User login
Zinc oxide
Zinc is a trace element, and it is not synthesized by the human body. The element was identified in the 1960s as being essential for human health and development. Zinc is a cofactor in more than 300 enzymes necessary for cell function. In the dermatologic realm, zinc deficiency has been associated with skin alterations, delayed wound healing, and hair loss.
Zinc oxide (ZnO) is a metal oxide that also has a broad profile in dermatology. It is perhaps best known as a physical sunscreen ingredient. ZnO and titanium dioxide (TiO2) have long been used in this manner. Both ZnO and TiO2 also have been increasingly used to replace large-particle compounds in numerous cosmetics and sunscreens. These two compounds have demonstrated effective protection against UV-induced damage, providing stronger protection against UV radiation while leaving less white residue than previous generations of physical sunscreens.
Particles of ZnO in earlier sunscreens were found to be too large to penetrate the stratum corneum and, thus, were deemed biologically inactive (J. Am. Acad. Dermatol. 1999;40:85-90). However, in novel nanoparticle form, such metal oxides absorb UV radiation, leading to photocatalysis and the release of reactive oxygen species (Australas. J. Dermatol. 2011;52:1-6). Indeed, nanoparticles exhibit new physiochemical properties as a result of increased surface area as compared to large-form products, and the potential adverse effects of the novel nanoparticle formulations in sunscreens cannot be adequately extrapolated from the effects of older-generation larger-particle skin care products (J. Drugs Dermatol. 2010;9:475-81; Int. J. Dermatol. 2011;50:247-54. The relative safety of ZnO nanoparticles will be discussed in a future column. The focus in this column will be a brief comparison with TiO2 and other indications for ZnO.
ZnO and TiO2
While numerous studies explore both TiO2 and ZnO, the latter is noted for greater versatility within the dermatologic armamentarium. In addition, ZnO is less photoactive and is associated with a lower refractive index in visible light than TiO2 (1.9 vs. 2.6, respectively) (J. Am. Acad. Dermatol. 1999;40:85-90); therefore, TiO2 appears whiter and is more difficult to incorporate into transparent products.
Another important difference is the spectrum of action. That is, only avobenzone (butyl methoxydibenzoylmethane) and ZnO are approved in the United States for broad-spectrum protection against UVA wavelengths greater than 360 nm, because TiO2 has been shown to be effective only against UV wavelengths less than 360 nm (UVA is 320-400 nm). In a study by Beasley and Meyer, TiO2 delivered neither the same level of UVA attenuation nor protection from UVA to human skin as did photostabilized formulations of avobenzone or ZnO. Therefore, TiO2 is not a suitable substitute for avobenzone and ZnO for strong UVA protection (Am. J. Clin. Dermatol. 2010;11:413-21).
Indications beyond photoprotection
More than 20 years ago, Hughes and McLean showed that a ZnO tape was effective in dressing fingertip and soft tissue injuries that were resistant to healing (Arch. Emerg. Med. 1988;5:223-7). More recently, Parboteeah and Brown demonstrated the efficacy of treating recalcitrant venous leg ulcers with ZnO paste bandages (Br. J. Nurs. 2008;17:S30, S32, S34-6). In addition, Treadwell has shown that the weekly application of ZnO compression dressings to surgical wounds of the lower leg promotes healing (Dermatol. Surg. 2011;37:166-7).
Micronized zinc oxide is included in a 4% hydroquinone/10% L-ascorbic acid treatment system recently found (in a small study of 34 females) to be effective in alleviating early signs of photodamage in normal to oily skin. Thirty patients, with minimal or mild facial photodamage and hyperpigmentation, completed the 12-week treatment regimen. All the participants were satisfied with the appearance of their skin after the study, with median scores for all assessment parameters significantly improved compared with baseline (J. Drugs Dermatol. 2011;10:1455-61). ZnO also is an active ingredient in formulations intended to support the healing of perianal eczema (Hautarzt. 2010;61:33-8).
A 2001 report on a series of blinded, randomized clinical trials conducted by Baldwin et al. showed that clinical benefits were derived from the continuous topical administration of a ZnO/petrolatum formulation in a diaper introduced at that time. The first study was undertaken to verify that the ZnO/petrolatum formulation was indeed transferred from the diaper to the child’s skin. Stratum corneum (SC) samples were analyzed from each child after the wearing of a single diaper for 3 hours or multiple diapers for 24 hours. The results indicated effective transfer, with ZnO increasing in the SC from 4.2 mcg/cm2 at 3 hours to more than 8 mcg/cm2 at 24 hours.
The second study of the formulation, in an adult arm model, assessed the prevention of irritation and SC damage induced by sodium laureth sulfate. The investigators found that the ZnO/petrolatum combination yielded significant reductions in SC damage and erythema. The third study, a 4-week trial in which 268 infants were assessed, considered the effects of the formulation on erythema and diaper rash. Half of the infants wore the test diaper and half used a control diaper lacking the ZnO/petrolatum product. Significant reductions in erythema and diaper rash were indeed observed in the test group (J. Eur. Acad. Dermatol. Venereol. 2001;15 Suppl 1:5-11).
A 2009 study showed that an unmedicated ZnO/petrolatum paste was effective in restoring the properties of the skin, allowing for balanced transepidermal water loss and water retention by SC previously compromised by diaper dermatitis. This skin condition affects approximately 50% of infants and a small percentage of the bedridden elderly (Int. J. Cosmet. Sci. 2009;31:369-74).
In 2010, a study that assessed the effectiveness of topical ZnO ointment using the rabbit ear hypertrophic scar model showed that the application of 40% ZnO significantly reduced clinical scar hypertrophy scores at 6 weeks compared with placebo. The researchers concluded that these results may suggest clinical applications for ZnO in the treatment of hypertrophic scars in humans (Burns 2010;36:1027-35). In addition, ZnO has demonstrated antibacterial properties, with nanoparticles exhibiting more potent antibacterial activity than bulk ZnO (Sci. Technol. Adv. Mater. 2008;9:1-7).
Products
ZnO is a key ingredient in calamine lotion, an antipruritic compound used to treat various mild conditions such as bites and stings from insects, eczema, poison ivy, rashes, and sunburn. It is also available over the counter in ointment or suppository form for healing hemorrhoids and fissures. In addition, ZnO is used widely in baby powders, barrier creams, moisturizers, antiseptic ointments, antidandruff shampoos, athletic bandage tape, and, of course, sunscreens.
Conclusion
ZnO is a versatile inorganic metal oxide with multiple indications in dermatology. Consequently, it is included in a wide array of skin care products, including shampoos, moisturizers, and sunscreens. Its use in nanoparticle form, along with the similar use of its physical sunscreen counterpart TiO2, represents one of the many subjects debated within the larger context of sunscreen use. The next edition of this column will focus on the relative safety of zinc oxide nanoparticles.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in Miami Beach. She founded the cosmetic dermatology center at the University of Miami in 1997. Dr. Baumann wrote the textbook "Cosmetic Dermatology: Principles and Practice" (McGraw-Hill, April 2002), and a book for consumers, "The Skin Type Solution" (Bantam, 2006). She has contributed to the Cosmeceutical Critique column in Skin & Allergy News since January 2001 and joined the editorial advisory board in 2004. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Galderma, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Stiefel, Topix Pharmaceuticals, and Unilever.
This column, "Cosmeceutical Critique," appears regularly in Skin & Allergy News, a publication of Frontline Medical News.
Zinc is a trace element, and it is not synthesized by the human body. The element was identified in the 1960s as being essential for human health and development. Zinc is a cofactor in more than 300 enzymes necessary for cell function. In the dermatologic realm, zinc deficiency has been associated with skin alterations, delayed wound healing, and hair loss.
Zinc oxide (ZnO) is a metal oxide that also has a broad profile in dermatology. It is perhaps best known as a physical sunscreen ingredient. ZnO and titanium dioxide (TiO2) have long been used in this manner. Both ZnO and TiO2 also have been increasingly used to replace large-particle compounds in numerous cosmetics and sunscreens. These two compounds have demonstrated effective protection against UV-induced damage, providing stronger protection against UV radiation while leaving less white residue than previous generations of physical sunscreens.
Particles of ZnO in earlier sunscreens were found to be too large to penetrate the stratum corneum and, thus, were deemed biologically inactive (J. Am. Acad. Dermatol. 1999;40:85-90). However, in novel nanoparticle form, such metal oxides absorb UV radiation, leading to photocatalysis and the release of reactive oxygen species (Australas. J. Dermatol. 2011;52:1-6). Indeed, nanoparticles exhibit new physiochemical properties as a result of increased surface area as compared to large-form products, and the potential adverse effects of the novel nanoparticle formulations in sunscreens cannot be adequately extrapolated from the effects of older-generation larger-particle skin care products (J. Drugs Dermatol. 2010;9:475-81; Int. J. Dermatol. 2011;50:247-54. The relative safety of ZnO nanoparticles will be discussed in a future column. The focus in this column will be a brief comparison with TiO2 and other indications for ZnO.
ZnO and TiO2
While numerous studies explore both TiO2 and ZnO, the latter is noted for greater versatility within the dermatologic armamentarium. In addition, ZnO is less photoactive and is associated with a lower refractive index in visible light than TiO2 (1.9 vs. 2.6, respectively) (J. Am. Acad. Dermatol. 1999;40:85-90); therefore, TiO2 appears whiter and is more difficult to incorporate into transparent products.
Another important difference is the spectrum of action. That is, only avobenzone (butyl methoxydibenzoylmethane) and ZnO are approved in the United States for broad-spectrum protection against UVA wavelengths greater than 360 nm, because TiO2 has been shown to be effective only against UV wavelengths less than 360 nm (UVA is 320-400 nm). In a study by Beasley and Meyer, TiO2 delivered neither the same level of UVA attenuation nor protection from UVA to human skin as did photostabilized formulations of avobenzone or ZnO. Therefore, TiO2 is not a suitable substitute for avobenzone and ZnO for strong UVA protection (Am. J. Clin. Dermatol. 2010;11:413-21).
Indications beyond photoprotection
More than 20 years ago, Hughes and McLean showed that a ZnO tape was effective in dressing fingertip and soft tissue injuries that were resistant to healing (Arch. Emerg. Med. 1988;5:223-7). More recently, Parboteeah and Brown demonstrated the efficacy of treating recalcitrant venous leg ulcers with ZnO paste bandages (Br. J. Nurs. 2008;17:S30, S32, S34-6). In addition, Treadwell has shown that the weekly application of ZnO compression dressings to surgical wounds of the lower leg promotes healing (Dermatol. Surg. 2011;37:166-7).
Micronized zinc oxide is included in a 4% hydroquinone/10% L-ascorbic acid treatment system recently found (in a small study of 34 females) to be effective in alleviating early signs of photodamage in normal to oily skin. Thirty patients, with minimal or mild facial photodamage and hyperpigmentation, completed the 12-week treatment regimen. All the participants were satisfied with the appearance of their skin after the study, with median scores for all assessment parameters significantly improved compared with baseline (J. Drugs Dermatol. 2011;10:1455-61). ZnO also is an active ingredient in formulations intended to support the healing of perianal eczema (Hautarzt. 2010;61:33-8).
A 2001 report on a series of blinded, randomized clinical trials conducted by Baldwin et al. showed that clinical benefits were derived from the continuous topical administration of a ZnO/petrolatum formulation in a diaper introduced at that time. The first study was undertaken to verify that the ZnO/petrolatum formulation was indeed transferred from the diaper to the child’s skin. Stratum corneum (SC) samples were analyzed from each child after the wearing of a single diaper for 3 hours or multiple diapers for 24 hours. The results indicated effective transfer, with ZnO increasing in the SC from 4.2 mcg/cm2 at 3 hours to more than 8 mcg/cm2 at 24 hours.
The second study of the formulation, in an adult arm model, assessed the prevention of irritation and SC damage induced by sodium laureth sulfate. The investigators found that the ZnO/petrolatum combination yielded significant reductions in SC damage and erythema. The third study, a 4-week trial in which 268 infants were assessed, considered the effects of the formulation on erythema and diaper rash. Half of the infants wore the test diaper and half used a control diaper lacking the ZnO/petrolatum product. Significant reductions in erythema and diaper rash were indeed observed in the test group (J. Eur. Acad. Dermatol. Venereol. 2001;15 Suppl 1:5-11).
A 2009 study showed that an unmedicated ZnO/petrolatum paste was effective in restoring the properties of the skin, allowing for balanced transepidermal water loss and water retention by SC previously compromised by diaper dermatitis. This skin condition affects approximately 50% of infants and a small percentage of the bedridden elderly (Int. J. Cosmet. Sci. 2009;31:369-74).
In 2010, a study that assessed the effectiveness of topical ZnO ointment using the rabbit ear hypertrophic scar model showed that the application of 40% ZnO significantly reduced clinical scar hypertrophy scores at 6 weeks compared with placebo. The researchers concluded that these results may suggest clinical applications for ZnO in the treatment of hypertrophic scars in humans (Burns 2010;36:1027-35). In addition, ZnO has demonstrated antibacterial properties, with nanoparticles exhibiting more potent antibacterial activity than bulk ZnO (Sci. Technol. Adv. Mater. 2008;9:1-7).
Products
ZnO is a key ingredient in calamine lotion, an antipruritic compound used to treat various mild conditions such as bites and stings from insects, eczema, poison ivy, rashes, and sunburn. It is also available over the counter in ointment or suppository form for healing hemorrhoids and fissures. In addition, ZnO is used widely in baby powders, barrier creams, moisturizers, antiseptic ointments, antidandruff shampoos, athletic bandage tape, and, of course, sunscreens.
Conclusion
ZnO is a versatile inorganic metal oxide with multiple indications in dermatology. Consequently, it is included in a wide array of skin care products, including shampoos, moisturizers, and sunscreens. Its use in nanoparticle form, along with the similar use of its physical sunscreen counterpart TiO2, represents one of the many subjects debated within the larger context of sunscreen use. The next edition of this column will focus on the relative safety of zinc oxide nanoparticles.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in Miami Beach. She founded the cosmetic dermatology center at the University of Miami in 1997. Dr. Baumann wrote the textbook "Cosmetic Dermatology: Principles and Practice" (McGraw-Hill, April 2002), and a book for consumers, "The Skin Type Solution" (Bantam, 2006). She has contributed to the Cosmeceutical Critique column in Skin & Allergy News since January 2001 and joined the editorial advisory board in 2004. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Galderma, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Stiefel, Topix Pharmaceuticals, and Unilever.
This column, "Cosmeceutical Critique," appears regularly in Skin & Allergy News, a publication of Frontline Medical News.
Zinc is a trace element, and it is not synthesized by the human body. The element was identified in the 1960s as being essential for human health and development. Zinc is a cofactor in more than 300 enzymes necessary for cell function. In the dermatologic realm, zinc deficiency has been associated with skin alterations, delayed wound healing, and hair loss.
Zinc oxide (ZnO) is a metal oxide that also has a broad profile in dermatology. It is perhaps best known as a physical sunscreen ingredient. ZnO and titanium dioxide (TiO2) have long been used in this manner. Both ZnO and TiO2 also have been increasingly used to replace large-particle compounds in numerous cosmetics and sunscreens. These two compounds have demonstrated effective protection against UV-induced damage, providing stronger protection against UV radiation while leaving less white residue than previous generations of physical sunscreens.
Particles of ZnO in earlier sunscreens were found to be too large to penetrate the stratum corneum and, thus, were deemed biologically inactive (J. Am. Acad. Dermatol. 1999;40:85-90). However, in novel nanoparticle form, such metal oxides absorb UV radiation, leading to photocatalysis and the release of reactive oxygen species (Australas. J. Dermatol. 2011;52:1-6). Indeed, nanoparticles exhibit new physiochemical properties as a result of increased surface area as compared to large-form products, and the potential adverse effects of the novel nanoparticle formulations in sunscreens cannot be adequately extrapolated from the effects of older-generation larger-particle skin care products (J. Drugs Dermatol. 2010;9:475-81; Int. J. Dermatol. 2011;50:247-54. The relative safety of ZnO nanoparticles will be discussed in a future column. The focus in this column will be a brief comparison with TiO2 and other indications for ZnO.
ZnO and TiO2
While numerous studies explore both TiO2 and ZnO, the latter is noted for greater versatility within the dermatologic armamentarium. In addition, ZnO is less photoactive and is associated with a lower refractive index in visible light than TiO2 (1.9 vs. 2.6, respectively) (J. Am. Acad. Dermatol. 1999;40:85-90); therefore, TiO2 appears whiter and is more difficult to incorporate into transparent products.
Another important difference is the spectrum of action. That is, only avobenzone (butyl methoxydibenzoylmethane) and ZnO are approved in the United States for broad-spectrum protection against UVA wavelengths greater than 360 nm, because TiO2 has been shown to be effective only against UV wavelengths less than 360 nm (UVA is 320-400 nm). In a study by Beasley and Meyer, TiO2 delivered neither the same level of UVA attenuation nor protection from UVA to human skin as did photostabilized formulations of avobenzone or ZnO. Therefore, TiO2 is not a suitable substitute for avobenzone and ZnO for strong UVA protection (Am. J. Clin. Dermatol. 2010;11:413-21).
Indications beyond photoprotection
More than 20 years ago, Hughes and McLean showed that a ZnO tape was effective in dressing fingertip and soft tissue injuries that were resistant to healing (Arch. Emerg. Med. 1988;5:223-7). More recently, Parboteeah and Brown demonstrated the efficacy of treating recalcitrant venous leg ulcers with ZnO paste bandages (Br. J. Nurs. 2008;17:S30, S32, S34-6). In addition, Treadwell has shown that the weekly application of ZnO compression dressings to surgical wounds of the lower leg promotes healing (Dermatol. Surg. 2011;37:166-7).
Micronized zinc oxide is included in a 4% hydroquinone/10% L-ascorbic acid treatment system recently found (in a small study of 34 females) to be effective in alleviating early signs of photodamage in normal to oily skin. Thirty patients, with minimal or mild facial photodamage and hyperpigmentation, completed the 12-week treatment regimen. All the participants were satisfied with the appearance of their skin after the study, with median scores for all assessment parameters significantly improved compared with baseline (J. Drugs Dermatol. 2011;10:1455-61). ZnO also is an active ingredient in formulations intended to support the healing of perianal eczema (Hautarzt. 2010;61:33-8).
A 2001 report on a series of blinded, randomized clinical trials conducted by Baldwin et al. showed that clinical benefits were derived from the continuous topical administration of a ZnO/petrolatum formulation in a diaper introduced at that time. The first study was undertaken to verify that the ZnO/petrolatum formulation was indeed transferred from the diaper to the child’s skin. Stratum corneum (SC) samples were analyzed from each child after the wearing of a single diaper for 3 hours or multiple diapers for 24 hours. The results indicated effective transfer, with ZnO increasing in the SC from 4.2 mcg/cm2 at 3 hours to more than 8 mcg/cm2 at 24 hours.
The second study of the formulation, in an adult arm model, assessed the prevention of irritation and SC damage induced by sodium laureth sulfate. The investigators found that the ZnO/petrolatum combination yielded significant reductions in SC damage and erythema. The third study, a 4-week trial in which 268 infants were assessed, considered the effects of the formulation on erythema and diaper rash. Half of the infants wore the test diaper and half used a control diaper lacking the ZnO/petrolatum product. Significant reductions in erythema and diaper rash were indeed observed in the test group (J. Eur. Acad. Dermatol. Venereol. 2001;15 Suppl 1:5-11).
A 2009 study showed that an unmedicated ZnO/petrolatum paste was effective in restoring the properties of the skin, allowing for balanced transepidermal water loss and water retention by SC previously compromised by diaper dermatitis. This skin condition affects approximately 50% of infants and a small percentage of the bedridden elderly (Int. J. Cosmet. Sci. 2009;31:369-74).
In 2010, a study that assessed the effectiveness of topical ZnO ointment using the rabbit ear hypertrophic scar model showed that the application of 40% ZnO significantly reduced clinical scar hypertrophy scores at 6 weeks compared with placebo. The researchers concluded that these results may suggest clinical applications for ZnO in the treatment of hypertrophic scars in humans (Burns 2010;36:1027-35). In addition, ZnO has demonstrated antibacterial properties, with nanoparticles exhibiting more potent antibacterial activity than bulk ZnO (Sci. Technol. Adv. Mater. 2008;9:1-7).
Products
ZnO is a key ingredient in calamine lotion, an antipruritic compound used to treat various mild conditions such as bites and stings from insects, eczema, poison ivy, rashes, and sunburn. It is also available over the counter in ointment or suppository form for healing hemorrhoids and fissures. In addition, ZnO is used widely in baby powders, barrier creams, moisturizers, antiseptic ointments, antidandruff shampoos, athletic bandage tape, and, of course, sunscreens.
Conclusion
ZnO is a versatile inorganic metal oxide with multiple indications in dermatology. Consequently, it is included in a wide array of skin care products, including shampoos, moisturizers, and sunscreens. Its use in nanoparticle form, along with the similar use of its physical sunscreen counterpart TiO2, represents one of the many subjects debated within the larger context of sunscreen use. The next edition of this column will focus on the relative safety of zinc oxide nanoparticles.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in Miami Beach. She founded the cosmetic dermatology center at the University of Miami in 1997. Dr. Baumann wrote the textbook "Cosmetic Dermatology: Principles and Practice" (McGraw-Hill, April 2002), and a book for consumers, "The Skin Type Solution" (Bantam, 2006). She has contributed to the Cosmeceutical Critique column in Skin & Allergy News since January 2001 and joined the editorial advisory board in 2004. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Galderma, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Stiefel, Topix Pharmaceuticals, and Unilever.
This column, "Cosmeceutical Critique," appears regularly in Skin & Allergy News, a publication of Frontline Medical News.
Peppermint and menthol
Mentha piperita, better known as peppermint, is used worldwide in many ways. Its use for culinary and medical purposes dates back to the ancient Greek and Roman civilizations. Peppermint is used in numerous forms (i.e., oil, leaf, leaf extract, and leaf water), with the oil as the most versatile (Dermatitis 2010;21:327-9). Peppermint has long been known for its beneficial gastrointestinal effects, and it has a well-established record of antimicrobial, antifungal, and analgesic activity (Mills S., Bone K. Principles and Practice of Phytotherapy: Modern Herbal Medicine. [London: Churchill Livingstone, 2000, pp 507-13]; J. Environ. Biol. 2011;32:23-9).
Menthol (C10H20O) is a naturally occurring monocyclic terpene alcohol derived from Mentha piperita as well as other mint oils (Skin Therapy Lett. 2010;15:5-9), and has been associated with several health benefits. Recently, anticancer properties have been ascribed to menthol (Biochim. Biophys. Acta 2009;1792:33-8). This column will discuss recent findings regarding the actual or potential cutaneous benefits of peppermint and menthol.
Various Mentha species, including M. piperita, have exhibited significant antioxidant activity (Toxicol. Ind. Health. 2012;28:83-9; Nat. Prod. Commun. 2009;4:1107-12; Nat. Prod. Commun. 2009;4:535-42). In a 2010 study of the antioxidant activity of the essential oils of six popular herbs, including lavender (Lavendular angustifolia), peppermint (M. piperita), rosemary (Rosmarius officinalis), lemon (Citrus limon), grapefruit (C. paradise), and frankincense (Boswellia carteri), investigators found, in testing free radical-scavenging capacity and lipid peroxidation in the linoleic acid system, that peppermint essential oil exhibited the greatest radical-scavenging activity against the 2,2\'-azinobis-(3-ethylbenzothiazoline-6-sulfonic acid) ABTS radical (Nat. Prod. Res. 2010;24:140-51).
In 2010, Baliga and Rao showed that M. piperita and M. arvensis (wild mint) protected mice against gamma-radiation–induced morbidity and mortality. Specifically, M. piperita protected murine testes as well as gastrointestinal and hemopoietic systems (J. Cancer Res. Ther. 2010;6:255-62).
Anticancer activity
Investigations by Jain et al. into the molecular mechanisms supporting the anticarcinogenic potential of M. piperita leaf extracts on six human cancer cell lines (HeLa, MCF-7, Jurkat, T24, HT-29, MIAPaCa-2) in 2011 revealed that chloroform and ethyl acetate extracts dose- and time-dependently displayed anticarcinogenic activity leading to G1 cell cycle arrest and mitochondrial-mediated apoptosis among the cascade of effects. The investigators identified their findings as the first evidence of direct anticarcinogenic activity of Mentha leaf extracts and suggested that future work might focus on isolating active constituents as a foundation for mechanistic and translational studies leading to new anticancer drugs, alone or in combination, to prevent and treat human cancers (Int. J. Toxicol. 2011;30:225-36).
Topical benefits of menthol
In a recent examination of the antibacterial and antifungal properties, as well as speculated anti-inflammatory activity of menthol as a topical treatment for diaper dermatitis, investigators conducted a pilot clinical trial in a hospital setting. The study involved 84 neonates with diagnosed candidal diaper dermatitis who required no critical care or systemic antifungal and anti-inflammatory medications. The menthol group (n = 42) received topical clotrimazole and topically applied menthol drops and the control group (n = 42) received topical clotrimazole and a placebo. Thirty-five infants in each group completed the study. The researchers found that complete healing was shorter in the menthol group, with significant relief of erythema and pustules observed in this group. They concluded that topically-applied menthol may be an effective agent in the treatment of candidal diaper dermatitis (World J. Pediatr. 2011;7:167-70).
In 2011, Qiu et al. showed, through various assays, that menthol, in low concentrations, could significantly suppress the expression of alpha-hemolysin, enterotoxins A and B, and toxic shock syndrome toxin 1 in Staphylococcus aureus. The investigators concluded that menthol may warrant inclusion in the armamentarium against S. aureus when combined with beta-lactam antibiotics, which, at subinhibitory concentrations, can actually augment S. aureus toxin secretion. They added that menthol may also have possible uses in novel anti-virulence drugs (Appl. Microbiol. Biotechnol. 2011;90:705-12). It should be noted that menthol is considered safe and effective, with concentrations up to 16% approved in OTC external products by the Food and Drug Administration (J. Am. Acad. Dermatol. 2007;57:873-8).
Pruritus, TRPM8, and melanoma
Topically applied menthol, in concentrations of 1%-3%, is often used to treat pruritus, particularly in the elderly (Skin Therapy Lett. 2010;15:5-9). In addition, recent evidence suggests that the presence of menthol can facilitate penetration of other agents in topical products (Int. J. Toxicol. 2001;20 Suppl 3:61-73; J. Am. Acad. Dermatol. 2007;57:873-8). Patel and Yosipovitch suggest that elderly patients who report diminished pruritus with cooling may stand to benefit from menthol-containing topical therapies (J. Am. Acad. Dermatol. 2007;57:873-8; Skin Therapy Lett. 2010;15:5-9). Interestingly, menthol, via the transient receptor potential melastatin subfamily 8 (TRPM8) receptor, a member of a family of excitatory ion channels, engenders the same cooling sensation as low temperature, though menthol is not linked to a reduction in skin temperature (J. Am. Acad. Dermatol. 2007;57:873-8; Skin Therapy Lett. 2010;15:5-9).
Although the exact mechanism by which menthol exerts its antipruritic and analgesic effects has yet to be determined, the discovery that the TRPM8 is its underlying receptor is proving to be significant, particularly in understanding the cooling effect of the botanical (J. Am. Acad. Dermatol. 2007;57:873-8). There are also indications that menthol has therapeutic potential for melanoma. Specifically, melanoma expresses TRPM8 receptors, the activation of which inhibits melanoma viability. Menthol appears to mediate this response through an influx of extracellular calcium ions (Am. J. Physiol. Cell Physiol. 2008;295:C296-301; Am. J. Physiol. Cell Physiol. 2008;295:C293-5).
Peppermint oil
In 2003, Schuhmacher et al. investigated the virucidal effect of peppermint oil and found that it had a direct effect against herpes simplex virus type 1 (HSV-1) and herpes simplex virus type 2 (HSV-2) as well as an acyclovir-resistant HSV-1 strain. The investigators concluded, noting the lipophilic nature of peppermint oil, that it might be an appropriate topical treatment for recurrent herpes outbreaks (Phytomedicine 2003;10:504-10).
Because of its flavor, aroma, and cooling qualities, peppermint oil is used in a wide range of products, including cosmeceuticals, personal hygiene products (e.g., bath preparations, mouthwashes, toothpastes, and topical formulations), foods, pharmaceutical products, and aromatherapy. Topical indications include pruritus, irritation, and inflammation. Peppermint oil can act as a skin sensitizer, though, particularly in impaired and sensitive skin (Dermatitis 2010;21:327-9). Although peppermint oil has been reported to be a sensitizer in isolated cases, peppermint oil 8% was not found to be a sensitizer in a recent test using a maximization protocol and the various forms of peppermint (i.e., oil, extract, leaves, and water) are considered to be safe in cosmetic formulations. In rinse-off products, peppermint oil is used in concentrations up to 3% and up to 0.2% in leave-on formulations (Int. J. Toxicol. 2001;20 Suppl 3:61-73).
Conclusion
Peppermint and menthol, its naturally occurring monocyclic terpene alcohol derivative, have long been used for medical purposes. Contemporary practice and continuing research continue to support various uses of M. piperita in the medical armamentarium, with specific and additional uses continually being found in the dermatologic realm.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in Miami Beach. She founded the cosmetic dermatology center at the University of Miami in 1997. Dr. Baumann wrote the textbook "Cosmetic Dermatology: Principles and Practice" (McGraw-Hill, April 2002), and a book for consumers, "The Skin Type Solution" (Bantam, 2006). She has contributed to the Cosmeceutical Critique column in Skin & Allergy News since January 2001 and joined the editorial advisory board in 2004. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Galderma, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Stiefel, Topix Pharmaceuticals, and Unilever.
Mentha piperita, better known as peppermint, is used worldwide in many ways. Its use for culinary and medical purposes dates back to the ancient Greek and Roman civilizations. Peppermint is used in numerous forms (i.e., oil, leaf, leaf extract, and leaf water), with the oil as the most versatile (Dermatitis 2010;21:327-9). Peppermint has long been known for its beneficial gastrointestinal effects, and it has a well-established record of antimicrobial, antifungal, and analgesic activity (Mills S., Bone K. Principles and Practice of Phytotherapy: Modern Herbal Medicine. [London: Churchill Livingstone, 2000, pp 507-13]; J. Environ. Biol. 2011;32:23-9).
Menthol (C10H20O) is a naturally occurring monocyclic terpene alcohol derived from Mentha piperita as well as other mint oils (Skin Therapy Lett. 2010;15:5-9), and has been associated with several health benefits. Recently, anticancer properties have been ascribed to menthol (Biochim. Biophys. Acta 2009;1792:33-8). This column will discuss recent findings regarding the actual or potential cutaneous benefits of peppermint and menthol.
Various Mentha species, including M. piperita, have exhibited significant antioxidant activity (Toxicol. Ind. Health. 2012;28:83-9; Nat. Prod. Commun. 2009;4:1107-12; Nat. Prod. Commun. 2009;4:535-42). In a 2010 study of the antioxidant activity of the essential oils of six popular herbs, including lavender (Lavendular angustifolia), peppermint (M. piperita), rosemary (Rosmarius officinalis), lemon (Citrus limon), grapefruit (C. paradise), and frankincense (Boswellia carteri), investigators found, in testing free radical-scavenging capacity and lipid peroxidation in the linoleic acid system, that peppermint essential oil exhibited the greatest radical-scavenging activity against the 2,2\'-azinobis-(3-ethylbenzothiazoline-6-sulfonic acid) ABTS radical (Nat. Prod. Res. 2010;24:140-51).
In 2010, Baliga and Rao showed that M. piperita and M. arvensis (wild mint) protected mice against gamma-radiation–induced morbidity and mortality. Specifically, M. piperita protected murine testes as well as gastrointestinal and hemopoietic systems (J. Cancer Res. Ther. 2010;6:255-62).
Anticancer activity
Investigations by Jain et al. into the molecular mechanisms supporting the anticarcinogenic potential of M. piperita leaf extracts on six human cancer cell lines (HeLa, MCF-7, Jurkat, T24, HT-29, MIAPaCa-2) in 2011 revealed that chloroform and ethyl acetate extracts dose- and time-dependently displayed anticarcinogenic activity leading to G1 cell cycle arrest and mitochondrial-mediated apoptosis among the cascade of effects. The investigators identified their findings as the first evidence of direct anticarcinogenic activity of Mentha leaf extracts and suggested that future work might focus on isolating active constituents as a foundation for mechanistic and translational studies leading to new anticancer drugs, alone or in combination, to prevent and treat human cancers (Int. J. Toxicol. 2011;30:225-36).
Topical benefits of menthol
In a recent examination of the antibacterial and antifungal properties, as well as speculated anti-inflammatory activity of menthol as a topical treatment for diaper dermatitis, investigators conducted a pilot clinical trial in a hospital setting. The study involved 84 neonates with diagnosed candidal diaper dermatitis who required no critical care or systemic antifungal and anti-inflammatory medications. The menthol group (n = 42) received topical clotrimazole and topically applied menthol drops and the control group (n = 42) received topical clotrimazole and a placebo. Thirty-five infants in each group completed the study. The researchers found that complete healing was shorter in the menthol group, with significant relief of erythema and pustules observed in this group. They concluded that topically-applied menthol may be an effective agent in the treatment of candidal diaper dermatitis (World J. Pediatr. 2011;7:167-70).
In 2011, Qiu et al. showed, through various assays, that menthol, in low concentrations, could significantly suppress the expression of alpha-hemolysin, enterotoxins A and B, and toxic shock syndrome toxin 1 in Staphylococcus aureus. The investigators concluded that menthol may warrant inclusion in the armamentarium against S. aureus when combined with beta-lactam antibiotics, which, at subinhibitory concentrations, can actually augment S. aureus toxin secretion. They added that menthol may also have possible uses in novel anti-virulence drugs (Appl. Microbiol. Biotechnol. 2011;90:705-12). It should be noted that menthol is considered safe and effective, with concentrations up to 16% approved in OTC external products by the Food and Drug Administration (J. Am. Acad. Dermatol. 2007;57:873-8).
Pruritus, TRPM8, and melanoma
Topically applied menthol, in concentrations of 1%-3%, is often used to treat pruritus, particularly in the elderly (Skin Therapy Lett. 2010;15:5-9). In addition, recent evidence suggests that the presence of menthol can facilitate penetration of other agents in topical products (Int. J. Toxicol. 2001;20 Suppl 3:61-73; J. Am. Acad. Dermatol. 2007;57:873-8). Patel and Yosipovitch suggest that elderly patients who report diminished pruritus with cooling may stand to benefit from menthol-containing topical therapies (J. Am. Acad. Dermatol. 2007;57:873-8; Skin Therapy Lett. 2010;15:5-9). Interestingly, menthol, via the transient receptor potential melastatin subfamily 8 (TRPM8) receptor, a member of a family of excitatory ion channels, engenders the same cooling sensation as low temperature, though menthol is not linked to a reduction in skin temperature (J. Am. Acad. Dermatol. 2007;57:873-8; Skin Therapy Lett. 2010;15:5-9).
Although the exact mechanism by which menthol exerts its antipruritic and analgesic effects has yet to be determined, the discovery that the TRPM8 is its underlying receptor is proving to be significant, particularly in understanding the cooling effect of the botanical (J. Am. Acad. Dermatol. 2007;57:873-8). There are also indications that menthol has therapeutic potential for melanoma. Specifically, melanoma expresses TRPM8 receptors, the activation of which inhibits melanoma viability. Menthol appears to mediate this response through an influx of extracellular calcium ions (Am. J. Physiol. Cell Physiol. 2008;295:C296-301; Am. J. Physiol. Cell Physiol. 2008;295:C293-5).
Peppermint oil
In 2003, Schuhmacher et al. investigated the virucidal effect of peppermint oil and found that it had a direct effect against herpes simplex virus type 1 (HSV-1) and herpes simplex virus type 2 (HSV-2) as well as an acyclovir-resistant HSV-1 strain. The investigators concluded, noting the lipophilic nature of peppermint oil, that it might be an appropriate topical treatment for recurrent herpes outbreaks (Phytomedicine 2003;10:504-10).
Because of its flavor, aroma, and cooling qualities, peppermint oil is used in a wide range of products, including cosmeceuticals, personal hygiene products (e.g., bath preparations, mouthwashes, toothpastes, and topical formulations), foods, pharmaceutical products, and aromatherapy. Topical indications include pruritus, irritation, and inflammation. Peppermint oil can act as a skin sensitizer, though, particularly in impaired and sensitive skin (Dermatitis 2010;21:327-9). Although peppermint oil has been reported to be a sensitizer in isolated cases, peppermint oil 8% was not found to be a sensitizer in a recent test using a maximization protocol and the various forms of peppermint (i.e., oil, extract, leaves, and water) are considered to be safe in cosmetic formulations. In rinse-off products, peppermint oil is used in concentrations up to 3% and up to 0.2% in leave-on formulations (Int. J. Toxicol. 2001;20 Suppl 3:61-73).
Conclusion
Peppermint and menthol, its naturally occurring monocyclic terpene alcohol derivative, have long been used for medical purposes. Contemporary practice and continuing research continue to support various uses of M. piperita in the medical armamentarium, with specific and additional uses continually being found in the dermatologic realm.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in Miami Beach. She founded the cosmetic dermatology center at the University of Miami in 1997. Dr. Baumann wrote the textbook "Cosmetic Dermatology: Principles and Practice" (McGraw-Hill, April 2002), and a book for consumers, "The Skin Type Solution" (Bantam, 2006). She has contributed to the Cosmeceutical Critique column in Skin & Allergy News since January 2001 and joined the editorial advisory board in 2004. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Galderma, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Stiefel, Topix Pharmaceuticals, and Unilever.
Mentha piperita, better known as peppermint, is used worldwide in many ways. Its use for culinary and medical purposes dates back to the ancient Greek and Roman civilizations. Peppermint is used in numerous forms (i.e., oil, leaf, leaf extract, and leaf water), with the oil as the most versatile (Dermatitis 2010;21:327-9). Peppermint has long been known for its beneficial gastrointestinal effects, and it has a well-established record of antimicrobial, antifungal, and analgesic activity (Mills S., Bone K. Principles and Practice of Phytotherapy: Modern Herbal Medicine. [London: Churchill Livingstone, 2000, pp 507-13]; J. Environ. Biol. 2011;32:23-9).
Menthol (C10H20O) is a naturally occurring monocyclic terpene alcohol derived from Mentha piperita as well as other mint oils (Skin Therapy Lett. 2010;15:5-9), and has been associated with several health benefits. Recently, anticancer properties have been ascribed to menthol (Biochim. Biophys. Acta 2009;1792:33-8). This column will discuss recent findings regarding the actual or potential cutaneous benefits of peppermint and menthol.
Various Mentha species, including M. piperita, have exhibited significant antioxidant activity (Toxicol. Ind. Health. 2012;28:83-9; Nat. Prod. Commun. 2009;4:1107-12; Nat. Prod. Commun. 2009;4:535-42). In a 2010 study of the antioxidant activity of the essential oils of six popular herbs, including lavender (Lavendular angustifolia), peppermint (M. piperita), rosemary (Rosmarius officinalis), lemon (Citrus limon), grapefruit (C. paradise), and frankincense (Boswellia carteri), investigators found, in testing free radical-scavenging capacity and lipid peroxidation in the linoleic acid system, that peppermint essential oil exhibited the greatest radical-scavenging activity against the 2,2\'-azinobis-(3-ethylbenzothiazoline-6-sulfonic acid) ABTS radical (Nat. Prod. Res. 2010;24:140-51).
In 2010, Baliga and Rao showed that M. piperita and M. arvensis (wild mint) protected mice against gamma-radiation–induced morbidity and mortality. Specifically, M. piperita protected murine testes as well as gastrointestinal and hemopoietic systems (J. Cancer Res. Ther. 2010;6:255-62).
Anticancer activity
Investigations by Jain et al. into the molecular mechanisms supporting the anticarcinogenic potential of M. piperita leaf extracts on six human cancer cell lines (HeLa, MCF-7, Jurkat, T24, HT-29, MIAPaCa-2) in 2011 revealed that chloroform and ethyl acetate extracts dose- and time-dependently displayed anticarcinogenic activity leading to G1 cell cycle arrest and mitochondrial-mediated apoptosis among the cascade of effects. The investigators identified their findings as the first evidence of direct anticarcinogenic activity of Mentha leaf extracts and suggested that future work might focus on isolating active constituents as a foundation for mechanistic and translational studies leading to new anticancer drugs, alone or in combination, to prevent and treat human cancers (Int. J. Toxicol. 2011;30:225-36).
Topical benefits of menthol
In a recent examination of the antibacterial and antifungal properties, as well as speculated anti-inflammatory activity of menthol as a topical treatment for diaper dermatitis, investigators conducted a pilot clinical trial in a hospital setting. The study involved 84 neonates with diagnosed candidal diaper dermatitis who required no critical care or systemic antifungal and anti-inflammatory medications. The menthol group (n = 42) received topical clotrimazole and topically applied menthol drops and the control group (n = 42) received topical clotrimazole and a placebo. Thirty-five infants in each group completed the study. The researchers found that complete healing was shorter in the menthol group, with significant relief of erythema and pustules observed in this group. They concluded that topically-applied menthol may be an effective agent in the treatment of candidal diaper dermatitis (World J. Pediatr. 2011;7:167-70).
In 2011, Qiu et al. showed, through various assays, that menthol, in low concentrations, could significantly suppress the expression of alpha-hemolysin, enterotoxins A and B, and toxic shock syndrome toxin 1 in Staphylococcus aureus. The investigators concluded that menthol may warrant inclusion in the armamentarium against S. aureus when combined with beta-lactam antibiotics, which, at subinhibitory concentrations, can actually augment S. aureus toxin secretion. They added that menthol may also have possible uses in novel anti-virulence drugs (Appl. Microbiol. Biotechnol. 2011;90:705-12). It should be noted that menthol is considered safe and effective, with concentrations up to 16% approved in OTC external products by the Food and Drug Administration (J. Am. Acad. Dermatol. 2007;57:873-8).
Pruritus, TRPM8, and melanoma
Topically applied menthol, in concentrations of 1%-3%, is often used to treat pruritus, particularly in the elderly (Skin Therapy Lett. 2010;15:5-9). In addition, recent evidence suggests that the presence of menthol can facilitate penetration of other agents in topical products (Int. J. Toxicol. 2001;20 Suppl 3:61-73; J. Am. Acad. Dermatol. 2007;57:873-8). Patel and Yosipovitch suggest that elderly patients who report diminished pruritus with cooling may stand to benefit from menthol-containing topical therapies (J. Am. Acad. Dermatol. 2007;57:873-8; Skin Therapy Lett. 2010;15:5-9). Interestingly, menthol, via the transient receptor potential melastatin subfamily 8 (TRPM8) receptor, a member of a family of excitatory ion channels, engenders the same cooling sensation as low temperature, though menthol is not linked to a reduction in skin temperature (J. Am. Acad. Dermatol. 2007;57:873-8; Skin Therapy Lett. 2010;15:5-9).
Although the exact mechanism by which menthol exerts its antipruritic and analgesic effects has yet to be determined, the discovery that the TRPM8 is its underlying receptor is proving to be significant, particularly in understanding the cooling effect of the botanical (J. Am. Acad. Dermatol. 2007;57:873-8). There are also indications that menthol has therapeutic potential for melanoma. Specifically, melanoma expresses TRPM8 receptors, the activation of which inhibits melanoma viability. Menthol appears to mediate this response through an influx of extracellular calcium ions (Am. J. Physiol. Cell Physiol. 2008;295:C296-301; Am. J. Physiol. Cell Physiol. 2008;295:C293-5).
Peppermint oil
In 2003, Schuhmacher et al. investigated the virucidal effect of peppermint oil and found that it had a direct effect against herpes simplex virus type 1 (HSV-1) and herpes simplex virus type 2 (HSV-2) as well as an acyclovir-resistant HSV-1 strain. The investigators concluded, noting the lipophilic nature of peppermint oil, that it might be an appropriate topical treatment for recurrent herpes outbreaks (Phytomedicine 2003;10:504-10).
Because of its flavor, aroma, and cooling qualities, peppermint oil is used in a wide range of products, including cosmeceuticals, personal hygiene products (e.g., bath preparations, mouthwashes, toothpastes, and topical formulations), foods, pharmaceutical products, and aromatherapy. Topical indications include pruritus, irritation, and inflammation. Peppermint oil can act as a skin sensitizer, though, particularly in impaired and sensitive skin (Dermatitis 2010;21:327-9). Although peppermint oil has been reported to be a sensitizer in isolated cases, peppermint oil 8% was not found to be a sensitizer in a recent test using a maximization protocol and the various forms of peppermint (i.e., oil, extract, leaves, and water) are considered to be safe in cosmetic formulations. In rinse-off products, peppermint oil is used in concentrations up to 3% and up to 0.2% in leave-on formulations (Int. J. Toxicol. 2001;20 Suppl 3:61-73).
Conclusion
Peppermint and menthol, its naturally occurring monocyclic terpene alcohol derivative, have long been used for medical purposes. Contemporary practice and continuing research continue to support various uses of M. piperita in the medical armamentarium, with specific and additional uses continually being found in the dermatologic realm.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in Miami Beach. She founded the cosmetic dermatology center at the University of Miami in 1997. Dr. Baumann wrote the textbook "Cosmetic Dermatology: Principles and Practice" (McGraw-Hill, April 2002), and a book for consumers, "The Skin Type Solution" (Bantam, 2006). She has contributed to the Cosmeceutical Critique column in Skin & Allergy News since January 2001 and joined the editorial advisory board in 2004. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Galderma, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Stiefel, Topix Pharmaceuticals, and Unilever.
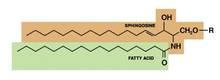
Stearic acid
Stearic acid, a waxlike fatty acid also known as octadecanoic acid, is an important component of stratum corneum lipids. Stearic acid is also found in cocoa butter, shea butter, and other vegetable fats, as well as animal tallow. As an FDA-approved ingredient in several cosmetic products, it is used as a surfactant and emulsifying agent for fragrance and as the base for other fatty acid ingredients that are synthesized into emollients and lubricants. Stearic acid is used most often to thicken and retain the shape of soaps (indirectly, through saponification of triglycerides composed of stearic acid esters), and it is also used in shampoos, shaving creams, and detergents.
There is limited evidence for the potential of exogenously produced stearic acid to play a significant role as a topical dermatologic therapeutic agent. Stearic acid is thought to be associated with behenyltrimethylammonium chloride through salt bridges, and the combination is believed to have the capacity to build bilayer vesicles with the aid of hinokitiol (beta-thujaplicin), a natural monoterpenoid found in the wood of trees in the Cupressaceae family that has been shown to exert topical inhibitory activity against Chlamydia trachomatis (Antimicrob. Agents Chemother. 2005;49:2519-21). These vesicles, used to enhance the skin permeation of hinokitiol, were tested in hairless mice and appear to have the potential to promote hair growth (Drug Dev. Ind. Pharm. 2010;36:556-62).
In 2000, Khalil et al. studied the effects of cream formulations on chemically induced burns in mice based on reports that the ingredients, docosanol or stearic acid, were associated with antiviral and anti-inflammatory activity. Burns were engendered by painting murine abdomens with a chloroform solution of phenol. Investigators then topically applied the test formulations 0.5, 3, and 6 hours after injury. They found that the docosanol- and stearic acid–containing creams significantly mitigated the severity and progression of skin lesions compared with untreated sites, yielding, respectively, 76% and 57% declines in mean lesion scores (Contact Dermatitis 2000;43:79-81).
In 2001, Fluhr et al. studied the effects of the free fatty acid pool on stratum corneum (SC) acidification and function by topically applying two phospholipase inhibitors – bromphenacylbromide and 1-hexadecyl-3-trifluoroethylglycero-sn-2-phosphomethanol – for 3 days to murine skin. This raised skin pH and yielded permeability barrier abnormality, altered SC integrity, and reduced SC cohesion. All malfunctions were normalized, including SC pH, with the coapplication of either palmitic, stearic, or linoleic acids along with the inhibiting agents (J. Invest. Dermatol. 2001;117:44-51).
In 2010, Mukherjee et al. evaluated a recently marketed mild, moisturizing body wash containing stearic acid and emollient soybean oil to ascertain the location and amount of stearic acid deposited in the SC after in vivo usage of the product. They conducted clinical cleansing studies for 1 and 5 consecutive days using the soybean product or petroleum jelly. The deuterated variant of stearic acid replaced the free stearic acid in the soybean formulation. The researchers detected deuterated stearic acid in all 10 consecutive layers of SC, with a total stearic acid level measured at 0.33 mcg/cm2 after five washes with the soybean oil product. They concluded that the estimated total fatty acid delivered to the skin from cleansing, probably incorporated into the SC lipid phase, is comparable to the fatty acid amount in an SC layer (J. Cosmet. Dermatol. 2010;9:202-10).
Stearic acid is incorporated into several over-the-counter products, including formulations by Aveda (Green Science Firming Face Cream), Yves Rocher (Les Plaisirs Nature), Kiss My Face (with alpha hydroxy acid), Valeant Pharmaceuticals’ Kinerase line (including Clear Skin Regulating Mask), Buster’s Skin Care for Men (peptide complex organic face moisturizer), and Dermalogica (Soothing Shaving Cream with Daily Defense Block), among others.
Conclusion
While stearic acid is an important component in stratum corneum lipids and a widely used ingredient in skin care products, there is a dearth of data on its significance, if any, in the topical dermatologic armamentarium beyond its primary activity as a surfactant and emulsifying agent. Specifically, it remains to be seen whether stearic acid can be replenished in the stratum corneum through topical treatment. Much more research is needed in this area to assess the potential of stearic acid as a therapeutic agent.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in Miami Beach. She founded the cosmetic dermatology center at the University of Miami in 1997. Dr. Baumann wrote the textbook "Cosmetic Dermatology: Principles and Practice" (McGraw-Hill, April 2009), and a book for consumers, "The Skin Type Solution" (Bantam, 2006). She has contributed to the Cosmeceutical Critique column in Skin & Allergy News since January 2001 and joined the editorial advisory board in 2004. She has received funding for clinical grants from Allergan, Aveeno, Avon Products, Galderma, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Stiefel, Topix Pharmaceuticals, and Unilever. E-mail [email protected] to contact Dr. Baumann or to suggest topics for a future column.
Stearic acid, a waxlike fatty acid also known as octadecanoic acid, is an important component of stratum corneum lipids. Stearic acid is also found in cocoa butter, shea butter, and other vegetable fats, as well as animal tallow. As an FDA-approved ingredient in several cosmetic products, it is used as a surfactant and emulsifying agent for fragrance and as the base for other fatty acid ingredients that are synthesized into emollients and lubricants. Stearic acid is used most often to thicken and retain the shape of soaps (indirectly, through saponification of triglycerides composed of stearic acid esters), and it is also used in shampoos, shaving creams, and detergents.
There is limited evidence for the potential of exogenously produced stearic acid to play a significant role as a topical dermatologic therapeutic agent. Stearic acid is thought to be associated with behenyltrimethylammonium chloride through salt bridges, and the combination is believed to have the capacity to build bilayer vesicles with the aid of hinokitiol (beta-thujaplicin), a natural monoterpenoid found in the wood of trees in the Cupressaceae family that has been shown to exert topical inhibitory activity against Chlamydia trachomatis (Antimicrob. Agents Chemother. 2005;49:2519-21). These vesicles, used to enhance the skin permeation of hinokitiol, were tested in hairless mice and appear to have the potential to promote hair growth (Drug Dev. Ind. Pharm. 2010;36:556-62).
In 2000, Khalil et al. studied the effects of cream formulations on chemically induced burns in mice based on reports that the ingredients, docosanol or stearic acid, were associated with antiviral and anti-inflammatory activity. Burns were engendered by painting murine abdomens with a chloroform solution of phenol. Investigators then topically applied the test formulations 0.5, 3, and 6 hours after injury. They found that the docosanol- and stearic acid–containing creams significantly mitigated the severity and progression of skin lesions compared with untreated sites, yielding, respectively, 76% and 57% declines in mean lesion scores (Contact Dermatitis 2000;43:79-81).
In 2001, Fluhr et al. studied the effects of the free fatty acid pool on stratum corneum (SC) acidification and function by topically applying two phospholipase inhibitors – bromphenacylbromide and 1-hexadecyl-3-trifluoroethylglycero-sn-2-phosphomethanol – for 3 days to murine skin. This raised skin pH and yielded permeability barrier abnormality, altered SC integrity, and reduced SC cohesion. All malfunctions were normalized, including SC pH, with the coapplication of either palmitic, stearic, or linoleic acids along with the inhibiting agents (J. Invest. Dermatol. 2001;117:44-51).
In 2010, Mukherjee et al. evaluated a recently marketed mild, moisturizing body wash containing stearic acid and emollient soybean oil to ascertain the location and amount of stearic acid deposited in the SC after in vivo usage of the product. They conducted clinical cleansing studies for 1 and 5 consecutive days using the soybean product or petroleum jelly. The deuterated variant of stearic acid replaced the free stearic acid in the soybean formulation. The researchers detected deuterated stearic acid in all 10 consecutive layers of SC, with a total stearic acid level measured at 0.33 mcg/cm2 after five washes with the soybean oil product. They concluded that the estimated total fatty acid delivered to the skin from cleansing, probably incorporated into the SC lipid phase, is comparable to the fatty acid amount in an SC layer (J. Cosmet. Dermatol. 2010;9:202-10).
Stearic acid is incorporated into several over-the-counter products, including formulations by Aveda (Green Science Firming Face Cream), Yves Rocher (Les Plaisirs Nature), Kiss My Face (with alpha hydroxy acid), Valeant Pharmaceuticals’ Kinerase line (including Clear Skin Regulating Mask), Buster’s Skin Care for Men (peptide complex organic face moisturizer), and Dermalogica (Soothing Shaving Cream with Daily Defense Block), among others.
Conclusion
While stearic acid is an important component in stratum corneum lipids and a widely used ingredient in skin care products, there is a dearth of data on its significance, if any, in the topical dermatologic armamentarium beyond its primary activity as a surfactant and emulsifying agent. Specifically, it remains to be seen whether stearic acid can be replenished in the stratum corneum through topical treatment. Much more research is needed in this area to assess the potential of stearic acid as a therapeutic agent.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in Miami Beach. She founded the cosmetic dermatology center at the University of Miami in 1997. Dr. Baumann wrote the textbook "Cosmetic Dermatology: Principles and Practice" (McGraw-Hill, April 2009), and a book for consumers, "The Skin Type Solution" (Bantam, 2006). She has contributed to the Cosmeceutical Critique column in Skin & Allergy News since January 2001 and joined the editorial advisory board in 2004. She has received funding for clinical grants from Allergan, Aveeno, Avon Products, Galderma, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Stiefel, Topix Pharmaceuticals, and Unilever. E-mail [email protected] to contact Dr. Baumann or to suggest topics for a future column.
Stearic acid, a waxlike fatty acid also known as octadecanoic acid, is an important component of stratum corneum lipids. Stearic acid is also found in cocoa butter, shea butter, and other vegetable fats, as well as animal tallow. As an FDA-approved ingredient in several cosmetic products, it is used as a surfactant and emulsifying agent for fragrance and as the base for other fatty acid ingredients that are synthesized into emollients and lubricants. Stearic acid is used most often to thicken and retain the shape of soaps (indirectly, through saponification of triglycerides composed of stearic acid esters), and it is also used in shampoos, shaving creams, and detergents.
There is limited evidence for the potential of exogenously produced stearic acid to play a significant role as a topical dermatologic therapeutic agent. Stearic acid is thought to be associated with behenyltrimethylammonium chloride through salt bridges, and the combination is believed to have the capacity to build bilayer vesicles with the aid of hinokitiol (beta-thujaplicin), a natural monoterpenoid found in the wood of trees in the Cupressaceae family that has been shown to exert topical inhibitory activity against Chlamydia trachomatis (Antimicrob. Agents Chemother. 2005;49:2519-21). These vesicles, used to enhance the skin permeation of hinokitiol, were tested in hairless mice and appear to have the potential to promote hair growth (Drug Dev. Ind. Pharm. 2010;36:556-62).
In 2000, Khalil et al. studied the effects of cream formulations on chemically induced burns in mice based on reports that the ingredients, docosanol or stearic acid, were associated with antiviral and anti-inflammatory activity. Burns were engendered by painting murine abdomens with a chloroform solution of phenol. Investigators then topically applied the test formulations 0.5, 3, and 6 hours after injury. They found that the docosanol- and stearic acid–containing creams significantly mitigated the severity and progression of skin lesions compared with untreated sites, yielding, respectively, 76% and 57% declines in mean lesion scores (Contact Dermatitis 2000;43:79-81).
In 2001, Fluhr et al. studied the effects of the free fatty acid pool on stratum corneum (SC) acidification and function by topically applying two phospholipase inhibitors – bromphenacylbromide and 1-hexadecyl-3-trifluoroethylglycero-sn-2-phosphomethanol – for 3 days to murine skin. This raised skin pH and yielded permeability barrier abnormality, altered SC integrity, and reduced SC cohesion. All malfunctions were normalized, including SC pH, with the coapplication of either palmitic, stearic, or linoleic acids along with the inhibiting agents (J. Invest. Dermatol. 2001;117:44-51).
In 2010, Mukherjee et al. evaluated a recently marketed mild, moisturizing body wash containing stearic acid and emollient soybean oil to ascertain the location and amount of stearic acid deposited in the SC after in vivo usage of the product. They conducted clinical cleansing studies for 1 and 5 consecutive days using the soybean product or petroleum jelly. The deuterated variant of stearic acid replaced the free stearic acid in the soybean formulation. The researchers detected deuterated stearic acid in all 10 consecutive layers of SC, with a total stearic acid level measured at 0.33 mcg/cm2 after five washes with the soybean oil product. They concluded that the estimated total fatty acid delivered to the skin from cleansing, probably incorporated into the SC lipid phase, is comparable to the fatty acid amount in an SC layer (J. Cosmet. Dermatol. 2010;9:202-10).
Stearic acid is incorporated into several over-the-counter products, including formulations by Aveda (Green Science Firming Face Cream), Yves Rocher (Les Plaisirs Nature), Kiss My Face (with alpha hydroxy acid), Valeant Pharmaceuticals’ Kinerase line (including Clear Skin Regulating Mask), Buster’s Skin Care for Men (peptide complex organic face moisturizer), and Dermalogica (Soothing Shaving Cream with Daily Defense Block), among others.
Conclusion
While stearic acid is an important component in stratum corneum lipids and a widely used ingredient in skin care products, there is a dearth of data on its significance, if any, in the topical dermatologic armamentarium beyond its primary activity as a surfactant and emulsifying agent. Specifically, it remains to be seen whether stearic acid can be replenished in the stratum corneum through topical treatment. Much more research is needed in this area to assess the potential of stearic acid as a therapeutic agent.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in Miami Beach. She founded the cosmetic dermatology center at the University of Miami in 1997. Dr. Baumann wrote the textbook "Cosmetic Dermatology: Principles and Practice" (McGraw-Hill, April 2009), and a book for consumers, "The Skin Type Solution" (Bantam, 2006). She has contributed to the Cosmeceutical Critique column in Skin & Allergy News since January 2001 and joined the editorial advisory board in 2004. She has received funding for clinical grants from Allergan, Aveeno, Avon Products, Galderma, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Stiefel, Topix Pharmaceuticals, and Unilever. E-mail [email protected] to contact Dr. Baumann or to suggest topics for a future column.
Mulberry
Often in this column, several species within a family might be discussed in relation to a broad range of health benefits. Licorice and mushrooms are good examples. In this case, and in this column, the focus will be on several species within a family that are thought to confer the same type of dermatologic benefit. The Morus genus within the Moraceae family appears to include several species that display skin-lightening properties.
Tyrosinase is the enzyme that controls the production of melanin. Suppressing tyrosinase activity to achieve skin lightening is a well-established method in dermatologic practice. The desire for products with fewer side effects than the mainstay, hydroquinone, or natural products such as kojic acid or arbutin, has led to investigations of several species in the Moraceae family. Notably, several Moraceae trees have been found to exhibit antioxidant activity (Int. J. Mol. Sci. 2012;13:2472-80; Biol. Pharm. Bull. 2002;25:1045-8; Biosci. Biotechnol. Biochem. 2010;74:2385-95; J. Pharm. Pharmacol. 2004;56:1291-8). The focus here, though, will be on the skin-lightening activity of various parts of Morus (commonly known as mulberry) trees.
In 2013, Singh et al. assessed the effects of mulberry, kiwi, and Sophora extracts on melanogenesis and melanin transfer in human melanocytes and in cocultures with phototype-matched normal adult epidermal keratinocytes. The extracts were evaluated against isobutylmethylxanthine, hydroquinone, vitamin C, and niacinamide. The investigators found that compared with unstimulated control, mulberry, kiwi, and Sophora extracts significantly reduced melanogenesis in normal adult epidermal melanocytes and human melanoma cells. Melanin transfer also was lowered, as was filopodia expression on melanocytes. The authors concluded that the test compounds compared well with standard-bearing depigmenting agents and warrant consideration as topical agents for diminishing hyperpigmentation (Exp. Dermatol. 2013;22:67-9).
Encouraging results in melasma treatment
A randomized, single-blind, placebo-controlled trial of 50 Filipino patients (49 women, 1 man) to examine the safety and efficacy of 75% Morus alba (white mulberry) extract oil was conducted by Alvin et al. in 2011. Patients were evaluated at weeks 4 and 8. The Melasma Area and Severity Index (MASI) score, Mexameter score, and Melasma Quality of Life (MelasQOL) score were measured, with the mulberry extract group performing significantly better than the placebo group according to all metrics.
The 25 patients treated with mulberry extract showed improvement in the MASI score, from 4.076 at baseline to 2.884 at week 8 (mean difference, 1.19); the mean difference for the placebo group was 0.06. The mean Mexameter reading revealed a significant difference, with a slight increase for the mulberry group (indicating lighter pigmentation), and the placebo group scored a slightly higher value. In addition, the MelasQOL score for the mulberry group improved markedly from baseline to week 8 (58.84 to 44.16), whereas the placebo group score improved only slightly, from 57.44 at baseline to 54.28 at week 8.
Adverse events were rare, with mild itching in 4 patients reported from the mulberry group, and 12 cases of either itching or erythema reported by the placebo group.
The investigators concluded that 75% mulberry extract oil objectively diminishes the hyperpigmentation of melasma in skin types III-V, although they recommend additional research with a larger sample size and longer treatment duration and follow-up (J. Drugs Dermatol. 2011;10:1025-31).
Paper mulberry
The bark of paper mulberry (Broussonetia papyrifera, also known as Morus papyrifera) is composed of extremely strong fibers used to produce high-quality paper and cloth. In China, the leaves, stem, leaf juice, roots, fruits, and bark have all been found to impart various health benefits, with the stem and leaf juice used to treat skin disorders and insect bites (Phytother. Res. 2012;26:1-10).
In one study, a 0.4% concentration of paper mulberry extract was demonstrated to suppress tyrosinase activity by 50% compared with 5.5% hydroquinone and 10% kojic acid. Notably, paper mulberry is not considered a significant irritant even at 1% concentration (J. Drugs Dermatol. 2009;8:s5-9).
White mulberry
In 2002, Lee et al. investigated the in vitro effects of an 85% methanol extract of dried white mulberry leaves on melanin biosynthesis. They found that one of the primary bioactive constituents, mulberroside F (moracin M-6, 3’-di-O-beta-D-glucopyranoside), inhibited the tyrosinase activity that converts dopa to dopachrome in the melanin synthesis process and also suppressed the melanin formation of melan-a cells. In addition, the mulberry extract inhibited tyrosinase activity more potently than did kojic acid (Biol. Pharm. Bull. 2002;25:1045-8).
The following year, a different team found that the young twigs of white mulberry also suppressed tyrosinase activity as well as melanin production in B-16 melanoma cells. In vivo, the extracts decreased melanin synthesis in a guinea pig model without displaying toxicity (J. Cosmet. Sci. 2003;54:133-42).
In 2006, Wang et al. investigated 25 traditional Chinese herbal medicines potentially useful in dermatology, particularly for skin whitening, and found that white mulberry was one of four species to potently inhibit tyrosinase activity, and more strongly than arbutin did (J. Ethnopharmacol. 2006;106:353-9).
Chinese mulberry/shimaguwa
In 2012, Zheng et al. isolated constituents from the roots of Chinese mulberry and found that several ingredients, including oxyresveratrol, moracenin D, sanggenon T, and kuwanon O, displayed more potent tyrosinase inhibition than kojic acid did. They concluded that Chinese mulberry is a good natural source of tyrosinase inhibitors and is potentially useful in cosmetic skin-lightening products as well as in foods as antibrowning agents (Fitoterapia 2012;83:1008-13).
Conclusion
Mulberry is actively used within the dermatologic armamentarium as one of the many options for skin lightening. A significant body of evidence has emerged over the past 15 years to establish the antityrosinase activity of various mulberry species, particularly white mulberry and paper mulberry.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in Miami Beach. She founded the cosmetic dermatology center at the University of Miami in 1997. Dr. Baumann wrote the textbook "Cosmetic Dermatology: Principles and Practice" (McGraw-Hill, 2009), and a book for consumers, "The Skin Type Solution" (Bantam, 2006). She has contributed to the Cosmeceutical Critique column in Skin & Allergy News since January 2001 and joined the editorial advisory board in 2004. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Galderma, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Stiefel, Topix Pharmaceuticals, and Unilever.
Often in this column, several species within a family might be discussed in relation to a broad range of health benefits. Licorice and mushrooms are good examples. In this case, and in this column, the focus will be on several species within a family that are thought to confer the same type of dermatologic benefit. The Morus genus within the Moraceae family appears to include several species that display skin-lightening properties.
Tyrosinase is the enzyme that controls the production of melanin. Suppressing tyrosinase activity to achieve skin lightening is a well-established method in dermatologic practice. The desire for products with fewer side effects than the mainstay, hydroquinone, or natural products such as kojic acid or arbutin, has led to investigations of several species in the Moraceae family. Notably, several Moraceae trees have been found to exhibit antioxidant activity (Int. J. Mol. Sci. 2012;13:2472-80; Biol. Pharm. Bull. 2002;25:1045-8; Biosci. Biotechnol. Biochem. 2010;74:2385-95; J. Pharm. Pharmacol. 2004;56:1291-8). The focus here, though, will be on the skin-lightening activity of various parts of Morus (commonly known as mulberry) trees.
In 2013, Singh et al. assessed the effects of mulberry, kiwi, and Sophora extracts on melanogenesis and melanin transfer in human melanocytes and in cocultures with phototype-matched normal adult epidermal keratinocytes. The extracts were evaluated against isobutylmethylxanthine, hydroquinone, vitamin C, and niacinamide. The investigators found that compared with unstimulated control, mulberry, kiwi, and Sophora extracts significantly reduced melanogenesis in normal adult epidermal melanocytes and human melanoma cells. Melanin transfer also was lowered, as was filopodia expression on melanocytes. The authors concluded that the test compounds compared well with standard-bearing depigmenting agents and warrant consideration as topical agents for diminishing hyperpigmentation (Exp. Dermatol. 2013;22:67-9).
Encouraging results in melasma treatment
A randomized, single-blind, placebo-controlled trial of 50 Filipino patients (49 women, 1 man) to examine the safety and efficacy of 75% Morus alba (white mulberry) extract oil was conducted by Alvin et al. in 2011. Patients were evaluated at weeks 4 and 8. The Melasma Area and Severity Index (MASI) score, Mexameter score, and Melasma Quality of Life (MelasQOL) score were measured, with the mulberry extract group performing significantly better than the placebo group according to all metrics.
The 25 patients treated with mulberry extract showed improvement in the MASI score, from 4.076 at baseline to 2.884 at week 8 (mean difference, 1.19); the mean difference for the placebo group was 0.06. The mean Mexameter reading revealed a significant difference, with a slight increase for the mulberry group (indicating lighter pigmentation), and the placebo group scored a slightly higher value. In addition, the MelasQOL score for the mulberry group improved markedly from baseline to week 8 (58.84 to 44.16), whereas the placebo group score improved only slightly, from 57.44 at baseline to 54.28 at week 8.
Adverse events were rare, with mild itching in 4 patients reported from the mulberry group, and 12 cases of either itching or erythema reported by the placebo group.
The investigators concluded that 75% mulberry extract oil objectively diminishes the hyperpigmentation of melasma in skin types III-V, although they recommend additional research with a larger sample size and longer treatment duration and follow-up (J. Drugs Dermatol. 2011;10:1025-31).
Paper mulberry
The bark of paper mulberry (Broussonetia papyrifera, also known as Morus papyrifera) is composed of extremely strong fibers used to produce high-quality paper and cloth. In China, the leaves, stem, leaf juice, roots, fruits, and bark have all been found to impart various health benefits, with the stem and leaf juice used to treat skin disorders and insect bites (Phytother. Res. 2012;26:1-10).
In one study, a 0.4% concentration of paper mulberry extract was demonstrated to suppress tyrosinase activity by 50% compared with 5.5% hydroquinone and 10% kojic acid. Notably, paper mulberry is not considered a significant irritant even at 1% concentration (J. Drugs Dermatol. 2009;8:s5-9).
White mulberry
In 2002, Lee et al. investigated the in vitro effects of an 85% methanol extract of dried white mulberry leaves on melanin biosynthesis. They found that one of the primary bioactive constituents, mulberroside F (moracin M-6, 3’-di-O-beta-D-glucopyranoside), inhibited the tyrosinase activity that converts dopa to dopachrome in the melanin synthesis process and also suppressed the melanin formation of melan-a cells. In addition, the mulberry extract inhibited tyrosinase activity more potently than did kojic acid (Biol. Pharm. Bull. 2002;25:1045-8).
The following year, a different team found that the young twigs of white mulberry also suppressed tyrosinase activity as well as melanin production in B-16 melanoma cells. In vivo, the extracts decreased melanin synthesis in a guinea pig model without displaying toxicity (J. Cosmet. Sci. 2003;54:133-42).
In 2006, Wang et al. investigated 25 traditional Chinese herbal medicines potentially useful in dermatology, particularly for skin whitening, and found that white mulberry was one of four species to potently inhibit tyrosinase activity, and more strongly than arbutin did (J. Ethnopharmacol. 2006;106:353-9).
Chinese mulberry/shimaguwa
In 2012, Zheng et al. isolated constituents from the roots of Chinese mulberry and found that several ingredients, including oxyresveratrol, moracenin D, sanggenon T, and kuwanon O, displayed more potent tyrosinase inhibition than kojic acid did. They concluded that Chinese mulberry is a good natural source of tyrosinase inhibitors and is potentially useful in cosmetic skin-lightening products as well as in foods as antibrowning agents (Fitoterapia 2012;83:1008-13).
Conclusion
Mulberry is actively used within the dermatologic armamentarium as one of the many options for skin lightening. A significant body of evidence has emerged over the past 15 years to establish the antityrosinase activity of various mulberry species, particularly white mulberry and paper mulberry.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in Miami Beach. She founded the cosmetic dermatology center at the University of Miami in 1997. Dr. Baumann wrote the textbook "Cosmetic Dermatology: Principles and Practice" (McGraw-Hill, 2009), and a book for consumers, "The Skin Type Solution" (Bantam, 2006). She has contributed to the Cosmeceutical Critique column in Skin & Allergy News since January 2001 and joined the editorial advisory board in 2004. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Galderma, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Stiefel, Topix Pharmaceuticals, and Unilever.
Often in this column, several species within a family might be discussed in relation to a broad range of health benefits. Licorice and mushrooms are good examples. In this case, and in this column, the focus will be on several species within a family that are thought to confer the same type of dermatologic benefit. The Morus genus within the Moraceae family appears to include several species that display skin-lightening properties.
Tyrosinase is the enzyme that controls the production of melanin. Suppressing tyrosinase activity to achieve skin lightening is a well-established method in dermatologic practice. The desire for products with fewer side effects than the mainstay, hydroquinone, or natural products such as kojic acid or arbutin, has led to investigations of several species in the Moraceae family. Notably, several Moraceae trees have been found to exhibit antioxidant activity (Int. J. Mol. Sci. 2012;13:2472-80; Biol. Pharm. Bull. 2002;25:1045-8; Biosci. Biotechnol. Biochem. 2010;74:2385-95; J. Pharm. Pharmacol. 2004;56:1291-8). The focus here, though, will be on the skin-lightening activity of various parts of Morus (commonly known as mulberry) trees.
In 2013, Singh et al. assessed the effects of mulberry, kiwi, and Sophora extracts on melanogenesis and melanin transfer in human melanocytes and in cocultures with phototype-matched normal adult epidermal keratinocytes. The extracts were evaluated against isobutylmethylxanthine, hydroquinone, vitamin C, and niacinamide. The investigators found that compared with unstimulated control, mulberry, kiwi, and Sophora extracts significantly reduced melanogenesis in normal adult epidermal melanocytes and human melanoma cells. Melanin transfer also was lowered, as was filopodia expression on melanocytes. The authors concluded that the test compounds compared well with standard-bearing depigmenting agents and warrant consideration as topical agents for diminishing hyperpigmentation (Exp. Dermatol. 2013;22:67-9).
Encouraging results in melasma treatment
A randomized, single-blind, placebo-controlled trial of 50 Filipino patients (49 women, 1 man) to examine the safety and efficacy of 75% Morus alba (white mulberry) extract oil was conducted by Alvin et al. in 2011. Patients were evaluated at weeks 4 and 8. The Melasma Area and Severity Index (MASI) score, Mexameter score, and Melasma Quality of Life (MelasQOL) score were measured, with the mulberry extract group performing significantly better than the placebo group according to all metrics.
The 25 patients treated with mulberry extract showed improvement in the MASI score, from 4.076 at baseline to 2.884 at week 8 (mean difference, 1.19); the mean difference for the placebo group was 0.06. The mean Mexameter reading revealed a significant difference, with a slight increase for the mulberry group (indicating lighter pigmentation), and the placebo group scored a slightly higher value. In addition, the MelasQOL score for the mulberry group improved markedly from baseline to week 8 (58.84 to 44.16), whereas the placebo group score improved only slightly, from 57.44 at baseline to 54.28 at week 8.
Adverse events were rare, with mild itching in 4 patients reported from the mulberry group, and 12 cases of either itching or erythema reported by the placebo group.
The investigators concluded that 75% mulberry extract oil objectively diminishes the hyperpigmentation of melasma in skin types III-V, although they recommend additional research with a larger sample size and longer treatment duration and follow-up (J. Drugs Dermatol. 2011;10:1025-31).
Paper mulberry
The bark of paper mulberry (Broussonetia papyrifera, also known as Morus papyrifera) is composed of extremely strong fibers used to produce high-quality paper and cloth. In China, the leaves, stem, leaf juice, roots, fruits, and bark have all been found to impart various health benefits, with the stem and leaf juice used to treat skin disorders and insect bites (Phytother. Res. 2012;26:1-10).
In one study, a 0.4% concentration of paper mulberry extract was demonstrated to suppress tyrosinase activity by 50% compared with 5.5% hydroquinone and 10% kojic acid. Notably, paper mulberry is not considered a significant irritant even at 1% concentration (J. Drugs Dermatol. 2009;8:s5-9).
White mulberry
In 2002, Lee et al. investigated the in vitro effects of an 85% methanol extract of dried white mulberry leaves on melanin biosynthesis. They found that one of the primary bioactive constituents, mulberroside F (moracin M-6, 3’-di-O-beta-D-glucopyranoside), inhibited the tyrosinase activity that converts dopa to dopachrome in the melanin synthesis process and also suppressed the melanin formation of melan-a cells. In addition, the mulberry extract inhibited tyrosinase activity more potently than did kojic acid (Biol. Pharm. Bull. 2002;25:1045-8).
The following year, a different team found that the young twigs of white mulberry also suppressed tyrosinase activity as well as melanin production in B-16 melanoma cells. In vivo, the extracts decreased melanin synthesis in a guinea pig model without displaying toxicity (J. Cosmet. Sci. 2003;54:133-42).
In 2006, Wang et al. investigated 25 traditional Chinese herbal medicines potentially useful in dermatology, particularly for skin whitening, and found that white mulberry was one of four species to potently inhibit tyrosinase activity, and more strongly than arbutin did (J. Ethnopharmacol. 2006;106:353-9).
Chinese mulberry/shimaguwa
In 2012, Zheng et al. isolated constituents from the roots of Chinese mulberry and found that several ingredients, including oxyresveratrol, moracenin D, sanggenon T, and kuwanon O, displayed more potent tyrosinase inhibition than kojic acid did. They concluded that Chinese mulberry is a good natural source of tyrosinase inhibitors and is potentially useful in cosmetic skin-lightening products as well as in foods as antibrowning agents (Fitoterapia 2012;83:1008-13).
Conclusion
Mulberry is actively used within the dermatologic armamentarium as one of the many options for skin lightening. A significant body of evidence has emerged over the past 15 years to establish the antityrosinase activity of various mulberry species, particularly white mulberry and paper mulberry.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in Miami Beach. She founded the cosmetic dermatology center at the University of Miami in 1997. Dr. Baumann wrote the textbook "Cosmetic Dermatology: Principles and Practice" (McGraw-Hill, 2009), and a book for consumers, "The Skin Type Solution" (Bantam, 2006). She has contributed to the Cosmeceutical Critique column in Skin & Allergy News since January 2001 and joined the editorial advisory board in 2004. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Galderma, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Stiefel, Topix Pharmaceuticals, and Unilever.
Tamanu oil
Calophyllum inophyllum is a large, nondeciduous tree native to a wide swath of regions including Central and East Africa; a north-to-south swath of India; Southeast Asia; Polynesia; the Philippines; and Australia. A member of the mangosteen family (Clusiaceae, also known as Guttiferae), C. inophyllum is now cultivated in much of the tropical world.
The oil derived from this abundant plant is known by a wide variety of names, including Alexandrian laurel, beach mahogany, beauty leaf, beach calophyllum, dilo, and kamani. But perhaps it is best known by the French Polynesian name: tamanu. Tamanu oil has been used for hundreds of years in cuisine and to treat various medical conditions. Ocular burn and cutaneous wound healing are some distinct conditions for which the oil of C. inophyllum has a long history of use in traditional folk medicine (Oncol. Rep. 2012;28:1096-102; Int. J. Cosmet. Sci. 2002;24:341-8).
Wound healing and eye protection
The C. inophyllum components to which wound-healing activity have been attributed include calophyllolide and inophyllum, as well as various polyphenols, many of which exert antioxidant effects (Int. J. Cosmet. Sci. 2002;24:341-8).
Modern research buttresses the use of tamanu oil for corneal protection from burns. In 2007, Said et al. explored the anti-UV activity of tamanu oil for eye protection. They found that the botanical oil displayed a significant capacity to absorb UV radiation, even at low concentrations (1/10,000, v/v), with a sun protection factor ranging from 18 to 22. Concentrations of C. inophyllum oil of up to 1% were not cytotoxic to human conjunctival epithelial cells, with the agent acting against oxidative stress and DNA damage. In light of the apparent antioxidant and cytoprotective effects of C. inophyllum oil in the study, the researchers concluded that the oil has potential as a natural UV filter in ophthalmic formulations (Eur. J. Pharm. Sci. 2007;30:203-10).
In 2009, Said et al. performed in vitro, in vivo, and ex vivo studies to assess the effects of different rinsing and healing protocols for alkali-induced ocular burn and inflammation in rabbits. The researchers used NaOH to induce corneal reactions in the rabbits, followed by rinses with NaCl 0.9% or controlled-ionization marine formula combined with N-acetylcysteine or vegetable oils (from C. inophyllum and Aleurites moluccana). The investigators assessed corneal epithelium regeneration and inflammatory cell infiltration using in vivo confocal microscopy and ex vivo histological cuts. They found that the combination of controlled-ionization marine solution with 10% C. inophyllum oil and 90% A. moluccana oil promoted corneal epithelium regeneration while reducing inflammatory cells, suggesting its viability as ocular burn therapy (Ophthalmologica 2009;223:52-9).
Other medical benefits
A wide range of health benefits have been ascribed to tamanu oil, and the ingredient has been found in an increasing number of topical products. It is thought to impart anti-inflammatory, antioxidant, antibacterial, antiviral, and photoprotective activity.
In 2011, Ayyanar et al. concluded a 4-year study intended to ascertain the herbs used in traditional medicine practiced by the Kani tribes in the Tirunelveli hills of Western Ghats, India. The researchers identified 90 species of plants used traditionally as ethnomedicinal treatments, with 65 different indications reported, particularly dermatologic conditions and gastrointestinal illnesses. Based on their study, they identified 16 species, including C. inophyllum, for additional ethnopharmacological investigation as potential sources of new drug agents (J. Ethnopharmacol. 2011;134:851-64).
In 2004, Yimdjo et al. investigated the chemical constituents of the root bark and nut of C. inophyllum, resulting in the isolation of several compounds and the discovery of antibacterial activity against several microbes (Phytochemistry 2004;65:2789-95).
C. inophyllum leaf extracts from the islands of French Polynesia have also been touted for several constituents that hold promise as anti-HIV-1 agents, including inophyllum B and P (Anal. Chim. Acta 2008;624:147-53). In addition, quantitative high-performance liquid chromatography (HPLC) analysis of callus cultures of C. inophyllum has revealed the anti-HIV activity of the dipyranocoumarins inophyllum B and P (J. Biotechnol. 2007;130:346-53).
Tamanu oil also has demonstrated potential use for humans and domestic animals as an insect repellent, specifically against the stable fly, Stomoxys calcitrans (J. Med. Entomol. 2010;47:575-80; Pest Manag. Sci. 2010;66:1191-8).
In 2012, Tsai et al. investigated the anti-inflammatory properties of an acetone extract of C. inophyllum leaves using lipopolysaccharide (LPS)-induced RAW 264.7 cells to assess the impact of the extract on nitric oxide (NO) expression and inducible nitric oxide synthase (iNOS). They found that C. inophyllum significantly inhibited, in dose-dependent fashion, the LPS-induced synthesis of NO, in addition to the expression of iNOS, cyclooxygenase (COX)-2, and nuclear factor–kappa B (NF-kappaB). The researchers concluded that the C. inophyllum extract exhibits anti-inflammatory activity and has potential application to inflammatory conditions in human beings (Oncol. Rep. 2012;28:1096-102).
Cancer
Recent work suggests the anti-cancer potential of C. inophyllum. In a study just over a decade ago, Itogawa et al. examined the potential inhibitory effects of C. inophyllum 4-phenylcoumarin isolates on Epstein-Barr virus early antigen (EBV-EA) activation caused by 12-O-tetradecanoylphorbol-13-acetate in Raji cells. All 10 of the isolates displayed inhibitory activity against EBV and no cytotoxicity. The strongest compound tested was calocoumarin-A (5), which also demonstrated a significant capacity to suppress murine skin tumor promotion in a two-stage cancer model. The investigators concluded that some 4-phenylcoumarin constituents of C. inophyllum warrant further study as possible antitumor agents (Cancer Lett. 2001;169:15-19).
C. inophyllum was one of 155 extracts from 93 plant species found on peninsular Malaysia during a screening by Ong et al. in 2009 for in vitro photocytotoxic activity using human leukemia cells (cell line HL60). Further, C. inophyllum was among the 29 plants to lower the in vitro cell viability by more than 50% after exposure to 9.6 J/cm2 of a broad-spectrum light when tested at a concentration of 20 mcg/mL (J. Photochem. Photobiol. B 2009;96:216-22). In addition, Li et al. isolated one new friedelane-type triterpene and seven previously discovered triterpenoids from the stems and leaves of C. inophyllum, and ascertained that they exhibited growth inhibitory activity against human leukemia HL-60 cells (Fitoterapia 2010;81:586-9).
In 2008, Xiao et al. isolated a new prenylated xanthone (caloxanthone) as well as two previously known xanthones from the ethanolic extract of C. inophyllum twigs and reported that two of the constituents (including the new xanthone) demonstrated cytotoxicity against myelogenous leukemia (cell line K562) (J. Asian Nat. Prod. Res. 2008;10:993-7).
C. inophyllum is known to contain an abundance of phytosterols – primarily stigmasterol and beta-sitosterol, which are steroids associated with several healthy benefits (stigmasterol is a potent antioxidant) – as well as delta-tocotrienol, a form of vitamin E that acts as an antioxidant and is associated with anticancer activity, particularly against murine melanoma (Phytochemistry 2005;66:1825-31; J. Nutr. 1997;127:668-74).
Conclusion
Tamanu oil certainly isn’t a passing fad for the numerous traditional societies in the mainly eastern and southern hemispheres who have used the botanical for medicinal and culinary purposes for centuries. As an ingredient in skin care products, though, more research is needed. While modern studies are promising, randomized, placebo-controlled clinical trials are necessary to establish a potential role of C. inophyllum in the large array of topical dermatologic formulations.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in Miami Beach. She has received funding for clinical grants from Allergan, Aveeno, Avon Products, Galderma, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Stiefel, Topix Pharmaceuticals, and Unilever. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
Calophyllum inophyllum is a large, nondeciduous tree native to a wide swath of regions including Central and East Africa; a north-to-south swath of India; Southeast Asia; Polynesia; the Philippines; and Australia. A member of the mangosteen family (Clusiaceae, also known as Guttiferae), C. inophyllum is now cultivated in much of the tropical world.
The oil derived from this abundant plant is known by a wide variety of names, including Alexandrian laurel, beach mahogany, beauty leaf, beach calophyllum, dilo, and kamani. But perhaps it is best known by the French Polynesian name: tamanu. Tamanu oil has been used for hundreds of years in cuisine and to treat various medical conditions. Ocular burn and cutaneous wound healing are some distinct conditions for which the oil of C. inophyllum has a long history of use in traditional folk medicine (Oncol. Rep. 2012;28:1096-102; Int. J. Cosmet. Sci. 2002;24:341-8).
Wound healing and eye protection
The C. inophyllum components to which wound-healing activity have been attributed include calophyllolide and inophyllum, as well as various polyphenols, many of which exert antioxidant effects (Int. J. Cosmet. Sci. 2002;24:341-8).
Modern research buttresses the use of tamanu oil for corneal protection from burns. In 2007, Said et al. explored the anti-UV activity of tamanu oil for eye protection. They found that the botanical oil displayed a significant capacity to absorb UV radiation, even at low concentrations (1/10,000, v/v), with a sun protection factor ranging from 18 to 22. Concentrations of C. inophyllum oil of up to 1% were not cytotoxic to human conjunctival epithelial cells, with the agent acting against oxidative stress and DNA damage. In light of the apparent antioxidant and cytoprotective effects of C. inophyllum oil in the study, the researchers concluded that the oil has potential as a natural UV filter in ophthalmic formulations (Eur. J. Pharm. Sci. 2007;30:203-10).
In 2009, Said et al. performed in vitro, in vivo, and ex vivo studies to assess the effects of different rinsing and healing protocols for alkali-induced ocular burn and inflammation in rabbits. The researchers used NaOH to induce corneal reactions in the rabbits, followed by rinses with NaCl 0.9% or controlled-ionization marine formula combined with N-acetylcysteine or vegetable oils (from C. inophyllum and Aleurites moluccana). The investigators assessed corneal epithelium regeneration and inflammatory cell infiltration using in vivo confocal microscopy and ex vivo histological cuts. They found that the combination of controlled-ionization marine solution with 10% C. inophyllum oil and 90% A. moluccana oil promoted corneal epithelium regeneration while reducing inflammatory cells, suggesting its viability as ocular burn therapy (Ophthalmologica 2009;223:52-9).
Other medical benefits
A wide range of health benefits have been ascribed to tamanu oil, and the ingredient has been found in an increasing number of topical products. It is thought to impart anti-inflammatory, antioxidant, antibacterial, antiviral, and photoprotective activity.
In 2011, Ayyanar et al. concluded a 4-year study intended to ascertain the herbs used in traditional medicine practiced by the Kani tribes in the Tirunelveli hills of Western Ghats, India. The researchers identified 90 species of plants used traditionally as ethnomedicinal treatments, with 65 different indications reported, particularly dermatologic conditions and gastrointestinal illnesses. Based on their study, they identified 16 species, including C. inophyllum, for additional ethnopharmacological investigation as potential sources of new drug agents (J. Ethnopharmacol. 2011;134:851-64).
In 2004, Yimdjo et al. investigated the chemical constituents of the root bark and nut of C. inophyllum, resulting in the isolation of several compounds and the discovery of antibacterial activity against several microbes (Phytochemistry 2004;65:2789-95).
C. inophyllum leaf extracts from the islands of French Polynesia have also been touted for several constituents that hold promise as anti-HIV-1 agents, including inophyllum B and P (Anal. Chim. Acta 2008;624:147-53). In addition, quantitative high-performance liquid chromatography (HPLC) analysis of callus cultures of C. inophyllum has revealed the anti-HIV activity of the dipyranocoumarins inophyllum B and P (J. Biotechnol. 2007;130:346-53).
Tamanu oil also has demonstrated potential use for humans and domestic animals as an insect repellent, specifically against the stable fly, Stomoxys calcitrans (J. Med. Entomol. 2010;47:575-80; Pest Manag. Sci. 2010;66:1191-8).
In 2012, Tsai et al. investigated the anti-inflammatory properties of an acetone extract of C. inophyllum leaves using lipopolysaccharide (LPS)-induced RAW 264.7 cells to assess the impact of the extract on nitric oxide (NO) expression and inducible nitric oxide synthase (iNOS). They found that C. inophyllum significantly inhibited, in dose-dependent fashion, the LPS-induced synthesis of NO, in addition to the expression of iNOS, cyclooxygenase (COX)-2, and nuclear factor–kappa B (NF-kappaB). The researchers concluded that the C. inophyllum extract exhibits anti-inflammatory activity and has potential application to inflammatory conditions in human beings (Oncol. Rep. 2012;28:1096-102).
Cancer
Recent work suggests the anti-cancer potential of C. inophyllum. In a study just over a decade ago, Itogawa et al. examined the potential inhibitory effects of C. inophyllum 4-phenylcoumarin isolates on Epstein-Barr virus early antigen (EBV-EA) activation caused by 12-O-tetradecanoylphorbol-13-acetate in Raji cells. All 10 of the isolates displayed inhibitory activity against EBV and no cytotoxicity. The strongest compound tested was calocoumarin-A (5), which also demonstrated a significant capacity to suppress murine skin tumor promotion in a two-stage cancer model. The investigators concluded that some 4-phenylcoumarin constituents of C. inophyllum warrant further study as possible antitumor agents (Cancer Lett. 2001;169:15-19).
C. inophyllum was one of 155 extracts from 93 plant species found on peninsular Malaysia during a screening by Ong et al. in 2009 for in vitro photocytotoxic activity using human leukemia cells (cell line HL60). Further, C. inophyllum was among the 29 plants to lower the in vitro cell viability by more than 50% after exposure to 9.6 J/cm2 of a broad-spectrum light when tested at a concentration of 20 mcg/mL (J. Photochem. Photobiol. B 2009;96:216-22). In addition, Li et al. isolated one new friedelane-type triterpene and seven previously discovered triterpenoids from the stems and leaves of C. inophyllum, and ascertained that they exhibited growth inhibitory activity against human leukemia HL-60 cells (Fitoterapia 2010;81:586-9).
In 2008, Xiao et al. isolated a new prenylated xanthone (caloxanthone) as well as two previously known xanthones from the ethanolic extract of C. inophyllum twigs and reported that two of the constituents (including the new xanthone) demonstrated cytotoxicity against myelogenous leukemia (cell line K562) (J. Asian Nat. Prod. Res. 2008;10:993-7).
C. inophyllum is known to contain an abundance of phytosterols – primarily stigmasterol and beta-sitosterol, which are steroids associated with several healthy benefits (stigmasterol is a potent antioxidant) – as well as delta-tocotrienol, a form of vitamin E that acts as an antioxidant and is associated with anticancer activity, particularly against murine melanoma (Phytochemistry 2005;66:1825-31; J. Nutr. 1997;127:668-74).
Conclusion
Tamanu oil certainly isn’t a passing fad for the numerous traditional societies in the mainly eastern and southern hemispheres who have used the botanical for medicinal and culinary purposes for centuries. As an ingredient in skin care products, though, more research is needed. While modern studies are promising, randomized, placebo-controlled clinical trials are necessary to establish a potential role of C. inophyllum in the large array of topical dermatologic formulations.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in Miami Beach. She has received funding for clinical grants from Allergan, Aveeno, Avon Products, Galderma, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Stiefel, Topix Pharmaceuticals, and Unilever. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
Calophyllum inophyllum is a large, nondeciduous tree native to a wide swath of regions including Central and East Africa; a north-to-south swath of India; Southeast Asia; Polynesia; the Philippines; and Australia. A member of the mangosteen family (Clusiaceae, also known as Guttiferae), C. inophyllum is now cultivated in much of the tropical world.
The oil derived from this abundant plant is known by a wide variety of names, including Alexandrian laurel, beach mahogany, beauty leaf, beach calophyllum, dilo, and kamani. But perhaps it is best known by the French Polynesian name: tamanu. Tamanu oil has been used for hundreds of years in cuisine and to treat various medical conditions. Ocular burn and cutaneous wound healing are some distinct conditions for which the oil of C. inophyllum has a long history of use in traditional folk medicine (Oncol. Rep. 2012;28:1096-102; Int. J. Cosmet. Sci. 2002;24:341-8).
Wound healing and eye protection
The C. inophyllum components to which wound-healing activity have been attributed include calophyllolide and inophyllum, as well as various polyphenols, many of which exert antioxidant effects (Int. J. Cosmet. Sci. 2002;24:341-8).
Modern research buttresses the use of tamanu oil for corneal protection from burns. In 2007, Said et al. explored the anti-UV activity of tamanu oil for eye protection. They found that the botanical oil displayed a significant capacity to absorb UV radiation, even at low concentrations (1/10,000, v/v), with a sun protection factor ranging from 18 to 22. Concentrations of C. inophyllum oil of up to 1% were not cytotoxic to human conjunctival epithelial cells, with the agent acting against oxidative stress and DNA damage. In light of the apparent antioxidant and cytoprotective effects of C. inophyllum oil in the study, the researchers concluded that the oil has potential as a natural UV filter in ophthalmic formulations (Eur. J. Pharm. Sci. 2007;30:203-10).
In 2009, Said et al. performed in vitro, in vivo, and ex vivo studies to assess the effects of different rinsing and healing protocols for alkali-induced ocular burn and inflammation in rabbits. The researchers used NaOH to induce corneal reactions in the rabbits, followed by rinses with NaCl 0.9% or controlled-ionization marine formula combined with N-acetylcysteine or vegetable oils (from C. inophyllum and Aleurites moluccana). The investigators assessed corneal epithelium regeneration and inflammatory cell infiltration using in vivo confocal microscopy and ex vivo histological cuts. They found that the combination of controlled-ionization marine solution with 10% C. inophyllum oil and 90% A. moluccana oil promoted corneal epithelium regeneration while reducing inflammatory cells, suggesting its viability as ocular burn therapy (Ophthalmologica 2009;223:52-9).
Other medical benefits
A wide range of health benefits have been ascribed to tamanu oil, and the ingredient has been found in an increasing number of topical products. It is thought to impart anti-inflammatory, antioxidant, antibacterial, antiviral, and photoprotective activity.
In 2011, Ayyanar et al. concluded a 4-year study intended to ascertain the herbs used in traditional medicine practiced by the Kani tribes in the Tirunelveli hills of Western Ghats, India. The researchers identified 90 species of plants used traditionally as ethnomedicinal treatments, with 65 different indications reported, particularly dermatologic conditions and gastrointestinal illnesses. Based on their study, they identified 16 species, including C. inophyllum, for additional ethnopharmacological investigation as potential sources of new drug agents (J. Ethnopharmacol. 2011;134:851-64).
In 2004, Yimdjo et al. investigated the chemical constituents of the root bark and nut of C. inophyllum, resulting in the isolation of several compounds and the discovery of antibacterial activity against several microbes (Phytochemistry 2004;65:2789-95).
C. inophyllum leaf extracts from the islands of French Polynesia have also been touted for several constituents that hold promise as anti-HIV-1 agents, including inophyllum B and P (Anal. Chim. Acta 2008;624:147-53). In addition, quantitative high-performance liquid chromatography (HPLC) analysis of callus cultures of C. inophyllum has revealed the anti-HIV activity of the dipyranocoumarins inophyllum B and P (J. Biotechnol. 2007;130:346-53).
Tamanu oil also has demonstrated potential use for humans and domestic animals as an insect repellent, specifically against the stable fly, Stomoxys calcitrans (J. Med. Entomol. 2010;47:575-80; Pest Manag. Sci. 2010;66:1191-8).
In 2012, Tsai et al. investigated the anti-inflammatory properties of an acetone extract of C. inophyllum leaves using lipopolysaccharide (LPS)-induced RAW 264.7 cells to assess the impact of the extract on nitric oxide (NO) expression and inducible nitric oxide synthase (iNOS). They found that C. inophyllum significantly inhibited, in dose-dependent fashion, the LPS-induced synthesis of NO, in addition to the expression of iNOS, cyclooxygenase (COX)-2, and nuclear factor–kappa B (NF-kappaB). The researchers concluded that the C. inophyllum extract exhibits anti-inflammatory activity and has potential application to inflammatory conditions in human beings (Oncol. Rep. 2012;28:1096-102).
Cancer
Recent work suggests the anti-cancer potential of C. inophyllum. In a study just over a decade ago, Itogawa et al. examined the potential inhibitory effects of C. inophyllum 4-phenylcoumarin isolates on Epstein-Barr virus early antigen (EBV-EA) activation caused by 12-O-tetradecanoylphorbol-13-acetate in Raji cells. All 10 of the isolates displayed inhibitory activity against EBV and no cytotoxicity. The strongest compound tested was calocoumarin-A (5), which also demonstrated a significant capacity to suppress murine skin tumor promotion in a two-stage cancer model. The investigators concluded that some 4-phenylcoumarin constituents of C. inophyllum warrant further study as possible antitumor agents (Cancer Lett. 2001;169:15-19).
C. inophyllum was one of 155 extracts from 93 plant species found on peninsular Malaysia during a screening by Ong et al. in 2009 for in vitro photocytotoxic activity using human leukemia cells (cell line HL60). Further, C. inophyllum was among the 29 plants to lower the in vitro cell viability by more than 50% after exposure to 9.6 J/cm2 of a broad-spectrum light when tested at a concentration of 20 mcg/mL (J. Photochem. Photobiol. B 2009;96:216-22). In addition, Li et al. isolated one new friedelane-type triterpene and seven previously discovered triterpenoids from the stems and leaves of C. inophyllum, and ascertained that they exhibited growth inhibitory activity against human leukemia HL-60 cells (Fitoterapia 2010;81:586-9).
In 2008, Xiao et al. isolated a new prenylated xanthone (caloxanthone) as well as two previously known xanthones from the ethanolic extract of C. inophyllum twigs and reported that two of the constituents (including the new xanthone) demonstrated cytotoxicity against myelogenous leukemia (cell line K562) (J. Asian Nat. Prod. Res. 2008;10:993-7).
C. inophyllum is known to contain an abundance of phytosterols – primarily stigmasterol and beta-sitosterol, which are steroids associated with several healthy benefits (stigmasterol is a potent antioxidant) – as well as delta-tocotrienol, a form of vitamin E that acts as an antioxidant and is associated with anticancer activity, particularly against murine melanoma (Phytochemistry 2005;66:1825-31; J. Nutr. 1997;127:668-74).
Conclusion
Tamanu oil certainly isn’t a passing fad for the numerous traditional societies in the mainly eastern and southern hemispheres who have used the botanical for medicinal and culinary purposes for centuries. As an ingredient in skin care products, though, more research is needed. While modern studies are promising, randomized, placebo-controlled clinical trials are necessary to establish a potential role of C. inophyllum in the large array of topical dermatologic formulations.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in Miami Beach. She has received funding for clinical grants from Allergan, Aveeno, Avon Products, Galderma, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Stiefel, Topix Pharmaceuticals, and Unilever. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
Blue light
Photodynamic light therapies (PDLs) have emerged as significant adjuvant approaches for treating acne. In particular, such therapies have been used for acne refractory to standard retinoid or combined retinoid and antimicrobial regimens. Why write about PDL in a column devoted to topical cosmeceutical products and ingredients? Blue light warrants inclusion because it has been studied in comparison to topical cosmeceutical treatments, and it is used in conjunction with other topical approaches.
Blue light exerts a phototoxic effect on the heme metabolism of Propionibacterium acnes, and it is considered effective by targeting part of the etiologic pathway of acne. It has become a widely used option for inflammatory acne (J. Drugs. Dermatol. 2006;5:605-10).
Early work
In 1990, Meffert et al. were the first to show that a blue light–type, high-pressure lamp could improve acne and seborrhea (10 10-minute treatments, cumulative light dose 325 J/cm2). Given the copious amounts of porphyrins stored in lipophilic P. acnes, the technology could be targeted to destroy propionibacteria, and the researchers observed a decline in the porphyrin content inside acne follicles. They concluded that short-range visible light (400-420 nm) was a viable option for acne treatment during the light-poor season of the year (Dermatol. Monatsschr. 1990;176:597-603). It was subsequently established that treatment with UV-free blue light in the range of 405-420 nm leads to the elimination of acne bacteria by virtue of the effects on the porphyrins generated naturally by P. acnes (J. Cosmet. Laser. Ther. 2003;5:111-7). Notably, blue light appears to photoinactivate P. acnes, but it does not penetrate deeply into the skin (Dermatol. Online J. 2011;17:2).
In an open study of the then-novel high-intensity, enhanced, narrow-band, blue-light phototherapy, Kawada et al. treated 30 acne patients (27 female, 3 male) twice a week for up to 5 weeks. A reduction of 64% was seen in acne lesions, and in vitro data showed a significant decline in P. acnes, but not in Staphylococcus epidermidis (J. Dermatol. Sci. 2002;30:129-35).
Mechanism of action
In 2006, Shnitkind et al. studied the effect of narrow-band blue light on the inflammatory process in the presence and absence of cytokines and ultraviolet B using interleukin-1 alpha (IL-1alpha) and intercellular adhesion molecule 1 (ICAM-1) as markers for inflammation. They found that blue light treatment of HaCaT and hTERT cells decreased levels of IL-1alpha by 82% in HaCaT and by 75% in hTERT. When blue light was combined with ultraviolet B, the respective reductions were 95% and 91%. Similar reductions in ICAM-1 expression were seen in HaCaT, but not in hTERT. The researchers concluded that narrow-band blue light exerts anti-inflammatory effects on keratinocytes by reducing cytokine-induced synthesis of IL-1alpha and ICAM-1. They suggested that these findings imply a broader range of effects is exerted on the inflammatory process by narrow-band blue light than previously understood (J. Drugs. Dermatol. 2006;5:605-10).
Comparison studies
In 2000, Papageorgiou et al. randomized 107 patients with mild to moderate acne to four treatment groups: blue light (peak at 415 nm), mixed blue and red light (peaks at 415 and 660 nm), cool white light, and 5% benzoyl peroxide cream, for 12 weeks of active treatment. Phototherapy using portable light sources was conducted daily for 15 minutes; comparative assessments among the three phototherapy groups were done with observers blinded. The investigators found that the greatest improvement in acne lesions occurred in the blue and red light combined group. The blue/red treatment was significantly superior to blue light alone at 4 and 8 weeks but not 12 weeks, benzoyl peroxide at weeks 8 and 12, and white light at all assessments (Br. J. Dermatol. 2000;142:973-8).
Gold et al. performed a multicenter clinical evaluation comparing blue light to topical 1% clindamycin solution with respect to safety and efficacy. They found that clindamycin was associated with a 14% reduction of inflammatory lesions, but blue light reduced such lesions by an average of 34% (J. Drugs. Dermatol. 2005;4:64-70).
In another study, 20 patients with moderate to severe facial acne were treated in four weekly sessions with topical aminolevulinic acid (ALA)-photodynamic therapy with blue light (415 nm) on the right side of the face, or blue light alone on the left side of the face. At 4, 8, 12, and 16 weeks after the start of treatment, the mean percent reductions in inflamed lesions were higher in the ALA-PDT areas (32%, 50.9%, 65.9%, and 71.1%, respectively) than in the blue light–only treatment areas (20.7%, 27%, 57.7%, and 56.7%), but the differences were not statistically significant. Side effects, which included pain, stinging, erythema, itching, peeling, oozing, and pustules, were more pronounced in the areas treated with ALA-PDT (Photodermatol. Photoimmunol. Photomed. 2007;23:186-90).
However, in a 2007 study of 22 patients with moderate to severe acne randomized to one of three ALA-PDT treatments – intense pulsed light (IPL; 600-850 nm), a combination of IPL (580-980 nm) and bipolar radiofrequency (RF) energies, or blue light (417 nm) – in three sessions at 2-week intervals, ALA-PDT with activation by IPL yielded the most consistent, lasting improvement in moderate to severe acne (J. Drugs Dermatol. 2007;6:1010-6).
In a study of 60 volunteers with facial acne (grades II and III), de Arruda et al. compared the safety and efficacy of blue light to topical benzoyl peroxide 5% over 4 weeks. Thirty patients received blue light treatment twice a week, and the other 30 self-applied the topical formulation twice daily. The improvements were similar in both groups, but side effects were milder in the blue light group (An. Bras. Dermatol. 2009;84:463-8).
Choi et al. compared the bactericidal effects of 5-aminolevulinic acid (ALA) with blue and red light on P. acnes and found that blue light was more effective than red light phototherapy in eliminating the bacteria unless ALA was added, which substantially augmented red light phototherapy efficacy (J. Dermatol. 2011;38:661-6).
In summarizing the off-label uses of light-based treatments and PDT using topical precursors of porphyrins, Sakamoto et al. observed that blue light alone lessens acne severity due to anti-inflammatory effects; PDT using 5-ALA or ALA derivatives provides antimicrobial and anti-inflammatory activity; and, at high doses, red-light PDT may suppress or eradicate sebaceous glands, yielding clinical improvement (J. Am. Acad. Dermatol. 2010;63:183-93).
Combination therapy
In 2011, Wheeland and Dhawan assessed the efficacy and tolerability of treating mild to moderate facial acne using a novel, handheld, light-emitting diode (LED) blue-light device, along with a foam cleanser containing 5% glycolic acid and 2% salicylic acid, plus a serum containing 1.25% salicylic acid, 0.5% niacinamide, 0.08% liposomal-based azelaic acid, and superoxide dismutase. In all, 28 of 35 adults aged 25-45 years completed the 8-week study, in which they used the device twice daily (in addition to the cleanser before treatments and the serum after nighttime treatments). Significant reductions in inflammatory lesion counts were seen from week 1 onward, and significant reductions in noninflammatory lesion counts were seen from week 4 onward compared with baseline counts. The number and severity of flares were significantly reduced from baseline as well.
Therapy was well received by patients, with more than 90% claiming improvement in overall skin appearance and other parameters. In addition, 86% described the treatment as gentler than other therapies. (J. Drugs Dermatol. 2011;10:596-602).
Products
The Skin Clarifying Blue Light device has a power density of 400 mW/cm2, which is 10 times the power of other LED acne devices. This high power density allows the Skin Clarifying Blue Light device to deliver high levels of efficacy with short treatment times. When used as stand-alone treatment, it delivered a 70% reduction in inflammatory lesions in 8 weeks. The success of products designed for self-administration has coincided with the rampant interest in the creation of smart phone applications (J. Cosmet. Laser. Ther. 2011;13:308-14; J. Clin. Aesthet. Dermatol. 2009;2:40-4; J. Clin. Aesthet. Dermatol. 2009;2:44-50). That is, blue-light therapy apps have been developed for the iPhone and the iPod touch. None, however, has been approved by the Food and Drug Administration, although at least one is said to be under investigation in a clinical trial. I am skeptical about the efficacy of these LED-backlit apps and concerned about potentially prolonged magnetic radiation exposure that would be required. The self-administered devices appear to be a more reliable alternative.
Conclusion
Blue light can effectively be used to treat mild to moderate acne by causing photodynamic destruction of P. acnes. It can be used alone or in combination with topical or other light regimens. Additional studies are needed before a consensus protocol can be established, and future research goals should include establishing the optimal incubation time, activating light source, and frequency of treatment.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
Photodynamic light therapies (PDLs) have emerged as significant adjuvant approaches for treating acne. In particular, such therapies have been used for acne refractory to standard retinoid or combined retinoid and antimicrobial regimens. Why write about PDL in a column devoted to topical cosmeceutical products and ingredients? Blue light warrants inclusion because it has been studied in comparison to topical cosmeceutical treatments, and it is used in conjunction with other topical approaches.
Blue light exerts a phototoxic effect on the heme metabolism of Propionibacterium acnes, and it is considered effective by targeting part of the etiologic pathway of acne. It has become a widely used option for inflammatory acne (J. Drugs. Dermatol. 2006;5:605-10).
Early work
In 1990, Meffert et al. were the first to show that a blue light–type, high-pressure lamp could improve acne and seborrhea (10 10-minute treatments, cumulative light dose 325 J/cm2). Given the copious amounts of porphyrins stored in lipophilic P. acnes, the technology could be targeted to destroy propionibacteria, and the researchers observed a decline in the porphyrin content inside acne follicles. They concluded that short-range visible light (400-420 nm) was a viable option for acne treatment during the light-poor season of the year (Dermatol. Monatsschr. 1990;176:597-603). It was subsequently established that treatment with UV-free blue light in the range of 405-420 nm leads to the elimination of acne bacteria by virtue of the effects on the porphyrins generated naturally by P. acnes (J. Cosmet. Laser. Ther. 2003;5:111-7). Notably, blue light appears to photoinactivate P. acnes, but it does not penetrate deeply into the skin (Dermatol. Online J. 2011;17:2).
In an open study of the then-novel high-intensity, enhanced, narrow-band, blue-light phototherapy, Kawada et al. treated 30 acne patients (27 female, 3 male) twice a week for up to 5 weeks. A reduction of 64% was seen in acne lesions, and in vitro data showed a significant decline in P. acnes, but not in Staphylococcus epidermidis (J. Dermatol. Sci. 2002;30:129-35).
Mechanism of action
In 2006, Shnitkind et al. studied the effect of narrow-band blue light on the inflammatory process in the presence and absence of cytokines and ultraviolet B using interleukin-1 alpha (IL-1alpha) and intercellular adhesion molecule 1 (ICAM-1) as markers for inflammation. They found that blue light treatment of HaCaT and hTERT cells decreased levels of IL-1alpha by 82% in HaCaT and by 75% in hTERT. When blue light was combined with ultraviolet B, the respective reductions were 95% and 91%. Similar reductions in ICAM-1 expression were seen in HaCaT, but not in hTERT. The researchers concluded that narrow-band blue light exerts anti-inflammatory effects on keratinocytes by reducing cytokine-induced synthesis of IL-1alpha and ICAM-1. They suggested that these findings imply a broader range of effects is exerted on the inflammatory process by narrow-band blue light than previously understood (J. Drugs. Dermatol. 2006;5:605-10).
Comparison studies
In 2000, Papageorgiou et al. randomized 107 patients with mild to moderate acne to four treatment groups: blue light (peak at 415 nm), mixed blue and red light (peaks at 415 and 660 nm), cool white light, and 5% benzoyl peroxide cream, for 12 weeks of active treatment. Phototherapy using portable light sources was conducted daily for 15 minutes; comparative assessments among the three phototherapy groups were done with observers blinded. The investigators found that the greatest improvement in acne lesions occurred in the blue and red light combined group. The blue/red treatment was significantly superior to blue light alone at 4 and 8 weeks but not 12 weeks, benzoyl peroxide at weeks 8 and 12, and white light at all assessments (Br. J. Dermatol. 2000;142:973-8).
Gold et al. performed a multicenter clinical evaluation comparing blue light to topical 1% clindamycin solution with respect to safety and efficacy. They found that clindamycin was associated with a 14% reduction of inflammatory lesions, but blue light reduced such lesions by an average of 34% (J. Drugs. Dermatol. 2005;4:64-70).
In another study, 20 patients with moderate to severe facial acne were treated in four weekly sessions with topical aminolevulinic acid (ALA)-photodynamic therapy with blue light (415 nm) on the right side of the face, or blue light alone on the left side of the face. At 4, 8, 12, and 16 weeks after the start of treatment, the mean percent reductions in inflamed lesions were higher in the ALA-PDT areas (32%, 50.9%, 65.9%, and 71.1%, respectively) than in the blue light–only treatment areas (20.7%, 27%, 57.7%, and 56.7%), but the differences were not statistically significant. Side effects, which included pain, stinging, erythema, itching, peeling, oozing, and pustules, were more pronounced in the areas treated with ALA-PDT (Photodermatol. Photoimmunol. Photomed. 2007;23:186-90).
However, in a 2007 study of 22 patients with moderate to severe acne randomized to one of three ALA-PDT treatments – intense pulsed light (IPL; 600-850 nm), a combination of IPL (580-980 nm) and bipolar radiofrequency (RF) energies, or blue light (417 nm) – in three sessions at 2-week intervals, ALA-PDT with activation by IPL yielded the most consistent, lasting improvement in moderate to severe acne (J. Drugs Dermatol. 2007;6:1010-6).
In a study of 60 volunteers with facial acne (grades II and III), de Arruda et al. compared the safety and efficacy of blue light to topical benzoyl peroxide 5% over 4 weeks. Thirty patients received blue light treatment twice a week, and the other 30 self-applied the topical formulation twice daily. The improvements were similar in both groups, but side effects were milder in the blue light group (An. Bras. Dermatol. 2009;84:463-8).
Choi et al. compared the bactericidal effects of 5-aminolevulinic acid (ALA) with blue and red light on P. acnes and found that blue light was more effective than red light phototherapy in eliminating the bacteria unless ALA was added, which substantially augmented red light phototherapy efficacy (J. Dermatol. 2011;38:661-6).
In summarizing the off-label uses of light-based treatments and PDT using topical precursors of porphyrins, Sakamoto et al. observed that blue light alone lessens acne severity due to anti-inflammatory effects; PDT using 5-ALA or ALA derivatives provides antimicrobial and anti-inflammatory activity; and, at high doses, red-light PDT may suppress or eradicate sebaceous glands, yielding clinical improvement (J. Am. Acad. Dermatol. 2010;63:183-93).
Combination therapy
In 2011, Wheeland and Dhawan assessed the efficacy and tolerability of treating mild to moderate facial acne using a novel, handheld, light-emitting diode (LED) blue-light device, along with a foam cleanser containing 5% glycolic acid and 2% salicylic acid, plus a serum containing 1.25% salicylic acid, 0.5% niacinamide, 0.08% liposomal-based azelaic acid, and superoxide dismutase. In all, 28 of 35 adults aged 25-45 years completed the 8-week study, in which they used the device twice daily (in addition to the cleanser before treatments and the serum after nighttime treatments). Significant reductions in inflammatory lesion counts were seen from week 1 onward, and significant reductions in noninflammatory lesion counts were seen from week 4 onward compared with baseline counts. The number and severity of flares were significantly reduced from baseline as well.
Therapy was well received by patients, with more than 90% claiming improvement in overall skin appearance and other parameters. In addition, 86% described the treatment as gentler than other therapies. (J. Drugs Dermatol. 2011;10:596-602).
Products
The Skin Clarifying Blue Light device has a power density of 400 mW/cm2, which is 10 times the power of other LED acne devices. This high power density allows the Skin Clarifying Blue Light device to deliver high levels of efficacy with short treatment times. When used as stand-alone treatment, it delivered a 70% reduction in inflammatory lesions in 8 weeks. The success of products designed for self-administration has coincided with the rampant interest in the creation of smart phone applications (J. Cosmet. Laser. Ther. 2011;13:308-14; J. Clin. Aesthet. Dermatol. 2009;2:40-4; J. Clin. Aesthet. Dermatol. 2009;2:44-50). That is, blue-light therapy apps have been developed for the iPhone and the iPod touch. None, however, has been approved by the Food and Drug Administration, although at least one is said to be under investigation in a clinical trial. I am skeptical about the efficacy of these LED-backlit apps and concerned about potentially prolonged magnetic radiation exposure that would be required. The self-administered devices appear to be a more reliable alternative.
Conclusion
Blue light can effectively be used to treat mild to moderate acne by causing photodynamic destruction of P. acnes. It can be used alone or in combination with topical or other light regimens. Additional studies are needed before a consensus protocol can be established, and future research goals should include establishing the optimal incubation time, activating light source, and frequency of treatment.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
Photodynamic light therapies (PDLs) have emerged as significant adjuvant approaches for treating acne. In particular, such therapies have been used for acne refractory to standard retinoid or combined retinoid and antimicrobial regimens. Why write about PDL in a column devoted to topical cosmeceutical products and ingredients? Blue light warrants inclusion because it has been studied in comparison to topical cosmeceutical treatments, and it is used in conjunction with other topical approaches.
Blue light exerts a phototoxic effect on the heme metabolism of Propionibacterium acnes, and it is considered effective by targeting part of the etiologic pathway of acne. It has become a widely used option for inflammatory acne (J. Drugs. Dermatol. 2006;5:605-10).
Early work
In 1990, Meffert et al. were the first to show that a blue light–type, high-pressure lamp could improve acne and seborrhea (10 10-minute treatments, cumulative light dose 325 J/cm2). Given the copious amounts of porphyrins stored in lipophilic P. acnes, the technology could be targeted to destroy propionibacteria, and the researchers observed a decline in the porphyrin content inside acne follicles. They concluded that short-range visible light (400-420 nm) was a viable option for acne treatment during the light-poor season of the year (Dermatol. Monatsschr. 1990;176:597-603). It was subsequently established that treatment with UV-free blue light in the range of 405-420 nm leads to the elimination of acne bacteria by virtue of the effects on the porphyrins generated naturally by P. acnes (J. Cosmet. Laser. Ther. 2003;5:111-7). Notably, blue light appears to photoinactivate P. acnes, but it does not penetrate deeply into the skin (Dermatol. Online J. 2011;17:2).
In an open study of the then-novel high-intensity, enhanced, narrow-band, blue-light phototherapy, Kawada et al. treated 30 acne patients (27 female, 3 male) twice a week for up to 5 weeks. A reduction of 64% was seen in acne lesions, and in vitro data showed a significant decline in P. acnes, but not in Staphylococcus epidermidis (J. Dermatol. Sci. 2002;30:129-35).
Mechanism of action
In 2006, Shnitkind et al. studied the effect of narrow-band blue light on the inflammatory process in the presence and absence of cytokines and ultraviolet B using interleukin-1 alpha (IL-1alpha) and intercellular adhesion molecule 1 (ICAM-1) as markers for inflammation. They found that blue light treatment of HaCaT and hTERT cells decreased levels of IL-1alpha by 82% in HaCaT and by 75% in hTERT. When blue light was combined with ultraviolet B, the respective reductions were 95% and 91%. Similar reductions in ICAM-1 expression were seen in HaCaT, but not in hTERT. The researchers concluded that narrow-band blue light exerts anti-inflammatory effects on keratinocytes by reducing cytokine-induced synthesis of IL-1alpha and ICAM-1. They suggested that these findings imply a broader range of effects is exerted on the inflammatory process by narrow-band blue light than previously understood (J. Drugs. Dermatol. 2006;5:605-10).
Comparison studies
In 2000, Papageorgiou et al. randomized 107 patients with mild to moderate acne to four treatment groups: blue light (peak at 415 nm), mixed blue and red light (peaks at 415 and 660 nm), cool white light, and 5% benzoyl peroxide cream, for 12 weeks of active treatment. Phototherapy using portable light sources was conducted daily for 15 minutes; comparative assessments among the three phototherapy groups were done with observers blinded. The investigators found that the greatest improvement in acne lesions occurred in the blue and red light combined group. The blue/red treatment was significantly superior to blue light alone at 4 and 8 weeks but not 12 weeks, benzoyl peroxide at weeks 8 and 12, and white light at all assessments (Br. J. Dermatol. 2000;142:973-8).
Gold et al. performed a multicenter clinical evaluation comparing blue light to topical 1% clindamycin solution with respect to safety and efficacy. They found that clindamycin was associated with a 14% reduction of inflammatory lesions, but blue light reduced such lesions by an average of 34% (J. Drugs. Dermatol. 2005;4:64-70).
In another study, 20 patients with moderate to severe facial acne were treated in four weekly sessions with topical aminolevulinic acid (ALA)-photodynamic therapy with blue light (415 nm) on the right side of the face, or blue light alone on the left side of the face. At 4, 8, 12, and 16 weeks after the start of treatment, the mean percent reductions in inflamed lesions were higher in the ALA-PDT areas (32%, 50.9%, 65.9%, and 71.1%, respectively) than in the blue light–only treatment areas (20.7%, 27%, 57.7%, and 56.7%), but the differences were not statistically significant. Side effects, which included pain, stinging, erythema, itching, peeling, oozing, and pustules, were more pronounced in the areas treated with ALA-PDT (Photodermatol. Photoimmunol. Photomed. 2007;23:186-90).
However, in a 2007 study of 22 patients with moderate to severe acne randomized to one of three ALA-PDT treatments – intense pulsed light (IPL; 600-850 nm), a combination of IPL (580-980 nm) and bipolar radiofrequency (RF) energies, or blue light (417 nm) – in three sessions at 2-week intervals, ALA-PDT with activation by IPL yielded the most consistent, lasting improvement in moderate to severe acne (J. Drugs Dermatol. 2007;6:1010-6).
In a study of 60 volunteers with facial acne (grades II and III), de Arruda et al. compared the safety and efficacy of blue light to topical benzoyl peroxide 5% over 4 weeks. Thirty patients received blue light treatment twice a week, and the other 30 self-applied the topical formulation twice daily. The improvements were similar in both groups, but side effects were milder in the blue light group (An. Bras. Dermatol. 2009;84:463-8).
Choi et al. compared the bactericidal effects of 5-aminolevulinic acid (ALA) with blue and red light on P. acnes and found that blue light was more effective than red light phototherapy in eliminating the bacteria unless ALA was added, which substantially augmented red light phototherapy efficacy (J. Dermatol. 2011;38:661-6).
In summarizing the off-label uses of light-based treatments and PDT using topical precursors of porphyrins, Sakamoto et al. observed that blue light alone lessens acne severity due to anti-inflammatory effects; PDT using 5-ALA or ALA derivatives provides antimicrobial and anti-inflammatory activity; and, at high doses, red-light PDT may suppress or eradicate sebaceous glands, yielding clinical improvement (J. Am. Acad. Dermatol. 2010;63:183-93).
Combination therapy
In 2011, Wheeland and Dhawan assessed the efficacy and tolerability of treating mild to moderate facial acne using a novel, handheld, light-emitting diode (LED) blue-light device, along with a foam cleanser containing 5% glycolic acid and 2% salicylic acid, plus a serum containing 1.25% salicylic acid, 0.5% niacinamide, 0.08% liposomal-based azelaic acid, and superoxide dismutase. In all, 28 of 35 adults aged 25-45 years completed the 8-week study, in which they used the device twice daily (in addition to the cleanser before treatments and the serum after nighttime treatments). Significant reductions in inflammatory lesion counts were seen from week 1 onward, and significant reductions in noninflammatory lesion counts were seen from week 4 onward compared with baseline counts. The number and severity of flares were significantly reduced from baseline as well.
Therapy was well received by patients, with more than 90% claiming improvement in overall skin appearance and other parameters. In addition, 86% described the treatment as gentler than other therapies. (J. Drugs Dermatol. 2011;10:596-602).
Products
The Skin Clarifying Blue Light device has a power density of 400 mW/cm2, which is 10 times the power of other LED acne devices. This high power density allows the Skin Clarifying Blue Light device to deliver high levels of efficacy with short treatment times. When used as stand-alone treatment, it delivered a 70% reduction in inflammatory lesions in 8 weeks. The success of products designed for self-administration has coincided with the rampant interest in the creation of smart phone applications (J. Cosmet. Laser. Ther. 2011;13:308-14; J. Clin. Aesthet. Dermatol. 2009;2:40-4; J. Clin. Aesthet. Dermatol. 2009;2:44-50). That is, blue-light therapy apps have been developed for the iPhone and the iPod touch. None, however, has been approved by the Food and Drug Administration, although at least one is said to be under investigation in a clinical trial. I am skeptical about the efficacy of these LED-backlit apps and concerned about potentially prolonged magnetic radiation exposure that would be required. The self-administered devices appear to be a more reliable alternative.
Conclusion
Blue light can effectively be used to treat mild to moderate acne by causing photodynamic destruction of P. acnes. It can be used alone or in combination with topical or other light regimens. Additional studies are needed before a consensus protocol can be established, and future research goals should include establishing the optimal incubation time, activating light source, and frequency of treatment.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
Blackberry
Endemic to Europe and North America, the blackberry (Rubus fruticosus) is naturally laden with an abundance of polyphenolic compounds, including ellagic acid, tannins, ellagitannins, quercetin, gallic acid, anthocyanins, and cyanidins, which have been associated with antioxidant and anticarcinogenic activity (J. Med. Food 2007;10:258-65; J. Agric. Food. Chem. 2002;50:3495-500; J. Agric. Food Chem. 2008;56:661-9). Indeed, the health benefits of consuming plants rich in anthocyanins have been known at least since the 1500s (Nat. Prod. Commun. 2011;6:149-56).
It is not surprising, then, that blackberries have long been part of traditional medicine. Rubus extracts have been used in traditional medicine for antimicrobial, anticonvulsant, and muscle relaxant indications, as well as for their ability to detect and inhibit free radicals (Int. J. Antimicrob. Agents. 2009;34:50-9). Rubus has been reported in traditional medicine on Sardinia for hemorrhoids, bleeding gums, and ulcers (J. Ethnobiol. Ethnomed. 2009;5:6). Phytotherapeutic uses have also been noted in Central Italy (Fitoterapia. 2005;76:1-25). Dermatologic applications of blackberry in southern Italy include use of the leaves to treat dog bites, and use of the roots in a hair-wash preparation (J. Ethnobiol. Ethnomed. 2008;4:5).
Data from other studies suggest additional potential uses for blackberry. For example, polyphenols and leaf extract of Rubus ulmifolius exhibited antibacterial activity against two strains of Helicobacter pylori (Int. J. Antimicrob. Agents. 2009;34:50-9). The antimicrobial activity of berries and other anthocyanin-containing fruits, which are typically more effective against Gram-positive than Gram-negative bacteria, is believed to result from various mechanisms and interactions associated with anthocyanins, weak organic acids, phenolic acids, and their mixtures of varying chemical composition (Nat. Prod. Commun. 2011;6:149-56; J. Ethnopharmacol. 2002;79:165-8).
Anti-inflammatory activity
In 2006, Pergola et al. examined whether the pharmacological activity of the anthocyanin fraction of a blackberry extract (cyanidin-3-O-glucoside, approximately 88% of the total anthocyanin content) could be attributed to the inhibition of nitric oxide production. The researchers found that the increased synthesis of nitrites spurred by the treatment of J774 cells with lipopolysaccharide over 24 hours was inhibited by anthocyanin, in a concentration-dependent manner. They concluded that the anti-inflammatory activity associated with blackberry extract can be partially ascribed to the blocking of nitric oxide synthesis by cyanidin-3-O-glucoside, the primary anthocyanin found in the extract (Nitric Oxide 2006;15:30-9).
In another study involving in vivo data and a mouse ear model, investigators assessed the antioxidant and topical anti-inflammatory activity of low- and high-molecular-weight phenolic fractions from three blackberry cultivars (i.e., Navaho, Kiowa, and Ouachita) bred for the warm and humid conditions of the southeastern United States. They found that all three formulations significantly mitigated TPA-induced inflammation. In addition, the researchers investigated mouse ear myeloperoxidase activity, an indicator of polymorphonuclear leukocyte infiltration, and noted that it was substantially diminished after topical application of both blackberry preparations as well as indomethacin (J. Agric. Food. Chem. 2010;58:6102-9).
Antioxidant activity
Blackberries consistently rank highly in oxygen radical absorbance capacity (ORAC), and they showed the strongest antioxidant activity among 1,000 antioxidant foods eaten in the United States in a study by Halvorsen et al. (Am. J. Clin. Nutr. 2006;84:95-135).
Investigators recently evaluated and compared the effect of extraction time (5 and 15 minutes) and hydrolysis on the qualitative and quantitative content of phenolic compounds and antioxidant capacity of six traditional medicinal plants, including blackberry (Rubus fruticosus), lemon balm (Melissa officinalis), thyme (Thymus serpyllum), lavender (Lavandula officinalis), stinging nettle (Urtica dioica), and olive (Olea europea). The distribution of phenolic compounds identified varied widely among the botanicals selected, and the extraction efficiency and antioxidant capacity of the extracts were influenced by prolonged extraction and hydrolysis. The hydrolyzed extract of blackberry leaves, obtained after 15 minutes of extraction, demonstrated the highest phenolic content and antioxidant capacity (Phytochem. Anal. 2011;22:172-80).
In 2007, Dai et al. obtained Hull blackberries grown in Kentucky and analyzed total anthocyanin and phenolic content, polymeric color, as well as anthocyanin composition and antioxidant capacity. Their in vitro cell culture work indicated that the blackberry extract suppressed HT-29 colon tumor cell growth by up to 66% after 72 hours, in a concentration-dependent manner. High-dose and low-dose lipid A-induced interleukin-12 release was also concentration-dependently inhibited from mouse bone marrow–derived dendritic cells by total anthocyanin concentrations (0-40 mcg/mL). The investigators concluded that the blackberry extract exhibits strong antioxidant, antiproliferative, and anti-inflammatory activities, and products based on the extract might be considered for the treatment or prevention of inflammatory conditions as well as cancer (J. Med. Food 2007;10:258-65).
Anticarcinogenic activity
In 2004, Feng et al. studied the effects of fresh blackberry extracts on cancer cell proliferation and neoplastic transformation induced by TPA. They confirmed, using electron spin resonance, that the extract effectively scavenges hydroxyl and superoxide free radicals. They also determined that pretreatment of the human cancer cell line A549 with blackberry extract suppressed cell proliferation and inhibited 8-hydroxy-2\'-deoxyguanosine (8-OHdG) formation induced by UVB. In addition, pretreatment with the extract reduced neoplastic transformation of JB6 P+ cells induced by TPA and blocked UVB- and TPA-induced AP-1 transactivation. The investigators concluded that fresh blackberry extract appears to have anticarcinogenic properties, and that associated activity may be derived from its antioxidant characteristics (Nutr. Cancer 2004;50:80-9).
In 2006, Ding et al. examined the chemopreventive and chemotherapeutic activity of cyanidin-3-glucoside (C3G), a key active ingredient in blackberry. C3G was shown to scavenge UVB-induced hydroxyl and superoxide radicals in cultured JB6 cells. The investigators observed reductions in the number of nonmalignant and malignant skin tumors per mouse induced by TPA in 7,12-dimethylbenz[a]anthracene-initiated mouse skin. In addition, UVB- and TPA-induced transactivation of NF-kappaB and AP-1 and expression of cyclooxygenase-2 and tumor necrosis factor–alpha were suppressed by the pretreatment with C3G of JB6 cells. The researchers suggested that the inhibition of MAPK activity may be important in mediating such effects. TPA-induced neoplastic transformation in JB6 cells was also hindered via C3G pretreatment. Further, C3G suppressed proliferation of the human lung carcinoma cell line A549, diminished the size of A549 tumor xenograft growth, and significantly limited metastasis in nude mice. The investigators concluded that C3G, an important constituent of blackberry, displays significant anticancer activity by dint of its capacity to scavenge free radicals. As such, they suggested that this blackberry derivative, which exhibits scant cytotoxicity to healthy tissue, warrants additional study as a preventive and therapeutic agent in human cancers (J. Biol. Chem. 2006;281:17359-68).
Conclusion
The most recent evidence suggests that blackberry warrants attention for medical applications, including dermatology. In fact, in a small (n = 33) single-center, open-label study led by the author, significant improvement in most metrics of photoaged skin was observed after the use of a day and night regimen containing blackberry leaf extract, dill extract, and Zn-Cu(II) bi-mineral complex in patients with mild to moderate photodamage. (Baumann LS, Figueras KA, Bell M, Flitter CJ. Assessing the efficacy and tolerance of a day and night regimen containing blackberry leaf extract, dill extract, and Cu-Zinc bi-mineral complex in subjects with mild to moderate photoaged skin. Unpublished results.) It remains to be seen if and when blackberry extract alone may be harnessed for dermatologic indications, but present data are promising, and justify continued study.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
Endemic to Europe and North America, the blackberry (Rubus fruticosus) is naturally laden with an abundance of polyphenolic compounds, including ellagic acid, tannins, ellagitannins, quercetin, gallic acid, anthocyanins, and cyanidins, which have been associated with antioxidant and anticarcinogenic activity (J. Med. Food 2007;10:258-65; J. Agric. Food. Chem. 2002;50:3495-500; J. Agric. Food Chem. 2008;56:661-9). Indeed, the health benefits of consuming plants rich in anthocyanins have been known at least since the 1500s (Nat. Prod. Commun. 2011;6:149-56).
It is not surprising, then, that blackberries have long been part of traditional medicine. Rubus extracts have been used in traditional medicine for antimicrobial, anticonvulsant, and muscle relaxant indications, as well as for their ability to detect and inhibit free radicals (Int. J. Antimicrob. Agents. 2009;34:50-9). Rubus has been reported in traditional medicine on Sardinia for hemorrhoids, bleeding gums, and ulcers (J. Ethnobiol. Ethnomed. 2009;5:6). Phytotherapeutic uses have also been noted in Central Italy (Fitoterapia. 2005;76:1-25). Dermatologic applications of blackberry in southern Italy include use of the leaves to treat dog bites, and use of the roots in a hair-wash preparation (J. Ethnobiol. Ethnomed. 2008;4:5).
Data from other studies suggest additional potential uses for blackberry. For example, polyphenols and leaf extract of Rubus ulmifolius exhibited antibacterial activity against two strains of Helicobacter pylori (Int. J. Antimicrob. Agents. 2009;34:50-9). The antimicrobial activity of berries and other anthocyanin-containing fruits, which are typically more effective against Gram-positive than Gram-negative bacteria, is believed to result from various mechanisms and interactions associated with anthocyanins, weak organic acids, phenolic acids, and their mixtures of varying chemical composition (Nat. Prod. Commun. 2011;6:149-56; J. Ethnopharmacol. 2002;79:165-8).
Anti-inflammatory activity
In 2006, Pergola et al. examined whether the pharmacological activity of the anthocyanin fraction of a blackberry extract (cyanidin-3-O-glucoside, approximately 88% of the total anthocyanin content) could be attributed to the inhibition of nitric oxide production. The researchers found that the increased synthesis of nitrites spurred by the treatment of J774 cells with lipopolysaccharide over 24 hours was inhibited by anthocyanin, in a concentration-dependent manner. They concluded that the anti-inflammatory activity associated with blackberry extract can be partially ascribed to the blocking of nitric oxide synthesis by cyanidin-3-O-glucoside, the primary anthocyanin found in the extract (Nitric Oxide 2006;15:30-9).
In another study involving in vivo data and a mouse ear model, investigators assessed the antioxidant and topical anti-inflammatory activity of low- and high-molecular-weight phenolic fractions from three blackberry cultivars (i.e., Navaho, Kiowa, and Ouachita) bred for the warm and humid conditions of the southeastern United States. They found that all three formulations significantly mitigated TPA-induced inflammation. In addition, the researchers investigated mouse ear myeloperoxidase activity, an indicator of polymorphonuclear leukocyte infiltration, and noted that it was substantially diminished after topical application of both blackberry preparations as well as indomethacin (J. Agric. Food. Chem. 2010;58:6102-9).
Antioxidant activity
Blackberries consistently rank highly in oxygen radical absorbance capacity (ORAC), and they showed the strongest antioxidant activity among 1,000 antioxidant foods eaten in the United States in a study by Halvorsen et al. (Am. J. Clin. Nutr. 2006;84:95-135).
Investigators recently evaluated and compared the effect of extraction time (5 and 15 minutes) and hydrolysis on the qualitative and quantitative content of phenolic compounds and antioxidant capacity of six traditional medicinal plants, including blackberry (Rubus fruticosus), lemon balm (Melissa officinalis), thyme (Thymus serpyllum), lavender (Lavandula officinalis), stinging nettle (Urtica dioica), and olive (Olea europea). The distribution of phenolic compounds identified varied widely among the botanicals selected, and the extraction efficiency and antioxidant capacity of the extracts were influenced by prolonged extraction and hydrolysis. The hydrolyzed extract of blackberry leaves, obtained after 15 minutes of extraction, demonstrated the highest phenolic content and antioxidant capacity (Phytochem. Anal. 2011;22:172-80).
In 2007, Dai et al. obtained Hull blackberries grown in Kentucky and analyzed total anthocyanin and phenolic content, polymeric color, as well as anthocyanin composition and antioxidant capacity. Their in vitro cell culture work indicated that the blackberry extract suppressed HT-29 colon tumor cell growth by up to 66% after 72 hours, in a concentration-dependent manner. High-dose and low-dose lipid A-induced interleukin-12 release was also concentration-dependently inhibited from mouse bone marrow–derived dendritic cells by total anthocyanin concentrations (0-40 mcg/mL). The investigators concluded that the blackberry extract exhibits strong antioxidant, antiproliferative, and anti-inflammatory activities, and products based on the extract might be considered for the treatment or prevention of inflammatory conditions as well as cancer (J. Med. Food 2007;10:258-65).
Anticarcinogenic activity
In 2004, Feng et al. studied the effects of fresh blackberry extracts on cancer cell proliferation and neoplastic transformation induced by TPA. They confirmed, using electron spin resonance, that the extract effectively scavenges hydroxyl and superoxide free radicals. They also determined that pretreatment of the human cancer cell line A549 with blackberry extract suppressed cell proliferation and inhibited 8-hydroxy-2\'-deoxyguanosine (8-OHdG) formation induced by UVB. In addition, pretreatment with the extract reduced neoplastic transformation of JB6 P+ cells induced by TPA and blocked UVB- and TPA-induced AP-1 transactivation. The investigators concluded that fresh blackberry extract appears to have anticarcinogenic properties, and that associated activity may be derived from its antioxidant characteristics (Nutr. Cancer 2004;50:80-9).
In 2006, Ding et al. examined the chemopreventive and chemotherapeutic activity of cyanidin-3-glucoside (C3G), a key active ingredient in blackberry. C3G was shown to scavenge UVB-induced hydroxyl and superoxide radicals in cultured JB6 cells. The investigators observed reductions in the number of nonmalignant and malignant skin tumors per mouse induced by TPA in 7,12-dimethylbenz[a]anthracene-initiated mouse skin. In addition, UVB- and TPA-induced transactivation of NF-kappaB and AP-1 and expression of cyclooxygenase-2 and tumor necrosis factor–alpha were suppressed by the pretreatment with C3G of JB6 cells. The researchers suggested that the inhibition of MAPK activity may be important in mediating such effects. TPA-induced neoplastic transformation in JB6 cells was also hindered via C3G pretreatment. Further, C3G suppressed proliferation of the human lung carcinoma cell line A549, diminished the size of A549 tumor xenograft growth, and significantly limited metastasis in nude mice. The investigators concluded that C3G, an important constituent of blackberry, displays significant anticancer activity by dint of its capacity to scavenge free radicals. As such, they suggested that this blackberry derivative, which exhibits scant cytotoxicity to healthy tissue, warrants additional study as a preventive and therapeutic agent in human cancers (J. Biol. Chem. 2006;281:17359-68).
Conclusion
The most recent evidence suggests that blackberry warrants attention for medical applications, including dermatology. In fact, in a small (n = 33) single-center, open-label study led by the author, significant improvement in most metrics of photoaged skin was observed after the use of a day and night regimen containing blackberry leaf extract, dill extract, and Zn-Cu(II) bi-mineral complex in patients with mild to moderate photodamage. (Baumann LS, Figueras KA, Bell M, Flitter CJ. Assessing the efficacy and tolerance of a day and night regimen containing blackberry leaf extract, dill extract, and Cu-Zinc bi-mineral complex in subjects with mild to moderate photoaged skin. Unpublished results.) It remains to be seen if and when blackberry extract alone may be harnessed for dermatologic indications, but present data are promising, and justify continued study.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
Endemic to Europe and North America, the blackberry (Rubus fruticosus) is naturally laden with an abundance of polyphenolic compounds, including ellagic acid, tannins, ellagitannins, quercetin, gallic acid, anthocyanins, and cyanidins, which have been associated with antioxidant and anticarcinogenic activity (J. Med. Food 2007;10:258-65; J. Agric. Food. Chem. 2002;50:3495-500; J. Agric. Food Chem. 2008;56:661-9). Indeed, the health benefits of consuming plants rich in anthocyanins have been known at least since the 1500s (Nat. Prod. Commun. 2011;6:149-56).
It is not surprising, then, that blackberries have long been part of traditional medicine. Rubus extracts have been used in traditional medicine for antimicrobial, anticonvulsant, and muscle relaxant indications, as well as for their ability to detect and inhibit free radicals (Int. J. Antimicrob. Agents. 2009;34:50-9). Rubus has been reported in traditional medicine on Sardinia for hemorrhoids, bleeding gums, and ulcers (J. Ethnobiol. Ethnomed. 2009;5:6). Phytotherapeutic uses have also been noted in Central Italy (Fitoterapia. 2005;76:1-25). Dermatologic applications of blackberry in southern Italy include use of the leaves to treat dog bites, and use of the roots in a hair-wash preparation (J. Ethnobiol. Ethnomed. 2008;4:5).
Data from other studies suggest additional potential uses for blackberry. For example, polyphenols and leaf extract of Rubus ulmifolius exhibited antibacterial activity against two strains of Helicobacter pylori (Int. J. Antimicrob. Agents. 2009;34:50-9). The antimicrobial activity of berries and other anthocyanin-containing fruits, which are typically more effective against Gram-positive than Gram-negative bacteria, is believed to result from various mechanisms and interactions associated with anthocyanins, weak organic acids, phenolic acids, and their mixtures of varying chemical composition (Nat. Prod. Commun. 2011;6:149-56; J. Ethnopharmacol. 2002;79:165-8).
Anti-inflammatory activity
In 2006, Pergola et al. examined whether the pharmacological activity of the anthocyanin fraction of a blackberry extract (cyanidin-3-O-glucoside, approximately 88% of the total anthocyanin content) could be attributed to the inhibition of nitric oxide production. The researchers found that the increased synthesis of nitrites spurred by the treatment of J774 cells with lipopolysaccharide over 24 hours was inhibited by anthocyanin, in a concentration-dependent manner. They concluded that the anti-inflammatory activity associated with blackberry extract can be partially ascribed to the blocking of nitric oxide synthesis by cyanidin-3-O-glucoside, the primary anthocyanin found in the extract (Nitric Oxide 2006;15:30-9).
In another study involving in vivo data and a mouse ear model, investigators assessed the antioxidant and topical anti-inflammatory activity of low- and high-molecular-weight phenolic fractions from three blackberry cultivars (i.e., Navaho, Kiowa, and Ouachita) bred for the warm and humid conditions of the southeastern United States. They found that all three formulations significantly mitigated TPA-induced inflammation. In addition, the researchers investigated mouse ear myeloperoxidase activity, an indicator of polymorphonuclear leukocyte infiltration, and noted that it was substantially diminished after topical application of both blackberry preparations as well as indomethacin (J. Agric. Food. Chem. 2010;58:6102-9).
Antioxidant activity
Blackberries consistently rank highly in oxygen radical absorbance capacity (ORAC), and they showed the strongest antioxidant activity among 1,000 antioxidant foods eaten in the United States in a study by Halvorsen et al. (Am. J. Clin. Nutr. 2006;84:95-135).
Investigators recently evaluated and compared the effect of extraction time (5 and 15 minutes) and hydrolysis on the qualitative and quantitative content of phenolic compounds and antioxidant capacity of six traditional medicinal plants, including blackberry (Rubus fruticosus), lemon balm (Melissa officinalis), thyme (Thymus serpyllum), lavender (Lavandula officinalis), stinging nettle (Urtica dioica), and olive (Olea europea). The distribution of phenolic compounds identified varied widely among the botanicals selected, and the extraction efficiency and antioxidant capacity of the extracts were influenced by prolonged extraction and hydrolysis. The hydrolyzed extract of blackberry leaves, obtained after 15 minutes of extraction, demonstrated the highest phenolic content and antioxidant capacity (Phytochem. Anal. 2011;22:172-80).
In 2007, Dai et al. obtained Hull blackberries grown in Kentucky and analyzed total anthocyanin and phenolic content, polymeric color, as well as anthocyanin composition and antioxidant capacity. Their in vitro cell culture work indicated that the blackberry extract suppressed HT-29 colon tumor cell growth by up to 66% after 72 hours, in a concentration-dependent manner. High-dose and low-dose lipid A-induced interleukin-12 release was also concentration-dependently inhibited from mouse bone marrow–derived dendritic cells by total anthocyanin concentrations (0-40 mcg/mL). The investigators concluded that the blackberry extract exhibits strong antioxidant, antiproliferative, and anti-inflammatory activities, and products based on the extract might be considered for the treatment or prevention of inflammatory conditions as well as cancer (J. Med. Food 2007;10:258-65).
Anticarcinogenic activity
In 2004, Feng et al. studied the effects of fresh blackberry extracts on cancer cell proliferation and neoplastic transformation induced by TPA. They confirmed, using electron spin resonance, that the extract effectively scavenges hydroxyl and superoxide free radicals. They also determined that pretreatment of the human cancer cell line A549 with blackberry extract suppressed cell proliferation and inhibited 8-hydroxy-2\'-deoxyguanosine (8-OHdG) formation induced by UVB. In addition, pretreatment with the extract reduced neoplastic transformation of JB6 P+ cells induced by TPA and blocked UVB- and TPA-induced AP-1 transactivation. The investigators concluded that fresh blackberry extract appears to have anticarcinogenic properties, and that associated activity may be derived from its antioxidant characteristics (Nutr. Cancer 2004;50:80-9).
In 2006, Ding et al. examined the chemopreventive and chemotherapeutic activity of cyanidin-3-glucoside (C3G), a key active ingredient in blackberry. C3G was shown to scavenge UVB-induced hydroxyl and superoxide radicals in cultured JB6 cells. The investigators observed reductions in the number of nonmalignant and malignant skin tumors per mouse induced by TPA in 7,12-dimethylbenz[a]anthracene-initiated mouse skin. In addition, UVB- and TPA-induced transactivation of NF-kappaB and AP-1 and expression of cyclooxygenase-2 and tumor necrosis factor–alpha were suppressed by the pretreatment with C3G of JB6 cells. The researchers suggested that the inhibition of MAPK activity may be important in mediating such effects. TPA-induced neoplastic transformation in JB6 cells was also hindered via C3G pretreatment. Further, C3G suppressed proliferation of the human lung carcinoma cell line A549, diminished the size of A549 tumor xenograft growth, and significantly limited metastasis in nude mice. The investigators concluded that C3G, an important constituent of blackberry, displays significant anticancer activity by dint of its capacity to scavenge free radicals. As such, they suggested that this blackberry derivative, which exhibits scant cytotoxicity to healthy tissue, warrants additional study as a preventive and therapeutic agent in human cancers (J. Biol. Chem. 2006;281:17359-68).
Conclusion
The most recent evidence suggests that blackberry warrants attention for medical applications, including dermatology. In fact, in a small (n = 33) single-center, open-label study led by the author, significant improvement in most metrics of photoaged skin was observed after the use of a day and night regimen containing blackberry leaf extract, dill extract, and Zn-Cu(II) bi-mineral complex in patients with mild to moderate photodamage. (Baumann LS, Figueras KA, Bell M, Flitter CJ. Assessing the efficacy and tolerance of a day and night regimen containing blackberry leaf extract, dill extract, and Cu-Zinc bi-mineral complex in subjects with mild to moderate photoaged skin. Unpublished results.) It remains to be seen if and when blackberry extract alone may be harnessed for dermatologic indications, but present data are promising, and justify continued study.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
NSAIDs
Nonsteroidal anti-inflammatory drugs (NSAIDs) have therapeutic applications that "have spanned several centuries," according to Rao and Knaus (J. Pharm. Pharm. Sci. 2008;11:81s-110s). NSAIDs are among the increasing number of anti-inflammatory agents used to target bioactive lipids produced from arachidonic acid. Although this drug class is one of the most often used in practice and has been well studied by investigators, the role of NSAIDs for cutaneous purposes has been relatively limited (J. Cutan. Med. Surg. 2002;6:241-56). Indeed, only three topical NSAIDs are approved for use in the United States, for a narrow range of conditions.
Diclofenac sodium 1.5% topical solution (containing dimethyl sulfoxide to enhance penetration) and diclofenac sodium gel 1% are currently approved in the United States for hand and knee osteoarthritis (Postgrad. Med. 2010;122:98-106). The diclofenac hydroxyethylpyrrolidine (epolamine) 1.3% patch was approved by the U.S. Food and Drug Administration for soft-tissue injuries in January 2007, although it has long been available in more than 40 countries (Int. J. Clin. Pract. 2010;64:1546-53; Clin. Ther. 2010;32:1001-14).
A winning adverse event profile
Significantly, topical NSAIDs have not been associated with the adverse events resulting from oral NSAIDs, which engender various dose-related side effects (Semin. Arthritis. Rheum. 2009;39:203-12). Mild and self-limiting local skin reactions are the most common adverse side effects from topical NSAID products. The diclofenac products are approved in the European Union, as are ibuprofen creams and gels, ketoprofen gel, felbinac gel and cutaneous foam, and piroxicam gel.
The efficacy and safety of these products have been established through meta-analyses. In a recent study, researchers cautioned that the patient, the drug, and the drug delivery mechanism should be considered in topical NSAID selection, because the pharmacokinetic absorption from topical preparations can vary with different formulations of the same drug, depending on the agent, the underlying disorder, and the application site (Am. J. Ther. 2012 Feb 22 [Epub ahead of print]).
Easing osteoarthritis
Although oral NSAIDs have been the mainstays of hand and knee osteoarthritis treatment regimens, their dose- and age-related side effect profiles (including adverse effects on the cardiovascular, renal, and gastrointestinal systems) have prompted the use of topical NSAIDs, which yield comparable efficacy with far less systemic risk. Results of a Jan. 1, 2005, to March 31, 2010, literature review showed that topical products exhibited superior efficacy compared with placebo, with similar adverse event profiles. Topicals also showed efficacy comparable to that of oral diclofenac, with side effects seen primarily at the application site and no ulcers, perforations, or bleeding (Postgrad. Med. 2010;122(6):98-106).
In 2009, Barthel et al. evaluated the efficacy and safety of topical diclofenac sodium gel (DSG) 1% in a randomized, double-blind, vehicle-controlled trial of 492 adults (aged 35 years and older) with mild to moderate symptomatic knee osteoarthritis lasting at least 6 months. Patients received 4 g of topical treatment of DSG or vehicle four times daily for 12 weeks. The investigators noted significant reductions in the DSG group compared with the vehicle group according to the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain and physical function subscales, as well as global rating of disease. They also observed significantly better efficacy results with DSG as early as week 1 of treatment. Gastrointestinal reactions occurred in 5.9% of the DSG group and 5.0% of the vehicle group, and application site reactions emerged in 5.1% of the DSG group and 2.5% of the vehicle group (Semin. Arthritis Rheum. 2009;39:203-12).
In 2010, Baraf et al. also conducted a 12-week efficacy and safety study of topical DSG 1% for symptomatic knee osteoarthritis. This randomized, double-blind, parallel-group, multicenter trial of patients at least 35 years of age with symptomatic Kellgren-Lawrence grade (KLG) 1 to 3 osteoarthritis in one or both knees for at least 6 months assigned 208 subjects to DSG treatment and 212 to vehicle. The investigators found significant improvement according to WOMAC metrics in the DSG patients compared with placebo patients. Unlike the Barthel report, no gastrointestinal upset was noted in this study. Application site reactions were the most common side effect, occurring in 4.8% of the DSG group and 0% of the vehicle group (Phys. Sportsmed. 2010;38:19-28).
In 2012, Baraf et al. extended their previous work and assessed the safety of topical DSG 1% for the treatment of knee and hand osteoarthritis in older and younger patients. They also compared the treatment in those with or without comorbid hypertension, type 2 diabetes, or cerebrovascular or cardiovascular disease. This post hoc analysis of pooled data from five randomized, double-blind, placebo-controlled trials included 1,426 patients 35 years of age and older with mild to moderate osteoarthritis of the knee and 783 patients 40 years of age and older with mild to moderate osteoarthritis of the hand. Participants applied 4 g of DSG or vehicle to affected knees q.i.d. for 12 weeks or 2 g of DSG or vehicle to affected hands q.i.d. for 8 weeks. The investigators found that the adverse event profile was similar across comparisons of patients with knee osteoarthritis. Among patients with hand osteoarthritis, the only differences were that the adverse event profile was lower in patients with type 2 diabetes than in patients without the condition, and higher in patients with cerebrovascular or cardiovascular disease than in patients without those conditions. The authors concluded that the rates of adverse side effects were similar and low between the two groups (Am. J. Geriatr. Pharmacother. 2012;10:47-60).
To further examine the efficacy and tolerability of the diclofenac epolamine topical patch (DETP), investigators reviewed data from eight studies from 1984 to 2009, including data on patients with acute pain from soft-tissue injuries or localized periarticular disorders. Significant reductions in spontaneous pain from baseline due to DETP were seen (range, 26%-88% on day 7 and 56%-61% on day 14). In addition, significant decreases in pain scores were linked to DETP use compared with a placebo patch in two studies and compared with diclofenac diethylammonium topical gel in one study. Adverse events were low across studies; reactions at the application site and nausea were the most common events (Clin. Ther. 2010;32:1001-14).
Oral ibuprofen and combination therapy
Notably, ibuprofen has demonstrated effectiveness in the treatment of acne, as inflammatory acne lesions are infiltrated with neutrophils and ibuprofen suppresses leukocyte chemotaxis (Dermatology. 2003;206:68-73). Ibuprofen is generally considered safe, with low potential for causing gastrointestinal, cardiovascular, or renal risks compared with other NSAIDs and selective cyclooxygenase-2 inhibitors (coxibs), which have been removed from the market (Inflammopharmacology 2009;17:275-342; J. Pharm. Pharm. Sci. 2008;11:81s-110s).
In a double-blind study of 60 patients aged 15-35 years with acne vulgaris, patients were randomly assigned to one of four groups: oral ibuprofen (600 mg) plus tetracycline (250 mg) four times daily; ibuprofen (600 mg) plus placebo four times daily; tetracycline (250 mg) plus placebo four times daily; and two placebos four times daily. Interestingly, the combination therapy was the only approach that yielded an effect statistically superior to that of placebo in reducing total lesion counts. The use of ibuprofen alone netted improvements comparable to those afforded by tetracycline but with fewer side effects (J. Am. Acad. Dermatol. 1984;11:1076-81).
NSAIDs are also used for the treatment of sunburn. In 1992, Hughes et al. investigated ameliorating UVB-induced skin injury by nonsteroidal drugs (oral ibuprofen or indomethacin) plus topical betamethasone dipropionate in 24 subjects. Measurements of erythema and increased skin blood flow, performed serially, revealed a synergistic effect of oral NSAIDs combined with topical corticosteroids to repair UVB-induced skin damage (Dermatology 1992;184:54-8).
Conclusion
An ideal anti-inflammatory agent has not yet been developed, but topical NSAIDs appear to fit the bill in terms of reducing or eliminating the adverse side effects associated with oral NSAID regimens. However, topical NSAIDs are approved for only a narrow range of indications, and more research is necessary to determine whether they are appropriate for a wider array of dermatologic conditions.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest.
Nonsteroidal anti-inflammatory drugs (NSAIDs) have therapeutic applications that "have spanned several centuries," according to Rao and Knaus (J. Pharm. Pharm. Sci. 2008;11:81s-110s). NSAIDs are among the increasing number of anti-inflammatory agents used to target bioactive lipids produced from arachidonic acid. Although this drug class is one of the most often used in practice and has been well studied by investigators, the role of NSAIDs for cutaneous purposes has been relatively limited (J. Cutan. Med. Surg. 2002;6:241-56). Indeed, only three topical NSAIDs are approved for use in the United States, for a narrow range of conditions.
Diclofenac sodium 1.5% topical solution (containing dimethyl sulfoxide to enhance penetration) and diclofenac sodium gel 1% are currently approved in the United States for hand and knee osteoarthritis (Postgrad. Med. 2010;122:98-106). The diclofenac hydroxyethylpyrrolidine (epolamine) 1.3% patch was approved by the U.S. Food and Drug Administration for soft-tissue injuries in January 2007, although it has long been available in more than 40 countries (Int. J. Clin. Pract. 2010;64:1546-53; Clin. Ther. 2010;32:1001-14).
A winning adverse event profile
Significantly, topical NSAIDs have not been associated with the adverse events resulting from oral NSAIDs, which engender various dose-related side effects (Semin. Arthritis. Rheum. 2009;39:203-12). Mild and self-limiting local skin reactions are the most common adverse side effects from topical NSAID products. The diclofenac products are approved in the European Union, as are ibuprofen creams and gels, ketoprofen gel, felbinac gel and cutaneous foam, and piroxicam gel.
The efficacy and safety of these products have been established through meta-analyses. In a recent study, researchers cautioned that the patient, the drug, and the drug delivery mechanism should be considered in topical NSAID selection, because the pharmacokinetic absorption from topical preparations can vary with different formulations of the same drug, depending on the agent, the underlying disorder, and the application site (Am. J. Ther. 2012 Feb 22 [Epub ahead of print]).
Easing osteoarthritis
Although oral NSAIDs have been the mainstays of hand and knee osteoarthritis treatment regimens, their dose- and age-related side effect profiles (including adverse effects on the cardiovascular, renal, and gastrointestinal systems) have prompted the use of topical NSAIDs, which yield comparable efficacy with far less systemic risk. Results of a Jan. 1, 2005, to March 31, 2010, literature review showed that topical products exhibited superior efficacy compared with placebo, with similar adverse event profiles. Topicals also showed efficacy comparable to that of oral diclofenac, with side effects seen primarily at the application site and no ulcers, perforations, or bleeding (Postgrad. Med. 2010;122(6):98-106).
In 2009, Barthel et al. evaluated the efficacy and safety of topical diclofenac sodium gel (DSG) 1% in a randomized, double-blind, vehicle-controlled trial of 492 adults (aged 35 years and older) with mild to moderate symptomatic knee osteoarthritis lasting at least 6 months. Patients received 4 g of topical treatment of DSG or vehicle four times daily for 12 weeks. The investigators noted significant reductions in the DSG group compared with the vehicle group according to the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain and physical function subscales, as well as global rating of disease. They also observed significantly better efficacy results with DSG as early as week 1 of treatment. Gastrointestinal reactions occurred in 5.9% of the DSG group and 5.0% of the vehicle group, and application site reactions emerged in 5.1% of the DSG group and 2.5% of the vehicle group (Semin. Arthritis Rheum. 2009;39:203-12).
In 2010, Baraf et al. also conducted a 12-week efficacy and safety study of topical DSG 1% for symptomatic knee osteoarthritis. This randomized, double-blind, parallel-group, multicenter trial of patients at least 35 years of age with symptomatic Kellgren-Lawrence grade (KLG) 1 to 3 osteoarthritis in one or both knees for at least 6 months assigned 208 subjects to DSG treatment and 212 to vehicle. The investigators found significant improvement according to WOMAC metrics in the DSG patients compared with placebo patients. Unlike the Barthel report, no gastrointestinal upset was noted in this study. Application site reactions were the most common side effect, occurring in 4.8% of the DSG group and 0% of the vehicle group (Phys. Sportsmed. 2010;38:19-28).
In 2012, Baraf et al. extended their previous work and assessed the safety of topical DSG 1% for the treatment of knee and hand osteoarthritis in older and younger patients. They also compared the treatment in those with or without comorbid hypertension, type 2 diabetes, or cerebrovascular or cardiovascular disease. This post hoc analysis of pooled data from five randomized, double-blind, placebo-controlled trials included 1,426 patients 35 years of age and older with mild to moderate osteoarthritis of the knee and 783 patients 40 years of age and older with mild to moderate osteoarthritis of the hand. Participants applied 4 g of DSG or vehicle to affected knees q.i.d. for 12 weeks or 2 g of DSG or vehicle to affected hands q.i.d. for 8 weeks. The investigators found that the adverse event profile was similar across comparisons of patients with knee osteoarthritis. Among patients with hand osteoarthritis, the only differences were that the adverse event profile was lower in patients with type 2 diabetes than in patients without the condition, and higher in patients with cerebrovascular or cardiovascular disease than in patients without those conditions. The authors concluded that the rates of adverse side effects were similar and low between the two groups (Am. J. Geriatr. Pharmacother. 2012;10:47-60).
To further examine the efficacy and tolerability of the diclofenac epolamine topical patch (DETP), investigators reviewed data from eight studies from 1984 to 2009, including data on patients with acute pain from soft-tissue injuries or localized periarticular disorders. Significant reductions in spontaneous pain from baseline due to DETP were seen (range, 26%-88% on day 7 and 56%-61% on day 14). In addition, significant decreases in pain scores were linked to DETP use compared with a placebo patch in two studies and compared with diclofenac diethylammonium topical gel in one study. Adverse events were low across studies; reactions at the application site and nausea were the most common events (Clin. Ther. 2010;32:1001-14).
Oral ibuprofen and combination therapy
Notably, ibuprofen has demonstrated effectiveness in the treatment of acne, as inflammatory acne lesions are infiltrated with neutrophils and ibuprofen suppresses leukocyte chemotaxis (Dermatology. 2003;206:68-73). Ibuprofen is generally considered safe, with low potential for causing gastrointestinal, cardiovascular, or renal risks compared with other NSAIDs and selective cyclooxygenase-2 inhibitors (coxibs), which have been removed from the market (Inflammopharmacology 2009;17:275-342; J. Pharm. Pharm. Sci. 2008;11:81s-110s).
In a double-blind study of 60 patients aged 15-35 years with acne vulgaris, patients were randomly assigned to one of four groups: oral ibuprofen (600 mg) plus tetracycline (250 mg) four times daily; ibuprofen (600 mg) plus placebo four times daily; tetracycline (250 mg) plus placebo four times daily; and two placebos four times daily. Interestingly, the combination therapy was the only approach that yielded an effect statistically superior to that of placebo in reducing total lesion counts. The use of ibuprofen alone netted improvements comparable to those afforded by tetracycline but with fewer side effects (J. Am. Acad. Dermatol. 1984;11:1076-81).
NSAIDs are also used for the treatment of sunburn. In 1992, Hughes et al. investigated ameliorating UVB-induced skin injury by nonsteroidal drugs (oral ibuprofen or indomethacin) plus topical betamethasone dipropionate in 24 subjects. Measurements of erythema and increased skin blood flow, performed serially, revealed a synergistic effect of oral NSAIDs combined with topical corticosteroids to repair UVB-induced skin damage (Dermatology 1992;184:54-8).
Conclusion
An ideal anti-inflammatory agent has not yet been developed, but topical NSAIDs appear to fit the bill in terms of reducing or eliminating the adverse side effects associated with oral NSAID regimens. However, topical NSAIDs are approved for only a narrow range of indications, and more research is necessary to determine whether they are appropriate for a wider array of dermatologic conditions.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest.
Nonsteroidal anti-inflammatory drugs (NSAIDs) have therapeutic applications that "have spanned several centuries," according to Rao and Knaus (J. Pharm. Pharm. Sci. 2008;11:81s-110s). NSAIDs are among the increasing number of anti-inflammatory agents used to target bioactive lipids produced from arachidonic acid. Although this drug class is one of the most often used in practice and has been well studied by investigators, the role of NSAIDs for cutaneous purposes has been relatively limited (J. Cutan. Med. Surg. 2002;6:241-56). Indeed, only three topical NSAIDs are approved for use in the United States, for a narrow range of conditions.
Diclofenac sodium 1.5% topical solution (containing dimethyl sulfoxide to enhance penetration) and diclofenac sodium gel 1% are currently approved in the United States for hand and knee osteoarthritis (Postgrad. Med. 2010;122:98-106). The diclofenac hydroxyethylpyrrolidine (epolamine) 1.3% patch was approved by the U.S. Food and Drug Administration for soft-tissue injuries in January 2007, although it has long been available in more than 40 countries (Int. J. Clin. Pract. 2010;64:1546-53; Clin. Ther. 2010;32:1001-14).
A winning adverse event profile
Significantly, topical NSAIDs have not been associated with the adverse events resulting from oral NSAIDs, which engender various dose-related side effects (Semin. Arthritis. Rheum. 2009;39:203-12). Mild and self-limiting local skin reactions are the most common adverse side effects from topical NSAID products. The diclofenac products are approved in the European Union, as are ibuprofen creams and gels, ketoprofen gel, felbinac gel and cutaneous foam, and piroxicam gel.
The efficacy and safety of these products have been established through meta-analyses. In a recent study, researchers cautioned that the patient, the drug, and the drug delivery mechanism should be considered in topical NSAID selection, because the pharmacokinetic absorption from topical preparations can vary with different formulations of the same drug, depending on the agent, the underlying disorder, and the application site (Am. J. Ther. 2012 Feb 22 [Epub ahead of print]).
Easing osteoarthritis
Although oral NSAIDs have been the mainstays of hand and knee osteoarthritis treatment regimens, their dose- and age-related side effect profiles (including adverse effects on the cardiovascular, renal, and gastrointestinal systems) have prompted the use of topical NSAIDs, which yield comparable efficacy with far less systemic risk. Results of a Jan. 1, 2005, to March 31, 2010, literature review showed that topical products exhibited superior efficacy compared with placebo, with similar adverse event profiles. Topicals also showed efficacy comparable to that of oral diclofenac, with side effects seen primarily at the application site and no ulcers, perforations, or bleeding (Postgrad. Med. 2010;122(6):98-106).
In 2009, Barthel et al. evaluated the efficacy and safety of topical diclofenac sodium gel (DSG) 1% in a randomized, double-blind, vehicle-controlled trial of 492 adults (aged 35 years and older) with mild to moderate symptomatic knee osteoarthritis lasting at least 6 months. Patients received 4 g of topical treatment of DSG or vehicle four times daily for 12 weeks. The investigators noted significant reductions in the DSG group compared with the vehicle group according to the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain and physical function subscales, as well as global rating of disease. They also observed significantly better efficacy results with DSG as early as week 1 of treatment. Gastrointestinal reactions occurred in 5.9% of the DSG group and 5.0% of the vehicle group, and application site reactions emerged in 5.1% of the DSG group and 2.5% of the vehicle group (Semin. Arthritis Rheum. 2009;39:203-12).
In 2010, Baraf et al. also conducted a 12-week efficacy and safety study of topical DSG 1% for symptomatic knee osteoarthritis. This randomized, double-blind, parallel-group, multicenter trial of patients at least 35 years of age with symptomatic Kellgren-Lawrence grade (KLG) 1 to 3 osteoarthritis in one or both knees for at least 6 months assigned 208 subjects to DSG treatment and 212 to vehicle. The investigators found significant improvement according to WOMAC metrics in the DSG patients compared with placebo patients. Unlike the Barthel report, no gastrointestinal upset was noted in this study. Application site reactions were the most common side effect, occurring in 4.8% of the DSG group and 0% of the vehicle group (Phys. Sportsmed. 2010;38:19-28).
In 2012, Baraf et al. extended their previous work and assessed the safety of topical DSG 1% for the treatment of knee and hand osteoarthritis in older and younger patients. They also compared the treatment in those with or without comorbid hypertension, type 2 diabetes, or cerebrovascular or cardiovascular disease. This post hoc analysis of pooled data from five randomized, double-blind, placebo-controlled trials included 1,426 patients 35 years of age and older with mild to moderate osteoarthritis of the knee and 783 patients 40 years of age and older with mild to moderate osteoarthritis of the hand. Participants applied 4 g of DSG or vehicle to affected knees q.i.d. for 12 weeks or 2 g of DSG or vehicle to affected hands q.i.d. for 8 weeks. The investigators found that the adverse event profile was similar across comparisons of patients with knee osteoarthritis. Among patients with hand osteoarthritis, the only differences were that the adverse event profile was lower in patients with type 2 diabetes than in patients without the condition, and higher in patients with cerebrovascular or cardiovascular disease than in patients without those conditions. The authors concluded that the rates of adverse side effects were similar and low between the two groups (Am. J. Geriatr. Pharmacother. 2012;10:47-60).
To further examine the efficacy and tolerability of the diclofenac epolamine topical patch (DETP), investigators reviewed data from eight studies from 1984 to 2009, including data on patients with acute pain from soft-tissue injuries or localized periarticular disorders. Significant reductions in spontaneous pain from baseline due to DETP were seen (range, 26%-88% on day 7 and 56%-61% on day 14). In addition, significant decreases in pain scores were linked to DETP use compared with a placebo patch in two studies and compared with diclofenac diethylammonium topical gel in one study. Adverse events were low across studies; reactions at the application site and nausea were the most common events (Clin. Ther. 2010;32:1001-14).
Oral ibuprofen and combination therapy
Notably, ibuprofen has demonstrated effectiveness in the treatment of acne, as inflammatory acne lesions are infiltrated with neutrophils and ibuprofen suppresses leukocyte chemotaxis (Dermatology. 2003;206:68-73). Ibuprofen is generally considered safe, with low potential for causing gastrointestinal, cardiovascular, or renal risks compared with other NSAIDs and selective cyclooxygenase-2 inhibitors (coxibs), which have been removed from the market (Inflammopharmacology 2009;17:275-342; J. Pharm. Pharm. Sci. 2008;11:81s-110s).
In a double-blind study of 60 patients aged 15-35 years with acne vulgaris, patients were randomly assigned to one of four groups: oral ibuprofen (600 mg) plus tetracycline (250 mg) four times daily; ibuprofen (600 mg) plus placebo four times daily; tetracycline (250 mg) plus placebo four times daily; and two placebos four times daily. Interestingly, the combination therapy was the only approach that yielded an effect statistically superior to that of placebo in reducing total lesion counts. The use of ibuprofen alone netted improvements comparable to those afforded by tetracycline but with fewer side effects (J. Am. Acad. Dermatol. 1984;11:1076-81).
NSAIDs are also used for the treatment of sunburn. In 1992, Hughes et al. investigated ameliorating UVB-induced skin injury by nonsteroidal drugs (oral ibuprofen or indomethacin) plus topical betamethasone dipropionate in 24 subjects. Measurements of erythema and increased skin blood flow, performed serially, revealed a synergistic effect of oral NSAIDs combined with topical corticosteroids to repair UVB-induced skin damage (Dermatology 1992;184:54-8).
Conclusion
An ideal anti-inflammatory agent has not yet been developed, but topical NSAIDs appear to fit the bill in terms of reducing or eliminating the adverse side effects associated with oral NSAID regimens. However, topical NSAIDs are approved for only a narrow range of indications, and more research is necessary to determine whether they are appropriate for a wider array of dermatologic conditions.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest.
Alstonia scholaris
Alstonia scholaris, a tree that grows 50-80 feet high and belongs to the Apocynaceae family, has a long history of use in traditional and homeopathic medicine, including Ayurvedic medicine in India, where it is known as sapthaparna (Integr. Cancer Ther. 2009;8:273-9), in traditional Chinese medicine (J. Ethnopharmacol. 2010;129:293-8; J. Ethnopharmacol. 2010;129:174-81), and in traditional medicine in Africa and Australia (Integr. Cancer Ther. 2010;9:261-9). The bark contains the alkaloids ditamine, echitamine (or ditaine), and echitanines; and decoctions or other preparations of the bark have been used to treat gastrointestinal conditions (Grieve M. A Modern Herbal (Vol. 1). New York, Dover Publications, 1971, p. 29). Often called the devil’s tree, the bark of A. scholaris also has been used to treat malaria, cutaneous diseases, tumors, ulcers, chronic respiratory conditions (such as asthma and bronchitis), helminthiasis, and agalactia (Chin. J. Integr. Med. 2012 Mar 28 [Epub ahead of print]).
In the study of A. scholaris most directly pertinent to potential dermatologic treatment, Lee et al. found that ethanolic bark extracts of A. scholaris significantly suppressed retinoid-induced skin irritation in vitro and in vivo, in human HaCat keratinocytes. The investigators identified echitamine and loganin as the primary components likely responsible for the anti-inflammatory effects.
Data showed that A. scholaris dose-dependently inhibited the all-trans retinoic acid–induced releases of the pro-inflammatory cytokines monocyte chemoattractant protein-1 (MCP-1) and interleukin-8 (IL-8) in vitro. Also in vitro, A. scholaris extract potently suppressed radiation-induced increases in matrix metalloproteinase-1 (MMP-1). Importantly, in a cumulative irritation patch test, the botanical extract diminished retinol-induced skin irritation while enhancing retinoid activity in blocking MMP-1 expression, which is linked closely to cutaneous aging. The authors concluded that A. scholaris appears to have the dual benefits of decreasing irritation associated with retinoids while augmenting their antiaging impact (Evid. Based Complement. Alternat. Med. 2012;2012:190370).
The leaf extract of A. scholaris has been used to treat cold symptoms and tracheitis, and it has been prescribed in hospitals and approved for commercial over-the-counter sale by the State Food and Drugs Administration of China (SFDA) (J. Ethnopharmacol. 2010;129:293-8; J. Ethnopharmacol. 2010;129:174-81). The broad range of biological properties associated with A. scholaris has been ascribed to particular constituent categories, including alkaloids, flavonoids, and terpenoids (specifically, phenolic acids) (Chin. J. Integr. Med. 2012 Mar 28 [Epub ahead of print]). These properties include, but are reportedly not limited to, antioxidant, anticancer, anti-inflammatory, antistress, analgesic, antimutagenic, hepatoprotective, immunomodulatory, and chemopreventive activity (Integr. Cancer Ther. 2010;9:261-9; Chin. J. Integr. Med. 2012 Mar 28 [Epub ahead of print]). Antineoplastic effects have been linked directly to phytochemical constituents including echitamine, alstonine, pleiocarpamine, O-methylmacralstonine, macralstonine, and lupeol (Integr. Cancer Ther. 2010;9:261-9).
In 2006, Jagetia and Baliga investigated the anticancer activity of A. scholaris alkaloid fractions in vitro in cultured human neoplastic cell lines. They also conducted in vivo studies in tumor-bearing mice. The in vitro data in HeLa cells revealed a time-dependent rise in antineoplastic activity after 24 hours of exposure (25 mcg/mL). Further, once-daily administration of A. scholaris (240 mg/kg) to tumor-bearing mice yielded dose-dependent remissions, although there were toxic presentations at this dosage. The next-lower dose of 210 mg/kg was found to be most effective, with 20% of the mice surviving for as long as 120 days after tumor cell inoculation, compared with none of the control animals treated with saline (Phytother. Res. 2006;20:103-9).
Using an acute-restraint stress model in mice in 2009, Kulkarni and Juvekar evaluated the effects of stress and the impact of a methanolic extract of A. scholaris bark. Pretreatments with the extract of 100, 250, and 500 mg/kg for 7 days were found to exert significant antistress effects. In addition, nootropic activities were observed, with memory functions clearly enhanced in learning tasks. A. scholaris also was associated with significant antioxidant properties. The extract at 200 mcg/mL exhibited maximum scavenging of the stable radical 1,1-diphenyl-2-picrylhydrazyl at 90.11% and the nitric oxide radical at 62.77% (Indian J. Exp. Biol. 2009;47:47-52).
Later in 2009, Jahan et al. reported on their investigation of potential antioxidant and chemopreventive activity displayed by A. scholaris in a two-stage murine model. Skin carcinogenesis development was initiated in Swiss albino mice through one application of 7, 12-dimethyabenz(a)anthrecene (DMBA) and then promoted two weeks later by repeated application of croton oil three times per week through 16 weeks. The investigators found a lower incidence of tumors, tumor yield, tumor burden, and number of papillomas in mice treated with A. scholaris extract as compared to untreated controls (Integr. Cancer Ther. 2009;8:273-9).
In 2010, Shang et al. conducted multiple studies using A. scholaris. In the first published report, they assessed the anti-inflammatory and analgesic properties of the ethanolic leaf extract to validate its use in traditional Chinese medicine and modern clinical medicine. The investigators first determined that analgesic activity was conferred as the ethyl acetate and alkaloid fractions significantly diminished acetic acid-induced reactions in mice and, along with the ethanolic extract, reduced xylene-induced ear edema.
The researchers also performed in vivo and in vitro assessments of anti-inflammatory activity again on xylene-induced ear edema and carrageenan-induced air pouch formation in mice, as well as cyclooxygenase (COX)-1, -2 and 5-LOX inhibition.
In the air pouch model, A. scholaris alkaloids were found to have significantly spurred superoxide dismutase activity while lowering nitric oxide, prostaglandin E2, and malondialdehyde levels. In vitro tests, supporting evidence from animal models, showed that the three primary alkaloids isolated from A. scholaris leaves (picrinine, vallesamine, and scholaricine) inhibited the inflammatory mediators COX-1, COX-2, and 5-LOX. The researchers also noted that the in vitro anti-inflammatory assay results reinforced the notion of these alkaloids as the bioactive fraction of the plant (J. Ethnopharmacol. 2010;129:174-81).
In their second published report that year, Shang et al. investigated the antitussive and anti-asthmatic activities of the ethanolic extract, fractions, and chief alkaloids of A. scholaris leaf.
The researchers tested for antitussive effects using ammonia-induced or sulfur dioxide-induced coughing in mice and citric acid-induced coughing in guinea pigs. They evaluated anti-asthmatic activity via histamine-induced bronchoconstriction in guinea pigs. They also measured phenol red volume in murine tracheas to assess expectorant activity.
The data indicated antitussive activity, with significant alkaloid suppression of ammonia-induced coughing frequency in mice. Latency periods of sulfur dioxide-induced cough in mice and citric acid-induced cough in guinea pigs increased, and cough frequency in guinea pigs decreased.
Anti-asthmatic effects, such as suppression of convulsion, were observed in guinea pigs. In the expectorant assessment, tracheal phenol red production was increased. The researchers identified picrinine as the primary alkaloid responsible for these activities (J. Ethnopharmacol. 2010;129:293-8).
In addition, Jahan and Goyal showed that pretreatment with A. scholaris bark extract protected the bone marrow of mice against radiation-induced chromosomal damage and micronuclei induction (J Environ. Pathol. Toxicol. Oncol. 2010;29:101-11).
Conclusion
Despite the dearth of research on A. scholaris, the existing data are intriguing, particularly the findings that A. scholaris may have the capacity to amplify the anti-aging activity of retinoids while blunting their irritating effects. Although more research is needed to determine the dermatologic value of A. scholaris, the pursuit may potentially prove fruitful.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
Alstonia scholaris, a tree that grows 50-80 feet high and belongs to the Apocynaceae family, has a long history of use in traditional and homeopathic medicine, including Ayurvedic medicine in India, where it is known as sapthaparna (Integr. Cancer Ther. 2009;8:273-9), in traditional Chinese medicine (J. Ethnopharmacol. 2010;129:293-8; J. Ethnopharmacol. 2010;129:174-81), and in traditional medicine in Africa and Australia (Integr. Cancer Ther. 2010;9:261-9). The bark contains the alkaloids ditamine, echitamine (or ditaine), and echitanines; and decoctions or other preparations of the bark have been used to treat gastrointestinal conditions (Grieve M. A Modern Herbal (Vol. 1). New York, Dover Publications, 1971, p. 29). Often called the devil’s tree, the bark of A. scholaris also has been used to treat malaria, cutaneous diseases, tumors, ulcers, chronic respiratory conditions (such as asthma and bronchitis), helminthiasis, and agalactia (Chin. J. Integr. Med. 2012 Mar 28 [Epub ahead of print]).
In the study of A. scholaris most directly pertinent to potential dermatologic treatment, Lee et al. found that ethanolic bark extracts of A. scholaris significantly suppressed retinoid-induced skin irritation in vitro and in vivo, in human HaCat keratinocytes. The investigators identified echitamine and loganin as the primary components likely responsible for the anti-inflammatory effects.
Data showed that A. scholaris dose-dependently inhibited the all-trans retinoic acid–induced releases of the pro-inflammatory cytokines monocyte chemoattractant protein-1 (MCP-1) and interleukin-8 (IL-8) in vitro. Also in vitro, A. scholaris extract potently suppressed radiation-induced increases in matrix metalloproteinase-1 (MMP-1). Importantly, in a cumulative irritation patch test, the botanical extract diminished retinol-induced skin irritation while enhancing retinoid activity in blocking MMP-1 expression, which is linked closely to cutaneous aging. The authors concluded that A. scholaris appears to have the dual benefits of decreasing irritation associated with retinoids while augmenting their antiaging impact (Evid. Based Complement. Alternat. Med. 2012;2012:190370).
The leaf extract of A. scholaris has been used to treat cold symptoms and tracheitis, and it has been prescribed in hospitals and approved for commercial over-the-counter sale by the State Food and Drugs Administration of China (SFDA) (J. Ethnopharmacol. 2010;129:293-8; J. Ethnopharmacol. 2010;129:174-81). The broad range of biological properties associated with A. scholaris has been ascribed to particular constituent categories, including alkaloids, flavonoids, and terpenoids (specifically, phenolic acids) (Chin. J. Integr. Med. 2012 Mar 28 [Epub ahead of print]). These properties include, but are reportedly not limited to, antioxidant, anticancer, anti-inflammatory, antistress, analgesic, antimutagenic, hepatoprotective, immunomodulatory, and chemopreventive activity (Integr. Cancer Ther. 2010;9:261-9; Chin. J. Integr. Med. 2012 Mar 28 [Epub ahead of print]). Antineoplastic effects have been linked directly to phytochemical constituents including echitamine, alstonine, pleiocarpamine, O-methylmacralstonine, macralstonine, and lupeol (Integr. Cancer Ther. 2010;9:261-9).
In 2006, Jagetia and Baliga investigated the anticancer activity of A. scholaris alkaloid fractions in vitro in cultured human neoplastic cell lines. They also conducted in vivo studies in tumor-bearing mice. The in vitro data in HeLa cells revealed a time-dependent rise in antineoplastic activity after 24 hours of exposure (25 mcg/mL). Further, once-daily administration of A. scholaris (240 mg/kg) to tumor-bearing mice yielded dose-dependent remissions, although there were toxic presentations at this dosage. The next-lower dose of 210 mg/kg was found to be most effective, with 20% of the mice surviving for as long as 120 days after tumor cell inoculation, compared with none of the control animals treated with saline (Phytother. Res. 2006;20:103-9).
Using an acute-restraint stress model in mice in 2009, Kulkarni and Juvekar evaluated the effects of stress and the impact of a methanolic extract of A. scholaris bark. Pretreatments with the extract of 100, 250, and 500 mg/kg for 7 days were found to exert significant antistress effects. In addition, nootropic activities were observed, with memory functions clearly enhanced in learning tasks. A. scholaris also was associated with significant antioxidant properties. The extract at 200 mcg/mL exhibited maximum scavenging of the stable radical 1,1-diphenyl-2-picrylhydrazyl at 90.11% and the nitric oxide radical at 62.77% (Indian J. Exp. Biol. 2009;47:47-52).
Later in 2009, Jahan et al. reported on their investigation of potential antioxidant and chemopreventive activity displayed by A. scholaris in a two-stage murine model. Skin carcinogenesis development was initiated in Swiss albino mice through one application of 7, 12-dimethyabenz(a)anthrecene (DMBA) and then promoted two weeks later by repeated application of croton oil three times per week through 16 weeks. The investigators found a lower incidence of tumors, tumor yield, tumor burden, and number of papillomas in mice treated with A. scholaris extract as compared to untreated controls (Integr. Cancer Ther. 2009;8:273-9).
In 2010, Shang et al. conducted multiple studies using A. scholaris. In the first published report, they assessed the anti-inflammatory and analgesic properties of the ethanolic leaf extract to validate its use in traditional Chinese medicine and modern clinical medicine. The investigators first determined that analgesic activity was conferred as the ethyl acetate and alkaloid fractions significantly diminished acetic acid-induced reactions in mice and, along with the ethanolic extract, reduced xylene-induced ear edema.
The researchers also performed in vivo and in vitro assessments of anti-inflammatory activity again on xylene-induced ear edema and carrageenan-induced air pouch formation in mice, as well as cyclooxygenase (COX)-1, -2 and 5-LOX inhibition.
In the air pouch model, A. scholaris alkaloids were found to have significantly spurred superoxide dismutase activity while lowering nitric oxide, prostaglandin E2, and malondialdehyde levels. In vitro tests, supporting evidence from animal models, showed that the three primary alkaloids isolated from A. scholaris leaves (picrinine, vallesamine, and scholaricine) inhibited the inflammatory mediators COX-1, COX-2, and 5-LOX. The researchers also noted that the in vitro anti-inflammatory assay results reinforced the notion of these alkaloids as the bioactive fraction of the plant (J. Ethnopharmacol. 2010;129:174-81).
In their second published report that year, Shang et al. investigated the antitussive and anti-asthmatic activities of the ethanolic extract, fractions, and chief alkaloids of A. scholaris leaf.
The researchers tested for antitussive effects using ammonia-induced or sulfur dioxide-induced coughing in mice and citric acid-induced coughing in guinea pigs. They evaluated anti-asthmatic activity via histamine-induced bronchoconstriction in guinea pigs. They also measured phenol red volume in murine tracheas to assess expectorant activity.
The data indicated antitussive activity, with significant alkaloid suppression of ammonia-induced coughing frequency in mice. Latency periods of sulfur dioxide-induced cough in mice and citric acid-induced cough in guinea pigs increased, and cough frequency in guinea pigs decreased.
Anti-asthmatic effects, such as suppression of convulsion, were observed in guinea pigs. In the expectorant assessment, tracheal phenol red production was increased. The researchers identified picrinine as the primary alkaloid responsible for these activities (J. Ethnopharmacol. 2010;129:293-8).
In addition, Jahan and Goyal showed that pretreatment with A. scholaris bark extract protected the bone marrow of mice against radiation-induced chromosomal damage and micronuclei induction (J Environ. Pathol. Toxicol. Oncol. 2010;29:101-11).
Conclusion
Despite the dearth of research on A. scholaris, the existing data are intriguing, particularly the findings that A. scholaris may have the capacity to amplify the anti-aging activity of retinoids while blunting their irritating effects. Although more research is needed to determine the dermatologic value of A. scholaris, the pursuit may potentially prove fruitful.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
Alstonia scholaris, a tree that grows 50-80 feet high and belongs to the Apocynaceae family, has a long history of use in traditional and homeopathic medicine, including Ayurvedic medicine in India, where it is known as sapthaparna (Integr. Cancer Ther. 2009;8:273-9), in traditional Chinese medicine (J. Ethnopharmacol. 2010;129:293-8; J. Ethnopharmacol. 2010;129:174-81), and in traditional medicine in Africa and Australia (Integr. Cancer Ther. 2010;9:261-9). The bark contains the alkaloids ditamine, echitamine (or ditaine), and echitanines; and decoctions or other preparations of the bark have been used to treat gastrointestinal conditions (Grieve M. A Modern Herbal (Vol. 1). New York, Dover Publications, 1971, p. 29). Often called the devil’s tree, the bark of A. scholaris also has been used to treat malaria, cutaneous diseases, tumors, ulcers, chronic respiratory conditions (such as asthma and bronchitis), helminthiasis, and agalactia (Chin. J. Integr. Med. 2012 Mar 28 [Epub ahead of print]).
In the study of A. scholaris most directly pertinent to potential dermatologic treatment, Lee et al. found that ethanolic bark extracts of A. scholaris significantly suppressed retinoid-induced skin irritation in vitro and in vivo, in human HaCat keratinocytes. The investigators identified echitamine and loganin as the primary components likely responsible for the anti-inflammatory effects.
Data showed that A. scholaris dose-dependently inhibited the all-trans retinoic acid–induced releases of the pro-inflammatory cytokines monocyte chemoattractant protein-1 (MCP-1) and interleukin-8 (IL-8) in vitro. Also in vitro, A. scholaris extract potently suppressed radiation-induced increases in matrix metalloproteinase-1 (MMP-1). Importantly, in a cumulative irritation patch test, the botanical extract diminished retinol-induced skin irritation while enhancing retinoid activity in blocking MMP-1 expression, which is linked closely to cutaneous aging. The authors concluded that A. scholaris appears to have the dual benefits of decreasing irritation associated with retinoids while augmenting their antiaging impact (Evid. Based Complement. Alternat. Med. 2012;2012:190370).
The leaf extract of A. scholaris has been used to treat cold symptoms and tracheitis, and it has been prescribed in hospitals and approved for commercial over-the-counter sale by the State Food and Drugs Administration of China (SFDA) (J. Ethnopharmacol. 2010;129:293-8; J. Ethnopharmacol. 2010;129:174-81). The broad range of biological properties associated with A. scholaris has been ascribed to particular constituent categories, including alkaloids, flavonoids, and terpenoids (specifically, phenolic acids) (Chin. J. Integr. Med. 2012 Mar 28 [Epub ahead of print]). These properties include, but are reportedly not limited to, antioxidant, anticancer, anti-inflammatory, antistress, analgesic, antimutagenic, hepatoprotective, immunomodulatory, and chemopreventive activity (Integr. Cancer Ther. 2010;9:261-9; Chin. J. Integr. Med. 2012 Mar 28 [Epub ahead of print]). Antineoplastic effects have been linked directly to phytochemical constituents including echitamine, alstonine, pleiocarpamine, O-methylmacralstonine, macralstonine, and lupeol (Integr. Cancer Ther. 2010;9:261-9).
In 2006, Jagetia and Baliga investigated the anticancer activity of A. scholaris alkaloid fractions in vitro in cultured human neoplastic cell lines. They also conducted in vivo studies in tumor-bearing mice. The in vitro data in HeLa cells revealed a time-dependent rise in antineoplastic activity after 24 hours of exposure (25 mcg/mL). Further, once-daily administration of A. scholaris (240 mg/kg) to tumor-bearing mice yielded dose-dependent remissions, although there were toxic presentations at this dosage. The next-lower dose of 210 mg/kg was found to be most effective, with 20% of the mice surviving for as long as 120 days after tumor cell inoculation, compared with none of the control animals treated with saline (Phytother. Res. 2006;20:103-9).
Using an acute-restraint stress model in mice in 2009, Kulkarni and Juvekar evaluated the effects of stress and the impact of a methanolic extract of A. scholaris bark. Pretreatments with the extract of 100, 250, and 500 mg/kg for 7 days were found to exert significant antistress effects. In addition, nootropic activities were observed, with memory functions clearly enhanced in learning tasks. A. scholaris also was associated with significant antioxidant properties. The extract at 200 mcg/mL exhibited maximum scavenging of the stable radical 1,1-diphenyl-2-picrylhydrazyl at 90.11% and the nitric oxide radical at 62.77% (Indian J. Exp. Biol. 2009;47:47-52).
Later in 2009, Jahan et al. reported on their investigation of potential antioxidant and chemopreventive activity displayed by A. scholaris in a two-stage murine model. Skin carcinogenesis development was initiated in Swiss albino mice through one application of 7, 12-dimethyabenz(a)anthrecene (DMBA) and then promoted two weeks later by repeated application of croton oil three times per week through 16 weeks. The investigators found a lower incidence of tumors, tumor yield, tumor burden, and number of papillomas in mice treated with A. scholaris extract as compared to untreated controls (Integr. Cancer Ther. 2009;8:273-9).
In 2010, Shang et al. conducted multiple studies using A. scholaris. In the first published report, they assessed the anti-inflammatory and analgesic properties of the ethanolic leaf extract to validate its use in traditional Chinese medicine and modern clinical medicine. The investigators first determined that analgesic activity was conferred as the ethyl acetate and alkaloid fractions significantly diminished acetic acid-induced reactions in mice and, along with the ethanolic extract, reduced xylene-induced ear edema.
The researchers also performed in vivo and in vitro assessments of anti-inflammatory activity again on xylene-induced ear edema and carrageenan-induced air pouch formation in mice, as well as cyclooxygenase (COX)-1, -2 and 5-LOX inhibition.
In the air pouch model, A. scholaris alkaloids were found to have significantly spurred superoxide dismutase activity while lowering nitric oxide, prostaglandin E2, and malondialdehyde levels. In vitro tests, supporting evidence from animal models, showed that the three primary alkaloids isolated from A. scholaris leaves (picrinine, vallesamine, and scholaricine) inhibited the inflammatory mediators COX-1, COX-2, and 5-LOX. The researchers also noted that the in vitro anti-inflammatory assay results reinforced the notion of these alkaloids as the bioactive fraction of the plant (J. Ethnopharmacol. 2010;129:174-81).
In their second published report that year, Shang et al. investigated the antitussive and anti-asthmatic activities of the ethanolic extract, fractions, and chief alkaloids of A. scholaris leaf.
The researchers tested for antitussive effects using ammonia-induced or sulfur dioxide-induced coughing in mice and citric acid-induced coughing in guinea pigs. They evaluated anti-asthmatic activity via histamine-induced bronchoconstriction in guinea pigs. They also measured phenol red volume in murine tracheas to assess expectorant activity.
The data indicated antitussive activity, with significant alkaloid suppression of ammonia-induced coughing frequency in mice. Latency periods of sulfur dioxide-induced cough in mice and citric acid-induced cough in guinea pigs increased, and cough frequency in guinea pigs decreased.
Anti-asthmatic effects, such as suppression of convulsion, were observed in guinea pigs. In the expectorant assessment, tracheal phenol red production was increased. The researchers identified picrinine as the primary alkaloid responsible for these activities (J. Ethnopharmacol. 2010;129:293-8).
In addition, Jahan and Goyal showed that pretreatment with A. scholaris bark extract protected the bone marrow of mice against radiation-induced chromosomal damage and micronuclei induction (J Environ. Pathol. Toxicol. Oncol. 2010;29:101-11).
Conclusion
Despite the dearth of research on A. scholaris, the existing data are intriguing, particularly the findings that A. scholaris may have the capacity to amplify the anti-aging activity of retinoids while blunting their irritating effects. Although more research is needed to determine the dermatologic value of A. scholaris, the pursuit may potentially prove fruitful.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
Ceramides
Structured in lamellar sheets, the primary lipids of the epidermis – ceramides, cholesterol, and free fatty acids – play a crucial role in the barrier function of the skin. Ceramides have come to be known as a complex family of lipids (sphingolipids – a sphingoid base and a fatty acid) involved in cell signaling in addition to their role in barrier homeostasis and water retention. In fact, ceramides are known to play a critical role in cell proliferation, differentiation, and apoptosis (Food Chem. Toxicol. 2009;47:681-6). Significantly, they cannot be replenished or obtained through natural sources, but synthetic ceramides, studied since the 1950s, are increasingly sophisticated and useful.
This column will review some key aspects of natural human ceramides as well as topically applied synthetic versions (also known as pseudoceramides), which are thought to ameliorate the structure and function of ceramide-depleted skin.
Ceramide structure and function
Lipids in the stratum corneum (SC) play an important role in the barrier function of the skin. The intercellular lipids of the SC are thought to be composed of approximately equal proportions of ceramides (J. Invest. Dermatol. 1987;88:2s-6s), cholesterol, and fatty acids (Am. J. Clin. Dermatol. 2003;4:107-29). Ceramides are not found in significant supply in lower levels of the epidermis, such as the stratum granulosum or basal layer. This implies that terminal differentiation is an important component of the natural production of ceramides, of which there are at least nine classes in the SC. Ceramide 1 was first identified in 1982. In addition to ceramides 1 to 9, there are two protein-bound ceramides classified as ceramides A and B, which are covalently bound to cornified envelope proteins, such as involucrin (Bouwstra JA, Pilgrim K, Ponec M. Structure of the skin barrier, in "Skin Barrier," Elias PM, Feingold KR, Eds. New York: Taylor & Francis, 2006, p. 65) .
Ceramides are named based on the polarity and composition of the molecule. As suggested above, the foundational ceramide structure is a fatty acid covalently bound to a sphingoid base. The various classes of ceramides are grouped according to the arrangements of sphingosine (S), phytosphingosine (P), or 6-hydroxysphingosine (H) bases, to which an alpha-hydroxy (A) or nonhydroxy (N) fatty acid is attached, in addition to the presence or absence of a discrete omega-esterified linoleic acid residue (J. Lipid. Res. 2004;45:923-32).
Ceramide 1 is unique in that it is nonpolar, and it contains linoleic acid. The special function of ceramide 1 in the SC is typically ascribed to its unique structure, which is thought to allow it to act as a molecular rivet, binding the multiple bilayers of the SC (J. Invest. Dermatol. 1987;88:2s-6s). This would explain the stacking of lipid bilayers in lamellar sheets observed in the barrier. Ceramides 1, 4, and 7 exhibit critical functions in terms of epidermal integrity by serving as the primary storage areas for linoleic acid, an essential fatty acid with significant roles in the epidermal lipid barrier (J. Invest. Dermatol. 1980;74:230-3). Although all epidermal ceramides are produced from a lamellar body–derived glucosylceramide precursor, sphingomyelin-derived ceramides (ceramides 2 and 5) are essential for maintaining the integrity of the SC (J. Lipid. Res. 2000;41:2071-82). It is worth noting that because an alkaline pH suppresses beta-glucocerebrosidase and acid sphingomyelinase activity (J. Invest. Dermatol. 2005;125:510-20), alkaline soaps can exacerbate poor barrier formation.
Exposure to UVB radiation and cytokines has been associated with an increase in the regulatory enzyme for ceramide synthesis, serine palmitoyltransferase, and it has been determined that in response to UVB exposure, the epidermis upregulates sphingolipid synthesis at the mRNA and protein levels (J. Lipid. Res. 1998;39:2031-8).
Synthetic ceramides
Skin conditions such as atopic dermatitis (AD), psoriasis, contact dermatitis, and some genetic disorders have been associated with depleted ceramide levels (Am. J. Clin. Dermatol. 2005;6:215-23), but these diseases can be ameliorated through the use of exogenous ceramides or their analogues (topical ceramide replacement therapy) (Curr. Med. Chem. 2010;17:2301-24; J. Dermatol. Sci. 2008;51:37-43; Am. J. Clin. Dermatol. 2005;6:215-23). Notably, the activities of enzymes in the SC, particularly ceramidase, sphingomyelin deacylase, and glucosylceramide deacylase, have been shown to be elevated in epidermal AD (Am. J. Clin. Dermatol. 2005;6:215-23).
Synthetic ceramides, or pseudoceramides, contain hydroxyl groups, two alkyl groups, and an amide bond – the same key structural components as natural ceramides. Consequently, various synthetic ceramides have been reported to form the multilamellar structure observed in the intercellular spaces of the SC (J. Lipid. Res. 1996;37:361-7).
Coderch et al., in a review of ceramides and skin function, endorsed the potential of topical therapy for several skin conditions using complete lipid mixtures and some ceramide supplementation, as well as the topical delivery of lipid precursors (Am. J. Clin. Dermatol. 2003;4:107-29). And, in fact, the topical application of synthetic ceramides has been shown to speed up the repair of impaired SC (J. Clin. Invest. 1994;94:89-96; Dermatology 2005;211:128-34). Recent reports by Tokudome et al. also indicate that the application of sphingomyelin-based liposomes effectively augments the levels of various ceramides in cultured human skin models (Skin Pharmacol. Physiol. 2011;24:218-23; J. Liposome Res. 2010;20:49-54).
In 2005, de Jager et al. used small-angle and wide-angle x-ray diffraction to show that lipid mixtures prepared with well-defined synthetic ceramides exhibit organization and lipid-phase behavior that are very similar to those of lamellar and lateral SC lipids, and can be used to further elucidate the molecular structure and roles of individual ceramides (J. Lipid. Res. 2005;46:2649-56).
In light of the uncertainty regarding the metabolic impact of pseudoceramides, in 2008, Uchida et al. compared the effects of two chemically unrelated, commercially available products to exogenous cell-permeant or natural ceramide on cell growth and apoptosis thresholds. Using cultured human keratinocytes, the investigators found that the commercial ceramides did not suppress keratinocyte growth or increase cell toxicity, as did the cell-permeant. The investigators suggested that these findings buttress the preclinical studies indicating that these pseudoceramides are safe for topical application (J. Dermatol. Sci. 2008;51:37-43).
Kang et al. recently conducted studies of synthetic ceramide derivatives of PC-9S (N-ethanol-2-mirystyl-3-oxostearamide), which, itself, has been shown to be effective in atopic and psoriatic patients. Both studies, conducted in NC/Nga mice, demonstrated that the topical application of the derivative K6PC-9 or the derivative K6PC-9p reduced skin inflammation and AD symptoms. According to the authors, K6PC-9 warrants consideration as a topical agent for AD, and K6PC-9p warrants consideration as a treatment for inflammatory skin diseases in general (Int. Immunopharmacol. 2007;7:1589-97; Exp. Dermatol. 2008;17:958-64).
Subsequently, Kang et al. studied the effects of another ceramide derivative of PC-9S, K112PC-5 (2-acetyl-N-(1,3-dihydroxyisopropyl)tetradecanamide), on macrophage and T-lymphocyte function in primary macrophages and splenocytes, respectively. The researchers also studied the impact of topically applied K112PC-5 on skin inflammation and AD in NC/Nga mice. Among several findings, the investigators noted that K112PC-5 suppressed AD induced by extracts of dust mites, Dermatophagoides pteronyssinus and Dermatophagoides farinae, with the pseudoceramide exhibiting in vitro and in vivo anti-inflammatory activity. They concluded that K112PC-5 is another synthetic ceramide derivative with potential as a topical agent for the treatment of AD (Arch. Pharm. Res. 2008;31:1004-9).
In 2009, Morita et al. studied the potential adverse effects of the synthetic pseudoceramide SLE66, which has demonstrated the capacity to improve xerosis, pruritus, and scaling of human skin. They found that the tested product failed to provoke cutaneous irritation or sensitization in animal and human studies. In addition, they did not observe any phototoxicity or photosensitization, and they established 1,000 mg/kg/day (the highest level tested) as the no-observed-adverse-effect (NOAEL) for systemic toxicity after oral administration or topical application (Food Chem. Toxicol. 2009;47:669-73).
Conclusion
Ceramides are among the primary lipid constituents, along with cholesterol and fatty acids, of the lamellar sheets found in the intercellular spaces of the SC. Together, these lipids maintain the water permeability barrier role of the skin. Ceramides also play an important role in cell signaling. Research over the last several decades, particularly the last 20 years, indicates that topically applied synthetic ceramide agents can effectively compensate for diminished ceramide levels associated with various skin conditions.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
Structured in lamellar sheets, the primary lipids of the epidermis – ceramides, cholesterol, and free fatty acids – play a crucial role in the barrier function of the skin. Ceramides have come to be known as a complex family of lipids (sphingolipids – a sphingoid base and a fatty acid) involved in cell signaling in addition to their role in barrier homeostasis and water retention. In fact, ceramides are known to play a critical role in cell proliferation, differentiation, and apoptosis (Food Chem. Toxicol. 2009;47:681-6). Significantly, they cannot be replenished or obtained through natural sources, but synthetic ceramides, studied since the 1950s, are increasingly sophisticated and useful.
This column will review some key aspects of natural human ceramides as well as topically applied synthetic versions (also known as pseudoceramides), which are thought to ameliorate the structure and function of ceramide-depleted skin.
Ceramide structure and function
Lipids in the stratum corneum (SC) play an important role in the barrier function of the skin. The intercellular lipids of the SC are thought to be composed of approximately equal proportions of ceramides (J. Invest. Dermatol. 1987;88:2s-6s), cholesterol, and fatty acids (Am. J. Clin. Dermatol. 2003;4:107-29). Ceramides are not found in significant supply in lower levels of the epidermis, such as the stratum granulosum or basal layer. This implies that terminal differentiation is an important component of the natural production of ceramides, of which there are at least nine classes in the SC. Ceramide 1 was first identified in 1982. In addition to ceramides 1 to 9, there are two protein-bound ceramides classified as ceramides A and B, which are covalently bound to cornified envelope proteins, such as involucrin (Bouwstra JA, Pilgrim K, Ponec M. Structure of the skin barrier, in "Skin Barrier," Elias PM, Feingold KR, Eds. New York: Taylor & Francis, 2006, p. 65) .
Ceramides are named based on the polarity and composition of the molecule. As suggested above, the foundational ceramide structure is a fatty acid covalently bound to a sphingoid base. The various classes of ceramides are grouped according to the arrangements of sphingosine (S), phytosphingosine (P), or 6-hydroxysphingosine (H) bases, to which an alpha-hydroxy (A) or nonhydroxy (N) fatty acid is attached, in addition to the presence or absence of a discrete omega-esterified linoleic acid residue (J. Lipid. Res. 2004;45:923-32).
Ceramide 1 is unique in that it is nonpolar, and it contains linoleic acid. The special function of ceramide 1 in the SC is typically ascribed to its unique structure, which is thought to allow it to act as a molecular rivet, binding the multiple bilayers of the SC (J. Invest. Dermatol. 1987;88:2s-6s). This would explain the stacking of lipid bilayers in lamellar sheets observed in the barrier. Ceramides 1, 4, and 7 exhibit critical functions in terms of epidermal integrity by serving as the primary storage areas for linoleic acid, an essential fatty acid with significant roles in the epidermal lipid barrier (J. Invest. Dermatol. 1980;74:230-3). Although all epidermal ceramides are produced from a lamellar body–derived glucosylceramide precursor, sphingomyelin-derived ceramides (ceramides 2 and 5) are essential for maintaining the integrity of the SC (J. Lipid. Res. 2000;41:2071-82). It is worth noting that because an alkaline pH suppresses beta-glucocerebrosidase and acid sphingomyelinase activity (J. Invest. Dermatol. 2005;125:510-20), alkaline soaps can exacerbate poor barrier formation.
Exposure to UVB radiation and cytokines has been associated with an increase in the regulatory enzyme for ceramide synthesis, serine palmitoyltransferase, and it has been determined that in response to UVB exposure, the epidermis upregulates sphingolipid synthesis at the mRNA and protein levels (J. Lipid. Res. 1998;39:2031-8).
Synthetic ceramides
Skin conditions such as atopic dermatitis (AD), psoriasis, contact dermatitis, and some genetic disorders have been associated with depleted ceramide levels (Am. J. Clin. Dermatol. 2005;6:215-23), but these diseases can be ameliorated through the use of exogenous ceramides or their analogues (topical ceramide replacement therapy) (Curr. Med. Chem. 2010;17:2301-24; J. Dermatol. Sci. 2008;51:37-43; Am. J. Clin. Dermatol. 2005;6:215-23). Notably, the activities of enzymes in the SC, particularly ceramidase, sphingomyelin deacylase, and glucosylceramide deacylase, have been shown to be elevated in epidermal AD (Am. J. Clin. Dermatol. 2005;6:215-23).
Synthetic ceramides, or pseudoceramides, contain hydroxyl groups, two alkyl groups, and an amide bond – the same key structural components as natural ceramides. Consequently, various synthetic ceramides have been reported to form the multilamellar structure observed in the intercellular spaces of the SC (J. Lipid. Res. 1996;37:361-7).
Coderch et al., in a review of ceramides and skin function, endorsed the potential of topical therapy for several skin conditions using complete lipid mixtures and some ceramide supplementation, as well as the topical delivery of lipid precursors (Am. J. Clin. Dermatol. 2003;4:107-29). And, in fact, the topical application of synthetic ceramides has been shown to speed up the repair of impaired SC (J. Clin. Invest. 1994;94:89-96; Dermatology 2005;211:128-34). Recent reports by Tokudome et al. also indicate that the application of sphingomyelin-based liposomes effectively augments the levels of various ceramides in cultured human skin models (Skin Pharmacol. Physiol. 2011;24:218-23; J. Liposome Res. 2010;20:49-54).
In 2005, de Jager et al. used small-angle and wide-angle x-ray diffraction to show that lipid mixtures prepared with well-defined synthetic ceramides exhibit organization and lipid-phase behavior that are very similar to those of lamellar and lateral SC lipids, and can be used to further elucidate the molecular structure and roles of individual ceramides (J. Lipid. Res. 2005;46:2649-56).
In light of the uncertainty regarding the metabolic impact of pseudoceramides, in 2008, Uchida et al. compared the effects of two chemically unrelated, commercially available products to exogenous cell-permeant or natural ceramide on cell growth and apoptosis thresholds. Using cultured human keratinocytes, the investigators found that the commercial ceramides did not suppress keratinocyte growth or increase cell toxicity, as did the cell-permeant. The investigators suggested that these findings buttress the preclinical studies indicating that these pseudoceramides are safe for topical application (J. Dermatol. Sci. 2008;51:37-43).
Kang et al. recently conducted studies of synthetic ceramide derivatives of PC-9S (N-ethanol-2-mirystyl-3-oxostearamide), which, itself, has been shown to be effective in atopic and psoriatic patients. Both studies, conducted in NC/Nga mice, demonstrated that the topical application of the derivative K6PC-9 or the derivative K6PC-9p reduced skin inflammation and AD symptoms. According to the authors, K6PC-9 warrants consideration as a topical agent for AD, and K6PC-9p warrants consideration as a treatment for inflammatory skin diseases in general (Int. Immunopharmacol. 2007;7:1589-97; Exp. Dermatol. 2008;17:958-64).
Subsequently, Kang et al. studied the effects of another ceramide derivative of PC-9S, K112PC-5 (2-acetyl-N-(1,3-dihydroxyisopropyl)tetradecanamide), on macrophage and T-lymphocyte function in primary macrophages and splenocytes, respectively. The researchers also studied the impact of topically applied K112PC-5 on skin inflammation and AD in NC/Nga mice. Among several findings, the investigators noted that K112PC-5 suppressed AD induced by extracts of dust mites, Dermatophagoides pteronyssinus and Dermatophagoides farinae, with the pseudoceramide exhibiting in vitro and in vivo anti-inflammatory activity. They concluded that K112PC-5 is another synthetic ceramide derivative with potential as a topical agent for the treatment of AD (Arch. Pharm. Res. 2008;31:1004-9).
In 2009, Morita et al. studied the potential adverse effects of the synthetic pseudoceramide SLE66, which has demonstrated the capacity to improve xerosis, pruritus, and scaling of human skin. They found that the tested product failed to provoke cutaneous irritation or sensitization in animal and human studies. In addition, they did not observe any phototoxicity or photosensitization, and they established 1,000 mg/kg/day (the highest level tested) as the no-observed-adverse-effect (NOAEL) for systemic toxicity after oral administration or topical application (Food Chem. Toxicol. 2009;47:669-73).
Conclusion
Ceramides are among the primary lipid constituents, along with cholesterol and fatty acids, of the lamellar sheets found in the intercellular spaces of the SC. Together, these lipids maintain the water permeability barrier role of the skin. Ceramides also play an important role in cell signaling. Research over the last several decades, particularly the last 20 years, indicates that topically applied synthetic ceramide agents can effectively compensate for diminished ceramide levels associated with various skin conditions.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
Structured in lamellar sheets, the primary lipids of the epidermis – ceramides, cholesterol, and free fatty acids – play a crucial role in the barrier function of the skin. Ceramides have come to be known as a complex family of lipids (sphingolipids – a sphingoid base and a fatty acid) involved in cell signaling in addition to their role in barrier homeostasis and water retention. In fact, ceramides are known to play a critical role in cell proliferation, differentiation, and apoptosis (Food Chem. Toxicol. 2009;47:681-6). Significantly, they cannot be replenished or obtained through natural sources, but synthetic ceramides, studied since the 1950s, are increasingly sophisticated and useful.
This column will review some key aspects of natural human ceramides as well as topically applied synthetic versions (also known as pseudoceramides), which are thought to ameliorate the structure and function of ceramide-depleted skin.
Ceramide structure and function
Lipids in the stratum corneum (SC) play an important role in the barrier function of the skin. The intercellular lipids of the SC are thought to be composed of approximately equal proportions of ceramides (J. Invest. Dermatol. 1987;88:2s-6s), cholesterol, and fatty acids (Am. J. Clin. Dermatol. 2003;4:107-29). Ceramides are not found in significant supply in lower levels of the epidermis, such as the stratum granulosum or basal layer. This implies that terminal differentiation is an important component of the natural production of ceramides, of which there are at least nine classes in the SC. Ceramide 1 was first identified in 1982. In addition to ceramides 1 to 9, there are two protein-bound ceramides classified as ceramides A and B, which are covalently bound to cornified envelope proteins, such as involucrin (Bouwstra JA, Pilgrim K, Ponec M. Structure of the skin barrier, in "Skin Barrier," Elias PM, Feingold KR, Eds. New York: Taylor & Francis, 2006, p. 65) .
Ceramides are named based on the polarity and composition of the molecule. As suggested above, the foundational ceramide structure is a fatty acid covalently bound to a sphingoid base. The various classes of ceramides are grouped according to the arrangements of sphingosine (S), phytosphingosine (P), or 6-hydroxysphingosine (H) bases, to which an alpha-hydroxy (A) or nonhydroxy (N) fatty acid is attached, in addition to the presence or absence of a discrete omega-esterified linoleic acid residue (J. Lipid. Res. 2004;45:923-32).
Ceramide 1 is unique in that it is nonpolar, and it contains linoleic acid. The special function of ceramide 1 in the SC is typically ascribed to its unique structure, which is thought to allow it to act as a molecular rivet, binding the multiple bilayers of the SC (J. Invest. Dermatol. 1987;88:2s-6s). This would explain the stacking of lipid bilayers in lamellar sheets observed in the barrier. Ceramides 1, 4, and 7 exhibit critical functions in terms of epidermal integrity by serving as the primary storage areas for linoleic acid, an essential fatty acid with significant roles in the epidermal lipid barrier (J. Invest. Dermatol. 1980;74:230-3). Although all epidermal ceramides are produced from a lamellar body–derived glucosylceramide precursor, sphingomyelin-derived ceramides (ceramides 2 and 5) are essential for maintaining the integrity of the SC (J. Lipid. Res. 2000;41:2071-82). It is worth noting that because an alkaline pH suppresses beta-glucocerebrosidase and acid sphingomyelinase activity (J. Invest. Dermatol. 2005;125:510-20), alkaline soaps can exacerbate poor barrier formation.
Exposure to UVB radiation and cytokines has been associated with an increase in the regulatory enzyme for ceramide synthesis, serine palmitoyltransferase, and it has been determined that in response to UVB exposure, the epidermis upregulates sphingolipid synthesis at the mRNA and protein levels (J. Lipid. Res. 1998;39:2031-8).
Synthetic ceramides
Skin conditions such as atopic dermatitis (AD), psoriasis, contact dermatitis, and some genetic disorders have been associated with depleted ceramide levels (Am. J. Clin. Dermatol. 2005;6:215-23), but these diseases can be ameliorated through the use of exogenous ceramides or their analogues (topical ceramide replacement therapy) (Curr. Med. Chem. 2010;17:2301-24; J. Dermatol. Sci. 2008;51:37-43; Am. J. Clin. Dermatol. 2005;6:215-23). Notably, the activities of enzymes in the SC, particularly ceramidase, sphingomyelin deacylase, and glucosylceramide deacylase, have been shown to be elevated in epidermal AD (Am. J. Clin. Dermatol. 2005;6:215-23).
Synthetic ceramides, or pseudoceramides, contain hydroxyl groups, two alkyl groups, and an amide bond – the same key structural components as natural ceramides. Consequently, various synthetic ceramides have been reported to form the multilamellar structure observed in the intercellular spaces of the SC (J. Lipid. Res. 1996;37:361-7).
Coderch et al., in a review of ceramides and skin function, endorsed the potential of topical therapy for several skin conditions using complete lipid mixtures and some ceramide supplementation, as well as the topical delivery of lipid precursors (Am. J. Clin. Dermatol. 2003;4:107-29). And, in fact, the topical application of synthetic ceramides has been shown to speed up the repair of impaired SC (J. Clin. Invest. 1994;94:89-96; Dermatology 2005;211:128-34). Recent reports by Tokudome et al. also indicate that the application of sphingomyelin-based liposomes effectively augments the levels of various ceramides in cultured human skin models (Skin Pharmacol. Physiol. 2011;24:218-23; J. Liposome Res. 2010;20:49-54).
In 2005, de Jager et al. used small-angle and wide-angle x-ray diffraction to show that lipid mixtures prepared with well-defined synthetic ceramides exhibit organization and lipid-phase behavior that are very similar to those of lamellar and lateral SC lipids, and can be used to further elucidate the molecular structure and roles of individual ceramides (J. Lipid. Res. 2005;46:2649-56).
In light of the uncertainty regarding the metabolic impact of pseudoceramides, in 2008, Uchida et al. compared the effects of two chemically unrelated, commercially available products to exogenous cell-permeant or natural ceramide on cell growth and apoptosis thresholds. Using cultured human keratinocytes, the investigators found that the commercial ceramides did not suppress keratinocyte growth or increase cell toxicity, as did the cell-permeant. The investigators suggested that these findings buttress the preclinical studies indicating that these pseudoceramides are safe for topical application (J. Dermatol. Sci. 2008;51:37-43).
Kang et al. recently conducted studies of synthetic ceramide derivatives of PC-9S (N-ethanol-2-mirystyl-3-oxostearamide), which, itself, has been shown to be effective in atopic and psoriatic patients. Both studies, conducted in NC/Nga mice, demonstrated that the topical application of the derivative K6PC-9 or the derivative K6PC-9p reduced skin inflammation and AD symptoms. According to the authors, K6PC-9 warrants consideration as a topical agent for AD, and K6PC-9p warrants consideration as a treatment for inflammatory skin diseases in general (Int. Immunopharmacol. 2007;7:1589-97; Exp. Dermatol. 2008;17:958-64).
Subsequently, Kang et al. studied the effects of another ceramide derivative of PC-9S, K112PC-5 (2-acetyl-N-(1,3-dihydroxyisopropyl)tetradecanamide), on macrophage and T-lymphocyte function in primary macrophages and splenocytes, respectively. The researchers also studied the impact of topically applied K112PC-5 on skin inflammation and AD in NC/Nga mice. Among several findings, the investigators noted that K112PC-5 suppressed AD induced by extracts of dust mites, Dermatophagoides pteronyssinus and Dermatophagoides farinae, with the pseudoceramide exhibiting in vitro and in vivo anti-inflammatory activity. They concluded that K112PC-5 is another synthetic ceramide derivative with potential as a topical agent for the treatment of AD (Arch. Pharm. Res. 2008;31:1004-9).
In 2009, Morita et al. studied the potential adverse effects of the synthetic pseudoceramide SLE66, which has demonstrated the capacity to improve xerosis, pruritus, and scaling of human skin. They found that the tested product failed to provoke cutaneous irritation or sensitization in animal and human studies. In addition, they did not observe any phototoxicity or photosensitization, and they established 1,000 mg/kg/day (the highest level tested) as the no-observed-adverse-effect (NOAEL) for systemic toxicity after oral administration or topical application (Food Chem. Toxicol. 2009;47:669-73).
Conclusion
Ceramides are among the primary lipid constituents, along with cholesterol and fatty acids, of the lamellar sheets found in the intercellular spaces of the SC. Together, these lipids maintain the water permeability barrier role of the skin. Ceramides also play an important role in cell signaling. Research over the last several decades, particularly the last 20 years, indicates that topically applied synthetic ceramide agents can effectively compensate for diminished ceramide levels associated with various skin conditions.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].