User login
Medicare Billing Regulations for Nonphysician Providers Vary by State, Facility
Nurse practitioners (NPs) and physician assistants (PAs), referred to as nonphysician providers (NPPs) in billing policy, provide many different services in the hospital setting. Roles include:
- Rounding independently and following patients of varying acuity with physician supervision. The NPP may ask the physician to see the patient, as necessary, if a change in the patient’s condition arises and warrants physician evaluation.
- Providing prompt consultative
- services when the physician is not
- readily available.
- Rounding alongside the physician and expediting the work of admission services through a combined effort.
Hospitalist programs may elect one model over another, or utilize NPPs according to existing need and shifting census. Employers must be aware of state and federal regulations, facility-imposed standards of care, and billing requirements surrounding NPP services.
Medicare Enrollment and Billing Eligibility
Certified PAs and NPs may provide covered services to Medicare beneficiaries in accordance with their state scope of practice under state law and corresponding supervision/collaboration requirements. They can submit claims for these services, providing they meet enrollment qualifications.1
PAs must have:
- Graduated from a PA educational program accredited by the Accreditation Review Commission on Education for the Physician Assistant (or its predecessor agencies, the Commission on Accreditation of Allied Health Education Programs (CAAHEP) and the Committee on Allied Health Education and Accreditation (CAHEA); or
- Passed the national certification examination administered by the National Commission on Certification of Physician Assistants (NCCPA); and
- A license as a PA in the practicing state.
NPs must:
- Be a registered nurse who is authorized and licensed by the state to practice as a nurse practitioner by Dec. 31, 2000; or
- After Jan. 1, 2001, be a registered nurse who is authorized and licensed by the state to practice as an NP and be certified by a recognized national certifying body that has established standards for NPs (e.g. American Academy of Nurse Practitioners, American Nurses Credentialing Center, AACN Certification Corp., or National Board on Certification of Hospice and Palliative Nurses); and
- Possess a master’s degree in nursing.
Independent Billing
NPPs can see patients in any setting without the presence of a physician. The physician is not required to see the patient but must be available by phone or beeper in accordance with supervisory/collaborative guidelines. Physician cosignature is not required unless mandated by state law or the facility.
NPPs document and report their services according to the Centers for Medicare & Medicaid Services (CMS) Documentation Guidelines (available at www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/EMDOC.html). The NPP should be listed as the rendering provider on the claim form. Currently, insurance programs Medicare and Aetna Inc. consistently enroll and recognize NPPs as billing providers and reimburse these services at 85% of the allowable physician rate.2
Shared/Split Billing
When two providers (a physician and NPP) from the same group (direct employment or a lease arrangement contractually linking the providers) perform a service for the same patient on the same calendar day, CMS allows the combined services to be reported under a single provider’s name.
Allowable services. NPPs are only limited by the state scope of practice under state law, and the facility rules in which the NPPs practice. Services must be performed under the appropriate level of supervision or collaboration. Medicare reimburses reasonable and necessary services not otherwise excluded from coverage.
However, shared/split rules restrict the services reported under this billing model, recognizing only evaluation and management (E/M) services (and not procedures) provided in the ED, outpatient hospital clinics, or inpatient hospital (i.e. facility-based services). Shared/split rules do not involve all types of E/M services. For hospitalist programs, critical-care services (99291-99292) are excluded.3
Physician requirement. Shared/split rules require a face-to-face patient encounter by each provider on the same calendar day. There are no billing mandates requiring the NPP to see the patient before the physician does, although practice style might govern this decision.4 CMS does not specify the extent of provider involvement, but it could be established by local Medicare contractor requirements. Some contractors reference physician participation as a “substantive” service without further elaboration on specific parameters. Therefore, the physician determines the critical or key portion of his/her personal service. Minimalistic documentation can be problematic for quality or medicolegal aspects of patient care, and physicians might benefit from a more detailed notation of participation.
Documentation. Physician documentation must include an attestation that supports the physician encounter (e.g. “Patient seen and examined by me”), the individual with whom the service is shared (e.g. “Agree with note by X”), their portion of the rendered service (e.g. “Pulse oximetry 94% on room air. Audible rhonchi at bilateral lung bases. Start O2 2L nasal cannula. Obtain CXR”), the date, and a legible signature. NPP documentation should include as similar reference to the physician with whom the service is being shared for better charge capture. It alerts coders, auditors, and payor representatives to consider both notes in support of the billed service and ensures that the correct notes are sent to the payor in the event of claim denial and subsequent appeal.
Although the visit level is supported by both provider services, only one claim may be submitted for a shared/split service. The rendering provider listed on the claim can be the physician (reimbursed at 100% of the Medicare allowable physician rate) or the NPP (reimbursed at 85% of the allowable physician rate).
Non-Medicare Claims
Shared/split billing policy only applies to Medicare beneficiaries, while independent billing policy applies to Medicare and Aetna. Excessive costs prevent most other non-Medicare insurers from credentialing and enrollment NPPs. Absence of payor policy does not disqualify reimbursement for shared services, but it does require additional measures to establish recognition of NPP services and a corresponding reimbursement model.
After determining payor mix, develop a reasonable guideline for those payors who do not enroll NPPs. Delineate, in writing, a predetermined time frame for guideline implementation unless the payor can provide an alternate billing option. Some experts suggest physician groups outline the following key issues when structuring a billing option5:
- Type of NPPs involved in patient care;
- Category of services provided;
- Service location(s);
- Physician involvement;
- Mechanism for reporting services; and
- Documentation requirements.
Guidelines can be developed for any of the billing options (independent, “incident-to,” shared/split). Be sure to obtain written payor response before initiating the billing process.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services. Medicare Benefit Policy Manual: Chapter 15, Section 190-200. Centers for Medicare & Medicaid website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/bp102c15.pdf. Accessed Nov. 5, 2012.
- Aetna Inc. Aetna office links updates. Reminder: Reimbursement change for mid-level practitioners. Aetna Inc. website. Available at www.aetna.com/provider/data/OLU_MA_JUN2010_final.pdf. Accessed Nov. 6, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. Centers for Medicare & Medicaid website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan 21, 2013.
- Pohlig, C. Nonphysician Providers in Your Practice. In: Coding for Chest Medicine 2011. Northbrook, Ill.: American College of Chest Physicians, 2010.
Nurse practitioners (NPs) and physician assistants (PAs), referred to as nonphysician providers (NPPs) in billing policy, provide many different services in the hospital setting. Roles include:
- Rounding independently and following patients of varying acuity with physician supervision. The NPP may ask the physician to see the patient, as necessary, if a change in the patient’s condition arises and warrants physician evaluation.
- Providing prompt consultative
- services when the physician is not
- readily available.
- Rounding alongside the physician and expediting the work of admission services through a combined effort.
Hospitalist programs may elect one model over another, or utilize NPPs according to existing need and shifting census. Employers must be aware of state and federal regulations, facility-imposed standards of care, and billing requirements surrounding NPP services.
Medicare Enrollment and Billing Eligibility
Certified PAs and NPs may provide covered services to Medicare beneficiaries in accordance with their state scope of practice under state law and corresponding supervision/collaboration requirements. They can submit claims for these services, providing they meet enrollment qualifications.1
PAs must have:
- Graduated from a PA educational program accredited by the Accreditation Review Commission on Education for the Physician Assistant (or its predecessor agencies, the Commission on Accreditation of Allied Health Education Programs (CAAHEP) and the Committee on Allied Health Education and Accreditation (CAHEA); or
- Passed the national certification examination administered by the National Commission on Certification of Physician Assistants (NCCPA); and
- A license as a PA in the practicing state.
NPs must:
- Be a registered nurse who is authorized and licensed by the state to practice as a nurse practitioner by Dec. 31, 2000; or
- After Jan. 1, 2001, be a registered nurse who is authorized and licensed by the state to practice as an NP and be certified by a recognized national certifying body that has established standards for NPs (e.g. American Academy of Nurse Practitioners, American Nurses Credentialing Center, AACN Certification Corp., or National Board on Certification of Hospice and Palliative Nurses); and
- Possess a master’s degree in nursing.
Independent Billing
NPPs can see patients in any setting without the presence of a physician. The physician is not required to see the patient but must be available by phone or beeper in accordance with supervisory/collaborative guidelines. Physician cosignature is not required unless mandated by state law or the facility.
NPPs document and report their services according to the Centers for Medicare & Medicaid Services (CMS) Documentation Guidelines (available at www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/EMDOC.html). The NPP should be listed as the rendering provider on the claim form. Currently, insurance programs Medicare and Aetna Inc. consistently enroll and recognize NPPs as billing providers and reimburse these services at 85% of the allowable physician rate.2
Shared/Split Billing
When two providers (a physician and NPP) from the same group (direct employment or a lease arrangement contractually linking the providers) perform a service for the same patient on the same calendar day, CMS allows the combined services to be reported under a single provider’s name.
Allowable services. NPPs are only limited by the state scope of practice under state law, and the facility rules in which the NPPs practice. Services must be performed under the appropriate level of supervision or collaboration. Medicare reimburses reasonable and necessary services not otherwise excluded from coverage.
However, shared/split rules restrict the services reported under this billing model, recognizing only evaluation and management (E/M) services (and not procedures) provided in the ED, outpatient hospital clinics, or inpatient hospital (i.e. facility-based services). Shared/split rules do not involve all types of E/M services. For hospitalist programs, critical-care services (99291-99292) are excluded.3
Physician requirement. Shared/split rules require a face-to-face patient encounter by each provider on the same calendar day. There are no billing mandates requiring the NPP to see the patient before the physician does, although practice style might govern this decision.4 CMS does not specify the extent of provider involvement, but it could be established by local Medicare contractor requirements. Some contractors reference physician participation as a “substantive” service without further elaboration on specific parameters. Therefore, the physician determines the critical or key portion of his/her personal service. Minimalistic documentation can be problematic for quality or medicolegal aspects of patient care, and physicians might benefit from a more detailed notation of participation.
Documentation. Physician documentation must include an attestation that supports the physician encounter (e.g. “Patient seen and examined by me”), the individual with whom the service is shared (e.g. “Agree with note by X”), their portion of the rendered service (e.g. “Pulse oximetry 94% on room air. Audible rhonchi at bilateral lung bases. Start O2 2L nasal cannula. Obtain CXR”), the date, and a legible signature. NPP documentation should include as similar reference to the physician with whom the service is being shared for better charge capture. It alerts coders, auditors, and payor representatives to consider both notes in support of the billed service and ensures that the correct notes are sent to the payor in the event of claim denial and subsequent appeal.
Although the visit level is supported by both provider services, only one claim may be submitted for a shared/split service. The rendering provider listed on the claim can be the physician (reimbursed at 100% of the Medicare allowable physician rate) or the NPP (reimbursed at 85% of the allowable physician rate).
Non-Medicare Claims
Shared/split billing policy only applies to Medicare beneficiaries, while independent billing policy applies to Medicare and Aetna. Excessive costs prevent most other non-Medicare insurers from credentialing and enrollment NPPs. Absence of payor policy does not disqualify reimbursement for shared services, but it does require additional measures to establish recognition of NPP services and a corresponding reimbursement model.
After determining payor mix, develop a reasonable guideline for those payors who do not enroll NPPs. Delineate, in writing, a predetermined time frame for guideline implementation unless the payor can provide an alternate billing option. Some experts suggest physician groups outline the following key issues when structuring a billing option5:
- Type of NPPs involved in patient care;
- Category of services provided;
- Service location(s);
- Physician involvement;
- Mechanism for reporting services; and
- Documentation requirements.
Guidelines can be developed for any of the billing options (independent, “incident-to,” shared/split). Be sure to obtain written payor response before initiating the billing process.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services. Medicare Benefit Policy Manual: Chapter 15, Section 190-200. Centers for Medicare & Medicaid website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/bp102c15.pdf. Accessed Nov. 5, 2012.
- Aetna Inc. Aetna office links updates. Reminder: Reimbursement change for mid-level practitioners. Aetna Inc. website. Available at www.aetna.com/provider/data/OLU_MA_JUN2010_final.pdf. Accessed Nov. 6, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. Centers for Medicare & Medicaid website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan 21, 2013.
- Pohlig, C. Nonphysician Providers in Your Practice. In: Coding for Chest Medicine 2011. Northbrook, Ill.: American College of Chest Physicians, 2010.
Nurse practitioners (NPs) and physician assistants (PAs), referred to as nonphysician providers (NPPs) in billing policy, provide many different services in the hospital setting. Roles include:
- Rounding independently and following patients of varying acuity with physician supervision. The NPP may ask the physician to see the patient, as necessary, if a change in the patient’s condition arises and warrants physician evaluation.
- Providing prompt consultative
- services when the physician is not
- readily available.
- Rounding alongside the physician and expediting the work of admission services through a combined effort.
Hospitalist programs may elect one model over another, or utilize NPPs according to existing need and shifting census. Employers must be aware of state and federal regulations, facility-imposed standards of care, and billing requirements surrounding NPP services.
Medicare Enrollment and Billing Eligibility
Certified PAs and NPs may provide covered services to Medicare beneficiaries in accordance with their state scope of practice under state law and corresponding supervision/collaboration requirements. They can submit claims for these services, providing they meet enrollment qualifications.1
PAs must have:
- Graduated from a PA educational program accredited by the Accreditation Review Commission on Education for the Physician Assistant (or its predecessor agencies, the Commission on Accreditation of Allied Health Education Programs (CAAHEP) and the Committee on Allied Health Education and Accreditation (CAHEA); or
- Passed the national certification examination administered by the National Commission on Certification of Physician Assistants (NCCPA); and
- A license as a PA in the practicing state.
NPs must:
- Be a registered nurse who is authorized and licensed by the state to practice as a nurse practitioner by Dec. 31, 2000; or
- After Jan. 1, 2001, be a registered nurse who is authorized and licensed by the state to practice as an NP and be certified by a recognized national certifying body that has established standards for NPs (e.g. American Academy of Nurse Practitioners, American Nurses Credentialing Center, AACN Certification Corp., or National Board on Certification of Hospice and Palliative Nurses); and
- Possess a master’s degree in nursing.
Independent Billing
NPPs can see patients in any setting without the presence of a physician. The physician is not required to see the patient but must be available by phone or beeper in accordance with supervisory/collaborative guidelines. Physician cosignature is not required unless mandated by state law or the facility.
NPPs document and report their services according to the Centers for Medicare & Medicaid Services (CMS) Documentation Guidelines (available at www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/EMDOC.html). The NPP should be listed as the rendering provider on the claim form. Currently, insurance programs Medicare and Aetna Inc. consistently enroll and recognize NPPs as billing providers and reimburse these services at 85% of the allowable physician rate.2
Shared/Split Billing
When two providers (a physician and NPP) from the same group (direct employment or a lease arrangement contractually linking the providers) perform a service for the same patient on the same calendar day, CMS allows the combined services to be reported under a single provider’s name.
Allowable services. NPPs are only limited by the state scope of practice under state law, and the facility rules in which the NPPs practice. Services must be performed under the appropriate level of supervision or collaboration. Medicare reimburses reasonable and necessary services not otherwise excluded from coverage.
However, shared/split rules restrict the services reported under this billing model, recognizing only evaluation and management (E/M) services (and not procedures) provided in the ED, outpatient hospital clinics, or inpatient hospital (i.e. facility-based services). Shared/split rules do not involve all types of E/M services. For hospitalist programs, critical-care services (99291-99292) are excluded.3
Physician requirement. Shared/split rules require a face-to-face patient encounter by each provider on the same calendar day. There are no billing mandates requiring the NPP to see the patient before the physician does, although practice style might govern this decision.4 CMS does not specify the extent of provider involvement, but it could be established by local Medicare contractor requirements. Some contractors reference physician participation as a “substantive” service without further elaboration on specific parameters. Therefore, the physician determines the critical or key portion of his/her personal service. Minimalistic documentation can be problematic for quality or medicolegal aspects of patient care, and physicians might benefit from a more detailed notation of participation.
Documentation. Physician documentation must include an attestation that supports the physician encounter (e.g. “Patient seen and examined by me”), the individual with whom the service is shared (e.g. “Agree with note by X”), their portion of the rendered service (e.g. “Pulse oximetry 94% on room air. Audible rhonchi at bilateral lung bases. Start O2 2L nasal cannula. Obtain CXR”), the date, and a legible signature. NPP documentation should include as similar reference to the physician with whom the service is being shared for better charge capture. It alerts coders, auditors, and payor representatives to consider both notes in support of the billed service and ensures that the correct notes are sent to the payor in the event of claim denial and subsequent appeal.
Although the visit level is supported by both provider services, only one claim may be submitted for a shared/split service. The rendering provider listed on the claim can be the physician (reimbursed at 100% of the Medicare allowable physician rate) or the NPP (reimbursed at 85% of the allowable physician rate).
Non-Medicare Claims
Shared/split billing policy only applies to Medicare beneficiaries, while independent billing policy applies to Medicare and Aetna. Excessive costs prevent most other non-Medicare insurers from credentialing and enrollment NPPs. Absence of payor policy does not disqualify reimbursement for shared services, but it does require additional measures to establish recognition of NPP services and a corresponding reimbursement model.
After determining payor mix, develop a reasonable guideline for those payors who do not enroll NPPs. Delineate, in writing, a predetermined time frame for guideline implementation unless the payor can provide an alternate billing option. Some experts suggest physician groups outline the following key issues when structuring a billing option5:
- Type of NPPs involved in patient care;
- Category of services provided;
- Service location(s);
- Physician involvement;
- Mechanism for reporting services; and
- Documentation requirements.
Guidelines can be developed for any of the billing options (independent, “incident-to,” shared/split). Be sure to obtain written payor response before initiating the billing process.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services. Medicare Benefit Policy Manual: Chapter 15, Section 190-200. Centers for Medicare & Medicaid website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/bp102c15.pdf. Accessed Nov. 5, 2012.
- Aetna Inc. Aetna office links updates. Reminder: Reimbursement change for mid-level practitioners. Aetna Inc. website. Available at www.aetna.com/provider/data/OLU_MA_JUN2010_final.pdf. Accessed Nov. 6, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. Centers for Medicare & Medicaid website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan 21, 2013.
- Pohlig, C. Nonphysician Providers in Your Practice. In: Coding for Chest Medicine 2011. Northbrook, Ill.: American College of Chest Physicians, 2010.
Hospital Medicine Group Leaders Strive to Balance Administrative, Clinical Tasks
Balance Is Key to HM Group Leaders’ Clinical Load
Should the leader of my hospitalist group have a lighter clinical load?
Cheryl Clinkenbeard, DO, MPH, Bartlesville, Okla.
Dr. Hospitalist responds:
This is an incredibly tough question, and it applies to pretty much every hospitalist program in existence. Big, small, private, teaching—every program needs leaders.
For starters, being a hospitalist program leader is generally a thankless job. It involves a heck of a lot of meetings, administrative hassles, and parsing of complaints. In my experience, it also tends to be a horrifically underpaid position. There generally is no waiting list of clinicians begging to be the group leader. Given all the time demands, I think it is perfectly reasonable to expect a leader to have a lighter clinical load. There is no way to fulfill both clinical and administrative duties while working full time, unless the group is very small (less than six FTEs). On the other hand, having a leader do no clinical work is pretty much a recipe for disaster. If your group leader is a clinician and does a lot less, or no clinical work, they will lose credibility with colleagues quickly. Group leaders focused solely on administration also lose sight of the day-to-day morale and activem issues facing the group.
The crux is trying to find the balance between admin and clinical duties. I think it is preferable to have a leader work fewer shifts but take an equivalent clinical load on those days. That allows group leaders to be viewed as “one of the team,” with the same shift responsibilities as everyone else—just not as many shifts. It’s a better way to understand the day-to-day variations and concerns of the job.
The other option is to have the leader work the same number of shifts but take a smaller census. I think this is a bad idea, mainly from the standpoint that HM is nothing if not unpredictable, and trying to protect one person’s census on a busy day is an impossible task. Either the leader will end up taking on too much clinical work (to help even the census) or the rest of the group will feel bitter that the group leader is not always available to help. I’ve seen both sides of this equation, and it is just not a good working environment.
Another factor to consider are the “undesirable” shifts. Whether it is nights or weekends, there are always shifts that folks would rather not do. A leader should continue to work these shifts, even at a reduced number, for the same reasons. Becoming an HM leader is not an excuse to design the perfect, protected schedule at the expense of the other physicians.
On balance, I think the hospitalist group leader ends up with more work, similar schedule obligations, and an inadequate pay structure. That does not make the position particularly attractive, as has been my experience over the years. However, given the opportunity to modify those variables, I think the shifts should be kept “whole” and reduced only in number, with the remainder of the compensation for the work coming in the form of increased pay. How much, you ask? Well, have a seat; this could take a while.
Balance Is Key to HM Group Leaders’ Clinical Load
Should the leader of my hospitalist group have a lighter clinical load?
Cheryl Clinkenbeard, DO, MPH, Bartlesville, Okla.
Dr. Hospitalist responds:
This is an incredibly tough question, and it applies to pretty much every hospitalist program in existence. Big, small, private, teaching—every program needs leaders.
For starters, being a hospitalist program leader is generally a thankless job. It involves a heck of a lot of meetings, administrative hassles, and parsing of complaints. In my experience, it also tends to be a horrifically underpaid position. There generally is no waiting list of clinicians begging to be the group leader. Given all the time demands, I think it is perfectly reasonable to expect a leader to have a lighter clinical load. There is no way to fulfill both clinical and administrative duties while working full time, unless the group is very small (less than six FTEs). On the other hand, having a leader do no clinical work is pretty much a recipe for disaster. If your group leader is a clinician and does a lot less, or no clinical work, they will lose credibility with colleagues quickly. Group leaders focused solely on administration also lose sight of the day-to-day morale and activem issues facing the group.
The crux is trying to find the balance between admin and clinical duties. I think it is preferable to have a leader work fewer shifts but take an equivalent clinical load on those days. That allows group leaders to be viewed as “one of the team,” with the same shift responsibilities as everyone else—just not as many shifts. It’s a better way to understand the day-to-day variations and concerns of the job.
The other option is to have the leader work the same number of shifts but take a smaller census. I think this is a bad idea, mainly from the standpoint that HM is nothing if not unpredictable, and trying to protect one person’s census on a busy day is an impossible task. Either the leader will end up taking on too much clinical work (to help even the census) or the rest of the group will feel bitter that the group leader is not always available to help. I’ve seen both sides of this equation, and it is just not a good working environment.
Another factor to consider are the “undesirable” shifts. Whether it is nights or weekends, there are always shifts that folks would rather not do. A leader should continue to work these shifts, even at a reduced number, for the same reasons. Becoming an HM leader is not an excuse to design the perfect, protected schedule at the expense of the other physicians.
On balance, I think the hospitalist group leader ends up with more work, similar schedule obligations, and an inadequate pay structure. That does not make the position particularly attractive, as has been my experience over the years. However, given the opportunity to modify those variables, I think the shifts should be kept “whole” and reduced only in number, with the remainder of the compensation for the work coming in the form of increased pay. How much, you ask? Well, have a seat; this could take a while.
Balance Is Key to HM Group Leaders’ Clinical Load
Should the leader of my hospitalist group have a lighter clinical load?
Cheryl Clinkenbeard, DO, MPH, Bartlesville, Okla.
Dr. Hospitalist responds:
This is an incredibly tough question, and it applies to pretty much every hospitalist program in existence. Big, small, private, teaching—every program needs leaders.
For starters, being a hospitalist program leader is generally a thankless job. It involves a heck of a lot of meetings, administrative hassles, and parsing of complaints. In my experience, it also tends to be a horrifically underpaid position. There generally is no waiting list of clinicians begging to be the group leader. Given all the time demands, I think it is perfectly reasonable to expect a leader to have a lighter clinical load. There is no way to fulfill both clinical and administrative duties while working full time, unless the group is very small (less than six FTEs). On the other hand, having a leader do no clinical work is pretty much a recipe for disaster. If your group leader is a clinician and does a lot less, or no clinical work, they will lose credibility with colleagues quickly. Group leaders focused solely on administration also lose sight of the day-to-day morale and activem issues facing the group.
The crux is trying to find the balance between admin and clinical duties. I think it is preferable to have a leader work fewer shifts but take an equivalent clinical load on those days. That allows group leaders to be viewed as “one of the team,” with the same shift responsibilities as everyone else—just not as many shifts. It’s a better way to understand the day-to-day variations and concerns of the job.
The other option is to have the leader work the same number of shifts but take a smaller census. I think this is a bad idea, mainly from the standpoint that HM is nothing if not unpredictable, and trying to protect one person’s census on a busy day is an impossible task. Either the leader will end up taking on too much clinical work (to help even the census) or the rest of the group will feel bitter that the group leader is not always available to help. I’ve seen both sides of this equation, and it is just not a good working environment.
Another factor to consider are the “undesirable” shifts. Whether it is nights or weekends, there are always shifts that folks would rather not do. A leader should continue to work these shifts, even at a reduced number, for the same reasons. Becoming an HM leader is not an excuse to design the perfect, protected schedule at the expense of the other physicians.
On balance, I think the hospitalist group leader ends up with more work, similar schedule obligations, and an inadequate pay structure. That does not make the position particularly attractive, as has been my experience over the years. However, given the opportunity to modify those variables, I think the shifts should be kept “whole” and reduced only in number, with the remainder of the compensation for the work coming in the form of increased pay. How much, you ask? Well, have a seat; this could take a while.
Automated Hospital Inpatient Assignment Program Increases Efficiency, Coordination of Care
A computerized patient assignment program to distribute new hospital admissions among 12 hospitalist-led, unit-based teams at Our Lady of the Lake Hospital in Baton Rouge, La., not only saves time and improves coordination of care, but also helps to build trust and satisfaction with patients, according to a poster presented at HM12.
Lead author and hospitalist Eric Wascome, MD, says the automated program takes into account patient medical intensity scores aggregated by hospital team in deciding who should get the next patient, thus smoothing out the referral process and minimizing hard feelings that some physicians are getting more than their fair share of work. The program also adjusts for particular units and room locations and incorporates physician preferences, then spits out the next referral within minutes. It also reduces the need to reassign rooms and allows patients to be told who their next-day hospitalist will be when they are admitted to the hospital overnight.
“It takes a complicated, head-scratching process and makes it a no-brainer,” Dr. Wascome says.
The Web-based, HIPAA-compliant program has thrived since Dr. Wascome’s presentation in April 2012. “A new twist is that we’ve added the capacity to bring in doctors who are not scheduled to work if they are needed on a voluntary basis, to address higher volumes of patients, and to have them on site within an hour,” he says.
Hospitalists say they approve of computerized patient scheduling, which was programmed by Dr. Wascome based on previous spreadsheet-based approaches to scheduling. Automation, he says, makes possible greater numbers of variables.
For more information, email Dr. Wascome at [email protected].
A computerized patient assignment program to distribute new hospital admissions among 12 hospitalist-led, unit-based teams at Our Lady of the Lake Hospital in Baton Rouge, La., not only saves time and improves coordination of care, but also helps to build trust and satisfaction with patients, according to a poster presented at HM12.
Lead author and hospitalist Eric Wascome, MD, says the automated program takes into account patient medical intensity scores aggregated by hospital team in deciding who should get the next patient, thus smoothing out the referral process and minimizing hard feelings that some physicians are getting more than their fair share of work. The program also adjusts for particular units and room locations and incorporates physician preferences, then spits out the next referral within minutes. It also reduces the need to reassign rooms and allows patients to be told who their next-day hospitalist will be when they are admitted to the hospital overnight.
“It takes a complicated, head-scratching process and makes it a no-brainer,” Dr. Wascome says.
The Web-based, HIPAA-compliant program has thrived since Dr. Wascome’s presentation in April 2012. “A new twist is that we’ve added the capacity to bring in doctors who are not scheduled to work if they are needed on a voluntary basis, to address higher volumes of patients, and to have them on site within an hour,” he says.
Hospitalists say they approve of computerized patient scheduling, which was programmed by Dr. Wascome based on previous spreadsheet-based approaches to scheduling. Automation, he says, makes possible greater numbers of variables.
For more information, email Dr. Wascome at [email protected].
A computerized patient assignment program to distribute new hospital admissions among 12 hospitalist-led, unit-based teams at Our Lady of the Lake Hospital in Baton Rouge, La., not only saves time and improves coordination of care, but also helps to build trust and satisfaction with patients, according to a poster presented at HM12.
Lead author and hospitalist Eric Wascome, MD, says the automated program takes into account patient medical intensity scores aggregated by hospital team in deciding who should get the next patient, thus smoothing out the referral process and minimizing hard feelings that some physicians are getting more than their fair share of work. The program also adjusts for particular units and room locations and incorporates physician preferences, then spits out the next referral within minutes. It also reduces the need to reassign rooms and allows patients to be told who their next-day hospitalist will be when they are admitted to the hospital overnight.
“It takes a complicated, head-scratching process and makes it a no-brainer,” Dr. Wascome says.
The Web-based, HIPAA-compliant program has thrived since Dr. Wascome’s presentation in April 2012. “A new twist is that we’ve added the capacity to bring in doctors who are not scheduled to work if they are needed on a voluntary basis, to address higher volumes of patients, and to have them on site within an hour,” he says.
Hospitalists say they approve of computerized patient scheduling, which was programmed by Dr. Wascome based on previous spreadsheet-based approaches to scheduling. Automation, he says, makes possible greater numbers of variables.
For more information, email Dr. Wascome at [email protected].
EHRs and medicolegal risk: How they help, when they could hurt
Survey: Many physicians plan to leave or scale down practice
Janelle Yates (February 2012)
Is private ObGyn practice on its way out?
Lucia DiVenere, MA (October 2011)
The medical record has evolved considerably since it originated in ancient Greece as a narrative of cure.1 For one thing, it’s now electronic. For another, it’s no longer a medical record but a health record. According to the US Department of Health and Human Services, the distinction is not a trivial one. A medical record is used by clinicians mostly for diagnosis and treatment, whereas the health record focuses on the total wellbeing of the patient.2 The medical record is used primarily within a practice. The electronic health record (EHR) reaches across borders to other offices, institutions, and clinicians.
Use of the EHR has been stimulated by the Health Information Technology for Economic and Clinical Health Act,3 which offers grants and incentives for “meaningful use” of electronic records.4 After 2014, medical practices that do not use EHRs will face a financial penalty that amounts to 2% of 2013 clinical revenue.
EHRs have been hailed as a panacea and derided as anathema. Whatever your perspective, there is no denying that they dramatically increase the immediate and easy availability of information and, therefore, influence decision-making in regard to medical care, cost-effectiveness, and patient safety. EHRs have the potential to improve communication, broaden access to information, and help guide clinical decision-making through the use of best-practice algorithms. When used properly—which means taking advantage of the EHR’s full potential and adapting to the way information is organized and analyzed—the EHR can reduce adverse events and help defend the appropriateness of the care provided. This lowers your medicolegal risk. When used improperly or haphazardly, they may increase that risk. In this article, we elaborate on both.
EHRs have many benefits
Improved communication. EHRs facilitate communication between healthcare providers. A primary care physician can access a consultant’s report practically as it is written. Providers also can carry on a dialogue electronically, planning together for care that will best serve the patient, with less redundancy and time.
The EHR also facilitates communication between physician and patient, allowing the physician to see the patient’s recent history and plan her management while speaking to her on the phone. Issues can be addressed with greater accuracy and expediency, leading to reduced anxiety for the patient and increased compliance.
Seamless integration. Information can be entered into the EHR and integrated into the full record more seamlessly than it is with written records. And data can be entered once and used many times.
Enhanced decision-making. Decision-making depends on careful analysis of a clinical scenario. Protocols, templates, and order sets embedded in the EHR can reduce medical errors by identifying scenarios for the physician to review.5,6
The EHR can also highlight adverse drug-drug interactions and help avoid potential allergic reactions. Murphy and colleagues reported a reduction of medical errors by utilizing a pharmacy-driven EHR component—a reduction from 90% to 47% on the surgical unit and from 57% to 33% on the medicine unit.7
Improved documentation. The EHR can enhance documentation by offering specific and detailed templates for informed consent, making it more comprehensive than a handwritten notation of the risks and benefits.
Decipherability is another strength of the EHR. Because physicians are notorious for poor handwriting skills, some hospitals now require a writing sample as part of their privileging process. The EHR avoids this issue entirely.8 Typos and grammatical errors are minimized by spellchecking and grammar-correcting programs written into the EHR.
Quality assurance. Timely evaluation of approaches to clinical care is available to physicians as well as hospitals that use EHRs.9 An individual physician can perform personal quality-assurance audits. And hospital management can gather cumulative statistics more quickly and easily.5,6,10,11
Patient data can be accessed independent of medical department, with lab tests, imaging studies, and pathology reports readily available for review. And accessibility is available regardless of geographic location.
EHRs are not perfect, and neither are their users. EHRs present the potential for problems related to absent or erroneous data entry, patient privacy issues, misunderstanding and misuse of software, and development of metadata.
With initial use, EHRs can create documentation gaps with the transition from paper to electronic records. In addition, inadequate provider training can create new error pathways, and a failure to use EHRs consistently can lead to loss of data and communication errors. These gaps and errors can increase medicolegal risk, as can the more extensive documentation often seen with early use, which creates more discoverable data. The temptation to cut and paste risks repeating earlier errors and omitting new information.
Another area of risk involves communication with the patient via email. A failure to reply could result in claims of negligence, and information overload could obscure pertinent pieces of information. And a departure from clinical decision support could be used by the patient to defend allegations of negligence.
With widespread use of EHRs, improved access to data could change the “duty” owed to the patient. In addition, clinical decision support embedded within the software could become the de facto “standard of care.”
The learning curve can be steep
The learning curve for EHRs may be steep and, at times, discouraging. One reason is that data are organized differently than in the conventional paper record, where information is read and analyzed in a progressive and stepwise manner, as in an analog or vertical system. The EHR is a digital format, so finding information requires digital (horizontal) inquiry. Information is, therefore, utilized in both horizontal and vertical formats in everyday situations. If data are entered incorrectly, all subsequent decisions could be flawed. And if the EHR suggests a plan, and that plan is not performed by the provider, the risk of liability could increase.
Inadvertent violation of the Health Insurance Portability and Accountability Act (HIPAA) with an EHR could increase medicolegal risk. For example, HIPAA allows for patients to make corrections to inaccurate information in their personal documents, but access by the patient could require the physician to review all records viewed by the patient after visit notes have been entered. This could drive up the cost of practice and reduce face-to-face time between physician and patient. Patients are not necessarily the best judges of which information is most important in their medical records.
Internet access raises concerns about the privacy of sensitive issues and misuse of information. Making a patient’s protected health information accessible electronically leaves physicians and hospitals at risk for a government fine or lawsuit. In several instances, the US Department of Health and Human Services (HHS) has levied fines against small practices and government agencies.
In one case, HHS fined Phoenix Cardiac Surgery in Phoenix, Arizona, $100,000 for posting surgery and appointment schedules on an Internet-based calendar that was accessible to the public.12 In another, HHS fined the Massachusetts Eye and Ear Infirmary in Boston $1.5 million after it reported the loss of an encrypted personal laptop containing the protected health information of patients and research subjects.13 The Alaska Department of Health and Social Services (DHSS) agreed to pay HHS $1.7 million after it reported the loss of a USB drive—possibly containing protected health information—from the vehicle of a DHSS employee.14
In traditional physician practices that employ handwritten records, the potential for compromise of patient information is limited. An organization may lose a few patient charts in the office and recover from the loss without incident. With the EHR, the loss poses a significant threat. The cases mentioned above were attributed to negligence or ignorance. The consequences could be worse if the compromise of EHR data is determined to be intentional. On September 4, 2010, hackers may have exposed the personal information of approximately 9,493 patients at Southwest Seattle Orthopaedics and Sports Medicine in Burien, Washington. Even with the best encryption technology, any electronic system remains vulnerable to external attack.
Metadata reveal how original data are used
Another concern regarding EHRs involves metadata—”data about data content.”15 Metadata is structured information that describes, locates, explains, or manages information. Metadata relevant to the EHR includes the data and time it was reviewed by the provider and whether it was manipulated in any way. Clearly, there is a potential for use and misuse by third-party reviewers.
Specialty-specific EHRs are recommended
Many ObGyns have found that most EHR systems are inadequate to the task of recording and analyzing information relevant to their specialty. Obstetric care is episodic and frequent. Data are added into the flow that must be considered at each visit, such as gestational age, fetal growth, labs (and normative values), prenatal diagnostic studies, and so on, representing both vertical and horizontal processing.16
The legal discovery process poses challenges that have not yet been resolved
The legal discovery process grants all parties to a lawsuit equal access to information. Under ideal circumstances, the EHR can provide comprehensive data more quickly than traditional records can. The problem is determining what constitutes relevant data and which party has the burden or benefit of making that decision. Uncontrolled access has the potential to violate privacy and privilege requirements.
Rules regarding discovery are still being debated in regard to their applicability to digital discovery.17 Even before a lawsuit is filed, the potential for “data mining” by third parties could lead to allegations of malpractice.
How to use EHRs responsibly without increasing risk
Good communication between patient and provider is paramount in the provision of quality medical care. Adherence to evidence-based standards with thorough documentation always serves the best interests of both patients and providers. The EHR can facilitate this process.
Our recommendations for appropriate use of your EHR include:
- Spend time learning the ins and outs of your particular EHR, and make sure your staff does the same. This will help reduce the likelihood that errors will be introduced into the record and ensure consistent use.
- Use individual sign-ons for anyone involved in data entry. This step facilitates the identification of users responsible for inaccurate use or errors, so that the situation can be addressed efficiently.
- Do not let third parties enter or manipulate data. This could jeopardize patient privacy, as well as the integrity of the record itself.
- Track all data entry on a regular basis. The frequency of tracking should be a function of routine as well as clinical circumstance. All new data from the previous interval should be reviewed at the time of the subsequent visit in order to direct care and ensure proper data entry.
Because of the considerable risk of liability claims in ObGyn practice, it is critical that the medical record accurately and precisely reflects the circumstances of each case. The EHR can be an effective and useful tool to document what occurred (and when) in a clinical scenario.18 As with all medical records, completeness and accuracy are the first and best defense against allegations of medical malpractice.
1. The Casebooks Project. History of Medical Record-keeping. http://www.magicandmedicine.hps.cam.ac.uk/on-astrological-medicine/further-reading/history-of-medical-record-keeping/. Accessed February 26 2013.
2. US Department of Health and Human Services. EMR vs EHR—What is the difference? Health IT Buzz. http://www.healthit.gov/buzz-blog/electronic-health-and-medical-records/emr-vs-ehr-difference/. Accessed February 20, 2013.
3. Health Information Technology for Economic and Clinical Health Act of 2009. HITECH Act. Pub L No 111-5 Div A tit XIII Div B tit IV Feb 17 2009, 123 stat 226, 467. Codified in scattered sections of 42 USCA.
4. Mangalmurti S, Murtagh L, Mello M. Medical malpractice liability in the age of electronic health records. N Engl J Med. 2010;363(21):2060-2067.
5. Reid P, Compton D, Grossman J, et al. Building a Better Delivery System: A New Engineering/Healthcare Partnership. Committee on Engineering and the Health Care System, Institute of Medicine and the National Academy of Engineering. Washington, DC: National Academies Press; 2005.
6. Grossman J. Disruptive innovation in healthcare: challenges for engineering. The Bridge. 2008;38:10-16.
7. Murphy E, Oxencis C, Klauck J, et al. Medication reconciliation at an academic medical center; implementation of a comprehensive program from admission to discharge. Am J Health-System Pharmacy. 2009;66(23):2126-2131.
8. Schuler R. The smart grid: a bridge between emerging technologies society and the environment. The Bridge. 2010;40:42-49.
9. Haberman S, Feldman J, Merhi Z, et al. Effect of clinical decision support on documentation compliance in an electronic medical record. Obstet Gynecol. 2009;114(2 Pt 1):311-317.
10. Hasley S. Decision support and patient safety: the time has come. Am J Obstet Gynecol. 2011;204(6):461-465.
11. Lagrew D, Stutman H, Sicaeros L. Voluntary physician adoption of an inpatient electronic medical record by obstetrician-gynecologists. Am J Obstet Gynecol. 2008;198(6):690.e1-e6.
12. Dolan PL. $100,000 HIPAA fine designed to send message to small physician practices. American Medical News. 2012. http://www.ama-assn.org/amednews/2012/04/30/bisd0502.htm. Accessed February 26, 2013.
13. US Department of Health and Human Services. Massachusetts provider settles HIPAA case for $1.5 million [news release]. September 17 2012. http://www.hhs.gov/news/press/2012pres/09/20120917a.html. Accessed February 26, 2013.
14. US Department of Health and Human Services. Alaska settles HIPAA security case for $1,700,000 [news release]. June 26, 2012. http://www.hhs.gov/news/press/2012pres/06/20120626a.html. Accessed February 26, 2013.
15. National Information Standards Organization. Understanding Metadata. Bethesda MD: NISO Press; 2004. http://www.niso.org/publications/press/UnderstandingMetadata.pdf. Accessed February 26, 2013.
16. McCoy M, Diamond A, Strunk A. Special requirements of electronic medical record systems in obstetrics and gynecology. Obstet Gynecol. 2010;116(1):140-143.
17. The Berkman Center for Internet and Society at Harvard Law School. The Federal Rules of Civil Procedure: The Impact of Digital Discovery. http://cyber.law.harvard.edu/digitaldiscovery/digdisc_library_4.html. Accessed February 26 2013.
18. Quinn M, Kats A, Kleinman K, et al. The relationship between electronic health records and malpractice claims. Arch Intern Med. 2012;172(15):1187-1188.
Survey: Many physicians plan to leave or scale down practice
Janelle Yates (February 2012)
Is private ObGyn practice on its way out?
Lucia DiVenere, MA (October 2011)
The medical record has evolved considerably since it originated in ancient Greece as a narrative of cure.1 For one thing, it’s now electronic. For another, it’s no longer a medical record but a health record. According to the US Department of Health and Human Services, the distinction is not a trivial one. A medical record is used by clinicians mostly for diagnosis and treatment, whereas the health record focuses on the total wellbeing of the patient.2 The medical record is used primarily within a practice. The electronic health record (EHR) reaches across borders to other offices, institutions, and clinicians.
Use of the EHR has been stimulated by the Health Information Technology for Economic and Clinical Health Act,3 which offers grants and incentives for “meaningful use” of electronic records.4 After 2014, medical practices that do not use EHRs will face a financial penalty that amounts to 2% of 2013 clinical revenue.
EHRs have been hailed as a panacea and derided as anathema. Whatever your perspective, there is no denying that they dramatically increase the immediate and easy availability of information and, therefore, influence decision-making in regard to medical care, cost-effectiveness, and patient safety. EHRs have the potential to improve communication, broaden access to information, and help guide clinical decision-making through the use of best-practice algorithms. When used properly—which means taking advantage of the EHR’s full potential and adapting to the way information is organized and analyzed—the EHR can reduce adverse events and help defend the appropriateness of the care provided. This lowers your medicolegal risk. When used improperly or haphazardly, they may increase that risk. In this article, we elaborate on both.
EHRs have many benefits
Improved communication. EHRs facilitate communication between healthcare providers. A primary care physician can access a consultant’s report practically as it is written. Providers also can carry on a dialogue electronically, planning together for care that will best serve the patient, with less redundancy and time.
The EHR also facilitates communication between physician and patient, allowing the physician to see the patient’s recent history and plan her management while speaking to her on the phone. Issues can be addressed with greater accuracy and expediency, leading to reduced anxiety for the patient and increased compliance.
Seamless integration. Information can be entered into the EHR and integrated into the full record more seamlessly than it is with written records. And data can be entered once and used many times.
Enhanced decision-making. Decision-making depends on careful analysis of a clinical scenario. Protocols, templates, and order sets embedded in the EHR can reduce medical errors by identifying scenarios for the physician to review.5,6
The EHR can also highlight adverse drug-drug interactions and help avoid potential allergic reactions. Murphy and colleagues reported a reduction of medical errors by utilizing a pharmacy-driven EHR component—a reduction from 90% to 47% on the surgical unit and from 57% to 33% on the medicine unit.7
Improved documentation. The EHR can enhance documentation by offering specific and detailed templates for informed consent, making it more comprehensive than a handwritten notation of the risks and benefits.
Decipherability is another strength of the EHR. Because physicians are notorious for poor handwriting skills, some hospitals now require a writing sample as part of their privileging process. The EHR avoids this issue entirely.8 Typos and grammatical errors are minimized by spellchecking and grammar-correcting programs written into the EHR.
Quality assurance. Timely evaluation of approaches to clinical care is available to physicians as well as hospitals that use EHRs.9 An individual physician can perform personal quality-assurance audits. And hospital management can gather cumulative statistics more quickly and easily.5,6,10,11
Patient data can be accessed independent of medical department, with lab tests, imaging studies, and pathology reports readily available for review. And accessibility is available regardless of geographic location.
EHRs are not perfect, and neither are their users. EHRs present the potential for problems related to absent or erroneous data entry, patient privacy issues, misunderstanding and misuse of software, and development of metadata.
With initial use, EHRs can create documentation gaps with the transition from paper to electronic records. In addition, inadequate provider training can create new error pathways, and a failure to use EHRs consistently can lead to loss of data and communication errors. These gaps and errors can increase medicolegal risk, as can the more extensive documentation often seen with early use, which creates more discoverable data. The temptation to cut and paste risks repeating earlier errors and omitting new information.
Another area of risk involves communication with the patient via email. A failure to reply could result in claims of negligence, and information overload could obscure pertinent pieces of information. And a departure from clinical decision support could be used by the patient to defend allegations of negligence.
With widespread use of EHRs, improved access to data could change the “duty” owed to the patient. In addition, clinical decision support embedded within the software could become the de facto “standard of care.”
The learning curve can be steep
The learning curve for EHRs may be steep and, at times, discouraging. One reason is that data are organized differently than in the conventional paper record, where information is read and analyzed in a progressive and stepwise manner, as in an analog or vertical system. The EHR is a digital format, so finding information requires digital (horizontal) inquiry. Information is, therefore, utilized in both horizontal and vertical formats in everyday situations. If data are entered incorrectly, all subsequent decisions could be flawed. And if the EHR suggests a plan, and that plan is not performed by the provider, the risk of liability could increase.
Inadvertent violation of the Health Insurance Portability and Accountability Act (HIPAA) with an EHR could increase medicolegal risk. For example, HIPAA allows for patients to make corrections to inaccurate information in their personal documents, but access by the patient could require the physician to review all records viewed by the patient after visit notes have been entered. This could drive up the cost of practice and reduce face-to-face time between physician and patient. Patients are not necessarily the best judges of which information is most important in their medical records.
Internet access raises concerns about the privacy of sensitive issues and misuse of information. Making a patient’s protected health information accessible electronically leaves physicians and hospitals at risk for a government fine or lawsuit. In several instances, the US Department of Health and Human Services (HHS) has levied fines against small practices and government agencies.
In one case, HHS fined Phoenix Cardiac Surgery in Phoenix, Arizona, $100,000 for posting surgery and appointment schedules on an Internet-based calendar that was accessible to the public.12 In another, HHS fined the Massachusetts Eye and Ear Infirmary in Boston $1.5 million after it reported the loss of an encrypted personal laptop containing the protected health information of patients and research subjects.13 The Alaska Department of Health and Social Services (DHSS) agreed to pay HHS $1.7 million after it reported the loss of a USB drive—possibly containing protected health information—from the vehicle of a DHSS employee.14
In traditional physician practices that employ handwritten records, the potential for compromise of patient information is limited. An organization may lose a few patient charts in the office and recover from the loss without incident. With the EHR, the loss poses a significant threat. The cases mentioned above were attributed to negligence or ignorance. The consequences could be worse if the compromise of EHR data is determined to be intentional. On September 4, 2010, hackers may have exposed the personal information of approximately 9,493 patients at Southwest Seattle Orthopaedics and Sports Medicine in Burien, Washington. Even with the best encryption technology, any electronic system remains vulnerable to external attack.
Metadata reveal how original data are used
Another concern regarding EHRs involves metadata—”data about data content.”15 Metadata is structured information that describes, locates, explains, or manages information. Metadata relevant to the EHR includes the data and time it was reviewed by the provider and whether it was manipulated in any way. Clearly, there is a potential for use and misuse by third-party reviewers.
Specialty-specific EHRs are recommended
Many ObGyns have found that most EHR systems are inadequate to the task of recording and analyzing information relevant to their specialty. Obstetric care is episodic and frequent. Data are added into the flow that must be considered at each visit, such as gestational age, fetal growth, labs (and normative values), prenatal diagnostic studies, and so on, representing both vertical and horizontal processing.16
The legal discovery process poses challenges that have not yet been resolved
The legal discovery process grants all parties to a lawsuit equal access to information. Under ideal circumstances, the EHR can provide comprehensive data more quickly than traditional records can. The problem is determining what constitutes relevant data and which party has the burden or benefit of making that decision. Uncontrolled access has the potential to violate privacy and privilege requirements.
Rules regarding discovery are still being debated in regard to their applicability to digital discovery.17 Even before a lawsuit is filed, the potential for “data mining” by third parties could lead to allegations of malpractice.
How to use EHRs responsibly without increasing risk
Good communication between patient and provider is paramount in the provision of quality medical care. Adherence to evidence-based standards with thorough documentation always serves the best interests of both patients and providers. The EHR can facilitate this process.
Our recommendations for appropriate use of your EHR include:
- Spend time learning the ins and outs of your particular EHR, and make sure your staff does the same. This will help reduce the likelihood that errors will be introduced into the record and ensure consistent use.
- Use individual sign-ons for anyone involved in data entry. This step facilitates the identification of users responsible for inaccurate use or errors, so that the situation can be addressed efficiently.
- Do not let third parties enter or manipulate data. This could jeopardize patient privacy, as well as the integrity of the record itself.
- Track all data entry on a regular basis. The frequency of tracking should be a function of routine as well as clinical circumstance. All new data from the previous interval should be reviewed at the time of the subsequent visit in order to direct care and ensure proper data entry.
Because of the considerable risk of liability claims in ObGyn practice, it is critical that the medical record accurately and precisely reflects the circumstances of each case. The EHR can be an effective and useful tool to document what occurred (and when) in a clinical scenario.18 As with all medical records, completeness and accuracy are the first and best defense against allegations of medical malpractice.
Survey: Many physicians plan to leave or scale down practice
Janelle Yates (February 2012)
Is private ObGyn practice on its way out?
Lucia DiVenere, MA (October 2011)
The medical record has evolved considerably since it originated in ancient Greece as a narrative of cure.1 For one thing, it’s now electronic. For another, it’s no longer a medical record but a health record. According to the US Department of Health and Human Services, the distinction is not a trivial one. A medical record is used by clinicians mostly for diagnosis and treatment, whereas the health record focuses on the total wellbeing of the patient.2 The medical record is used primarily within a practice. The electronic health record (EHR) reaches across borders to other offices, institutions, and clinicians.
Use of the EHR has been stimulated by the Health Information Technology for Economic and Clinical Health Act,3 which offers grants and incentives for “meaningful use” of electronic records.4 After 2014, medical practices that do not use EHRs will face a financial penalty that amounts to 2% of 2013 clinical revenue.
EHRs have been hailed as a panacea and derided as anathema. Whatever your perspective, there is no denying that they dramatically increase the immediate and easy availability of information and, therefore, influence decision-making in regard to medical care, cost-effectiveness, and patient safety. EHRs have the potential to improve communication, broaden access to information, and help guide clinical decision-making through the use of best-practice algorithms. When used properly—which means taking advantage of the EHR’s full potential and adapting to the way information is organized and analyzed—the EHR can reduce adverse events and help defend the appropriateness of the care provided. This lowers your medicolegal risk. When used improperly or haphazardly, they may increase that risk. In this article, we elaborate on both.
EHRs have many benefits
Improved communication. EHRs facilitate communication between healthcare providers. A primary care physician can access a consultant’s report practically as it is written. Providers also can carry on a dialogue electronically, planning together for care that will best serve the patient, with less redundancy and time.
The EHR also facilitates communication between physician and patient, allowing the physician to see the patient’s recent history and plan her management while speaking to her on the phone. Issues can be addressed with greater accuracy and expediency, leading to reduced anxiety for the patient and increased compliance.
Seamless integration. Information can be entered into the EHR and integrated into the full record more seamlessly than it is with written records. And data can be entered once and used many times.
Enhanced decision-making. Decision-making depends on careful analysis of a clinical scenario. Protocols, templates, and order sets embedded in the EHR can reduce medical errors by identifying scenarios for the physician to review.5,6
The EHR can also highlight adverse drug-drug interactions and help avoid potential allergic reactions. Murphy and colleagues reported a reduction of medical errors by utilizing a pharmacy-driven EHR component—a reduction from 90% to 47% on the surgical unit and from 57% to 33% on the medicine unit.7
Improved documentation. The EHR can enhance documentation by offering specific and detailed templates for informed consent, making it more comprehensive than a handwritten notation of the risks and benefits.
Decipherability is another strength of the EHR. Because physicians are notorious for poor handwriting skills, some hospitals now require a writing sample as part of their privileging process. The EHR avoids this issue entirely.8 Typos and grammatical errors are minimized by spellchecking and grammar-correcting programs written into the EHR.
Quality assurance. Timely evaluation of approaches to clinical care is available to physicians as well as hospitals that use EHRs.9 An individual physician can perform personal quality-assurance audits. And hospital management can gather cumulative statistics more quickly and easily.5,6,10,11
Patient data can be accessed independent of medical department, with lab tests, imaging studies, and pathology reports readily available for review. And accessibility is available regardless of geographic location.
EHRs are not perfect, and neither are their users. EHRs present the potential for problems related to absent or erroneous data entry, patient privacy issues, misunderstanding and misuse of software, and development of metadata.
With initial use, EHRs can create documentation gaps with the transition from paper to electronic records. In addition, inadequate provider training can create new error pathways, and a failure to use EHRs consistently can lead to loss of data and communication errors. These gaps and errors can increase medicolegal risk, as can the more extensive documentation often seen with early use, which creates more discoverable data. The temptation to cut and paste risks repeating earlier errors and omitting new information.
Another area of risk involves communication with the patient via email. A failure to reply could result in claims of negligence, and information overload could obscure pertinent pieces of information. And a departure from clinical decision support could be used by the patient to defend allegations of negligence.
With widespread use of EHRs, improved access to data could change the “duty” owed to the patient. In addition, clinical decision support embedded within the software could become the de facto “standard of care.”
The learning curve can be steep
The learning curve for EHRs may be steep and, at times, discouraging. One reason is that data are organized differently than in the conventional paper record, where information is read and analyzed in a progressive and stepwise manner, as in an analog or vertical system. The EHR is a digital format, so finding information requires digital (horizontal) inquiry. Information is, therefore, utilized in both horizontal and vertical formats in everyday situations. If data are entered incorrectly, all subsequent decisions could be flawed. And if the EHR suggests a plan, and that plan is not performed by the provider, the risk of liability could increase.
Inadvertent violation of the Health Insurance Portability and Accountability Act (HIPAA) with an EHR could increase medicolegal risk. For example, HIPAA allows for patients to make corrections to inaccurate information in their personal documents, but access by the patient could require the physician to review all records viewed by the patient after visit notes have been entered. This could drive up the cost of practice and reduce face-to-face time between physician and patient. Patients are not necessarily the best judges of which information is most important in their medical records.
Internet access raises concerns about the privacy of sensitive issues and misuse of information. Making a patient’s protected health information accessible electronically leaves physicians and hospitals at risk for a government fine or lawsuit. In several instances, the US Department of Health and Human Services (HHS) has levied fines against small practices and government agencies.
In one case, HHS fined Phoenix Cardiac Surgery in Phoenix, Arizona, $100,000 for posting surgery and appointment schedules on an Internet-based calendar that was accessible to the public.12 In another, HHS fined the Massachusetts Eye and Ear Infirmary in Boston $1.5 million after it reported the loss of an encrypted personal laptop containing the protected health information of patients and research subjects.13 The Alaska Department of Health and Social Services (DHSS) agreed to pay HHS $1.7 million after it reported the loss of a USB drive—possibly containing protected health information—from the vehicle of a DHSS employee.14
In traditional physician practices that employ handwritten records, the potential for compromise of patient information is limited. An organization may lose a few patient charts in the office and recover from the loss without incident. With the EHR, the loss poses a significant threat. The cases mentioned above were attributed to negligence or ignorance. The consequences could be worse if the compromise of EHR data is determined to be intentional. On September 4, 2010, hackers may have exposed the personal information of approximately 9,493 patients at Southwest Seattle Orthopaedics and Sports Medicine in Burien, Washington. Even with the best encryption technology, any electronic system remains vulnerable to external attack.
Metadata reveal how original data are used
Another concern regarding EHRs involves metadata—”data about data content.”15 Metadata is structured information that describes, locates, explains, or manages information. Metadata relevant to the EHR includes the data and time it was reviewed by the provider and whether it was manipulated in any way. Clearly, there is a potential for use and misuse by third-party reviewers.
Specialty-specific EHRs are recommended
Many ObGyns have found that most EHR systems are inadequate to the task of recording and analyzing information relevant to their specialty. Obstetric care is episodic and frequent. Data are added into the flow that must be considered at each visit, such as gestational age, fetal growth, labs (and normative values), prenatal diagnostic studies, and so on, representing both vertical and horizontal processing.16
The legal discovery process poses challenges that have not yet been resolved
The legal discovery process grants all parties to a lawsuit equal access to information. Under ideal circumstances, the EHR can provide comprehensive data more quickly than traditional records can. The problem is determining what constitutes relevant data and which party has the burden or benefit of making that decision. Uncontrolled access has the potential to violate privacy and privilege requirements.
Rules regarding discovery are still being debated in regard to their applicability to digital discovery.17 Even before a lawsuit is filed, the potential for “data mining” by third parties could lead to allegations of malpractice.
How to use EHRs responsibly without increasing risk
Good communication between patient and provider is paramount in the provision of quality medical care. Adherence to evidence-based standards with thorough documentation always serves the best interests of both patients and providers. The EHR can facilitate this process.
Our recommendations for appropriate use of your EHR include:
- Spend time learning the ins and outs of your particular EHR, and make sure your staff does the same. This will help reduce the likelihood that errors will be introduced into the record and ensure consistent use.
- Use individual sign-ons for anyone involved in data entry. This step facilitates the identification of users responsible for inaccurate use or errors, so that the situation can be addressed efficiently.
- Do not let third parties enter or manipulate data. This could jeopardize patient privacy, as well as the integrity of the record itself.
- Track all data entry on a regular basis. The frequency of tracking should be a function of routine as well as clinical circumstance. All new data from the previous interval should be reviewed at the time of the subsequent visit in order to direct care and ensure proper data entry.
Because of the considerable risk of liability claims in ObGyn practice, it is critical that the medical record accurately and precisely reflects the circumstances of each case. The EHR can be an effective and useful tool to document what occurred (and when) in a clinical scenario.18 As with all medical records, completeness and accuracy are the first and best defense against allegations of medical malpractice.
1. The Casebooks Project. History of Medical Record-keeping. http://www.magicandmedicine.hps.cam.ac.uk/on-astrological-medicine/further-reading/history-of-medical-record-keeping/. Accessed February 26 2013.
2. US Department of Health and Human Services. EMR vs EHR—What is the difference? Health IT Buzz. http://www.healthit.gov/buzz-blog/electronic-health-and-medical-records/emr-vs-ehr-difference/. Accessed February 20, 2013.
3. Health Information Technology for Economic and Clinical Health Act of 2009. HITECH Act. Pub L No 111-5 Div A tit XIII Div B tit IV Feb 17 2009, 123 stat 226, 467. Codified in scattered sections of 42 USCA.
4. Mangalmurti S, Murtagh L, Mello M. Medical malpractice liability in the age of electronic health records. N Engl J Med. 2010;363(21):2060-2067.
5. Reid P, Compton D, Grossman J, et al. Building a Better Delivery System: A New Engineering/Healthcare Partnership. Committee on Engineering and the Health Care System, Institute of Medicine and the National Academy of Engineering. Washington, DC: National Academies Press; 2005.
6. Grossman J. Disruptive innovation in healthcare: challenges for engineering. The Bridge. 2008;38:10-16.
7. Murphy E, Oxencis C, Klauck J, et al. Medication reconciliation at an academic medical center; implementation of a comprehensive program from admission to discharge. Am J Health-System Pharmacy. 2009;66(23):2126-2131.
8. Schuler R. The smart grid: a bridge between emerging technologies society and the environment. The Bridge. 2010;40:42-49.
9. Haberman S, Feldman J, Merhi Z, et al. Effect of clinical decision support on documentation compliance in an electronic medical record. Obstet Gynecol. 2009;114(2 Pt 1):311-317.
10. Hasley S. Decision support and patient safety: the time has come. Am J Obstet Gynecol. 2011;204(6):461-465.
11. Lagrew D, Stutman H, Sicaeros L. Voluntary physician adoption of an inpatient electronic medical record by obstetrician-gynecologists. Am J Obstet Gynecol. 2008;198(6):690.e1-e6.
12. Dolan PL. $100,000 HIPAA fine designed to send message to small physician practices. American Medical News. 2012. http://www.ama-assn.org/amednews/2012/04/30/bisd0502.htm. Accessed February 26, 2013.
13. US Department of Health and Human Services. Massachusetts provider settles HIPAA case for $1.5 million [news release]. September 17 2012. http://www.hhs.gov/news/press/2012pres/09/20120917a.html. Accessed February 26, 2013.
14. US Department of Health and Human Services. Alaska settles HIPAA security case for $1,700,000 [news release]. June 26, 2012. http://www.hhs.gov/news/press/2012pres/06/20120626a.html. Accessed February 26, 2013.
15. National Information Standards Organization. Understanding Metadata. Bethesda MD: NISO Press; 2004. http://www.niso.org/publications/press/UnderstandingMetadata.pdf. Accessed February 26, 2013.
16. McCoy M, Diamond A, Strunk A. Special requirements of electronic medical record systems in obstetrics and gynecology. Obstet Gynecol. 2010;116(1):140-143.
17. The Berkman Center for Internet and Society at Harvard Law School. The Federal Rules of Civil Procedure: The Impact of Digital Discovery. http://cyber.law.harvard.edu/digitaldiscovery/digdisc_library_4.html. Accessed February 26 2013.
18. Quinn M, Kats A, Kleinman K, et al. The relationship between electronic health records and malpractice claims. Arch Intern Med. 2012;172(15):1187-1188.
1. The Casebooks Project. History of Medical Record-keeping. http://www.magicandmedicine.hps.cam.ac.uk/on-astrological-medicine/further-reading/history-of-medical-record-keeping/. Accessed February 26 2013.
2. US Department of Health and Human Services. EMR vs EHR—What is the difference? Health IT Buzz. http://www.healthit.gov/buzz-blog/electronic-health-and-medical-records/emr-vs-ehr-difference/. Accessed February 20, 2013.
3. Health Information Technology for Economic and Clinical Health Act of 2009. HITECH Act. Pub L No 111-5 Div A tit XIII Div B tit IV Feb 17 2009, 123 stat 226, 467. Codified in scattered sections of 42 USCA.
4. Mangalmurti S, Murtagh L, Mello M. Medical malpractice liability in the age of electronic health records. N Engl J Med. 2010;363(21):2060-2067.
5. Reid P, Compton D, Grossman J, et al. Building a Better Delivery System: A New Engineering/Healthcare Partnership. Committee on Engineering and the Health Care System, Institute of Medicine and the National Academy of Engineering. Washington, DC: National Academies Press; 2005.
6. Grossman J. Disruptive innovation in healthcare: challenges for engineering. The Bridge. 2008;38:10-16.
7. Murphy E, Oxencis C, Klauck J, et al. Medication reconciliation at an academic medical center; implementation of a comprehensive program from admission to discharge. Am J Health-System Pharmacy. 2009;66(23):2126-2131.
8. Schuler R. The smart grid: a bridge between emerging technologies society and the environment. The Bridge. 2010;40:42-49.
9. Haberman S, Feldman J, Merhi Z, et al. Effect of clinical decision support on documentation compliance in an electronic medical record. Obstet Gynecol. 2009;114(2 Pt 1):311-317.
10. Hasley S. Decision support and patient safety: the time has come. Am J Obstet Gynecol. 2011;204(6):461-465.
11. Lagrew D, Stutman H, Sicaeros L. Voluntary physician adoption of an inpatient electronic medical record by obstetrician-gynecologists. Am J Obstet Gynecol. 2008;198(6):690.e1-e6.
12. Dolan PL. $100,000 HIPAA fine designed to send message to small physician practices. American Medical News. 2012. http://www.ama-assn.org/amednews/2012/04/30/bisd0502.htm. Accessed February 26, 2013.
13. US Department of Health and Human Services. Massachusetts provider settles HIPAA case for $1.5 million [news release]. September 17 2012. http://www.hhs.gov/news/press/2012pres/09/20120917a.html. Accessed February 26, 2013.
14. US Department of Health and Human Services. Alaska settles HIPAA security case for $1,700,000 [news release]. June 26, 2012. http://www.hhs.gov/news/press/2012pres/06/20120626a.html. Accessed February 26, 2013.
15. National Information Standards Organization. Understanding Metadata. Bethesda MD: NISO Press; 2004. http://www.niso.org/publications/press/UnderstandingMetadata.pdf. Accessed February 26, 2013.
16. McCoy M, Diamond A, Strunk A. Special requirements of electronic medical record systems in obstetrics and gynecology. Obstet Gynecol. 2010;116(1):140-143.
17. The Berkman Center for Internet and Society at Harvard Law School. The Federal Rules of Civil Procedure: The Impact of Digital Discovery. http://cyber.law.harvard.edu/digitaldiscovery/digdisc_library_4.html. Accessed February 26 2013.
18. Quinn M, Kats A, Kleinman K, et al. The relationship between electronic health records and malpractice claims. Arch Intern Med. 2012;172(15):1187-1188.
Obese mother gains another 60 lb before delivery … and more

AN OBESE WOMAN with a family history of diabetes had previously given birth to a large baby. Even though she expressed her concern that this fetus would also be macrosomic, the ObGyn planned for spontaneous vaginal delivery. At 39 weeks’ gestation, after gaining 60 lb, she went to the hospital requesting induction of labor; the ObGyn reluctantly agreed. Labor was lengthy, forceps-assisted delivery was performed, and a shoulder dystocia was encountered. The baby was born with respiratory distress, a brachial plexus injury, bruises on his right cheek and both ears, and multiple rib fractures. After transfer to a children’s hospital, surgical exploration revealed avulsion of the C6 root nerve from the spinal cord and damage to C5, C7, and C8 nerve roots. Several surgical repairs and physical therapy have led to some improvement, but the child is permanently injured. His right arm is shorter than the left, his right hand is smaller, and he has less strength and range of motion in the right arm. He also has excessive tearing in the right eye and his right eyelid droops.
PARENTS’ CLAIM The ObGyn failed to recognize the risk of delivering a macrosomic baby and did not consider cesarean delivery. The brachial plexus injury was due to downward traction applied during delivery.
PHYSICIAN’S DEFENSE There was no negligence. The brachial plexus injury was not caused by downward traction.
VERDICT A $4.1 million Indiana verdict was returned, but was reduced to the state cap of $1.25 million.
Failure to follow-up on mass: $1.97M verdict
AFTER STAGE II OVARIAN CANCER was found in 1999, a woman underwent surgery and chemotherapy, and was told she was cancer-free. She had regular visits between 2000 and 2008 with another surgical oncologist after her first surgeon moved. In 2004, the oncologist documented finding a round fullness during a pelvic exam. A CT scan confirmed a mass in the pelvic cul-de-sac.
In August 2008, the patient was treated for deep venous thrombosis in her leg. The attending physician saw the pelvic mass on imaging, and a biopsy indicated a recurrence of ovarian cancer. After chemotherapy, the patient underwent surgery, but the tumor was unresectable. In early 2011, testing revealed metastasis to the spine, sternum, pelvic bone, arm, and lung.
PATIENT’S CLAIM The surgeon did not properly investigate the mass resulting in a delayed diagnosis of cancer recurrence. The patient alleged that the surgical oncologist repeatedly stated that the mass had not changed and was most likely fluid; it was nothing to worry about. Radiology reports indicated a suspicion of cancer.
DEFENDANTS’ DEFENSE The oncologist repeatedly told the patient that the mass should be biopsied, but the patient refused because she was dealing with other medical issues. The radiologist argued that reports to the oncologist included everything needed to diagnose the cancer.
VERDICT A Pennsylvania jury found the surgical oncologist fully at fault and returned a $1,971,455 verdict.
Incomplete tubal ligation
BEFORE DELIVERY OF HER THIRD CHILD, a 26-year-old woman requested sterilization using tubal ligation. After delivery, the ObGyn performed a bilateral tubal ligation. The pathologist’s report indicated that the ligation was incomplete: the left fallopian tube had not been fully removed. The ObGyn failed to note the report’s results in the patient’s record, nor did he advise the patient. Two years later, the patient delivered a fourth child.
PATIENT’S CLAIM The patient alleged wrongful birth against both the ObGyn and pathologist. The ObGyn was negligent for not reacting to the pathologist’s report of incomplete tubal ligation, and for not informing the patient. The pathologist should have verbally confirmed receipt of the report with the ObGyn.
PHYSICIANS’ DEFENSE The ObGyn settled before trial. The pathologist claimed he had properly interpreted the specimen and reported the results.
VERDICT A Louisiana jury found the ObGyn fully at fault and assessed additional damages of $56,252 to the $100,000 settlement.

A WOMAN SUFFERED FROM PELVIC PAIN caused by adhesions following two cesarean deliveries and a hysterectomy. In January 2003, her ObGyn performed laparotomy to reduce adhesions from prior surgeries and place Gore-Tex mesh to prevent future adhesions. In October 2010, the patient reported epigastric pain, and went to a different surgeon (her insurance changed). A CT scan identified a foreign body encapsulated in scar tissue in the patient’s lower abdomen/pelvis. The surgeon removed the foreign body.
PATIENT’S CLAIM The ObGyn and hospital were negligent in conducting the 2003 procedure; the foreign object was a retained surgical sponge.
DEFENDANTS’ DEFENSE The foreign body removed in 2010 was the Gore-Tex mesh placed in 2003. The mesh became encapsulated in scar tissue due to the patient’s propensity to develop adhesions, and then moved within the patient’s body. Surgical sponges have embedded radiopaque tracers; CT scans in 2003 and 2010 did not detect any radiopaque tracers.
VERDICT A California defense verdict was returned.
Massive bleed during sacrocolpopexy
AFTER A 72-YEAR-OLD WOMAN developed pelvic organ prolapse, her urologist performed an abdominal sacrocolpopexy. As the urologist attempted to gain access to the sacral prominence, a tear in the median sacral vein expanded to involve the inferior vena cava and left iliac vein. Massive bleeding occurred and multiple units of blood were transfused. A general surgeon successfully repaired the vascular injuries. The patient was hospitalized for 16 days, received home healthcare, and fully recovered.
PATIENT’S CLAIM The urologist was negligent in overaggressive manipulation of the median sacral vein, causing it to avulse.
PHYSICIAN’S DEFENSE Bleeds of this type are a known complication of the procedure.
VERDICT A Michigan defense verdict was returned.
Was it hypoxia or autism?
AFTER SEVERAL HOURS IN LABOR, a fetal heart-rate monitor indicated decreasing fetal heart rate that led to terminal bradycardia. The ObGyn was called and performed an emergency cesarean delivery. The child was diagnosed with brain damage at 2 years of age.
PARENTS’ CLAIM A cesarean delivery should have been planned because of the fetal weight (8 lb 11 oz). A hypoxic event occurred during labor. Ultrasonography would have shown that the fetus was inverted and that the baby’s face was covered by one of its hands. Delivery was not properly managed, and fetal distress was not reported to the ObGyn in a timely manner.
DEFENDANTS’ DEFENSE The infant’s weight was not sufficient to warrant a cesarean delivery. The infant did not suffer hypoxia. The child’s abnormalities only emerged in the second year of life. An MRI at that time did not indicate brain damage. The child’s development with subsequent regression suggests autism.
VERDICT A New York defense verdict was returned.
Should mammography have been diagnostic?
A 46-YEAR-OLD WOMAN with a family history of breast cancer had regular annual screenings. In December 2006, the patient reported pain, hardness, and burning in her left breast to her gynecologist. A radiologist interpreted the mammography as normal. In May 2007, the patient found a lump in her left breast. Testing indicated she had stage IV breast cancer. She died 2 months after the trial concluded.
PATIENT’S CLAIM The 2006 mammogram was performed as a screening mammography, but should have been diagnostic, considering her family history and reported symptoms. The radiologist improperly interpreted the films.
DEFENDANTS’ DEFENSE The hospital staff testified that the patient did not report pain, hardness, and burning in her left breast when she presented for the 2006 mammography. The radiologist claimed his screening and interpretation were appropriate.
VERDICT The Louisiana court granted the patient’s motion for judgment, and awarded $558,000 in medical costs and $1.3 million in noneconomic damages, totalling $1.808 million. This was reduced to the $500,000 statutory cap.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
We want to hear from you! Tell us what you think.

AN OBESE WOMAN with a family history of diabetes had previously given birth to a large baby. Even though she expressed her concern that this fetus would also be macrosomic, the ObGyn planned for spontaneous vaginal delivery. At 39 weeks’ gestation, after gaining 60 lb, she went to the hospital requesting induction of labor; the ObGyn reluctantly agreed. Labor was lengthy, forceps-assisted delivery was performed, and a shoulder dystocia was encountered. The baby was born with respiratory distress, a brachial plexus injury, bruises on his right cheek and both ears, and multiple rib fractures. After transfer to a children’s hospital, surgical exploration revealed avulsion of the C6 root nerve from the spinal cord and damage to C5, C7, and C8 nerve roots. Several surgical repairs and physical therapy have led to some improvement, but the child is permanently injured. His right arm is shorter than the left, his right hand is smaller, and he has less strength and range of motion in the right arm. He also has excessive tearing in the right eye and his right eyelid droops.
PARENTS’ CLAIM The ObGyn failed to recognize the risk of delivering a macrosomic baby and did not consider cesarean delivery. The brachial plexus injury was due to downward traction applied during delivery.
PHYSICIAN’S DEFENSE There was no negligence. The brachial plexus injury was not caused by downward traction.
VERDICT A $4.1 million Indiana verdict was returned, but was reduced to the state cap of $1.25 million.
Failure to follow-up on mass: $1.97M verdict
AFTER STAGE II OVARIAN CANCER was found in 1999, a woman underwent surgery and chemotherapy, and was told she was cancer-free. She had regular visits between 2000 and 2008 with another surgical oncologist after her first surgeon moved. In 2004, the oncologist documented finding a round fullness during a pelvic exam. A CT scan confirmed a mass in the pelvic cul-de-sac.
In August 2008, the patient was treated for deep venous thrombosis in her leg. The attending physician saw the pelvic mass on imaging, and a biopsy indicated a recurrence of ovarian cancer. After chemotherapy, the patient underwent surgery, but the tumor was unresectable. In early 2011, testing revealed metastasis to the spine, sternum, pelvic bone, arm, and lung.
PATIENT’S CLAIM The surgeon did not properly investigate the mass resulting in a delayed diagnosis of cancer recurrence. The patient alleged that the surgical oncologist repeatedly stated that the mass had not changed and was most likely fluid; it was nothing to worry about. Radiology reports indicated a suspicion of cancer.
DEFENDANTS’ DEFENSE The oncologist repeatedly told the patient that the mass should be biopsied, but the patient refused because she was dealing with other medical issues. The radiologist argued that reports to the oncologist included everything needed to diagnose the cancer.
VERDICT A Pennsylvania jury found the surgical oncologist fully at fault and returned a $1,971,455 verdict.
Incomplete tubal ligation
BEFORE DELIVERY OF HER THIRD CHILD, a 26-year-old woman requested sterilization using tubal ligation. After delivery, the ObGyn performed a bilateral tubal ligation. The pathologist’s report indicated that the ligation was incomplete: the left fallopian tube had not been fully removed. The ObGyn failed to note the report’s results in the patient’s record, nor did he advise the patient. Two years later, the patient delivered a fourth child.
PATIENT’S CLAIM The patient alleged wrongful birth against both the ObGyn and pathologist. The ObGyn was negligent for not reacting to the pathologist’s report of incomplete tubal ligation, and for not informing the patient. The pathologist should have verbally confirmed receipt of the report with the ObGyn.
PHYSICIANS’ DEFENSE The ObGyn settled before trial. The pathologist claimed he had properly interpreted the specimen and reported the results.
VERDICT A Louisiana jury found the ObGyn fully at fault and assessed additional damages of $56,252 to the $100,000 settlement.

A WOMAN SUFFERED FROM PELVIC PAIN caused by adhesions following two cesarean deliveries and a hysterectomy. In January 2003, her ObGyn performed laparotomy to reduce adhesions from prior surgeries and place Gore-Tex mesh to prevent future adhesions. In October 2010, the patient reported epigastric pain, and went to a different surgeon (her insurance changed). A CT scan identified a foreign body encapsulated in scar tissue in the patient’s lower abdomen/pelvis. The surgeon removed the foreign body.
PATIENT’S CLAIM The ObGyn and hospital were negligent in conducting the 2003 procedure; the foreign object was a retained surgical sponge.
DEFENDANTS’ DEFENSE The foreign body removed in 2010 was the Gore-Tex mesh placed in 2003. The mesh became encapsulated in scar tissue due to the patient’s propensity to develop adhesions, and then moved within the patient’s body. Surgical sponges have embedded radiopaque tracers; CT scans in 2003 and 2010 did not detect any radiopaque tracers.
VERDICT A California defense verdict was returned.
Massive bleed during sacrocolpopexy
AFTER A 72-YEAR-OLD WOMAN developed pelvic organ prolapse, her urologist performed an abdominal sacrocolpopexy. As the urologist attempted to gain access to the sacral prominence, a tear in the median sacral vein expanded to involve the inferior vena cava and left iliac vein. Massive bleeding occurred and multiple units of blood were transfused. A general surgeon successfully repaired the vascular injuries. The patient was hospitalized for 16 days, received home healthcare, and fully recovered.
PATIENT’S CLAIM The urologist was negligent in overaggressive manipulation of the median sacral vein, causing it to avulse.
PHYSICIAN’S DEFENSE Bleeds of this type are a known complication of the procedure.
VERDICT A Michigan defense verdict was returned.
Was it hypoxia or autism?
AFTER SEVERAL HOURS IN LABOR, a fetal heart-rate monitor indicated decreasing fetal heart rate that led to terminal bradycardia. The ObGyn was called and performed an emergency cesarean delivery. The child was diagnosed with brain damage at 2 years of age.
PARENTS’ CLAIM A cesarean delivery should have been planned because of the fetal weight (8 lb 11 oz). A hypoxic event occurred during labor. Ultrasonography would have shown that the fetus was inverted and that the baby’s face was covered by one of its hands. Delivery was not properly managed, and fetal distress was not reported to the ObGyn in a timely manner.
DEFENDANTS’ DEFENSE The infant’s weight was not sufficient to warrant a cesarean delivery. The infant did not suffer hypoxia. The child’s abnormalities only emerged in the second year of life. An MRI at that time did not indicate brain damage. The child’s development with subsequent regression suggests autism.
VERDICT A New York defense verdict was returned.
Should mammography have been diagnostic?
A 46-YEAR-OLD WOMAN with a family history of breast cancer had regular annual screenings. In December 2006, the patient reported pain, hardness, and burning in her left breast to her gynecologist. A radiologist interpreted the mammography as normal. In May 2007, the patient found a lump in her left breast. Testing indicated she had stage IV breast cancer. She died 2 months after the trial concluded.
PATIENT’S CLAIM The 2006 mammogram was performed as a screening mammography, but should have been diagnostic, considering her family history and reported symptoms. The radiologist improperly interpreted the films.
DEFENDANTS’ DEFENSE The hospital staff testified that the patient did not report pain, hardness, and burning in her left breast when she presented for the 2006 mammography. The radiologist claimed his screening and interpretation were appropriate.
VERDICT The Louisiana court granted the patient’s motion for judgment, and awarded $558,000 in medical costs and $1.3 million in noneconomic damages, totalling $1.808 million. This was reduced to the $500,000 statutory cap.

AN OBESE WOMAN with a family history of diabetes had previously given birth to a large baby. Even though she expressed her concern that this fetus would also be macrosomic, the ObGyn planned for spontaneous vaginal delivery. At 39 weeks’ gestation, after gaining 60 lb, she went to the hospital requesting induction of labor; the ObGyn reluctantly agreed. Labor was lengthy, forceps-assisted delivery was performed, and a shoulder dystocia was encountered. The baby was born with respiratory distress, a brachial plexus injury, bruises on his right cheek and both ears, and multiple rib fractures. After transfer to a children’s hospital, surgical exploration revealed avulsion of the C6 root nerve from the spinal cord and damage to C5, C7, and C8 nerve roots. Several surgical repairs and physical therapy have led to some improvement, but the child is permanently injured. His right arm is shorter than the left, his right hand is smaller, and he has less strength and range of motion in the right arm. He also has excessive tearing in the right eye and his right eyelid droops.
PARENTS’ CLAIM The ObGyn failed to recognize the risk of delivering a macrosomic baby and did not consider cesarean delivery. The brachial plexus injury was due to downward traction applied during delivery.
PHYSICIAN’S DEFENSE There was no negligence. The brachial plexus injury was not caused by downward traction.
VERDICT A $4.1 million Indiana verdict was returned, but was reduced to the state cap of $1.25 million.
Failure to follow-up on mass: $1.97M verdict
AFTER STAGE II OVARIAN CANCER was found in 1999, a woman underwent surgery and chemotherapy, and was told she was cancer-free. She had regular visits between 2000 and 2008 with another surgical oncologist after her first surgeon moved. In 2004, the oncologist documented finding a round fullness during a pelvic exam. A CT scan confirmed a mass in the pelvic cul-de-sac.
In August 2008, the patient was treated for deep venous thrombosis in her leg. The attending physician saw the pelvic mass on imaging, and a biopsy indicated a recurrence of ovarian cancer. After chemotherapy, the patient underwent surgery, but the tumor was unresectable. In early 2011, testing revealed metastasis to the spine, sternum, pelvic bone, arm, and lung.
PATIENT’S CLAIM The surgeon did not properly investigate the mass resulting in a delayed diagnosis of cancer recurrence. The patient alleged that the surgical oncologist repeatedly stated that the mass had not changed and was most likely fluid; it was nothing to worry about. Radiology reports indicated a suspicion of cancer.
DEFENDANTS’ DEFENSE The oncologist repeatedly told the patient that the mass should be biopsied, but the patient refused because she was dealing with other medical issues. The radiologist argued that reports to the oncologist included everything needed to diagnose the cancer.
VERDICT A Pennsylvania jury found the surgical oncologist fully at fault and returned a $1,971,455 verdict.
Incomplete tubal ligation
BEFORE DELIVERY OF HER THIRD CHILD, a 26-year-old woman requested sterilization using tubal ligation. After delivery, the ObGyn performed a bilateral tubal ligation. The pathologist’s report indicated that the ligation was incomplete: the left fallopian tube had not been fully removed. The ObGyn failed to note the report’s results in the patient’s record, nor did he advise the patient. Two years later, the patient delivered a fourth child.
PATIENT’S CLAIM The patient alleged wrongful birth against both the ObGyn and pathologist. The ObGyn was negligent for not reacting to the pathologist’s report of incomplete tubal ligation, and for not informing the patient. The pathologist should have verbally confirmed receipt of the report with the ObGyn.
PHYSICIANS’ DEFENSE The ObGyn settled before trial. The pathologist claimed he had properly interpreted the specimen and reported the results.
VERDICT A Louisiana jury found the ObGyn fully at fault and assessed additional damages of $56,252 to the $100,000 settlement.

A WOMAN SUFFERED FROM PELVIC PAIN caused by adhesions following two cesarean deliveries and a hysterectomy. In January 2003, her ObGyn performed laparotomy to reduce adhesions from prior surgeries and place Gore-Tex mesh to prevent future adhesions. In October 2010, the patient reported epigastric pain, and went to a different surgeon (her insurance changed). A CT scan identified a foreign body encapsulated in scar tissue in the patient’s lower abdomen/pelvis. The surgeon removed the foreign body.
PATIENT’S CLAIM The ObGyn and hospital were negligent in conducting the 2003 procedure; the foreign object was a retained surgical sponge.
DEFENDANTS’ DEFENSE The foreign body removed in 2010 was the Gore-Tex mesh placed in 2003. The mesh became encapsulated in scar tissue due to the patient’s propensity to develop adhesions, and then moved within the patient’s body. Surgical sponges have embedded radiopaque tracers; CT scans in 2003 and 2010 did not detect any radiopaque tracers.
VERDICT A California defense verdict was returned.
Massive bleed during sacrocolpopexy
AFTER A 72-YEAR-OLD WOMAN developed pelvic organ prolapse, her urologist performed an abdominal sacrocolpopexy. As the urologist attempted to gain access to the sacral prominence, a tear in the median sacral vein expanded to involve the inferior vena cava and left iliac vein. Massive bleeding occurred and multiple units of blood were transfused. A general surgeon successfully repaired the vascular injuries. The patient was hospitalized for 16 days, received home healthcare, and fully recovered.
PATIENT’S CLAIM The urologist was negligent in overaggressive manipulation of the median sacral vein, causing it to avulse.
PHYSICIAN’S DEFENSE Bleeds of this type are a known complication of the procedure.
VERDICT A Michigan defense verdict was returned.
Was it hypoxia or autism?
AFTER SEVERAL HOURS IN LABOR, a fetal heart-rate monitor indicated decreasing fetal heart rate that led to terminal bradycardia. The ObGyn was called and performed an emergency cesarean delivery. The child was diagnosed with brain damage at 2 years of age.
PARENTS’ CLAIM A cesarean delivery should have been planned because of the fetal weight (8 lb 11 oz). A hypoxic event occurred during labor. Ultrasonography would have shown that the fetus was inverted and that the baby’s face was covered by one of its hands. Delivery was not properly managed, and fetal distress was not reported to the ObGyn in a timely manner.
DEFENDANTS’ DEFENSE The infant’s weight was not sufficient to warrant a cesarean delivery. The infant did not suffer hypoxia. The child’s abnormalities only emerged in the second year of life. An MRI at that time did not indicate brain damage. The child’s development with subsequent regression suggests autism.
VERDICT A New York defense verdict was returned.
Should mammography have been diagnostic?
A 46-YEAR-OLD WOMAN with a family history of breast cancer had regular annual screenings. In December 2006, the patient reported pain, hardness, and burning in her left breast to her gynecologist. A radiologist interpreted the mammography as normal. In May 2007, the patient found a lump in her left breast. Testing indicated she had stage IV breast cancer. She died 2 months after the trial concluded.
PATIENT’S CLAIM The 2006 mammogram was performed as a screening mammography, but should have been diagnostic, considering her family history and reported symptoms. The radiologist improperly interpreted the films.
DEFENDANTS’ DEFENSE The hospital staff testified that the patient did not report pain, hardness, and burning in her left breast when she presented for the 2006 mammography. The radiologist claimed his screening and interpretation were appropriate.
VERDICT The Louisiana court granted the patient’s motion for judgment, and awarded $558,000 in medical costs and $1.3 million in noneconomic damages, totalling $1.808 million. This was reduced to the $500,000 statutory cap.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
We want to hear from you! Tell us what you think.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
We want to hear from you! Tell us what you think.
Four pillars of a successful practice: 1. Keep your current patients happy
Dr. Baum describes his number one strategy to retain patients (Audiocast, March 2013)
Pillar 2: Attract new patients (May 2013)
Pillar 3: Obtain and maintain physician referrals (June 2013)
Pillar 4: Motivate your staff (August 2013)
The medical landscape has changed. No one is quite certain what the future will hold. One thing we do know: 20 million more Americans, half of them women, will enter the health-care system in the very near future, as the Affordable Care Act continues to unfold. This flood of new patients will affect nearly every ObGyn practice in the country because we lack an adequate increase in the number of physicians to care for them. In the meantime, what can you do to ensure the continued success of your practice? This series focuses on four key areas. I call them the “four pillars”:
- Keep existing patients happy
- Attract new patients
- Nurture relationships with your medical colleagues and other health-care providers, such as physician assistants and nurse practitioners
- Maintain the morale of your staff.
No pillar is more important than the others; all four are necessary to guarantee success.
It is more cost-effective to keep an existing customer than to attract
a new one
In this article, I explain why it is vital to ensure that every patient has a positive experience of your practice, from the moment they make their first telephone call for an appointment, through their wait in the reception area, to the moment they are seen by the staff or the physician, and beyond—when they tell others about their stellar experience.
It’s nice to get new patients, but it is more important to keep the ones you already have. In most professions and businesses, the cost of keeping an established customer is one-fifth the cost of acquiring a new one. Medical practices are no exception. If you are not doing a good job with the patients you already have, spending thousands of dollars on a marketing plan to bring in new patients is pointless. The patients you have right now are the backbone of your practice.
Give your practice a checkup
Look at your practice from your patients’ perspective
Today, it is critical to know the needs and expectations of your patients and referring physicians. The best way to do this is to ask your patients what they think, which also will reveal your practice’s strengths and weaknesses. This information can be obtained easily by surveying patients about various aspects of your practice. (Even practices that are full or closed need to evaluate their services periodically and listen to their patients. Changes always occur, and the cup may not “runneth over” forever.)
Tom Peters, the nationally renowned author of In Search of Excellence, has described two keys to success in business:
- Find out what the customer (patient) wants and give him or her more of it
- Find out what the customer (patient) does not want and be sure to avoid it.
Techniques to gather the patient’s perspective
There are five effective techniques for determining how patients perceive your practice and for evaluating your performance and reputation:
- Conduct personal interviews
- Conduct patient surveys
- Create a focus group
- Use a suggestion box
- Commission evaluation by a mystery shopper.
Although I have used all five techniques, my favorite and most cost-effective involves a survey card that is given to every patient on every office visit (FIGURE 1). The card is given to the patient when she checks in, and she can complete it in the reception area or exam room and return it to the receptionist before leaving the practice. The cards are reviewed by a nurse, who addresses positive and negative comments. Most negative comments are addressed with a phone call. If necessary, I respond to the patient’s complaint.
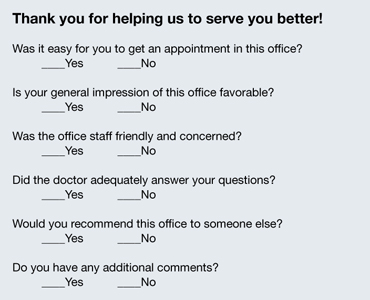
FIGURE 1: Patient survey card
There is another benefit to the survey card. The flip side of the card prompts the patient to write down the three questions she would like you to address on her current visit to the office (FIGURE 2). Conducting the appointment according to these concerns can help keep patients from initiating a last-minute discussion, often after you have closed the chart or electronic medical record, that you don’t have time to address adequately. Since my office has implemented use of this survey card, we seldom get follow-up phone calls from patients about issues they forgot to ask about. The survey card demonstrates that we are listening to the patient and want to be certain that all her questions have been answered at the time of her office visit.
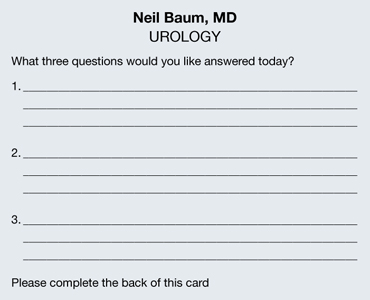
FIGURE 2: Focus of the appointment
Develop an on-time practice philosophy
You know the adage: Timeliness is next to godliness. (Actually, it’s cleanliness that’s next to godliness, but timeliness is vital, too.) The most common complaint patients have about the health-care experience is “waiting for the doctor.” Spending time in the reception area probably accounts for more patient dissatisfaction than any other aspect of medical care. In one recent survey, nearly one in four patients (24%) claimed to have waited 30 minutes or longer. With so many more women entering the marketplace, this statistic is only going to get worse.
In order to gain an accurate picture of what is happening in regard to the schedule in your practice, I suggest conducting a “time and motion” study. For a period of 3 to 5 days, place a sheet on each patient’s record or superbill and log in the following:
- time of her appointment
- time she arrived
- time she left the office
- how much time she spent with her physician.
You will be amazed to discover that patients are waiting 1 or 2 hours or longer to see the physician, and that the physician is spending only 5 minutes with the patient. Ask any patient on a survey if she feels she is getting bang for her buck, and she will answer, “No!”
By conducting a time and motion study, you will discover that there are predictable periods when backlogs occur. Often, these delays are the result of “working a patient in” to the schedule. Unscheduled patients who call to report vaginal bleeding, pelvic pain, urinary tract infection, or another problem are often told to come in without an appointment, but they inevitably displace women already scheduled and delay their visit. This problem affects almost every ObGyn.
One way to avoid this scenario is to create “sacred” time slots. These are 15-minute intervals at the end of the morning or afternoon in which unscheduled patients can be worked into the round of visits. Instead of telling the patient to “just come in,” I tell her to report at a specific time. These time slots cannot be filled with routine appointments. Nor can they be filled prior to 9 am each day. This leaves two or three slots open for patients who must be seen immediately.
Few ObGyns can change health-care policy. But all of us can be more sensitive to our patients’ time and make an effort to see them as soon as possible, thereby eliminating one of patients’ most common complaints: the long wait to see their doctor.
Make the patient’s experience memorable
All of us can provide a diagnosis and treatment strategy for most women’s medical problems. But how many of us can make the experience memorable for the woman? Often, it is a few little things that can be easily and inexpensively performed that make a big difference.
Go with cloth, not paper. There’s a sharp contrast between a paper sheet, a paper gown, and a soft robe. You don’t step out of the shower in a fine hotel and put on a paper robe. If you are offering five-star service, you need to offer five-star amenities. If you want to attract special patients, treat your patients special. It doesn’t cost that much to add a few dozen robes to your office supplies, laundering them after each use and placing them on hangers or in a plastic bag that each patient can use during her visit. I can assure you that this single idea will set you apart from most other ObGyns in your community.
Stirrups are cold! Here’s another idea: Use pads to cover the metal of the stirrups for the pelvic exam. Those stirrups are cold steel, and no woman who is already naked and concerned about her dignity wants to place her feet on those chilly structures. You can have lamb’s wool pads created by a seamstress for a few dollars—or if you prefer to go low-tech, you can use potholders to cover the stirrups.
Warm the speculum. My wife shared with me how uncomfortable it is to have a metal speculum inserted and how much she appreciated her gynecologist warming the instrument with tap water before its insertion. I have found that this saves on the use of lubricant jelly, too, because the water serves as a lubricant!
Keep the temperature in mind. Most medical offices are kept at 70° to 72° F to keep the doctor and staff comfortable. However, when a woman puts on her gown or robe, she often becomes cold and uncomfortable. On days when it is cold outside or the office is cold, use an inexpensive heater to make the room comfortable for the patient.
Talk to your patient “eyeball to eyeball.” You make big points with your patient if you speak to her when she is fully dressed and when your eyes are at the same level as hers. A woman lying on her back in a gown or robe does not hear or recall what her doctor is telling her. However, if the doctor and nurse leave the room and allow the patient to get dressed, and if the doctor sits with the patient without barriers between them, she is far more likely to listen and recall what has been discussed.
Pick up the telephone. I am often asked for my “best” idea to keep patients happy. My numero uno suggestion is to take a few minutes to call the patient at home. Which patients should you call? Women undergoing outpatient studies or procedures, those recently discharged from the hospital, and those who require a little more hand holding and attention. You can be sure that every patient who undergoes a procedure or is discharged from the hospital has questions about the findings, any precautions, medications, and follow-up. A call from a nurse or doctor does a lot to allay her apprehension—and it often keeps the patient from calling the office with her questions and concerns.
My nurse identifies key patients and contacts them at the end of the workday. She is usually able to answer all the questions but may identify two or three that require my attention. She tells the patient what time I will call so she can keep the phone line free.
Calling patients usually takes no more than 5 to 10 minutes a day and provides me with great satisfaction. Patients are usually shocked—and happy—that their physician is calling them at home. The advantages of this strategy include:
- fewer calls from your patients
- more efficient use of your time
- deep appreciation by the patient.
One patient I called at home wrote me a note that I think is worth mentioning: “This is the first time a member of your profession has taken the time to call me at home and check on my condition. Undoubtedly, it will foster a better relationship between you and me.”
Results of an informal poll indicate the answer is mostly “Yes”
As outlined in the article by Neil Baum, MD, the need to keep existing patients happy—and to determine how they’re feeling about your practice—seems as though it should occupy a berth rather high on your list of priorities. To gauge how widespread the practice of measuring patient satisfaction is among ObGyns, we polled our Virtual Board of Editors (VBE) on the subject. Because these physicians range from private practitioners to academic professionals and hospital employees, we find them to be one bellwether of wider practice patterns.
When we asked, 65% of our VBE members reported that they regularly measure the satisfaction of their patients. Among the reasons given for this tactic were corporate policy, but the vast majority of respondents indicated that they “need to know what patients like and don’t like” in order to “improve our services.” As one physician noted, “all practices can improve in some respects.” Regular inquiries about patient satisfaction provide a method and rationale for improvement.
Another respondent observed that the information gained from assessments of patient satisfaction is useful during insurance contracting. Another said, simply, “It’s the right thing to do.”
When asked exactly how they measure patient satisfaction, almost 60% of respondents who regularly assess this component of practice said they use surveys to do so, compared with 14% who use interviews, 17% who make a suggestion box available, and 11% who employ a “mystery shopper” (The percentages add up to more than 100% because some VBE members employ more than one approach.) None of the VBE members reported convening a focus group.
When asked to rate the importance of patient-satisfaction assessments, just over half of all respondents characterized it as “very important.” Only one physician reported that the practice of measuring patient satisfaction is “not important.”
“It is critical—especially for doctors with younger practices who are trying to build a reputation or practice—to get feedback to improve care and increase their patient load,” noted one respondent. Another reported: “We do a detailed satisfaction survey after every surgery on every patient. We actively seek feedback and use our Web site and social media to find ways to improve.”
“We are in a large city (over 500,000 population), so there is competition, and patients have choices,” wrote another VBE member. “In smaller communities, patients may have fewer options and have to accept the few available providers. My basic method of achieving patient satisfaction is outdated: I spend a lot of time per patient, see few patients per day, and try to help with whatever issues they have (not just breast and pelvic). I make less money practicing this way—I accepted a long time ago that really caring for patients means spending more time and being paid less for it.”
Another VBE member said, “I promise what I’ll do for patients, and I keep that promise! I use the telephone as a tool. Patients are very impressed and thankful when I talk to them about their problems and test results.”
—Janelle Yates, Senior Editor
The bottom line
Word of mouth was the time-honored method of attracting new patients for thousands of years. That method still works today. Ensuring that your patients have an outstanding experience during their visit is one of the smartest strategies to market and promote your practice.
We want to hear from you! Tell us what you think.
CLICK HERE to access 10 recent articles on managing your ObGyn practice.
Dr. Baum describes his number one strategy to retain patients (Audiocast, March 2013)
Pillar 2: Attract new patients (May 2013)
Pillar 3: Obtain and maintain physician referrals (June 2013)
Pillar 4: Motivate your staff (August 2013)
The medical landscape has changed. No one is quite certain what the future will hold. One thing we do know: 20 million more Americans, half of them women, will enter the health-care system in the very near future, as the Affordable Care Act continues to unfold. This flood of new patients will affect nearly every ObGyn practice in the country because we lack an adequate increase in the number of physicians to care for them. In the meantime, what can you do to ensure the continued success of your practice? This series focuses on four key areas. I call them the “four pillars”:
- Keep existing patients happy
- Attract new patients
- Nurture relationships with your medical colleagues and other health-care providers, such as physician assistants and nurse practitioners
- Maintain the morale of your staff.
No pillar is more important than the others; all four are necessary to guarantee success.
It is more cost-effective to keep an existing customer than to attract
a new one
In this article, I explain why it is vital to ensure that every patient has a positive experience of your practice, from the moment they make their first telephone call for an appointment, through their wait in the reception area, to the moment they are seen by the staff or the physician, and beyond—when they tell others about their stellar experience.
It’s nice to get new patients, but it is more important to keep the ones you already have. In most professions and businesses, the cost of keeping an established customer is one-fifth the cost of acquiring a new one. Medical practices are no exception. If you are not doing a good job with the patients you already have, spending thousands of dollars on a marketing plan to bring in new patients is pointless. The patients you have right now are the backbone of your practice.
Give your practice a checkup
Look at your practice from your patients’ perspective
Today, it is critical to know the needs and expectations of your patients and referring physicians. The best way to do this is to ask your patients what they think, which also will reveal your practice’s strengths and weaknesses. This information can be obtained easily by surveying patients about various aspects of your practice. (Even practices that are full or closed need to evaluate their services periodically and listen to their patients. Changes always occur, and the cup may not “runneth over” forever.)
Tom Peters, the nationally renowned author of In Search of Excellence, has described two keys to success in business:
- Find out what the customer (patient) wants and give him or her more of it
- Find out what the customer (patient) does not want and be sure to avoid it.
Techniques to gather the patient’s perspective
There are five effective techniques for determining how patients perceive your practice and for evaluating your performance and reputation:
- Conduct personal interviews
- Conduct patient surveys
- Create a focus group
- Use a suggestion box
- Commission evaluation by a mystery shopper.
Although I have used all five techniques, my favorite and most cost-effective involves a survey card that is given to every patient on every office visit (FIGURE 1). The card is given to the patient when she checks in, and she can complete it in the reception area or exam room and return it to the receptionist before leaving the practice. The cards are reviewed by a nurse, who addresses positive and negative comments. Most negative comments are addressed with a phone call. If necessary, I respond to the patient’s complaint.
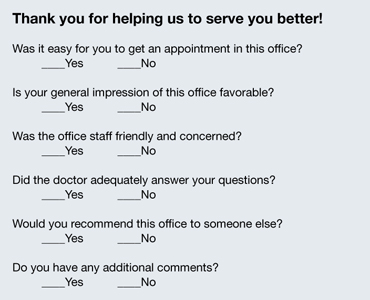
FIGURE 1: Patient survey card
There is another benefit to the survey card. The flip side of the card prompts the patient to write down the three questions she would like you to address on her current visit to the office (FIGURE 2). Conducting the appointment according to these concerns can help keep patients from initiating a last-minute discussion, often after you have closed the chart or electronic medical record, that you don’t have time to address adequately. Since my office has implemented use of this survey card, we seldom get follow-up phone calls from patients about issues they forgot to ask about. The survey card demonstrates that we are listening to the patient and want to be certain that all her questions have been answered at the time of her office visit.
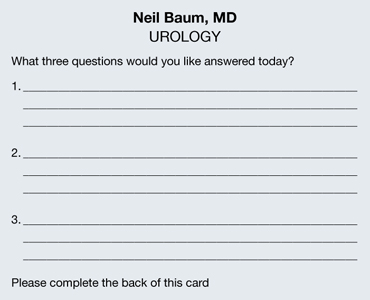
FIGURE 2: Focus of the appointment
Develop an on-time practice philosophy
You know the adage: Timeliness is next to godliness. (Actually, it’s cleanliness that’s next to godliness, but timeliness is vital, too.) The most common complaint patients have about the health-care experience is “waiting for the doctor.” Spending time in the reception area probably accounts for more patient dissatisfaction than any other aspect of medical care. In one recent survey, nearly one in four patients (24%) claimed to have waited 30 minutes or longer. With so many more women entering the marketplace, this statistic is only going to get worse.
In order to gain an accurate picture of what is happening in regard to the schedule in your practice, I suggest conducting a “time and motion” study. For a period of 3 to 5 days, place a sheet on each patient’s record or superbill and log in the following:
- time of her appointment
- time she arrived
- time she left the office
- how much time she spent with her physician.
You will be amazed to discover that patients are waiting 1 or 2 hours or longer to see the physician, and that the physician is spending only 5 minutes with the patient. Ask any patient on a survey if she feels she is getting bang for her buck, and she will answer, “No!”
By conducting a time and motion study, you will discover that there are predictable periods when backlogs occur. Often, these delays are the result of “working a patient in” to the schedule. Unscheduled patients who call to report vaginal bleeding, pelvic pain, urinary tract infection, or another problem are often told to come in without an appointment, but they inevitably displace women already scheduled and delay their visit. This problem affects almost every ObGyn.
One way to avoid this scenario is to create “sacred” time slots. These are 15-minute intervals at the end of the morning or afternoon in which unscheduled patients can be worked into the round of visits. Instead of telling the patient to “just come in,” I tell her to report at a specific time. These time slots cannot be filled with routine appointments. Nor can they be filled prior to 9 am each day. This leaves two or three slots open for patients who must be seen immediately.
Few ObGyns can change health-care policy. But all of us can be more sensitive to our patients’ time and make an effort to see them as soon as possible, thereby eliminating one of patients’ most common complaints: the long wait to see their doctor.
Make the patient’s experience memorable
All of us can provide a diagnosis and treatment strategy for most women’s medical problems. But how many of us can make the experience memorable for the woman? Often, it is a few little things that can be easily and inexpensively performed that make a big difference.
Go with cloth, not paper. There’s a sharp contrast between a paper sheet, a paper gown, and a soft robe. You don’t step out of the shower in a fine hotel and put on a paper robe. If you are offering five-star service, you need to offer five-star amenities. If you want to attract special patients, treat your patients special. It doesn’t cost that much to add a few dozen robes to your office supplies, laundering them after each use and placing them on hangers or in a plastic bag that each patient can use during her visit. I can assure you that this single idea will set you apart from most other ObGyns in your community.
Stirrups are cold! Here’s another idea: Use pads to cover the metal of the stirrups for the pelvic exam. Those stirrups are cold steel, and no woman who is already naked and concerned about her dignity wants to place her feet on those chilly structures. You can have lamb’s wool pads created by a seamstress for a few dollars—or if you prefer to go low-tech, you can use potholders to cover the stirrups.
Warm the speculum. My wife shared with me how uncomfortable it is to have a metal speculum inserted and how much she appreciated her gynecologist warming the instrument with tap water before its insertion. I have found that this saves on the use of lubricant jelly, too, because the water serves as a lubricant!
Keep the temperature in mind. Most medical offices are kept at 70° to 72° F to keep the doctor and staff comfortable. However, when a woman puts on her gown or robe, she often becomes cold and uncomfortable. On days when it is cold outside or the office is cold, use an inexpensive heater to make the room comfortable for the patient.
Talk to your patient “eyeball to eyeball.” You make big points with your patient if you speak to her when she is fully dressed and when your eyes are at the same level as hers. A woman lying on her back in a gown or robe does not hear or recall what her doctor is telling her. However, if the doctor and nurse leave the room and allow the patient to get dressed, and if the doctor sits with the patient without barriers between them, she is far more likely to listen and recall what has been discussed.
Pick up the telephone. I am often asked for my “best” idea to keep patients happy. My numero uno suggestion is to take a few minutes to call the patient at home. Which patients should you call? Women undergoing outpatient studies or procedures, those recently discharged from the hospital, and those who require a little more hand holding and attention. You can be sure that every patient who undergoes a procedure or is discharged from the hospital has questions about the findings, any precautions, medications, and follow-up. A call from a nurse or doctor does a lot to allay her apprehension—and it often keeps the patient from calling the office with her questions and concerns.
My nurse identifies key patients and contacts them at the end of the workday. She is usually able to answer all the questions but may identify two or three that require my attention. She tells the patient what time I will call so she can keep the phone line free.
Calling patients usually takes no more than 5 to 10 minutes a day and provides me with great satisfaction. Patients are usually shocked—and happy—that their physician is calling them at home. The advantages of this strategy include:
- fewer calls from your patients
- more efficient use of your time
- deep appreciation by the patient.
One patient I called at home wrote me a note that I think is worth mentioning: “This is the first time a member of your profession has taken the time to call me at home and check on my condition. Undoubtedly, it will foster a better relationship between you and me.”
Results of an informal poll indicate the answer is mostly “Yes”
As outlined in the article by Neil Baum, MD, the need to keep existing patients happy—and to determine how they’re feeling about your practice—seems as though it should occupy a berth rather high on your list of priorities. To gauge how widespread the practice of measuring patient satisfaction is among ObGyns, we polled our Virtual Board of Editors (VBE) on the subject. Because these physicians range from private practitioners to academic professionals and hospital employees, we find them to be one bellwether of wider practice patterns.
When we asked, 65% of our VBE members reported that they regularly measure the satisfaction of their patients. Among the reasons given for this tactic were corporate policy, but the vast majority of respondents indicated that they “need to know what patients like and don’t like” in order to “improve our services.” As one physician noted, “all practices can improve in some respects.” Regular inquiries about patient satisfaction provide a method and rationale for improvement.
Another respondent observed that the information gained from assessments of patient satisfaction is useful during insurance contracting. Another said, simply, “It’s the right thing to do.”
When asked exactly how they measure patient satisfaction, almost 60% of respondents who regularly assess this component of practice said they use surveys to do so, compared with 14% who use interviews, 17% who make a suggestion box available, and 11% who employ a “mystery shopper” (The percentages add up to more than 100% because some VBE members employ more than one approach.) None of the VBE members reported convening a focus group.
When asked to rate the importance of patient-satisfaction assessments, just over half of all respondents characterized it as “very important.” Only one physician reported that the practice of measuring patient satisfaction is “not important.”
“It is critical—especially for doctors with younger practices who are trying to build a reputation or practice—to get feedback to improve care and increase their patient load,” noted one respondent. Another reported: “We do a detailed satisfaction survey after every surgery on every patient. We actively seek feedback and use our Web site and social media to find ways to improve.”
“We are in a large city (over 500,000 population), so there is competition, and patients have choices,” wrote another VBE member. “In smaller communities, patients may have fewer options and have to accept the few available providers. My basic method of achieving patient satisfaction is outdated: I spend a lot of time per patient, see few patients per day, and try to help with whatever issues they have (not just breast and pelvic). I make less money practicing this way—I accepted a long time ago that really caring for patients means spending more time and being paid less for it.”
Another VBE member said, “I promise what I’ll do for patients, and I keep that promise! I use the telephone as a tool. Patients are very impressed and thankful when I talk to them about their problems and test results.”
—Janelle Yates, Senior Editor
The bottom line
Word of mouth was the time-honored method of attracting new patients for thousands of years. That method still works today. Ensuring that your patients have an outstanding experience during their visit is one of the smartest strategies to market and promote your practice.
We want to hear from you! Tell us what you think.
CLICK HERE to access 10 recent articles on managing your ObGyn practice.
Dr. Baum describes his number one strategy to retain patients (Audiocast, March 2013)
Pillar 2: Attract new patients (May 2013)
Pillar 3: Obtain and maintain physician referrals (June 2013)
Pillar 4: Motivate your staff (August 2013)
The medical landscape has changed. No one is quite certain what the future will hold. One thing we do know: 20 million more Americans, half of them women, will enter the health-care system in the very near future, as the Affordable Care Act continues to unfold. This flood of new patients will affect nearly every ObGyn practice in the country because we lack an adequate increase in the number of physicians to care for them. In the meantime, what can you do to ensure the continued success of your practice? This series focuses on four key areas. I call them the “four pillars”:
- Keep existing patients happy
- Attract new patients
- Nurture relationships with your medical colleagues and other health-care providers, such as physician assistants and nurse practitioners
- Maintain the morale of your staff.
No pillar is more important than the others; all four are necessary to guarantee success.
It is more cost-effective to keep an existing customer than to attract
a new one
In this article, I explain why it is vital to ensure that every patient has a positive experience of your practice, from the moment they make their first telephone call for an appointment, through their wait in the reception area, to the moment they are seen by the staff or the physician, and beyond—when they tell others about their stellar experience.
It’s nice to get new patients, but it is more important to keep the ones you already have. In most professions and businesses, the cost of keeping an established customer is one-fifth the cost of acquiring a new one. Medical practices are no exception. If you are not doing a good job with the patients you already have, spending thousands of dollars on a marketing plan to bring in new patients is pointless. The patients you have right now are the backbone of your practice.
Give your practice a checkup
Look at your practice from your patients’ perspective
Today, it is critical to know the needs and expectations of your patients and referring physicians. The best way to do this is to ask your patients what they think, which also will reveal your practice’s strengths and weaknesses. This information can be obtained easily by surveying patients about various aspects of your practice. (Even practices that are full or closed need to evaluate their services periodically and listen to their patients. Changes always occur, and the cup may not “runneth over” forever.)
Tom Peters, the nationally renowned author of In Search of Excellence, has described two keys to success in business:
- Find out what the customer (patient) wants and give him or her more of it
- Find out what the customer (patient) does not want and be sure to avoid it.
Techniques to gather the patient’s perspective
There are five effective techniques for determining how patients perceive your practice and for evaluating your performance and reputation:
- Conduct personal interviews
- Conduct patient surveys
- Create a focus group
- Use a suggestion box
- Commission evaluation by a mystery shopper.
Although I have used all five techniques, my favorite and most cost-effective involves a survey card that is given to every patient on every office visit (FIGURE 1). The card is given to the patient when she checks in, and she can complete it in the reception area or exam room and return it to the receptionist before leaving the practice. The cards are reviewed by a nurse, who addresses positive and negative comments. Most negative comments are addressed with a phone call. If necessary, I respond to the patient’s complaint.
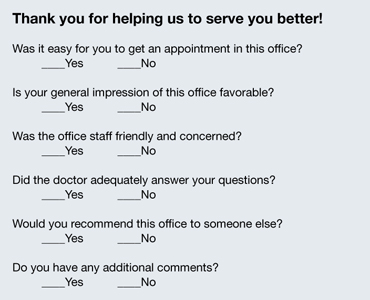
FIGURE 1: Patient survey card
There is another benefit to the survey card. The flip side of the card prompts the patient to write down the three questions she would like you to address on her current visit to the office (FIGURE 2). Conducting the appointment according to these concerns can help keep patients from initiating a last-minute discussion, often after you have closed the chart or electronic medical record, that you don’t have time to address adequately. Since my office has implemented use of this survey card, we seldom get follow-up phone calls from patients about issues they forgot to ask about. The survey card demonstrates that we are listening to the patient and want to be certain that all her questions have been answered at the time of her office visit.
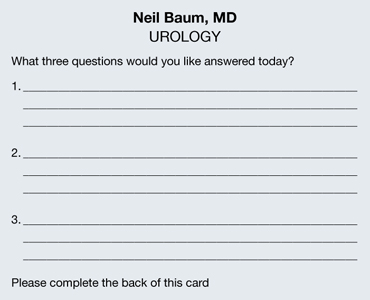
FIGURE 2: Focus of the appointment
Develop an on-time practice philosophy
You know the adage: Timeliness is next to godliness. (Actually, it’s cleanliness that’s next to godliness, but timeliness is vital, too.) The most common complaint patients have about the health-care experience is “waiting for the doctor.” Spending time in the reception area probably accounts for more patient dissatisfaction than any other aspect of medical care. In one recent survey, nearly one in four patients (24%) claimed to have waited 30 minutes or longer. With so many more women entering the marketplace, this statistic is only going to get worse.
In order to gain an accurate picture of what is happening in regard to the schedule in your practice, I suggest conducting a “time and motion” study. For a period of 3 to 5 days, place a sheet on each patient’s record or superbill and log in the following:
- time of her appointment
- time she arrived
- time she left the office
- how much time she spent with her physician.
You will be amazed to discover that patients are waiting 1 or 2 hours or longer to see the physician, and that the physician is spending only 5 minutes with the patient. Ask any patient on a survey if she feels she is getting bang for her buck, and she will answer, “No!”
By conducting a time and motion study, you will discover that there are predictable periods when backlogs occur. Often, these delays are the result of “working a patient in” to the schedule. Unscheduled patients who call to report vaginal bleeding, pelvic pain, urinary tract infection, or another problem are often told to come in without an appointment, but they inevitably displace women already scheduled and delay their visit. This problem affects almost every ObGyn.
One way to avoid this scenario is to create “sacred” time slots. These are 15-minute intervals at the end of the morning or afternoon in which unscheduled patients can be worked into the round of visits. Instead of telling the patient to “just come in,” I tell her to report at a specific time. These time slots cannot be filled with routine appointments. Nor can they be filled prior to 9 am each day. This leaves two or three slots open for patients who must be seen immediately.
Few ObGyns can change health-care policy. But all of us can be more sensitive to our patients’ time and make an effort to see them as soon as possible, thereby eliminating one of patients’ most common complaints: the long wait to see their doctor.
Make the patient’s experience memorable
All of us can provide a diagnosis and treatment strategy for most women’s medical problems. But how many of us can make the experience memorable for the woman? Often, it is a few little things that can be easily and inexpensively performed that make a big difference.
Go with cloth, not paper. There’s a sharp contrast between a paper sheet, a paper gown, and a soft robe. You don’t step out of the shower in a fine hotel and put on a paper robe. If you are offering five-star service, you need to offer five-star amenities. If you want to attract special patients, treat your patients special. It doesn’t cost that much to add a few dozen robes to your office supplies, laundering them after each use and placing them on hangers or in a plastic bag that each patient can use during her visit. I can assure you that this single idea will set you apart from most other ObGyns in your community.
Stirrups are cold! Here’s another idea: Use pads to cover the metal of the stirrups for the pelvic exam. Those stirrups are cold steel, and no woman who is already naked and concerned about her dignity wants to place her feet on those chilly structures. You can have lamb’s wool pads created by a seamstress for a few dollars—or if you prefer to go low-tech, you can use potholders to cover the stirrups.
Warm the speculum. My wife shared with me how uncomfortable it is to have a metal speculum inserted and how much she appreciated her gynecologist warming the instrument with tap water before its insertion. I have found that this saves on the use of lubricant jelly, too, because the water serves as a lubricant!
Keep the temperature in mind. Most medical offices are kept at 70° to 72° F to keep the doctor and staff comfortable. However, when a woman puts on her gown or robe, she often becomes cold and uncomfortable. On days when it is cold outside or the office is cold, use an inexpensive heater to make the room comfortable for the patient.
Talk to your patient “eyeball to eyeball.” You make big points with your patient if you speak to her when she is fully dressed and when your eyes are at the same level as hers. A woman lying on her back in a gown or robe does not hear or recall what her doctor is telling her. However, if the doctor and nurse leave the room and allow the patient to get dressed, and if the doctor sits with the patient without barriers between them, she is far more likely to listen and recall what has been discussed.
Pick up the telephone. I am often asked for my “best” idea to keep patients happy. My numero uno suggestion is to take a few minutes to call the patient at home. Which patients should you call? Women undergoing outpatient studies or procedures, those recently discharged from the hospital, and those who require a little more hand holding and attention. You can be sure that every patient who undergoes a procedure or is discharged from the hospital has questions about the findings, any precautions, medications, and follow-up. A call from a nurse or doctor does a lot to allay her apprehension—and it often keeps the patient from calling the office with her questions and concerns.
My nurse identifies key patients and contacts them at the end of the workday. She is usually able to answer all the questions but may identify two or three that require my attention. She tells the patient what time I will call so she can keep the phone line free.
Calling patients usually takes no more than 5 to 10 minutes a day and provides me with great satisfaction. Patients are usually shocked—and happy—that their physician is calling them at home. The advantages of this strategy include:
- fewer calls from your patients
- more efficient use of your time
- deep appreciation by the patient.
One patient I called at home wrote me a note that I think is worth mentioning: “This is the first time a member of your profession has taken the time to call me at home and check on my condition. Undoubtedly, it will foster a better relationship between you and me.”
Results of an informal poll indicate the answer is mostly “Yes”
As outlined in the article by Neil Baum, MD, the need to keep existing patients happy—and to determine how they’re feeling about your practice—seems as though it should occupy a berth rather high on your list of priorities. To gauge how widespread the practice of measuring patient satisfaction is among ObGyns, we polled our Virtual Board of Editors (VBE) on the subject. Because these physicians range from private practitioners to academic professionals and hospital employees, we find them to be one bellwether of wider practice patterns.
When we asked, 65% of our VBE members reported that they regularly measure the satisfaction of their patients. Among the reasons given for this tactic were corporate policy, but the vast majority of respondents indicated that they “need to know what patients like and don’t like” in order to “improve our services.” As one physician noted, “all practices can improve in some respects.” Regular inquiries about patient satisfaction provide a method and rationale for improvement.
Another respondent observed that the information gained from assessments of patient satisfaction is useful during insurance contracting. Another said, simply, “It’s the right thing to do.”
When asked exactly how they measure patient satisfaction, almost 60% of respondents who regularly assess this component of practice said they use surveys to do so, compared with 14% who use interviews, 17% who make a suggestion box available, and 11% who employ a “mystery shopper” (The percentages add up to more than 100% because some VBE members employ more than one approach.) None of the VBE members reported convening a focus group.
When asked to rate the importance of patient-satisfaction assessments, just over half of all respondents characterized it as “very important.” Only one physician reported that the practice of measuring patient satisfaction is “not important.”
“It is critical—especially for doctors with younger practices who are trying to build a reputation or practice—to get feedback to improve care and increase their patient load,” noted one respondent. Another reported: “We do a detailed satisfaction survey after every surgery on every patient. We actively seek feedback and use our Web site and social media to find ways to improve.”
“We are in a large city (over 500,000 population), so there is competition, and patients have choices,” wrote another VBE member. “In smaller communities, patients may have fewer options and have to accept the few available providers. My basic method of achieving patient satisfaction is outdated: I spend a lot of time per patient, see few patients per day, and try to help with whatever issues they have (not just breast and pelvic). I make less money practicing this way—I accepted a long time ago that really caring for patients means spending more time and being paid less for it.”
Another VBE member said, “I promise what I’ll do for patients, and I keep that promise! I use the telephone as a tool. Patients are very impressed and thankful when I talk to them about their problems and test results.”
—Janelle Yates, Senior Editor
The bottom line
Word of mouth was the time-honored method of attracting new patients for thousands of years. That method still works today. Ensuring that your patients have an outstanding experience during their visit is one of the smartest strategies to market and promote your practice.
We want to hear from you! Tell us what you think.
CLICK HERE to access 10 recent articles on managing your ObGyn practice.
Keep your staff current
It goes without saying that, as a physician, it’s essential to keep your knowledge and skills current. But too many private practitioners overlook the similar needs of their employees.
Continuing education is as important for your staff as for you. Like you, staff members provide better care to patients when they know the latest findings and techniques. They also provide better information: When patients ask questions of your staff, either in the office or over the phone (which happens more often than you probably think), you certainly want their answers to be accurate and up to date.
There are lots of other good reasons to invest in ongoing staff training. It’s a win-win strategy for you, your staff, and for your practice.
The more your employees know, the more productive they will be. Not only will they complete everyday duties more efficiently, they will be stimulated to learn new tasks and accept more responsibility.
Staffers who have learned new skills are more willing to take on new challenges. And the better their skills and the greater their confidence, the less supervision they need from you and the more they become involved in their work.
They also will be happier in their jobs. Investing in your employees’ competence makes them feel valued and appreciated. This leads to reduced turnover, which is often enough to pay for the training.
You probably already do some ongoing education: You do your yearly OSHA training because the law requires it, you run HIPAA updates as necessary (more on those two next month), and you have everyone recertified periodically in basic or advanced CPR (or you should). I’m talking about going beyond the basic stuff, which may satisfy legal requirements but does not motivate your people to loftier goals.
An obvious example is sending your insurance people annually to coding and insurance processing courses – or at the very least, on-line refreshers – so they are always current on the latest third-party changes. The use of outdated or obsolete codes can cost you thousands of dollars every month. Other opportunities include keyboarding and computer courses for staff who work with your computers, and Excel and QuickBooks updates for your bookkeepers.
Continuing education does not have to be costly, and in some cases it can be free. For example, pharmaceutical representatives will be happy to run an in-service for your staff on a new medication or procedure or instrument, or to refresh their memories on an established one. Be sure to make clear to the rep that the presentation must be as objective and impartial as possible, given the obvious potential conflicts of interest involved.
Your office manager should join the Association of Dermatology Administrators & Managers (ADAM). It holds annual meetings at the same time and place as the American Academy of Dermatology winter meetings, with a good selection of refresher courses and lots of opportunities for networking with other managers, either personally or virtually.
Many other venues are available for employee education, either in the cloud and in conventional classrooms. Courses are offered in many relevant subjects – a quick Google search turns up an eclectic mix, including medical terminology, recordkeeping and accounting, laboratory skills, diagnostic tests and procedures, pharmacology and medication administration, patient relations, medical law and ethics, and many others.
By far the most common question I receive on this issue is this: "What if I pay for all that training and the employees leave?" My invariable answer is this: "What if you don’t, and they stay?"
Well-trained employees are vastly preferable to untrained ones, even with the small risk of the occasional staffer who accepts training and then moves on. But in 31 years, it has never happened in my office. In my experience, well-trained employees will stay. Education fosters loyalty. Employees who know that you care enough about them to advance their skills will sense that they have a stake in the practice, and thus will be less likely to want to leave. Furthermore, continuing education will always be cheaper than training new employees from scratch.
In any case, everyone will benefit from a well-trained staff: you, your employees, your practice, and – most importantly – your patients.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J.
It goes without saying that, as a physician, it’s essential to keep your knowledge and skills current. But too many private practitioners overlook the similar needs of their employees.
Continuing education is as important for your staff as for you. Like you, staff members provide better care to patients when they know the latest findings and techniques. They also provide better information: When patients ask questions of your staff, either in the office or over the phone (which happens more often than you probably think), you certainly want their answers to be accurate and up to date.
There are lots of other good reasons to invest in ongoing staff training. It’s a win-win strategy for you, your staff, and for your practice.
The more your employees know, the more productive they will be. Not only will they complete everyday duties more efficiently, they will be stimulated to learn new tasks and accept more responsibility.
Staffers who have learned new skills are more willing to take on new challenges. And the better their skills and the greater their confidence, the less supervision they need from you and the more they become involved in their work.
They also will be happier in their jobs. Investing in your employees’ competence makes them feel valued and appreciated. This leads to reduced turnover, which is often enough to pay for the training.
You probably already do some ongoing education: You do your yearly OSHA training because the law requires it, you run HIPAA updates as necessary (more on those two next month), and you have everyone recertified periodically in basic or advanced CPR (or you should). I’m talking about going beyond the basic stuff, which may satisfy legal requirements but does not motivate your people to loftier goals.
An obvious example is sending your insurance people annually to coding and insurance processing courses – or at the very least, on-line refreshers – so they are always current on the latest third-party changes. The use of outdated or obsolete codes can cost you thousands of dollars every month. Other opportunities include keyboarding and computer courses for staff who work with your computers, and Excel and QuickBooks updates for your bookkeepers.
Continuing education does not have to be costly, and in some cases it can be free. For example, pharmaceutical representatives will be happy to run an in-service for your staff on a new medication or procedure or instrument, or to refresh their memories on an established one. Be sure to make clear to the rep that the presentation must be as objective and impartial as possible, given the obvious potential conflicts of interest involved.
Your office manager should join the Association of Dermatology Administrators & Managers (ADAM). It holds annual meetings at the same time and place as the American Academy of Dermatology winter meetings, with a good selection of refresher courses and lots of opportunities for networking with other managers, either personally or virtually.
Many other venues are available for employee education, either in the cloud and in conventional classrooms. Courses are offered in many relevant subjects – a quick Google search turns up an eclectic mix, including medical terminology, recordkeeping and accounting, laboratory skills, diagnostic tests and procedures, pharmacology and medication administration, patient relations, medical law and ethics, and many others.
By far the most common question I receive on this issue is this: "What if I pay for all that training and the employees leave?" My invariable answer is this: "What if you don’t, and they stay?"
Well-trained employees are vastly preferable to untrained ones, even with the small risk of the occasional staffer who accepts training and then moves on. But in 31 years, it has never happened in my office. In my experience, well-trained employees will stay. Education fosters loyalty. Employees who know that you care enough about them to advance their skills will sense that they have a stake in the practice, and thus will be less likely to want to leave. Furthermore, continuing education will always be cheaper than training new employees from scratch.
In any case, everyone will benefit from a well-trained staff: you, your employees, your practice, and – most importantly – your patients.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J.
It goes without saying that, as a physician, it’s essential to keep your knowledge and skills current. But too many private practitioners overlook the similar needs of their employees.
Continuing education is as important for your staff as for you. Like you, staff members provide better care to patients when they know the latest findings and techniques. They also provide better information: When patients ask questions of your staff, either in the office or over the phone (which happens more often than you probably think), you certainly want their answers to be accurate and up to date.
There are lots of other good reasons to invest in ongoing staff training. It’s a win-win strategy for you, your staff, and for your practice.
The more your employees know, the more productive they will be. Not only will they complete everyday duties more efficiently, they will be stimulated to learn new tasks and accept more responsibility.
Staffers who have learned new skills are more willing to take on new challenges. And the better their skills and the greater their confidence, the less supervision they need from you and the more they become involved in their work.
They also will be happier in their jobs. Investing in your employees’ competence makes them feel valued and appreciated. This leads to reduced turnover, which is often enough to pay for the training.
You probably already do some ongoing education: You do your yearly OSHA training because the law requires it, you run HIPAA updates as necessary (more on those two next month), and you have everyone recertified periodically in basic or advanced CPR (or you should). I’m talking about going beyond the basic stuff, which may satisfy legal requirements but does not motivate your people to loftier goals.
An obvious example is sending your insurance people annually to coding and insurance processing courses – or at the very least, on-line refreshers – so they are always current on the latest third-party changes. The use of outdated or obsolete codes can cost you thousands of dollars every month. Other opportunities include keyboarding and computer courses for staff who work with your computers, and Excel and QuickBooks updates for your bookkeepers.
Continuing education does not have to be costly, and in some cases it can be free. For example, pharmaceutical representatives will be happy to run an in-service for your staff on a new medication or procedure or instrument, or to refresh their memories on an established one. Be sure to make clear to the rep that the presentation must be as objective and impartial as possible, given the obvious potential conflicts of interest involved.
Your office manager should join the Association of Dermatology Administrators & Managers (ADAM). It holds annual meetings at the same time and place as the American Academy of Dermatology winter meetings, with a good selection of refresher courses and lots of opportunities for networking with other managers, either personally or virtually.
Many other venues are available for employee education, either in the cloud and in conventional classrooms. Courses are offered in many relevant subjects – a quick Google search turns up an eclectic mix, including medical terminology, recordkeeping and accounting, laboratory skills, diagnostic tests and procedures, pharmacology and medication administration, patient relations, medical law and ethics, and many others.
By far the most common question I receive on this issue is this: "What if I pay for all that training and the employees leave?" My invariable answer is this: "What if you don’t, and they stay?"
Well-trained employees are vastly preferable to untrained ones, even with the small risk of the occasional staffer who accepts training and then moves on. But in 31 years, it has never happened in my office. In my experience, well-trained employees will stay. Education fosters loyalty. Employees who know that you care enough about them to advance their skills will sense that they have a stake in the practice, and thus will be less likely to want to leave. Furthermore, continuing education will always be cheaper than training new employees from scratch.
In any case, everyone will benefit from a well-trained staff: you, your employees, your practice, and – most importantly – your patients.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J.
Tips to Help Hospital Medicine Group Leaders Know When to Grow Their Service
SHM board member Burke Kealey, MD, SFHM, medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn., says there is no easy way to know when it is the right time to grow. He offers four tips to hospitalist group leaders grappling with the question:
- Benchmark: Use the SHM survey, MGMA data, or local analyses to determine best practices. But don’t be a slave to data that don’t account for the particulars of your payor mix, patient population, etc.
- Network: Meet with group leaders in nearby practices. Talk to administrators. Understand the competitive set for your hospital and know what their data sets are.
- Communicate: Talk to doctors, C-suite executives, and everyone in between. Front-line physicians and nurses often know better than practice heads which resources are needed, and where.
- Stay flexible: Don’t be wedded to needing to grow. Maybe a group has physicians who want extra shifts to handle a new schedule. Maybe the installation of new technology will improve efficiency and eliminate the need for a new physician.
SHM board member Burke Kealey, MD, SFHM, medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn., says there is no easy way to know when it is the right time to grow. He offers four tips to hospitalist group leaders grappling with the question:
- Benchmark: Use the SHM survey, MGMA data, or local analyses to determine best practices. But don’t be a slave to data that don’t account for the particulars of your payor mix, patient population, etc.
- Network: Meet with group leaders in nearby practices. Talk to administrators. Understand the competitive set for your hospital and know what their data sets are.
- Communicate: Talk to doctors, C-suite executives, and everyone in between. Front-line physicians and nurses often know better than practice heads which resources are needed, and where.
- Stay flexible: Don’t be wedded to needing to grow. Maybe a group has physicians who want extra shifts to handle a new schedule. Maybe the installation of new technology will improve efficiency and eliminate the need for a new physician.
SHM board member Burke Kealey, MD, SFHM, medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn., says there is no easy way to know when it is the right time to grow. He offers four tips to hospitalist group leaders grappling with the question:
- Benchmark: Use the SHM survey, MGMA data, or local analyses to determine best practices. But don’t be a slave to data that don’t account for the particulars of your payor mix, patient population, etc.
- Network: Meet with group leaders in nearby practices. Talk to administrators. Understand the competitive set for your hospital and know what their data sets are.
- Communicate: Talk to doctors, C-suite executives, and everyone in between. Front-line physicians and nurses often know better than practice heads which resources are needed, and where.
- Stay flexible: Don’t be wedded to needing to grow. Maybe a group has physicians who want extra shifts to handle a new schedule. Maybe the installation of new technology will improve efficiency and eliminate the need for a new physician.
Fundamentals of Highly Reliable Organizations Could Benefit Hospitalists
Reliability. This sounds like a decent trait. Who wouldn’t want to be described as “reliable”? It sounds reputable whether you’re a person, a car, or a dishwasher. So how does one become or emulate the trait of being reliable, one who is predictable, punctua—“reproducible,” if you will?
Organizational reliability has received a fair bit of press these days. The industries that have come to embrace reliability concepts are those in which failure is easy to come by, and those in which failure is likely to be catastrophic if it occurs. In the medical industry, failure occurs to people, not widgets or machines, so by definition it tends to be catastrophic. These failures generally come in three flavors:
- The expected fails to occur (i.e. a patient with pneumonia does not receive their antibiotics on time);
- The unexpected occurs (i.e. a patient falls and breaks their hip); or
- The unexpected was not previously thought of (i.e. low-risk patient has a PEA arrest).
A fair bit of research has been done on how organizations can become more reliable. In their book “Managing the Unexpected: Assuring High Performance in an Age of Complexity,”1 Karl Weick and Kathleen Sutcliffe studied firefighting, workers on aircraft carriers, and nuclear power plant employees. They all have in common the fundamental similarity that failure in their workplace is catastrophically dangerous, and that they must continuously strive to reduce the risk and/or mitigate effectively. The Agency for Healthcare Research and Quality (AHRQ) specifically studied, through case studies and site visits, how some healthcare organizations have achieved some success in the different domains of reliability.2
What both studies found is that there are five prerequisites that, if done well, lead to an organizational “state of mindfulness.” What they and others have found in their research of highly reliable organizations (HROs) is not that they have failure-free operations, but that they continuously and “mindfully” think about how to be failure-free. Inattention and complacency are the biggest threats to reliability.
The Fundamentals
The first prerequisite is sensitivity to operations. This refers to actively seeking information on how things actually are working, instead of how they are supposed to be working. It is being acutely aware of all operations, including the smallest details: Does the patient have an armband on? Is the nurse washing their hands? Is the whiteboard information correct? Is the bed alarm enabled? It is the state of mind when everyone knows how things should work, look, feel, sound, and can recognize when something is out of bounds.
The next prerequisite is a preoccupation with failure. This refers to a system in which failure and near-misses are completely transparent, and openly and honestly discussed (without inciting individual blame or punitive action), and learned from communally. This “group thought” continually reaffirms the fact that systems, and everyone in them, are completely fallible to errors. It is the complete opposite of inattention and complacency. It is continuously asking “What can go wrong, how can it go wrong, when will it go wrong, and how can I stop it?”
The next prerequisite is reluctance to oversimplify. This does not imply that simplicity is bad, but that oversimplicity is lethal. It forces people and organizations to avoid shortcuts and to not rely on simplistic explanations for situations that need to be complicated. Think of this as making a complicated soufflé; if you leave out a step or an ingredient, the product will be far from a soufflé.
The next prerequisite is deference to expertise. This principle recognizes that authority and/or rank are not equivalent to expertise. This assumes that people and organizations are willing and able to defer decision-making to the person who will make the best decision, not to who ranks highest in the organizational chart. A junior hospitalist might be much more likely to make a good decision on building a new order set than the hospitalist director is.
The last prerequisite is resilience. Webster’s defines resilience as “the capability of a strained body to recover its size and shape after deformation caused especially by compressive stress … an ability to recover from or adjust easily to misfortune or change.” The “compressive stresses” and “misfortune or change” can present in a number of different ways, including bad patient outcomes, bad national press, or bad hospital rankings. A good HRO is not one that does not experience unexpected events, but is one that is not disabled by them. They routinely train and practice for worst-case scenarios. It is easy to “audit” resilience by looking at the organizational response to unexpected events. Are they handled with grace, ease, and speed, or with panic, anxiety, and ongoing uncertainty? Resilience involves adequately functioning despite adversity, recovering well, and learning from the experience.
Take-Home Message
The first three principles relate to how organizations can anticipate and reduce the risk of failure; the last two principles relate to how organizations mitigate the extent or severity of failure when it occurs. Together, they create the state of mindfulness, in which all senses are open and alert for signs of aberrations in the system, and where there is continuous learning of how to make the system function better.
What does this mean for a hospitalist to function in an HRO? Most hospitalists are on the front lines, where they routinely see where and how things can fail. They need to resist the urge to become complacent and remain continuously alert to signals that the system is not functioning for the safety of the patient. And when things do go awry, they need to be part of the resilience plan, to work with their teams to swiftly and effectively mitigate ongoing risks, and defer decision to expertise and not necessarily authority.
It also requires that each of us work within multidisciplinary teams in which all members add to the “state of mindfulness,” including the patient and their families (who very often note “aberrancies” before anyone else does). Think of your hospital as ascribed by Gordon Bethune, the former CEO of Continental Airlines. When asked why all employees received a bonus for on-time departure (instead of only employees on the front line), he held up his wristwatch and said, “What part of this watch don’t you think we need?”
Hospitalists can be powerful motivators for a culture change that empowers all hospital employees to be engaged in anticipating and managing failures—just by being mindful. This is a great place to start.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
References
- Weick KE, Sutcliffe KM. Managing the unexpected: Resilient performance in an age of uncertainty, 2nd ed. 2007: Hoboken, NJ: John Wiley & Sons Inc.
- Agency for Healthcare Research and Quality. Becoming a high reliability organization: operational advice for hospital leaders. Agency for Healthcare Research and Quality website. Available at: http://www.ahrq.gov/qual/hroadvice/. Accessed Dec. 10, 2012.
Reliability. This sounds like a decent trait. Who wouldn’t want to be described as “reliable”? It sounds reputable whether you’re a person, a car, or a dishwasher. So how does one become or emulate the trait of being reliable, one who is predictable, punctua—“reproducible,” if you will?
Organizational reliability has received a fair bit of press these days. The industries that have come to embrace reliability concepts are those in which failure is easy to come by, and those in which failure is likely to be catastrophic if it occurs. In the medical industry, failure occurs to people, not widgets or machines, so by definition it tends to be catastrophic. These failures generally come in three flavors:
- The expected fails to occur (i.e. a patient with pneumonia does not receive their antibiotics on time);
- The unexpected occurs (i.e. a patient falls and breaks their hip); or
- The unexpected was not previously thought of (i.e. low-risk patient has a PEA arrest).
A fair bit of research has been done on how organizations can become more reliable. In their book “Managing the Unexpected: Assuring High Performance in an Age of Complexity,”1 Karl Weick and Kathleen Sutcliffe studied firefighting, workers on aircraft carriers, and nuclear power plant employees. They all have in common the fundamental similarity that failure in their workplace is catastrophically dangerous, and that they must continuously strive to reduce the risk and/or mitigate effectively. The Agency for Healthcare Research and Quality (AHRQ) specifically studied, through case studies and site visits, how some healthcare organizations have achieved some success in the different domains of reliability.2
What both studies found is that there are five prerequisites that, if done well, lead to an organizational “state of mindfulness.” What they and others have found in their research of highly reliable organizations (HROs) is not that they have failure-free operations, but that they continuously and “mindfully” think about how to be failure-free. Inattention and complacency are the biggest threats to reliability.
The Fundamentals
The first prerequisite is sensitivity to operations. This refers to actively seeking information on how things actually are working, instead of how they are supposed to be working. It is being acutely aware of all operations, including the smallest details: Does the patient have an armband on? Is the nurse washing their hands? Is the whiteboard information correct? Is the bed alarm enabled? It is the state of mind when everyone knows how things should work, look, feel, sound, and can recognize when something is out of bounds.
The next prerequisite is a preoccupation with failure. This refers to a system in which failure and near-misses are completely transparent, and openly and honestly discussed (without inciting individual blame or punitive action), and learned from communally. This “group thought” continually reaffirms the fact that systems, and everyone in them, are completely fallible to errors. It is the complete opposite of inattention and complacency. It is continuously asking “What can go wrong, how can it go wrong, when will it go wrong, and how can I stop it?”
The next prerequisite is reluctance to oversimplify. This does not imply that simplicity is bad, but that oversimplicity is lethal. It forces people and organizations to avoid shortcuts and to not rely on simplistic explanations for situations that need to be complicated. Think of this as making a complicated soufflé; if you leave out a step or an ingredient, the product will be far from a soufflé.
The next prerequisite is deference to expertise. This principle recognizes that authority and/or rank are not equivalent to expertise. This assumes that people and organizations are willing and able to defer decision-making to the person who will make the best decision, not to who ranks highest in the organizational chart. A junior hospitalist might be much more likely to make a good decision on building a new order set than the hospitalist director is.
The last prerequisite is resilience. Webster’s defines resilience as “the capability of a strained body to recover its size and shape after deformation caused especially by compressive stress … an ability to recover from or adjust easily to misfortune or change.” The “compressive stresses” and “misfortune or change” can present in a number of different ways, including bad patient outcomes, bad national press, or bad hospital rankings. A good HRO is not one that does not experience unexpected events, but is one that is not disabled by them. They routinely train and practice for worst-case scenarios. It is easy to “audit” resilience by looking at the organizational response to unexpected events. Are they handled with grace, ease, and speed, or with panic, anxiety, and ongoing uncertainty? Resilience involves adequately functioning despite adversity, recovering well, and learning from the experience.
Take-Home Message
The first three principles relate to how organizations can anticipate and reduce the risk of failure; the last two principles relate to how organizations mitigate the extent or severity of failure when it occurs. Together, they create the state of mindfulness, in which all senses are open and alert for signs of aberrations in the system, and where there is continuous learning of how to make the system function better.
What does this mean for a hospitalist to function in an HRO? Most hospitalists are on the front lines, where they routinely see where and how things can fail. They need to resist the urge to become complacent and remain continuously alert to signals that the system is not functioning for the safety of the patient. And when things do go awry, they need to be part of the resilience plan, to work with their teams to swiftly and effectively mitigate ongoing risks, and defer decision to expertise and not necessarily authority.
It also requires that each of us work within multidisciplinary teams in which all members add to the “state of mindfulness,” including the patient and their families (who very often note “aberrancies” before anyone else does). Think of your hospital as ascribed by Gordon Bethune, the former CEO of Continental Airlines. When asked why all employees received a bonus for on-time departure (instead of only employees on the front line), he held up his wristwatch and said, “What part of this watch don’t you think we need?”
Hospitalists can be powerful motivators for a culture change that empowers all hospital employees to be engaged in anticipating and managing failures—just by being mindful. This is a great place to start.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
References
- Weick KE, Sutcliffe KM. Managing the unexpected: Resilient performance in an age of uncertainty, 2nd ed. 2007: Hoboken, NJ: John Wiley & Sons Inc.
- Agency for Healthcare Research and Quality. Becoming a high reliability organization: operational advice for hospital leaders. Agency for Healthcare Research and Quality website. Available at: http://www.ahrq.gov/qual/hroadvice/. Accessed Dec. 10, 2012.
Reliability. This sounds like a decent trait. Who wouldn’t want to be described as “reliable”? It sounds reputable whether you’re a person, a car, or a dishwasher. So how does one become or emulate the trait of being reliable, one who is predictable, punctua—“reproducible,” if you will?
Organizational reliability has received a fair bit of press these days. The industries that have come to embrace reliability concepts are those in which failure is easy to come by, and those in which failure is likely to be catastrophic if it occurs. In the medical industry, failure occurs to people, not widgets or machines, so by definition it tends to be catastrophic. These failures generally come in three flavors:
- The expected fails to occur (i.e. a patient with pneumonia does not receive their antibiotics on time);
- The unexpected occurs (i.e. a patient falls and breaks their hip); or
- The unexpected was not previously thought of (i.e. low-risk patient has a PEA arrest).
A fair bit of research has been done on how organizations can become more reliable. In their book “Managing the Unexpected: Assuring High Performance in an Age of Complexity,”1 Karl Weick and Kathleen Sutcliffe studied firefighting, workers on aircraft carriers, and nuclear power plant employees. They all have in common the fundamental similarity that failure in their workplace is catastrophically dangerous, and that they must continuously strive to reduce the risk and/or mitigate effectively. The Agency for Healthcare Research and Quality (AHRQ) specifically studied, through case studies and site visits, how some healthcare organizations have achieved some success in the different domains of reliability.2
What both studies found is that there are five prerequisites that, if done well, lead to an organizational “state of mindfulness.” What they and others have found in their research of highly reliable organizations (HROs) is not that they have failure-free operations, but that they continuously and “mindfully” think about how to be failure-free. Inattention and complacency are the biggest threats to reliability.
The Fundamentals
The first prerequisite is sensitivity to operations. This refers to actively seeking information on how things actually are working, instead of how they are supposed to be working. It is being acutely aware of all operations, including the smallest details: Does the patient have an armband on? Is the nurse washing their hands? Is the whiteboard information correct? Is the bed alarm enabled? It is the state of mind when everyone knows how things should work, look, feel, sound, and can recognize when something is out of bounds.
The next prerequisite is a preoccupation with failure. This refers to a system in which failure and near-misses are completely transparent, and openly and honestly discussed (without inciting individual blame or punitive action), and learned from communally. This “group thought” continually reaffirms the fact that systems, and everyone in them, are completely fallible to errors. It is the complete opposite of inattention and complacency. It is continuously asking “What can go wrong, how can it go wrong, when will it go wrong, and how can I stop it?”
The next prerequisite is reluctance to oversimplify. This does not imply that simplicity is bad, but that oversimplicity is lethal. It forces people and organizations to avoid shortcuts and to not rely on simplistic explanations for situations that need to be complicated. Think of this as making a complicated soufflé; if you leave out a step or an ingredient, the product will be far from a soufflé.
The next prerequisite is deference to expertise. This principle recognizes that authority and/or rank are not equivalent to expertise. This assumes that people and organizations are willing and able to defer decision-making to the person who will make the best decision, not to who ranks highest in the organizational chart. A junior hospitalist might be much more likely to make a good decision on building a new order set than the hospitalist director is.
The last prerequisite is resilience. Webster’s defines resilience as “the capability of a strained body to recover its size and shape after deformation caused especially by compressive stress … an ability to recover from or adjust easily to misfortune or change.” The “compressive stresses” and “misfortune or change” can present in a number of different ways, including bad patient outcomes, bad national press, or bad hospital rankings. A good HRO is not one that does not experience unexpected events, but is one that is not disabled by them. They routinely train and practice for worst-case scenarios. It is easy to “audit” resilience by looking at the organizational response to unexpected events. Are they handled with grace, ease, and speed, or with panic, anxiety, and ongoing uncertainty? Resilience involves adequately functioning despite adversity, recovering well, and learning from the experience.
Take-Home Message
The first three principles relate to how organizations can anticipate and reduce the risk of failure; the last two principles relate to how organizations mitigate the extent or severity of failure when it occurs. Together, they create the state of mindfulness, in which all senses are open and alert for signs of aberrations in the system, and where there is continuous learning of how to make the system function better.
What does this mean for a hospitalist to function in an HRO? Most hospitalists are on the front lines, where they routinely see where and how things can fail. They need to resist the urge to become complacent and remain continuously alert to signals that the system is not functioning for the safety of the patient. And when things do go awry, they need to be part of the resilience plan, to work with their teams to swiftly and effectively mitigate ongoing risks, and defer decision to expertise and not necessarily authority.
It also requires that each of us work within multidisciplinary teams in which all members add to the “state of mindfulness,” including the patient and their families (who very often note “aberrancies” before anyone else does). Think of your hospital as ascribed by Gordon Bethune, the former CEO of Continental Airlines. When asked why all employees received a bonus for on-time departure (instead of only employees on the front line), he held up his wristwatch and said, “What part of this watch don’t you think we need?”
Hospitalists can be powerful motivators for a culture change that empowers all hospital employees to be engaged in anticipating and managing failures—just by being mindful. This is a great place to start.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
References
- Weick KE, Sutcliffe KM. Managing the unexpected: Resilient performance in an age of uncertainty, 2nd ed. 2007: Hoboken, NJ: John Wiley & Sons Inc.
- Agency for Healthcare Research and Quality. Becoming a high reliability organization: operational advice for hospital leaders. Agency for Healthcare Research and Quality website. Available at: http://www.ahrq.gov/qual/hroadvice/. Accessed Dec. 10, 2012.
Hospital Medicine Experts Outline Criteria To Consider Before Growing Your Group
—Brian Hazen, MD, medical director, Inova Fairfax Hospital Group, Fairfax, Va.
Ilan Alhadeff, MD, SFHM, program medical director for Cogent HMG at Hackensack University Medical Center in Hackensack, N.J., pays a lot of attention to the work relative-value units (wRVUs) his hospitalists are producing and the number of encounters they’re tallying. But he’s not particularly worried about what he sees on a daily, weekly, or even monthly basis; he takes a monthslong view of his data when he wants to forecast whether he is going to need to think about adding staff.
“When you look at months, you can start seeing trends,” Dr. Alhadeff says. “Let’s say there’s 16 to 18 average encounters. If your average is 16, you’re saying, ‘OK, you’re on the lower end of your normal.’ And if your average is 18, you’re on the higher end of normal. But if you start seeing 18 every month, odds are you’re going to start getting to 19. So at that point, that’s raising the thought that we need to start thinking about bringing someone else on.”
It’s a dance HM group leaders around the country have to do when confronted with the age-old question: Should we expand our service? The answer is more art than science, experts say, as there is no standardized formula for knowing when your HM group should request more support from administration to add an FTE—or two or three. And, in a nod to the HM adage that if you’ve seen one HM group (HMG), then you’ve seen one HMG, the roadmap to expansion varies from place to place. But in a series of interviews with The Hospitalist, physicians, consultants, and management experts suggest there are broad themes that guide the process, including:
- Data. Dashboard metrics, such as average daily census (ADC), wRVUs, patient encounters, and length of stay (LOS), must be quantified. No discussion on expansion can be intelligibly made without a firm understanding of where a practice currently stands.
- Benchmarking. Collating figures isn’t enough. Measure your group against other local HMGs, regional groups, and national standards. SHM’s 2012 State of Hospital Medicine report is a good place to start.
- Scope or schedule. Pushing into new business lines (e.g. orthopedic comanagement) often requires new staff, as does adding shifts to provide 24-hour on-site coverage. Those arguments are different from the case to be made for expanding based on increased patient encounters.
- Physician buy-in. Group leaders cannot unilaterally determine it’s time to add staff, particularly in small-group settings in which hiring a new physician means taking revenue away from the existing group, if only in the short term. Talk with group members before embarking on expansion. Keep track of physician turnover. If hospitalists are leaving often, it could be a sign the group is understaffed.
- Administrative buy-in. If a group leader’s request for a new hire comes without months of conversation ahead of it, it’s likely too late. Prepare C-suite executives in advance about potential growth needs so the discussion does not feel like a surprise.
- Know your market. Don’t wait until a new active-adult community floods the hospital with patients to begin analyzing the impact new residents might have. The same goes for companies that are bringing thousands of new workers to an area.
- Prepare to do nothing. Too often, group leaders think the easiest solution is hiring a physician to lessen workload. Instead, exhaust improved efficiency options and infrastructure improvements that could accomplish the same goal.
“There is no one specific measure,” says Burke Kealey, MD, SFHM, medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn., and an SHM board member. “You have to look at it from several different aspects, and all or most need to line up and say that, yes, you could use more help.”
Practice Analysis
Dr. Kealey, board liaison to SHM’s Practice Analysis Committee, says that benchmarking might be among the most important first steps in determining the right time to grow a practice. Group leaders should keep in mind, though, that comparative analysis to outside measures is only step one of gauging a group’s performance.
“The external benchmarking is easy,” he says. “You can look at SHM survey data. There are a lot of places that will do local market surveys; that’s easy stuff to look at. It’s the internal stuff that’s a bit harder to make the case for, ‘OK, yes, I am a little below the national benchmarks, but here’s why.’”
In those instances, group leaders need to “look at the value equation” and engage hospital administrators in a discussion on why such metrics as wRVUs and ADC might not match local, regional, or national standards. Perhaps a hospital has a lower payor mix than the sample pool, or comparable regional institutions have a better mix of medical and surgical comanagement populations. Regardless of the details of the tailored explanation, the conversation must be one that’s ongoing between a group leader and the C-suite or it is likely to fail, Dr. Kealey says.
“It really gets to the partnership between the hospital and the hospitalist group and working together throughout the whole year, and not just looking at staffing needs, but looking at the hospital’s quality,” he adds. “It’s looking at [the hospital’s] ability to retain the surgeons and the specialists. It’s the leadership that you’re providing. It’s showing that you’re a real partner, so that when it does come time to make that value argument, that we need to grow...there is buy-in.
“If you’re not a true partner and you just come in as an adversary, I think your odds of success are not very high.”
Steve Sloan, MD, a partner at AIM Hospitalist Group of Westmont, Ill., says that group leaders would be wise to obtain input from all of their physicians before adding a new doctor, as each new hire impacts compensation for existing staff members. In Dr. Sloan’s 16-member group, 11 physicians are partners who discuss growth plans. The other doctors are on partnership tracks. And while that makes discussions more difficult than when nine physicians formed the group in 2007, up-front dialogue is crucial, Dr. Sloan says.
“We try to get all the partners together to make major decisions, such as hiring,” he says. “We don’t need everyone involved in every decision, but it’s not just one or two people making the decision.”
The conversation about growth also differs if new hires are needed to move the group into a new business line or if the group is adding staff to deal with its current patient load. Both require a business case for expansion to be made, but either way, codifying expectations with hospital clients is another way to streamline the growth process, says Dr. Alhadeff. His group contracts with his hospital to provide services and has the ability to autonomously add or delete staff as needed. Although personnel moves don’t require prior approval from the hospital, there is “an expected fiscal responsibility on our end and predetermined agreement do so.”
The group also keeps administrative stakeholders updated to make sure everyone is on the same page. Other groups might delineate in a contract what thresholds need to be met for expansion to be viable.
“It needs to be agreed upon,” Dr. Alhadeff says. “I like the flexibility of being able to determine within our company what we’re doing. But in answer to that, there are unintentional consequences. If we determine that we’re going to bring on someone else, and then we see after a few months that there is not enough volume to support this new physician, we could run into a problem. We will then have to make a financial decision, and the worst thing is to have to fire someone.”
Dr. Alhadeff also worries about the flipside: failing to hire when staff is overworked.
“We run that risk also,” he says. “We are walking a tightrope all the time, and we need to balance that tightrope.”

—Kenneth Hertz, FACMPE, principal, Medical Group Management Association Health Care Consulting Group, Denver
The Long View
Another tightrope is timing. Kenneth Hertz, FACMPE, principal of the Medical Group Management Association’s Health Care Consulting Group, says that it can take six months or longer to hire a physician, which means group leaders need to have a continual focus on whether growth is needed or will soon be needed. He suggests forecasting at least 12 to 18 months in advance to stay ahead of staffing needs.
Unfortunately, he says, analysis often gets put on hold in the shuffle of dealing with daily duties. “This is kind of generic to practice administrators, who are putting out fires almost every day. And when you’re putting out fires every day, you don’t have the luxury and the time to look out there and see what’s happening and know everything that’s going on,” he says. “They need to understand the importance of it and how all the pieces tie in together.”
Brian Hazen, MD, medical director of Inova Fairfax Hospital Group in Fairfax, Va., says an important approach is to realize growth isn’t always a good thing. HM group leaders often want to grow before they have stabilized their existing business lines, he says, and that can be the worst tack to take. He also notes that a group leader should ingratiate their program into the fabric of their hospital and not just rely on data to make the argument of the group’s value. That means putting hospitalists on committees, spearheading safety programs, and being seen as a partner in the institution.
“Job One is always patient safety and physician sanity,” he says. “If you are careful about growth and buy-in, and you do the committee work and support everybody so that you’re firmly entrenched in the hospital as a value, it’s much safer to grow. Growing for the sake of growing, you risk overexpansion, and that’s dangerous.”
Many hospitalist groups looking to grow will use locum tenens to bridge the staffing gap while they hire new employees (see “No Strings Attached,” December 2012, p. 36), but Dr. Hazen says without a longer view, that only serves as a Band-Aid.
Hertz, the consultant, often uses an analogy to show how important it is to be constantly planning ahead of the growth curve.
“It is a little bit like building roads,” he says. “Once you decide you need to add two lanes, by the time those are finished, you realize we really need to add two more lanes.”
Richard Quinn is a freelance writer in New Jersey.
—Brian Hazen, MD, medical director, Inova Fairfax Hospital Group, Fairfax, Va.
Ilan Alhadeff, MD, SFHM, program medical director for Cogent HMG at Hackensack University Medical Center in Hackensack, N.J., pays a lot of attention to the work relative-value units (wRVUs) his hospitalists are producing and the number of encounters they’re tallying. But he’s not particularly worried about what he sees on a daily, weekly, or even monthly basis; he takes a monthslong view of his data when he wants to forecast whether he is going to need to think about adding staff.
“When you look at months, you can start seeing trends,” Dr. Alhadeff says. “Let’s say there’s 16 to 18 average encounters. If your average is 16, you’re saying, ‘OK, you’re on the lower end of your normal.’ And if your average is 18, you’re on the higher end of normal. But if you start seeing 18 every month, odds are you’re going to start getting to 19. So at that point, that’s raising the thought that we need to start thinking about bringing someone else on.”
It’s a dance HM group leaders around the country have to do when confronted with the age-old question: Should we expand our service? The answer is more art than science, experts say, as there is no standardized formula for knowing when your HM group should request more support from administration to add an FTE—or two or three. And, in a nod to the HM adage that if you’ve seen one HM group (HMG), then you’ve seen one HMG, the roadmap to expansion varies from place to place. But in a series of interviews with The Hospitalist, physicians, consultants, and management experts suggest there are broad themes that guide the process, including:
- Data. Dashboard metrics, such as average daily census (ADC), wRVUs, patient encounters, and length of stay (LOS), must be quantified. No discussion on expansion can be intelligibly made without a firm understanding of where a practice currently stands.
- Benchmarking. Collating figures isn’t enough. Measure your group against other local HMGs, regional groups, and national standards. SHM’s 2012 State of Hospital Medicine report is a good place to start.
- Scope or schedule. Pushing into new business lines (e.g. orthopedic comanagement) often requires new staff, as does adding shifts to provide 24-hour on-site coverage. Those arguments are different from the case to be made for expanding based on increased patient encounters.
- Physician buy-in. Group leaders cannot unilaterally determine it’s time to add staff, particularly in small-group settings in which hiring a new physician means taking revenue away from the existing group, if only in the short term. Talk with group members before embarking on expansion. Keep track of physician turnover. If hospitalists are leaving often, it could be a sign the group is understaffed.
- Administrative buy-in. If a group leader’s request for a new hire comes without months of conversation ahead of it, it’s likely too late. Prepare C-suite executives in advance about potential growth needs so the discussion does not feel like a surprise.
- Know your market. Don’t wait until a new active-adult community floods the hospital with patients to begin analyzing the impact new residents might have. The same goes for companies that are bringing thousands of new workers to an area.
- Prepare to do nothing. Too often, group leaders think the easiest solution is hiring a physician to lessen workload. Instead, exhaust improved efficiency options and infrastructure improvements that could accomplish the same goal.
“There is no one specific measure,” says Burke Kealey, MD, SFHM, medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn., and an SHM board member. “You have to look at it from several different aspects, and all or most need to line up and say that, yes, you could use more help.”
Practice Analysis
Dr. Kealey, board liaison to SHM’s Practice Analysis Committee, says that benchmarking might be among the most important first steps in determining the right time to grow a practice. Group leaders should keep in mind, though, that comparative analysis to outside measures is only step one of gauging a group’s performance.
“The external benchmarking is easy,” he says. “You can look at SHM survey data. There are a lot of places that will do local market surveys; that’s easy stuff to look at. It’s the internal stuff that’s a bit harder to make the case for, ‘OK, yes, I am a little below the national benchmarks, but here’s why.’”
In those instances, group leaders need to “look at the value equation” and engage hospital administrators in a discussion on why such metrics as wRVUs and ADC might not match local, regional, or national standards. Perhaps a hospital has a lower payor mix than the sample pool, or comparable regional institutions have a better mix of medical and surgical comanagement populations. Regardless of the details of the tailored explanation, the conversation must be one that’s ongoing between a group leader and the C-suite or it is likely to fail, Dr. Kealey says.
“It really gets to the partnership between the hospital and the hospitalist group and working together throughout the whole year, and not just looking at staffing needs, but looking at the hospital’s quality,” he adds. “It’s looking at [the hospital’s] ability to retain the surgeons and the specialists. It’s the leadership that you’re providing. It’s showing that you’re a real partner, so that when it does come time to make that value argument, that we need to grow...there is buy-in.
“If you’re not a true partner and you just come in as an adversary, I think your odds of success are not very high.”
Steve Sloan, MD, a partner at AIM Hospitalist Group of Westmont, Ill., says that group leaders would be wise to obtain input from all of their physicians before adding a new doctor, as each new hire impacts compensation for existing staff members. In Dr. Sloan’s 16-member group, 11 physicians are partners who discuss growth plans. The other doctors are on partnership tracks. And while that makes discussions more difficult than when nine physicians formed the group in 2007, up-front dialogue is crucial, Dr. Sloan says.
“We try to get all the partners together to make major decisions, such as hiring,” he says. “We don’t need everyone involved in every decision, but it’s not just one or two people making the decision.”
The conversation about growth also differs if new hires are needed to move the group into a new business line or if the group is adding staff to deal with its current patient load. Both require a business case for expansion to be made, but either way, codifying expectations with hospital clients is another way to streamline the growth process, says Dr. Alhadeff. His group contracts with his hospital to provide services and has the ability to autonomously add or delete staff as needed. Although personnel moves don’t require prior approval from the hospital, there is “an expected fiscal responsibility on our end and predetermined agreement do so.”
The group also keeps administrative stakeholders updated to make sure everyone is on the same page. Other groups might delineate in a contract what thresholds need to be met for expansion to be viable.
“It needs to be agreed upon,” Dr. Alhadeff says. “I like the flexibility of being able to determine within our company what we’re doing. But in answer to that, there are unintentional consequences. If we determine that we’re going to bring on someone else, and then we see after a few months that there is not enough volume to support this new physician, we could run into a problem. We will then have to make a financial decision, and the worst thing is to have to fire someone.”
Dr. Alhadeff also worries about the flipside: failing to hire when staff is overworked.
“We run that risk also,” he says. “We are walking a tightrope all the time, and we need to balance that tightrope.”

—Kenneth Hertz, FACMPE, principal, Medical Group Management Association Health Care Consulting Group, Denver
The Long View
Another tightrope is timing. Kenneth Hertz, FACMPE, principal of the Medical Group Management Association’s Health Care Consulting Group, says that it can take six months or longer to hire a physician, which means group leaders need to have a continual focus on whether growth is needed or will soon be needed. He suggests forecasting at least 12 to 18 months in advance to stay ahead of staffing needs.
Unfortunately, he says, analysis often gets put on hold in the shuffle of dealing with daily duties. “This is kind of generic to practice administrators, who are putting out fires almost every day. And when you’re putting out fires every day, you don’t have the luxury and the time to look out there and see what’s happening and know everything that’s going on,” he says. “They need to understand the importance of it and how all the pieces tie in together.”
Brian Hazen, MD, medical director of Inova Fairfax Hospital Group in Fairfax, Va., says an important approach is to realize growth isn’t always a good thing. HM group leaders often want to grow before they have stabilized their existing business lines, he says, and that can be the worst tack to take. He also notes that a group leader should ingratiate their program into the fabric of their hospital and not just rely on data to make the argument of the group’s value. That means putting hospitalists on committees, spearheading safety programs, and being seen as a partner in the institution.
“Job One is always patient safety and physician sanity,” he says. “If you are careful about growth and buy-in, and you do the committee work and support everybody so that you’re firmly entrenched in the hospital as a value, it’s much safer to grow. Growing for the sake of growing, you risk overexpansion, and that’s dangerous.”
Many hospitalist groups looking to grow will use locum tenens to bridge the staffing gap while they hire new employees (see “No Strings Attached,” December 2012, p. 36), but Dr. Hazen says without a longer view, that only serves as a Band-Aid.
Hertz, the consultant, often uses an analogy to show how important it is to be constantly planning ahead of the growth curve.
“It is a little bit like building roads,” he says. “Once you decide you need to add two lanes, by the time those are finished, you realize we really need to add two more lanes.”
Richard Quinn is a freelance writer in New Jersey.
—Brian Hazen, MD, medical director, Inova Fairfax Hospital Group, Fairfax, Va.
Ilan Alhadeff, MD, SFHM, program medical director for Cogent HMG at Hackensack University Medical Center in Hackensack, N.J., pays a lot of attention to the work relative-value units (wRVUs) his hospitalists are producing and the number of encounters they’re tallying. But he’s not particularly worried about what he sees on a daily, weekly, or even monthly basis; he takes a monthslong view of his data when he wants to forecast whether he is going to need to think about adding staff.
“When you look at months, you can start seeing trends,” Dr. Alhadeff says. “Let’s say there’s 16 to 18 average encounters. If your average is 16, you’re saying, ‘OK, you’re on the lower end of your normal.’ And if your average is 18, you’re on the higher end of normal. But if you start seeing 18 every month, odds are you’re going to start getting to 19. So at that point, that’s raising the thought that we need to start thinking about bringing someone else on.”
It’s a dance HM group leaders around the country have to do when confronted with the age-old question: Should we expand our service? The answer is more art than science, experts say, as there is no standardized formula for knowing when your HM group should request more support from administration to add an FTE—or two or three. And, in a nod to the HM adage that if you’ve seen one HM group (HMG), then you’ve seen one HMG, the roadmap to expansion varies from place to place. But in a series of interviews with The Hospitalist, physicians, consultants, and management experts suggest there are broad themes that guide the process, including:
- Data. Dashboard metrics, such as average daily census (ADC), wRVUs, patient encounters, and length of stay (LOS), must be quantified. No discussion on expansion can be intelligibly made without a firm understanding of where a practice currently stands.
- Benchmarking. Collating figures isn’t enough. Measure your group against other local HMGs, regional groups, and national standards. SHM’s 2012 State of Hospital Medicine report is a good place to start.
- Scope or schedule. Pushing into new business lines (e.g. orthopedic comanagement) often requires new staff, as does adding shifts to provide 24-hour on-site coverage. Those arguments are different from the case to be made for expanding based on increased patient encounters.
- Physician buy-in. Group leaders cannot unilaterally determine it’s time to add staff, particularly in small-group settings in which hiring a new physician means taking revenue away from the existing group, if only in the short term. Talk with group members before embarking on expansion. Keep track of physician turnover. If hospitalists are leaving often, it could be a sign the group is understaffed.
- Administrative buy-in. If a group leader’s request for a new hire comes without months of conversation ahead of it, it’s likely too late. Prepare C-suite executives in advance about potential growth needs so the discussion does not feel like a surprise.
- Know your market. Don’t wait until a new active-adult community floods the hospital with patients to begin analyzing the impact new residents might have. The same goes for companies that are bringing thousands of new workers to an area.
- Prepare to do nothing. Too often, group leaders think the easiest solution is hiring a physician to lessen workload. Instead, exhaust improved efficiency options and infrastructure improvements that could accomplish the same goal.
“There is no one specific measure,” says Burke Kealey, MD, SFHM, medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn., and an SHM board member. “You have to look at it from several different aspects, and all or most need to line up and say that, yes, you could use more help.”
Practice Analysis
Dr. Kealey, board liaison to SHM’s Practice Analysis Committee, says that benchmarking might be among the most important first steps in determining the right time to grow a practice. Group leaders should keep in mind, though, that comparative analysis to outside measures is only step one of gauging a group’s performance.
“The external benchmarking is easy,” he says. “You can look at SHM survey data. There are a lot of places that will do local market surveys; that’s easy stuff to look at. It’s the internal stuff that’s a bit harder to make the case for, ‘OK, yes, I am a little below the national benchmarks, but here’s why.’”
In those instances, group leaders need to “look at the value equation” and engage hospital administrators in a discussion on why such metrics as wRVUs and ADC might not match local, regional, or national standards. Perhaps a hospital has a lower payor mix than the sample pool, or comparable regional institutions have a better mix of medical and surgical comanagement populations. Regardless of the details of the tailored explanation, the conversation must be one that’s ongoing between a group leader and the C-suite or it is likely to fail, Dr. Kealey says.
“It really gets to the partnership between the hospital and the hospitalist group and working together throughout the whole year, and not just looking at staffing needs, but looking at the hospital’s quality,” he adds. “It’s looking at [the hospital’s] ability to retain the surgeons and the specialists. It’s the leadership that you’re providing. It’s showing that you’re a real partner, so that when it does come time to make that value argument, that we need to grow...there is buy-in.
“If you’re not a true partner and you just come in as an adversary, I think your odds of success are not very high.”
Steve Sloan, MD, a partner at AIM Hospitalist Group of Westmont, Ill., says that group leaders would be wise to obtain input from all of their physicians before adding a new doctor, as each new hire impacts compensation for existing staff members. In Dr. Sloan’s 16-member group, 11 physicians are partners who discuss growth plans. The other doctors are on partnership tracks. And while that makes discussions more difficult than when nine physicians formed the group in 2007, up-front dialogue is crucial, Dr. Sloan says.
“We try to get all the partners together to make major decisions, such as hiring,” he says. “We don’t need everyone involved in every decision, but it’s not just one or two people making the decision.”
The conversation about growth also differs if new hires are needed to move the group into a new business line or if the group is adding staff to deal with its current patient load. Both require a business case for expansion to be made, but either way, codifying expectations with hospital clients is another way to streamline the growth process, says Dr. Alhadeff. His group contracts with his hospital to provide services and has the ability to autonomously add or delete staff as needed. Although personnel moves don’t require prior approval from the hospital, there is “an expected fiscal responsibility on our end and predetermined agreement do so.”
The group also keeps administrative stakeholders updated to make sure everyone is on the same page. Other groups might delineate in a contract what thresholds need to be met for expansion to be viable.
“It needs to be agreed upon,” Dr. Alhadeff says. “I like the flexibility of being able to determine within our company what we’re doing. But in answer to that, there are unintentional consequences. If we determine that we’re going to bring on someone else, and then we see after a few months that there is not enough volume to support this new physician, we could run into a problem. We will then have to make a financial decision, and the worst thing is to have to fire someone.”
Dr. Alhadeff also worries about the flipside: failing to hire when staff is overworked.
“We run that risk also,” he says. “We are walking a tightrope all the time, and we need to balance that tightrope.”

—Kenneth Hertz, FACMPE, principal, Medical Group Management Association Health Care Consulting Group, Denver
The Long View
Another tightrope is timing. Kenneth Hertz, FACMPE, principal of the Medical Group Management Association’s Health Care Consulting Group, says that it can take six months or longer to hire a physician, which means group leaders need to have a continual focus on whether growth is needed or will soon be needed. He suggests forecasting at least 12 to 18 months in advance to stay ahead of staffing needs.
Unfortunately, he says, analysis often gets put on hold in the shuffle of dealing with daily duties. “This is kind of generic to practice administrators, who are putting out fires almost every day. And when you’re putting out fires every day, you don’t have the luxury and the time to look out there and see what’s happening and know everything that’s going on,” he says. “They need to understand the importance of it and how all the pieces tie in together.”
Brian Hazen, MD, medical director of Inova Fairfax Hospital Group in Fairfax, Va., says an important approach is to realize growth isn’t always a good thing. HM group leaders often want to grow before they have stabilized their existing business lines, he says, and that can be the worst tack to take. He also notes that a group leader should ingratiate their program into the fabric of their hospital and not just rely on data to make the argument of the group’s value. That means putting hospitalists on committees, spearheading safety programs, and being seen as a partner in the institution.
“Job One is always patient safety and physician sanity,” he says. “If you are careful about growth and buy-in, and you do the committee work and support everybody so that you’re firmly entrenched in the hospital as a value, it’s much safer to grow. Growing for the sake of growing, you risk overexpansion, and that’s dangerous.”
Many hospitalist groups looking to grow will use locum tenens to bridge the staffing gap while they hire new employees (see “No Strings Attached,” December 2012, p. 36), but Dr. Hazen says without a longer view, that only serves as a Band-Aid.
Hertz, the consultant, often uses an analogy to show how important it is to be constantly planning ahead of the growth curve.
“It is a little bit like building roads,” he says. “Once you decide you need to add two lanes, by the time those are finished, you realize we really need to add two more lanes.”
Richard Quinn is a freelance writer in New Jersey.