User login
Scott Gottlieb to step down as FDA commissioner
According to reports, he is stepping down to spend more time with his family, who live in Westport, Conn. He splits time between there and Washington. He was confirmed by the Senate in May 2017 with five Democrats and one independent joining Republicans in voting him in.
President Trump confirmed Dr. Gottlieb’s resignation, praising him in a tweet for the “terrific job” he has done in this role and commending his efforts to help “us to lower drug prices, get a record number of generic drugs approved and onto the market, and so many other things. ”
Dr. Gottlieb’s legacy may be his work on regulating e-cigarettes, although that work is unfinished. His passion for this subject can be found in a statement made in Nov. 2018, announcing an advanced notice of proposed rule making to regulate e-cigarettes.
“Today, I’m pursuing actions aimed at addressing the disturbing trend of youth nicotine use and continuing to advance the historic declines we’ve achieved in recent years in the rates of combustible cigarette use among kids,” Dr. Gottlieb said in the statement.
More recently, the agency announced March 4 enforcement actions aimed at both retailers and manufacturers, including requesting a meeting with Walgreens to discuss the nearly 1,800 violations the chain has amassed across the country for selling tobacco products to minors.
“Because tobacco use is almost always initiated and established during adolescence, early intervention ‒ including making sure tobacco products aren’t being marketed to, sold to, or used by kids ‒ is critical,” he said in announcing the enforcement actions. He added that the FDA will “continue vigorous enforcement activities, with a sustained campaign to monitor, penalize, and help prevent e-cigarette sales to minors in retail locations, including manufacturers’ Internet storefronts, as well as take additional steps to tackle other concerns related to the youth access and appeal of these products. The FDA is also exploring additional enforcement avenues to target violative sales and marketing practices by manufacturers and retailers.”
The American Heart Association praised Dr. Gottlieb’s work.
“Commissioner Gottlieb departs the FDA having established himself as a tireless champion of tobacco control,” the organization said in a statement. “He elevated the war on tobacco use – and particularly the epidemic of electronic cigarette use among youth – to unprecedented levels. Because of his efforts, millions more people nationwide are aware of the grave threats posed by e-cigarettes and other tobacco products that are addicting a new generation of youth. We urge the FDA in the strongest possible terms to move forward with effective regulation of an industry that continues to prioritize profits over the lives of consumers.”
Department of Health & Human Services Secretary Alex Azar acknowledged Dr. Gottlieb’s work in combating youth e-cigarette use among a number of areas that the outgoing official has had a positive impact on.
“Scott’s leadership inspired historic results from the FDA team, which delivered record approvals of both innovative treatments and affordable generic drugs, while advancing important policies to confront opioid addiction, tobacco and youth e-cigarette use, chronic disease, and more,” Secretary Azar said in a statement. “The public health of our country is better off for the work Scott and the entire FDA team have done over the last two years.”
Under his leadership, FDA has approved a record number of generic drugs, although many still are not on the market yet.
In the area of opioids, his tenure could be a mixed bag as the FDA on the one hand removed an opioid product from the market, but on the other, controversially approved a new, powerful one.
According to reports, he is stepping down to spend more time with his family, who live in Westport, Conn. He splits time between there and Washington. He was confirmed by the Senate in May 2017 with five Democrats and one independent joining Republicans in voting him in.
President Trump confirmed Dr. Gottlieb’s resignation, praising him in a tweet for the “terrific job” he has done in this role and commending his efforts to help “us to lower drug prices, get a record number of generic drugs approved and onto the market, and so many other things. ”
Dr. Gottlieb’s legacy may be his work on regulating e-cigarettes, although that work is unfinished. His passion for this subject can be found in a statement made in Nov. 2018, announcing an advanced notice of proposed rule making to regulate e-cigarettes.
“Today, I’m pursuing actions aimed at addressing the disturbing trend of youth nicotine use and continuing to advance the historic declines we’ve achieved in recent years in the rates of combustible cigarette use among kids,” Dr. Gottlieb said in the statement.
More recently, the agency announced March 4 enforcement actions aimed at both retailers and manufacturers, including requesting a meeting with Walgreens to discuss the nearly 1,800 violations the chain has amassed across the country for selling tobacco products to minors.
“Because tobacco use is almost always initiated and established during adolescence, early intervention ‒ including making sure tobacco products aren’t being marketed to, sold to, or used by kids ‒ is critical,” he said in announcing the enforcement actions. He added that the FDA will “continue vigorous enforcement activities, with a sustained campaign to monitor, penalize, and help prevent e-cigarette sales to minors in retail locations, including manufacturers’ Internet storefronts, as well as take additional steps to tackle other concerns related to the youth access and appeal of these products. The FDA is also exploring additional enforcement avenues to target violative sales and marketing practices by manufacturers and retailers.”
The American Heart Association praised Dr. Gottlieb’s work.
“Commissioner Gottlieb departs the FDA having established himself as a tireless champion of tobacco control,” the organization said in a statement. “He elevated the war on tobacco use – and particularly the epidemic of electronic cigarette use among youth – to unprecedented levels. Because of his efforts, millions more people nationwide are aware of the grave threats posed by e-cigarettes and other tobacco products that are addicting a new generation of youth. We urge the FDA in the strongest possible terms to move forward with effective regulation of an industry that continues to prioritize profits over the lives of consumers.”
Department of Health & Human Services Secretary Alex Azar acknowledged Dr. Gottlieb’s work in combating youth e-cigarette use among a number of areas that the outgoing official has had a positive impact on.
“Scott’s leadership inspired historic results from the FDA team, which delivered record approvals of both innovative treatments and affordable generic drugs, while advancing important policies to confront opioid addiction, tobacco and youth e-cigarette use, chronic disease, and more,” Secretary Azar said in a statement. “The public health of our country is better off for the work Scott and the entire FDA team have done over the last two years.”
Under his leadership, FDA has approved a record number of generic drugs, although many still are not on the market yet.
In the area of opioids, his tenure could be a mixed bag as the FDA on the one hand removed an opioid product from the market, but on the other, controversially approved a new, powerful one.
According to reports, he is stepping down to spend more time with his family, who live in Westport, Conn. He splits time between there and Washington. He was confirmed by the Senate in May 2017 with five Democrats and one independent joining Republicans in voting him in.
President Trump confirmed Dr. Gottlieb’s resignation, praising him in a tweet for the “terrific job” he has done in this role and commending his efforts to help “us to lower drug prices, get a record number of generic drugs approved and onto the market, and so many other things. ”
Dr. Gottlieb’s legacy may be his work on regulating e-cigarettes, although that work is unfinished. His passion for this subject can be found in a statement made in Nov. 2018, announcing an advanced notice of proposed rule making to regulate e-cigarettes.
“Today, I’m pursuing actions aimed at addressing the disturbing trend of youth nicotine use and continuing to advance the historic declines we’ve achieved in recent years in the rates of combustible cigarette use among kids,” Dr. Gottlieb said in the statement.
More recently, the agency announced March 4 enforcement actions aimed at both retailers and manufacturers, including requesting a meeting with Walgreens to discuss the nearly 1,800 violations the chain has amassed across the country for selling tobacco products to minors.
“Because tobacco use is almost always initiated and established during adolescence, early intervention ‒ including making sure tobacco products aren’t being marketed to, sold to, or used by kids ‒ is critical,” he said in announcing the enforcement actions. He added that the FDA will “continue vigorous enforcement activities, with a sustained campaign to monitor, penalize, and help prevent e-cigarette sales to minors in retail locations, including manufacturers’ Internet storefronts, as well as take additional steps to tackle other concerns related to the youth access and appeal of these products. The FDA is also exploring additional enforcement avenues to target violative sales and marketing practices by manufacturers and retailers.”
The American Heart Association praised Dr. Gottlieb’s work.
“Commissioner Gottlieb departs the FDA having established himself as a tireless champion of tobacco control,” the organization said in a statement. “He elevated the war on tobacco use – and particularly the epidemic of electronic cigarette use among youth – to unprecedented levels. Because of his efforts, millions more people nationwide are aware of the grave threats posed by e-cigarettes and other tobacco products that are addicting a new generation of youth. We urge the FDA in the strongest possible terms to move forward with effective regulation of an industry that continues to prioritize profits over the lives of consumers.”
Department of Health & Human Services Secretary Alex Azar acknowledged Dr. Gottlieb’s work in combating youth e-cigarette use among a number of areas that the outgoing official has had a positive impact on.
“Scott’s leadership inspired historic results from the FDA team, which delivered record approvals of both innovative treatments and affordable generic drugs, while advancing important policies to confront opioid addiction, tobacco and youth e-cigarette use, chronic disease, and more,” Secretary Azar said in a statement. “The public health of our country is better off for the work Scott and the entire FDA team have done over the last two years.”
Under his leadership, FDA has approved a record number of generic drugs, although many still are not on the market yet.
In the area of opioids, his tenure could be a mixed bag as the FDA on the one hand removed an opioid product from the market, but on the other, controversially approved a new, powerful one.
Take stronger steps to prevent staph infections and sepsis
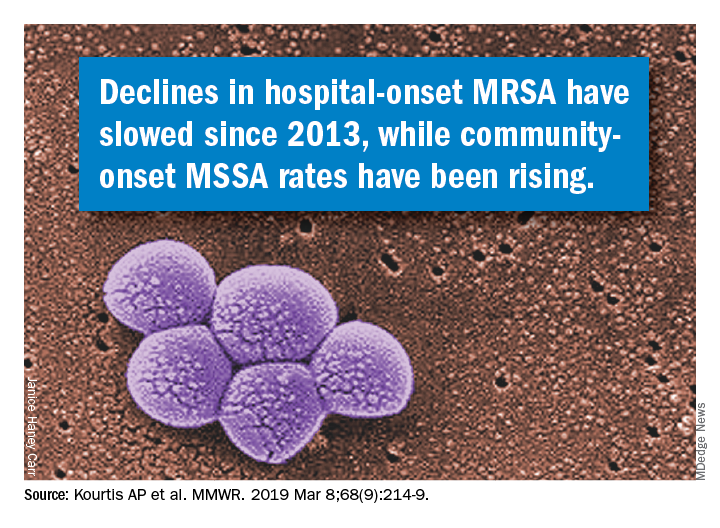
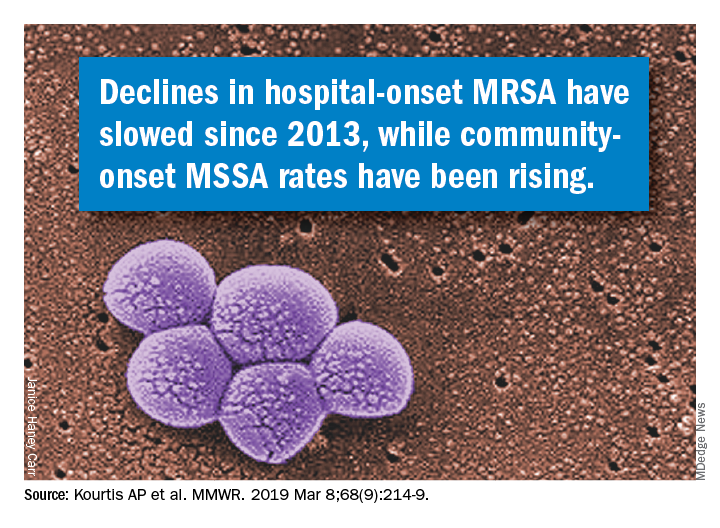
according to data from a Vital Signs report issued by the Centers for Disease Control and Prevention. The data include both methicillin-resistant S. aureus (MRSA) and methicillin-susceptible S. aureus (MSSA).
Although MRSA infections in health care settings declined by approximately 17% during 2005-2012, rates plateaued during 2012-2017, Anne Schuchat, MD, principal deputy director of the CDC, said in a teleconference March 5 to present the findings. The report emphasizes the potential for serious illness and death with any staph infection and the need for ongoing vigilance on the part of clinicians, she said.
In addition, community-onset MSSA infections increased by 3.9%/year during 2012-2017. Data from previous studies suggest that this increase may be connected to the opioid epidemic, said Dr. Schuchat.
“People who inject drugs are 16% more likely to develop a staph infection” than are those who don’t inject drugs, she said.
Community-onset MRSA declined by 6.9% during 2001-2016, attributed to declines in health care–associated infections, according to Vital Signs author Athena P. Kourtis, MD, of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases, and her colleagues. Rates of hospital-associated MSSA infection remained essentially unchanged (P = .11). The overall unadjusted in-hospital mortality among patients with S. aureus bloodstream infections over the study period was 18%.
The data for the report were collected from electronic health records at more than 400 acute care hospitals, as well as population-based surveillance data from the CDC’s Emerging Infections Program.
Most people carry staph on their skin with no ill effects, but the bacteria become dangerous when they enter the bloodstream, Dr. Schuchat emphasized. “We hope the new data today will refocus the nation’s efforts to protect patients from staph infections,” she said.
Dr. Schuchat advised clinicians and hospital administrators to review their data and step up their safety protocols to prevent staph infections. Precautions include wearing gowns and gloves, following proper hand washing protocols, cautious use of antibiotics, and treating infections rapidly when they occur, she said. Dr. Schuchat noted that lack of adherence to these recommendations may have declined in recent years if clinicians and hospital administrators were wondering whether their protocols have an effect and have value. However, “this is a very serious infection, and we think it is very much worth preventing,” she emphasized.
Other strategies to prevent staph infections in health care settings include reviewing infection data regularly, exploring new approaches to prevent infections, and educating patients about when they may be at increased risk for infection, such as when invasive devices are in place or during surgical procedures. Also, clinicians should be aware of the increased risk for patients who inject drugs, Dr. Schuchat said.
Dr. Schuchat commended the Department of Veterans Affairs Medical Centers (VAMC), which overall reduced their rate of staph infections by 43% during the period from 2005 through 2017 in contrast to the national trend. These findings also appeared in the MMWR on March 5. The VAMC implemented additional interventions and increased their adherence to CDC recommendations during this period, she noted.
The Vital Signs data were published March 5 in the CDC’s Morbidity and Mortality Weekly Report; read the full report here.
The CDC researchers had no financial conflicts to disclose.
SOURCE: Kourtis AP et al. MMWR. 2019 Mar 5; 68:1-6.
according to data from a Vital Signs report issued by the Centers for Disease Control and Prevention. The data include both methicillin-resistant S. aureus (MRSA) and methicillin-susceptible S. aureus (MSSA).
Although MRSA infections in health care settings declined by approximately 17% during 2005-2012, rates plateaued during 2012-2017, Anne Schuchat, MD, principal deputy director of the CDC, said in a teleconference March 5 to present the findings. The report emphasizes the potential for serious illness and death with any staph infection and the need for ongoing vigilance on the part of clinicians, she said.
In addition, community-onset MSSA infections increased by 3.9%/year during 2012-2017. Data from previous studies suggest that this increase may be connected to the opioid epidemic, said Dr. Schuchat.
“People who inject drugs are 16% more likely to develop a staph infection” than are those who don’t inject drugs, she said.
Community-onset MRSA declined by 6.9% during 2001-2016, attributed to declines in health care–associated infections, according to Vital Signs author Athena P. Kourtis, MD, of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases, and her colleagues. Rates of hospital-associated MSSA infection remained essentially unchanged (P = .11). The overall unadjusted in-hospital mortality among patients with S. aureus bloodstream infections over the study period was 18%.
The data for the report were collected from electronic health records at more than 400 acute care hospitals, as well as population-based surveillance data from the CDC’s Emerging Infections Program.
Most people carry staph on their skin with no ill effects, but the bacteria become dangerous when they enter the bloodstream, Dr. Schuchat emphasized. “We hope the new data today will refocus the nation’s efforts to protect patients from staph infections,” she said.
Dr. Schuchat advised clinicians and hospital administrators to review their data and step up their safety protocols to prevent staph infections. Precautions include wearing gowns and gloves, following proper hand washing protocols, cautious use of antibiotics, and treating infections rapidly when they occur, she said. Dr. Schuchat noted that lack of adherence to these recommendations may have declined in recent years if clinicians and hospital administrators were wondering whether their protocols have an effect and have value. However, “this is a very serious infection, and we think it is very much worth preventing,” she emphasized.
Other strategies to prevent staph infections in health care settings include reviewing infection data regularly, exploring new approaches to prevent infections, and educating patients about when they may be at increased risk for infection, such as when invasive devices are in place or during surgical procedures. Also, clinicians should be aware of the increased risk for patients who inject drugs, Dr. Schuchat said.
Dr. Schuchat commended the Department of Veterans Affairs Medical Centers (VAMC), which overall reduced their rate of staph infections by 43% during the period from 2005 through 2017 in contrast to the national trend. These findings also appeared in the MMWR on March 5. The VAMC implemented additional interventions and increased their adherence to CDC recommendations during this period, she noted.
The Vital Signs data were published March 5 in the CDC’s Morbidity and Mortality Weekly Report; read the full report here.
The CDC researchers had no financial conflicts to disclose.
SOURCE: Kourtis AP et al. MMWR. 2019 Mar 5; 68:1-6.
according to data from a Vital Signs report issued by the Centers for Disease Control and Prevention. The data include both methicillin-resistant S. aureus (MRSA) and methicillin-susceptible S. aureus (MSSA).
Although MRSA infections in health care settings declined by approximately 17% during 2005-2012, rates plateaued during 2012-2017, Anne Schuchat, MD, principal deputy director of the CDC, said in a teleconference March 5 to present the findings. The report emphasizes the potential for serious illness and death with any staph infection and the need for ongoing vigilance on the part of clinicians, she said.
In addition, community-onset MSSA infections increased by 3.9%/year during 2012-2017. Data from previous studies suggest that this increase may be connected to the opioid epidemic, said Dr. Schuchat.
“People who inject drugs are 16% more likely to develop a staph infection” than are those who don’t inject drugs, she said.
Community-onset MRSA declined by 6.9% during 2001-2016, attributed to declines in health care–associated infections, according to Vital Signs author Athena P. Kourtis, MD, of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases, and her colleagues. Rates of hospital-associated MSSA infection remained essentially unchanged (P = .11). The overall unadjusted in-hospital mortality among patients with S. aureus bloodstream infections over the study period was 18%.
The data for the report were collected from electronic health records at more than 400 acute care hospitals, as well as population-based surveillance data from the CDC’s Emerging Infections Program.
Most people carry staph on their skin with no ill effects, but the bacteria become dangerous when they enter the bloodstream, Dr. Schuchat emphasized. “We hope the new data today will refocus the nation’s efforts to protect patients from staph infections,” she said.
Dr. Schuchat advised clinicians and hospital administrators to review their data and step up their safety protocols to prevent staph infections. Precautions include wearing gowns and gloves, following proper hand washing protocols, cautious use of antibiotics, and treating infections rapidly when they occur, she said. Dr. Schuchat noted that lack of adherence to these recommendations may have declined in recent years if clinicians and hospital administrators were wondering whether their protocols have an effect and have value. However, “this is a very serious infection, and we think it is very much worth preventing,” she emphasized.
Other strategies to prevent staph infections in health care settings include reviewing infection data regularly, exploring new approaches to prevent infections, and educating patients about when they may be at increased risk for infection, such as when invasive devices are in place or during surgical procedures. Also, clinicians should be aware of the increased risk for patients who inject drugs, Dr. Schuchat said.
Dr. Schuchat commended the Department of Veterans Affairs Medical Centers (VAMC), which overall reduced their rate of staph infections by 43% during the period from 2005 through 2017 in contrast to the national trend. These findings also appeared in the MMWR on March 5. The VAMC implemented additional interventions and increased their adherence to CDC recommendations during this period, she noted.
The Vital Signs data were published March 5 in the CDC’s Morbidity and Mortality Weekly Report; read the full report here.
The CDC researchers had no financial conflicts to disclose.
SOURCE: Kourtis AP et al. MMWR. 2019 Mar 5; 68:1-6.
FROM THE MORBIDITY AND MORTALITY WEEKLY REPORT
Hospitalists on the Hill
Advocating for HM in DC
Another Hill Day is coming – the all-day advocacy event on Capitol Hill is scheduled in conjunction with the Society of Hospital Medicine’s Annual Conference whenever it is held in Washington, DC. In 2019, Hill Day will take place on March 27, the final day of HM19.
This will be the fourth Hill Day, and the last for some time, said Ron Greeno, MD, FCCP, MHM, senior advisor for government affairs at SHM and the society’s immediate past president. For at least the next 5 years, SHM’s annual conferences won’t be held in Washington, so there will not be any opportunities to plan a Hill Day during that time. “Members may want to take advantage of this opportunity,” Dr. Greeno said. “The people who do this never forget it.”
How Hill Day works
Sign up for Hill Day and you’ll spend a day visiting legislators and their health care staffers to educate them on what hospital medicine is, what a hospitalist does, and some of the pressing issues that affect the profession, said Joshua Lenchus, DO, RPh, FACP, SFHM, chair of the SHM Public Policy Committee. “We try to leverage participants’ work and home addresses to pair them up with legislators from that area. Some hospitalists have personal or professional relationships with some of the legislators, and even if they’re not in their area, we’ll try to leverage that. And for people who have expertise in a particular topic, we try to arrange an audience with a member of Congress who may be promoting or sponsoring a bill related to that.”
Hill Day volunteers will attend an orientation to learn more about what the day will look like and what they’ll be talking about in their meetings. “We’ll only have time to cover one or two issues, and we’re in the process now of choosing the issues we want to address. We orient participants on those subjects so everybody is kind of saying the same thing,” Dr. Greeno said. “People shouldn’t be afraid of not being conversant with the issues because we do sufficient orientation that everybody gets comfortable enough to do a good job.”
Registration for Hill Day is happening online now. HM19 attendees can register at https://s1.goeshow.com/shm/annual/2019/registration_form.cfm.
“We beg people: If you sign up, show up, because we have many more people trying to participate than we can accommodate,” Dr. Greeno said. “If you change your mind, that’s fine because we have a waiting list, but please let us know because somebody else wants to take your place.”
The purpose of Hill Day
Educating legislators and their health care staff is the goal of the day, and it’s an important job. “Hospital medicine is still a relatively new field,” Dr. Lenchus said. “There are a fair number of legislators who still don’t know what a hospitalist is or what hospital medicine is. Part of our visits is always to educate them about what we do and what our impact is on the health care landscape of the country.” He added that educating Hill staff about the most pressing issues is another primary goal.
“Finally, and this is what separates us from other organizations that do legislative advocacy, we try to leave them with the idea that we’re here to help,” Dr. Lenchus said. “If there’s an issue or a particular bill that we’re asking them to sponsor or cosponsor, that’s one part of a visit. But by and large, we are trying to leave them with the sense that SHM is a resource when it comes to health care–related issues. We want to be there for legislators so that they can understand our position accurately from the outset.”
In short, Hill Day offers a rare opportunity to have direct access to the people who are voting on new legislation affecting hospitalists and affecting the implementation of existing legislation. “This is where the rubber meets the road,” Dr. Lenchus said. Each time a Hill Day is held, he noted, attendance increases. “That’s a true testament to the level of involvement and the interest that hospitalists have across the country. If you’re at all interested, you should absolutely sign up. This will be an amazing experience.”
The lasting impact
Though it’s just one day, Hill Day’s effects are significant.
“Before I started doing this work, I often thought, ‘What impact could someone have going into a legislator’s office?’ ” Dr. Greeno said. “But the answer is ‘A lot.’ The members and staff really do listen – especially if an advocate is highly educated and represent what legislators consider an important constituency, like health care providers. Health care is a hot topic, and it’s probably going to be one of the hot topics in the next election. Hospitalists have good ideas, and as a result these meetings are extremely influential; we wouldn’t do it otherwise. It is fun, but we’re not doing it for fun. We’re doing it because we know we can make a difference.”
In fact, in terms of impact on Capitol Hill, SHM punches above its weight, he added.
“We’re a relatively new society; we’re not huge. There are lots of societies that are much bigger than us and have many more resources, but people on the Hill have told us they like talking with us because they know we’re not looking at things the same way,” Dr. Greeno revealed. “We’re trying to help, and the issues that we’re addressing are not necessarily self-serving. We’re not saying, ‘You need to do this because it will make more money for our doctors.’ Instead, we’re saying, ‘You need to do this because the way it’s being done now is hurting patients. It’s hurting the health care system, and we have ideas about how to make that better.’ ”
SHM’s impressive track record has earned the society a positive reputation that will underlie the Hill Day meetings. “When we first set up the policy shop at SHM, we wanted to be seen as providers who cared about the American health care system and our patients,” Dr. Greeno said. “We have established that reputation, and that has led members on Capitol Hill to recognize us as being well intentioned and knowledgeable. So we have an outsize influence in Congress for our age and our size. When 200 hospitalists go to Capitol Hill, it’s an important thing.”
For more information about Hill Day, including details about participation, visit shmannualconference.org/hill-day/.
Advocating for HM in DC
Advocating for HM in DC
Another Hill Day is coming – the all-day advocacy event on Capitol Hill is scheduled in conjunction with the Society of Hospital Medicine’s Annual Conference whenever it is held in Washington, DC. In 2019, Hill Day will take place on March 27, the final day of HM19.
This will be the fourth Hill Day, and the last for some time, said Ron Greeno, MD, FCCP, MHM, senior advisor for government affairs at SHM and the society’s immediate past president. For at least the next 5 years, SHM’s annual conferences won’t be held in Washington, so there will not be any opportunities to plan a Hill Day during that time. “Members may want to take advantage of this opportunity,” Dr. Greeno said. “The people who do this never forget it.”
How Hill Day works
Sign up for Hill Day and you’ll spend a day visiting legislators and their health care staffers to educate them on what hospital medicine is, what a hospitalist does, and some of the pressing issues that affect the profession, said Joshua Lenchus, DO, RPh, FACP, SFHM, chair of the SHM Public Policy Committee. “We try to leverage participants’ work and home addresses to pair them up with legislators from that area. Some hospitalists have personal or professional relationships with some of the legislators, and even if they’re not in their area, we’ll try to leverage that. And for people who have expertise in a particular topic, we try to arrange an audience with a member of Congress who may be promoting or sponsoring a bill related to that.”
Hill Day volunteers will attend an orientation to learn more about what the day will look like and what they’ll be talking about in their meetings. “We’ll only have time to cover one or two issues, and we’re in the process now of choosing the issues we want to address. We orient participants on those subjects so everybody is kind of saying the same thing,” Dr. Greeno said. “People shouldn’t be afraid of not being conversant with the issues because we do sufficient orientation that everybody gets comfortable enough to do a good job.”
Registration for Hill Day is happening online now. HM19 attendees can register at https://s1.goeshow.com/shm/annual/2019/registration_form.cfm.
“We beg people: If you sign up, show up, because we have many more people trying to participate than we can accommodate,” Dr. Greeno said. “If you change your mind, that’s fine because we have a waiting list, but please let us know because somebody else wants to take your place.”
The purpose of Hill Day
Educating legislators and their health care staff is the goal of the day, and it’s an important job. “Hospital medicine is still a relatively new field,” Dr. Lenchus said. “There are a fair number of legislators who still don’t know what a hospitalist is or what hospital medicine is. Part of our visits is always to educate them about what we do and what our impact is on the health care landscape of the country.” He added that educating Hill staff about the most pressing issues is another primary goal.
“Finally, and this is what separates us from other organizations that do legislative advocacy, we try to leave them with the idea that we’re here to help,” Dr. Lenchus said. “If there’s an issue or a particular bill that we’re asking them to sponsor or cosponsor, that’s one part of a visit. But by and large, we are trying to leave them with the sense that SHM is a resource when it comes to health care–related issues. We want to be there for legislators so that they can understand our position accurately from the outset.”
In short, Hill Day offers a rare opportunity to have direct access to the people who are voting on new legislation affecting hospitalists and affecting the implementation of existing legislation. “This is where the rubber meets the road,” Dr. Lenchus said. Each time a Hill Day is held, he noted, attendance increases. “That’s a true testament to the level of involvement and the interest that hospitalists have across the country. If you’re at all interested, you should absolutely sign up. This will be an amazing experience.”
The lasting impact
Though it’s just one day, Hill Day’s effects are significant.
“Before I started doing this work, I often thought, ‘What impact could someone have going into a legislator’s office?’ ” Dr. Greeno said. “But the answer is ‘A lot.’ The members and staff really do listen – especially if an advocate is highly educated and represent what legislators consider an important constituency, like health care providers. Health care is a hot topic, and it’s probably going to be one of the hot topics in the next election. Hospitalists have good ideas, and as a result these meetings are extremely influential; we wouldn’t do it otherwise. It is fun, but we’re not doing it for fun. We’re doing it because we know we can make a difference.”
In fact, in terms of impact on Capitol Hill, SHM punches above its weight, he added.
“We’re a relatively new society; we’re not huge. There are lots of societies that are much bigger than us and have many more resources, but people on the Hill have told us they like talking with us because they know we’re not looking at things the same way,” Dr. Greeno revealed. “We’re trying to help, and the issues that we’re addressing are not necessarily self-serving. We’re not saying, ‘You need to do this because it will make more money for our doctors.’ Instead, we’re saying, ‘You need to do this because the way it’s being done now is hurting patients. It’s hurting the health care system, and we have ideas about how to make that better.’ ”
SHM’s impressive track record has earned the society a positive reputation that will underlie the Hill Day meetings. “When we first set up the policy shop at SHM, we wanted to be seen as providers who cared about the American health care system and our patients,” Dr. Greeno said. “We have established that reputation, and that has led members on Capitol Hill to recognize us as being well intentioned and knowledgeable. So we have an outsize influence in Congress for our age and our size. When 200 hospitalists go to Capitol Hill, it’s an important thing.”
For more information about Hill Day, including details about participation, visit shmannualconference.org/hill-day/.
Another Hill Day is coming – the all-day advocacy event on Capitol Hill is scheduled in conjunction with the Society of Hospital Medicine’s Annual Conference whenever it is held in Washington, DC. In 2019, Hill Day will take place on March 27, the final day of HM19.
This will be the fourth Hill Day, and the last for some time, said Ron Greeno, MD, FCCP, MHM, senior advisor for government affairs at SHM and the society’s immediate past president. For at least the next 5 years, SHM’s annual conferences won’t be held in Washington, so there will not be any opportunities to plan a Hill Day during that time. “Members may want to take advantage of this opportunity,” Dr. Greeno said. “The people who do this never forget it.”
How Hill Day works
Sign up for Hill Day and you’ll spend a day visiting legislators and their health care staffers to educate them on what hospital medicine is, what a hospitalist does, and some of the pressing issues that affect the profession, said Joshua Lenchus, DO, RPh, FACP, SFHM, chair of the SHM Public Policy Committee. “We try to leverage participants’ work and home addresses to pair them up with legislators from that area. Some hospitalists have personal or professional relationships with some of the legislators, and even if they’re not in their area, we’ll try to leverage that. And for people who have expertise in a particular topic, we try to arrange an audience with a member of Congress who may be promoting or sponsoring a bill related to that.”
Hill Day volunteers will attend an orientation to learn more about what the day will look like and what they’ll be talking about in their meetings. “We’ll only have time to cover one or two issues, and we’re in the process now of choosing the issues we want to address. We orient participants on those subjects so everybody is kind of saying the same thing,” Dr. Greeno said. “People shouldn’t be afraid of not being conversant with the issues because we do sufficient orientation that everybody gets comfortable enough to do a good job.”
Registration for Hill Day is happening online now. HM19 attendees can register at https://s1.goeshow.com/shm/annual/2019/registration_form.cfm.
“We beg people: If you sign up, show up, because we have many more people trying to participate than we can accommodate,” Dr. Greeno said. “If you change your mind, that’s fine because we have a waiting list, but please let us know because somebody else wants to take your place.”
The purpose of Hill Day
Educating legislators and their health care staff is the goal of the day, and it’s an important job. “Hospital medicine is still a relatively new field,” Dr. Lenchus said. “There are a fair number of legislators who still don’t know what a hospitalist is or what hospital medicine is. Part of our visits is always to educate them about what we do and what our impact is on the health care landscape of the country.” He added that educating Hill staff about the most pressing issues is another primary goal.
“Finally, and this is what separates us from other organizations that do legislative advocacy, we try to leave them with the idea that we’re here to help,” Dr. Lenchus said. “If there’s an issue or a particular bill that we’re asking them to sponsor or cosponsor, that’s one part of a visit. But by and large, we are trying to leave them with the sense that SHM is a resource when it comes to health care–related issues. We want to be there for legislators so that they can understand our position accurately from the outset.”
In short, Hill Day offers a rare opportunity to have direct access to the people who are voting on new legislation affecting hospitalists and affecting the implementation of existing legislation. “This is where the rubber meets the road,” Dr. Lenchus said. Each time a Hill Day is held, he noted, attendance increases. “That’s a true testament to the level of involvement and the interest that hospitalists have across the country. If you’re at all interested, you should absolutely sign up. This will be an amazing experience.”
The lasting impact
Though it’s just one day, Hill Day’s effects are significant.
“Before I started doing this work, I often thought, ‘What impact could someone have going into a legislator’s office?’ ” Dr. Greeno said. “But the answer is ‘A lot.’ The members and staff really do listen – especially if an advocate is highly educated and represent what legislators consider an important constituency, like health care providers. Health care is a hot topic, and it’s probably going to be one of the hot topics in the next election. Hospitalists have good ideas, and as a result these meetings are extremely influential; we wouldn’t do it otherwise. It is fun, but we’re not doing it for fun. We’re doing it because we know we can make a difference.”
In fact, in terms of impact on Capitol Hill, SHM punches above its weight, he added.
“We’re a relatively new society; we’re not huge. There are lots of societies that are much bigger than us and have many more resources, but people on the Hill have told us they like talking with us because they know we’re not looking at things the same way,” Dr. Greeno revealed. “We’re trying to help, and the issues that we’re addressing are not necessarily self-serving. We’re not saying, ‘You need to do this because it will make more money for our doctors.’ Instead, we’re saying, ‘You need to do this because the way it’s being done now is hurting patients. It’s hurting the health care system, and we have ideas about how to make that better.’ ”
SHM’s impressive track record has earned the society a positive reputation that will underlie the Hill Day meetings. “When we first set up the policy shop at SHM, we wanted to be seen as providers who cared about the American health care system and our patients,” Dr. Greeno said. “We have established that reputation, and that has led members on Capitol Hill to recognize us as being well intentioned and knowledgeable. So we have an outsize influence in Congress for our age and our size. When 200 hospitalists go to Capitol Hill, it’s an important thing.”
For more information about Hill Day, including details about participation, visit shmannualconference.org/hill-day/.
Malpractice suits are less frequent – but more costly
Lawsuits against physicians declined across virtually all specialties by more than a quarter over a 10-year span, but the cost to manage legal challenges went up, a recent analysis finds.
From 2007 to 2016, the rate of claims dropped by 27% per 100 doctors from 5.1 to 3.7, according to a review of 124,000 cases by CRICO Strategies, a division of CRICO, the medical liability insurance provider for the Harvard medical community. CRICO’s database of claims contains about 30% of legal cases filed against health providers across the U.S.
For internists, the rate of lawsuits decreased by 35% between 2007 and 2016, according to CRICO data provided to MDedge News. Ob.gyns. saw a 44% drop in claims over the 10-year period, and surgeons experienced a 23% rate decrease. The analysis did not break down the rate of claims by other single subspecialists. Claims decreased by a combined 29% for cardiologists, dermatologists, endocrinologists, family physicians, gastroenterologists, hematologists/oncologists, hospitalists, infectious disease specialists, internists, nephrologists, neurologists, pulmonologists, and rheumatologists/immunologists, according to the report published in February 2019 on CRICO’s website.
The findings are consistent with prior research on claim trends, said Seth Seabury, PhD, a medical liability researcher and director of the Keck-Schaeffer Initiative for Population Health Policy at the University of Southern California, Los Angeles.
“Malpractice claim frequency has been falling pretty steadily for a while now, reflecting a number of factors including the widespread adoption of tort reform and other measures to shield physicians from malpractice risk,” Dr. Seabury said in an interview. “Interestingly, the decline seems greatest in the claims with lower potential stakes, as you see average indemnity holding flat or rising. Some of this likely reflects the unwillingness of attorneys to take cases with lower potential payouts, because of the high cost of litigating a malpractice case.”
While frequency went down, the cost to manage a legal claim went up, according to CRICO data. The price of defending a malpractice lawsuit rose an average of 3.5% annually over the 10-year period from $36,000 to $46,000. For cases that ended with no payment (indemnity) to plaintiffs, the cost to manage a case rose an average of 5% annually.
The upward trends in case management expenses are striking, particularly since the time to resolve cases has decreased, said Michelle Mello, PhD, a health research and policy professor at Stanford (Calif.) University. From 2007 to 2016, the average time to resolve a case dropped from 29 to 27 months, the CRICO report found.
“CRICO nods to disclosure and apology approaches as perhaps underlying the more encouraging trend in time to resolution, but it was surprising to me that such approaches have not translated into lower defense costs,” Dr. Mello said in an interview. “In particular, a lot is still being spent to manage cases that never result in a payment to the patient. My hope was that, as hospitals got better at communicating with patients about adverse events, including the fact that about three-quarters of them are not due to substandard care, there would be fewer claims involving such events and also less money spent dealing with such claims when they do arise.”
For cases that do end in payment, high payouts are on the rise. Cases that ended in payments of $1 million or more increased 4% over the 10-year time frame, while payments of $3 million to $11 million increased 7% annually, according to the CRICO report. Cases that ended in payment lower than $1 million dropped over the 10-year span.
The reasons behind increasing plaintiff payouts is uncertain, Dr. Seabury said.
“It’s hard to say exactly why high payouts are on the rise, as payout levels reflect a number of factors – [such as] economic damages, clinical severity, pain and suffering – that can be difficult to disentangle,” he said. “But it is probably concerning for doctors in the sense that, while claims are becoming less likely, when they do happen, it could be more catastrophic in the sense of having large damages that exceed the policy limit.”
Lawsuits against physicians declined across virtually all specialties by more than a quarter over a 10-year span, but the cost to manage legal challenges went up, a recent analysis finds.
From 2007 to 2016, the rate of claims dropped by 27% per 100 doctors from 5.1 to 3.7, according to a review of 124,000 cases by CRICO Strategies, a division of CRICO, the medical liability insurance provider for the Harvard medical community. CRICO’s database of claims contains about 30% of legal cases filed against health providers across the U.S.
For internists, the rate of lawsuits decreased by 35% between 2007 and 2016, according to CRICO data provided to MDedge News. Ob.gyns. saw a 44% drop in claims over the 10-year period, and surgeons experienced a 23% rate decrease. The analysis did not break down the rate of claims by other single subspecialists. Claims decreased by a combined 29% for cardiologists, dermatologists, endocrinologists, family physicians, gastroenterologists, hematologists/oncologists, hospitalists, infectious disease specialists, internists, nephrologists, neurologists, pulmonologists, and rheumatologists/immunologists, according to the report published in February 2019 on CRICO’s website.
The findings are consistent with prior research on claim trends, said Seth Seabury, PhD, a medical liability researcher and director of the Keck-Schaeffer Initiative for Population Health Policy at the University of Southern California, Los Angeles.
“Malpractice claim frequency has been falling pretty steadily for a while now, reflecting a number of factors including the widespread adoption of tort reform and other measures to shield physicians from malpractice risk,” Dr. Seabury said in an interview. “Interestingly, the decline seems greatest in the claims with lower potential stakes, as you see average indemnity holding flat or rising. Some of this likely reflects the unwillingness of attorneys to take cases with lower potential payouts, because of the high cost of litigating a malpractice case.”
While frequency went down, the cost to manage a legal claim went up, according to CRICO data. The price of defending a malpractice lawsuit rose an average of 3.5% annually over the 10-year period from $36,000 to $46,000. For cases that ended with no payment (indemnity) to plaintiffs, the cost to manage a case rose an average of 5% annually.
The upward trends in case management expenses are striking, particularly since the time to resolve cases has decreased, said Michelle Mello, PhD, a health research and policy professor at Stanford (Calif.) University. From 2007 to 2016, the average time to resolve a case dropped from 29 to 27 months, the CRICO report found.
“CRICO nods to disclosure and apology approaches as perhaps underlying the more encouraging trend in time to resolution, but it was surprising to me that such approaches have not translated into lower defense costs,” Dr. Mello said in an interview. “In particular, a lot is still being spent to manage cases that never result in a payment to the patient. My hope was that, as hospitals got better at communicating with patients about adverse events, including the fact that about three-quarters of them are not due to substandard care, there would be fewer claims involving such events and also less money spent dealing with such claims when they do arise.”
For cases that do end in payment, high payouts are on the rise. Cases that ended in payments of $1 million or more increased 4% over the 10-year time frame, while payments of $3 million to $11 million increased 7% annually, according to the CRICO report. Cases that ended in payment lower than $1 million dropped over the 10-year span.
The reasons behind increasing plaintiff payouts is uncertain, Dr. Seabury said.
“It’s hard to say exactly why high payouts are on the rise, as payout levels reflect a number of factors – [such as] economic damages, clinical severity, pain and suffering – that can be difficult to disentangle,” he said. “But it is probably concerning for doctors in the sense that, while claims are becoming less likely, when they do happen, it could be more catastrophic in the sense of having large damages that exceed the policy limit.”
Lawsuits against physicians declined across virtually all specialties by more than a quarter over a 10-year span, but the cost to manage legal challenges went up, a recent analysis finds.
From 2007 to 2016, the rate of claims dropped by 27% per 100 doctors from 5.1 to 3.7, according to a review of 124,000 cases by CRICO Strategies, a division of CRICO, the medical liability insurance provider for the Harvard medical community. CRICO’s database of claims contains about 30% of legal cases filed against health providers across the U.S.
For internists, the rate of lawsuits decreased by 35% between 2007 and 2016, according to CRICO data provided to MDedge News. Ob.gyns. saw a 44% drop in claims over the 10-year period, and surgeons experienced a 23% rate decrease. The analysis did not break down the rate of claims by other single subspecialists. Claims decreased by a combined 29% for cardiologists, dermatologists, endocrinologists, family physicians, gastroenterologists, hematologists/oncologists, hospitalists, infectious disease specialists, internists, nephrologists, neurologists, pulmonologists, and rheumatologists/immunologists, according to the report published in February 2019 on CRICO’s website.
The findings are consistent with prior research on claim trends, said Seth Seabury, PhD, a medical liability researcher and director of the Keck-Schaeffer Initiative for Population Health Policy at the University of Southern California, Los Angeles.
“Malpractice claim frequency has been falling pretty steadily for a while now, reflecting a number of factors including the widespread adoption of tort reform and other measures to shield physicians from malpractice risk,” Dr. Seabury said in an interview. “Interestingly, the decline seems greatest in the claims with lower potential stakes, as you see average indemnity holding flat or rising. Some of this likely reflects the unwillingness of attorneys to take cases with lower potential payouts, because of the high cost of litigating a malpractice case.”
While frequency went down, the cost to manage a legal claim went up, according to CRICO data. The price of defending a malpractice lawsuit rose an average of 3.5% annually over the 10-year period from $36,000 to $46,000. For cases that ended with no payment (indemnity) to plaintiffs, the cost to manage a case rose an average of 5% annually.
The upward trends in case management expenses are striking, particularly since the time to resolve cases has decreased, said Michelle Mello, PhD, a health research and policy professor at Stanford (Calif.) University. From 2007 to 2016, the average time to resolve a case dropped from 29 to 27 months, the CRICO report found.
“CRICO nods to disclosure and apology approaches as perhaps underlying the more encouraging trend in time to resolution, but it was surprising to me that such approaches have not translated into lower defense costs,” Dr. Mello said in an interview. “In particular, a lot is still being spent to manage cases that never result in a payment to the patient. My hope was that, as hospitals got better at communicating with patients about adverse events, including the fact that about three-quarters of them are not due to substandard care, there would be fewer claims involving such events and also less money spent dealing with such claims when they do arise.”
For cases that do end in payment, high payouts are on the rise. Cases that ended in payments of $1 million or more increased 4% over the 10-year time frame, while payments of $3 million to $11 million increased 7% annually, according to the CRICO report. Cases that ended in payment lower than $1 million dropped over the 10-year span.
The reasons behind increasing plaintiff payouts is uncertain, Dr. Seabury said.
“It’s hard to say exactly why high payouts are on the rise, as payout levels reflect a number of factors – [such as] economic damages, clinical severity, pain and suffering – that can be difficult to disentangle,” he said. “But it is probably concerning for doctors in the sense that, while claims are becoming less likely, when they do happen, it could be more catastrophic in the sense of having large damages that exceed the policy limit.”
Advancing coherence: Your “meta-leadership” objective
Learn to balance organizational priorities
For the many people who expect you to lead, your role – among others – is to create coherence. That coherence characterizes the logic and consistency of what you do in your organization. It assembles the individual work of many different people into a whole that functions well. Coherence in your workplace helps people make sense of what they are doing and why it matters.
Our very rational brain craves coherence. We assemble facts, emotions, ambitions and our life stories into narratives that define who we are, what we are doing, and why it is important. An effective organizational “metaleader” encourages that process for followers. It helps people make sense of the work side of their life.
When coherence is absent, the workplace is riddled with contradictions, unpredictability, and dissonance. People are expected to accomplish tasks for which the time, tools, and talent are missing. There is a perplexed swirl of high activity and low productivity. Expectations for high quality of care and patient satisfaction are contradicted by an overbearing workload, reams of paper work, and the low morale that leaves the work force lethargic. “What we are doing here and how we are doing it doesn’t make sense,” exemplifies the exasperation of working amid incoherence. The department does not drive together toward success-oriented performance. Instead, different people, priorities, and opportunities will be positioned in conflict with one another. For people in your group and those surrounding it, morale and motivation suffer. There is the risk that people will descend into malaise.
Creating coherence is a complex metaleadership process. A large health care center is a cacophony of priorities, of which advancing quality of care is but one. There are other objectives, some contradictory, that also absorb time and attention: achievement of financial benchmarks, promotion of professional careers, and the individual hopes and desires of patients. Systematically aligning those many priorities and objectives is a process of both design and leadership.
The metaleadership model is a strategy for building coherence amid the complexity of health care operations. For those unfamiliar with metaleadership: The prefix “meta-” refers to a wider perspective on what is happening, the people involved, and the overall combination of objectives. The three dimensions of practice are: 1) the Person of the metaleader – your own priorities, values and emotional intelligence; 2) the Situation – what is happening and what ought to be done about it; and 3) Connectivity of Effort, which leads down to subordinates, up to bosses, across to other internal departments, and beyond to external organizations and professionals.
In building connectivity of effort, the metaleader links the many sides of the work being accomplished. The intent is to balance – purposefully – different organizational objectives into a combined whole that gets the jobs done. Furthermore, that coherence links and adapts what people are doing to the situation at hand. And in essence, the person of the leader cannot lead broader coherence if not coherent in her or his own thinking, attitudes, and behaviors, so achievement of personal and professional clarity of purpose is important.
The question for you: How do you as a hospitalist leader create coherence in what you are leading given the changing priorities, actions, and turbulence of current health policy and the market?
The answers lie in the communication you foster and clarify. That communication demands clarity and diplomacy. It is multidirectional such that messages and information in your leading down, up, across, and beyond complement and inform one another.
An illustration of one pathway: You learn from senior management about cuts in the budget. You reflect with them on the choices implicit in those cuts. Perhaps there are better ways to reduce expenditures and increase revenues that offer an alternative pathway to a balanced budget? When communicating with your subordinates, you open conversation on ways to enhance efficiencies and assure quality. You explore avenues to partner with other departments within your institution on how you can link and leverage services and capabilities. And you consider your marketplace and the actions you can take to reinforce your department and assure the volume necessary to achieve budget and quality objectives. And through it all, you monitor the situation. What are the effects of the budget adjustments, and what can be done to sustain the coherence of the work and output of the department? It is a leadership process of constant situational awareness, personal commitment, and connectivity of effort.
An illustration of another pathway: Resist the change and argue forcefully for holding onto the current budget and workforce. Though you do not possess the authority to control larger budgetary decisions, you employ influence well beyond your authority. You recruit allies to your cause, advocates who believe in the purpose you are promoting. You build an alternative coherence, mindful of fostering friendship and minimizing alienation. You are recognized for the passion of your professional commitment and your capacity to uphold quality care and organizational balance.
Two very different pathways to crafting coherence. Leaders of each perceive their actions to advance priority coherence objectives. Apply this question to your own complex problem solving.
Metaleaders forge coherence through the narratives they build and the consistency with those themes and priorities. When everyone on your staff, from physicians to housekeeping personnel, can say “I am here to help save lives,” you know that your followers are on board with a shared mission. They recognize that their efforts contribute to that overall mission. Each person has a role to play, and her or his work fits with the efforts of others, and the bottom line accomplishments of the department.
The coherence you forge assists your followers to make sense of what they are doing and how it fits what others are doing. Work is fulfilling. Beyond that, in a turbulent health care system, you anticipate both problems and opportunities with strategies to meet them. You stay ahead of the game to ensure that people within and outside the department are aligned to maximize opportunities for success.
This is particularly important for the hospitalist. Your job is to fashion coherence on many levels. First, coherent patient care for the patient. Second, coherent interactions among professionals. Finally, organizational coherence, so one piece of the puzzle fits with others. And, when there is a need to recalculate, you adapt and develop solutions that fit the people and situation at hand.
Dr. Marcus is coauthor of Renegotiating Health Care: Resolving Conflict to Build Collaboration, Second Edition (San Francisco: Jossey-Bass Publishers, 2011) and is Director of the Program for Health Care Negotiation and Conflict Resolution, Harvard T.H. Chan School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected].
Learn to balance organizational priorities
Learn to balance organizational priorities
For the many people who expect you to lead, your role – among others – is to create coherence. That coherence characterizes the logic and consistency of what you do in your organization. It assembles the individual work of many different people into a whole that functions well. Coherence in your workplace helps people make sense of what they are doing and why it matters.
Our very rational brain craves coherence. We assemble facts, emotions, ambitions and our life stories into narratives that define who we are, what we are doing, and why it is important. An effective organizational “metaleader” encourages that process for followers. It helps people make sense of the work side of their life.
When coherence is absent, the workplace is riddled with contradictions, unpredictability, and dissonance. People are expected to accomplish tasks for which the time, tools, and talent are missing. There is a perplexed swirl of high activity and low productivity. Expectations for high quality of care and patient satisfaction are contradicted by an overbearing workload, reams of paper work, and the low morale that leaves the work force lethargic. “What we are doing here and how we are doing it doesn’t make sense,” exemplifies the exasperation of working amid incoherence. The department does not drive together toward success-oriented performance. Instead, different people, priorities, and opportunities will be positioned in conflict with one another. For people in your group and those surrounding it, morale and motivation suffer. There is the risk that people will descend into malaise.
Creating coherence is a complex metaleadership process. A large health care center is a cacophony of priorities, of which advancing quality of care is but one. There are other objectives, some contradictory, that also absorb time and attention: achievement of financial benchmarks, promotion of professional careers, and the individual hopes and desires of patients. Systematically aligning those many priorities and objectives is a process of both design and leadership.
The metaleadership model is a strategy for building coherence amid the complexity of health care operations. For those unfamiliar with metaleadership: The prefix “meta-” refers to a wider perspective on what is happening, the people involved, and the overall combination of objectives. The three dimensions of practice are: 1) the Person of the metaleader – your own priorities, values and emotional intelligence; 2) the Situation – what is happening and what ought to be done about it; and 3) Connectivity of Effort, which leads down to subordinates, up to bosses, across to other internal departments, and beyond to external organizations and professionals.
In building connectivity of effort, the metaleader links the many sides of the work being accomplished. The intent is to balance – purposefully – different organizational objectives into a combined whole that gets the jobs done. Furthermore, that coherence links and adapts what people are doing to the situation at hand. And in essence, the person of the leader cannot lead broader coherence if not coherent in her or his own thinking, attitudes, and behaviors, so achievement of personal and professional clarity of purpose is important.
The question for you: How do you as a hospitalist leader create coherence in what you are leading given the changing priorities, actions, and turbulence of current health policy and the market?
The answers lie in the communication you foster and clarify. That communication demands clarity and diplomacy. It is multidirectional such that messages and information in your leading down, up, across, and beyond complement and inform one another.
An illustration of one pathway: You learn from senior management about cuts in the budget. You reflect with them on the choices implicit in those cuts. Perhaps there are better ways to reduce expenditures and increase revenues that offer an alternative pathway to a balanced budget? When communicating with your subordinates, you open conversation on ways to enhance efficiencies and assure quality. You explore avenues to partner with other departments within your institution on how you can link and leverage services and capabilities. And you consider your marketplace and the actions you can take to reinforce your department and assure the volume necessary to achieve budget and quality objectives. And through it all, you monitor the situation. What are the effects of the budget adjustments, and what can be done to sustain the coherence of the work and output of the department? It is a leadership process of constant situational awareness, personal commitment, and connectivity of effort.
An illustration of another pathway: Resist the change and argue forcefully for holding onto the current budget and workforce. Though you do not possess the authority to control larger budgetary decisions, you employ influence well beyond your authority. You recruit allies to your cause, advocates who believe in the purpose you are promoting. You build an alternative coherence, mindful of fostering friendship and minimizing alienation. You are recognized for the passion of your professional commitment and your capacity to uphold quality care and organizational balance.
Two very different pathways to crafting coherence. Leaders of each perceive their actions to advance priority coherence objectives. Apply this question to your own complex problem solving.
Metaleaders forge coherence through the narratives they build and the consistency with those themes and priorities. When everyone on your staff, from physicians to housekeeping personnel, can say “I am here to help save lives,” you know that your followers are on board with a shared mission. They recognize that their efforts contribute to that overall mission. Each person has a role to play, and her or his work fits with the efforts of others, and the bottom line accomplishments of the department.
The coherence you forge assists your followers to make sense of what they are doing and how it fits what others are doing. Work is fulfilling. Beyond that, in a turbulent health care system, you anticipate both problems and opportunities with strategies to meet them. You stay ahead of the game to ensure that people within and outside the department are aligned to maximize opportunities for success.
This is particularly important for the hospitalist. Your job is to fashion coherence on many levels. First, coherent patient care for the patient. Second, coherent interactions among professionals. Finally, organizational coherence, so one piece of the puzzle fits with others. And, when there is a need to recalculate, you adapt and develop solutions that fit the people and situation at hand.
Dr. Marcus is coauthor of Renegotiating Health Care: Resolving Conflict to Build Collaboration, Second Edition (San Francisco: Jossey-Bass Publishers, 2011) and is Director of the Program for Health Care Negotiation and Conflict Resolution, Harvard T.H. Chan School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected].
For the many people who expect you to lead, your role – among others – is to create coherence. That coherence characterizes the logic and consistency of what you do in your organization. It assembles the individual work of many different people into a whole that functions well. Coherence in your workplace helps people make sense of what they are doing and why it matters.
Our very rational brain craves coherence. We assemble facts, emotions, ambitions and our life stories into narratives that define who we are, what we are doing, and why it is important. An effective organizational “metaleader” encourages that process for followers. It helps people make sense of the work side of their life.
When coherence is absent, the workplace is riddled with contradictions, unpredictability, and dissonance. People are expected to accomplish tasks for which the time, tools, and talent are missing. There is a perplexed swirl of high activity and low productivity. Expectations for high quality of care and patient satisfaction are contradicted by an overbearing workload, reams of paper work, and the low morale that leaves the work force lethargic. “What we are doing here and how we are doing it doesn’t make sense,” exemplifies the exasperation of working amid incoherence. The department does not drive together toward success-oriented performance. Instead, different people, priorities, and opportunities will be positioned in conflict with one another. For people in your group and those surrounding it, morale and motivation suffer. There is the risk that people will descend into malaise.
Creating coherence is a complex metaleadership process. A large health care center is a cacophony of priorities, of which advancing quality of care is but one. There are other objectives, some contradictory, that also absorb time and attention: achievement of financial benchmarks, promotion of professional careers, and the individual hopes and desires of patients. Systematically aligning those many priorities and objectives is a process of both design and leadership.
The metaleadership model is a strategy for building coherence amid the complexity of health care operations. For those unfamiliar with metaleadership: The prefix “meta-” refers to a wider perspective on what is happening, the people involved, and the overall combination of objectives. The three dimensions of practice are: 1) the Person of the metaleader – your own priorities, values and emotional intelligence; 2) the Situation – what is happening and what ought to be done about it; and 3) Connectivity of Effort, which leads down to subordinates, up to bosses, across to other internal departments, and beyond to external organizations and professionals.
In building connectivity of effort, the metaleader links the many sides of the work being accomplished. The intent is to balance – purposefully – different organizational objectives into a combined whole that gets the jobs done. Furthermore, that coherence links and adapts what people are doing to the situation at hand. And in essence, the person of the leader cannot lead broader coherence if not coherent in her or his own thinking, attitudes, and behaviors, so achievement of personal and professional clarity of purpose is important.
The question for you: How do you as a hospitalist leader create coherence in what you are leading given the changing priorities, actions, and turbulence of current health policy and the market?
The answers lie in the communication you foster and clarify. That communication demands clarity and diplomacy. It is multidirectional such that messages and information in your leading down, up, across, and beyond complement and inform one another.
An illustration of one pathway: You learn from senior management about cuts in the budget. You reflect with them on the choices implicit in those cuts. Perhaps there are better ways to reduce expenditures and increase revenues that offer an alternative pathway to a balanced budget? When communicating with your subordinates, you open conversation on ways to enhance efficiencies and assure quality. You explore avenues to partner with other departments within your institution on how you can link and leverage services and capabilities. And you consider your marketplace and the actions you can take to reinforce your department and assure the volume necessary to achieve budget and quality objectives. And through it all, you monitor the situation. What are the effects of the budget adjustments, and what can be done to sustain the coherence of the work and output of the department? It is a leadership process of constant situational awareness, personal commitment, and connectivity of effort.
An illustration of another pathway: Resist the change and argue forcefully for holding onto the current budget and workforce. Though you do not possess the authority to control larger budgetary decisions, you employ influence well beyond your authority. You recruit allies to your cause, advocates who believe in the purpose you are promoting. You build an alternative coherence, mindful of fostering friendship and minimizing alienation. You are recognized for the passion of your professional commitment and your capacity to uphold quality care and organizational balance.
Two very different pathways to crafting coherence. Leaders of each perceive their actions to advance priority coherence objectives. Apply this question to your own complex problem solving.
Metaleaders forge coherence through the narratives they build and the consistency with those themes and priorities. When everyone on your staff, from physicians to housekeeping personnel, can say “I am here to help save lives,” you know that your followers are on board with a shared mission. They recognize that their efforts contribute to that overall mission. Each person has a role to play, and her or his work fits with the efforts of others, and the bottom line accomplishments of the department.
The coherence you forge assists your followers to make sense of what they are doing and how it fits what others are doing. Work is fulfilling. Beyond that, in a turbulent health care system, you anticipate both problems and opportunities with strategies to meet them. You stay ahead of the game to ensure that people within and outside the department are aligned to maximize opportunities for success.
This is particularly important for the hospitalist. Your job is to fashion coherence on many levels. First, coherent patient care for the patient. Second, coherent interactions among professionals. Finally, organizational coherence, so one piece of the puzzle fits with others. And, when there is a need to recalculate, you adapt and develop solutions that fit the people and situation at hand.
Dr. Marcus is coauthor of Renegotiating Health Care: Resolving Conflict to Build Collaboration, Second Edition (San Francisco: Jossey-Bass Publishers, 2011) and is Director of the Program for Health Care Negotiation and Conflict Resolution, Harvard T.H. Chan School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected].
Helping quality improvement teams succeed
QI coaches may be the answer
Hospitalists understand the need for quality improvement (QI) as an important part of health care, and they take active roles in – or personally drive – many of the QI efforts at their own facilities. But too often the results are inconsistent and the adoption of new practices slow.
Help can come from a QI Coach, according to a recent paper describing a model of successful coaching. “We wanted to be able to help novice QI teams to be successful,” said the paper’s lead author Danielle Olds, PhD. “Unfortunately, most QI projects are not successful for a variety of reasons including inadequate project planning, a lack of QI skills, a lack of leadership and stakeholder buy-in, and inappropriate measures and methods.”
The coaching model outlined comes from the VAQS program, launched in 1998 to provide structured training around QI and the care of veterans. The seven-step process outlined in the paper provides a road map to overcoming typical QI stumbling blocks and create more successful projects.
“Improvement should be a part of everyone’s practice, however most clinicians have not been trained in how to successfully lead a formal QI project,” said Dr. Olds, who is based at the University of Kansas Medical Center in Kansas City. “Hospitals can bridge this gap by providing QI coaches as a resource to guide teams through the process.”
The model offers a new way for hospitalists to take the lead on QI. “Hospitalists who may have extensive experience in conducting QI could use a model, such as ours, to guide their coaching of teams within their facility,” she said. “Because of the nature of hospitalist practice, they are in an ideal position to understand improvement needs at a systems level within their facility. I would strongly encourage hospitalists to engage in QI because of the wealth of knowledge and experience that they could bring.”
Reference
Olds DM et al. “VA Quality Scholars Quality Improvement Coach Model to Facilitate Learning and Success.” Qual Manag Healthcare. 2018;27(2):87-92. doi: 10.1097/QMH.0000000000000164. Accessed 2018 Jun 11.
QI coaches may be the answer
QI coaches may be the answer
Hospitalists understand the need for quality improvement (QI) as an important part of health care, and they take active roles in – or personally drive – many of the QI efforts at their own facilities. But too often the results are inconsistent and the adoption of new practices slow.
Help can come from a QI Coach, according to a recent paper describing a model of successful coaching. “We wanted to be able to help novice QI teams to be successful,” said the paper’s lead author Danielle Olds, PhD. “Unfortunately, most QI projects are not successful for a variety of reasons including inadequate project planning, a lack of QI skills, a lack of leadership and stakeholder buy-in, and inappropriate measures and methods.”
The coaching model outlined comes from the VAQS program, launched in 1998 to provide structured training around QI and the care of veterans. The seven-step process outlined in the paper provides a road map to overcoming typical QI stumbling blocks and create more successful projects.
“Improvement should be a part of everyone’s practice, however most clinicians have not been trained in how to successfully lead a formal QI project,” said Dr. Olds, who is based at the University of Kansas Medical Center in Kansas City. “Hospitals can bridge this gap by providing QI coaches as a resource to guide teams through the process.”
The model offers a new way for hospitalists to take the lead on QI. “Hospitalists who may have extensive experience in conducting QI could use a model, such as ours, to guide their coaching of teams within their facility,” she said. “Because of the nature of hospitalist practice, they are in an ideal position to understand improvement needs at a systems level within their facility. I would strongly encourage hospitalists to engage in QI because of the wealth of knowledge and experience that they could bring.”
Reference
Olds DM et al. “VA Quality Scholars Quality Improvement Coach Model to Facilitate Learning and Success.” Qual Manag Healthcare. 2018;27(2):87-92. doi: 10.1097/QMH.0000000000000164. Accessed 2018 Jun 11.
Hospitalists understand the need for quality improvement (QI) as an important part of health care, and they take active roles in – or personally drive – many of the QI efforts at their own facilities. But too often the results are inconsistent and the adoption of new practices slow.
Help can come from a QI Coach, according to a recent paper describing a model of successful coaching. “We wanted to be able to help novice QI teams to be successful,” said the paper’s lead author Danielle Olds, PhD. “Unfortunately, most QI projects are not successful for a variety of reasons including inadequate project planning, a lack of QI skills, a lack of leadership and stakeholder buy-in, and inappropriate measures and methods.”
The coaching model outlined comes from the VAQS program, launched in 1998 to provide structured training around QI and the care of veterans. The seven-step process outlined in the paper provides a road map to overcoming typical QI stumbling blocks and create more successful projects.
“Improvement should be a part of everyone’s practice, however most clinicians have not been trained in how to successfully lead a formal QI project,” said Dr. Olds, who is based at the University of Kansas Medical Center in Kansas City. “Hospitals can bridge this gap by providing QI coaches as a resource to guide teams through the process.”
The model offers a new way for hospitalists to take the lead on QI. “Hospitalists who may have extensive experience in conducting QI could use a model, such as ours, to guide their coaching of teams within their facility,” she said. “Because of the nature of hospitalist practice, they are in an ideal position to understand improvement needs at a systems level within their facility. I would strongly encourage hospitalists to engage in QI because of the wealth of knowledge and experience that they could bring.”
Reference
Olds DM et al. “VA Quality Scholars Quality Improvement Coach Model to Facilitate Learning and Success.” Qual Manag Healthcare. 2018;27(2):87-92. doi: 10.1097/QMH.0000000000000164. Accessed 2018 Jun 11.
Opportunities missed for advance care planning for elderly ICU patients
SAN DIEGO – A nationally representative survey of the problem is more pronounced among some blacks and Hispanics and those with lower net worth. The study also found that these patients see physicians an average of 20 times in the year preceding the ICU visit, which suggests that there are plenty of opportunities to put ACP in place.
“Over two-thirds were seen by a doctor in the last 2 weeks. So they’re seeing doctors, but they’re still not doing advance care planning,” said Brian Block, MD, during a presentation of the study at the Critical Care Congress sponsored by the Society of Critical Care Medicine. Dr. Block is with the University of California, San Francisco.
Lack of advance planning can put major road blocks in front of patient care in the ICU, as well as complicate communication between physicians and family members. The findings underscore the need to encourage conversations about end-of-life care between physicians and their patients – before the patients wind up in intensive care.
One audience member believes these conversations are already happening. Paul Yodice, MD, chairman of medicine at Saint Barnabas Medical Center in Livingston, N.J., suggested that physicians are attempting to engage older patients and family members in ACP, but many are unready to make decisions. “In my experience, it is happening much more frequently than is captured either in the medical record or in the research that we’ve been publishing. I’ve been a part of those conversations. Those individuals who are faced with those toughest of choices choose to delay making the decision or speaking about it further because it’s just too painful to consider, and they hold out hope of being the one to beat the odds, to have one more day,” said Dr. Yodice.
He called for further research to document whether ACP conversations are happening and to identify barriers to decisions and the means to overcome them. “A next good study would be to send out a respectful survey to the families of those who have lost people they love and ask: Has someone in the past year spoken with you or offered to have a discussion about end-of-life issues? We could get a better handle on [how often] the discussion is being had, and then find a solution,” said Dr. Yodice.
ACP can also be difficult for the provider, he added. Family members and patients, desperate for another treatment option, will often ask if there’s anything else that can be done. “In medicine, the answer almost always is ‘Well, we can try something else even though I know it’s not going to work.’ And people hold on to that, including us,” said Dr. Yodice.
The study analyzed data from a Medicare cohort of 1,109 patients who died during 2000-2013 and had an ICU admission within the last 30 days of their life. Ages were fairly evenly distributed, with 29% aged 65-74 years, 39% aged 75-84, and 32% aged 85 and over. Fifty-four percent were women, 26% were nonwhite, 42% had not completed high school, and 11% were in skilled nursing facilities.
About 35% had no ACP in 2000-2001, and that percentage gradually declined, to about 20% in 2012-2013 (slope, –1.6%/year; P = .009).
Seventeen percent of white participants had no ACP, compared with 51% of blacks and 49% of Hispanics. Net worth was also strongly associated with having ACP: The top quartile had 13% lacking ACP, compared with 43% of the bottom quartile.
The study found that 94% of patients who had no ACP had visited a health care provider in the past year. The average number of visits in the past year was 20, and 83% had seen a provider within the past 30 days.
Dr. Block did not declare a source of funding or potential conflicts. Dr. Yodice had no disclosures.
SOURCE: Block B et al. CCC48, Abstract 401.
SAN DIEGO – A nationally representative survey of the problem is more pronounced among some blacks and Hispanics and those with lower net worth. The study also found that these patients see physicians an average of 20 times in the year preceding the ICU visit, which suggests that there are plenty of opportunities to put ACP in place.
“Over two-thirds were seen by a doctor in the last 2 weeks. So they’re seeing doctors, but they’re still not doing advance care planning,” said Brian Block, MD, during a presentation of the study at the Critical Care Congress sponsored by the Society of Critical Care Medicine. Dr. Block is with the University of California, San Francisco.
Lack of advance planning can put major road blocks in front of patient care in the ICU, as well as complicate communication between physicians and family members. The findings underscore the need to encourage conversations about end-of-life care between physicians and their patients – before the patients wind up in intensive care.
One audience member believes these conversations are already happening. Paul Yodice, MD, chairman of medicine at Saint Barnabas Medical Center in Livingston, N.J., suggested that physicians are attempting to engage older patients and family members in ACP, but many are unready to make decisions. “In my experience, it is happening much more frequently than is captured either in the medical record or in the research that we’ve been publishing. I’ve been a part of those conversations. Those individuals who are faced with those toughest of choices choose to delay making the decision or speaking about it further because it’s just too painful to consider, and they hold out hope of being the one to beat the odds, to have one more day,” said Dr. Yodice.
He called for further research to document whether ACP conversations are happening and to identify barriers to decisions and the means to overcome them. “A next good study would be to send out a respectful survey to the families of those who have lost people they love and ask: Has someone in the past year spoken with you or offered to have a discussion about end-of-life issues? We could get a better handle on [how often] the discussion is being had, and then find a solution,” said Dr. Yodice.
ACP can also be difficult for the provider, he added. Family members and patients, desperate for another treatment option, will often ask if there’s anything else that can be done. “In medicine, the answer almost always is ‘Well, we can try something else even though I know it’s not going to work.’ And people hold on to that, including us,” said Dr. Yodice.
The study analyzed data from a Medicare cohort of 1,109 patients who died during 2000-2013 and had an ICU admission within the last 30 days of their life. Ages were fairly evenly distributed, with 29% aged 65-74 years, 39% aged 75-84, and 32% aged 85 and over. Fifty-four percent were women, 26% were nonwhite, 42% had not completed high school, and 11% were in skilled nursing facilities.
About 35% had no ACP in 2000-2001, and that percentage gradually declined, to about 20% in 2012-2013 (slope, –1.6%/year; P = .009).
Seventeen percent of white participants had no ACP, compared with 51% of blacks and 49% of Hispanics. Net worth was also strongly associated with having ACP: The top quartile had 13% lacking ACP, compared with 43% of the bottom quartile.
The study found that 94% of patients who had no ACP had visited a health care provider in the past year. The average number of visits in the past year was 20, and 83% had seen a provider within the past 30 days.
Dr. Block did not declare a source of funding or potential conflicts. Dr. Yodice had no disclosures.
SOURCE: Block B et al. CCC48, Abstract 401.
SAN DIEGO – A nationally representative survey of the problem is more pronounced among some blacks and Hispanics and those with lower net worth. The study also found that these patients see physicians an average of 20 times in the year preceding the ICU visit, which suggests that there are plenty of opportunities to put ACP in place.
“Over two-thirds were seen by a doctor in the last 2 weeks. So they’re seeing doctors, but they’re still not doing advance care planning,” said Brian Block, MD, during a presentation of the study at the Critical Care Congress sponsored by the Society of Critical Care Medicine. Dr. Block is with the University of California, San Francisco.
Lack of advance planning can put major road blocks in front of patient care in the ICU, as well as complicate communication between physicians and family members. The findings underscore the need to encourage conversations about end-of-life care between physicians and their patients – before the patients wind up in intensive care.
One audience member believes these conversations are already happening. Paul Yodice, MD, chairman of medicine at Saint Barnabas Medical Center in Livingston, N.J., suggested that physicians are attempting to engage older patients and family members in ACP, but many are unready to make decisions. “In my experience, it is happening much more frequently than is captured either in the medical record or in the research that we’ve been publishing. I’ve been a part of those conversations. Those individuals who are faced with those toughest of choices choose to delay making the decision or speaking about it further because it’s just too painful to consider, and they hold out hope of being the one to beat the odds, to have one more day,” said Dr. Yodice.
He called for further research to document whether ACP conversations are happening and to identify barriers to decisions and the means to overcome them. “A next good study would be to send out a respectful survey to the families of those who have lost people they love and ask: Has someone in the past year spoken with you or offered to have a discussion about end-of-life issues? We could get a better handle on [how often] the discussion is being had, and then find a solution,” said Dr. Yodice.
ACP can also be difficult for the provider, he added. Family members and patients, desperate for another treatment option, will often ask if there’s anything else that can be done. “In medicine, the answer almost always is ‘Well, we can try something else even though I know it’s not going to work.’ And people hold on to that, including us,” said Dr. Yodice.
The study analyzed data from a Medicare cohort of 1,109 patients who died during 2000-2013 and had an ICU admission within the last 30 days of their life. Ages were fairly evenly distributed, with 29% aged 65-74 years, 39% aged 75-84, and 32% aged 85 and over. Fifty-four percent were women, 26% were nonwhite, 42% had not completed high school, and 11% were in skilled nursing facilities.
About 35% had no ACP in 2000-2001, and that percentage gradually declined, to about 20% in 2012-2013 (slope, –1.6%/year; P = .009).
Seventeen percent of white participants had no ACP, compared with 51% of blacks and 49% of Hispanics. Net worth was also strongly associated with having ACP: The top quartile had 13% lacking ACP, compared with 43% of the bottom quartile.
The study found that 94% of patients who had no ACP had visited a health care provider in the past year. The average number of visits in the past year was 20, and 83% had seen a provider within the past 30 days.
Dr. Block did not declare a source of funding or potential conflicts. Dr. Yodice had no disclosures.
SOURCE: Block B et al. CCC48, Abstract 401.
REPORTING FROM CCC48
The ever-evolving scope of hospitalists’ clinical services
More care ‘beyond the walls’ of the hospital
The 2018 State of Hospital Medicine (SoHM) Report provides indispensable data about the scope of clinical services routinely provided by adult and pediatric hospitalists. This year’s SoHM report reveals that a growing number of Hospital Medicine Groups (HMGs) serving adults are involved in roles beyond the inpatient medical wards, including various surgical comanagement programs, outpatient care, and post-acute care services.
The survey also compares services provided by academic and nonacademic HMGs, which remain markedly different in some areas. As the landscape of health care continues to evolve, hospitalists transform their scope of services to meet the needs of the institutions and communities they serve.
In the previous three SoHM reports, it was well established that more than 87% of adult hospital medicine groups play some role in comanaging surgical patients. In this year’s SoHM report, that role was further stratified to capture the various subspecialties represented, and to identify whether the hospitalists generally served as admitting/attending physician or consultant.
Hospitalists’ roles in comanagement are most prominent for care of orthopedic and general surgery patients, but more than 50% of surveyed HMGs reported being involved in comanagement in some capacity with neurosurgery, obstetrics, and cardiovascular surgery. Additionally, almost 95% of surveyed adult HMGs reported that they provided comanagement services for at least one other surgical specialty that was not listed in the survey.
The report also displays comanagement services provided to various medical subspecialties, including neurology, GI/liver, oncology, and more. Of the medical subspecialties represented, adult HMGs comanaged GI/liver (98.2%) and oncology (97.7%) services more often than others.
Interestingly, more HMGs are providing care for patients beyond the walls of the hospital. In the 2018 SoHM report, over 17% of surveyed HMG respondents reported providing care in an outpatient setting, representing an increase of 6.5 percentage points over 2016. Most strikingly, from 2016 to 2018, there was a 12 percentage point increase in adult HMGs reporting services provided to post-acute care facilities (from 13.1% to 24.8%).
These trends were most notable in the Midwest region where nearly 28% of HMGs provide patient care in an outpatient setting and up to 34% in post-acute care facilities. In part, this trend may result from the increased emphasis on improving transitions of care, by providing prehospital preoperative services, postdischarge follow-up encounters, or offering posthospitalization extensivist care.
Within the hospital itself, there remain striking differences in certain services provided by academic and nonacademic HMGs serving adults. Nonacademic HMGs are far more likely to cover patients in an ICU than their academic counterparts (72.0% vs. 34.3%). In contrast, academic hospitalist groups were significantly more inclined to perform procedures. However, the report also showed that there was an overall downtrend of percentage of HMGs that cover patients in an ICU or perform procedures.
As the scope of hospitalist services continues to change over time, should there be concern for scope creep? It depends on how one might view the change. As health care becomes ever more complex, high-functioning HMGs are needed to navigate it, both within and beyond the hospital. Some might consider scope evolution to be a reflection of hospitalists being recognized for their ability to provide high-quality, efficient, and comprehensive care. Hospital medicine groups will likely continue to evolve to meet the needs of an ever-changing health care environment.
Dr. Kurian is chief of the academic division of hospital medicine at Northwell Health in New York. She is a member of the SHM Practice Analysis Committee.
More care ‘beyond the walls’ of the hospital
More care ‘beyond the walls’ of the hospital
The 2018 State of Hospital Medicine (SoHM) Report provides indispensable data about the scope of clinical services routinely provided by adult and pediatric hospitalists. This year’s SoHM report reveals that a growing number of Hospital Medicine Groups (HMGs) serving adults are involved in roles beyond the inpatient medical wards, including various surgical comanagement programs, outpatient care, and post-acute care services.
The survey also compares services provided by academic and nonacademic HMGs, which remain markedly different in some areas. As the landscape of health care continues to evolve, hospitalists transform their scope of services to meet the needs of the institutions and communities they serve.
In the previous three SoHM reports, it was well established that more than 87% of adult hospital medicine groups play some role in comanaging surgical patients. In this year’s SoHM report, that role was further stratified to capture the various subspecialties represented, and to identify whether the hospitalists generally served as admitting/attending physician or consultant.
Hospitalists’ roles in comanagement are most prominent for care of orthopedic and general surgery patients, but more than 50% of surveyed HMGs reported being involved in comanagement in some capacity with neurosurgery, obstetrics, and cardiovascular surgery. Additionally, almost 95% of surveyed adult HMGs reported that they provided comanagement services for at least one other surgical specialty that was not listed in the survey.
The report also displays comanagement services provided to various medical subspecialties, including neurology, GI/liver, oncology, and more. Of the medical subspecialties represented, adult HMGs comanaged GI/liver (98.2%) and oncology (97.7%) services more often than others.
Interestingly, more HMGs are providing care for patients beyond the walls of the hospital. In the 2018 SoHM report, over 17% of surveyed HMG respondents reported providing care in an outpatient setting, representing an increase of 6.5 percentage points over 2016. Most strikingly, from 2016 to 2018, there was a 12 percentage point increase in adult HMGs reporting services provided to post-acute care facilities (from 13.1% to 24.8%).
These trends were most notable in the Midwest region where nearly 28% of HMGs provide patient care in an outpatient setting and up to 34% in post-acute care facilities. In part, this trend may result from the increased emphasis on improving transitions of care, by providing prehospital preoperative services, postdischarge follow-up encounters, or offering posthospitalization extensivist care.
Within the hospital itself, there remain striking differences in certain services provided by academic and nonacademic HMGs serving adults. Nonacademic HMGs are far more likely to cover patients in an ICU than their academic counterparts (72.0% vs. 34.3%). In contrast, academic hospitalist groups were significantly more inclined to perform procedures. However, the report also showed that there was an overall downtrend of percentage of HMGs that cover patients in an ICU or perform procedures.
As the scope of hospitalist services continues to change over time, should there be concern for scope creep? It depends on how one might view the change. As health care becomes ever more complex, high-functioning HMGs are needed to navigate it, both within and beyond the hospital. Some might consider scope evolution to be a reflection of hospitalists being recognized for their ability to provide high-quality, efficient, and comprehensive care. Hospital medicine groups will likely continue to evolve to meet the needs of an ever-changing health care environment.
Dr. Kurian is chief of the academic division of hospital medicine at Northwell Health in New York. She is a member of the SHM Practice Analysis Committee.
The 2018 State of Hospital Medicine (SoHM) Report provides indispensable data about the scope of clinical services routinely provided by adult and pediatric hospitalists. This year’s SoHM report reveals that a growing number of Hospital Medicine Groups (HMGs) serving adults are involved in roles beyond the inpatient medical wards, including various surgical comanagement programs, outpatient care, and post-acute care services.
The survey also compares services provided by academic and nonacademic HMGs, which remain markedly different in some areas. As the landscape of health care continues to evolve, hospitalists transform their scope of services to meet the needs of the institutions and communities they serve.
In the previous three SoHM reports, it was well established that more than 87% of adult hospital medicine groups play some role in comanaging surgical patients. In this year’s SoHM report, that role was further stratified to capture the various subspecialties represented, and to identify whether the hospitalists generally served as admitting/attending physician or consultant.
Hospitalists’ roles in comanagement are most prominent for care of orthopedic and general surgery patients, but more than 50% of surveyed HMGs reported being involved in comanagement in some capacity with neurosurgery, obstetrics, and cardiovascular surgery. Additionally, almost 95% of surveyed adult HMGs reported that they provided comanagement services for at least one other surgical specialty that was not listed in the survey.
The report also displays comanagement services provided to various medical subspecialties, including neurology, GI/liver, oncology, and more. Of the medical subspecialties represented, adult HMGs comanaged GI/liver (98.2%) and oncology (97.7%) services more often than others.
Interestingly, more HMGs are providing care for patients beyond the walls of the hospital. In the 2018 SoHM report, over 17% of surveyed HMG respondents reported providing care in an outpatient setting, representing an increase of 6.5 percentage points over 2016. Most strikingly, from 2016 to 2018, there was a 12 percentage point increase in adult HMGs reporting services provided to post-acute care facilities (from 13.1% to 24.8%).
These trends were most notable in the Midwest region where nearly 28% of HMGs provide patient care in an outpatient setting and up to 34% in post-acute care facilities. In part, this trend may result from the increased emphasis on improving transitions of care, by providing prehospital preoperative services, postdischarge follow-up encounters, or offering posthospitalization extensivist care.
Within the hospital itself, there remain striking differences in certain services provided by academic and nonacademic HMGs serving adults. Nonacademic HMGs are far more likely to cover patients in an ICU than their academic counterparts (72.0% vs. 34.3%). In contrast, academic hospitalist groups were significantly more inclined to perform procedures. However, the report also showed that there was an overall downtrend of percentage of HMGs that cover patients in an ICU or perform procedures.
As the scope of hospitalist services continues to change over time, should there be concern for scope creep? It depends on how one might view the change. As health care becomes ever more complex, high-functioning HMGs are needed to navigate it, both within and beyond the hospital. Some might consider scope evolution to be a reflection of hospitalists being recognized for their ability to provide high-quality, efficient, and comprehensive care. Hospital medicine groups will likely continue to evolve to meet the needs of an ever-changing health care environment.
Dr. Kurian is chief of the academic division of hospital medicine at Northwell Health in New York. She is a member of the SHM Practice Analysis Committee.
Medicare’s two-midnight rule
What hospitalists must know
Most hospitalists’ training likely included caring for patients in the ambulatory clinic, urgent care, and ED settings. One of the most important aspects of medical training is deciding which of the patients seen in these settings need to “be admitted” to a hospital because of risk, severity of illness, and/or need for certain medical services. In this context, “admit” is a synonym for “hospitalize.”
However, in today’s health care system, in which hospitalization costs are usually borne by a third-party payer, “admit” can have a very different meaning. For most payers, “admit” means “hospitalize as inpatient.” This is distinct from “hospitalize as an outpatient.” (“Observation” or “obs” is the most common example of a hospitalization as an outpatient.) In the medical payer world, inpatient and outpatient are often referred to as “statuses.” The distinction between inpatient versus outpatient status can affect payment and is based on rules that a hospital and payer have agreed upon. (Inpatient hospital care is generally paid at a higher rate than outpatient hospital care.) It is important for hospitalists to have a basic understanding of these rules because it can affect hospital billing, the hospitalist’s professional fees, beneficiary liability, and payer denials of inpatient care.
For years, Medicare’s definition of an inpatient hospitalization was primarily based on an expectation of a hospitalization of at least 24 hours and a physician’s judgment of the beneficiary’s need for inpatient hospital services. This judgment was to be based on the physician’s assessment of the patient’s severity of illness, the risk of an adverse outcome, and the hospital services required. (The exact definition by Centers for Medicare & Medicaid Services is much longer and can be found in the Medicare Benefits Policy Manual.1) Under Medicare, defining a hospitalization as inpatient versus outpatient is especially important because they are billed to different Medicare programs (Part A for inpatient, Part B for outpatient), and both hospital reimbursement and the patient liability can vary significantly.
Not surprisingly, CMS found that how physicians were making status decisions for medically similar hospitalized patients varied greatly. CMS noted two major concerns: an overuse of inpatient for patients hospitalized overnight leading to increased charges to CMS and multiday observation hospitalizations for lower-acuity patients leading to excessive liability for Medicare beneficiaries. (Observation stays are billed under Part B, under which the beneficiary generally has a 20% copay.)
To address these concerns, in October 2013, CMS adjusted the definition of inpatient to include “the two-midnight rule.” Basically, CMS said that, in order to qualify for inpatient, the admitting physician should expect the beneficiary to require hospital care spanning at least two midnights, rather than the previous 24-hour benchmark, regardless of the severity of illness or risk of adverse outcome. (There are exceptions and exemptions to the two-midnight rule, which are discussed later in this article.)
The idea of the two-midnight rule was to address the two concerns noted above. Under this rule, most expected overnight hospitalizations should be outpatients, even if they are more than 24 hours in length, and any medically necessary outpatient hospitalization should be “converted” to inpatient if and when it is clear that a second midnight of hospitalization is medically necessary.
In January 2016, CMS amended the two-midnight rule to recognize, as it had done prior to October 2013, that some hospitalizations, based on physician judgment, would be appropriate for inpatient without an expectation of a hospitalization that spans at least two midnights. Unfortunately, CMS has not been forthcoming with guidance of examples of which hospitalizations would fall into this new category, other than to say they expect the use of this new provision would generally not be appropriate for a hospital stay of less than 24 hours.
As of today, physicians should order inpatient services under the following three situations:
- The physician expects the beneficiary to require hospital care spanning at least two midnights.
- The physician provides a service on Medicare’s inpatient-only list.
- The physician expects the beneficiary to require hospital care for less than two midnights but feels that inpatient services are nevertheless appropriate.
This most recently updated version of the two-midnight rule can be found in Section 42 CFR §412.3 of the Code of Federal Regulations.2 Each of these three situations warrants additional discussion.
Care expected to span two midnights
The first situation is the one most applicable to hospitalists. In this circumstance there are three key points to remember.
The first point is that the two-midnight rule is based on a reasonable expectation of a need for hospitalization for at least two nights, not the actual length of hospitalization. Auditors, based on long-standing guidance from the CMS, should consider only the information known (or that should have been known) to the provider at the time the inpatient decision is made.
For example, if the expectation of the need for hospitalization of at least 2 midnights is well documented in the admission note, but the beneficiary improves more rapidly than expected and can be discharged before the second midnight, billing Medicare under Part A for inpatient admission remains appropriate. Auditors may look for provider documentation describing the unexpected improvement, and while such documentation is not an absolute requirement, its presence can be helpful in defending inpatient billing.
Other situations in which there can be an expectation of hospitalization of at least two midnights, but the actual length of stay does not meet this benchmark, are death, patients leaving against medical advice, or transfer to another hospital. For example, if a patient is hospitalized as an inpatient for bacterial endocarditis, and the documented plan of care includes at least 2 days of IV antibiotics and monitoring of cultures, inpatient remains appropriate even if the patient signs out against medical advice the following day.
The second key point to understand is that a night must be “medically necessary” to count toward the two-midnight benchmark. Hospital time spent receiving custodial care, because of excessive delays, or incurred because of the convenience of the beneficiary or provider does not count toward the two-midnight benchmark. For example, imagine a patient hospitalized with chest pain on Saturday evening and the attending physician determines that the patient requires serial cardiac isoenzymes and ECGs followed, most likely, by a noninvasive stress test. The attending physician, knowing that the hospital does not offer stress testing on Sunday, expects the patient to remain hospitalized at least until Monday, thus two midnights. However, in this situation, the second midnight (Sunday night) was not medically necessary and does not count toward the two midnight expectation.
The third key point to know is that the clock for calculating the two-midnight rule begins when the beneficiary starts receiving hospital care, not when the inpatient order is placed. Further, care that starts in the ED or at another hospital counts, too. In contrast, care at an outpatient clinic, an urgent care facility, or waiting-room time in an ED does not count.
When CMS implemented the two-midnight rule in 2013, they said that they would be open to exceptions. The first and only exception to date to the two-midnight rule is newly initiated and unanticipated mechanical ventilation. (This excludes anticipated intubations related to other care, such as procedures.) For example, inpatient is appropriate for a patient who requires hospitalization for an anaphylactic reaction or a drug overdose and needs intubation and mechanical ventilation, even if discharge is expected before a second midnight of hospital care.
CMS’s inpatient-only list
Each year, CMS publishes a list of procedures that CMS will pay only under Part A (that is, as inpatient). This list is updated quarterly (Addendum E) and can be found on the CMS website.3 Hospitalizations associated with the procedures on this list should always be inpatient, regardless of the expected length of stay.
It is important to note that the inpatient-only list is dynamic; it is revised annually, and procedures can come on or off the list. Notably, in January 2018, elective total knee replacements and laparoscopic radical prostatectomies came off the inpatient-only list. Most surgeons and proceduralists know whether the procedure they are performing is on this list, and they should advise hospitalists accordingly if the hospitalist is to be the attending of record and will be writing the admission order.
Inpatient services are nevertheless appropriate
The third situation, in which an inpatient admission is appropriate even when the admitting provider does not expect a two-midnight stay, was added to the two-midnight rule in January 2016. CMS states that the factors used in making this determination can be based on physician judgment and documented in the medical record.
At first reading, one might think that CMS is, in effect, returning to the definition of an inpatient prior to the two-midnight rule’s implementation in 2013. However, CMS has not offered clear guidance for its use, and they did not remove any of the previous two-midnight rule guidance. In the absence of clear guidance, hospitalists may be best served by not using this latest change to the two-midnight rule in determining which Medicare beneficiary hospitalizations are appropriate for inpatient designation.
A final, and critical, point about the two-midnight rule is that it only applies to traditional Medicare, and it does not apply to other payers, including commercial insurance and Medicaid. Medicare Advantage plans may or may not follow the two-midnight rule, depending on their contract with the hospital. Which patients are appropriate for inpatient designations are usually determined by the individual contract that the hospital has signed with that payer.
A better understanding of the two-midnight rule including to whom it applies, when it applies, and how to apply it will help you accurately determine which hospitalizations are appropriate for inpatient payment. With this understanding you will quickly become the hero of your hospital’s case managers and billing department.
Dr. Locke is senior physician advisor at the Johns Hopkins Hospital in Baltimore and president-elect of the American College of Physician Advisors. Dr. Hu is executive director of physician advisor services at the University of North Carolina Health Care System, Chapel Hill, and president of the American College of Physician Advisors.
References
1. Medicare Benefit Policy Manual. Chapter 1 - Inpatient Hospital Services Covered Under Part A. https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/bp102c01.pdf.
2. Code of Federal Regulations. https://www.ecfr.gov/cgi-bin/text-idx?SID=958ee67a826285698204a34e1e5d6406&node=42:2.0.1.2.12.1.47.3&rgn=div8.
3. Current Procedural Terminology, Fourth Edition. https://www.cms.gov/apps/ama/license.asp?file=/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/Downloads/CMS-1695-FC-2019-OPPS-FR-Addenda.zip.
What hospitalists must know
What hospitalists must know
Most hospitalists’ training likely included caring for patients in the ambulatory clinic, urgent care, and ED settings. One of the most important aspects of medical training is deciding which of the patients seen in these settings need to “be admitted” to a hospital because of risk, severity of illness, and/or need for certain medical services. In this context, “admit” is a synonym for “hospitalize.”
However, in today’s health care system, in which hospitalization costs are usually borne by a third-party payer, “admit” can have a very different meaning. For most payers, “admit” means “hospitalize as inpatient.” This is distinct from “hospitalize as an outpatient.” (“Observation” or “obs” is the most common example of a hospitalization as an outpatient.) In the medical payer world, inpatient and outpatient are often referred to as “statuses.” The distinction between inpatient versus outpatient status can affect payment and is based on rules that a hospital and payer have agreed upon. (Inpatient hospital care is generally paid at a higher rate than outpatient hospital care.) It is important for hospitalists to have a basic understanding of these rules because it can affect hospital billing, the hospitalist’s professional fees, beneficiary liability, and payer denials of inpatient care.
For years, Medicare’s definition of an inpatient hospitalization was primarily based on an expectation of a hospitalization of at least 24 hours and a physician’s judgment of the beneficiary’s need for inpatient hospital services. This judgment was to be based on the physician’s assessment of the patient’s severity of illness, the risk of an adverse outcome, and the hospital services required. (The exact definition by Centers for Medicare & Medicaid Services is much longer and can be found in the Medicare Benefits Policy Manual.1) Under Medicare, defining a hospitalization as inpatient versus outpatient is especially important because they are billed to different Medicare programs (Part A for inpatient, Part B for outpatient), and both hospital reimbursement and the patient liability can vary significantly.
Not surprisingly, CMS found that how physicians were making status decisions for medically similar hospitalized patients varied greatly. CMS noted two major concerns: an overuse of inpatient for patients hospitalized overnight leading to increased charges to CMS and multiday observation hospitalizations for lower-acuity patients leading to excessive liability for Medicare beneficiaries. (Observation stays are billed under Part B, under which the beneficiary generally has a 20% copay.)
To address these concerns, in October 2013, CMS adjusted the definition of inpatient to include “the two-midnight rule.” Basically, CMS said that, in order to qualify for inpatient, the admitting physician should expect the beneficiary to require hospital care spanning at least two midnights, rather than the previous 24-hour benchmark, regardless of the severity of illness or risk of adverse outcome. (There are exceptions and exemptions to the two-midnight rule, which are discussed later in this article.)
The idea of the two-midnight rule was to address the two concerns noted above. Under this rule, most expected overnight hospitalizations should be outpatients, even if they are more than 24 hours in length, and any medically necessary outpatient hospitalization should be “converted” to inpatient if and when it is clear that a second midnight of hospitalization is medically necessary.
In January 2016, CMS amended the two-midnight rule to recognize, as it had done prior to October 2013, that some hospitalizations, based on physician judgment, would be appropriate for inpatient without an expectation of a hospitalization that spans at least two midnights. Unfortunately, CMS has not been forthcoming with guidance of examples of which hospitalizations would fall into this new category, other than to say they expect the use of this new provision would generally not be appropriate for a hospital stay of less than 24 hours.
As of today, physicians should order inpatient services under the following three situations:
- The physician expects the beneficiary to require hospital care spanning at least two midnights.
- The physician provides a service on Medicare’s inpatient-only list.
- The physician expects the beneficiary to require hospital care for less than two midnights but feels that inpatient services are nevertheless appropriate.
This most recently updated version of the two-midnight rule can be found in Section 42 CFR §412.3 of the Code of Federal Regulations.2 Each of these three situations warrants additional discussion.
Care expected to span two midnights
The first situation is the one most applicable to hospitalists. In this circumstance there are three key points to remember.
The first point is that the two-midnight rule is based on a reasonable expectation of a need for hospitalization for at least two nights, not the actual length of hospitalization. Auditors, based on long-standing guidance from the CMS, should consider only the information known (or that should have been known) to the provider at the time the inpatient decision is made.
For example, if the expectation of the need for hospitalization of at least 2 midnights is well documented in the admission note, but the beneficiary improves more rapidly than expected and can be discharged before the second midnight, billing Medicare under Part A for inpatient admission remains appropriate. Auditors may look for provider documentation describing the unexpected improvement, and while such documentation is not an absolute requirement, its presence can be helpful in defending inpatient billing.
Other situations in which there can be an expectation of hospitalization of at least two midnights, but the actual length of stay does not meet this benchmark, are death, patients leaving against medical advice, or transfer to another hospital. For example, if a patient is hospitalized as an inpatient for bacterial endocarditis, and the documented plan of care includes at least 2 days of IV antibiotics and monitoring of cultures, inpatient remains appropriate even if the patient signs out against medical advice the following day.
The second key point to understand is that a night must be “medically necessary” to count toward the two-midnight benchmark. Hospital time spent receiving custodial care, because of excessive delays, or incurred because of the convenience of the beneficiary or provider does not count toward the two-midnight benchmark. For example, imagine a patient hospitalized with chest pain on Saturday evening and the attending physician determines that the patient requires serial cardiac isoenzymes and ECGs followed, most likely, by a noninvasive stress test. The attending physician, knowing that the hospital does not offer stress testing on Sunday, expects the patient to remain hospitalized at least until Monday, thus two midnights. However, in this situation, the second midnight (Sunday night) was not medically necessary and does not count toward the two midnight expectation.
The third key point to know is that the clock for calculating the two-midnight rule begins when the beneficiary starts receiving hospital care, not when the inpatient order is placed. Further, care that starts in the ED or at another hospital counts, too. In contrast, care at an outpatient clinic, an urgent care facility, or waiting-room time in an ED does not count.
When CMS implemented the two-midnight rule in 2013, they said that they would be open to exceptions. The first and only exception to date to the two-midnight rule is newly initiated and unanticipated mechanical ventilation. (This excludes anticipated intubations related to other care, such as procedures.) For example, inpatient is appropriate for a patient who requires hospitalization for an anaphylactic reaction or a drug overdose and needs intubation and mechanical ventilation, even if discharge is expected before a second midnight of hospital care.
CMS’s inpatient-only list
Each year, CMS publishes a list of procedures that CMS will pay only under Part A (that is, as inpatient). This list is updated quarterly (Addendum E) and can be found on the CMS website.3 Hospitalizations associated with the procedures on this list should always be inpatient, regardless of the expected length of stay.
It is important to note that the inpatient-only list is dynamic; it is revised annually, and procedures can come on or off the list. Notably, in January 2018, elective total knee replacements and laparoscopic radical prostatectomies came off the inpatient-only list. Most surgeons and proceduralists know whether the procedure they are performing is on this list, and they should advise hospitalists accordingly if the hospitalist is to be the attending of record and will be writing the admission order.
Inpatient services are nevertheless appropriate
The third situation, in which an inpatient admission is appropriate even when the admitting provider does not expect a two-midnight stay, was added to the two-midnight rule in January 2016. CMS states that the factors used in making this determination can be based on physician judgment and documented in the medical record.
At first reading, one might think that CMS is, in effect, returning to the definition of an inpatient prior to the two-midnight rule’s implementation in 2013. However, CMS has not offered clear guidance for its use, and they did not remove any of the previous two-midnight rule guidance. In the absence of clear guidance, hospitalists may be best served by not using this latest change to the two-midnight rule in determining which Medicare beneficiary hospitalizations are appropriate for inpatient designation.
A final, and critical, point about the two-midnight rule is that it only applies to traditional Medicare, and it does not apply to other payers, including commercial insurance and Medicaid. Medicare Advantage plans may or may not follow the two-midnight rule, depending on their contract with the hospital. Which patients are appropriate for inpatient designations are usually determined by the individual contract that the hospital has signed with that payer.
A better understanding of the two-midnight rule including to whom it applies, when it applies, and how to apply it will help you accurately determine which hospitalizations are appropriate for inpatient payment. With this understanding you will quickly become the hero of your hospital’s case managers and billing department.
Dr. Locke is senior physician advisor at the Johns Hopkins Hospital in Baltimore and president-elect of the American College of Physician Advisors. Dr. Hu is executive director of physician advisor services at the University of North Carolina Health Care System, Chapel Hill, and president of the American College of Physician Advisors.
References
1. Medicare Benefit Policy Manual. Chapter 1 - Inpatient Hospital Services Covered Under Part A. https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/bp102c01.pdf.
2. Code of Federal Regulations. https://www.ecfr.gov/cgi-bin/text-idx?SID=958ee67a826285698204a34e1e5d6406&node=42:2.0.1.2.12.1.47.3&rgn=div8.
3. Current Procedural Terminology, Fourth Edition. https://www.cms.gov/apps/ama/license.asp?file=/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/Downloads/CMS-1695-FC-2019-OPPS-FR-Addenda.zip.
Most hospitalists’ training likely included caring for patients in the ambulatory clinic, urgent care, and ED settings. One of the most important aspects of medical training is deciding which of the patients seen in these settings need to “be admitted” to a hospital because of risk, severity of illness, and/or need for certain medical services. In this context, “admit” is a synonym for “hospitalize.”
However, in today’s health care system, in which hospitalization costs are usually borne by a third-party payer, “admit” can have a very different meaning. For most payers, “admit” means “hospitalize as inpatient.” This is distinct from “hospitalize as an outpatient.” (“Observation” or “obs” is the most common example of a hospitalization as an outpatient.) In the medical payer world, inpatient and outpatient are often referred to as “statuses.” The distinction between inpatient versus outpatient status can affect payment and is based on rules that a hospital and payer have agreed upon. (Inpatient hospital care is generally paid at a higher rate than outpatient hospital care.) It is important for hospitalists to have a basic understanding of these rules because it can affect hospital billing, the hospitalist’s professional fees, beneficiary liability, and payer denials of inpatient care.
For years, Medicare’s definition of an inpatient hospitalization was primarily based on an expectation of a hospitalization of at least 24 hours and a physician’s judgment of the beneficiary’s need for inpatient hospital services. This judgment was to be based on the physician’s assessment of the patient’s severity of illness, the risk of an adverse outcome, and the hospital services required. (The exact definition by Centers for Medicare & Medicaid Services is much longer and can be found in the Medicare Benefits Policy Manual.1) Under Medicare, defining a hospitalization as inpatient versus outpatient is especially important because they are billed to different Medicare programs (Part A for inpatient, Part B for outpatient), and both hospital reimbursement and the patient liability can vary significantly.
Not surprisingly, CMS found that how physicians were making status decisions for medically similar hospitalized patients varied greatly. CMS noted two major concerns: an overuse of inpatient for patients hospitalized overnight leading to increased charges to CMS and multiday observation hospitalizations for lower-acuity patients leading to excessive liability for Medicare beneficiaries. (Observation stays are billed under Part B, under which the beneficiary generally has a 20% copay.)
To address these concerns, in October 2013, CMS adjusted the definition of inpatient to include “the two-midnight rule.” Basically, CMS said that, in order to qualify for inpatient, the admitting physician should expect the beneficiary to require hospital care spanning at least two midnights, rather than the previous 24-hour benchmark, regardless of the severity of illness or risk of adverse outcome. (There are exceptions and exemptions to the two-midnight rule, which are discussed later in this article.)
The idea of the two-midnight rule was to address the two concerns noted above. Under this rule, most expected overnight hospitalizations should be outpatients, even if they are more than 24 hours in length, and any medically necessary outpatient hospitalization should be “converted” to inpatient if and when it is clear that a second midnight of hospitalization is medically necessary.
In January 2016, CMS amended the two-midnight rule to recognize, as it had done prior to October 2013, that some hospitalizations, based on physician judgment, would be appropriate for inpatient without an expectation of a hospitalization that spans at least two midnights. Unfortunately, CMS has not been forthcoming with guidance of examples of which hospitalizations would fall into this new category, other than to say they expect the use of this new provision would generally not be appropriate for a hospital stay of less than 24 hours.
As of today, physicians should order inpatient services under the following three situations:
- The physician expects the beneficiary to require hospital care spanning at least two midnights.
- The physician provides a service on Medicare’s inpatient-only list.
- The physician expects the beneficiary to require hospital care for less than two midnights but feels that inpatient services are nevertheless appropriate.
This most recently updated version of the two-midnight rule can be found in Section 42 CFR §412.3 of the Code of Federal Regulations.2 Each of these three situations warrants additional discussion.
Care expected to span two midnights
The first situation is the one most applicable to hospitalists. In this circumstance there are three key points to remember.
The first point is that the two-midnight rule is based on a reasonable expectation of a need for hospitalization for at least two nights, not the actual length of hospitalization. Auditors, based on long-standing guidance from the CMS, should consider only the information known (or that should have been known) to the provider at the time the inpatient decision is made.
For example, if the expectation of the need for hospitalization of at least 2 midnights is well documented in the admission note, but the beneficiary improves more rapidly than expected and can be discharged before the second midnight, billing Medicare under Part A for inpatient admission remains appropriate. Auditors may look for provider documentation describing the unexpected improvement, and while such documentation is not an absolute requirement, its presence can be helpful in defending inpatient billing.
Other situations in which there can be an expectation of hospitalization of at least two midnights, but the actual length of stay does not meet this benchmark, are death, patients leaving against medical advice, or transfer to another hospital. For example, if a patient is hospitalized as an inpatient for bacterial endocarditis, and the documented plan of care includes at least 2 days of IV antibiotics and monitoring of cultures, inpatient remains appropriate even if the patient signs out against medical advice the following day.
The second key point to understand is that a night must be “medically necessary” to count toward the two-midnight benchmark. Hospital time spent receiving custodial care, because of excessive delays, or incurred because of the convenience of the beneficiary or provider does not count toward the two-midnight benchmark. For example, imagine a patient hospitalized with chest pain on Saturday evening and the attending physician determines that the patient requires serial cardiac isoenzymes and ECGs followed, most likely, by a noninvasive stress test. The attending physician, knowing that the hospital does not offer stress testing on Sunday, expects the patient to remain hospitalized at least until Monday, thus two midnights. However, in this situation, the second midnight (Sunday night) was not medically necessary and does not count toward the two midnight expectation.
The third key point to know is that the clock for calculating the two-midnight rule begins when the beneficiary starts receiving hospital care, not when the inpatient order is placed. Further, care that starts in the ED or at another hospital counts, too. In contrast, care at an outpatient clinic, an urgent care facility, or waiting-room time in an ED does not count.
When CMS implemented the two-midnight rule in 2013, they said that they would be open to exceptions. The first and only exception to date to the two-midnight rule is newly initiated and unanticipated mechanical ventilation. (This excludes anticipated intubations related to other care, such as procedures.) For example, inpatient is appropriate for a patient who requires hospitalization for an anaphylactic reaction or a drug overdose and needs intubation and mechanical ventilation, even if discharge is expected before a second midnight of hospital care.
CMS’s inpatient-only list
Each year, CMS publishes a list of procedures that CMS will pay only under Part A (that is, as inpatient). This list is updated quarterly (Addendum E) and can be found on the CMS website.3 Hospitalizations associated with the procedures on this list should always be inpatient, regardless of the expected length of stay.
It is important to note that the inpatient-only list is dynamic; it is revised annually, and procedures can come on or off the list. Notably, in January 2018, elective total knee replacements and laparoscopic radical prostatectomies came off the inpatient-only list. Most surgeons and proceduralists know whether the procedure they are performing is on this list, and they should advise hospitalists accordingly if the hospitalist is to be the attending of record and will be writing the admission order.
Inpatient services are nevertheless appropriate
The third situation, in which an inpatient admission is appropriate even when the admitting provider does not expect a two-midnight stay, was added to the two-midnight rule in January 2016. CMS states that the factors used in making this determination can be based on physician judgment and documented in the medical record.
At first reading, one might think that CMS is, in effect, returning to the definition of an inpatient prior to the two-midnight rule’s implementation in 2013. However, CMS has not offered clear guidance for its use, and they did not remove any of the previous two-midnight rule guidance. In the absence of clear guidance, hospitalists may be best served by not using this latest change to the two-midnight rule in determining which Medicare beneficiary hospitalizations are appropriate for inpatient designation.
A final, and critical, point about the two-midnight rule is that it only applies to traditional Medicare, and it does not apply to other payers, including commercial insurance and Medicaid. Medicare Advantage plans may or may not follow the two-midnight rule, depending on their contract with the hospital. Which patients are appropriate for inpatient designations are usually determined by the individual contract that the hospital has signed with that payer.
A better understanding of the two-midnight rule including to whom it applies, when it applies, and how to apply it will help you accurately determine which hospitalizations are appropriate for inpatient payment. With this understanding you will quickly become the hero of your hospital’s case managers and billing department.
Dr. Locke is senior physician advisor at the Johns Hopkins Hospital in Baltimore and president-elect of the American College of Physician Advisors. Dr. Hu is executive director of physician advisor services at the University of North Carolina Health Care System, Chapel Hill, and president of the American College of Physician Advisors.
References
1. Medicare Benefit Policy Manual. Chapter 1 - Inpatient Hospital Services Covered Under Part A. https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/bp102c01.pdf.
2. Code of Federal Regulations. https://www.ecfr.gov/cgi-bin/text-idx?SID=958ee67a826285698204a34e1e5d6406&node=42:2.0.1.2.12.1.47.3&rgn=div8.
3. Current Procedural Terminology, Fourth Edition. https://www.cms.gov/apps/ama/license.asp?file=/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/Downloads/CMS-1695-FC-2019-OPPS-FR-Addenda.zip.
New handoff tool can improve safety
Standardization of process reduces variation
Hospitalists know all too well that a significant source of medical errors is miscommunication during transitions: By interrupting the continuity of care, handoffs can increase the risk of adverse events.
Yet the transfer of patients from the ED to the hospitalist inpatient service has not been well studied, said Carmen Gonzalez, MD, lead author of a recent paper that examined the issue. “The scope of this study was to develop and test a handoff communication tool and a standardized process for transitioning patients from the ED to the hospitalist service at a comprehensive cancer center,” she explained.
In the study, the researchers found that the number of ICU transfers within 24 hours of admission and the number of rapid-response calls decreased after the implementation of a customized handoff tool. “The tool was named DE-PASS (DE-PASS: Decisive problem requiring admission, Evaluation time, Patient summary, Acute issues/action list, Situation unfinished/awareness, Signed out to), which was a modification of the I-PASS, and adapted to our workflow,” reported Dr. Gonzalez, who is based at the University of Texas MD Anderson Cancer Center, Houston. DE-PASS stratifies patients as stable/urgent/emergent and establishes requirements for communications between providers.
Results from the 1-month pilot revealed that, within a 24-hour period, DE-PASS reduced the number of intensive care unit transfers by 58%, the number of rapid-response team calls by 39%, and time to inpatient order by 31%.
“The standardization of the language and format of the handoff process of admission from the ED to the hospitalist service reduced handoff variations, increased provider satisfaction, and improved patient safety,” she noted.
The hospitalists expressed satisfaction with the tool. “This handoff tool helps stratify newly admitted patients based on their illness acuity, hence, assists the busy admitting hospitalist in prioritizing which patient needs to be attended first,” said study coauthor Norman Brito-Dellan, MD, also of MD Anderson Cancer Center. “In this study, DE-PASS reduced admission-to-evaluation times for unstable patients. These patients tend to be evaluated earlier, improving safety.”
Reference
1. Gonzalez CE et al. Handoff tool enabling standardized transitions between the emergency department and the hospitalist inpatient service at a major cancer center. American Journal of Medical Quality. 2018 May 21. doi: 10.1177/1062860618776096.
Standardization of process reduces variation
Standardization of process reduces variation
Hospitalists know all too well that a significant source of medical errors is miscommunication during transitions: By interrupting the continuity of care, handoffs can increase the risk of adverse events.
Yet the transfer of patients from the ED to the hospitalist inpatient service has not been well studied, said Carmen Gonzalez, MD, lead author of a recent paper that examined the issue. “The scope of this study was to develop and test a handoff communication tool and a standardized process for transitioning patients from the ED to the hospitalist service at a comprehensive cancer center,” she explained.
In the study, the researchers found that the number of ICU transfers within 24 hours of admission and the number of rapid-response calls decreased after the implementation of a customized handoff tool. “The tool was named DE-PASS (DE-PASS: Decisive problem requiring admission, Evaluation time, Patient summary, Acute issues/action list, Situation unfinished/awareness, Signed out to), which was a modification of the I-PASS, and adapted to our workflow,” reported Dr. Gonzalez, who is based at the University of Texas MD Anderson Cancer Center, Houston. DE-PASS stratifies patients as stable/urgent/emergent and establishes requirements for communications between providers.
Results from the 1-month pilot revealed that, within a 24-hour period, DE-PASS reduced the number of intensive care unit transfers by 58%, the number of rapid-response team calls by 39%, and time to inpatient order by 31%.
“The standardization of the language and format of the handoff process of admission from the ED to the hospitalist service reduced handoff variations, increased provider satisfaction, and improved patient safety,” she noted.
The hospitalists expressed satisfaction with the tool. “This handoff tool helps stratify newly admitted patients based on their illness acuity, hence, assists the busy admitting hospitalist in prioritizing which patient needs to be attended first,” said study coauthor Norman Brito-Dellan, MD, also of MD Anderson Cancer Center. “In this study, DE-PASS reduced admission-to-evaluation times for unstable patients. These patients tend to be evaluated earlier, improving safety.”
Reference
1. Gonzalez CE et al. Handoff tool enabling standardized transitions between the emergency department and the hospitalist inpatient service at a major cancer center. American Journal of Medical Quality. 2018 May 21. doi: 10.1177/1062860618776096.
Hospitalists know all too well that a significant source of medical errors is miscommunication during transitions: By interrupting the continuity of care, handoffs can increase the risk of adverse events.
Yet the transfer of patients from the ED to the hospitalist inpatient service has not been well studied, said Carmen Gonzalez, MD, lead author of a recent paper that examined the issue. “The scope of this study was to develop and test a handoff communication tool and a standardized process for transitioning patients from the ED to the hospitalist service at a comprehensive cancer center,” she explained.
In the study, the researchers found that the number of ICU transfers within 24 hours of admission and the number of rapid-response calls decreased after the implementation of a customized handoff tool. “The tool was named DE-PASS (DE-PASS: Decisive problem requiring admission, Evaluation time, Patient summary, Acute issues/action list, Situation unfinished/awareness, Signed out to), which was a modification of the I-PASS, and adapted to our workflow,” reported Dr. Gonzalez, who is based at the University of Texas MD Anderson Cancer Center, Houston. DE-PASS stratifies patients as stable/urgent/emergent and establishes requirements for communications between providers.
Results from the 1-month pilot revealed that, within a 24-hour period, DE-PASS reduced the number of intensive care unit transfers by 58%, the number of rapid-response team calls by 39%, and time to inpatient order by 31%.
“The standardization of the language and format of the handoff process of admission from the ED to the hospitalist service reduced handoff variations, increased provider satisfaction, and improved patient safety,” she noted.
The hospitalists expressed satisfaction with the tool. “This handoff tool helps stratify newly admitted patients based on their illness acuity, hence, assists the busy admitting hospitalist in prioritizing which patient needs to be attended first,” said study coauthor Norman Brito-Dellan, MD, also of MD Anderson Cancer Center. “In this study, DE-PASS reduced admission-to-evaluation times for unstable patients. These patients tend to be evaluated earlier, improving safety.”
Reference
1. Gonzalez CE et al. Handoff tool enabling standardized transitions between the emergency department and the hospitalist inpatient service at a major cancer center. American Journal of Medical Quality. 2018 May 21. doi: 10.1177/1062860618776096.