User login
Uterine rupture, child stillborn: $3.8M net award
Uterine rupture, child stillborn: $3.8M net award
At 35 weeks' gestation, a woman went to the emergency department (ED) with abdominal pain, fast heartbeat, and irregular contractions. Her history included three cesarean deliveries, including one with a vertical incision. She was admitted, and a cesarean delivery was planned for the next day. After 8 hours, during which the patient’s condition worsened, an emergency cesarean delivery was undertaken. A full rupture of the uterus was found; the baby’s body had extruded into the mother’s abdomen. The child was stillborn.
PARENTS’ CLAIM The stillbirth could have been avoided if the nurses had communicated the mother’s worsening condition to the physicians.
DEFENDANTS’ DEFENSE After the hospital and physicians settled prior to trial, the case continued against the nurse in charge of the mother’s care and the nurse-staffing group. Negligence was denied; all protocols were followed.
VERDICT A $2.9 million Illinois verdict was returned. With a $900,000 settlement from the hospital and physicians, the net award was $3.8 million.
_______________
Where did rare strep A infection come from?
A 36-year-old woman reported heavy vaginal bleeding to her ObGyn. She underwent endometrial ablation in her physician’s office.
The next day, the woman called the office to report abdominal pain. She was told to stop the medication she was taking, and if the pain continued to the next day, to go to an ED. The next day, the patient went to the ED and was found to be in septic shock. During emergency laparotomy, 50 mL of purulent fluid were drained and an emergency hysterectomy was performed. Three days later, the patient died from pulmonary arrest caused by toxic shock syndrome. An autopsy revealed that the patient’s sepsis was caused by group A streptococci (GAS) infection.
ESTATE’S CLAIM The patient was not a proper candidate for endometrial ablation because of her history of chronic cervical infection. The ObGyn perforated the cervix during the procedure and tried to conceal it. At autopsy, bone wax was found in the rectal lumen that had been used to cover up damage to the cervix. The ObGyn introduced GAS bacteria into the patient’s system. The ObGyn’s staff failed to ask the proper questions when she called the day after the procedure. She should have been told to go directly to the ED.
DEFENDANTS’ DEFENSE The ObGyn did not perforate the cervix or uterus during the procedure. GAS infection is so rare that it would have been difficult to foresee or diagnose. Potentially, the patient had a chronic
cervical infection before ablation.
VERDICT A Texas defense verdict was returned.
_______________
DURING INSERTION, IUD PERFORATES UTERINE WALL; LATER FOUND BELOW LIVER
On July 21, a 46-year-old woman went to an ObGyn for placement of an intrauterine device (IUD). Shortly after the ObGyn inserted the levonorgestrel-releasing intrauterine system (Mirena, Bayer HealthCare), the patient reported severe pelvic and abdominal pain. On July 26, the patient underwent surgical removal of the IUD.
She was discharged on July 29 but continued to report pain. She was readmitted to the hospital the next day and treated for pain. She was bed ridden for 3 weeks after IUD-removal surgery, and had a 3-month recovery before feeling pain free.
PATIENT’S CLAIM The ObGyn was negligent in perforating the patient’s uterine wall during IUD insertion, causing the device to ultimately migrate under the patient’s liver.
DEFENDANTS’ DEFENSE Uterine perforation is a known complication of IUD insertion. The IUD escaped from the patient’s uterus at a later time and not during the insertion procedure.
VERDICT A Florida verdict of $208,839 was returned; the amount was reduced to $161,058 because the medical expenses were written off by the health-care providers.
_______________
Was travel appropriate for this pregnant woman?
A woman with a history of two premature deliveries and one miscarriage became pregnant again. She received prenatal care at an Army hospital. She traveled to Spain, where the baby was born at 31 weeks’ gestation. The baby required treatment in a neonatal intensive care unit (NICU) for 17 days. The child has cerebral palsy, with tetraplegia of all four extremities. She cannot walk without assistance and suffers severe cognitive and vision impairment.
PARENTS’ CLAIM The ObGyn at the Army hospital should not have approved the mother’s request for travel; he did so, despite knowing that the mother was at high risk for premature birth. The military medical hospital to which she was assigned in Spain could not manage a high-risk pregnancy, didn’t have a NICU, and didn’t have specialists to treat premature infants.
DEFENDANTS’ DEFENSE The ObGyn argued that he did not have access to the medical records showing the mother’s history. The patient countered that the ObGyn did indeed have the patient’s records, as he had discussed them with her.
VERDICT A $10,409,700 California verdict was returned against the ObGyn and the government facility.
_______________
Triple-negative BrCa not diagnosed until metastasized: $5.2M
After finding lumps in both breasts, a woman in her 30s saw a nurse practitioner (NP) at an Army hospital. A radiologist reported no mass in the right breast and multiple benign-appearing anechoic lesions in the left breast after bilateral mammography and ultrasonography (US) in July 2008. The Chief of Mammography Services recommended referral to a breast surgeon, but the patient never received the letter. It was placed in her mammography file, not in the treatment file.
In November 2008, the patient returned to the clinic. Bilateral diagnostic mammography and US were ordered, but for unknown reasons, cancelled. US of the left breast was interpreted as benign in January 2009.
After imaging in March 2010, followed by a needle biopsy of the right breast, a radiologist reported finding intermediate-grade infiltrating ductal carcinoma.
The patient sought care outside the military medical system at a large university hospital. In April 2010, stage 3 triple-negative invasive ductal carcinoma (IDC) was identified. The patient underwent chemotherapy, a double mastectomy, removal of 21 lymph nodes, and breast reconstruction. She was given a 60% chance of recurrence in 5–7 years.
PATIENT’S CLAIM It was negligent to not inform her of imaging results. Biopsy should have been performed in 2008, when the IDC was likely at stage 1; treatment would have been far less aggressive. Electronic medical records showed that the 2008 mammography and US results had been “signed off” by an NP at the clinic.
DEFENDANTS’ DEFENSE While unable to concede liability, the government agency did not contest the point.
VERDICT A $5.2 million Tennessee federal court bench verdict was returned, citing failures in communication, poor and improper record keeping and retention, failure to follow-up, and an unexplained cancellation of a medical order.
_______________
Woman dies from cervical cancer: $2.3M
In 2001, a 41-year-old woman had abnormal Pap smear results but her gynecologist did not order more testing. The patient was told to return in 3 months, but she did not return until 2007—reporting abnormal bleeding, vaginal discharge, and pain. Her Pap results were normal, however, and the gynecologist did not order further testing. In 2009, the patient was found to have advanced cervical cancer. She died 2 years later.
ESTATE’S CLAIM Further testing should have been ordered in 2001, which would have likely revealed dysplasia, which can lead to cancer. The laboratory incorrectly interpreted the 2007 Pap test; if the results had been properly reported, additional testing could have been ordered.
DEFENDANTS’ DEFENSE The laboratory and patient’s estate settled for a confidential amount before trial. The gynecologist denied negligence.
VERDICT A New Jersey jury found the gynecologist 40% at fault for his actions in 2007. The jury found the laboratory 50% at fault, and the patient 10% at fault. A gross verdict of $2.33 million was returned.
_______________
Bowel injury after cesarean delivery; mother dies of sepsis
At 40 4/7 weeks' gestation, a 37-year-old woman gave birth to a healthy child by cesarean delivery. The next day, the patient had an elevated white blood cell (WBC) count with a left shift, her abdomen was tympanic but soft, and she was passing flatus and belching. The ObGyn ordered a Fleet enema; only flatus was released. A covering ObGyn ordered an abdominal radiograph, which the radiologist reported as showing postoperative ileus and mild constipation. The patient was given a second Fleet enema the next day, resulting in watery stool. She vomited 300 mL of dark green fluid.
After a rectal tube was placed 2 days later, one hard brown stool and several brown, pasty, loose, and liquid stools were returned. She vomited several times that day, and was found to have hypoactive bowel sounds with continued tympanic quality in the upper quadrants. Laboratory testing revealed continued elevated WBC count with left shift. The next day, she had hypoactive bowel sounds with brown liquid stools. Later that morning, she was able to tolerate clear liquids. The ObGyn decided to discharge her home with instructions to continue on a clear liquid diet for 2 more days before advancing her diet.
The day after discharge, she was found unresponsive at home. She was taken to the hospital, but resuscitation attempts failed. She died. An autopsy revealed that the cause of death was sepsis.
ESTATE’S CLAIM The ObGyn was negligent in failing to diagnose and treat a postoperative intra-abdominal infection caused by bowel perforation. A surgical consult should have been obtained. The woman was prematurely discharged. The radiologist failed to report the presence of free air on the abdominal x-ray.
DEFENDANTS’ DEFENSE The case was settled during trial.
VERDICT A $1 million Maryland settlement was reached.
_______________
Right ureter injury detected and repaired
During laparoscopic-assisted vaginal hysterectomy, the ObGyn detected and repaired an injury to the right ureter. The patient’s recovery was delayed by the injury.
PATIENT’S CLAIM The ObGyn was negligent in using a Kleppinger bipolar cauterizing instrument to cauterize the vaginal cuff. Thermal overspray from the instrument or the instrument itself damaged the ureter. The ObGyn was also negligent in not performing diagnostic cystoscopy to confirm patency of the ureter after the repair was made.
PHYSICIAN’S DEFENSE Ureter injury is a known risk of the procedure. All procedures were performed according to protocol.
VERDICT A Florida defense verdict was returned.
_______________
Failure to detect inflammatory BrCa; woman dies
A 42-year-old woman underwent mammography in February 2002 after reporting pain, discoloration, inflammation, and swelling in her left breast. The radiologist who interpreted the mammography suggested a biopsy for a differential diagnosis of mastitis or inflammatory carcinoma. The biopsy results were negative.
The patient’s symptoms persisted, and she underwent US in late May 2002. Another radiologist interpreted the US, noting that the patient could not tolerate compression, which led to less than optimal evaluation. The radiologist suggested that mastitis was the likely cause of the patient’s symptoms.
The patient then consulted a surgeon, who ordered mammography and magnetic resonance imaging (MRI) followed by biopsy, which indicated cancer. The patient underwent a mastectomy but metastasis had already occurred. She died at age 50 prior to the trial.
ESTATE’S CLAIM If the cancer had been diagnosed earlier, the outcome would have been better. Both radiologists misinterpreted the mammographies.
DEFENDANTS’ DEFENSE The mammographies had been properly interpreted. Any missed diagnosis would not have impacted the outcome due to the type of cancer. The scans had been released to the patient, but were subsequently lost; an adverse interference instruction was given to the jury.
VERDICT A New York defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Uterine rupture, child stillborn: $3.8M net award
At 35 weeks' gestation, a woman went to the emergency department (ED) with abdominal pain, fast heartbeat, and irregular contractions. Her history included three cesarean deliveries, including one with a vertical incision. She was admitted, and a cesarean delivery was planned for the next day. After 8 hours, during which the patient’s condition worsened, an emergency cesarean delivery was undertaken. A full rupture of the uterus was found; the baby’s body had extruded into the mother’s abdomen. The child was stillborn.
PARENTS’ CLAIM The stillbirth could have been avoided if the nurses had communicated the mother’s worsening condition to the physicians.
DEFENDANTS’ DEFENSE After the hospital and physicians settled prior to trial, the case continued against the nurse in charge of the mother’s care and the nurse-staffing group. Negligence was denied; all protocols were followed.
VERDICT A $2.9 million Illinois verdict was returned. With a $900,000 settlement from the hospital and physicians, the net award was $3.8 million.
_______________
Where did rare strep A infection come from?
A 36-year-old woman reported heavy vaginal bleeding to her ObGyn. She underwent endometrial ablation in her physician’s office.
The next day, the woman called the office to report abdominal pain. She was told to stop the medication she was taking, and if the pain continued to the next day, to go to an ED. The next day, the patient went to the ED and was found to be in septic shock. During emergency laparotomy, 50 mL of purulent fluid were drained and an emergency hysterectomy was performed. Three days later, the patient died from pulmonary arrest caused by toxic shock syndrome. An autopsy revealed that the patient’s sepsis was caused by group A streptococci (GAS) infection.
ESTATE’S CLAIM The patient was not a proper candidate for endometrial ablation because of her history of chronic cervical infection. The ObGyn perforated the cervix during the procedure and tried to conceal it. At autopsy, bone wax was found in the rectal lumen that had been used to cover up damage to the cervix. The ObGyn introduced GAS bacteria into the patient’s system. The ObGyn’s staff failed to ask the proper questions when she called the day after the procedure. She should have been told to go directly to the ED.
DEFENDANTS’ DEFENSE The ObGyn did not perforate the cervix or uterus during the procedure. GAS infection is so rare that it would have been difficult to foresee or diagnose. Potentially, the patient had a chronic
cervical infection before ablation.
VERDICT A Texas defense verdict was returned.
_______________
DURING INSERTION, IUD PERFORATES UTERINE WALL; LATER FOUND BELOW LIVER
On July 21, a 46-year-old woman went to an ObGyn for placement of an intrauterine device (IUD). Shortly after the ObGyn inserted the levonorgestrel-releasing intrauterine system (Mirena, Bayer HealthCare), the patient reported severe pelvic and abdominal pain. On July 26, the patient underwent surgical removal of the IUD.
She was discharged on July 29 but continued to report pain. She was readmitted to the hospital the next day and treated for pain. She was bed ridden for 3 weeks after IUD-removal surgery, and had a 3-month recovery before feeling pain free.
PATIENT’S CLAIM The ObGyn was negligent in perforating the patient’s uterine wall during IUD insertion, causing the device to ultimately migrate under the patient’s liver.
DEFENDANTS’ DEFENSE Uterine perforation is a known complication of IUD insertion. The IUD escaped from the patient’s uterus at a later time and not during the insertion procedure.
VERDICT A Florida verdict of $208,839 was returned; the amount was reduced to $161,058 because the medical expenses were written off by the health-care providers.
_______________
Was travel appropriate for this pregnant woman?
A woman with a history of two premature deliveries and one miscarriage became pregnant again. She received prenatal care at an Army hospital. She traveled to Spain, where the baby was born at 31 weeks’ gestation. The baby required treatment in a neonatal intensive care unit (NICU) for 17 days. The child has cerebral palsy, with tetraplegia of all four extremities. She cannot walk without assistance and suffers severe cognitive and vision impairment.
PARENTS’ CLAIM The ObGyn at the Army hospital should not have approved the mother’s request for travel; he did so, despite knowing that the mother was at high risk for premature birth. The military medical hospital to which she was assigned in Spain could not manage a high-risk pregnancy, didn’t have a NICU, and didn’t have specialists to treat premature infants.
DEFENDANTS’ DEFENSE The ObGyn argued that he did not have access to the medical records showing the mother’s history. The patient countered that the ObGyn did indeed have the patient’s records, as he had discussed them with her.
VERDICT A $10,409,700 California verdict was returned against the ObGyn and the government facility.
_______________
Triple-negative BrCa not diagnosed until metastasized: $5.2M
After finding lumps in both breasts, a woman in her 30s saw a nurse practitioner (NP) at an Army hospital. A radiologist reported no mass in the right breast and multiple benign-appearing anechoic lesions in the left breast after bilateral mammography and ultrasonography (US) in July 2008. The Chief of Mammography Services recommended referral to a breast surgeon, but the patient never received the letter. It was placed in her mammography file, not in the treatment file.
In November 2008, the patient returned to the clinic. Bilateral diagnostic mammography and US were ordered, but for unknown reasons, cancelled. US of the left breast was interpreted as benign in January 2009.
After imaging in March 2010, followed by a needle biopsy of the right breast, a radiologist reported finding intermediate-grade infiltrating ductal carcinoma.
The patient sought care outside the military medical system at a large university hospital. In April 2010, stage 3 triple-negative invasive ductal carcinoma (IDC) was identified. The patient underwent chemotherapy, a double mastectomy, removal of 21 lymph nodes, and breast reconstruction. She was given a 60% chance of recurrence in 5–7 years.
PATIENT’S CLAIM It was negligent to not inform her of imaging results. Biopsy should have been performed in 2008, when the IDC was likely at stage 1; treatment would have been far less aggressive. Electronic medical records showed that the 2008 mammography and US results had been “signed off” by an NP at the clinic.
DEFENDANTS’ DEFENSE While unable to concede liability, the government agency did not contest the point.
VERDICT A $5.2 million Tennessee federal court bench verdict was returned, citing failures in communication, poor and improper record keeping and retention, failure to follow-up, and an unexplained cancellation of a medical order.
_______________
Woman dies from cervical cancer: $2.3M
In 2001, a 41-year-old woman had abnormal Pap smear results but her gynecologist did not order more testing. The patient was told to return in 3 months, but she did not return until 2007—reporting abnormal bleeding, vaginal discharge, and pain. Her Pap results were normal, however, and the gynecologist did not order further testing. In 2009, the patient was found to have advanced cervical cancer. She died 2 years later.
ESTATE’S CLAIM Further testing should have been ordered in 2001, which would have likely revealed dysplasia, which can lead to cancer. The laboratory incorrectly interpreted the 2007 Pap test; if the results had been properly reported, additional testing could have been ordered.
DEFENDANTS’ DEFENSE The laboratory and patient’s estate settled for a confidential amount before trial. The gynecologist denied negligence.
VERDICT A New Jersey jury found the gynecologist 40% at fault for his actions in 2007. The jury found the laboratory 50% at fault, and the patient 10% at fault. A gross verdict of $2.33 million was returned.
_______________
Bowel injury after cesarean delivery; mother dies of sepsis
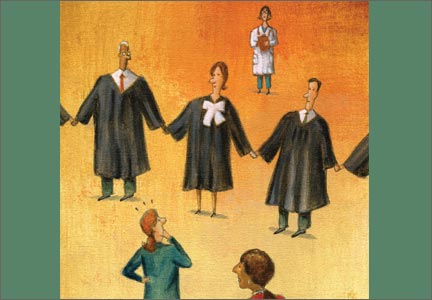
At 40 4/7 weeks' gestation, a 37-year-old woman gave birth to a healthy child by cesarean delivery. The next day, the patient had an elevated white blood cell (WBC) count with a left shift, her abdomen was tympanic but soft, and she was passing flatus and belching. The ObGyn ordered a Fleet enema; only flatus was released. A covering ObGyn ordered an abdominal radiograph, which the radiologist reported as showing postoperative ileus and mild constipation. The patient was given a second Fleet enema the next day, resulting in watery stool. She vomited 300 mL of dark green fluid.
After a rectal tube was placed 2 days later, one hard brown stool and several brown, pasty, loose, and liquid stools were returned. She vomited several times that day, and was found to have hypoactive bowel sounds with continued tympanic quality in the upper quadrants. Laboratory testing revealed continued elevated WBC count with left shift. The next day, she had hypoactive bowel sounds with brown liquid stools. Later that morning, she was able to tolerate clear liquids. The ObGyn decided to discharge her home with instructions to continue on a clear liquid diet for 2 more days before advancing her diet.
The day after discharge, she was found unresponsive at home. She was taken to the hospital, but resuscitation attempts failed. She died. An autopsy revealed that the cause of death was sepsis.
ESTATE’S CLAIM The ObGyn was negligent in failing to diagnose and treat a postoperative intra-abdominal infection caused by bowel perforation. A surgical consult should have been obtained. The woman was prematurely discharged. The radiologist failed to report the presence of free air on the abdominal x-ray.
DEFENDANTS’ DEFENSE The case was settled during trial.
VERDICT A $1 million Maryland settlement was reached.
_______________
Right ureter injury detected and repaired
During laparoscopic-assisted vaginal hysterectomy, the ObGyn detected and repaired an injury to the right ureter. The patient’s recovery was delayed by the injury.
PATIENT’S CLAIM The ObGyn was negligent in using a Kleppinger bipolar cauterizing instrument to cauterize the vaginal cuff. Thermal overspray from the instrument or the instrument itself damaged the ureter. The ObGyn was also negligent in not performing diagnostic cystoscopy to confirm patency of the ureter after the repair was made.
PHYSICIAN’S DEFENSE Ureter injury is a known risk of the procedure. All procedures were performed according to protocol.
VERDICT A Florida defense verdict was returned.
_______________
Failure to detect inflammatory BrCa; woman dies
A 42-year-old woman underwent mammography in February 2002 after reporting pain, discoloration, inflammation, and swelling in her left breast. The radiologist who interpreted the mammography suggested a biopsy for a differential diagnosis of mastitis or inflammatory carcinoma. The biopsy results were negative.
The patient’s symptoms persisted, and she underwent US in late May 2002. Another radiologist interpreted the US, noting that the patient could not tolerate compression, which led to less than optimal evaluation. The radiologist suggested that mastitis was the likely cause of the patient’s symptoms.
The patient then consulted a surgeon, who ordered mammography and magnetic resonance imaging (MRI) followed by biopsy, which indicated cancer. The patient underwent a mastectomy but metastasis had already occurred. She died at age 50 prior to the trial.
ESTATE’S CLAIM If the cancer had been diagnosed earlier, the outcome would have been better. Both radiologists misinterpreted the mammographies.
DEFENDANTS’ DEFENSE The mammographies had been properly interpreted. Any missed diagnosis would not have impacted the outcome due to the type of cancer. The scans had been released to the patient, but were subsequently lost; an adverse interference instruction was given to the jury.
VERDICT A New York defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Uterine rupture, child stillborn: $3.8M net award
At 35 weeks' gestation, a woman went to the emergency department (ED) with abdominal pain, fast heartbeat, and irregular contractions. Her history included three cesarean deliveries, including one with a vertical incision. She was admitted, and a cesarean delivery was planned for the next day. After 8 hours, during which the patient’s condition worsened, an emergency cesarean delivery was undertaken. A full rupture of the uterus was found; the baby’s body had extruded into the mother’s abdomen. The child was stillborn.
PARENTS’ CLAIM The stillbirth could have been avoided if the nurses had communicated the mother’s worsening condition to the physicians.
DEFENDANTS’ DEFENSE After the hospital and physicians settled prior to trial, the case continued against the nurse in charge of the mother’s care and the nurse-staffing group. Negligence was denied; all protocols were followed.
VERDICT A $2.9 million Illinois verdict was returned. With a $900,000 settlement from the hospital and physicians, the net award was $3.8 million.
_______________
Where did rare strep A infection come from?
A 36-year-old woman reported heavy vaginal bleeding to her ObGyn. She underwent endometrial ablation in her physician’s office.
The next day, the woman called the office to report abdominal pain. She was told to stop the medication she was taking, and if the pain continued to the next day, to go to an ED. The next day, the patient went to the ED and was found to be in septic shock. During emergency laparotomy, 50 mL of purulent fluid were drained and an emergency hysterectomy was performed. Three days later, the patient died from pulmonary arrest caused by toxic shock syndrome. An autopsy revealed that the patient’s sepsis was caused by group A streptococci (GAS) infection.
ESTATE’S CLAIM The patient was not a proper candidate for endometrial ablation because of her history of chronic cervical infection. The ObGyn perforated the cervix during the procedure and tried to conceal it. At autopsy, bone wax was found in the rectal lumen that had been used to cover up damage to the cervix. The ObGyn introduced GAS bacteria into the patient’s system. The ObGyn’s staff failed to ask the proper questions when she called the day after the procedure. She should have been told to go directly to the ED.
DEFENDANTS’ DEFENSE The ObGyn did not perforate the cervix or uterus during the procedure. GAS infection is so rare that it would have been difficult to foresee or diagnose. Potentially, the patient had a chronic
cervical infection before ablation.
VERDICT A Texas defense verdict was returned.
_______________
DURING INSERTION, IUD PERFORATES UTERINE WALL; LATER FOUND BELOW LIVER
On July 21, a 46-year-old woman went to an ObGyn for placement of an intrauterine device (IUD). Shortly after the ObGyn inserted the levonorgestrel-releasing intrauterine system (Mirena, Bayer HealthCare), the patient reported severe pelvic and abdominal pain. On July 26, the patient underwent surgical removal of the IUD.
She was discharged on July 29 but continued to report pain. She was readmitted to the hospital the next day and treated for pain. She was bed ridden for 3 weeks after IUD-removal surgery, and had a 3-month recovery before feeling pain free.
PATIENT’S CLAIM The ObGyn was negligent in perforating the patient’s uterine wall during IUD insertion, causing the device to ultimately migrate under the patient’s liver.
DEFENDANTS’ DEFENSE Uterine perforation is a known complication of IUD insertion. The IUD escaped from the patient’s uterus at a later time and not during the insertion procedure.
VERDICT A Florida verdict of $208,839 was returned; the amount was reduced to $161,058 because the medical expenses were written off by the health-care providers.
_______________
Was travel appropriate for this pregnant woman?
A woman with a history of two premature deliveries and one miscarriage became pregnant again. She received prenatal care at an Army hospital. She traveled to Spain, where the baby was born at 31 weeks’ gestation. The baby required treatment in a neonatal intensive care unit (NICU) for 17 days. The child has cerebral palsy, with tetraplegia of all four extremities. She cannot walk without assistance and suffers severe cognitive and vision impairment.
PARENTS’ CLAIM The ObGyn at the Army hospital should not have approved the mother’s request for travel; he did so, despite knowing that the mother was at high risk for premature birth. The military medical hospital to which she was assigned in Spain could not manage a high-risk pregnancy, didn’t have a NICU, and didn’t have specialists to treat premature infants.
DEFENDANTS’ DEFENSE The ObGyn argued that he did not have access to the medical records showing the mother’s history. The patient countered that the ObGyn did indeed have the patient’s records, as he had discussed them with her.
VERDICT A $10,409,700 California verdict was returned against the ObGyn and the government facility.
_______________
Triple-negative BrCa not diagnosed until metastasized: $5.2M
After finding lumps in both breasts, a woman in her 30s saw a nurse practitioner (NP) at an Army hospital. A radiologist reported no mass in the right breast and multiple benign-appearing anechoic lesions in the left breast after bilateral mammography and ultrasonography (US) in July 2008. The Chief of Mammography Services recommended referral to a breast surgeon, but the patient never received the letter. It was placed in her mammography file, not in the treatment file.
In November 2008, the patient returned to the clinic. Bilateral diagnostic mammography and US were ordered, but for unknown reasons, cancelled. US of the left breast was interpreted as benign in January 2009.
After imaging in March 2010, followed by a needle biopsy of the right breast, a radiologist reported finding intermediate-grade infiltrating ductal carcinoma.
The patient sought care outside the military medical system at a large university hospital. In April 2010, stage 3 triple-negative invasive ductal carcinoma (IDC) was identified. The patient underwent chemotherapy, a double mastectomy, removal of 21 lymph nodes, and breast reconstruction. She was given a 60% chance of recurrence in 5–7 years.
PATIENT’S CLAIM It was negligent to not inform her of imaging results. Biopsy should have been performed in 2008, when the IDC was likely at stage 1; treatment would have been far less aggressive. Electronic medical records showed that the 2008 mammography and US results had been “signed off” by an NP at the clinic.
DEFENDANTS’ DEFENSE While unable to concede liability, the government agency did not contest the point.
VERDICT A $5.2 million Tennessee federal court bench verdict was returned, citing failures in communication, poor and improper record keeping and retention, failure to follow-up, and an unexplained cancellation of a medical order.
_______________
Woman dies from cervical cancer: $2.3M
In 2001, a 41-year-old woman had abnormal Pap smear results but her gynecologist did not order more testing. The patient was told to return in 3 months, but she did not return until 2007—reporting abnormal bleeding, vaginal discharge, and pain. Her Pap results were normal, however, and the gynecologist did not order further testing. In 2009, the patient was found to have advanced cervical cancer. She died 2 years later.
ESTATE’S CLAIM Further testing should have been ordered in 2001, which would have likely revealed dysplasia, which can lead to cancer. The laboratory incorrectly interpreted the 2007 Pap test; if the results had been properly reported, additional testing could have been ordered.
DEFENDANTS’ DEFENSE The laboratory and patient’s estate settled for a confidential amount before trial. The gynecologist denied negligence.
VERDICT A New Jersey jury found the gynecologist 40% at fault for his actions in 2007. The jury found the laboratory 50% at fault, and the patient 10% at fault. A gross verdict of $2.33 million was returned.
_______________
Bowel injury after cesarean delivery; mother dies of sepsis
At 40 4/7 weeks' gestation, a 37-year-old woman gave birth to a healthy child by cesarean delivery. The next day, the patient had an elevated white blood cell (WBC) count with a left shift, her abdomen was tympanic but soft, and she was passing flatus and belching. The ObGyn ordered a Fleet enema; only flatus was released. A covering ObGyn ordered an abdominal radiograph, which the radiologist reported as showing postoperative ileus and mild constipation. The patient was given a second Fleet enema the next day, resulting in watery stool. She vomited 300 mL of dark green fluid.
After a rectal tube was placed 2 days later, one hard brown stool and several brown, pasty, loose, and liquid stools were returned. She vomited several times that day, and was found to have hypoactive bowel sounds with continued tympanic quality in the upper quadrants. Laboratory testing revealed continued elevated WBC count with left shift. The next day, she had hypoactive bowel sounds with brown liquid stools. Later that morning, she was able to tolerate clear liquids. The ObGyn decided to discharge her home with instructions to continue on a clear liquid diet for 2 more days before advancing her diet.
The day after discharge, she was found unresponsive at home. She was taken to the hospital, but resuscitation attempts failed. She died. An autopsy revealed that the cause of death was sepsis.
ESTATE’S CLAIM The ObGyn was negligent in failing to diagnose and treat a postoperative intra-abdominal infection caused by bowel perforation. A surgical consult should have been obtained. The woman was prematurely discharged. The radiologist failed to report the presence of free air on the abdominal x-ray.
DEFENDANTS’ DEFENSE The case was settled during trial.
VERDICT A $1 million Maryland settlement was reached.
_______________
Right ureter injury detected and repaired
During laparoscopic-assisted vaginal hysterectomy, the ObGyn detected and repaired an injury to the right ureter. The patient’s recovery was delayed by the injury.
PATIENT’S CLAIM The ObGyn was negligent in using a Kleppinger bipolar cauterizing instrument to cauterize the vaginal cuff. Thermal overspray from the instrument or the instrument itself damaged the ureter. The ObGyn was also negligent in not performing diagnostic cystoscopy to confirm patency of the ureter after the repair was made.
PHYSICIAN’S DEFENSE Ureter injury is a known risk of the procedure. All procedures were performed according to protocol.
VERDICT A Florida defense verdict was returned.
_______________
Failure to detect inflammatory BrCa; woman dies
A 42-year-old woman underwent mammography in February 2002 after reporting pain, discoloration, inflammation, and swelling in her left breast. The radiologist who interpreted the mammography suggested a biopsy for a differential diagnosis of mastitis or inflammatory carcinoma. The biopsy results were negative.
The patient’s symptoms persisted, and she underwent US in late May 2002. Another radiologist interpreted the US, noting that the patient could not tolerate compression, which led to less than optimal evaluation. The radiologist suggested that mastitis was the likely cause of the patient’s symptoms.
The patient then consulted a surgeon, who ordered mammography and magnetic resonance imaging (MRI) followed by biopsy, which indicated cancer. The patient underwent a mastectomy but metastasis had already occurred. She died at age 50 prior to the trial.
ESTATE’S CLAIM If the cancer had been diagnosed earlier, the outcome would have been better. Both radiologists misinterpreted the mammographies.
DEFENDANTS’ DEFENSE The mammographies had been properly interpreted. Any missed diagnosis would not have impacted the outcome due to the type of cancer. The scans had been released to the patient, but were subsequently lost; an adverse interference instruction was given to the jury.
VERDICT A New York defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
More inclusions:
- Where did rare strep A infection come from?
- During insertion, IUD perforates uterine wall; Later found below liver
- Was travel appropriate for this pregnant woman?
- Triple-negative BrCa not diagnosed until metastasized: $5.2M
- Woman dies from cervical cancer: $2.3M
- Bowel injury after cesarean delivery; mother dies of sepsis
- Right ureter injury detected and repaired
- Failure to detect inflammatory BrCa; woman dies
The Affordable Care Act: What’s the latest?
mmmm
When I last wrote about the Affordable Care Act (ACA), in May 2014, I focused on the contraception issue. Since then, the US Supreme Court ruled, in Burwell v. Hobby Lobby, that closely held, for-profit companies with religious objections to covering birth control can opt out of the requirement to provide contraceptive coverage to their employees.
In this article, I explore that decision and what it means for women’s health. I also present data on the uninsured rate in the United States, which has dropped significantly since enactment of the ACA, and I discuss one increasingly common barrier to access to care—the use of narrow networks by insurers.
A corporation now can hold a religious belief
The Supreme Court’s majority 5-4 ruling recognized, for the first time, that a for-profit corporation can hold a religious belief, but the Court limited this claim to closely held corporations. The Court also decided that the ACA placed a substantial burden on the corporations’ religious beliefs and concluded that there are less burdensome ways to accomplish the law’s intent, rendering the contraceptive coverage provision in the ACA in violation of the Religious Freedom Restoration Act (RFRA). The Court limited its ruling to the contraceptive coverage requirement, essentially turning the requirement into an option for many employers.
Are contraceptives abortifacients?
The religious belief at the center of Burwell v. Hobby Lobby was that life begins at conception, which the Green family—the owners of Hobby Lobby—equate to fertilization. Hobby Lobby’s attorneys also asserted that four contraceptives approved by the US Food and Drug Administration and included in the ACA mandate may prevent implantation of a fertilized egg, thereby constituting abortion.
Although there is no scientific answer as to when life begins, ACOG and the medical community agree that pregnancy begins at implantation. In its amicus brief to the US Supreme Court, ACOG asserted the medical community’s consensus that the four contraceptives prevent pregnancy rather than end it, and are not abortifacients:
- emergency contraceptive pills: levonorgestrel (Plan B) and its generic equivalents and ulipristal acetate (ella)
- the copper IUD (ParaGard)
- levonorgestrel-releasing intrauterine systems (Mirena, Skyla).
What is a closely held corporation?
In general, according to the Pew Research Center, a closely held corporation is a private company (not publicly traded) with a limited number of shareholders. The Internal Revenue Service (IRS), an important source, defines a closely held corporation as one in which more than half of the stock is owned (directly or indirectly) by five or fewer individuals at any time in the second half of the year.
“S” corporations are also considered closely held. These are corporations with 100 or fewer shareholders, with all members of the same family counted as one shareholder. “S” corporations don’t pay income tax; their shareholders pay tax on their personal returns, based on the corporations’ profits and losses.
Hobby Lobby is organized as an “S” corporation. According to the IRS, in 2011, there were 4,158,572 “S” corporations, 99.4% of them with 10 or fewer shareholders.1
The US Census Bureau estimates that, in 2012, about 2.9 million “S” corporations employed more than 29 million people. Many closely held corporations are quite large.2 According to the Pew Research Center, family-owned Cargill employs 140,000 people and had $136.7 billion in revenue in fiscal 2013. Hobby Lobby has estimated revenues of $3.3 billion and 23,000 employees.2
What’s next?
ACOG helped secure coverage of contraceptives in the ACA and is working with the US Congress and our women’s health partners to restore this important care. Days after the Supreme Court decision, Senator Patty Murray (D-WA) introduced the Protect Women’s Health from Corporate Interference Act, S. 2578, with 46 cosponsors as of this writing. ACOG fully supports this bill, also known as the “Not My Boss’ Business Bill,” which would reestablish the contraceptive coverage mandate as well as other care required by federal law. This bill still maintains the exemption from contraceptive coverage for houses of worship and the accommodation for religious nonprofits.
In introducing her bill, Senator Murray pointed out that “the contraceptive coverage requirement has already made a tremendous difference in women’s lives—24 million more prescriptions for oral contraceptives were filled with no copay in 2013 than in 2012, and women have saved $483 million in out-of-pocket costs for oral contraceptives.”3
Uninsured rate is declining
The Commonwealth Fund shows that, from July–September 2013 to April–June 2014, the nation’s uninsured rate fell from 20% to 15%, resulting in 9.5 million fewer uninsured adults.4 The biggest drop occurred among young adults, with the uninsured rate falling from 28% to 18%, and in states that adopted the Medicaid expansion, where uninsured rates fell from 28% to 17%.4
States that didn’t expand their Medicaid program didn’t show any noticeable change, with the uninsured rate declining only two points, from 38% to 36%.4
Coverage resulted in access to care for the majority of the newly covered. Sixty percent of people with new coverage visited a provider or hospital or paid for a prescription. Sixty-two percent of these individuals said they wouldn’t have been able to access this care before getting this coverage. Eighty-one percent of people with new coverage said they were better off now than before.4
ACA works better in some states than others
The Kaiser Family Foundation looked at four successful states—Colorado, Connecticut, Kentucky, and Washington state—to see what lessons can be learned. Important commonalities include the fact that the states run their own marketplace, adopted the Medi-caid expansion, and conducted extensive outreach and public education, including engaging providers in patient outreach and enrollment.5
Other tools of success were developing good marketing and branding, providing consumer-friendly assistance, and attention to systems and operations.5
How the Hobby Lobby decision affects individual states
Because the Supreme Court’s decision concerned interpretation of a federal law—the Religious Freedom Restoration Act (RFRA)—it does not supersede state laws that mandate coverage of contraceptives.
Twenty-eight states have laws or rulings requiring insurers to cover contraceptives, most of them dating from the 1990s and providing some exemption for religious insurers or plans. Only Illinois allows an exemption for secular bodies.
Although these state laws remain in effect, state officials may opt to stop enforcing them with regard to certain companies. For example, after the Hobby Lobby decision, Wisconsin officials announced that they no longer will enforce contraceptive coverage when a company has a religious objection.
For companies that self-fund or self-insure worker health coverage, the state coverage laws don’t apply—only federal law does. These companies do not have to adhere to state insurance mandates.
Some states have their own version of the RFRA. See the chart at right for details on a state-by-state basis.
The Supreme Court ruling also has no effect on state laws that guarantee access to emergency contraception in hospital emergency departments and that require pharmacists to dispense contraceptives.
| State | Contraceptive equity law? | Employer/insurer exemption to equity law? | Religious freedom law? |
| Alabama | ✔ | ||
| Alaska | |||
| Arizona | ✔ | ✔ | ✔ |
| Arkansas | ✔ | ✔ | |
| California | ✔ | ✔ | |
| Colorado | ✔ | ||
| Connecticut | ✔ | ✔ | ✔ |
| Delaware | ✔ | ✔ | |
| Florida | ✔ | ||
| Georgia | ✔ | ||
| Hawaii | ✔ | ✔ | |
| Idaho | ✔ | ||
| Illinois | ✔ | ✔ | ✔ |
| Indiana | |||
| Iowa | ✔ | ||
| Kansas | |||
| Kentucky | ✔ | ||
| Louisiana | ✔ | ||
| Maine | ✔ | ✔ | |
| Maryland | ✔ | ✔ | |
| Massachusetts | ✔ | ✔ | |
| Michigan | ✔ | ✔ | |
| Minnesota | |||
| Mississippi | ✔ | ||
| Missouri | ✔ | ✔ | ✔ |
| Montana | ✔ | ||
| Nebraska | |||
| Nevada | ✔ | ✔ | |
| New Hampshire | ✔ | ||
| New Jersey | ✔ | ✔ | |
| New Mexico | ✔ | ✔ | ✔ |
| New York | ✔ | ✔ | |
| North Carolina | ✔ | ✔ | |
| North Dakota | |||
| Ohio | |||
| Oklahoma | ✔ | ||
| Oregon | ✔ | ✔ | |
| Pennsylvania | ✔ | ||
| Rhode Island | ✔ | ✔ | ✔ |
| South Carolina | ✔ | ||
| South Dakota | |||
| Tennessee | ✔ | ||
| Texas | ✔ | ||
| Utah | |||
| Vermont | ✔ | ||
| Virginia | ✔ | ||
| Washington | ✔ | ||
| West Virginia | ✔ | ✔ | |
| Wisconsin | ✔ | ||
| Wyoming | |||
| TOTAL | 28 | 20 | 18 |
Narrow networks limit access to care
Huge concerns abound regarding implementation and real-life experiences related to the ACA. A number of them—high deductibles, low payment rates, limited access to physicians, long drive and wait times—can be related to “narrow networks.” Insurers exclude certain providers and offer all providers lower payment rates (which leads some physicians to drop out of the plan); they also create tiers (charging consumers lower copays and deductibles for using inner-tier preferred providers and high out-of-pocket costs for using other providers, even though they may be in the network).
Narrow networks work for insurers as an effective tool for lowering provider payment rates to keep premiums low and gain market share. The narrower the network, the lower are physician payments and premiums.
The ACA promises expanded access to high-quality, affordable health care for millions of Americans—a promise being compromised in many areas of the country through narrow networks. In these instances, insurers offering new plans in a health-care marketplace limit patient access to the numbers, types, and locations of physicians and hospitals covered under certain plans. Insurers typically offer patients low premiums, offer selected providers a high volume of patients at low payment levels, and exclude other providers whom the insurer deems to be high-cost.
Narrow networks aren’t new
As with so many elements of the ACA, narrow networks aren’t a new phenomenon. Many of us remember the public relations price that HMOs paid in the 1980s and 1990s for exceedingly limiting patients’ access to care while charging low premiums. The consumer outcry led the National Association of Insurance Commissioners to urge states to require managed-care plans to maintain adequate networks, the approach adopted by the federal government in the ACA.6
The pendulum swung in the next decade to broader networks in which consumers had much greater access, but premiums increased by an average of 11% per year.6 Employers then pushed insurers to reduce premium costs, leading back to narrow networks in the years just before the ACA. Narrow network plans accounted for 23% of all employer-sponsored plans in 2012, up from 15% in 2007.6
Increasing consolidation contributes to narrow networks
The trend toward narrower networks is also linked to increasing consolidation in health care. As health systems grow and individual or small group practices disappear, insurers rely on being able to credibly threaten to exclude systems and big groups from their networks as leverage in payment negotiations. By restricting the choice of providers in a plan, the insurer can promise more customers for the doctors and hospitals that are included, and negotiate lower payments to those providers.
The downside for physicians is clear:
- low payment rates
- exclusion from networks and coverage
- inability to refer patients to providers the physician determines to be best for that patient’s needs.
- The downside for patients:
- If they have to go out of network to get needed care, they may end up paying high out-of-pocket costs
- If they delay or forego care, their health may suffer significantly.
The insurance industry’s position is that patients have choices. Plans with access to more hospitals and specialists are available but usually at a higher price.
Narrow networks are one way to achieve low premiums
In the months leading up to ACA enactment, insurers got to work developing plans designed to be sold on the exchanges that would attract consumers through low-cost premiums and still maximize profits, especially now that insurers, under the ACA, are barred from excluding sick enrollees or increasing premiums for women, in addition to other important protections.
In previous articles, we’ve explored these landmark protections. Insurers in the individual market used to be able to keep premiums relatively low, and profits up, through use of preexisting coverage exclusions, benefit exclusions including noncoverage for maternity care or prescription drugs, and high cost sharing. Not anymore.
Since enactment of the ACA, narrow networks seem to be the preferred, and most effective, payment negotiation tool of many insurers offering plans through the exchanges, reflecting the trend we’re already seeing in the private health insurance marketplace.
NPR spotlights the difficulty of finding a specialist
The consumer and provider problems of narrow networks have been gaining attention in the media. In July, the National Public Radio (NPR) Web site carried an article entitled, “Patients with low-cost insurance struggle to find specialists,” with a key subtitle: “So you found an exchange plan. But can you find a provider?”7
In the NPR article, author Carrie Feibel reported on the situation in a majority-immigrant area of southwest Houston.
There, many patients at the local clinic have health insurance coverage for the first time, an important step toward healthier lives for themselves and their families. But many people in need of a specialist are learning that their insurance card doesn’t guarantee them access to a needed surgeon or hospital. They’ve purchased a narrow-network insurance plan, with a low premium but few specialists who accept that insurance.7
The two largest hospital chains in Houston—Houston Methodist and Memorial Hermann—as well as Houston’s MD Anderson Cancer Center, don’t participate in the Blue Cross Blue Shield HMO Silver plan, a plan popular with low-income consumers because of its low premium.7
Will the government take action?
The ACA actually guards against overly narrow networks and established the first national standard for network adequacy—a standard that needs fuller development, for sure. Plans sold on the exchanges are required to establish networks that include, among other providers, essential community providers, who typically care for mostly low-income and medically underserved populations. Networks also must include sufficient numbers and types of providers, including “providers that specialize in mental health and substance abuse services, to assure that all services will be accessible without unreasonable delay.”8
Insurers also must provide people who are considering purchasing their products with an accurate directory—both online and a hard copy—identifying providers not accepting new patients in the network. And plans are prohibited from charging out-of-network cost-sharing for emergency services.
Much of the oversight and many of the details—how much is adequate? what is unreasonable?—are left to the states, many of which have years of experience grappling with the downsides and delicate balance of networks.
The Urban Institute points out that Vermont and Delaware set standards for maximum geographic distance and drive times for primary care services. In California, plans must make it easy for consumers to reach urban providers on public transportation.6
Professional societies are taking note
Today, the misuse of narrow networks by exchange plans also has gotten the attention of the American Medical Association, ACOG, and many other national medical specialty societies, in addition to the states and federal government.
The trick, many health-care policy experts agree, is to find the right balance. How broad can the network be before premiums soar? Most agree that consumers must be able to choose between plans with confidence, without any cost or access surprises, meaning much better transparency. And many agree that provider quality, in addition to cost, has to find its way into the equation.
This year, the Center for Consumer Information and Insurance Oversight, a part of the federal Department of Health and Human Services created by the ACA to investigate these kinds of issues, is investigating access to hospital systems, mental health services, oncology, and primary care providers and is developing time, distance, and other standards that insurers will have to adhere to.
Employer groups oppose strong standards or limits on narrow networks. Recently, representatives of the US Chamber of Commerce, the National Retail Federation, and others warned Congress to stay out of this fight. They understand that more generous networks mean higher premiums. These employer representative groups prefer to strengthen consumer protections like directories and keep low the cost of health insurance that they provide for their employees.
Acknowledgment
The author acknowledges the work and expertise of ACOG's state government affairs team for the state analysis—Kathryn Moore, Director, and Kate Vlach, Senior Manager—as well as advocacy partners.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Internal Revenue Service. SOI Tax States, Table 1, Returns of Active Corporations, Form 1120S. http://www.irs.gov/uac/SOI-Tax-Stats-Table-1-Returns-of-Active-Corporations,-Form-1120S. Updated June 27, 2014. Accessed September 4, 2014.
2. DeSilver D. What is a ‘closely held corporation,’ anyway, and how many are there? Pew Research Center: Fact Tank. http://www.pewresearch.org/fact-tank/2014/07/07/what-is-a-closely-held-corporation-anyway-and-how-many-are-there/. Published July 7, 2014. Accessed September 4, 2014.
3. Murray P. Protect Women’s Health From Corporate Interference Act: Summary. http://www.murray.senate.gov/public/_cache/files/30554052-0f84-485a-babc-ccc04af85bb6/protect-women-s-health-from-corporate-interference-act---one-page-summary---final.pdf. Accessed September 4, 2014.
4. The Commonwealth Fund. New Survey: After First ACA Enrollment Period, Uninsured Rate Dropped from 20% to 15%; Largest Declines Among Young Adults, Latinos, and Low-Income People. http://www.commonwealthfund.org/publications/press-releases/2014/jul/after-first-aca -enrollment-period. Published July 10,2014. Accessed September 4, 2014.
5. Artiga S, Stephens J, Rudowitz R, Perry M. What Worked and What’s Next? Strategies in Four States Leading ACA Enrollment Efforts. Kaiser Family Foundation. http://kff.org/health-reform/issue-brief/what-worked-and-whats-next-strategies-in-four-states-leading-aca-enrollment-efforts/. Published July 16, 2014. Accessed September 4, 2014.
6. Corlette S, Volk J. Narrow Provider Networks in New Health Plans: Balancing Affordability with Access to Quality Care. Urban Institute: Georgetown University Center on Health Insurance Reforms. http://www.urban.org/UploadedPDF/413135-New-Provider-Networks-in-New-Health-Plans.pdf. Published May 2014. Accessed September 4, 2014.
7. Feibel C. Patients With Low-Cost Insurance Struggle to Find Specialists. National Public Radio. http://www.npr.org/blogs/health/2014/07/16/331419293/patients-with-low-cost-insurance-struggle-to-find-specialists. Published July 16, 2014. Accessed September 4, 2014.
8. Patient Protection and Affordable Care Act: Preexisting Condition Exclusions, Lifetime and Annual Limits, Rescissions, and Patient Protections. US Department of Health and Human Services. http://www.regulations.go/#!documentDetail;D=HHS-OS-2010-0014-0001. Published June 28, 2010. Accessed September 9, 2014.
mmmm
When I last wrote about the Affordable Care Act (ACA), in May 2014, I focused on the contraception issue. Since then, the US Supreme Court ruled, in Burwell v. Hobby Lobby, that closely held, for-profit companies with religious objections to covering birth control can opt out of the requirement to provide contraceptive coverage to their employees.
In this article, I explore that decision and what it means for women’s health. I also present data on the uninsured rate in the United States, which has dropped significantly since enactment of the ACA, and I discuss one increasingly common barrier to access to care—the use of narrow networks by insurers.
A corporation now can hold a religious belief
The Supreme Court’s majority 5-4 ruling recognized, for the first time, that a for-profit corporation can hold a religious belief, but the Court limited this claim to closely held corporations. The Court also decided that the ACA placed a substantial burden on the corporations’ religious beliefs and concluded that there are less burdensome ways to accomplish the law’s intent, rendering the contraceptive coverage provision in the ACA in violation of the Religious Freedom Restoration Act (RFRA). The Court limited its ruling to the contraceptive coverage requirement, essentially turning the requirement into an option for many employers.
Are contraceptives abortifacients?
The religious belief at the center of Burwell v. Hobby Lobby was that life begins at conception, which the Green family—the owners of Hobby Lobby—equate to fertilization. Hobby Lobby’s attorneys also asserted that four contraceptives approved by the US Food and Drug Administration and included in the ACA mandate may prevent implantation of a fertilized egg, thereby constituting abortion.
Although there is no scientific answer as to when life begins, ACOG and the medical community agree that pregnancy begins at implantation. In its amicus brief to the US Supreme Court, ACOG asserted the medical community’s consensus that the four contraceptives prevent pregnancy rather than end it, and are not abortifacients:
- emergency contraceptive pills: levonorgestrel (Plan B) and its generic equivalents and ulipristal acetate (ella)
- the copper IUD (ParaGard)
- levonorgestrel-releasing intrauterine systems (Mirena, Skyla).
What is a closely held corporation?
In general, according to the Pew Research Center, a closely held corporation is a private company (not publicly traded) with a limited number of shareholders. The Internal Revenue Service (IRS), an important source, defines a closely held corporation as one in which more than half of the stock is owned (directly or indirectly) by five or fewer individuals at any time in the second half of the year.
“S” corporations are also considered closely held. These are corporations with 100 or fewer shareholders, with all members of the same family counted as one shareholder. “S” corporations don’t pay income tax; their shareholders pay tax on their personal returns, based on the corporations’ profits and losses.
Hobby Lobby is organized as an “S” corporation. According to the IRS, in 2011, there were 4,158,572 “S” corporations, 99.4% of them with 10 or fewer shareholders.1
The US Census Bureau estimates that, in 2012, about 2.9 million “S” corporations employed more than 29 million people. Many closely held corporations are quite large.2 According to the Pew Research Center, family-owned Cargill employs 140,000 people and had $136.7 billion in revenue in fiscal 2013. Hobby Lobby has estimated revenues of $3.3 billion and 23,000 employees.2
What’s next?
ACOG helped secure coverage of contraceptives in the ACA and is working with the US Congress and our women’s health partners to restore this important care. Days after the Supreme Court decision, Senator Patty Murray (D-WA) introduced the Protect Women’s Health from Corporate Interference Act, S. 2578, with 46 cosponsors as of this writing. ACOG fully supports this bill, also known as the “Not My Boss’ Business Bill,” which would reestablish the contraceptive coverage mandate as well as other care required by federal law. This bill still maintains the exemption from contraceptive coverage for houses of worship and the accommodation for religious nonprofits.
In introducing her bill, Senator Murray pointed out that “the contraceptive coverage requirement has already made a tremendous difference in women’s lives—24 million more prescriptions for oral contraceptives were filled with no copay in 2013 than in 2012, and women have saved $483 million in out-of-pocket costs for oral contraceptives.”3
Uninsured rate is declining
The Commonwealth Fund shows that, from July–September 2013 to April–June 2014, the nation’s uninsured rate fell from 20% to 15%, resulting in 9.5 million fewer uninsured adults.4 The biggest drop occurred among young adults, with the uninsured rate falling from 28% to 18%, and in states that adopted the Medicaid expansion, where uninsured rates fell from 28% to 17%.4
States that didn’t expand their Medicaid program didn’t show any noticeable change, with the uninsured rate declining only two points, from 38% to 36%.4
Coverage resulted in access to care for the majority of the newly covered. Sixty percent of people with new coverage visited a provider or hospital or paid for a prescription. Sixty-two percent of these individuals said they wouldn’t have been able to access this care before getting this coverage. Eighty-one percent of people with new coverage said they were better off now than before.4
ACA works better in some states than others
The Kaiser Family Foundation looked at four successful states—Colorado, Connecticut, Kentucky, and Washington state—to see what lessons can be learned. Important commonalities include the fact that the states run their own marketplace, adopted the Medi-caid expansion, and conducted extensive outreach and public education, including engaging providers in patient outreach and enrollment.5
Other tools of success were developing good marketing and branding, providing consumer-friendly assistance, and attention to systems and operations.5
How the Hobby Lobby decision affects individual states
Because the Supreme Court’s decision concerned interpretation of a federal law—the Religious Freedom Restoration Act (RFRA)—it does not supersede state laws that mandate coverage of contraceptives.
Twenty-eight states have laws or rulings requiring insurers to cover contraceptives, most of them dating from the 1990s and providing some exemption for religious insurers or plans. Only Illinois allows an exemption for secular bodies.
Although these state laws remain in effect, state officials may opt to stop enforcing them with regard to certain companies. For example, after the Hobby Lobby decision, Wisconsin officials announced that they no longer will enforce contraceptive coverage when a company has a religious objection.
For companies that self-fund or self-insure worker health coverage, the state coverage laws don’t apply—only federal law does. These companies do not have to adhere to state insurance mandates.
Some states have their own version of the RFRA. See the chart at right for details on a state-by-state basis.
The Supreme Court ruling also has no effect on state laws that guarantee access to emergency contraception in hospital emergency departments and that require pharmacists to dispense contraceptives.
| State | Contraceptive equity law? | Employer/insurer exemption to equity law? | Religious freedom law? |
| Alabama | ✔ | ||
| Alaska | |||
| Arizona | ✔ | ✔ | ✔ |
| Arkansas | ✔ | ✔ | |
| California | ✔ | ✔ | |
| Colorado | ✔ | ||
| Connecticut | ✔ | ✔ | ✔ |
| Delaware | ✔ | ✔ | |
| Florida | ✔ | ||
| Georgia | ✔ | ||
| Hawaii | ✔ | ✔ | |
| Idaho | ✔ | ||
| Illinois | ✔ | ✔ | ✔ |
| Indiana | |||
| Iowa | ✔ | ||
| Kansas | |||
| Kentucky | ✔ | ||
| Louisiana | ✔ | ||
| Maine | ✔ | ✔ | |
| Maryland | ✔ | ✔ | |
| Massachusetts | ✔ | ✔ | |
| Michigan | ✔ | ✔ | |
| Minnesota | |||
| Mississippi | ✔ | ||
| Missouri | ✔ | ✔ | ✔ |
| Montana | ✔ | ||
| Nebraska | |||
| Nevada | ✔ | ✔ | |
| New Hampshire | ✔ | ||
| New Jersey | ✔ | ✔ | |
| New Mexico | ✔ | ✔ | ✔ |
| New York | ✔ | ✔ | |
| North Carolina | ✔ | ✔ | |
| North Dakota | |||
| Ohio | |||
| Oklahoma | ✔ | ||
| Oregon | ✔ | ✔ | |
| Pennsylvania | ✔ | ||
| Rhode Island | ✔ | ✔ | ✔ |
| South Carolina | ✔ | ||
| South Dakota | |||
| Tennessee | ✔ | ||
| Texas | ✔ | ||
| Utah | |||
| Vermont | ✔ | ||
| Virginia | ✔ | ||
| Washington | ✔ | ||
| West Virginia | ✔ | ✔ | |
| Wisconsin | ✔ | ||
| Wyoming | |||
| TOTAL | 28 | 20 | 18 |
Narrow networks limit access to care
Huge concerns abound regarding implementation and real-life experiences related to the ACA. A number of them—high deductibles, low payment rates, limited access to physicians, long drive and wait times—can be related to “narrow networks.” Insurers exclude certain providers and offer all providers lower payment rates (which leads some physicians to drop out of the plan); they also create tiers (charging consumers lower copays and deductibles for using inner-tier preferred providers and high out-of-pocket costs for using other providers, even though they may be in the network).
Narrow networks work for insurers as an effective tool for lowering provider payment rates to keep premiums low and gain market share. The narrower the network, the lower are physician payments and premiums.
The ACA promises expanded access to high-quality, affordable health care for millions of Americans—a promise being compromised in many areas of the country through narrow networks. In these instances, insurers offering new plans in a health-care marketplace limit patient access to the numbers, types, and locations of physicians and hospitals covered under certain plans. Insurers typically offer patients low premiums, offer selected providers a high volume of patients at low payment levels, and exclude other providers whom the insurer deems to be high-cost.
Narrow networks aren’t new
As with so many elements of the ACA, narrow networks aren’t a new phenomenon. Many of us remember the public relations price that HMOs paid in the 1980s and 1990s for exceedingly limiting patients’ access to care while charging low premiums. The consumer outcry led the National Association of Insurance Commissioners to urge states to require managed-care plans to maintain adequate networks, the approach adopted by the federal government in the ACA.6
The pendulum swung in the next decade to broader networks in which consumers had much greater access, but premiums increased by an average of 11% per year.6 Employers then pushed insurers to reduce premium costs, leading back to narrow networks in the years just before the ACA. Narrow network plans accounted for 23% of all employer-sponsored plans in 2012, up from 15% in 2007.6
Increasing consolidation contributes to narrow networks
The trend toward narrower networks is also linked to increasing consolidation in health care. As health systems grow and individual or small group practices disappear, insurers rely on being able to credibly threaten to exclude systems and big groups from their networks as leverage in payment negotiations. By restricting the choice of providers in a plan, the insurer can promise more customers for the doctors and hospitals that are included, and negotiate lower payments to those providers.
The downside for physicians is clear:
- low payment rates
- exclusion from networks and coverage
- inability to refer patients to providers the physician determines to be best for that patient’s needs.
- The downside for patients:
- If they have to go out of network to get needed care, they may end up paying high out-of-pocket costs
- If they delay or forego care, their health may suffer significantly.
The insurance industry’s position is that patients have choices. Plans with access to more hospitals and specialists are available but usually at a higher price.
Narrow networks are one way to achieve low premiums
In the months leading up to ACA enactment, insurers got to work developing plans designed to be sold on the exchanges that would attract consumers through low-cost premiums and still maximize profits, especially now that insurers, under the ACA, are barred from excluding sick enrollees or increasing premiums for women, in addition to other important protections.
In previous articles, we’ve explored these landmark protections. Insurers in the individual market used to be able to keep premiums relatively low, and profits up, through use of preexisting coverage exclusions, benefit exclusions including noncoverage for maternity care or prescription drugs, and high cost sharing. Not anymore.
Since enactment of the ACA, narrow networks seem to be the preferred, and most effective, payment negotiation tool of many insurers offering plans through the exchanges, reflecting the trend we’re already seeing in the private health insurance marketplace.
NPR spotlights the difficulty of finding a specialist
The consumer and provider problems of narrow networks have been gaining attention in the media. In July, the National Public Radio (NPR) Web site carried an article entitled, “Patients with low-cost insurance struggle to find specialists,” with a key subtitle: “So you found an exchange plan. But can you find a provider?”7
In the NPR article, author Carrie Feibel reported on the situation in a majority-immigrant area of southwest Houston.
There, many patients at the local clinic have health insurance coverage for the first time, an important step toward healthier lives for themselves and their families. But many people in need of a specialist are learning that their insurance card doesn’t guarantee them access to a needed surgeon or hospital. They’ve purchased a narrow-network insurance plan, with a low premium but few specialists who accept that insurance.7
The two largest hospital chains in Houston—Houston Methodist and Memorial Hermann—as well as Houston’s MD Anderson Cancer Center, don’t participate in the Blue Cross Blue Shield HMO Silver plan, a plan popular with low-income consumers because of its low premium.7
Will the government take action?
The ACA actually guards against overly narrow networks and established the first national standard for network adequacy—a standard that needs fuller development, for sure. Plans sold on the exchanges are required to establish networks that include, among other providers, essential community providers, who typically care for mostly low-income and medically underserved populations. Networks also must include sufficient numbers and types of providers, including “providers that specialize in mental health and substance abuse services, to assure that all services will be accessible without unreasonable delay.”8
Insurers also must provide people who are considering purchasing their products with an accurate directory—both online and a hard copy—identifying providers not accepting new patients in the network. And plans are prohibited from charging out-of-network cost-sharing for emergency services.
Much of the oversight and many of the details—how much is adequate? what is unreasonable?—are left to the states, many of which have years of experience grappling with the downsides and delicate balance of networks.
The Urban Institute points out that Vermont and Delaware set standards for maximum geographic distance and drive times for primary care services. In California, plans must make it easy for consumers to reach urban providers on public transportation.6
Professional societies are taking note
Today, the misuse of narrow networks by exchange plans also has gotten the attention of the American Medical Association, ACOG, and many other national medical specialty societies, in addition to the states and federal government.
The trick, many health-care policy experts agree, is to find the right balance. How broad can the network be before premiums soar? Most agree that consumers must be able to choose between plans with confidence, without any cost or access surprises, meaning much better transparency. And many agree that provider quality, in addition to cost, has to find its way into the equation.
This year, the Center for Consumer Information and Insurance Oversight, a part of the federal Department of Health and Human Services created by the ACA to investigate these kinds of issues, is investigating access to hospital systems, mental health services, oncology, and primary care providers and is developing time, distance, and other standards that insurers will have to adhere to.
Employer groups oppose strong standards or limits on narrow networks. Recently, representatives of the US Chamber of Commerce, the National Retail Federation, and others warned Congress to stay out of this fight. They understand that more generous networks mean higher premiums. These employer representative groups prefer to strengthen consumer protections like directories and keep low the cost of health insurance that they provide for their employees.
Acknowledgment
The author acknowledges the work and expertise of ACOG's state government affairs team for the state analysis—Kathryn Moore, Director, and Kate Vlach, Senior Manager—as well as advocacy partners.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
mmmm
When I last wrote about the Affordable Care Act (ACA), in May 2014, I focused on the contraception issue. Since then, the US Supreme Court ruled, in Burwell v. Hobby Lobby, that closely held, for-profit companies with religious objections to covering birth control can opt out of the requirement to provide contraceptive coverage to their employees.
In this article, I explore that decision and what it means for women’s health. I also present data on the uninsured rate in the United States, which has dropped significantly since enactment of the ACA, and I discuss one increasingly common barrier to access to care—the use of narrow networks by insurers.
A corporation now can hold a religious belief
The Supreme Court’s majority 5-4 ruling recognized, for the first time, that a for-profit corporation can hold a religious belief, but the Court limited this claim to closely held corporations. The Court also decided that the ACA placed a substantial burden on the corporations’ religious beliefs and concluded that there are less burdensome ways to accomplish the law’s intent, rendering the contraceptive coverage provision in the ACA in violation of the Religious Freedom Restoration Act (RFRA). The Court limited its ruling to the contraceptive coverage requirement, essentially turning the requirement into an option for many employers.
Are contraceptives abortifacients?
The religious belief at the center of Burwell v. Hobby Lobby was that life begins at conception, which the Green family—the owners of Hobby Lobby—equate to fertilization. Hobby Lobby’s attorneys also asserted that four contraceptives approved by the US Food and Drug Administration and included in the ACA mandate may prevent implantation of a fertilized egg, thereby constituting abortion.
Although there is no scientific answer as to when life begins, ACOG and the medical community agree that pregnancy begins at implantation. In its amicus brief to the US Supreme Court, ACOG asserted the medical community’s consensus that the four contraceptives prevent pregnancy rather than end it, and are not abortifacients:
- emergency contraceptive pills: levonorgestrel (Plan B) and its generic equivalents and ulipristal acetate (ella)
- the copper IUD (ParaGard)
- levonorgestrel-releasing intrauterine systems (Mirena, Skyla).
What is a closely held corporation?
In general, according to the Pew Research Center, a closely held corporation is a private company (not publicly traded) with a limited number of shareholders. The Internal Revenue Service (IRS), an important source, defines a closely held corporation as one in which more than half of the stock is owned (directly or indirectly) by five or fewer individuals at any time in the second half of the year.
“S” corporations are also considered closely held. These are corporations with 100 or fewer shareholders, with all members of the same family counted as one shareholder. “S” corporations don’t pay income tax; their shareholders pay tax on their personal returns, based on the corporations’ profits and losses.
Hobby Lobby is organized as an “S” corporation. According to the IRS, in 2011, there were 4,158,572 “S” corporations, 99.4% of them with 10 or fewer shareholders.1
The US Census Bureau estimates that, in 2012, about 2.9 million “S” corporations employed more than 29 million people. Many closely held corporations are quite large.2 According to the Pew Research Center, family-owned Cargill employs 140,000 people and had $136.7 billion in revenue in fiscal 2013. Hobby Lobby has estimated revenues of $3.3 billion and 23,000 employees.2
What’s next?
ACOG helped secure coverage of contraceptives in the ACA and is working with the US Congress and our women’s health partners to restore this important care. Days after the Supreme Court decision, Senator Patty Murray (D-WA) introduced the Protect Women’s Health from Corporate Interference Act, S. 2578, with 46 cosponsors as of this writing. ACOG fully supports this bill, also known as the “Not My Boss’ Business Bill,” which would reestablish the contraceptive coverage mandate as well as other care required by federal law. This bill still maintains the exemption from contraceptive coverage for houses of worship and the accommodation for religious nonprofits.
In introducing her bill, Senator Murray pointed out that “the contraceptive coverage requirement has already made a tremendous difference in women’s lives—24 million more prescriptions for oral contraceptives were filled with no copay in 2013 than in 2012, and women have saved $483 million in out-of-pocket costs for oral contraceptives.”3
Uninsured rate is declining
The Commonwealth Fund shows that, from July–September 2013 to April–June 2014, the nation’s uninsured rate fell from 20% to 15%, resulting in 9.5 million fewer uninsured adults.4 The biggest drop occurred among young adults, with the uninsured rate falling from 28% to 18%, and in states that adopted the Medicaid expansion, where uninsured rates fell from 28% to 17%.4
States that didn’t expand their Medicaid program didn’t show any noticeable change, with the uninsured rate declining only two points, from 38% to 36%.4
Coverage resulted in access to care for the majority of the newly covered. Sixty percent of people with new coverage visited a provider or hospital or paid for a prescription. Sixty-two percent of these individuals said they wouldn’t have been able to access this care before getting this coverage. Eighty-one percent of people with new coverage said they were better off now than before.4
ACA works better in some states than others
The Kaiser Family Foundation looked at four successful states—Colorado, Connecticut, Kentucky, and Washington state—to see what lessons can be learned. Important commonalities include the fact that the states run their own marketplace, adopted the Medi-caid expansion, and conducted extensive outreach and public education, including engaging providers in patient outreach and enrollment.5
Other tools of success were developing good marketing and branding, providing consumer-friendly assistance, and attention to systems and operations.5
How the Hobby Lobby decision affects individual states
Because the Supreme Court’s decision concerned interpretation of a federal law—the Religious Freedom Restoration Act (RFRA)—it does not supersede state laws that mandate coverage of contraceptives.
Twenty-eight states have laws or rulings requiring insurers to cover contraceptives, most of them dating from the 1990s and providing some exemption for religious insurers or plans. Only Illinois allows an exemption for secular bodies.
Although these state laws remain in effect, state officials may opt to stop enforcing them with regard to certain companies. For example, after the Hobby Lobby decision, Wisconsin officials announced that they no longer will enforce contraceptive coverage when a company has a religious objection.
For companies that self-fund or self-insure worker health coverage, the state coverage laws don’t apply—only federal law does. These companies do not have to adhere to state insurance mandates.
Some states have their own version of the RFRA. See the chart at right for details on a state-by-state basis.
The Supreme Court ruling also has no effect on state laws that guarantee access to emergency contraception in hospital emergency departments and that require pharmacists to dispense contraceptives.
| State | Contraceptive equity law? | Employer/insurer exemption to equity law? | Religious freedom law? |
| Alabama | ✔ | ||
| Alaska | |||
| Arizona | ✔ | ✔ | ✔ |
| Arkansas | ✔ | ✔ | |
| California | ✔ | ✔ | |
| Colorado | ✔ | ||
| Connecticut | ✔ | ✔ | ✔ |
| Delaware | ✔ | ✔ | |
| Florida | ✔ | ||
| Georgia | ✔ | ||
| Hawaii | ✔ | ✔ | |
| Idaho | ✔ | ||
| Illinois | ✔ | ✔ | ✔ |
| Indiana | |||
| Iowa | ✔ | ||
| Kansas | |||
| Kentucky | ✔ | ||
| Louisiana | ✔ | ||
| Maine | ✔ | ✔ | |
| Maryland | ✔ | ✔ | |
| Massachusetts | ✔ | ✔ | |
| Michigan | ✔ | ✔ | |
| Minnesota | |||
| Mississippi | ✔ | ||
| Missouri | ✔ | ✔ | ✔ |
| Montana | ✔ | ||
| Nebraska | |||
| Nevada | ✔ | ✔ | |
| New Hampshire | ✔ | ||
| New Jersey | ✔ | ✔ | |
| New Mexico | ✔ | ✔ | ✔ |
| New York | ✔ | ✔ | |
| North Carolina | ✔ | ✔ | |
| North Dakota | |||
| Ohio | |||
| Oklahoma | ✔ | ||
| Oregon | ✔ | ✔ | |
| Pennsylvania | ✔ | ||
| Rhode Island | ✔ | ✔ | ✔ |
| South Carolina | ✔ | ||
| South Dakota | |||
| Tennessee | ✔ | ||
| Texas | ✔ | ||
| Utah | |||
| Vermont | ✔ | ||
| Virginia | ✔ | ||
| Washington | ✔ | ||
| West Virginia | ✔ | ✔ | |
| Wisconsin | ✔ | ||
| Wyoming | |||
| TOTAL | 28 | 20 | 18 |
Narrow networks limit access to care
Huge concerns abound regarding implementation and real-life experiences related to the ACA. A number of them—high deductibles, low payment rates, limited access to physicians, long drive and wait times—can be related to “narrow networks.” Insurers exclude certain providers and offer all providers lower payment rates (which leads some physicians to drop out of the plan); they also create tiers (charging consumers lower copays and deductibles for using inner-tier preferred providers and high out-of-pocket costs for using other providers, even though they may be in the network).
Narrow networks work for insurers as an effective tool for lowering provider payment rates to keep premiums low and gain market share. The narrower the network, the lower are physician payments and premiums.
The ACA promises expanded access to high-quality, affordable health care for millions of Americans—a promise being compromised in many areas of the country through narrow networks. In these instances, insurers offering new plans in a health-care marketplace limit patient access to the numbers, types, and locations of physicians and hospitals covered under certain plans. Insurers typically offer patients low premiums, offer selected providers a high volume of patients at low payment levels, and exclude other providers whom the insurer deems to be high-cost.
Narrow networks aren’t new
As with so many elements of the ACA, narrow networks aren’t a new phenomenon. Many of us remember the public relations price that HMOs paid in the 1980s and 1990s for exceedingly limiting patients’ access to care while charging low premiums. The consumer outcry led the National Association of Insurance Commissioners to urge states to require managed-care plans to maintain adequate networks, the approach adopted by the federal government in the ACA.6
The pendulum swung in the next decade to broader networks in which consumers had much greater access, but premiums increased by an average of 11% per year.6 Employers then pushed insurers to reduce premium costs, leading back to narrow networks in the years just before the ACA. Narrow network plans accounted for 23% of all employer-sponsored plans in 2012, up from 15% in 2007.6
Increasing consolidation contributes to narrow networks
The trend toward narrower networks is also linked to increasing consolidation in health care. As health systems grow and individual or small group practices disappear, insurers rely on being able to credibly threaten to exclude systems and big groups from their networks as leverage in payment negotiations. By restricting the choice of providers in a plan, the insurer can promise more customers for the doctors and hospitals that are included, and negotiate lower payments to those providers.
The downside for physicians is clear:
- low payment rates
- exclusion from networks and coverage
- inability to refer patients to providers the physician determines to be best for that patient’s needs.
- The downside for patients:
- If they have to go out of network to get needed care, they may end up paying high out-of-pocket costs
- If they delay or forego care, their health may suffer significantly.
The insurance industry’s position is that patients have choices. Plans with access to more hospitals and specialists are available but usually at a higher price.
Narrow networks are one way to achieve low premiums
In the months leading up to ACA enactment, insurers got to work developing plans designed to be sold on the exchanges that would attract consumers through low-cost premiums and still maximize profits, especially now that insurers, under the ACA, are barred from excluding sick enrollees or increasing premiums for women, in addition to other important protections.
In previous articles, we’ve explored these landmark protections. Insurers in the individual market used to be able to keep premiums relatively low, and profits up, through use of preexisting coverage exclusions, benefit exclusions including noncoverage for maternity care or prescription drugs, and high cost sharing. Not anymore.
Since enactment of the ACA, narrow networks seem to be the preferred, and most effective, payment negotiation tool of many insurers offering plans through the exchanges, reflecting the trend we’re already seeing in the private health insurance marketplace.
NPR spotlights the difficulty of finding a specialist
The consumer and provider problems of narrow networks have been gaining attention in the media. In July, the National Public Radio (NPR) Web site carried an article entitled, “Patients with low-cost insurance struggle to find specialists,” with a key subtitle: “So you found an exchange plan. But can you find a provider?”7
In the NPR article, author Carrie Feibel reported on the situation in a majority-immigrant area of southwest Houston.
There, many patients at the local clinic have health insurance coverage for the first time, an important step toward healthier lives for themselves and their families. But many people in need of a specialist are learning that their insurance card doesn’t guarantee them access to a needed surgeon or hospital. They’ve purchased a narrow-network insurance plan, with a low premium but few specialists who accept that insurance.7
The two largest hospital chains in Houston—Houston Methodist and Memorial Hermann—as well as Houston’s MD Anderson Cancer Center, don’t participate in the Blue Cross Blue Shield HMO Silver plan, a plan popular with low-income consumers because of its low premium.7
Will the government take action?
The ACA actually guards against overly narrow networks and established the first national standard for network adequacy—a standard that needs fuller development, for sure. Plans sold on the exchanges are required to establish networks that include, among other providers, essential community providers, who typically care for mostly low-income and medically underserved populations. Networks also must include sufficient numbers and types of providers, including “providers that specialize in mental health and substance abuse services, to assure that all services will be accessible without unreasonable delay.”8
Insurers also must provide people who are considering purchasing their products with an accurate directory—both online and a hard copy—identifying providers not accepting new patients in the network. And plans are prohibited from charging out-of-network cost-sharing for emergency services.
Much of the oversight and many of the details—how much is adequate? what is unreasonable?—are left to the states, many of which have years of experience grappling with the downsides and delicate balance of networks.
The Urban Institute points out that Vermont and Delaware set standards for maximum geographic distance and drive times for primary care services. In California, plans must make it easy for consumers to reach urban providers on public transportation.6
Professional societies are taking note
Today, the misuse of narrow networks by exchange plans also has gotten the attention of the American Medical Association, ACOG, and many other national medical specialty societies, in addition to the states and federal government.
The trick, many health-care policy experts agree, is to find the right balance. How broad can the network be before premiums soar? Most agree that consumers must be able to choose between plans with confidence, without any cost or access surprises, meaning much better transparency. And many agree that provider quality, in addition to cost, has to find its way into the equation.
This year, the Center for Consumer Information and Insurance Oversight, a part of the federal Department of Health and Human Services created by the ACA to investigate these kinds of issues, is investigating access to hospital systems, mental health services, oncology, and primary care providers and is developing time, distance, and other standards that insurers will have to adhere to.
Employer groups oppose strong standards or limits on narrow networks. Recently, representatives of the US Chamber of Commerce, the National Retail Federation, and others warned Congress to stay out of this fight. They understand that more generous networks mean higher premiums. These employer representative groups prefer to strengthen consumer protections like directories and keep low the cost of health insurance that they provide for their employees.
Acknowledgment
The author acknowledges the work and expertise of ACOG's state government affairs team for the state analysis—Kathryn Moore, Director, and Kate Vlach, Senior Manager—as well as advocacy partners.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Internal Revenue Service. SOI Tax States, Table 1, Returns of Active Corporations, Form 1120S. http://www.irs.gov/uac/SOI-Tax-Stats-Table-1-Returns-of-Active-Corporations,-Form-1120S. Updated June 27, 2014. Accessed September 4, 2014.
2. DeSilver D. What is a ‘closely held corporation,’ anyway, and how many are there? Pew Research Center: Fact Tank. http://www.pewresearch.org/fact-tank/2014/07/07/what-is-a-closely-held-corporation-anyway-and-how-many-are-there/. Published July 7, 2014. Accessed September 4, 2014.
3. Murray P. Protect Women’s Health From Corporate Interference Act: Summary. http://www.murray.senate.gov/public/_cache/files/30554052-0f84-485a-babc-ccc04af85bb6/protect-women-s-health-from-corporate-interference-act---one-page-summary---final.pdf. Accessed September 4, 2014.
4. The Commonwealth Fund. New Survey: After First ACA Enrollment Period, Uninsured Rate Dropped from 20% to 15%; Largest Declines Among Young Adults, Latinos, and Low-Income People. http://www.commonwealthfund.org/publications/press-releases/2014/jul/after-first-aca -enrollment-period. Published July 10,2014. Accessed September 4, 2014.
5. Artiga S, Stephens J, Rudowitz R, Perry M. What Worked and What’s Next? Strategies in Four States Leading ACA Enrollment Efforts. Kaiser Family Foundation. http://kff.org/health-reform/issue-brief/what-worked-and-whats-next-strategies-in-four-states-leading-aca-enrollment-efforts/. Published July 16, 2014. Accessed September 4, 2014.
6. Corlette S, Volk J. Narrow Provider Networks in New Health Plans: Balancing Affordability with Access to Quality Care. Urban Institute: Georgetown University Center on Health Insurance Reforms. http://www.urban.org/UploadedPDF/413135-New-Provider-Networks-in-New-Health-Plans.pdf. Published May 2014. Accessed September 4, 2014.
7. Feibel C. Patients With Low-Cost Insurance Struggle to Find Specialists. National Public Radio. http://www.npr.org/blogs/health/2014/07/16/331419293/patients-with-low-cost-insurance-struggle-to-find-specialists. Published July 16, 2014. Accessed September 4, 2014.
8. Patient Protection and Affordable Care Act: Preexisting Condition Exclusions, Lifetime and Annual Limits, Rescissions, and Patient Protections. US Department of Health and Human Services. http://www.regulations.go/#!documentDetail;D=HHS-OS-2010-0014-0001. Published June 28, 2010. Accessed September 9, 2014.
1. Internal Revenue Service. SOI Tax States, Table 1, Returns of Active Corporations, Form 1120S. http://www.irs.gov/uac/SOI-Tax-Stats-Table-1-Returns-of-Active-Corporations,-Form-1120S. Updated June 27, 2014. Accessed September 4, 2014.
2. DeSilver D. What is a ‘closely held corporation,’ anyway, and how many are there? Pew Research Center: Fact Tank. http://www.pewresearch.org/fact-tank/2014/07/07/what-is-a-closely-held-corporation-anyway-and-how-many-are-there/. Published July 7, 2014. Accessed September 4, 2014.
3. Murray P. Protect Women’s Health From Corporate Interference Act: Summary. http://www.murray.senate.gov/public/_cache/files/30554052-0f84-485a-babc-ccc04af85bb6/protect-women-s-health-from-corporate-interference-act---one-page-summary---final.pdf. Accessed September 4, 2014.
4. The Commonwealth Fund. New Survey: After First ACA Enrollment Period, Uninsured Rate Dropped from 20% to 15%; Largest Declines Among Young Adults, Latinos, and Low-Income People. http://www.commonwealthfund.org/publications/press-releases/2014/jul/after-first-aca -enrollment-period. Published July 10,2014. Accessed September 4, 2014.
5. Artiga S, Stephens J, Rudowitz R, Perry M. What Worked and What’s Next? Strategies in Four States Leading ACA Enrollment Efforts. Kaiser Family Foundation. http://kff.org/health-reform/issue-brief/what-worked-and-whats-next-strategies-in-four-states-leading-aca-enrollment-efforts/. Published July 16, 2014. Accessed September 4, 2014.
6. Corlette S, Volk J. Narrow Provider Networks in New Health Plans: Balancing Affordability with Access to Quality Care. Urban Institute: Georgetown University Center on Health Insurance Reforms. http://www.urban.org/UploadedPDF/413135-New-Provider-Networks-in-New-Health-Plans.pdf. Published May 2014. Accessed September 4, 2014.
7. Feibel C. Patients With Low-Cost Insurance Struggle to Find Specialists. National Public Radio. http://www.npr.org/blogs/health/2014/07/16/331419293/patients-with-low-cost-insurance-struggle-to-find-specialists. Published July 16, 2014. Accessed September 4, 2014.
8. Patient Protection and Affordable Care Act: Preexisting Condition Exclusions, Lifetime and Annual Limits, Rescissions, and Patient Protections. US Department of Health and Human Services. http://www.regulations.go/#!documentDetail;D=HHS-OS-2010-0014-0001. Published June 28, 2010. Accessed September 9, 2014.
Inside the article:
Are contraceptives abortifacients?
How the Hobby Lobby decision affects individual states
Narrow networks limit access to care
License to slip up?
The Food and Drug Administration recently approved another weight-loss drug (Contrave), a combination of naltrexone (indicated for opioid dependence) and bupropion (indicated for depression). This is the third weight-loss drug approved in the past 2 years. The FDA previously approved lorcaserin (Belviq) and topiramate/phentermine (Qsymia). This approval activity signals pharmaceutical interest in a multibillion dollar weight loss industry and perhaps, maybe less so, the FDA’s recognition of our public health crisis.
For patients who meet criteria for the use of these medications, they should be offered if they can be afforded. However, these medications may make patients behave differently.
It’s called “license.”
License is the psychological phenomenon in which people who feel they have made progress toward a goal feel liberated to make an incongruent choice. Think of a patient interested in losing weight who now takes a weight-loss pill. Despite not having lost any weight yet and perhaps just after taking the first pill, the patient then makes a choice to consume a high-calorie dessert.
Here are some data that support that this could be happening.
One team of investigators randomized subjects to being informed they were taking a placebo or a weight-loss supplement (which was actually the same placebo tablet as in the other study arm). After receiving the supplement, participants were allowed access to a reward buffet lunch at which their food consumption was recorded. Compared with controls, participants receiving a purported weight-loss supplement ate more food at the reward buffet. This effect seemed to occur through a perceived sense that they were making progress toward their weight-loss goal by taking the pill (Nutrition 2014;30:1007-14).
This is critical for us to think about and incorporate into our clinical teaching when prescribing these medications. Psychological liberation threatens any health gains we can make at a population level with any weight-loss approach. We need to help our patients understand that these medications should be used in combination with sustainable lifestyle changes or they may as well be taking a placebo.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician.
The Food and Drug Administration recently approved another weight-loss drug (Contrave), a combination of naltrexone (indicated for opioid dependence) and bupropion (indicated for depression). This is the third weight-loss drug approved in the past 2 years. The FDA previously approved lorcaserin (Belviq) and topiramate/phentermine (Qsymia). This approval activity signals pharmaceutical interest in a multibillion dollar weight loss industry and perhaps, maybe less so, the FDA’s recognition of our public health crisis.
For patients who meet criteria for the use of these medications, they should be offered if they can be afforded. However, these medications may make patients behave differently.
It’s called “license.”
License is the psychological phenomenon in which people who feel they have made progress toward a goal feel liberated to make an incongruent choice. Think of a patient interested in losing weight who now takes a weight-loss pill. Despite not having lost any weight yet and perhaps just after taking the first pill, the patient then makes a choice to consume a high-calorie dessert.
Here are some data that support that this could be happening.
One team of investigators randomized subjects to being informed they were taking a placebo or a weight-loss supplement (which was actually the same placebo tablet as in the other study arm). After receiving the supplement, participants were allowed access to a reward buffet lunch at which their food consumption was recorded. Compared with controls, participants receiving a purported weight-loss supplement ate more food at the reward buffet. This effect seemed to occur through a perceived sense that they were making progress toward their weight-loss goal by taking the pill (Nutrition 2014;30:1007-14).
This is critical for us to think about and incorporate into our clinical teaching when prescribing these medications. Psychological liberation threatens any health gains we can make at a population level with any weight-loss approach. We need to help our patients understand that these medications should be used in combination with sustainable lifestyle changes or they may as well be taking a placebo.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician.
The Food and Drug Administration recently approved another weight-loss drug (Contrave), a combination of naltrexone (indicated for opioid dependence) and bupropion (indicated for depression). This is the third weight-loss drug approved in the past 2 years. The FDA previously approved lorcaserin (Belviq) and topiramate/phentermine (Qsymia). This approval activity signals pharmaceutical interest in a multibillion dollar weight loss industry and perhaps, maybe less so, the FDA’s recognition of our public health crisis.
For patients who meet criteria for the use of these medications, they should be offered if they can be afforded. However, these medications may make patients behave differently.
It’s called “license.”
License is the psychological phenomenon in which people who feel they have made progress toward a goal feel liberated to make an incongruent choice. Think of a patient interested in losing weight who now takes a weight-loss pill. Despite not having lost any weight yet and perhaps just after taking the first pill, the patient then makes a choice to consume a high-calorie dessert.
Here are some data that support that this could be happening.
One team of investigators randomized subjects to being informed they were taking a placebo or a weight-loss supplement (which was actually the same placebo tablet as in the other study arm). After receiving the supplement, participants were allowed access to a reward buffet lunch at which their food consumption was recorded. Compared with controls, participants receiving a purported weight-loss supplement ate more food at the reward buffet. This effect seemed to occur through a perceived sense that they were making progress toward their weight-loss goal by taking the pill (Nutrition 2014;30:1007-14).
This is critical for us to think about and incorporate into our clinical teaching when prescribing these medications. Psychological liberation threatens any health gains we can make at a population level with any weight-loss approach. We need to help our patients understand that these medications should be used in combination with sustainable lifestyle changes or they may as well be taking a placebo.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician.
Managing Your Practice: What is your practice worth?
At least once during your career, you probably will have to put a value on your practice. The need arises more often than you might think – if you sell it, of course (more on that next month); but also for estate planning, preparation of financial statements, or divorce negotiations; or when an associate joins or leaves your office; or if you have occasion to combine or partner your practice with one or more others, as I will discuss in detail in a future issue.
As you might guess, a medical practice is trickier to value than an ordinary business, and usually requires the services of an experienced professional appraiser. Entire books have been written about the process, so I can’t hope to cover it completely in a few hundred words, but three basic yardsticks are essential for a practice appraisal:
Tangible assets: equipment, cash, accounts receivable, and other property owned by the practice.
Liabilities: accounts payable, outstanding loans, and anything else owed to others.
Intangible assets: sometimes called “good will” – the reputation of the physicians, the location and name recognition of the practice, the loyalty and volume of patients, and other, well, intangibles.
Armed with those numbers, an appraiser can then determine the “equity,” or book value, of the practice.
Valuing tangible assets is comparatively straightforward, but there are several ways to do it, and when reviewing a practice appraisal you should ask which of them was used. Depreciated value is the book value of equipment and supplies as determined by their purchase price, less the amount their value has decreased since purchase. Remaining useful life value estimates how long the equipment can be expected to last. Market (or replacement) value is the amount it would cost on the open market to replace all equipment and supplies.
Intangible assets are more difficult to value. Many components are analyzed, including location, interior and exterior decor, accessibility to patients, age and functional status of equipment, systems in place to promote efficiency, reasons patients come back (if they do), and the overall reputation of the practice in the community. Other important factors include the “payer mix” (what percentage pays cash, how many third-party contracts are in place and how well they pay, etc.), the extent and strength of the referral base, and the presence of clinical studies or other supplemental income streams.
It is also important to determine to what extent intangible assets are transferrable. For example, unique skills with a laser, neurotoxins, or filler substances (or extraordinary personal charisma) may increase your practice’s value to you, but they are worthless to the next owner, and he or she will be unwilling to pay for them unless your services become part of the deal.
Once again, there are many ways to estimate intangible asset value, and once again you should ask which were used. Cash flow analysis works on the assumption that cash flow is a measure of intangible value. Capitalization of earnings puts a value, or capitalization, on the practice’s income streams using a variety of assumptions. Guideline comparison uses various databases to compare your practice with other, similar ones that have changed hands in the past.
Two newer techniques, which some consider to provide a better estimate of intangible assets, are the replacement method, which estimates the costs of starting the practice over again in the current market; and the excess earnings method, which measures how far above average your practice’s earnings are (and thus its overall value).
Asset-based valuation is the most popular, but by no means the only, method available. Income-based valuation looks at the source and strength of a practice’s income stream as a creator of value, as well as whether or not the income stream under a different owner would mirror its present one. This in turn becomes the basis for an understanding of the fair market value of both tangible and intangible assets. Market valuation combines the asset-based and income-based approaches, along with an analysis of sales and mergers of comparable practices in the community, to determine the value of a practice in its local market.
Whatever methods are used, it is important that the appraisal be done by an experienced financial consultant, that all techniques used in the valuation be divulged and explained, and that documentation is supplied to support the conclusions reached. This is especially important if the appraisal will be relied upon in the sale or merger of the practice. I’ll talk about sales and mergers over the next several columns.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Skin & Allergy News.
At least once during your career, you probably will have to put a value on your practice. The need arises more often than you might think – if you sell it, of course (more on that next month); but also for estate planning, preparation of financial statements, or divorce negotiations; or when an associate joins or leaves your office; or if you have occasion to combine or partner your practice with one or more others, as I will discuss in detail in a future issue.
As you might guess, a medical practice is trickier to value than an ordinary business, and usually requires the services of an experienced professional appraiser. Entire books have been written about the process, so I can’t hope to cover it completely in a few hundred words, but three basic yardsticks are essential for a practice appraisal:
Tangible assets: equipment, cash, accounts receivable, and other property owned by the practice.
Liabilities: accounts payable, outstanding loans, and anything else owed to others.
Intangible assets: sometimes called “good will” – the reputation of the physicians, the location and name recognition of the practice, the loyalty and volume of patients, and other, well, intangibles.
Armed with those numbers, an appraiser can then determine the “equity,” or book value, of the practice.
Valuing tangible assets is comparatively straightforward, but there are several ways to do it, and when reviewing a practice appraisal you should ask which of them was used. Depreciated value is the book value of equipment and supplies as determined by their purchase price, less the amount their value has decreased since purchase. Remaining useful life value estimates how long the equipment can be expected to last. Market (or replacement) value is the amount it would cost on the open market to replace all equipment and supplies.
Intangible assets are more difficult to value. Many components are analyzed, including location, interior and exterior decor, accessibility to patients, age and functional status of equipment, systems in place to promote efficiency, reasons patients come back (if they do), and the overall reputation of the practice in the community. Other important factors include the “payer mix” (what percentage pays cash, how many third-party contracts are in place and how well they pay, etc.), the extent and strength of the referral base, and the presence of clinical studies or other supplemental income streams.
It is also important to determine to what extent intangible assets are transferrable. For example, unique skills with a laser, neurotoxins, or filler substances (or extraordinary personal charisma) may increase your practice’s value to you, but they are worthless to the next owner, and he or she will be unwilling to pay for them unless your services become part of the deal.
Once again, there are many ways to estimate intangible asset value, and once again you should ask which were used. Cash flow analysis works on the assumption that cash flow is a measure of intangible value. Capitalization of earnings puts a value, or capitalization, on the practice’s income streams using a variety of assumptions. Guideline comparison uses various databases to compare your practice with other, similar ones that have changed hands in the past.
Two newer techniques, which some consider to provide a better estimate of intangible assets, are the replacement method, which estimates the costs of starting the practice over again in the current market; and the excess earnings method, which measures how far above average your practice’s earnings are (and thus its overall value).
Asset-based valuation is the most popular, but by no means the only, method available. Income-based valuation looks at the source and strength of a practice’s income stream as a creator of value, as well as whether or not the income stream under a different owner would mirror its present one. This in turn becomes the basis for an understanding of the fair market value of both tangible and intangible assets. Market valuation combines the asset-based and income-based approaches, along with an analysis of sales and mergers of comparable practices in the community, to determine the value of a practice in its local market.
Whatever methods are used, it is important that the appraisal be done by an experienced financial consultant, that all techniques used in the valuation be divulged and explained, and that documentation is supplied to support the conclusions reached. This is especially important if the appraisal will be relied upon in the sale or merger of the practice. I’ll talk about sales and mergers over the next several columns.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Skin & Allergy News.
At least once during your career, you probably will have to put a value on your practice. The need arises more often than you might think – if you sell it, of course (more on that next month); but also for estate planning, preparation of financial statements, or divorce negotiations; or when an associate joins or leaves your office; or if you have occasion to combine or partner your practice with one or more others, as I will discuss in detail in a future issue.
As you might guess, a medical practice is trickier to value than an ordinary business, and usually requires the services of an experienced professional appraiser. Entire books have been written about the process, so I can’t hope to cover it completely in a few hundred words, but three basic yardsticks are essential for a practice appraisal:
Tangible assets: equipment, cash, accounts receivable, and other property owned by the practice.
Liabilities: accounts payable, outstanding loans, and anything else owed to others.
Intangible assets: sometimes called “good will” – the reputation of the physicians, the location and name recognition of the practice, the loyalty and volume of patients, and other, well, intangibles.
Armed with those numbers, an appraiser can then determine the “equity,” or book value, of the practice.
Valuing tangible assets is comparatively straightforward, but there are several ways to do it, and when reviewing a practice appraisal you should ask which of them was used. Depreciated value is the book value of equipment and supplies as determined by their purchase price, less the amount their value has decreased since purchase. Remaining useful life value estimates how long the equipment can be expected to last. Market (or replacement) value is the amount it would cost on the open market to replace all equipment and supplies.
Intangible assets are more difficult to value. Many components are analyzed, including location, interior and exterior decor, accessibility to patients, age and functional status of equipment, systems in place to promote efficiency, reasons patients come back (if they do), and the overall reputation of the practice in the community. Other important factors include the “payer mix” (what percentage pays cash, how many third-party contracts are in place and how well they pay, etc.), the extent and strength of the referral base, and the presence of clinical studies or other supplemental income streams.
It is also important to determine to what extent intangible assets are transferrable. For example, unique skills with a laser, neurotoxins, or filler substances (or extraordinary personal charisma) may increase your practice’s value to you, but they are worthless to the next owner, and he or she will be unwilling to pay for them unless your services become part of the deal.
Once again, there are many ways to estimate intangible asset value, and once again you should ask which were used. Cash flow analysis works on the assumption that cash flow is a measure of intangible value. Capitalization of earnings puts a value, or capitalization, on the practice’s income streams using a variety of assumptions. Guideline comparison uses various databases to compare your practice with other, similar ones that have changed hands in the past.
Two newer techniques, which some consider to provide a better estimate of intangible assets, are the replacement method, which estimates the costs of starting the practice over again in the current market; and the excess earnings method, which measures how far above average your practice’s earnings are (and thus its overall value).
Asset-based valuation is the most popular, but by no means the only, method available. Income-based valuation looks at the source and strength of a practice’s income stream as a creator of value, as well as whether or not the income stream under a different owner would mirror its present one. This in turn becomes the basis for an understanding of the fair market value of both tangible and intangible assets. Market valuation combines the asset-based and income-based approaches, along with an analysis of sales and mergers of comparable practices in the community, to determine the value of a practice in its local market.
Whatever methods are used, it is important that the appraisal be done by an experienced financial consultant, that all techniques used in the valuation be divulged and explained, and that documentation is supplied to support the conclusions reached. This is especially important if the appraisal will be relied upon in the sale or merger of the practice. I’ll talk about sales and mergers over the next several columns.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Skin & Allergy News.
Negotiation Skills for Physicians
Summary
Physicians suffer from “arrested development,” said Dr. Chiang, a hospitalist and chief of inpatient services at Boston Children’s Hospital, during a PHM2014 workshop on the basics of negotiation. Dr. Chiang was referring to the fact that in several professional realms, including negotiation, most physicians have not had the traditional experience of interviewing and negotiating for jobs after high school or college.
An understanding of several negotiation concepts can help the negotiator achieve an agreeable solution. Awareness of values and limits prior to the actual discussion or negotiation will increase the chance of a successful negotiation. Examples of some of these concepts are:
- Best alternative to a negotiation agreement (BATNA). This is the course of action if negotiations fail. The negotiator should not accept a worse resolution than the BATNA.
- Reservation value (RV). This is the lowest value a negotiator will accept in a deal.
- Zone of possible agreement (ZOPA). This is the intellectual zone between two parties in a negotiation where an agreement can be reached.
The twin tasks of negotiation are a) learning about the true ZOPA in advance and b) determining how to influence the other person’s perception of this zone.
There are several negotiation methods and strategies of influence that can be used to support your position or goals. For example, status quo bias is very common. Addressing the specific reason a person is not willing to change from the status quo enables progress.
While it is important to advocate for one’s position, fairness is an important variable in reaching an agreement. Fairness often is not universally defined. Communication is essential in understanding each group’s position.
Summary
Physicians suffer from “arrested development,” said Dr. Chiang, a hospitalist and chief of inpatient services at Boston Children’s Hospital, during a PHM2014 workshop on the basics of negotiation. Dr. Chiang was referring to the fact that in several professional realms, including negotiation, most physicians have not had the traditional experience of interviewing and negotiating for jobs after high school or college.
An understanding of several negotiation concepts can help the negotiator achieve an agreeable solution. Awareness of values and limits prior to the actual discussion or negotiation will increase the chance of a successful negotiation. Examples of some of these concepts are:
- Best alternative to a negotiation agreement (BATNA). This is the course of action if negotiations fail. The negotiator should not accept a worse resolution than the BATNA.
- Reservation value (RV). This is the lowest value a negotiator will accept in a deal.
- Zone of possible agreement (ZOPA). This is the intellectual zone between two parties in a negotiation where an agreement can be reached.
The twin tasks of negotiation are a) learning about the true ZOPA in advance and b) determining how to influence the other person’s perception of this zone.
There are several negotiation methods and strategies of influence that can be used to support your position or goals. For example, status quo bias is very common. Addressing the specific reason a person is not willing to change from the status quo enables progress.
While it is important to advocate for one’s position, fairness is an important variable in reaching an agreement. Fairness often is not universally defined. Communication is essential in understanding each group’s position.
Summary
Physicians suffer from “arrested development,” said Dr. Chiang, a hospitalist and chief of inpatient services at Boston Children’s Hospital, during a PHM2014 workshop on the basics of negotiation. Dr. Chiang was referring to the fact that in several professional realms, including negotiation, most physicians have not had the traditional experience of interviewing and negotiating for jobs after high school or college.
An understanding of several negotiation concepts can help the negotiator achieve an agreeable solution. Awareness of values and limits prior to the actual discussion or negotiation will increase the chance of a successful negotiation. Examples of some of these concepts are:
- Best alternative to a negotiation agreement (BATNA). This is the course of action if negotiations fail. The negotiator should not accept a worse resolution than the BATNA.
- Reservation value (RV). This is the lowest value a negotiator will accept in a deal.
- Zone of possible agreement (ZOPA). This is the intellectual zone between two parties in a negotiation where an agreement can be reached.
The twin tasks of negotiation are a) learning about the true ZOPA in advance and b) determining how to influence the other person’s perception of this zone.
There are several negotiation methods and strategies of influence that can be used to support your position or goals. For example, status quo bias is very common. Addressing the specific reason a person is not willing to change from the status quo enables progress.
While it is important to advocate for one’s position, fairness is an important variable in reaching an agreement. Fairness often is not universally defined. Communication is essential in understanding each group’s position.
Put Key Principles, Characteristics of Effective Hospital Medicine Groups to Work
I hope you’re already familiar with “The Key Principles and Characteristics of an Effective Hospital Medicine Group: An Assessment Guide for Hospitals and Hospitalists” [www.hospitalmedicine.org/keychar] and have spent at least a few minutes reviewing the list of 10 “principles” and 47 “characteristics” thought to be associated with effective hospital medicine groups (HMGs). (Full disclosure: I was one of the authors of the article published in February 2014 in the Journal of Hospital Medicine.) Most of us are very busy, so the temptation might be high to set the article aside and risk forgetting it. But I hope many in our field, both clinicians and administrators, will look at it more carefully. There are a number of ways you could use the guide to stimulate thinking or change in your practice.
Grading Our Specialty
I just returned from a meeting of about 10 hospitalist leaders from different organizations around the country. Attendees represented the diversity of our field, including hospital-employed HMGs, large hospitalist management companies, and academic programs. We spent a portion of the meeting discussing what grade we as a group would give the whole specialty of hospital medicine on each of the 10 “principles.” Essentially, we generated a report card for the U.S. hospitalist movement.
This wasn’t a rigorous scientific exercise; instead, it was a robust and thought-provoking discussion around what grade to assign. Opinions regarding the appropriate grade varied significantly, but a common theme was that our specialty really “owns” the importance of pursuing many or most of the principles listed in the article and is devoting time and resources to them even if many individual HMGs might have a long way to go to perform optimally.
For example, meeting attendees thought our field has for a long time worked diligently to “support care coordination across the care continuum” (Principle 6). No one thought that all HMGs do this optimally, but the consensus was that most HMGs have invested effort to do it well. And most were concerned that many HMGs still lack “adequate resources” (Principle 3) and sufficiently “engaged hospitalists” (Principle 2)—and that the former contributes to the latter.
The opinion of the hospitalist leaders who happened to attend the meeting where this conversation took place doesn’t represent the final word on how our specialty is performing, but I think all involved found value in having the conversation, hearing different perspectives about what we’re doing well and where we should focus energy and resources to improve.
Grading Your HM Group
You might want to do something similar within your own group, but make it more relevant by grading how your own practice performs on each of the 10 principles. You could do this on your own just to stimulate your thinking, or you could have each member of your HMG generate a report card of your group’s performance—then discuss where there is agreement or disagreement within the group.
You could structure this sort of individual or group assessment simply as an exercise to generate ideas and conversation about the practice, or your group could take a more formal approach and use it as part of a planning process to determine future practice management-related goals. I know of some groups that scheduled strategic planning meetings specifically to discuss which of the elements to make a priority.
Discussion Document for Leadership
In addition to using the article to generate conversation among hospitalists within your group, it can be a really valuable tool in guiding conversations with hospital leaders and the entity that employs the hospitalists. For example, you could use the article to generate or update the job description of the lead hospitalist or practice manager. Or during annual budgeting for the hospitalist practice, the guide could be used as a checklist to think about whether there are important areas that would benefit from more resources.
Of course, there is a risk that hospital leaders or those who employ the hospitalists could use the article primarily to criticize a hospitalist group and its leader for not already having excellent performance on every one of the principles and characteristics listed. That would be pretty unfortunate; there probably isn’t a single group that performs well on every domain, and the real value of the article is to “be aspirational, helping to raise the bar” for each HMG and our specialty as a whole.
And, as discussed in the article, an HMG doesn’t need to be a stellar performer on all 47 characteristics to be effective. Some of the characteristics listed in the article may not apply to all groups, so all involved in the management of any individual HMG should think about whether to set some aside when assessing their own group.
Where to Go from Here
The article is based on expert opinion, with the help of many more people than those listed as author, and I’m hopeful it will stimulate researchers to study some of these principles and characteristics. For many reasons, we will probably never have robust data, but I’d be happy for whatever we can get.
There is a pretty good chance that the evolution in the work we do and the nature of the hospital setting mean that the principles and characteristics may need to be revised periodically. I would love to know how they might be different in 10 or 20 years.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
I hope you’re already familiar with “The Key Principles and Characteristics of an Effective Hospital Medicine Group: An Assessment Guide for Hospitals and Hospitalists” [www.hospitalmedicine.org/keychar] and have spent at least a few minutes reviewing the list of 10 “principles” and 47 “characteristics” thought to be associated with effective hospital medicine groups (HMGs). (Full disclosure: I was one of the authors of the article published in February 2014 in the Journal of Hospital Medicine.) Most of us are very busy, so the temptation might be high to set the article aside and risk forgetting it. But I hope many in our field, both clinicians and administrators, will look at it more carefully. There are a number of ways you could use the guide to stimulate thinking or change in your practice.
Grading Our Specialty
I just returned from a meeting of about 10 hospitalist leaders from different organizations around the country. Attendees represented the diversity of our field, including hospital-employed HMGs, large hospitalist management companies, and academic programs. We spent a portion of the meeting discussing what grade we as a group would give the whole specialty of hospital medicine on each of the 10 “principles.” Essentially, we generated a report card for the U.S. hospitalist movement.
This wasn’t a rigorous scientific exercise; instead, it was a robust and thought-provoking discussion around what grade to assign. Opinions regarding the appropriate grade varied significantly, but a common theme was that our specialty really “owns” the importance of pursuing many or most of the principles listed in the article and is devoting time and resources to them even if many individual HMGs might have a long way to go to perform optimally.
For example, meeting attendees thought our field has for a long time worked diligently to “support care coordination across the care continuum” (Principle 6). No one thought that all HMGs do this optimally, but the consensus was that most HMGs have invested effort to do it well. And most were concerned that many HMGs still lack “adequate resources” (Principle 3) and sufficiently “engaged hospitalists” (Principle 2)—and that the former contributes to the latter.
The opinion of the hospitalist leaders who happened to attend the meeting where this conversation took place doesn’t represent the final word on how our specialty is performing, but I think all involved found value in having the conversation, hearing different perspectives about what we’re doing well and where we should focus energy and resources to improve.
Grading Your HM Group
You might want to do something similar within your own group, but make it more relevant by grading how your own practice performs on each of the 10 principles. You could do this on your own just to stimulate your thinking, or you could have each member of your HMG generate a report card of your group’s performance—then discuss where there is agreement or disagreement within the group.
You could structure this sort of individual or group assessment simply as an exercise to generate ideas and conversation about the practice, or your group could take a more formal approach and use it as part of a planning process to determine future practice management-related goals. I know of some groups that scheduled strategic planning meetings specifically to discuss which of the elements to make a priority.
Discussion Document for Leadership
In addition to using the article to generate conversation among hospitalists within your group, it can be a really valuable tool in guiding conversations with hospital leaders and the entity that employs the hospitalists. For example, you could use the article to generate or update the job description of the lead hospitalist or practice manager. Or during annual budgeting for the hospitalist practice, the guide could be used as a checklist to think about whether there are important areas that would benefit from more resources.
Of course, there is a risk that hospital leaders or those who employ the hospitalists could use the article primarily to criticize a hospitalist group and its leader for not already having excellent performance on every one of the principles and characteristics listed. That would be pretty unfortunate; there probably isn’t a single group that performs well on every domain, and the real value of the article is to “be aspirational, helping to raise the bar” for each HMG and our specialty as a whole.
And, as discussed in the article, an HMG doesn’t need to be a stellar performer on all 47 characteristics to be effective. Some of the characteristics listed in the article may not apply to all groups, so all involved in the management of any individual HMG should think about whether to set some aside when assessing their own group.
Where to Go from Here
The article is based on expert opinion, with the help of many more people than those listed as author, and I’m hopeful it will stimulate researchers to study some of these principles and characteristics. For many reasons, we will probably never have robust data, but I’d be happy for whatever we can get.
There is a pretty good chance that the evolution in the work we do and the nature of the hospital setting mean that the principles and characteristics may need to be revised periodically. I would love to know how they might be different in 10 or 20 years.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
I hope you’re already familiar with “The Key Principles and Characteristics of an Effective Hospital Medicine Group: An Assessment Guide for Hospitals and Hospitalists” [www.hospitalmedicine.org/keychar] and have spent at least a few minutes reviewing the list of 10 “principles” and 47 “characteristics” thought to be associated with effective hospital medicine groups (HMGs). (Full disclosure: I was one of the authors of the article published in February 2014 in the Journal of Hospital Medicine.) Most of us are very busy, so the temptation might be high to set the article aside and risk forgetting it. But I hope many in our field, both clinicians and administrators, will look at it more carefully. There are a number of ways you could use the guide to stimulate thinking or change in your practice.
Grading Our Specialty
I just returned from a meeting of about 10 hospitalist leaders from different organizations around the country. Attendees represented the diversity of our field, including hospital-employed HMGs, large hospitalist management companies, and academic programs. We spent a portion of the meeting discussing what grade we as a group would give the whole specialty of hospital medicine on each of the 10 “principles.” Essentially, we generated a report card for the U.S. hospitalist movement.
This wasn’t a rigorous scientific exercise; instead, it was a robust and thought-provoking discussion around what grade to assign. Opinions regarding the appropriate grade varied significantly, but a common theme was that our specialty really “owns” the importance of pursuing many or most of the principles listed in the article and is devoting time and resources to them even if many individual HMGs might have a long way to go to perform optimally.
For example, meeting attendees thought our field has for a long time worked diligently to “support care coordination across the care continuum” (Principle 6). No one thought that all HMGs do this optimally, but the consensus was that most HMGs have invested effort to do it well. And most were concerned that many HMGs still lack “adequate resources” (Principle 3) and sufficiently “engaged hospitalists” (Principle 2)—and that the former contributes to the latter.
The opinion of the hospitalist leaders who happened to attend the meeting where this conversation took place doesn’t represent the final word on how our specialty is performing, but I think all involved found value in having the conversation, hearing different perspectives about what we’re doing well and where we should focus energy and resources to improve.
Grading Your HM Group
You might want to do something similar within your own group, but make it more relevant by grading how your own practice performs on each of the 10 principles. You could do this on your own just to stimulate your thinking, or you could have each member of your HMG generate a report card of your group’s performance—then discuss where there is agreement or disagreement within the group.
You could structure this sort of individual or group assessment simply as an exercise to generate ideas and conversation about the practice, or your group could take a more formal approach and use it as part of a planning process to determine future practice management-related goals. I know of some groups that scheduled strategic planning meetings specifically to discuss which of the elements to make a priority.
Discussion Document for Leadership
In addition to using the article to generate conversation among hospitalists within your group, it can be a really valuable tool in guiding conversations with hospital leaders and the entity that employs the hospitalists. For example, you could use the article to generate or update the job description of the lead hospitalist or practice manager. Or during annual budgeting for the hospitalist practice, the guide could be used as a checklist to think about whether there are important areas that would benefit from more resources.
Of course, there is a risk that hospital leaders or those who employ the hospitalists could use the article primarily to criticize a hospitalist group and its leader for not already having excellent performance on every one of the principles and characteristics listed. That would be pretty unfortunate; there probably isn’t a single group that performs well on every domain, and the real value of the article is to “be aspirational, helping to raise the bar” for each HMG and our specialty as a whole.
And, as discussed in the article, an HMG doesn’t need to be a stellar performer on all 47 characteristics to be effective. Some of the characteristics listed in the article may not apply to all groups, so all involved in the management of any individual HMG should think about whether to set some aside when assessing their own group.
Where to Go from Here
The article is based on expert opinion, with the help of many more people than those listed as author, and I’m hopeful it will stimulate researchers to study some of these principles and characteristics. For many reasons, we will probably never have robust data, but I’d be happy for whatever we can get.
There is a pretty good chance that the evolution in the work we do and the nature of the hospital setting mean that the principles and characteristics may need to be revised periodically. I would love to know how they might be different in 10 or 20 years.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
State of Hospital Medicine Report: Pre-Order Yours Today
Recruiting and retaining hospitalists are major challenges for hospital medicine groups across the country, and the State of Hospital Medicine report can be the roadmap for helping them keep the hospitalists they need.
The State of Hospital Medicine, available in September from SHM, provides a comprehensive data set on compensation and productivity for hospitalists across the country—and across sub-specialties in HM. Using data from the State of Hospital Medicine report, hospitalists everywhere compare their own compensation strategies against those in their region and throughout the U.S.
The latest issue, published by SHM every other year, will be available later this month but can be pre-ordered today. For more information, or to pre-order, visit www.hospitalmedicine.org/sohm.
Recruiting and retaining hospitalists are major challenges for hospital medicine groups across the country, and the State of Hospital Medicine report can be the roadmap for helping them keep the hospitalists they need.
The State of Hospital Medicine, available in September from SHM, provides a comprehensive data set on compensation and productivity for hospitalists across the country—and across sub-specialties in HM. Using data from the State of Hospital Medicine report, hospitalists everywhere compare their own compensation strategies against those in their region and throughout the U.S.
The latest issue, published by SHM every other year, will be available later this month but can be pre-ordered today. For more information, or to pre-order, visit www.hospitalmedicine.org/sohm.
Recruiting and retaining hospitalists are major challenges for hospital medicine groups across the country, and the State of Hospital Medicine report can be the roadmap for helping them keep the hospitalists they need.
The State of Hospital Medicine, available in September from SHM, provides a comprehensive data set on compensation and productivity for hospitalists across the country—and across sub-specialties in HM. Using data from the State of Hospital Medicine report, hospitalists everywhere compare their own compensation strategies against those in their region and throughout the U.S.
The latest issue, published by SHM every other year, will be available later this month but can be pre-ordered today. For more information, or to pre-order, visit www.hospitalmedicine.org/sohm.
Was fetus’ wrist injured during cesarean delivery?
Was fetus’ wrist injured during cesarean delivery?
At 34 weeks’ gestation, a 39-year-old woman went to the hospital in preterm labor. Her history included a prior cesarean delivery. Ultrasonography (US) showed that the fetus was in a double-footling breech position. The ObGyn decided to perform a cesarean delivery when the fetal heart-rate monitor indicated distress.
After making a midline incision through the earlier scar, the ObGyn created a low transverse uterine incision with a scalpel. The mother’s uterus was thick because labor had not progressed. When the ObGyn was unable to deliver the baby through the low transverse incision, she performed a T-extension of the incision using bandage scissors while placing her free hand inside the uterus to shield the fetus from injury. After extensive manipulation, the baby was delivered and immediately handed to a neonatologist. After surgery, the neonatologist told the mother that the baby had sustained two lacerations to the ulnar side of the right wrist. The newborn was airlifted to another hospital for treatment of sepsis. There, an orthopedic hand surgeon examined the child and determined that the lacerations were superficial and only required sutures. The orthopedist saw the infant a month later and believed there was no significant wrist injury.
When the child began preschool, she started to experience cold intolerance and difficulty writing with her right hand. The child was referred to a pediatric neurologist, who found no nerve damage and ordered occupational therapy.
The original orthopedic surgeon examined the child when she was 7 years old and determined that the flexor carpi ulnaris tendon had been completely severed with a partial injury to the ulnar nerve. He recommended a return visit at age 14 for full assessment of the wrist injury.
PARENTS’ CLAIM The ObGyn did not properly shield the fetus when performing the T-extension incision during cesarean delivery. The child’s weakness will increase with age, ruling out some occupations.
PHYSICIAN’S DEFENSE The ObGyn was not negligent; she had provided adequate protection of the fetus during both incisions.
VERDICT An Illinois defense verdict was returned.
Woman dies after tubal ligation
After a 42-year-old woman underwent tubal ligation, her surgeon was concerned about a possible bowel perforation and admitted her to the hospital. The next morning, a computed tomography (CT) scan of the abdomen did not reveal bowel injury.
That afternoon, when the patient reported shortness of breath, the surgeon called the hospitalist with concern for pulmonary embolism (PE). The hospitalist immediately ordered a CT scan of the chest, initiated PE protocol, and wrote “r/o PE” on the chart. A radiologist reminded the hospitalist of the earlier CT scan with concern for kidney damage from another dye study. The hospitalist cancelled the CT scan and PE protocol. After waiting 17 hours to run any further tests, a CT scan revealed massive bilateral PE. The patient was transferred to the ICU, but died the next day.
PATIENT’S CLAIM The 17-hour delay was negligent.
PHYSICIAN’S DEFENSE There was no negligence. The patient died of septic shock, not PE.
VERDICT A $4 million Virginia verdict was returned.
Child born without hand and forearm
During prenatal care, a mother underwent US at 20 and 36 weeks; both studies were reported as normal. The child was born missing his left hand and part of his left forearm due to a congenital amputation. The child will require prosthetics for life.
PATIENT’S CLAIM The condition should have been seen during prenatal US; an abortion was still an option at 20 weeks.
DEFENDANTS’ DEFENSE US was properly performed and evaluated. It can be difficult to differentiate the right from left extremities.
VERDICT A California defense verdict was returned.
After starting Yasmin, woman has stroke with permanent paralysis: $16.5M total award
When a 37-year-old woman reported irregular menstruation, her ObGyn prescribed drospirenone/ethinyl estradiol (Yasmin; Bayer). Thirteen days after starting the drug, the patient had a stroke. She is paralyzed on her left side, has limited ability to speak, cannot use her left arm and leg, and requires 24-hour care.
PATIENT’S CLAIM The ObGyn should have recognized that Yasmin was not appropriate for this patient because of the drug’s clotting risks. The patient’s risk factors included her age (over 35), borderline hypertension, overweight, history of smoking, and high cholesterol. The ObGyn should have offered safer alternatives, such as a progesterone-only pill. The US Food and Drug Administration (FDA) issued a safety warning that all drospirenone-containing drugs may be associated with a higher risk of venous thrombosis during the first 6 months of use.
DEFENDANTS’ DEFENSE According to Bayer, Yasmin is safe, and remains on the market. It was an appropriate drug to treat her irregular bleeding.
VERDICT Claims against the medical center that referred the patient to the ObGyn were settled for $2.5 million before trial. A $14 million Illinois verdict was returned against the ObGyn, for a total award of $16.5 million.
Who is at fault when pelvic mesh erodes?
In January 2011, an ObGyn implanted the Gynecare TVT Obturator System (TVT‑O; Ethicon) during a midurethral sling procedure to treat stress urinary incontinence (SUI) in a woman in her 60s. Shortly thereafter, the ObGyn left practice because of early-onset Alzheimer’s disease, and the patient’s care was taken over by a gynecologist.
At the 2-month postoperative visit, the gynecologist found that the mesh had eroded into the patient’s vagina. The gynecologist simply cut the mesh with a scissor, charted that a small erosion was present, and prescribed estrogen cream.
The patient continued to report pain, discomfort, pressure, difficulty voiding urine, continued incontinence, vaginal discharge, scarring, infection, odor, and bleeding.
PATIENT’S CLAIM The polypropylene mesh used during the midurethral sling procedure has been shown to be incompatible with human tissue. It promotes an immune response, which stimulates degradation of the pelvic tissue and can contribute to the development of severe adverse reactions to the mesh. Ethicon negligently designed, manufactured, marketed, labeled, and packaged the pelvic mesh products.
DEFENDANTS’ DEFENSE Proper warnings were provided about the health risks associated with polypropylene mesh products. The medical device was not properly sized.
VERDICT A Texas jury rejected the patient’s claims that Ethicon did not provide proper warnings about the sling’s health risks and declined to award punitive damages.
However, the jury decided that the mesh implant was defectively designed, and returned a $1.2 million verdict against Ethicon.
Was suspected bowel injury treated properly?
A 40-year-old woman was referred to an ObGyn after reporting abnormal uterine bleeding to her primary care physician. The patient had very light menses every few weeks. The ObGyn performed an ablation procedure, without relief. A month later, the ObGyn performed robot-assisted laparoscopic hysterectomy. The next day, the patient reported abdominal pain. Suspecting a bowel injury, the ObGyn ordered a CT scan; the bowel appeared normal, so the ObGyn referred the patient to a surgeon. During exploratory laparotomy, the surgeon found and repaired a bowel injury. The patient developed significant complications from a necrotizing infection that included respiratory distress and ongoing wound care.
PATIENT’S CLAIM Conservative treatment should have been offered before surgery. The ObGyn should have waited longer after the ablation procedure before doing the hysterectomy. The ObGyn should have checked for a possible bowel injury before closing the hysterectomy.
PHYSICIAN’S DEFENSE The bowel injury is a known complication of the procedure and was recognized and repaired in a timely manner.
VERDICT A Kentucky defense verdict was returned.
Pap smear improperly interpreted: Woman dies from cervical cancer
A 37-year-old woman underwent a pap smear in 2008 that was read by a cytotechnologist as normal. Two years later, the patient was found to have a golf-ball–sized cancerous tumor. She died from cervical cancer in 2011.
ESTATE’S CLAIM The cytotechnologist was negligent in misreading the 2008 Pap smear. If treatment had been started in 2008, the cancer could have been resolved with a simple conization biopsy.
DEFENDANTS’ DEFENSE The Pap smear interpretation was reasonable. The cancer could not have been diagnosed in 2008. The patient was at fault for failing to follow-up Pap smears during the next 2 years.
VERDICT After assigning 75% fault to the cytotechnologist and 25% fault to the patient, a Florida jury returned a $20,870,200 verdict, which was reduced to $15,816,699.
Disastrous off-label use of anticoagulation
When a pelvic abscess was found, a 50-year-old woman was admitted to the hospital for treatment. She was taking warfarin due to a history of venous thromboembolism.
Before the procedure, her physicians attempted to temporarily reverse her anticoagulation by administering Factor IX Complex (Profilnine SD, Grifols Biologicals). The dose ordered for the patient was nearly double the maximum recommended weight-based dose. Almost immediately after receiving the infusion, the patient went into cardiopulmonary arrest and died. An autopsy found the cause of death to be pulmonary emboli (PE).
ESTATE’S CLAIM An excessive dose of Profilnine caused PE. At the time of the incident, Profilnine was not FDA approved for warfarin reversal, although some off-label uses were recognized in emergent situations, such as intracranial bleeds.
DEFENDANTS’ DEFENSE The case was settled during the trial.
VERDICT A $1.25 million Virginia settlement was reached.
Vesicovaginal fistula from ureteral injury
At a women’s health clinic, a patient reported continuous, heavy vaginal bleeding; pain; and shortness of breath when walking. She had a history of endometritis and multiple abdominal surgeries. Examination disclosed a profuse vaginal discharge, a normal cervix, and an enlarged uterus. The patient consented to abdominal hysterectomy and bilateral salpingo-oophorectomy performed by an ObGyn assisted by a resident.
During surgery, the ObGyn found that the patient’s uterus was at 16 to 20 weeks’ gestation size, with multiple serosal uterine fibroids and frank pus and necrosed fibroid tumors within the uterine cavity. The procedure took longer than planned because of extensive adhesions. After surgery, the patient was anemic and was given a beta-blocker for tachycardia. She was discharged 3 days later with 48 hours’ worth of intravenous antibiotics.
A month later, the patient reported urinary incontinence. She saw a urologist, who found a vesicovaginal fistula. The patient underwent nephrostomy-tube placement. Right ureterolysis and a right ureteral reimplant was performed 4 months later.
PATIENT’S CLAIM The ObGyn injured the right ureter during surgery.
DEFENDANTS’ DEFENSE The ureter injury is a known risk of the procedure. The injury was due to an infection or delayed effects of ischemia. The patient had a good recovery with no residual injury.
VERDICT A Michigan defense verdict was returned.
Why did mother die after delivering twins?
After a 35-year-old woman gave birth to twins by cesarean delivery, she died. At autopsy, 4 liters of blood were found in her abdomen.
ESTATE’S CLAIM The ObGyn failed to recognize and treat an arterial or venous bleed during surgery.
DEFENDANTS’ DEFENSE The patient died from amniotic fluid embolism. Autopsy results showed right ventricular heart failure, respiratory failure, and disseminated intravascular coagulation.
VERDICT A Florida defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Was fetus’ wrist injured during cesarean delivery?
At 34 weeks’ gestation, a 39-year-old woman went to the hospital in preterm labor. Her history included a prior cesarean delivery. Ultrasonography (US) showed that the fetus was in a double-footling breech position. The ObGyn decided to perform a cesarean delivery when the fetal heart-rate monitor indicated distress.
After making a midline incision through the earlier scar, the ObGyn created a low transverse uterine incision with a scalpel. The mother’s uterus was thick because labor had not progressed. When the ObGyn was unable to deliver the baby through the low transverse incision, she performed a T-extension of the incision using bandage scissors while placing her free hand inside the uterus to shield the fetus from injury. After extensive manipulation, the baby was delivered and immediately handed to a neonatologist. After surgery, the neonatologist told the mother that the baby had sustained two lacerations to the ulnar side of the right wrist. The newborn was airlifted to another hospital for treatment of sepsis. There, an orthopedic hand surgeon examined the child and determined that the lacerations were superficial and only required sutures. The orthopedist saw the infant a month later and believed there was no significant wrist injury.
When the child began preschool, she started to experience cold intolerance and difficulty writing with her right hand. The child was referred to a pediatric neurologist, who found no nerve damage and ordered occupational therapy.
The original orthopedic surgeon examined the child when she was 7 years old and determined that the flexor carpi ulnaris tendon had been completely severed with a partial injury to the ulnar nerve. He recommended a return visit at age 14 for full assessment of the wrist injury.
PARENTS’ CLAIM The ObGyn did not properly shield the fetus when performing the T-extension incision during cesarean delivery. The child’s weakness will increase with age, ruling out some occupations.
PHYSICIAN’S DEFENSE The ObGyn was not negligent; she had provided adequate protection of the fetus during both incisions.
VERDICT An Illinois defense verdict was returned.
Woman dies after tubal ligation
After a 42-year-old woman underwent tubal ligation, her surgeon was concerned about a possible bowel perforation and admitted her to the hospital. The next morning, a computed tomography (CT) scan of the abdomen did not reveal bowel injury.
That afternoon, when the patient reported shortness of breath, the surgeon called the hospitalist with concern for pulmonary embolism (PE). The hospitalist immediately ordered a CT scan of the chest, initiated PE protocol, and wrote “r/o PE” on the chart. A radiologist reminded the hospitalist of the earlier CT scan with concern for kidney damage from another dye study. The hospitalist cancelled the CT scan and PE protocol. After waiting 17 hours to run any further tests, a CT scan revealed massive bilateral PE. The patient was transferred to the ICU, but died the next day.
PATIENT’S CLAIM The 17-hour delay was negligent.
PHYSICIAN’S DEFENSE There was no negligence. The patient died of septic shock, not PE.
VERDICT A $4 million Virginia verdict was returned.
Child born without hand and forearm
During prenatal care, a mother underwent US at 20 and 36 weeks; both studies were reported as normal. The child was born missing his left hand and part of his left forearm due to a congenital amputation. The child will require prosthetics for life.
PATIENT’S CLAIM The condition should have been seen during prenatal US; an abortion was still an option at 20 weeks.
DEFENDANTS’ DEFENSE US was properly performed and evaluated. It can be difficult to differentiate the right from left extremities.
VERDICT A California defense verdict was returned.
After starting Yasmin, woman has stroke with permanent paralysis: $16.5M total award
When a 37-year-old woman reported irregular menstruation, her ObGyn prescribed drospirenone/ethinyl estradiol (Yasmin; Bayer). Thirteen days after starting the drug, the patient had a stroke. She is paralyzed on her left side, has limited ability to speak, cannot use her left arm and leg, and requires 24-hour care.
PATIENT’S CLAIM The ObGyn should have recognized that Yasmin was not appropriate for this patient because of the drug’s clotting risks. The patient’s risk factors included her age (over 35), borderline hypertension, overweight, history of smoking, and high cholesterol. The ObGyn should have offered safer alternatives, such as a progesterone-only pill. The US Food and Drug Administration (FDA) issued a safety warning that all drospirenone-containing drugs may be associated with a higher risk of venous thrombosis during the first 6 months of use.
DEFENDANTS’ DEFENSE According to Bayer, Yasmin is safe, and remains on the market. It was an appropriate drug to treat her irregular bleeding.
VERDICT Claims against the medical center that referred the patient to the ObGyn were settled for $2.5 million before trial. A $14 million Illinois verdict was returned against the ObGyn, for a total award of $16.5 million.
Who is at fault when pelvic mesh erodes?
In January 2011, an ObGyn implanted the Gynecare TVT Obturator System (TVT‑O; Ethicon) during a midurethral sling procedure to treat stress urinary incontinence (SUI) in a woman in her 60s. Shortly thereafter, the ObGyn left practice because of early-onset Alzheimer’s disease, and the patient’s care was taken over by a gynecologist.
At the 2-month postoperative visit, the gynecologist found that the mesh had eroded into the patient’s vagina. The gynecologist simply cut the mesh with a scissor, charted that a small erosion was present, and prescribed estrogen cream.
The patient continued to report pain, discomfort, pressure, difficulty voiding urine, continued incontinence, vaginal discharge, scarring, infection, odor, and bleeding.
PATIENT’S CLAIM The polypropylene mesh used during the midurethral sling procedure has been shown to be incompatible with human tissue. It promotes an immune response, which stimulates degradation of the pelvic tissue and can contribute to the development of severe adverse reactions to the mesh. Ethicon negligently designed, manufactured, marketed, labeled, and packaged the pelvic mesh products.
DEFENDANTS’ DEFENSE Proper warnings were provided about the health risks associated with polypropylene mesh products. The medical device was not properly sized.
VERDICT A Texas jury rejected the patient’s claims that Ethicon did not provide proper warnings about the sling’s health risks and declined to award punitive damages.
However, the jury decided that the mesh implant was defectively designed, and returned a $1.2 million verdict against Ethicon.
Was suspected bowel injury treated properly?
A 40-year-old woman was referred to an ObGyn after reporting abnormal uterine bleeding to her primary care physician. The patient had very light menses every few weeks. The ObGyn performed an ablation procedure, without relief. A month later, the ObGyn performed robot-assisted laparoscopic hysterectomy. The next day, the patient reported abdominal pain. Suspecting a bowel injury, the ObGyn ordered a CT scan; the bowel appeared normal, so the ObGyn referred the patient to a surgeon. During exploratory laparotomy, the surgeon found and repaired a bowel injury. The patient developed significant complications from a necrotizing infection that included respiratory distress and ongoing wound care.
PATIENT’S CLAIM Conservative treatment should have been offered before surgery. The ObGyn should have waited longer after the ablation procedure before doing the hysterectomy. The ObGyn should have checked for a possible bowel injury before closing the hysterectomy.
PHYSICIAN’S DEFENSE The bowel injury is a known complication of the procedure and was recognized and repaired in a timely manner.
VERDICT A Kentucky defense verdict was returned.
Pap smear improperly interpreted: Woman dies from cervical cancer
A 37-year-old woman underwent a pap smear in 2008 that was read by a cytotechnologist as normal. Two years later, the patient was found to have a golf-ball–sized cancerous tumor. She died from cervical cancer in 2011.
ESTATE’S CLAIM The cytotechnologist was negligent in misreading the 2008 Pap smear. If treatment had been started in 2008, the cancer could have been resolved with a simple conization biopsy.
DEFENDANTS’ DEFENSE The Pap smear interpretation was reasonable. The cancer could not have been diagnosed in 2008. The patient was at fault for failing to follow-up Pap smears during the next 2 years.
VERDICT After assigning 75% fault to the cytotechnologist and 25% fault to the patient, a Florida jury returned a $20,870,200 verdict, which was reduced to $15,816,699.
Disastrous off-label use of anticoagulation
When a pelvic abscess was found, a 50-year-old woman was admitted to the hospital for treatment. She was taking warfarin due to a history of venous thromboembolism.
Before the procedure, her physicians attempted to temporarily reverse her anticoagulation by administering Factor IX Complex (Profilnine SD, Grifols Biologicals). The dose ordered for the patient was nearly double the maximum recommended weight-based dose. Almost immediately after receiving the infusion, the patient went into cardiopulmonary arrest and died. An autopsy found the cause of death to be pulmonary emboli (PE).
ESTATE’S CLAIM An excessive dose of Profilnine caused PE. At the time of the incident, Profilnine was not FDA approved for warfarin reversal, although some off-label uses were recognized in emergent situations, such as intracranial bleeds.
DEFENDANTS’ DEFENSE The case was settled during the trial.
VERDICT A $1.25 million Virginia settlement was reached.
Vesicovaginal fistula from ureteral injury
At a women’s health clinic, a patient reported continuous, heavy vaginal bleeding; pain; and shortness of breath when walking. She had a history of endometritis and multiple abdominal surgeries. Examination disclosed a profuse vaginal discharge, a normal cervix, and an enlarged uterus. The patient consented to abdominal hysterectomy and bilateral salpingo-oophorectomy performed by an ObGyn assisted by a resident.
During surgery, the ObGyn found that the patient’s uterus was at 16 to 20 weeks’ gestation size, with multiple serosal uterine fibroids and frank pus and necrosed fibroid tumors within the uterine cavity. The procedure took longer than planned because of extensive adhesions. After surgery, the patient was anemic and was given a beta-blocker for tachycardia. She was discharged 3 days later with 48 hours’ worth of intravenous antibiotics.
A month later, the patient reported urinary incontinence. She saw a urologist, who found a vesicovaginal fistula. The patient underwent nephrostomy-tube placement. Right ureterolysis and a right ureteral reimplant was performed 4 months later.
PATIENT’S CLAIM The ObGyn injured the right ureter during surgery.
DEFENDANTS’ DEFENSE The ureter injury is a known risk of the procedure. The injury was due to an infection or delayed effects of ischemia. The patient had a good recovery with no residual injury.
VERDICT A Michigan defense verdict was returned.
Why did mother die after delivering twins?
After a 35-year-old woman gave birth to twins by cesarean delivery, she died. At autopsy, 4 liters of blood were found in her abdomen.
ESTATE’S CLAIM The ObGyn failed to recognize and treat an arterial or venous bleed during surgery.
DEFENDANTS’ DEFENSE The patient died from amniotic fluid embolism. Autopsy results showed right ventricular heart failure, respiratory failure, and disseminated intravascular coagulation.
VERDICT A Florida defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Was fetus’ wrist injured during cesarean delivery?
At 34 weeks’ gestation, a 39-year-old woman went to the hospital in preterm labor. Her history included a prior cesarean delivery. Ultrasonography (US) showed that the fetus was in a double-footling breech position. The ObGyn decided to perform a cesarean delivery when the fetal heart-rate monitor indicated distress.
After making a midline incision through the earlier scar, the ObGyn created a low transverse uterine incision with a scalpel. The mother’s uterus was thick because labor had not progressed. When the ObGyn was unable to deliver the baby through the low transverse incision, she performed a T-extension of the incision using bandage scissors while placing her free hand inside the uterus to shield the fetus from injury. After extensive manipulation, the baby was delivered and immediately handed to a neonatologist. After surgery, the neonatologist told the mother that the baby had sustained two lacerations to the ulnar side of the right wrist. The newborn was airlifted to another hospital for treatment of sepsis. There, an orthopedic hand surgeon examined the child and determined that the lacerations were superficial and only required sutures. The orthopedist saw the infant a month later and believed there was no significant wrist injury.
When the child began preschool, she started to experience cold intolerance and difficulty writing with her right hand. The child was referred to a pediatric neurologist, who found no nerve damage and ordered occupational therapy.
The original orthopedic surgeon examined the child when she was 7 years old and determined that the flexor carpi ulnaris tendon had been completely severed with a partial injury to the ulnar nerve. He recommended a return visit at age 14 for full assessment of the wrist injury.
PARENTS’ CLAIM The ObGyn did not properly shield the fetus when performing the T-extension incision during cesarean delivery. The child’s weakness will increase with age, ruling out some occupations.
PHYSICIAN’S DEFENSE The ObGyn was not negligent; she had provided adequate protection of the fetus during both incisions.
VERDICT An Illinois defense verdict was returned.
Woman dies after tubal ligation
After a 42-year-old woman underwent tubal ligation, her surgeon was concerned about a possible bowel perforation and admitted her to the hospital. The next morning, a computed tomography (CT) scan of the abdomen did not reveal bowel injury.
That afternoon, when the patient reported shortness of breath, the surgeon called the hospitalist with concern for pulmonary embolism (PE). The hospitalist immediately ordered a CT scan of the chest, initiated PE protocol, and wrote “r/o PE” on the chart. A radiologist reminded the hospitalist of the earlier CT scan with concern for kidney damage from another dye study. The hospitalist cancelled the CT scan and PE protocol. After waiting 17 hours to run any further tests, a CT scan revealed massive bilateral PE. The patient was transferred to the ICU, but died the next day.
PATIENT’S CLAIM The 17-hour delay was negligent.
PHYSICIAN’S DEFENSE There was no negligence. The patient died of septic shock, not PE.
VERDICT A $4 million Virginia verdict was returned.
Child born without hand and forearm
During prenatal care, a mother underwent US at 20 and 36 weeks; both studies were reported as normal. The child was born missing his left hand and part of his left forearm due to a congenital amputation. The child will require prosthetics for life.
PATIENT’S CLAIM The condition should have been seen during prenatal US; an abortion was still an option at 20 weeks.
DEFENDANTS’ DEFENSE US was properly performed and evaluated. It can be difficult to differentiate the right from left extremities.
VERDICT A California defense verdict was returned.
After starting Yasmin, woman has stroke with permanent paralysis: $16.5M total award
When a 37-year-old woman reported irregular menstruation, her ObGyn prescribed drospirenone/ethinyl estradiol (Yasmin; Bayer). Thirteen days after starting the drug, the patient had a stroke. She is paralyzed on her left side, has limited ability to speak, cannot use her left arm and leg, and requires 24-hour care.
PATIENT’S CLAIM The ObGyn should have recognized that Yasmin was not appropriate for this patient because of the drug’s clotting risks. The patient’s risk factors included her age (over 35), borderline hypertension, overweight, history of smoking, and high cholesterol. The ObGyn should have offered safer alternatives, such as a progesterone-only pill. The US Food and Drug Administration (FDA) issued a safety warning that all drospirenone-containing drugs may be associated with a higher risk of venous thrombosis during the first 6 months of use.
DEFENDANTS’ DEFENSE According to Bayer, Yasmin is safe, and remains on the market. It was an appropriate drug to treat her irregular bleeding.
VERDICT Claims against the medical center that referred the patient to the ObGyn were settled for $2.5 million before trial. A $14 million Illinois verdict was returned against the ObGyn, for a total award of $16.5 million.
Who is at fault when pelvic mesh erodes?
In January 2011, an ObGyn implanted the Gynecare TVT Obturator System (TVT‑O; Ethicon) during a midurethral sling procedure to treat stress urinary incontinence (SUI) in a woman in her 60s. Shortly thereafter, the ObGyn left practice because of early-onset Alzheimer’s disease, and the patient’s care was taken over by a gynecologist.
At the 2-month postoperative visit, the gynecologist found that the mesh had eroded into the patient’s vagina. The gynecologist simply cut the mesh with a scissor, charted that a small erosion was present, and prescribed estrogen cream.
The patient continued to report pain, discomfort, pressure, difficulty voiding urine, continued incontinence, vaginal discharge, scarring, infection, odor, and bleeding.
PATIENT’S CLAIM The polypropylene mesh used during the midurethral sling procedure has been shown to be incompatible with human tissue. It promotes an immune response, which stimulates degradation of the pelvic tissue and can contribute to the development of severe adverse reactions to the mesh. Ethicon negligently designed, manufactured, marketed, labeled, and packaged the pelvic mesh products.
DEFENDANTS’ DEFENSE Proper warnings were provided about the health risks associated with polypropylene mesh products. The medical device was not properly sized.
VERDICT A Texas jury rejected the patient’s claims that Ethicon did not provide proper warnings about the sling’s health risks and declined to award punitive damages.
However, the jury decided that the mesh implant was defectively designed, and returned a $1.2 million verdict against Ethicon.
Was suspected bowel injury treated properly?
A 40-year-old woman was referred to an ObGyn after reporting abnormal uterine bleeding to her primary care physician. The patient had very light menses every few weeks. The ObGyn performed an ablation procedure, without relief. A month later, the ObGyn performed robot-assisted laparoscopic hysterectomy. The next day, the patient reported abdominal pain. Suspecting a bowel injury, the ObGyn ordered a CT scan; the bowel appeared normal, so the ObGyn referred the patient to a surgeon. During exploratory laparotomy, the surgeon found and repaired a bowel injury. The patient developed significant complications from a necrotizing infection that included respiratory distress and ongoing wound care.
PATIENT’S CLAIM Conservative treatment should have been offered before surgery. The ObGyn should have waited longer after the ablation procedure before doing the hysterectomy. The ObGyn should have checked for a possible bowel injury before closing the hysterectomy.
PHYSICIAN’S DEFENSE The bowel injury is a known complication of the procedure and was recognized and repaired in a timely manner.
VERDICT A Kentucky defense verdict was returned.
Pap smear improperly interpreted: Woman dies from cervical cancer
A 37-year-old woman underwent a pap smear in 2008 that was read by a cytotechnologist as normal. Two years later, the patient was found to have a golf-ball–sized cancerous tumor. She died from cervical cancer in 2011.
ESTATE’S CLAIM The cytotechnologist was negligent in misreading the 2008 Pap smear. If treatment had been started in 2008, the cancer could have been resolved with a simple conization biopsy.
DEFENDANTS’ DEFENSE The Pap smear interpretation was reasonable. The cancer could not have been diagnosed in 2008. The patient was at fault for failing to follow-up Pap smears during the next 2 years.
VERDICT After assigning 75% fault to the cytotechnologist and 25% fault to the patient, a Florida jury returned a $20,870,200 verdict, which was reduced to $15,816,699.
Disastrous off-label use of anticoagulation
When a pelvic abscess was found, a 50-year-old woman was admitted to the hospital for treatment. She was taking warfarin due to a history of venous thromboembolism.
Before the procedure, her physicians attempted to temporarily reverse her anticoagulation by administering Factor IX Complex (Profilnine SD, Grifols Biologicals). The dose ordered for the patient was nearly double the maximum recommended weight-based dose. Almost immediately after receiving the infusion, the patient went into cardiopulmonary arrest and died. An autopsy found the cause of death to be pulmonary emboli (PE).
ESTATE’S CLAIM An excessive dose of Profilnine caused PE. At the time of the incident, Profilnine was not FDA approved for warfarin reversal, although some off-label uses were recognized in emergent situations, such as intracranial bleeds.
DEFENDANTS’ DEFENSE The case was settled during the trial.
VERDICT A $1.25 million Virginia settlement was reached.
Vesicovaginal fistula from ureteral injury
At a women’s health clinic, a patient reported continuous, heavy vaginal bleeding; pain; and shortness of breath when walking. She had a history of endometritis and multiple abdominal surgeries. Examination disclosed a profuse vaginal discharge, a normal cervix, and an enlarged uterus. The patient consented to abdominal hysterectomy and bilateral salpingo-oophorectomy performed by an ObGyn assisted by a resident.
During surgery, the ObGyn found that the patient’s uterus was at 16 to 20 weeks’ gestation size, with multiple serosal uterine fibroids and frank pus and necrosed fibroid tumors within the uterine cavity. The procedure took longer than planned because of extensive adhesions. After surgery, the patient was anemic and was given a beta-blocker for tachycardia. She was discharged 3 days later with 48 hours’ worth of intravenous antibiotics.
A month later, the patient reported urinary incontinence. She saw a urologist, who found a vesicovaginal fistula. The patient underwent nephrostomy-tube placement. Right ureterolysis and a right ureteral reimplant was performed 4 months later.
PATIENT’S CLAIM The ObGyn injured the right ureter during surgery.
DEFENDANTS’ DEFENSE The ureter injury is a known risk of the procedure. The injury was due to an infection or delayed effects of ischemia. The patient had a good recovery with no residual injury.
VERDICT A Michigan defense verdict was returned.
Why did mother die after delivering twins?
After a 35-year-old woman gave birth to twins by cesarean delivery, she died. At autopsy, 4 liters of blood were found in her abdomen.
ESTATE’S CLAIM The ObGyn failed to recognize and treat an arterial or venous bleed during surgery.
DEFENDANTS’ DEFENSE The patient died from amniotic fluid embolism. Autopsy results showed right ventricular heart failure, respiratory failure, and disseminated intravascular coagulation.
VERDICT A Florida defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Using the Internet in your practice. Part 3: Maximizing your online reach through SEO and pay-per-click
It’s high time to go beyond relying on YellowPages.com to attract patients to your practice. According to research and analysis company BIA/Kelsey, “nearly all consumers (97%) now use online media to shop locally.”1 Today’s patients are Internet savvy and expect their ObGyn not only to be a good physician who diagnoses and treats their conditions but also to demonstrate his or her electronic technical abilities, through online communication, a Web site, email newsletter outreach, and, yes, a social media presence.
Yet, being the best in your field or having an incredible Web site won’t matter if your existing patients and potential new patients can’t find you on the Internet. The solution? Get your Web site onto the first page of Google’s search results. Why? Google is still by far the dominant search engine in the United States, and it has the overwhelming ability to offer you an endless supply of patients. And can your practice survive without a steady flow of new patients?
Type a keyword into the Google search window and dozens, hundreds, or thousands of sites may become visible. Google lists 10 sites per page, however, and when was the last time you went to the second, third, or fourth results page looking for something? If your Web site does not appear on the first results page, you are essentially invisible. The good news is that you can easily and inexpensively reach the top of a search engine’s results page by knowing and applying best practices for effective search engine optimization (SEO; a free endeavor, although your time investment should considered) and/or utilizing a pay-per-click (PPC) service (for a fee that’s comparable to what you used to pay for your old Yellow Pages listing). In this article, we aim to provide to you the know-how to embark on these endeavors by defining SEO and PPC and relaying effective principles for marketing your practice to potential new patients.
What is SEO?
SEO refers to techniques that help your Web site rank higher in organic (natural) results, which helps your site, and you, become more visible to people who are seeking your services. Search engines specialize in offering Web surfers the best information about their search terms, or keywords. To do this, Google uses more than 200 different algorithms, some of which we know but most of which are not published.
The algorithms are used to determine where your Web site ranks according to a number of factors relevant to the content and set-up of each page of your Web site (on-page SEO) as well as everything you do outside of your Web site (off-page SEO) to enhance your SEO rankings. This relevance is calculated by looking at both on-page and off-page factors, including:
- what you are doing in relation to your competition
- how long your Web site has been active
- search engine submission
- article submission
- directory submission
- linking strategies.
You have to work on both on-page and off-page factors many times a month to convince the search engines that you are a Web site worth visiting. Over time, your site will start to rise in the rankings and gain qualified traffic. Then you can concentrate on converting those Web site visitors to office-based patients.
A warning: If you use unethical tactics to get your Web site on the first page of the search results, Google will catch up to you—and your Web-site rankings will plummet.
Five important steps to increase SEO
There’s a system to reach the top of any search engine’s results page. The most important steps are to:
- Use keywords in your Web site coding, or page description (called meta tags).
- Use keywords in your Web site copy.
- Develop in-bound links.
- Post new keyword-related content regularly—typically accomplished through a blog.
- Integrate your keywords in social media postings.
1 and 2. Keywords are key
Keywords are what an Internet surfer enters into a search function and what the search engine crawlers hunt for. The crawlers then direct the surfer to the Web site that is perceived as the best source of information.
Here are the most popular keywords used by potential patients looking for ObGyns: obstetrician, gynecologist, gynecology, vaginal discharge, vaginal dryness, breast self-exam, breast cancer screening, prolapsed bladder, pelvic pain, and adolescent gynecology. You also should include your city’s name as a keyword.
Use keywords in Web site coding and copy. Unless you are experienced in Web development, you’re better off hiring a professional who knows Internet coding to help you develop HTML meta tags, anchor text, a sitemap, etc. You easily can incorporate keywords in the copy on your Web site, but the keyword density should be no more than approximately 3% to 5% of the copy. (If it is more than 5%, it is considered “stuffing,” and not looked on kindly by Google.)
3. In-bound links: Who’s linking to you?
As the search engine crawlers scan Web pages for indexing, they also look for links from other Web sites. The greater number of quality in-bound links a Web site has, the stronger influence or authority it accrues.
In-bound links are weighted differently: a link from a highly authoritative Web site like NYTimes.com will give a Web site a bigger boost than a link from a small blog site. Links from high-ranking sites, such as city directories, hospitals, and online medical directories, improve your Web-site ranking. You should be submitting your Web site address and keyword description to these appropriate directories for in-bound links on a weekly or monthly basis.
4. Develop new content by blogging
Search engines place a high value on new content, and the easiest way to add new keyword-related content is to blog. Writing a 400-word keyword–relevant blog on a regular basis will provide the search engine crawlers with new content to graze.
As an added bonus, there are many medical ezines—small magazines and newsletters distributed by any electronic method—that regularly need content. Publication of your blog article will provide additional back-links to your Web site and improve your SEO rankings. This is your opportunity to go “viral,” have your material read by thousands, and increase visits to your Web site. When your name appears on multiple sites, you create the perception of demonstrating your expertise in various topics, techniques, and therapeutic options.
5. Search engines love social media
Newer technologies are given greater weight in determining Web page ranking. Start with blogging and then add Facebook, YouTube, and Twitter. Always remember to link from these sites with relevant keywords to the exact page on your site that contains the best information for those keywords.
Advertise your practice using PPC (Google AdWords)
Google, Yahoo, and other Internet portals make their money by selling advertisements on search-results pages. Both paid and organic listings appear on the search results pages, but they are displayed in different locations. On Google, PPC listings are found on the top and right side of each page under the header “Ads” (FIGURE 1). The organic or natural search (no payment required) is on the left below the ads.
On Google, the PPC function is called “AdWords” (http://www.google.com/adwords). On the AdWords page, a listing is found that offers how many times people type in certain words or phrases—keywords. Google AdWords allows the marketplace to bid on keywords; the higher the bid, the closer to the top position on the first page of the Google search results. Depending on monthly search volume, popularity, and competition, you can pay anywhere from pennies to $25 each time a Web surfer clicks on your ad. In FIGURE 2, you can see that a suggested bid for “Gynecologist Miami” is $2.96.
You must constantly monitor and manage your AdWords account. Test different landing pages, adjust your copy, and change offerings to make sure you are converting your paid traffic to patients. Otherwise, you can spend hundreds of dollars each month without achieving the desired outcome.
By doing your own research with Google AdWords’ keyword planner, you will see the variations of keywords that you can use in the copy of your Web site and related content for organic SE
Patient conversion: Your ultimate goal
Google is only one piece of the Internet marketing puzzle. Once you have invested in mastering the SEO rankings (by doing it yourself or by paying for professional help), it’s up to your Web site to convert the visitor to a paying patient. To maximize your return on investment (ROI), implement marketing strategies and a patient conversion system on your Web site. When a prospective patient lands there, you have less than 10 seconds to engage her. In Part 1of this series, we discuss features that will keep your visitor involved while she navigates the site and make it easy for her to make an appointment. Don’t lose her because she can’t find your contact information hidden at the bottom of the page.2
If you don’t want to spend the time and effort to do it yourself, outsourcing is a cost-effective solution, and a trackable and measurable way for you to calculate your ROI.
Bottom line: Be seen on the Internet. We are all connected to the Internet every waking moment. This is where we go for information; this is how we communicate with each other; and this is where we create relationships. If you want to build your practice, you have to be where your patient can find you—on the top of an Internet search results page.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Pacheco E, Udowitz R. Nearly all consumers (97%) now use online media to shop locally, according to BIA/Kelsey and ConStat [press release]. BIA/Kelsey Web site. http://www.biakelsey.com/company/press-releases/100310-nearly-all-consumers-now-use-online-media-to-shop-locally.asp. Published March 10, 2010. Accessed August 12, 2014.
2. Baum NH, Romano R. Using the Internet in your practice. Part 1: why social media are important and how to get started. OBG Manag. 2014;26(2):25–36.
It’s high time to go beyond relying on YellowPages.com to attract patients to your practice. According to research and analysis company BIA/Kelsey, “nearly all consumers (97%) now use online media to shop locally.”1 Today’s patients are Internet savvy and expect their ObGyn not only to be a good physician who diagnoses and treats their conditions but also to demonstrate his or her electronic technical abilities, through online communication, a Web site, email newsletter outreach, and, yes, a social media presence.
Yet, being the best in your field or having an incredible Web site won’t matter if your existing patients and potential new patients can’t find you on the Internet. The solution? Get your Web site onto the first page of Google’s search results. Why? Google is still by far the dominant search engine in the United States, and it has the overwhelming ability to offer you an endless supply of patients. And can your practice survive without a steady flow of new patients?
Type a keyword into the Google search window and dozens, hundreds, or thousands of sites may become visible. Google lists 10 sites per page, however, and when was the last time you went to the second, third, or fourth results page looking for something? If your Web site does not appear on the first results page, you are essentially invisible. The good news is that you can easily and inexpensively reach the top of a search engine’s results page by knowing and applying best practices for effective search engine optimization (SEO; a free endeavor, although your time investment should considered) and/or utilizing a pay-per-click (PPC) service (for a fee that’s comparable to what you used to pay for your old Yellow Pages listing). In this article, we aim to provide to you the know-how to embark on these endeavors by defining SEO and PPC and relaying effective principles for marketing your practice to potential new patients.
What is SEO?
SEO refers to techniques that help your Web site rank higher in organic (natural) results, which helps your site, and you, become more visible to people who are seeking your services. Search engines specialize in offering Web surfers the best information about their search terms, or keywords. To do this, Google uses more than 200 different algorithms, some of which we know but most of which are not published.
The algorithms are used to determine where your Web site ranks according to a number of factors relevant to the content and set-up of each page of your Web site (on-page SEO) as well as everything you do outside of your Web site (off-page SEO) to enhance your SEO rankings. This relevance is calculated by looking at both on-page and off-page factors, including:
- what you are doing in relation to your competition
- how long your Web site has been active
- search engine submission
- article submission
- directory submission
- linking strategies.
You have to work on both on-page and off-page factors many times a month to convince the search engines that you are a Web site worth visiting. Over time, your site will start to rise in the rankings and gain qualified traffic. Then you can concentrate on converting those Web site visitors to office-based patients.
A warning: If you use unethical tactics to get your Web site on the first page of the search results, Google will catch up to you—and your Web-site rankings will plummet.
Five important steps to increase SEO
There’s a system to reach the top of any search engine’s results page. The most important steps are to:
- Use keywords in your Web site coding, or page description (called meta tags).
- Use keywords in your Web site copy.
- Develop in-bound links.
- Post new keyword-related content regularly—typically accomplished through a blog.
- Integrate your keywords in social media postings.
1 and 2. Keywords are key
Keywords are what an Internet surfer enters into a search function and what the search engine crawlers hunt for. The crawlers then direct the surfer to the Web site that is perceived as the best source of information.
Here are the most popular keywords used by potential patients looking for ObGyns: obstetrician, gynecologist, gynecology, vaginal discharge, vaginal dryness, breast self-exam, breast cancer screening, prolapsed bladder, pelvic pain, and adolescent gynecology. You also should include your city’s name as a keyword.
Use keywords in Web site coding and copy. Unless you are experienced in Web development, you’re better off hiring a professional who knows Internet coding to help you develop HTML meta tags, anchor text, a sitemap, etc. You easily can incorporate keywords in the copy on your Web site, but the keyword density should be no more than approximately 3% to 5% of the copy. (If it is more than 5%, it is considered “stuffing,” and not looked on kindly by Google.)
3. In-bound links: Who’s linking to you?
As the search engine crawlers scan Web pages for indexing, they also look for links from other Web sites. The greater number of quality in-bound links a Web site has, the stronger influence or authority it accrues.
In-bound links are weighted differently: a link from a highly authoritative Web site like NYTimes.com will give a Web site a bigger boost than a link from a small blog site. Links from high-ranking sites, such as city directories, hospitals, and online medical directories, improve your Web-site ranking. You should be submitting your Web site address and keyword description to these appropriate directories for in-bound links on a weekly or monthly basis.
4. Develop new content by blogging
Search engines place a high value on new content, and the easiest way to add new keyword-related content is to blog. Writing a 400-word keyword–relevant blog on a regular basis will provide the search engine crawlers with new content to graze.
As an added bonus, there are many medical ezines—small magazines and newsletters distributed by any electronic method—that regularly need content. Publication of your blog article will provide additional back-links to your Web site and improve your SEO rankings. This is your opportunity to go “viral,” have your material read by thousands, and increase visits to your Web site. When your name appears on multiple sites, you create the perception of demonstrating your expertise in various topics, techniques, and therapeutic options.
5. Search engines love social media
Newer technologies are given greater weight in determining Web page ranking. Start with blogging and then add Facebook, YouTube, and Twitter. Always remember to link from these sites with relevant keywords to the exact page on your site that contains the best information for those keywords.
Advertise your practice using PPC (Google AdWords)
Google, Yahoo, and other Internet portals make their money by selling advertisements on search-results pages. Both paid and organic listings appear on the search results pages, but they are displayed in different locations. On Google, PPC listings are found on the top and right side of each page under the header “Ads” (FIGURE 1). The organic or natural search (no payment required) is on the left below the ads.
On Google, the PPC function is called “AdWords” (http://www.google.com/adwords). On the AdWords page, a listing is found that offers how many times people type in certain words or phrases—keywords. Google AdWords allows the marketplace to bid on keywords; the higher the bid, the closer to the top position on the first page of the Google search results. Depending on monthly search volume, popularity, and competition, you can pay anywhere from pennies to $25 each time a Web surfer clicks on your ad. In FIGURE 2, you can see that a suggested bid for “Gynecologist Miami” is $2.96.
You must constantly monitor and manage your AdWords account. Test different landing pages, adjust your copy, and change offerings to make sure you are converting your paid traffic to patients. Otherwise, you can spend hundreds of dollars each month without achieving the desired outcome.
By doing your own research with Google AdWords’ keyword planner, you will see the variations of keywords that you can use in the copy of your Web site and related content for organic SE
Patient conversion: Your ultimate goal
Google is only one piece of the Internet marketing puzzle. Once you have invested in mastering the SEO rankings (by doing it yourself or by paying for professional help), it’s up to your Web site to convert the visitor to a paying patient. To maximize your return on investment (ROI), implement marketing strategies and a patient conversion system on your Web site. When a prospective patient lands there, you have less than 10 seconds to engage her. In Part 1of this series, we discuss features that will keep your visitor involved while she navigates the site and make it easy for her to make an appointment. Don’t lose her because she can’t find your contact information hidden at the bottom of the page.2
If you don’t want to spend the time and effort to do it yourself, outsourcing is a cost-effective solution, and a trackable and measurable way for you to calculate your ROI.
Bottom line: Be seen on the Internet. We are all connected to the Internet every waking moment. This is where we go for information; this is how we communicate with each other; and this is where we create relationships. If you want to build your practice, you have to be where your patient can find you—on the top of an Internet search results page.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
It’s high time to go beyond relying on YellowPages.com to attract patients to your practice. According to research and analysis company BIA/Kelsey, “nearly all consumers (97%) now use online media to shop locally.”1 Today’s patients are Internet savvy and expect their ObGyn not only to be a good physician who diagnoses and treats their conditions but also to demonstrate his or her electronic technical abilities, through online communication, a Web site, email newsletter outreach, and, yes, a social media presence.
Yet, being the best in your field or having an incredible Web site won’t matter if your existing patients and potential new patients can’t find you on the Internet. The solution? Get your Web site onto the first page of Google’s search results. Why? Google is still by far the dominant search engine in the United States, and it has the overwhelming ability to offer you an endless supply of patients. And can your practice survive without a steady flow of new patients?
Type a keyword into the Google search window and dozens, hundreds, or thousands of sites may become visible. Google lists 10 sites per page, however, and when was the last time you went to the second, third, or fourth results page looking for something? If your Web site does not appear on the first results page, you are essentially invisible. The good news is that you can easily and inexpensively reach the top of a search engine’s results page by knowing and applying best practices for effective search engine optimization (SEO; a free endeavor, although your time investment should considered) and/or utilizing a pay-per-click (PPC) service (for a fee that’s comparable to what you used to pay for your old Yellow Pages listing). In this article, we aim to provide to you the know-how to embark on these endeavors by defining SEO and PPC and relaying effective principles for marketing your practice to potential new patients.
What is SEO?
SEO refers to techniques that help your Web site rank higher in organic (natural) results, which helps your site, and you, become more visible to people who are seeking your services. Search engines specialize in offering Web surfers the best information about their search terms, or keywords. To do this, Google uses more than 200 different algorithms, some of which we know but most of which are not published.
The algorithms are used to determine where your Web site ranks according to a number of factors relevant to the content and set-up of each page of your Web site (on-page SEO) as well as everything you do outside of your Web site (off-page SEO) to enhance your SEO rankings. This relevance is calculated by looking at both on-page and off-page factors, including:
- what you are doing in relation to your competition
- how long your Web site has been active
- search engine submission
- article submission
- directory submission
- linking strategies.
You have to work on both on-page and off-page factors many times a month to convince the search engines that you are a Web site worth visiting. Over time, your site will start to rise in the rankings and gain qualified traffic. Then you can concentrate on converting those Web site visitors to office-based patients.
A warning: If you use unethical tactics to get your Web site on the first page of the search results, Google will catch up to you—and your Web-site rankings will plummet.
Five important steps to increase SEO
There’s a system to reach the top of any search engine’s results page. The most important steps are to:
- Use keywords in your Web site coding, or page description (called meta tags).
- Use keywords in your Web site copy.
- Develop in-bound links.
- Post new keyword-related content regularly—typically accomplished through a blog.
- Integrate your keywords in social media postings.
1 and 2. Keywords are key
Keywords are what an Internet surfer enters into a search function and what the search engine crawlers hunt for. The crawlers then direct the surfer to the Web site that is perceived as the best source of information.
Here are the most popular keywords used by potential patients looking for ObGyns: obstetrician, gynecologist, gynecology, vaginal discharge, vaginal dryness, breast self-exam, breast cancer screening, prolapsed bladder, pelvic pain, and adolescent gynecology. You also should include your city’s name as a keyword.
Use keywords in Web site coding and copy. Unless you are experienced in Web development, you’re better off hiring a professional who knows Internet coding to help you develop HTML meta tags, anchor text, a sitemap, etc. You easily can incorporate keywords in the copy on your Web site, but the keyword density should be no more than approximately 3% to 5% of the copy. (If it is more than 5%, it is considered “stuffing,” and not looked on kindly by Google.)
3. In-bound links: Who’s linking to you?
As the search engine crawlers scan Web pages for indexing, they also look for links from other Web sites. The greater number of quality in-bound links a Web site has, the stronger influence or authority it accrues.
In-bound links are weighted differently: a link from a highly authoritative Web site like NYTimes.com will give a Web site a bigger boost than a link from a small blog site. Links from high-ranking sites, such as city directories, hospitals, and online medical directories, improve your Web-site ranking. You should be submitting your Web site address and keyword description to these appropriate directories for in-bound links on a weekly or monthly basis.
4. Develop new content by blogging
Search engines place a high value on new content, and the easiest way to add new keyword-related content is to blog. Writing a 400-word keyword–relevant blog on a regular basis will provide the search engine crawlers with new content to graze.
As an added bonus, there are many medical ezines—small magazines and newsletters distributed by any electronic method—that regularly need content. Publication of your blog article will provide additional back-links to your Web site and improve your SEO rankings. This is your opportunity to go “viral,” have your material read by thousands, and increase visits to your Web site. When your name appears on multiple sites, you create the perception of demonstrating your expertise in various topics, techniques, and therapeutic options.
5. Search engines love social media
Newer technologies are given greater weight in determining Web page ranking. Start with blogging and then add Facebook, YouTube, and Twitter. Always remember to link from these sites with relevant keywords to the exact page on your site that contains the best information for those keywords.
Advertise your practice using PPC (Google AdWords)
Google, Yahoo, and other Internet portals make their money by selling advertisements on search-results pages. Both paid and organic listings appear on the search results pages, but they are displayed in different locations. On Google, PPC listings are found on the top and right side of each page under the header “Ads” (FIGURE 1). The organic or natural search (no payment required) is on the left below the ads.
On Google, the PPC function is called “AdWords” (http://www.google.com/adwords). On the AdWords page, a listing is found that offers how many times people type in certain words or phrases—keywords. Google AdWords allows the marketplace to bid on keywords; the higher the bid, the closer to the top position on the first page of the Google search results. Depending on monthly search volume, popularity, and competition, you can pay anywhere from pennies to $25 each time a Web surfer clicks on your ad. In FIGURE 2, you can see that a suggested bid for “Gynecologist Miami” is $2.96.
You must constantly monitor and manage your AdWords account. Test different landing pages, adjust your copy, and change offerings to make sure you are converting your paid traffic to patients. Otherwise, you can spend hundreds of dollars each month without achieving the desired outcome.
By doing your own research with Google AdWords’ keyword planner, you will see the variations of keywords that you can use in the copy of your Web site and related content for organic SE
Patient conversion: Your ultimate goal
Google is only one piece of the Internet marketing puzzle. Once you have invested in mastering the SEO rankings (by doing it yourself or by paying for professional help), it’s up to your Web site to convert the visitor to a paying patient. To maximize your return on investment (ROI), implement marketing strategies and a patient conversion system on your Web site. When a prospective patient lands there, you have less than 10 seconds to engage her. In Part 1of this series, we discuss features that will keep your visitor involved while she navigates the site and make it easy for her to make an appointment. Don’t lose her because she can’t find your contact information hidden at the bottom of the page.2
If you don’t want to spend the time and effort to do it yourself, outsourcing is a cost-effective solution, and a trackable and measurable way for you to calculate your ROI.
Bottom line: Be seen on the Internet. We are all connected to the Internet every waking moment. This is where we go for information; this is how we communicate with each other; and this is where we create relationships. If you want to build your practice, you have to be where your patient can find you—on the top of an Internet search results page.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Pacheco E, Udowitz R. Nearly all consumers (97%) now use online media to shop locally, according to BIA/Kelsey and ConStat [press release]. BIA/Kelsey Web site. http://www.biakelsey.com/company/press-releases/100310-nearly-all-consumers-now-use-online-media-to-shop-locally.asp. Published March 10, 2010. Accessed August 12, 2014.
2. Baum NH, Romano R. Using the Internet in your practice. Part 1: why social media are important and how to get started. OBG Manag. 2014;26(2):25–36.
1. Pacheco E, Udowitz R. Nearly all consumers (97%) now use online media to shop locally, according to BIA/Kelsey and ConStat [press release]. BIA/Kelsey Web site. http://www.biakelsey.com/company/press-releases/100310-nearly-all-consumers-now-use-online-media-to-shop-locally.asp. Published March 10, 2010. Accessed August 12, 2014.
2. Baum NH, Romano R. Using the Internet in your practice. Part 1: why social media are important and how to get started. OBG Manag. 2014;26(2):25–36.