health benefits to the host when present or administered at appropriate levels (J. Appl. Bacteriol. 1989;66:365-78). Intestinal microflora are better understood and more frequently used than cutaneous microbiota, but researchers have recently applied the concepts underlying the efficacy of intestinal probiotics to investigate potential benefits in the dermatologic realm. This work has also been spurred by the flurry of investigations on probiotics for the treatment of atopic dermatitis (AD).
In one of the earlier studies of possible uses of probiotics for the skin, Ouwehand et al. identified strains that adhere to keratin. However, the tested microbes (Propionibacteria, selected because they are among the normal microbiota of the skin) were not found to inhibit cutaneous pathogen adhesion to human keratin. Nevertheless, the researchers concluded that additional study was warranted to identify strains that adhere in vivo and exhibit activity against potential skin pathogens (Lett. Appl. Microbiol. 2003;36:327-31).
Clearly, some probiotic strains have been shown to exhibit strong immunomodulatory activity at the cutaneous level (Eur. J. Dermatol. 2010;20:731-7). In addition, some topical skin products now contain probiotic strains as active ingredients, including Clinique Medical, which incorporates lactobacillus cultures to yield molecules that help ameliorate skin barrier effects from laser treatments or chemical peels (Facial Plast. Surg. 2009;25:285-9). Probiotics have also been used successively as adjuvant therapy to treat suppurative inflammatory conditions (i.e., boils and abscesses) in the maxilla-facial region (Stomatologiia (Mosk) 2009;88:50-2).
This column will consider some of the most current AD studies as well as other recent research. History is not to be disregarded, though. After all, the notion of topical probiotics conferring cutaneous benefits against acne and seborrhea was considered in 1912 (Gut Pathog. 2011;3:1). Current findings may, indeed, bear this out.
Atopic Dermatitis
The safety of probiotic, as well as prebiotic, treatments for AD in children was established in a long-term, randomized, double-blind trial (Clin. Dermatol. 2010;28:57-61; Pediatrics 2008;122:8-1). But questions remain regarding efficacy, with conflicting data emerging from recent studies. Given increasing interest in the use of probiotics for the treatment of AD, Boyle et al. conducted an extensive literature search up to 2008 and found that 12 trials, including 781 subjects (all children), met their inclusion criteria, with probiotics not emerging as an effective treatment for eczema (Cochrane Database Syst. Rev. 2008;CD006135).
In 2008, Betsi et al. reviewed the results of 13 relevant randomized, placebo-controlled trials, 10 of which assessed probiotics as treatment and 3 for prevention of AD. Overall, they found that probiotics, particularly Lactobacillus rhamnosus GG, appear to be effective for preventing AD, lowering its severity in half of the trials assessed though inflammatory markers were not significantly affected. The authors called for more research to determine the usefulness of probiotics in AD treatment or prevention (Am. J. Clin. Dermatol. 2008;9:93-103).
In a 2010 analysis of systematic reviews indexed between August 2007 and August 2008 covering disease prevention and atopic eczema treatment, Williams and Grindlay found two independent systematic reviews suggesting that ingestion of probiotics by mothers during pregnancy might lower the incidence of subsequent eczema. However, they noted that a review of 13 studies of probiotics for treating established eczema revealed no convincing support for its clinical use, a stance that was buttressed by a later Cochrane Review (Clin. Exp. Dermatol. 2010;35:223-7).
In 2010, Gerasimov et al. conducted a randomized, double-blind, placebo-controlled, prospective study of 90 children (1-3 years old) with moderate to severe AD treated with a mixture of L. acidophilus DDS-1 and Bifidobacterium lactis UABLA-12 with fructo-oligosaccharide (5 billion colony-forming units twice daily for 8 weeks vs. placebo). The researchers found that the use of the probiotic compound correlated with significant clinical improvement in children with AD, and suggested that additional research is necessary to assess the efficacy of probiotics in adults with AD (Am. J. Clin. Dermatol. 2010;11:351-61).
In another recent study, investigators isolated L. plantarum strains from the Korean fermented food kimchi, and found that they hindered the dermatitis promoted by house-dust mites in a mouse model representative of human AD (J. Appl. Microbiol. 2011;110:1195-202). Overall, clinical trials conducted to test the use of probiotics to treat AD over the last 15 years have yielded conflicting results, though it appears that there is not enough evidence to warrant support for such therapy (Clin. Rev. Allergy Immunol. 2011;41:267-71).
Mechanism of Action
Presently, the mechanism of action whereby skin benefits are manifested through the oral ingestion of probiotics is thought to be a downstream result of the boost in systemic immune response, especially T-cell subsets such as Th1 cells that may ultimately enhance immune responses in organs beyond the digestive tract (Clin. Plast. Surg. 2012;39:59-64; Clin. Dermatol. 2008;26:4-11).
In discussing an alternative to antibacterial products for imbalances in cutaneous microorganisms that result in mild acne, xerosis, or AD, Simmering and Breves suggest that "prebiotic actives rebalance the skin microflora while probiotic approaches predominantly consist of applying an inactivated microbial biomass of beneficial bacteria" (Hautarzt. 2009;60:809-14).
Cutaneous Immune Homeostasis
In a 2009 randomized, double-blind, placebo-controlled clinical trial with 54 volunteers, Guéniche et al. set out to ascertain whether the probiotic bacterium L. johnsonii (La1) could influence cutaneous immune homeostasis in humans after solar-simulated UV exposure (twice 1.5 MED [minimal erythema dose]). They showed that La1 consumption contributed to hastening the recovery of allostimulatory function in epidermal cells (Dermatoendocrinol. 2009;1:275-9).
Previously, in 2008, Peguet-Navarro et al. conducted a randomized, double-blind, placebo-controlled clinical trial in 54 healthy volunteers to study the potential impact of oral supplementation with La1 on skin immune status after UV exposure. Subjects received either La1 or placebo during the 6 weeks prior to solar-simulated UV exposure. The investigators found on day 4 after exposure that the allostimulatory capacity of epidermal cells had completely recovered in the La1 group correlating with the normalization of epidermal CD1a expression. They concluded that ingested probiotic bacteria hasten the recovery of skin immune homeostasis after UV-provoked immunosuppression (Eur. J. Dermatol. 2008;18:504-11).
Anti-inflammatory Activity
In 2010, Guéniche et al. demonstrated that B. longum can reduce skin inflammation mediated by substance P (Exp. Dermatol. 2010;19:e1-8). In a separate study, some of the same investigators found that L. paracasei appears to have the capacity to confer benefits related to barrier function and skin reactivity, also blunting the effects of substance P–induced skin inflammation (Eur. J. Dermatol. 2010;20:731-7).
Antiphotoaging Activity
In 2010, Bouilly-Gauthier et al. evaluated the effects of a dietary supplement combining L. johnsonii (La1), which is thought to protect the skin immune system after UV exposure, and nutritional doses of carotenoids on early UV-induced skin damage. They performed three clinical trials using various UV sources (non–extreme UV with a high UVA irradiance, extreme simulated solar radiation, and natural sunlight) in 139 healthy women over age 18 with skin type II-IV. The investigators found over the 10 weeks of the study that the combination of probiotic (La1) and nutritional doses of carotenoids lowered early UV-induced skin damage caused by simulated or natural sun exposure. Further study of the possible long-term effects against UV exposure and photoaging is warranted, they concluded (Br. J. Dermatol. 2010;163:536-43).
Topical Uses
In a study more than a decade ago, Di Marzio et al. showed that the topical application of a cream containing Streptococcus thermophilus, an organism found in most yogurts, raised the production of ceramides, which is notable given the anti-inflammatory activity and antimicrobial activity of some ceramides against Proprionibacterium acnes (J. Invest. Dermatol. 1999;113:98-106;Gut Pathog. 2011;3:1). Two recent in vitro studies have also revealed that probiotics can have antibacterial activity against P. acnes (Int. J. Cosmet. Sci. 2010;32:139-42; J. Microbiol. 2009;47:101-9). The prospects for efficacy of topically applied probiotics in the prevention and treatment of pro-inflammatory immune reactions are considered, by some, to be promising, however (Hautarzt. 2009;60:795-801). And, in fact, Guéniche et al. have found that the topical application of Vitreoscilla filiformis demonstrated efficacy against seborrheic dermatitis and AD (J. Eur. Acad. Dermatol. Venereol. 2008;22:1014-5; Eur. J. Dermatol. 2006;16:380-4).
Conclusion
While still controversial, the findings of probiotics’ effects in the treatment of atopic dermatitis remain compelling. Even more interesting, though, is the current work that suggests additional potential applications of probiotics in the dermatologic armamentarium. The work is in its early stages, but results warrant additional research, at the very least, if not cause for optimism over the prospect of more supportive evidence.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest.
Probiotics are live microorganisms that impart health benefits to the host when present or administered at appropriate levels (J. Appl. Bacteriol. 1989;66:365-78). Intestinal microflora are better understood and more frequently used than cutaneous microbiota, but researchers have recently applied the concepts underlying the efficacy of intestinal probiotics to investigate potential benefits in the dermatologic realm. This work has also been spurred by the flurry of investigations on probiotics for the treatment of atopic dermatitis (AD).
In one of the earlier studies of possible uses of probiotics for the skin, Ouwehand et al. identified strains that adhere to keratin. However, the tested microbes (Propionibacteria, selected because they are among the normal microbiota of the skin) were not found to inhibit cutaneous pathogen adhesion to human keratin. Nevertheless, the researchers concluded that additional study was warranted to identify strains that adhere in vivo and exhibit activity against potential skin pathogens (Lett. Appl. Microbiol. 2003;36:327-31).
Clearly, some probiotic strains have been shown to exhibit strong immunomodulatory activity at the cutaneous level (Eur. J. Dermatol. 2010;20:731-7). In addition, some topical skin products now contain probiotic strains as active ingredients, including Clinique Medical, which incorporates lactobacillus cultures to yield molecules that help ameliorate skin barrier effects from laser treatments or chemical peels (Facial Plast. Surg. 2009;25:285-9). Probiotics have also been used successively as adjuvant therapy to treat suppurative inflammatory conditions (i.e., boils and abscesses) in the maxilla-facial region (Stomatologiia (Mosk) 2009;88:50-2).
This column will consider some of the most current AD studies as well as other recent research. History is not to be disregarded, though. After all, the notion of topical probiotics conferring cutaneous benefits against acne and seborrhea was considered in 1912 (Gut Pathog. 2011;3:1). Current findings may, indeed, bear this out.
Atopic Dermatitis
The safety of probiotic, as well as prebiotic, treatments for AD in children was established in a long-term, randomized, double-blind trial (Clin. Dermatol. 2010;28:57-61; Pediatrics 2008;122:8-1). But questions remain regarding efficacy, with conflicting data emerging from recent studies. Given increasing interest in the use of probiotics for the treatment of AD, Boyle et al. conducted an extensive literature search up to 2008 and found that 12 trials, including 781 subjects (all children), met their inclusion criteria, with probiotics not emerging as an effective treatment for eczema (Cochrane Database Syst. Rev. 2008;CD006135).
In 2008, Betsi et al. reviewed the results of 13 relevant randomized, placebo-controlled trials, 10 of which assessed probiotics as treatment and 3 for prevention of AD. Overall, they found that probiotics, particularly Lactobacillus rhamnosus GG, appear to be effective for preventing AD, lowering its severity in half of the trials assessed though inflammatory markers were not significantly affected. The authors called for more research to determine the usefulness of probiotics in AD treatment or prevention (Am. J. Clin. Dermatol. 2008;9:93-103).
In a 2010 analysis of systematic reviews indexed between August 2007 and August 2008 covering disease prevention and atopic eczema treatment, Williams and Grindlay found two independent systematic reviews suggesting that ingestion of probiotics by mothers during pregnancy might lower the incidence of subsequent eczema. However, they noted that a review of 13 studies of probiotics for treating established eczema revealed no convincing support for its clinical use, a stance that was buttressed by a later Cochrane Review (Clin. Exp. Dermatol. 2010;35:223-7).
In 2010, Gerasimov et al. conducted a randomized, double-blind, placebo-controlled, prospective study of 90 children (1-3 years old) with moderate to severe AD treated with a mixture of L. acidophilus DDS-1 and Bifidobacterium lactis UABLA-12 with fructo-oligosaccharide (5 billion colony-forming units twice daily for 8 weeks vs. placebo). The researchers found that the use of the probiotic compound correlated with significant clinical improvement in children with AD, and suggested that additional research is necessary to assess the efficacy of probiotics in adults with AD (Am. J. Clin. Dermatol. 2010;11:351-61).
In another recent study, investigators isolated L. plantarum strains from the Korean fermented food kimchi, and found that they hindered the dermatitis promoted by house-dust mites in a mouse model representative of human AD (J. Appl. Microbiol. 2011;110:1195-202). Overall, clinical trials conducted to test the use of probiotics to treat AD over the last 15 years have yielded conflicting results, though it appears that there is not enough evidence to warrant support for such therapy (Clin. Rev. Allergy Immunol. 2011;41:267-71).
Mechanism of Action
Presently, the mechanism of action whereby skin benefits are manifested through the oral ingestion of probiotics is thought to be a downstream result of the boost in systemic immune response, especially T-cell subsets such as Th1 cells that may ultimately enhance immune responses in organs beyond the digestive tract (Clin. Plast. Surg. 2012;39:59-64; Clin. Dermatol. 2008;26:4-11).
In discussing an alternative to antibacterial products for imbalances in cutaneous microorganisms that result in mild acne, xerosis, or AD, Simmering and Breves suggest that "prebiotic actives rebalance the skin microflora while probiotic approaches predominantly consist of applying an inactivated microbial biomass of beneficial bacteria" (Hautarzt. 2009;60:809-14).
Cutaneous Immune Homeostasis
In a 2009 randomized, double-blind, placebo-controlled clinical trial with 54 volunteers, Guéniche et al. set out to ascertain whether the probiotic bacterium L. johnsonii (La1) could influence cutaneous immune homeostasis in humans after solar-simulated UV exposure (twice 1.5 MED [minimal erythema dose]). They showed that La1 consumption contributed to hastening the recovery of allostimulatory function in epidermal cells (Dermatoendocrinol. 2009;1:275-9).
Previously, in 2008, Peguet-Navarro et al. conducted a randomized, double-blind, placebo-controlled clinical trial in 54 healthy volunteers to study the potential impact of oral supplementation with La1 on skin immune status after UV exposure. Subjects received either La1 or placebo during the 6 weeks prior to solar-simulated UV exposure. The investigators found on day 4 after exposure that the allostimulatory capacity of epidermal cells had completely recovered in the La1 group correlating with the normalization of epidermal CD1a expression. They concluded that ingested probiotic bacteria hasten the recovery of skin immune homeostasis after UV-provoked immunosuppression (Eur. J. Dermatol. 2008;18:504-11).
Anti-inflammatory Activity
In 2010, Guéniche et al. demonstrated that B. longum can reduce skin inflammation mediated by substance P (Exp. Dermatol. 2010;19:e1-8). In a separate study, some of the same investigators found that L. paracasei appears to have the capacity to confer benefits related to barrier function and skin reactivity, also blunting the effects of substance P–induced skin inflammation (Eur. J. Dermatol. 2010;20:731-7).
Antiphotoaging Activity
In 2010, Bouilly-Gauthier et al. evaluated the effects of a dietary supplement combining L. johnsonii (La1), which is thought to protect the skin immune system after UV exposure, and nutritional doses of carotenoids on early UV-induced skin damage. They performed three clinical trials using various UV sources (non–extreme UV with a high UVA irradiance, extreme simulated solar radiation, and natural sunlight) in 139 healthy women over age 18 with skin type II-IV. The investigators found over the 10 weeks of the study that the combination of probiotic (La1) and nutritional doses of carotenoids lowered early UV-induced skin damage caused by simulated or natural sun exposure. Further study of the possible long-term effects against UV exposure and photoaging is warranted, they concluded (Br. J. Dermatol. 2010;163:536-43).
Topical Uses
In a study more than a decade ago, Di Marzio et al. showed that the topical application of a cream containing Streptococcus thermophilus, an organism found in most yogurts, raised the production of ceramides, which is notable given the anti-inflammatory activity and antimicrobial activity of some ceramides against Proprionibacterium acnes (J. Invest. Dermatol. 1999;113:98-106;Gut Pathog. 2011;3:1). Two recent in vitro studies have also revealed that probiotics can have antibacterial activity against P. acnes (Int. J. Cosmet. Sci. 2010;32:139-42; J. Microbiol. 2009;47:101-9). The prospects for efficacy of topically applied probiotics in the prevention and treatment of pro-inflammatory immune reactions are considered, by some, to be promising, however (Hautarzt. 2009;60:795-801). And, in fact, Guéniche et al. have found that the topical application of Vitreoscilla filiformis demonstrated efficacy against seborrheic dermatitis and AD (J. Eur. Acad. Dermatol. Venereol. 2008;22:1014-5; Eur. J. Dermatol. 2006;16:380-4).
Conclusion
While still controversial, the findings of probiotics’ effects in the treatment of atopic dermatitis remain compelling. Even more interesting, though, is the current work that suggests additional potential applications of probiotics in the dermatologic armamentarium. The work is in its early stages, but results warrant additional research, at the very least, if not cause for optimism over the prospect of more supportive evidence.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest.
Probiotics are live microorganisms that impart health benefits to the host when present or administered at appropriate levels (J. Appl. Bacteriol. 1989;66:365-78). Intestinal microflora are better understood and more frequently used than cutaneous microbiota, but researchers have recently applied the concepts underlying the efficacy of intestinal probiotics to investigate potential benefits in the dermatologic realm. This work has also been spurred by the flurry of investigations on probiotics for the treatment of atopic dermatitis (AD).
In one of the earlier studies of possible uses of probiotics for the skin, Ouwehand et al. identified strains that adhere to keratin. However, the tested microbes (Propionibacteria, selected because they are among the normal microbiota of the skin) were not found to inhibit cutaneous pathogen adhesion to human keratin. Nevertheless, the researchers concluded that additional study was warranted to identify strains that adhere in vivo and exhibit activity against potential skin pathogens (Lett. Appl. Microbiol. 2003;36:327-31).
Clearly, some probiotic strains have been shown to exhibit strong immunomodulatory activity at the cutaneous level (Eur. J. Dermatol. 2010;20:731-7). In addition, some topical skin products now contain probiotic strains as active ingredients, including Clinique Medical, which incorporates lactobacillus cultures to yield molecules that help ameliorate skin barrier effects from laser treatments or chemical peels (Facial Plast. Surg. 2009;25:285-9). Probiotics have also been used successively as adjuvant therapy to treat suppurative inflammatory conditions (i.e., boils and abscesses) in the maxilla-facial region (Stomatologiia (Mosk) 2009;88:50-2).
This column will consider some of the most current AD studies as well as other recent research. History is not to be disregarded, though. After all, the notion of topical probiotics conferring cutaneous benefits against acne and seborrhea was considered in 1912 (Gut Pathog. 2011;3:1). Current findings may, indeed, bear this out.
Atopic Dermatitis
The safety of probiotic, as well as prebiotic, treatments for AD in children was established in a long-term, randomized, double-blind trial (Clin. Dermatol. 2010;28:57-61; Pediatrics 2008;122:8-1). But questions remain regarding efficacy, with conflicting data emerging from recent studies. Given increasing interest in the use of probiotics for the treatment of AD, Boyle et al. conducted an extensive literature search up to 2008 and found that 12 trials, including 781 subjects (all children), met their inclusion criteria, with probiotics not emerging as an effective treatment for eczema (Cochrane Database Syst. Rev. 2008;CD006135).
In 2008, Betsi et al. reviewed the results of 13 relevant randomized, placebo-controlled trials, 10 of which assessed probiotics as treatment and 3 for prevention of AD. Overall, they found that probiotics, particularly Lactobacillus rhamnosus GG, appear to be effective for preventing AD, lowering its severity in half of the trials assessed though inflammatory markers were not significantly affected. The authors called for more research to determine the usefulness of probiotics in AD treatment or prevention (Am. J. Clin. Dermatol. 2008;9:93-103).
In a 2010 analysis of systematic reviews indexed between August 2007 and August 2008 covering disease prevention and atopic eczema treatment, Williams and Grindlay found two independent systematic reviews suggesting that ingestion of probiotics by mothers during pregnancy might lower the incidence of subsequent eczema. However, they noted that a review of 13 studies of probiotics for treating established eczema revealed no convincing support for its clinical use, a stance that was buttressed by a later Cochrane Review (Clin. Exp. Dermatol. 2010;35:223-7).
In 2010, Gerasimov et al. conducted a randomized, double-blind, placebo-controlled, prospective study of 90 children (1-3 years old) with moderate to severe AD treated with a mixture of L. acidophilus DDS-1 and Bifidobacterium lactis UABLA-12 with fructo-oligosaccharide (5 billion colony-forming units twice daily for 8 weeks vs. placebo). The researchers found that the use of the probiotic compound correlated with significant clinical improvement in children with AD, and suggested that additional research is necessary to assess the efficacy of probiotics in adults with AD (Am. J. Clin. Dermatol. 2010;11:351-61).
In another recent study, investigators isolated L. plantarum strains from the Korean fermented food kimchi, and found that they hindered the dermatitis promoted by house-dust mites in a mouse model representative of human AD (J. Appl. Microbiol. 2011;110:1195-202). Overall, clinical trials conducted to test the use of probiotics to treat AD over the last 15 years have yielded conflicting results, though it appears that there is not enough evidence to warrant support for such therapy (Clin. Rev. Allergy Immunol. 2011;41:267-71).
Mechanism of Action
Presently, the mechanism of action whereby skin benefits are manifested through the oral ingestion of probiotics is thought to be a downstream result of the boost in systemic immune response, especially T-cell subsets such as Th1 cells that may ultimately enhance immune responses in organs beyond the digestive tract (Clin. Plast. Surg. 2012;39:59-64; Clin. Dermatol. 2008;26:4-11).
In discussing an alternative to antibacterial products for imbalances in cutaneous microorganisms that result in mild acne, xerosis, or AD, Simmering and Breves suggest that "prebiotic actives rebalance the skin microflora while probiotic approaches predominantly consist of applying an inactivated microbial biomass of beneficial bacteria" (Hautarzt. 2009;60:809-14).
Cutaneous Immune Homeostasis
In a 2009 randomized, double-blind, placebo-controlled clinical trial with 54 volunteers, Guéniche et al. set out to ascertain whether the probiotic bacterium L. johnsonii (La1) could influence cutaneous immune homeostasis in humans after solar-simulated UV exposure (twice 1.5 MED [minimal erythema dose]). They showed that La1 consumption contributed to hastening the recovery of allostimulatory function in epidermal cells (Dermatoendocrinol. 2009;1:275-9).
Previously, in 2008, Peguet-Navarro et al. conducted a randomized, double-blind, placebo-controlled clinical trial in 54 healthy volunteers to study the potential impact of oral supplementation with La1 on skin immune status after UV exposure. Subjects received either La1 or placebo during the 6 weeks prior to solar-simulated UV exposure. The investigators found on day 4 after exposure that the allostimulatory capacity of epidermal cells had completely recovered in the La1 group correlating with the normalization of epidermal CD1a expression. They concluded that ingested probiotic bacteria hasten the recovery of skin immune homeostasis after UV-provoked immunosuppression (Eur. J. Dermatol. 2008;18:504-11).
Anti-inflammatory Activity
In 2010, Guéniche et al. demonstrated that B. longum can reduce skin inflammation mediated by substance P (Exp. Dermatol. 2010;19:e1-8). In a separate study, some of the same investigators found that L. paracasei appears to have the capacity to confer benefits related to barrier function and skin reactivity, also blunting the effects of substance P–induced skin inflammation (Eur. J. Dermatol. 2010;20:731-7).
Antiphotoaging Activity
In 2010, Bouilly-Gauthier et al. evaluated the effects of a dietary supplement combining L. johnsonii (La1), which is thought to protect the skin immune system after UV exposure, and nutritional doses of carotenoids on early UV-induced skin damage. They performed three clinical trials using various UV sources (non–extreme UV with a high UVA irradiance, extreme simulated solar radiation, and natural sunlight) in 139 healthy women over age 18 with skin type II-IV. The investigators found over the 10 weeks of the study that the combination of probiotic (La1) and nutritional doses of carotenoids lowered early UV-induced skin damage caused by simulated or natural sun exposure. Further study of the possible long-term effects against UV exposure and photoaging is warranted, they concluded (Br. J. Dermatol. 2010;163:536-43).
Topical Uses
In a study more than a decade ago, Di Marzio et al. showed that the topical application of a cream containing Streptococcus thermophilus, an organism found in most yogurts, raised the production of ceramides, which is notable given the anti-inflammatory activity and antimicrobial activity of some ceramides against Proprionibacterium acnes (J. Invest. Dermatol. 1999;113:98-106;Gut Pathog. 2011;3:1). Two recent in vitro studies have also revealed that probiotics can have antibacterial activity against P. acnes (Int. J. Cosmet. Sci. 2010;32:139-42; J. Microbiol. 2009;47:101-9). The prospects for efficacy of topically applied probiotics in the prevention and treatment of pro-inflammatory immune reactions are considered, by some, to be promising, however (Hautarzt. 2009;60:795-801). And, in fact, Guéniche et al. have found that the topical application of Vitreoscilla filiformis demonstrated efficacy against seborrheic dermatitis and AD (J. Eur. Acad. Dermatol. Venereol. 2008;22:1014-5; Eur. J. Dermatol. 2006;16:380-4).
Conclusion
While still controversial, the findings of probiotics’ effects in the treatment of atopic dermatitis remain compelling. Even more interesting, though, is the current work that suggests additional potential applications of probiotics in the dermatologic armamentarium. The work is in its early stages, but results warrant additional research, at the very least, if not cause for optimism over the prospect of more supportive evidence.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest.
Cosmeceutical Critique: Safflower Oil
Safflower (Carthamus tinctorius), a thistlelike annual, is one of the oldest cultivated crops, its use dating back to ancient Egypt. It was traditionally grown for its seeds, which were used in foods and folk medicine. Safflower is now primarily cultivated for its vegetable oil, which is extracted from its seeds. Safflower oil has been found to exert notable health benefits when consumed through the diet and also when used in topical formulations.
Linoleic acid is a primary constituent of safflower seeds, and is the component to which the oil’s cutaneous benefits are typically ascribed. In fact, safflower oil is one of the richest sources of linoleic acid, which is necessary for the endogenous production of ceramides, key components of the epidermal layer that play a crucial role in barrier function and help the skin retain water.
In skin care products, safflower oil is incorporated in moisturizing agents for its occlusive properties. Occlusive agents coat the stratum corneum to slow transepidermal water loss. Typically, such substances have the capacity to dissolve fats and are therefore used in many skin care cosmetics.
Research on Topical Applications
In an early study on the antiproliferative potential of C. tinctorius extracts, Yasukawa et al., in 1996, isolated erythro-alkane-6,8-diols from the flowers of C. tinctorius and applied the tumor-promoting agent 12-O-tetradecanoylphorbol-13-acetate (TPA) to the ears of mice (1 mcg/ear) to induce inflammation. The investigators reported that five of the eight alkane-6,8-diols assayed suppressed inflammation, and the mixture of erythro-alkane-6,8-diols significantly inhibited TPA-induced skin tumor formation in mice after initiation with 7,12-dimethylbenz[a]anthracene (Oncology 1996;53:133-6).
In 2004, Roh et al. investigated the melanogenesis-suppressing activity of safflower seeds to develop a novel skin-whitening agent. They reported that an 80% aqueous methanol extract and ethyl acetate fraction from the seeds significantly inhibited mushroom tyrosinase, and the researchers identified three active constituents [N-feruloylserotonin, N-(p-coumaroyl)serotonin, and acacetin]. Of these, N-feruloylserotonin and N-(p-coumaroyl)serotonin were found to more potently suppress the melanin synthesis of Streptomyces bikiniensis and B16 melanoma cells than arbutin, a well-known inhibitor of melanogenesis (Biol. Pharm. Bull. 2004;27:1976-8).
In 2005, Solanki et al. conducted a short, randomized controlled study in a tertiary-care neonatal intensive care unit (NICU) of a large teaching hospital, to assess the transcutaneous absorption of oil traditionally used in massage of newborns, and to compare the effects of safflower oil and coconut oil on fatty acid profiles of massaged babies. The investigators randomly assigned 120 babies to three groups – safflower oil, coconut oil, or no-oil controls (40 in each group). The babies were massaged with 5 mL of oil four times daily for 5 days. Blood triglyceride levels were significantly elevated in all groups, though much more so in the noncontrol groups. Significant increases in essential fatty acids (linolenic and arachidonic) were seen in the safflower oil group, and similar increases in saturated fats were seen in the coconut oil group, with changes more evident in term babies. The researchers concluded that topically applied oil is absorbed in neonates and is likely available nutritionally. Consequently, they deemed the fatty acid constituents of the massage oils significant in potentially impacting the fatty acid profiles of patients (Indian Pediatr. 2005;42:998-1005). Safflower oil is rich in essential fatty acids, and coconut oil is rife with saturated fat.
Potential Dietary Benefits
Safflower oil has also been found, as has olive oil, to confer dietary benefits on diabetic pregnant rats and their embryos, preventing diabetes-induced developmental harm during early organogenesis (Mol. Hum. Reprod. 2010;16:286-95). Supplementation with either oil has also been demonstrated to prevent excessive activity by matrix metalloproteinases (specifically MMP-2 and MMP-9) in the placenta of diabetic rats, with salubrious effects manifesting in the sera (Placenta 2012;33:8-16). In addition, in a recent study, safflower oil and folic acid supplementations were shown to interact, protecting rat embryos from diabetes-induced harm through reductions in proinflammatory mediators (Mol. Hum. Reprod. 2012;18:253-64).
As mentioned above, safflower oil is available in several topical products, but it is more likely beneficial through diet. Topically, safflower oil, as found in a Neutrogena bath oil, for example, contains linoleic acid and may be useful when added to bathwater or applied to wet skin. Of course, oils in general are not suitable for all skin types. Safflower oil is indicated for individuals with dry or damaged skin.
Conclusion
Safflower oil, rich in the essential omega-6 fatty acid linoleic acid, is known to confer health benefits via diet. It is also included in skin care products, such as bath oils, which anecdotally appear to be effective. Nevertheless, there is a dearth of data on the use of safflower oil for dermatologic purposes. Much more research is necessary, including randomized controlled clinical trials in humans, to establish the potential for more extensive uses of safflower oil for skin health.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
Safflower (Carthamus tinctorius), a thistlelike annual, is one of the oldest cultivated crops, its use dating back to ancient Egypt. It was traditionally grown for its seeds, which were used in foods and folk medicine. Safflower is now primarily cultivated for its vegetable oil, which is extracted from its seeds. Safflower oil has been found to exert notable health benefits when consumed through the diet and also when used in topical formulations.
Linoleic acid is a primary constituent of safflower seeds, and is the component to which the oil’s cutaneous benefits are typically ascribed. In fact, safflower oil is one of the richest sources of linoleic acid, which is necessary for the endogenous production of ceramides, key components of the epidermal layer that play a crucial role in barrier function and help the skin retain water.
In skin care products, safflower oil is incorporated in moisturizing agents for its occlusive properties. Occlusive agents coat the stratum corneum to slow transepidermal water loss. Typically, such substances have the capacity to dissolve fats and are therefore used in many skin care cosmetics.
Research on Topical Applications
In an early study on the antiproliferative potential of C. tinctorius extracts, Yasukawa et al., in 1996, isolated erythro-alkane-6,8-diols from the flowers of C. tinctorius and applied the tumor-promoting agent 12-O-tetradecanoylphorbol-13-acetate (TPA) to the ears of mice (1 mcg/ear) to induce inflammation. The investigators reported that five of the eight alkane-6,8-diols assayed suppressed inflammation, and the mixture of erythro-alkane-6,8-diols significantly inhibited TPA-induced skin tumor formation in mice after initiation with 7,12-dimethylbenz[a]anthracene (Oncology 1996;53:133-6).
In 2004, Roh et al. investigated the melanogenesis-suppressing activity of safflower seeds to develop a novel skin-whitening agent. They reported that an 80% aqueous methanol extract and ethyl acetate fraction from the seeds significantly inhibited mushroom tyrosinase, and the researchers identified three active constituents [N-feruloylserotonin, N-(p-coumaroyl)serotonin, and acacetin]. Of these, N-feruloylserotonin and N-(p-coumaroyl)serotonin were found to more potently suppress the melanin synthesis of Streptomyces bikiniensis and B16 melanoma cells than arbutin, a well-known inhibitor of melanogenesis (Biol. Pharm. Bull. 2004;27:1976-8).
In 2005, Solanki et al. conducted a short, randomized controlled study in a tertiary-care neonatal intensive care unit (NICU) of a large teaching hospital, to assess the transcutaneous absorption of oil traditionally used in massage of newborns, and to compare the effects of safflower oil and coconut oil on fatty acid profiles of massaged babies. The investigators randomly assigned 120 babies to three groups – safflower oil, coconut oil, or no-oil controls (40 in each group). The babies were massaged with 5 mL of oil four times daily for 5 days. Blood triglyceride levels were significantly elevated in all groups, though much more so in the noncontrol groups. Significant increases in essential fatty acids (linolenic and arachidonic) were seen in the safflower oil group, and similar increases in saturated fats were seen in the coconut oil group, with changes more evident in term babies. The researchers concluded that topically applied oil is absorbed in neonates and is likely available nutritionally. Consequently, they deemed the fatty acid constituents of the massage oils significant in potentially impacting the fatty acid profiles of patients (Indian Pediatr. 2005;42:998-1005). Safflower oil is rich in essential fatty acids, and coconut oil is rife with saturated fat.
Potential Dietary Benefits
Safflower oil has also been found, as has olive oil, to confer dietary benefits on diabetic pregnant rats and their embryos, preventing diabetes-induced developmental harm during early organogenesis (Mol. Hum. Reprod. 2010;16:286-95). Supplementation with either oil has also been demonstrated to prevent excessive activity by matrix metalloproteinases (specifically MMP-2 and MMP-9) in the placenta of diabetic rats, with salubrious effects manifesting in the sera (Placenta 2012;33:8-16). In addition, in a recent study, safflower oil and folic acid supplementations were shown to interact, protecting rat embryos from diabetes-induced harm through reductions in proinflammatory mediators (Mol. Hum. Reprod. 2012;18:253-64).
As mentioned above, safflower oil is available in several topical products, but it is more likely beneficial through diet. Topically, safflower oil, as found in a Neutrogena bath oil, for example, contains linoleic acid and may be useful when added to bathwater or applied to wet skin. Of course, oils in general are not suitable for all skin types. Safflower oil is indicated for individuals with dry or damaged skin.
Conclusion
Safflower oil, rich in the essential omega-6 fatty acid linoleic acid, is known to confer health benefits via diet. It is also included in skin care products, such as bath oils, which anecdotally appear to be effective. Nevertheless, there is a dearth of data on the use of safflower oil for dermatologic purposes. Much more research is necessary, including randomized controlled clinical trials in humans, to establish the potential for more extensive uses of safflower oil for skin health.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
Safflower (Carthamus tinctorius), a thistlelike annual, is one of the oldest cultivated crops, its use dating back to ancient Egypt. It was traditionally grown for its seeds, which were used in foods and folk medicine. Safflower is now primarily cultivated for its vegetable oil, which is extracted from its seeds. Safflower oil has been found to exert notable health benefits when consumed through the diet and also when used in topical formulations.
Linoleic acid is a primary constituent of safflower seeds, and is the component to which the oil’s cutaneous benefits are typically ascribed. In fact, safflower oil is one of the richest sources of linoleic acid, which is necessary for the endogenous production of ceramides, key components of the epidermal layer that play a crucial role in barrier function and help the skin retain water.
In skin care products, safflower oil is incorporated in moisturizing agents for its occlusive properties. Occlusive agents coat the stratum corneum to slow transepidermal water loss. Typically, such substances have the capacity to dissolve fats and are therefore used in many skin care cosmetics.
Research on Topical Applications
In an early study on the antiproliferative potential of C. tinctorius extracts, Yasukawa et al., in 1996, isolated erythro-alkane-6,8-diols from the flowers of C. tinctorius and applied the tumor-promoting agent 12-O-tetradecanoylphorbol-13-acetate (TPA) to the ears of mice (1 mcg/ear) to induce inflammation. The investigators reported that five of the eight alkane-6,8-diols assayed suppressed inflammation, and the mixture of erythro-alkane-6,8-diols significantly inhibited TPA-induced skin tumor formation in mice after initiation with 7,12-dimethylbenz[a]anthracene (Oncology 1996;53:133-6).
In 2004, Roh et al. investigated the melanogenesis-suppressing activity of safflower seeds to develop a novel skin-whitening agent. They reported that an 80% aqueous methanol extract and ethyl acetate fraction from the seeds significantly inhibited mushroom tyrosinase, and the researchers identified three active constituents [N-feruloylserotonin, N-(p-coumaroyl)serotonin, and acacetin]. Of these, N-feruloylserotonin and N-(p-coumaroyl)serotonin were found to more potently suppress the melanin synthesis of Streptomyces bikiniensis and B16 melanoma cells than arbutin, a well-known inhibitor of melanogenesis (Biol. Pharm. Bull. 2004;27:1976-8).
In 2005, Solanki et al. conducted a short, randomized controlled study in a tertiary-care neonatal intensive care unit (NICU) of a large teaching hospital, to assess the transcutaneous absorption of oil traditionally used in massage of newborns, and to compare the effects of safflower oil and coconut oil on fatty acid profiles of massaged babies. The investigators randomly assigned 120 babies to three groups – safflower oil, coconut oil, or no-oil controls (40 in each group). The babies were massaged with 5 mL of oil four times daily for 5 days. Blood triglyceride levels were significantly elevated in all groups, though much more so in the noncontrol groups. Significant increases in essential fatty acids (linolenic and arachidonic) were seen in the safflower oil group, and similar increases in saturated fats were seen in the coconut oil group, with changes more evident in term babies. The researchers concluded that topically applied oil is absorbed in neonates and is likely available nutritionally. Consequently, they deemed the fatty acid constituents of the massage oils significant in potentially impacting the fatty acid profiles of patients (Indian Pediatr. 2005;42:998-1005). Safflower oil is rich in essential fatty acids, and coconut oil is rife with saturated fat.
Potential Dietary Benefits
Safflower oil has also been found, as has olive oil, to confer dietary benefits on diabetic pregnant rats and their embryos, preventing diabetes-induced developmental harm during early organogenesis (Mol. Hum. Reprod. 2010;16:286-95). Supplementation with either oil has also been demonstrated to prevent excessive activity by matrix metalloproteinases (specifically MMP-2 and MMP-9) in the placenta of diabetic rats, with salubrious effects manifesting in the sera (Placenta 2012;33:8-16). In addition, in a recent study, safflower oil and folic acid supplementations were shown to interact, protecting rat embryos from diabetes-induced harm through reductions in proinflammatory mediators (Mol. Hum. Reprod. 2012;18:253-64).
As mentioned above, safflower oil is available in several topical products, but it is more likely beneficial through diet. Topically, safflower oil, as found in a Neutrogena bath oil, for example, contains linoleic acid and may be useful when added to bathwater or applied to wet skin. Of course, oils in general are not suitable for all skin types. Safflower oil is indicated for individuals with dry or damaged skin.
Conclusion
Safflower oil, rich in the essential omega-6 fatty acid linoleic acid, is known to confer health benefits via diet. It is also included in skin care products, such as bath oils, which anecdotally appear to be effective. Nevertheless, there is a dearth of data on the use of safflower oil for dermatologic purposes. Much more research is necessary, including randomized controlled clinical trials in humans, to establish the potential for more extensive uses of safflower oil for skin health.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
Ajuga turkestanica
A perennial herb found primarily in Central Asia, Ajuga turkestanica is known to contain several bioactive compounds and has been used in traditional medicine to treat heart disease, and stomach and muscle aches (Chem. Nat. Compd. 1998;34:150-4; Chem. Nat. Compd. 2004;40:85-6). It is one of the many species of Ajuga gaining attention for exhibiting medicinal properties with the potential for commercial applications (Phytochem. Lett. 2008;1:81-4).
Clerodane diterpenes, recognized sources of antimicrobial, antiviral, antitumor, antibiotic, and amoebicidal activities (Phytochem. Rev. 2008;7:25-49), are among the three classes of potentially bioactive compounds, along with phytoecdysteroids and iridoid glycosides found in the Ajuga genus (Phytochem. Lett. 2008;1:81-4). Phytoecdysteroids are known to display significant physiological activities in insects and mammals; and iridoid glycosides, especially abundant in A. decumbens, have exhibited anticancer activity (Cancer Lett. 2000;157:87-92).
A. turkestanica reportedly contains several phytoecdysteroids (turkesterone, 20-hydroxyecdysone, cyasterone, cyasterone 22-acetate, ajugalactone, ajugasterone B, alpha-ecdysone, and ecdysone 2,3-monoacetonide), as well as the iridoids harpagide and harpagide 8-acetate (Chem. Nat. Compd. 2005;41:361-9; Chem. Nat. Compd. 1978;14:175-8; Chem. Nat. Compd. 1975;11:484-7; Chem. Nat. Compd. 1973;9:125-6; Chem. Nat. Compd. 1971;7:520; Phytochem. Lett. 2008;1:81-4).
Aquaporins
Aquaporins (AQPs) are integral membrane proteins that facilitate water transport in several organs, including the skin, brain, eyes, and digestive tract, as well as in the renal tubules. Thirteen isoforms of aquaporins (AQPs 0-12) are found in mammals. Of these, there are two functional subtype classifications: AQPs 1, 2, 4, 5, and 8 conduct only water, and AQPs 3, 7, 9, and 10 transport water and other substances including glycerol and urea (Prog. Histochem. Cytochem. 2004;39:1-83). AQP-3, permeable to water and glycerol, is the main water channel in human epidermis. Glycerol acts as an endogenous humectant, thereby facilitating hydration of the stratum corneum (SC) (J. Invest. Dermatol. 2005;125:288-93).
Defects in AQP-3 in mice models have been demonstrated to lead to epidermal xerosis and to reductions in SC hydration and epidermal glycerol content, followed by diminished elasticity and impaired skin barrier recovery (J. Biol. Chem. 2002;277:46616-21; Proc. Natl. Acad. Sci. 2003;100:7360-5). Such findings underscore the important role of glycerol in cutaneous hydration. Significantly, AQPs, particularly AQP-3, contribute to the transport of water, glycerol, and solutes between keratinocytes.
Dumas et al. note that the role of AQPs in hydrating the living layers of the epidermis where keratinocyte differentiation occurs and in barrier development and recovery suggests that they are significant protein targets for improving the quality and resistance of the skin surface, as well as ameliorating aging- and UV-induced xerosis (J. Drugs Dermatol. 2007;6(6 Suppl):s20-4).
A. turkestanica and Aquaporins
Patented extracts of A. turkestanica have been shown to contain sufficient ecdysteroids and other active ingredients to improve the differentiation of keratinocytes, thus facilitating skin hydration and yielding antiaging effects (U.S. Patent 7,060,693 B1, June 13, 2006). The patent inventors Dumas et al. observed that the extracts are especially effective in regulating epidermal water transport, achieving improved hydration of the basal layer by working in concert with or enhancing AQP-3 (Cosmet. Toil. 2008;123:22-7).
In 2007, Dumas et al. conducted in vitro and in vivo studies of active ingredients capable of raising AQP-3 levels to enhance hydration in human skin keratinocytes, with the understanding that improving hydration in keratinocytes would ultimately improve epidermal hydration (Eur. J. Dermatol. 2002;12:XXV-XXVI). They used an ethanol/water (70/30 v/v) extract of A. turkestanica as the hydrating agent (2.5 mcg/mL), and found that after 17 days of in vitro treatment every 2 days in human reconstructed epidermis, AQP-3 expression measured at the protein level was significantly elevated. Increased epidermal proliferation and differentiation were also noted. Electron microscopy showed a significantly thicker, compact SC and more clearly differentiated desmosomes. Constituents of the A. turkestanica extract revealed by chemical analysis included iridoids (chiefly harpagoside and 8-O-acetylharpagoside), ajugasterone B, ajugalactone, turkesterone, 22-acetylcyasterone, and phenols (J. Drugs. Dermatol. 2007;6:s20-4).
The investigators prepared an oil-water emulsion infused with A. turkestanica extract (0.3% w/w) for an in vivo study in which 15 healthy female volunteers (22-56 years old) applied the formulation twice daily to their forearms for 21 days. Significant reductions in transepidermal water loss were seen in the treated area compared with the control area on days 7 and 21. The researchers concluded that the tested A. turkestanica extract formulation enhanced AQP-3 expression and human epidermal differentiation in vitro, and ameliorated epidermal barrier structure and human skin recovery in vivo (J. Drugs. Dermatol. 2007;6:s20-4).
Conclusion
There is a dearth of research on A. turkestanica. But what exists is particularly favorable, insofar as the botanical appears to impact AQP-3, a compound whose significance has been recognized during the past 2 decades. Thus, A. turkestanica appears to have the potential to play an effective role in cosmetic products for treating dry skin. Much more research is necessary, however.
A perennial herb found primarily in Central Asia, Ajuga turkestanica is known to contain several bioactive compounds and has been used in traditional medicine to treat heart disease, and stomach and muscle aches (Chem. Nat. Compd. 1998;34:150-4; Chem. Nat. Compd. 2004;40:85-6). It is one of the many species of Ajuga gaining attention for exhibiting medicinal properties with the potential for commercial applications (Phytochem. Lett. 2008;1:81-4).
Clerodane diterpenes, recognized sources of antimicrobial, antiviral, antitumor, antibiotic, and amoebicidal activities (Phytochem. Rev. 2008;7:25-49), are among the three classes of potentially bioactive compounds, along with phytoecdysteroids and iridoid glycosides found in the Ajuga genus (Phytochem. Lett. 2008;1:81-4). Phytoecdysteroids are known to display significant physiological activities in insects and mammals; and iridoid glycosides, especially abundant in A. decumbens, have exhibited anticancer activity (Cancer Lett. 2000;157:87-92).
A. turkestanica reportedly contains several phytoecdysteroids (turkesterone, 20-hydroxyecdysone, cyasterone, cyasterone 22-acetate, ajugalactone, ajugasterone B, alpha-ecdysone, and ecdysone 2,3-monoacetonide), as well as the iridoids harpagide and harpagide 8-acetate (Chem. Nat. Compd. 2005;41:361-9; Chem. Nat. Compd. 1978;14:175-8; Chem. Nat. Compd. 1975;11:484-7; Chem. Nat. Compd. 1973;9:125-6; Chem. Nat. Compd. 1971;7:520; Phytochem. Lett. 2008;1:81-4).
Aquaporins
Aquaporins (AQPs) are integral membrane proteins that facilitate water transport in several organs, including the skin, brain, eyes, and digestive tract, as well as in the renal tubules. Thirteen isoforms of aquaporins (AQPs 0-12) are found in mammals. Of these, there are two functional subtype classifications: AQPs 1, 2, 4, 5, and 8 conduct only water, and AQPs 3, 7, 9, and 10 transport water and other substances including glycerol and urea (Prog. Histochem. Cytochem. 2004;39:1-83). AQP-3, permeable to water and glycerol, is the main water channel in human epidermis. Glycerol acts as an endogenous humectant, thereby facilitating hydration of the stratum corneum (SC) (J. Invest. Dermatol. 2005;125:288-93).
Defects in AQP-3 in mice models have been demonstrated to lead to epidermal xerosis and to reductions in SC hydration and epidermal glycerol content, followed by diminished elasticity and impaired skin barrier recovery (J. Biol. Chem. 2002;277:46616-21; Proc. Natl. Acad. Sci. 2003;100:7360-5). Such findings underscore the important role of glycerol in cutaneous hydration. Significantly, AQPs, particularly AQP-3, contribute to the transport of water, glycerol, and solutes between keratinocytes.
Dumas et al. note that the role of AQPs in hydrating the living layers of the epidermis where keratinocyte differentiation occurs and in barrier development and recovery suggests that they are significant protein targets for improving the quality and resistance of the skin surface, as well as ameliorating aging- and UV-induced xerosis (J. Drugs Dermatol. 2007;6(6 Suppl):s20-4).
A. turkestanica and Aquaporins
Patented extracts of A. turkestanica have been shown to contain sufficient ecdysteroids and other active ingredients to improve the differentiation of keratinocytes, thus facilitating skin hydration and yielding antiaging effects (U.S. Patent 7,060,693 B1, June 13, 2006). The patent inventors Dumas et al. observed that the extracts are especially effective in regulating epidermal water transport, achieving improved hydration of the basal layer by working in concert with or enhancing AQP-3 (Cosmet. Toil. 2008;123:22-7).
In 2007, Dumas et al. conducted in vitro and in vivo studies of active ingredients capable of raising AQP-3 levels to enhance hydration in human skin keratinocytes, with the understanding that improving hydration in keratinocytes would ultimately improve epidermal hydration (Eur. J. Dermatol. 2002;12:XXV-XXVI). They used an ethanol/water (70/30 v/v) extract of A. turkestanica as the hydrating agent (2.5 mcg/mL), and found that after 17 days of in vitro treatment every 2 days in human reconstructed epidermis, AQP-3 expression measured at the protein level was significantly elevated. Increased epidermal proliferation and differentiation were also noted. Electron microscopy showed a significantly thicker, compact SC and more clearly differentiated desmosomes. Constituents of the A. turkestanica extract revealed by chemical analysis included iridoids (chiefly harpagoside and 8-O-acetylharpagoside), ajugasterone B, ajugalactone, turkesterone, 22-acetylcyasterone, and phenols (J. Drugs. Dermatol. 2007;6:s20-4).
The investigators prepared an oil-water emulsion infused with A. turkestanica extract (0.3% w/w) for an in vivo study in which 15 healthy female volunteers (22-56 years old) applied the formulation twice daily to their forearms for 21 days. Significant reductions in transepidermal water loss were seen in the treated area compared with the control area on days 7 and 21. The researchers concluded that the tested A. turkestanica extract formulation enhanced AQP-3 expression and human epidermal differentiation in vitro, and ameliorated epidermal barrier structure and human skin recovery in vivo (J. Drugs. Dermatol. 2007;6:s20-4).
Conclusion
There is a dearth of research on A. turkestanica. But what exists is particularly favorable, insofar as the botanical appears to impact AQP-3, a compound whose significance has been recognized during the past 2 decades. Thus, A. turkestanica appears to have the potential to play an effective role in cosmetic products for treating dry skin. Much more research is necessary, however.
A perennial herb found primarily in Central Asia, Ajuga turkestanica is known to contain several bioactive compounds and has been used in traditional medicine to treat heart disease, and stomach and muscle aches (Chem. Nat. Compd. 1998;34:150-4; Chem. Nat. Compd. 2004;40:85-6). It is one of the many species of Ajuga gaining attention for exhibiting medicinal properties with the potential for commercial applications (Phytochem. Lett. 2008;1:81-4).
Clerodane diterpenes, recognized sources of antimicrobial, antiviral, antitumor, antibiotic, and amoebicidal activities (Phytochem. Rev. 2008;7:25-49), are among the three classes of potentially bioactive compounds, along with phytoecdysteroids and iridoid glycosides found in the Ajuga genus (Phytochem. Lett. 2008;1:81-4). Phytoecdysteroids are known to display significant physiological activities in insects and mammals; and iridoid glycosides, especially abundant in A. decumbens, have exhibited anticancer activity (Cancer Lett. 2000;157:87-92).
A. turkestanica reportedly contains several phytoecdysteroids (turkesterone, 20-hydroxyecdysone, cyasterone, cyasterone 22-acetate, ajugalactone, ajugasterone B, alpha-ecdysone, and ecdysone 2,3-monoacetonide), as well as the iridoids harpagide and harpagide 8-acetate (Chem. Nat. Compd. 2005;41:361-9; Chem. Nat. Compd. 1978;14:175-8; Chem. Nat. Compd. 1975;11:484-7; Chem. Nat. Compd. 1973;9:125-6; Chem. Nat. Compd. 1971;7:520; Phytochem. Lett. 2008;1:81-4).
Aquaporins
Aquaporins (AQPs) are integral membrane proteins that facilitate water transport in several organs, including the skin, brain, eyes, and digestive tract, as well as in the renal tubules. Thirteen isoforms of aquaporins (AQPs 0-12) are found in mammals. Of these, there are two functional subtype classifications: AQPs 1, 2, 4, 5, and 8 conduct only water, and AQPs 3, 7, 9, and 10 transport water and other substances including glycerol and urea (Prog. Histochem. Cytochem. 2004;39:1-83). AQP-3, permeable to water and glycerol, is the main water channel in human epidermis. Glycerol acts as an endogenous humectant, thereby facilitating hydration of the stratum corneum (SC) (J. Invest. Dermatol. 2005;125:288-93).
Defects in AQP-3 in mice models have been demonstrated to lead to epidermal xerosis and to reductions in SC hydration and epidermal glycerol content, followed by diminished elasticity and impaired skin barrier recovery (J. Biol. Chem. 2002;277:46616-21; Proc. Natl. Acad. Sci. 2003;100:7360-5). Such findings underscore the important role of glycerol in cutaneous hydration. Significantly, AQPs, particularly AQP-3, contribute to the transport of water, glycerol, and solutes between keratinocytes.
Dumas et al. note that the role of AQPs in hydrating the living layers of the epidermis where keratinocyte differentiation occurs and in barrier development and recovery suggests that they are significant protein targets for improving the quality and resistance of the skin surface, as well as ameliorating aging- and UV-induced xerosis (J. Drugs Dermatol. 2007;6(6 Suppl):s20-4).
A. turkestanica and Aquaporins
Patented extracts of A. turkestanica have been shown to contain sufficient ecdysteroids and other active ingredients to improve the differentiation of keratinocytes, thus facilitating skin hydration and yielding antiaging effects (U.S. Patent 7,060,693 B1, June 13, 2006). The patent inventors Dumas et al. observed that the extracts are especially effective in regulating epidermal water transport, achieving improved hydration of the basal layer by working in concert with or enhancing AQP-3 (Cosmet. Toil. 2008;123:22-7).
In 2007, Dumas et al. conducted in vitro and in vivo studies of active ingredients capable of raising AQP-3 levels to enhance hydration in human skin keratinocytes, with the understanding that improving hydration in keratinocytes would ultimately improve epidermal hydration (Eur. J. Dermatol. 2002;12:XXV-XXVI). They used an ethanol/water (70/30 v/v) extract of A. turkestanica as the hydrating agent (2.5 mcg/mL), and found that after 17 days of in vitro treatment every 2 days in human reconstructed epidermis, AQP-3 expression measured at the protein level was significantly elevated. Increased epidermal proliferation and differentiation were also noted. Electron microscopy showed a significantly thicker, compact SC and more clearly differentiated desmosomes. Constituents of the A. turkestanica extract revealed by chemical analysis included iridoids (chiefly harpagoside and 8-O-acetylharpagoside), ajugasterone B, ajugalactone, turkesterone, 22-acetylcyasterone, and phenols (J. Drugs. Dermatol. 2007;6:s20-4).
The investigators prepared an oil-water emulsion infused with A. turkestanica extract (0.3% w/w) for an in vivo study in which 15 healthy female volunteers (22-56 years old) applied the formulation twice daily to their forearms for 21 days. Significant reductions in transepidermal water loss were seen in the treated area compared with the control area on days 7 and 21. The researchers concluded that the tested A. turkestanica extract formulation enhanced AQP-3 expression and human epidermal differentiation in vitro, and ameliorated epidermal barrier structure and human skin recovery in vivo (J. Drugs. Dermatol. 2007;6:s20-4).
Conclusion
There is a dearth of research on A. turkestanica. But what exists is particularly favorable, insofar as the botanical appears to impact AQP-3, a compound whose significance has been recognized during the past 2 decades. Thus, A. turkestanica appears to have the potential to play an effective role in cosmetic products for treating dry skin. Much more research is necessary, however.
Red Light for Acne
Several light devices based on red light–emitting diodes (LEDs) have made their way to the market in recent years. Although red light is not truly a cosmeceutical, it is a significant emerging adjuvant therapy that, like blue light, has been studied in comparison to and in conjunction with topical options primarily to treat acne. Of course, acne is the most common skin disorder prompting visits to the dermatologist, with an estimated 85% of adolescents affected, many into adulthood (J. Am. Acad. Dermatol. 2008;58:56-9).
This discussion will consider red light when used alone and when used in combination with blue light. Blue light is the most effective light to target Propionibacterium acnes (specifically at wavelengths of 407-420 nm). However, many devices are utilizing red light because it has a purported anti-inflammatory effect and penetrates deeper into the skin (Dermatol. Ther. 2005;18:253-66).
Erythrasma
Darras-Vercambre et al. evaluated the effects of red light for the treatment of erythrasma (a superficial skin infection provoked by Corynebacterium minutissimum) in 13 patients. One treatment (80 J/cm2) by red light (broadband, peak at 635 nm) without exogenous photosensitizing molecules was administered to each subject. Therapy was effective and well tolerated, with three patients experiencing complete recovery, and significant reduction of lesions in most other cases. The authors noted that the key to their study, given the absence of an exogenous photosensitizing agent, was capitalizing on the presence of porphyrins in the lesions. They concluded that the use of red light alone for this localized infection is easy and inexpensive, but that an optimal method has not yet been established (Photodermatol. Photoimmunol. Photomed. 2006;22:153-6).
Acne
In 2007, Na and Suh evaluated the efficacy of red light phototherapy with a portable device in 28 volunteers with mild to moderate acne in a split-face randomized trial. Phototherapy was performed twice daily for 15 minutes for a total of 8 weeks to one side of the face. The investigators concluded that red light phototherapy alone is an effective therapeutic option for acne, as they noted significant reductions in noninflammatory and inflammatory lesion counts on the treated side versus the untreated side, a drop from 3.9 to 1.9 in the visual analog scale on the treatment side, and significant disparities between the treatment and control sides after 8 weeks (Dermatol. Surg. 2007;33:1228-33, discussion 1233).
A 2006 article in the British Journal of Dermatology reported good clinical results from acne treatment with photodynamic therapy (PDT) using methyl aminolevulinate (MAL) and red light, but there were adverse side effects that prompted 7 of 19 subjects to discontinue the study (Br. J. Dermatol. 2006;154:969-76). In response to the study, Mavilia et al. wrote a letter to the journal acknowledging their more effective combination therapy using a lower concentration of MAL and low doses of red light. All 16 patients completed the study, in which the count of inflammatory lesions fell an average of 66% with mild but tolerable side effects, including a subtle sensation of heat, then minimal erythema during the procedure and slight scaling that began 3 days after treatment (Br. J. Dermatol. 2007;157:810-1).
In a small study of patients with moderate facial acne, Zane et al. exposed 15 women to 20 J/cm2 of broadband red light (600-750 nm) twice weekly for 4 weeks. They also measured skin sebum, pH, hydration, and transepidermal water loss (TEWL). Untreated lesions of the trunk served as controls. The investigators found the treatment safe, well tolerated, and effective, with significant improvement in acne lesions and reduction of sebum excretion and TEWL after 4 weeks of therapy and at the 3-month follow-up visit. They speculated that the improvement was due to the decreased colonization of P. acnes, decimated by photoactivated endogenous porphyrin, and concluded that this inexpensive therapy warrants inclusion among treatment options for moderate acne (Photodermatol. Photoimmunol. Photomed. 2008;24:244-8).
In a 2009 study of 19 patients with moderate to severe facial acne who received a single treatment of low-dose, red-light PDT on the left cheek and MAL 3 hours before red light on the right cheek, both therapies yielded significant reductions in acne score. Red light was found to be as effective as MAL-PDT (Acta Derm. Venereol. 2009;89:372-8).
Combined Blue and Red Light Phototherapy
In 2006, Goldberg and Russell evaluated the combination of blue (415 nm) and red (633 nm) LED phototherapy in 24 patients with Fitzpatrick skin types II-V and mild to severe symmetric facial acne. Twenty-two patients completed the trial, which included two sessions per week (separated by 3 days) alternating between blue and red light for a total of eight sessions. Mild microdermabrasion was used at the start of each session. The mean decrease in lesion count was significant after 4 weeks (46%) and 12 weeks (81%). Inflammatory lesions responded better than did noninflammatory ones, and severe acne responded slightly better than mild acne. The investigators concluded that the combination of blue and red LED phototherapy is free of side effects and pain, and exhibits great potential for the treatment of mild to severe acne (J. Cosmet. Laser Ther. 2006;8:71-5).
In 2007, Lee et al. set out to examine the efficacy of combining blue and red LED phototherapy for acne in a study of 24 patients with mild to moderately severe facial acne. Twice weekly for 4 weeks, patients were treated with quasi-monochromatic LED devices, alternating blue (415 nm) and red (633 nm) light. Fourteen patients self-reported improvements in skin tone and texture. Improvements in noninflammatory and inflammatory lesions were substantial (34.28% and 77.93%, respectively). The researchers concluded that combined blue and red LED phototherapy is a safe and effective option, especially for papulopustular acne (Lasers Surg. Med. 2007;39:180-8).
In 2009, Sadick evaluated the efficacy of the combination of blue (415 nm) and near-infrared (830 nm) LED therapy for moderate acne in 13 females and 4 males ranging in skin type from II to VI and in Burton acne grade at baseline from 1 to 5. Twice-weekly 20-minute sessions were conducted for 4 weeks, alternating between blue and near-infrared light. Eleven patients exhibited improvement ranging from 0% to 83.3%, and 6 patients discontinued the study. A decreasing trend was observed in the Burton grade. Noninflammatory lesion counts improved in seven patients but increased in four. Sadick noted that these results paled in comparison to the effectiveness of the blue and red combination at lowering inflammatory lesions seen previously, but encouraged the study of the combination phototherapy in a much larger population (J. Cosmet. Laser Ther. 2009;11:125-8).
Several recent reviews have found that red light–activated MAL-PDT, the combination of blue and red light, and aminolevulinic acid as a photosensitizing agent before treatment with blue light, red light, or the 595-nm pulsed dye laser are among the most promising evidence-based laser- and light-based therapies for acne (Semin. Cutan. Med. Surg. 2008;27:207-11; J. Eur. Acad. Dermatol. Venereol. 2008;22:267-78; Dermatol. Surg. 2007;33:1005-26).
In a systematic literature review of randomized controlled trials of light and laser therapies for acne vulgaris (using the Cochrane Central Register of Controlled Trials, MEDLINE, Embase, CINAHL, PsycINFO, LILACS, ISI Science Citation Index, and Dissertation Abstracts International), Hamilton et al. found that trials of blue light, blue-red light, and infrared radiation were more successful, especially when multiple treatments were used. Notably, blue-red light demonstrated better short-term effectiveness than did topical 5% benzoyl peroxide cream (Br. J. Dermatol. 2009;160:1273-85).
Kim and Armstrong have noted that blue light has been demonstrated to photoinactivate P. acnes, but it does not penetrate deeply into the skin. It is believed to work synergistically, however, with red light, which is less effective than blue light at exciting porphyrins but can reach deeper sebaceous glands and may impart an anti-inflammatory effect by inciting cytokine release from macrophages (Dermatol. Surg. 2007;33:1005-26). Indeed, Kim and Armstrong found that combined blue-red light therapy was more effective at lowering the number of inflammatory acne lesions than were benzoyl peroxide monotherapy and blue light monotherapy (Lasers Surg. Med. 1989;9:497-505).
Conclusions
A lengthy review of the literature and personal experience treating patients have convinced me that blue light is an effective treatment for acne. P. acnes is most susceptible to the blue light wavelengths of 407-420 nm. Addition of red light may help speed resolution of inflammatory lesions through an anti-inflammatory effect. Blue and red light devices are efficacious when used in the office if the devices deliver enough joules.
Many at-home devices and iPhone apps have hit the market. These are a great alternative to irritating topicals and antibiotics, and they may help increase compliance. However, many at-home light devices are too weak (do not emit enough joules), or emit a broad range of light (rather than 407-420 nm). The manufacturers of some of these products claim that the heat produced by the devices improves acne, but there is a paucity of research proving this point. In my opinion, using an at-home device twice a day that delivers 407-420 nm (with or without the addition of red light), and delivers enough joules (at least 25 J/cm2), is an effective method of treating acne. For comparison purposes, the in-office Omnilux delivers around 49 J/cm2 but is used only two or three times per week. Know your wavelengths and joules when trying to decide which device to sell in your practice or recommend to patients.
Several light devices based on red light–emitting diodes (LEDs) have made their way to the market in recent years. Although red light is not truly a cosmeceutical, it is a significant emerging adjuvant therapy that, like blue light, has been studied in comparison to and in conjunction with topical options primarily to treat acne. Of course, acne is the most common skin disorder prompting visits to the dermatologist, with an estimated 85% of adolescents affected, many into adulthood (J. Am. Acad. Dermatol. 2008;58:56-9).
This discussion will consider red light when used alone and when used in combination with blue light. Blue light is the most effective light to target Propionibacterium acnes (specifically at wavelengths of 407-420 nm). However, many devices are utilizing red light because it has a purported anti-inflammatory effect and penetrates deeper into the skin (Dermatol. Ther. 2005;18:253-66).
Erythrasma
Darras-Vercambre et al. evaluated the effects of red light for the treatment of erythrasma (a superficial skin infection provoked by Corynebacterium minutissimum) in 13 patients. One treatment (80 J/cm2) by red light (broadband, peak at 635 nm) without exogenous photosensitizing molecules was administered to each subject. Therapy was effective and well tolerated, with three patients experiencing complete recovery, and significant reduction of lesions in most other cases. The authors noted that the key to their study, given the absence of an exogenous photosensitizing agent, was capitalizing on the presence of porphyrins in the lesions. They concluded that the use of red light alone for this localized infection is easy and inexpensive, but that an optimal method has not yet been established (Photodermatol. Photoimmunol. Photomed. 2006;22:153-6).
Acne
In 2007, Na and Suh evaluated the efficacy of red light phototherapy with a portable device in 28 volunteers with mild to moderate acne in a split-face randomized trial. Phototherapy was performed twice daily for 15 minutes for a total of 8 weeks to one side of the face. The investigators concluded that red light phototherapy alone is an effective therapeutic option for acne, as they noted significant reductions in noninflammatory and inflammatory lesion counts on the treated side versus the untreated side, a drop from 3.9 to 1.9 in the visual analog scale on the treatment side, and significant disparities between the treatment and control sides after 8 weeks (Dermatol. Surg. 2007;33:1228-33, discussion 1233).
A 2006 article in the British Journal of Dermatology reported good clinical results from acne treatment with photodynamic therapy (PDT) using methyl aminolevulinate (MAL) and red light, but there were adverse side effects that prompted 7 of 19 subjects to discontinue the study (Br. J. Dermatol. 2006;154:969-76). In response to the study, Mavilia et al. wrote a letter to the journal acknowledging their more effective combination therapy using a lower concentration of MAL and low doses of red light. All 16 patients completed the study, in which the count of inflammatory lesions fell an average of 66% with mild but tolerable side effects, including a subtle sensation of heat, then minimal erythema during the procedure and slight scaling that began 3 days after treatment (Br. J. Dermatol. 2007;157:810-1).
In a small study of patients with moderate facial acne, Zane et al. exposed 15 women to 20 J/cm2 of broadband red light (600-750 nm) twice weekly for 4 weeks. They also measured skin sebum, pH, hydration, and transepidermal water loss (TEWL). Untreated lesions of the trunk served as controls. The investigators found the treatment safe, well tolerated, and effective, with significant improvement in acne lesions and reduction of sebum excretion and TEWL after 4 weeks of therapy and at the 3-month follow-up visit. They speculated that the improvement was due to the decreased colonization of P. acnes, decimated by photoactivated endogenous porphyrin, and concluded that this inexpensive therapy warrants inclusion among treatment options for moderate acne (Photodermatol. Photoimmunol. Photomed. 2008;24:244-8).
In a 2009 study of 19 patients with moderate to severe facial acne who received a single treatment of low-dose, red-light PDT on the left cheek and MAL 3 hours before red light on the right cheek, both therapies yielded significant reductions in acne score. Red light was found to be as effective as MAL-PDT (Acta Derm. Venereol. 2009;89:372-8).
Combined Blue and Red Light Phototherapy
In 2006, Goldberg and Russell evaluated the combination of blue (415 nm) and red (633 nm) LED phototherapy in 24 patients with Fitzpatrick skin types II-V and mild to severe symmetric facial acne. Twenty-two patients completed the trial, which included two sessions per week (separated by 3 days) alternating between blue and red light for a total of eight sessions. Mild microdermabrasion was used at the start of each session. The mean decrease in lesion count was significant after 4 weeks (46%) and 12 weeks (81%). Inflammatory lesions responded better than did noninflammatory ones, and severe acne responded slightly better than mild acne. The investigators concluded that the combination of blue and red LED phototherapy is free of side effects and pain, and exhibits great potential for the treatment of mild to severe acne (J. Cosmet. Laser Ther. 2006;8:71-5).
In 2007, Lee et al. set out to examine the efficacy of combining blue and red LED phototherapy for acne in a study of 24 patients with mild to moderately severe facial acne. Twice weekly for 4 weeks, patients were treated with quasi-monochromatic LED devices, alternating blue (415 nm) and red (633 nm) light. Fourteen patients self-reported improvements in skin tone and texture. Improvements in noninflammatory and inflammatory lesions were substantial (34.28% and 77.93%, respectively). The researchers concluded that combined blue and red LED phototherapy is a safe and effective option, especially for papulopustular acne (Lasers Surg. Med. 2007;39:180-8).
In 2009, Sadick evaluated the efficacy of the combination of blue (415 nm) and near-infrared (830 nm) LED therapy for moderate acne in 13 females and 4 males ranging in skin type from II to VI and in Burton acne grade at baseline from 1 to 5. Twice-weekly 20-minute sessions were conducted for 4 weeks, alternating between blue and near-infrared light. Eleven patients exhibited improvement ranging from 0% to 83.3%, and 6 patients discontinued the study. A decreasing trend was observed in the Burton grade. Noninflammatory lesion counts improved in seven patients but increased in four. Sadick noted that these results paled in comparison to the effectiveness of the blue and red combination at lowering inflammatory lesions seen previously, but encouraged the study of the combination phototherapy in a much larger population (J. Cosmet. Laser Ther. 2009;11:125-8).
Several recent reviews have found that red light–activated MAL-PDT, the combination of blue and red light, and aminolevulinic acid as a photosensitizing agent before treatment with blue light, red light, or the 595-nm pulsed dye laser are among the most promising evidence-based laser- and light-based therapies for acne (Semin. Cutan. Med. Surg. 2008;27:207-11; J. Eur. Acad. Dermatol. Venereol. 2008;22:267-78; Dermatol. Surg. 2007;33:1005-26).
In a systematic literature review of randomized controlled trials of light and laser therapies for acne vulgaris (using the Cochrane Central Register of Controlled Trials, MEDLINE, Embase, CINAHL, PsycINFO, LILACS, ISI Science Citation Index, and Dissertation Abstracts International), Hamilton et al. found that trials of blue light, blue-red light, and infrared radiation were more successful, especially when multiple treatments were used. Notably, blue-red light demonstrated better short-term effectiveness than did topical 5% benzoyl peroxide cream (Br. J. Dermatol. 2009;160:1273-85).
Kim and Armstrong have noted that blue light has been demonstrated to photoinactivate P. acnes, but it does not penetrate deeply into the skin. It is believed to work synergistically, however, with red light, which is less effective than blue light at exciting porphyrins but can reach deeper sebaceous glands and may impart an anti-inflammatory effect by inciting cytokine release from macrophages (Dermatol. Surg. 2007;33:1005-26). Indeed, Kim and Armstrong found that combined blue-red light therapy was more effective at lowering the number of inflammatory acne lesions than were benzoyl peroxide monotherapy and blue light monotherapy (Lasers Surg. Med. 1989;9:497-505).
Conclusions
A lengthy review of the literature and personal experience treating patients have convinced me that blue light is an effective treatment for acne. P. acnes is most susceptible to the blue light wavelengths of 407-420 nm. Addition of red light may help speed resolution of inflammatory lesions through an anti-inflammatory effect. Blue and red light devices are efficacious when used in the office if the devices deliver enough joules.
Many at-home devices and iPhone apps have hit the market. These are a great alternative to irritating topicals and antibiotics, and they may help increase compliance. However, many at-home light devices are too weak (do not emit enough joules), or emit a broad range of light (rather than 407-420 nm). The manufacturers of some of these products claim that the heat produced by the devices improves acne, but there is a paucity of research proving this point. In my opinion, using an at-home device twice a day that delivers 407-420 nm (with or without the addition of red light), and delivers enough joules (at least 25 J/cm2), is an effective method of treating acne. For comparison purposes, the in-office Omnilux delivers around 49 J/cm2 but is used only two or three times per week. Know your wavelengths and joules when trying to decide which device to sell in your practice or recommend to patients.
Several light devices based on red light–emitting diodes (LEDs) have made their way to the market in recent years. Although red light is not truly a cosmeceutical, it is a significant emerging adjuvant therapy that, like blue light, has been studied in comparison to and in conjunction with topical options primarily to treat acne. Of course, acne is the most common skin disorder prompting visits to the dermatologist, with an estimated 85% of adolescents affected, many into adulthood (J. Am. Acad. Dermatol. 2008;58:56-9).
This discussion will consider red light when used alone and when used in combination with blue light. Blue light is the most effective light to target Propionibacterium acnes (specifically at wavelengths of 407-420 nm). However, many devices are utilizing red light because it has a purported anti-inflammatory effect and penetrates deeper into the skin (Dermatol. Ther. 2005;18:253-66).
Erythrasma
Darras-Vercambre et al. evaluated the effects of red light for the treatment of erythrasma (a superficial skin infection provoked by Corynebacterium minutissimum) in 13 patients. One treatment (80 J/cm2) by red light (broadband, peak at 635 nm) without exogenous photosensitizing molecules was administered to each subject. Therapy was effective and well tolerated, with three patients experiencing complete recovery, and significant reduction of lesions in most other cases. The authors noted that the key to their study, given the absence of an exogenous photosensitizing agent, was capitalizing on the presence of porphyrins in the lesions. They concluded that the use of red light alone for this localized infection is easy and inexpensive, but that an optimal method has not yet been established (Photodermatol. Photoimmunol. Photomed. 2006;22:153-6).
Acne
In 2007, Na and Suh evaluated the efficacy of red light phototherapy with a portable device in 28 volunteers with mild to moderate acne in a split-face randomized trial. Phototherapy was performed twice daily for 15 minutes for a total of 8 weeks to one side of the face. The investigators concluded that red light phototherapy alone is an effective therapeutic option for acne, as they noted significant reductions in noninflammatory and inflammatory lesion counts on the treated side versus the untreated side, a drop from 3.9 to 1.9 in the visual analog scale on the treatment side, and significant disparities between the treatment and control sides after 8 weeks (Dermatol. Surg. 2007;33:1228-33, discussion 1233).
A 2006 article in the British Journal of Dermatology reported good clinical results from acne treatment with photodynamic therapy (PDT) using methyl aminolevulinate (MAL) and red light, but there were adverse side effects that prompted 7 of 19 subjects to discontinue the study (Br. J. Dermatol. 2006;154:969-76). In response to the study, Mavilia et al. wrote a letter to the journal acknowledging their more effective combination therapy using a lower concentration of MAL and low doses of red light. All 16 patients completed the study, in which the count of inflammatory lesions fell an average of 66% with mild but tolerable side effects, including a subtle sensation of heat, then minimal erythema during the procedure and slight scaling that began 3 days after treatment (Br. J. Dermatol. 2007;157:810-1).
In a small study of patients with moderate facial acne, Zane et al. exposed 15 women to 20 J/cm2 of broadband red light (600-750 nm) twice weekly for 4 weeks. They also measured skin sebum, pH, hydration, and transepidermal water loss (TEWL). Untreated lesions of the trunk served as controls. The investigators found the treatment safe, well tolerated, and effective, with significant improvement in acne lesions and reduction of sebum excretion and TEWL after 4 weeks of therapy and at the 3-month follow-up visit. They speculated that the improvement was due to the decreased colonization of P. acnes, decimated by photoactivated endogenous porphyrin, and concluded that this inexpensive therapy warrants inclusion among treatment options for moderate acne (Photodermatol. Photoimmunol. Photomed. 2008;24:244-8).
In a 2009 study of 19 patients with moderate to severe facial acne who received a single treatment of low-dose, red-light PDT on the left cheek and MAL 3 hours before red light on the right cheek, both therapies yielded significant reductions in acne score. Red light was found to be as effective as MAL-PDT (Acta Derm. Venereol. 2009;89:372-8).
Combined Blue and Red Light Phototherapy
In 2006, Goldberg and Russell evaluated the combination of blue (415 nm) and red (633 nm) LED phototherapy in 24 patients with Fitzpatrick skin types II-V and mild to severe symmetric facial acne. Twenty-two patients completed the trial, which included two sessions per week (separated by 3 days) alternating between blue and red light for a total of eight sessions. Mild microdermabrasion was used at the start of each session. The mean decrease in lesion count was significant after 4 weeks (46%) and 12 weeks (81%). Inflammatory lesions responded better than did noninflammatory ones, and severe acne responded slightly better than mild acne. The investigators concluded that the combination of blue and red LED phototherapy is free of side effects and pain, and exhibits great potential for the treatment of mild to severe acne (J. Cosmet. Laser Ther. 2006;8:71-5).
In 2007, Lee et al. set out to examine the efficacy of combining blue and red LED phototherapy for acne in a study of 24 patients with mild to moderately severe facial acne. Twice weekly for 4 weeks, patients were treated with quasi-monochromatic LED devices, alternating blue (415 nm) and red (633 nm) light. Fourteen patients self-reported improvements in skin tone and texture. Improvements in noninflammatory and inflammatory lesions were substantial (34.28% and 77.93%, respectively). The researchers concluded that combined blue and red LED phototherapy is a safe and effective option, especially for papulopustular acne (Lasers Surg. Med. 2007;39:180-8).
In 2009, Sadick evaluated the efficacy of the combination of blue (415 nm) and near-infrared (830 nm) LED therapy for moderate acne in 13 females and 4 males ranging in skin type from II to VI and in Burton acne grade at baseline from 1 to 5. Twice-weekly 20-minute sessions were conducted for 4 weeks, alternating between blue and near-infrared light. Eleven patients exhibited improvement ranging from 0% to 83.3%, and 6 patients discontinued the study. A decreasing trend was observed in the Burton grade. Noninflammatory lesion counts improved in seven patients but increased in four. Sadick noted that these results paled in comparison to the effectiveness of the blue and red combination at lowering inflammatory lesions seen previously, but encouraged the study of the combination phototherapy in a much larger population (J. Cosmet. Laser Ther. 2009;11:125-8).
Several recent reviews have found that red light–activated MAL-PDT, the combination of blue and red light, and aminolevulinic acid as a photosensitizing agent before treatment with blue light, red light, or the 595-nm pulsed dye laser are among the most promising evidence-based laser- and light-based therapies for acne (Semin. Cutan. Med. Surg. 2008;27:207-11; J. Eur. Acad. Dermatol. Venereol. 2008;22:267-78; Dermatol. Surg. 2007;33:1005-26).
In a systematic literature review of randomized controlled trials of light and laser therapies for acne vulgaris (using the Cochrane Central Register of Controlled Trials, MEDLINE, Embase, CINAHL, PsycINFO, LILACS, ISI Science Citation Index, and Dissertation Abstracts International), Hamilton et al. found that trials of blue light, blue-red light, and infrared radiation were more successful, especially when multiple treatments were used. Notably, blue-red light demonstrated better short-term effectiveness than did topical 5% benzoyl peroxide cream (Br. J. Dermatol. 2009;160:1273-85).
Kim and Armstrong have noted that blue light has been demonstrated to photoinactivate P. acnes, but it does not penetrate deeply into the skin. It is believed to work synergistically, however, with red light, which is less effective than blue light at exciting porphyrins but can reach deeper sebaceous glands and may impart an anti-inflammatory effect by inciting cytokine release from macrophages (Dermatol. Surg. 2007;33:1005-26). Indeed, Kim and Armstrong found that combined blue-red light therapy was more effective at lowering the number of inflammatory acne lesions than were benzoyl peroxide monotherapy and blue light monotherapy (Lasers Surg. Med. 1989;9:497-505).
Conclusions
A lengthy review of the literature and personal experience treating patients have convinced me that blue light is an effective treatment for acne. P. acnes is most susceptible to the blue light wavelengths of 407-420 nm. Addition of red light may help speed resolution of inflammatory lesions through an anti-inflammatory effect. Blue and red light devices are efficacious when used in the office if the devices deliver enough joules.
Many at-home devices and iPhone apps have hit the market. These are a great alternative to irritating topicals and antibiotics, and they may help increase compliance. However, many at-home light devices are too weak (do not emit enough joules), or emit a broad range of light (rather than 407-420 nm). The manufacturers of some of these products claim that the heat produced by the devices improves acne, but there is a paucity of research proving this point. In my opinion, using an at-home device twice a day that delivers 407-420 nm (with or without the addition of red light), and delivers enough joules (at least 25 J/cm2), is an effective method of treating acne. For comparison purposes, the in-office Omnilux delivers around 49 J/cm2 but is used only two or three times per week. Know your wavelengths and joules when trying to decide which device to sell in your practice or recommend to patients.
Cosmeceutical Critique: Ginkgo Biloba
In the East, the nut from the inedible fruit of the Ginkgo biloba tree, believed to be the oldest living tree species, has been a popular medical elixir, as well as food item, for many years. People in the West may be most familiar with Ginkgo biloba for the fetid odor of its fruit. During the last 15 years, though, the plant has become well known here for its use as a dietary supplement to treat dementia and memory loss (Arch. Neurol. 1998;55:1409-15; Public Health Nutr. 2000;3:495-9). Ginkgo is also believed to possess properties capable of imparting healthy benefits to human skin.
Medical Uses
In China and Japan, the leaves and nuts of the ginkgo tree have been used for thousands of years to treat various medical conditions, including poor circulation; hypertension; poor memory, dementia, and depression, particularly among the aged; male impotence; and disorders related to an inner-ear imbalance, such as deafness, tinnitus, and vertigo (Hori T, et al. Ginkgo Biloba: A Global Treasure. Berlin, Springer-Verlag, 1997).
Currently, ginkgo is used globally to treat depression, usually in the elderly, and circulatory problems (for example, cerebrovascular and peripheral vascular insufficiency).
G. biloba contains quercetin, which is one of the most abundant natural flavonoids (Clin. Exp. Dermatol. 2001;26:536-9; Free Radic. Biol. Med. 1998;25:196-200). Discussed in a recent column, quercetin is gaining a reputation as a potent antioxidant, conferring significant anti-inflammatory activity. Ginkgo also contains various other flavonoids with demonstrated antioxidant and anti-inflammatory activities against cyclooxygenase (COX) and lipoxygenase (J. Pharm. Pharmacol. 1988;40:787-92; Biochem. Pharmacol. 1993;45:13-9).
It is not surprising, then, that ginkgo is developing a similar reputation as a significant antioxidant and anti-inflammatory agent (Br. J. Dermatol. 2003;149:681-91).
The G. biloba extract EGb 761, prepared from the tree’s leaves, is a natural mixture containing flavone glycosides (33%), mostly quercetin and kaempferol derivatives, and terpenes (6%), that has been used or evaluated for the treatment of stroke, aging, and some adverse drug effects (Biomed. Papers 2003;147:137-45).
This extract has also exhibited the capacity to halt lipoperoxidation by scavenging peroxyl radicals (Photodermatol. Photoimmunol. Photomed. 2002;18:117-20; Pharm. Pharmacol. 1999;51:1435-40; Biochem. Pharmacol. 1995;49:1649-55) and reduce the number of UVB-induced sunburn cells in mice (Photodermatol. Photoimmunol. Photomed. 2002;18:117-20).
In a study of the effects of ginkgetin, a biflavone component of G. biloba leaves reported to confer significant antiarthritic and analgesic activity in rats, ginkgetin down-regulated COX-2 in the dorsal skin of ICR mice treated with 12-O-tetradecanoylphorbol 13-acetate (TPA) and the topical application of both ginkgetin and a mostly 1:1 biflavonoid mixture of ginkgetin and isoginkgetin, from G. biloba leaves, dose-dependently inhibited skin inflammation of croton oil–induced ear edema in mice. Researchers concluded that the capacity of this biflavone constituent of ginkgo leaves to down-regulate COX-2 indicates anti-inflammatory activity against cutaneous inflammation (Planta Med. 2002;68:316-21).
Established in earlier research, the discrete effects of G. biloba extracts such as quercetin and sciadopitysin on UVB-irradiated cultured normal human skin fibroblasts were investigated by researchers using a neutral red dye uptake assay and a lactic dehydrogenase (LDH) release assay. The reduced cytotoxicity observed suggested that the structure-related activity might account for the antioxidant potential of biflavones of G. biloba as well as hydroxy- and methyl-substitutions on the basic structure of these flavonoids (J. Dermatol. 2001;28:193-9).
Anti-Inflammatory and Antioxidant Properties
With the fairly expansive range of applications associated with antioxidant and anti-inflammatory agents, it seems reasonable to expect that ginkgo will join the legion of popular botanical products studied as potential therapies for numerous conditions. In a double-blind placebo-controlled trial in which 47 patients were evaluated, investigators assessed the efficacy of G. biloba extract in controlling limited and slow-spreading vitiligo and promoting repigmentation in affected areas. One group of patients was administered 40 mg G. biloba extract three times daily the other group received the same doses of placebo. Researchers observed a statistically significant cessation of depigmentation in patients treated with G. biloba, with notable to complete repigmentation seen in 10 patients from the treated group, but only two patients in the placebo group. This study lends support to the notion that G. biloba extract may be an effective, safe approach to arresting the progression of vitiligo (Clin. Exp. Dermatol. 2003;28:285-7).
In a study evaluating the effect of orally administered G. biloba extract on UVB-irradiated mouse skin, investigators measured superoxide dismutase (SOD) activity and zinc levels. Zinc, an essential element that acts as a cofactor in some metabolic processes, has reported antioxidant activity and is typically found in high concentrations in the skin. Both SOD activity and zinc levels decreased after UVB exposure in comparison to the control group; after ginkgo treatment, measurement increased, compared with untreated UVB-exposed group (Biol. Trace Elem. Res. 2001;80:175-9). In a previous study, ginkgo extracts exhibited SOD-like activity (Experientia 1989;45:708-12).
Researchers conducted in vitro and in vivo studies of the activity of terpene-free G. biloba extract containing 33% ginkgo flavone glycosides, mostly quercetin and kaempferol derivatives, with the antioxidant SOD as a positive control. Results of both the in vitro electron spin resonance (ESR) assays and in vivo experiments on anti-inflammatory models with cutaneous blood flux measured by a laser Doppler perfusion imager, corroborated the antioxidant and anti-inflammatory properties of the ginkgo extract and its capacity for protecting skin from free radical damage. This study also indicated an optimal concentration for ginkgo extract, above or below which its beneficial actions subside (J. Pharm. Pharmacol. 1999;51:1435-40).
In an earlier study, ginkgo extracts, particularly the flavonoid components quercetin, kaempferol, sciadopitysin, ginkgetin, and isoginkgetin, were shown to enhance the proliferation of normal human skin fibroblast in vitro as measured by MTT (3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyl-tetrazolium bromide) assay and direct hemocytometer cell count. Various additional assays of fibroblasts incubated with G. biloba extracts and ascorbic acid and controls incubated only with ascorbic acid demonstrated increased collagen and extracellular fibronectin synthesis in the treatment group (Skin Pharmacol. 1997;10:200-5).
Products
Like many herbal ingredients, ginkgo is used in a small but growing number of topical products. The Hydramax Ginkgo Biloba PhytoSerum (1 fl. oz./$15.50) is a moisturizer intended to restore chapped and severely dehydrated skin. The product is formulated with 2% standardized time-released phytoliposomes of G. biloba and buttressed by a cocktail of organic herb concentrates of white willow bark, ivy, comfrey, chamomile, mallow, and G. biloba as well as numerous emollient and essential oils in an organic aloe vera serum.
The Rejuvenex Body Lotion (6 oz./$21.60) features a highly purified alpha-glycolic acid, but includes ginkgo extract and vitamin E to protect against the skin irritation that high concentrations of glycolic acid can engender.
Ginkgo extract is increasingly found among the lists of the unadvertised or inactive ingredients in more and more topical skin care products. For example, two of the three products in the emerginC Crease Ease Kit ($250) – the emerginC crease ease emulsion (50 ml) and the emerginC crease ease gel (eye/lip area – 30 mL) – contain G. biloba along with a long list of other herbal ingredients.
Conclusion
Whether in oral or topical form, G. biloba extracts do not reek like the fruit of the tree; otherwise, such products might never make their way to the shelf. Use in aromatherapy would also be precluded. Fortunately, the offensive odor dissipates after separation of the nut from the seed shell and subsequent cleaning.
In topical products, various components of ginkgo are used more often as ancillary ingredients, though some formulations now feature this increasingly popular herbal ingredient. Preliminary research suggests reasons for optimism and should spur further investigation as to the overall health benefits conferred by G. biloba.
The research on vitiligo is particularly compelling from a dermatologic perspective. More study is required to ascertain whether topical formulations can harness the apparent antioxidant and anti-inflammatory effects to confer significant cutaneous benefits. More randomized controlled trials will build on what is currently a small but intriguing body of evidence.
In the East, the nut from the inedible fruit of the Ginkgo biloba tree, believed to be the oldest living tree species, has been a popular medical elixir, as well as food item, for many years. People in the West may be most familiar with Ginkgo biloba for the fetid odor of its fruit. During the last 15 years, though, the plant has become well known here for its use as a dietary supplement to treat dementia and memory loss (Arch. Neurol. 1998;55:1409-15; Public Health Nutr. 2000;3:495-9). Ginkgo is also believed to possess properties capable of imparting healthy benefits to human skin.
Medical Uses
In China and Japan, the leaves and nuts of the ginkgo tree have been used for thousands of years to treat various medical conditions, including poor circulation; hypertension; poor memory, dementia, and depression, particularly among the aged; male impotence; and disorders related to an inner-ear imbalance, such as deafness, tinnitus, and vertigo (Hori T, et al. Ginkgo Biloba: A Global Treasure. Berlin, Springer-Verlag, 1997).
Currently, ginkgo is used globally to treat depression, usually in the elderly, and circulatory problems (for example, cerebrovascular and peripheral vascular insufficiency).
G. biloba contains quercetin, which is one of the most abundant natural flavonoids (Clin. Exp. Dermatol. 2001;26:536-9; Free Radic. Biol. Med. 1998;25:196-200). Discussed in a recent column, quercetin is gaining a reputation as a potent antioxidant, conferring significant anti-inflammatory activity. Ginkgo also contains various other flavonoids with demonstrated antioxidant and anti-inflammatory activities against cyclooxygenase (COX) and lipoxygenase (J. Pharm. Pharmacol. 1988;40:787-92; Biochem. Pharmacol. 1993;45:13-9).
It is not surprising, then, that ginkgo is developing a similar reputation as a significant antioxidant and anti-inflammatory agent (Br. J. Dermatol. 2003;149:681-91).
The G. biloba extract EGb 761, prepared from the tree’s leaves, is a natural mixture containing flavone glycosides (33%), mostly quercetin and kaempferol derivatives, and terpenes (6%), that has been used or evaluated for the treatment of stroke, aging, and some adverse drug effects (Biomed. Papers 2003;147:137-45).
This extract has also exhibited the capacity to halt lipoperoxidation by scavenging peroxyl radicals (Photodermatol. Photoimmunol. Photomed. 2002;18:117-20; Pharm. Pharmacol. 1999;51:1435-40; Biochem. Pharmacol. 1995;49:1649-55) and reduce the number of UVB-induced sunburn cells in mice (Photodermatol. Photoimmunol. Photomed. 2002;18:117-20).
In a study of the effects of ginkgetin, a biflavone component of G. biloba leaves reported to confer significant antiarthritic and analgesic activity in rats, ginkgetin down-regulated COX-2 in the dorsal skin of ICR mice treated with 12-O-tetradecanoylphorbol 13-acetate (TPA) and the topical application of both ginkgetin and a mostly 1:1 biflavonoid mixture of ginkgetin and isoginkgetin, from G. biloba leaves, dose-dependently inhibited skin inflammation of croton oil–induced ear edema in mice. Researchers concluded that the capacity of this biflavone constituent of ginkgo leaves to down-regulate COX-2 indicates anti-inflammatory activity against cutaneous inflammation (Planta Med. 2002;68:316-21).
Established in earlier research, the discrete effects of G. biloba extracts such as quercetin and sciadopitysin on UVB-irradiated cultured normal human skin fibroblasts were investigated by researchers using a neutral red dye uptake assay and a lactic dehydrogenase (LDH) release assay. The reduced cytotoxicity observed suggested that the structure-related activity might account for the antioxidant potential of biflavones of G. biloba as well as hydroxy- and methyl-substitutions on the basic structure of these flavonoids (J. Dermatol. 2001;28:193-9).
Anti-Inflammatory and Antioxidant Properties
With the fairly expansive range of applications associated with antioxidant and anti-inflammatory agents, it seems reasonable to expect that ginkgo will join the legion of popular botanical products studied as potential therapies for numerous conditions. In a double-blind placebo-controlled trial in which 47 patients were evaluated, investigators assessed the efficacy of G. biloba extract in controlling limited and slow-spreading vitiligo and promoting repigmentation in affected areas. One group of patients was administered 40 mg G. biloba extract three times daily the other group received the same doses of placebo. Researchers observed a statistically significant cessation of depigmentation in patients treated with G. biloba, with notable to complete repigmentation seen in 10 patients from the treated group, but only two patients in the placebo group. This study lends support to the notion that G. biloba extract may be an effective, safe approach to arresting the progression of vitiligo (Clin. Exp. Dermatol. 2003;28:285-7).
In a study evaluating the effect of orally administered G. biloba extract on UVB-irradiated mouse skin, investigators measured superoxide dismutase (SOD) activity and zinc levels. Zinc, an essential element that acts as a cofactor in some metabolic processes, has reported antioxidant activity and is typically found in high concentrations in the skin. Both SOD activity and zinc levels decreased after UVB exposure in comparison to the control group; after ginkgo treatment, measurement increased, compared with untreated UVB-exposed group (Biol. Trace Elem. Res. 2001;80:175-9). In a previous study, ginkgo extracts exhibited SOD-like activity (Experientia 1989;45:708-12).
Researchers conducted in vitro and in vivo studies of the activity of terpene-free G. biloba extract containing 33% ginkgo flavone glycosides, mostly quercetin and kaempferol derivatives, with the antioxidant SOD as a positive control. Results of both the in vitro electron spin resonance (ESR) assays and in vivo experiments on anti-inflammatory models with cutaneous blood flux measured by a laser Doppler perfusion imager, corroborated the antioxidant and anti-inflammatory properties of the ginkgo extract and its capacity for protecting skin from free radical damage. This study also indicated an optimal concentration for ginkgo extract, above or below which its beneficial actions subside (J. Pharm. Pharmacol. 1999;51:1435-40).
In an earlier study, ginkgo extracts, particularly the flavonoid components quercetin, kaempferol, sciadopitysin, ginkgetin, and isoginkgetin, were shown to enhance the proliferation of normal human skin fibroblast in vitro as measured by MTT (3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyl-tetrazolium bromide) assay and direct hemocytometer cell count. Various additional assays of fibroblasts incubated with G. biloba extracts and ascorbic acid and controls incubated only with ascorbic acid demonstrated increased collagen and extracellular fibronectin synthesis in the treatment group (Skin Pharmacol. 1997;10:200-5).
Products
Like many herbal ingredients, ginkgo is used in a small but growing number of topical products. The Hydramax Ginkgo Biloba PhytoSerum (1 fl. oz./$15.50) is a moisturizer intended to restore chapped and severely dehydrated skin. The product is formulated with 2% standardized time-released phytoliposomes of G. biloba and buttressed by a cocktail of organic herb concentrates of white willow bark, ivy, comfrey, chamomile, mallow, and G. biloba as well as numerous emollient and essential oils in an organic aloe vera serum.
The Rejuvenex Body Lotion (6 oz./$21.60) features a highly purified alpha-glycolic acid, but includes ginkgo extract and vitamin E to protect against the skin irritation that high concentrations of glycolic acid can engender.
Ginkgo extract is increasingly found among the lists of the unadvertised or inactive ingredients in more and more topical skin care products. For example, two of the three products in the emerginC Crease Ease Kit ($250) – the emerginC crease ease emulsion (50 ml) and the emerginC crease ease gel (eye/lip area – 30 mL) – contain G. biloba along with a long list of other herbal ingredients.
Conclusion
Whether in oral or topical form, G. biloba extracts do not reek like the fruit of the tree; otherwise, such products might never make their way to the shelf. Use in aromatherapy would also be precluded. Fortunately, the offensive odor dissipates after separation of the nut from the seed shell and subsequent cleaning.
In topical products, various components of ginkgo are used more often as ancillary ingredients, though some formulations now feature this increasingly popular herbal ingredient. Preliminary research suggests reasons for optimism and should spur further investigation as to the overall health benefits conferred by G. biloba.
The research on vitiligo is particularly compelling from a dermatologic perspective. More study is required to ascertain whether topical formulations can harness the apparent antioxidant and anti-inflammatory effects to confer significant cutaneous benefits. More randomized controlled trials will build on what is currently a small but intriguing body of evidence.
In the East, the nut from the inedible fruit of the Ginkgo biloba tree, believed to be the oldest living tree species, has been a popular medical elixir, as well as food item, for many years. People in the West may be most familiar with Ginkgo biloba for the fetid odor of its fruit. During the last 15 years, though, the plant has become well known here for its use as a dietary supplement to treat dementia and memory loss (Arch. Neurol. 1998;55:1409-15; Public Health Nutr. 2000;3:495-9). Ginkgo is also believed to possess properties capable of imparting healthy benefits to human skin.
Medical Uses
In China and Japan, the leaves and nuts of the ginkgo tree have been used for thousands of years to treat various medical conditions, including poor circulation; hypertension; poor memory, dementia, and depression, particularly among the aged; male impotence; and disorders related to an inner-ear imbalance, such as deafness, tinnitus, and vertigo (Hori T, et al. Ginkgo Biloba: A Global Treasure. Berlin, Springer-Verlag, 1997).
Currently, ginkgo is used globally to treat depression, usually in the elderly, and circulatory problems (for example, cerebrovascular and peripheral vascular insufficiency).
G. biloba contains quercetin, which is one of the most abundant natural flavonoids (Clin. Exp. Dermatol. 2001;26:536-9; Free Radic. Biol. Med. 1998;25:196-200). Discussed in a recent column, quercetin is gaining a reputation as a potent antioxidant, conferring significant anti-inflammatory activity. Ginkgo also contains various other flavonoids with demonstrated antioxidant and anti-inflammatory activities against cyclooxygenase (COX) and lipoxygenase (J. Pharm. Pharmacol. 1988;40:787-92; Biochem. Pharmacol. 1993;45:13-9).
It is not surprising, then, that ginkgo is developing a similar reputation as a significant antioxidant and anti-inflammatory agent (Br. J. Dermatol. 2003;149:681-91).
The G. biloba extract EGb 761, prepared from the tree’s leaves, is a natural mixture containing flavone glycosides (33%), mostly quercetin and kaempferol derivatives, and terpenes (6%), that has been used or evaluated for the treatment of stroke, aging, and some adverse drug effects (Biomed. Papers 2003;147:137-45).
This extract has also exhibited the capacity to halt lipoperoxidation by scavenging peroxyl radicals (Photodermatol. Photoimmunol. Photomed. 2002;18:117-20; Pharm. Pharmacol. 1999;51:1435-40; Biochem. Pharmacol. 1995;49:1649-55) and reduce the number of UVB-induced sunburn cells in mice (Photodermatol. Photoimmunol. Photomed. 2002;18:117-20).
In a study of the effects of ginkgetin, a biflavone component of G. biloba leaves reported to confer significant antiarthritic and analgesic activity in rats, ginkgetin down-regulated COX-2 in the dorsal skin of ICR mice treated with 12-O-tetradecanoylphorbol 13-acetate (TPA) and the topical application of both ginkgetin and a mostly 1:1 biflavonoid mixture of ginkgetin and isoginkgetin, from G. biloba leaves, dose-dependently inhibited skin inflammation of croton oil–induced ear edema in mice. Researchers concluded that the capacity of this biflavone constituent of ginkgo leaves to down-regulate COX-2 indicates anti-inflammatory activity against cutaneous inflammation (Planta Med. 2002;68:316-21).
Established in earlier research, the discrete effects of G. biloba extracts such as quercetin and sciadopitysin on UVB-irradiated cultured normal human skin fibroblasts were investigated by researchers using a neutral red dye uptake assay and a lactic dehydrogenase (LDH) release assay. The reduced cytotoxicity observed suggested that the structure-related activity might account for the antioxidant potential of biflavones of G. biloba as well as hydroxy- and methyl-substitutions on the basic structure of these flavonoids (J. Dermatol. 2001;28:193-9).
Anti-Inflammatory and Antioxidant Properties
With the fairly expansive range of applications associated with antioxidant and anti-inflammatory agents, it seems reasonable to expect that ginkgo will join the legion of popular botanical products studied as potential therapies for numerous conditions. In a double-blind placebo-controlled trial in which 47 patients were evaluated, investigators assessed the efficacy of G. biloba extract in controlling limited and slow-spreading vitiligo and promoting repigmentation in affected areas. One group of patients was administered 40 mg G. biloba extract three times daily the other group received the same doses of placebo. Researchers observed a statistically significant cessation of depigmentation in patients treated with G. biloba, with notable to complete repigmentation seen in 10 patients from the treated group, but only two patients in the placebo group. This study lends support to the notion that G. biloba extract may be an effective, safe approach to arresting the progression of vitiligo (Clin. Exp. Dermatol. 2003;28:285-7).
In a study evaluating the effect of orally administered G. biloba extract on UVB-irradiated mouse skin, investigators measured superoxide dismutase (SOD) activity and zinc levels. Zinc, an essential element that acts as a cofactor in some metabolic processes, has reported antioxidant activity and is typically found in high concentrations in the skin. Both SOD activity and zinc levels decreased after UVB exposure in comparison to the control group; after ginkgo treatment, measurement increased, compared with untreated UVB-exposed group (Biol. Trace Elem. Res. 2001;80:175-9). In a previous study, ginkgo extracts exhibited SOD-like activity (Experientia 1989;45:708-12).
Researchers conducted in vitro and in vivo studies of the activity of terpene-free G. biloba extract containing 33% ginkgo flavone glycosides, mostly quercetin and kaempferol derivatives, with the antioxidant SOD as a positive control. Results of both the in vitro electron spin resonance (ESR) assays and in vivo experiments on anti-inflammatory models with cutaneous blood flux measured by a laser Doppler perfusion imager, corroborated the antioxidant and anti-inflammatory properties of the ginkgo extract and its capacity for protecting skin from free radical damage. This study also indicated an optimal concentration for ginkgo extract, above or below which its beneficial actions subside (J. Pharm. Pharmacol. 1999;51:1435-40).
In an earlier study, ginkgo extracts, particularly the flavonoid components quercetin, kaempferol, sciadopitysin, ginkgetin, and isoginkgetin, were shown to enhance the proliferation of normal human skin fibroblast in vitro as measured by MTT (3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyl-tetrazolium bromide) assay and direct hemocytometer cell count. Various additional assays of fibroblasts incubated with G. biloba extracts and ascorbic acid and controls incubated only with ascorbic acid demonstrated increased collagen and extracellular fibronectin synthesis in the treatment group (Skin Pharmacol. 1997;10:200-5).
Products
Like many herbal ingredients, ginkgo is used in a small but growing number of topical products. The Hydramax Ginkgo Biloba PhytoSerum (1 fl. oz./$15.50) is a moisturizer intended to restore chapped and severely dehydrated skin. The product is formulated with 2% standardized time-released phytoliposomes of G. biloba and buttressed by a cocktail of organic herb concentrates of white willow bark, ivy, comfrey, chamomile, mallow, and G. biloba as well as numerous emollient and essential oils in an organic aloe vera serum.
The Rejuvenex Body Lotion (6 oz./$21.60) features a highly purified alpha-glycolic acid, but includes ginkgo extract and vitamin E to protect against the skin irritation that high concentrations of glycolic acid can engender.
Ginkgo extract is increasingly found among the lists of the unadvertised or inactive ingredients in more and more topical skin care products. For example, two of the three products in the emerginC Crease Ease Kit ($250) – the emerginC crease ease emulsion (50 ml) and the emerginC crease ease gel (eye/lip area – 30 mL) – contain G. biloba along with a long list of other herbal ingredients.
Conclusion
Whether in oral or topical form, G. biloba extracts do not reek like the fruit of the tree; otherwise, such products might never make their way to the shelf. Use in aromatherapy would also be precluded. Fortunately, the offensive odor dissipates after separation of the nut from the seed shell and subsequent cleaning.
In topical products, various components of ginkgo are used more often as ancillary ingredients, though some formulations now feature this increasingly popular herbal ingredient. Preliminary research suggests reasons for optimism and should spur further investigation as to the overall health benefits conferred by G. biloba.
The research on vitiligo is particularly compelling from a dermatologic perspective. More study is required to ascertain whether topical formulations can harness the apparent antioxidant and anti-inflammatory effects to confer significant cutaneous benefits. More randomized controlled trials will build on what is currently a small but intriguing body of evidence.