User login
Should gynecologists receive the HPV vaccine?
Gynecologists have experience managing human papillomavirus–associated diseases of the lower genital tract. However, HPV also causes warty disease, dysplasia, and carcinoma of the head and neck. Risk factors for head and neck cancer include smoking and smokeless tobacco use, alcohol consumption, periodontal disease, radiation exposure, and HPV. The incidence of HPV-associated head and neck cancer is rising, particularly among men, at a rate of 2.7% per year.1 The incidence of HPV-associated squamous cell carcinoma of the oropharynx now surpasses that of cervical cancer. Concerns exist regarding occupational exposure to HPV by health care providers (HCP) who perform smoke-generating procedures on HPV-infected tissues, and the potential for them to develop head and neck pathology.
In March of 2020, the American Society for Colposcopy and Cervical Pathology made the recommendation that clinicians who are routinely exposed to HPV should protect themselves against the sequela of occupationally acquired HPV by receiving the HPV vaccine.2 They advocate for the “complete provider team” including physicians, advanced practice providers, nurses, operative technicians, and residents and fellows to be considered for protective vaccination.
Similar to disease patterns in the genital tract, different strains of HPV have differing propensity to cause benign, premalignant, and malignant disease states. HPV 6 and 11 are more commonly associated with warty disease in the nares, pharynx, and tonsillar tissues. HPV 16, 18, 31, and 33 (most commonly 16) are considered high risk for carcinoma formation, particularly of the tonsils and base of the tongue.
The procedures most implicated in occupational HPV exposure include ablative procedures for anogenital warts, laser ablation of vaginal and vulvar dysplasia, and electrosurgical excisional procedures for cervical dysplasia. Smoke plumes from HPV-associated procedures are known to contain HPV for both laser and electrocautery sources.3 A study of 134 patients undergoing surgical procedures for laser ablation of HPV-infected tissues detected concordant strains of HPV in approximately 30% of smoke plumes and approximately 1.5% of surgeons’ nares.4 Not all procedures appear to carry the same risk. Electrocoagulation procedures appear to yield fewer postprocedural positive mucosal swabs for HPV, compared with those taken after CO2 laser.5
Animal studies have shown that papilloma virus procured from smoke plume has the capacity to generate disease. When 10 calves were inoculated with bovine papillary virus obtained from smoke plumes from laser ablation of bovine papillomavirus lesions, all calves manifested BPV fibropapilloma lesions at the sites of inoculation.6
There appears to be an increased incidence of HPV-associated head and neck disease among surgeons who perform procedures on HPV tissues, and there have been multiple case reports that have cited examples of HPV-associated benign and malignant disease among HCPs with frequent occupational exposure to HPV anogenital ablative and excisional procedures.7 While these observations are not proof of causation, they are cause for concern.
While the ASCCP guidelines advocate for HPV vaccination as a strategy for prevention of occupationally related HPV-associated disease, there are other strategies in place to minimize risk. The CDC guidelines for environmental infection control in health care facilities include the following recommendations:
- In settings where surgical lasers are used, wear appropriate personnel protective equipment (PPE), including N95 or N100 respirators to minimize exposure to laser plumes.
- Use central wall suction units with in-line filters to evacuate minimal laser plumes.
- Use a mechanical smoke evaluation system with a high efficiency filter to manage the generation of large amounts of laser plume, when ablating tissue infected with HPV.
- Use local exhaust ventilation (LEV).8
When closely adhered to, these methods appear to provide high-level protection. Data suggest that, when HCPs can access appropriate protective equipment, risks for HPV exposure are low. However, this is more feasible for larger hospital facilities, and may be more limited in outpatient settings. This has led to the consideration of background protection in the form of HPV vaccination for at-risk HCPs. This is analogous to mandates for HCPs to receive hepatitis B vaccination despite the concomitant practice of universal precautions in health care settings. Preventative strategies are typically most efficacious when performed in concert.
After nearly 2 decades of widespread use, we have confidence in the safety of the HPV vaccination. Its benefit through age 45 has been established, leading to the 2018 FDA approval for the 9-valent HPV vaccine, Guardisil-9, for this expanded age group. It would seem logical that systematic administration of the HPV vaccine for at-risk HCPs would be both feasible and safe. There are well-established systems for administering vaccines for HCPs in all health care systems. Perhaps health system administrators should consider routinely offering HPV vaccination for at-risk employees as part of their occupational health care responsibilities. One important caveat being the cost and efficacy of HPV vaccination in this group has not been not established.
In the meantime, it is critical that gynecology providers be aware of their risk for occupational exposure to HPV when using laser and electrocautery techniques on HPV-infected tissues and the potential for them developing head and neck pathology. They should strictly adhere to preventative measures such as use of fit-tested N-95 respirators, mechanical smoke evacuators with high-efficiency filters and work in environments with adequate room ventilation. We all should individually evaluate what role HPV vaccination may play for us in augmenting our own safety.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Van Dyne EA et al. MMWR Morb Mortal Wkly Rep. 2018 Aug 24;67(33):918-24.
2. ASCCP. ASCCP recommends HPV vaccination for providers.
3. Fox-Lewis A et al. Occup Environ Med. 2020 Dec;77(12):809-17.
4. Zhou Q et al. Cancer Manag Res. 2019;11:3643-54
5. Bergbrant I et al. Acta Derm Venereol. 1994 Sep;74(5):393-5.
6. Garden J et al. Arch Dermatol. 2002 Oct;138(10):1303-7.
7. Harrison R, Huh W. Obstet Gynecol. 2020;136:663-5.
8. CDC. 1996. DHHS (NIOSH) Publication Number 96-128.
Gynecologists have experience managing human papillomavirus–associated diseases of the lower genital tract. However, HPV also causes warty disease, dysplasia, and carcinoma of the head and neck. Risk factors for head and neck cancer include smoking and smokeless tobacco use, alcohol consumption, periodontal disease, radiation exposure, and HPV. The incidence of HPV-associated head and neck cancer is rising, particularly among men, at a rate of 2.7% per year.1 The incidence of HPV-associated squamous cell carcinoma of the oropharynx now surpasses that of cervical cancer. Concerns exist regarding occupational exposure to HPV by health care providers (HCP) who perform smoke-generating procedures on HPV-infected tissues, and the potential for them to develop head and neck pathology.
In March of 2020, the American Society for Colposcopy and Cervical Pathology made the recommendation that clinicians who are routinely exposed to HPV should protect themselves against the sequela of occupationally acquired HPV by receiving the HPV vaccine.2 They advocate for the “complete provider team” including physicians, advanced practice providers, nurses, operative technicians, and residents and fellows to be considered for protective vaccination.
Similar to disease patterns in the genital tract, different strains of HPV have differing propensity to cause benign, premalignant, and malignant disease states. HPV 6 and 11 are more commonly associated with warty disease in the nares, pharynx, and tonsillar tissues. HPV 16, 18, 31, and 33 (most commonly 16) are considered high risk for carcinoma formation, particularly of the tonsils and base of the tongue.
The procedures most implicated in occupational HPV exposure include ablative procedures for anogenital warts, laser ablation of vaginal and vulvar dysplasia, and electrosurgical excisional procedures for cervical dysplasia. Smoke plumes from HPV-associated procedures are known to contain HPV for both laser and electrocautery sources.3 A study of 134 patients undergoing surgical procedures for laser ablation of HPV-infected tissues detected concordant strains of HPV in approximately 30% of smoke plumes and approximately 1.5% of surgeons’ nares.4 Not all procedures appear to carry the same risk. Electrocoagulation procedures appear to yield fewer postprocedural positive mucosal swabs for HPV, compared with those taken after CO2 laser.5
Animal studies have shown that papilloma virus procured from smoke plume has the capacity to generate disease. When 10 calves were inoculated with bovine papillary virus obtained from smoke plumes from laser ablation of bovine papillomavirus lesions, all calves manifested BPV fibropapilloma lesions at the sites of inoculation.6
There appears to be an increased incidence of HPV-associated head and neck disease among surgeons who perform procedures on HPV tissues, and there have been multiple case reports that have cited examples of HPV-associated benign and malignant disease among HCPs with frequent occupational exposure to HPV anogenital ablative and excisional procedures.7 While these observations are not proof of causation, they are cause for concern.
While the ASCCP guidelines advocate for HPV vaccination as a strategy for prevention of occupationally related HPV-associated disease, there are other strategies in place to minimize risk. The CDC guidelines for environmental infection control in health care facilities include the following recommendations:
- In settings where surgical lasers are used, wear appropriate personnel protective equipment (PPE), including N95 or N100 respirators to minimize exposure to laser plumes.
- Use central wall suction units with in-line filters to evacuate minimal laser plumes.
- Use a mechanical smoke evaluation system with a high efficiency filter to manage the generation of large amounts of laser plume, when ablating tissue infected with HPV.
- Use local exhaust ventilation (LEV).8
When closely adhered to, these methods appear to provide high-level protection. Data suggest that, when HCPs can access appropriate protective equipment, risks for HPV exposure are low. However, this is more feasible for larger hospital facilities, and may be more limited in outpatient settings. This has led to the consideration of background protection in the form of HPV vaccination for at-risk HCPs. This is analogous to mandates for HCPs to receive hepatitis B vaccination despite the concomitant practice of universal precautions in health care settings. Preventative strategies are typically most efficacious when performed in concert.
After nearly 2 decades of widespread use, we have confidence in the safety of the HPV vaccination. Its benefit through age 45 has been established, leading to the 2018 FDA approval for the 9-valent HPV vaccine, Guardisil-9, for this expanded age group. It would seem logical that systematic administration of the HPV vaccine for at-risk HCPs would be both feasible and safe. There are well-established systems for administering vaccines for HCPs in all health care systems. Perhaps health system administrators should consider routinely offering HPV vaccination for at-risk employees as part of their occupational health care responsibilities. One important caveat being the cost and efficacy of HPV vaccination in this group has not been not established.
In the meantime, it is critical that gynecology providers be aware of their risk for occupational exposure to HPV when using laser and electrocautery techniques on HPV-infected tissues and the potential for them developing head and neck pathology. They should strictly adhere to preventative measures such as use of fit-tested N-95 respirators, mechanical smoke evacuators with high-efficiency filters and work in environments with adequate room ventilation. We all should individually evaluate what role HPV vaccination may play for us in augmenting our own safety.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Van Dyne EA et al. MMWR Morb Mortal Wkly Rep. 2018 Aug 24;67(33):918-24.
2. ASCCP. ASCCP recommends HPV vaccination for providers.
3. Fox-Lewis A et al. Occup Environ Med. 2020 Dec;77(12):809-17.
4. Zhou Q et al. Cancer Manag Res. 2019;11:3643-54
5. Bergbrant I et al. Acta Derm Venereol. 1994 Sep;74(5):393-5.
6. Garden J et al. Arch Dermatol. 2002 Oct;138(10):1303-7.
7. Harrison R, Huh W. Obstet Gynecol. 2020;136:663-5.
8. CDC. 1996. DHHS (NIOSH) Publication Number 96-128.
Gynecologists have experience managing human papillomavirus–associated diseases of the lower genital tract. However, HPV also causes warty disease, dysplasia, and carcinoma of the head and neck. Risk factors for head and neck cancer include smoking and smokeless tobacco use, alcohol consumption, periodontal disease, radiation exposure, and HPV. The incidence of HPV-associated head and neck cancer is rising, particularly among men, at a rate of 2.7% per year.1 The incidence of HPV-associated squamous cell carcinoma of the oropharynx now surpasses that of cervical cancer. Concerns exist regarding occupational exposure to HPV by health care providers (HCP) who perform smoke-generating procedures on HPV-infected tissues, and the potential for them to develop head and neck pathology.
In March of 2020, the American Society for Colposcopy and Cervical Pathology made the recommendation that clinicians who are routinely exposed to HPV should protect themselves against the sequela of occupationally acquired HPV by receiving the HPV vaccine.2 They advocate for the “complete provider team” including physicians, advanced practice providers, nurses, operative technicians, and residents and fellows to be considered for protective vaccination.
Similar to disease patterns in the genital tract, different strains of HPV have differing propensity to cause benign, premalignant, and malignant disease states. HPV 6 and 11 are more commonly associated with warty disease in the nares, pharynx, and tonsillar tissues. HPV 16, 18, 31, and 33 (most commonly 16) are considered high risk for carcinoma formation, particularly of the tonsils and base of the tongue.
The procedures most implicated in occupational HPV exposure include ablative procedures for anogenital warts, laser ablation of vaginal and vulvar dysplasia, and electrosurgical excisional procedures for cervical dysplasia. Smoke plumes from HPV-associated procedures are known to contain HPV for both laser and electrocautery sources.3 A study of 134 patients undergoing surgical procedures for laser ablation of HPV-infected tissues detected concordant strains of HPV in approximately 30% of smoke plumes and approximately 1.5% of surgeons’ nares.4 Not all procedures appear to carry the same risk. Electrocoagulation procedures appear to yield fewer postprocedural positive mucosal swabs for HPV, compared with those taken after CO2 laser.5
Animal studies have shown that papilloma virus procured from smoke plume has the capacity to generate disease. When 10 calves were inoculated with bovine papillary virus obtained from smoke plumes from laser ablation of bovine papillomavirus lesions, all calves manifested BPV fibropapilloma lesions at the sites of inoculation.6
There appears to be an increased incidence of HPV-associated head and neck disease among surgeons who perform procedures on HPV tissues, and there have been multiple case reports that have cited examples of HPV-associated benign and malignant disease among HCPs with frequent occupational exposure to HPV anogenital ablative and excisional procedures.7 While these observations are not proof of causation, they are cause for concern.
While the ASCCP guidelines advocate for HPV vaccination as a strategy for prevention of occupationally related HPV-associated disease, there are other strategies in place to minimize risk. The CDC guidelines for environmental infection control in health care facilities include the following recommendations:
- In settings where surgical lasers are used, wear appropriate personnel protective equipment (PPE), including N95 or N100 respirators to minimize exposure to laser plumes.
- Use central wall suction units with in-line filters to evacuate minimal laser plumes.
- Use a mechanical smoke evaluation system with a high efficiency filter to manage the generation of large amounts of laser plume, when ablating tissue infected with HPV.
- Use local exhaust ventilation (LEV).8
When closely adhered to, these methods appear to provide high-level protection. Data suggest that, when HCPs can access appropriate protective equipment, risks for HPV exposure are low. However, this is more feasible for larger hospital facilities, and may be more limited in outpatient settings. This has led to the consideration of background protection in the form of HPV vaccination for at-risk HCPs. This is analogous to mandates for HCPs to receive hepatitis B vaccination despite the concomitant practice of universal precautions in health care settings. Preventative strategies are typically most efficacious when performed in concert.
After nearly 2 decades of widespread use, we have confidence in the safety of the HPV vaccination. Its benefit through age 45 has been established, leading to the 2018 FDA approval for the 9-valent HPV vaccine, Guardisil-9, for this expanded age group. It would seem logical that systematic administration of the HPV vaccine for at-risk HCPs would be both feasible and safe. There are well-established systems for administering vaccines for HCPs in all health care systems. Perhaps health system administrators should consider routinely offering HPV vaccination for at-risk employees as part of their occupational health care responsibilities. One important caveat being the cost and efficacy of HPV vaccination in this group has not been not established.
In the meantime, it is critical that gynecology providers be aware of their risk for occupational exposure to HPV when using laser and electrocautery techniques on HPV-infected tissues and the potential for them developing head and neck pathology. They should strictly adhere to preventative measures such as use of fit-tested N-95 respirators, mechanical smoke evacuators with high-efficiency filters and work in environments with adequate room ventilation. We all should individually evaluate what role HPV vaccination may play for us in augmenting our own safety.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Van Dyne EA et al. MMWR Morb Mortal Wkly Rep. 2018 Aug 24;67(33):918-24.
2. ASCCP. ASCCP recommends HPV vaccination for providers.
3. Fox-Lewis A et al. Occup Environ Med. 2020 Dec;77(12):809-17.
4. Zhou Q et al. Cancer Manag Res. 2019;11:3643-54
5. Bergbrant I et al. Acta Derm Venereol. 1994 Sep;74(5):393-5.
6. Garden J et al. Arch Dermatol. 2002 Oct;138(10):1303-7.
7. Harrison R, Huh W. Obstet Gynecol. 2020;136:663-5.
8. CDC. 1996. DHHS (NIOSH) Publication Number 96-128.
Advice on biopsies, workups, and referrals
Over the next 2 months we will dedicate this column to some general tips and pearls from the perspective of a gynecologic oncologist to guide general obstetrician gynecologists in the workup and management of preinvasive or invasive gynecologic diseases. The goal of these recommendations is to minimize misdiagnosis or delayed diagnosis and avoid unnecessary or untimely referrals.
Perform biopsy, not Pap smears, on visible cervical and vaginal lesions
The purpose of the Pap smear is to screen asymptomatic patients for cervical dysplasia or microscopic invasive disease. Cytology is an unreliable diagnostic tool for visible, symptomatic lesions in large part because of sampling errors, and the lack of architectural information in cytologic versus histopathologic specimens. Invasive lesions can be mischaracterized as preinvasive on a Pap smear. This can result in delayed diagnosis and unnecessary diagnostic procedures. For example, if a visible, abnormal-appearing, cervical lesion is seen during a routine visit and a Pap smear is performed (rather than a biopsy of the mass), the patient may receive an incorrect preliminary diagnosis of “high-grade dysplasia, carcinoma in situ” as it can be difficult to distinguish invasive carcinoma from carcinoma in situ on cytology. If the patient and provider do not understand the limitations of Pap smears in diagnosing invasive cancers, they may be falsely reassured and possibly delay or abstain from follow-up for an excisional procedure. If she does return for the loop electrosurgical excision procedure (LEEP), there might still be unnecessary delays in making referrals and definitive treatment while waiting for results. Radical hysterectomy may not promptly follow because, if performed within 6 weeks of an excisional procedure, it is associated with a significantly higher risk for perioperative complication, and therefore, if the excisional procedure was unnecessary to begin with, there may be additional time lost that need not be.1
Some clinicians avoid biopsy of visible lesions because they are concerned about bleeding complications that might arise in the office. Straightforward strategies to control bleeding are readily available in most gynecology offices, especially those already equipped for procedures such as LEEP and colposcopy. Prior to performing the biopsy, clinicians should ensure that they have supplies such as gauze sponges and ring forceps or packing forceps, silver nitrate, and ferric subsulfate solution (“Monsel’s solution”) close at hand. In the vast majority of cases, direct pressure for 5 minutes with gauze sponges and ferric subsulfate is highly effective at resolving most bleeding from a cervical or vaginal biopsy site. If this does not bring hemostasis, cautery devices or suture can be employed. If all else fails, be prepared to place vaginal packing (always with the insertion of a urinary Foley catheter to prevent urinary retention). In my experience, this is rarely needed.
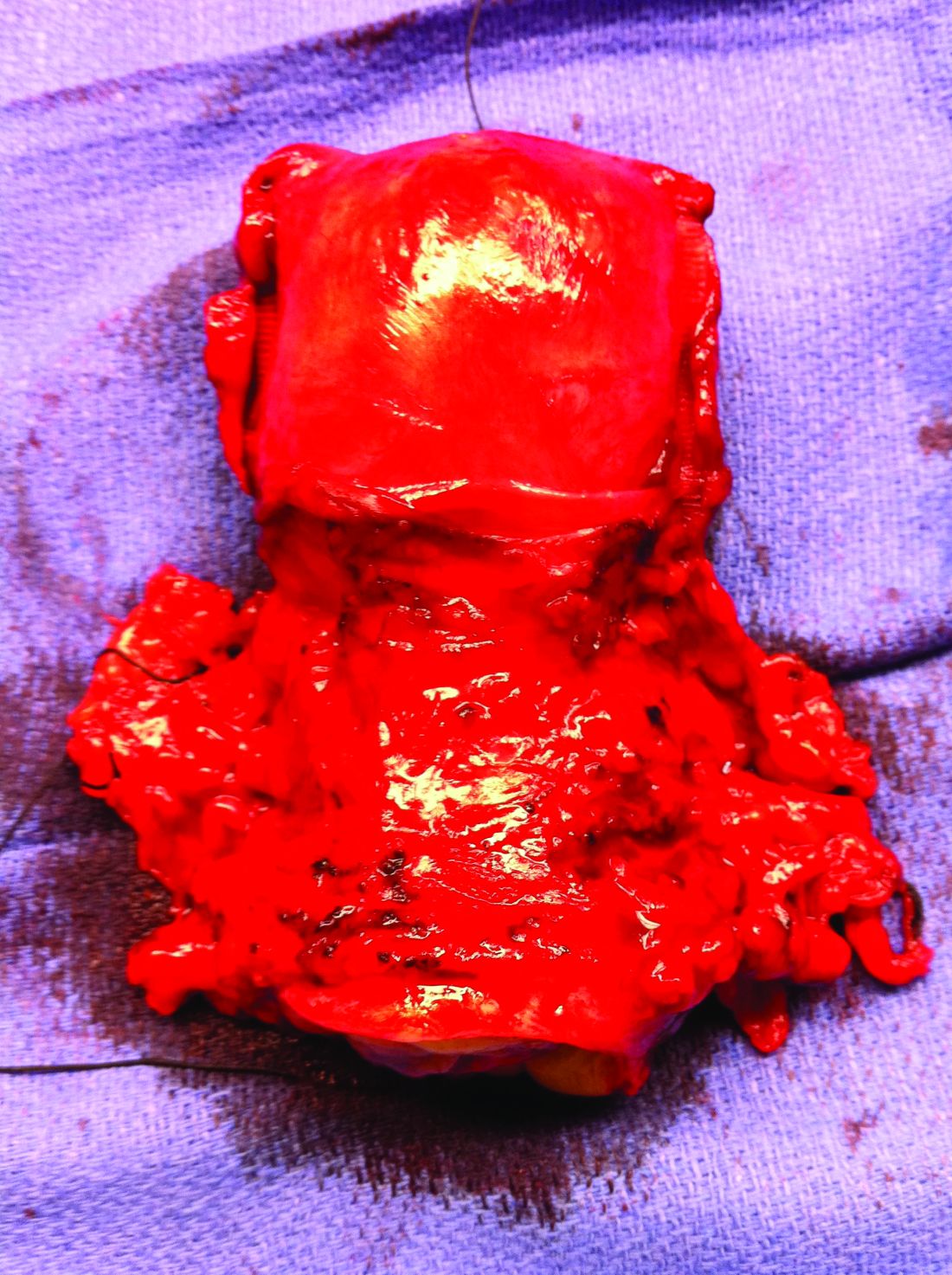
Wherever possible, visible cervical or vaginal (or vulvar, see below) lesions should be biopsied for histopathology, sampling representative areas of the most concerning portion, in order to minimize misdiagnosis and expedite referral and definitive treatment. For necrotic-appearing lesions I recommend taking multiple samples of the tumor, as necrotic, nonviable tissue can prevent accurate diagnosis of a cancer. In general, Pap smears should be reserved as screening tests for asymptomatic women without visible pathology.
Don’t treat or refer low-grade dysplasia, even if persistent
Increasingly we are understanding that low-grade dysplasia of the lower genital tract (CIN I, VAIN I, VIN I) is less a precursor for cancer, and more a phenomenon of benign HPV-associated changes.2 This HPV change may be chronically persistent, may require years of observation and serial Pap smears, and may be a general nuisance for the patient. However, current guidelines do not recommend intervention for low-grade dysplasia of the lower genital tract.2 Interventions to resect these lesions can result in morbidity, including perineal pain, vaginal scarring, and cervical stenosis or insufficiency. Given the extremely low risk for progression to cancer, these morbidities do not outweigh any small potential benefit.
When I am conferring with patients who have chronic low-grade dysplasia I spend a great deal of time exploring their understanding of the diagnosis and its pathophysiology, their fears, and their expectation regarding “success” of treatment. I spend the time educating them that this is a sequela of chronic viral infection that will not be eradicated with local surgical excisions, that their cancer risk and need for surveillance would persist even if surgical intervention were offered, and that the side effects of treatment would outweigh any benefit from the small risk of cancer or high-grade dysplasia.
In summary, the treatment of choice for persistent low-grade dysplasia of the lower genital tract is comprehensive patient education, not surgical resection or referral to gynecologic oncology.
Repeat sampling if there’s a discordance between imaging and biopsy results
Delay in cancer diagnosis is one of the greatest concerns for front-line gynecology providers. One of the more modifiable strategies to avoid missed or delayed diagnosis is to ensure that there is concordance between clinical findings and testing results. Otherwise said: The results and findings should make sense in aggregate. An example was cited above in which a visible cervical mass demonstrated CIN III on cytologic testing. Another common example is a biopsy result of “scant benign endometrium” in a patient with postmenopausal bleeding and thickened endometrial stripe on ultrasound. In both of these cases there is clear discordance between physical findings and the results of pathology sampling. A pathology report, in all of its black and white certitude, seems like the most reliable source of information. However, always trust your clinical judgment. If the clinical picture is suggesting something far worse than these limited, often random or blind samplings, I recommend repeated or more extensive sampling (for example, dilation and curettage). At the very least, schedule close follow-up with repeated sampling if the symptom or finding persists. The emphasis here is on scheduled follow-up, rather than “p.r.n.,” because a patient who was given a “normal” pathology result to explain her abnormal symptoms may not volunteer that those symptoms are persistent as she may feel that anything sinister was already ruled out. Make certain that you explain the potential for misdiagnosis as the reason for why you would like to see her back shortly to ensure the issue has resolved.
Biopsy vulvar lesions, minimize empiric treatment
Vulvar cancer is notoriously associated with delayed diagnosis. Unfortunately, it is commonplace for gynecologic oncologists to see women who have vulvar cancers that have been empirically treated, sometimes for months or years, with steroids or other topical agents. If a lesion on the vulva is characteristically benign in appearance (such as condyloma or lichen sclerosis), it may be reasonable to start empiric treatment. However, all patients who are treated without biopsy should be rescheduled for a planned follow-up appointment in 2-3 months. If the lesion/area remains unchanged, or worse, the lesion should be biopsied before proceeding with a change in therapy or continued therapy. Once again, don’t rely on patients to return for evaluation if the lesion doesn’t improve. Many patients assume that our first empiric diagnosis is “gospel,” and therefore may not return if the treatment doesn’t work. Meanwhile, providers may assume that patients will know that there is uncertainty in our interpretation and that they will know to report if the initial treatment didn’t work. These assumptions are the recipe for delayed diagnosis. If there is too great a burden on the patient to schedule a return visit because of social or financial reasons then the patient should have a biopsy prior to initiation of treatment. As a rule, empiric treatment is not a good strategy for patients without good access to follow-up.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at [email protected].
References
1. Sullivan S. et al Gynecol Oncol. 2017 Feb;144(2):294-8.
2. Perkins R .et al J Low Genit Tract Dis. 2020 Apr;24(2):102-31.
Over the next 2 months we will dedicate this column to some general tips and pearls from the perspective of a gynecologic oncologist to guide general obstetrician gynecologists in the workup and management of preinvasive or invasive gynecologic diseases. The goal of these recommendations is to minimize misdiagnosis or delayed diagnosis and avoid unnecessary or untimely referrals.
Perform biopsy, not Pap smears, on visible cervical and vaginal lesions
The purpose of the Pap smear is to screen asymptomatic patients for cervical dysplasia or microscopic invasive disease. Cytology is an unreliable diagnostic tool for visible, symptomatic lesions in large part because of sampling errors, and the lack of architectural information in cytologic versus histopathologic specimens. Invasive lesions can be mischaracterized as preinvasive on a Pap smear. This can result in delayed diagnosis and unnecessary diagnostic procedures. For example, if a visible, abnormal-appearing, cervical lesion is seen during a routine visit and a Pap smear is performed (rather than a biopsy of the mass), the patient may receive an incorrect preliminary diagnosis of “high-grade dysplasia, carcinoma in situ” as it can be difficult to distinguish invasive carcinoma from carcinoma in situ on cytology. If the patient and provider do not understand the limitations of Pap smears in diagnosing invasive cancers, they may be falsely reassured and possibly delay or abstain from follow-up for an excisional procedure. If she does return for the loop electrosurgical excision procedure (LEEP), there might still be unnecessary delays in making referrals and definitive treatment while waiting for results. Radical hysterectomy may not promptly follow because, if performed within 6 weeks of an excisional procedure, it is associated with a significantly higher risk for perioperative complication, and therefore, if the excisional procedure was unnecessary to begin with, there may be additional time lost that need not be.1
Some clinicians avoid biopsy of visible lesions because they are concerned about bleeding complications that might arise in the office. Straightforward strategies to control bleeding are readily available in most gynecology offices, especially those already equipped for procedures such as LEEP and colposcopy. Prior to performing the biopsy, clinicians should ensure that they have supplies such as gauze sponges and ring forceps or packing forceps, silver nitrate, and ferric subsulfate solution (“Monsel’s solution”) close at hand. In the vast majority of cases, direct pressure for 5 minutes with gauze sponges and ferric subsulfate is highly effective at resolving most bleeding from a cervical or vaginal biopsy site. If this does not bring hemostasis, cautery devices or suture can be employed. If all else fails, be prepared to place vaginal packing (always with the insertion of a urinary Foley catheter to prevent urinary retention). In my experience, this is rarely needed.
Wherever possible, visible cervical or vaginal (or vulvar, see below) lesions should be biopsied for histopathology, sampling representative areas of the most concerning portion, in order to minimize misdiagnosis and expedite referral and definitive treatment. For necrotic-appearing lesions I recommend taking multiple samples of the tumor, as necrotic, nonviable tissue can prevent accurate diagnosis of a cancer. In general, Pap smears should be reserved as screening tests for asymptomatic women without visible pathology.
Don’t treat or refer low-grade dysplasia, even if persistent
Increasingly we are understanding that low-grade dysplasia of the lower genital tract (CIN I, VAIN I, VIN I) is less a precursor for cancer, and more a phenomenon of benign HPV-associated changes.2 This HPV change may be chronically persistent, may require years of observation and serial Pap smears, and may be a general nuisance for the patient. However, current guidelines do not recommend intervention for low-grade dysplasia of the lower genital tract.2 Interventions to resect these lesions can result in morbidity, including perineal pain, vaginal scarring, and cervical stenosis or insufficiency. Given the extremely low risk for progression to cancer, these morbidities do not outweigh any small potential benefit.
When I am conferring with patients who have chronic low-grade dysplasia I spend a great deal of time exploring their understanding of the diagnosis and its pathophysiology, their fears, and their expectation regarding “success” of treatment. I spend the time educating them that this is a sequela of chronic viral infection that will not be eradicated with local surgical excisions, that their cancer risk and need for surveillance would persist even if surgical intervention were offered, and that the side effects of treatment would outweigh any benefit from the small risk of cancer or high-grade dysplasia.
In summary, the treatment of choice for persistent low-grade dysplasia of the lower genital tract is comprehensive patient education, not surgical resection or referral to gynecologic oncology.
Repeat sampling if there’s a discordance between imaging and biopsy results
Delay in cancer diagnosis is one of the greatest concerns for front-line gynecology providers. One of the more modifiable strategies to avoid missed or delayed diagnosis is to ensure that there is concordance between clinical findings and testing results. Otherwise said: The results and findings should make sense in aggregate. An example was cited above in which a visible cervical mass demonstrated CIN III on cytologic testing. Another common example is a biopsy result of “scant benign endometrium” in a patient with postmenopausal bleeding and thickened endometrial stripe on ultrasound. In both of these cases there is clear discordance between physical findings and the results of pathology sampling. A pathology report, in all of its black and white certitude, seems like the most reliable source of information. However, always trust your clinical judgment. If the clinical picture is suggesting something far worse than these limited, often random or blind samplings, I recommend repeated or more extensive sampling (for example, dilation and curettage). At the very least, schedule close follow-up with repeated sampling if the symptom or finding persists. The emphasis here is on scheduled follow-up, rather than “p.r.n.,” because a patient who was given a “normal” pathology result to explain her abnormal symptoms may not volunteer that those symptoms are persistent as she may feel that anything sinister was already ruled out. Make certain that you explain the potential for misdiagnosis as the reason for why you would like to see her back shortly to ensure the issue has resolved.
Biopsy vulvar lesions, minimize empiric treatment
Vulvar cancer is notoriously associated with delayed diagnosis. Unfortunately, it is commonplace for gynecologic oncologists to see women who have vulvar cancers that have been empirically treated, sometimes for months or years, with steroids or other topical agents. If a lesion on the vulva is characteristically benign in appearance (such as condyloma or lichen sclerosis), it may be reasonable to start empiric treatment. However, all patients who are treated without biopsy should be rescheduled for a planned follow-up appointment in 2-3 months. If the lesion/area remains unchanged, or worse, the lesion should be biopsied before proceeding with a change in therapy or continued therapy. Once again, don’t rely on patients to return for evaluation if the lesion doesn’t improve. Many patients assume that our first empiric diagnosis is “gospel,” and therefore may not return if the treatment doesn’t work. Meanwhile, providers may assume that patients will know that there is uncertainty in our interpretation and that they will know to report if the initial treatment didn’t work. These assumptions are the recipe for delayed diagnosis. If there is too great a burden on the patient to schedule a return visit because of social or financial reasons then the patient should have a biopsy prior to initiation of treatment. As a rule, empiric treatment is not a good strategy for patients without good access to follow-up.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at [email protected].
References
1. Sullivan S. et al Gynecol Oncol. 2017 Feb;144(2):294-8.
2. Perkins R .et al J Low Genit Tract Dis. 2020 Apr;24(2):102-31.
Over the next 2 months we will dedicate this column to some general tips and pearls from the perspective of a gynecologic oncologist to guide general obstetrician gynecologists in the workup and management of preinvasive or invasive gynecologic diseases. The goal of these recommendations is to minimize misdiagnosis or delayed diagnosis and avoid unnecessary or untimely referrals.
Perform biopsy, not Pap smears, on visible cervical and vaginal lesions
The purpose of the Pap smear is to screen asymptomatic patients for cervical dysplasia or microscopic invasive disease. Cytology is an unreliable diagnostic tool for visible, symptomatic lesions in large part because of sampling errors, and the lack of architectural information in cytologic versus histopathologic specimens. Invasive lesions can be mischaracterized as preinvasive on a Pap smear. This can result in delayed diagnosis and unnecessary diagnostic procedures. For example, if a visible, abnormal-appearing, cervical lesion is seen during a routine visit and a Pap smear is performed (rather than a biopsy of the mass), the patient may receive an incorrect preliminary diagnosis of “high-grade dysplasia, carcinoma in situ” as it can be difficult to distinguish invasive carcinoma from carcinoma in situ on cytology. If the patient and provider do not understand the limitations of Pap smears in diagnosing invasive cancers, they may be falsely reassured and possibly delay or abstain from follow-up for an excisional procedure. If she does return for the loop electrosurgical excision procedure (LEEP), there might still be unnecessary delays in making referrals and definitive treatment while waiting for results. Radical hysterectomy may not promptly follow because, if performed within 6 weeks of an excisional procedure, it is associated with a significantly higher risk for perioperative complication, and therefore, if the excisional procedure was unnecessary to begin with, there may be additional time lost that need not be.1
Some clinicians avoid biopsy of visible lesions because they are concerned about bleeding complications that might arise in the office. Straightforward strategies to control bleeding are readily available in most gynecology offices, especially those already equipped for procedures such as LEEP and colposcopy. Prior to performing the biopsy, clinicians should ensure that they have supplies such as gauze sponges and ring forceps or packing forceps, silver nitrate, and ferric subsulfate solution (“Monsel’s solution”) close at hand. In the vast majority of cases, direct pressure for 5 minutes with gauze sponges and ferric subsulfate is highly effective at resolving most bleeding from a cervical or vaginal biopsy site. If this does not bring hemostasis, cautery devices or suture can be employed. If all else fails, be prepared to place vaginal packing (always with the insertion of a urinary Foley catheter to prevent urinary retention). In my experience, this is rarely needed.
Wherever possible, visible cervical or vaginal (or vulvar, see below) lesions should be biopsied for histopathology, sampling representative areas of the most concerning portion, in order to minimize misdiagnosis and expedite referral and definitive treatment. For necrotic-appearing lesions I recommend taking multiple samples of the tumor, as necrotic, nonviable tissue can prevent accurate diagnosis of a cancer. In general, Pap smears should be reserved as screening tests for asymptomatic women without visible pathology.
Don’t treat or refer low-grade dysplasia, even if persistent
Increasingly we are understanding that low-grade dysplasia of the lower genital tract (CIN I, VAIN I, VIN I) is less a precursor for cancer, and more a phenomenon of benign HPV-associated changes.2 This HPV change may be chronically persistent, may require years of observation and serial Pap smears, and may be a general nuisance for the patient. However, current guidelines do not recommend intervention for low-grade dysplasia of the lower genital tract.2 Interventions to resect these lesions can result in morbidity, including perineal pain, vaginal scarring, and cervical stenosis or insufficiency. Given the extremely low risk for progression to cancer, these morbidities do not outweigh any small potential benefit.
When I am conferring with patients who have chronic low-grade dysplasia I spend a great deal of time exploring their understanding of the diagnosis and its pathophysiology, their fears, and their expectation regarding “success” of treatment. I spend the time educating them that this is a sequela of chronic viral infection that will not be eradicated with local surgical excisions, that their cancer risk and need for surveillance would persist even if surgical intervention were offered, and that the side effects of treatment would outweigh any benefit from the small risk of cancer or high-grade dysplasia.
In summary, the treatment of choice for persistent low-grade dysplasia of the lower genital tract is comprehensive patient education, not surgical resection or referral to gynecologic oncology.
Repeat sampling if there’s a discordance between imaging and biopsy results
Delay in cancer diagnosis is one of the greatest concerns for front-line gynecology providers. One of the more modifiable strategies to avoid missed or delayed diagnosis is to ensure that there is concordance between clinical findings and testing results. Otherwise said: The results and findings should make sense in aggregate. An example was cited above in which a visible cervical mass demonstrated CIN III on cytologic testing. Another common example is a biopsy result of “scant benign endometrium” in a patient with postmenopausal bleeding and thickened endometrial stripe on ultrasound. In both of these cases there is clear discordance between physical findings and the results of pathology sampling. A pathology report, in all of its black and white certitude, seems like the most reliable source of information. However, always trust your clinical judgment. If the clinical picture is suggesting something far worse than these limited, often random or blind samplings, I recommend repeated or more extensive sampling (for example, dilation and curettage). At the very least, schedule close follow-up with repeated sampling if the symptom or finding persists. The emphasis here is on scheduled follow-up, rather than “p.r.n.,” because a patient who was given a “normal” pathology result to explain her abnormal symptoms may not volunteer that those symptoms are persistent as she may feel that anything sinister was already ruled out. Make certain that you explain the potential for misdiagnosis as the reason for why you would like to see her back shortly to ensure the issue has resolved.
Biopsy vulvar lesions, minimize empiric treatment
Vulvar cancer is notoriously associated with delayed diagnosis. Unfortunately, it is commonplace for gynecologic oncologists to see women who have vulvar cancers that have been empirically treated, sometimes for months or years, with steroids or other topical agents. If a lesion on the vulva is characteristically benign in appearance (such as condyloma or lichen sclerosis), it may be reasonable to start empiric treatment. However, all patients who are treated without biopsy should be rescheduled for a planned follow-up appointment in 2-3 months. If the lesion/area remains unchanged, or worse, the lesion should be biopsied before proceeding with a change in therapy or continued therapy. Once again, don’t rely on patients to return for evaluation if the lesion doesn’t improve. Many patients assume that our first empiric diagnosis is “gospel,” and therefore may not return if the treatment doesn’t work. Meanwhile, providers may assume that patients will know that there is uncertainty in our interpretation and that they will know to report if the initial treatment didn’t work. These assumptions are the recipe for delayed diagnosis. If there is too great a burden on the patient to schedule a return visit because of social or financial reasons then the patient should have a biopsy prior to initiation of treatment. As a rule, empiric treatment is not a good strategy for patients without good access to follow-up.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at [email protected].
References
1. Sullivan S. et al Gynecol Oncol. 2017 Feb;144(2):294-8.
2. Perkins R .et al J Low Genit Tract Dis. 2020 Apr;24(2):102-31.
Surgery for early-stage cervical cancer: Are we still too radical?
It has been more than 120 years since Ernst Wertheim, a Viennese surgeon, performed and described what is considered to have been the first radical total hysterectomy with lymphadenectomy for early-stage cervical cancer, yet this morbid procedure remains the standard of care for most early-stage cervical cancers. The rationale for this procedure, which included removal of the parametrial tissue, uterosacral and cardinal ligaments, and upper vagina en bloc with the cervix and uterus, was to obtain margins around a cancer that has a dominant radial growth pattern. The morbidity associated with this procedure is substantial. The parametrium houses important vascular, neural, and urologic structures. Unlike extrafascial hysterectomy, often referred to as “simple” hysterectomy, in which surgeons follow a fascial plane, and therefore a relatively avascular dissection, surgeons performing radical hysterectomy must venture outside of these embryologic fusion planes into less well–defined anatomy. Therefore, surgical complications are relatively common including hemorrhage, ureteral and bladder injury, as well as late-onset devastating complications such as fistula, urinary retention, or incontinence, and sexual dysfunction.1 More recently, variations of the Wertheim-Meigs radical hysterectomy have been described, and objective classifications created, which include modified radical procedures (removing less parametria) and nerve-sparing procedures to facilitate standardized nomenclature for tailoring the most appropriate procedure for any given tumor.2
The trend, and a positive one at that, over the course of the past century, has been a move away from routine radical surgical procedures for most clinical stage 1 cancers. No better example exists than breast cancer, in which the Halsted radical mastectomy has been largely replaced by less morbid breast-conserving or nonradical procedures with adjunct medical and radiation therapies offered to achieve high rates of cure with far more acceptable patient-centered outcomes.3 And so why is it that radical hysterectomy is still considered the standard of care for all but the smallest of microscopic cervical cancers?
The risk of lymph node metastases or recurrence is exceptionally low for women with microscopic (stage IA1) cervical cancers that are less than 3 mm in depth. Therefore, the National Comprehensive Cancer Network guidelines recommend nonradical surgical remedies (such as extrafascial hysterectomy, or cone biopsy or trachelectomy if fertility preservation is desired) for this earlier stage of disease.4 If there is lymphovascular space invasion (an indicator of poor prognosis and potential lymphatic involvement), a lymphadenectomy or sentinel lymph node biopsy is also recommended. For women with stage IA2 or IB lesions, radical excisions (either trachelectomy or hysterectomy) are considered the standard of care. However, this “gold standard” was achieved largely through legacy, and not a result of randomized trials comparing its outcomes with nonradical procedures.
Initial strides away from radical cervical cancer surgery focused on the goal of fertility preservation via radical trachelectomy which allowed women to preserve an intact uterine fundus. This was initially met with skepticism and concern that surgeons could be sacrificing oncologic outcomes in order to preserve a woman’s fertility. Thanks to pioneering work, including prospective research studies by surgeon innovators it has been shown that, in appropriately selected candidates with tumors less than 2 cm, it is an accepted standard of care.4 Radical vaginal or abdominal trachelectomy is associated with cancer recurrence rates of less than 5% and successful pregnancy in approximately three-quarters of patients in whom this is desired.5,6 However, full-term pregnancy is achieved in 50%-75% of cases, reflecting increased obstetric risk, and radical trachelectomy still subjects patients to the morbidity of a radical parametrial resection, despite the fact that many of them will have no residual carcinoma in their final pathological specimens.
Therefore, can we be even more conservative in our surgery for these patients? Are simple hysterectomy or conization potentially adequate treatments for small (<2 cm) stage IA2 and IB1 lesions that have favorable histology (<10 mm stromal invasion, low-risk histology, no lymphovascular space involvement, negative margins on conization and no lymph node metastases)? In patients whose tumor exhibits these histologic features, the likelihood of parametrial involvement is approximately 1%, calling into question the virtue of parametrial resection.7 Observational studies have identified mixed results on the safety of conservative surgical techniques in early-stage cervical cancer. In a study of the National Cancer Database, the outcomes of 2,543 radical hysterectomies and 1,388 extrafascial hysterectomies for women with stage IB1 disease were evaluated and observed a difference in 5-year survival (92.4% vs. 95.3%) favoring the radical procedure.8 Unfortunately, database analyses such as these are limited by potential confounders and discordance between the groups such as rates of lymphadenectomy, known involvement of oncologic surgeon specialists, and margin status. An alternative evaluation of the Surveillance, Epidemiology, and End Results database including 2,571 patients with stage IB1 disease, all of whom had lymphadenectomy performed, showed no difference in 10-year disease-specific survival between the two surgical approaches.9
Ultimately, whether conservative procedures (such as conization or extrafascial hysterectomy) can be offered to women with small, low-risk IB1 or IA2 cervical cancers will be best determined by prospective single-arm or randomized trials. Fortunately, these are underway. Preliminary results from the ConCerv trial in which 100 women with early-stage, low-risk stage IA2 and IB1 cervical cancer were treated with either repeat conization or extrafascial hysterectomy with sentinel lymph node biopsy showed acceptably low rates of recurrence (3%) with this approach.10 If the mature data supports this finding, it seems that, for appropriately selected and well-counseled patients, conservative surgery may become more broadly accepted as a reasonable option for treatment that spares women not only loss of fertility, but also the early and late surgical morbidity from radical procedures.
In the meantime, until more is known about the oncologic safety of nonradical procedures for stage IA2 and IB1 cervical cancer, this option should not be considered standard of care, and only offered to patients with favorable tumor factors who are well counseled regarding the uncertainty of this approach. It is critical that patients with early-stage cervical cancer be evaluated by a gynecologic cancer specialist prior to definitive surgical treatment as they are best equipped to evaluate risk profiles and counsel about her options for surgery, its known and unknown consequences, and the appropriateness of fertility preservation or radicality of surgery. We eagerly await the results of trials evaluating the safety of conservative cervical cancer surgery, which promise to advance us from 19th-century practices, preserving not only fertility, but also quality of life.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no disclosures and can be contacted at [email protected].
References
1. Trimbos JB et al. Eur J Cancer. 2004;40(3):375-8.
2. Querleu D and Morrow CP. Lancet Oncol. 2008;9:297-303.
3. Sakorafas GH and Safioleas M. Eur J Cancer Care. 2010 Mar;19(2):145-66.
4. National Comprehensive Cancer Network. Cervical Cancer (Version 1.2021). https://www.nccn.org/professionals/physician_gls/pdf/cervical.pdf. Accessed 2021 Apr 21.
5. Plante M et al. Gynecol Oncol. 2011;121:290-7.
6. Wethington SL et al. Int J Gynecol Cancer. 2012;22:1251-7.
7. Domgue J and Schmeler K. Best Pract Res Clin Obstet Gynaecol. 2019 Feb;55:79-92.
8. Sia TY et al. Obstet Gyenecol. 2019;134(6):1132.
9. Tseng J et al. Gynecol Oncol. 2018;150(1):44.
10. Schmeler K et al. Int J Gynecol Cancer. 2019;29:A14-5.
It has been more than 120 years since Ernst Wertheim, a Viennese surgeon, performed and described what is considered to have been the first radical total hysterectomy with lymphadenectomy for early-stage cervical cancer, yet this morbid procedure remains the standard of care for most early-stage cervical cancers. The rationale for this procedure, which included removal of the parametrial tissue, uterosacral and cardinal ligaments, and upper vagina en bloc with the cervix and uterus, was to obtain margins around a cancer that has a dominant radial growth pattern. The morbidity associated with this procedure is substantial. The parametrium houses important vascular, neural, and urologic structures. Unlike extrafascial hysterectomy, often referred to as “simple” hysterectomy, in which surgeons follow a fascial plane, and therefore a relatively avascular dissection, surgeons performing radical hysterectomy must venture outside of these embryologic fusion planes into less well–defined anatomy. Therefore, surgical complications are relatively common including hemorrhage, ureteral and bladder injury, as well as late-onset devastating complications such as fistula, urinary retention, or incontinence, and sexual dysfunction.1 More recently, variations of the Wertheim-Meigs radical hysterectomy have been described, and objective classifications created, which include modified radical procedures (removing less parametria) and nerve-sparing procedures to facilitate standardized nomenclature for tailoring the most appropriate procedure for any given tumor.2
The trend, and a positive one at that, over the course of the past century, has been a move away from routine radical surgical procedures for most clinical stage 1 cancers. No better example exists than breast cancer, in which the Halsted radical mastectomy has been largely replaced by less morbid breast-conserving or nonradical procedures with adjunct medical and radiation therapies offered to achieve high rates of cure with far more acceptable patient-centered outcomes.3 And so why is it that radical hysterectomy is still considered the standard of care for all but the smallest of microscopic cervical cancers?
The risk of lymph node metastases or recurrence is exceptionally low for women with microscopic (stage IA1) cervical cancers that are less than 3 mm in depth. Therefore, the National Comprehensive Cancer Network guidelines recommend nonradical surgical remedies (such as extrafascial hysterectomy, or cone biopsy or trachelectomy if fertility preservation is desired) for this earlier stage of disease.4 If there is lymphovascular space invasion (an indicator of poor prognosis and potential lymphatic involvement), a lymphadenectomy or sentinel lymph node biopsy is also recommended. For women with stage IA2 or IB lesions, radical excisions (either trachelectomy or hysterectomy) are considered the standard of care. However, this “gold standard” was achieved largely through legacy, and not a result of randomized trials comparing its outcomes with nonradical procedures.
Initial strides away from radical cervical cancer surgery focused on the goal of fertility preservation via radical trachelectomy which allowed women to preserve an intact uterine fundus. This was initially met with skepticism and concern that surgeons could be sacrificing oncologic outcomes in order to preserve a woman’s fertility. Thanks to pioneering work, including prospective research studies by surgeon innovators it has been shown that, in appropriately selected candidates with tumors less than 2 cm, it is an accepted standard of care.4 Radical vaginal or abdominal trachelectomy is associated with cancer recurrence rates of less than 5% and successful pregnancy in approximately three-quarters of patients in whom this is desired.5,6 However, full-term pregnancy is achieved in 50%-75% of cases, reflecting increased obstetric risk, and radical trachelectomy still subjects patients to the morbidity of a radical parametrial resection, despite the fact that many of them will have no residual carcinoma in their final pathological specimens.
Therefore, can we be even more conservative in our surgery for these patients? Are simple hysterectomy or conization potentially adequate treatments for small (<2 cm) stage IA2 and IB1 lesions that have favorable histology (<10 mm stromal invasion, low-risk histology, no lymphovascular space involvement, negative margins on conization and no lymph node metastases)? In patients whose tumor exhibits these histologic features, the likelihood of parametrial involvement is approximately 1%, calling into question the virtue of parametrial resection.7 Observational studies have identified mixed results on the safety of conservative surgical techniques in early-stage cervical cancer. In a study of the National Cancer Database, the outcomes of 2,543 radical hysterectomies and 1,388 extrafascial hysterectomies for women with stage IB1 disease were evaluated and observed a difference in 5-year survival (92.4% vs. 95.3%) favoring the radical procedure.8 Unfortunately, database analyses such as these are limited by potential confounders and discordance between the groups such as rates of lymphadenectomy, known involvement of oncologic surgeon specialists, and margin status. An alternative evaluation of the Surveillance, Epidemiology, and End Results database including 2,571 patients with stage IB1 disease, all of whom had lymphadenectomy performed, showed no difference in 10-year disease-specific survival between the two surgical approaches.9
Ultimately, whether conservative procedures (such as conization or extrafascial hysterectomy) can be offered to women with small, low-risk IB1 or IA2 cervical cancers will be best determined by prospective single-arm or randomized trials. Fortunately, these are underway. Preliminary results from the ConCerv trial in which 100 women with early-stage, low-risk stage IA2 and IB1 cervical cancer were treated with either repeat conization or extrafascial hysterectomy with sentinel lymph node biopsy showed acceptably low rates of recurrence (3%) with this approach.10 If the mature data supports this finding, it seems that, for appropriately selected and well-counseled patients, conservative surgery may become more broadly accepted as a reasonable option for treatment that spares women not only loss of fertility, but also the early and late surgical morbidity from radical procedures.
In the meantime, until more is known about the oncologic safety of nonradical procedures for stage IA2 and IB1 cervical cancer, this option should not be considered standard of care, and only offered to patients with favorable tumor factors who are well counseled regarding the uncertainty of this approach. It is critical that patients with early-stage cervical cancer be evaluated by a gynecologic cancer specialist prior to definitive surgical treatment as they are best equipped to evaluate risk profiles and counsel about her options for surgery, its known and unknown consequences, and the appropriateness of fertility preservation or radicality of surgery. We eagerly await the results of trials evaluating the safety of conservative cervical cancer surgery, which promise to advance us from 19th-century practices, preserving not only fertility, but also quality of life.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no disclosures and can be contacted at [email protected].
References
1. Trimbos JB et al. Eur J Cancer. 2004;40(3):375-8.
2. Querleu D and Morrow CP. Lancet Oncol. 2008;9:297-303.
3. Sakorafas GH and Safioleas M. Eur J Cancer Care. 2010 Mar;19(2):145-66.
4. National Comprehensive Cancer Network. Cervical Cancer (Version 1.2021). https://www.nccn.org/professionals/physician_gls/pdf/cervical.pdf. Accessed 2021 Apr 21.
5. Plante M et al. Gynecol Oncol. 2011;121:290-7.
6. Wethington SL et al. Int J Gynecol Cancer. 2012;22:1251-7.
7. Domgue J and Schmeler K. Best Pract Res Clin Obstet Gynaecol. 2019 Feb;55:79-92.
8. Sia TY et al. Obstet Gyenecol. 2019;134(6):1132.
9. Tseng J et al. Gynecol Oncol. 2018;150(1):44.
10. Schmeler K et al. Int J Gynecol Cancer. 2019;29:A14-5.
It has been more than 120 years since Ernst Wertheim, a Viennese surgeon, performed and described what is considered to have been the first radical total hysterectomy with lymphadenectomy for early-stage cervical cancer, yet this morbid procedure remains the standard of care for most early-stage cervical cancers. The rationale for this procedure, which included removal of the parametrial tissue, uterosacral and cardinal ligaments, and upper vagina en bloc with the cervix and uterus, was to obtain margins around a cancer that has a dominant radial growth pattern. The morbidity associated with this procedure is substantial. The parametrium houses important vascular, neural, and urologic structures. Unlike extrafascial hysterectomy, often referred to as “simple” hysterectomy, in which surgeons follow a fascial plane, and therefore a relatively avascular dissection, surgeons performing radical hysterectomy must venture outside of these embryologic fusion planes into less well–defined anatomy. Therefore, surgical complications are relatively common including hemorrhage, ureteral and bladder injury, as well as late-onset devastating complications such as fistula, urinary retention, or incontinence, and sexual dysfunction.1 More recently, variations of the Wertheim-Meigs radical hysterectomy have been described, and objective classifications created, which include modified radical procedures (removing less parametria) and nerve-sparing procedures to facilitate standardized nomenclature for tailoring the most appropriate procedure for any given tumor.2
The trend, and a positive one at that, over the course of the past century, has been a move away from routine radical surgical procedures for most clinical stage 1 cancers. No better example exists than breast cancer, in which the Halsted radical mastectomy has been largely replaced by less morbid breast-conserving or nonradical procedures with adjunct medical and radiation therapies offered to achieve high rates of cure with far more acceptable patient-centered outcomes.3 And so why is it that radical hysterectomy is still considered the standard of care for all but the smallest of microscopic cervical cancers?
The risk of lymph node metastases or recurrence is exceptionally low for women with microscopic (stage IA1) cervical cancers that are less than 3 mm in depth. Therefore, the National Comprehensive Cancer Network guidelines recommend nonradical surgical remedies (such as extrafascial hysterectomy, or cone biopsy or trachelectomy if fertility preservation is desired) for this earlier stage of disease.4 If there is lymphovascular space invasion (an indicator of poor prognosis and potential lymphatic involvement), a lymphadenectomy or sentinel lymph node biopsy is also recommended. For women with stage IA2 or IB lesions, radical excisions (either trachelectomy or hysterectomy) are considered the standard of care. However, this “gold standard” was achieved largely through legacy, and not a result of randomized trials comparing its outcomes with nonradical procedures.
Initial strides away from radical cervical cancer surgery focused on the goal of fertility preservation via radical trachelectomy which allowed women to preserve an intact uterine fundus. This was initially met with skepticism and concern that surgeons could be sacrificing oncologic outcomes in order to preserve a woman’s fertility. Thanks to pioneering work, including prospective research studies by surgeon innovators it has been shown that, in appropriately selected candidates with tumors less than 2 cm, it is an accepted standard of care.4 Radical vaginal or abdominal trachelectomy is associated with cancer recurrence rates of less than 5% and successful pregnancy in approximately three-quarters of patients in whom this is desired.5,6 However, full-term pregnancy is achieved in 50%-75% of cases, reflecting increased obstetric risk, and radical trachelectomy still subjects patients to the morbidity of a radical parametrial resection, despite the fact that many of them will have no residual carcinoma in their final pathological specimens.
Therefore, can we be even more conservative in our surgery for these patients? Are simple hysterectomy or conization potentially adequate treatments for small (<2 cm) stage IA2 and IB1 lesions that have favorable histology (<10 mm stromal invasion, low-risk histology, no lymphovascular space involvement, negative margins on conization and no lymph node metastases)? In patients whose tumor exhibits these histologic features, the likelihood of parametrial involvement is approximately 1%, calling into question the virtue of parametrial resection.7 Observational studies have identified mixed results on the safety of conservative surgical techniques in early-stage cervical cancer. In a study of the National Cancer Database, the outcomes of 2,543 radical hysterectomies and 1,388 extrafascial hysterectomies for women with stage IB1 disease were evaluated and observed a difference in 5-year survival (92.4% vs. 95.3%) favoring the radical procedure.8 Unfortunately, database analyses such as these are limited by potential confounders and discordance between the groups such as rates of lymphadenectomy, known involvement of oncologic surgeon specialists, and margin status. An alternative evaluation of the Surveillance, Epidemiology, and End Results database including 2,571 patients with stage IB1 disease, all of whom had lymphadenectomy performed, showed no difference in 10-year disease-specific survival between the two surgical approaches.9
Ultimately, whether conservative procedures (such as conization or extrafascial hysterectomy) can be offered to women with small, low-risk IB1 or IA2 cervical cancers will be best determined by prospective single-arm or randomized trials. Fortunately, these are underway. Preliminary results from the ConCerv trial in which 100 women with early-stage, low-risk stage IA2 and IB1 cervical cancer were treated with either repeat conization or extrafascial hysterectomy with sentinel lymph node biopsy showed acceptably low rates of recurrence (3%) with this approach.10 If the mature data supports this finding, it seems that, for appropriately selected and well-counseled patients, conservative surgery may become more broadly accepted as a reasonable option for treatment that spares women not only loss of fertility, but also the early and late surgical morbidity from radical procedures.
In the meantime, until more is known about the oncologic safety of nonradical procedures for stage IA2 and IB1 cervical cancer, this option should not be considered standard of care, and only offered to patients with favorable tumor factors who are well counseled regarding the uncertainty of this approach. It is critical that patients with early-stage cervical cancer be evaluated by a gynecologic cancer specialist prior to definitive surgical treatment as they are best equipped to evaluate risk profiles and counsel about her options for surgery, its known and unknown consequences, and the appropriateness of fertility preservation or radicality of surgery. We eagerly await the results of trials evaluating the safety of conservative cervical cancer surgery, which promise to advance us from 19th-century practices, preserving not only fertility, but also quality of life.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no disclosures and can be contacted at [email protected].
References
1. Trimbos JB et al. Eur J Cancer. 2004;40(3):375-8.
2. Querleu D and Morrow CP. Lancet Oncol. 2008;9:297-303.
3. Sakorafas GH and Safioleas M. Eur J Cancer Care. 2010 Mar;19(2):145-66.
4. National Comprehensive Cancer Network. Cervical Cancer (Version 1.2021). https://www.nccn.org/professionals/physician_gls/pdf/cervical.pdf. Accessed 2021 Apr 21.
5. Plante M et al. Gynecol Oncol. 2011;121:290-7.
6. Wethington SL et al. Int J Gynecol Cancer. 2012;22:1251-7.
7. Domgue J and Schmeler K. Best Pract Res Clin Obstet Gynaecol. 2019 Feb;55:79-92.
8. Sia TY et al. Obstet Gyenecol. 2019;134(6):1132.
9. Tseng J et al. Gynecol Oncol. 2018;150(1):44.
10. Schmeler K et al. Int J Gynecol Cancer. 2019;29:A14-5.
The significance of mismatch repair deficiency in endometrial cancer
Women with Lynch syndrome are known to carry an approximately 60% lifetime risk of endometrial cancer. These cancers result from inherited deleterious mutations in genes that code for mismatch repair proteins. However, mismatch repair deficiency (MMR-d) is not exclusively found in the tumors of patients with Lynch syndrome, and much is being learned about this group of endometrial cancers, their behavior, and their vulnerability to targeted therapies.
During the processes of DNA replication, recombination, or chemical and physical damage, mismatches in base pairs frequently occurs. Mismatch repair proteins function to identify and repair such errors, and the loss of their function causes the accumulation of the insertions or deletions of short, repetitive sequences of DNA. This phenomenon can be measured using polymerase chain reaction (PCR) screening of known microsatellites to look for the accumulation of errors, a phenotype which is called microsatellite instability (MSI). The accumulation of errors in DNA sequences is thought to lead to mutations in cancer-related genes.
The four predominant mismatch repair genes include MLH1, MSH2, MSH 6, and PMS2. These genes may possess loss of function through a germline/inherited mechanism, such as Lynch syndrome, or can be sporadically acquired. Approximately 20%-30% of endometrial cancers exhibit MMR-d with acquired, sporadic losses in function being the majority of cases and only approximately 10% a result of Lynch syndrome. Mutations in PMS2 are the dominant genotype of Lynch syndrome, whereas loss of function in MLH1 is most frequent aberration in sporadic cases of MMR-d endometrial cancer.1
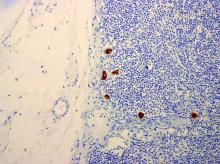
Endometrial cancers can be tested for MMR-d by performing immunohistochemistry to look for loss of expression in the four most common MMR genes. If there is loss of expression of MLH1, additional triage testing can be performed to determine if this loss is caused by the epigenetic phenomenon of hypermethylation. When present, this excludes Lynch syndrome and suggests a sporadic form origin of the disease. If there is loss of expression of the MMR genes (including loss of MLH1 and subsequent negative testing for promotor methylation), the patient should receive genetic testing for the presence of a germline mutation indicating Lynch syndrome. As an adjunct or alternative to immunohistochemistry, PCR studies or next-generation sequencing can be used to measure the presence of microsatellite instability in a process that identifies the expansion or reduction in repetitive DNA sequences of the tumor, compared with normal tumor.2
It is of the highest importance to identify endometrial cancers caused by Lynch syndrome because this enables providers to offer cascade testing of relatives, and to intensify screening or preventative measures for the many other cancers (such as colon, upper gastrointestinal, breast, and urothelial) for which these patients are at risk. Therefore, routine screening for MMR-d tumors is recommended in all cases of endometrial cancer, not simply those of a young age at diagnosis or for whom a strong family history exists.3 Using family history factors, primary tumor site, and age as a trigger for screening for Lynch syndrome, such as the Bethesda Guidelines, is associated with a 82% sensitivity in identifying Lynch syndrome. In a meta-analysis including testing results from 1,159 women with endometrial cancer, 43% of patients who were diagnosed with Lynch syndrome via molecular analysis would have been missed by clinical screening using Bethesda Guidelines.2
Discovering cases of Lynch syndrome is not the only benefit of routine testing for MMR-d in endometrial cancers. There is also significant value in the characterization of sporadic mismatch repair–deficient tumors because this information provides prognostic information and guides therapy. Tumors with a microsatellite-high phenotype/MMR-d were identified as one of the four distinct molecular subgroups of endometrial cancer by the Cancer Genome Atlas.4 Patients with this molecular profile exhibited “intermediate” prognostic outcomes, performing better than the “serous-like” cancers with p53 mutations, yet worse than patients with a POLE ultramutated group who rarely experience recurrences or death, even in the setting of unfavorable histology.
Beyond prognostication, the molecular profile of endometrial cancers also influence their responsiveness to therapeutics, highlighting the importance of splitting, not lumping endometrial cancers into relevant molecular subgroups when designing research and practicing clinical medicine. The PORTEC-3 trial studied 410 women with high-risk endometrial cancer, and randomized participants to receive either adjuvant radiation alone, or radiation with chemotherapy.5 There were no differences in progression-free survival between the two therapeutic strategies when analyzed in aggregate. However, when analyzed by Cancer Genome Atlas molecular subgroup, it was noted that there was a clear benefit from chemotherapy for patients with p53 mutations. For patients with MMR-d tumors, no such benefit was observed. Patients assigned this molecular subgroup did no better with the addition of platinum and taxane chemotherapy over radiation alone. Unfortunately, for patients with MMR-d tumors, recurrence rates remained high, suggesting that we can and need to discover more effective therapies for these tumors than what is available with conventional radiation or platinum and taxane chemotherapy. Targeted therapy may be the solution to this problem. Through microsatellite instability, MMR-d tumors create somatic mutations which result in neoantigens, an immunogenic environment. This state up-regulates checkpoint inhibitor proteins, which serve as an actionable target for anti-PD-L1 antibodies, such as the drug pembrolizumab which has been shown to be highly active against MMR-d endometrial cancer. In the landmark, KEYNOTE-158 trial, patients with advanced, recurrent solid tumors that exhibited MMR-d were treated with pembrolizumab.6 This included 49 patients with endometrial cancer, among whom there was a 79% response rate. Subsequently, pembrolizumab was granted Food and Drug Administration approval for use in advanced, recurrent MMR-d/MSI-high endometrial cancer. Trials are currently enrolling patients to explore the utility of this drug in the up-front setting in both early- and late-stage disease with a hope that this targeted therapy can do what conventional cytotoxic chemotherapy has failed to do.
Therefore, given the clinical significance of mismatch repair deficiency, all patients with endometrial cancer should be investigated for loss of expression in these proteins, and if present, considered for the possibility of Lynch syndrome. While most will not have an inherited cause, this information regarding their tumor biology remains critically important in both prognostication and decision-making surrounding other therapies and their eligibility for promising clinical trials.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no conflicts of interest to declare. Email her at [email protected].
References
1. Simpkins SB et al. Hum. Mol. Genet. 1999;8:661-6.
2. Kahn R et al. Cancer. 2019 Sep 15;125(18):2172-3183.
3. SGO Clinical Practice Statement: Screening for Lynch Syndrome in Endometrial Cancer. https://www.sgo.org/clinical-practice/guidelines/screening-for-lynch-syndrome-in-endometrial-cancer/
4. Kandoth et al. Nature. 2013;497(7447):67-73.
5. Leon-Castillo A et al. J Clin Oncol. 2020 Oct 10;38(29):3388-97.
6. Marabelle A et al. J Clin Oncol. 2020 Jan 1;38(1):1-10.
Women with Lynch syndrome are known to carry an approximately 60% lifetime risk of endometrial cancer. These cancers result from inherited deleterious mutations in genes that code for mismatch repair proteins. However, mismatch repair deficiency (MMR-d) is not exclusively found in the tumors of patients with Lynch syndrome, and much is being learned about this group of endometrial cancers, their behavior, and their vulnerability to targeted therapies.
During the processes of DNA replication, recombination, or chemical and physical damage, mismatches in base pairs frequently occurs. Mismatch repair proteins function to identify and repair such errors, and the loss of their function causes the accumulation of the insertions or deletions of short, repetitive sequences of DNA. This phenomenon can be measured using polymerase chain reaction (PCR) screening of known microsatellites to look for the accumulation of errors, a phenotype which is called microsatellite instability (MSI). The accumulation of errors in DNA sequences is thought to lead to mutations in cancer-related genes.
The four predominant mismatch repair genes include MLH1, MSH2, MSH 6, and PMS2. These genes may possess loss of function through a germline/inherited mechanism, such as Lynch syndrome, or can be sporadically acquired. Approximately 20%-30% of endometrial cancers exhibit MMR-d with acquired, sporadic losses in function being the majority of cases and only approximately 10% a result of Lynch syndrome. Mutations in PMS2 are the dominant genotype of Lynch syndrome, whereas loss of function in MLH1 is most frequent aberration in sporadic cases of MMR-d endometrial cancer.1
Endometrial cancers can be tested for MMR-d by performing immunohistochemistry to look for loss of expression in the four most common MMR genes. If there is loss of expression of MLH1, additional triage testing can be performed to determine if this loss is caused by the epigenetic phenomenon of hypermethylation. When present, this excludes Lynch syndrome and suggests a sporadic form origin of the disease. If there is loss of expression of the MMR genes (including loss of MLH1 and subsequent negative testing for promotor methylation), the patient should receive genetic testing for the presence of a germline mutation indicating Lynch syndrome. As an adjunct or alternative to immunohistochemistry, PCR studies or next-generation sequencing can be used to measure the presence of microsatellite instability in a process that identifies the expansion or reduction in repetitive DNA sequences of the tumor, compared with normal tumor.2
It is of the highest importance to identify endometrial cancers caused by Lynch syndrome because this enables providers to offer cascade testing of relatives, and to intensify screening or preventative measures for the many other cancers (such as colon, upper gastrointestinal, breast, and urothelial) for which these patients are at risk. Therefore, routine screening for MMR-d tumors is recommended in all cases of endometrial cancer, not simply those of a young age at diagnosis or for whom a strong family history exists.3 Using family history factors, primary tumor site, and age as a trigger for screening for Lynch syndrome, such as the Bethesda Guidelines, is associated with a 82% sensitivity in identifying Lynch syndrome. In a meta-analysis including testing results from 1,159 women with endometrial cancer, 43% of patients who were diagnosed with Lynch syndrome via molecular analysis would have been missed by clinical screening using Bethesda Guidelines.2
Discovering cases of Lynch syndrome is not the only benefit of routine testing for MMR-d in endometrial cancers. There is also significant value in the characterization of sporadic mismatch repair–deficient tumors because this information provides prognostic information and guides therapy. Tumors with a microsatellite-high phenotype/MMR-d were identified as one of the four distinct molecular subgroups of endometrial cancer by the Cancer Genome Atlas.4 Patients with this molecular profile exhibited “intermediate” prognostic outcomes, performing better than the “serous-like” cancers with p53 mutations, yet worse than patients with a POLE ultramutated group who rarely experience recurrences or death, even in the setting of unfavorable histology.
Beyond prognostication, the molecular profile of endometrial cancers also influence their responsiveness to therapeutics, highlighting the importance of splitting, not lumping endometrial cancers into relevant molecular subgroups when designing research and practicing clinical medicine. The PORTEC-3 trial studied 410 women with high-risk endometrial cancer, and randomized participants to receive either adjuvant radiation alone, or radiation with chemotherapy.5 There were no differences in progression-free survival between the two therapeutic strategies when analyzed in aggregate. However, when analyzed by Cancer Genome Atlas molecular subgroup, it was noted that there was a clear benefit from chemotherapy for patients with p53 mutations. For patients with MMR-d tumors, no such benefit was observed. Patients assigned this molecular subgroup did no better with the addition of platinum and taxane chemotherapy over radiation alone. Unfortunately, for patients with MMR-d tumors, recurrence rates remained high, suggesting that we can and need to discover more effective therapies for these tumors than what is available with conventional radiation or platinum and taxane chemotherapy. Targeted therapy may be the solution to this problem. Through microsatellite instability, MMR-d tumors create somatic mutations which result in neoantigens, an immunogenic environment. This state up-regulates checkpoint inhibitor proteins, which serve as an actionable target for anti-PD-L1 antibodies, such as the drug pembrolizumab which has been shown to be highly active against MMR-d endometrial cancer. In the landmark, KEYNOTE-158 trial, patients with advanced, recurrent solid tumors that exhibited MMR-d were treated with pembrolizumab.6 This included 49 patients with endometrial cancer, among whom there was a 79% response rate. Subsequently, pembrolizumab was granted Food and Drug Administration approval for use in advanced, recurrent MMR-d/MSI-high endometrial cancer. Trials are currently enrolling patients to explore the utility of this drug in the up-front setting in both early- and late-stage disease with a hope that this targeted therapy can do what conventional cytotoxic chemotherapy has failed to do.
Therefore, given the clinical significance of mismatch repair deficiency, all patients with endometrial cancer should be investigated for loss of expression in these proteins, and if present, considered for the possibility of Lynch syndrome. While most will not have an inherited cause, this information regarding their tumor biology remains critically important in both prognostication and decision-making surrounding other therapies and their eligibility for promising clinical trials.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no conflicts of interest to declare. Email her at [email protected].
References
1. Simpkins SB et al. Hum. Mol. Genet. 1999;8:661-6.
2. Kahn R et al. Cancer. 2019 Sep 15;125(18):2172-3183.
3. SGO Clinical Practice Statement: Screening for Lynch Syndrome in Endometrial Cancer. https://www.sgo.org/clinical-practice/guidelines/screening-for-lynch-syndrome-in-endometrial-cancer/
4. Kandoth et al. Nature. 2013;497(7447):67-73.
5. Leon-Castillo A et al. J Clin Oncol. 2020 Oct 10;38(29):3388-97.
6. Marabelle A et al. J Clin Oncol. 2020 Jan 1;38(1):1-10.
Women with Lynch syndrome are known to carry an approximately 60% lifetime risk of endometrial cancer. These cancers result from inherited deleterious mutations in genes that code for mismatch repair proteins. However, mismatch repair deficiency (MMR-d) is not exclusively found in the tumors of patients with Lynch syndrome, and much is being learned about this group of endometrial cancers, their behavior, and their vulnerability to targeted therapies.
During the processes of DNA replication, recombination, or chemical and physical damage, mismatches in base pairs frequently occurs. Mismatch repair proteins function to identify and repair such errors, and the loss of their function causes the accumulation of the insertions or deletions of short, repetitive sequences of DNA. This phenomenon can be measured using polymerase chain reaction (PCR) screening of known microsatellites to look for the accumulation of errors, a phenotype which is called microsatellite instability (MSI). The accumulation of errors in DNA sequences is thought to lead to mutations in cancer-related genes.
The four predominant mismatch repair genes include MLH1, MSH2, MSH 6, and PMS2. These genes may possess loss of function through a germline/inherited mechanism, such as Lynch syndrome, or can be sporadically acquired. Approximately 20%-30% of endometrial cancers exhibit MMR-d with acquired, sporadic losses in function being the majority of cases and only approximately 10% a result of Lynch syndrome. Mutations in PMS2 are the dominant genotype of Lynch syndrome, whereas loss of function in MLH1 is most frequent aberration in sporadic cases of MMR-d endometrial cancer.1
Endometrial cancers can be tested for MMR-d by performing immunohistochemistry to look for loss of expression in the four most common MMR genes. If there is loss of expression of MLH1, additional triage testing can be performed to determine if this loss is caused by the epigenetic phenomenon of hypermethylation. When present, this excludes Lynch syndrome and suggests a sporadic form origin of the disease. If there is loss of expression of the MMR genes (including loss of MLH1 and subsequent negative testing for promotor methylation), the patient should receive genetic testing for the presence of a germline mutation indicating Lynch syndrome. As an adjunct or alternative to immunohistochemistry, PCR studies or next-generation sequencing can be used to measure the presence of microsatellite instability in a process that identifies the expansion or reduction in repetitive DNA sequences of the tumor, compared with normal tumor.2
It is of the highest importance to identify endometrial cancers caused by Lynch syndrome because this enables providers to offer cascade testing of relatives, and to intensify screening or preventative measures for the many other cancers (such as colon, upper gastrointestinal, breast, and urothelial) for which these patients are at risk. Therefore, routine screening for MMR-d tumors is recommended in all cases of endometrial cancer, not simply those of a young age at diagnosis or for whom a strong family history exists.3 Using family history factors, primary tumor site, and age as a trigger for screening for Lynch syndrome, such as the Bethesda Guidelines, is associated with a 82% sensitivity in identifying Lynch syndrome. In a meta-analysis including testing results from 1,159 women with endometrial cancer, 43% of patients who were diagnosed with Lynch syndrome via molecular analysis would have been missed by clinical screening using Bethesda Guidelines.2
Discovering cases of Lynch syndrome is not the only benefit of routine testing for MMR-d in endometrial cancers. There is also significant value in the characterization of sporadic mismatch repair–deficient tumors because this information provides prognostic information and guides therapy. Tumors with a microsatellite-high phenotype/MMR-d were identified as one of the four distinct molecular subgroups of endometrial cancer by the Cancer Genome Atlas.4 Patients with this molecular profile exhibited “intermediate” prognostic outcomes, performing better than the “serous-like” cancers with p53 mutations, yet worse than patients with a POLE ultramutated group who rarely experience recurrences or death, even in the setting of unfavorable histology.
Beyond prognostication, the molecular profile of endometrial cancers also influence their responsiveness to therapeutics, highlighting the importance of splitting, not lumping endometrial cancers into relevant molecular subgroups when designing research and practicing clinical medicine. The PORTEC-3 trial studied 410 women with high-risk endometrial cancer, and randomized participants to receive either adjuvant radiation alone, or radiation with chemotherapy.5 There were no differences in progression-free survival between the two therapeutic strategies when analyzed in aggregate. However, when analyzed by Cancer Genome Atlas molecular subgroup, it was noted that there was a clear benefit from chemotherapy for patients with p53 mutations. For patients with MMR-d tumors, no such benefit was observed. Patients assigned this molecular subgroup did no better with the addition of platinum and taxane chemotherapy over radiation alone. Unfortunately, for patients with MMR-d tumors, recurrence rates remained high, suggesting that we can and need to discover more effective therapies for these tumors than what is available with conventional radiation or platinum and taxane chemotherapy. Targeted therapy may be the solution to this problem. Through microsatellite instability, MMR-d tumors create somatic mutations which result in neoantigens, an immunogenic environment. This state up-regulates checkpoint inhibitor proteins, which serve as an actionable target for anti-PD-L1 antibodies, such as the drug pembrolizumab which has been shown to be highly active against MMR-d endometrial cancer. In the landmark, KEYNOTE-158 trial, patients with advanced, recurrent solid tumors that exhibited MMR-d were treated with pembrolizumab.6 This included 49 patients with endometrial cancer, among whom there was a 79% response rate. Subsequently, pembrolizumab was granted Food and Drug Administration approval for use in advanced, recurrent MMR-d/MSI-high endometrial cancer. Trials are currently enrolling patients to explore the utility of this drug in the up-front setting in both early- and late-stage disease with a hope that this targeted therapy can do what conventional cytotoxic chemotherapy has failed to do.
Therefore, given the clinical significance of mismatch repair deficiency, all patients with endometrial cancer should be investigated for loss of expression in these proteins, and if present, considered for the possibility of Lynch syndrome. While most will not have an inherited cause, this information regarding their tumor biology remains critically important in both prognostication and decision-making surrounding other therapies and their eligibility for promising clinical trials.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no conflicts of interest to declare. Email her at [email protected].
References
1. Simpkins SB et al. Hum. Mol. Genet. 1999;8:661-6.
2. Kahn R et al. Cancer. 2019 Sep 15;125(18):2172-3183.
3. SGO Clinical Practice Statement: Screening for Lynch Syndrome in Endometrial Cancer. https://www.sgo.org/clinical-practice/guidelines/screening-for-lynch-syndrome-in-endometrial-cancer/
4. Kandoth et al. Nature. 2013;497(7447):67-73.
5. Leon-Castillo A et al. J Clin Oncol. 2020 Oct 10;38(29):3388-97.
6. Marabelle A et al. J Clin Oncol. 2020 Jan 1;38(1):1-10.
Neoadjuvant chemotherapy for advanced ovarian cancer
Historically the standard treatment approach for advanced ovarian cancer has been to perform up-front primary cytoreduction surgery or primary “debulking” surgery (PDS) followed by adjuvant chemotherapy. The goal of surgery was to establish cytoreduction of the tumor to optimal (<1 cm3 disease) or, ideally, complete (no gross residual disease). While PDS has long been considered the default treatment approach, neoadjuvant chemotherapy (NACT) followed by interval cytoreductive surgery, typically after three or four cycles of chemotherapy, was the alternative strategy if it was anticipated or known that an “optimal” cytoreduction was not possible, feasible, or associated with acceptable morbidity. However, NACT was, and to some degree still is, widely considered the inferior strategy, reserved for patients with the worst prognosis. While mounting data challenges the inherent superiority of PDS, it still largely remains the default.
Why was PDS considered superior?
Why was PDS for advanced ovarian cancer considered a superior sequencing when it is so rarely considered appropriate for other disseminated cancers? This was born from the observation among retrospective data showing that survival was best when surgery was performed first, and when surgery was able to remove most or all visible disease (“complete” or “optimal” cytoreduction), NACT was performed.1 Several theories were proposed to explain the observations. These included the theory that bulky tumors contained avascular regions that would be less well accessed by chemotherapy, as well as the notion that chemotherapy exerts a constant fraction of kill on tumor cells, and if there is a lower burden of tumor cells to begin with, fewer cycles of chemotherapy will be necessary to eliminate all cells. Coupled with this was the notion that, if fewer cycles of chemotherapy are necessary, there would be less opportunity for development of drug resistance. Other theories such as the inflammatory effects of surgery impacting immune-mediated kill of malignant cells also are reported. These theories were largely found in the pages of textbooks, only supported by heavily biased observational series and not in the results of elegant translational studies. Of course, the observed superiority of PDS in these cohort studies was not surprising given that the patients who were historically selected for NACT had their treatment course chosen specifically for their poor prognostic factors (large volume, unresectable disease, poor performance status, and comorbidities). These “studies” were self-fulfilling prophecies.
Anecdotally I can attest that most patients are enthusiastic about a primary surgical approach to their advanced cancer. There is something concretely satisfying for patient and surgeon alike in the physical act of removing disease. As surgeons, if we believe that our added surgical effort will be rewarded with better outcomes for the patients, we will “try harder” in the operating room in order for them to do better. However, mounting data challenges whether it is our aggressive surgical effort as much as it is primary tumor biology that is the driver of prognosis in this disease. And aggressive primary surgery may add little other than perioperative morbidity.
Why that perspective may be changing
A culmination of many years of sophisticated translational research led by Anil Sood, MD, from the University of Texas MD Anderson Cancer Center, Houston, established there are fundamental biologic differences in the tumors of patients with ovarian cancer whose disease is amenable or not to a complete cytoreduction with PDS.2 In their work, the researchers sampled tumors from patients with advanced ovarian cancer who had been triaged either to PDS or NACT based on a standardized, validated laparoscopic algorithm that predicted a high probability of complete surgical resection. They performed pretreatment biopsies in both groups of patients and conducted a range of “omics” analyses to stratify these two subsets of patients – those who had a disease burden amenable to complete surgical resection versus those whose presenting disease burden exceeded an acceptable surgical effort). They identified several key molecular differences in the pretreatment biopsies of these two groups of patients, including alterations which might explain better or worse responses to therapy. These results suggest that the tumors of patients who go on to have successful PDS to no gross residual disease have different tumor biology to begin with. Otherwise said, perhaps it is favorable tumor biology that is associated with both a disease burden that is more amenable to both primary complete cytoreduction and better oncologic outcomes, rather than the surgical effort in and of itself.
This finding is supported by a study in which ovarian cancer survival outcomes were stratified by disease burden, surgical complexity scores, and postoperative residual disease among patients who were enrolled in GOG-182.3 Investigators led by Neil Horowitz, MD, created scores for surgical complexity, disease burden, and residual disease. They observed that the radicality of surgery (complexity score) was not an independent determinant of survival, but rather, patients who presented with a lower disease burden that required a less radical surgery had the best oncologic outcomes.
If the complexity of surgery does not influence outcomes as much as the predetermined, unmodifiable tumor biology, how should surgeons make decisions about the sequencing of treatment? Over the past 10 years, four randomized trials have been completed including more than 1,600 patients randomized to either PDS or NACT.4-7 All four have found no difference in the oncologic outcomes (progression-free or overall survival) between patients when randomized to PDS or NACT. While the statistical designs vary slightly, some being designed to look for noninferiority and others for superiority, they all showed that the sequence in which surgery and chemotherapy was performed mattered less than whether optimal cytoreduction was achieved when surgery was performed. As stated above, this phenomenon seems to be best determined by unmodifiable tumor biology. Unsurprisingly, these studies also have consistently found that perioperative outcomes (e.g., surgical complications, length of stay, death) were worse with PDS because of the higher surgical complexity that it demands. In the most recent SCORPION trial, rates of major postoperative complications in the PDS group were 25.9%, compared with only 7.6% in the NACT group (P < .0001) and all of the deaths from postoperative complications occurred in the PDS group at a rate of 8.3% (7 of 84 patients).7
Therefore, the wealth of data supports that oncologic outcomes are equivalent, and perioperative outcomes are improved for patients who undergo NACT for advanced, bulky ovarian cancer.
Why physicians still are questioning
Unfortunately, because ofthe nature of the disease, these prospective trials include heterogeneous populations of disease presentation, surgeon skill, and hospital settings. They have been criticized for achieving “low” rates of complete or optimal cytoreduction in the PDS arm. They also identified subgroups of patients who may do better with PDS (such as those with lower-volume stage IIIC disease) and those who have better outcomes with NACT (patients with stage IV disease). Therefore, not satisfied that we have definitively answered the question, a fifth randomized study, the TRUST trial, is underway.8 This study includes surgeons at high-volume institutions, purported to have the highest degree of skill and quality in executing radical debulking procedures. Perhaps this fifth trial will show that, if performed in the most skilled hands and quality settings, PDS is preferable to NACT. Perhaps. However, the generalizability of these results will be poor for all patients with advanced ovarian cancer, most of whom will have limited access to these highest-volume surgeons.
What can be agreed upon is that an individualized and nuanced approach is best for advanced ovarian cancer. There will be some patients who benefit from PDS (e.g., healthy, young patients with low-volume disease). However, for most patients, the bulk of prospective and translational research supports NACT as the default treatment course, associated with noninferior survival and superior perioperative outcomes (including postoperative death). While it may not be a one-size-fits-all approach, one could argue that NACT should be the default strategy, and surgeons should look for reasons to “opt in” to PDS in special circumstances guided by biomarkers such as imaging, tumor markers, clinical factors, and surgical findings.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at [email protected].
References
1. Gynecol Oncol. 2006 Dec. doi: 10.1016/j.ygyno.2006.06.025.
2. Cell Rep. 2020 Apr 14. doi: 10.1016/j.celrep.2020.03.066.
3. J Clin Oncol. 2015 Mar 10. doi: 10.1200/JCO.2014.56.3106.
4. N Engl J Med. 2010 Sep 2. doi: 10.1056/NEJMoa0908806.
5. Lancet. 2015 Jul 18. doi: 10.1016/S0140-6736(14)62223-6.
6. Eur J Cancer. 2020. doi: 10.1016/j.ejca.2020.02.020.
7. Int J Gynecol Cancer. 2020. doi: 10.1136/ijgc-2020-001640.
8. Int J Gynecol Cancer. 2019. doi: 10.1136/ijgc-2019-000682.
Historically the standard treatment approach for advanced ovarian cancer has been to perform up-front primary cytoreduction surgery or primary “debulking” surgery (PDS) followed by adjuvant chemotherapy. The goal of surgery was to establish cytoreduction of the tumor to optimal (<1 cm3 disease) or, ideally, complete (no gross residual disease). While PDS has long been considered the default treatment approach, neoadjuvant chemotherapy (NACT) followed by interval cytoreductive surgery, typically after three or four cycles of chemotherapy, was the alternative strategy if it was anticipated or known that an “optimal” cytoreduction was not possible, feasible, or associated with acceptable morbidity. However, NACT was, and to some degree still is, widely considered the inferior strategy, reserved for patients with the worst prognosis. While mounting data challenges the inherent superiority of PDS, it still largely remains the default.
Why was PDS considered superior?
Why was PDS for advanced ovarian cancer considered a superior sequencing when it is so rarely considered appropriate for other disseminated cancers? This was born from the observation among retrospective data showing that survival was best when surgery was performed first, and when surgery was able to remove most or all visible disease (“complete” or “optimal” cytoreduction), NACT was performed.1 Several theories were proposed to explain the observations. These included the theory that bulky tumors contained avascular regions that would be less well accessed by chemotherapy, as well as the notion that chemotherapy exerts a constant fraction of kill on tumor cells, and if there is a lower burden of tumor cells to begin with, fewer cycles of chemotherapy will be necessary to eliminate all cells. Coupled with this was the notion that, if fewer cycles of chemotherapy are necessary, there would be less opportunity for development of drug resistance. Other theories such as the inflammatory effects of surgery impacting immune-mediated kill of malignant cells also are reported. These theories were largely found in the pages of textbooks, only supported by heavily biased observational series and not in the results of elegant translational studies. Of course, the observed superiority of PDS in these cohort studies was not surprising given that the patients who were historically selected for NACT had their treatment course chosen specifically for their poor prognostic factors (large volume, unresectable disease, poor performance status, and comorbidities). These “studies” were self-fulfilling prophecies.
Anecdotally I can attest that most patients are enthusiastic about a primary surgical approach to their advanced cancer. There is something concretely satisfying for patient and surgeon alike in the physical act of removing disease. As surgeons, if we believe that our added surgical effort will be rewarded with better outcomes for the patients, we will “try harder” in the operating room in order for them to do better. However, mounting data challenges whether it is our aggressive surgical effort as much as it is primary tumor biology that is the driver of prognosis in this disease. And aggressive primary surgery may add little other than perioperative morbidity.
Why that perspective may be changing
A culmination of many years of sophisticated translational research led by Anil Sood, MD, from the University of Texas MD Anderson Cancer Center, Houston, established there are fundamental biologic differences in the tumors of patients with ovarian cancer whose disease is amenable or not to a complete cytoreduction with PDS.2 In their work, the researchers sampled tumors from patients with advanced ovarian cancer who had been triaged either to PDS or NACT based on a standardized, validated laparoscopic algorithm that predicted a high probability of complete surgical resection. They performed pretreatment biopsies in both groups of patients and conducted a range of “omics” analyses to stratify these two subsets of patients – those who had a disease burden amenable to complete surgical resection versus those whose presenting disease burden exceeded an acceptable surgical effort). They identified several key molecular differences in the pretreatment biopsies of these two groups of patients, including alterations which might explain better or worse responses to therapy. These results suggest that the tumors of patients who go on to have successful PDS to no gross residual disease have different tumor biology to begin with. Otherwise said, perhaps it is favorable tumor biology that is associated with both a disease burden that is more amenable to both primary complete cytoreduction and better oncologic outcomes, rather than the surgical effort in and of itself.
This finding is supported by a study in which ovarian cancer survival outcomes were stratified by disease burden, surgical complexity scores, and postoperative residual disease among patients who were enrolled in GOG-182.3 Investigators led by Neil Horowitz, MD, created scores for surgical complexity, disease burden, and residual disease. They observed that the radicality of surgery (complexity score) was not an independent determinant of survival, but rather, patients who presented with a lower disease burden that required a less radical surgery had the best oncologic outcomes.
If the complexity of surgery does not influence outcomes as much as the predetermined, unmodifiable tumor biology, how should surgeons make decisions about the sequencing of treatment? Over the past 10 years, four randomized trials have been completed including more than 1,600 patients randomized to either PDS or NACT.4-7 All four have found no difference in the oncologic outcomes (progression-free or overall survival) between patients when randomized to PDS or NACT. While the statistical designs vary slightly, some being designed to look for noninferiority and others for superiority, they all showed that the sequence in which surgery and chemotherapy was performed mattered less than whether optimal cytoreduction was achieved when surgery was performed. As stated above, this phenomenon seems to be best determined by unmodifiable tumor biology. Unsurprisingly, these studies also have consistently found that perioperative outcomes (e.g., surgical complications, length of stay, death) were worse with PDS because of the higher surgical complexity that it demands. In the most recent SCORPION trial, rates of major postoperative complications in the PDS group were 25.9%, compared with only 7.6% in the NACT group (P < .0001) and all of the deaths from postoperative complications occurred in the PDS group at a rate of 8.3% (7 of 84 patients).7
Therefore, the wealth of data supports that oncologic outcomes are equivalent, and perioperative outcomes are improved for patients who undergo NACT for advanced, bulky ovarian cancer.
Why physicians still are questioning
Unfortunately, because ofthe nature of the disease, these prospective trials include heterogeneous populations of disease presentation, surgeon skill, and hospital settings. They have been criticized for achieving “low” rates of complete or optimal cytoreduction in the PDS arm. They also identified subgroups of patients who may do better with PDS (such as those with lower-volume stage IIIC disease) and those who have better outcomes with NACT (patients with stage IV disease). Therefore, not satisfied that we have definitively answered the question, a fifth randomized study, the TRUST trial, is underway.8 This study includes surgeons at high-volume institutions, purported to have the highest degree of skill and quality in executing radical debulking procedures. Perhaps this fifth trial will show that, if performed in the most skilled hands and quality settings, PDS is preferable to NACT. Perhaps. However, the generalizability of these results will be poor for all patients with advanced ovarian cancer, most of whom will have limited access to these highest-volume surgeons.
What can be agreed upon is that an individualized and nuanced approach is best for advanced ovarian cancer. There will be some patients who benefit from PDS (e.g., healthy, young patients with low-volume disease). However, for most patients, the bulk of prospective and translational research supports NACT as the default treatment course, associated with noninferior survival and superior perioperative outcomes (including postoperative death). While it may not be a one-size-fits-all approach, one could argue that NACT should be the default strategy, and surgeons should look for reasons to “opt in” to PDS in special circumstances guided by biomarkers such as imaging, tumor markers, clinical factors, and surgical findings.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at [email protected].
References
1. Gynecol Oncol. 2006 Dec. doi: 10.1016/j.ygyno.2006.06.025.
2. Cell Rep. 2020 Apr 14. doi: 10.1016/j.celrep.2020.03.066.
3. J Clin Oncol. 2015 Mar 10. doi: 10.1200/JCO.2014.56.3106.
4. N Engl J Med. 2010 Sep 2. doi: 10.1056/NEJMoa0908806.
5. Lancet. 2015 Jul 18. doi: 10.1016/S0140-6736(14)62223-6.
6. Eur J Cancer. 2020. doi: 10.1016/j.ejca.2020.02.020.
7. Int J Gynecol Cancer. 2020. doi: 10.1136/ijgc-2020-001640.
8. Int J Gynecol Cancer. 2019. doi: 10.1136/ijgc-2019-000682.
Historically the standard treatment approach for advanced ovarian cancer has been to perform up-front primary cytoreduction surgery or primary “debulking” surgery (PDS) followed by adjuvant chemotherapy. The goal of surgery was to establish cytoreduction of the tumor to optimal (<1 cm3 disease) or, ideally, complete (no gross residual disease). While PDS has long been considered the default treatment approach, neoadjuvant chemotherapy (NACT) followed by interval cytoreductive surgery, typically after three or four cycles of chemotherapy, was the alternative strategy if it was anticipated or known that an “optimal” cytoreduction was not possible, feasible, or associated with acceptable morbidity. However, NACT was, and to some degree still is, widely considered the inferior strategy, reserved for patients with the worst prognosis. While mounting data challenges the inherent superiority of PDS, it still largely remains the default.
Why was PDS considered superior?
Why was PDS for advanced ovarian cancer considered a superior sequencing when it is so rarely considered appropriate for other disseminated cancers? This was born from the observation among retrospective data showing that survival was best when surgery was performed first, and when surgery was able to remove most or all visible disease (“complete” or “optimal” cytoreduction), NACT was performed.1 Several theories were proposed to explain the observations. These included the theory that bulky tumors contained avascular regions that would be less well accessed by chemotherapy, as well as the notion that chemotherapy exerts a constant fraction of kill on tumor cells, and if there is a lower burden of tumor cells to begin with, fewer cycles of chemotherapy will be necessary to eliminate all cells. Coupled with this was the notion that, if fewer cycles of chemotherapy are necessary, there would be less opportunity for development of drug resistance. Other theories such as the inflammatory effects of surgery impacting immune-mediated kill of malignant cells also are reported. These theories were largely found in the pages of textbooks, only supported by heavily biased observational series and not in the results of elegant translational studies. Of course, the observed superiority of PDS in these cohort studies was not surprising given that the patients who were historically selected for NACT had their treatment course chosen specifically for their poor prognostic factors (large volume, unresectable disease, poor performance status, and comorbidities). These “studies” were self-fulfilling prophecies.
Anecdotally I can attest that most patients are enthusiastic about a primary surgical approach to their advanced cancer. There is something concretely satisfying for patient and surgeon alike in the physical act of removing disease. As surgeons, if we believe that our added surgical effort will be rewarded with better outcomes for the patients, we will “try harder” in the operating room in order for them to do better. However, mounting data challenges whether it is our aggressive surgical effort as much as it is primary tumor biology that is the driver of prognosis in this disease. And aggressive primary surgery may add little other than perioperative morbidity.
Why that perspective may be changing
A culmination of many years of sophisticated translational research led by Anil Sood, MD, from the University of Texas MD Anderson Cancer Center, Houston, established there are fundamental biologic differences in the tumors of patients with ovarian cancer whose disease is amenable or not to a complete cytoreduction with PDS.2 In their work, the researchers sampled tumors from patients with advanced ovarian cancer who had been triaged either to PDS or NACT based on a standardized, validated laparoscopic algorithm that predicted a high probability of complete surgical resection. They performed pretreatment biopsies in both groups of patients and conducted a range of “omics” analyses to stratify these two subsets of patients – those who had a disease burden amenable to complete surgical resection versus those whose presenting disease burden exceeded an acceptable surgical effort). They identified several key molecular differences in the pretreatment biopsies of these two groups of patients, including alterations which might explain better or worse responses to therapy. These results suggest that the tumors of patients who go on to have successful PDS to no gross residual disease have different tumor biology to begin with. Otherwise said, perhaps it is favorable tumor biology that is associated with both a disease burden that is more amenable to both primary complete cytoreduction and better oncologic outcomes, rather than the surgical effort in and of itself.
This finding is supported by a study in which ovarian cancer survival outcomes were stratified by disease burden, surgical complexity scores, and postoperative residual disease among patients who were enrolled in GOG-182.3 Investigators led by Neil Horowitz, MD, created scores for surgical complexity, disease burden, and residual disease. They observed that the radicality of surgery (complexity score) was not an independent determinant of survival, but rather, patients who presented with a lower disease burden that required a less radical surgery had the best oncologic outcomes.
If the complexity of surgery does not influence outcomes as much as the predetermined, unmodifiable tumor biology, how should surgeons make decisions about the sequencing of treatment? Over the past 10 years, four randomized trials have been completed including more than 1,600 patients randomized to either PDS or NACT.4-7 All four have found no difference in the oncologic outcomes (progression-free or overall survival) between patients when randomized to PDS or NACT. While the statistical designs vary slightly, some being designed to look for noninferiority and others for superiority, they all showed that the sequence in which surgery and chemotherapy was performed mattered less than whether optimal cytoreduction was achieved when surgery was performed. As stated above, this phenomenon seems to be best determined by unmodifiable tumor biology. Unsurprisingly, these studies also have consistently found that perioperative outcomes (e.g., surgical complications, length of stay, death) were worse with PDS because of the higher surgical complexity that it demands. In the most recent SCORPION trial, rates of major postoperative complications in the PDS group were 25.9%, compared with only 7.6% in the NACT group (P < .0001) and all of the deaths from postoperative complications occurred in the PDS group at a rate of 8.3% (7 of 84 patients).7
Therefore, the wealth of data supports that oncologic outcomes are equivalent, and perioperative outcomes are improved for patients who undergo NACT for advanced, bulky ovarian cancer.
Why physicians still are questioning
Unfortunately, because ofthe nature of the disease, these prospective trials include heterogeneous populations of disease presentation, surgeon skill, and hospital settings. They have been criticized for achieving “low” rates of complete or optimal cytoreduction in the PDS arm. They also identified subgroups of patients who may do better with PDS (such as those with lower-volume stage IIIC disease) and those who have better outcomes with NACT (patients with stage IV disease). Therefore, not satisfied that we have definitively answered the question, a fifth randomized study, the TRUST trial, is underway.8 This study includes surgeons at high-volume institutions, purported to have the highest degree of skill and quality in executing radical debulking procedures. Perhaps this fifth trial will show that, if performed in the most skilled hands and quality settings, PDS is preferable to NACT. Perhaps. However, the generalizability of these results will be poor for all patients with advanced ovarian cancer, most of whom will have limited access to these highest-volume surgeons.
What can be agreed upon is that an individualized and nuanced approach is best for advanced ovarian cancer. There will be some patients who benefit from PDS (e.g., healthy, young patients with low-volume disease). However, for most patients, the bulk of prospective and translational research supports NACT as the default treatment course, associated with noninferior survival and superior perioperative outcomes (including postoperative death). While it may not be a one-size-fits-all approach, one could argue that NACT should be the default strategy, and surgeons should look for reasons to “opt in” to PDS in special circumstances guided by biomarkers such as imaging, tumor markers, clinical factors, and surgical findings.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at [email protected].
References
1. Gynecol Oncol. 2006 Dec. doi: 10.1016/j.ygyno.2006.06.025.
2. Cell Rep. 2020 Apr 14. doi: 10.1016/j.celrep.2020.03.066.
3. J Clin Oncol. 2015 Mar 10. doi: 10.1200/JCO.2014.56.3106.
4. N Engl J Med. 2010 Sep 2. doi: 10.1056/NEJMoa0908806.
5. Lancet. 2015 Jul 18. doi: 10.1016/S0140-6736(14)62223-6.
6. Eur J Cancer. 2020. doi: 10.1016/j.ejca.2020.02.020.
7. Int J Gynecol Cancer. 2020. doi: 10.1136/ijgc-2020-001640.
8. Int J Gynecol Cancer. 2019. doi: 10.1136/ijgc-2019-000682.
Should all patients with advanced ovarian cancer receive frontline maintenance therapy?
The current standard frontline therapy for advanced epithelial ovarian, fallopian tube, and primary peritoneal cancer includes a combination of surgical cytoreduction and at least six cycles of platinum-based chemotherapy. While this achieves a complete clinical response (“remission”) in most, 85% of patients will recur and eventually succumb to the disease. This suggests that treatments are good at inducing remission, but poor at eradicating the disease altogether. This has motivated the consideration of maintenance therapy: extended treatment beyond completion of chemotherapy during the period of time when patients are clinically disease free.
Maintenance therapy is an appealing concept for clinicians who desperately want to “hold” their patients in a disease-free state for longer periods. It is also a profitable way to administer therapy as there is more compensation to the pharmaceutical industry from chronic, long-term drug administration rather than episodic treatment courses. However, the following question must be asked: Is this extended therapy worthwhile for all patients, and is it good value?
In the past 12 months, three major industry-sponsored clinical trials have been published (PRIMA, PAOLA-1, and VELIA)which suggest a benefit for all patients with advanced epithelial ovarian cancer in receiving prolonged poly (ADP-ribose) polymerase inhibitor (PARPi) therapy after primary chemotherapy.1-3 This has resulted in Food and Drug Administration approval for some of these agents as maintenance therapy. Despite differences in the drugs tested and the timing of therapy, these studies observed that treatment of advanced ovarian cancer with the addition of a PARPi during and/or after carboplatin and paclitaxel chemotherapy for up to an additional 3 years resulted in a longer progression-free survival (PFS) of approximately 6 months. PFS is defined as the time to measurable recurrence or death. However, this positive effect was not equally distributed across the whole population; rather, it appeared to be created by a substantial response in a smaller subgroup.
PARP inhibitor therapies such as olaparib, niraparib, veliparib, and rucaparib target a family of enzymes that repair DNA and stabilize the human genome through the repair of single-stranded DNA breaks. Inhibiting these enzymes facilitates the accumulation of single-stranded breaks, allowing the development of double-strand breaks, which in turn cannot be repaired if the cell has deficient homologous recombination (HRD) such as through a germline or somatic BRCA mutation, or alternative relevant mutation that confers a similar effect. The opportunistic pairing of a drug interaction with a pathway specific to the cancer is an example of a targeted therapy.
In order to improve the value of cancer drug therapy, there has been emphasis by cooperative research groups, such as the Gynecologic Oncology Group, to study the efficacy of targeted therapies, such as PARPi, in patients identified by biomarkers such as tumors that possess germline or somatic HRD in whom they are most likely to work. This approach makes good common sense and promises to deliver a large magnitude of clinical benefit in a smaller focused population. Therefore, even if drug costs are high, the treatment may still have value. Consistent with that principle, the recently published VELIA, PRIMA, and PAOLA-1 trials all showed impressive benefit in PFS (on average 11-12 months) for the subgroup of patients with HRD. However, these studies were designed and funded by the pharmaceutical industry, and abandoned the principle of biomarker-driven targeted therapy. They did not limit their studies to the HRD-positive population most likely to benefit, but instead included and reported on the impact on all-comers (patients with both HRD and HR-proficient tumors). Subsequently their final conclusions could be extrapolated to the general population of ovarian cancer patients, and in doing so, a larger share of the marketplace.
Only 30% of the general population of ovarian, fallopian tube and primary peritoneal cancer patients carry a germline or somatic BRCA mutation and less than half carry this or alternative mutations which confer HRD. The remaining majority are HR-proficient tumors. However, the three study populations in the aforementioned trials were enriched for HRD tumors with 50%-60% subjects carrying germline or somatic HRD. Therefore, it is likely that the observed benefits in the “intent-to-treat” group were larger than what a clinician would observe in their patient population. Additionally, the large (11-12 month) gains in the HRD-positive group may have been so significant that they compensated for the subtle impact in the HR-proficient population (less than 3 months), resulting in an average total effect that, while being statistically significant for “all comers,” was actually only clinically significant for the HRD group. The positive impact for HRD tumors effectively boosted the results for the group as a whole.
The use of PFS as a primary endpoint raises another significant concern with the design of these PARPi maintenance trials. Much has been written about the importance of PFS as an endpoint for ovarian cancer because of confounding effects of subsequent therapy and to minimize the costs and duration of clinical trials.4 PFS is a quicker, less expensive endpoint to capture than overall survival. It usually correlates with overall survival, but typically only when there is a large magnitude of benefit in PFS. These arguments are fair when considering episodic drug therapies in the setting of measurable, active disease. However, maintenance therapy is given during a period of what patients think of as remission. Remission is valued by patients because it is a gateway to cure, and also because it is a time devoid of symptoms of disease, toxicity (therapeutic and financial), and the burden of frequent medical visits and interventions. While PFS is a measure of the length of remission, it is not a measure of cure. We should ask: What does it mean to a patient if she has a longer remission but needs to be on drug therapy (with its associated burdens and toxicities) in order to maintain that remission? We know that an increase in PFS with maintenance therapy does not always result in a commensurate increase in survival. One does not always precede the other. An example of this is the use of maintenance bevacizumab following upfront chemotherapy which improves PFS by 4 months, but is not associated with an increase in survival.5
When considering the value and ethics of maintenance therapy, it should be associated with a proven survival benefit or an improvement in quality of life. With respect to PARPi maintenance, we lack the data regarding the former, and have contrary evidence regarding the latter. In these three trials, PARPi maintenance was associated with significantly more toxicity than placebo including the commonly observed nausea and fatigue. Most of us would not like to be on a drug therapy for 3 years that made us feel nauseated or fatigued if it didn’t also increase our chance of cure or a longer life. While the significant PFS benefit of maintenance PARPi that is consistently observed in HRD-positive ovarian cancers suggests there will also likely be a clinically significant improvement in survival and cure in that specific subpopulation, this is less likely true for the majority of women with HR-proficient ovarian cancers. Time will tell this story, but as yet, we don’t know.
The use of maintenance PARPi therapy during and/or after primary cytotoxic chemotherapy for advanced epithelial ovarian, primary peritoneal, and fallopian tube cancer is associated with a substantial benefit in time to recurrence in a population with HRD tumors and a small benefit among the majority who don’t. However, it comes at the cost of toxicity at a time when patients would otherwise be free of disease and treatment. I propose that, until a survival benefit for all women has been observed, we should consider a targeted and biomarker-driven approach to maintenance PARPi prescription, favoring prescription for those with germline or somatic HRD mutations.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She said she had no relevant financial disclosures. Email Dr. Rossi at [email protected].
References
1. González-Martín A et al. N Engl J Med. 2019 Dec 19;381(25):2391-402.
2. Ray-Coquard I et al. N Engl J Med. 2019 Dec 19;381(25):2416-28.
3. Coleman RL et al. N Engl J Med. 2019 Dec 19;381(25):2403-15.
4. Herzog TJ et al. Gynecol Oncol. 2014 Jan;132(1):8-17.
5. Tewari KS et al. J Clin Oncol. 2019 Sep 10;37(26):2317-28.
The current standard frontline therapy for advanced epithelial ovarian, fallopian tube, and primary peritoneal cancer includes a combination of surgical cytoreduction and at least six cycles of platinum-based chemotherapy. While this achieves a complete clinical response (“remission”) in most, 85% of patients will recur and eventually succumb to the disease. This suggests that treatments are good at inducing remission, but poor at eradicating the disease altogether. This has motivated the consideration of maintenance therapy: extended treatment beyond completion of chemotherapy during the period of time when patients are clinically disease free.
Maintenance therapy is an appealing concept for clinicians who desperately want to “hold” their patients in a disease-free state for longer periods. It is also a profitable way to administer therapy as there is more compensation to the pharmaceutical industry from chronic, long-term drug administration rather than episodic treatment courses. However, the following question must be asked: Is this extended therapy worthwhile for all patients, and is it good value?
In the past 12 months, three major industry-sponsored clinical trials have been published (PRIMA, PAOLA-1, and VELIA)which suggest a benefit for all patients with advanced epithelial ovarian cancer in receiving prolonged poly (ADP-ribose) polymerase inhibitor (PARPi) therapy after primary chemotherapy.1-3 This has resulted in Food and Drug Administration approval for some of these agents as maintenance therapy. Despite differences in the drugs tested and the timing of therapy, these studies observed that treatment of advanced ovarian cancer with the addition of a PARPi during and/or after carboplatin and paclitaxel chemotherapy for up to an additional 3 years resulted in a longer progression-free survival (PFS) of approximately 6 months. PFS is defined as the time to measurable recurrence or death. However, this positive effect was not equally distributed across the whole population; rather, it appeared to be created by a substantial response in a smaller subgroup.
PARP inhibitor therapies such as olaparib, niraparib, veliparib, and rucaparib target a family of enzymes that repair DNA and stabilize the human genome through the repair of single-stranded DNA breaks. Inhibiting these enzymes facilitates the accumulation of single-stranded breaks, allowing the development of double-strand breaks, which in turn cannot be repaired if the cell has deficient homologous recombination (HRD) such as through a germline or somatic BRCA mutation, or alternative relevant mutation that confers a similar effect. The opportunistic pairing of a drug interaction with a pathway specific to the cancer is an example of a targeted therapy.
In order to improve the value of cancer drug therapy, there has been emphasis by cooperative research groups, such as the Gynecologic Oncology Group, to study the efficacy of targeted therapies, such as PARPi, in patients identified by biomarkers such as tumors that possess germline or somatic HRD in whom they are most likely to work. This approach makes good common sense and promises to deliver a large magnitude of clinical benefit in a smaller focused population. Therefore, even if drug costs are high, the treatment may still have value. Consistent with that principle, the recently published VELIA, PRIMA, and PAOLA-1 trials all showed impressive benefit in PFS (on average 11-12 months) for the subgroup of patients with HRD. However, these studies were designed and funded by the pharmaceutical industry, and abandoned the principle of biomarker-driven targeted therapy. They did not limit their studies to the HRD-positive population most likely to benefit, but instead included and reported on the impact on all-comers (patients with both HRD and HR-proficient tumors). Subsequently their final conclusions could be extrapolated to the general population of ovarian cancer patients, and in doing so, a larger share of the marketplace.
Only 30% of the general population of ovarian, fallopian tube and primary peritoneal cancer patients carry a germline or somatic BRCA mutation and less than half carry this or alternative mutations which confer HRD. The remaining majority are HR-proficient tumors. However, the three study populations in the aforementioned trials were enriched for HRD tumors with 50%-60% subjects carrying germline or somatic HRD. Therefore, it is likely that the observed benefits in the “intent-to-treat” group were larger than what a clinician would observe in their patient population. Additionally, the large (11-12 month) gains in the HRD-positive group may have been so significant that they compensated for the subtle impact in the HR-proficient population (less than 3 months), resulting in an average total effect that, while being statistically significant for “all comers,” was actually only clinically significant for the HRD group. The positive impact for HRD tumors effectively boosted the results for the group as a whole.
The use of PFS as a primary endpoint raises another significant concern with the design of these PARPi maintenance trials. Much has been written about the importance of PFS as an endpoint for ovarian cancer because of confounding effects of subsequent therapy and to minimize the costs and duration of clinical trials.4 PFS is a quicker, less expensive endpoint to capture than overall survival. It usually correlates with overall survival, but typically only when there is a large magnitude of benefit in PFS. These arguments are fair when considering episodic drug therapies in the setting of measurable, active disease. However, maintenance therapy is given during a period of what patients think of as remission. Remission is valued by patients because it is a gateway to cure, and also because it is a time devoid of symptoms of disease, toxicity (therapeutic and financial), and the burden of frequent medical visits and interventions. While PFS is a measure of the length of remission, it is not a measure of cure. We should ask: What does it mean to a patient if she has a longer remission but needs to be on drug therapy (with its associated burdens and toxicities) in order to maintain that remission? We know that an increase in PFS with maintenance therapy does not always result in a commensurate increase in survival. One does not always precede the other. An example of this is the use of maintenance bevacizumab following upfront chemotherapy which improves PFS by 4 months, but is not associated with an increase in survival.5
When considering the value and ethics of maintenance therapy, it should be associated with a proven survival benefit or an improvement in quality of life. With respect to PARPi maintenance, we lack the data regarding the former, and have contrary evidence regarding the latter. In these three trials, PARPi maintenance was associated with significantly more toxicity than placebo including the commonly observed nausea and fatigue. Most of us would not like to be on a drug therapy for 3 years that made us feel nauseated or fatigued if it didn’t also increase our chance of cure or a longer life. While the significant PFS benefit of maintenance PARPi that is consistently observed in HRD-positive ovarian cancers suggests there will also likely be a clinically significant improvement in survival and cure in that specific subpopulation, this is less likely true for the majority of women with HR-proficient ovarian cancers. Time will tell this story, but as yet, we don’t know.
The use of maintenance PARPi therapy during and/or after primary cytotoxic chemotherapy for advanced epithelial ovarian, primary peritoneal, and fallopian tube cancer is associated with a substantial benefit in time to recurrence in a population with HRD tumors and a small benefit among the majority who don’t. However, it comes at the cost of toxicity at a time when patients would otherwise be free of disease and treatment. I propose that, until a survival benefit for all women has been observed, we should consider a targeted and biomarker-driven approach to maintenance PARPi prescription, favoring prescription for those with germline or somatic HRD mutations.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She said she had no relevant financial disclosures. Email Dr. Rossi at [email protected].
References
1. González-Martín A et al. N Engl J Med. 2019 Dec 19;381(25):2391-402.
2. Ray-Coquard I et al. N Engl J Med. 2019 Dec 19;381(25):2416-28.
3. Coleman RL et al. N Engl J Med. 2019 Dec 19;381(25):2403-15.
4. Herzog TJ et al. Gynecol Oncol. 2014 Jan;132(1):8-17.
5. Tewari KS et al. J Clin Oncol. 2019 Sep 10;37(26):2317-28.
The current standard frontline therapy for advanced epithelial ovarian, fallopian tube, and primary peritoneal cancer includes a combination of surgical cytoreduction and at least six cycles of platinum-based chemotherapy. While this achieves a complete clinical response (“remission”) in most, 85% of patients will recur and eventually succumb to the disease. This suggests that treatments are good at inducing remission, but poor at eradicating the disease altogether. This has motivated the consideration of maintenance therapy: extended treatment beyond completion of chemotherapy during the period of time when patients are clinically disease free.
Maintenance therapy is an appealing concept for clinicians who desperately want to “hold” their patients in a disease-free state for longer periods. It is also a profitable way to administer therapy as there is more compensation to the pharmaceutical industry from chronic, long-term drug administration rather than episodic treatment courses. However, the following question must be asked: Is this extended therapy worthwhile for all patients, and is it good value?
In the past 12 months, three major industry-sponsored clinical trials have been published (PRIMA, PAOLA-1, and VELIA)which suggest a benefit for all patients with advanced epithelial ovarian cancer in receiving prolonged poly (ADP-ribose) polymerase inhibitor (PARPi) therapy after primary chemotherapy.1-3 This has resulted in Food and Drug Administration approval for some of these agents as maintenance therapy. Despite differences in the drugs tested and the timing of therapy, these studies observed that treatment of advanced ovarian cancer with the addition of a PARPi during and/or after carboplatin and paclitaxel chemotherapy for up to an additional 3 years resulted in a longer progression-free survival (PFS) of approximately 6 months. PFS is defined as the time to measurable recurrence or death. However, this positive effect was not equally distributed across the whole population; rather, it appeared to be created by a substantial response in a smaller subgroup.
PARP inhibitor therapies such as olaparib, niraparib, veliparib, and rucaparib target a family of enzymes that repair DNA and stabilize the human genome through the repair of single-stranded DNA breaks. Inhibiting these enzymes facilitates the accumulation of single-stranded breaks, allowing the development of double-strand breaks, which in turn cannot be repaired if the cell has deficient homologous recombination (HRD) such as through a germline or somatic BRCA mutation, or alternative relevant mutation that confers a similar effect. The opportunistic pairing of a drug interaction with a pathway specific to the cancer is an example of a targeted therapy.
In order to improve the value of cancer drug therapy, there has been emphasis by cooperative research groups, such as the Gynecologic Oncology Group, to study the efficacy of targeted therapies, such as PARPi, in patients identified by biomarkers such as tumors that possess germline or somatic HRD in whom they are most likely to work. This approach makes good common sense and promises to deliver a large magnitude of clinical benefit in a smaller focused population. Therefore, even if drug costs are high, the treatment may still have value. Consistent with that principle, the recently published VELIA, PRIMA, and PAOLA-1 trials all showed impressive benefit in PFS (on average 11-12 months) for the subgroup of patients with HRD. However, these studies were designed and funded by the pharmaceutical industry, and abandoned the principle of biomarker-driven targeted therapy. They did not limit their studies to the HRD-positive population most likely to benefit, but instead included and reported on the impact on all-comers (patients with both HRD and HR-proficient tumors). Subsequently their final conclusions could be extrapolated to the general population of ovarian cancer patients, and in doing so, a larger share of the marketplace.
Only 30% of the general population of ovarian, fallopian tube and primary peritoneal cancer patients carry a germline or somatic BRCA mutation and less than half carry this or alternative mutations which confer HRD. The remaining majority are HR-proficient tumors. However, the three study populations in the aforementioned trials were enriched for HRD tumors with 50%-60% subjects carrying germline or somatic HRD. Therefore, it is likely that the observed benefits in the “intent-to-treat” group were larger than what a clinician would observe in their patient population. Additionally, the large (11-12 month) gains in the HRD-positive group may have been so significant that they compensated for the subtle impact in the HR-proficient population (less than 3 months), resulting in an average total effect that, while being statistically significant for “all comers,” was actually only clinically significant for the HRD group. The positive impact for HRD tumors effectively boosted the results for the group as a whole.
The use of PFS as a primary endpoint raises another significant concern with the design of these PARPi maintenance trials. Much has been written about the importance of PFS as an endpoint for ovarian cancer because of confounding effects of subsequent therapy and to minimize the costs and duration of clinical trials.4 PFS is a quicker, less expensive endpoint to capture than overall survival. It usually correlates with overall survival, but typically only when there is a large magnitude of benefit in PFS. These arguments are fair when considering episodic drug therapies in the setting of measurable, active disease. However, maintenance therapy is given during a period of what patients think of as remission. Remission is valued by patients because it is a gateway to cure, and also because it is a time devoid of symptoms of disease, toxicity (therapeutic and financial), and the burden of frequent medical visits and interventions. While PFS is a measure of the length of remission, it is not a measure of cure. We should ask: What does it mean to a patient if she has a longer remission but needs to be on drug therapy (with its associated burdens and toxicities) in order to maintain that remission? We know that an increase in PFS with maintenance therapy does not always result in a commensurate increase in survival. One does not always precede the other. An example of this is the use of maintenance bevacizumab following upfront chemotherapy which improves PFS by 4 months, but is not associated with an increase in survival.5
When considering the value and ethics of maintenance therapy, it should be associated with a proven survival benefit or an improvement in quality of life. With respect to PARPi maintenance, we lack the data regarding the former, and have contrary evidence regarding the latter. In these three trials, PARPi maintenance was associated with significantly more toxicity than placebo including the commonly observed nausea and fatigue. Most of us would not like to be on a drug therapy for 3 years that made us feel nauseated or fatigued if it didn’t also increase our chance of cure or a longer life. While the significant PFS benefit of maintenance PARPi that is consistently observed in HRD-positive ovarian cancers suggests there will also likely be a clinically significant improvement in survival and cure in that specific subpopulation, this is less likely true for the majority of women with HR-proficient ovarian cancers. Time will tell this story, but as yet, we don’t know.
The use of maintenance PARPi therapy during and/or after primary cytotoxic chemotherapy for advanced epithelial ovarian, primary peritoneal, and fallopian tube cancer is associated with a substantial benefit in time to recurrence in a population with HRD tumors and a small benefit among the majority who don’t. However, it comes at the cost of toxicity at a time when patients would otherwise be free of disease and treatment. I propose that, until a survival benefit for all women has been observed, we should consider a targeted and biomarker-driven approach to maintenance PARPi prescription, favoring prescription for those with germline or somatic HRD mutations.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She said she had no relevant financial disclosures. Email Dr. Rossi at [email protected].
References
1. González-Martín A et al. N Engl J Med. 2019 Dec 19;381(25):2391-402.
2. Ray-Coquard I et al. N Engl J Med. 2019 Dec 19;381(25):2416-28.
3. Coleman RL et al. N Engl J Med. 2019 Dec 19;381(25):2403-15.
4. Herzog TJ et al. Gynecol Oncol. 2014 Jan;132(1):8-17.
5. Tewari KS et al. J Clin Oncol. 2019 Sep 10;37(26):2317-28.
What is the significance of isolated tumor cells in endometrial cancer?
Over the past decade gynecologic oncology surgeons have increasingly adopted the technique of sentinel lymph node (SLN) biopsy to stage endometrial cancer. This is supported by evidence that selective removal of the few lymph nodes which are the first to drain the uterus can accurately detect metastatic disease, sparing the patient a complete lymphadenectomy and its associated risks, such as lymphedema.1 The proposed benefits of SLN biopsy are not just its ability to spare the patient removal of dozens of unnecessary lymph nodes, but also the ability to improve upon the detection of previously unrecognized nodal metastases in locations not routinely sampled by lymphadenectomy and by identifying very-low-volume metastatic disease. This is beneficial only, however, if that previously overlooked low-volume disease is clinically significant.

When pathologists evaluate lymph nodes as part of conventional lymphadenectomy, they typically bivalve the lymph node and evaluate with hematoxylin and eosin (H&E) stains. This technique is capable of detecting metastatic lesions greater than 2 mm, but can miss low-volume disease. In contrast, pathologists process SLNs with much finer sectioning (no greater than 2 mm), and, if the node is larger than 4 mm, they will section it perpendicular to the long axis in a bread-loaf fashion. It is not feasible to perform this ultrasectioning on the large numbers of lymph nodes of a complete lymphadenectomy specimen, but when applied to an SLN it allows pathologists to detect much smaller metastatic foci, the so-called “micrometastases” that are between 0.2 and 2 mm in size, and which typically arise in the subcapsular region of the node. The graphic depicts how a traditional longitudinal cut (a) might miss the micrometastasis that could be identified on the finer perpendicular cuts of ultra-sectioning (b). In addition to the ultrasectioning of the node into smaller slices, the pathologist performs additional immunohistochemistry stains for cytokeratin on sentinel nodes which appear negative on preliminary H&E stains. This allows the pathologist to identify even smaller clusters of malignant cells that are less than 0.2 mm, or individual cancer cells, so-called “isolated tumor cells” (ITCs) as shown in the photo. Most SLN series identify that approximately half of their “positive” lymph nodes are low-volume disease (micrometastases and ITCs). ITCs make up the majority of these cases, typically three-quarters.
Clinicians might be reassured by the discovery of low-volume metastatic disease, perceiving that the added attention afforded by the SLN approach helped them to identify metastases that might otherwise have been missed and therefore not treated. This is because node-positive (stage IIIC) disease is not cured by surgery or radiation alone and requires the addition of chemotherapy for survival benefit.2 Alternatively, there is no clear survival benefit derived from treating stage I high/intermediate cancers with chemotherapy, and therefore, the prescription of chemotherapy hinges upon reliable identification of extrauterine disease on pathology.3
It would make sense that if SLNs are more effective in identifying metastatic disease, clinicians who practice SLN biopsy would identify it more of the time. This appears to be the case with a trend towards upstaging in patients who undergo SLN biopsy, compared with those undergoing complete lymphadenectomy.4 It should also follow that if this increased detection of metastatic disease was clinically relevant, we would observe a corresponding improvement in survival outcomes. If not, then the additional identification of low-volume disease may not be value added: imparting toxicity of adjuvant therapy without survival benefit.
Micrometastases (foci sized 0.2-2 mm) are not a new phenomenon to the SLN era. Low-volume lesions were occasionally detected with routine nodal processing and H&E stains. Attention wasn’t paid to nodal volume categorization in pathology reports prior to the SLN era. These were usually reported collectively as stage IIIC disease. It would make sense to continue to approach micrometastases in a manner similar to what we have always done, recognizing that it may represent a continuum of nodal macrometastases. In contrast, ITCs are rarely detected with routine pathologic processing. Perhaps they are less within a continuum of nodal metastases, and more within the continuum of lymphovascular space invasion. We know that ITCs are significantly associated with the cofinding of this uterine phenomenon, which itself is considered a significant risk factor for local recurrence.5
Series have consistently shown the outcomes of women with ITCs to be favorable, compared with those with micrometastases or macrometastases.5,6 However, most retrospective series that evaluated the outcomes of patients with respect to volume of metastatic disease have high rates of treatment of ITCs with chemotherapy, radiotherapy, or both.6 This may mask and confuse whether there is any intrinsically favorable prognostic virtue of ITCs, compared with larger metastatic foci. When ITCs are untreated, it would appear that the rates and patterns of recurrence appear similar to those with negative SLNs, with the caveat that these series all include small numbers.5,7 This would suggest that women with ITCs do not need additional therapy beyond what would be prescribed for their uterine risk factors.
Further supporting the notion that ITCs have more favorable prognosis is that, while SLN biopsy is associated with a higher detection of nodal metastatic disease, it is not necessarily associated with improved survival when compared with complete lymphadenectomy in retrospective series.8 This suggests that finding and treating ITCs may not positively affect outcomes. Or possibly it is a result of inadequate statistical power to show a small benefit should one exist. It is especially difficult to differentiate micrometastases and ITCs with respect to treatment outcomes. Given that ITCs make up the majority of low-volume nodal disease detected through the SLN technique, any potential benefit of increased capture and treatment of the more substantial micrometastases is not likely to be captured. As a result, most series tend to lump patients with micrometastases with those with ITCs in their analysis of patient outcomes. This may be a mistake.
Clearly more research needs to be performed to definitively address the clinical significance of ITCs. While it would be ideal to conduct a prospective trial in which patients with ITCs are randomized to therapy or observation, in reality the scope of such a trial makes it impractical. ITCs are detected in only approximately 5% of all the patients with endometrial cancer, and given that outcomes for this group are, in general, good, it would require enrollment of tens of thousands of patients to establish a statistically satisfactory result. Therefore it is likely that we will need to rely on the results of large retrospective, population-based, observational series to determine if the identification and treatment of ITCs adds value and superior outcomes to patients. In addition, we are making leaps in better understanding the molecular profile of endometrial cancers and how we might incorporate this data with histology and staging results to create treatment algorithms, much like what has been developed for breast cancer. This is likely where the future lies in interpreting the results of staging. In the meantime, it seems reasonable to collect the data regarding volume of metastatic disease including the presence of ITCs, making shared treatment decisions with the patient regarding the addition of adjuvant therapy, recognizing that
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no conflicts of interest to declare. Email her at [email protected].
References
1. Lancet Oncol. 2017 Mar;18(3):384-92.
2. J Clin Oncol. 2006 Jan 1;24(1):36-44.
3. J Clin Oncol. 2019 Jul 20;37(21):1810-8.
4. Clin Transl Oncol. 2019. doi: 10.1007/s12094-019-02249-x.
5. Gynecol Oncol. 2017 Aug;146(2):240-6.
6. Ann Surg Oncol. 2016 May;23(5):1653-9.
7. Gynecol Oncol. 2019 Jun;153(3):496-9.
8. Gynecol Oncol. 2018 Nov;151(2):235-42.
Over the past decade gynecologic oncology surgeons have increasingly adopted the technique of sentinel lymph node (SLN) biopsy to stage endometrial cancer. This is supported by evidence that selective removal of the few lymph nodes which are the first to drain the uterus can accurately detect metastatic disease, sparing the patient a complete lymphadenectomy and its associated risks, such as lymphedema.1 The proposed benefits of SLN biopsy are not just its ability to spare the patient removal of dozens of unnecessary lymph nodes, but also the ability to improve upon the detection of previously unrecognized nodal metastases in locations not routinely sampled by lymphadenectomy and by identifying very-low-volume metastatic disease. This is beneficial only, however, if that previously overlooked low-volume disease is clinically significant.

When pathologists evaluate lymph nodes as part of conventional lymphadenectomy, they typically bivalve the lymph node and evaluate with hematoxylin and eosin (H&E) stains. This technique is capable of detecting metastatic lesions greater than 2 mm, but can miss low-volume disease. In contrast, pathologists process SLNs with much finer sectioning (no greater than 2 mm), and, if the node is larger than 4 mm, they will section it perpendicular to the long axis in a bread-loaf fashion. It is not feasible to perform this ultrasectioning on the large numbers of lymph nodes of a complete lymphadenectomy specimen, but when applied to an SLN it allows pathologists to detect much smaller metastatic foci, the so-called “micrometastases” that are between 0.2 and 2 mm in size, and which typically arise in the subcapsular region of the node. The graphic depicts how a traditional longitudinal cut (a) might miss the micrometastasis that could be identified on the finer perpendicular cuts of ultra-sectioning (b). In addition to the ultrasectioning of the node into smaller slices, the pathologist performs additional immunohistochemistry stains for cytokeratin on sentinel nodes which appear negative on preliminary H&E stains. This allows the pathologist to identify even smaller clusters of malignant cells that are less than 0.2 mm, or individual cancer cells, so-called “isolated tumor cells” (ITCs) as shown in the photo. Most SLN series identify that approximately half of their “positive” lymph nodes are low-volume disease (micrometastases and ITCs). ITCs make up the majority of these cases, typically three-quarters.
Clinicians might be reassured by the discovery of low-volume metastatic disease, perceiving that the added attention afforded by the SLN approach helped them to identify metastases that might otherwise have been missed and therefore not treated. This is because node-positive (stage IIIC) disease is not cured by surgery or radiation alone and requires the addition of chemotherapy for survival benefit.2 Alternatively, there is no clear survival benefit derived from treating stage I high/intermediate cancers with chemotherapy, and therefore, the prescription of chemotherapy hinges upon reliable identification of extrauterine disease on pathology.3
It would make sense that if SLNs are more effective in identifying metastatic disease, clinicians who practice SLN biopsy would identify it more of the time. This appears to be the case with a trend towards upstaging in patients who undergo SLN biopsy, compared with those undergoing complete lymphadenectomy.4 It should also follow that if this increased detection of metastatic disease was clinically relevant, we would observe a corresponding improvement in survival outcomes. If not, then the additional identification of low-volume disease may not be value added: imparting toxicity of adjuvant therapy without survival benefit.
Micrometastases (foci sized 0.2-2 mm) are not a new phenomenon to the SLN era. Low-volume lesions were occasionally detected with routine nodal processing and H&E stains. Attention wasn’t paid to nodal volume categorization in pathology reports prior to the SLN era. These were usually reported collectively as stage IIIC disease. It would make sense to continue to approach micrometastases in a manner similar to what we have always done, recognizing that it may represent a continuum of nodal macrometastases. In contrast, ITCs are rarely detected with routine pathologic processing. Perhaps they are less within a continuum of nodal metastases, and more within the continuum of lymphovascular space invasion. We know that ITCs are significantly associated with the cofinding of this uterine phenomenon, which itself is considered a significant risk factor for local recurrence.5
Series have consistently shown the outcomes of women with ITCs to be favorable, compared with those with micrometastases or macrometastases.5,6 However, most retrospective series that evaluated the outcomes of patients with respect to volume of metastatic disease have high rates of treatment of ITCs with chemotherapy, radiotherapy, or both.6 This may mask and confuse whether there is any intrinsically favorable prognostic virtue of ITCs, compared with larger metastatic foci. When ITCs are untreated, it would appear that the rates and patterns of recurrence appear similar to those with negative SLNs, with the caveat that these series all include small numbers.5,7 This would suggest that women with ITCs do not need additional therapy beyond what would be prescribed for their uterine risk factors.
Further supporting the notion that ITCs have more favorable prognosis is that, while SLN biopsy is associated with a higher detection of nodal metastatic disease, it is not necessarily associated with improved survival when compared with complete lymphadenectomy in retrospective series.8 This suggests that finding and treating ITCs may not positively affect outcomes. Or possibly it is a result of inadequate statistical power to show a small benefit should one exist. It is especially difficult to differentiate micrometastases and ITCs with respect to treatment outcomes. Given that ITCs make up the majority of low-volume nodal disease detected through the SLN technique, any potential benefit of increased capture and treatment of the more substantial micrometastases is not likely to be captured. As a result, most series tend to lump patients with micrometastases with those with ITCs in their analysis of patient outcomes. This may be a mistake.
Clearly more research needs to be performed to definitively address the clinical significance of ITCs. While it would be ideal to conduct a prospective trial in which patients with ITCs are randomized to therapy or observation, in reality the scope of such a trial makes it impractical. ITCs are detected in only approximately 5% of all the patients with endometrial cancer, and given that outcomes for this group are, in general, good, it would require enrollment of tens of thousands of patients to establish a statistically satisfactory result. Therefore it is likely that we will need to rely on the results of large retrospective, population-based, observational series to determine if the identification and treatment of ITCs adds value and superior outcomes to patients. In addition, we are making leaps in better understanding the molecular profile of endometrial cancers and how we might incorporate this data with histology and staging results to create treatment algorithms, much like what has been developed for breast cancer. This is likely where the future lies in interpreting the results of staging. In the meantime, it seems reasonable to collect the data regarding volume of metastatic disease including the presence of ITCs, making shared treatment decisions with the patient regarding the addition of adjuvant therapy, recognizing that
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no conflicts of interest to declare. Email her at [email protected].
References
1. Lancet Oncol. 2017 Mar;18(3):384-92.
2. J Clin Oncol. 2006 Jan 1;24(1):36-44.
3. J Clin Oncol. 2019 Jul 20;37(21):1810-8.
4. Clin Transl Oncol. 2019. doi: 10.1007/s12094-019-02249-x.
5. Gynecol Oncol. 2017 Aug;146(2):240-6.
6. Ann Surg Oncol. 2016 May;23(5):1653-9.
7. Gynecol Oncol. 2019 Jun;153(3):496-9.
8. Gynecol Oncol. 2018 Nov;151(2):235-42.
Over the past decade gynecologic oncology surgeons have increasingly adopted the technique of sentinel lymph node (SLN) biopsy to stage endometrial cancer. This is supported by evidence that selective removal of the few lymph nodes which are the first to drain the uterus can accurately detect metastatic disease, sparing the patient a complete lymphadenectomy and its associated risks, such as lymphedema.1 The proposed benefits of SLN biopsy are not just its ability to spare the patient removal of dozens of unnecessary lymph nodes, but also the ability to improve upon the detection of previously unrecognized nodal metastases in locations not routinely sampled by lymphadenectomy and by identifying very-low-volume metastatic disease. This is beneficial only, however, if that previously overlooked low-volume disease is clinically significant.

When pathologists evaluate lymph nodes as part of conventional lymphadenectomy, they typically bivalve the lymph node and evaluate with hematoxylin and eosin (H&E) stains. This technique is capable of detecting metastatic lesions greater than 2 mm, but can miss low-volume disease. In contrast, pathologists process SLNs with much finer sectioning (no greater than 2 mm), and, if the node is larger than 4 mm, they will section it perpendicular to the long axis in a bread-loaf fashion. It is not feasible to perform this ultrasectioning on the large numbers of lymph nodes of a complete lymphadenectomy specimen, but when applied to an SLN it allows pathologists to detect much smaller metastatic foci, the so-called “micrometastases” that are between 0.2 and 2 mm in size, and which typically arise in the subcapsular region of the node. The graphic depicts how a traditional longitudinal cut (a) might miss the micrometastasis that could be identified on the finer perpendicular cuts of ultra-sectioning (b). In addition to the ultrasectioning of the node into smaller slices, the pathologist performs additional immunohistochemistry stains for cytokeratin on sentinel nodes which appear negative on preliminary H&E stains. This allows the pathologist to identify even smaller clusters of malignant cells that are less than 0.2 mm, or individual cancer cells, so-called “isolated tumor cells” (ITCs) as shown in the photo. Most SLN series identify that approximately half of their “positive” lymph nodes are low-volume disease (micrometastases and ITCs). ITCs make up the majority of these cases, typically three-quarters.
Clinicians might be reassured by the discovery of low-volume metastatic disease, perceiving that the added attention afforded by the SLN approach helped them to identify metastases that might otherwise have been missed and therefore not treated. This is because node-positive (stage IIIC) disease is not cured by surgery or radiation alone and requires the addition of chemotherapy for survival benefit.2 Alternatively, there is no clear survival benefit derived from treating stage I high/intermediate cancers with chemotherapy, and therefore, the prescription of chemotherapy hinges upon reliable identification of extrauterine disease on pathology.3
It would make sense that if SLNs are more effective in identifying metastatic disease, clinicians who practice SLN biopsy would identify it more of the time. This appears to be the case with a trend towards upstaging in patients who undergo SLN biopsy, compared with those undergoing complete lymphadenectomy.4 It should also follow that if this increased detection of metastatic disease was clinically relevant, we would observe a corresponding improvement in survival outcomes. If not, then the additional identification of low-volume disease may not be value added: imparting toxicity of adjuvant therapy without survival benefit.
Micrometastases (foci sized 0.2-2 mm) are not a new phenomenon to the SLN era. Low-volume lesions were occasionally detected with routine nodal processing and H&E stains. Attention wasn’t paid to nodal volume categorization in pathology reports prior to the SLN era. These were usually reported collectively as stage IIIC disease. It would make sense to continue to approach micrometastases in a manner similar to what we have always done, recognizing that it may represent a continuum of nodal macrometastases. In contrast, ITCs are rarely detected with routine pathologic processing. Perhaps they are less within a continuum of nodal metastases, and more within the continuum of lymphovascular space invasion. We know that ITCs are significantly associated with the cofinding of this uterine phenomenon, which itself is considered a significant risk factor for local recurrence.5
Series have consistently shown the outcomes of women with ITCs to be favorable, compared with those with micrometastases or macrometastases.5,6 However, most retrospective series that evaluated the outcomes of patients with respect to volume of metastatic disease have high rates of treatment of ITCs with chemotherapy, radiotherapy, or both.6 This may mask and confuse whether there is any intrinsically favorable prognostic virtue of ITCs, compared with larger metastatic foci. When ITCs are untreated, it would appear that the rates and patterns of recurrence appear similar to those with negative SLNs, with the caveat that these series all include small numbers.5,7 This would suggest that women with ITCs do not need additional therapy beyond what would be prescribed for their uterine risk factors.
Further supporting the notion that ITCs have more favorable prognosis is that, while SLN biopsy is associated with a higher detection of nodal metastatic disease, it is not necessarily associated with improved survival when compared with complete lymphadenectomy in retrospective series.8 This suggests that finding and treating ITCs may not positively affect outcomes. Or possibly it is a result of inadequate statistical power to show a small benefit should one exist. It is especially difficult to differentiate micrometastases and ITCs with respect to treatment outcomes. Given that ITCs make up the majority of low-volume nodal disease detected through the SLN technique, any potential benefit of increased capture and treatment of the more substantial micrometastases is not likely to be captured. As a result, most series tend to lump patients with micrometastases with those with ITCs in their analysis of patient outcomes. This may be a mistake.
Clearly more research needs to be performed to definitively address the clinical significance of ITCs. While it would be ideal to conduct a prospective trial in which patients with ITCs are randomized to therapy or observation, in reality the scope of such a trial makes it impractical. ITCs are detected in only approximately 5% of all the patients with endometrial cancer, and given that outcomes for this group are, in general, good, it would require enrollment of tens of thousands of patients to establish a statistically satisfactory result. Therefore it is likely that we will need to rely on the results of large retrospective, population-based, observational series to determine if the identification and treatment of ITCs adds value and superior outcomes to patients. In addition, we are making leaps in better understanding the molecular profile of endometrial cancers and how we might incorporate this data with histology and staging results to create treatment algorithms, much like what has been developed for breast cancer. This is likely where the future lies in interpreting the results of staging. In the meantime, it seems reasonable to collect the data regarding volume of metastatic disease including the presence of ITCs, making shared treatment decisions with the patient regarding the addition of adjuvant therapy, recognizing that
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no conflicts of interest to declare. Email her at [email protected].
References
1. Lancet Oncol. 2017 Mar;18(3):384-92.
2. J Clin Oncol. 2006 Jan 1;24(1):36-44.
3. J Clin Oncol. 2019 Jul 20;37(21):1810-8.
4. Clin Transl Oncol. 2019. doi: 10.1007/s12094-019-02249-x.
5. Gynecol Oncol. 2017 Aug;146(2):240-6.
6. Ann Surg Oncol. 2016 May;23(5):1653-9.
7. Gynecol Oncol. 2019 Jun;153(3):496-9.
8. Gynecol Oncol. 2018 Nov;151(2):235-42.
How long is it safe to delay gynecologic cancer surgery?
As I write this column, there are more than 25,000 current cases of COVID-19 in the United States with an expected exponential rise in these numbers. Hospitals are issuing directives to cancel or postpone “elective” surgery to preserve the finite essential personal protective equipment (PPE), encourage social distancing, prevent exposure of at-risk patients within the hospital, and ensure bed and ventilator capacity for the impending surge in COVID-19 patients.
Many health systems have defined which surgeries they consider permissible, typically by using time parameters such as would not cause patient harm if not performed within 4 weeks, or 7 days, or 24 hours. This leaves surgeons in the unfamiliar position of rationing health care, a role with which, over the coming months, we may have to become increasingly comfortable. This is an enormous responsibility, the shift of resources between one population in need and another, and decisions should be based on data, not bias or hunch. We know that untreated cancer is life threatening, but there is a difference between untreated and delayed. What is a safe time to wait for gynecologic cancer surgery after diagnosis without negatively affecting survival from that cancer?
As I looked through my own upcoming surgical schedule, I sought guidance from the American College of Surgeons’ website, updated on March 17, 2020. In this site they tabulate an “Elective Surgery Acuity Scale” in which “most cancers” fit into tier 3a, which corresponds to high acuity surgery – “do not postpone.” This definition is fairly generalized and blunt; it does not account for the differences in cancers and occasional voluntary needs to postpone a patient’s cancer surgery for health optimization. There are limited data that measure the impact of surgical wait times on survival from gynecologic cancer. Most of this research is observational, and therefore, is influenced by confounders causing delay in surgery (e.g., comorbid conditions or socioeconomic factors that limit access to care). However, the current enforced delays are involuntary; driven by the system, not the patient; and access is universally restricted.
Endometrial cancer
Most data regarding outcomes and gynecologic cancer delay come from endometrial cancer. In 2016, Shalowitz et al. evaluated 182,000 endometrial cancer cases documented within the National Cancer Database (NCDB), which captures approximately 70% of cancer surgeries in the United States.1 They separated these patients into groups of low-grade (grade 1 and 2 endometrioid) and high-grade (grade 3 endometrioid and nonendometrioid) cancers, and evaluated the groups for their overall survival, stratified by the time period between diagnosis and surgery. Interestingly, those whose surgery was performed under 2 weeks from diagnosis had worse perioperative mortality and long-term survival. This seems to be a function of lack of medical optimization; low-volume, nonspecialized centers having less wait time; and the presentation of more advanced and symptomatic disease demanding a more urgent surgery. After those initial 2 weeks of worse outcomes, there was a period of stable outcomes and safety in waiting that extended up to 8 weeks for patients with low-grade cancers and up to 18 weeks for patients with high-grade cancers.
It may be counterintuitive to think that surgical delay affects patients with high-grade endometrial cancers less. These are more aggressive cancers, and there is patient and provider concern for metastatic spread with time elapsed. But an expedited surgery does not appear to be necessary for this group. The Shalowitz study demonstrated no risk for upstaging with surgical delay, meaning that advanced stage was not more likely to be identified in patients whose surgery was delayed, compared with those performed earlier. This observation suggests that the survival from high-grade endometrial cancers is largely determined by factors that cannot be controlled by the surgeon such as the stage at diagnosis, occult spread, and decreased responsiveness of the tumor to adjuvant therapy. In other words, fast-tracking these patients to surgery has limited influence on the outcomes for high-grade endometrial cancers.
For low-grade cancers, adverse outcomes were seen with a surgical delay of more than 8 weeks. But this may not have been caused by progression of disease (low-grade cancers also were not upstaged with delays), but rather may reflect that, in normal times, elective delays of more than 8 weeks are a function of necessary complex medical optimization of comorbidities (such as obesity-related disease). The survival that is measured by NCDB is not disease specific, and patients with comorbidities will be more likely to have impaired overall survival.
A systematic review of all papers that looked at endometrial cancer outcomes associated with surgical delay determined that it is reasonable to delay surgery for up to 8 weeks.2
Ovarian cancer
The data for ovarian cancer surgery is more limited. Most literature discusses the impact of delay in the time between surgery and the receipt of adjuvant chemotherapy, but there are limited data exploring how a delay in primary debulking negatively affects patients. This is perhaps because advanced ovarian cancer surgery rarely is delayed because of symptoms and apparent advanced stage at diagnosis. When a patient’s surgery does need to be voluntarily delayed, for example for medical optimization, there is the option of neoadjuvant chemotherapy (NACT) in which surgery is performed after three or more cycles of chemotherapy. NACT has been shown in multiple studies to have noninferior cancer outcomes, compared with primary debulking surgery.3,4
Perhaps in this current environment in which access to operating rooms and supplies is rationed, we should consider offering more, or all, patients NACT? Hospital stays after primary cytoreductive surgeries are typically 3-7 days in length, and these patients are at a higher risk, compared with other gynecologic cancer surgeries, of ICU admission and blood transfusions, both limited resources in this current environment. The disadvantage of this approach is that, while chemotherapy can keep patients out of the hospital so that they can practice social distancing, this particular therapy adds to the immunocompromised population. However, even patients who undergo primary surgical cytoreductive surgery will need to rapidly transition to immunosuppressive cytotoxic therapy; therefore it is unlikely that this can be avoided entirely during this time.
Lower genital tract cancers
Surgery for patients with lower genital tract cancers – such as cervical and vulvar cancer – also can probably be safely delayed for a 4-week period, and possibly longer. A Canadian retrospective study looked collectively at cervical, vaginal, and vulvar cancers evaluating for disease progression associated with delay to surgery, using 28 days as a benchmark for delayed surgery.5 They found no significant increased progression associated with surgical delay greater than 28 days. This study evaluated progression of cancer and did not measure cancer survival, although it is unlikely we would see impaired survival without a significant increase in disease progression.
We also can look to outcomes from delayed radical hysterectomy for stage I cervical cancer in pregnancy to provided us with some data. A retrospective cohort study observed no difference in survival when 28 women with early-stage cervical cancer who were diagnosed in pregnancy (average wait time 20 weeks from diagnosis to treatment) were compared with the outcomes of 52 matched nonpregnant control patients (average wait time 8 weeks). Their survival was 89% versus 94% respectively (P = .08).6
Summary
Synthesizing this data, it appears that, in an environment of competing needs and resources, it is reasonable and safe to delay surgery for patients with gynecologic cancers for 4-6 weeks and potentially longer. This includes patients with high-grade endometrial cancers. Clearly, these decisions should be individualized to patients and different health systems. For example, a patient who presents with a cancer-associated life-threatening bowel obstruction or hemorrhage may need an immediate intervention, and communities minimally affected by the coronavirus pandemic may have more allowances for surgery. With respect to patient anxiety, most patients with cancer are keen to have surgery promptly, and breaking the news to them that their surgery may be delayed because of institutional and public health needs will be difficult. However, the data support that this is likely safe.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She had no relevant financial disclosures. Email Dr. Rossi at [email protected].
References
1. Am J Obstet Gynecol 2017;216(3):268 e1-68 e18.
2. Eur J Obstet Gynecol Reprod Biol 2020;246:1-6. doi: 10.1016/j.ejogrb.2020.01.004.
3. N Engl J Med 2010;363(10):943-53.
4. Lancet 2015;386(9990):249-57.
5. J Obstet Gynaecol Can 2015;37(4):338-44.
6. Am J Obstet Gynecol 2017;216(3):276 e1-76 e6. doi: 10.1016/j.ajog.2016.10.034.
As I write this column, there are more than 25,000 current cases of COVID-19 in the United States with an expected exponential rise in these numbers. Hospitals are issuing directives to cancel or postpone “elective” surgery to preserve the finite essential personal protective equipment (PPE), encourage social distancing, prevent exposure of at-risk patients within the hospital, and ensure bed and ventilator capacity for the impending surge in COVID-19 patients.
Many health systems have defined which surgeries they consider permissible, typically by using time parameters such as would not cause patient harm if not performed within 4 weeks, or 7 days, or 24 hours. This leaves surgeons in the unfamiliar position of rationing health care, a role with which, over the coming months, we may have to become increasingly comfortable. This is an enormous responsibility, the shift of resources between one population in need and another, and decisions should be based on data, not bias or hunch. We know that untreated cancer is life threatening, but there is a difference between untreated and delayed. What is a safe time to wait for gynecologic cancer surgery after diagnosis without negatively affecting survival from that cancer?
As I looked through my own upcoming surgical schedule, I sought guidance from the American College of Surgeons’ website, updated on March 17, 2020. In this site they tabulate an “Elective Surgery Acuity Scale” in which “most cancers” fit into tier 3a, which corresponds to high acuity surgery – “do not postpone.” This definition is fairly generalized and blunt; it does not account for the differences in cancers and occasional voluntary needs to postpone a patient’s cancer surgery for health optimization. There are limited data that measure the impact of surgical wait times on survival from gynecologic cancer. Most of this research is observational, and therefore, is influenced by confounders causing delay in surgery (e.g., comorbid conditions or socioeconomic factors that limit access to care). However, the current enforced delays are involuntary; driven by the system, not the patient; and access is universally restricted.
Endometrial cancer
Most data regarding outcomes and gynecologic cancer delay come from endometrial cancer. In 2016, Shalowitz et al. evaluated 182,000 endometrial cancer cases documented within the National Cancer Database (NCDB), which captures approximately 70% of cancer surgeries in the United States.1 They separated these patients into groups of low-grade (grade 1 and 2 endometrioid) and high-grade (grade 3 endometrioid and nonendometrioid) cancers, and evaluated the groups for their overall survival, stratified by the time period between diagnosis and surgery. Interestingly, those whose surgery was performed under 2 weeks from diagnosis had worse perioperative mortality and long-term survival. This seems to be a function of lack of medical optimization; low-volume, nonspecialized centers having less wait time; and the presentation of more advanced and symptomatic disease demanding a more urgent surgery. After those initial 2 weeks of worse outcomes, there was a period of stable outcomes and safety in waiting that extended up to 8 weeks for patients with low-grade cancers and up to 18 weeks for patients with high-grade cancers.
It may be counterintuitive to think that surgical delay affects patients with high-grade endometrial cancers less. These are more aggressive cancers, and there is patient and provider concern for metastatic spread with time elapsed. But an expedited surgery does not appear to be necessary for this group. The Shalowitz study demonstrated no risk for upstaging with surgical delay, meaning that advanced stage was not more likely to be identified in patients whose surgery was delayed, compared with those performed earlier. This observation suggests that the survival from high-grade endometrial cancers is largely determined by factors that cannot be controlled by the surgeon such as the stage at diagnosis, occult spread, and decreased responsiveness of the tumor to adjuvant therapy. In other words, fast-tracking these patients to surgery has limited influence on the outcomes for high-grade endometrial cancers.
For low-grade cancers, adverse outcomes were seen with a surgical delay of more than 8 weeks. But this may not have been caused by progression of disease (low-grade cancers also were not upstaged with delays), but rather may reflect that, in normal times, elective delays of more than 8 weeks are a function of necessary complex medical optimization of comorbidities (such as obesity-related disease). The survival that is measured by NCDB is not disease specific, and patients with comorbidities will be more likely to have impaired overall survival.
A systematic review of all papers that looked at endometrial cancer outcomes associated with surgical delay determined that it is reasonable to delay surgery for up to 8 weeks.2
Ovarian cancer
The data for ovarian cancer surgery is more limited. Most literature discusses the impact of delay in the time between surgery and the receipt of adjuvant chemotherapy, but there are limited data exploring how a delay in primary debulking negatively affects patients. This is perhaps because advanced ovarian cancer surgery rarely is delayed because of symptoms and apparent advanced stage at diagnosis. When a patient’s surgery does need to be voluntarily delayed, for example for medical optimization, there is the option of neoadjuvant chemotherapy (NACT) in which surgery is performed after three or more cycles of chemotherapy. NACT has been shown in multiple studies to have noninferior cancer outcomes, compared with primary debulking surgery.3,4
Perhaps in this current environment in which access to operating rooms and supplies is rationed, we should consider offering more, or all, patients NACT? Hospital stays after primary cytoreductive surgeries are typically 3-7 days in length, and these patients are at a higher risk, compared with other gynecologic cancer surgeries, of ICU admission and blood transfusions, both limited resources in this current environment. The disadvantage of this approach is that, while chemotherapy can keep patients out of the hospital so that they can practice social distancing, this particular therapy adds to the immunocompromised population. However, even patients who undergo primary surgical cytoreductive surgery will need to rapidly transition to immunosuppressive cytotoxic therapy; therefore it is unlikely that this can be avoided entirely during this time.
Lower genital tract cancers
Surgery for patients with lower genital tract cancers – such as cervical and vulvar cancer – also can probably be safely delayed for a 4-week period, and possibly longer. A Canadian retrospective study looked collectively at cervical, vaginal, and vulvar cancers evaluating for disease progression associated with delay to surgery, using 28 days as a benchmark for delayed surgery.5 They found no significant increased progression associated with surgical delay greater than 28 days. This study evaluated progression of cancer and did not measure cancer survival, although it is unlikely we would see impaired survival without a significant increase in disease progression.
We also can look to outcomes from delayed radical hysterectomy for stage I cervical cancer in pregnancy to provided us with some data. A retrospective cohort study observed no difference in survival when 28 women with early-stage cervical cancer who were diagnosed in pregnancy (average wait time 20 weeks from diagnosis to treatment) were compared with the outcomes of 52 matched nonpregnant control patients (average wait time 8 weeks). Their survival was 89% versus 94% respectively (P = .08).6
Summary
Synthesizing this data, it appears that, in an environment of competing needs and resources, it is reasonable and safe to delay surgery for patients with gynecologic cancers for 4-6 weeks and potentially longer. This includes patients with high-grade endometrial cancers. Clearly, these decisions should be individualized to patients and different health systems. For example, a patient who presents with a cancer-associated life-threatening bowel obstruction or hemorrhage may need an immediate intervention, and communities minimally affected by the coronavirus pandemic may have more allowances for surgery. With respect to patient anxiety, most patients with cancer are keen to have surgery promptly, and breaking the news to them that their surgery may be delayed because of institutional and public health needs will be difficult. However, the data support that this is likely safe.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She had no relevant financial disclosures. Email Dr. Rossi at [email protected].
References
1. Am J Obstet Gynecol 2017;216(3):268 e1-68 e18.
2. Eur J Obstet Gynecol Reprod Biol 2020;246:1-6. doi: 10.1016/j.ejogrb.2020.01.004.
3. N Engl J Med 2010;363(10):943-53.
4. Lancet 2015;386(9990):249-57.
5. J Obstet Gynaecol Can 2015;37(4):338-44.
6. Am J Obstet Gynecol 2017;216(3):276 e1-76 e6. doi: 10.1016/j.ajog.2016.10.034.
As I write this column, there are more than 25,000 current cases of COVID-19 in the United States with an expected exponential rise in these numbers. Hospitals are issuing directives to cancel or postpone “elective” surgery to preserve the finite essential personal protective equipment (PPE), encourage social distancing, prevent exposure of at-risk patients within the hospital, and ensure bed and ventilator capacity for the impending surge in COVID-19 patients.
Many health systems have defined which surgeries they consider permissible, typically by using time parameters such as would not cause patient harm if not performed within 4 weeks, or 7 days, or 24 hours. This leaves surgeons in the unfamiliar position of rationing health care, a role with which, over the coming months, we may have to become increasingly comfortable. This is an enormous responsibility, the shift of resources between one population in need and another, and decisions should be based on data, not bias or hunch. We know that untreated cancer is life threatening, but there is a difference between untreated and delayed. What is a safe time to wait for gynecologic cancer surgery after diagnosis without negatively affecting survival from that cancer?
As I looked through my own upcoming surgical schedule, I sought guidance from the American College of Surgeons’ website, updated on March 17, 2020. In this site they tabulate an “Elective Surgery Acuity Scale” in which “most cancers” fit into tier 3a, which corresponds to high acuity surgery – “do not postpone.” This definition is fairly generalized and blunt; it does not account for the differences in cancers and occasional voluntary needs to postpone a patient’s cancer surgery for health optimization. There are limited data that measure the impact of surgical wait times on survival from gynecologic cancer. Most of this research is observational, and therefore, is influenced by confounders causing delay in surgery (e.g., comorbid conditions or socioeconomic factors that limit access to care). However, the current enforced delays are involuntary; driven by the system, not the patient; and access is universally restricted.
Endometrial cancer
Most data regarding outcomes and gynecologic cancer delay come from endometrial cancer. In 2016, Shalowitz et al. evaluated 182,000 endometrial cancer cases documented within the National Cancer Database (NCDB), which captures approximately 70% of cancer surgeries in the United States.1 They separated these patients into groups of low-grade (grade 1 and 2 endometrioid) and high-grade (grade 3 endometrioid and nonendometrioid) cancers, and evaluated the groups for their overall survival, stratified by the time period between diagnosis and surgery. Interestingly, those whose surgery was performed under 2 weeks from diagnosis had worse perioperative mortality and long-term survival. This seems to be a function of lack of medical optimization; low-volume, nonspecialized centers having less wait time; and the presentation of more advanced and symptomatic disease demanding a more urgent surgery. After those initial 2 weeks of worse outcomes, there was a period of stable outcomes and safety in waiting that extended up to 8 weeks for patients with low-grade cancers and up to 18 weeks for patients with high-grade cancers.
It may be counterintuitive to think that surgical delay affects patients with high-grade endometrial cancers less. These are more aggressive cancers, and there is patient and provider concern for metastatic spread with time elapsed. But an expedited surgery does not appear to be necessary for this group. The Shalowitz study demonstrated no risk for upstaging with surgical delay, meaning that advanced stage was not more likely to be identified in patients whose surgery was delayed, compared with those performed earlier. This observation suggests that the survival from high-grade endometrial cancers is largely determined by factors that cannot be controlled by the surgeon such as the stage at diagnosis, occult spread, and decreased responsiveness of the tumor to adjuvant therapy. In other words, fast-tracking these patients to surgery has limited influence on the outcomes for high-grade endometrial cancers.
For low-grade cancers, adverse outcomes were seen with a surgical delay of more than 8 weeks. But this may not have been caused by progression of disease (low-grade cancers also were not upstaged with delays), but rather may reflect that, in normal times, elective delays of more than 8 weeks are a function of necessary complex medical optimization of comorbidities (such as obesity-related disease). The survival that is measured by NCDB is not disease specific, and patients with comorbidities will be more likely to have impaired overall survival.
A systematic review of all papers that looked at endometrial cancer outcomes associated with surgical delay determined that it is reasonable to delay surgery for up to 8 weeks.2
Ovarian cancer
The data for ovarian cancer surgery is more limited. Most literature discusses the impact of delay in the time between surgery and the receipt of adjuvant chemotherapy, but there are limited data exploring how a delay in primary debulking negatively affects patients. This is perhaps because advanced ovarian cancer surgery rarely is delayed because of symptoms and apparent advanced stage at diagnosis. When a patient’s surgery does need to be voluntarily delayed, for example for medical optimization, there is the option of neoadjuvant chemotherapy (NACT) in which surgery is performed after three or more cycles of chemotherapy. NACT has been shown in multiple studies to have noninferior cancer outcomes, compared with primary debulking surgery.3,4
Perhaps in this current environment in which access to operating rooms and supplies is rationed, we should consider offering more, or all, patients NACT? Hospital stays after primary cytoreductive surgeries are typically 3-7 days in length, and these patients are at a higher risk, compared with other gynecologic cancer surgeries, of ICU admission and blood transfusions, both limited resources in this current environment. The disadvantage of this approach is that, while chemotherapy can keep patients out of the hospital so that they can practice social distancing, this particular therapy adds to the immunocompromised population. However, even patients who undergo primary surgical cytoreductive surgery will need to rapidly transition to immunosuppressive cytotoxic therapy; therefore it is unlikely that this can be avoided entirely during this time.
Lower genital tract cancers
Surgery for patients with lower genital tract cancers – such as cervical and vulvar cancer – also can probably be safely delayed for a 4-week period, and possibly longer. A Canadian retrospective study looked collectively at cervical, vaginal, and vulvar cancers evaluating for disease progression associated with delay to surgery, using 28 days as a benchmark for delayed surgery.5 They found no significant increased progression associated with surgical delay greater than 28 days. This study evaluated progression of cancer and did not measure cancer survival, although it is unlikely we would see impaired survival without a significant increase in disease progression.
We also can look to outcomes from delayed radical hysterectomy for stage I cervical cancer in pregnancy to provided us with some data. A retrospective cohort study observed no difference in survival when 28 women with early-stage cervical cancer who were diagnosed in pregnancy (average wait time 20 weeks from diagnosis to treatment) were compared with the outcomes of 52 matched nonpregnant control patients (average wait time 8 weeks). Their survival was 89% versus 94% respectively (P = .08).6
Summary
Synthesizing this data, it appears that, in an environment of competing needs and resources, it is reasonable and safe to delay surgery for patients with gynecologic cancers for 4-6 weeks and potentially longer. This includes patients with high-grade endometrial cancers. Clearly, these decisions should be individualized to patients and different health systems. For example, a patient who presents with a cancer-associated life-threatening bowel obstruction or hemorrhage may need an immediate intervention, and communities minimally affected by the coronavirus pandemic may have more allowances for surgery. With respect to patient anxiety, most patients with cancer are keen to have surgery promptly, and breaking the news to them that their surgery may be delayed because of institutional and public health needs will be difficult. However, the data support that this is likely safe.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She had no relevant financial disclosures. Email Dr. Rossi at [email protected].
References
1. Am J Obstet Gynecol 2017;216(3):268 e1-68 e18.
2. Eur J Obstet Gynecol Reprod Biol 2020;246:1-6. doi: 10.1016/j.ejogrb.2020.01.004.
3. N Engl J Med 2010;363(10):943-53.
4. Lancet 2015;386(9990):249-57.
5. J Obstet Gynaecol Can 2015;37(4):338-44.
6. Am J Obstet Gynecol 2017;216(3):276 e1-76 e6. doi: 10.1016/j.ajog.2016.10.034.
Molar pregnancy: The next steps after diagnosis
Molar pregnancy is an uncommon but serious condition that affects young women of reproductive age. The diagnosis and management of molar pregnancy is familiar to most gynecologists. However, in the days and weeks following evacuation of molar pregnancy, clinicians face a critical time period in which they must be vigilant for the development of postmolar gestational trophoblastic neoplasia (GTN). If recognized early and treated appropriately, it almost always can be cured; however, errors or delays in the management of this condition can have catastrophic consequences for patients, including decreasing the likelihood of cure. Here we will review some of the steps and actions that can be taken immediately following the diagnosis of a molar pregnancy to expeditiously identify postmolar GTN and ensure patients are appropriately prepared for further consultation and intervention.
Postmolar GTN includes the diagnoses of invasive mole and choriocarcinoma that contain highly atypical trophoblasts with the capacity for local invasion and metastasis. Typically, the diagnosis is made clinically and not distinguished with histology. While molar pregnancies are a benign condition, invasive moles and choriocarcinoma are malignant conditions in which the molar tissue infiltrates the uterine myometrium, vasculature, and frequently is associated with hematogenous spread with distant metastases. It is a highly chemosensitive disease, and cure with chemotherapy typically is achieved with the ability to preserve fertility if desired even in advanced stage disease.1
After evacuation of a molar pregnancy, gynecologists should be on alert for the development of postmolar GTN if the following known risk factors are present: a history of a prior GTN diagnosis, complete mole on pathology (as opposed to partial mole), serum human chorionic gonadotropin (hCG) levels greater than 100,000 mIU/mL, age greater than 40 years, an enlarged uterus or large ovarian theca lutein cysts, and slow to normalize (more than 2 months) hCG. Symptoms for the development of postmolar GTN include persistent vaginal bleeding after evacuation, a persistently enlarged or enlarging uterine size, and adnexal masses. Ultimately, the diagnosis is made through plateaued or rising serum hCG assessments.2 (See graphic.)
Following the evacuation of a molar pregnancy, hCG levels should be drawn at the same laboratory every 1-2 weeks until normalization and then three consecutive normal values. Once this has been achieved, hCG levels should be tested once at 3 months and again at 6 months. During this 6 month period, patients should use reliable contraception, ideally, and through oral contraceptive pills that suppress the secretion of pituitary hCG if not contraindicated. Should a woman become pregnant during this 6-month surveillance, it becomes impossible to rule out occult postmolar GTN.
Typically after evacuation of a molar pregnancy, there is rapid fall in hCG levels, but this does not occur when the molar pregnancy has become invasive or is associated with choriocarcinoma. In these cases, after an initial drop in hCG levels, there is an observed rise or plateau in levels (as defined in the accompanying table), and this establishes the diagnosis of postmolar GTN. It is common for hCG to fall in fits and starts, rather than have a smooth, consistent diminution, and this can be worrying for gynecologists; however, provided there is a consistent reduction in values in accordance with the stated definitions, observation can continue.
Another source of confusion and concern is an HCG level that fails to completely normalize during observation, yet reaches a very low level. If this is observed, clinicians should consider the diagnosis of quiescent hCG, pituitary hCG, or phantom hCG.3 These can be difficult to distinguish from postmolar GTN, and consultation with a gynecologic oncologist with experience in the diagnosis and management of these rare tumors is helpful to determine if the persistent low levels in hCG require intervention.
Once a clinician has observed a plateau or rise in hCG levels, a gynecologic examination should be performed because the lower genital tract is a common site for metastatic postmolar GTN. If during this evaluation, a suspicious lesion is identified (typically a blue-black, slightly raised, hemorrhagic-appearing lesion), it should not be biopsied, but rather assumed to be a metastatic site. The vasculature of metastatic sites is extremely fragile, and biopsy or disruption can result in catastrophic hemorrhage, even from very small lesions.
In addition to physical examination, several diagnostic studies should be performed which may expedite the triage and management of the case. A pelvic ultrasound should evaluate the endometrial cavity for a new viable pregnancy, and residual molar tissue; sometimes, myometrial invasion consistent with an invasive mole can be appreciated. Chest x-ray or CT scan should be ordered to evaluate for pulmonary metastatic lesions. Additionally, CT scans of the abdomen and pelvis should be ordered, and if lung metastases are present, brain imaging with either MRI or CT scan also should be obtained. These imaging studies will provide the necessary information to stage the GTN (as metastatic or not).
Treatment for postmolar GTN is determined based on further prognostic categorization (“high risk” or “low risk”) in accordance with the WHO classification, which is derived using several prognostic clinical variables including age, antecedent pregnancy, interval from index pregnancy, pretreatment hCG, largest tumor size, sites and number of metastases, and response to previous chemotherapy.4 These assignments are necessary to determine whether single-agent or multiagent chemotherapy should be prescribed.
Laboratory studies are helpful to obtain at this time and include metabolic panels (which can ensure that renal and hepatic function are within normal limits in anticipation of future chemotherapy), and complete blood count ,which can establish viable bone marrow function prior to chemotherapy.
Once postmolar GTN has been diagnosed, it is most appropriate to refer the patient to a gynecologic oncologist with experience in the treatment of these relatively rare malignancies. At that point, the patient will be formally staged, and offered treatment based on these staging results.
Among women with low-risk, nonmetastatic GTN who desire future fertility it is appropriate to offer a repeat dilation and curettage (D&C) procedure rather than immediately proceeding with chemotherapy. Approximately two-thirds of women with low risk disease can avoid chemotherapy with repeat curettage.5 Risk factors for needing chemotherapy after repeat D&C include the presence of trophoblastic disease in the pathology specimen and urinary hCG levels greater than 1,500 mIU/mL at the time of curettage. In my experience, many women appreciate this option to potentially avoid toxic chemotherapy.
For women with low-risk, nonmetastatic postmolar GTN who do not desire future fertility, and hope to avoid chemotherapy, hysterectomy also is a reasonable first option. This can be performed via either minimally invasive, laparotomy, or vaginal route. If performing a minimally invasive procedure in the setting of GTN, there should be caution or avoidance of use of a uterine manipulator because the uterine wall typically is soft and prone to perforation, and bleeding can be significant secondary to disruption of the tumor.
If repeat D&C or hysterectomy are adopted instead of chemotherapy, it is important that patients are very closely monitored post operatively to ensure normalization of their hCG levels (as described above). If it fails to normalize, restaging scans and examinations should be performed, and referral for the appropriate chemotherapy regimen should be initiated without delay.
Postmolar GTN is a serious condition that usually can be cured with chemotherapy or, if appropriate, surgery. and refer to a gynecologic oncologist when criteria are met to ensure that overtreatment is avoided and essential therapy is ensured.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She said she had no relevant financial disclosures. Email her at [email protected].
References
1. Lancet Oncol. 2007 Aug;8(8):715-24.
2. J Natl Compr Canc Netw. 2019 Nov 1;17(11):1374-91.
3. Gynecol Oncol. 2009 Mar;112(3):663-72.
4. World Health Organ Tech Rep Ser. 1983;692:7-81.
5. Obstet Gynecol. 2016;128(3):535-42.
Molar pregnancy is an uncommon but serious condition that affects young women of reproductive age. The diagnosis and management of molar pregnancy is familiar to most gynecologists. However, in the days and weeks following evacuation of molar pregnancy, clinicians face a critical time period in which they must be vigilant for the development of postmolar gestational trophoblastic neoplasia (GTN). If recognized early and treated appropriately, it almost always can be cured; however, errors or delays in the management of this condition can have catastrophic consequences for patients, including decreasing the likelihood of cure. Here we will review some of the steps and actions that can be taken immediately following the diagnosis of a molar pregnancy to expeditiously identify postmolar GTN and ensure patients are appropriately prepared for further consultation and intervention.
Postmolar GTN includes the diagnoses of invasive mole and choriocarcinoma that contain highly atypical trophoblasts with the capacity for local invasion and metastasis. Typically, the diagnosis is made clinically and not distinguished with histology. While molar pregnancies are a benign condition, invasive moles and choriocarcinoma are malignant conditions in which the molar tissue infiltrates the uterine myometrium, vasculature, and frequently is associated with hematogenous spread with distant metastases. It is a highly chemosensitive disease, and cure with chemotherapy typically is achieved with the ability to preserve fertility if desired even in advanced stage disease.1
After evacuation of a molar pregnancy, gynecologists should be on alert for the development of postmolar GTN if the following known risk factors are present: a history of a prior GTN diagnosis, complete mole on pathology (as opposed to partial mole), serum human chorionic gonadotropin (hCG) levels greater than 100,000 mIU/mL, age greater than 40 years, an enlarged uterus or large ovarian theca lutein cysts, and slow to normalize (more than 2 months) hCG. Symptoms for the development of postmolar GTN include persistent vaginal bleeding after evacuation, a persistently enlarged or enlarging uterine size, and adnexal masses. Ultimately, the diagnosis is made through plateaued or rising serum hCG assessments.2 (See graphic.)
Following the evacuation of a molar pregnancy, hCG levels should be drawn at the same laboratory every 1-2 weeks until normalization and then three consecutive normal values. Once this has been achieved, hCG levels should be tested once at 3 months and again at 6 months. During this 6 month period, patients should use reliable contraception, ideally, and through oral contraceptive pills that suppress the secretion of pituitary hCG if not contraindicated. Should a woman become pregnant during this 6-month surveillance, it becomes impossible to rule out occult postmolar GTN.
Typically after evacuation of a molar pregnancy, there is rapid fall in hCG levels, but this does not occur when the molar pregnancy has become invasive or is associated with choriocarcinoma. In these cases, after an initial drop in hCG levels, there is an observed rise or plateau in levels (as defined in the accompanying table), and this establishes the diagnosis of postmolar GTN. It is common for hCG to fall in fits and starts, rather than have a smooth, consistent diminution, and this can be worrying for gynecologists; however, provided there is a consistent reduction in values in accordance with the stated definitions, observation can continue.
Another source of confusion and concern is an HCG level that fails to completely normalize during observation, yet reaches a very low level. If this is observed, clinicians should consider the diagnosis of quiescent hCG, pituitary hCG, or phantom hCG.3 These can be difficult to distinguish from postmolar GTN, and consultation with a gynecologic oncologist with experience in the diagnosis and management of these rare tumors is helpful to determine if the persistent low levels in hCG require intervention.
Once a clinician has observed a plateau or rise in hCG levels, a gynecologic examination should be performed because the lower genital tract is a common site for metastatic postmolar GTN. If during this evaluation, a suspicious lesion is identified (typically a blue-black, slightly raised, hemorrhagic-appearing lesion), it should not be biopsied, but rather assumed to be a metastatic site. The vasculature of metastatic sites is extremely fragile, and biopsy or disruption can result in catastrophic hemorrhage, even from very small lesions.
In addition to physical examination, several diagnostic studies should be performed which may expedite the triage and management of the case. A pelvic ultrasound should evaluate the endometrial cavity for a new viable pregnancy, and residual molar tissue; sometimes, myometrial invasion consistent with an invasive mole can be appreciated. Chest x-ray or CT scan should be ordered to evaluate for pulmonary metastatic lesions. Additionally, CT scans of the abdomen and pelvis should be ordered, and if lung metastases are present, brain imaging with either MRI or CT scan also should be obtained. These imaging studies will provide the necessary information to stage the GTN (as metastatic or not).
Treatment for postmolar GTN is determined based on further prognostic categorization (“high risk” or “low risk”) in accordance with the WHO classification, which is derived using several prognostic clinical variables including age, antecedent pregnancy, interval from index pregnancy, pretreatment hCG, largest tumor size, sites and number of metastases, and response to previous chemotherapy.4 These assignments are necessary to determine whether single-agent or multiagent chemotherapy should be prescribed.
Laboratory studies are helpful to obtain at this time and include metabolic panels (which can ensure that renal and hepatic function are within normal limits in anticipation of future chemotherapy), and complete blood count ,which can establish viable bone marrow function prior to chemotherapy.
Once postmolar GTN has been diagnosed, it is most appropriate to refer the patient to a gynecologic oncologist with experience in the treatment of these relatively rare malignancies. At that point, the patient will be formally staged, and offered treatment based on these staging results.
Among women with low-risk, nonmetastatic GTN who desire future fertility it is appropriate to offer a repeat dilation and curettage (D&C) procedure rather than immediately proceeding with chemotherapy. Approximately two-thirds of women with low risk disease can avoid chemotherapy with repeat curettage.5 Risk factors for needing chemotherapy after repeat D&C include the presence of trophoblastic disease in the pathology specimen and urinary hCG levels greater than 1,500 mIU/mL at the time of curettage. In my experience, many women appreciate this option to potentially avoid toxic chemotherapy.
For women with low-risk, nonmetastatic postmolar GTN who do not desire future fertility, and hope to avoid chemotherapy, hysterectomy also is a reasonable first option. This can be performed via either minimally invasive, laparotomy, or vaginal route. If performing a minimally invasive procedure in the setting of GTN, there should be caution or avoidance of use of a uterine manipulator because the uterine wall typically is soft and prone to perforation, and bleeding can be significant secondary to disruption of the tumor.
If repeat D&C or hysterectomy are adopted instead of chemotherapy, it is important that patients are very closely monitored post operatively to ensure normalization of their hCG levels (as described above). If it fails to normalize, restaging scans and examinations should be performed, and referral for the appropriate chemotherapy regimen should be initiated without delay.
Postmolar GTN is a serious condition that usually can be cured with chemotherapy or, if appropriate, surgery. and refer to a gynecologic oncologist when criteria are met to ensure that overtreatment is avoided and essential therapy is ensured.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She said she had no relevant financial disclosures. Email her at [email protected].
References
1. Lancet Oncol. 2007 Aug;8(8):715-24.
2. J Natl Compr Canc Netw. 2019 Nov 1;17(11):1374-91.
3. Gynecol Oncol. 2009 Mar;112(3):663-72.
4. World Health Organ Tech Rep Ser. 1983;692:7-81.
5. Obstet Gynecol. 2016;128(3):535-42.
Molar pregnancy is an uncommon but serious condition that affects young women of reproductive age. The diagnosis and management of molar pregnancy is familiar to most gynecologists. However, in the days and weeks following evacuation of molar pregnancy, clinicians face a critical time period in which they must be vigilant for the development of postmolar gestational trophoblastic neoplasia (GTN). If recognized early and treated appropriately, it almost always can be cured; however, errors or delays in the management of this condition can have catastrophic consequences for patients, including decreasing the likelihood of cure. Here we will review some of the steps and actions that can be taken immediately following the diagnosis of a molar pregnancy to expeditiously identify postmolar GTN and ensure patients are appropriately prepared for further consultation and intervention.
Postmolar GTN includes the diagnoses of invasive mole and choriocarcinoma that contain highly atypical trophoblasts with the capacity for local invasion and metastasis. Typically, the diagnosis is made clinically and not distinguished with histology. While molar pregnancies are a benign condition, invasive moles and choriocarcinoma are malignant conditions in which the molar tissue infiltrates the uterine myometrium, vasculature, and frequently is associated with hematogenous spread with distant metastases. It is a highly chemosensitive disease, and cure with chemotherapy typically is achieved with the ability to preserve fertility if desired even in advanced stage disease.1
After evacuation of a molar pregnancy, gynecologists should be on alert for the development of postmolar GTN if the following known risk factors are present: a history of a prior GTN diagnosis, complete mole on pathology (as opposed to partial mole), serum human chorionic gonadotropin (hCG) levels greater than 100,000 mIU/mL, age greater than 40 years, an enlarged uterus or large ovarian theca lutein cysts, and slow to normalize (more than 2 months) hCG. Symptoms for the development of postmolar GTN include persistent vaginal bleeding after evacuation, a persistently enlarged or enlarging uterine size, and adnexal masses. Ultimately, the diagnosis is made through plateaued or rising serum hCG assessments.2 (See graphic.)
Following the evacuation of a molar pregnancy, hCG levels should be drawn at the same laboratory every 1-2 weeks until normalization and then three consecutive normal values. Once this has been achieved, hCG levels should be tested once at 3 months and again at 6 months. During this 6 month period, patients should use reliable contraception, ideally, and through oral contraceptive pills that suppress the secretion of pituitary hCG if not contraindicated. Should a woman become pregnant during this 6-month surveillance, it becomes impossible to rule out occult postmolar GTN.
Typically after evacuation of a molar pregnancy, there is rapid fall in hCG levels, but this does not occur when the molar pregnancy has become invasive or is associated with choriocarcinoma. In these cases, after an initial drop in hCG levels, there is an observed rise or plateau in levels (as defined in the accompanying table), and this establishes the diagnosis of postmolar GTN. It is common for hCG to fall in fits and starts, rather than have a smooth, consistent diminution, and this can be worrying for gynecologists; however, provided there is a consistent reduction in values in accordance with the stated definitions, observation can continue.
Another source of confusion and concern is an HCG level that fails to completely normalize during observation, yet reaches a very low level. If this is observed, clinicians should consider the diagnosis of quiescent hCG, pituitary hCG, or phantom hCG.3 These can be difficult to distinguish from postmolar GTN, and consultation with a gynecologic oncologist with experience in the diagnosis and management of these rare tumors is helpful to determine if the persistent low levels in hCG require intervention.
Once a clinician has observed a plateau or rise in hCG levels, a gynecologic examination should be performed because the lower genital tract is a common site for metastatic postmolar GTN. If during this evaluation, a suspicious lesion is identified (typically a blue-black, slightly raised, hemorrhagic-appearing lesion), it should not be biopsied, but rather assumed to be a metastatic site. The vasculature of metastatic sites is extremely fragile, and biopsy or disruption can result in catastrophic hemorrhage, even from very small lesions.
In addition to physical examination, several diagnostic studies should be performed which may expedite the triage and management of the case. A pelvic ultrasound should evaluate the endometrial cavity for a new viable pregnancy, and residual molar tissue; sometimes, myometrial invasion consistent with an invasive mole can be appreciated. Chest x-ray or CT scan should be ordered to evaluate for pulmonary metastatic lesions. Additionally, CT scans of the abdomen and pelvis should be ordered, and if lung metastases are present, brain imaging with either MRI or CT scan also should be obtained. These imaging studies will provide the necessary information to stage the GTN (as metastatic or not).
Treatment for postmolar GTN is determined based on further prognostic categorization (“high risk” or “low risk”) in accordance with the WHO classification, which is derived using several prognostic clinical variables including age, antecedent pregnancy, interval from index pregnancy, pretreatment hCG, largest tumor size, sites and number of metastases, and response to previous chemotherapy.4 These assignments are necessary to determine whether single-agent or multiagent chemotherapy should be prescribed.
Laboratory studies are helpful to obtain at this time and include metabolic panels (which can ensure that renal and hepatic function are within normal limits in anticipation of future chemotherapy), and complete blood count ,which can establish viable bone marrow function prior to chemotherapy.
Once postmolar GTN has been diagnosed, it is most appropriate to refer the patient to a gynecologic oncologist with experience in the treatment of these relatively rare malignancies. At that point, the patient will be formally staged, and offered treatment based on these staging results.
Among women with low-risk, nonmetastatic GTN who desire future fertility it is appropriate to offer a repeat dilation and curettage (D&C) procedure rather than immediately proceeding with chemotherapy. Approximately two-thirds of women with low risk disease can avoid chemotherapy with repeat curettage.5 Risk factors for needing chemotherapy after repeat D&C include the presence of trophoblastic disease in the pathology specimen and urinary hCG levels greater than 1,500 mIU/mL at the time of curettage. In my experience, many women appreciate this option to potentially avoid toxic chemotherapy.
For women with low-risk, nonmetastatic postmolar GTN who do not desire future fertility, and hope to avoid chemotherapy, hysterectomy also is a reasonable first option. This can be performed via either minimally invasive, laparotomy, or vaginal route. If performing a minimally invasive procedure in the setting of GTN, there should be caution or avoidance of use of a uterine manipulator because the uterine wall typically is soft and prone to perforation, and bleeding can be significant secondary to disruption of the tumor.
If repeat D&C or hysterectomy are adopted instead of chemotherapy, it is important that patients are very closely monitored post operatively to ensure normalization of their hCG levels (as described above). If it fails to normalize, restaging scans and examinations should be performed, and referral for the appropriate chemotherapy regimen should be initiated without delay.
Postmolar GTN is a serious condition that usually can be cured with chemotherapy or, if appropriate, surgery. and refer to a gynecologic oncologist when criteria are met to ensure that overtreatment is avoided and essential therapy is ensured.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She said she had no relevant financial disclosures. Email her at [email protected].
References
1. Lancet Oncol. 2007 Aug;8(8):715-24.
2. J Natl Compr Canc Netw. 2019 Nov 1;17(11):1374-91.
3. Gynecol Oncol. 2009 Mar;112(3):663-72.
4. World Health Organ Tech Rep Ser. 1983;692:7-81.
5. Obstet Gynecol. 2016;128(3):535-42.
How should we monitor for ovarian cancer recurrence?
Several practice-changing developments in the treatment of ovarian cancer were seen in 2019, including the results of the pivotal trial Gynecologic Oncology Group (GOG)-213, which were published in November in the New England Journal of Medicine.1 This trial randomly assigned women with ovarian cancer who had achieved a remission of more than 6 months after primary therapy (“platinum sensitive”) to either a repeat surgical cytoreduction followed by chemotherapy versus chemotherapy alone. It found that the addition of surgery provided no benefit in overall survival, challenging the notion that repeat surgical “debulking” should be routinely considered for the treatment of women with platinum-sensitive ovarian cancer.
The primary treatment of ovarian cancer includes a combination of surgery and chemotherapy, after which the vast majority of patients will experience a complete clinical response, a so-called “remission.” At that time patients enter surveillance care, in which their providers evaluate them, typically every 3 months in the first 2-3 years. These visits are designed to address ongoing toxicities of therapy in addition to evaluation for recurrence. At these visits, it is common for providers to assess tumor markers, such as CA 125 (cancer antigen 125), if they had been elevated at original diagnosis. As a gynecologic oncologist, I can vouch for the fact that patients “sweat” on this lab result the most. No matter how reassuring my physical exams or their symptom profiles are, there is nothing more comforting as a normal, stable CA 125 value in black and white. However, and may, in fact, be harmful.
Providers have drawn tumor markers at surveillance exams under the working premise that abnormal or rising values signal the onset of asymptomatic recurrence, and that earlier treatment will be associated with better responses to salvage therapy. However, this has not been shown to be the case in randomized, controlled trials. In a large European cooperative-group trial, more than 500 patients with a history of completely treated ovarian cancer were randomized to either reinitiation of chemotherapy (salvage therapy) when CA 125 values first doubled or to reinitiation of therapy when they became symptomatic without knowledge of their CA 125 values.2 In this trial the mean survival of both groups was the same (26 months for the early initiation of chemotherapy vs. 27 for late initiation). However, what did differ were the quality of life scores, which were lower for the group who initiated chemotherapy earlier, likely because they received toxic therapies for longer periods of time.
The results of this trial were challenged by those who felt that this study did not evaluate the role that surgery might play. Their argument was that surgery in the recurrent setting would improve the outcomes from chemotherapy for certain patients with long platinum-free intervals (duration of remission since last receiving a platinum-containing drug), oligometastatic disease, and good performance status, just as it had in the primary setting. Retrospective series seemed to confirm this phenomenon, particularly if surgeons were able to achieve a complete resection (no residual measurable disease).3,4 By detecting asymptomatic patients with early elevations in CA 125, they proposed they might identify patients with lower disease burden in whom complete debulking would be more feasible. Whereas, in waiting for symptoms alone, they might “miss the boat,” and discover recurrence when it was too advanced to be completely resected.
The results of the GOG-213 study significantly challenge this line of thought, although with some caveats. Because this new trial showed no survival benefit for women with secondary debulking prior to chemotherapy, one could question whether there is any benefit in screening for asymptomatic, early recurrence. The authors of the study looked in subgroup analyses to attempt to identify groups who might benefit over others, such as women who had complete surgical cytoreduction (no residual disease) but still did not find a benefit to surgery. The trial population as a whole included women who had very favorable prognostic factors, including very long disease-free intervals (median, 20.4 months), and most women had only one or two sites of measurable recurrence. Yet it is remarkable that, in this group of patients who were predisposed to optimal outcomes, no benefit from surgery was observed.
However, it is important to recognize that the equivalent results of single-modality chemotherapy were achieved with the majority of women receiving bevacizumab with their chemotherapy regimen. An additional consideration is that the chemotherapy for platinum-sensitive, recurrent ovarian cancer has changed in recent years as we have learned the benefit of poly (ADP-ribose) polymerase (PARP) inhibitor drugs as maintenance therapy following complete or partial response to chemotherapy.5 It is unclear how the addition of PARP inhibitor maintenance therapy might have influenced the results of GOG-213. Further advancements in targeted therapies and consideration of hyperthermic intraperitoneal chemotherapy at the time of surgery also are being developed, and so, the answer of optimal therapy for platinum-sensitive ovarian cancer is a fluid one and might include a role for surgery for some of these patients.
However, in the meantime, before routinely ordering that tumor marker assessment in the surveillance period, it is important to remember that, if secondary cytoreduction is not beneficial and early initiation of chemotherapy is not helpful either, then these tumor marker results might provide more hindrance than help. Why search for recurrence at an earlier time point with CA 125 elevations if there isn’t a benefit to the patient in doing so? There certainly appears to be worse quality of life in doing so, and most likely also additional cost. Perhaps we should wait for clinical symptoms to confirm recurrence?
In the meantime, we will continue to have discussions with patients after primary therapy regarding how to best monitor them in the surveillance period. We will educate them about the limitations of early initiation of chemotherapy and the potentially limited role for surgery. Hopefully with individualized care and shared decision making, patients can guide us as to how they best be evaluated. While receiving a normal CA 125 result is powerfully reassuring, it is just as powerfully confusing and difficult for a patient to receive an abnormal one followed by a period of “doing nothing,” otherwise known as expectant management, if immediate treatment is not beneficial.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She had no relevant financial disclosures. Email her at [email protected].
References
1. N Engl J Med. 2019 Nov 14;381(20):1929-39.
2. Lancet. 2010 Oct 2;376(9747):1155-63.
3. Gynecol Oncol. 2009 Jan;112(1):265-74.
4. Br J Cancer. 2011 Sep 27;105(7):890-6.
5. N Engl J Med. 2016 Dec 1;375(22):2154-64.
Several practice-changing developments in the treatment of ovarian cancer were seen in 2019, including the results of the pivotal trial Gynecologic Oncology Group (GOG)-213, which were published in November in the New England Journal of Medicine.1 This trial randomly assigned women with ovarian cancer who had achieved a remission of more than 6 months after primary therapy (“platinum sensitive”) to either a repeat surgical cytoreduction followed by chemotherapy versus chemotherapy alone. It found that the addition of surgery provided no benefit in overall survival, challenging the notion that repeat surgical “debulking” should be routinely considered for the treatment of women with platinum-sensitive ovarian cancer.
The primary treatment of ovarian cancer includes a combination of surgery and chemotherapy, after which the vast majority of patients will experience a complete clinical response, a so-called “remission.” At that time patients enter surveillance care, in which their providers evaluate them, typically every 3 months in the first 2-3 years. These visits are designed to address ongoing toxicities of therapy in addition to evaluation for recurrence. At these visits, it is common for providers to assess tumor markers, such as CA 125 (cancer antigen 125), if they had been elevated at original diagnosis. As a gynecologic oncologist, I can vouch for the fact that patients “sweat” on this lab result the most. No matter how reassuring my physical exams or their symptom profiles are, there is nothing more comforting as a normal, stable CA 125 value in black and white. However, and may, in fact, be harmful.
Providers have drawn tumor markers at surveillance exams under the working premise that abnormal or rising values signal the onset of asymptomatic recurrence, and that earlier treatment will be associated with better responses to salvage therapy. However, this has not been shown to be the case in randomized, controlled trials. In a large European cooperative-group trial, more than 500 patients with a history of completely treated ovarian cancer were randomized to either reinitiation of chemotherapy (salvage therapy) when CA 125 values first doubled or to reinitiation of therapy when they became symptomatic without knowledge of their CA 125 values.2 In this trial the mean survival of both groups was the same (26 months for the early initiation of chemotherapy vs. 27 for late initiation). However, what did differ were the quality of life scores, which were lower for the group who initiated chemotherapy earlier, likely because they received toxic therapies for longer periods of time.
The results of this trial were challenged by those who felt that this study did not evaluate the role that surgery might play. Their argument was that surgery in the recurrent setting would improve the outcomes from chemotherapy for certain patients with long platinum-free intervals (duration of remission since last receiving a platinum-containing drug), oligometastatic disease, and good performance status, just as it had in the primary setting. Retrospective series seemed to confirm this phenomenon, particularly if surgeons were able to achieve a complete resection (no residual measurable disease).3,4 By detecting asymptomatic patients with early elevations in CA 125, they proposed they might identify patients with lower disease burden in whom complete debulking would be more feasible. Whereas, in waiting for symptoms alone, they might “miss the boat,” and discover recurrence when it was too advanced to be completely resected.
The results of the GOG-213 study significantly challenge this line of thought, although with some caveats. Because this new trial showed no survival benefit for women with secondary debulking prior to chemotherapy, one could question whether there is any benefit in screening for asymptomatic, early recurrence. The authors of the study looked in subgroup analyses to attempt to identify groups who might benefit over others, such as women who had complete surgical cytoreduction (no residual disease) but still did not find a benefit to surgery. The trial population as a whole included women who had very favorable prognostic factors, including very long disease-free intervals (median, 20.4 months), and most women had only one or two sites of measurable recurrence. Yet it is remarkable that, in this group of patients who were predisposed to optimal outcomes, no benefit from surgery was observed.
However, it is important to recognize that the equivalent results of single-modality chemotherapy were achieved with the majority of women receiving bevacizumab with their chemotherapy regimen. An additional consideration is that the chemotherapy for platinum-sensitive, recurrent ovarian cancer has changed in recent years as we have learned the benefit of poly (ADP-ribose) polymerase (PARP) inhibitor drugs as maintenance therapy following complete or partial response to chemotherapy.5 It is unclear how the addition of PARP inhibitor maintenance therapy might have influenced the results of GOG-213. Further advancements in targeted therapies and consideration of hyperthermic intraperitoneal chemotherapy at the time of surgery also are being developed, and so, the answer of optimal therapy for platinum-sensitive ovarian cancer is a fluid one and might include a role for surgery for some of these patients.
However, in the meantime, before routinely ordering that tumor marker assessment in the surveillance period, it is important to remember that, if secondary cytoreduction is not beneficial and early initiation of chemotherapy is not helpful either, then these tumor marker results might provide more hindrance than help. Why search for recurrence at an earlier time point with CA 125 elevations if there isn’t a benefit to the patient in doing so? There certainly appears to be worse quality of life in doing so, and most likely also additional cost. Perhaps we should wait for clinical symptoms to confirm recurrence?
In the meantime, we will continue to have discussions with patients after primary therapy regarding how to best monitor them in the surveillance period. We will educate them about the limitations of early initiation of chemotherapy and the potentially limited role for surgery. Hopefully with individualized care and shared decision making, patients can guide us as to how they best be evaluated. While receiving a normal CA 125 result is powerfully reassuring, it is just as powerfully confusing and difficult for a patient to receive an abnormal one followed by a period of “doing nothing,” otherwise known as expectant management, if immediate treatment is not beneficial.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She had no relevant financial disclosures. Email her at [email protected].
References
1. N Engl J Med. 2019 Nov 14;381(20):1929-39.
2. Lancet. 2010 Oct 2;376(9747):1155-63.
3. Gynecol Oncol. 2009 Jan;112(1):265-74.
4. Br J Cancer. 2011 Sep 27;105(7):890-6.
5. N Engl J Med. 2016 Dec 1;375(22):2154-64.
Several practice-changing developments in the treatment of ovarian cancer were seen in 2019, including the results of the pivotal trial Gynecologic Oncology Group (GOG)-213, which were published in November in the New England Journal of Medicine.1 This trial randomly assigned women with ovarian cancer who had achieved a remission of more than 6 months after primary therapy (“platinum sensitive”) to either a repeat surgical cytoreduction followed by chemotherapy versus chemotherapy alone. It found that the addition of surgery provided no benefit in overall survival, challenging the notion that repeat surgical “debulking” should be routinely considered for the treatment of women with platinum-sensitive ovarian cancer.
The primary treatment of ovarian cancer includes a combination of surgery and chemotherapy, after which the vast majority of patients will experience a complete clinical response, a so-called “remission.” At that time patients enter surveillance care, in which their providers evaluate them, typically every 3 months in the first 2-3 years. These visits are designed to address ongoing toxicities of therapy in addition to evaluation for recurrence. At these visits, it is common for providers to assess tumor markers, such as CA 125 (cancer antigen 125), if they had been elevated at original diagnosis. As a gynecologic oncologist, I can vouch for the fact that patients “sweat” on this lab result the most. No matter how reassuring my physical exams or their symptom profiles are, there is nothing more comforting as a normal, stable CA 125 value in black and white. However, and may, in fact, be harmful.
Providers have drawn tumor markers at surveillance exams under the working premise that abnormal or rising values signal the onset of asymptomatic recurrence, and that earlier treatment will be associated with better responses to salvage therapy. However, this has not been shown to be the case in randomized, controlled trials. In a large European cooperative-group trial, more than 500 patients with a history of completely treated ovarian cancer were randomized to either reinitiation of chemotherapy (salvage therapy) when CA 125 values first doubled or to reinitiation of therapy when they became symptomatic without knowledge of their CA 125 values.2 In this trial the mean survival of both groups was the same (26 months for the early initiation of chemotherapy vs. 27 for late initiation). However, what did differ were the quality of life scores, which were lower for the group who initiated chemotherapy earlier, likely because they received toxic therapies for longer periods of time.
The results of this trial were challenged by those who felt that this study did not evaluate the role that surgery might play. Their argument was that surgery in the recurrent setting would improve the outcomes from chemotherapy for certain patients with long platinum-free intervals (duration of remission since last receiving a platinum-containing drug), oligometastatic disease, and good performance status, just as it had in the primary setting. Retrospective series seemed to confirm this phenomenon, particularly if surgeons were able to achieve a complete resection (no residual measurable disease).3,4 By detecting asymptomatic patients with early elevations in CA 125, they proposed they might identify patients with lower disease burden in whom complete debulking would be more feasible. Whereas, in waiting for symptoms alone, they might “miss the boat,” and discover recurrence when it was too advanced to be completely resected.
The results of the GOG-213 study significantly challenge this line of thought, although with some caveats. Because this new trial showed no survival benefit for women with secondary debulking prior to chemotherapy, one could question whether there is any benefit in screening for asymptomatic, early recurrence. The authors of the study looked in subgroup analyses to attempt to identify groups who might benefit over others, such as women who had complete surgical cytoreduction (no residual disease) but still did not find a benefit to surgery. The trial population as a whole included women who had very favorable prognostic factors, including very long disease-free intervals (median, 20.4 months), and most women had only one or two sites of measurable recurrence. Yet it is remarkable that, in this group of patients who were predisposed to optimal outcomes, no benefit from surgery was observed.
However, it is important to recognize that the equivalent results of single-modality chemotherapy were achieved with the majority of women receiving bevacizumab with their chemotherapy regimen. An additional consideration is that the chemotherapy for platinum-sensitive, recurrent ovarian cancer has changed in recent years as we have learned the benefit of poly (ADP-ribose) polymerase (PARP) inhibitor drugs as maintenance therapy following complete or partial response to chemotherapy.5 It is unclear how the addition of PARP inhibitor maintenance therapy might have influenced the results of GOG-213. Further advancements in targeted therapies and consideration of hyperthermic intraperitoneal chemotherapy at the time of surgery also are being developed, and so, the answer of optimal therapy for platinum-sensitive ovarian cancer is a fluid one and might include a role for surgery for some of these patients.
However, in the meantime, before routinely ordering that tumor marker assessment in the surveillance period, it is important to remember that, if secondary cytoreduction is not beneficial and early initiation of chemotherapy is not helpful either, then these tumor marker results might provide more hindrance than help. Why search for recurrence at an earlier time point with CA 125 elevations if there isn’t a benefit to the patient in doing so? There certainly appears to be worse quality of life in doing so, and most likely also additional cost. Perhaps we should wait for clinical symptoms to confirm recurrence?
In the meantime, we will continue to have discussions with patients after primary therapy regarding how to best monitor them in the surveillance period. We will educate them about the limitations of early initiation of chemotherapy and the potentially limited role for surgery. Hopefully with individualized care and shared decision making, patients can guide us as to how they best be evaluated. While receiving a normal CA 125 result is powerfully reassuring, it is just as powerfully confusing and difficult for a patient to receive an abnormal one followed by a period of “doing nothing,” otherwise known as expectant management, if immediate treatment is not beneficial.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She had no relevant financial disclosures. Email her at [email protected].
References
1. N Engl J Med. 2019 Nov 14;381(20):1929-39.
2. Lancet. 2010 Oct 2;376(9747):1155-63.
3. Gynecol Oncol. 2009 Jan;112(1):265-74.
4. Br J Cancer. 2011 Sep 27;105(7):890-6.
5. N Engl J Med. 2016 Dec 1;375(22):2154-64.