User login
The perils of CA-125 as a diagnostic tool in patients with adnexal masses
CA-125, or cancer antigen 125, is an epitope (antigen) on the transmembrane glycoprotein MUC16, or mucin 16. This protein is expressed on the surface of tissue derived from embryonic coelomic and Müllerian epithelium including the reproductive tract. CA-125 is also expressed in other tissue such as the pleura, lungs, pericardium, intestines, and kidneys. MUC16 plays an important role in tumor proliferation, invasiveness, and cell motility.1 In patients with epithelial ovarian cancer (EOC), CA-125 may be found on the surface of ovarian cancer cells. It is shed in the bloodstream and can be quantified using a serum test.
There are a number of CA-125 assays in commercial use, and although none have been deemed to be clinically superior, there can be some differences between assays. It is important, if possible, to use the same assay when following serial CA-125 values. Most frequently, this will mean getting the test through the same laboratory.
CA-125 has Food and Drug Administration approval for use in patients with a current or prior diagnosis of ovarian cancer to monitor treatment response, progression of disease, or disease recurrence.
It is frequently used off label in the workup of adnexal masses, while not FDA approved. CA-125 and other serum biomarkers may help determine the etiology of an adnexal mass; however, they are not diagnostic and should be used thoughtfully. It is important to have conversations with patients before ordering a CA-125 (or other serum biomarkers) about potential results and their effect on diagnosis and treatment. This will lessen some patient anxiety when tests results become available, especially in the setting of autoreleasing results under the Cures Act.
One of the reasons that CA-125 can be difficult to interpret when used as a diagnostic tool is the number of nonmalignant disease processes that can result in CA-125 elevations. CA-125 can be elevated in inflammatory and infectious disease states, including but not limited to, chronic obstructive pulmonary disease, pelvic inflammatory disease, diverticulitis, and pneumonia. Severe/critical COVID-19 infection has recently been found to be associated with increased levels of CA-125.2 It is important to obtain a complete medical history and to take specific note of any current or recent flares in inflammatory or infectious processes that could contribute to CA-125 elevations.
Special caution should be taken in premenopausal patients. The sensitivity and specificity of CA-125 are lower in this cohort of patients compared to postmenopausal women. This is multifactorial but in part due to gynecologic conditions that can increase CA-125, such as uterine fibroids and endometriosis, and the higher incidence of nonepithelial ovarian cancers (which frequently have different serum biomarkers) in younger patients. A patient’s gynecologic history, her age, and ultrasound or other imaging findings should help determine what, if any, serum biomarkers are appropriate for workup of an adnexal mass rather than the default ordering of CA-125 to determine need for referral to gynecologic oncology. If the decision has been made to take the patient to the operating room, CA-125 is not approved as a triage tool to guide who best to perform the surgery. In this case, one of two serum tumor marker panel tests that has received FDA approval for triage after the decision for surgery has been made (the multivariate index assay or the risk of ovarian malignancy algorithm) should be used.
When considering its ability to serve as a diagnostic test for ovarian cancer, the sensitivity of CA-125 is affected by the number of patients with epithelial ovarian cancer who have a test result that falls within the normal range (up to 50% of patients with stage I disease).3 The specificity of CA-125 is affected by the large number of nonmalignant conditions that can cause its elevation. Depending on the age of the patient, her menopausal status, comorbid conditions, and reason for obtaining serum biomarkers (e.g., decision for surgery has already been made), CA-125 (or CA-125 alone) may not be the best tool to use in the workup of an adnexal mass and can cause significant patient anxiety. In the setting of acute disease, such as COVID-19 infection, it may be better to delay obtaining serum biomarkers for the work-up of an adnexal mass. If delay is not feasible, then repeat serum biomarkers once the acute phase of illness has passed.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Thériault C et al. Gynecol Oncol. 2011 Jun 1;121(3):434-43.
2. Wei X et al. J Med Virol. 2020;92(10):2036-41.
3. Zurawski VR Jr et al. Int J Cancer. 1988;42:677-80.
CA-125, or cancer antigen 125, is an epitope (antigen) on the transmembrane glycoprotein MUC16, or mucin 16. This protein is expressed on the surface of tissue derived from embryonic coelomic and Müllerian epithelium including the reproductive tract. CA-125 is also expressed in other tissue such as the pleura, lungs, pericardium, intestines, and kidneys. MUC16 plays an important role in tumor proliferation, invasiveness, and cell motility.1 In patients with epithelial ovarian cancer (EOC), CA-125 may be found on the surface of ovarian cancer cells. It is shed in the bloodstream and can be quantified using a serum test.
There are a number of CA-125 assays in commercial use, and although none have been deemed to be clinically superior, there can be some differences between assays. It is important, if possible, to use the same assay when following serial CA-125 values. Most frequently, this will mean getting the test through the same laboratory.
CA-125 has Food and Drug Administration approval for use in patients with a current or prior diagnosis of ovarian cancer to monitor treatment response, progression of disease, or disease recurrence.
It is frequently used off label in the workup of adnexal masses, while not FDA approved. CA-125 and other serum biomarkers may help determine the etiology of an adnexal mass; however, they are not diagnostic and should be used thoughtfully. It is important to have conversations with patients before ordering a CA-125 (or other serum biomarkers) about potential results and their effect on diagnosis and treatment. This will lessen some patient anxiety when tests results become available, especially in the setting of autoreleasing results under the Cures Act.
One of the reasons that CA-125 can be difficult to interpret when used as a diagnostic tool is the number of nonmalignant disease processes that can result in CA-125 elevations. CA-125 can be elevated in inflammatory and infectious disease states, including but not limited to, chronic obstructive pulmonary disease, pelvic inflammatory disease, diverticulitis, and pneumonia. Severe/critical COVID-19 infection has recently been found to be associated with increased levels of CA-125.2 It is important to obtain a complete medical history and to take specific note of any current or recent flares in inflammatory or infectious processes that could contribute to CA-125 elevations.
Special caution should be taken in premenopausal patients. The sensitivity and specificity of CA-125 are lower in this cohort of patients compared to postmenopausal women. This is multifactorial but in part due to gynecologic conditions that can increase CA-125, such as uterine fibroids and endometriosis, and the higher incidence of nonepithelial ovarian cancers (which frequently have different serum biomarkers) in younger patients. A patient’s gynecologic history, her age, and ultrasound or other imaging findings should help determine what, if any, serum biomarkers are appropriate for workup of an adnexal mass rather than the default ordering of CA-125 to determine need for referral to gynecologic oncology. If the decision has been made to take the patient to the operating room, CA-125 is not approved as a triage tool to guide who best to perform the surgery. In this case, one of two serum tumor marker panel tests that has received FDA approval for triage after the decision for surgery has been made (the multivariate index assay or the risk of ovarian malignancy algorithm) should be used.
When considering its ability to serve as a diagnostic test for ovarian cancer, the sensitivity of CA-125 is affected by the number of patients with epithelial ovarian cancer who have a test result that falls within the normal range (up to 50% of patients with stage I disease).3 The specificity of CA-125 is affected by the large number of nonmalignant conditions that can cause its elevation. Depending on the age of the patient, her menopausal status, comorbid conditions, and reason for obtaining serum biomarkers (e.g., decision for surgery has already been made), CA-125 (or CA-125 alone) may not be the best tool to use in the workup of an adnexal mass and can cause significant patient anxiety. In the setting of acute disease, such as COVID-19 infection, it may be better to delay obtaining serum biomarkers for the work-up of an adnexal mass. If delay is not feasible, then repeat serum biomarkers once the acute phase of illness has passed.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Thériault C et al. Gynecol Oncol. 2011 Jun 1;121(3):434-43.
2. Wei X et al. J Med Virol. 2020;92(10):2036-41.
3. Zurawski VR Jr et al. Int J Cancer. 1988;42:677-80.
CA-125, or cancer antigen 125, is an epitope (antigen) on the transmembrane glycoprotein MUC16, or mucin 16. This protein is expressed on the surface of tissue derived from embryonic coelomic and Müllerian epithelium including the reproductive tract. CA-125 is also expressed in other tissue such as the pleura, lungs, pericardium, intestines, and kidneys. MUC16 plays an important role in tumor proliferation, invasiveness, and cell motility.1 In patients with epithelial ovarian cancer (EOC), CA-125 may be found on the surface of ovarian cancer cells. It is shed in the bloodstream and can be quantified using a serum test.
There are a number of CA-125 assays in commercial use, and although none have been deemed to be clinically superior, there can be some differences between assays. It is important, if possible, to use the same assay when following serial CA-125 values. Most frequently, this will mean getting the test through the same laboratory.
CA-125 has Food and Drug Administration approval for use in patients with a current or prior diagnosis of ovarian cancer to monitor treatment response, progression of disease, or disease recurrence.
It is frequently used off label in the workup of adnexal masses, while not FDA approved. CA-125 and other serum biomarkers may help determine the etiology of an adnexal mass; however, they are not diagnostic and should be used thoughtfully. It is important to have conversations with patients before ordering a CA-125 (or other serum biomarkers) about potential results and their effect on diagnosis and treatment. This will lessen some patient anxiety when tests results become available, especially in the setting of autoreleasing results under the Cures Act.
One of the reasons that CA-125 can be difficult to interpret when used as a diagnostic tool is the number of nonmalignant disease processes that can result in CA-125 elevations. CA-125 can be elevated in inflammatory and infectious disease states, including but not limited to, chronic obstructive pulmonary disease, pelvic inflammatory disease, diverticulitis, and pneumonia. Severe/critical COVID-19 infection has recently been found to be associated with increased levels of CA-125.2 It is important to obtain a complete medical history and to take specific note of any current or recent flares in inflammatory or infectious processes that could contribute to CA-125 elevations.
Special caution should be taken in premenopausal patients. The sensitivity and specificity of CA-125 are lower in this cohort of patients compared to postmenopausal women. This is multifactorial but in part due to gynecologic conditions that can increase CA-125, such as uterine fibroids and endometriosis, and the higher incidence of nonepithelial ovarian cancers (which frequently have different serum biomarkers) in younger patients. A patient’s gynecologic history, her age, and ultrasound or other imaging findings should help determine what, if any, serum biomarkers are appropriate for workup of an adnexal mass rather than the default ordering of CA-125 to determine need for referral to gynecologic oncology. If the decision has been made to take the patient to the operating room, CA-125 is not approved as a triage tool to guide who best to perform the surgery. In this case, one of two serum tumor marker panel tests that has received FDA approval for triage after the decision for surgery has been made (the multivariate index assay or the risk of ovarian malignancy algorithm) should be used.
When considering its ability to serve as a diagnostic test for ovarian cancer, the sensitivity of CA-125 is affected by the number of patients with epithelial ovarian cancer who have a test result that falls within the normal range (up to 50% of patients with stage I disease).3 The specificity of CA-125 is affected by the large number of nonmalignant conditions that can cause its elevation. Depending on the age of the patient, her menopausal status, comorbid conditions, and reason for obtaining serum biomarkers (e.g., decision for surgery has already been made), CA-125 (or CA-125 alone) may not be the best tool to use in the workup of an adnexal mass and can cause significant patient anxiety. In the setting of acute disease, such as COVID-19 infection, it may be better to delay obtaining serum biomarkers for the work-up of an adnexal mass. If delay is not feasible, then repeat serum biomarkers once the acute phase of illness has passed.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Thériault C et al. Gynecol Oncol. 2011 Jun 1;121(3):434-43.
2. Wei X et al. J Med Virol. 2020;92(10):2036-41.
3. Zurawski VR Jr et al. Int J Cancer. 1988;42:677-80.
Hormones after cancer: Are they safe?
The impact of a gynecologic cancer diagnosis reaches beyond the obvious side effects of surgery, chemotherapy, and radiation. Many of our patients experience the quality-of-life–limiting side effects of abrupt hormone withdrawal as a consequence of our treatments. Assumptions are common, by both patients and providers, that hormonal therapy is unsafe after a gynecologic cancer diagnosis and that it is associated with an increased risk for recurrence. This sentiment likely originates from the fallout of the Womens’ Health Initiative (WHI) studies which showed an increased risk of breast cancer among users of combined estrogen and progesterone therapy.1 While this may be true for breast cancer risk, when initiated early, hormonal therapy is safe, even beneficial, for many patients with a history of gynecologic cancer, and can significantly improve their quality of life in addition to reducing all-cause mortality and incidence of osteoporosis, dementia, and cardiovascular disease.2
Premenopausal women undergoing surgery for endometrial cancer or preinvasive hyperplasia should be considered for ovarian preservation at the time of surgery. This strategy has been shown to be safe and not associated with an increased risk of recurrence. If oophorectomy is performed, hormonal therapy has been shown to be a safe remedy to the side effects of surgical menopause and the deleterious acceleration of bone loss and cardiovascular aging. The safety of hormone therapy for early-stage endometrial cancer has been thoroughly studied, including in a randomized controlled trial of more than 1,200 patients.3 This study showed no difference in the recurrence rate in users when compared with nonusers.
While hormone therapy is safe, from an oncologic standpoint, for women with a history of early-stage endometrial cancer other risks must also be considered. Given the association between endometrial cancer and obesity, these patients are at higher risk for venous thromboembolic (VTE) events, more so with the addition of exogenous hormone therapy. While not an overt contraindication to hormone prescription, obese patients who are prescribed these agents should be counseled regarding their risks for VTE.
The subgroup of patients with endometrial cancer in whom hormones should not be prescribed are those with advanced or recurrent disease. It is common for these tumors to express estrogen receptors, as evidenced by the responsiveness of these tumors to progesterone and antiestrogen treatments. Therefore, there is a theoretical risk for progression while using estrogen. In addition, as stated above, the risk of VTE is particularly elevated for women with metastatic malignancy receiving systemic therapies.
Cervical cancer commonly affects women of premenopausal age; therefore, early ovarian failure is particularly deleterious for this group of patients. Early-stage cervical cancer is most commonly treated with radical or extrafascial hysterectomy. Oophorectomy is not obligatory for the majority of these cases, and can be omitted in pre-, or perimenopausal patients to prevent surgical menopause. Ovarian metastases have been reported in cases of cervical adenocarcinoma, which led to the concern that ovarian preservation was not safe for this histology. However, recent data dispute this concern. A contemporary retrospective series of 105 patients with cervical adenocarcinoma identified no significant difference in overall survival when comparing those who had undergone ovarian preservation versus bilateral salpingo-oophorectomy.4
Ovarian preservation during cervical cancer surgery may not be enough to prevent early menopause. Approximately 20% of cervical cancer patients may require postoperative radiation for high- or intermediate-risk disease (such as positive lymph nodes, or adverse features in the tumor). For these women, ovarian ablation results, even if the ovaries were preserved at the time of surgery. Transposition of the ovaries to a location outside of the potential radiation fields is a strategy to mitigate this risk. To achieve this, the preserved ovaries and their vascular pedicles are skeletonized. The ovaries are then sutured to the paracolic gutter peritoneum or similar location above the pelvic brim, taking care to ensure that the vascular pedicle is not compromised or twisted. Placement of radio-opaque surgical clips on the caudad aspect of the transposed ovary aids in their identification by radiation oncologists when planning their treatment fields.
Ovarian transposition is most commonly used for women who are undergoing definitive surgery for cervical cancer. However, this strategy can also be used as a lead-in procedure for young women with advanced cervical cancer in whom definitive chemoradiation is planned. If the ovaries cannot be spared or moved out of “harm’s way” for premenopausal women undergoing treatment with definitive radiation, hormone therapy may be necessary and is safe for patients with cervical cancer, including those with adenocarcinoma. If the patient has not undergone hysterectomy, a regimen that includes a combination of estrogen and progesterone is necessary to avoid carcinogenic effects of unopposed estrogen on an intact endometrium, even after radiation has ablated those tissues.
When ovarian and fallopian cancers arise in premenopausal patients and appear confined to a single adnexa, contralateral ovarian preservation can be considered. However, for advanced disease, this is usually not possible or appropriate. Given that most ovarian cancers arise in a postmenopausal population, these patients may be preexisting users of hormone therapy. The data, including a randomized controlled trial, would suggest that it is safe to continue to use hormone therapy during or following a diagnosis of ovarian, fallopian tube, or primary peritoneal cancer and that it is not associated with worse outcomes from their cancer.5
Once again, patients should be carefully counseled about the additive risks for VTE that come from metastatic ovarian cancer, surgery via laparotomy, and exogenous hormonal therapy. However, these patients need not be subjected to an abrupt transition to menopause, because level I evidence suggests that these therapies are not associated with worse oncologic outcomes. All patients with ovarian, fallopian tube, and primary peritoneal cancer should receive genetic testing, and if deleterious mutations are found in BRCA 1 or 2 genes indicating an elevated risk for breast cancer, decision making regarding continued exogenous hormonal therapy is complicated. The most contemporary data, including long-term follow-up from the Women’s Health Initiative clinical trials, do not suggest an increased risk for breast cancer with estrogen-only preparations of hormone therapy.6 Given that most women with gynecologic cancers have undergone hysterectomy as part of their treatment, these estrogen-only preparations are appropriate for most.
For patients with rare tumors, such as endometrial stromal tumors or uterine leiomyosarcoma, the safety of exogenous hormone therapy should be dictated by the receptor profile of their particular cancer. Many of these cancers express estrogen receptors; therefore, current guidelines recommend against the use of hormones after these diagnoses when estrogen receptors are expressed.
Gynecologic cancer treatments induce many toxicities with long-term deleterious effects on quality of life. Use of hormones to mitigate the symptoms of menopause is an important tool in the toolkit for gynecologists. Assumptions should not be made that hormonal therapies are always unsafe for all of these patients. It is important to closely evaluate the patient’s tumor and other risk factors before withholding potentially valuable therapies.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at [email protected].
References
1. Chlebowski R et al. JAMA. 2010 Oct 20;304(15):1684-92.
2. Sinno AK et al. Gynecol Oncol. 2020;157(2):303-6.
3. Barakat et al. J Clin Oncol. 2006;24(4):587-92.
4. Hu Jun et al. J Obstet Gynaecol. 2017 Nov;37(8):1065-9.
5. Eeles R et al. J Clin Oncol. 2015 Dec 10;33(35):4138-44.
6. Chlebowski R et al. JAMA Jul 28 2020;324(4):369-80.
The impact of a gynecologic cancer diagnosis reaches beyond the obvious side effects of surgery, chemotherapy, and radiation. Many of our patients experience the quality-of-life–limiting side effects of abrupt hormone withdrawal as a consequence of our treatments. Assumptions are common, by both patients and providers, that hormonal therapy is unsafe after a gynecologic cancer diagnosis and that it is associated with an increased risk for recurrence. This sentiment likely originates from the fallout of the Womens’ Health Initiative (WHI) studies which showed an increased risk of breast cancer among users of combined estrogen and progesterone therapy.1 While this may be true for breast cancer risk, when initiated early, hormonal therapy is safe, even beneficial, for many patients with a history of gynecologic cancer, and can significantly improve their quality of life in addition to reducing all-cause mortality and incidence of osteoporosis, dementia, and cardiovascular disease.2
Premenopausal women undergoing surgery for endometrial cancer or preinvasive hyperplasia should be considered for ovarian preservation at the time of surgery. This strategy has been shown to be safe and not associated with an increased risk of recurrence. If oophorectomy is performed, hormonal therapy has been shown to be a safe remedy to the side effects of surgical menopause and the deleterious acceleration of bone loss and cardiovascular aging. The safety of hormone therapy for early-stage endometrial cancer has been thoroughly studied, including in a randomized controlled trial of more than 1,200 patients.3 This study showed no difference in the recurrence rate in users when compared with nonusers.
While hormone therapy is safe, from an oncologic standpoint, for women with a history of early-stage endometrial cancer other risks must also be considered. Given the association between endometrial cancer and obesity, these patients are at higher risk for venous thromboembolic (VTE) events, more so with the addition of exogenous hormone therapy. While not an overt contraindication to hormone prescription, obese patients who are prescribed these agents should be counseled regarding their risks for VTE.
The subgroup of patients with endometrial cancer in whom hormones should not be prescribed are those with advanced or recurrent disease. It is common for these tumors to express estrogen receptors, as evidenced by the responsiveness of these tumors to progesterone and antiestrogen treatments. Therefore, there is a theoretical risk for progression while using estrogen. In addition, as stated above, the risk of VTE is particularly elevated for women with metastatic malignancy receiving systemic therapies.
Cervical cancer commonly affects women of premenopausal age; therefore, early ovarian failure is particularly deleterious for this group of patients. Early-stage cervical cancer is most commonly treated with radical or extrafascial hysterectomy. Oophorectomy is not obligatory for the majority of these cases, and can be omitted in pre-, or perimenopausal patients to prevent surgical menopause. Ovarian metastases have been reported in cases of cervical adenocarcinoma, which led to the concern that ovarian preservation was not safe for this histology. However, recent data dispute this concern. A contemporary retrospective series of 105 patients with cervical adenocarcinoma identified no significant difference in overall survival when comparing those who had undergone ovarian preservation versus bilateral salpingo-oophorectomy.4
Ovarian preservation during cervical cancer surgery may not be enough to prevent early menopause. Approximately 20% of cervical cancer patients may require postoperative radiation for high- or intermediate-risk disease (such as positive lymph nodes, or adverse features in the tumor). For these women, ovarian ablation results, even if the ovaries were preserved at the time of surgery. Transposition of the ovaries to a location outside of the potential radiation fields is a strategy to mitigate this risk. To achieve this, the preserved ovaries and their vascular pedicles are skeletonized. The ovaries are then sutured to the paracolic gutter peritoneum or similar location above the pelvic brim, taking care to ensure that the vascular pedicle is not compromised or twisted. Placement of radio-opaque surgical clips on the caudad aspect of the transposed ovary aids in their identification by radiation oncologists when planning their treatment fields.
Ovarian transposition is most commonly used for women who are undergoing definitive surgery for cervical cancer. However, this strategy can also be used as a lead-in procedure for young women with advanced cervical cancer in whom definitive chemoradiation is planned. If the ovaries cannot be spared or moved out of “harm’s way” for premenopausal women undergoing treatment with definitive radiation, hormone therapy may be necessary and is safe for patients with cervical cancer, including those with adenocarcinoma. If the patient has not undergone hysterectomy, a regimen that includes a combination of estrogen and progesterone is necessary to avoid carcinogenic effects of unopposed estrogen on an intact endometrium, even after radiation has ablated those tissues.
When ovarian and fallopian cancers arise in premenopausal patients and appear confined to a single adnexa, contralateral ovarian preservation can be considered. However, for advanced disease, this is usually not possible or appropriate. Given that most ovarian cancers arise in a postmenopausal population, these patients may be preexisting users of hormone therapy. The data, including a randomized controlled trial, would suggest that it is safe to continue to use hormone therapy during or following a diagnosis of ovarian, fallopian tube, or primary peritoneal cancer and that it is not associated with worse outcomes from their cancer.5
Once again, patients should be carefully counseled about the additive risks for VTE that come from metastatic ovarian cancer, surgery via laparotomy, and exogenous hormonal therapy. However, these patients need not be subjected to an abrupt transition to menopause, because level I evidence suggests that these therapies are not associated with worse oncologic outcomes. All patients with ovarian, fallopian tube, and primary peritoneal cancer should receive genetic testing, and if deleterious mutations are found in BRCA 1 or 2 genes indicating an elevated risk for breast cancer, decision making regarding continued exogenous hormonal therapy is complicated. The most contemporary data, including long-term follow-up from the Women’s Health Initiative clinical trials, do not suggest an increased risk for breast cancer with estrogen-only preparations of hormone therapy.6 Given that most women with gynecologic cancers have undergone hysterectomy as part of their treatment, these estrogen-only preparations are appropriate for most.
For patients with rare tumors, such as endometrial stromal tumors or uterine leiomyosarcoma, the safety of exogenous hormone therapy should be dictated by the receptor profile of their particular cancer. Many of these cancers express estrogen receptors; therefore, current guidelines recommend against the use of hormones after these diagnoses when estrogen receptors are expressed.
Gynecologic cancer treatments induce many toxicities with long-term deleterious effects on quality of life. Use of hormones to mitigate the symptoms of menopause is an important tool in the toolkit for gynecologists. Assumptions should not be made that hormonal therapies are always unsafe for all of these patients. It is important to closely evaluate the patient’s tumor and other risk factors before withholding potentially valuable therapies.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at [email protected].
References
1. Chlebowski R et al. JAMA. 2010 Oct 20;304(15):1684-92.
2. Sinno AK et al. Gynecol Oncol. 2020;157(2):303-6.
3. Barakat et al. J Clin Oncol. 2006;24(4):587-92.
4. Hu Jun et al. J Obstet Gynaecol. 2017 Nov;37(8):1065-9.
5. Eeles R et al. J Clin Oncol. 2015 Dec 10;33(35):4138-44.
6. Chlebowski R et al. JAMA Jul 28 2020;324(4):369-80.
The impact of a gynecologic cancer diagnosis reaches beyond the obvious side effects of surgery, chemotherapy, and radiation. Many of our patients experience the quality-of-life–limiting side effects of abrupt hormone withdrawal as a consequence of our treatments. Assumptions are common, by both patients and providers, that hormonal therapy is unsafe after a gynecologic cancer diagnosis and that it is associated with an increased risk for recurrence. This sentiment likely originates from the fallout of the Womens’ Health Initiative (WHI) studies which showed an increased risk of breast cancer among users of combined estrogen and progesterone therapy.1 While this may be true for breast cancer risk, when initiated early, hormonal therapy is safe, even beneficial, for many patients with a history of gynecologic cancer, and can significantly improve their quality of life in addition to reducing all-cause mortality and incidence of osteoporosis, dementia, and cardiovascular disease.2
Premenopausal women undergoing surgery for endometrial cancer or preinvasive hyperplasia should be considered for ovarian preservation at the time of surgery. This strategy has been shown to be safe and not associated with an increased risk of recurrence. If oophorectomy is performed, hormonal therapy has been shown to be a safe remedy to the side effects of surgical menopause and the deleterious acceleration of bone loss and cardiovascular aging. The safety of hormone therapy for early-stage endometrial cancer has been thoroughly studied, including in a randomized controlled trial of more than 1,200 patients.3 This study showed no difference in the recurrence rate in users when compared with nonusers.
While hormone therapy is safe, from an oncologic standpoint, for women with a history of early-stage endometrial cancer other risks must also be considered. Given the association between endometrial cancer and obesity, these patients are at higher risk for venous thromboembolic (VTE) events, more so with the addition of exogenous hormone therapy. While not an overt contraindication to hormone prescription, obese patients who are prescribed these agents should be counseled regarding their risks for VTE.
The subgroup of patients with endometrial cancer in whom hormones should not be prescribed are those with advanced or recurrent disease. It is common for these tumors to express estrogen receptors, as evidenced by the responsiveness of these tumors to progesterone and antiestrogen treatments. Therefore, there is a theoretical risk for progression while using estrogen. In addition, as stated above, the risk of VTE is particularly elevated for women with metastatic malignancy receiving systemic therapies.
Cervical cancer commonly affects women of premenopausal age; therefore, early ovarian failure is particularly deleterious for this group of patients. Early-stage cervical cancer is most commonly treated with radical or extrafascial hysterectomy. Oophorectomy is not obligatory for the majority of these cases, and can be omitted in pre-, or perimenopausal patients to prevent surgical menopause. Ovarian metastases have been reported in cases of cervical adenocarcinoma, which led to the concern that ovarian preservation was not safe for this histology. However, recent data dispute this concern. A contemporary retrospective series of 105 patients with cervical adenocarcinoma identified no significant difference in overall survival when comparing those who had undergone ovarian preservation versus bilateral salpingo-oophorectomy.4
Ovarian preservation during cervical cancer surgery may not be enough to prevent early menopause. Approximately 20% of cervical cancer patients may require postoperative radiation for high- or intermediate-risk disease (such as positive lymph nodes, or adverse features in the tumor). For these women, ovarian ablation results, even if the ovaries were preserved at the time of surgery. Transposition of the ovaries to a location outside of the potential radiation fields is a strategy to mitigate this risk. To achieve this, the preserved ovaries and their vascular pedicles are skeletonized. The ovaries are then sutured to the paracolic gutter peritoneum or similar location above the pelvic brim, taking care to ensure that the vascular pedicle is not compromised or twisted. Placement of radio-opaque surgical clips on the caudad aspect of the transposed ovary aids in their identification by radiation oncologists when planning their treatment fields.
Ovarian transposition is most commonly used for women who are undergoing definitive surgery for cervical cancer. However, this strategy can also be used as a lead-in procedure for young women with advanced cervical cancer in whom definitive chemoradiation is planned. If the ovaries cannot be spared or moved out of “harm’s way” for premenopausal women undergoing treatment with definitive radiation, hormone therapy may be necessary and is safe for patients with cervical cancer, including those with adenocarcinoma. If the patient has not undergone hysterectomy, a regimen that includes a combination of estrogen and progesterone is necessary to avoid carcinogenic effects of unopposed estrogen on an intact endometrium, even after radiation has ablated those tissues.
When ovarian and fallopian cancers arise in premenopausal patients and appear confined to a single adnexa, contralateral ovarian preservation can be considered. However, for advanced disease, this is usually not possible or appropriate. Given that most ovarian cancers arise in a postmenopausal population, these patients may be preexisting users of hormone therapy. The data, including a randomized controlled trial, would suggest that it is safe to continue to use hormone therapy during or following a diagnosis of ovarian, fallopian tube, or primary peritoneal cancer and that it is not associated with worse outcomes from their cancer.5
Once again, patients should be carefully counseled about the additive risks for VTE that come from metastatic ovarian cancer, surgery via laparotomy, and exogenous hormonal therapy. However, these patients need not be subjected to an abrupt transition to menopause, because level I evidence suggests that these therapies are not associated with worse oncologic outcomes. All patients with ovarian, fallopian tube, and primary peritoneal cancer should receive genetic testing, and if deleterious mutations are found in BRCA 1 or 2 genes indicating an elevated risk for breast cancer, decision making regarding continued exogenous hormonal therapy is complicated. The most contemporary data, including long-term follow-up from the Women’s Health Initiative clinical trials, do not suggest an increased risk for breast cancer with estrogen-only preparations of hormone therapy.6 Given that most women with gynecologic cancers have undergone hysterectomy as part of their treatment, these estrogen-only preparations are appropriate for most.
For patients with rare tumors, such as endometrial stromal tumors or uterine leiomyosarcoma, the safety of exogenous hormone therapy should be dictated by the receptor profile of their particular cancer. Many of these cancers express estrogen receptors; therefore, current guidelines recommend against the use of hormones after these diagnoses when estrogen receptors are expressed.
Gynecologic cancer treatments induce many toxicities with long-term deleterious effects on quality of life. Use of hormones to mitigate the symptoms of menopause is an important tool in the toolkit for gynecologists. Assumptions should not be made that hormonal therapies are always unsafe for all of these patients. It is important to closely evaluate the patient’s tumor and other risk factors before withholding potentially valuable therapies.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at [email protected].
References
1. Chlebowski R et al. JAMA. 2010 Oct 20;304(15):1684-92.
2. Sinno AK et al. Gynecol Oncol. 2020;157(2):303-6.
3. Barakat et al. J Clin Oncol. 2006;24(4):587-92.
4. Hu Jun et al. J Obstet Gynaecol. 2017 Nov;37(8):1065-9.
5. Eeles R et al. J Clin Oncol. 2015 Dec 10;33(35):4138-44.
6. Chlebowski R et al. JAMA Jul 28 2020;324(4):369-80.
The medical management of early-stage endometrial cancer: When surgery isn’t possible, or desired
The standard management for early-stage endometrial cancer involves surgery with hysterectomy, salpingectomy with or without oophorectomy, and staging lymph node sampling. Surgery serves as both a therapeutic and diagnostic intervention because surgical pathology results are in turn used to predict the likelihood of relapse and guide adjuvant therapy decisions. However, in some cases, surgical intervention is not feasible or desired, particularly if fertility preservation is a goal. Fortunately, there are nonsurgical options that are associated with favorable outcomes to offer these patients.
Endometrial cancer is associated with obesity attributable to causative mechanisms that promote endometrial hyperplasia, cellular proliferation, and heightened hormonal and growth factor signaling. Not only does obesity drive the development of endometrial cancer, but it also complicates the treatment of the disease. For example, endometrial cancer staging surgery is less successfully completed through a minimally invasive route as body mass index increases, primarily because of limitations in surgical exposure.1 In fact, obesity can prevent surgery from being offered through any route. In addition to body habitus, determination of inoperability is also significantly influenced by the presence of coronary artery disease, hypertension, and diabetes.2 Given that these comorbidities are more commonly experienced by women who are overweight, obesity creates a perfect storm of causative and complicating factors for optimal treatment.
While surgeons may determine the candidacy of patients for hysterectomy, patients themselves also drive this decision-making, particularly in the case of young patients who desire fertility preservation. Approximately 10% of patients with endometrial cancer are premenopausal, a number that is increasing over time. These women may have experienced infertility prior to their diagnosis, yet still strongly desire the attempt to conceive, particularly if they have suffered from anovulatory menstrual cycles or polycystic ovarian disease. Women with Lynch syndrome are at a higher risk for developing their cancer in premenopausal years. Therefore, it is critical that gynecologic oncologists consider nonsurgical remedies for these women and understand their potential for success.
Certain criteria should be met for women undergoing nonsurgical management of endometrial cancer, particularly if chosen electively for fertility preservation. Diagnosis should be obtained with a curettage specimen (rather than a pipelle) to optimize the accuracy of establishing tumor grade and to “debulk” the endometrial tissue. Pretreatment imaging is necessary to rule out distant metastatic disease. MRI is particularly helpful in approximating the depth of myometrial invasion of the malignancy and is recommended for patients desiring fertility preservation. Patients who have an endometrial cancer that is deeply invasive into the myometrium are poor candidates for fertility preservation and have a higher risk for metastatic disease, particularly to lymph nodes, and treatment decisions (such as surgery, or, if inoperable, radiation which treats nodal basins) should be considered for these women.
Hormonal therapy has long been identified as a highly effective systemic therapy for endometrial cancers, particularly those that are low grade and express estrogen and progesterone receptors. Progesterone can be administered orally in preparations such as megestrol or medroxyprogesterone or “locally” with levonorgestrel-releasing intrauterine devices. Oral preparations are straightforward, typically low-cost agents. Likelihood of success is 50%-75%. However, the systemic side effects of these agents, which include increased venous thromboembolism risk and appetite stimulation, are particularly problematic in this population. Therefore, many providers prefer to place progestin-releasing intrauterine devices to “bypass” these side effects, avoid issues with adherence to dosing, and provide some preventative endometrial coverage after resolution of the cancer. Recent trials have observed elimination of endometrial cancer on repeat sampling in 67%-76% of cases.3-5 This strategy may be more successful when it is paired with the addition of GnRH agonists.4
When hormonal therapy is chosen for primary endometrial cancer treatment, it is typically monitored for efficacy with repeat endometrial samplings, most commonly with pipelle biopsies to avoid displacement of an intrauterine device, though repeat D&C may be more effective in achieving a complete pathologic response to treatment. Most providers recommend resampling the endometrium at 3-month intervals until resolution of the malignancy has been documented, and thereafter if any new bleeding events develop. For women who have demonstrated resolution of carcinoma on repeat sampling, data are lacking to guide decision-making regarding resumption of conception efforts, ongoing surveillance, and completion hysterectomy after they finish childbearing. If malignancy continues to be identified after 6 months of hormonal therapy, consideration should be made of a more definitive treatment (such as surgery, if feasible, or radiation if not). Continued hormonal therapy can also be considered, as delayed responses remain common even 1 year after starting therapy.6 If hormonal therapy is prolonged for persistent disease, repeat MRI is recommended at 6 months to document lack of progression.
Radiation, preferably with both intracavitary and external beam treatment, is the most definitive intervention for inoperable early-stage endometrial cancer. Unfortunately, fertility is not preserved with this approach. However, for patients with high-grade tumors that are less likely to express hormone receptors or respond to hormonal therapies, this may be the only treatment option available. Typical treatment courses include 5 weeks of external beam radiation treatments, focused on treating the pelvis as a whole, including occult metastases not identified on imaging. Optimal therapy also includes placement of intracavitary radiation implants, such as Heymans capsules, to concentrate the dose at the uterine fundus, while minimizing toxicity to the adjacent bladder and bowel structures. While definitive radiation is considered inferior to a primary surgical effort, disease-specific survival can be observed in more than 80% of patients treated this way.7
While surgery remains the standard intervention for women with early-stage endometrial cancer, hormonal therapy or radiation remain viable options with high rates of success for women who are not surgical candidates or who desire fertility preservation.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Walker JL et al. J Clin Oncol. 2009;27(32):5331-6.
2. Ertel M et al. Ann Surg Oncol. 2021;28(13):8987-95.
3. Janda M et al. Gynecol Oncol. 2021;161(1):143-51.
4. Novikova OV et al. Gynecol Oncol. 2021;161(1):152-9.
5. Westin SN et al. Am J Obstet Gynecol. 2021;224(2):191.e1-15.
6. Cho A et al. Gynecol Oncol. 2021;160(2):413-17.
7. Dutta SW et al. Brachytherapy. 2017;16(3):526-33.
The standard management for early-stage endometrial cancer involves surgery with hysterectomy, salpingectomy with or without oophorectomy, and staging lymph node sampling. Surgery serves as both a therapeutic and diagnostic intervention because surgical pathology results are in turn used to predict the likelihood of relapse and guide adjuvant therapy decisions. However, in some cases, surgical intervention is not feasible or desired, particularly if fertility preservation is a goal. Fortunately, there are nonsurgical options that are associated with favorable outcomes to offer these patients.
Endometrial cancer is associated with obesity attributable to causative mechanisms that promote endometrial hyperplasia, cellular proliferation, and heightened hormonal and growth factor signaling. Not only does obesity drive the development of endometrial cancer, but it also complicates the treatment of the disease. For example, endometrial cancer staging surgery is less successfully completed through a minimally invasive route as body mass index increases, primarily because of limitations in surgical exposure.1 In fact, obesity can prevent surgery from being offered through any route. In addition to body habitus, determination of inoperability is also significantly influenced by the presence of coronary artery disease, hypertension, and diabetes.2 Given that these comorbidities are more commonly experienced by women who are overweight, obesity creates a perfect storm of causative and complicating factors for optimal treatment.
While surgeons may determine the candidacy of patients for hysterectomy, patients themselves also drive this decision-making, particularly in the case of young patients who desire fertility preservation. Approximately 10% of patients with endometrial cancer are premenopausal, a number that is increasing over time. These women may have experienced infertility prior to their diagnosis, yet still strongly desire the attempt to conceive, particularly if they have suffered from anovulatory menstrual cycles or polycystic ovarian disease. Women with Lynch syndrome are at a higher risk for developing their cancer in premenopausal years. Therefore, it is critical that gynecologic oncologists consider nonsurgical remedies for these women and understand their potential for success.
Certain criteria should be met for women undergoing nonsurgical management of endometrial cancer, particularly if chosen electively for fertility preservation. Diagnosis should be obtained with a curettage specimen (rather than a pipelle) to optimize the accuracy of establishing tumor grade and to “debulk” the endometrial tissue. Pretreatment imaging is necessary to rule out distant metastatic disease. MRI is particularly helpful in approximating the depth of myometrial invasion of the malignancy and is recommended for patients desiring fertility preservation. Patients who have an endometrial cancer that is deeply invasive into the myometrium are poor candidates for fertility preservation and have a higher risk for metastatic disease, particularly to lymph nodes, and treatment decisions (such as surgery, or, if inoperable, radiation which treats nodal basins) should be considered for these women.
Hormonal therapy has long been identified as a highly effective systemic therapy for endometrial cancers, particularly those that are low grade and express estrogen and progesterone receptors. Progesterone can be administered orally in preparations such as megestrol or medroxyprogesterone or “locally” with levonorgestrel-releasing intrauterine devices. Oral preparations are straightforward, typically low-cost agents. Likelihood of success is 50%-75%. However, the systemic side effects of these agents, which include increased venous thromboembolism risk and appetite stimulation, are particularly problematic in this population. Therefore, many providers prefer to place progestin-releasing intrauterine devices to “bypass” these side effects, avoid issues with adherence to dosing, and provide some preventative endometrial coverage after resolution of the cancer. Recent trials have observed elimination of endometrial cancer on repeat sampling in 67%-76% of cases.3-5 This strategy may be more successful when it is paired with the addition of GnRH agonists.4
When hormonal therapy is chosen for primary endometrial cancer treatment, it is typically monitored for efficacy with repeat endometrial samplings, most commonly with pipelle biopsies to avoid displacement of an intrauterine device, though repeat D&C may be more effective in achieving a complete pathologic response to treatment. Most providers recommend resampling the endometrium at 3-month intervals until resolution of the malignancy has been documented, and thereafter if any new bleeding events develop. For women who have demonstrated resolution of carcinoma on repeat sampling, data are lacking to guide decision-making regarding resumption of conception efforts, ongoing surveillance, and completion hysterectomy after they finish childbearing. If malignancy continues to be identified after 6 months of hormonal therapy, consideration should be made of a more definitive treatment (such as surgery, if feasible, or radiation if not). Continued hormonal therapy can also be considered, as delayed responses remain common even 1 year after starting therapy.6 If hormonal therapy is prolonged for persistent disease, repeat MRI is recommended at 6 months to document lack of progression.
Radiation, preferably with both intracavitary and external beam treatment, is the most definitive intervention for inoperable early-stage endometrial cancer. Unfortunately, fertility is not preserved with this approach. However, for patients with high-grade tumors that are less likely to express hormone receptors or respond to hormonal therapies, this may be the only treatment option available. Typical treatment courses include 5 weeks of external beam radiation treatments, focused on treating the pelvis as a whole, including occult metastases not identified on imaging. Optimal therapy also includes placement of intracavitary radiation implants, such as Heymans capsules, to concentrate the dose at the uterine fundus, while minimizing toxicity to the adjacent bladder and bowel structures. While definitive radiation is considered inferior to a primary surgical effort, disease-specific survival can be observed in more than 80% of patients treated this way.7
While surgery remains the standard intervention for women with early-stage endometrial cancer, hormonal therapy or radiation remain viable options with high rates of success for women who are not surgical candidates or who desire fertility preservation.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Walker JL et al. J Clin Oncol. 2009;27(32):5331-6.
2. Ertel M et al. Ann Surg Oncol. 2021;28(13):8987-95.
3. Janda M et al. Gynecol Oncol. 2021;161(1):143-51.
4. Novikova OV et al. Gynecol Oncol. 2021;161(1):152-9.
5. Westin SN et al. Am J Obstet Gynecol. 2021;224(2):191.e1-15.
6. Cho A et al. Gynecol Oncol. 2021;160(2):413-17.
7. Dutta SW et al. Brachytherapy. 2017;16(3):526-33.
The standard management for early-stage endometrial cancer involves surgery with hysterectomy, salpingectomy with or without oophorectomy, and staging lymph node sampling. Surgery serves as both a therapeutic and diagnostic intervention because surgical pathology results are in turn used to predict the likelihood of relapse and guide adjuvant therapy decisions. However, in some cases, surgical intervention is not feasible or desired, particularly if fertility preservation is a goal. Fortunately, there are nonsurgical options that are associated with favorable outcomes to offer these patients.
Endometrial cancer is associated with obesity attributable to causative mechanisms that promote endometrial hyperplasia, cellular proliferation, and heightened hormonal and growth factor signaling. Not only does obesity drive the development of endometrial cancer, but it also complicates the treatment of the disease. For example, endometrial cancer staging surgery is less successfully completed through a minimally invasive route as body mass index increases, primarily because of limitations in surgical exposure.1 In fact, obesity can prevent surgery from being offered through any route. In addition to body habitus, determination of inoperability is also significantly influenced by the presence of coronary artery disease, hypertension, and diabetes.2 Given that these comorbidities are more commonly experienced by women who are overweight, obesity creates a perfect storm of causative and complicating factors for optimal treatment.
While surgeons may determine the candidacy of patients for hysterectomy, patients themselves also drive this decision-making, particularly in the case of young patients who desire fertility preservation. Approximately 10% of patients with endometrial cancer are premenopausal, a number that is increasing over time. These women may have experienced infertility prior to their diagnosis, yet still strongly desire the attempt to conceive, particularly if they have suffered from anovulatory menstrual cycles or polycystic ovarian disease. Women with Lynch syndrome are at a higher risk for developing their cancer in premenopausal years. Therefore, it is critical that gynecologic oncologists consider nonsurgical remedies for these women and understand their potential for success.
Certain criteria should be met for women undergoing nonsurgical management of endometrial cancer, particularly if chosen electively for fertility preservation. Diagnosis should be obtained with a curettage specimen (rather than a pipelle) to optimize the accuracy of establishing tumor grade and to “debulk” the endometrial tissue. Pretreatment imaging is necessary to rule out distant metastatic disease. MRI is particularly helpful in approximating the depth of myometrial invasion of the malignancy and is recommended for patients desiring fertility preservation. Patients who have an endometrial cancer that is deeply invasive into the myometrium are poor candidates for fertility preservation and have a higher risk for metastatic disease, particularly to lymph nodes, and treatment decisions (such as surgery, or, if inoperable, radiation which treats nodal basins) should be considered for these women.
Hormonal therapy has long been identified as a highly effective systemic therapy for endometrial cancers, particularly those that are low grade and express estrogen and progesterone receptors. Progesterone can be administered orally in preparations such as megestrol or medroxyprogesterone or “locally” with levonorgestrel-releasing intrauterine devices. Oral preparations are straightforward, typically low-cost agents. Likelihood of success is 50%-75%. However, the systemic side effects of these agents, which include increased venous thromboembolism risk and appetite stimulation, are particularly problematic in this population. Therefore, many providers prefer to place progestin-releasing intrauterine devices to “bypass” these side effects, avoid issues with adherence to dosing, and provide some preventative endometrial coverage after resolution of the cancer. Recent trials have observed elimination of endometrial cancer on repeat sampling in 67%-76% of cases.3-5 This strategy may be more successful when it is paired with the addition of GnRH agonists.4
When hormonal therapy is chosen for primary endometrial cancer treatment, it is typically monitored for efficacy with repeat endometrial samplings, most commonly with pipelle biopsies to avoid displacement of an intrauterine device, though repeat D&C may be more effective in achieving a complete pathologic response to treatment. Most providers recommend resampling the endometrium at 3-month intervals until resolution of the malignancy has been documented, and thereafter if any new bleeding events develop. For women who have demonstrated resolution of carcinoma on repeat sampling, data are lacking to guide decision-making regarding resumption of conception efforts, ongoing surveillance, and completion hysterectomy after they finish childbearing. If malignancy continues to be identified after 6 months of hormonal therapy, consideration should be made of a more definitive treatment (such as surgery, if feasible, or radiation if not). Continued hormonal therapy can also be considered, as delayed responses remain common even 1 year after starting therapy.6 If hormonal therapy is prolonged for persistent disease, repeat MRI is recommended at 6 months to document lack of progression.
Radiation, preferably with both intracavitary and external beam treatment, is the most definitive intervention for inoperable early-stage endometrial cancer. Unfortunately, fertility is not preserved with this approach. However, for patients with high-grade tumors that are less likely to express hormone receptors or respond to hormonal therapies, this may be the only treatment option available. Typical treatment courses include 5 weeks of external beam radiation treatments, focused on treating the pelvis as a whole, including occult metastases not identified on imaging. Optimal therapy also includes placement of intracavitary radiation implants, such as Heymans capsules, to concentrate the dose at the uterine fundus, while minimizing toxicity to the adjacent bladder and bowel structures. While definitive radiation is considered inferior to a primary surgical effort, disease-specific survival can be observed in more than 80% of patients treated this way.7
While surgery remains the standard intervention for women with early-stage endometrial cancer, hormonal therapy or radiation remain viable options with high rates of success for women who are not surgical candidates or who desire fertility preservation.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Walker JL et al. J Clin Oncol. 2009;27(32):5331-6.
2. Ertel M et al. Ann Surg Oncol. 2021;28(13):8987-95.
3. Janda M et al. Gynecol Oncol. 2021;161(1):143-51.
4. Novikova OV et al. Gynecol Oncol. 2021;161(1):152-9.
5. Westin SN et al. Am J Obstet Gynecol. 2021;224(2):191.e1-15.
6. Cho A et al. Gynecol Oncol. 2021;160(2):413-17.
7. Dutta SW et al. Brachytherapy. 2017;16(3):526-33.
Optimizing ‘optimal’ in ovarian cancer cytoreduction
The goal of advanced ovarian cancer surgery is to remove all gross disease, or all visible and palpable disease implants. This became the established standard when improved survival was consistently observed among patients who had undergone complete surgical resection. Traditionally, definitions of no gross residual disease have been left in the hands, and eyes, of the surgeon. However, new technology has emerged which affords surgeons the ability to visualize ovarian cancer deposits that are imperceptible to the naked eye. But will this improve upon the poor cure rates for advanced ovarian cancer?
Many are familiar with the traditional definitions of “optimal” (less than 1 cm–sized deposits at any one location) and “suboptimal” (greater than 1 cm–sized deposits remaining) when referring to surgical cytoreduction of ovarian cancer. This nomenclature was introduced to define, categorize, and prognosticate patient groups after surgery. In recent years we have moved away from these descriptive definitions of ovarian cancer resection, borrowing from surgical oncology measures of surgical outcomes where “R0” defines surgical resection with negative margins, “R1” includes resection with positive microscopic margins (negative for tumor intraoperatively, but positive on microscopic pathology), and “R2” refers to macroscopic residual disease remaining.1
In ovarian cancer, surgeons have adopted the expression R0 to include patients in whom there is no gross visible or palpable residual disease, a special, favorable subgrouping of the previous “optimal” group. R1 is applied to patients with macroscopic, residual disease that fits within the traditional “optimal” cytoreduction classification (<1 cm in any one location). Obviously, these are significant variations to the traditional surgical oncology definitions, but not without supporting data. For example, patients with no gross residual disease (now defined as “R0”) have been observed to have improved survival, compared with patients who are “optimally” debulked but with R1 (<1 cm) residual disease.2 Therefore, this new goal of complete surgical resection has replaced the previous standard of “optimal” cytoreduction in which small macroscopic residual disease was acceptable.
Whether or not a surgery is completed with no gross residual disease is a subjective assessment made by the surgeon, and in practice, highly inaccurate. When a posttrial ad hoc analysis of 1,873 patients with advanced ovarian cancer who had been enrolled in a Gynecologic Oncology Group cooperative trial correlated surgeons’ assessments of “optimal” cytoreduction with objective postoperative radiographic findings (performed, on average, less than 1 month postoperatively) they found that postoperative CT scans identified lesions >1 cm in 40% of cases that had been characterized by surgeons as an “optimal” cytoreduction.3 Most commonly, discrepant lesions were identified in the upper abdominal quadrants and retroperitoneal aortic nodal regions. Therefore, surgeons’ subjective assessment of cytoreduction is prone to error, and given how important the completeness of cytoreduction is for clinical outcomes, there is interest in discovering methods to improve upon surgeons’ ability to discriminate volume of disease.
Pafolacianine (Cytalux, On Target Laboratories) is a novel drug that binds a fluorescent molecule to folic acid targeting the folate alpha receptors which are overexpressed on nonmucinous epithelial ovarian cancer cells compared with adjacent nonmalignant tissues.4 The drug is intravenously infused preoperatively and then visualized with companion near-infrared imaging devices during surgery to visualize its fluorescent signal where it is bound to ovarian cancer implants. In a phase 2 study of 178 patients with confirmed or suspected ovarian cancer, pafolacianine was able to detect implants of ovarian cancer in 26.9% of cases where the surgeon’s visual inspection was negative.5 Of note, the false-positive rate of this drug was not trivial, at 20%. Based on this efficacy data, the drug has been granted FDA approved for use in ovarian cancer surgery to augment the surgeon’s visualization of cancer. However, important questions remain unanswered by these preliminary data.
Will removal of additional microscopic ovarian cancer implants, only seen by pafolacianine, improve the survival of patients with ovarian cancer, and what effect will the addition of this extra surgery have on their surgical morbidity and risk? The use of pafolacianine to augment ovarian cancer debulking surgeries pivots on the premise that ovarian cancer outcomes are determined by surgical “effort” more than the biology of the disease. Otherwise said: The more we surgically remove, the more we cure. But this seems an old-fashioned notion, increasingly challenged by data. It has been shown that, when ovarian cancer debulking surgeries are necessarily more radical because of extensive disease distribution, prognosis is worse, compared with those patients with less extensive disease distribution.6 The effect of surgical effort contributes less than that of predetermined patterns of disease presentation. Additionally, genomic traits are different in tumors that are objectively determined to be not amenable to optimal cytoreduction, compared with resectable tumors.7 These data suggest that it is the disease, more than the surgeon, that most influences outcomes.
Additionally, the question of whether surgical removal of microscopic disease improves ovarian cancer survival has already been addressed with negative findings. The LION trial randomized 647 women with advanced ovarian cancer to primary cytoreductive surgery either with or without routine lymphadenectomy of clinically negative nodes.8 This study found no survival benefit to resecting clinically negative, microscopically positive nodes. In light of these data, it is difficult to imagine that there would be different results with the resection of microscopic peritoneal disease implants identified by pafolacianine.
While pafolacianine promises to move us closer to a true “R0” (negative margins) resection of ovarian cancer, is this even a feasible goal in a disease that is widely metastatic, particularly in the peritoneal cavity? What do “negative margins” mean in the peritoneal cavity? The sensitivity of pafolacianine in detecting microscopic disease is obviously not so high that it can guarantee patients a complete resection of a disseminated disease, and we still do not know what absolute benefit is derived from moving a little bit further on the continuum of surgical resection.
Perhaps augmentation of debulking is not the only, or best, use of pafolacianine for ovarian cancer surgery. Perhaps it might serve a role in diagnostics or staging of the disease rather than for a therapeutic purpose. In the meantime, we await ongoing clinical trials in this space to better inform clinicians what benefits, or harms, they might expect from the addition of this new drug as we continue to define the “optimal” surgical procedure for advanced ovarian cancer.
Dr. Emma Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no conflicts of interest.
References
1. Hermanek P, Wittekind C. Semin Surg Oncol 1994;10:12-20.
2. Elattar A et al. Cochrane Database Syst Rev 2011 Aug 10;2011(8):CD007565.
3. Eskander RN et al. Gynecol Oncol 2018;149:525-30.
4. Randall LM et al. Gynecol Oncol 2019;155:63-8.
5. Food and Drug Administration. FDA approves pafolacianine for identifying malignant ovarian cancer lesions. 2021 Dec 1.
6. Horowitz NS et al. J Clin Oncol 2015;33:937-43.
7. Lee S et al. Cell Rep. 2020;31:107502.
8. Harter P et al. N Engl J Med 2019;380:822-32.
The goal of advanced ovarian cancer surgery is to remove all gross disease, or all visible and palpable disease implants. This became the established standard when improved survival was consistently observed among patients who had undergone complete surgical resection. Traditionally, definitions of no gross residual disease have been left in the hands, and eyes, of the surgeon. However, new technology has emerged which affords surgeons the ability to visualize ovarian cancer deposits that are imperceptible to the naked eye. But will this improve upon the poor cure rates for advanced ovarian cancer?
Many are familiar with the traditional definitions of “optimal” (less than 1 cm–sized deposits at any one location) and “suboptimal” (greater than 1 cm–sized deposits remaining) when referring to surgical cytoreduction of ovarian cancer. This nomenclature was introduced to define, categorize, and prognosticate patient groups after surgery. In recent years we have moved away from these descriptive definitions of ovarian cancer resection, borrowing from surgical oncology measures of surgical outcomes where “R0” defines surgical resection with negative margins, “R1” includes resection with positive microscopic margins (negative for tumor intraoperatively, but positive on microscopic pathology), and “R2” refers to macroscopic residual disease remaining.1
In ovarian cancer, surgeons have adopted the expression R0 to include patients in whom there is no gross visible or palpable residual disease, a special, favorable subgrouping of the previous “optimal” group. R1 is applied to patients with macroscopic, residual disease that fits within the traditional “optimal” cytoreduction classification (<1 cm in any one location). Obviously, these are significant variations to the traditional surgical oncology definitions, but not without supporting data. For example, patients with no gross residual disease (now defined as “R0”) have been observed to have improved survival, compared with patients who are “optimally” debulked but with R1 (<1 cm) residual disease.2 Therefore, this new goal of complete surgical resection has replaced the previous standard of “optimal” cytoreduction in which small macroscopic residual disease was acceptable.
Whether or not a surgery is completed with no gross residual disease is a subjective assessment made by the surgeon, and in practice, highly inaccurate. When a posttrial ad hoc analysis of 1,873 patients with advanced ovarian cancer who had been enrolled in a Gynecologic Oncology Group cooperative trial correlated surgeons’ assessments of “optimal” cytoreduction with objective postoperative radiographic findings (performed, on average, less than 1 month postoperatively) they found that postoperative CT scans identified lesions >1 cm in 40% of cases that had been characterized by surgeons as an “optimal” cytoreduction.3 Most commonly, discrepant lesions were identified in the upper abdominal quadrants and retroperitoneal aortic nodal regions. Therefore, surgeons’ subjective assessment of cytoreduction is prone to error, and given how important the completeness of cytoreduction is for clinical outcomes, there is interest in discovering methods to improve upon surgeons’ ability to discriminate volume of disease.
Pafolacianine (Cytalux, On Target Laboratories) is a novel drug that binds a fluorescent molecule to folic acid targeting the folate alpha receptors which are overexpressed on nonmucinous epithelial ovarian cancer cells compared with adjacent nonmalignant tissues.4 The drug is intravenously infused preoperatively and then visualized with companion near-infrared imaging devices during surgery to visualize its fluorescent signal where it is bound to ovarian cancer implants. In a phase 2 study of 178 patients with confirmed or suspected ovarian cancer, pafolacianine was able to detect implants of ovarian cancer in 26.9% of cases where the surgeon’s visual inspection was negative.5 Of note, the false-positive rate of this drug was not trivial, at 20%. Based on this efficacy data, the drug has been granted FDA approved for use in ovarian cancer surgery to augment the surgeon’s visualization of cancer. However, important questions remain unanswered by these preliminary data.
Will removal of additional microscopic ovarian cancer implants, only seen by pafolacianine, improve the survival of patients with ovarian cancer, and what effect will the addition of this extra surgery have on their surgical morbidity and risk? The use of pafolacianine to augment ovarian cancer debulking surgeries pivots on the premise that ovarian cancer outcomes are determined by surgical “effort” more than the biology of the disease. Otherwise said: The more we surgically remove, the more we cure. But this seems an old-fashioned notion, increasingly challenged by data. It has been shown that, when ovarian cancer debulking surgeries are necessarily more radical because of extensive disease distribution, prognosis is worse, compared with those patients with less extensive disease distribution.6 The effect of surgical effort contributes less than that of predetermined patterns of disease presentation. Additionally, genomic traits are different in tumors that are objectively determined to be not amenable to optimal cytoreduction, compared with resectable tumors.7 These data suggest that it is the disease, more than the surgeon, that most influences outcomes.
Additionally, the question of whether surgical removal of microscopic disease improves ovarian cancer survival has already been addressed with negative findings. The LION trial randomized 647 women with advanced ovarian cancer to primary cytoreductive surgery either with or without routine lymphadenectomy of clinically negative nodes.8 This study found no survival benefit to resecting clinically negative, microscopically positive nodes. In light of these data, it is difficult to imagine that there would be different results with the resection of microscopic peritoneal disease implants identified by pafolacianine.
While pafolacianine promises to move us closer to a true “R0” (negative margins) resection of ovarian cancer, is this even a feasible goal in a disease that is widely metastatic, particularly in the peritoneal cavity? What do “negative margins” mean in the peritoneal cavity? The sensitivity of pafolacianine in detecting microscopic disease is obviously not so high that it can guarantee patients a complete resection of a disseminated disease, and we still do not know what absolute benefit is derived from moving a little bit further on the continuum of surgical resection.
Perhaps augmentation of debulking is not the only, or best, use of pafolacianine for ovarian cancer surgery. Perhaps it might serve a role in diagnostics or staging of the disease rather than for a therapeutic purpose. In the meantime, we await ongoing clinical trials in this space to better inform clinicians what benefits, or harms, they might expect from the addition of this new drug as we continue to define the “optimal” surgical procedure for advanced ovarian cancer.
Dr. Emma Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no conflicts of interest.
References
1. Hermanek P, Wittekind C. Semin Surg Oncol 1994;10:12-20.
2. Elattar A et al. Cochrane Database Syst Rev 2011 Aug 10;2011(8):CD007565.
3. Eskander RN et al. Gynecol Oncol 2018;149:525-30.
4. Randall LM et al. Gynecol Oncol 2019;155:63-8.
5. Food and Drug Administration. FDA approves pafolacianine for identifying malignant ovarian cancer lesions. 2021 Dec 1.
6. Horowitz NS et al. J Clin Oncol 2015;33:937-43.
7. Lee S et al. Cell Rep. 2020;31:107502.
8. Harter P et al. N Engl J Med 2019;380:822-32.
The goal of advanced ovarian cancer surgery is to remove all gross disease, or all visible and palpable disease implants. This became the established standard when improved survival was consistently observed among patients who had undergone complete surgical resection. Traditionally, definitions of no gross residual disease have been left in the hands, and eyes, of the surgeon. However, new technology has emerged which affords surgeons the ability to visualize ovarian cancer deposits that are imperceptible to the naked eye. But will this improve upon the poor cure rates for advanced ovarian cancer?
Many are familiar with the traditional definitions of “optimal” (less than 1 cm–sized deposits at any one location) and “suboptimal” (greater than 1 cm–sized deposits remaining) when referring to surgical cytoreduction of ovarian cancer. This nomenclature was introduced to define, categorize, and prognosticate patient groups after surgery. In recent years we have moved away from these descriptive definitions of ovarian cancer resection, borrowing from surgical oncology measures of surgical outcomes where “R0” defines surgical resection with negative margins, “R1” includes resection with positive microscopic margins (negative for tumor intraoperatively, but positive on microscopic pathology), and “R2” refers to macroscopic residual disease remaining.1
In ovarian cancer, surgeons have adopted the expression R0 to include patients in whom there is no gross visible or palpable residual disease, a special, favorable subgrouping of the previous “optimal” group. R1 is applied to patients with macroscopic, residual disease that fits within the traditional “optimal” cytoreduction classification (<1 cm in any one location). Obviously, these are significant variations to the traditional surgical oncology definitions, but not without supporting data. For example, patients with no gross residual disease (now defined as “R0”) have been observed to have improved survival, compared with patients who are “optimally” debulked but with R1 (<1 cm) residual disease.2 Therefore, this new goal of complete surgical resection has replaced the previous standard of “optimal” cytoreduction in which small macroscopic residual disease was acceptable.
Whether or not a surgery is completed with no gross residual disease is a subjective assessment made by the surgeon, and in practice, highly inaccurate. When a posttrial ad hoc analysis of 1,873 patients with advanced ovarian cancer who had been enrolled in a Gynecologic Oncology Group cooperative trial correlated surgeons’ assessments of “optimal” cytoreduction with objective postoperative radiographic findings (performed, on average, less than 1 month postoperatively) they found that postoperative CT scans identified lesions >1 cm in 40% of cases that had been characterized by surgeons as an “optimal” cytoreduction.3 Most commonly, discrepant lesions were identified in the upper abdominal quadrants and retroperitoneal aortic nodal regions. Therefore, surgeons’ subjective assessment of cytoreduction is prone to error, and given how important the completeness of cytoreduction is for clinical outcomes, there is interest in discovering methods to improve upon surgeons’ ability to discriminate volume of disease.
Pafolacianine (Cytalux, On Target Laboratories) is a novel drug that binds a fluorescent molecule to folic acid targeting the folate alpha receptors which are overexpressed on nonmucinous epithelial ovarian cancer cells compared with adjacent nonmalignant tissues.4 The drug is intravenously infused preoperatively and then visualized with companion near-infrared imaging devices during surgery to visualize its fluorescent signal where it is bound to ovarian cancer implants. In a phase 2 study of 178 patients with confirmed or suspected ovarian cancer, pafolacianine was able to detect implants of ovarian cancer in 26.9% of cases where the surgeon’s visual inspection was negative.5 Of note, the false-positive rate of this drug was not trivial, at 20%. Based on this efficacy data, the drug has been granted FDA approved for use in ovarian cancer surgery to augment the surgeon’s visualization of cancer. However, important questions remain unanswered by these preliminary data.
Will removal of additional microscopic ovarian cancer implants, only seen by pafolacianine, improve the survival of patients with ovarian cancer, and what effect will the addition of this extra surgery have on their surgical morbidity and risk? The use of pafolacianine to augment ovarian cancer debulking surgeries pivots on the premise that ovarian cancer outcomes are determined by surgical “effort” more than the biology of the disease. Otherwise said: The more we surgically remove, the more we cure. But this seems an old-fashioned notion, increasingly challenged by data. It has been shown that, when ovarian cancer debulking surgeries are necessarily more radical because of extensive disease distribution, prognosis is worse, compared with those patients with less extensive disease distribution.6 The effect of surgical effort contributes less than that of predetermined patterns of disease presentation. Additionally, genomic traits are different in tumors that are objectively determined to be not amenable to optimal cytoreduction, compared with resectable tumors.7 These data suggest that it is the disease, more than the surgeon, that most influences outcomes.
Additionally, the question of whether surgical removal of microscopic disease improves ovarian cancer survival has already been addressed with negative findings. The LION trial randomized 647 women with advanced ovarian cancer to primary cytoreductive surgery either with or without routine lymphadenectomy of clinically negative nodes.8 This study found no survival benefit to resecting clinically negative, microscopically positive nodes. In light of these data, it is difficult to imagine that there would be different results with the resection of microscopic peritoneal disease implants identified by pafolacianine.
While pafolacianine promises to move us closer to a true “R0” (negative margins) resection of ovarian cancer, is this even a feasible goal in a disease that is widely metastatic, particularly in the peritoneal cavity? What do “negative margins” mean in the peritoneal cavity? The sensitivity of pafolacianine in detecting microscopic disease is obviously not so high that it can guarantee patients a complete resection of a disseminated disease, and we still do not know what absolute benefit is derived from moving a little bit further on the continuum of surgical resection.
Perhaps augmentation of debulking is not the only, or best, use of pafolacianine for ovarian cancer surgery. Perhaps it might serve a role in diagnostics or staging of the disease rather than for a therapeutic purpose. In the meantime, we await ongoing clinical trials in this space to better inform clinicians what benefits, or harms, they might expect from the addition of this new drug as we continue to define the “optimal” surgical procedure for advanced ovarian cancer.
Dr. Emma Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no conflicts of interest.
References
1. Hermanek P, Wittekind C. Semin Surg Oncol 1994;10:12-20.
2. Elattar A et al. Cochrane Database Syst Rev 2011 Aug 10;2011(8):CD007565.
3. Eskander RN et al. Gynecol Oncol 2018;149:525-30.
4. Randall LM et al. Gynecol Oncol 2019;155:63-8.
5. Food and Drug Administration. FDA approves pafolacianine for identifying malignant ovarian cancer lesions. 2021 Dec 1.
6. Horowitz NS et al. J Clin Oncol 2015;33:937-43.
7. Lee S et al. Cell Rep. 2020;31:107502.
8. Harter P et al. N Engl J Med 2019;380:822-32.
Should gynecologists receive the HPV vaccine?
Gynecologists have experience managing human papillomavirus–associated diseases of the lower genital tract. However, HPV also causes warty disease, dysplasia, and carcinoma of the head and neck. Risk factors for head and neck cancer include smoking and smokeless tobacco use, alcohol consumption, periodontal disease, radiation exposure, and HPV. The incidence of HPV-associated head and neck cancer is rising, particularly among men, at a rate of 2.7% per year.1 The incidence of HPV-associated squamous cell carcinoma of the oropharynx now surpasses that of cervical cancer. Concerns exist regarding occupational exposure to HPV by health care providers (HCP) who perform smoke-generating procedures on HPV-infected tissues, and the potential for them to develop head and neck pathology.
In March of 2020, the American Society for Colposcopy and Cervical Pathology made the recommendation that clinicians who are routinely exposed to HPV should protect themselves against the sequela of occupationally acquired HPV by receiving the HPV vaccine.2 They advocate for the “complete provider team” including physicians, advanced practice providers, nurses, operative technicians, and residents and fellows to be considered for protective vaccination.
Similar to disease patterns in the genital tract, different strains of HPV have differing propensity to cause benign, premalignant, and malignant disease states. HPV 6 and 11 are more commonly associated with warty disease in the nares, pharynx, and tonsillar tissues. HPV 16, 18, 31, and 33 (most commonly 16) are considered high risk for carcinoma formation, particularly of the tonsils and base of the tongue.
The procedures most implicated in occupational HPV exposure include ablative procedures for anogenital warts, laser ablation of vaginal and vulvar dysplasia, and electrosurgical excisional procedures for cervical dysplasia. Smoke plumes from HPV-associated procedures are known to contain HPV for both laser and electrocautery sources.3 A study of 134 patients undergoing surgical procedures for laser ablation of HPV-infected tissues detected concordant strains of HPV in approximately 30% of smoke plumes and approximately 1.5% of surgeons’ nares.4 Not all procedures appear to carry the same risk. Electrocoagulation procedures appear to yield fewer postprocedural positive mucosal swabs for HPV, compared with those taken after CO2 laser.5
Animal studies have shown that papilloma virus procured from smoke plume has the capacity to generate disease. When 10 calves were inoculated with bovine papillary virus obtained from smoke plumes from laser ablation of bovine papillomavirus lesions, all calves manifested BPV fibropapilloma lesions at the sites of inoculation.6
There appears to be an increased incidence of HPV-associated head and neck disease among surgeons who perform procedures on HPV tissues, and there have been multiple case reports that have cited examples of HPV-associated benign and malignant disease among HCPs with frequent occupational exposure to HPV anogenital ablative and excisional procedures.7 While these observations are not proof of causation, they are cause for concern.
While the ASCCP guidelines advocate for HPV vaccination as a strategy for prevention of occupationally related HPV-associated disease, there are other strategies in place to minimize risk. The CDC guidelines for environmental infection control in health care facilities include the following recommendations:
- In settings where surgical lasers are used, wear appropriate personnel protective equipment (PPE), including N95 or N100 respirators to minimize exposure to laser plumes.
- Use central wall suction units with in-line filters to evacuate minimal laser plumes.
- Use a mechanical smoke evaluation system with a high efficiency filter to manage the generation of large amounts of laser plume, when ablating tissue infected with HPV.
- Use local exhaust ventilation (LEV).8
When closely adhered to, these methods appear to provide high-level protection. Data suggest that, when HCPs can access appropriate protective equipment, risks for HPV exposure are low. However, this is more feasible for larger hospital facilities, and may be more limited in outpatient settings. This has led to the consideration of background protection in the form of HPV vaccination for at-risk HCPs. This is analogous to mandates for HCPs to receive hepatitis B vaccination despite the concomitant practice of universal precautions in health care settings. Preventative strategies are typically most efficacious when performed in concert.
After nearly 2 decades of widespread use, we have confidence in the safety of the HPV vaccination. Its benefit through age 45 has been established, leading to the 2018 FDA approval for the 9-valent HPV vaccine, Guardisil-9, for this expanded age group. It would seem logical that systematic administration of the HPV vaccine for at-risk HCPs would be both feasible and safe. There are well-established systems for administering vaccines for HCPs in all health care systems. Perhaps health system administrators should consider routinely offering HPV vaccination for at-risk employees as part of their occupational health care responsibilities. One important caveat being the cost and efficacy of HPV vaccination in this group has not been not established.
In the meantime, it is critical that gynecology providers be aware of their risk for occupational exposure to HPV when using laser and electrocautery techniques on HPV-infected tissues and the potential for them developing head and neck pathology. They should strictly adhere to preventative measures such as use of fit-tested N-95 respirators, mechanical smoke evacuators with high-efficiency filters and work in environments with adequate room ventilation. We all should individually evaluate what role HPV vaccination may play for us in augmenting our own safety.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Van Dyne EA et al. MMWR Morb Mortal Wkly Rep. 2018 Aug 24;67(33):918-24.
2. ASCCP. ASCCP recommends HPV vaccination for providers.
3. Fox-Lewis A et al. Occup Environ Med. 2020 Dec;77(12):809-17.
4. Zhou Q et al. Cancer Manag Res. 2019;11:3643-54
5. Bergbrant I et al. Acta Derm Venereol. 1994 Sep;74(5):393-5.
6. Garden J et al. Arch Dermatol. 2002 Oct;138(10):1303-7.
7. Harrison R, Huh W. Obstet Gynecol. 2020;136:663-5.
8. CDC. 1996. DHHS (NIOSH) Publication Number 96-128.
Gynecologists have experience managing human papillomavirus–associated diseases of the lower genital tract. However, HPV also causes warty disease, dysplasia, and carcinoma of the head and neck. Risk factors for head and neck cancer include smoking and smokeless tobacco use, alcohol consumption, periodontal disease, radiation exposure, and HPV. The incidence of HPV-associated head and neck cancer is rising, particularly among men, at a rate of 2.7% per year.1 The incidence of HPV-associated squamous cell carcinoma of the oropharynx now surpasses that of cervical cancer. Concerns exist regarding occupational exposure to HPV by health care providers (HCP) who perform smoke-generating procedures on HPV-infected tissues, and the potential for them to develop head and neck pathology.
In March of 2020, the American Society for Colposcopy and Cervical Pathology made the recommendation that clinicians who are routinely exposed to HPV should protect themselves against the sequela of occupationally acquired HPV by receiving the HPV vaccine.2 They advocate for the “complete provider team” including physicians, advanced practice providers, nurses, operative technicians, and residents and fellows to be considered for protective vaccination.
Similar to disease patterns in the genital tract, different strains of HPV have differing propensity to cause benign, premalignant, and malignant disease states. HPV 6 and 11 are more commonly associated with warty disease in the nares, pharynx, and tonsillar tissues. HPV 16, 18, 31, and 33 (most commonly 16) are considered high risk for carcinoma formation, particularly of the tonsils and base of the tongue.
The procedures most implicated in occupational HPV exposure include ablative procedures for anogenital warts, laser ablation of vaginal and vulvar dysplasia, and electrosurgical excisional procedures for cervical dysplasia. Smoke plumes from HPV-associated procedures are known to contain HPV for both laser and electrocautery sources.3 A study of 134 patients undergoing surgical procedures for laser ablation of HPV-infected tissues detected concordant strains of HPV in approximately 30% of smoke plumes and approximately 1.5% of surgeons’ nares.4 Not all procedures appear to carry the same risk. Electrocoagulation procedures appear to yield fewer postprocedural positive mucosal swabs for HPV, compared with those taken after CO2 laser.5
Animal studies have shown that papilloma virus procured from smoke plume has the capacity to generate disease. When 10 calves were inoculated with bovine papillary virus obtained from smoke plumes from laser ablation of bovine papillomavirus lesions, all calves manifested BPV fibropapilloma lesions at the sites of inoculation.6
There appears to be an increased incidence of HPV-associated head and neck disease among surgeons who perform procedures on HPV tissues, and there have been multiple case reports that have cited examples of HPV-associated benign and malignant disease among HCPs with frequent occupational exposure to HPV anogenital ablative and excisional procedures.7 While these observations are not proof of causation, they are cause for concern.
While the ASCCP guidelines advocate for HPV vaccination as a strategy for prevention of occupationally related HPV-associated disease, there are other strategies in place to minimize risk. The CDC guidelines for environmental infection control in health care facilities include the following recommendations:
- In settings where surgical lasers are used, wear appropriate personnel protective equipment (PPE), including N95 or N100 respirators to minimize exposure to laser plumes.
- Use central wall suction units with in-line filters to evacuate minimal laser plumes.
- Use a mechanical smoke evaluation system with a high efficiency filter to manage the generation of large amounts of laser plume, when ablating tissue infected with HPV.
- Use local exhaust ventilation (LEV).8
When closely adhered to, these methods appear to provide high-level protection. Data suggest that, when HCPs can access appropriate protective equipment, risks for HPV exposure are low. However, this is more feasible for larger hospital facilities, and may be more limited in outpatient settings. This has led to the consideration of background protection in the form of HPV vaccination for at-risk HCPs. This is analogous to mandates for HCPs to receive hepatitis B vaccination despite the concomitant practice of universal precautions in health care settings. Preventative strategies are typically most efficacious when performed in concert.
After nearly 2 decades of widespread use, we have confidence in the safety of the HPV vaccination. Its benefit through age 45 has been established, leading to the 2018 FDA approval for the 9-valent HPV vaccine, Guardisil-9, for this expanded age group. It would seem logical that systematic administration of the HPV vaccine for at-risk HCPs would be both feasible and safe. There are well-established systems for administering vaccines for HCPs in all health care systems. Perhaps health system administrators should consider routinely offering HPV vaccination for at-risk employees as part of their occupational health care responsibilities. One important caveat being the cost and efficacy of HPV vaccination in this group has not been not established.
In the meantime, it is critical that gynecology providers be aware of their risk for occupational exposure to HPV when using laser and electrocautery techniques on HPV-infected tissues and the potential for them developing head and neck pathology. They should strictly adhere to preventative measures such as use of fit-tested N-95 respirators, mechanical smoke evacuators with high-efficiency filters and work in environments with adequate room ventilation. We all should individually evaluate what role HPV vaccination may play for us in augmenting our own safety.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Van Dyne EA et al. MMWR Morb Mortal Wkly Rep. 2018 Aug 24;67(33):918-24.
2. ASCCP. ASCCP recommends HPV vaccination for providers.
3. Fox-Lewis A et al. Occup Environ Med. 2020 Dec;77(12):809-17.
4. Zhou Q et al. Cancer Manag Res. 2019;11:3643-54
5. Bergbrant I et al. Acta Derm Venereol. 1994 Sep;74(5):393-5.
6. Garden J et al. Arch Dermatol. 2002 Oct;138(10):1303-7.
7. Harrison R, Huh W. Obstet Gynecol. 2020;136:663-5.
8. CDC. 1996. DHHS (NIOSH) Publication Number 96-128.
Gynecologists have experience managing human papillomavirus–associated diseases of the lower genital tract. However, HPV also causes warty disease, dysplasia, and carcinoma of the head and neck. Risk factors for head and neck cancer include smoking and smokeless tobacco use, alcohol consumption, periodontal disease, radiation exposure, and HPV. The incidence of HPV-associated head and neck cancer is rising, particularly among men, at a rate of 2.7% per year.1 The incidence of HPV-associated squamous cell carcinoma of the oropharynx now surpasses that of cervical cancer. Concerns exist regarding occupational exposure to HPV by health care providers (HCP) who perform smoke-generating procedures on HPV-infected tissues, and the potential for them to develop head and neck pathology.
In March of 2020, the American Society for Colposcopy and Cervical Pathology made the recommendation that clinicians who are routinely exposed to HPV should protect themselves against the sequela of occupationally acquired HPV by receiving the HPV vaccine.2 They advocate for the “complete provider team” including physicians, advanced practice providers, nurses, operative technicians, and residents and fellows to be considered for protective vaccination.
Similar to disease patterns in the genital tract, different strains of HPV have differing propensity to cause benign, premalignant, and malignant disease states. HPV 6 and 11 are more commonly associated with warty disease in the nares, pharynx, and tonsillar tissues. HPV 16, 18, 31, and 33 (most commonly 16) are considered high risk for carcinoma formation, particularly of the tonsils and base of the tongue.
The procedures most implicated in occupational HPV exposure include ablative procedures for anogenital warts, laser ablation of vaginal and vulvar dysplasia, and electrosurgical excisional procedures for cervical dysplasia. Smoke plumes from HPV-associated procedures are known to contain HPV for both laser and electrocautery sources.3 A study of 134 patients undergoing surgical procedures for laser ablation of HPV-infected tissues detected concordant strains of HPV in approximately 30% of smoke plumes and approximately 1.5% of surgeons’ nares.4 Not all procedures appear to carry the same risk. Electrocoagulation procedures appear to yield fewer postprocedural positive mucosal swabs for HPV, compared with those taken after CO2 laser.5
Animal studies have shown that papilloma virus procured from smoke plume has the capacity to generate disease. When 10 calves were inoculated with bovine papillary virus obtained from smoke plumes from laser ablation of bovine papillomavirus lesions, all calves manifested BPV fibropapilloma lesions at the sites of inoculation.6
There appears to be an increased incidence of HPV-associated head and neck disease among surgeons who perform procedures on HPV tissues, and there have been multiple case reports that have cited examples of HPV-associated benign and malignant disease among HCPs with frequent occupational exposure to HPV anogenital ablative and excisional procedures.7 While these observations are not proof of causation, they are cause for concern.
While the ASCCP guidelines advocate for HPV vaccination as a strategy for prevention of occupationally related HPV-associated disease, there are other strategies in place to minimize risk. The CDC guidelines for environmental infection control in health care facilities include the following recommendations:
- In settings where surgical lasers are used, wear appropriate personnel protective equipment (PPE), including N95 or N100 respirators to minimize exposure to laser plumes.
- Use central wall suction units with in-line filters to evacuate minimal laser plumes.
- Use a mechanical smoke evaluation system with a high efficiency filter to manage the generation of large amounts of laser plume, when ablating tissue infected with HPV.
- Use local exhaust ventilation (LEV).8
When closely adhered to, these methods appear to provide high-level protection. Data suggest that, when HCPs can access appropriate protective equipment, risks for HPV exposure are low. However, this is more feasible for larger hospital facilities, and may be more limited in outpatient settings. This has led to the consideration of background protection in the form of HPV vaccination for at-risk HCPs. This is analogous to mandates for HCPs to receive hepatitis B vaccination despite the concomitant practice of universal precautions in health care settings. Preventative strategies are typically most efficacious when performed in concert.
After nearly 2 decades of widespread use, we have confidence in the safety of the HPV vaccination. Its benefit through age 45 has been established, leading to the 2018 FDA approval for the 9-valent HPV vaccine, Guardisil-9, for this expanded age group. It would seem logical that systematic administration of the HPV vaccine for at-risk HCPs would be both feasible and safe. There are well-established systems for administering vaccines for HCPs in all health care systems. Perhaps health system administrators should consider routinely offering HPV vaccination for at-risk employees as part of their occupational health care responsibilities. One important caveat being the cost and efficacy of HPV vaccination in this group has not been not established.
In the meantime, it is critical that gynecology providers be aware of their risk for occupational exposure to HPV when using laser and electrocautery techniques on HPV-infected tissues and the potential for them developing head and neck pathology. They should strictly adhere to preventative measures such as use of fit-tested N-95 respirators, mechanical smoke evacuators with high-efficiency filters and work in environments with adequate room ventilation. We all should individually evaluate what role HPV vaccination may play for us in augmenting our own safety.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Van Dyne EA et al. MMWR Morb Mortal Wkly Rep. 2018 Aug 24;67(33):918-24.
2. ASCCP. ASCCP recommends HPV vaccination for providers.
3. Fox-Lewis A et al. Occup Environ Med. 2020 Dec;77(12):809-17.
4. Zhou Q et al. Cancer Manag Res. 2019;11:3643-54
5. Bergbrant I et al. Acta Derm Venereol. 1994 Sep;74(5):393-5.
6. Garden J et al. Arch Dermatol. 2002 Oct;138(10):1303-7.
7. Harrison R, Huh W. Obstet Gynecol. 2020;136:663-5.
8. CDC. 1996. DHHS (NIOSH) Publication Number 96-128.
Evaluating phantom hCG and low-level hCG elevations in the nonpregnant patient
A human chorionic gonadotropin (hCG) test is commonly ordered by gynecologists prior to surgical procedures, in the workup of bleeding abnormalities, and in the follow-up of ectopic and molar pregnancies, to name a few indications. In doing so, occasionally clinicians will find themselves in the diagnostic dilemma of discovering an inexplicable low-level elevation in hCG, such as in a postmenopausal patient. This clinical picture can be confusing and can be concerning for conditions such as postmolar gestational trophoblastic neoplasia (GTN). However, there can be benign causes of this phenomenon.1 To prevent unnecessary worry, investigation of treatments is important. In fact, misdiagnosis and inappropriate treatment of benign, low-level hCG levels with unnecessary chemotherapy is problematic mismanagement of gestational trophoblastic disease (GTD), and a major cause of litigation.
Human chorionic gonadotropin is a glycoprotein hormone with two subunits (alpha and beta). It can come from multiple sources, including trophoblastic cells, malignant trophoblastic cells, the pituitary gland, and exogenous sources.1 Its alpha-subunit is identical to that of follicle stimulating hormone (FSH), luteinizing hormone (LH), and thyroid-stimulating hormone (TSH). Its beta-subunit is unique, though very similar to that of LH. The free hCG beta subunit can be produced by nontrophoblastic neoplasms. The gene for the beta subunit of hCG is in close proximity to the beta subunit of LH and increases in gonadotropin-releasing hormone (GnRH) in menopause can result in the stimulation of both genes. Understanding the sources of hCG-like glycoproteins and mechanisms for testing is important when considering possible causes for falsely elevated hCG.
Most commercially available serum hCG assays detect normal intact hCG and free beta subunits. They are typically sandwich assays utilizing antibody binding sites in which a solid-phase anti-hCG antibody to a specific hCG target is then mixed with the patient’s serum, trapping or binding the hCG, which is then treated with an indicator antibody. After being washed with the indicator or “capture” antibody, its relative (quantitative) levels can be measured.1
Urine hCG testing (such as urine pregnancy tests) work through capillary action, drawing the patient’s urine across absorbent pads before reaching a pad which contains anti-hCG antibodies (the detection zone) in the test line. These tests are less sensitive than serum tests, but many can detect hCG levels <15-20 mIU/mL.1
When ob.gyns. are asked to consult on or evaluate persistently low-level elevations of hCG in nonpregnant patients they should consider both malignant and nonmalignant etiologies. Malignant causes include GTN or quiescent GTD (e.g., after treatment of a molar pregnancy or GTN), choriocarcinoma (e.g., ovarian germ cell tumors), and nonchoriocarcinoma malignancies (such as cervical, pancreatic, breast, renal). Nonmalignant causes of hCG elevations in nonpregnant patients include pituitary hCG (in postmenopausal patients), exogenous hCG, and phantom hCG.
The first step in diagnostic workup is to perform a urine pregnancy test. Provided that the serum hCG level is > 20 mIU/mL, the urine HCG should be positive unless the cause of elevated levels is “phantom hCG” from heterophilic antibodies. When patients are exposed to animal antigens (such as in vaccines) they can develop antibodies such as human anti-mouse antibody. These antibodies have affinity to the binding antibodies used in many hCG sandwich assays and form a linkage between the solid phase antibody and the detection antibody creating a false-positive result. This false-positive test is only present in serum testing but not urine tests because the patient’s heterophilic antibodies are not excreted by the kidney and thus not available to create a false-positive result. An alternative method to make the diagnosis of phantom hCG is to request that the hCG testing be run at a different lab with a different assay (which may not react with the same affinity to the patient’s anti-animal heterophile antibodies), or to request that the lab perform serial dilutions. If phantom hCG from heterophile antibodies is at play, serial dilutions will result in a nonlinear dilution response.
If the patient’s urine hCG test is positive, then pregnancy should be ruled out with a transvaginal ultrasound. If negative, an ectopic pregnancy should still be considered (unless not medically plausible, such as in postmenopausal women or women who have undergone hysterectomy). In the absence of an intrauterine or ectopic pregnancy, a positive serum and urine pregnancy test could be from exogenous hCG, from malignancy or pituitary hCG. Use of exogenous hCG can be ruled out by taking a thorough history, with particular focus on asking about weight loss medications and muscle building therapies.
If pregnancy and exogenous hCG are ruled out, clinicians should assess for an occult hCG-secreting malignancy. The lab should be asked to measure the proportion of the free beta subunit of hCG, as this is typically what is secreted by malignancies. CT imaging of the chest, abdomen, and pelvis to search for an occult primary tumor should take place. If the patient has been recently treated for molar pregnancy or GTN, and serum hCG levels reside between 100 and 300 mIU/mL, quiescent GTD should be considered the diagnosis. Determination of the proportion of hyperglycosylated hCG to total hCG can help differentiate active choriocarcinoma from quiescent GTD. After restaging imaging has been done to confirm no measurable metastatic foci, observation can follow with monthly hCG measurements. The majority of these cases will eventually resolve without intervention within a year. Quiescent GTD and persistent low-level HCG in the absence of measurable GTN on imaging or symptoms does not require treatment with chemotherapy or hysterectomy, particularly in women who desire future fertility.2
Once occult malignancy has been ruled out, the remaining potential source of hCG is the pituitary gland. As mentioned earlier, hCG shares its morphology with TSH, LH, and FSH. This can result in cross reactivity and false positives. In the menopausal state, GnRH levels increase and thus so do pituitary LH and hCG levels. To confirm that the pituitary is the source of the low-level hCG levels, the provider should prescribe a course of hormonal treatment such as an oral contraceptive pill for a 2- to 3-month period. This should result in suppression of pituitary hCG, and serum hCG levels, as part of a negative feedback loop. Pituitary source of hCG is a benign condition, and, like quiescent GTD, phantom hCG or exogenous hCG does not require intervention.
Getting to the bottom of persistent low-level hCG elevations can be challenging. By following the step-wise algorithm listed here, clinicians can sequentially test for urine hCG, heterophilic antibodies, elevated free beta-subunit, occult malignancy, and pituitary hCG.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no conflicts of interest. Email her at [email protected].
References
1. Oyatogun O et al. Ther Adv Reprod Health 2021 Jun 13. doi: 10.1177/2F26334941211016412.
2. Soper JT. Obstet Gynecol. 2021 Feb 1;137(2):355-70.
A human chorionic gonadotropin (hCG) test is commonly ordered by gynecologists prior to surgical procedures, in the workup of bleeding abnormalities, and in the follow-up of ectopic and molar pregnancies, to name a few indications. In doing so, occasionally clinicians will find themselves in the diagnostic dilemma of discovering an inexplicable low-level elevation in hCG, such as in a postmenopausal patient. This clinical picture can be confusing and can be concerning for conditions such as postmolar gestational trophoblastic neoplasia (GTN). However, there can be benign causes of this phenomenon.1 To prevent unnecessary worry, investigation of treatments is important. In fact, misdiagnosis and inappropriate treatment of benign, low-level hCG levels with unnecessary chemotherapy is problematic mismanagement of gestational trophoblastic disease (GTD), and a major cause of litigation.
Human chorionic gonadotropin is a glycoprotein hormone with two subunits (alpha and beta). It can come from multiple sources, including trophoblastic cells, malignant trophoblastic cells, the pituitary gland, and exogenous sources.1 Its alpha-subunit is identical to that of follicle stimulating hormone (FSH), luteinizing hormone (LH), and thyroid-stimulating hormone (TSH). Its beta-subunit is unique, though very similar to that of LH. The free hCG beta subunit can be produced by nontrophoblastic neoplasms. The gene for the beta subunit of hCG is in close proximity to the beta subunit of LH and increases in gonadotropin-releasing hormone (GnRH) in menopause can result in the stimulation of both genes. Understanding the sources of hCG-like glycoproteins and mechanisms for testing is important when considering possible causes for falsely elevated hCG.
Most commercially available serum hCG assays detect normal intact hCG and free beta subunits. They are typically sandwich assays utilizing antibody binding sites in which a solid-phase anti-hCG antibody to a specific hCG target is then mixed with the patient’s serum, trapping or binding the hCG, which is then treated with an indicator antibody. After being washed with the indicator or “capture” antibody, its relative (quantitative) levels can be measured.1
Urine hCG testing (such as urine pregnancy tests) work through capillary action, drawing the patient’s urine across absorbent pads before reaching a pad which contains anti-hCG antibodies (the detection zone) in the test line. These tests are less sensitive than serum tests, but many can detect hCG levels <15-20 mIU/mL.1
When ob.gyns. are asked to consult on or evaluate persistently low-level elevations of hCG in nonpregnant patients they should consider both malignant and nonmalignant etiologies. Malignant causes include GTN or quiescent GTD (e.g., after treatment of a molar pregnancy or GTN), choriocarcinoma (e.g., ovarian germ cell tumors), and nonchoriocarcinoma malignancies (such as cervical, pancreatic, breast, renal). Nonmalignant causes of hCG elevations in nonpregnant patients include pituitary hCG (in postmenopausal patients), exogenous hCG, and phantom hCG.
The first step in diagnostic workup is to perform a urine pregnancy test. Provided that the serum hCG level is > 20 mIU/mL, the urine HCG should be positive unless the cause of elevated levels is “phantom hCG” from heterophilic antibodies. When patients are exposed to animal antigens (such as in vaccines) they can develop antibodies such as human anti-mouse antibody. These antibodies have affinity to the binding antibodies used in many hCG sandwich assays and form a linkage between the solid phase antibody and the detection antibody creating a false-positive result. This false-positive test is only present in serum testing but not urine tests because the patient’s heterophilic antibodies are not excreted by the kidney and thus not available to create a false-positive result. An alternative method to make the diagnosis of phantom hCG is to request that the hCG testing be run at a different lab with a different assay (which may not react with the same affinity to the patient’s anti-animal heterophile antibodies), or to request that the lab perform serial dilutions. If phantom hCG from heterophile antibodies is at play, serial dilutions will result in a nonlinear dilution response.
If the patient’s urine hCG test is positive, then pregnancy should be ruled out with a transvaginal ultrasound. If negative, an ectopic pregnancy should still be considered (unless not medically plausible, such as in postmenopausal women or women who have undergone hysterectomy). In the absence of an intrauterine or ectopic pregnancy, a positive serum and urine pregnancy test could be from exogenous hCG, from malignancy or pituitary hCG. Use of exogenous hCG can be ruled out by taking a thorough history, with particular focus on asking about weight loss medications and muscle building therapies.
If pregnancy and exogenous hCG are ruled out, clinicians should assess for an occult hCG-secreting malignancy. The lab should be asked to measure the proportion of the free beta subunit of hCG, as this is typically what is secreted by malignancies. CT imaging of the chest, abdomen, and pelvis to search for an occult primary tumor should take place. If the patient has been recently treated for molar pregnancy or GTN, and serum hCG levels reside between 100 and 300 mIU/mL, quiescent GTD should be considered the diagnosis. Determination of the proportion of hyperglycosylated hCG to total hCG can help differentiate active choriocarcinoma from quiescent GTD. After restaging imaging has been done to confirm no measurable metastatic foci, observation can follow with monthly hCG measurements. The majority of these cases will eventually resolve without intervention within a year. Quiescent GTD and persistent low-level HCG in the absence of measurable GTN on imaging or symptoms does not require treatment with chemotherapy or hysterectomy, particularly in women who desire future fertility.2
Once occult malignancy has been ruled out, the remaining potential source of hCG is the pituitary gland. As mentioned earlier, hCG shares its morphology with TSH, LH, and FSH. This can result in cross reactivity and false positives. In the menopausal state, GnRH levels increase and thus so do pituitary LH and hCG levels. To confirm that the pituitary is the source of the low-level hCG levels, the provider should prescribe a course of hormonal treatment such as an oral contraceptive pill for a 2- to 3-month period. This should result in suppression of pituitary hCG, and serum hCG levels, as part of a negative feedback loop. Pituitary source of hCG is a benign condition, and, like quiescent GTD, phantom hCG or exogenous hCG does not require intervention.
Getting to the bottom of persistent low-level hCG elevations can be challenging. By following the step-wise algorithm listed here, clinicians can sequentially test for urine hCG, heterophilic antibodies, elevated free beta-subunit, occult malignancy, and pituitary hCG.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no conflicts of interest. Email her at [email protected].
References
1. Oyatogun O et al. Ther Adv Reprod Health 2021 Jun 13. doi: 10.1177/2F26334941211016412.
2. Soper JT. Obstet Gynecol. 2021 Feb 1;137(2):355-70.
A human chorionic gonadotropin (hCG) test is commonly ordered by gynecologists prior to surgical procedures, in the workup of bleeding abnormalities, and in the follow-up of ectopic and molar pregnancies, to name a few indications. In doing so, occasionally clinicians will find themselves in the diagnostic dilemma of discovering an inexplicable low-level elevation in hCG, such as in a postmenopausal patient. This clinical picture can be confusing and can be concerning for conditions such as postmolar gestational trophoblastic neoplasia (GTN). However, there can be benign causes of this phenomenon.1 To prevent unnecessary worry, investigation of treatments is important. In fact, misdiagnosis and inappropriate treatment of benign, low-level hCG levels with unnecessary chemotherapy is problematic mismanagement of gestational trophoblastic disease (GTD), and a major cause of litigation.
Human chorionic gonadotropin is a glycoprotein hormone with two subunits (alpha and beta). It can come from multiple sources, including trophoblastic cells, malignant trophoblastic cells, the pituitary gland, and exogenous sources.1 Its alpha-subunit is identical to that of follicle stimulating hormone (FSH), luteinizing hormone (LH), and thyroid-stimulating hormone (TSH). Its beta-subunit is unique, though very similar to that of LH. The free hCG beta subunit can be produced by nontrophoblastic neoplasms. The gene for the beta subunit of hCG is in close proximity to the beta subunit of LH and increases in gonadotropin-releasing hormone (GnRH) in menopause can result in the stimulation of both genes. Understanding the sources of hCG-like glycoproteins and mechanisms for testing is important when considering possible causes for falsely elevated hCG.
Most commercially available serum hCG assays detect normal intact hCG and free beta subunits. They are typically sandwich assays utilizing antibody binding sites in which a solid-phase anti-hCG antibody to a specific hCG target is then mixed with the patient’s serum, trapping or binding the hCG, which is then treated with an indicator antibody. After being washed with the indicator or “capture” antibody, its relative (quantitative) levels can be measured.1
Urine hCG testing (such as urine pregnancy tests) work through capillary action, drawing the patient’s urine across absorbent pads before reaching a pad which contains anti-hCG antibodies (the detection zone) in the test line. These tests are less sensitive than serum tests, but many can detect hCG levels <15-20 mIU/mL.1
When ob.gyns. are asked to consult on or evaluate persistently low-level elevations of hCG in nonpregnant patients they should consider both malignant and nonmalignant etiologies. Malignant causes include GTN or quiescent GTD (e.g., after treatment of a molar pregnancy or GTN), choriocarcinoma (e.g., ovarian germ cell tumors), and nonchoriocarcinoma malignancies (such as cervical, pancreatic, breast, renal). Nonmalignant causes of hCG elevations in nonpregnant patients include pituitary hCG (in postmenopausal patients), exogenous hCG, and phantom hCG.
The first step in diagnostic workup is to perform a urine pregnancy test. Provided that the serum hCG level is > 20 mIU/mL, the urine HCG should be positive unless the cause of elevated levels is “phantom hCG” from heterophilic antibodies. When patients are exposed to animal antigens (such as in vaccines) they can develop antibodies such as human anti-mouse antibody. These antibodies have affinity to the binding antibodies used in many hCG sandwich assays and form a linkage between the solid phase antibody and the detection antibody creating a false-positive result. This false-positive test is only present in serum testing but not urine tests because the patient’s heterophilic antibodies are not excreted by the kidney and thus not available to create a false-positive result. An alternative method to make the diagnosis of phantom hCG is to request that the hCG testing be run at a different lab with a different assay (which may not react with the same affinity to the patient’s anti-animal heterophile antibodies), or to request that the lab perform serial dilutions. If phantom hCG from heterophile antibodies is at play, serial dilutions will result in a nonlinear dilution response.
If the patient’s urine hCG test is positive, then pregnancy should be ruled out with a transvaginal ultrasound. If negative, an ectopic pregnancy should still be considered (unless not medically plausible, such as in postmenopausal women or women who have undergone hysterectomy). In the absence of an intrauterine or ectopic pregnancy, a positive serum and urine pregnancy test could be from exogenous hCG, from malignancy or pituitary hCG. Use of exogenous hCG can be ruled out by taking a thorough history, with particular focus on asking about weight loss medications and muscle building therapies.
If pregnancy and exogenous hCG are ruled out, clinicians should assess for an occult hCG-secreting malignancy. The lab should be asked to measure the proportion of the free beta subunit of hCG, as this is typically what is secreted by malignancies. CT imaging of the chest, abdomen, and pelvis to search for an occult primary tumor should take place. If the patient has been recently treated for molar pregnancy or GTN, and serum hCG levels reside between 100 and 300 mIU/mL, quiescent GTD should be considered the diagnosis. Determination of the proportion of hyperglycosylated hCG to total hCG can help differentiate active choriocarcinoma from quiescent GTD. After restaging imaging has been done to confirm no measurable metastatic foci, observation can follow with monthly hCG measurements. The majority of these cases will eventually resolve without intervention within a year. Quiescent GTD and persistent low-level HCG in the absence of measurable GTN on imaging or symptoms does not require treatment with chemotherapy or hysterectomy, particularly in women who desire future fertility.2
Once occult malignancy has been ruled out, the remaining potential source of hCG is the pituitary gland. As mentioned earlier, hCG shares its morphology with TSH, LH, and FSH. This can result in cross reactivity and false positives. In the menopausal state, GnRH levels increase and thus so do pituitary LH and hCG levels. To confirm that the pituitary is the source of the low-level hCG levels, the provider should prescribe a course of hormonal treatment such as an oral contraceptive pill for a 2- to 3-month period. This should result in suppression of pituitary hCG, and serum hCG levels, as part of a negative feedback loop. Pituitary source of hCG is a benign condition, and, like quiescent GTD, phantom hCG or exogenous hCG does not require intervention.
Getting to the bottom of persistent low-level hCG elevations can be challenging. By following the step-wise algorithm listed here, clinicians can sequentially test for urine hCG, heterophilic antibodies, elevated free beta-subunit, occult malignancy, and pituitary hCG.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no conflicts of interest. Email her at [email protected].
References
1. Oyatogun O et al. Ther Adv Reprod Health 2021 Jun 13. doi: 10.1177/2F26334941211016412.
2. Soper JT. Obstet Gynecol. 2021 Feb 1;137(2):355-70.
Management of advanced endometrial cancer
Endometrial cancer is most commonly diagnosed at an early stage. Unfortunately, there is a trend toward the diagnosis of more advanced disease, for which cure is rare, and this is an important contributing factor toward the overall increasing mortality trend for endometrial cancer.
Histology is a major risk factor for advanced disease. For example, serous carcinoma, which accounts for approximately only 10% of all endometrial cancer diagnoses, comprises 25% of cases of advanced cases. Similarly, carcinosarcoma, a cell type known to be particularly aggressive, is relatively overrepresented among cases of advanced disease.
Advanced endometrial cancer includes cases of stage III (involvement of lymph nodes, ovaries, and vagina) and stage IV disease (with direct extension into pelvic viscera and distant metastases). In most cases of stage III disease, extrauterine metastases are microscopic and are detected only at the time of surgical staging. Bulky nodal disease within the pelvic and para-aortic nodal basins is less common but associated with worse prognosis than for patients with microscopic nodal metastases. Stage IV disease usually presents with peritoneal spread of disease including carcinomatosis, omental disease, and involvement of the small and large intestine.
Once advanced, endometrial cancer requires more than surgery alone, relying heavily on adjuvant therapies to achieve responses, particularly systemic therapy with platinum and taxane chemotherapy. In some cases, molecularly targeted therapy (such as trastuzumab for serous carcinomas that demonstrate overexpression of HER2) has been shown to be superior in efficacy.1 Surgery may involve either radical nodal dissections to the infrarenal aortic basin, and/or peritoneal debulking procedures similar to that required for ovarian cancer. Perhaps because of patterns of disease distribution so similar to ovarian cancer, historically, sequencing of therapy focused on radical primary debulking surgery (PDS) followed by chemotherapy.
In 2000, a retrospective series from Johns Hopkins University documented the outcomes of 65 patients with advanced endometrial cancer who had undergone primary debulking surgery followed by chemotherapy.2 They noted that survival was directly associated with degree of cytoreduction, with the best outcomes seen for those patients whose surgery resulted in no gross residual disease. Following these data, PDS with complete resection of all disease became the goal of primary therapy.
However, unlike ovarian cancer (which shares a similar disease distribution with advanced endometrial cancer) patients with endometrial cancer are more obese, older, and typically have more comorbidities. Therefore, radical primary debulking surgeries may be associated with poor patient perioperative outcomes, and feasibility of complete cytoreduction, particularly in very obese patients, can be limited. For this reason, neoadjuvant chemotherapy (NACT) has been explored as an option. The potential virtue of NACT is that it allows for tumor deposits to decrease in size, or be eliminated, prior to surgery, resulting in a less morbid procedure for the patient.
Observed outcomes for NACT relative to PDS are mixed. When small series have compared the two for the treatment of advanced serous endometrial cancer, NACT was associated with decreased perioperative morbidity, with similar overall survival observed.3,4
However, in larger series exploring patients within the National Cancer Database (a collection of over 1,500 hospitals accredited by the Commission on Cancer) outcomes appear different for the two approaches.5,6 While PDS was initially associated with worse survival, at approximately 5-6 months from diagnosis, this changed and survival was observed to be consistently superior for this group. These data suggest that patients undergoing primary surgical cytoreduction may experience an early mortality risk, possibly secondary to the impact of surgery, but that if they are to survive beyond this point, they experience better outcomes. While the researchers attempted to control for risk factors of poor outcomes that might have systematically differed between the two groups, this specific database is limited in its ability to account for all fundamental differences between them. Only approximately 15% of women with advanced endometrial cancer were offered NACT during those time periods. This observation alone suggests that this likely represents a group specially selected for their poor candidacy for upfront debulking surgery, and inherently increased risk for death from all causes.
The question remains, is NACT appropriate for all patients or just those who are considered poor surgical candidates? Could all patients benefit from the decreased morbidity associated with surgery after NACT without compromising survival? Randomized controlled trials are necessary to answer this question as they are the only way to ensure that risk factors for poor outcomes (such as histology, disease distribution, medical comorbidities) are equally distributed among both groups.
In the meantime, gynecologic oncologists should take a cautious approach to decision making regarding sequencing of surgery and chemotherapy in the setting of a new diagnosis of advanced endometrial cancer. Arguably more important than surgical interventions, access to molecularly targeted systemic therapy is likely to bring the best outcomes for advanced endometrial cancer. Carboplatin and paclitaxel are the current gold standard of care for frontline systemic therapy; however, response rates with this regimen are less favorable for endometrial cancer than for ovarian cancer. Work is being done to test novel therapies against actionable targets to use as alternatives or as adjuncts to traditional chemotherapy regimens. In doing so, clinicians are learning to distinguish endometrial cancers by more than simply their histologic features, but also by their molecular profiles.
Advanced endometrial cancer is a serious disease with high lethality. Future research should focus on ways to ensure toxicities of therapy, including surgery, are minimized while improving upon existing poor clinical outcomes.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no financial disclosures.
References
1. Fader AN et al. J Clin Oncol 2018;36(20):2044-51.
2. Bristow RE et al. Gynecol Oncol 2000;78(2):85-91.
3. Bogani G et al. Tumori 2019;105(1):92-97.
4. Wilkinson-Ryan I et al. Int J Gynecol Cancer. 2015;25(1):63-8.
5. Tobias CJ et al. JAMA Netw Open 2020;3(12):e2028612.
6. Chambers LM et al. Gynecol Oncol 2021;160(2):405-12.
Endometrial cancer is most commonly diagnosed at an early stage. Unfortunately, there is a trend toward the diagnosis of more advanced disease, for which cure is rare, and this is an important contributing factor toward the overall increasing mortality trend for endometrial cancer.
Histology is a major risk factor for advanced disease. For example, serous carcinoma, which accounts for approximately only 10% of all endometrial cancer diagnoses, comprises 25% of cases of advanced cases. Similarly, carcinosarcoma, a cell type known to be particularly aggressive, is relatively overrepresented among cases of advanced disease.
Advanced endometrial cancer includes cases of stage III (involvement of lymph nodes, ovaries, and vagina) and stage IV disease (with direct extension into pelvic viscera and distant metastases). In most cases of stage III disease, extrauterine metastases are microscopic and are detected only at the time of surgical staging. Bulky nodal disease within the pelvic and para-aortic nodal basins is less common but associated with worse prognosis than for patients with microscopic nodal metastases. Stage IV disease usually presents with peritoneal spread of disease including carcinomatosis, omental disease, and involvement of the small and large intestine.
Once advanced, endometrial cancer requires more than surgery alone, relying heavily on adjuvant therapies to achieve responses, particularly systemic therapy with platinum and taxane chemotherapy. In some cases, molecularly targeted therapy (such as trastuzumab for serous carcinomas that demonstrate overexpression of HER2) has been shown to be superior in efficacy.1 Surgery may involve either radical nodal dissections to the infrarenal aortic basin, and/or peritoneal debulking procedures similar to that required for ovarian cancer. Perhaps because of patterns of disease distribution so similar to ovarian cancer, historically, sequencing of therapy focused on radical primary debulking surgery (PDS) followed by chemotherapy.
In 2000, a retrospective series from Johns Hopkins University documented the outcomes of 65 patients with advanced endometrial cancer who had undergone primary debulking surgery followed by chemotherapy.2 They noted that survival was directly associated with degree of cytoreduction, with the best outcomes seen for those patients whose surgery resulted in no gross residual disease. Following these data, PDS with complete resection of all disease became the goal of primary therapy.
However, unlike ovarian cancer (which shares a similar disease distribution with advanced endometrial cancer) patients with endometrial cancer are more obese, older, and typically have more comorbidities. Therefore, radical primary debulking surgeries may be associated with poor patient perioperative outcomes, and feasibility of complete cytoreduction, particularly in very obese patients, can be limited. For this reason, neoadjuvant chemotherapy (NACT) has been explored as an option. The potential virtue of NACT is that it allows for tumor deposits to decrease in size, or be eliminated, prior to surgery, resulting in a less morbid procedure for the patient.
Observed outcomes for NACT relative to PDS are mixed. When small series have compared the two for the treatment of advanced serous endometrial cancer, NACT was associated with decreased perioperative morbidity, with similar overall survival observed.3,4
However, in larger series exploring patients within the National Cancer Database (a collection of over 1,500 hospitals accredited by the Commission on Cancer) outcomes appear different for the two approaches.5,6 While PDS was initially associated with worse survival, at approximately 5-6 months from diagnosis, this changed and survival was observed to be consistently superior for this group. These data suggest that patients undergoing primary surgical cytoreduction may experience an early mortality risk, possibly secondary to the impact of surgery, but that if they are to survive beyond this point, they experience better outcomes. While the researchers attempted to control for risk factors of poor outcomes that might have systematically differed between the two groups, this specific database is limited in its ability to account for all fundamental differences between them. Only approximately 15% of women with advanced endometrial cancer were offered NACT during those time periods. This observation alone suggests that this likely represents a group specially selected for their poor candidacy for upfront debulking surgery, and inherently increased risk for death from all causes.
The question remains, is NACT appropriate for all patients or just those who are considered poor surgical candidates? Could all patients benefit from the decreased morbidity associated with surgery after NACT without compromising survival? Randomized controlled trials are necessary to answer this question as they are the only way to ensure that risk factors for poor outcomes (such as histology, disease distribution, medical comorbidities) are equally distributed among both groups.
In the meantime, gynecologic oncologists should take a cautious approach to decision making regarding sequencing of surgery and chemotherapy in the setting of a new diagnosis of advanced endometrial cancer. Arguably more important than surgical interventions, access to molecularly targeted systemic therapy is likely to bring the best outcomes for advanced endometrial cancer. Carboplatin and paclitaxel are the current gold standard of care for frontline systemic therapy; however, response rates with this regimen are less favorable for endometrial cancer than for ovarian cancer. Work is being done to test novel therapies against actionable targets to use as alternatives or as adjuncts to traditional chemotherapy regimens. In doing so, clinicians are learning to distinguish endometrial cancers by more than simply their histologic features, but also by their molecular profiles.
Advanced endometrial cancer is a serious disease with high lethality. Future research should focus on ways to ensure toxicities of therapy, including surgery, are minimized while improving upon existing poor clinical outcomes.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no financial disclosures.
References
1. Fader AN et al. J Clin Oncol 2018;36(20):2044-51.
2. Bristow RE et al. Gynecol Oncol 2000;78(2):85-91.
3. Bogani G et al. Tumori 2019;105(1):92-97.
4. Wilkinson-Ryan I et al. Int J Gynecol Cancer. 2015;25(1):63-8.
5. Tobias CJ et al. JAMA Netw Open 2020;3(12):e2028612.
6. Chambers LM et al. Gynecol Oncol 2021;160(2):405-12.
Endometrial cancer is most commonly diagnosed at an early stage. Unfortunately, there is a trend toward the diagnosis of more advanced disease, for which cure is rare, and this is an important contributing factor toward the overall increasing mortality trend for endometrial cancer.
Histology is a major risk factor for advanced disease. For example, serous carcinoma, which accounts for approximately only 10% of all endometrial cancer diagnoses, comprises 25% of cases of advanced cases. Similarly, carcinosarcoma, a cell type known to be particularly aggressive, is relatively overrepresented among cases of advanced disease.
Advanced endometrial cancer includes cases of stage III (involvement of lymph nodes, ovaries, and vagina) and stage IV disease (with direct extension into pelvic viscera and distant metastases). In most cases of stage III disease, extrauterine metastases are microscopic and are detected only at the time of surgical staging. Bulky nodal disease within the pelvic and para-aortic nodal basins is less common but associated with worse prognosis than for patients with microscopic nodal metastases. Stage IV disease usually presents with peritoneal spread of disease including carcinomatosis, omental disease, and involvement of the small and large intestine.
Once advanced, endometrial cancer requires more than surgery alone, relying heavily on adjuvant therapies to achieve responses, particularly systemic therapy with platinum and taxane chemotherapy. In some cases, molecularly targeted therapy (such as trastuzumab for serous carcinomas that demonstrate overexpression of HER2) has been shown to be superior in efficacy.1 Surgery may involve either radical nodal dissections to the infrarenal aortic basin, and/or peritoneal debulking procedures similar to that required for ovarian cancer. Perhaps because of patterns of disease distribution so similar to ovarian cancer, historically, sequencing of therapy focused on radical primary debulking surgery (PDS) followed by chemotherapy.
In 2000, a retrospective series from Johns Hopkins University documented the outcomes of 65 patients with advanced endometrial cancer who had undergone primary debulking surgery followed by chemotherapy.2 They noted that survival was directly associated with degree of cytoreduction, with the best outcomes seen for those patients whose surgery resulted in no gross residual disease. Following these data, PDS with complete resection of all disease became the goal of primary therapy.
However, unlike ovarian cancer (which shares a similar disease distribution with advanced endometrial cancer) patients with endometrial cancer are more obese, older, and typically have more comorbidities. Therefore, radical primary debulking surgeries may be associated with poor patient perioperative outcomes, and feasibility of complete cytoreduction, particularly in very obese patients, can be limited. For this reason, neoadjuvant chemotherapy (NACT) has been explored as an option. The potential virtue of NACT is that it allows for tumor deposits to decrease in size, or be eliminated, prior to surgery, resulting in a less morbid procedure for the patient.
Observed outcomes for NACT relative to PDS are mixed. When small series have compared the two for the treatment of advanced serous endometrial cancer, NACT was associated with decreased perioperative morbidity, with similar overall survival observed.3,4
However, in larger series exploring patients within the National Cancer Database (a collection of over 1,500 hospitals accredited by the Commission on Cancer) outcomes appear different for the two approaches.5,6 While PDS was initially associated with worse survival, at approximately 5-6 months from diagnosis, this changed and survival was observed to be consistently superior for this group. These data suggest that patients undergoing primary surgical cytoreduction may experience an early mortality risk, possibly secondary to the impact of surgery, but that if they are to survive beyond this point, they experience better outcomes. While the researchers attempted to control for risk factors of poor outcomes that might have systematically differed between the two groups, this specific database is limited in its ability to account for all fundamental differences between them. Only approximately 15% of women with advanced endometrial cancer were offered NACT during those time periods. This observation alone suggests that this likely represents a group specially selected for their poor candidacy for upfront debulking surgery, and inherently increased risk for death from all causes.
The question remains, is NACT appropriate for all patients or just those who are considered poor surgical candidates? Could all patients benefit from the decreased morbidity associated with surgery after NACT without compromising survival? Randomized controlled trials are necessary to answer this question as they are the only way to ensure that risk factors for poor outcomes (such as histology, disease distribution, medical comorbidities) are equally distributed among both groups.
In the meantime, gynecologic oncologists should take a cautious approach to decision making regarding sequencing of surgery and chemotherapy in the setting of a new diagnosis of advanced endometrial cancer. Arguably more important than surgical interventions, access to molecularly targeted systemic therapy is likely to bring the best outcomes for advanced endometrial cancer. Carboplatin and paclitaxel are the current gold standard of care for frontline systemic therapy; however, response rates with this regimen are less favorable for endometrial cancer than for ovarian cancer. Work is being done to test novel therapies against actionable targets to use as alternatives or as adjuncts to traditional chemotherapy regimens. In doing so, clinicians are learning to distinguish endometrial cancers by more than simply their histologic features, but also by their molecular profiles.
Advanced endometrial cancer is a serious disease with high lethality. Future research should focus on ways to ensure toxicities of therapy, including surgery, are minimized while improving upon existing poor clinical outcomes.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no financial disclosures.
References
1. Fader AN et al. J Clin Oncol 2018;36(20):2044-51.
2. Bristow RE et al. Gynecol Oncol 2000;78(2):85-91.
3. Bogani G et al. Tumori 2019;105(1):92-97.
4. Wilkinson-Ryan I et al. Int J Gynecol Cancer. 2015;25(1):63-8.
5. Tobias CJ et al. JAMA Netw Open 2020;3(12):e2028612.
6. Chambers LM et al. Gynecol Oncol 2021;160(2):405-12.
Recommendations from a gynecologic oncologist to a general ob.gyn., part 2
In this month’s column we continue to discuss recommendations from the gynecologic oncologist to the general gynecologist.
Don’t screen average-risk women for ovarian cancer.
Ovarian cancer is most often diagnosed at an advanced stage, which limits the curability of the disease. Consequently, there is a strong focus on attempting to diagnose the disease at earlier, more curable stages. This leads to the impulse by some well-intentioned providers to implement screening tests, such as ultrasounds and tumor markers, for all women. Unfortunately, the screening of “average risk” women for ovarian cancer is not recommended. Randomized controlled trials of tens of thousands of women have not observed a clinically significant decrease in ovarian cancer mortality with the addition of screening with tumor markers and ultrasound.1 These studies did observe a false-positive rate of 5%. While that may seem like a low rate of false-positive testing, the definitive diagnostic test which follows is a major abdominal surgery (oophorectomy) and serious complications are encountered in 15% of patients undergoing surgery for false-positive ovarian cancer screening.1 Therefore, quite simply, the harms are not balanced by benefits.
The key to offering patients appropriate and effective screening is case selection. It is important to identify which patients are at higher risk for ovarian cancer and offer those women testing for germline mutations and screening strategies. An important component of a well-woman visit is to take a thorough family history of cancer. Women are considered at high risk for having hereditary predisposition to ovarian cancer if they have a first- or second-degree relative with breast cancer younger than 45-50 years, or any age if Ashkenazi Jewish, triple-negative breast cancer younger than 60 years of age, two or more primary breast cancers with the first diagnosed at less than 50 years of age, male breast cancer, ovarian cancer, pancreatic cancer, a known BRCA 1/2 mutation, or a personal history of those same conditions. These women should be recommended to undergo genetic testing for BRCA 1, 2, and Lynch syndrome. They should not automatically be offered ovarian cancer screening. If a patient has a more remote family history for ovarian cancer, their personal risk may be somewhat elevated above the baseline population risk, however, not substantially enough to justify implementing screening in the absence of a confirmed genetic mutation.
While screening tests may not be appropriate for all patients, all patients should be asked about the early symptoms of ovarian cancer because these are consistently present, and frequently overlooked, prior to the eventual diagnosis of advanced disease. Those symptoms include abdominal discomfort, abdominal swelling and bloating, and urinary urgency.2 Consider offering all patients a dedicated ovarian cancer specific review of systems that includes inquiries about these symptoms at their annual wellness visits.
Opt for vertical midline incisions when surgery is anticipated to be complex
What is the first thing gynecologic oncologists do when called in to assist in a difficult gynecologic procedure? Get better exposure. Exposure is the cornerstone of safe, effective surgery. Sometimes this simply means placing a more effective retractor. In other cases, it might mean extending the incision. However, if the incision is a low transverse incision (the go-to for many gynecologists because of its favorable cosmetic and pain-producing profile) this proves to be difficult. Attempting to assist in a complicated case, such as a frozen pelvis, severed ureter or rectal injury, through a pfannensteil incision can be extraordinarily difficult, and while these incisions can be extended by incising the rectus muscle bellies, upper abdominal visualization remains elusive in most patients. This is particularly problematic if the ureter or splenic flexure need to be mobilized, or if extensive lysis of adhesions is necessary to ensure there is no occult enterotomy. As my mentor Dr. John Soper once described to me: “It’s like trying to scratch your armpit by reaching through your fly.”
While pfannensteil incisions come naturally, and comfortably, to most gynecologists, likely because of their frequent application during cesarean section, all gynecologists should be confident in the steps and anatomy for vertical midline, or paramedian incisions. This is not only beneficial for complex gynecologic cases, but also in the event of vascular emergency. In the hands of an experienced abdominal/pelvic surgeon, the vertical midline incision is the quickest way to safely enter the abdomen, and provides the kind of exposure that may be critical in safely repairing or controlling hemorrhage from a major vessel.
While low transverse incisions may be more cosmetic, less painful, and associated with fewer wound complications, our first concern as surgeons should be mitigating complications. In situations where risks of complications are high, it is best to not handicap ourselves with the incision location. And always remember, wound complications are highest when a transverse incision needs to be converted to a vertical one with a “T.”
It’s not just about diagnosis of cancer, it’s also prevention
Detection of cancer is an important role of the obstetrician gynecologist. However, equally important is being able to seize opportunities for cancer prevention. Cervical, vulvar, endometrial and ovarian cancer are all known to have preventative strategies.
All patients up to the age of 45 should be offered vaccination against HPV. Initial indications for HPV vaccination were for women up to age 26; however, recent data support the safety and efficacy of the vaccine in older women.3 HPV vaccination is most effective at preventing cancer when administered prior to exposure (ideally age 9-11), leaving this in the hands of our pediatrician colleagues. However, we must be vigilant to inquire about vaccination status for all our patients and encourage vaccines for those who were missed earlier in their life.
Patients should be counseled regarding the significant risk reduction for cancer that is gained from use of oral hormonal contraceptives and progestin-releasing IUDs (especially for endometrial and ovarian cancers). Providing them with knowledge of this information when considering options for contraception or menstrual cycle management is important in their decision-making process.
Endometrial cancer incidence is sadly on the rise in the United States, likely secondary to increasing rates of obesity. Pregnancy is a time when many women begin to gain, and accumulate, weight and therefore obstetric providers have a unique opportunity to assist patients in strategies to normalize their weight after pregnancy. Many of my patients with endometrial cancer state that they have never heard that it is associated with obesity. This suggests that more can be done to educate patients on the carcinogenic effect of obesity (for both endometrial and breast cancer), which may aid in motivating change of modifiable behaviors.
The fallopian tubes are the source of many ovarian cancers and knowledge of this has led to the recommendation to perform opportunistic salpingectomy as a cancer risk-reducing strategy. Hysterectomy and sterilization procedures are most apropos for this modification. While prospective data to confirm a reduced risk of ovarian cancer with opportunistic salpingectomy are lacking, a reduced incidence of cancer has been observed when the tubes have been removed for indicated surgeries; there appear to be no significant deleterious sequelae.4,5 A focus should be made on removal of the entire distal third of the tube, particularly the fimbriated ends, as this is the portion most implicated in malignancy.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant disclosures. Contact her at [email protected].
References
1. Buys SS et al. JAMA. 2011;305(22):2295.
2. Goff BA et al. JAMA. 2004;291(22):2705.
3. Castellsagué X et al. Br J Cancer. 2011;105(1):28.
4. Yoon SH et al. Eur J Cancer. 2016 Mar;55:38-46.
5. Hanley GE et al. Am J Obstet Gynecol. 2018;219(2):172.
In this month’s column we continue to discuss recommendations from the gynecologic oncologist to the general gynecologist.
Don’t screen average-risk women for ovarian cancer.
Ovarian cancer is most often diagnosed at an advanced stage, which limits the curability of the disease. Consequently, there is a strong focus on attempting to diagnose the disease at earlier, more curable stages. This leads to the impulse by some well-intentioned providers to implement screening tests, such as ultrasounds and tumor markers, for all women. Unfortunately, the screening of “average risk” women for ovarian cancer is not recommended. Randomized controlled trials of tens of thousands of women have not observed a clinically significant decrease in ovarian cancer mortality with the addition of screening with tumor markers and ultrasound.1 These studies did observe a false-positive rate of 5%. While that may seem like a low rate of false-positive testing, the definitive diagnostic test which follows is a major abdominal surgery (oophorectomy) and serious complications are encountered in 15% of patients undergoing surgery for false-positive ovarian cancer screening.1 Therefore, quite simply, the harms are not balanced by benefits.
The key to offering patients appropriate and effective screening is case selection. It is important to identify which patients are at higher risk for ovarian cancer and offer those women testing for germline mutations and screening strategies. An important component of a well-woman visit is to take a thorough family history of cancer. Women are considered at high risk for having hereditary predisposition to ovarian cancer if they have a first- or second-degree relative with breast cancer younger than 45-50 years, or any age if Ashkenazi Jewish, triple-negative breast cancer younger than 60 years of age, two or more primary breast cancers with the first diagnosed at less than 50 years of age, male breast cancer, ovarian cancer, pancreatic cancer, a known BRCA 1/2 mutation, or a personal history of those same conditions. These women should be recommended to undergo genetic testing for BRCA 1, 2, and Lynch syndrome. They should not automatically be offered ovarian cancer screening. If a patient has a more remote family history for ovarian cancer, their personal risk may be somewhat elevated above the baseline population risk, however, not substantially enough to justify implementing screening in the absence of a confirmed genetic mutation.
While screening tests may not be appropriate for all patients, all patients should be asked about the early symptoms of ovarian cancer because these are consistently present, and frequently overlooked, prior to the eventual diagnosis of advanced disease. Those symptoms include abdominal discomfort, abdominal swelling and bloating, and urinary urgency.2 Consider offering all patients a dedicated ovarian cancer specific review of systems that includes inquiries about these symptoms at their annual wellness visits.
Opt for vertical midline incisions when surgery is anticipated to be complex
What is the first thing gynecologic oncologists do when called in to assist in a difficult gynecologic procedure? Get better exposure. Exposure is the cornerstone of safe, effective surgery. Sometimes this simply means placing a more effective retractor. In other cases, it might mean extending the incision. However, if the incision is a low transverse incision (the go-to for many gynecologists because of its favorable cosmetic and pain-producing profile) this proves to be difficult. Attempting to assist in a complicated case, such as a frozen pelvis, severed ureter or rectal injury, through a pfannensteil incision can be extraordinarily difficult, and while these incisions can be extended by incising the rectus muscle bellies, upper abdominal visualization remains elusive in most patients. This is particularly problematic if the ureter or splenic flexure need to be mobilized, or if extensive lysis of adhesions is necessary to ensure there is no occult enterotomy. As my mentor Dr. John Soper once described to me: “It’s like trying to scratch your armpit by reaching through your fly.”
While pfannensteil incisions come naturally, and comfortably, to most gynecologists, likely because of their frequent application during cesarean section, all gynecologists should be confident in the steps and anatomy for vertical midline, or paramedian incisions. This is not only beneficial for complex gynecologic cases, but also in the event of vascular emergency. In the hands of an experienced abdominal/pelvic surgeon, the vertical midline incision is the quickest way to safely enter the abdomen, and provides the kind of exposure that may be critical in safely repairing or controlling hemorrhage from a major vessel.
While low transverse incisions may be more cosmetic, less painful, and associated with fewer wound complications, our first concern as surgeons should be mitigating complications. In situations where risks of complications are high, it is best to not handicap ourselves with the incision location. And always remember, wound complications are highest when a transverse incision needs to be converted to a vertical one with a “T.”
It’s not just about diagnosis of cancer, it’s also prevention
Detection of cancer is an important role of the obstetrician gynecologist. However, equally important is being able to seize opportunities for cancer prevention. Cervical, vulvar, endometrial and ovarian cancer are all known to have preventative strategies.
All patients up to the age of 45 should be offered vaccination against HPV. Initial indications for HPV vaccination were for women up to age 26; however, recent data support the safety and efficacy of the vaccine in older women.3 HPV vaccination is most effective at preventing cancer when administered prior to exposure (ideally age 9-11), leaving this in the hands of our pediatrician colleagues. However, we must be vigilant to inquire about vaccination status for all our patients and encourage vaccines for those who were missed earlier in their life.
Patients should be counseled regarding the significant risk reduction for cancer that is gained from use of oral hormonal contraceptives and progestin-releasing IUDs (especially for endometrial and ovarian cancers). Providing them with knowledge of this information when considering options for contraception or menstrual cycle management is important in their decision-making process.
Endometrial cancer incidence is sadly on the rise in the United States, likely secondary to increasing rates of obesity. Pregnancy is a time when many women begin to gain, and accumulate, weight and therefore obstetric providers have a unique opportunity to assist patients in strategies to normalize their weight after pregnancy. Many of my patients with endometrial cancer state that they have never heard that it is associated with obesity. This suggests that more can be done to educate patients on the carcinogenic effect of obesity (for both endometrial and breast cancer), which may aid in motivating change of modifiable behaviors.
The fallopian tubes are the source of many ovarian cancers and knowledge of this has led to the recommendation to perform opportunistic salpingectomy as a cancer risk-reducing strategy. Hysterectomy and sterilization procedures are most apropos for this modification. While prospective data to confirm a reduced risk of ovarian cancer with opportunistic salpingectomy are lacking, a reduced incidence of cancer has been observed when the tubes have been removed for indicated surgeries; there appear to be no significant deleterious sequelae.4,5 A focus should be made on removal of the entire distal third of the tube, particularly the fimbriated ends, as this is the portion most implicated in malignancy.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant disclosures. Contact her at [email protected].
References
1. Buys SS et al. JAMA. 2011;305(22):2295.
2. Goff BA et al. JAMA. 2004;291(22):2705.
3. Castellsagué X et al. Br J Cancer. 2011;105(1):28.
4. Yoon SH et al. Eur J Cancer. 2016 Mar;55:38-46.
5. Hanley GE et al. Am J Obstet Gynecol. 2018;219(2):172.
In this month’s column we continue to discuss recommendations from the gynecologic oncologist to the general gynecologist.
Don’t screen average-risk women for ovarian cancer.
Ovarian cancer is most often diagnosed at an advanced stage, which limits the curability of the disease. Consequently, there is a strong focus on attempting to diagnose the disease at earlier, more curable stages. This leads to the impulse by some well-intentioned providers to implement screening tests, such as ultrasounds and tumor markers, for all women. Unfortunately, the screening of “average risk” women for ovarian cancer is not recommended. Randomized controlled trials of tens of thousands of women have not observed a clinically significant decrease in ovarian cancer mortality with the addition of screening with tumor markers and ultrasound.1 These studies did observe a false-positive rate of 5%. While that may seem like a low rate of false-positive testing, the definitive diagnostic test which follows is a major abdominal surgery (oophorectomy) and serious complications are encountered in 15% of patients undergoing surgery for false-positive ovarian cancer screening.1 Therefore, quite simply, the harms are not balanced by benefits.
The key to offering patients appropriate and effective screening is case selection. It is important to identify which patients are at higher risk for ovarian cancer and offer those women testing for germline mutations and screening strategies. An important component of a well-woman visit is to take a thorough family history of cancer. Women are considered at high risk for having hereditary predisposition to ovarian cancer if they have a first- or second-degree relative with breast cancer younger than 45-50 years, or any age if Ashkenazi Jewish, triple-negative breast cancer younger than 60 years of age, two or more primary breast cancers with the first diagnosed at less than 50 years of age, male breast cancer, ovarian cancer, pancreatic cancer, a known BRCA 1/2 mutation, or a personal history of those same conditions. These women should be recommended to undergo genetic testing for BRCA 1, 2, and Lynch syndrome. They should not automatically be offered ovarian cancer screening. If a patient has a more remote family history for ovarian cancer, their personal risk may be somewhat elevated above the baseline population risk, however, not substantially enough to justify implementing screening in the absence of a confirmed genetic mutation.
While screening tests may not be appropriate for all patients, all patients should be asked about the early symptoms of ovarian cancer because these are consistently present, and frequently overlooked, prior to the eventual diagnosis of advanced disease. Those symptoms include abdominal discomfort, abdominal swelling and bloating, and urinary urgency.2 Consider offering all patients a dedicated ovarian cancer specific review of systems that includes inquiries about these symptoms at their annual wellness visits.
Opt for vertical midline incisions when surgery is anticipated to be complex
What is the first thing gynecologic oncologists do when called in to assist in a difficult gynecologic procedure? Get better exposure. Exposure is the cornerstone of safe, effective surgery. Sometimes this simply means placing a more effective retractor. In other cases, it might mean extending the incision. However, if the incision is a low transverse incision (the go-to for many gynecologists because of its favorable cosmetic and pain-producing profile) this proves to be difficult. Attempting to assist in a complicated case, such as a frozen pelvis, severed ureter or rectal injury, through a pfannensteil incision can be extraordinarily difficult, and while these incisions can be extended by incising the rectus muscle bellies, upper abdominal visualization remains elusive in most patients. This is particularly problematic if the ureter or splenic flexure need to be mobilized, or if extensive lysis of adhesions is necessary to ensure there is no occult enterotomy. As my mentor Dr. John Soper once described to me: “It’s like trying to scratch your armpit by reaching through your fly.”
While pfannensteil incisions come naturally, and comfortably, to most gynecologists, likely because of their frequent application during cesarean section, all gynecologists should be confident in the steps and anatomy for vertical midline, or paramedian incisions. This is not only beneficial for complex gynecologic cases, but also in the event of vascular emergency. In the hands of an experienced abdominal/pelvic surgeon, the vertical midline incision is the quickest way to safely enter the abdomen, and provides the kind of exposure that may be critical in safely repairing or controlling hemorrhage from a major vessel.
While low transverse incisions may be more cosmetic, less painful, and associated with fewer wound complications, our first concern as surgeons should be mitigating complications. In situations where risks of complications are high, it is best to not handicap ourselves with the incision location. And always remember, wound complications are highest when a transverse incision needs to be converted to a vertical one with a “T.”
It’s not just about diagnosis of cancer, it’s also prevention
Detection of cancer is an important role of the obstetrician gynecologist. However, equally important is being able to seize opportunities for cancer prevention. Cervical, vulvar, endometrial and ovarian cancer are all known to have preventative strategies.
All patients up to the age of 45 should be offered vaccination against HPV. Initial indications for HPV vaccination were for women up to age 26; however, recent data support the safety and efficacy of the vaccine in older women.3 HPV vaccination is most effective at preventing cancer when administered prior to exposure (ideally age 9-11), leaving this in the hands of our pediatrician colleagues. However, we must be vigilant to inquire about vaccination status for all our patients and encourage vaccines for those who were missed earlier in their life.
Patients should be counseled regarding the significant risk reduction for cancer that is gained from use of oral hormonal contraceptives and progestin-releasing IUDs (especially for endometrial and ovarian cancers). Providing them with knowledge of this information when considering options for contraception or menstrual cycle management is important in their decision-making process.
Endometrial cancer incidence is sadly on the rise in the United States, likely secondary to increasing rates of obesity. Pregnancy is a time when many women begin to gain, and accumulate, weight and therefore obstetric providers have a unique opportunity to assist patients in strategies to normalize their weight after pregnancy. Many of my patients with endometrial cancer state that they have never heard that it is associated with obesity. This suggests that more can be done to educate patients on the carcinogenic effect of obesity (for both endometrial and breast cancer), which may aid in motivating change of modifiable behaviors.
The fallopian tubes are the source of many ovarian cancers and knowledge of this has led to the recommendation to perform opportunistic salpingectomy as a cancer risk-reducing strategy. Hysterectomy and sterilization procedures are most apropos for this modification. While prospective data to confirm a reduced risk of ovarian cancer with opportunistic salpingectomy are lacking, a reduced incidence of cancer has been observed when the tubes have been removed for indicated surgeries; there appear to be no significant deleterious sequelae.4,5 A focus should be made on removal of the entire distal third of the tube, particularly the fimbriated ends, as this is the portion most implicated in malignancy.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant disclosures. Contact her at [email protected].
References
1. Buys SS et al. JAMA. 2011;305(22):2295.
2. Goff BA et al. JAMA. 2004;291(22):2705.
3. Castellsagué X et al. Br J Cancer. 2011;105(1):28.
4. Yoon SH et al. Eur J Cancer. 2016 Mar;55:38-46.
5. Hanley GE et al. Am J Obstet Gynecol. 2018;219(2):172.
Advice on biopsies, workups, and referrals
Over the next 2 months we will dedicate this column to some general tips and pearls from the perspective of a gynecologic oncologist to guide general obstetrician gynecologists in the workup and management of preinvasive or invasive gynecologic diseases. The goal of these recommendations is to minimize misdiagnosis or delayed diagnosis and avoid unnecessary or untimely referrals.
Perform biopsy, not Pap smears, on visible cervical and vaginal lesions
The purpose of the Pap smear is to screen asymptomatic patients for cervical dysplasia or microscopic invasive disease. Cytology is an unreliable diagnostic tool for visible, symptomatic lesions in large part because of sampling errors, and the lack of architectural information in cytologic versus histopathologic specimens. Invasive lesions can be mischaracterized as preinvasive on a Pap smear. This can result in delayed diagnosis and unnecessary diagnostic procedures. For example, if a visible, abnormal-appearing, cervical lesion is seen during a routine visit and a Pap smear is performed (rather than a biopsy of the mass), the patient may receive an incorrect preliminary diagnosis of “high-grade dysplasia, carcinoma in situ” as it can be difficult to distinguish invasive carcinoma from carcinoma in situ on cytology. If the patient and provider do not understand the limitations of Pap smears in diagnosing invasive cancers, they may be falsely reassured and possibly delay or abstain from follow-up for an excisional procedure. If she does return for the loop electrosurgical excision procedure (LEEP), there might still be unnecessary delays in making referrals and definitive treatment while waiting for results. Radical hysterectomy may not promptly follow because, if performed within 6 weeks of an excisional procedure, it is associated with a significantly higher risk for perioperative complication, and therefore, if the excisional procedure was unnecessary to begin with, there may be additional time lost that need not be.1
Some clinicians avoid biopsy of visible lesions because they are concerned about bleeding complications that might arise in the office. Straightforward strategies to control bleeding are readily available in most gynecology offices, especially those already equipped for procedures such as LEEP and colposcopy. Prior to performing the biopsy, clinicians should ensure that they have supplies such as gauze sponges and ring forceps or packing forceps, silver nitrate, and ferric subsulfate solution (“Monsel’s solution”) close at hand. In the vast majority of cases, direct pressure for 5 minutes with gauze sponges and ferric subsulfate is highly effective at resolving most bleeding from a cervical or vaginal biopsy site. If this does not bring hemostasis, cautery devices or suture can be employed. If all else fails, be prepared to place vaginal packing (always with the insertion of a urinary Foley catheter to prevent urinary retention). In my experience, this is rarely needed.
Wherever possible, visible cervical or vaginal (or vulvar, see below) lesions should be biopsied for histopathology, sampling representative areas of the most concerning portion, in order to minimize misdiagnosis and expedite referral and definitive treatment. For necrotic-appearing lesions I recommend taking multiple samples of the tumor, as necrotic, nonviable tissue can prevent accurate diagnosis of a cancer. In general, Pap smears should be reserved as screening tests for asymptomatic women without visible pathology.
Don’t treat or refer low-grade dysplasia, even if persistent
Increasingly we are understanding that low-grade dysplasia of the lower genital tract (CIN I, VAIN I, VIN I) is less a precursor for cancer, and more a phenomenon of benign HPV-associated changes.2 This HPV change may be chronically persistent, may require years of observation and serial Pap smears, and may be a general nuisance for the patient. However, current guidelines do not recommend intervention for low-grade dysplasia of the lower genital tract.2 Interventions to resect these lesions can result in morbidity, including perineal pain, vaginal scarring, and cervical stenosis or insufficiency. Given the extremely low risk for progression to cancer, these morbidities do not outweigh any small potential benefit.
When I am conferring with patients who have chronic low-grade dysplasia I spend a great deal of time exploring their understanding of the diagnosis and its pathophysiology, their fears, and their expectation regarding “success” of treatment. I spend the time educating them that this is a sequela of chronic viral infection that will not be eradicated with local surgical excisions, that their cancer risk and need for surveillance would persist even if surgical intervention were offered, and that the side effects of treatment would outweigh any benefit from the small risk of cancer or high-grade dysplasia.
In summary, the treatment of choice for persistent low-grade dysplasia of the lower genital tract is comprehensive patient education, not surgical resection or referral to gynecologic oncology.
Repeat sampling if there’s a discordance between imaging and biopsy results
Delay in cancer diagnosis is one of the greatest concerns for front-line gynecology providers. One of the more modifiable strategies to avoid missed or delayed diagnosis is to ensure that there is concordance between clinical findings and testing results. Otherwise said: The results and findings should make sense in aggregate. An example was cited above in which a visible cervical mass demonstrated CIN III on cytologic testing. Another common example is a biopsy result of “scant benign endometrium” in a patient with postmenopausal bleeding and thickened endometrial stripe on ultrasound. In both of these cases there is clear discordance between physical findings and the results of pathology sampling. A pathology report, in all of its black and white certitude, seems like the most reliable source of information. However, always trust your clinical judgment. If the clinical picture is suggesting something far worse than these limited, often random or blind samplings, I recommend repeated or more extensive sampling (for example, dilation and curettage). At the very least, schedule close follow-up with repeated sampling if the symptom or finding persists. The emphasis here is on scheduled follow-up, rather than “p.r.n.,” because a patient who was given a “normal” pathology result to explain her abnormal symptoms may not volunteer that those symptoms are persistent as she may feel that anything sinister was already ruled out. Make certain that you explain the potential for misdiagnosis as the reason for why you would like to see her back shortly to ensure the issue has resolved.
Biopsy vulvar lesions, minimize empiric treatment
Vulvar cancer is notoriously associated with delayed diagnosis. Unfortunately, it is commonplace for gynecologic oncologists to see women who have vulvar cancers that have been empirically treated, sometimes for months or years, with steroids or other topical agents. If a lesion on the vulva is characteristically benign in appearance (such as condyloma or lichen sclerosis), it may be reasonable to start empiric treatment. However, all patients who are treated without biopsy should be rescheduled for a planned follow-up appointment in 2-3 months. If the lesion/area remains unchanged, or worse, the lesion should be biopsied before proceeding with a change in therapy or continued therapy. Once again, don’t rely on patients to return for evaluation if the lesion doesn’t improve. Many patients assume that our first empiric diagnosis is “gospel,” and therefore may not return if the treatment doesn’t work. Meanwhile, providers may assume that patients will know that there is uncertainty in our interpretation and that they will know to report if the initial treatment didn’t work. These assumptions are the recipe for delayed diagnosis. If there is too great a burden on the patient to schedule a return visit because of social or financial reasons then the patient should have a biopsy prior to initiation of treatment. As a rule, empiric treatment is not a good strategy for patients without good access to follow-up.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at [email protected].
References
1. Sullivan S. et al Gynecol Oncol. 2017 Feb;144(2):294-8.
2. Perkins R .et al J Low Genit Tract Dis. 2020 Apr;24(2):102-31.
Over the next 2 months we will dedicate this column to some general tips and pearls from the perspective of a gynecologic oncologist to guide general obstetrician gynecologists in the workup and management of preinvasive or invasive gynecologic diseases. The goal of these recommendations is to minimize misdiagnosis or delayed diagnosis and avoid unnecessary or untimely referrals.
Perform biopsy, not Pap smears, on visible cervical and vaginal lesions
The purpose of the Pap smear is to screen asymptomatic patients for cervical dysplasia or microscopic invasive disease. Cytology is an unreliable diagnostic tool for visible, symptomatic lesions in large part because of sampling errors, and the lack of architectural information in cytologic versus histopathologic specimens. Invasive lesions can be mischaracterized as preinvasive on a Pap smear. This can result in delayed diagnosis and unnecessary diagnostic procedures. For example, if a visible, abnormal-appearing, cervical lesion is seen during a routine visit and a Pap smear is performed (rather than a biopsy of the mass), the patient may receive an incorrect preliminary diagnosis of “high-grade dysplasia, carcinoma in situ” as it can be difficult to distinguish invasive carcinoma from carcinoma in situ on cytology. If the patient and provider do not understand the limitations of Pap smears in diagnosing invasive cancers, they may be falsely reassured and possibly delay or abstain from follow-up for an excisional procedure. If she does return for the loop electrosurgical excision procedure (LEEP), there might still be unnecessary delays in making referrals and definitive treatment while waiting for results. Radical hysterectomy may not promptly follow because, if performed within 6 weeks of an excisional procedure, it is associated with a significantly higher risk for perioperative complication, and therefore, if the excisional procedure was unnecessary to begin with, there may be additional time lost that need not be.1
Some clinicians avoid biopsy of visible lesions because they are concerned about bleeding complications that might arise in the office. Straightforward strategies to control bleeding are readily available in most gynecology offices, especially those already equipped for procedures such as LEEP and colposcopy. Prior to performing the biopsy, clinicians should ensure that they have supplies such as gauze sponges and ring forceps or packing forceps, silver nitrate, and ferric subsulfate solution (“Monsel’s solution”) close at hand. In the vast majority of cases, direct pressure for 5 minutes with gauze sponges and ferric subsulfate is highly effective at resolving most bleeding from a cervical or vaginal biopsy site. If this does not bring hemostasis, cautery devices or suture can be employed. If all else fails, be prepared to place vaginal packing (always with the insertion of a urinary Foley catheter to prevent urinary retention). In my experience, this is rarely needed.
Wherever possible, visible cervical or vaginal (or vulvar, see below) lesions should be biopsied for histopathology, sampling representative areas of the most concerning portion, in order to minimize misdiagnosis and expedite referral and definitive treatment. For necrotic-appearing lesions I recommend taking multiple samples of the tumor, as necrotic, nonviable tissue can prevent accurate diagnosis of a cancer. In general, Pap smears should be reserved as screening tests for asymptomatic women without visible pathology.
Don’t treat or refer low-grade dysplasia, even if persistent
Increasingly we are understanding that low-grade dysplasia of the lower genital tract (CIN I, VAIN I, VIN I) is less a precursor for cancer, and more a phenomenon of benign HPV-associated changes.2 This HPV change may be chronically persistent, may require years of observation and serial Pap smears, and may be a general nuisance for the patient. However, current guidelines do not recommend intervention for low-grade dysplasia of the lower genital tract.2 Interventions to resect these lesions can result in morbidity, including perineal pain, vaginal scarring, and cervical stenosis or insufficiency. Given the extremely low risk for progression to cancer, these morbidities do not outweigh any small potential benefit.
When I am conferring with patients who have chronic low-grade dysplasia I spend a great deal of time exploring their understanding of the diagnosis and its pathophysiology, their fears, and their expectation regarding “success” of treatment. I spend the time educating them that this is a sequela of chronic viral infection that will not be eradicated with local surgical excisions, that their cancer risk and need for surveillance would persist even if surgical intervention were offered, and that the side effects of treatment would outweigh any benefit from the small risk of cancer or high-grade dysplasia.
In summary, the treatment of choice for persistent low-grade dysplasia of the lower genital tract is comprehensive patient education, not surgical resection or referral to gynecologic oncology.
Repeat sampling if there’s a discordance between imaging and biopsy results
Delay in cancer diagnosis is one of the greatest concerns for front-line gynecology providers. One of the more modifiable strategies to avoid missed or delayed diagnosis is to ensure that there is concordance between clinical findings and testing results. Otherwise said: The results and findings should make sense in aggregate. An example was cited above in which a visible cervical mass demonstrated CIN III on cytologic testing. Another common example is a biopsy result of “scant benign endometrium” in a patient with postmenopausal bleeding and thickened endometrial stripe on ultrasound. In both of these cases there is clear discordance between physical findings and the results of pathology sampling. A pathology report, in all of its black and white certitude, seems like the most reliable source of information. However, always trust your clinical judgment. If the clinical picture is suggesting something far worse than these limited, often random or blind samplings, I recommend repeated or more extensive sampling (for example, dilation and curettage). At the very least, schedule close follow-up with repeated sampling if the symptom or finding persists. The emphasis here is on scheduled follow-up, rather than “p.r.n.,” because a patient who was given a “normal” pathology result to explain her abnormal symptoms may not volunteer that those symptoms are persistent as she may feel that anything sinister was already ruled out. Make certain that you explain the potential for misdiagnosis as the reason for why you would like to see her back shortly to ensure the issue has resolved.
Biopsy vulvar lesions, minimize empiric treatment
Vulvar cancer is notoriously associated with delayed diagnosis. Unfortunately, it is commonplace for gynecologic oncologists to see women who have vulvar cancers that have been empirically treated, sometimes for months or years, with steroids or other topical agents. If a lesion on the vulva is characteristically benign in appearance (such as condyloma or lichen sclerosis), it may be reasonable to start empiric treatment. However, all patients who are treated without biopsy should be rescheduled for a planned follow-up appointment in 2-3 months. If the lesion/area remains unchanged, or worse, the lesion should be biopsied before proceeding with a change in therapy or continued therapy. Once again, don’t rely on patients to return for evaluation if the lesion doesn’t improve. Many patients assume that our first empiric diagnosis is “gospel,” and therefore may not return if the treatment doesn’t work. Meanwhile, providers may assume that patients will know that there is uncertainty in our interpretation and that they will know to report if the initial treatment didn’t work. These assumptions are the recipe for delayed diagnosis. If there is too great a burden on the patient to schedule a return visit because of social or financial reasons then the patient should have a biopsy prior to initiation of treatment. As a rule, empiric treatment is not a good strategy for patients without good access to follow-up.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at [email protected].
References
1. Sullivan S. et al Gynecol Oncol. 2017 Feb;144(2):294-8.
2. Perkins R .et al J Low Genit Tract Dis. 2020 Apr;24(2):102-31.
Over the next 2 months we will dedicate this column to some general tips and pearls from the perspective of a gynecologic oncologist to guide general obstetrician gynecologists in the workup and management of preinvasive or invasive gynecologic diseases. The goal of these recommendations is to minimize misdiagnosis or delayed diagnosis and avoid unnecessary or untimely referrals.
Perform biopsy, not Pap smears, on visible cervical and vaginal lesions
The purpose of the Pap smear is to screen asymptomatic patients for cervical dysplasia or microscopic invasive disease. Cytology is an unreliable diagnostic tool for visible, symptomatic lesions in large part because of sampling errors, and the lack of architectural information in cytologic versus histopathologic specimens. Invasive lesions can be mischaracterized as preinvasive on a Pap smear. This can result in delayed diagnosis and unnecessary diagnostic procedures. For example, if a visible, abnormal-appearing, cervical lesion is seen during a routine visit and a Pap smear is performed (rather than a biopsy of the mass), the patient may receive an incorrect preliminary diagnosis of “high-grade dysplasia, carcinoma in situ” as it can be difficult to distinguish invasive carcinoma from carcinoma in situ on cytology. If the patient and provider do not understand the limitations of Pap smears in diagnosing invasive cancers, they may be falsely reassured and possibly delay or abstain from follow-up for an excisional procedure. If she does return for the loop electrosurgical excision procedure (LEEP), there might still be unnecessary delays in making referrals and definitive treatment while waiting for results. Radical hysterectomy may not promptly follow because, if performed within 6 weeks of an excisional procedure, it is associated with a significantly higher risk for perioperative complication, and therefore, if the excisional procedure was unnecessary to begin with, there may be additional time lost that need not be.1
Some clinicians avoid biopsy of visible lesions because they are concerned about bleeding complications that might arise in the office. Straightforward strategies to control bleeding are readily available in most gynecology offices, especially those already equipped for procedures such as LEEP and colposcopy. Prior to performing the biopsy, clinicians should ensure that they have supplies such as gauze sponges and ring forceps or packing forceps, silver nitrate, and ferric subsulfate solution (“Monsel’s solution”) close at hand. In the vast majority of cases, direct pressure for 5 minutes with gauze sponges and ferric subsulfate is highly effective at resolving most bleeding from a cervical or vaginal biopsy site. If this does not bring hemostasis, cautery devices or suture can be employed. If all else fails, be prepared to place vaginal packing (always with the insertion of a urinary Foley catheter to prevent urinary retention). In my experience, this is rarely needed.
Wherever possible, visible cervical or vaginal (or vulvar, see below) lesions should be biopsied for histopathology, sampling representative areas of the most concerning portion, in order to minimize misdiagnosis and expedite referral and definitive treatment. For necrotic-appearing lesions I recommend taking multiple samples of the tumor, as necrotic, nonviable tissue can prevent accurate diagnosis of a cancer. In general, Pap smears should be reserved as screening tests for asymptomatic women without visible pathology.
Don’t treat or refer low-grade dysplasia, even if persistent
Increasingly we are understanding that low-grade dysplasia of the lower genital tract (CIN I, VAIN I, VIN I) is less a precursor for cancer, and more a phenomenon of benign HPV-associated changes.2 This HPV change may be chronically persistent, may require years of observation and serial Pap smears, and may be a general nuisance for the patient. However, current guidelines do not recommend intervention for low-grade dysplasia of the lower genital tract.2 Interventions to resect these lesions can result in morbidity, including perineal pain, vaginal scarring, and cervical stenosis or insufficiency. Given the extremely low risk for progression to cancer, these morbidities do not outweigh any small potential benefit.
When I am conferring with patients who have chronic low-grade dysplasia I spend a great deal of time exploring their understanding of the diagnosis and its pathophysiology, their fears, and their expectation regarding “success” of treatment. I spend the time educating them that this is a sequela of chronic viral infection that will not be eradicated with local surgical excisions, that their cancer risk and need for surveillance would persist even if surgical intervention were offered, and that the side effects of treatment would outweigh any benefit from the small risk of cancer or high-grade dysplasia.
In summary, the treatment of choice for persistent low-grade dysplasia of the lower genital tract is comprehensive patient education, not surgical resection or referral to gynecologic oncology.
Repeat sampling if there’s a discordance between imaging and biopsy results
Delay in cancer diagnosis is one of the greatest concerns for front-line gynecology providers. One of the more modifiable strategies to avoid missed or delayed diagnosis is to ensure that there is concordance between clinical findings and testing results. Otherwise said: The results and findings should make sense in aggregate. An example was cited above in which a visible cervical mass demonstrated CIN III on cytologic testing. Another common example is a biopsy result of “scant benign endometrium” in a patient with postmenopausal bleeding and thickened endometrial stripe on ultrasound. In both of these cases there is clear discordance between physical findings and the results of pathology sampling. A pathology report, in all of its black and white certitude, seems like the most reliable source of information. However, always trust your clinical judgment. If the clinical picture is suggesting something far worse than these limited, often random or blind samplings, I recommend repeated or more extensive sampling (for example, dilation and curettage). At the very least, schedule close follow-up with repeated sampling if the symptom or finding persists. The emphasis here is on scheduled follow-up, rather than “p.r.n.,” because a patient who was given a “normal” pathology result to explain her abnormal symptoms may not volunteer that those symptoms are persistent as she may feel that anything sinister was already ruled out. Make certain that you explain the potential for misdiagnosis as the reason for why you would like to see her back shortly to ensure the issue has resolved.
Biopsy vulvar lesions, minimize empiric treatment
Vulvar cancer is notoriously associated with delayed diagnosis. Unfortunately, it is commonplace for gynecologic oncologists to see women who have vulvar cancers that have been empirically treated, sometimes for months or years, with steroids or other topical agents. If a lesion on the vulva is characteristically benign in appearance (such as condyloma or lichen sclerosis), it may be reasonable to start empiric treatment. However, all patients who are treated without biopsy should be rescheduled for a planned follow-up appointment in 2-3 months. If the lesion/area remains unchanged, or worse, the lesion should be biopsied before proceeding with a change in therapy or continued therapy. Once again, don’t rely on patients to return for evaluation if the lesion doesn’t improve. Many patients assume that our first empiric diagnosis is “gospel,” and therefore may not return if the treatment doesn’t work. Meanwhile, providers may assume that patients will know that there is uncertainty in our interpretation and that they will know to report if the initial treatment didn’t work. These assumptions are the recipe for delayed diagnosis. If there is too great a burden on the patient to schedule a return visit because of social or financial reasons then the patient should have a biopsy prior to initiation of treatment. As a rule, empiric treatment is not a good strategy for patients without good access to follow-up.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at [email protected].
References
1. Sullivan S. et al Gynecol Oncol. 2017 Feb;144(2):294-8.
2. Perkins R .et al J Low Genit Tract Dis. 2020 Apr;24(2):102-31.
Decision making regarding LEEP versus cone biopsy for excision of cervical dysplasia
Loop electrosurgical excision procedure (LEEP) or cold knife conization of the cervix (CKC) is the standard of care approach for women with cervical intra-epithelial neoplasia (CIN 3) because it achieves both disease control and diagnostic evaluation to rule out invasive carcinoma. While both techniques are associated with equivalent efficacy in disease control, each has its virtues and advantages, and clinical judgment is necessary when choosing a technique.1
LEEP, or large loop electrosurgical excision of the transformation zone (LLETZ) involves use of electrosurgical current directed through wire loops to excise pieces of cervical tissue. The equipment for this technique is widely available and this procedure can most often be performed safely and comfortably in an outpatient office setting, making it a cost-effective strategy. Its ease of access means that it can be employed in “see-and-treat” programs where there is concern regarding follow-up. The loop from the device has a tendency to take more shallow pieces of tissue, preserving more cervical stroma. This may be why LEEP has been associated with decreased risk for obstetric complications associated with cervical insufficiency when compared with CKC.2,3
The shallowness and standardized, preset shapes of the loops present challenges with this technique. It can be more difficult to tailor the shape of the excision for particular lesions, and surgeons may need to add a second “top hat” endocervical LEEP after the first ectocervical excision to adequately excise the endocervical canal. If the “coagulation” setting is used instead of “blend” or “cut,” excessive drag and resistance can develop during the procedure, which can result in the specimen’s being amputated, fragmented, or interrupted mid-sweep. This can severely limit pathologic interpretation of the specimen. Orienting these multiple fragments for pathology to specify margin status can be limited or impossible. Electrosurgical effect (“thermal effect”) at the margins of the specimen can limit accurate interpretation of adequacy of the excision.
CKC of the cervix is a procedure in which a narrow scalpel (typically an 11-blade) is used to excise the ecto- and endocervical tissues in a cone-shaped specimen that ensures maximal inclusion of ectocervical and endocervical mucosa but minimization of stromal excision. Absence of electrosurgery in the primary excision means that pathologists have clean edges to evaluate for margin status. Because the shape of the incision is unique for each patient, the surgeon can tailor the shape and extent of the cone to focus on known or suspected areas of disease. It is particularly useful when there is an endocervical lesion, such as in cases of adenocarcinoma in situ and in postmenopausal women whose transformation zone is frequently within the canal. In cases of a distorted, atrophic cervix, or one that is flush with the vagina, a conization procedure in the operating room affords surgeons greater control and precision. Major limitations of this procedure are that it is typically performed in an operating room setting because of the potential for intraoperative bleeding, and its increased risk for early and late complications. The conization procedure is associated with increased obstetric risk in later pregnancies, possibly because of more significant disturbance of cervical stroma.2,3
As mentioned earlier, both procedures are associated with equivalent outcomes with respect to control of disease.1 CKC procedures are associated with more complications, including bleeding (intraoperatively and postoperatively) than are LEEPs. Traditionally, adenocarcinoma in situ (AIS) has been preferentially treated with CKC because of the propensity of this lesion to reside within the endocervical canal, a region more readily and extensively sampled with the CKC. However, provided that the LEEP specimen achieves negative margin status, there is no specific benefit of CKC over LEEP. Guidelines recommend that AIS is excised as a single specimen (without a “top hat”) to achieve accurate pathology regarding margins in the endocervical canal.4 Considering that a specimen depth between 10 and 20 mm is ideal in the setting of AIS, it may be difficult to achieve this depth with a single-pass LEEP depending upon the dimensions of the cervix. It is due to these technical challenges associated with LEEP that CKC is typically preferred in the treatment of AIS.
Ultimately, the decision regarding when to choose LEEP versus CKC is nuanced and should be tailored for each patient. Factors to consider include the patient’s ease of follow-up, financial limitations, preexisting distortion of anatomy, and the need to minimize obstetrics risks or achieve wider margins. For example, a young, nulliparous patient with an ectocervical lesion of squamous dysplasia would likely best be served by a LEEP, which preserves her cervical stroma and affords her easy access and affordability of the procedure. A patient with a bleeding diathesis including iatrogenic anticoagulant therapy may also benefit from a LEEP to achieve better hemostasis and lower risk of bleeding complications.
A postmenopausal woman with a narrow upper vagina and cervix flush with the vagina from prior excisional procedures may benefit from a conization in the operating room where adequate retraction and exposure can minimize the risk of damage to adjacent structures, and the shape and size of the excision can be tailored to the long, narrow segment that is indicated. The table highlights some of the factors to consider when choosing these options. 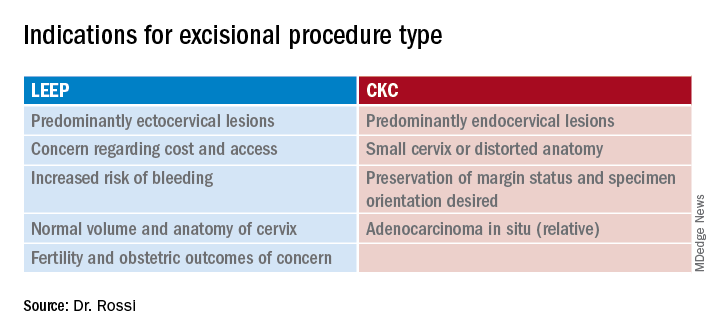
In summary, LEEP and CKC are both highly effective excisional procedures that can be considered for all patients with cervical dysplasia. Decisions regarding which is preferred for patients are nuanced and should consider individualized anatomic, pathologic, functional and financial implications.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no conflicts of interest. Contact her at [email protected].
References
1. Martin-Hirsch PL et al. Cochrane Database Syst Rev 2000;(2):CD001318.
2. Arbyn M et al. BMJ. 2008;337:a1284.
3. Jin G et al. Arch Gynecol Obstet. 2014 Jan;289(1):85-99.
4. Perkins RB et al. J Low Genit Tract Dis. 2020;24(2):102.
Loop electrosurgical excision procedure (LEEP) or cold knife conization of the cervix (CKC) is the standard of care approach for women with cervical intra-epithelial neoplasia (CIN 3) because it achieves both disease control and diagnostic evaluation to rule out invasive carcinoma. While both techniques are associated with equivalent efficacy in disease control, each has its virtues and advantages, and clinical judgment is necessary when choosing a technique.1
LEEP, or large loop electrosurgical excision of the transformation zone (LLETZ) involves use of electrosurgical current directed through wire loops to excise pieces of cervical tissue. The equipment for this technique is widely available and this procedure can most often be performed safely and comfortably in an outpatient office setting, making it a cost-effective strategy. Its ease of access means that it can be employed in “see-and-treat” programs where there is concern regarding follow-up. The loop from the device has a tendency to take more shallow pieces of tissue, preserving more cervical stroma. This may be why LEEP has been associated with decreased risk for obstetric complications associated with cervical insufficiency when compared with CKC.2,3
The shallowness and standardized, preset shapes of the loops present challenges with this technique. It can be more difficult to tailor the shape of the excision for particular lesions, and surgeons may need to add a second “top hat” endocervical LEEP after the first ectocervical excision to adequately excise the endocervical canal. If the “coagulation” setting is used instead of “blend” or “cut,” excessive drag and resistance can develop during the procedure, which can result in the specimen’s being amputated, fragmented, or interrupted mid-sweep. This can severely limit pathologic interpretation of the specimen. Orienting these multiple fragments for pathology to specify margin status can be limited or impossible. Electrosurgical effect (“thermal effect”) at the margins of the specimen can limit accurate interpretation of adequacy of the excision.
CKC of the cervix is a procedure in which a narrow scalpel (typically an 11-blade) is used to excise the ecto- and endocervical tissues in a cone-shaped specimen that ensures maximal inclusion of ectocervical and endocervical mucosa but minimization of stromal excision. Absence of electrosurgery in the primary excision means that pathologists have clean edges to evaluate for margin status. Because the shape of the incision is unique for each patient, the surgeon can tailor the shape and extent of the cone to focus on known or suspected areas of disease. It is particularly useful when there is an endocervical lesion, such as in cases of adenocarcinoma in situ and in postmenopausal women whose transformation zone is frequently within the canal. In cases of a distorted, atrophic cervix, or one that is flush with the vagina, a conization procedure in the operating room affords surgeons greater control and precision. Major limitations of this procedure are that it is typically performed in an operating room setting because of the potential for intraoperative bleeding, and its increased risk for early and late complications. The conization procedure is associated with increased obstetric risk in later pregnancies, possibly because of more significant disturbance of cervical stroma.2,3
As mentioned earlier, both procedures are associated with equivalent outcomes with respect to control of disease.1 CKC procedures are associated with more complications, including bleeding (intraoperatively and postoperatively) than are LEEPs. Traditionally, adenocarcinoma in situ (AIS) has been preferentially treated with CKC because of the propensity of this lesion to reside within the endocervical canal, a region more readily and extensively sampled with the CKC. However, provided that the LEEP specimen achieves negative margin status, there is no specific benefit of CKC over LEEP. Guidelines recommend that AIS is excised as a single specimen (without a “top hat”) to achieve accurate pathology regarding margins in the endocervical canal.4 Considering that a specimen depth between 10 and 20 mm is ideal in the setting of AIS, it may be difficult to achieve this depth with a single-pass LEEP depending upon the dimensions of the cervix. It is due to these technical challenges associated with LEEP that CKC is typically preferred in the treatment of AIS.
Ultimately, the decision regarding when to choose LEEP versus CKC is nuanced and should be tailored for each patient. Factors to consider include the patient’s ease of follow-up, financial limitations, preexisting distortion of anatomy, and the need to minimize obstetrics risks or achieve wider margins. For example, a young, nulliparous patient with an ectocervical lesion of squamous dysplasia would likely best be served by a LEEP, which preserves her cervical stroma and affords her easy access and affordability of the procedure. A patient with a bleeding diathesis including iatrogenic anticoagulant therapy may also benefit from a LEEP to achieve better hemostasis and lower risk of bleeding complications.
A postmenopausal woman with a narrow upper vagina and cervix flush with the vagina from prior excisional procedures may benefit from a conization in the operating room where adequate retraction and exposure can minimize the risk of damage to adjacent structures, and the shape and size of the excision can be tailored to the long, narrow segment that is indicated. The table highlights some of the factors to consider when choosing these options. 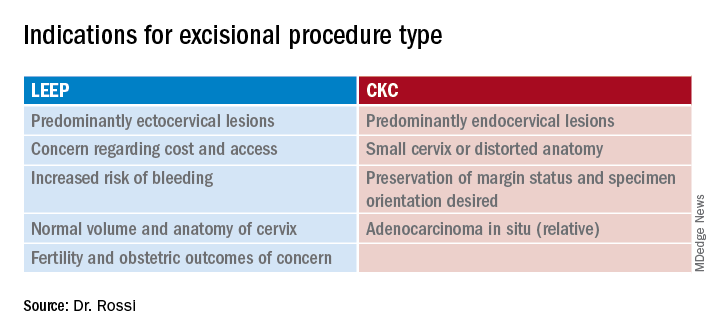
In summary, LEEP and CKC are both highly effective excisional procedures that can be considered for all patients with cervical dysplasia. Decisions regarding which is preferred for patients are nuanced and should consider individualized anatomic, pathologic, functional and financial implications.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no conflicts of interest. Contact her at [email protected].
References
1. Martin-Hirsch PL et al. Cochrane Database Syst Rev 2000;(2):CD001318.
2. Arbyn M et al. BMJ. 2008;337:a1284.
3. Jin G et al. Arch Gynecol Obstet. 2014 Jan;289(1):85-99.
4. Perkins RB et al. J Low Genit Tract Dis. 2020;24(2):102.
Loop electrosurgical excision procedure (LEEP) or cold knife conization of the cervix (CKC) is the standard of care approach for women with cervical intra-epithelial neoplasia (CIN 3) because it achieves both disease control and diagnostic evaluation to rule out invasive carcinoma. While both techniques are associated with equivalent efficacy in disease control, each has its virtues and advantages, and clinical judgment is necessary when choosing a technique.1
LEEP, or large loop electrosurgical excision of the transformation zone (LLETZ) involves use of electrosurgical current directed through wire loops to excise pieces of cervical tissue. The equipment for this technique is widely available and this procedure can most often be performed safely and comfortably in an outpatient office setting, making it a cost-effective strategy. Its ease of access means that it can be employed in “see-and-treat” programs where there is concern regarding follow-up. The loop from the device has a tendency to take more shallow pieces of tissue, preserving more cervical stroma. This may be why LEEP has been associated with decreased risk for obstetric complications associated with cervical insufficiency when compared with CKC.2,3
The shallowness and standardized, preset shapes of the loops present challenges with this technique. It can be more difficult to tailor the shape of the excision for particular lesions, and surgeons may need to add a second “top hat” endocervical LEEP after the first ectocervical excision to adequately excise the endocervical canal. If the “coagulation” setting is used instead of “blend” or “cut,” excessive drag and resistance can develop during the procedure, which can result in the specimen’s being amputated, fragmented, or interrupted mid-sweep. This can severely limit pathologic interpretation of the specimen. Orienting these multiple fragments for pathology to specify margin status can be limited or impossible. Electrosurgical effect (“thermal effect”) at the margins of the specimen can limit accurate interpretation of adequacy of the excision.
CKC of the cervix is a procedure in which a narrow scalpel (typically an 11-blade) is used to excise the ecto- and endocervical tissues in a cone-shaped specimen that ensures maximal inclusion of ectocervical and endocervical mucosa but minimization of stromal excision. Absence of electrosurgery in the primary excision means that pathologists have clean edges to evaluate for margin status. Because the shape of the incision is unique for each patient, the surgeon can tailor the shape and extent of the cone to focus on known or suspected areas of disease. It is particularly useful when there is an endocervical lesion, such as in cases of adenocarcinoma in situ and in postmenopausal women whose transformation zone is frequently within the canal. In cases of a distorted, atrophic cervix, or one that is flush with the vagina, a conization procedure in the operating room affords surgeons greater control and precision. Major limitations of this procedure are that it is typically performed in an operating room setting because of the potential for intraoperative bleeding, and its increased risk for early and late complications. The conization procedure is associated with increased obstetric risk in later pregnancies, possibly because of more significant disturbance of cervical stroma.2,3
As mentioned earlier, both procedures are associated with equivalent outcomes with respect to control of disease.1 CKC procedures are associated with more complications, including bleeding (intraoperatively and postoperatively) than are LEEPs. Traditionally, adenocarcinoma in situ (AIS) has been preferentially treated with CKC because of the propensity of this lesion to reside within the endocervical canal, a region more readily and extensively sampled with the CKC. However, provided that the LEEP specimen achieves negative margin status, there is no specific benefit of CKC over LEEP. Guidelines recommend that AIS is excised as a single specimen (without a “top hat”) to achieve accurate pathology regarding margins in the endocervical canal.4 Considering that a specimen depth between 10 and 20 mm is ideal in the setting of AIS, it may be difficult to achieve this depth with a single-pass LEEP depending upon the dimensions of the cervix. It is due to these technical challenges associated with LEEP that CKC is typically preferred in the treatment of AIS.
Ultimately, the decision regarding when to choose LEEP versus CKC is nuanced and should be tailored for each patient. Factors to consider include the patient’s ease of follow-up, financial limitations, preexisting distortion of anatomy, and the need to minimize obstetrics risks or achieve wider margins. For example, a young, nulliparous patient with an ectocervical lesion of squamous dysplasia would likely best be served by a LEEP, which preserves her cervical stroma and affords her easy access and affordability of the procedure. A patient with a bleeding diathesis including iatrogenic anticoagulant therapy may also benefit from a LEEP to achieve better hemostasis and lower risk of bleeding complications.
A postmenopausal woman with a narrow upper vagina and cervix flush with the vagina from prior excisional procedures may benefit from a conization in the operating room where adequate retraction and exposure can minimize the risk of damage to adjacent structures, and the shape and size of the excision can be tailored to the long, narrow segment that is indicated. The table highlights some of the factors to consider when choosing these options. 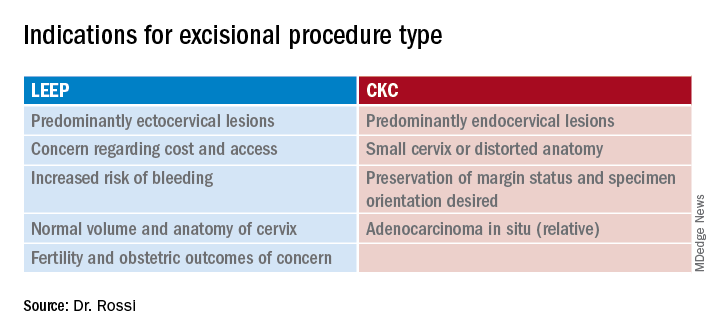
In summary, LEEP and CKC are both highly effective excisional procedures that can be considered for all patients with cervical dysplasia. Decisions regarding which is preferred for patients are nuanced and should consider individualized anatomic, pathologic, functional and financial implications.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no conflicts of interest. Contact her at [email protected].
References
1. Martin-Hirsch PL et al. Cochrane Database Syst Rev 2000;(2):CD001318.
2. Arbyn M et al. BMJ. 2008;337:a1284.
3. Jin G et al. Arch Gynecol Obstet. 2014 Jan;289(1):85-99.
4. Perkins RB et al. J Low Genit Tract Dis. 2020;24(2):102.



